

How Does Technology Affect Mental Health?
View all blog posts under Articles | View all blog posts under Counseling Resources

Upon completion of a Master of Arts in Counseling degree , individuals can choose to work as mental health counselors — individuals who help clients living with varying mental health and/or interpersonal issues. For example, a mental health counselor may meet with a bereaved woman in the morning who recently has lost her husband, and then a young man in his 20s in the afternoon who is living with an anxiety disorder. The role is challenging and rewarding, and necessitates understanding and expertise for a whole spectrum of mental health concerns.
Given the ubiquity of technology in daily life — particularly the internet and internet-based platforms such as social media sites and smartphone apps — mental health counselors working today likely will encounter clients who are experiencing issues that may be directly or indirectly linked to the use of digital media. According to Dr. Igor Pantic, writing in the literature review “Online Social Networking and Mental Health,” published by the U.S. National Library of Medicine, there is little doubt that the internet and social media platforms such as Facebook have had a notable impact on the way that individuals communicate.
Pantic further explained that a number of recent studies have observed a link between social media use and certain mental health problems, including anxiety and depression. Pantic is quick to assert, however, that the studies are by no means conclusive and that endeavors to understand the relationship between mental health and technology remain in their infancy.
Still, it is useful for mental health counselors to have an understanding of the research and insights into technology’s impact on mental health, which extends to the positive impacts, as well. After all, drawbacks aside, technology continues to improve many aspects of daily life for the better, and the arena of mental health is no exception: there are a number of observable areas in which the development of technology has helped clients take charge of their mental health care in a positive way.
Technology: A force for good?
Despite progress in terms of mental health awareness, journalist Conor Farrington, writing for the Guardian, explained how mental health care still receives a notable lack of funding from international governments. For example, Farrington reported that the per capita expenses on mental health care in industrialized nations such as the U.S. and U.K. amounts to just over $33, which equates to a little under £33. The amount is considerably less in developing countries. Consequently, Farrington argued that technology holds promise as a vehicle for improving access to mental health care, particularly in nations where such services are elementary at best.
Technology is improving mental health care in a number of ways, Lena H. Sun explained, writing for the Los Angeles Times, and it is primarily through platforms such as apps based on smartphones and computers that can help provide services and information to clients in a more cost-effective way. For example, Sun explained how there are now, in addition to smartphone apps that promote mental wellness, certain platforms available that allow patients to complete courses of cognitive behavioral therapy online. In her article, Sun profiled a British-based service known as the Big White Wall, which has been endorsed by the U.K.’s government-funded National Health Service. Big White Wall is an online platform that enables users living with mental health problems such as anxiety and depression to manage their symptoms from home via tools such as educational resources, online conversations and virtual classes on issues of mental health. The efficacy of Big White Wall is conspicuous — Sun reported on a 2009 study that found that a vast majority of the service’s users —some 95 percent —noted an improvement in their symptoms.

How can counselors harness technology?
Mental health counselors can play an important role in facilitating access to services such as Big White Wall and also can help promote smartphone apps and other online services that can be used to help improve general mental health. Technology can be used alongside in-person counseling, as opposed to being employed as a substitution. Counselors even may find that digital platforms allow the development of deeper working relationships with clients, particularly younger clients who are used to utilizing technology on a daily basis. Bethany Bay, writing in an article for Counseling Today, interviewed Sarah Spiegelhoff, a counselor from Syracuse, N.Y., who elaborated on this important point :
“I find technology resources to be great tools to supplement traditional counseling services, as well as a way for counselors to reach larger populations than we typically serve on an individual basis […] I find that college students are quicker to check Facebook and Twitter statuses than their email, so using social media has been one way for us to promote and distribute information on healthy living and outreach events […] I also share information related to new apps that promote wellness both through our social media accounts and directly in counseling sessions. For example, during alcohol awareness programming, we encouraged students to download free blood alcohol calculator apps. We also offer free mindfulness meditation MP3s through iTunes. I find the MP3s to be a great resource because I am able to present them to clients in session, talk about their experiences listening to and practicing the meditations and then develop a treatment plan that includes their use of the meditations outside of the counseling sessions.”
Counselors also can use platforms to connect with clients who may be situated in underserved or rural areas and are unable to travel for in-person meetings. As Farrington explained, some studies, including one from Oxford University, have found that text messaging and phone calls can be effective ways for counselors to connect with clients. Furthermore, telehealth platforms, which include instant messaging or video calling, already are proving useful in primary care settings for helping counselors reach clients. For example, Rob Reinhardt, writing for Counseling Today, interviewed Tasha Holland-Kornegay, a counseling professional who primarily provides counseling services to clients living with HIV via a messaging platform, which incorporates the option for video and audio calls.
Reinhardt, writing in a different piece published by Tame Your Practice, explained how the use of telemedicine platforms in mental health counseling has been shown to be beneficial in a number of ways. Perhaps most importantly, Reinhardt cited a study from researchers based at the University of Zurich, as detailed by Science Daily, which found that counseling conducted online actually can be more effective than face-to-face sessions. Researchers examined two groups of clients — one group received in-person therapy and the other received therapy via a telemedicine platform. Researchers found that the clients who received counseling sessions online actually experienced better outcomes — 53 percent reported that their depression had abated, compared to 50 percent reporting the same in the group that received in-person counseling. Other benefits include the fact that it is cheaper and allows a wider net of clients to be seen and treated, particularly those who are unable to access mental health services in person, whether due to geography, lack of funds or issues such as social anxiety disorder.
A point of clarification needs to be made, however. Whereas counselors may indeed use online technologies to aid the counseling process or to provide counseling services, they always must abide by the ethical guidelines on the use of technologies. These guidelines can be found in the Ethics Code of American Counseling Association and through the National Board for Certified Counselors’ website. Furthermore, counselors are required by law to be licensed in the locations where their clients reside.
Can technology have an adverse impact on mental health?
Although the use of technology can have a positive impact in terms of helping clients manage and get treated for certain mental health conditions, some research has indicated that the use of technology in general — and especially the internet — actually can be connected with the development of mental health conditions, such as anxiety and depression in some individuals. As Pantic noted, while more research is needed in this area, it is useful to take a closer look at what has been published on this topic so far:
Internet addiction
As detailed by Dr. Romeo Vitelli, writing in an article published by Psychology Today, research has indicated that addiction to the internet , particularly among younger demographics such as adolescents, is becoming a notable issue. Vitelli explained that internet addiction disorder shares many similar features when compared with other forms of addiction, such as withdrawal symptoms when online access is precluded. While the internet can be an agent for good in terms of education and the strengthening of interpersonal relationships, internet addiction can be problematic because it can negatively impact academic success and one’s ability to communicate effectively in person. Vitalli noted that research also has observed a link between certain mental illnesses and internet addiction, including depression, low self-esteem and loneliness.
The link between social media use and mental illness
In his literature review, Pantic explained how several studies have shown a link between depression and the use of social media sites, such as Facebook, Twitter and Instagram. Pantic is quick to caution that much more research is needed before the conclusions reached in the aforementioned studies are widely accepted as fact within the counseling community. Still, the findings are worth examining. Pantic reported on one study from 2013, which found that younger adults who frequently used the social networking site Facebook tended to report feeling less happy, with the use of the social platform possibly to blame. Pantic also reported on a study that he personally was involved with that found among high school students, rates of depression tended to be higher among those who regularly utilized social media sites.
Pantic proffered some possible reasons for the findings, explaining that social media sites, for some individuals, can trigger feelings of low self-esteem. For example, a social media site user may see other people on the site and assume those individuals are more successful, beautiful, intelligent and so on. Pantic explained that a study examining students at a Utah university found those who routinely used social media sites tended to feel as though their peers were more successful and happier than they were. Pantic noted that although these feelings are not necessarily linked to depression, there can be a relationship between them, particularly if the individuals in question already experience or are likely to experience mental health problems.
Dr. Saju Mathew was interviewed for an article by Piedmont Health, wherein he elaborated on this important point : “When we get on social media, we are looking for affirmation and consciously or not, we are comparing our life to the lives of others. As a result, we may not enjoy what’s in the moment.”
In conclusion
The impact of technology has extended into the realm of health care, and it is clear that technology also is making positive changes in terms of mental health care. Research has indicated, however, that the very tools that can help alleviate mental health issues, such as smartphone apps, may be linked with the experience of mental health problems in different contexts. As Pantic stressed, more research is needed before definitive conclusions are drawn. Still, for mental health counselors entering the field, a comprehensive understanding of the nuanced relationship between technology and mental health is necessary for effective practice. Counselors are compelled to expand their technological competencies but always in compliance with their respective ethical guidelines and the rule of law.
Consider Bradley University
If you are interested in pursuing a career as a mental health counselor, consider applying to Bradley University’s online Master of Arts in Counseling — Clinical Mental Health Counseling program. Designed with a busy schedule in mind, completion of the degree program will put you on a direct path to becoming licensed to practice.
Recommended Readings
Substance abuse counseling: What you can learn in a MAC program
What are the Clinical Mental Health specialty courses?
Bradley University Online Counseling Programs
- #5 Among Regional Universities (Midwest) – U.S. News & World Report: Best Colleges (2021)
- #5 Best Value Schools, Regional Universities (Midwest) – U.S. News & World Report (2019)
- Bradley Ranked Among Nation’s Best Universities – The Princeton Review: The Best 384 Colleges (2019). Only 15% of all four-year colleges receive this distinction each year, and Bradley has regularly been included on the list.
- Bradley University has been named a Military Friendly School – a designation honoring the top 20% of colleges, universities and trade schools nationwide that are doing the most to embrace U.S. military service members, veterans and spouses to ensure their success as students.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- NEWS & VIEWS FORUM
- 10 February 2020
Scrutinizing the effects of digital technology on mental health
- Jonathan Haidt &
You can also search for this author in PubMed Google Scholar
You have full access to this article via your institution.
The topic in brief
• There is an ongoing debate about whether social media and the use of digital devices are detrimental to mental health.
• Adolescents tend to be heavy users of these devices, and especially of social media.
• Rates of teenage depression began to rise around 2012, when adolescent use of social media became common (Fig. 1).
• Some evidence indicates that frequent users of social media have higher rates of depression and anxiety than do light users.
• But perhaps digital devices could provide a way of gathering data about mental health in a systematic way, and make interventions more timely.
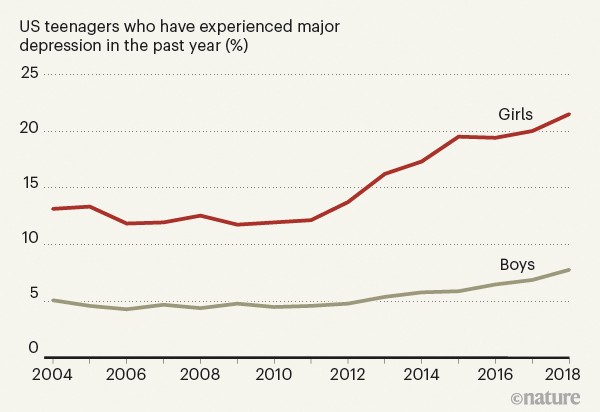
Figure 1 | Depression on the rise. Rates of depression among teenagers in the United States have increased steadily since 2012. Rates are higher and are increasing more rapidly for girls than for boys. Some researchers think that social media is the cause of this increase, whereas others see social media as a way of tackling it. (Data taken from the US National Survey on Drug Use and Health, Table 11.2b; go.nature.com/3ayjaww )
JONATHAN HAIDT: A guilty verdict
A sudden increase in the rates of depression, anxiety and self-harm was seen in adolescents — particularly girls — in the United States and the United Kingdom around 2012 or 2013 (see go.nature.com/2up38hw ). Only one suspect was in the right place at the right time to account for this sudden change: social media. Its use by teenagers increased most quickly between 2009 and 2011, by which point two-thirds of 15–17-year-olds were using it on a daily basis 1 . Some researchers defend social media, arguing that there is only circumstantial evidence for its role in mental-health problems 2 , 3 . And, indeed, several studies 2 , 3 show that there is only a small correlation between time spent on screens and bad mental-health outcomes. However, I present three arguments against this defence.
First, the papers that report small or null effects usually focus on ‘screen time’, but it is not films or video chats with friends that damage mental health. When research papers allow us to zoom in on social media, rather than looking at screen time as a whole, the correlations with depression are larger, and they are larger still when we look specifically at girls ( go.nature.com/2u74der ). The sex difference is robust, and there are several likely causes for it. Girls use social media much more than do boys (who, in turn, spend more of their time gaming). And, for girls more than boys, social life and status tend to revolve around intimacy and inclusion versus exclusion 4 , making them more vulnerable to both the ‘fear of missing out’ and the relational aggression that social media facilitates.
Second, although correlational studies can provide only circumstantial evidence, most of the experiments published in recent years have found evidence of causation ( go.nature.com/2u74der ). In these studies, people are randomly assigned to groups that are asked to continue using social media or to reduce their use substantially. After a few weeks, people who reduce their use generally report an improvement in mood or a reduction in loneliness or symptoms of depression.
The best way forward
Third, many researchers seem to be thinking about social media as if it were sugar: safe in small to moderate quantities, and harmful only if teenagers consume large quantities. But, unlike sugar, social media does not act just on those who consume it. It has radically transformed the nature of peer relationships, family relationships and daily activities 5 . When most of the 11-year-olds in a class are on Instagram (as was the case in my son’s school), there can be pervasive effects on everyone. Children who opt out can find themselves isolated. A simple dose–response model cannot capture the full effects of social media, yet nearly all of the debate among researchers so far has been over the size of the dose–response effect. To cite just one suggestive finding of what lies beyond that model: network effects for depression and anxiety are large, and bad mental health spreads more contagiously between women than between men 6 .
In conclusion, digital media in general undoubtedly has many beneficial uses, including the treatment of mental illness. But if you focus on social media, you’ll find stronger evidence of harm, and less exculpatory evidence, especially for its millions of under-age users.
What should we do while researchers hash out the meaning of these conflicting findings? I would urge a focus on middle schools (roughly 11–13-year-olds in the United States), both for researchers and policymakers. Any US state could quickly conduct an informative experiment beginning this September: randomly assign a portion of school districts to ban smartphone access for students in middle school, while strongly encouraging parents to prevent their children from opening social-media accounts until they begin high school (at around 14). Within 2 years, we would know whether the policy reversed the otherwise steady rise of mental-health problems among middle-school students, and whether it also improved classroom dynamics (as rated by teachers) and test scores. Such system-wide and cross-school interventions would be an excellent way to study the emergent effects of social media on the social lives and mental health of today’s adolescents.
NICK ALLEN: Use digital technology to our advantage
It is appealing to condemn social media out of hand on the basis of the — generally rather poor-quality and inconsistent — evidence suggesting that its use is associated with mental-health problems 7 . But focusing only on its potential harmful effects is comparable to proposing that the only question to ask about cars is whether people can die driving them. The harmful effects might be real, but they don’t tell the full story. The task of research should be to understand what patterns of digital-device and social-media use can lead to beneficial versus harmful effects 7 , and to inform evidence-based approaches to policy, education and regulation.
Long-standing problems have hampered our efforts to improve access to, and the quality of, mental-health services and support. Digital technology has the potential to address some of these challenges. For instance, consider the challenges associated with collecting data on human behaviour. Assessment in mental-health care and research relies almost exclusively on self-reporting, but the resulting data are subjective and burdensome to collect. As a result, assessments are conducted so infrequently that they do not provide insights into the temporal dynamics of symptoms, which can be crucial for both diagnosis and treatment planning.
By contrast, mobile phones and other Internet-connected devices provide an opportunity to continuously collect objective information on behaviour in the context of people’s real lives, generating a rich data set that can provide insight into the extent and timing of mental-health needs in individuals 8 , 9 . By building apps that can track our digital exhaust (the data generated by our everyday digital lives, including our social-media use), we can gain insights into aspects of behaviour that are well-established building blocks of mental health and illness, such as mood, social communication, sleep and physical activity.

Stress and the city
These data can, in turn, be used to empower individuals, by giving them actionable insights into patterns of behaviour that might otherwise have remained unseen. For example, subtle shifts in patterns of sleep or social communication can provide early warning signs of deteriorating mental health. Data on these patterns can be used to alert people to the need for self-management before the patterns — and the associated symptoms — become more severe. Individuals can also choose to share these data with health professionals or researchers. For instance, in the Our Data Helps initiative, individuals who have experienced a suicidal crisis, or the relatives of those who have died by suicide, can donate their digital data to research into suicide risk.
Because mobile devices are ever-present in people’s lives, they offer an opportunity to provide interventions that are timely, personalized and scalable. Currently, mental-health services are mainly provided through a century-old model in which they are made available at times chosen by the mental-health practitioner, rather than at the person’s time of greatest need. But Internet-connected devices are facilitating the development of a wave of ‘just-in-time’ interventions 10 for mental-health care and support.
A compelling example of these interventions involves short-term risk for suicide 9 , 11 — for which early detection could save many lives. Most of the effective approaches to suicide prevention work by interrupting suicidal actions and supporting alternative methods of coping at the moment of greatest risk. If these moments can be detected in an individual’s digital exhaust, a wide range of intervention options become available, from providing information about coping skills and social support, to the initiation of crisis responses. So far, just-in-time approaches have been applied mainly to behaviours such as eating or substance abuse 8 . But with the development of an appropriate research base, these approaches have the potential to provide a major advance in our ability to respond to, and prevent, mental-health crises.
These advantages are particularly relevant to teenagers. Because of their extensive use of digital devices, adolescents are especially vulnerable to the devices’ risks and burdens. And, given the increases in mental-health problems in this age group, teens would also benefit most from improvements in mental-health prevention and treatment. If we use the social and data-gathering functions of Internet-connected devices in the right ways, we might achieve breakthroughs in our ability to improve mental health and well-being.
Nature 578 , 226-227 (2020)
doi: https://doi.org/10.1038/d41586-020-00296-x
Twenge, J. M., Martin, G. N. & Spitzberg, B. H. Psychol. Pop. Media Culture 8 , 329–345 (2019).
Article Google Scholar
Orben, A. & Przybylski, A. K. Nature Hum. Behav. 3 , 173–182 (2019).
Article PubMed Google Scholar
Odgers, C. L. & Jensen, M. R. J. Child Psychol. Psychiatry https://doi.org/10.1111/jcpp.13190 (2020).
Maccoby, E. E. The Two Sexes: Growing Up Apart, Coming Together Ch. 2 (Harvard Univ. Press, 1999).
Google Scholar
Nesi, J., Choukas-Bradley, S. & Prinstein, M. J. Clin. Child. Fam. Psychol. Rev. 21 , 267–294 (2018).
Rosenquist, J. N., Fowler, J. H. & Christakis, N. A. Molec. Psychiatry 16 , 273–281 (2011).
Orben, A. Social Psychiatry Psychiatr. Epidemiol. https://doi.org/10.1007/s00127-019-01825-4 (2020).
Mohr, D. C., Zhang, M. & Schueller, S. M. Annu. Rev. Clin. Psychol. 13 , 23–47 (2017).
Nelson, B. W. & Allen, N. B. Perspect. Psychol. Sci. 13 , 718–733 (2018).
Nahum-Shani, I. et al. Ann. Behav. Med. 52 , 446–462 (2018).
Allen, N. B., Nelson, B. W., Brent, D. & Auerbach, R. P. J. Affect. Disord. 250 , 163–169 (2019).
Download references
Reprints and permissions
Competing Interests
N.A. has an equity interest in Ksana Health, a company he co-founded and which has the sole commercial licence for certain versions of the Effortless Assessment of Risk States (EARS) mobile-phone application and some related EARS tools. This intellectual property was developed as part of his research at the University of Oregon’s Center for Digital Mental Health (CDMH).
Related Articles

See all News & Views
- Human behaviour

How a tree-hugging protest transformed Indian environmentalism
Comment 26 MAR 24

Scientists under arrest: the researchers taking action over climate change
News Feature 21 FEB 24

Gender bias is more exaggerated in online images than in text
News & Views 14 FEB 24
Use fines from EU social-media act to fund research on adolescent mental health
Correspondence 09 APR 24

Circulating myeloid-derived MMP8 in stress susceptibility and depression
Article 07 FEB 24

Only 0.5% of neuroscience studies look at women’s health. Here’s how to change that
World View 21 NOV 23

Rwanda 30 years on: understanding the horror of genocide
Editorial 09 APR 24

After the genocide: what scientists are learning from Rwanda
News Feature 05 APR 24

Right- or left-handed? Protein in embryo cells might help decide
News 02 APR 24
Junior Group Leader Position at IMBA - Institute of Molecular Biotechnology
The Institute of Molecular Biotechnology (IMBA) is one of Europe’s leading institutes for basic research in the life sciences. IMBA is located on t...
Austria (AT)
IMBA - Institute of Molecular Biotechnology
Research Group Head, BeiGene Institute
A cross-disciplinary research organization where cutting-edge science and technology drive the discovery of impactful Insights
Pudong New Area, Shanghai
BeiGene Institute
Open Rank Faculty, Center for Public Health Genomics
Center for Public Health Genomics & UVA Comprehensive Cancer Center seek 2 tenure-track faculty members in Cancer Precision Medicine/Precision Health.
Charlottesville, Virginia
Center for Public Health Genomics at the University of Virginia
Husbandry Technician I
Memphis, Tennessee
St. Jude Children's Research Hospital (St. Jude)
Lead Researcher – Department of Bone Marrow Transplantation & Cellular Therapy
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
For Better or Worse, Technology Is Taking Over the Health World
Sarah Fielding is a freelance writer covering a range of topics with a focus on mental health and women's issues.
:max_bytes(150000):strip_icc():format(webp)/SarahFieldingHeadshot1-afe3609d152d4e409fc179f68c17e652-0ddbe13118414f25ae9e00030fea1fae.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Nick Blackmer is a librarian, fact-checker, and researcher with more than 20 years’ experience in consumer-oriented health and wellness content. He keeps a DSM-5 on hand just in case.
:max_bytes(150000):strip_icc():format(webp)/NickBlackmer-1a9957221fee406e85bcdefd1b05a136.jpg)
For many people over the past year and a half, the world has existed primarily through a screen. With social distancing measures in place to protect individuals from becoming infected with the coronavirus, technology has stepped in to fill the void of physical connections. It’s also become a space for navigating existing and new mental health conditions through virtual therapy sessions, meditation apps, mental health influencers, and beyond.
“Over the years, mental health and technology have started touching each other more and more, and the pandemic accelerated that in an unprecedented way,” says Naomi Torres-Mackie, PhD , the head of research at The Mental Health Coalition , a clinical psychologist at Lenox Hill Hospital, and an adjunct professor at Columbia University. “This is especially the case because the pandemic has highlighted the importance of mental health for everyone as we struggle to make sense of an overwhelming new world and can find mental health information and services online.”
This shift is especially critical, with a tremendous spike occurring in mental health conditions. In the period between January and June 2019, 11% of US adults reported experiencing symptoms of an anxiety or depressive disorder. In January 2021, 10 months into the pandemic, in one survey that number increased to 41.1%. Research also points to a potential connection for some between having COVID-19 and developing a mental health condition—whether or not you previously had one.
The pandemic’s bridge between mental health and technology has helped to “meet the needs of many suffering from depression, anxiety, life transition, grief, family conflict, and addiction,” says Miyume McKinley, MSW, LCSW , a psychotherapist and founder of Epiphany Counseling, Consulting & Treatment Services.
Naomi Torres-Mackie, PhD
The risk of greater access is that the floodgates are open for anyone to say anything about mental health, and there’s no vetting process or way to truly check credibility.
This increased reliance on technology to facilitate mental health care and support appears to be a permanent one. Torres-Mackie has witnessed mental health clinicians drop their apprehension around virtual services throughout the pandemic and believes they will continue for good.
“Almost all therapists seem to be at least offering virtual sessions, and a good portion have transitioned their practices to be entirely virtual, giving up their traditional in-person offices,” adds Carrie Torn, MSW, LCSW , a licensed clinical social worker and psychotherapist in private practice in Charlotte, North Carolina.
The general public is also more receptive to technology’s expanded role in mental health care. “The pandemic has created a lasting relationship between technology, and it has helped increase access to mental health services across the world,” says McKinley. “There are lots of people seeking help who would not have done so prior to the pandemic, either due to the discomfort or because they simply didn’t know it was possible to obtain such services via technology.”
Accessibility Is a Tremendous Benefit of Technology
Every expert interviewed agreed: Accessibility is an undeniable and indispensable benefit of mental health’s increasing presence online. Torn points out, “We can access information, including mental health information and treatment like never before, and it’s low cost.”
A 2018 study found that, at the time, 74% of Americans didn’t view mental health as accessible to everyone. Participants cited long wait times, a lack of affordable options, low awareness, and social stigma as barriers to mental health care. The evolution of mental health and technology has alleviated some of these issues—whether it be through influencers creating open discussions around mental health and normalizing it or low-cost therapy apps . In addition, wait times may reduce when people are no longer tied to seeing a therapist in their immediate area.
While some people may still be apprehensive about trying digital therapy, research has shown that it is an effective strategy for managing your mental health. A 2020 review of 17 studies published in EClinicalMedicine found that online cognitive-behavioral therapy sessions were at least as effective at reducing the severity of depression symptoms than in-person sessions. There wasn’t a significant difference in participant satisfaction between the two options.
There Are Limitations to Mental Health and Technology’s Increasing Closeness
One of the most prevalent limitations of technology-fueled mental health care and awareness is the possibility of misleading or inaccurate information.
If you’re attending digital sessions with a therapist, it’s easy to check their qualifications and reviews. However, for most other online mental health resources, it can be more challenging but remains just as critical to verify their expertise and benefits. “The risk of greater access is that the floodgates are open for anyone to say anything about mental health, and there’s no vetting process or way to truly check credibility,” says Torres-Mackle.
To that point, James Giordano, PhD, MPhil , professor of neurology and ethics at Georgetown University Medical Center and author of the book “Neurotechnology: Premises, Potential, and Problems,” cautions that, while there are guiding institutions, the market still contains “unregulated products, resources, and services, many of which are available via the internet. Thus, it’s very important to engage due diligence when considering the use of any mental health technology .”
Verywell / Alison Czinkota
McKinley raises another valuable point: A person’s home is not always a space they can securely explore their mental health. “For many individuals, home is not a safe place due to abuse, addiction, toxic family, or unhealthy living environments,” she says. “Despite technology offering a means of support, if the home is not a safe place, many people won’t seek the help or mental health treatment that they need. For some, the therapy office is the only safe place they have.” Due to the pandemic and a general limit on private places outside of the home to dive into your personal feelings, someone in this situation may struggle to find opportunities for help.
Miyume McKinley, MSW, LCSW
There are lots of people seeking help that would not have done so prior to the pandemic, either due to the discomfort or because they simply didn’t know it was possible to obtain such services via technology.
Torn explains that therapists who work for tech platforms can also suffer due to burnout and low pay. She claims that some of these platforms prioritize seeing new clients instead of providing time for existing clients to grow their relationship. “I’ve heard about clients having to jump from one therapist to the next, or therapists who can’t even leave stops open for their existing clients, and instead their schedule gets filled with new clients,” she says. “Therapists are burning out in general right now, and especially on these platforms, which leads to a lower quality of care for clients.”
Screen Time Can Also Have a Negative Impact
As mental health care continues to spread into online platforms, clinicians and individuals must contend with society’s growing addiction to tech and extended screen time’s negative aspects.
Social media, in particular, has been shown to impact an individual’s mental health negatively. A 2019 study looked at how social media affected feelings of social isolation in 1,178 students aged 18 to 30. While having a positive experience on social media didn’t improve it, each 10% increase in negative experiences elevated social isolation feelings by 13%.
Verywell / Alison Czinkota
While certain aspects like Zoom therapy and mental health influencers require looking at a screen, you can use other digital options such as meditation apps without constantly staring at your device.
What to Be Mindful of as You Explore Mental Health Within Technology
Nothing is all bad or all good and that stands true for mental health’s increased presence within technology. What’s critical is being aware that “technology is a tool, and just like any tool, its impact depends on how it's used,” says Torres-Mackie.
For example, technology can produce positive results if you use the digital space to access treatment that you may have struggled to otherwise, support your mental well-being, or gather helpful—and credible—information about mental health. In contrast, she explains that diving into social media or other avenues only to compare yourself with others and avoid your responsibilities can have negative repercussions on your mental health and relationships.
Giordano expresses the importance of staying vigilant about your relationship with and reliance on tech and your power to control it.
With that in mind, pay attention to how much time you spend online. “We are spending less time outside, and more time glued to our screens. People are constantly comparing their lives to someone else's on social media, making it harder to be present in the moment and actually live our lives,” says Torn.
Between the increase in necessary services moving online and trying to connect with people through a screen, it’s critical to take time away from your devices. According to a 2018 study, changing your social media habits, in particular, can improve your overall well-being . Participants limited Instagram, Facebook, and Snapchat use to 10 minutes a day per platform for three weeks. At the end of the study, they showed significant reductions in depression and loneliness compared to the control group. However, even the increased awareness of their social media use appeared to help the control group lower feelings of anxiety and fear of missing out.
“Remember, it’s okay to turn your phone off. It’s okay to turn notifications off for news, apps, and emails,” says McKinley. Take opportunities to step outside, spend time with loved ones, and explore screen-free self-care activities. She adds, “Most of the things in life that make life worthwhile cannot be found on our devices, apps, or through technology—it’s found within ourselves and each other.”
Kaiser Family Foundation. The implications of COVID-19 for mental health and substance use .
Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA . Lancet Psychiatry . 2021;8(2):130-140. doi:10.1016/S2215-0366(20)30462-4
Luo C, Sanger N, Singhal N, et al. A comparison of electronically-delivered and face to face cognitive behavioural therapies in depressive disorders: a systematic review and meta-analysis . EClinicalMedicine . 2020;24:100442. doi:10.1016/j.eclinm.2020.100442
Primack BA, Karim SA, Shensa A, Bowman N, Knight J, Sidani JE. Positive and negative experiences on social media and perceived social isolation . Am J Health Promot . 2019;33(6):859-868. doi:10.1177/0890117118824196
Hunt MG, Marx R, Lipson C, Young J. No more FOMO: Limiting social media decreases loneliness and depression . J Soc Clin Psychol . 2018;37(10):751-768. doi:10.1521/jscp.2018.37.10.751
🎉 Enhance web accessibility and compliance with our new Bundles - Check out our special pricing today! 👉
Digital Therapy: Can Technology Support Mental Health?
Technology touches our lives in more ways than we might realize—it extends far beyond the glow of our devices, and has the power to shape our mental and emotional well-being in significant ways. We take a look at the relationship between our digital interactions and mental health. We’ll discuss how technology and mental health interconnect, enhancing our access to information and support networks while offering new avenues for mental health advocacy. We’ll also consider some of the challenges, including exclusion and barriers to digital spaces that can all have an impact on peoples’ mental health.
What is mental health?
Mental health is the holistic state of our emotional, mental, and social wellness, affecting how we think, feel, and act. It’s defined not just by the lack of mental health disorders but also by positive attributes, like coping with stress, maintaining productivity, and engaging positively with our communities.
Each year, 1 in 4 people will encounter some form of mental health issue , and on a weekly basis, 1 in 6 individuals report facing common mental health challenges such as anxiety and depression.
Throughout an individual’s lifetime, their mental health diagnosis can change multiple times. Some complex conditions are quantified by the number of people who receive a particular diagnosis at any point in their lives or within a specific year.
There are many different types of mental health illnesses with some of the most common including:
- Depression: Depression is a prevalent and significant health condition that impacts mood, thought processes, and behavior. However, it’s important to note that treatment options are available.
- Anxiety: Anxiety disorders are the most common mental illness in the United States, affecting 40 million adults in the United States age 18 and older, or 18.1% of the population every year.
- Post-traumatic stress disorder (PTSD): PTSD is a psychiatric disorder that can occur in people who have experienced or witnessed a life-threatening event, like combat, a natural disaster, a car accident, or sexual assault.
- Schizophrenia: Schizophrenia is a chronic and severe mental disorder that affects a person’s ability to think, feel, and behave normally.
- Eating disorders: Eating disorders are mental illnesses that involve abnormal eating habits and distorted body image.
Recognizing the varied landscape of challenges, it’s important to consider how the reach of tech for mental health intersects with these conditions, shaping and sometimes shifting our mental health experiences in today’s connected world. Let’s explore the multifaceted impact of tech on mental health.
How does technology affect mental health?
The integration of technology in supporting mental health stretches back to the 20th century. But it wasn’t until the personal computer and internet revolution of the 1990s that its role became truly transformative in mental health care. Initially, computer-based applications were limited to providing psychoeducation and self-assessment tools.
With technological advancements over time, the collection of digital mental health tools has broadened considerably, now encompassing a wide range of applications designed to offer a wide spectrum of mental health interventions including:
Mobile Apps and Self-Help Tools
Several mobile apps have been developed to provide resources and self-help strategies for managing anxiety and depression. These apps often include mood tracking, relaxation exercises, cognitive-behavioral therapy (CBT) exercises, and psychoeducation to empower individuals to monitor and improve their mental well-being.
Online Therapy and Telehealth
Telehealth platforms enable individuals to access therapy and counseling services remotely, overcoming barriers like geographical distance and stigma. Online therapy is effective for a range of mental health conditions, including depression and anxiety. It allows individuals to receive evidence-based treatments like CBT through video calls or messaging.
Wearable Devices
Wearable technology, such as smartwatches and fitness trackers, can monitor physiological signals like heart rate, sleep patterns, and activity levels. These data can be valuable for identifying trends and triggers related to anxiety and depression and providing individuals with insights to manage their condition.
Virtual Reality (VR) Therapy
VR technology is increasingly used for exposure therapy in treating anxiety disorders like phobias and post-traumatic stress disorder (PTSD). VR creates controlled and immersive environments where individuals can confront and gradually desensitize themselves to their fears or triggers.
Artificial Intelligence (AI) and Chatbots
AI-powered chatbots and virtual assistants can provide immediate support and resources to individuals experiencing anxiety or depression symptoms. These tools can engage in text-based conversations, offering coping strategies, psychoeducation, and referrals to mental health professionals.
Digital Therapeutics
These are evidence-based, software-driven interventions designed to treat specific mental health conditions. They often involve interactive modules and assessments that guide individuals through therapeutic exercises.
7 apps revolutionizing mental health accessibility
In a time where many of us are deeply connected by technology, innovative companies are harnessing the potential to support mental health. By blending technological advancements with the professional expertise of mental health professionals, these organizations are shaping a new landscape for mental health support.
Let’s explore some of these pioneering companies and their cutting-edge solutions that are making mental well-being more accessible and effective than ever before:
1. Calm: Calm is a meditation and mindfulness app that offers a variety of guided meditations, breathing exercises, and sleep stories to help people reduce stress, improve sleep, and manage anxiety.
2. Headspace: Headspace is another popular meditation app that offers a variety of guided meditations, mindfulness exercises, and sleep stories. Headspace also has a dedicated focus on workplace mental health, offering programs for businesses to help their employees manage stress and improve their well-being.
3. Happify: Happify is a gamified mental health app that uses positive psychology techniques to help people increase their happiness and resilience. Happify offers a variety of games and activities that are designed to teach people positive thinking skills and help them develop a more positive outlook on life.
4. Talkspace: Talkspace is an online therapy platform that connects people with licensed therapists for video or text-based therapy sessions. Talkspace makes therapy more affordable and accessible by offering a variety of subscription plans to choose from.
5. BetterHelp: BetterHelp is another online therapy platform that connects people with licensed therapists for video or text-based therapy sessions. BetterHelp offers a variety of features, including a matching tool to help you find the right therapist for your needs.
6. SonderMind: SonderMind is a non-profit organization that provides free and low-cost mental health care to people in need. SonderMind offers a variety of services, including therapy, medication management, and case management.
7. The Trevor Project: The Trevor Project is a non-profit organization that provides crisis intervention and suicide prevention services to LGBTQ youth. The Trevor Project offers a variety of services, including a hotline, chat, and text messaging.
How do awareness initiatives support mental health?
Beyond technological advancements, societal awareness of mental health is also on the rise, illustrated by initiatives such as Mental Health Awareness Week in May, which confronts stigma and educates the public on mental health matters. World Mental Health Day, observed on October 10th, serves as a call to action for mental health awareness and stigma elimination, while International Self-Care Day on July 24th champions the importance of self-care for well-being. These observances are vital in advocating for proactive mental health measures.
Fundraising during awareness events is also essential, as it secures resources for creating and distributing these tech tools, making them widely available.
There are also training opportunities, workshops and conferences such as the Mental Health America Conference, where meaningful dialogues on how to strengthen commitments to promote well-being are generated.
Organizations like Lifeline utilize awareness campaigns to highlight crucial crisis support, including hotlines and text services, enabling instant access to help via technology, thus reinforcing the mental health support system.
Web accessibility: opening digital doors for people with disabilities
As we celebrate innovations in mental health technologies, it’s vital to pivot towards the often overlooked issue of accessibility for people with disabilities.
As technology advances, its potential to support many individuals is evident, yet it’s imperative that it remains accessible and functional for all, particularly for the estimated 1.3 billion people who experience significant disability , This inclusivity ensures that mental health technologies are equally beneficial to those with visual, auditory, motor, or cognitive impairments, embracing a truly universal design.
How can you ensure digital mental health services are accessible?
Creating mental health platforms that are accessible to individuals with disabilities requires thoughtful design and a commitment to universal usability. Here are some key considerations:
1. Simplicity and Clarity: Employ a clear, uncluttered layout with straightforward navigation to avoid overwhelming users with cognitive challenges like anxiety or ADHD.
2. Customizable Interfaces: Incorporate features that allow users to control visual elements, such as adjusting colors or font sizes, to accommodate visual impairments and reduce sensory overload for those with sensory processing issues.
3. Alternative Text: Use alt text for images and provide transcripts for videos, aiding those with visual or auditory disabilities in accessing information.
4. Keyboard Navigation: Ensure that all functions can be accessed with a keyboard alone, benefiting users with motor disabilities who cannot use a mouse.
5. Consistent Structure: Maintain a consistent layout throughout the platform, with predictable patterns for content and menus, which is especially helpful for users with cognitive difficulties.
6. Avoiding Automatic Media: Refrain from using auto-playing audio or video, which can be startling or difficult for individuals with sensory processing disorders or autism.
7. Clear Language: Use plain language to communicate effectively, making content more digestible for all users, including those with cognitive disabilities or depression.
Accessible design illustrates to users with disabilities that their requirements are recognized, their challenges understood, and their well-being valued. It is through this lens that we must view the development of mental health technology: as a tool that is by design empathetic, approachable, and empowering for all.
By committing to these principles, we can create a digital environment where support is not only available but also accessible, allowing everyone the opportunity to seek help, engage in self-care, and enjoy the benefits of technology’s vast potential to improve mental health outcomes.
For a deeper understanding of accessible design principles, we invite you to explore the wealth of information available on the Web Content Accessibility Guidelines (WCAG ). These guidelines offer a comprehensive framework for creating technology that’s inclusive for all.
UserWay: powering accessible mental health tech
UserWay stands at the forefront of combining AI-powered technology with accessibility, deploying artificial intelligence to seamlessly correct code errors to enhance web and app accessibility. Our approach blends compliance with usability and ethical responsibility. UserWay’s commitment to universal accessibility, ensuring everything from websites to apps and other digital assets are available to everyone, reflects the powerful that tech can have on making mental health platforms accessible to everyone, including individuals with disabilities. Request a demo and get started with making your digital spaces accessible today.
How can technology support mental health?
Technology supports mental health through apps for meditation, online therapy services, and digital support communities.
How can technology enhance accessibility for people with disabilities?
Technology enhances accessibility by providing assistive devices and software that enable people with disabilities to navigate, communicate, and learn more independently.
How does accessible design in mental health technology empower users with disabilities?
Accessible design in mental health technology empowers users with disabilities by ensuring the tools are empathetic, approachable, and tailored to their specific needs for better support and independence.

Check Your Site for Accessibility Issues
Ensure your site complies with WCAG standards.
Are College Websites Meeting ADA Standards?
How to build accessibility into mobile apps, how inclusive is the entertainment industry, putting rent-a-car websites on the road to accessibility, uber ordered to pay $1.1 million to a blind woman. what can we learn from this case, california’s unruh civil rights act and web accessibility: key insights, creating inclusive spaces: showcasing artists with disabilities, embracing adaptive fitness: digitally accessible online workouts, ai-powered accessibility: the future for online retailers, embracing inclusive web design for digital accessibility, how to make education inclusive with digital textbooks, usability testing for websites: accessibility on real terms, best practices for accessible & engaging for dental websites.
Request a demo from UserWay
See how easy it is to become ADA and WCAG 2.1 AA compliant with UserWay accessibility solutions
- Skip to main content
- Skip to "About this site"
Language selection
- Français
- Search and menus
Digital Insights Digital well-being: the relationship between technology use, mental health and interpersonal relationships
by Gabrielle Asselin , Howard Bilodeau and Aisha Khalid
Skip to text
Introduction
Younger canadians spend the most time online, taking a break from the internet was not associated with better mental health, but spending less time online was, smartphone use is steadily increasing among canadians, increased smartphone use was linked to lower mental health and satisfaction in relationships with friends and family in 2020, the majority of canadians communicate with others online at least once per week, weekly online communications with friends and family were associated with more frequent in-person interactions in 2022, other articles based on the 2022 cius, digital economy and society statistics portal, methodology, acknowledgements, external references, internal references.
Text begins
Digital technologies have created many new opportunities for individuals to overcome barriers and challenges in their personal lives and at work. As the utility of digital technologies, like smartphones, continues to rise, individuals are spending an increasing amount of time online. The 2022 Canadian Internet Use Survey (CIUS) found that one-quarter of Canadians spent 20 hours or more per week using the Internet for general purposes, up at least 4 percentage points from 2018 (21%) and down only slightly from the beginning of the COVID-19 pandemic in 2020 (27%). Note
In the 2022 CIUS , Canadians reported that their online activities helped them make more informed decisions (51%) and saved them time (47%). However, the use of digital technologies was not always associated with positive outcomes; Canadians also reported that their online activities sometimes made them feel anxious, depressed or envious of the lives of others (22%), interfered with their relationships (8%) and interfered with other aspects of their lives, such as sleep, physical activity, and work- or school-related activities (24%).
This article highlights new data from the 2020 and 2022 CIUS , examining the complex relationship between digital technology use and various measures of well-being. Section 1 explores the relationship between time spent online and self-reported mental health, Section 2 examines how increased smartphone use is related to satisfaction with interpersonal relationships and self-reported mental health, and Section 3 explores the relationship between online communications and in-person interactions.
Section 1: Time spent online and self-reported mental health
About two-fifths of Canadians aged 15 to 24 (42%) reported spending 20 hours or more per week on general Internet use in 2022, the highest among all age groups, followed by those aged 25 to 34 (38%). The percentage of Canadians aged 15 to 24 spending this amount of time online for general purposes was about the same as during the pandemic in 2020 (43%), but at least 10 percentage points higher than before the pandemic in 2018 (32%).
Almost 9 in 10 Canadians watched content online in 2022 (87%) and 17% watched content online for 20 hours or more in a typical week. Watching online content includes activities such as watching television series or movies, watching eSports or other video game streaming services, or watching user-generated content on platforms such as YouTube or TikTok. Again, use was highest for younger Canadians, with 26% of those aged 15 to 24 and 23% of those aged 25 to 34 spending 20 hours or more per week watching online content.
About 37% of Canadians played video games online in 2022, with only 6% doing so for 20 hours or more per week. As with other online activities, those aged 15 to 24 were the most likely to play online video games during a typical week (73%) and spend 20 hours or more per week on this activity (15%).
In 2022, just over 1 in 5 Canadians (22%) reported taking a break from using the Internet or decreasing their time spent on the Internet because they felt they were using it too often or for too long. This was not significantly different from 2020 (24%) or 2018 (21%). In 2022, Canadians aged 15 to 24 (36%) were the age group most likely to report taking a break from or reducing time spent on the Internet.
Of those who took a break from the Internet in 2022, 44% reported having very good or excellent mental health. Conversely, among those who didn’t take a break from the Internet, the percentage reporting very good or excellent mental health was almost 10 percentage points higher (53%). The 2022 CIUS also found that the percentage of Canadians who spent 20 hours or more per week online (regardless of activity) was not significantly different between those who took breaks from the Internet and those who did not. This could be related to a disconnect between the desire to take a break from the Internet and the willingness to actually do so. In the Young Canadians in a Wireless World study conducted by MediaSmarts in 2021, most surveyed school-aged children reported that they were worried about spending too much time online, and also that they would be unhappy if they couldn’t use the Internet for a week. Note
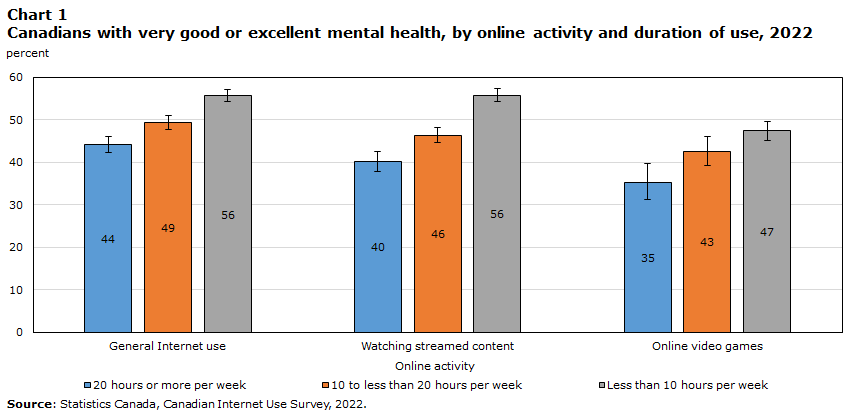
Although taking a break from the Internet wasn’t found to be associated with better mental health in the 2022 CIUS , a correlation between less time spent online and better mental health was identified. The percentage of Canadians reporting very good or excellent mental health was 16 percentage points higher for those who watched content online for less than 10 hours per week, compared with those who watched online content for 20 hours or more per week. Note For general Internet use, the percentage of Canadians reporting very good or excellent mental health was 12 percentage points higher among those who spent less than 10 hours per week online, compared with those who spent 20 hours or more online per week. Note
The percentage of Canadians reporting very good or excellent mental health was significantly lower for all amounts of time spent playing video games online, compared with general Internet use. For example, nearly half (44%) of Canadians who spent 20 hours or more per week on general Internet use reported very good or excellent mental health, compared with 35% of those who spent 20 hours or more per week playing video games online. These findings demonstrate that factors other than time spent online can contribute to the relationship between Internet use and mental health, such as the type of online activity, and the age, sex and gender of the user.
In another study recently conducted by Statistics Canada, which examined data on mental health in adolescents aged 12 to 17 from the 2019 Canadian Health Survey on Children and Youth, video game use by girls was found to be associated with lower self-reported mental health, even when controlling for other factors. For boys, no relationship between video game use and mental health could be identified. Similarly, for social media or instant messaging use, no differences in mental health could be identified when controlling for other factors, regardless of sex. Note These findings further demonstrate the importance of considering the type of activity and personal characteristics when examining the relationship between Internet use and mental health.
Section 2: Smartphone use, relationship satisfaction and self-reported mental health
The 2020 CIUS found that most Canadians (84%) had a smartphone for personal use, up 4 percentage points from 2018 (80%). Note The increase was even larger for seniors aged 65 and older (+11 percentage points), despite lower overall use (54%). Meanwhile, smartphone use by teenagers and adults aged 15 to 24 (96%), 25 to 34 (97%) and 35 to 44 (96%) was nearly universal in 2020.
Almost two-thirds of Canadians (64%) used their smartphone at least once per hour in 2020, including to check messages, use social networks and news sites, and check notifications, while one-fifth (20%) used their smartphone a few times per day or less. Younger individuals were more likely to check their smartphone more often—88% of those aged 15 to 24 and those aged 25 to 34 reported using their smartphone at least once per hour, with those aged 35 to 44 not far behind (82%). Many teenagers and young adults aged 15 to 24 (46%) and 25 to 34 (33%) reported using their smartphone as frequently as every 15 minutes.
As smartphone use grows steadily, some Canadians are trying to control their use. The 2022 CIUS found that 20% of Canadians reported modifying smartphone or application settings to manage time spent on their smartphone. This behaviour was most prevalent for those aged 15 to 24 and those aged 25 to 34, with 32% reporting they tried to control their smartphone use.
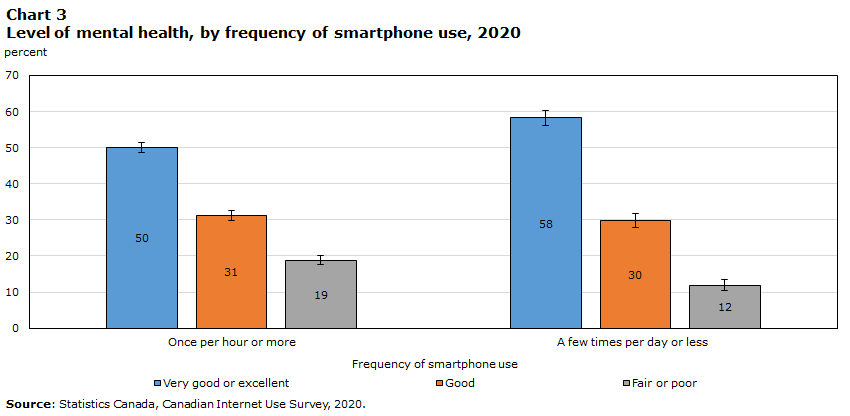
In 2020, Canadians who checked their smartphone once per hour or more were less likely to report being completely satisfied with their relationships with friends (46%) than those who checked their phone a few times per day or less (54%). Note The same pattern was found when examining relationships with relatives or family members, excluding those the respondent lived with.
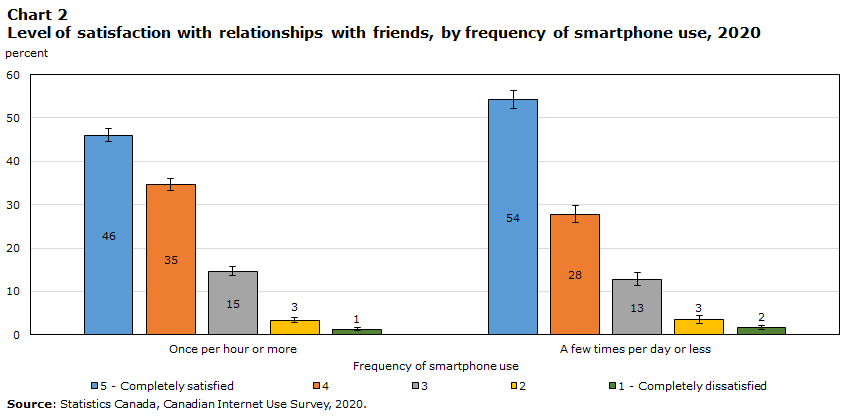
Checking one’s smartphone more frequently was also associated with lower reported levels of very good or excellent mental health. Among Canadians who checked their phone a few times per day or less, almost 6 in 10 (58%) reported very good or excellent mental health, compared with 5 in 10 of those who checked their phone at least once per hour or more. The most frequent smartphone users also reported the highest level of fair or poor health (19%), compared with 12% of the least frequent users.
Section 3: Online communications and in-person interactions
As new digital technologies have become more readily accessible, Canadians have increasingly integrated new communication methods into their lives. The 2022 CIUS found that almost 8 in 10 Canadians (77%) communicated with friends online at least once per week (e.g., iMessage, FaceTime, Facebook Messenger, WhatsApp), and over 6 in 10 (65%) communicated with relatives or family members online at least once per week. Online communications with friends (+4 percentage points) and family (+2 percentage points) increased modestly from 2020 to 2022.
In 2022, teenagers and young adults aged 15 to 24 were most likely to communicate with friends via the Internet at least once per week (93%), with the likelihood decreasing among older age groups. However, for online communications with family, the likelihood of weekly interactions peaked with individuals aged 25 to 34 (79%) and then decreased for older age groups.
The use of video conferencing has also been growing in importance, particularly since the start of the COVID-19 pandemic. Over 6 in 10 (65%) individuals made online voice or video calls in 2022 (excluding business- and school-related use), up 17 percentage points from 2018 (47%) and seemingly stable since 2020 (64%).
Although there may be a connection between rising technology use and decreasing relationship satisfaction and mental health, the relationship between these factors may not be causal. Researchers have proposed that it’s not the amount of time spent with technology that matters most when understanding the impact of technology on well-being, but rather the quality or content of the activities a person engages in. Note Studies on social connectedness through technology have shown that technology use can be associated with positive outcomes; for example, during the COVID-19 pandemic, individuals who communicated more with others online were more likely to engage in positive behaviours, such as maintaining their physical health. Note
Similarly, the 2022 CIUS found a correlation between the frequency of online and in-person interactions. Note Among Canadians who said they interacted with their friends online weekly, over half (52%) reported seeing friends in person outside of work or school at least weekly as well. By comparison, among those who said they interacted with their friends online a few times per month or less, only 22% reported seeing friends in person at least weekly.
For interactions with relatives or family members, the same pattern was observed, but to a lesser extent. For those interacting weekly with family online, just under half (47%) saw family in person (excluding those they live with) at least weekly. Meanwhile, among those who interacted with family online a few times or less per month, only 16% saw their family at least weekly. These findings provide evidence that online interactions aren’t necessarily replacing in-person interactions.
Compared with the overall population (52%), a higher percentage of individuals aged 15 to 24 who interacted weekly with their friends online reported seeing them in person at least weekly (61%). This is likely partly related to younger Canadians using the Internet to communicate with friends more often than older Canadians, and the fact that younger Canadians tend to have more opportunities to see their friends on a weekly basis.
Overall, regardless of the frequency of online interactions, a larger percentage of Canadians reported spending time in person with both friends (+21 percentage points) and family (+15 percentage points) at least weekly in 2022, compared with 2020. A large part of this trend can likely be attributed to the reduction of COVID-19 pandemic restrictions that limited in-person interactions in 2020.
Results from the 2020 and 2022 CIUS demonstrate a complex relationship between technology use and measures of well-being, such as mental health, satisfaction in interpersonal relationships and time spent with others in person. The survey found that increased time spent online and smartphone use were associated with lower self-reported mental health and that increased smartphone use was also associated with lower satisfaction in interpersonal relationships. However, the survey also showed that spending more time with others online was linked to an increased likelihood of seeing others in person, and that the correlation between time spent engaging in online activities and self-reported mental health differed by type of online activity. As other studies have proposed, the quality of time spent online may be a better predictor of digital well-being than time spent online alone.
The CIUS is a rich source of information for understanding the impact of technology on the lives of Canadians. Further research could go beyond the analysis in this article by simultaneously controlling for multiple variables that may impact well-being, such as aggregate time spent online and the personal characteristics of technology users.
Results for the 2022 CIUS were released in The Daily on July 20, 2023.
Visit the Digital economy and society statistics portal to find data, publications, and interactive tools related to the digital economy and society in one convenient location.
This article uses data from the 2018, 2020 and 2022 iterations of the Canadian Internet Use Survey (CIUS) . The CIUS aims to measure the adoption and use of digital technologies by Canadians aged 15 years and older, living in the 10 provinces.
Data for the CIUS were collected through an electronic questionnaire during the following periods:
- 2018: December 15, 2018 to March 21, 2019
- 2020: November 3, 2020 to March 3, 2021
- 2022: December 29, 2022 to April 5, 2023
In the 2018 survey, a sample of approximately 33,000 individuals was used and the response rate was 43.7%. In the 2020 survey, the sample size consisted of approximately 44,800 individuals and the response rate was 41.6%. Finally, in the 2022 survey, the sample size was approximately 55,700 individuals and the response rate was 45.3%.
Error bars on charts represent the 95% confidence interval.
The authors would like to thank Nicole Minnema, Karine Garneau, Mark Uhrbach and Christoph Schimmele for their feedback on an earlier version of this paper.
Boers, E., Afzali M.H., Newton N., & Conrod P. (2019). Association of Screen Time and Depression in Adolescence. JAMA Pediatrics . 173(9):853–859. Retrieved March 16, 2023.
MediaSmarts (2023). Young Canadians in a Wireless World, Phase IV: Trends and Recommendations . Retrieved October 30, 2023.
Royal, C., Wasik, S., Horne, R., Dames, L. S., & Newsome, G. (2017). Digital Wellness: Integrating Wellness in Everyday Life with Digital Content and Learning Technologies. In J. Keengwe & P. Bull (Eds.), Handbook of Research on Transformative Digital Content and Learning Technologies (pp. 103–117). IGI Global. Retrieved March 16, 2023.
Charnock, S., Heisz, A., Kaddatz, J., Spinks, N., & Mann, R. (2021). Canadians' Well-being in Year One of the COVID-19 Pandemic . Income Research Paper Series . Statistics Canada. Retrieved October 30, 2023.
Kerr, S., & Kingsbury, M. (2023). Online digital media use and adolescent mental health . Health Reports . Statistics Canada. Retrieved October 30, 2023.
More information
Note of appreciation.
Canada owes the success of its statistical system to a long-standing partnership between Statistics Canada, the citizens of Canada, its businesses, governments and other institutions. Accurate and timely statistical information could not be produced without their continued co-operation and goodwill.
Standards of service to the public
Statistics Canada is committed to serving its clients in a prompt, reliable and courteous manner. To this end, the Agency has developed standards of service which its employees observe in serving its clients.
Published by authority of the Minister responsible for Statistics Canada.
© His Majesty the King in Right of Canada, as represented by the Minister of Industry, 2024
Use of this publication is governed by the Statistics Canada Open Licence Agreement .
Catalogue no. 22-20-0001
Frequency: Occasional
Is something not working? Is there information outdated? Can't find what you're looking for?
Please contact us and let us know how we can help you.
Privacy notice
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Technology and Mental Health: State of the Art for Assessment and Treatment
- Philip D. Harvey , Ph.D. ,
- Colin A. Depp , Ph.D. ,
- Albert A. Rizzo , Ph.D. ,
- Gregory P. Strauss , Ph.D. ,
- David Spelber , M.D. ,
- Linda L. Carpenter , M.D. ,
- Ned H. Kalin , M.D. ,
- John H. Krystal , M.D. ,
- William M. McDonald , M.D. ,
- Charles B. Nemeroff , M.D., Ph.D. ,
- Carolyn I. Rodriguez , M.D., Ph.D. ,
- Alik S. Widge , M.D., Ph.D. ,
- John Torous , M.D.
Search for more papers by this author
Technology is ubiquitous in society and is now being extensively used in mental health applications. Both assessment and treatment strategies are being developed and deployed at a rapid pace. The authors review the current domains of technology utilization, describe standards for quality evaluation, and forecast future developments. This review examines technology-based assessments of cognition, emotion, functional capacity and everyday functioning, virtual reality approaches to assessment and treatment, ecological momentary assessment, passive measurement strategies including geolocation, movement, and physiological parameters, and technology-based cognitive and functional skills training. There are many technology-based approaches that are evidence based and are supported through the results of systematic reviews and meta-analyses. Other strategies are less well supported by high-quality evidence at present, but there are evaluation standards that are well articulated at this time. There are some clear challenges in selection of applications for specific conditions, but in several areas, including cognitive training, randomized clinical trials are available to support these interventions. Some of these technology-based interventions have been approved by the U.S. Food and Drug administration, which has clear standards for which types of applications, and which claims about them, need to be reviewed by the agency and which are exempt.
Technology is ubiquitous in society and now mediates many forms of interpersonal and societal communication. It is no surprise that the numbers of technology-based interventions and strategies for treating psychiatric disorders are rapidly increasing. These technologies include evaluation of nearly all features of psychiatric disorders, including symptoms, cognitive performance, and everyday functioning. In fact, while technology-based assessments and intervention strategies initially were administered in-person at office visits, many of these strategies are now administered remotely using cloud-based applications.
Current technology allows for the structured delivery of material used for assessment and training in cognitive, social cognitive, and functional domains; two-way communication with video, short message services (SMS), such as Twitter and other software platforms, including remote therapy applications; paging using various technologies for assessment and intervention purposes using ecological momentary assessment (EMA) strategies; continuous passive monitoring of location and behavior (including activity and physiological signals such as heart rate and skin conductance); and presentation of reality-based computer simulations. These simulations include both immersive virtual reality (VR) simulations and more static simulations that allow performance assessment and, in some cases, training on veridical representations of technology-based tasks such as shopping, banking, traveling, and placing online orders. The devices on which such applications are now delivered range from computers to tablets to smartphones to wearable devices. Thus, technology in the context of this review refers to an array of different functions (messaging, monitoring) across a number of different platforms and operating systems (Windows, iOS, and Android).
In this review, we describe technology relevant to mental health applications, including both assessment and intervention applications. In the assessment domain, we focus on assessment of cognitive abilities, emotion regulation capacity, functional skills, and clinical symptoms, including thorough sampling of individual symptoms and activities through structured queries or observed experiences. Assessment technologies involve observational strategies, including EMA, paging, and passive measurement, and cues to engage in performance-based assessments in cognitive, social cognitive, or functional domains. We generally focus here on adult populations, with some mention of interventions for attention deficit hyperactivity disorder (ADHD) in children that may also apply to adults.
In the treatment domain, we present information on applications designed to deliver interventions as well as applications that are designed to augment other treatments. Examples of direct treatment delivery include performance-based training in cognition and functional skills, which are available across conditions ranging from ADHD to mild cognitive impairment to substance use disorders. Other therapeutic applications include immersive VR simulations as well as cognitive-behavioral therapy applications. Technology-based augmentation strategies include tools for self-monitoring between therapy sessions, delivery of reminders to reinforce therapeutic goals, and various ways to track adherence to treatments. This leads to a very broad-based review, which itself is only a shadow of the field of mental health assessment and treatment and technological interfaces.
Our review of these applications and technologies includes data on their efficacy (when they are employed as treatments or assessment tools) as well as data on user tolerability. Any disparities between clinical trial results obtained with digital health technologies and outcomes arising from traditional in-person clinical trials require reconciliation and interpretation, and are likely related to factors of 1) real-world engagement challenges for patients and 2) workflow challenges for clinicians ( 1 , 2 ). Considering data on real-world effectiveness beyond just efficacy data will be critical to ensure that the field makes optimal use of emerging technologies ( 3 ).
Technology-Based Assessment of Cognition and Everyday Functioning
Cognitive assessments.
Computerized cognitive assessment strategies have been used for several decades. Multiple testing batteries are currently available, and these have been reviewed in detail elsewhere ( 4 – 6 ). Computerized assessments are appealing for several reasons, including systematic delivery of instructions and collection of responses, as well as automated scoring and norming of response data.
Computerized cognitive testing has been used in multiple clinical trials, and its use in routine clinical practice is also becoming more common. Certain tests have always been available exclusively in a fully computerized format ( 7 ). Other assessments, initially developed for administration using paper and pencil (e.g., the Brief Assessment of Cognition [ 8 ] and the Wechsler Intelligence Scales) were subsequently released as computerized applications ( 9 , 10 ) developed to be convergent with the widely used paper versions. A significant advantage offered by many of these computer-based assessment tools is that the tester does not have to be a licensed professional; indeed, subprofessional clinical trainees can acquire the skills required to administer most computerized assessments and collect valid data. However, evaluation of whether results from computer-based cognitive assessments are convergent with the results of traditional in-person assessments remains an important consideration ( 11 ). Some recent data suggest substantial challenges with certain tasks, particularly if there is an attempt to sustain fidelity to paper-and-pencil assessments while performing a remote assessment ( 12 ). As a result, there is a need for careful consideration of whether all legacy cognitive assessments can be performed remotely.
Functional Capacity Assessments
A variety of computer-based strategies examine the ability to perform skills that are critical for everyday functioning, referred to as functional capacity. Available assessment tools evaluate performance on a range of tasks through structured simulations of everyday activities, veridical simulations of everyday tasks, and VR-based simulations. The stand-alone task batteries usually have a structured assessment sequence with individually scorable tasks and are normable in a manner similar to that applied to responses on neuropsychological tests. While the VR assessments (described below) are commonly more realistic and more flexible, they are, in many cases, less amenable to normative standards. In the stand-alone tests, such as the Virtual Reality Functional Capacity Assessment Tool (VRFCAT) ( 13 ), touch-screen responses are used to assess the subject’s ability to perform a sequence of skilled acts using simulation formats (e.g., looking in cabinets for specific target items, developing a shopping list, utilizing public transportation, and navigating a shopping experience in a virtual retail store). In another, the computerized functional skills assessment and training system (CFSAT) ( 14 ), the specific components of skilled acts are examined, such as entering a personal identification number on an automatic teller machine screen, selecting the correct ticket choice on a computer kiosk, and using the keypad on a simulated mobile phone to enter responses to a telephone voice menu. Data have consistently shown that performance on these computerized simulations of everyday activities is correlated with cognitive function ( 12 , 13 ) measured with standard or digital strategies. These assessments have a variety of functions, including use in clinical trials of cognitive enhancement where evidence of functional relevance is required and in clinical settings to directly measure improvements in functional skills in individuals receiving rehabilitative interventions ( 15 , 16 ).
Remote Delivery of Technology-Based Cognitive and Functional Assessments
As the assessment technology reviewed here is already available for either remote or in-person assessment settings, we briefly address the feasibility of remote delivery of cognitive assessments. Several different formats are used for remote assessment, including tester administration of tasks over a videoconferencing application and remote, exclusively self-administration of all assessments by the subject. There are several challenges inherent in each approach. For exclusively remote, self-administered assessments, the participant needs to be comfortable with, and capable of using, the required technology.
Videoconference administration of tests that were designed to be administered in-person requires consideration of the technological demands of the conferencing application and the ability of participants to use the technology as well as to perform the critical skills. It is certainly possible to perform certain types of cognitive assessments over the telephone (e.g., measurement of verbal responses in tests of working memory or episodic memory, and measurement of auditory processing speed on tasks such as the Oral Trail Making Task [ 17 ]). For videoconferencing applications in cases where the participant is asked to perform cognitive tests on the device while simultaneously receiving remote instructions and supervision, the participant need only be able to manage the technology-based delivery of the assessment program, which can possibly be facilitated by another person who is on-site with the participant at the time of testing ( 18 ). These challenges may be difficult to eliminate entirely.
In the case of assessments designed for fully remote self-administration, there are other potential challenges. Several such studies have found significantly more missing data than observed with in-person, paper-and-pencil assessments ( 19 , 20 ). One possibility is that some participants, particularly those with severe mental illness or other forms of cognitive impairment, find the computerized assessments difficult to comprehend and/or are less motivated, particularly without another person present to receive instructions and facilitate subject engagement. We recently validated methods for remote delivery of neurocognition ( 21 ) and social cognition (i.e., emotion recognition) ( 22 ) testing embedded in an EMA application. Participants were seen in person and trained on the use of the technology at the start of participation. In a sample that demonstrated the baseline ability to utilize this technology, we found that subsequent adherence to the EMA cognitive assessments (75% for neurocognition [N=168] and 80% for emotion recognition [N=86]) was high and data quality was on average excellent. Adherence was not correlated with diagnosis (major depression, bipolar disorder, schizophrenia), age, sex, or presence of psychosis, negative symptoms, or suicidal ideation. Although these data are quite positive, strategies for determination of an individual’s capacity to be assessed remotely seems to be an important clinical topic.
Clinical Virtual Reality
Over the past 25 years, researchers and clinicians have pursued the use of VR as a tool to advance clinical assessment, intervention, and scientific research ( 23 – 31 ). This effort was inspired by the intuitively obvious opportunity for VR environments to address specific challenges inherent in the provision of usual clinical strategies for mental health, rehabilitation, and general medical care. At its core, VR technology, along with other related simulation-based formats (e.g., augmented/mixed reality), offers new capabilities that did not exist a decade ago. Many recently developed VR-based testing, training, teaching, and treatment approaches would be difficult, if not impossible, to deliver without leveraging the power of modern computing, three-dimensional (3D) graphics, body tracking sensors, novel user interfaces, gaming/narrative principles, big data analytics, and artificial intelligence. Such VR-enabling technologies allow for the creation of highly realistic, interactive, engaging, and systematically controllable digital simulation environments. Users can be immersed in VR simulations and interact with content for the purposes of clinical assessment and intervention. VR technology is thus well matched to the requirements of various clinical targets and psychiatric contexts.
Defining Virtual Reality
Since the inception of VR, a large and evolving scientific literature has emerged regarding the outcomes and effects associated with what we now refer to as clinical VR applications that target psychological, cognitive, motor, and functional impairments or symptoms across a wide range of health conditions. Continuing advances in the underlying enabling technologies for creating and delivering VR applications have resulted in their widespread availability as consumer products, sometimes at a very low cost (e.g., Oculus Quest 2).
The concept and definition of VR has been debated over the years. VR has been very generally defined as a way to visualize, manipulate, and interact with technology and complex data in a more naturalistic and intuitive manner ( 32 ). From this baseline perspective, VR can be seen as an advanced form of human-computer interaction that allows a user to interact with computers beyond what is typically afforded by standard mouse–keyboard–touchscreen interface devices. An engaged VR user experience can be created through unique combinations of interaction devices, sensory display systems, and the type of content presented in the virtual environment. Thus, there are two common types of VR. The automated observation of these interactions constitutes the assessment components of VR therapies.
Nonimmersive VR is the most basic format and is similar to the experience of playing a video game. Virtual content is delivered on a standard computer monitor, tablet, mobile phone, or television as users interact with 3D computer graphics using a game pad, joystick, mouse, keyboard, or specialized interface devices (e.g., other handheld devices, data gloves, treadmills). Modern computer games that support user interaction and navigation within 3D graphics can be considered to be VR environments. Tasks such as the VRFCAT described above are nonimmersive VR assessment strategies.
Immersive VR integrates head-mounted displays, body-tracking sensors, specialized interface devices, and 3D graphics ( 33 ). Users operate within a simulated environment that changes in a natural or intuitive way based on the user’s motion and interaction. The head-mounted display occludes the user’s view of the outside world while head- and body-tracking technology senses the user’s position and movement. These user movement data are rapidly sent to a computing system, which uses the movement and interaction data to update the sensory stimuli, which are presented to the user via the head-mounted display. When users are immersed in computer-generated visual imagery and sounds of a simulated virtual scene, their interaction produces an experience that corresponds to what they would see and hear if the scene were real.
Regardless of the technical approach, the key aim of these immersive systems is to perceptually replace the outside world with the virtual world to psychologically engage users with simulated digital content designed to create a specific user experience. Immersive VR is typically the choice for applications where a controlled stimulus environment is desirable for constraining a user’s perceptual experience to a synthetic world. This format has been often used in clinical VR applications for assessment of anxiety disorder or PTSD severity and subsequent exposure therapy, as distraction for patients undergoing acutely painful medical procedures, and in the physical/cognitive assessment/rehabilitation domain. The research potential—for example, studying neural processes during brain imaging or neurosurgery—are also clear.
In a related domain, recent work has involved the creation of virtual human characters (sometimes called avatars or autonomous agents) that allow users to engage in clinical interactions within both nonimmersive and immersive simulations. The creation of virtual humans has evolved from research showing their clinical usefulness as stimuli for exposure therapy for social phobias ( 34 , 35 ), for role-play training for social skills in people on the autism spectrum ( 36 – 38 ), for activities for addressing intimate partner violence ( 39 ), and for teaching self-compassion in persons with depression ( 40 ). More complex virtual humans infused with varying levels of natural language processing and artificial intelligence have shown effectiveness in the role of virtual patients that novice clinicians can use in practicing the skills required for challenging diagnostic interviews ( 41 ) and motivational interviewing ( 42 ). They have also been created to produce online virtual human health care guides ( 43 , 44 ) and as clinical interviewers, with automated sensing of facial, gestural, and vocal behaviors that are useful for inferring the state of the user interacting with these virtual human entities ( 45 ) and for assessing clinician empathetic behavior ( 46 ).
Current VR Clinical Treatment Areas
The field of clinical VR has expanded dramatically as the technology has evolved. Clinical VR has been shown to be effective in fear reduction in persons with specific phobias (e.g., 47 , 48 ), treatment for posttraumatic stress disorder (e.g., 49 – 52 ), and cue exposure for addiction treatment and relapse prevention ( 53 – 55 ). VR has also been effective in treating depression ( 40 ), paranoid delusions ( 56 ), and body image disturbances in patients with eating disorders ( 27 , 28 ). Cognitive and physical rehabilitation research using VR has produced promising results when applied to navigation and spatial training in children and adults with motor impairments ( 57 ), functional skill training and motor rehabilitation in patients with central nervous system dysfunction (e.g., stroke, traumatic brain injury, cerebral palsy, multiple sclerosis) ( 58 ), and for the rehabilitation of attention, memory, spatial skills, and other cognitive functions ( 59 , 60 ).

VR Assets for Advancing Clinical Interventions: Expose, Distract, Motivate, Measure, and Engage
On a very general level, VR leverages core processes that are relevant across a variety of clinical domains. These processes can be summarized as the capacity to expose, distract, motivate, measure, and engage users. Expose refers to clinical applications designed to provide exposure therapy for anxiety disorders and PTSD, to practice social interactions in order to reduce paranoid delusions, and cue-exposure approaches for addiction treatment and relapse prevention. VR used for exposure therapy offers strong evidence, with a recent meta-analysis suggesting efficacy across a wide range of phobias, anxiety, and trauma- and stressor-related disorders ( 61 ). Further meta-analysis supports the efficacy of virtual reality for anxiety-related disorders, although the research base is still relatively small ( 62 ). Distract refers to methods for distracting attention from painful medical procedures to reduce pain perception, promote reduction of discomfort, and provide respite from bleak hospital settings. A recent systematic review supported the potential of VR for pain management but noted that the studied effects are often for acute pain, and less is known about longitudinal analgesia for chronic pain ( 63 ). Motivate refers to the practice of promoting patient adherence to repetitive and sometimes boring or frustrating training tasks that need to be performed for cognitive or physical rehabilitation and chronic pain management by embedding these activities within game-like contexts. Measure underscores the capability that VR simulations provide for quantifying activity and/or performance in response to controlled simulations of fearful experiences. Finally, engage is generally seen as the end result of capturing attention or action that is useful for encouraging participation with clinical applications where users relate to and interact with virtual content as if it were physically real—sometimes referred to as the sense of presence ( 64 ). For example, learning the “skill” of achieving a “mindful” state typically requires multiple sessions before the user perceives a rewarding change in their mental or emotional state. VR has been used to create engaging experiences within which users may be more compelled to practice and learn this skill.
The Future of Clinical VR
Scientific support for the clinical use of VR for mental health and rehabilitation has evolved as the costs and complexity of developing VR applications have gone down and the capacity of the technology has increased. A complex VR headset and hand controllers that might have cost tens of thousands of dollars in 2000 now cost well under $800. This trend should be accelerated by recent developments in “standalone” VR headsets (e.g., Oculus Quest, Pico Neo, Vive Focus, etc.). Such low-cost VR display systems do not require a tethered computer, as all the graphic and interaction processing take place onboard the device. These lower-cost devices will promote adoption and enable larger-scale clinical studies that can help build the effectiveness data necessary for VR to build out a solid evidence base for guiding future clinical implementation. As we look to the future, we also see growing clinician awareness, acceptance, and adoption of clinical VR methods. For example, Norcross et al. ( 65 ) surveyed 70 psychotherapy experts regarding interventions they predicted to increase in the next decade; VR was ranked 4th out of 45 options, with other computer-supported methods (teletherapy, mobile apps, online cognitive-behavioral therapy self-help) occupying three of the other top five positions. Moreover, the COVID-19 crisis has certainly accelerated the exploration and acceptance of these technologies to amplify access to care, and that interest will likely continue after the pandemic has passed ( 66 ). Thus, in view of the current enthusiasm for VR generally across society, and specifically in the clinical community, coupled with emerging scientific support and lower system costs, it is likely that clinical VR applications have the potential to become standard tools for psychiatry researchers and possibly to be utilized more widely by practitioners.
Ecological Momentary Assessment (EMA)
Ecological momentary assessment (EMA), also referred to as the experience sampling method (ESM), has been a tool for understanding fluctuating phenomena and within-person dynamics, and the ubiquity of the smartphone has greatly accelerated the accessibility of this method for clinical applications ( 67 ). Programs for the delivery of EMA surveys have become more widely available, and the tools for analysis of intensive longitudinal data have proliferated. At the earlier stages of EMA, the focus was typically on the recording of behaviors (e.g., activity, sleep, smoking) or daily life experiences, such as stressors, through diaries ( 68 – 70 ). The data gathered enabled examination of within-person change, but required user input and did little to reduce the biases inherent to self-report ( 70 ). These older assessment strategies had no way to accurately time-stamp the reports that were collected. Anecdotal reports of people arriving 20 minutes early for their appointments and completing 14 days’ worth of assessments are confirmed by the results of research studies comparing reported and observed adherence to paper diary assessments ( 71 ).
Personal digital assistants such as early Palm Pilot–like devices automated these processes ( 72 , 73 ). Moreover, prompts to complete surveys could now be timed and momentary responses could be time-stamped ( 74 ). With the translation of EMA to smartphones, surveys could be delivered according to different contexts experienced by the individual (and indexed by the geolocation features of the device), thus enabling more personalized information to be gathered. The ability to tailor probes based on the individual’s momentary state generated a new field of ecological momentary intervention ( 75 ), and several trials have evaluated personalized automated interventions that leverage momentary data ( 76 , 77 ). Some researchers have moved beyond self-reports to intensively repeated objective measures, including brief cognitive tests embedded in the EMA programs as described above ( 21 , 22 ).
The kinds of questions that researchers have been able to ask with these new tools have led to new insights in fundamental questions in mental health. Sometimes these findings are at odds with prevailing theories. It is commonly believed that smokers relapse because of nicotine withdrawal symptoms. Shiffman et al. ( 78 ) evaluated smoking behavior in non-daily smokers and found that negative affect was more important than withdrawal symptoms in relapse, which is critical for understanding which factors to target to sustain smoking cessation. It is commonly believed that suicidal ideation arises from feelings of hopelessness. Kleiman et al. ( 79 ) found that suicidal thoughts varied markedly throughout the day and that variation in candidate predictors (e.g., hopelessness) did not predict the emergence of this ideation, a finding that had been produced previously in a hospitalized sample ( 80 ). Depp et al. ( 81 ) found that social isolation and number of social interactions did not predict onset of suicidal ideation in people with schizophrenia, but that the anticipation of being alone later was associated with an increase in ideation. Granholm et al. ( 82 ) found that people with schizophrenia (N=100) spent considerably more time home and alone than healthy control subjects (N=71) and, even when home and alone, engaged in fewer productive behaviors. In a follow-up analysis of this sample, Strassnig et al. ( 83 ) found that people with schizophrenia reported fewer activities, spent considerably more time sitting and less time standing, and were considerably more likely to sleep during the daytime hours. However, listening to music and watching television were not differentially common in healthy and schizophrenia participants, suggesting that activities less productive than passive recreation are among the things that were more common in participants with schizophrenia.
More general lifespan questions can also be addressed by EMA. Using a measurement burst design in which bouts of EMA are integrated with a longitudinal follow-up period, Koffer et al. ( 84 ) found that older age was associated with greater ability to buffer against the effect of stress on affect.
These are just a few examples from a burgeoning field, highlighting the degree to which active EMA paradigms can be used to advance understanding of the dynamic processes underlying psychiatric diagnoses, extending and sometimes challenging prevailing theories. EMA is a useful strategy to identify targeted features of different conditions on a momentary basis. For example, repeated assessment can identify the proportion of prompts that are answered at home versus away and in the presence of other people versus alone. As these are the central indices of social isolation and social avoidance, the socially relevant impact of negative symptoms in schizophrenia ( 85 ) and current depression in mood disorders can be directly indexed. Research suggests excellent correlations between clinical ratings of symptoms from structured interviews and EMA data, while identifying fluctuations in symptoms that are missed by more widely spaced assessments ( 86 , 87 ). These strategies can also be used to examine health-relevant behaviors in mental health populations, as described above. Given the reduced life expectancy associated with severe mental illness and the high prevalence of metabolic syndrome, EMA can be used to estimate the amount of time spent sitting versus standing or otherwise engaged in active behaviors. Given that contemporary EMA can collect the occurrence of multiple different activities since the last survey, it is quite easy to see whether only one activity has occurred since the last survey or whether participants are engaging in multiple concurrent activities, including physical activities ( 88 ). When paired with the passive digital phenotyping described below, a comprehensive EMA assessment can examine location and social context, refine measurements of activity (exercise vs. agitation), detect sleeping during the daytime and not at night, and assess concurrent subjective emotional responses to these activities.
Passive Digital Phenotyping
A more recent breakthrough involves quantifying clinical outcomes using “passive” digital phenotyping (i.e., unobtrusively collecting data via the internal sensors of a smartphone, a wrist-worn smart band, or another device). Passive measures can reduce certain limitations associated with interview- and questionnaire-based clinical assessments (e.g., cognitive impairment, social desirability, cultural biases [ 89 ]). Numerous passive measures have been evaluated in psychiatric populations (e.g., geolocation, accelerometry, ambient speech recorded from the environment, phone call and text logs, screen on/off time, social media activity, Bluetooth-based proximity social sensing) ( 90 – 96 ). However, the validity of these passive measures is only beginning to be established. Goldsack et al. ( 97 ) proposed the V3 framework for determining the validity of passive digital biomarkers, which involves three components: verification, analytical validation, and clinical validation. These components, as reviewed below, provide a useful heuristic for determining whether the level of validity achieved for various passive measures meets clinical standards.
The first component of the V3 model, verification (i.e., efficacy), is a quality-control step for the device of interest that is performed by the manufacturer. It occurs before testing is conducted on human subjects. The goal is to determine whether the sensor captures data accurately and to verify that the software accurately outputs data within a predetermined range of values. For example, accelerometry could be verified by placing a smart band on an object programmed to accelerate at a prespecified rate. Verification is typically done by device/software manufacturers against a reference standard. However, the results of these tests and the analytic methods supporting the devices are typically not published or made available for evaluation, which presents replication challenges. Additionally, common standards do not exist for verifying passive digital phenotyping sensors of interest, and sensors embedded in different models will often be different. Since devices and sensors may require differing levels of verification (e.g., required accuracy) for various clinical purposes, evaluating verification data is a critical step that should occur before passive digital phenotyping measures are applied in studies in clinical populations. For medical devices, such as medical decision-making software, this process may be handled by the U.S. Food and Drug Administration (FDA) as part of Good Manufacturing Practice (GMP) standards. Making test results and analytic methods underlying devices accessible to researchers will help disentangle whether failures of replication are true problems with reproducibility across clinical populations or simply differences in the technical quality of different devices used in studies.
The second component, analytical validation (i.e., effectiveness), involves behavioral or physiological validation of a device in human subjects in the real world. A key first step in this process is determining whether sample-level data output by the device is properly received and that algorithms calculated on that data perform as expected. The metric resulting from the algorithm, applied in real time or post hoc, should be evaluated against a relevant reference. Although agreed-upon reference standards have not been determined for validating passive digital phenotyping measures, there has been initial analytical validation of some passive measures. For example, phone-based geolocation and accelerometry recorded on the ExpoApp have been validated in relation to a reference wrist-worn actigraph and a travel/activity diary; time in microenvironments and physical activity from the diary demonstrated high agreement with phone-based geolocation and accelerometry measures ( 98 ). Huang and Onnela ( 92 ) analytically validated a phone accelerometer and gyroscope using a ground-truth standard. They had human participants engage in specific physical activities (e.g., sitting, standing, walking, and ascending and descending stairs) with a phone in their front and back pockets. Behavior was filmed throughout as an objective reference. The sensors accurately predicted video-recorded behavior in the reference standard. One ongoing challenge is that as smartphones are updated with new software and phone models with new sensors, prior validation efforts cannot be assumed to be valid.
The third component, clinical validation (i.e., implementation), involves determining whether the passive digital phenotyping variable of interest adequately predicts a specific clinical outcome within the population of interest. Preliminary evidence for clinical validation exists for several passive measures—although at times results have also been contradictory ( 99 ). For example, in bipolar disorder, incipient depressive symptoms have been predicted by changes in the number of outgoing text messages, the duration of incoming phone calls, geolocation-based mobility measures, and vocal features extracted during phone calls. Manic symptoms of bipolar disorder have been predicted by more outgoing texts and calls, acoustic properties of speech extracted during phone calls (e.g., standard deviation of pitch), and increased movement detected via accelerometry ( 100 , 101 ). Clinically elevated and subthreshold depressive symptoms have been predicted by geolocation-derived measures of circadian rhythm, normalized entropy, and location variance, as well as phone usage frequency and speech-derived audio volume ( 102 – 105 ). Social anxiety has been predicted by reduced movement on accelerometry and fewer outgoing calls and texts ( 106 ). Relapse of psychotic disorders has been predicted by geolocation mobility metrics and text/call behavior ( 90 ). Negative symptoms of schizophrenia measured via EMA or clinical ratings have been predicted by geolocation-based mobility metrics, voice activity, and actigraphy-based metrics of gesture and activity level ( 99 , 107 – 110 ). Combining passive measures with EMA surveys may further enhance clinical validation. For example, Raugh et al. ( 111 ) found that the combination of geolocation and EMA surveys was a stronger predictor of clinically rated negative symptoms in schizophrenia than either measure alone. Similarly, Faurholt-Jepsen et al. ( 101 ) found that combining vocal acoustic features extracted from phone calls with EMA reports improved the correct classification of mixed or manic mood states in bipolar disorder beyond either measure alone. Henson et al. ( 112 ) reported that a combination of EMA and passive data, when analyzed for congruence with anomaly detection methods, was associated with early warnings of relapse in people with schizophrenia. Thus, studies suggest that passive measures are promising tools for measuring clinical outcomes. However, there are numerous inconsistencies regarding the predictive value of specific metrics and measures for classifying individual disorders or symptom states, including geolocation, accelerometry, ambient speech, and ambulatory psychophysiology ( 113 – 116 ). For example, clinical data on sleep did not match sensor report in one study ( 94 ), and results are not comparable across studies because of differences in sensors utilized, in the clinical targets, in time frames for calculating associations across assessment modalities (e.g., daily or monthly), and in the populations studied. There are also fundamental differences across studies in methods and analyses, such as controlling for multiple comparisons when examining correlational data.
Clinical validation (i.e., implementation) is of particular concern for using passive measures as outcomes for clinical interventions. Unlike traditional interview- or questionnaire-based clinical outcome measures, standards for the level of psychometric evidence needed to say that a measure is clinically validated have not yet been determined for passive digital phenotyping. Proprietary data collection via devices (e.g., a custom wearable device [ 117 ]) and proprietary methods for analysis (e.g., a custom machine learning algorithm [ 118 ]) offer both innovation and a challenge to reproducible clinical research. Further complexity arises from the trend toward using more complex analytic methods with passive digital phenotyping because of the multilevel nature of the data. For example, machine learning is an increasingly common tool in the clinical validation process, and studies have employed various algorithms to predict a range of clinical outcomes (e.g., classification, regression, unsupervised clustering) ( 119 ). However, common standards for judging the level of psychometric evidence that constitutes clinical validation for machine learning are not yet uniformly applied across the field. Is predictive accuracy of 70% enough to declare clinical validation, or should a higher standard be set (e.g., 90% accuracy) ( 104 , 106 )? Similar considerations affect simpler analytic methods, such as simple correlations for passive data aggregated across a range of time (e.g., 1 week) to form a single value that can be correlated with clinical outcomes. It seems important that such aggregated values be adjusted for the extent of daily or time of day variation. These adjusted correlations tend to be statistically significant but lower (r values ∼0.3–0.5) than typical standards for convergent validity that would be applied within clinical rating scales or questionnaires (e.g., r values >0.80) ( 103 , 104 , 111 ). Do these lower correlations reflect inadequate convergent validity, even though they are statistically significant? Or is the lower correlation to be expected (and therefore acceptable) because of the fact that it averages across differences in temporal variation across measures or method variance? We suggest that common guidelines for judging what constitutes clinical validation are clearly needed for passive digital phenotyping. There should also be an effort to ensure that clinical validation studies include a representative sample with diverse individuals to ensure that algorithms are not primarily trained to be accurate in populations whose demographic and personal characteristics do not overlap with the clinical populations of interest and that methodological and analytic approaches are valid and consistent throughout the population.
Feasibility of implementation is the next consideration, and barriers and facilitators such as cost, accessibility, tolerability, ease of use, and data failure rates are among the relevant factors. Few studies have evaluated user experience of interactions with passive measures. However, qualitative studies employing interviews designed to assess patient perceptions have indicated that while many see these technologies as holding promise for clinical detection and self-management, there may also be unintended barriers to use, such as increased stigma or anxiety ( 120 , 121 ). One would expect that most passive measures would not be viewed by participants as burdensome, given that they are collected unobtrusively by the background sensors of their device and do not require direct participant action. However, there may be some instances where device interface proves problematic in clinical populations. For example, in a study on outpatients with chronic schizophrenia, the participants had considerable difficulty with remedying Bluetooth unpairing of a smart band and smartphone ( 112 ). People with schizophrenia found this pairing issue more burdensome than did control subjects. It is also unclear whether certain clinical symptoms interact with the willingness to consent to participating in digital phenotyping studies. For example, by their nature, continuous geolocation and ambient speech monitoring raise questions about privacy and agency. It is unclear whether clinical populations, such as individuals with schizophrenia who have delusions of suspicion, experience such technologies as intrusive and whether they exacerbate symptoms or result in the individual not consenting to participate out of fear of being monitored. Some data suggest that the prevalence of answering prompts while acknowledging concurrent psychotic symptoms is reasonably high ( 86 ) and that EMA reports of location have been validated using GPS coordinates ( 108 ). More generally, issues of systemic racism and mistrust of how passive digital phenotyping information could be (mis)used by the law enforcement or other systems of power may influence implementation of these methods in participants who are racial minorities. Thus, user experience should be carefully evaluated when administering these technologies in clinical populations. As we mention below, the general issue of access to the Internet and experience with any technology is a barrier that will need continuous attention.
Combinations of EMA and passive digital phenotyping seem likely to improve interventions and assessment. GPS location coordinates provide information about where one is, but not who is with them. Proximity detection can determine whether another individual with a device is present, and ambient sound sampling can tell whether individuals are interacting or are simply in proximity to each other. Smart bands can detect activity but not the motivation for the activity (exercise vs. agitation). Combining mood sampling with geolocation information and EMA can help determine whether social isolation is due to depression or lack of motivation, and facial and vocal affect assessment from participant-captured samples can provide validation information for mood reports. A recent example ( 122 ) suggested that the combination of passive phenotyping and EMA prompts was feasible, with multiple different prompted responses collected, in conjunction with data regarding location, psychophysiological responses, and ambulatory acoustics (44 participants with schizophrenia and 19 with bipolar disorder). Thus, an array of different elements of functioning can be captured simultaneously and used to generate a wide-ranging picture of momentary functioning.
A challenge in the domain of passive digital phenotyping is that application developers and scientific utilizers are commonly at the mercy of the manufacturers, who can restrict access to phone features for applications or push out operating system upgrades that cause software to fail. Further, applications that monitor access to social media may also encounter restricted access or requirements that access be granted for each time the application attempts to capture data. This is an area where collaboration with manufacturers will be required.
Adherence Monitoring
One of the major approaches using technology in mental health treatment is in adjuncts to therapies. In particular, treatment adherence monitoring is a clear area of need and has been a focus of both clinical trials and clinical treatments. For example, several studies have used mobile monitoring to check in with patients at high risk for nonadherence, including early-course psychosis patients ( 123 ) and patients with bipolar disorder ( 124 ). Some applications have been approved as medical devices by the FDA. For example, an application that monitors adherence to aripiprazole was approved by the FDA in 2017 ( 125 ) and involves an embedded sensor in a pill. Other strategies used in clinical trials include the use of digital photography to capture the moment of pill taking or other chemical tags that can be detected after a medication is taken ( 126 ). Systematic studies are under way to examine the usefulness of these strategies for real-world adherence support.
One of the issues with adherence monitoring is that this cannot be a passive measurement strategy. Individuals whose adherence is monitored, in either research or clinical treatment, need to be fully informed and to agree to this monitoring, and their consent must be valid.
Smartphone Therapeutic Applications
There are many mobile apps designed around the principles of cognitive-behavioral therapy (CBT) or other evidence-based interventions but few randomized controlled trials demonstrating their efficacy for any disorder. There are a huge number of applications available that attempt to promote mindfulness or induce relaxation. As many of these applications are not tested empirically at all, we have focused on the translation of CBT strategies into applications. As CBT has a long history of being systematically manualized, the comparison of efficacy of applications to legacy in-person treatment is facilitated. The majority of existing data on the efficacy of mobile app-based interventions comes from randomized controlled trials assessing symptoms associated with a defined disorder or other mental health outcomes such as stress levels, well-being, and quality of life. There are some data to suggest that smartphone interventions can be effective in reducing depressive symptoms. A 2017 meta-analysis by Firth et al. ( 127 ) identified a small number of randomized controlled trials (N=18) that examined the efficacy of smartphone-based interventions in improving symptoms of depression. They found a significant reduction in depressive symptoms with smartphone interventions compared with waiting list or inactive control conditions (g=0.56) and a smaller effect in comparison to active control conditions (g=0.22). The use of interventions based on cognitive-behavioral techniques offered greater benefits for depression than computerized cognitive training applications. In a 2019 meta-analysis of randomized controlled trials assessing the efficacy of app-supported smartphone interventions for mental health disorders, Linardon et al. ( 128 ) found that smartphone interventions significantly outperformed control conditions in improving depressive symptoms. Similar to the Firth et al. meta-analysis, the effect size was larger when waiting list (g=0.32) or informational resources (g=0.39) were used as control conditions compared with attention or placebo control conditions, such as checking the weather on the phone (g=0.12). Of the 54 comparisons (smartphone vs. control) analyzed, 26 involved a CBT-based app; however, a subgroup analysis did not show them to be associated with larger effect sizes. CBT is an empirically and meta-analytically supported treatment for depression, but some researchers have suggested a low level of adherence to the core principles of CBT models and identified highly variable usability among CBT-based smartphone interventions as reasons for their lack of superiority ( 129 ). A 2021 review of studies of CBT smartphone apps for depression featuring a control group reported that results remain too heterogeneous to recommend for front-line care ( 130 ).
Similarly, a small but growing body of data suggest that smartphone interventions may be efficacious in the treatment of anxiety symptoms. Another meta-analysis from 2017 ( 131 ), focused on randomized controlled trials involving smartphone-supported interventions to reduce anxiety symptoms and found significantly greater reductions in anxiety scores from smartphone interventions compared with control conditions across nine eligible randomized controlled trials. Effect sizes were significantly greater when studies made use of a waiting-list or inactive control conditions (g=0.45) compared with those that used active control conditions (g=0.19). This discrepancy in effect sizes—like that seen in studies assessing depressive symptoms, as noted above—suggests the complexity of conducting digital mental health research and the possibility of a digital placebo effect by which use of a digital device in itself confers a degree of psychological benefit. The Linardon et al. meta-analysis ( 128 ) found 29 studies assessing efficacy in treating generalized anxiety symptoms, with eight studies specifically designed to target generalized anxiety symptoms. Across the 39 comparisons within the identified studies, the pooled effect size (g) was found to be 0.30 and statistically significant across all sensitivity analyses. Subgroup analyses again showed a smaller effect size for comparisons using an active comparison intervention (g=0.09) and a larger effect size with studies that used a CBT-based app, which included 16 of the 39 comparisons analyzed.
An intervention strategy that combines EMA principles with interactive smartphone technology is referred to as “just-in-time adaptive interventions” ( 132 ). These strategies involve consistent monitoring of behavior, activities, moods, and symptoms, using EMA strategies, but they also interactively offer interventions in real time. An example of such a strategy is the FOCUS intervention ( 133 ), which uses a mix of prompts directed to the participant and self-activated tools. The goal of this class of interventions is to sustain engagement while offering interventions in real time. As noted in several reviews, this strategy is being widely used, but the data are not yet at the stage where global statements about efficacy can be made.
Two other examples of smartphone-based interventions that have FDA-approved elements are recently introduced devices to promote smoking cessation and to reduce opioid abuse. PIVOT is a digital smoking cessation app that includes human coaching with text messages, combined with smartphone-based carbon monoxide (CO) monitoring ( 134 ). The CO sensor is an FDA-cleared medical device, and the program includes a multistage intervention following standard human-delivered smoking cessation strategies as well as nicotine supplementation.
R-Set-O ( 135 ) is an application that is designed to be paired with buprenorphine treatment for opioid addition. In a randomized clinical trial, 82% of participants who were randomized to the device remained in treatment, compared with 68% of those in treatment as usual.
Abstinence was also higher in the active treatment group (77% vs. 63%). Given the typical attrition rates for opioid use disorder treatment (about 50% or more) ( 136 ), these are encouraging results. One of the challenges in these interventions is adherence and engagement. For example, in a naturalistic study of the R-Set-O intervention in which data from 3,144 individuals with opioid use disorder were evaluated, 80% completed at least eight of the 67 possible therapeutic modules, 66% completed half of all modules, and 49% completed all modules ( 137 ). Although abstinence rates were quite good (about 65%), there is a clear difference in adherence compared with the randomized controlled trials that led to FDA approval. In a large-scale review of device-based interventions, Linardon and Fuller-Tyszkiewicz ( 128 ) reported that adherence was challenging in many of these interventions. The types of strategies that succeeded in increasing adherence were clearly associated with attempts to promote engagement at the outset of the intervention. Interventions that used online enrollment were particularly susceptible to poor adherence and dropout, while in-person and telephone recruitment strategies were better.
Computerized Cognitive Training and Cognitive Remediation Therapy
The core of computerized cognitive training (CCT) is software designed to engage and practice cognitive functions. Cognitive functioning is commonly defined in these applications as the set of abilities that would be measured with neuropsychological assessments and relate consistently to everyday functional outcomes. Some programs are explicitly aimed at a single cognitive domain, while others target an array of domains. A central feature of successful CCT programs is adaptive presentation of training stimuli, such that the level of difficulty tracks the participant’s current performance. The goal is to train increasingly more difficult tasks while ensuring a success rate of about 80% of the target stimuli.
Computerized cognitive training has been widely studied in the past two decades, along with concurrent advances in computer technology, which has allowed for great strides forward in terms of control over the learning environment. Multiple studies have demonstrated CCT’s efficacy for improvement of cognition in multiple populations, with the bulk of the evidence in severe mental illness ( 138 , 139 ) and supported by large-scale studies of healthy older people ( 140 – 142 ). There is considerably less information outside of schizophrenia, but studies in bipolar disorder ( 143 ) and major depression ( 144 ) have been published. For evaluation of CCT as a mental health treatment, there are several central considerations. These include the range of efficacy expected, how the intervention needs to be delivered, the dose required, and whether there are specific subpopulations who stand to make the most treatment gains. Further, there are several considerations about concurrent treatments that may be required to translate cognitive gains into improvements in everyday functioning. Finally, remote delivery of cognitive training has been studied in the past with some success.
As described in the meta-analyses, cognitive changes induced with CCT have generally been shown to have minimal efficacy for the improvement of everyday functioning in the absence of a targeted intervention aimed at functional skills. When CCT is combined with structured intervention programs, the term cognitive remediation therapy (CRT) is generally applied. CRT has been shown in meta-analyses to produce both cognitive and functional gains ( 139 ). There are multiple approaches to delivering CRT, but they all share common features. The intervention is delivered in person by a trainer, and other skills training is delivered as well, typically with a focus on vocational or social functioning. CCT combined with supported employment programs has proven in multiple studies to provide considerable benefits (e.g., 145 ), even in previous nonresponders ( 146 ). Hence, when delivered in a structured CRT program, the range of expected efficacy includes cognition and everyday functioning. Some studies have also trained social cognitive abilities, leading to improved social outcomes ( 15 ), and some have found that combined CCT and computerized social cognitive training (CSCT) lead to more substantial gains than CCT alone ( 147 ). However, a recent study using compensatory cognitive training combined with supported employment did not find employment gains ( 148 ).
Dosing of CCT has varied considerably across studies. In studies of severe mental illness, doses ranging from 15 to 135 training sessions have been delivered. One factor that may mediate the effect of dose is the extent of training engagement. Several studies have suggested that training engagement predicts the extent of training gains in CCT ( 149 , 150 ). Even large doses of CCT may be ineffective if participants are not actually participating in the procedure ( 151 ). Thus, monitoring of engagement, easily accomplished through the software in most training programs, is clearly recommended. There are insufficient data to draw conclusions regarding the likelihood that training engagement will either improve in poorly engaged patients or worsen in those who are initially engaged.
In terms of specific subpopulations with potential to benefit from CRT, prodromal ( 152 ), first-episode ( 153 ), and chronic ( 154 ) schizophrenia patients show equivalent cognitive gains when trained with a single CCT system. In a reanalysis of a larger randomized trial, patients with a shorter illness duration had a greater cognitive and functional response to a comprehensive CRT program ( 155 ). In contrast, several studies of patients with extended institutional stays ( 156 , 157 ) have suggested that benefits are common and include both cognitive and functional improvements. Similarly, in mood disorders, patients with a history of major depression and treatment resistance, both older and younger, have received benefits from CRT ( 158 , 159 ). Thus, there are no clear indicators for illness characteristics that define which patients will achieve maximum benefit. Engagement has a much stronger signal than age in research to date.
Some rehabilitation facilities may not have access to computers for all participants, and some participants may prefer to train at home. Although the majority of structured CRT has been studied with in-person training, several studies suggest that home-based CCT can be accomplished with reasonable levels of adherence (70%) and with cognitive and social cognitive benefits ( 15 , 152 , 153 ). Train-at-home studies with nonpsychotic community-based populations have also been conducted ( 160 ). A sample of 2,912 older community dwellers participated in an entirely online training program, with evidence of gains in both composite scores on cognitive performance and everyday functioning. The dropout rate was considerably larger than seen in the studies noted above, with rates exceeding 50% at the 6-month follow-up.
A treatment for ADHD recently approved by the FDA, EndeavorRx (generic name, AKL-T01), also used a train-at-home performance-based training intervention ( 161 ). In a large-scale trial, AKL-T01 was delivered to children with ADHD in a video game–like interface via at-home play for 25 minutes per day, 5 days per week for 4 weeks. The outcome measure was performance on an ADHD-relevant cognitive task, the Test of Variables of Attention (TOVA) ( 162 ). The treatment was significantly superior to a video game control condition. AKL-T01 thus received approval to improve attention function as measured by computer-based testing in children ages 8–12 with primarily inattentive or combined-type ADHD who have a demonstrated attention issue. The sponsors of the treatment clearly state that it is designed to be used as augmentation therapy in addition to other treatments. One reason for this suggestion is that scores on ADHD rating scales did not show improvement after training. Thus, this intervention is very similar in terms of strategy to previous studies using CRT to improve cognitive functioning in other conditions, such as schizophrenia.
Pharmacological Augmentation of CRT
An important recent development been systematic studies of pharmacological augmentation of cognitive training ( 163 ). These augmentation strategies have been found to be successful for the use of stimulants ( 164 ), guanfacine ( 165 ), alertness promotion agents ( 166 ), and memantine ( 167 ) in schizophrenia, and for vortioxetine in age-related cognitive decline ( 168 ). Interestingly, modafinil and memantine have been much less effective as monotherapies for cognitive impairments ( 169 , 170 ). Other studies are examining compounds that have shown preliminary efficacy as monotherapy treatment to improve cognition in schizophrenia ( 171 ) and as an adjunct to CRT ( 172 ), and these therapies may have promise as augmentations.
An additional important recent finding in the area of pharmacological augmentation of cognitive training is that of the combination of long-acting injectable antipsychotic medications and CRT. In a study of first-episode patients randomized to either oral or long-acting medications as well as to either CRT or another augmented psychosocial intervention, an important interaction effect was found ( 173 ). The combination of long-acting medication and CRT led to considerably greater cognitive gains than seen with CRT and oral medications. Further, the cognitive changes directly translated into functional gains, including work function. As this intervention also included vocational rehabilitation for all participants, the effects of cognitive gains associated with CRT on work outcomes in more chronic patients was reproduced. This is, to our knowledge, the first study demonstrating that clinical stability may be a factor that is associated with the efficacy of CRT.
Level of Evidence and Approval
As digital mental health technologies evolve, so do questions regarding the level of evidence to support their claims of efficacy. In response, some have proposed that digital health technologies may benefit from alternative endpoints and novel study designs in order to best capture their efficacy ( 174 ). The FDA’s Digital Health Software Precertification (Pre-Cert) Pilot Program is an attempt to reenvision how it approves such technologies ( 175 ), although questions remain about the real-world practicality of this approach, given that it remains a pilot project. In short, Pre-Cert seeks to expedite approval of software as a medical device through preapproving technology developers and using real-world data to assess the performance of the software after approval. Still, as noted above, there are smartphones apps, computer programs, and devices that have all been granted FDA marketing approval through more traditional pathways (section 510(k) and de novo) and trial designs.
Software functions that help patients with diagnosed psychiatric conditions (e.g., post-traumatic stress disorder (PTSD), depression, anxiety, obsessive compulsive disorder) maintain their behavioral coping skills by providing a “Skill of the Day” behavioral technique or audio messages that the user can access when experiencing increased anxiety ( 176 , p. 23).
Thus, devices that do not attempt to replace an approved treatment or attempt to eliminate the need for medical care fall under this heading. Clearance of technology under general wellness applications or medical devices that fall under enforcement discretion are not likely to be eligible for direct insurance reimbursement, although they could be part of other bundled services. While in many clinical settings this would not be relevant because therapeutic activities are not billed on a session-by-session basis, in some practice settings this would be more of a challenge. For example, computerized cognitive training is covered by some insurance plans for neurological conditions, such as persistent traumatic brain injury, but not for psychotic or depressive disorders. Similarly, certain adherence applications have been approved by the FDA, but they are linked only to a single medication because the software actually detects the presence of a chip that is ingested along with the pill. Finally, as noted above, the AKL-T01 application for ADHD was approved only as an adjunctive treatment, not a stand-alone.
As regulation seeks to catch up to the mental health technology space, clinicians and patients must make choices today. Various frameworks have been proposed for such evaluation, including one endorsed by APA ( 177 ). Several score-based databases have also emerged, although research suggests low rates of concordance between such scoring systems as well as an inability to update at the rate of technology changes ( 178 ). Newer educational initiatives offer to help patients and clinicians make informed decisions based on available data ( 179 ). The Federal Trade Commission (FTC) continues to sue technology vendors for false marketing claims (notably Lumosity, in relation to brain training in 2016 [ 180 ] and a menstrual period tracking app in 2021 [ 181 ]) and offers consumer guidance as well.
Conclusions
Technology-based assessment and intervention strategies are proliferating, and the COVID-19 pandemic has accelerated the process. These strategies are based on technology that is newly developed and continuing to evolve. Technological strategies are likely to allow for expansion of clinical assessment and intervention potential and for clinicians’ ability to deliver more service in the same time frame. Even purportedly nontechnological interventions involve technology today, including electronic health records and video conferences, but this review addresses some of the ways that technology will continue to expand in the immediate future.
Development is faster than validation, and advertisements are less expensive than research. A reasonable idea would be to consider the evidence for using applications, keeping in mind that exaggerated claims are common in the technology area. While some of these claims have been the target of investigations by the FTC, the more common challenge is applications that are marketed without extravagant claims but also without adequate data. As a field, we need to develop our standards for what we utilize now and what we wait until later for.
There are several issues to follow into the future. One is the research–clinical deployment gap. Clearly, many technologies are well validated in research settings but are not as actively used in the clinic. Over time, this situation can change; the case for CCT is a perfect example: the advent of better computer technology and the feasibility of remote administration of training has enabled the expansion of general community access to CCT. This process may have been kicked off by CCT providers who made exaggerated efficacy claims, as described above, but the result is that the general community is quite aware of CCT now.
Another critical issue is access. While both age and socioeconomic status used to be barriers to technology access, many more older people have access to the Internet and use smartphone technology. The lack of access on the part of lower-income and rural populations was clearly highlighted during the COVID-19 pandemic, and until the access disparity is resolved, many people will not be reachable with these interventions. Importantly, these are the same factors that create access barriers to mental services in general; given the promise of technology increasing access to mental health services, increasing access to technology will be a critical first step.
In summary, these technological developments are exciting, and they show efficacy in controlled studies and are increasingly designed to be acceptable to patients. There is likely more to come in this broad area, and assessments and interventions that would have seemed like science fiction in the past are entirely commonplace now.
Dr. Harvey has served as a consultant for or received travel reimbursements from Acadia, Alkermes, BioExcel, Boehringer Ingelheim, Karuna Pharma, Merck Pharma, Minerva Pharma, Roche Pharma, and Sunovion (DSP) Pharma; he receives royalties for the Brief Assessment of Cognition in Schizophrenia (owned by WCG Verasci, Inc., and contained in the MATRICS Consensus Cognitive Battery); he is chief scientific officer of i-Function, and serves as a scientific consultant for EMA Wellness; he owns stock options in Mindstrong and equity interest in i-Function and EMA Wellness; he is compensated as an editor-in-chief by Elsevier; and he serves on the board of Skyland Trail. Dr. Rizzo has served as a consultant for Penumbra and Cognitive Leap. Dr. Strauss has served as a consultant for Acadia, Boehringer Ingelheim, Lundbeck, Minerva Neuroscience, Otsuka, and Sunovion; he is a research adviser at Quantic Innovations; he receives royalties in relation to commercial use of the Brief Negative Symptom Scale (BNSS), which are donated to the Brain and Behavior Research Foundation, and he has conducted trainings for MedAvante-ProPhase in conjunction with use of the BNSS. Dr. Carpenter has research grant or clinical trials contracts with Affect Neuro, Janssen, NIH, Neuronetics, and Neurolief; she has served as a consultant for Affect Neuro, Janssen, Neuronetics, Neurolief, Nexstim, Otsuka, Sage Therapeutics, and Sunovion; has she has received in-kind support for research projects from Affect Neuro, Janssen, Neuronetics, and Neurolief, and equipment loan from Nexstim. Dr. Kalin is Editor-in-Chief of the American Journal of Psychiatry , and Drs. McDonald and Rodriguez are Deputy Editors; the Editors’ disclosures are reported in the April issue of the Journal . Dr. Krystal has served as a consultant for Aptinyx, Biogen Bionomics, Boehringer Ingelheim, Epiodyne, EpiVario, Janssen Research and Development, Jazz Pharmaceuticals, Otsuka America Pharmaceutical, Spring Care, and Sunovion Pharmaceuticals; he is listed as co-inventor on a patent licensed by Yale to Spring Health; he serves on the board of directors of Freedom Biosciences and on scientific advisory boards for Biohaven Pharmaceuticals, BioXcel Therapeutics (clinical advisory board), Cerevel Therapeutics, Delix Therapeutics, Eisai, EpiVario, Jazz Pharmaceuticals, Neumora Therapeutics, Neurocrine Biosciences, Novartis, PsychoGenics, Tempero Bio, and Terran Biosciences; he holds stock in Biohaven Pharmaceuticals and Spring Care and stock options in Biohaven Pharmaceuticals Medical Sciences, EpiVario, Neumora Therapeutics, Tempero Bio, and Terran Biosciences; he serves on the editorial board of Biological Psychiatry ; he is named on U.S. patents 5,447,948, 8,778,979, and 9592207, patent application nos. 15/379,013, 61/973/961, 62/444,552, 62/719,935, and 63/125,181, and USPTO docket number Y0087.70116US00; and he has received study medications from AstraZeneca, Cerevel, and Novartis. Dr. Nemeroff has served as a consultant for AbbVie, Acadia Pharmaceuticals, Alfasigma, ANeuroTech (division of Anima BV), BioXcel Therapeutics, Corcept Therapeutics Pharmaceuticals Company, EcoR1, EMA Wellness, Engrail Therapeutics, GoodCap Pharmaceuticals, Intra-Cellular Therapies, Magstim, Navitor Pharmaceuticals, Neuritek, Pasithea Therapeutic Corp., Sage, Senseye, Signant Health, Silo Pharma, SK Life Science, and XW Pharma and on scientific advisory boards for ANeuroTech, the Anxiety and Depression Association of America (ADAA), the Brain and Behavior Research Foundation, Heading Health, the Laureate Institute for Brain Research, Magnolia CNS, Pasithea Therapeutics, Sage, Skyland Trail, Signant Health, and TRUUST Neuroimaging; he serves on boards of directors for ADAA, Gratitude America, Lucy Scientific Discovery, and Xhale Smart; he is a stockholder in Antares, BI Gen Holdings, Corcept Therapeutics Pharmaceuticals Company, EMA Wellness, Seattle Genetics, Naki Health, TRUUST Neuroimaging, and Xhale; and he holds patents on a method and devices for transdermal delivery of lithium (US 6,375,990B1) and on a method of assessing antidepressant drug therapy via transport inhibition of monoamine neurotransmitters by ex vivo assay (US 7,148,027B2). Dr. Widge has served as a consultant for Dandelion Science; he has received device donations from Medtronic; and he has unlicensed patents in the area of biomarkers and methods for tracking mental health symptoms. Dr. Torous has received support from Otsuka and is a cofounder of Precision Mental Wellness. The other authors report no financial relationships with commercial interests.
1. Linardon J, Cuijpers P, Carlbring P, et al. : The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials . World Psychiatry 2019 ; 18:325–336 Crossref , Medline , Google Scholar
2. Torous J, Firth J : Bridging the dichotomy of actual versus aspirational digital health . World Psychiatry 2018 ; 17:108–109 Crossref , Medline , Google Scholar
3. Firth J, Torous J, Nicholas J, et al. : The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials . World Psychiatry 2017 ; 16:287–298 Crossref , Medline , Google Scholar
4. Arrieux JP, Cole WR, Ahrens AP : A review of the validity of computerized neurocognitive assessment tools in mild traumatic brain injury assessment . Concussion 2017 ; 2:CNC31 Crossref , Medline , Google Scholar
5. Buckley RF, Sparks KP, Papp KV, et al. : Computerized cognitive testing for use in clinical trials: a comparison of the NIH Toolbox and Cogstate C3 batteries . J Prev Alzheimers Dis 2017 ; 4:3–11 Medline , Google Scholar
6. Wild K, Howieson D, Webbe F, et al. : Status of computerized cognitive testing in aging: a systematic review . Alzheimers Dement 2008 ; 4:428–437 Crossref , Medline , Google Scholar
7. Robbins TW, James M, Owen AM, et al. : Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers . Dementia 1994 ; 5:266–281 Medline , Google Scholar
8. Keefe RSE, Goldberg TE, Harvey PD, et al. : The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery . Schizophr Res 2004 ; 68:283–297 Crossref , Medline , Google Scholar
9. Atkins AS, Tseng T, Vaughan A, et al. : Validation of the tablet-administered Brief Assessment of Cognition (BAC App) . Schizophr Res 2017 ; 181:100–106 Crossref , Medline , Google Scholar
10. Pearson : Q-interactive: easily administer and score clinical assessments using 2 iPads . https://www.pearsonassessments.com/professional-assessments/digital-solutions/q-interactive/about.html Google Scholar
11. Cole WR, Arrieux JP, Ivins BJ, et al. : A comparison of four computerized neurocognitive assessment tools to a traditional neuropsychological test battery in service members with and without mild traumatic brain injury . Arch Clin Neuropsychol 2018 ; 33:102–119 Crossref , Medline , Google Scholar
12. Russell MT, Funsch KM, Springfield CR, et al. : Validity of remote administration of the MATRICS Consensus Cognitive Battery for individuals with severe mental illness . Schizophr Res Cogn 2021 ; 27:100226 Crossref , Medline , Google Scholar
13. Keefe RSE, Davis VG, Atkins AS, et al. : Validation of a computerized test of functional capacity . Schizophr Res 2016 ; 175:90–96 Crossref , Medline , Google Scholar
14. Harvey PD, Forero DB, Ahern LB, et al. : The computerized functional skills assessment and training program: sensitivity to global cognitive impairment, correlations with cognitive abilities, and factor structure . Am J Geriatr Psychiatry 2021 ; 29:395–404 Crossref , Medline , Google Scholar
15. Nahum M, Lee H, Fisher M, et al. : Online social cognition training in schizophrenia: a double-blind, randomized, controlled multi-site clinical trial . Schizophr Bull 2021 ; 47:108–117 Crossref , Medline , Google Scholar
16. Czaja SJ, Kallestrup P, Harvey PD : Evaluation of a novel technology-based program designed to assess and train everyday skills in older adults . Innov Aging 2020 ; 4:igaa052 Crossref , Medline , Google Scholar
17. Kaemmerer T, Riordan P : Oral adaptation of the Trail Making Test: a practical review . Appl Neuropsychol Adult 2016 ; 23:384–389 Crossref , Medline , Google Scholar
18. Salinas CM, Bordes Edgar V, Berrios Siervo G, et al. : Transforming pediatric neuropsychology through video-based teleneuropsychology: an innovative private practice model pre-COVID-19 . Arch Clin Neuropsychol 2020 ; 35:1189–1195 Crossref , Medline , Google Scholar
19. Keefe RSE, Bilder RM, Davis SM, et al. : Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial . Arch Gen Psychiatry 2007 ; 64:633–647 Crossref , Medline , Google Scholar
20. Silverstein SM, Jaeger J, Donovan-Lepore AM, et al. : A comparative study of the MATRICS and IntegNeuro cognitive assessment batteries [published correction appears in J Clin Exp Neuropsychol 2010; 32:1149] . J Clin Exp Neuropsychol 2010 ; 32:937–952 Crossref , Medline , Google Scholar
21. Parrish EM, Kamarsu S, Harvey PD, et al. : Remote ecological momentary testing of learning and memory in adults with serious mental illness . Schizophr Bull 2021 ; 47:740–750 Crossref , Medline , Google Scholar
22. Depp CA, Kamarsu S, Filip TF, et al. : Ecological momentary facial emotion recognition in psychotic disorders . Psychol Med (Online ahead of print, January 12, 2021) Google Scholar
23. Hoffman HG, Patterson DR, Carrougher GJ, et al. : Effectiveness of virtual reality–based pain control with multiple treatments . Clin J Pain 2001 ; 17:229–235 Crossref , Medline , Google Scholar
24. Hoffman HG, Meyer WJ III, Drever SA, et al. : Virtual reality distraction to help control acute pain during medical procedures , in Virtual Reality for Psychological and Neurocognitive Interventions: Virtual Reality Technologies for Health and Clinical Applications . Edited by Rizzo A, Bouchard S . New York, Springer, 2019 , pp 195–208 Crossref , Google Scholar
25. Rizzo AA, Buckwalter JG : Theoretical and practical issues for the use of virtual reality in the cognitive rehabilitation of persons with acquired brain injuries: an update , in Proceedings of the 3rd International Conference on Virtual Reality and Persons With Disabilities . Edited by Murphy HJ . California State University Northridge, 1995 . http://www.csun.edu/∼hfdss006/conf/1995/proceedings/0004.htm Google Scholar
26. Rizzo AS, Koenig ST : Is clinical virtual reality ready for primetime? Neuropsychology 2017 ; 31:877–899 Crossref , Medline , Google Scholar
27. Riva G : Virtual environment for body image modification: virtual reality system for the treatment of body image disturbances . Comput Hum Behav 1998 ; 14:477–490 Crossref , Google Scholar
28. Riva G, Gutiérrez-Maldonado J, Dakanalis A, et al. : Virtual reality in the assessment and treatment of weight-related disorders , in Virtual Reality for Psychological and Neurocognitive Interventions: Virtual Reality Technologies for Health and Clinical Applications . Edited by Rizzo A, Bouchard S . New York, Springer, 2019 , pp 163–194 Crossref , Google Scholar
29. Rothbaum BO, Hodges LF, Kooper R, et al. : Virtual reality graded exposure in the treatment of acrophobia: a case report . Behav Ther 1995 ; 26:547–554 Crossref , Google Scholar
30. Rothbaum BO, Price M, Jovanovic T, et al. : A randomized, double-blind evaluation of d -cycloserine or alprazolam combined with virtual reality exposure therapy for posttraumatic stress disorder in Iraq and Afghanistan War veterans . Am J Psychiatry 2014 ; 171:640–648 Link , Google Scholar
31. Slater M, Neyret S, Johnston T, et al. : An experimental study of a virtual reality counselling paradigm using embodied self-dialogue . Sci Rep 2019 ; 9:10903 Crossref , Medline , Google Scholar
32. Aukstakalnis S, Blatner D : Silicon Mirage: The Art and Science of Virtual Reality . Berkeley, Calif, Peachpit Press, 1992 Google Scholar
33. Slater M, Wilbur S : A framework for immersive virtual environments (FIVE): speculations on the role of presence in virtual environments . Teleoperators Virtual Environments 1997 ; 6:603–616 Crossref , Google Scholar
34. Bouchard S, Dumoulin S, Robillard G, et al. : Virtual reality compared with in vivo exposure in the treatment of social anxiety disorder: a three-arm randomised controlled trial . Br J Psychiatry 2017 ; 210:276–283 Crossref , Medline , Google Scholar
35. Botella C, García‐Palacios A, Villa H, et al. : Virtual reality exposure in the treatment of panic disorder and agoraphobia: a controlled study . Clin Psychol Psychotherapy 2007 ; 14:164–175 Crossref , Google Scholar
36. Burke SL, Bresnahan TL, Li T, et al. : Using Virtual Interactive Training Agents (ViTA) with adults with autism and other developmental disabilities . J Autism Dev Disord 2018 ; 48:905–912 Crossref , Medline , Google Scholar
37. Rutten A, Cobb S, Neale H, et al. : The AS interactive project: single‐user and collaborative virtual environments for people with high‐functioning autistic spectrum disorders . J Visualization Computer Anim 2003 ; 14:233–241 Crossref , Google Scholar
38. Yang YJD, Allen T, Abdullahi SM, et al. : Neural mechanisms of behavioral change in young adults with high‐functioning autism receiving virtual reality social cognition training: a pilot study . Autism Res 2018 ; 11:713–725 Crossref , Medline , Google Scholar
39. Gonzalez-Liencres C, Zapata LE, Iruretagoyena G, et al. : Being the victim of intimate partner violence in virtual reality: first- versus third-person perspective . Front Psychol 2020 ; 11:820 Crossref , Medline , Google Scholar
40. Falconer CJ, Rovira A, King JA, et al. : Embodying self-compassion within virtual reality and its effects on patients with depression . BrJPsych Open 2016 ; 2:74–80 Crossref , Medline , Google Scholar
41. Talbot T, Rizzo A : Virtual human standardized patients for clinical training , in Virtual Reality for Psychological and Neurocognitive Interventions: Virtual Reality Technologies for Health and Clinical Applications . Edited by Rizzo A, Bouchard S . New York, Springer, 2019 , pp 387–405 Crossref , Google Scholar
42. Reger GM, Norr AM, Rizzo AS, et al. : Virtual standardized patients vs academic training for learning motivational interviewing skills in the US Department of Veterans Affairs and the US military: a randomized trial . JAMA Netw Open 2020 ; 3:e2017348 Crossref , Medline , Google Scholar
43. Mozgai S, Hartholt A, Rizzo A : An adaptive agent–based interface for personalized health interventions , in Proceedings of the 2020 ACM Intelligent User Interfaces Conference . Association for Computing Machinery, 2020 , pp 118–119 Google Scholar
44. Rizzo AA, Shilling R, Forbell ED, et al. : Autonomous virtual human agents for healthcare information support and clinical interviewing , in Artificial Intelligence in Mental Healthcare Practice . Edited by Luxton DD . Oxford, Academic Press, 2015 , pp 53–80 Google Scholar
45. Rizzo AA, Scherer S, DeVault D, et al. : Detection and computational analysis of psychological signals using a virtual human interviewing agent . J Pain Manage 2016 ; 9:311–321 Google Scholar
46. Yao H, de Siqueira AG, Foster A, et al. : Toward automated evaluation of empathetic responses in virtual human interaction systems for mental health scenarios , in Proceedings of the 20th ACM International Conference on Intelligent Virtual Agents . Association for Computing Machinery, 2020 , pp 1–8 Google Scholar
47. Parsons TD, Rizzo AA : Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis . J Behav Ther Exp Psychiatry 2008 ; 39:250–261 Crossref , Medline , Google Scholar
48. Powers MB, Rothbaum BO : Recent advances in virtual reality therapy for anxiety and related disorders: introduction to the special issue . J Anxiety Disord 2019 ; 61:1–2 Crossref , Medline , Google Scholar
49. Rizzo AS, Difede J, Rothbaum BO, et al. : Development and early evaluation of the Virtual Iraq/Afghanistan exposure therapy system for combat-related PTSD . Ann N Y Acad Sci 2010 ; 1208:114–125 Crossref , Medline , Google Scholar
50. Rizzo AA, John B, Newman B, et al. : Virtual reality as a tool for delivering PTSD exposure therapy and stress resilience training . J Militar Behav Health 2013 ; 1:48–54 Google Scholar
51. Rizzo AA, Cukor J, Gerardi M, et al. : Virtual reality exposure therapy for PTSD due to military combat and terrorist attacks . J Contemp Psychother 2015 ; 45:255–264 Crossref , Google Scholar
52. Rothbaum BO, Hodges LF, Ready D, et al. : Virtual reality exposure therapy for Vietnam veterans with posttraumatic stress disorder . J Clin Psychiatry 2001 ; 62:617–622 Crossref , Medline , Google Scholar
53. Bordnick PS, Washburn M : Virtual environments for substance abuse assessment and treatment , in Virtual Reality for Psychological and Neurocognitive Interventions: Virtual Reality Technologies for Health and Clinical Applications . Edited by Rizzo A, Bouchard S . New York, Springer, 2019 , pp 131–162 Crossref , Google Scholar
54. Hone-Blanchet A, Wensing T, Fecteau S : The use of virtual reality in craving assessment and cue-exposure therapy in substance use disorders . Front Hum Neurosci 2014 ; 8:844 Crossref , Medline , Google Scholar
55. Yoon JH, Ii RDLG, Bordnick PS, et al. : A pilot study examining the efficacy of virtual-reality based relapse prevention among alcohol-dependent veterans with traumatic brain injury . Drug Alcohol Depend 2014 ; 140:e247 Crossref , Google Scholar
56. Freeman D, Bradley J, Antley A, et al. : Virtual reality in the treatment of persecutory delusions: randomised controlled experimental study testing how to reduce delusional conviction . Br J Psychiatry 2016 ; 209:62–67 Crossref , Medline , Google Scholar
57. John NW, Pop SR, Day TW, et al. : The implementation and validation of a virtual environment for training powered wheelchair manoeuvres . IEEE Trans Vis Comput Graph 2018 ; 24:1867–1878 Crossref , Medline , Google Scholar
58. Maggio MG, Latella D, Maresca G, et al. : Virtual reality and cognitive rehabilitation in people with stroke: an overview . J Neurosci Nurs 2019 ; 51:101–105 Crossref , Medline , Google Scholar
59. Rizzo AA, Bowerly T, Buckwalter JG, et al. : A virtual reality scenario for all seasons: the virtual classroom . CNS Spectrums 2006 ; 11:35–44 Crossref , Medline , Google Scholar
60. Rizzo AA, Chen JZ, Wang J, et al. : Normative data for a next generation virtual classroom for attention assessment in children with ADHD and beyond , in Proceedings of the International Conference on Disability, Virtual Reality, and Associated Technologies . http://studio.hei-lab.ulusofona.pt/archive/2021/ICDVRAT2021_Full_Proceedings_13thConf_FinalVersion.pdf Google Scholar
61. Dellazizzo L, Potvin S, Luigi M, et al. : Evidence on virtual reality–based therapies for psychiatric disorders: meta-review of meta-analyses . J Med Internet Res 2020 ; 22:e20889 Crossref , Medline , Google Scholar
62. Carl E, Stein AT, Levihn-Coon A, et al. : Virtual reality exposure therapy for anxiety and related disorders: a meta-analysis of randomized controlled trials . J Anxiety Disord 2019 ; 61:27–36 Crossref , Medline , Google Scholar
63. Mallari B, Spaeth EK, Goh H, et al. : Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis . J Pain Res 2019 ; 12:2053–2085 Crossref , Medline , Google Scholar
64. Skarbez R, Brooks FP Jr, Whitton MC : A survey of presence and related concepts . ACM Comput Surv (CSUR) 2017 ; 50:1–39 Crossref , Google Scholar
65. Norcross JC, Pfund RA, Prochaska JO : Psychotherapy in 2022: a Delphi poll on its future . Prof Psychol Res Pract 2013 ; 44:363–370 Crossref , Google Scholar
66. Rizzo A, Hartholt A, Mozgai S : From combat to COVID-19: managing the impact of trauma using virtual reality . J Tech Hum Serv 2021 ; 39:341–347 Crossref , Google Scholar
67. Doherty K, Balaskas A, Doherty G : The design of ecological momentary assessment technologies . Interact Comput 2020 ; 32:257–278 Crossref , Google Scholar
68. Stone AA, Schwartz JE, Neale JM, et al. : A comparison of coping assessed by ecological momentary assessment and retrospective recall . J Pers Soc Psychol 1998 ; 74:1670–1680 Crossref , Medline , Google Scholar
69. O’Connell KA, Gerkovich MM, Cook MR, et al. : Coping in real time: using ecological momentary assessment techniques to assess coping with the urge to smoke . Res Nurs Health 1998 ; 21:487–497 Crossref , Medline , Google Scholar
70. Kamarck TW, Schwartz JE, Shiffman S, et al. : Psychosocial stress and cardiovascular risk: what is the role of daily experience? J Pers 2005 ; 73:1749–1774 Crossref , Medline , Google Scholar
71. Stone AA, Shiffman S, Schwartz JE, et al. : Patient compliance with paper and electronic diaries . Control Clin Trials 2003 ; 24:182–199 Crossref , Medline , Google Scholar
72. Dunton GF, Huh J, Leventhal AM, et al. : Momentary assessment of affect, physical feeling states, and physical activity in children . Health Psychol 2014 ; 33:255–263 Crossref , Medline , Google Scholar
73. Weinstein SM, Mermelstein RJ, Hedeker D, et al. : The time-varying influences of peer and family support on adolescent daily positive and negative affect . J Clin Child Adolesc Psychol 2006 ; 35:420–430 Crossref , Medline , Google Scholar
74. Depp CA, Kim DH, de Dios LV, et al. : A pilot study of mood ratings captured by mobile phone versus paper-and-pencil mood charts in bipolar disorder . J Dual Diagn 2012 ; 8:326–332 Crossref , Medline , Google Scholar
75. Myin-Germeys I, Klippel A, Steinhart H, et al. : Ecological momentary interventions in psychiatry . Curr Opin Psychiatry 2016 ; 29:258–263 Crossref , Medline , Google Scholar
76. Depp CA, Mausbach B, Granholm E, et al. : Mobile interventions for severe mental illness: design and preliminary data from three approaches . J Nerv Ment Dis 2010 ; 198:715–721 Crossref , Medline , Google Scholar
77. Moore DJ, Montoya JL, Blackstone K, et al. : Preliminary evidence for feasibility, use, and acceptability of individualized texting for adherence building for antiretroviral adherence and substance use assessment among HIV-infected methamphetamine users . AIDS Res Treat 2013 ; 2013:585143 Medline , Google Scholar
78. Shiffman S, Scholl SM, Mao J, et al. : Ecological momentary assessment of temptations and lapses in non-daily smokers . Psychopharmacology (Berl) 2020 ; 237:2353–2365 Crossref , Medline , Google Scholar
79. Kleiman EM, Turner BJ, Fedor S, et al. : Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies . J Abnorm Psychol 2017 ; 126:726–738 Crossref , Medline , Google Scholar
80. Ben-Zeev D, Young MA, Depp CA : Real-time predictors of suicidal ideation: mobile assessment of hospitalized depressed patients . Psychiatry Res 2012 ; 197:55–59 Crossref , Medline , Google Scholar
81. Depp CA, Moore RC, Perivoliotis D, et al. : Social behavior, interaction appraisals, and suicidal ideation in schizophrenia: the dangers of being alone . Schizophr Res 2016 ; 172:195–200 Crossref , Medline , Google Scholar
82. Granholm E, Holden JL, Mikhael T, et al. : What do people with schizophrenia do all day? Ecological momentary assessment of real-world functioning in schizophrenia . Schizophr Bull 2020 ; 46:242–251 Medline , Google Scholar
83. Strassnig MT, Harvey PD, Miller ML, et al. : Real world sedentary behavior and activity levels in patients with schizophrenia and controls: an ecological momentary assessment study . Mental Health Phys Act 2021 ; 20:100364 Crossref , Google Scholar
84. Koffer R, Drewelies J, Almeida DM, et al. : The role of general and daily control beliefs for affective stressor-reactivity across adulthood and old age . J Gerontol B Psychol Sci Soc Sci 2019 ; 74:242–253 Crossref , Medline , Google Scholar
85. Harvey PD, Miller ML, Moore RC, et al. : Capturing clinical symptoms with ecological momentary assessment: convergence of momentary reports of psychotic and mood symptoms with diagnoses and standard clinical assessments . Innov Clin Neurosci 2021 ; 18:24–30 Medline , Google Scholar
86. Cohen AS, Schwartz E, Le TP, et al. : Digital phenotyping of negative symptoms: the relationship to clinician ratings . Schizophr Bull 2021 ; 47:44–53 Crossref , Medline , Google Scholar
87. Targum SD, Sauder C, Evans M, et al. : Ecological momentary assessment as a measurement tool in depression trials . J Psychiatr Res 2021 ; 136:256–264 Crossref , Medline , Google Scholar
88. Durand D, Strassnig MT, Moore RC, et al. : Self-reported social functioning and social cognition in schizophrenia and bipolar disorder: using ecological momentary assessment to identify the origin of bias . Schizophr Res 2021 ; 230:17–23 Crossref , Medline , Google Scholar
89. Insel TR : Digital phenotyping: a global tool for psychiatry . World Psychiatry 2018 ; 17:276–277 Crossref , Medline , Google Scholar
90. Barnett I, Onnela JP : Inferring mobility measures from GPS traces with missing data . Biostatistics 2020 ; 21:e98–e112 Crossref , Medline , Google Scholar
91. Fulford D, Mote J, Gonzalez R, et al. : Smartphone sensing of social interactions in people with and without schizophrenia . J Psychiatr Res 2021 ; 137:613–620 Crossref , Medline , Google Scholar
92. Huang EJ, Onnela J-P : Augmented movelet method for activity classification using smartphone gyroscope and accelerometer data . Sensors (Basel) 2020 ; 20:3706 Crossref , Medline , Google Scholar
93. Hswen Y, Gopaluni A, Brownstein JS, et al. : Using Twitter to detect psychological characteristics of self-identified persons with autism spectrum disorder: a feasibility study . JMIR Mhealth Uhealth 2019 ; 7:e12264 Crossref , Medline , Google Scholar
94. Staples P, Torous J, Barnett I, et al. : A comparison of passive and active estimates of sleep in a cohort with schizophrenia . NPJ Schizophrenia 2017 ; 3:37 Crossref , Medline , Google Scholar
95. Yan Z, Yang J, Tapia EM : Smartphone Bluetooth based social sensing , in Proceedings of the 2013 ACM conference on pervasive and ubiquitous computing adjunct publication . Association for Computing Machinery, 2013 , pp 95–98 Google Scholar
96. Wang Y, Ren X, Liu X, et al. : Examining the correlation between depression and social behavior on smartphones through usage metadata: empirical study . JMIR Mhealth Uhealth 2021 ; 9:e19046 Crossref , Medline , Google Scholar
97. Goldsack JC, Coravos A, Bakker JP, et al. : Verification, analytical validation, and clinical validation (V3): the foundation of determining fit-for-purpose for biometric monitoring technologies (BioMeTs) . NPJ Digit Med 2020 ; 3:55 Crossref , Medline , Google Scholar
98. Donaire-Gonzalez D, Valentín A, van Nunen E, et al. : ExpoApp: an integrated system to assess multiple personal environmental exposures . Environ Int 2019 ; 126:494–503 Crossref , Medline , Google Scholar
99. Adler DA, Ben-Zeev D, Tseng VWS, et al. : Predicting early warning signs of psychotic relapse from passive sensing data: an approach using encoder-decoder neural networks . JMIR Mhealth Uhealth 2020 ; 8:e19962 Crossref , Medline , Google Scholar
100. Ebner-Priemer UW, Mühlbauer E, Neubauer AB, et al. : Digital phenotyping: towards replicable findings with comprehensive assessments and integrative models in bipolar disorders . Int J Bipol Disord 2020 ; 8:35 Crossref , Medline , Google Scholar
101. Faurholt-Jepsen M, Busk J, Frost M, et al. : Voice analysis as an objective state marker in bipolar disorder . Transl Psychiatry 2016 ; 6:e856 Crossref , Medline , Google Scholar
102. Saeb S, Zhang M, Karr CJ, et al. : Mobile phone sensor correlates of depressive symptom severity in daily-life behavior: an exploratory study . J Med Internet Res 2015 ; 17:e175 Crossref , Medline , Google Scholar
103. Saeb S, Lattie EG, Schueller SM, et al. : The relationship between mobile phone location sensor data and depressive symptom severity . PeerJ 2016 ; 4:e2537 Crossref , Medline , Google Scholar
104. Sarda A, Munuswamy S, Sarda S, et al. : Using passive smartphone sensing for improved risk stratification of patients with depression and diabetes: cross-sectional observational study . JMIR Mhealth Uhealth 2019 ; 7:e11041 Crossref , Medline , Google Scholar
105. Di Matteo D, Fotinos K, Lokuge S, et al. : The relationship between smartphone-recorded environmental audio and symptomatology of anxiety and depression: exploratory study . JMIR Form Res 2020 ; 4:e18751 Crossref , Medline , Google Scholar
106. Jacobson NC, Summers B, Wilhelm S : Digital biomarkers of social anxiety severity: digital phenotyping using passive smartphone sensors . J Med Internet Res 2020 ; 22:e16875 Crossref , Medline , Google Scholar
107. Parrish EM, Depp CA, Moore RC, et al. : Emotional determinants of life-space through GPS and ecological momentary assessment in schizophrenia: what gets people out of the house? Schizophr Res 2020 ; 224:67–73 Crossref , Medline , Google Scholar
108. Depp CA, Bashem J, Moore RC, et al. : GPS mobility as a digital biomarker of negative symptoms in schizophrenia: a case control study . NPJ Digit Med 2019 ; 2:108 Crossref , Medline , Google Scholar
109. Umbricht D, Cheng WY, Lipsmeier F, et al. : Deep learning–based human activity recognition for continuous activity and gesture monitoring for schizophrenia patients with negative symptoms . Front Psychiatry 2020 ; 11:574375 Crossref , Medline , Google Scholar
110. Wee ZY, Yong SWL, Chew QH, et al. : Actigraphy studies and clinical and biobehavioural correlates in schizophrenia: a systematic review . J Neural Transm (Vienna) 2019 ; 126:531–558 Crossref , Medline , Google Scholar
111. Raugh IM, James SH, Gonzalez CM, et al. : Geolocation as a digital phenotyping measure of negative symptoms and functional outcome . Schizophr Bull 2020 ; 46:1596–1607 Crossref , Medline , Google Scholar
112. Henson P, D’Mello R, Vaidyam A, et al. : Anomaly detection to predict relapse risk in schizophrenia . Transl Psychiatry 2021 ; 11:28 Crossref , Medline , Google Scholar
113. Fraccaro P, Beukenhorst A, Sperrin M, et al. : Digital biomarkers from geolocation data in bipolar disorder and schizophrenia: a systematic review . J Am Med Inform Assoc 2019 ; 26:1412–1420 Crossref , Medline , Google Scholar
114. Or F, Torous J, Onnela JP : High potential but limited evidence: using voice data from smartphones to monitor and diagnose mood disorders . Psychiatr Rehabil J 2017 ; 40:320–324 Crossref , Medline , Google Scholar
115. Raugh IM, Chapman HC, Bartolomeo LA, et al. : A comprehensive review of psychophysiological applications for ecological momentary assessment in psychiatric populations . Psychol Assess 2019 ; 31:304–317 Crossref , Medline , Google Scholar
116. Tazawa Y, Wada M, Mitsukura Y, et al. : Actigraphy for evaluation of mood disorders: a systematic review and meta-analysis . J Affect Disord 2019 ; 253:257–269 Crossref , Medline , Google Scholar
117. Moshe I, Terhorst Y, Opoku Asare K, et al. : Predicting symptoms of depression and anxiety using smartphone and wearable data . Front Psychiatry 2021 ; 12:625247 Crossref , Medline , Google Scholar
118. Dagum P : Digital biomarkers of cognitive function . NPJ Digit Med 2018 ; 1:10 Crossref , Medline , Google Scholar
119. Benoit J, Onyeaka H, Keshavan M, et al. : Systematic review of digital phenotyping and machine learning in psychosis spectrum illnesses . Harv Rev Psychiatry 2020 ; 28:296–304 Crossref , Medline , Google Scholar
120. Simblett SK, Bruno E, Siddi S, et al. : Patient perspectives on the acceptability of mHealth technology for remote measurement and management of epilepsy: a qualitative analysis . Epilepsy Behav 2019 ; 97:123–129 Crossref , Medline , Google Scholar
121. Torous J, Wisniewski H, Bird B, et al. : Creating a digital health smartphone app and digital phenotyping platform for mental health and diverse healthcare needs: an interdisciplinary and collaborative approach . J Technol Behav Sci 2019 ; 4:73–85 Crossref , Google Scholar
122. Raugh IM, James SH, Gonzalez CM, et al. : Geolocation as a digital phenotyping measure of negative symptoms and functional outcome . Schizophr Bull 2020 ; 46:1596–1607 Crossref , Medline , Google Scholar
123. Bonet L, Torous J, Arce D, et al. : ReMindCare, an app for daily clinical practice in patients with first episode psychosis: a pragmatic real-world study protocol . Early Interv Psychiatry 2021 ; 15:183–192 Crossref , Medline , Google Scholar
124. Menon V, Selvakumar N, Kattimani S, et al. : Therapeutic effects of mobile-based text message reminders for medication adherence in bipolar I disorder: are they maintained after intervention cessation? J Psychiatr Res 2018 ; 104:163–168 Crossref , Medline , Google Scholar
125. US Food and Drug Administration : FDA approves pill with sensor that digitally tracks if patients have ingested their medication . https://www.fda.gov/news-events/press-announcements/fda-approves-pill-sensor-digitally-tracks-if-patients-have-ingested-their-medication . November 13, 2017 Google Scholar
126. Morey TE, Booth M, Wasdo S, et al. : Oral adherence monitoring using a breath test to supplement highly active antiretroviral therapy . AIDS Behav 2013 ; 17:298–306 Crossref , Medline , Google Scholar
127. Firth J, Torous J, Nicholas J, et al. : The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials . World Psychiatry 2017 ; 16:287–298 Crossref , Medline , Google Scholar
128. Linardon J, Fuller-Tyszkiewicz M : Attrition and adherence in smartphone-delivered interventions for mental health problems: a systematic and meta-analytic review . J Consult Clin Psychol 2020 ; 88:1–13 Crossref , Medline , Google Scholar
129. Huguet A, Rao S, McGrath PJ, et al. : A systematic review of cognitive behavioral therapy and behavioral activation apps for depression . PLoS One 2016 ; 11:e0154248 Crossref , Medline , Google Scholar
130. Hrynyschyn R, Dockweiler C : Effectiveness of smartphone-based cognitive behavioral therapy among patients with major depression: systematic review of health implications . JMIR Mhealth Uhealth 2021 ; 9:e24703 Crossref , Medline , Google Scholar
131. Firth J, Torous J, Nicholas J, et al. : Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials . J Affect Disord 2017 ; 218:15–22 Crossref , Medline , Google Scholar
132. Nahum-Shani I, Smith SN, Spring BJ, et al. : Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support . Ann Behav Med 2018 ; 52:446–462 Crossref , Medline , Google Scholar
133. Ben-Zeev D, Scherer EA, Gottlieb JD, et al. : mHealth for schizophrenia: patient engagement with a mobile phone intervention following hospital discharge . JMIR Ment Health 2016 ; 3:e34 Crossref , Medline , Google Scholar
134. Marler JD, Fujii CA, Utley DS, et al. : Initial assessment of a comprehensive digital smoking cessation program that incorporates a mobile app, breath sensor, and coaching: cohort study . JMIR Mhealth Uhealth 2019 ; 7:e12609 Crossref , Medline , Google Scholar
135. Maricich YA, Bickel WK, Marsch LA, et al. : Safety and efficacy of a prescription digital therapeutic as an adjunct to buprenorphine for treatment of opioid use disorder . Curr Med Res Opin 2021 ; 37:167–173 Crossref , Medline , Google Scholar
136. Hser YI, Evans E, Huang D, et al. : Long-term outcomes after randomization to buprenorphine/naloxone versus methadone in a multi-site trial . Addiction 2016 ; 111:695–705 Crossref , Medline , Google Scholar
137. Maricich YA, Xiong X, Gerwien R, et al. : Real-world evidence for a prescription digital therapeutic to treat opioid use disorder . Curr Med Res Opin 2021 ; 37:175–183 Crossref , Medline , Google Scholar
138. McGurk SR, Twamley EW, Sitzer D, et al. : A meta-analysis of cognitive remediation in schizophrenia . Am J Psychiatry 2007 ; 164:1791–1802 Link , Google Scholar
139. Wykes T, Huddy V, Cellard C, et al. : A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes . Am J Psychiatry 2011 ; 168:472–485 Link , Google Scholar
140. Rebok GW, Ball K, Guey LT, et al. : Ten-year effects of the Advanced Cognitive Training for Independent and Vital Elderly Cognitive Training Trial on cognition and everyday functioning in older adults . J Am Geriatr Soc 2014 ; 62:16–24 Crossref , Medline , Google Scholar
141. Wolinsky FD, Vander Weg MW, Howren MB, et al. : The effect of cognitive speed of processing training on the development of additional IADL difficulties and the reduction of depressive symptoms results from the IHAMS randomized controlled trial . J Aging Health 2015 ; 27:334–354 Crossref , Medline , Google Scholar
142. Smith GE, Housen P, Yaffe K, et al. : A cognitive training program based on principles of brain plasticity: results from the Improvement in Memory With Plasticity-Based Adaptive Cognitive Training (IMPACT) study . J Am Geriatr Soc 2009 ; 57:594–603 Crossref , Medline , Google Scholar
143. Bellani M, Biagianti B, Zovetti N, et al. : The effects of cognitive remediation on cognitive abilities and real-world functioning among people with bipolar disorder: a systematic review . J Affect Disord 2019 ; 257:691–697 Crossref , Medline , Google Scholar
144. Motter JN, Grinberg A, Lieberman DH, et al. : Computerized cognitive training in young adults with depressive symptoms: effects on mood, cognition, and everyday functioning . J Affect Disord 2019 ; 245:28–37 Crossref , Medline , Google Scholar
145. McGurk SR, Mueser KT, Feldman K, et al. : Cognitive training for supported employment: 2–3 year outcomes of a randomized controlled trial . Am J Psychiatry 2007 ; 164:437–441 Link , Google Scholar
146. McGurk SR, Mueser KT, Xie H, et al. : Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial . Am J Psychiatry 2015 ; 172:852–861 Link , Google Scholar
147. Lindenmayer JP, Khan A, McGurk SR, et al. : Does social cognition training augment response to computer-assisted cognitive remediation for schizophrenia? Schizophr Res 2018 ; 201:180–186 Crossref , Medline , Google Scholar
148. Twamley EW, Thomas KR, Burton CZ, et al. : Compensatory cognitive training for people with severe mental illnesses in supported employment: a randomized controlled trial . Schizophr Res 2019 ; 203:41–48 Crossref , Medline , Google Scholar
149. Harvey PD, Balzer AM, Kotwicki RJ : Training engagement, baseline cognitive functioning, and cognitive gains with computerized cognitive training: a cross-diagnostic study . Schizophr Res Cogn 2020 ; 19:100150 Crossref , Medline , Google Scholar
150. Biagianti B, Fisher M, Neilands TB, et al. : Engagement with the auditory processing system during targeted auditory cognitive training mediates changes in cognitive outcomes in individuals with schizophrenia . Neuropsychology 2016 ; 30:998–1008 Crossref , Medline , Google Scholar
151. Mahncke HW, Kim SJ, Rose A, et al. : Evaluation of a plasticity-based cognitive training program in schizophrenia: results from the eCaesar trial . Schizophr Res 2019 ; 208:182–189 Crossref , Medline , Google Scholar
152. Loewy R, Fisher M, Schlosser DA, et al. : Intensive auditory cognitive training improves verbal memory in adolescents and young adults at clinical high risk for psychosis . Schizophr Bull 2016 ; 42(suppl 1):S118–S126 Crossref , Medline , Google Scholar
153. Fisher M, Loewy R, Carter C, et al. : Neuroplasticity-based auditory training via laptop computer improves cognition in young individuals with recent onset schizophrenia . Schizophr Bull 2015 ; 41:250–258 Crossref , Medline , Google Scholar
154. Fisher M, Mellon SH, Wolkowitz O, et al. : Neuroscience-informed auditory training in schizophrenia: a final report of the effects on cognition and serum brain-derived neurotrophic factor . Schizophr Res Cogn 2016 ; 3:1–7 Crossref , Medline , Google Scholar
155. Bowie CR, Grossman M, Gupta M, et al. : Cognitive remediation in schizophrenia: efficacy and effectiveness in patients with early versus long-term course of illness . Early Interv Psychiatry 2014 ; 8:32–38 Crossref , Medline , Google Scholar
156. Lindenmayer JP, McGurk SR, Mueser KT, et al. : A randomized controlled trial of cognitive remediation among inpatients with persistent mental illness . Psychiatr Serv 2008 ; 59:241–247 Link , Google Scholar
157. Thomas ML, Bismark AW, Joshi YB, et al. : Targeted cognitive training improves auditory and verbal outcomes among treatment refractory schizophrenia patients mandated to residential care . Schizophr Res 2018 ; 202:378–384 Crossref , Medline , Google Scholar
158. Morimoto SS, Altizer RA, Gunning FM, et al. : Targeting cognitive control deficits with neuroplasticity-based computerized cognitive remediation in patients with geriatric major depression: a randomized, double-blind, controlled trial . Am J Geriatr Psychiatry 2020 ; 28:971–980 Crossref , Medline , Google Scholar
159. Bowie CR, Gupta M, Holshausen K, et al. : Cognitive remediation for treatment-resistant depression: effects on cognition and functioning and the role of online homework . J Nerv Ment Dis 2013 ; 201:680–685 Crossref , Medline , Google Scholar
160. Corbett A, Owen A, Hampshire A, et al. : The effect of an online cognitive training package in healthy older adults: an online randomized controlled trial . J Am Med Dir Assoc 2015 ; 16:990–997 Crossref , Medline , Google Scholar
161. Kollins SH, DeLoss DJ, Cañadas E, et al. : A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): a randomised controlled trial . Lancet Digit Health 2020 ; 2:e168–e178 Crossref , Medline , Google Scholar
162. Leark RA, Dupuy TR, Greenberg LM, et al. : Test of Visual Attention: Professional Manual (Edition Number 9.1-12-g63538d5) . Los Alamitos, Calif, TOVA Corporation, December 30, 2020 Google Scholar
163. Swerdlow NR : Beyond antipsychotics: pharmacologically augmented cognitive therapies (PACTs) for schizophrenia . Neuropsychopharmacology 2012 ; 37:310–311 Crossref , Medline , Google Scholar
164. Swerdlow NR, Tarasenko M, Bhakta SG, et al. : Amphetamine enhances gains in auditory discrimination training in adult schizophrenia patients . Schizophr Bull 2017 ; 43:872–880 Medline , Google Scholar
165. McClure MM, Graff F, Triebwasser J, et al. : Guanfacine augmentation of a combined intervention of computerized cognitive remediation therapy and social skills training for schizotypal personality disorder . Am J Psychiatry 2019 ; 176:307–314 Link , Google Scholar
166. Michalopoulou PG, Lewis SW, Drake RJ, et al. : Modafinil combined with cognitive training: pharmacological augmentation of cognitive training in schizophrenia . Eur Neuropsychopharmacol 2015 ; 25:1178–1189 Crossref , Medline , Google Scholar
167. Swerdlow NR, Bhakta SG, Talledo J, et al. : Memantine effects on auditory discrimination and training in schizophrenia patients . Neuropsychopharmacology 2020 ; 45:2180–2188 Crossref , Medline , Google Scholar
168. Lenze EJ, Stevens A, Waring JD, et al. : Augmenting computerized cognitive training with vortioxetine for age-related cognitive decline: a randomized controlled trial . Am J Psychiatry 2020 ; 177:548–555 Link , Google Scholar
169. Bhakta SG, Chou HH, Rana B, et al. : Effects of acute memantine administration on MATRICS Consensus Cognitive Battery performance in psychosis: testing an experimental medicine strategy . Psychopharmacology (Berl) 2016 ; 233:2399–2410 Crossref , Medline , Google Scholar
170. Ortiz-Orendain J, Covarrubias-Castillo SA, Vazquez-Alvarez AO, et al. : Modafinil for people with schizophrenia or related disorders . Cochrane Database Syst Rev 2019 ; 12:CD008661 Medline , Google Scholar
171. Fleischhacker WW, Podhorna J, Gröschl M, et al. : Efficacy and safety of the novel glycine transporter inhibitor BI 425809 once daily in patients with schizophrenia: a double-blind, randomised, placebo-controlled phase 2 study . Lancet Psychiatry 2021 ; 8:191–201 Crossref , Medline , Google Scholar
172. Harvey PD, Bowie CR, McDonald S, et al. : Evaluation of the efficacy of BI 425809 pharmacotherapy in patients with schizophrenia receiving computerized cognitive training: methodology for a double-blind, randomized, parallel-group trial . Clin Drug Investig 2020 ; 40:377–385 Crossref , Medline , Google Scholar
173. Nuechterlein KH, Ventura J, Subotnik KL, et al. : A randomized controlled trial of cognitive remediation and long-acting injectable risperidone after a first episode of schizophrenia: improving cognition and work/school functioning . Psychol Med 2022 ; 8:1517–1526 Crossref , Google Scholar
174. Coravos A, Goldsack JC, Karlin DR, et al. : Digital medicine: a primer on measurement . Digital Biomarkers 2019 ; 3:31–71 Crossref , Medline , Google Scholar
175. US Food and Drug Administration : Digital Health Software Precertification (Pre-Cert) Program . https://www.fda.gov/medical-devices/digital-health-center-excellence/digital-health-software-precertification-pre-cert-program . May 6, 2021 Google Scholar
176. US Food and Drug Administration : Mobile Medical Applications: Guidance for industry and FDA Staff . Washington, DC, US Food and Drug Administration, February 9, 2015 Google Scholar
177. Torous JB, Chan SR, Gipson SYMT, et al. : A hierarchical framework for evaluation and informed decision making regarding smartphone apps for clinical care . Psychiatr Serv 2018 ; 69:498–500 Link , Google Scholar
178. Carlo AD, Hosseini Ghomi R, Renn BN, et al. : By the numbers: ratings and utilization of behavioral health mobile applications . NPJ Digit Med 2019 ; 2:54–58 Crossref , Medline , Google Scholar
179. Lagan S, Aquino P, Emerson MR, et al. : Actionable health app evaluation: translating expert frameworks into objective metrics . NPJ Digit Med 2020 ; 3:100 Crossref , Medline , Google Scholar
180. Federal Trade Commission : Lumosity to pay $2 million to settle FTC deceptive advertising charges for its “brain training” program . January 5, 2016 . https://www.ftc.gov/news-events/press-releases/2016/01/lumosity-pay-2-million-settle-ftc-deceptive-advertising-charges Google Scholar
181. Federal Trade Commission : Developer of popular women’s fertility-tracking app settles FTC allegations that it misled consumers about the disclosure of their health data . January 13, 2021 . https://www.ftc.gov/news-events/press-releases/2021/01/developer-popular-womens-fertility-tracking-app-settles-ftc Google Scholar
- Perspectives on heterogeneity-informed cognitive training for attention-deficit/hyperactivity disorder 12 January 2023 | Frontiers in Psychiatry, Vol. 13
- Ned H. Kalin , M.D.
- Cognition/Learning/Memory
- Psychotherapy
- Assessment and Interviewing
- Neurodevelopmental Disorders
- Attention Deficit Hyperactivity Disorder (ADHD)
- Posttraumatic Stress Disorder (PTSD)
- Depressive Disorders
- Bipolar and Related Disorders
- Schizophrenia Spectrum and Other Psychotic Disorders
OPINION article
The need for a mental health technology revolution in the covid-19 pandemic.
Part of this article's content has been mentioned in:
Leveraging Technology for the Wellbeing of Individuals With Autism Spectrum Disorder and Their Families During Covid-19
- Read opinion

- 1 School of Social Welfare, University of California, Berkeley, Berkeley, CA, United States
- 2 Department of Psychiatry, Zuckerberg San Francisco General Hospital, University of California, San Francisco, San Francisco, CA, United States
Introduction
The current coronavirus 2019 (COVID-19) pandemic not only poses a large threat to the physical health of our population, if we fail to act now, it will also have detrimental long-term consequences for mental health.
Though social distancing is a crucial intervention to slow down the destructive effects of the pandemic, it can lead to isolation, decreased physical activity, and increased rumination, which might particularly hurt those with pre-existing mental illness. Further, the stream of disheartening COVID-19 news provides fodder for increased worry and distress, which can be detrimental for people with anxiety disorders. Early cross-sectional surveys in the United States, Canada, and Europe show an increase in symptoms of depression and anxiety for the general population, associated with COVID-19 concerns ( 1 ). Thus, this crisis is exacerbating existing mental health conditions and creating conditions for the development of new ones. Further, if lessons from other outbreaks such as Ebola ( 2 ) and SARS (Severe Acute Respiratory Syndrome) ( 3 ) are any indication, even after an outbreak is controlled, there will likely be a substantial increase in need for psychological support.
Crucially, this public health crisis will magnify and deepen existing shortcomings of mental health care systems. The US was already facing a mental health crisis before the pandemic: less than half of those with mental illness receive the care that they need ( 4 ). Underserved populations, such as low-income or ethnic minority populations, are disproportionately affected; they show the lowest utilization of mental health services ( 5 ). Early data suggest that underserved populations pay a larger health toll from COVID-19: they show higher mortality rates ( 6 , 7 ). They are more likely to work in essential jobs putting them at greater risk of contracting COVID-19, and suffer greater economic consequences. All these factors lead to increased stress and anxiety. We will therefore be faced with an even greater relative shortage of trained professionals and means to mental health care during and after this pandemic.
We argue that what we need during a public health crisis like this is a digital mental health revolution: scaling up the delivery of confidential mental health services to patients across a wide range of platforms, from telemental health to mobile interventions such as apps and text messaging. Here, we provide an overview of technological tools which could help to decrease the mental health burden of COVID-19, provide recommendations on how they could be used and scaled-up, and discuss considerations and limitations of mental health technology applications.
There is a crucial role for the use of teleconferencing software for therapy sessions during the COVID-19 pandemic. Most studies of teleconferencing services showed that effectiveness is comparable to in-person services across disorders including depression, posttraumatic stress disorder, and anxiety disorders ( 8 ). China has had some success with this approach. Researchers recently wrote in a Lancet Commentary that during the worst of the outbreak in January, China successfully provided online psychological counseling and self-help was widely rolled out by mental health professionals in medical institutions, universities, and academic societies ( 9 ).
In the US, the pandemic has also catalyzed a rapid adoption of telehealth ( 10 ). Medicare now allows for billing for telehealth. Further, the Health Insurance Portability and Accountability Act (HIPAA) has been revisited to permit more medical providers to use HIPAA compliant platforms to communicate with patients. This removes a major barrier to wider adoption of telemedicine and could also provide an outstanding opportunity for patients who previously did not feel comfortable seeking mental health care to now approach these services.
However, it is important to attend to disparities in technology access and digital literacy. Before the pandemic, only one in ten patients in the US used telehealth, and 75% said that they were unaware of telehealth options or how to access it ( 11 ). Recent data from primary care clinics showed that, though video care consults went up by 80% in late March and early April, minority groups represented a smaller portions of these visits ( 12 ). This is partly explained because of a lack of Internet availability, which varies due to limited data plans and lack of Wi-Fi, and inability to use smartphone features such as downloading apps ( 13 ). At the moment, some US telecom providers are offering free Internet services ( 14 ). However, longer-term strategies need to be developed to prevent further widening of the digital divide ( 15 ), including providing affordable, high speed Internet access, improving usability of telehealth programs, and providing appropriate guidance/training for patients using these services.
Mental Health Smartphone Applications
Importantly, the use of personal mobile phones presents an opportunity for broad scaling of interventions. Over 90% of Americans have some type of mobile phone and over 80% have smartphones ( 16 ). Even among low-income Americans (71%) and older adults (53%) smartphone ownership is high. Mental health apps have shown effectiveness in decreasing symptoms of depression ( 17 ) and anxiety ( 18 ). Because of COVID-19, multiple meditation and wellness apps designed by the private sector have now temporarily opened up free memberships to aid in easing anxiety, the majority of these being mindfulness apps ( 19 ).
However, there are over 10,000 consumer-available mental health apps in app stores and many of these are not evidence-based ( 20 ). Further, though many people download mental health apps, research shows low rates of continued use over longer periods of time ( 21 ). It is crucial that mental health providers recommend apps that are backed up by evidence. One helpful resource is Psyberguide ( www.psyberguide.org ), a non-profit that rates apps based on the strength of the scientific research that supports it, ease of use, and its privacy policies ( 22 ). Lastly, in order to improve engagement, providers should follow up with patients on their usage of these apps and integrate the app content into their treatment.
Texting Applications
In addition to apps, text-messaging platforms could be leveraged to help people cope with mental health challenges evoked by COVID-19. Because texts are also delivered via individuals' devices, they are easy to provide to many at once using automated text-messaging platforms. Text-messaging interventions have demonstrated effectiveness in behavioral health promotion and disease management ( 23 ). Importantly, text-messaging is an appropriate tool for low digital literacy populations and underserved groups ( 24 ). For instance, our own HIPAA approved texting platform, HealthySMS, was developed with and for low-income populations (mostly Spanish speakers) and shows high acceptability in underserved populations ( 25 ). We recently rolled-out a text-messaging study to provide wide-scale support to interested individuals in the US via daily automated text-messages, containing tips on coping with social distancing and COVID-19 anxiety.
For crisis situations, Crisis Text Line provides free confidential help via text-message. This platform has seen the mention of “coronavirus” in 24% of conversations from March 30th to April 6th ( 26 ). Furthermore, Caremessage, a non-profit organization, has temporarily provided free access to their messaging platform and COVID-19 template text-messaging library with health information ( 27 ). In addition, reliable information can also be delivered by health and government organizations automated via text messages. Scaling of information delivery to patients and the public could also relieve health professionals and public health departments, who are already understaffed, underfunded, and overburdened ( 14 ).
Social Media
Social media plays a complicated role in the management of mental health. On the one hand, it can provide positive and supportive connections during a time of physical isolation. Earlier work shows that many people with mental illness are increasingly turning to social media to share their experiences and seek mental health information and advice ( 28 ). On the other hand, it can also serve to increase depression and anxiety symptoms based on negative social comparisons and the spread of distressing information ( 29 ). For instance, in a recent cross-sectional survey of almost 5,000 participants in China, increased social media exposure on COVID-19 was associated with increases in anxiety and depression symptoms ( 30 ).
Social media has played a large role in the spread of information since the start of the COVID-19 outbreaks, including misinformation and “fake news”. Large social media platforms are now reportedly taking steps to remove false content or conspiracy theories about the pandemic, using artificial intelligence (AI); and distribute reliable information, such as developed by the World Health Organization ( 31 ).
In China, the government provided online mental health education through popular social media platforms, such as WeChat, Weibo, and TikTok during the height of the outbreak in January ( 9 ). In the UK, the National Health Service (NHS) is working with Google, Twitter, Instagram, and Facebook to provide the public with accurate information about COVID-19 ( 32 ).
Social media also provides a unique opportunity for health professionals to distribute accurate information to their patients and the public, or to highlight available mental health resources. In Wuhan China, mental health professionals uploaded videos of mental health education for the general public through WeChat and other Internet platforms at the early stage of the outbreak ( 9 ). In the US and Europe, many physicians have turned to Twitter to share medical information. The social media site has now implemented a mechanism to verify physicians and other scientific experts in an effort to counteract coronavirus misinformation ( 33 ).
However, because of the overload of information on social media, misinformation might still spread too fast to be intercepted by AI algorithms ( 34 , 35 ). A recent report of responses from more than 8,000 people from six countries showed that one third reported seeing a significant amount of false or misleading COVID-19 information on social media or messaging platforms ( 36 ).
Further, posting information on social media raises the question of how health professionals should respond to the information posted by patients, and how that can impact the therapeutic relationship. Currently, there are no clear guidelines for health professionals, to determine how to act on social media. This calls for a push in quickly establishing such a consensus ( 37 ).
The COVID-19 crisis has fast-forwarded the use of technology in mental health care. Technology is crucial in scaling up access to mental health services during and after COVID-19. Given that people interact differently with technology, people of various ages, technical abilities, languages, and levels of literacy will need distinct types of interventions ( 38 ).
Older people are particularly vulnerable during this pandemic and already suffer from high rates of loneliness ( 39 ). This is strongly associated with greater symptoms of depression and anxiety ( 40 ), and physical morbidities and mortality ( 41 ). Previous work shows that older adults are interested in using technology to support their mental health, and that mobile health technology is feasible and reliable for assessing cognitive and mental illness ( 42 ).
However, older adults and those with low digital literacy might lack prior knowledge of digital technology to fully benefit from these tools ( 43 ). Digital health tools suffer from usability issues: they do not always consider digital literacy, health literacy, age, or English proficiency in their design ( 44 ). For instance, previous work showed that even the most basic functions of apps are difficult to use for diverse populations ( 45 ). Top-funded digital health companies test only 30% of their apps in people with clinical conditions ( 46 ). These factors are important because individuals with lower health literacy have worse health outcomes over time due to difficulty making informed health choices ( 47 ).
Therefore, interventions should be specifically targeted toward vulnerable groups, and adapted to their specific needs. This includes design choices such as easy to navigate user interfaces and tailoring vocabulary to older adults or those with low English proficiency ( 48 ). Training for individuals with low-tech skills, through outreach programs by healthcare staff may help patients to understand and use digital tools ( 49 ). Health systems should prioritize implementation of this crucial service ( 12 ).
Further, the right infrastructure needs to be set up to provide digital interventions securely, without personal privacy violations and minimizing the risk of data breaches. Apps and text-messaging must not only be effective, but also safe, secure, and responsible, similar to how therapists are held to standards of responsible practice and confidentiality ( 42 ). Therefore, it is imperative that cybersecurity specialists also become involved in ensuring safe technological services ( 50 ). Finally, just as they have now shown flexibility with telehealth, insurance companies and health systems should begin covering digital and mobile health interventions.
We are now in the midst of an acute health crisis which calls for a grand upscaling of mental health resources. Technology provides a medium for delivering mental health services remotely and on a wide scale, which is particularly important during social distancing measures. Even when the worst of the COVID-19 pandemic has subsided, it is likely that a large need for mental health support and services delivered through technology will remain. Digital mental health tools should be affordable, accessible, and appropriate for a wide group of individuals with varying ages, languages, and digital literacy. The time to massively invest in high quality and accessible online and mobile mental health in the face of the COVID-19 pandemic, and possible future pandemics, is now.
Author Contributions
CF wrote the first draft of the article. AA contributed to the writing and editing of the manuscript. Both authors contributed to the editing of the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Nelson B, Pettitt AK, Flannery J, Allen N. Psychological and Epidemiological Predictors of COVID-19 Concern and Health-Related Behaviors. Psyarxiv (preprint) (2012). doi: 10.31234/osf.io/jftze
CrossRef Full Text | Google Scholar
2. Mohammed A, Sheikh TL, Poggensee G, Nguku P, Olayinka A, Ohuabunwo C, et al. Mental health in emergency response: lessons from Ebola. Lancet Psychiatry (2015) 2(11):955–7. doi: 10.1016/S2215-0366(15)00451-4
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry (2009) 31(4):318–26. doi: 10.1016/j.genhosppsych.2009.03.001
4. Mental Health America. The state of mental health in America. Author Alexandria, VA: Mental Health America, Inc. (2019).
Google Scholar
5. Clancy C, Munier W, Brady J, Moy E, Chaves K, Freeman W, et al. 2012 National Healthcare Quality & Disparities Report. Rockville, Washington, DC: AHRQ Publications (2013).
6. Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respiratory Med (2020). doi: 10.1016/S2213-2600(20)30228-9
7. Yancy CW. COVID-19 and African Americans. Jama (2020) 323(19):1891–2. doi: 10.1001/jama.2020.6548
8. Ralston AL, Andrews AR III, Hope DA. Fulfilling the promise of mental health technology to reduce public health disparities: Review and research agenda. Clin Psychol: Sci Practice (2019) 26(1):e12277. doi: 10.1111/cpsp.12277
9. Liu S, Yang L, Zhang C, Xiang Y-T, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry (2020) 7(4):e17–e8. doi: 10.1016/S2215-0366(20)30077-8
10. Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth Transformation: COVID-19 and the rise of Virtual Care. J Am Med Inf Assoc : JAMIA (2020) ocaa067. doi: 10.1093/jamia/ocaa067
11. Power JD. U.S. Telehealth Satisfaction Study. SM, J.D. Power (2019).
12. Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. Catalyst non-issue content. NEJM Catalyst (2020) 1(3).
13. Anderson M, Perrin A, Jiang J. 13% of Americans don"t use the internet. Who are they. Pew Research Center. (2016). p. 7.
14. New York Times. (2020). [Available from: https://www.usatoday.com/story/money/2020/03/16/utility-cable-internet-phone-coronavirus-covid-19/5060084002/ .
15. Yoon H, Jang Y, Vaughan PW, Garcia M. Older adults' Internet use for health information: Digital divide by race/ethnicity and socioeconomic status. J Appl Gerontol (2020) 39(1):105–10. doi: 10.1177/0733464818770772
16. Pew Research Center. Mobile Fact Sheet: Pew Research Center. Pew Research Center: Internet. Science & Tech. (2018). [Available from: https://www.pewinternet.org/fact-sheet/mobile/ .
17. Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry : Off J World Psychiatr Assoc (WPA) (2017) 16(3):287–98. doi: 10.1002/wps.20472
18. Firth J, Torous J, Nicholas J, Carney R, Rosenbaum S, Sarris J. Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. J Affect Disord (2017) 218:15–22. doi: 10.1016/j.jad.2017.04.046
19. Techcrunch. (2020). [Available from: https://techcrunch.com/2020/03/18/meditation-apps-offer-free-mindfulness-as-social-distancing-takes-a-toll/ .
20. Larsen ME, Huckvale K, Nicholas J, Torous J, Birrell L, Li E, et al. Using science to sell apps: evaluation of mental health app store quality claims. NPJ Digit Med (2019) 2(1):1–6. doi: 10.1038/s41746-019-0093-1
21. Baumel A, Muench F, Edan S, Kane JM. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J Med Internet Res (2019) 21(9):e14567. doi: 10.2196/14567
22. Lipczynska S. Psyberguide: a path through the app jungle. J Ment Health (2019) 28(1):104–. doi: 10.1080/09638237.2017.1417574
23. Berrouiguet S, Baca-García E, Brandt S, Walter M, Courtet P. Fundamentals for future mobile-health (mHealth): a systematic review of mobile phone and web-based text messaging in mental health. J Med Internet Res (2016) 18(6):e135. doi: 10.2196/jmir.5066
24. Pew Research Center. Smartphone Ownership Is Growing Rapidly Around the World, but Not Always Equally. Pew Research Center’s Global Attitudes Project (2019).
25. Aguilera A, Berridge C. Qualitative Feedback From a Text Messaging Intervention for Depression: Benefits, Drawbacks, and Cultural Differences. JMIR mHealth uHealth (2014) 2(4):e46. doi: 10.2196/mhealth.3660
26. Crisis Textline. (2020). [Available from: https://www.crisistextline.org/mental-health/notes-on-coronavirus-how-is-america-feeling-part-4/ .
27. CareMessage. (2020). [Available from: https://www.caremessage.org/covid-19-response-messaging-safety-net-providers .
28. Naslund JA, Aschbrenner KA, McHugo GJ, Unützer J, Marsch LA, Bartels SJ. Exploring opportunities to support mental health care using social media: A survey of social media users with mental illness. Early Intervent Psychiatry (2019) 13(3):405–13. doi: 10.1111/eip.12496
29. Primack BA, Shensa A, Escobar-Viera CG, Barrett EL, Sidani JE, Colditz JB, et al. Use of multiple social media platforms and symptoms of depression and anxiety: A nationally-representative study among US young adults. Comput Hum Behav (2017) 69:1–9. doi: 10.1016/j.chb.2016.11.013
30. Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental Health Problems and Social Media Exposure During COVID-19 Outbreak. Plos one (2020) 15(4):e0231924.
31. Lawfare. (2020). [Available from: https://www.lawfareblog.com/covid-19-and-social-media-content-moderation .
32. Healthcare IT News. (2020). [Available from: https://www.healthcareitnews.com/news/europe/nhs-joins-forces-tech-firms-stop-spread-covid-19-misinformation .
33. Medscape. . https://www.medscape.com/viewarticle/930360 . [Available from: https://www.medscape.com/viewarticle/930360 .
34. Politico. (2020). [Available from: https://www.politico.com/news/2020/03/12/social-media-giants-are-fighting-coronavirus-fake-news-its-still-spreading-like-wildfire-127038 .
35. Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science (2018) 359(6380):1146–51. doi: 10.1126/science.aap9559
36. Nielsen RK, Fletcher R, Newman N, Brennen JS, Howard PN. Navigating the ‘Infodemic': How People in Six Countries Access and Rate News and Information about Coronavirus. In: Misinformation, science, and media. The Reuters Institute for the Study of Journalism and University of Oxford (2020). p. 2020–04.
37. American Psychiatric Association Annual Meeting. Social media and psychiatry: challenges and opportunities. San Francisco, CA (2019). [press release]. https://www.psychcongress.com/ .
38. Hall AK, Bernhardt JM, Dodd V, Vollrath MW. The digital health divide: evaluating online health information access and use among older adults. Health Educ Behav (2015) 42(2):202–9. doi: 10.1177/1090198114547815
39. In Time of Social Distancing, Report's Call for Health Care System to Address Isolation and Loneliness Among Seniors Resonates. JAMA Health Forum (2020) 1(3):e200342–e200342. American Medical Association.
40. Santini ZI, Jose PE, Cornwell EY, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health (2020) 5(1):e62–70. doi: 10.1016/S2468-2667(19)30230-0
41. Perissinotto CM, Cenzer IS, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Internal Med (2012) 172(14):1078–84. doi: 10.1001/archinternmed.2012.1993
42. Moussa Y, Mahdanian AA, Yu C, Segal M, Looper KJ, Vahia IV, et al. Mobile health technology in late-life mental illness: a focused literature review. Am J Geriatr Psychiatry (2017) 25(8):865–72. doi: 10.1016/j.jagp.2017.04.003
43. Schreurs K, Quan-Haase A, Martin K. Problematizing the digital literacy paradox in the context of older adults' ICT use: Aging, media discourse, and self-determination. Can J Commun (2017) 42(2):1–34. doi: 10.22230/cjc.2017v42n2a3130
44. Schueller SM, Hunter JF, Figueroa C, Aguilera A. Use of Digital Mental Health for Marginalized and Underserved Populations. Curr Treat Options Psychiatry (2019) 6(3):243–55.
45. Sarkar U, Gourley GI, Lyles CR, Tieu L, Clarity C, Newmark L, et al. Usability of commercially available mobile applications for diverse patients. J Gen Internal Med (2016) 31(12):1417–26. doi: 10.1007/s11606-016-3771-6
46. Van Winkle B, Carpenter N, Moscucci M. Why Aren't Our Digital Solutions Working for Everyone? AMA J Ethics (2017) 19(11):1116–24. doi: 10.1001/journalofethics.2017.19.11.stas2-1711
47. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med (2011) 155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-0005
48. De Barros AC, Leitão R, Ribeiro J. Design and evaluation of a mobile user interface for older adults: navigation, interaction and visual design recommendations. Proc Comput Sci (2014) 27(27):369–78. doi: 10.1016/j.procs.2014.02.041
49. Grossman LV, Masterson Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inf Assoc (2019) 26(8-9):855–70. doi: 10.1093/jamia/ocz023
50. Alami H, Gagnon M-P, Ahmed MAA, Fortin J-P. Digital health: Cybersecurity is a value creation lever, not only a source of expenditure. Health Policy Technol (2019) 8(4):319–21. doi: 10.1016/j.hlpt.2019.09.002
Keywords: mobile health (mHealth), COVID-19, apps and smartphones, telemental health, public mental health, psychological therapies, depression, anxiety
Citation: Figueroa CA and Aguilera A (2020) The Need for a Mental Health Technology Revolution in the COVID-19 Pandemic. Front. Psychiatry 11:523. doi: 10.3389/fpsyt.2020.00523
Received: 02 April 2020; Accepted: 21 May 2020; Published: 03 June 2020.
Reviewed by:
Copyright © 2020 Figueroa and Aguilera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caroline A. Figueroa, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
How Does Technology Affect Mental Health? Essay Example
Did you know that there are over 3.36 Billion Active smartphones around the world! Over the past few decades technology has evolved to be something so much greater than what we come to realize. We use technology every single day of our lives in some way or another whether it is to communicate, for work, school, or social media. Americans tend to believe that technology such as phones has bad effects on us; varying from mental and physical behaviors and mental. I agree with this statement. This leads us to beg the question of, do smartphones degrade our minds like we think they do? Research around the world says that they do, but some say it does not. Mental behaviors such as depression, anxiety, and loneliness are all factors of phones and with further aid, we will find out how and why this happens.
To begin, Technology is very useful to us humans and has become very important to our world; however, what it does to our brains is a different story, relating to the research question. In the article Impact of smartphone addiction on depression and self-esteem among nursing students written by Mahamed Sayeda, a researcher in mental health at Cairo University as well as others conducted explaining the effects of smartphones. According to Mohamed Sayeda, “Smartphone addicted people tend to feel depressed and isolated without their smartphones; besides, they can experience other symptoms of addiction such as preoccupation, tolerance, lack of control, withdrawal, mood modification, conflict, lies, excessive use, and loss of interest. Depression and low self-esteem are general reflections of psychological well-being”( Sayeda 1347). In other words, Mohamed believes that Smartphones cause Addiction which then leads to depression. Concurring with what Mohamed makes a connection to addiction and depression in smartphones is reasonable. When you are addicted to something and lose that thing you are addicted to you tend to get sad and then depressed. On the topic of depression, that’s pretty mind degrading if you ask me.
Continuing, Smartphones have an instrumental effect on people of all ages. Especially college students. College students are more than likely to use their phones more than anybody, especially nowadays. People have become more reliant on phones than ever. Mohamed agrees in his study when he writes “In this study, there was a positive correlation between smartphone addiction and depression”( Sayeda 1351). Mohamed’s point is that phones can cause depression and will. The evidence listed backs the Research question. With depression being high among teens and college students in these recent years phones contribute to it. Nowadays because people are so attached to their phones Sayeda says “While the physical consequences of the overuse of smartphones can be easily diagnosed and managed, mental health issues are statistically significant concerns with smartphone overuse” (Sayeda 1347). Sayeda brings up a great point about how physical phones don’t harm us as much but mentally it’s a different story. Technology will continue to affect us until we limit our screen times and overall usage of it. Spending an abundance of time on smartphones and technology can also lead to other mental issues.
As a result of this, another way technology is affecting us is anxiety. Anxiety can come in many forms nevertheless it should never be looked over. Technology has its problems and anxiety is one of them. Nicholas Carr, a Pulitzer Prize winner who writes articles on technology, wrote the article How Smartphones Hijack Our Minds explaining how smartphones have taken over the human body in a bad way. Nicholas complicates the matter further when he writes “But while our phones offer convenience and diversion, they also breed anxiety. Their extraordinary usefulness gives them an unprecedented hold on our attention and vast influence over our thinking and behavior”(Carr 598). Carr is warning that because phones have taken over the world they have also overtaken our emotions. This directly affects our daily lives for the reason that phones are everywhere. A single buzz from your phone will get your heart rate racing and if you can't immediately look at the reason why it buzzed it makes the anxiety even worse. Carr relates by saying “even hearing one ring or vibrate, produces a welter of distractions that makes it harder to concentrate on a difficult problem or job”(598). Carr’s point specifically is that smartphone use every day brings an unprecedented amount of stress and anxiety and overall affects us daily. Having constant anxiety will regress your mind and lead to other issues such as loneliness.
Furthermore, Loneliness is a factor of technology as well. Being infatuated with a screen all day will affect your social life. It makes it easier to deny someone from hanging out and creating short condensed conversions with no meaning. As you can see technology really does hurt your mind. Carr advances on how technology hinders us by saying “Social skills and relationships seem to suffer as well. Because smartphones serve as constant reminders of all the friends we could be chatting with electronically, they pull at our minds when we’re talking with people in person, leaving our conversations shallower and less satisfying”(Carr 601). Moore is establishing that because we are so involved with our phones and being faced down into the fabricated world we tend to be less empathetic and lacking in social life. I completely agree since this happens all the time. We see kids and adults nowadays becoming more and more antisocial and lonely due to the constant reliance on technology. This isn’t good in the long run for Humans. It will create less communication and will allow us to further distance ourselves from others. Humans are social creatures and need constant interaction. “lol” as well as “idk” don't count as interactions in my book. Despite all this, there are still people out there who will disagree with the idea that technology degrades our mental state. Carr Brings up an excellent point when he says “The evidence that our phones can get inside our heads so forcefully is unsettling. It suggests that our thoughts and feelings, far from being sequestered in our skulls, can be skewed by external forces we’re not even aware of”(Carr 601-602). Carr puts it perfectly by describing an underlying issue with phones and technology by saying that our phones hinder our ability to process information and we are not aware of it. This is crazy because this means that not only is it making our mental state weaker, it's making our way of processing information much worse.
Moreover, People believe that there are merits and benefits to technology. Nicholas Brody a professor of communications at the University of Puget sound corresponds with this in his article It Turns Out Our Tech Gadgets Aren’t as Isolating as Experts Say. He presumes that this is true. Nicholas writes “The truth of the matter is that social media and smartphones never drove us away from one another. Rather, these tools highlight the most fundamental need of all to be connected”( Brody 594). By focusing just on being connected Nicholas overlooks the fact that being connected isn't just the problem. Yes, you can be connected but it doesn't solve depression, anxiety. For example, someone posts on social media and it show them living a happy life and you see it and it makes you jealous and sad realizing that you are not like them. To sum up, it's not just being connected there is plenty of other factors.
In addition to this, Near the end of Nicholas's article, he says “Expressing affection helps us better deal with stress”(Brody 594). I disagree with Nicholas’s view that affection reduces stress because studies have shown that expressing affection online does not parallel in-person affection. Therefore Nicholas’s claim is false.
To conclude, You may be asking yourself, if technology is so bad then why has it helped the world so much? This is because you only see the good side of it. There are millions of people that are having problems related to technology. These include depression, anxiety, and loneliness. So going back to the research question of whether phones degrade our minds. I can strongly say yes. Technology affects us exponentially in bad ways. Are you gonna let this happen to your mind?
Related Samples
- Health Effects of Video Games Essay Sample
- Systemic Lupus Erythematosus Autoimmune Disorder
- Why Should Humans Explore Space? Essay Example
- Blue-Stain Fungi Research Paper Example
- Positive Outcomes of COVID-19 Essay Example
- Essay Sample on Dealing With Stress in College: Spring Semester Edition
- Essay Sample on Nursing as a Profession
- Essay Sample: What Makes a Good Blog
- Essay Sample about Spirogyra
- Principles Of User Interface Design Research Paper
Didn't find the perfect sample?

You can order a custom paper by our expert writers
The Impact of Technology on Mental Health
In the contemporary world, symptoms of depression, stress, anxiety, and other mental disorders have become more prevalent among university students. Researchers have proven that time spent on social media, videos, and Instant messaging is directly associated with psychological distress. This bibliography examines different literature discussing how technology affects mental wellness.
The scope of this research is to uncover the consequences of technology use on mental health. The research question above will help examine the relationship between technology use and how this action results in mental illnesses such as anxiety and depression. Information used in this study includes both primary and secondary sources focusing on their observational and experimental data analysis.
The article explores how web-based social networking is a significant limitation to mental health. Deepa and Priya (2020) introduce a concept of time whereby they explain that the hours spent on social networking platforms promote depression and anxiety (Deepa & Priya, 2020). Some of the digital technology students use are Instagram, Facebook, Twitter, YouTube, and other web-based sites platforms, which have become a threat to mental health (Deepa & Priya, 2020). The authors explain that researchers discovered that excessive social media use was linked to mental illnesses during schooling. However, it may be alleviated by dialectical thinking, positivity, meditation, and active coping.
The authors used descriptive research using simple sampling questionnaires and ANOVA to study different groups of students and the social media platforms they use. This system provided mixed results based on these groups and examinations (Deepa & Priya, 2020). The research findings revealed a relationship between being active on social media and depression. The authors contradict a study done by Gordon et al. (2007) that mentions that the time spent on the internet has nothing to do with depression (Deepa & Priya, 2020). Instead, it is what students engage in when they are active online. This study is credible because it is not outdated and involved many participants, which helped strengthen the hypothesis created. This source will be integral in answering the types of technology students use and their consequences on mental wellness. Additionally, the journal’s credibility is guaranteed, considering that the article is an international publication. This title indicates that the journal has been peer-reviewed by many other scholars to ensure the information provided is accurate.
The article examines how internet use affects well-being by analyzing the rate of internet use among college students. Gordon et al. (2007) mention that technology use is triggered by self-expression, consumptive motives, and sharing information. In this study, Gordon et al. (2007) posit that frequency of internet use does not affect mental illness. Instead, they mention that what students do on those platforms is the factor that contributes to mental illness.
First, they mention that the internet has provided ways for students to get new acquaintances, find intimate partners, and conduct research for their college assignments, among other things. This factor indicates that these students’ daily life has become increasingly reliant on the internet (Gordon et al., 2007). Therefore, increased internet use has formed a new environment, full of peer pressure. This explanation is an indication of what they do on the internet. The reason is that they see, admire, and adopt new habits which increase stress and depressive symptoms. Additionally, overdependence on technology has affected family cohesion and social connectedness.
The article provides similar ideologies as Junco et al. (2011) that technology causes social isolation by keeping students from the realities in their environment. It explains that students live a fictional life by actively engaging in technology to hide their true selves (Gordon et al., 2007). The research is valid considering it applies rationales from different authors to justify their deduction that technology use has become an avenue for peer pressure among students. This article is essential since it explains the negative impact of technology on mental health, which is explored in this research. It is also a scholarly article considering that these authors have doctors of philosophy in education, indicating vast knowledge and command to undertake this research.
These researchers use unique survey data to investigate the adverse effects of instant messaging on academic achievement. They explain that instant messaging is not destructive since it can provide company when needed. However, excessive use of instant messaging reduces concentration by diverting the mind’s attention away from the facts of the surroundings. Students lose focus when multitasking activities like chatting while studying (Junco & Cotten, 2011). It also impacts the essential, incidental, and representational processing systems, the foundation for learning and memory. When they fail their tests, they become withdrawn with significant effects, such as anxiety and depression.
Additionally, the authors mention that students using IM become socially disengaged since IM becomes their point of contact with others. Considering all these effects, it is evident that IM can cause anxiety, depression, and social isolation if not regulated. Unlike Gordon et al. (2007), who mention only the detrimental effects of using technology, these authors mention that IM, an example of technology, helps students manage stress (Junco & Cotten, 2011). They explain that through a survey of a target group whereby students reported that IM and other online platforms such as video games had provided contact with the outside world, which relieves stress.
This article’s viability is uncertain because most arguments presented are derived from other researchers’ work (Junco & Cotten, 2011). However, the article is helpful for my research because it provides the negative and positive effects of using technology. The position of this research is that IM can help deal with stress. The viability of this research is verified considering the research has been reviewed by Mendeley Company which generates citations for scholarly articles.
Karim et al. (2020) explore how social media impacts mental health. They begin by conducting a qualitative analysis of 16 different studies provided by various researchers on the topic (Karim et al., 2020). First, they listed different types of social media platforms, including Twitter, Linkedin, Facebook, Instagram, and Snapchat, to be the most widely used social media platforms among the youth. They also mention that social media has become an influential technology in the contemporary world (Karim et al., 2020). Although social media has incredible benefits, it is linked to various mental health issues such as depression and anxiety. Some works agreed that social media use is detrimental to mental well-being, and the timing does not matter (Karim et al., 2020). In contrast, other studies suggested that no evidence justifies the maximum time one should be active on social media. None of the research provided the limit of time recommended for anyone to be active on social media.
The credibility of the piece is jeopardized because the researchers did not conduct their study to identify the correlation between mental health and technology (Karim et al., 2020). However, it provides substantial ideas drawn from other credible sources, which are essential in providing information addressing this topic. For example, their position is that long hours of social media use contribute to depression and anxiety (Karim et al., 2020). This focus is integral in my research since it addresses the impact of technology on mental health by explaining the possible avenues for mental health crises.
Lattie et al. (2019) investigate how the rise in mental disorders such as anxiety and depression correlates with computing technologies. According to these authors, personal computing technologies such as smartphones have become the source of mental health crises since they provide access to social media (Lattie et al., 2019). This platform has promoted harmful ideas that make people experience peer comparison. For instance, “fear of missing out (FOMO) is a pressure promoted by media which dictates how people interact, behave and talk within these platforms” (Lattie et al., 2019, para. 8). FOMO is when people feel the need to fit in with a specific trend by emulating verbatim how their internet friends behave, dress or talk. For instance, if all the girls on social media put on branded clothes for attention, every girl on the platform would also want to be like them. This pressure will result in stress to keep up with the standards set, promoting mental health disorders. These authors conclude that the pressure to feel accepted has increased the number of students negatively affected by technology.
However, the authors also mention that this digital platform has played a significant role in promoting mental health wellness. In addition, some of the interventions available such as the Headspace and Pacifica applications, are technology-enabled and provide coping skills when students face a crisis (Lattie et al., 2019). Lattie et al. (2019) provide similar sentiments as Junco et al. (2011), who also stated that technology is not entirely to blame for mental crises considering that activities such as assimilation of culture affect well-being. Additionally, this article is relevant since it has applied different up-to-date scholarly reasoning to create a hypothesis (Lattie et al., 2019). Finally, the article’s position is that social media promotes mental health by providing coping skills while also deteriorating it by contributing to disorders such as depression. However, this information is contrary to what Junco et al. (2011) mention that technology has the power to relieve stress by providing a coping mechanism.
The article provides informative discussions on the risks that digital presence has promoted. Skillbred-Fjeld et al. (2020) mention that many people have experienced harassment online based on their appearance, ethnicity, age, race, and religion. This exposure to bullying has resulted in psychological distress such as depression and suicidal thoughts. The authors indicate that most students spend more hours on digital media than how they spend with families and friends while also being more exposed to harassment. This disconnect is also a challenge to maintaining mental health, considering it breaks the bond between families and friends.
These authors stress that cyberbullying is a prevalent occurrence in online engagement and has detrimental effects on individuals. This article does not share similar rationales with other articles in this search since it focuses on proving how cyberbullying results in mental illness. The article answers the proposed research question, and its position is that cyberbullying affects most students using digital communication systems (Skilbred-Fjeld et al., 2020). The article is credible for this research since the author engaged in intensive searches, which enhanced the viability of the information provided.
In her article “Cyberspace and Identity,” Turkle (1999) posits that the development of cyberspace interactions has extended the range of identities. The author establishes her case with four essential points. Her first observation is that digital presence is based on fiction and not reality. Second, she claims that digital profile results from a digital exhibition that does not last. The third point made by Turkle (1999) is that online identity affects real self-considering the fact that it affects thoughts and behaviors). Finally, she claims that online identity exemplifies a cultural conception of diversity.
This author introduces the aspect of role-playing promoted by digital presence. She mentions that people are given a chance to portray themselves in a different light from reality on digital platforms considering the anonymity established when altering self-image through textual construction (Turkle, 1999). The research by Gordon et al. (2007) reinforced this claim when they mentioned that digital engagement does not cause mental illness. Instead, what students do on those platforms is the primary factor contributing to mental illness (Turkle, 1999). This factor is relatable in the current digital world since people share their adventurous moments, making others who cannot enjoy such things feel unworthy, posing a significant threat to mental wellness. The article’s position is that images portrayed on digital platforms are illusions, and they have promoted peer pressure, anxiety, and depression in people who believe them to be true (Turkle, 1999). The same sentiments are shared by Skilbred-Fjeld et al. (2020) since they mention that social media has become a site to dehumanize others who are less privileged. This occurrence promotes fear, self-hate, and depression, indicating a match in reasoning among these authors.
Deepa, M., & Priya, K. (2020). Impact of social media on mental health of students. International Journal of Scientific & Technology Research , 9 (03). Web.
Gordon, C., Juang, L., & Syed, M. (2007). Internet use and well-being among college students: Beyond frequency of use. Journal of College Student Development , 48( 6), 674-688. Web.
Junco, R., & Cotten, S. R. (2011). Perceived academic effects of instant messaging use.
Computer & Education , 56 (2), 370-378. Web.
Karim, F., Oyewande, A. A., Abdalla, L. F., Ehsanullah, R. C., & Khan, S. (2020). Social media use and its connection to mental health: A systematic review. Cureus , 12 (6). Web.
Lattie, E. G., Lipson, S. K., & Eisenberg, D. (2019). Technology and college student mental health: Challenges and opportunities. Frontiers in psychiatry , (10) , 246. Web.
Skilbred-Fjeld, S., Reme, S. E., & Mossige, S. (2020). Cyberbullying involvement and mental health problems among late adolescents. Cyberpsychology: Journal of Psychosocial Research on Cyberspace , 14 (1). Web.
Turkle, S. (1999). Looking toward cyberspace: Beyond grounded sociology. Cyberspace and identity. Contemporary Sociology , 28 (6), Web.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, December 10). The Impact of Technology on Mental Health. https://studycorgi.com/the-impact-of-technology-on-mental-health/
"The Impact of Technology on Mental Health." StudyCorgi , 10 Dec. 2022, studycorgi.com/the-impact-of-technology-on-mental-health/.
StudyCorgi . (2022) 'The Impact of Technology on Mental Health'. 10 December.
1. StudyCorgi . "The Impact of Technology on Mental Health." December 10, 2022. https://studycorgi.com/the-impact-of-technology-on-mental-health/.
Bibliography
StudyCorgi . "The Impact of Technology on Mental Health." December 10, 2022. https://studycorgi.com/the-impact-of-technology-on-mental-health/.
StudyCorgi . 2022. "The Impact of Technology on Mental Health." December 10, 2022. https://studycorgi.com/the-impact-of-technology-on-mental-health/.
This paper, “The Impact of Technology on Mental Health”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: December 10, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Introduction of Technology to Support Young People’s Care and Mental Health—A Rapid Evidence Review
1 The Kolvin Service, Specialist Children & Young People’s Services CBU, Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust, St Nicholas House, St Nicholas Hospital, Newcastle upon Tyne, NE33XT UK
2 Aycliffe Secure Centre, Durham County Council, Newton Aycliffe, DL5 6JB UK
3 MegaNexus Ltd, Tavistock House, North-West Wing, Tavistock Square, London, WC1H 9JZ UK
P. J. Kennedy
Associated data.
For queries regarding data, contact the ‘author for correspondence’.
Technology and its use within mental health services has advanced dramatically over recent years. Opportunities for mental health services to utilise technology to introduce novel, effective, and more efficient means of delivering assessment, and treatment are increasing.
The current rapid-evidence paper reviews evidence regarding the introduction of novel technology to support young people’s mental health and psychological well-being.
A rapid evidence review was conducted. PSYCHINFO and CINAHL were searched for research articles between 2016 and 2021 that were specific to young people, mental health, and technology developments within this domain. N = 27 studies which explored the introduction, feasibility, and value of technology for mental health purposes were included in a narrative synthesis. Quality or risk of bias analyses were not completed.
Overall, technological advancements in young people’s care were considered positive and engaging for young people. Factors including resources, efficiency of care, engagement, therapeutic effectiveness, ethical considerations, therapeutic alliance, and flexibility were considered within this review. Nevertheless, potential barriers include clinician concerns, socioeconomic factors, and motivation.
Effective and sustained use of technology within young people’s mental health services will depend on the technology’s usability, efficiency, and ability to engage young people. This paper expands on existing research by reviewing a broader range of technology proposed to support young people’s mental health and well-being. This will assist in the application of novel technological advancements by indicating effectiveness, preferences, potential barriers, and recommendations for the feasibility and efficacy of introducing technology into young people’s services.
Introduction
Technology and its use within psychiatric services has advanced dramatically since the infamous television link between Nebraska Psychiatric Institute and Norfolk State Hospital was established for psychiatric consultations over fifty years ago (Nesbitt, 2012 ). Technological developments have also become increasingly necessary due to the effects of the COVID-19 pandemic (Comer et al., 2021 ). ‘Telehealth’ or ‘tele-psychotherapy’ is well established within mental health services and is a validated method of conducting psychotherapy, as measured by the National Institute of Mental Health (Magnavita, 2018 ).
Services can now use devices to collect biometric data, such as heart rate or sleep, and electronic health record apps are now used routinely to collate and securely store data exchanges between service-users and health practitioners (Magnavita, 2018 ). The frequency of publications regarding ‘connected mental health’ examining electronic methods of delivering mental-health orientated support has increased from fewer than five publications per year in 2011, to over 70 publications in the year of 2019; with researchers anticipating that this trend will continue (Ouhbi et al., 2020 ). Abundant opportunities are available for mental health services to introduce novel, effective, and more efficient means of delivering assessment, intervention, and treatment using technology.
Mobile-based technologies have increasingly been examined for supporting the care of both young people and adults (Inal et al., 2020 ). Systematic reviews and meta-analyses have provided evidence for the effectiveness of internet-based Cognitive Behavioural Therapy (iCBT) for the treatment of depression and anxiety in adults (e.g., Etzelmueller et al., 2020 ; Luo et al., 2020 ). Similarly, a systematic review examining online mental health support for young people found that 64% of telehealth interventions were effective in managing anxiety and depression in young people, in comparison to control conditions (Zhou et al., 2021 ).
In a review conducted by Hollis and colleagues ( 2017 ) it was argued that out of all of the fields within mental health, the opportunities in relation to digital transformation are the greatest within child and adolescent services. Young people are increasingly being invited to be involved in testing new technology that could support or assist with psychosocial provision (Drissi et al. 2020 ). A systematic review of randomised control trials (RCTs) also found that digital interventions supporting treatment of depression in young people were more effective than no treatment (Garrido et al., 2019 ). Despite concerns that technology may have socially isolating effects, there are now evolving applications (apps) for supporting with loneliness (Ramo & Lim, 2021 ).
Practitioners are also encouraged to implement internet-based technology into their work in supporting youth mental health, as it can be a valuable forum for enabling and maintaining social connectedness (Wu et al., 2016 ). This is further emphasised within the NHS Long Term Plan (NHS, 2019 ) which highlights the importance of technology development within healthcare. The NHS Long Term Plan refers to technology as the digitisation of care using computers and smartphones to provide patients with fast and convenient access to care. Virtual services can be used to provide advice and connect people to healthcare professionals. The plan also highlights the use of apps and online resources for mental health provision. With this in mind, the current paper defines technology as the use of digital resources to promote engagement in the context of mental health care. The Division of Clinical Psychology (DCP) Guidelines also indicate the necessity of technology developments within the context of COVID-19 (DCP, 2020 ).
A previous systematic review examining how technology has been used in mental health settings highlighted services can adopt novel advancements to support with obtaining patients’ attitudes, to support patient learning, reminders for service users, information, supportive messages, self-monitoring procedures, and to facilitate the operation of mental health services generally (Berrouiguet et al., 2016 ; Inal et al., 2020 ).
Not only can novel technology support individuals with health and social care needs, but technologies such as phone apps can also be used for psychological interventions (Inal et al., 2020 ). One example of this is the Wellness Recovery Action Plan (WRAP, Copeland, 2002 ) app. WRAP was developed by individuals with mental health difficulties and is currently recognised as an evidence-based practice designed to support individuals to develop strategies to create and maintain wellness within their lives. In 2018, the WRAP app was introduced to promote global implementation of WRAP wellness strategies, and has received positive feedback from users (WRAP, 2018 ). Mobile-based procedures have also been examined in relation to supporting people with schizophrenia, affective disorders, suicide prevention, substance abuse, eating disorders, anger, psychosis, headaches, sleep problems, stress, and neurodevelopmental disabilities among other psychiatric concerns (Inal et al., 2020 ). This further highlights the growing evidence-base in this area.
Analysis of user reviews, interviews and surveys has found that depression, technical issues, and fatigue can be barriers to use of technology that is designed to support mental health (Bourgouts et al., 2021 ). Contrastingly, having positive beliefs about mental health and help-seeking, the ability to integrate the technology into one’s daily life, as well as participating in user-research are known to facilitate engagement (Bourgouts et al., 2021 ; Jagosh et al., 2012 ; Orlowski et al., 2015 ). Customisable information, the ability to connect with others, guided interventions, activities of an appropriate length, good understanding of how to use technology, and confidence in the privacy and anonymity of the site are also factors that encourage engagement (Bourghouts et al., 2021 ).
One especially pertinent challenge for young people in terms of introducing new pieces of technology is ensuring that they are accessible and engaging. Engagement and adherence rates from young people can be low, and young people have been found to enjoy a “ game-like” interactivity when using a device or app. Despite services promoting the use of technology to teach young people about mental health topics, educational materials can be perceived as less engaging by young people (Garrido et al., 2019 ). Although the “gamification” of mental health and wellbeing apps commonly overlaps with behaviour change frameworks, most of the gamification is not theory-driven (Cheng et al., 2019 ). It is important, therefore, that services do not focus only on the engagement and accessibility of the technology, at the detriment of theoretical integrity.
The emergence of the COVID-19 pandemic has precipitated rapid technological adaptation by many mental health services, as stipulated by the DCP COVID-19 guidance (DCP, 2020 ). Using video technology, team meetings and consultations have been able to continue remotely throughout the pandemic, with enhanced efficiency and attendance for some (DeFilippis et al., 2020 ; Oz & Crooks, 2020 ).
Psychologists have been advised to use digital alternatives to continue clinical work, but to be aware of any disadvantages that this could pose to different client groups. (The British Psychological Society, 2020 ). For example, psychologists are encouraged to facilitate access to relevant technology for service-users in instances where they do not have the correct equipment available, to use social media appropriately, and to ensure apps are safe, secure, and confidential (The British Psychological Society, 2020 ).
Undoubtedly, technological developments are occurring at a rapid rate within mental health care. In combination, the above evidence implies that the rapid adoption of novel technology should proceed with caution; considering both the utility and potential barriers involved in using technology to support young people’s care. Given the increasingly rapid adoption of technology due to the COVID-19 pandemic, and the drive for digitalisation of mental health care (NHS, 2019 ), services will benefit from an awareness of the existing literature prior to the implementation of new technologies within their services. The current rapid evidence review sought to collate existing research regarding the introduction of new technology for young people’s mental health and social care services. It was anticipated that the research will indicate any potential barriers, preferences, and recommendations for the feasibility and efficacy of introducing new technology into young people’s services.
The qualitative rapid evidence review design used in the current study is based upon the provisional recommendations suggested by the Cochrane Rapid Reviews Methods Group (Garritty et al., 2020 ). Such recommendations originate from a team of methodologists with experience in review methods such as rapid reviews and systematic reviews. Rapid evidence reviews are a form of data synthesis that follow similar steps to systematic reviews but are designed to be completed under limited time constraints.
This study met criteria for service evaluation under criteria outlined by the Health Research Authority (HRA, 2021 ) and therefore did not require NHS Research Ethics Committee (REC) approvals. The study received local approval from CNTW NHS Foundation Trust Research, Innovation & Clinical Effectiveness team (Reference: SER-21–045). There are no conflicts of interest identified within this paper.
Inclusion Criteria
The following inclusion criteria was used to screen relevant research:
- (i) Must be a published research or evaluation article within a peer-reviewed journal that is relevant to child health and social care, or child psychology,
- (ii) Must be published within the last five years (July 2016–July 2021),
- (iii) Must be written in English language,
- (iv) Authors must be able to access the full text publicly or via their institution,
- (v) Must have a focus upon the introduction of technology that is new to a service (i.e., technology such as an App or tablet that a service has not used before) or technological developments (e.g., a different way of using a piece of technology within a service), that are designed to assist or support with mental health, or psychosocial care,
- (vi) Must be specific to young people (samples within the ages of school age to eighteen years, with an extension of this to twenty-five years for intellectual disability services).
Due to the aim of obtaining generalisable findings, the following studies were excluded:
- (i) Studies examining technology for specific health conditions (e.g., diabetes) and sensory impairments (e.g., hearing impairments or blindness).
- (ii) Studies examining technology for physical disabilities, or multiple and severe disabilities.
Search Terms
The following search terms were used for the two different databases searched: (‘child*’ or ‘young pe*’ or ‘adolescent*’) and (‘New’ or ‘Novel’) and (‘Technol*’ or ‘Device*’)r and (‘psychiatr*’ or ‘mental health’ or ‘psychol*’ or ‘learn*’).
Search Strategy
The search was limited to two databases: PSYCHINFO and CINAHL. One author conducted the search and screening process to prioritise time constraints for completion of the study. Using guidance from NHS trust Clinical Effectiveness Librarians, the search of the databases was conducted using the NICE Healthcare Databases Advanced Search resource. Search limits were applied in relation to date (July 2016–July 2021), format (research articles only), and language (English only). Titles and abstracts were screened to gauge whether the study met the inclusion criteria. The studies that were left after this process were screened as a full text. Full texts that could not be obtained via the trust resources were excluded. Reasons for exclusion during the full text screening phase were recorded.
Quality appraisal of the included research was not conducted due to the limited time available within an active clinical service.
Data was extracted using the following categories: design; setting; aims; participants; type of technology; whether the study was focusing upon feasibility/acceptability/efficacy or exploring how the piece of technology could be used; intervention (if applicable); outcome measures, and results. The extracted data was tabulated using the categories as headings. Studies that had similarities in relation to technology or outcomes were grouped together during the tabulation process. Due to the heterogeneous nature of the research, findings were collated within the form of a narrative synthesis, following the guidelines of the Cochrane Rapid Reviews Methods Group (Garritty et al., 2020 ). The authors chose not to conduct a meta-analysis due to the anticipation that there would be insufficient quantitative data utilising the same outcome measures.
A total of n = 27 studies met the inclusion criteria and were included within the narrative synthesis. An overview of the included studies can be found within Appendix A. Appendix B outlines the number of studies excluded via a PRISMA flow chart. Studies explored the introduction, feasibility, and value of technology for mental health purposes. Studies excluded at the full-text stage of screening (n = 19) were excluded mostly due to the age group of the participants, including individuals that were older than eighteen years, and younger than UK school age (four years). One study was excluded as it examined technology specifically for the assessment of young people within countries experiencing war (Hashemi et al., 2017 ). The environmental specificities of this were not deemed sufficiently generalisable to include within this review.
Online platforms and websites appeared to be the most frequently examined within the literature for young people in relation to mental health, with 11 studies examining online platforms or websites specifically. Other studies utilised apps/games (n = 7), video-related technology (n = 2), SMS/phone calls (n = 2), other PC software (n = 1), a mixture of technology (n = 3), or other technology (n = 1). Most technologies facilitated some form of assessment, psychoeducation, mental health-oriented activities for young people, or a structured therapy.
For online and virtual therapies, interventions were mostly Cognitive Behavioural Therapy (CBT)-oriented. For example, Babiano-Espinosa and colleagues ( 2019 ) examined the feasibility and efficacy of internet-based CBT for young people with obsessive compulsive disorder (OCD), whilst Wozney and colleagues ( 2017 ) focused upon treatment outcomes for internet-based CBT and interpersonal therapy for young people with depression.
Young Person Engagement
Resources and activities.
One of the most apparent uses and benefits of the mental health-oriented technologies examined was the ability for young people to engage in interactive therapeutic activities, and in some instances to do this within their own time and space. Two studies described exercises to support coping skills and self-reflection on a web-based platform (Gabrielli et al., 2020 ; Kurki et al., 2018 ). For a wellness-promoting chatbot, such activities were oriented around emotional self-awareness, social awareness, interpersonal relationships, assertive communication, and other life skills (Gabrielli et al., 2020 ). General mental wellness activities were also featured, such as breathing techniques, muscle relaxation, and affective regulation (Davidson et al., 2019 ). Further activities were designed to solidify learning material, which was observed in relation to substance misuse prevention (Snijder et al., 2021 ), and in learning Dialectical Behaviour Therapy (DBT) skills (O’Grady et al., 2020 ).
Interactive and engaging activities also supported young person involvement and motivation. One study described engaging activities in relation to mood monitoring, encouraging young people to reflect upon their emotional triggers and the activities they had engaged in so far (Wozney et al., 2017 ). Similarly, O’Grady and colleagues ( 2020 ) described how the utilisation of a diary was adopted within their app for self-reflection during a therapeutic programme. In relation to activities, young people appeared to request motivational messages, relaxing videos, less text, and less detailed information generally (O’Grady et al., 2020 ). Activities that were game-like received particularly positive feedback from the young people; for instance, one young person described, “I liked this one [‘Affective Modulation’ chapter] because I got to spin the wheel and act the feeling … I really liked that one! I also liked the card game [‘What Do You Know?’] because they helped me get my feelings out.” (pg. 9–10, Davidson et al., 2019 ).
Enhancing Engagement
When considering engagement, there were apparent advantages in relation to technology’s ability to enhance therapeutic engagement when used as an adjunct to face-to-face therapy sessions. For example, this was pertinently demonstrated during an intervention examining TechConnect—an SMS messaging and telephone initiative for young people with depression who were receiving structured therapy sessions (Gearing et al., 2021 ). The initiative involved young people receiving SMS personalised messaging, consisting of eight weekly messages designed to target health beliefs that influence decision making in relation to engagement (e.g., self-efficacy and perceived barriers). This also involved three telephone calls made by facilitators to the young person’s parents following a semi-structured script. Almost all (90 percent) of the young people receiving TechConnect attended all eight therapy sessions, in comparison to 40 percent of young people that were part of a control group, illustrating the potential positive impact of technology on engagement.
Using technology to facilitate psychological assessment could also promote greater engagement from young people. An app for tablets was used to deliver the WellSEQ (Wellbeing in Special Education Questionnaire), a novel questionnaire for individuals with special educational needs, which examines mental health, peer relations and conflict, school environment, and the family environment (Boström et al., 2016 ). High response rates were received from the young people when testing the app, indicating positive engagement. Technology-assisted interactions may also reduce feelings of embarrassment or shame. For example, a review of technology-empowered CBT for individuals with OCD highlighted that parents and practitioners believed this would be a useful tool for young people that were embarrassed to talk to a practitioner about their problems (Wolters et al., 2017 ). It was thought that the technology could enhance adherence via enriching the therapeutic experience and supporting motivation.
Technological interventions can also offer enhanced engagement due to the game-like nature that can be adopted, contrasting what can be perceived as invasive traditional paper methods. For example, a wellness initiative created as an online game was specifically designed to offer non-invasive and effective assessment of socio-emotional functioning without the laboriousness of standard traditional psychometrics (Day et al., 2019 ). Encouragingly, the authors concluded that the game appeared successful in serving this function. Similarly, digital phenotyping has been highlighted as a non-invasive measure, demonstrating how assessment and intervention can occur without the need for interview-style questioning (Sequeira et al., 2019 ). This method uses accelerometers and other smart devices to support in the prediction of depression relapses in young people, without the need for invasive or time-consuming psychometric assessments. The review highlighted that the current research on digital phenotyping is too diverse in terms of outcome measures for results to be conclusive, however, the potential advantages of this method appear to warrant further research (Sequeira et al., 2019 ).
The development of the technology itself also relied on the engagement of young people in some cases. For instance, co-production from young people of specific ethnic origin enabled an informative substance-misuse prevention app to be culturally sensitive (Aboriginal and Torres Strait Islander young people; Snijder et al., 2021 ). A life-skills and wellness coaching intervention was also developed from young person input and focus groups (Gabrielli et al., 2020 ). Young people also supported in the development of a platform incorporating assessment, shared decision making, and routine evaluations (Rowe et al., 2020 ). Input from young people who access services can also facilitate the accessibility and personalisation of substance misuse online platforms or websites (Marsch & Borodovsky, 2016 ).
Nevertheless, technology-based interventions are not exempt from the challenges of non-adherence and drop-out. Wolters et al., ( 2017 ) listed compliance and non-respondence as pertinent challenges of technologically empowered CBT interventions. Additionally, social media was described as an untapped resource that could be valuable in capturing the engagement of young people, however, it does not appear to be widely used currently (Marsch & Borodovsky, 2016 ). Thus, there are several advantages in relation to technology for engagement of young people, however this requires further exploration and the existing engagement issues are not completely resolved.
Efficiency of Care
Technologies such as apps, websites, and other online platforms were described as effectively assessing and managing risk for vulnerable young people, in some ways in a superior manner to traditional methods. Practitioners described being able to identify risk factors rapidly and alert necessary professionals with post-assessment notifications (Rowe et al., 2020 ). Faster responding was also highlighted as an advantage for technology-based monitoring and assessment (Marsch & Borodovsky, 2016 ). Through using apps, young people can access urgent support when there is not a therapist present, potentially enhancing safety. For instance, the SafePlan App which has passed initial usability testing was designed for individuals that are of high-risk regarding suicidality (O’Grady et al., 2020 ), whilst the WRAP App promotes general wellbeing for individuals with various life experiences and mental health difficulties (WRAP, 2018 ). Young people can also access therapeutic support from a distance, which could be significant for settings that may struggle with accessibility of clinical provision (Batastini, 2016 ; Wolters et al., 2017 ). Certain technologies were also identified as valuable when there is insufficient staff, with benefits in relation to reducing cost and time (Marsch & Borodovsky, 2016 ).
Through data being stored online, it was identified how technologies such as apps can enable multiple teams, for example healthcare services at schools, to access the same server and hence access the same information. This was described by Merry and colleagues ( 2020 ) who detailed an app that could be flexibly developed to meet the changing needs of young people, for example, through providing pandemic-oriented support. Evidence suggests that having a clinically governed approach to information sharing resources can be advantageous within settings where there could be multiple systems. This is reflected within the Healthcare Standards for Children and Young People in Secure Settings (Royal College of Paediatrics and Child Health, 2019 ) which highlights the importance of appropriate information sharing between multi-disciplinary teams.
On the other hand, implementing novel technology into mental health services that are facing high-stress and high-pressure could be perceived as burdensome. Owens and Charles ( 2016 ) discovered this when conducting a feasibility study researching a novel SMS text-messaging intervention for young self-harmers. The feasibility study was unable to recruit sufficient numbers due to the CAMHS 1 service being ‘in crisis’, and staff experiencing heavy workloads.
Therapeutic Effectiveness
The effectiveness of technology-assisted therapeutic interventions has received mixed results. A systematic review examining internet-based CBT for young people found that all but one of their included studies demonstrated significant relative symptom reduction, and overall displayed high feasibility and good acceptability (Babiano-Espinosa et al., 2019 ). Two examples were self-help resources, whilst the rest were in conjunction with one-to-one therapist sessions (i.e., after or between sessions with a therapist). Further, a long-term study within a custodial setting found that psychiatric care delivered by videoconferencing was effective in reducing symptoms of distress (Batastini, 2016 ). Nevertheless, this is only a small number of studies, and a different review summarised that the effectiveness of technology-assisted CBT is not well established (Wolters et al., 2017 ). This review also found that having the physical presence of a therapist was deemed to be more beneficial for young people in comparison to technology-based alternatives. For other technological modalities, such as those used for digital phenotyping, the outcomes within the literature are too heterogeneous to summarise into a coherent conclusion regarding effectiveness (Sequeira et al., 2019 ).
The results from studies examining general wellness initiatives rather than specific psychological intervention appear more ubiquitously positive. For example, an online life skills coaching intervention co-designed by young people and delivered by cartoon avatars was rated easy to use by 90 percent of the young people that participated, with 76 percent identifying it as useful (Gabrielli et al., 2020 ). Another non-specific wellness initiative in the form of an online game assessing socio-emotional functioning in young people at school was also found to be well received and accepted by young people from various backgrounds (Day et al., 2019 ), highlighting positive feedback for general wellbeing technologies.
Ethical Considerations
There are several possible ethical barriers to using technology in mental health services (e.g., data protection, right to withdraw, transparent instructions), which were considered by some of the reviewed papers. Positively, one study concluded that the use of tablets was in fact more beneficial in relation to superior data protection security than traditional paper and pen recording methods (Wall et al., 2018 ). Tablets can also enable young people to skip questions and withdraw from any online application discretely (Wall et al., 2018 ).
In relation to conducting mental health research, it was highlighted within a review that young people that have witnessed violence are more likely to experience additional challenges in relation to engagement with technology (Wall et al., 2018 ). There may also be additional ethical barriers to consider when conducting technology-based research for this population, and the authors advised greater scrutiny of app developers in relation to ensuring instructions are clear for young people. Using technology to facilitate mental health research should also be interactive and enable young people to exit the application when they desire. Within a research context, the authors also recommended that services conduct needs-based assessments and consider whether they have the capacity and resources to use an app that may need to be updated and developed over time (Wall et al., 2018 ).
Within custodial settings, reportedly tele-mental health care can be readily implemented and provides advantages from a security perspective (Batastini, 2016 ). For example, workers reported being able to monitor group conversations more effectively if they were tech-facilitated. However, there are considerations needed in relation to confidentiality—if the young person cannot be left unsupervised with the technology, then this could limit the privacy of the therapeutic session (Batastini, 2016 ).
Risks in Relation to Therapeutic Alliance
It has been suggested that therapeutic alliance (Crum & Comer, 2016 ) and the emotional connectedness between the professional and the service-user could be compromised by use of technology (Batastini, 2016 ). For family-orientated therapy in particular, consideration is needed in relation to therapeutic alliance, privacy, safety, childcare logistics, and technological literacy varying across generations (Crum & Comer, 2016 ). Eapen et al. ( 2021 ) also highlighted the importance of considering privacy and internet access. Therapeutic alliance was listed as a particular difficulty for individuals with challenging behaviour, when facilitating technology-augmented therapies (Wolters et al., 2017 ), and when conducting psychiatric assessments for young people (Eapen et al., 2021 ). Clinicians expressed a need for therapies to be tailored to each individual, and voiced concerns in relation to the feasibility or effectiveness of technology-assisted therapy for individuals with more severe needs (Wolters et al., 2017 ).
Application of Technology to Mental Health Care
Flexible application of technology.
Evidence suggests that some practitioners appear to have philosophical and personal challenges with using technology to facilitate one-to-one therapeutic sessions. When the domain of staff non-engagement with a community mental health online platform for young people was explored, CAMHSweb practitioners expressed that the platform interfered with the therapeutic process and was challenging to implement into their daily practice. It was detailed that the platform interfered with the therapists’ personal style of therapy and their ability to be spontaneous during therapeutic sessions. Difficulty of use was not a complaint, suggesting that the barriers appeared to be more values-oriented towards how the therapists’ believed therapy should be conducted (Town et al., 2017 ). When comparing CAMHSweb to other CBT-oriented interventions that were perceived to be feasible and acceptable (e.g., Babiano-Espinosa et al., 2019 ), the difference appears to be whether the technology dictates the therapeutic session or whether the technology is perceived as an adjunct to the therapeutic session. In Babiano-Espinosa and colleagues’ ( 2019 ) review for instance, the online platforms were used in conjunction to the therapist’s own sessions with the young person, or as the sole delivery of therapy through self-help (i.e., without therapist involvement). Therefore, the use of technology to collaborate in-session may be challenging in some cases to the values of some practitioners.
These concerns were mirrored in a review conducted by Wolters and colleagues ( 2017 ), where practitioner views illustrated a reluctance to the standardised nature of technology-assisted structured interventions. Alternatively, an app for trauma-focused CBT was found to have high acceptability and satisfaction from providers and families during a pilot study, during which practitioners were informed that the chapters were non-prescriptive and that they could flexibly utilise any activities that they felt may be useful for a specific young person (Davidson et al., 2019 ). This highlights that flexibility may indeed be an important factor.
Optimising the Use of Technology
It has been suggested that particularly for vulnerable young people, using technology for psychological purposes should not be a time-burden (Wall et al., 2018 ). Young people and practitioners suggested short sessions as the optimum for this medium (e.g., 5 to 10 min for a cartoon chat box intervention; Gabrielli et al., 2020 ). Regarding improving usability and user-experience for young people, it was recommended in a review that touch screen be adopted as opposed to using a mouse, and text-based input should be minimised or avoided (Schueller et al., 2017 ). Providing challenges and feedback during the online interventions facilitates ‘flow’, sustaining engagement and motivation to engage for young people. It is also beneficial if the challenges and feedback are tailored to the young person’s needs and goals. Interaction with other young people on the online platform, or a remote agent, is also a valuable tool to enhance motivation and prevent drop-out (Schueller et al., 2017 ).
A systematic review highlighted that studies that resulted in positive therapeutic outcomes and engagement had a tendency to incorporate specific technological elements onto their online platform or website. This included a competent look and feel that was aesthetically pleasing for young people in-person supportive dialogue during the intervention, interventions that reduced therapeutic content into simple tasks, and the inclusion of self-monitoring tools (Wozney et al., 2017 ). Gamification appeared to be popular within the therapeutic forums deemed more acceptable by young people. For instance, a gaming programme that followed structures of CBT and Interpersonal Therapy for young people with depression was deemed positive by young people and practitioners, who believed it would be a useful addition to existing in-person therapy (Carrasco, 2016 ).
A further systematic review examining multiple modes of digital mental health interventions, (including websites, apps, games and computer-assisted programs, robots, digital devices, virtual reality, and text messaging) found that young people preferred digital interventions that included videos, less text, personalisation, having the ability to connect with other people, and text message reminders (Liverpool et al., 2020 ). Barriers included whether the technology was suitable, usable, the acceptability of the intervention, and patient motivation. Additional barriers to engagement included practical difficulties for individuals who may not have access to the technology in their younger years and may not have family members that can respond with technology (Batastini, 2016 ).
From a psychiatry perspective, clinicians disclosed concerns in relation to their ability to conduct comprehensive assessments of a young person, their development, and any risk factors when this was conducted through a technological medium such as videoconference (Eapen et al., 2021 ). Negative professional attitudes towards structured online courses were also a potential barrier to engagement (Kurki et al., 2018 ). These barriers should be considered when attempting to optimise the use of technology to support young people’s care.
For implementation within primary care, due to GPs having minimal capacity, practitioners from primary care recommended that online platforms, specifically ones that target engagement with therapeutic intervention for young people with anxiety and depression, should be advertised through physical patient reminders, and the use of champions in surgeries (Radovic et al., 2020 ). This highlights that consideration in relation to the practicalities of buy-in are important. Prior to implementing technology such as videoconferencing into a mental health service, considerations are also needed in relation to installation, maintenance, data storage and cost (Chou et al., 2016 ).
This review identified 27 papers examining the use of technology to support young people’s care, the majority focusing on technology which facilitated some form of assessment, psychoeducation, mental health activity, or structured therapy. In combination, the evidence presented suggests that the introduction of technology to support young people’s care has the potential to enhance engagement, increase efficiency of care and improve therapeutic effectiveness. Indeed, the increase of sophisticated technology into young people’s lives in modern society offers an opportunity to utilise these advancements to support mental health and wellbeing (Wolters et al., 2017 ). The findings presented within this review support Babiano-Espinosa and colleagues’ ( 2019 ) hypothesis that the use of technological modalities could address barriers for therapy by adjusting treatment to the technologically advanced modern life of young people and enhancing opportunities to improve cost-effectiveness. As argued by Day and colleagues ( 2019 ), technological advancements offer first-stage approaches for multiple-level assessments, or the opportunity to collect research data to inform practice. The evidence presented in this rapid review supports this claim.
It has been suggested that in order for technology to fully support young people’s care, it must be feasible and engaging to young people, whilst upholding validity and reliability (Day et al., 2019 ). Encouragingly, the majority of papers included in this review examined aspects of the acceptability, feasibility and efficacy of technology and highlighted several positive characteristics.
Young people provided positive feedback regarding the acceptability of technology (e.g., Davidson et al., 2019 ; Gabrielli et al., 2020 ; Snijder et al., 2021 ) and several studies also highlighted good reliability (e.g., Boström et al., 2016 ; Day et al., 2019 ). The current review also builds on recommendations made by Liverpool and colleagues ( 2020 ) for future research to investigate engagement as a component of effectiveness and to consider young people’s preferences relating to the various modes of delivery.
This review highlighted potential barriers, preferences, and recommendations for the feasibility and efficacy of introducing new technology into young people’s services. Barriers which should be considered when attempting to optimise the use of technology include service user motivation (Liverpool et al., 2020 ), socioeconomic factors relating to access to technology (Batastini, 2016 ), clinician concerns in relation to their ability to conduct comprehensive assessments using technology (Eapen et al., 2021 ), and negative professional attitudes (Kurki et al., 2018 ). Young people also offered useful suggestions to enhance engagement, such as using less text, personalisation, having the ability to connect with other people, and text message reminders (Liverpool et al., 2020 ). Motivational messages and relaxing videos were also a request from young people (O’Grady et al., 2020 ).
Strengths and Limitations
This review adhered to established guidelines for conducting rapid evidence reviews and highlighted 27 papers contributing to the research base on the use of technology to support young people’s care. Positively, this review highlighted the range of available methods of delivery, factors influencing engagement, and recommendations based on young person preferences. The findings provide a useful foundation to understand the potential benefits involved in introducing technology to support young people’s care.
However, the current paper is limited in that the review includes findings from before and during the COVID-19 pandemic. The impact of the pandemic on the use of technology in care settings is not yet fully understood. It is possible that this could have had some impact on the current findings, and post-pandemic research would be useful to further explore this. Additionally, a rapid evidence review was conducted in place of a meta-analysis due to the anticipation that there would be insufficient quantitative data or consistency of outcome measures. It has been argued that shortening the review process in the form of a rapid review could result in publication bias or inconsistencies being overlooked (Grant & Booth, 2009 ). As the current search was limited to only two databases, this is a potential limitation of the current review. Nevertheless, as argued by Grant and Booth ( 2009 ), it is important that producing the evidence within a rapid timescale is balanced against the risk of bias.
Quality appraisal was not conducted due to the limited time constraints of the authors. This limits the strength of the findings and clinicians should note that the quality of the studies included within this review may not have been to an equal standard. One author conducted the literature search and screening. The findings were therefore potentially at risk of greater bias as a result of this limitation. Future research with greater time and funding may have value in conducting a more comprehensive review with a method that mitigates against such limitations.
Implications and Recommendations
New technology is continually and rapidly being developed and implemented for therapeutic purposes. The current review highlights the value in collating and summarising recent evidence within this domain to inform mental health services and provision for young people. Effective and sustained use of technology within young people’s mental health services will depend on the technology’s usability, efficiency, and ability to engage young people.
Attention should be given to the design of the technology to ensure it is simple and engaging, making use of videos and motivational content. Clinicians’ concerns should also be taken into account, and professionals should be supported to use technology to enhance the services they offer. Consideration of socioeconomic factors is also needed, particularly with regards to supporting young people and their families to access technology. Developers should work collaboratively with clinicians and service users to create technology which is accessible, engaging, and suitable for young people.
In relation to generalisability and diversity, despite most of the research captured in the current review being predominantly from Westernised cultures, a diverse range of backgrounds and developmental needs were recruited. For instance, Hollis et al. ( 2017 ) conducted a systematic review including any young people accessing mental health services (including diagnoses such as Attention Deficit Hyperactivity Disorder [ADHD], Autism Spectrum Disorder [ASD], psychosis, eating disorders, and Post Traumatic Stress Disorder [PTSD]). The research included also indicated that technology can be specifically developed to be culturally sensitive and appropriate (Snijder et al., 2021 ). Additional research in relation to other cultures is needed to consolidate the efficacy of this approach. Intuitively, some of the benefits witnessed with the introduction of technology into young people’s mental health services, such as reductions in costing (Marsch & Borodovsky, 2016 ).), and reducing travel for appointments (Batastini, 2016 ; Wolters et al., 2017 ), may be beneficial for marginalised communities, or individuals that face more challenges in accessing appropriate mental health care.
Further research is needed to understand the long-term impact of using technology to support young people’s care. Enhanced understanding of whether the advantages acquired by using technology to support treatment will be maintained over time would be beneficial.
It would also be useful for future research to further investigate the possible adverse effects of technology use, for example, relating to confidentiality and patient safety. Additional research could further investigate the impact of the COVID-19 pandemic on technology use in care settings. It is possible that restrictions on social interaction could have increased young people’s reliance on technology, resulting in individuals being more likely to engage with treatment via apps or online forums.
As argued by Comer and colleagues ( 2021 ), the COVID-19 pandemic has created a sense of urgency to resolve the issues that have previously limited technological advancements within the public health sector. The current review suggests that the introduction of technology to support young people’s care is feasible, acceptable, and engaging. Factors that affect engagement were identified alongside young person preferences, allowing for future consideration of strategies to overcome barriers and successfully implement technology to enhance young people’s care. Further research is needed to investigate the long-term benefits of using technology to enhance young people’s care.
Flow Diagram detailing search numbers (PRISMA, 2009).

From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). P referred R eporting I tems for S ystematic Reviews and M eta- A nalyses: The PRISMA Statement. PLoS Med 6(7): e1000097. 10.1371/journal.pmed1000097
For more information, visit www.prisma-statement.org
Data availability, declarations.
The authors declare that they have no conflict of interest.
1 Children and Adolescent Mental Health Services.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
G. Ramshaw, Email: [email protected] .
A. McKeown, Email: [email protected] .
R. Lee, Email: [email protected] .
A. Conlon, Email: [email protected] .
D. Brown, Email: [email protected] .
P. J. Kennedy, Email: [email protected] .
- Babiano-Espinosa L, Wolters LH, Weidle B, op de Beek V, Pedersen SA, Compton S, Skokauskas N. Acceptability, feasibility, and efficacy of Internet cognitive behavioral therapy (iCBT) for pediatric obsessive-compulsive disorder: A systematic review. Systematic Reviews. 2019; 8 (1):1–16. doi: 10.1186/s13643-019-1166-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Batastini AB. Improving rehabilitative efforts for juvenile offenders through the use of telemental healthcare. Journal of Child and Adolescent Psychopharmacology. 2016; 26 (3):273–277. doi: 10.1089/cap.2015.0011. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Berrouiguet S, Baca-García E, Brandt S, Walter M, Courtet P. Fundamentals for future mobile-health (mHealth): A systematic review of mobile phone and web-based text messaging in mental health. Journal of Medical Internet Research. 2016; 18 (6):e135. doi: 10.2196/jmir.5066. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Borghouts J, Eikey E, Mark G, De Leon C, Schueller SM, Schneider M, Stadnick N, Zheng K, Mukamel D, Sorkin DH. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. Journal of Medical Internet Research. 2021; 23 (3):e24387. doi: 10.2196/24387. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boström P, Johnels JÅ, Thorson M, Broberg M. Subjective mental health, peer relations, family, and school environment in adolescents with intellectual developmental disorder: A first report of a new questionnaire administered on tablet PCs. Journal of Mental Health Research in Intellectual Disabilities. 2016; 9 (4):207–231. doi: 10.1080/19315864.2016.1186254. [ CrossRef ] [ Google Scholar ]
- Carrasco, Á. E. (2016). Acceptability of an adventure video game in the treatment of female adolescents with symptoms of depression. Research in Psychotherapy: Psychopathology, Process and Outcome, 19 (1), 10–18.
- Cheng VWS, Davenport T, Johnson D, Vella K, Hickie IB. Gamification in apps and technologies for improving mental health and well-being: Systematic review. JMIR Mental Health. 2019; 6 (6):e13717. doi: 10.2196/13717. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chou T, Comer JS, Turvey CL, Karr A, Spargo G. Technological considerations for the delivery of real-time child telemental healthcare. Journal of Child and Adolescent Psychopharmacology. 2016; 26 (3):192–197. doi: 10.1089/cap.2015.0043. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Comer JS, Furr JM, del Busto C, Silva K, Hong N, Poznanski B, Sanchez A, Cornacchio D, Herrera A, Coxe S, Miguel E, Georgiadis C, Conroy K, Puliafico A. Therapist-led, internet-delivered treatment for early child social anxiety: A waitlist-controlled evaluation of the iCALM telehealth program. Behavior Therapy. 2021; 52 (2021):1171–1187. doi: 10.1016/j.beth.2021.01.004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Copeland ME. Overview of WRAP: Wellness recovery action plan. Mental Health Recovery Newsletter. 2002; 3 :1–9. [ Google Scholar ]
- Crum KI, Comer JS. Using synchronous videoconferencing to deliver family-based mental healthcare. Journal of Child and Adolescent Psychopharmacology. 2016; 26 (3):229–234. doi: 10.1089/cap.2015.0012. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davidson TM, Bunnell BE, Saunders BE, Hanson RF, Danielson CK, Cook D, Chu BC, Dorsey S, Adams ZW, Andrews III AR, Walker JH, Soltis KE, Cohen JA, Deblinger E, Ruggiero KJ. Pilot evaluation of a tablet-based application to improve quality of care in child mental health treatment. Behavior Therapy. 2019; 50 (2):367–379. doi: 10.1016/j.beth.2018.07.005. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Day J, Freiberg K, Hayes A, Homel R. Towards scalable, integrative assessment of children’s self-regulatory capabilities: New applications of digital technology. Clinical Child and Family Psychology Review. 2019; 22 (1):90–103. doi: 10.1007/s10567-019-00282-4. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- DeFilippis E, Impink SM, Singell M, Polzer JT, Sadun R. Collaborating during coronavirus: The impact of COVID-19 on the nature of work. National Bureau of Economic Research. 2020 doi: 10.3386/w27612. [ CrossRef ] [ Google Scholar ]
- Division of Clinical Psychology. (2020, September). DCP Covid-19 strategy: A live document (version 1). https://www.bps.org.uk/sites/www.bps.org.uk/files/Member%20Networks/Divisions/DCP/DCP%20Covid-19%20Strategy.pdf
- Drissi N, Ouhbi S, Janati Idrissi MA, Fernandez-Luque L, Ghogho M. Connected Mental Health: Systematic Mapping Study. Journal of Medical Internet Research. 2020; 22 (8):e19950. doi: 10.2196/19950. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eapen, V., Dadich, A., Balachandran, S., Dani, A., Howari, R., Sequeria, A. Z., & Singer, J. D. (2021). E-mental health in child psychiatry during COVID-19: an initial attitudinal study. Australasian Psychiatry, 10398562211022748. [ PubMed ]
- Etzelmueller A, Vis C, Karyotaki E, Baumeister H, Titov N, Berking M, Cuijpers P, Riper H, Ebert DD. Effects of internet-based cognitive behavioral therapy in routine care for adults in treatment for depression and anxiety: Systematic review and meta-analysis. Journal of Medical Internet Research. 2020; 22 (8):e18100. doi: 10.2196/18100. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gabrielli S, Rizzi S, Carbone S, Donisi V. A chatbot-based coaching intervention for adolescents to promote life skills: Pilot study. JMIR Human Factors. 2020; 7 (1):e16762. doi: 10.2196/16762. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Garrido S, Millington C, Cheers D, Boydell K, Schubert E, Meade T, Nguyen QV. What works and what doesn’t work? A systematic review of digital mental health interventions for depression and anxiety in young people. Frontiers in Psychiatry. 2019; 10 :759. doi: 10.3389/fpsyt.2019.00759. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, Affengruber L, Stevens A. Cochrane rapid reviews methods group offers evidence-informed guidance to conduct rapid reviews. Journal of Clinical Epidemiology. 2020; 130 :13–22. doi: 10.1016/j.jclinepi.2020.10.007. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gearing RE, Attia-Guetta R, Moore K, Gorroochurn P, Olson L, Malekoff A. Tech connect: An intervention to promote treatment engagement for adolescents with depression. Community Mental Health Journal. 2021; 57 (5):880–883. doi: 10.1007/s10597-020-00663-y. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information & Libraries Journal. 2009; 26 (2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hashemi B, Ali S, Awaad R, Soudi L, Housel L, Sosebee SJ. Facilitating mental health screening of war-torn populations using mobile applications. Social Psychiatry and Psychiatric Epidemiology. 2017; 52 (1):27–33. doi: 10.1007/s00127-016-1303-7. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, Davies EB. Annual Research Review: Digital health interventions for children and young people with mental health problems—A systematic and meta-review. Journal of Child Psychology and Psychiatry. 2017; 58 (4):474–503. doi: 10.1111/jcpp.12663. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- HRA (Health Research Authority, 2021), Is My Study Research? http://www.hra-decisiontools.org.uk/research/ . Retrieved 29 Jan 21
- Inal Y, Wake JD, Guribye F, Nordgreen T. Usability evaluations of mobile mental health technologies: Systematic review. Journal of Medical Internet Research. 2020; 22 (1):e15337. doi: 10.2196/15337. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jagosh J, Macaulay AC, Pluye P, Salsberg JON, Bush PL, Henderson JIM, Sirett E, Wong G, Cargo M, Herbert CP, Seifer SD, Green LW, Greenhalgh T. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. The Milbank Quarterly. 2012; 90 (2):311–346. doi: 10.1111/j.1468-0009.2012.00665.x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kurki M, Anttila M, Koivunen M, Marttunen M, Välimäki M. Nurses’ experiences of the use of an Internet-based support system for adolescents with depressive disorders. Informatics for Health and Social Care. 2018; 43 (3):234–247. doi: 10.1080/17538157.2016.1269110. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liverpool S, Mota CP, Sales CM, Čuš A, Carletto S, Hancheva C, Edbrooke-Childs J, et al. Engaging children and young people in digital mental health interventions: Systematic review of modes of delivery, facilitators, and barriers. Journal of Medical Internet Research. 2020; 22 (6):e16317. doi: 10.2196/16317. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Luo, C., Sanger, N., Singhal, N., Pattrick, K., Shams, I., Shahid, H., ... & Samaan, Z. (2020). A comparison of electronically-delivered and face to face cognitive behavioural therapies in depressive disorders: A systematic review and meta-analysis. EClinicalMedicine, 24, 100442. [ PMC free article ] [ PubMed ]
- Magnavita, J. J. (2018). Introduction: How can technology advance mental health treatment? In J.J. Magnavita (Ed.), Using technology in mental health practice (pp. 3-10). American Psychological Association
- Marsch LA, Borodovsky JT. Technology-based interventions for preventing and treating substance use among youth. Child and Adolescent Psychiatric Clinics. 2016; 25 (4):755–768. doi: 10.1016/j.chc.2016.06.005. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Merry SN, Cargo T, Christie G, Donkin L, Hetrick S, Fleming T, Holt-Quick C, Hopkins S, Stasiak K, Warren J. Debate: Supporting the mental health of school students in the COVID-19 pandemic in New Zealand–a digital ecosystem approach. Child and Adolescent Mental Health. 2020; 25 (4):267–269. doi: 10.1111/camh.12429. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Health Service. (2019, August 21). The NHS Long Term Plan. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf
- Nesbitt, T. S. (2012). The evolution of telehealth: Where have we been and where are we going. In The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. Washington, DC: Institute of Medicine . [ PubMed ]
- O'Grady C, Melia R, Bogue J, O'Sullivan M, Young K, Duggan J. A mobile health approach for improving outcomes in suicide prevention (SafePlan) Journal of Medical Internet Research. 2020; 22 (7):e17481. doi: 10.2196/17481. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Orlowski SK, Lawn S, Venning A, Winsall M, Jones GM, Wyld K, Damarell RA, Antezana G, Schrader G, Smith D, Collin P, Bidargaddi N. Participatory research as one piece of the puzzle: a systematic review of consumer involvement in design of technology-based youth mental health and well-being interventions. JMIR Human Factors. 2015; 2 (2):e4361. doi: 10.2196/humanfactors.4361. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ouhbi S, Drissi N, Idrissi MAJ, Luque LF, Ghogho M. Connected mental health: Systematic mapping study. Journal of Medical Internet Research. 2020; 22 (8):e19950. doi: 10.2196/19950. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Owens C, Charles N. Implementation of a text-messaging intervention for adolescents who self-harm (TeenTEXT): A feasibility study using normalisation process theory. Child and Adolescent Psychiatry and Mental Health. 2016; 10 (1):1–9. doi: 10.1186/s13034-016-0101-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oz T, Crooks A. Exploring the impact of mandatory remote work during the COVID-19 pandemic. George Mason University. 2020 doi: 10.1111/bjop.12468. [ CrossRef ] [ Google Scholar ]
- Radovic A, Odenthal K, Flores AT, Miller E, Stein BD. Prescribing technology to increase uptake of depression treatment in primary care: A Pre-implementation focus group study of SOVA (supporting our valued adolescents) Journal of Clinical Psychology in Medical Settings. 2020; 27 (4):766–782. doi: 10.1007/s10880-019-09669-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ramo D, Lim MH. Technology Matters: Using apps to address loneliness in adolescents and young adults-leveraging tech engagement among digital natives. Child and Adolescent Mental Health. 2021; 26 (2):186–188. doi: 10.1111/camh.12465. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rowe SC, Davenport TA, Easton MA, Jackson TA, Melsness J, Ottavio A, Sinclair J, Hickie AM IB. Co-designing the InnoWell Platform to deliver the right mental health care first time to regional youth. Australian Journal of Rural Health. 2020; 28 (2):190–194. doi: 10.1111/ajr.12617. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Royal College of Paediatrics and Child Health (RCPCH). (2019, June). Healthcare Standards for Children and Young People in Secure Settings. www.rcpch.ac.uk/cypss
- Schueller SM, Stiles-Shields C, Yarosh L. Online treatment and virtual therapists in child and adolescent psychiatry. Child and Adolescent Psychiatric Clinics. 2017; 26 (1):1–12. doi: 10.1016/j.chc.2016.07.011. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sequeira L, Battaglia M, Perrotta S, Merikangas K, Strauss J. Digital phenotyping with mobile and wearable devices: Advanced symptom measurement in child and adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2019; 58 :841–845. doi: 10.1016/j.jaac.2019.04.011. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Snijder, M., Stapinski, L., Ward, J., Lees, B., Chapman, C., Champion, K., ... & Newton, N. (2021). Strong and Deadly Futures: Co-Development of a Web-Based Wellbeing and Substance Use Prevention Program for Aboriginal and Torres Strait Islander and Non-Aboriginal Adolescents . International Journal of Environmental Research and Public Health, 18(4), 2176. [ PMC free article ] [ PubMed ]
- The British Psychological Society (2020). Adaptations to psychological practice: Continuing guidance during Covid-19 Pandemic. https://www.bps.org.uk/sites/www.bps.org.uk/files/Policy/Policy%20-%20Files/Adaptations%20to%20psychological%20practice%20-%20interim%20guidance%20during%20Covid-19.pdf
- Town R, Midgley N, Ellis L, Tempest R, Wolpert M. A qualitative investigation of staff's practical, personal and philosophical barriers to the implementation of a web-based platform in a child mental health setting. Counselling and Psychotherapy Research. 2017; 17 (3):218–226. doi: 10.1002/capr.12129. [ CrossRef ] [ Google Scholar ]
- Wall MA, Jenney A, Walsh M. Conducting evaluation research with children exposed to violence: How technological innovations in methodologies and data collection may enhance the process. Child Abuse & Neglect. 2018; 85 :202–208. doi: 10.1016/j.chiabu.2018.01.007. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wolters LH, op de Beek V, Weidle B, Skokauskas N. How can technology enhance cognitive behavioral therapy: The case of pediatric obsessive compulsive disorder. BMC Psychiatry. 2017; 17 (1):1–9. doi: 10.1186/s12888-017-1377-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wozney L, Huguet A, Bennett K, Radomski AD, Hartling L, Dyson M, McGrath PJ, Newton AS. How do eHealth programs for adolescents with depression work? A realist review of persuasive system design components in internet-based psychological therapies. Journal of Medical Internet Research. 2017; 19 (8):e7573. doi: 10.2196/jmir.7573. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- WRAP. (2018). Wellness Recovery Action Plan: WRAP in action, WRAP App. https://www.wellnessrecoveryactionplan.com/wrap-in-action/wrap-app/
- Wu YJ, Outley C, Matarrita-Cascante D, Murphrey TP. A systematic review of recent research on adolescent social connectedness and mental health with internet technology use. Adolescent Research Review. 2016; 1 (2):153–162. doi: 10.1007/s40894-015-0013-9. [ CrossRef ] [ Google Scholar ]
- Zhou X, Edirippulige S, Bai X, Bambling M. Are online mental health interventions for youth effective? A systematic review. Journal of Telemedicine and Telecare. 2021; 27 (10):638–666. doi: 10.1177/1357633X211047285. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Essay Editor
Mental Health Essay
Introduction
Mental health, often overshadowed by its physical counterpart, is an intricate and essential aspect of human existence. It envelops our emotions, psychological state, and social well-being, shaping our thoughts, behaviors, and interactions. With the complexities of modern life—constant connectivity, societal pressures, personal expectations, and the frenzied pace of technological advancements—mental well-being has become increasingly paramount. Historically, conversations around this topic have been hushed, shrouded in stigma and misunderstanding. However, as the curtains of misconception slowly lift, we find ourselves in an era where discussions about mental health are not only welcomed but are also seen as vital. Recognizing and addressing the nuances of our mental state is not merely about managing disorders; it's about understanding the essence of who we are, how we process the world around us, and how we navigate the myriad challenges thrown our way. This essay aims to delve deep into the realm of mental health, shedding light on its importance, the potential consequences of neglect, and the spectrum of mental disorders that many face in silence.
Importance of Mental Health
Mental health plays a pivotal role in determining how individuals think, feel, and act. It influences our decision-making processes, stress management techniques, interpersonal relationships, and even our physical health. A well-tuned mental state boosts productivity, creativity, and the intrinsic sense of self-worth, laying the groundwork for a fulfilling life.
Negative Impact of Mental Health
Neglecting mental health, on the other hand, can lead to severe consequences. Reduced productivity, strained relationships, substance abuse, physical health issues like heart diseases, and even reduced life expectancy are just some of the repercussions of poor mental health. It not only affects the individual in question but also has a ripple effect on their community, workplace, and family.
Mental Disorders: Types and Prevalence
Mental disorders are varied and can range from anxiety and mood disorders like depression and bipolar disorder to more severe conditions such as schizophrenia.
- Depression: Characterized by persistent sadness, lack of interest in activities, and fatigue.
- Anxiety Disorders: Encompass conditions like generalized anxiety disorder, panic attacks, and specific phobias.
- Schizophrenia: A complex disorder affecting a person's ability to think, feel, and behave clearly.
The prevalence of these disorders has been on the rise, underscoring the need for comprehensive mental health initiatives and awareness campaigns.
Understanding Mental Health and Its Importance
Mental health is not merely the absence of disorders but encompasses emotional, psychological, and social well-being. Recognizing the signs of deteriorating mental health, like prolonged sadness, extreme mood fluctuations, or social withdrawal, is crucial. Understanding stems from awareness and education. Societal stigmas surrounding mental health have often deterred individuals from seeking help. Breaking these barriers, fostering open conversations, and ensuring access to mental health care are imperative steps.
Conclusion: Mental Health
Mental health, undeniably, is as significant as physical health, if not more. In an era where the stressors are myriad, from societal pressures to personal challenges, mental resilience and well-being are essential. Investing time and resources into mental health initiatives, and more importantly, nurturing a society that understands, respects, and prioritizes mental health is the need of the hour.
- World Leaders: Several influential personalities, from celebrities to sports stars, have openly discussed their mental health challenges, shedding light on the universality of these issues and the importance of addressing them.
- Workplaces: Progressive organizations are now incorporating mental health programs, recognizing the tangible benefits of a mentally healthy workforce, from increased productivity to enhanced creativity.
- Educational Institutions: Schools and colleges, witnessing the effects of stress and other mental health issues on students, are increasingly integrating counseling services and mental health education in their curriculum.
In weaving through the intricate tapestry of mental health, it becomes evident that it's an area that requires collective attention, understanding, and action.
Short Essay about Mental Health
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life. Yet, its impact is pervasive, influencing our productivity, relationships, and overall quality of life.
Sadly, mental health issues have long been stigmatized, seen as a sign of weakness or dismissed as mere mood swings. However, they are as real and significant as any physical ailment. From anxiety to depression, these disorders have touched countless lives, often in silence due to societal taboos.
But change is on the horizon. As awareness grows, conversations are shifting from hushed whispers to open discussions, fostering understanding and support. Institutions, workplaces, and communities are increasingly acknowledging the importance of mental health, implementing programs, and offering resources.
In conclusion, mental health is not a peripheral concern but a central one, crucial to our holistic well-being. It's high time we prioritize it, eliminating stigma and fostering an environment where everyone feels supported in their mental health journey.
Frequently Asked Questions
- What is the primary focus of a mental health essay?
Answer: The primary focus of a mental health essay is to delve into the intricacies of mental well-being, its significance in our daily lives, the various challenges people face, and the broader societal implications. It aims to shed light on both the psychological and emotional aspects of mental health, often emphasizing the importance of understanding, empathy, and proactive care.
- How can writing an essay on mental health help raise awareness about its importance?
Answer: Writing an essay on mental health can effectively articulate the nuances and complexities of the topic, making it more accessible to a wider audience. By presenting facts, personal anecdotes, and research, the essay can demystify misconceptions, highlight the prevalence of mental health issues, and underscore the need for destigmatizing discussions around it. An impactful essay can ignite conversations, inspire action, and contribute to a more informed and empathetic society.
- What are some common topics covered in a mental health essay?
Answer: Common topics in a mental health essay might include the definition and importance of mental health, the connection between mental and physical well-being, various mental disorders and their symptoms, societal stigmas and misconceptions, the impact of modern life on mental health, and the significance of therapy and counseling. It may also delve into personal experiences, case studies, and the broader societal implications of neglecting mental health.
Recent articles
Aithor's new brand identity.
Hello Aithors! We're here to share some exciting news with you. We've given ourselves a makeover, and we're thrilled to unveil our new brand identity! Our brand has always been about making AI-writing a seamless and secure experience. But we wanted our brand to really represent what we're all about: ease of use, speed, innovation, reliability, and a bit of rebelliousness. So, we’ve updated our look! Our new logo is a visual metaphor that uniquely combines the concepts of undetectability and sc ...
Interface is now available in Portuguese and Spanish
Hey aithors! We're excited to share with you that our interface is now available in Portuguese and Spanish. With more than 500 million Spanish and more than 250 million Portuguese speakers, we believe that this new update will enhance the experience on our platform. Our team worked closely with native speakers to make sure the translations considered all the nuances and peculiarities of the languages. For us, it’s a great opportunity to make Aithor as accessible as possible for users across th ...

25,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- Speech Writing /
5 Minutes Speech on Technology and Mental Health
- Updated on
- Jan 11, 2024

Technology and Mental Health Speech: Can you live without your smartphone for a minute? You know want my answer will be to this question? You guessed it right. We all have an addiction to our gadgets and it almost seems impossible to live without them.
Technology has overcome us. On one hand, technology has improved and lessened the workload on our shoulders, but on the other hand, it has become one of the ways to get distracted from work. Checking notifications every minute, worrying about the specifications of recently launched gadgets, and many other activities indicate this addiction. All this dependency somewhere leads to mental unrest as well.
Also Read: Essay on Advantages And Disadvantages of Social Media
Speech on Technology and Mental Health
‘Greetings to all teachers and students gathered here. Today, I stand before you to deliver my point of view on the trending topic in society, which is technology and mental health.
As students, we are growing in an environment where technology is slowly and steadily becoming the core of our private lives. Whether it is social media, smartphones, or any electronic amenities, everywhere we are surrounded by a digital panorama.
So shall we say that these robotics are bringing positive changes to us as well as to the community?
In the first place, advances in medical technology help in better diagnosis and treatment; conversely, telemedicine, robotic surgery, and telehealth help individuals without any geographical boundaries. Patients can easily get access to medical consultations, receive diagnoses, and even undergo surgeries without the physical availability of health consultants.
However, the same technology that showered these unexpected miracles also has a flip side. The absence of smartphones, and social media, contributes to the feeling of loneliness and social isolation. It is therefore suggested to maintain a balance the virtual and real-world interactions. Engaging with people face-to-face not only helps in quality connection and communication but also contributes positive impacts to healthy mental conditions.
One major concern about the impact of technology through social media is the constant exposure of carefully selected visuals and refined lifestyles on platforms like Facebook, Instagram and likewise. Students need to understand that whatever they are seeing online is not the full picture.
Another noteworthy issue of the impact of technology is the rise of cyberbullying. Anonymous people by online platforms harm individuals to engage in harmful behaviour. Students should be aware of the potential results of cyberbullying and try to connect with people whom they know well.
Apart from this online mode of communication, the prevalence of gaming and screen time among students is again a crucial area which requires attention. While video games can be entertaining and even educational too, excessive gaming may lead children to sedentary behaviour and lack of physical activity which can negatively impact mental health at last.
Moreover, the constant gaming and screen time among students also matter as gaming excessiveness may lead to sedentary behavior and a lack of physical activity can negatively impact the mental health of the students. The practice of encouraging outdoor activities and a balanced approach to screen time can help for overall well-being of the students.
While covering every aspect of the negative effects, how can we forget about the constant notification and overloaded information that keeps on ringing and can students stress and create hurdles in concentration?
As students, we must learn to utilise the power of digital technology positively. Creating a healthy relationship with technology has a positive impact on mental health. It is important to prioritise self-care, with adequate sleep, physical activity, and maintaining real-world connections. You should remember that taking breaks from the digital world is a strong signal of strength and not weakness.
In helping the students learn about the drawbacks of technology school can also play an important role. Incorporation of digital literacy and mental health into the curriculum can empower the students to understand digital technology positively. Teachers and parents should keep an open conversation about technology, mental health, and the importance of finding a balance between the two.
In conclusion, technology and mental health are complex. While technology offers opportunities and conveniences, it also poses challenges that require thoughtful consideration. As a student, you are the architect of the future, and it depends on how you want to handle this digital age which will not only help to shape your future but also the well-being of generations to come.
Stay connected with technology to enhance knowledge rather than hinder mental health. Do not be afraid to take support whenever need to get out of this addiction after all, everything comes with a boon as well as a bane.
Also Read: Speech on Future of Technology in India
10 Lines Speech on Technology and Mental Health
Here is the short and simple 10-line on technology and mental health.
- The constant connectivity with overloaded information through various technical gadgets can lead to stress and anxiety.
- As a part of technology, social media also contributes to cyberbullying, unrealistic beauty standards,s and the omnipresent fear of missing out.
- The pressure of creating an online persona likes, and comments can also pressure the mental well-being of the individual.
- It is a difficult task for students to recognize the fake images and lifestyles on social media.
- Excessive screen time on smartphones, tablets, or computers is the source of various mental issues.
- Long exposure to gadgets and screens, especially before bedtime, disturbs the sleeping pattern of a person and also affects mood as well as mental health.
- It is seen that students who are addicted to online video games and social media pose a risk to their mental health.
- Digital detox is necessary to detoxify from the constant stimuli of technology.
- Students should be encouraged to take periodic breaks from screens and should be engaging more in outdoor activities.
- Technology can be used to make use of mediate sessions and mental health resources.
Spending maximum time on social media and other online platforms can make you feel isolated. Also, constant notifications and pressure to keep one connected can lead to burnout.
The five ways to improve mental health are as follows: Try to spend more time in the natural environment. Do not isolate yourself. Instead, attend social activities and connect with others. It is suggested to give time to physical activities such as jogging, long walks, and regular exercise. Take complete sleep. Learn to be creative in every small thing you do.
Excessive screen time affects sleeping disturbance and can create strain in the eye. All these disturbances can affect the mental health of a person.
Yes, technology influences the behaviour of an individual. For example, social media affects self-esteem, and online interaction can impact real-world social skills.
The five negative effects of science and technology are environmental degradation, privacy breaches, social inequalities, and misuse of user rights and creative common licences.
Related Articles
For more information on such interesting speech topics for your school, visit our speech writing page and follow Leverage Edu .
Deepika Joshi
Deepika Joshi is an experienced content writer with expertise in creating educational and informative content. She has a year of experience writing content for speeches, essays, NCERT, study abroad and EdTech SaaS. Her strengths lie in conducting thorough research and ananlysis to provide accurate and up-to-date information to readers. She enjoys staying updated on new skills and knowledge, particulary in education domain. In her free time, she loves to read articles, and blogs with related to her field to further expand her expertise. In personal life, she loves creative writing and aspire to connect with innovative people who have fresh ideas to offer.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
25,000+ students realised their study abroad dream with us. Take the first step today.

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out
Essay on the Impact of Technology on Health Care
Technology has grown to become an integral part of health. Healthcare organizations in different parts of the world are using technology to monitor their patients’ progress while others are using technology to store patients’ data (Bonato 37). Patient outcomes have improved due to technology, and health organizations that sought profits have significantly increased their income because of technology. It is no doubt that technology has influenced medical services in varied ways. Therefore, it would be fair to conclude that technology has positively affected healthcare.
First, technology has improved access to medical information and data (Mettler 33). One of the most significant advantages triggered by technology is the ability to store and access patient data. Medical professionals can now track patients’ progress by retrieving data from anywhere. At the same time, the internet has allowed doctors to share medical information rapidly amongst themselves, an instance that leads to more efficient patient care.
Second, technology has allowed clinicians to gather big data in a limited time (Chen et al. 72). Digital technology allows instant data collection for professionals engaged in epidemiological studies, clinical trials, and those in research. The collection of data, in this case, allows for meta-analysis and permits healthcare organizations to stay on top of cutting edge technological trends.
In addition to allowing quick access to medical data and big data technology has improved medical communication (Free et al. 54). Communication is a critical part of healthcare; nurses and doctors must communicate in real-time, and technology allows this instance to happen. Also, healthcare professionals can today make their videos, webinars and use online platforms to communicate with other professionals in different parts of the globe.
Technology has revolutionized how health care services are rendered. But apart from improving healthcare, critics argue that technology has increased or added extra jobs for medical professionals (de Belvis et al. 11). Physicians need to have excellent clinical skills and knowledge of the human body. Today, they are forced to have knowledge of both the human body and technology, which makes it challenging for others. Technology has also improved access to data, and this has allowed physicians to study and understand patients’ medical history. Nevertheless, these instances have opened doors to unethical activities such as computer hacking (de Belvis et al. 13). Today patients risk losing their medical information, including their social security numbers, address and other critical information.
Despite the improvements that have come with adopting technology, there is always the possibility that digital technological gadgets might fail. If makers of a given technology do not have a sustainable business process or a good track record, their technologies might fail. Many people, including patients and doctors who solely rely on technology, might be affected when it does. Apart from equipment failure, technology has created the space for laziness within hospitals.
Doctors and patients heavily rely on medical technology for problem-solving. In like manner, medical technologies that use machine learning have removed decision-making in different hospitals; today, medical tools are solving people’s problems. Technology has been great for our hospitals, but the speed at which different hospitals are adapting to technological processes is alarming. Technology often fails, and when it does, health care may be significantly affected. Doctors and patients who use technology may be forced to go back to traditional methods of health care services.
Bonato, P. “Advances in Wearable Technology and Its Medical Applications.” 2010 Annual International Conference of The IEEE Engineering in Medicine and Biology , 2010, pp. 33-45.
Chen, Min et al. “Disease Prediction by Machine Learning Over Big Data from Healthcare Communities.” IEEE Access , vol. 5, 2017, pp. 69-79.
De Belvis, Antonio Giulio et al. “The Financial Crisis in Italy: Implications for The Healthcare Sector.” Health Policy , vol. 106, no. 1, 2012, pp. 10-16.
Free, Caroline et al. “The Effectiveness of M-Health Technologies for Improving Health and Health Services: A Systematic Review Protocol.” BMC Research Notes , vol. 3, no. 1, 2010, pp. 42-78.
Mettler, Matthias. “Blockchain Technology in Healthcare: The Revolution Starts Here.” 2016 IEEE 18Th International Conference On E-Health Networking, Applications and Services (Healthcom) , 2016, pp. 23-78.
Cite this page
Similar essay samples.
- Essay on Nationalism in China and Its Effect on Hong Kong
- The Multidisciplinary Approach to Medicine
- Essay on Orofacial Development Problems
- Essay on Financing Political Campaigns in America
- Research design: business intelligence
- Essay on Police Wearing Body Worn Cameras (BWC’s) Can in Turn Prove ...

IMAGES
VIDEO
COMMENTS
Background: Research increasingly shows how selective and targeted use of technology within care and welfare can have several advantages including improved quality of care and active user involvement. Purpose: The current overview of reviews aims to summarize the research on the effectiveness of technology for mental health and wellbeing. The goal is to highlight and structure the diverse ...
The impact of technology has extended into the realm of health care, and it is clear that technology also is making positive changes in terms of mental health care. Research has indicated, however, that the very tools that can help alleviate mental health issues, such as smartphone apps, may be linked with the experience of mental health ...
Debating digital-technology use and teenage mental health. ... but it is not films or video chats with friends that damage mental health. When research papers allow us to zoom in on social media, ...
Accessibility Is a Tremendous Benefit of Technology. Every expert interviewed agreed: Accessibility is an undeniable and indispensable benefit of mental health's increasing presence online. Torn points out, "We can access information, including mental health information and treatment like never before, and it's low cost.".
This editorial introduces the special issue on digital mental health. The promise of digital, mobile, and connected technologies to advance mental health, and especially psychiatric rehabilitation, continues to rapidly evolve. New sensors and data, such as those derived from increasingly ubiquitous smartphones, offer a new window into the functional, social, and emotional experiences of ...
The integration of technology in supporting mental health stretches back to the 20th century. But it wasn't until the personal computer and internet revolution of the 1990s that its role became truly transformative in mental health care. Initially, computer-based applications were limited to providing psychoeducation and self-assessment tools.
The Impact of Technology on Mental Health. August 2019. DOI: 10.1201/9780429325632-4. In book: Electrical Brain Stimulation for the Treatment of Neurological Disorders (pp.353-402) Authors: Bahman ...
In another study recently conducted by Statistics Canada, which examined data on mental health in adolescents aged 12 to 17 from the 2019 Canadian Health Survey on Children and Youth, video game use by girls was found to be associated with lower self-reported mental health, even when controlling for other factors.
The intersection of technology and mental health is a rapidly evolving field, offering new possibilities for improving mental health care. From mental health apps and wearable technology to AI and machine learning, technology is transforming the way we understand, treat, and manage mental health conditions. As we continue to navigate this new ...
Technology is ubiquitous in society and is now being extensively used in mental health applications. Both assessment and treatment strategies are being developed and deployed at a rapid pace. The authors review the current domains of technology utilization, describe standards for quality evaluation, and forecast future developments. This review examines technology-based assessments of ...
Bowers, Hitt, Hoeft, and Dunn (2003), modified Kirk-. patrick's (1959a, 1959b, 1960a, 1960b, 1976) training. model for application to clinical settings. Training in. the area of mental health is ...
Introduction. The current coronavirus 2019 (COVID-19) pandemic not only poses a large threat to the physical health of our population, if we fail to act now, it will also have detrimental long-term consequences for mental health. Though social distancing is a crucial intervention to slow down the destructive effects of the pandemic, it can lead ...
Having constant anxiety will regress your mind and lead to other issues such as loneliness. Furthermore, Loneliness is a factor of technology as well. Being infatuated with a screen all day will affect your social life. It makes it easier to deny someone from hanging out and creating short condensed conversions with no meaning.
For example, their position is that long hours of social media use contribute to depression and anxiety (Karim et al., 2020). This focus is integral in my research since it addresses the impact of technology on mental health by explaining the possible avenues for mental health crises. Lattie et al. (2019) investigate how the rise in mental ...
Introduction. Technology and its use within psychiatric services has advanced dramatically since the infamous television link between Nebraska Psychiatric Institute and Norfolk State Hospital was established for psychiatric consultations over fifty years ago (Nesbitt, 2012).Technological developments have also become increasingly necessary due to the effects of the COVID-19 pandemic (Comer et ...
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life.
lack of attention. low creativity. delays in language development. delays in social and emotional development. physical inactivity and obesity. poor sleep quality. social issues, such as social ...
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
Here is the short and simple 10-line on technology and mental health. The constant connectivity with overloaded information through various technical gadgets can lead to stress and anxiety. As a part of technology, social media also contributes to cyberbullying, unrealistic beauty standards,s and the omnipresent fear of missing out.
Essay on the Negative Effects of Technology on Mental Health. This essay sample was donated by a student to help the academic community. Papers provided by EduBirdie writers usually outdo students' samples. Technology runs the world and at this point, technological advances in any field are inevitable. Imagining a world without technology would ...
Therefore, it would be fair to conclude that technology has positively affected healthcare. First, technology has improved access to medical information and data (Mettler 33). One of the most significant advantages triggered by technology is the ability to store and access patient data. Medical professionals can now track patients' progress ...
Technology And Mental Health Essay. 1629 Words4 Pages. Technology is not mentally beneficial. Technology is truly taking a turn for the worst on mental health. Technology is the future, it's supposed to be the greatest thing to ever happen. Although technology may be helping the world out, it is hurting the people who use it.