Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- Inductive vs. Deductive Research Approach | Steps & Examples

Inductive vs. Deductive Research Approach | Steps & Examples
Published on April 18, 2019 by Raimo Streefkerk . Revised on June 22, 2023.
The main difference between inductive and deductive reasoning is that inductive reasoning aims at developing a theory while deductive reasoning aims at testing an existing theory .
In other words, inductive reasoning moves from specific observations to broad generalizations . Deductive reasoning works the other way around.
Both approaches are used in various types of research , and it’s not uncommon to combine them in your work.
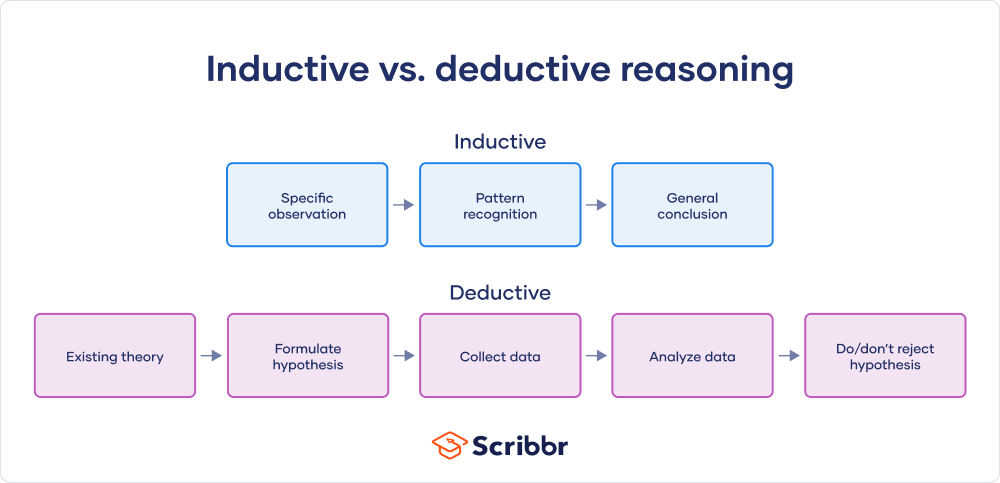
Table of contents
Inductive research approach, deductive research approach, combining inductive and deductive research, other interesting articles, frequently asked questions about inductive vs deductive reasoning.
When there is little to no existing literature on a topic, it is common to perform inductive research , because there is no theory to test. The inductive approach consists of three stages:
- A low-cost airline flight is delayed
- Dogs A and B have fleas
- Elephants depend on water to exist
- Another 20 flights from low-cost airlines are delayed
- All observed dogs have fleas
- All observed animals depend on water to exist
- Low cost airlines always have delays
- All dogs have fleas
- All biological life depends on water to exist
Limitations of an inductive approach
A conclusion drawn on the basis of an inductive method can never be fully proven. However, it can be invalidated.
Prevent plagiarism. Run a free check.
When conducting deductive research , you always start with a theory. This is usually the result of inductive research. Reasoning deductively means testing these theories. Remember that if there is no theory yet, you cannot conduct deductive research.
The deductive research approach consists of four stages:
- If passengers fly with a low cost airline, then they will always experience delays
- All pet dogs in my apartment building have fleas
- All land mammals depend on water to exist
- Collect flight data of low-cost airlines
- Test all dogs in the building for fleas
- Study all land mammal species to see if they depend on water
- 5 out of 100 flights of low-cost airlines are not delayed
- 10 out of 20 dogs didn’t have fleas
- All land mammal species depend on water
- 5 out of 100 flights of low-cost airlines are not delayed = reject hypothesis
- 10 out of 20 dogs didn’t have fleas = reject hypothesis
- All land mammal species depend on water = support hypothesis
Limitations of a deductive approach
The conclusions of deductive reasoning can only be true if all the premises set in the inductive study are true and the terms are clear.
- All dogs have fleas (premise)
- Benno is a dog (premise)
- Benno has fleas (conclusion)
Many scientists conducting a larger research project begin with an inductive study. This helps them develop a relevant research topic and construct a strong working theory. The inductive study is followed up with deductive research to confirm or invalidate the conclusion. This can help you formulate a more structured project, and better mitigate the risk of research bias creeping into your work.
Remember that both inductive and deductive approaches are at risk for research biases, particularly confirmation bias and cognitive bias , so it’s important to be aware while you conduct your research.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Chi square goodness of fit test
- Degrees of freedom
- Null hypothesis
- Discourse analysis
- Control groups
- Mixed methods research
- Non-probability sampling
- Quantitative research
- Inclusion and exclusion criteria
Research bias
- Rosenthal effect
- Implicit bias
- Cognitive bias
- Selection bias
- Negativity bias
- Status quo bias
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Inductive reasoning is a bottom-up approach, while deductive reasoning is top-down.
Inductive reasoning takes you from the specific to the general, while in deductive reasoning, you make inferences by going from general premises to specific conclusions.
Inductive reasoning is a method of drawing conclusions by going from the specific to the general. It’s usually contrasted with deductive reasoning, where you proceed from general information to specific conclusions.
Inductive reasoning is also called inductive logic or bottom-up reasoning.
Deductive reasoning is a logical approach where you progress from general ideas to specific conclusions. It’s often contrasted with inductive reasoning , where you start with specific observations and form general conclusions.
Deductive reasoning is also called deductive logic.
Exploratory research aims to explore the main aspects of an under-researched problem, while explanatory research aims to explain the causes and consequences of a well-defined problem.
Explanatory research is used to investigate how or why a phenomenon occurs. Therefore, this type of research is often one of the first stages in the research process , serving as a jumping-off point for future research.
Exploratory research is often used when the issue you’re studying is new or when the data collection process is challenging for some reason.
You can use exploratory research if you have a general idea or a specific question that you want to study but there is no preexisting knowledge or paradigm with which to study it.
A research project is an academic, scientific, or professional undertaking to answer a research question . Research projects can take many forms, such as qualitative or quantitative , descriptive , longitudinal , experimental , or correlational . What kind of research approach you choose will depend on your topic.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Streefkerk, R. (2023, June 22). Inductive vs. Deductive Research Approach | Steps & Examples. Scribbr. Retrieved April 8, 2024, from https://www.scribbr.com/methodology/inductive-deductive-reasoning/
Is this article helpful?
Raimo Streefkerk
Other students also liked, qualitative vs. quantitative research | differences, examples & methods, explanatory research | definition, guide, & examples, exploratory research | definition, guide, & examples, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

2.3: Inductive or Deductive? Two Different Approaches
- Last updated
- Save as PDF
- Page ID 12547

Learning Objectives
- Describe the inductive approach to research, and provide examples of inductive research.
- Describe the deductive approach to research, and provide examples of deductive research.
- Describe the ways that inductive and deductive approaches may be complementary.
Theories structure and inform sociological research. So, too, does research structure and inform theory. The reciprocal relationship between theory and research often becomes evident to students new to these topics when they consider the relationships between theory and research in inductive and deductive approaches to research. In both cases, theory is crucial. But the relationship between theory and research differs for each approach. Inductive and deductive approaches to research are quite different, but they can also be complementary. Let’s start by looking at each one and how they differ from one another. Then we’ll move on to thinking about how they complement one another.
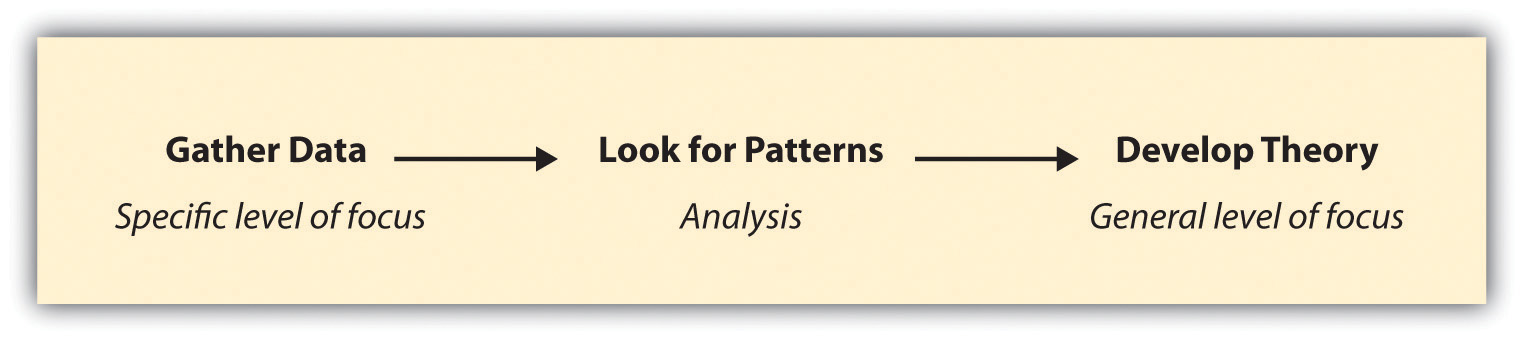
Inductive Approaches and Some Examples
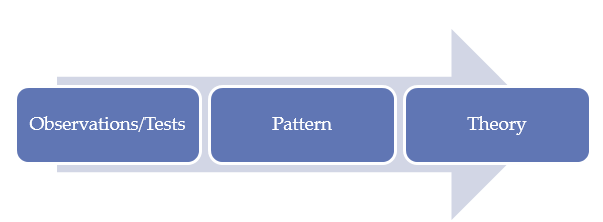
In an inductive approach to research, a researcher begins by collecting data that is relevant to his or her topic of interest. Once a substantial amount of data have been collected, the researcher will then take a breather from data collection, stepping back to get a bird’s eye view of her data. At this stage, the researcher looks for patterns in the data, working to develop a theory that could explain those patterns. Thus when researchers take an inductive approach, they start with a set of observations and then they move from those particular experiences to a more general set of propositions about those experiences. In other words, they move from data to theory, or from the specific to the general. Figure 2.5 outlines the steps involved with an inductive approach to research.
Figure 2.5 Inductive Research
There are many good examples of inductive research, but we’ll look at just a few here. One fascinating recent study in which the researchers took an inductive approach was Katherine Allen, Christine Kaestle, and Abbie Goldberg’s study (2011)Allen, K. R., Kaestle, C. E., & Goldberg, A. E. (2011). More than just a punctuation mark: How boys and young men learn about menstruation. Journal of Family Issues, 32 , 129–156. of how boys and young men learn about menstruation. To understand this process, Allen and her colleagues analyzed the written narratives of 23 young men in which the men described how they learned about menstruation, what they thought of it when they first learned about it, and what they think of it now. By looking for patterns across all 23 men’s narratives, the researchers were able to develop a general theory of how boys and young men learn about this aspect of girls’ and women’s biology. They conclude that sisters play an important role in boys’ early understanding of menstruation, that menstruation makes boys feel somewhat separated from girls, and that as they enter young adulthood and form romantic relationships, young men develop more mature attitudes about menstruation.
In another inductive study, Kristin Ferguson and colleagues (Ferguson, Kim, & McCoy, 2011)Ferguson, K. M., Kim, M. A., & McCoy, S. (2011). Enhancing empowerment and leadership among homeless youth in agency and community settings: A grounded theory approach. Child and Adolescent Social Work Journal, 28 , 1–22. analyzed empirical data to better understand how best to meet the needs of young people who are homeless. The authors analyzed data from focus groups with 20 young people at a homeless shelter. From these data they developed a set of recommendations for those interested in applied interventions that serve homeless youth. The researchers also developed hypotheses for people who might wish to conduct further investigation of the topic. Though Ferguson and her colleagues did not test the hypotheses that they developed from their analysis, their study ends where most deductive investigations begin: with a set of testable hypotheses.
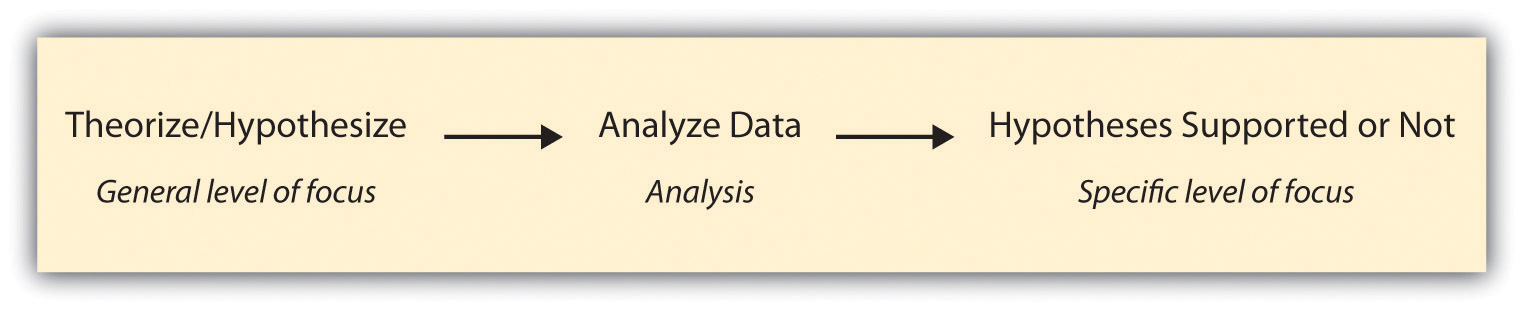
Deductive Approaches and Some Examples
Researchers taking a deductive approach take the steps described earlier for inductive research and reverse their order. They start with a social theory that they find compelling and then test its implications with data. That is, they move from a more general level to a more specific one. A deductive approach to research is the one that people typically associate with scientific investigation. The researcher studies what others have done, reads existing theories of whatever phenomenon he or she is studying, and then tests hypotheses that emerge from those theories. Figure 2.6 outlines the steps involved with a deductive approach to research.
Figure 2.6 Deductive Research
While not all researchers follow a deductive approach, as you have seen in the preceding discussion, many do, and there are a number of excellent recent examples of deductive research. We’ll take a look at a couple of those next.
In a study of US law enforcement responses to hate crimes, Ryan King and colleagues (King, Messner, & Baller, 2009)King, R. D., Messner, S. F., & Baller, R. D. (2009). Contemporary hate crimes, law enforcement, and the legacy of racial violence. American Sociological Review, 74 , 291–315.hypothesized that law enforcement’s response would be less vigorous in areas of the country that had a stronger history of racial violence. The authors developed their hypothesis from their reading of prior research and theories on the topic. Next, they tested the hypothesis by analyzing data on states’ lynching histories and hate crime responses. Overall, the authors found support for their hypothesis.
In another recent deductive study, Melissa Milkie and Catharine Warner (2011)Milkie, M. A., & Warner, C. H. (2011). Classroom learning environments and the mental health of first grade children. Journal of Health and Social Behavior, 52 , 4–22. studied the effects of different classroom environments on first graders’ mental health. Based on prior research and theory, Milkie and Warner hypothesized that negative classroom features, such as a lack of basic supplies and even heat, would be associated with emotional and behavioral problems in children. The researchers found support for their hypothesis, demonstrating that policymakers should probably be paying more attention to the mental health outcomes of children’s school experiences, just as they track academic outcomes (American Sociological Association, 2011).The American Sociological Association wrote a press release on Milkie and Warner’s findings: American Sociological Association. (2011). Study: Negative classroom environment adversely affects children’s mental health. Retrieved from asanet.org/press/Negative_Cla...tal_Health.cfm
Complementary Approaches?
While inductive and deductive approaches to research seem quite different, they can actually be rather complementary. In some cases, researchers will plan for their research to include multiple components, one inductive and the other deductive. In other cases, a researcher might begin a study with the plan to only conduct either inductive or deductive research, but then he or she discovers along the way that the other approach is needed to help illuminate findings. Here is an example of each such case.
In the case of my collaborative research on sexual harassment, we began the study knowing that we would like to take both a deductive and an inductive approach in our work. We therefore administered a quantitative survey, the responses to which we could analyze in order to test hypotheses, and also conducted qualitative interviews with a number of the survey participants. The survey data were well suited to a deductive approach; we could analyze those data to test hypotheses that were generated based on theories of harassment. The interview data were well suited to an inductive approach; we looked for patterns across the interviews and then tried to make sense of those patterns by theorizing about them.
For one paper (Uggen & Blackstone, 2004),Uggen, C., & Blackstone, A. (2004). Sexual harassment as a gendered expression of power. American Sociological Review, 69 , 64–92. we began with a prominent feminist theory of the sexual harassment of adult women and developed a set of hypotheses outlining how we expected the theory to apply in the case of younger women’s and men’s harassment experiences. We then tested our hypotheses by analyzing the survey data. In general, we found support for the theory that posited that the current gender system, in which heteronormative men wield the most power in the workplace, explained workplace sexual harassment—not just of adult women but of younger women and men as well. In a more recent paper (Blackstone, Houle, & Uggen, 2006),Blackstone, A., Houle, J., & Uggen, C. “At the time I thought it was great”: Age, experience, and workers’ perceptions of sexual harassment. Presented at the 2006 meetings of the American Sociological Association. Currently under review. we did not hypothesize about what we might find but instead inductively analyzed the interview data, looking for patterns that might tell us something about how or whether workers’ perceptions of harassment change as they age and gain workplace experience. From this analysis, we determined that workers’ perceptions of harassment did indeed shift as they gained experience and that their later definitions of harassment were more stringent than those they held during adolescence. Overall, our desire to understand young workers’ harassment experiences fully—in terms of their objective workplace experiences, their perceptions of those experiences, and their stories of their experiences—led us to adopt both deductive and inductive approaches in the work.
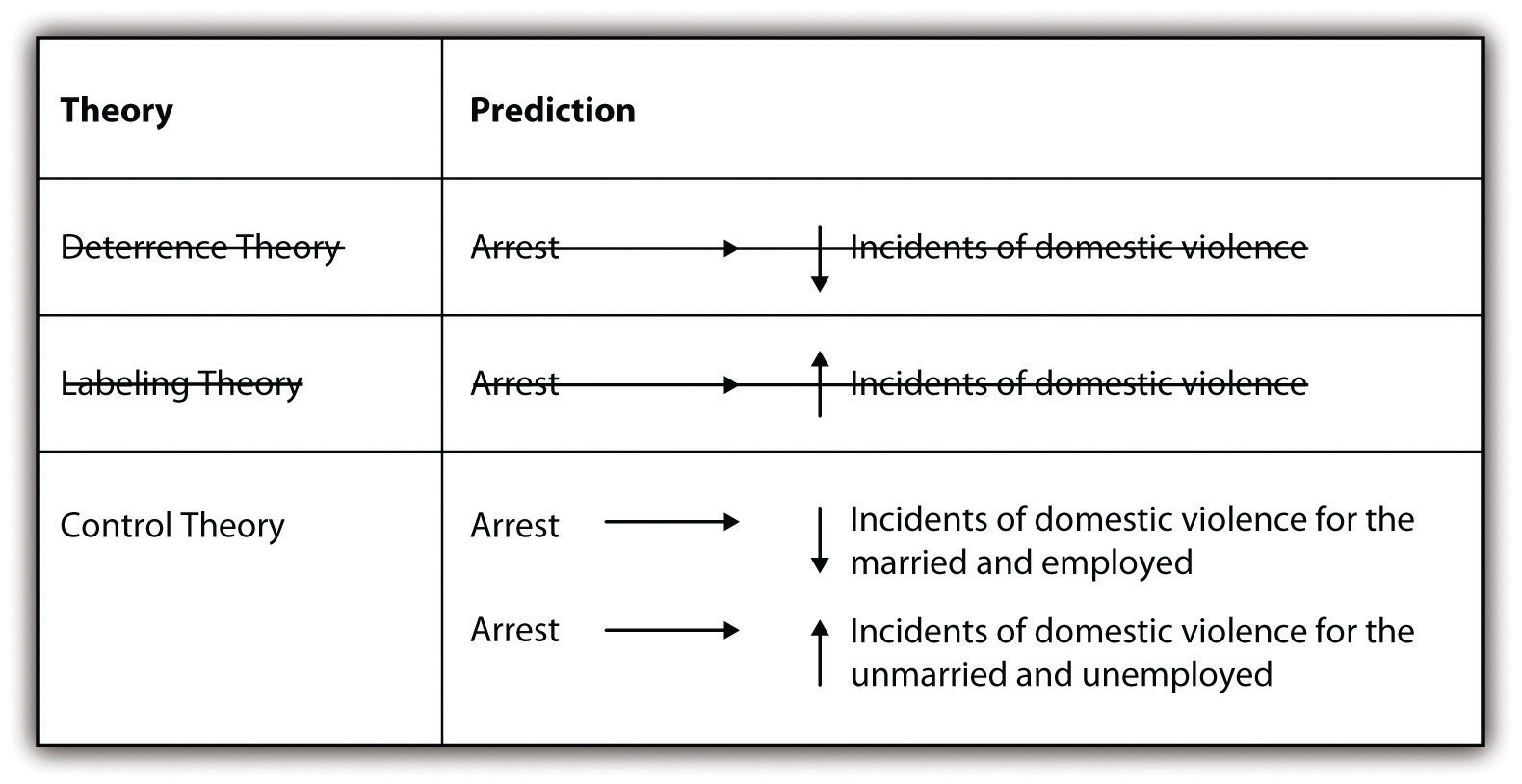
Researchers may not always set out to employ both approaches in their work but sometimes find that their use of one approach leads them to the other. One such example is described eloquently in Russell Schutt’s Investigating the Social World (2006).Schutt, R. K. (2006). Investigating the social world: The process and practice of research . Thousand Oaks, CA: Pine Forge Press. As Schutt describes, researchers Lawrence Sherman and Richard Berk (1984)Sherman, L. W., & Berk, R. A. (1984). The specific deterrent effects of arrest for domestic assault. American Sociological Review, 49 , 261–272. conducted an experiment to test two competing theories of the effects of punishment on deterring deviance (in this case, domestic violence). Specifically, Sherman and Berk hypothesized that deterrence theory would provide a better explanation of the effects of arresting accused batterers than labeling theory . Deterrence theory predicts that arresting an accused spouse batterer will reduce future incidents of violence. Conversely, labeling theory predicts that arresting accused spouse batterers will increase future incidents. Figure 2.7 summarizes the two competing theories and the predictions that Sherman and Berk set out to test.
Figure 2.7 Predicting the Effects of Arrest on Future Spouse Battery
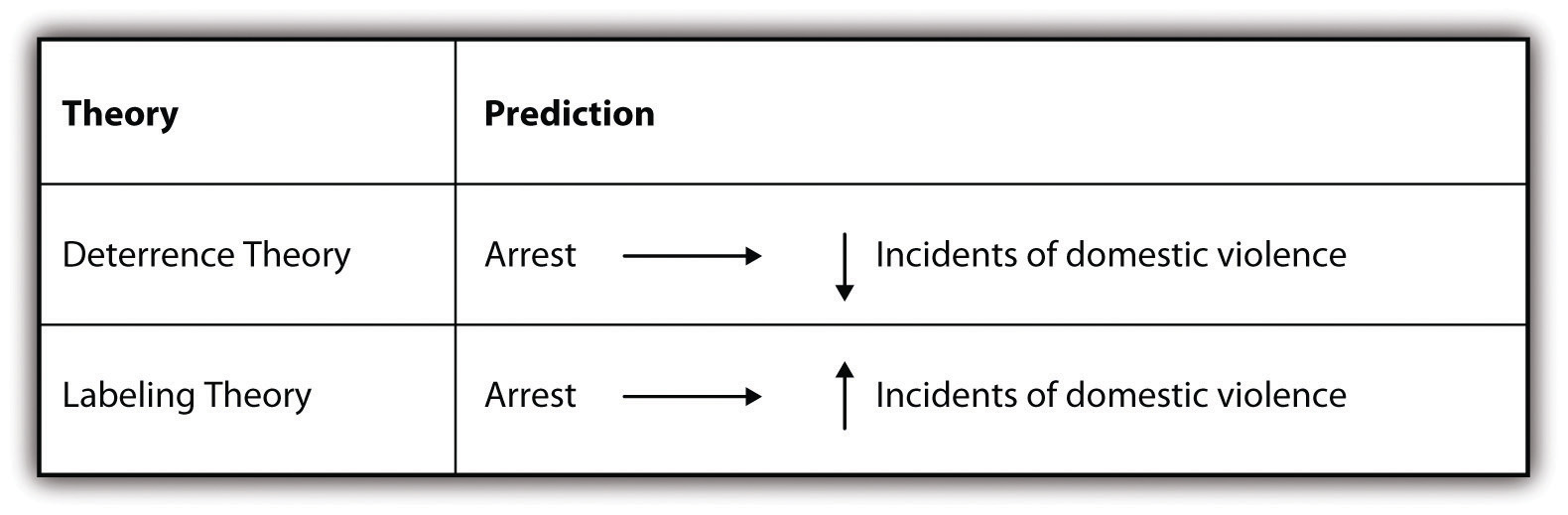
Sherman and Berk found, after conducting an experiment with the help of local police in one city, that arrest did in fact deter future incidents of violence, thus supporting their hypothesis that deterrence theory would better predict the effect of arrest. After conducting this research, they and other researchers went on to conduct similar experimentsThe researchers did what’s called replication. We’ll learn more about replication in Chapter 3. in six additional cities (Berk, Campbell, Klap, & Western, 1992; Pate & Hamilton, 1992; Sherman & Smith, 1992).Berk, R., Campbell, A., Klap, R., & Western, B. (1992). The deterrent effect of arrest in incidents of domestic violence: A Bayesian analysis of four field experiments. American Sociological Review, 57 , 698–708; Pate, A., & Hamilton, E. (1992). Formal and informal deterrents to domestic violence: The Dade county spouse assault experiment. American Sociological Review, 57 , 691–697; Sherman, L., & Smith, D. (1992). Crime, punishment, and stake in conformity: Legal and informal control of domestic violence. American Sociological Review, 57 , 680–690. Results from these follow-up studies were mixed. In some cases, arrest deterred future incidents of violence. In other cases, it did not. This left the researchers with new data that they needed to explain. The researchers therefore took an inductive approach in an effort to make sense of their latest empirical observations. The new studies revealed that arrest seemed to have a deterrent effect for those who were married and employed but that it led to increased offenses for those who were unmarried and unemployed. Researchers thus turned to control theory, which predicts that having some stake in conformity through the social ties provided by marriage and employment, as the better explanation.
Figure 2.8 Predicting the Effects of Arrest on Future Spouse Battery: A New Theory
What the Sherman and Berk research, along with the follow-up studies, shows us is that we might start with a deductive approach to research, but then, if confronted by new data that we must make sense of, we may move to an inductive approach. Russell Schutt depicts this process quite nicely in his text, and I’ve adapted his depiction here, in Figure 2.9.
KEY TAKEAWAYS
- The inductive approach involves beginning with a set of empirical observations, seeking patterns in those observations, and then theorizing about those patterns.
- The deductive approach involves beginning with a theory, developing hypotheses from that theory, and then collecting and analyzing data to test those hypotheses.
- Inductive and deductive approaches to research can be employed together for a more complete understanding of the topic that a researcher is studying.
- Though researchers don’t always set out to use both inductive and deductive strategies in their work, they sometimes find that new questions arise in the course of an investigation that can best be answered by employing both approaches.
Monty Python and Holy Grail :
(click to see video)
Do the townspeople take an inductive or deductive approach to determine whether the woman in question is a witch? What are some of the different sources of knowledge (recall Chapter 1) they rely on?
- Think about how you could approach a study of the relationship between gender and driving over the speed limit. How could you learn about this relationship using an inductive approach? What would a study of the same relationship look like if examined using a deductive approach? Try the same thing with any topic of your choice. How might you study the topic inductively? Deductively?
To read this content please select one of the options below:
Please note you do not have access to teaching notes, qualitative research: deductive and inductive approaches to data analysis.
Qualitative Research Journal
ISSN : 1443-9883
Article publication date: 31 October 2018
Issue publication date: 15 November 2018
The purpose of this paper is to explain the rationale for choosing the qualitative approach to research human resources practices, namely, recruitment and selection, training and development, performance management, rewards management, employee communication and participation, diversity management and work and life balance using deductive and inductive approaches to analyse data. The paper adopts an emic perspective that favours the study of transfer of human resource management practices from the point of view of employees and host country managers in subsidiaries of western multinational enterprises in Ghana.
Design/methodology/approach
Despite the numerous examples of qualitative methods of data generation, little is known particularly to the novice researcher about how to analyse qualitative data. This paper develops a model to explain in a systematic manner how to methodically analyse qualitative data using both deductive and inductive approaches.
The deductive and inductive approaches provide a comprehensive approach in analysing qualitative data. The process involves immersing oneself in the data reading and digesting in order to make sense of the whole set of data and to understand what is going on.
Originality/value
This paper fills a serious gap in qualitative data analysis which is deemed complex and challenging with limited attention in the methodological literature particularly in a developing country context, Ghana.
- Qualitative
- Emic interviews documents
Azungah, T. (2018), "Qualitative research: deductive and inductive approaches to data analysis", Qualitative Research Journal , Vol. 18 No. 4, pp. 383-400. https://doi.org/10.1108/QRJ-D-18-00035
Emerald Publishing Limited
Copyright © 2018, Emerald Publishing Limited
Related articles
We’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here

Inductive Approach (Inductive Reasoning)
Inductive approach, also known in inductive reasoning, starts with the observations and theories are proposed towards the end of the research process as a result of observations [1] . Inductive research “involves the search for pattern from observation and the development of explanations – theories – for those patterns through series of hypotheses” [2] . No theories or hypotheses would apply in inductive studies at the beginning of the research and the researcher is free in terms of altering the direction for the study after the research process had commenced.
It is important to stress that inductive approach does not imply disregarding theories when formulating research questions and objectives. This approach aims to generate meanings from the data set collected in order to identify patterns and relationships to build a theory; however, inductive approach does not prevent the researcher from using existing theory to formulate the research question to be explored. [3] Inductive reasoning is based on learning from experience. Patterns, resemblances and regularities in experience (premises) are observed in order to reach conclusions (or to generate theory).
Application of Inductive Approach (Inductive Reasoning) in Business Research
Inductive reasoning begins with detailed observations of the world, which moves towards more abstract generalisations and ideas [4] . When following an inductive approach, beginning with a topic, a researcher tends to develop empirical generalisations and identify preliminary relationships as he progresses through his research. No hypotheses can be found at the initial stages of the research and the researcher is not sure about the type and nature of the research findings until the study is completed.
As it is illustrated in figure below, “inductive reasoning is often referred to as a “bottom-up” approach to knowing, in which the researcher uses observations to build an abstraction or to describe a picture of the phenomenon that is being studied” [5]
Here is an example:
My nephew borrowed $100 last June but he did not pay back until September as he had promised (PREMISE). Then he assured me that he will pay back until Christmas but he didn’t (PREMISE). He also failed in to keep his promise to pay back in March (PREMISE). I reckon I have to face the facts. My nephew is never going to pay me back (CONCLUSION).
Generally, the application of inductive approach is associated with qualitative methods of data collection and data analysis, whereas deductive approach is perceived to be related to quantitative methods . The following table illustrates such a classification from a broad perspective:
However, the statement above is not absolute, and in some instances inductive approach can be adopted to conduct a quantitative research as well. The following table illustrates patterns of data analysis according to type of research and research approach .
When writing a dissertation in business studies it is compulsory to specify the approach of are adopting. It is good to include a table comparing inductive and deductive approaches similar to one below [6] and discuss the impacts of your choice of inductive approach on selection of primary data collection methods and research process.
My e-book, The Ultimate Guide to Writing a Dissertation in Business Studies: a step by step assistance contains discussions of theory and application of research approaches. The e-book also explains all stages of the research process starting from the selection of the research area to writing personal reflection. Important elements of dissertations such as research philosophy , research design , methods of data collection , data analysis and sampling are explained in this e-book in simple words.
John Dudovskiy
[1] Goddard, W. & Melville, S. (2004) “Research Methodology: An Introduction” 2nd edition, Blackwell Publishing
[2] Bernard, H.R. (2011) “Research Methods in Anthropology” 5 th edition, AltaMira Press, p.7
[3] Saunders, M., Lewis, P. & Thornhill, A. (2012) “Research Methods for Business Students” 6 th edition, Pearson Education Limited
[4] Neuman, W.L. (2003) “Social Research Methods: Qualitative and Quantitative Approaches” Allyn and Bacon
[5] Lodico, M.G., Spaulding, D.T &Voegtle, K.H. (2010) “Methods in Educational Research: From Theory to Practice” John Wiley & Sons, p.10
[6] Source: Alexandiris, K.T. (2006) “Exploring Complex Dynamics in Multi Agent-Based Intelligent Systems” Pro Quest
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol
Quantitative and Qualitative Approaches to Generalization and Replication–A Representationalist View
In this paper, we provide a re-interpretation of qualitative and quantitative modeling from a representationalist perspective. In this view, both approaches attempt to construct abstract representations of empirical relational structures. Whereas quantitative research uses variable-based models that abstract from individual cases, qualitative research favors case-based models that abstract from individual characteristics. Variable-based models are usually stated in the form of quantified sentences (scientific laws). This syntactic structure implies that sentences about individual cases are derived using deductive reasoning. In contrast, case-based models are usually stated using context-dependent existential sentences (qualitative statements). This syntactic structure implies that sentences about other cases are justifiable by inductive reasoning. We apply this representationalist perspective to the problems of generalization and replication. Using the analytical framework of modal logic, we argue that the modes of reasoning are often not only applied to the context that has been studied empirically, but also on a between-contexts level. Consequently, quantitative researchers mostly adhere to a top-down strategy of generalization, whereas qualitative researchers usually follow a bottom-up strategy of generalization. Depending on which strategy is employed, the role of replication attempts is very different. In deductive reasoning, replication attempts serve as empirical tests of the underlying theory. Therefore, failed replications imply a faulty theory. From an inductive perspective, however, replication attempts serve to explore the scope of the theory. Consequently, failed replications do not question the theory per se , but help to shape its boundary conditions. We conclude that quantitative research may benefit from a bottom-up generalization strategy as it is employed in most qualitative research programs. Inductive reasoning forces us to think about the boundary conditions of our theories and provides a framework for generalization beyond statistical testing. In this perspective, failed replications are just as informative as successful replications, because they help to explore the scope of our theories.
Introduction
Qualitative and quantitative research strategies have long been treated as opposing paradigms. In recent years, there have been attempts to integrate both strategies. These “mixed methods” approaches treat qualitative and quantitative methodologies as complementary, rather than opposing, strategies (Creswell, 2015 ). However, whilst acknowledging that both strategies have their benefits, this “integration” remains purely pragmatic. Hence, mixed methods methodology does not provide a conceptual unification of the two approaches.
Lacking a common methodological background, qualitative and quantitative research methodologies have developed rather distinct standards with regard to the aims and scope of empirical science (Freeman et al., 2007 ). These different standards affect the way researchers handle contradictory empirical findings. For example, many empirical findings in psychology have failed to replicate in recent years (Klein et al., 2014 ; Open Science, Collaboration, 2015 ). This “replication crisis” has been discussed on statistical, theoretical and social grounds and continues to have a wide impact on quantitative research practices like, for example, open science initiatives, pre-registered studies and a re-evaluation of statistical significance testing (Everett and Earp, 2015 ; Maxwell et al., 2015 ; Shrout and Rodgers, 2018 ; Trafimow, 2018 ; Wiggins and Chrisopherson, 2019 ).
However, qualitative research seems to be hardly affected by this discussion. In this paper, we argue that the latter is a direct consequence of how the concept of generalizability is conceived in the two approaches. Whereas most of quantitative psychology is committed to a top-down strategy of generalization based on the idea of random sampling from an abstract population, qualitative studies usually rely on a bottom-up strategy of generalization that is grounded in the successive exploration of the field by means of theoretically sampled cases.
Here, we show that a common methodological framework for qualitative and quantitative research methodologies is possible. We accomplish this by introducing a formal description of quantitative and qualitative models from a representationalist perspective: both approaches can be reconstructed as special kinds of representations for empirical relational structures. We then use this framework to analyze the generalization strategies used in the two approaches. These turn out to be logically independent of the type of model. This has wide implications for psychological research. First, a top-down generalization strategy is compatible with a qualitative modeling approach. This implies that mainstream psychology may benefit from qualitative methods when a numerical representation turns out to be difficult or impossible, without the need to commit to a “qualitative” philosophy of science. Second, quantitative research may exploit the bottom-up generalization strategy that is inherent to many qualitative approaches. This offers a new perspective on unsuccessful replications by treating them not as scientific failures, but as a valuable source of information about the scope of a theory.
The Quantitative Strategy–Numbers and Functions
Quantitative science is about finding valid mathematical representations for empirical phenomena. In most cases, these mathematical representations have the form of functional relations between a set of variables. One major challenge of quantitative modeling consists in constructing valid measures for these variables. Formally, to measure a variable means to construct a numerical representation of the underlying empirical relational structure (Krantz et al., 1971 ). For example, take the behaviors of a group of students in a classroom: “to listen,” “to take notes,” and “to ask critical questions.” One may now ask whether is possible to assign numbers to the students, such that the relations between the assigned numbers are of the same kind as the relations between the values of an underlying variable, like e.g., “engagement.” The observed behaviors in the classroom constitute an empirical relational structure, in the sense that for every student-behavior tuple, one can observe whether it is true or not. These observations can be represented in a person × behavior matrix 1 (compare Figure 1 ). Given this relational structure satisfies certain conditions (i.e., the axioms of a measurement model), one can assign numbers to the students and the behaviors, such that the relations between the numbers resemble the corresponding numerical relations. For example, if there is a unique ordering in the empirical observations with regard to which person shows which behavior, the assigned numbers have to constitute a corresponding unique ordering, as well. Such an ordering coincides with the person × behavior matrix forming a triangle shaped relation and is formally represented by a Guttman scale (Guttman, 1944 ). There are various measurement models available for different empirical structures (Suppes et al., 1971 ). In the case of probabilistic relations, Item-Response models may be considered as a special kind of measurement model (Borsboom, 2005 ).

Constructing a numerical representation from an empirical relational structure; Due to the unique ordering of persons with regard to behaviors (indicated by the triangular shape of the relation), it is possible to construct a Guttman scale by assigning a number to each of the individuals, representing the number of relevant behaviors shown by the individual. The resulting variable (“engagement”) can then be described by means of statistical analyses, like, e.g., plotting the frequency distribution.
Although essential, measurement is only the first step of quantitative modeling. Consider a slightly richer empirical structure, where we observe three additional behaviors: “to doodle,” “to chat,” and “to play.” Like above, one may ask, whether there is a unique ordering of the students with regard to these behaviors that can be represented by an underlying variable (i.e., whether the matrix forms a Guttman scale). If this is the case, we may assign corresponding numbers to the students and call this variable “distraction.” In our example, such a representation is possible. We can thus assign two numbers to each student, one representing his or her “engagement” and one representing his or her “distraction” (compare Figure 2 ). These measurements can now be used to construct a quantitative model by relating the two variables by a mathematical function. In the simplest case, this may be a linear function. This functional relation constitutes a quantitative model of the empirical relational structure under study (like, e.g., linear regression). Given the model equation and the rules for assigning the numbers (i.e., the instrumentations of the two variables), the set of admissible empirical structures is limited from all possible structures to a rather small subset. This constitutes the empirical content of the model 2 (Popper, 1935 ).

Constructing a numerical model from an empirical relational structure; Since there are two distinct classes of behaviors that each form a Guttman scale, it is possible to assign two numbers to each individual, correspondingly. The resulting variables (“engagement” and “distraction”) can then be related by a mathematical function, which is indicated by the scatterplot and red line on the right hand side.
The Qualitative Strategy–Categories and Typologies
The predominant type of analysis in qualitative research consists in category formation. By constructing descriptive systems for empirical phenomena, it is possible to analyze the underlying empirical structure at a higher level of abstraction. The resulting categories (or types) constitute a conceptual frame for the interpretation of the observations. Qualitative researchers differ considerably in the way they collect and analyze data (Miles et al., 2014 ). However, despite the diverse research strategies followed by different qualitative methodologies, from a formal perspective, most approaches build on some kind of categorization of cases that share some common features. The process of category formation is essential in many qualitative methodologies, like, for example, qualitative content analysis, thematic analysis, grounded theory (see Flick, 2014 for an overview). Sometimes these features are directly observable (like in our classroom example), sometimes they are themselves the result of an interpretative process (e.g., Scheunpflug et al., 2016 ).
In contrast to quantitative methodologies, there have been little attempts to formalize qualitative research strategies (compare, however, Rihoux and Ragin, 2009 ). However, there are several statistical approaches to non-numerical data that deal with constructing abstract categories and establishing relations between these categories (Agresti, 2013 ). Some of these methods are very similar to qualitative category formation on a conceptual level. For example, cluster analysis groups cases into homogenous categories (clusters) based on their similarity on a distance metric.
Although category formation can be formalized in a mathematically rigorous way (Ganter and Wille, 1999 ), qualitative research hardly acknowledges these approaches. 3 However, in order to find a common ground with quantitative science, it is certainly helpful to provide a formal interpretation of category systems.
Let us reconsider the above example of students in a classroom. The quantitative strategy was to assign numbers to the students with regard to variables and to relate these variables via a mathematical function. We can analyze the same empirical structure by grouping the behaviors to form abstract categories. If the aim is to construct an empirically valid category system, this grouping is subject to constraints, analogous to those used to specify a measurement model. The first and most important constraint is that the behaviors must form equivalence classes, i.e., within categories, behaviors need to be equivalent, and across categories, they need to be distinct (formally, the relational structure must obey the axioms of an equivalence relation). When objects are grouped into equivalence classes, it is essential to specify the criterion for empirical equivalence. In qualitative methodology, this is sometimes referred to as the tertium comparationis (Flick, 2014 ). One possible criterion is to group behaviors such that they constitute a set of specific common attributes of a group of people. In our example, we might group the behaviors “to listen,” “to take notes,” and “to doodle,” because these behaviors are common to the cases B, C, and D, and they are also specific for these cases, because no other person shows this particular combination of behaviors. The set of common behaviors then forms an abstract concept (e.g., “moderate distraction”), while the set of persons that show this configuration form a type (e.g., “the silent dreamer”). Formally, this means to identify the maximal rectangles in the underlying empirical relational structure (see Figure 3 ). This procedure is very similar to the way we constructed a Guttman scale, the only difference being that we now use different aspects of the empirical relational structure. 4 In fact, the set of maximal rectangles can be determined by an automated algorithm (Ganter, 2010 ), just like the dimensionality of an empirical structure can be explored by psychometric scaling methods. Consequently, we can identify the empirical content of a category system or a typology as the set of empirical structures that conforms to it. 5 Whereas the quantitative strategy was to search for scalable sub-matrices and then relate the constructed variables by a mathematical function, the qualitative strategy is to construct an empirical typology by grouping cases based on their specific similarities. These types can then be related to one another by a conceptual model that describes their semantic and empirical overlap (see Figure 3 , right hand side).

Constructing a conceptual model from an empirical relational structure; Individual behaviors are grouped to form abstract types based on them being shared among a specific subset of the cases. Each type constitutes a set of specific commonalities of a class of individuals (this is indicated by the rectangles on the left hand side). The resulting types (“active learner,” “silent dreamer,” “distracted listener,” and “troublemaker”) can then be related to one another to explicate their semantic and empirical overlap, as indicated by the Venn-diagram on the right hand side.
Variable-Based Models and Case-Based Models
In the previous section, we have argued that qualitative category formation and quantitative measurement can both be characterized as methods to construct abstract representations of empirical relational structures. Instead of focusing on different philosophical approaches to empirical science, we tried to stress the formal similarities between both approaches. However, it is worth also exploring the dissimilarities from a formal perspective.
Following the above analysis, the quantitative approach can be characterized by the use of variable-based models, whereas the qualitative approach is characterized by case-based models (Ragin, 1987 ). Formally, we can identify the rows of an empirical person × behavior matrix with a person-space, and the columns with a corresponding behavior-space. A variable-based model abstracts from the single individuals in a person-space to describe the structure of behaviors on a population level. A case-based model, on the contrary, abstracts from the single behaviors in a behavior-space to describe individual case configurations on the level of abstract categories (see Table 1 ).
Variable-based models and case-based models.
From a representational perspective, there is no a priori reason to favor one type of model over the other. Both approaches provide different analytical tools to construct an abstract representation of an empirical relational structure. However, since the two modeling approaches make use of different information (person-space vs. behavior-space), this comes with some important implications for the researcher employing one of the two strategies. These are concerned with the role of deductive and inductive reasoning.
In variable-based models, empirical structures are represented by functional relations between variables. These are usually stated as scientific laws (Carnap, 1928 ). Formally, these laws correspond to logical expressions of the form
In plain text, this means that y is a function of x for all objects i in the relational structure under consideration. For example, in the above example, one may formulate the following law: for all students in the classroom it holds that “distraction” is a monotone decreasing function of “engagement.” Such a law can be used to derive predictions for single individuals by means of logical deduction: if the above law applies to all students in the classroom, it is possible to calculate the expected distraction from a student's engagement. An empirical observation can now be evaluated against this prediction. If the prediction turns out to be false, the law can be refuted based on the principle of falsification (Popper, 1935 ). If a scientific law repeatedly withstands such empirical tests, it may be considered to be valid with regard to the relational structure under consideration.
In case-based models, there are no laws about a population, because the model does not abstract from the cases but from the observed behaviors. A case-based model describes the underlying structure in terms of existential sentences. Formally, this corresponds to a logical expression of the form
In plain text, this means that there is at least one case i for which the condition XYZ holds. For example, the above category system implies that there is at least one active learner. This is a statement about a singular observation. It is impossible to deduce a statement about another person from an existential sentence like this. Therefore, the strategy of falsification cannot be applied to test the model's validity in a specific context. If one wishes to generalize to other cases, this is accomplished by inductive reasoning, instead. If we observed one person that fulfills the criteria of calling him or her an active learner, we can hypothesize that there may be other persons that are identical to the observed case in this respect. However, we do not arrive at this conclusion by logical deduction, but by induction.
Despite this important distinction, it would be wrong to conclude that variable-based models are intrinsically deductive and case-based models are intrinsically inductive. 6 Both types of reasoning apply to both types of models, but on different levels. Based on a person-space, in a variable-based model one can use deduction to derive statements about individual persons from abstract population laws. There is an analogous way of reasoning for case-based models: because they are based on a behavior space, it is possible to deduce statements about singular behaviors. For example, if we know that Peter is an active learner, we can deduce that he takes notes in the classroom. This kind of deductive reasoning can also be applied on a higher level of abstraction to deduce thematic categories from theoretical assumptions (Braun and Clarke, 2006 ). Similarly, there is an analog for inductive generalization from the perspective of variable-based modeling: since the laws are only quantified over the person-space, generalizations to other behaviors rely on inductive reasoning. For example, it is plausible to assume that highly engaged students tend to do their homework properly–however, in our example this behavior has never been observed. Hence, in variable-based models we usually generalize to other behaviors by means of induction. This kind of inductive reasoning is very common when empirical results are generalized from the laboratory to other behavioral domains.
Although inductive and deductive reasoning are used in qualitative and quantitative research, it is important to stress the different roles of induction and deduction when models are applied to cases. A variable-based approach implies to draw conclusions about cases by means of logical deduction; a case-based approach implies to draw conclusions about cases by means of inductive reasoning. In the following, we build on this distinction to differentiate between qualitative (bottom-up) and quantitative (top-down) strategies of generalization.
Generalization and the Problem of Replication
We will now extend the formal analysis of quantitative and qualitative approaches to the question of generalization and replicability of empirical findings. For this sake, we have to introduce some concepts of formal logic. Formal logic is concerned with the validity of arguments. It provides conditions to evaluate whether certain sentences (conclusions) can be derived from other sentences (premises). In this context, a theory is nothing but a set of sentences (also called axioms). Formal logic provides tools to derive new sentences that must be true, given the axioms are true (Smith, 2020 ). These derived sentences are called theorems or, in the context of empirical science, predictions or hypotheses . On the syntactic level, the rules of logic only state how to evaluate the truth of a sentence relative to its premises. Whether or not sentences are actually true, is formally specified by logical semantics.
On the semantic level, formal logic is intrinsically linked to set-theory. For example, a logical statement like “all dogs are mammals,” is true if and only if the set of dogs is a subset of the set of mammals. Similarly, the sentence “all chatting students doodle” is true if and only if the set of chatting students is a subset of the set of doodling students (compare Figure 3 ). Whereas, the first sentence is analytically true due to the way we define the words “dog” and “mammal,” the latter can be either true or false, depending on the relational structure we actually observe. We can thus interpret an empirical relational structure as the truth criterion of a scientific theory. From a logical point of view, this corresponds to the semantics of a theory. As shown above, variable-based and case-based models both give a formal representation of the same kinds of empirical structures. Accordingly, both types of models can be stated as formal theories. In the variable-based approach, this corresponds to a set of scientific laws that are quantified over the members of an abstract population (these are the axioms of the theory). In the case-based approach, this corresponds to a set of abstract existential statements about a specific class of individuals.
In contrast to mathematical axiom systems, empirical theories are usually not considered to be necessarily true. This means that even if we find no evidence against a theory, it is still possible that it is actually wrong. We may know that a theory is valid in some contexts, yet it may fail when applied to a new set of behaviors (e.g., if we use a different instrumentation to measure a variable) or a new population (e.g., if we draw a new sample).
From a logical perspective, the possibility that a theory may turn out to be false stems from the problem of contingency . A statement is contingent, if it is both, possibly true and possibly false. Formally, we introduce two modal operators: □ to designate logical necessity, and ◇ to designate logical possibility. Semantically, these operators are very similar to the existential quantifier, ∃, and the universal quantifier, ∀. Whereas ∃ and ∀ refer to the individual objects within one relational structure, the modal operators □ and ◇ range over so-called possible worlds : a statement is possibly true, if and only if it is true in at least one accessible possible world, and a statement is necessarily true if and only if it is true in every accessible possible world (Hughes and Cresswell, 1996 ). Logically, possible worlds are mathematical abstractions, each consisting of a relational structure. Taken together, the relational structures of all accessible possible worlds constitute the formal semantics of necessity, possibility and contingency. 7
In the context of an empirical theory, each possible world may be identified with an empirical relational structure like the above classroom example. Given the set of intended applications of a theory (the scope of the theory, one may say), we can now construct possible world semantics for an empirical theory: each intended application of the theory corresponds to a possible world. For example, a quantified sentence like “all chatting students doodle” may be true in one classroom and false in another one. In terms of possible worlds, this would correspond to a statement of contingency: “it is possible that all chatting students doodle in one classroom, and it is possible that they don't in another classroom.” Note that in the above expression, “all students” refers to the students in only one possible world, whereas “it is possible” refers to the fact that there is at least one possible world for each of the specified cases.
To apply these possible world semantics to quantitative research, let us reconsider how generalization to other cases works in variable-based models. Due to the syntactic structure of quantitative laws, we can deduce predictions for singular observations from an expression of the form ∀ i : y i = f ( x i ). Formally, the logical quantifier ∀ ranges only over the objects of the corresponding empirical relational structure (in our example this would refer to the students in the observed classroom). But what if we want to generalize beyond the empirical structure we actually observed? The standard procedure is to assume an infinitely large, abstract population from which a random sample is drawn. Given the truth of the theory, we can deduce predictions about what we may observe in the sample. Since usually we deal with probabilistic models, we can evaluate our theory by means of the conditional probability of the observations, given the theory holds. This concept of conditional probability is the foundation of statistical significance tests (Hogg et al., 2013 ), as well as Bayesian estimation (Watanabe, 2018 ). In terms of possible world semantics, the random sampling model implies that all possible worlds (i.e., all intended applications) can be conceived as empirical sub-structures from a greater population structure. For example, the empirical relational structure constituted by the observed behaviors in a classroom would be conceived as a sub-matrix of the population person × behavior matrix. It follows that, if a scientific law is true in the population, it will be true in all possible worlds, i.e., it will be necessarily true. Formally, this corresponds to an expression of the form
The statistical generalization model thus constitutes a top-down strategy for dealing with individual contexts that is analogous to the way variable-based models are applied to individual cases (compare Table 1 ). Consequently, if we apply a variable-based model to a new context and find out that it does not fit the data (i.e., there is a statistically significant deviation from the model predictions), we have reason to doubt the validity of the theory. This is what makes the problem of low replicability so important: we observe that the predictions are wrong in a new study; and because we apply a top-down strategy of generalization to contexts beyond the ones we observed, we see our whole theory at stake.
Qualitative research, on the contrary, follows a different strategy of generalization. Since case-based models are formulated by a set of context-specific existential sentences, there is no need for universal truth or necessity. In contrast to statistical generalization to other cases by means of random sampling from an abstract population, the usual strategy in case-based modeling is to employ a bottom-up strategy of generalization that is analogous to the way case-based models are applied to individual cases. Formally, this may be expressed by stating that the observed qualia exist in at least one possible world, i.e., the theory is possibly true:
This statement is analogous to the way we apply case-based models to individual cases (compare Table 1 ). Consequently, the set of intended applications of the theory does not follow from a sampling model, but from theoretical assumptions about which cases may be similar to the observed cases with respect to certain relevant characteristics. For example, if we observe that certain behaviors occur together in one classroom, following a bottom-up strategy of generalization, we will hypothesize why this might be the case. If we do not replicate this finding in another context, this does not question the model itself, since it was a context-specific theory all along. Instead, we will revise our hypothetical assumptions about why the new context is apparently less similar to the first one than we originally thought. Therefore, if an empirical finding does not replicate, we are more concerned about our understanding of the cases than about the validity of our theory.
Whereas statistical generalization provides us with a formal (and thus somehow more objective) apparatus to evaluate the universal validity of our theories, the bottom-up strategy forces us to think about the class of intended applications on theoretical grounds. This means that we have to ask: what are the boundary conditions of our theory? In the above classroom example, following a bottom-up strategy, we would build on our preliminary understanding of the cases in one context (e.g., a public school) to search for similar and contrasting cases in other contexts (e.g., a private school). We would then re-evaluate our theoretical description of the data and explore what makes cases similar or dissimilar with regard to our theory. This enables us to expand the class of intended applications alongside with the theory.
Of course, none of these strategies is superior per se . Nevertheless, they rely on different assumptions and may thus be more or less adequate in different contexts. The statistical strategy relies on the assumption of a universal population and invariant measurements. This means, we assume that (a) all samples are drawn from the same population and (b) all variables refer to the same behavioral classes. If these assumptions are true, statistical generalization is valid and therefore provides a valuable tool for the testing of empirical theories. The bottom-up strategy of generalization relies on the idea that contexts may be classified as being more or less similar based on characteristics that are not part of the model being evaluated. If such a similarity relation across contexts is feasible, the bottom-up strategy is valid, as well. Depending on the strategy of generalization, replication of empirical research serves two very different purposes. Following the (top-down) principle of generalization by deduction from scientific laws, replications are empirical tests of the theory itself, and failed replications question the theory on a fundamental level. Following the (bottom-up) principle of generalization by induction to similar contexts, replications are a means to explore the boundary conditions of a theory. Consequently, failed replications question the scope of the theory and help to shape the set of intended applications.
We have argued that quantitative and qualitative research are best understood by means of the structure of the employed models. Quantitative science mainly relies on variable-based models and usually employs a top-down strategy of generalization from an abstract population to individual cases. Qualitative science prefers case-based models and usually employs a bottom-up strategy of generalization. We further showed that failed replications have very different implications depending on the underlying strategy of generalization. Whereas in the top-down strategy, replications are used to test the universal validity of a model, in the bottom-up strategy, replications are used to explore the scope of a model. We will now address the implications of this analysis for psychological research with regard to the problem of replicability.
Modern day psychology almost exclusively follows a top-down strategy of generalization. Given the quantitative background of most psychological theories, this is hardly surprising. Following the general structure of variable-based models, the individual case is not the focus of the analysis. Instead, scientific laws are stated on the level of an abstract population. Therefore, when applying the theory to a new context, a statistical sampling model seems to be the natural consequence. However, this is not the only possible strategy. From a logical point of view, there is no reason to assume that a quantitative law like ∀ i : y i = f ( x i ) implies that the law is necessarily true, i.e.,: □(∀ i : y i = f ( x i )). Instead, one might just as well define the scope of the theory following an inductive strategy. 8 Formally, this would correspond to the assumption that the observed law is possibly true, i.e.,: ◇(∀ i : y i = f ( x i )). For example, we may discover a functional relation between “engagement” and “distraction” without referring to an abstract universal population of students. Instead, we may hypothesize under which conditions this functional relation may be valid and use these assumptions to inductively generalize to other cases.
If we take this seriously, this would require us to specify the intended applications of the theory: in which contexts do we expect the theory to hold? Or, equivalently, what are the boundary conditions of the theory? These boundary conditions may be specified either intensionally, i.e., by giving external criteria for contexts being similar enough to the ones already studied to expect a successful application of the theory. Or they may be specified extensionally, by enumerating the contexts where the theory has already been shown to be valid. These boundary conditions need not be restricted to the population we refer to, but include all kinds of contextual factors. Therefore, adopting a bottom-up strategy, we are forced to think about these factors and make them an integral part of our theories.
In fact, there is good reason to believe that bottom-up generalization may be more adequate in many psychological studies. Apart from the pitfalls associated with statistical generalization that have been extensively discussed in recent years (e.g., p-hacking, underpowered studies, publication bias), it is worth reflecting on whether the underlying assumptions are met in a particular context. For example, many samples used in experimental psychology are not randomly drawn from a large population, but are convenience samples. If we use statistical models with non-random samples, we have to assume that the observations vary as if drawn from a random sample. This may indeed be the case for randomized experiments, because all variation between the experimental conditions apart from the independent variable will be random due to the randomization procedure. In this case, a classical significance test may be regarded as an approximation to a randomization test (Edgington and Onghena, 2007 ). However, if we interpret a significance test as an approximate randomization test, we test not for generalization but for internal validity. Hence, even if we use statistical significance tests when assumptions about random sampling are violated, we still have to use a different strategy of generalization. This issue has been discussed in the context of small-N studies, where variable-based models are applied to very small samples, sometimes consisting of only one individual (Dugard et al., 2012 ). The bottom-up strategy of generalization that is employed by qualitative researchers, provides such an alternative.
Another important issue in this context is the question of measurement invariance. If we construct a variable-based model in one context, the variables refer to those behaviors that constitute the underlying empirical relational structure. For example, we may construct an abstract measure of “distraction” using the observed behaviors in a certain context. We will then use the term “distraction” as a theoretical term referring to the variable we have just constructed to represent the underlying empirical relational structure. Let us now imagine we apply this theory to a new context. Even if the individuals in our new context are part of the same population, we may still get into trouble if the observed behaviors differ from those used in the original study. How do we know whether these behaviors constitute the same variable? We have to ensure that in any new context, our measures are valid for the variables in our theory. Without a proper measurement model, this will be hard to achieve (Buntins et al., 2017 ). Again, we are faced with the necessity to think of the boundary conditions of our theories. In which contexts (i.e., for which sets of individuals and behaviors) do we expect our theory to work?
If we follow the rationale of inductive generalization, we can explore the boundary conditions of a theory with every new empirical study. We thus widen the scope of our theory by comparing successful applications in different contexts and unsuccessful applications in similar contexts. This may ultimately lead to a more general theory, maybe even one of universal scope. However, unless we have such a general theory, we might be better off, if we treat unsuccessful replications not as a sign of failure, but as a chance to learn.
Author Contributions
MB conceived the original idea and wrote the first draft of the paper. MS helped to further elaborate and scrutinize the arguments. All authors contributed to the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Annette Scheunpflug for helpful comments on an earlier version of the manuscript.
1 A person × behavior matrix constitutes a very simple relational structure that is common in psychological research. This is why it is chosen here as a minimal example. However, more complex structures are possible, e.g., by relating individuals to behaviors over time, with individuals nested within groups etc. For a systematic overview, compare Coombs ( 1964 ).
2 This notion of empirical content applies only to deterministic models. The empirical content of a probabilistic model consists in the probability distribution over all possible empirical structures.
3 For example, neither the SAGE Handbook of qualitative data analysis edited by Flick ( 2014 ) nor the Oxford Handbook of Qualitative Research edited by Leavy ( 2014 ) mention formal approaches to category formation.
4 Note also that the described structure is empirically richer than a nominal scale. Therefore, a reduction of qualitative category formation to be a special (and somehow trivial) kind of measurement is not adequate.
5 It is possible to extend this notion of empirical content to the probabilistic case (this would correspond to applying a latent class analysis). But, since qualitative research usually does not rely on formal algorithms (neither deterministic nor probabilistic), there is currently little practical use of such a concept.
6 We do not elaborate on abductive reasoning here, since, given an empirical relational structure, the concept can be applied to both types of models in the same way (Schurz, 2008 ). One could argue that the underlying relational structure is not given a priori but has to be constructed by the researcher and will itself be influenced by theoretical expectations. Therefore, abductive reasoning may be necessary to establish an empirical relational structure in the first place.
7 We shall not elaborate on the metaphysical meaning of possible worlds here, since we are only concerned with empirical theories [but see Tooley ( 1999 ), for an overview].
8 Of course, this also means that it would be equally reasonable to employ a top-down strategy of generalization using a case-based model by postulating that □(∃ i : XYZ i ). The implications for case-based models are certainly worth exploring, but lie beyond the scope of this article.
- Agresti A. (2013). Categorical Data Analysis, 3rd Edn. Wiley Series In Probability And Statistics . Hoboken, NJ: Wiley. [ Google Scholar ]
- Borsboom D. (2005). Measuring the Mind: Conceptual Issues in Contemporary Psychometrics . Cambridge: Cambridge University Press; 10.1017/CBO9780511490026 [ CrossRef ] [ Google Scholar ]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology . Qual. Res. Psychol . 3 , 77–101. 10.1191/1478088706qp063oa [ CrossRef ] [ Google Scholar ]
- Buntins M., Buntins K., Eggert F. (2017). Clarifying the concept of validity: from measurement to everyday language . Theory Psychol. 27 , 703–710. 10.1177/0959354317702256 [ CrossRef ] [ Google Scholar ]
- Carnap R. (1928). The Logical Structure of the World . Berkeley, CA: University of California Press. [ Google Scholar ]
- Coombs C. H. (1964). A Theory of Data . New York, NY: Wiley. [ Google Scholar ]
- Creswell J. W. (2015). A Concise Introduction to Mixed Methods Research . Los Angeles, CA: Sage. [ Google Scholar ]
- Dugard P., File P., Todman J. B. (2012). Single-Case and Small-N Experimental Designs: A Practical Guide to Randomization Tests 2nd Edn . New York, NY: Routledge; 10.4324/9780203180938 [ CrossRef ] [ Google Scholar ]
- Edgington E., Onghena P. (2007). Randomization Tests, 4th Edn. Statistics. Hoboken, NJ: CRC Press; 10.1201/9781420011814 [ CrossRef ] [ Google Scholar ]
- Everett J. A. C., Earp B. D. (2015). A tragedy of the (academic) commons: interpreting the replication crisis in psychology as a social dilemma for early-career researchers . Front. Psychol . 6 :1152. 10.3389/fpsyg.2015.01152 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flick U. (Ed.). (2014). The Sage Handbook of Qualitative Data Analysis . London: Sage; 10.4135/9781446282243 [ CrossRef ] [ Google Scholar ]
- Freeman M., Demarrais K., Preissle J., Roulston K., St. Pierre E. A. (2007). Standards of evidence in qualitative research: an incitement to discourse . Educ. Res. 36 , 25–32. 10.3102/0013189X06298009 [ CrossRef ] [ Google Scholar ]
- Ganter B. (2010). Two basic algorithms in concept analysis , in Lecture Notes In Computer Science. Formal Concept Analysis, Vol. 5986 , eds Hutchison D., Kanade T., Kittler J., Kleinberg J. M., Mattern F., Mitchell J. C., et al. (Berlin, Heidelberg: Springer Berlin Heidelberg; ), 312–340. 10.1007/978-3-642-11928-6_22 [ CrossRef ] [ Google Scholar ]
- Ganter B., Wille R. (1999). Formal Concept Analysis . Berlin, Heidelberg: Springer Berlin Heidelberg; 10.1007/978-3-642-59830-2 [ CrossRef ] [ Google Scholar ]
- Guttman L. (1944). A basis for scaling qualitative data . Am. Sociol. Rev . 9 :139 10.2307/2086306 [ CrossRef ] [ Google Scholar ]
- Hogg R. V., Mckean J. W., Craig A. T. (2013). Introduction to Mathematical Statistics, 7th Edn . Boston, MA: Pearson. [ Google Scholar ]
- Hughes G. E., Cresswell M. J. (1996). A New Introduction To Modal Logic . London; New York, NY: Routledge; 10.4324/9780203290644 [ CrossRef ] [ Google Scholar ]
- Klein R. A., Ratliff K. A., Vianello M., Adams R. B., Bahník Š., Bernstein M. J., et al. (2014). Investigating variation in replicability . Soc. Psychol. 45 , 142–152. 10.1027/1864-9335/a000178 [ CrossRef ] [ Google Scholar ]
- Krantz D. H., Luce D., Suppes P., Tversky A. (1971). Foundations of Measurement Volume I: Additive And Polynomial Representations . New York, NY; London: Academic Press; 10.1016/B978-0-12-425401-5.50011-8 [ CrossRef ] [ Google Scholar ]
- Leavy P. (2014). The Oxford Handbook of Qualitative Research . New York, NY: Oxford University Press; 10.1093/oxfordhb/9780199811755.001.0001 [ CrossRef ] [ Google Scholar ]
- Maxwell S. E., Lau M. Y., Howard G. S. (2015). Is psychology suffering from a replication crisis? what does “failure to replicate” really mean? Am. Psychol. 70 , 487–498. 10.1037/a0039400 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miles M. B., Huberman A. M., Saldaña J. (2014). Qualitative Data Analysis: A Methods Sourcebook, 3rd Edn . Los Angeles, CA; London; New Delhi; Singapore; Washington, DC: Sage. [ Google Scholar ]
- Open Science, Collaboration (2015). Estimating the reproducibility of psychological science . Science 349 :Aac4716. 10.1126/science.aac4716 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Popper K. (1935). Logik Der Forschung . Wien: Springer; 10.1007/978-3-7091-4177-9 [ CrossRef ] [ Google Scholar ]
- Ragin C. (1987). The Comparative Method : Moving Beyond Qualitative and Quantitative Strategies . Berkeley, CA: University Of California Press. [ Google Scholar ]
- Rihoux B., Ragin C. (2009). Configurational Comparative Methods: Qualitative Comparative Analysis (Qca) And Related Techniques . Thousand Oaks, CA: Sage Publications, Inc; 10.4135/9781452226569 [ CrossRef ] [ Google Scholar ]
- Scheunpflug A., Krogull S., Franz J. (2016). Understanding learning in world society: qualitative reconstructive research in global learning and learning for sustainability . Int. Journal Dev. Educ. Glob. Learn. 7 , 6–23. 10.18546/IJDEGL.07.3.02 [ CrossRef ] [ Google Scholar ]
- Schurz G. (2008). Patterns of abduction . Synthese 164 , 201–234. 10.1007/s11229-007-9223-4 [ CrossRef ] [ Google Scholar ]
- Shrout P. E., Rodgers J. L. (2018). Psychology, science, and knowledge construction: broadening perspectives from the replication crisis . Annu. Rev. Psychol . 69 , 487–510. 10.1146/annurev-psych-122216-011845 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith P. (2020). An Introduction To Formal Logic . Cambridge: Cambridge University Press. 10.1017/9781108328999 [ CrossRef ] [ Google Scholar ]
- Suppes P., Krantz D. H., Luce D., Tversky A. (1971). Foundations of Measurement Volume II: Geometrical, Threshold, and Probabilistic Representations . New York, NY; London: Academic Press. [ Google Scholar ]
- Tooley M. (Ed.). (1999). Necessity and Possibility. The Metaphysics of Modality . New York, NY; London: Garland Publishing. [ Google Scholar ]
- Trafimow D. (2018). An a priori solution to the replication crisis . Philos. Psychol . 31 , 1188–1214. 10.1080/09515089.2018.1490707 [ CrossRef ] [ Google Scholar ]
- Watanabe S. (2018). Mathematical Foundations of Bayesian Statistics. CRC Monographs On Statistics And Applied Probability . Boca Raton, FL: Chapman And Hall. [ Google Scholar ]
- Wiggins B. J., Chrisopherson C. D. (2019). The replication crisis in psychology: an overview for theoretical and philosophical psychology . J. Theor. Philos. Psychol. 39 , 202–217. 10.1037/teo0000137 [ CrossRef ] [ Google Scholar ]
The Spectrum of Inductive and Deductive Research Approaches Using Quantitative and Qualitative Data
Affiliation.
- 1 associate professor, Institute of Health Sciences Education and Department of Medicine, McGill University professor, Department of Medicine, Uniformed Services University of the Health Sciences professor, Department of Medicine, Uniformed Services University of the Health Sciences assistant professor and Canada Research Chair, Collaborative Healthcare Practice, The Wilson Centre, University Health Network, Leslie Dan Faculty of Pharmacy and Department of Sociology, University of Toronto.
- PMID: 31833855
- DOI: 10.1097/ACM.0000000000003101
- Open access
- Published: 08 April 2024
What may encourage or deter health services utilization by people living with or at the risk of HIV/AIDS in special health centers? Qualitative evidence from a stigmatized community
- Mohammad Bazyar 1 ,
- Samaneh Tahmasebi Ghorabi 2 ,
- Jamil Sadeghifar 1 , 3 ,
- Mohammad Ranjbar 4 ,
- Reza Pakzad 5 ,
- Fatemeh Bonyadi 6 ,
- Keyvan Khasi 7 ,
- Ebrahim Shakiba 7 ,
- Mahtab Nourbakhsh 6 ,
- Leila Rezeghian 7 ,
- Boshra Noshadi 6 ,
- Mehrdad Bavandpour 7 ,
- Azim HasanBeigi 8 &
- Anahita Behzadi ORCID: orcid.org/0000-0002-6988-3759 9 , 10
BMC Public Health volume 24 , Article number: 981 ( 2024 ) Cite this article
Metrics details
Behavioral Diseases Counseling Centers (BDCCs) and Vulnerable Women’s Counseling Centers (VWCCs) in Iran are the main peripheral centers that offer educational, counseling, diagnostic, preventive, curative and protective services to individuals living with or at high risk of contracting HIV/AIDS and female sex workers respectively. Due to the social stigma surrounding HIV in Iran, this study aims to identify the factors that may hinder or encourage HIV/AIDS patients and women with risky sexual behaviors from visiting these centers.
Conducted in 2023, this qualitative study involved individuals visiting BDCCs and VWCCs in two western provinces of Iran, Ilam and Kermanshah. The study participants included 21 health staff members working in BDCCs and VWCCs and 20 HIV/AIDS patients and vulnerable women with unsafe sexual behaviors referring to these centers. Purposive, snowball and maximum variation sampling techniques were applied to interview the participants. Interviews were conducted between January 5th and May 21st, 2023, using a semi-structure guideline. Interviews were transcribed and content analysis approach was applied to analyze data using MAXQDA20 software.
According to the findings, the barriers and facilitators of visiting specialized centers for HIV/AIDS patients and vulnerable women were categorized into three main categories, 10 subcategories and 35 sub-subcategories including: Medical and operational processes (4 subcategories and 12 sub-subcategories), mutual interactions between the personnel and visitors (people living with and at the risk of getting HIV/AIDS) (3 subcategory and 13 sub-subcategories), and physical characteristics of the centers (3 subcategories and 10 sub-subcategories).
Conclusions
To improve the performance of BDCCs and VWCCs and encourage people living with and at the risk of contracting HIV/AIDS to visit these centers regularly, health policy makers should consider modifying clinical processes, physical features, personnel behaviors and visitors’ concerns raised by the interviewees and the issues identified in this study.
Peer Review reports
According to the latest report of the Joint United Nations Program on HIV/AIDS (UNAIDS), in 2019, 38.0 million people globally were living with HIV, and around 690,000 people died from AIDS-related illnesses [ 1 ]. This threat is dominant for countries in East Mediterranean Region, such as Iran [ 2 ]. In 2019, 59,000 [33,000–130,000] adults and children were living with HIV in Iran. The number of men aged 15 and over living with HIV was estimated at 43,000 [23,000– 91,000], while that of women stood at 16,000 [8800–32,000] [ 3 , 4 ]. Injection drug use is considered the main cause of HIV transmission in Iran [ 5 ]. According to a previous study, there were about 230.000 people injecting drug in Iran in 2016 [ 6 ].
Since finding the first case of HIV/AIDS in the country, Iran has established different national and provincial institutions and has implemented different programs aiming to put the disease under control. For example, in 2003, the Supreme Council for HIV/AIDS Prevention Planning (SCHAPP) was formed [ 7 , 8 , 9 ]. Accordingly, at national and provincial level, the department for Controlling Communicable Diseases was created within Ministry of Health and Public Health Deputy of Medical Universities. Besides, at district level, the peripheral institutions to provide specialized health services for HIV/AIDS patients are called “Behavioral Diseases Counseling Centers” (BDCCs). These centers are governmental and operate as a part of District Health Network under supervision of Public Health Deputy. BDCCs provide educational, counseling, diagnostic, preventive, and curative services to those who live with or are at the high risk of contracting HIV/AIDS [ 6 , 10 , 11 ]. Following groups can use the services of BDCCs: people who inject drugs; individuals with sexually transmitted diseases; people with risky sexual behaviors like homosexuals and vulnerable women with unsafe sexual behaviors; health workers and other professions who are in contact with high risk groups or are the risk of encountering sharp and infectious tools; and also individuals looking for counseling services. A group of health staff including infectious diseases specialist, psychologist, general physician, public health technician and midwifes work in these centers.
However, emerging evidence indicates that vulnerable women and female having uncontrolled and unsafe sex behaviors are becoming increasingly a leading source of HIV incidence [ 12 ]. For this reason, female sex workers are considered the second most at risk population for HIV transmission [ 13 ]. As prostitution and sex work are illegal and extremely stigmatized in Iran [ 14 ], it has affected the process of diagnosis and treatment of HIV/AIDS adversely and consequently has posed major challenges to cope with it in Iran [ 5 , 15 ]. To encourage safe sexual behaviors and control spread of HIV/AIDS in this part of population, other centers so-called “Vulnerable Women’s Counseling Centers” were created separately to provide counseling services, and distribute preventive and protective services for female at the risk of getting HIV (women live with HIV/AIDS use their curative services from BDCCs).
Additionally, several other supportive institutions such as “Drop in Centers”, “Outreach Team”, “Methadone Maintenance Therapy”, “Hot Lines”, and “Positive Clubs” have been established which provide supportive and empowering services for addicted, unprivileged and marginalized groups [ 9 ]. However, Iran is still struggling reaching national and international health indicators regarding HIV/AIDS control. For example, the reduction of HIV/AIDS cases in Iran is lower than the global rate. Since 2010, the worldwide reduction in new HIV infections was 18%, while it was 10% for Iran [ 16 , 17 ]. Other indicators such as the rate of adherence to antiretroviral therapy (ART) which are crucial for successful HIV treatment shows that the situation is not promising. For example, the rate of ART regimens among Iranian people living with HIV/AIDS (PLWHA) is so as low as 20% and only 17% are ART adherent and virally suppressed [ 5 ].
Various factors can hinder appropriate service delivery to people living with HIV/AIDS which in turn can impede implementing health program for HIV/AIDS, including diagnosis of new cases and adherence to treatment. Multiple structural, social, and psychological challenges contribute to non-adherence to treatment which stems from different causes [ 18 , 19 , 20 ]. Among the most robust predictors of ART non-adherence is social stigmatization of HIV [ 18 ]. HIV stigma affects working on HIV/AIDS objectives adversely and undermine all phases of health care provision from late diagnoses of HIV by discouraging high risk individuals from taking test [ 21 , 22 ], to suppressing antiretroviral treatment (ART) coverage and viral suppression rates as it impedes individuals from looking for the healthcare services they need and from attending medical appointments and taking their medication [ 23 , 24 ]. Other findings from various contexts suggest that different factors related to the health centers and health personnel may hinder HIV/AIDS individuals from accessing services. These include concerns about lack of privacy and confidentiality during HIV testing, distrust of healthcare workers’ ability to keep personal information confidential, stigma associated with being seen at health services, fear of punishment or criminalization, transportation costs, and financial barriers. These barriers and facilitators vary across different populations and settings, highlighting the need for more studies to identify other context based deterrents and facilitators [ 25 , 26 , 27 , 28 , 29 , 30 ].
Previous studies in Iran have addressed other aspects of health status of people living with HIV/AIDS such as antiretroviral therapy adherence and determining factors in general [ 5 , 31 ], their quality of life [ 32 , 33 , 34 ], factors affecting their survival [ 35 ] and late diagnosis [ 36 ], and etc. However, to the authors’ best knowledge, no study has still been carried out specifically on Behavioral Diseases Counseling Centers and Vulnerable Women’s Counseling Centers in Iran to reveal what may hinder or encourage people living with and at the risk of getting HIV/AIDS coming to these centers at the first step as they are the main peripheral centers that should attract people to take test, get their treatment, receive medications and other protective and preventive services, follow-up their health status, and adhere to treatment for the rest of their life. Conducting this study in Iran, as an Islamic country with strict laws and heavy social stigma against HIV/AIDS and sexual promiscuity, can provide new insights and reveal hidden angles on barriers to accessing services specialized for populations at the risk of HIV/AIDS that can be applicable to other countries with similar constrains.
Study setting
This article presents the findings of qualitative section of a larger mix-method study done in 2023. The study population consisted of everyone visiting Behavioral Diseases Counseling (BDCCs) and Vulnerable Women’ Counseling Centers (VWCCs) in two western provinces in Iran, namely Ilam and Kermanshah, in 2023. These two regions were selected as they generally have similar cultural and social context and the members of research team are from these two provinces. Another reason to mention is that Ilam province (the initial place for the purpose of the study) is a small region and the number of patients to participate was not enough to cover both qualitative and quantitative phases of the main study, so it was decided to extend the study to the neighboring metropolis of Kermanshah aiming to have adequate number of participants to run the study (The distance between these two cities is about 170 km). Although this decision enriched findings of the study because the BDCCs and VWCCs of these cities are located in different geographical regions and there are potential differences among them in terms of physical and structural conditions of the centers, service provision processes, staff performance, and etc. These differences provided a better opportunity to extract the most factors affecting the clients’ trust as possible. Kermanshah has two BDCCs and two VWCCs and Ilam has only one BDCC. All of these five centers were selected to recruit interviewees. For better understanding of the health facilities as a part of the study context, the number and composition of health staff working in these centers in 2023 are shown in Table 1 .
-Number of active and inactive HIV/AIDS patients and female sex workers were not provided for confidentiality reasons.
Sample size, sampling method, and interview guide
The study population composed of two main groups: (1) HIV/AIDS patients and people visiting BDCCs, and vulnerable women coming to VWCCs, (2) the health staff members working in these centers. So purposive sampling was applied to select interviewees from the above groups.
Moreover, since the researchers were not familiar with all the knowledgeable people at the beginning of the study, further samples were identified using snowball sampling. To do so, at the end of each interview, the participants (mainly health workers) were asked to introduce other people with relevant knowledge and experience for interview, even if they worked in other organizations. Using snowball sampling, two experts from other organizations working with vulnerable groups such as the State Welfare Organization (Sazman-e Behzisti) and two experts with previous experience in DBCCs were identified. Furthermore, we tried to apply maximum variation sampling by selecting interviewees from 5 BDCCs and VWCCs located in different geographical regions; interviewing people from different groups including health staffs with different professions from different organizations, people living with HIV/AIDS and vulnerable women; and recruiting interviewees from both sexes. Apart from old patients, we tried to interview new cases if possible. The sample size is directly associated with data saturation and interviews continued until no new data or idea was revealed, and interviewees repeat the subjects already mentioned. A semi-structured qualitative interview guide was used to do the interviews. The questions were based on the study objectives. The initial version of the questions was approved through discussions among the research team members and feedback that we get from the key informants (health workers working BDCCs and VWCCs) during the first interviews. These were the main questions outlined in the interview guide: What were your initial concerns when considering a visit to the center? What about the next visits? Which attributes of the healthcare staff motivated or dissuaded you from continuing to visit the center? What aspects of the clinical and administrative procedures instilled confidence or apprehension in you regarding the utilization of healthcare services at the center? What is your assessment of the center’s location and infrastructure? What precautions do you take to address any concerns prior to visiting the center? While the main questions remained consistent, additional questions were introduced in subsequent interviews as new ideas and inquiries emerged throughout the research process. It is important to highlight that unlike quantitative studies, qualitative research allows for flexibility in the interview guide, enabling researchers to adapt and refine questions as they deepen their understanding of the topic over the course of the study.
Individual interviews and focus group discussions
The interviews were initiated after official correspondence with the Public Health Deputies of Ilam and Kermanshah Medical Universities. An interview guide was used to conduct the interviews. The interviews normally began with simple and general subjects and moved toward more specific questions. Also, probing questions were employed to obtain more accurate and in-depth information by encouraging the interviewees to give more explanations. At the beginning of each interview, after explaining the importance of recording the interview and assuring them of the confidentiality of the contents, the interview was recorded using two voice recorders. At the end of each interview, the interviewee was asked to introduce experts and people with knowledge in the field of this study to be interviewed to gain complementary information. The main researcher (MB), interviewed all health staff members from Kermanshah and Ilam. Whenever possible, these interviews were conducted face to face at the BDCCs and VWCCs. In 8 cases, personnel from Kermanshah were interviewed over the phone due to physical distance. The phone interviews were conducted at home in privacy, with the speakerphone on and the audio recorded using a recorder. In-depth individual interviews were utilized in, 14 cases, involving a range of health professionals such as general physicians, psychologists, midwives, laboratory technicians, and public health experts. Table 2 displays key characteristics of the health staff interviewed, including their position, gender, age, work experience, years in the field of HIV/AIDS and the duration of the interviews. There was no repeated long interviews but we asked the initial interviewees additional questions in-person or on the phone later on during the research as new questions arose. In two cases, despite multiple follow-ups and setting time to interview over phone, we were unable to conduct interviews due to the busy schedules of the interviewees. To foster deeper discussions and extract more nuanced insights about the subject, focus group discussions (FGDs) were employed whenever possible. Two FGDs were conducted, one with four health staff members at the Ilam BDCC and another with three employees at BDCC number 1 in Kermanshah. These FGDs took place in the psychologist’s room at midday to ensure a quiet and conducive environment for open dialogue without interruptions. The main investigator (MB) facilitated the discussions, each lasting for an hour. The use of group discussions created an interactive setting that encouraged participants to recall and share additional details regarding the factors influencing people’s trust in visiting the BDCCs and VWCCs. In total, 21 personnel were engaged in the study, with 14 individuals participating in in-depth individual interviews and 7 taking part in FGDs.
However in regard with the HIV/AIDS patients and women coming to the BDCCs and VWCCs, another approach was applied. In accordance to confidentiality principles, one of the staff members from each center, was selected to conduct the interviews on behalf of the research team. To do so, three health workers from three centers were selected, BDCC number 2 and VWCC number 2 from Kermanshah and the only BDCC from Ilam. All of these health staff who agreed to collaborate were female. In other centers, no health staff agreed to participate in doing the interviews. Having a close relationship with patients and being interested in research project were the criteria to select the interviewers. The selected health staff were interviewed as key informants which enabled them to gain a thorough understanding of the research objectives and qualitative interview techniques. Moreover, the selected members were trained about the main ethical principles and how to conduct interviews. Additionally, the recorded interviews conducted by the health staff were heard and analyzed several times by the main investigator (BM). Constructive feedback was provided to the interviewers to improve the quality of subsequent interviews. Notably two of these staff held Master of Science degrees in relevant health fields and possessed a solid understanding of fundamental health research methodologies. In total, health staff could interview 20 HIV/AIDS patients and female sex workers, including 6 individuals from Ilam BDCC, 12 and 6 individuals from Kermanshah BDCCs and VWCCs respectively. Patients were mainly male and the interviews lasted from 10 min to 35 min (20 min on average). The duration of interviews with patients was normal as they had specific and limited but different concerns for visiting or not visiting health centers. On the other hand, one of the limitations of the interviews was that some of participants wanted to finish the interview quickly and leave the center. Only three of cases in BDCCs were new visitors while the rest were regular and routine visitors of the BDCCs and VWCCs. In 8 cases, mainly female sex workers, they did not allowed recording their voice, so interviewers took notes of the main points. Furthermore, according to the interviewers, approximately 7 visitors refused to participate in the study due to inappropriate mental conditions, being in rush, and fear of their identity being revealed by recording their voices. Interviews were done within the time period between January 5th and May 21st, 2023. For the confidentiality purposes, no detailed demographic information of the patients was provided. In both groups (personnel and visitors), we reached saturation at about 17th interviewee, but we conducted 6 extra interviews, 3 for each group, to ensure not missing new data. Literature review was done from 10 July 2022 to 25 June 2023, no time limitation was applied for extracting the related articles.
Ethical issues
This study was approved by Ethics Committee of Ilam University of Medical Sciences. Also, a reference letter was provided by the Ethics Committee for the Security Departments, and Infectious Diseases Departments of Health Deputies of Ilam and Kermanshah Medical Universities, and their approvals to start the project were obtained. Moreover, research team were introduced by Infectious Diseases Departments in both universities to the BDCCs and VWCCs for doing interviews. Considering the sensitivity of the subject and the necessity of observing all ethical issues, the required permissions were also obtained from the Infectious Disease Control Center and the HIV office of the Health Deputy of the Iranian Ministry of Health and Medical Education. In addition, in line with confidentiality principles, the research team were not allowed to interview the HIV/AIDS patients and women coming to BDCCs and VWCCs directly. To do so, one of the staff members from each center, preferably the counselor, was selected to conduct the interviews.
Qualitative data analysis
Each interview was transcribed and analyzed immediately before doing the next one. This contributed to the conduction of later interviews as the researchers were able to have a more comprehensive view of the subject under studying. One author (MB) initially analyzed and indexed the transcribed interviews. Content analysis was used to analyze the interviews according to the six-step framework of Braun and Clarke including familiarizing with data, generating initial coding, searching for themes, reviewing of themes, defining and naming of themes, and reporting the findings [ 37 ]. Using inductive approach, we categorized the emerging codes according to the patterns and similarities between them. The categories were generated from the patterns within the codes, frequency and repetition, and their importance to the participants. In the next step, categories were further grouped into more general categories according to the research objectives. The emerging categories and sub-categories, appropriateness of titles chosen for them, and choosing right category for each sub-categories were constantly discussed among the research team and amendments were made whenever necessary. The codes were classified into three layers including categories, subcategories, and sub-subcategories. The final classification was shown to the health staff members in Ilam BDCC once again and few further codes were identified. All the processes related to data coding and emerging themes were carried out using MAXQDA20 software (VERBI Software. MAXQDA20. Berlin: VERBI Software, 2020).
Trustworthiness
To ensure the trustworthiness of our findings, we adhered to four criteria outlined by Lincoln and Guba (1986) which encompass credibility, transferability, dependability, and confirmability [ 38 , 39 ]. “Credibility”, focusing on the question of how well the findings reflect reality, was achieved through the following techniques. The primary researcher (MB) spent nearly 4 months constantly reviewing and analyzing qualitative data to enhance credibility. Additionally, member-checking validation was utilized by sharing initial categories and sub-categories with the healthcare staff at Ilam BDCC. During interviews, clarifying questions such as ‘What do you mean?’ or “do you mean….?” were posed to address any ambiguity in responses, ensuring a clear understanding of the interviewees’ intentions. Feedback was provided during interviews to confirm mutual understanding and interpretation between interviewers and interviewees. Peer review was employed as a method to enhance credibility through ongoing discussions between two authors (MB and JS) regarding the accuracy and categorization of emerging categories and sub-categories. Negative cases were also highlighted to showcase instances where there was a discrepancy in perspectives among interviewees, further bolstering credibility. To ensure the findings’ applicability to other settings, the researchers employed purposive and maximum variation sampling in line with the concept of “transferability.” Furthermore, the technique of “thick description” was utilized to offer a comprehensive portrayal of the context (including the HIV/AIDS situation in Iran, the cities of Ilam and Kermanshah, and the characteristics of the healthcare personnel in the selected facilities) to bolster transferability. Furthermore, we implemented an audit trail by meticulously detailing and documenting each step of the research process, along with explaining the rationale behind the research decisions made at various stages of the study, in order to guarantee “dependability”. Additionally, we utilized “peer debriefing” to enhance dependability by engaging a colleague who works in the HIV/AIDS field in Ahwaz as an external auditor to review and provide feedback on the finalized classification of codes. “Confirmability”, the final criterion for trustworthiness, focuses on ensuring that “the researcher’s interpretations and findings are clearly rooted in the data, necessitating the researcher to demonstrate how conclusions and interpretations were reached.” To achieve this, we employed methodological triangulation and included quotations. For example, we conducted in-depth individual interviews, focus group discussions and field notes concurrently to enrich data collection. The primary researcher diligently recorded field notes before and during the research process to capture every relevant phenomenon, such as observations, conversations, personal experiences, emerging thoughts, insights gained, and new questions that arose during the study. For example, notes taken during visits to the research sites and informal discussions with healthcare staff yielded valuable insights that prompted further inquiry into the topic. Furthermore, we included quotations from patients and healthcare staff members to confirm that the findings were derived directly from the data [ 38 , 40 , 41 , 42 , 43 ].
According to the views of the interviewees, at the open coding phase, about 600 codes were identified. These codes were categorized into three main categories, 10 sub-categories and 35 sub-subcategories including: Medical and operational processes (4 subcategories, 12 sub-subcategories), Mutual interactions between personnel and visitors (people living with and at the risk of getting HIV/AIDS) (3 subcategory, 13 sub-subcategories), and Physical characteristics of the centers (3 subcategories, 10 sub-subcategories)(see Table 3 ).
Medical and operational processes
Counseling services considerations, counseling the clients even before admission and administrative operations on their first visit to bdccs and vwccs.
Counseling clients before admission and administrative operations on their first visit to BDCCs and VWCCs is crucial. Interviewees suggested guiding patients directly to the counseling room without any questions or admission processes, allowing them to receive consultation services immediately. It was also recommended to have the counseling room located near the entrance to minimize contact with the personnel or other patients, reducing concerns and increasing their trust in the center’s services.
“” When a person comes to the center for the first time, it is better not request for any demographic information, instead he or she should be referred directly to the counselor’s room” (One of the psychologist in BDCCs) .
counseling in a room with the doors closed to keep the client calm
Conducting counseling in a closed room or with the door partly open (if the counselor and the client are not of the same sex or if the client requests it) is important for HIV/AIDS patients in DBCCs and vulnerable women in VWCCs. This ensures confidentiality during conversations. They also highlighted that to maintain the patient’s calmness, other personnel should avoid entering the room unless necessary.
“Another reason I trust you (female psychologist in one of the BDCCs) was that you closed the door and I felt secure that no one can hear my statements” (a young man looking for HIV/AIDS test on his first visit) .
Identity information considerations
Not insisting on receiving identification information of hiv/aids patients and sex workers.
Given the social stigma associated with AIDS, one of the most frequently mentioned statements by interviewees was that the centers must not insist on receiving identity information at least in first visits, including first and last name, national ID number, address, age, etc. In addition, the patients are even encouraged to use nicknames instead of providing personal information. This helps build trust between patients and the health staff, and patients may be willing to provide their real information in subsequent visits once they trust the center. Interviewees also mentioned that no notes should be taken during the first counseling sessions, and personnel should not enter patient information into the computer simultaneously, further building patient trust.
“They resist giving the right information about themselves. For example they don’t give their telephone number or their numbers are wrong. The addresses they give are not precise at all and it is not possible for us to follow up or send reminder” (one of the health workforces from VWCCs) .
Considering the fear of patient regarding disclosure of their disease and the importance of following confidentiality principles by the personnel
Maintaining confidentiality is crucial to address patient fears regarding the disclosure of their disease. Personnel should emphasize confidentiality and assure patients that their information will not be shared with anyone, including their closest family members, without their permission. In cases where patients and personnel know each other, clear assurances should be given regarding confidentiality. Personnel should also try to avoid drawing attention to familiar clients and should refrain from calling patients by their names to uphold confidentiality principles.
“Some patients may come at the same time, and we assign them to different rooms. We try to refer one of them to the doctor’s office, one to the psychologist’s, and another to other wards so they do not see each other. For instance, two of them might be from the same city, so they are afraid of being recognized.” (One of the midwives in BDCCs with 6 years’ work experience in HIV/AIDS) .
Moreover, some of the patients suggested that if they need health services in hospitals or other medical centers, their companions must not be involved in the treatment process. For instance, their companion should not be asked to get the patient’s test results, and everything should be done by the personnel in order not to increase the risk of the disease being revealed to their families. In this regard, some of the patients believed that if the HIV/AIDS test results are positive, no one else must be informed, and if needed, their families or relatives should be told that the results were negative.
Requirements of storing identity information of HIV/AIDS patients and sex workers and how to keep them safe
In BDCCs, each patient is assigned a code for their medical procedures. However, patients who give their real identity information, such as their national code or the cause of the disease, are worried about who may get access to this information. To address these concerns, some centers have implemented measures to improve information security. For example, only select staff members, such as the doctor or counselor, can have access to patients’ files and in some cases, on patients’ request, other staff members only have access to the necessary information (e.g., patients requiring special treatment without disclosing the cause of their disease). Patients also expressed concerns about storage of their information, and the possibility of it being revealed if the computers are hacked.
“No one else except the health forces working here (BDCC) should access to our files and the computer. It is risky to store the identity information of patients in the computer. There are people who are intelligent and can access to our information by hacking the computer” (A regular old male HIV/AIDS patient) .
Providing remote services for patients
Reaching health services to hiv/aids patients without coming to bdccs and vwccs in person as much as possible.
In an effort to improve the services and gain patients’ trust, BDCCs have implemented measures to reduce unnecessary in-person visits while maintaining confidentiality and medical protocols. For example, on the patient’s request, tests can be performed outside the center such as in the car, during the first visits. Some patients may also prefer to receive their medication outside the center or for a longer period of time. In certain cases, the medication can be posted to patients’ addresses, or trusted individuals, such as friends or family members, can be designated to receive medication.
“I remember one of new visitors asked us to take a test from her in her car without registering her name”. (A male counselor) (A male counselor with 6 years’ work experience in the field of HIV/AIDS) .
Consideration and requirements of using phone for follow-ups
Another important consideration continuing treatment is the requirements and sensitivities surrounding phone calls to contact patients. According to the interviewees, many patients initially refuse to provide their phone numbers on first visits and strongly resist follow-up phone calls due to concerns about unintentionally revealing their disease to their families. As a result, patients are only willing to give their phone numbers if they trust the center and if personnel take necessary precautions when making calls. For example, personnel can phone specified family members if the patients is not accessible, or they can introduce themselves as calling from the health center rather than the BDCCs. Patients strongly disagree with the centers giving their phone numbers to other governmental institutions without prior permission. Interviewees suggested that only one personnel member should make contact with patients for follow-up to help patients feel secure. Some patients, particularly those who have been in contact with the center for a longer period or those who are less conservative, were satisfied with the follow-up calls and considered them a positive sign of the personnel’s commitment. Having an active phone line in the center can help patients receive the services more conveniently and securely as they can call the center and m check for any potential acquaintances before going.
“Some of the patients call before coming to the center. Some of them have my own number and call me directly and ask if the center is crowded or quiet. Although patients’ having my number increases my work labor but I believe this has been effective in trusting the center” (A male counselor in BDCCs with 6 years’ work experience in the field of HIV/AIDS) .
“I wanted to call before visiting the BDCC because it was my first time coming to these kinds of centers, but I could not find any telephone number” (A young male HIV/AIDS patient) .
Enhancement and diversification of services and reducing social stigma
Providing services, regardless of the cause of the hiv/aids, and not focusing on the real cause.
According to the interviewees, usually during the first visits, health staff members do not focus on the cause of HIV/AIDS and provide services without insisting on knowing the real cause. Sometimes, morally acceptable causes of HIV/AIDS may be reported to family members to protect patients’ dignity. Patients reveal the real cause when they have established trust in the center and the personnel’s confidentiality. In some cases, an unreal cause for HIV/AIDS is recorded in patients’ file at their request to further gain their trust.
Diversifying the range of diseases covered by the BDCCs, not only HIV/AIDS patients
One thing that causes patients to be cautious about visiting these centers in-person is that the BDCCs provide services exclusively to HIV patients, and this increases patients’ concerns about visiting these centers. The interviewees, both the personnel and the patients, suggested that health services for other related diseases such as hepatitis, HPV, and other blood diseases should be provided so that patients can visit the centers with better excuses.
“I wish we could also cover other diseases like HPV or Hepatitis B, so the patients can say “I am here for Hepatitis B if they see someone familiar in the center. We are working exclusively on HIV now and it is one of the drawbacks of our BDCC” (A female general practitioner with 4 years’ work experience in HIV/AIDS) .
Providing complementary specialized diagnostic tests and supportive non-medical services
According to one of health staff with 10 years’ experience in field of HIV/AIDS, one factor that increases patients’ motivation is providing complementary and free specialized services. The patients stated that if an HIV viral load test is performed in addition to cd4 in every visit and patients are informed of the success of their treatment, they would have higher motivation to continue treatment and visit the centers more. Also, some patients need specialized services such as seeing gynecologists and other specialists and having pap smears and ultrasonography, and they cannot afford the expenses. Therefore, if the services are provided free of charge, they will be motivated to come back. The availability of supplementary medication and supportive packages including food packages in the centers is another factor encouraging patients to visit the centers again.
Avoiding provision of specialized health services in specific weekdays and preventing gathering of patients in the BDCCs
One concern raised by patients was the availability of specialists on specific days at some centers which leads to overcrowding and increases the fear of being seen by acquaintances. This can discourage patients from visiting these centers.
“Sometimes here becomes so crowded, because the specialist comes here just two days a week” (An adolescent male HIV/AIDS patient with a history of 10 years visiting the center) .
Giving patients hope of having a normal life and ensuring them of the effectiveness of the medication and treatment
Health personnel insisted that in first visit when patients face the reality of having HIV/AIDS, they get desperate and become confused. So it is crucial for personnel to revive their hope assure them that a normal and long life is still possible with effective medication and adherence to medical recommendations. Creating such a feeling in patients establishes trust in the quality of the services and increases their adherence to treatment and regular visits to the BDCCs.
Mutual interactions between personnel and visitors (people living with and at the risk of getting HIV/AIDS)
Personnel behavior, not judging and reproaching hiv/aids patients and sex workers.
Personnel repeatedly emphasized the need to avoid judging or blaming patients during treatment. The focus should be on educating patients about healthy behaviors to improve their overall health and manage their disease, rather than moral judgments. Female sex workers, in particular, expressed fear of being judged during initial visits as a reason for their reluctance to seek care. It is important for personnel with strong religious values to consider whether they are suitable for working in these centers.
Personnel repeatedly emphasized the need to avoid judging or blaming HIV/AIDS patients during treatment. The focus should be on educating patients about healthy behaviors to improve their overall health and manage their disease, rather than reminding them of what is right and what is wrong morally. Female sex workers, in particular, expressed fear of being judged, during the initial visits, as a reason for their reluctance to seek care. This can be challenging for the personnel with strong religious values. It is important for personnel with strong religious values to consider whether they are suitable for working in these centers as it may discourage patients and sex workers from visiting health centers as well.
“Those who work in Vulnerable Women Counseling Centers, no matter a psychologist or midwife, if they have a judgmental mind, or if they wants to bring their religious values into the work or blame women for what they do, or they look at them badly, the patients will definitely feel it, even if you don’t say anything. In this case, the patients will not come back” (one of the midwifes with 2 years’ work experience in VWCCs) .
Having normal and friendly behavior with HIV/AIDS patients
Establishing a strong staff-patient relationship involves treating patients like normal individuals and avoiding physical distance. Interviewees recommended that it is better minimize the use of masks or gloves during examination and counseling as much as possible while still adhering to safety guidelines, in order to build trust with patients. They may also offer food, sweets, water, and tea to the patients, shake hands with patients of the same sex, place their hands on their shoulders, or even care for their child during counseling or testing. All these behaviors can create a sense of intimacy and trust in patients and reduce the stigma and help them feel that their disease is harmless. Treating patients with respect and kindness is another key components of effective communication.
“The personnel treat us really well without any expectations, like the way a mother treats her child” (An old male HIV/AIDS patient regularly visiting the BDCC) .
Previous patients satisfied with and trusted in BDCCs and VWCCs as a key factor to assure new cases to visit these centers
The interviewees consistently emphasized that satisfied and trusting current clients play a crucial role in attracting new patients. According to the interviewees, Most of new female sex workers are introduced to VWCCs by their friends and those who have visited the centers before. These peers assure them that there are no threatens and the services provided are completely confidential.
“The final point that we used is peer group. When someone comes and trusts the center, they realize that there is no judgment here, and health services are provided. They receive education. Then we tell them that we do not have access to others, please introduce this place to your friends, and they bring their friends with them in the next visit. Peer group works very well. When a new person comes, their stress has been already reduced to great extent because of their friends” (A midwife with 8 years’ experience with female sex workers in VWCCs) .
Training the personnel regarding the principles of interaction with HIV/AIDS patients
Interviewees emphasized the importance of providing training to personnel on how to interact with HIV/AIDS patients before they are employed in these centers. These patients require specialized care due to social stigma associated with their disease, their high-risk status, and the need for unique treatments and psychological understanding to establish trust during their initial visit. Unfortunately, many personnel do not possess this knowledge when they begin working and must learn through trial and error.
“When I first started working in this center, I did not even dare to make any move. I was afraid of the patients. I was really stressed, but after a while, when I saw the kindness between my colleagues and the patients, I felt better, and I changed my attitude” (A midwife with 6 years’ experience in DBCC) .
Getting a better physical and mental feeling in each visit
One of the most recurrent subjects the interviewees pointed out was that the patients should feel better, more cheerful, and more hopeful about their future when they leave the center after each visit. This can highly influence patients’ trust and is one of the responsibilities and issues the personnel should be aware of.
“One of the doctors talked to me and said there were people who had been living and combating with this disease for almost thirty years, but they had no problems and no one found out about their disease.” (One of regular male HIV/AIDS patients) .
“ When they call me, I come here with joy, because when personnel talk to me, I get inspired”. (One of regular old male HIV/AIDS patients)
Wearing a formal uniform
Wearing a uniform and following the principles and dress codes such as wearing name tags were among the issues that some patients mentioned as factors that help them feel secure in these centers. One of the interviewees that it was his first visit to BDCC expressed that he did not trust in female psychologist until she has worn her uniform.
“The second thing that frightened me was that you were wearing a coat and not a uniform, and you put on a uniform after knowing about my presence. Then, I understood you were an official staff member. You had a name tag and your appearance became professional.”(A young male visitor on his first visit to BDCC) .
Concerns of visitors
Patients’ concerns about seeing familiar personnel.
In small cities, chances of people knowing each other to see one another in the street or in public places are high, which can become a concern for HIV/AIDS patients and sex workers. Therefore, the accent and language of personnel may negatively affect patients’ trust. Patients feel secure more with personnel from other cities because risk of seeing familiar personnel will make them reluctant to return to the centers. However, some of the interviewees stated that most of the patients are from vulnerable groups or sometimes from a particular neighborhood or minority groups, and therefore, know that none of their relatives has a high academic degree or works in public medical centers. Consequently, they are not concerned about the possibility of encountering familiar faces in these centers.
“Usually, when people go to medical centers, they look for familiar personnel so that they can ask for favors, but in the BDCCs and VWCCs, the clients avoid being seen by their acquaintances or relatives. If we see a patient we know, we should pretend that we did not see anything” (An old male counselor with 6 years’ work experience in BDCCs) .
Concerning about legal problems
A major concerns among HIV/AID patients and especially female sex workers is the fear of legal issues, and potential disclosure of their information to the police or other security institutions. It was also stated that patients feel secure when they know the centers are state-owned and run by the government and that no HIV/AID patients and female sex workers has ever been caught or faced any problem in the past.
“The first thing that concerns them is the fear that legal and judicial issues may arise, and their personal information may be easily accessed. They worry that they may encounter legal problems. However, we explain to them that the center is a governmental and the government has established this center, and they will not face legal issues. We say that this is just a health center, and so far, no legal problem has arisen. Most of the time, they trust the center with our explanations” (One of personnel with 6 years of working in VWCC) .
Avoiding changing the personnel working in BDCCs and VWCCs
As previously mentioned, one concern for patients, particularly during their initial visits, is the fear of running into familiar faces at the center. Additionally, building trust and intimate relationships between the patient and the personnel takes time. To address these issues, it is recommended that staff members who display good behavior and establish positive communication with the patients should not be transferred unnecessarily. This allows for continuity of care and avoids disrupting the patients’ treatment process. Furthermore, it is important for personnel in these centers to have a close relationship with each other. In crowded centers, if possible, there should be both male and female staff member to provide patients with the option to choose.
“” Now that this new lady has come to the center, I have to come here at least several times to be able to have a proper conversation with her, but when I talk to you, it’s like I’m talking to my family members.” (One of male HIV/AIDS patients with more than 8 years visiting the center) .
Concerns about taking medications
One of the patients’ concerns is that their disease will be revealed through the drugs they take, so patients have many challenges with taking medicine, and in turn, use different tricks take them secretly. For example, they do not keep the medicines in a special packaging for AIDS medicine, they put them in multivitamin containers or they keep them inside a locked cupboard. Some of the interviewees stated that the high number of drugs used in the past was one of the challenges of regular drug use and increased the possibility of revealing these patients’ diseases. Nowadays, however, with the advancement of medicine and the reduction in the number of medicines used, as well as the reduction of the number of times the medicine is taken during the day, it has become easier for patients to take them secretly.
Precautions by visitors
Excuses and tricks used by patients and vulnerable women in their first visit.
Patients take extreme precautions before their initial visits due to their fear of encountering familiar faces, especially among the personnel. They use many tricks so that if they meet someone they know in the center, they can use a plausible excuse to cover up the main reason for their visit. For example, they ask questions such as what are behavioral diseases? Or I have a friend who has problems in his/her family, can I bring them here? Some also use vaccination, check-ups, or receiving harm-reduction equipment as excuses for their visits. They might also ask “Does Mr. or Ms. X work here?” or some others come with their friends and act as the companion of another person” (A male psychologist with 5 years’ work experience in BDCCs) .
Using disguise or protective equipment to remain anonymous during visits
The interviewees mentioned that sometimes some patients try to change their appearance as much as possible using things such as sunglasses, face masks, hats, or even veils. This increases their security, and reduce the possibility of being recognized by other familiar patients or personnel.
Going to the BDCCs and VWCCs during the last working hours: Spending the minimum possible time in the center
Due to the fact that these patients are always afraid of being seen by the others, when they visit the center, they try to receive services in the shortest possible time and without delay; therefore, they use some tricks. For example, some patients come so late at the end of office hours as they know there are not a lot of people in the center and the personnel are leaving, so that they do not have to spend much time for counseling or retests and the personnel only have time to give them their medications. According to the health personnel, some patients insist on the personnel to get their work done in the center as quickly as possible with excuses such as that the taxi is waiting for them outside.
“I remember two cases. They brought their husbands to get tested outside office hours.”(A male psychologist with 6 years of working in BDCCs) .
Physical characteristics of the centers
Location of bdccs and vwccs, area of operation: in a quiet or crowded place.
The location of BDCCs and VWCCs is a significant factor that can influence the patient experience. There are differing opinions among patients and personnel regarding whether these centers should be located in quiet, remote areas or in crowded places near other high-traffic organizations such as health centers, hospitals, schools, and banks. Some patients argue that quiet areas are preferable to minimize the likelihood of encountering familiar individuals. On the other hand, some believe that proximity to crowded places, including other health centers, facilitates easier access for patients without explicitly revealing the purpose of their visit. Being close to other health centers allows patients to use getting vaccinated or receiving other health services as a cover for visiting BDCCs and VWCCs. Once they are confident that there are no familiar faces around, they can discuss their real needs. Although the probability of encountering familiar people is obviously higher in these areas, there are more excuses available to conceal the real reason for the visits. However, locating these centers next to or near security organizations such as the police station may instill fear in patients and deter them from seeking care. “The center used to be in a crowded area. Whenever I was going to BDCC, it was likely to see a few familiar faces, but I made excuses by saying that I am going to the bank, but new BDCC is located in a remote area, so there are few familiar people and less traffic (which is good).” (An adolescent HIV/AIDS patient with regular visits to BDCC) .
Working as independent and separate BDCCs and VWCCs or as a part of a larger building?
Another factor that can significantly impacts patients’ feelings of fear and worry regarding their visits to the BDCCs and VWCCs is whether these centers should operate independently or as part of a larger health center. Interviewees expressed varying opinions on this matter. Some believed that the integrating these centers within other health centers would negatively affect getting routine public health services by ordinary people. This is because some of HIV/AIDS patients have an appearance that is perceived as untidy and disheveled, which could discourage other people from seeking their routine health services. Furthermore, some stated that the integration would increase the likelihood of encountering familiar personnel or people seeking routine health services, as they had personally experienced such encounters. However, most of the interviewees believed that having an independent DBCC or VWCC from the outset brings stigma. If people are seen going to these centers, there will be no excuse to conceal their visits. They argued that integrating these centers into a larger health center with the same entrance, allows patients or female sex workers to conceal the true reason for their visits, making them more comfortable visiting the centers. It was also suggested that having separate entrance and exist in different sides of the building can help HIV/AIDS patients and sex workers to reduce the risk of encountering familiar individuals.
“I strongly disagree (with integration of BDCCs in health centers) because some patients carry knives with them, some of them are clearly drug addicts, or have an extremely unpleasant appearance, which frightens other patients… HIV/AIDS patients are even opposed to installing CCTV cameras in the center, let alone merging it with a health center” (One of the public health experts with about 5 years’ experience in HIV/AIDS) .
It should be noted that the State Welfare Organization (SWO) manages the supportive services provided for poor, isolated, and marginalized groups and families with handicapped members. This organization runs centers for training and supporting vulnerable groups including HIV/AIDS patients called Positive Clubs. Since a wide range of people with various needs refer to these centers and most of them are healthy, it appears that the integration of BDCCs and VWCCs into the SWO as a supportive institution rather than a medical center could encourage HIV/AIDS patients to visit these centers compared to the integration of these centers into health centers.
“One of the advantages of our center (Welfare Organization Counseling Center) is that it has the title “Welfare Organization” on its signboard. A lot of visitors including healthy people come here… its signboard doesn’t have a negative connotation and doesn’t make anyone suspicious.”(A counselor working in the Welfare Organization with more than 15 years’ experience in HIV/AIDS) .
Establishing fixed centers and not changing the location of BDCCs and VWCCs
Since the majority of patients refuse to give their identity and contact information, the relocation of the BDCCs and VWCCs, especially if the centers are rented and not owned, can strongly affect the number of patients and sex workers. According to the interviewees, each relocation leads to a significant reduction in the number of patients and sex workers, and therefore, their treatment will be disrupted.
“If the building of BDCCs and WCCs is owned by the medical university, there would be no relocation, which is great. It is not easy to encourage vulnerable women to come to the center, and now if we relocated, exactly two-thirds of the cases and maybe even more would be lost.”(One of the psychologists with more than 6 years of work in VWCCs) .
The physical space (size) of the BDCCs and VWCCs
The interviewees also highlighted the importance of the physical space and the physical layout of the centers and patients and female sex workers’ fear of encountering acquaintances as factors affecting their willingness to visit the centers. Patients prefer to receive services with minimal contact with others. Therefore, the physical space of the center can either hinder or facilitate visiting the centers. Overall, the majority of interviewees criticized the small physical space of the centers and the potential issues it could cause. Some of the personnel mentioned difficulties in storing a large number of files due to increasingly number of clients. Having a larger space would reduce the chances of encountering other patients, and private areas could be designated for those who wish to wait or conceal themselves from familiar patients.
“If we had more space and knew that for example, Ms. X is sensitive, we would ask her to wait in a separate room and when it was less crowded, we would visit her privately, but that’s not possible now.” (One of midwives with 8 years of work in VWCCs) .
“There were one or two cases who were relatives, and because of not having enough space the unavoidable encounters are increasing among them, which is causing concerns.” (One of psychologists with 2 years’ work experience in VWCCs) .
“Sometimes, when I see someone I know from afar, I hide so that they don’t see me and they don’t get anxious, but it’s not possible for all patients because of this small space.”(A female general practitioner with 3 years’ work in BDCCs) .
Geographical distribution of BDCCs and VWCCs
Physical distance between bdccs and vwccs and living place of people.
According to the interviewees, since most of the clients are from vulnerable groups, it is very important to distribute the centers in such a way that they are closest to the patients’ places of residence so that they can find the centers easily and do not have to spend too much for transportation expenses.
Not having a catchment area and no geographical division for BDCCs and VWCCs
One of the current benefits of BDCCs and VWCCs is that there is no catchment area and the population of the city is not divided between them based on geographical distribution, and any patient from any part of the city can go to any center in which they feel more secure and less likely to be seen by their relatives, friends, family members, colleagues and other familiar people.
“People who live near here ( BDCC number 2) can visit our center if they’d like to, even those who live near BDCC number 1 but know that they have relatives in that area and aren’t willing to go to that center can visit our center too.” (One of female personnel with 4 years’ working in BDCC number 2) .
Increasing the number of BDCCs and VWCCs
Another factor that can greatly affect patients’ trust and encourage them to visit is increasing the number of these centers in the city. This, especially in bigger cities, would not only make it more convenient for patients to access the centers due to easier access, but it also allow them to choose a center in which they are less concerned about being seen by acquaintances.
Physical evidence
The signboard of the bdccs and vwccs.
Different opinions were expressed regarding the appropriateness or the repulsion caused by the title written on the signboard of these centers. Some stated that the title “Behavioral Disorders Counseling Center” is a neutral title because there is no mention of the words HIV or AIDS, and at the same time, it is not very ambiguous, and people in need of services can figure out what services these centers provide and get the services they need. On the other hand, some others found this title repulsive and believed that the title itself specifies the reason for the visits and a more neutral title should be sought.
“The title of these centers is inappropriate. My niece told me that from the title ‘Behavioral Disorders Counseling Center’ she understood that I was ill.”(A young male HIV/AIDS patient on his first visit) .
Not having surveillance cameras installed
One of the key issues greatly affecting patients’ willingness to visit these centers is that they are very sensitive about the CCTV, which can make them paranoid and afraid of referring to the BDCCs and VWCCs.
“Because of the equipment here, several times it was suggested that CCTVs should be installed, but it was rejected each time because seeing them can negatively affect patients’ trust” (A male counselor with 5 years’ experience in DBCCs) .
“Women keep asking if there are any CCTVs here and we have to reassure them that there are not” (one of the midwives with two years’ experience in VWCCs) .
Not using signs of HIV/AIDS in the BDCCs
To maintain confidentiality and ensure patients’ peace of mind, it was suggested to avoid hanging banners or educational announcements containing HIV/AIDS content in the centers. Some patients even recommended that the lab kits used in the centers should not have the name AIDS or any sign indicating that the majority of clients are HIV/AIDS patients.
To maintain confidentiality and ensure patients’ peace of mind, it was suggested to avoid hanging banners or educational announcements containing HIV/AIDS content in these centers. Some patients even recommended that the lab kits used in the centers should not have the name AIDS and any sign indicating that the majority of clients are HIV/AIDS patients.
“There is no brochure or any sign of HIV/AIDS on the walls in the center” ( A consultant working in counseling centers affiliated with the Welfare Organization with 5 years’ experience with HIV/AIDS patients) .
“It was written on the laboratory kits “KITS FOR DIAGNOSING HIV/AIDS”. It should not be like that” (A young male HIV/AIDS patient with regular visits to BDCC) .
This study investigated the most important factors affecting HIV/AIDS patients and vulnerable women visiting BDCCs and VWCCs respectively. The factors were categorized into three categories including medical and operational processes, mutual interactions between the personnel and visitors (people living with and at the risk of getting HIV/AIDS), and the physical characteristics of the centers. This section provides a discussion of the findings.
Due to the significant social stigma associated with HIV/AIDS in Iran in general and in Ilam and Kermanshah in particular, it is crucial for BDCCs and VWCCs to carefully consider the clinical processes and the provision of medical and counseling services to these patients. The success of the treatment process relies on providing services that meet the clients’ needs and are based on their preferences. The findings of the study indicate that within the current context of Iran, it is important to avoid asking too many questions or focusing on the cause of the disease during the initial visits in order to increase the patient’s interest in continuing their visits to the centers and adhering to the medical instructions. Accordingly, the personnel should not insist on receiving identity information, at least in the first visits, and it can be postponed until trust is established. Using codes instead of personal information can help patients to feel secure, particularly in small towns where familiarity is more likely.
Confidentiality is of utmost importance in BDCCs and VWCCs and the building design should provide a safe environment for clients to feel secure about their privacy. Colleagues should also avoid interrupting the counseling process and create a comfortable atmosphere for all clients. Similarly, studies from Ghana and Sub-Saharan Africa showed that pregnant women and other groups stated doing HIV test in an open and not private space and not trusting health workers’ being confidential as the reasons for refuting taking HIV test [ 25 , 26 ]. Moreover, studies of the Global Fund to Fight AIDS, Tuberculosis and Malaria showed lack of confidentiality and gossiping as common behaviors among healthcare workers. These behaviors can make HIV patients and sex workers highly worried about no secrecy of their personal information, their HIV status, or sexual activities in the society [ 27 ].
Moreover, to address concerns about answering questions regarding the cause and history of visitors’ disease, personnel should wear a uniform with a tag displaying their first and last name and position. Additionally, according to the interviews, some patients may prefer to avoid in-person visits, especially in small provinces, to minimize the chance of encountering familiar faces. Another factor contributing to creation of a positive view of BDCCs is the management of fear of death among HIV/AIDS patients and helping them hope the possibility of living a normal life through regular taking medication. Remote services, such as electronic services and phone calls, can be developed to minimize in-person visits. These services can allow patients to confirm that no familiar or new individuals are present at the centers while visiting the centers. Other relevant studies also indicate that deterioration of physical health and/or death of sexual partner or child are among the enabling factors for up-taking HIV test [ 26 ].
Phone or virtual counseling can also ensure confidentiality is maintained. Such facilities can enable patients to make sure no familiar person or new person is in the centers before going there. During the time period that this study was conducted, there were not strong remote and friendly-used online or telephone services in the studied centers, for HIV/AIDS patients or female with risky sexual behaviors to rely on. It definitely make it difficult for visitors, especially new cases, to visit the centers. The stigma of being seen at health services has been stated by previous studies as a major barrier to utilizing health services by HIV patients [ 28 ]. To improve health services utilization for HIV/AIDS patients in Iran, it may be useful to create a website with information about the responsibilities, exact address, contact information, and personnel working in the BDCCs. This may reduce patients’ concerns and contribute to more convenient visits, especially, during their first visits. In this regard, social media can also be utilized to promote the website and availability of such centers.
Another crucial factor improving the quality of health services in BDCCs and VWCCs is the employment of personnel who are flexible, patient, and accessible, with effective communicative skills and specialized counseling knowledge for individuals living with or at risk of HIV/AIDS. The personnel should treat clients with dignity and respect, convey medical instructions accurately and motivate and assure patients to continue their treatment. Continuous training courses should be provided to maintain their skills, and the personnel should be selected carefully and not transferred frequently. Additionally, according to our findings, it is advisable to avoid employing health forces with strict religious beliefs and religious appearance in BDCCs and especially in VWCCs as their religious beliefs may hinder effective communication, especially with female sex workers. Personnel should avoid making clients feel blamed or shamed behave normally when encountering the HIV/AIDS patients outside of the center. According to the findings from Ghana and San Francisco, women and drug users mentioned that not being treated well by the nurses and snobby attitude of the staff discouraged them from participating in the facilities for HIV testing and counseling [ 25 , 29 , 30 ]. Other studies also referred to lack of training for medical staff on medical ethics as a reason exacerbating the problem [ 28 ]. Feelings of blame and shame and confronting stereotypes of HIV are strong among HIV positive and sex workers and can prevent them from coming to health centers at the first step [ 44 ]. Personnel should be aware of that and try to reduce these feelings in their patients.
Findings of our study revealed that patients and sex workers in particular are afraid of being prosecuted by security and legal agencies. Other studies shows similar findings, for example drug users were afraid of “punishment and being locked up” if their HIV test was positive [ 29 ] and also in Denmark criminalization hinders women who use drugs from access to harm reduction services [ 27 ]. An effective factor in gaining other patients’ trust is the satisfaction of the current and previous clients. Therefore, using this capacity can be effective in expanding the services, identifying other patients, and providing services to a larger population in severe need of these services.
The physical properties and location of the centers are also important considerations. Counseling rooms should be soundproofed to ensure patient conversation cannot be overheard. Similar to standards for building rural and urban comprehensive health centers in Iran, a building plan with defined standards should be developed for BDCCs and VWCCs to address all the concerns raised in this study. Furthermore, financial support should be provided at the national and provincial levels to establish an adequate number of these centers across the country. Insufficient space in some centers for providing a safe waiting area, maintaining confidentiality, reducing unnecessary encounters between the clients, and archiving their files was a major concern among interviewees. Establishing larger centers, especially in small cities, can help alleviate these concerns.
Another important factor rooted in the context of research site which affects health care utilization by people is the location of the of the BDCCs and VWCCs and their operation as independent centers or centers integrated into other medical facilities. According to the findings, it is better to establish BDCCs and VWCCs in crowded areas and near other medical centers. This allows HIV/AIDS patients and vulnerable women to visit the BDCCs and VWCCs more conveniently without drawing attention. Also, most of the interviewees expressed a preference for the centers to be integrated into larger facilities or separate buildings within a larger environment with a common entrance, rather than operating as independent centers. This allows patients to blend in with other clients and conceal the reason for their visit. Although this has been considered in the BDCC booklet, the centers in this study operate as a separate buildings, which creates a barrier to patient visits. Although this may adversely affects health services utilization by other groups. In many countries, such as the US, Sweden, New Zealand, India, Lebanon, Mozambique and Zimbabwe, health centers for HIV/AIDS are located in rural and urban areas, and the public and private sectors work together in this field [ 45 , 46 ]. However, in Iran, situation is different and these centers are located only in cities and are only run by the governmental sector. Cities are preferred as people are less likely to know each other. Even a part of patients prefer not use health services available in their cities and go to other cities due to social stigma and fear of seeing acquaintances. Due to the substantial stigma associated with this disease in Iran, establishing these centers in rural areas is neither recommended nor possible. In order to preserve the confidentiality of HIV/AIDS patients in Iran, and to properly manage the distribution of specialized medications and diagnostic tests for these patient, all diagnostic and treatment measures for HIV/AIDS patients are centralized and provided free of charge in the public sector through the Behavioral Diseases Counseling Centers. The private sector currently only has the responsibility of referring suspected HIV cases to the BDCCs.
Another notable issue to consider is the establishment of BDCCs and VWCCs in easily accessible locations with the aim of reducing transportation expenses for patients, especially those from poor and vulnerable groups. Increasing the number of these centers in various urban regions not only facilitates patients’ visits and reduces their transportation costs, but also provides them with more options to choose from, thereby addressing concerns about encountering acquaintances during visits. Financial difficulties were identified as a barrier to regular visits to BDCCs and VWCCs. To encourage clients to visit these centers more frequently, interviewees mentioned the importance of proposing financial and food support. Additionally, one positive aspect of these centers in Iran is that there are no geographical restrictions, allowing patients to visit any center they feel comfortable with, regardless of their place of residence. According to the findings of the study and considering the current limitations which exist in Ilam and Kermanshah, it is recommended to avoid using HIV and AIDS signs within the facilities. Furthermore, it was also proposed that diversifying services and offering services for a variety of patients such as tuberculosis, diabetes, thalassemia, hypertension, etc., can provide a better environment for HIV/AIDS people to continue their treatment conveniently. Installing educational banners about other diseases outside the centers and on websites, while highlighting the availability of these facilities, may also increase patients’ visits. Similarly, the study by Downing in San Francisco showed that convenience, increasing the number of HIV test sites, free transportation and monetary incentives were among the main structural motivating factors for drug’ users to take HIV test [ 29 ]. Removing financial barriers and convenient access to HIV test were among the facilitators helping people take HIV test in Sub-Saharan Africa [ 26 ].
Study limitations
There were limitations in conducting interviews, as the research team was not allowed to interview HIV/AIDS patients or vulnerable women referring to the BDCCs and VWCCs directly and had to rely on health staff working in the centers instead. This may have affected the quality of the interviews, as patients may not have felt comfortable revealing certain challenges or difficulties to health staff. Additionally, some clients were reluctant to be interviewed or have their voices recorded, so the interviewers had to take notes instead. It is also difficult to have deep interviews with patients, especially on general issues like motives or obstacles of health care utilization.
In order to enhance the performance of BDCCs and VWCCs and encourage regular visits from HIV/AIDS patients, vulnerable women and those at the risk of getting HIV/AIDS, it is crucial for policy makers and public health officials to address the concerns and issues mentioned in this paper. The clinical processes, physical features, and the way personnel treat patients should change and improve in a way that make patients less afraid of coming to the centers and ensure them that everything has been arranged in order to keep their disease confidential. Further studies are required to measure the value and importance of the factors revealed in this study. For example a survey can measure the weight of each factor in terms of creating trust in people living with HIV/AIDS and sex workers about the performance and secrecy principles of the centers. Moreover, different new features can be extracted from the findings which can be applied to run a new project using conjoint analysis and discrete choice experiments to understand the preferences of visitors and targeted population to know what kind of centers they prefer more and what kinds of changes should be made in these centers to fulfill their expectations.
Data availability
All data generated during the current study are in Persian and not publicly available as it is not allowed by the Ethics Committee, but would be available from the corresponding author on reasonable request.
Abbreviations
Behavioral Diseases Counseling Centers
Vulnerable Women’ Counseling Centers
UNAIDS, Global HIV. & AIDS Statistics — 2020 Fact Sheet. 2021. https://www.unaidsorg/en/resources/fact-sheet . 2021.
Zadeh AOT, SeyedAlinaghi S, Hassanzad FF, Hajizadeh M, Mohamadi S, Emamzadeh-Fard S, et al. Prevalence of HIV infection and the correlates among homeless in Tehran, Iran. Asian Pac J Trop Biomed. 2014;4(1):65–8.
Article PubMed PubMed Central Google Scholar
UNAIDS, HIV, Estimates AIDS. 2019. https://www.unaidsorg/en/regionscountries/countries/islamicrepublicofiran
Khodayari-Zarnaq R, Ravaghi H, Mosaddegh‐rad AM, Jalilian H, Bazyar M. HIV/AIDS policy‐making in Iran: a stakeholder analysis. Int J Health Plann Manag. 2021;36(6):2351–65.
Article Google Scholar
Bazrafshani A, Panahi S, Sharifi H, Merghati-Khoei E. The role of online social networks in improving health literacy and medication adherence among people living with HIV/AIDS in Iran: development of a conceptual model. PLoS ONE. 2022;17(6):e0261304.
Article CAS PubMed PubMed Central Google Scholar
Armoon B, Noroozi M, Jorjoran Shushtari Z, Sharhani A, Ahounbar E, Karimi S, et al. Factors associated with HIV risk perception among people who inject drugs: findings from a cross-sectional behavioral survey in Kermanshah, Iran. J Subst Use. 2018;23(1):63–6.
Khodayari-Zarnaq R, Ravaghi H, Mosaddeghrad AM, Sedaghat A, Mohraz M. HIV/AIDS policy agenda setting in Iran. Med J Islamic Repub Iran. 2016;30:392.
Google Scholar
Moradi G, Mohraz M, Gouya MM, Dejman M, Seyedalinaghi S, Khoshravesh S, et al. Health needs of people living with HIV/AIDS: from the perspective of policy makers, physicians and consultants, and people living with HIV/AIDS. Iran J Public Health. 2014;43(10):1424.
PubMed PubMed Central Google Scholar
Khodayari-Zarnaq R, Mosaddeghrad AM, Nadrian H, Kabiri N, Ravaghi H. Comprehensive analysis of the HIV/AIDS policy-making process in Iran. Health Res Policy Syst. 2019;17:1–12.
Radfar R, Taheri K, Tabar HN. Executive instructions on how to provide services in behavioral diseases counseling centers. Tehran, Iran: Public Health Deputy of Ministry of Health and Medical Education.
Moradi G, Ghaderi E, Sargolzaei M, Fallahi H, Eybpoosh S, Tayeri K et al. HIV/AIDS surveillance system in the Islamic Republic of Iran: history, structures and processes. Iran J Epidemiol. 2019;15(2).
Sharifi H, Karamouzian M, Baneshi MR, Shokoohi M, Haghdoost A, McFarland W, et al. Population size estimation of female sex workers in Iran: synthesis of methods and results. PLoS ONE. 2017;12(8):e0182755.
Ahmadi S, Khezri M, Roshanfekr P, Karimi SE, Vameghi M, Ali D et al. HIV testing and its associated factors among street-based female sex workers in Iran: results of a national rapid assessment and response survey. Substance abuse treatment, prevention, and policy. 2021;16(1):43.
Sajadi L, Mirzazadeh A, Navadeh S, Osooli M, Khajehkazemi R, Gouya MM, et al. HIV prevalence and related risk behaviours among female sex workers in Iran: results of the national biobehavioural survey, 2010. Sex Transm Infect. 2013;89(Suppl 3):iii37–40.
Article PubMed Google Scholar
Farhoudi B, Ghalekhani N, Afsar Kazerooni P, Namdari Tabar H, Tayeri K, Gouya MM, et al. Cascade of care in people living with HIV in Iran in 2019; how far to reach UNAIDS/WHO targets. AIDS Care. 2022;34(5):590–6.
WHO. Iran (Islamic Republic of) HIV Country Profile; 2017.
UNAIDS, Sheet DATA. AIDSinfo, Trend of New of New HIV Infections; 2018.
Camacho G, Kalichman S, Katner H. Anticipated HIV-related stigma and HIV treatment adherence: the indirect effect of medication concerns. AIDS Behav. 2020;24:185–91.
Shubber Z, Mills EJ, Nachega JB, Vreeman R, Freitas M, Bock P, et al. Patient-reported barriers to adherence to antiretroviral therapy: a systematic review and meta-analysis. PLoS Med. 2016;13(11):e1002183.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta‐synthesis. J Int AIDS Soc. 2013;16:18640.
Yu F, Hsiao Y-H, Park S, Kambara K, Allan B, Brough G, et al. The influence of anticipated HIV stigma on health-related behaviors, self-rated health, and treatment preferences among people living with HIV in east Asia. AIDS Behav. 2023;27(4):1287–303.
Threats M, Boyd DT, Diaz JE, Adebayo OW. Deterrents and motivators of HIV testing among young Black men who have sex with men in North Carolina. AIDS Care. 2021;33(7):943–51.
Pearson CA, Johnson MO, Neilands TB, Dilworth SE, Sauceda JA, Mugavero MJ, et al. Internalized HIV stigma predicts suboptimal retention in care among people living with HIV in the United States. AIDS Patient Care STDs. 2021;35(5):188–93.
Zeng C, Li X, Qiao S, Yang X, Shen Z, Zhou Y. Anticipated stigma and medication adherence among people living with HIV: the mechanistic roles of medication support and ART self-efficacy. AIDS Care. 2020;32(8):1014–22.
Kwapong GD, Boateng D, Agyei-Baffour P, Addy EA. Health service barriers to HIV testing and counseling among pregnant women attending Antenatal Clinic; a cross-sectional study. BMC Health Serv Res. 2014;14:1–10.
Musheke M, Ntalasha H, Gari S, Mckenzie O, Bond V, Martin-Hilber A, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-saharan Africa. BMC Public Health. 2013;13(1):1–16.
Fund G. Global fund breaking down barriers initiative summary of key findings of the baseline assessments in 20 countries. The Global Fund Geneva; 2020.
Shirley-Beavan S, Roig A, Burke-Shyne N, Daniels C, Csak R. Women and barriers to harm reduction services: a literature review and initial findings from a qualitative study in Barcelona, Spain. Harm Reduct J. 2020;17(1):1–13.
Downing M, Knight K, Reiss T, Vernon K, Mulia N, Ferreboeuf M, et al. Drug users talk about HIV testing: motivating and deterring factors. AIDS Care. 2001;13(5):561–77.
Article CAS PubMed Google Scholar
Turan J, Miller S, Bukusi E, Sande J, Cohen C. HIV/AIDS and maternity care in Kenya: how fears of stigma and discrimination affect uptake and provision of labor and delivery services. AIDS Care. 2008;20(8):938–45.
Morowatisharifabad MA, Movahed E, Farokhzadian J, Nikooie R, Hosseinzadeh M, Askarishahi M, et al. Antiretroviral therapy adherence and its determinant factors among people living with HIV/AIDS: a case study in Iran. BMC Res Notes. 2019;12(1):1–5.
Ebrahimi Kalan M, Han J, Ben Taleb Z, Fennie KP, Asghari Jafarabadi M, Dastoorpoor M et al. Quality of life and stigma among people living with HIV/AIDS in Iran. HIV/AIDS-Research and Palliative Care. 2019:287– 98.
Khademi N, Saeidi S, Zangeneh A, Saeidi F, Choobtashani M. The relationship between life satisfaction and quality of life among people living with HIV/AIDS in Kermanshah-West of Iran. Health Soc Care Commun. 2020;28(6):2218–24.
Maleki MR, Derakhshani N, Azami-Aghdash S, Naderi M, Nikoomanesh M. Quality of life of people with HIV/AIDS in Iran: a systematic review and meta-analysis. Iran J Public Health. 2020;49(8):1399.
Akbari M, Fararouei M, Haghdoost AA, Gouya MM, Kazerooni PA. Survival and associated factors among people living with HIV/AIDS: a 30-year national survey in Iran. J Res Med Sciences: Official J Isfahan Univ Med Sci. 2019;24.
Mohammadi Y, Mirzaei M, Shirmohammadi-Khorram N, Farhadian M. Identifying risk factors for late HIV diagnosis and survival analysis of people living with HIV/AIDS in Iran (1987–2016). BMC Infect Dis. 2021;21(1):1–9.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Stahl NA, King JR. Expanding approaches for research: understanding and using trustworthiness in qualitative research. J Dev Educ. 2020;44(1):26–8.
Lincoln Y, Guba. E.(1985). Naturalistic inquiry. Beverly Hills: Sage LincolnNaturalistic Inquiry1985. 1980.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qualitative Methods. 2017;16(1):1609406917733847.
Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative content analysis: a focus on trustworthiness. SAGE open. 2014;4(1):2158244014522633.
Yadav D. Criteria for good qualitative research: a comprehensive review. Asia-Pacific Educ Researcher. 2022;31(6):679–89.
Triangulation DS, editor. Editor the use of triangulation in qualitative research. Oncol Nurs Forum; 2014.
Sayles JN, Ryan GW, Silver JS, Sarkisian CA, Cunningham WE. Experiences of social stigma and implications for healthcare among a diverse population of HIV positive adults. J Urb Health. 2007;84:814–28.
Nasiripour AA, Raeissi P, Tabibi SJ, Majidpour A. Designing a Domestic Model for Resource Management at Counseling Centers for Behavioral Illnesses in Iran. J Ardabil Univ Med Sci. 2012;12(2):190–203.
Pfeiffer J, Montoya P, Baptista AJ, Karagianis M, Pugas MM, Micek M, et al. Integration of HIV/AIDS services into African primary health care: lessons learned for health system strengthening in Mozambique-a case study. J Int AIDS Soc. 2010;13:1–9.
Download references
Acknowledgements
We thanks to all patients and key informants who participated in the study and enriched our study by their valuable comments.
This study was supported financially by Ilam University of Medical Sciences.
Author information
Authors and affiliations.
Health Management and Economics Department, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran
Mohammad Bazyar & Jamil Sadeghifar
Clinical Research Development Unit, Emam Khomeini Hospital, Ilam University of Medical Sciences, Ilam, Iran
Samaneh Tahmasebi Ghorabi
Health and Environment Research Center, Ilam University of Medical Sciences, Ilam, Iran
Jamil Sadeghifar
Health Policy & Management Research Center, Department of Health Management and Economics, School of Public Health, Shahid Sadoughi University of Medical sciences, Yazd, Iran
Mohammad Ranjbar
Department of Epidemiology, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran
Reza Pakzad
Department of Public Health, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran
Fatemeh Bonyadi, Mahtab Nourbakhsh & Boshra Noshadi
Behavioral Diseases Research Center, Public Health Deputy, Kermanshah University of Medical Sciences, Kermanshah, Iran
Keyvan Khasi, Ebrahim Shakiba, Leila Rezeghian & Mehrdad Bavandpour
Communicable Diseases Department, Public Health Deputy, Ilam University of Medical Sciences, Ilam,, Iran
Azim HasanBeigi
Health Services Management Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
Anahita Behzadi
Department of Health Management, Policy and Economics, Faculty of Management and Medical Informatics Sciences, Kerman University of Medical Sciences, Kerman, Iran
You can also search for this author in PubMed Google Scholar
Contributions
MB, JS, KK, ESh and RP participated in designing the study; MB, LR, and MN did the interviews; MR, FB, ST, BN, AH reviewed the literature and transcribed the interviews. MB, AB and MR analyzed the interviews. MB and AB and JS prepared the manuscript. All authors read and approve the manuscript for submission.
Corresponding author
Correspondence to Anahita Behzadi .

Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from research ethics committee at Ilam University of Medical Sciences with the ethics code IR.MEDILAM.REC.1401.120. Informed consent was obtained from all participants to do interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bazyar, M., Ghorabi, S.T., Sadeghifar, J. et al. What may encourage or deter health services utilization by people living with or at the risk of HIV/AIDS in special health centers? Qualitative evidence from a stigmatized community. BMC Public Health 24 , 981 (2024). https://doi.org/10.1186/s12889-024-18480-3
Download citation
Received : 05 September 2023
Accepted : 28 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1186/s12889-024-18480-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Behavioral diseases Counseling centers
- Vulnerable women’s Counseling centers
- Facilitators
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 05 January 2024
Acceptability, values, and preferences of older people for chronic low back pain management; a qualitative evidence synthesis
- Heather Ames 1 ,
- Christine Hillestad Hestevik 1 &
- Andrew M. Briggs 2 , 3
BMC Geriatrics volume 24 , Article number: 24 ( 2024 ) Cite this article
950 Accesses
4 Altmetric
Metrics details
Chronic primary low back pain (CPLBP) and other musculoskeletal conditions represent a sizable attribution to the global burden of disability, with rates greatest in older age. There are multiple and varied interventions for CPLBP, delivered by a wide range of health and care workers. However, it is not known if these are acceptable to or align with the values and preferences of care recipients. The objective of this synthesis was to understand the key factors influencing the acceptability of, and values and preferences for, interventions/care for CPLBP from the perspective of people over 60 and their caregivers.
We searched MEDLINE, CINAHL and OpenAlex, for eligible studies from inception until April 2022. We included studies that used qualitative methods for data collection and analysis; explored the perceptions and experiences of older people and their caregivers about interventions to treat CPLBP; from any setting globally. We conducted a best fit framework synthesis using a framework developed specifically for this review. We assessed our certainty in the findings using GRADE-CERQual.
All 22 included studies represented older people’s experiences and had representation across a range of geographies and economic contexts. No studies were identified on caregivers. Older people living with CPLBP express values and preferences for their care that relate to therapeutic encounters and the importance of therapeutic alliance, irrespective of the type of treatment, choice of intervention, and intervention delivery modalities. Older people with CPLBP value therapeutic encounters that validate, legitimise, and respect their pain experience, consider their context holistically, prioritise their needs and preferences, adopt a person-centred and tailored approach to care, and are supported by interprofessional communication. Older people valued care that provided benefit to them, included interventions beyond analgesic medicines alone and was financially and geographically accessible.
Conclusions
These findings provide critical context to the implementation of clinical guidelines into practice, particularly related to how care providers interact with older people and how components of care are delivered, their location and their cost. Further research is needed focusing on low- and middle-income settings, vulnerable populations, and caregivers.
Peer Review reports
Low back pain (LBP) and other musculoskeletal conditions represent a sizable contribution to the global burden of disability [ 1 , 2 , 3 , 4 , 5 ]. While the prevalence and impact of LBP are relevant across the life-course, global estimates for prevalence and disability show rates to be greatest in older age. The high prevalence of LBP in older people accounts for frequent care seeking for LBP [ 6 ], particularly among older adults experiencing recurrent LBP [ 7 ]. The number of older people experiencing and seeking care for LBP is expected to increase due to population ageing and an increasing prevalence of risk factors for noncommunicable diseases [ 8 ]. Despite this, intervention trials and clinical guidelines for LBP disproportionately underrepresent older people [ 9 , 10 ], potentially leaving an important knowledge gap for optimal care of LBP in older people.
Clinical management of LBP is characterized by multiple and varied interventions, delivered by a wide range of health and care workers [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 ]. In many contexts the interventions delivered may not be aligned with best evidence leading to unwarranted care variation and potential harm. Further, interventions may not be aligned with the values, preferences and acceptability attitudes among care recipients (and/or their carers), substantiating the need for global guidelines in this area [ 21 ]. Importantly, values and preferences of older people likely differ to younger adults. From the perspective of healthy ageing, carers are an essential workforce for supporting functional ability in older people and enabling ageing in place. The perspectives of carers are therefore critical to ensure care planning and delivery for any health condition experienced by an older people is feasible and acceptable and does not negatively impact on the quality of life of the carer [ 22 , 23 ] . For example, recent work has also identified the need to sample perspectives of carers related to delivery of care for people living with chronic pain [ 24 ].
In response to this context and the priority to support healthy ageing, the World Health Organization (WHO) initiated the development of standard clinical guideline for the non-surgical management of chronic primary LBP (CPLBP) in adults, including older people, in primary and community care settings in 2020 [ 21 ]. The guidelines were published in December 2023 [ 25 ].
This qualitative evidence synthesis was commissioned in parallel to several systematic reviews of evidence of benefits and harms of prioritized interventions for the Guideline, synthesized from randomized controlled trials (RCTs) [ 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ]. These interventions were broad in scope, intensity and setting for delivery (reflected in the inclusion criteria for this synthesis). The aim of all the interventions is to improve health and wellbeing outcomes for people living with CPLBP. However, it is important to explore how this broad variation in interventions is perceived and experienced by older people with CPLBP and/or their caregivers (formal or informal, family members). Are some interventions more accepted than others? Are there differences between the interventions and/or access to them related to equity (gender, culture, place of residence, socio economic status) or setting (geographic or health care setting)? These important context questions can only be comprehensively answered using qualitative research methods. These contextual data are intended to support the development of the WHO guideline and complement additional perspectives brought to the development process by other stakeholders involved in the guideline development, consistent with WHO guideline development methods [ 45 ].
It is important to consider people’s preferences around interventions when formulating and implementing clinical management guidelines. In this paper we use the concept of person-centred care, in order to encompass a broader perspective than those related to being a patient. We have adopted the definition of person-centred care that is used in the WHO Guideline, that is “Person-centred care means eliciting an individual’s values, preferences and priorities: once expressed, they should guide all aspects of that person’s health care, supporting their personalized health and life goals” [ 46 , 47 ].
An intervention may be proven effective but if it is not accepted by people living with the condition (and/or their carers) or they feel it causes burden or harm, it will not be adopted. An important step in a WHO guidelines development process is to consider what people living with CPLBP and their caregivers find acceptable? Feasible? Valued? [ 45 ] For example, there is a need to understand preferences and perspectives concerning accessibility, availability, affordability, perceived quality, burden [time, distance, frequency of visits], stigma, duration of therapeutic effect, person/patient’s role (passive or active role), immediacy of treatment effect, configuration of the care team– single practitioner or team approach, influence on comorbid health conditions, and symptoms related to the treatment. Some of these dimensions of value, preference and acceptability have been identified as previously as important to decision-making around treatments among older adults with osteoarthritis [ 48 ]. To date there has been some research conducted that considers people’s preferences for treatment for CPLBP [ 49 , 50 , 51 , 52 , 53 , 54 , 55 ]. However, to our knowledge, there has been no synthesis of primary qualitative research exploring the key factors influencing the implementation, uptake, and experience of interventions designed to manage CPLBP from the perspective of people aged over 60 and their caregivers.
The objective of this qualitative evidence synthesis (QES) was to understand the key factors influencing the acceptability of, and values and preferences/perspectives for, interventions/care for CPLBP from the perspective of people over 60 and their caregivers. The purpose of the QES was to inform the development of the WHO guideline [ 25 ].
This QES followed the best practice as described by the Cochrane collaboration in their handbook [ 56 , 57 ]. The protocol was registered on PROSPERO at inception ( https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=328469 ).
We included primary studies with qualitative study designs. We included mixed-methods studies when it was possible to extract the data that were collected and analysed using qualitative methods. The inclusion criteria are described in Table 1 .
We searched in two databases (MEDLINE and CINAHL powered by Ovid) (April 28, 2022) and supplemented the search with a search in an open-source dataset, OpenAlex [ 59 , 60 ] (May 3, 2022) through the EPPI-Reviewer platform [ 59 ]. We also screened the references of the included studies. Finally, we asked members of the WHO Guideline Development Group to recommend any relevant research they were aware of.
To maximise efficiency of the study selection process, we used the machine learning function “priority screening” in the systematic review software EPPI-reviewer [ 61 ].
Two review authors (HA and CHH) independently assessed eligibility of the titles and abstracts. We retrieved the full text of all the papers identified as potentially relevant. Two authors (HA and CHH) then assessed the eligibility of these papers independently. Discrepancies in decisions were resolved by discussion among the authors.
Data extraction was performed using a data extraction form designed specifically for this review. One author performed the data extraction and a second author checked for accuracy against the source paper and any discordances were resolved through consensus discussion. We extracted the following information from the studies; author, year of publication, geographic setting, description of context, data collection methods (sampling, collection, and analysis), description of participants covering the aspects named in the inclusion table (see Table 1 ) and if ethics approval was given for the study.
We assessed the methodological limitations of the included studies using a list of domains iteratively developed by the Cochrane EPOC group [ 62 , 63 , 64 , 65 ]. We did not exclude studies based on our assessment of methodological limitations but used the information about methodological limitations to assess our confidence in the review findings.
We analysed the data by conducting a best fit framework synthesis [ 66 , 67 , 68 , 69 ]. Best fit framework synthesis is a qualitative synthesis method that blends deductive and inductive synthesis and analysis processes. As part of the synthesis method, review authors identify a conceptual framework that fits at least 50% of the data. After data extraction, data that does not fit within the framework is further analysed in order to develop a new framework that includes all of the data. We used the themes identified in the scoping review on older adults’ perceptions and experiences of integrated care by Lawless et al. [ 70 ], a conceptual framework from Chua et al. on choosing interventions for hip or knee osteoarthritis [ 48 ] as well as the PROGRESS Plus framework that addresses issues related to equity [ 71 ] to generate an a priori theoretical framework. We chose these frameworks as they were relevant to the topic we were exploring and expected to cover at least 50% of the data. The PROGRESS+ framework [ 71 ] was added to address the specific needs of the WHO guidelines process around equity, gender and human rights. HA moved the extracted data into the framework and CHH checked the data. We then analysed the data within each framework section and developed our findings. Relevant data that did not fit into the framework were analysed thematically. We used a thematic analysis approach as described by Miles and Huberman [ 72 ] as referred to in Carroll 2013 [ 66 ] in their paper on best fit framework synthesis. New themes were generated based on our interpretation of the evidence and constant comparison of the new themes across the included studies. In accordance with best fit framework synthesis methods, we inductively expanded the a priori framework to include a section on person-centred care and communication to reflect the breadth of all our findings.
Findings were then organized according to the domains defined in the WHO Handbook for Guideline Development that inform the determination of a recommendation, derived from qualitative evidence, including values and preferences, resource implications, equity and human rights, acceptability and feasibility (See Table 2 ).
Finally, we assessed our confidence in the findings using GRADE-CERQual [ 73 ]. We present detailed descriptions of our confidence assessment in Evidence Profile(s) [ 74 ].
In each section we present the summary of findings table and a summary of the main points discussed in the findings. For specific findings and our confidence in them please refer to Tables 4 - 9 (Summary of Qualitative Evidence Tables).
Review author reflexivity
Neither Heather Ames (HA), Christine Hillestad Hestevik (CHH) or Andrew Briggs (AMB) have reached the age of 60, so we do not understand the lived experience of being an older adult. HA is a previous elite athlete who has experience with chronic musculoskeletal pain and interventions due to injury and AMB has experience of chronic musculoskeletal pain. Both HA and AMB’s parents are over 60, have experienced chronic pain and have discussed their treatments with them. All authors support an evidence-based medicine approach to care. AMB is a clinician, researcher, and health systems professional in the field of chronic musculoskeletal pain. CHH does not have personal experience with chronic musculoskeletal pain or treatment interventions. She did her PhD on healthcare provided to older people from the perspectives of older persons, their family caregivers and healthcare professionals and has some experience with older persons experiences with encounters when in need of healthcare. These prior experiences, particularly a lived experience of chronic musculoskeletal pain, lead us to believe in the difficulties older people are facing. It also felt like the topics that were being raised were familiar from the perspective of personal and research experience.
From a yield of 1878 unique citations, 22 studies were included in this review, reflected in 24 reports. See Fig. 1 for the study selection process. For a description of the included studies see Table 3 .
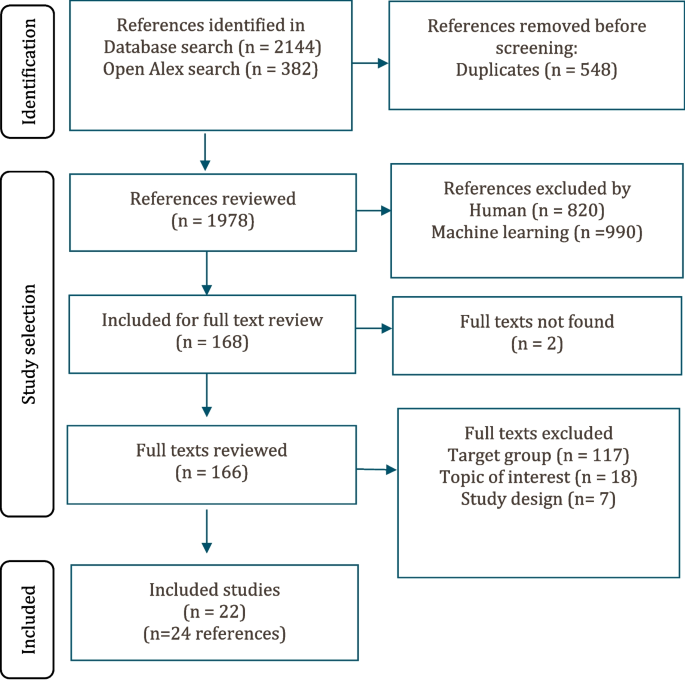
Study selection flowchart
The included studies were conducted in the United States ( n = 8) [ 53 , 54 , 78 , 90 , 91 , 93 , 94 , 96 ], United Kingdom ( n = 3) [ 77 , 79 , 92 ], Germany ( n = 2) [ 85 , 86 ], Sweden ( n = 2) [ 75 , 87 ], Australia ( n = 2) [ 84 , 88 , 89 ], Canada ( n = 1) [ 80 ], Chile ( n = 1) [ 95 ], Brazil ( n = 1) [ 76 ], and Nigeria ( n = 2) [ 81 , 82 , 83 ]. One study focused on Aboriginal Australians, a vulnerable population [ 88 , 89 ]. In 14 of the studies all participants were aged 60 or older [ 53 , 54 , 77 , 80 , 84 , 85 , 86 , 87 , 90 , 91 , 93 , 94 , 95 , 96 ]. In five, the mean or median age of the participants were 60 or older [ 75 , 76 , 78 , 79 , 92 ]. Three studies were included under the inclusion criteria for age for a low or middle-income country or identified vulnerable population [ 75 , 81 , 82 , 83 , 88 , 89 ]. In these studies, the age of the participants ranged from 26 to 72 years, but we only used disaggregated results from participants aged 40 or above.
In 16 of the studies, the participants were community-dwelling older adults [ 53 , 54 , 76 , 77 , 78 , 80 , 81 , 82 , 83 , 87 , 88 , 89 , 90 , 91 , 93 , 94 , 95 , 96 ]. Three of the studies were conducted in a primary health care setting but the residence of the participants was not discussed [ 75 , 85 , 86 ]. In three studies, the setting was unclear so we could not define the residence of the participants [ 79 , 84 , 92 ]. Nine of the studies were nested in a trial or a larger feasibility study [ 53 , 54 , 84 , 86 , 90 , 91 , 92 , 93 , 94 ].
We did not identify any studies that explored the perceptions or experiences of caregivers (formal or informal, family members).
Acceptability, values, and preferences
Since there was a large overlap in evidence related to values and preferences and acceptability, the findings are presented pooled. Values and preferences extended to interactions with health care providers, interventions for CPLBP and the modes of care delivery for CPLBP. Sixteen studies from 11 countries contributed to these findings (USA, Germany, Australia, United Kingdom, England, Scotland, Canada, Nigeria, Sweden, Brazil, and Chile). Participants in nine studies were all over 60 [ 54 , 77 , 80 , 85 , 87 , 91 , 93 , 95 , 96 ]. Four studies had participants with a mean or average age of 60 or older [ 75 , 76 , 79 , 92 ] and four studies were from LMICs or vulnerable populations [ 76 , 81 , 82 , 83 , 88 , 89 ] of which three were included based on a lowered age threshold [ 81 , 82 , 83 , 88 , 89 ]. In 13 of the studies most of the participants were women (53–83%) [ 54 , 75 , 76 , 77 , 79 , 80 , 81 , 82 , 85 , 87 , 91 , 93 , 95 , 96 ]. In two studies [ 83 , 92 ] there was an equal distribution of men and women. In one study most participants were men (52–66% men) [ 88 , 89 ].
Interactions with health care providers
Most participants wanted their health care providers to collaborate and work together to provide holistic care for their CPLBP. There was a preference among participants for providers who were respectful, caring, person-centred, collaborative, open to discussing treatment options and provided individualized care. They preferred health care providers who recognized them and their pain as individual and unique. This type of care allowed them to feel safe and feel they had meaningful relationships. When this was lacking, they could feel frustrated, vulnerable and experience a sense of aloneness (high confidence) [ 75 , 79 , 83 , 88 , 89 , 91 , 93 , 95 , 96 ].
Participants generally emphasized the care should be person-centred and provide continuity. They also identified a preference for a collaborative communication style which meant involving the older person in discussions about diagnosis and treatment options and viewing them as the expert on their own body (low confidence) [ 77 , 79 , 80 , 88 , 91 ].
Participants wanted collaboration and communication across their care teams to ensure co-ordinated care delivery and avoid duplication in care or diagnostics (moderate confidence) [ 75 , 88 , 91 ]. Some participants felt that they often received conflicting advice or information from health care providers. Participants valued receiving a diagnosis as this influenced their treatment decisions. The way the diagnosis was communicated could also shape their beliefs and responses to pain (moderate confidence) [ 76 , 79 , 81 , 83 , 85 , 89 , 91 , 92 , 95 ]. Some participants expressed dissatisfaction with health care providers for being unwilling to discuss treatment options other than medication (low confidence) [ 75 , 93 , 96 ]. The summary of findings is presented in Table 4 .
Values and preferences for CPLBP interventions in older people
Participants had clear values and preferences for how they chose a specific treatment for CPLBP. A choice of treatment could be influenced by previous experiences. Participants valued treatments that they viewed as effective, beneficial, and credible and fit them as individuals (high confidence) [ 53 , 54 , 79 , 80 , 81 , 82 , 84 , 85 , 86 , 87 , 93 , 95 , 96 ].
Most participants used and valued medication for its ability to provide short-term pain relief. However, many participants did not like the side effects associated with medications or the way the medication(s) made them feel (moderate confidence) [ 53 , 78 , 79 , 91 , 93 , 96 ]. Many also feared addiction, especially in relation to opioid analgesics. In some cases, participants adjusted or stopped medication without consulting their health care provider because of fears of adverse events (moderate confidence) [ 53 , 79 , 91 , 96 , 97 ].
Mindfulness and meditation encouraged participants to examine, assess, understand, and accept their pain rather than avoid it. Participants were able to use mindfulness and meditation for pain management and coping to varying degrees (moderate confidence) [ 54 , 90 , 94 ]. The summary of the findings is presented in Table 5 .
Format of interventions and educational materials for CPLBP in older people
Participants discussed their experiences with, and views of, organized and unorganized physical therapies and activities. Specific physical interventions were rarely mentioned. For many participants, physical activity was an important aspect of coping with their CPLBP. Many participants preferred a group format for physical exercises as it facilitated social support, collaboration and encouraged increased attendance (moderate confidence) [ 54 , 79 , 80 , 81 , 82 , 85 ]. Some participants also expressed preferences for educational material for physical interventions which had drawings and descriptions of the exercises. This made them more comprehensible, easier to follow and helpful for present and future reference (low confidence) [ 79 , 81 , 82 , 85 , 86 ].
Peer support interventions appeared to be acceptable and valued by some older people. They were seen as an acceptable way of gaining support and sharing information or advice. Participants mostly viewed peer support as feasible as it could be delivered through several different modalities (for example, face to face, in groups or online) that would fit individual preferences and lifestyles. However, it was clear that peer support was difficult to find and access in some settings, although appeared to be valued as a component of overall self-management of a CPLBP experience (low confidence) [ 77 , 78 , 80 , 92 , 96 ] [ 77 , 78 , 80 , 92 , 96 ].. The summary of the findings is presented in Table 6 .
Cost/resources related to CPLBP care in older people
Seven studies from five countries contributed to these findings (USA, Australia, England, Nigeria, and Sweden). Participants in three studies were all over 60 [ 53 , 84 , 91 ], two studies had participants with a mean or average age of 60 or older [ 75 , 79 ] and two studies were from LMICs or vulnerable populations of which both were included based on a lowered age threshold [ 83 , 88 , 89 ]. In five of the studies most of the participants where women (55–100%) [ 53 , 75 , 79 , 84 , 91 ]. In one study there was an equal distribution between men and women [ 83 ]. In one study most participants were men (66%) [ 88 , 89 ].
We found that cost and resources could be a barrier to accessing care for CPLBP for some participants. High costs (financial, time and travel) could render treatments inaccessible to participants or acts as a deterrent (moderate confidence) [ 53 , 79 , 83 , 91 ]. Many also preferred health care providers near where they lived to minimise travel burden. However, some participants were willing to travel if a trusted or favoured provider relocated, or they wanted to explore new treatment options. Others chose to find a new practitioner closer to them in this situation (moderate confidence) [ 53 , 75 , 79 , 83 , 84 , 88 , 91 ]. The summary of the findings is presented in Table 7 .
Feasibility
Twelve studies from eight countries contributed to these findings (USA, Canada, UK, Australia, England, Scotland, Nigeria, Chile). Participants in seven studies were all over 60 [ 53 , 77 , 80 , 84 , 91 , 95 , 96 ]. Three studies had participants with a mean or average age of 60 or older [ 78 , 79 , 92 ] and two studies were from LMICs or vulnerable populations of which both were included based on a lowered age threshold [ 81 , 82 , 83 ]. In 10 of the studies most of the participants where women (62–100%) [ 53 , 77 , 78 , 79 , 80 , 81 , 82 , 84 , 91 , 95 , 96 ]. In two studies there was about an equal distribution between men and women [ 83 , 92 ].
Some participants found information about treatments difficult to access and wanted help finding it or navigating the information from a health or care worker or through a peer support system. They felt that this could help them make decisions (low confidence) [ 78 , 79 , 84 , 92 , 96 ].
Physical activity and/or exercise was used a part of a self-management strategy for many participants. Activities such as swimming and walking were often mentioned as being done in their own time and when it fit their schedule. Some participants adopted physical exercise, assistive products, or alternative forms of treatment to supplement the conventional treatments they were receiving or when they felt “conventional treatments” failed. However, some did not inform their health care providers about their self-management strategies or changes they had made (moderate confidence). The summary of findings is presented in Table 8 .
Equity and human rights
Seven studies from six countries contributed to this finding (USA, Canada, UK, England, Scotland, and Sweden, Brazil). Participants in four studies were all over 60 [ 77 , 80 , 91 , 93 ] and three studies had participants with a mean or average age of 60 or older [ 75 , 79 , 92 ]. In six of the studies most of the participants were women [ 75 , 77 , 79 , 80 , 91 , 93 ]. In one study there was an equal distribution of men and women [ 92 ].
Some participants perceived age-related stigma or bias when accessing healthcare for their CPLBP. They reported feeling that they were treated differently, dismissed, or discriminated against because of their age. They felt they were not taken seriously. This perceived stigma could deter them from seeking further treatment. However, in other cases participants believed that they were taken more seriously as they aged (Low confidence). The summary of the finding is presented in Table 9 .
Additions to the framework
To incorporate all the data we analysed we expanded the framework to include a section we labelled person centred care.
Main findings
Based on this synthesis of qualitative evidence derived from more than 650 older participants across 22 studies with representation across a range of geographies and economic contexts, we identified that older people living with CPLBP express values and preferences for their care that relate to therapeutic encounters and the importance of therapeutic alliance, irrespective of the type of treatment offered or delivered, choice of intervention, and intervention delivery modalities. Older people with CPLBP value therapeutic encounters that validate, legitimise, and respect their pain experience; that consider their context holistically and prioritise their needs and preferences; that adopt a person-focused and tailored approach to care; and that are supported by interprofessional communication. Older people value care that provides benefit to them, that includes a suite of interventions beyond analgesic medicines alone, and that is financially and geographically accessible. These findings provide critical context to service delivery models for older people; formulation of recommendations for guidelines that relate to older people; and service considerations for the implementation of clinical guidelines into practice, particularly related to how health care workers interact with older people, with attention to potential age-related bias, and how components of care are delivered.
Person-centred care for older adults living with CPLBP
Many older people felt that healthcare providers did not legitimise their pain and that pain was deprioritised relative to other health conditions. Musculoskeletal pain, including CPLBP, is a common experience in older people [ 98 , 99 ] and a very frequent co-morbidity with other noncommunicable diseases [ 100 ]. Therefore, pain assessment is a key component of the WHO Integrated Care for Older People (ICOPE) assessment and care pathway [ 101 ]. Comorbidities more strongly associated with mortality or acute health declines can make it difficult for health professionals to prioritise symptoms of CPLBP in time-limited clinical encounters. There seems to be a difference between patient and care provider priorities when it comes to pain management and our findings point to the need to legitimise and respond to pain as this clearly is a priority for older people, consistent with recently reported evidence [ 55 ]. Our findings point to the importance of the therapeutic relationship and communication between older people and care providers to understand the impact of, and preference for, CPLBP care. Older people also experienced issues linked to equity during the therapeutic encounter. These could be expressed through ageism and stigma associated with CPLBP. Being told to ‘just live with it’, or the idea that CPLBP was an inevitable part of ageing were common and suggest a potential age-related bias among healthcare providers. Being aware of potential clinician bias related to chronic pain in older people is important, since ageism is associated with poorer health outcomes, particularly in low resource settings [ 102 ].
The needs and priorities of older people may well differ to younger adults (e.g. return to work, taking care of dependents, intensity of everyday activities or sport may be less important for older people). There are previous findings of the perceived needs of adult groups with CPLBP [ 103 , 104 ]. Consistent with other reviews among adults, we identified that older people value clear and consistent information, a clear diagnosis, prognosis, and a communication style that is meaningful and avoids jargon [ 105 ]. Communication that emphasises disability or impairments can be unhelpful to fostering pain self-efficacy, contribute to fear, unhelpful care seeking and further compound disability [ 106 , 107 , 108 , 109 ], which will foster healthy ageing. Rather, providing empowering and positive communication that is validating, helping to make sense of pain and the likelihood of a positive prognosis, providing cognitive reassurance and clear information about benefits and harms of interventions (in particular, medicines) can support shared decision-making, positive behaviour change towards effective self-management, and better engagement in meaningful activities [ 110 ]; all important for supporting healthy ageing.
We identified a preference for integrated and coordinated CPLBP care across care providers and facilities, consistent with the WHO ICOPE model [ 101 ]. This includes holistic care planning with comprehensive assessments and care plans aligned with the person’s values, priorities and preferences concerning their care. The older person should be involved with decision-making and goal-setting from the the start of their care journey. The care should be regular and include sustained follow-up, with integration and communication across different levels of care. This approach to care can help to avoid unnecessary treatments, polypharmacy and other potential harms [ 47 , 110 ]. Our findings about fears of side effects, dependency and medicine withdrawal or non-adherence also points to the need for clinicians to take time to explain risk-benefits of different medicines so that older people understand what medicines are for and how to use them safely.
Values and preferences were largely agnostic to intervention modality, other than values relating to medicines, where specific issues related to fear of adverse events were observed. Although analgesic medicines were considered important for CPLBP care, older people preferred care packages that extend beyond analgesia so that care is more holistic and considers safety (e.g. issues of dependency for opioid analgesics) and that were meaningful and personally enjoyable – such as social benefits of group exercise. Recent evidence points to the importance of considering pharmacologic and non-pharmacologic therapies for CPLBP care, consistent with the experiences, values and preferences of older people [ 97 ]. Other evidence highlights care needs also extend beyond biomedical domains [ 24 , 103 ]. Specifcally, tailoring components of care that addresses pain, emotional and social wellbeing, consistent with WHO ICOPE [ 101 ] model for improving functional ability, is important.
Implementing and delivering care for older people living with CPLBP
When developing, implementing, and delivering interventions for older people who experience functional disability related to musculoskeletal pain (or other co-morbidities), consideration of economic, social, and cultural contexts is critical. Many experienced financial and geographic barriers to care. Access to care that is expensive (or not included in UHC or insurance rebates), that requires travel, or accessing buildings that are not adapted for people experiencing functional disability can be problematic. This threat is more severe for those living in poverty without access to healthcare or who cannot afford to access healthcare near them, such as in low-resource settings. This lack of access may lead to worse outcomes for older people living in these settings, widening inequities in access to health care and health outcomes. Services also need to consider the user’s social context [ 111 ]. If not taken into account, pain care is likely to be inequitable and inaccessible. Support needs to go beyond the purely biomedical (especially focusing on medication) and encompass interventions that address peer support and socialization as well as issues around acceptability and stigma. Interventions should be tailored to local contexts to increase social and cultural approval. Some of the interventions included in this synthesis, such as exercise, were stigmatized in some settings [ 81 , 82 , 83 ]. Other research has also found that stigma can be associated with gender [ 112 ] or with interventions targeted at older people [ 113 ].
Older people also wanted support for the implementation of interventions such as guidance on how to perform exercises in the form of drawings and text. None of the studies we included talked about digital supports except for those related to peer support where digital meetings were discussed. While some formative evidence exists around the role of digital technologies to support healthy ageing [ 114 , 115 , 116 ], further research is required to understand users’ perspectives, benefits and harms in different contexts and among different population groups. Other research has also shown the acceptability of peer support in older adults with CPLBP [ 117 ]. Research on older people has found that they access digital tools but may face barriers such as physical mobility, sight and hearing impairment and low digital literacy when trying to use them [ 118 , 119 , 120 ]. Studies examining the use of digital tools for interventions for low back pain not limited to older people have found that users value models that are easily understandable, provide an opening to further communication with health care providers, family and colleagues and can provide prompts, reassurance, ongoing support and interaction with other users [ 121 , 122 ].
These empirical findings hold direct relevance to the formulation of recommendations in guidelines and implementation of recommended care within service models and local care pathways. In this context, the current QES has informed the development of the WHO Guideline for non-surgical management of chronic primary low back pain in adults in primary and community care settings [ 25 ]. Without consideration of the fundamental EtD factors (Table 2 ) and the evidence underpinning each when formulating recommendations for guidelines or implementation plans for service models, as presented in our QES, care recipients (and in some cases, care providers) may not accept or be able to access care, manifesting as an enduring disease burden and inequity in health outcomes. The QES findings, when coupled with evidence for benefit, harm, cost effectiveness and implementation feasibility and lived experience perspectives that contribute to co-creation of solutions (care recommendations, service models, care pathways) that are more likely to be implemented, sustainable and acceptable [ 123 ]. Indeed, consideration of qualitative evidence anchored to EtD domains is common practice for WHO guidelines [ 45 ].
Implications for research
There was a clear lack of research from low- and middle-income settings as well as vulnerable populations in all settings. Most of the included studies explored the perceptions of community dwelling older adults. More research on the experiences of older adults living in residential care or other settings could help to broaden our understanding. Very few of the studies explored perceptions of specific interventions. Most looked at treatment across interventions and participants did not differentiate between interventions in the same way a health care provider would. For example, participants viewed the visit to the physiotherapist as the intervention whereas health care providers would view each of the treatments received as individual interventions. One topic not frequently discussed in the included studies was cost and out of pocket expenses. This may be because several studies were conducted as part of a trial where participants did not pay to access the intervention. Cost was also rarely discussed in studies taking place in publicly funded health care systems. Understanding affordability of care, willingness to pay and inequities in access to care due to cost will be important in planning implementation of health services for CPLBP care for older people. Further research is also needed on the perspectives and experiences of caregivers as there were no studies identified that explored this topic of interest.
Implications for practice
The questions that form our implications for practice are derived from our findings with moderate or high confidence. They may help health system or program managers to plan, implement or manage interventions for CPLBP. It is important to consider local contextual factors including gender, age, cultural group, and education when implementing interventions.
Is the burden to access services low (financial, time and travel)? Have issues related to burden and equity of access been considered?
When planning, implementing, or managing an intervention for CPLBP or communicating with people over 60 with CPLBP:
◦ have participants values and preferences been explored and taken into consideration?
◦ are participants informed about the physical exercise or physical supports available to them?
When communicating with adults over 60 with CPLBP, have values and preferences been considered, regarding:
◦ communication, cultural preferences, and health care provider collaboration?
◦ receiving a diagnosis and preferences for information?
When prescribing medication, do health care workers provide open and honest communication with their patients about medications, the risk of side effects, and the risk of dependency, inviting them to return with concerns and informing of the importance of working together to manage their medications?
Older people with CPLBP value therapeutic encounters that legitimise and respect their pain experience, that consider their context holistically and prioritises their needs and preferences, that is tailored, and that is supported by interprofessional communication. Older people value care that provides benefit, that includes interventions beyond analgesic medicines alone, and that is financially and geographically accessible. These findings provide critical context to the implementation of clinical guidelines and service models into practice, particularly related to how care providers interact with older people and how components of care are delivered and their accessibility.
Availability of data and materials
All the studies in this synthesis are published and available. The data that is in each finding is available in an interactive Summary of Qualitative Findings table. For access to this tool please send an email to the corresponding author.
Abbreviations
Chronic primary low back pain
- Low back pain
- Qualitative evidence synthesis
Randomised controlled trial
Universal health coverage
Integrated care for older people
World health organization
Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10267):2006–17.
Article CAS PubMed PubMed Central Google Scholar
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–22.
Article Google Scholar
Ferreira ML, de Luca K, Haile LM, Steinmetz JD, Culbreth GT, Cross M, et al. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. 2023;5(6):e316-ee29.
Article CAS Google Scholar
Gill TK, Mittinty MM, March LM, Steinmetz JD, Culbreth GT, Cross M, et al. Global, regional, and national burden of other musculoskeletal disorders, 1990–2020, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. 2023;5(11):e670-ee82.
Black RJ, Cross M, Haile LM, Culbreth GT, Steinmetz JD, Hagins H, et al. Global, regional, and national burden of rheumatoid arthritis, 1990–2020, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. 2023;5(10):e594–610.
Beyera GK, O’Brien J, Campbell S. Health-care utilisation for low back pain: a systematic review and meta-analysis of population-based observational studies. Rheumatol Int. 2019;39(10):1663–79.
Article PubMed Google Scholar
Vigdal ØN, Storheim K, Killingmo RM, Småstuen MC, Grotle M. Characteristics of older adults with back pain associated with choice of first primary care provider: a cross-sectional analysis from the BACE-N cohort study. BMJ Open. 2021;11(9):e053229.
Article PubMed PubMed Central Google Scholar
Wong AY, Karppinen J, Samartzis D. Low back pain in older adults: risk factors, management options and future directions. Scoliosis Spinal Disord. 2017;12(1):1–23.
Paeck T, Ferreira ML, Sun C, Lin CWC, Tiedemann A, Maher CG. Are older adults missing from low back pain clinical trials? A systematic review and meta-analysis. Arthritis Care Res. 2014;66(8):1220–6.
Carvalho do Nascimento PR, Ferreira ML, Poitras S, Bilodeau M. Exclusion of older adults from ongoing clinical trials on low back pain: a review of the WHO trial registry database. J Am Geriatr Soc. 2019;67(3):603–8.
Rittweger J, Just K, Kautzsch K, Reeg P, Felsenberg D. Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise: a randomized controlled trial. Spine. 2002;27(17):1829–34.
Hutchinson AJ, Ball S, Andrews JC, Jones GG. The effectiveness of acupuncture in treating chronic non-specific low back pain: a systematic review of the literature. J Orthop Surg Res. 2012;7(1):1–8.
Yerlikaya M, Saracoglu İ. The attitudes and beliefs of physiotherapists, family physicians and physiatrists concerning chronic low back pain. J Health Sci Med. 5(2):393–8.
La Touche R, Escalante K, Linares MT. Treating non-specific chronic low back pain through the Pilates method. J Bodyw Mov Ther. 2008;12(4):364–70.
Senderovich H, Wagman H, Zhang D, Vinoraj D, Waicus S. The effectiveness of Cannabis and Cannabis derivatives in treating lower Back pain in the aged population: a systematic review. Gerontology. 2021;68:1–13.
Google Scholar
Netchanok S, Wendy M, Marie C. The effectiveness of Swedish massage and traditional Thai massage in treating chronic low back pain: a review of the literature. Complement Ther Clin Pract. 2012;18(4):227–34.
Wu L-C, Weng P-W, Chen C-H, Huang Y-Y, Tsuang Y-H, Chiang C-J. Literature review and meta-analysis of transcutaneous electrical nerve stimulation in treating chronic back pain. Reg Anesth Pain Med. 2018;43(4):425–33.
Owen PJ, Miller CT, Mundell NL, Verswijveren SJ, Tagliaferri SD, Brisby H, et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2020;54(21):1279–87.
Kolber MR, Ton J, Thomas B, Kirkwood J, Moe S, Dugré N, et al. PEER systematic review of randomized controlled trials: management of chronic low back pain in primary care. Can Fam Physician. 2021;67(1):e20–30.
Pillastrini P, Gardenghi I, Bonetti F, Capra F, Guccione A, Mugnai R, et al. An updated overview of clinical guidelines for chronic low back pain management in primary care. Joint Bone Spine. 2012;79(2):176–85.
World Health Organization. Development of WHO Guideline on management of chronic primary low back pain in adults. 2022. Available from: https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/ageing-and-health/integrated-care-for-older-people-icope/development-of-who-guideline-on-management-of-chronic-primary-low-back-pain-in-adults . Accessed 1 Sept 2023.
Cesari M, Sumi Y, Han ZA, Perracini M, Jang H, Briggs A, et al. Implementing care for healthy ageing. BMJ Glob Health. 2022;7(2):e007778.
Lee D-CA, Burton E, Slatyer S, Jacinto A, Oliveira D, Bryant C, et al. Understanding the role, quality of life and strategies used by older carers of older people to maintain their own health and well-being: a national Australian survey. Clin Interv Aging. 2022;17:1549–67.
Slater H, Jordan JE, O’Sullivan PB, Schütze R, Goucke R, Chua J, et al. ‘Listen to me, learn from me’: a priority setting partnership for shaping interdisciplinary pain training to strengthen chronic pain care. Pain. 2022;163.
WHO guideline for non-surgical management of chronic primary low back pain in adults in primary and community care settings. Geneva: World Health Organization; 2023. https://www.who.int/publications/i/item/9789240081789 . Licence: CC BY-NC-SA 3.0 IGO.
Cancelliere C, Hincapié C, Bussières A, Gross D, Pereira P, Mior S, et al. Education or advice for chronic primary low back pain in adults; A systematic review protocol. PROSPERO; 2022.
Cancelliere C, Hayden J, Ogilvie R, Hincapié C, Bussières A, Gross D, et al. Exercise therapy for chronic primary low back pain in adults; A systematic review protocol. PROSPERO; 2022.
Rubinstein S, de Zoete A, Innocenti T, Maas E, Pellekooren S, Chiarotto A, et al. Systematic review on the effect of spinal manipulative therapy in people with chronic primary low back pain (protocol). PROSPERO; 2022.
Maas E, Pellekooren S, Ostelo R, Innocenti T, Chiarotto A, de Zoete A, et al. Systematic review on the effect of massage therapy in people with chronic primary low back pain (protocol). PROSPERO; 2022.
Pellekooren S, Maas E, Wegner I, Ostelo R, Innocenti T, Chiarotto A, et al. Systematic review on the effect of traction in people with chronic primary low back pain (protocol). PROSPERO; 2022.
Cancelliere C, Hincapié C, Bussières A, Gross D, Pereira P, Mior S, et al. Acupuncture for chronic primary low back pain in adults (protocol). PROSPERO; 2022.
Cancelliere C, Hincapié C, Bussières A, Gross D, Pereira P, Mior S, et al. Transcutaneous electrical nerve stimulation (TENS) for chronic primary low back pain in adults (protocol). PROSPERO; 2022.
Probyn K, Petkovic J, Cogo E, Bergman H, Arienti C, Negrini S, et al. Protocolfor a systematic review on therapeutic ultrasound for chronic primary low back painin adults. Open science framework; 2022.
Probyn K, Villannueva G, Cogo E, Bergman H, Petkovic J, Conde M, et al. Protocolfor a systematic review on psychosocial therapies for chronic primary low back painin adults. Open science framework; 2022.
Chou R, Dana T. Pharmacotherapies for chronic primary low back pain: systematic review to inform the WHO global guideline on chronic primary low back pain in adults (protocol). PROSPERO; 2022.
Wewege M, Bagg M, Jones M, McAuley J. Analgesic medicines for adults with low back pain: a systematic review and network meta-analysis (protocol). PROSPERO.; 2019.
Chou R, Hartung D, Turner J, Blazina I, Chan B, Levander X, et al. Opioid treatments for chronic pain. Comparative Effectiveness Review No. 229. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2015-00009-I.) 2020.
McDonagh MS, Selph SS, Buckley DI, Holmes RS, Mauer K, Ramirez S, et al. Nonopioid pharmacologic treatments for chronic pain. Comparative Effectiveness Review No. 228.; 2020.
Chou R, Pinto RZ, Fu R, Lowe RA, Henschke N, McAuley JH, et al. Systemic corticosteroids for radicular and non-radicular low back pain. Cochrane Database Syst Rev. 2022;10.
Probyn K, Villannueva G, Cogo E, Bergman H, Conde M, Negrini S, et al. Protocolfor a systematic review on localanaesthetic agents for chronic primary lowback painin adults. Open science framework; 2022.
McDonagh M, Wagner J, Ahmed AY, Fu R, Morasco B, Kansagara D, et al. Living systematic review on Cannabis and other plant-based treatments for chronic pain. Comparative Effectiveness Review No. 250. . 2021.
Probyn K, Villannueva G, Chi Y, Cogo E, Conde M, Berman B, et al. Protocolfor a systematic review on herbal medicinesfor chronic primary low back painin adults. Open science framework; 2022.
Williams C, Tutty A, Cashin A, McAuley J, Kamper S, Michaleff Z, et al. Effectiveness of weight management intervention for chronic primary low back pain care: protocol for a systematic review and meta-analysis to inform the WHO global guideline on low back pain in adults. PROSPERO; 2022.
Probyn K, Villannueva G, Bergman H, Arienti C, Minozzi S, Lazzarini SG, et al. Protocolfor a systematic review on biopsychosocial rehabilitationfor chronic primary low back painin adults. Open science framework; 2022.
World Health Organization. WHO handbook for guideline development. World Health Organization; 2014.
Care AGSEPoPC, Brummel-Smith K, Butler D, Frieder M, Gibbs N, Henry M, et al. Person-centered care: a definition and essential elements. J Am Geriatr Soc. 2016;64(1):15–8.
Hutting N, Caneiro J, Ong'wen OM, Miciak M, Roberts L. Person-centered care for musculoskeletal pain: Putting principles into practice. Musculoskelet Sci Pract.. 2022:102663.
Chua J, Briggs AM, Hansen P, Chapple C, Abbott JH. Choosing interventions for hip or knee osteoarthritis-what matters to stakeholders? A mixed-methods study. Osteoarthr Cartil Open. 2020;2(3):100062.
Kløjgaard ME, Manniche C, Pedersen LB, Bech M, Søgaard R. Patient preferences for treatment of low back pain—a discrete choice experiment. Value Health. 2014;17(4):390–6.
Staats P, Deer T, Ottestad E, Erdek M, Spinner D, Gulati A. Understanding the role of patient preference in the treatment algorithm for chronic low back pain: results from a survey-based study. Pain Manag. 2021;12.
Walsh DA, Boeri M, Abraham L, Atkinson J, Bushmakin AG, Cappelleri JC, et al. Exploring patient preference heterogeneity for pharmacological treatments for chronic pain: a latent class analysis. Eur J Pain. 2022;26(3):648–67.
Rutgers KM. Shared decision making in physical therapy treatments of people with intermittent claudication, before and after the implementation of KomPas; a pre-post study. 2021. Master's Thesis.
Stensland M. Managing the incurable: older pain clinic Patients’ experiences of managing treatment-resistant chronic low Back pain. J Gerontol Soc Work. 2021;64(4):405–22.
Lee TLSK, Hawkes RJ, Phelan EA, Turner JA. The benefits of T'ai Chi for older adults with chronic Back pain: a qualitative study. J Altern Complement Med. 2020;26(6):456–62.
Slater H, Jordan JE, O'Sullivan PB, Schütze R, Goucke R, Chua J, et al. “Listen to me, learn from me”: a priority setting partnership for shaping interdisciplinary pain training to strengthen chronic pain care. Pain. 2022;10(1097).
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2019.
Book Google Scholar
Noyes J, Booth A, Cargo M, Flemming K, Harden A, Harris J, et al. Qualitative evidence. Cochrane Handbook for systematic reviews of interventions; 2019. p. 525–45.
Nicholas M, Vlaeyen JW, Rief W, Barke A, Aziz Q, Benoliel R, et al. The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain. 2019;160(1):28–37.
OpenAlex. OpenAlex documentation 2022 [Available from: https://docs.openalex.org/ .
Priem J, Piwowar H, Orr R. OpenAlex: A fully-open index of scholarly works, authors, venues, institutions, and concepts. arXiv preprint arXiv:220501833. 2022.
Thomas J, Brunton J, Graziosi S. EPPI-reviewer 4: software for research synthesis. EPPI-Centre software. London: Social Science Research Unit, UCL Institute of Education; 2010.
Ames HM, Glenton C, Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database Syst Rev. 2017;2.
Ames HM, Glenton C, Lewin S, Tamrat T, Akama E, Leon N. Clients’ perceptions and experiences of targeted digital communication accessible via mobile devices for reproductive, maternal, newborn, child, and adolescent health: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2019;10.
Munabi-Babigumira S, Glenton C, Lewin S, Fretheim A, Nabudere H. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low-and middle-income countries: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2017;11.
Glenton C, Carlsen B, Lewin S, Wennekes MD, Winje BA, Eilers R. Healthcare workers’ perceptions and experiences of communicating with people over 50 years of age about vaccination: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2021;7.
Carroll C, Booth A, Leaviss J, Rick J. “Best fit” framework synthesis: refining the method. BMC Med Res Methodol. 2013;13(1):1–16.
Booth A, Carroll C. How to build up the actionable knowledge base: the role of ‘best fit’framework synthesis for studies of improvement in healthcare. BMJ Qual Saf. 2015;24(11):700–8.
Carroll C, Booth A, Cooper K. A worked example of" best fit" framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. 2011;11(1):1–9.
Brunton G, Oliver S, Thomas J. Innovations in framework synthesis as a systematic review method. Res Synth Methods. 2020;11(3):316–30.
Lawless MT, Marshall A, Mittinty MM, Harvey G. What does integrated care mean from an older person’s perspective? A scoping review. BMJ Open. 2020;10(1):e035157.
O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol. 2014;67(1):56–64.
Huberman M, Miles MB. The qualitative researcher’s companion. Sage; 2002.
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. BioMed Central; 2018.
Lewin S, Bohren M, Rashidian A, Munthe-Kaas H, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings—paper 2: how to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implement Sci. 2018;13(1):11–23.
Allvin R, Fjordkvist E, Blomberg K. Struggling to be seen and understood as a person - chronic back pain patients’ experiences of encounters in health care: an interview study. Nurs Open. 2019;6(3):1047–54.
Bonfim IDS, Correa LA, Nogueira LAC, Meziat-Filho N, Reis FJJ, de Almeida RS. Your spine is so worn out - the influence of clinical diagnosis on beliefs in patients with non-specific chronic low back pain - a qualitative study. Braz J Phys Ther. 2021;25(6):811–8.
Cooper K, Schofield P, Klein S, Smith BH, Jehu LM. Exploring peer-mentoring for community dwelling older adults with chronic low back pain: a qualitative study. Physiotherapy. 2017;103(2):138–45.
Cummings EC, van Schalkwyk GI, Grunschel BD, Snyder MK, Davidson L. Self-efficacy and paradoxical dependence in chronic back pain: a qualitative analysis. Chronic Illness. 2017;13(4):251–61.
Dima A, Lewith GT, Little P, Moss-Morris R, Foster NE, Bishop FL. Identifying patients’ beliefs about treatments for chronic low back pain in primary care: a focus group study. Br J Gen Pract. 2013;63(612):e490–8.
Hay ME, Connelly DM. Exploring the experience of exercise in older adults with chronic Back pain. J Aging Phys Act. 2020;28(2):294–305.
Igwesi-Chidobe CN, Godfrey EL, Kitchen S, Onwasigwe CN, Sorinola IO. Community-based self-management of chronic low back pain in a rural African primary care setting: a feasibility study. Primary Health Care Res Dev. 2019;20:e45.
Igwesi-Chidobe CN, Kitchen S, Sorinola IO, Godfrey EL. Evidence, theory and context: using intervention mapping in the development of a community-based self-management program for chronic low back pain in a rural African primary care setting - the good back program. BMC Public Health. 2020;20(1):343.
Igwesi-Chidobe CN, Kitchen S, Sorinola IO, Godfrey EL. “a life of living death”: the experiences of people living with chronic low back pain in rural Nigeria. Disabil Rehabil. 2017;39(8):779–90.
Kirby ER, Broom AF, Adams J, Sibbritt DW, Refshauge KM. A qualitative study of influences on older women’s practitioner choices for back pain care. BMC Health Serv Res. 2014;14:131.
Kuss K, Leonhardt C, Quint S, Seeger D, Pfingsten M, Wolf P, et al. Graded activity for older adults with chronic low Back pain: program development and mixed methods feasibility cohort study. Pain Med. 2016;17(12):2218–29.
Leonhardt C, Kuss K, Becker A, Basler H-D, de Jong J, Flatau B, et al. Graded exposure for chronic low Back pain in older adults: a pilot study. J Geriatr Phys Ther. 2017;40(1):51–9.
Lilje SC, Olander E, Berglund J, Skillgate E, Anderberg P. Experiences of older adults with Mobile phone text messaging as reminders of home exercises after specialized manual therapy for recurrent low Back pain: a qualitative study. JMIR MHealth UHealth. 2017;5(3):e39.
Lin I, O’Sullivan P, Coffin J, Mak DB, Toussaint S, Straker L. “I can sit and talk to her”: Aboriginal people, chronic low back pain and healthcare practitioner communication. Aust Fam Physician. 2014;43(5):320–4.
Lin IB, O'Sullivan PB, Coffin JA, Mak DB, Toussaint S, Straker LM. Disabling chronic low back pain as an iatrogenic disorder: a qualitative study in Aboriginal Australians. BMJ Open. 2013;3(4).
Luiggi-Hernandez JG, Woo J, Hamm M, Greco CM, Weiner DK, Morone NE. Mindfulness for chronic low Back pain: a qualitative analysis. Pain Med. 2018;19(11):2138–45.
Lyons Kevin J, Salsbury Stacie A, Hondras Maria A, Hondras Maria A, Jones Mark E, Andresen Andrew A, et al. Perspectives of older adults on co-management of low back pain by doctors of chiropractic and family medicine physicians: a focus group study. BMC Complement Altern Med. 2013;13(1):225.
MacKichan F, Paterson C, Britten N. GP support for self-care: the views of people experiencing long-term back pain. Fam Pract. 2013;30(2):212–8.
Makris Una E, Makris Una E, Higashi Robin T, Marks Emily G, Fraenkel L, Fraenkel L, et al. Ageism, negative attitudes, and competing co-morbidities – why older adults may not seek care for restricting back pain: a qualitative study. Bmc Geriatrics. 2015;15(1):39.
Morone NE, Lynch CS, Greco CM, Tindle HA, Weiner DK. “I felt like a new person” the effects of mindfulness meditation on older adults with chronic pain: qualitative narrative analysis of diary entries. J Pain. 2008;9(9):841–8.
Rodriguez I, Abarca E, Herskovic V, Campos M. Living with chronic pain: a qualitative study of the daily life of older people with chronic pain in Chile. Pain Res Manag. 2019;2019:8148652.
Teh Carrie F, Karp Jordan F, Kleinman Arthur M, Reynolds Charles F, Weiner Debra L, Cleary PD. Older People’s experiences of patient-centered treatment for chronic pain: a qualitative study. Pain Med. 2009;10(3):521–30.
Makris UE, Higashi RT, Marks EG, Fraenkel L, Gill TM, Friedly JL, et al. Physical, emotional, and social impacts of restricting back pain in older adults: a qualitative study. Pain Med. 2016;18(7):1225–35.
PubMed Central Google Scholar
Wong CK, Mak RY, Kwok TS, Tsang JS, Leung MY, Funabashi M, et al. Prevalence, incidence, and factors associated with non-specific chronic low back pain in community-dwelling older adults aged 60 years and older: a systematic review and meta-analysis. J Pain. 2022;23(4):509–34.
De Souza IMB, Sakaguchi TF, Yuan SLK, Matsutani LA, do Espírito-Santo AdS, Pereira CAdB, et al. Prevalence of low back pain in the elderly population: a systematic review. Clinics. 2019;74.
Simões D, Araújo FA, Severo M, Monjardino T, Cruz I, Carmona L, et al. Patterns and consequences of multimorbidity in the general population: there is no chronic disease management without rheumatic disease management. Arthritis Care Res. 2017;69(1):12–20.
World Health Organization. Integrated care for older people (ICOPE): guidance for person-centred assessment and pathways in primary care. World Health Organization; 2019.
Chang ES, Kannoth S, Levy S, Wang SY, Lee JE, Levy BR. Global reach of ageism on older persons’ health: a systematic review. PLoS One. 2020;15(1):e0220857.
Chou L, Cicuttini FM, Urquhart DM, Anthony SN, Sullivan K, Seneviwickrama M, et al. People with low back pain perceive needs for non-biomedical services in workplace, financial, social and household domains: a systematic review. J Phys. 2018;64(2):74–83.
Van Rysewyk S, Blomkvist R, Chuter A, Crighton R, Hodson F, Roomes D, et al. Understanding the lived experience of chronic pain: a systematic review and synthesis of qualitative evidence syntheses. Br J Pain. 2023;17:20494637231196424.
Lim YZ, Chou L, Au RT, Seneviwickrama KMD, Cicuttini FM, Briggs AM, et al. People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: a systematic review. J Physiother. 2019;65(3):124–35.
O’Keeffe M, Ferreira GE, Harris IA, Darlow B, Buchbinder R, Traeger AC, et al. Effect of diagnostic labelling on management intentions for non-specific low back pain: a randomized scenario-based experiment. Eur J Pain. 2022;26(7):1532–45.
O’Keeffe M, Michaleff ZA, Harris IA, Buchbinder R, Ferreira GE, Zadro JR, et al. Public and patient perceptions of diagnostic labels for non-specific low back pain: a content analysis. Eur Spine J. 2022;31(12):3627–39.
Sloan TJ, Walsh DA. Explanatory and diagnostic labels and perceived prognosis in chronic low Back pain. Spine. 2010;35(21).
Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain. 2012;16(1):3–17.
Article CAS PubMed Google Scholar
Belton J, Birkinshaw H, Pincus T. Patient-centered consultations for persons with musculoskeletal conditions. Chiropr Man Ther. 2022;30(1):53.
Ashton-James CE, Anderson SR, Mackey SC, Darnall BD. Beyond pain, distress, and disability: the importance of social outcomes in pain management research and practice. Pain. 2022;163(3):e426-ee31.
Ruissen GR, Liu Y, Schmader T, Lubans DR, Harden SM, Wolf SA, et al. Effects of group-based exercise on flourishing and stigma consciousness among older adults: findings from a randomised controlled trial. Appl Psychol: Health Well-Being. 2020;12(2):559–83.
PubMed Google Scholar
Bunn F, Dickinson A, Barnett-Page E, Mcinnes E, Horton K. A systematic review of older people’s perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing Soc. 2008;28(4):449–72.
Ienca M, Schneble C, Kressig RW, Wangmo T. Digital health interventions for healthy ageing: a qualitative user evaluation and ethical assessment. BMC Geriatr. 2021;21:1–10.
De Santis KK, Mergenthal L, Christianson L, Busskamp A, Vonstein C, Zeeb H. Digital Technologies for Health Promotion and Disease Prevention in older people: scoping review. J Med Internet Res. 2023;25:e43542.
Pan American Health Organization and International Telecommunication Union. The role of digital Technologies in Aging and Health. Washington, D.C.; 2023.
Cooper K, Schofield P, Smith BH, Klein S. PALS: peer support for community dwelling older people with chronic low back pain: a feasibility and acceptability study. Physiotherapy. 2020;106:154–62.
Terp R, Kayser L, Lindhardt T. Older patients’ competence, preferences, and attitudes toward digital technology use: explorative study. JMIR Hum Factors. 2021;8(2):e27005.
Fenge L-A, Melacca D, Lee S, Rosenorn-Lanng E. Older peoples’ preferences and challenges when using digital technology: a systematic review with particular reference to digital games. Int J Educ Ageing. 2019;5(1):61–78.
Airola E. Learning and use of eHealth among older adults living at home in rural and nonrural settings: systematic review. J Med Internet Res. 2021;23(12):e23804.
Svendsen MJ, Wood KW, Kyle J, Cooper K, Rasmussen CDN, Sandal LF, et al. Barriers and facilitators to patient uptake and utilisation of digital interventions for the self-management of low back pain: a systematic review of qualitative studies. BMJ Open. 2020;10(12):e038800.
Geraghty AW, Roberts LC, Stanford R, Hill JC, Yoganantham D, Little P, et al. Exploring patients’ experiences of internet-based self-management support for low back pain in primary care. Pain Med. 2020;21(9):1806–17.
Belton JL, Slater H, Ravindran TS, Briggs AM. Harnessing People’s lived experience to strengthen health systems and support equitable musculoskeletal health care. J Orthop Sports Phys Ther. 2023;53(4):162–71.
Download references
Acknowledgements
We would like to acknowledge our search specialist Elisabet Hafstad for her expertise in developing and conducting the search for this synthesis.
Open access funding provided by Norwegian Institute of Public Health (FHI) This synthesis was commissioned and funded by the WHO to contribute to a guidelines process. The lead authors (HA and CHH) discussed the synthesis objectives and inclusion criteria with the commissioner. HA and CHH independently conducted the synthesis and came to the findings.
Author information
Authors and affiliations.
The Norwegian Institute of Public Health, PO Box 222, 0213, Oslo, Skøyen, Norway
Heather Ames & Christine Hillestad Hestevik
Ageing and Health Unit, Department of Maternal, Newborn, Child & Adolescent Health and Ageing, World Health Organization, Avenue Appia 20, 1211, Geneva, Switzerland
Andrew M. Briggs
Faculty of Health Sciences, Curtin University, PO Box U1987, Perth, 6845, Western Australia
You can also search for this author in PubMed Google Scholar
Contributions
All authors conceptualised the synthesis and wrote the protocol. HA and CHH conducted the search, study selection, analysis, and decision on findings. AMB was not involved in data extraction or synthesis. AMB acted as a subject expert during the synthesis process and connecting the findings of the synthesis to the broader field. All authors were involved in drafting this manuscript.
Authors’ information
HA is an anthropologist and health systems research who has been working with qualitative evidence synthesis since 2013. She is a senior researcher at the Norwegian Institute of Public Health and an Associate convener with the Cochrane Qualitative and Implementation Methods Group.
CHH is a health systems researcher with a speciality within nutrition. She has been working with qualitative evidence synthesis since 2018. She is a senior advisor at the Norwegian Institute of Public Health where she specialises in conducting systematic reviews.
AMB is a consultant to the WHO, supporting the development of the WHO Guideline on chronic primary low back pain in adults. He is also a health systems and services researcher and practicing physiotherapist.
Corresponding author
Correspondence to Heather Ames .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
HA and CHH declare that they have no competing interests. AMB declares he works as a consultant to the WHO.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search strategy.
Additional file 2.
Machine learning plan.
Additional file 3.
Excluded full text studies with reason.
Additional file 4.
Evidence profile table.
Additional file 5.
Final adapted framework.
Additional file 6.
ENTREQ Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ames, H., Hestevik, C.H. & Briggs, A.M. Acceptability, values, and preferences of older people for chronic low back pain management; a qualitative evidence synthesis. BMC Geriatr 24 , 24 (2024). https://doi.org/10.1186/s12877-023-04608-4
Download citation
Received : 29 March 2023
Accepted : 16 December 2023
Published : 05 January 2024
DOI : https://doi.org/10.1186/s12877-023-04608-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Interventions
- Older adults
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 08 April 2024
Transformational nurse leadership attributes in German hospitals pursuing organization-wide change via Magnet® or Pathway® principles: results from a qualitative study
- Joan Kleine ORCID: orcid.org/0009-0005-1727-3683 1 ,
- Julia Köppen ORCID: orcid.org/0000-0001-7941-641X 1 , 2 ,
- Carolin Gurisch ORCID: orcid.org/0009-0008-3763-7220 3 &
- Claudia B. Maier ORCID: orcid.org/0000-0002-7734-2258 2
BMC Health Services Research volume 24 , Article number: 440 ( 2024 ) Cite this article
Metrics details
Budget constraints, staff shortages and high workloads pose challenges for German hospitals. Magnet® and Pathway® are concepts for implementing organization-wide change and redesigning work environments. There is limited research on the key elements that characterize nurse leaders driving the implementation of Magnet®/Pathway® principles outside the U.S. We explored the key attributes of nurse leaders driving organization-wide change through Magnet®/Pathway® principles in German hospitals.
Using a qualitative study design, semi-structured interviews ( n = 18) were conducted with nurse leaders, managers, and clinicians, in five German hospitals known as having started implementing Magnet® or Pathway® principles. The interviews were recorded and transcribed verbatim. Data were analyzed in Atlas.ti using content analysis. For the analysis, a category system was created using a deductive-inductive approach.
Five leadership attributes and eleven sub-attributes were identified as main themes and sub-themes: Visionary leaders who possess and communicate a strong vision and serve as role models to inspire change. Strategic leaders who focus on strategic planning and securing top management support. Supportive leaders who empower, emphasizing employee motivation, individualized support, and team collaboration. Stamina highlights courage, assertiveness, and resilience in the face of challenges. Finally, agility which addresses a leader’s presence, accessibility, and rapid responsiveness, fostering adaptability.
Conclusions
The study demonstrates leadership attributes explicitly focusing on instigating and driving organization-wide change through Magnet®/Pathway® principles in five German hospitals. The findings suggest a need for comprehensive preparation and ongoing development of nurse leaders aimed at establishing and sustaining a positive hospital work environment.
Peer Review reports
European hospitals are facing multiple challenges, including economic pressure, cost containment strategies, technological advancements, and shortages of healthcare professionals, which require constant adaptation [ 1 , 2 , 3 , 4 ]. Particularly concerning is the high burden of mental distress reported by nurses and other healthcare professionals [ 5 , 6 ]. It is increasingly recognized that the root causes of increased stress and burnout among nurses are linked to the work environment in hospitals and other healthcare settings, that is why hospitals should strive to change their working conditions [ 7 , 8 ].
The Magnet Recognition Program® (Magnet) and the Pathway to Excellence® Program (Pathway), both originating in the United States (U.S.) and held at the American Nurses Credentialing Center (ANCC), are designed to facilitate organizational-wide change of work environments, enhancing employee well-being, retention, productivity, and patient outcomes [ 9 , 10 , 11 ]. These concepts can provide a structured approach for European hospitals to tackle the challenges of the future effectively.
Research on Magnet hospitals, primarily conducted in the U.S., suggests that Magnet can enhance working conditions, job satisfaction, and nurse well-being in hospitals [ 12 , 13 , 14 , 15 ], while also improving patient outcomes [ 14 , 15 , 16 ]. However, findings across studies and outcomes vary. In contrast, the impact of Pathway has received less attention in research. Nevertheless, some studies have indicated that Pathway promotes increased nurse autonomy and decision-making authority, fosters leadership development, improves safety and quality standards, enhances employee well-being, and supports professional growth [ 17 , 18 ].
As of December 2023, 591 organizations worldwide had Magnet designation [ 19 ], and 214 had Pathway designation [ 20 ], with the majority in the U.S. Internationally, only 17 hospitals hold Magnet designation [ 19 ] and 16 have Pathway designation [ 20 ]. While none of them are in Germany, some German hospitals have proactively started implementing Magnet/Pathway principles to drive organization-wide changes aiming at enhancing job satisfaction, attracting and retaining healthcare professionals [ 21 , 22 , 23 , 24 ]. Hence, the inclusion of Magnet and Pathway principles as comparable case examples of organization-wide change in the current study is justified by the growing proactive adoption of these concepts by some German hospitals.
Magnet and Pathway focus on promoting nurse engagement and supporting professional nursing practice environments. The difference lies in their specific objectives: Magnet emphasizes sustained quality patient care, nursing excellence, and innovations in professional practice, while Pathway highlights creating supportive practice environments that empower and engage staff and is known for having less stringent data requirements [ 25 , 26 ]. However, both aim to cultivate a culture of nursing care excellence, supported by a transformational leadership style [ 25 ], which is the central focus of the present study.
Leadership skills do play a crucial role in successfully promoting organization-wide change [ 27 , 28 , 29 ] and has also been shown to have a profound impact on employee stress and emotional well-being [ 30 ]. Transformational leadership was identified as one effective leadership style in healthcare settings [ 29 , 31 , 32 , 33 ]. Transformational leaders motivate employees towards an organizational vision by inspiring and empowering them to continuously develop themselves and addressing their individual needs [ 34 , 35 ]. The theoretical framework for transformational leadership was first conceptualized in the 1970s, defining it as a relationship between leaders and employees who motivate, empower, and elevate each other’s moral values in pursuit of fulfilling common interests [ 36 ]. Further expansion by Bass and Avolio introduced four subcategories that represent the characteristics of transformational leaders: Idealized influence, inspirational motivation, intellectual stimulation, and individualized consideration [ 34 , 35 ].
Several U.S. studies have analyzed the relationship between transformational leadership and the implementation of Magnet principles [ 37 , 38 , 39 ]. In a southern U.S. nonprofit acute care hospital seeking Magnet designation, a survey of 115 staff nurses showed that transformational leadership style was positively associated with nurses’ job satisfaction and satisfaction with promotion opportunities [ 37 ]. Magnet hospital CNOs rated their transformational leadership practices highly and reported a strong positive correlation between engagement and leadership practice, with empowering others as the most important practice [ 38 ]. A study of clinical nurse leaders, who attended the 2016 Magnet Conference in Orlando, Florida, showed a positive relationship between transformational leadership practices and work engagement, but observed differences in leadership practices and work engagement based on varying levels of education [ 39 ].
The majority of research conducted outside of the U.S. has focused on investigating the impact of transformational leadership style within healthcare settings, with no focus on the implementation of Magnet/Pathway [ 29 , 31 , 32 , 33 , 37 , 40 , 41 , 42 , 43 , 44 , 45 ]. Several studies found that forms of transformational leadership styles resulted in positive organizational performance, such as improved staff retention, lower turnover, and better quality of care [ 31 , 32 , 33 , 37 , 40 , 41 ]. A systematic review including 12 studies from the US, Canada, Saudi Arabia, China, Ethiopia, Italy, and Jordan, showed a positive correlation between transformational leadership and nurses’ job satisfaction in the hospital setting [ 29 ].
To date, most of the qualitative studies analyzed transformational leadership style from the nurse leaders’ perspective. A study from Finland used a qualitative design to examine nurses’ leadership skills in leading change [ 44 ]. They identified three main roles: First, ‘leading interpersonal relationships’ including competencies of being a team player, coach, and parental figure. Second, ‘leading processes’ including competencies such as organizing, coordinating, and being a conductor based on the organization’s mission. And third, ‘leading a culture’ is defined as advocating values and norms and creating an open, resilient, and evidence-based culture [ibid.]. Another study from 2016 explored senior nurses’ experiences of organization-wide change leadership in three NHS acute hospitals in England through in-depth interviews [ 43 ]. The aspect of leadership was frequently discussed in relation to organization-wide change. An effective nurse leader was characterized as a strong, inspiring, and supportive leader with novel and heroic approaches [ibid.]. Weak leaders were those who did not encourage their teams, had poor presence and were unresponsive to the need for change [ibid]. Another qualitative study used a grounded theory approach to examine the processes nursing management uses to promote change on their wards in five hospitals in Japan [ 45 ]. According to the interviewees, the change management process led by nurse managers consists of having beliefs and being able to empathize with the nursing staff to achieve common goals [ibid.]. Four characteristics of nurse leaders were reported as indispensable factors for change: having both a micro and macro perspective; respecting their own beliefs and external standards; being proactive; having empathy for nursing staff [ibid.]. A 2020 study conducted in a university hospital in Brazil, examined the challenges of exercising transformational leadership and strategies nurses leaders used to address these challenges include being role models for the team, proactively maintaining dialogue with co-workers, and building empathetic relationships [ 42 ].
In German hospitals, a cross-sectional study investigated nursing leadership styles, analyzing the self-assessment of 93 ward managers and the external evaluation of 1,567 employees with the multifactorial leadership questionnaire (MLQ-5X), revealing the presence of transformational leadership practices [ 46 ]. The ward management consistently achieved mean values above the scale mean in all dimensions of transformational leadership, both in the self-assessment and in the external evaluation [ibid.]. However, despite the acknowledged existence of transformational leadership practices in nursing within German hospitals, research on the attributes of nurse leaders that support organization-wide change through implementation of Magnet/Pathway principles remains scarce. This study aims to identify beneficial attributes of nurse leaders from German hospitals, shedding light on their role in driving organization-wide change through Magnet/Pathway and advancing the understanding of leadership practices’ impact within the German healthcare systems. Research on this topic is critical to fill a gap in the literature regarding nurse leader attributes that facilitate organization-wide change and can provides insights that could inform nursing leadership development initiatives tailored to the needs of German hospitals seeking Magnet/Pathway designation.
Design and setting
This study was conducted as part of the German Magnet pioneer study, based on a qualitative research design in five pioneer hospitals. Semi-structured interviews were conducted between March and October 2020 with nurse leaders, managers, and clinicians involved in introducing Magnet or Pathway principles in five German hospitals. Inclusion criteria were as follows: (i) hospitals known as pioneers, defined as early adopters of the Magnet or Pathway principles, (ii) having started the implementation on their own initiative prior to 2020. For the purposes of this study, the primary focus was on the leadership attributes of nurses driving organization-wide change using Magnet/Pathway principles. The research protocol was approved by the Ethics Committee of the Charité (No. EA4/185/19). This study used the consolidated qualitative research reporting criteria (COREQ) [ 47 ].
The semi-structured interview guide contained a total of nine question with a set of probing questions. Topics covered motivation and rationale for implementing Magnet/Pathway, the identification of facilitators and barriers, of which one question was specifically on the role of leadership. However, interviewees referred to leadership attributes and practices throughout the interview in various instances. All interviewees filled out a short questionnaire on demographic characteristics and information about their role in the hospital, position, and years of work experience.
Sample recruitment
The purposive sample consisted of 18 persons from the five hospitals. Hospital size ranged between 200 and 2000 beds. Interviewees were nurse leaders, managers, and clinicians who had gained experience with the implementation of Magnet/Pathway. All requested interview partners agreed to be interviewed.
Data collection and analysis
Interviews were conducted in German and face-to-face by three members of the research team, following the semi-structured interview guide. The interviews lasted between 30 and 135 min. The interviews were anonymized and transcribed verbatim and were coded with ID01-ID18. The analysis of the anonymized transcripts was carried out in a multi-stage procedure based on content analysis, with a content structuring and summarising approach according to Mayring [ 48 ].
A deductive-inductive approach was chosen. The transcripts were coded using the data analysis software ATLAS.ti. For the deductive coding a coding guide was developed prior to the analysis based on the five components of the Magnet model [ 10 ]. Subsequently, the content of the deductive code leadership was re-analyzed in-depth inductively to answer the research question.
Several measures were applied to ensure transparency and quality. This involved investigator triangulation whereby the three researchers were involved in the data collection, analysis, and interpretation of the study [ 49 ].
Prior to the interviews, the three researchers conducted pilot interviews among themselves to ensure consistency. The coding of the interviews was performed by the three researchers who also conducted the interviews. Each coder was familiar with all 18 transcripts. After a pilot analysis phase with three interviews which were coded together and discussed at length to achieve high interrater agreement, the transcripts were randomly allocated. In regularly scheduled meetings, the coders reported the interim status and discussed problems or questions regarding the analysis and reviewed sample content of the codes together. In the next step, themes and sub-themes were formed by the researchers and discussed. Examples of quotes from interviewees are provided in the results section to enhance understanding of the interpretation of the results.
Interviewee characteristics
The 18 interviewees had a mean age of 48.9 (SD: 10.0) years, seven were female and eleven male. The majority ( n = 16) had a degree in nursing and two a degree in medicine. Leadership and/or staff responsibilities had 17 interviewees and on average they had five (SD: 2.8) years of experience with implementing Magnet/Pathway (see Table 1 ).
All 18 transcripts were included in the analysis, regardless of whether direct quotes are shown in this study. Five main leadership attributes (subsequently referred to as main themes) driving organization-wide change using the Magnet/Pathway principles were identified: visionary, strategic, supportive, stamina, and agility. The main themes consist of eleven sub-themes (see Table 2 ).
Main theme 1: Visionary
Two sub-themes were clustered as the main theme visionary. It emerged that having a vision and acting as a role model were identified as requirement to implement organization-wide change.
Having a vision
Most interviewees agreed that leaders need a vision that they carry with conviction and strive to realize with high motivation. Interviewees suggested that a leader who is visionary would inspire employees for the change process. Furthermore, some interviewees mentioned that it is beneficial if leaders communicate well their vision of the future to their employees.
“With a vision I can inspire people. So, I need something that is strong enough, that really radiates energy, that […] gives people courage.” (ID9) .
It was seen as essential that the visions should be catchy, based on clinical practice and reflect the needs of clinical practitioners. One of the interviewees also mentioned the involvement of employees in the practical elaboration of the vision.
“So, I […] presented the vision to my team. […] And we went into working groups on how we can implement it, how we can live it. We have three keywords in there: human, competent, pioneering.” (ID14) .
The interviewees described the need for people who serve as role models that adhere to their vision, ideals, and values and stand up for them. Leaders acting as role models were identified as being less concerned with fulfilling specific criteria for maintaining a label or certificate but focused on improving the well-being of employees and quality of care. Interviewees explained a role model function of leaders as beneficial when employees could identify with their leaders, as this makes it easier to formulate and accept the vision and values as common goals. One interviewee stressed the importance of the personality of the leader and their manner of communicating with their staff.
“I would almost reduce it to the personalities that drive the whole thing. So, it always depends on how you transmit something, how do you communicate, how do you deal with your staff.” (ID4) .
A role model as an inspiration was suggested to increase the motivation of the employees to develop themselves and eventually to work towards the achievement of common goals.
“For me it was […] exciting to have a nursing director who brought special knowledge and an enthusiasm that I sometimes missed in the nursing field. […] just ahead of the times and […] powerful with motivation and of course that caught me.” (ID2) .
Main theme 2: Strategic
Two sub-themes were identified under the main theme strategic: Critical attributes as strategic planning and convincing top management contribute to effective implementation of positive change.
Strategic planning
Interviewees mentioned that leadership attributes included the ability to plan strategically to meet the goals of the hospital. For example, one of the interviewees described that the implementation of transformational leadership had been the key to driving further changes in the direction of Magnet.
“I think that the key component to live the Magnet concept is transformational leadership. […] I first must manage through leadership to keep people and attract new ones. And if that succeeds, […] then I can bring the other components into life […].” (ID9) .
Some interviewees highlighted the relevance of strategic resource allocation to be able to initiate and sustain the hospital-wide change via Magnet/Pathway principles. This included investing in human resources, e.g. nursing scientists or project coordinators, and in structural development, e.g. data management or digitalization. One interviewee described the strategy of providing budget or other cost-related information for the top management and the board required for Magnet/Pathway implementation.
“There needs to be at least […] an overarching Magnet project manager or director. […] last year I made an initial rough calculation for the board […] as a template, what it would cost the hospital. […] because that is of course indispensable.” (ID7) .
Convincing top management
Most interviewees addressed the importance of seeking and gaining the support of top management to advance change processes.
“The first step, […], was to convince the executive director, because the combination is simply necessary to do anything at all.” (ID4) .
One interviewee underscored the importance of active involvement and dedication from top-level decision makers and management in driving organization-wide change processes.
“So, I think you definitely need […] - the decision makers, the management - they must commit themselves clearly to it, and they must have a vision in this direction […].” (ID5) .
Main theme 3: Supportive
Three sub-themes were clustered under the main theme supportive. To be a supportive leader who fosters an empowering workplace to meet Magnet/Pathway principles, it was described as important to inspire and motivate employees to evolve professionally, support employees individually in developing themselves and their ideas further and cultivate a strong team spirit as a team player to pursue common goals.
Inspiration and motivation
Some of the interviewees talked about encouraging and inspiring employees to go beyond themselves. Increasing employees’ self-confidence enabled them to make their own decisions and motivated them to evolve professionally. This increased the motivation to drive positive change within the organization. One of the interviewees further explained that the higher the motivation in the team, the faster positive changes could be implemented.
“The half of it is […] that you get moving forward and, of course, the more motivated you are, the faster and the better you get moving forward. So, it’s about strengthening motivation and this for the whole team and making sure that you get better professionally.” (ID2) .
A leader should have a passion for the intended changes to persuade and motivate all employees and should take into account the time component of implementing organization-wide change using the Magnet/Pathway concept.
“And you have to be passionate about the topic, otherwise the concept won’t work either. That takes time at first. And then the biggest task is to get all the employees on board.” (ID4) .
Individual support of employees
The individual support of employees by leaders was recognized as indispensable when it comes to empowering them. According to the interviewees it was important to create a trusting working environment and to make employees feel that they are supported in developing themselves and their ideas further.
“[T]he employees must feel something is getting better for me. Managers are standing up for me, they are behind me. That is what is important for employees.” (ID9) .
However, finding the right support for each employee required individual consultation. Only in this way special circumstances and needs could be considered in a targeted manner. In particular, support for the academic training of bedside nurses is mentioned by interviewees as an example which underscores the significance of management’s role in facilitating and encouraging such endeavors.
“[…] there was […] a young [male nurse] sitting there […] who says, ‘Yeah, did I get this right, you want us all to have academic degrees?’ And he says, ‘Listen, I’m 35, I have three kids, I can’t afford to give up one euro right now at all.’ And [the CNO] understands, of course, there are priorities. But then you must see how you can support someone like that. […] If someone wants the [bachelor in nursing] […] then there is massive support, especially at the management level.” (ID7) .
Team player
The interviewees shared the idea that inspiration, motivation, and support of staff succeed more effectively when leaders are perceived as team players. According to the interviewees, a strong team spirit strengthens motivation to pursue common goals and helps not to give up. It also supports the well-being of all employees in their daily work.
“The team spirit is so important because if you motivate a team, if you win a team, and if you, as the leader of such a team, ensure that people enjoy working together and that the day-to-day problems can be sorted out, and if it says at the top and at the front: We are a team, we do this together, and together we are strong, Then you have already won half of everything that can be won.” (ID2) .
An interviewee at a higher managerial level additionally stated that it is important to always maintain a friendly atmosphere and show appreciation to receive important information about current issues and concerns in the teams. Decisions should not be made alone, but should always be considered with the teams, as they know more about the day-to-day matters of the staff members.
“We have […] a very, very friendly interaction, because I think that they are not my subordinates, they are my ward managers and they are the most important source of work for me, so to speak. Without them, I wouldn’t need to show up here to work, without my ward managers interacting with their teams, knowing exactly what’s going on here right now […], where’s the tension right now? What’s going well right now, what’s not going well right now?” (ID17) .
Main theme 4: Stamina
Two of the sub-themes were clustered as the main theme stamina. It emerged that implementing organization-wide change requires leaders who have strong personalities with courage and assertiveness.
The interviews showed that courage and a willingness to take risks in a context of uncertainty, which requires change, is experienced as a beneficial leader attribute. For the interviewees, courage meant being committed to the community and pursuing a vision and goals and being persistent about them. The step of opting for the implementation of organization-wide change with the Magnet/Pathway is described by some interviewees as a dare and leaders should be prepared for negative effects and to face resistance.
“I would say: Yes, you can always change something. And I didn’t let myself be discouraged […]. Sometimes people have said that we can’t really implement the Magnet concept here. And for me it was always important which ideas from the concept can be implemented and this I want to implement […], but I don’t let that stop me. […] And of course you also need leaders who are strong enough to say: ‘I know, even if it sounds crazy, we’re going in that direction now’.” (ID9) .
Nevertheless, especially in times of nursing shortages and high workload, it was important to have a sense of achievement to summon up courage. One of the CNOs interviewed reported that due to a high number of applicants to study nursing in the interviewee’s initial phase at the hospital, the interviewee had gained the courage to believe in the change concept and continued to pursue the interviewee’s vision despite high workloads and poor moods among the nursing staff and continued to pursue their vision.
“[…] despite reports of work overload, which reached me in droves at that time in my starting phase […], and then I was talking about academic training, actually I almost got a slap in the face, but at the same time [many] applied [to study nursing]. And then that was again the point where I had confidence: ‘You’re sticking to it; you have the courage’.” (ID3) .
Assertiveness
Interviewees agreed that implementing organization-wide change requires a high level of commitment and that leaders should have assertiveness. It was mentioned that it is important to prepare for the long term and to be aware of the length of time required to drive change processes using the Magnet/Pathway concept.
“I think the concepts themselves are very, very complex and take an incredible amount of time to implement. But it is possible. You just need someone who has stamina and who stands there and says, ‘So, and I want this, and this is the way, and this is my way, and I’m going to follow through.‘” (ID14) .
A sufficient individual resilience of leaders in hospitals was described as crucial to be able to overcome past failures, learn from them and stay positive. An interviewee described that initial rejection of new intervention plans by employees was initially perceived as a setback, but the leaders remained strong and learned from it.
“Well, that certainly took its time. [The CNO] came back [from U.S.] to the hospital with lots of new ideas and everyone who hears something new first says: ‘Stop, hold this. […], English words, now we only use English words. What does Magnet mean at all?’ and there was already a lot of distance from the employees […]. But then [the CNO] was able to convince […] at least the mangement level.” (ID4) .
Convincing top management was also described as an endeavor and requires the attributes of assertiveness and courage. One example is to advocate for one’s employees.
“And my job as a CNO, of course, is to fight to make sure that my nurse leaders have the resources, from time, to space, to other things, to be able to do good leadership.” (ID9) .
Main theme 5: Agility
In the context of this study, agility means the ability to adapt flexibly and quickly to changing tasks, circumstances, and demands as well as fostering a sense of team spirit. Two of the sub-themes were clustered as the main theme agility; showing presence and demonstrate well and fast accessibility and responsiveness.
Showing presence
It emerged from the statements of the interviewees that showing presence and direct personal contact of the leaders towards the employees was an important competence to keep up the commitment of the employees for implementing positive change within the hospital.
“Of course, I’m also in favour of the director of nursing not working at the bedside anymore […], but they should also not forget the direct contact to those who do the frontline work.“(ID2) .
With personal presence the leader’s appreciation of frontline workers and the interest in their well-being could become more tangible. It would also be a better way to transmit enthusiasm for the overarching, common goal to employees. Likewise, communication lines would be shortened, and employee concerns and needs could be addressed quicker. One of the interviewees shared a key moment when the CNO introduced himself unannounced at a staff meeting, and this sparked a sense of optimism among the employees.
“And I don’t think there’s ever been anything like this before, where a team meets for a dialogue and all of a sudden the CNO comes in and introduces himself and also says something about his philosophy and how he would like it to be. […] And that was the first jolt, because the employees realized, there’s someone who’s not untouchable, but there’s someone who’s like us.” (ID14) .
Another interviewee stated that they were expected as a nurse leader to know as many of the employees personally as possible. This was an essential factor for equal interaction between the professional groups.
“I know a lot of our nurses […], I know all the academic nurses, […] people expect me to take an interest in them. The whole eye-level system means that you really give everyone a name as well, not just a number anymore.” (ID1) .
One of the interviewees acknowledged that a lack of presence at the frontline work, as well as a lack of interest in the processes by the leader, had negatively impacted the success of implementing change processes.
“He [CNO] wasn’t on the wards; he didn’t see that as his responsibility either. It was more like; he gives the strategy and then the others are supposed to do the implementation. That just didn’t work out well. […] it was certainly a barrier that the [CNO] had little understanding of the daily operational problems. […] It would still have been easier if the employees had experienced him as being a little closer to the employees.” (ID10) .
Accessibility and responsiveness
In addition, interviewees explained that by showing presence outside of their own office, leaders should also cultivate an “open door”-culture and be available to meet with employees at short notice. This includes accessibility via various communication channels but also quick responsiveness.
“My door is open all day. I am not the leader who is available once a year for one hour […], but I am permanently there for dialogue, I do have time.” (ID6) . “We do a topical hour with the nursing directorate where they can come and get in touch with science here. [AND] Cappuccino with the nursing directors; where everyone can come without an appointment and also have individual talks […].” (ID3) .
Another interviewee used a current occurrence to stress the importance of responding to employee requests as soon as possible to keep them motivated.
“Right before you came in, there was a colleague who asked me […] if he could do a work shadowing. Within three minutes he got his answer […]. What use has a rigid structure, if you let someone like him wait for two weeks and say ‘Well, I was overworked’? You have to address these things.” (ID2) .
The findings of this study shed light on the attributes of nurse leaders in German hospitals that drive organization-wide change using Magnet/Pathway, which are aimed at improving employee well-being, productivity, and patient outcomes. A key component of the concepts is the practice of transformational leadership [ 9 ]. The results highlight five main themes that encompass beneficial leadership attributes: visionary, strategic, supportive, stamina, and agility.
The theme of visionary underscores the significance of visionary leadership in driving organization-wide change towards Magnet/Pathway. Having a clear and compelling vision that is communicated effectively to employees emerged as a key factor. The role of leaders as role models who embody vision and values was also emphasized. This aligns with existing literature on transformational leadership, which emphasizes the importance of idealized influence and inspirational motivation [ 34 , 35 ]. Leaders who serve as role models and inspire others create a sense of identification and motivation among employees to work towards common goals.
The theme of strategic highlights the role of strategic planning and resource allocation in Magnet/Pathway implementation. Several studies confirmed that strategic thinkers are among the most effective leaders. People with the ability to think strategically are more likely to ensure the sustainable success of an organization and are better able to put existing strategic plans into execution [ 50 , 51 , 52 , 53 ]. Furthermore, this study emphasizes the importance of leaders advocating for Magnet/Pathway principles to gain the support and commitment of the top management. Convincing the top management was seen as crucial for the success of change efforts.
The supportive theme emphasizes the significance of individualized support for employees’ development and well-being. This includes empowering employees to pursue further education, addressing their unique needs, and fostering a trusting work environment. This study highlights the role of leaders in providing resources and support for academic advancement, which aligns with the Magnet key component on structural empowerment. Furthermore, the importance of team spirit and collaboration was emphasized, echoing the Magnet/Pathway principle of exemplary professional practice and a collaborative work environment. Supportive leaders act as team players and inspire and motivate their staff to perform beyond the norm [ 38 , 54 ]. They support staff nurses to assessing their own performance, working out their goals and defining their responsibilities [ 38 , 43 , 44 ]. As a result, nurse leaders can promote knowledge building, intrinsic motivation and innovative work behavior among nurses [ 54 ].
In the German healthcare system, it is noteworthy that not every nursing director automatically holds a position on the hospital’s executive board, underscoring the importance of engaging top management in organizational change initiatives. Additionally, given that lifelong learning and continuous professional development are not standard practices in nursing in Germany, contrasting with the conditions required for Magnet/Pathway implementation, it highlights the crucial role of CNOs in empowering their staff and fostering a culture of lifelong learning and professional growth.
Results of previous qualitative studies analyzing transformational leadership style from the nurse leaders’ perspective confirm these findings. They include competencies such as a strong, inspiring, and supportive leader with novel approaches. The leaders serve as role models and are able to empathize with nursing staff to achieve common goals [ 42 , 43 , 44 , 45 ]. By cultivating a visionary outlook and a supportive stance, nurse leaders can effectively foster work engagement, address burnout, and create a motivating environment for healthcare professionals. Importantly, these leadership qualities can be learned and improved over time among nurses through targeted educational interventions, training, mentoring, and hands-on experiences [ 55 , 56 , 57 ]. Nevertheless, while some leadership skills can be developed through training and experience, certain innate character traits may provide an inherent advantage in the cultivation of effective leadership [ 58 ]. For instance, personality traits such as emotional intelligence, empathy, and authenticity have been linked to leadership effectiveness [ibid.]. Although these traits may not be directly teachable, they may serve as foundational elements that contribute to the development of successful transformational leadership practices.
The alignment between the findings of this study and those from various international contexts raises important implications for both the Magnet/Pathway implementation process and the broader understanding of transformational leadership. The resemblance between the identified leadership attributes and those found in studies conducted in different countries suggests a level of universality in the leadership qualities required for successful organization-wide change, particularly in healthcare settings. Furthermore, the consensus between the leadership attributes identified in this study and those from international research may imply that studies solely focused on transformational leadership can offer relevant insights for organizations pursuing Magnet/Pathway designation.
Given the diversity of leadership approaches across other sectors (including industry), it is important to recognize the contextual relativity of specific leadership traits. While the leadership attributes identified in this study are tailored specifically to nursing within hospitals, they may be relevant in other sectors, but require further evaluations in different contexts. While a leader’s ability to communicate a clear vision and motivate employees is as crucial in the business sector as in healthcare, the best way of communication and motivation may vary.
New insights that expand the understanding of the role of leadership in driving organization-wide change that emerge from this study is the perspective on the themes of stamina and agility in the context of transformational leadership and Magnet/Pathway implementation.
The theme of stamina reflects the perseverance and resilience required for implementing Magnet/Pathway principles. Leaders need courage to navigate uncertainty and take calculated risks. Leaders should want to make changes and push them forward with stamina and assertiveness, and who are not afraid to speak up and ask for support from higher authorities. In the context of transformational leadership, stamina has often been discussed as a leader’s perseverance, determination, and resilience in the face of challenges [ 34 ]. However, the findings of this study emphasize a more profound dimension of stamina as the leader’s ability not only to persevere, but also to inspire and sustain momentum during complex, long-term endeavors such as Magnet/Pathway implementation.
The concept of agility as an essential leadership skill has gained attention in recent years and refers to a leader’s ability to adapt quickly to changing circumstances. This aligns with the dynamic nature of healthcare settings, where leaders must respond to changing demands [ 59 ]. Interviewees in this study emphasized the positive impact of agile leadership, which enables leaders to respond rapidly, purposefully, and individually to different situations [ 59 , 60 , 61 ]. By adapting task structures and difficulty levels to match employees’ needs and commitment, leaders can prevent both under- and over-challenging their team members, thereby facilitating their professional development [ 59 , 60 , 61 ]. With the sub-themes showing presence as well as accessibility and responsiveness, it became clear that leaders should be in regular exchange with their employees to be able to react agilely to the requirements and needs [ 62 ]. In contrast, the findings confirm that the lack of frontline presence as well as the leader’s lack of interest in the processes negatively impacted the success of Magnet/Pathway implementation. However, in the context of Magnet/Pathway implementation, agility goes beyond flexibility to include a dynamic responsiveness to evolving healthcare challenges. The results show that leaders need to be flexible not only in their decision-making, but also in their accessibility and responsiveness to employees. This reflects a proactive approach that not only supports the implementation of the Magnet/Pathway principles, but also ensures that employees remain engaged and motivated throughout the transformation process.
Limitations
This study has several limitations. Firstly, the interviews were conducted in only five German hospitals, yet they were the first ones known to have started introducing Magnet or Pathway in Germany. While these hospitals provided valuable insights into the implementation process, the perspectives shared by leaders and staff are not representative of all hospitals in Germany, limiting the generalizability of the findings. Secondly, the majority of interviewees in this study were nurse managers or individuals with leadership responsibilities. As a result, the findings primarily reflect the management and leadership perspective, potentially overlooking the viewpoints and experiences of frontline nurses. It is important to consider a wider range of perspectives to gain a comprehensive understanding of the challenges and opportunities associated with leadership while implementing Magnet/Pathway principles.
This study provides in-depth insights into the leadership attributes that drives the implementation of organization-wide change through Magnet/Pathway principles in German. It offers guidance for nurse leaders seeking to drive positive organization-wide change and enhance employee well-being.
The interviewees in this study emphasized the importance of leadership competencies such as visionary direction, strategic planning, personalized support, resolute stamina, and adaptive agility. The themes of stamina and agility offer new insights, showcasing the need for courage, assertiveness, and adaptability in leaders driving long-term organization-wide change towards Magnet/Pathway.
Given the vital role of transformational leadership in driving organization-wide change, as well as the fact that transformational leadership skills can be trained, a comprehensive preparation and ongoing development of nurse leaders toward transformational leadership skills may support establishing and sustaining a positive work environment in hospitals.
Data availability
A 32-item checklist for interviews and focus groups (COREQ) and the coding tree are provided as supplementary material. The transcripts used and analyzed during the Magnet pioneer study are available from the corresponding author on reasonable request.
Abbreviations
American Nurses Association
American Nurses Credentialing Center
Chief Nursing Officer
Consolidated Criteria for Reporting Qualitative
Interviewee Identification
Multifactor Leadership Questionnaire
National Health Service
Standard deviation
United Sates of America
Rafferty AE, Griffin MA. Perceptions of organizational change: a stress and coping perspective. J Appl Psychol. 2006;91:1154–62. https://doi.org/10.1037/0021-9010.91.5.1154 .
Article PubMed Google Scholar
Duncan S, Rodney PA, Thorne S. Forging a strong nursing future: insights from the Canadian context. J Res Nurs. 2014;19:621–33. https://doi.org/10.1177/1744987114559063 .
Article Google Scholar
Alonso JM, Clifton J, Díaz-Fuentes D. The impact of New Public Management on efficiency: an analysis of Madrid’s hospitals. Health Policy. 2015;119:333–40. https://doi.org/10.1016/j.healthpol.2014.12.001 .
Nilsen P, Seing I, Ericsson C, Birken SA, Schildmeijer K. Characteristics of successful changes in health care organizations: an interview study with physicians, registered nurses and assistant nurses. BMC Health Serv Res. 2020;20:147. https://doi.org/10.1186/s12913-020-4999-8 .
Article PubMed PubMed Central Google Scholar
Kim M-S, Kim T, Lee D, Yook J-H, Hong Y-C, Lee S-Y, et al. Mental disorders among workers in the healthcare industry: 2014 national health insurance data. Ann Occup Environ Med. 2018;30:31. https://doi.org/10.1186/s40557-018-0244-x .
Skoda E-M, Teufel M, Stang A, Jöckel K-H, Junne F, Weismüller B, et al. Psychological burden of healthcare professionals in Germany during the acute phase of the COVID-19 pandemic: differences and similarities in the international context. J Public Health. 2020;42:688–95. https://doi.org/10.1093/pubmed/fdaa124 .
Nowrouzi B, Lightfoot N, Larivière M, Carter L, Rukholm E, Schinke R, Belanger-Gardner D. Occupational Stress Management and Burnout Interventions in nursing and their implications for healthy work environments: a Literature Review. Workplace Health Saf. 2015;63:308–15. https://doi.org/10.1177/2165079915576931 .
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–81. https://doi.org/10.1016/S0140-6736(16)31279-X .
ANCC. 2023 MAGNET Application Manual; 2021.
Magnet Model ANA. 2017. https://www.nursingworld.org/organizational-programs/magnet/magnet-model/ . Accessed 19 Mar 2023.
Pabico C, Cadmus E. Using the pathway to Excellence® Framework to create a culture of sustained Organizational Engagement. Nurse Lead. 2016;14:203–6. https://doi.org/10.1016/j.mnl.2016.01.005 .
Kelly LA, McHugh MD, Aiken LH. Nurse outcomes in Magnet® and non-magnet hospitals. J Nurs Adm. 2012;42:S44–9. https://doi.org/10.1097/01.NNA.0000420394.18284.4f .
Kutney-Lee A, Stimpfel AW, Sloane DM, Cimiotti JP, Quinn LW, Aiken LH. Changes in patient and nurse outcomes associated with magnet hospital recognition. Med Care. 2015;53:550–7. https://doi.org/10.1097/MLR.0000000000000355 .
Petit Dit Dariel O, Regnaux J-P. Do Magnet®-accredited hospitals show improvements in nurse and patient outcomes compared to non-magnet hospitals: a systematic review. JBI Database Syst Rev Implement Rep. 2015;13:168–219. https://doi.org/10.11124/jbisrir-2015-2262 .
Rodríguez-García MC, Márquez-Hernández VV, Belmonte-García T, Gutiérrez-Puertas L, Granados-Gámez G. Original Research: how Magnet Hospital Status affects nurses, patients, and organizations: a systematic review. Am J Nurs. 2020;120:28–38. https://doi.org/10.1097/01.NAJ.0000681648.48249.16 .
McHugh MD, Kelly LA, Smith HL, Wu ES, Vanak JM, Aiken LH. Lower mortality in magnet hospitals. Med Care. 2013;51:382–8. https://doi.org/10.1097/MLR.0b013e3182726cc5 .
Hume L, Hall M. Sustaining a positive practice environment after pathway to Excellence® designation. Nurs Manage. 2020;51:6–9. https://doi.org/10.1097/01.NUMA.0000651208.47176.91 .
Sepe P, Hargreaves J. Responding to the COVID-19 pandemic with the pathway to Excellence® framework. Nurs Manage. 2020;51:6–8. https://doi.org/10.1097/01.NUMA.0000688980.49993.c0 .
ANA, Find a Magnet. Organization. 2017. https://www.nursingworld.org/organizational-programs/magnet/find-a-magnet-organization/ . Accessed 20 Feb 2024.
ANA, Find a Pathway. Organization. 2017. https://www.nursingworld.org/organizational-programs/pathway/find-a-pathway-organization/ . Accessed 20 Feb 2024.
Schweiger J. Das Magnet-Krankenhaus — Anziehend durch Qualität und Transparenz. Pflegez. 2017;70:18–21. https://doi.org/10.1007/s41906-017-0090-4 .
Osterloh F. Zusammenarbeit Von Ärzten Und Pflegekräften: Der Kulturwandel hat begonnen. Deutsches Ärzteblatt. 2019;116:930–1.
Google Scholar
Maier C, Köppen J, Kleine J. Das Arbeitsumfeld in Krankenhäusern verbessern - das Magnet4Europe-Projekt. Die Schwester Der Pfleger. 2022:84–7.
Kleine J, Maier CB, Köppen J, Busse R. Magnet®-Krankenhäuser: Eine Chance für Deutschland? In: Klauber J, Wasem J, Beivers A, Mostert C, editors. Schwerpunkt Personal. Berlin: Springer; 2023. pp. 107–17. https://doi.org/10.1007/978-3-662-66881-8_7 .
Chapter Google Scholar
Graystone R, Pabico C. Magnet® or Pathway® recognition: comparing and contrasting. J Nurs Adm. 2018;48:233–4. https://doi.org/10.1097/NNA.0000000000000606 .
Lal MM, Pabico CG. Magnet® and pathway: partners for nursing Excellence. J Nurs Adm. 2021;51:175–6. https://doi.org/10.1097/NNA.0000000000000992 .
Mororó DDS, Enders BC, Lira ALBC, Da Silva CMB, de Menezes RMP. Concept analysis of nursing care management in the hospital context. Acta Paul Enferm. 2017;30:323–32. https://doi.org/10.1590/1982-0194201700043 .
de Moura AA, Bernardes A, Balsanelli AP, Zanetti ACB, Gabriel CS. Liderança E satisfação no trabalho da enfermagem: revisão integrativa. Acta Paul Enferm. 2017;30:442–50. https://doi.org/10.1590/1982-0194201700055 .
Specchia ML, Cozzolino MR, Carini E, Di Pilla A, Galletti C, Ricciardi W, Damiani G. Leadership styles and nurses’ job satisfaction. Results of a systematic review. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph18041552 .
Schaufeli W. Engaging Leadership: how to promote Work Engagement? Front Psychol. 2021;12:754556. https://doi.org/10.3389/fpsyg.2021.754556 .
Wang X, Chontawan R, Nantsupawat R. Transformational leadership: effect on the job satisfaction of registered nurses in a hospital in China. J Adv Nurs. 2012;68:444–51. https://doi.org/10.1111/j.1365-2648.2011.05762.x .
Cummings GG, Tate K, Lee S, Wong CA, Paananen T, Micaroni SPM, Chatterjee GE. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud. 2018;85:19–60. https://doi.org/10.1016/j.ijnurstu.2018.04.016 .
Moon SE, van Dam PJ, Kitsos A. Measuring transformational Leadership in establishing nursing Care Excellence. Healthc (Basel). 2019. https://doi.org/10.3390/healthcare7040132 .
Bass B, Avolio B. Improving Organisational Eectiveness through transformational Leadership. Thousand Oaks, CA, USA: Sage; 1994.
Avolio B. Full range leadership development. 2nd ed. Thousand Oaks, CA: SAGE; 2011.
Book Google Scholar
Burns JM. Leadership. New York. NY, USA: Harper & Row; 1978.
Bormann L, Abrahamson K. Do staff nurse perceptions of nurse leadership behaviors influence staff nurse job satisfaction? The case of a hospital applying for Magnet® designation. J Nurs Adm. 2014;44:219–25. https://doi.org/10.1097/nna.0000000000000053 .
Prado-Inzerillo M, Clavelle JT, Fitzpatrick JJ. Leadership practices and Engagement among Magnet® Hospital Chief nursing officers. J Nurs Adm. 2018;48:502–7. https://doi.org/10.1097/NNA.0000000000000658 .
Shaughnessy MK, Quinn Griffin MT, Bhattacharya A, Fitzpatrick JJ. Transformational Leadership practices and Work Engagement among Nurse leaders. J Nurs Adm. 2018;48:574–9. https://doi.org/10.1097/NNA.0000000000000682 .
Labrague LJ, Nwafor CE, Tsaras K. Influence of toxic and transformational leadership practices on nurses’ job satisfaction, job stress, absenteeism and turnover intention: a cross-sectional study. J Nurs Manag. 2020;28:1104–13. https://doi.org/10.1111/jonm.13053 .
Suliman M, Aljezawi M, Almansi S, Musa A, Alazam M. Ta’an WF. Identifying the nurse characteristics that affect anticipated turnover. Nurs Manag (Harrow). 2020. https://doi.org/10.7748/nm.2020.e1956 .
Ferreira VB, Amestoy SC, Da Silva GTR, Trindade LL, Santos IARD, Varanda PAG. Transformational leadership in nursing practice: challenges and strategies. Rev Bras Enferm. 2020;73:e20190364. https://doi.org/10.1590/0034-7167-2019-0364 .
Boyal A, Hewison A. Exploring senior nurses’ experiences of leading organizational change. Leadersh Health Serv (Bradf Engl). 2016;29:37–51. https://doi.org/10.1108/LHS-03-2015-0005 .
Salmela S, Eriksson K, Fagerström L. Leading change: a three-dimensional model of nurse leaders’ main tasks and roles during a change process. J Adv Nurs. 2012;68:423–33. https://doi.org/10.1111/j.1365-2648.2011.05802.x .
Kodama Y, Fukahori H. Nurse managers’ attributes to promote change in their wards: a qualitative study. Nurs Open. 2017;4:209–17. https://doi.org/10.1002/nop2.87 .
Kilian R. Transformationale Führung in der Pflege als Beitrag zur Managemententwicklung [Dissertation]. Private Universität für Gesundheitswissenschaften: Medizinische Informatik u. Technik Hall in Tirol (UMIT); 2013.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. https://doi.org/10.1093/intqhc/mzm042 .
Mayring P. Qualitative inhaltsanalyse: Grundlagen Und Techniken. 11th ed. Weinheim: Beltz; 2010.
Golafshani N. Understanding reliability and validity in qualitative research. TQR. 2015. https://doi.org/10.46743/2160-3715/2003.1870 .
Gavetti G. PERSPECTIVE—Toward a behavioral theory of strategy. Organ Sci. 2012;23:267–85. https://doi.org/10.1287/orsc.1110.0644 .
Gavetti G, Levinthal DA, Rivkin JW. Strategy making in novel and complex worlds: the power of analogy. Strat Mgmt J. 2005;26:691–712. https://doi.org/10.1002/smj.475 .
Moon B-J. Antecedents and outcomes of strategic thinking. J Bus Res. 2013;66:1698–708. https://doi.org/10.1016/j.jbusres.2012.11.006 .
Smriti V, Dhir S, Dhir S. Strategic thinking in Professional Environment: a review of the literature. IJBIR. 2020;1:1. https://doi.org/10.1504/IJBIR.2020.10028592 .
Masood M, Afsar B. Transformational leadership and innovative work behavior among nursing staff. Nurs Inq. 2017. https://doi.org/10.1111/nin.12188 .
Hamdani MR. Learning how to be a transformational leader through a skill-building, role-play exercise. Int J Manage Educ. 2018;16:26–36. https://doi.org/10.1016/j.ijme.2017.11.003 .
Cummings GG, Lee S, Tate K, Penconek T, Micaroni SPM, Paananen T, Chatterjee GE. The essentials of nursing leadership: a systematic review of factors and educational interventions influencing nursing leadership. Int J Nurs Stud. 2021;115:103842. https://doi.org/10.1016/j.ijnurstu.2020.103842 .
Cohrs C, Bormann KC, Diebig M, Millhoff C, Pachocki K, Rowold J. Transformational leadership and communication. LODJ. 2020;41:101–17. https://doi.org/10.1108/LODJ-02-2019-0097 .
Avolio BJ, Walumbwa FO, Weber TJ. Leadership: current theories, research, and future directions. Annu Rev Psychol. 2009;60:421–49. https://doi.org/10.1146/annurev.psych.60.110707.163621 .
Ahmed Mohamed Ibrahim S, Mohammed Araby Ebraheem S, Hassan EL-S, Mahfouz H. Effect of Educational Program about Head nurses’ Agile Leadership on Staff nurses’ Workplace spirituality and job reputation. Egypt J Health Care. 2022;13:1638–58. https://doi.org/10.21608/ejhc.2022.231783 .
Aij KH, Teunissen M. Lean leadership attributes: a systematic review of the literature. J Health Organ Manag. 2017;31:713–29. https://doi.org/10.1108/JHOM-12-2016-0245 .
Simonovich SD, Spurlark RS, Badowski D, Krawczyk S, Soco C, Ponder TN, et al. Examining effective communication in nursing practice during COVID-19: a large-scale qualitative study. Int Nurs Rev. 2021;68:512–23. https://doi.org/10.1111/inr.12690 .
Bailey KD, Losty LS, Albert D, Rodenhausen N, Santis JP. de. Leadership presence: A concept analysis. Nurs Forum. 2022;57:1069–79. https://doi.org/10.1111/nuf.12784 .
Download references
Acknowledgements
We extend our thanks to the 18 interviewees for their time and valuable insights, especially considering the challenges posed by the COVID-19 pandemic during the interview data collection period. Their willingness to participate in this study is greatly appreciated and has significantly contributed to our research. We also thank the consortium of the Magnet4Europe study.
The Magnet pioneer study was funded by the B. Braun Foundation (Grant No. 18001021). Additional time on the study was funded by a grant from Robert Bosch Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Department of Healthcare Management, Technische Universität Berlin, Straße des 17. Juni 135, 10623, Berlin, Germany
Joan Kleine & Julia Köppen
School of Public Health, Universität Bielefeld, Universitätsstraße 25, 33615, Bielefeld, Germany
Julia Köppen & Claudia B. Maier
BQS Institute for Quality & Patient Safety GmbH, Wendenstraße 375, 20537, Hamburg, Germany
Carolin Gurisch
You can also search for this author in PubMed Google Scholar
Contributions
CBM was the PI of the Magnet pioneer study and planned the study and its methodology. CBM and JuK contributed to the study’s design. CBM, JuK and JoK performed data collection and conducted the deductive analysis of the data. JoK conducted the main inductive analyses for the purpose of the current study. CBM and JuK provided critical review and discussion of inductive coding. JoK wrote the first draft manuscript, and prepared tables. CBM, JuK and CG were involved in subsequent iterations and conducted critical review of the manuscript.
Corresponding author
Correspondence to Joan Kleine .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
This research has been performed in accordance with the Declaration of Helsinki with ethics approval through the Ethics Committee of the Charité (No. EA4/185/19). Written informed consent was obtained from all interviewees prior to the interviews. For interviewees, neither advantages nor disadvantages resulted from participation or non-participation in the study. Participation could be withdrawn at any time without consequences till anonymizations.
Consent for publication
Not applicable.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kleine, J., Köppen, J., Gurisch, C. et al. Transformational nurse leadership attributes in German hospitals pursuing organization-wide change via Magnet® or Pathway® principles: results from a qualitative study. BMC Health Serv Res 24 , 440 (2024). https://doi.org/10.1186/s12913-024-10862-y
Download citation
Received : 27 November 2023
Accepted : 13 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1186/s12913-024-10862-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nurse leadership
- Transformational leadership
- Organization-wide change
- German hospitals
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
ORIGINAL RESEARCH article
Challenges and support needs in psychological and physical health among pilots: a qualitative study.

- 1 School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 2 Other, Shanghai, China
- 3 National Center For Global Health and Medicine, Shinjuku, Tokyo, Japan
- 4 School of Public Health, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 5 School of Nursing, Shanghai Jiao Tong University, Shanghai, Shanghai, China
- 6 International Peace Maternity and Child Health Hospital, Shanghai, Shanghai Municipality, China
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
Abstract Introduction Physical and mental health problems among pilots affect their working state and impact flight safety. Although pilots’ physical and mental health problems have become increasingly prominent, their health has not been taken seriously. This study aimed to clarify challenges and support needs related to psychological and physical health among pilots to inform development of a more scientific and comprehensive physical and mental health system for civil aviation pilots. Methods This qualitative study recruited pilots from nine civil aviation companies. Focus group interviews via an online conference platform were conducted in August 2022. Colaizzi analysis was used to derive themes from the data and explore pilots’ experiences, challenges, and support needs. Results The main sub-themes capturing pilots’ psychological and physical health challenges were: 1) imbalance between family life and work; 2) pressure from assessment and physical examination eligibility requirements; 3) pressure from worries about being infected with COVID-19; 4) nutrition deficiency during working hours; 5) changes in eating habits because of the COVID-19 pandemic; 6) sleep deprivation; 7) occupational diseases; 8) lack of support from the company in coping with stress; 9) pilots’ yearly examination standards; 10) support with sports equipment; 11) respecting planned rest time; and 12) isolation periods. Discussion The interviewed pilots experienced major psychological pressure from various sources, and their physical health condition was concerning. We offer several suggestions that could be addressed to improve pilots’ physical and mental health. However, more research is needed to compare standard health measures for pilots around the world in order to improve their physical and mental health and contribute to overall aviation safety.
Keywords: Occupational Health, Mental Health, physical health, qualitative study, Pilots and cabin crew, COVID-19
Received: 06 Dec 2023; Accepted: 05 Apr 2024.
Copyright: © 2024 Xu, Bao, Zhang, Li, Zhang, Li, Jin, Chen, Duan, Shi, Wang, Lu, Chen, Gao, Han, Ren, Su and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Yuyan Bao, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Lin Zhang, Other, Shanghai, China Qingqing Jin, Other, Shanghai, China Yan Chen, Other, Shanghai, China Qingqing Duan, Other, Shanghai, China Feng Shi, Other, Shanghai, China Linlin Wang, Other, Shanghai, China Ziyang Lu, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Xuhua Chen, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Qijing Gao, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Bin Ren, Other, Shanghai, China Ya Su, School of Nursing, Shanghai Jiao Tong University, Shanghai, Shanghai, China Mi Xiang, School of Public Health, School of Medicine, Shanghai Jiao Tong University, Shanghai, 200240, China
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
A general inductive approach for analysis of qualitative evaluation data is described. The purposes for using an inductive approach are to (a) condense raw textual data into a brief, summary format; (b) establish clear links between the evaluation or research objectives and the summary findings derived from the raw data; and (c) develop a framework of the underlying structure of experiences or ...
In short, a data analysis process that draws on both deductive and inductive analysis supports a more organized, rigorous, and analytically sound qualitative study. See below for an example of how I organize deductive and inductive analytic practices into cycles. This figure, adapted from Bingham & Witkowsky (2022) and Bingham (2023), gives an ...
The inductive approach reflects frequently reported patterns used in qualitative data analysis. Most inductive studies report a model that has between three and eight main categories in the ...
Revised on June 22, 2023. The main difference between inductive and deductive reasoning is that inductive reasoning aims at developing a theory while deductive reasoning aims at testing an existing theory. In other words, inductive reasoning moves from specific observations to broad generalizations. Deductive reasoning works the other way around.
Generic inductive approach is a qualitative research approach only identified within the past decade, and has not been extensively discussed in the relevant literature although some scholars have described it (Maxwell, 2005; Silverman, 2005). However, it has become a growing trend in qualitative scholarship.
The Spectrum of Inductive and Deductive Research Approaches Using Quantitative and Qualitative Data. Young, Meredith PhD; Varpio, Lara PhD; Uijtdehaage, Sebastian PhD; Paradis, Elise PhD. Author Information. associate professor, Institute of Health Sciences Education and Department of Medicine, McGill University.
The deductive approach involves beginning with a theory, developing hypotheses from that theory, and then collecting and analyzing data to test those hypotheses. Inductive and deductive approaches to research can be employed together for a more complete understanding of the topic that a researcher is studying.
Primarily inductive to develop the theory or hypothesis. Focus: Concerned with the outcomes and prediction of the causal relationships. ... The ultimate strength of the qualitative research approach lies in the richness of the data and the descriptions and depth of exploration it makes. Hence, qualitative methods are considered as the most ...
Purpose. The purpose of this paper is to explain the rationale for choosing the qualitative approach to research human resources practices, namely, recruitment and selection, training and development, performance management, rewards management, employee communication and participation, diversity management and work and life balance using deductive and inductive approaches to analyse data.
A fourth issue is that the "implicit use of methods in qualitative research makes the field far less standardized than the quantitative ... for instance, an exceptional flexibility, an inductive approach (Strauss and Corbin 1998:31-33; 1990; Esterberg 2002:7), an ability to step back and critically analyze situations, recognize ...
Inductive approach, also known in inductive reasoning, starts with the observations and theories are proposed towards the end of the research process as a result of observations [1]. Inductive research "involves the search for pattern from observation and the development of explanations - theories - for those patterns through series of ...
point that the polarization of quantitative and qualitative research methods began. In the later part of the 20th century the post-structuralists and post-modernists believed in the ... use of the inductive approach to research, the researcher begins with specific observations and measures, and then moves to detecting themes and patterns in the ...
We conclude that quantitative research may benefit from a bottom-up generalization strategy as it is employed in most qualitative research programs. Inductive reasoning forces us to think about the boundary conditions of our theories and provides a framework for generalization beyond statistical testing.
Purpose. The purpose of this paper is to explain the rationale for choosing the qualitative approach to research human resources practices, namely, recruitment and selection, training and development, performance management, rewards management, employee communication and participation, diversity management and work and life balance using deductive and inductive approaches to analyse data.
The Spectrum of Inductive and Deductive Research Approaches Using Quantitative and Qualitative Data. Acad Med. 2020 Jul;95 (7):1122. doi: 10.1097/ACM.0000000000003101.
Content analysis is a research approach that can be used in both qualitative and quantitative research. At a top-level, content analysis simply looks at the meaning of information (content) in textual data "by isolating small pieces of the data that represent salient concepts." ... As one approach to qualitative content analysis, inductive ...
The author developed a model to explain how interview and documentary data are analysed using deductive and inductive methods. The qualitative approach highlights "contextual understanding" with an emphasis that researchers usually seek to understand the "behaviour, values, beliefs, and so on in terms of the context in which the research ...
Using inductive approach, we categorized the emerging codes according to the patterns and similarities between them. The categories were generated from the patterns within the codes, frequency and repetition, and their importance to the participants. ... Yadav D. Criteria for good qualitative research: a comprehensive review. Asia-Pacific Educ ...
Data analysis included a deductive followed by an inductive approach. This dual analysis adheres to Levesque's framework for qualitative methods, which is discussed in the Definition of Analytic Domains sub-section below. Original synthesis of the literature informed the development of our initial deductive codebook.
These important context questions can only be comprehensively answered using qualitative research methods. ... Best fit framework synthesis is a qualitative synthesis method that blends deductive and inductive synthesis and analysis processes. As part of the synthesis method, review authors identify a conceptual framework that fits at least 50% ...
For the analysis, a category system was created using a deductive-inductive approach. Five leadership attributes and eleven sub-attributes were identified as main themes and sub-themes: Visionary leaders who possess and communicate a strong vision and serve as role models to inspire change. ... This study used the consolidated qualitative ...
Methods This qualitative study recruited pilots from nine civil aviation companies. Focus group interviews via an online conference platform were conducted in August 2022. ... However, more research is needed to compare standard health measures for pilots around the world in order to improve their physical and mental health and contribute to ...
Part 1: Identifying Qualitative and Quantitative Research Characteristics: Qualitative The topic chosen speaks on the approaches of vocational peer support: research of qualitative study. The characteristic of this study is deemed to be of qualitative research because it discusses the Peer support services for individuals with psychiatric disabilities proliferated in the past two decades and ...