20 DBT Worksheets and Dialectical Behavior Therapy Skills

If you’re as lost as I was when I first heard the term, then you’ve come to the right place. In this piece, you will learn what DBT is, how it works, and some of the most useful and applicable components of treatment.
Whether you are someone who is thinking about participating in Dialectical Behavior Therapy, a therapist who is looking for DBT worksheets to use with clients, or just a curious individual, read on to learn more about it.
Mindfulness is critical to DBT. Before you read on, we thought you might like to download our three Mindfulness Exercises for free . These science-based, comprehensive exercises will not only help you cultivate a sense of inner peace throughout your daily life but will also give you the tools to enhance the mindfulness of your clients, students or employees.

This Article Contains:
- What is Dialectical Behavior Therapy? A Definition
- About the Founder by Marsha Linehan
DBT vs. CBT: How Do They Differ?
4 essential dbt skills & techniques to master.
- 4 DBT Worksheets, Handout and Manuals (PDF)
What Is The Diary Card All About?
The 4 best books on dbt, treatment methods based on dbt and emotion regulation, certification possibilities & courses.
- What is DBT’s Role in Mindfulness?
A Take-Home Message
What is dialectical behavior therapy a definition..
Dialectical Behavior Therapy (DBT) is a type of cognitive-behavioral therapy that focuses on the psychosocial aspects of therapy, emphasizing the importance of a collaborative relationship, support for the client, and the development of skills for dealing with highly emotional situations (Psych Central, 2016).
DBT was created for the treatment of individuals struggling with suicidal thoughts but has matured into a treatment for a range of other conditions that involve dysfunctional emotional regulation. It is currently considered the “gold standard” for borderline personality disorder and has even been applied to the treatment of substance abuse and eating disorders (Linehan Institute, n.d.).
DBT is generally characterized by its two main components:
- Individual weekly therapy sessions;
- Weekly group therapy sessions.
Individual Weekly Therapy Sessions
These individual sessions are an opportunity for the therapist and client to address the issues and solutions that came up over the last week, with special attention paid to self-destructive or potentially self-harmful behaviors. These behaviors are targeted not only because they are inherently worrisome, but also because they can seriously disrupt the treatment process and undermine treatment goals.
Clients and therapists work as a team in these individual sessions, with the focus on learning and improving social and coping skills . They may also discuss more general issues relevant to improving the client’s quality of life, or more specific issues like post-traumatic stress disorder .
Weekly Group Therapy Sessions

These sessions are usually scheduled for two and a half hours and generally focus on developing skills from one of four skill areas:
- Interpersonal effectiveness ;
- Distress tolerance/reality acceptance skills;
- Emotion regulation;
- Mindfulness skills.
Skill Modules
These four skill modules cover a wide range of useful skills that can be applied in daily life:
1. Interpersonal Effectiveness Module
The skills in this module are related to interacting with others, especially in difficult or potentially damaging situations.
These skills are intended to help clients function effectively when trying to change something (e.g., making a request) or in trying to resist changes (e.g., refusing a request). The intention is to aid the client in meeting their goals in each situation while avoiding any damage to the relationship or to the client’s self-respect (Psych Central, 2016).
2. Distress Tolerance Module
This module includes skills that are extremely important yet often overlooked: skills relating to accepting, tolerating, and learning from suffering.
Many other mental health treatment regimens focus on avoiding pain, changing difficult situations, or walking away from circumstances that cause suffering, but the distress tolerance skills taught through Dialectical Behavior Therapy focus on dealing with the pain and suffering that is inevitable to the human condition.
The distress tolerance module is split into four crisis survival strategies:
- Distracting;
- Self-soothing;
- Improving the moment;
- Thinking of pros and cons.
In addition, there are many skills that relate to accepting and tolerating the current situation, like radical acceptance and willingness vs. willfulness.
3. Emotion Regulation Module
Many clients who participate in DBT are struggling with personality or mood disorders and can benefit immensely from emotion regulation skills.
Some of these skills that can help clients deal with their emotions include:
- Identifying and labeling emotions;
- Identifying obstacles to changing emotions;
- Reducing vulnerability to “emotion mind;”
- Increasing positive emotional events;
- Increasing mindfulness to current emotions;
- Taking the opposite action;
- Applying distress tolerance techniques (Psych Central, 2016).
4. Mindfulness Module
Readers of this blog are likely already aware of the numerous mindfulness-related skills that can benefit them in their daily life.
These skills include “what” skills or skills that answer the question “What do I do to practice core mindfulness skills?” like observing, describing, and participating. There are also “how” skills or skills that answer the question “How do I practice core mindfulness skills?”, like non-judgment and practicing “One-mindfully” effectively.
Many of these mindfulness skills feed into skills from the other modules; for example, the nonjudgment encouraged in mindfulness is also encouraged in distress tolerance, and the observing and describing skills can be helpful in identifying and labeling emotions.
About the Founder Marsha Linehan

Dialectical Behavior Therapy was developed by Dr. Marsha Linehan.
She is a Professor of Psychology and adjunct Professor of Psychiatry and Behavioral Sciences at the University of Washington and Director of the Behavioral Research and Therapy Clinics, a research consortium that explores treatments for severely disordered and suicidal individuals (The Linehan Institute, n.d.).
Dr. Linehan is dedicated to promoting effective and accessible resources for the treatment of individuals who are struggling.
Dr. Linehan founded Behavioral Tech LLC, an institute focused on developing and sharing treatment tools for DBT training, consultation, and treatment. Behavioral Tech Research, Inc., was also established by Dr. Linehan in an effort to incorporate online and mobile technology into the successful practice of DBT.
Dr. Linehan approaches her scientific research and development from a perspective that is relatively uncommon in the sciences: one based in spirituality. She has trained with a number of spiritual leaders and influential thinkers, including a Zen master.
This may help explain her affinity for mindfulness, which grew to prominence through a collaboration of traditional Buddhist philosophy and the modern scientific paradigm (The Linehan Institute, n.d.).

Of course, DBT is a type of CBT, so similarities are understandable. But DBT also has distinct features that set it apart from most CBT approaches.
DBT, like CBT, focuses on helping people address their dysfunctional thinking and behavior through modification of their thought patterns and, through changing their thoughts, their behavior as well. However, CBT is usually confined to a limited period of time and is often applied with one or two specific goals in mind.
On the other hand, DBT narrows the focus to psychosocial aspects of daily life. Many people have trouble with their thought and behavior patterns, but these issues are often at their most disruptive in the context of relationships with others. DBT was created to approach treatment from this angle, one that is often incorporated in general CBT but is not typically the main focus (Grohol, 2016).
This emphasis on relating to others is what explains the DBT-specific treatment component of group therapy sessions. The benefits of additional therapy to the treatment of severe emotion regulation dysfunction are clear, but it’s the group aspect that really helps explain its importance.
Adding group dynamics to the learning setting offers clients an opportunity to practice relational skills in a safe and supportive environment, a practice that has been shown to be extremely effective.
DBT also differs from general CBT in the use of clients’ history. Both incorporate the past in striving for a healthier future, but this discussion is not a focus of the therapy in DBT as it often is in CBT (Grohol, 2016). The perspective of DBT is that one can learn from their past, but that problems are inevitably rooted in current thoughts and behaviors, and the present is where these will be addressed.

We won’t go into all of them in detail, but these are the main skills and techniques applied in DBT.
Interpersonal Effective Skills
1) objectiveness effectiveness “dear man” skills.
- Appear confident;
2) Relationship Effectiveness “GIVE” Skills
- Interested;
- Easy manner.
3) Self-Respect Effectiveness “FAST” Skills
- Apologies / no apologies;
- Stick to value;
Distress Tolerance Skills
1) crisis survival “accepts” skills.
- Activities;
- Contributing;
- Comparisons;
- Pushing away;
- Sensations.
2) Self-Soothing Skills
3) improve the moment “improve” skills.
- Relaxation;
- One thing at a time;
- Encouragement.
4) Pros and Cons / Accepting Reality Skills
- Willingness;
- Turning your mind;
- Radical acceptance.
Download 3 Free Mindfulness Exercises (PDF)
These detailed, science-based exercises will help you or your clients enjoy the benefits of mindfulness and create positive shifts in their mental, physical, and emotional health.
Download 3 Free Mindfulness Tools Pack (PDF)
By filling out your name and email address below.
Emotion Regulation Skills
1) reducing vulnerability skills.
- Treat physical illness;
- Altering drugs (only those prescribed by a doctor);
2) Build Mastery Skills
- Build positive experiences;
- Be mindful of current emotion;
- Opposite to emotion action.
Mindfulness Skills
1) “what” skills.
- Participate.
2) “How” skills
- Non-judgmentally;
- One-mindfully;
- Effectively (Dietz, 2012).
As you can see, acronyms are front and center in DBT treatment, in part because it makes remembering these skills in important moments easier.
You may also notice that many of these skills are generally considered effective skills , rather than specific skills for specific problems. While Dialectical Behavior Therapy focuses on the treatment of severely distressed individuals, the means of working towards these goals are not mystical or mysterious. The methods of furthering treatment are grounded in common sense and the straightforward practice of skills.
In fact, these skills are so generally applicable that many of them have practical applications for everyone.
Mindfulness
Mindfulness is such a simple and beneficial practice that it’s hard to sum up the potential positive impacts in one section, let alone one article (but we gave it a shot anyway – see our piece on the benefits of mindfulness ).
“Mindfulness can be described as simply living your life in the present instead of being stuck in the past or the future. Practicing mindfulness helps us become more aware of our thought patterns, our emotions, and how our thoughts and feelings affect our reactions to events” (Tartakovsky, 2015A).
If your mind has you jumping on the thought train (i.e., one thought leads to another, which often leads to a “should” thought, which can lead to judgment), try to detach yourself from the thought by telling yourself about the thought you are having (e.g., “There’s a thought about the errand I need to run after work”).
This can help you refocus on your current practice and remind yourself that you have thoughts, but you are not your thoughts (Tartakovsky, 2015A).
If you’re interested in learning more about how to practice mindfulness, check out our post on mindfulness exercises and techniques .
Reality Acceptance

Accepting reality is an effective antidote for a common problem in our society: struggling against the pain and suffering that is inherent to life as a human. DBT and Acceptance and Commitment Therapy (ACT) have this in common – both teach that accepting our reality, including the unpleasant aspects of it, is the only way to thrive.
This skill can be harder to practice and build than it seems since there are all sorts of sneaky ways we find to deny the reality of our situation.
These examples from Psych Central can shed some light on when we fight reality and how we can stop this tendency:
- You need to rush home, but you’re catching every red light. Instead of getting frustrated, you take a deep breath and tell yourself: “ It is what it is. I’ll get home when I get there .”
- You need to fill up your car, but gas prices have skyrocketed. Again, you breathe deeply, and say to yourself: “ There’s nothing I can do about it. I need gas. Getting angry isn’t going to help. ”
- You have to walk to work because your car is in the shop. It’s not far, but it’s pouring. You take a deep breath and say: “ It’s just rain. I’ll bring a towel, and I’ll dry off when I get to work ” (Tartakovsky, 2015A).
The part-humorous, part-helpful Tumblr blog “ Shit Borderlines Do ” provides some steps towards practicing this skill in the moment:
- Observe that you are fighting the reality of your situation. Acknowledge that you are reacting to something that you cannot change;
- Remind yourself what the reality is, even if it’s difficult or upsetting;
- Consider the causes of the current reality and incorporate the skill of non-judgment to remind yourself that this is a random occurrence set in motion by a million other factors that are outside of your control;
- Accept this reality with your whole being, or your mind, body, and spirit. Pay attention to the bodily signs of fighting reality (e.g., posture, “fight-or-flight” response) as well as the spiritual signs (you may “know” that this is real, but you don’t “feel” like it’s real).
These steps are by no means exhaustive or required to accept reality, but they can be helpful in the moment.
Radical Acceptance
Dialectical Behavior Therapy’s radical acceptance technique can help in these situations.
Radical acceptance is simply acknowledging the reality of your circumstances instead of fighting it by thinking “ This shouldn’t be happening ” or “ This isn’t fair. ”
It can be difficult to accept pain, but fighting the reality of your pain only creates more pain, and this pain is optional. Instead of fighting pain, radical acceptance offers a way to accept it and address it.
In the words of psychotherapist Sheri Van Dijk:
“If you don’t like something, you first have to accept that it is the way it is before you can try to [change] it. If you’re not accepting something, you’ll be so busy fighting that reality that you don’t have the energy to put towards trying to change it” (Tartakovsky, 2015).
This explanation shows us that not only can radical acceptance help us accept the reality of things that we cannot change, it can also help us to realize what can be changed.
Non-judgmental Stance

Being non-judgmental means that you avoid assigning value to events and feelings.
Instead of facing a difficult situation and thinking “ This is awful ,” practicing non-judgment allows us to take a step back and realize that the value judgments we make are based on facts (the facts of what is happening) and the emotions we are feeling in reaction (Tartakovsky, 2015B).
For example, you may be stuck in accident-related traffic and thinking “People are such idiots.” If you make an effort to be nonjudgmental, this may translate to “ I’m stuck at a standstill in traffic because of an accident up ahead. This makes me frustrated and upset. ”
When you break a judgment down into a fact and your emotional reaction, you not only reduce the emotion(s) you are feeling, you can also be empowered to think about ways to solve the problem and make healthy decisions.
Say you are thinking about how selfish your significant other is being right now. Instead of stopping at “ My partner is so selfish ,” practicing non-judgment may lead to articulating the issue (“ My partner is not helping me with this problem, and that makes me angry and disappointed ”) and finding a way to solve it (“ This is not a wise use of my time and energy. I will talk to my partner about how his/her unwillingness to help me with this problem makes me feel, and try to negotiate a solution with him/her ”).
Handling emotional situations in this manner can not only help you reduce your emotional reaction and find smart solutions to problems, it can also improve your self-esteem and self-respect when you handle the issue in a way that makes you proud of yourself (Tartakovsky, 2015B).
4 DBT Worksheets, Handout, and Manuals (PDF)

This is where Dialectical Behavior Therapy worksheets, handouts, and manuals can prove to be extremely effective tools in building your skills and improving your ability to accept your situation, deal with difficulty, and solve problems.
We’ll go over some of the most popular and effective ones below.
DBT Interpersonal Effectiveness Skills
This handout lists and describes the interpersonal effectiveness skills we outlined earlier, and also provides useful tips to put these skills into practice.
For example, the section on objective effectiveness (the DEAR MAN skills) lists the following tips:
- Use clear and concrete terms to describe what you want;
- Don’t say: “Could you please clean?”;
- Do say: “Could you do the dishes before going to bed?”
- Let others know how a situation makes you feel by clearly expressing your feelings;
- Don’t expect others to read your mind;
- Try using this line: “I feel ___ because ___.”
- Don’t beat around the bush—say what you need to say;
- Don’t say: “Oh, well, I don’t know if I can cook tonight or not;”
- Do say: “I won’t be able to cook because I’m working late.”
- Reward people who respond well, and reinforce why your desired outcome is positive;
- This can be as simple as a smile and a “thank you.”
- Don’t forget the objective of the interaction;
- It can be easy to get sidetracked into harmful arguments and lose focus.
- Consider your posture, tone, eye contact, and body language.
- No one can have everything they want out of an interaction all the time;
- Be open to negotiation;
- Do say: “If you wash the dishes, I’ll put them away.”
The Wise Mind
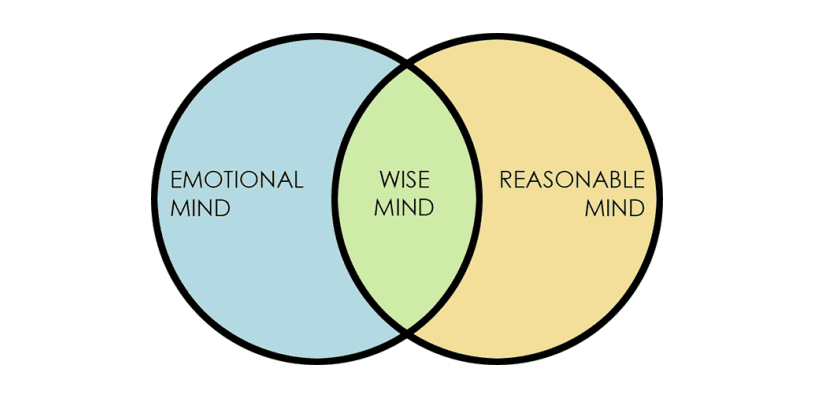
It is a balance between the two minds and is characterized by the ability to recognize and respect your feelings, but also respond to them in a rational manner .
The worksheet offers space to describe an experience that you have had with each of these three “minds” to further your understanding of the minds and how they have come into play in your life.
Function of Emotion Worksheet
The Function of Emotion Regulation worksheet helps you to identify the function of an emotional reaction you have had over the last week.
The worksheet moves through the following questions and steps:
- What was the prompting event?
- What was your interpretation?
- What was the emotion and intensity (0-100)?
Use the following to identify the function(s) of the emotion:
- Did the emotion communicate something to others or influence their behavior? If so, describe;
- Did the emotion organize or motivate you to do something? If so, describe;
- Did the emotion give you information, color your perception, or lead you to any conclusions? If so, describe.
These questions aid the individual in making the connections between a galvanizing event and the reaction s/he had to the event, as well as understanding how the emotional reaction impacts the self and others.
DBT Skills Training Manual: Second Edition
For a resource that can help you apply general DBT treatment, check out this manual from Dr. Linehan herself. It’s not free, but it is an extremely valuable resource for applying DBT with your clients.
This manual is separated into two parts: the first describes DBT and provides instructions on how to set up a treatment program and manage the problems that can arise, while the second gives detailed notes on teaching each DBT skill.
Check out the manual, buying options, and reviews from some very satisfied readers here .

According to dbtselfhelp.com :
“You use the card to track your urges, moods, how you did or did not use DBT Skills, your feelings, and whatever else is helpful to you. You bring these cards with you to your DBT therapist every week to help you look for behavior patterns and triggers that occur in your life. Such information is invaluable to help you to help yourself live a life worth living.”
There are many possible layouts for a diary card (see here , here , and here ), but they generally contain the same fields:
- Day/date of urge or behavior;
- Emotions felt;
- Actions taken or skills used (or not used);
- Triggers for the urges.
The diary card may also include space for a general rating for the day and any medications or substances used (legal or illegal).
The client is encouraged to fill out this card regularly and faithfully. While it is important that the client does so, they should know that no one is going to score them or judge them based on their diary card. It is not an assignment to be completed and graded, but a way for them to track their experience and evaluate their progression through DBT treatment and, hopefully, self-improvement.
Diary Card App
As with most problems or issues, technology is making an impact on how people keep diary cards.
If you hate to waste paper, don’t like getting ink on your hands, or just get tired of writing, there’s a diary card app that you can use instead.
Check out the app created by a licensed clinical psychologist here .
If you’re interested in learning more about Dialectical Behavior Therapy, as a client, therapist, or just a curious person, there are several books available.
Listed below are some of the most popular and highly reviewed books on DBT out there, and they’re all available for purchase on Amazon.com:
1. The Dialectical Behavior Therapy Skills Workbook – Matthew McKay, Jeffrey C. Wood, and Jeffrey Brantley
It walks the reader through descriptions of DBT and how it can help, introductory exercises, and more advanced skill chapters. This can be an excellent resource for any individual considering DBT or for therapists to recommend to their clients.
Available on Amazon .
2. DBT Made Simple: A Step-by-Step Guide to Dialectical Behavior Therapy – Sheri Van Dijk
It includes a section on the theory and research behind DBT and how it grew from traditional CBT approaches, as well as strategies for working with clients, an explanation of the four skill modules, and several handouts, case examples, and some sample therapy dialogue.
3. The Mindfulness Solution for Intense Emotions: Take Control of Borderline Personality Disorder with DBT – Cedar R. Koons and Marsha M. Linehan
It teaches readers about the seven powerful skills related to mindfulness and emotion regulation that can help people cope with a borderline personality disorder (BPD), post-traumatic stress disorder (PTSD), severe depression, and other emotion regulation problems.
4. Calming the Emotional Storm: Using Dialectical Behavior Therapy Skills to Manage Your Emotions and Balance Your Life – Sheri Van Dijk
With a rating of over 4.5 out of 5 stars from nearly 50 customers, it sounds like the description is accurate.
These books are an excellent start to learning about DBT and applying the skills in your clients’ lives, but if you’re looking for even more, visit this website to learn about other helpful books.

- Understanding one’s emotions;
- Reducing emotional vulnerability;
- Decreasing emotional suffering (Bray, 2013B).
There are several ways to work toward these goals.
One of the websites we mentioned earlier, dbtselfhelp.com , offers an outline of how to build emotion regulation skills:
Interpreting Emotions
We all have emotions, but there is a theory that there are only a few basic emotions while the rest is interpretation and evaluation.
You can work on your skills related to interpreting emotions by completing a writing challenge described here .
Describing Emotions
Emotions involve action urges, prompts to perform certain behaviors. These urges are not part of the emotion but can feel like they are. There is often a prompting event, followed by interpretation, body changes in response to the emotions, and action urges.
This can lead to an effective or dysfunctional expression of emotions, which can have a wide range of consequences. To work on describing emotions, try to describe the qualities of your emotions and pay attention to things that may interfere, like secondary emotions that spring from the original emotion.
Follow this link for more information on describing emotions.
Function of Emotions
Emotions have three major functions in DBT:
- They communicate to and influence others;
- They organize and motivate action, and;
- They can be self-validating.
You can learn about the function of emotions by answering questions like “What are some examples of situations where your expressions of emotion were misread?” and “Can you think of some times when you misread the emotions of someone else?”
See this page for more information.
Reducing Vulnerability
We are all vulnerable to negative emotions, but we can build our skills related to reducing vulnerability. You can keep track of the factors that affect your physical and mental wellbeing, like your diet, any mood-altering drugs, sleep, and exercise.
Refer to these skills in the emotion regulation module for more information.
Paying Attention to Positives
Increasing positive emotions can be an effective method for dealing with difficult emotions. To build this skill, focus on the positive experiences you have throughout the day (short-term experiences) and the bigger, more impactful ones (long-term experiences).
Focus on building and maintaining positive relationships, and give mindfulness a try to savor positive experiences.
Letting Go of Painful Emotions
On the flipside of savoring the positive, letting go of the negative also has a place in emotion regulation. While accepting that pain happens is healthy, dwelling on negative emotions is dysfunctional.
Practice observing your emotions, describing and accepting them but not allowing yourself to be overwhelmed by them.
See this page for more information on letting go.
Opposite to Emotion Action
This technique is used to change painful emotions that are harmful rather than helpful. It is not about suppressing our emotions, but accepting the emotion and using it to take a different action.
To practice this technique, list some examples of when you have acted opposite to your current emotion. Describe a situation in which it is not appropriate to act opposite to your emotion to help you learn about the difference between each situation.
Check out this handout for more information.
What is Dialectical Behavior Therapy for adolescents (DBT)? – UC San Francisco
Dialectical Behavior Therapy is a recognized treatment that is well supported by the evidence. There are many ways to learn about applying DBT, but getting certified is a great option. There are courses and online DBT training for both individuals interested in practicing DBT and for therapists and other mental health professionals who wish to apply DBT in their work.
For Therapists and Other Mental Health Professionals
Dr. Linehan’s Behavioral Tech Research Institute provides information on Dialectical Behavior Therapy certification for therapists. The certification is available through the DBT-Linehan Board of Certification and requires the following:
- A graduate degree in a mental health-related field from a regionally accredited institution of higher education;
- A mental health practitioner license;
- A minimum of 40 didactic training hours specific to DBT Clinical experience with DBT (at least three clients);
- DBT team experiences (at least 12 months of preparation and current participation on a DBT team);
- DBT skills knowledge/experience;
- You must have read the Skills Training Manual for Treating Borderline Personality Disorder by Marsha Linehan, completed all the homework assignments in the manual, and taught or participated in all modules of skill training;
- Successful pass of exam based on the Cognitive-Behavioral Treatment of Borderline Personality Disorder by Marsha Linehan;
- Letter of recommendation from your team leader;
- Work product demonstration (videotapes of three consecutive live therapy sessions);
- Mindfulness experience (at least one of the following: a mindfulness retreat, formal practice community participation, formally a student of a recognized Zen/contemplative teacher, or at least one formal training in mindfulness).
You can also become certified through the Dialectical Behavior Therapy National Certification and Accreditation Association (DBTNCAA). This allows you to list a specialized certification in DBT when you apply to Health Care Providers and HMO networks.
What is DBT’s Role in Mindfulness?

While DBT and mindfulness are not synonymous, they are certainly linked.
DBT is a therapy based on identifying, describing, and modifying thoughts and feelings. Mindfulness has clear applicability in this therapy, through its ability to help practitioners to become more aware of their feelings, thoughts, impulses, and behaviors (Bray, 2013A).
One description of the benefit of mindfulness in Dialectical Behavior Therapy is that it provides the individual with the ability to take control of the mind instead of having the mind control the individual.
Practicing mindfulness helps the individual in DBT to direct their attention to observing, describing, and participating in a nonjudgmental way, which enhances the individual’s skills and leads to improved ability to focus on the positive, let go of the negative, and regulate emotions.
As we’ve said before, mindfulness is an extremely useful skill for individuals dealing with difficult emotions or situations, but it can be an even more effective tool for people struggling with a diagnosis.
Top 17 Exercises for Mindfulness & Meditation
Use these 17 Mindfulness & Meditation Exercises [PDF] to help others build life-changing habits and enhance their wellbeing with the physical and psychological benefits of mindfulness.
Created by Experts. 100% Science-based.
The intention of this piece was to provide an overview of Dialectical Behavior Therapy and outline the skills and tools that can help you or your clients to address emotion regulation issues. I hope it has met this goal, and that you know much more about Dialectical Behavior Therapy than you did when you started!
I hope you also keep in mind that the skills involved in DBT are applicable for those that are not suffering from a diagnosed mental health issue as well. Skills like mindfulness, focusing on the positive, letting go of the negative, and accepting the reality of your situation have clear benefits for everyone, not just those who are in the midst of suffering.
Have you tried DBT? Have you applied DBT with your clients? As always, please let us know about your experiences in the comments.
Thanks for reading!
We hope you enjoyed reading this article. Don’t forget to download our three Mindfulness Exercises for free .
- Bray, S. (2013A). Core mindfulness in Dialectical Behavior Therapy. GoodTherapy. Retrieved from http://www.goodtherapy.org/blog/core-mindfulness-dialectical-behavior-therapy-0215134
- Bray, S. (2013B). Emotion regulation in Dialectical Behavior Therapy. GoodTherapy. Retrieved from www.goodtherapy.org/blog/emotion-regulation-dialectical-behavior-therapy-dbt-0318135
- Dietz, L. (2012). DBT skills list. DBT Self Help. Retrieved from www.dbtselfhelp.com/html/dbt_skills_list.html
- Grohol, J. (2016). What’s the difference Between CBT and DBT? Psych Central. Retrieved from https://psychcentral.com/lib/whats-the-difference-between-cbt-and-dbt/ Linehan Institute
- Psych Central. (2016). An overview of Dialectical Behavior Therapy. Psych Central. Retrieved from https://psychcentral.com/lib/an-overview-of-dialectical-behavior-therapy/
- Tartakovsky, M. (2015A). 3 DBT skills everyone can benefit from. Psych Central. Retrieved from https://psychcentral.com/blog/archives/2015/08/28/3-dbt-skills-everyone-can-benefit-from/
- Tartakovsky, M. (2015B). What it really means to practice radical acceptance. Psych Central. Retrieved from https://psychcentral.com/blog/archives/2015/10/04/what-it-really-means-to-practice-radical-acceptance/
- The Linehan Institute. (n.d.). Linehan Institute. Retrieved from http://www.linehaninstitute.org/about-Linehan.php
Share this article:
Article feedback
What our readers think.
I appreciate you giving this information. In our online treatment, dialectical behavioral therapy is used. It works incredibly well for depression, substance abuse, and borderline personality disorder. Even the most serious cases respond very well to DBT, and we treat a wide range of clients.
I’ve been looking for this info!!! DBT saved my life and I believe EVERYONE could benefit from it. The reason I’ve been searching is for my boys. I never meant to pass that part of me to any of my children but I see it in them. I’m trying for them to avoid the wrong roads I took. I barely escaped the darkness. I couldn’t bare to see them in that place. So ty!! I can’t say it enough.
I have recently completed a DBT group therapy course which I found extremely helpful in managing my BPD and PTSD.
I would love to teach these skills to others worldwide, is it a requirement that you have a certain level of certification to teach cbt/dbt and if so what qualifications are required to go on to teach these skills to others online?
I believe I have enough personal experience, understanding and now knowledge of the skills and mental illness, but am confused on the law of teaching these skills without official certification, or even if that’s a must?
Please help
That’s great your experience was so helpful for you! To teach CBT and DBT skills to support people with mental illnesses, you need to become a licensed therapist or psychologist. This requires that you complete a master’s qualification. You can learn more about the process in our dedicated blog post: https://positivepsychology.com/how-to-become-a-therapist/
Hope this helps!
– Nicole | Community Manager
I have the same question. I work in mental health as a life coach and yoga instructior. I do not want to teach the program. My intention is to use the “My life Vision” worksheet and the wise mind model. What is the legal implications? I would sight the source while being clear on my role and title. The client would be provided resources for a licensed therapist.
This is outstanding!!!!!!
Just curious, you mention in the section – Working with Primary and Secondary Emotions While – “this webpage” but then there is no link to the webpage the article is referencing. I am wondering if you would direct me to the webpage please for further reference. As well, in the following paragraph on Emotion Regulation, again you mention “this worksheet” but don’t link a worksheet. Are you able to reference these for follow-up, please and thank you?
Hi Heather,
Thank you so much for being so observant and bringing this to our attention.
These links went to other websites, which may have restructured their content and caused dead links on our side. I have unfortunately not been able to trace the original worksheets discussed, but have amended our copy to prevent any further confusion.
Apologies for not being able to help you further.
Regards, Annelé
I wish DBT was more available in standard mental health services. In the UK, it’s thin on the ground.
BPD is prolific and causes so much suffering. Yet still much ignorance and stigma remains.
I hate the way so many blame and shame such lonely and fragile people.
We want love, but are terrified of our vulnerability being abused. I wish I could’ve got this treatment. My partners would not have had to put up with so much, maybe.
Damaged people damage people.
Thank you for sharing your thoughts on the availability of Dialectical Behavior Therapy (DBT) and the challenges faced by individuals with Borderline Personality Disorder (BPD). It is indeed disheartening to hear that access to this valuable treatment is limited in the UK and that stigma continues to surround BPD.
The importance of raising awareness about mental health conditions and advocating for better access to evidence-based treatments, such as DBT, cannot be overstated. It is essential to create a more understanding and compassionate society that supports individuals with mental health challenges instead of perpetuating shame and blame.
I encourage you to check out Psychology Today! It has a great directory you can use to find therapists in your local area. Usually, the therapists provide a summary in their profile with their areas of expertise and types of issues they are used to working with.
Please know that your voice matters and your experiences can contribute to raising awareness, challenging stigmas, and ultimately improving mental health care for those who need it most.
Warm regards, Julia | Community Manager
I have been waiting a very long time for DBT therapy for diagnosed Borderline Personality Disorder, being unable to work for 20 months now. I have finally been assigned a place but am unable to purchase DBT Skills Training Handouts and Worksheets Second Edition. Seeking help from so many places, I can’t even find a Microsoft Word version of the worksheets that I can complete online in order to participate in the group therapy. As a result, I cannot have the therapy I desperately need. I know this is a long shot, but does anyone have a version in Word (or Open.Office) that they can send to me?? Otherwise, I will continue to suffer as the NHS has taken so long to help me with a condition I have had for decades, together with my depression and anxiety. Thanking you in advance.
I’m sorry to hear you’ve had so much trouble receiving support. Please let me know which specific worksheet(s) you are trying to open, and I will let you know the best way to do so with free software.
Thank you for providing this information.
This sums up the group therapy session I have just graduated from! Modalities were based from Marsha’s core theories; it is alot of skills to practice.
Courtney, everything you wrote on this page IS TRUE, well written for any level audience. Well done.
Radical Acceptance, and Emotional identification is THE HARDEST part of BPD and DBT. I find it hard now to identify why I am in an “emotional crisis”, since I want to “Name it, to Tame it”. I really can’t identify why I become so deeply emotional (rage, crying, worthless…) but the emotions are EXTREME. I can’t identify what I was so emotional about, why I became so emotional in the first place ONCE I GET CAUGHT IN “THE DARK HOLE” as my husband refers to my “emotional crises”.
Just thought I would share my own personal experience; FYI I am an ongoing work in progress. Still have many ups and downs; however I can reflect on these events (usually AFTER the fact, but LIVE AND LEARN).
Super frustrting that it says “We hope you enjoyed reading this article. Don’t forget to download our 3 Mindfulness Exercises for free.” but you enter your information and then it tells you it cost $27.00. Why the false advertising…why say free just to get another person email to spam?
My apologies! Please try visiting this link to access the free downloads. The three exercises are definitely free! But if there’s a link in the text that tries to point you toward a paid resources, please let us know where it is so we can correct this 🙂
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Non-Sleep Deep Rest (NSDR): Exploring a World Beyond Sleep
In our relentless quest for productivity and success, we often fall prey to the misconception that rest is a reward for hard work. But what [...]

35 DBT Interventions & Resources for Your Therapy Sessions
Dialectical Behavior Therapy (DBT) is not your average therapy session; it’s like a toolbox filled with colorful tools to tame the unruliest of emotions and [...]

Equanimity: The Holy Grail of Calmness & Grace?
How can we find a calm harbor within ourselves amid life’s storms? How can we develop our ability to remain composed and centered when faced [...]
Read other articles by their category
- Body & Brain (48)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (27)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (17)
- Positive Parenting (0)
- Positive Psychology (33)
- Positive Workplace (36)
- Productivity (16)
- Relationships (49)
- Resilience & Coping (35)
- Self Awareness (21)
- Self Esteem (37)
- Strengths & Virtues (30)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
3 Mindfulness Exercises Pack (PDF)
- Free Therapy Techniques
- Anxiety Treatment
- Business and Marketing
- CBT Techniques
- Client Motivation
- Dealing With Difficult Clients
- Hypnotherapy Techniques
- Insomnia and Sleep
- Personal Skills
- Practitioner in Focus
- Psychology Research
- Psychotherapy Techniques
- PTSD, Trauma and Phobias
- Relationships
- Self Esteem
- Sensible Psychology Dictionary
- Smoking Cessation and Addiction
- The Dark Side of Your Emotional Needs
- Uncommon Philosophy
10 of the Best Sites for DBT Worksheets and Resources
The best dialectical behavior therapy resources, activities and assignments all in one place.
Hi, it’s Rosie here, Content Manager at Uncommon Knowledge. Continuing our series of ‘Top 10s’, which started with ‘ Top Ten CBT Worksheets ‘, we’ve put together this piece on DBT. I hope it’s useful!
Dialectical behavior therapy (DBT) is one of the most effective therapeutic treatment approaches for issues related to emotional dysregulation 1 . Focusing on the psychosocial aspects of therapy, DBT emphasizes a collaborative approach, with support for the client and development of skills for dealing with highly charged emotional situations.
DBT was originally created for treating clients diagnosed with borderline personality disorder and struggling with chronic suicidal ideation. But over time, DBT has shown efficacy in the treatment of a range of issues involving dysfunction of emotional regulation and has become the gold standard for treating borderline personality disorder.
Navigating the ocean of resources
As a practitioner, you are probably always on the lookout for clinically sound, cost-effective, easily accessible resources and tools. But Google “DBT worksheets” and you’ll get almost a million hits. (I’m not exaggerating!) How do you know what’s legit and what is just an attempt to sell you something that may not be clinically sound? And, more importantly, who has time to sift through that many links?
Here’s the article you’ve been waiting for! We’ve done the searches, sifted through the results, and gathered ten of the best DBT resources out there for information and worksheets. You’re sure to find something (probably many things!) you can use to help your clients.
1. The Linehan Institute
You can’t talk about DBT without mentioning Dr Marsha Linehan and the Linehan Institute. At the institute’s website you will find a number of informative articles and resources for clients, families, and clinicians.
One of the highlights of the site is a free two-hour video that addresses how using the principles of DBT can help teens manage intense feelings. It is a great resource for clinicians and parents to learn how they can help.
Visit the institute’s sister site, Behavioral Tech , for even more information and resources.
2. PsychPoint
PsychPoint is a great mental health resource that offers a large selection of free DBT worksheets for therapists in PDF format. At the time of writing, 29 worksheets are available for download. Topics include:
- Distress Tolerance Skills: Radical Acceptance Worksheet
- DBT Interpersonal Effectiveness Skills: FAST Worksheet
- DBT Interpersonal Effectiveness Skills DEARMAN Worksheet
- Emotion Regulation Skills: Opposite Action Worksheet
- Emotion Regulation Skills: PLEASE Worksheet.
3. Therapist Aid
This website has long been a favorite of therapists, providing a large selection of free, simple-to-use worksheets that are easy to understand and jargon-free. Search for “DBT” and you’ll find a range of great worksheets on a variety of topics, including:
- DBT Distress Tolerance Skills
- DBT Emotion Regulation Skills
- The Wise Mind
- DBT Mindfulness Skills.
You will also find articles and some very reasonably priced resources for purchase.
4. Positive Psychology Program
You’ve probably seen this awesome website mentioned in other articles, and for good reason! This site has compiled some of the best resources available for a variety of clinical needs, including, of course, DBT . You may find some overlap with other sites, but the Positive Psychology Program website is one of the most comprehensive resources for tools and information related to the positive, person-centred approach.
In addition, the Positive Psychology Program offers a free e-book containing exercises that you can use with your clients. When you join their mailing list, you’ll also receive additional resources, including free PDFs and downloads.
FREE Reframing Book! Just subscribe to my therapy techniques newsletter below.
Download my book on reframing, "New Ways of Seeing", when you subscribe for free email updates
Click to subscribe free now
5. DBT Self Help
This interesting website was built by and for people who have experience with or are interested in DBT. Here you will find a variety of tools, such as:
- Diary cards
- DBT skills information
- Flash cards
- And so much more.
There are also links to a number of other resources that clients may find helpful. This is a great site for your more self-motivated clients to learn more about DBT and how it can be useful in their lives.
6. GetSelfHelp
This is another website that you’ve probably seen mentioned before for its plethora of CBT-focused resources. Now they’ve added a DBT-specific section that offers a good overview of DBT and the Wise Mind theory. Here you’ll also find a number of free worksheets and educational handouts, such as:
- Wise Mind Worksheet
- Dealing With Distress Worksheets
- Mindfulness
- Emotional Regulation.
7. Pinterest
Pinterest might not be the first place you think of when you’re looking for DBT worksheets. But believe it or not, this site is becoming one of the go-to places for therapists to find all kinds of helpful resources.
When you search for “DBT Worksheets” on Pinterest, you’ll find a myriad of pins and some great resources. You may even want to join some Pinterest Groups focused specifically on the types of tools you’re looking for. Some groups are more self-help based, while others are aimed at clinicians.
On Pinterest, you’re bound to find something that will help your client. And the best part? It’s free to use!
8. Psychology Tools
This website offers so many useful resources for both clinicians and self-motivated clients. There are plenty of free self-help tools and information available here, including:
- A Guide to Emotions
- Thought Records
- Symptom Monitoring
- Behavioral Activation
- And much more.
The site also offers a wide assortment of more clinically focused materials, including assessments and worksheets, workbooks, e-books, techniques, and more. Some of these materials are free to use, while others are available to subscribers only. The subscription fee is very reasonable, but if you’re not sure just opt for a free trial to see what’s available.
9. The Centre for Clinical Interventions (CCI)
This Australian mental health organization has developed a number of DBT-related resources. Free resources available on the website include programs and educational materials on topics such as:
- Distress Tolerance/Emotional Regulation
- Assertiveness
- Interpersonal Effectiveness.
The site also offers a number of workbooks and manuals for clinicians. Some of these are free to download; others are available for a reasonable fee. To start with, it’s worth checking out the Distress Tolerance workbook .
The resources on this site are some of the best out there, and not just for DBT. This is one site you’ll want to bookmark, as you will return again and again.
10. Mark Purcell, PsyD
This is a gem of a website. Dr. Purcell is a clinician experienced in the practice of DBT with youth. His website offers an entire section of resources available for professionals. Here you will find an excellent DBT Workbook and sample Diary Card.
What makes this site a standout are the many PowerPoint presentations available for use by clinicians. You’ll find a number of training presentations, including a great overview of the principles and therapeutic strategies of working with youth using DBT. What a great tool for your DBT toolbox!
So, DBT practitioners, there you have it: some of the very best DBT-related resources the internet has to offer. I hope you find this list useful in your practice and helpful for your clients. Of course, you probably have a few of your own little gems that you go to again and again, but if there’s one thing I know, it’s that you can never have too many great tools in that toolbox!
Check these out and find the ones that work for you. Be well!
For more articles on therapy worksheets and more, subscribe to our co-founder Mark Tyrrell’s therapy tips newsletter .
Watch Mark conduct live therapy
Hundreds of practitioners are watching Mark Tyrrell conduct therapy with dozens of clients and a multitude of issues in Uncommon Practitioners TV right now. Join them here .
About Mark Tyrrell
Psychology is my passion. I've been a psychotherapist trainer since 1998, specializing in brief, solution focused approaches. I now teach practitioners all over the world via our online courses .
You can get my book FREE when you subscribe to my therapy techniques newsletter. Click here to subscribe free now.
You can also get my articles on YouTube , find me on Instagram , Amazon , Twitter , and Facebook .
- https://behavioraltech.org/wp-content/uploads/2019/04/ResearchUpdatesJanuaryFebruaryMarch2019.pdf

Related articles:
There are no related articles.
Read more CBT Techniques therapy techniques »
Search for more therapy techniques:
- Odnoklassniki
- Facebook Messenger
- LiveJournal

Clinical psychology
- Anxiety disorders
- Feeding and eating disorders
- Mood disorders
- Neuro-developmental disorders
- Personality disorders
- Affirmations
- Cover Letters
- Relationships
- Resignation & Leave letters
Psychotherapy
Personality.
Table of Contents
Borderline Personality Disorder Self Help Worksheets (5)
As a BetterHelp affiliate, we may receive compensation from BetterHelp if you purchase products or services through the links provided.
The Optimistminds editorial team is made up of psychologists, psychiatrists and mental health professionals. Each article is written by a team member with exposure to and experience in the subject matter. The article then gets reviewed by a more senior editorial member. This is someone with extensive knowledge of the subject matter and highly cited published material.
This page displays borderline personality disorder self-help worksheets.
Some of these worksheets have been created by us while some of them have been curated from reputable third party websites, after reviewing relevant content in bulk.
These borderline personality disorder self help worksheets aid individuals with borderline personality disorder in regulating their emotions efficiently.
It teaches them deep thinking techniques to help them manage their intense mood shifts.
Narcisim and paranoia are few of the different types of personality disorders.
Borderline Personality Disorder Self Help Worksheet- Mood Buttons
A borderline personality disorder is referred to as a dysfunctional emotional state.
Borderline personality disorder is also known as emotionally unstable personality disorder (EUPD).
This psychological disorder is characterized by long term issues in an individual’s relationships, misinterpretation about one’s image and encounter of intense emotions.
Individuals with borderline personality disorder get triggered easily.
The most common triggers of these individuals include problems in one’s relationships and distress resulting from those relations.
The relationships of such people make them feel abandoned, rejected or criticized. They experience intense emotions like fear, anger, worthlessness etcetera and may indulge in self-harm behaviors.
Thus, it is important for an individual to recognize his emotional triggers, so he could work on them to prevent their negative results.

Borderline Personality Disorder Self Help Worksheet- Justifying Mood Shifts
Individuals with borderline personality disorder find it very difficult to manage their emotions as they experience them with greater intensity than others do.
Such individuals think on the extremes only and ignore the grey part between white and black.
This is why their thinking is sometimes referred to as black or white thinking.
Their inability to think in between extremes makes it difficult for them to regulate their emotions efficiently.
Though emotion regulation seems difficult for individuals with borderline personality disorder it is not impossible.
Exploring the situation in detail can help him manage his intense emotions.

Borderline Personality Disorder Self Help Worksheet- Pre-Planned Coping
Dealing with uncomfortable feelings resulting from intense emotions like anger and fear is a challenging but achievable task.
Individuals with borderline personality disorder experience emotions with greater intensity and thus struggle to regulate their emotions.
When such individuals are aware of their triggers they can successfully work on their triggers and adopt pre-planned coping strategies to deal with uncomfortable emotions emerging in the future with efficiency.
Some of the pre-planned coping strategies include writing down phone numbers on your diary or cell phone to call them when you feel worthless and wish to harm yourself, keeping a diary to write down your feelings when your experience intense emotions like anger, making a list of things you would do to distract yourself when you encounter intense emotions such as anxiety and so forth.

Borderline Personality Disorder Self Help Worksheet- Anger Diary
Anger management can be difficult at times when an individual is experiencing it with greater intensity.
Writing down feelings on a paper can help an individual prevent their negative outcomes.
Anger diary worksheet is an effective technique for dealing with anger emotion.
The individuals are directed to write down the anger causing the incident and their feelings.
Writing down the whole incident and their feelings can help an individual review the whole situation and figure out where the real problem is.
Anger diary not only helps an individual calm down but also aids in identifying the problem.
This worksheet is an effective source of managing anger . You can download it from here .
Borderline Personality Disorder Self Help Worksheet- Triggers and Coping Skills
Borderline personality disorder can be treated by managing the triggers that give rise to intense emotions in an individual.
Acknowledging the triggers and working on them can help deal with the negative outcomes produced by the triggers.
The worksheet, triggers and coping skills, by a reputable website, aims to help individuals identify the things that trigger intense emotions in them and thinking of the skills and strategies that can help deal with them.
This worksheet is an effective source of identifying and managing emotions.
It can be downloaded from this link.
Borderline Personality Disorder Self Help Worksheet- Emotion Regulation Handout 10
Emotion regulation handout 10 is a great, detailed resource for learning ways of dealing with intense emotions.
This worksheet teaches individuals effective ways of managing common emotions such as fear, justified nd unjustified guilt or shame, sadness or depression and anger.
This worksheet is easily available on the internet and can also be printed.
It can be accessed from here .
Borderline Personality Disorder Self Help Worksheet- Rank Order of BDP Intrusion
Different people experience different emotions that make them feel sad, depressed, anxious, abandoned and creates an urge to commit suicide.
Rand order of BDP intrusion worksheet is a good resource for identifying one’s triggers and work on them.
This worksheet provides individuals with the most common triggers of BPD and directs the individuals to rank them in order, starting from the greatest BPD issue they are facing.
Then the individuals are asked to find the root causes of why these issues trigger intense emotions in them.
This helps them recognize their triggers and work on them to eliminate their negative effects on themselves.
This worksheet can be downloaded in the form of pdf through this link.
Borderline Personality Disorder Self Help Worksheet- Six Steps of the Self-Mutilation Sequence
The six steps of the mutilation sequence worksheet is an effective worksheet for helping the individuals identify their self-harm patterns and enable them to control their behavior efficiently.
This worksheet consists of six questions that inquire about the tendency to get harmed from others, harm oneself and getting detached from oneself.
The individuals are then asked about the ways the can prevent self-harm.
This worksheet is helpful in preventing self-mutilating behavior.
The worksheet can be downloaded in the form pdf from here.
This page provides you with some of the best borderline personality disorder self-help worksheets .
Some of these worksheets have been made by us while some of them have been curated from reputable third-party websites.
If you have any questions or queries regarding these worksheets, let us know through your comments, we will be glad to assist you.
Enjoyed this article? Then Repin to your own inspiration board so others can too!
Was this helpful?
Related posts, building resilience: psychological strategies for helping children cope with challenges, counseling compass: mapping your route to emotional well-being, how to deal with political anxiety in an election year.
Daniel J. Fox, Ph.D
- BPD Symptom Tracker
- Anger Meter
- Facts & Fears Worksheet
- Trigger = Response worksheet
- Personality Traits List
- Optimism v Pessimism
- Anger Sequence Handout
- Distress Tolerance Worksheets
- My Stress Signs and Symptoms
- Coping Sequence
- Goals & Resolutions Worksheet
- Loneliness to Connection
- Defense Mechanism Worksheet
- 6 Steps of the Self-Harm Sequence
- BPD Intrusion Worksheet
- Anger Questionnaire
- Control Your Emotions Worksheets
- ACE Anxiety Worksheet
- BPD and Unstable Self-Image Worksheet
- Borderline & Narcissistic System Worksheet
- Depression Awareness PHQ-9
- 3-Parts of the Narcissistic Relationship Cycle
- Weekly Mood Tracker
- BPD & Splitting Treatment Scale
- Changing your attachment type
- Holiday Survival Tips Worksheet
- Escape Valve Emotions Worksheet
- Paranoid Personality Disorder Checklist
- Cluster B Client Assessment
- Emotions Exercise
- Perspectives of LIFE
- Antisocial PD - Can They Collaborate?
- Histrionic PD - Emotional Spectrum
- Narcissistic PD - Surmount Power Struggles
- Borderline PD - Identifying Maladaptive Patterns
- DBT - Ready, Breathe, Draw
- Behavioral Stress Tolerance Plan Worksheet
- Feeling Connected and Understood Worksheet
Daniel J. Fox
I’m dedicated and honored to be able to help people help themselves through the identification of personality components
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Coping Skills for Borderline Personality Disorder
Amy Morin, LCSW, is a psychotherapist and international bestselling author. Her books, including "13 Things Mentally Strong People Don't Do," have been translated into more than 40 languages. Her TEDx talk, "The Secret of Becoming Mentally Strong," is one of the most viewed talks of all time.
:max_bytes(150000):strip_icc():format(webp)/VW-MIND-Amy-2b338105f1ee493f94d7e333e410fa76.jpg)
Benefits of Coping Skills
Engage in an activity, find support, ride it out, ground yourself, breathe deeply, help someone else, how to learn bpd coping skills.
If you have borderline personality disorder (BPD), your emotions can be overwhelming. Symptoms of BPD , include erratic mood shifts, self-harming behaviors, suicidality, intense emotional experiences, sensitivity to problems in your relationships, and problems with impulsive behaviors . These symptoms may all be related to one core feature: emotion dysregulation.
Because of emotion dysregulation, you may have very strong emotional responses and difficulty managing those responses. Unfortunately, many people with BPD turn to unhealthy behaviors to cope with emotional pain, such as violence , self-harm, or substance abuse.
This article discusses coping skills that can help to reduce emotion dysregulation and other symptoms of BPD.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
Since emotion dysregulation is such an important feature of BPD, many treatments for this personality disorder emphasize the importance of building coping skills to better manage emotions when they arise.
What exactly are coping skills? They are healthier ways of addressing situations and their resulting emotions.
Learning new ways to cope provides possible benefits. These techniques may:
- Build confidence in your ability to handle difficult situations
- Improve your ability to be able to continue to function well even when in stressful circumstances
- Reduce the intensity of the emotional distress you feel
- Reduce the likelihood that you will do something harmful (e.g., engage in self-harming behaviors) to attempt to escape from the emotional distress
- Reduce the likelihood that you will engage in behaviors that destroy relationships (e.g., physical aggression) when you are upset
- Ultimately reduce your overall experience of emotion dysregulation
If you are having suicidal thoughts, contact the National Suicide Prevention Lifeline at 988 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database .
There are literally thousands of different coping skills that people use to manage stressful situations and the emotions that result. Here are a few types of coping skills that work for many people.
Music can be a helpful way to explore emotions. This can be particularly helpful when people are not really quite sure to describe what they are feeling.
Research has also supported the idea that music can make a difference in mood. For example, when people are experiencing feelings of sadness, they tend to prefer somber music.
One study published in the Journal of Positive Psychology found that listening to upbeat songs can help improve people's moods and increase happiness .
Play Music Incongruent With Your Mood
Play music that creates an emotion opposite to the one you are struggling with. For example, play happy, upbeat music if you are feeling very sad. If you are feeling anxious, play slow, relaxing music.
Exercise can have a positive impact on mood and emotion. One 2022 study in pre-print found that physical activity could effectively improve emotional regulation ability. However, the researchers noted that the duration of exercise sessions might impact the effects.
However, another study looking specifically at BPD found that a single 20-minute exercise session did not significantly impact negative affect in BPD.
More research is needed to understand how exercise affects emotional regulation in people with borderline personality disorder. Regular exercise can be a useful coping skill when struggling with difficult emotions.
It may also be helpful to combine mindfulness practices with aerobic activity. One study found that an eight-week intervention utilizing mindfulness-based yoga and aerobic jogging improved implicit emotional regulation.
Behavioral activiation is a strategy that involves changing the behaviors that play a role in feeding emotional responses. It is often used in cognitive-behavioral therapy (CBT) to help people with depression, but it can also help people with borderline personality disorder.
Researchers suggest that people with BPD engage in maladaptive behaviors in response to life's challenges. Utilizing behavioral activation may help people with the condition develop more effective coping strategies that aid in emotional regulation.
To utilize behavioral activation, engage in a highly engaging activity when you are having trouble managing your emotions. Television or computer activities do not count here—these are too passive.
Behavioral activation might involve taking a walk , dancing, cleaning your house, or doing some other activity that gets you engaged and distracts you from your current emotions.
One study found that social support could be essential in mediating symptoms of perceived stress and depression in people with BPD.
Unfortunately, people with borderline personality disorder often experience a range of social disadvantages and relationship problems.
People with BPD have poorer social support, more frequent negative interactions with others, and worse integration within their social network. Poor relationships and early trauma are also believed to contribute to the condition's development.
If you have BPD, take steps such as:
- Spending time with others
- Working on your relationship skills
- Seek professional treatment to improve your relationship skills
Reaching out to others can help when you are struggling with strong emotions. Call a supportive friend or family member. Call a helpline if you don’t have someone in mind that is supportive and you are in a crisis.
Press Play for Advice On Dealing With Crisis Fatigue
This episode of The Verywell Mind Podcast shares strategies for dealing with crisis fatigue. Click below to listen now.
Follow Now : Apple Podcasts / Spotify / Google Podcasts / Amazon Music
The ability to control impulsive behaviors is an essential part of emotional regulation. People with BPD, however, often struggle to do this effectively. Building your ability to tolerate distress and ride out an emotion until it passes can help prevent emotional outbursts from happening.
With practice, you can build your distress tolerance skills:
- Be aware of the emotion and try to identify what you are feeling
- Remind yourself that what you are feeling won't last forever
- Accept what you are feeling
- Remember that your thoughts don't dictate your actions
The peak of most strong emotional reactions and the urges to engage in harmful activities last for a few minutes and then begin to subside. Grab an egg timer from the kitchen, and set it for 10 minutes. Wait for 10 minutes and practice riding out the emotion .
Mindfulness involves focusing fully on the present moment while calmly accepting your own thoughts and feelings. This practice is a core component of dialectical behavior therapy (DBT), a type of therapy that was specifically developed to treat borderline personality disorder.
You can become more aware of your internal states by learning to be more mindful. By better understanding your feelings, you can also become more aware of automatic negative thoughts that often contribute to emotional problems and impulsive behavior.
How to Practice Mindfulness
Practice mindfulness of your emotions. Notice the emotion you are having and let yourself experience it as a wave without trying to block it, suppress it, or hold onto it. Try to accept the emotion for what it is. Try to stay in the moment so you do not carry the past emotions along with it.
Grounding is a strategy that can help you cope with feelings of distress and anxiety. If you feel overwhelmed by emotions, grounding techniques can help put your mind back in the here and now.
When emotions seem to be taking you out of the current moment, such as when you start feeling “zoned out,” do something to ground yourself . Grab an ice cube and hold it in your hand for a few moments or snap a rubber band against your wrist to bring yourself out of negative thoughts.
Other sensory-based grounding techniques can include holding an object, listening to noises in your environment, smelling flowers or food, or taking a warm bath.
Try to lose yourself in the sensations. Allow the sensations to distract you from the situation you are upset about. Instead, focus on relaxing your mind and body.
Deep breathing can significantly impact emotions, mood, and anxiety levels. Research suggests that utilizing deep breathing strategies can help decrease acute distress and promote long-term well-being. This technique is often utilized as part of distress tolerance skills practiced in DBT.
Breathing deeply is one of the simplest relaxation methods. Sit or lie somewhere quiet and bring your attention to your breathing. Breathe evenly, slowly, and deeply. Watch your stomach rise and fall with each breath. This can help you stay grounded in the present.
If breathing deeply isn't enough to relax you, try another relaxation exercise like progressive muscle relaxation .
Are you a religious or spiritual person? If you are or have considered attending religious ceremonies, praying and attending weekly congregations can be tremendously helpful in times of extreme stress.
Research has found that spirituality may positively impact coping, emotions, and well-being. In one study, people who had regular spiritual experiences had fewer negative emotions and more positive feelings.
Helping others can not only help you feel good; it can also distract you from feelings of stress. One study found that people who engaged in regular acts of kindness experienced less stress and negativity.
Do something nice for someone else. It doesn't have to be something big; you can walk to the nearest store, buy a pack of gum, smile at the cashier, and say, "Have a great day."
Even small gestures of kindness can reduce emotional pain and connect you to the outside world.
Ready to learn some new, healthier ways of coping? One way to do this is by seeking treatment. Many psychological treatments for BPD, including cognitive behavioral treatments such as dialectical behavior therapy (DBT), focus on teaching healthier coping skills to manage strong emotions.
There are online resource pages that can help you find a cognitive behavioral therapist or a DBT provider.
A Word From Verywell
Borderline personality disorder is characterized by problems with emotional regulation. Fortunately, there are ways that you can better manage your emotional responses. Strategies that help you become more mindful of your emotions, build your tolerance to distress, and provide distraction until the emotion passes can be highly effective.
While you can practice many of these coping strategies on your own, working with a therapist can also be very effective. By learning how to take greater control over your emotional experiences, you can lessen the potential adverse effects your condition might have on your life and relationships.
Dixon-Gordon KL, Peters JR, Fertuck EA, Yen S. Emotional Processes in Borderline Personality Disorder: An Update for Clinical Practice . J Psychother Integr. 2017;27(4):425-438. doi:10.1037/int0000044
Lee CJ, Andrade EB, Palmer SE. I nterpersonal relationships and preferences for mood-congruency in aesthetic experiences . J Consum Res . 2013;40(2):382-391. doi:10.1086/670609
Ferguson YL, Sheldon KM. Trying to be happier really can work: Two experimental studies . The Journal of Positive Psychology . 2013;8(1):23-33. doi:10.1080/17439760.2012.747000
Liu J, Gao S, Zhang L. Effects of physical exercises on emotion regulation: a meta-analysis . Sports Medicine ; 2022. doi:10.1101/2022.07.04.22277120
St-Amour S, Cailhol L, Ruocco AC, Bernard P. Acute Effect of physical exercise on negative affect in borderline personality disorder: a pilot study . Clin Psychol Eur . 2022;4(2):e7495. doi:10.32872/cpe.7495
Zhang Y, Fu R, Sun L, Gong Y, Tang D. How does exercise improve implicit emotion regulation ability: preliminary evidence of mind-body exercise intervention combined with aerobic jogging and mindfulness-based yoga . Front Psychol . 2019;10:1888. doi:10.3389/fpsyg.2019.01888
Dimaggio G, Salvatore G, Lysaker PH, Ottavi P, Popolo R. Behavioral activation revisited as a key principle of change in personality disorders psychotherapy . Journal of Psychotherapy Integration . 2015;25(1):30-38. doi:10.1037/a0038769
Ingkachotivanich N, Wongpakaran T, Wongpakaran N, et al. Different effects of perceived social support on the relationship between perceived stress and depression among university students with borderline personality disorder symptoms: a multigroup mediation analysis . Healthcare (Basel) . 2022;10(11):2212. doi:10.3390/healthcare10112212
Beeney JE, Hallquist MN, Clifton AD, Lazarus SA, Pilkonis PA. Social disadvantage and borderline personality disorder: A study of social networks . Personal Disord . 2018;9(1):62-72. doi:10.1037/per0000234
Schaich A, Braakmann D, Rogg M, et al. How do patients with borderline personality disorder experience Distress Tolerance Skills in the context of dialectical behavioral therapy?-A qualitative study . PLoS One . 2021;16(6):e0252403.
Feliu-Soler A, Pascual JC, Borràs X, Portella MJ, Martín-Blanco A, Armario A, Alvarez E, Pérez V, Soler J. Effects of dialectical behaviour therapy-mindfulness training on emotional reactivity in borderline personality disorder: Preliminary results . Clin Psychol Psychother . 2014;21(4):363-70. doi:10.1002/cpp.1837
Kaur M, Murphy D, Smith KV. An adapted imaginal exposure approach to traditional methods used within trauma-focused cognitive behavioural therapy, trialled with a veteran population . Cogn Behav Therap . 2016;9:e10. doi:10.1017/S1754470X16000052
Zaccaro A, Piarulli A, Laurino M, et al. How breath-control can change your life: a systematic review on psycho-physiological correlates of slow breathing . Front Hum Neurosci . 2018;12:353. doi:10.3389/fnhum.2018.00353
Whitehead BR, Bergeman CS. Coping with daily stress: Differential role of spiritual experience on daily positive and negative affect . J Gerontol B Psychol Sci Soc Sci . 2012;67(4):456-459. doi:10.1093/geronb/gbr136
Raposa EB, Laws HB, Ansell EB. Prosocial behavior mitigates the negative effects of stress in everyday life . Clinical Psychological Science . 2016;4(4):691-698. doi:10.1177/2167702615611073
National Alliance on Mental Health. Borderline personality disorder .
By Kristalyn Salters-Pedneault, PhD Kristalyn Salters-Pedneault, PhD, is a clinical psychologist and associate professor of psychology at Eastern Connecticut State University.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ment Health Clin
- v.6(2); 2016 Mar

Dialectical behavior therapy as treatment for borderline personality disorder
Jennifer m. may.
1 Resident, Combined Internal Medicine and Psychiatry Program, Medical University of South Carolina, Charleston, South Carolina
Toni M. Richardi
2 Postdoctoral Fellow, Department of Psychiatry, Biobehavioral Medicine Division, Medical University of South Carolina, Charleston, South Carolina
Kelly S. Barth
3 Associate Professor, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, South Carolina, ude.csum@nehpets
Dialectical behavior therapy (DBT) is a structured outpatient treatment developed by Dr Marsha Linehan for the treatment of borderline personality disorder (BPD). Dialectical behavior therapy is based on cognitive-behavioral principles and is currently the only empirically supported treatment for BPD. Randomized controlled trials have shown the efficacy of DBT not only in BPD but also in other psychiatric disorders, such as substance use disorders, mood disorders, posttraumatic stress disorder, and eating disorders. Traditional DBT is structured into 4 components, including skills training group, individual psychotherapy, telephone consultation, and therapist consultation team. These components work together to teach behavioral skills that target common symptoms of BPD, including an unstable sense of self, chaotic relationships, fear of abandonment, emotional lability, and impulsivity such as self-injurious behaviors. The skills include mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance. Given the often comorbid psychiatric symptoms with BPD in patients participating in DBT, psychopharmacologic interventions are oftentimes considered appropriate adjunctive care. This article aims to outline the basic principles of DBT as well as comment on the role of pharmacotherapy as adjunctive treatment for the symptoms of BPD.
Introduction to Dialectical Behavior Therapy
Dialectical behavior therapy (DBT) is a structured outpatient treatment based on cognitive-behavioral principles developed by Dr Marsha Linehan in the early 1990s for the treatment of parasuicidal behavior in women with borderline personality disorder (BPD). 1 Linehan defines parasuicidal behavior as “any intentional, acute self-injurious behavior with or without suicidal intent, including both suicide attempts and self-mutilative behaviors.” 2 Borderline personality disorder, as outlined by the Diagnostic and Statistical Manual, 5th Edition (DSM-5) , is a chronic disorder that includes symptoms such as frantic efforts to avoid real or imagined abandonment, unstable relationships, identity disturbance, impulsive and dangerous behaviors, recurrent suicidal threats or self-mutilating behaviors, affective instability, feelings of emptiness, difficulties controlling anger, and/or stress-related paranoid thoughts or dissociation. 3 The lifetime prevalence of BPD is approximately 6%. 4 Borderline personality disorder accounts for significantly higher health care costs than both major depressive disorder and other personality disorders. 5 These high medical costs can be attributed to a greater number of hospitalizations, more frequent emergency room visits, and greater use of outpatient services. 5
The term “dialectical” means the interaction of conflicting ideas. Within DBT, “dialectical” refers to the integration of both acceptance and change as necessities for improvement. 6 Dialectical behavior therapy aims to address the symptoms of BPD by replacing maladaptive behaviors with healthier coping skills, such as mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance. It is currently the only empirically supported treatment for BPD as demonstrated by the Cochrane Collaborative Review. 7 Research has also shown it be effective in treatment of substance use disorders, mood disorders, posttraumatic stress disorder (PTSD), and eating disorders in both adults and adolescents. 8 Given the often comorbid psychiatric symptoms with BPD in patients participating in DBT, psychopharmacologic interventions are oftentimes considered appropriate adjunctive care. This article aims to outline the basic principles of DBT as well as comment on the role of pharmacotherapy as adjunctive treatment for the symptoms of BPD.
The Efficacy of DBT in Borderline Personality Disorder and Other Psychiatric Disorders
There have been several randomized controlled trials (RCTs) studying the efficacy of DBT in BPD. The Linehan Institute compiled a list of RCTs reviewing studies on DBT since 1991. 8 This compilation shows that DBT has been more effective than community-based treatment-as-usual in numerous areas, including reducing parasuicidal behaviors, increasing adherence to treatment, and reducing the number of hospitalizations. Dialectical behavior therapy has also been efficacious in comorbid substance use disorders, binge eating disorder, depression, and bulimia nervosa. 8 In addition, it has been studied with primary diagnoses of trichotillomania, bipolar disorder, attention-deficit hyperactivity disorder, eating disorders (eg, binge eating, bulimia nervosa, anorexia nervosa), adolescents with behavioral disorders, and PTSD. 8 Noticeably, many of the aforementioned psychiatric disorders share diagnostic criteria with BPD, such as impulsivity, labile mood, interpersonal difficulties, suicidal behaviors, and/or engagement in risky behaviors. These shared target symptoms likely contribute to DBT's efficacy across disorders.
DBT Structure
Traditional DBT consists of 4 components: skills training group, individual psychotherapy, telephone consultation, and therapist consultation team. This treatment structure was used in the RCTs validating its effectiveness; however, DBT can be modified or shortened to accommodate any treatment setting, including solo private practices or inpatient facilities. 1 , 6
Skills Training Group
Linehan's DBT manual explains that the skills training group is designed to target behavioral skill deficits that are common to patients with BPD, including an unstable sense of self, chaotic relationships, fear of abandonment, emotional lability, and impulsivity. The group focuses on teaching psychosocial skills that target these deficits through 4 skills training modules: core mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance. The group typically meets weekly for approximately 2 hours, and it takes about 6 months to complete all of the modules. Individuals can choose to repeat the modules, and it is recommended that patients who are new to DBT stay in the skills training group for at least 1 year. Patients are assigned homework to reinforce skills and given diary cards to keep track of how they are using the skills outside of the group. Although patients can discuss with the group how they are using the skills, they are encouraged to process their diary cards primarily with their individual therapists. 6
Core Mindfulness
The core mindfulness skills are central to all of the skills taught in DBT and are frequently revisited within the other 3 modules. Many of these skills have been adopted from Eastern meditation practices. The mindfulness skills are divided into “what” skills and “how” skills. The “what” skills teach patients to observe, describe, and participate fully in the present moment. These skills are meant to target the tendency of patients to participate without awareness through impulsive and emotion-driven behaviors. The “how” skills teach patients to be present in the moment with a nonjudgmental mindset, focusing on one thing at a time, and in an effective manner. These skills target the tendency of patients to idealize and devalue both themselves and other people as well as the tendency for patients to ruminate about the past or worry about the future instead of living in the present moment. 6
Interpersonal Effectiveness
The interpersonal effectiveness module focuses on teaching and practicing social skills that are effective in relationships. Many patients with BPD have a history of childhood abuse, neglect, or other forms of invalidation that made it difficult for them to form secure attachments early in life. They therefore often experience intense, unstable relationships in which they have trouble asserting themselves. Although these patients fear abandonment, they frequently end relationships prematurely because of difficulties tolerating conflict. The interpersonal strategies teach patients how to ask for what they need, say “no” to inappropriate demands, and cope with interpersonal conflict. The focus of these strategies is in learning to keep meaningful relationships, while also maintaining self-respect. 6
Emotion Regulation
The emotion regulation skills are strategies for enhancing control over personal emotions. For individuals with BPD, emotions can be intense and labile. This often leads to the development of dysfunctional behaviors that are aimed at avoiding negative emotions. The emotion regulation skills first work on identifying and labeling emotions so that patients can understand how emotions can lead to behaviors affecting their overall functioning. The patients also learn to identify obstacles to changing their emotions, which often include parasuicidal and other dysfunctional behaviors that have been used by a patient for communication or validation of their experience. Patients are taught to avoid vulnerable situations that often lead to negative emotions and taught to increase events in their life that frequently lead to positive emotions. Patients are encouraged to use mindfulness techniques to accept and tolerate painful emotions in a nonjudgmental way. 6
Distress Tolerance
The distress tolerance skills teach patients that pain and distress are an inevitable part of life, and unwillingness to accept this fact often leads to greater suffering. This module shows patients how to experience their current situation nonjudgmentally without attempting to change it. It is important to note that accepting their current situation does not mean that they must approve of their current situation. The distress tolerance skills include both crisis survival and acceptance strategies. The crisis survival skills teach patients techniques for distracting, self-soothing, and adjusting their thoughts in the moment. The acceptance skills work on transforming intolerable suffering into pain that can be tolerated. 6
Individual Psychotherapy
Within the weekly individual therapy module of treatment, there are 6 main areas of focus: parasuicidal behaviors, therapy-interfering behaviors, behaviors that interfere with quality of life, behavioral skills acquisition, posttraumatic stress behaviors, and self-respect behaviors. 9 These are meant to supplement and enhance the group therapy module of treatment. Individual therapy is conducted by the patient's primary therapist on the patient's treatment team and is usually someone selected by the patient. 1
Parasuicidal behaviors, whether those with actual suicidal intent or not, are never to be ignored in DBT. Parasuicidal behaviors are explored in detail, and emphasis is also placed on problem-solving behaviors, engaging in active coping, and using short-term distress management techniques. Previous trauma may need to be addressed if posttraumatic stress behaviors occur, as it can influence parasuicidal behaviors. However, the focus should initially be on current parasuicidal behaviors. 9
Therapy-interfering behaviors can occur on the behalf of both therapist and patient. Patient interference includes anything that may interfere with receiving therapy or lead to therapist burnout (eg, nonadherence, inattentive behavior, breaking agreements with the therapist that are repeatedly addressed). By reducing therapy-interfering behaviors, drop-out rates can be significantly reduced. 9
Behaviors that interfere with quality of life include any behaviors that may seriously interfere with development of an improved lifestyle for the patient. Some examples are substance abuse, high-risk sexual behaviors, financial or employment concerns, and/or any behaviors with potential legal, interpersonal, or health issues. 9
Behavioral skills are considered those skills that will be used in the patient's daily life. These behaviors specifically address BPD traits defined in the DSM-5 . Mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness skills are explained in further detail and applied to the patient's everyday life. In addition, new self-management skills (eg, learning/maintaining healthy behaviors, eliminating unhealthy behaviors) are taught and reinforced throughout individual therapy. 9
Most patients, particularly those with BPD, enter therapy with a trauma history. 9 Although trauma and posttraumatic symptoms may initially remain unaddressed because of the priority of suicidal behaviors, it is important that the therapist address trauma history when the patient appears ready. This focus includes remembering the abuse (eg, validation of memories, acknowledging emotions related to abuse), reducing self-blame and stigmatization, ending denial and intrusive thoughts regarding abuse (eg, exposure techniques), and reducing polarization or dialectical view of the self and the abuser. 9
Last, self-respect behaviors are designed to enhance the patient's ability to validate him or herself. It is important for the patient to build greater self-reliance. The therapist will need to consistently reinforce self-respect behaviors throughout the therapy process. 9
Telephone Consultation
Telephone consultation allows the patient to contact the individual therapist for in-the-moment guidance. Phone calls are designed to teach patients how to ask for help effectively and to apply skills learned in therapy to everyday life, especially during times of crisis. Patients with BPD often do not ask for help because they feel invalidated and instead harm themselves as a cry for help. At other times, they may ask for help in an abusive manner leaving others feeling manipulated. Phone coaching is meant to help change these dysfunctional behaviors. 1
The strategies used for telephone consultation are designed to minimize reinforcement of parasuicidal behaviors. For that reason, patients are told at the beginning of therapy that they are expected to call their individual therapist before engaging in parasuicidal behavior. In addition, the patient is not allowed to call the therapist for 24 hours after engaging in parasuicidal behavior unless there are life-threatening injuries. The 24-hour rule is meant to encourage patients to seek help from the therapist at earlier stages of a crisis while the therapist can still offer assistance and not after the patient has already chosen maladaptive behaviors. 1
Many therapists are fearful and overwhelmed by the idea of being available to their patients at all hours of the day and night. For this reason, many therapists limit when they are available or choose not to participate in this part of DBT treatment. Nevertheless, this part of the treatment module is strongly recommended in order to reduce parasuicidal behaviors. The length and frequency of permissible phone conversations vary for different therapists and different patients. Many therapists quickly realize that many of the patients do not utilize the phone coaching as often as they should. For patients who abuse the telephone conversations, this becomes a therapy-interfering behavior that is addressed during individual therapy sessions. When DBT is restructured in various outpatient or inpatient settings, other providers such as mental health technicians, nurses, or on-call psychiatrists may fill this role. 1
Therapist Consultation Team
The therapist consultation team is a weekly meeting of all individual and group therapists who are currently providing DBT. Working with patients with BPD who are highly suicidal can be challenging and stressful. Significant stress can lead therapists to react in problematic ways during treatment. The therapist consultation team functions to maintain motivation and commitment among all providers in order to provide optimal treatment. 1 It can also be used to promote empathy within the therapist, focusing on accepting the patient rather than forcing change upon the patient, that will ultimately help reduce parasuicidal behaviors in the patient. 9 If a group setting is not possible, all DBT therapists are strongly encouraged to be a part of some form of consultation or supervision relationship. 1
Pharmacologic Considerations for Treatment of BPD
In general, psychotherapy is the treatment of choice for BPD over psychotropic medications. 10 In fact, the National Institute of Health and Clinical Excellence (NICE) has published guidelines that medication should not be used specifically for BPD or symptoms associated with BPD. 11 However, patients with personality disorders are prescribed medications more frequently than any other diagnostic group, 12 and the American Psychiatric Association declared pharmacotherapy as having an important “adjunctive role” in treatment of personality disorders. 13
In a 2012 multicenter study in the United Kingdom, researchers showed that within a sample of 161 patients with BPD, approximately 45% were prescribed second-generation antipsychotics (other than clozapine), 40% were prescribed mood stabilizers, and 20% were prescribed clozapine. Polypharmacy (including antidepressants, mood stabilizers, antipsychotics, benzodiazepines, and “other” medications) was also shown to be common, with approximately 62% of patients on 2 or more medications and approximately 24% on 3 or more medications. In this study, approximately 80% of patients with BPD had past or current comorbid psychiatric disorders, including schizophrenia, PTSD, depression, bipolar disorder, and/or anxiety. Additionally, approximately 60% of the 14 “consultants” involved in management of these subjects with BPD disagreed with the NICE guidelines, and none completely agreed with the guidelines. 10
In the scientific literature, there appears to be mixed evidence on the efficacy of medications for the management of BPD, and psychopharmacologic interventions usually have nonspecific results. 14 A 2011 meta-analysis evaluated the effectiveness of medications in treating impulsivity, aggression, depression, anxiety, anger, and suicidal behavior in patients with BPD, and concluded the following: (1) selective serotonin reuptake inhibitors (SSRIs) can improve impulsivity and aggression but have little effect on other symptoms; (2) mood stabilizers and anticonvulsants have a moderate effect on depression and can improve aggression and impulsivity; (3) first-generation antipsychotics can reduce anger and suicidal behavior in patients with BPD but have little effect on psychosis and anxiety; and (4) second-generation antipsychotics can have an effect on aggression, but there are mixed results for other symptoms. 12 Benzodiazepine use by patients with BPD has been greatly discouraged, as it may be abused (ie, used to self-medicate intrapersonal issues) and exacerbate BPD symptoms. 12 Other research has supported this finding, as 87% of psychiatrists interviewed cited medication misuse, including overdose, as a common problem among their BPD patients. 15 Despite continued use of pharmacotherapy, researchers have concluded that conservative use should be considered best practice, given potential lethality of most medications, with the exception of SSRIs. 14
There is some evidence that DBT is effective in lowering psychotropic medication use in patients. One study noticed significant decrease in psychotropic medication use among college students with parasuicidal behaviors following DBT treatment. 16 One particular study focusing on adolescent DBT during long-term inpatient therapy also found a reduction in psychotropic medications prescribed. 17 However, there were no comparison group results with which to run a statistical analysis on the significance in the DBT group's reduction in medication. This is an area that deserves further consideration, given the mixed evidence for medication effectiveness, medication side effects, and potential for misuse of psychotropic medications.
There are several overall implications of medication in the treatment of BPD. While medications may be helpful for some comorbid psychiatric symptoms in patients with BPD, their efficacy for treatment of BPD should not be assumed. 18 For example, research shows that SSRIs may show improvement in depression or anxiety on a variety of self-report measures in patients with BPD; however, these measures are not designed to assess changes in symptoms of BPD, as depression and anxiety are comorbid issues. 18 In addition, medications in BPD often create more problems than they solve owing to the potential for adverse side effects, addiction, and lethal overdose. 14 Therefore, it is recommended to use caution when prescribing medications to this population. When medications are prescribed, they should only be used in conjunction with psychotherapy. 19 In general, DBT is first-line treatment for BPD and has been shown to reduce the need for medications and medical care by up to 90%. 8 , 19
Although medications can provide adjunctive treatment in patients with BPD and comorbid psychiatric symptoms, DBT is currently the only empirically supported treatment for BPD. For that reason, it is important that all patient providers understand when a patient could potentially benefit from DBT. Pharmacists, in particular, have the unique opportunity to speak to patients and providers in both formal contexts (eg, medication management appointments, medication reconciliation and education, inpatient consultation, medical rounds) and informal contexts (eg, conversation while a patient pays for a prescription, patient chart review in a medical setting). Within these contexts, a patient provider may discover behaviors consistent with those of BPD, including impulsivity, affective instability, interpersonal or intrapersonal conflict, parasuicidal behaviors, substance abuse (alcohol, prescription drugs, or illicit drugs), or polypharmacy. If a pharmacist notices any of these symptoms, it would be beneficial to provide the patient with a referral to a local community mental health center for DBT in addition to providing direct services such as assessing current medication efficacy or safety concerns, reducing unnecessary polypharmacy, and/or addressing prescription drug abuse concerns.
Disclosures: The authors have no relevant financial or nonfinancial relationships to disclose.

Borderline Personality Disorder & DBT Resources
Books, workbooks, worksheets, classes, movies, and more!
Featured BPD & DBT Resources

Borderline Personality & DBT Resources
Please note that I do my best to do due diligence before accepting any listings for the following sections by qualifying the resources with some or all of the following: phone interviews, email correspondence, credential checks, and when possible, references. That being said, please contact/use these services at your own risk, as I am not responsible for any interactions you may engage in with any resource listed here.
Mental Health Hotlines
National BPD Hotline (TARA): 888-4-TARA APD (888-482-7227) 12 am – 5 pm EST
Suicide Prevention Telephone Numbers (worldwide)
Samaritans Helplines Suicide Prevention (Confidential & Anonymous)
Peer Staffed Hotlines By State
Befrienders (Help for suicidal and self-harm thoughts, worldwide)
Mental Health Chat
Crisis Chat (Domestic, USA)
Lifeline Chat is a service of the National Suicide Prevention Lifeline, connecting individuals with counselors for emotional support and other services via web chat. All chat centers in the Lifeline network are accredited by CONTACT USA. Lifeline Chat is available 24/7 across the U.S.
Dialectical Behavior Therapy Skills (DBT Skills)
DBT – Dialectical Behavior Therapy
Online DBT Courses
DBT Path – Worldwide, online DBT Skills Course
DBT Skills Focused Websites
M y Daily DBT (by same author of this blog)
DBT Resources for Clinicians and those seeking services
Behavioral Tech, LLC. (via Dr. Marsha Linehan, who founded DBT)
Fulton State Hospital DBT Workbook
Tons of Therapy Worksheets (many on BPD/DBT, but not limited to these)
DBT Cheat Sheets and Carry Cards
DBT “The Decider” Skills Card by Michelle Ayres and Carol Vivyan
Printable DBT Skills Cheat Sheet
Feelings Wheel (Be Mindful of Current Emotion)
Kaiser Permanente Podcasts: Anxiety, stress, coping and more.
DBT for Children
Dialectical Behavior Therapy Validation Strategies for Parents
Worksheet for Coping with Anger
Using DBT to Reduce Emotion Dysregulation in Children & Adolescents
Meditation Video
Urge Surfing
BPD & DBT Therapists, Consultants, & Referral Specialists
Find a DBT Therapist
Behavioral Tech, LLC.
Entirely Online Weekly DBT Course Group
Wondering if our online DBT informed course is right for you? Check out Peggy’s video on how our classes helped her reclaim her life and confidence. We’re so proud of Peggy. Her share is a testament to her hard work and dedication to skillfulness and self-compassion. Way to go, Peggy! For more information on our online, Real-time DBT informed courses, visit ► www.emotionallysensitive.com ♥
Books for Those With BPD & Their Therapists
Memoirs and Lived Experience of Borderline Personality Disorder:
“Stronger than BPD: The Girl’s Guide to Taking Control of Intense Emotions, Drama, and Chaos using DBT” by Debbie Corso, Foreword by Gillian Galen, PsyD (My book)
The Buddha and the Borderline: My Recovery from Borderline Personality Disorder through Dialectical Behavior Therapy, Buddhism, and Online Dating
Get Me Out of Here: My Recovery from Borderline Personality Disorder
Girl in Need of a Tourniquet
Girl, Interrupted
Healing from Borderline Personality Disorder: My Journey Out of Hell Through Dialectical Behavior Therapy (My book)
I Hate You–Don’t Leave Me: Understanding the Borderline Personality
Lost in The Mirror: An Inside Look at Borderline Personality Disorder
Loud in the House of Myself
New Hope for People with Borderline Personality Disorder: Your Friendly, Authoritative Guide to the Latest in Traditional and Complementary Solutions
Sometimes I Act Crazy: Living with Borderline Personality Disorder
Workbooks and Guidebooks
Mindfulness for Borderline Personality Disorder
Coping with BPD
Borderline Personality Disorder Demystified: Essential Guide for Understanding and Living with BPD
Borderline Personality Disorder for Dummies
Borderline Personality Disorder Survival Guide
The Borderline Personality Disorder Survival Guide: Everything You Need to Know About Living With BPD
Calming the emotional storm – using dialectical behavior therapy skills to manage your emotions and balance your life
Depressed and Anxious: The Dialectical Behavior Therapy Workbook for Overcoming Depression & Anxiety
The Dialectical Behavior Therapy Diary: Monitoring Your Emotional Regulation Day by Day
Dialectical Behavior Therapy Skills, 101 Mindfulness Exercises and Other Fun Activities for Children and Adolescents: A Learning Supplement
The Dialectical Behavior Therapy Skills Workbook (Peer Recommended!)
Dialectical Behavior Therapy: Volume 2 – Companion Worksheets
Doing Dialectical Behavior Therapy: A Practical Guide (Guides to Individualized Evidence- Based Treatment)
Freedom from Selfharm: Overcoming Self-Injury with Skills from DBT and Other Treatments
Mindfulness for Borderline Personality Disorder: Relieve Your Suffering Using the Core Skill of Dialectical Behavior Therapy
Overcoming Borderline Personality Disorder : A Family Guide For Healing and Change
Skills Training Manual for Treating Borderline Personality Disorder
Stop Sabotaging: A 31 Day DBT Challenge to Change Your Life (My book)
Boundaries Where You End And I Begin: How To Recognize And Set Healthy Boundaries
Specific Spiritual Perspectives
Unglued (by Christian author Lysa TerKuerst)
Borderline Personality: A Scriptural Perspective (Gospel for Real Life)
For Helping Children through DBT
Dialectical Behavior Therapy: Children & Adolescents
Don’t Let Your Emotions Run Your Life for Teens: Dialectical Behavior Therapy Skills for Helping You Manage Mood Swings, Control Angry Outbursts, and Get Along with Others
Books for Family Members & Loved Ones of Those With Borderline Personality Disorder
Overcoming Borderline Personality Disorder:A Family Guide for Healing and Change
Borderline Personality Disorder in Adolescents: A Complete Guide to Understanding and Coping When Your Adolescent Has BPD
Loving Someone With Borderline Personality Disorder: How to Keep Out-of-Control Emotions from Destroying Your Relationship
Surviving a Borderline Parent: How to Heal Your Childhood Wounds and Build Trust, Boundaries, and Self-Esteem
Overcoming Borderline Personality Disorder: A Family Guide for Healing and Change
When Love is Not Enough: The Chronicles of LauraJo
Helping Teens Who Cut
Movies That Deal With BPD
Characters described as having or believed to have BPD:
Girl, Interrupted online rental version – Starring Winona Ryder & Angelina Jolie
Girl, Interrupted DVD version – Starring Winona Ryder & Angelina Jolie
Prozac Nation online rental version – Starring Christina Ricci
Prozac Nation DVD version – Starring Christina Ricci
Runaway Bride online rental version – Starring Julia Roberts
Runaway Bride DVD version – Starring Julia Roberts
Young Adult – online rental version – Starring Charlize Theron
Young Adult – DVD version – Starring Charlize Theron
Free BPD Documentary
Border_ : A Compassionate Documentary on Borderline Personality Disorder (About 20 minutes in length)
DBT Diary Card and Skills Coach
List of DBT Apps for Android and IOS
Guided Meditations
Guided Meditation:
The Healing Waterfall
The Healing Waterfall II: Tropical Paradise
Time for Healing: Relaxation for Mind and Body
Total Relation with accompanying book
Intensive help for Anxiety and Depression
Attacking Anxiety and Depression by Lucinda Bassett
The Healing Waterfall: A Guided Meditation
The Healing Waterfall 2: Guided Meditation
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com
Learn DBT Skills
Learn DBT Skills Online at EmotionallySensitive.com These are the skills that helped this blog’s author overcome BPD!

This site uses cookies to give you the best, most relevant experience. Using this website means you're okay with this. For more information, visit our Terms of Service & Privacy Policy page.
Cookie and Privacy Settings
We may request cookies to be set on your device. We use cookies to let us know when you visit our websites, how you interact with us, to enrich your user experience, and to customize your relationship with our website.
Click on the different category headings to find out more. You can also change some of your preferences. Note that blocking some types of cookies may impact your experience on our websites and the services we are able to offer.
These cookies are strictly necessary to provide you with services available through our website and to use some of its features.
Because these cookies are strictly necessary to deliver the website, refusing them will have impact how our site functions. You always can block or delete cookies by changing your browser settings and force blocking all cookies on this website. But this will always prompt you to accept/refuse cookies when revisiting our site.
We fully respect if you want to refuse cookies but to avoid asking you again and again kindly allow us to store a cookie for that. You are free to opt out any time or opt in for other cookies to get a better experience. If you refuse cookies we will remove all set cookies in our domain.
We provide you with a list of stored cookies on your computer in our domain so you can check what we stored. Due to security reasons we are not able to show or modify cookies from other domains. You can check these in your browser security settings.
These cookies collect information that is used either in aggregate form to help us understand how our website is being used or how effective our marketing campaigns are, or to help us customize our website and application for you in order to enhance your experience.
If you do not want that we track your visit to our site you can disable tracking in your browser here:
We also use different external services like Google Webfonts, Google Maps, and external Video providers. Since these providers may collect personal data like your IP address we allow you to block them here. Please be aware that this might heavily reduce the functionality and appearance of our site. Changes will take effect once you reload the page.
Google Webfont Settings:
Google Map Settings:
Google reCaptcha Settings:
Vimeo and Youtube video embeds:
The following cookies are also needed - You can choose if you want to allow them:
You can read about our cookies and privacy settings in detail on our Privacy Policy Page.

Why Do People with BPD Self-Victimize?
Sometimes they blame you..
Posted December 13, 2020 | Reviewed by Devon Frye

Many individuals with symptoms of Borderline Personality Disorder (BPD) engage in different types of self-victimization. In this blog we will explore three forms of self-victimization that are common in individuals with symptoms of BPD and explore why they do it.
Direct self-Harm
Self-mutilation occurs frequently with people who suffer from BPD. Perhaps the most common form is cutting or burning themselves with razor blades, knives or cigarettes. These actions often occur during periods of very high emotion . These individuals describe the cutting or burning as a way of minimizing emotional pain and claim that it has a calming effect on them.
Sometimes individuals with symptoms of BPD self-harm directly for manipulative purposes. In the following example, Mindy, an adolescent sufferer of BPD, is arguing with her mother Sally because her mother will not allow her to go to an unchaperoned party at a friend’s house.
Mindy: I have to eat early tonight. I am going to Ginger’s house to hang out tonight.
Sally: Will there be other kids there?
Mindy: Just a few close friends.
Sally: Boys?
Mindy: I hope so.
Sally: Will Ginger’s parents be there?
Mindy: We can’t have fun with her parents standing over us.
Sally: Where are her parents?
Mindy: They are going away for the weekend.
Sally: You can’t go to a party unless there is a parent there.
Mindy: Mom, all my friends are going.
Sally: Not unless there is parental supervision.
Mindy: They are expecting me.
Sally: You can call them and tell them you can’t go.
Mindy: Everyone will think I am a dork.
Sally: They will get over it.
Mindy: I have to go.
Sally: Not without supervision.
Mindy: If you don’t let me go, I will kill myself.
While it is not common for a child to actually kill herself under these circumstances it is common for them to make a gesture. These gestures often include cutting themselves with a knife or possibly taking a bunch of pills, if they have access. One child drank bleach in front of her parents when not allowed to do what she wanted to do.
Indirect Self-harm
This is a very large category of behavior, all of which involve engaging in activities that are unhealthy. This includes substance abuse as well as engaging in high-risk activities such as promiscuity or breaking the law. It also includes self-neglect, such as eating poorly, not going to school/work or not getting proper medical/dental care. Indirect self-harmful behaviors generally serve the function of expressing their self-loathing . They show the world that they feel unworthy of care and that they don’t care what happens to them.
Projected Self-harm
This is the type of self-harm that causes the most instability in relationships. This involves projecting feelings of self-loathing onto others and then feeling victimized by them. In the following example, Robert is confronting his son Gene for not doing his homework and getting a failing grade. Gene projects onto his father that he is a perpetrator so as to feel victimized by his father. He then blames his father for his poor performance.
Robert: Gene, I heard from your teacher today. He told me that you are failing Biology.
Gene: Yeah. He hates me.
Robert: He said that you have not handed in a single homework assignment this term.
Robert: Is it true?
Gene: I can’t get my work done with you and mom on my case all of the time.
Robert: We are on your case all of the time?
Gene: Yes. “Gene put out the garbage. Gene, do your homework. Gene, clean your room.”
Robert: You didn’t do your homework because Mom and I got on your case to do your homework?
Gene: You are on my case all of the time. You make me feel like I want to die.
In the above example, Gene explains to his father that the reason he is failing Biology is because his parents mistreat him by making him study and keep his room clean (and hence he is a victim). This type of self-blame serves two functions for Gene:

· It helps him avoid taking responsibility for failing his class by blaming his parents.
· It justifies other behaviors, such as lashing out at his parents, because they have ‘victimized’ him.
Many people in Sally and Gene’s position give into the threats of self-harm out of fear that if they don’t, someone they care about will hurt themselves. Unfortunately, when you give into threats of self-harm or suicide you increase the power of making such threats, and increase the likelihood that this mechanism will be used more in the future. It gets them what they want.
Self-victimization is never healthy. Individuals who use this mechanism as a way of getting what they want are sick and need help to find healthier ways of getting what they want. Giving into these threats makes them sicker. The proper response is to recognize self-harm as being a symptom of serious mental illness and get them professional help. This is the only way to truly help someone you love who suffers with this problem.

Daniel S. Lobel, Ph.D. , is a clinical psychologist in private practice in Katonah, NY, as well as an Assistant Clinical Professor at Mount Sinai School of Medicine in the Department of Psychiatry.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

Borderline Personality Disorder
15 unexpected ways borderline personality disorder affects everyday tasks.
When asked what everyday tasks borderline personality disorder (BPD) unexpectedly affects, Mighty community member Alicia M. said, “I’ll just be the person to openly admit this: everything .”
She’s not the only one. When you live with a condition like BPD that affects your emotional regulation, it’s hard to keep it from affecting your daily functioning. Classic symptoms like frantic efforts to avoid fear of abandonment, “splitting” and dissociation undoubtedly affect daily parts of life like getting chores done, communicating with others and your job.
No matter what your experience with BPD is, we want you to know you’re not alone and there is help available. For more information on managing BPD, check out our in-depth explainer that answers frequently asked questions about BPD.
We wanted to know the unexpected ways BPD can affect daily tasks, so we turned to our BPD community to share their experiences. Below you can read what they shared.
How does BPD affect your daily functioning? Click on the image below to share your answer!
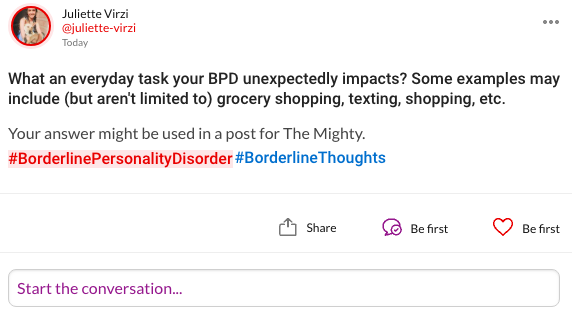
Here’s what our community shared with us:
“I would say texting. I want to tell all that’s going on in my mind, but it’s absolutely impossible to do.” — Laura D.
“Texting. I want/crave talking to people at times but then continuing the conversation or friendship I initiated suddenly becomes just too much . At times it feels like my fingers weigh tons and I can’t manage to type anything. I’ve begun to avoid opening messages, sometimes for only hours, but also for days as well. When I’m in the mood for people, I can overdo it and message everyone, yet the moment I’ve lost interest and feel down, I block up on all sides from socializing.” — Omar L.
“Driving. I’m totally paranoid about what other drivers think of me. If I let someone out and they don’t thank me, I get disproportionately angry. If someone is behind me, I worry they’re judging my speed. I worry the person in front thinks I’m following them and the list goes on. I’m also quite erratic as a driver, sometimes overly-cautious and anxious and other times reckless and speedy. All dependent on mood!” — Kim A.
“Driving! I have an irrational fear of having an accident, thinking something is wrong with my car or everyone else is out to get me and drive aggressively.” — Susan L.
“Working. I have such a hard time finding and keeping a job because of my anxiety. I constantly feel like I won’t be good enough and I’ll be let go under pressure.” — Bree C.
“Working. I have a hard enough time manufacturing reasons for me to care about doing things for myself that actually benefit my life. As I get older, it is nearly impossible to do useless tasks assigned by someone else simply to justify the amount of hours I’m forced to leave my home.” — Thomas D.
4. Cleaning
“Right now BPD triggers have me so upset, mad, angry, depressed, dejected, teeth grinding and crying that I’m afraid to do dishes. [I’m afraid] I might break them because I’m distracted and dizzy.” — Corina S.
“Cleaning for sure. I try but once my mood changes to something negative/stressful, my day is shot. I’m so embarrassed my house is filthy but sometimes I just can’t force myself to get it done.” — Marissa P.
“I find daily chores incredibly daunting. I will plan to do them, but once I’m there, all motivation and energy is drained from me. I stare at crumbs on the table and cannot find it in myself to care enough to grab a simple washcloth to wipe them up.” — Heather M.
5. Maintaining Relationships
“ The mood swings make it so hard to go through my daily life, especially working or maintaining relationships. The smallest things set me off into rage that is basically impossible to come back from, I lash out at customers or my significant other. And when I’m finally able to bring myself out of it, I’m immediately greeted with [debilitating] shame and guilt so strong that I can’t help but cry, even at work.” — Kierstyn D.
“Communication… Sometimes, I am overly enthusiastic to speak to my friends but then some days, I don’t wanna hear from any of them and end up feeling as though they don’t truly care and are just using me.” — Shalena V.
“Talking to people. I’m either overly excited and annoying or awkwardly and aggressively quiet.” — Aurorah B.
6. Talking on the Phone
“I absolutely dread talking on the phone, sending voice memos, voice chat or FaceTime. I don’t even know why… I think I’m scared of sounding ‘stupid’ because I don’t have as much time to think of what to say like I do with texting. It literally fills me with anxiety to the point that I have a panic attack and feel like I could throw up.” — Victoria R.
7. Walking the Dog
“Walking the dog. It can be so frustrating when she pulls and I don’t have much patience but I’m I’m too firm with her. I’ll feel crazy guilty and have more problems after…” — Rishele S.
8. Taking Care of Kids
“Caring for my kids. I have my mom staying with us because I can’t even get them ready for school or be around because they are too loud and I can’t deal with it… I feel like the worst mom… so debilitating.” — Joanne M.
“ Picking up my daughter from school… Some days I feel so disconnected from everything and everyone in my life that the very act of going to the school and waiting in the parking lot for 45 minutes (I have to get there that early for a parking spot) is a nightmare. I sit with my feelings of emptiness and loneliness and disconnection and cry.” — Julianne J.
9. Shopping
“I hate going to busy stores, the mall, grocery stores etc. I get overstimulated and hyper-anxious. I’ve definitely disassociated in the mall before. Once I got my diagnosis and started DBT, I was able to notice these patterns and avoid them or cope ahead.” — Erin B.
“Grocery shopping can be a real issue for me, as I disassociate, get confused and have a lot of anxiety.” — Su K.
10. Opening Emails
“Opening replies to texts and emails. Just always scared of what the reply will be. Will they hate me for asking this question? Will they laugh at me? Was I acting ‘crazy’ or paranoid? Did I just get everything wrong again? Did I unnecessarily worry someone?” — Fiona M.
“I’m scared of getting emails. I always think it’s going to be bad news about me, from my boss or friends. I have terrible anxiety when starting up my computer in the morning. The suspense of not knowing what’s in there is overpowering. I’ve had to turn off the email alert tone as it was scaring me during the day.” — Sam F.
“Work emailing — really easy to misread them and take things personally that weren’t about you at all.” — Laurie E.
11. Getting Out of Bed
“Generally getting out of bed… With no motivation, it’s hard to do anything I need to do — and I automatically think there’s no point in anything, so I may as well stay in bed.” — Abby A.
“Getting out of bed is one of the biggest challenges that comes with my BPD. Before I even open my eyes to check what time it is, I’m already worried about what could make my day go wrong.” — Holly B.
12. Doing Homework
“It’s really hard to study and read because of my symptoms sometimes. If I’m dissociating, I can’t focus on the words in front of me. If I’m shaking with rage, my thoughts are racing, and I can’t slow down to get my homework and studying done. If I’m preoccupied with thoughts of abandonment or flashbacks of times I’ve been treated badly in the past, it seems like my mind keeps switching away from the task at hand, and I keep getting angry and depressed. I have disability accommodations at college, and when I absolutely need it, assignment due dates can be extended. The symptoms are both psychologically and physically painful. The intensity at which the symptoms hit is totally underestimated.” — Kellyann N.
“Homework, it makes it really hard to be able to get anything done. I know I can do it but it makes me feel impossible to achieve.” — Rose L.
13. Exercising
“Exercising. I rarely get off the couch or even out of the house. And going to the gym basically doesn’t happen because I can’t/won’t go alone.” — Tess B.
14. Cooking
“Cooking… I want to, I am hungry but I don’t want to. [When] I finally do it, I dread the clean up. My anxiety spirals…. the next time I don’t do it at all…” — Jenna R.
“Eating and hygiene. My brain has so much trouble with impulse control.” — Amy H.
“Eating. I find myself apologizing because I’m anxious about eating, and the fact I need to eat. Then I hate myself because I’ve eaten. And apologize for that.” — Cassy C.
If BPD negatively impacts your daily functioning, you’re not alone. No matter what symptoms you are currently battling , there is help available to you. Dialectical behavior therapy (DBT) is the gold standard treatment for folks with BPD. You can read more about it here .
What everyday tasks does your BPD affect? Let us know in the comments.
Want to talk about your feelings with other people with borderline personality disorder? Download our free app to follow #BorderlineThoughts and more easily join in the conversation.
Unsplash photo via Avery Klein
Hi, I'm Juliette. I'm the former Mental Health Editor at The Mighty. I joined The Mighty because I believe storytelling is a powerful tool in raising awareness about mental health and trauma. I'm inspired every day by the brave vulnerability of our community. #MightyTogether
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
What Does Euthymic Mean?
:max_bytes(150000):strip_icc():format(webp)/7cZXd_5cLI7mNtZRS31XzPzGTeA8lh_k24WTXKJk-mo-3956d73663764f15bce8e3e4ea4d59fa.jpeg)
Characteristics of a Euthymic Mood
Euthymia and bipolar disorder, other conditions with periods of euthymia, benefits of experiencing euthymia, how to reach and maintain euthymia.
Klaus Vedfelt / Getty Images
Euthymia is a state of tranquility and well-being. Someone experiencing euthymia is considered to be in a euthymic mood. The term euthymic is often used in the context of bipolar disorder—someone with the mood disorder is considered to be in a euthymic mood when they are experiencing neither mania nor depression.
Being in a euthymic mood is not the same as being happy or optimistic. Instead, euthymia defines the time a person with a mood disorder isn't showing significant distress. Someone in a euthymic mood is no longer experiencing the extremes of the disorder and so appears more stabilized based on specific rating scales and diagnostic criteria. They have enhanced functioning and behavior.
Thankfully, there are things people with bipolar disorder or other mood disorders can do to reach and maintain euthymia.
Editor's Note: The word "euthymia" is derived from the Greek terms eu , which means well, and thymos , which means soul.
There are certain factors someone must meet to be considered in a euthymic mood. A mental health professional can determine whether you are in euthymia based on rating scales and other diagnostic criteria.
When someone is experiencing a euthymic mood, they will have these key characteristics:
- Displays a lack of mood disturbances and is considered in full remission of a mood disorder (using diagnostic tools to verify)
- Experiences negative emotions like sadness, irritability, or anxiety only if a specific situation calls for it; the emotions are temporary and don't interfere with daily life
- Exhibits positive affects like cheerfulness and calmness
- Appears to be active and interested in things around them
- Gets quality sleep that feels restorative and refreshing
- Exhibits a positive well-being and is resilient in the face of stress, frustration, or anxiety
When someone is being treated for bipolar disorder, their healthcare provider will often develop a treatment plan with the goal of euthymia in mind. Bipolar disorder can cause extreme highs and significant lows and impact a person's ability to function. When euthymia is achieved, the person can have a more stable mood and a dramatic reduction in symptoms of bipolar disorder .
Because the moods of people with bipolar disorder can change throughout their lives, an euthymic mood is a goal but not always a constant. In other words, how long an euthymic mood lasts will depend on the person, how well they respond to treatment, and the severity of their condition.
Some people with bipolar disorder who have euthymia will relapse frequently while others will have a significant span of time between extreme moods. One study suggests the average timespan between episodes is about 18 months. Another study found that nearly 40% of people with bipolar disorder stayed euthymic for two to five years, and almost 12% of people went six to 10 years without an episode.
Many mental health professionals suggest viewing euthymia as a neutral state rather than classifying it as a positive mood to be attained. Euthymia also doesn't mean that the person will no longer experience sadness, anger, or other negative feelings. It is simply a more stable period in a person with bipolar disorder's life where they do not meet the criteria for another mood (like mania or depression).
Euthymia can also be used to describe periods of well-being or tranquility in people with other mood disorders. For instance, mental health professionals may strive for euthymia in people with borderline personality disorder and major depressive disorder .
Although there is limited research on achieving euthymia in these mental health disorders, researchers are starting to explore euthymia's potential impact. For instance, one study found that slight decreases in euthymia may serve as a warning that depression could be returning.
Researchers also noted that working toward euthymia during the treatment of depression may improve well-being, an important component in dealing with negative emotions. That said, additional research is needed to determine the role euthymia plays in depression.
When a person experiences euthymia, this means that they are no longer experiencing any extreme moods associated with a diagnosed mental health condition like bipolar disorder, borderline personality disorder, or major depression. They also may experience emotional well-being and psychological flexibility.
During euthymia, any sadness, anger, or irritability they experience is likely in response to everyday life events and not associated with a mood disorder. Likewise, feelings of happiness, calmness, and thankfulness are also in relation to life events and not extreme.
People in a euthymic state also experience resilience and deal with stress in more productive ways.
Reaching euthymia may also have some preventative factors. One study found that people who had experienced depression but reached euthymia were less likely to experience another episode of depression. However, the researchers noted that more studies are needed to determine how the findings should dictate depression management .
Researchers are also exploring whether trying to achieve euthymia may be helpful for people who have had a stroke or spinal cord injury—especially since rates of depression among these groups are as high as 60% six months after their event. The researchers theorize that if healthcare providers make euthymia a goal in treatment, people with these conditions may do better in rehab.
To reach and maintain euthymia, it's important to work closely with your mental health professional and healthcare provider to develop a treatment plan. While this plan may include medications, lifestyle changes, and therapy , it will typically be unique to your particular symptoms, diagnosis, and personality.
Ongoing treatment is often needed to keep mood disturbances from recurring or to address those that re-emerge during treatment, so it's important to continue your treatment even if you feel better.
Here are some of the common ways euthymia is achieved and maintained:
- Medication: Typically, medications known as mood stabilizers, such as lithium, are the cornerstone of treatment for bipolar disorder, the goal of which is to reach euthymia.
- Well-being therapy: This approach to therapy involves keeping a structured diary that emphasizes self-observation of moods, feelings, sleep, and other parameters. This information may then be used in therapy sessions alongside cognitive restructuring and homework assignments to help maintain euthymia.
- Mindfulness-based cognitive therapy (MBCT): Designed to prevent the relapse of depression, MBCT is a variation of cognitive therapy that uses mindfulness as a tool to keep your thoughts in the present and avoid negative thought patterns that can derail your mood.
- Acceptance and commitment therapy: This intervention is a form of cognitive behavioral therapy (CBT) that uses acceptance, mindfulness, and commitment techniques as well as behavior changes to create psychological flexibility. By being psychologically flexible, you can better acknowledge and accept any negative feelings, as well as more successfully handle challenges.
- Electroconvulsive therapy (ECT): If medications and other treatments don't work, ECT might be useful in bipolar disorder or depression. When you receive ECT, you will be under general anesthesia , meaning you won't feel anything or be aware. During the treatment, brief electrical currents are applied to the scalp and cause short, controlled seizures . Seizures brought on by ECT are thought to help with certain conditions since they remodel brain signaling pathways.
Family members also may benefit from resources like health advocacy groups and support groups, especially since mood changes can cause stress for loved ones, too.
A Quick Review
When someone experiences euthymia, they are in a state of being that is characterized by calmness and improved functioning. Achieving a euthymic mood is the goal of treatment for mood disorders like bipolar disorder. You can reach and maintain euthymia with medications and therapy.
Some people may remain in euthymia for years while others may only experience a euthymic mood for a few months. Even if you feel better, you should continue with your treatment so you can try to maintain euthymia for as long as possible.
American Psychological Association. Euthymia .
Fava GA, Guidi J. The pursuit of euthymia . World Psychiatry . 2020 Feb;19(1):40-50. doi:10.1002/wps.20698
American Psychiatric Association. What are bipolar disorders? .
Ossola P, Garrett N, Sharot T, Marchesi C. Belief updating in bipolar disorder predicts time of recurrence . eLife . 2020;9:e58891. doi:10.7554/eLife.58891
Vidal-Rubio SLL, Balanzá-Martínez V, Cuenca M, Vila-Francés J, Vieta E, Romeu JE. Duration of euthymia and predominant polarity in bipolar disorder . Journal of Affective Disorders . 2018;241:356-359. doi:10.1016/j.jad.2018.08.001
Bąk W, Łysiak M. Euthymia: A neglected aspect of trait depression and its role in predicting subjective well-being . Curr Issues Personal Psychol. 2021 Apr 10;9(4):281-288. doi:10.5114/cipp.2021.104801
Guidi J, Fava GA. The emerging role of euthymia in psychotherapy research and practice . Clinical Psychology Review . 2020;82:101941. doi:10.1016/j.cpr.2020.101941
Sasaki N, Nishi D. Euthymia scale as a protective factor for depressive symptoms: A one-year follow-up longitudinal study . BMC Res Notes. 2023 Sep 22;16(1):230. doi:10.1186/s13104-023-06512-x
Nierenberg BP. Euthymia and disabling health conditions . World Psychiatry. 2020 Feb;19(1):58-59. doi:10.1002/wps.20721
Ferguson A, Dinh-Williams LA, Segal Z. Mindfulness-based cognitive therapy. In: Wenzel A, ed. Handbook of Cognitive Behavioral Therapy: Overview and Approaches (Vol. 1). American Psychological Association ; 2021:595-615. doi:10.1037/0000218-020
American Psychological Association. Acceptance and commitment therapy .

COMMENTS
In turn, negative feelings contribute to harmful behavior and can worsen mood disorders. That is why it is important to know how […] Free Borderline Personality Disorder (BPD) worksheets for therapists to download. Use these BPD worksheets and exercises with your patients as session work or homework.
You must have read the Skills Training Manual for Treating Borderline Personality Disorder by Marsha Linehan, completed all the homework assignments in the manual, and taught or participated in all modules of skill training; Successful pass of exam based on the Cognitive-Behavioral Treatment of Borderline Personality Disorder by Marsha Linehan;
Ini7ally, women with borderline personality disorder were treated. Over the years, DBT has proved its effec7veness in trea7ng individuals with anxiety, substance abuse problems, PTSD, ... Match the homework assignments to the client's learning style, taking into account how they learn and processes informa7on. Addi7onally, the client's ...
DBT Skill: IMPROVE. worksheet. Dialectical behavior therapy (DBT) takes a structured, skills-driven approach to managing anxiety and improving emotion regulation. A key focus of these interventions is distress tolerance, which is the ability to accept and allow uncomfortable emotions. Our IMPROVE the Moment worksheet introduces a range of DBT ...
2. PsychPoint. PsychPoint is a great mental health resource that offers a large selection of free DBT worksheets for therapists in PDF format. At the time of writing, 29 worksheets are available for download. Topics include: Distress Tolerance Skills: Radical Acceptance Worksheet.
Borderline Personality Disorder Self Help Worksheet- Emotion Regulation Handout 10 Emotion regulation handout 10 is a great, detailed resource for learning ways of dealing with intense emotions. This worksheet teaches individuals effective ways of managing common emotions such as fear, justified nd unjustified guilt or shame, sadness or ...
Dialectical behavioral therapy (DBT) may improve symptoms of borderline personality disorder (BPD) by teaching skills that include mindfulness and emotion regulation. Marked by difficulties with ...
Worksheets BPD Symptom Tracker Anger Meter Facts & Fears Worksheet Trigger = Response worksheet Personality Traits List Optimism v Pessimism Anger Sequence Handout Distress Tolerance Worksheets My Stress Signs and Symptoms Coping Sequence Goals & Resolutions Worksheet Loneliness to Connection Defense Mechanism Worksheet 6 Steps of the Self-Harm Sequence BPD Intrusion Worksheet Anger ...
Are ready to fully commit to therapy and do homework assignments. Are ready to focus mostly on your present and future, rather than your past. Feel able to do some sessions in a group with others. ... Many therapists believe that the treatment for borderline personality disorder, in particular, can often take several years. ...
Coping Skills for Borderline Personality Disorder. If you have borderline personality disorder (BPD), your emotions can be overwhelming. Symptoms of BPD, include erratic mood shifts, self-harming behaviors, suicidality, intense emotional experiences, sensitivity to problems in your relationships, and problems with impulsive behaviors.
Borderline personality disorder (BPD) is a mental disorder characterized by a persistent pattern of emotional dysregulation, self‐image and interpersonal relationship instability, and marked impulsivity. ... in‐session practice of the strategies, and weekly homework assignments. The skills taught in a given week were reviewed at the ...
Dialectical behavior therapy (DBT) is a structured outpatient treatment based on cognitive-behavioral principles developed by Dr Marsha Linehan in the early 1990s for the treatment of parasuicidal behavior in women with borderline personality disorder (BPD). Linehan defines parasuicidal behavior as "any intentional, acute self-injurious ...
Borderline Personality. Borderline personality disorder (BPD) is a condition characterized by chronic instability in relationships, extreme emotional reactions, and chronic fear of abandonment ...
Last updated: 08/19/2021. Borderline personality disorder is a chronic condition that may include mood instability, difficulty with interpersonal relationships, and high rates of self-injury and ...
Mental Health Hotlines. National BPD Hotline (TARA): 888-4-TARA APD (888-482-7227) 12 am - 5 pm EST. Suicide Prevention Telephone Numbers (worldwide) Samaritans Helplines Suicide Prevention (Confidential & Anonymous) Peer Staffed Hotlines By State.
Borderline personality disorder; Chronic bipolar II disorder, most recent episode major depressive; ... and facilitate incorporation into the client's everyday life (e.g., homework assignments). ... Assign the client a homework exercise in which he/she identifies fearful self-talk and creates reality-based alternatives; review and reinforce ...
How do therapists treat borderline personality disorder? ... DBT is an active program, and homework assignments often encourage patients to practice concrete self-management skills between sessions.
Personality disorders, including borderline personality disorder; Self-harm; Post-traumatic stress disorder; Bulimia; ... Patients can expect homework assignments, which might, for example, focus ...
Homework assignments in relational psychoanalytic treatment of personality disorders: A case study of a patient with narcissistic personality disorder. ... As a result, therapy was stalled and progress was limited. At this point, the therapist asked him to complete homework assignments that encouraged him to refrain from his compulsive ...
Self-mutilation occurs frequently with people who suffer from BPD. Perhaps the most common form is cutting or burning themselves with razor blades, knives or cigarettes. These actions often occur ...
Mental Health portion case study: borderline personality disorder nancy, age 23, has just been hospitalized after she reported to her college roommate, carol, Skip to document. University; High School. Books; ... Homework Assignment Ch24; Homework Assignment Ch25; Homework Assignment Ch27; Healthcare; Careplan for Advanced Adult Health Care course.
When asked what everyday tasks borderline personality disorder ... assignment due dates can be extended. The symptoms are both psychologically and physically painful. The intensity at which the symptoms hit is totally underestimated." — Kellyann N. Advertisement "Homework, it makes it really hard to be able to get anything done. I know I ...
A euthymic mood is strived for in bipolar disorder and other mood disorders. ... borderline personality disorder, or major depression. ... sessions alongside cognitive restructuring and homework ...