
- Free Study Planner
- Residency Consulting
- Free Resources
- Med School Blog
- 1-888-427-7737

The Ultimate Patient Case Presentation Template for Med Students
- by Neelesh Bagrodia
- Apr 06, 2024
- Reviewed by: Amy Rontal, MD

Knowing how to deliver a patient presentation is one of the most important skills to learn on your journey to becoming a physician. After all, when you’re on a medical team, you’ll need to convey all the critical information about a patient in an organized manner without any gaps in knowledge transfer.
One big caveat: opinions about the correct way to present a patient are highly personal and everyone is slightly different. Additionally, there’s a lot of variation in presentations across specialties, and even for ICU vs floor patients.
My goal with this blog is to give you the most complete version of a patient presentation, so you can tailor your presentations to the preferences of your attending and team. So, think of what follows as a model for presenting any general patient.
Here’s a breakdown of what goes into the typical patient presentation.

7 Ingredients for a Patient Case Presentation Template
1. the one-liner.
The one-liner is a succinct sentence that primes your listeners to the patient.
A typical format is: “[Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y].
2. The Chief Complaint
This is a very brief statement of the patient’s complaint in their own words. A common pitfall is when medical students say that the patient had a chief complaint of some medical condition (like cholecystitis) and the attending asks if the patient really used that word!
An example might be, “Patient has chief complaint of difficulty breathing while walking.”
3. History of Present Illness (HPI)
The goal of the HPI is to illustrate the story of the patient’s complaint.
I remember when I first began medical school, I had a lot of trouble determining what was relevant and ended up giving a lot of extra details. Don’t worry if you have the same issue. With time, you’ll learn which details are important.
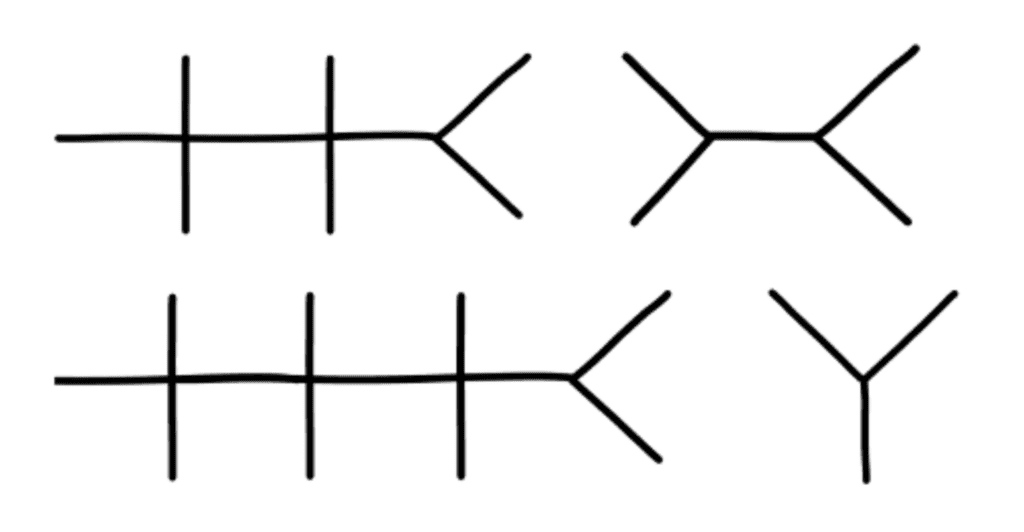
The OPQRST Framework
In the beginning of your clinical experience, a helpful framework to use is OPQRST:
Describe when the issue started, and if it occurs during certain environmental or personal exposures.
P rovocative
Report if there are any factors that make the pain better or worse. These can be broad, like noting their shortness of breath worsened when lying flat, or their symptoms resolved during rest.
Relay how the patient describes their pain or associated symptoms. For example, does the patient have a burning versus a pressure sensation? Are they feeling weakness, stiffness, or pain?
R egion/Location
Indicate where the pain is located and if it radiates anywhere.
Talk about how bad the pain is for the patient. Typically, a 0-10 pain scale is useful to provide some objective measure.
Discuss how long the pain lasts and how often it occurs.
A Case Study
While the OPQRST framework is great when starting out, it can be limiting.
Let’s take an example where the patient is not experiencing pain and comes in with altered mental status along with diffuse jaundice of the skin and a history of chronic liver disease. You will find that certain sections of OPQRST do not apply.
In this event, the HPI is still a story, but with a different framework. Try to go in chronological order. Include relevant details like if there have been any changes in medications, diet, or bowel movements.
Pertinent Positive and Negative Symptoms
Regardless of the framework you use, the name of the game is pertinent positive and negative symptoms the patient is experiencing.
I’d like to highlight the word “pertinent.” It’s less likely the patient’s chronic osteoarthritis and its management is related to their new onset shortness of breath, but it’s still important for knowing the patient’s complete medical picture. A better place to mention these details would be in the “Past Medical History” section, and reserve the HPI portion for more pertinent history.
As you become exposed to more illness scripts, experience will teach you which parts of the history are most helpful to state. Also, as you spend more time on the wards, you will pick up on which questions are relevant and important to ask during the patient interview.
By painting a clear picture with pertinent positives and negatives during your presentation, the history will guide what may be higher or lower on the differential diagnosis.
Some other important components to add are the patient’s additional past medical/surgical history, family history, social history, medications, allergies, and immunizations.
The HEADSSS Method
Particularly, the social history is an important time to describe the patient as a complete person and understand how their life story may affect their present condition.
One way of organizing the social history is the HEADSSS method:
– H ome living situation and relationships – E ducation and employment – A ctivities and hobbies – D rug use (alcohol, tobacco, cocaine, etc.) Note frequency of use, and if applicable, be sure to add which types of alcohol consumption (like beer versus hard liquor) and forms of drug use. – S exual history (partners, STI history, pregnancy plans) – S uicidality and depression – S piritual and religious history
Again, there’s a lot of variation in presenting social history, so just follow the lead of your team. For example, it’s not always necessary/relevant to obtain a sexual history, so use your judgment of the situation.
4. Review of Symptoms
Oftentimes, most elements of this section are embedded within the HPI. If there are any additional symptoms not mentioned in the HPI, it’s appropriate to state them here.
5. Objective
Vital signs.
Some attendings love to hear all five vital signs: temperature, blood pressure (mean arterial pressure if applicable), heart rate, respiratory rate, and oxygen saturation. Others are happy with “afebrile and vital signs stable.” Just find out their preference and stick to that.
Physical Exam
This is one of the most important parts of the patient presentation for any specialty. It paints a picture of how the patient looks and can guide acute management like in the case of a rigid abdomen. As discussed in the HPI section, typically you should report pertinent positives and negatives. When you’re starting out, your attending and team may prefer for you to report all findings as part of your learning.
For example, pulmonary exam findings can be reported as: “Regular chest appearance. No abnormalities on palpation. Lungs resonant to percussion. Clear to auscultation bilaterally without crackles, rhonchi, or wheezing.”
Typically, you want to report the physical exams in a head to toe format: General Appearance, Mental Status, Neurologic, Eyes/Ears/Nose/Mouth/Neck, Cardiovascular, Pulmonary, Breast, Abdominal, Genitourinary, Musculoskeletal, and Skin. Depending on the situation, additional exams can be incorporated as applicable.
Now comes reporting pertinent positive and negative labs. Several labs are often drawn upon admission. It’s easy to fall into the trap of reading off all the labs and losing everyone’s attention. Here are some pieces of advice:
You normally can’t go wrong sticking to abnormal lab values.
One qualification is that for a patient with concern for acute coronary syndrome, reporting a normal troponin is essential. Also, stating the normalization of previously abnormal lab values like liver enzymes is important.
Demonstrate trends in lab values.
A lab value is just a single point in time and does not paint the full picture. For example, a hemoglobin of 10g/dL in a patient at 15g/dL the previous day is a lot more concerning than a patient who has been stable at 10g/dL for a week.
Try to avoid editorializing in this section.
Save your analysis of the labs for the assessment section. Again, this can be a point of personal preference. In my experience, the team typically wants the raw objective data in this section.
This is also a good place to state the ins and outs of your patient (if applicable). In some patients, these metrics are strictly recorded and are typically reported as total fluid in and out over the past day followed by the net fluid balance. For example, “1L in, 2L out, net -1L over the past 24 hours.”
6. Diagnostics/Imaging
Next, you’ll want to review any important diagnostic tests and imaging. For example, describe how the EKG and echo look in a patient presenting with chest pain or the abdominal CT scan in a patient with right lower quadrant abdominal pain.
Try to provide your own interpretation to develop your skills and then include the final impression. Also, report if a diagnostic test is still pending.
7. Assessment/Plan
This is the fun part where you get to use your critical thinking (aka doctor) skills! For the scope of this blog, we’ll review a problem-based plan.
It’s helpful to begin with a summary statement that incorporates the one-liner, presenting issue(s)/diagnosis(es), and patient stability.
Then, go through all the problems relevant to the admission. You can impress your audience by casting a wide differential diagnosis and going through the elements of your patient presentation that support one diagnosis over another.
Following your assessment, try to suggest a management plan. In a patient with congestive heart failure exacerbation, initiating a diuresis regimen and measuring strict ins/outs are good starting points.
You may even suggest a follow-up on their latest ejection fraction with an echo and check if they’re on guideline-directed medical therapy. Again, with more time on the clinical wards you’ll start to pick up on what management plan to suggest.
One pointer is to talk about all relevant problems, not just the presenting issue. For example, a patient with diabetes may need to be put on a sliding scale insulin regimen or another patient may require physical/occupational therapy. Just try to stay organized and be comprehensive.
A Note About Patient Presentation Skills
When you’re doing your first patient presentations, it’s common to feel nervous. There may be a lot of “uhs” and “ums.”
Here’s the good news: you don’t have to be perfect! You just need to make a good faith attempt and keep on going with the presentation.
With time, your confidence will build. Practice your fluency in the mirror when you have a chance. No one was born knowing medicine and everyone has gone through the same stages of learning you are!
Practice your presentation a couple times before you present to the team if you have time. Pull a resident aside if they have the bandwidth to make sure you have all the information you need.
One big piece of advice: NEVER LIE. If you don’t know a specific detail, it’s okay to say, “I’m not sure, but I can look that up.” Someone on your team can usually retrieve the information while you continue on with your presentation.
Example Patient Case Presentation Template
Here’s a blank patient case presentation template that may come in handy. You can adapt it to best fit your needs.
Chief Complaint:
History of Present Illness:
Past Medical History:
Past Surgical History:
Family History:
Social History:
Medications:
Immunizations:
Vital Signs : Temp ___ BP ___ /___ HR ___ RR ___ O2 sat ___
Physical Exam:
General Appearance:
Mental Status:
Neurological:
Eyes, Ears, Nose, Mouth, and Neck:
Cardiovascular:
Genitourinary:
Musculoskeletal:
Most Recent Labs:
Previous Labs:
Diagnostics/Imaging:
Impression/Interpretation:
Assessment/Plan:
One-line summary:
#Problem 1:
Assessment:
#Problem 2:
Final Thoughts on Patient Presentations
I hope this post demystified the patient presentation for you. Be sure to stay organized in your delivery and be flexible with the specifications your team may provide.
Something I’d like to highlight is that you may need to tailor the presentation to the specialty you’re on. For example, on OB/GYN, it’s important to include a pregnancy history. Nonetheless, the aforementioned template should set you up for success from a broad overview perspective.
Stay tuned for my next post on how to give an ICU patient presentation. And if you’d like me to address any other topics in a blog, write to me at [email protected] !
Looking for more (free!) content to help you through clinical rotations? Check out these other posts from Blueprint tutors on the Med School blog:
- How I Balanced My Clinical Rotations with Shelf Exam Studying
- How (and Why) to Use a Qbank to Prepare for USMLE Step 2
- How to Study For Shelf Exams: A Tutor’s Guide
About the Author
Hailing from Phoenix, AZ, Neelesh is an enthusiastic, cheerful, and patient tutor. He is a fourth year medical student at the Keck School of Medicine of the University of Southern California and serves as president for the Class of 2024. He is applying to surgery programs for residency. He also graduated as valedictorian of his high school and the USC Viterbi School of Engineering, obtaining a B.S. in Biomedical Engineering in 2020. He discovered his penchant for teaching when he began tutoring his friends for the SAT and ACT in the summer of 2015 out of his living room. Outside of the academic sphere, Neelesh enjoys surfing at San Onofre Beach and hiking in the Santa Monica Mountains. Twitter: @NeeleshBagrodia LinkedIn: http://www.linkedin.com/in/neelesh-bagrodia

Related Posts

The Ultimate ICU Patient Presentation Template for Med Students

How Long Does It Take to Become a Surgeon?

Navigating the ERAS Residency Application Timeline: The Ultimate Guide
Search the blog, try blueprint med school study planner.
Create a personalized study schedule in minutes for your upcoming USMLE, COMLEX, or Shelf exam. Try it out for FREE, forever!
Could You Benefit from Tutoring?
Sign up for a free consultation to get matched with an expert tutor who fits your board prep needs
Find Your Path in Medicine
A side by side comparison of specialties created by practicing physicians, for you!
Popular Posts

Need a personalized USMLE/COMLEX study plan?
We use essential cookies to make Venngage work. By clicking “Accept All Cookies”, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts.
Manage Cookies
Cookies and similar technologies collect certain information about how you’re using our website. Some of them are essential, and without them you wouldn’t be able to use Venngage. But others are optional, and you get to choose whether we use them or not.
Strictly Necessary Cookies
These cookies are always on, as they’re essential for making Venngage work, and making it safe. Without these cookies, services you’ve asked for can’t be provided.
Show cookie providers
- Google Login
Functionality Cookies
These cookies help us provide enhanced functionality and personalisation, and remember your settings. They may be set by us or by third party providers.
Performance Cookies
These cookies help us analyze how many people are using Venngage, where they come from and how they're using it. If you opt out of these cookies, we can’t get feedback to make Venngage better for you and all our users.
- Google Analytics
Targeting Cookies
These cookies are set by our advertising partners to track your activity and show you relevant Venngage ads on other sites as you browse the internet.
- Google Tag Manager
- Infographics
- Daily Infographics
- Template Lists
- Graphic Design
- Graphs and Charts
- Data Visualization
- Human Resources
- Beginner Guides
Blog Business How to Present a Case Study like a Pro (With Examples)
How to Present a Case Study like a Pro (With Examples)
Written by: Danesh Ramuthi Sep 07, 2023

Okay, let’s get real: case studies can be kinda snooze-worthy. But guess what? They don’t have to be!
In this article, I will cover every element that transforms a mere report into a compelling case study, from selecting the right metrics to using persuasive narrative techniques.
And if you’re feeling a little lost, don’t worry! There are cool tools like Venngage’s Case Study Creator to help you whip up something awesome, even if you’re short on time. Plus, the pre-designed case study templates are like instant polish because let’s be honest, everyone loves a shortcut.
Click to jump ahead:
What is a case study presentation?
What is the purpose of presenting a case study, how to structure a case study presentation, how long should a case study presentation be, 5 case study presentation examples with templates, 6 tips for delivering an effective case study presentation, 5 common mistakes to avoid in a case study presentation, how to present a case study faqs.
A case study presentation involves a comprehensive examination of a specific subject, which could range from an individual, group, location, event, organization or phenomenon.
They’re like puzzles you get to solve with the audience, all while making you think outside the box.
Unlike a basic report or whitepaper, the purpose of a case study presentation is to stimulate critical thinking among the viewers.
The primary objective of a case study is to provide an extensive and profound comprehension of the chosen topic. You don’t just throw numbers at your audience. You use examples and real-life cases to make you think and see things from different angles.

The primary purpose of presenting a case study is to offer a comprehensive, evidence-based argument that informs, persuades and engages your audience.
Here’s the juicy part: presenting that case study can be your secret weapon. Whether you’re pitching a groundbreaking idea to a room full of suits or trying to impress your professor with your A-game, a well-crafted case study can be the magic dust that sprinkles brilliance over your words.
Think of it like digging into a puzzle you can’t quite crack . A case study lets you explore every piece, turn it over and see how it fits together. This close-up look helps you understand the whole picture, not just a blurry snapshot.
It’s also your chance to showcase how you analyze things, step by step, until you reach a conclusion. It’s all about being open and honest about how you got there.
Besides, presenting a case study gives you an opportunity to connect data and real-world scenarios in a compelling narrative. It helps to make your argument more relatable and accessible, increasing its impact on your audience.
One of the contexts where case studies can be very helpful is during the job interview. In some job interviews, you as candidates may be asked to present a case study as part of the selection process.
Having a case study presentation prepared allows the candidate to demonstrate their ability to understand complex issues, formulate strategies and communicate their ideas effectively.
The way you present a case study can make all the difference in how it’s received. A well-structured presentation not only holds the attention of your audience but also ensures that your key points are communicated clearly and effectively.
In this section, let’s go through the key steps that’ll help you structure your case study presentation for maximum impact.
Let’s get into it.
Open with an introductory overview
Start by introducing the subject of your case study and its relevance. Explain why this case study is important and who would benefit from the insights gained. This is your opportunity to grab your audience’s attention.

Explain the problem in question
Dive into the problem or challenge that the case study focuses on. Provide enough background information for the audience to understand the issue. If possible, quantify the problem using data or metrics to show the magnitude or severity.
Detail the solutions to solve the problem
After outlining the problem, describe the steps taken to find a solution. This could include the methodology, any experiments or tests performed and the options that were considered. Make sure to elaborate on why the final solution was chosen over the others.
Key stakeholders Involved
Talk about the individuals, groups or organizations that were directly impacted by or involved in the problem and its solution.
Stakeholders may experience a range of outcomes—some may benefit, while others could face setbacks.
For example, in a business transformation case study, employees could face job relocations or changes in work culture, while shareholders might be looking at potential gains or losses.
Discuss the key results & outcomes
Discuss the results of implementing the solution. Use data and metrics to back up your statements. Did the solution meet its objectives? What impact did it have on the stakeholders? Be honest about any setbacks or areas for improvement as well.
Include visuals to support your analysis
Visual aids can be incredibly effective in helping your audience grasp complex issues. Utilize charts, graphs, images or video clips to supplement your points. Make sure to explain each visual and how it contributes to your overall argument.
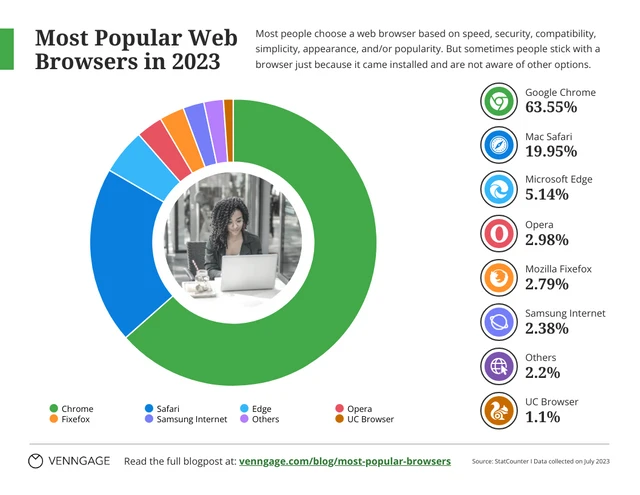
Pie charts illustrate the proportion of different components within a whole, useful for visualizing market share, budget allocation or user demographics.
This is particularly useful especially if you’re displaying survey results in your case study presentation.
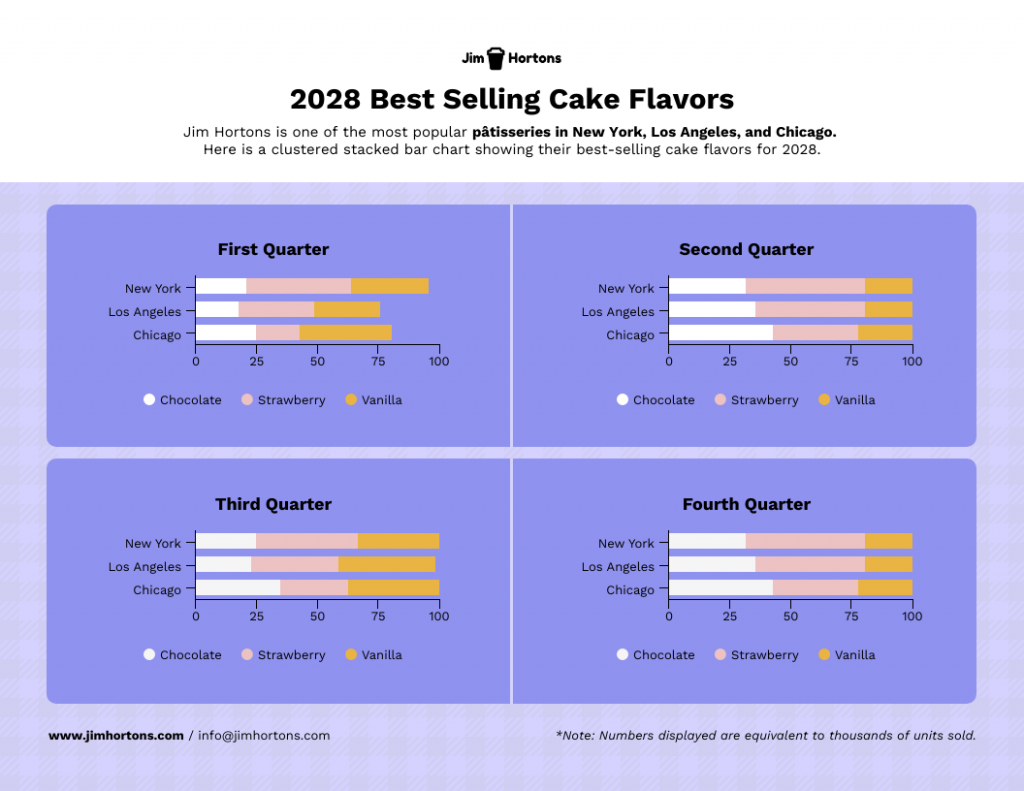
Stacked charts on the other hand are perfect for visualizing composition and trends. This is great for analyzing things like customer demographics, product breakdowns or budget allocation in your case study.
Consider this example of a stacked bar chart template. It provides a straightforward summary of the top-selling cake flavors across various locations, offering a quick and comprehensive view of the data.
Not the chart you’re looking for? Browse Venngage’s gallery of chart templates to find the perfect one that’ll captivate your audience and level up your data storytelling.
Recommendations and next steps
Wrap up by providing recommendations based on the case study findings. Outline the next steps that stakeholders should take to either expand on the success of the project or address any remaining challenges.
Acknowledgments and references
Thank the people who contributed to the case study and helped in the problem-solving process. Cite any external resources, reports or data sets that contributed to your analysis.
Feedback & Q&A session
Open the floor for questions and feedback from your audience. This allows for further discussion and can provide additional insights that may not have been considered previously.
Closing remarks
Conclude the presentation by summarizing the key points and emphasizing the takeaways. Thank your audience for their time and participation and express your willingness to engage in further discussions or collaborations on the subject.

Well, the length of a case study presentation can vary depending on the complexity of the topic and the needs of your audience. However, a typical business or academic presentation often lasts between 15 to 30 minutes.
This time frame usually allows for a thorough explanation of the case while maintaining audience engagement. However, always consider leaving a few minutes at the end for a Q&A session to address any questions or clarify points made during the presentation.
When it comes to presenting a compelling case study, having a well-structured template can be a game-changer.
It helps you organize your thoughts, data and findings in a coherent and visually pleasing manner.
Not all case studies are created equal and different scenarios require distinct approaches for maximum impact.
To save you time and effort, I have curated a list of 5 versatile case study presentation templates, each designed for specific needs and audiences.
Here are some best case study presentation examples that showcase effective strategies for engaging your audience and conveying complex information clearly.
1 . Lab report case study template
Ever feel like your research gets lost in a world of endless numbers and jargon? Lab case studies are your way out!
Think of it as building a bridge between your cool experiment and everyone else. It’s more than just reporting results – it’s explaining the “why” and “how” in a way that grabs attention and makes sense.
This lap report template acts as a blueprint for your report, guiding you through each essential section (introduction, methods, results, etc.) in a logical order.
Want to present your research like a pro? Browse our research presentation template gallery for creative inspiration!
2. Product case study template
It’s time you ditch those boring slideshows and bullet points because I’ve got a better way to win over clients: product case study templates.
Instead of just listing features and benefits, you get to create a clear and concise story that shows potential clients exactly what your product can do for them. It’s like painting a picture they can easily visualize, helping them understand the value your product brings to the table.
Grab the template below, fill in the details, and watch as your product’s impact comes to life!
3. Content marketing case study template
In digital marketing, showcasing your accomplishments is as vital as achieving them.
A well-crafted case study not only acts as a testament to your successes but can also serve as an instructional tool for others.
With this coral content marketing case study template—a perfect blend of vibrant design and structured documentation, you can narrate your marketing triumphs effectively.

4. Case study psychology template
Understanding how people tick is one of psychology’s biggest quests and case studies are like magnifying glasses for the mind. They offer in-depth looks at real-life behaviors, emotions and thought processes, revealing fascinating insights into what makes us human.
Writing a top-notch case study, though, can be a challenge. It requires careful organization, clear presentation and meticulous attention to detail. That’s where a good case study psychology template comes in handy.
Think of it as a helpful guide, taking care of formatting and structure while you focus on the juicy content. No more wrestling with layouts or margins – just pour your research magic into crafting a compelling narrative.
5. Lead generation case study template
Lead generation can be a real head-scratcher. But here’s a little help: a lead generation case study.
Think of it like a friendly handshake and a confident resume all rolled into one. It’s your chance to showcase your expertise, share real-world successes and offer valuable insights. Potential clients get to see your track record, understand your approach and decide if you’re the right fit.
No need to start from scratch, though. This lead generation case study template guides you step-by-step through crafting a clear, compelling narrative that highlights your wins and offers actionable tips for others. Fill in the gaps with your specific data and strategies, and voilà! You’ve got a powerful tool to attract new customers.
Related: 15+ Professional Case Study Examples [Design Tips + Templates]
So, you’ve spent hours crafting the perfect case study and are now tasked with presenting it. Crafting the case study is only half the battle; delivering it effectively is equally important.
Whether you’re facing a room of executives, academics or potential clients, how you present your findings can make a significant difference in how your work is received.
Forget boring reports and snooze-inducing presentations! Let’s make your case study sing. Here are some key pointers to turn information into an engaging and persuasive performance:
- Know your audience : Tailor your presentation to the knowledge level and interests of your audience. Remember to use language and examples that resonate with them.
- Rehearse : Rehearsing your case study presentation is the key to a smooth delivery and for ensuring that you stay within the allotted time. Practice helps you fine-tune your pacing, hone your speaking skills with good word pronunciations and become comfortable with the material, leading to a more confident, conversational and effective presentation.
- Start strong : Open with a compelling introduction that grabs your audience’s attention. You might want to use an interesting statistic, a provocative question or a brief story that sets the stage for your case study.
- Be clear and concise : Avoid jargon and overly complex sentences. Get to the point quickly and stay focused on your objectives.
- Use visual aids : Incorporate slides with graphics, charts or videos to supplement your verbal presentation. Make sure they are easy to read and understand.
- Tell a story : Use storytelling techniques to make the case study more engaging. A well-told narrative can help you make complex data more relatable and easier to digest.

Ditching the dry reports and slide decks? Venngage’s case study templates let you wow customers with your solutions and gain insights to improve your business plan. Pre-built templates, visual magic and customer captivation – all just a click away. Go tell your story and watch them say “wow!”
Nailed your case study, but want to make your presentation even stronger? Avoid these common mistakes to ensure your audience gets the most out of it:
Overloading with information
A case study is not an encyclopedia. Overloading your presentation with excessive data, text or jargon can make it cumbersome and difficult for the audience to digest the key points. Stick to what’s essential and impactful. Need help making your data clear and impactful? Our data presentation templates can help! Find clear and engaging visuals to showcase your findings.
Lack of structure
Jumping haphazardly between points or topics can confuse your audience. A well-structured presentation, with a logical flow from introduction to conclusion, is crucial for effective communication.
Ignoring the audience
Different audiences have different needs and levels of understanding. Failing to adapt your presentation to your audience can result in a disconnect and a less impactful presentation.
Poor visual elements
While content is king, poor design or lack of visual elements can make your case study dull or hard to follow. Make sure you use high-quality images, graphs and other visual aids to support your narrative.
Not focusing on results
A case study aims to showcase a problem and its solution, but what most people care about are the results. Failing to highlight or adequately explain the outcomes can make your presentation fall flat.
How to start a case study presentation?
Starting a case study presentation effectively involves a few key steps:
- Grab attention : Open with a hook—an intriguing statistic, a provocative question or a compelling visual—to engage your audience from the get-go.
- Set the stage : Briefly introduce the subject, context and relevance of the case study to give your audience an idea of what to expect.
- Outline objectives : Clearly state what the case study aims to achieve. Are you solving a problem, proving a point or showcasing a success?
- Agenda : Give a quick outline of the key sections or topics you’ll cover to help the audience follow along.
- Set expectations : Let your audience know what you want them to take away from the presentation, whether it’s knowledge, inspiration or a call to action.
How to present a case study on PowerPoint and on Google Slides?
Presenting a case study on PowerPoint and Google Slides involves a structured approach for clarity and impact using presentation slides :
- Title slide : Start with a title slide that includes the name of the case study, your name and any relevant institutional affiliations.
- Introduction : Follow with a slide that outlines the problem or situation your case study addresses. Include a hook to engage the audience.
- Objectives : Clearly state the goals of the case study in a dedicated slide.
- Findings : Use charts, graphs and bullet points to present your findings succinctly.
- Analysis : Discuss what the findings mean, drawing on supporting data or secondary research as necessary.
- Conclusion : Summarize key takeaways and results.
- Q&A : End with a slide inviting questions from the audience.
What’s the role of analysis in a case study presentation?
The role of analysis in a case study presentation is to interpret the data and findings, providing context and meaning to them.
It helps your audience understand the implications of the case study, connects the dots between the problem and the solution and may offer recommendations for future action.
Is it important to include real data and results in the presentation?
Yes, including real data and results in a case study presentation is crucial to show experience, credibility and impact. Authentic data lends weight to your findings and conclusions, enabling the audience to trust your analysis and take your recommendations more seriously
How do I conclude a case study presentation effectively?
To conclude a case study presentation effectively, summarize the key findings, insights and recommendations in a clear and concise manner.
End with a strong call-to-action or a thought-provoking question to leave a lasting impression on your audience.
What’s the best way to showcase data in a case study presentation ?
The best way to showcase data in a case study presentation is through visual aids like charts, graphs and infographics which make complex information easily digestible, engaging and creative.
Don’t just report results, visualize them! This template for example lets you transform your social media case study into a captivating infographic that sparks conversation.

Choose the type of visual that best represents the data you’re showing; for example, use bar charts for comparisons or pie charts for parts of a whole.
Ensure that the visuals are high-quality and clearly labeled, so the audience can quickly grasp the key points.
Keep the design consistent and simple, avoiding clutter or overly complex visuals that could distract from the message.
Choose a template that perfectly suits your case study where you can utilize different visual aids for maximum impact.
Need more inspiration on how to turn numbers into impact with the help of infographics? Our ready-to-use infographic templates take the guesswork out of creating visual impact for your case studies with just a few clicks.
Related: 10+ Case Study Infographic Templates That Convert
Congrats on mastering the art of compelling case study presentations! This guide has equipped you with all the essentials, from structure and nuances to avoiding common pitfalls. You’re ready to impress any audience, whether in the boardroom, the classroom or beyond.
And remember, you’re not alone in this journey. Venngage’s Case Study Creator is your trusty companion, ready to elevate your presentations from ordinary to extraordinary. So, let your confidence shine, leverage your newly acquired skills and prepare to deliver presentations that truly resonate.
Go forth and make a lasting impact!
Discover popular designs
Brochure maker
White paper online

Newsletter creator

Flyer maker
Timeline maker
Letterhead maker
Mind map maker

Ebook maker
Home Blog Business How to Present a Case Study: Examples and Best Practices
How to Present a Case Study: Examples and Best Practices
Marketers, consultants, salespeople, and all other types of business managers often use case study analysis to highlight a success story, showing how an exciting problem can be or was addressed. But how do you create a compelling case study and then turn it into a memorable presentation? Get a lowdown from this post!
Table of Content s
- Why Case Studies are a Popular Marketing Technique
Popular Case Study Format Types
How to write a case study: a 4-step framework, how to do a case study presentation: 3 proven tips, how long should a case study be, final tip: use compelling presentation visuals, business case study examples, what is a case study .
Let’s start with this great case study definition by the University of South Caroline:
In the social sciences, the term case study refers to both a method of analysis and a specific research design for examining a problem, both of which can generalize findings across populations.
In simpler terms — a case study is investigative research into a problem aimed at presenting or highlighting solution(s) to the analyzed issues.
A standard business case study provides insights into:
- General business/market conditions
- The main problem faced
- Methods applied
- The outcomes gained using a specific tool or approach
Case studies (also called case reports) are also used in clinical settings to analyze patient outcomes outside of the business realm.
But this is a topic for another time. In this post, we’ll focus on teaching you how to write and present a business case, plus share several case study PowerPoint templates and design tips!
Why Case Studies are a Popular Marketing Technique
Besides presenting a solution to an internal issue, case studies are often used as a content marketing technique . According to a 2020 Content Marketing Institute report, 69% of B2B marketers use case studies as part of their marketing mix.
A case study informs the reader about a possible solution and soft-sells the results, which can be achieved with your help (e.g., by using your software or by partnering with your specialist).
For the above purpose, case studies work like a charm. Per the same report:
- For 9% of marketers, case studies are also the best method for nurturing leads.
- 23% admit that case studies are beneficial for improving conversions.
Moreover, case studies also help improve your brand’s credibility, especially in the current fake news landscape and dubious claims made without proper credit.
Ultimately, case studies naturally help build up more compelling, relatable stories and showcase your product benefits through the prism of extra social proof, courtesy of the case study subject.
Most case studies come either as a slide deck or as a downloadable PDF document.
Typically, you have several options to distribute your case study for maximum reach:
- Case study presentations — in-person, virtual, or pre-recorded, there are many times when a case study presentation comes in handy. For example, during client workshops, sales pitches, networking events, conferences, trade shows, etc.
- Dedicated website page — highlighting case study examples on your website is a great way to convert middle-on-the-funnel prospects. Google’s Think With Google case study section is a great example of a web case study design done right.
- Blog case studies — data-driven storytelling is a staunch way to stand apart from your competition by providing unique insights, no other brand can tell.
- Video case studies — video is a great medium for showcasing more complex business cases and celebrating customer success stories.
Once you decide on your case study format, the next step is collecting data and then translating it into a storyline. There are different case study methods and research approaches you can use to procure data.
But let’s say you already have all your facts straight and need to organize them in a clean copy for your presentation deck. Here’s how you should do it.
1. Identify the Problem
Every compelling case study research starts with a problem statement definition. While in business settings, there’s no need to explain your methodology in-depth; you should still open your presentation with a quick problem recap slide.
Be sure to mention:
- What’s the purpose of the case study? What will the audience learn?
- Set the scene. Explain the before, aka the problems someone was facing.
- Advertise the main issues and findings without highlighting specific details.
The above information should nicely fit in several paragraphs or 2-3 case study template slides
2. Explain the Solution
The bulk of your case study copy and presentation slides should focus on the provided solution(s). This is the time to speak at length about how the subject went from before to the glorious after.
Here are some writing prompts to help you articulate this better:
- State the subject’s main objective and goals. What outcomes were they after?
- Explain the main solution(s) provided. What was done? Why this, but not that?
- Mention if they tried any alternatives. Why did those work? Why were you better?
This part may take the longest to write. Don’t rush it and reiterate several times. Sprinkle in some powerful words and catchphrases to make your copy more compelling.
3. Collect Testimonials
Persuasive case studies feature the voice of customer (VoC) data — first-party testimonials and assessments of how well the solution works. These provide extra social proof and credibility to all the claims you are making.
So plan and schedule interviews with your subjects to collect their input and testimonials. Also, design your case study interview questions in a way that lets you obtain quantifiable results.
4. Package The Information in a Slide Deck
Once you have a rough first draft, try different business case templates and designs to see how these help structure all the available information.
As a rule of thumb, try to keep one big idea per slide. If you are talking about a solution, first present the general bullet points. Then give each solution a separate slide where you’ll provide more context and perhaps share some quantifiable results.
For example, if you look at case study presentation examples from AWS like this one about Stripe , you’ll notice that the slide deck has few texts and really focuses on the big picture, while the speaker provides extra context.
Need some extra case study presentation design help? Download our Business Case Study PowerPoint template with 100% editable slides.
Your spoken presentation (and public speaking skills ) are equally if not more important than the case study copy and slide deck. To make a strong business case, follow these quick techniques.
Focus on Telling a Great Story
A case study is a story of overcoming a challenge, and achieving something grand. Your delivery should reflect that. Step away from the standard “features => benefits” sales formula. Instead, make your customer the hero of the study. Describe the road they went through and how you’ve helped them succeed.
The premises of your story can be as simple as:
- Help with overcoming a hurdle
- Gaining major impact
- Reaching a new milestone
- Solving a persisting issue no one else code
Based on the above, create a clear story arc. Show where your hero started. Then explain what type of journey they went through. Inject some emotions into the mix to make your narrative more relatable and memorable.
Experiment with Copywriting Formulas
Copywriting is the art and science of organizing words into compelling and persuasive combinations that help readers retain the right ideas.
To ensure that the audience retains the right takeaways from your case study presentation, you can try using some of the classic copywriting formulas to structure your delivery. These include:
- AIDCA — short for A ttention, I nterest, D esire, C onviction, and A ction. First, grab the audience’s attention by addressing the major problem. Next, pique their interest with some teaser facts. Spark their desire by showing that you know the right way out. Then, show a conviction that you know how to solve the issue—finally, prompt follow-up action such as contacting you to learn more.
- PADS — is short for Problem, Agitation, Discredit, or Solution. This is more of a sales approach to case study narration. Again, you start with a problem, agitate about its importance, discredit why other solutions won’t cut it, and then present your option.
- 4Ps — short for P roblem, P romise, P roof, P roposal. This is a middle-ground option that prioritizes storytelling over hard pitches. Set the scene first with a problem. Then make a promise of how you can solve it. Show proof in the form of numbers, testimonials, and different scenarios. Round it up with a proposal for getting the same outcomes.
Take an Emotion-Inducing Perspective
The key to building a strong rapport with an audience is showing that you are one of them and fully understand what they are going through.
One of the ways to build this connection is by speaking from an emotion-inducing perspective. This is best illustrated with an example:
- A business owner went to the bank
- A business owner came into a bank branch
In the second case, the wording prompts listeners to paint a mental picture from the perspective of the bank employees — a role you’d like them to relate to. By placing your audience in the right visual perspective, you can make them more receptive to your pitches.
One common question that arises when creating a case study is determining its length. The length of a case study can vary depending on the complexity of the problem and the level of detail you want to provide. Here are some general guidelines to help you decide how long your case study should be:
- Concise and Informative: A good case study should be concise and to the point. Avoid unnecessary fluff and filler content. Focus on providing valuable information and insights.
- Tailor to Your Audience: Consider your target audience when deciding the length. If you’re presenting to a technical audience, you might include more in-depth technical details. For a non-technical audience, keep it more high-level and accessible.
- Cover Key Points: Ensure that your case study covers the key points effectively. These include the problem statement, the solution, and the outcomes. Provide enough information for the reader to understand the context and the significance of your case.
- Visuals: Visual elements such as charts, graphs, images, and diagrams can help convey information more effectively. Use visuals to supplement your written content and make complex information easier to understand.
- Engagement: Keep your audience engaged. A case study that is too long may lose the reader’s interest. Make sure the content is engaging and holds the reader’s attention throughout.
- Consider the Format: Depending on the format you choose (e.g., written document, presentation, video), the ideal length may vary. For written case studies, aim for a length that can be easily read in one sitting.
In general, a written case study for business purposes often falls in the range of 1,000 to 2,000 words. However, this is not a strict rule, and the length can be shorter or longer based on the factors mentioned above.
Our brain is wired to process images much faster than text. So when you are presenting a case study, always look for an opportunity to tie in some illustrations such as:
- A product demo/preview
- Processes chart
- Call-out quotes or numbers
- Custom illustrations or graphics
- Customer or team headshots
Use icons to minimize the volume of text. Also, opt for readable fonts that can look good in a smaller size too.
To better understand how to create an effective business case study, let’s explore some examples of successful case studies:
Apple Inc.: Apple’s case study on the launch of the iPhone is a classic example. It covers the problem of a changing mobile phone market, the innovative solution (the iPhone), and the outstanding outcomes, such as market dominance and increased revenue.
Tesla, Inc.: Tesla’s case study on electric vehicles and sustainable transportation is another compelling example. It addresses the problem of environmental concerns and the need for sustainable transportation solutions. The case study highlights Tesla’s electric cars as the solution and showcases the positive impact on reducing carbon emissions.
Amazon.com: Amazon’s case study on customer-centricity is a great illustration of how the company transformed the e-commerce industry. It discusses the problem of customer dissatisfaction with traditional retail, Amazon’s customer-focused approach as the solution, and the remarkable outcomes in terms of customer loyalty and market growth.
Coca-Cola: Coca-Cola’s case study on brand evolution is a valuable example. It outlines the challenge of adapting to changing consumer preferences and demographics. The case study demonstrates how Coca-Cola continually reinvented its brand to stay relevant and succeed in the global market.
Airbnb: Airbnb’s case study on the sharing economy is an intriguing example. It addresses the problem of travelers seeking unique and affordable accommodations. The case study presents Airbnb’s platform as the solution and highlights its impact on the hospitality industry and the sharing economy.
These examples showcase the diversity of case studies in the business world and how they effectively communicate problems, solutions, and outcomes. When creating your own business case study, use these examples as inspiration and tailor your approach to your specific industry and target audience.
Finally, practice your case study presentation several times — solo and together with your team — to collect feedback and make last-minute refinements!
1. Business Case Study PowerPoint Template

To efficiently create a Business Case Study it’s important to ask all the right questions and document everything necessary, therefore this PowerPoint Template will provide all the sections you need.
Use This Template
2. Medical Case Study PowerPoint Template
3. Medical Infographics PowerPoint Templates
4. Success Story PowerPoint Template
5. Detective Research PowerPoint Template

6. Animated Clinical Study PowerPoint Templates

Like this article? Please share
Business Intelligence, Business Planning, Business PowerPoint Templates, Content Marketing, Feasibility Study, Marketing, Marketing Strategy Filed under Business
Related Articles
Filed under Business • April 22nd, 2024
Setting SMART Goals – A Complete Guide (with Examples + Free Templates)
This guide on SMART goals introduces the concept, explains the definition and its meaning, along the main benefits of using the criteria for a business.

Filed under Business • February 2nd, 2024
Business Plan Presentations: A Guide
Learn all that’s required to produce a high-quality business plan presentation in this guide. Suggested templates and examples are included.
Filed under Business • January 16th, 2024
The OODA Loop Decision-Making Model and How to Use it for Presentations
OODA Loop is a model that supports people and companies when defining important decisions in teams or individuals. See here how to apply it in presentation slide design.
Leave a Reply
How to make an oral case presentation to healthcare colleagues
The content and delivery of a patient case for education and evidence-based care discussions in clinical practice.

BSIP SA / Alamy Stock Photo
A case presentation is a detailed narrative describing a specific problem experienced by one or more patients. Pharmacists usually focus on the medicines aspect , for example, where there is potential harm to a patient or proven benefit to the patient from medication, or where a medication error has occurred. Case presentations can be used as a pedagogical tool, as a method of appraising the presenter’s knowledge and as an opportunity for presenters to reflect on their clinical practice [1] .
The aim of an oral presentation is to disseminate information about a patient for the purpose of education, to update other members of the healthcare team on a patient’s progress, and to ensure the best, evidence-based care is being considered for their management.
Within a hospital, pharmacists are likely to present patients on a teaching or daily ward round or to a senior pharmacist or colleague for the purpose of asking advice on, for example, treatment options or complex drug-drug interactions, or for referral.
Content of a case presentation
As a general structure, an oral case presentation may be divided into three phases [2] :
- Reporting important patient information and clinical data;
- Analysing and synthesising identified issues (this is likely to include producing a list of these issues, generally termed a problem list);
- Managing the case by developing a therapeutic plan.

Specifically, the following information should be included [3] :
Patient and complaint details
Patient details: name, sex, age, ethnicity.
Presenting complaint: the reason the patient presented to the hospital (symptom/event).
History of presenting complaint: highlighting relevant events in chronological order, often presented as how many days ago they occurred. This should include prior admission to hospital for the same complaint.
Review of organ systems: listing positive or negative findings found from the doctor’s assessment that are relevant to the presenting complaint.
Past medical and surgical history
Social history: including occupation, exposures, smoking and alcohol history, and any recreational drug use.
Medication history, including any drug allergies: this should include any prescribed medicines, medicines purchased over-the-counter, any topical preparations used (including eye drops, nose drops, inhalers and nasal sprays) and any herbal or traditional remedies taken.
Sexual history: if this is relevant to the presenting complaint.
Details from a physical examination: this includes any relevant findings to the presenting complaint and should include relevant observations.
Laboratory investigation and imaging results: abnormal findings are presented.
Assessment: including differential diagnosis.
Plan: including any pharmaceutical care issues raised and how these should be resolved, ongoing management and discharge planning.
Any discrepancies between the current management of the patient’s conditions and evidence-based recommendations should be highlighted and reasons given for not adhering to evidence-based medicine ( see ‘Locating the evidence’ ).
Locating the evidence
The evidence base for the therapeutic options available should always be considered. There may be local guidance available within the hospital trust directing the management of the patient’s presenting condition. Pharmacists often contribute to the development of such guidelines, especially if medication is involved. If no local guidelines are available, the next step is to refer to national guidance. This is developed by a steering group of experts, for example, the British HIV Association or the National Institute for Health and Care Excellence . If the presenting condition is unusual or rare, for example, acute porphyria, and there are no local or national guidelines available, a literature search may help locate articles or case studies similar to the case.
Giving a case presentation
Currently, there are no available acknowledged guidelines or systematic descriptions of the structure, language and function of the oral case presentation [4] and therefore there is no standard on how the skills required to prepare or present a case are taught. Most individuals are introduced to this concept at undergraduate level and then build on their skills through practice-based learning.
A case presentation is a narrative of a patient’s care, so it is vital the presenter has familiarity with the patient, the case and its progression. The preparation for the presentation will depend on what information is to be included.
Generally, oral case presentations are brief and should be limited to 5–10 minutes. This may be extended if the case is being presented as part of an assessment compared with routine everyday working ( see ‘Case-based discussion’ ). The audience should be interested in what is being said so the presenter should maintain this engagement through eye contact, clear speech and enthusiasm for the case.
It is important to stick to the facts by presenting the case as a factual timeline and not describing how things should have happened instead. Importantly, the case should always be concluded and should include an outcome of the patient’s care [5] .
An example of an oral case presentation, given by a pharmacist to a doctor, is available here .
A successful oral case presentation allows the audience to garner the right amount of patient information in the most efficient way, enabling a clinically appropriate plan to be developed. The challenge lies with the fact that the content and delivery of this will vary depending on the service, and clinical and audience setting [3] . A practitioner with less experience may find understanding the balance between sufficient information and efficiency of communication difficult, but regular use of the oral case presentation tool will improve this skill.
Tailoring case presentations to your audience
Most case presentations are not tailored to a specific audience because the same type of information will usually need to be conveyed in each case.
However, case presentations can be adapted to meet the identified learning needs of the target audience, if required for training purposes. This method involves varying the content of the presentation or choosing specific cases to present that will help achieve a set of objectives [6] . For example, if a requirement to learn about the management of acute myocardial infarction has been identified by the target audience, then the presenter may identify a case from the cardiology ward to present to the group, as opposed to presenting a patient reviewed by that person during their normal working practice.
Alternatively, a presenter could focus on a particular condition within a case, which will dictate what information is included. For example, if a case on asthma is being presented, the focus may be on recent use of bronchodilator therapy, respiratory function tests (including peak expiratory flow rate), symptoms related to exacerbation of airways disease, anxiety levels, ability to talk in full sentences, triggers to worsening of symptoms, and recent exposure to allergens. These may not be considered relevant if presenting the case on an unrelated condition that the same patient has, for example, if this patient was admitted with a hip fracture and their asthma was well controlled.
Case-based discussion
The oral case presentation may also act as the basis of workplace-based assessment in the form of a case-based discussion. In the UK, this forms part of many healthcare professional bodies’ assessment of clinical practice, for example, medical professional colleges.
For pharmacists, a case-based discussion forms part of the Royal Pharmaceutical Society (RPS) Foundation and Advanced Practice assessments . Mastery of the oral case presentation skill could provide useful preparation for this assessment process.
A case-based discussion would include a pharmaceutical needs assessment, which involves identifying and prioritising pharmaceutical problems for a particular patient. Evidence-based guidelines relevant to the specific medical condition should be used to make treatment recommendations, and a plan to monitor the patient once therapy has started should be developed. Professionalism is an important aspect of case-based discussion — issues must be prioritised appropriately and ethical and legal frameworks must be referred to [7] . A case-based discussion would include broadly similar content to the oral case presentation, but would involve further questioning of the presenter by the assessor to determine the extent of the presenter’s knowledge of the specific case, condition and therapeutic strategies. The criteria used for assessment would depend on the level of practice of the presenter but, for pharmacists, this may include assessment against the RPS Foundation or Pharmacy Frameworks .
Acknowledgement
With thanks to Aamer Safdar for providing the script for the audio case presentation.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal . You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
[1] Onishi H. The role of case presentation for teaching and learning activities. Kaohsiung J Med Sci 2008;24:356–360. doi: 10.1016/s1607-551x(08)70132–3
[2] Edwards JC, Brannan JR, Burgess L et al . Case presentation format and clinical reasoning: a strategy for teaching medical students. Medical Teacher 1987;9:285–292. doi: 10.3109/01421598709034790
[3] Goldberg C. A practical guide to clinical medicine: overview and general information about oral presentation. 2009. University of California, San Diego. Available from: https://meded.ecsd.edu/clinicalmed.oral.htm (accessed 5 December 2015)
[4] Chan MY. The oral case presentation: toward a performance-based rhetorical model for teaching and learning. Medical Education Online 2015;20. doi: 10.3402/meo.v20.28565
[5] McGee S. Medicine student programs: oral presentation guidelines. Learning & Scholarly Technologies, University of Washington. Available from: https://catalyst.uw.edu/workspace/medsp/30311/202905 (accessed 7 December 2015)
[6] Hays R. Teaching and Learning in Clinical Settings. 2006;425. Oxford: Radcliffe Publishing Ltd.
[7] Royal Pharmaceutical Society. Tips for assessors for completing case-based discussions. 2015. Available from: http://www.rpharms.com/help/case_based_discussion.htm (accessed 30 December 2015)
You might also be interested in…

How to demonstrate empathy and compassion in a pharmacy setting

Be more proactive to convince medics, pharmacists urged

How pharmacists can encourage patient adherence to medicines
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Writing a case report...
Writing a case report in 10 steps
- Related content
- Peer review
- Victoria Stokes , foundation year 2 doctor, trauma and orthopaedics, Basildon Hospital ,
- Caroline Fertleman , paediatrics consultant, The Whittington Hospital NHS Trust
- victoria.stokes1{at}nhs.net
Victoria Stokes and Caroline Fertleman explain how to turn an interesting case or unusual presentation into an educational report
It is common practice in medicine that when we come across an interesting case with an unusual presentation or a surprise twist, we must tell the rest of the medical world. This is how we continue our lifelong learning and aid faster diagnosis and treatment for patients.
It usually falls to the junior to write up the case, so here are a few simple tips to get you started.
First steps
Begin by sitting down with your medical team to discuss the interesting aspects of the case and the learning points to highlight. Ideally, a registrar or middle grade will mentor you and give you guidance. Another junior doctor or medical student may also be keen to be involved. Allocate jobs to split the workload, set a deadline and work timeframe, and discuss the order in which the authors will be listed. All listed authors should contribute substantially, with the person doing most of the work put first and the guarantor (usually the most senior team member) at the end.
Getting consent
Gain permission and written consent to write up the case from the patient or parents, if your patient is a child, and keep a copy because you will need it later for submission to journals.
Information gathering
Gather all the information from the medical notes and the hospital’s electronic systems, including copies of blood results and imaging, as medical notes often disappear when the patient is discharged and are notoriously difficult to find again. Remember to anonymise the data according to your local hospital policy.
Write up the case emphasising the interesting points of the presentation, investigations leading to diagnosis, and management of the disease/pathology. Get input on the case from all members of the team, highlighting their involvement. Also include the prognosis of the patient, if known, as the reader will want to know the outcome.
Coming up with a title
Discuss a title with your supervisor and other members of the team, as this provides the focus for your article. The title should be concise and interesting but should also enable people to find it in medical literature search engines. Also think about how you will present your case study—for example, a poster presentation or scientific paper—and consider potential journals or conferences, as you may need to write in a particular style or format.
Background research
Research the disease/pathology that is the focus of your article and write a background paragraph or two, highlighting the relevance of your case report in relation to this. If you are struggling, seek the opinion of a specialist who may know of relevant articles or texts. Another good resource is your hospital library, where staff are often more than happy to help with literature searches.
How your case is different
Move on to explore how the case presented differently to the admitting team. Alternatively, if your report is focused on management, explore the difficulties the team came across and alternative options for treatment.
Finish by explaining why your case report adds to the medical literature and highlight any learning points.
Writing an abstract
The abstract should be no longer than 100-200 words and should highlight all your key points concisely. This can be harder than writing the full article and needs special care as it will be used to judge whether your case is accepted for presentation or publication.
Discuss with your supervisor or team about options for presenting or publishing your case report. At the very least, you should present your article locally within a departmental or team meeting or at a hospital grand round. Well done!
Competing interests: We have read and understood BMJ’s policy on declaration of interests and declare that we have no competing interests.

Researched by Consultants from Top-Tier Management Companies

Powerpoint Templates
Icon Bundle
Kpi Dashboard
Professional
Business Plans
Swot Analysis
Gantt Chart
Business Proposal
Marketing Plan
Project Management
Business Case
Business Model
Cyber Security
Business PPT
Digital Marketing
Digital Transformation
Human Resources
Product Management
Artificial Intelligence
Company Profile
Acknowledgement PPT
PPT Presentation
Reports Brochures
One Page Pitch
Interview PPT
All Categories
Top 7 Medical Case Presentation Templates with Samples and Examples


Sarojit Hazra
How does information expand beyond essential recollection? Facts alone can diminish in value over time. Context and implementation are crucial to form deep connections and roots. Here comes the role of case studies for clinical personnel in the medical field.
In the always-growing healthcare industry, medical case presentation is essential as it is a suggestion for new researchers. A medical case study is a report where a medical practitioner shares a patient's case. It comprises every detail related to patients. It is beneficial for describing a new medical condition, management options, or treatment for diseases.
Medical case presentations contribute significantly to the evolution of medical knowledge and research.
Case study analysis is essential for every business or industry, like the medical industry. It helps in managing the twists and turns of the industry. Want to take some ideas? Have a look at SlideTeam’s blog Case Analysis Templates .
Let us highlight some significant benefits of medical case presentation:
- Case study presentations are extremely good at depicting realistic clinical frameworks.
- It helps to enhance student participation alongside the joy of learning.
- These are ideal for sharing the latest information on the clinical landscape.
- It promotes critical thinking.
- It can also make better clinical outcomes.
If you are in the healthcare sector, another important tool is the medical dashboard. For a deeper insight, quickly take a look at Medical dashboard Templates .
Each of the slides is 100% editable and customizable. The 100% customizable nature of the templates allows you to edit your presentations. The content-ready slides give you the much-needed structure. Below, let’s explore a wide array of ready to use, content ready medical case presentation templates fit for your organization.
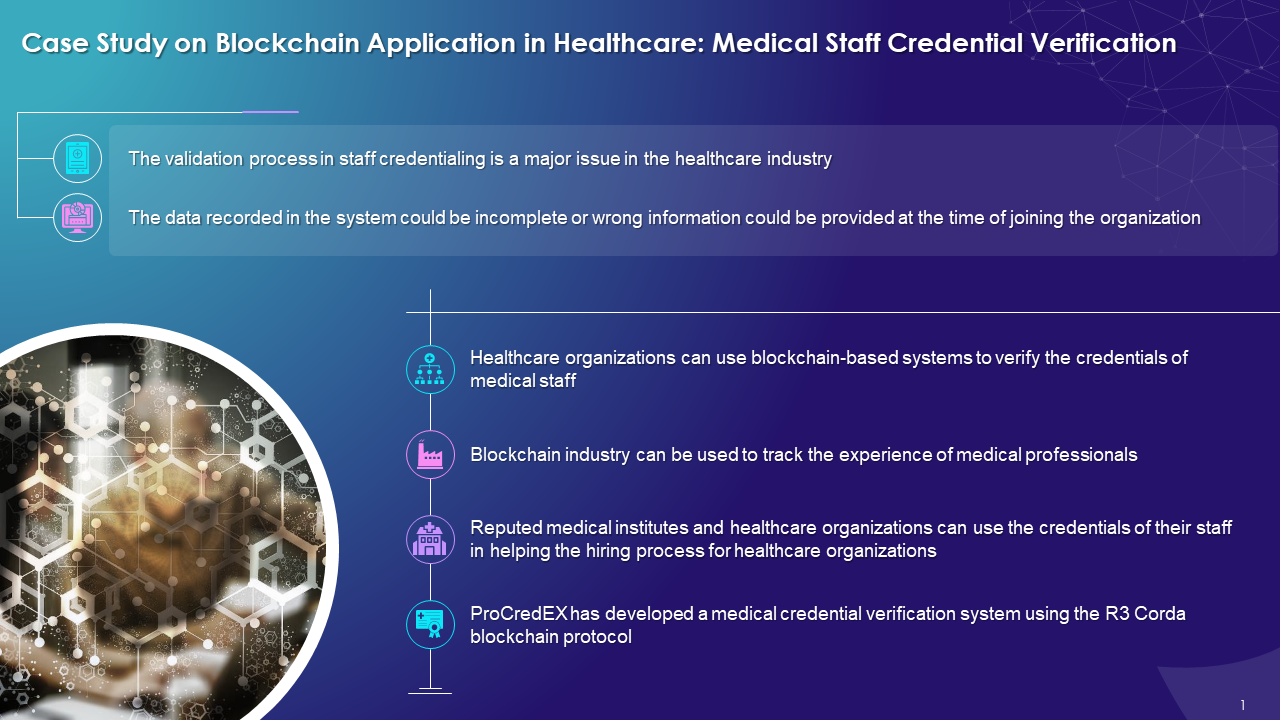
Template 1: Case Study on Blockchain Application in Healthcare: Medical Staff Credential Verification
Blockchain is becoming a potential solution to verify medical credentials. Though these are open to the public, they can be restricted through permissions. Are you finding it difficult to understand and implement? SlideTeam introduces this PPT Template that highlights how to operationalize medical staff verification process using blockchain technology. It explains that healthcare-based systems can also be used to verify the credentials of medical staff. Solutions-based blockchain to track the experiences of medical professionals. The PPT slides are designed with suitable icons, designs, graphs and other relevant material. Grab it quickly and draft your case study as per the client’s requirements.
Click to Download
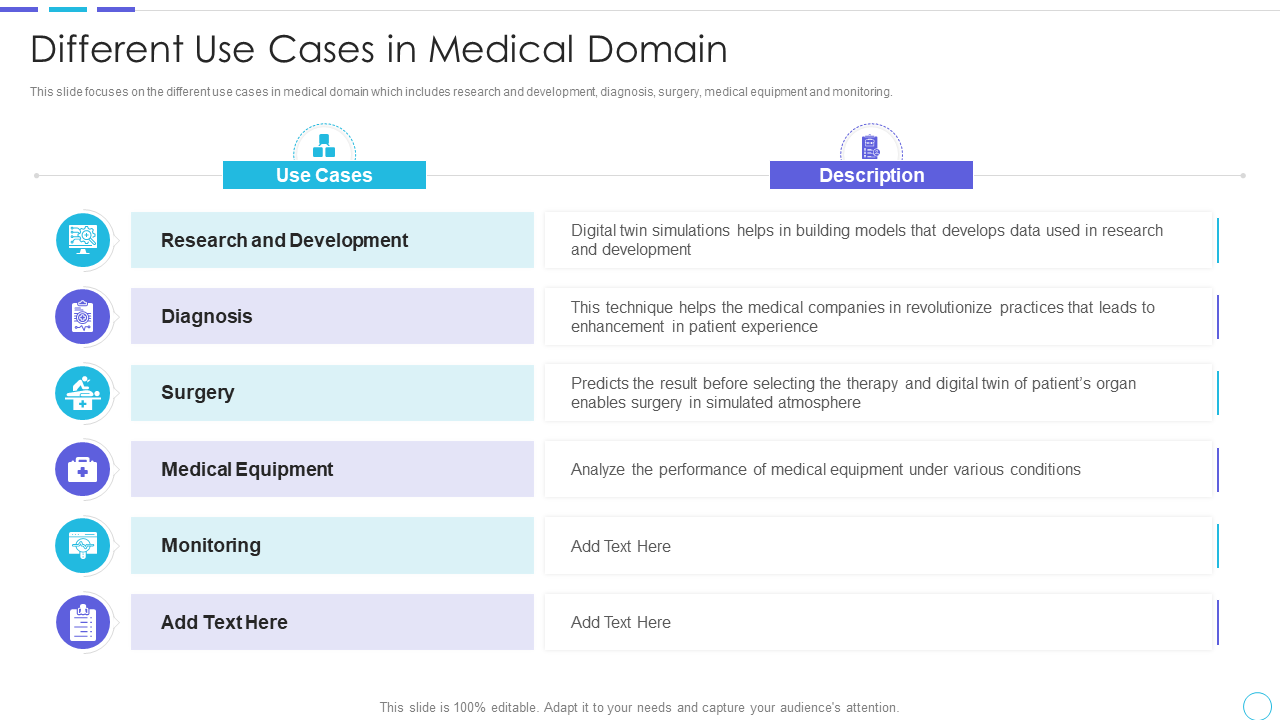
Template 2: Cost Benefits IOT Digital Twins Implementation Use Cases in the Medical Domain
This PPT template is designed to focus on the use cases in the medical domain, including research and development, diagnosis, surgery, medical equipment, etc. The slide offers a brief description of the mentioned use cases to understand the scenario better. Use it as an essential tool and captivate your audience. Get it Now!
Template 3: Major Use Cases for Tracking Medical Assets Asset Tracking and Management IoT
Want to simplify medical complexities? The asset tracking solution is here to accompany you. It enables the medical sector to locate patients, clinicians, and medications more accurately and quickly. IoT development has made this task much more accessible by guiding you through every significant aspect of a medical asset-tracking solution. Introducing our slide exhibiting use cases of medical tools that can be tracked with IoT technology . Medical assets, including medical tools, medical equipment tracking, medications , etc., are shown in the layout with their use cases and impacts. Each topic is depicted in separate tables with appropriate icons.
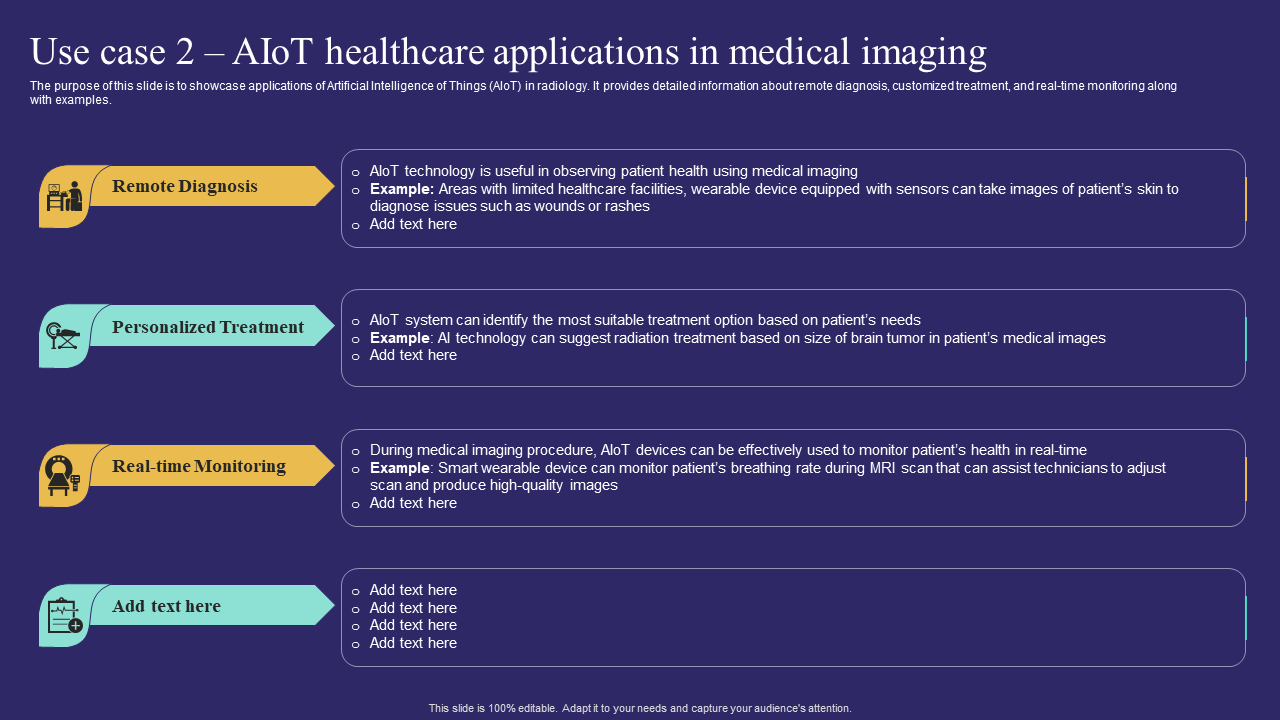
Template 4: AIoT Healthcare Applications in Medical Imaging
AIoT is making the medical sector smarter and wiser to improve data management and human-machine interaction. When AIoT is applied to healthcare, enables virtual monitoring and accurate diagnosis of patients to develop a personalized patient experience. Here, we introduce our premium PPT Templates showcasing applications of Artificial Intelligence of Things (AIoT) in radiology. You can provide detailed information about remote diagnosis , personalized treatment , and real-time monitoring. Adapt it now to increase your presentation threshold and educate your audience.
Template 5: Case Study of Leading Medical Devices Manufacturing Organization
An array of disruptive themes is shaping the medical device industry, and cloud computing is one of them. Soon, cloud computing will have a more significant impact on this industry. So, for your convenience, we are presenting our slide covering a case study of blue cloud with lending medical devices manufacturing organization. It covers significant topics like client objective, problem, our solution, and results chronologically. Consisting of three essential stages, this template is excellent for educating and enticing your audience.

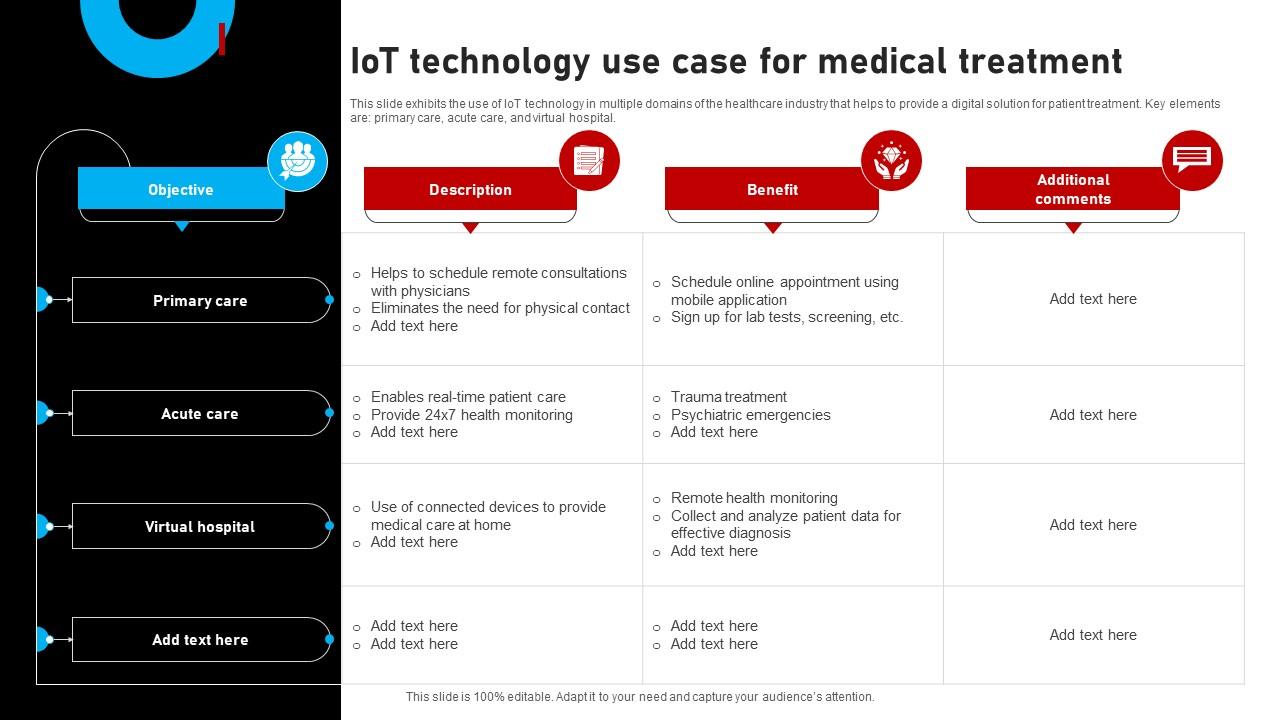
Template 6: IoT Technology Use Case for Medical Treatment
IoT, or the Internet of Things, is gaining significance across industries, and the medical sector is no exception. It has taken medical treatment to a new level. This custom-built PowerPoint Template exhibits the use of IoT technology in domains of the healthcare industry. It provides a digital solution for patient treatment. The key elements are primary care, acute care, virtual hospital, etc., which are depicted along with descriptions, benefits, and additional comments. Each illustration is highlighted, colored and has a relevant icon for instantaneous identification.
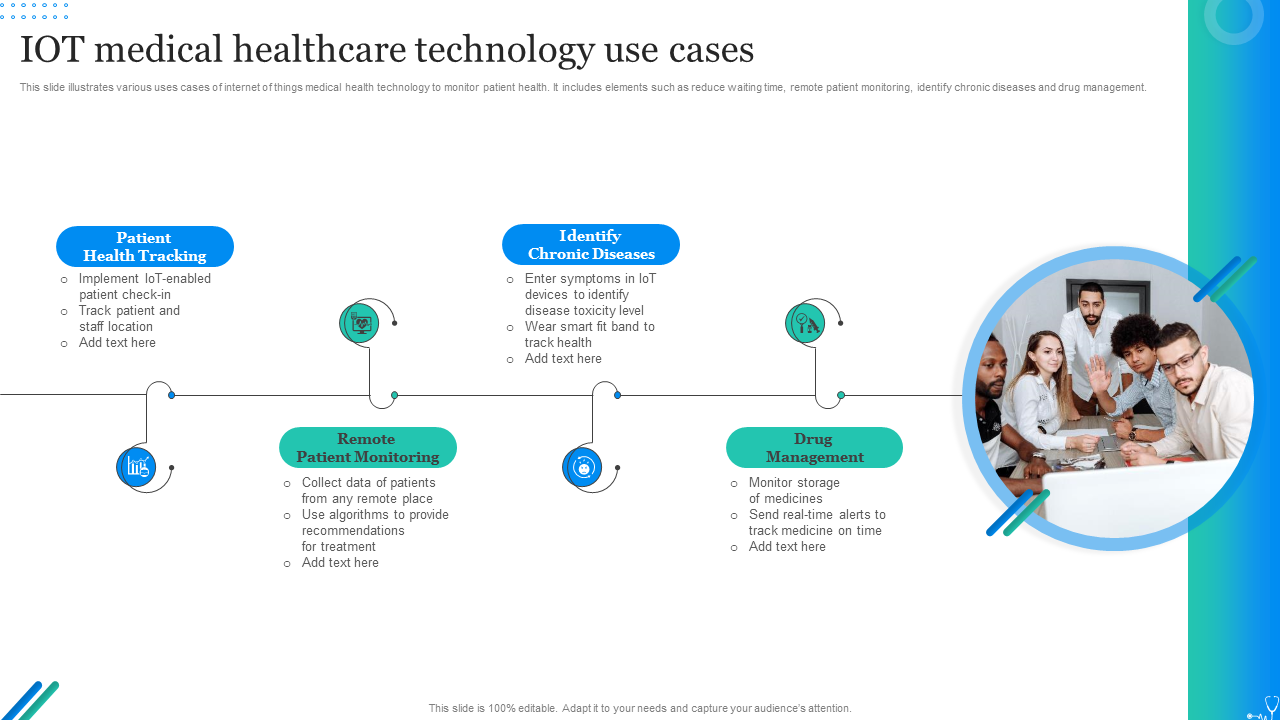
Template 7: IoT Medical Healthcare Technology Use Cases
The transformation of healthcare into digital healthcare has resulted in the rise of IoMT, or medical IoT . It refers to connected devices in medical healthcare and has become one of the fastest-growing industries in the IoT market. It would help if you dived deeper to manage, monitor, and preserve IoT devices in medical healthcare. This PPT presentation demonstrates uses of IoT Medical Healthcare Technology in monitoring patient health. Moreover, the slide includes remote patient monitoring, reduced waiting time, identifying chronic diseases, and drug management. Download this template design and present your case study with ultimate professionalism.
HEALTH CONSULTATION WILL BE QUICKER, SAFER AND SECURE
Case studies have a great history as an educational tool for clinicians. These are highly beneficial for nurturing deeper insights and learning. Access to such visually appealing and comprehensively presented Top 7 Medical Case Presentation Templates enables medical professionals to quickly present their patients' case studies. Be it tracking of medical assets, application of IoT in the clinical field, IoT medical healthcare technology uses, and so on, these templates serve as essential equipment in implementing all.
P.S. For perfection and success, you should dig into SlideTeam's fantastic blog, Medical Report Templates .
Related posts:
- How to Design the Perfect Service Launch Presentation [Custom Launch Deck Included]
- Quarterly Business Review Presentation: All the Essential Slides You Need in Your Deck
- [Updated 2023] How to Design The Perfect Product Launch Presentation [Best Templates Included]
- 99% of the Pitches Fail! Find Out What Makes Any Startup a Success
Liked this blog? Please recommend us

Top 10 Training Framework Templates with Examples and Samples

Top 5 Product Strategy Framework Templates with Samples and Examples
This form is protected by reCAPTCHA - the Google Privacy Policy and Terms of Service apply.

Digital revolution powerpoint presentation slides

Sales funnel results presentation layouts
3d men joinning circular jigsaw puzzles ppt graphics icons
Business Strategic Planning Template For Organizations Powerpoint Presentation Slides
Future plan powerpoint template slide

Project Management Team Powerpoint Presentation Slides

Brand marketing powerpoint presentation slides

Launching a new service powerpoint presentation with slides go to market

Agenda powerpoint slide show
Four key metrics donut chart with percentage

Engineering and technology ppt inspiration example introduction continuous process improvement

Meet our team representing in circular format

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Case study: 24-year-old male presenting with polyarthralgias.
Anusha Vakiti ; Saad Javed ; Kevin C. King .
Affiliations
Last Update: February 20, 2023 .
- Case Presentation
A 24-year-old white male with no known medical history presented to the hospital with chief complaints of 2 weeks of progressively worsening pain and swelling of his right wrist and left ankle joints. He did not report any fevers, chills, night sweats, weight loss or rash. He was employed as a fireman. He denied alcohol use disorder, smoking cigarettes, or any recreational drugs. Family history was significant for hypertension in father and ovarian cancer in the mother. His vital signs were within normal limits on presentation. On physical examination, the patient had significant swelling of multiple joints including the right wrist, right elbow, and left ankle. The joints were erythematous and tender to touch. Due to severe pain, he had limited range in the involved joints.
- Initial Evaluation
Initial laboratory workup for the swollen joints included a complete blood count which revealed an elevated white blood cell count (WBC) of 14000/microliter with neutrophil predominance, ESR of 118 mm per hour, and CRP of 8 mg/dL. A comprehensive metabolic panel was within normal limits. Infectious workup, which included blood and urine cultures, was negative. Immunological workup revealed elevated ANA titer (1:320), positive lupus anticoagulant, and high dsDNA antibodies. Ultrasound of the right elbow and left ankle joints revealed effusion in the joints and the surrounding soft tissue swelling. MRI of the right wrist revealed heterogeneous signal and enhancement of multiple carpal bones involving the second through fifth metacarpals, subcutaneous and deep soft tissue of the wrist and proximal hand. Based on the clinical and laboratory evidence, the patient was diagnosed with systemic lupus erythematosus (SLE) by the rheumatologist and was started on steroids, Plaquenil, and methotrexate. The patient’s clinical condition initially improved with the regimen, but his symptoms relapsed when weaning the steroids. He was discharged on a slow tapering dose of prednisone.
- Differential Diagnosis
The differential diagnosis for a young male (before fourth decade) with polyarthralgia is more inclined towards rheumatologic conditions like SLE, sarcoid arthritis, scleroderma, or gout. If associated with signs and symptoms of infection, gonococcal joint infection is high on the differential. Rheumatoid arthritis and polymyalgia rheumatica usually affect the older population (after the fourth decade). Based on the distribution of the joints, duration of symptoms, and association with other organ systems the classification of polyarthralgia is very broad and makes for a very challenging diagnosis. The most common differentials for a patient presenting with polyarthralgia are Rheumatoid arthritis, Lupus, Lyme, Septic arthritis, Gonorrheal joint arthritis, or Gout.
- Confirmatory Evaluation
During a follow-up appointment a few weeks later, he complained of multiple subcutaneous nodules. On physical exam, multiple, tender, non-erythematous subcutaneous nodules were noted along with a palpable, non-tender mass on the left side of the abdomen. CT abdomen showed a large heterogeneous mass measuring 20.1 by 10.7 by 18.1 cm, in the left quadrant of the abdomen along with a poorly defined low attenuation mass measuring 2.9 by 3 cm in the right hepatic lobe. CT guided biopsy of the left-sided abdominal mass was non-diagnostic. He underwent exploratory laparotomy, with excision of the left-sided abdominal mass along with splenectomy and distal pancreatectomy. There were multiple abnormal areas in the liver concerning for metastases. Pathology of the resected mass revealed sheets of malignant acinar cells with no intervening ductal structures or islets. Tumor cells were positive for trypsin and cytokeratin and were negative for CD117 and synaptophysin, consistent with pancreatic acinar cell carcinoma. Serum CA 19-9 levels were high. Lipase levels were elevated at 40,000U/dL. At this point, based on the biopsy and staging, the patient was diagnosed with stage IV pancreatic acinar cell carcinoma, but the cause of his polyarthralgia was still uncertain. Adjuvant chemotherapy was initiated with leucovorin, 5-fluorouracil (5-FU) and oxaliplatin for the carcinoma. During his treatment, his joint swelling and pain progressed and involved new joints of right ankle and left knee. Imaging studies of the joints showed joint effusion and soft tissue swelling. Arthrocentesis of the right ankle joint was performed, and the synovial fluid studies were consistent with infection and cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas. He was treated with antibiotics including vancomycin and piperacillin–tazobactam without any improvement. Due to progressive worsening of the right ankle joint, he required irrigation and debridement with arthrotomy. Repeat cultures were negative, but his symptoms continued to worsen, and he had persistent drainage of milky colored fluid from the surgical site and eventually required a below-knee amputation. Surgical pathology of the right knee joint revealed acute on chronic inflammation with the presence of granulation and fibrin tissue, without any evidence of malignancy. For further evaluation, arthrocentesis of left knee, left ankle, and right wrist was done and yielded milky colored fluid. His lipase levels continued to remain above 20,000 U/dL despite being treated with chemotherapy.
The persistent drainage of milky colored fluid from all the involved joints led to diagnosing the cause of polyarthralgia in this patient. Based on the diagnosis of metastatic acinar cell pancreatic carcinoma, evidence of elevated lipase levels, subcutaneous nodules, and the arthrocentesis yielding milky colored fluid, the patient’s polyarthralgia were believed to be due to hyperlipasemia, a rare paraneoplastic manifestation of pancreatic acinar cell carcinoma. The painful subcutaneous lesions are caused by an inflammatory process known as panniculitis which has been studied to be associated with polyarthralgia in a patient with pancreatic acinar cell carcinoma. Pancreatic polyarthritis and panniculitis are hypothesized to be caused by the peripheral lipolytic activity of lipase circulating systemically due to the pancreatic disease. [1] [2]
Initial adjuvant chemotherapy was with leucovorin, 5-fluorouracil (5-FU) and oxaliplatin but given the lack of response, his chemotherapy was switched to capecitabine and subsequently to gemcitabine and Abraxane. In spite of chemotherapy, the patient did not have any response, and his clinical condition worsened. After goals of care discussion with the patient and his family, he was transitioned to hospice care given his poor prognosis and chemotherapy was discontinued.
Paraneoplastic syndromes are a rare group of heterogeneous disorders that are triggered by an altered immune system response to a neoplasm. The symptoms may involve any organ system ranging from cutaneous manifestations to involvement of the neuromuscular or musculoskeletal systems. As seen in this patient, the paraneoplastic syndrome can be the initial presentation of the malignancy and can lead to delayed diagnosis and treatment. It is of great significance to understand the various paraneoplastic syndromes associated with a neoplasm. Few examples of common paraneoplastic syndromes are hypercalcemia of malignancy associated with breast cancer, SIADH associated with small cell carcinoma of the lung. Hyperlipasemia syndrome is a rare paraneoplastic syndrome associated with acinar cell carcinomas. Few cases have been reported of pancreatic panniculitis and polyarthralgia caused by hyperlipasemia. [3] [4]
Acinar cell carcinomas fall into the category of malignant epithelial neoplasms with an incidence of about 1% to 2% of the pancreatic neoplasms. The usual presentation of these tumors is solid, but they can also present either as cystic lesions or mixed with both solid and cystic components. They can present at any age but are often seen in older patients (sixth decade) and predominant in males than in females. Most patients present with vague symptoms such as abdominal pain, weight loss, fatigue or nausea. They are characterized by the production of zymogen granules containing pancreatic exocrine enzymes, in the tumor cells. A consequence of this is a rare paraneoplastic syndrome called hyperlipasemia or lipase hypersecretion syndrome. Serum lipase levels in such cases are usually above 10,000 U/dl and can result in multiple subcutaneous fat nodules and necrosis, termed as pancreatic panniculitis and polyarthralgia due to effusions and sclerotic lesions in the bones. This syndrome can be the initial manifestation of the neoplasm and is associated with poor prognosis. Histologically, these neoplasms are characterized by malignant cells with acinar cell differentiation, which stain positive for immunohistochemical stains such as trypsin, chymotrypsin, elastase, or lipase. Zymogen granules can be noted on the ultrastructure examination. KRAS, SMAD4, the mutations commonly associated with ductal adenocarcinomas are not seen in acinar cell carcinomas. Compared to patients with ductal adenocarcinoma, the overall prognosis for patients with acinar cell carcinoma is better. However, the presence of paraneoplastic syndrome association can worsen the prognosis and affect the quality of life as seen in this case. [5]
Hyperlipasemia syndrome is associated with poor prognosis of the acinar cell carcinoma, and the management modalities vary. Surgical resection is often the curative option for cases with local early-stage acinar cell carcinomas. However, often these acinar cell carcinomas are diagnosed in advanced or metastatic stages, and such cases often require adjuvant chemotherapy. Given the presence of APC gene/beta-catenin pathway genetic alterations, as seen in colorectal carcinomas, acinar cell carcinomas are often treated with 5-FU/leucovorin. Other chemotherapeutic agents that can be used include irinotecan, doxorubicin, erlotinib, gemcitabine, cisplatin, docetaxel, capecitabine, oxaliplatin, sunitinib, and sirolimus. Lowery et al. published a study in 2011 that highlighted the use of combination therapy, to use gemcitabine or 5-FU-based combination chemotherapy along with platinum analogs such as irinotecan in patients with advanced studies validated to have improved chemosensitivity. [6] [7] [8]
- Pearls of Wisdom
- Pancreatic acinar cell cancer is a rare malignancy of the pancreas and often seen in the elderly population.
- Usually dominated by symptoms of abdominal pain, and less frequently jaundice.
- The hypersecretion subtype may present with fever, arthralgia, rash, hypereosinophilia, and panniculitis.
- Imaging will usually reveal large lesions with sharp boundaries.
- Tissue is required to confirm diagnosis.
- Surgery is the treatment of localized lesions.
- For metastasis lesions, various chemotherapy protocols have been developed, which can result in long-term survival.
- Current day suggests that oxaliplatin-based chemotherapy is most effective.
- Compared to pancreatic adenocarcinomas, these malignancies carry a better prognosis.
It is important to be aware of the various paraneoplastic manifestations of malignancies, as the paraneoplastic presentation might be the initial sign of malignancy and could be misleading.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
CT abdomen image obtained from owner
Disclosure: Anusha Vakiti declares no relevant financial relationships with ineligible companies.
Disclosure: Saad Javed declares no relevant financial relationships with ineligible companies.
Disclosure: Kevin King declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Vakiti A, Javed S, King KC. Case Study: 24-Year-Old Male Presenting With Polyarthralgias. [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Cases from the Osler Medical Service at Johns Hopkins University. [Am J Med. 2004] Cases from the Osler Medical Service at Johns Hopkins University. Blank S, Le D, Hemnes A. Am J Med. 2004 Jul 1; 117(1):55-7.
- Cases from the Osler Medical Service at Johns Hopkins University. Diagnosis: P. carinii pneumonia and primary pulmonary sporotrichosis. [Am J Med. 2004] Cases from the Osler Medical Service at Johns Hopkins University. Diagnosis: P. carinii pneumonia and primary pulmonary sporotrichosis. Losman JA, Cavanaugh K. Am J Med. 2004 Sep 1; 117(5):353-6.
- A 34-Year-Old Man With Bilateral Paraspinal Masses and Shortness of Breath. [Chest. 2019] A 34-Year-Old Man With Bilateral Paraspinal Masses and Shortness of Breath. White K, Blay C, Ataya A, Alnuaimat H, Reddy R. Chest. 2019 Nov; 156(5):e99-e102.
- Review Clinical Case of the Month: A 57-Year-Old Man with an Axillary Mass. [J La State Med Soc. 2017] Review Clinical Case of the Month: A 57-Year-Old Man with an Axillary Mass. Desai P, Myers A, Boulmay B, Lopez FA. J La State Med Soc. 2017 May-Jun; 169(3):78-82. Epub 2017 Jun 23.
- Review With this eruption, there is not a second to lues. [Skinmed. 2005] Review With this eruption, there is not a second to lues. Burdette SD, Waibel JS, Bernstein JM, Trevino JJ. Skinmed. 2005 May-Jun; 4(3):179-82.
Recent Activity
- Case Study: 24-Year-Old Male Presenting With Polyarthralgias - StatPearls Case Study: 24-Year-Old Male Presenting With Polyarthralgias - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Patient Mrs. B.C. is a 56 year old female who is presenting to her WHNP for her annual exam. She had to cancel her appointment two months ago and didn’t reschedule until now. Her last pap smear and mammogram were normal. Today, while performing her breast exam, her nurse practitioner notices dimpling in the left breast as the patient raises her arms over her head. When the NP mentions it to Mrs. B.C. she is surprised and denies noticing it before today. A firm, non-tender, immobile nodule is palpated in the upper quadrant of her breast . The NP then asks Mrs. B.C. how frequently she is performing breast self-exams, she admits to only doing them randomly when she remembers, which is about every few months. She reports no recent or abnormal drainage from her breast. Further examination reveals palpable axillary lymph nodes.
Mrs. B.C. is about 30 pounds overweight and walks her dog around her neighborhood every morning before work and every evening when she gets home. She reports drinking a glass of white wine before bed each night. She denies any history of tobacco use. She reports use of a combination birth control pill on and off for 25 years until she reached menopause. She is not currently taking any prescription medications.
Past Medical History
- Menarche (Age 10)
- Post-menopausal (Age 53)
- No other pertinent medical history
Family History:
- Father George- deceased from stroke (75 years old), history of hypertension, CAD, HLD
- Mother Maryanne alive- 76 years old, history of dementia, osteoporosis
- Brother Michael- alive, 57 years old, history of hypertension, CAD and cardiac stent placement (54 years old)
- Sister, Michelle- alive 53 years old, history of GERD, Asthma
- Brother- Jimmy- alive 50 years old, no past medical history
Social History:
Mrs. B.C. works Monday-Friday 8am-5pm at the local dentist’s office at the front desk as a schedule coordinator. She is planning to retire in a few years. In her spare time, she is involved in various community efforts to feed the homeless and helps to prepare dinners at her local church one night a week. She also enjoys cooking and baking at home, gardening, and nature photography.
Mrs. B.C. has two children. Her oldest son, Patrick, is 21 years old and is in his final year of pre-med. He is attending a public university about 2 hours away from home where he lives year-round. As an infant, Patrick was breastfed until 18 months when he self-weaned. Her daughter, Veronica, is 19 years old and lives at home while attending the local branch campus of a state university. She is in her second year of a business degree and then plans to transfer to the main campus next year. When Veronica was an infant she had difficulty latching onto the breast due to an undiagnosed tongue and lip ties resulting in Mrs. BC exclusively pumping and bottle feeding for six months. After six months, Mrs. B.C. was having a hard time keeping up while working and her found her supply diminished. Veronica had begun eating solid foods so Mrs. B.C. switched to supplemental formula, which was a big relief.
Mrs. B.C. was married to her now ex-husband Kent for 26 years. They divorced two years ago when Veronica was a senior in high school. They have remained friends and Kent lives 25 minutes away in a condo with his girlfriend. She also has two brothers who live nearby and a sister who lives out of state. Her 7 nieces and nephews range in age from 9 years old to 26 years old. Her father, George, passed away from a sudden stroke 4 years ago. Her mother, Maryanne, has dementia and is living in a nearby memory care facility. She also has many close friends.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
memorial day
12 templates

17 templates
26 templates

20 templates
american history
73 templates

11 templates
Clinical Case 01-2023
Clinical case 01-2023 presentation, free google slides theme, powerpoint template, and canva presentation template.
Present your clinical case to the medical community with this dynamic and engaging presentation by Slidesgo. Who said science can’t be creative and fun?
This presentation has been created combining a traditional structure with flat illustrations to get a professional and original template. We’ve selected blue as the primary color since it’s generally used to represent the healthcare sector. Besides, the typography used is understandable and readable so that you can present your content clearly. Follow the prescription of our designers and make a difference!
Features of this template
- 100% editable and easy to modify
- 19 different slides
- Available in five colors: pink, yellow, green, blue and orange
- Contains editable graphics and maps
- Includes 1000+ icons divided into 11 different themes for customizing your slides
- Designed to be used in Google Slides, Canva and PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Available colors.
Original Color
Related posts on our blog

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.
Premium template
Unlock this template and gain unlimited access

- Reference Manager
- Simple TEXT file
People also looked at
Case report article, old woman with sheehan's syndrome suffered severe hyponatremia following percutaneous coronary intervention: a case report and review of literature.

- 1 School of Clinical Medicine, Shandong Second Medical University, Weifang, Shandong, China
- 2 Cardiology Department and Experimental Animal Center, Liaocheng People’s Hospital of Shandong University and Liaocheng Hospital Affiliated to Shandong First Medical University, Liaocheng, Shandong, China
- 3 Department of Central Laboratory, Liaocheng People’s Hospital, Liaocheng, Shandong, China
- 4 Department of Cardiology, Shandong Corps Hospital of Chinese People’s Armed Police Forces, Jinan, China
Glucocorticoid deficiency can lead to hypoglycemia, hypotension, and electrolyte disorders. Acute glucocorticoid deficiency under stress is very dangerous. Here, we present a case study of an elderly patient diagnosed with Sheehan's syndrome, manifesting secondary adrenal insufficiency and secondary hypothyroidism, managed with daily prednisone and levothyroxine therapy. She was admitted to our hospital due to acute non-ST segment elevation myocardial infarction. The patient developed nausea and limb twitching post-percutaneous coronary intervention, with subsequent diagnosis of hyponatremia. Despite initial intravenous sodium supplementation failed to rectify the condition, and consciousness disturbances ensued. However, administration of 50 mg hydrocortisone alongside 6.25 mg sodium chloride rapidly ameliorated symptoms and elevated blood sodium levels. Glucocorticoid deficiency emerged as the primary etiology of hyponatremia in this context, exacerbated by procedural stress during percutaneous coronary intervention. Contrast agent contributed to blood sodium dilution. Consequently, glucocorticoid supplementation emerges as imperative, emphasizing the necessity of stress-dose administration of glucocorticoid before the procedure. Consideration of shorter intervention durations and reduced contrast agent dosages may mitigate severe hyponatremia risks. Moreover, it is crucial for this patient to receive interdisciplinary endocrinologist management. In addition, Sheehan's syndrome may pose a risk for coronary atherosclerotic disease.
Introduction
In developed countries, studies have revealed varying prevalence rates of Sheehan's syndrome (SHS) among women, ranging from 0.0051% ( 1 ) to 3.1% ( 2 ). There were also studies showing that the prevalence of SHS ranged from 1% to 2% among women who experienced hypotension due to blood loss of 1–2 L ( 3 , 4 ). Contrastingly, in undeveloped nations, the prevalence varies from 3.1% to 27.6% ( 5 – 7 ). The diagnostic journey for SHS patients spans a considerable duration of 7–19 years from symptom onset to definitive diagnosis ( 8 ). Sheehan's syndrome arises from ischemic necrosis of the anterior pituitary gland triggered by postpartum hemorrhage ( 8 ), leading to pituitary hormone dysfunction, including insufficient secretion of growth hormone, thyroid stimulating hormone, gonadotropin, prolactin, and adrenocorticotropin (ACTH) ( 7 , 9 ). Predominant symptoms are associated with dysfunction of the gonads, thyroid, and adrenal cortex due to insufficient secretion of gonadotropins, thyroid stimulating hormones, and ACTH, respectively. The latter is the most prominent and sometimes life-threatening. Supplementing various deficient hormones is the primary treatment for SHS.
Glucocorticoids, pivotal adrenal cortex hormones, play crucial roles in regulating glucose metabolism, blood pressure, and electrolyte balance. Deficiency in glucocorticoids can lead to hypoglycemia, hypotension, and electrolyte disturbances. Lifetime glucocorticoid replacement therapy stands as a cornerstone in managing SHS patients. Fluctuations in neuroendocrine system activity necessitate adjustments in glucocorticoid supplementation, while metabolic disruptions from other etiologies also dictate dosage alterations. Inadequate comprehension of these dynamics among healthcare professionals may impact the prognosis of SHS patients and predispose them to risks. Surgical treatments, including interventional procedures, represent significant stressors in medical care. Failure to administer preoperative stress doses of glucocorticoids to SHS patients can engender serious consequences. To our knowledge, this article represents the first documented case of severe hyponatremia in an SHS patient following percutaneous coronary intervention (PCI).
Case presentation
A 70-year-old female patient presented with paroxysmal exertional chest tightness persisting for one month, alleviated by a few minutes of rest. Forty years ago, the patient suffered from postpartum hemorrhage, without blood transfusion, subsequently developing lactation failure and amenorrhea. Five years later, she was diagnosed with SHS at the Affiliated Hospital of Shandong University. Management included 5 mg of prednisone acetate in the morning for secondary adrenal insufficiency, and 50 ug of levothyroxine for secondary hypothyroidism. Apart from medication adherence, the patient lacked awareness regarding adrenal insufficiency. The patient had a decade-long history of hypertension, controlled with 5 mg of telmisartan and 5 mg of amlodipine daily. This patient had a weight of 46 kl, a height of 1.57 m, and a BMI of 18.66 kg/m 2 . Upon hospital admission, her vital signs were stable with a blood pressure of 122/58 mmHg, and a heart rate of 65 beats per minute. Physical examination revealed no pulmonary rales, cardiac murmurs, lower limb edema. Laboratory finding indicated elevated blood troponin I (0.5487 ng/ml, 0–0.0175 ng/ml), normal blood sodium (141.5 mmol/L, 137 mmol/L–147 mmol/L), and elevated fasting total cholesterol (6.28 mmol/L, 3 mmol/L–5.7 mmol/L). Thyroid function tests revealed low level of free thyroxine (FT4) (6.77 pmol/L, 7.98 pmol/L–16.02 pmol/L), with normal levels of free triiodothyronine (FT3) and thyroid stimulating hormone. Electrocardiogram indicated sinus bradycardia. We diagnosed the patient with acute non-ST segment elevation myocardial infarction (NSTEMI) and performed percutaneous coronary angiography (CAG) and intravascular ultrasound (IVUS) examination. We found that the stenosis degree was 40%, 80%, and 60%, 98%, and almost completely occluded, respectively, in the left main trunk (LM), the proximal and middle segments of the left anterior descending branch (LAD), the proximal segments of the left circumflex branch (LCX), and the middle segment of the right coronary artery (RCA) ( Figures 1A–C ). The minimum lumen area at the distal stenosis of the LM was 4.51 mm 2 ( Figure 1E ), the plaque load at the most severe stenosis of the proximal LAD was 80%, with a minimum lumen area of 2.88 mm 2 ( Figure 1F ). Due to the patient's refusal to undergo coronary artery bypass grafting, two stents were inserted in the middle segment of the RCA ( Figure 1D ). The intervention lasted for 2 h, including coronary angiography, bilateral intravascular ultrasound examination, patient involvement in treatment decision-making based on examination results, and subsequent coronary intervention treatment, utilizing 130 ml of iodixanol. The patient did not experience any chest discomfort, but was nervous and had a blood pressure rise to 190/100 mmHg, managed with sublingual nifedipine tablets and intravenous isosorbide nitrate. Following percutaneous intervention (PCI), the patient experienced a sequence of symptoms from the 12th to the 50th h, including nausea and loss of appetite, profuse sweating, mild limb twitching, and drowsiness in sequence ( Table 1 ). Limb twitching persisited for 18 h from the 38th to the 56th h post-PCI. On the 24th h post-PCI, the patient was diagnosed with hyponatremia ( Table 1 ), and 2%−3% sodium chloride was intermittently administered intravenously. Despite increased sodium chloride supplementation, symptoms persisted until administration of hydrocortisone, leading to symptom resolution and rapid improvement in blood sodium levels ( Table 1 ). By the 62nd h post-PCI, symptoms of hyponatremia completely resolved, with blood sodium level increasing from 114.2 mmol/L to 132 mmol/L ( Table 1 ). At the 86th h post-PCI, blood sodium level returned to normal. After 40 h, blood tests revealed low levels of cortisol (2.76 ug/dl, 6.7ug/dl–22.6 ug/dl), ACTH (4.26 pg/ml, 10.1 pg/ml–57.6 pg/ml), FT3 (3.41 pmol/L, 3.53 pmol/L−7.37 pmol/L), and FT4 (7.12 pmol/L, 7.98 pmol/L–16.02 pmol/L). Following discharge, the patient continued oral medication with 2.5 mg prednisone acetate and 50 ug levothyroxine sodium daily, as well as dual antiplatelet drugs, statins, and antihypertensive agents. During the next nine-month follow-up period, the patient did not experience ischemic symptoms or hyponatremia.
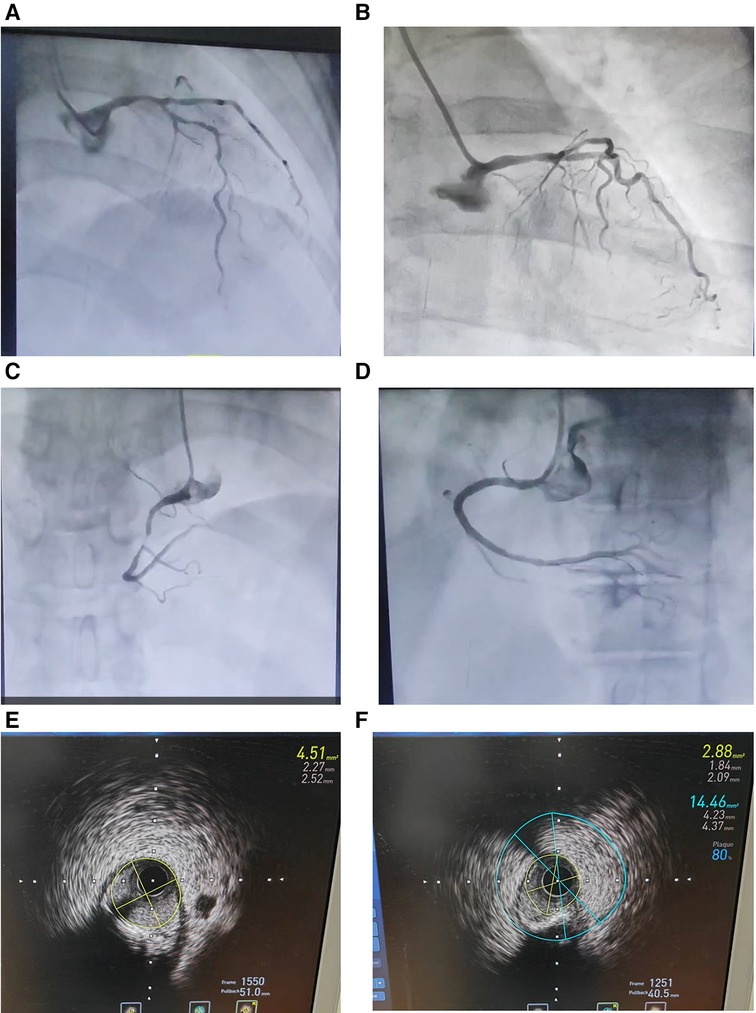
Figure 1 . Coronary angiography ( A – D ) and intravascular ultrasound examination ( E and F ) in an elderly patient with Sheehan's syndrome. ( A ) The stenosis degree is 40%, 80%, and 60%, respectively, at the end of the left main trunk, the proximal and middle segments of the left anterior descending branch. ( B ) The stenosis degree is 98% at the proximal segments of the left circumflex branch. ( C ) The stenosis degree is almost completely occluded at the middle segment of the right coronary artery. ( D ) Two stents are inserted in the middle segment of the RCA. ( E ) The minimum lumen area at the distal stenosis of the left main trunk is 4.51 mm 2 . ( F ) The plaque load at the most severe stenosis of the proximal left anterior descending branch is 80%, and the minimum lumen area is 2.88 mm 2 .
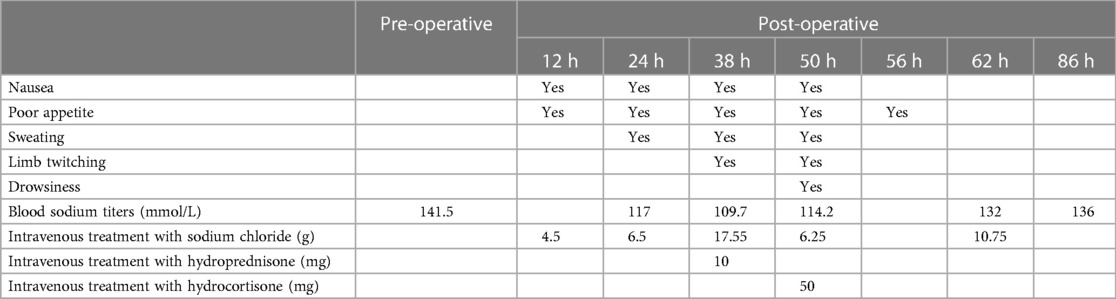
Table 1 . Timeline of changes in symptoms, blood sodium titers, and hyponatremia treatment in this patient at 12, 24, 38, 50, 56, 62 and 86 h after percutaneous intervention. normal titer blood sodium reference value: 137 mmol/L to 147 mmol/L.
SHS and hyponatremia
Sheehan's syndrome is characterized by insufficient secretion of ACTH due to pituitary necrosis, resulting in decreased synthesis and secretion of adrenocortical hormones, particularly glucocorticoids. Glucocorticoids play a vital role in regulating sodium and water excretion and maintaining electrolyte balance in the body. Insufficient glucocorticoid levels lead to diminished renal free water clearance, causing water retention and dilutional hyponatremia, resulting in reduced plasma osmolality. Furthermore, despite low osmolality, there is inappropriate secretion of antidiuretic hormone (vasopressin) due to the absence of cortisol's tonic inhibition ( 10 ).
Clinical presentation and management
In this case, the patient had a medical history of a SHS diagnosis, presenting with secondary adrenal insufficiency and secondary thyrotrophin deficiency necessitating hormone replacement therapy. Secondary adrenal insufficiency arises from pituitary impairment, causing decreased production of ACTH and subsequent reduction in adrenal stimulation, leading to decreased cortisol production. Glucocorticoid deficiency emerged as the primary mechanism of hyponatremia in this patient. During the 2-h of coronary diagnosis and treatment, the patient was anxious, had high blood pressure, and was in a severe stress state, which required additional cortisol to cope with. The specific amount could be evaluated by a specialist doctor. However, due to secondary adrenal insufficiency, the patient could not suddenly increase the secretion of glucocorticoids to copy with the stress. Additionally, glucocorticoids were not pre increased before the procedure. Therefore, the patient was at risk of acute and severe adrenal cortical hormone deficiency, leading to excessive sodium loss, water retention, and subsequent hyponatremia.
Treatment response
Despite intravenous supplementation of 24.05 g sodium chloride within 26 h, hyponatremia persisted, accompanied limb twitching and drowsiness, indicating an exacerbation of hyponatremia and the formation of hypotonic brain edema. Administration of 50 mg hydrocortisone effectively relieved excessive sodium excretion and water retention. Even with 6.25 g sodium chloride treatment, the patient's symptoms almost disappeared after 6 h, and blood sodium increased from 114.2 mmol/L to 132 mmol/L after 12 h. The subsequent increase in blood sodium levels highlights the importance of glucocorticoid replacement therapy in managing hyponatremia secondary to SHS.
Management considerations
The case underscores the importance of preoperative stress dose glucocorticoid therapy in SHS patients undergoing procedures such as PCI. However, we were unaware the importance. Additionally, awareness of the potential for contrast agents to induce dilutional hyponatremia and stress response caused by PCI is crucial. Lack of endocrinologist consultation before the procedure and inadequate patient education regarding adrenal insufficiency contributed to the suboptimal management of this patient. Inappropriately administered sublingual nifedipine treatment, intended to manage transient hypertension, not only increased the risk of acute cardiovascular and cerebrovascular disease, but also increased the risks of further activating the sympathetic nervous ( 11 ) and exacerbating stress. Therefore, the interdisciplinary management involving endocrinologists is crucial for optimizing the treatment for patients with complex endocrine disorders like SHS, facilitating appropriate examinations, treatment and health education to prevent adrenal crisis and improve long-term outcomes ( 12 , 13 ).
Prolonged limb twitching and sodium correction
Unlike the transient symptoms of epilepsy, the patient experienced persistent limb twitching for up to 18 h, possibly due to prolonged lower blood sodium levels. This prolonged imbalance could have led to sustained electrical instability in brain cells, resulting in repetitive abnormal electro-discharge and impaired brain function, posing significant risks to the patient. However, our approach to correcting hyponatremia may not have followed optimal guidelines. Our method of correcting hyponatremia may not have followed the best guidelines. The target value for increasing serum sodium was not set to not exceed 8–10 mmol/L/24 h ( 14 ). Our treatment rapidly increased the patient's blood sodium from 114 mmol/L to 132 mmol/L in 12 h, and then continued to supplement with hypertonic sodium chloride. Within 26 h after identifying hyponatremia, 24.05 g of sodium chloride was administered intravenously. These treatments are unreasonable, and the overly rapid correction of hyponatremia may be a risk factor for osmotic demyelination syndrome. Proper management should aim to increase blood sodium concentration gradually, with close monitoring to prevent such complications.
Other proposed mechanisms of hyponatremia
Contrast agents have been implicated in inducing hyponatremia, particularly in women ( 15 – 18 ). Following administration, the contrast agents elevate the osmotic pressure of extracellular fluid, leading to passive water transfer of intracellular to extracellular compartments and resultant diluted hyponatremia ( 15 , 16 ). Sweating caused by sympathetic nerve stimulation and sweating caused by adverse reactions to iodixanol injection may also contribute to sodium loss.
Role of hypothyroidism
The patient's thyroid hormone levels were low before and after the procedure, indicating the presence of secondary hypothyroidism. Hypothyroidism may have contributed to hyponatremia mainly through the reduced ability to excretal free water, caused by higher levels of ADH. The elevation in ADH levels is largely due to the decrease in cardiac output that stimulates the carotid sinus baroreceptors, prompting the release of ADH. In addition, hypothyroidism can promote hyaluronic acid deposition in extravascular tissues, leading to increased water retention and reduced blood volume. This not only reduces glomerular filtration, but also increases the secretion of antidiuretic hormone, thereby increasing the risk of diluted hyponatremia ( 19 – 22 ). Therefore, optimizing levothyroxine therapy to restore normal thyroid hormone levels may help mitigate the risk of hyponatremia in such cases.
SHS and coronary artery disease
Previous studies have indicated a higher mortality rate in patients with pituitary dysfunction, primarily attributed to cardiovascular diseases ( 23 – 25 ). Due to chronic inflammation, dyslipidemia, and abdominal obesity, patients with SHS tend to develop coronary artery disease (CAD) ( 26 ). This NSTEMI patient suffered from severe coronary atherosclerosis, with traditional risk factors including hypertension and hypercholesterolemia. Long-term oral administration of glucocorticoids may be associated with hypertension and hyperlipidemia in such patients ( 27 , 28 ). In addition, hypothyroidism, which is common in SHS, can also contribute to hyperlipidemia ( 29 ).
Although severe hyponatremia following PCI in SHS patients is not extensively reported, there are cases of female patients exhibiting life-threatening adrenal dysfunction post-PCI ( 30 , 31 ). The lowest blood sodium level in these cases is 122 mmol/L, and there is no hypoglycemia. Glucocorticoids have good therapeutic effects. The difference is that these patients exhibit significant hypotension, shock, and even Takotsubo syndrome ( 30 , 31 ).
Conclusions
The deficiency of glucocorticoids caused by secondary adrenal insufficiency is the primary mechanism for severe hyponatremia in this patient with SHS. The stress induced by PCI exacerbates glucocorticoid deficiency. The contrast agent further contributes to dilutional hyponatremia. The preoperative stress dose of glucocorticoid is crucial to avoid this complication. Glucocorticoids were crucial in correcting severe hyponatremia in this SHS patient with secondary adrenal insufficiency. Shortening the duration of PCI and minimizing the dosage of contrast agents may be beneficial for preventing severe hyponatremia. Meanwhile, it is also crucial for this SHS patient to receive interdisciplinary management involving endocrinologists before and after the procedure. Additionally, SHS may serve as a potential risk factor for CAD.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of Liaocheng People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JG: Data curation, Writing – review & editing. YW: Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing, Software, Methodology, Project administration, Supervision. AZ: Writing – review & editing. HP: Writing – review & editing, Data curation. FW: Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
The work was supported by Shandong Province Traditional Chinese Medicine Science and Technology Development Plan Project (No. 20190906).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kristjansdottir HL, Bodvarsdottir SP, Sigurjonsdottir HA. Sheehan’s syndrome in modern times: a nationwide retrospective study in Iceland. Eur J Endocrinol . (2011) 164(3):349–54. doi: 10.1530/EJE-10-1004
PubMed Abstract | Crossref Full Text | Google Scholar
2. Abs R, Bengtsson BA, Hernberg-Stâhl E, Monson JP, Tauber JP, Wilton P, et al. GH replacement in 1034 growth hormone deficient hypopituitary adults: demographic and clinical characteristics, dosing and safety. Clin Endocrinol (Oxf) . (1999) 50(6):703–13. doi: 10.1046/j.1365-2265.1999.00695.x
3. Vaphiades MS, Simmons D, Archer RL, Stringer W. Sheehan syndrome: a splinter of the mind. Surv Ophthalmol . (2003) 48(2):230–3. doi: 10.1016/s0039-6257(02)00459-9
4. Keleştimur F. Sheehan’s syndrome. Pituitary . (2003) 6(4):181–8. doi: 10.1023/b:pitu.0000023425.20854.8e
Crossref Full Text | Google Scholar
5. Tanriverdi F, Dokmetas HS, Kebapcı N, Kilicli F, Atmaca H, Yarman S, et al. Etiology of hypopituitarism in tertiary care institutions in Turkish population: analysis of 773 patients from pituitary study group database. Endocrine . (2014) 47(1):198–205. doi: 10.1007/s12020-013-0127-4
6. Diri H, Karaca Z, Tanriverdi F, Unluhizarci K, Kelestimur F. Sheehan’s syndrome: new insights into an old disease. Endocrine . (2016) 51(1):22–31. doi: 10.1007/s12020-015-0726-3
7. Zargar AH, Singh B, Laway BA, Masoodi SR, Wani AI, Bashir MI. Epidemiologic aspects of postpartum pituitary hypofunction (Sheehan’s syndrome). Fertil Steril . (2005) 84(2):523–8. doi: 10.1016/j.fertnstert.2005.02.022
8. Diri H, Tanriverdi F, Karaca Z, Senol S, Unluhizarci K, Durak AC, et al. Extensive investigation of 114 patients with Sheehan’s syndrome: a continuing disorder. Eur J Endocrinol . (2014) 171(3):311–8. doi: 10.1530/EJE-14-0244
9. Laway BA, Misgar RA, Mir SA, Wani AI. Clinical, hormonal and radiological features of partial Sheehan’s syndrome: an Indian experience. Arch Endocrinol Metab . (2016) 60(2):125–9. doi: 10.1590/2359-3997000000137
10. Garrahy A, Thompson CJ. Hyponatremia and glucocorticoid deficiency. Front Horm Res . (2019) 52:80–92. doi: 10.1159/000493239
11. Ragueneau I, Sao AB, Démolis JL, Darné B, Funck-Brentano C, Jaillon P. Comparison of sympathetic modulation induced by single oral doses of mibefradil, amlodipine, and nifedipine in healthy volunteers. Clin Pharmacol Ther . (2001) 69(3):122–9. doi: 10.1067/mcp.2001.113406
12. Arlt W, Society for Endocrinology Clinical Committee. SOCIETY FOR ENDOCRINOLOGY ENDOCRINE EMERGENCY GUIDANCE: emergency management of acute adrenal insufficiency (adrenal crisis) in adult patients. Endocr Connect . (2016) 5(5):G1–3. doi: 10.1530/EC-16-0054
13. Fleseriu M, Hashim IA, Karavitaki N, Melmed S, Murad MH, Salvatori R, et al. Hormonal replacement in hypopituitarism in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab . (2016) 101(11):3888–921. doi: 10.1210/jc.2016-2118
14. Lindner G, Schwarz C, Haidinger M, Ravioli S. Hyponatremia in the emergency department. Am J Emerg Med . (2022) 60:1–8. doi: 10.1016/j.ajem.2022.07.023
15. Lim LY, Mohd Firdaus CA, Fam XI, Goh EH. Acute symptomatic hyponatremia after computed tomography renal protocol. J Comput Assist Tomogr . (2017) 41(1):65–6. doi: 10.1097/RCT.0000000000000487
16. Sirken G, Raja R, Garces J, Bloom E, Fumo P. Contrast-induced translocational hyponatremia and hyperkalemia in advanced kidney disease. Am J Kidney Dis . (2004) 43(2):e31–5. doi: 10.1053/j.ajkd.2003.10.028. Erratum in: Am J Kidney Dis. 2004 Dec; 44(6):1127. Fumo, Peter [added]. PMID: 14750123.14750123
17. Sankaran S, Saharia GK, Naik S, Mangaraj M. Effect of iodinated contrast media on serum electrolyte concentrations in patients undergoing routine contrast computed tomography scan procedure. Int J Appl Basic Med Res . (2019) 9(4):217–20. doi: 10.4103/ijabmr.IJABMR_69_19
18. Gucun M, Kahyaoglu M, Celik M, Guner A, Akyuz O, Yilmaz Y. Predictive value of post-procedural hyponatremia on contrast-induced nephropathy in patients who underwent coronary angiography or percutaneous coronary intervention. Acta Cardiol . (2022) 77(3):215–21. doi: 10.1080/00015385.2021.1901022
19. Tomlinson JW, Holden N, Hills RK, Wheatley K, Clayton RN, Bates AS, et al. Association between premature mortality and hypopituitarism. West midlands prospective hypopituitary study group. Lancet . (2001) 357(9254):425–31. doi: 10.1016/S0140-6736(00)04006-X
20. Schmitt R, Klussmann E, Kahl T, Ellison DH, Bachmann S. Renal expression of sodium transporters and aquaporin-2 in hypothyroid rats. Am J Physiol Renal Physiol . (2003) 284(5):F1097–104. doi: 10.1152/ajprenal.00368.2002
21. Liamis G, Filippatos TD, Liontos A, Elisaf MS. Management of endocrine disease: hypothyroidism-associated hyponatremia: mechanisms, implications and treatment. Eur J Endocrinol . (2017) 176(1):R15–20. doi: 10.1530/EJE-16-0493
22. Macaron C, Famuyiwa O. Hyponatremia of hypothyroidism. Appropriate suppression of antidiuretic hormone levels. Arch Intern Med . (1978) 138(5):820–2. doi: 10.1001/archinte.138.5.820
23. Nakano M, Higa M, Ishikawa R, Yamazaki T, Yamamuro W. Hyponatremia with increased plasma antidiuretic hormone in a case of hypothyroidism. Intern Med . (2000) 39(12):1075–8. doi: 10.2169/internalmedicine.39.1075
24. Pappachan JM, Raskauskiene D, Kutty VR, Clayton RN. Excess mortality associated with hypopituitarism in adults: a meta-analysis of observational studies. J Clin Endocrinol Metab . (2015) 100(4):1405–11. doi: 10.1210/jc.2014-3787
25. McCallum RW, Petrie JR, Dominiczak AF, Connell JMC. Growth hormone deficiency and vascular risk. Clin Endocrinol (Oxf) . (2002) 57(1):11–24. doi: 10.1046/j.1365-2265.2002.01559.x
26. Laway BA, Rasool A, Baba MS, Misgar RA, Bashir MI, Wani AI, et al. High prevalence of coronary artery calcification and increased risk for coronary artery disease in patients with Sheehan syndrome-A case-control study. Clin Endocrinol (Oxf) . (2023) 98(3):375–82. doi: 10.1111/cen.14871
27. Khan NA, Donatelli CV, Tonelli AR, Wiesen J, Ribeiro Neto ML, Sahoo D, et al. Toxicity risk from glucocorticoids in sarcoidosis patients. Respir Med . (2017) 132:9–14. doi: 10.1016/j.rmed.2017.09.003
28. Hemmer MC, Wierer M, Schachtrup K, Downes M, Hübner N, Evans RM, et al. E47 modulates hepatic glucocorticoid action. Nat Commun . (2019) 10(1):306. doi: 10.1038/s41467-018-08196-5
29. Matlock CL, Vanhoof AR, Rangrej SB, Rathore R. Comparison between levothyroxine and lifestyle intervention on subclinical hypothyroidism in women: a review. Cureus . (2023) 15(4):e38309. doi: 10.7759/cureus.38309
30. Kumar B, Kodliwadmath A, Singh A, Duggal B. Acute adrenal insufficiency as a mysterious cause of shock following percutaneous coronary intervention: a cardiologist’s nightmare. BMJ Case Rep . (2020) 13(3):e233585. doi: 10.1136/bcr-2019-233585
31. Falcetta A, Bonfanti E, Rossini R, Lauria G. A case of shock after STEMI: think beyond the cardiogenic one. Clin Case Rep . (2023) 11(1):e6792. doi: 10.1002/ccr3.6792
Keywords: Sheehan’s syndrome, percutaneous coronary intervention, severe hyponatremia, glucocorticoid deficiency, stress, contrast agent, coronary atherosclerotic disease
Citation: Gao J, Wang Y, Zhang A, Pang H and Wang F (2024) Old woman with Sheehan's syndrome suffered severe hyponatremia following percutaneous coronary intervention: a case report and review of literature. Front. Cardiovasc. Med. 11:1353392. doi: 10.3389/fcvm.2024.1353392
Received: 15 December 2023; Accepted: 17 April 2024; Published: 29 April 2024.
Reviewed by:
© 2024 Gao, Wang, Zhang, Pang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuehai Wang [email protected]
† These authors have contributed equally to this work
This article is part of the Research Topic
Case Reports in General Cardiovascular Medicine: 2023
- Open access
- Published: 02 May 2024
Use of the International IFOMPT Cervical Framework to inform clinical reasoning in postgraduate level physiotherapy students: a qualitative study using think aloud methodology
- Katie L. Kowalski 1 ,
- Heather Gillis 1 ,
- Katherine Henning 1 ,
- Paul Parikh 1 ,
- Jackie Sadi 1 &
- Alison Rushton 1
BMC Medical Education volume 24 , Article number: 486 ( 2024 ) Cite this article
Metrics details
Vascular pathologies of the head and neck are rare but can present as musculoskeletal problems. The International Federation of Orthopedic Manipulative Physical Therapists (IFOMPT) Cervical Framework (Framework) aims to assist evidence-based clinical reasoning for safe assessment and management of the cervical spine considering potential for vascular pathology. Clinical reasoning is critical to physiotherapy, and developing high-level clinical reasoning is a priority for postgraduate (post-licensure) educational programs.
To explore the influence of the Framework on clinical reasoning processes in postgraduate physiotherapy students.
Qualitative case study design using think aloud methodology and interpretive description, informed by COnsolidated criteria for REporting Qualitative research. Participants were postgraduate musculoskeletal physiotherapy students who learned about the Framework through standardized delivery. Two cervical spine cases explored clinical reasoning processes. Coding and analysis of transcripts were guided by Elstein’s diagnostic reasoning components and the Postgraduate Musculoskeletal Physiotherapy Practice model. Data were analyzed using thematic analysis (inductive and deductive) for individuals and then across participants, enabling analysis of key steps in clinical reasoning processes and use of the Framework. Trustworthiness was enhanced with multiple strategies (e.g., second researcher challenged codes).
For all participants ( n = 8), the Framework supported clinical reasoning using primarily hypothetico-deductive processes. It informed vascular hypothesis generation in the patient history and testing the vascular hypothesis through patient history questions and selection of physical examination tests, to inform clarity and support for diagnosis and management. Most participant’s clinical reasoning processes were characterized by high-level features (e.g., prioritization), however there was a continuum of proficiency. Clinical reasoning processes were informed by deep knowledge of the Framework integrated with a breadth of wider knowledge and supported by a range of personal characteristics (e.g., reflection).
Conclusions
Findings support use of the Framework as an educational resource in postgraduate physiotherapy programs to inform clinical reasoning processes for safe and effective assessment and management of cervical spine presentations considering potential for vascular pathology. Individualized approaches may be required to support students, owing to a continuum of clinical reasoning proficiency. Future research is required to explore use of the Framework to inform clinical reasoning processes in learners at different levels.
Peer Review reports
Introduction
Musculoskeletal neck pain and headache are highly prevalent and among the most disabling conditions globally that require effective rehabilitation [ 1 , 2 , 3 , 4 ]. A range of rehabilitation professionals, including physiotherapists, assess and manage musculoskeletal neck pain and headache. Assessment of the cervical spine can be a complex process. Patients can present to physiotherapy with vascular pathology masquerading as musculoskeletal pain and dysfunction, as neck pain and/or headache as a common first symptom [ 5 ]. While vascular pathologies of the head and neck are rare [ 6 ], they are important considerations within a cervical spine assessment to facilitate the best possible patient outcomes [ 7 ]. The International IFOMPT (International Federation of Orthopedic Manipulative Physical Therapists) Cervical Framework (Framework) provides guidance in the assessment and management of the cervical spine region, considering the potential for vascular pathologies of the neck and head [ 8 ]. Two separate, but related, risks are considered: risk of misdiagnosis of an existing vascular pathology and risk of serious adverse event following musculoskeletal interventions [ 8 ].
The Framework is a consensus document iteratively developed through rigorous methods and the best contemporary evidence [ 8 ], and is also published as a Position Statement [ 7 ]. Central to the Framework are clinical reasoning and evidence-based practice, providing guidance in the assessment of the cervical spine region, considering the potential for vascular pathologies in advance of planned interventions [ 7 , 8 ]. The Framework was developed and published to be a resource for practicing musculoskeletal clinicians and educators. It has been implemented widely within IFOMPT postgraduate (post-licensure) educational programs, influencing curricula by enabling a comprehensive and systemic approach when considering the potential for vascular pathology [ 9 ]. Frequently reported curricula changes include an emphasis on the patient history and incorporating Framework recommended physical examination tests to evaluate a vascular hypothesis [ 9 ]. The Framework aims to assist musculoskeletal clinicians in their clinical reasoning processes, however no study has investigated students’ use of the Framework to inform their clinical reasoning.
Clinical reasoning is a critical component to physiotherapy practice as it is fundamental to assessment and diagnosis, enabling physiotherapists to provide safe and effective patient-centered care [ 10 ]. This is particularly important for postgraduate physiotherapy educational programs, where developing a high level of clinical reasoning is a priority for educational curricula [ 11 ] and critical for achieving advanced practice physiotherapy competency [ 12 , 13 , 14 , 15 ]. At this level of physiotherapy, diagnostic reasoning is emphasized as an important component of a high level of clinical reasoning, informed by advanced use of domain-specific knowledge (e.g., propositional, experiential) and supported by a range of personal characteristics (e.g., adaptability, reflective) [ 12 ]. Facilitating the development of clinical reasoning improves physiotherapist’s performance and patient outcomes [ 16 ], underscoring the importance of clinical reasoning to physiotherapy practice. Understanding students’ use of the Framework to inform their clinical reasoning can support optimal implementation of the Framework within educational programs to facilitate safe and effective assessment and management of the cervical spine for patients.
To explore the influence of the Framework on the clinical reasoning processes in postgraduate level physiotherapy students.
Using a qualitative case study design, think aloud case analyses enabled exploration of clinical reasoning processes in postgraduate physiotherapy students. Case study design allows evaluation of experiences in practice, providing knowledge and accounts of practical actions in a specific context [ 17 ]. Case studies offer opportunity to generate situationally dependent understandings of accounts of clinical practice, highlighting the action and interaction that underscore the complexity of clinical decision-making in practice [ 17 ]. This study was informed by an interpretive description methodological approach with thematic analysis [ 18 , 19 ]. Interpretive description is coherent with mixed methods research and pragmatic orientations [ 20 , 21 ], and enables generation of evidence-based disciplinary knowledge and clinical understanding to inform practice [ 18 , 19 , 22 ]. Interpretive description has evolved for use in educational research to generate knowledge of educational experiences and the complexities of health care education to support achievement of educational objectives and professional practice standards [ 23 ]. The COnsolidated criteria for REporting Qualitative research (COREQ) informed the design and reporting of this study [ 24 ].
Research team
All research team members hold physiotherapy qualifications, and most hold advanced qualifications specializing in musculoskeletal physiotherapy. The research team is based in Canada and has varying levels of academic credentials (ranging from Clinical Masters to PhD or equivalent) and occupations (ranging from PhD student to Director of Physical Therapy). The final author (AR) is also an author of the Framework, which represents international and multiprofessional consensus. Authors HG and JS are lecturers on one of the postgraduate programs which students were recruited from. The primary researcher and first author (KK) is a US-trained Physical Therapist and Postdoctoral Research Associate investigating spinal pain and clinical reasoning in the School of Physical Therapy at Western University. Authors KK, KH and PP had no prior relationship with the postgraduate educational programs, students, or the Framework.
Study setting
Western University in London, Ontario, Canada offers a one-year Advanced Health Care Practice (AHCP) postgraduate IFOMPT-approved Comprehensive Musculoskeletal Physiotherapy program (CMP) and a postgraduate Sport and Exercise Medicine (SEM) program. Think aloud case analyses interviews were conducted using Zoom, a viable option for qualitative data collection and audio-video recording of interviews that enables participation for students who live in geographically dispersed areas across Canada [ 25 ]. Interviews with individual participants were conducted by one researcher (KK or KH) in a calm and quiet environment to minimize disruption to the process of thinking aloud [ 26 ].
Participants
AHCP postgraduate musculoskeletal physiotherapy students ≥ 18 years of age in the CMP and SEM programs were recruited via email and an introduction to the research study during class by KK, using purposive sampling to ensure theoretical representation. The purposive sample ensured key characteristics of participants were included, specifically gender, ethnicity, and physiotherapy experience (years, type). AHCP students must have attended standardized teaching about the Framework to be eligible to participate. Exclusion criteria included inability to communicate fluently in English. As think-aloud methodology seeks rich, in-depth data from a small sample [ 27 ], this study sought to recruit 8–10 AHCP students. This range was informed by prior think aloud literature and anticipated to balance diversity of participant characteristics, similarities in musculoskeletal physiotherapy domain knowledge and rich data supporting individual clinical reasoning processes [ 27 , 28 ].
Learning about the IFOMPT Cervical Framework
CMP and SEM programs included standardized teaching of the Framework to inform AHCP students’ clinical reasoning in practice. Delivery included a presentation explaining the Framework, access to the full Framework document [ 8 ], and discussion of its role to inform practice, including a case analysis of a cervical spine clinical presentation, by research team members AR and JS. The full Framework document that is publicly available through IFOMPT [ 8 ] was provided to AHCP students as the Framework Position Statement [ 7 ] was not yet published. Discussion and case analysis was led by AHCP program leads in November 2021 (CMP, including research team member JS) and January 2022 (SEM).
Think aloud case analyses data collection
Using think aloud methodology, the analytical processes of how participants use the Framework to inform clinical reasoning were explored in an interview with one research team member not involved in AHCP educational programs (KK or KH). The think aloud method enables description and explanation of complex information paralleling the clinical reasoning process and has been used previously in musculoskeletal physiotherapy [ 29 , 30 ]. It facilitates the generation of rich verbal [ 27 ]as participants verbalize their clinical reasoning protocols [ 27 , 31 ]. Participants were aware of the aim of the research study and the research team’s clinical and research backgrounds, supporting an open environment for depth of data collection [ 32 ]. There was no prior relationship between participants and research team members conducting interviews.
Participants were instructed to think aloud their analysis of two clinical cases, presented in random order (Supplementary 1 ). Case information was provided in stages to reflect the chronology of assessment of patients in practice (patient history, planning the physical examination, physical examination, treatment). Use of the Framework to inform clinical reasoning was discussed at each stage. The cases enabled participants to identify and discuss features of possible vascular pathology, treatment indications and contraindications/precautions, etc. Two research study team members (HG, PP) developed cases designed to facilitate and elicit clinical reasoning processes in neck and head pain presentations. Cases were tested against the research team to ensure face validity. Cases and think aloud prompts were piloted prior to use with three physiotherapists at varying levels of practice to ensure they were fit for purpose.
Data collection took place from March 30-August 15, 2022, during the final terms of the AHCP programs and an average of 5 months after standardized teaching about the Framework. During case analysis interviews, participants were instructed to constantly think aloud, and if a pause in verbalizations was sustained, they were reminded to “keep thinking aloud” [ 27 ]. As needed, prompts were given to elicit verbalization of participants’ reasoning processes, including use of the Framework to inform their clinical reasoning at each stage of case analysis (Supplementary 2 ). Aside from this, all interactions between participants and researchers minimized to not interfere with the participant’s thought processes [ 27 , 31 ]. When analysis of the first case was complete, the researcher provided the second case, each lasting 35–45 min. A break between cases was offered. During and after interviews, field notes were recorded about initial impressions of the data collection session and potential patterns appearing to emerge [ 33 ].
Data analysis
Data from think aloud interviews were analyzed using thematic analysis [ 30 , 34 ], facilitating identification and analysis of patterns in data and key steps in the clinical reasoning process, including use of the Framework to enable its characterization (Fig. 1 ). As established models of clinical reasoning exist, a hybrid approach to thematic analysis was employed, incorporating inductive and deductive processes [ 35 ], which proceeded according to 5 iterative steps: [ 34 ]
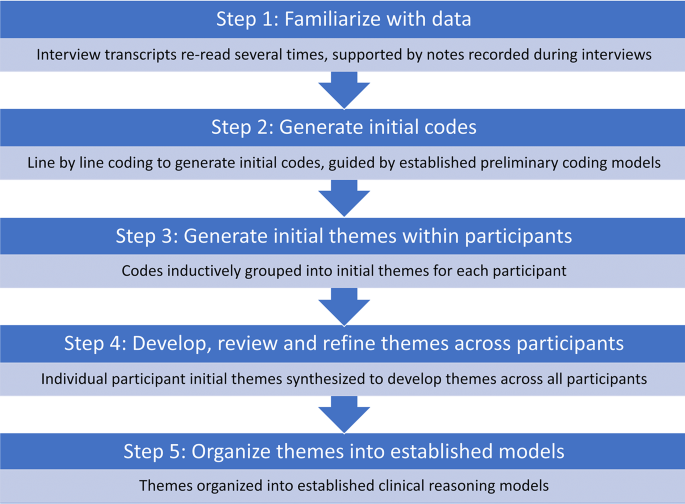
Data analysis steps
Familiarize with data: Audio-visual recordings were transcribed verbatim by a physiotherapist external to the research team. All transcripts were read and re-read several times by one researcher (KK), checking for accuracy by reviewing recordings as required. Field notes supported depth of familiarization with data.
Generate initial codes: Line-by-line coding of transcripts by one researcher (KK) supported generation of initial codes that represented components, patterns and meaning in clinical reasoning processes and use of the Framework. Established preliminary coding models were used as a guide. Elstein’s diagnostic reasoning model [ 36 ] guided generating initial codes of key steps in clinical reasoning processes (Table 1 a) [ 29 , 36 ]. Leveraging richness of data, further codes were generated guided by the Postgraduate Musculoskeletal Physiotherapy Practice model, which describes masters level clinical practice (Table 1 b) [ 12 ]. Codes were refined as data analysis proceeded. All codes were collated within participants along with supporting data.
Generate initial themes within participants: Coded data was inductively grouped into initial themes within each participant, reflecting individual clinical reasoning processes and use of the Framework. This inductive stage enabled a systematic, flexible approach to describe each participant’s unique thinking path, offering insight into the complexities of their clinical reasoning processes. It also provided a comprehensive understanding of the Framework informing clinical reasoning and a rich characterization of its components, aiding the development of robust, nuanced insights [ 35 , 37 , 38 ]. Initial themes were repeatedly revised to ensure they were grounded in and reflected raw data.
Develop, review and refine themes across participants: Initial themes were synthesized across participants to develop themes that represented all participants. Themes were reviewed and refined, returning to initial themes and codes at the individual participant level as needed.
Organize themes into established models: Themes were deductively organized into established clinical reasoning models; first into Elstein’s diagnostic reasoning model, second into the Postgraduate Musculoskeletal Physiotherapy Practice model to characterize themes within each diagnostic reasoning component [ 12 , 36 ].
Trustworthiness of findings
The research study was conducted according to an a priori protocol and additional steps were taken to establish trustworthiness of findings [ 39 ]. Field notes supported deep familiarization with data and served as a means of data source triangulation during analysis [ 40 ]. One researcher coded transcripts and a second researcher challenged codes, with codes and themes rigorously and iteratively reviewed and refined. Frequent debriefing sessions with the research team, reflexive discussions with other researchers and peer scrutiny of initial findings enabled wider perspectives and experiences to shape analysis and interpretation of findings. Several strategies were implemented to minimize the influence of prior relationships between participants and researchers, including author KK recruiting participants, KK and KH collecting/analyzing data, and AR, JS, HG and PP providing input on de-identified data at the stage of synthesis and interpretation.
Nine AHCP postgraduate level students were recruited and participated in data collection. One participant was withdrawn because of unfamiliarity with the standardized teaching session about use of the Framework (no recall of session), despite confirmation of attendance. Data from eight participants were used for analysis (CMP: n = 6; SEM: n = 2; Table 2 ), which achieved sample size requirements for think aloud methodology of rich and in-depth data [ 27 , 28 ].
Diagnostic reasoning components
Informed by the Framework, all components of Elstein’s diagnostic reasoning processes [ 36 ] were used by participants, including use of treatment with physiotherapy interventions to aid diagnostic reasoning. An illustrative example is presented in Supplement 3 . Clinical reasoning used primarily hypothetico-deductive processes reflecting a continuum of proficiency, was informed by deep Framework knowledge and breadth of prior knowledge (e.g., experiential), and supported by a range of personal characteristics (e.g., justification for decisions).
Cue acquisition
All participants sought to acquire additional cues early in the patient history, and for some this persisted into the medical history and physical examination. Cue acquisition enabled depth and breadth of understanding patient history information to generate hypotheses and factors contributing to the patient’s pain experience (Table 3 ). All participants asked further questions to understand details of the patients’ pain and their presentation, while some also explored the impact of pain on patient functioning and treatments received to date. There was a high degree of specificity to questions for most participants. Ongoing clinical reasoning processes through a thorough and complete assessment, even if the patient had previously received treatment for similar symptoms, was important for some participants. Cue acquisition was supported by personal characteristics including a patient-centered approach (e.g., understanding the patient’s beliefs about pain) and one participant reflected on their approach to acquiring patient history cues.
Hypothesis generation
Participants generated an average of 4.5 hypotheses per case (range: 2–8) and most hypotheses (77%) were generated rapidly early in the patient history. Knowledge from the Framework about patient history features of vascular pathology informed vascular hypothesis generation in the patient history for all participants in both cases (Table 4 ). Vascular hypotheses were also generated during the past medical history, where risk factors for vascular pathology were identified and interpreted by some participants who had high levels of suspicion for cervical articular involvement. Non-vascular hypotheses were generated during the physical examination by some participants to explain individual physical examination or patient history cues. Deep knowledge of the patient history section in the Framework supported high level of cue identification and interpretation for generating vascular hypotheses. Initial hypotheses were prioritized by some participants, however the level of specificity of hypotheses varied.
Cue evaluation
All participants evaluated cues throughout the patient history and physical examination in relationship to hypotheses generated, indicating use of hypothetico-deductive reasoning processes (Table 5 ). Framework knowledge of patient history features of vascular pathology was used to test vascular hypotheses and aid differential diagnosis. The patient history section supported high level of cue identification and interpretation of patient history features for all but one participant, and generation of further patient history questions for all participants. The level of specificity of these questions was high for all but one participant. Framework knowledge of recommended physical examination tests, including removal of positional testing, supported planning a focused and prioritized physical examination to further test vascular hypotheses for all participants. No participant indicated intention to use positional testing as part of their physical examination. Treatment with physiotherapy interventions served as a form of cue evaluation, and cues were evaluated to inform prognosis for some participants. At times during the physical examination, some participants demonstrated occasional errors or difficulty with cue evaluation by omitting key physical exam tests (e.g., no cranial nerve assessment despite concerns for trigeminal nerve involvement), selecting physical exam tests in advance of hypothesis generation (e.g., cervical spine instability testing), difficulty interpreting cues, or late selection of a physical examination test. Cue acquisition was supported by a range of personal characteristics. Most participants justified selection of physical examination tests, and some self-reflected on their ability to collect useful physical examination information to inform selection of tests. Precaution to the physical examination was identified by all participants but one, which contributed to an adaptable approach, prioritizing patient safety and comfort. Critical analysis of physical examination information aided interpretation within the context of the patient for most participants.
Hypothesis evaluation
All participants used the Framework to evaluate their hypotheses throughout the patient history and physical examination, continuously shifting their level of support for hypotheses (Table 6 , Supplement 4 ). This informed clarity in the overall level of suspicion for vascular pathology or musculoskeletal diagnoses, which were specific for most participants. Response to treatment with physiotherapy interventions served as a form of hypothesis evaluation for most participants who had low level suspicion for vascular pathology, highlighting ongoing reasoning processes. Hypotheses evaluated were prioritized by ranking according to level of suspicion by some participants. Difficulties weighing patient history and physical examination cues to inform judgement on overall level of suspicion for vascular pathology was demonstrated by some participants who reported that incomplete physical examination data and not being able to see the patient contributed to difficulties. Hypothesis evaluation was supported by the personal characteristic of reflection, where some students reflected on the Framework’s emphasis on the patient history to evaluate a vascular hypothesis.
The Framework supported all participants in clinical reasoning related to treatment (Table 7 ). Treatment decisions were always linked to the participant’s overall level of suspicion for vascular pathology or musculoskeletal diagnosis. Framework knowledge supported participants with high level of suspicion for vascular pathology to refer for further investigations. Participants with a musculoskeletal diagnosis kept the patient for physiotherapy interventions. The Framework patient history section supported patient education about symptoms of vascular pathology and safety netting for some participants. Framework knowledge influenced informed consent processes and risk-benefit analysis to support the selection of musculoskeletal physiotherapy interventions, which were specific and prioritized for some participants. Less Framework knowledge related to treatment was demonstrated by some students, generating unclear recommendations regarding the urgency of referral and use of the Framework to inform musculoskeletal physiotherapy interventions. Treatment was supported by a range of personal characteristics. An adaptable approach that prioritized patient safety and was supported by justification was demonstrated in all participants except one. Shared decision-making enabled the selection of physiotherapy interventions, which were patient-centered (individualized, considered whole person, identified future risk for vascular pathology). Communication with the patient’s family doctor facilitated collaborative patient-centered care for most participants.
This is the first study to explore the influence of the Framework on clinical reasoning processes in postgraduate physiotherapy students. The Framework supported clinical reasoning that used primarily hypothetico-deductive processes. The Framework informed vascular hypothesis generation in the patient history and testing the vascular hypothesis through patient history questions and selection of physical examination tests to inform clarity and support for diagnosis and management. Most postgraduate students’ clinical reasoning processes were characterized by high-level features (e.g. specificity, prioritization). However, some demonstrated occasional difficulties or errors, reflecting a continuum of clinical reasoning proficiency. Clinical reasoning processes were informed by deep knowledge of the Framework integrated with a breadth of wider knowledge and supported by a range of personal characteristics (e.g., justification for decisions, reflection).
Use of the Framework to inform clinical reasoning processes
The Framework provided a structured and comprehensive approach to support postgraduate students’ clinical reasoning processes in assessment and management of the cervical spine region, considering the potential for vascular pathology. Patient history and physical examination information was evaluated to inform clarity and support the decision to refer for further vascular investigations or proceed with musculoskeletal physiotherapy diagnosis/interventions. The Framework is not intended to lead to a vascular pathology diagnosis [ 7 , 8 ], and following the Framework does not guarantee vascular pathologies will be identified [ 41 ]. Rather, it aims to support a process of clinical reasoning to elicit and interpret appropriate patient history and physical examination information to estimate the probability of vascular pathology and inform judgement about the need to refer for further investigations [ 7 , 8 , 42 ]. Results of this study suggest the Framework has achieved this aim for postgraduate physiotherapy students.
The Framework supported postgraduate students in using primarily hypothetico-deductive diagnostic reasoning processes. This is expected given the diversity of vascular pathology clinical presentations precluding a definite clinical pattern and inherent complexity as a potential masquerader of a musculoskeletal problem [ 7 ]. It is also consistent with prior research investigating clinical reasoning processes in musculoskeletal physiotherapy postgraduate students [ 12 ] and clinical experts [ 29 ] where hypothetico-deductive and pattern recognition diagnostic reasoning are employed according to the demands of the clinical situation [ 10 ]. Diagnostic reasoning of most postgraduate students in this study demonstrated features suggestive of high-level clinical reasoning in musculoskeletal physiotherapy [ 12 ], including ongoing reasoning with high-level cue identification and interpretation, specificity and prioritization during assessment and treatment, use of physiotherapy interventions to aid diagnostic reasoning, and prognosis determination [ 12 , 29 , 43 ]. Expert physiotherapy practice has been further described as using a dialectical model of clinical reasoning with seamless transitions between clinical reasoning strategies [ 44 ]. While diagnostic reasoning was a focus in this study, postgraduate students considered a breadth of information as important to their reasoning (e.g., patient’s perspectives of the reason for their pain). This suggests wider reasoning strategies (e.g., narrative, collaborative) were employed to enable shared decision-making within the context of patient-centered care.
Study findings also highlighted a continuum of proficiency in use of the Framework to inform clinical reasoning processes. Not all students demonstrated all characteristics of high-level clinical reasoning and there are suggestions of incomplete reasoning processes, for example occasional errors in evaluating cues. Some students offered explanations such as incomplete case information as factors contributing to difficulties with clinical reasoning processes. However, the ability to critically evaluate incomplete and potentially conflicting clinical information is consistently identified as an advanced clinical practice competency [ 14 , 43 ]. A continuum of proficiency in clinical reasoning in musculoskeletal physiotherapy is supported by wider healthcare professions describing acquisition and application of clinical knowledge and skills as a developmental continuum of clinical competence progressing from novice to expert [ 45 , 46 ]. The range of years of clinical practice experience in this cohort of students (3–14 years) or prior completed postgraduate education may have contributed to the continuum of proficiency, as high-quality and diverse experiential learning is essential for the development of high-level clinical reasoning [ 14 , 47 ].
Deep knowledge of the Framework informs clinical reasoning processes
Postgraduate students demonstrated deep Framework knowledge to inform clinical reasoning processes. All students demonstrated knowledge of patient history features of vascular pathology, recommended physical examination tests to test a vascular hypothesis, and the need to refer if there is a high level of suspicion for vascular pathology. A key development in the recent Framework update is the removal of the recommendation to perform positional testing [ 8 ]. All students demonstrated knowledge of this development, and none wanted to test a vascular hypothesis with positional testing. Most also demonstrated Framework knowledge about considerations for planning treatment with physiotherapy interventions (e.g., risk-benefit analysis, informed consent), though not all, which underscores the continuum of proficiency in postgraduate students. Rich organization of multidimensional knowledge is a required component for high level clinical reasoning and is characteristic of expert physiotherapy practice [ 10 , 48 , 49 ]. Most postgraduate physiotherapy students displayed this expert practice characteristic through integration of deep Framework knowledge with a breadth of prior knowledge (e.g., experiential, propositional) to inform clinical reasoning processes. This highlights the utility of the Framework in postgraduate physiotherapy education to develop advanced level evidence-based knowledge informing clinical reasoning processes for safe assessment and management of the cervical spine, considering the potential for vascular pathology [ 9 , 8 , 50 , 51 , 52 ].
Framework supports personal characteristics to facilitate integration of knowledge and clinical reasoning
The Framework supported personal characteristics of postgraduate students, which are key drivers for the complex integration of advanced knowledge and high-level clinical reasoning [ 10 , 12 , 48 ]. For all students, the Framework supported justification for decisions and patient-centered care, emphasizing a whole-person approach and shared decision-making. Further demonstrating a continuum of proficiency, the Framework supported a wider breadth of personal characteristics for some students, including critical analysis, reflection, self-analysis, and adaptability. These personal characteristics illustrate the interwoven cognitive and metacognitive skills that influence and support a high level of clinical reasoning [ 10 , 12 ] and the development of clinical expertise [ 48 , 53 ]. For example [ 54 ], reflection is critical to developing high-level clinical reasoning and advanced level practice [ 12 , 55 ]. Postgraduate students reflected on prior knowledge, experiences, and action within the context of current Framework knowledge, emphasizing active engagement in cognitive processes to inform clinical reasoning processes. Reflection-in-action is highlighted by self-analysis and adaptability. These characteristics require continuous cognitive processing to consider personal strengths and limitations in the context of the patient and evidence-based practice, adapting the clinical encounter as required [ 53 , 55 ]. These findings highlight use of the Framework in postgraduate education to support development of personal characteristics that are indicative of an advanced level of clinical practice [ 12 ].
Synthesis of findings
Derived from synthesis of research study findings and informed by the Postgraduate Musculoskeletal Physiotherapy Practice model [ 12 ], use of the Framework to inform clinical reasoning processes in postgraduate students is illustrated in Fig. 2 . Overlapping clinical reasoning, knowledge and personal characteristic components emphasize the complex interaction of factors contributing to clinical reasoning processes. Personal characteristics of postgraduate students underpin clinical reasoning and knowledge, highlighting their role in facilitating the integration of these two components. Bolded subcomponents indicate convergence of results reflecting all postgraduate students and underscores the variability among postgraduate students contributing to a continuum of clinical reasoning proficiency. The relative weighting of the components is approximately equal to balance the breadth and convergence of subcomponents. Synthesis of findings align with the Postgraduate Musculoskeletal Physiotherapy Practice model [ 12 ], though some differences exist. Limited personal characteristics were identified in this study with little convergence across students, which may be due to the objective of this study and the case analysis approach.
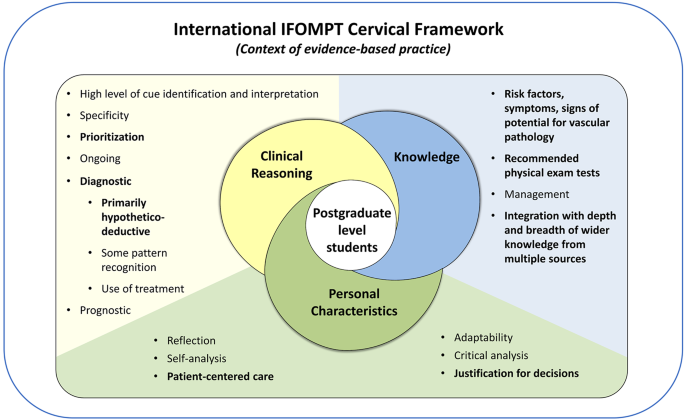
Use of the Framework to inform clinical reasoning in postgraduate level musculoskeletal physiotherapy students. Adapted from the Postgraduate Musculoskeletal Physiotherapy Practice model [ 12 ].
Strengths and limitations
Think aloud case analyses enabled situationally dependent understanding of the Framework to inform clinical reasoning processes in postgraduate level students [ 17 ], considering the rare potential for vascular pathology. A limitation of this approach was the standardized nature of case information provided to students, which may have influenced clinical reasoning processes. Future research studies may consider patient case simulation to address this limitation [ 30 ]. Interviews were conducted during the second half of the postgraduate educational program, and this timing could have influenced clinical reasoning processes compared to if interviews were conducted at the end of the program. Future research can explore use of the Framework to inform clinical reasoning processes in established advanced practice physiotherapists. The sample size of this study aligns with recommendations for think aloud methodology [ 27 , 28 ], achieved rich data, and purposive sampling enabled wide representation of key characteristics (e.g., gender, ethnicity, country of training, physiotherapy experiences), which enhances transferability of findings. Students were aware of the study objective in advance of interviews which may have contributed to a heightened level of awareness of vascular pathology. The prior relationship between students and researchers may have also influenced results, however several strategies were implemented to minimize this influence.
Implications
The Framework is widely implemented within IFOMPT postgraduate educational programs and has led to important shifts in educational curricula [ 9 ]. Findings of this study support use of the Framework as an educational resource in postgraduate physiotherapy programs to inform clinical reasoning processes for safe and effective assessment and management of cervical spine presentations considering the potential for vascular pathology. Individualized approaches may be required to support each student, owing to a continuum of clinical reasoning proficiency. As the Framework was written for practicing musculoskeletal clinicians, future research is required to explore use of the Framework to inform clinical reasoning in learners at different levels, for example entry-level physiotherapy students.
The Framework supported clinical reasoning that used primarily hypothetico-deductive processes in postgraduate physiotherapy students. It informed vascular hypothesis generation in the patient history and testing the vascular hypothesis through patient history questions and selection of physical examination tests, to inform clarity and support for diagnosis and management. Most postgraduate students clinical reasoning processes were characterized as high-level, informed by deep Framework knowledge integrated with a breadth of wider knowledge, and supported by a range of personal characteristics to facilitate the integration of advanced knowledge and high-level clinical reasoning. Future research is required to explore use of the Framework to inform clinical reasoning in learners at different levels.
Data availability
The dataset used and analyzed during the current study are available from the corresponding author on reasonable request.
Safiri S, Kolahi AA, Hoy D, Buchbinder R, Mansournia MA, Bettampadi D et al. Global, regional, and national burden of neck pain in the general population, 1990–2017: systematic analysis of the global burden of Disease Study 2017. BMJ. 2020;368.
Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Neurol. 2018;17:954–76.
Article Google Scholar
Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:2006–17.
Côté P, Yu H, Shearer HM, Randhawa K, Wong JJ, Mior S et al. Non-pharmacological management of persistent headaches associated with neck pain: A clinical practice guideline from the Ontario protocol for traffic injury management (OPTIMa) collaboration. European Journal of Pain (United Kingdom). 2019;23.
Diamanti S, Longoni M, Agostoni EC. Leading symptoms in cerebrovascular diseases: what about headache? Neurological Sciences. 2019.
Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, Majersik JJ, et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015;14:640–54.
Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for examination of the Cervical Region for potential of vascular pathologies of the Neck Prior to Musculoskeletal intervention: International IFOMPT Cervical Framework. J Orthop Sports Phys Therapy. 2023;53:7–22.
Rushton A, Carlesso LC, Flynn T, Hing WA, Kerry R, Rubinstein SM, et al. International framework for examination of the cervical region for potential of vascular pathologies of the neck prior to orthopaedic manual therapy (OMT) intervention: International IFOMPT Cervical Framework. International IFOMPT Cervical Framework; 2020.
Hutting N, Kranenburg R, Taylor A, Wilbrink W, Kerry R, Mourad F. Implementation of the International IFOMPT Cervical Framework: a survey among educational programmes. Musculoskelet Sci Pract. 2022;62:102619.
Jones MA, Jensen G, Edwards I. Clinical reasoning in physiotherapy. In: Campbell S, Watkins V, editors. Clinical reasoning in the health professions. Third. Philadelphia: Elsevier; 2008. pp. 245–56.
Google Scholar
Fennelly O, Desmeules F, O’Sullivan C, Heneghan NR, Cunningham C. Advanced musculoskeletal physiotherapy practice: informing education curricula. Musculoskelet Sci Pract. 2020;48:102174.
Rushton A, Lindsay G. Defining the construct of masters level clinical practice in manipulative physiotherapy. Man Ther. 2010;15.
Rushton A, Lindsay G. Defining the construct of masters level clinical practice in healthcare based on the UK experience. Med Teach. 2008;30:e100–7.
Noblet T, Heneghan NR, Hindle J, Rushton A. Accreditation of advanced clinical practice of musculoskeletal physiotherapy in England: a qualitative two-phase study to inform implementation. Physiotherapy (United Kingdom). 2021;113.
Tawiah AK, Stokes E, Wieler M, Desmeules F, Finucane L, Lewis J, et al. Developing an international competency and capability framework for advanced practice physiotherapy: a scoping review with narrative synthesis. Physiotherapy. 2023;122:3–16.
Williams A, Rushton A, Lewis JJ, Phillips C. Evaluation of the clinical effectiveness of a work-based mentoring programme to develop clinical reasoning on patient outcome: a stepped wedge cluster randomised controlled trial. PLoS ONE. 2019;14.
Miles R. Complexity, representation and practice: case study as method and methodology. Issues Educational Res. 2015;25.
Thorne S, Kirkham SR, MacDonald-Emes J. Interpretive description: a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health. 1997;20.
Thorne S, Kirkham SR, O’Flynn-Magee K. The Analytic challenge in interpretive description. Int J Qual Methods. 2004;3.
Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. Sage; 2003.
Dolan S, Nowell L, Moules NJ. Interpretive description in applied mixed methods research: exploring issues of fit, purpose, process, context, and design. Nurs Inq. 2023;30.
Thorne S. Interpretive description. In: Routledge International Handbook of Qualitative Nursing Research. 2013. pp. 295–306.
Thompson Burdine J, Thorne S, Sandhu G. Interpretive description: a flexible qualitative methodology for medical education research. Med Educ. 2021;55.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus group. Int J Qual Health Care. 2007;19:349–57.
Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using zoom videoconferencing for qualitative data Collection: perceptions and experiences of researchers and participants. Int J Qual Methods. 2019;18.
Van Someren M, Barnard YF, Sandberg J. The think aloud method: a practical approach to modelling cognitive. Volume 11. London: Academic; 1994.
Fonteyn ME, Kuipers B, Grobe SJ. A description of think aloud Method and Protocol Analysis. Qual Health Res. 1993;3:430–41.
Lundgrén-Laine H, Salanterä S. Think-Aloud technique and protocol analysis in clinical decision-making research. Qual Health Res. 2010;20:565–75.
Doody C, McAteer M. Clinical reasoning of expert and novice physiotherapists in an outpatient orthopaedic setting. Physiotherapy. 2002;88.
Gilliland S. Physical therapist students’ development of diagnostic reasoning: a longitudinal study. J Phys Therapy Educ. 2017;31.
Ericsson KA, Simon HA. How to study thinking in Everyday Life: contrasting think-aloud protocols with descriptions and explanations of thinking. Mind Cult Act. 1998;5:178–86.
Dwyer SC, Buckle JL. The space between: on being an insider-outsider in qualitative research. Int J Qual Methods. 2009;8.
Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inform. 2004;22:63–75.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Fereday J, Muir-Cochrane E. Demonstrating Rigor using thematic analysis: a Hybrid Approach of Inductive and deductive coding and theme development. Int J Qual Methods. 2006;5.
Elstein ASLSS. Medical problem solving: an analysis of clinical reasoning. Harvard University Press; 1978.
Proudfoot K. Inductive/Deductive Hybrid Thematic Analysis in mixed methods research. J Mix Methods Res. 2023;17.
Charters E. The use of think-aloud methods in qualitative research an introduction to think-aloud methods. Brock Educ J. 2003;12.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness Criteria. Int J Qual Methods. 2017;16:1–13.
Thurmond VA. The point of triangulation. J Nurs Scholarsh. 2001;33.
Hutting N, Wilbrink W, Taylor A, Kerry R. Identifying vascular pathologies or flow limitations: important aspects in the clinical reasoning process. Musculoskelet Sci Pract. 2021;53:102343.
de Best RF, Coppieters MW, van Trijffel E, Compter A, Uyttenboogaart M, Bot JC, et al. Risk assessment of vascular complications following manual therapy and exercise for the cervical region: diagnostic accuracy of the International Federation of Orthopaedic Manipulative physical therapists framework (the Go4Safe project). J Physiother. 2023;69:260–6.
Petty NJ. Becoming an expert: a masterclass in developing clinical expertise. Int J Osteopath Med. 2015;18:207–18.
Edwards I, Jones M, Carr J, Braunack-Mayer A, Jensen GM. Clinical reasoning strategies in physical therapy. Phys Ther. 2004;84.
Carraccio CL, Benson BJ, Nixon LJ, Derstine PL. Clinical teaching from the Educational Bench to the clinical Bedside: Translating the Dreyfus Developmental Model to the Learning of Clinical Skills.
Benner P. Using the Dreyfus Model of Skill Acquisition to describe and interpret Skill Acquisition and Clinical Judgment in nursing practice and education. Bull Sci Technol Soc. 2004;24:188–99.
Benner P. From novice to expert: Excellence and power in clinical nursing practice. Upper Saddle River, New Jersey: Prentice Hall;: Commemorative Ed; 2001.
Jensen GM, Gwyer J, Shepard KF, Hack LM. Expert practice in physical therapy. Phys Ther. 2000;80.
Huhn K, Gilliland SJ, Black LL, Wainwright SF, Christensen N. Clinical reasoning in physical therapy: a Concept Analysis. Phys Ther. 2019;99.
Hutting N, Kranenburg HA, Rik KR. Yes, we should abandon pre-treatment positional testing of the cervical spine. Musculoskelet Sci Pract. 2020;49:102181.
Kranenburg HA, Tyer R, Schmitt M, Luijckx GJ, Schans C, Van Der, Hutting N, et al. Effects of head and neck positions on blood flow in the vertebral, internal carotid, and intracranial arteries: a systematic review. J Orthop Sports Phys Ther. 2019;49:688–97.
Hutting N, Kerry R, Coppieters MW, Scholten-Peeters GGM. Considerations to improve the safety of cervical spine manual therapy. Musculoskelet Sci Pract. 2018;33.
Wainwright SF, Shepard KF, Harman LB, Stephens J. Novice and experienced physical therapist clinicians: a comparison of how reflection is used to inform the clinical decision-making process. Phys Ther. 2010;90:75–88.
Dy SM, Purnell TS. Key concepts relevant to quality of complex and shared decision-making in health care: a literature review. Soc Sci Med. 2012;74:582–7.
Christensen N, Jones MA, Higgs J, Edwards I. Dimensions of clinical reasoning capability. In: Campbell S, Watkins V, editors. Clinical reasoning in the health professions. 3rd edition. Philadelphia: Elsevier; 2008. pp. 101–10.
Download references
Acknowledgements
The authors would like to acknowledge study participants and the transcriptionist for their time in completing and transcribing think aloud interviews.
No funding was received to conduct this research study.
Author information
Authors and affiliations.
School of Physical Therapy, Western University, London, Ontario, Canada
Katie L. Kowalski, Heather Gillis, Katherine Henning, Paul Parikh, Jackie Sadi & Alison Rushton
You can also search for this author in PubMed Google Scholar
Contributions
Katie Kowalski: Conceptualization, methodology, validation, formal analysis, investigation, data curation, writing– original draft, visualization, project administration. Heather Gillis: Validation, resources, writing– review & editing. Katherine Henning: Investigation, formal analysis, writing– review & editing. Paul Parikh: Validation, resources, writing– review & editing. Jackie Sadi: Validation, resources, writing– review & editing. Alison Rushton: Conceptualization, methodology, validation, writing– review & editing, supervision.
Corresponding author
Correspondence to Katie L. Kowalski .
Ethics declarations
Ethics approval and consent to participate.
Western University Health Science Research Ethics Board granted ethical approval (Project ID: 119934). Participants provided written informed consent prior to participating in think aloud interviews.
Consent for publication
Not applicable.
Competing interests
Author AR is an author of the IFOMPT Cervical Framework. Authors JS and HG are lecturers on the AHCP CMP program. AR and JS led standardized teaching of the Framework. Measures to reduce the influence of potential competing interests on the conduct and results of this study included: the Framework representing international and multiprofessional consensus, recruitment of participants by author KK, data collection and analysis completed by KK with input from AR, JS and HG at the stage of data synthesis and interpretation, and wider peer scrutiny of initial findings. KK, KH and PP have no potential competing interests.
Authors’ information
The lead author of this study (AR) is the first author of the International IFOMPT Cervical Framework.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kowalski, K.L., Gillis, H., Henning, K. et al. Use of the International IFOMPT Cervical Framework to inform clinical reasoning in postgraduate level physiotherapy students: a qualitative study using think aloud methodology. BMC Med Educ 24 , 486 (2024). https://doi.org/10.1186/s12909-024-05399-x
Download citation
Received : 11 February 2024
Accepted : 08 April 2024
Published : 02 May 2024
DOI : https://doi.org/10.1186/s12909-024-05399-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- International IFOMPT Cervical Framework
- Clinical reasoning
- Postgraduate students
- Physiotherapy
- Educational research
- Qualitative research
- Think aloud methodology
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
The Dialysis Social Worker Perspective: Case Studies Discussion
Session 5 in the Navigating Transplant : A Guide to Empowering Your Patients series, we welcome two dialysis social workers as they share their clinical experiences. Through case presentation and discussion, we will focus in on the challenges and opportunities that face social workers and their patients during the transplant education, referral, and work up stages of the journey. Equally important, through these examples, we will share strategies and resources that will help you address barriers and empower your patients and their care partners forward through the transplant process. This virtual session will be on May 22, 2024 at 12pm PT / 2pm CT / 3pm ET and is not for CE credit.
Wed, 05/22/2024 - 12:00pm

IMAGES
VIDEO
COMMENTS
7 Ingredients for a Patient Case Presentation Template. 1. The One-Liner. The one-liner is a succinct sentence that primes your listeners to the patient. A typical format is: " [Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y]. 2.
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Keywords. How to Present a Patient Case. Created Date. 8/5/2019 9:48:12 PM.
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
Case Presentation. History of Present Illness: A 33-year-old white female presents after admission to the general medical/surgical hospital ward with a chief complaint of shortness of breath on exertion. She reports that she was seen for similar symptoms previously at her primary care physician's office six months ago.
To save you time and effort, I have curated a list of 5 versatile case study presentation templates, each designed for specific needs and audiences. Here are some best case study presentation examples that showcase effective strategies for engaging your audience and conveying complex information clearly. 1. Lab report case study template.
Case Presentation. The patient is a 60-year-old white female presenting to the emergency department with acute onset shortness of breath. Symptoms began approximately 2 days before and had progressively worsened with no associated, aggravating, or relieving factors noted. She had similar symptoms approximately 1 year ago with an acute, chronic ...
Learn how to deliver oral case presentations for internal medicine inpatients with this comprehensive guide. Find out the key elements of a strong oral case presentation, such as opener, history of present illness, review of systems, past medical history, family history, social history, physical exam, and more.
An 81-year-old man presented with fever, cough, and shortness of breath. Within a few hours after presentation, chest pain and respiratory distress developed. A chest radiograph showed bilateral pa...
Presentation of Case. ... Finally, among patients with Covid-19, chest imaging studies may show peripheral lung opacities without radiographically significant alveolar edema; it is possible that ...
The above information should nicely fit in several paragraphs or 2-3 case study template slides. 2. Explain the Solution. The bulk of your case study copy and presentation slides should focus on the provided solution (s). This is the time to speak at length about how the subject went from before to the glorious after.
A case presentation is a narrative of a patient's care, so it is vital the presenter has familiarity with the patient, the case and its progression. The preparation for the presentation will depend on what information is to be included. Generally, oral case presentations are brief and should be limited to 5-10 minutes.
Writing up. Write up the case emphasising the interesting points of the presentation, investigations leading to diagnosis, and management of the disease/pathology. Get input on the case from all members of the team, highlighting their involvement. Also include the prognosis of the patient, if known, as the reader will want to know the outcome.
Clinical Case Study Presentation Template. Number of slides: 10. Signup Free to download. A clinical case study is a report where medical practitioners share a patient's case. Generally, clinical case studies are valuable tools for medical research as they provide detailed information on the development of a disease or illness in particular ...
Download the Climacteric Syndrome Case Study presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...
Here comes the role of case studies for clinical personnel in the medical field. In the always-growing healthcare industry, medical case presentation is essential as it is a suggestion for new researchers. A medical case study is a report where a medical practitioner shares a patient's case. It comprises every detail related to patients.
A 24-year-old white male with no known medical history presented to the hospital with chief complaints of 2 weeks of progressively worsening pain and swelling of his right wrist and left ankle joints. He did not report any fevers, chills, night sweats, weight loss or rash. He was employed as a fireman. He denied alcohol use disorder, smoking cigarettes, or any recreational drugs. Family ...
Patient Case Presentation. Figure 1. Blue and silver stethoscope (Pixabay, N.D.) Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness.
Thenew england journal ofmedicine. Presentation of Case. Dr. Mathew S. Lopes:A 65-year-old woman was transferred to this hospital because of chest pain. Six months before the current presentation ...
Patient Case Presentation. A 61-year-old American woman was referred to a Gastroenterology Clinic from primary care provider due to consistent discomfort and significant weight loss. She looked for a PCP's advice as she had a tarry stool in the early morning which she had never experienced before. She presented with a 2-month history of ...
Patient Case Presentation. Patient Mrs. B.C. is a 56 year old female who is presenting to her WHNP for her annual exam. She had to cancel her appointment two months ago and didn't reschedule until now. Her last pap smear and mammogram were normal. Today, while performing her breast exam, her nurse practitioner notices dimpling in the left ...
This presentation has been created combining a traditional structure with flat illustrations to get a professional and original template. We've selected blue as the primary color since it's generally used to represent the healthcare sector. Besides, the typography used is understandable and readable so that you can present your content clearly.
Glucocorticoid deficiency can lead to hypoglycemia, hypotension, and electrolyte disorders. Acute glucocorticoid deficiency under stress is very dangerous. Here, we present a case study of an elderly patient diagnosed with Sheehan's syndrome, manifesting secondary adrenal insufficiency and secondary hypothyroidism, managed with daily prednisone and levothyroxine therapy. She was admitted to ...
In this study, we describe a patient of primary cutaneous acral CD8-positive lymphoproliferative disorder located in a nonacral region. A 65-year-old male presented with an ill-defined lesion of rubbery consistency and a maximum diameter of 2.5 cm localized in the right thigh.
On examination, the patient appeared to be in respiratory distress. The temperature was 35.9°C, the pulse 98 beats per minute, the blood pressure 129/58 mm Hg, the respiratory rate 24 breaths per ...
Qualitative case study design using think aloud methodology and interpretive description, informed by COnsolidated criteria for REporting Qualitative research. ... All participants asked further questions to understand details of the patients' pain and their presentation, while some also explored the impact of pain on patient functioning and ...
Session 5 in the Navigating Transplant: A Guide to Empowering Your Patients series, we welcome two dialysis social workers as they share their clinical experiences.Through case presentation and discussion, we will focus in on the challenges and opportunities that face social workers and their patients during the transplant education, referral, and work up stages of the journey.