- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
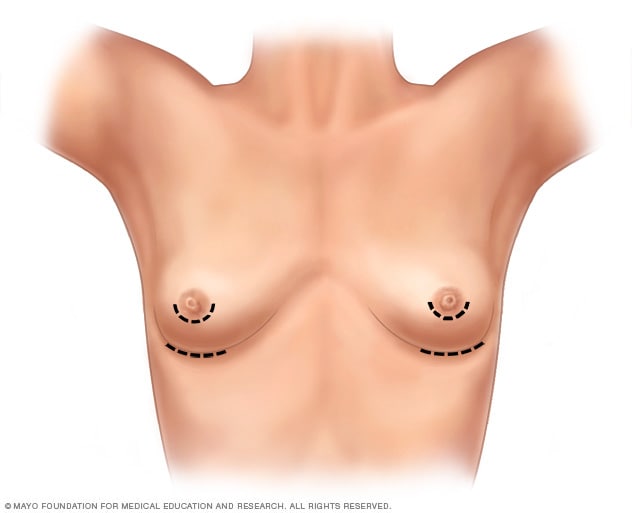
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
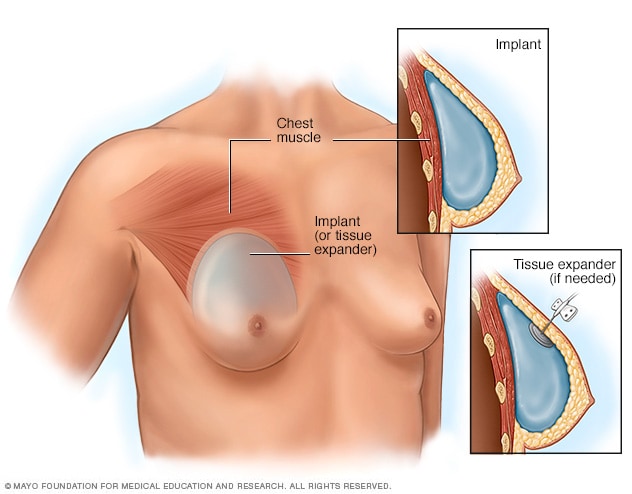
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
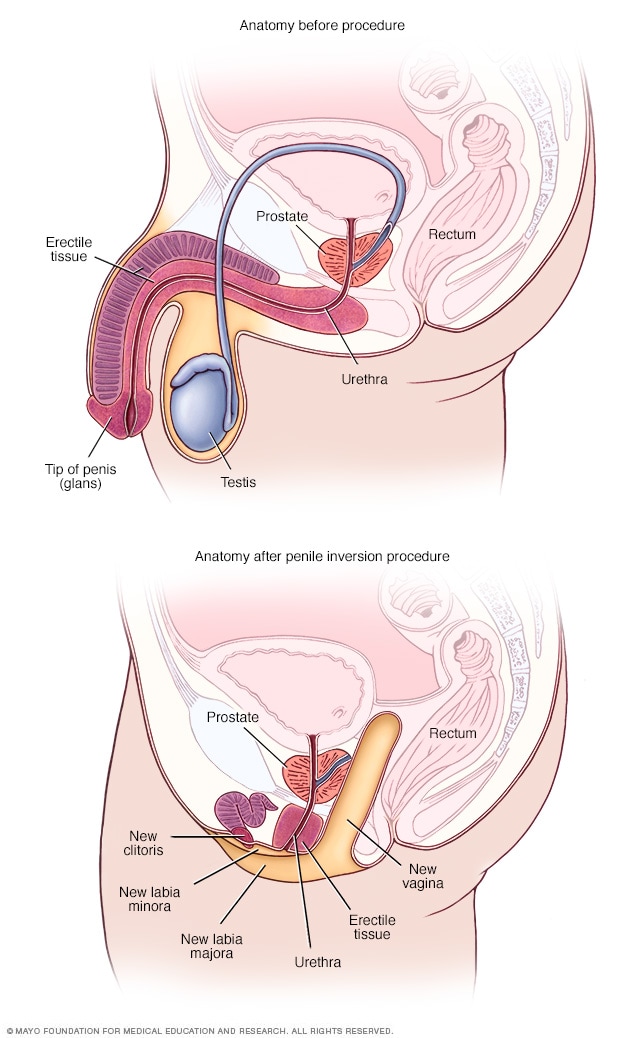
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
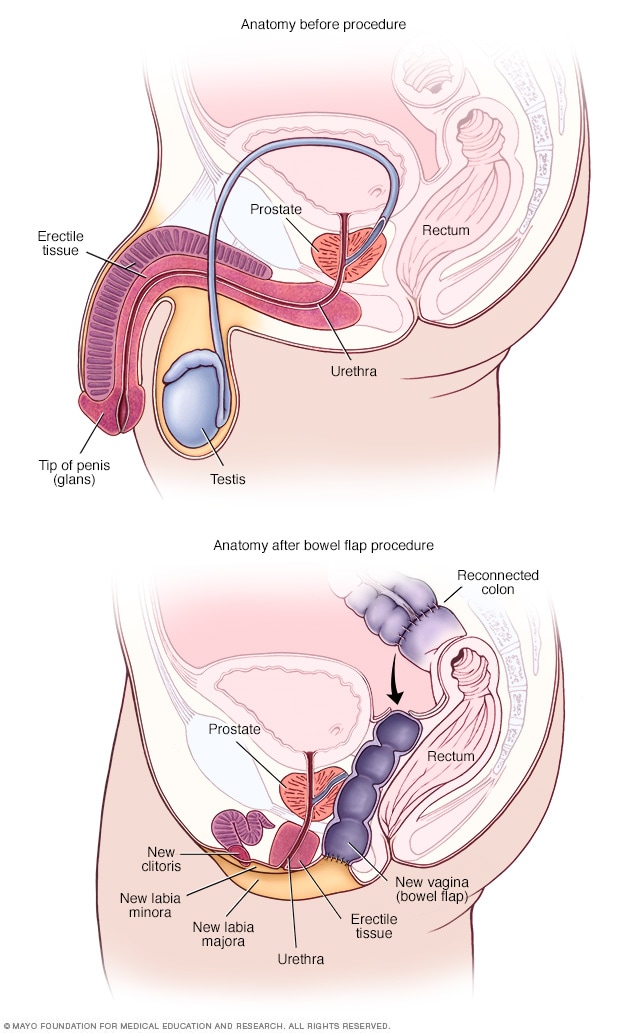
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Gender Confirmation Surgery (GCS)
What is Gender Confirmation Surgery?
- Transfeminine Tr
Transmasculine Transition
- Traveling Abroad
Choosing a Surgeon
Gender confirmation surgery (GCS), known clinically as genitoplasty, are procedures that surgically confirm a person's gender by altering the genitalia and other physical features to align with their desired physical characteristics. Gender confirmation surgeries are also called gender affirmation procedures. These are both respectful terms.
Gender dysphoria , an experience of misalignment between gender and sex, is becoming more widely diagnosed. People diagnosed with gender dysphoria are often referred to as "transgender," though one does not necessarily need to experience gender dysphoria to be a member of the transgender community. It is important to note there is controversy around the gender dysphoria diagnosis. Many disapprove of it, noting that the diagnosis suggests that being transgender is an illness.
Ellen Lindner / Verywell
Transfeminine Transition
Transfeminine is a term inclusive of trans women and non-binary trans people assigned male at birth.
Gender confirmation procedures that a transfeminine person may undergo include:
- Penectomy is the surgical removal of external male genitalia.
- Orchiectomy is the surgical removal of the testes.
- Vaginoplasty is the surgical creation of a vagina.
- Feminizing genitoplasty creates internal female genitalia.
- Breast implants create breasts.
- Gluteoplasty increases buttock volume.
- Chondrolaryngoplasty is a procedure on the throat that can minimize the appearance of Adam's apple .
Feminizing hormones are commonly used for at least 12 months prior to breast augmentation to maximize breast growth and achieve a better surgical outcome. They are also often used for approximately 12 months prior to feminizing genital surgeries.
Facial feminization surgery (FFS) is often done to soften the lines of the face. FFS can include softening the brow line, rhinoplasty (nose job), smoothing the jaw and forehead, and altering the cheekbones. Each person is unique and the procedures that are done are based on the individual's need and budget,
Transmasculine is a term inclusive of trans men and non-binary trans people assigned female at birth.
Gender confirmation procedures that a transmasculine person may undergo include:
- Masculinizing genitoplasty is the surgical creation of external genitalia. This procedure uses the tissue of the labia to create a penis.
- Phalloplasty is the surgical construction of a penis using a skin graft from the forearm, thigh, or upper back.
- Metoidioplasty is the creation of a penis from the hormonally enlarged clitoris.
- Scrotoplasty is the creation of a scrotum.
Procedures that change the genitalia are performed with other procedures, which may be extensive.
The change to a masculine appearance may also include hormone therapy with testosterone, a mastectomy (surgical removal of the breasts), hysterectomy (surgical removal of the uterus), and perhaps additional cosmetic procedures intended to masculinize the appearance.
Paying For Gender Confirmation Surgery
Medicare and some health insurance providers in the United States may cover a portion of the cost of gender confirmation surgery.
It is unlawful to discriminate or withhold healthcare based on sex or gender. However, many plans do have exclusions.
For most transgender individuals, the burden of financing the procedure(s) is the main difficulty in obtaining treatment. The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed.
A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019.
Traveling Abroad for GCS
Some patients seek gender confirmation surgery overseas, as the procedures can be less expensive in some other countries. It is important to remember that traveling to a foreign country for surgery, also known as surgery tourism, can be very risky.
Regardless of where the surgery will be performed, it is essential that your surgeon is skilled in the procedure being performed and that your surgery will be performed in a reputable facility that offers high-quality care.
When choosing a surgeon , it is important to do your research, whether the surgery is performed in the U.S. or elsewhere. Talk to people who have already had the procedure and ask about their experience and their surgeon.
Before and after photos don't tell the whole story, and can easily be altered, so consider asking for a patient reference with whom you can speak.
It is important to remember that surgeons have specialties and to stick with your surgeon's specialty. For example, you may choose to have one surgeon perform a genitoplasty, but another to perform facial surgeries. This may result in more expenses, but it can result in a better outcome.
A Word From Verywell
Gender confirmation surgery is very complex, and the procedures that one person needs to achieve their desired result can be very different from what another person wants.
Each individual's goals for their appearance will be different. For example, one individual may feel strongly that breast implants are essential to having a desirable and feminine appearance, while a different person may not feel that breast size is a concern. A personalized approach is essential to satisfaction because personal appearance is so highly individualized.
Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review . Transgend Health . 2018;3(1):159-169. doi:10.1089/trgh.2018.0014
Morrison SD, Vyas KS, Motakef S, et al. Facial Feminization: Systematic Review of the Literature . Plast Reconstr Surg. 2016;137(6):1759-70. doi:10.1097/PRS.0000000000002171
Hadj-moussa M, Agarwal S, Ohl DA, Kuzon WM. Masculinizing Genital Gender Confirmation Surgery . Sex Med Rev . 2019;7(1):141-155. doi:10.1016/j.sxmr.2018.06.004
Dowshen NL, Christensen J, Gruschow SM. Health Insurance Coverage of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information . Transgend Health . 2019;4(1):131-135. doi:10.1089/trgh.2018.0055
American Society of Plastic Surgeons. Rhinoplasty nose surgery .
Rights Group: More U.S. Companies Covering Cost of Gender Reassignment Surgery. CNS News. http://cnsnews.com/news/article/rights-group-more-us-companies-covering-cost-gender-reassignment-surgery
The Sex Change Capital of the US. CBS News. http://www.cbsnews.com/2100-3445_162-4423154.html
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health
What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, male-to-female gender-affirming surgery: 20-year review of technique and surgical results.

- 1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

Figure 1 . The initial circumferential subcoronal incision.

Figure 2 . The de-gloved penis being passed through the scrotal opening.

Figure 3 . The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.
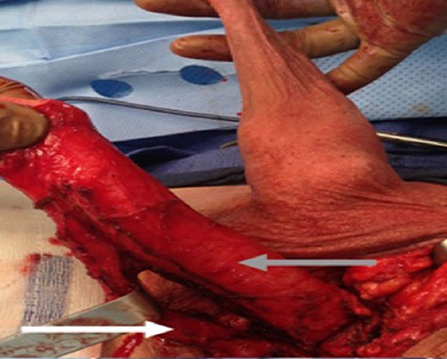
Figure 4 . The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

Figure 5 . The inverted penile skin flap.
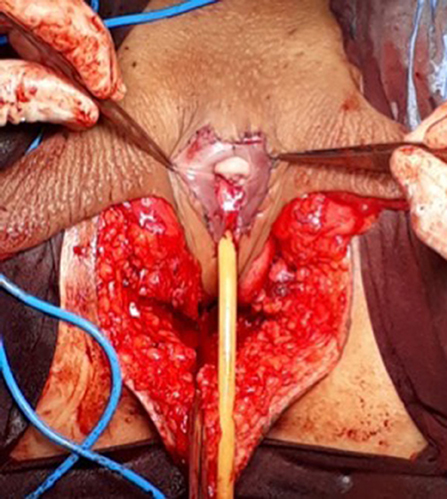
Figure 6 . The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.
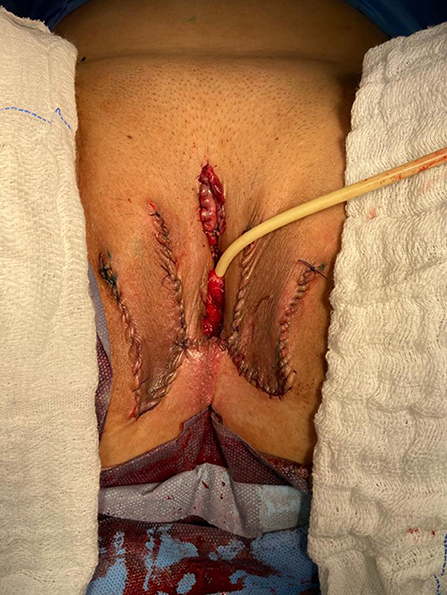
Figure 7 . The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Figure 8 . Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
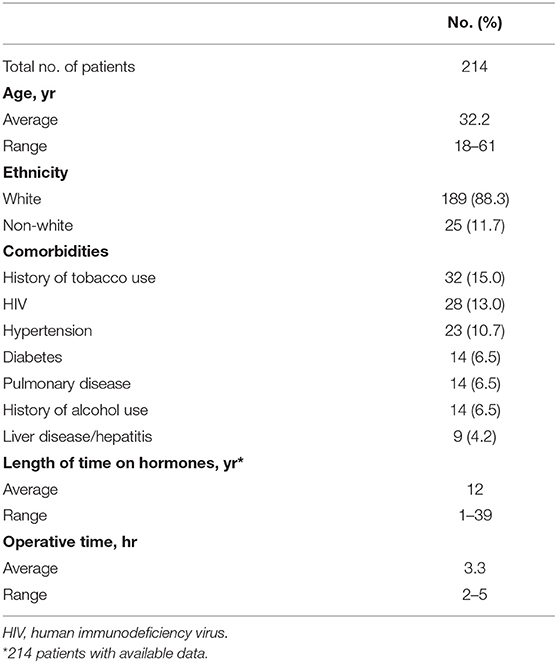
Table 1 . Patient demographics.
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
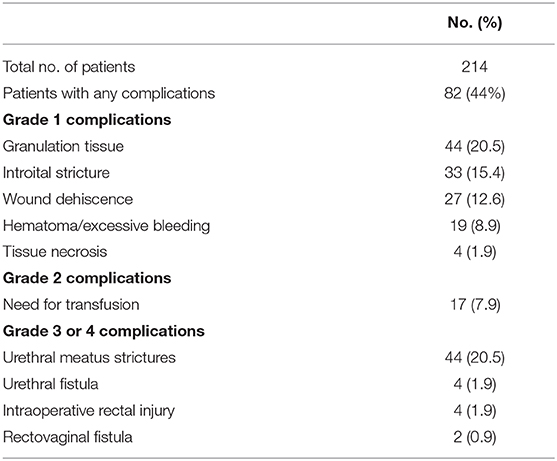
Table 2 . Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.

Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-non-conforming people, version 7. Int J Transgend. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
CrossRef Full Text | Google Scholar
2. Massie JP, Morrison SD, Maasdam JV, Satterwhite T. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstruct Surg. (2018) 141:911–921. doi: 10.1097/PRS.0000000000004427
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep . (2018) 19:62. doi: 10.1007/s11934-018-0809-9
4. Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int . (2007) 100:607–13. doi: 10.1111/j.1464-410X.2007.07017.x
5. Rossi NR, Hintz F, Krege S, Rübben H, Vom DF, Hess J. Gender reassignment surgery – a 13 year review of surgical outcomes. Eur Urol Suppl . (2013) 12:e559. doi: 10.1016/S1569-9056(13)61042-8
6. Silva RUM, Abreu FJS, Silva GMV, Santos JVQV, Batezini NSS, Silva Neto B, et al. Step by step male to female transsexual surgery. Int Braz J Urol. (2018) 44:407–8. doi: 10.1590/s1677-5538.ibju.2017.0044
7. Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender surgery in Denmark from 1994 to 2015: 20-year follow-up study. J Sex Med. (2016) 13:720–5. doi: 10.1016/j.jsxm.2016.01.012
8. Perovic SV, Stanojevic DS, Djordjevic MLJ. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. (2001) 86:843–50. doi: 10.1046/j.1464-410x.2000.00934.x
9. Krege S, Bex A, Lümmen G, Rübben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. (2001) 88:396–402. doi: 10.1046/j.1464-410X.2001.02323.x
10. Wagner S, Greco F, Hoda MR, Inferrera A, Lupo A, Hamza A, et al. Male-to-female transsexualism: technique, results and 3-year follow-up in 50 patients. Urol International. (2010) 84:330–3. doi: 10.1159/000288238
11. Reed H. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin PlasticSurg. (2011) 25:163–74. doi: 10.1055/s-0031-1281486
12. Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. (2015) 12:1837–45. doi: 10.1111/jsm.12936
13. Sigurjonsson H, Rinder J, Möllermark C, Farnebo F, Lundgren TK. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. (2015) 6:69–73. doi: 10.1016/j.jpra.2015.09.003
14. Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. (2018) 199:760–5. doi: 10.1016/j.juro.2017.10.013
15. Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr. Urol. Rep. (2018) 19:36. doi: 10.1007/s11934-018-0795-y
16. Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. (2013) 64:141–9. doi: 10.1016/j.eururo.2012.12.030
17. Horbach SER, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med . (2015) 12:1499–512. doi: 10.1111/jsm.12868
18. Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. (2018) 6:457–68.e2. doi: 10.1016/j.sxmr.2017.11.005
19. Salim A, Poh M. Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. (2018) 45:343–50. doi: 10.1016/j.cps.2018.04.001
20. Hess J, Rossi NR, Panic L, Rubben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. DtschArztebl Int. (2014) 111:795–801. doi: 10.3238/arztebl.2014.0795
21. Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. (2016) 13:988–93. doi: 10.1016/j.jsxm.2016.03.370
22. Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol . (2010) 72:214–31. doi: 10.1111/j.1365-2265.2009.03625.x
23. Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest . (2015) 38:1373–81. doi: 10.1007/s40618-015-0398-0
24. Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, et al. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J Sex Med . (2015) 12:180–8. doi: 10.1111/jsm.12758
Keywords: transsexualism, gender dysphoria, gender-affirming genital surgery, penile inversion vaginoplasty, surgical outcome
Citation: Moisés da Silva GV, Lobato MIR, Silva DC, Schwarz K, Fontanari AMV, Costa AB, Tavares PM, Gorgen ARH, Cabral RD and Rosito TE (2021) Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Front. Surg. 8:639430. doi: 10.3389/fsurg.2021.639430
Received: 17 December 2020; Accepted: 22 March 2021; Published: 05 May 2021.
Reviewed by:
Copyright © 2021 Moisés da Silva, Lobato, Silva, Schwarz, Fontanari, Costa, Tavares, Gorgen, Cabral and Rosito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Veber Moisés da Silva, veber.gabriel@gmail.com
This article is part of the Research Topic
Gender Dysphoria: Diagnostic Issues, Clinical Aspects and Health Promotion
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
The Go-To Guide to Gender Surgeons
Find a qualified surgeon for gender-affirming care.
Start Your Search
Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps
The Go-To Guide To Gender Surgeons

How Gender Reassignment Surgery Works (Infographic)
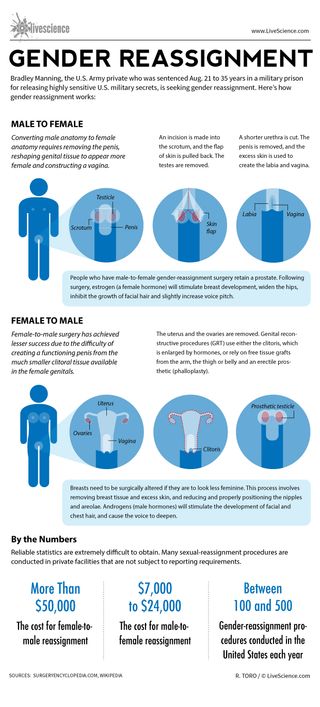
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Man's years of premature ejaculation had a rare cause
Viagra alternatives? Study of mouse erections hints at new ways to treat erectile dysfunction
Pet fox with 'deep relationship with the hunter-gatherer society' buried 1,500 years ago in Argentina
Most Popular
By Anna Gora December 27, 2023
By Anna Gora December 26, 2023
By Anna Gora December 25, 2023
By Emily Cooke December 23, 2023
By Victoria Atkinson December 22, 2023
By Anna Gora December 16, 2023
By Anna Gora December 15, 2023
By Anna Gora November 09, 2023
By Donavyn Coffey November 06, 2023
By Anna Gora October 31, 2023
By Anna Gora October 26, 2023
- 2 How and where to watch the April 8 solar eclipse online for free
- 3 NASA engineers discover why Voyager 1 is sending a stream of gibberish from outside our solar system
- 4 Giant coyote killed in southern Michigan turns out to be a gray wolf — despite the species vanishing from region 100 years ago
- 5 When is the next total solar eclipse after 2024 in North America?
- 2 Giant 'toe biter' water bugs discovered in Cyprus for the 1st time
- 3 Watch live! The total solar eclipse has begun over North America.
- 4 8,200-year-old campsite of 'Paleo-Archaic' peoples discovered on US Air Force base in New Mexico
Advocates blast Vatican's new position on gender-affirming surgery as 'dangerously ignorant'
Doctrine says gender-affirming surgery and surrogacy reject god's plan for human life.

Social Sharing
Transgender activists and allies on Monday decried the Vatican's new doctrine against gender-affirming surgery as "hurtful" and devoid of the voices and experiences of trans, non-binary and gender-diverse people, especially in its distinction between transgender and intersex people.
"The suggestion that gender-affirming health care — which has saved the lives of so many wonderful trans people and enabled them to live in harmony with their bodies, their communities and (God) — might risk or diminish trans people's dignity is not only hurtful but dangerously ignorant," said Mara Klein, a non-binary, transgender activist who has participated in Germany's church reform project.
"Seeing that, in contrast, surgical interventions on intersex people — which if performed without consent especially on minors often cause immense physical and psychological harm for many intersex people to date — are assessed positively just seems to expose the underlying hypocrisy further," Klein said.
The Vatican on Monday declared gender-affirming surgery as well as surrogacy as grave violations of "human dignity," putting them on par with abortion and euthanasia as practices that it says rejects God's plan for human life.
The Vatican's doctrine office issued "Infinite Dignity," a 20-page declaration that has been in the works for five years. After substantial revision in recent months, it was approved March 25 by Pope Francis, who ordered its publication.

How trans content creators are fighting back against hate online
In its most eagerly anticipated section, the Vatican repeated its rejection of what it calls "gender theory," or the idea that one's gender can be changed. Gender theory, often called gender ideology by its detractors, suggests that gender is more complex and fluid than the binary categories of male and female, and depends on more than visible sex characteristics.
The term "gender theory" is often used to suggest that trans and non-binary people have a political agenda.
- Hundreds of Canadian artists denounce 'alarming' anti-trans legislation in open letter
- Queer Interfaith Coalition co-founded by N.S. rabbi aims to fight 2SLGBTQ+ hate
"It follows that any sex-change intervention, as a rule, risks threatening the unique dignity the person has received from the moment of conception," the document said.
It distinguished between gender-affirming surgeries, which it rejected, and what it called "genital abnormalities" that are present at birth or that develop later. Those abnormalities can be "resolved" with the help of health-care professionals, it said.

The Vatican's use of "sex-change" is also considered a loaded term by transgender advocates. The Trans Journalists Association notes that "sex-change" and "sex reassignment" are outdated terms and "are now generally considered offensive, though some medical literature still uses them. Some organizations with anti-trans political goals also use these phrases in lieu of gender-affirming care."
Warnings document could fuel hate and violence
Advocates for 2SLGBTQ+ Catholics immediately criticized the document as outdated, harmful and contrary to the stated goal of recognizing the "infinite dignity" of all of God's children. They warned it could have real-world effects on trans people, fuelling anti-trans violence and discrimination.
"While it lays out a wonderful rationale for why each human being, regardless of condition in life, must be respected, honoured, and loved, it does not apply this principle to gender-diverse people," said Francis DeBernardo of New Ways Ministry, which advocates for 2SLGBTQ+ Catholics.
- Pope says gender theory is 'ugly ideology' that threatens humanity
- Pope appeals for peace in Gaza and Ukraine as he presides over Easter Mass
The document's existence, rumoured since 2019, was confirmed in recent weeks by the new prefect of the Dicastery for the Doctrine of the Faith, Argentine Cardinal Víctor Manuel Fernández, a close Francis confidant.
The document comes at a time of some backlash against transgender people, including in the United States where Republican-led state legislatures are considering a new round of bills restricting medical care for transgender youths — and in some cases, adults.

Pope's stance on gender angers some Catholics
In addition, bills to govern youths' pronouns, sports teams and bathrooms at school are also under consideration, as well as some books and school curriculums.
"On top of the rising hostility toward our communities, we are faced with a church that does not listen and refuses to see the beauty of creation that can be found in our biographies," Klein said.
Francis has made reaching out to 2SLGBTQ+ people a hallmark of his papacy, ministering to trans Catholics and insisting that the Catholic Church must welcome all children of God.
But he has also denounced "gender theory" as the "worst danger" facing humanity today, an "ugly ideology" that threatens to cancel out what the church considers as God-given differences between man and woman.
He has blasted in particular what he calls the "ideological colonization" of the West in the developing world, where development aid is sometimes conditioned on adopting Western ideas about gender and reproductive health.
With files from CBC News
Hong Kong Amends Its Surgery Requirements to Change Gender Markers on IDs

H ong Kong no longer requires transgender people to undergo full gender-affirming surgery to change their legal gender markers in their IDs, more than a year after the Chinese enclave’s top court called the requirement unconstitutional.
The government announced the change on Wednesday, “having prudently considered the objective of the policy, relevant legal and medical advice, as well as drawing reference from the relevant practices overseas.”
Under the new rules, Hong Kong residents who have not undergone full sex reassignment surgery [SRS] who want to have their gender marker on their ID changed still must have completed select surgical treatment to modify their sexual characteristics—removal of the breasts for transgender men, removal of the penis and testes for transgender women—along with medical documentation. Previous guidelines required the removal of the uterus and ovaries or the construction of a penis or “some form” of it for female-to-male transition, and the removal of the penis and testes and the construction of a vagina for male-to-female transition.
“We are still concerned about the heavy emphasis on sex reassignment surgeries being a requirement,” Wong Hiu-chong, the lawyer for transgender activist Henry Tse , whose case led to the policy change, told TIME. “SRS can be life threatening.”
Those who wish to change their gender markers must also statutorily declare that they have gender dysphoria—the medical term for the psychological distress a person feels when their gender identity does not match with their assigned sex at birth—and have lived as the opposite sex for at least two years before their application. They must also show proof of receiving hormonal treatment throughout the previous two years, and will be subjected to random blood tests to check their hormonal profile.
“Our clients have waited a very long time for such an unconstitutional policy to be revised, and for them, the wait has been painful,” Wong said in a statement. She also questioned the need for blood tests, calling this requirement, among others that remain for gender marker changes, “potentially discriminatory” as it does not apply to other Hong Kong ID card holders.
A government spokesperson clarified in the announcement that the gender marker change will only apply to the Hong Kong Identity Card and that “the sex entry on a Hong Kong identity card does not represent the holder’s sex as a matter of law. It does not affect any other policies of the Government or the handling of any other gender-related matters under the law in Hong Kong or relevant legal procedures.”
The policy change comes years after Tse filed a case in 2017 to question the full gender-affirming surgery requirement. Despite the city’s Court of Final Appeal issuing a ruling deeming the requirement unconstitutional in February 2023, implementation of the ruling was long-delayed, which Tse also challenged . The ruling said “such surgical procedures are at the most invasive end of the treatment spectrum” and that “full SRS is not medically required by many transgender persons whose gender dysphoria has been effectively treated.”
More Must-Reads From TIME
- Exclusive: Google Workers Revolt Over $1.2 Billion Contract With Israel
- Jane Fonda Champions Climate Action for Every Generation
- Stop Looking for Your Forever Home
- The Sympathizer Counters 50 Years of Hollywood Vietnam War Narratives
- The Bliss of Seeing the Eclipse From Cleveland
- Hormonal Birth Control Doesn’t Deserve Its Bad Reputation
- The Best TV Shows to Watch on Peacock
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
You May Also Like
Transgender inclusion? World’s major religions take varying stances

The Vatican has issued a new document rejecting the concept of changing one’s biological sex — a setback for transgender people who had hoped Pope Francis might be setting the stage for a more welcoming approach from the Catholic Church.
Around the world, major religions have diverse approaches to gender identity, and the inclusion or exclusion of transgender people. Some examples:
Christianity
The Catholic Church’s disapproving stance toward gender transition is shared by some other denominations. For example, the Southern Baptist Convention — the largest Protestant denomination in the United States — adopted a resolution in 2014 stating that “God’s design was the creation of two distinct and complementary sexes, male and female.” It asserts that gender identity “is determined by biological sex, not by one’s self-perception”
However, numerous mainline Protestant denominations welcome trans people as members and as clergy. The Evangelical Lutheran Church in America elected an openly transgender man as a bishop in 2021.
In Islam, there isn’t a single central religious authority and policies can vary in different regions.
Abbas Shouman, secretary-general of Al-Azhar’s Council of Senior Scholars in Cairo, said that “for us ... sex conversion is completely rejected.”
“It is God who has determined the ... sex of the fetus and intervening to change that is a change of God’s creation, which is completely rejected,” Shouman added.
In Iran, the Shiite theocracy’s founder, Ayatollah Ruhollah Khomeini, issued a religious decree, or fatwa, decades ago, opening the way for official support for gender transition surgery.
In Hindu society in South Asia, while traditional roles were and are still prescribed for men and women, people of non-binary gender expression have been recognized for millennia and played important roles in holy texts. Third gender people have been revered throughout South Asian history with many rising to significant positions of power under Hindu and Muslim rulers. One survey in 2014 estimated that around 3 million third gender people live in India alone.
Sanskrit, the ancient language of Hindu scriptures, has the vocabulary to describe three genders — masculine, feminine and gender-neutral.
The most common group of third gender people in India are known as the “hijras.” While some choose to undergo gender reassignment surgery, others are born intersex. Most consider themselves neither male or female.
Some Hindus believe third gender people have special powers and the ability to bless or curse, which has led to stereotyping causing the community to be feared and marginalized. Many live in poverty without proper access to healthcare, housing and employment.
In 2014, India, Nepal and Bangladesh, which is a Muslim-majority country, officially recognized third gender people as citizens deserving of equal rights. The Supreme Court of India stated that “it is the right of every human being to choose their gender,” and that recognition of the group “is not a social or medical issue, but a human rights issue.”
Buddhism has traditionally adhered to binary gender roles, particularly in its monastic traditions where men and women are segregated and assigned specific roles.
These beliefs remain strong in the Theravada tradition, as seen in the attempt of the Thai Sangha Council, the governing Buddhist body in Thailand, to ban ordinations of transgender people. More recently, the Theravada tradition has somewhat eased restrictions against gender nonconforming people by ordaining them in their sex recorded at birth.
However, the Mahayana, and Vajrayana schools of Buddhism have allowed more exceptions while the Jodo Shinshu sect has been even more inclusive in ordaining transgender monks both in Japan and North America. In Tibetan Buddhism, Tashi Choedup, an openly queer monk, was ordained after their teacher refrained from asking about their gender identity as prescribed by Buddhist doctrine. Many Buddhist denominations, particularly in the West, are intentionally inclusive of transgender people in their sanghas or gatherings.
Reform Judaism is accepting of transgender people and allows for the ordination of trans rabbis. According to David J. Meyer, who served for many years as a rabbi in Marblehead, Massachusetts, Jewish traditional wisdom allowed possibilities of gender identity and expression that differed from those typically associated with the sex assigned at birth.
“Our mystical texts, the Kabbalah, address the notion of transitioning from one gender to another,” he wrote on a Reform-affiliated website.
It’s different, for the most part, in Orthodox Judaism. “Most transgender people will find Orthodox communities extremely difficult to navigate,” says the Human Rights Campaign, a major U.S. LGBTQ-rights advocacy group.
“Transgender people are further constrained by Orthodox Judaism’s emphasis on binary gender and strict separation between men and women,” the HRC says. “For example, a transgender person who has not medically transitioned poses a challenge for a rabbi who must decide whether that person will sit with men or women during worship.”
Rabbi Avi Shafran, spokesman for the Orthodox Jewish organization Agudath Israel of America, wrote a blog post last year after appearing on an Israeli television panel to discuss transgender-related issues.
“There can be no denying that there are people who are deeply conflicted about their gender identities. They deserve to be safe from harm and, facing challenges the rest of us don’t, deserve empathy and compassion,” Shafran wrote. “But the Torah and its extension, halacha, or Jewish religious law, are unequivocal about the fact that being born in a male body requires living the life of a man, and being born female entails living as a woman.”
“In Judaism, each gender has its particular life-role to play,” he added. “The bodies God gave us are indications of what we are and what we are not, and of how He wants us to live our lives.”
The Associated Press
- Share full article
Advertisement
Supported by
Four Takeaways From the Vatican’s Document on Human Dignity
The document restated the Roman Catholic Church’s rejection of abortion, gender fluidity and transition surgery.

By Jason Horowitz and Elisabetta Povoledo
Jason Horowitz reported from Rome, and Elisabetta Povoledo from Verbania, Italy.
The document issued on Monday by the Vatican puts human dignity at the center of Catholic life , but in doing so, it broaches some of the most difficult and sensitive social issues, those that Pope Francis has spent his papacy avoiding.
On Monday, though, his church leaned hard into them in the document, called “Infinite Dignity.” It argued that the exploitation of the poor, the outcast and the vulnerable amounted to an erosion of human dignity. But it was the restating of the church’s rejection of abortion, the death penalty and euthanasia, and especially gender fluidity, transition surgery and surrogacy, that church liberals worried would be used as ammunition by the right.
Here are four takeaways.
The pope’s inclusivity has limits.
Pope Francis’ inclusive message, which has included allowing L.G.B.T.Q. Catholics to receive blessings from priests and transgender people to be baptized and act as godparents , has a limit: Catholic doctrine.
The pope’s conservative critics have for a decade argued that his tendency to speak off the cuff and in overly welcoming ways toward L.G.B.T.Q. people, the divorced and remarried, along with others who sin in the church’s eyes, had sent the wrong signal.
But the document released on Monday, and remarks by Cardinal Víctor Manuel Fernández, the prefect of the Vatican department with oversight over doctrine, underlined that the pope’s message was just that — a signal that the church was more open to the world, but that the substance, what it considers immutable “truth,” remained the same.
That dissonance, though, between Francis’ style and his defense of Catholic doctrine was highlighted by the document, and for many supporters of great change within the church, it amounted to a declaration that they would not get what they want.
As if to highlight that tension, Cardinal Fernández responded to a question on Monday about the church’s teaching that homosexual acts are “intrinsically disordered” — what many supporters of L.G.B.T.Q. faithful consider the insurmountable obstacle to true acceptance — by saying that the problem may be the terminology, not the meaning.
It was, he said, a “very strong expression” and that perhaps “more suitable words” could be found to express the thought that homosexual sex could not produce the “mystery” of childbirth.
Gender fluidity erodes human dignity, the document says.
The Vatican argues that gender fluidity, or the idea that people can decide their own sex, erodes human dignity because it blurs the difference between men and women, which it considers a gift from God.
Francis, while personally welcoming to transgender people — he has met many throughout his papacy — is convinced that powerful lobbies are pushing what the Vatican calls “gender theory” as a form of “cultural colonization” on more traditionalist societies.
This ideology, the Vatican said in the document issued on Monday, “envisages a society without sexual differences, thereby eliminating the anthropological basis of the family.” It was unacceptable, the Vatican said, that such ideologies managed to “assert themselves as absolute and unquestionable, even dictating how children should be raised.”
The Vatican ties surrogacy to commercialization.
The Vatican document reiterates its opposition to surrogacy, arguing that even though the process may fulfill the wishes of couples longing to have children, it does so at the cost of a wider human dignity because it reduces women, in the Vatican’s view, to simply carriers and children to what Francis has called products of “commercialization.”
The church’s opposition to surrogacy and in vitro fertilization stems from its ethical and theological teachings on the issue of life. Though Francis has made it clear that while the church opposes surrogacy, children born from surrogacy can be baptized.
“First and foremost, the practice of surrogacy violates the dignity of the child,” who “has the right to have a fully human (and not artificially induced) origin and to receive the gift of a life that manifests both the dignity of the giver and that of the receiver,” the document states.
“Surrogacy also violates the dignity of the woman, whether she is coerced into it or chooses to subject herself to it freely,” as it detaches the women “from the child growing in her and becomes a mere means subservient to the arbitrary gain or desire of others.”
The sex a person is born with is seen as a gift from God.
The Vatican document is adamant in its rejection of transition surgeries, what it calls “Sex Change.” It argues that the physical sex a person is born with — male or female — is an equal gift from God, who has made the human in his image. It is not a gift you can give back, the Vatican says.
Changing sex, the church argues, is to put individualism before “the need to respect the natural order of the human person,” and “any sex-change intervention, as a rule, risks threatening the unique dignity the person has received from the moment of conception.”
The church, however, made an exception for people with “genital abnormalities that are already evident at birth or that develop later,” which could be resolved through “health care professionals” because it would “not constitute a sex change in the sense intended here.”
Jason Horowitz is the Rome bureau chief for The Times, covering Italy, the Vatican, Greece and other parts of Southern Europe. More about Jason Horowitz
Elisabetta Povoledo is a reporter based in Rome, covering Italy, the Vatican and the culture of the region. She has been a journalist for 35 years. More about Elisabetta Povoledo
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Biomed Res Int

Sexuality after Male-to-Female Gender Affirmation Surgery
1 Department of Urology, University Hospital Essen, University Duisburg-Essen, Germany
2 Department of Urology, Kliniken Essen-Mitte, Essen, Germany
3 General Practice van Hal, Essen, Germany
R. Rossi Neto
4 Clinica Urologia, General Hospital Ernesto Simoes Filho, Salvador, Brazil
B. Hadaschik
Male-to-Female (MtF) gender affirmation surgery (GAS) comprises the creation of a functional and aesthetic perineogenital complex. This study aimed to evaluate the effect of GAS on sexuality. We retrospectively surveyed all 254 MtF transsexual patients who had undergone GAS with penile inversion vaginoplasty at the Department of Urology, University Hospital Essen, Germany, between 2004 and 2010. In total, we received 119 completed questionnaires after a median of 5.05 years since surgery. Of the study participants, 33.7% reported a heterosexual, 37.6% a lesbian, and 22.8% a bisexual orientation related to the self-perceived gender. Of those who had sexual intercourse, 55.8% rated their orgasms to be more intensive than before, with 20.8% who felt no difference. Most patients were satisfied with the sensitivity of the neoclitoris (73.9%) and with the depth of the neovaginal canal (67.1%). The self-estimated pleasure of sexual activity correlated significantly with neoclitoral sensitivity but not with neovaginal depth. There was a significant correlation between the ease with which patients were able to become sexually aroused and their ability to achieve orgasms. In conclusion, orgasms after surgery were experienced more intensely than before in the majority of women in our cohort and neoclitoral sensitivity seems to contribute to enjoyment of sexual activity to a greater extent than neovaginal depth.
1. Introduction
Male-to-female (MtF) gender affirmation surgery (GAS) comprises the resection of all clearly defining features of male genitalia. The aim is the formation of a perineogenital complex in appearance and function as feminine as possible [ 1 ] with a sensitive clitoris to enable orgasms. GAS should be performed by a surgeon with specialized competence in genital reconstructive techniques [ 2 ]. The aim is to “create a perineogenital complex as feminine in appearance and function as possible” [ 1 ]. There is a broad agreement that GAS has a positive impact on gender dysphoria [ 3 – 13 ]. The inversion of penile skin is used by most gender surgeons. While some trans ∗ and gender nonconforming people do not require surgical therapy to express their preferred gender role and identity, others see GAS as a pivotal step to relieve their gender dysphoria [ 14 ]. GAS might reduce risk of stigmatization and discrimination in venues like swimming pools and health clubs or when dealing with authorities [ 2 , 15 ]. Without doubt surgery has a positive effect on subjective wellbeing and sexual function [ 16 – 18 ].
Sexual orientation can change after GAS [ 19 ] but little is known about changes of orgasmic experience after GAS. Bartolucci et al. found a positive impact of cross gender hormone replacement therapy on sexual quality of life in transgender who had not undergone GAS yet [ 20 ]. However effects of GAS in this field remain unclear so far. This study aimed to evaluate the effect of GAS on sexuality and satisfaction with sexual life of MtF-transgender patients.
2. Material and Methods
2.1. participants.
Our study cohort comprised all 254 MtF patients who had undergone GAS with penile inversion vaginoplasty at the Department of Urology, University Hospital Essen, Germany, between 2004 and 2010, as has been previously reported [ 6 ]. Transsexualism was diagnosed by two independent mental healthcare professionals competent to work with gender dysphoric adults in accordance with 10th version of the International Classification of Diseases (ICD-10). All patients were contacted by mail using their last known address and asked if they would be willing to answer the questionnaire. In cases of invalid addresses the local residents' registration offices were contacted in order to reconsign a new questionnaire. Patients who had not sent back the questionnaire could not be followed up due to previous anonymization.
2.2. Statistics
Statistical calculation was performed using Statistical Package for the Social Sciences (SPSS 21.0). Fisher's exact test and Chi Square were used to compare categorical and ordinal variables in independent samples. The Mann–Whitney U test was used to compare satisfaction scale distribution of two independent samples. This nonparametric test was used in preference to the t-test because the Shapiro–Wilk test indicated that distribution was not normal. Spearman's correlation analysis was performed.
In total, 119 completed questionnaires were received, all of which were included in the evaluation (response rate 46.9%). Due to anonymization of the questionnaires, it was not possible to obtain information on patients' ages. However, the average age of a comparable cohort of patients at our department between 1995 and 2008 [ 21 ] was 36.7 years (16 to 68 years). Not all patients completed the questionnaire, so for some questions the total number of responses was not 119. The results are given in absolute numbers and percentage in relation to total participants or number of answers. After a median of 5.05 years (standard deviation: 1.6 years; range: 1 to 7 years) since surgery, 67 participants (56.3% of the total cohort) did not encounter sexual intercourse on a regular basis at the time of questioning (which depicts 67.7% of those who answered that question). Twenty of the 119 patients (16.8%) did not answer this question. Of those who answered the question nearly a quarter (n = 24; 24.2%) reported a mean frequency of one to three times per month, seven (7.1%) stated a frequency of one to three times per week, and one woman (1.0%) stated a frequency of over three times per week. Time since GAS did not correlate with the frequency of intercourse and the self-rated intensity of orgasms. There was neither an association of the extent to which women felt female themselves nor with the degree to which they felt considered as women with time since surgery.
In our cohort, 18 (15.1% of all participants) patients refused to answer regarding sexual attraction related to the self-perceived gender. Of those who answered (n = 101), slightly more of the patients (n = 38; 37.6%) indicated a sexual attraction towards women than towards men (n = 34; 33.7%). 23 women (22.8%) were attracted by both men and women and six (5.9%) neither by men nor by women ( Figure 1 ). In total, 38 subjects (41.3%) were highly satisfied, 30 (32.6%) were satisfied, 18 (19.6%) were not satisfied, and six (6.5%) were highly unsatisfied with the sensitivity of the neoclitoris ( Figure 2 ). This question was not answered by 27 individuals (22.7% of all participants). When asked how satisfied the women were with the depth of the neovaginal canal, 19 were very satisfied (20.9%), 42 (46.2%) were satisfied, 23 (25.3%) were unsatisfied, and seven (7.7%) were very unsatisfied, with 28 (23.5% of all participants) not answering the question ( Figure 3 ). We asked our patients whether it was easy to get sexually aroused. In total 91 women responded to this question, and about a quarter (n = 28; 23.5% of all participants) declined to answer. Of these 91 women 22 (24.2%) stated that this was always easy; for 43 (47.3%) it was mostly easy; for 15 (16.5%) it was seldom easy; and for eleven women (12.1%) it was never easy to get sexually aroused. The modality as to how orgasms were achieved is shown in Figure 4(a) (absolute numbers of patients; n = 119) and Figure 4(b) (percentages expressed in relation to total answers; n = 126). The majority of participants achieved an orgasm with masturbation, followed by sexual intercourse and “other” not further specified sexual practices. 29 women (24.4% of all participants) did not answer that question. Of those who answered that question (n = 77), 43 women (55.8%) quoted that orgasms were more intense after GAS compared with those experienced before surgery, 18 (23.4%) women stated that it was less intense than before, and 16 (20.8%) felt no difference. Frequency of achieved orgasms changed in our cohort after GAS. Of all 119 patients 41 (34.5%) refused to answer that question. Of the residual 78 women 41 (52.6%) indicated that orgasms were achieved less frequently, 21 women (26.9%) reported more frequent orgasms, and for 16 women (20.5%), frequency did not change. In order to gather information on patients' general satisfaction with their sex lives, they were asked to place themselves on a Likert scale ranging from 0 (“very dissatisfied”) to 10 (“very satisfied”). Nearly a quarter of participants either selected scores from 0 to 3 (n = 29; 24.4%), from 4 to 6 (n = 30; 25.2%), or from 7 to 10 (n = 29; 24.4%) or refused to answer (n = 31; 26.1%). Figure 5 shows a detailed illustration. We received feedback regarding pleasure of sexual activity from 88 women (73.9%). Of these respondents 31 (35.2%) stated that sexual activity was always pleasurable; 44 (50.0%) said it was sometimes pleasurable and 13 (14.8%) never felt pleasure with sexual activity. In our cohort, there was a significant correlation between the ease of getting sexually aroused and the ability to achieve an orgasm (r s = 0.616, p = 0.01). The better the sexual arousal, the easier it was to achieve an orgasm. The correlation between arousal and sensitivity of the neoclitoris was less distinctive but still significant (r s = 0.506, p = 0.01). The self-estimated pleasure of sexual activity was significantly correlated with the sensitivity of the neoclitoris (r s = 0.508, p = 0.01) but not with the depth of the neovaginal canal (r s = 0.198, p = 0.079); i.e., neoclitoral sensitivity seems to contribute to the enjoyment of sexual activity to a greater extent than the depth of the neovagina.

Sexual orientation related to the self-perceived gender.

Satisfaction with neoclitoral sensitivity.

Satisfaction with neovaginal depth.

Modality as to how orgasms were achieved (multiple answers possible). (a) Absolute number of patients. MB = masturbation; SI = sexual intercourse; OT = other (not further specified); NO = no orgasm; NA = no answer. (b) Modality as percentage of answers.

Patients' general satisfaction with their sex lives. Likert scale ranging from 0 (“very dissatisfied”) to 10 (“very satisfied”).
4. Discussion
Overall, subjective satisfaction rates can be expected to be 80% and higher after GAS [ 22 ]. Löwenberg reported a general satisfaction with the outcome of GAS to be even over 90% [ 10 ]. Studies often stress the emphasis on functional or aesthetic aspects after GAS [ 5 – 7 , 23 – 25 ] or, at best, on sexual quality of life before GAS [ 20 , 26 ]. To our best knowledge, this is the first study placing a particular focus on sexual life after MtF GAS.
In our study, sexual attraction was referred to the self-perceived sexual identity on the basis of self-identification. Accordingly, we used the term “heterosexual” or “homosexual” when participants reported on sexual attraction towards men (natal men as well as transmen) and women, respectively. Due to the existing stigmatization of homosexual and lesbian individuals in a heteronormative community or to patients' wish for social desirability, it is possible that reports on the prevalence of homosexuality (gay and lesbian) are underestimations. A representative study with over 14.000 men and women in Germany reported on a prevalence of 4% of men and 3% of women who self-identified as “gays”. Another 9% of male and 20% of female heterosexual participants felt sexually attracted by the same sex without identifying themselves as gay [ 27 ]. International surveys found a prevalence of homosexuality in up to 3% with regional and age-dependent variations [ 28 – 32 ]. In our study, the percentage of homosexuality (gay and lesbian) related to self-perceived gender was much higher. This could be because the interviewees knew the interrogators well, had generally revealed their sexual orientation beforehand, and had no fear of societal stigmatization. There is also the possibility that the rate of homo- and bisexuality is, in fact, higher in transsexuals compared with nontranssexuals. [ 33 ] Lawrence found a change in predominant sexual attraction in 232 MtF transsexuals before and after genital reassignment [ 19 ]. In her study, 54% and 25% of participants reported a gynephile orientation before and after surgery, respectively. Androphilic orientation changed from 9% preoperatively to 34% postoperatively. Regarding asexuality, we followed the definition of Prause and Graham who found that asexuality is defined to be a lack of sexual interest or desire, rather than a lack of sexual experience [ 34 ]. In our cohort, in total 6% of the women self-identified as asexual. Bogaert reported on approximately 1% asexual individuals of a total sample size of over 18.000 (nontranssexual) British residents, with more women being asexual than men [ 35 ]. He found both biological and psychosocial factors contributing to the development of asexuality. Prause and Graham found significantly lower sexual arousability and lower sexual excitation in asexual individuals with a prevalence of 4% [ 34 ]. A reduced sensitivity of the neoclitoris could therefore be a prognostic factor for asexuality. Our results support this assumption. The sensitivity of the neoclitoris correlated with the ability of sexual arousal and achieving an orgasm, as well as with the self-estimated pleasure of sexual activity. In our cohort, satisfaction with the sensitivity of the neoclitoris was higher than with the depth of the neovaginal canal. This could be due to the time of questioning, which was a median of 5.05 years after GAS. While neoclitoral sensitivity is unlikely to diminish, it is more likely that the neovaginal canal shrinks over time. Of the subjects 6% reported a stenosis of the neovagina and 45% a loss of initial neovaginal depth [ 25 ]. The longer the period after GAS is, the more prevalent the stenosis of the neovaginal canal seems to be [ 36 ]. Ineffective dilatation of the neovaginal canal is obviously a key factor contributing to neovaginal stenosis. Over half of all patients (58%) do not use vaginal dilators appropriately, which is a major reason for this kind of long-term complication [ 36 ].
Postsurgical sexuality plays an important role in overall satisfaction and depends substantially on the functionality of the neovagina [ 5 , 6 ]. Satisfaction with functionality ranges between 56% and 84% [ 7 , 9 , 10 , 37 , 38 ]. Previously, we reported a satisfaction rate with functionality, including satisfaction with depth and breadth of the neovagina and the satisfaction with penetration or intercourse, to be 72% (“very satisfied” and “satisfied”) or 91% (including also “mostly satisfied”) [ 6 ]. The self-reported enjoyment of sexual activity correlated significantly and to a greater extent with neoclitoral sensitivity than with neovaginal dimensions, which was not significant. Though genital dimensions were not surveyed in our study, penile size often exceeds the depth of the vaginal canal in natal women without causing problems with, or pain during, sexual intercourse. However in contrast to a skin derived vaginal canal of transgender women the vagina of natal women is able to expand 2.5 to 3.5 cm in length when sexually stimulated [ 39 ]. Neoclitoral sensitivity is usually assessed by means simply of asking the women and can be biased by the patients' wish for social desirability. In this retrospective study we could not rule this out. However, we previously introduced a measurement tool to assess semiquantitatively the sensitivity with a customary brush and a tuning fork [ 40 ] which could be used for future studies on this topic. Though the rate of women, who were able to achieve an orgasm, was lower in the present study than in an earlier cohort from our department [ 9 ], our data aligns well with comparable studies of a similar size [ 11 , 19 , 41 – 43 ]. Interestingly, Dunn et al. found a similar rate of natal women who were unsure or not able to achieve an orgasm during intercourse (16%) or masturbation (14%) [ 44 ]. In total 55.8% of the women in our study rated their orgasms postoperatively as more intense than before surgery, one in five women (20.8%) felt no difference, and 23.4% reported less intense orgasms after surgery. These results are roughly in line with a study by Buncamper et al. [ 45 ]. Since it is very unlikely that handling of the neurovascular bundle during surgery will make the neoclitoris more sensitive than the glans penis was before, a possible explanation could be that postoperative patients were able to experience orgasm for the first time in a body that matched their perception. Furthermore, a decline in sexual desire after sex reassignment therapy (hormonal and surgical) could contribute to an altered orgasmic experience [ 46 ]. Interestingly, in their systematic review, Guillamon et al. reported on results of three longitudinal studies showing a transformation in the brain morphology of MtF after initiation of cross sex hormonal therapy towards a more female morphology [ 47 ]. Moreover, receiving hormonal treatment was one of the factors related to a better subjective perception of sexual quality of life [ 20 ]. Rolle et al. registered a cerebral modification after sex reassignment in fifteen MtF transsexual individuals towards a more female cognitive response [ 48 ]. It is unclear whether this could explain differences in subjective orgasm experience before and after GAS. Further prospective studies with a larger sample size are needed to validate this preliminary aspect.
5. Limitations
The study was limited by its retrospective character with a response rate below 50%. Suicide is a very unlikely reason for nonparticipation since the suicide rate after successful GAS is not higher than in the general population [ 49 ]. However, contacting trans-female patients for long-term follow-up is generally difficult [ 3 , 37 , 50 – 54 ] particularly in countries like Germany where there is no central registration. Another reason is that patients often move following successful surgery [ 5 ]. Response rates to surveys in retrospective research in this field are between 19% [ 54 ] and 79% [ 55 ]. With 49%, Löwenberg et al. achieved a similar response rate in a follow-up inquiry of a comparable cohort [ 10 ]. Another bias could be that the answers represent patients' wishes for social desirability, rather than the reality of their situation. However, this cannot be verified retrospectively.
6. Conclusion
To our best knowledge, this was the first study to survey sexuality after MtF GAS in a very detailed way. In the majority of women, orgasms after surgery were experienced more intense than before. In our cohort, neoclitoral sensitivity seems to contribute to enjoyment of sexual activity to a greater extent than the depth of the neovaginal canal.
Acknowledgments
The authors acknowledge support by the Open Access Publication Fund of the University of Duisburg-Essen. This study has been conducted without external funding. Expenses have been financed by the Clinic for Urology, University Hospital Essen, University Duisburg-Essen, Germany.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Ethical Approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Parts of the data were presented as an abstract at the 2nd Biennial Conference “Contemporary TransHealth in Europe: Focus on Challenges and Improvements” 2017 in Belgrade, Serbia.
Vatican says sex reassignment surgery, surrogacy and gender theory threaten human 'dignity'
The Vatican has declared gender confirmation operations and surrogacy as grave threats to human "dignity", putting them on par with abortion and euthanasia as practices that violate God's plan for human life.
The Vatican's doctrine office on Monday published a 20-page declaration titled Infinite Dignity that was in the works for the past five years.
It was approved for publication by Pope Francis on March 25 after substantial revision in recent months.
In its most eagerly anticipated section, the Vatican reiterated its rejection of "gender theory" or the idea that one's gender can be "a self-determination".
It said God created man and woman as biologically different, separate beings, and said they must not tinker with that plan or try to "make oneself God".
"It follows that any sex-change intervention, as a rule, risks threatening the unique dignity the person has received from the moment of conception," the document said.
It distinguished between transitioning surgeries, which it rejected, and "genital abnormalities" that are present at birth or that develop later. Those abnormalities can be "resolved" with the help of health care professionals, it said.
The document's existence, rumoured since 2019, was confirmed in recent weeks by the new prefect of the Dicastery for the Doctrine of the Faith, Argentine Cardinal Víctor Manuel Fernández, a close confidante of Pope Francis.
He had cast it as something of a nod to conservatives after he authored a more explosive document approving blessings for same-sex couples that sparked criticism from conservative bishops around the world, especially in Africa.
While the new document rejected gender theory, it took pointed aim at countries — including many in Africa — that criminalise homosexuality.
It echoed Pope Francis's assertion in a 2023 interview that "being homosexual is not a crime", making the assertion now part of the Vatican's doctrinal teaching.
It denounced "as contrary to human dignity the fact that, in some places, not a few people are imprisoned, tortured, and even deprived of the good of life solely because of their sexual orientation".
The document restated well-known Catholic doctrine opposing abortion and euthanasia.
It also added to the list some of Pope Francis's main concerns as pope: the threats to human dignity posed by poverty, war, human trafficking and forced migration.
A child's right to 'a fully human origin'
In a newly articulated position, the declaration said surrogacy violated both the dignity of the surrogate mother and the child.
While much attention on surrogacy has focused on possible exploitation of poor women as surrogates, the Vatican document focuses more on the resulting child.
"The child has the right to have a fully human (and not artificially induced) origin and to receive the gift of a life that manifests both the dignity of the giver and that of the receiver," the document said.
"Considering this, the legitimate desire to have a child cannot be transformed into a 'right to a child' that fails to respect the dignity of that child as the recipient of the gift of life."
The Vatican published its most articulated position on gender in 2019, when the Congregation for Catholic Education rejected the idea that people can choose or change their genders.
It insisted on the complementary nature of biologically male and female sex organs to create new life.
Gender fluidity was described as a symptom of the "confused concept of freedom" and "momentary desires" that characterise post-modern culture.
The new document from the more authoritative Dicastery for the Doctrine of the Faith quoted from that 2019 education document but tempered the tone.
Significantly, it did not repurpose the 1986 language of a previous doctrinal document saying that homosexual people deserve to be treated with dignity and respect but that homosexual actions are "intrinsically disordered".
Francis has made reaching out to LGBTQ+ people a hallmark of his papacy, ministering to trans Catholics and insisting that the Catholic Church must welcome all children of God.
But he has also denounced "gender theory" as the "worst danger" facing humanity today, describing it as an "ugly ideology" that threatens to cancel out God-given differences between man and woman.
"It needs to be emphasised that biological sex and the sociocultural role of sex (gender) can be distinguished but not separated," the new document said.
- X (formerly Twitter)
Related Stories
Pope presides over easter vigil service after pulling out of good friday procession to 'conserve his health'.
Pope Francis approves blessings for Catholic same-sex couples in reversal of 2021 decision
The Catholic church has relaxed rules on cremation. Here's what has changed
- Community and Society
- Gender Discrimination
- Gender Roles
- Holy See (Vatican City State)
- Reproduction and Contraception
- Skip to main content
- Keyboard shortcuts for audio player
The Vatican says surrogacy and gender theory are 'grave threats' to human dignity

Jason DeRose

The crowd looks in direction of the window of the apostolic palace overlooking St. Peter's square during Pope Francis' prayer on April 1 in The Vatican. TizianaI Fabi/AFP via Getty Images hide caption
The crowd looks in direction of the window of the apostolic palace overlooking St. Peter's square during Pope Francis' prayer on April 1 in The Vatican.
The Vatican has released a new document calling poverty, war and the plight of migrants "threats to human dignity." But it also calls abortion, surrogacy and gender theory "grave threats" facing humanity today.
The document, titled " Infinite Dignity " says that each person's dignity comes from the love of the creator "who has imprinted the indelible features of his image on every person." This language is familiar to Christians accustomed to hearing that humans are all made in God's image.
The document goes on to say that this dignity is inalienable, beyond any circumstance or situation the person might encounter. Simply put, because a person exists, a human has intrinsic dignity.
"Infinite Dignity" details a long list of what it calls grave threats to that dignity, some of which might be expected given other Catholic teachings. It talks about the drama of poverty and how the unequal distribution of wealth denies humans their God-given dignity. It also describes war, the abuse of migrants, sexual abuse, violence against women, the marginalizing of people with disabilities, assisted suicide and abortion all as affronts to human dignity.
But then the document turns to other issues that have become more highly politicized in recent years: surrogacy, gender theory, and what it calls "sex change."

The pope wants surrogacy banned. Here's why one advocate says that's misguided
The document's framework holds that if a person is made in God's image, gender theory and gender reassignment surgery call into question why God would create a person with the wrong gender.
It says that the understanding of humanity as divided into two sexes — male and female — is biblical and deeply meaningful, especially in terms of procreation. Gender theory argues that a person's gender can be different from the sex that person was assigned at birth.
"Infinite Dignity" says the concept of human dignity can be misused to justify what it calls an "arbitrary proliferation of new rights," describing those, rather, as "individual preference" or "desire." That language is very similar to how conservatives often talk about being transgender as a choice, which is something major medical and psychological groups dispute.
The document makes a clear distinction between the issue of sexual orientation (whether a person is gay, lesbian or bisexual) and the issue of gender identity (whether a person's sex assigned at birth matches what that person understands his or her gender to be).
The document will be seen by some more conservative Catholic as a win after years of feeling embattled during Pope Francis's leadership. Just last year, the Vatican said priests could baptize transgender Catholics and allowed for priests to bless people in same-sex relationships .

Catholic Church works to explain what same-sex blessings are and are not
But many transgender Catholics and their families as well as more progressive Catholics are displeased with "Infinite Dignity."
Executive director of the LGBTQ Catholic group New Ways Ministry, Francis DeBernardo says of the document, "When it gets to the section on people who are transgender or non-binary, it doesn't apply the principles of human dignity to them."
New Ways Ministry's mission is, in part, to help pastors and religious teachers better understand gender identity and sexuality. It also fosters, "holiness and wholeness within the Catholic LGBTQ+ community."
DeBernardo argues "Infinite Dignity" does not live up to its own name. "In a sense, it's not infinite dignity," he says. "It's a very limited dignity that the church is offering."
He fears this document will be used to further persecute transgender people, and he thinks it will cause transgender Catholics and their families to leave the church.

The Vatican says priests can baptize transgender people
DeBernardo also worries the sections on gender theory and what it calls "sex change" will eclipse what he describes as the very good parts of the document on war, poverty and migrants.
The group Catholics for Choice, is also disappointed and calls into question how the document was created. "Yet again," said the group's president Jamie Manson in a written statement, "a group of all-male, celibate clergymen are telling women and gender-expansive people that their lived experiences are not real or valid."
Catholics for Choice advocates within the church on a variety of issues regarding sexual and reproductive health, including abortion rights. The group holds – and argues that Catholic teaching supports – people's individual consciences should be their guide in such decisions.
"It is clear to me that the women and trans people who continue to identify as Catholic — despite documents like this completely disregarding our experiences — only do so because of a deep love for our faith and its traditions," continues Manson in her statement. "It is devastating that our leaders do not offer the same respect and love in return."
- gender confirmation surgery

IMAGES
VIDEO
COMMENTS
Sex and sexual health tips for transgender women after gender-affirming surgery. Sex after surgery. Achieving orgasm. Libido. Vaginal depth and lubrication. Aftercare. Contraceptions and STIs ...
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a feminine-appearing outer genital area with a shallow vaginal canal.
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly ...
Female-to-male surgery is a type of gender-affirmation or gender-affirming surgery. There are multiple forms of gender-affirming surgery, including altering the genital region, known as "bottom ...
Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria. Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX ...
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current ...
A trans person can choose from multiple procedures to make their appearance match their self-identified gender identity. Doctors refer to this as gender "affirmation" surgery. Trans people might ...
A Pioneering Approach to Gender Affirming Surgery From a World Leader in the Field. Miroslav Djordjevic, MD, PhD, an internationally renowned surgeon and a leading authority on surgery for transgender individuals, is developing a procedure to match two patients undergoing transgender surgery—one male-to-female, the other female-to-male—and ...
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected]. We will assist you in obtaining what you need to qualify for surgery. University of Michigan Comprehensive Gender Services Program brings ...
The Crane Center for Transgender Surgery has announced the launch of a gender-affirming hormone clinic at their transgender wellness center in Austin, Texas. The new clinic offers hormone replacement therapy for transgender and non-binary adults through an informed consent model. Both in-office and telemedicine appointments are available.
The two major sex reassignment surgery (SRS) interventions in the female-to-male transsexual patients that will be addressed here are (1) the subcutaneous mastectomy (SCM), often combined with a hysterectomy/ ovariectomy; and (2) the actual genital transformation consisting of vaginectomy, reconstruction of the fixed part of the urethra (if ...
A US study showed that from 2000 to 2011, the rate of surgical sex reassignment measures among trans persons rose from 72% to 83.9% ().These data move the question of the effectiveness of such operations increasingly into the focus of clinical attention and awareness (8- 11).In the context of evidence-based medicine, the consensus is now that the success of medical procedures should not be ...
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000. Between 100 to 500 gender-reassignment procedures are ...
The objective of this video is to familiarize gynecologists with gender dysphoria and the basic steps of male-to-female transgender surgery using the penile ...
Ettore Ferrari/EPA, via Shutterstock. The Vatican on Monday issued a new document approved by Pope Francis stating that the church believes that gender fluidity and transition surgery, as well as ...
Transgender activists and allies on Monday decried the Vatican's new doctrine against gender-affirming surgery as "hurtful" and devoid of the voices and experiences of trans, non-binary and gender ...
April 3, 2024 7:15 AM EDT. H ong Kong no longer requires transgender people to undergo full gender-affirming surgery to change their legal gender markers in their IDs, more than a year after the ...
During this period, 214 patients underwent penile inversion vaginoplasty. Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18-61 years); the average of operative time was 3.3 h (range 2-5 h); the average duration of hormone therapy before surgery was 12 years (range 1-39).
The Vatican has issued a strong warning against "gender theory" and said that any gender-affirming surgery risks threatening "the unique dignity" of a person, in a new document signed off ...
The Vatican has issued a new document rejecting the concept of changing one's biological sex — a setback for transgender people who had hoped Pope Francis might be setting the stage for a more ...
The document restated the Roman Catholic Church's rejection of abortion, gender fluidity and transition surgery. By Jason Horowitz and Elisabetta Povoledo Jason Horowitz reported from Rome, and ...
Abstract. Male-to-Female (MtF) gender affirmation surgery (GAS) comprises the creation of a functional and aesthetic perineogenital complex. This study aimed to evaluate the effect of GAS on sexuality. We retrospectively surveyed all 254 MtF transsexual patients who had undergone GAS with penile inversion vaginoplasty at the Department of ...
The Vatican declares sex reassignment operations and surrogacy as grave threats to human "dignity", putting them on par with abortion and euthanasia as practices that violate God's plan for human ...
The document's framework holds that if a person is made in God's image, gender theory and gender reassignment surgery call into question why God would create a person with the wrong gender.