- NLN Certification
- Assessment Services
- CNEA Accreditation
- NLN Foundation
- Mission & Core Values
- History & Archives
- Board of Governors
- Senior Management
- Consultants & Speakers Bureau
- NLN Elections
- NLN Nominations
- Career Center

Faculty Toolkit for Innovation in Curriculum Design
In 2008, the NLN Task Group on Innovations in Curriculum Design was formed with the mission of promoting excellence and innovation in curriculum design. The task group included the following experts in nursing education: Linda Benedict, MA, RN; M. Sharon Boni, PhD, RN; Pat Bradley, PhD, RN, CNE; Linda Carpenter, PhD, RN, CNE; Jean Giddens, PhD, RN; Janet Grady, DrPH, RN, ANEF; Marian Kovatchitch, MS, RN; Lynne P. Lewallen, PhD, RN, CNE; Barbara McLaughlin, DNSc, RN, CNE; Janet Phillips, PhD, RN; Jerelyn Resnick, PhD, RN; Judith P. Ruland, PhD, RN, CNE; and Nancy Stuever, EdD, RN. Linda Benedict chaired the task group. The group was divided into two work groups: one work group developed a repository of current curriculum innovations and the other work group developed the Faculty Toolkit for Innovation in Curriculum Design. The authors of this toolkit are: Linda Carpenter, Marian Kovatchitch, Lynne Lewallen, and Jean Giddens. This toolkit comprises three sections:
- A curriculum report card (DOC)
- A resources section (DOC)
- A section containing exemplars in teaching strategies and curriculum (DOC)
The first two sections were developed using the curriculum and innovation indicators in the NLN Hallmarks of Excellence in Nursing Education. The exemplars were chosen based on a task group study of schools self-identified as having innovative curricula. The report card is designed to be used by nursing programs to assess their curricula. If you are assessing more than one nursing program, assess each one separately. Answer the questions in each section with your curriculum in mind. Each item can be ranked from “0” (no implementation in your curriculum) to “4” (full implementation in your curriculum).
Although there are no specific numerical cut-points, the areas where your curriculum scores highest are the areas where it most aligns with the curriculum and innovation hallmarks in the NLN Hallmarks of Excellence. Areas where your curriculum scores lowest are areas for your faculty to work on. Each section of the report card is linked to a specific part of the resources section. Note the number of the section of the report card where your curriculum scores lowest, and go to the corresponding area of the resources section for articles, books, and websites that address this hallmark. The exemplars at the end of the resources section represent general innovative ideas and do not correspond directly to a report card section.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. Washington (DC): National Academies Press (US); 2011.

The Future of Nursing: Leading Change, Advancing Health.
- Hardcopy Version at National Academies Press
4 Transforming Education
Key Message #2 : Nurses should achieve higher lev els of education and training through an improved education system that promotes seamless academic progression.
Major changes in the U.S. health care system and practice environ ments will require equally profound changes in the education of nurses both before and after they receive their licenses. Nursing education at all levels needs to provide a better understanding of and experience in care management, quality improvement methods, systems-level change management, and the reconceptualized roles of nurses in a reformed health care system. Nursing education should serve as a platform for continued lifelong learning and include opportunities for seamless tran sition to higher degree programs. Accrediting, licensing, and certifying organizations need to mandate demonstrated mastery of core skills and competencies to complement the completion of degree programs and written board examinations. To respond to the underrepresentation of racial and ethnic minority groups and men in the nursing workforce, the nursing student body must become more diverse. Finally, nurses should be educated with physicians and other health professionals as students and throughout their careers.
Major changes in the U.S. health care system and practice environments will require equally profound changes in the education of nurses both before and after they receive their licenses. In Chapter 1 , the committee set forth a vision of health care that depends on a transformation of the roles and responsibilities of nurses. This chapter outlines the fundamental transformation of nurse education that must occur if this vision is to be realized.
The primary goals of nursing education remain the same: nurses must be prepared to meet diverse patients’ needs; function as leaders; and advance science that benefits patients and the capacity of health professionals to deliver safe, quality patient care. At the same time, nursing education needs to be transformed in a number of ways to prepare nursing graduates to work collaboratively and effectively with other health professionals in a complex and evolving health care system in a variety of settings (see Chapter 3 ). Entry-level nurses, for example, need to be able to transition smoothly from their academic preparation to a range of practice environments, with an increased emphasis on community and public health settings. And advanced practice registered nurses (APRNs) need graduate programs that can prepare them to assume their roles in primary care, acute care, long-term care, and other settings, as well as specialty practices.
This chapter addresses key message #2 set forth in Chapter 1 : Nurses should achieve higher levels of education and training through an improved education system that promotes seamless academic progression. The chapter begins by focusing on nurses’ undergraduate education, emphasizing the need for a greater number of nurses to enter the workforce with a baccalaureate degree or to progress to this degree early in their career. This section also outlines some of the challenges to meeting undergraduate educational needs. The chapter then turns to graduate nursing education, stressing the need to increase significantly the numbers and preparation of nurse faculty and researchers at the doctoral level. The third section explores the need to establish, maintain, and expand new competencies throughout a nurse’s education and career. The chapter next addresses the challenge of underrepresentation of racial and ethnic minority groups and men in the nursing profession and argues that meeting this challenge will require increasing the diversity of the nursing student body. The fifth section describes some creative solutions that have been devised for addressing concerns about educational capacity and the need to transform nursing curricula. The final section presents the committee’s conclusions regarding the improvements needed to transform nursing education.
The committee could have devoted this entire report to the topic of nursing education—the subject is rich and widely debated. However, the committee’s statement of task required that it examine a range of issues in the field, rather than delving deeply into the many challenges involved in and solutions required to advance the nursing education system. Several comprehensive reports and analyses addressing nursing education have recently been published. They include a 2009 report from the Carnegie Foundation that calls for a “radical transforma tion” of nursing education (Benner et al., 2009); a 2010 report from a conference sponsored by the Macy Foundation that charts a course for “life-long learning” that is assessed by the “demonstration of competency [as opposed to written assessment] in both academic programs and in continuing education” (AACN and AAMC, 2010); two consensus reports from the Institute of Medicine (IOM) that call for greater interprofessional education of physicians, nurses, and other health professionals, as well as new methods of improving and demonstrating competency throughout one’s career (IOM, 2003b, 2009); and other articles and reports on necessary curriculum changes, faculty development, and new partnerships in education (Erickson, 2002; Lasater and Nielsen, 2009; Mitchell et al., 2006; Orsolini-Hain and Waters, 2009; Tanner et al., 2008). Additionally, in February 2009, the committee hosted a forum on the future of nursing in Houston, Texas, that focused on nursing education. Discussion during that forum informed the committee’s deliberations and this chapter; a summary of that forum is included on the CD-ROM in the back of this report. 1 Finally, Appendix A highlights other recent reports relevant to the nursing profession. The committee refers readers wishing to explore the subject of nursing education in greater depth to these publications.
- UNDERGRADUATE EDUCATION
This section begins with an overview of current undergraduate nursing education, including educational pathways, the distribution of undergraduate degrees, the licensing exam, and costs (see Appendix E for additional background information on undergraduate education). The discussion then focuses on the need for more nurses prepared at the baccalaureate level. Finally, barriers to meeting undergraduate educational needs are reviewed.
Overview of Current Undergraduate Education
Educational pathways.
Nursing is unique among the health care professions in the United States in that it has multiple educational pathways leading to an entry-level license to practice (see the annexes to Chapter 1 and Appendix E ). For the past four decades, nursing students have been able to pursue three different educational pathways to become registered nurses (RNs): the bachelor’s of science in nursing (BSN), the associate’s degree in nursing (ADN), and the diploma in nursing. More recently, an accelerated, second-degree bachelor’s program for students who possess a baccalaureate degree in another field has become a popular option. This multiplicity of options has fragmented the nursing community and has created confusion among the public and other health professionals about the expectations for these educational options. However, these pathways also provide numerous opportunities for women and men of modest means and diverse backgrounds to access careers in an economically stable field.
In addition to the BSN, ADN, or diploma received by RNs, another undergraduate-level program available is the licensed practical/vocational diploma in nursing. Licensed practical/vocational nurses (LPNs/LVNs) are especially important because of their contributions to care in long-term care facilities and nursing homes. 2 LPNs/LVNs receive a diploma after completion of a 12-month program. They are not educated or licensed for independent decision making for complex care, but obtain basic training in anatomy and physiology, nutrition, and nursing techniques. Some LPNs/LVNs continue their education to become RNs; in fact, approximately 17.9 percent of RNs were once licensed as LPNs/LVNs (HRSA, 2010b). While most LPNs/LVNs have an interest in advancing their education, a number of barriers to their doing so have been cited, including financial concerns, lack of capacity and difficulty getting into ADN and BSN programs, and family commitments (HRSA, 2004). Although this chapter focuses primarily on the education of RNs and APRNs, the committee recognizes the contributions of LPNs/LVNs in improving the quality of health care. The committee also recognizes the opportunity the LPN/LVN diploma creates as a possible pathway toward further education along the RN and APRN tracks for the diverse individuals who hold that diploma.
Distribution of Undergraduate Degrees
At present, the most common way to become an RN is to pursue an ADN at a community college. Associate’s degree programs in nursing were launched in the mid-20th century in response to the nursing shortage that followed World War II (Lynaugh, 2008; Lynaugh and Brush, 1996). The next most common undergraduate nursing degree is the BSN, a 4-year degree typically offered at a university. Baccalaureate nursing programs emphasize liberal arts, advanced sciences, and nursing coursework across a wider range of settings than are addressed by ADN programs, along with formal coursework that emphasizes both the acquisition of leadership development and the exposure to community and public health competencies. The least common route to becoming an RN currently is the diploma program, which is offered at a hospital-based school and generally lasts 3 years. During the 20th century, as nursing gained a stronger theoretical foundation and other types of nursing programs increased in number, the number of diploma programs declined remarkably except in a few states, such as New Jersey, Ohio, and Pennsylvania. Figure 4-1 gives an overview of trends in the distribution of nursing graduates by initial nursing degree.
Trends in graduation from basic RN programs, by type, 2002–2008. SOURCE: NLN, 2010b.
Entry into Practice: The Licensing Exam 3
Regardless of which educational pathway nursing students pursue, those working toward an RN must ultimately pass the National Council Licensure Examination for Registered Nurses (NCLEX-RN), which is administered by the National Council of State Boards of Nursing (NCSBN), before they are granted a license to practice. Rates of success on the NCLEX-RN are often used for rating schools or for marketing to potential students. As with many entry-level licensing exams, however, the NCLEX-RN uses multiple-choice, computer-based methods to test the minimum competency required to practice nursing safely. The exam is administered on a pass/fail basis and, although rigorous, is not meant to be a test of optimal performance. Following passage of the exam, individual state boards of nursing grant nurses their license to practice.
The content of the NCLEX-RN is based on surveys of what new nurses need to know to begin their practice. As with most entry-level licensing exams, the content of the NCLEX-RN directly influences the curricula used to educate nursing students. Currently, the exam is skewed toward acute care settings because this is where the majority of nurses are first employed and where most work throughout their careers. To keep pace with the changing demands of the health care system and patient populations, including the shift toward increasing care in community settings (see Chapter 2 ), the focus of the exam will need to shift as well. Greater emphasis must be placed on competencies related to community health, public health, primary care, geriatrics, disease prevention, health promotion, and other topics beyond the provision of nursing care in acute care settings to ensure that nurses are ready to practice in an evolving health care system.
Costs of Nursing Education
Although a limited number of educational grants and scholarships are available, most of individuals seeking nursing education must finance their own education at any level of preparation. Costs vary based on the pathway selected for basic preparation and through to doctoral preparation. The LPN degree is the least expensive to attain, followed by the ADN, BSN (accelerated program), BSN, master’s of science in nursing (MSN), and PhD/doctor of nursing practice (DNP) degrees. It is no surprise that educational costs and living expenses play a major role in determining which degree is pursued and the numbers of nurses who seek advanced degrees.
To better understand the costs of nursing education, the committee asked the Robert Wood Johnson Foundation (RWJF) Nursing Research Network to estimate the various costs associated with pursuing nursing education, specifically at the advanced practice level, in comparison with those for a medical doctor (MD) or doctor of osteopathy (DO). The RWJF Nursing Research Network produced several comparison charts in an attempt to convey accurately the differences in costs between alternative nursing degrees and the MD or DO degree. This task required making assumptions about public versus private and proprietary/for-profit education options, prerequisites for entry, and years required to complete each degree. An area of particular difficulty arose in assessing costs associated with obtaining an ADN degree. In most non–health care disciplines, the associates degree takes 2 years to complete. In nursing, however, surveys have found that it takes students 3 to 4 years to complete an ADN program because of the need to fulfill prerequisites necessary to prepare students for entry into degree programs and the lack of adequate faculty, which lead to long waiting lists for many programs and classes (Orsolini-Hain, 2008). Box 4-1 illustrates the challenges of this task by outlining the difficulty of comparing the cost of becoming a physician with the cost of becoming an APRN. The task of comparing the increasing “sticker costs” of nursing and medical education was complicated further because much of the data needed to compute those costs is either missing or drawn from incomparable years. In the end, the committee decided not to include detailed discussion of the costs of nursing education in this report.
Costs of Health Professional Education. Depending on the method used, the number of advanced practice registered nurses (APRNs) that can be trained for the cost of training 1 physician is between 3 and 14. Assessing the costs of education is a multidimensional (more...)
Why More BSN-Prepared Nurses Are Needed
The qualifications and level of education required for entry into the nursing profession have been widely debated by nurses, nursing organizations, academics, and a host of other stakeholders for more than 40 years (NLN, 2007). The causal relationship between the academic degree obtained by RNs and patient outcomes is not conclusive in the research literature. However, several studies support a significant association between the educational level of RNs and outcomes for patients in the acute care setting, including mortality rates (Aiken et al., 2003; Estabrooks et al., 2005; Friese et al., 2008; Tourangeau et al., 2007; Van den Heede et al., 2009). Other studies argue that clinical experience, qualifications before entering a nursing program (e.g., SAT scores), and the number of BSN-prepared RNs that received an earlier degree confound the value added through the 4-year educational program. One study found that the level of experience of nurses was more important than their education level in mitigating medication errors in hospitals (Blegen et al., 2001). Another study performed within the Department of Veterans Affairs (VA) system found no significant association between the proportion of RNs with a baccalaureate degree and patient outcomes at the hospital level (Sales et al., 2008).
This debate aside, an all-BSN workforce at the entry level would provide a more uniform foundation for the reconceptualized roles for nurses and new models of care that are envisioned in Chapters 1 and 2 . Although a BSN education is not a panacea for all that is expected of nurses in the future, it does, relative to other educational pathways, introduce students to a wider range of competencies in such arenas as health policy and health care financing, leadership, quality improvement, and systems thinking. One study found that new BSN graduates reported significantly higher levels of preparation in evidence-based practice, research skills, and assessment of gaps in areas such as teamwork, collaboration, and practice (Kovner et al., 2010)—other important competencies for a future nursing workforce. Moreover, as more nurses are being called on to lead care coordination efforts, they should have the competencies requisite for this task, many of which are included in the American Association of Colleges of Nursing’s (AACN’s) Essentials of Baccalaureate Education for Professional Nursing Practice . 4
Care within the hospital setting continues to grow more complex, and nurses must make critical decisions associated with care for sicker, frailer patients. Care in this setting depends on sophisticated, life-saving technology coupled with complex information management systems that require skills in analysis and synthesis. Care outside the hospital is becoming more complex as well. Nurses are being called upon to coordinate care among a variety of clinicians and community agencies; to help patients manage chronic illnesses, thereby preventing acute care episodes and disease progression; and to use a variety of technological tools to improve the quality and effectiveness of care. A more educated nursing workforce would be better equipped to meet these demands.
An all-BSN workforce would also be poised to achieve higher levels of education at the master’s and doctoral levels, required for nurses to serve as primary care providers, nurse researchers, and nurse faculty—positions currently in great demand as discussed later in this chapter. Shortages of nurses in these positions continue to be a barrier to advancing the profession and improving the delivery of care to patients.
Some health care organizations in the United States are already leading the way by requiring more BSN-prepared nurses for entry-level positions. A growing number of hospitals, particularly teaching and children’s hospitals and those that have been recognized by the American Nurses Credentialing Center Magnet Recognition Program (see Chapter 5 ), favor the BSN for employment (Aiken, 2010). Depending on the type of hospital, the goal for the proportion of BSN-prepared nurses varies; for example, teaching hospitals aim for 90 percent, whereas community hospitals seek at least 50 percent (Goode et al., 2001). Absent a nursing shortage, then, nurses holding a baccalaureate degree are usually the preferred new-graduate hires in acute care settings (Cronenwett, 2010). Likewise, in a recent survey of 100 physician members of Sermo.com (see Chapter 3 for more information on this online community), conducted by the RWJF Nursing Research Network, 76 percent of physicians strongly or somewhat agreed that nurses with a BSN are more competent than those with an ADN. Seventy percent of the physicians surveyed also either strongly or somewhat agreed that all nurses who provide care in a hospital should hold a BSN, although when asked about the characteristics they most value in nurses they work with, the physicians placed a significantly higher value on compassion, efficiency, and experience than on years of nursing education and caliber of nursing school (RWJF, 2010c).
In community and public health settings, the BSN has long been the preferred minimum requirement for nurses, given the competencies, knowledge of community-based interventions, and skills that are needed in these settings (ACHNE, 2009; ASTDN, 2003). The U.S. military and the VA also are taking steps to ensure that the nurses making up their respective workforces are more highly educated. The U.S. Army, Navy, and Air Force require all active duty RNs to have a baccalaureate degree to practice, and the U.S. Public Health Service has the same requirement for its Commissioned Officers. Additionally, as the largest employer of RNs in the country, the VA has established a requirement that nurses must have a BSN to be considered for promotion beyond entry level (AACN, 2010c). As Table 4-1 shows, however, the average earnings of BSN-prepared nurses are not substantially higher than those of ADN- or diploma-prepared nurses.
Average Earnings of Full-Time RNs, by Highest Nursing or Nursing-Related Education and Job Title.
Decades of “blue ribbon panels” and reports to Congress on the health care workforce have found that there is a significant shortage of nurses with baccalaureate and higher degrees to respond to the nation’s health needs (Aiken, 2010). Almost 15 years ago, the National Advisory Council on Nurse Education and Practice, which advises Congress and the secretary of Health and Human Services on areas relevant to nursing, called for the development of policy actions that would ensure a minimum of 66 percent of RNs who work as nurses would have a BSN or higher degree by 2010 (Aiken et al., 2009). The result of policy efforts of the past decade has been a workforce in which approximately 50 percent of RNs hold a BSN degree or higher, a figure that includes ADN- and diploma-educated RNs who have gone on to obtain a BSN (HRSA, 2010b). Of significant note, the Tri-Council for Nursing, which consists of the American Nurses Association, American Organization of Nurse Executives, National League for Nursing (NLN), and AACN, recently released a consensus policy statement calling for a more highly educated nursing workforce, citing the need to increase the number of BSN-prepared nurses to deliver safer and more effective care (AACN, 2010a).
In sum, an increase in the percentage of nurses with a BSN is imperative as the scope of what the public needs from nurses grows, expectations surrounding quality heighten, and the settings where nurses are needed proliferate and become more complex. The formal education associated with obtaining the BSN is desirable for a variety of reasons, including ensuring that the next generation of nurses will master more than basic knowledge of patient care, providing a stronger foundation for the expansion of nursing science, and imparting the tools nurses need to be effective change agents and to adapt to evolving models of care. As discussed later in this chapter, the committee’s recommendation for a more highly educated nursing workforce must be paired with overall improvements to the education system and must include competencies in such areas as leadership, basic health policy, evidence-based care, quality improvement, and systems thinking. Moreover, even as the breadth and depth of content increase within prelicensure curricula, the caring essence and human connectedness nurses bring to patient care must be preserved. Nurses need to continue to provide holistic, patient-centered care that goes beyond physical health needs to recognize and respond to the social, mental, and spiritual needs of patients and their families. Other fundamental elements of nursing education, such as ethics and integrity, need to remain intact as well.
The Goal and a Plan for Achieving It
In the committee’s view, increasing the percentage of the current nursing workforce holding a BSN from 50 to 100 percent in the near term is neither practical nor achievable. Setting a goal of increasing the percentage to 80 percent by 2020 is, however, bold, achievable, and necessary to move the nursing workforce to an expanded set of competencies, especially in the domains of community and public health, leadership, systems improvement and change, research, and health policy.
The committee believes achieving the goal of 80 percent of the nursing workforce having a BSN is possible in part because much of the educational capacity needed to meet this goal exists. RNs with an ADN or diploma degree have a number of options for completing the BSN, as presented below. The combination of these options and others yet to be developed will be needed to meet the 80 percent goal—no one strategy will provide a universal solution. Technologies, such as the use of simulation and distance learning through online courses, will have to play a key role as well. Above all, what is needed to achieve this goal is the will of nurses to return to higher education, support from nursing employers and others to help fund nursing education, the elevation of educational standards, an education system that recognizes the experience and previous learning of returning students, and regional collaboratives of schools of nursing and employers to share financial and human resources.
While there are challenges associated with shortages of nurse faculty and clinical education sites (discussed below), these challenges are less problematic for licensed RNs pursuing a BSN than for prelicensure students, who require more intense oversight and monitoring by faculty. Additionally, most of what ADN-prepared nurses need to move on to a baccalaureate degree can be taught in a classroom or online, with additional tailored clinical experience. Online education creates flexibility and provides an additional skill set to students who will use technology into the future to retrieve and manage information.
Over the course of its deliberations and during the forum on education held in Houston, the committee learned about several pathways that are available to achieve the goal of 80 percent of the nursing workforce having a BSN (additional innovations discussed at the forum on education can be found in the forum summary on the CD-ROM in the back of this report). For RNs returning to obtain their BSN, a number of options are possible, including traditional RN-to-BSN programs. Many hospitals also have joint arrangements with local universities and colleges to offer onsite classes. Hospitals generally provide stipends to employees as an incentive to continue their education. Online education programs make courses available to all students regardless of where they live. For prospective nursing students, there are traditional 4-year BSN programs at a university, but there are also community colleges now offering 4-year baccalaureate degrees in some states (see the next section). Educational collaboratives between universities and community colleges, such as the Oregon Consortium for Nursing Education (described in Box 4-2 ), allow for automatic and seamless transition from an ADN to a BSN program, with all schools sharing curriculum, simulation facilities, and faculty. As described below, this type of model is goes beyond the conventional articulation agreement between community colleges and universities. Beyond traditional nursing schools, new providers of nursing education are entering the market, such as proprietary/for-profit schools. These programs are offering new models and alternatives for delivering curriculum and reaching RNs and prospective students, although each of these schools should be evaluated for its ability to meet nursing accreditation standards, including the provision of clinical experiences required to advance the profession.
Case Study: The Oregon Consortium for Nursing Education (OCNE). Sharing Resources to Prepare the Next Generation of Nurses I n 2006, when Basilia Basin, BSN, RN, entered nursing school at Mount Hood Community College in Gresham, Oregon, near Portland, (more...)
Two other important programs designed to facilitate academic progression to higher levels of education are the LPN-to-BSN and ADN-to-MSN programs. The ADN-to-MSN program, in particular, is establishing a significant pathway to advanced practice and faculty positions, especially at the community college level. Financial support to help build capacity for these programs will be important, including funding for grants and scholarships for nurses wishing to pursue these pathways. By the same token, the committee believes that diploma programs should be phased out over the next 10 years and should consolidate their resources with those of community college or preferably university programs offering the baccalaureate degree. Additionally, there are federal resources currently being used to support diploma schools that could better be used to expand baccalaureate and higher education programs.
The committee anticipates that it will take a few years to build the educational capacity needed to achieve the goal of 80 percent of the nursing workforce being BSN-prepared by 2020, but also emphasizes that existing BSN completion programs have capacity that is far from exhausted. Regional networks of schools working together, along with health care organizations, may best facilitate reaching this goal. Moreover, the committee believes this clearly defined goal will stimulate stakeholders to take action. Examples of such action include academic and health care organizations/employers partnering to achieve strategic alignment around workforce development; government and foundations introducing funding opportunities for scholarships to build faculty and provide tuition relief; state boards of nursing increasing the use of earmarks on licensure fees to offset the cost of education; and states developing statewide policy agendas and political action plans with identified leaders in nursing, government, and business to adopt measures to meet the goal.
The Role of Community Colleges
Community colleges play a key role in attracting students to the nursing education pipeline. Specifically, they provide an opportunity for students who may not have access to traditional university baccalaureate programs because of those programs’ lack of enrollment capacity, distance, or cost.
Community colleges have an important role to play in ensuring that more BSN-prepared nurses are available in all regions of the United States and that nursing education at the associate level is high quality and affordable and prepares ADN nurses to move on to higher levels of education. Currently, ADN- and BSN-prepared nurses are not evenly distributed nationwide. BSN-prepared RNs are found more commonly in urban areas, while many rural and other medically underserved communities depend heavily on nurses with associate’s degrees to staff their hospitals, clinics, and long-term care facilities (Cronenwett, 2010). Figure 4-2 shows the highest nursing or nursing-related education by urban/rural residence. According to a study by the Urban Institute, “medical personnel, including nurses, tend to work near where they were trained” (Bovjberg, 2009; see Figure 4-3 ). This suggests that state and community investments in nursing education (e.g., building nursing school capacity, building infrastructure to support that capacity, funding the purchase of technology, and offering scholarships) may be an effective way to reduce local and regional shortages. Community colleges are the predominant educational institutions in rural and medically underserved areas. Therefore, they must either join educational collaboratives or develop innovative and easily accessible programs that seamlessly connect students to schools offering the BSN and higher degrees, or they must develop their own BSN programs (if feasible within state laws and regulations). Community colleges must foster a culture that promotes and values academic progression and should encourage their students to continue their education through strategies that include making them aware of the full range of educational pathways and opportunities available to them (e.g., ADN-to-MSN and online RN-to-BSN programs). Box 4-3 describes a community college in Florida where nursing students can take advantage of lower costs and online classes to receive a BSN degree.
Highest nursing or nursing-related education by urban/rural residence. SOURCE: Calculations performed using the data and documentation for the 2004 National Sample of Registered Nurses, available from the Health Resources and Services Administration’s (more...)
Distance between nursing education program and workplace for early-career nurses (graduated 2007–2008) SOURCE: RWJF, 2010a. Reprinted with permission from Lori Melichar, RWJF.
Case Study: Community Colleges Offering the BSN. The College of Nursing at St. Petersburg College and Others Open the Door to the Bachelor’s Degree in Nursing T amela Monroe was 33 and working in sales in 1997 when she decided to pursue a career (more...)
Barriers to Meeting Undergraduate Educational Needs
Although the committee believes the capacity needed to ensure a nursing workforce that is 80 percent BSN-prepared by 2020 can be attained using the approaches outlined above, getting there will not be easy. Nursing schools across the United States collectively turn away tens of thousands of qualified applicants each year because of a lack of capacity (Kovner and Djukic, 2009)—a situation that makes filling projected needs for more and different types of nurses difficult. Figure 4-4 shows the breakdown of numbers of qualified applicants who are turned away from ADN and BSN programs.
Numbers of qualified applicants not accepted in ADN and BSN programs. NOTES:
An examination of the root causes of the education system’s insufficient capacity to meet undergraduate educational needs reveals four major barriers: (1) the aging and shortage of nursing faculty; (2) insufficient clinical placement opportunities of the right kind or duration for prelicensure nurses to learn their profession; (3) nursing education curricula that fail to impart relevant competencies needed to meet the future needs of patients and to prepare nurses adequately for academic progression to higher degrees; and (4) inadequate workforce planning, which stems from a lack of the communications, data sources, and information systems needed to align educational capacity with market demands. This final root cause—inadequate workforce planning—affects all levels of nursing education and is the subject of Chapter 6 .
Aging and Shortage of Nursing Faculty
There are not enough nursing faculty to teach the current number of nursing students, let alone the number of qualified applicants who wish to pursue nursing. The same forces that are leading to deficits in the numbers and competencies of bedside nurses affect the capacity of nursing faculty as well (Allan and Aldebron, 2008). According to a survey by the NLN, 84 percent of U.S. nursing schools tried to hire new faculty in the 2007–2008 academic year; of those, four out of five found it “difficult” 5 to recruit faculty, and one out of three found it “very difficult.” The principal difficulties included “not enough qualified candidates” (cited by 46 percent) and the inability to offer competitive salaries (cited by 38 percent). The survey concluded that “post-licensure programs were much more likely to cite a shortage of faculty, whereas pre-licensure programs reported that lack of clinical placement settings were [sic] the biggest impediment to admitting more students. Specifically, almost two thirds (64 percent) of doctoral programs and one half of RN-BSN and master’s programs identified an insufficient faculty pool to draw from as the major constraint to expansion, in contrast to one third of prelicensure programs” (NLN, 2010a).
Age is also a contributing factor to faculty shortages. Nursing faculty tend to be older than clinical nurses because they must meet requirements for an advanced degree in order to teach. Figure 4-5 shows that the average age of nurses who work as faculty as their principal nursing position—the position in which a nurse spends the majority of his or her working hours 6 —is 50 to 54. By contrast, the median age of the total RN workforce is 46. More than 19 percent of RNs whose principal position is faculty are aged 60 or older, while only 8.7 percent of nurses who have a secondary position as faculty—those who hold a nonfaculty (e.g., clinical) principal position—are aged 60 or older. Nurses who work as faculty as their secondary position tend to be younger; among nurses under age 50, more work as faculty as their secondary than as their principal position (HRSA, 2010b). Moreover, the average retirement age for nursing faculty is 62.5 (Berlin and Sechrist, 2002); as a result, many full-time faculty will be ready to retire soon. Given the landscape of the health care system and the fragmented nursing education system, the current pipeline cannot easily replenish this loss, let alone meet the potential demand for more educators. In addition to the innovative strategies of the Veterans Affairs Nursing Academy (VANA) and Gulf Coast Health Services Steering Committee for responding to faculty shortages (discussed later in this chapter), a potential opportunity to relieve faculty shortages could involve the creation of programs that would allow MSN, DNP, and PhD students to teach as nursing faculty interns, with mentoring by full-time faculty. Box 4-4 presents a nurse profile of one assistant professor and her experience moving into an academic career.
Age distribution of nurses who work as faculty. SOURCE: HRSA, 2010b.
Nurse Profile: Jennifer Wenzel. Pursuing an Academic Career A lthough she believes that “all nurses make a difference, wherever we practice, whatever we do,” Jennifer Wenzel, PhD, RN, CCM, said that her primary motivation in choosing an (more...)
Effects of the first degree at entry into the profession Nurses who enter the profession with an associate’s degree are less likely than those who enter with a bachelor’s degree to advance to the graduate level over the course of their career (Cleary et al., 2009). Figure 4-6 gives an overview of the highest educational degree obtained by women and men who hold the RN license. It includes RNs who are working as nurses and those who have retired, have changed professions, or are no longer working. According to an analysis by Aiken and colleagues (2009), nurses whose initial degree is the ADN are just as likely as BSN-prepared nurses to seek another degree. Approximately 80 percent of the time, however, ADN graduates fail to move beyond a BSN. Therefore, the greatest number of nurses with a master’s or doctorate, a prerequisite for serving as faculty, received a BSN as their initial degree. Since two-thirds of current RNs received the ADN as their initial degree, Aiken’s analysis suggests that currently “having enough faculty (and other master’s prepared nurses) to enable nursing schools to expand enrollment is a mathematical improbability” (Aiken et al., 2009). A separate analysis of North Carolina nurses led to a similar conclusion (Bevill et al., 2007). Table 4-2 shows the length of time it takes those nurses who do move on to higher levels of education to progress from completing initial nursing education to completing the highest nursing degree achieved.
Distribution of the registered nurse population by highest nursing or nursing-related educational preparation, 1980–2008 NOTES: The totals in each bar may not equal the estimated numbers for RNs in each survey year because of incomplete information (more...)
Years Between Completion of Initial and Highest RN Degrees.
Salary disparities Another factor that contributes to the current nursing faculty shortage is salary disparities between nurses working in education and those working in clinical service (Gilliss, 2010). As shown in Table 4-3 , the average annual earnings of nurses who work full time as faculty (most with either a master’s or doctoral degree) total $63,949. By contrast, nurse practitioners (NPs) (with either a master’s or doctoral degree) average just over $85,000 (see Table 4-4 ). Section 5311 of the Affordable Care Act (ACA) offers an incentive designed to offset lower faculty salaries by providing up to $35,000 in loan repayments and scholarships for eligible nurses who complete an advanced nursing degree and serve “as a full-time member of the faculty of an accredited school of nursing, for a total period, in the aggregate, of at least 4 years.” 7 However, the ACA does not provide incentives for nurses to develop the specific educational and clinical competencies required to teach.
Average Annual Earnings of Nurses Who Work Full Time as Faculty in Their Principal Nursing Position, 2008.
Average Earnings by Job Title of Principal Position for Nurses Working Full Time.
Projections of future faculty demand To establish a better understanding of future needs, the committee asked the RWJF Nursing Research Network to proj ect faculty demand for the next 15 years. After reviewing data from the AACN 8 and the NLN (Kovner et al., 2006), the network estimated that between 5,000 and 5,500 faculty positions will remain unfilled in associate’s, baccalaureate, and higher degree programs. This projection is based on historical nurse faculty retirement rates and on graduation trends in research-focused nursing PhD programs. Although a doctoral degree is often required or preferred for all current faculty vacancies, some of these positions can be filled with faculty holding DNP or master’s degrees.
If faculty retirement rates decrease and/or new faculty positions are created to meet future demands (resulting, for example, from provisions for loan repayment in the ACA), these factors will affect the shortage estimates. Additionally, the faculty supply may be affected positively by growing numbers of graduates with a DNP degree (discussed later in this chapter) who, as noted above, may be eligible for faculty positions in some academic institutions.
Insufficient Clinical Placement Opportunities
As nursing education has moved out of hospital-based programs and into mainstream colleges and universities, integrating opportunities for clinical experience into coursework has become more difficult (Cronenwett, 2010). Nursing leaders continue to confront challenges associated with the separation of the academic and practice worlds in ensuring that nursing students develop the competencies required to enter the workforce and function effectively in health care settings (Cronenwett and Redman, 2003; Fagin, 1986). While efforts are being made to expand placements in the community and more care is being delivered in community settings, the bulk of clinical education for students still occurs in acute care settings.
The required number of clinical hours varies widely from one program to another, and most state boards of nursing do not specify a minimum number of clinical hours in prelicensure programs (NCSBN, 2008). It is likely, moreover, that many of the clinical hours fail to result in productive learning. Students spend much of their clinical time performing routine care tasks repeatedly, which may not contribute significantly to increased learning. Faculty report spending most of their time supervising students in hands-on procedures, leaving little time focused on fostering the development of clinical reasoning skills (McNelis and Ironside, 2009). 9
Some advances in clinical education have been made through strong academic–service partnerships. An example of such partnerships in community settings is nurse-managed health centers (discussed in Chapter 3 ), which serve a dual role as safety net practices and clinical education sites. Another, commonly used model is having skilled and experienced practitioners in the field oversee student clinical experiences. According to a recent integrative review, using these skilled practitioners, called preceptors, in a clinical setting is at least as effective as traditional approaches while conserving scarce faculty resources (Udlis, 2006). A variety of other clinical partnerships have been designed to increase capacity in the face of nursing faculty shortages (Baxter, 2007; DeLunas and Rooda, 2009; Kowalski et al., 2007; Kreulen et al., 2008; Kruger et al., 2010).
In addition to academic–service partnerships and preceptor models, the use of high-fidelity simulation offers a potential solution to the problem of limited opportunities for clinical experience, with early studies suggesting the effectiveness of this approach (Harder, 2010). The NLN, for example, has established an online community called the Simulation Innovation Resource Center, where nurse faculty can learn how to “design, implement, and evaluate the use of simulation” in their curriculum. 10 However, there is little evidence that simulation expands faculty capacity, and no data exist to define what portion of clinical experience it can replace. To establish uniform guidelines for educators, accreditation requirements should be evaluated and revised to allow simulation to fulfill the requirement for a standard number of clinical hours. The use of simulation in relationship to the promotion of interprofessional education is discussed below.
Increased attention is being focused on the dedicated education unit (DEU) as a viable alternative for expanding clinical education capacity (Moscato et al., 2007). In this model, health care units are dedicated to the instruction of students from one program. Staff nurses who want to serve as clinical instructors are prepared to do so, and faculty expertise is used to support their development and comfort in this role. DEUs were developed in Australia and launched in the United States at the University of Portland in Oregon in 2003. Since then, the University of Portland has helped at least a dozen other U.S. nursing schools establish DEUs. In programs that offer DEUs, students perform two 6-week rotations per semester, each instructor/staff nurse teaches no more than two students at a time, and a university faculty member oversees the instruction. Early results suggest the DEU can dramatically increase capacity and have a positive effect on satisfaction among students and nursing staff. A multisite study funded by RWJF is currently under way to evaluate outcomes of the DEU model.
DEUs offer benefits for the nursing schools, the hospitals, the faculty, and the students. Because the hospital employs the clinical instructors, the nursing school can increase its enrollment without increasing costs. The hospital benefits by training students it can hire after their graduation and licensure. Students benefit by having consistent clinical instructors each day, something not guaranteed under the traditional preceptorship model. As the case study in Box 4-5 shows, the benefits of DEUs extend beyond the academic environment to the practice setting as well.
Case Study: The Dedicated Education Unit. A New Model of Education to Increase Enrollment Without Raising Costs J amie Sharp, a 21-year-old University of Portland (UP) nursing student who has performed clinical rotations in a variety of units, remembers (more...)
Need for Updated and Adaptive Curricula
A look at the way nursing students are educated at the prelicensure level 11 shows that most schools are not providing enough nurses with the required competencies in such areas as geriatrics and culturally relevant care to meet the changing health needs of the U.S. population (as outlined in Chapter 2 ) (AACN and Hartford, 2000). The majority of nursing schools still educate students primarily for acute care rather than community settings, including public health and long-term care. Most curricula are organized around traditional medical specialties (e.g., maternal–child, pediatrics, medical–surgical, or adult health) (McNelis and Ironside, 2009). The intricacies of care coordination are not adequately addressed in most prelicensure programs. Nursing students may gain exposure to leading health care disciplines and know something about basic health policy and available health and social service programs, such as Medicaid. However, their education often does not promote the skills needed to negotiate with the health care team, navigate the regulatory and access stipulations that determine patients’ eligibility for enrollment in health and social service programs, or understand how these programs and health policies impact health outcomes. Nursing curricula need to be reexamined and updated. They need to be adaptive enough to undergo continuous evaluation and improvement based on new evidence and a changing science base, changes and advances in technology, and changes in the needs of patients and the health care system.
Many nursing schools have dealt with the rapid growth of health research and knowledge by adding layers of content that require more instruction (Ironside, 2004). A wide range of new competencies also are being incorporated into requirements for accreditation (CCNE, 2009; NLNAC, 2008). For example, new competencies have been promulgated to address quality and patient safety goals (Cronenwett et al., 2007; IOM, 2003a). Greater emphasis on prevention, wellness, and improved health outcomes has led to new competency requirements as well (Allan et al., 2005). New models of care being promulgated as a result of health care reform will need to be introduced into students’ experiences and will require competencies in such areas as care coordination. These models, many of which could be focused in alternative settings such as schools and workplaces, will create new student placement options that will need to be tested for scalability and compared for effectiveness with more traditional care settings. (See also the discussion of competencies later in the chapter.)
The explosion of knowledge and decision-science technology also is changing the way health professionals access, process, and use information. No longer is rote memorization an option. There simply are not enough hours in the day or years in an undergraduate program to continue compressing all available information into the curriculum. New approaches must be developed for evaluating curricula and presenting fundamental concepts that can be applied in many different situations rather than requiring students to memorize different lists of facts and information for each situation.
Just as curricula must be assessed and rethought, so, too, must teaching–learning strategies. Most nurse faculty initially learned to be nurses through highly structured curricula that were laden with content (NLN Board of Governors, 2003), and too few have received advanced formal preparation in curriculum development, instructional design, or performance assessment. Faculty, tending to teach as they were taught, focus on covering content (Benner et al., 2009; Duchscher, 2003). They also see curriculum-related requirements as a barrier to the creation of learning environments that are both engaging and student-centered (Schaefer and Zygmont, 2003; Tanner, 2007).
- GRADUATE NURSING EDUCATION
Even absent passage of the ACA, the need for APRNs, nurse faculty, and nurse researchers would have increased dramatically under any scenario (Cronenwett, 2010). Not only must schools of nursing build their capacity to prepare more students at the graduate level, but they must do so in a way that fosters a unified, competency-based approach with the highest possible standards. Therefore, building the science of nursing education research, or how best to teach students, is an important emphasis for the field of nursing education. For APRNs, graduate education should ensure that they can contribute to primary care and help respond to shortages, especially for those populations who are most underserved. For nurse researchers, a focus on fundamental improvements in the delivery of nursing care to improve patient safety and quality is key.
Numbers and Distribution of Graduate-Level Nurses
As of 2008, more than 375,000 women and men in the workforce had received a master’s degree in nursing or a nursing-related field, and more than 28,000 had gone on to receive either a doctorate in nursing or a nursing-related doctoral degree in a field such as public health, public administration, sociology, or education 12 (see Table 4-5 ) (HRSA, 2010b). Master’s degrees prepare RNs for roles in nursing administration and clinical leadership or for work in advanced practice roles (discussed below) (AARP, 2010 [see Annex 1-1 ]). Many nursing faculty, particularly clinical instructors, are prepared at the master’s level. Doctoral degrees include the DNP and PhD. A PhD in nursing is a research-oriented degree designed to educate nurses in a wide range of scientific areas that may include clinical science, social science, policy, and education. Traditionally, PhD-educated nurses teach in university settings and conduct research to expand knowledge and improve care, although they can also work in clinical settings and assume leadership and administrative roles in health care systems and academic settings.
Estimated Distribution of Master’s and Doctoral Degrees as Highest Nursing or Nursing-Related Educational Preparation, 2000–200.
The DNP is the complement to other practice doctorates, such as the MD, PharmD, doctorate of physical therapy, and others that require highly rigorous clinical training. Nurses with DNPs are clinical scholars who have the capacity to translate research, shape systems of care, potentiate individual care into care needed to serve populations, and ask the clinical questions that influence organizational-level research to improve performance using informatics and quality improvement models. The DNP is a relatively new degree that offers nurses an opportunity to become practice scholars in such areas as clinical practice, leadership, quality improvement, and health policy. The core curriculum for DNPs is guided by the AACN’s Essentials of Doctoral Education for Advanced Nursing Practice . 13
Schools of nursing have been developing DNP programs since 2002, but only in the last 5 years have the numbers of graduates approached a substantial level (Raines, 2010). Between 2004 and 2008 the number of programs offering the degree increased by nearly 40 percent, as is shown in Figure 4-7 . At this point, more evidence is needed to examine the impact DNP nurses will have on patient outcomes, costs, quality of care, and access in clinical settings. It is also difficult to discern how DNP nurses could affect the provision of nursing education and whether they will play a significant role in easing faculty shortages. While the DNP provides a promising opportunity to advance the nursing profession, and some nursing organizations are promoting this degree as the next step for APRNs, the committee cannot comment directly on the potential role of DNP nurses because of the current lack of evidence on outcomes.
Growth trends in different nursing programs. NOTE: BSN = bachelor’s of science in nursing; DNP = doctor of nursing practice.
Although 13 percent of nurses hold a graduate degree, fewer than 1 percent (28,369 nurses) have a doctoral degree in nursing or a nursing-related field, the qualification needed to conduct independent research (HRSA, 2010b). In fact, only 555 students graduated with a PhD in nursing in 2009, a number that has remained constant for the past decade (AACN, 2009a). As noted, key roles for PhD nurses include teaching future generations of nurses and conducting research that becomes the basis for improvements in nursing practice. As the need for nursing education and research and for nurses to engage with interprofessional research teams has grown, the numbers of nurses with a PhD in nursing or a related field have not kept pace (see Figure 4-7 for trends in the various nursing programs). The main reasons for this lag are (1) an inadequate pool of nurses with advanced nursing degrees to draw upon, (2) faculty salaries and benefits that are not comparable to those of nurses with advanced nursing degrees working in clinical settings, and (3) a culture that promotes obtaining clinical experience prior to continuing graduate education.
Preparation of Advanced Practice Registered Nurses
Nurses prepared at the graduate level to provide advanced practice services include those with master’s and doctoral degrees. APRNs serve as NPs, certified nurse midwives (CNMs), clinical nurse specialists (CNSs), and certified registered nurse anesthetists (CRNAs). To gain certification in one of these advanced practice areas, nurses must take specialized courses in addition to a basic core curriculum. Credit requirements vary from program to program and from specialty to specialty, but typically range from a minimum of 40 credits for a master’s to more than 80 credits for a DNP. Upon completion of required coursework and clinical hours, students must take a certification exam that is administered by a credentialing organization relevant to the specific specialization, such as the American Nursing Credentialing Center (for NPs and CNSs), the American Midwifery Certification Board (for CNMs), or the National Board on Certification and Recertification of Nurse Anesthetists (for CRNAs).
Nurses who receive certification, including those serving in all advanced practice roles, provide added assurance to the public that they have acquired the specialized professional development, training, and competencies required to provide safe, quality care for specific patient populations. For example, NPs and CNSs may qualify for certification after completing a master’s degree, post-master’s coursework, or doctoral degree through an accredited nursing program, with specific advanced coursework in areas such as health assessment, pharmacology, and pathophysiology; additional content in health promotion, disease prevention, differential diagnosis, and disease management; and at least 500 hours of faculty-supervised clinical training within a program of study (ANCC, 2010a, 2010c).
Certification is time-limited, and maintenance of certification requires ongoing acquisition of both knowledge and experience in practice. For example, most advanced practice certification must be renewed every 5 years (NPs, CNSs); requirements include a minimum of 1,000 practice hours in the specific certification role and population/specialty. These requirements must be fulfilled within the 5 years preceding submission of the renewal application (ANCC, 2010b). CRNAs are recertified every 2 years and must be substantially engaged in the practice of nurse anesthesia during those years, in addition to completing continuing education credits (NBCRNA, 2009). Recertification for CNMs is shifting from 8 to 5 years and also involves a continuing education requirement (AMCB, 2009).
As the health care system grows in complexity, expectations are that APRNs will have competence in expanding areas such as technology, genetics, quality improvement, and geriatrics. Coursework and clinical experience requirements are increasing to keep pace with these changes. Jean Johnson, Dean of the School of Nursing at The George Washington University, notes that in terms of education, this is a time of major transition for APRNs. 14 With the DNP, some nursing education institutions are now able to offer professional parity with other health disciplines that are shifting, or have already shifted, to require doctorates in their areas of practice, such as pharmacy, occupational and physical therapy, and speech pathology. As discussed above, DNP programs allow nurses to hone their expertise in roles related to nurse executive practice, health policy, informatics, and other practice specialties. (It should be noted, however, that throughout this report, the discussion of APRNs does not distinguish between those with master’s and DNP degrees who have graduated from an accredited program.)
Research Roles
Graduate-level education produces nurses who can assume roles in advanced practice, leadership, teaching, and research. For the latter role, a doctoral degree is required, yet as noted above, fewer than 1 percent of nurses have achieved this level of education. This number is insufficient to meet the crucial need for research in two key areas: nursing education and nursing science.
Research on Nursing Education
At no time in recent history has there been a greater need for research on nursing education. As health care reform progresses, basic and advanced nursing practices are being defined by the new competencies alluded to above and discussed in the next section, yet virtually no evidence exists to support the teaching approaches used in nursing education. 15
Additionally, little research has focused on clinical education models or clinical experiences that can help students achieve these competencies, even though clinical education constitutes the largest portion of nurses’ educational costs. Likewise, little evidence supports appropriate student/faculty ratios. Yet current clinical education models and student/faculty ratios are limiting capacity at a time when the need for new nurses is projected to increase. The paucity of evidence in nursing education and pedagogy calls for additional research and funding to ascertain the efficiency and effectiveness of approaches to nursing education, advancing evidence-based teaching and interprofessional knowledge. Chapter 7 outlines specific research priorities that could shape improvements to nursing education.
In a recent editorial, Broome (2009) highlighted the need for three critical changes required to “systematically build a … science that could guide nurse educators to develop high quality, relevant, and cost-effective models of education that produce graduates who can make a difference in the health system”:
- funding to support nursing education research, potentially via mechanisms through the Health Resources and Services Administration;
- multidisciplinary research training programs, including postdoctoral training to prepare a cadre of nurses dedicated to developing the science of nursing education; and
- efforts to foster the development of PhD programs that have faculty expertise to mentor a new generation of nursing education researchers.
Research on Nursing Science
The expansion of knowledge about the science of nursing is key to providing better patient care, improving health, and evaluating outcomes. Along with an adequate supply of qualified nurses, meeting the nation’s growing health care needs requires continued growth in the science of delivering effective care for people and populations and designing health systems. Nurse scientists are a critical link in the discovery and translation of knowledge that can be generated by nurses and other health scientists. To carry out this crucial work, a sustainable supply of and support for nurse scientists will be necessary (IOM, 2010).
The research conducted by nurse scientists has led to many fundamental improvements in the provision of care. Advances have been realized, for example, in the prevention of pressure ulcers; the reduction of high blood pressure among African American males; and the models described elsewhere in this report for providing transitional care after hospital discharge and for promoting health and well-being among young, disadvantaged mothers and their newborns. Yet nursing’s research capacity has been largely overlooked in the development of strategies for responding to the shortage of nurses or effecting the necessary transformation of the nursing profession. The result has been a serious mismatch between the urgent need for knowledge and innovation to improve care and the nursing profession’s ability to respond to that need, as well as a limitation on what nursing schools can include in their curricula and what is disseminated in the clinical settings where nurses engage.
A chapter of the National Research Council’s 2005 report, Advancing the Nation’s Health Needs: NIH’s Research Training Program , focuses on nursing research; it identified factors that would likely influence its future, for example: an aging cadre of nursing science researchers, longer times required to complete doctoral degrees, increasing demands on nursing faculty to also meet workforce demands, and the emergence of clinical doctoral programs (NRC, 2005). Evaluating these and other factors will be essential to achieving the transformation of the nursing profession that this report argues is essential to a transformed health care system.
- COMPETENCY-BASED EDUCATION
Competencies that are well known to the nursing profession, such as care management and coordination, patient education, public health intervention, and transitional care, are likely to dominate in a reformed health care system. As Edward O’Neil, Director, Center for the Health Professions at the University of California, San Francisco, pointed out however, “these traditional competencies must be reinterpreted for students into the settings of the emergent care system, not the one that is being left behind. This will require faculty to not only teach to these competencies but also creatively apply them to health environments that are only now emerging” (O’Neil, 2009). Emerging new competencies in decision making, quality improvement, systems thinking, and team leadership must become part of every nurse’s professional formation from the prelicensure through the doctoral level.
A review of medical school education found that evidence in favor of competency-based education is limited but growing (Carraccio et al., 2002). Nursing schools also have embraced the notion of competency-based education, as noted earlier in the chapter in the case study on the Oregon Consortium for Nursing Education ( Box 4-2 ). In addition, Western Governors University uses competency-based education exclusively, allowing nursing students to move through their program of study at their own pace. Mastery of the competency is achieved to the satisfaction of the faculty without the normal time-bound semester structure (IOM, 2010).
Defining Core Competencies
The value of competency-based education in nursing is that it can be strongly linked to clinically based performance expectations. It should be noted that “competencies” here denotes not task-based proficiencies but higher-level competencies that represent the ability to demonstrate mastery over care management knowledge domains and that provide a foundation for decision-making skills under variety of clinical situations across all care settings.
Numerous sets of core competencies for nursing education are available from a variety of sources. It has proven difficult to establish a single set of competencies that cover all clinical situations, across all settings, for all levels of students. However, there is significant overlap among the core competencies that exist because many of them are derived from such landmark reports as Recreating Health Professional Practice for a New Century (O’Neil and Pew Health Professions Commission, 1998) and Health Professions Education: A Bridge to Quality (IOM, 2003b). The competencies in these reports focus on aspects of professional behavior (e.g., ethical standards, cultural competency) and emphasize areas of care (e.g., prevention, primary care), with overarching goals of (1) providing patient-centered care, (2) applying quality improvement principles, (3) working in interprofessional teams, (4) using evidence-based practices, and (5) using health information technologies.
Two examples of sets of core competencies come from the Oregon Consortium for Nursing Education 16 and the AACN. The former set features competencies that promote nurses’ abilities in such areas as clinical judgment and critical thinking; evidence-based practice; relationship-centered care; interprofessional collaboration; leadership; assistance to individuals and families in self-care practices for promotion of health and management of chronic illness; and teaching, delegation, and supervision of caregivers. The AACN’s set of competencies is outlined in Essentials for Baccalaureate Education and highlights such areas as “patient-centered care, interprofessional teams, evidence-based practice, quality improvement, patient safety, informatics, clinical reasoning/critical thinking, genetics and genomics, cultural sensitivity, professionalism, practice across the lifespan, and end-of-life care” (AACN, 2008b). While students appear to gradu ate with ample factual knowledge of these types of core competencies, however, they often appear to have little sense of how the competencies can be applied or integrated into real-world practice situations (Benner et al., 2009).
Imparting emerging competencies, such as quality improvement and systems thinking, is also key to developing a more highly educated workforce. Doing so will require performing a thorough evaluation and redesign of educational content, not just adding content to existing curricula. An exploration of the educational changes required to teach all the emerging competencies required to meet the needs of diverse patient populations is beyond the scope of this report.
Defining an agreed-upon set of core competencies across health professions could lead to better communication and coordination among disciplines (see the discussion of the Interprofessional Education Collaborative below for an example of one such effort). Additionally, the committee supports the development of a unified set of core competencies across the nursing profession and believes it would help provide direction for standards across nursing education. Defining these core competencies must be a collaborative effort among nurse educators, professional organizations, and health care organizations and providers. This effort should be ongoing and should inform regular updates of nursing curricula to ensure that graduates at all levels are prepared to meet the current and future health needs of the population.
Assessing Competencies
Changes in the way competencies are assessed are also needed. In 2003, the IOM’s Health Professions Education: A Bridge to Quality called for systemwide changes in the education of health professionals, including a move on the part of accrediting and certifying organizations for all health professionals toward mandating a competency-based approach to education (IOM, 2003a). Steps are already being taken to establish competency-based assessments in medical education. In its 2009 report to Congress on Improving Incentives in the Medicare Program , the Medicare Payment Advisory Commission highlighted an initiative of the Accreditation Council for Graduate Medical Education to require greater competency-based assessment of all residency programs that train physicians in the United States (MedPAC, 2009). The NCSBN has considered various challenges related to competency assessment and is considering approaches to ensure that RNs can demonstrate competence in the full range of areas that are required for the practice of nursing. 17
A competency-based approach to education strives to make the competencies for a particular course explicit to students and requires them to demonstrate mastery of those competencies (Harden, 2002). Performance-based assessment then shows whether students have both a theoretical grasp of what they have learned and the ability to apply that knowledge in a real-world or realistically simulated situation. The transition-to-practice or nurse residency programs discussed in Chapter 3 could offer an extended opportunity to reinforce and test core competencies in real-world settings that are both safe and monitored.
Lifelong Learning and Continuing Competence
Many professions, such as nursing, that depend heavily on knowledge are becoming increasingly technical and complex (The Lewin Group, 2009). No individual can know all there is to know about providing safe and effective care, which is why nurses must be integral members of teams that include other health professionals. Nor can a single initial degree provide a nurse with all she or he will need to know over an entire career. Creating an expectation and culture of lifelong learning for nurses is therefore essential.
From Continuing Education to Continuing Competence
Nurses, physicians, and other health professionals have long depended on continuing education programs to maintain and develop new competencies over the course of their careers. Yet the 2009 IOM study Redesigning Continuing Education in the Health Professions cites “major flaws in the way [continuing education] is conducted, financed, regulated, and evaluated” and states that the evidence base underlying current continuing education programs is “fragmented and undeveloped.” These shortcomings, the report suggests, have hindered the identification of effective educational methods and their integration into coordinated, comprehensive programs that meet the needs of all health professionals (IOM, 2009). Likewise, the NCSBN has found that there is no clear link between continuing education requirements and continued competency. 18 A new vision of professional development is needed that enables learning both individually and from a collaborative, team perspective and ensures that “all health professionals engage effectively in a process of lifelong learning aimed squarely at improving patient care and population health” (IOM, 2009).
This new comprehensive vision is often termed “continuing competence.” The practice setting, like the academic setting, is challenged by the need to integrate traditional and emerging competencies. Therefore, building the capacity for lifelong learning—which encompasses both continuing competence and advanced degrees—requires ingenuity on the part of employers, businesses, schools, community and government leaders, and philanthropies. The case study in Box 4-6 describes a program that extends the careers of nurses by training them to transition from the acute care to the community setting.
Case Study: Nursing for Life—The RN Career Transition Program. A New Program Extends the Working Life of Aging Nurses By Training Them to Work in Community Settings A t age 62 Jackie Tibbetts, MS, RN, CAGS, was thinking, naturally, about retirement. (more...)
Interprofessional Education
The importance of interprofessional collaboration and education has been recognized since the 1970s (Alberto and Herth, 2009). What is new is the introduction of simulation and web-based learning—solutions that can be used to can break down traditional barriers to learning together, such as the conflicting schedules of medical and APRN students or their lack of joint clinical learning opportunities. Simulation technology offers a safe environment in which to learn (and make mistakes), while web-based learning makes schedule conflicts more manageable and content more repeatable. If all nursing and medical students are educated in aspects of interprofessional collaboration, such as knowledge of professional roles and responsibilities, effective communication, conflict resolution, and shared decision making, and are exposed to working with other health professional students through simulation and web-based training, they may be more likely to engage in collaboration in future work settings. Further, national quality and safety agendas, including requirements set by the Joint Commission, the Commission on Collegiate Nursing Education, the NLN, and the Association of American Medical Colleges (AAMC), along with studies that link disruptive behavior between RNs and MDs to negative patient and worker outcomes (Rosenstein and O’Daniel, 2005, 2008), create a strong incentive to not just talk about but actually work on implementing interprofessional collaboration.
England, Canada, and the United States have made strides to improve interprofessional education by bringing students together from academic health science universities and medical centers (e.g., students of nursing, medicine, pharmacy, social work, physical therapy, and public health, among others) in shared learning environments (Tilden, 2010). Defined as “occasions when two or more professions learn with, from, and about each other to improve collaboration and the quality of care” (Barr et al., 2005), such education is based on the premise that students’ greater familiarity with each other’s roles, competencies, nomenclatures, and scopes of practice will result in more collaborative graduates. It is expected that graduates of programs with interprofessional education will be ready to work effectively in patient-centered teams where miscommunication and undermining behaviors are minimized or eliminated, resulting in safer, more effective care and greater clinician and patient satisfaction. Interprofessional education is thought to foster collaboration in implementing policies and improving services, prepare students to solve problems that exceed the capacity of any one profession, improve future job satisfaction, create a more flexible workforce, modify negative attitudes and perceptions, and remedy failures of trust and communication (Barr, 2002). 19
The AAMC, the American of Association of Colleges of Osteopathic Medicine, the American Dental Education Association, the American Association of Colleges of Pharmacy, the Association of Schools of Public Health, and the AACN recently formed a partnership called the Interprofessional Education Collaborative. This collaborative is committed to the development of models of collaboration that will provide the members’ individual communities with the standards and tools needed to achieve productive interprofessional education practices. These organizations are committed to fulfilling the social contract that every nursing, pharmacy, dental, public health, and medical graduate is proficient in the core competencies required for interprofessional, team-based care, including preventive, acute, chronic, and catastrophic care. The collaborative is also committed to facilitating the identification, development, and deployment of the resources essential to achieving this vision. As a first step, the collaborative is developing a shared and mutually endorsed set of core competencies that will frame the education of the six represented health professions. 20
Efforts have been made to evaluate the effectiveness of interprofessional education in improving outcomes, including increased student satisfaction, modified negative stereotypes of other disciplines, increased collaborative behavior, and improved patient outcomes. However, the effect of interprofessional education is not easily verified since control group designs are expensive, reliable measures are few, and time lapses can be long between interprofessional education and the behavior of graduates. Barr and colleagues (2005) reviewed 107 evaluations of interprofessional education in published reports and found support for three outcomes: interprofessional education creates positive interaction among students and faculty; encourages collaboration between professions; and results in improvements in aspects of patient care, such as more targeted health promotion advice, higher immunization rates, and reduced blood pressure for patients with chronic heart disease. Reeves and colleagues (2008) reviewed six later studies of varying designs. Four of the studies found that interprofessional education improved aspects of how clinicians worked together, while the remaining two found that it had no effect (Reeves et al., 2008). Although empirical evidence is mixed, widespread theoretical agreement and anecdotal evidence suggest that students who demonstrate teamwork skills in the simulation laboratory or in a clinical education environment with patients will apply those skills beyond the confines of their academic programs. 21
- THE NEED TO INCREASE THE DIVERSITY OF THE NURSING WORKFORCE
Chapter 3 highlighted a variety of challenges facing the nursing profession in meeting the changing needs of patients and the health care system. A major challenge for the nursing workforce is the underrepresentation of racial and ethnic minority groups and men in the profession. To better meet the current and future health needs of the public and to provide more culturally relevant care, the nursing workforce will need to grow more diverse. And to meet this need, efforts to increase nurses’ levels of educational attainment must emphasize increasing the diversity of the student body. This is a crucial concern that needs to be addressed across all levels of nursing education.
Racial and Ethnic Diversity
Although the composition of the nursing student body is more racially and ethnically diverse than that of the current workforce, diversity continues to be a challenge. Figure 4-8 shows the distribution of minority students enrolled in nursing programs by race/ethnicity and by program type. Their underrepresentation is greatest for pathways associated with higher levels of education. In academic year 2008–2009, for example, ethnic minority groups made up 28.2 percent of ADN, 23.6 percent of BSN, 24.4 percent of master’s, and 20.3 percent of doctoral students (NLN, 2009). Even less evidence of diversity is present among nurses in faculty positions (AACN, 2010b).
Percentage of minority students enrolled in nursing programs by race/ethnicity and program type, 2008–2009 NOTE: ADN = associate’s degree programs; BSN = bachelor’s of science programs; BSRN = RN-to-BSN programs; DIP = diploma (more...)
In 2003, the Sullivan Commission on Diversity in the Healthcare Workforce was established to develop recommendations that would “bring about systemic change … [to] address the scarcity of minorities in our health professions.” The commission’s report, Missing Persons: Minorities in the Health Professions (Sullivan Commission on Diversity in the Healthcare Workforce, 2004), offered strategies to increase the diversity of the medical, nursing, and dentistry professions and included recommendations designed to remove barriers to health professions education for underrepresented minority students. The commission’s 37 recommendations called for leadership, commitment, and accountability among a wide range of stakeholders—from institutions responsible for educating health professionals, to professional organizations and health systems, to state and federal agencies and Congress. The recommendations focused on expediting strategies to increase the number of minorities in health professions, improving the education pipeline for health professionals, financing education for minority students, and establishing leadership and accountability to realize the commission’s vision of increasing the diversity of health professionals. The committee believes the implementation of these recommendations holds promise for ensuring a more diverse health care workforce in the future.
In the nursing profession, creating bridge programs and educational pathways between undergraduate and graduate programs—specifically programs such as LPN to BSN, ADN to BSN, and ADN to MSN—appears to be one way of increasing the overall diversity of the student body and nurse faculty with respect to not only race/ethnicity, but also geography, background, and personal experience. Mentoring programs that support minority nursing students are another promising approach. One example of such a program is the National Coalition of Ethnic Minority Nursing Associations, a group made up of five ethnic minority nursing associations that aims to build the cadre and preparation of ethnic minority nurses and promote equity in health care across ethnic minority populations (NCEMNA, 2010). This program is described at greater length in Chapter 5 . Another example of a successful program that has promoted racial and ethnic diversity is the ANA Minority Fellowship Program, 22 started in 1974 under the leadership of Dr. Hattie Bessent. This program has played a crucial role in supporting minority nurses with predoctoral and postdoctoral fellowships to advance research and clinical practice (Minority Fellowship Program, 2010). Programs to recruit and retain more individuals from racial and ethnic minority groups in nursing education programs are needed. A necessary first step toward accomplishing this goal is to create policies that increase the overall educational attainment of ethnic minorities (Coffman et al., 2001).
Gender Diversity
As noted in Chapter 3 , the nursing workforce historically has been composed predominantly of women. While the number of men who become nurses has grown dramatically in the last two decades, men still make up just 7 percent of all RNs (HRSA, 2010b). While most disciplines within the health professional workforce have become more gender balanced, the same has not been true for nursing. For example, in 2009 nearly half of medical school graduates were female (The Kaiser Family Foundation— statehealthfacts.org , 2010), a significant achievement of gender parity in a traditionally male-dominated profession. Stereotypes, academic acceptance, and role support are challenges for men entering the nursing profession. These barriers must be overcome if men are to be recruited in larger numbers to help offset the shortage of nurses and fill advanced and expanded nursing roles. Compounding the gender diversity problem of the nursing profession is the fact that fewer men in general are enrolling in higher education programs (Mather and Adams, 2007). While more men are being drawn to nursing, especially as a second career, the profession needs to continue efforts to recruit men; their unique perspectives and skills are important to the profession and will help contribute additional diversity to the workforce.
One professional organization that works to encourage men to join the nursing profession and supports men who do so is the American Assembly for Men in Nursing (AAMN). 23 To increase opportunities for men interested in joining the profession, the AAMN Foundation, in partnership with Johnson & Johnson, has awarded more than $50,000 in scholarships to undergraduate and graduate male nursing students since 2004 (AAMN, 2010b). Additionally, each year the AAMN recognizes the best school or college of nursing for men; in 2009, the honor was given to Monterey Peninsula College in Monterey, California, and Excelsior College in Albany, New York, for their “efforts in recruiting and retaining men in nursing, in providing men a supportive educational environment, and in educating faculty, students and the community about the contributions men have and do make to the nursing profession” (AAMN, 2010a).
- SOLUTIONS FROM THE FIELD
This chapter has outlined a number of challenges facing nursing education. These challenges have been the subject of much documentation, analysis, and debate (Benner et al., 2009; Erickson, 2002; IOM, 2003a, 2009; Lasater and Nielsen, 2009; Mitchell et al., 2006; Orsolini-Hain and Waters, 2009; Tanner et al., 2008). Various approaches to responding to these challenges and transforming curricula have been proposed, and several are being tested. The committee reviewed the literature on educational capacity and redesign, heard testimony about various challenges and potential solutions at the public forum in Houston, and chose a number of exemplars for closer examination. Three of these models are described in this section. The committee found that each of these models provided important insight into creative approaches to maximizing faculty resources, encouraging the establishment and funding of new faculty positions, maximizing the effectiveness of clinical education, and redesigning nursing curricula.
Veterans Affairs Nursing Academy
In 2007, the VA launched the VANA—a 5-year, $40 million pilot program—with the primary goals of developing partnerships with academic nursing institutes; expanding the number of faculty for baccalaureate programs; establishing partnerships to enhance faculty development; and increasing baccalaureate enrollment to increase the supply of nurses, not solely for the VA, but for the country at large. VANA also was aimed at encouraging interprofessional programs and increasing the retention and recruitment of VA nurses. 24
Since the program’s inception, three cycles of requests for proposals have been sent to more than 600 colleges and schools of nursing, as well as to institutions within the VA system. Fifteen geographically and demographically diverse pilot sites were selected to participate in VANA based on the strength of their proposals.
Each funded VANA partnership is required to have a rigorous evaluation plan to measure outcomes. Outcomes are expected to include increased staff, patient, student, and faculty satisfaction; greater scholarly output; enhanced professional development; better continuity and coordination of care; more reliance on evidence-based practice; and enhanced interprofessional learning. Each selected school is also expected to increase enrollment by at least 20 students a year.
The program has already resulted in 2,700 new students, with 620 receiving the majority of their clinical rotation experiences at the VA. The graduates of this program may include students who have pursued a traditional prelicensure BSN, a BSN through a second-degree program, or a BSN through an RN-to-BSN program. The number of nursing school faculty has increased by 176 and the number of VA faculty by 264.
In addition to the new nurses and faculty, educational innovations have encompassed curriculum revision, including quality and safety standards; DEUs (described earlier in Box 4-4 ); and a postgraduate baccalaureate nurse residency (see Chapter 3 ). Other changes include interprofessional simulation training and the development of evidence-based practice committees and programs. Beyond these specific changes and accomplishments, the VANA faculty has worked to develop the program into a single community of learning and to prepare students in a genuinely collaborative practice environment with clinically proficient staff and educators.
Carondolet Health Network
The Carondolet Health Network of Tucson, Arizona, is an example of how employers can offer educational benefits that improve both patient outcomes and the bottom line. Carondelet, which includes four hospitals and other facilities and employs approximately 1,650 nurses, is featured as one of seven cases studies in the Lewin Group’s 2009 report Wisdom at Work: Retaining Experienced RNs and Their Knowledge—Case Studies of Top Performing Organizations .
After Carondelet became part of Ascension Health in 2002, the Tucson organization embarked on a strategic plan to recruit and retain more nurses. Arizona faces some of the severest nursing shortages in the nation, and most nurses prefer to live and work in higher-paying markets, such as Phoenix or southern California. When Carondelet instituted an on-site BSN program, which it subsidized in exchange for a 2-year work commitment, the response was dramatic. Instead of an anticipated class size of 20 nurses in the first semester of the program, it enrolled 104. Of interest, it was the business case—the opportunity to decrease the amount of money the organization was spending on costly temporary nurses—that tipped the balance in favor of action (The Lewin Group, 2009).
Hospital Employee Education and Training
The Hospital Employee Education and Training (HEET) program was developed through a joint effort of the 1199NW local affiliate of the Service Employees International Union and the Washington State Hospital Association Work Force Institute to help address shortages in nursing and nursing-related positions through education and upgrading of incumbent workers. The program is administered through the Washington State Board for Community and Technical Colleges. Across the state, HEET-funded programs support industry-based reform of the education system and include preparation and completion of nursing career ladder programs. HEET seeks to develop educational opportunities that support both employer needs and the career aspirations of health care workers. It features cohort-based programs, distance learning, worksite classes, use of a simulation laboratory for nursing prerequisites, case management, tutoring support for those reentering academia, and nontraditional scheduling of classes to enable working adults to attend and address employee barriers to education.
The findings for this union-inspired initiative demonstrate its potential to increase racial/ethnic diversity in the nursing population. HEET participants represent a pool of potential nurses who are more diverse than the current nursing workforce. Providing on-site classes at hospitals appears to support the participation of working adults who are enrolled in nursing school while continuing to work at least part time. Workers participating in the HEET program have had lower attrition rates and higher rates of course completion compared with community college students in nursing career tracks. The curriculum also blends academic preparation with health care career education, thereby opening the doors of college to workers who might not otherwise enroll or succeed (Moss and Weinstein, 2009).
The future of access to basic primary care and nursing education will depend on increasing the number of BSN-prepared nurses. Unless this goal is met, the committee’s recommendations for greater access to primary care; enhanced, expanded, and reconceptualized roles for nurses; and updated nursing scopes of practice (see Chapter 7 ) cannot be achieved. The committee believes that increasing the proportion of the nursing workforce with a BSN from the current 50 percent to 80 percent by 2020 is bold but achievable. Achieving this target will help meet future demand for nurses qualified for advanced practice positions and possessing competencies in such areas as community care, public health, health policy, evidence-based practice, research, and leadership. The committee concludes further that the number of nurses holding a doctorate must be increased to produce a greater pool of nurses prepared to assume faculty and research positions. The committee believes a target of doubling the number of nurses with a doctorate by 2020 would meet this need and is achievable.
To achieve these targets, however, will require overcoming a number of barriers. The numbers of educators and clinical placements are insufficient for all the qualified applicants who wish to enter nursing school. There also is a shortage of faculty to teach nurses at all levels. Incentives for nurses at any level to pursue further education are few, and there are active disincentives against advanced education. Nurses and physicians—not to mention pharmacists and social workers—typically are not educated together and yet are increasingly required to cooperate and collaborate more closely in the delivery of care.
To address these barriers, innovative new programs to attract nursing faculty and provide a wider range of clinical education placements must clear long-stand ing bottlenecks. To this end, market-based salary adjustments must be made for faculty, and more scholarships must be provided to help nursing students advance their education. Accrediting and certifying organizations must mandate demonstrated mastery of clinical skills, managerial competencies, and professional development at all levels. Mandated skills, competencies, and professional development milestones must be updated on a more timely basis to keep pace with the rapidly changing demands of health care. All health professionals should receive more of their education in concert with students from other disciplines. Efforts also must be made to increase the diversity of the nursing workforce.
The nursing profession must adopt a framework of continuous lifelong learning that includes basic education, academic progression, and continuing competencies. More nurses must receive a solid education in how to manage complex conditions and coordinate care with multiple health professionals. They must demonstrate new competencies in systems thinking, quality improvement, and care management and a basic understanding of health care policy. Graduate-level nurses must develop an even deeper understanding of care coordination, quality improvement, systems thinking, and policy.
The committee emphasizes further that, as discussed in Chapter 2 , the ACA is likely to accelerate the shift in care from the hospital to the community setting. This transition will have a particularly strong impact on nurses, more than 60 percent of whom are currently employed in hospitals (HRSA, 2010b). Nurses may turn to already available positions in primary or chronic care or in public or community health, or they may pursue entirely new careers in emerging fields that they help create. Continuing and graduate education programs must support the transition to a future that rewards flexibility. In addition, the curriculum at many nursing schools, which places heavy emphasis on preparing students for employment in the acute care setting, will need to be rethought (Benner et al., 2009).
- AACN (American Association of Colleges of Nursing). 2005. Enrollment and graduations in bac calaureate and graduate programs in nursing, 2004-05 . Washington, DC: AACN.
- AACN. 2006. Enrollment and graduations in baccalaureate and graduate programs in nursing, 2005-06 . Washington, DC: AACN.
- AACN. 2007. Enrollment and graduations in baccalaureate and graduate programs in nursing, 2006-07 . Washington, DC: AACN.
- AACN. 2008. a. Enrollment and graduations in baccalaureate and graduate programs in nursing, 2007-08 . Washington, DC: AACN.
- AACN. 2008. b. The essentials of baccalaureate education for professional nursing practice . Washington, DC: AACN. Available from http://www .aacn.nche .edu/education/pdf/BaccEssentials08.pdf .
- AACN. 2009. a. Advancing higher education in nursing: 2009 annual report . Washington, DC: AACN.
- AACN. 2009. b. Enrollment and graduations in baccalaureate and graduate programs in nursing, 2008-09 . Washington, DC: AACN.
- AACN. 2009c. Student enrollment expands at U.S. Nursing colleges and universities for the 9th year despite financial challenges and capacity restraints . http://www .aacn.nche .edu/Media/NewsReleases /2009/StudentEnrollment.html (accessed March 13, 2010).
- AACN. 2010. a. Education policy: New policy statement from the Tri-Council for Nursing on the educational advancement of registered nurses . http://www .aacn.nche.edu/Education/ (accessed September 7, 2010).
- AACN. 2010. b. Enhancing diversity in the nursing workforce: Fact sheet updated March 2010 . http://www .aacn.nche .edu/Media/FactSheets/diversity.htm (accessed July 1, 2010).
- AACN. 2010. c. The impact of education on nursing practice . http://www .aacn.nche .edu/media/factsheets/impactednp.htm (accessed September 7, 2010).
- AACN and AAMC (Association of American Medical Colleges). 2010. Lifelong learning in medicine and nursing: Final conference report . Washington, DC: AACN and AAMC.
- AACN and Hartford (The John A. Hartford Foundation Institute for Geriatric Nursing). 2000. Older adults: Recommended baccalaureate competencies and curricular guidelines for geriatric nursing care . Washington, DC and New York: AACN and The John A. Hartford Foundation Institute for Geriatric Nursing.
- AAMN (American Assembly for Men in Nursing). 2010. a. Awards: Best nursing school/college for men in nursing . http://www .aamn.org/awschool.html (accessed September 10, 2010).
- AAMN. 2010. b. Scholarships . http://www .aamn.org/scholarships.html (accessed September 10, 2010).
- AARP. 2010. Preparation and roles of nursing care providers in America . http: //championnursing .org/resources/preparation-and-roles-nursing-care-providers-america (accessed August 17, 2010).
- ACHNE (Association of Community Health Nursing Educators). 2009. Essentials of baccalaure ate nursing education for entry level community/public health nursing . Wheat Ridge, CO: ACHNE.
- Aiken, L. H. 2010. Nursing education policy priorities . Paper commissioned by the Committee on the RWJF Initiative on the Future of Nursing, at the IOM (see Appendix I on CD-ROM).
- Aiken, L. H., S. P. Clarke, R. B. Cheung, D. M. Sloane, and J. H. Silber. 2003. Educational levels of hospital nurses and surgical patient mortality . JAMA 290(12):1617-1623. [ PMC free article : PMC3077115 ] [ PubMed : 14506121 ]
- Aiken, L. H., R. B. Cheung, and D. M. Olds. 2009. Education policy initiatives to address the nurse shortage in the United States . Health Affairs 28(4):w646-w656. [ PMC free article : PMC2718732 ] [ PubMed : 19525285 ]
- Alberto, J., and K. Herth. 2009. Interprofessional collaboration within faculty roles: Teaching, service, and research . OJIN: The Online Journal of Issues in Nursing 14(2).
- Allan, J., and J. Aldebron. 2008. A systematic assessment of strategies to address the nursing faculty shortage, U.S. Nursing Outlook 56(6):286-297. [ PubMed : 19041450 ]
- Allan, J., J. Stanley, M. Crabtree, K. Werner, and M. Swenson. 2005. Clinical prevention and population health curriculum framework: The nursing perspective . Journal of Professional Nursing 21(5):259-267. [ PubMed : 16179238 ]
- AMCB (American Midwifery Certification Board). 2009. Letter to certified nurse-midwives and certi fied midwives from B.W. Graves, president, AMCB . http://www .amcbmidwife .org/assets/documents /FINAL%20CMP%20LETTER3.pdf (accessed September 27, 2010).
- ANCC (American Nurses Credentialing Center). 2010. a. Adult nurse practitioner certification eligi bility criteria . http://www .nursecredentialing .org/Eligibility /AdultNPEligibility.aspx (accessed September 27, 2010).
- ANCC. 2010. b. ANCC nurse certification . http://www .nursecredentialing .org/Certification.aspx (accessed September 8, 2010).
- ANCC. 2010. c. Clinical nurse specialist in adult health certification eligibility criteria . http://www .nursecredentialing .org/Eligibility /AdultHealthCNSEligibility.aspx (accessed September 27, 2010).
- ASTDN (Association of State and Territorial Directors of Nursing). 2003. Quad council PHN com petencies . http://www .astdn.org /publication_quad_council _phn_competencies.htm (accessed September 7, 2010).
- Barr, H. 2002. Interprofessional education today, yesterday and tomorrow: A review . London: LTSN Hs&P.
- Barr, H., I. Koppel, S. Reeves, M. Hammick, and D. Freeth. 2005. Effective interprofessional educa tion: Argument, assumption & evidence . Oxford, England: Blackwell Publishing, Ltd.
- Baxter, P. 2007. The CCARE model of clinical supervision: Bridging the theory-practice gap . Nurse Education in Practice 7:103-111. [ PubMed : 17689431 ]
- Benner, P., M. Sutphen, V. Leonard, and L. Day. 2009. Educating nurses: A call for radical transfor mation . San Francisco, CA: Jossey-Bass.
- Berlin, L. E., and K. R. Sechrist. 2002. The shortage of doctorally prepared nursing faculty: A dire situation . Nursing Outlook 50(2):50-56. [ PubMed : 12029296 ]
- Bevill, J. W., Jr., B. L. Cleary, L. M. Lacey, and J. G. Nooney. 2007. Educational mobility of RNs in North Carolina: Who will teach tomorrow’s nurses? A report on the first study to longitudinally examine educational mobility among nurses . American Journal of Nursing 107(5):60-70; quiz 71. [ PubMed : 17443081 ]
- Blegen, M. A., T. E. Vaughn, and C. J. Goode. 2001. Nurse experience and education: Effect on quality of care . Journal of Nursing Administration 31(1):33-39. [ PubMed : 11198839 ]
- Bovjberg, R. 2009. The nursing workforce challenge: Public policy for a dynamic and complex market . Washington, DC: Urban Institute.
- Broome, M. E. 2009. Building the science for nursing education: Vision or improbable dream . Nurs ing Outlook 57(4):177-179. [ PubMed : 19631056 ]
- Carraccio, C. M. D., S. D. M. D. Wolfsthal, R. M. D. M. P. H. Englander, K. M. D. Ferentz, and C. P. Martin. 2002. Shifting paradigms: From Flexner to competencies . Academic Medicine 77(5):361-367. [ PubMed : 12010689 ]
- CCNE (Commission on Collegiate Nursing Education). 2009. Standards for accreditation of bac calaureate and graduate degree nursing programs . Washington, DC: CCNE.
- Cleary, B. L., A. B. McBride, M. L. McClure, and S. C. Reinhard. 2009. Expanding the capacity of nursing education . Health Affairs 28(4):w634-w645. [ PubMed : 19525284 ]
- Coffman, J. M., E. Rosenoff, and K. Grumbach. 2001. Racial/ethnic disparities in nursing . Health Affairs 20(3):263-272. [ PubMed : 11585176 ]
- Cronenwett, L. R. 2010. The future of nursing education . Paper commissioned by the Committee on the RWJF Initiative on the Future of Nursing, at the IOM (see Appendix I on CD-ROM).
- Cronenwett, L. R., and R. Redman. 2003. Partners in action: Nursing education and nursing practice . Journal of Nursing Administration 33(3):131-133. [ PubMed : 12629297 ]
- Cronenwett, L., G. Sherwood, J. Barnsteiner, J. Disch, J. Johnson, and P. Mitchell. 2007. Quality and safety education for nurses . Nursing Outlook 55(3):122-131. [ PubMed : 17524799 ]
- DeLunas, L. R., and L. A. Rooda. 2009. A new model for the clinical instruction of undergraduate nursing students . Nursing Education Perspectives 30(6):377-380. [ PubMed : 19999940 ]
- Duchscher, J. E. 2003. Critical thinking: Perceptions of newly graduated female baccalaureate nurses . Journal of Nursing Education 42(1):14-27. [ PubMed : 12555818 ]
- Erickson, H. 2002. Concept-based curriculum and instruction: Teaching beyond the facts . Thousand Oaks, CA: Corwin Press.
- Estabrooks, C. A., W. K. Midodzi, G. G. Cummings, K. L. Ricker, and P. Giovannetti. 2005. The impact of hospital nursing characteristics on 30-day mortality . Nursing Research 54(2):74-84. [ PubMed : 15778649 ]
- Fagin, C. M. 1986. Institutionalizing faculty practice . Nursing Outlook 34(3):140-144. [ PubMed : 3635036 ]
- Florida Center for Nursing. 2010. Florida nursing education capacity and nurse faculty supply/ demand: 2007-2009 trends . http://www .flcenterfornursing .org/files/2010 _Education_Report.pdf (accessed March 29, 2010).
- Friese, C. R., E. T. Lake, L. H. Aiken, J. H. Silber, and J. Sochalski. 2008. Hospital nurse practice environments and outcomes for surgical oncology patients . Health Services Research 43(4):1145-1163. [ PMC free article : PMC2517272 ] [ PubMed : 18248404 ]
- Gilliss, C. L. 2010. Nursing education: Leading into the future . Cronenwett, L. R. 2010. The future of nursing education. Paper commissioned by the Committee on the RWJF Initiative on the Future of Nursing, at the IOM (see Appendix I on CD-ROM).
- Gonyea, M. A. 1998. Assessing resource requirements and financing for health professions education . In Mission management: A new synthesis , edited by E. R. Rubin, editor. . Washington, DC: Association of Academic Health Centers. Pp.217-233.
- Goode, C. J., S. Pinkerton, M. P. McCausland, P. Southard, R. Graham, and C. Krsek. 2001. Documenting chief nursing officers’ preference for BSN-prepared nurses . Journal of Nursing Ad ministration 31(2):55-59. [ PubMed : 11271678 ]
- Gubrud-Howe, P., K. Shaver, C. Tanner, J. Bennett-Stillmaker, S. Davidson, M. Flaherty-Robb, K. Goudreau, L. Hardham, C. Hayden, S. Hendy, S. Omel, K. Potempa, L. Shores, S. Theis, and P. Wheeler. 2003. A challenge to meet the future: Nursing education in Oregon, 2010 . Journal of Nursing Education 42(4):163-167. [ PubMed : 12710807 ]
- Harden, R. M. 2002. Developments in outcome-based education . Medical Teacher 24 (2):117-120. [ PubMed : 12098427 ]
- Harder, B. N. 2010. Use of simulation in teaching and learning in health sciences: A systematic review . Journal of Nursing Education 49(1):23-28. [ PubMed : 19731886 ]
- HRSA (Health Resources and Services Administration). 2004. Supply, demand, and use of licensed practical nurses . Rockville, MD: HRSA.
- HRSA. 2006. The registered nurse population: Findings from the National Sample Survey of Regis tered Nurses, March 2004 . Rockville, MD: HRSA.
- HRSA. 2010. a. HRSA Geospatial Data Warehouse (HGDW) . http: //datawarehouse .hrsa.gov/nursingsurvey.aspx (accessed September 2, 2010).
- HRSA. 2010. b. The registered nurse population: Findings from the 2008 National Sample Survey of Registered Nurses . Rockville, MD: HRSA.
- IOM (Institute of Medicine). 2003. a. Health professions education: A bridge to quality . Washington, DC: The National Academies Press. [ PubMed : 25057657 ]
- IOM. 2003. b. Health professions education: A bridge to quality . Washington, DC: The National Academies Press. [ PubMed : 25057657 ]
- IOM. 2009. Redesigning continuing education in the health professions . Washington, DC: The National Academies Press. [ PubMed : 25032352 ]
- IOM. 2010. A summary of the February 2010 Forum on the Future of Nursing: Education . Washington, DC: The National Academies Press. [ PubMed : 25032390 ]
- Ironside, P. 2004. “Covering content” and teaching thinking: Deconstructing the additive curriculum . Journal of Nursing Education 43(1):5-12. [ PubMed : 14748529 ]
- The Kaiser Family Foundation—statehealthfacts.org. 2010. Distribution of medical school graduates by gender, 2009 . http://www .statehealthfacts .org/comparetable .jsp?ind=435&cat =8&sub =101&yr=92&typ=1 (accessed September 10, 2010).
- Kovner, C., and M. Djukic. 2009. The nursing career process from application through the first 2 years of employment . Journal of Professional Nursing 25(4):197-203. [ PubMed : 19616187 ]
- Kovner, C. T., S. Fairchild, and L. Jacobson. 2006. Nurse educators 2006: A report of the faculty census survey of RN and graduate programs . Washington, DC: NLN.
- Kovner, C. T., C. S. Brewer, S. Yingrengreung, and S. Fairchild. 2010. New nurses’ views of quality improvement education . Joint Commission Journal on Quality and Patient Safety 36(1):29-35. [ PubMed : 20112663 ]
- Kowalski, K., M. Horner, K. Carroll, D. Center, K. Foss, and S. Jarrett. 2007. Nursing clinical faculty revisited: The benefits of developing staff nurses as clinical scholars . Journal of Continuing Education in Nursing 38:69-75. [ PubMed : 17402378 ]
- Kreulen, G. J., P. K. Bednarz, T. Wehrwein, and J. Davis. 2008. Clinical education partnership: A model for school district and college of nursing collaboration . The Jour n al of Schoo l Nursing 24(6):360-369. [ PubMed : 19114466 ]
- Kruger, B. J., C. Roush, B. J. Olinzock, and K. Bloom. 2010. Engaging nursing students in long-term relationships with a home-base community . Journal of Nursing Education 49(1):10-16. [ PubMed : 19731887 ]
- Lane, A. 2009. Battle of degrees heats up: Universities, community colleges spar over four-year pro grams . http://www .crainsdetroit .com/article/20091129/FREE/311299958 (accessed November 29, 2009).
- Lasater, K., and A. Nielsen. 2009. The influence of concept-based learning activities on students’ clinical judgment development Journal of Nursing Education 48(8):441-446. [ PubMed : 19681533 ]
- The Lewin Group. 2009. Wisdom at work: Retaining experienced RNs and their knowledge—case studies of top performing organizations . Falls Church, VA.
- Lynaugh, J. E. 2008. Kate Hurd-Mead lecture. Nursing the great society: The impact of the Nurse Training Act of 1964 . Nursing History Review 16:13-28. [ PubMed : 18595339 ]
- Lynaugh, J. E., and B. L. Brush. 1996. American nursing: From hospitals to health systems . Cambridge, MA and Oxford, U.K.: Blackwell Press.
- Manno, B. V. 1998. Vocabulary lesson: Cost, price, and subsidy in American higher education . Busi ness Officer 31(10):22-25.
- Mather, M., and D. Adams. 2007. The crossover in female-male college enrollment rates . http://www .prb.org/articles /2007/crossoverinfemalemalecollegeenrollmentrates .aspx (accessed September 10, 2010).
- McNelis, A. M., and P. M. Ironside. 2009. National survey on clinical education in prelicensure nursing education programs . In Clinical nursing education: Current reflections , edited by N. Ard, editor; and T. M. Valiga, editor. . New York: National League for Nursing.
- MedPAC (Medicare Payment Advisory Commission). 2009. Report to the Congress: Improving incen tives in the Medicare program . Washington, DC: MedPAC.
- Minority Fellowship Program. 2010. Background . http://www .emfp.org/MainMenuCategory /AboutMFP/Background .aspx (accessed September 8, 2010).
- Mitchell, P. H., B. Belza, D. C. Schaad, L. S. Robins, F. J. Gianola, P. S. Odegard, D. Kartin, and R. A. Ballweg. 2006. Working across the boundaries of health professions disciplines in education, research, and service: The University of Washington experience . Academic Medicine 81(10):891-896. [ PubMed : 16985349 ]
- Moscato, S. R., J. Miller, K. Logsdon, S. Weinberg, and L. Chorpenning. 2007. Dedicated education unit: An innovative clinical partner education model . Nursing Outlook 55(1):31-37. [ PubMed : 17289465 ]
- Moss, H., and M. Weinstein. 2009. Addressing the skills shortage in healthcare through the develop ment of incumbent employees: Hospital employee education and training (HEET) program . Eugene, OR: University of Oregon Labor Education and Research Center.
- NBCRNA (National Board on Certification and Recertification of Nurse Anesthetists). 2009. Recerti fication . http://www .nbcrna.com/recertification .html (accessed September 28, 2010).
- NCEMNA (National Coalition of Ethnic Minority Nurse Associations). 2010. About NCEMNA . http://www .ncemna.org/about.asp (accessed July 2, 2010).
- NCSBN (National Council of State Boards of Nursing). 2008. Member board profiles National Council of State Boards of Nursing . https://www .ncsbn.org/MBP_PDF.pdf (accessed September 3, 2010).
- NCSBN. 2009. NCLEX examination pass rates, 2009 . https://www .ncsbn.org /Table_of_Pass_Rates_2009.pdf (accessed March 30, 2010).
- NLN (National League for Nursing). 2007. Reflection & dialogue: Academic/professional progression in nursing . http://www .nln.org/aboutnln /reflection_dialogue/refl_dial_2 .htm (accessed September 8, 2010).
- NLN. 2009. Annual survey of schools of nursing academic year 2008-2009 . New York: NLN.
- NLN. 2010. a. 2010 NLN nurse educator shortage fact sheet . http://www .nln.org/governmentaffairs /pdf /NurseFacultyShortage.pdf (accessed July 2, 2010).
- NLN. 2010. b. Nursing education research: Graduations from RN programs . http://www .nln.org/research /slides/topic_graduations_rn.htm (accessed September 8, 2010).
- NLN. 2010. c. Percentage of minority students enrolled in nursing programs by race-ethnicity and program type, 2008-2009 . http://www .nln.org/research /slides/pdf/AS0809_F14.pdf (accessed September 5, 2010.
- NLN Board of Governors. 2003. Position statement: Innovation in nursing education: A call to reform . http://www .nln.org/aboutnln /positionstatements /innovation082203.pdf (accessed September 27, 2010).
- NLNAC (National League for Nursing Accrediting Commission). 2008. NLNAC 2008 standards and criteria . http://www .nlnac.org/manuals/SC2008.htm (accessed March 11, 2010).
- NRC (National Research Council). 2005. Advancing the nation’s health needs: NIH research training programs . Washington, DC: National Academy of Sciences. [ PubMed : 20669451 ]
- O’Neil, E. H., and Pew Health Professions Commission. 1998. Recreating health professional prac tice for a new century: The fourth report of the Pew Health Professions Commission . San Francisco: CA.
- O’Neil, E. 2009. Four factors that guarantee health care change . Journal of Professional Nursing 25(6):317-321. [ PubMed : 19942196 ]
- Oregon Center for Nursing. 2009. Oregon’s nurse faculty workforce: A report from the oregon center for nursing . http://www .oregoncenterfornursing .org/documents /OCN%20Nurse%20Faculty %20Workforce%20Report%202009 .pdf (accessed March 22, 2010).
- Orsolini-Hain, L. 2008. An interpretive phenomenological study on the influences on associate degree prepared nurses to return to school to earn a higher degree in nursing , Department of Nursing, University of California, San Francisco.
- Orsolini-Hain, L., and V. Waters. 2009. Education evolution: A historical perspective of associate degree nursing . Journal of Nursing Education 48(5):266-271. [ PubMed : 19476031 ]
- Raines, C. F. 2010. The doctor of nursing practice: A report on progress . Paper presented at AACN Spring Annual Meeting 2010.
- Reeves, S., M. Zwarenstein, J. Goldman, H. Barr, D. Freeth, M. Hammick, and I. Koppel. 2008. Interprofessional education: Effects on professional practice and health care outcomes . Cochrane Database of Systematic Reviews (1):CD002213. [ PubMed : 18254002 ]
- Rosenstein, A. H., and M. O’Daniel. 2005. Disruptive behavior and clinical outcomes: Perceptions of nurses and physicians . American Journal of Nursing 105(1):54-64; quiz 64-55. [ PubMed : 15659998 ]
- Rosenstein, A. H., and M. O’Daniel. 2008. A survey of the impact of disruptive behaviors and communication defects on patient safety . Joint Commission Journal on Quality and Patient Safety 34(8):464-471. [ PubMed : 18714748 ]
- RWJF (Robert Wood Johnson Foundation). 2010. a. Distance between nursing education program and workplace for early career nurses (graduated 2007-2008) . http: //thefutureofnursing .org/NursingResearchNetwork5 (accessed December 6, 2010).
- RWJF. 2010. b. Qualified applicants not accepted in Associate (AD) and Baccalaureate (BS) RN programs . http: //thefutureofnursing .org/NursingResearchNetwork6 (accessed December 15, 2010).
- RWJF. 2010. c. Sermo.Com survey data on physicians’ opinions of nurse practitioners and nurses’ educational preparation . http: //thefutureofnursing .org/NursingResearchNetwork8 (accessed December 15, 2010).
- Sales, A., N. Sharp, Y. F. Li, E. Lowy, G. Greiner, C. F. Liu, A. Alt-White, C. Rick, J. Sochalski, P. H. Mitchell, G. Rosenthal, C. Stetler, P. Cournoyer, and J. Needleman. 2008. The association between nursing factors and patient mortality in the Veterans Health Administration: The view from the nursing unit level . Medical Care 46(9):938-945. [ PubMed : 18725848 ]
- Schaefer, K. M., and D. Zygmont. 2003. Analyzing the teaching style of nursing faculty. Does it promote a student-centered or teacher-centered learning environment? Nursing Education Per spectives 24(5):238-245. [ PubMed : 14535144 ]
- Starck, P. L. 2005. The cost of doing business in nursing education . Journal of Professional Nursing 21(3):183-190. [ PubMed : 16021562 ]
- Sullivan Commission on Diversity in the Healthcare Workforce. 2004. Missing persons: Minorities in the health professions: A report of the Sullivan Commission on Diversity in the Healthcare Workforce . Washington, DC: The Sullivan Commission.
- Tanner, C. A. 2007. The curriculum revolution revisited . Journal of Nursing Education 46(2):51-52. [ PubMed : 17315561 ]
- Tanner, C. A., P. Gubrud-Howe, and L. Shores. 2008. The Oregon Consortium for Nursing Education: A response to the nursing shortage . Policy, Politics & Nursing Practice 9(3):203-209. [ PubMed : 18829605 ]
- Tilden, V. 2010. The future of nursing education . Paper commissioned by the Committee on the RWJF Initiative on the Future of Nursing, at the IOM (see Appendix I on CD-ROM).
- Tourangeau, A. E., D. M. Doran, L. McGillis Hall, L. O’Brien Pallas, D. Pringle, J. V. Tu, and L. A. Cranley. 2007. Impact of hospital nursing care on 30-day mortality for acute medical patients . Journal of Advanced Nursing 57(1):32-44. [ PubMed : 17184372 ]
- Udlis, K. A. 2006. Preceptorship in undergraduate nursing education: An intergrative review . Journal of Nursing Education 47(1):20-29. [ PubMed : 18232611 ]
- Valberg, L. S., M. A. Gonyea, D. G. Sinclair, and J. Wade. 1994. Planning the future academic medical centre . Canadian Medical Association Journal 151(11):1581-1587. [ PMC free article : PMC1337369 ] [ PubMed : 7954157 ]
- Van den Heede, K., E. Lesaffre, L. Diya, A. Vleugels, S. P. Clarke, L. H. Aiken, and W. Sermeus. 2009. The relationship between inpatient cardiac surgery mortality and nurse numbers and educational level: Analysis of administrative data . International Journal of Nursing Studies 46(6):796-803. [ PMC free article : PMC2856596 ] [ PubMed : 19201407 ]
The summary also can be downloaded at http://www .iom.edu .
While titles for LPNs and LVNs vary from state to state, their responsibilities and education are relatively consistent. LPNs/LVNs are required to pass the National Council Licensure Examination for Practical Nurses (NCLEX-PN) to secure a license to practice.
See https://www .ncsbn.org/nclex.htm .
See http://www .aacn.nche .edu/education/pdf/BaccEssentials08.pdf .
“Difficult” is the sum of schools responding either “somewhat difficult” or “very difficult.” Personal communication, Kathy A. Kaufman, Senior Research Scientist, Public Policy, National League for Nursing, September 8, 2010.
Personal communication, Joanne Spetz, Professor, Community Health Systems, University of California, San Francisco, September 2, 2010.
Patient Protection and Affordable Care Act , HR 3590 § 5311, 111th Congress.
Personal communication, Di Fang, Director of Research and Data Services, AACN, March 3, 2010.
This paragraph, and the three that follow, were adapted from a paper commissioned by the committee on “Transforming Pre-Licensure Nursing Education: Preparing the New Nurse to Meet Emerging Health Care Needs,” prepared by Christine A. Tanner, Oregon Health & Science University School of Nursing (see Appendix I on CD-ROM).
See http://sirc .nln.org/ .
Available evidence is based on evaluation of BSN programs and curricula. Evidence was not available for ADN or diploma programs.
Nursing-related doctoral degrees are defined by the National Sample Survey of Registered Nurses as non-nursing degrees that are directly related to a nurse’s career in the nursing profession. “Nursing-related degrees include public health, health administration, social work, education, and other fields” (HRSA, 2010b).
See http://www .aacn.nche .edu/dnp/pdf/essentials.pdf .
Personal communication, Jean Johnson, Dean, School of Nursing, George Washington University, September 3, 2010.
Some faculty development programs and training opportunities are offered through universities and professional organizations, such as the AACN and the NLN. Additionally, the NLN offers a certification program for nurse educators, who can publically confirm knowledge in the areas of pedagogy, learning, and the complex encounter between educator and student. This certification program can provide a basis for innovation and the continuous quality improvement of nursing education.
See http://www .ocne.org/ .
Personal communication, Kathy Apple, CEO, NCSBN, May 30, 2010.
This paragraph draws upon a paper commissioned by the committee on “The Future of Nursing Education,” prepared by Virginia Tilden, University of Nebraska Medical Center College of Nursing (see Appendix I on CD-ROM).
Personal communication, Geraldine Bednash, CEO, AACN, August 12, 2010.
See http://www .emfp.org/ .
See http://www .aamn.org/ .
This paragraph, and the three that follow, draw upon a presentation made by Cathy Rick, chief nursing officer for the VA, at the Forum on the Future of Nursing: Education, held in Houston, TX on February 22, 2010 (see Appendix C ) and published in A Summary of the February 2010 Forum on the Future of Nursing: Education (IOM, 2010).
- Cite this Page Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. Washington (DC): National Academies Press (US); 2011. 4, Transforming Education.
- PDF version of this title (6.0M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Transforming Education - The Future of Nursing Transforming Education - The Future of Nursing
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
8 templates
memorial day
12 templates

ocean theme
44 templates
environmental science
36 templates

art portfolio
82 templates
49 templates
Nursing Presentation templates
They draw your blood when you have a blood test. they give you vaccinations. they assist doctors with critical tasks and help the elderly if they need it. that's right, we're talking about nurses take a look at these designs about nursing..

It seems that you like this template!
Aquatic and physical therapy center.
The way we present our company says a lot about it. This time we bring you a perfect template for aquatic therapy centers. Its background is white, which contrasts with the waves in blue and gray tones, simulating the movement of water. Edit the graphics, show your milestones and explain...
Premium template
Unlock this template and gain unlimited access
Pregnancy Breakthrough
Giving birth to a baby is a beautiful occasion, a manifestation of love between two people. Obstetrics are key during pregnancy, so how about giving a presentation about the latest breakthrough in this field? Our free medical template will come in handy.

Patients and Nurses Medical Theme
As the backbone of every healthcare system, nurses play an integral role in providing top-notch patient care. Whether it's administering medication, monitoring vital signs, or simply holding a hand, these dedicated professionals are the ones keeping our loved ones safe and comfortable during their time of need. But let's not...

Pastel Palette Doctor Theme
Presentations on health and medical topics can be challenging to create, but this Google Slides & PowerPoint template is here to rescue you! This multi-purpose layout is designed with blue pastel tones, providing a professional and calm environment to showcase your medical expertise to colleagues, students, or patients. The template...

Medical Imaging Techniques Breakthrough

Cream & Pastel Palette Healthcare Center Characters
Let us introduce you to a new way of presenting healthcare centers. Did you think that we were going to use blue? Tut-tut! This time, the palette revolves around cream (the color of the backgrounds) and other pastel tones. As you explain in detail (or in brief) your healthcare services,...

National Library of Medicine
How many books about medicine can there be? And medical centers? We can't give you an exact number, but what we can offer you is a template for Google Slides and PowerPoint to present your medical center. In a simple, but direct style, you can talk about your center, where...

STI Case Report: HPV
Download the STI Case Report: HPV presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...

Idiopathic Aplastic Anemia Case Report
Download the Idiopathic Aplastic Anemia Case Report presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals...
Hand Drawn Style Healthcare Center
If you need to present a healthcare center, the overall aesthetic you might be looking for is something peaceful and pretty. Something that makes your center look approachable and safe. In that case, we have the perfect template for you! These slides will make your presentation super calm and attractive:...

Cervical Cancer Disease
Download the Cervical Cancer Disease presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking medical...

Clinical Case 06-2023
Slidesgo is back with a new free medical template, perfect for a presentation about a clinical case. The design is very appealing, so these slides are a nice tool to provide a lot of useful information for doctors and researchers.

Health Problems due to Air Pollution Breakthrough
Download the Health Problems due to Air Pollution Breakthrough presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news....

Bronchitis Cough Breakthrough
Download the Bronchitis Cough Breakthrough presentation for PowerPoint or Google Slides. Gone are the days of dreary, unproductive meetings. Check out this sophisticated solution that offers you an innovative approach to planning and implementing meetings! Detailed yet simplified, this template ensures everyone is on the same page, contributing to a...

Alcoholism Treatment Drugs Breakthrough
Drug addictions are a difficult condition to treat, but thanks to the investigations and studies conducted by health professionals, new breakthroughs are appearing to help people who suffer them. Speak about it with this visual design for breakthrough news and share the treatment you have discovered with the medical community!...
Clinical Case 04-2023
When trying to prevent diseases, information is key, and if it’s reliable, all the better. With this new free medical template, you can show the results of a clinical case, including the symptoms, the patient monitoring, the treatment and all the important data. Its design will help you grab your...

Electrocardiogram (EKG) Test Breakthrough
Download the Electrocardiogram (EKG) Test Breakthrough presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news. Should there be...

Clinical Case 01-2023
Present your clinical case to the medical community with this dynamic and engaging presentation by Slidesgo. Who said science can’t be creative and fun?
- Page 1 of 163
Great presentations, faster
Slidesgo for Google Slides :
The easy way to wow
Register for free and start editing online
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Handwashing
- Hand Hygiene as a Family Activity
- Hand Hygiene FAQs
- Handwashing Facts
- Publications, Data, & Statistics
- Health Promotion Materials
- Global Handwashing Day
- Clean Hands and Spaces: Handwashing and Cleaning in Educational Facilities
- Life is Better with Clean Hands Campaign
- Clinical Safety
- Healthcare Training
- Clean Hands Count Materials
About Hand Hygiene for Patients in Healthcare Settings
- Patients in healthcare settings are at risk of getting infections while receiving treatment for other conditions.
- Cleaning your hands can prevent the spread of germs, including those that are resistant to antibiotics, and protects healthcare personnel and patients.
- Patients and their loved ones can play a role in asking and reminding healthcare personnel to clean their hands.
Your hands can spread germs.
- Hands have good germs that your body needs to stay healthy. Hands can also have bad germs on them that make you sick.
Alcohol-based hand sanitizer kills most of the bad germs that make you sick.
- Alcohol-based hand sanitizers kill the good and bad germs, but the good germs quickly come back on your hands.
Alcohol-based hand sanitizer does not create antimicrobial-resistant germs.
- Alcohol-based hand sanitizers kill germs quickly and in a different way than antibiotics.
- Using alcohol-based hand sanitizers to clean your hands does not cause antimicrobial resistance.
Steps to take
When patients and visitors should clean their hands.
- Before preparing or eating food.
- Before touching your eyes, nose, or mouth.
- Before and after changing wound dressings or bandages.
- After using the restroom.
- After blowing your nose, coughing, or sneezing.
- After touching hospital surfaces such as bed rails, bedside tables, doorknobs, remote controls, or the phone.
How to clean hands
With an alcohol-based hand sanitizer:.
- Put product on hands and rub hands together.
- Cover all surfaces until hands feel dry.
- This should take around 20 seconds.
With soap and water:
- Wet your hands with warm water. Use liquid soap if possible. Apply a nickel- or quarter-sized amount of soap to your hands.
- Rub your hands together until the soap forms a lather and then rub all over the top of your hands, in between your fingers and the area around and under the fingernails.
- Continue rubbing your hands for at least 15 seconds. Need a timer? Imagine singing the "Happy Birthday" song twice.
- Rinse your hands well under running water.
- Dry your hands using a paper towel if possible. Then use your paper towel to turn off the faucet and to open the door if needed.
Clean Hands Count Campaign Materials
Ask your healthcare provider to clean their hands.
- Wearing gloves alone is not enough for your healthcare provider to prevent the spread of infection.
- "Before you start the exam, would you mind cleaning your hands again?"
- "Would it be alright if you cleaned your hands before changing my bandages?"
- "I didn't see you clean your hands when you came in, would you mind cleaning them again before you examine me?"
- "I'm worried about germs spreading in the hospital. Will you please clean your hands once more before you start my treatment?"
Speak up for clean hands in healthcare settings
- Clean your own hands and ask those around you to do the same.
- Don't be afraid to use your voice: it's okay to ask your healthcare provider to clean their hands.
- "I saw you clean your hands when you arrived some time ago, but would you mind cleaning them again?"
Frequently asked questions
Is there such a thing as too clean.
- Germs are everywhere. They are within and on our bodies and on every surface you touch. But not all germs are bad. We need some of these germs to keep us healthy and our immune system strong.
- Your hands have good germs on them that your body needs to stay healthy. These germs live under the deeper layers of the skin.
- Your hands can also have bad germs on them that make you sick. These germs live on the surface and are easily killed/wiped away by the alcohol-based hand sanitizer.
- Using an alcohol-based hand sanitizer is the preferred way for to keep your hands clean.
Washing with soap and water: 15 versus 20 seconds
- Wash your hands for more than 15 seconds, not exactly 15 seconds.
- The time it takes is less important than making sure you clean all areas of your hands.
- Alcohol-based hand sanitizers are the preferred way to clean your hands in healthcare facilities.
Which one? Soap and water versus alcohol-based hand sanitizer
An alcohol-based hand sanitizer is the preferred method for cleaning your hands when they are not visibly dirty because it:
- Is more effective at killing potentially deadly germs on hands than soap.
- when moving from soiled to clean activities with the same patient or resident.
- when moving between patients or residents in shared rooms or common areas.
- Improves skin condition with less irritation and dryness than soap and water.
Guidelines for Hand Hygiene in Healthcare Settings Published 2002
Core Infection Prevention and Control Practices for Safe Healthcare Delivery in All Settings

What CDC is doing
CDC's Clean Hands Count campaign offers posters, factsheets, and brochures for healthcare providers and patients.
Keep reading: Clean Hands Count materials
Healthcare personnel
When and how to practice hand hygiene. Learn more .
New Training and Education Resources available for Healthcare Professionals.
Hand Hygiene in Healthcare Settings Video Series link: Education Courses | Hand Hygiene | CDC
Clean Hands
Having clean hands is one of the best ways to avoid getting sick and prevent the spread of germs to others.
For Everyone
Health care providers.
- Open access
- Published: 14 May 2024
Evaluation of the feasibility of a midwifery educator continuous professional development (CPD) programme in Kenya and Nigeria: a mixed methods study
- Duncan N. Shikuku 1 , 2 ,
- Hauwa Mohammed 3 ,
- Lydia Mwanzia 4 ,
- Alice Norah Ladur 2 ,
- Peter Nandikove 5 ,
- Alphonce Uyara 6 ,
- Catherine Waigwe 7 ,
- Lucy Nyaga 1 ,
- Issak Bashir 8 ,
- Eunice Ndirangu 9 ,
- Carol Bedwell 2 ,
- Sarah Bar-Zeev 10 &
- Charles Ameh 2 , 11 , 12
BMC Medical Education volume 24 , Article number: 534 ( 2024 ) Cite this article
196 Accesses
9 Altmetric
Metrics details
Midwifery education is under-invested in developing countries with limited opportunities for midwifery educators to improve/maintain their core professional competencies. To improve the quality of midwifery education and capacity for educators to update their competencies, a blended midwifery educator-specific continuous professional development (CPD) programme was designed with key stakeholders. This study evaluated the feasibility of this programme in Kenya and Nigeria.
This was a mixed methods intervention study using a concurrent nested design. 120 randomly selected midwifery educators from 81 pre-service training institutions were recruited. Educators completed four self-directed online learning (SDL) modules and three-day practical training of the blended CPD programme on teaching methods (theory and clinical skills), assessments, effective feedback and digital innovations in teaching and learning. Pre- and post-training knowledge using multiple choice questions in SDL; confidence (on a 0–4 Likert scale) and practical skills in preparing a teaching a plan and microteaching (against a checklist) were measured. Differences in knowledge, confidence and skills were analysed. Participants’ reaction to the programme (relevance and satisfaction assessed on a 0–4 Likert scale, what they liked and challenges) were collected. Key informant interviews with nursing and midwifery councils and institutions’ managers were conducted. Thematic framework analysis was conducted for qualitative data.
116 (96.7%) and 108 (90%) educators completed the SDL and practical components respectively. Mean knowledge scores in SDL modules improved from 52.4% (± 10.4) to 80.4% (± 8.1), preparing teaching plan median scores improved from 63.6% (IQR 45.5) to 81.8% (IQR 27.3), and confidence in applying selected pedagogy skills improved from 2.7 to 3.7, p < 0.001. Participants rated the SDL and practical components of the programme high for relevance and satisfaction (median, 4 out of 4 for both). After training, 51.4% and 57.9% of the participants scored 75% or higher in preparing teaching plans and microteaching assessments. Country, training institution type or educator characteristics had no significant associations with overall competence in preparing teaching plans and microteaching ( p > 0.05). Qualitatively, educators found the programme educative, flexible, convenient, motivating, and interactive for learning. Internet connectivity, computer technology, costs and time constraints were potential challenges to completing the programme.
The programme was feasible and effective in improving the knowledge and skills of educators for effective teaching/learning. For successful roll-out, policy framework for mandatory midwifery educator specific CPD programme is needed.
Peer Review reports
Introduction
Quality midwifery education underpins the provision of quality midwifery care and is vital for the health and well-being of women, infants, and families [ 1 ]. The recent State of the World’s Midwifery report (SoWMy) (2021) indicates that urgent investments are needed in midwifery, especially quality midwifery education, to improve health outcomes for women and neonates. Despite evidence to support midwifery, midwifery education and training is grossly underfunded in low- and middle-income countries (LMICs) with variation in the quality, content and duration of content between and within countries [ 2 ]. Barriers to achieving quality education are: inadequate content, lack of learning and teaching materials, insufficient and poorly trained educators and weak regulation, midwifery educators having no connection with clinical practice or opportunities for updating their knowledge or skills competencies [ 3 , 4 ].
The WHO, UNFPA, UNICEF and the International Confederation of Midwives’ (ICM) seven-step action plan to strengthen quality midwifery education, and ICM’s four pillars for midwives to achieve their potential emphasize strengthening midwifery faculty to teach students as a key priority [ 4 , 5 ]. Consequently, ICM recommends that (i) at least 50% of midwifery education curriculum should be practise-based with opportunities for clinical experience, (ii) midwifery faculty should use fair, valid and reliable formative and summative assessment methods to measure student performance and progress in learning and (iii) midwifery programmes have sufficient and up-to-date teaching and learning resources and technical support for virtual/distance learning to meet programme needs [ 6 ]. To achieve this, WHO’s Midwifery Educator Core Competencies and ICM’s Global Standards for Midwifery Education provide core competencies that midwifery educators must possess for effective practice [ 6 , 7 ]. The WHO’s global midwifery educator survey in 2018–2019 reported that fewer than half of the educators (46%) were trained or accredited as educators [ 5 ]. Educators are important determinants of quality graduates from midwifery programmes [ 7 ]. However, the survey identified that none of the educators felt confident in all of WHO’s midwifery educator core competencies [ 5 ]. Further evidence shows that many midwifery educators are more confident with theoretical classroom teaching than clinical teaching despite advances in teaching methods and have low confidence in facilitating online/virtual teaching and learning [ 4 , 8 , 9 ]. To remain competent, design and deliver competency-based curriculum and strengthen midwifery practice, ICM and WHO emphasize that midwifery faculty should engage in ongoing professional development as a midwifery practitioner, teacher/lecturer and leader [ 6 , 10 , 11 ]. However in many settings there is inadequate provision or access to faculty development opportunities [ 12 ].
Continuous professional development (CPD)
Continuous professional development has been defined as the means by which members of the profession maintain, improve and broaden their knowledge, expertise, and competence, and develop the personal and professional qualities required throughout their professional lives [ 13 ]. This can be achieved through multiple formal educational pathways based on the ICM Global Standards for Midwifery Education whilst incorporating the ICM Essential Competencies for Basic Midwifery Practice [ 6 , 14 ]. There are formal CPD activities where there is structured learning that often follows set curricula, usually approved by independent accreditation services or informal CPD that is usually self-directed learning. Participating in accredited CPD programmes is beneficial to the profession. A requirement of regular CPD renewal by a country to maintain licensure ensures an up-to-date, relevant nursing and midwifery workforce [ 15 ] and increases the legitimacy of CPD [ 16 ]. Structured learning (direct or distant), mandatory training, attending workshops and conferences, accredited college/university courses and trainings, research and peer review activities are opportunities for CPD [ 17 ]. Importantly, these CPD programmes are essential for safe, competent and effective practice that is essential to the universal health coverage (UHC) & maternal and newborn health SDGs agenda particularly in developing countries [ 18 , 19 ].
Whilst regulatory bodies and employers in many countries have requirements for midwives to complete CPD programmes and activities, these programmes and supporting activities are found to be ineffective if CPD is irrelevant to the practitioners’ practice setting, attended only because of monetary or non-monetary benefits, geared towards improving a skill for which there is no demonstrated need, and taken only to meet regulatory requirements rather than to close a competency gap [ 20 ]. In most LMICs, midwifery licensure is permanent, without obligation to demonstrate ongoing education or competence [ 15 ]. Consequently, CPD processes are not in place, and if in place, not fully utilised. A systematic review on CPD status in WHO regional office for Africa member states reported that nurses and midwives are required to attend formalised programmes delivered face-to-face or online, but only16 out of 46 (34.7%) member states had mandatory CPD programmes [ 15 ]. This underscores the need for designing regulator approved midwifery educator CPD programmes to improve the quality of midwifery education in LMICs.
Modes and approaches for delivery of CPD
Face-to-face contact is a common mode of delivery of CPD although mHealth is an emerging platform that increases access, particularly to nurses and midwives in rural areas [ 12 , 21 ]. Emerging platforms and organisations such as World Continuing Education Alliance (WCEA) offer mHealth learning opportunities in LMICs for skilled health personnel to access CPD resources that can improve health care provider knowledge and skills and potentially positively impact healthcare outcomes [ 22 ]. Although there is evidence of capacity building initiatives and CPD for midwifery educators in LMICs [ 23 ], these have been largely delivered as part of long duration (2-year) fellowship programmes and led by international organisations. In addition, these programmes have largely focused on curriculum design, leadership, management, research, project management and programme evaluation skills in health professions education with little on teaching and learning approaches and assessment for educators [ 24 , 25 , 26 ]. Successful CPD initiatives should be (i) accredited by the national regulatory bodies (Nursing and Midwifery Councils); (ii) multifaceted and provide different types of formal and informal learning opportunities and support; (iii) combine theory and clinical practice to develop the knowledge, skills and attitudes and (iv) must be adapted to fit the local context in which participants work and teach to ensure local ownership and sustainability of the initiatives [ 16 ].
Short competency-based blended trainings for educators improve their competence and confidence in delivering the quality midwifery teaching. However, systems for regular updates to sustain the competencies are lacking [ 27 , 28 ]. Evidence on effectiveness of the available CPD initiatives is limited. Even where these initiatives have been evaluated, this has largely focused on the outcomes of the programmes and little attention on the feasibility and sustainability of such programmes in low-resourced settings [ 24 , 25 , 29 ]. As part of global investments to improve the quality of midwifery education and training, Liverpool School of Tropical Medicine (LSTM) in collaboration with the UNFPA Headquarters Global Midwifery Programme and Kenya midwifery educators developed a blended midwifery educator CPD programme (described in detail in the methods section). The CPD programme modules in this programme are aligned to the WHO’s midwifery educators’ core competencies [ 7 ] and ICM essential competencies for midwifery practice [ 14 ]. The programme is also aligned to the nursing and midwifery practice national regulatory requirements of Nursing and Midwifery Councils in LMICs such as Kenya and Nigeria, and relevant national policy [ 30 , 31 , 32 ].This programme aimed at sustaining and improving the educators’ competencies in delivery of their teaching, assessments, mentoring and feedback to students. To promote uptake, there is need to test the relevance and practicability of the CPD programme. Feasibility studies are used to determine whether an intervention is appropriate for further testing, relevant and sustainable in answering the question – Can it work [ 33 ]? The key focus of these studies are acceptability of the intervention, resources and ability to manage and implement intervention (availability, requirements, sustainability), practicality, adaptation, integration into the system, limited efficacy testing of the intervention in controlled settings and preliminary evaluation of participant responses to the intervention [ 33 , 34 , 35 ].
This study evaluated the feasibility of the LSTM/UNFPA midwifery educator CPD programme using the Kirkpatrick’s model for evaluating training programmes [ 36 ]. This model is an effective tool with four levels for evaluating training programmes. Level 1 (Participants’ reaction to the programme experience) helps to understand how satisfying, engaging and relevant participants find the experience. Level 2 (Learning) measures the changes in knowledge, skills and confidence after training. Level 3 (Behaviour) measures the degree to which participants apply what they learned during training when they are back on job and this can be immediately and several months after the training. This level is critical as it can also reveal where participants might need help to transfer learning during the training to practice afterwards. Level 4 (Results) measures the degree to which targeted outcomes occur because of training. In this study, participants’ reaction to the programme – satisfaction and relevance of the programme to meeting their needs (level 1) and change in knowledge, confidence and skills after the CPD programme (level 2) were assessed. Also, user perspectives and barriers to implementing the CPD programme were explored.
Study design
This was a mixed methods intervention study using a concurrent nested/embedded/convergent design conducted in Kenya and Nigeria in May and June 2023. This was designed to evaluate the feasibility of the midwifery educator CPD programme. The goal was to obtain different but complementary data to better understand the CPD programme with the data collected from the same participants or similar target populations [ 37 ].
The quantitative component of the evaluation used a quasi-experimental pre-post and post-test only designs to evaluate the effectiveness of the blended CPD programme intervention among midwifery educators from mid-level training colleges and universities from the two countries. Pre and post evaluation of knowledge (online self-directed component) and skills (developing a teaching plan during the face-to-face component) was performed. Post intervention evaluation on programme satisfaction, relevance of CPD programme and microteaching sessions for educators was conducted.
The qualitative component of the evaluation included open-ended written responses from the midwifery educators and master trainers to describe what worked well (enablers), challenges/barriers experienced in the blended programme and key recommendations for improvement were collected. In addition, key informant interviews with the key stakeholders (nursing and midwifery councils and the national heads of training institutions) were conducted. Data on challenges anticipated in the scale up of the programme and measures to promote sustainability, access and uptake of the programme were collected from both educators and key stakeholders.
A mixed methods design was used for its strengths in (i) collecting the two types of data (quantitative and qualitative) simultaneously, during a single data collection phase, (ii) provided the study with the advantages of both quantitative and qualitative data and (iii) helped gain perspectives and contextual experiences from the different types of data or from different levels (educators, master trainers, heads of training institutions and nursing and midwifery councils) within the study [ 38 , 39 ].
The study was conducted in Kenya and Nigeria. Kenya has over 121 mid-level training colleges and universities offering nursing and midwifery training while Nigeria has about 300. Due to the vastness in Nigeria, representative government-owned nursing and midwifery training institutions were randomly selected from each of the six geo-political zones in the country and the Federal Capital Territory. Mid-level training colleges offer the integrated nursing and midwifery training at diploma level while universities offer integrated nursing and midwifery training at bachelor/master degree level in the two countries (three universities in Kenya offer midwifery training at bachelor level). All nurse-midwives and midwives trained at both levels are expected to possess ICM competencies to care for the woman and newborn. Midwifery educators in Kenya and Nigeria are required to have at least advanced diploma qualifications although years of clinical experience are not specified.
It is a mandatory requirement of the Nursing and Midwifery Councils for nurse/midwives and midwifery educators in both countries to demonstrate evidence of CPD for renewal of practising license in both countries [ 40 , 41 ]. A minimum of 20 CPD points (equivalent to 20 credit hours) is recommended annually for Kenya and 60 credit hours for Nigeria every three years. However, there are no specific midwifery educator CPD that incorporated both face-to-face and online modes of delivery, available for Kenya and Nigeria and indeed for many countries in the region. Nursing and midwifery educators are registered and licensed to practice nursing and midwifery while those from other disciplines who teach in the midwifery programme are qualified in the content they teach.
Study sites
In Kenya, a set of two mid-level colleges (Nairobi and Kakamega Kenya Medical Training Colleges (KMTCs) and two universities (Nairobi and Moi Universities), based on the geographical distribution of the training institutions were identified as CPD Centres of Excellence (COEs)/hubs. In Nigeria, two midwifery schools (Centre of Excellence for Midwifery and Medical Education, College of Nursing and Midwifery, Illorin, Kwara State and Centre of Excellence for Midwifery and Medical Education, School of Nursing Gwagwalada, Abuja, FCT) were identified. These centres were equipped with teaching and EmONC training equipment for the practical components of the CPD programme. The centres were selected based on the availability of spacious training labs/classes specific for skills training and storage of equipment and an emergency obstetrics and newborn care (EmONC) master trainer among the educators in the institution. They were designated as host centres for the capacity strengthening of educators in EmONC and teaching skills.
Intervention
Nursing and midwifery educators accessed and completed 20 h of free, self-directed online modules on the WCEA portal and face-to-face practical sessions in the CPD centres of excellence.
The design of the midwifery educator CPD programme
The design of the CPD modules was informed by the existing gap for professional development for midwifery educators in Kenya and other LMICs and the need for regular updates in knowledge and skills competencies in delivery of teaching [ 9 , 15 , 23 , 28 ]. Liverpool School of Tropical Medicine led the overall design of the nursing and midwifery educator CPD programme (see Fig. 1 for summarised steps taken in the design of the blended programme).
This was a two-part blended programme with a 20-hour self-directed online learning component (accessible through the WCEA platform at no cost) and a 3-day face-to-face component designed to cover theoretical and practical skills components respectively. The 20-hour self-directed online component had four 5-hour modules on reflection practice, teaching/learning theories and methods, student assessments and effective feedback and mentoring. These modules had pretest and post-test questions and were interactive with short videos, short quizzes within modules, links for further directed reading and resources to promote active learning. This online component is also available on the WCEA platform as a resource for other nurses and midwifery educators across the globe ( https://wcea.education/2022/05/05/midwifery-educator-cpd-programme/ ).
Practical aspects of competency-based teaching pedagogy, clinical teaching skills including selected EmONC skills, giving effective feedback, applying digital innovations in teaching and learning for educators and critical thinking and appraisal were delivered through a 3-day residential face-to-face component in designated CPD centres of excellence. Specific skills included: planning and preparing teaching sessions (lesson plans), teaching practical skills methodologies (lecture, simulation, scenario and role plays), selected EmONC skills, managing teaching and learning sessions, assessing students, providing effective feedback and mentoring and use of online applications such as Mentimeter and Kahoot in formative classroom assessment of learning. Selected EmONC skills delivered were shoulder dystocia, breech delivery, assisted vaginal delivery (vacuum assisted birth), managing hypovolemic shock and pre-eclampsia/eclampsia and newborn resuscitation. These were designed to reinforce the competencies of educators in using contemporary teaching pedagogies. The goal was to combine theory and practical aspects of effective teaching as well as provide high quality, evidence-based learning environment and support for students in midwifery education [ 4 ]. These modules integrated the ICM essential competencies for midwifery practice to provide a high quality, evidence-based learning environment for midwifery students. The pre and post tests form part of the CPD programme as a standard assessment of the educators.
As part of the design, this programme was piloted among 60 midwifery educators and regulators from 16 countries across Africa at the UNFPA funded Alliance to Improve Midwifery Education (AIME) Africa regional workshop in Nairobi in November 2022. They accessed and completed the self-directed online modules on the WCEA platform, participated in selected practical sessions, self-evaluated the programme and provided useful feedback for strengthening the modules.
The Nursing and Midwifery Councils of Kenya and Nigeria host the online CPD courses from individual or organisation entities on the WCEA portal. In addition, the Nursing Council of Kenya provides opportunities for self-reporting for various CPD events including accredited online CPD activities/programmes, skill development workshops, attending conferences and seminars, in-service short courses, practice-based research projects (as learner, principal investigator, principal author, or co-author) among others. In Nigeria, a certificate of attendance for Mandatory Continuing Professional Development Programme (MCPDP) is required as evidence for CPD during license renewal. However, the accredited CPD programmes specific for midwifery educators are not available in both countries and Africa region [ 15 , 42 ].
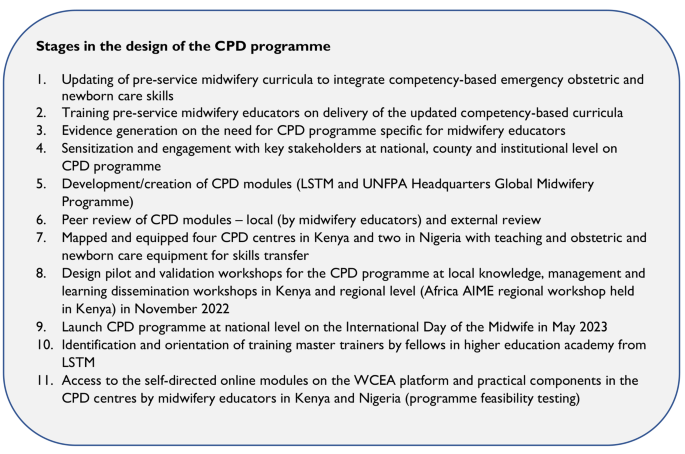
Midwifery educator CPD programme design stages
Participants and sample size
Bowen and colleagues suggest that many feasibility studies are designed to test an intervention in a limited way and such tests may be conducted in a convenience sample, with intermediate rather than final outcomes, with shorter follow-up periods, or with limited statistical power [ 34 ].
A convenience random sample across the two countries was used. Sample size calculations were performed using the formula for estimation of a proportion: a 95% confidence interval for estimation of a proportion can be estimated using the formula: \(p\pm 1.96\sqrt{\frac{\text{p}(1-\text{p})}{n}}\) The margin of error (d) is the second term in the equation. For calculation of the percentage change in competence detectable Stata’s power paired proportion function was used.
To achieve the desired level of low margin of error of 5% and a 90% power (value of proportion) to detect competence change after the training, a sample of 120 participants was required. Using the same sample to assess competence before and after training, so that the improvement in percentage competent can be derived and 2.5% are assessed as competent prior to training but not after training (regress), a 90% power would give a 12% improvement change in competence after the training.
A random sample of 120 educators (60 each from Kenya & Nigeria; 30 each from mid-level training colleges and universities) were invited to participate via an email invitation in the two components of the CPD programme (Fig. 2 ). Importantly, only participants who completed the self-directed online modules were eligible to progress to the face-to-face practical component.
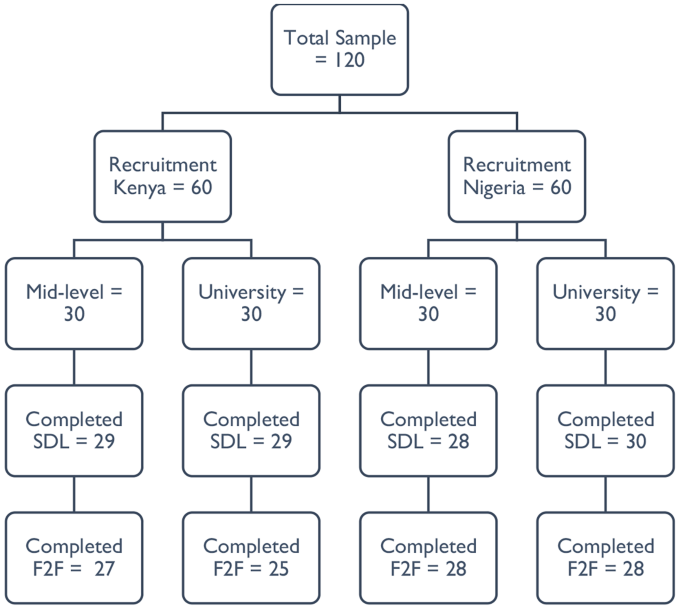
Flow of participants in the CPD programme (SDL = self-directed online learning; F2F = face-to-face practical)
For qualitative interviews, eight key informant interviews were planned with a representative each from the Nursing and Midwifery Councils, mid-level training institutions’ management, university and midwifery associations in both countries. Interviews obtained data related to challenges anticipated in the scale up of the programme and measures to promote sustainability, access and uptake of the programme.
Participant recruitment
Only nursing and midwifery educators registered and licensed by the Nursing and Midwifery Councils were eligible and participated. This was because they can access the WCEA website with the self-directed online programme via the Nursing and Midwifery Councils’ websites, only accessible to registered and licensed nurses and midwives.
The recruitment process was facilitated through the central college management headquarters (for mid-level training colleges’ educators) and Nursing and Midwifery Councils (for university participants). Training institutions’ heads of nursing and midwifery departments were requested to share the contact details of all educators teaching midwifery modules, particularly the antepartum, intrapartum, postpartum and newborn care modules in the two countries. A list of 166 midwifery educators from 81 universities and mid-level training colleges was obtained through the Heads of the Department in the institutions.
The research lead, with the assistance by the co-investigator from Nigeria then randomly sampled 120 educators based on institution type and region for representativeness across the countries. Following the selection of participants, the two investigators shared the electronic detailed participant study information sheet and consent form to the potential participants one week before the start of the self-directed online modules. Clear guidance and emphasis on the conduct of the two-part program including completing the mandatory four self-directed online modules was provided. Due to the large number of eligible participants, the recruitment and consenting process was closed after reaching the first 30 participants consenting per institution type and region, with 1–2 educators per institution randomly recruited. This allowed as many institutions to be represented across the country as possible. Participants received a study information sheet and an auto-generated copy of the electronic consent form completed in their emails. Other opportunities for participating in the two-part programme were provided as appropriate for those who missed out. Only those who completed the four online modules were invited for the practical component. A WhatsApp community group for the recruited participants was formed for clarifications about the study, troubleshooting on challenges with online access and completion of the modules before and during the programme.
Self-directed online component
Upon consenting, the contact details of the educators from each level were shared with WCEA program director for generation of a unique identification code to access the self-directed online modules on the WCEA portal. Educators completed their baseline characteristics (demographic and academic) in the online platform just before the modules. Each self-directed online module was estimated to be completed in five hours. Only after completing a module was the participant allowed to progress to the next module. The modules were available for participants to complete at their own time/schedule. An autogenerated certificate of completion with the participant’s post-completion score was awarded as evidence of completing a module. Participants completed a set of 20 similar pretest and posttest multiple choice questions in each module for knowledge check. A dedicated staff from WCEA actively provided technical support for educators to register, access and complete the online modules. At the end of each module, participants completed a self-evaluation on a 5-point Likert scale for satisfaction (0 = very unsatisfied, 1 = unsatisfied, 2 = neutral, 3 = satisfied and 4 = very satisfied) and relevance of the modules (0 = very irrelevant, 1 = irrelevant, 2 = neutral, 3 = relevant and 4 = very relevant). This provided participants’ reactions to the different components of the modules on whether they met the individual educator’s development needs. In addition, participants responded to the open-ended questions at the end of the modules. These were on what they liked about the modules, challenges encountered in completing the modules and suggestions for improvement of the modules. A maximum period of two weeks was given for educators to complete the modules before progressing to the practical component.
Practical component
The practical component was delivered by a pool of 18 master trainers who received a 1-day orientation from the research lead before the training. The master trainers were a blend of experienced midwifery and obstetrics faculty in teaching and clinical practice actively engaged in facilitating EmONC trainings selected from Kenya and Nigeria. Four of these master trainers from Kenya participated in the delivery of both sets of trainings in Kenya and Nigeria.
Only educator participants who completed the self-directed online modules and certified were invited to participate in a 3-day residential practical component. Two separate classes were trained (mid-level and university level educators) per country by the same group of eight master trainers. The sessions were delivered through short interactive lectures; small group and plenary discussions; skills demonstrations/simulations and scenario teaching in small breakout groups; role plays and debrief sessions. Sessions on digital innovations in teaching and learning were live practical sessions with every participant using own laptop. Nursing and Midwifery Councils representatives and training institutions’ managers were invited to participate in both components of the programme.
Participant costs for participating in the two-part CPD programme were fully sponsored by the study. These were internet data for completing the self-directed online component and residential costs – transport, accommodation, and meals during the practical component.
Data collection
Self-directed online knowledge pretests and post-tests results, self-rated measures of satisfaction and relevance of the modules including what they liked about the modules, challenges encountered in accessing and completing the modules and suggestions for improvement data was extracted from the WCEA platform in Microsoft Excel.
On day 1 of the practical component, participants using their personal computers developed a teaching plan. On the last day (day 3), participants prepared a teaching plan and powerpoint presentation for the microteaching sessions. No teaching plan template from the trainers was provided to the participants before the training. However, they used formats from their institutions if available. A standard teaching plan template was provided at the end of the training.
The group of master trainers and participants were divided into groups for the microteaching sessions which formed part of the formative assessment. Each participant delivered a powerpoint presentation on a topic of interest (covered in the teaching plan) to the small group of 13–15 participants. This was followed by a structured session of constructive feedback that started with a self-reflection and assessment. This was followed by peer supportive and constructive feedback from the audience participants and faculty/master trainers identifying areas of effective practice and opportunities for further development. Each microteaching session lasted 10–15 min. Each of the microteaching session presentation and teaching plan were evaluated against a pre-determined electronic checklist by two designated faculty members independently during/immediately after the microteaching session. The checklist was adapted from LSTM’s microteaching assessment of the United Kingdom’s Higher Education Academy (HEA)’s Leading in Global Health Teaching (LIGHT) programme. The evaluation included preparing a teaching plan, managing a teaching and learning session using multiple interactive activities, designing and conducting formative assessments for learning using digital/online platforms, and giving effective feedback and critical appraisal. The master trainers received an orientation training on the scoring checklist by the lead researcher/corresponding author.
Self-rated confidence in different teaching pedagogy skills were evaluated before (on day 1) and after (day 3) the training on a 5-point Likert scale (0 = not at all confident, 1 = slightly confident, 2 = somewhat confident, 3 = quite confident and 4 = very confident). A satisfaction and relevance of practical component evaluation on a 5-point Likert scale was completed by the participants on an online designed form on day 3 after the microteaching sessions of the practical component. This form also had a similar qualitative survey with open-ended questions on what they liked about the practical component, challenges encountered in completing the practical component and suggestions for improvement of the component.
Using a semi-structured interview guide, six qualitative key informant interviews, each lasting about 30–45 min, were conducted by the lead researcher with the Nursing and Midwifery Councils focal persons and training institutions’ managers. These were audio recorded in English, anonymized, and deleted after transcription. These interviews were aimed at getting their perspectives on the programme design, anticipated barriers/enablers with the CPD programme and strategies for promoting uptake of the CPD programme. These interviews were considered adequate due to their information power (indicating that the more information the sample holds, relevant for the actual study, the lower amount of participants is needed) [ 43 ] and upon obtaining data saturation, considered the cornerstone of rigor in qualitative research [ 44 , 45 ].
Assessment of outcomes
Participants’ reaction to the programme (satisfaction and relevance) (Kirkpatrick level 1) was tested using the self-rated 5-point Likert scales. Change in knowledge, confidence and skills (Kirkpatrick level 2) was tested as follows: knowledge through 20 pretest and post-test multiple choice questions per module in the self-directed online modules; confidence in applying different pedagogy skills through the self-rated 5-point Likert scale; and teaching skills through the observed microteaching sessions using a checklist.
Reliability and validity of the data collection tools
The internal consistency (a measure of the reliability, generalizability or reproducibility of a test) of the Likert scales/tools assessing the relevance of the online and practical modules and satisfaction of educators with the two blended modules were tested using the Cronbach’s alpha statistic. The Cronbach’s alpha statistics for the four Likert scales/tools ranged from 0.835 to 0.928, all indicating acceptably good to excellent level of reliability [ 46 ]. Validity (which refers to the accuracy of a measure) of the Likert scales were tested using the Pearson correlation coefficient statistic. Obtained correlation values were compared to the critical values and p-values reported at 95% confidence intervals. All the scales were valid with obtained Pearson correlation coefficients reported − 0.1946, which were all greater than the critical values ( p < 0.001) [ 46 ]. The semi-structured interview guides for the qualitative interviews with the training institutions’ managers and midwifery councils (regulators) were developed and reviewed by expert study team members with experience in qualitative research.
Data management and analysis
Data from the online/electronic tools was extracted in Microsoft Excel and exported to SPSS version 28 for cleaning and analysis. Normality of data was tested using the Kolmogorov-Smirnov test suitable for samples above 50. Proportions of educator characteristics in the two countries were calculated. Differences between the educator characteristics in the two countries were tested using chi-square tests (and Fishers-exact test for cells with counts of less than 5).
For self-rated relevance of CPD programme components and satisfaction with the programme on the 0–4 Likert scales, descriptive statistics were calculated (median scores and proportions). Results are presented as bar graphs and tables. Cronbach alpha and Pearson correlation coefficients were used to test the reliability and validity of the test items respectively.
Change in knowledge in online modules, confidence in pedagogy skills and preparing teaching plans among educators was assessed by comparing pre-training scores and post-training scores. Descriptive statistics are reported based on normality of data. Differences in the scores were analysed using the Wilcoxon signed ranks tests, a non-parametric equivalent of the paired t-test. Differences between educators scores in microteaching by country and institution type were performed by Mann-Whitney U test. Level of competence demonstrated in the teaching plan and microteaching skill was defined as the percentage of the desired characteristics present in the teaching plan and microteaching session, set at 75% and above. The proportion of participants that achieved the desired level of competence in their teaching plan and microteaching skill was calculated. Binary logistic regression models were used to assess for the strengths of associations between individual educator and institutional characteristics (age, gender, qualifications, length of time as educator, training institution and country) and the overall dichotomised competent score (proportion achieved competence in teaching plan and microteaching skills). P-values less than 0.05 at 95% confidence interval were considered statistically significant.
Preparation for qualitative data analysis involved a rigorous process of transcription of recorded interviews with key informants. In addition, online free text responses by midwifery educators on what worked well, challenges encountered, and recommendations were extracted in Microsoft Excel format and exported to Microsoft Word for data reduction (coding) and theme development. Qualitative data was analysed using thematic framework analysis by Braun and Clarke (2006) as it provides clear steps to follow, is flexible and uses a very structured process and enables transparency and team working [ 47 ]. Due to the small number of transcripts, computer assisted coding in Microsoft Word using the margin and comments tool were used. The six steps by Braun and Clarke in thematic analysis were conducted: (i) familiarising oneself with the data through transcription and reading transcripts, looking for recurring issues/inconsistencies and, identifying possible categories and sub-categories of data; (ii) generating initial codes – both deductive (using topic guides/research questions) and inductive coding (recurrent views, phrases, patterns from the data) was conducted for transparency; (iii) searching for themes by collating initial codes into potential sub-themes/themes; (iv) reviewing themes by generating a thematic map (code book) of the analysis; (v) defining and naming themes (ongoing analysis to refine the specifics of each sub-theme/theme, and the overall story the analysis tells); and (vi) writing findings/producing a report. Confidentiality was maintained by using pseudonyms for participant identification in the study. Trustworthiness was achieved by (i) respondent validation/check during the interviews for accurate data interpretation; (ii) using a criterion for thematic analysis; (iii) returning to the data repeatedly to check for accuracy in interpretation; (iv) quality checks and discussions with the study team with expertise in mixed methods research [ 39 , 47 ].
Integration of findings used the parallel-databases variant and are synthesised in the discussion section. In this common approach, two parallel strands of data are collected and analysed independently and are only brought together during interpretation. The two sets of independent results are then synthesized or compared during the discussion [ 39 ].
Quantitative findings
Midwifery educators’ characteristics.
A total of 116 (96.7%) and 108 (90.0%) educators from 81 institutions completed the self-directed online learning and practical component respectively from the two countries. There were no significant differences between countries in educators’ qualifications, when last taught a midwifery class and whether attended any CPD training in the preceding year before the study ( p > 0.05). Overall, only 28.7% of the educators had a midwifery related CPD training in the preceding year before the study. Midwifery educator characteristics are outlined below (Table 1 ).
Change in knowledge
This was assessed in each of the four self-directed online modules. The results from ranked scores based on Wilcoxon signed ranks test showed significant improvements in educators’ knowledge in all the four online modules completed ( p < 0.001). The highest mean score improvement was observed in students’ assessment module, 48.1% (SD ± 15.1) to 85.2% (SD ± 15.7), a 37.1% improvement. Improvements in knowledge in the other modules were as follows: reflective practice (27.6%), mentoring and giving effective feedback (27.4%) and teaching methods (19.2%). Overall knowledge score for all modules improved from 52.4% (SD ± 10.4) to 80.4 (SD ± 8.1), p < 0.001 (Table 2 ).
Relevance of self-directed online modules
The internal consistency of each of the four modules was tested with Cronbach’s alpha. The overall Cronbach’s alpha for the four items was 0.837, a good and acceptable level of reliability. All the four modules assessed were valid with calculated Pearson correlation coefficient values greater than the critical value of 0.1946 ( p < 0.001) at 95% confidence interval.
Educators from the two countries, on a scale of 0–4 rated the online modules as very relevant with a median score of 4 out of 4 (IQR 0) for each of the four modules: reflective practice, teaching methods, students’ assessments and mentoring and giving effective feedback. There were no ratings of 0, 1 and 2 for all the modules (Fig. 3 ).

Educators’ ratings of the relevance of self-directed online modules
Satisfaction with the self-directed online modules
The internal consistency of each of the eight items was tested with Cronbach’s alpha. The overall Cronbach’s alpha for the eight items was 0.928, an excellent level of reliability. All the eight items assessed were valid with their obtained Pearson correlation coefficient values greater than the critical value of 0.1946 ( p < 0.001) at 95% confidence interval.
Each of the eight items rated on satisfaction had a median score of 4 out of 4 (IQR 0). Over 80% of the educators were very satisfied with the online modules’ content as presented in a logical format and informative. Also, the modules helped them to learn something new, updated their knowledge and the materials were useful and valuable for their practice. Over 70% were very satisfied with the modules as they helped them refresh their knowledge and skills with the links and activities embedded in the modules useful in adding to their learning. None of the educators were dissatisfied (rated 0 or 1) with the online modules (Table 3 ).
Change in confidence in different pedagogy skills
The internal consistency of each of the eight items assessed was tested with Cronbach’s alpha using the baseline data. The overall Cronbach’s alpha for the eight items was 0.893, a good level of reliability. All the eight items assessed were valid with their obtained Pearson correlation coefficient values greater than the critical value of 0.1946 ( p < 0.001) at 95% confidence interval.
Changes in confidence before and after the training were compared using the Wilcoxon signed rank test, a parametric equivalent of the paired t-test when data is not normally distributed. The mean score of self-rated confidence of educators on a scale of 0–4 for all the eight skills significantly improved after the training from 2.73 (SD ± 0.68) to 3.74 (SD ± 0.34) ( p < 0.001). Mean confidence was highest in facilitating a lecture (3.23, SD ± 0.8) and lowest on using digital innovations (Mentimeter) in formative assessment of teaching/learning (1.75, SD ± 1.15) before the training. These improved significantly after the training to 3.84 (SD ± 0.41) for facilitating a lecture and 3.50 (SD ± 0.63) for using digital innovations (Mentimeter) in formative assessment of teaching/learning, p < 0.001. The mean confidence of educators was largely average before the training and significantly improved after the training in six skills ( p < 0.001). These were designing learning outcomes using measurable Bloom’s taxonomy verbs, preparing a teaching plan, identifying relevant resources to enhance learning, facilitating a scenario teaching, facilitating a practical simulation/demonstration and giving effective feedback for learning (Table 4 ).
Preparing a teaching plan and microteaching skills
The overall median score in preparing a teaching plan was 63.6% (IQR 45.5) before the training and improved significantly to 81.8% (IQR 27.3) after the training, p < 0.001. The median scores differed significantly by country before and after the training. Before the training, Kenyan educators had higher median scores (72.7%, IQR 27.3) compared to Nigeria counterparts (54.5%, IQR 36.4), p < 0.001. After the training, Kenyan educators had significantly higher median scores (81.2%, IQR 18.2) than Nigerian counterparts (72.7%, IQR 18.2), p = 0.024. However, there were no significant differences in the median scores between the training institutions before and after the training, p > 0.05. For microteaching, the overall median score was 76.5% (IQR 29.4). There were no significant differences between countries and training institutions in the microteaching scores, p > 0.05. Kenya educators (82.4%, IQR 29.4) had slightly higher scores than Nigeria (76.5%, IQR 29.4), p = 0.78. Mid-level educators (79.4%, IQR 29.4) had slightly higher scores than university educators (76.5%, IQR 28.7), p = 0.515 (Table 5 ).
The inter-rater reliability/agreement of the eight pairs of assessors in both countries were assessed by Cohen Kappa statistic. The Kappa statistics for the eight pairs ranged between 0.806 and 0.917, p < 0.001, showing near perfect agreement between the pairs of assessors.
Association between independent educator and institutional characteristics and the microteaching skill scores
Categorised skills scores (≥ 75% mean score as competent) showed that 55 (51.4%) and 62 (57.9%) of the educators scored 75% or higher in the teaching plan preparation and microteaching skill assessments respectively. Logistic regression analysis showed that educator’s country, age, gender, qualifications, training institution type and length as educator were not significantly associated with the overall categorised teaching plan or microteaching scores ( p > 0.05).
Relevance of the practical component
The internal consistency of each of the six skills items was tested with Cronbach’s alpha. The overall Cronbach’s alpha for the six items was 0.866, a good level of reliability. All the six skills items assessed were valid with their obtained Pearson correlation coefficient values greater than the critical value of 0.1946 ( p < 0.001) at 95% confidence interval.
On a self-rating Likert scale of 0–4, the median score for each of the six skills assessed and trained was 4 out of a maximum of 4, indicating that the educators found the different pedagogy skills very relevant after the training. Over 80% of the educators rated the sessions on teaching plan (85.2%), scenario teaching (87.0%), simulation/demonstration teaching (82.4%) and giving effective feedback (85.2%) as very relevant. Over three-quarters (77.8%) of the educators rated the sessions on lecture teaching and use of digital innovations (Mentimeter) in assessment as very relevant (Fig. 4 ).
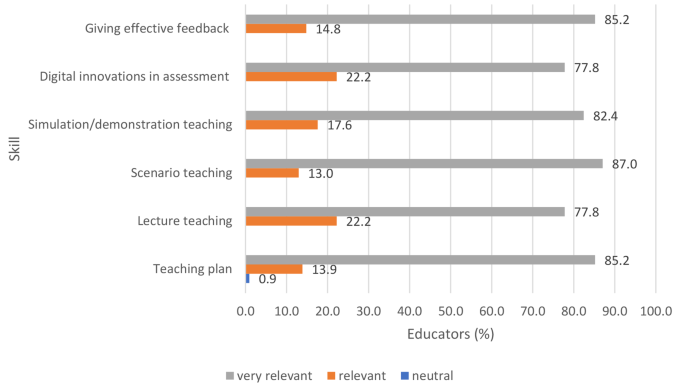
Relevance of the practical components
Satisfaction with the practical component
The internal consistency of each of the six skills items was tested with Cronbach’s alpha. The overall Cronbach’s alpha for the six items was 0.835, a good level of reliability. All the six skills items assessed were valid with their obtained Pearson correlation coefficient values greater than the critical value of 0.1946 ( p < 0.001) at 95% confidence interval.
On a self-rating Likert scale of 0–4, the median score for each of the six skills assessed was 4 out of a maximum of 4, indicating that educators were very satisfied with the practical skills sessions. Over 70% of the educators were very satisfied with the sessions on giving effective feedback (79.6%), lecture teaching (75.9%), scenario and simulation teaching (73.1% each). Two-thirds of the educators (67.6%) were very satisfied with the digital innovations in teaching (use of Mentimeter) for formative assessment in teaching and learning. All educators were satisfied with the preparing of teaching plan in teaching and learning with the majority (63.0%) as very satisfied while the remaining 37.0% satisfied. None of the educators were dissatisfied with the practical component of the training (Fig. 5 ).
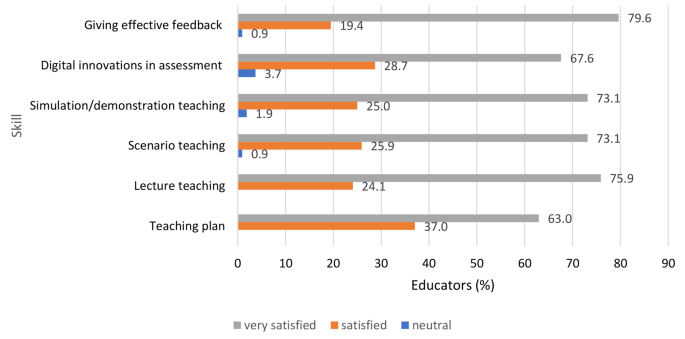
Satisfaction with practical skills
Qualitative findings
What educators liked about the self-directed online modules.
Educators from both levels and countries had similar views on the online component. These are broadly summarised under the sub-themes: (i) educative and relevant for practice, (ii) flexible and convenient learning and (iii) motivating, interesting and interactive.
Educative and relevant for practice
Educators reported the online modules as educative and informative and, improved their knowledge in teaching, assessments, reflective practice and providing effective feedback to students to promote learning as well as increasing their self-confidence and critical thinking skills. Besides, educators found the modules valuable and relevant for their professional growth and practice.
“The modules were well organized, they were relevant to my practice and met my expectations” university midwifery educator, Kenya. “The materials are very rich with current information to guide. Very informative & valuable to my professional growth” university midwifery educator, Nigeria.
Flexible and convenient learning
Educators reported that they could access and complete the online modules at their flexible and convenient time. This flexibility enhanced and stimulated them to complete the informative modules at their comfort times either at home or office without disruption to their schedules.
“(The modules) gave me ample time to read at my own pace and time without any hurry to understand the content well. They were well organised. Also, flexibility of learning and the access to materials was excellent” university midwifery educator, Kenya. “It is flexible and convenient. It empowers the learner to take ownership of the learning process. Learning is personalized” mid-level training college midwifery educator, Nigeria.
Motivating, interesting and interactive
Educators reported that the online modules were well structured, motivating, interesting and had components that promoted interaction for learning. For example, pretests, various quizzes within the modules and posttest questions and the added specific short extra reading segments promoted interaction and learning.
“The intermittent assessment questions. It helped maintain my focus” university midwifery educator, Nigeria . “Very interactive. They were very informative and extra reading assignments complemented the content” university midwifery educator, Kenya .
Challenges encountered with the self-directed online learning modules
Four sub-themes emerged that summarised the challenges experienced by midwifery educators in the two countries to access and complete the self-directed online modules. These are (i) network/internet connectivity, (ii) technology challenges, (iii) electricity power supply and power outages and, (iv) time constraints.
Network/internet connectivity
Network and internet connectivity difficulties and fluctuations was the commonest reported challenge in completing the self-directed online modules by educators from both countries. This affected the access, progress, downloading extra resources embedded within the modules and completing the integrated evaluations within the modules.
“Accessing the modules, problem with submitting forms and exams, had network problem” mid-level training college midwifery educator, Nigeria . “I kept going offline and I would have to restart every time. They were too internet dependent” university midwifery educator, Kenya.
Technology challenges
Technological challenges were observed as well as reported among educators from both countries. These ranged from poor access to emails due to forgotten email addresses, usernames or passwords, difficult access and navigation through the online modules, completing the matching questions that required dragging items, completing the evaluations and downloading certificates after completion of the modules.
“I am not very good with ICT, so I had issues using my laptop” mid-level training college midwifery educator, Nigeria. “Accessibility was difficult. I had to restart the process a number of times. The modules would sometimes take you back more than 20 slides which delayed the completion rate” university midwifery educator, Kenya.
Electricity power supply interruptions and fluctuations
Power interruptions, fluctuations and outages especially in Nigeria were cited as a challenge to complete the online modules. This delayed the completion of the modules as electric power was critical to access and complete the modules on either WCEA app on mobile phones or computers.
“The modules should not start from beginning whenever there is interrupted power supply” MLC midwifery educator, Nigeria. “Network failure due to interrupted power supply” university midwifery educator, Nigeria.
Time constraints
Although educators commented the flexibility with which to complete the online modules, time to complete the online modules was also cited as a challenge in both countries.
“It requires a lot of time, this is a challenge because I am also involved with other activities at the place of work which require my attention” university midwifery educator, Kenya.
What educators liked about the practical component
Educators written feedback on what they liked about the practical component of the CPD programme was categorised into the four sub-themes: new knowledge and relevant for practice; improved knowledge, skills and confidence to teach; enhanced participatory and active learning; individualised support in learning.
New knowledge and relevant for practice
The practical component provided new learning particularly on the use of digital platforms (Mentimeter and Kahoot) for formative assessment to evaluate learning during classroom teaching. In their integrated teaching using both online and face-to-face delivery, use of technology (Mentimeter and Kahoot) in classroom assessment was not a common practice as most of them had not heard about the available online platforms. They found Mentimeter (and Kahoot) to be interesting resources for formative assessments in class to facilitate teaching and learning. The techniques of giving effective feedback using the sandwich and ‘stop, start, continue’ methods were viewed to promote interaction between the educator and the learner for effective learning. Educators also acknowledged new knowledge and skills updates on EmONC relevant for their practice.
“Giving feedback, innovation of the online formative assessment, the teaching plan. I wish we would adapt them for daily application rather than the traditional teacher centered one.” Mid-level training college educator, Kenya . “(I liked) Everything, especially the technological innovations for assessment” Mid-level training college educator, Nigeria .
Improved knowledge, skills and confidence to teach
Educators reported that the practical sessions were interactive and engaging with good combination of theory and practice which facilitated learning. They reported that participating in the practical component enabled them to update and improve their knowledge, skills and confidence in planning and delivering theoretical and practical teaching using multiple methods. Similar improvements were reported on preparing and conducting students’ assessments and giving effective feedback to promote learning. On use of technology in formative assessments, the interactive practical sessions boosted the confidence of educators in using Mentimeter (and Kahoot) online platforms during classroom teaching.
“It helped build my confidence, had hands on practice on clinical skills and teaching skills, learnt about outdated practices and current evidence based clinical and teaching skills.” Mid-level training college educator, Nigeria . “They were very interesting especially the scenarios and skills. I was able to enhance my practical skills and technology in evaluating learning.” University midwifery educator, Kenya .
Enhanced participatory and active learning
The practical component complemented the self-directed online learning for educators. They highly commented and benefitted from the hands-on opportunities to actively engage through return demonstrations during the practical programme. This component also enabled them to brainstorm and contribute actively during the sessions. They highlighted that the practical component enhanced and reinforced learning through active participation in demonstrations, questions, group discussions and plenary sessions.
“This face-to-face module provided me with the opportunity to brainstorm with other educators, facilitators and resource persons. This will enhance my teaching skills.” Mid-level training college midwifery educator, Nigeria . “Interaction with facilitators who could clarify points that I had earlier not understood, interaction with other participants and was also able to learn from them.” University midwifery educator, Kenya .
Individualised support in learning
Educators received individualised peer support and learning during the practical component. They had opportunities within the small breakout groups for peer learning and one-to-one support from the facilitators to update and learn new knowledge and skills.
“A chance to get immediate feedback was availed by the presenters.” University midwifery educator, Kenya . “Facilitators were well informed and gave learners opportunity for return demonstration and support.” Mid-level training college midwifery educator, Kenya .
Challenges encountered with the practical component
Key challenges reported by the mixed group of educators and master trainers across the two countries include: inadequate time, computer technology challenges and poor internet connectivity for practical components.
Inadequate time
Although small breakout sessions were utilised to provide each educator with an opportunity to practice the skills, it was commonly reported that time was inadequate for skills demonstrations and return demonstrations by all educators. This was especially for areas educators had inadequate knowledge and new skills that were observed thus adequate time for teaching and repeat demonstrations for mastery was required. Similar observations were made by the master trainers who felt that some educators had never encountered some of the basic EmONC skills demonstrated or never practised and thus required a longer duration for familiarisation and practice.
“Time was short hence not enough to return demo” Mid-level training college midwifery educator, Kenya . “Some of the things were new and required more time for demonstration and practice.” Mid-level training college midwifery educator, Nigeria .
Computer technology challenges and poor internet connectivity for practical components
Some educators encountered technical difficulties in using computers during the practical component. In some cases, this was compounded by poor network/internet connectivity. This delayed completion of practical components requiring the use of computers including pretests, preparing teaching plans and presentations, post-tests and classroom demonstrations using digital innovations in teaching and learning. However, assistance was provided by the trainers as appropriate to those who needed technical support.
“(There were) technical challenges with use of computers for few participants.” Master trainer, Nigeria . “Slow internet can hinder smooth flow of sessions.” Master trainer, Kenya .
Key areas for additional support
For quality education and training, master trainers generally recommended that all educators should be trained and regularly supported in the basic EmONC course to strengthen their competencies for effective teaching of EmONC skills. Further support in computer technology use including basics in navigation around windows/programmes, formatting in Microsoft Office Word and Powerpoint, literature searching, and referencing were other critical components to be strengthened.
Perspectives from training institutions managers and midwifery regulators
Measures to ensure midwifery educators take specific cpds that have been designed to improve their teaching competencies.
Key informant interviews with the pre-service training institutions’ managers and nursing and midwifery councils from the two countries were conducted and revealed key strategies outlined below that should ensure access and completion of the blended CPD programme specific for educators’ teaching competencies.
Awareness creation, integrating programme into policy and performance appraisal
The aspect of online CPD was highlighted as a new concept in Nigeria. Due to this novelty, the country was reluctant to accredit many online CPD programmes for in-service and pre-service nursing and midwifery personnel. However, the regulatory Nursing and Midwifery Council of Nigeria had established monitoring mechanisms to evaluate its uptake to meet the definition of CPD and is still work in progress.
“For the online, it’s actually a relatively new concept, in fact because of monitoring and evaluation, we have struggled with accepting online CPDs… So, we’re struggling on how to develop a guideline for online CPDs. So, we’re now starting with the WCEA. So far, only the WCEA has that approval to provide CPD…We said let’s look at how this works out before we can extend it to other providers.” Nursing and Midwifery Council, Nigeria .
Both countries emphasized the need to create awareness of the CPD programme for midwifery educators and a policy framework for CPD. Regulators emphasized the need to have the CPD programme as mandatory for all midwifery educators through a policy directive. They suggested that the blended CPD programme should form a mandatory specified proportion of the content addressing their specific competencies. Besides, the training institution recommended that the programme should form part of the educator’s performance appraisal on a regular basis. Active monitoring systems were suggested to be in place to ensure compliance of participation and completion to acquire specific relevant competencies in pedagogy.
“…Ensure that educators take the particular modules before license renewal. Tie modules that are related to midwifery education to the educators and make them mandatory. Yes, we make it as a matter of policy that you should be taking these courses over and over again.” Nursing and Midwifery Council, Nigeria .
It was strongly suggested that attaching incentives as motivators to completing the programme would attract educators to complete the CPD programme. These incentives include certification, recognition for participation in curriculum reviews, national examination setting, facilitating national examinations, promotion and service and eligibility as trainers of trainers to colleagues.
“You attach a course, one training, you cannot guarantee that these courses will be taken. So we find a way to attach something to it. You must have evidence that you attended these programs. So once you attach something like that, they will all flock because there is an incentive to it. Because we say, as an educator, before you go after every examination to examine students, you must have taken these courses.” Nursing and Midwifery Council, Nigeria .
Internet connectivity
Training institutions’ managers suggested investments in internet connectivity for training institutions to support educators access and complete the self-directed online programme. This was also highlighted as a critical challenge for the online component by the educators in both countries.
“The issues of internet connectivity and I think we need to be proactive about it so that we have a way to constantly bring it to the forefront especially in our policies. But connectivity would be a major area to look at as people are using their money.” Mid-level training college manager, Kenya .
Anticipated challenges in the scale-up of the CPD programme
Key challenges anticipated in the roll-out and scale-up of the blended CPD programme were identified as inadequate skills of the educators in the use of information and communication technology during the practical component (including preparation of powerpoint presentations and completing tasks using a computer), and participant costs to attend the practical component (including participants’ residential costs and investments in proctor technology for ensuring academic integrity and monitoring and evaluation tool for educators’ compliance.) It was also emphasized that due to low remuneration of the educators, additional costs from their pocket to undertake the CPD could be a limiting factor for the intended faculty development initiatives. Other challenges included maintaining quality and academic integrity of the programme, potential bias in the selection of educators to attend future CPD programmes that is based on pre-existing relationships and ensuring an adequate pool of in-country trainers of trainers with midwifery competencies to deliver the practical component of the CPD programme.
There were strong suggestions that personal commitment by educators was required for personal and professional development. There were observations that educators sometimes completed the professional development programmes purely for relicensing and not necessarily for professional development. Regulators and institutional managers emphasized that educators need to understand the value of continuous professional development and create time to participate in the targeted CPD programmes to improve their competencies.
“We do advise our nurses, or we continue to inform them that taking these courses shouldn’t be tied to license renewal. It shouldn’t be tied to licence expiration or renewal of licences. You should continue to take these courses to develop yourself and not waiting until your licence expired before you take the courses. Yes, we actually try as much as possible to dissociate the renewal of licences with these courses.” Nursing and Midwifery Council, Nigeria .
Key results
Our study evaluated the feasibility of what the authors believe to be the first blended programme with online and face-to-face learning available in Africa, as a tool to reach midwifery educators in both urban and rural low-resource areas. In addition, our study is in line to an important call by WHO, UNFPA, UNICEF and ICM for an effective midwifery educator with formal preparation for teaching and engages in ongoing development as a midwifery practitioner, teacher/lecturer and leader [ 6 , 7 ]. Consequently, our intervention is part of investments for improving and strengthening the capacity of midwifery educators for quality and competent midwifery workforce as recommended by multiple global reports [ 4 , 5 , 11 ] and other publications [ 12 , 15 , 23 , 42 ]. Our study findings showed that the midwifery educators were very satisfied with the blended CPD programme. Educators rated the programme as highly relevant, educative, flexible, interesting and interactive, improved their knowledge, confidence and practical skills in their professional competencies for practice. Use of digital technology in teaching and students’ assessment was found to be an effective and innovative approach in facilitating teaching and learning. Key challenges experienced by educators included deficiencies in computer technology use, internet/network connectivity for online components, time constraints to complete the blended programme and isolated electric power outages and fluctuations which affected completion of the self-directed online components. Costs for participating and completing the programme, motivation, investments in information and communication technology, quality assurance and academic integrity were highlighted as critical components for the scale-up of the programme by institutional managers and training regulators. Establishment of a policy framework for educators to complete mandatory specific and relevant CPD was recommended for a successful roll-out in the countries.
Interpretation of our findings
Our study findings demonstrated that educators found the theoretical and practical content educative, informative and relevant to their practice. Recent evidence showed that midwifery educators had no/limited connection with clinical practice or opportunities for updating their knowledge or skills [ 15 , 42 ]. This underscores the value and importance of regular opportunities of CPD specific for educators to improve their professional competencies. It has provided these educators with a flexible educational model that allows them to continue working while developing their professional practice.
The use of a blended programme was beneficial as educators’ needs were met. It provided opportunities for educators to reflect, critically think, internalise and complement what was learned in the self-directed online component during the practical phase. This approach has been considered a means to adequately prepare midwifery faculty and improving national midwifery programmes in low-resource and remote settings [ 48 , 49 ]. Use of self-directed online platforms has emerged as a key strategy to improve access to CPD with flexibility and convenience as educators take responsibility for their own learning. Evidence suggests that the flexibility of net-based learning offers the midwifery educators a new and effective educational opportunity that they previously did not have [ 50 , 51 ]. A practical – based learning is important in pre-service education settings where the capacity of midwifery educators needs to be strengthened [ 52 , 53 ]. However, without continuous regular training, the midwives’ competence deteriorate and this in turn threaten the quality of pre-service midwifery education [ 52 , 54 ]. Implementation of this flexible blended educational model allows educators to continue working while developing their professional practice.
The quality of educators is an important factor affecting the quality of graduates from midwifery programmes to provide quality maternal and newborn health services [ 7 ]. Evidence suggests that many midwifery educators are more confident with theoretical classroom teaching than clinical practice teaching and that they also struggle to maintain their own midwifery clinical skills [ 4 , 5 ]. Our findings showed that the programme was effective, and educators improved their knowledge, confidence and skills in teaching, students’ assessment, effective feedback, reflective practice, mentoring and use of digital innovations in teaching and assessments. Our findings are similar to other related models of capacity building midwifery educators in other developing countries [ 24 , 50 , 53 , 55 , 56 , 57 ]. It is expected that educators will apply the learning in their planning for teaching, delivery of interactive and stimulatory teaching, monitoring learning through formative and summative assessments and mentoring their students into competent midwives. This is a pathway for accelerating the achievement of maternal and newborn health SDGs, universal health coverage, ending preventable maternal mortalities and every newborn action plan targets.
The value for CPD on educators’ knowledge, confidence and skills has been demonstrated with opportunities for improvement. Specific CPD targeted to relevant professional competencies is beneficial to the profession, quality of graduates for maternal and newborn health care and global targets. However, further investments in strengthening capacity of educators in EmONC skills and information and communication technology for effective teaching and learning is mandatory. Related challenges with individual technical capacity, technological deficiencies and infrastructure to support the technological advancement have been reported in other studies that have used a blended learning approach [ 58 ]. Resource constraints – financial and infrastructural (e.g. computers) as well as internet access are key challenges to participation in CPD activities especially the self-directed learning [ 16 ]. Designing self-directed modules that can be accessed and completed offline will increase access especially in poorly connected settings with electric power and network coverage.
Strengths and limitations
This study assessed the feasibility a blended midwifery educator CPD programme in low resource settings. This was conducted in a multi-country and multi-site context which provided opportunities for learning across the two countries, two levels of training institutions and specific in-country experiences [ 20 ]. The study served to improve awareness of the availability of the CPD programme so that (1) regulators can ensure that midwifery educators take this as part of mandatory CPD required for relicensing and (2) training institutions can plan to support their educators access/participate in the practical components of the programme after the study. It is a mandatory requirement of the Nursing and Midwifery Councils of Kenya and Nigeria for nurse/midwives and midwifery educators to demonstrate evidence of CPD for renewal of practising license [ 40 , 41 ]. The use of mixed methods research design with multiple evaluations was relevant to address the aims and objectives of the study and ensure methodological rigour, depth and scientific validity as recommended for good practice in designing pilot studies [ 37 , 38 ]. This also enhanced triangulation of findings and enabled the capturing of broad perspectives important in strengthening sustainable implementation of the blended CPD programme [ 39 ]. Preliminary findings were disseminated to participant stakeholders from Kenya and Nigeria at the knowledge management and learning event in Nairobi. This approach enhanced the credibility and trustworthiness of the final findings reported. We believe our study findings from different participants using multiple data collection methods are robust, transparent and trustworthy for generalization to other contexts [ 38 ].The self-directed learning component of the blended CPD programme is hosted on the WCEA platform which is accessible to healthcare professionals in over 60 countries in Africa, Asia and Middle East and accredited for continuous professional development (59). Although our sample size was small, it is sufficient, geographically representative for training institutions across the countries and acceptable for feasibility studies [ 34 ].
The additional cost analysis of implementing the blended midwifery educator CPD programme is relevant and key to the uptake, scale-up and sustainability of the programme but this was not conducted due to limited funding. Different CPD programme funding models exist. In Nigeria, educators are required to meet the costs for accessing and completing the CPD programme components, while in Kenya the cost of accessing the online component is minimal (internet access costs only) and the face-to-face component has to be funded. The cost of implementing the programme should be explored in future studies and optional models for sustainable funding explored with stakeholders.
Implications
Our findings show demand for the CPD programme. Regular continuous professional development could help to bridge the gap between theory and practice and improve the quality of teaching by midwifery educators. A blended CPD programme is effective in improving the teaching and clinical skills of midwifery educators and increasing their confidence in effective teaching. However, midwifery educators require motivation and close support (individual capacity, time, technological infrastructure and policy) if the blended CPD approach is to be mandatory and successfully implemented in resource limited settings. Besides, regular quality assurance modalities including review of content, monitoring and evaluation of uptake of the CPD programme should be undertaken to ensure that updated and relevant content is available.
For quality CPD programmes, hands-on teaching is more effective than didactic classroom teaching and should be used when feasible to transfer clinical skills. Distance education models (self-directed learning) in combination with short residential training and mentoring should be embraced to strengthen capacity strengthening of midwifery educators; and CPD programmes must consider the local context in which participants work and teach [ 16 , 23 ]. Evidence has shown that knowledge and clinical skills are retained for up to 12 months after training [ 54 ]. Taking the CPD programme annually will potentially maintain/improve knowledge, skills and practice by midwifery educators for quality teaching and learning leading to a competent midwifery workforce.
For quality midwifery education and practice, educators need contact with clinical practice to strengthen classroom teaching [ 6 , 7 ]. This will promote and enable students to acquire the skills, knowledge, and behaviours essential to become autonomous midwifery practitioners. Therefore, demonstrating relevant practical clinical CPD should be included in midwifery educator CPD policy. In addition, a business case by the CPD hubs on the sustainability of the face-to-face practical components in the centres is necessary. Stakeholder engagement on cost and sustainability are required as key policy components for the scale-up of the blended midwifery educator CPD programme for impact.
The blended CPD programme was relevant, acceptable and feasible to implement. Midwifery educators reacted positively to its content as they were very satisfied with the modules meeting their needs and rated the content as relevant to their practice. The programme also improved their knowledge, confidence and skills in teaching, students’ assessments and providing effective feedback for learning and using digital/technological innovations for effective teaching and learning. Investments in information and communication technology, quality assurance and academic integrity were highlighted as critical components for the scale-up of the programme. For successful and mandatory implementation of the specific midwifery educator CPD programme to enhance practice, a policy framework by midwifery training regulators is required by countries.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the confidentiality of the data but are available from the corresponding author on request.
Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014;384(9948):1129–45.
Article Google Scholar
World Health Organization, United Nations Population Fund, International Confederation of Midwives. The State of the World’s Midwifery 2021: Building a health workforce to meet the needs of women, newborns and adolescents everywhere 2021. https://www.unfpa.org/publications/sowmy-2021 .
Filby A, McConville F, Portela A. What prevents quality midwifery care? A systematic mapping of barriers in low and middle income countries from the provider perspective. PLoS ONE. 2016;11(5):e0153391.
WHO. Strengthening quality midwifery education for Universal Health Coverage 2030: Framework for action 2019. https://www.who.int/publications/i/item/9789241515849 .
United Nations Population Fund, International Confederation of Midwives, World Health Organization. The State of the World’s Midwifery 2021: Building a health workforce to meet the needs of women, newborns and adolescents everywhere 2021. https://www.unfpa.org/publications/sowmy-2021 .
International Confederation of Midwives. ICM Global Standards for Midwifery Education. (Revised 2021) 2021. https://www.internationalmidwives.org/assets/files/education-files/2021/10/global-standards-for-midwifery-education_2021_en-1.pdf .
WHO. Midwifery educator core competencies: building capacities of midwifery educators 2014. https://www.who.int/hrh/nursing_midwifery/14116_Midwifery_educator_web.pdf .
Gavine A, MacGillivray S, McConville F, Gandhi M, Renfrew MJ. Pre-service and in-service education and training for maternal and newborn care providers in low-and middle-income countries: an evidence review and gap analysis. Midwifery. 2019;78:104–13.
Shikuku DN, Tallam E, Wako I, Mualuko A, Waweru L, Nyaga L, et al. Evaluation of capacity to deliver Emergency Obstetrics and Newborn Care updated midwifery and reproductive health training curricula in Kenya: before and after study. Int J Afr Nurs Sci. 2022;17:100439.
Google Scholar
International Confederation of Midwives. Global Standards for Midwifery Regulation. 2011. https://www.internationalmidwives.org/assets/files/regulation-files/2018/04/global-standards-for-midwifery-regulation-eng.pdf .
World Health Organization. Global strategic directions for nursing and midwifery 2021–2025. Geneva: World Health Organization. 2021. https://iris.who.int/bitstream/handle/10665/344562/9789240033863-eng.pdf?sequence=1 .
Smith RM, Gray JE, Homer CSE. Common content, delivery modes and outcome measures for faculty development programs in nursing and midwifery: a scoping review. Nurse Educ Pract. 2023:103648.
Nursing and Midwifery Board of Australia. Registration standard: Continuing professional development 2016 3rd January 2022. https://www.nursingmidwiferyboard.gov.au/Registration-Standards/Continuing-professional-development.aspx .
International Confederation of Midwives. Essential competencies for midwifery practice: 2019 Update. 2019.
Baloyi OB, Jarvis MA. Continuing Professional Development status in the World Health Organisation, Afro-region member states. Int J Afr Nurs Sci. 2020;13:100258.
Mack HG, Golnik KC, Murray N, Filipe HP. Models for implementing continuing professional development programs in low-resource countries. MedEdPublish. 2017;6(1).
Lucas A. Continuous professional development, friend or foe? Br J Midwifery. 2012;20(8):576–81.
Ingwu JA, Efekalam J, Nwaneri A, Ohaeri B, Israel C, Chikeme P, et al. Perception towards mandatory continuing professional development programme among nurses working at University of Nigeria Teaching Hospital, Enugu-Nigeria. Int J Afr Nurs Sci. 2019;11:100169.
Hasumi T, Jacobsen KH. Healthcare service problems reported in a national survey of South africans. Int J Qual Health Care. 2014;26(4):482–9.
Giri K, Frankel N, Tulenko K, Puckett A, Bailey R, Ross H. Keeping up to date: continuing professional development for health workers in developing countries. IntraHealth Int. 2012.
Botha A, Booi V, editors. mHealth implementation in South Africa. 2016 IST-Africa Week Conference; 2016: IEEE.
World Continuing Education Alliance (WCEA). World Continuing Education Alliance: About us2022 3rd January 2022. https://lmic.wcea.education/about-us/ .
West F, Homer C, Dawson A. Building midwifery educator capacity in teaching in low and lower-middle income countries. A review of the literature. Midwifery. 2016;33:12–23.
van Wyk JM, Wolvaardt JE, Nyoni CN. Evaluating the outcomes of a faculty capacity development programme on nurse educators in sub-saharan Africa. Afr J Health Professions Educ. 2020;12(4):201–5.
Frantz JM, Bezuidenhout J, Burch VC, Mthembu S, Rowe M, Tan C, et al. The impact of a faculty development programme for health professions educators in sub-saharan Africa: an archival study. BMC Med Educ. 2015;15(1):1–8.
Fullerton JT, Johnson PG, Thompson JB, Vivio D. Quality considerations in midwifery pre-service education: exemplars from Africa. Midwifery. 2011;27(3):308–15.
Shikuku DN, Tallam, E., Wako, I., Mualuko, A., Waweru, L., Nyaga, L., ... & Ameh, C. Evaluation of capacity to deliver Emergency Obstetrics and Newborn Care updated midwifery and reproductive health training curricula in Kenya: Before and after study. 2022
Shikuku DN, Jebet J, Nandikove P, Tallam E, Ogoti E, Nyaga L, et al. Improving midwifery educators’ capacity to teach emergency obstetrics and newborn care in Kenya universities: a pre-post study. BMC Med Educ. 2022;22(1):1–10.
Akiode A, Fetters T, Daroda R, Okeke B, Oji E. An evaluation of a national intervention to improve the postabortion care content of midwifery education in Nigeria. Int J Gynecol Obstet. 2010;110(2):186–90.
Nursing Council of Kenya. Continuing Professional Development guidelines. Nursing Council of Kenya; 2021.
Nursing and Midwifery Council of Nigeria. Promoting & Maintaining Excellence in Nursing Education and Practice: Functions2022. https://www.nmcn.gov.ng/function.html .
Ministry of Health. Kenya Health Policy 2014–2030: Towards attaining the highest standard of health 2014. http://publications.universalhealth2030.org/uploads/kenya_health_policy_2014_to_2030.pdf .
Orsmond GI, Cohn ES. The distinctive features of a feasibility study: objectives and guiding questions. OTJR: Occupation Participation Health. 2015;35(3):169–77.
Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–7.
Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol. 2010;10(1):1–7.
Kirkpatrick DL. Implementing the four levels: A practical guide for effective evaluation of training programs: Easyread super large 24pt edition: ReadHowYouWant. com; 2009.
Warfa A-RM. Mixed-methods design in biology education research: Approach and uses. CBE—Life Sci Educ. 2016;15(4):rm5.
Creswell JW, Creswell JD. Research design: qualitative, quantitative, and mixed methods approaches. Sage; 2017.
Creswell JW, Clark VLP. Designing and conducting mixed methods research. Third ed: Sage; 2018.
NCK Online CPD Portal: Continuous Professional Development [Internet]. 2021. https://osp.nckenya.com/cpd? .
Nursing and Midwifery Council of Nigeria. Promoting & maintaining Excellence in nursing education and practice: Renewal of License. 2022. Available from. https://www.nmcn.gov.ng/renewal.html .
Warren N, Gresh A, Mkhonta NR, Kazembe A, Engelbrecht S, Feraud J et al. Pre-service midwifery education in sub-saharan Africa: a scoping review. Nurse Educ Pract. 2023:103678.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Muellmann S, Brand T, Jürgens D, Gansefort D, Zeeb H. How many key informants are enough? Analysing the validity of the community readiness assessment. BMC Res Notes. 2021;14(1):1–6.
Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med. 2022;292:114523.
Shumway JM, Harden RM. AMEE Guide 25: the assessment of learning outcomes for the competent and reflective physician. Med Teach. 2003;25(6):569–84.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77.
Erlandsson K, Doraiswamy S, Wallin L, Bogren M. Capacity building of midwifery faculty to implement a 3-years midwifery diploma curriculum in Bangladesh: A process evaluation of a mentorship programme. Nurse Educ Pract. 2018;29:212–8.
Erlandsson K, Byrskog U, Osman F, Pedersen C, Hatakka M, Klingberg-Allvin M. Evaluating a model for the capacity building of midwifery educators in Bangladesh through a blended, web-based master’s programme. Global Health Action. 2019;12(1):1652022.
Hatakka M, Osman F, Erlandsson K, Byrskog U, Egal J, Klingberg-Allvin M. Change-makers in midwifery care: exploring the differences between expectations and outcomes—A qualitative study of a midwifery net-based education programme in the Somali region. Midwifery. 2019;69:135–42.
Erlandsson K, Osman F, Hatakka M, Egal JA, Byrskog U, Pedersen C, et al. Evaluation of an online master’s programme in Somaliland. A phenomenographic study on the experience of professional and personal development among midwifery faculty. Nurse Educ Pract. 2017;25:96–103.
Bogren M, Rosengren J, Erlandsson K, Berg M. Build professional competence and equip with strategies to empower midwifery students–an interview study evaluating a simulation-based learning course for midwifery educators in Bangladesh. Nurse Educ Pract. 2019;35:27–31.
Msosa A, Msiska M, Mapulanga P, Mtambo J, Mwalabu G. Simulation-based education in classroom and clinical settings in sub-saharan Africa: a systematic review. Higher Education, Skills and Work-Based Learning; 2023.
Ameh CA, White S, Dickinson F, Mdegela M, Madaj B, van den Broek N. Retention of knowledge and skills after emergency Obstetric Care training: a multi-country longitudinal study. PLoS ONE. 2018;13(10):e0203606.
Evans C, Razia R, Cook E. Building nurse education capacity in India: insights from a faculty development programme in Andhra Pradesh. BMC Nurs. 2013;12(1):1–8.
Koto-Shimada K, Yanagisawa S, Boonyanurak P, Fujita N. Building the capacity of nursing professionals in Cambodia: insights from a bridging programme for faculty development. Int J Nurs Pract. 2016;22:22–30.
Kitema GF, Laidlaw A, O’Carroll V, Sagahutu JB, Blaikie A. The status and outcomes of interprofessional health education in sub-saharan Africa: a systematic review. J Interprof Care. 2023:1–23.
Ladur AN, Kumah EA, Egere U, Mgawadere F, Murray C, Ravit M et al. A blended learning approach for capacity strengthening to improve the quality of integrated HIV, TB, and Malaria services during antenatal and postnatal care in LMICs: a feasibility study. medRxiv. 2023:2023.05. 04.23289508.
World Continuing Education Alliance (WCEA). Improving Health Outcomes: WCEA delivering sustainable solutions for CPD & lifelong learning2023 26th December 2023. https://wcea.education/ .
Download references
Acknowledgements
The study was made possible through the financial support of the Johnson and Johnson Foundation for the three-year “Design, implementation and evaluation of Nursing/Midwifery CPD Educator Programme in Kenya” (2021 – 2023) and the Alliance to Improve Midwifery Education through UNFPA Headquarters. Special acknowledgement to nursing and midwifery educators from mid-level training colleges and universities in Kenya and Nigeria, Ministries of Health, Nursing Council of Kenya, Nursing and Midwifery Council of Nigeria, KMTC headquarters management who participated in the study. Also, we specially appreciate the World Continuing Education Alliance for the dedicated support with the online modules and expert trainers who participated in the delivery of the face-to-face training component: Aisha Hassan, Dr. Mojisola Ojibara, Dr. Eniola Risikat Kadir, Aminat Titi Kadir, Benson Milimo, Esther Ounza, Marthar Opisa, Millicent Kabiru, Sylvia Kimutai, Dr. Joyce Jebet, Dr. Steve Karangau, Dr. Moses Lagat and Dr. Evans Ogoti. Gratitude to Boslam Adacha and Roselynne Githinji for their dedicated support with data preparation for analysis and Dr. Sarah White for her statistical analysis expert guidance and support. Thank you also to Geeta Lal at UNFPA Headquarters. Lastly, the authors would like to acknowledge the special technical and logistical support provided by the LSTM – Kenya team (Onesmus Maina, Martin Eyinda, David Ndakalu, Diana Bitta, Esther Wekesa and Evans Koitaba) and LSTM Nigeria team (Dr. Michael Adeyemi and Deborah Charles) during the trainings.
The study was funded by the Johnson and Johnson Foundation as part of the three-year “Design, implementation and evaluation of Nursing/Midwifery CPD Educator Programme in Kenya” and the Alliance to Improve Midwifery Education through UNFPA. The Johnson and Johnson Foundation were not involved in the research – study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and affiliations.
Liverpool School of Tropical Medicine (Kenya), P.O. Box 24672-00100, Nairobi, Kenya
Duncan N. Shikuku & Lucy Nyaga
Liverpool School of Tropical Medicine (UK), Liverpool, L3 5QA, UK
Duncan N. Shikuku, Alice Norah Ladur, Carol Bedwell & Charles Ameh
Liverpool School of Tropical Medicine (Nigeria), Utako District, P.O Box 7745, Abuja, Nigeria
Hauwa Mohammed
Moi University, P.O. Box 4606-30100, Eldoret, Kenya
Lydia Mwanzia
Masinde Muliro University of Science and Technology, P.O. Box 190-50100, Kakamega, Kenya
Peter Nandikove
Maseno University, P.O. Box 3275-40100, Kisumu, Kenya
Alphonce Uyara
Kenya Medical Training College, P.O Box 30195-00100, Nairobi, Kenya
Catherine Waigwe
Department of Family Health, Ministry of Health (Kenya), P.O. Box 30016-00100, Nairobi, Kenya
Issak Bashir
Aga Khan University of East Africa, P.O Box 39340-00623, Nairobi, Kenya
Eunice Ndirangu
Burnet Institute, 85 Commercial Road Prahran Victoria, Melbourne, Australia
Sarah Bar-Zeev
University of Nairobi, P. O. Box 19676-00100, Nairobi, Kenya
Charles Ameh
Diponegoro University, JI. Prof Sudarto No 13, Temalang, Kec, Tembalang, Kota, Semarang, Jawa Tengah, 50275, Indonesia
You can also search for this author in PubMed Google Scholar
Contributions
DNS, SBZ and CA conceived the idea and designed the study protocol; DNS designed the online data collection tools/checklists/assessments, performed data extraction, cleaning, analysis and interpretation of the results, drafted the primary manuscript, reviewed and prepared it for publication; DNS, HM, LM, PN and AU conducted the training intervention, collected data and reviewed the drafts and final manuscript; AL participated in the design of the study, qualitative data analysis, interpretation of findings and reviewed draft manuscripts; CW, LN, IB, EN, CB and SBZ participated in the design of the study procedures and substantively reviewed the drafts and final manuscript. CA reviewed study procedures, data collection tools, provided oversight in investigation, analysis, interpretation and substantively reviewed the manuscript drafts. SBZ and CA obtained funding for the study. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Duncan N. Shikuku .
Ethics declarations
Ethics approval and consent to participate.
Ethics review and approvals were obtained from Liverpool School of Tropical Medicine’s Research Ethics Committee (LSTM REC No. 23 − 004) and in-country ethical approvals from Kenya (MTRH/MU – IREC FAN 0004383; NACOSTI License No: NACOSTI/P/23/25498) and Nigeria (NHREC Approval Number NHREC/01/01/2007- 31/03/2023). Participation in the study was strictly voluntary and did not form part of the educator’s performance appraisals. Not taking part in the study did not disadvantage some educators who consented but missed out. Informed electronic and written consent was obtained from all participants. Unique participant codes were used for identification and all the data collection tools/forms and datasets were de-identified with no participant identifying information. All interviews were conducted at the offices of the respective stakeholders maintaining privacy during data collection process.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shikuku, D.N., Mohammed, H., Mwanzia, L. et al. Evaluation of the feasibility of a midwifery educator continuous professional development (CPD) programme in Kenya and Nigeria: a mixed methods study. BMC Med Educ 24 , 534 (2024). https://doi.org/10.1186/s12909-024-05524-w
Download citation
Received : 24 January 2024
Accepted : 06 May 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12909-024-05524-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Continuous professional development
- Feasibility
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Master rotation plan is the overall plan of rotation of all students in a particular educational institution, showing the placement of the students belonging to total programme (4 years in B.Sc.(N) and 3 years in GNM) includes both theory and practice denoting the study block, partial block, placement of student in clinical blocks, team nursing, examinations, vacation, co-curricular activities ...
In your teaching presentation, you described the learning outcomes for the audience and explained why medication safety is important. You went through the four steps in your safety checklist (taking as prescribed, storage, side effects and interactions, and keeping a med list) and gave examples to illustrate each.
Similarly, the ability for nurses to predict change, employ improvement strategies, and exercise fiscal prudence are critical skills. System awareness, innovation, and design also are needed to address such issues as structural racism and systemic inequity. Entry-Level Professional Nursing Education.
The report card is designed to be used by nursing programs to assess their curricula. If you are assessing more than one nursing program, assess each one separately. Answer the questions in each section with your curriculum in mind. Each item can be ranked from "0" (no implementation in your curriculum) to "4" (full implementation in ...
CONTENT FOR A COURSE PLAN •State the objectives to be achieved or outcomes to be attained through the given course. •Specify the levels of learners ( I, II ,III, IV Yr). •Mention the placement of the course within the curriculum. •Eg:-A course in Nursing foundation is placed in the I st yr of nursing curriculum.
This document provides a course plan for a Nursing Education course. The course is 240 hours of theory and 300 hours of practical work for a Master's program. The course aims to help students understand fundamental principles of nursing education including teaching and learning processes, instructional methods and media, curriculum development, evaluation and standards. Some key objectives are ...
in nursing education, even in schools of nursing with established curricula. The extent of the ... A plan or program for all the experiences that the learner encounters under the direction of the ... be a unit, a course, a sequence of courses, the school's entire program of studies—and may be encountered inside or outside class or school ...
The document discusses the principles and process of course planning for nursing educational programs. It explains that a course combines interrelated units to achieve program objectives. When planning a course, the objectives should be stated behaviorally and the content sequenced logically. The teacher must consider what and how students will learn. A course plan should describe the course ...
Despite the increased discussion of and evidence for active learning, it is not clear how frequently nurse educators choose to use lectures or active learning in their classes. This study examined the extent to which nursing faculty across schools of nurs-ing use lecture versus active learning. Of the 438 faculty, only a few used solely active ...
Writing Learning Objectives for Nursing When you are writing learning objectives, think of them as being connected to a larger, overarching goal that you want to achieve in your learning. Your learning objectives are the smaller steps (e.g. strategies or actions) you will take to reach your goal. Each learning
The Essentials documents published by the American Association of Colleges of Nursing (AACN) have guided curricular development across baccalaureate and higher degree programs since the mid-1980s (AACN, 2019a).In response to shifts within healthcare delivery, AACN began revisions to the Essentials documents in 2018. Since that time, collaboration between academe and practice has resulted in a ...
course plan - Download as a PDF or view online for free. Submit Search. Upload. course plan ... Lesson plan, Nursing Education . ... Instructional design nsg edu topic ppt.
The document is a lesson plan for teaching nursing students about the concept of teaching and learning. It outlines the objectives to introduce the topic, define teaching and learning, and explain the stages of teaching. The plan details the content, teaching methods such as using PowerPoint slides and a blackboard, as well as evaluation for each segment. It aims to help students understand ...
summative evaluation in nursing education1 1Goh HS et al. Value of nursing objective structured clinical examinations: a scoping review. Nurse Educa. [epub ahead of print] doi: 10.1097/NNE.0000000000000620 Simulation for Assessment cont High stakes assessment: students need to pass assessment to pass the course Critical steps to follow: 1.
The Report's Key Messages. For our country to advance health equity for all, the systems that educate, pay, and employ nurses need to: Permanently remove nurse practice barriers. Value nurses' contributions. Prepare nurses to tackle and understand health equity. Fully support nurses. 13.
Key Message #2: Nurses should achieve higher levels of education and training through an improvededucation system that promotes seamless academicprogression.. Major changes in the U.S. health care system and practice environments will require equally profound changes in the education of nurses both before and after they receive their licenses.Nursing education at all levels needs to provide a ...
Presentations on health and medical topics can be challenging to create, but this Google Slides & PowerPoint template is here to rescue you! This multi-purpose layout is designed with blue pastel tones, providing a professional and calm environment to showcase your medical expertise to colleagues, students, or patients.
Perfect for individuals pursuing a career in nursing or education, this elegant and minimalistic PowerPoint and Google Slides template radiates professionalism. Specializing in college degrees, short courses, and other vocational learning, it utilizes a gentle blend of blue and pink hues to create a visually appealing design. Whether you're ...
Is easier to use during the course of care, especially: when moving from soiled to clean activities with the same patient or resident. when moving between patients or residents in shared rooms or common areas. Improves skin condition with less irritation and dryness than soap and water. Guidelines for Hand Hygiene in Healthcare Settings ...
Midwifery education is under-invested in developing countries with limited opportunities for midwifery educators to improve/maintain their core professional competencies. To improve the quality of midwifery education and capacity for educators to update their competencies, a blended midwifery educator-specific continuous professional development (CPD) programme was designed with key stakeholders.
This week the University of Arkansas - Fort Smith announced the return of its 2-year Associate of Applied Science (AAS) Nursing degree in the Carolyn McKelvey Moore School of Nursing. The Arkansas State Board of Nursing approved the new degree plan on Thursday, May 16, 2024, following earlier approvals from the Arkansas Department of Higher Education and the University of Arkansas Board of ...