- How It Works
- PhD thesis writing
- Master thesis writing
- Bachelor thesis writing
- Dissertation writing service
- Dissertation abstract writing
- Thesis proposal writing
- Thesis editing service
- Thesis proofreading service
- Thesis formatting service
- Coursework writing service
- Research paper writing service
- Architecture thesis writing
- Computer science thesis writing
- Engineering thesis writing
- History thesis writing
- MBA thesis writing
- Nursing dissertation writing
- Psychology dissertation writing
- Sociology thesis writing
- Statistics dissertation writing
- Buy dissertation online
- Write my dissertation
- Cheap thesis
- Cheap dissertation
- Custom dissertation
- Dissertation help
- Pay for thesis
- Pay for dissertation
- Senior thesis
- Write my thesis

226 Hot Public Health Thesis Topics For Top Grades
Are you stuck trying to get the best current public health research topics for thesis and writing it? If yes, know you are not alone. A lot of students find the tasks challenging, but we are here to help. Keep reading our informative guide that demonstrates how to prepare an engaging public health paper.
We will also highlight hot 226 health policy topics for paper and other public health ideas for dissertation that you can use for top grades. Why settle for less when we can help you select the best college or university papers?
What Is Public Health?
Before looking at the top public health statistics undergraduate thesis topics or other public health research ideas, let’s start with the definition. So, what is public health?
According to the World Health Organization (WHO), public health is “the art and science of preventing diseases, helping to prolong life and promote health using organized efforts. Good examples of public health efforts include preventing outbreaks, educating the public on health choices, promoting fitness, preparing for emergencies, and avoiding the spread of infectious diseases. Public health
How To Write A Great Public Health Dissertation
If you are a graduate or masters student, one of the most comprehensive documents that you need to prepare is the dissertation. It is an expansive paper and comes at the end of your course. Remember that you need to ensure it is prepared well because a team of professors will ultimately evaluate it. So, here are the main steps that you need to follow to prepare a high quality dissertation:
Identify the topic of study Comprehensively research the topic and identify the main points to support it Develop the thesis statement for the dissertation (this thesis will ultimately be tested after gathering your data) Develop an outline for the dissertation. This guide should tell you what to write at what specific instance. Here is a sample outline: Topic of the study Introduction. Start with the thesis statement, followed by the objectives of the study. Then, the rest of the introduction should be used to set the background for the study. Literature review: Review relevant resources about the topic. Methodology: Explain the methodology that was used during the study. Is Results and analysis: Provide the results gathered during the study. Discussion and conclusion: Here, you should discuss the study results and demonstrate whether they approve or disapprove the thesis statement. If you found any gaps in the previous studies, highlight them too and call for further studies. Bibliography: This is a list of all the resources you used to prepare the paper. Write the first draft following the outline we have just listed above. Write the final copy by refining the first draft, proofreading, and editing it.
Awesome Public Health Thesis Topics
Here are the leading thesis topics in public health for top grades. You can use them as they are or tweak a little to suit your preference.
Public Health Thesis Topics In Mental Issues
- What is the role of public health in addressing mental issues in society?
- Seasonal affective disorder: A review of the disorder’s prevalence rates.
- Society should always listen to the needs of mentally ill persons.
- Eating disorders in adults: A review of the treatment strategies used for adults in the UK.
- What is the relation between climate change and emerging public health issues?
- Comparing depression prevalence rates in the UK to those of the US.
- What are the main causes of anxiety disorders in society?
- A review of the connection between HIV/AIDS and mental health issues in society.
- Running a public health facility: What is the most important equipment?
- Emerging public health issues in developing countries.
- Analyzing the psychological problems of breast cancer.
- What strategies should people use to prevent their mental health from social media dangers?
- A review of the public health benefits associated with active lifestyles.
- Stress: Why is it a major risk factor for mental health in many communities?
- What are the most common mental health issues in society today?
- Comparing the rates of depression and stress in China and the UK.
- Addressing anxiety-related disorders: Is cognitive-behavior therapy the best treatment method?
- A review of the economic burden of living with a person suffering from anxiety disorders.
- How does depression impact the quality of life?
- Comparing training of public health officers in the US to India.
Unique Research Topics In Public Health
- Surrogacy: A review of associated ethical issues.
- Prevalence of medical errors in hospitals: A review of the policies used to prevent the problem in the United States.
- Blood transfusion: What are the side effects?
- A review of doctors’ roles in promoting healthy lifestyles.
- Maintaining healthy body weight: Comparing the effectiveness of the recommended methods.
- A review of organ donation trends in Europe and Asia.
- Analyzing the ethical factors around cloning: When should it be allowed?
- The ethics of human experimentation.
- Comparing the rates of heart attacks in women to men in the United States.
- What are the main causes of heart attacks? Can it be prevented?
- Progress in diabetes studies and treatment: Is it possible to get a cure in the future?
- Biological weapons and their impacts on society: A review of the Leukemia rates in Japan.
- Pre-diabetes in children: What are the main symptoms, and how can it be addressed?
Public Health Paper Topics On COVID-19
- How will COVID-19 change life?
- What are the advantages and disadvantages of self-isolation?
- Life lessons that you learned during the COVID-19 pandemic.
- What challenges has your community faced during COVID-19 pandemic?
- School life during COVID-19 pandemic.
- A review of mass media operations during pandemic.
- What projects did you undertake during the pandemic?
- A review of projects that your community undertook during the COVID-19 pandemic.
- A closer look at the backlash against Asians in Europe at the start COVID-19 pandemic period.
- Preparing for the next pandemic: What lessons did the world learn from the COVID-19 pandemic?
- The best strategies for staying healthy during a pandemic.
- Is there anything that we could have done to prevent the COVID-19 pandemic?
- Comparing the effectiveness of Europe and American healthcare preparedness for tackling disasters.
- A review of mental health status in a community of your choice during the COVID-19 pandemic.
- A review of COVID-19 emergence theories: Which one do you think is more credible?
- Comparing the impacts of the COVID-19 pandemic to Ebola.
- Vaccines development for viral infections: What made the development of the COVID-19 vaccine possible so fast, whereas that of HIV/AIDS has taken so long?
- A review of the vaccine development process.
- Time for review: How effectively do you think your government responded to the COVID-19 pandemic?
- Rethinking public health on a global scale: Demonstrating why effective healthcare is only possible when looked at globally.
Interesting Public Health Research Topic Ideas
- What is the importance of learning public health in school?
- Identify and review a common public health issue in your community.
- The history of human health: Comparing what was considered healthy in ancient times to what is referred to as healthy today.
- Going vegan: How can it impact your health?
- Excessive weight: Is it the new threat to human civilization?
- Is bodybuilding healthy?
- Body positive: Is it a new health standard or ignorance of body issues?
- Things to consider when selecting healthy food to eat.
- Why psychological health should be part of every community in society.
- The health of newborns: What is the difference between their healthcare and that of adults?
- Emerging trends in the healthcare industry: How can the latest trends benefit society?
- Comparing depression and anxiety in two countries of your choice.
- Physical wellness must include healthy behavioral patterns and nutrition.
- A sense of belonging is paramount to personal and community health.
- What is the relationship between spirituality and public health?
- A review of stigmatization of mental health issues in a community of your choice.
- Is it possible to prevent depression?
- At what point should children start learning sex-related education?
- Comparing the two main public health issues in two cities: London and New York.
- What is the relationship between poverty and public health?
Hot Researchable Topics In Public Health
- The resurgence of measles in society: The best guidance for clinicians.
- Tackling the growing national drug problem.
- Bioterrorism preparedness for global disasters.
- A review of recent vitamin D recommendations for older adults.
- Strategies for maintaining maternal mortality at low levels across the globe.
- Efforts by Asian governments to reduce infections from using unsafe water.
- Over-the-counter drug abuse in Europe: Compare two countries of your choice.
- Health care providers’ roles in preventing bullying in society.
- Knowledge management in the UK healthcare organizations.
- The health benefits of good healthcare waste management.
- Characteristics of dental wastes in hospitals.
- Comparing the most prevalent public health issues in developed and developing nations.
- Latest trends in financing public health.
- The relevance of clinical epidemiology in public health.
- Evidence based public health.
- Epidemiological burden of HIV/AIDS in developing countries.
- Addressing cervical cancer in developing countries: Is it possible to eliminate it completely?
- Ethics in public health clinical research.
- Comparing the strategies used in teaching and motivating public health professionals in developing and developed countries.
Research Topics In Public Health For Masters
- Advertising and impacts on food choices in the community.
- The use of stem cell technologies for cancer treatment: What are the latest trends?
- Bio-printing: Is it the future of organ transplants?
- Nutrition education: How does it promote healthy diets?
- Exercising: What role does it play in promoting strength and balance in the elderly?
- Weight loss surgery: What are the key advantages and disadvantages?
- Heart disease is a major public health issue in society.
- Alternative strategies for treating depression in society: Are they effective?
- Healthcare leadership and its importance in public health.
- Legal aspects of public health care in the society.
- Mental disabilities in patients: A review of the emerging trends in the UK.
- How does the United States promote the development of public health?
- Inequalities in medicine: What impact does it have in public health?
- The most controversial issues in public health in the UK.
- What are the most preferred storage systems for medical supplies in the UK public health facilities?
- Reimagining the public health systems on the globe: Where do you see the UK health system in the next 20 years?
Top Thesis Topics In Dental Public Health
- Common oral health issues in Ireland.
- A review of common problems of endodontically treated teeth.
- The role of good leadership skills in dental education.
- Child management techniques between male and female practitioners.
- What role does ergonomics play in dentistry?
- Dental material and bio-engineering: What are the latest trends?
- A review of the relationship between diabetes and oral health in the society.
- The role of electronic health care record systems used in public health.
- Comparing dental health issues in the developing and developed countries.
- A review of public awareness of dental health issues in a community of choice.
- How can you ensure that all the food you buy is safe and healthy?
- What strategies are used by your local health community to promote dental awareness?
- Dental health management in California: What do you think should be done differently?
- Are you satisfied with the strategies used to address dental issues?
Hot Thesis Topics Public Health
- Mandatory overtime work for medical staff: How does it impact their commitment to their job?
- Nursing shortage and its impact in public health.
- Strategies for improving public health in the EU.
- Mental health issues among asylum seekers in the United States.
- Common mental issues among veterans returning from war: A case study of the United States.
- What functions does management play in healthcare settings when handling key public health issues?
- How poor relationships between nurses and doctors can impact public health services delivery.
- Third-party players in public health and their roles.
- Financial reporting standards in public health facilities.
- What is the correlation between revenue collection in society and the quality of patient services?
- Reviewing the coordination of public health officials during disasters.
- The importance of staff training on quality of health services.
- Comparing the differences between alternative medicine and conventional medicine in addressing public health issues in society.
- Obesity: What are the main causes in child-going age?
- A review of health consequences of caffeine.
- Medical marijuana: What are the main pros and cons?
- A review of the US Farm Bill Amendments that legalized use of cannabis in the US.
- Doing sports: Is it always healthy?
- Low-fat or low-carb diet: Which one is better in addressing overweight and diabetes issues?
- Preventing communicable diseases: Evaluating the prevention strategies used in Asia.
- What is the estimated cost of treating heart problems?
Controversial Public Health Dissertation Topics
- Smoking and impacts of current efforts to address cancer in the society.
- A review of the main causes of heart attacks in society today.
- Tobacco ads: Evaluating their impacts and the relationship to the current cancer trends in the society.
- Sleep disorders: Explain why they should be considered a public health issue.
- Staffing shortage and the impacts in fighting COVID-19 pandemic in Asia.
- Analyzing risk management of treating different diseases in the community.
- COVID-19 pandemic in numbers: Comparing the infection rates in the developed and developing countries.
- Reviewing strategies used in the US public health system to achieve equity: How effective are they?
- Analyzing the main challenges in the UK medical care system.
- Rising cases of suicides in the society: What are the main causes?
- A comprehensive review of strategies used to prevent suicides in the 21st century in the US.
- Use of vaccines to prevent diseases: Do adults still need the vaccines?
- Heat-related deaths: What strategies should be adopted?
- Chronic-diseases prevention: Comparing the strategies used in developing and developed countries.
- Are we becoming too dependent on antibiotics in fighting diseases?
- Opioid crisis: Are the doctors to blame for it?
- Use of blockchain in growing accuracy of clinical trials in medicine.
- What dangers are posed by nuclear wastes in society?
- Assessing US industrial facilities compliance rates to cut down emissions.
- Using clean energy as a strategy of improving public health: What are the expectations?
- What is the healthiest country?
- Evaluating the correlation between gaming and deviant behavior among children in society.
- COVID-19 could have been prevented if WHO was more vigilant?
Public Health Research Questions
- Is the high cost of medical healthcare in the United States justified?
- What is the correlation between poverty and poor health in society?
- Should health care for homeless people be free?
- Unconventional medicine: Should it be part of the UK healthcare system?
- Should doctors be responsible for medical errors?
- Should medical officers or health facilities be allowed to promote selective medical products?
- Should all healthcare facilities in the UK be required to have translators for non-English speaking clients?
- Mental health issues associated with domestic violence: A case study of France.
- Is it a good idea to legalize euthanasia?
- What are the benefits of using surgical masks in public?
- What are the most important lessons from the different waves of the COVID-19 pandemic reported on the globe?
- Who is more responsible for the COVID-19 pandemic?
- Ebola or COVID-19 pandemic: Which is worse?
- What are the main causes of epidemics on the globe?
- Public health planning: What are the most important things to think about?
- Should governments pay the cost of rehabilitating drug addicts in society?
- Teaching children healthy lifestyles: What are the best strategies?
- What problems do people with autism face in society?
- What are the leading causes of child mortality in your community?
- Gun violence in the United States: Should it be considered a public health issue?
- What illnesses are considered foodborne?
Easy Topics In Public Health
- All workplaces should support breastfeeding.
- What are the best strategies to reduce pollution in society?
- Public health benefits of recycling waste in society.
- Reviewing the causes of poor water quality in the developing world.
- Comparing water quality standards policies in the UK and US.
- Health impacts of the rapid depletion of o-zone depletion.
- Better planning of infrastructural development is important for healthier societies: Discuss.
- The US is better prepared to handle pandemics that might arise after the COVID-19 pandemic. Discuss.
- A review of common diseases spread by vectors.
- A review of key policies installed to protect employee health.
- Legal age for consuming energy drinks should be set by the government to address the problem of diabetes.
- Smoking: Should it be banned in public?
- What are the best strategies for raising awareness in public?
- Can reducing the workload of employees in manufacturing facilities improve their health?
- Sunbathing should be restricted to prevent the risk of cancer: Discuss.
- Should abortion be banned in society?
- School-related stress: How can it be prevented?
- Should birth control be made available and free for all teenagers?
- What should be categorized as a bad health habit?
- Compare and contrast two common treatment methods for treating behavioral disorders.
- Internet addiction: What are the main dangers of internet addiction?
Other Public Health Topics For Research
- How to stay healthy and safe during a pandemic.
- Using a bicycle instead of driving is healthier.
- Common mental disorders in India.
- What is the biggest health issue among young people?
- The impact of exercising in teenagers.
- Why do teenagers experiment with drugs?
- What impact does dispositional violence have on mental disorders?
- Is telemedicine helpful in promoting better healthcare?
- Unproven alternative medicine: What are the associated risks?
- What alternatives do we have for antibiotics?
- What is the difference between private and public healthcare?
- A review of the main health issues associated with puberty.
- What is the most dangerous disease of the 21st century?
- Why are some people still afraid of vaccines?
- Experimental treatment: Why do people agree to undergo it?
- How can we improve the health of people living with chronic illnesses?
- The best strategies to make people aware of the basics of healthcare.
- A review of the growing awareness about reproductive health in the society.
Seek Thesis Help from Experts
As we indicated earlier, writing a dissertation or other advanced papers is never easy. However, you should not give up or get content with poor quality work. If you do, defending the paper in front of a team of professors will be challenging. The best way out is to pay master thesis help .
We work with the best writers who are always ready to help you craft A-rated papers. They are educated in top schools and have a lot of experience in preparing both undergraduate papers and masters thesis. When you buy medical thesis , we also offer editing and proofreading services to guarantee students of highly refined work. Our services are also affordable and we also use secure communication to guarantee every student high confidentiality. When your teacher issues the assignment prompt, whether for a research paper or dissertation, let our professionals help you to get the best grades.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Comment * Error message
Name * Error message
Email * Error message
Save my name, email, and website in this browser for the next time I comment.
As Putin continues killing civilians, bombing kindergartens, and threatening WWIII, Ukraine fights for the world's peaceful future.
Ukraine Live Updates
100+ ICMR Research Topics: Unlocking Health Insights
The landscape of healthcare research in India has been significantly shaped by the endeavors of the Indian Council of Medical Research (ICMR). Established in 1911, the ICMR has played a pivotal role in advancing medical knowledge, informing health policies, and fostering collaborations to address pressing health challenges in the country.
In this blog, we embark on a journey through the corridors of ICMR research topics, shedding light on the council’s current and noteworthy research topics that are contributing to the nation’s health and well-being.
The Role of ICMR in Health Research
Table of Contents
The Indian Council of Medical Research operates as the apex body in India for the formulation, coordination, and promotion of biomedical research. With a mission to nurture and harness the potential of medical research for the benefit of society, ICMR has become a cornerstone in shaping health policies and practices.
By fostering collaborations with researchers and institutions across the nation, ICMR has emerged as a driving force in advancing healthcare knowledge and outcomes.
| Unlock the secrets of the microbial world without breaking the bank! Elevate your academic journey with affordable – because knowledge should be accessible to all students, regardless of budget constraints. |
Understanding ICMR Research Methodology
The success of ICMR’s research lies not only in its expansive scope but also in its rigorous methodology and ethical considerations. ICMR has established guidelines that researchers must adhere to, ensuring that studies funded by the council are not only scientifically sound but also ethically conducted.
This commitment to ethical research practices has been a cornerstone in building public trust and confidence in the findings generated by ICMR-funded studies.
100+ ICMR Research Topics For All Level Students
- Infectious Diseases: Emerging pathogens and control strategies.
- Non-Communicable Diseases (NCDs): Diabetes, cardiovascular research.
- Maternal and Child Health: Strategies for mortality reduction.
- Biomedical Research: Molecular insights into diseases.
- Cancer Research: Innovative approaches for treatment.
- Epidemiology: Studying disease patterns and trends.
- Vaccination Strategies: Enhancing immunization programs.
- Public Health Interventions: Effective community health measures.
- Antibiotic Resistance: Combating microbial resistance.
- Genetic Studies: Understanding genetic contributions to diseases.
- Neurological Disorders: Research on neurological conditions.
- Mental Health: Addressing mental health challenges.
- Nutrition and Health: Studying dietary impacts on health.
- Health Systems Research: Improving healthcare delivery.
- Ayurveda Research: Integrating traditional medicine practices.
- Environmental Health: Impact of environment on health.
- Emerging Technologies: Utilizing tech for healthcare innovations.
- Pharmacological Research: Advancements in drug discovery.
- Global Health Collaborations: International health partnerships.
- Waterborne Diseases: Prevention and control strategies.
- Health Policy Research: Shaping evidence-based policies.
- Health Economics: Studying economic aspects of healthcare.
- Telemedicine: Harnessing technology for remote healthcare.
- Rare Diseases: Understanding and treating rare disorders.
- Community Health: Promoting health at the grassroots level.
- HIV/AIDS Research: Advancements in HIV prevention and treatment.
- Aging and Health: Research on geriatric health issues.
- Cardiovascular Health: Preventive measures and treatments.
- Respiratory Diseases: Understanding lung-related conditions.
- Zoonotic Diseases: Investigating diseases transmitted from animals.
- Stem Cell Research: Applications in regenerative medicine.
- Yoga and Health: Studying the health benefits of yoga.
- Gender and Health: Research on gender-specific health issues.
- Oral Health: Preventive measures and treatments for oral diseases.
- Health Informatics: Utilizing data for healthcare improvements.
- Health Education: Promoting awareness for better health.
- Drug Resistance: Research on antimicrobial resistance.
- Hepatitis Research: Prevention and treatment strategies.
- Telehealth: Remote healthcare services and accessibility.
- Diabetes Management: Strategies for diabetes prevention and control.
- Tuberculosis Research: Advancements in TB diagnosis and treatment.
- Fertility Research: Understanding reproductive health issues.
- Artificial Intelligence in Healthcare: Integrating AI for diagnostics.
- Health Disparities: Addressing inequalities in healthcare access.
- Mental Health Stigma: Research on reducing stigma.
- Mobile Health (mHealth): Applications for mobile-based healthcare.
- Vector-Borne Diseases: Prevention and control measures.
- Nanotechnology in Medicine: Applications in healthcare.
- Occupational Health: Research on workplace health issues.
- Biobanking: Storing and utilizing biological samples for research.
- Telepsychiatry: Providing mental health services remotely.
- Health Equity: Promoting fairness in healthcare delivery.
- Community-Based Participatory Research: Engaging communities in research.
- E-health: Electronic methods for healthcare delivery.
- Sleep Disorders: Understanding and treating sleep-related conditions.
- Health Communication: Effective communication in healthcare.
- Global Burden of Disease: Research on disease prevalence and impact.
- Traditional Medicine: Studying traditional healing practices.
- Nutraceuticals: Research on health-promoting food components.
- Health Data Security: Ensuring privacy and security of health data.
- Regenerative Medicine: Advancements in tissue engineering.
- Social Determinants of Health: Studying social factors affecting health.
- Pharmacovigilance: Monitoring and ensuring drug safety.
- Gerontology: Research on aging and the elderly.
- Mobile Apps in Healthcare: Applications for health monitoring.
- Genetic Counseling: Supporting individuals with genetic conditions.
- Community Health Workers: Role in improving healthcare access.
- Health Behavior Change: Strategies for promoting healthier habits.
- Palliative Care Research: Enhancing end-of-life care.
- Nanomedicine: Applications of nanotechnology in medicine.
- Climate Change and Health: Impact on public health.
- Health Literacy: Promoting understanding of health information.
- Antibody Therapeutics: Advancements in antibody-based treatments.
- Digital Health Records: Electronic health record systems.
- Microbiome Research: Understanding the role of microorganisms in health.
- Disaster Preparedness: Research on health response during disasters.
- Food Safety and Health: Ensuring safe food consumption.
- Artificial Organs: Advancements in organ transplantation.
- Telepharmacy: Remote pharmaceutical services.
- Environmental Epidemiology: Studying the link between environment and health.
- E-mental Health: Digital tools for mental health support.
- Precision Medicine: Tailoring treatments based on individual characteristics.
- Health Impact Assessment: Evaluating the consequences of policies on health.
- Genome Editing: Applications in modifying genetic material.
- Mobile Clinics: Bringing healthcare to underserved areas.
- Telecardiology: Remote cardiac care services.
- Health Robotics: Utilizing robots in healthcare settings.
- Precision Agriculture and Health: Linking agriculture practices to health outcomes.
- Community-Based Rehabilitation: Supporting rehabilitation at the community level.
- Nanotoxicology: Studying the toxicological effects of nanomaterials.
- Community Mental Health: Strategies for promoting mental well-being.
- Health Financing: Research on funding models for healthcare.
- Augmented Reality in Healthcare: Applications in medical training and diagnostics.
- One Health Approach: Integrating human, animal, and environmental health.
- Disaster Mental Health: Addressing mental health issues after disasters.
- Mobile Laboratory Units: Rapid response in disease outbreaks.
- Health Impact Investing: Investing for positive health outcomes.
- Rehabilitation Robotics: Assisting in physical therapy.
- Human Microbiota: Understanding the microorganisms living in and on the human body.
- 3D Printing in Medicine: Applications in medical device manufacturing.
Success Stories from ICMR-Funded Research
Highlighting the impact of ICMR-funded research is essential in appreciating the council’s contribution to healthcare in India. From breakthrough discoveries to successful interventions, ICMR-supported studies have led to tangible improvements in health outcomes.
Case studies showcasing the journey from ICMR research topics and findings to real-world applications serve as inspiring examples of how scientific knowledge can translate into positive societal impacts.
Challenges and Opportunities in ICMR Research
While ICMR has achieved remarkable success in advancing health research, it is not without its challenges. Researchers face obstacles in conducting studies, ranging from resource constraints to logistical issues.
Acknowledging these challenges is crucial in finding solutions and optimizing the impact of ICMR-funded research. Additionally, there are opportunities for collaboration, both nationally and internationally, that can further enrich the research landscape and accelerate progress in addressing health challenges.
The Future of Health Research in India: ICMR’s Vision
Looking ahead, ICMR envisions a future where health research continues to play a central role in shaping the well-being of the nation. Strategic goals include harnessing the power of technology and innovation to drive research advancements, fostering interdisciplinary collaborations, and addressing emerging health challenges.
The vision extends beyond the laboratory, emphasizing the translation of research findings into practical solutions that can positively impact the lives of individuals and communities across India.
In conclusion, the Indian Council of Medical Research stands as a beacon in the realm of healthcare research, tirelessly working towards advancements that contribute to the well-being of the nation.
By exploring ICMR research topics, understanding its methodology, and reflecting on success stories, we gain insight into the transformative power of scientific inquiry.
As ICMR continues to forge ahead, the future of health research in India looks promising, guided by a vision of innovation, collaboration, and a steadfast commitment to improving the health of all citizens.
Related Posts

Step by Step Guide on The Best Way to Finance Car

The Best Way on How to Get Fund For Business to Grow it Efficiently
Public Health Education, Practice, and Research in India
- Living reference work entry
- First Online: 25 March 2024
- Cite this living reference work entry

- Yaser Mohammed Al-Worafi ORCID: orcid.org/0000-0002-5752-2913 2 , 3 ,
- Abubakar Siddique 4 ,
- Long Chiau Ming 5 , 6 &
- Abdullah Ahmed Dhabali 7 , 8
This chapter aims to discuss public health education, practice, and research-related issues in India. Moreover, it described the achievement in education, practice, and research in the country. This chapter will describe the challenges facing education in the country and suggest the recommendations to overcome these challenges; challenges facing the practice in the country and suggest the recommendations to overcome these challenges; and challenges facing the research in the country and suggest the recommendations to overcome these challenges. Moreover, online education, practice, and research will be discussed in this chapter; facilitators for the best online education, practice, and research will be explained; and finally the barriers to the implementation of online education, practice, and research will be discussed with the recommendations to overcome it.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Abd Rahim, N. H., Ming, L. C., Al-Worafi, Y. M. A., & Sarker, M. M. R. (2016). A regulatory review for products containing glutathione. Archives of Pharmacy Practice, 7 (5), S57.
Article Google Scholar
Ahmed, A., Lee, K. S., Bukhsh, A., Al-Worafi, Y. M., Sarker, M. M. R., Ming, L. C., & Khan, T. M. (2018). Outbreak of vaccine-preventable diseases in Muslim majority countries. Journal of Infection and Public Health, 11 (2), 153–155.
Article PubMed Google Scholar
Akkawi, M. E., Al-Shami, N., Al-Worafi, Y. M., Ahmed, A. A. A., & Al-Shami, A. M. (2022). Knowledge, attitude, and practice towards antibiotic use among the public in the City of Kuantan, Pahang State, Malaysia. Journal of Pharmacy, 2 (2), 149–158.
Google Scholar
Alakhali, K. M., Alshahrani, S. M., Al-Worafi, Y. M., & Irawati, L. (2020). A case report of COVID-19 in Yemen: Detailed clinical observations. Journal of Pharmaceutical Research International, 32 (26), 1–5.
Al-Meman, A., Al-Worafi, Y. M., & Saeed, M. S. (2014). Team-based learning as a new learning strategy in pharmacy college, Saudi Arabia: Students’ perceptions. Universal Journal of Pharmacy, 3 (3), 57–65.
Al-Mohamadi, A., Halboup, A. M., Ibrahim, M. I. M., Abdulghani, M., Al-Worafi, Y. M., Otham, G., … & Ansari, M. (2018). Medical and pharmacy students’ perceptions regarding generic medicines in Yemen. Journal of Pharmacy Practice and Community Medicine, 4 , 47–50.
Al-Qahtani, I., Almoteb, T. M., & Al-Warafi, Y. (2015). Competency of metered-dose inhaler use among Saudi community pharmacists: A simulation method study. RRJPPS, 4 (2), 37–31.
Alshahrani, S. M., Alakhali, K. M., & Al-Worafi, Y. M. (2019a). Medication errors in a health care facility in southern Saudi Arabia. Tropical Journal of Pharmaceutical Research, 18 (5), 1119–1122.
Alshahrani, S. M., Alavudeen, S. S., Alakhali, K. M., Al-Worafi, Y. M., Bahamdan, A. K., & Vigneshwaran, E. (2019b). Self-medication among King Khalid University students, Saudi Arabia. Risk Management and Healthcare Policy, 12 , 243–249.
Article PubMed PubMed Central Google Scholar
Alshahrani, S. M., Alakhali, K. M., Al-Worafi, Y. M., & Alshahrani, N. Z. (2020a). Awareness and use of over the counter analgesic medication: A survey in the Aseer region population, Saudi Arabia. International Journal of Advanced and Applied Sciences, 7 (3), 130–134.
Alshahrani, S. M., Alzahran, M., Alakhali, K., Vigneshwaran, E., Iqbal, M. J., Khan, N. A., … & Alavudeen, S. S. (2020b). Association between diabetes consequences and quality of life among patients with diabetes mellitus in the Aseer Province of Saudi Arabia. Open Access Macedonian Journal of Medical Sciences, 8 (E), 325–330.
Al-Worafi, Y. M. (2013a). Pharmacy education in Yemen. American Journal of Pharmaceutical Education, 77 (3), 65.
Al-Worafi, Y. M. (2013b). Do community pharmacists need a workshop about MDI use? Journal of Pharmacy Practice and Research, 43 (2), 165.
Al-Worafi, Y. (2013c). Towards supporting clinical pharmacy research in Arabic countries. Journal of Pharmacy Practice & Research, 43 (3), 247–248.
Al-Worafi, Y. M. (2014a). The challenges of pharmacy education in Yemen. American Journal of Pharmaceutical Education, 78 (8), 146.
Al-Worafi, Y. M. (2014b). Pharmacy practice and its challenges in Yemen. The Australasian Medical Journal, 7 (1), 17.
Al-Worafi, Y. M. (2014c). Prescription writing errors at a tertiary care hospital in Yemen: Prevalence, types, causes and recommendations. American Journal of Pharmacy and Health Research, 2 , 134–140.
Al-Worafi, Y. M. (2014d). Comment on: “Pharmacovigilance in the Middle East”. Drug Safety, 37 (8), 651.
Al-Worafi, Y. M. A. (2015). Appropriateness of metered-dose inhaler use in the Yemeni community pharmacies. Journal of Taibah University Medical Sciences, 10 (3), 353–358.
Al-Worafi, Y. M. A. (2016). Pharmacy practice in Yemen. In Pharmacy practice in developing countries (pp. 267–287). Academic.
Chapter Google Scholar
Al-Worafi, Y. M. (2017). Pharmacoeconomics education in Yemen. Currents in Pharmacy Teaching & Learning, 9 (5), 945.
Al-Worafi, Y. M. (2018a). Knowledge, attitude and practice of Yemeni physicians toward pharmacovigilance: A mixed method study. International Journal of Pharmacy and Pharmaceutical Sciences., 10 (10), 74–77.
Al-Worafi, Y. M. (2018b). Dispensing errors observed by community pharmacy dispensers in IBB–Yemen. Asian Journal of Pharmaceutical and Clinical Research, 11 (11), 478.
Al-Worafi, Y. M. (2018c). Evaluation of inhaler technique among patients with asthma and COPD in Yemen. Journal of Taibah University Medical Sciences, 13 (5), 488–490.
Al-Worafi, Y. M. (Ed.). (2020a). Drug safety in developing countries: Achievements and challenges . Academic.
Al-Worafi, Y. M. (2020b). Medications safety research issues. In Drug safety in developing countries (pp. 213–227). Academic.
Al-Worafi, Y. M. (2020c). Medications safety-related terminology. In Drug safety in developing countries (pp. 7–19). Academic.
Al-Worafi, Y. M. (2020d). Medications registration and marketing: Safety-related issues. In Drug safety in developing countries (pp. 21–28). Academic.
Al-Worafi, Y. M. (2020e). Pharmacovigilance. In Drug safety in developing countries (pp. 29–38). Academic.
Al-Worafi, Y. M. (2020f). Medication errors. In Drug safety in developing countries (pp. 59–71). Academic.
Al-Worafi, Y. M. (2020g). Adverse drug reactions. In Drug safety in developing countries (pp. 39–57). Academic.
Al-Worafi, Y. M. (2020h). Self-medication. In Drug safety in developing countries (pp. 73–86). Academic.
Al-Worafi, Y. M. (2020i). Antibiotics safety issues. In Drug safety in developing countries (pp. 87–103). Academic.
Al-Worafi, Y. M. (2020j). Drug-related problems. In Drug safety in developing countries (pp. 105–117). Academic.
Al-Worafi, Y. M. (2020k). Counterfeit and substandard medications. In Drug safety in developing countries (pp. 119–126). Academic.
Al-Worafi, Y. M. (2020l). Medication abuse and misuse. In Drug safety in developing countries (pp. 127–135). Academic.
Al-Worafi, Y. M. (2020m). Storage and disposal of medications. In Drug safety in developing countries (pp. 137–142). Academic.
Al-Worafi, Y. M. (2020n). Safety of medications in special population. In Drug safety in developing countries (pp. 143–162). Academic.
Al-Worafi, Y. M. (2020o). Herbal medicines safety issues. In Drug safety in developing countries (pp. 163–178). Academic.
Al-Worafi, Y. M. (2020p). Medications safety pharmacoeconomics-related issues. In Drug safety in developing countries (pp. 187–195). Academic.
Al-Worafi, Y. M. (2020q). Evidence-based medications safety practice. In Drug safety in developing countries (pp. 197–201). Academic.
Al-Worafi, Y. M. (2020r). Quality indicators for medications safety. In Drug safety in developing countries (pp. 229–242). Academic.
Al-Worafi, Y. M. (2020s). Drug safety in Yemen. In Drug safety in developing countries (pp. 391–405). Academic.
Al-Worafi, Y. M. (2020t). Drug safety in Saudi Arabia. In Drug safety in developing countries (pp. 407–417). Academic.
Al-Worafi, Y. M. (2020u). Drug safety in United Arab Emirates. In Drug safety in developing countries (pp. 419–428). Academic.
Al-Worafi, Y. M. (2020v). Drug safety in Indonesia. In Drug safety in developing countries (pp. 279–285). Academic.
Al-Worafi, Y. M. (2020w). Drug safety in Palestine. In Drug safety in developing countries (pp. 471–480). Academic.
Al-Worafi, Y. M. (2020x). Drug safety: Comparison between developing countries. In Drug safety in developing countries (pp. 603–611). Academic.
Al-Worafi, Y. M. (2020y). Drug safety in developing versus developed countries. In Drug safety in developing countries (pp. 613–615). Academic.
Al-Worafi, Y. (2022a). A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Book Google Scholar
Al-Worafi, Y. (2022b). Pharmacy education: Learning styles. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022c). Competencies and learning outcomes. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022d). Social media, social-networking sites, and webinar and video conferencing platforms. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022e). Teaching the practice and tutorial. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022f). Self-learning and self-directed learning. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022g). Traditional and active strategies. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022h). Team-based learning in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022i). Problem-based learning in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022j). Case-based learning in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022k). Simulation in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022l). Project-based learning in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022m). Flipped classes in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022n). Educational games in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022o). Web-based learning in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022p). Mobile health technologies. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022q). Blended learning in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022r). Assessment methods in pharmacy education: Strengths and limitations. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022s). Assessment methods in pharmacy education: Direct assessment. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022t). Access and equitable access. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022u). Assessment methods in pharmacy education: Formative assessment. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022v). Objective structured clinical examination (OSCE) in pharmacy education. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022w). Pharmacists’ prescribing. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2022x). Technologies and tools. In A guide to online pharmacy education: Teaching strategies and assessment methods . CRC Press.
Al-Worafi, Y. (2023a). Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023b). Patient safety-related issues: History and importance. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023c). Patient safety-related issues: Patient care errors and related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023d). Patient care errors and related problems: Preventive medicine errors & related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023e). Patient care errors and related problems: Patient assessment and diagnostic errors & related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023f). Patient care errors and related problems: Non-pharmacological errors & related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023g). Patient care errors and related problems: Medical errors & related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023h). Patient care errors and related problems: Surgical errors & related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023i). Patient care errors and related problems: Complementary and alternative medicines (CAM) errors & related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023j). Patient care errors and related problems: Nutrition errors & related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023k). Patient care errors and related problems: Pharmacological errors & related problems (medication errors and related problems). In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023l). Patient safety research in developing countries achievements, challenges, and recommendations. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023m). Patient care errors and related problems: Monitoring errors & related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023n). Patient care errors and related problems: Patient education and counselling errors and related problems. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023o). Patient safety resources and tools. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023p). Patient safety culture. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023q). Nosocomial infections in developing countries. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023r). Patient safety in pharmacies. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023s). Patient safety for special populations: Geriatrics. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023t). Patient safety for special populations: Paediatrics. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023u). Patient safety for special populations: Pregnancy. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023v). Patient safety for special populations: Lactation. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023w). Patient safety for special populations: Adolescents. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023x). Patient safety during pandemics. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023y). Patient safety: Antimicrobial-resistance and interventions. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. (2023z). Patient safety education: Competencies and learning outcomes. In Patient safety in developing countries: Education, research, case studies . CRC Press.
Al-Worafi, Y. M. (Ed.). (2023aa). Clinical case studies on medication safety . Academic.
Al-Worafi, Y. M. (2023ab). Technology for drug safety: Current status and future developments . Springer Nature.
Al-Worafi, Y. M. (Ed.). (2023ac). Comprehensive healthcare simulation: Pharmacy education, practice and research . Springer Nature.
Al-Worafi, Y. M. (2023ad). Artificial intelligence and machine learning for drug safety. In Technology for drug safety: Current status and future developments (pp. 69–80). Springer International Publishing.
Al-Worafi, Y. M. (2023ae). Technology for drug safety: Challenges. In Technology for drug safety: Current status and future developments (pp. 129–152). Springer International Publishing.
Al-Worafi, Y. M. (2023af). Development and validation of the pharmacist care model and definitions. https://doi.org/10.21203/rs.3.rs-3128130/v1
Al-Worafi, Y. M. (2023ag). Health care systems in the Arab world: Achievements, challenges, and recommendations. https://doi.org/10.13140/RG.2.2.14972.82562
Al-Worafi, Y. M. (2023ah). Migration of health care professionals from the Arabic countries: A mixed method study. https://doi.org/10.13140/RG.2.2.11427.32808
Al-Worafi, Y. M. (2023ai). Patient and public satisfaction towards health care services in the Arab world. https://doi.org/10.13140/RG.2.2.23867.69924
Al-Worafi, Y. M. (2023aj). Pharmacy education in the Arab world: Achievements, challenges, and recommendations. https://doi.org/10.13140/RG.2.2.24546.81600
Al-Worafi, Y. M. (2023ak). Public health education in the Arab world: Achievements, challenges, and recommendations. https://doi.org/10.13140/RG.2.2.26643.96802
Al-Worafi, Y. M. (2023al). Nursing education in the Arab world: Achievements, challenges, and recommendations. https://doi.org/10.13140/RG.2.2.29160.55044
Al-Worafi, Y. M. (2023am). Medical education in the Arab world: Achievements, challenges, and recommendations. https://doi.org/10.13140/RG.2.2.29422.69444
Al-Worafi, Y. M. (2023an). Dentistry education in the Arab world. https://doi.org/10.13140/RG.2.2.31257.70245
Al-Worafi, Y. (2024). Handbook of complementary, alternative, and integrative medicine: Education, practice and research . CRC Press.
Al-Worafi, Y. M., & Ming, L. C. (2022). Attitude and practice of Yemeni physicians toward the integration of herbal medicines into patient care practice. https://doi.org/10.21203/rs.3.rs-2351211/v1
Al-Worafi, Y. M., Kassab, Y. W., Alseragi, W. M., Almutairi, M. S., Ahmed, A., Ming, L. C., Alkhoshaiban, A. S., & Hadi, M. A. (2017). Pharmacovigilance and adverse drug reaction reporting: A perspective of community pharmacists and pharmacy technicians in Sana’a, Yemen. Therapeutics and Clinical Risk Management, 13 , 1175.
Al-Worafi, Y. M., Patel, R. P., Zaidi, S. T. R., Alseragi, W. M., Almutairi, M. S., Alkhoshaiban, A. S., & Ming, L. C. (2018a). Completeness and legibility of handwritten prescriptions in Sana’a, Yemen. Medical Principles and Practice, 27 , 290–292.
Al-Worafi, Y. M., Alseragi, W. M., Seng, L. K., Kassab, Y. W., Yeoh, S. F., Chiau, L., … & Husain, K. (2018b). Dispensing errors in community pharmacies: A prospective study in Sana’a, Yemen. Archives of Pharmacy Practice, 9 (4), 1–3.
Al-Worafi, Y. M., Alseragi, W. M., & Mahmoud, M. A. (2019). Competency of metered-dose inhaler use among community pharmacy dispensers in Ibb, Yemen: A simulation method study. Latin American Journal of Pharmacy, 38 (3), 489–494.
Al-Worafi, Y. M., Alseragi, W. M., Ming, L. C., & Alakhali, K. M. (2020a). Drug safety in China. In Drug safety in developing countries (pp. 381–388). Academic.
Al-Worafi, Y. M., Alseragi, W. M., Alakhali, K. M., Ming, L. C., Othman, G., Halboup, A. M., … & Elkalmi, R. M. (2020b). Knowledge, beliefs and factors affecting the use of generic medicines among patients in Ibb, Yemen: A mixed-method study. Journal of Pharmacy Practice and Community Medicine, 6 (4), 53.
Al-Worafi, Y. M., Elkalmi, R. M., Ming, L. C., Othman, G., Halboup, A. M., Battah, M. M., … & Mani, V. (2021a). Dispensing errors in hospital pharmacies: A prospective study in Yemen. https://doi.org/10.21203/rs.3.rs-153952/v1
Al-Worafi, Y. M., Hasan, S., Hassan, N. M., & Gaili, A. A. (2021b). Knowledge, attitude and experience of pharmacist in the UAE towards pharmacovigilance. Research Journal of Pharmacy and Technology, 14 (1), 265–269.
Al-Worafi, Y., Ming, L., Alseragi, W., Dhabali, A., & Al-Shami, A. (2021c). Adverse reactions of COVID-19 vaccine among frontline workers in Fujairah, UAE. https://doi.org/10.21203/rs.3.rs-137445/v1
Al-Worafi, Y. M., Hermansyah, A., Goh, K. W., & Ming, L. C. (2023a). Artificial intelligence use in university: Should we ban ChatGPT?. https://doi.org/10.20944/preprints202302.0400.v1
Al-Worafi, Y. M., Ming, L. C., & Al-Shami, A. M. (2023b). Vaccines safety case studies. In Clinical case studies on medication safety (pp. 487–497). Academic.
Ang, L. P., Ng, P. W., Lean, Y. L., Kotra, V., Kifli, N., Goh, H. P., … & Ming, L. C. (2021). Herbal products containing aristolochic acids: A call to revisit the context of safety. Journal of Herbal Medicine, 28 , 100447.
Atif, M., Ahmed, W., Nouman Iqbal, M., Ahmad, N., Ahmad, W., Malik, I., & Al-Worafi, Y. M. (2022a). Frequency and factors associated with adverse events among multi-drug resistant tuberculosis patients in Pakistan: A retrospective study. Frontiers in Medicine, 8 , 790718.
Atif, M., Munir, K., Malik, I., Al-Worafi, Y. M., Mushtaq, I., & Ahmad, N. (2022b). Perceptions of healthcare professionals and patients on the role of the pharmacist in TB management in Pakistan: A qualitative study. Frontiers in Pharmacology, 13 , 965806.
Baig, M. R., Al-Worafi, Y. M., Alseragi, W. M., Ming, L. C., & Siddique, A. (2020). Drug safety in India. In Drug safety in developing countries (pp. 327–334). Academic.
Begum, R., Choudhry, F. R., Khan, T. M., Bakrin, F. S., Al-Worafi, Y. M., & Munawar, K. (2020). Mental health literacy in Pakistan: A narrative review. Mental Health Review Journal, 25 (1), 63–74.
Choudhry, F. R., Munawar, K., Kassab, Y. W., Bakrin, F. S., Al-Worafi, Y. M., & Khan, T. M. (2021). Public perception about the Zika virus in working professionals: A qualitative inquiry. International Quarterly of Community Health Education, 41 (2), 199–207.
Elangovan, D., Long, C. S., Bakrin, F. S., Tan, C. S., Goh, K. W., Hussain, Z., … & Ming, L. C. (2020). Application of blockchain technology in hospital information system. In Mathematical modeling and soft computing in epidemiology (pp. 231–246). Taylor & Francis Group.
Elkalmi, R. M., Al-Worafi, Y. M., Alseragi, W. M., Ming, L. C., & Siddique, A. (2020). Drug safety in Malaysia. In Drug safety in developing countries (pp. 245–253). Academic.
Elsayed, T., & Al-Worafi, Y. M. (2020). Drug safety in Egypt. In Drug safety in developing countries (pp. 511–523). Academic.
Guella, I., Hassan, N., Shahwan, M., Al-Worafi, Y. M., & Alkhoujah, S. (2021). Patients’ beliefs towards generic medicines in The United Arab Emirates. Research Journal of Pharmacy and Technology, 14 (6), 3343–3346.
Hamdan, N. K. A., Lean, Q. Y., Neoh, C. F., Abdullah, A. H., Lim, S. M., Ramasamy, K., … & Lua, P. L. (2020). Knowledge and perception of facial candling for allergic rhinitis among university staff and students. Evidence-Based Complementary and Alternative Medicine , 2020 , 1.
Hasan, S., Al-Omar, M. J., Al-Zubaidy, H., & Al-Worafi, Y. M. (2019). Use of medications in Arab countries. In Handbook of healthcare in the Arab world (p. 42). Springer.
Hassan, Y., Abd Aziz, N., Kassab, Y. W., Elgasim, I., Shaharuddin, S., Al-Worafi, Y. M. A., … & Ming, L. C. (2014). How to help patients to control their blood pressure? Blood pressure control and its predictor. Archives of Pharmacy Practice, 5 (4), 153.
Hossain, M. S., Kader, M. A., Goh, K. W., Islam, M., Khan, M. S., Harun-Ar, M. R., … & Ming, L. C. (2022). Herb and spices in colorectal cancer prevention and treatment: A narrative review. Frontiers in Pharmacology, 13 , 865801.
Izahar, S., Lean, Q. Y., Hameed, M. A., Murugiah, M. K., Patel, R. P., Al-Worafi, Y. M., … & Ming, L. C. (2017). Content analysis of mobile health applications on diabetes mellitus. Frontiers in Endocrinology, 8 , 318.
Jaber, A. A. S., Al-Worafi, Y. M., & Dhabali, A. A. (2022). Patients’ beliefs toward generic medication in Yemen. Journal of Generic Medicines, 18 (2), 110–115.
Jefri, U. H. N. M., Khan, A., Lim, Y. C., Lee, K. S., Liew, K. B., Kassab, Y. W., … & Kalusalingam, A. (2022). A systematic review on chlorine dioxide as a disinfectant. Journal of Medicine and Life, 15 (3), 313.
Khan, T. M., Tahir, H., Salman, M., Mustafa, Z. U., Raza, M. H., Asif, N., … & Baig, M. R. (2021). General anxiety predictors among frontline warriors of COVID: Cross-sectional study among nursing staff in Punjab, Pakistan. Archives of Pharmacy Practice, 1 , 40.
Kharaba, Z., Farhat, J., Mahboub, B. S., Buabeid, M. A., Alfoteih, Y., Al-Worafi, Y., … & Al-Ahmad, M. (2022). Current views of community and hospital pharmacists on pharmaceutical care services in the United Arab Emirates: A mixed methodological study. F1000Research, 11 , 694.
Kouider, D. A. R., Hassan, N. A. G., & Al-Worafi, Y. M. (2019). A study investigating the association between vitamin D and depression among university students in 39 countries. Biomedical Research, 30 (4), 655–659.
Kumaran, H., Long, C. S., Bakrin, F. S., Tan, C. S., Goh, K. W., Al-Worafi, Y. M., … & Ming, L. C. (2020). Online pharmacies: Desirable characteristics and regulations. Drugs & Therapy Perspectives, 36 , 243–245.
Lee, K. S., Yee, S. M., Zaidi, S. T. R., Patel, R. P., Yang, Q., Al-Worafi, Y. M., & Ming, L. C. (2017). Combating sale of counterfeit and falsified medicines online: A losing battle. Frontiers in Pharmacology, 8 , 268.
Loy, M. J., Goh, K. W., Osili, N., Ming, L. C., Dhaliwal, J. S., Hermansyah, A., … & Lee, K. S. (2022). Features and functionalities of medical mobile applications for the endemic phase of COVID-19: Review and content analysis. Progress in Microbes & Molecular Biology, 5 (1), 1–17.
Mahleyuddin, N. N., Moshawih, S., Ming, L. C., Zulkifly, H. H., Kifli, N., Loy, M. J., … & Goh, H. P. (2021). Coriandrum sativum L.: A review on ethnopharmacology, phytochemistry, and cardiovascular benefits. Molecules, 27 (1), 209.
Mahmoud, M. A., Wajid, S., Naqvi, A. A., Samreen, S., Althagfan, S. S., & Al-Worafi, Y. (2020). Self-medication with antibiotics: A cross-sectional community-based study. Latin American Journal of Pharmacy, 39 (2), 348–353.
Manan, M. M., Rusli, R. A., Ang, W. C., Al-Worafi, Y. M., & Ming, L. C. (2014). Assessing the pharmaceutical care issues of antiepileptic drug therapy in hospitalised epileptic patients. Journal of Pharmacy Practice and Research, 44 (3), 83–88.
Manan, M. M., Ibrahim, N. A., Aziz, N. A., Zulkifly, H. H., Al-Worafi, Y. M. A., & Long, C. M. (2016). Empirical use of antibiotic therapy in the prevention of early onset sepsis in neonates: A pilot study. Archives of Medical Science, 12 (3), 603–613.
Article CAS PubMed Google Scholar
Ming, L. C., Hameed, M. A., Lee, D. D., Apidi, N. A., Lai, P. S. M., Hadi, M. A., Al-Worafi, Y. M. A., & Khan, T. M. (2016). Use of medical mobile applications among hospital pharmacists in Malaysia. Therapeutic Innovation & Regulatory Science, 50 (4), 419–426.
Ming, L. C., Untong, N., Aliudin, N. A., Osili, N., Kifli, N., Tan, C. S., … & Goh, H. P. (2020). Mobile health apps on COVID-19 launched in the early days of the pandemic: Content analysis and review. JMIR mHealth and uHealth, 8 (9), e19796.
Moshawih, S., Abdullah Juperi, R. A. N. A., Paneerselvam, G. S., Ming, L. C., Liew, K. B., Goh, B. H., … & Kifli, N. (2022). General health benefits and pharmacological activities of Triticum aestivum L. Molecules, 27 (6), 1948.
Othman, G., Ali, F., Ibrahim, M. I. M., Al-Worafi, Y. M., Ansari, M., & Halboup, A. M. (2020). Assessment of anti-diabetic medications adherence among diabetic patients in Sana’a City, Yemen: A cross sectional study. Journal of Pharmaceutical Research International, 32 (21), 114–122.
Saeed, M. S., Alkhoshaiban, A. S., Al-Worafi, Y. M. A., & Long, C. M. (2014). Perception of self-medication among university students in Saudi Arabia. Archives of Pharmacy Practice, 5 (4), 149.
Saher, T., Al-Worafi, Y. M., Iqbal, M. N., Wahid, A., Iqbal, Q., Khan, A., … & Ahmad, N. (2022). Doctors’ adherence to guidelines recommendations and glycaemic control in diabetic patients in Quetta, Pakistan: Findings from an observational study. Frontiers in Medicine, 9 , 978345.
Shahid, I., Khan, K. M., Khan, T. M., Imran, M. S., Shahid, N., Alnafoosi, F. N., … & Al-Worafi, Y. M. (2021). Clinical efficacy of LivPro® herbal medicine among hepatitis C patients Pakistan: Longitudinal Interventional Study. Archives of Pharmacy Practice, 12 (4), 55.
Voo, J. Y. H., Lean, Q. Y., Ming, L. C., Al-Worafi, Y. M., & Ibrahim, B. (2021). Vaccine knowledge, awareness and hesitancy: A cross sectional survey among parents residing at Sandakan district, Sabah. Vaccine, 9 (11), 1348.
Wahid, A., Ghafoor, A., Khan, A. W., Al-Worafi, Y. M., Latif, A., Shahwani, N. A., … & Ahmad, N. (2022). Comparative effectiveness of individualized longer and standardized shorter regimens in the treatment of multidrug resistant tuberculosis in a high burden country. Frontiers in Pharmacology, 13 , 973713.
Yaseen, M. O., Saif, A., Khan, T. M., Yaseen, M., Saif, A., Bukhsh, A., … & Jaber, A. A. (2022). A qualitative insight into the perceptions and COVID-19 vaccine hesitancy among Pakistani pharmacists. Human Vaccines & Immunotherapeutics, 18 (1), 2031455.
Download references
Author information
Authors and affiliations.
College of Pharmacy, University of Science and Technology of Fujairah, Fujairah, UAE
Yaser Mohammed Al-Worafi
College of Medical Sciences, Azal University for Human Development, Sana’a, Yemen
School of Pharmaceutical Sciences, Universiti Sains Malaysia (USM), Pulau Pinang, Malaysia
Abubakar Siddique
PAP Rashidah Sa’adatul Bolkiah Institute of Health Sciences, Universiti Brunei Darussalam, Gadong, Brunei Darussalam
Long Chiau Ming
School of Medical and Life Sciences, Sunway University, Selangor, Malaysia
Faculty of Pharmacy, Sana’a University, Sana’a, Yemen
Abdullah Ahmed Dhabali
School of Clinical Pharmacy, Lebanese International University, Sana’a, Yemen
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
College of Pharmacy, University of Science and Technology of Fujairah, Fujairah, United Arab Emirates
Rights and permissions
Reprints and permissions
Copyright information
© 2024 Springer Nature Switzerland AG
About this entry
Cite this entry.
Al-Worafi, Y.M., Siddique, A., Ming, L.C., Dhabali, A.A. (2024). Public Health Education, Practice, and Research in India. In: Al-Worafi, Y.M. (eds) Handbook of Medical and Health Sciences in Developing Countries. Springer, Cham. https://doi.org/10.1007/978-3-030-74786-2_540-1
Download citation
DOI : https://doi.org/10.1007/978-3-030-74786-2_540-1
Received : 07 October 2023
Accepted : 07 October 2023
Published : 25 March 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-74786-2
Online ISBN : 978-3-030-74786-2
eBook Packages : Springer Reference Medicine Reference Module Medicine
- Publish with us
Policies and ethics
- Find a journal
- Track your research

Most Searched
- Birth Certificate
- Driving Licence
Website of Integrated Health Information Platform

The Integrated Health Information Platform (IHIP) is a comprehensive digital initiative by the Ministry of Health and Family Welfare, Government of India, aimed at transforming India's public health surveillance system. The platform integrates and streamlines health information from various sources to provide real-time, actionable insights into public health data. It is designed to enhance the collection, management, and analysis of health data across the country, ultimately improving the quality and timeliness of health services and responses.
Related Links
Family welfare activities of ministry of health and family welfare.
Find detailed information about the family welfare activities regulated by Ministry of Health and Family Welfare. Details of various programmes and schemes are available. Manuals and guidelines for schemes and programmes are also available.
Website of Ministry of Health and Family Welfare
Website of national medical register (nmr), website of directorate general of health services.
The Directorate General of Health Services (Dte.GHS) is a repository of technical knowledge concerning Public Health, Medical Education and Health Care. It is an attached organisation of the Ministry of Health & Family Welfare.
Website of My Hospital
My Hospital is Ministry of Health, Government of India initiative to capture patient feedback for the services received at the hospital through user-friendly multiple channels such as Short Message Service (SMS), Outbound Dialling (OBD) mobile application and web portal.
Website of MyHealthRecord
Get more information related to Personal Health Record Locker. Services like as Citizen-contrilled Personal Health Record accessible over web and mobile, comprehensive dashboard for health monitoring, Provision for Tele-Consulation and many mores.
Information of Yoga
Yoga is an Art and Science of healthy living. It is a spiritual discipline based on an extremely subtle science, which focuses on bringing harmony between mind and body. The holistic approach of Yoga is well established and it brings harmony in all walks of life and thus, known for disease prevention, promotion of health and management of many lifestyle –related disorders.
Information of Unani
The Unani System of Medicine offers treatment of diseases related to all the systems and organs of the human body. The treatments for chronic ailments and diseases of skin, liver, musculo-skeletal and reproductive systems, immunological and lifestyle disorders have been found to be highly effective and acceptable.
Information of Siddha
Siddha is one of the earliest traditional medicine systems in the world which treats not only the body but also the mind and the soul. The word Siddha has its origin in the Tamil word Siddhi which means "an object to be attained" or "perfection" or "heavenly bliss".
Information of Homoeopathy
Homeopathy can be defined as a “dynamic, holistic and vitalistic system of individualistic drug therapeutics, based on the law of similars, potentially capable to cure diseases that are curable and relieves symptoms of incurable nature”.
Clinical Establishments (Registration and Regulation) ACT, 2010
National art & surrogacy portal.
The National ART & Surrogacy Registry hosted at Department of Health Research, under Ministry of Health and Family Welfare (Govt. of India). This National ART and Surrogacy Registry (NARTSR) is a online public record system of ART Clinics/Banks and Surrogacy Clinics in India
National ART & Surrogacy Registry
You can get detailed information about the National ART & Surrogacy Registry under Ministry of Health and Family Welfare. Step to be taken for registration under the National Assisted Reproductive Technology and Surrogacy Registry.
Website of Heal in India
Hub for Medical and Wellness Tourism globally, inviting the world to "Heal in India" with the mandate of 'Seva' coupled with 'Atithi Devo Bhava' on mission mode.
Website of National Medical Commission
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
New Research Sheds Light on Treatment and Harm Reduction Gaps Among Drug Users
Amidst rising stimulant drug use and an increasingly contaminated drug supply, there is a need for broader communication and fewer barriers to access of harm-reduction strategies
Lindsey Culli
The overdose crisis in the U.S. continues to escalate, with over 100,000 deaths in 2023 and more than one million since 1999. As the drug supply has changed, the crisis has evolved, and opioid overdose deaths now overwhelmingly involve illicitly manufactured synthetic opioids like fentanyl. There has also been a sharp rise in overdose deaths involving stimulants such as cocaine and methamphetamine, and other toxic adulterants like xylazine . Drug overdose mortality has risen most rapidly in marginalized communities.
A new study led by Sachini Bandara, PhD , assistant professor in Mental Health , and Brendan Saloner, PhD , professor in Health Policy and Management , published in August in JAMA Network Open, revealed significant gaps in access to treatment and harm reduction services, as well as disparities in use of services, and suggests that targeted interventions are urgently needed to address the overdose crisis effectively. Conducted across Wisconsin, Michigan, and New Jersey, this study adds to what is known about overdose risk with the current drug supply because of the recency of data collection and targeted sampling of key populations with increasingly higher risk for overdose, including Black and Hispanic populations, older adults, and people who use stimulants. Similar surveys of people who use drugs (PWUD) have historically been small in scale, limited to clients of a small number of service providers, limited to certain types of drug use (e.g., opioids), and have been predominately comprised of younger, white non-Hispanic respondents.
The study, known as VOICES, was supported by the Bloomberg Overdose Prevention Initiative funded by Bloomberg Philanthropies, and conducted in partnership with Vital Strategies. It aimed to understand how access to treatment and harm reduction services varies by overdose history and drug type among a racially and ethnically diverse population of drug users. It involved a cross-sectional telephone survey conducted between January and July 2023, with 1,240 participants recruited from 39 different treatment, harm reduction, and social service provider organizations.
Researchers found that 37% of respondents who had experienced an overdose in the past year reported using fentanyl test strips, compared to only 23.4% of those who had not experienced an overdose. Despite heightened awareness of test strips among overdose survivors, use was low among both groups. As Bandara noted, “Our findings highlight the need for reducing barriers to accessing critical overdose prevention tools.”
Approximately 48% of all participants had received treatment in the past 30 days, indicating that while nearly half were accessing treatment, a substantial portion remained untreated. People who had overdosed were more likely to possess naloxone and use harm reduction services compared to those who had not overdosed. However, there was no significant difference in treatment use between these groups.
Notably, stimulant-only users were less likely to possess naloxone compared to opioid-only users and polysubstance users. Among stimulant-only users, 51.4% possessed naloxone compared to 77.3% of opioid-only users and 77.6% of polysubstance users. There were similar disparities between those different types of drug users in their use of fentanyl test strips with only 16% of stimulant-only users currently using fentanyl test strips.
The study’s results highlight critical gaps in the use of evidence-based treatment and harm reduction services that could significantly reduce overdose risks. Despite the availability of these services, many individuals, especially stimulant users, are not accessing them, suggesting a need for enhanced communication and outreach to promote these lifesaving services.
The study also identified several barriers to accessing treatment and harm reduction services, which include not being ready for treatment, a lack of perceived need for harm reduction services, and a lack of awareness or availability, as many participants said they were unaware of fentanyl test strips or how to obtain them.
“There are substantial gaps in the use of treatment and harm reduction services that could reduce overdose risk,” Bandara said. “In particular, we found low use of harm reduction and treatment services among people who use stimulants, and additional communication around their importance and efforts to remove barriers to access may help increase the use of these services amidst an increasingly contaminated stimulant drug supply.”
The findings suggest that targeted public health campaigns and outreach programs are essential to increase awareness and utilization of treatment and harm reduction services. The research underscores the urgent need for improved access to and utilization of harm reduction and treatment services to save lives. Addressing gaps in harm reduction practices through targeted interventions and increased awareness could significantly mitigate the overdose crisis, particularly in marginalized communities.
- Xylazine: The New Overdose Crisis
- Do Overdose Prevention Sites Make Their Communities Less Safe? (Podcast)
- Nearly One-Third of U.S. Adults Know Someone Who’s Died of Drug Overdose
Related Content

Xylazine: The Emerging Threat in the U.S. Drug Supply and Policy Responses

Understanding the Impact of Economic and Social Conditions on Health

Study Reveals Significant Barriers for TGNC Adults Accessing Healthcare in the U.S.
Medical Misinformation Harms People from Communities that are Marginalized

‘Heat Poverty’: A Growing Threat in India
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 13, Issue 10
- Barriers to climate change and health research in India: a qualitative study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-9647-7855 Shreya Shrikhande 1 , 2 ,
- Sonja Merten 1 , 2 ,
- Olga Cambaco 1 , 2 , 3 ,
- Tristan T Lee 1 , 2 ,
- Ravivarman Lakshmanasamy 4 , 5 ,
- http://orcid.org/0000-0002-7475-1531 Martin Röösli 1 , 2 ,
- Mohammad Aqiel Dalvie 6 ,
- Jürg Utzinger 1 , 2 ,
- Guéladio Cissé 1 , 2
- 1 Epidemiology and Public Health Department , Swiss Tropical and Public Health Institute , Allschwil , Switzerland
- 2 University of Basel , Basel , Switzerland
- 3 Manhiça Health Research Centre , Maputo , Mozambique
- 4 Department of Health and Family Welfare Services , Goverment of Puducherry , Puducherry , India
- 5 Non-communicable Diseases Team , World Health Organization Country Office for India , New Delhi , India
- 6 Centre for Environmental and Occupational Health Research, School of Public Health , University of Cape Town , Rondebosch , Western Cape , South Africa
- Correspondence to Shreya Shrikhande; shreya.shrikhande{at}swisstph.ch
Objectives Almost a quarter of the global burden of disease and mortalities is attributable to environmental causes, the magnitude of which is projected to increase in the near future. However, in many low- and middle-income settings, there remains a large gap in the synthesis of evidence on climate-sensitive health outcomes. In India, now the world’s most populous country, little remains known about the impacts of climate change on various health outcomes. The objective of this study is to better understand the challenges faced in conducting climate change and health research in Puducherry, India.
Design and setting In this study, we employed key informant interviews to deepen the understanding of the perceived research barriers in Puducherry. The findings were analysed using data-driven qualitative thematic analysis to elaborate the major perceived barriers to conducting environmental health research.
Participants This study was conducted among 16 public health professionals, including medical researchers, and professionals involved in environmental policies and planning in Puducherry.
Results We identify three key barriers faced by public health professionals as key stakeholders, namely: (1) political and institutional barriers; (2) education and awareness barriers; and (3) technical research barriers. We show there is a need, from the professionals’ perspective, to improve community and political awareness on climate change and health; strengthen technical research capacity and collaboration among researchers; and strengthen health surveillance, resource allocation and access to health data for research.
Conclusion Evidence informed policies and interventions are a key element in the adaptation response for countries. In the context of the paucity of data on environmental health from India, despite recognised climate change related health vulnerabilities, these findings could contribute to the development and improvement of relevant interventions conducive to a strong research environment.
- public health
- qualitative research
- epidemiology
Data availability statement
No data are available. All data relevant to the study are included in the article or uploaded as supplementary information. All relevant data from this study have been included in the Supplementary material. As this is a qualitative study with a small number of key informants, making the full dataset and interview transcripts available to a wider audience could potentially breach the confidentiality commitment made to the participants during the process of obtaining informed consent as well as to the ethics committees that approved this study. Therefore, these data will not be made available.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2023-073381
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
STRENGTHS AND LIMITATIONS OF THIS STUDY
This study identifies crucial challenges faced in conducting environmental health research by public health professionals for the first time.
The findings draw on the experiences of respected experts who are well placed in the climate change and health sphere.
The sample was restricted to Puducherry district and not representative of the entire Union Territory of Puducherry, much less India as a whole.
The sample is restricted to the opinions of a selected group of experts and we could not include the experiences and perspectives of other public health professionals or stakeholders.
Introduction
An ever-growing body of research has irrefutably shown the global health impacts of climate change through both direct and indirect exposure pathways. 1 2 Multiple risk and vulnerability factors determine the population resilience and adaptive capacity, from sociopolitical, demographic and biological factors to infrastructure, urban planning, health information systems and health workforce. 2 3 Given the regional variations in climate systems, the health impacts of climate change differ between and within countries and communities, mediated by interconnected socioeconomic and environmental determinants of health. 4 5 Non-communicable diseases, such as respiratory diseases, cardiovascular diseases (CVDs) and mental health conditions, have been recognised as growing climate-sensitive health outcomes, in addition to other communicable diseases like vector-borne and water-borne diseases and malnutrition. 3 6
With the rapid pace of climate change, the health impacts attributable to it are also projected to increase. 7 Strengthening the adaptive capacity of countries is therefore an essential component of the climate change response. 8 Timely public health interventions can do much to protect population health from the potential adverse health impacts of climate change. 9 Low- and middle-income countries (LMICs), such as India, remain disproportionately affected by climate impacts, with a critical need to strengthen the healthcare response to climate impacts. 10 11 One of the key steps in the regional or local adaptation response is assessing the true burden of the health impacts within the population of that location. 12 However, owing to the complexity of the relationship between climate change and health, identifying and estimating this association remain one of the biggest global and environmental health challenges, especially in LMICs. 11
In India, the existing health and social disparities within the population make it one of the most vulnerable to climate change impacts, compounded by climatic diversity. 13–16 There have been recent efforts from the Government of India to focus on climate change and health, as evinced by the recent addition of a health mission to the National Action Plan on Climate Change (NAPCC). This led to the formulation of the National Action Plan on Climate Change and Human Health (NAPCCHH) and the drive for State Action Plans for Climate Change and Human Health (SAPCCHH). 17 18 The government recognises several diseases as climate sensitive in these official documents. However, public health engagement, action and research on health impacts of climate change are limited in India, especially given the magnitude of climate impacts to which it is vulnerable. 19 20
Medical and public health professionals, hereafter referred to as health professionals, play an important role in researching, managing and responding to climate change impacts on health. Along with being considered credible sources of information, these groups of professionals also have the capacity for scientific inquiries into the climate change attributable impacts of health. 21–24 Globally, there is an acknowledged need to train health professionals to engage in, study and manage health impacts of climate change. There are few studies assessing stakeholder perceptions on climate change and health, 14 25 26 and even fewer studies looking at specific barriers to research on this topic. 27 28 Given the present gaps in this domain, especially in LMICs, it is particularly salient to better understand research barriers and needs, as perceived by health professionals. 25–27 29
The aim of this study is to understand some of the contextual barriers to environmental health action and research among two relevant professional groups in Puducherry, India. We focused our study on: (1) medical professionals, both in active research and practising; and (2) members of the Department of Science, Technology and Environment (DSTE) working on climate change in Puducherry. As this study is a part of a larger project on CVDs and climate change in India, we also highlighted the specific challenges and barriers to conducting research on CVDs.
Study setting
This study employed key informant interviews following a semistructured interview guide. The methods have been described in detail elsewhere. Briefly, the geographical focus of our study was Puducherry district, which lies on the south-eastern coast of India, with a population of 950 289, as per the Government of India 2011 Census. 30 Puducherry has one main State government run tertiary care hospital and medical college, along with several private clinics and primary care health centres. It is also home to the Central Government Jawaharlal Institute of Postgraduate Medical Education and Research, an ‘Institute of National Importance’ and tertiary care referral hospital. Within the DSTE, there also exists a specialised Puducherry Climate Change Cell with the aim to integrate knowledge about climate change and facilitate the NAPCC implementation, including the state specific Action Plan. 31
Data collection and analysis
Sixteen semistructured interviews were conducted between January and March 2022 with participants from Puducherry. Fourteen interviews were conducted in-person and two were conducted virtually over Zoom. Using purposive sampling based on prior connections followed by snowball sampling, we invited medical professionals (research or practicing) and DSTE staff working on the Puducherry State Action Plan for Climate Change (hereon referred to as environmentalists). Interviews continued until information saturation was reached in the interviews or we had interviewed all the relevant target participants, as in the case of the DSTE staff. The full interview guide and framework with the main categories has been given in the online supplemental table S1 .
Supplemental material
Eleven of the participants had a medical background and were working as either practising physicians or researchers. Within the doctors, we mainly targeted cardiologists, emergency medicine or general medicine physicians who were involved in areas relevant to our study. The majority of the participants was male, with only three females, out of which only one had a medical background. Half of the participants were practising physicians, while the other half were researchers. The participant profile is presented in table 1 and further described in Ref 32 .
- View inline
Profile of participants interviewed in this study
The interviews, conducted by S.S., lasted between 15 to 50 min and were audio recorded with informed consent using a voice recorder. Field notes taken to optimise the interview guide and note key topics. R.L. was a passive observer and facilitator for three interviews. We used an a priori developed interview guide with broad and open-ended questions to allow participants to freely bring up and discuss relevant topics. All interview recordings were assigned a number prior to transcription to ensure anonymity throughout the analysis process. Verbatim transcription and analysis was done using the MaxQDA software V.2018.1 (VERBI Software, Berlin, Germany) by S.S.
For the analysis, a combination of deductive and inductive thematic analysis was used as described by Gale et al . 33 Broad themes were developed based on the aim, framework and interview guide, as discussed below. During analysis, major themes were inductively developed for emerging topics, which we then clearly defined. After familiarisation with the transcripts, an initial codebook was developed from coding the three interviews with the richest data; the remaining interviews were indexed and coded further. The codes were classified into categories, subthemes and themes. The final analytical matrix included three themes. S.S. and T.L. independently validated the codebook with the three main interviews and agreed on the final framework matrix that considered all relevant codes. The matrix was then used to chart relevant quotes supporting our findings and draw comparisons between participants.
The conceptual framework for climate change risk perceptions developed by van Eck et al 34 and the framework for health inequalities proposed by Rudolph et al 35 were used as a base for our analytical framework, shown in figure 1 . While there are three major themes, this paper focuses only on the theme of ‘Institutional determinants’. The findings from the two other themes have been elaborated elsewhere. Within the context of this paper, ‘institution’ is used as a broad term covering all governmental structures, including policy, education and occupation. We identify how these determinants can be perceived as barriers to environmental health research. The framework matrix with relevant themes and categories has been provided in online supplemental table S2 . Additional supporting quotes have also been provided in the online supplemental material .
- Download figure
- Open in new tab
- Download powerpoint
A framework for health adaptation action in the context of climate change based on level of knowledge, perceived health risks, policy and institutional support and public engagement. The circled part highlights the thematic areas we focus on in this work, namely institutional determinants and its challenges.
Ethical consideration
There was no prior relationship between the researchers and participants. Before the interview, the researcher went over the informed consent form, which was then signed by both parties. S.S., the main researcher, is an Indian PhD candidate supervised by a team of international experts based mainly in Switzerland. R.L. is also Indian national based in Puducherry. Additionally, all the quotes presented in this analysis have been assigned only by serial number to ensure anonymity.
Patient and public involvement
As we employed a combination of purposive and snowball sampling, some participants were involved in helping us identify suitable participants to interview. Beyond that, no members of the public were involved in the design, conduct, reporting or dissemination plan of our research.
Overall, there are four main themes that emerged from this research, which are presented in figure 2 . We first report participants’ knowledge regarding climate change and health policies, followed by their perceived institutional barriers to research, namely political, educational and technical barriers. As this study is part of a larger study examining climate change impacts on CVDs, we also highlight barriers specific to climate change and CVD research.
An overview of the thematic framework and salient findings for the four themes explored in this paper. The four main themes are: (1) institutional framework: knowledge on policies; (2) political and institutional; (3) educational and informational; and (4) technical research barriers.
Institutional framework: knowledge on policies
Limited knowledge and awareness on climate change and health related policies.
We found limited awareness among the participants about climate change and health-related policies, such as the NAPCC, NAPCCHH and SAPCCHH. Aside from the environmentalists, who worked on it, only three medical professionals who worked on one of the Action Plans were aware of it. Four participants expressed belief about the non-inclusion of climate change in disease-specific policies and the lack of integrated climate change and health policies and guidelines.
Our country has different policy, environmental policy, health policy. But I have doubt whether health policy has any component of climate change. So, it needs to be incorporated in a health policy of national importance as well as the state, but currently, this element is not in place, that is my feeling. #8, Environmentalist.
One of the environmentalist also mentioned challenges in integrating climate change in development plans. These were thought to be made primarily from a socioeconomic development perspective, although there were ongoing efforts to include the economic co-benefits of climate change adaptation in the development plans.
The challenge is that the government sectoral officers are not aware of how the climate adaptations need to be integrated into their developmental plans. Because whenever they plan for a project, they plan it from the socioeconomic development perspective. #7, Environmentalist.
Political and institutional barriers
Disengaged leadership and low political prioritisation of climate change and health.
Political leadership that did not consider health impacts of climate change as a pressing matter was perceived as one of the barriers to conducting research on the topic. Several participants mentioned how climate change was seen as future concern by policy-makers and the general public, rather than viewed as a cause for immediate concern. A few participants also mentioned the slim likelihood of decision-makers actually being aware of it. One participant described the issue as being ‘not mainstream enough’ to warrant focused work, contributing to the perceived low priority assigned to environmental health research.
Many participants felt that the governmental focus was inclined towards non-health impacts of climate change. The most pressing climate change impacts, which also influence research focus, were thought to be pollution, coastal sensitivity and natural resource depletion and degradation, especially in the context of Puducherry as a coastal region. Additionally, existing sectoral programmes already running were seen as a hindrance to focusing on climate change related programmes by one participant.
The problem is everybody has to understand at the level of the minister or the secretaries. So many programmes are there. Not only about climate change, other programmes are there so they do not focus much on (climate change) programmes… Actually, what I have seen for the past 2–3 years, they don’t care much about climate. #1, Practicing physician/policy advisor.
Despite climate change being recognised as a health risk factor, there was a clear disconnect between on-paper government plans and practice when it came to environmental health research. The challenges India faces from other vulnerabilities, including unmet nutritional and economic needs, were perceived to outrank climate risks to health.
I'm an adviser to government of India on health related research. We did discuss a lot of things but we also touched upon climate and the effects of climate on health… That was considered as an important topic, but we didn't dwell much upon how to take it forward because there are more pressing problems. #15, Practicing physician/academic.
Weak interdepartmental integration and coordination for climate change and health
The compartmentalisation of topics within institutes or sectors was seen as a barrier to conducting interdisciplinary research by the participants. One participant discussed the newly formed Puducherry Climate Change and Health Action Plan (2022), which aims to bring together a multisectoral team, under the leadership of the health ministry, to focus on health impacts of climate change.
However, apart from one participant, most others voiced a perceived need for an independent, coordinating body focused on environmental health, incorporating a research agenda. Partially, this was due to climate change being thought of an added responsibility for health professionals and vice versa for environmentalists, especially for those working in the government. As highlighted by a few participants, officials were likely to prioritise their primary work profile over the added responsibility of climate change and health research. Another concern in the existing scenario was intersectoral, collaborative research being dependant on higher officials being receptive to their junior employees researching a topic not entirely within the scope of their respective department.
Especially government departments, they are loaded with a lot of work. Today, an officer comes in, he has to do his own work, not the work that other departments asks us to do… #9, Environmentalist.
Several participants mentioned the Puducherry Climate Change cell created in response to address climate change impacts. However, despite that, one medical researcher mentioned the current difficulties in collaborating on climate change and health. Several participants also mentioned the need to improving coordination between the sectors, with a dedicated head of climate change and health.
Intersectoral body and there should be one decision maker. So now, everybody is like the leader in the particular sector, but if they need the support from other one, that coordination may be lacking… There won't be any one dedicated person for the climate change. So they will be in charge of multiple departments. For example, somebody’s going to be in charge of immunization or the child health. So their priority will be child health obviously. #3, Medical doctor/academic.
Educational and informational barriers
Gaps in climate change and health in higher education curricula.
One of the strongest emergent themes, referred to by most participants, was the need for environmental health education, either by incorporating climate change in the health curriculum or health impacts of climate change in the environmental curriculum in universities and schools. The prevalent feeling was the source of climate change and health literacy needs to be from multiple sources, with formal education being the most important one. Most participants also felt that at present there was a disconnect between environmental and health education, as a result of which there was a relatively low level of awareness on climate change impacts on health.
Education system need to be addressed from beginning… Even the medical college students who are completing five years courses, I do not see any syllabus which contains impact on health by the climate change even though it is very important…my son is studying medical-medicine, but I guess I just go through the syllabus, but nothing is there. #8, Environmentalist.
All the environmentalists professed to never having specifically studied health impacts of climate change during the course of their education. On the other hand, the health professionals expressed incongruent views on climate change-health education. While one mentioned having studied climate sensitive diseases in medical school, another denied ever having been taught the link between climate change and various diseases.
Continuing education courses specific for health impacts of climate change were suggested by a few participants as potential options to bridge the gap between the environment and health. Two participants also suggested including short courses on this topic for all people working on topics related to climate change, health, adaptation and resilience.
Weakness in intersectoral information dissemination
Many of the participants mentioned having little to no awareness on climate change-health related research unless actively searching for it, pointing to the scope for improving related education and science dissemination, especially among the scientific community. Environmental risk factors were not commonly associated with health inherently, partially attributed the low scientific exposure on the topic.
CVDs were seen as a ‘silent’ disease, with many people are not trained to look for symptoms, much less correlate them to weather conditions, all suggesting the need for improved CVD literacy and awareness on the topic. On the other hand, many participants were open to changing theirs current schools of thought on risk factors for health to include climate change, conditional to being informed by global research on the topic.
If there is research or it’s already proven in other countries, ’so this is a risk factor it is a good idea to add’ but [before adding anything], I think some data or there should be some routine surveillance or monitoring system should be there. … even within the medical circle, people may not be aware how much is the contribution of climate change to the heart disease or for any disease for that case… I don't think our administrators or even our clinicians are that much thinking about the impact of climate change, and [heart disease]. #3, Medical doctor/academic.
Scepticism and low awareness on non-conventional health impacts of climate change
As alluded to previously, health impacts of climate change are often not explicit, making it a challenge to research or focus the research agenda on for several reasons. One participant described how the slow pace of climate impacts leads people to think it will not immediately affect health, unless the impacts are drastic.
…The problem has to become so severe, like you have air pollution in Delhi, then people will act. Climate change affects the life slowly it’s not drastic… that is one of the reasons I feel. And slowly if you get some data and keep on generating awareness not only among the public, but also within the scientific community, then slowly things will be better. #3, Medical doctor/academic.
For researchers, an additional challenge of convincing funders or collaborators on the health impacts of climate change also emerged. One participant described the difficulty researchers had separating environmental risks from other common health risk factors. Scepticism when attempting to research health impacts of climate change was also encountered. Confounding from other risk factors and potential ecological bias was seen as the roots of this uncertainty.
Maybe for six, seven years, I have been trying to do some work on climate change and environmental health. Every time I write a proposal I'm criticized largely telling that "how is it going to work?… And one other problem I see with the research with climate change or any environmental thing, it’s ecological effects. So people ask “how can you attribute this to only this, why not to this?“, " Why not to lifestyle, why only to climate change?” So this direct relationship is not there. #4, Medical doctor/ academic.
Diseases such as malaria, with historical links to stagnant water as breeding grounds, have been etched into public knowledge and further perpetrated through mass awareness campaigns, intervention programmes and research. The slow developing nature of CVDs and the prevalent categorisation of CVDs as solely lifestyle diseases was mentioned by many participants as potential barriers to research. One participant described how CVDs are commonly reduced to lifestyle diseases with the onus of risk management on the individual rather than a “willingness to see the invisible factors”. The multifactorial nature of CVDs was thought to add to the difficulty of identifying climate attributable impacts. Another participant described how clinicians especially do not see the need to focus on environmental risk factors for CVDs, believing it ineffective in reducing the overall burden.
Non-communicable diseases, because we are not quantifying that and because of the long latent period of the incident, you're not able to quantify directly to environment or climate change. So definitely, hypertension, cardiovascular disease, all these probably diabetes also because of the changing food pattern, but I don't think—you cannot separate climate change from any of the health effects or any of the non-communicable diseases. Also related to stress caused by climate change. #2, Medical doctor/ academic.
The need for regional studies was also stressed on as there seemed likely to be a disconnect in comparing national-level or global-level problems with health impacts of climate change on a local level. Participants described the attitude of “this does not affect us” among the public when it came to climate change especially. A few participants expressed belief and hope that the temperature-CVD association was an upcoming topic of interest for the government and public alike.
Technical barriers to research
Insufficient resources and workforce dedicated to research.
Resource allocation, especially financial, for climate change-health research was described as a barrier, especially by researchers. Along with inconsistent funding from the government, one of the problems mentioned was lack of adequate trained personnel. This was partially linked to the need to relieve the research expectations from already overburdened doctors. There was also a need to have trained personnel for digitalisation and categorisation of health data in order to create a digital state-level health database.
Some participants, referred to the low percentage of the annual budget of India allocated to health along with the need to increase this. One participant described funds earmarked for climate change-health research institutionally, along with optimism that this would lead to future research opportunities.
Yes, for recent years even ICMR (Indian Council of Medical Research) has called for proposals on this environment related, uh, this one. ICMR is one of the largest body which is for the research organisation as well as for the academic institutes like us. So, clearly, they are given a separate block of funding for climate change and [health]. That means the funds are available. #3, Medical doctor/academic.
However, this was countered by the notion that most of the funds are directed to central government institutes as opposed to smaller research institutes. A participant also alluded to misappropriation of research funding at an institutional level. Another participant spoke about the need to involve university students in research along with concern that most students do not get access to funding or research opportunities. There was a feeling that most students remain unaware of opportunities for funding or that funds do not ultimately reach the students aiming to conduct research. Another participant also described the prioritisation of more immediate health burdens and curative research as opposed to preventative research for the directing of funds or resources. This was supported by the opinion expressed by an environmentalist on climate change being viewed as a problem for the future as opposed to the present.
So though we focus on vaccination and other things, but still, the budget still flows more for the curative aspects rather than the preventive part. So for instance, the climate change is more of like, you prevent this—the future heart attacks or some other diseases. You have to focus on the prevention. #3, Medical doctor/academic.
Underdeveloped transdisciplinary research capacity
Alongside education, the need to build more technical capacity among researchers was also mentioned as one of the biggest challenges by participants. Despite a potential interest and willingness from researchers, the lack of training and expertise in climate change-health research was strongly expressed. This was tied in with the expressed desire for mentorship, both to facilitate increased awareness among the scientific and medical community as well as increased regional research on health impacts of climate change.
Yeah, more than research, I would tell it as people are aware and willing to do it, but here is more of capacity building… Let’s say if I want to work on vector-borne disease, I know who to approach…but when it comes to climate change, that linking is absent. … So actually, even if I'm interested and I want to work on it, there are a lot of hurdles which have to be crossed… So I have to be given an opportunity to work on it, or I feel somebody has to mentor me to work on it. So what we call as, starting trouble, you know is there. Once I think somebody starts, we will be going into it…. #4, Medical doctor/ academic.
Some participants had the belief that larger research institutes or relevant ministries could be drafted to provide training to the smaller educational institutes or local government bodies. There was a sense of “duty” attached to studying all aspects of climate change impacts for the environmentalists in Puducherry tied in with a search for a starting point.
Research slowed by unavailability and limited access to quality data
Participants described critical gaps in monitoring, surveillance and database development, all of which were perceived to hamper research conduction, especially for health data. First, merging health data from the many healthcare facilities within Puducherry was seen as a challenge. There was an expressed need to bring together health data for the entire UT in a single system, including public and private healthcare facilities.
Second, some participants mentioned the state-level government health-monitoring database. However, participants described this as being limited to selected diseases from all the government run primary healthcare centres, with limited information on the private sector or secondary and tertiary care hospitals. A few participants described the lack of disease-specific categorisation of health outcomes, making it an added challenge in conducting health-related research.
Third, participants also perceived private medical colleges and healthcare facilities as reluctant to share data with the government, with a felt need to enhance governmental efforts to work on the state-wide database. Fourth, on a related note, concerns about data quality were mentioned by several participants. Part of the reason for an unwillingness to share data by healthcare facilities was thought to be due to potentially inaccurate or poor quality data.
They're all afraid of like somebody will find a fault with that. So because they don't have manpower to look at the accurate or clean the data, okay, so somebody shares and later they find their mistake, and they will be answerable to the higher authority. So that’s the usual reason we do not to share the data, the insecurity. #3, Medical doctor/academic.
Another challenge shared was the slow, ongoing effort to digitalise the data. Participants described as feeling unmotivated to start research at the cost of manually sorting through thousands of paper records, unless there was a way to guarantee research output. This was also relate to a challenge of medical professionals being overburdened with work.
There is not even a digitalization… Many hospital doesn't have digitalized MRD [medical records department]. For example, I was doing a study, retrospective study, collecting infective endocarditis data for past 10 years, there are more than 1000 files. How can I go through the 1000 files? It’s not possible. #13, Practicing physician.
Surveillance of diseases was mentioned as ongoing work. Diabetes, hypertension, cervical cancer and other ‘notifiable’ diseases like infectious diseases were described as being under surveillance.
This research examined barriers faced in conducting climate change and health research by key stakeholders in Puducherry. The localised findings relatively remain relevant for India and can be extrapolated to other LMIC settings. 28 Four main themes emerged from this research, which are discussed below.
First, we found limited knowledge of relevant policies, especially among the participants with a medical background. In recent years, there have been a lot of strides taken in the Indian policy space with pertaining to climate change and health, such as the addition of the Health Pillar to the NAPCC and the subsequent development of the NAPCCHH and mandates for the development of the state-level action plans for climate change and health. 17 18 Although the Health Pillar is a relatively recent addition (2015), there was still a substantial lack of awareness on the NAPCC as well as the health mission in general, which we present as a key area for strengthening. Knowledge of such policies, especially if they can provide a framework to support-related research, is a useful tool to advance the research agenda on climate change and health. 36 37 Health system vulnerabilities are already being seen in Puducherry and active knowledge of such policies can also be used by relevant stakeholders to develop resilience focused interventions. This includes communicating the severity of the problem to the policy-makers, who generally lack the political will to divert resources to non-apparent problems, alluded to by the participants in this study and identified in other studies. 38 39
Second, participants perceived climate change and health as a topic lacking political support and prioritisation. Most political efforts are thought to be focused on mitigation measures such as air pollution control, with little importance given to health adaptation and healthcare resilience. The participants believed that the health impacts of climate change were not a political priority or seen as urgent. Similar findings have been elucidated in other studies which also found public health leadership on climate change to be fragmented. 27 40 Further efforts to inform the decision-makers on the importance of health adaptation might contribute to more evidence informed climate change and health policies. 41 42 As an added justification for health cobenefits of mitigation can be introduced through multiple pathways, including air pollution, lifestyle modification, health surveillance or research programmes in development or related policies. 43 44
Participants also highlighted weaknesses in interdepartmental coordination for working on climate change and health. We found almost unanimous support for a separate intersectoral body focused specifically on climate change and health. Methodological challenges in the light of limited technical knowledge and adequate intersectorial coordination and support for transdisciplinary capacity that we found have also been reported elsewhere. 29 45 A recent study on the knowledge, attitudes and practices related to climate change and health among the Indian health workforce found intermediate or delayed health impacts of climate change less commonly identified. 26 This could also support the development of regional, national or even international research networks facilitating knowledge sharing and transfer, including research methodology support. 29
The siloed operations of ‘health’ and ‘climate change’ were also seen as a research barrier. This was partially due to the unclear division of responsibilities and fragmented institutional focus, as also seen in other studies. 29 40 46 A study examining the challenges for the Californian public health sector in climate change found the compartmentalisation and lack of intersectorial coordination to limit work on intersectoral issues such as climate change and health. 27 Our findings point to the need to have regular national level conferences or improved science dissemination systems to communicate climate adaptation related research or plans between and across sectors.
Third, participants perceived gaps in formal education and training on climate change and health. Our respondents had varied views regarding education on climate change or its health impacts; however, the need to improve this was clearly described by participants in this study. The need for strengthening capacity and education has been a common finding in several other studies. Globally, there is a critical gap and scope for improvement in the education on health impacts of climate change, especially for medical practitioners. 25 27 47–54 A study comparing medical curriculums across the world found inconsistencies between environmental changes, health and community needs, with Indian and Chinese students especially having a gap in the inclusion of planetary health in medical schools. 50 The inclusion of planetary health from an early stage for medical students leads to a more active role of physicians in educating their patients about climate risks. 50 55 However, there is a need to validate the results in future studies given the inconsistencies in the views we found on climate change-health education. The emphasis on cure rather that prevention, which has shown to reduce long-term healthcare costs, could support the need for Puducherry to focus on the preventative aspects, largely through education and awareness. 24 We also found scepticism and low awareness on the non-conventional health impacts of climate change, such as CVDs. These health impacts were thought to be viewed as ‘invisible’ compared with more conventional or immediate impacts, such as air pollution or extreme events. This is also a commonly identified challenge to climate change and health research, accompanied by insufficient education about climate systems during the course of school or university education. 26 56
Fourth, technical research barriers we found included insufficient data, capacity, human and financial resources. Data barriers remain common challenges in public health research, despite efforts to facilitate improvements. 57 58 As Puducherry has the advantage of a relatively small size and well-connected healthcare facilities, efforts need to be taken to improve a central, disease-specific data collection system, incorporating all the healthcare facilities in the state. 59 Facilitating training to build local data analysis expertise and capacity would contribute to more region specific research on the topic. 60 As was also made apparent in this study, other studies have shown that health impacts of climate change are a relatively new concept and not inherently associated with climate, potentially explaining the uncertainties and scepticism expressed by our participants, especially for diseases that do not warrant a visit to the doctor. 61 62 On the positive side, the expressed desire of participants to learn more about it and make changes to the healthcare system and policies based on robust, conclusive evidence implies a willingness to adapt and implement changes in how the region tackles health impacts of climate change. 49 63 Resource and funding constraints are one of the most common barriers to public health research, especially in LMICs and there remains a critical need to address this gap. 64
At present, little is known on CVD impacts of climate change in India. Our related study from Puducherry found a high attributable burden of non-optimal temperature to CVD mortality, suggesting a need for similar studies from around the country. 65 66 The CVD-specific challenges we identified here are comparable to the general health challenges. Awareness among the medical community on the environmental risk factors of CVDs will be instrumental in furthering this research agenda, while awareness among policy-makers will help raise the political prioritisation of CVD impacts of climate change. 24 67 68
Limitations
First, the sample was restricted to Puducherry district and not representative of the entire Union Territory of Puducherry, much less India as a whole, although the projected population for Puducherry is 1.25 million in 2021, comparable to a few smaller countries or global regions. 69 The results might thus only reflect the studied context and participants. Second, while we chose to focus on the medical community and DSTE representatives working on climate change, we did not include the experiences and perspectives of other public health professionals or stakeholders. Third, we do not highlight the opportunities for increasing research on climate change and health as many of these are very often interconnected with barriers. However, we do discuss potential recommendations given by stakeholders. Nonetheless, the results of this study could be useful for the research community and policy-makers alike to strengthen climate change and health research and engagement.
There is a great need to fill the gap in research on the impacts of climate change on various health outcomes in India, especially in light of the vulnerabilities it faces. By highlighting some crucial barriers to environmental health research faced by relevant professionals, we present potential intervention points for consideration. Insufficient awareness on health impacts of climate change and perceived need to improve research capacity through collaborative work; and challenges in data availability emerged as the largest barriers to conducting research on this topic in Puducherry. We outlined the gaps and scope for addressing these through improved policy awareness; informed leadership and evidence informed climate change and health policies; research capacity strengthening and transdisciplinary research and communication network; improved education on climate change and health on all levels; and addressing data barriers in climate change through improved monitoring and evaluation systems. The key findings could contribute to supporting and strengthening evidence-informed climate resilient healthcare systems. In addition, it would also serve to inform and strengthen the research and institutional support for environmental health research in the future both in India and globally.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study was approved by the Institute Ethics Committee (Human Studies) of the Indira Gandhi Medical College and Research Institute (A Government of Puducherry Institution); No. 318/IEC-31/IGM&RI/PP/2021 and by the Ethics Committee Northwest and Central Switzerland; Statement ID- AO_2020_00034. The methodology used in this project abided by the principles laid out in the Declaration of Helsinki and the Consolidated criteria for Reporting Qualitative research checklist. All participants were verbally explained the project and its objectives as well as being provided information sheets. All participants were made aware of their right to refuse participation at any point prior to publication of the study. Signed informed consent was obtained from all participants prior to the interviews, with participants retaining one copy.
Acknowledgments
The authors would like to extend their sincere gratitude to all the participants who made this study possible.
- Rocque RJ ,
- Beaudoin C ,
- Ndjaboue R , et al
- McLeman R ,
- Adams H , et al
- Campbell-Lendrum D ,
- Holloway T , et al
- Arnell N , et al
- Stafford Smith M , et al
- Smith KR , et al
- Kjellstrom T
- Scheelbeek PFD ,
- Dangour AD ,
- Jarmul S , et al
- Kovats RS ,
- Scheffran J
- Tripathi V ,
- Dagdeviren H ,
- Elangovan A ,
- Parimalavalli R
- National Action Plan for Climate Change and Human Health, G.o.I
- Kotha SR , et al
- Roberts I ,
- Stott R , Climate and Health Council executive
- Stigler FL ,
- Sainsbury P ,
- Charlesworth K ,
- Madden L , et al
- Hathaway J ,
- Sambath V ,
- Narayan S ,
- Kumar P , et al
- Joseph HA ,
- McLaughlin M , et al
- Leal Filho W ,
- Morgan EA ,
- Godoy ES , et al
- Shrikhande SS ,
- Cambaco O , et al
- Cameron E , et al
- van Eck CW ,
- Mulder BC ,
- van der Linden S
- Rudolph L ,
- Crouzat E ,
- Brunet L , et al
- van Valkengoed AM ,
- Perlaviciute G ,
- Hussey LK ,
- Austin SE ,
- Berrang-Ford L , et al
- Biesbroek R ,
- Klostermann J ,
- Termeer C , et al
- Lavis JN , et al
- Uzochukwu B ,
- Onwujekwe O ,
- Mbachu C , et al
- McMichael AJ ,
- Michael E , et al
- Eisenack K ,
- Hoffmann E , et al
- Liu C , et al
- Kotcher J ,
- Maibach E ,
- Miller J , et al
- Omrani OE ,
- Dafallah A ,
- Paniello Castillo B , et al
- Whitley CT ,
- Takahashi B ,
- Zwickle A , et al
- Chaplin G ,
- Greibe Andersen J ,
- Karekezi C ,
- Ali Z , et al
- Case P , et al
- McMichael AJ
- van Panhuis WG ,
- Emerson C , et al
- Sheikhtaheri A
- Lakshmanasamy Ravivarman PK
- Levison MM ,
- Butler AJ ,
- Rebellato S , et al
- Ouellet C , et al
- Herrmann A ,
- Sauerborn R
- Paterson J ,
- Ebi K , et al
- Shumba CS ,
- Lusambili AM
- Röösli M , et al
- Kumar M , et al
- Sheffield PE ,
- Durante KT ,
- Rahona E , et al
- GovernmentOfPuducherry
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors SS, MR, MAD, JU and GC conceptualised and planned the study. SS and RL acquired and provided access to the data. RL facilitated the interviews. SM and SS designed the study. TTL validated the codes and codebook. OC, SS and SM conceptualised and structured the framework. SS wrote the main manuscript with inputs from all authors. The final manuscript has been revised by all authors.GC and SS are the guarantors of this study.
Funding SS has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 801076, through the SSPH+ Global PhD Fellowship Programme in Public Health Sciences (GlobalP3HS) of the Swiss School of Public Health and from the Joint South Africa and Swiss Chair in Global Environmental Health. OC has been funded by the Swiss Government Excellence Scholarship (ESKAS) (reference no. 2020 0742).
Competing interests None declared.
Patient and public involvement Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Public health research in India in the new millennium: a bibliometric analysis
Affiliations.
- 1 Department of Population Health, IKP Trust, New Delhi, India.
- 2 Sangath, Goa, India.
- 3 London School of Hygiene and Tropical Medicine, London, United Kingdom.
- 4 Public Health Foundation of India, New Delhi, India; [email protected].
- PMID: 26282573
- PMCID: PMC4539388
- DOI: 10.3402/gha.v8.27576
Background: Public health research has gained increasing importance in India's national health policy as the country seeks to address the high burden of disease and its inequitable distribution, and embarks on an ambitious agenda towards universalising health care.
Objective: This study aimed at describing the public health research output in India, its focus and distribution, and the actors involved in the research system. It makes recommendations for systematically promoting and strengthening public health research in the country.
Design: The study was a bibliometric analysis of PubMed and IndMed databases for years 2000-2010. The bibliometric data were analysed in terms of biomedical focus based on the Global Burden of Disease, location of research, research institutions, and funding agencies.
Results: A total of 7,893 eligible articles were identified over the 11-year search period. The annual research output increased by 42% between 2000 and 2010. In total, 60.8% of the articles were related to communicable diseases, newborn, maternal, and nutritional causes, comparing favourably with the burden of these causes (39.1%). While the burdens from non-communicable diseases and injuries were 50.2 and 10.7%, respectively, only 31.9 and 7.5% of articles reported research for these conditions. The north-eastern states and the Empowered-Action-Group states of India were the most under-represented for location of research. In total, 67.2% of papers involved international collaborations and 49.2% of these collaborations were with institutions in the UK or USA; 35.4% of the publications involved international funding and 71.2% of funders were located in the UK or USA.
Conclusions: While public health research output in India has increased significantly, there are marked inequities in relation to the burden of disease and the geographic distribution of research. Systematic priority setting, adequate funding, and institutional capacity building are needed to address these inequities.
Keywords: India; bibliometry; health research funding; public health research; research capacity; research systems.
PubMed Disclaimer
The process of data collection…
The process of data collection for bibliometric analysis.
Absolute research output from India…
Absolute research output from India during the decade 2000–2010.
Publication research focus relative to…
Publication research focus relative to the burden of disease in India during 2000–2010.…
Trends in publications from India…
Trends in publications from India by global burden of disease categories from 2000…
Per capita distribution of research…
Per capita distribution of research studies in India.
Similar articles
- The lack of public health research output from India. Dandona L, Sivan YS, Jyothi MN, Bhaskar VS, Dandona R. Dandona L, et al. BMC Public Health. 2004 Nov 25;4:55. doi: 10.1186/1471-2458-4-55. BMC Public Health. 2004. PMID: 15563377 Free PMC article.
- Trends of public health research output from India during 2001-2008. Dandona L, Raban MZ, Guggilla RK, Bhatnagar A, Dandona R. Dandona L, et al. BMC Med. 2009 Oct 14;7:59. doi: 10.1186/1741-7015-7-59. BMC Med. 2009. PMID: 19828017 Free PMC article.
- Health status and epidemiological capacity and prospects: WHO Western Pacific Region. Blakely T, Pega F, Nakamura Y, Beaglehole R, Lee L, Tukuitonga CF. Blakely T, et al. Int J Epidemiol. 2011 Aug;40(4):1109-21. doi: 10.1093/ije/dyr014. Epub 2011 Feb 22. Int J Epidemiol. 2011. PMID: 21343183
- Health systems research in the time of health system reform in India: a review. Rao KD, Arora R, Ghaffar A. Rao KD, et al. Health Res Policy Syst. 2014 Aug 9;12:37. doi: 10.1186/1478-4505-12-37. Health Res Policy Syst. 2014. PMID: 25106759 Free PMC article. Review.
- A bibliometric analysis of the published road traffic injuries research in India, post-1990. Sharma N, Bairwa M, Gowthamghosh B, Gupta SD, Mangal DK. Sharma N, et al. Health Res Policy Syst. 2018 Mar 1;16(1):18. doi: 10.1186/s12961-018-0298-9. Health Res Policy Syst. 2018. PMID: 29490646 Free PMC article. Review.
- Challenges in the execution of public health research: Reflections from Public Health Research Initiative (PHRI) grant management in India. Saxena D, Trivedi P, Bhatt R, Yasobant S, Bhavsar P, Kansara K, Memon F, Mavalankar D. Saxena D, et al. Dialogues Health. 2022 May 30;1:100020. doi: 10.1016/j.dialog.2022.100020. eCollection 2022 Dec. Dialogues Health. 2022. PMID: 38515896 Free PMC article.
- Awareness of Medical Research among the Resident Doctors in a Tertiary Care Hospital in India. Divya G, Kundal VK, Debnath PR, Kundal R. Divya G, et al. J Indian Assoc Pediatr Surg. 2022 Nov-Dec;27(6):673-676. doi: 10.4103/jiaps.jiaps_13_22. Epub 2022 Nov 14. J Indian Assoc Pediatr Surg. 2022. PMID: 36714480 Free PMC article.
- Health research in the state of Odisha, India: A decadal bibliometric analysis (2011-2020). Kshatri JS, Satpathy P, Sharma S, Bhoi T, Mishra SP, Sahoo SS. Kshatri JS, et al. J Family Med Prim Care. 2022 Jul;11(7):3771-3776. doi: 10.4103/jfmpc.jfmpc_2192_21. Epub 2022 Jul 22. J Family Med Prim Care. 2022. PMID: 36387708 Free PMC article.
- How does academia respond to the burden of infectious and parasitic disease? Zhao W, Wang L, Zhang L. Zhao W, et al. Health Res Policy Syst. 2022 Aug 13;20(1):89. doi: 10.1186/s12961-022-00889-0. Health Res Policy Syst. 2022. PMID: 35964031 Free PMC article.
- Dyslexia: A Bibliometric and Visualization Analysis. Wu Y, Cheng Y, Yang X, Yu W, Wan Y. Wu Y, et al. Front Public Health. 2022 Jun 23;10:915053. doi: 10.3389/fpubh.2022.915053. eCollection 2022. Front Public Health. 2022. PMID: 35812514 Free PMC article.
- WHO. Geneva: World Health Organization; 2008. NBD summary tables, health statistics and informatics – information, evidence and research (IER/HIS)
- Benzer A, Pomaroli A, Hauffe H, Schmutzhard E. Geographical analysis of medical publications in 1990. Lancet. 1993;341:247. - PubMed
- Hefler L, Tempfer C, Kainz C. Geography of biomedical publications in the European Union, 1990–98. Lancet. 1999;353:1856. - PubMed
- Thompson DF, Geography of U.S. biomedical publications, 1990 to 1997. N Engl J Med. 1999;340:817–18. - PubMed
- Soteriades ES, Rosmarakis ES, Paraschakis K, Falagas ME. Research contribution of different world regions in the top 50 biomedical journals (1995–2002) FASEB J. 2006;20:29–34. - PubMed
Publication types
- Search in MeSH
Related information
Grants and funding.
- WT_/Wellcome Trust/United Kingdom
- 091834/WT_/Wellcome Trust/United Kingdom
- 100714/WT_/Wellcome Trust/United Kingdom
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- PubMed Central
- Taylor & Francis
Other Literature Sources
- scite Smart Citations
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Welcome About The Center

A Communication Implementation Guide Read and Share

कोविड- 19 हिंदी में पढ़े

Projects Read about our work
The Harvard T.H. Chan School of Public Health has had active research and educational programs in India since the 1960s. However, the Mumbai-based India Research Center, an office of Harvard Global Research Support Centre India, is designed to broaden and coordinate the School’s existing collaborations and create new relationships with organizations and agencies across India. The ultimate goal is to improve health in India and around the world through the strategic goals of research, training, and knowledge translation and communication.
Center researchers are engaged in a number of diverse projects , developing cases for the School’s DrPH program, convening workshops and symposiums on important public health topics, and designing a national communication strategy on mental health for the Indian ministry of health and family welfare, among many others.
We invite you to explore the India Research Center website and learn about our projects and collaborators.

Improving Health in India
As the world’s second-most-populous country and one of its fastest-growing economies, India faces both unique challenges and unprecedented opportunities in the sphere of public health.
For more than a decade, India has experienced record-breaking economic growth that has been accompanied by significant reductions in poverty. According to the World Bank, infant mortality in India fell from 66 to 38 per 1,000 live births from 2000 to 2015. Life expectancy at birth has increased from 63 to 68 years, and the maternal mortality ratio has fallen from 374 to 174 per 100,000 live births over the same period.
India also has dynamic pharmaceutical and biotechnology industries; world-class scientists, including a burgeoning clinical trials industry; and leading hospitals that attract foreign patients and treat its better-off citizens.
Yet Indian government and public health officials agree that the country also faces persistent and daunting public health challenges, particularly for the poor. These include child undernutrition and low birth weights that often lead to premature death or lifelong health problems; high rates of neonatal and maternal mortality; growth in noncommunicable diseases such as obesity, diabetes, and tobacco use, leading to cancer and other diseases; and high rates of road traffic accidents that result in injuries and deaths.
As the Indian government strives to provide comprehensive health coverage for all, the country’s rapidly developing health system remains an area of concern. There are disparities in health and health care systems between poorer and richer states and underfunded health care systems that in many cases are inefficiently run and underregulated. New government-financed health insurance programs are increasing coverage, but insurance remains limited.
Public and private health systems are placing huge demands on the country’s capacity to train exceptional health leaders and professionals. Rising to meet these challenges, the people of India have an opportunity to have a major influence on their own future health and on the future of public health and medical efforts globally.
Supporting Development of India’s Health Workforce
The Harvard T.H. Chan School of Public Health is collaborating with partners across India to address those challenges. Together, the School and its partners are introducing educational innovations to India to expand skills training, degree programs, and leadership development at new schools and institutes of public health. We seek to leverage the School’s resources to help strengthen public health training and build capacity across the health sector in India.
Public Health Foundation of India
- Management Team
- Financial Information
- Right to Information
- Awards and Recognitions
- Academic Programs
- Our Supporters
- Research Collaborations
- IIPH Gandhinagar
- IIPH Hyderabad
- IIPH Bhubaneswar
- IIPH Shillong
- The Ramalingaswami Centre on Equity and Social Determinants of Health
- Centre for Chronic Conditions & Injuries (CCCI)
- South Asia Centre for Disability Inclusive Development and Research (SACDIR), Hyderabad
- Centre for Environmental Health (CEH)
- Adjunct Faculty (National)
- Adjunct Faculty (International)
- WORK WITH US
- Ways to give and partner
- Focus your CSR on Preventive Healthcare
- Reports A compilation of PHFI Research and Project reports
- Journals List of Journal articles where PHFI and IIPH researchers and faculty have published
- Books A listing of Book and Book chapters by PHFI and IIPH researchers and faculty have published
- Policy Briefs PHFI regularly disseminates policy briefs on various public health subjects
- Covid-19 Publications
- Research Training Programmes
- India State-Level Disease Burden Initiative
- Centre for Ethics Humanities and Public Health
- Health technologies @PHFI
- Work with SEAO countries
- Routine Health Information Systems Work at PHFI
Prof. Monika Arora is a public health scientist working in the area of Non-Communicable Disease (NCD) prevention and control and adolescent health. She is the Vice President (Research and Health Promotion) at the Public Health Foundation of India (PHFI). She is the President of the NCD Alliance (2023-25), was the founding Chairperson of the South East Asia NCD Alliance (2020-23), and a Founding GB member of the Healthy India Alliance. She coordinates a multi-disciplinary research team at PHFI. She Chairs the Research Management Committee of PHFI and is also a Member Secretary of the External Research Advisory Council of PHFI.
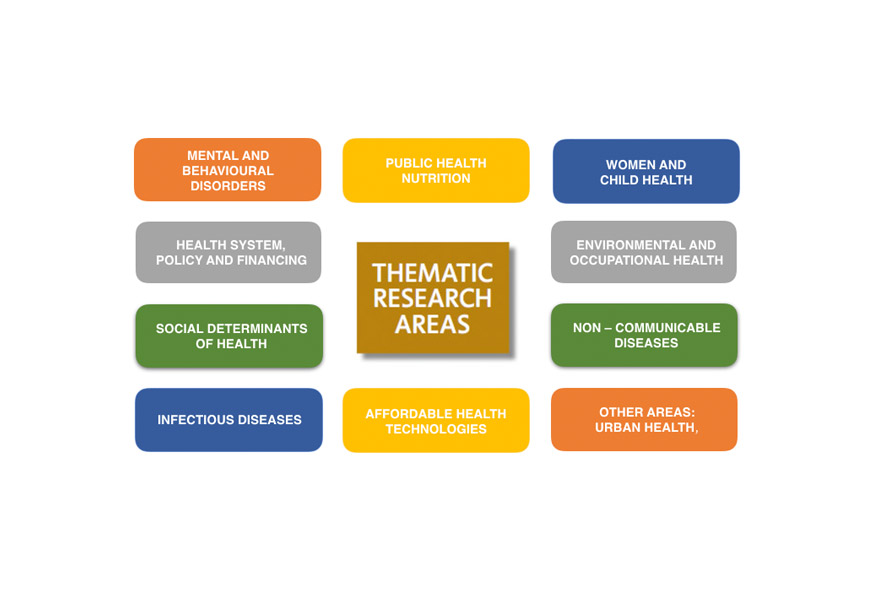
Research at PHFI
Since its inception PHFI has worked to establish a robust evidence base for public health, in partnership with national and international institutions, by advancing policy and programme relevant research in prioritised health areas. PHFI has been undertaking projects in multiple areas including epidemiology and control of infectious and chronic diseases, maternal and child health, health systems, and social determinants of health.

Centres of Excellence
PHFI has set up five Centres of Excellence to raise awareness and strengthen research, training and education in the high priority area of public health in India.

Research Governance
PHFI has a strong research governance mechanism that has evolved over a decade and outlines the principles of good governance that apply to all research undertaken within the remit of PHFI.

Research Collaborations (National & International)
PHFI researchers are collaborating with a range of stakeholders including the national and state governments, academia, civil society, global foundations and the private sector.

Research Recognitions and Awards
PHFI’s multi-disciplinary talent pool is well recognised and our colleague and teams win some very competitive bids for grants and are also recognised at the individual level for the work in contributing towards public health.

Training Division
The Training Division at PHFI focuses on implementing various capacity building initiatives that aim to upgrade the knowledge, skills and core competencies of Healthcare Professionals since the year 2010. Various initiatives have been formalized and implemented for healthcare professionals from diverse backgrounds in the areas of chronic conditions, palliative care, healthcare quality, health program management, health technology, occupational health and evaluation & monitoring of health programs.

Training Programmes in Chronic Conditions
Research infrastructure.
The laboratory at PHFI is equipped to deal with all aspects of clinical biochemistry and basic genetics research. The lab is equipped with: Chemistry analyzers c311, immunochemistry analyzer e411 from ROCHE, D-10 from Bio-Rad, Electrolyte analyzer from Caretium, microplate reader from Bio-Rad, Spectrophotometer from Thermo, Gas chromatography from Agilent.
About Health Promotion Division (HPD)
The Health Promotion Division at the Public Health Foundation of India (PHFI) aims to nurture interdisciplinary health promotion research, programming and practice and focuses on promoting multi-sectoral coordination. The Division adopts a settings based approach to design health communication, health literacy, and community outreach activities that mainstream health promotion policy and practice. The Division works on designing theory-based interventions to develop healthy settings in diverse contexts and generates evidence to support effective messaging, programming and policy development. The Division brings together approaches ranging from health education, advocacy, community empowerment, legislative reforms, fiscal policy change to organizational change and strengthening health services to address social inequalities in health.
The Division undertakes rigorous evaluation of outcomes and processes to assess impact of these health promotion interventions on population health and wellbeing. Research on impact of programmes in influencing health of individuals and population is a core activity undertaken at the Health Promotion Division. Represented by multi-disciplinary team of Epidemiologists, public health experts, clinicians, behavioral scientists, nutritionists, qualitative researchers and heath communication experts.
Brochure Implementation of Peer Education Programme in i-Saathiya
Impact Stories
Sex selection in pregnancy.
Dr. Sutapa B. Neogi (Principal Investigator), IIPH-Delhi (Relevance to MDG 3A and 5A)
Objective: Sex selection is a major social concern in India. The use of indigenous medicines purportedly influencing the probability of having a son is reported to be a common practice... Read More
Programme for Improving Mental Health CarE (PRIME)
Dr. Rahul Shidhaye (Principal Investigator), CCCI, PHFI
Objective: The Programme for Improving Mental Health CarE (PRIME) was launched in 2011 to generate evidence on the implementation and scaling up of... Read More
mHealthcare
Dr. Ajay Vamadevan (Project Coordinator), CCCI, PHFI
Objective: The rising burden of chronic diseases, and their co-morbidity are a major challenge for the Indian health system, requiring life-long therapy. Innovative approaches such as task-shifting/sharing... Read More
Diabetic Retinopathy
Prof. GVS Murthy (Principal Investigator), Director, IIPH-Hyderabad
Objective: Of the projected 69 million people with diabetes in India, 6 million people are estimated to have sight threatening Diabetic Retinopathy (DR). This is an important and avoidable cause of blindness... Read More
Global burden of Disease
Dr. Lalit Dandona (Principal Investigator), PHFI
Objective: While programmes for disease prevention and control as well as health promotion are underway in many countries, often, they are historically and politically shaped, rather than reflecting... Read More

India’s tobacco-related fiscal policies
Dr. Sakthivel Selvaraj (Principal Investigator), PHFI
Objective: India has a complex tobacco tax structure; there has been a growing interest from state governments to increase taxes on tobacco products as a measure to curtail consumption, although the impact of the same on revenue and consumption was unexplored... Read More
Yoga-CaRe trial
Prof. Prabhakaran D (Principal Investigator), CCCI, PHFI
Objective: Many of the ancient traditions of India such as Yoga can be an answer to the spiralling health care costs and can be used innovatively to address the emerging epidemic of chronic diseases in India... Read More
Yoga for Tobacco Cessation
Dr. Bidyut Sarkar (Principal Investigator), PHFI
Objective: To evaluate, if a brief community outreach intervention (a single session advice of 15 min to stop tobacco use combined with training in yogic breathing exercise) delivered by health workers to promote tobacco cessation in India... Read More
Donate to a Healthier India : Collective effort is required to address the public health challenges we face today. Partner with PHFI and support initiatives to strengthen public health initiatives in India.

- Social Media
- Events Calendar
- DWIH Network
- DWIH New York
- DWIH New Delhi
- DWIH Moscow
- DWIH San Francisco
- DWIH São Paulo
- Organisation
- DWIH Focus Topic 2024
- DWIH Focus Topic 2023
- DWIH Focus Topic 2022
- Researching the Corona Crisis: The Social Science Discourse in Germany and India
COVID-19 and Public Health in India
- Civil Society in the Corona Crisis in Germany – Which Implications for Cohesion and Polarisation?
- DWIH Focus Topic 2021
- Indo-German Cooperation: Focus – Green Mobility
- Climate Research in Germany
- Climate Research in India
- DWIH Focus Topic 2020
- DWIH Focus Topic for 2019
- Artificial Intelligence (AI) in Germany
- Artificial Intelligence (AI) in India
- Supporting Science-based Start-ups and Entrepreneurship
- Falling Walls Lab and Venture (India)
- Science-based Start-ups and Entrepreneurship in Germany
- Science-based Start-ups and Entrepreneurship in India
- Quantum Computing – An International Challenge
- India: Making Strides in the Second Quantum Revolution
- Updates from the Quantum Research Landscape in India and Germany
- Rethinking the Way we Work
- Indo German Symposium: Future of Work
- Why frugal innovations are also changing the world of work
- “The Role Played by Humans Will Change Considerably”
- Industry 4.0: the Future of Production
- “Knowledge Sharing Is Important”
- Network Partners
- The Research and Innovation Landscape in Germany
- Research Careers in Germany
- Research and Innovation Organisations
- Research and Innovation Funding & Support
- Indo-German Research Cooperation
- Downloads and Publications
- Annual Reports
- DWIH Annual Report 2023
- DWIH Annual Report 2022
- DWIH Annual Report 2021
- DWIH Annual Report 2020
- Older DWIH Annual Reports
- Society in Transition: Impacts of the Pandemic
The COVID-19 pandemic in India caused considerable suffering, along with economic and social disruption. Till October 2021, 34.3 million people were infected by COVID-19, and an estimated 0.45 million people died. One of the defining features of the pandemic was a public reckoning of the state of the health system. Was the healthcare system in India capable of responding to a large-scale pandemic? What were the economic costs of the lockdowns imposed to control the pandemic? And what is the direction of public healthcare in India?
The Indian Healthcare System
The good news is public health expenditure in India has increased. Revised estimates for 2020-21 place the share of overall spending on health at 1.8% of GDP. The SDG India Index Report (2019-20) by NITI Aayog reports that India aims to increase health expenditure to 2.5% of GDP by 2025. Furthermore, important health schemes such as Ayushman Bharat , launched by the National Health Policy 2017, aim to widen tertiary health coverage.
While these measures are promising, India lags in public health investments and infrastructure, both in contrast to its international peers as well as compared to its own aspirations. Current health expenditure in India is lower than the world average of 9.8% of GDP as of 2018. According to World Bank data, current health expenditure (% of GDP) was 9.51% for Brazil, 5.32% for Russia, 4.12% for Turkey and 2.18% for Indonesia in 2018. India’s federal structure implies that both the centre and state governments spend on healthcare. However, state health expenditure in India is highly divergent, ranging from 3.4% to 12.66% of state budgets, as of 2020-21.
What is more concerning is the health infrastructure investments in India – which fall short of the demands of its large population, and the expenditure levels as well. Total number of government hospital beds per thousand vary widely across states. In 2019, for instance, Karnataka and Kerala had 67 and 61 government hospital beds per thousand, respectively, while states like Punjab and Uttar Pradesh had 22 and 11 government hospital beds per thousand people respectively. Indeed, the covid facility camps and beds may have increased during the pandemic (data not yet available on this), yet disparity in health infrastructure across states is a standing issue.
Economic Costs of the First Lockdown
During the first wave of infections in India in March-May 2020, the Government of India implemented the “world’s strictest lockdown” ( Hale et al. 2020 ). This lockdown severely disrupted business activity and mobility, with millions of migrants traveling back to their villages as opportunities for work in the cities dried up.
The rationale behind implementing this lockdown was to curtail the spread of Covid-19 and to reduce the consequent burden on the healthcare system to save lives. The government hoped that the lockdown would allow for a quicker resumption of normal economic activity over time. However, the trade-off from the lockdowns was short-run reductions in economic activity. In contrast to wealthier countries, the lockdown potentially affected the Indian economy more as per capita incomes were lower; remote working was less prevalent; the extent of digitisation was lower, and social protection was weaker.
What was the economic cost of this lockdown? One perspective is that Gross Domestic Product (GDP) contracted by 24.4% in the second quarter of 2020. However, this headline number conflates both lockdown effects, as well as potentially self-imposed restrictions as citizens restrict their own activities due to the spread of Covid-19 infections. To isolate the impact of government-imposed restrictions (separately from other factors), Beyer, Jain and Sinha 2020 examined the economic implications of a graded ‘unlock’ in May and June 2020, when the central government decided to vary containment rules across districts in the country).
The Impact of Zonal Containment on Economic Activity
The Government of India announced a comprehensive nationwide lockdown on 25 March 2020, which was implemented uniformly across all states and districts. During this phase, nearly all offices, commercial and private establishments, industrial units, as well as public services were closed. Most transportation services – including international and domestic flights, railways, and roadways – were suspended. Hospitality services and educational institutions were shut. This nationwide lockdown lasted until 3 May 2020.
To facilitate a gradual resumption of economic activity, the government announced in May 2020 a differentiated unlock of districts, with some districts retaining strict restrictions, some with intermediate measures, and the remaining districts returning to “business as usual”. The authors of this article contrasted how these districts fared on a range of outcomes – individual mobility (measured by location tracking on cell phones), economic activity (measured by satellites from outer space), and household consumption and income (measured by household surveys).
What were the findings? First, phone location data corroborated that the restrictions were indeed effective in reducing mobility, as the government mandated. The main finding is that the economic recovery was lower by 9.3% in districts with the maximum restrictions relative to districts with minimal restrictions. The recovery was 1.6% lower in districts with intermediate restrictions compared to districts with minimal restrictions. These results are not driven by India’s large metropolitan cities and hold even when they are excluded from the analysis. Some districts were more impacted by the restrictions than others. More developed districts with above-median population density, share of employment in services, credit per capita, and average age, experienced larger impacts.
Households reported both lower income as well as reduced consumption as a consequence of the lockdowns, worrying for the long run if this impacts human capital investments in nutrition, health, and education.
India suffered a lot less economically during the second wave of the pandemic due to imposition of micro-containment zones, in contrast to nationwide lockdown during the first wave. Policymakers can continue to follow similar approaches and maintain preventive measures and protocols which could enable least disruption to economic activity, trade, and travel even as threats of further variants emerge.
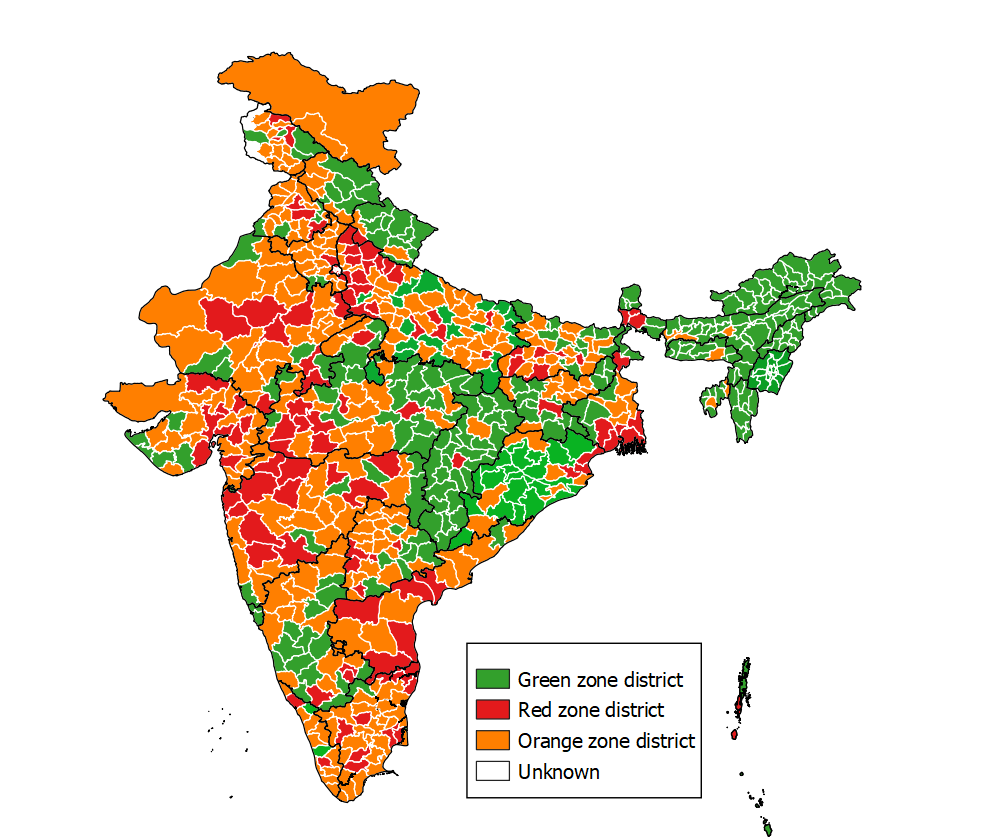
Policy Trade-offs
Could greater public health expenditures insure against the need for large scale lockdowns in future health emergencies? For policymakers, GDP decline estimates offer a useful benchmark to contrast with public health expenditures.
India’s economic policymakers well understand the value of increased investments in healthcare. During the pandemic, Indian public health expenditure rose from 1.5% of GDP to 1.8% of GDP. The PM Ayushman Bharat Health Infrastructure Mission scheme aims to increase infrastructure, with financing from the central government. Furthermore, the private sector played a major role during the pandemic, from the development and manufacture of vaccines, to diagnosis of COVID-19 infections and vaccination. To prevent high prices, the government regulated private sector with extensive price controls. Whether this expansion of private sector activities sustains (both in COVID-19 related and other healthcare needs) is an open question.
The way forward should involve building public consensus on the importance of healthcare investments and recognizing the potential economic gains from greater investments.
Disclaimer: The views expressed in the article are those of Dr. Sinha and Prof. Jain and not the Reserve Bank of India. The usual disclaimer applies.
|
, Economist, Reserve Bank of India |
|
, Associate Professor of Economics, Indian Institute of Management Ahmedabad |
Further Reading:
Beyer, R., T. Jain and. S Sinha (2020), ‘ Lights out? COVID-19 containment policies and economic activity ’, World Bank Policy Research Working Paper 9485.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 23 August 2024
Nationwide surveys of awareness of tuberculosis in India uncover a gender gap in tuberculosis awareness
- Ranganath Thimmanahalli Sobagaiah 1 ,
- Nitu Kumari 2 ,
- Divya Bharathi Gattam 3 &
- Mohammed Shoyaib Khazi ORCID: orcid.org/0000-0003-4682-0306 4
Communications Medicine volume 4 , Article number: 168 ( 2024 ) Cite this article
656 Accesses
3 Altmetric
Metrics details
- Epidemiology
- Tuberculosis
Tuberculosis remains a major challenge in India, with an estimated 2.69 million cases each year. Although men are more affected than women, gender differences and related factors affect awareness of tuberculosis and thus impact tuberculosis diagnosis and access to treatment. Understanding the gender-specific needs and complexities when diagnosing and treating tuberculosis is essential to manage cases in India.
We undertook a comparative study using data from three National Family and Health Surveys (NFHS), specifically NFHS-3, NFHS-4 and NFHS-5. We investigated the prevalence and gender disparity in awareness about tuberculosis, and associated factors, using regression analysis.
Most men and women surveyed are between the ages of 15 and 19. Across the surveys, the proportion of men and women who are unaware of spreading of tuberculosis decreases from 44.9% during NFHS 3 to 29.6% during NFHS 5. However, the prevalence ratio of men to women with no knowledge about modes of transmission of Tuberculosis increases from 0.92 during NFHS 3 to 0.98 during NFHS 5. Higher odds with younger age (NFHS 5, aOR: 1.07 (1.01–1.13)) and rural residency (NFHS 5, aOR: 1.12 (1.06–1.18)), and lower odds with unmarried marital status (NFHS 5, aOR: 0.92 (0.86–0.98)) are noteworthy associations. Women and men have differences in knowledge.
Conclusions
Gender disparity associated with awareness about tuberculosis in India is observed across all three nationwide surveys. Being aged fifteen to nineteen years and residing in rural area are risk factors. Being unmarried is a protective factor for women, but not for men.
Plain Language Summary
Lack of awareness of the spread of tuberculosis may be an important factor contributing to the current burden of disease. We used datasets from three rounds of the National Family Health Survey conducted in India to determine the proportion of men and women who knew how tuberculosis spreads. Using a predictive model, we showed that misconceptions are more common among both men and women. For women, younger age and living in rural areas were risk factors for lack of awareness, which was not the case for men. Such differences may represent a barrier to reducing the burden of disease. These findings can be used to develop gender-specific, comprehensive people awareness programs to raise awareness about tuberculosis.
Similar content being viewed by others
Drivers of sex differences in the South African adult tuberculosis incidence and mortality trends, 1990–2019
Identification and Prediction of Tuberculosis in Eastern China: Analyses from 10-year Population-based Notification Data in Zhejiang Province, China
Long-term trends of tuberculosis incidence and mortality in four central African countries
Introduction.
Tuberculosis (TB) is a disease vastly influenced and prevented by the social factors in the community. Lack of knowledge regarding the disease can contribute to underuse of medical services, delay in diagnosis and poor treatment adherence in people living with tuberculosis. Enhancing the dissemination of information on tuberculosis to increase the public awareness and health promotion is crucial to achieve the global targets for reduction in disease burden of tuberculosis. Studies have revealed that irrespective of a general overview about the disease, there is a breach in knowledge regarding the transmission, diagnosis, management, and its prevention. Also, poor knowledge or comprehension of tuberculosis disease and its treatment frequently contributes to non-adherence to therapy 1 , 2 , 3 .
Currently in India, the National Tuberculosis Elimination Programme (NTEP) with the development of National Strategic Plan 2017–25 is an ambitious attempt by the Government to eliminate tuberculosis by 2025 4 . Despite being a preventable and curable disease, tuberculosis is the most infectious killer disease attributing to almost 10 million cases per year globally, out of which 1.9 million cases are from India 5 , 6 . Numerous guidelines and tools have been released and made accessible by the Ministry of Health and Family Welfare (MoHFW) to tackle the problem of tuberculosis. The policies have been constantly updated after gathering considerable implementation-related learnings and the expansion of programme activities is still happening 7 .
Lack of knowledge about TB is a continuing problem and pose a risk for its prevention and care in China 8 . Similar situation can also be expected in India. In addition, because of the lack of knowledge about the disease and fear of being ostracized, persons with TB often hide their symptoms and fail to receive appropriate treatment which is a stumbling block in the prevention and care of the disease 9 .
The trend analysis of National Family Health Survey (NFHS) 10 aids to give us key themes to improve the National Tuberculosis Elimination Programme’s (NTEP) coverage, quality, equity, efficiency, and effectiveness.
Internationally, in countries with high disease burden of tuberculosis, the routine diagnosis of tuberculosis, treatment compliance and health seeking habits are observed to be affected by gender and their knowledge and perception towards the disease 11 , 12 . The overall misconceptions about the transmission of TB ranges from 43–68 percent of women and 35–66 percent of men in all subgroups of background characteristics 13 , 14 .
With the disease burden of 1,933,381 cases from India in 2021 6 , out of which 6% were children aged 0 to 14 years, 58% were men and 36% were women, it becomes even more crucial to address the gap in awareness of transmission of TB among the two genders. Therefore, the Central TB Division formed the National Framework for Gender Responsive Approach to TB in India guidelines which reports that gender differences and inequalities play a crucial role in how people access and receive healthcare due to TB 15 . Gender is an important variable in the incidence, exposure, risks, health seeking behaviour and in treatment outcomes of tuberculosis.
Globally, studies have also shown that men may repress their illnesses knowingly or unknowingly in an effort to avoid being perceived as weak or feminine, or as a form of compensation. They achieve this, among other things, by believing that they are physically superior to women. They ignore disease as they work to fulfil their obligations to support and uplift their families, something many people are finding harder and harder to accomplish 7 . Men perceive control as a fundamental component of acceptable manhood and efforts to obtain it have also led men to put their health on the back burner, men were afraid of being perceived as being less than men 11 , 16 .
In countries like Malawi, role constructions as primary material providers for their immediate family along with the opportunity costs of acknowledging illness seem important barriers to care-seeking. Upon that, Men’s sense of adequacy as providers was influenced by limited employment opportunities and small incomes. It has been suggested that there is a need to address harmful masculinity and promote gender equality to support interventions for TB and chronic cough 16 .
In India, men are more affected with TB compared to women, but women are at a higher risk of manifesting the disease easily due to undernutrition mainly because of social norms which prevent prioritizing of their nutrition, health, and well-being. Whereas men are at the risk of developing TB due to their employment like mining and construction industries 15 .
Moreover, the factors affecting the health seeking due to gender remains the same as that found globally and access to services is greatly impacted by gender disparities that affect care-seeking, as well as health system variables such access restrictions, a lower index of suspicion of TB in women, and the provision of insufficient information to care-seekers 17 .
Across the globe, there has been a trend that the female participation in the surveys exceeded male participation in TB related surveys 18 . During NFHS less number of men were interviewed when compared to women. Hence, gender-specific factors in tuberculosis prevention and treatment can have a wide range such as differences in care-seeking behavior, diagnostic challenges, risk factors, disease burden of HIV and tuberculosis coinfection, and delayed treatment. Addressing these factors is crucial for achieving equity in tuberculosis care and reducing the burden of the disease among both men and women 19 . Another important factor that can be considered is the sex assortativity among the contacts of the existing patients that might have contributed to sex disparities in disease burden of tuberculosis among adults 20 . According to the NFHS-5 data, although, gender influence in knowledge and perception towards the disease affects the tuberculosis management and care, the extent of the influence is not explicitly explored in India.
This study observes the trends in gender influence in awareness of transmission of tuberculosis at national level to understand the factors that affect this. Noteworthy variation in awareness regarding transmission of tuberculosis is observed among men and women at the national level. On exploring the factors that influence TB awareness, interesting results are obtained which have major implications for TB prevention and care initiatives such as the NTEP in India. The most important factors among women are socioeconomic status, rural residence, age, and education. Our results suggest empowering women and promoting the education of mothers could improve TB awareness, a goal of the TB prevention and care program in India.
Study design
It is a cross-sectional study that compares three complex sample surveys of nationally representative population.
Data sources
Datasets of Demographic Health Survey (DHS) which is also known as National Family Health Survey (NFHS) in India. After permission we obtained the recoded datasets for all three NFHS from DHS. Individual Recode file that contains the data on all the women and Mens Recode file that contains data on all men interviewed during NFHS were used in data analysis. These files shall be referred as Womens dataset and Mens dataset in the article.
For NFHS 3 conducted during 2005 to 2006, the survey included participants from 29 states. For NFHS 4 conducted during 2015 to 2016 and NFHS 5 conducted during 2019 to 2021, the survey included participants from all states and union territories.
Sample characteristics
For NFHS surveys, the multistage cluster sampling is adopted along with population proportion to sampling technique.
Participants
NFHS-3 and NFHS-4 adopted different sample designs for data collection. NFHS-3 used a two-stage approach for rural areas and a three-stage approach for urban areas. In rural areas, the first stage involved selecting villages as Primary Sampling Units (PSUs) using probability proportional to population size (PPS), and in the second stage, households were systematically chosen within each village. In urban areas, three stages were used, with the selection of wards, Census Enumeration Blocks (CEBs), and households 21 . NFHS-4 employed a stratified two-stage sample design with the 2011 census serving as the sampling frame. In rural areas, PSUs (villages) were selected using PPS, and the strata were defined based on the number of households and the percentage of the population belonging to scheduled castes and tribes. In urban areas, CEBs were selected using PPS, considering the SC/ST population percentage. Complete household mapping was conducted in selected PSUs, which were segmented into clusters. Random sampling was used to choose clusters, and within each selected cluster, 22 households were randomly selected in the second stage of data collection. This design resulted in NFHS-4 clusters being either complete PSUs or segments of PSUs 22 . NFHS-5 used the same sample design as that of NFHS-4 21 . From each household one woman from the eligible age group was selected randomly for interview. However for men, during NFHS 3, only those men were interviewed who were usual residents of the sample household or visitors who stayed in the sample household the night before the survey 21 . However, during NFHS 4 and NFHS 5, only men who were selected only in the subsample of households selected for the state module 22 , 23 . In addition to the above, during NFHS 3, the union territories were not considered. Moreover, Telangana was formed in June 2014. Therefore, it is not available as a separate state in NFHS 3. Similarly, Ladakh as a union territory was formed in October 2019. Hence it is not available as a separate state or union territory in NFHS 4.
A total of 74369 cases in Mens dataset and 124385 cases in Womens dataset during NFHS 3, 112122 cases in Mens dataset and 169686 cases in Womens dataset during NFHS 4 and 101839 cases in Mens dataset and 724115 cases in Womens dataset during NFHS 5 were available. Inclusion criteria for analysis for our research was, first: age group of the respondent between 15 to 45 years of age, and second was “Yes” as response to the question: Ever heard about tuberculosis. Detailed inclusion criteria are given in Supplementary Figs. 1 and 2 .
We created the variable on awareness about tuberculosis based on the respondent’s response as “Yes” or “No” to the following questions that were asked during NFHS survey:
Q1: Tuberculosis spread by: Air when coughing or sneezing.
Q2: Tuberculosis spread by: Sharing utensils.
Q3: Tuberculosis spread by: Touching a person with tuberculosis.
Q4: Tuberculosis spread by: Food.
Q5: Tuberculosis spread by: Sexual contact.
Q6: Tuberculosis spread by: Mosquito bites.
Based on the responses, we derived four categories in the dependent variable which are as follows: Category 1: Knowledge without misconceptions: if the response was “Yes” to Q1 and “No” to all other questions. Category 2: Knowledge with misconceptions: if the response was “Yes” to Q1 and “Yes” to any other questions from Q2 to Q6. Category 3: No knowledge without misconceptions: if the response was “No” to all questions from Q1 to Q6. Category 4: No knowledge with misconceptions: if the response was “No” to Q1 and “Yes” to any other questions from Q2 to Q6. For data representation and analysis, Category 3 and Category 4 were added and was considered as single category. Category 1 was used as reference for regression analysis. The categorization in the dependent variable was made based on previous study 24 .
Independent
Based on the review of literature 15 , we selected the following variables for the regression model.
Age in five-year groups
The current age of the respondent was divided into groups of five years each. The participants from all surveys selected in the study were belonging to the age group of fifteen to forty-five years of age. Age group of 45 to 49 years was used as reference category.
Type of place of residence
It is where the respondent was interviewed as either urban or rural which was created based on whether the cluster or sample point number is defined as urban or rural and urban area was considered as a reference category.
Region in which the respondent was interviewed. During NFHS 3, only twenty-nine states were included. However, during NFHS 4 and NFHS 5, states along with Union Territories were also included in the survey. Kerala state was taken as a reference category.
Highest education level
This is a standardized variable providing level of education in the following categories: No education, Primary, Secondary, and Higher which was used as reference category.
Wealth Index
The wealth index is a composite measure of a household’s cumulative living standard. The wealth index is calculated using easy-to-collect data on a household’s ownership of selected assets, such as televisions and bicycles; materials used for housing construction; and types of water access and sanitation facilities. Richest category was used for reference in regression analysis.
Current marital status
It is the current marital status of the respondent. The original variable in the dataset was recoded to form three categories as the distribution of data among various categories in the original variable was skewed. The recoded variable had three categories: “Never married”, “Married” and “Others” which was used as reference category.
Response to the question
Tuberculosis can be cured: The response had three categories: “No”, “Yes” and “Don’t know”. The response “Yes” was taken as reference category.
Keep secret if family member gets tuberculosis: The response had three categories: “No”, “Yes, remain a secret” and “Don’t know/Not sure/It depends”. Response “No” was taken as reference category.
Frequency of reading newspaper or magazine
The response had four categories: “Not at all”, “Less than once a week”, “at least once a week” and “almost every day”.
Frequency of listening to radio
The response was had four categories like those of frequency of reading newspaper or magazine.
Frequency of watching television
The response was had four categories like those of frequency of reading newspaper or magazine. Reference category for frequency of reading newspaper or magazine, listening to radio and watching television was “at least once a week” for regression analysis.
During NFHS 3, the Men’s Questionnaire was employed to interview men aged 15–54 who were usual residents of the sample household or visitors who stayed in the sample household the night before the survey 21 . However, during NFHS 4 and NFHS 5, the Men’s Questionnaire was administered only in the subsample of households selected for the state module 14 , 21 . Hence, the number of cases in the Mens dataset are less in number when compared to those in Womens dataset. Moreover, those who were not interviewed may have contributed notably to the results of our study.
64,212 cases from Mens dataset and 109,032 cases from Womens dataset file for NFHS 3, 91,293 cases from Mens dataset and 61,8274 cases from Womens dataset for NFHS 4 and 85,751 cases from Mens dataset and 671,750 cases from Womens dataset for NFHS 5 were included in the study for further analysis.
Ethical considerations
Our study used secondary data for analysis from the datasets provided by the Demographic Health Surveys Program (DHS). We applied for access, and this was granted based on us providing information about our planned use. All the datasets provided were re coded and already anonymized to completely protect the privacy of the survey participants. Informed consent was obtained from the participant or guardian (for children) before the interview for all surveys by DHS 25 . We did not obtain approval from institutional review boards as the data we were using was deidentified and recoded, that has already been reviewed for privacy and ethical concerns before by DHS. Moreover, this data is available public domain in form of datasets and national and state level reports. The authors were not allowed to share the datasets with each other. Hence all authors have obtained authorization to use the datasets separately from DHS.
Statistics and reproducibility
The datasets were imported to STATA® MP 4 core v17, and declaration for survey design for each dataset was done for weights, primary sampling unit and strata as per instructions by DHS in order to accommodate for stratification by province and state, size group. Dependent variables were computed and required independent variables were recoded. Association between categorical variables was assessed using design adjusted Chi square test. Further, Multinominal Logistic Regression analysis was used to derive adjusted odds ratio with Category 1 as the reference category in the dependent variable. The regression models were derived separately for men and women. Subsequently Poissons Regression analysis was used to derive adjusted prevalence ratio for similar models as it is difficult to interpret an odds ratio for a cross-sectional study as there is confusion between risk or odds leading to incorrect quantitative interpretation 26 . Moreover, the prevalence of no knowledge was higher than 10% and the odds ratio would overestimate the prevalence ratio. However, due to the limitation of Poissons regression with svy commands, in the dependent variable was converted into binomial variable combining Category 1 and Category 2 into a single category as “Knowledge about the spread of Tuberculosis” and Category 3 and Category 4 into a single category as “No knowledge about the spread of Tuberculosis”. All the statistical analysis was carried out under the subset of svy commands that has inherent property for measures similar to robust measures for poisons regression 27 . Microsoft® Excel 365 was used to make line charts. QGIS® Desktop 3.30.1 was used to make maps for prevalence ratio of Men: Women of No knowledge about spreading tuberculosis among men and women. To limit the length of the manuscript, the details on odds ratio are given in the main manuscript and details on prevalence ratio are given in the Supplementary Table No. 7 to Supplementary Table No. 10 .
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
In NFHS 3, 64,212 cases from Mens dataset (containing data from interview of eligible men at household) and 109,032 cases from Womens dataset (containing data from interview of eligible women at household) were included as they fulfilled inclusion criteria. Similarly, from NFHS 4, 91,293 cases from Mens dataset and 618,274 cases from Womens dataset were included for analysis. In addition to the above, from NFHS 5, 85,751 cases from Mens dataset and 691,750 cases from Womens dataset were included for analysis.
Descriptive data
In NFHS 3, 18.26% men and 19.93% women were from the age group fifteen to nineteen years. 38.00% of the men were residing in urban area whereas 64.53% women were residing in rural areas. Most of the men and women had Secondary level of education and belonged to richest level of wealth index. More than half of them were married. While highest proportion of the men belonged from Central zone followed by South zone, most of the women were from Central zone followed by East and South zone in similar proportion. 36.41% men read newspaper or magazine, 25.23% listened to the radio, and 47.83% watched television almost every day. However, for most of the women watching television daily was the only mode of exposure to mass media on almost daily basis. More than 50% of the women never read newspaper or magazine or listened to radio. More than 75% believed that tuberculosis can be cured and would not keep a secret if family member gets tuberculosis.
In NFHS 4, the proportions for age group, level of education, wealth index, current marital status, belief that tuberculosis can be cured, belonging to zone and response for keeping secret if family member gets tuberculosis, were like those in NFHS 3 among men. However, most of the women belonged to the age group twenty to twenty-four years followed by fifteen to nineteen years. Among women similar proportions as that of NFHS 3 were seen with respect to reading newspaper or magazine, listening to radio, and watching television. However, more than 60% of both men and women resided in rural area. In addition to that, among men only 34.53% red newspaper or magazine, and only 6.98% listened to radio and 63.28% watched television almost every day. There was a major change in proportion among men for frequency of mode of exposure to mass media with respect to and listening to radio and watching television.
In NFHS 5, like that in NFHS 4, the proportion of majority of men and women remained unchanged in terms of, type of place of residence, education level, current marital status, belief that tuberculosis can be cured, and response to the question that will they keep secret if family member gets tuberculosis. Among women most of them belonged to the age group of fifteen to nineteen years. In addition to that, most of the men belonged from East zone followed by West zone. Also, there was an increase in proportion of men and women who would never read a newspaper or magazine and listen to radio. In addition to that, there were no respondents who would read newspaper or magazine, listen to radio, or watch television almost every day among both men and women who participated in NFHS 5.
The detailed distribution of eligible men and women during three NFHS surveys are given in Tables 1 and 2 respectively. Moreover, the state and union territory wise distribution for eligible men and women is given in Supplementary Table No. 1 and Supplementary Table No. 2 respectively.
Trend of Knowledge and Misconceptions about spreading to tuberculosis:
Across three surveys, there has been a decrease in the proportion of men who had “No knowledge” and consequently rise in proportion of those who had knowledge about spreading of tuberculosis. Moreover, during NFHS 4, the proportion of those with “No Knowledge” was less than that of those who “Had Knowledge”. In addition to that, from NFHS 4 to NFHS 5, there is an increase in proportion of those who “Had knowledge with misconceptions” but decrease in the proportion of those men who “Had knowledge without misconceptions” about the spread of tuberculosis. Hence there was an increase of misconceptions among men. (Fig. 1 ).
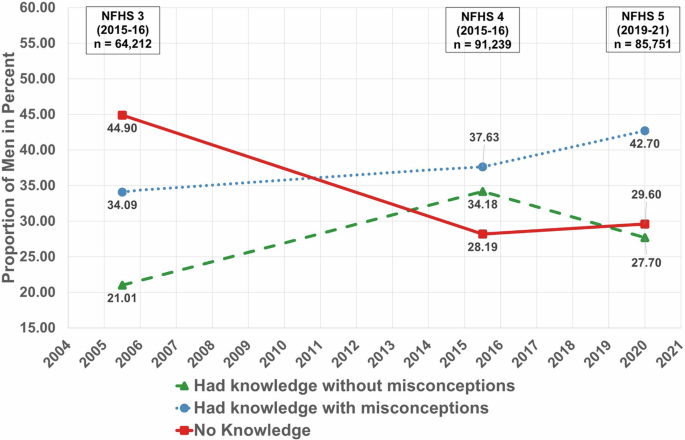
Proportion of knowledge and misconceptions about spreading of tuberculosis among men.
Across three surveys, there has been a decrease in the proportion of women who had “No knowledge” and consequently rise proportion of women who “Had knowledge” about the spread of tuberculosis. However, the proportion of women with “No Knowledge” has always been higher than that of those who “Had knowledge without misconception”. The difference between those who “Had knowledge without misconception” and those who “Had knowledge with misconceptions” about the spread of tuberculosis had been increasing. Hence, there was an increase of misconceptions among women. (Fig. 2 ).

Proportion of knowledge and misconceptions about spreading of tuberculosis among women.
For comparison of prevalence of “No knowledge” about spreading tuberculosis among men and women across the states, during NFHS 3, NFHS 4 and NFHS 5 are presented as Prevalence Ratio on geographical basis on map of India with political boundaries denoting state and union territories. (Figs. 3 , 4 and 5 respectively)
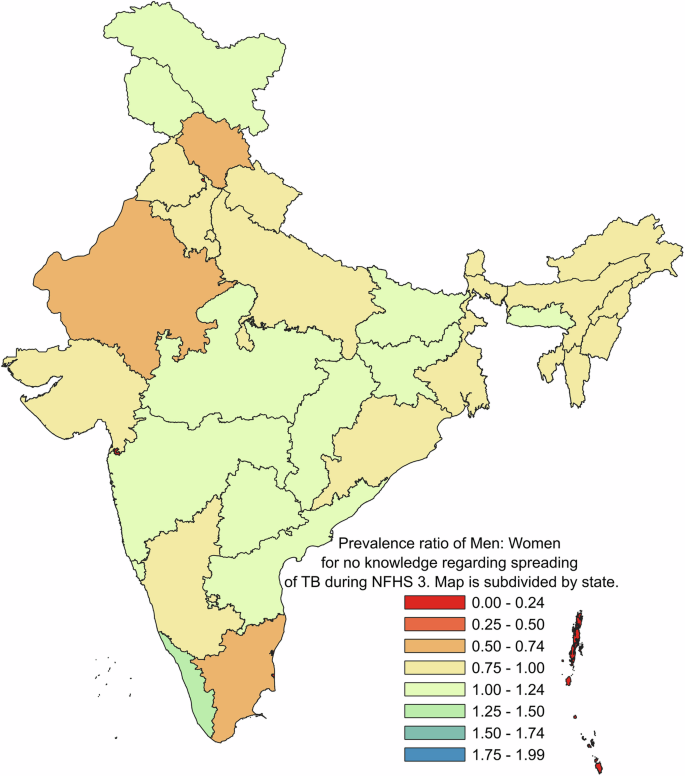
Prevalence ratio of men: women for no knowledge regarding spreading of TB during NFHS 3.
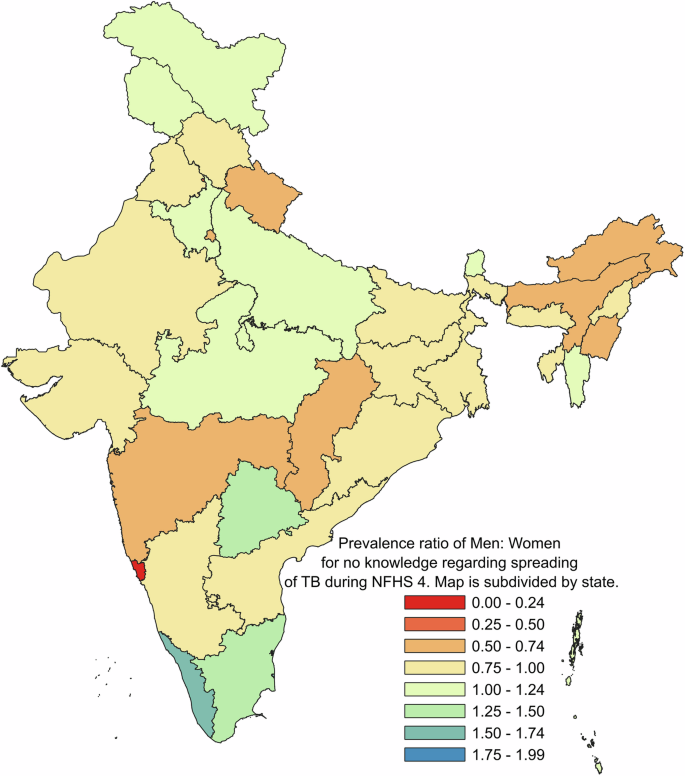
Prevalence ratio of men: women for no knowledge regarding spreading of TB during NFHS 4.
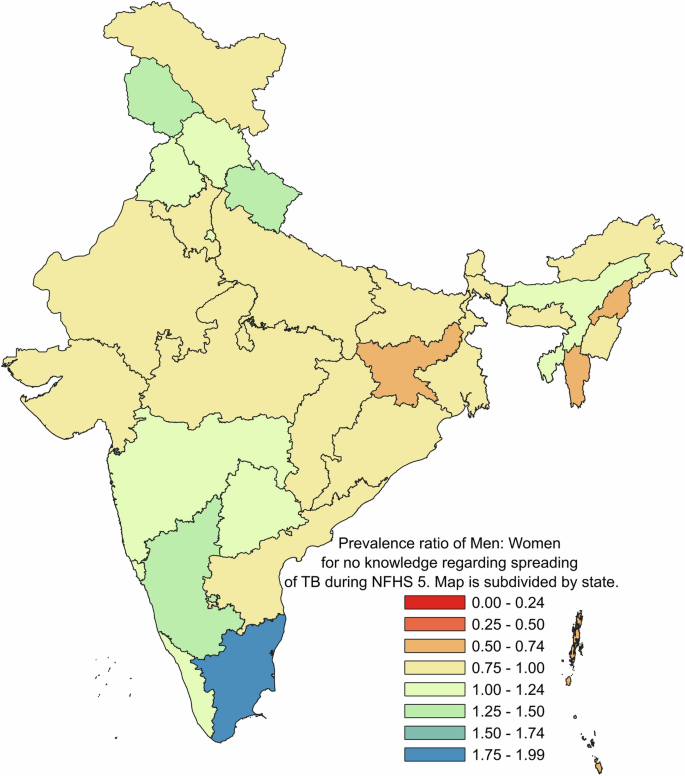
Prevalence ratio of men: women for no knowledge regarding spreading of TB during NFHS 5.
Outcome data
Adjusted odds ratio for men and women for various factors affecting the response as “No knowledge” about spreading of tuberculosis.
Main results
The Crude odds ratio for the independent variables for men and women during three rounds of NFHS is given in Supplementary Table No. 3 and Supplementary Table No. 4 respectively. While any age group was not a significant factor among men, among women the age group of fifteen to twenty four years had higher odds of having “No knowledge” about the spread of tuberculosis during NFHS 3 (aOR: 1.28 (1.12–1.44) for age group fifteen to nineteen years and 1.15 (1.03–1.28) for age group of twenty to twenty four years) and NFHS 5 (aOR: 1.07 (1.01–1.13) for both age groups) and it was statistically significant.
Like the age groups, residing in rural areas was not a significant factor among men. However, women had the higher odds ratio of “No knowledge” who were residing in rural areas and the odds had marginal change across three surveys (aOR: 1.18 (1.07–1.30) during NFHS 3, aOR: 1.09 (1.03–1.14) during NFHS 4 and aOR: 1.12 (1.06–1.18) during NFHS 5) and it was statistically significant. It shows that there has been a disparity between men and women with respect to residing in rural areas.
Education level
No education has constantly been associated significantly with higher odds ratio of having “No knowledge” about spread of tuberculosis among both men and women, however the odds ratio were higher among women (aOR: 2.72 (2.37–3.11) during NFHS 3, aOR: 2.08 (1.96–2.22) during NFHS 4 aOR: 1.66 (1.57–1.76) during NFHS 5) when compared to men through three surveys and the difference of odds ratio between men and women have been decreasing.
For both genders, all categories of wealth index were associated significantly with higher odds ratio of “No Knowledge” about spread of tuberculosis and the odds ratio were highest among the respondents belonging to the poorest category of wealth index during NFHS 3 and NFHS 4. However, during NFHS 5, among men only those belonging to the poorest category of wealth index were associated with higher odds ratio.
For men the marital status was not a significant factor. However, among women never married had lesser odds ratio of “No knowledge” about spreading tuberculosis during NFHS 3 and NFHS 5 which was statistically significant.
Tuberculosis can be cured
Both among men and women those who believed that tuberculosis cannot be cured, were associated with higher odds ratio of having “No knowledge” about spreading of tuberculosis. Among men the odds ratio had increased during NFHS 5 (aOR: 1.95 (1.62–2.34)) when compared to NFHS 3 (aOR: 1.74 (1.51–2.00)). However, among women the odds ratio had decreased during NFHS 5 (aOR: 1.62 (1.54–1.71)) when compared to NFHS 3 (aOR: 1.76 (1.57–1.98)) and these findings were statistically significant.
Would keep secret if family member gets tuberculosis
For men, only during NFHS 5 had higher odds ratio (aOR: 1.21 (1.05–1.39)) for “No knowledge” about spreading of tuberculosis if they wanted keep secret if family member gets tuberculosis. However, for women, the odds ratio of “No knowledge” about spreading of tuberculosis were higher during all three surveys. Moreover, the odds ratio among women have reduced over time marginally. ((aOR 1.27 (1.16–1.38) in NFSH 3, aOR: 1.23 (1.17–1.30) in NFHS 4 and aOR: 1.26 (1.16–1.38) in NFHS 5).
Not reading newspaper or magazine at all among men was associated with increased odds ratio of having “No knowledge” about spreading tuberculosis among men during NFHS 3 (aOR: 1.33 (1.16–1.50)) and NFHS 4 (aOR: 1.24 (1.12–1.36)) only. However, the odds ratio was insignificant during NFHS 5. Among women not reading newspaper or magazine at all was associated with increased odds ratio of having “No knowledge” about spreading of tuberculosis during three surveys. In addition to that the odds ratio had decreased from NFHS 3 (aOR: 1.23 (1.12–1.35)) to NFHS 5 (aOR: 1.16 (1.10–1.22)).
Among both genders, not listening to radio was associated with higher odds ratio of having “No knowledge” about spreading of tuberculosis during NFHS 3. How ever during NFHS 5, the odds ratio were insignificant in males and protective among females (aOR: 0.93 (0.86–0.99)).
For men not watching television at was associated with increased odds ratio of “No knowledge” about spread of tuberculosis during NFHS 4 (aOR: 1.14 (1.02–1.27)). However, among females, not watching television at all was associated with increased odds ratio during NFHS 3 (aOR: 1.12 (1.01–1.24)) and NFHS 5 (aOR: 1.08 (1.04–1.12)).
The detailed adjusted odds ratio for men and women are given in Tables 3 and 4 respectively.
Other analyses
In our regression model for all three surveys, we included the State or Union Territory of residence of respondents to derive aOR for residents of other states and union territories when compared to the residents of the state Kerala. During NFHS 3 for men, the highest odds ratio for “No knowledge” about spreading of tuberculosis was among those who were residing in Jharkhand (aOR: 11.02 (6.71–18.10)) followed by Madhya Pradesh (aOR: 4.96 (3.43–7.17)). Similarly, during NFHS 4 the highest odds ratio was among those who were residing in Uttarakhand (aOR: 7.33 (5.07–10.58)) followed by Himachal Pradesh (aOR: 6.04 (4.44–8.21)). However, during NFHS 5, Dadra & Nagar Haveli and Daman & Diu (aOR: 47.76 (24.25–94.07)) had the highest odds ratio followed by Bihar (aOR: 14.49 (10.02–20.97)). For women, during NFHS 3, the highest odds ratio for having “No knowledge” about spreading of tuberculosis was among those who were residing in Bihar (aOR: 15.00 (10.52–21.38)) followed by Assam (aOR: 10.07 (7.82–12.96)). Similarly, during NFHS 4, the highest odds ratio was among those who were residing in Jharkhand (aOR: 14.93 (13.18–16.90)) followed by Assam (aOR 8.49 (7.47–9.63)). However, during NFHS 5, the highest odds ratio was in those women who were residing in Bihar (aOR: 31.36 (27.65–35.57)) followed by Jharkhand (aOR: 25.46 (22.16–29.25)).
The detailed adjusted odds ratio for men and women for state and union territories is given in Supplementary Table 5 and Supplementary Table 6 respectively.
The details on unadjusted and adjusted Prevalence Ratio for Men and Women are given in Supplementary Table 7 to Supplementary Table 10 .
India being a signatory to the 2030 Agenda for Sustainable Development 28 , we are currently implementing National Strategic Plan (NSP – 2017–2025) 29 , 30 and envision tuberculosis free India by 2025. In order to achieve this goal, there is a need to adopt a comprehensive approach to gender specific and gender sensitive interventions 15 . This study was undertaken to find out gender disparity and its associated factors regarding awareness of tuberculosis in India by comparing data of three nationwide surveys viz. NFHS-3, NFHS-4 and NFHS-5.
Across the three surveys comparison, we found that there has been a decrease in the proportion of men with “no knowledge” about the spread of tuberculosis and consequently rise in proportion of those who had knowledge over the stretch of years in India. This depicts success of various strategies involved to increase public awareness viz. availability of health information sources in vernacular language and according to local needs; regular training of concerned human resources and promotion of e- learning modes. Moreover, the decrease in the proportion of women who had “no knowledge” was more as compared to men, may be due to improved access of women to electronic media via mobile and internet usage, which could not be assessed due to limitations of the study and may also be due to inclusion of females in health manpower. Moreover, the proportion of men and women with knowledge about the spread of tuberculosis was associated with misconception regarding awareness of tuberculosis transmission which can be attributed to easier access to electronic media via mobile and internet and also lack of awareness of trusted sources of correct information regarding health-related states, particularly TB. In addition, it points towards gender being an important social construct which influences the level of awareness of people about health and illness. As per social norms men have a greater public involvement and hence greater exposure to information, which leads to greater awareness about tuberculosis among men 31 . A previous study from Gujarat showed similar findings of higher proportion of men with better knowledge. It was seen that men were more aware about the mode of transmission and symptoms of tuberculosis 32 . Another study from Nanded, Maharashtra showed similar finding of higher knowledge (33.6%) and more positive attitude (53%) in men about tuberculosis compared to women 33 .
In present study, age was an important risk factor which is associated with gender disparity in awareness regarding tuberculosis transmission. Women in age group of fifteen to nineteen years age and twenty to twenty-four years of age were having “no knowledge” about the spread of tuberculosis when compared to men in same age group. Our analysis was concordant to previous similar studies which showed that women with higher age group are more aware and knowledgeable about TB 34 , 35 , 36 . Increase in age may add more health experience, hence, better aware about TB and identify the mode of infection. In addition to that, culturally higher aged women in India enjoy greater autonomy and freedom than younger one, thus find little or no hindrance in order to seek medical help for self thus more aware and knowledgeable than younger one 37 .
Overall, the analysis shows that the odds among those with “no education” having lesser awareness of tuberculosis transmission have reduced in both men and women but still the odds were more in women as compared to men over the years. As women with higher education have higher odds for awareness and correct knowledge regarding spread of TB, it was in the line with other studies 38 , 39 . It could be that educated people have greater access to various sources of information leading to more awareness about health, availability of healthcare services and use this awareness and information in accessing the health care services 40 , 41 .
Furthermore, women residing in rural area and belonging to low income households were acting as a risk factor for decreased awareness on transmission of tuberculosis, while, such was not the case among men, which is in line with similar other studies 42 , 43 , 44 , 45 . Women with better socio-economic status and those in urban areas are more likely to have better access to health, better media access to TB information, as well as good communication, transportation, and other necessities 35 , 46 . In addition, the rural-urban divide in knowledge and awareness can also attribute to awareness disparity depending upon the place of residence. Therefore, urbanized women and from higher socioeconomic backgrounds have a much better chance than women from rural areas and lower socioeconomic backgrounds of meeting their needs and demands thus knowledge and awareness regarding TB 47 .
It is also found that women who would like to keep it a secret if any member suffers from tuberculosis have higher odds of having no knowledge about spread of tuberculosis than men during NFHS 3 and NFHS 4 which was not so during NFHS 5. Its probable explanation could be that women with more hindrance feel lesser autonomy in terms of medical seeking behaviour thus do not easily disclose a family member’s tuberculosis 47 . During NFHS 5 there was an overlap in the odds for men and women thus eliminating the gender disparity. Usually, NFHS is completed within a year. However, NFHS 5 was completed in three years that is from 2019 to 2021. The duration of completion of survey was increased due to lockdown. However, we are of the opinion that the pandemic has not affected awareness about the methods of spreading tuberculosis in a notable way. The results can be generalised to whole population of the country as the NFHS was conducted among the nationally representative population in the country.
Various strategies to improve access to knowledge regarding tuberculosis and its transmission include creating a culture of evidence-based decision-making by the use of ICT based applications from grass root level upwards, supporting integration and improvement in TB information systems, including NIKSHAY for achievement of TB elimination goals and establishing a TB Knowledge Network (TBKN), inter-connecting all knowledge and research institutions in the country through a virtual network. The overarching role will be to establish a backbone connectivity which will enable knowledge and information sharing amongst TBKN connected institutes, enabling collaborative research, development and innovation amongst TBKN connected institutes, facilitating advanced distance education in specialized sub-areas of TB, facilitating connection between different sectoral networks in the field of research.
The key strategy is to move towards an e-learning mode utilizing the web based and mobile based learning experiences and translating the content to vernacular language and adding relevant content as per local needs at the State level. There has been also high visibility media campaign involving Amitabh Bacchan, India’s biggest film star and an ex-TB patient, as the TB brand ambassador, a big impact on conveying the threat of TB to the public at large. Moreover, TB Champions from amongst patients, technical experts, political representatives, public figures, sportsperson, and celebrities added their voice to increase visibility and action on TB. Substantial efforts have been made towards capacity building of programme managers, state IEC officers and communication facilitators with dedicated national, regional and state level trainings and workshops, to increase awareness about TB 29 .
This study has few limitations such as since it is secondary data analysis, all aspects about knowledge and awareness of tuberculosis could not be explored. Secondly, NFHS which produced the data for this study, was based on respondents’ self-reported information, with no objective validation of the information provided. Furthermore, the dataset of women used in the analysis is limited to the reproductive age group women (fifteen years to forty-nine years of age), which is insufficient to generalize the result for all the women. Similarly, elderly men dataset is not available for analysis. The proportion of men included in the survey was not comparable to that of women. Lastly, since the data for this study came from a cross-sectional survey, we were only able to look at the association between independent and dependent variables and hence any conclusions about causality could not be drawn. In the models derived using Poisson’s Regression providing Prevalence Ratio, multiple independent variables can be seen having a varied level of significance, when compared with Odds Ratio Logistic Regression providing Relative Risk Ratio. This can be attributed to the fact that Poisson’s Regression was derived after converting the dependent variable into a binomial variable for the feasibility of the statistical analysis based on the available expertise of the authors.
Based upon our study, we recommend increased usage of mass media and social media platforms for disseminating health education, since television and radio as media of communication does not hold much value in today’s era. Future research should investigate the reasons that could explain the unexplained differences in tuberculosis awareness, knowledge, and attitude amongst men and women. Moreover, frequent community health contact activities considering gender- specific needs in tuberculosis prevention and care initiatives should be promoted. Furthermore, the fear of stigma and discrimination in different ways at their homes, workplaces, healthcare settings and in communities may prevent people, women, and transgenders, from seeking healthcare. This can be tackled by adopting social behaviour change communication (SBCC) campaigns, especially targeting women, may yield greater results in tuberculosis awareness and knowledge, leading to better tuberculosis notification rates, hence, achieve the goal of ending tuberculosis in India by 2025.
Data availability
The datasets that support the findings of this study are available from DHS at https://dhsprogram.com/ but restrictions apply to the availability of these data, which were used under license for the current study. Though the datasets are available in the public domain, a formal request is required to be placed with DHS which should mention the project details such as Title, Objectives and description of tentative analysis that will be carried out. The numerical data for the Figs. 1 and 2 can be found in file named Supplementary Table 11 . Further, the numerical data for Figs. 3 , 4 and 5 is provided in Supplementary Tables 12 , 13 and 14 respectively.
Mbuthia, G. W., Olungah, C. O. & Ondicho, T. G. Knowledge and perceptions of tuberculosis among patients in a pastoralist community in Kenya: A qualitative study. Pan Afr Med J 30 , 287 (2018).
Article PubMed PubMed Central Google Scholar
Matakanye H., Tshitangano T. G., Mabunda J. T. & Maluleke T. X. Knowledge, beliefs, and perceptions of tb and its treatment amongst tb patients in the limpopo province, South Africa. Int J Environ Res Public Health . 18 , 10404, (2021). Available from: /pmc/articles/PMC8508321/
Mondal, M. N., Nazrul, H. M., Chowdhury, M. R. K. & Howard, J. Socio-demographic factors affecting knowledge level of Tuberculosis patients in Rajshahi City, Bangladesh. Afr Health Sci [Internet] 14 , 855 (2014).
Article CAS PubMed Google Scholar
Family N. & Survey H. Government of India Ministry of Health and Family Welfare COMPENDIUM OF FACT SHEETS INDIA AND 14 STATES/UTs (Phase-11).
Khanna, A., Saha, R. & Ahmad, N. National TB elimination programme - What has changed. Indian J Med Microbiol [Internet] 42 , 103 (2023).
Tuberculosis. [cited 2023 Apr 25]. https://www.who.int/health-topics/tuberculosis#tab=tab_1
Mavhu, W. et al. Chronic cough and its association with TB–HIV co‐infection: factors affecting help‐seeking behaviour in Harare, Zimbabwe. Tropical Medicine & International Health 15 , 574–579 (2010).
Google Scholar
Chen, W. et al. Is tuberculosis health education reaching the public in China? A cross-sectional survey in Guizhou Province. Bmj Open 6 , e013534 (2016).
Mathew, A. S. & Takalkar, A. M. Living with tuberculosis: the myths and the stigma from the Indian perspective. Clinical infectious diseases 45 , 1247 (2007).
Article PubMed Google Scholar
TB statistics - India.: https://tbfacts.org/tb-statistics-india/
Chikovore, J. et al. Missing men with tuberculosis: the need to address structural influences and implement targeted and multidimensional interventions. BMJ Global Health 5 , e002255 (2020).
Chikovore, J., Hart, G., Kumwenda, M., Chipungu, G. A. & Corbett, L. For a mere cough, men must just chew Conjex, gain strength, and continue working’: the provider construction and tuberculosis care-seeking implications in Blantyre, Malawi. Global Health Action 8 , 26292 (2015).
India announces plan to end tuberculosis by 2025 [Internet]. Bill & Melinda Gates Foundation. Available from: https://www.gatesfoundation.org/ideas/articles/india-announces-plan-to-end-tuberculosis-by-2025
International Institute for Population Sciences. National Family Health Survey(NFHS-5) India 2019-21. Minist Heal Fam Welf Natl . 1 , 1–714 (2022).
National Framework For a Gender-responsive approach to TB in India [Internet]. [cited 2023 Aug 23]. Available from: https://tbcindia.mohfw.gov.in/wp-content/uploads/2023/05/388838054811-NTEP-Gender-Responsive-Framework_311219.pdf
Chikovore, J. et al. Control, struggle, and emergent masculinities: a qualitative study of men’s care-seeking determinants for chronic cough and tuberculosis symptoms in Blantyre, Malawi. BMC Public Health 14 , 1–2 (2014).
Article Google Scholar
National Family Health Survey. http://rchiips.org/nfhs/
Horton, K. C., MacPherson, P., Houben, R. M., White, R. G. & Corbett, E. L. Sex differences in tuberculosis burden and notifications in low-and middle-income countries: a systematic review and meta-analysis. PLoS Medicine 13 , e1002119 (2016).
Ledesma, J. R. et al. Global, regional, and national sex differences in the global burden of tuberculosis by HIV status, 1990–2019: results from the Global Burden of Disease Study 2019. The Lancet Infectious Diseases 22 , 222–241 (2022).
Horton, K. C., Hoey, A. L., Béraud, G., Corbett, E. L. & White, R. G. Systematic review and meta-analysis of sex differences in social contact patterns and implications for tuberculosis transmission and control. Emerging Infectious Diseases 26 , 910 (2020).
Danarastri, S., Perry, K. E., Hastomo, Y. E., Kurniawati & Priyonugroho, K. Gender differences in health-seeking behaviour, diagnosis and treatment for TB. Int J Tuberc Lung Dis 26 , 568–570 (2022).
Article CAS PubMed PubMed Central Google Scholar
International Institute for Population Sciences. 1, National Family Health Survey (NFHS-3) 2005-06 India . 12–13. (Mumbai, International Institute for Population Sciences, 2007).
International Institute for Population Sciences. 1, National Family Health Survey (NFHS-4) 2015-2016 India . 1–2. (Mumbai, International Institute for Population Sciences, 2017).
Khandoker, A., Khan, M. M., Krämer, A. & Mori, M. Knowledge about tuberculosis transmission among ever-married women in Bangladesh. The International Journal of Tuberculosis and Lung Disease 15 , 379–384 (2011).
CAS PubMed Google Scholar
International Institute for Population Sciences. 1, National Family Health Survey (NFHS-5) 2019-2021 India . 2–3. (Mumbai, International Institute for Population Sciences, 2022).
Krishnamoorthy, Y. & Ganesh, K. Prevalence and determinants of physical violence and its impact on birth outcomes during pregnancy in India: evidence from a nationally representative survey. Journal of Interpersonal Violence 37 , 2615–2632 (2022).
StataCorp. [stata.com]. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC, (2021). https://www.stata.com/manuals/svy.pdf
The DHS program [Internet]. The DHS Program - Protecting the Privacy of DHS Survey Respondents. The Demographic and Health Surveys (DHS) Program. https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm
Sustainable Development Goals. United Nations India Annual Report 2021.
National Strategic Plan for Tuberculosis 2017 - 25: Elimination by 2025 [Internet]. Central Tuberculosis Division National Tuberculosis Elimination Programme. Ministry of Health and Family Welfare; 2017 [cited 2023 Aug 24]. Available from: https://tbcindia-wp.azurewebsites.net/wp-content/uploads/2023/05/National-Strategic-Plan-2017-25.pdf
World Health Organization. Gender and tuberculosis . (World Health Organization, 2002)
Bhalla, S., Chndwani, H., Chudasama, R., Somasundaram, C. & Pathi, S. Awareness regarding pulmonary Tuberculosis In a rural population of Gujrat. Health and Population 27 , 29–39 (2004).
Pichamuthu, B., Putthawar, P. & Akinola, A. Gender differences in knowledge and attitude about tuberculosis among rural population in Nanded district Maharashtra State India. IOSR Journal of Humanities and Social Science 19 , 81–84 (2014).
Agho, K. E., Hall, J. & Ewald, B. Determinants of the knowledge of and attitude towards tuberculosis in Nigeria. J Heal Popul Nutr 32 , 520–538 (2014).
CAS Google Scholar
Pengpid, S. & Peltzer, K. Knowledge, attitudes, and practices regarding tuberculosis in Timor-Leste: Results from the demographic and health Survey 2016. J Prev Med Public Heal 52 , 115–122 (2019).
Navio, J. L. P., Yuste, M. R. & Pasicatan, M. A. Socio-economic determinants of knowledge and attitudes about tuberculosis among the general population of Metro Manila, Philippines. Int J Tuberc Lung Dis 6 , 301–306 (2002).
All, U. T. C. Evidence of women’s empowerment in India: a study of socio-spatial disparities. GeoJournal 65 , 365–380 (2016).
Tolossa, D., Medhin, G. & Legesse, M. Community knowledge, attitude, and practices towards tuberculosis in Shinile town, Somali regional state, eastern Ethiopia: A cross-sectional study. BMC Public Health 14 , 1–13 (2014).
Datiko, D. G., Habte, D., Jerene, D. & Suarez, P. Knowledge, attitudes, and practices related to TB among the general population of Ethiopia: Findings from a national cross-sectional survey. PLoS One 14 , 1–16 (2019).
Mazumdar, S., Satyanarayana, S. & Pai, M. Self-reported tuberculosis in India: Evidence from NFHS-4. BMJ Glob Heal 4 , 1–8 (2019).
Feuser T. Investigation of Tuberculosis Stigma in 2008 Ghana. Thesis https://scholarworks.gsu.edu/cgi/viewcontent.cgi?article=1351&context=iph_theses (2014).
Pengpid, S. et al. Knowledge, attitudes, and practices about tuberculosis and choice of communication channels in Thailand. J Infect Dev Ctries 10 , 687–693 (2016).
Hoa, N. P., Chuc, N. T. K. & Thorson, A. Knowledge, attitudes, and practices about tuberculosis and choice of communication channels in a rural community in Vietnam. Health Policy (New York) 90 , 8–12 (2009).
de Freitas, I. M. et al. Fatores associados ao conhecimento sobre tuberculose e atitudes das famílias de pacientes com a doença em Ribeirão Preto, São Paulo. Rev Bras. Epidemiol. 18 , 326–340 (2015).
Turk, T., Newton, F. J., Netwon, J. D., Naureen, F. & Bokhari, J. Evaluating the efficacy of tuberculosis Advocacy, Communication and Social Mobilization (ACSM) activities in Pakistan: A cross-sectional study. BMC Public Health 13 , 887 (2013).
Gautam, N., Karki, R. R. & Khanam, R. Knowledge on tuberculosis and utilization of DOTS service by tuberculosis patients in Lalitpur District, Nepal. PLoS One 16 , 1–14 (2021).
Mondal, D., Karmakar, S. & Banerjee, A. Women’s autonomy and utilization of maternal healthcare in India: Evidence from a recent national survey. PLoS One 15 , 1 (2020).
Download references
Acknowledgements
We would like to thank DHS for approving the authorization to use datasets and providing datasets free of cost upon request. The authors would like to state that we did not receive any external funding for our work. This research project was entirely self-funded, and we did not have the support of any grants or other funding sources.
Author information
Authors and affiliations.
Bangalore Medical College and Research Institute, Bengaluru, India
Ranganath Thimmanahalli Sobagaiah
World College of Medical Sciences and Research, Jhajjar, India
Nitu Kumari
Kempegowda Institute Medical Sciences, Bengaluru, India
Divya Bharathi Gattam
All India Institute of Medical Sciences, Mangalagiri, India
Mohammed Shoyaib Khazi
You can also search for this author in PubMed Google Scholar
Contributions
Ranganath T S (R.T.S.) conceptualized the study. In addition to that, he performed a review of literature, and supervised the research team. Nitu Kumari (N.K.) and Divya Bharathi G (D.B.G.) curated the data, conducted the investigation for filtering the variables, developed, and validated the methodology, and created the visualizations. K Md Shoyaib (K.M.D.S.) conducted the final statistical analysis on the final datasets. N.K., D.B.G. and K.M.D.S. drafted the manuscript and all authors reviewed, edited, and approved the final manuscript. All authors had complete access to the D.H.S. datasets, which were accessed upon approval of individual requests, by D.H.S. All authors have verified the data.
Corresponding author
Correspondence to Mohammed Shoyaib Khazi .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
: Communications Medicine thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplement file, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Thimmanahalli Sobagaiah, R., Kumari, N., Bharathi Gattam, D. et al. Nationwide surveys of awareness of tuberculosis in India uncover a gender gap in tuberculosis awareness. Commun Med 4 , 168 (2024). https://doi.org/10.1038/s43856-024-00592-x
Download citation
Received : 08 June 2023
Accepted : 14 August 2024
Published : 23 August 2024
DOI : https://doi.org/10.1038/s43856-024-00592-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Queensland research finds young people 'burnt out and in need of help'
By Claudia Williams
Topic: Mental Health
New research shows almost nine out of 10 young Queenslanders have seen a negative change in their health and wellbeing in the past year. ( ABC News: Stephanie Anderson )
It is impossible to ignore the negative impacts of smartphones and social media on the mental health and wellbeing of young people, Queensland’s chief health officer says.
The comments come as new research shows almost nine out of 10 young Queenslanders have seen a negative change in their health and wellbeing in the past year.
The survey of 1,424 young people conducted by the state's prevention agency, Health and Wellbeing Queensland, found more than half of respondents reported feeling stressed or anxious.
Chief Health Officer Dr John Gerrard said while less people were dying from heart disease and strokes, the mental health of young people was "getting worse very rapidly".
"It appears to be a real phenomenon and not the result of better reporting," he said. "I believe this is a very significant concern.
"One of the most dramatic indicators is the instances of hospitalisation due to self-harm in young children aged 10 to 14 has almost [tripled] over the last decade."
John Gerrard says the mental ill-health of young people is a very real phenomenon being seen across the world. ( ABC News: Claudia Williams )
Dr Gerrard said the mental health decline in young people had been seen on a global scale since 2010, in the years following the release of the first smartphone.
He said there were no simple solutions, adding the community at-large has not spoken about "this enough".
"It is not clear at this stage what to do about this specific problem, but I have been meeting with Commonwealth agencies to discuss these issues."
'Burnt out and in need of help'
The research, commissioned by the Queensland government, found more than half of those aged 15 to 24 reported feeling tired for no reason or that everything was an effort in the four weeks prior to being surveyed.
Health and Wellbeing Queensland deputy chief executive Gemma Hodgetts said these were the warning signs of a generation "burnt out and in need of help".
"Young Queenslanders who should be our most vibrant, energetic and hopeful generation are struggling," she said.
Gemma Hodgetts says the research shows young people are struggling. ( ABC News: Claudia Williams )
"Almost one in two Queenslanders will experience mental ill-health in their lifetime ... about 75 per cent of mental disorders emerge before the age of 24 years, so we need to act now."
The research found those experiencing mental health challenges were more likely to rate their health significantly lower.
The report said the findings suggest increased stress, along with poorer diets, may be negatively impacting the mental health of young Queenslanders, particularly young adults.
According to the research, women, girls and mothers are also more likely to experience negative impacts, which may in part be due to their lower activity levels.
Ms Hodgetts said the report laid the foundation for an Australian-first strategy which would take a deliberate wellbeing approach to mental health.
- Search Menu
- Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Prehistoric Archaeology
- Browse content in Art
- History of Art
- Browse content in Classical Studies
- Classical History
- Classical Literature
- Classical Reception
- Greek and Roman Archaeology
- Digital Humanities
- Browse content in History
- Diplomatic History
- Environmental History
- Genocide and Ethnic Cleansing
- History by Period
- Legal and Constitutional History
- Regional and National History
- Social and Cultural History
- Theory, Methods, and Historiography
- World History
- Browse content in Language Teaching and Learning
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Language Families
- Language Evolution
- Lexicography
- Browse content in Literature
- Bibliography
- Literary Studies (American)
- Literary Studies (20th Century onwards)
- Literary Studies (British and Irish)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Medicine and Music
- Music Theory and Analysis
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Philosophy of Science
- Philosophy of Mind
- Philosophy of Mathematics and Logic
- Practical Ethics
- Browse content in Religion
- Christianity
- Judaism and Jewish Studies
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Ethical Issues and Debates
- Browse content in Law
- Arbitration
- Company and Commercial Law
- Comparative Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Parliamentary and Legislative Practice
- Employment and Labour Law
- Environment and Energy Law
- Financial Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Society
- Legal System and Practice
- Medical and Healthcare Law
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Dietetics and Nutrition
- Physiotherapy
- Radiography
- Anaesthetics
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Geriatric Medicine
- Infectious Diseases
- Medical Oncology
- Medical Toxicology
- Rheumatology
- Sleep Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Forensic Medicine
- History of Medicine
- Browse content in Medical Dentistry
- Restorative Dentistry and Orthodontics
- Medical Ethics
- Medical Skills
- Medical Statistics and Methodology
- Browse content in Neurology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
Occupational Medicine
- Paediatrics
- Browse content in Pathology
- Clinical Cytogenetics and Molecular Genetics
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Preclinical Medicine
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- Neurosurgery
- Plastic and Reconstructive Surgery
- Trauma and Orthopaedic Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Physical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Human-Computer Interaction
- Mathematical Theory of Computation
- Browse content in Computing
- Computer Security
- Computer Networking and Communications
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Meteorology and Climatology
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- Transport Technology and Trades
- Browse content in Environmental Science
- Environmental Sustainability
- Management of Land and Natural Resources (Environmental Science)
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- Mathematical Education
- Mathematical Analysis
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Neuroscientific Techniques
- Browse content in Physics
- Astronomy and Astrophysics
- Classical Mechanics
- Relativity and Gravitation
- Browse content in Psychology
- Clinical Psychology
- Cognitive Neuroscience
- Cognitive Psychology
- Health Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Human Evolution
- Browse content in Business and Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- Organizational Theory and Behaviour
- Public and Nonprofit Management
- Browse content in Criminology and Criminal Justice
- Criminology
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- Health, Education, and Welfare
- Labour and Demographic Economics
- Law and Economics
- Public Economics
- Urban, Rural, and Regional Economics
- Browse content in Education
- Schools Studies
- Teaching of Specific Groups and Special Educational Needs
- Environment
- Browse content in Human Geography
- Economic Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- Foreign Policy
- Gender and Politics
- International Relations
- International Organization (Politics)
- Political Sociology
- Political Theory
- Political Behaviour
- Political Economy
- Political Institutions
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Security Studies
- Browse content in Regional and Area Studies
- African Studies
- Japanese Studies
- Research and Information
- Browse content in Social Work
- Addictions and Substance Misuse
- Browse content in Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Migration Studies
- Race and Ethnicity
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Urban and Rural Studies
- Journals A to Z
- Books on Oxford Academic
What are the trending topics in Public Health and related disciplines?
You can identify some of the most discussed and influential topics with the help of Altmetric attention scores, which take into account several outlets including social media, news articles, and policy documents.
Drawing from a selection of Public Health and Medicine journals, we have compiled a list of the articles that have been mentioned the most over the past few months.
Discover the articles that are trending right now, and catch up on current topics in Public Health and related disciplines. We will update our collection every few weeks; come back to this page to be on top of the latest conversations in Public Health and Medicine. Previously featured articles are listed here .
You can also sign up for e-alerts to make sure you never miss the latest research from our journals.
*Last updated October 2021*
Age and Ageing
Alcohol and alcoholism, american journal of epidemiology, annals of work exposures and health, epidemiologic reviews, european journal of public health, family practice, health education research, health policy and planning, health promotion international, international health, international journal of epidemiology, international journal for quality in health care, journal of public health, journal of travel medicine, journal of tropical pediatrics, nicotine & tobacco research, transactions of the royal society of tropical medicine & hygiene.
There is moderate-certainty evidence that behaviour change interventions are associated with increased physical activity levels among older hospitalised patients.
This study from Canada found that one in three young adults with ADHD had a lifetime alcohol use disorder, and that young adults with ADHD were also three times more likely to develop a substance use disorder. Targeted outreach and interventions for this extremely vulnerable population are warranted.
According to this study, resuming evictions in summer 2020 was associated with increased COVID-19 incidence and mortality in US states, with an estimated 433,700 excess cases and 10,700 excess deaths. Explore more research on COVID-19 in a curated collection from the AJE: https://academic.oup.com/aje/pages/covid-19
The British Occupational Hygiene Society (BOHS) developed a control banding matrix for employers and others to help assess the risks of COVID-19 infection, and calls for further work to validate the reliability of the tool. Browse the Annals' collection on occupational hygiene for virus protection: https://academic.oup.com/annweh/pages/covid-19
In 1777, George Washington ordered a mandatory inoculation program for his troops, in what would become the first mass immunization mandate in the US. This archival article discussess and contextualizes immunization practices for US Armed Forces.
Responding to concerns that that face mask use could elicit a false sense of security and lead to riskier behaviours, this study from Denmark found that mask use overall correlated positively with protective behaviours.
While medical practice is often undermined by subsequent investigation, randomized trials relevant to primary care generally hold up over time.
This study shows the potential for using social media influencers to inspire positive engagements on pro-vaccine health messaging. For more content on accurate information's importance for public health, browse the latest article collection from HER: https://academic.oup.com/her/pages/covid-19
Current emergency response planning does not have adequate coverage to maintain health systems functionality for essential health service delivery alongside emergency-specific interventions and healthcare. The findings from this study can help align health emergency planning with broader population health needs.
This case study shows that that ongoing efforts are needed to improve sustainability of nutrition policy and programmes to address all diet-related diseases.
This review article outlines evidence for a range of institutional measures and behaviour-change measures, and highlights research and knowledge gaps.
The COVID-19 pandemic triggered significant mortality increases in 2020 of a magnitude not witnessed since World War II in Western Europe or the breakup of the Soviet Union in Eastern Europe.
The authors propose an update to the Equator’s Consolidated criteria for reporting qualitative research (COREQ) checklist, with the aim of enhancing inclusivity.
This study confirms previous findings on a low risk of SARS-CoV-2 reinfection. If confirmed, these findings suggest that more targeted restriction policies can be applied to the subjects that recovered after a first infection. Read highly cited papers on COVID-19 from the Journal of Public Health: https://academic.oup.com/jpubhealth/pages/covid-19
Given the Delta variant's high reproductive number associated with higher transmissibility, in a context of globally still low vaccine coverage rates and lower vaccine effectiveness, public health and social measures will need to be substantially strengthened. A high reproductive number also means that much higher vaccine coverage rates need to be achieved compared to the originally assumed.
Neurological complications are rare in children suffering from COVID-19. Still, these children are at risk of developing seizures and encephalopathy, more in those suffering from severe illness.
The researchers examined support for and perceived impact of e-cigarette sales restrictions. Findings suggest that bans on flavored vape products could have a positive impact on lower-risk users, but that other young adult user subgroups may not experience benefit.
An editorial from the earlier stages of the pandemic highlights the importance of properly fitted respirators for worker safety and outlines occupational hygiene measures.
Guidelines for safe mass drug administration for neglected tropical diseases were developed in a COVID-19 context; training and implementation were assessed through an observation checklist.
For more research on the impact of COVID-19 on NTDs, explore the March 2021 special issue: https://academic.oup.com/trstmh/issue/115/3
Previously featured
Age and frailty are independently associated with increased COVID-19 mortality and increased care needs in survivors: results of an international multi-centre study
Trajectories of Alcohol Use and Related Harms for Managed Alcohol Program Participants over 12 Months Compared with Local Controls: A Quasi-Experimental Study
Estimating the Effect of Social Distancing Interventions on COVID-19 in the United States
Selecting Controls for Minimizing SARS-CoV-2 Aerosol Transmission in Workplaces and Conserving Respiratory Protective Equipment Supplies
What Do We Know About the Association Between Firearm Legislation and Firearm-Related Injuries?
Denialism: what is it and how should scientists respond?
Acute cooling of the feet and the onset of common cold symptoms
The effect of falsely balanced reporting of the autism–vaccine controversy on vaccine safety perceptions and behavioral intentions
Climate change: an urgent priority for health policy and systems research
Power, control, communities and health inequalities I: theories, concepts and analytical frameworks
Research ethics in context: understanding the vulnerabilities, agency and resourcefulness of research participants living along the Thai–Myanmar border
Tobacco smoking and mortality among Aboriginal and Torres Strait Islander adults in Australia
Quality and safety in the time of Coronavirus: design better, learn faster
Years of life lost associated with COVID-19 deaths in the United States
In-flight transmission of SARS-CoV-2: a review of the attack rates and available data on the efficacy of face masks
Stability of the Initial Diagnosis of Autism Spectrum Disorder by DSM-5 in Children: A Short-Term Follow-Up Study
Impact of Tobacco Smoking on the Risk of COVID-19: A Large Scale Retrospective Cohort Study
Mental health of staff working in intensive care during COVID-19
The benefits and costs of social distancing in high- and low-income countries
A classification tree to assist with routine scoring of the Clinical Frailty Scale
Recent Advances in the Potential of Positive Allosteric Modulators of the GABAB Receptor to Treat Alcohol Use Disorder
The recent oubreak of smallpox in Meschede, West Germany
Your Hair or Your Service: An Issue of Faith for Sikh Healthcare Professionals During the COVID-19 Pandemic
Emerging Infections: Pandemic Influenza
Identifying the views of adolescents in five European countries on the drivers of obesity using group model building
Novel multi-virus rapid respiratory microbiological point-of-care testing in primary care: a mixed-methods feasibility evaluation
Public health crisis in the refugee community: little change in social determinants of health preserve health disparities
In search of ‘community’: a critical review of community mental health services for women in African settings
COVID-19, a tale of two pandemics: novel coronavirus and fake news messaging
Disrupting vaccine logistics
Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations
Measurement and monitoring patient safety in prehospital care: a systematic review
Black Lives Matter protests and COVID-19 cases: relationship in two databases
The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China
Severe Malnutrition and Anemia Are Associated with Severe COVID in Infants
A Single-Arm, Open-Label, Pilot, and Feasibility Study of a High Nicotine Strength E-Cigarette Intervention for Smoking Cessation or Reduction for People With Schizophrenia Spectrum Disorders Who Smoke Cigarettes
Healthcare workers and protection against inhalable SARS-CoV-2 aerosols
Affiliations
- Copyright © 2024
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
The current state of public health education in India: A scoping review
Ashish joshi.
1 Graduate School of Public Health and Health Policy, City University of New York, New York, NY, United States
Ashruti Bhatt
2 Foundation of Healthcare Technologies Society, New Delhi, India
Mansi Gupta
Ashoo grover.
3 Division of Non Communicable Diseases, Indian Council of Medical Research, New Delhi, India
Sofia Rani Saggu
Isha vikas malik, associated data.
With the creation of public health management cadre in the state, district, and block levels of India, there is a need for a comprehensive, synergistic education system to ensure efficient public health across the country. This scoping review, therefore, aims to examine the characteristics of public health education programs available in India's varied geographical and regional contexts. It examines 16 program-related descriptors across public health Doctoral, Masters, Bachelors, Post-graduate Diploma, and Diploma education programs offered. Data was retrieved through institutional websites. Results of our analysis showed 84 unique institutions in 20 states and 3 UTs currently offering 116 public health programs across India's 28 states and 8 UTs. Private and public institutes were 65% ( n = 75) and 35% ( n = 41) respectfully. The majority of universities mainly provided Masters of Public Health ( n = 73, 63%) programs followed by Postgraduate Diploma (PGD) and Diploma ( n = 17, 15%), BPHSc ( n = 14, 12%), and Ph.D. ( n = 12, 10%). The majority of Ph.D. programs in public health are offered in Maharashtra, Karnataka, and Haryana, while Masters in Public Health programs are offered highest in Karnataka, Bachelors in Public Health programs in Rajasthan, Post Graduate Diploma in Public Health program in Delhi, and Tamil Nadu had the most number of Diploma in Public Health programs. Thirty-one percent ( n = 36) of the public health programs are offered across the south, 28% ( n = 32) across the north, and 22% ( n = 26) across the west Analyzed descriptors provide comprehensive information on program characteristics, mainly admission, format, and tuition fee. The review offers five suggestions to improve collaborative public health education and prepare a workforce with the skills, knowledge, and expertise to respond to the twentyfirst century's public health threats and challenges in India.
Introduction
The COVID-19 pandemic continues to be a major public health problem globally. The public health workforce has been undermined by decades of underinvestment. State and local health departments across countries have failed to attract, recruit and retain skilled health professionals required to respond to health threats due to inadequate funding. Lagging skills among workers due to changing technology, lack of systems and data to assess the existing gaps for the required workforce, and various hiring barriers that exist at federal, state, and local levels have resulted in several challenges affecting workforce development. There is a need for pro-activeness in planning for tomorrow's workforce through today's actions. Of the various lessons taught by COVID-19, the need for investment in a robust public health workforce has come up strongly ( 1 ).
One of the six building blocks of the World Health Organization (WHO's) framework for health is a strong health workforce. There is a need for health professionals with sound technical knowledge ( 2 ).
The current pandemic has its own novelty and scope which has exposed a gap in the competency and the surge capacity of the public health workforce ( 3 ). The COVID-19 pandemic has brought the public health workforce in limelight. A significant shift was observed in the years prior to the pandemic across various specializations of the public health workforce. The pandemic has increased the calling for epidemiologists and statisticians to play a leading role in COVID-19 response ( 4 ). There is a need for capacity building and identifying gaps in academic programs and the requirements of employers. An adequately trained workforce protects and promotes health, advocates for disparities, and responds rapidly to various health challenges ( 5 ).
India with a 1.3 billion population, is second-largest in the world and spread over 3,287,259 km 2 making it the seventh-largest country in the world. The population is approximately one-sixth of the world's population ( 6 , 7 ). In India, understaffed health systems, inadequate distribution of qualified workers, workforce shortages, and undersubscribed training programs along with an inadequate number of workforce and workers with a limited appropriate mix of skills have always been a challenge in solving complex health system challenges ( 8 ). Many nationwide programs to control or eliminate diseases have been established in the country. Public health in India is growing at a relatively slow rate. Adequate public health workforce training with the required skills to address complex public health challenges is the need of the hour, however, insufficient national standards for public health education, including curriculum and methods have resulted in a limited public health workforce ( 9 ). This situation results in ill-equipped public health workers with insufficient competencies, not online in the medical and nursing disciplines, but also among public health engineers, veterinarians specializing in public health, social scientists working in public health, statisticians working with public health-related databases, health workers and ground-level workers such as Accredited Social Health Activists (ASHAs), who are responsible for health promotion, health education, and other key responsibilities ( 10 ).
India's health care delivery system faces multiple shortages in the backdrop of poor health indicators across the country. The existing workforces that do not have requisite training are loaded with managerial functions. This needs to be replaced by a professional public health managerial cadre to ensure a safe, effective, and accountable health system. The extent to which public health can be enhanced is mainly determined by the quality of the public health workforce, which is determined by the relevance and quality of its training and educational opportunities ( 10 ). The availability of multidisciplinary public health professionals would enhance the equity and efficiency of healthcare delivery and would also relieve the burden on clinical professionals to cope with managerial functions. There are extremely few public health institutes in India, and national requirements for public health education are inadequate This situation results in ill-equipped public health workers with inadequate competencies, not only from the nursing and medical disciplines, but also from public health engineers, veterinarians specializing in public health, social scientists employed in community health, data analysts working with public health related database systems, health workers and ground level workers such as Accredited Social Health Activists (ASHAs), who are responsible for health promotion, health education, and many other responsibilities ( 10 ). The High-Level Expert Group, (HLEG) emphasized the need for the establishment of public health institutes across India ( 11 ). The National Health Policy 2017 envisages the creation of a Public Health management cadre in all states. The learning from the COVID-19 pandemic highlighted the need for a robust Public Health cadre. The surveillance and expert committee were held in 2020 wherein members participated and endorsed the creation of the Public Health Management cadre.
At the state, district, and block levels, the health ministry has recommended four verticals: specialist cadre, public health cadre, health management cadre, and teaching cadre. This highlights the need for a comprehensive synergistic system to ensure efficient public health in India. The most important challenge is to develop a framework that facilitates such public health management cadre to be accepted into the system ( 12 ).
Recent studies have reviewed public programs such as Masters in public health, Bachelors in public health, and certificate and diploma courses across the country. The program format and offerings have changed over the years as institutes try to deliver programs of high quality. Seminal contributions have been made by recent literature in charting public programs across India. Health education developments, notably the establishment of departments of preventive and social medicine in medical schools and health electives in other courses such as social work, enhanced India's ability for studying health inequalities ( 13 ). As public health is multidisciplinary, the Medical colleges in India only include public health as part of curriculums but do not have independent departments ( 14 ). Several authors have recognized the growing public health sphere and the need to meet the qualitative demand ( 15 – 17 ). More recent examples of studies in the arena of public health education in India can be found in the works of public health faculties in India ( 17 – 19 ), however their methodological approaches vary. The studies discuss competencies and course curriculums and do not capture the geographical distribution across India.
There has been a rapid increase in the number of public health programs offered in India given the increased demand for the public health workforce. Several institutes offer public health programs but due to a lack of council for regulating the programs, there is limited information available about these programs. Analysis of the various public health programs in India will help understand the public health education landscape in India.The study's objectives are to examine the characteristics of public health programmes offered across India. The study will evaluate program-related descriptors such as mode of delivery, program duration, program fee, program content, internship opportunities, scholarship, and competencies that students acquire to prepare this workforce that has the skills, knowledge, and expertise to respond to the public health emerging threats and challenges of the twentyfirst century.
Methodology
Search methodology.
A search was conducted from August 2021 to November 2021 using the “Google search engine”. The keywords used for the search are as follows; “Public health education” AND, “public health training,” OR “BPH in India,” OR “Bachelors in Public health programs in India,” OR “MPH in India,” “Masters in Public health in India,” OR “Ph.D. in public health in India,” OR “Diploma in Public health in India” OR “Postgraduate diploma in public health in India,” AND/OR “public health universities and institutes.” The search results showed the website links of the institutes offering the courses and various third-party websites and, career counseling websites showing a listing of respective programs offered. The first 20 result pages were adapted in our study. The listing of institutes and programs was done by referring to these websites. A centralized database of public health programs was developed, and duplicates were removed and filtered through a criteria ( Appendix 1 ). The inclusion criteria included only those public health programs to be included in the analysis that was offered by a recognized institute or a University. Third-party websites, links or proxy websites, and websites with missing and incomplete information were excluded. Institutes that no longer offered the program were excluded.
Variable extraction
Each program website was carefully studied to extract the variables of interest. These 16 variables have been listed and described in Table 1 .
Variable description.
| 1. | University name | Name of the university offering the public health training program. |
| 2. | Institute name | Name of the institute offering the program. |
| 3 | State/Union territory | The State/Union territory in which the Institute/University offering the public health program is located. |
| 4. | City | The city in which the Institute/University offering the public health program is located. |
| 5. | Institute type | Institutes offering public health programs classified as Public or Private institutes. |
| 6. | Official website | The official website of the public health program being offered by the Institute/University. |
| 7. | Programs offered | The information was recorded on the various public health programs offered by the Institute/University. |
| 8. | Program fees or tuition | Total fees for the various public health programs offered by the institute/University. |
| 10. | Eligibility criteria | Prerequisites for the various public health programs recorded. |
| 11. | Admission procedure | The process of admission and whether the candidate needs to appear for an exam, interview, or group discussion. |
| 12. | Mode of delivery of the program | Whether the program is conducted online, on-campus, in hybrid mode, full-time, or part-time. |
| 13. | Internship requirement | Whether there is an internship requirement for completion of the program and its tenure is mentioned. |
| 14 | Specializations | Whether there are any specializations offered. |
| 15 | Fees | Averages fees per semester/year as provided. |
| 16 | Course duration | Period of offering the course in years. |
Overview of public health programs across Indian states and UTs
Out of all the 28 states and 8 UTs of India, 84 unique universities in 20 states and 3 UTs are providing 116 Public health programs ( Figure 1 ; Table 2 ). The majority of universities mainly provided Masters of Public Health ( n = 73, 63%) programs followed by Postgraduate Diploma (PGD) and Diploma ( n = 17, 15%), BPHSc ( n = 14, 12%), and Ph.D. ( n = 12, 10%). The eight states including Andhra Pradesh, Assam, Bihar, Goa, Manipur, Mizoram, Punjab, Tripura, and five UTs Andaman and Nicobar Island, Dadra and Nagar Haveli & Daman and Diu, Jammu and Kashmir, Lakshadweep, and Leh-Ladakh do not have any public health programs. States like Karnataka, Rajasthan, and Tamil Nadu offered most of the public health programs. Fifty percent of the doctoral programs are offered each by both the public ( n = 6) and private Universities ( n = 6). While in the case of master's in public health programs ( n = 73), the majority of them (74%; n = 54) are offered by the private institutes compared to 26% ( n = 19) that are offered by public institutes. In the case of bachelor's programs in public health ( n = 14), 78% ( n = 11) were offered by private universities compared to 21% ( n = 3) of them that were offered by public institutes. Eighty-six percent of the ( n = 12) postgraduate diploma program in public health is offered by public universities and only 14% ( n = 2) of the private universities offered postgraduate diploma in public health programs. Similarly, the diploma program ( N = 3) is only offered by one public university and two private universities.

Distribution of public health programs across different states in India.
List of unique institutes/universities offering public health programs across India ( n = 84).
| . | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Academy of scientific and innovative research | Northern | Delhi | Delhi | Private | No | Yes | No | No | No |
| AIPH University | Eastern | Odisha | Bhubaneshwar | Private | Yes | Yes | No | No | No |
| Amity University | Northern | Haryana/Uttar Pradesh | Gurugram/Noida | Private | Yes | Yes | No | No | No |
| Amrita Vishwa Vidyapeetham | Southern | Kerala | Cochin | Private | No | Yes | No | No | No |
| Government Medical University | Eastern | West Bengal | Kolkata | Public | No | No | No | Yes | No |
| Arunodaya university | North-Eastern | Arunachal Pradesh | Itanagar | Private | No | Yes | No | No | No |
| Chitkara University | Northern | Chandigarh | Chandigarh | Private | No | Yes | No | No | No |
| Apex University | Western | Rajasthan | Jaipur | Private | No | No | Yes | No | No |
| Christian Medical College (affiliated to Shree Chitra Tirunal Institute for Medical Sciences and Technology) | Southern | Tamil Nadu | Vellore | Private | No | Yes | No | No | No |
| Career Point University | Western | Rajasthan | Alaniya/Kota | Private | No | Yes | Yes | No | No |
| Datta Meghe Institute Of Medical Science | Western | Maharashtra | Wardha | Private | No | Yes | No | No | No |
| Post Graduate Institute of medical education and research | Northern | Chandigarh | Chandigarh | Public | No | No | No | Yes | No |
| DY Patil University | Western | Maharashtra | Pune | Private | No | Yes | No | No | No |
| Eternal University | Northern | Himachal Pradesh | Baru Sahib/Sirmaur | Private | Yes | Yes | No | No | No |
| G D Goenka University | Northern | Haryana | Gurugram | Private | No | Yes | No | No | No |
| Galgotias University | Northern | Uttar Pradesh | Greater Noida | Private | No | Yes | No | No | No |
| Gurugram University | Northern | Haryana | Gurugram | Private | No | Yes | No | No | No |
| Himalyan Garhwal University | Northern | Uttarakhand | Garhwal | Private | No | Yes | No | No | No |
| Indian School of Business Management And Administration | Southern | TamilNadu | Chennai | Private | No | Yes | No | No | No |
| Johns Hopkins University | Western | Rajasthan | Jaipur | Private | No | Yes | No | No | No |
| JSS University | Southern | Karnataka | Mysore | Private | No | Yes | No | No | No |
| Kaloji Narayana Rao University of Health Sciences, Warangal | Southern | Telangana | Hyderabad | Private | No | Yes | No | No | No |
| Post graduate institute of medical sciences | Northern | Punjab/Haryana | Chandigarh | Public | Yes | No | No | No | No |
| Institute of Public Health | Southern | Karnataka | Bengaluru | Private | Yes | No | No | No | No |
| Krishna Institute of Medical Sciences | Central | Madhya Pradesh | Chhatarpur | Private | No | Yes | No | No | No |
| Manipal University | Southern | Karnataka | Mangalore | Private | No | Yes | No | No | No |
| Maulana Abul Kalam Azad University of Technology, West Bengal | Eastern | West Bengal | Kolkata/Haldia | Private | No | Yes | No | No | No |
| MIT World Peace University | Western | Maharashtra | Pune | Private | No | Yes | No | No | No |
| NITTE Education Trust | Southern | Karnataka | Mangalore | Private | No | Yes | No | No | No |
| NM (University partners) | Not mentioned | Multiple locations | Multiple locations | Private | No | Yes | No | No | No |
| Noida International University | Northern | Uttar Pradesh | Gautam Buddha Nagar | Private | No | Yes | No | No | No |
| SRM Institute of Science and Technology | Southern | Tamil Nadu | Chennai | Private | Yes | No | Yes | No | No |
| Indira Gandhi open university | Northern | Delhi | Delhi | Public | No | No | No | Yes | No |
| North East Frontier Technical University | North-Eastern | Arunachal Pradesh | Aalo | Private | No | Yes | No | No | No |
| NSHM College Of Management And Technology, Kolkata | Eastern | West Bengal | Kolkata | Private | No | Yes | No | No | No |
| Pavara institute of medical science | Western | Maharashtra | Ahmednagar | Private | No | Yes | No | No | No |
| Poornima University | Western | Rajasthan | Vidhani | Private | No | Yes | No | No | No |
| Om Sterling Global University | Northern | Haryana | Hisar | Private | No | Yes | Yes | No | No |
| Parul University | Western | Gujarat | Vadodara | Private | No | Yes | Yes | No | No |
| Poornima University School of Public Health | Western | Rajasthan | Jaipur | Private | No | Yes | Yes | No | No |
| Rajiv Gandhi University Of Health Sciences | Southern | Karnataka | Bangalore | Private | No | Yes | Yes | No | No |
| Ramaiah University | Southern | Karnataka | Banglore | Private | No | Yes | No | No | No |
| Sai Business And Media School, Sai Group Of Institutions | Northern | Uttarakhand | Dehradun | Private | No | Yes | No | No | No |
| SGT University | Northern | Haryana | Gurugram | Private | No | Yes | No | No | No |
| SRM University | North-Eastern | Sikkim/Tamil Nadu | Gangtok/Kattankalathur | Private | No | Yes | No | No | No |
| Lachoo Memorial College of Science and Technology | Western | Rajasthan | Jodhpur | Private | No | No | Yes | No | No |
| Sushant University | Northern | Haryana | Gurugram | Private | No | Yes | No | No | No |
| Symbiosis University | Western | Maharashtra | Pune | Private | No | Yes | No | No | No |
| Mahatma Jyoti Rao Phoole University | Western | Rajasthan | Jaipur | Private | No | No | Yes | No | No |
| Ministry of health and family welfare | Northern | Delhi | Delhi | Public | No | No | No | Yes | No |
| Indian Institute of skill development | Not mentioned | Not mentioned | Not mentioned | Public | No | No | No | Yes | No |
| Martin Luther Christian University | North-Eastern | Meghalaya | Shillong | Private | No | No | Yes | No | No |
| Vocational Institution of Ministry of HRD, Government of India (AVI no-710367) and all the courses of IGMPI are approved for lifetime empanelment under Ministry of Horticulture and Food Processing, Government of Uttar Pradesh | Not mentioned | Not mentioned | Not mentioned | Public | No | No | No | Yes | No |
| The Global Open University | North-Eastern | Nagaland | Dimapur | Private | No | Yes | No | No | No |
| The Y.B. University | Eastern | Jharkhand | Ranchi | Private | No | Yes | No | No | No |
| University Of Technology | Western | Rajasthan | Jaipur | Private | No | Yes | No | No | No |
| Vinayaka Missions University | Southern | Tamil Nadu | Salem | Private | No | Yes | No | No | No |
| Yenepoya University | Southern | Karnataka | Mangalore | Private | No | Yes | Yes | No | No |
| All India Institute of Medical Sciences | Western/Northern/ Central | Rajasthan/ Uttarakhand/ Chattisgarh | Jodhpur/Rishikesh/ Raipur | Public | No | Yes | No | No | No |
| Central University Of Kerala | Southern | Kerala | Kasaragod | Public | No | Yes | No | No | No |
| Singhania University | Western | Rajasthan | Jhunjhunu | Public | No | No | Yes | Yes | No |
| Delhi Pharmaceuticals Sciences And Research University | Northern | Delhi | Delhi | Public | No | Yes | No | No | No |
| Guru Gobind Singh Indraprastha University | Northern | Delhi | Delhi | Public | No | Yes | No | No | No |
| James Lind Institute | Southern | Karnataka | Bengaluru | Private | No | No | No | Yes | No |
| Indian Council of Medical Research and NIE | Southern | TamilNadu | Chennai | Public | No | Yes | No | No | No |
| Jamia Hamdard University | Northern | Delhi | Delhi | Public | No | Yes | No | No | No |
| Jawahar Lal Nehru University | Northern | Delhi | New Delhi | Public | No | Yes | No | No | No |
| Jawaharlal Institute of Postgraduate Medical Education and Research | Southern | Pondicherry | Pondicherry | Public | No | Yes | No | No | No |
| KLE Academy of Higher Education and Research | Southern | Karnataka | Belagavi | Public | Yes | Yes | Yes | No | No |
| Kalinga Institute of Industrial Technology | Eastern | Odisha | Bhubaneshwar | Public | No | Yes | No | No | No |
| The Tamil Nadu Dr. M.G.R Medical University | Southern | Tamil Nadu | Not mentioned | Private | No | No | No | No | Yes |
| Karnataka State Rural Development And Panchayat Raj University | Southern | Karnataka | Bengaluru | Public | No | Yes | No | No | No |
| Kerala University of Health Sciences | Southern | Kerala | Kottayam/ Thiruvananthapuram | Public | No | Yes | No | No | No |
| NIMHANS | Southern | Karnataka | Bengaluru | Public | No | Yes | No | No | No |
| Sree Chitra Tirunal Institute for Medical Sciences and Technology | Southern | Kerala | Trivandrum | Public | Yes | Yes | No | No | Yes |
| Punjab University | Northern | Chandigarh | Chandigarh | Public | No | Yes | No | No | No |
| Sam Higginbottom University Of Agriculture, Technology And Sciences | Northern | Uttar Pradesh | Allahabad | Public | No | Yes | No | No | No |
| Tata Institute of Social Sciences | Western | Maharashtra | Mumbai | Private | Yes | Yes | No | No | No |
| Sri Ramchandra Institute Of Medical Sciences | Southern | Tamil Nadu | Chennai | Public | No | Yes | No | No | No |
| University Of Hyderabad | Southern | Telangana | Hyderabad | Public | No | Yes | No | No | No |
| University Of Lucknow | Northern | Uttar Pradesh | Lucknow | Public | No | Yes | No | No | No |
| West Bengal University of Health Sciences | Eastern | West Bengal | Kolkata | Public | No | Yes | No | Yes | Yes |
| Public health foundation of India | Western | Gujarat/Delhi | Gandhinagar/Delhi | Public | Yes | No | No | Yes | No |
| Savitribai Phule Pune University | Western | Maharashtra | Pune | Public | Yes | Yes | No | No | No |
Geographical distribution of public health programs
All Indian states and UTs were categorized into six regions including North East, East, West, South, Central, and North Regional coverage was calculated by dividing the overall number of public health programme offerings in each region by the total number of public health programme offerings in India. Thirty-one percent ( n = 36) of the public health programs are offered across the south, 28% ( n = 32) across the north, and 22% ( n = 26) across the west. The lowest number of public health program offerings were across the central and North East region of India ( Figure 2 ). Geographical coverage was calculated by dividing the total number of states offering public health programs in each region by the total number of states in that region.

Percentage distribution of all public health programs across different geographical areas and regions of India.
Madhya Pradesh in the Central, West Bengal in the East, Arunachal Pradesh in the North East, Karnataka in the South, Delhi in the North, and Rajasthan in the West were the states that offered most of the public health program offerings within their own regions ( Figure 3 ).

States offering most of the public health programs within their regions.
Geographical coverage of program types across states and UTs of India
Masters of Public Health programs were offered the most across all the regions of India ( Figure 4 ). The states of Karnataka (South) (12%) Maharashtra (West) (10%), and Harayana (North) (8%) contributed the highest percentage toward the master of public health programs. Karnataka (17%) and Maharashtra (17%) also offered the highest percentage of doctoral programs in public health. Rajasthan (43%) and Karnataka (29%) offered the most bachelors in public health programs while the post-graduate diploma and diploma programs in public health were offered the highest across the states of Delhi (24%), Odisha (18%), West Bengal (12%) and Tamil Nadu (12%) ( Figure 5 ).

Distribution of public health programs across different regions in India.

A comparison of all the different types of public health programs across different States/UTs in India.
Analysis by programs
Doctorate in philosophy in public health (ph.d.), regional distribution.
Nearly twelve universities are providing Ph.D. programs in public health across India. The doctoral programs are offered mostly in the Southern (33%; n = 4) and Northern states (33%; n = 4) of India ( Figure 5 ). Seventeen percent ( n = 2) of the programs were been offered in the state of Maharashtra, Haryana, and Karnataka ( Table 3 ).
Ph.D. programs in public health in different states/UTs in India ( N = 12).
| Mode of delivery | Full-time and Part-time | 5 (42) |
| Full time | 3 (25) | |
| Not mentioned | 4 (33) | |
| Type | Private | 6 (50) |
| Public | 6 (50) | |
| Odisha | AIPH University | 1 (8) |
| Maharashtra | Savitribai Phule Pune University | 1 (8) |
| Tata Institute of Social Sciences | 1 (8) | |
| Karnataka | Institute of Public Health | 1 (8) |
| KLE Academy of Higher Education and Research | 1 (8) | |
| Uttar Pradesh | Amity University | 1 (8) |
| Haryana | Amity University | 1 (8) |
| Post Graduate Institute of medical sciences | 1 (8) | |
| Tamil Nadu | SRM Institute of Science and Technology | 1 (8) |
| Kerala | Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum | 1 (8) |
| Himachal Pradesh | Eternal University | 1 (8) |
| Gujarat | Public health foundation of India | 1 (8) |
A.1 Total number of programs
Forty-two percent ( n = 5) of the doctoral programs in public health are offered both part-time and full-time while 25% ( n = 3) of them were offered only full-time. Thirty-three percent ( n = 4) of the doctoral programs did not mention the modality of offering. Fifty percent ( n = 6) of the doctoral programs in public health were offered by both public as well as private institutes.
A.2 Program fees
Of the 12 universities offering a doctoral program in public health, only half of them mentioned the fees details (50%; n = 6). Among the universities where the information was available, the average fee for each semester of the doctoral program is nearly INR 44,889 (Range: INR 14,833–INR 81,000), for the private universities the average fee is nearly INR 55,750 (Range: INR 42,000–INR 81,000) and whereas for the public universities the average fees are nearly INR 23,167 (Range: INR 14,833–INR 31,500).
A.3 Program format
Among the 12 universities, four are offering doctoral programs in public health in the fields of Biostatistics, Epidemiology, Health system research, Health promotion, health behavior, Global health, Migration, Urbanization, Public health, and health economics.
A.4 Program admission
Only two universities ( n = 2, 17%) have mentioned the frequency of seat intake for doctoral programs in public health. Forty-two percent ( n = 5) of the universities required for those applying from non-health backgrounds a minimum of 2–5 years of post-graduation work experience while those with a health background were required to have field experience, and prior experience in research, and teaching. Only two universities ( n = 2, 17%) required publications as an essential criterion for admission to the doctoral program in public health. Fifty-eight percent of universities had an admission test ( n = 7, 58%), 17% interview ( n = 2, 17%), and 25% included both an admission test and an interview ( n = 3, 25%) to be the criteria for admission. Eighty-three percent ( n = 10) of the universities had a master's or equivalent degree awarded by an accredited university in India or abroad as the minimum academic qualification criteria for admission to the Ph.D. programs.
A.5 Additional details
None of the 12 universities presented any details on the website regarding course competencies the students will acquire. Four of the 12 universities offering doctoral programs in public health provided information related to the course curriculum indicating them to be designed as per the UGC choice-based credit system. However, only one out of these four universities shared a semester-wise Ph.D. program curriculum along with desired field/practical work. Only one university offers a fellowship for the Ph.D. program ( Table 3 ).
Master's in public health (MPH)
The majority of the master's in public health programs are offered in the southern region ( n = 23, 32%) followed by nothern ( n = 22, 30%), western ( n = 14, 19%), eastern ( n = 7, 10%), north-eastern ( n = 4, 6%) and central region ( n = 2, 3%). The geographical distribution of universities offering master's programs in public health highlights that in Karnataka ( n = 9, 12%), Maharashtra ( n = 7, 10%), and Tamil Nadu ( n = 6, 8%) ( Table 4 ).
MPH programs delivered by the different states/UTs of India ( N = 73).
| Course duration (in years) | >2 years | 2 (3) |
| 2 years | 71 (97) | |
| Type of universities | Public | 19 (26) |
| Private | 54 (74) | |
| States | Arunachal Pradesh | 2 (3) |
| Chhattisgarh | 1 (1) | |
| Haryana | 6 (8) | |
| Gujarat | 2 (3) | |
| Uttar Pradesh | 5 (7) | |
| Himachal Pradesh | 1 (1) | |
| Jharkhand | 1 (1) | |
| Karnataka | 9 (12) | |
| Kerala | 5 (7) | |
| Maharashtra | 7 (10) | |
| Madhya Pradesh | 1 (1) | |
| Nagaland | 1 (1) | |
| Odisha | 2 (3) | |
| Rajasthan | 5 (7) | |
| Sikkim | 1 (1) | |
| Tamil Nadu | 6 (8) | |
| Telangana | 2 (3) | |
| Uttarakhand | 3 (4) | |
| West Bengal | 4 (6) | |
| Union territories | Universities | |
| Chandigarh | 2 (3) | |
| Delhi | 5 (7) | |
| Pondicherry | 1 (1) |
B.1 Total number of programs
Of the 73 universities providing Master's programs in public health across India, 95% ( n = 69, 95%) offered the program on campus. Nearly, Two-third ( n = 54, 74%) of the public health programs were offered by private universities ( Table 4 ).
B.2 Program fees
More than half of the programs (58%, n = 42) mentioned the program fee details on their website. Among the universities where the information was available, the average fee for the complete MPH program offered was INR 2,21,993 (Range: INR 5,865–INR 17,07,376). The average program fee for the private institute was INR 2,70,039 (Range: INR 34,150–INR17,07,376) and INR 1,08,233 (Range: INR 5,865–INR 2,50,000) for public universities.
B.3 Program format
More than half of the universities ( n = 62, 85%) provided no information regarding specializations in public health. Only 15 percent of the programs listed ( n = 11, 15%) mentioned their specializations ranging from the field of Epidemiology, Health Economics and Outcomes Research, Health Care Quality and Safety.
Admission requirements
Less than half of the institutes (38%, n = 28) mentioned seat intake for the masters in public health programs. Eighty-nine percent ( n = 65) of the institutes offering Masters in public health programs required preferably a bachelor's degree with 50% marks in any discipline such as MBBS, BDS, AYUSH, B.Sc. Nursing, B. Pharma, BPT, BPH, B.Sc. Micro, B.Sc. Lab Tech (Med), B.Sc. For admission to the master's in public health degree, 15% of the universities ( n = 11) required at least 1 year of work experience. Less than half of the institutions (42%, n = 31) required students to complete an internship as a course completion criterion. Twenty-five percent ( n = 18) of colleges needed a written exam as part of the admissions process, 19% ( n = 14) required interviews, and 14% ( n = 10) required a combination of entrance test and interview.
Additional details
The course curriculum was presented on the institute website in 48% ( n = 35) of the cases while <10% ( n = 6) of universities provided details on the course competencies. The scholarship is offered by nine universities ( n = 9, 12%) ( Table 4 ).
Bachelors in public health sciences (BPHSc)
Fourteen universities offering BPHSc programs, most of them are offered in the western region ( n = 7, 50%) followed by the southern region (36% n = 5) ( Table 5 ).
Frequency of universities providing BPHSc in different states of India ( N = 14).
| Course duration (in years) | 3 years | 8 (57) |
| Between 3 and 4 years | 1 (7) | |
| 4 years | 4 (29) | |
| Not mentioned | 1 (7) | |
| Course category | BPH | 10 (71) |
| BSc | 4 (29) | |
| Type of universities | Public | 3 (21) |
| Private | 11 (79) | |
| Karnataka | Yenepoya University | 1 (7) |
| Rajiv Gandhi University of Health Sciences recognized by Govt. of Karnataka | 2 (14) | |
| KLE Academy of Higher Education and Research | 1 (7) | |
| Tamil Nadu | SRM Institute of Science and Technology | 1 (7) |
| Gujarat | Parul University | 1 (7) |
| Rajasthan | Apex University | 1 (7) |
| Mahatma Jyoti Rao Phoole University | 1 (7) | |
| Lachoo Memorial College of Science and Technology | 1 (7) | |
| Career Point University | 1 (7) | |
| Poornima University School of Public Health | 1 (7) | |
| Singhania University | 1 (7) | |
| Meghalaya | Martin Luther Christian University | 1 (7) |
| Haryana | Om Sterling Global University | 1 (7) |
C.1 Total number of programs
The majority of the bachelor's in public health programs were offered in Rajasthan (43%; n = 6) followed by Karnataka (29%, n = 4). More than half of these programs (79%, n = 11) were offered by private universities. The BPHSc course duration varied from 3 to 4 years. More than fifty percent of universities provided a complete course for 3 years (57%, n = 8) followed by 4 years (29%, n = 4) ( Table 4 ). More than half of the programs are offered as Bachelor in Public Health (BPH) (71%, n = 10) while the remaining 29% ( n = 4) of the programs are offered as BSc in Public Health.
C.2 Program fees
The average fee for a complete BPHSc program is around 1,56,000 (Range: INR 81,000–INR 2,40,000). The average fee of the BPHSc program for the public universities is INR 1,50,000 (Range: INR 0–INR 1,50,000) compared to private universities which is INR 1,57,000 (Range: INR 81,000–INR 2,40,000).
C.3 Program format
Almost all the BPHSc programs have been offered in a general format with no specializations and field of the study mentioned.
C.4 Program admission
Among all the 14 universities, 10 of them were admitted based on academic merit ( n = 10, 71%). All the universities required educational qualification of higher secondary level or pre-university college in any stream, preferably science with physics, chemistry, and biology as main subjects as a minimum academic qualification for admission to the BPHSc programs. Fourteen percent of universities ( n = 2) included interviews as one of the criterias for admission while 7% ( n = 1) involved both an admission test and an interview for consideration of admission to the program.
C.5 Additional details
Fourteen percent ( n = 2) of the universities provided details on course competencies while 35% ( n = 5) of them provided information on course curriculum. Only one institute provided some form of scholarship ( Table 5 ).
Postgraduate diploma in public health (PGDPh)
The majority of the post-graduate diploma in public health programs are offered by universities in the western region ( n = 2, 40%) followed by the southern region ( n = 2, 29%).
D.1 Total number of programs
Of the 14 universities in different States/UTs of India, 29% ( n = 4) of the universities in Delhi provide PGDPh programs followed by in eastern region Odisha and West Bengal ( n = 2, 14%) each, and other states (Gujarat; Telangana; Madhya Pradesh; Chandigarh; Rajasthan, and Karnataka) offering one PGD program ( n = 1, 7%) each. Among all universities offering PGD, ( n = 2, 14%) were private and ( n = 12, 86%) were public. Among the 12 public universities, ( n = 7, 58%) provided courses as regular on-campus programs and ( n = 4, 33%) in online mode whereas ( n = 1, 8%) provided the course education in hybrid mode, that is, both online and on-campus. However, the two private universities run the course in off-campus ( n = 1, 50%) and online ( n = 1, 50%) mode, respectively ( Table 6 ).
Frequency of PGD programs provided by universities in the different states ( N = 14).
| Mode of delivery | On-campus | 7 (50) |
| Online | 5 (36) | |
| Hybrid (On campus/Online/Distance) | 1 (7) | |
| Off-campus | 1 (7) | |
| Type of universities | Public (On-campus/Online/Hybrid) | 12 (86) |
| Private | 2 (14) | |
| Odisha | Public health foundation of India | 2 (14) |
| Gujarat | Public health foundation of India | 1 (7) |
| Telangana | Public health foundation of India | 1 (7) |
| West Bengal | West Bengal University of health sciences | 1 (7) |
| Government medical university | 1 (7) | |
| Madhya Pradesh | Indian Institute of skill development | 1 (7) |
| Rajasthan | Singhania University | 1 (7) |
| Karnataka | James Lind Institute | 1 (7) |
| Delhi | Public health foundation of India | 1 (7) |
| Vocational Institution of Ministry of HRD, Government of India | 1(7) | |
| Ministry of health and family welfare | 1 (7) | |
| Indira Gandhi open university | 1 (7) | |
| Chandigarh | Post Graduate Institute of medical education and research | 1 (7) |
D.2 Program fees
The average fee for a complete PGDPh program offered by both private and public universities in different states is around one lakh (INR 1,02,240) (Range: INR 3,620–INR 2,75,000). For private universities, the average fee for a complete PGDPh program is around INR 32,750 (Range: INR 27,000–INR 38,500) and for public universities, the complete fee of the PGDPh program is nearly INR 1,07,551 (Range: INR 3,620–INR 2,75,000).
D.3 Program format
All of the PGD Ph programs are provided in a general format with no details on specializations and fields of study.
D.4 Program admission
Only 14% ( n = 2) of the universities mentioned the frequency of admission intake. The minimum eligibility criteria required for admission to the PGDPh programs is to graduate in any discipline preferably MBBS, BDS, AYUSH, allied sciences, nursing, health science, natural science, or post-graduation in Social Sciences or an equivalent qualification. Additional qualifications include candidates who were working with the central, state, or local governments with at least 3 years of experience in the health sector, nursing staff, municipal corporation officers, and other professionals in health-related. More than half of the universities (86%; n = 12) offered admissions based on academic merit, entrance tests, interview performance, or both. Fifty-seven percent ( n = 8) of the universities require at least 1 year of work experience.
D.5 Additional details
Of the 14 universities, 21% ( n = 3) shared details on program competencies, while 36% ( n = 5) mentioned the course curriculum ( Table 6 ).
Diploma programs
Two out of the three diploma programs are offered in the Southern part of India while one program is offered in the eastern region ( Table 7 ).
Frequency of diploma programs provided by universities in the different states ( N = 3).
| Type of universities | Public (On campus/Online/Hybrid) | 1 (33) |
| Private | 2 (67) | |
| Tamil Nadu | The Tamil Nadu Dr. M.G.R Medical University | 1 (33) |
| Kerala | Sree Chitra Tirunal Institute of Medical Sciences and Technologies | 1 (33) |
| West Bengal | West Bengal University of Health Sciences | 1 (33) |
Each diploma program is offered in the states of Tamil Nadu, Kerala, and West Bengal. Among all the three universities offering a Diploma in Public Health, two of the private universities are present in the state of Tamil Nadu and Kerala whereas the public university is in the state of West Bengal ( Table 7 ).
E.2 Program fees
No fees were mentioned for any of the Diploma programs offered by either private or public universities.
E.3 Program format
Two out of the three programs listed on their website the duration of the diploma program in public health.
E.4 Program admission
None of the universities mentioned the frequency of seat intake in the diploma program. Different universities require different levels of prior work experience. e.g., the university in Kerala required at least 3 years of work experience for in-service candidates, and the university in West Bengal requires 1 year of continuous rotational internship training in any Medical College. Candidates' admission to one of the diploma programs offered by a University in West Bengal is based not only on academic merit but also on the entrance test conducted by the central or state government (if any) and the performance of the candidate in the interview.
E.5 Additional details
None of the Universities provided any information related to program competencies, course curriculum, or scholarships ( Table 7 ).
Results of our analysis showed that the majority of Ph.D. programs in Public Health are offered in the states of Maharashtra, Karnataka, and Haryana while Masters in Public Health programs are offered highest in Karnataka, Bachelors in Public Health programs highest in Rajasthan, Post Graduate Diploma in Public Health program is highest in Delhi, and Diploma in Public Health program highest in the state of Tamil Nadu ( Table 2 ).
The current study presents an overview of the various public health program offerings across various states and UTs of India. From the recent available literature, the unique institutes offering public health programs have increased from 59 institutes ( 8 ) to 84 unique institutes. Institutes offering Masters in Public Health have increased from 44 institutes in the years 2017 and 2018 ( 15 ) to 73 institutes according to our study in the year 2022.
Key findings of our study are: Of the 28 states and 8 UTs of India, 20 states and 3 UTs offered a public health-related program, the geographical concentration was highest in the southern states ( n = 36, 31%) followed by the northern ( n = 32, 28%) western ( n = 26, 22%), eastern ( n = 13, 11%), north-eastern ( n = 5, 4%) and lastly, central regions of India ( n = 3, 3%). Course competencies for Ph.D. and diploma programs are not mentioned by the universities, however, competencies were mentioned by one university offering a bachelor's program and 3 universities offering postgraduate programs. Of the programs studied, 35, 48, and 36% of institutes of doctoral, masters, and post-graduate programs respectively mentioned their course curriculum, other programs did not disclose their detailed curriculum. Few programs stated that their curriculum is as per the UGC choice-based credit system. Findings of our study show a lack of curriculum competencies as well as the mention of core concentration and cross-cutting fields on the website of the institutes ( 20 , 21 ). A study by Miller et al.; reviewed the landscape of public health training and conducted a qualitative SWOT analysis among selected institutions. The study identified collaborations, lack of career pathways, and incentives as weaknesses and the strengths to be the tuition, innovation, and the available infrastructure for research ( 8 ). This finding correlates with our analyses, where program fees are kept affordable for quality education, this can be an advantage to increase student enrolment in public health programs. However, only 12% of MPH institutes and 7% of BPHSc institutes offered scholarships, this dearth of provision of scholarships and lack of public-private partnership is also reported among public health colleges across the globe as reviewed by Effa et al. ( 22 ) and Indian public health education by Scheiff et al. ( 23 ).
Findings of this review suggest (1) the need for additional public health incentive programs to be implemented to encourage public health workers to join local and state governments. (2) The requirement for well-trained public health workers should correspond to the new paradigm of place-led, which is at the heart of economic development strategy. (3) Aspirants in public health must be skilled in twentyfirst-century skills such as communication, informatics, leadership, policy, governance, and effective design and development of public health interventions. (4) To improve access to learning, public health initiatives should be equitably distributed throughout the country. The absence of educational facilities in certain regions can be attributed to per capita income. A good example from our analysis is the North Eastern, Eastern, and Central regions of India that have a low concentration of public health programs and notably nill doctorate programs; interestingly these states are reported to have the lowest per capita income and poor health indicators. There is a high disparity in health outcomes at regional and state levels. The backward states continue to have a high disease and mortality indices ( 24 ). (5) Aside from course-based curriculums, students should engage in experiential learning through internships, training, or research exposure to enhance their skills post their education.
The present review has the following limitations: Each program website was carefully searched for the enlisted variables. Owing to the differences in website content and lack of search engine optimization certain institute websites were not displayed in the results. The differences in content and format of the programs on respective websites resulted in some variables were not captured. The information gathered was unstructured on the official website pages, some information was found on the program page, some in a brochure, and some on the admissions page. On account of the dynamic nature of websites and updates in the content periodically there might be a difference in values extracted from August 2021 to November 2021 to date. The main drawback is the lack of a central counsel or regulating board for public health programs in India, there is no comprehensive data on all the institutes that offer public health courses in India.
The COVID-19 epidemic taught us the importance of an autonomous emergency system staffed by trained public health workers. While the past 2 years have profoundly raised public awareness of health, it has challenged the State, local and academic departments to substantially increase their capacity and contribute to the health workforce. To enable future preparedness, institutes across the country are to promptly work on capacity building for a future workforce that includes public health graduates ( 25 ).
The present review concurs with the view that public health education in India must now enhance health system performance by adapting core professional competencies to varied settings, which need to be revisited to deliver high-quality comprehensive public health services that are vital to improving population health equity ( 10 ). Our recommendations based on our observations are that the public health programs from universities and institutions can provide concise and clear information on student outcomes such as graduation rates, employment, career and placement opportunities, current alumni record, their roles, functions, and skills, and most importantly use of competencies gained in the field. With the increase in demand of job market coupled with the recent emphasis on public health cadre in states of India, career and placement services need to be a focus in public health program features. Additional information on the fee structure of different programs and on the salary structure of graduating students should be stated.
The recent proposal by the government of India's Ministry of Health and Family Welfare (MoHFW) aimed to create a cadre across all states under the 2017 National Health Policy, this elucidates the urgent need to strengthen public health care delivery across India. To fulfill this, the workforce pool should be generated from institutes or universities having standardized programs with efficient curricula that equip them with necessary competencies. The public health programs across institutes have varied discrepancies in their deliverance and hence a synergistic effort across institutes can complement each other and equip the public health professional workforce in India.
Author contributions
AJ and AG contributed to the conception and design of the study. MG collected and prepared the database. AJ, AB, and IVM performed the statistical analysis and interpretation. AJ, AB, and SSR prepared the draft of the manuscript. All authors were involved in manuscript revision and have approved the final version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.970617/full#supplementary-material
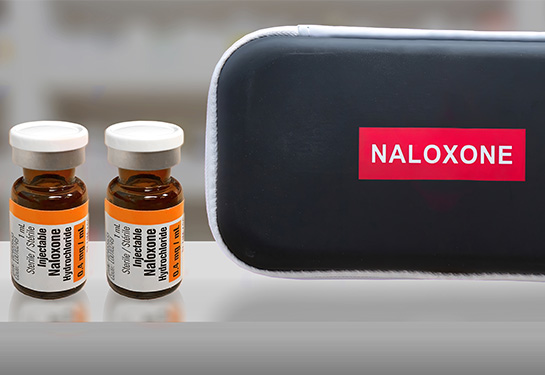
Can naloxone improve survival rates of patients with cardiac arrest?
Uc davis health study identifies link between naloxone administration and outcomes of certain cardiac arrests..
Patients who overdose on opioids and have a pulse are often given naloxone (Narcan) by first responders, a common life-saving measure.
However, emergency medical service (EMS) agencies have different protocols for administering naloxone, so there is little evidence to support its use in patients without a pulse who experienced opioid-associated out of hospital cardiac arrest (OHCA).
A recent study by UC Davis Health researchers set out to assess the effects of giving naloxone administration by paramedics to patients with OHCA.
The study, published in Jama Open Network , concluded there was an association between naloxone administration, and both return of spontaneous circulation and survival to hospital discharge.
“The incidence of drug-related cardiac arrests has skyrocketed in the past two decades, and there is an urgent need for evidence to guide possible naloxone use in this circumstance,” said David Dillon , assistant professor of Emergency Medicine and one of the study’s authors.
The incidence of drug-related cardiac arrests has skyrocketed in the past two decades, and there is an urgent need for evidence to guide possible naloxone use in this circumstance.” — David Dillon
What is naloxone?
Naloxone is a medicine that rapidly reverses an opioid overdose. It is an antagonist — meaning it attaches to opioid receptors and reverses and blocks the effects of other opioids. Naloxone can quickly restore normal breathing to a person whose breathing has slowed or stopped because of an opioid overdose. Researchers hypothesize that naloxone may also help patients who are experiencing opioid-related cardiac arrest.
Naloxone has no effect on someone who does not have opioids in their system, nor does it harm them, and it is not a treatment for opioid use disorder.
Opioid-associated cardiac arrests
Cardiac arrest occurs when the heart suddenly stops beating. Roughly 350,000 cardiac arrests occur outside the hospital each year, according to the American Heart Association . The majority of these are due to heart attacks or electrical issues with the heart, but opioid overdose-related cardiac arrests are a major cause of death for adults 25 to 64 years old.
Recent studies estimate 17.6% of all OHCA, and 34% of OHCA in those under 60 years of age, are the result of opioid toxicity.
Study results
For this retrospective study, researchers collected data from San Francisco, Sacramento and Yolo county EMS agencies between 2015-2023. In total, 8,195 patients with OHCA were treated by the three agencies.
The results showed EMS administration of naloxone was associated with significantly improved outcomes. The number needed to treat with naloxone, which represents the number of patients that need to be given naloxone to observe one additional positive outcome, was nine patients for return of spontaneous circulation and 26 patients who survived and were discharged from the hospital.
“Surprisingly, our findings showed that naloxone was associated with improved clinical outcomes in both drug-related cardiac arrests and non-drug related cardiac arrests,” explained Dillon. “This is important because it adds to our understanding about the effectiveness of naloxone for drug related out of hospital cardiac arrest.”
The researchers noted that these finding warrant further investigation, given the growing opioid epidemic in the United States and the potential benefits of naloxone as part of cardiac arrest care.
Related stories:
- Why you should carry naloxone (Narcan) to combat opioid overdoses
- Naloxone and Opioid Overdose
- Can fentanyl be absorbed through your skin?
Explore related topics

UC Davis Health emergency department receives prestigious Lantern Award

UC Davis Health and the Department of Defense create prototype for temporary surge facility

Research findings could help children reduce exposure to radiation after cervical spine injury
Connect with us.

IMAGES
VIDEO
COMMENTS
Comparing training of public health officers in the US to India. Unique Research Topics In Public Health. Surrogacy: A review of associated ethical issues. Prevalence of medical errors in hospitals: A review of the policies used to prevent the problem in the United States. Blood transfusion: What are the side effects?
Indian states are in different phases of epidemiological transition, resulting in large variations in disease burden across the states.1 However, the public health priorities across the country remain similar. Addressing the availability of relevant and robust data for meaningful planning of programmes and policies is a gap that needs urgent consideration to improve population health and the ...
The landscape of healthcare research in India has been significantly shaped by the endeavors of the Indian Council of Medical Research (ICMR). Established in 1911, the ICMR has played a pivotal role in advancing medical knowledge, informing health policies, and fostering collaborations to address pressing health challenges in the country.
The public health research situation in India is characteristic of the low priority to public health more generally. A recent review by Dandona et al. ( 8) observed that only 3.3% of the 4,876 health research studies published from India during 2002 were devoted to public health.
Vital statistics of Delhi 2023: The updates. The Annual Report on "Registration of Births and Deaths in N.C.T. of Delhi for the year 2023", released in August shows an increase in birth rate and death rate while a decrease in infant mortality rate, maternal mortality ratio and sex ratio from 2022 to 2023. Content Editor: Dr. Urmimala.
The Public Health Foundation of India and the Indian Institutes of Public Health disseminates its research findings through dissemination workshops, seminars, print and online media. The PHFI Online Knowledge Repository lists all the publications of PHFI, IIPHs, and Centers of Excellence. Publications such as articles in peer reviewed journals, book and book chapters, policy briefs, […]
The Harvard Chan India Research Center is providing seed grant funding to early career researchers from the Harvard T.H. Chan School of Public Health. For the year 2022-23, pioneering research projects led by Dr Manish Kumar and Dr Matthew Shupler have been funded. 'Identification of histone lactylation in Plasmodium falciparum as an ...
Abstract. This chapter aims to discuss public health education, practice, and research-related issues in India. Moreover, it described the achievement in education, practice, and research in the country. This chapter will describe the challenges facing education in the country and suggest the recommendations to overcome these challenges ...
are notable public health goals of the new millennium, both globally and in India. In India, public health research. has been emphasised as a core investment and tool to guide. policy and practice ...
National Portal of India provides a single-window access to information and services that are electronically delivered from all Government Departments, Institutions and Organizations. It has been a popular source of information to a wide range of stakeholders - from citizens, to government, business and Indian Diasporas. It is a gateway to access Indian Government websites at Centre, State and ...
The Health Challenges. In health sector, India has made enormous strides over the past decades. The life expectancy has crossed 67 years, infant and under-five mortality rates are declining as is the rate of disease incidence. Many diseases, such as polio, guinea worm disease, yaws, and tetanus, have been eradicated.
The findings suggest that targeted public health campaigns and outreach programs are essential to increase awareness and utilization of treatment and harm reduction services. The research underscores the urgent need for improved access to and utilization of harm reduction and treatment services to save lives. ... A Growing Threat in India. July ...
Public Health Challenges is a multidisciplinary journal addressing all areas of public health research, policy, and practice, and supporting the One Health agenda. Abstract The year 2022 saw COVID-19 as the primary public health concern, with vaccine rollout and mandates at the forefront. Other viral infectious diseases, such as Monkeypox and ...
Results We identify three key barriers faced by public health professionals as key stakeholders, namely: (1) political and institutional barriers; (2) education and awareness barriers; and (3) technical research barriers. We show there is a need, from the professionals' perspective, to improve community and political awareness on climate change and health; strengthen technical research ...
Background: Public health research has gained increasing importance in India's national health policy as the country seeks to address the high burden of disease and its inequitable distribution, and embarks on an ambitious agenda towards universalising health care. Objective: This study aimed at describing the public health research output in India, its focus and distribution, and the actors ...
The Public Health Foundation of India is a positive step to redress the limited institutional capacity in India by strengthening training, research and policy development in public health. Preservice training is essential to train the medical workforce in public health leadership and to impart skills required for the practice of public health.
The Harvard T.H. Chan School of Public Health has had active research and educational programs in India since the 1960s. However, the Mumbai-based India Research Center, an office of Harvard Global Research Support Centre India, is designed to broaden and coordinate the School's existing collaborations and create new relationships with organizations and agencies across India.
The COVID-19 pandemic and response are having profound impacts on India's people, leading to myriad health-care challenges, a looming economic recession, and humanitarian crises.1 The long-standing need for universal health coverage (UHC) in India has been brought into sharp focus by the pandemic. The mission of the Lancet Citizens' Commission on reimagining India's health system is to lay ...
Public health priorities for India. Indian states are in diferent phases of epidemiological transition, resulting in large variations in disease burden across the states.1 However, the public health priorities across the country remain similar. Addressing the availability of relevant and robust data for meaningful planning of programmes and ...
Prof. Monika Arora is a public health scientist working in the area of Non-Communicable Disease (NCD) prevention and control and adolescent health. She is the Vice President (Research and Health Promotion) at the Public Health Foundation of India (PHFI). She is the President of the NCD Alliance (2023-25), was the founding Chairperson of the ...
The COVID-19 pandemic in India caused considerable suffering, along with economic and social disruption. Till October 2021, 34.3 million people were infected by COVID-19, and an estimated 0.45 million people died. One of the defining features of the pandemic was a public reckoning of the state of the health system.
Tuberculosis remains a major challenge in India, with an estimated 2.69 million cases each year. Although men are more affected than women, gender differences and related factors affect awareness ...
Impact Factor: 1.6 5-Year Impact Factor: 2.0. Journal Homepage. The Journal of Public Health Research is an online Open Access, peer-reviewed scholarly journal in the field of public health science. The aim of the journal is to stimulate debate and dissemination of knowledge in the public health field in order to improve … | View full journal ...
John Gerrard says the mental ill-health of young people is a very real phenomenon being seen across the world. (ABC News: Claudia Williams)Dr Gerrard said the mental health decline in young people ...
Discover the articles that are trending right now, and catch up on current topics in Public Health and related disciplines. We will update our collection every few weeks; come back to this page to be on top of the latest conversations in Public Health and Medicine. ... Health Education Research, Volume 36, Issue 3, June 2021, Pages 286-294 ...
Household income levels are also a strong predictor of obesity levels - obesity is more common among poorer households. For example, national data for England shows that the prevalence of 10- and 11-year-old children living with severe obesity was over four times as high for children living in the most deprived areas (9.4%) compared with those living in the least deprived areas (2.1%).
Maharashtra, India's richest state and ruled by a BJP coalition, has raised its fiscal deficit target to 2.6% of state GDP for the current fiscal year from 2.3% in an interim budget in February.
Results of our analysis showed 84 unique institutions in 20 states and 3 UTs currently offering 116 public health programs across India's 28 states and 8 UTs. Private and public institutes were 65% (n = 75) and 35% (n = 41) respectfully. The majority of universities mainly provided Masters of Public Health (n = 73, 63%) programs followed by ...
A recent study by UC Davis Health researchers set out to assess the effects of giving naloxone administration by paramedics to patients with OHCA. The study, published in Jama Open Network , concluded there was an association between naloxone administration, and both return of spontaneous circulation and survival to hospital discharge.
While other scholars have pointed India as the top LMIC contributor to health inequalities research in general (Cash-Gibson et al. 2018), the present study reveals that India is now the new global ...