An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-.


InformedHealth.org [Internet].
In brief: cognitive behavioral therapy (cbt).
Last Update: June 2, 2022 ; Next update: 2025.
Cognitive behavioral therapy (CBT) is one of the most common and best studied forms of psychotherapy. It is a combination of two therapeutic approaches, known as cognitive therapy and behavioral therapy.
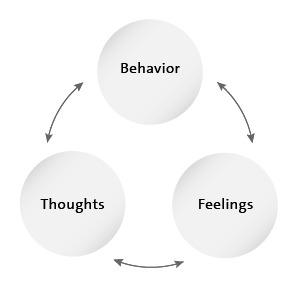
The exact treatment approaches used will depend on the illness or problem to be treated. But the basic idea behind the therapy is always the same: What we think, how we behave, and how other people make us feel are all closely related – and they all affect our wellbeing.
- What is cognitive therapy?
The term cognitive comes from the Latin "cognoscere," meaning "to recognize." Cognitive therapy is about forming a clear idea of your own thoughts, attitudes and expectations. The goal is to recognize and change false and distressing beliefs. It is often not only the things and situations themselves that cause problems, but the sometimes exaggerated importance that we attach to them, too.
One example of a distressing thought pattern is when somebody immediately draws negative conclusions from a certain situation, generalizes them and applies them to other similar situations. In psychology, this generalized way of thinking is called “over-generalizing.” Another distressing way of thinking is known as “catastrophizing”: Something unsettling happens, and people immediately start worrying that it will turn into a disaster.
Such thought patterns can sometimes develop into self-fulfilling prophecies and make life difficult for those affected. If you think that other people don't like you, for instance, then you're likely to put your guard up when you're around them. As a result, they will be less friendly towards you too.
Cognitive therapy helps people learn to replace these thought patterns with more realistic and less harmful thoughts. It also helps people think more clearly and control their own thoughts better.
- How does behavioral therapy work?
Behavioral therapy has its origins in “behaviorism.” This theory assumes that human behavior is learned and can therefore be changed or learned differently. Behavioral therapy aims to find out whether certain behavioral patterns make your life more difficult or make problems worse. In the second step, you work on changing those behavioral patterns.
For example, people who have developed depressive thoughts often tend to become withdrawn and give up their hobbies. As a result, they feel even more unhappy and isolated. Behavioral therapy helps to identify this pattern and find ways to become more active again.
In anxiety disorders , behavioral therapy often includes learning about things that can help you feel calmer. For example, you can learn to reduce anxiety by consciously breathing in and out deeply so that your breathing is calmer and your body can relax. When doing this, you concentrate on your breathing instead of the thing that is causing your anxiety. These kinds of techniques can help you to calm down instead of letting your anxiety overwhelm you.
- Which thoughts and behavioral patterns are harmful, and which are not?
Harmful thoughts or behavioral habits can make people feel bad about themselves. Picture the following situation: You see somebody you know on the street and say hello, but they don't say hello back. Your own reaction to that very much depends on how you assess the situation:
Table: Example of harmful and neutral thoughts and behavioral patterns
View in own window
- How is CBT different from other psychological treatments?
Cognitive behavioral therapy (CBT) is problem-oriented. It focuses on working through specific current problems and finding solutions for them. Unlike psychoanalysis, for example, it doesn't mainly deal with the past. CBT is much more concerned with dealing with problems in the here-and-now. The most important thing is helping people to help themselves: They should be able to cope with their lives again without therapy as soon as possible. This doesn't mean that cognitive behavioral therapy completely ignores the influence of past events. But it mainly deals with identifying and changing current distressing thoughts and behavioral patterns.
Analytic psychotherapy, which has its origin in classic Freudian psychoanalysis, uses a different approach. Here the therapist tries to help the patient discover and understand problems and their deeper causes.
- When is CBT considered?
Cognitive behavioral therapy is used to treat mental health conditions such as depression , anxiety , obsessive-compulsive disorder and addictions. But it can also be used to treat physical conditions such as chronic pain, tinnitus and rheumatism . Here it can help people to cope better with the symptoms.
To really benefit from cognitive behavioral therapy, you have to be committed and willing to put in enough effort. The therapy can only help if you actively take part in it, you are open and honest with the therapist, and also work on your problems between the sessions. This can be quite exhausting, especially with severe psychological conditions such as severe depression or anxiety disorders. For this reason, medication is sometimes used at first to relieve the worst symptoms so that psychological treatment can be started.
When trying to find the right kind of psychotherapy, the specific goals play an important role. If you would like to look deeper into the cause of your problems, CBT is probably not the right choice. It is particularly useful if you are mainly interested in tackling specific problems, and are less interested in the causes.
- How does CBT work and how long does it take?
It is important that you and your therapist have a close and trusting working relationship. It can sometimes take a while to find the right therapist .
In the first session, you briefly describe your current problems and outline your expectations of the therapy. Then you define the goals of your therapy and make a therapy plan together with the therapist. The plan can be adjusted if your personal goals change over the course of therapy.
Therapy often includes writing down your own thoughts in a journal over a certain period of time. The therapist will then check the following things with you: Do you see things realistically? What happens if you behave differently than you normally do in a certain situation? In the therapy sessions, you will regularly discuss any problems you may have and progress that you have made.
Relaxation exercises, stress-reducing and pain-relieving techniques are often used in cognitive behavioral therapy, too. You also learn problem-solving strategies.
Compared to analytical psychotherapy approaches, cognitive behavioral therapy is a short-term treatment. But there is no "standard" length of treatment here. Some people already feel much better after a few sessions, while others need treatment for several months. This depends on various factors, such as the kind and severity of the problems. An individual session typically lasts about one hour. Sessions usually take place once a week. Cognitive behavioral therapy is offered in psychotherapy practices, hospitals and rehabilitation clinics. It is sometimes also offered as group therapy, or online.
- Can CBT also have side effects?
Psychological treatments can have side effects, too: Facing your problems or anxieties head on may be distressing or make you feel quite "wobbly" at first, and can negatively affect relationships with other people. It is important to speak openly with your therapist about any difficulties that come up during therapy.
There is hardly any scientific research on the possible side effects of psychotherapy.
- Who covers the costs?
In Germany, statutory health insurers pay for cognitive behavioral therapy to treat mental illnesses such as depression , anxiety, obsessive-compulsive disorder and addictions. The costs of cognitive behavioral therapy can also be covered for the treatment of severe psychological distress that is caused by a chronic physical illness. But it can sometimes take several weeks or months until you can see a therapist or until the insurance company approves the therapy.
In Germany, a psychotherapy practice can bill the statutory health insurer directly for two to four trial sessions at first – and up to six trial sessions for children, teenagers and people with learning difficulties. This allows the psychotherapist and client to get to know each other, find out what the problems are and whether therapy would be worthwhile. After the trial sessions, you and the therapist have to prepare an application explaining why therapy is needed. You have to submit this application to your health insurance company before therapy can begin. Besides this application, you also have to give your health insurer a medical report from your doctor stating that the symptoms aren't caused by a physical problem, and that there are no medical reasons not to have psychotherapy. The statutory health insurance company then decides whether to approve therapy based on an evaluation.
- Gemeinsamer Bundesausschuss (G-BA). Richtlinie des Gemeinsamen Bundesausschusses über die Durchführung der Psychotherapie (Psychotherapie-Richtlinie) . 2021.
- Pschyrembel Online . 2022.
- Robert Koch Institute (RKI), Statistisches Bundesamt (Destatis). Psychotherapeutische Versorgung . (Gesundheitsberichterstattung des Bundes; Heft 41). 2008.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
- Cite this Page InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. In brief: Cognitive behavioral therapy (CBT) [Updated 2022 Jun 2].
- Disable Glossary Links
In this Page
Informed health links, recent activity.
- In brief: Cognitive behavioral therapy (CBT) - InformedHealth.org In brief: Cognitive behavioral therapy (CBT) - InformedHealth.org
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
10 Best Problem-Solving Therapy Worksheets & Activities

Cognitive science tells us that we regularly face not only well-defined problems but, importantly, many that are ill defined (Eysenck & Keane, 2015).
Sometimes, we find ourselves unable to overcome our daily problems or the inevitable (though hopefully infrequent) life traumas we face.
Problem-Solving Therapy aims to reduce the incidence and impact of mental health disorders and improve wellbeing by helping clients face life’s difficulties (Dobson, 2011).
This article introduces Problem-Solving Therapy and offers techniques, activities, and worksheets that mental health professionals can use with clients.
Before you continue, we thought you might like to download our three Positive Psychology Exercises for free . These science-based exercises explore fundamental aspects of positive psychology, including strengths, values, and self-compassion, and will give you the tools to enhance the wellbeing of your clients, students, or employees.
This Article Contains:
What is problem-solving therapy, 14 steps for problem-solving therapy, 3 best interventions and techniques, 7 activities and worksheets for your session, fascinating books on the topic, resources from positivepsychology.com, a take-home message.
Problem-Solving Therapy assumes that mental disorders arise in response to ineffective or maladaptive coping. By adopting a more realistic and optimistic view of coping, individuals can understand the role of emotions and develop actions to reduce distress and maintain mental wellbeing (Nezu & Nezu, 2009).
“Problem-solving therapy (PST) is a psychosocial intervention, generally considered to be under a cognitive-behavioral umbrella” (Nezu, Nezu, & D’Zurilla, 2013, p. ix). It aims to encourage the client to cope better with day-to-day problems and traumatic events and reduce their impact on mental and physical wellbeing.
Clinical research, counseling, and health psychology have shown PST to be highly effective in clients of all ages, ranging from children to the elderly, across multiple clinical settings, including schizophrenia, stress, and anxiety disorders (Dobson, 2011).
Can it help with depression?
PST appears particularly helpful in treating clients with depression. A recent analysis of 30 studies found that PST was an effective treatment with a similar degree of success as other successful therapies targeting depression (Cuijpers, Wit, Kleiboer, Karyotaki, & Ebert, 2020).
Other studies confirm the value of PST and its effectiveness at treating depression in multiple age groups and its capacity to combine with other therapies, including drug treatments (Dobson, 2011).
The major concepts
Effective coping varies depending on the situation, and treatment typically focuses on improving the environment and reducing emotional distress (Dobson, 2011).
PST is based on two overlapping models:
Social problem-solving model
This model focuses on solving the problem “as it occurs in the natural social environment,” combined with a general coping strategy and a method of self-control (Dobson, 2011, p. 198).
The model includes three central concepts:
- Social problem-solving
- The problem
- The solution
The model is a “self-directed cognitive-behavioral process by which an individual, couple, or group attempts to identify or discover effective solutions for specific problems encountered in everyday living” (Dobson, 2011, p. 199).
Relational problem-solving model
The theory of PST is underpinned by a relational problem-solving model, whereby stress is viewed in terms of the relationships between three factors:
- Stressful life events
- Emotional distress and wellbeing
- Problem-solving coping
Therefore, when a significant adverse life event occurs, it may require “sweeping readjustments in a person’s life” (Dobson, 2011, p. 202).

- Enhance positive problem orientation
- Decrease negative orientation
- Foster ability to apply rational problem-solving skills
- Reduce the tendency to avoid problem-solving
- Minimize the tendency to be careless and impulsive
D’Zurilla’s and Nezu’s model includes (modified from Dobson, 2011):
- Initial structuring Establish a positive therapeutic relationship that encourages optimism and explains the PST approach.
- Assessment Formally and informally assess areas of stress in the client’s life and their problem-solving strengths and weaknesses.
- Obstacles to effective problem-solving Explore typically human challenges to problem-solving, such as multitasking and the negative impact of stress. Introduce tools that can help, such as making lists, visualization, and breaking complex problems down.
- Problem orientation – fostering self-efficacy Introduce the importance of a positive problem orientation, adopting tools, such as visualization, to promote self-efficacy.
- Problem orientation – recognizing problems Help clients recognize issues as they occur and use problem checklists to ‘normalize’ the experience.
- Problem orientation – seeing problems as challenges Encourage clients to break free of harmful and restricted ways of thinking while learning how to argue from another point of view.
- Problem orientation – use and control emotions Help clients understand the role of emotions in problem-solving, including using feelings to inform the process and managing disruptive emotions (such as cognitive reframing and relaxation exercises).
- Problem orientation – stop and think Teach clients how to reduce impulsive and avoidance tendencies (visualizing a stop sign or traffic light).
- Problem definition and formulation Encourage an understanding of the nature of problems and set realistic goals and objectives.
- Generation of alternatives Work with clients to help them recognize the wide range of potential solutions to each problem (for example, brainstorming).
- Decision-making Encourage better decision-making through an improved understanding of the consequences of decisions and the value and likelihood of different outcomes.
- Solution implementation and verification Foster the client’s ability to carry out a solution plan, monitor its outcome, evaluate its effectiveness, and use self-reinforcement to increase the chance of success.
- Guided practice Encourage the application of problem-solving skills across multiple domains and future stressful problems.
- Rapid problem-solving Teach clients how to apply problem-solving questions and guidelines quickly in any given situation.
Success in PST depends on the effectiveness of its implementation; using the right approach is crucial (Dobson, 2011).
Problem-solving therapy – Baycrest
The following interventions and techniques are helpful when implementing more effective problem-solving approaches in client’s lives.
First, it is essential to consider if PST is the best approach for the client, based on the problems they present.
Is PPT appropriate?
It is vital to consider whether PST is appropriate for the client’s situation. Therapists new to the approach may require additional guidance (Nezu et al., 2013).
Therapists should consider the following questions before beginning PST with a client (modified from Nezu et al., 2013):
- Has PST proven effective in the past for the problem? For example, research has shown success with depression, generalized anxiety, back pain, Alzheimer’s disease, cancer, and supporting caregivers (Nezu et al., 2013).
- Is PST acceptable to the client?
- Is the individual experiencing a significant mental or physical health problem?
All affirmative answers suggest that PST would be a helpful technique to apply in this instance.
Five problem-solving steps
The following five steps are valuable when working with clients to help them cope with and manage their environment (modified from Dobson, 2011).
Ask the client to consider the following points (forming the acronym ADAPT) when confronted by a problem:
- Attitude Aim to adopt a positive, optimistic attitude to the problem and problem-solving process.
- Define Obtain all required facts and details of potential obstacles to define the problem.
- Alternatives Identify various alternative solutions and actions to overcome the obstacle and achieve the problem-solving goal.
- Predict Predict each alternative’s positive and negative outcomes and choose the one most likely to achieve the goal and maximize the benefits.
- Try out Once selected, try out the solution and monitor its effectiveness while engaging in self-reinforcement.
If the client is not satisfied with their solution, they can return to step ‘A’ and find a more appropriate solution.

Download 3 Free Positive Psychology Exercises (PDF)
Enhance wellbeing with these free, science-based exercises that draw on the latest insights from positive psychology.
Download 3 Free Positive Psychology Tools Pack (PDF)
By filling out your name and email address below.
Positive self-statements
When dealing with clients facing negative self-beliefs, it can be helpful for them to use positive self-statements.
Use the following (or add new) self-statements to replace harmful, negative thinking (modified from Dobson, 2011):
- I can solve this problem; I’ve tackled similar ones before.
- I can cope with this.
- I just need to take a breath and relax.
- Once I start, it will be easier.
- It’s okay to look out for myself.
- I can get help if needed.
- Other people feel the same way I do.
- I’ll take one piece of the problem at a time.
- I can keep my fears in check.
- I don’t need to please everyone.

5 Worksheets and workbooks
Problem-solving self-monitoring form.
Answering the questions in the Problem-Solving Self-Monitoring Form provides the therapist with necessary information regarding the client’s overall and specific problem-solving approaches and reactions (Dobson, 2011).
Ask the client to complete the following:
- Describe the problem you are facing.
- What is your goal?
- What have you tried so far to solve the problem?
- What was the outcome?
Reactions to Stress
It can be helpful for the client to recognize their own experiences of stress. Do they react angrily, withdraw, or give up (Dobson, 2011)?
The Reactions to Stress worksheet can be given to the client as homework to capture stressful events and their reactions. By recording how they felt, behaved, and thought, they can recognize repeating patterns.
What Are Your Unique Triggers?
Helping clients capture triggers for their stressful reactions can encourage emotional regulation.
When clients can identify triggers that may lead to a negative response, they can stop the experience or slow down their emotional reaction (Dobson, 2011).
The What Are Your Unique Triggers ? worksheet helps the client identify their triggers (e.g., conflict, relationships, physical environment, etc.).
Problem-Solving worksheet
Imagining an existing or potential problem and working through how to resolve it can be a powerful exercise for the client.
Use the Problem-Solving worksheet to state a problem and goal and consider the obstacles in the way. Then explore options for achieving the goal, along with their pros and cons, to assess the best action plan.
Getting the Facts
Clients can become better equipped to tackle problems and choose the right course of action by recognizing facts versus assumptions and gathering all the necessary information (Dobson, 2011).
Use the Getting the Facts worksheet to answer the following questions clearly and unambiguously:
- Who is involved?
- What did or did not happen, and how did it bother you?
- Where did it happen?
- When did it happen?
- Why did it happen?
- How did you respond?
2 Helpful Group Activities
While therapists can use the worksheets above in group situations, the following two interventions work particularly well with more than one person.
Generating Alternative Solutions and Better Decision-Making
A group setting can provide an ideal opportunity to share a problem and identify potential solutions arising from multiple perspectives.
Use the Generating Alternative Solutions and Better Decision-Making worksheet and ask the client to explain the situation or problem to the group and the obstacles in the way.
Once the approaches are captured and reviewed, the individual can share their decision-making process with the group if they want further feedback.
Visualization
Visualization can be performed with individuals or in a group setting to help clients solve problems in multiple ways, including (Dobson, 2011):
- Clarifying the problem by looking at it from multiple perspectives
- Rehearsing a solution in the mind to improve and get more practice
- Visualizing a ‘safe place’ for relaxation, slowing down, and stress management
Guided imagery is particularly valuable for encouraging the group to take a ‘mental vacation’ and let go of stress.
Ask the group to begin with slow, deep breathing that fills the entire diaphragm. Then ask them to visualize a favorite scene (real or imagined) that makes them feel relaxed, perhaps beside a gently flowing river, a summer meadow, or at the beach.
The more the senses are engaged, the more real the experience. Ask the group to think about what they can hear, see, touch, smell, and even taste.
Encourage them to experience the situation as fully as possible, immersing themselves and enjoying their place of safety.
Such feelings of relaxation may be able to help clients fall asleep, relieve stress, and become more ready to solve problems.
We have included three of our favorite books on the subject of Problem-Solving Therapy below.
1. Problem-Solving Therapy: A Treatment Manual – Arthur Nezu, Christine Maguth Nezu, and Thomas D’Zurilla
This is an incredibly valuable book for anyone wishing to understand the principles and practice behind PST.
Written by the co-developers of PST, the manual provides powerful toolkits to overcome cognitive overload, emotional dysregulation, and the barriers to practical problem-solving.
Find the book on Amazon .
2. Emotion-Centered Problem-Solving Therapy: Treatment Guidelines – Arthur Nezu and Christine Maguth Nezu
Another, more recent, book from the creators of PST, this text includes important advances in neuroscience underpinning the role of emotion in behavioral treatment.
Along with clinical examples, the book also includes crucial toolkits that form part of a stepped model for the application of PST.
3. Handbook of Cognitive-Behavioral Therapies – Keith Dobson and David Dozois
This is the fourth edition of a hugely popular guide to Cognitive-Behavioral Therapies and includes a valuable and insightful section on Problem-Solving Therapy.
This is an important book for students and more experienced therapists wishing to form a high-level and in-depth understanding of the tools and techniques available to Cognitive-Behavioral Therapists.
For even more tools to help strengthen your clients’ problem-solving skills, check out the following free worksheets from our blog.
- Case Formulation Worksheet This worksheet presents a four-step framework to help therapists and their clients come to a shared understanding of the client’s presenting problem.
- Understanding Your Default Problem-Solving Approach This worksheet poses a series of questions helping clients reflect on their typical cognitive, emotional, and behavioral responses to problems.
- Social Problem Solving: Step by Step This worksheet presents a streamlined template to help clients define a problem, generate possible courses of action, and evaluate the effectiveness of an implemented solution.
If you’re looking for more science-based ways to help others enhance their wellbeing, check out this signature collection of 17 validated positive psychology tools for practitioners. Use them to help others flourish and thrive.
17 Top-Rated Positive Psychology Exercises for Practitioners
Expand your arsenal and impact with these 17 Positive Psychology Exercises [PDF] , scientifically designed to promote human flourishing, meaning, and wellbeing.
Created by Experts. 100% Science-based.
While we are born problem-solvers, facing an incredibly diverse set of challenges daily, we sometimes need support.
Problem-Solving Therapy aims to reduce stress and associated mental health disorders and improve wellbeing by improving our ability to cope. PST is valuable in diverse clinical settings, ranging from depression to schizophrenia, with research suggesting it as a highly effective treatment for teaching coping strategies and reducing emotional distress.
Many PST techniques are available to help improve clients’ positive outlook on obstacles while reducing avoidance of problem situations and the tendency to be careless and impulsive.
The PST model typically assesses the client’s strengths, weaknesses, and coping strategies when facing problems before encouraging a healthy experience of and relationship with problem-solving.
Why not use this article to explore the theory behind PST and try out some of our powerful tools and interventions with your clients to help them with their decision-making, coping, and problem-solving?
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free .
- Cuijpers, P., Wit, L., Kleiboer, A., Karyotaki, E., & Ebert, D. (2020). Problem-solving therapy for adult depression: An updated meta-analysis. European P sychiatry , 48 (1), 27–37.
- Dobson, K. S. (2011). Handbook of cognitive-behavioral therapies (3rd ed.). Guilford Press.
- Dobson, K. S., & Dozois, D. J. A. (2021). Handbook of cognitive-behavioral therapies (4th ed.). Guilford Press.
- Eysenck, M. W., & Keane, M. T. (2015). Cognitive psychology: A student’s handbook . Psychology Press.
- Nezu, A. M., & Nezu, C. M. (2009). Problem-solving therapy DVD . Retrieved September 13, 2021, from https://www.apa.org/pubs/videos/4310852
- Nezu, A. M., & Nezu, C. M. (2018). Emotion-centered problem-solving therapy: Treatment guidelines. Springer.
- Nezu, A. M., Nezu, C. M., & D’Zurilla, T. J. (2013). Problem-solving therapy: A treatment manual . Springer.
Share this article:
Article feedback
What our readers think.
Thanks for your information given, it was helpful for me something new I learned
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

The Empty Chair Technique: How It Can Help Your Clients
Resolving ‘unfinished business’ is often an essential part of counseling. If left unresolved, it can contribute to depression, anxiety, and mental ill-health while damaging existing [...]

29 Best Group Therapy Activities for Supporting Adults
As humans, we are social creatures with personal histories based on the various groups that make up our lives. Childhood begins with a family of [...]
47 Free Therapy Resources to Help Kick-Start Your New Practice
Setting up a private practice in psychotherapy brings several challenges, including a considerable investment of time and money. You can reduce risks early on by [...]
Read other articles by their category
- Body & Brain (50)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (29)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (18)
- Positive Parenting (4)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (17)
- Relationships (46)
- Resilience & Coping (38)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (32)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)

Get weekly notifications for new group therapy session times.
Are you interested in joining an online group therapy session? Subscribe and receive weekly updates for new group therapy session times at Grouport.
Thank you for your interest.
We’ll keep you updated on our schedule weekly.
.png)
Learn DBT Skills In A Group
Weekly sessions are available. Grouport offers therapist-led dialectical behavior therapy skills groups online. The first 12 weeks covers fundamental DBT skills.
Problem-Solving with Dialectical Behavior Therapy: A Guide to Effective Strategies

Dialectical behavior therapy (DBT) is a well-regarded therapeutic approach that has been proven effective in addressing various mental health issues, such as depression, anxiety, and borderline personality disorder. At its core, DBT emphasizes developing essential skills for emotional regulation and interpersonal effectiveness, which can be applied to problem-solving in various aspects of life. In this article, we will explore the role of problem-solving in DBT and discuss how this therapeutic approach can help individuals navigate life's challenges with greater emotional resilience and balance.
DBT is a type of cognitive-behavioral therapy that focuses on teaching skills in four key areas: mindfulness, distress tolerance, emotional regulation, and interpersonal effectiveness. By learning and practicing these skills, individuals can better manage emotional challenges, develop healthier relationships, and improve their overall well-being. Furthermore, DBT encourages applying these skills to real-life situations, enabling individuals to address and resolve problems that arise effectively.
With numerous resources available to those interested in DBT, individuals can easily access valuable tools and guidance for mastering these essential skills. From beginner guides to advanced materials, a wealth of resources is suitable for individuals at all stages of their DBT journey. By engaging with these materials, individuals can deepen their understanding of DBT, hone their skills, and ultimately achieve more excellent emotional balance and well-being.
The Role of Problem-Solving in Dialectical Behavior Therapy
Problem-solving is a fundamental aspect of dialectical behavior therapy, as it involves applying the skills learned in DBT to address and resolve real-life challenges. By developing effective problem-solving strategies, individuals can better navigate life's difficulties, reduce emotional distress, and foster greater personal empowerment and control.
One of the primary ways in which DBT facilitates problem-solving is through the application of mindfulness skills. Individuals can develop greater self-awareness and clarity in the face of challenges by cultivating present-moment awareness and non-judgmental acceptance of their thoughts, emotions, and bodily sensations. This heightened self-awareness can enable individuals to identify problems more effectively, evaluate potential solutions, and make informed decisions about addressing them.
Another important aspect of problem-solving within DBT is the development of distress tolerance skills. By effectively coping with emotional pain and distress, individuals can better manage the emotional turbulence that often accompanies problem-solving efforts. This increased emotional resilience can, in turn, lead to more effective problem-solving strategies, as individuals are better able to maintain focus and persevere through challenging situations.
Developing Effective Problem-Solving Strategies with DBT
To effectively address and resolve life's challenges, it is essential to develop problem-solving strategies grounded in the principles of dialectical behavior therapy. By incorporating DBT skills into one's problem-solving approach, individuals can cultivate greater emotional resilience, improve interpersonal effectiveness, and achieve more successful outcomes.
One key strategy for problem-solving within DBT is to employ mindfulness techniques to maintain present-moment awareness and non-judgmental acceptance throughout the problem-solving process. This can help individuals stay focused on the task rather than becoming overwhelmed by emotional reactions or unhelpful thought patterns. Additionally, mindfulness can enable individuals to approach problems with greater curiosity, openness, and flexibility, facilitating creative and effective solutions.
Another important DBT-based problem-solving strategy is to draw upon emotional regulation skills to maintain emotional balance and stability during problem-solving. This emotional balance promotes clearer thinking and more effective decision-making, ultimately leading to more successful problem-solving outcomes. By identifying and labeling emotions, understanding the function of emotions, and employing strategies to modify emotional responses, individuals can better manage their emotional reactions to challenging situations.
Interpersonal effectiveness skills also play a crucial role in problem-solving, as many challenges in life involve navigating relationships and communicating with others. By developing and applying assertiveness, active listening, and negotiation skills, individuals can more effectively address interpersonal conflicts, collaborate with others to generate solutions and establish healthy boundaries. This can lead to improved relationships, reduced stress, and a greater well-being.
Section 3: The Long-Term Benefits of Problem-Solving with DBT
Consistent problem-solving with dialectical behavior therapy can lead to numerous long-term benefits for mental health and overall well-being. By honing problem-solving skills rooted in DBT principles, individuals can develop greater emotional resilience, improve interpersonal relationships, and foster a stronger sense of personal empowerment.
One of the primary long-term benefits of problem-solving with DBT is the development of emotional resilience. By effectively managing emotional reactions and coping with distress, individuals can better navigate life's challenges and bounce back from setbacks more quickly. This emotional resilience can increase confidence, self-esteem, and overall mental health.
Improved interpersonal relationships are another significant long-term benefit of problem-solving with DBT. By applying interpersonal effectiveness skills to address conflicts and communicate more effectively, individuals can cultivate healthier, more satisfying relationships with others. This can lead to increased social support, reduced feelings of isolation, and enhanced overall well-being.
Finally, problem-solving with DBT can foster a greater sense of personal empowerment and control. By developing and refining problem-solving strategies grounded in DBT principles, individuals can gain increased confidence in their ability to address and resolve life's challenges. This sense of personal empowerment can contribute to a more positive outlook on life, reduce feelings of helplessness, and improve overall mental health.

Final Thoughts
Dialectical behavior therapy offers a powerful problem-solving approach, equipping individuals with the skills and strategies to address and resolve life's challenges effectively. By incorporating DBT principles into problem-solving, individuals can cultivate emotional resilience, improve interpersonal relationships, and foster greater personal empowerment. Consistent problem-solving with DBT can ultimately lead to lasting improvements in mental health, emotional stability, and overall quality of life.
Grouport Offers Online DBT Skills Groups
If you're struggling with daily life and relationship issues due to negative behaviors and emotions, consider enrolling in the Grouport DBT series by Grouport Therapy. Our 12-week program can help equip you with new skills to improve your mental health and well-being.
Our group meets once a week at a scheduled time, and you'll receive access to session links via email after enrolling and paying for the program. By joining our DBT skills group , you can improve relationships, manage anxiety, and reduce emotional suffering, regaining hope for the future.
Don't hesitate to take the first step towards a better life. Our next session is waiting for you. Join our Grouport DBT series today and start improving your mental health alongside a supportive group of individuals.
Join a DBT Group Support Session
We offer DBT group therapy online to improve emotion regulation, distress tolerance, mindfulness, & interpersonal skills. Get effective and affordable treatment.
Space is limited, so reserve your seat today.
Share This Post:
Exploring the Range of OCD Treatment Resources in Minneapolis
Understanding discouraged borderline personality disorder: key signs, causes, and treatments, becoming a mental health ally: 7 essential tips for providing support, get started with grouport today.
E9: Problem Solving
Introduction
In the previous exercises from this module we worked on recognizing certain situations that are triggering and causing us to feel overwhelming emotions. This is helpful because once we know that certain situation can be potentially problematic for us, then we can also work on doing something before the situation happens again - a type of preparation. This is exactly what we are going to be working on in this exercise. Getting prepared beforehand can give us a sense of control over the triggering situation that is about to happen. We will go through four steps that are going to help you solve the problematic situation before it happens.
Instructions
Step one: behavior analysis.
Take your time and try to remember what usually causes you to feel ineffectively overwhelmed. Is it an event with your family, a work situation, your kids or your friends? Next, write down the emotion that you are usually experiencing. Maybe you feel intensively angry, rejected or abandoned, or depressed and anxious. Try to remember how the situation usually takes place and what your ongoing fleeting feelings and thoughts are while the situation is happening.
Example : Event : My husband criticizes my looks. He makes a subtle comment that I should lose weight and that I should dress differently. Main emotion : Anger Other emotions and thoughts during the event : At first, I low-key agree with him and I think how fat and ugly I look. I've always hated my body. Before my anger strikes I feel ashamed and sad.
Step Two: What Can I Change?
What out of the three elements from the previous step can you change? Bear in mind that the change that you can potentially make should eventually improve your emotional health and your immediate overwhelming emotion.
Sometimes it's impossible to change the external event, but we can work on our thoughts and how we talk to ourselves internally during the situation. Pick two things out of the elements in the previous step that you think are the most suitable for you to try to change.
In the previous example, the person cannot control what her husband says to her. What she can work on though, is the messages she directs towards herself about her appearance. At the same time, she will also work on the feelings of shame and sadness that are occurring during the event.
Step Three: Brainstorming Alternatives
Now that you have identified the two aspects that you can and would like to change, it's time to brainstorm for alternative ideas. If you chose to work on the occurring thoughts, what else can you say to yourself about the situation? What can you remind yourself of in order to objectify the all-or-nothing thinking or the generalizations you make? Perhaps you want to change the event and do something differently than what you usually does.
In the example we presented, the alternative and objective thoughts that the woman can remind herself of would be: - "He has no right to make such aggressive comments and body shame me." - "Even though his tone was seemingly polite, it is not okay to say things like that to your significant other. It's still passive aggressive." - "I don't have to look a certain way unless I want to. My body serves me in great ways and I am grateful that I am physically healthy." - "There are many great aspects about me, I am sociable and charming." - "This trend to be thin will probably have a cultural shift and it will change. It's just a societal pressure and conditioning and I really am smarter than that!"
Step Four: Put the Solution into Action
After you have brainstormed for ideas about what you can do to change the aspects that are changeable, choose what works best for you and try to put the solution into action. Actively decide and remind yourself to act the way you decided to next time you find yourself in the situation.
For example: "Now that I've straightened some of the incorrect ways in which I am thinking about my body, I want to try and remind myself more often of what I actually believe in. Maybe next time this happens I can communicate to my husband what my thoughts are in a polite way and not get angry and make mean comments to hurt him back. I will assertively put boundaries about what is acceptable and what is not."
Use the worksheet to help you prepare for situations that you expect to be difficult.
DBT Emotional Regulation: Problem Solving
How should I know which aspect of the situation should I work on changing? I am not sure which one is the most suitable.
Start with the things you have control over. For example, our thoughts and the resulting feelings are usually something we can work on (trying to straighten the cognitive distortions present). You can benefit from the exercise about cognitive vulnerability that we previously worked on in this module. Sometimes the way in which other people consistently behave is out of our control. That is not to say that we shouldn't try to communicate our boundaries. You can also work on changing the way you behave in and do something differently. For example you can walk out of a situation that is harmful to you (if possible).
I can't think of alternatives, my brainstorming session is a little dry.
You can try asking somebody you trust and you know has your back about ideas about the situation. If you regularly put yourself down with the way you think about yourself and the way you interpret the events around you, then you can try thinking about what advice you would give a friend of yours who is in the same situation. Remember that the potential solution to the problem should eventually improve the situation for you and help you with the overwhelming emotion you usually experience. For example, in the body-shaming example we presented, if the woman shamed herself into losing a lot of weight, she would still end up with negative emotions, so that would not be the best solution for her.
What if I can't remember to try the solution I've come up with next time I find myself in the problematic situation?
It is okay if you need some time to get used to implementing the solution. Quality change doesn't come with little effort. If you don't remember to implement the solution the first time, just remind yourself that that is totally fine, be patient and try it again next time. Maybe the first couple of times you won't end up with the emotion you would eventually like to feel, but remember that this is a skill and it can be learned through practice.
Comments About Problem Solving
Hey im here postpartum depression
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

"Going through all the DBT worksheets really helped me rethink the way I was approaching my life. Thank you!"
- Tillie S.
"Life changer! I struggled with depression and anxiety before I did this course. Do it!"
- Suzanne R.
"I started doing your worksheets a month ago. My therapist says they helped us make faster progress in our sessions."
- Eduardo D.
"Stick with it. It really works. Doing these exercises every day helped me get over a really bad spell of depression."
- Juliana D.
- MINDFULNESS
- INTERPERSONAL

- Previous Article
- Next Article
Origins of Problem Solving as a Behavioral Treatment
Application of pst to diabetes: what is the evidence, example of traditional pst applied to diabetes self-management, current and future research directions, article information, evidence-based behavioral treatments for diabetes: problem-solving therapy.
Problem solving is an essential skill for effective diabetes self-management. Evidence suggests that problem-solving therapy (PST) approaches, used in the context of broader diabetes educational or lifestyle interventions, may be effective for mood and select diabetes outcomes. As a stand-alone treatment, formal PST adapted for diabetes self-management is a promising behavioral intervention for improving health-related problem-solving, diabetes self-care behaviors, and disease control.
All of the authors are based in Baltimore, Md. Kristina P. Schumann, MA, June A. Sutherland, MS, and Haseeb M. Majid, MA, are lifestyle interventionists in the Division of General Internal Medicine at Johns Hopkins School of Medicine. Felicia Hill-Briggs, PhD, ABPP, is an associate professor in the Departments of Medicine; Health, Behavior & Society; and Physical Medicine & Rehabilitation at the Johns Hopkins Medical Institutions and director of the cognition and behavior sub-core of the Johns Hopkins/University of Maryland Diabetes Research and Training Center.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Kristina P. Schumann , June A. Sutherland , Haseeb M. Majid , Felicia Hill-Briggs; Evidence-Based Behavioral Treatments for Diabetes: Problem-Solving Therapy. Diabetes Spectr 1 May 2011; 24 (2): 64–69. https://doi.org/10.2337/diaspect.24.2.64
Download citation file:
- Ris (Zotero)
- Reference Manager
Problem solving is a basic human thinking process. Many general counseling and psychotherapy approaches, such as cognitive behavioral therapy, include problem solving as a component of treatment for managing life problems and emotional disorders. 1 Similarly, educational and lifestyle interventions in diabetes often include elements of problem solving as part of broader intervention approaches. 2
Among diabetes educators, problem solving is identified as necessary for patient mastery of diabetes self-management and as the skill most difficult to teach patients. 3 This article describes the origins of problem-solving therapy (PST) as a formal, stand-alone intervention approach for behavior change; application of this technique to diabetes care; and evidence of its effectiveness in improving diabetes outcomes.
Problem solving, which has its origins in the behavioral and cognitive basic sciences, 4 – 8 is an identified intervention approach for behavior change. 9 , 10 Cognitive psychology defines problem solving as involving the following components: the individual is goal-directed; reaching the goal requires a series of mental processes; and those processes are cognitive rather than automatic. 6 , 7 Problem solving can perhaps be described more simply as a series of cognitive operations used to figure out what to do when the way to reach a goal is not apparent.
Although problem solving is a counseling approach that may be incorporated within other intervention models, PST is a stand-alone intervention with a longstanding history. PST took root in clinical and counseling psychology in the 1960s and 1970s to address a variety of mental health disorders, including schizophrenia and psychotic disorders, depression and suicidality, social phobia, generalized anxiety disorder, and posttraumatic stress disorder. 11 , 12 PST has also been used to address marital/family distress, lifestyle management in people with mental retardation, stress management, ineffective coping, and substance abuse. 11
There is a substantial evidence base for the effectiveness of PST in reducing symptoms of depression, anxiety, and stress. 12 Moreover, problem-solving approaches have been found effective in helping patients cope with cancer, enhancing weight loss maintenance, reducing pain, and lowering blood pressure. 12 – 16
The PST model proposed by D'Zurilla and Goldfried 9 and refined by D'Zurilla and Nezu 11 is perhaps the most recognized PST approach. This intervention approach is based on the premise that humans are innate problem solvers but that there are significant individual differences in problem-solving abilities.
PST has historical roots in four different areas: 1 ) increased focus on human creativity, creativity research, and creative problem solving; 2 ) a positive approach to clinical intervention, which moves away from the medical model of pathology and focuses on building social competence through enhancing problem-solving abilities; 3 ) recognition of the importance of cognitive processes and self-control in behavior therapy, in which PST intends to teach patients a skill set they can apply across all life situations, resulting in generalized and lasting behavior change; and 4 ) Lazarus's relational model of stress, which describes stress as a result of person-environment interactions where the demands of the interaction exceed the individual's coping resources. 17
D'Zurilla and Nezu 11 describe three levels of variables influencing the cognitive-behavioral process of problem solving. PST is effective in facilitating behavior change by intervening on these three levels. First, orienting responses refer to how individuals respond to problematic situations in terms of their thoughts and emotions. PST intervenes on these responses by teaching individuals how to effectively recognize and appraise problems while increasing their self-efficacy to cope with challenging situations. Second, problem-solving skills refer to the specific tasks that must be completed before a problem can be solved successfully. PST intends to teach problem-solving skills, thereby improving individuals' ability to manage challenging situations. Finally, basic cognitive abilities refer to specific abilities that directly affect individuals' capacity to learn and perform problem-solving skills. Examples of basic cognitive abilities include causal thinking, consequential thinking, and perspective taking.
Interventions often focus primarily on the first two levels because it is typically assumed that individuals come to treatment with basic cognitive abilities intact. This assumption may be incorrect for specific populations (e.g., people with schizophrenia), in which case deficits in this area should be included in the intervention. 11 PST also intervenes on individuals' emotional responses to life situations, which have a significant effect on all aspects of problem solving. PST aims to facilitate positive emotional reactions and reduce or eliminate negative emotional reactions (e.g., anxiety and anger). 11
Traditional PST

Key components of PST are provided in Table 1 . The D'Zurilla and Nezu 11 PST uses a five-dimensional model of social problem solving, which includes two problem-orientation styles (positive and negative) and three problem-solving styles (rational, impulsive/careless, and avoidant). The model also identifies four rational problem-solving skills: problem definition and formulation, generation of alternatives, decision making, and solution implementation and verification. PST must be conducted in a sequential order, and a series of problem-solving therapy modules is available. 11
The number of sessions required to complete PST varies depending on the purpose of the training, but ranges from 8 to 16 sessions. 11 , 12 The interventionist conducting PST uses didactic approaches, coaching, modeling, shaping, rehearsal, performance feedback, and positive reinforcement. Nezu et al. 18 have developed a user-friendly self-help guidebook to assist in training professionals in PST and to serve as a supporting reference for patients engaging in therapist-led PST. Successful implementation depends on adequate development of rapport between the facilitator and the patient(s). To evaluate success of PST, an assessment tool such as the Social Problem-Solving Inventory–Revised 19 is also recommended.
The American Association of Diabetes Educators (AADE) has identified problem solving as one of seven core diabetes self-management behaviors (AADE-7). 20 AADE defines problem solving as a learned behavior that includes generating a set of potential strategies for problem resolution, selecting the most appropriate strategy, applying the strategy, and evaluating the effectiveness of the strategy. In the AADE-7 framework, problem solving is conceptualized as intervening on barriers to self-care 21 , 22 and thereby enabling patients to carry out all other self-management behaviors (i.e., healthy eating, physical activity, self-monitoring, medication taking, risk reduction, and healthy coping). 2
Hill-Briggs 21 proposed a model for understanding problem solving in the context of diabetes self-management. Based on the D'Zurilla and Nezu framework combined with theories of problem solving from cognitive psychology and education/learning theory, the model highlights four key components of problem solving that are particularly salient in disease self-management. First, problem-solving skill refers to the approach an individual takes to solving problems (i.e., rational, impulsive/careless, or avoidant), with a rational approach being most effective. Second, problem-solving orientation refers to individuals' attitudes and beliefs about their disease and the problems they encounter. Problem-solving orientation can be positive (e.g., problems viewed as a challenge) or negative (e.g., problems viewed as a threat). Third, transfer of past experience/learning refers to the use of previous experience in attempting to solve novel problems. This transfer of past experience can also be effective (e.g., using a solution that was effective in a similar situation in the past) or ineffective (e.g., trying an ineffective solution repeatedly in the same situation). The fourth component of problem solving is disease-specific knowledge . To solve problems related to disease self-management effectively, individuals must have a working knowledge base about the disease and its management. Each key component of problem solving operates within the problem environment , composed of the social/physical context and characteristics of the problem itself. 23
The evidence base for problem solving as a diabetes self-management intervention approach was examined in a 2007 systematic review. 2 This review revealed problem solving as a frequently used component of interventions within diabetes education and care. Research with adult populations has demonstrated some effectiveness of interventions with a problem-solving component on outcomes including disease control, depressive symptoms, self-management behaviors, weight loss, self-efficacy, and quality of life. Research with children/adolescents has demonstrated effectiveness of problem-solving training in improving some self-management behaviors and psychosocial outcomes. 2
Specifically, the review 2 yielded 36 quantitative, 11 conceptual, and 5 qualitative studies of problem solving in diabetes self-management and control. Studies examined in the review were conducted with children/adolescents (43%) and adults (57%). The samples were varied in terms of race and ethnicity, with Caucasian (25%), multiple ethnicities (most often Caucasian, African-American, and Latino) (22%), African-American (11%), and international (Japanese, Italian) (8%) populations represented.
Intervention studies were conducted with children/adolescents ( n = 8) and adults ( n = 8). The extent to which problem solving was involved in the intervention varied, but in most cases, problem solving was one component of a larger diabetes self-management intervention and was not the main focus of treatment. Outcomes reported in the systematic review included problem solving, self-management behaviors, physiological outcomes, and psychosocial outcomes. 2 Two of five studies with children and both studies with adults in which problem solving was assessed demonstrated a positive effect of the intervention on problem-solving ability. The studies with adults demonstrated maintenance of problem-solving abilities at follow-up (6 months and 5 years later). 2
Twelve studies reported use of an intervention that was problem-solving based or included problem solving in a broader package of intervention approaches. Three of six studies with children demonstrated a positive effect of the intervention on dietary intake, self-monitoring of blood glucose (SMBG), and general treatment adherence, with effects lasting for up to 12 months. Additionally, four of six studies in adults demonstrated positive effects of the intervention on dietary behaviors (most common), SMBG, and exercise. Findings related to medication adherence in adults were mixed, and one study demonstrated no link between problem solving and foot inspections. 2
All but two intervention studies assessed the effect of problem-solving training on glycemic control. Half of the adult studies demonstrated a positive effect of the intervention on A1C. The results in children/adolescents were even more mixed, with two studies showing a decrease in A1C, three studies showing no effect on glycemic control, and one study reporting higher A1C at follow-up in both the intervention and control groups. 2
Two studies demonstrated a positive effect of the intervention on weight loss in adults, whereas one study demonstrated no effect on weight loss. Finally, two studies demonstrated a positive effect of the intervention on cardiovascular disease (CVD) markers (cholesterol and triglycerides). 2
Three intervention studies assessed psychosocial outcomes in children/adolescents. Results indicated a positive effect of the intervention on self-efficacy, adjustment, parent-adolescent relationships, diabetes-related conflict, ability to use sick-day self-management guidelines, and quality of life. One study conducted with adults demonstrated a positive effect of the intervention on self-efficacy, whereas the other showed no effect on self-efficacy. Three studies with adults reported improvements in depressive symptoms post-intervention. Of the three studies that investigated quality of life in adults, two found no differences between the intervention and control groups in quality of life, whereas one showed improved quality of life in the intervention group. 2
Several limitations in the research reviewed affected the conclusions that could be drawn regarding the effectiveness of PST for diabetes self-management. In the diabetes interventions reported to date, problem solving generally was added to self-management training as a very small, informal, or unstructured component within a package of intervention techniques and without incorporating all elements that constitute PST as a behavior-change intervention. Therefore, it has been difficult to determine to what extent problem solving (compared to the other offered interventions) contributed to outcomes. Moreover, few studies provided a description of the problem-solving component of the intervention package. Nonetheless, as a whole, evidence suggests that problem solving–related interventions are effective for select diabetes outcomes.
Not previously tested was whether traditional PST as a stand-alone intervention rather than a small component of a broader intervention package is effective for diabetes self-management and disease control. This was the focus of a recent investigation and is the subject of an ongoing trial.
Project DECIDE (Decision-making Education for Choices In Diabetes Everyday) began as a study funded by the National Institutes of Health (NIH) to translate traditional PST into a problem-based diabetes self-management training program. The DECIDE intervention centers on a series of learning modules that train patients in the problem-solving process as a life skill applied to diabetes self-management. This skill-training approach allows health/diabetes educators to relinquish the role of patients' problem-solver, a role that inadvertently disempowers patients. 24 For patients, the problem-based self-management approach allows them to identify and work toward solutions for daily barriers, life challenges, and competing priorities that directly impede their effective application of diabetes knowledge and self-management of diabetes in real life.
DECIDE Diabetes PST

Key components of the DECIDE self-management training are provided in Table 2 . The DECIDE program consists of a diabetes and CVD education module, which provides the booster patient education needed as a prerequisite for diabetes-related problem solving, followed by health-related problem-solving training modules modeled on the described D'Zurilla and Nezu approach. 11 Patients receive two workbooks: Diabetes and Your Heart: Your Facts and Information Workbook , which accompanies the education module, and Hitting the Targets for Diabetes and Your Heart: Your Problem-Solving Workbook , which accompanies the problem-solving training. The problem-solving modules also include take-home exercises, which provide opportunities for patients to practice newly learned problem-solving skills in their natural environments. Both patient workbooks were developed using guidelines for accessibility and usability for vulnerable adult populations 25 – 28 and have been found to be accessible and understandable to people with low and average literacy, 29 as well as people with mild to moderate visual and cognitive impairment. 30
The pilot study tested a comprehensive DECIDE PST intervention (as shown in Table 2) and a condensed version, which consisted of the diabetes and CVD education module followed by one PST session. The condensed PST intervention and patient workbook covered all the problem-solving topics with abbreviated exercises. The study used two measures designed to assess problem solving in the context of health: the Diabetes Problem-Solving Scale 31 and the Health Problem-Solving Scale. 32
The pilot study was conducted with an underserved patient population. Participants were 56 African Americans (59% female, mean age 61 years, 57% living in poverty) with a mean diabetes duration of 14 years. The vast majority of patients (86%) had suboptimal A1C (defined as > 7.0%). 33 Participants were randomized to the intensive ( n = 29) or condensed ( n = 27) DECIDE programs, which were delivered in group format.
At 3 months after intervention completion (6 months to 1 year from baseline), the intensive DECIDE PST resulted in improved diabetes knowledge, problem solving, and self-care and a reduction in A1C of 0.71%. For participants with suboptimal blood pressure or LDL cholesterol, benefits in these parameters were seen as well. The condensed intervention resulted in knowledge gain but not problem solving or clinical improvements. The study demonstrated that a diabetes PST delivered with the intensity of traditional PST (eight problem-solving sessions) was an effective intervention in a challenging adult patient population. 34 Participants in both the intensive and condensed interventions rated the problem solving–based self-management training as highly satisfactory, helpful, and easy to understand. 34
Investigations are underway to test the effectiveness of different formats for delivery of the DECIDE approach to PST (i.e., self-study, individual, and group formats) and for greater dissemination (e.g., Internet-based and electronic education platforms) to patients who may benefit from this approach across clinic and community settings. Additionally, a search of active, federally funded research grants using the NIH RePORT database revealed a number of current research projects investigating problem solving among children/adolescents, ethnic minorities, and families. These studies generally describe use of problem solving as an intervention component rather than PST as a stand-alone intervention.
Future research should provide evidence of the effectiveness of PST across populations (e.g., different age-groups, sexes, and racial/ethnic minority groups for whom effectiveness of this approach has not yet been reported, including Asians, Latinos, and Native Americans). Additional research is needed to evaluate and disseminate effective tools for health care professionals' use in implementing problem-solving training and to establish best practices for training health care professionals in the delivery of problem-solving education to patients.
PST, both in its traditional format and in formats adapted for diabetes self-management, can be effective for multiple outcomes of interest to health care professionals treating patients with diabetes. A recent statement from a panel convened by AADE on the current state of the science of problem solving concluded that evidence supports problem solving as an important process, intervention, and skill in diabetes self-management. 35 It teaches patients the skills necessary to achieve goals related to recommended self-care behaviors.
Teaching the problem-solving process to patients is an important role health care professionals can play. Further attention is needed to the skills, experiences, and expectations health care professionals bring to problem-solving interventions and to ensuring that professionals are able to conduct thorough assessments and interventions using this approach. 35
Although the activities of problem solving tend to be included routinely in clinical encounters, it is important that clinicians be able to distinguish between using the problem solving process with patients and teaching patients problem-solving as a self-management and life skill. Training patients in problem solving can be done using diabetes-focused PST. There remains a need for dissemination of effective problem-solving training materials and increased formal training opportunities for health care professionals interested in using this approach.
Preparation of this article was supported by National Institute of Diabetes and Digestive and Kidney Disease Diabetes Research and Training Center grant P60 DK079637 and National Heart, Lung, and Blood Institute grant R01 HL089751.
Email alerts
- Behavioral Interventions to Promote Diabetes Self-Management
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is Rational Emotive Behavior Therapy (REBT)?
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
- How It Works
- Beliefs Addressed
- Effectiveness
- Factors to Consider
- Getting Started
Rational emotive behavior therapy (REBT) is a type of cognitive behavioral therapy (CBT) developed by psychologist Albert Ellis . REBT is an action-oriented approach that’s focused on helping people deal with irrational beliefs and learn how to manage their emotions , thoughts, and behaviors in a healthier, more realistic way.
When people hold irrational beliefs about themselves or the world, problems can result. REBT helps people recognize and alter those beliefs and negative thinking patterns in order to overcome psychological problems and mental distress.
How Rational Emotive Therapy Works
According to REBT, our cognition, emotions, and behavior are connected. In order to understand the impact of events and situations that people encounter throughout life, it’s essential to look at the beliefs people hold about these experiences and the emotions that arise as a result of those beliefs.
The main goal of REBT is to help people respond rationally to situations that would typically cause stress, depression, or other negative feelings. When faced with this type of situation in the future, the emotionally healthy response would be to realize that it is not realistic to expect success in every endeavor. All you can do is learn from the situation and move on.
Main Beliefs
Rational emotive behavior therapy operates under a few main beliefs. The three main beliefs of REBT are:
- You are worthy of self-acceptance no matter what even when you struggle or make mistakes; there is no need for shame or guilt.
- Others are also worthy of acceptance, even when their behavior involves something that you don’t like.
- Negative things will sometimes happen in life, and that doesn’t mean that things are happening in a way they shouldn’t be. Life is not positive all of the time, and there’s no rational reason to expect it to be.
A core concept of REBT is the ABC model. This model explains how, while we may blame external events for our unhappiness, it is our interpretation of these events that truly lies at the heart of our psychological distress.
"ABC" is an acronym for:
- A : Activating event, which is when something happens in the environment around you
- B : Belief, which describes your thoughts about the event or situation
- C : Consequence, which is your emotional response to your belief
During REBT, your therapist will help you learn how to apply the ABC model to your daily life.
If you’re feeling depressed due to a conflict in your relationship , for example, a rational emotive behavior therapist may help you identify the activating event for your problem before encouraging you to figure out which beliefs led to your negative feelings. They would then work with you to change those beliefs and, ultimately, your emotional response to the conflict.
Common Irrational Beliefs Addressed With REBT
An important step in the therapeutic process is recognizing the underlying beliefs that lead to psychological distress. In many cases, these are reflected as absolutes, as in "I must," "I should," or "I can’t."
Some of the most common irrational beliefs addressed in rational emotive behavior therapy include:
- Feeling excessively upset over other people’s mistakes or misconduct
- Believing that you must be perfectly competent and successful in everything to be valued and worthwhile
- Believing that you will be happier if you avoid life’s difficulties or challenges
- Feeling that you have no control over your own happiness; that your contentment and joy are dependent upon external forces
Holding unyielding beliefs like these makes it almost impossible to respond to activating situations in a psychologically healthy way. Possessing rigid expectations of ourselves and others only leads to disappointment, recrimination, regret, and anxiety.
Rational Emotive Behavior Therapy Techniques
A couple of different techniques can be used during rational emotive behavior therapy.
Disputation
One step toward changing your beliefs is undergoing a process called disputation . Disputation is meant to teach you life-long skills to help you manage your emotional response and overall mental health.
During disputation, your therapist will challenge your irrational beliefs using direct methods. They may question your beliefs head-on, causing you to rethink them, or they could ask you to imagine another point of view that you haven’t considered before.
While each therapist may approach disputation differently, challenging your beliefs is part of the process. Ellis suggested that rather than simply being warm and supportive, therapists need to be blunt, honest, and logical in order to push people toward changing their thoughts and behaviors.
Targeting Emotional Responses
An important part of the REBT process is learning how to replace your irrational beliefs with healthier ones. This process can be daunting and upsetting, and it’s normal to feel some discomfort or to worry that you’ve made a mistake.
While REBT uses cognitive strategies, it focuses on emotions and behaviors as well. In addition to identifying and disputing irrational beliefs, therapists and clients also work together to target the emotional responses that accompany problematic thoughts.
Techniques that might be encouraged include:
- Guided imagery
Conditions REBT Can Help With
REBT has some data to support its benefit for a variety of conditions, including:
- Anxiety and distress
- Disruptive behavior in children
- Obsessive-compulsive disorder (OCD)
- Social anxiety disorder
- Psychotic symptoms
REBT has also shown promise in sports psychology , where it can be used to help athletes overcome irrational beliefs that may be negatively impacting their mental health and performance.
Benefits of Rational Emotive Behavior Therapy
When developing REBT, Ellis’s goal was to create an action-oriented approach to psychotherapy that produced results by helping people manage their emotions, cognitions, and behaviors. Indeed, research suggests that REBT is effective at reducing irrational beliefs and changing behavior.
We see the same results in sports psychology, where REBT can decrease irrational beliefs and reduce anxiety for athletes.
Overall, REBT offers several behavioral benefits, like:
- Reduced feelings of anger, anxiety, depression, and distress
- Improved health and quality of life
- Better school performance and social skills
Effectiveness of REBT
REBT has a wide range of potential applications. Because it’s focused on education and taking action, it may be effective for a variety of situations and mental health conditions. It may even lead to lasting change in those who undergo this form of therapy.
Burnout at School or Work
Researchers have studied the impact that REBT has on professional and academic performance. One 2018 study showed that this approach was effective in reducing symptoms of burnout for undergraduate students and continued to help even months after therapy concluded.
Another 2018 study showed similar results for nurses. Group REBT reduced their job-related stress and burnout while increasing their job satisfaction and commitment to their organization.
Depression and Anxiety
REBT may be effective in reducing symptoms for people with depression or anxiety. The positive effects also appear to last even after therapy ends.
REBT has also shown promising results for adolescents experiencing depression. This may be due to its emphasis on teaching techniques like:
- Identifying cognitive errors
- Challenging irrational beliefs
- Separating individuals from their behaviors
- Practicing acceptance
Sports-Related Issues
REBT is quickly gaining popularity as a treatment option for athletes who are experiencing mental health issues. It can be used to restore and maintain athletes’ mental health, helping them learn how to change their outlook and manage their emotions. This often improves their athletic performance, though the goal of REBT in sports psychology is to care for the athlete’s mental well-being first and foremost.
Factors to Consider With REBT
REBT can be a daunting process. For some, disputation may feel aggressive or confrontational, and facing irrational thought patterns can be difficult, as it’s not easy to accept these beliefs as unhealthy. The process of changing these thoughts can be even more challenging, as it may involve learning to let go of long-held beliefs.
REBT is meant to teach you life-long skills and, as such, it’s not a passive process. Your sessions may involve reading assignments and homework , and you’ll likely have to step out of your comfort zone to get the benefits of this form of therapy.
How to Get Started With Rational Emotive Behavior Therapy
To begin REBT, check with your doctor for any recommendations of local therapists or search for mental healthcare professionals who offer this approach either in person or online .
During your first session, your therapist will likely discuss your goals and the activating event (or events) that prompted you to seek treatment. They may want to delve into REBT techniques right away; this form of therapy is very active and focused, so your therapist is not likely to spend a lot of time on casual conversation.
Throughout your treatment, you will probably receive homework assignments to complete and new behaviors to experiment with. Your willingness to try out new beliefs and different behaviors will impact how beneficial REBT is for you.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
Turner MJ. Rational emotive behavior therapy (REBT), irrational and rational beliefs, and the mental health of athletes . Front Psychol . 2016;7:1423. doi:10.3389/fpsyg.2016.01423
Russo-Netzer P, Ameli M. Optimal sense-making and resilience in times of pandemic: Integrating rationality and meaning in psychotherapy . Front Psychol . 2021;12:772. doi:10.3389/fpsyg.2021.645926
Ellis A, Ellis DJ. Rational Emotive Behavior Therapy, Second Edition . Washington, DC; 2019. doi:10.1037/0000134-001
David D, Cotet C, Matu S, Mogoase C, Stefan S. 50 years of rational-emotive and cognitive-behavioral therapy: A systematic review and meta-analysis . J Clin Psychol . 2018;74(3):304-318. doi:10.1002/jclp.22514
Turner M, Barker JB. Examining the efficacy of rational-emotive behavior therapy (REBT) on irrational beliefs and anxiety in elite youth cricketers . J Appl Sport Psychol . 2013;25(1):131-147. doi:10.1080/10413200.2011.574311
Ogbuanya TC, Eseadi C, Orji CT, et al. Effect of rational-emotive behavior therapy program on the symptoms of burnout syndrome among undergraduate electronics work students in Nigeria . Psychol Rep . 2019;122(1):4-22. doi:10.1177/0033294117748587
Kim H-L, Yoon S-H. Effects of group rational emotive behavior therapy on the nurses’ job stress, burnout, job satisfaction, organizational commitment and turnover intention . J Korean Acad Nurs . 2018;48(4):432-442. doi:10.4040/jkan.2018.48.4.432
Zhaleh N, Zarbakhsh M, Faramarzi M, Branch AA. Effectiveness of rational-emotive behavior therapy on the level of depression among female adolescents . 2014;4(4):102-107 J Appl Environ Biol Sci .
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."

3 Ways to Help Clients Learn DBT Skills
How to customize dialectical behavior therapy skills training..
Posted April 9, 2024 | Reviewed by Gary Drevitch
- What Is Therapy?
- Find a therapist near me

If you utilize dialectical behavior therapy (DBT) in your clinical work, you already know that this modality can be extremely helpful to clients. In some cases, DBT literally saves lives. You may also be familiar with how it can be difficult for some clients to tolerate learning DBT concepts and skills.
When teaching DBT-informed skills groups, I have witnessed a range of reactions from clients exposed to this modality. While some become DBT lovers (like me), I have seen others groan or protest as I pass out handouts from the DBT Skills Training Handouts and Worksheets manual. (To better understand why some clients struggle to access DBT, see this post .)
“So I’m Supposed to Customize It?”
Marsha Linehan, author of the DBT Skills Training Manual , acknowledges the difficulties of teaching these skills. She understands the potential barriers and encourages facilitators to use whatever resources, strengths, and skills they have to customize the modality to best meet a client's needs. In her manual, she provides examples of creative ways to support clients. But at the same time, the process of “customization” can be confusing and overwhelming for many facilitators. They may be asking themselves:
- Is there guidance on best practices for modifying DBT so I can ensure that I am not decreasing treatment efficacy?
- How do I come up with creative exercises in my 10 minutes between sessions?
- How much time do I actually need to come up with these exercises or improve the ones I am already using?
- Will changing things improve engagement?
- I’m running a group… How can I customize the skills to benefit all of its members?
Following is what the literature says about improving engagement in skills training and interventions from action-based DBT.
1. Supportive Spaces
As therapists, we know that magic happens in cohesive, supportive groups . This applies to psychoeducation groups as well. Research indicates that a connected, supportive environment in DBT skills training can help individuals who are experiencing strong, unwanted emotions, particularly feelings of anxiety and shame . According to Barnicot and colleagues (2015), participants found learning much easier when there was a “fun, light-hearted atmosphere in the group." These researchers also illuminated how it is beneficial for all participants to feel included in the group process, even those less inclined to volunteer spontaneously.
Most therapists have had the experience of being in the following version of a psychoeducation group: A worksheet is passed out, the facilitator teaches, and then asks for feedback. The facilitator “calls on” certain group members if the room is silent. Group members do not respond to one another, and you can hear the crickets chirping.
Suppose you have participated in or facilitated one of these groups. Imagine the relief you may have felt when the session was over. As you left the group room, you may have asked yourself, "What just happened?”
One of the reasons that psychoeducation groups run in this format can feel a bit cringe is that group members likely feel disconnected from the content, facilitator, and each other. Finding ways for the participants to connect, perhaps by splitting members into dyads for conversations or engaging in an experiential mirroring exercise, can build cohesion. The research indicates that developing a sense of connection and community within a positive environment leads to better outcomes (Cancian et al., 2019). Finding ways to break up the group and create opportunities for connection between participants can greatly increase cohesion and shift the group from “When will this end?” to “We have so much more to discuss!” One pathway to generating a supportive space is helping group members connect with one another—a strategy that can shift the entire energy of the group.
2. Personalization
Personalizing skills for each group member may support participants in better understanding and internalizing information. You likely already know this, as it was a concept taught in graduate school. When teaching DBT skills, “leaders often have to be creative in demonstrating how particular sets of skills apply to particular problems” (Linehan, 2015).
Research emphasizes the personalization of skills and highlights that the understanding of each client's specific challenges is the first step toward personalization. This can be quite a challenge when managing an entire group of clients with varied skills and needs. That being said, prompting clients with directives that allow them to apply the skills to their own life is a great place to start.

If teaching the DEAR MAN skill , for example, use the client’s experience (not an example from a handout). If the clients are too overwhelmed to provide personal experiences with the group, encourage them to write one down or break the group into dyads so they can share with another individual. If that is still overwhelming, just have them write about a personal experience. Assess each of their unique struggles and try to pinpoint the precise triggers, behavior patterns, or emotions that need specific attention .
By tailoring the delivery of these skills to the individual needs and preferences of each client, you can greatly improve their engagement in the therapeutic process and overall results for everyone.
3. Creativity
The ability to foster a sense of creativity within your group can also strongly impact engagement in these settings. For example, give each participant a chance to think on their own before a group brainstorm. Research suggests that clients will come up with more creative ideas if they can respond to facilitator prompts independently before sharing them with others (D’Zurilla & Nezu, 1999; Paulus & Brown, 2007). In other words, it can be more effective to have the clients jot down ideas on their own and then bring the group together to brainstorm.
Linehan knew about the importance of getting creative with DBT, and the research has supported this. Cancian and colleagues (2019) suggested that experiential and creative exercises, particularly ones that included “stories, metaphors, and practical exercises,” facilitated client engagement and comprehension. Some creative arts therapists have found that psychoeducation groups are more effective when clinicians teach skills in creative ways (Clark, 2017; Heckwolf et al., 2014; Huckvale & Learmonth, 2009; Morris, 2018; von Daler & Schwanbeck, 2014; Walters, 2018; Roohan & Trottier, 2021). While going through the many ways creative interventions have been infused into DBT skills training is not within the scope of this page, I think it is essential to acknowledge that this work is happening.
Barnicot, K., Couldrey, L., Sandhu, S., & Priebe, S. (2015). Overcoming Barriers to Skills Training in Borderline Personality Disorder: A Qualitative Interview Study. PLOS One, 10(10).
Cancian, A. C. M., de Souza, L. S., & da Silva Oliveira, M. (2019). Qualitative analysis of a Dialectical Behavior Therapy adapted Skills Training group for women with obesity. Contextos Clínicos, 12(3), 707.
Clark, S. M. (2017). DBT-informed art therapy: Mindfulness, cognitive behavior therapy, and the creative process. Jessica Kingsley Publishers.
D’Zurilla, T. J., & Nezu, A. M. (1999). Problem- solving therapy: A social competence approach to clinical intervention (2nd ed.). New York: Springer.
Heckwolf, J. I., Bergland, M. C., & Mouratidis, M. (2014). Coordinating principles of art therapy and DBT. The Arts in Psychotherapy, 41(4), 329-335.
Huckvale, K., & Learmonth, M. (2009). A case example of art therapy in relation to dialectical behaviour therapy. International Journal of Art Therapy, 14(2), 52-63.
Linehan, M.M. (2015). DBT skills training manual (2nd ed.). Guilford Press.
Morris, N. (2018). Dramatherapy for borderline personality disorder: Empowering and nurturing people through creativity. Routledge.
Paulus, P. B., & Brown, V. R. (2007). Toward more creative and innovative group idea generation: A cognitive–social–motivational perspective of brainstorming. Social and Personality Psychology Compass, 1, 248–265.
Von Daler, K., and Schwanbeck, L. (2014). Creative mindfulness: Dialectical behavior therapy and expressive arts therapy. In L. Rappaport (Ed.), Mindfulness and the arts therapies: Theory and practice (pp. 107-116). Jessica Kingsley Publishers.

Mary Kate Roohan, Psy.D., is a licensed psychologist and drama therapist and the founder of Thrive and Feel, a therapy practice that supports clients in managing emotional sensitivity.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

IMAGES
VIDEO
COMMENTS
Problem-solving therapy is a brief intervention that provides people with the tools they need to identify and solve problems that arise from big and small life stressors. It aims to improve your overall quality of life and reduce the negative impact of psychological and physical illness. Problem-solving therapy can be used to treat depression ...
Key points. Problem-solving is one technique used on the behavioral side of cognitive-behavioral therapy. The problem-solving technique is an iterative, five-step process that requires one to ...
Problem-solving therapy (PST) is an intervention with cognitive and behavioral influences used to assist individuals in managing life problems. Therapists help clients learn effective skills to address their issues directly and make positive changes. PST is used in various settings to address mental health concerns such as depression, anxiety, and more.
Cognitive behavior therapy (CBT) is a type of mental health treatment that helps identify and change thought patterns that contribute to psychological distress. ... Problem-Solving . Learning problem-solving skills during cognitive behavioral therapy can help you learn how to identify and solve problems that may arise from life stressors, both ...
Cognitive behavioral therapy or CBT is a popular psychotherapy that helps you change your negative thoughts to improve your mood and relationships. ... like problem-solving, personal interaction ...
Problem-solving therapy is a cognitive-behavioral intervention geared to improve an individual's ability to cope with stressful life experiences. The underlying assumption of this approach is that symptoms of psychopathology can often be understood as the negative consequences of ineffective or maladaptive coping.
Cognitive behavioral therapy (CBT) is a short-term form of psychotherapy based on the idea that the way someone thinks and feels affects the way he or she behaves. CBT aims to help clients resolve ...
Cognitive behavioral therapy (CBT) is a form of psychological treatment that has been demonstrated to be effective for a range of problems including depression, anxiety disorders, alcohol and drug use problems, marital problems, eating disorders, and severe mental illness. Numerous research studies suggest that CBT leads to significant ...
Cognitive behavioral therapy (CBT) is a structured, goal-oriented type of psychotherapy (talk therapy). Mental health professionals, including psychologists, therapists and counselors, use it to treat or manage mental health conditions and emotional concerns. It's one of the most common and best-studied forms of psychotherapy.
Cognitive behavioral therapy (CBT) is one of the most common and best studied forms of psychotherapy. It is a combination of two therapeutic approaches, known as cognitive therapy and behavioral therapy. The exact treatment approaches used will depend on the illness or problem to be treated. But the basic idea behind the therapy is always the same: What we think, how we behave, and how other ...
"Problem-solving therapy (PST) is a psychosocial intervention, generally considered to be under a cognitive-behavioral umbrella" (Nezu, Nezu, & D'Zurilla, 2013, p. ix). It aims to encourage the client to cope better with day-to-day problems and traumatic events and reduce their impact on mental and physical wellbeing.
This book represents the culmination of decades of research and clinical experience regarding various problem-solving-based interventions. These interventions, primarily known as problem-solving therapy (PST), have been in existence since the 1970s. Historically, the "first wave" of behavior therapy or modification was based very heavily on principles of respondent learning and operant learning.
This article provides an overview of this literature and especially highlights the flexible nature of problem-solving therapy with regard to targeted problems and populations, clinical treatment goals, and modes of implementation. ... Nezu, A. M. (2004). Problem solving and behavior therapy revisited. Behavior Therapy, 35(1), 1-33. https://
Problem-solving is a fundamental aspect of dialectical behavior therapy, as it involves applying the skills learned in DBT to address and resolve real-life challenges. By developing effective problem-solving strategies, individuals can better navigate life's difficulties, reduce emotional distress, and foster greater personal empowerment and ...
BEHAVIOR THERAPY 35, 1--33, 2004 Problem Solving and Behavior Therapy Revisited ARTHUR M. NEZU Drexel University Over three decades ago, D'Zurilla and Goldfried (1971) published a seminal article delineating a model of problem-solving training geared to enhance social competence and decrease psychological distress. Since that time, a ...
Cognitive behavioural therapy (CBT) explores the links between thoughts, emotions and behaviour. It is a directive, time-limited, structured approach used to treat a variety of mental health disorders. It aims to alleviate distress by helping patients to develop more adaptive cognitions and behaviours. It is the most widely researched and ...
Step Four: Put the Solution into Action. After you have brainstormed for ideas about what you can do to change the aspects that are changeable, choose what works best for you and try to put the solution into action. Actively decide and remind yourself to act the way you decided to next time you find yourself in the situation.
worksheet. Guide your clients and groups through the problem solving process with the help of the Problem Solving Packet. Each page covers one of five problem solving steps with a rationale, tips, and questions. The steps include defining the problem, generating solutions, choosing one solution, implementing the solution, and reviewing the ...
Problem solving is a basic human thinking process. Many general counseling and psychotherapy approaches, such as cognitive behavioral therapy, include problem solving as a component of treatment for managing life problems and emotional disorders. 1 Similarly, educational and lifestyle interventions in diabetes often include elements of problem solving as part of broader intervention approaches. 2
Behavior Therapy: Basics and Beyond, 3rd ed. (2020), and Beck, J. S. Cognitive Therapy for Challenging Problems (2005). As noted in these books, the decision to use any given worksheet is based on the
Getting Started. Rational emotive behavior therapy (REBT) is a type of cognitive behavioral therapy (CBT) developed by psychologist Albert Ellis. REBT is an action-oriented approach that's focused on helping people deal with irrational beliefs and learn how to manage their emotions, thoughts, and behaviors in a healthier, more realistic way.
How to customize dialectical behavior therapy skills training. Posted April 9, 2024 | ... A. M. (1999). Problem- solving therapy: A social competence approach to clinical intervention (2nd ed.). ...