- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram

Researchers solve mystery of how statins improve blood vessel health
Statins designed to lower cholesterol have long been noted to work in mysterious ways to improve other aspects of cardiovascular health. A Stanford Medicine-led study uncovers how they do it.
May 8, 2023 - By Nina Bai

Researchers at Stanford Medicine and their colleagues have discovered how statins improve cardiovascular health beyond lowering cholesterol. roger ashford/Shutterstock.com
Using new genetic tools to study statins in human cells and mice, Stanford Medicine researchers and collaborators have uncovered how the cholesterol-lowering drugs protect the cells that line blood vessels.
The findings provide new insight into statins’ curiously wide-ranging benefits, for conditions ranging from arteriosclerosis to diabetes, that have long been observed in the clinic.
“The study gives us an understanding, at a very deep mechanistic level, of why statins have such a positive effect outside of reducing LDL,” said professor of medicine Joseph Wu , MD, PhD, referring to low-density lipoprotein, or “bad” cholesterol. “Given how many people take statins, I think the implications are pretty profound.”
Statins are the most prescribed medications in the country, with more than 40 million Americans taking them. Developed in the 1980s from compounds found in mold and fungi, statins target an enzyme that regulates cholesterol production in the liver. But clinical trials have shown that they also seem to safeguard against cardiovascular disease beyond their ability to lower cholesterol.
Heart failure patients who take statins, for example, are less likely to suffer a second heart attack. They have also been shown to prevent the clogging of arteries, reduce inflammation and even lower cancer risk. Yet these underlying mechanisms are poorly understood.
“Statins were invented to lower cholesterol by targeting the liver. But we didn’t know the targets or the pathways in the cardiovascular system,” said Chun Liu , PhD, an instructor at the Stanford Cardiovascular Institute and co-lead author of the study published May 8 in Nature Cardiovascular Research . Mengcheng Shen , PhD, and Wilson Tan, PhD, postdoctoral scholars at the Stanford Cardiovascular Institute, are the other co-lead authors, and Wu is the senior author.

Hints from a dish
To take a closer look at statins’ effect on blood vessels, Liu and colleagues tested a common statin, simvastatin, on lab-grown human endothelial cells derived from induced pluripotent stem cells. Endothelial cells make up the lining of blood vessels, but in many diseases they transform into a different cell type, known as mesenchymal cells, which are poor substitutes.
“Mesenchymal cells are less functional and make tissues stiffer so they cannot relax or contract correctly,” Liu said.
The researchers suspected that statins could reduce this harmful transition. Indeed, endothelial cells treated with simvastatin in a dish formed more capillary-like tubes, a sign of their enhanced ability to grow into new blood vessels.
RNA sequencing of the treated cells offered few clues. The researchers saw some changes in gene expression, but they “didn’t find anything interesting,” Liu said.
It was not until they employed a newer technique called ATAC-seq that the role of statins became apparent. ATAC-seq reveals what happens at the epigenetic level, meaning the changes to gene expression that do not involve changes to the genetic sequence.
They found that the changes in gene expression stemmed from the way strings of DNA are packaged inside the cell nucleus. DNA exists in our cells not as loose strands but as a series of tight spools around proteins, together known as chromatin. Whether particular DNA sequences are exposed or hidden in these spools determines how much they are expressed.
“When we adopted the ATAC-seq technology, we were quite surprised to find a really robust epigenetic change of the chromatin,” Liu said.
ATAC-seq revealed that simvastatin-treated cells had closed chromatin structures that reduced the expression of genes that cause the endothelial-to-mesenchymal transition. Working backward, the researchers found that simvastatin prevents a protein known as YAP from entering the nucleus and opening chromatin.
The YAP protein is known to play important roles in development, such as regulating the size of our organs, but also has been implicated in the abnormal cell growth seen in cancer.
A look at diabetes
To see the drug in context, the researchers tested simvastatin on diabetic mice. Diabetes causes subtle changes to blood vessels that mimic the damage commonly seen in people who are prescribed statins — older patients who do not have a cardiovascular condition, Liu said.
They found that after eight weeks on simvastatin, the diabetic mice had significantly improved vascular function, with arteries that more easily relaxed and contracted.
“If we can understand the mechanism, we can fine-tune this drug to be more specific to rescuing vascular function,” Liu said.
The findings also provide a more detailed picture of the vascular disease process, which could help doctors identify and treat early signs of vascular damage.
“I’ve been taking statins for the past 10 years to keep my cholesterol down. I also knew it has good vascular effects. I just didn’t know how it does it,” said Wu, the Simon H. Stertzer, MD, Professor who is also the director of the Stanford Cardiovascular Institute. “This study explains how.”
Researchers from the University of North Texas and the Ohio State University College of Medicine contributed to this study.
The study was supported by funding from the National Institutes of Health (grants R01 HL130020, R01 HL150693, R01 HL163680, R01 HL145676, P01 HL141084, R01 HL141371, R01 HL126527, R01 HL15864, R01 HL161002, R01 HL155282 and 18CDA34110293), an American Heart Association SFRN grant, an AHA Career Development Award and the Tobacco-Related Disease Research Program.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care


An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- News and Events
- < Back To All News
Study challenges “good” cholesterol’s role in universally predicting heart disease risk

Lower levels of HDL cholesterol were associated with increased risks for heart attacks in white but not Black adults, and higher levels were not protective for either group
A National Institutes of Health-supported study found that high-density lipoprotein (HDL) cholesterol, often called the “good cholesterol,” may not be as effective as scientists once believed in uniformly predicting cardiovascular disease risk among adults of different racial and ethnic backgrounds. The research, which published in the Journal of the American College of Cardiology , found that while low levels of HDL cholesterol predicted an increased risk of heart attacks or related deaths for white adults – a long-accepted association – the same was not true for Black adults. Additionally, higher HDL cholesterol levels were not associated with reduced cardiovascular disease risk for either group.
“The goal was to understand this long-established link that labels HDL as the beneficial cholesterol, and if that’s true for all ethnicities,” said Nathalie Pamir, Ph.D., a senior author of the study and an associate professor of medicine within the Knight Cardiovascular Institute at Oregon Health & Science University, Portland. “It’s been well accepted that low HDL cholesterol levels are detrimental, regardless of race. Our research tested those assumptions.”
To do that, Pamir and her colleagues reviewed data from 23,901 United States adults who participated in the Reasons for Geographic and Racial Differences in Stroke Study (REGARDS). Previous studies that shaped perceptions about “good” cholesterol levels and heart health were conducted in the 1970s through research with a majority of white adult study participants. For the current study, researchers were able to look at how cholesterol levels from Black and white middle-aged adults without heart disease who lived throughout the country overlapped with future cardiovascular events. Study participants enrolled in REGARDS between 2003-2007 and researchers analyzed information collected throughout a 10- to 11-year period. Black and white study participants shared similar characteristics, such as age, cholesterol levels, and underlying risk factors for heart disease, including having diabetes, high blood pressure, or smoking. During this time, 664 Black adults and 951 white adults experienced a heart attack or heart attack-related death. Adults with increased levels of LDL cholesterol and triglycerides had modestly increased risks for cardiovascular disease, which aligned with findings from previous research.
However, the study was the first to find that lower HDL cholesterol levels only predicted increased cardiovascular disease risk for white adults. It also expands on findings from other studies showing that high HDL cholesterol levels are not always associated with reduced cardiovascular events. The REGARDS analysis was the largest U.S. study to show that this was true for both Black and white adults, suggesting that higher than optimal amounts of “good” cholesterol may not provide cardiovascular benefits for either group.
“What I hope this type of research establishes is the need to revisit the risk-predicting algorithm for cardiovascular disease,” Pamir said. “It could mean that in the future we don’t get a pat on the back by our doctors for having higher HDL cholesterol levels.”
Pamir explained that as researchers study HDL cholesterol’s role in supporting heart health, they are exploring different theories. One is quality over quantity. That is, instead of having more HDL, the quality of HDL’s function – in picking up and transporting excess cholesterol from the body – may be more important for supporting cardiovascular health . They are also taking a microscopic look at properties of HDL cholesterol, including analyzing hundreds of proteins associated with transporting cholesterol and how varying associations, based on one protein or groups of proteins, may improve cardiovascular health predictions.
“HDL cholesterol has long been an enigmatic risk factor for cardiovascular disease,” explained Sean Coady, a deputy branch chief of epidemiology within the National Heart, Lung, and Blood Institute (NHLBI)’s Division of Cardiovascular Sciences. “The findings suggest that a deeper dive into the epidemiology of lipid metabolism is warranted, especially in terms of how race may modify or mediate these relationships.” The authors conclude that in addition to supporting ongoing and future research with diverse populations to explore these connections, the findings suggest that cardiovascular disease risk calculators using HDL cholesterol could lead to inaccurate predictions for Black adults.
“When it comes to risk factors for heart disease, they cannot be limited to one race or ethnicity,” said Pamir. “They need to apply to everyone.”
The REGARDS study is co-funded by the National Institute of Neurological Disorders and Stroke and the National Institute of Aging and received additional support from NHLBI. To learn more about cholesterol and heart health, visit https://www.nhlbi.nih.gov/health/blood-cholesterol . To learn about heart-healthy living, visit https://www.nhlbi.nih.gov/health/heart-healthy-living . Study: Zakai NA, Minnier J, Safford MM, et al. Race-dependent association of high-density lipoprotein cholesterol levels with incident coronary artery disease. J Am Coll Cardiol . 2022; doi: 10.1016/j.jacc.2022.09.027.
About the National Heart, Lung, and Blood Institute (NHLBI): NHLBI is the global leader in conducting and supporting research in heart, lung, and blood diseases and sleep disorders that advances scientific knowledge, improves public health, and saves lives. For more information, visit www.nhlbi.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
More Information
Related health topics, health education, related news.

In two studies, experimental drugs for cholesterol show ‘revolutionary’ promise
New, experimental drugs designed to drive down dangerous levels of cholesterol were shown to be safe and effective in two groundbreaking bodies of research presented Sunday at an annual meeting of the American Heart Association.
Both medications target people born with a genetic predisposition to high cholesterol. While drugs like statins , as well as diet and exercise, can help these individuals manage cholesterol, they cannot change the underlying genetic cause.
The two new approaches work in different ways, but with a singular mission: go after genes responsible for raising cholesterol to change the trajectory of a person’s risk for heart attack and stroke .
Neither treatment had ever been tested in humans before. And both will need years of additional research before they'd be considered for approval by the Food and Drug Administration. Still, experts are impressed with the results.
"There is no way to categorize this other than revolutionary," said Dr. Hugh Cassiere, director for critical care services at South Shore University Hospital, Northwell Cardiovascular Institute in New York. Cassiere was not involved with either study.
A tiny change to a gene
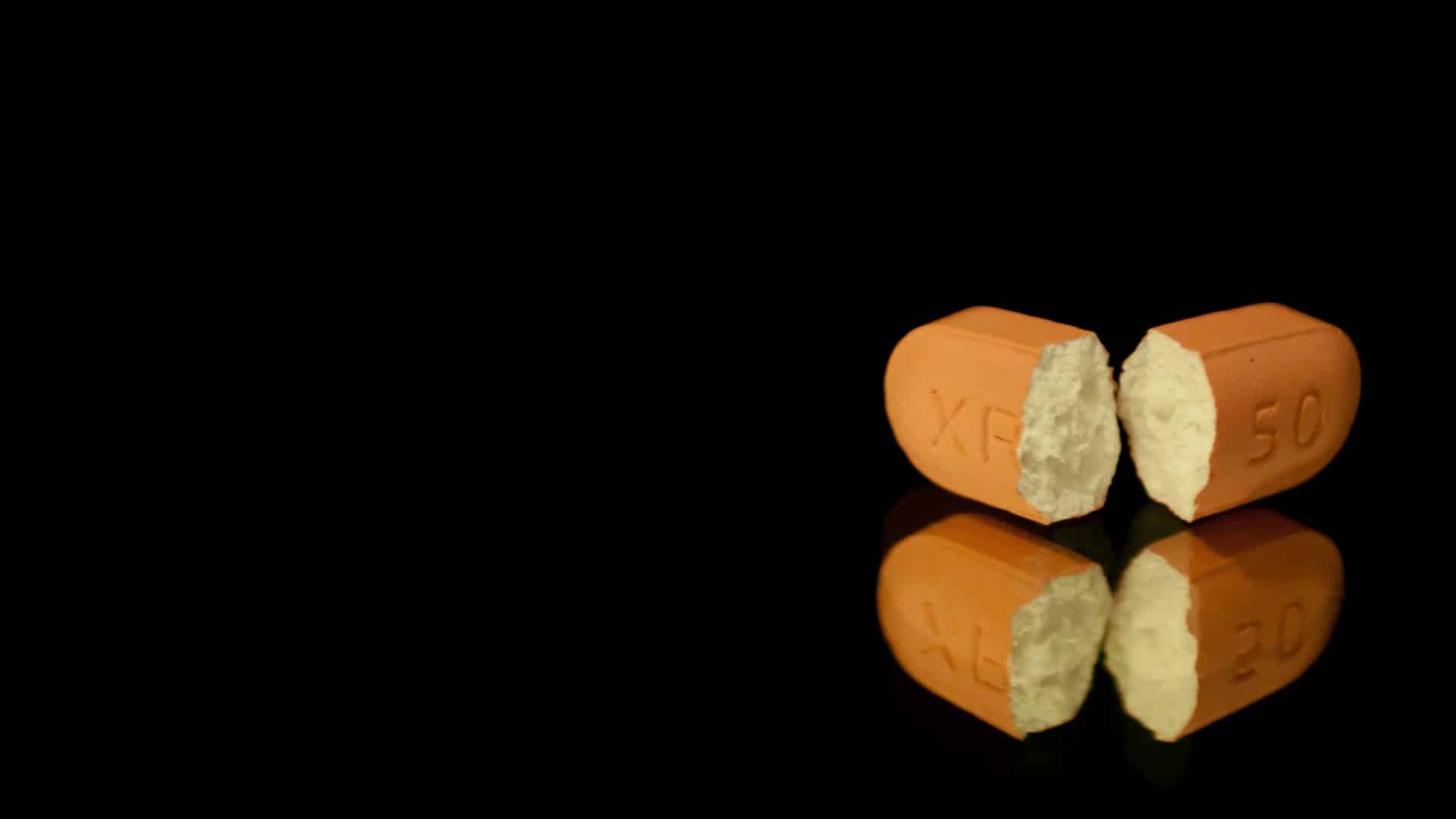
One of the treatments, from Boston-based Verve Therapeutics, uses a gene-editing approach called base editing. It involves an IV infusion of a drug that targets the PCSK9 gene, which is instrumental in the production of LDL, often called "bad" cholesterol .
When the drug zeroes in on PCSK9, it makes a tiny change to the gene. The effect is akin to a permanent eraser, removing its ability to raise cholesterol, said Dr. Sekar Kathiresan, Verve's co-founder and chief executive officer.
In theory, the one-time treatment should last a lifetime. Patients so far have only been followed for six months.
Verve's preliminary study, which was presented on Sunday, was meant to test the safety of the drug. Ten patients participated. Most received doses that didn't make a measurable difference in their LDL levels, but were found to be safe.
Three patients, however, were given higher doses — and their LDL cholesterol levels were reduced by more than half. Additional studies will be needed to ensure the treatment remains safe, without unexpected side effects, and effective.
Verve's research was limited to people with a genetic condition called heterozygous familial hypercholesterolemia , in which cholesterol levels are sky-high from birth. Many people affected suffer heart attacks at young ages, in their 30s or 40s.
Kathiresan, a cardiologist who previously worked at Massachusetts General Hospital and was a professor of medicine at Harvard Medical School, has long focused his research on understanding why some people have heart attacks at young ages, and why others do not. He has a strong family history of high cholesterol. In 2012, his brother died from a heart attack at age 40.
That's when Kathiresan decided "to try to develop a therapy that could avert tragedies like what's happened in my family."
It is unclear whether the approach will make a measurable impact on heart attack and stroke risk — that remains to be seen in future studies.
Experts were still optimistic about the technology.
"While larger and longer-term studies are required to assess both effectiveness, durability and safety, this should be the dawn of an era of therapeutic gene targeting for cardiovascular disease," said Dr. Sahil Parikh, director of endovascular services at Columbia University Irving Medical Center in New York. Parikh was not involved with Verve's research.
Shooting the messenger
Findings on a second novel therapy were also presented on Sunday.
The results, though early, offer a promising glimpse of what could be the first treatment for a particularly dangerous type of cholesterol called lipoprotein(a).
People with high levels of Lp(a) are at extremely high risk of having fats and cholesterol build up in their arteries.
That's because Lp(a) gloms onto LDL cholesterol, making those LDL particles even stickier and more likely to cause plaque.
It's like adding super glue to duct tape. And it's purely genetic, meaning that people are born with this elevated risk. Diet and exercise have no impact on Lp(a) levels.
"It is essentially untreatable," said study author Dr. Steven Nissen, chief academic officer of the Heart, Vascular & Thoracic Institute at Cleveland Clinic. "The only way to target such a genetic risk factor is to find a way to interfere with the product of the gene."
Nissen and colleagues used a novel approach to correcting how that gene acts.
They used a drug called lepodisiran, which targets mRNA. If that sounds familiar, it should: Most Covid vaccines use mRNA to prompt the body to make an antibody against SARS-CoV-2.
In this case, the mRNA in question tells the body to produce Lp(a). The drug stops this from happening, essentially shooting the messenger.
Nissen's study was meant to test the safety of lepodisiran. It was small, including just 48 adults in the U.S. and Singapore. All had very high levels of Lp(a). Overall, the drug was found to be safe, with no major side effects, Nissen said.
But it also dramatically lowered their Lp(a) levels. A single shot of lepodisiran drove down Lp(a) by more than 94% for nearly one year, the study found.
The results of the study, which was sponsored by drugmaker Eli Lilly, were published Sunday in the Journal of the American Medical Association .
"This really offers a lot of hope for patients with elevated lipoprotein(a)," Nissen said. "We're working as fast as we can because there are patients dying every day because of this disorder. We've not been able to treat it, and we need to change that."
As many as 64 million Americans have elevated Lp(a) levels, most commonly people of African and South Asian descent.
Additional research is critical. An important question moving forward is whether lowering Lp(a) actually cuts heart risks.
"We've had to wait until this generation of therapeutics where we can directly and specifically target Lp(a) and do it safely to see whether that will also result in fewer heart attacks and strokes," said Dr. Donald Lloyd-Jones, professor and chair of the department of preventive medicine Northwestern Feinberg School of Medicine in Chicago. Lloyd-Jones, also a past president of the American Heart Association, was not involved with the lepodisiran study.
Nissen predicts that the treatment could someday be used as an "annual vaccine-like treatment for this previously untreatable disorder."
While many heart problems may be avoided with lifestyle changes such as exercise and healthy diets, Lloyd-Jones said, the medical community needs therapies to help people whose genes put them at greater risk for heart attacks and stroke.
"We'll always need some medication for people who are at very high risk," he said.
Follow NBC HEALTH on Twitter & Facebook .
Erika Edwards is a health and medical news writer and reporter for NBC News and "TODAY."
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Exercise cuts heart disease risk in part by lowering stress, study finds

How to realize immense promise of gene editing

Women rarely die from heart problems, right? Ask Paula.
Don’t need high cholesterol to benefit from statins.
Miles Martin
BWH Communications
Studies find drug protects against heart disease in high-risk groups
Two new studies found that statins, the most prescribed class of drugs to treat high cholesterol, are protective for high-risk groups who haven’t yet had a heart attack or stroke but could be at risk of one, according to Harvard-affiliated Brigham and Women’s Hospital.
The results provide additional context to a longstanding debate among the medical community about whether there are benefits to initiating statin use in people who don’t already have high cholesterol or cardiovascular disease. The studies appear in the JAMA Network Open and the Journal of the American Geriatrics Society.
“Statins are a first line class of drugs that can lower cholesterol and lower the risk of a second heart attack or stroke in people who have already had one — there’s no question about that,” said corresponding author Ariela Orkaby of the Brigham’s Division of Aging . “However, many clinicians still don’t agree on whether statins should be used as a preventative treatment for people who haven’t had a heart attack or stroke yet but are at high risk due to age or other factors.
“Our findings demonstrate statins have a protective effect even in people who haven’t had their first major cardiac event, which means there are still benefits to prescribing these medications for primary prevention of heart disease,” said Orkaby, who is also an investigator in the Veterans Affairs Geriatric Research Education and Clinical Center.
For most people, statins are well-tolerated and don’t have significant side-effects. However, some doctors over the last few years have called for these medications to stop being prescribed for certain people, including those with chronic kidney disease. Notably, cardiovascular disease is the leading cause of death for older adults with kidney disease.
“Our results suggest that for statins, frailty status doesn’t decrease benefit, and it may be the frailest older adults who benefit the most.” Ariela Orkaby, Brigham and Women’s Hospital
“There has been some chatter about statins causing muscle pains but, for the vast majority of people, these are very safe and effective medications,” said Orkaby. “The problem is that we’re still missing a lot of clinical evidence about their effectiveness in certain groups, which has made some doctors deprescribe statins out of caution.”
In their study of 14,828 people with chronic kidney disease, the researchers found that starting statins was associated with 9 percent reduced mortality and a 4 percent lower risk of heart attack or stroke. The team also looked at a much larger group of older adults without kidney disease, of whom 12 percent were frail. Among this group of 710,313 people, they found that statin therapy was associated with a 39 percent lower risk of mortality and 14 percent lower risk of a first heart attack or stroke. Both studies used data from the Veteran’s Affairs Healthcare System.
Notably, the researchers found that these reductions in mortality and disease risk were independent of frailty, which the researchers measured through a score that accounted for dozens of age-related health conditions.
“When we’re talking about the risk-benefit analysis of using a certain medication in older populations, we need to consider frailty because medications may not work as well or may cause more side effects in people who are frailer,” said Orkaby. “Our results suggest that for statins, frailty status doesn’t decrease benefit, and it may be the frailest older adults who benefit the most.”
While the two studies benefited from the large patient population and long-term follow-up afforded by working with VA data, the researchers caution that their conclusions drawn from past patient data should be validated in new clinical trials that prospectively address these questions.
“We’re still missing some of the evidence we need to fully understand the scope of what these medications do,” said Orkaby. “However, these studies tell us that until we have clinical data that suggests otherwise, statins are safe and effective for older people and those with chronic kidney disease.”
Disclosures: Ariela Orkaby accepted personal fees from Anthos Therapeutics during this research, unrelated to this work. Luc Djosse reports current research funding from Novartis, unrelated to this work.
This research was supported by grants from the National Institute on Aging (R03-AG060169) and Veterans Affairs (IK2-CX001800, I01 CX001025) .
Share this article
You might like.
Benefits nearly double for people with depression

Nobel-winning CRISPR pioneer says approval of revolutionary sickle-cell therapy shows need for more efficient, less expensive process

New book traces how medical establishment’s sexism, focus on men over centuries continues to endanger women’s health, lives
Finding right mix on campus speech policies
Legal, political scholars discuss balancing personal safety, constitutional rights, academic freedom amid roiling protests, cultural shifts
Good genes are nice, but joy is better
Harvard study, almost 80 years old, has proved that embracing community helps us live longer, and be happier
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Research Highlight
- Published: 16 April 2024
Gut microbiota
Gut bacteria can break down cholesterol
- Irene Fernández-Ruiz 1
Nature Reviews Cardiology ( 2024 ) Cite this article
25 Accesses
Metrics details
- Dyslipidaemias
Alterations in the gut microbiome have been associated with an increased risk of cardiovascular disease (CVD), but the underlying mechanisms are not fully understood. A study published in Cell now identifies a group of gut bacteria that can metabolize cholesterol and are associated with lower plasma cholesterol levels. Thus, these gut bacteria could have potential benefits for lipid homeostasis and cardiovascular health.
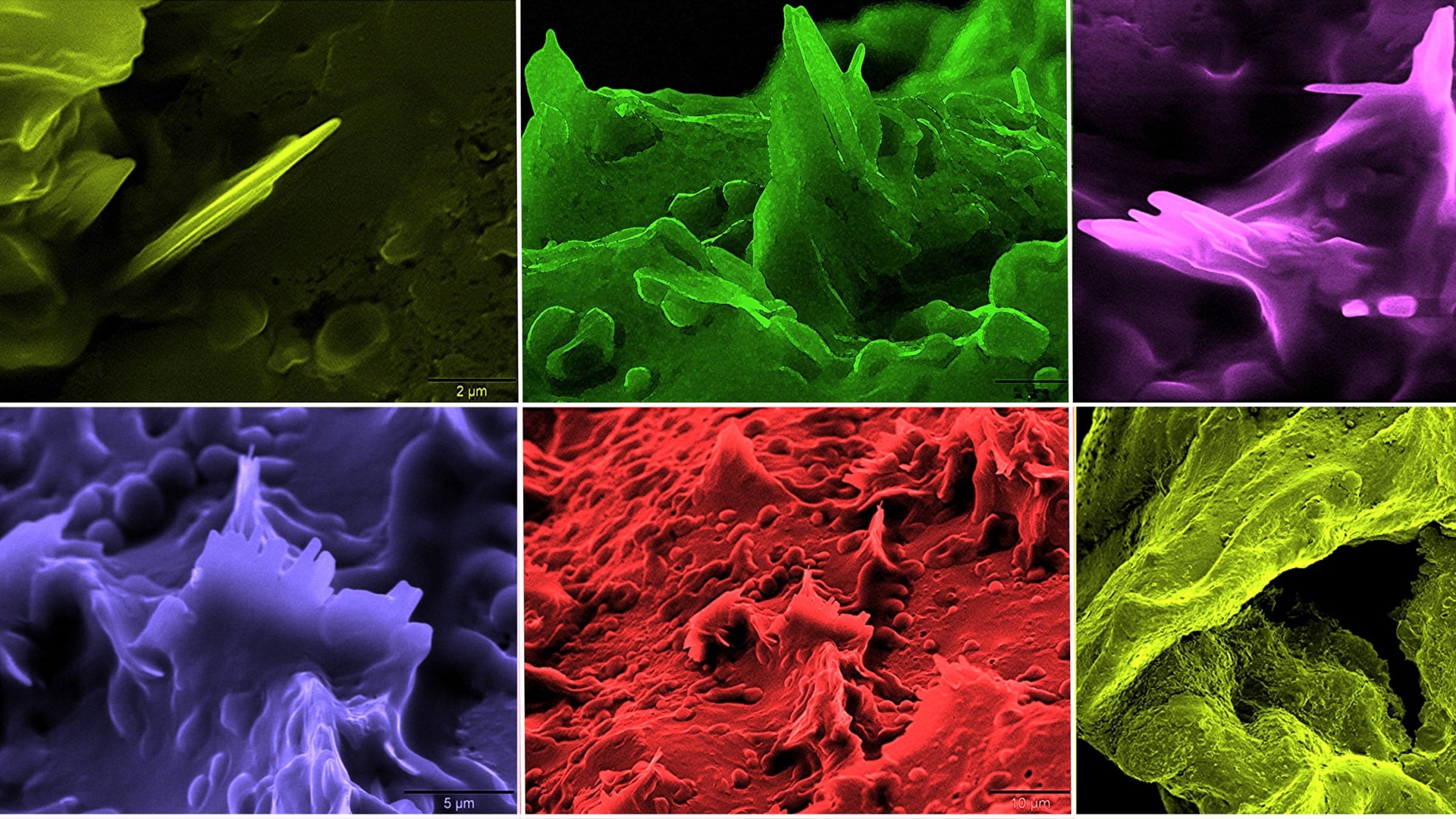
Next, the investigators showed that Oscillibacter can metabolize cholesterol through multiple pathways. Molecular networking and structural similarity searches using a protein language model identified several candidate genes involved in cholesterol metabolism in Oscillibacter . Functional prediction and in vitro assays of multiple gut Oscillibacter isolates from human samples demonstrated that Oscillibacter have conserved cholesterol-metabolizing capacity, with efficient cholesterol uptake and transformation into cholestenone, glycosylated cholesterol and hydroxycholesterol.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Original article
Li, C. et al. Gut microbiome and metabolome profiling in Framingham Heart Study reveals cholesterol-metabolizing bacteria. Cell 187 , 1834–1852.e19 (2024)
Article PubMed Google Scholar
Related article
Chakaroun, R. M. et al. The potential of tailoring the gut microbiome to prevent and treat cardiometabolic disease. Nat. Rev. Cardiol. 20 , 217–235 (2023)
Download references
Author information
Authors and affiliations.
Nature Reviews Cardiology http://www.nature.com/nrcardio/
Irene Fernández-Ruiz
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Irene Fernández-Ruiz .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Fernández-Ruiz, I. Gut bacteria can break down cholesterol. Nat Rev Cardiol (2024). https://doi.org/10.1038/s41569-024-01026-w
Download citation
Published : 16 April 2024
DOI : https://doi.org/10.1038/s41569-024-01026-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

New heart disease calculator could save lives by identifying high-risk patients missed by current tools
Collaborative research, led from the University of Oxford and published today in Nature Medicine , has developed a new tool called QR4 that more accurately predicts an individual's 10-year risk of cardiovascular diseases, like heart disease and stroke, particularly identifying high-risk patients that current prediction tools miss.
Cardiovascular disease is a leading cause of death globally. The new tool, QR4 can be thought of as a type of calculator that lets doctors use an individual’s health data, such as blood pressure, age and medical history, to estimate their likelihood of developing a cardiovascular disease over the next 10 years, allowing them to intervene early to prevent illness.
QR4 includes seven new risk factors applicable to all adults: chronic obstructive pulmonary disease (COPD), learning disabilities, Down syndrome and four cancer types (blood, lung, oral and brain), highlighting how other significant diseases impact on heart health.
QR4 also identified factors specific to women's health that were predictive of future heart disease risk, such as complications from high blood pressure during pregnancy, and postnatal depression.
'While traditional cardiovascular risk factors such as smoking and high cholesterol are well-recognised, our latest research identifies less obvious, yet crucial risk indicators,' said Professor Julia Hippisley-Cox , lead author, Professor of Clinical Epidemiology and General Practice, at the University of Oxford’s Nuffield Department of Primary Care Health Sciences . 'For instance, conditions like postnatal depression and Down’s syndrome significantly contribute to cardiovascular risk, underscoring the complex interplay between mental health, genetic factors, and heart health. QR4 also helps to address inequalities in health, particularly around learning disabilities, which often coincide with barriers to effective health management and access, leading to an increased risk.
'We believe that these findings are important to both patients and policy makers,' said P rofessor Hippisley-Cox . 'They indicate that more groups of people are at increased risk for heart and circulatory diseases than previously recognised. These people could and should now benefit from treatments and other preventive measures to reduce their risk.'
'Our findings also reveal that women with COPD are at a higher risk of cardiovascular diseases than previously understood,' said Professor Mona Bafadhel , co-author, Chair of Respiratory Medicine, King’s College, London and Asthma + Lung UK Professor. 'This underscores the critical need for targeted cardiovascular monitoring and interventions in these patients, which begins with an early diagnosis.'
As part of a comprehensive evaluation, the QR4 algorithm was rigorously tested against some of the most well-established cardiovascular risk assessment tools currently used in both the United States and Europe. It outperformed the most widely used heart disease risk calculators, including QRISK3 recommended by the National Institute for Health and Care Excellence (NICE) in the UK, accurately identifying more high-risk patients.
'This important update to the QRISK tool will allow clinicians to build the clearest picture yet of individuals’ risk of developing heart and circulatory diseases,' said Professor Bryan Williams , Chief Scientific and Medical Officer at the British Heart Foundation . 'Informed by large amounts of data from diverse populations, the new and improved algorithm takes vital steps towards improving risk assessment in populations where cardiovascular risk may often go under-detected. The QR4 tool will offer a much-needed, renewed focus on better identifying people at risk and improving the prevention of cardiovascular diseases.'
'Cardiovascular risk has been under-recognised in some populations, which through QR4 we can now better address,' said Professor Keith Channon , BHF Professor of Cardiovascular Medicine at the University of Oxford. 'The new findings will help identify more diverse groups of people who have high cardiovascular risk, enabling them to access interventions and treatments to reduce their risk.'
'The QR4 model potentially sets a new standard in cardiovascular risk assessment,' said Dr Carol Coupland , senior researcher at the University of Oxford and Professor of Medical Statistics in Primary Care at the University of Nottingham and co-author of the study. 'Our head-to-head comparisons with established models show that QR4 provides a more detailed risk profile for each individual, allowing for earlier and more precise intervention strategies. This is crucial in a field where early detection can save lives and could significantly impact how we approach prevention on a global scale.'
This new algorithm builds on almost two decades of work and global leadership in the field of risk algorithms, and cardiovascular risk algorithms in particular. QR4’s predecessor, QRISK is widely used in the NHS to assess over 5 million patients a year, often as part of NHS Health Checks.
The researchers hope that clinicians, advisory bodies, regulators, and health and care policymakers consider the implications of QR4's advanced predictive capabilities on national health guidelines and support its adoption in clinical settings to improve cardiovascular health outcomes.
The study ' Development and validation of a new algorithm for improved cardiovascular risk prediction ' is published in Nature Medicine .
DISCOVER MORE
- Support Oxford's research
- Partner with Oxford on research
- Study at Oxford
- Research jobs at Oxford
You can view all news or browse by category
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
April 16, 2024
Gut bacteria may reduce cholesterol and lower heart disease risk
At a glance.
- Researchers pinpointed gut bacteria that affect levels of cholesterol and other compounds linked to heart disease.
- The findings suggest that the risk of heart disease might be lowered with strategies to alter the levels of specific gut bacteria.

Different people have different resident microbes in and on their bodies. The trillions of microbes in the human intestines influence not just digestion and gut health, but how organs throughout the body function. Levels of certain microbes in the gut have been associated with the risk of health conditions like diabetes, liver disease, and cancer.
Scientists have thought that certain gut microbes may also play a role in cardiovascular disease (CVD). But which microbes might affect the risk of CVD—and how they might do this—has been unclear. Much remains unknown about how gut microbes process, or metabolize, compounds like cholesterol that affect CVD risk.
In a new study, funded in part by NIH, researchers led by Dr. Ramnik Xavier from the Broad Institute, Massachusetts General Hospital, and Harvard studied bacteria in the stool of more than 1,400 people participating in the Framingham Heart Study, a long-term study of heart health.
The team analyzed the bacterial genomes (the complete sets of genes) in the stool samples. They also studied blood samples and cardiovascular health measurements from the participants to identify microbes and metabolic pathways that are associated with CVD. The results were published on April 2, 2024, in Cell .
The researchers identified several species of bacteria whose levels were associated with blood markers of CVD. Such markers included cholesterol, triglyceride, and blood glucose levels.

Higher levels of one group of bacteria called Oscillibacter were strongly associated with lower levels of cholesterol, both in the stool and the blood. Oscillibacter were also linked with other blood markers of reduced CVD risk, such as lower triglycerides and glucose and higher HDL (high-density lipoprotein).
The reductions in cholesterol by Oscillibacter appeared to be related to genes for enzymes that break down cholesterol in the intestines. This might lead to less cholesterol making its way into the bloodstream.
To confirm that Oscillibacte r could process cholesterol, the researchers grew several Oscillibacter strains from the stool samples and then fed them cholesterol. The bacteria took up the cholesterol and broke it down into smaller molecules that don’t raise the risk of CVD.
The team identified enzymes from other bacteria that were also associated with lower cholesterol levels. A detailed knowledge of the microbes and metabolic pathways that affect CVD risk may eventually lead to personalized therapies that manipulate gut bacteria.
“Our research integrates findings from human subjects with experimental validation to ensure we achieve actionable mechanistic insight that will serve as starting points to improve cardiovascular health,” Xavier says.
—by Sharon Reynolds
Related Links
- Gut Microbes May Affect Motivation to Exercise
- COVID-19 Disrupts Gut Microbiome
- Gut Bacteria May Contribute to Abnormal Blood Vessel Formation
- Gut Microbe Drives Autoimmunity
- When HDL Cholesterol Doesn’t Protect Against Heart Disease
- Gut Microbe Provokes Release of Inflammatory Substance
- Your Body’s Bugs: Nurturing Healthy Microbes
- The Microbiome
- NIH Human Microbiome Project
- Blood Cholesterol
- Framingham Heart Study
References: Gut microbiome and metabolome profiling in Framingham heart study reveals cholesterol-metabolizing bacteria. Li C, Stražar M, Mohamed AMT, Pacheco JA, Walker RL, Lebar T, Zhao S, Lockart J, Dame A, Thurimella K, Jeanfavre S, Brown EM, Ang QY, Berdy B, Sergio D, Invernizzi R, Tinoco A, Pishchany G, Vasan RS, Balskus E, Huttenhower C, Vlamakis H, Clish C, Shaw SY, Plichta DR, Xavier RJ. Cell . 2024 Apr 11;187(8):1834-1852.e19. doi: 10.1016/j.cell.2024.03.014. Epub 2024 Apr 2. PMID: 38569543.
Funding: NIH’s National Heart, Lung, and Blood Institute (NHLBI) and National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); Center for Microbiome Informatics and Therapeutics.
Connect with Us
- More Social Media from NIH
Cholesterol
Cholesterol is a vital component of our cells, which is why our body makes all that we need.
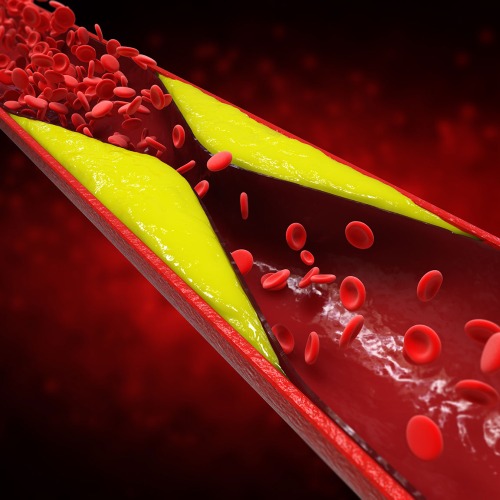
For most Americans eating a conventional diet, plaque accumulates inside the coronary arteries that feed our heart muscle. This plaque buildup, known as atherosclerosis, is the hardening of the arteries by pockets of cholesterol-rich fatty material that builds up beneath the inner linings of the blood vessels. This process seems to occur over decades, slowly bulging into the space inside the arteries, narrowing the path for blood to flow.
The restriction of blood circulation to the heart may lead to chest pain and pressure when people try to exert themselves. If the plaque ruptures, a blood clot may form within the artery. This sudden blockage of blood flow may cause a heart attack, damaging or even killing part of the heart.
A large body of evidence shows there were once enormous swaths of the world where the coronary heart disease epidemic seemed to be almost non-existent, such as rural China and sub-Saharan Africa . It’s not genetics: When people move from low- to high-risk areas, their disease rates appear to skyrocket as they adopt the diet and lifestyle habits of their new homes. The extraordinarily low rates of heart disease in rural China and Africa have been attributed to the extraordinarily low cholesterol levels among these populations. Though Chinese and African diets are very different, they are both centered on plant-derived foods, such as grains and vegetables . By eating so much fiber and so little animal fat, their total cholesterol levels averaged under 150 mg/dL, similar to people eating contemporary strictly plant-based diets .
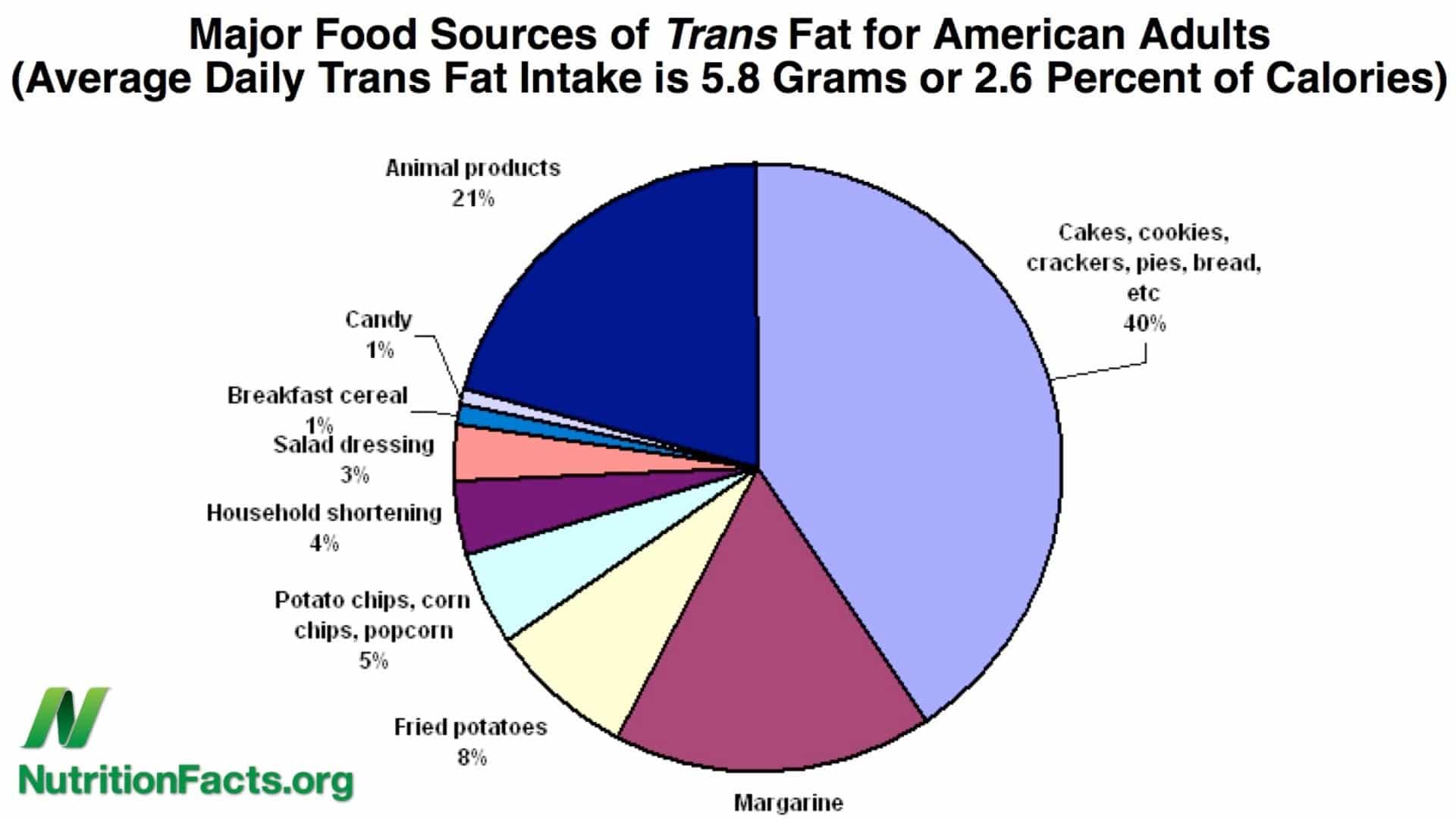
According to William C. Roberts, editor in chief of the American Journal of Cardiology , the only critical risk factor for atherosclerotic plaque buildup is cholesterol, specifically elevated LDL cholesterol in our blood. To drastically reduce LDL cholesterol levels, it appears we need to drastically reduce our intake of trans fat , which comes from processed foods and naturally from meat and dairy; saturated fat , found mainly in animal products and junk foods; and, playing a lesser role, dietary cholesterol, found exclusively in animal-derived foods, especially eggs .
Notice the pattern? The three boosters of bad cholesterol—the number-one risk factor for our number-one killer—all stem from eating processed foods and animal products . This likely explains why populations living on traditional diets revolving around whole plant foods have largely remained free from the epidemic of heart disease.
For substantiation of any statements of fact from the peer-reviewed medical literature, please see the associated videos below.
Subscribe to our free newsletter and receive the preface of Dr. Greger’s upcoming book How Not to Age .
Popular Videos for Cholesterol

Cholesterol and Heart Disease: Why Has There Been So Much Controversy?
Can Cholesterol Get Too Low?
How Low Should You Go for Ideal Cholesterol Levels?

Dietary Cholesterol and Cancer
Trans Fat, Saturated Fat, & Cholesterol: Tolerable Upper Intake of Zero

Cholesterol and Alzheimer’s Disease
Cholesterol Crystals May Tear Through Our Artery Lining

Optimal Cholesterol Level
The Actual Benefit of Diet vs. Drugs

Back in Circulation: Sciatica & Cholesterol

Does Cholesterol Size Matter?
How the Egg Board Designs Misleading Studies

When Low-Risk Means High-Risk

Cholesterol Feeds Breast Cancer Cells

Eggs and Cholesterol: Patently False and Misleading Claims
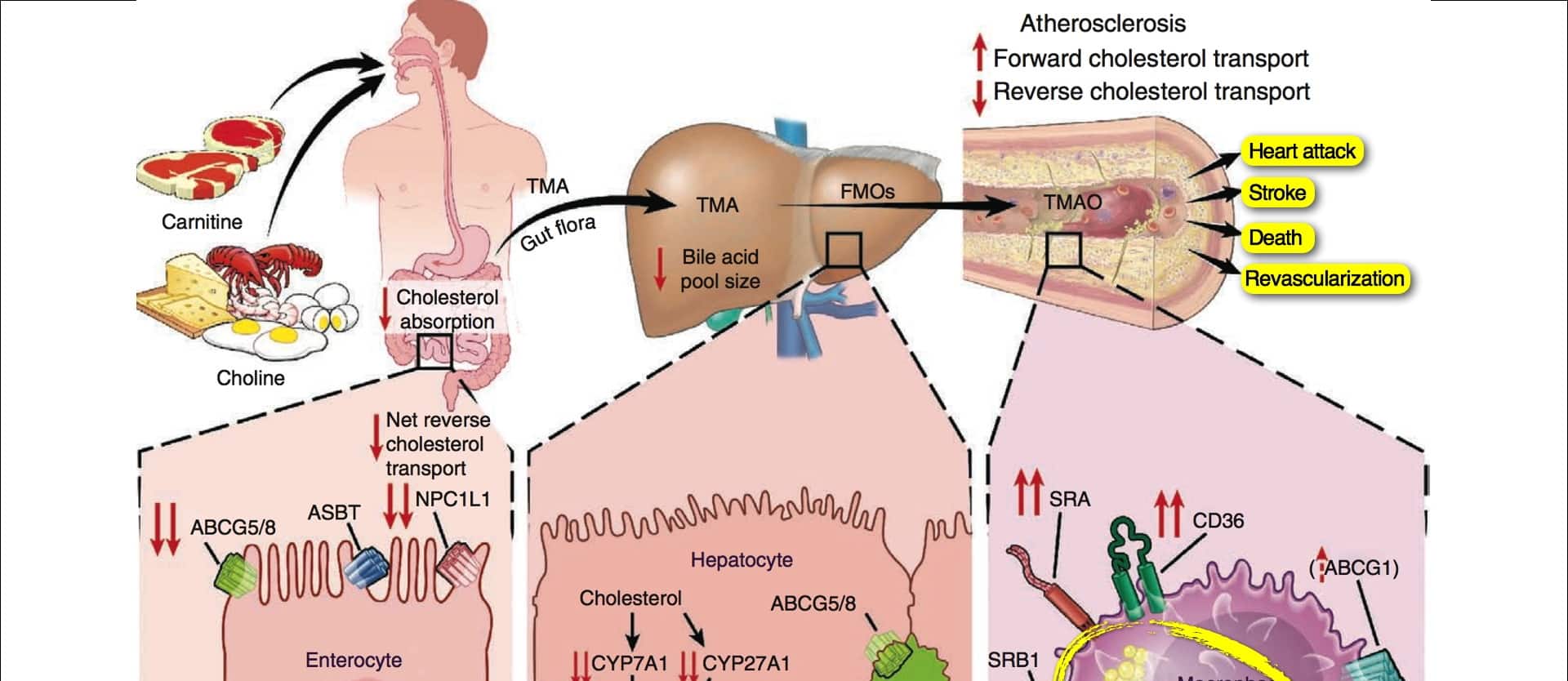
Carnitine, Choline, Cancer, & Cholesterol: The TMAO Connection

How to Prevent Non-Alcoholic Fatty Liver Disease
All videos for cholesterol.

APOE—The Single Most Important Gene for Longevity
APOE is the primary cholesterol carrier in the brain and plays a major role in packaging and transporting LDL cholesterol throughout the body.

How to Boost Your Endothelial Progenitor Cells (EPCs) for Heart Health
How can we improve the capacity of our blood vessels to repair themselves?

How Not To Age – Live Presentation
In this live lecture, Dr. Greger offers a sneak peek into his latest book, How Not to Age, a New York Times Best Seller.

Soy Foods for Menopause Hot Flash Symptoms
Soy can be considered a first-line treatment for menopausal hot flash and night sweat symptoms.

The Diet Shown to Slow Age-Related Hearing Loss
An interventional trial found that dietary changes may slow or even reverse the loss of hearing.

Book Trailer for How Not to Age
Learn about my newest book, How Not to Age, a New York Times Best Seller.

Is Soy Milk the Most Nutritious Non-Dairy Milk?
Soy milk is compared to dairy milk and other plant-based milks.

Are Beyond Meat Plant-Based Meat Alternatives Healthy?
The SWAP-MEAT study puts Beyond Meat products to the test.

Plant-Based Diet for Minimal Change Disease of the Kidney
What are the three reasons plant protein is preferable to animal protein for kidney protection?

Dietary Cholesterol and Inflammation from Abdominal Obesity
The optimal intake of dietary cholesterol may be zero.

Improving VO2 Max: A Look at Vegetarian and Vegan Athletes
Plant-based diets improve the performance of athletes and nonathletes alike.

The Negative Effects and Benefits of Plant-Based Diets
What are the pros and cons of plant-based eating?

Fat-Blocking Benefits of Hibiscus Tea
What did a randomized, double-blind, placebo-controlled trial of hibiscus tea for weight loss find?

Plant-Based Diet for Treating and Reversing Stage 3 Kidney Disease
I share a touching story of the power of plant-based eating for chronic kidney failure.

Dietary Guidelines: “Eat as Little Dietary Cholesterol as Possible”
Why do the official federal Dietary Guidelines for Americans recommend limiting the intake of dietary cholesterol (found mostly in eggs) as much as possible?

Soul Food That’s Good for the Soul
The best of soul food’s origins are tied to the plant-centric West African diet.

How Does Oatmeal Help with Blood Sugars?
The prebiotic fiber in oats helps to explain why oatmeal can improve diabetic control.

Is Oatmeal Good for People with Diabetes?
Before there was insulin, there was the “oatmeal cure.”

The Role of Endotoxins in Alzheimer’s and Dementia
Why can a single meal high in saturated fat impair cognition?

The Best Diet for Fibromyalgia and Other Chronic Pain Relief
Anti-inflammatory diets can be effective in alleviating chronic pain syndromes.

The Fat-Blocking and Appetite-Suppressing Effects of Thylakoids
What is a natural way to cut down on unhealthy food cravings?

Answering Your Questions About Cholesterol and Diabetes
I answer some common questions I’ve been asked about cholesterol and diabetes, such as “What is the ideal LDL?” “What’s going on when someone eats healthfully but their glucose is still out of control?”

Does Dietary Cholesterol (Eggs) Raise Blood Cholesterol?
Even nine out of ten studies funded by the egg industry show that eggs raise cholesterol.

Is the role of cholesterol in heart disease settled beyond a reasonable doubt?

The Benefits of Fenugreek for Preventing and Treating Diabetes
The spice fenugreek contains 4-hydroxyisoleucine, a peculiar amino acid that may explain its benefits for controlling blood sugar.

Is Allulose a Healthy Sweetener?
Are rare sugars like allulose a healthy alternative for traditional sweeteners?

Are the Health Benefits of Nuts Limited to Those Eating Bad Diets?
Do nut eaters live longer simply because they swap in protein from plants in place of animal protein?

Exercising to Protect Your Arteries from Fast Food
There is a window of time in which sufficient physical activity can help mediate some of the damage caused by eating an unhealthy meal.
Saturated Fat Causes Artery and Lung Inflammation
What happens within hours of eating a high-fat meal?

Should You Get Personalized Genetic Risk Testing?
Overrated “precision medicine” may just be serving vested interests, and consumer DNA testing can be useless—or even worse.

Do the Health Benefits of Peanut Butter Include Longevity?
Why are nuts associated with decreased mortality, but not peanut butter?

How to Boost FGF21 with Diet for Longevity
Fasting and exercise can boost the longevity hormone FGF21, but what can we eat—or avoid eating—to get similar effects?

Life Extension with FGF21
What can we do to boost the longevity hormone FGF21?

Which Foods Are Anti-Inflammatory?
Foods that reduce inflammation. What does an anti-inflammatory diet look like?

Foods That Cause Inflammation
Inflammatory markers can double within six hours of eating a pro-inflammatory meal. Which foods are the worst?

Pomegranate: A Natural Treatment for Rheumatoid Arthritis
Pomegranates are put to the test for weight loss, diabetes, COPD, prostate cancer, osteoarthritis, and rheumatoid arthritis.

Onions Put to the Test for Weight Loss, Cholesterol, and PCOS Treatment
Weight loss, cholesterol, and PCOS treatment with diet. What can an eighth of a teaspoon a day of onion powder do for body fat, and what can raw red onion do for cholesterol?

Are PCSK9 Inhibitors for LDL Cholesterol Safe and Effective?
Those with genetic mutations that leave them with an LDL cholesterol of 30 live exceptionally long lives. Can we duplicate that effect with drugs?
Why might healthy lifestyle choices wipe out 90 percent of our risk for having a heart attack, whereas drugs may only reduce risk by 20 to 30 percent?

Are Baruka Nuts the Healthiest Nut?
How do barukas, also known as baru almonds, compare with other nuts?
Pin It on Pinterest
New research underway on monthly shot to treat high cholesterol
by Liz Bonis & Megan Burgasser, WKRC

CINCINNATI (WKRC) - A new therapy could help a person lower his or her risk of having a heart attack. New research is explaining how.
This new research showed that a single shot taken once a month can drop cholesterol significantly. It’s a PCSK9 inhibitor.
“What it is, is a drug to lower LDL-C cholesterol, which in layman’s terms is the bad cholesterol,” said Katie Vale-Freeburg, a sub-investigator at Velocity Clinical Research.
Cholesterol is a waxy substance found in the blood. As it deposits in a person’s blood vessels, it reduces blood flow and raises the risk of a heart attack. Vale-Freeburg said these new PCSK9 shots can actually reduce that risk by giving the body a bit of a boost.
“So, the way that this drug works is that your liver makes a protein called PCSK9, and what that protein does is it makes it hard for your liver to get that cholesterol out of your body. What this drug does is it blocks that protein, and it makes it easier for your body to get rid of the cholesterol,” Vale-Freeburg said.
A study that was just presented at the annual meeting of the American College of Cardiology found that a new kind of PCSK9 inhibitor reduced bad (LDL) cholesterol in nine out of 10 patients by 50%. The placebo group dropped just 16%.
“15 years ago, we were doing research on the statins. Which at the time, we thought was gonna be the best thing that ever happened to cholesterol research, and how could we ever get better than that. Here we are 15 years later doing PCSK9 research,” said Kurt Percy, Executive Director of Regional Operations at Velocity Clinical Research.
The research on these new monthly shots showed that PCSK9s may help those who don't respond well to therapies, such as statins, currently on the market. Vale-Freeburg said the goal now is to get bad cholesterol levels to 70 mg/dL or lower.
“This drug really aids with that goal,” said Vale-Freeburg.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10285014

Eggs and Cardiovascular Disease Risk: An Update of Recent Evidence
Sharayah carter.
1 Alliance for Research in Exercise, Nutrition and Activity (ARENA), Allied Health & Human Performance, University of South Australia, GPO Box 2471, Adelaide, 5001 Australia
Elizabeth S. Connole
Alison m. hill.
2 Alliance for Research in Exercise, Nutrition and Activity (ARENA), Clinical and Health Sciences, University of South Australia, Adelaide, Australia
Jonathan D. Buckley
Alison m. coates, associated data, purpose of review.
This review summarizes recent evidence published since a previous review in 2018 on the association between egg consumption and risk of cardiovascular disease (CVD) mortality, CVD incidence, and CVD risk factors.
Recent Findings
No recent randomized controlled trials were identified. Evidence from observational studies is mixed, with studies reporting either an increased risk or no association of highest egg consumption with CVD mortality, and a similar spread of increased risk, decreased risk, or no association between egg intake and total CVD incidence. Most studies reported a reduced risk or no association between egg consumption and CVD risk factors. Included studies reported low and high egg intake as between 0 and 1.9 eggs/week and 2 and ≥14 eggs/week, respectively. Ethnicity may influence the risk of CVD with egg consumption, likely due to differences in how eggs are consumed in the diet rather than eggs themselves.
Recent findings are inconsistent regarding the possible relationship between egg consumption and CVD mortality and morbidity. Dietary guidance should focus on improving the overall quality of the diet to promote cardiovascular health.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11883-023-01109-y.
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality globally [ 1 ]. Early studies, which indicated that elevated serum cholesterol was associated with an increased risk of heart disease [ 2 , 3 ], led to the American Heart Association (AHA) recommending limiting dietary cholesterol to less than 300 mg/day with specific recommendations to restrict egg consumption, which are high in cholesterol, to a maximum of three eggs per week [ 4 ]. A later analysis from the Framingham study found no association between egg intake and blood cholesterol or heart disease [ 5 ], and in 2002, the AHA removed its advice to limit egg intake while retaining its recommendation to consume less than 300 mg/day of dietary cholesterol [ 6 ]. During this time, findings surfaced indicating that increased intake of dietary cholesterol was associated with decreased synthesis of endogenous cholesterol [ 7 ], and in 2013, the AHA announced that “there is insufficient evidence to determine whether lowering dietary cholesterol reduces low-density lipoproteins (LDL) cholesterol” [ 8 ]. As a result, the 2015–2020 Dietary Guidelines for Americans removed the recommendation of setting a limit to the maximum intake of 300 mg/day of cholesterol. However, the controversy around the impact of consuming foods high in cholesterol, including eggs, on CVD risk remains.
A possible explanation for the controversy is that foods high in cholesterol are also typically high in saturated fat [ 9 ], which is well documented to increase LDL cholesterol and CVD risk [ 10 ]. Thus, it is difficult to determine the independent effects of dietary cholesterol on the blood lipid profile. Based on nutrient profiles from Australian food databases, eggs are high in cholesterol but low in saturated fat, with the average large whole egg (50 g) containing 244 mg of cholesterol but only 1.2 g of saturated fat [ 11 ]. However, eggs, like any individual food, are not consumed in isolation, but as part of an overall diet, which can influence total cholesterol and saturated fat intake. For example, in the American diet, intakes of cholesterol and saturated fat increase in parallel, which may be due to eggs being frequently consumed with bacon or sausage which are high in saturated fat [ 12 ]. Previous reviews considering egg consumption and blood lipids have reported contradictory findings, with a 2018 review of randomized controlled trials (RCT) finding that consuming eggs does not adversely affect the blood lipid profile [ 13 ]. However, in contrast, a subsequent meta-analysis of RCTs reported a positive relationship between changes in dietary cholesterol (all sources, including eggs) and changes in LDL cholesterol, after controlling for saturated fat [ 14 ], and so, the relationship remains unclear.
When the relationship between egg consumption and CVD risk has been reviewed, there have also been mixed findings. The majority of systematic reviews and meta-analyses observed no association between egg consumption and CVD risk [ 15 – 20 ], but a small number of studies identified an increased risk [ 21 , 22 ], particularly in people with diabetes [ 17 , 18 , 23 ]. These inconsistencies in study findings continue to fuel the controversy around the impact of egg consumption on CVD risk.
This review aims to update current evidence identified from a systematic search and narrative review of observational studies and RCTs from 2019 onwards to explore the association between egg consumption and CVD risk, specifically, CVD mortality, incidence, and risk factors in adults. In addition, confounding factors that may play a role in the associations found will be discussed.
Search Strategy
An electronic search of PubMed, Web of Science, and Embase was conducted from January 1, 2019, to September 14, 2022, to identify the potentially eligible studies recent studies with the following search strategy: “[(egg OR eggs) AND (cardiovascular diseases OR cardiovascular OR coronary heart disease OR CHD OR CVD OR stroke OR myocardial infarction OR ischemic heart disease OR ischemic stroke OR hemorrhagic stroke) AND (randomized control trial OR RCT OR cohort OR prospective OR longitudinal OR follow-up OR case-cohort OR nested case control).” Studies were selected if they met the following inclusion criteria: (i) they were conducted on human adults; (ii) evaluated associations between egg intake and risk of CVD (fatal and nonfatal); (iii) evaluated associations between egg intake and CVD risk factors (e.g., hypertension, blood lipid profile, body fat mass). All references were evaluated by two independent reviewers (all by ESC, half each by SC and AMC) with an independent reviewer (either SC or AMC) resolving any disagreement.
Data Extraction
Data were extracted by two independent reviewers (ESC and SC) from each identified study using a standardized extraction form. The following information was collected: (i) author names; (ii) year of publication; (iii) study cohort name and country; (iv) sample size, sex, and age (mean or range) of participants; (v) study aim and design; (vi) follow-up period; (vii) exposure type/dose/frequency; (viii) CVD outcome measures; (ix) CVD results; (x) covariates used in adjustments.
Out of 269 references published during the four-year search period, 209 abstracts were screened, 75 were eligible for full-text screening, and 30 studies (35 data sets) were identified to review (all observational, no RCTs) (See Fig. 1 ). From the 30 studies, 13 were conducted with data from populations living in the USA [ 24 , 25 ••, 26 – 29 , 30 •, 31 – 34 , 35 •, 36 ], eight from China [ 15 , 35 •, 37 , 38 ••, 39 – 42 ], eight from Europe [ 43 – 50 ], one from Iran [ 51 ], and one was a multinational cohort study [ 52 •].

Flow Diagram of search strategy and included articles
The majority (> 50%) of studies controlled for age, gender, education, smoking status, alcohol consumption, physical activity, energy intake, BMI, hypertension, and diabetes. Two studies (7%) controlled for saturated fat intake [ 25 ••, 30 •], eleven studies (37%) controlled for vegetable intake [ 28 , 29 , 36 , 38 ••, 39 , 41 , 42 , 48 – 50 , 52 •], six studies (20%) controlled for meat intake [ 26 , 38 ••, 39 , 41 , 50 , 52 •] (two (6%) for processed meat [ 26 , 50 ]), three (10%) for Mediterranean diet score [ 28 , 44 , 46 ], three (10%) for dietary approaches to stop hypertension (DASH) score [ 31 – 33 ], and six (20%) for diet quality [ 24 , 26 , 34 , 35 •, 37 , 51 ]. Three (10%) studies which were across multiple countries controlled for center or region but not ethnicity [ 45 , 48 , 52 •].
Eggs and CVD Mortality
In the past 4 years, 11 observational studies [ 15 , 24 , 27 , 29 , 30 •, 34 , 35 •, 43 , 44 , 46 , 52 •] have examined the associations between eggs and CVD mortality (See Supplementary Table 1 ). Of these, six publications reported on CVD mortality [ 24 , 29 , 30 •, 34 , 43 , 46 ], and all except one [ 43 ] reported a higher risk of CVD mortality with the highest egg intake vs. the lowest egg intake (hazard ratio (HR) ranging from 1.14–1.75). Four out of five studies reporting a higher risk were from the USA [ 24 , 29 , 30 •, 34 ] with the remaining study from Italy [ 46 ]. One of these five studies [ 30 •] was a substitution study that reported a reduced risk of CVD mortality (total, heart disease, and stroke [males only]) when 3% of energy from plant protein was substituted for egg protein (HR range 0.72–0.76). In one study [ 24 ], the significant association was lost after adjusting for dietary cholesterol, and no association was found for egg white consumption. Five publications [ 15 , 27 , 35 •, 44 , 52 •] reported no association between eggs and CVD mortality (one reported on heart disease mortality only [ 27 ]). One study [ 35 •], after grouping cardiometabolic subtypes (coronary heart disease (CHD), stroke, and diabetes) together, found that the highest egg intake in the White American cohort was associated with higher cardiometabolic mortality, reduced risk was found with moderate egg intake in the Chinese cohort, and no association was found in the Black American cohort.
Eggs and CVD Incidence (Non-Fatal CVD)
Fifteen observational studies reported on egg consumption and CVD incidence (non-fatal CVD) in the last 4 years [ 25 ••, 26 , 28 , 31 – 34 , 38 ••, 39 , 45 , 48 – 51 , 52 •] (See Supplementary Table 1 ). Eight reported on total CVD incidence [ 25 ••, 26 , 28 , 34 , 38 ••, 39 , 51 , 52 •] with four studies finding an increased incidence (HR ranging from 1.06–1.39) with the highest (≥ 7 eggs/week) vs. lowest egg intake (< 1 egg/week) [ 34 ], high (> 6 eggs/week) and low intake (< 3 eggs/week) [ 38 ••], or with a 0.5 egg/day continuous intake [ 25 ••], noting that in this last study, significance was lost after adjusting for dietary cholesterol. The fourth study was a substitution study that reported that substituting eggs with fish, nuts, legumes, or whole grains was associated with 2–3% lower relative risks for incident CVD when the substitution amount was one serving per week and 15–21% lower relative risks when the substitution amount was one serving per day [ 26 ]. Two studies found a decreased incidence (HR ranging from 0.78–0.89) [ 39 , 52 •] (data from the PURE study [ 52 •]), and three found no association [ 28 , 51 , 52 •] (data from the ONTARGET/TRANSCEND study [ 52 •]).
Five studies reported on egg intake and stroke incidence with three finding no association [ 49 , 51 , 52 •] and two finding an increased risk (HR ranging from 1.07–1.34). One study reported an increased risk of total stroke and ischemic stroke with high and low egg intake (> 6 and < 3 eggs/week for total stroke, and > 6 and < 1 egg/week for ischemic stroke) and an increased risk of hemorrhagic stroke with low egg intake (< 3 eggs/week) [ 38 ••]. The other study found an increased risk of 7% for total stroke and 25% for hemorrhagic stroke with 20 g egg/day continuous intake (total: 95% CI 1.01–1.14, P trend = 0.031, hemorrhagic: 95% CI 1.09–1.43, P trend = 0.002) but no association for ischemic stroke [ 45 ].
Individual studies investigating heart disease reported on the incidence of ischemic heart disease, coronary heart disease, myocardial infarction, or venous thromboembolism. Two studies reported on ischemic heart disease, one reporting an increased association with highest (≥ 7 eggs/week) vs. lowest egg intake (< 1 egg/week) [ 34 ] and the other showing a 7% decreased risk for continuous 20 g egg/day intake (95% CI 0.88–0.99, P trend = 0.023) [ 48 ]. Coronary heart disease incidence was reported in three studies, two finding no association [ 33 , 51 ] except in a sub-analysis where an increased risk of 30% (95% CI 1.03–1.56) was found in the older cohort [ 33 ], and one finding an increased risk with highest (> 6 eggs/week) vs. moderate egg consumption (3 < 6 eggs/week) [ 38 ••]. Three studies reported on myocardial infarction incidence, one reported an 11–13% increased risk [ 32 ], one found no association [ 51 ], and one study with two data sets found a 17% reduced risk (data from the PURE study) and no association (data from the ONTARGET/TRANSCEND study) [ 52 •]. No association was found for the incidence of heart disease [ 52 •] or the incidence of venous thromboembolism [ 50 ].
Eggs and CVD Risk Factors
Nine observational studies [ 15 , 36 , 37 , 40 , 42 , 47 , 49 , 52 •, 53 ] were identified in the last 4 years that examined the associations between egg consumption and CVD risk factors including lipid and lipoprotein concentrations, blood pressure (including the presence of hypertension), and adiposity (See Supplementary Table 1 ). Four publications examined the association between eggs and lipid profile [ 15 , 36 , 37 , 52 •]. Two studies found no association [ 36 , 52 •], one study found a decrease in lipid profile (with no association for high-density lipoprotein (HDL) cholesterol) [ 15 ], and one study found an increase in total cholesterol (TC) and LDL cholesterol but a decrease in triglycerides (TG) and an increase in HDL cholesterol [ 37 ]. One study [ 40 ] reported on the association between eggs and lipoprotein particle concentrations and found reduced risk [ 40 ].
Four studies examined eggs and blood pressure [ 15 , 36 , 49 , 52 •]. Two studies found reduced systolic blood pressure [ 15 , 52 •] (data set from the PURE study [ 52 •]), and three studies found reduced diastolic blood pressure [ 15 , 49 , 52 •] (data set from the PURE study [ 52 •]) with the highest egg intake (> 45 g/day or ≥ 7 eggs/week). In contrast, one study reported increased systolic and diastolic blood pressure (data set from ONTARGET/TRANSCEND study [ 52 •]). One study found no association between eggs and systolic blood pressure [ 49 ], and one study found no association for both diastolic and systolic blood pressure [ 36 ]. Two studies reported on the association between eggs and hypertension [ 42 , 47 ]. No association was found for the highest (≥ 7 eggs/week) vs. the lowest (< 1 egg/week) egg intake, but an increased risk was found for lower egg intakes (2–6.9 eggs/week) [ 47 ]. A decreased risk was noted in a substitution study where eggs were substituted for meat [ 42 ].
Three studies described the associations between eggs and adiposity (BMI, body fat, waist circumference) [ 15 , 36 , 41 ]. One study [ 41 ] completed analysis by sex and found a decreased risk of adiposity for females with the highest (approximately 50 g/day) vs. lowest egg intake (0 g/day) but no association for males, and two studies found no association with eggs and waist circumference [ 15 , 36 ].
The majority of research included in this review was from cohort data collected in three geographical regions, with population ethnicity influencing the direction of associations between egg consumption and CVD outcomes. Thirteen publications were from studies conducted in populations residing in the USA [ 24 , 25 ••, 26 – 29 , 30 •, 31 – 34 , 35 •, 36 ]; twelve studies reported on eggs and non-fatal and fatal CVD [ 24 , 25 ••, 26 – 29 , 30 •, 31 – 34 , 35 •] and one on risk factors [ 36 ], with seven identifying an increased risk [ 24 , 25 ••, 26 , 29 , 30 •, 31 , 34 ], five indicating no association [ 27 , 28 , 32 , 33 , 36 ] and one indicating an increased risk (White Americans) or no association (Black Americans) [ 35 •]. Eight studies used data from cohorts residing in China [ 15 , 35 •, 37 , 38 ••, 39 – 42 ] with four studies reporting on eggs and non-fatal and fatal CVD [ 15 , 35 •, 38 ••, 39 ] and five reporting on eggs and CVD risk factors [ 15 , 37 , 40 – 42 ]. In contrast to the US findings, only one of these studies reported an increased risk [ 38 ••], six showed reduced risk [ 35 •, 37 , 39 – 42 ], and one found no association [ 15 ]. Eight studies used cohort data from Europe reporting on eggs and non-fatal and fatal CVD as well as CVD risk factors [ 43 – 50 ]. Three confirmed an increased risk [ 45 – 47 ], one found a reduced risk [ 43 ], and four found no association [ 44 , 48 – 50 ]. One study from Iran found no association with non-fatal CVD [ 51 ]. A final study including cohort data from 21 countries also found no association between fatal CVD and CVD risk factors [ 52 •].
Eleven studies conducted subgroup analyses on eggs and CVD mortality, incidence, and/or risk factors [ 25 ••, 31 , 32 , 34 , 38 ••, 39 , 46 – 49 , 52 •]. Six studies evaluated sex differences: six for men [ 25 ••, 31 , 38 ••, 39 , 48 , 49 ] and four for women [ 31 , 38 ••, 39 , 48 ]. All but two studies found no association or no difference to the overall study outcomes. One study, which reported no association in the total cohort, found a reduced risk of IHD in males [ 48 ], and another study that reported a reduced risk of total CVD and hypertension in the total cohort found no association for males but confirmed reduced risk for females [ 39 ]. Eight studies assessed BMI in a sub-analysis [ 31 , 32 , 34 , 38 ••, 39 , 46 – 48 ] with the majority (seven studies) reporting no association or no difference to the overall study findings. One study reported an increased risk of MI incidence for people with a BMI over 25 kg/m 2 but found no association in the total cohort [ 32 ]. Nine completed sub-analyses for type 2 diabetes, and all but two found no association [ 25 ••, 31 , 32 , 34 , 38 ••, 46 – 48 ]. The two studies [ 31 ] reporting an increased risk of CVD incidence in persons with type 2 diabetes (one specific to ischemic stroke [ 31 ]) also reported increased risk in their overall findings.
Eggs are a highly nutritious food; they offer a complete source of protein, containing all essential amino acids and a complement of vitamins and minerals [ 54 ]. However, the high cholesterol content in eggs makes them a food of concern, which has led to a plethora of studies over the last few decades investigating egg consumption and the risk of CVD.
In this narrative review (with studies identified by a systematic search), we summarized recent evidence from studies published from 2019 to September 2022 with regard to the impact of egg consumption on CVD risk. The studies were all observational, and the findings were mixed. For CVD mortality, an equal number of studies reported an increased risk or no association with the highest egg intake. This was similar to earlier reviews which also found mixed results. A meta-analysis of 39 observational studies including nearly 2 million individuals found no association between the highest intake of eggs and CVD mortality [ 55 ], and similar findings were presented in another meta-analysis of 24 observational studies of over 11 million individuals that found no association between highest intake of eggs and CVD mortality [ 56 ]. However, contrasting findings were reported in a meta-analysis of 19 observational studies that found a nonlinear dose–response association between egg consumption and CVD mortality, although the certainty of the evidence for these observations was rated as very low [ 57 ]. In this latter review, the majority (80%) of studies reporting an increased risk were studied from US populations. Similarly, in a meta-analysis which found no association in the total population, an increased risk was reported in a sub-analysis by ethnicity in the American population [ 56 ].
It is difficult to study food in isolation without considering the effect of foods consumed in the whole diet and the nutrients they collectively contribute. In Western populations, eggs are typically consumed with meat (often processed) which is high in saturated fat, while in Asian cultures, eggs are frequently consumed in meals with vegetables [ 27 ]. It is also possible that Western populations consume more cholesterol from other sources (e.g., red meat, full-fat dairy, and discretionary foods), as compared to people from Asian cultures [ 12 , 58 , 59 ]. In the American diet for example, due to dietary patterns, dietary cholesterol and saturated fat increase in parallel, e.g., eggs with bacon and sausage [ 12 ]. Cooking methods are also different, with higher temperatures and longer cooking time leading to oxidative damage to vitamins [ 60 ]. Furthermore, while nutrition databases have an average for the cholesterol content of eggs, this commonly differs by country and can be influenced by multiple factors including feed composition [ 61 – 63 ], housing systems (free range vs. caged) [ 64 ], and age of the laying hens [ 65 ]. These factors may contribute to the observed country differences. Very few studies in this review controlled for saturated fat; no studies have considered cooking methods, whether eggs were from free-range or caged chickens, or the feed they were provided; and only 37% controlled for vegetable intake, 20% controlled for red meat, and 6% controlled for processed meat which may confound associations.
Regarding CVD incidence (non-fatal), the findings of this review were also mixed. Almost an equal spread of increase, decrease, and no association between egg intake and total CVD incidence was found. Of the eight studies reporting an increased risk of a CVD event, six (75%) were from the USA, and in two of these studies, the populations were majority (92%) male. Therefore, similar to the mortality findings, there is a potential effect of ethnicity, sex, and dietary patterns. Although not consistently so, studies reporting increased incidence of CVD were often from older cohorts or studies with longer duration and hence an aging cohort, both of which would predispose to an increased risk of CVD incidence. Similar mixed findings have been reported in earlier review studies. A meta-analysis of 17 observational studies found no association with CHD or stroke and an increased risk of heart failure with high compared to low egg consumption [ 16 ]. In a meta-analysis of nine observation studies, eating one egg daily was not associated with an increased risk of ischemic heart disease (IHD) and was associated with a small reduction in stroke [ 15 ]. Similarly, a meta-analysis of 21 observational studies also found no association between egg consumption and CVD risk and found beneficial effects toward stroke risk [ 66 ]. An umbrella review of seven systematic reviews and 15 meta-analyses concluded that increased egg consumption is not associated with CVD risk in the general population [ 67 ].
In this review, most studies assessing egg consumption and CVD risk factors found a reduced risk or no association. Interestingly, the majority (56%) of studies were from Chinese cohorts, and only one study was from the USA. However, due to the exploratory nature of observational studies, these studies are unable to establish a causal relationship between egg intake and CVD risk factors. Randomized controlled trials are required to provide evidence of causation, and as there were no RCTs during the defined period of this review, our discussion will focus on review studies of earlier RCTs that examined eggs and CVD risk factors. A systematic review of 23 RCTs found nonsignificant effects of increasing the consumption of eggs on risk markers for CVD [ 13 ]. In a meta-analysis of 28 RCTs, high egg consumption increased total cholesterol, LDL, and HDL cholesterol, but not LDL-to-HDL or TC-to-HDL ratios or triglycerides compared with low egg control diets [ 68 ]. In another meta-analysis of eight RCTs comparing greater than four eggs/week to less than 4 eggs/week, egg consumption was not associated with differences in blood lipid profile or blood pressure [ 69 ] and in two meta-analyses looking at the effects of different food groups on hypertension, regular egg consumption was associated with a lower risk of hypertension [ 70 , 71 ].
In summary, recent data on the associations between egg consumption and risk of CVD mortality, incidence, and risk factors is mixed. With observational data, it is difficult to assess the relationship of any individual food independently of a dietary pattern. The risk associations reported in the reviewed observational studies are likely to be attributed to the dietary pattern accompanying high egg intake (e.g., eating eggs with bacon and sausage or as part of a meal with vegetables) and/or other risk factors present in people with high egg consumption. For example, in Asian cultures, egg consumption is positively associated with socioeconomic status and physical activity, inversely associated with smoking, and generally correlated with other aspects of a healthy dietary pattern (e.g., higher intake of fiber, vegetables, and fruit) [ 15 ]. In the USA, egg consumption is correlated with low physical activity, smoking, and dietary patterns high in saturated fat (e.g., full-fat dairy, red meat, and processed meat) [ 72 ]. Very few of the studies reviewed adjusted analyses for dietary confounders like meat, processed meat, vegetables, and saturated fat, and this could have impacted outcomes. Therefore, the suggestion that egg consumption by itself promotes the risk and development of CVD is questionable compared with the overall complexity of the dietary pattern, physical activity, and genetic predisposition. There is, however, evidence suggesting higher egg consumption could be associated with a higher risk of CVD in people with diabetes [ 17 , 18 , 73 ], but not all studies confirm these findings, specifically after adjusting for background diet [ 74 ]; further studies are needed. The best evidence for CVD prevention supports adopting a change in overall dietary pattern [ 75 ], and therefore, dietary guidance to reduce CVD risk should focus on implementing a healthy dietary pattern rather than removing a single food, such as eggs.
Below is the link to the electronic supplementary material.
Open Access funding enabled and organized by CAUL and its Member Institutions
Declarations
JDB is currently funded by the American Egg Board’s Egg Nutrition Center. They have also received grant support from the Almond Board of California, the Almond Board of Australia, the International Nut and Dried Fruit Council, and Dried Fruit Australia. AMC is currently funded by the American Egg Board’s Egg Nutrition Center. AMC is the immediate past president of the Nutrition Society of Australia. They have also received grant support from the Almond Board of California, the Almond Board of Australia, the International Nut and Dried Fruit Council, and Dried Fruit Australia. And they have been a consultant for Nuts for Life. AMH is currently funded by the American Egg Board’s Egg Nutrition Center. They have also received grant support from the Almond Board of California, the Almond Board of Australia, the International Nut and Dried Fruit Council, and the Dried Fruit Australia. SC and ESC declare that they have no conflicts of interest or funding to disclose.
The article does not contain any studies with human or animal subjects performed by any of the authors.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Research explores how a father's diet could shape the health of his offspring
New research, published in Nature Communications , finds that the macronutrient balance in the diet of male mice affects the level of anxiety-like behaviour of sons and the metabolic health of daughters.
The research provides a step towards understanding how the effect of diet can transmit from one generation to the next via a father's sperm. It could ultimately inform dietary guidelines for fathers-to-be, with the goal of lowering the risk of metabolic disease and mood disorders in the next generation.
Parents like to believe they can shape the interests and behaviour of their children, with mixed success. But a new study from an international team of researchers confirms this is the case for mice, with father's shaping their offspring's health through their own diet.
Scientists have already discovered that a mouse father's diet can have an impact not only on his own reproductive health but on that of his offspring. Over- or under-feeding male mice can affect their offspring's metabolism and behaviour, as well as their risk of cancer. What is less understood is whether there are diverse types of health impacts on the health of offspring, depending on the type and composition of the diet of male mice before conception.
This was the starting point for the research by scientists in the international GECKO consortium, with lead investigators in Copenhagen, Sydney, and Chicago.
At the University of Sydney's Charles Perkins Centre in Australia researchers fed male mice one of ten diets differing in the proportions of protein, fats, and carbohydrates, then allowed them to mate with females reared on standard diet. The behaviour and physiology of the resulting pups were then studied.
Dietary composition as important as number of calories
The scientists discovered that male mice fed low protein and high carbohydrate diets were more likely to have male offspring with higher levels of anxiety, as measured by time spent in the safety zones of their maze. They also found that male mice that were fed high fat diets were more likely to have daughters with higher levels of body fat and markers of metabolic disease.
"Our study shows that the type of diet eaten before conception can program specific characteristics of the next generation," says co-senior author and leader of the GECKO consortium Professor Romain Barrès, from the University of Copenhagen and Université Côte d'Azur, Nice.
"It is extraordinary that by titrating mixtures of protein, fat and carbs in the father's diet we could influence specific features of his sons and daughters health and behaviour. There is some important biology at play here," said Professor Stephen Simpson, co-senior author and Academic Director of the Charles Perkins Centre at the University of Sydney.
The team also observed that males on a low protein diet also ate more food overall. However, thanks to the study design, they could determine that both the amount of calories, and the macronutrient composition of the males' diets, influenced the health of their offspring.
"Our study shows that it's not just eating too much or too little, but the composition of the diet that can have an impact on future children," says Professor Romain Barrès.
The work was conducted in mice and has opened the way for the team to study the molecular mechanisms involved. The mouse work is part of a broader series of studies within the GECKO consortium, involving humans and other mammals at partner institutions.
"We think our study is a step towards establishing dietary guidelines for fathers to be, with the ultimate goal of lowering the risk of metabolic disease and mood disorders in the next generation," says Professor Romain Barrès.
- Diet and Weight Loss
- Cholesterol
- Mating and Breeding
- Healthy diet
- Health science
- Atkins Diet
- Epidemiology
- Personalized medicine
- House mouse
- Separation anxiety disorder
Story Source:
Materials provided by University of Sydney . Note: Content may be edited for style and length.
Journal Reference :
- Angela Jane Crean, Alistair McNair Senior, Therese Freire, Thomas Daniel Clark, Flora Mackay, Gracie Austin, Tamara Jayne Pulpitel, Marcelo Aguiar Nobrega, Romain Barrès, Stephen James Simpson. Paternal dietary macronutrient balance and energy intake drive metabolic and behavioral differences among offspring . Nature Communications , 2024; 15 (1) DOI: 10.1038/s41467-024-46782-y
Cite This Page :
Explore More
- Warming Antarctic Deep-Sea and Sea Level Rise
- Octopus Inspires New Suction Mechanism for ...
- Cities Sinking: Urban Populations at Risk
- Puzzle Solved About Ancient Galaxy
- How 3D Printers Can Give Robots a Soft Touch
- Combo of Multiple Health Stressors Harming Bees
- Methane Emission On a Cold Brown Dwarf
- Remarkable Memories of Mountain Chickadees
- Predicting Future Marine Extinctions
- Drain On Economy Due to Climate Change
Trending Topics
Strange & offbeat.

IMAGES
COMMENTS
Why has dietary cholesterol advice changed over the years? Scientists learn stuff. Decades ago, nutrition research was focused on an isolated nutrient or a specific food, Van Horn said. "Nutrition research has shifted that focus to the broader totality of eating patterns and food frequency," she said.
New guidelines from the American Heart Association advise sitting less and moving more as the first treatment. Physical activity can reduce LDL (low-density lipoprotein, or "bad") cholesterol ...
Aug. 28, 2023 — New research details the first oral drug for the treatment of a type of high cholesterol -- called Lp(a) -- that is a potentially more dangerous version of the so called 'bad ...
A new study is deepening researchers' understanding of how dietary cholesterol enters the bloodstream. Researchers say these findings could pave the way for new cholesterol medications. Experts ...
Aug. 28, 2023 — New research details the first oral drug for the treatment of a type of high cholesterol -- called Lp(a) -- that is a potentially more dangerous version of the so called 'bad ...
"Statins were invented to lower cholesterol by targeting the liver. But we didn't know the targets or the pathways in the cardiovascular system," said Chun Liu, PhD, an instructor at the Stanford Cardiovascular Institute and co-lead author of the study published May 8 in Nature Cardiovascular Research.
A National Institutes of Health-supported study has found that high-density lipoprotein (HDL) cholesterol, often called the "good cholesterol," may not be as effective as scientists once believed in uniformly predicting cardiovascular disease risk among adults of different racial and ethnic backgrounds. The research, which published in the Journal of the American College of Cardiology ...
New research, presented at the American Heart Association's annual conference, could usher in a new era of cholesterol control. IE 11 is not supported. For an optimal experience visit our site on ...
Research published in Science provides a breakthrough in understanding how dietary cholesterol is absorbed from the gut into the bloodstream. Aster proteins are involved in the non-vesicular ...
Aug. 28, 2023 — New research details the first oral drug for the treatment of a type of high cholesterol -- called Lp(a) -- that is a potentially more dangerous version of the so called 'bad ...
Thus, in recent studies about serum cholesterol, the interest in the role of LDL-C is increasing. There are many studies that show that LDL-C, one of the cholesterols constituting TC, causes atherosclerosis-related disease. ... are thought to influence the ideal serum cholesterol level, so further research is needed. Funding Statement. This ...
The elimination of specific dietary cholesterol target recommendations in recent guidelines has raised questions about its role with respect to cardiovascular disease. This advisory was developed aft. ... Lipid Research Clinics Prevalence Follow-up Study (US and Canada) 4546 men and women: 408: CHD death, 1.0 (10 mg) per 5000 kJ (0.99-1.02)
However, if the cholesterol sources are consumed with saturated and trans fats, as happens in the Western diet pattern, increases in plasma cholesterol may be observed. The most recent epidemiological data and clinical interventions for the most part continue to support the USDA 2015 dietary guidelines that removed the upper limit of dietary ...
The research, which published in the Journal of the American College of Cardiology, found that while low levels of HDL cholesterol predicted an increased risk of heart attacks or related deaths for white adults - a long-accepted association - the same was not true for Black adults. Additionally, higher HDL cholesterol levels were not ...
Abstract. Cardiovascular disease (CVD) is the leading cause of death in the United States. For years, dietary cholesterol was implicated in increasing blood cholesterol levels leading to the elevated risk of CVD. To date, extensive research did not show evidence to support a role of dietary cholesterol in the development of CVD.
Studies find drug protects against heart disease in high-risk groups. Two new studies found that statins, the most prescribed class of drugs to treat high cholesterol, are protective for high-risk groups who haven't yet had a heart attack or stroke but could be at risk of one, according to Harvard-affiliated Brigham and Women's Hospital.
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. When you have too much of this fatty substance, it's considered hyperlipidemia, hypercholesterolemia or high blood cholesterol—a major risk factor for heart attack, heart disease and stroke.
A new study identifies a group of gut bacteria that can metabolize cholesterol and are associated with lower plasma cholesterol levels. ... research highlights.
Collaborative research, led from the University of Oxford and published today in Nature Medicine, has developed a new tool called QR4 that more accurately predicts an individual's 10-year risk of cardiovascular diseases, like heart disease and stroke, particularly identifying high-risk patients that current prediction tools miss.
Higher levels of one group of bacteria called Oscillibacter were strongly associated with lower levels of cholesterol, both in the stool and the blood.Oscillibacter were also linked with other blood markers of reduced CVD risk, such as lower triglycerides and glucose and higher HDL (high-density lipoprotein).. The reductions in cholesterol by Oscillibacter appeared to be related to genes for ...
Childhood abuse may raise cholesterol, diabetes risk in some adults . Apr 27, 2022. Some children who experience abuse may have higher risk for high cholesterol and Type 2 diabetes as adults, new research shows. But some risks may be offset by having "well-organized" households.
By eating so much fiber and so little animal fat, their total cholesterol levels averaged under 150 mg/dL, similar to people eating contemporary strictly plant-based diets. According to William C. Roberts, editor in chief of the American Journal of Cardiology, the only critical risk factor for atherosclerotic plaque buildup is cholesterol ...
New research is explaining how. This new research showed that a single shot taken once a month can drop cholesterol significantly. It's a PCSK9 inhibitor. "What it is, is a drug to lower LDL-C ...
New Research Confirms We Got Cholesterol All Wrong. The U.S. government has pushed a lot of bad nutrition advice over the years. Maybe it should stop advising us on what to eat. A comprehensive ...
Recent research has found a link between certain metabolic factors — such as blood sugar and 'good' cholesterol — and different levels of risk for anxiety, depression, and other mental health ...
Introduction. Cardiovascular disease (CVD) is the leading cause of mortality globally [].Early studies, which indicated that elevated serum cholesterol was associated with an increased risk of heart disease [2, 3], led to the American Heart Association (AHA) recommending limiting dietary cholesterol to less than 300 mg/day with specific recommendations to restrict egg consumption, which are ...
Statins are drugs that lower your body's cholesterol level. They work by reducing the production of cholesterol in the liver and therefore reduce your risk of heart disease. Reliable research? The total number of people involved in the study was nearly 70,000, but only 9 of the 19 studies actually included deaths from heart and circulatory ...
CLEVELAND: Cleveland Clinic has announced the launch of its new Women's Comprehensive Health and Research Center, an initiative dedicated to helping women during midlife and beyond thrive and easily receive the specialized care they need.The center is focused on four key areas: access, connectivity, education, and research and innovation to empower women to navigate their health journey with ...
Research explores how a father's diet could shape the health of his offspring. ScienceDaily . Retrieved April 17, 2024 from www.sciencedaily.com / releases / 2024 / 04 / 240417131002.htm