- Neurology Specialists
- Pediatricians

Education & Research
MaineHealth is advancing the practice of medicine and training the next generation of clinicians through high-quality research and education programs.
Maine Medical Center Department of Medical Education
Maine Medical Center (MMC) is Maine’s only academic medical center conducting cutting edge biomedical research that provides the most advanced treatment options for our patients. Since 1874, MMC has maintained a proud tradition of high-quality medical education and training. We are committed to providing medical students , residents and fellows with the knowledge and skills needed to become future leaders in medicine. MMC also partners with Tufts University School of Medicine (TUSM) to offer the Maine Track Program , an innovative curriculum that includes the unique aspects of rural clinical practice as well as training at major tertiary medical center. Learn more about medical education.
MaineHealth Institute for Research (MHIR)
MaineHealth Institute for Research supports and encourages a broad spectrum of research at MaineHealth ranging from basic laboratory-based research through translational research, which works to apply basic discoveries to medical problems, to clinical research, which studies the direct application of new drugs, devices and treatment protocols to patients, to health services research which seeks to use research methods to help improve and evaluate health care delivery programs and new technologies. View our annual report or visit the MHIR website .
MaineHealth Innovation
MaineHealth drives a culture of innovation by nurturing and funding innovative ideas across our system. Together we are solving health care challenges through new care team models, products, technology and services. Learn more about our innovation program.
MHIR supports and encourages a broad spectrum of research at, ranging from basic laboratory-based research to translational research, clinical research and health services research.

Students, Residents & Fellows
We support over 240 residents and fellows in over 20 ACGME approved programs.

Hannaford Simulation Center
The Hannaford Center for Safety, Innovation and Simulation offers high-tech and realistic simulation.

Continuing Medical Education
Our mission is to promote excellence in medical education in Maine.
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- Health & Well-being
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Funding Opportunities
- Join Our Voluntary Faculty
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Medical Education (MHS-MedEd) Track
This two-year degree program in the Medical Education track features an education research project and includes a comprehensive curriculum for individuals interested in developing a career in the field of medical health.
The degree course work includes a research project, core curriculum and elective courses. Students work within an individualized learning plan that is designed to facilitate their development as educators, scholars, and leaders in medical education.
Graduates of the program will be prepared to contribute to the education community at Yale School of Medicine and the broader field of medical education, both nationally and internationally.
On this Page
Program objectives, course & graduation requirements, time allowance & department commitment.
- Current Students & Alumni
Contact Us & Track Leadership
- Design, implement, and disseminate an education research project.
- Gain practical educational experience though active involvement in graduate and undergraduate medical education activities.
- Develop proficiency to serve as a leader in medical education and medical education research.
MHS Required Courses
- IMED 625 – Principles of Clinical Research – Summer Semester (July)
- IMED 630– Ethical Issues in Biomedical Research, which is offered during the fall semester on Tuesdays 3:30-5:00 pm, and conflicts with MD506.
- Med Ed Track Students take: SecEd 511 – Responsible Conduct of Research (RCR) offered on various dates beginning in the fall semester through the spring semester. Six total sessions, each two hours long.
- IMED 645 – Introduction to Biostatistics in Clinical Investigation – offered during summer semester July-August
Medical Education Track Required Courses
First-year student requirements:.
MD506 – Medical Education: Theory Research and Practice – primarily Tuesdays 4-7:00 pm
- Summer Semester, including seven classes in July and August
- Fall Semester, including 13 classes with 5 Research in Progress Sessions
- Spring Semester, including 13 classes with 3 Research in Progress Sessions
Second-year Student Requirements:
- Fall semester: 5 Research in Progress Sessions
- Spring semester: 3 Research in Progress Sessions
- Leadership development: There is also a leadership development course shared across MHS tracks.
Additional Graduation Requirements:
Tracked by the Center for Medical Education on the Individual Learning Plan form:
- Write and defend a thesis
- Graduate research presentation attended by all current students
- Manuscript ready for publication
- Scheduled meetings with mentors and Center for Medical Education faculty, as specified
- Submission of information on research products that stem from the MHS-Medical Education work (e.g., manuscript, publication, presentations, grants)
- Submission of updated Yale CV Parts 1 and 2 with any products (e.g., presentations, talks, workshops, and publications) resulting from the research highlighted
This is a two-year program requiring a 35% time commitment, which must be approved by your department chair or division chief in writing. This program is intended for those who plan to pursue a career at Yale. While this is not a strict requirement, because of Yale’s investment in the participant, it will be an important consideration.
If a participant is unable to complete the degree in two years, approval of an extension is required by the Yale MHS Degree Program and the Track Academic Director.
Graduation Candidates - May 2025
Clinical Fellow
Associate Professor of Medicine (General Medicine); Director of Diversity, Equity and Inclusivity, GME, VA; Associate Program Director, Internal Medicine Residency Program, Department of Medicine; Vice-Chair of DEI at VACHS, Veterans Affairs Healthcare System of CT
Jennifer Rockfeld, MD View Full Profile
Graduation Candidates - May 2024
Assistant Professor of Psychiatry; Director of Social Justice and Health Equity (SJHE) Education, Adult Psychiatry
Hospital Resident
Clinical Associate
Assistant Professor of Anesthesiology; Co-Director Yale Adult ECMO Program, Cardiac Anesthesiology Leadership; Associate Director Adult Cardiothoracic Anesthesiology Fellowship, Cardiac Anesthesiology Leadership
Assistant Professor of Medicine (Medical Oncology)
Assistant Professor of Surgery (Plastic); Plastic Surgery Residency, Associate Program Director, Plastic & Reconstructive Surgery; Plastic Surgery Clerkship Director, Department of Surgery
Instructor of Medicine (General Medicine)
Please contact Center for Medical Education Director of Programs, Dorothy DeBernardo , with questions.
Professor of Pediatrics (General Pediatrics); Associate Dean for Teaching and Learning, General Pediatrics; Director of the Center for Medical Education, Pediatrics
Coronavirus (COVID-19): Latest Updates | Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies | COVID-19 Testing | Vaccine Information Vaccine Information Vaccine Information
Department of Medicine
Medical education research and scholarship.

Advancing the process of educating the people who care for our community
The University of Rochester Department of Medicine is a leader in medical education innovation. We’re here to support scholars to develop, investigate, and disseminate this work. Our goal is to move the field of medical education forward at the undergraduate, graduate, and continuing professional education level, incorporating our interprofessional learners, and supporting an environment where diverse learners and faculty can thrive.
Request a Consult
Request a consult on your medical education research or scholarly project.
Request a consult
Resource Center
Developing your research question, methods, writing, dissemination
- Our curated collection of resources in Miner Library to support medical education scholars (coming soon!)
- Research Subjects Review Board
Upcoming Events
Department of medicine medical education works-in-progress.
Presenter: Alec O'Connor, MD, MPH
Friday, March 29, 2024 Noon-12:50pm
Contact [email protected] or [email protected] for zoom info
Annual Faculty Development Colloquium
Wedmesday, June 5, 2024 8am-1:00pm More information
Learn more about the Ritchie Fellowships
Scholar Highlight
Meet christopher mooney, phd, mph, ma.

Chris’ education scholarship focuses on evaluating and improving the quality of narrative assessments of learners, and education research methods. In response to the limited reliability and meaningfulness of numerical (e.g. Likert scale) evaluations, there has been a shift in medical education toward improving the quality and usefulness of narrative (free text) evaluations. Chris worked with a team to develop an instrument to evaluate the quality of narrative evaluations, then led studies revealing important factors that correlate with the quality of narrative evaluations. In addition to his own research program, Chris has long been a sought-after collaborator on medical education research. He has chaired the NEGEA Medical Education Scholarship, Research, and Evaluation Committee and directed the AAMC’s Medical Education Research Certificate program, where he teaches quantitative methods. Currently serving as the President-elect of the Society of Directors of Research in Medical Education (SDRME), Chris holds several roles at the University of Rochester School of Medicine including Director of Assessment and Director of the students' Medical Education Pathway. Outside of these pursuits, he is a husband and father of four children—the bulk of which are growing tired of his corny puns and dad jokes. The Mooney family motto is “Well, that escalated quickly.”
Medical Education
Make the AAMC your medical education home. Explore what we have to offer, from learning events, trainings, and professional development conferences to programs, initiatives, and scholarship on key and emerging topics. Get involved, advance your career, and help move the field of medical education forward.
Areas of Focus
'Qualitative' and 'quantitative' methods and approaches across subject fields: implications for research values, assumptions, and practices
Nick Pilcher & Martin Cortazzi
Carrying out research in Nepal: perceptions of scholars about research environment and challenges
Prakash Kumar Paudel & Basant Giri

A Medical Science Educator’s Guide to Selecting a Research Paradigm: Building a Basis for Better Research
Megan E.L. Brown & Angelique N. Dueñas
Avoid common mistakes on your manuscript.
Introduction
Is the field of medical education (Med Ed) research an interdisciplinary field? This question may sound odd to members of the field as it is generally presumed that Med Ed research draws on the insights, methods, and knowledge from multiple disciplines and research domains (e.g. Sociology, Anthropology, Education, Humanities, Psychology) (Albert et al. 2020 ). This common view of Med Ed research is echoed and reinforced by the narrative used by leading Med Ed departments and research centres to describe their activities. Words and expressions such as “interdisciplinarity,” “multidisciplinary perspective,” and “opportunities for interdisciplinary collaboration” are frequently used to depict their mission, goals, and the academic training they provide to their students. Footnote 1 Researchers in Med Ed also often characterise the field as being a hybrid domain, building on various methodologies and disciplines (Gruppen 2014 ; Gwee et al. 2013 ; O’Sullivan et al. 2010 ; Teodorczuk et al. 2017 ).
In this article, we examine the assumption that Med Ed research is an interdisciplinary field. This wide-spread assumption has not yet been investigated. To date, there is no empirical evidence that either supports or calls into question that the field is interdisciplinary. Answering this question may impact the development of Med Ed research as members of the field will be able to make an informed decision about how they would like to see the field develop. In this article, we define interdisciplinarity, following the National Academy of Science’s definition ( 2005 ), as communication and collaboration between researchers across academic disciplines and research domains.
One effective method to investigate whether Med Ed research is interdisciplinary is to conduct a bibliometric analysis (Larivière and Gingras 2014 ) of articles and journals cited by Med Ed researchers. Bibliometrics offer a “set of methods and measures for studying the structure and process of scholarly communication” (Borgman and Furner 2002 , p. 2). Bibliometric data can shed light on the knowledge that informs Med Ed academics in their published work and, concurrently, trace the contour of the intellectual landscape of the Med Ed research field. By using bibliometric data, we are studying cross-disciplinary communication. We are not attempting to make any claims about the collaborative dimension of interdisciplinarity, as that is beyond the scope of this methodology and this paper. We examined one facet of cross-disciplinary communication, which is the flow of ideas, concepts, and knowledge from other disciplines into the Med Ed field.
A growing body of research shows that cross-disciplinary exchange is a common feature of academic life. Rob Moore coined the term “routine interdisciplinary” to capture this practice ( 2009 ). Jacobs and Frickel ( 2009 ), Jacobs ( 2014 ), Larivieres and Gingras ( 2014 ), and Van Noorden ( 2015 ) used bibliometrics to show that it is a customary practice for scientists to cite the work from colleagues outside their discipline. We build on this body of work in this study by examining Med Ed researchers’ distinct citation practice. We use these citation practices as a way to trace which disciplines and domains of knowledge are drawn upon by Med Ed researchers to inform their work.
Journals and research articles sampling rationale and procedure
The first step in our bibliometric analysis was identifying the five Med Ed journals with the highest impact factor by using the 2017 Journal Citation Reports (JCR) (2018 was not available at the time of data collection). The JCR category used was “Education, Scientific Disciplines,” which is where Med Ed journals are classified by Clarivate Analytics. The five journals with the highest impact factor in Med Ed (at the time we conducted our research) were: Academic Medicine , Medical Education , Advances in Health Sciences Education , Medical Teacher , and BMC Medical Education (see Table 1 ). Our goal was not to create a sample of journals representative of the whole range of publications in the Med Ed research field, but to select the most cited journals, i.e., those that are the most influential in the field.
The second step was selecting a sample of articles published within these five journals. Since the goal of our project was to study the patterns of knowledge circulation within Med Ed research, we included research articles published in 2017 in the five journals. The research articles from 2017 from each journal were exported from Web of Science and cross-checked manually with each journal’s Table of Contents. For feasibility, we included only a subset of the total research articles published in 2017. Using a random number generator (random.org), we selected 10% of the research articles published in each journal (see Table 1 ). The procedure we followed for each journal is exemplified by the steps we took to select articles from the journal Academic Medicine which published 134 research articles in 2017. First, we numbered 1–134 all the research articles published in the journal in 2017. Second, we set the number generator minimum as 1 and maximum as 134, and then we generated 13 random numbers (i.e., 10% of the 134 research articles). For our study dataset, we used the 13 articles that matched the randomly generated numbers. We repeated this procedure for all selected journals. In total, 64 articles were selected to be included in our sample across the five journals. Table 1 outlines the number of research articles published in each of the five targeted journals in 2017 and the number of articles randomly selected per journal based on the 10% ratio. Reviews, commentaries, letters, editorials, and other non-primary research formats were excluded from our sample as they are not research (e.g. Academic Medicine Last Page, Medical Teacher Twelve Tips, Advances in Health Sciences Education Reflection articles, Medical Education When I Say).
We decided to sample 10% of the research articles published in each journal for feasibility reasons. Our goal was not to be exhaustive but to ensure a reasonable representation of the work without skewing the selection in favour of any one research area or discipline. We have no reason to believe that the articles included in our sample are meaningfully different in terms of reference patterns from those not included.
References sampling
The third methodological step was constructing our references dataset from the 64 randomly selected research articles. We exported the references for each of the 64 articles from Web of Science and cross-checked manually with the article PDFs to ensure all references were captured. We included references (n = 1412) from peer-reviewed journals as our unit of analysis.
In total, 153 references cited books across the 64 articles included in our sample, in comparison with 1412 references which cited peer-reviewed journal articles. The ratio of book references to journal references is therefore: 1412:153 which is just over nine. Proportionally, this means that there are nearly nine times more references from journals than from books. We did, however, review the titles of these books as part of our initial analysis. There was no particular trend arising from the book references that significantly alter the patterns observed across the articles. For the remainder of this paper, we will focus on the analysis of the 1412 journal articles referenced, which was our dataset. Figure 1 outlines the steps we took constructing our references dataset.
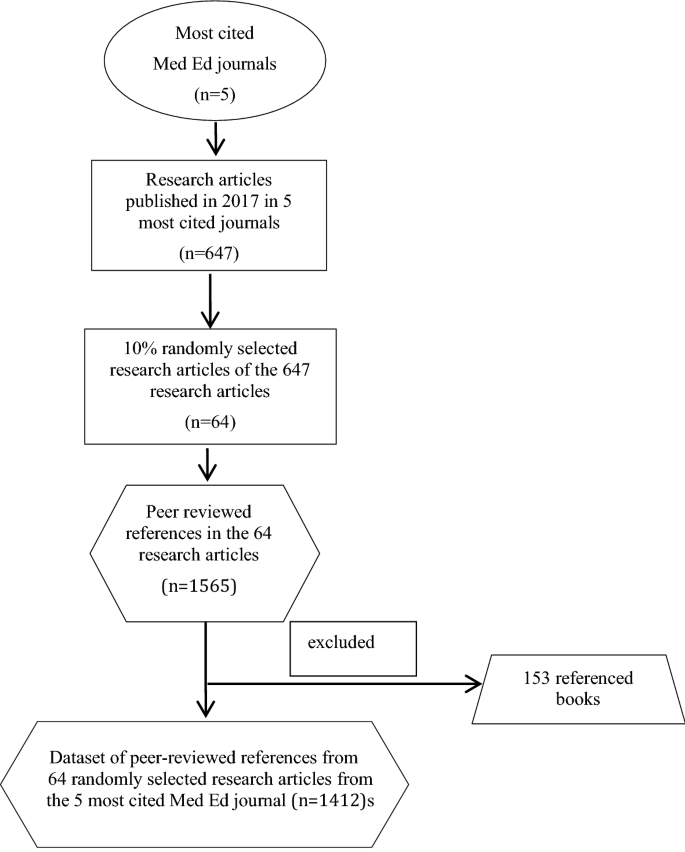
Procedure used to construct the dataset of peer-reviewed cited references from the five most cited Med Ed journals
Data analysis
To analyse the references and examine which disciplines Med Ed researchers draw from, we inductively developed a typology of six knowledge orientations, which we labelled knowledge clusters (see Table 2 ). These knowledge clusters were developed by examining the “Aims and Scope” of the journals cited by the 1412 references. All journals have a web page dedicated to their “Aims and Scope” where they describe their mandate and the type(s) of research they consider in alignment with their editorial orientation. The details provided typically list what discipline(s), topic(s), research area(s), and method(s) fall within their scope. The categorisation procedure we followed is similar to the one followed by qualitative researchers when conducting thematic analysis: in both types of research, categories, or clusters, are gradually developed through an iterative process of inclusion, exclusion, expansion, and division. Clusters take their final shape only when the analysis of new data (quotes in qualitative research, journals in our study) is completed. This inductive procedure should not be confused with the statistical cluster analysis method used in quantitative studies.
The six inductively developed knowledge clusters served as our conceptual map to categorise the 1412 references. For example, a reference from the journals Journal of the American Medical Association (JAMA) or the New England Journal of Medicine ( NEJM ) was classified within the Applied Health Research knowledge cluster because JAMA and NEJM , based on their aims and scope, are two journals whose primary research orientation is applied health research (in contrast, for example, to basic or disciplinary health research). Another example is the journal Simulation in Healthcare . We categorised this journal within the Interdisciplinary Health knowledge cluster because its main focus is healthcare simulation technology (which is a research topic, not a discipline) and it defines itself as a multidisciplinary publication. In cases where the information posted on the aims and scope web page was insufficiently detailed or unclear, members of the research team (MA and SL) read articles published in the recent issues of the referenced journals before categorising. In order to provide as much detail as possible on the journal categorisation, we list in Table 2 the six journals with the highest number of references for each cluster. The detailed list will help elucidate the groupings made therein and the knowledge orientation of each cluster.
We chose to design our groupings of journals as inductively developed “clusters” instead of “categories” since the type of data we are working with (i.e., references, journals, and ultimately areas of knowledge production) is inherently porous. The notion of cluster, more than category, better reflects this porosity. All journals within a cluster share a key characteristic (for example, being topic-centered, disciplinary, or education-focused); however, a number of journals may also share aspects with, or overlap onto, a neighboring cluster. For example, the journal Educational and Psychological Measurement was included in the Topic-Centered knowledge cluster because its primary focus is measurement; however, articles in this journal may tangentially address educational or psychological issues. The assignment of any journal to a knowledge cluster was based on its predominant characteristics. The clustering was performed by MA and SL.
Citation patterns in medical education journals
The most striking finding is the steep discrepancy between, on the one hand, the Applied Health Research and Med Ed knowledge clusters and, on the other hand, the other four clusters (see Fig. 2 ). The Applied Health and Med Ed clusters cover 81% of all references, leaving 19% distributed among the other knowledge clusters. This pattern suggests that the field of Med Ed research stands predominantly on two knowledge pillars. These pillars are health services research and clinical research (which represent 41% of the references) and Med Ed (which represents 40% of the references). The quasi-hegemonic position held by these two knowledge clusters confines the other sources of knowledge to a peripheral role within the Med Ed research field.
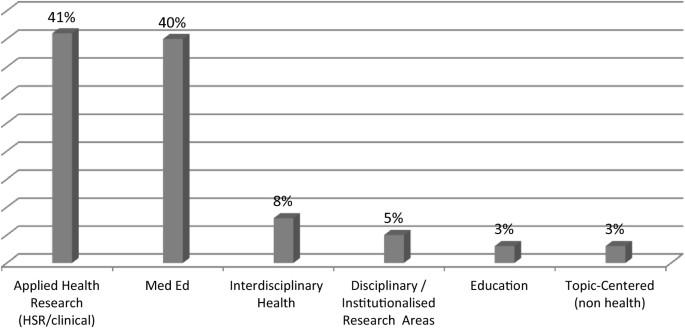
Distribution of peer-reviewed references (n = 1412) per knowledge cluster. Data presented in %
When Med Ed researchers seek knowledge from outside their field and the applied health research field, they primarily turn to interdisciplinary health research (see Interdisciplinary Health in Fig. 2 ). The journals included in this cluster cover a wide spectrum of topics, from drugs and alcohol dependence to women’s health, health policy, simulation, and religion and health. One key characteristic of the journals in this cluster is that some of the articles draw on the knowledge developed in the core disciplines and institutionalised research areas (organisation studies, cognitive sciences, sociology, etc.). While their mandate is usually not to expand theory (but rather to report on empirical research), it is not uncommon for a number of these journals, such as Social Science & Medicine , to publish articles offering a conceptual understanding of phenomena. Therefore, through the journals included in the Interdisciplinary Health knowledge cluster, Med Ed researchers have a connection with a more comprehensive source of knowledge that is both basic and applied.
As shown in Fig. 2 , the Interdisciplinary Health knowledge cluster stands in third position in terms of its overall volume of references. Yet, this volume represents only 8% (n = 115 references) of the 1412 references in our sample used by Med Ed researchers. It follows that the capacity of this body of knowledge to influence the Med Ed academic culture is likely to be relatively marginal.
The bodies of literature cited by Med Ed researchers decreases substantially when these references come from journals outside health research. The next three clusters in Fig. 2 (the Disciplinary and Institutionalised Research Areas cluster, the Education cluster, and the Topic-Centered (non-health) cluster) respectively represent only 5%, 3%, and 3% of all references. One would expect that Med Ed researchers draw upon these research areas more—especially education, as it is a cognate field. Our data suggest that, to the contrary, Med Ed researchers tend to marginally engage with this literature.
In order to paint a more detailed picture of the disciplinary knowledge entering the Med Ed intellectual space, we examine the Disciplinary and Institutionalised Research Areas knowledge cluster more closely. We noticed that one discipline (psychology) largely exceeded the others, which has the effect of further narrowing down the range of disciplinary knowledge entering the Med Ed field. Among the 77 references contained in this cluster, 55 (71%) are from psychology journals (including seven from psychology journals applied to education). The remaining references are distributed across nine disciplines and research areas: sociology (n = 6), business, management and organisations studies (n = 5), social psychology (n = 3), biology (n = 2), the humanities (n = 2), neuropsychology (n = 1), physiology (n = 1), statistics (n = 1), and cognitive science (n = 1).
One of the common goals of the journals included in the Disciplinary and Institutionalised Research Areas knowledge cluster is to advance both basic and applied disciplinary and interdisciplinary knowledge through cross-communication between empirical research and theory. Based on the citation patterns revealed by our data, it seems that this mix of disciplinary, basic/applied, and theoretical knowledge does not easily find its way into the Med Ed research field. While psychology may be utilized by Med Ed researchers, the other disciplines are essentially absent.
Our findings suggest that when Med Ed researchers seek knowledge from outside their field, they predominantly draw from one research area (i.e., applied health). This practice seems to show some discrepancy in regard to the commonly accepted definition of interdisciplinarity, which emphasizes knowledge flow between various research communities (National Academy of Science 2005 ). The high percentage of citations from just one knowledge cluster outside Med Ed suggests that the knowledge landscape of the field could be portrayed as being only tangentially interdisciplinary. With 41% of the references coming from health services research and clinical journals, the academic group with whom Med Ed researchers have the closest connection is the applied health research community. This privileged connection risks excluding other research communities and these other robust bodies of knowledge. These other research communities are the social scientists, the natural scientists, and the humanities scholars. It seems, therefore, that interdisciplinarity for Med Ed researchers means, first and foremost, drawing on and being inspired by clinical and health services research and by the medical epistemic culture underpinning these knowledge domains. Basic, (inter)-disciplinary, and theory-based knowledge seems to be infrequently used by Med Ed researchers and therefore is unlikely to influence the field in a meaningful way. In light of this, one wonders how the Med Ed research field may best be characterised: as an interdisciplinary sub-field of education or as a sub-field of health research? The difference is potentially subtle, but reflecting on this positioning draws attention to how we might think about the dynamics of knowledge production and the future of Med Ed.
If Med Ed researchers predominantly use knowledge developed in health services research and the clinical sciences, it is legitimate to ask whether there could be a misalignment between the body of knowledge drawn from and their research object—education—which is primarily a social science object. If education is a multifaceted phenomenon, how can it be comprehensively studied if researchers draw on a relatively narrow range of knowledge sources, methods, and approaches? Specifically, how can the sociological, psychological, political, cultural, and historical dimensions embedded in the practice of education be studied and understood, without substantive inputs from the academic disciplines focusing on understanding these aspects (Bridges 2017 ; Furlong 2013 )?
Further, the lack of engagement with wider developments in disciplinary knowledge may raise a number of challenges: Med Ed researchers may not have an in-depth understanding of the literature coming from these fields and have difficulty teaching disciplinary knowledge to their students, further hindering knowledge communication with scholars outside Med Ed. Because of the health orientation and relative insularity of the field (as our data suggest), Med Ed researchers could also find themselves asking questions that researchers and practitioners within the Med Ed field may find interesting and novel, but that might have already been investigated by researchers in the social and natural sciences. This would be a lost opportunity to build Med Ed knowledge upon existing foundations, and could potentially undermine the status of the Med Ed field in the broader academic market where it is common practice to borrow ideas, concepts, and methods from other disciplines (Albert et al. 2020 ; Jacobs 2014 , Larivière and Gingras 2014 ; Moore 2011 ). Research fields with a low participation in knowledge exchange across the university may potentially be at risk of being left behind when new theoretical and methodological developments occur (Jacobs 2014 ). Being “out of the loop” may also result in Med Ed researchers potentially applying a theoretical framing or methodological approach that has already been debated, dismissed, or evolved in other disciplines.
The goal of this study was to examine the widespread assumption that Med Ed research is an interdisciplinary field. Our findings show that this belief is not convincingly supported by empirical data and that the knowledge entering, circulating, and informing Med Ed research comes mostly from the health research domain. It behooves members of the Med Ed field to reflect on the current knowledge flow: is the health orientation of the field appropriate and sufficient to pursue education research in health care or is a diversification of knowledge needed? We see this as a contribution to the understanding of what the Med Ed field is, and what could be done to further its development.
Our study is not without limitations. A larger sample may have offered a more refined picture of the citation practices of Med Ed researchers. Also, since we have not used a comparative design, we cannot interpret our findings in comparison with the knowledge flow occurring in other research communities. This is something worth studying in future projects.
Further research should also explore the reasons why Med Ed researchers tend to predominantly cite literature from health rather than from non-health disciplines. Perhaps Med Ed researchers build their rationale for education research from the observation of clinical problems (i.e. the needs of a particular patient population indicate a need for further clinical education), but do not go far beyond the clinical rationale in their literature searches. Another reason could be that clinical and health services research journals are the most familiar to Med Ed researchers, perhaps the most easily accessible and discussed in their academic environment. It could also be that researchers in the Med Ed field view Education and the social sciences as having little to contribute to education in health care settings. Investigating these questions will help develop a better understanding of the factors influencing knowledge production in Med Ed research and situate the field among other education research fields. The types of knowledge drawn upon have implications for how education interventions are designed and how we train future generations of Med Ed researchers.
The two following quotes illustrate the interdisciplinary narrative used by Med Ed departments and research centres to describe the nature of their core activities: “The Centre for Education Research and Innovation is an interdisciplinary, collaborative research group exploring health professions education research” (Centre for Education Research and Innovation, Western University 2019 ). “Health sciences education research draws on theories and methodologies from across myriad research traditions.” (Centre for Medical Education, McGill University 2019 ). Other examples of interdisciplinary narratives can be found on the web site of the School of Health Profession Education, Maastricht University ( 2019 ), the Centre for Health Education Scholarship, University of British Columbia ( 2019 ), the Health Professions Education Research PhD Program, University of Toronto ( 2019 ), the Department of Innovation in Medical Education, University of Ottawa ( 2019 ) and Chang Gung Medical Education Research Center, Chang Gung University ( 2019 ).
Albert, M., Friesen, F., Rowland, P., & Laberge, S. (2020). Problematizing assumptions about interdisciplinary research: Implications for health professions education research. Advances in Health Sciences Education .
Borgman, C. L., & Furner, J. (2002). Scholarly communication and bibliometrics. Annual Review of Information Science and Technology, 36 (1), 3–72.
Google Scholar
Bridges, D. (2017). Philosophy in educational research. Epistemology, ethics, politics and quality . Cham: Springer.
Centre for Health Education Scholarship, University of British Columbia. Retrieved August 26, 2019, from https://ches.med.ubc.ca/about-ches/strategic-plan/ .
Centre for Medical Education, McGill University. Retrieved August 26, 2019, from https://www.mcgill.ca/centreformeded/research-activities/cross-cutting-goals-and-strategies .
Centre of Education Research & Innovation, W. University. Retrieved August 26, 2019, from https://www.schulich.uwo.ca/ceri/research/index.html .
Chang Gung Medical Education Research Center, Chang Gung University. Retrieved August 26, 2019, from https://www1.cgmh.org.tw/cgmerc/view/about.aspx?tMenuNameId=9 .
Department of Innovation in Medical Education, University of Ottawa. Retrieved August 26, 2019, from https://med.uottawa.ca/department-innovation/research/support-your-research .
Furlong, J. (2013). Education. An anatomy of the discipline . New York: Routledge.
Book Google Scholar
Health Professions Education Research PhD Program, University of Toronto. Retrieved August 26, 2019, from https://ihpme.utoronto.ca/academics/rd/hper-phd/ .
Gruppen, L. D. (2014). Humility and respect: Core values in medical education. Medical Education, 48 (1), 53–58.
Article Google Scholar
Gwee, M. C. E., Samarasekera, D. D., & Chong, Y. (2013). APMEC 2014: Optimising collaboration in medical education: Building bridges connecting minds. Medical Education, 47 (s2), iii–iv.
Jacobs, J. A. (2014). In defense of disciplines interdisciplinarity and specialization in the research university . Chicago: University of Chicago Press.
Jacobs, J. A., & Frickel, S. (2009). Interdisciplinarity: A critical assessment. Annual Review of Sociology , 35 , 43–65.
Larivière, V., & Gingras, Y. (2014). Measuring interdisciplinarity. In B.Cronin, & C. Sugimoto (Eds.), Beyond bibliometrics: Harnessing multidimensional indicators of scholarly impact (pp. 187–200). Cambridge: MIT Press.
Moore, R. (2011). Making the break: Disciplines and interdisciplinarity. In F. Christie & K. Maton (Eds.), Disciplinarity: Functional linguistic and sociological perspectives (pp. 87–105). London: Continuum.
National Academy of Sciences. (2005). Facilitating Interdisciplinary research . Washinton: The National Academies Press.
O’Sullivan, P. S., Stoddard, H. A., & Kalishman, S. (2010). Collaborative research in medical education: A discussion of theory and practice. Medical Education, 44 (12), 1175–1184.
School of Health Profession Education, Maastricht University. Retrieved August 26, 2019, from https://she.mumc.maastrichtuniversity.nl/mission-vision-societal-impact-0 .
Teodorczuk, A., Yardley, S., Patel, R., Rogers, G. D., Billett, S., Worley, P., Hirsh, D., & Illing, J. (2017). Medical education research should extend further into clinical practice. Medical Education, 51 (11), 1092–1100.
Van Noorden, R. (2015). Interdisciplinary research by the numbers. Nature, 525 , 306–307.
Download references
Social Sciences and Humanities Research Council of Canada (Grant Nos. 435-2016-0111 and 611-2017-0493).
Author information
Authors and affiliations.
Wilson Centre, Department of Psychiatry, University of Toronto, University Health Network, Toronto, Canada
Mathieu Albert
Wilson Centre, Department of Occupational Science and Occupational Therapy, University of Toronto, University Health Network, Toronto, Canada
Paula Rowland
Centre for Faculty Development, Faculty of Medicine, University of Toronto at St. Michael’s Hospital, Unity Health Toronto, Toronto, Canada
Farah Friesen
School of kinesiology and physical activity sciences, Université de Montréal, Montreal, Canada
Suzanne Laberge
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mathieu Albert .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Albert, M., Rowland, P., Friesen, F. et al. Interdisciplinarity in medical education research: myth and reality. Adv in Health Sci Educ 25 , 1243–1253 (2020). https://doi.org/10.1007/s10459-020-09977-8
Download citation
Received : 23 September 2019
Accepted : 15 June 2020
Published : 24 June 2020
Issue Date : December 2020
DOI : https://doi.org/10.1007/s10459-020-09977-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Interdisciplinarity
- Disciplines
- Medical education research
- Citation analysis
- Find a journal
- Publish with us
- Track your research

- ACGME Accredited Programs
- CPME Accredited Programs
- AEGD Dental Accredited Program
- Medical Clerkships
- Postgraduate Sub-Internships
- Department of Research
- Faculty-Scholar
- Resident-Scholar
- Team 11 Volunteers
- Research Rotation – Fellows
- Research Partner Organizations
- Continuing Medical Education
- Institutional Review Board (IRB)
- Miami Lifestyle
- Department of Research and Academic Affairs
- About the Department of Research and Academic Affairs
- Department Achievements
- Program Spotlight
- Residents & Fellows
- Templates for Research and Scholarly Work
- Global Research Collaboration Network
- Research Internship Opportunity
- Faculty Development
- Department Newsletters
ABOUT THE DEPARTMENT
Our department’s mission is to foster programs that shall promote the interest of clinicians to conduct research, generate knowledge, and advance healthcare. We assist medical Residents and Fellows in:
- Developing skills for the formulation of scholarly work such as posters, presentations, review of literature, and quality improvement.
- Developing foundation skills for research inclusive of formulation of a research question, access and analyze data, review pertinent literature as well as prepare a well-organized research presentation.
- Promote the research and scholarly work of residents, fellows and faculty of Larkin Community Hospital.
- Work on a Research Project from conception through publication.
- Preparing research presentations for Annual Scientific Conferences.
- Promote understanding of Institutional Review Board and relates processes.
- Providing learning experiences and resources for residents and fellows to help them complete their own research projects.
MEET OUR TEAM MEMBERS

Martha Echols, PhD Vice President Department of Research and Academic Affairs

Sultan S. Ahmed, MD Associate Vice President & Ombudsman for GME Department of Research and Academic Affairs

Joseph Hasselbach Coordinator Department of Research and Academic Affairs

Sujan Poudel, M.D Coordinator Department of Research and Academic Affairs
Reach Out To Us Email: [email protected] Phone: 305-284-7567 Office: Room 601, 7000 SW 62nd St. Miami FL
REACH OUT TO THE OMBUDSMAN
The position of Ombudsman for Graduate Medical Education was created to promote a positive climate for residency and fellowship education by providing an independent, impartial, informal, and confidential resource for residents, fellows, and faculty with training-related concerns. You can confidentially call Dr. Sultan S. Ahmed at 786-253-8741 as well as email him at [email protected] . All anonymous concerns and complaints can also be addressed through correspondence at the following e-mail: [email protected] .
Ombudsman Policy
JOIN THE TEAM
This fellowship opportunity is for post-grad and under-grad applicants to develop hands-on research project development and implementation. The term of this fellowship shall be for (3) Months , (6) Months , or (1) Year .
Essential Requirements:
- Must have interpersonal skills needed to develop relationships with clinical departments, international research volunteers, and research liaisons in the Larkin Health System.
- Must be familiar with basics of research and methods application to work with reliable clinical evidence and data, having previous research collaborations that was resulted in publications would be preferred.
- In-person work at DRAA office at least three days a week is preferred.
What You Will Do:
- Participate in DRAA activities as a team member.
- Complete Citi Certificate.
- Complete the Research Training Lab and receive a “Certificate of Completion”.
- Complete and publish a Clinical Case Report.
- Work directly with residents and fellows to complete required research work, such as manuscripts, and quality improvement projects.
- Participate in the development of the Research Department newsletter and Research Symposium.
- Complete a presentation at a continuing medical education conference.
For Application and Requirements click here
Larkin team 11.
Sponsored by Larkin Community Hospital Research Services South Miami, Florida
TEAM 11 OVERVIEW
As background, Team 11 was originally formed during the COVID pandemic and provided invaluable research opportunities during these unprecedented times when sharing of information was critical. As a result of the purpose and connection, the members wanted to stay together and formed the Global Research Collaboration Network.
Recognizing the value of the program, Global Research Collaboration Network, also known as Team 11, Larkin Community Hospital sponsors the program and has integrated it into the Department of Research and Academic Affairs. The platform is open for everyone to bring any research and global health-related issues upfront to make a difference in the world and is free of cost. Team 11 creates opportunities to carry out research projects at both the local and international levels. From its inception, we have had more than 1400 plus researchers worldwide, including medical students, medical graduates, residents, and fellows with multiple successful publications who represent over 100 countries from every continent.

Department of Research & Academic Affairs
7000 SW 62 nd Ave | Suite #601 | Miami, FL 33143
Phone: 305-284-7567 | Email: [email protected]
Most Visited
- AEGD Accredited Program

Let's Get Connected
- Open access
- Published: 19 June 2020
Development and maintenance of a medical education research registry
- Jeffrey A. Wilhite ORCID: orcid.org/0000-0003-4096-8473 1 ,
- Lisa Altshuler 1 ,
- Sondra Zabar 1 ,
- Colleen Gillespie 1 , 2 &
- Adina Kalet 1 , 3
BMC Medical Education volume 20 , Article number: 199 ( 2020 ) Cite this article
6524 Accesses
7 Citations
1 Altmetric
Metrics details
Medical Education research suffers from several methodological limitations including too many single institution, small sample-sized studies, limited access to quality data, and insufficient institutional support. Increasing calls for medical education outcome data and quality improvement research have highlighted a critical need for uniformly clean and easily accessible data. Research registries may fill this gap. In 2006, the Research on Medical Education Outcomes (ROMEO) unit of the Program for Medical Innovations and Research (PrMEIR) at New York University’s (NYU) Robert I. Grossman School of Medicine established the Database for Research on Academic Medicine (DREAM). DREAM is a database of routinely collected, de-identified undergraduate (UME, medical school leading up to the Medical Doctor degree) and graduate medical education (GME, residency also known as post graduate education leading to eligibility for specialty board certification) outcomes data available, through application, to researchers. Learners are added to our database through annual consent sessions conducted at the start of educational training. Based on experience, we describe our methods in creating and maintaining DREAM to serve as a guide for institutions looking to build a new or scale up their medical education registry.
At present, our UME and GME registries have consent rates of 90% ( n = 1438/1598) and 76% ( n = 1988/2627), respectively, with a combined rate of 81% ( n = 3426/4225). 7% ( n = 250/3426) of these learners completed both medical school and residency at our institution. DREAM has yielded a total of 61 individual studies conducted by medical education researchers and a total of 45 academic journal publications.
We have built a community of practice through the building of DREAM and hope, by persisting in this work the full potential of this tool and the community will be realized. While researchers with access to the registry have focused primarily on curricular/ program evaluation, learner competency assessment, and measure validation, we hope to expand the output of the registry to include patient outcomes by linking learner educational and clinical performance across the UME-GME continuum and into independent practice. Future publications will reflect our efforts in reaching this goal and will highlight the long-term impact of our collaborative work.
Peer Review reports
Medical education research (MER) should and could improve the health of the public by informing policy and practice but it suffers from many methodological limitations including small sample sizes, cross sectional designs, and lack of attention to important context variables. There are increasing calls for medical education research, a poorly funded field, to go beyond the proximate outcomes of training to study more distal clinical outcomes using “big data” strategies [ 1 , 2 ]. And yet, even within the same institution, data is collected using different systems and a wide range of formats, without a shared ontology or structured language and therefore is not organized to enable longitudinal tracking of learners, learning, or linking with outcomes.
While medical trainees must be afforded the same ethical and legal protections as any research subjects and U.S. federal regulations allow the use of educational data collected in the routine conduct of a required curriculum for research without written consent from learners, medical school research ethics review boards are not consistent in their approach to trainees as study subjects, complicating the ethical conduct of this type of research [ 3 ]. Establishing research registries can help overcome some of these barriers and facilitate higher impact, ethically rigorous programs of medical education research [ 4 ].
Research registries compile and maintain multiple-source, standardized information on potential study participants longitudinally for many purposes [ 5 ]. The National Leprosy Registry in Norway established in 1856, was the earliest disease specific registry, and the number of disease specific registries has increased steadily since [ 6 ]. More recently, research registries have focused on data integrity and quality improvement, following in the footprints of the Framingham Heart Study-style that began in 1970 [ 5 , 7 ]. In 2006, the Research on Education Outcomes (ROMEO) unit of the Program for Medical Innovations and Research (PrMEIR) at New York University’s (NYU) School of Medicine established the Database for Research on Academic Medicine (DREAM) with funding from the Bureau of Health Professions (BHPr) of the department of Human Resource Services Administration (HRSA # D54HP05446). Borrowing from the constructs underlying disease registries, the goal of DREAM is to enable ethical, longitudinal study of outcomes in medical education through the collection of routine trainee and educational context data [ 8 ]. DREAM, a potential database assembled as needed to ask and answer specific research questions, is structured as two research registries - one for Medical Students (established in 2008, with 1438 current individuals enrolled) and the second, a Graduate Medical Education Registry (established 2006, with 1988 current individuals enrolled), for trainees in the twenty participating residency and fellowship programs in our institution.
With approval from NYU’s Institutional Review Board (IRB) for our medical student and resident/fellow registries, we have been collecting written informed consent from medical trainees (students, residents, and fellows) using highly structured, transparent procedures. We request permission to compile data collected as a routine, required part of the trainee’s education for use in medical education research. Consenting subjects are informed both verbally and in writing that only data that has been de-identified by DREAM’s Honest Broker- a specific individual is responsible for serving as the data steward for the registries and who has absolutely no involvement in the selection, recruitment, employment, evaluation or education of the potential subjects- will be made available for the purposes of research. The consenting process is conducted by core members of the research team serving as Honest Brokers to ensure that the students’ and residents’ decision to consent is private and will not have repercussions (perceived or actual) for their standing in medical school.
DREAM is a collection of routinely gathered educational data spanning the undergraduate medical education (UME, medical school leading up to the Medical Doctor degree)-graduate medical education (GME, residency training also known as post graduate education leading to eligibility for specialty board certification) continuum. Available data at the UME level includes admissions data (e.g., Medical College Admission Test (MCAT) scores, Bachelor’s Degree Grade Point Average (GPA) and field of study (also referred to as major), medical school admissions multiple-mini interview scores), academic performance data (e.g., medical knowledge exam scores, clinical clerkship grades, clinical and workplace-based assessments), performance-based assessments (e.g., Objective Structured Clinical Examinations (OSCEs) and simulations), national licensing exams (Specialty Shelf, Step 1 and Step 2 Exams), and assessments of professional development. Available data at the GME level depends on the participating residency program but generally includes admissions data (medical school, Step 1 and Step 2 Clinical Knowledge (CK) exam scores), attitude and clinical experience/training surveys, milestone assessments, performance-based assessments (OSCEs and simulations), national exams (specialty certification board scores) and clinical assessments (e.g., workplace-based assessments, clinical and procedural skill assessments, and Unannounced Standardized Patient visits). We are currently engaged in several initiatives to incorporate clinical process and outcome data, at least partly attributable to residents, including primary care panel process and outcome variables, laboratory test ordering, and relevant practice quality metrics. As part of the GME Registry, we ask permission to join UME and GME data of learners who graduated from both levels at NYU School of Medicine, and currently maintain a database of 250 continuum learners.
As far as we know the DREAM registries are the longest standing comprehensive medical education registries globally. To date 61 studies have been approved that utilize DREAM data (Table 1 ). Of these studies, there have been 45 publications, answering research questions focused on evaluation of trainings or curriculum, assessment of learner core competencies, and/ or validation of measures (Table 1 , Table 2 ). Routine Registry processes and flow have developed longitudinally through continual internal review and improvement (Fig. 1 , Fig. 2 ). Based on this accumulated experience and scholarly productivity, we propose 3 overarching principles and related practical advice to the larger medical education community on how to develop, implement, maintain and maximize the productivity of a MER registry. While our registries, and the data privacy issue examples provided are specific to the United States context, we suspect that the underlying goals, objectives, principles and guidance provided can be applied in general to the international MER community.
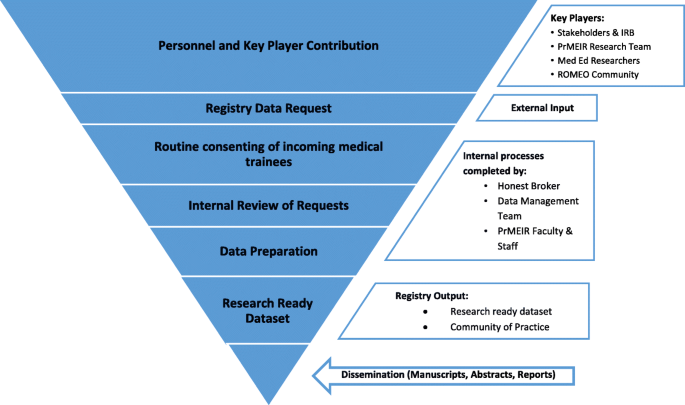
Registry Component Funnel
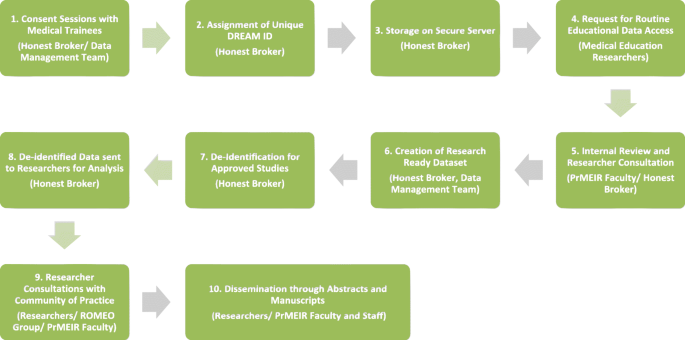
The Research Registry Roadmap (Responsible Party)
Principle 1: ensure the MER registry is addressing an important research mission
Invite broad input from stakeholders.
Assembling a broadly representative team of key stakeholders early in the project ensures long-term buy-in and maximizes resource support and registry productivity [ 9 ]. During initial planning phases, our discussions with community members, including medical education researchers, trainees, information technology (IT) experts, and course, clerkship and residency program directors honed registry objectives and built a case for a medical education research registry at the School of Medicine. A major objective of the registry, developed in collaboration with stakeholders, is to provide clean, easily accessible, de-identified data to the medical education community at NYU while maintaining strict confidentiality and data security. These types of data sets are exceedingly rare in medical education compared to other fields [ 10 , 11 ].
Stakeholder relationships continue to deepen because projects using DREAM data are regularly discussed at weekly, multi-disciplinary sessions where work in progress is shared and collaborations are nurtured. In addition, our review and approval processes include consultations and advising on available data resources, research design and methods, analytic approaches and opportunities for collaboration and therefore there is a great deal of informal MER faculty development that has helped build and sustain a community of Medical Education Researchers (Fig. 2 ).
Identify the scope and purpose of the registry
It is critical to define the scope and purpose of the MER registry [ 5 ]. Given our funding and particular areas of interest, the long term goal of DREAM is to establish the evidence base to guide medical education policy, innovation and practice by directly linking medical education with care quality and safety outcomes for patients. Our registries incorporate selective demographic and descriptive data about learners (e.g. Admissions), all routinely collected assessment and performance data, and selected education-focused survey data. For residents and fellows, we collect de-identified patient data directly attributable to those clinicians (e.g. ambulatory care-based patient panel data), and research utilizing this data is in progress [ 8 ].
Our registry was developed in close collaboration with NYU’s Human Subjects Institutional Review Board (IRB), the Office of Medical Education responsible for running the medical school, and individual residency and fellowship program directors [ 8 ]. Carefully articulating the purpose of a medical education registry helps to maximize stake-holder involvement and buy-in (e.g. trainees, faculty, administrators, patients, the community, the IRB), and to avoid potential misunderstandings of the registry process [ 12 ]. While building the argument for the need for the registry, creators should identify, become conversant with and address critical issues relevant to implementation including the privacy rights and concerns of trainees and legal concerns of the educational and training programs. In the U.S. this means being familiar with both the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and The Family Educational Rights and Privacy Act of 1974 (FERPA) federal laws addressing relevant privacy rights. Data for the registry is maintained by institutional entities and housed on highly secure Medical Center Information Technology (MCIT) servers. The DREAM registries protocols describe how researchers can obtain research-ready curated sets of data (fully de-identified data for only those learners that have provided consent).
Ultimately, the DREAM registries not only serve to advance medical education research globally, they also have contributed substantially to educational scholarship locally, supported promotion and career advancement for our education faculty, and helped faculty and education leaderships answer important – and almost always generalizable – questions about our local curriculum.
Establish a vision and set goals related to future data needs
Registry creators should remain aspirational and regularly brainstorm new research questions and protocols. Our initial plans, which included a focus on collecting performance-based assessment data (e.g. mostly from OSCEs), has grown to include additional assessment data (e.g. knowledge tests, peer assessments, mid-clerkship formative feedback). We also document the nature and timing of significant admissions and curriculum changes. Through regular registry data requests, the PrMEIR team has identified and addressed barriers to filling these requests. These barriers include technical issues such as a variety of data naming, storage, format and complexity concerns, as well as differing views on data use from course and curriculum leadership, registrar, human resources and clinical administrators despite consent from trainees (e.g. “who’s data is it?”). With increasing awareness of the registry and clarification of its purpose we are seeing an increase in the number and complexity of data requests. This has pushed us to continuously improve our communication with stakeholders, clarify our written materials, and enhance our capacity for data wrangling and management [ 13 ]. For instance, we have identified a goal of creating and implementing a standardized education research data warehouse with complete sets of data by student cohort [ 8 , 11 ]. Ideally this warehouse, or mart, will become a one-stop-shop for commonly requested data elements [ 8 ] that would permit aggregate data queries for planning studies and extraction of de-identified data sets for research. The Honest Broker, in more of a Data Steward role (see Principle 2 below) would help maintain the warehouse and routinely adjust its contents, structure, and data definitions to meet demands of an enlarging MER community. In our case, because financial support for DREAM staff has been provided through a combination of research and data infrastructure grants updating to a more robust and comprehensive data architecture is not yet possible. We are optimistic that as institutional data/ information technology resources become steadily more sophisticated more support will become available.
Principle 2: utilize best practice policies and procedures in establishing a MER
Assign a honest broker.
A registry should be managed by a data steward, or an individual positioned as the Honest Broker of research data. In clinical research, Honest Brokers are HIPAA compliant data preparers with a detailed understanding of the role of privacy, confidentiality and data security as regulated by legal requirement and sound moral judgement [ 14 ]. A steward should be capable of carrying out routine data management practices and able to maintain IRB and collaborator communication [ 14 ]. Ideally, Honest Brokers serve as a neutral intermediary between researchers and research participants and in the context of medical education, are responsible for safeguarding a participant’s protected education and training data [ 15 , 16 ]
PrMEIR’s Honest Broker is usually an individual with master’s level education and training specific to adhering to the rules of medical trainee privacy protection. The Broker conducts informed consent procedures with potential participants, prepares clean, de-identified data, communicates with interested collaborators, maintains a relationship with the IRB, is present during all registry related discussions, disseminates appropriate pieces of information to stakeholders, and most importantly, holds, privately and securely, the information on trainees’ decision to consent. Salary support for this function (e.g. calculated as % of a full-time equivalent (FTE)) is provided by a combination of external grants and institutional operating budget.
Establish appropriate funding channels and designate faculty and staff time
Creation of the DREAM registries was funded primarily through three successive Academic Administrative Unit grants from the US Health Resources and Services Administration (HRSA) running from 2011 to 2017. The aim of these grants was, among other things, to build the evidence base for medical education by supporting the data infrastructure necessary for linking educational efforts to patient outcomes in primary care. During the initial days of the registry, several core faculty members spent about a year designing the UME and GME registries and working with the NYU Robert I. Grossman School of Medicine’s IRB to finalize the protocol, consent materials and standard operating procedures. During this period, a small portion of funding was used to obtain the input of a data scientist, with the remainder going toward salary support of PrMEIR staff and faculty. Data storage was, and remains supported through NYU’s MCIT. Since then, grant funding has gone directly to PrMEIR faculty and staff (Honest Broker, Data Management Team) support in the realms of consenting, data cleaning, and upkeep of the registry.
Maintaining the two registries involves annual IRB continuation applications, consenting new learners each year, logging those consents, processing requests to participate in the registry, and overseeing data management. PrMEIR’s Honest Broker (author JW) spends approximately .40 FTE on registry upkeep. Data management, including data cleaning, rationalization (variable labeling, building and maintaining data dictionaries), merging/linking of data sets, and secure data storage, requires the greatest share of resources and currently includes .50 FTE of a Data Manager and .25 FTE of a Data Analyst. When grant-funded studies use core data from the Registries, small amounts of funding have been allocated to supporting Registry Data Management. The Principal Investigator (PI), or lead PrMEIR faculty for each Registry’s IRB protocol (authors CG and SZ), ensures that protocol is followed and participates as part of a small advisory committee that reviews and approves Registry requests, advises on data management practices, and makes use of the data for education research locally. This represents an estimated .05 FTE effort for each of the PIs and for each of the three advisory committee faculty members. A PrMEIR Program Administrator provides supervision to the Honest Broker and Data Management Team (.10 FTE). Therefore, the full team represents about 1.5 total FTE annually. Upkeep of the registry has since been supported in small ways through philanthropy-based funds and portions of other grants from external sources including AHRQ and foundation funding. There was little buy-in from the institution during early development phases, but this has shifted due to the meaningful output of research from those who utilize registry data.
Create rigorous, regulatory-compliant consent materials and processes
IRB approved consent forms (stamped with the approval date) describe the project, anticipated benefits and potential risks as well as processes for consenting, withdrawal of consent and reporting of coercion and breaches of privacy [ 17 ]. The Honest Broker (or delegated research team member) obtains trainee consents by attending new medical trainee program orientations to conduct a brief (< 30 min) information session. He or she briefly describes the project, allows time for trainees to read the consent form, answers questions, and collects signed, written consents from incoming learners. Trainees place their consent forms, whether they provided consent or not, in an envelope and all are asked to return the envelope in order to preserve the privacy and confidentiality of their decision to consent. Beforehand, the Honest Broker coordinates attendance with departmental leadership, collects rosters of incoming students for registry record keeping and prepares materials (printed consent forms, rosters, and attendance tracking materials).
The names of all trainees who consent to a registry are entered into the secure database (REDCap) within 24 h of collection from learners [ 18 ]. Each consenting learner is assigned a unique DREAM Identification number (DREAM ID). The Honest Broker maintains this “cross walk” database connecting subject names and DREAM IDs which is kept on a secure, firewall-protected server to which only a very limited set of research team members have access (currently, n = 2). Signed consent forms are organized consecutively and kept in a locked file cabinet. No one but the Honest Broker and core research team has access to information on the consent status of any individual trainee. Institutional collaborators are then able to request, from the PrMEIR team, curated sets of this data for research studies [ 8 ]. Collaborators must meet strict guidelines for usage. Namely, their study cannot be experimental, must be for education evaluation, assessment, or improvement purposes, and must identify each individual (Table 4 ).
Approximately 90% of medical students (UME) and 76% of residents and fellows (GME) consent to the DREAM registries annually (Table 3 ). Registry personnel complete and maintain all required research staff training. At our institution this includes the Collaborative Institutional Training Initiative (CITI Program) training on biomedical and social/ behavioral research, and good clinical practice. The PrMEIR faculty must maintain Principal Investigator Development and Resources (PINDAR) training completion certificates. These are research ethics trainings that are required for faculty doing research in the United States and are certified by the US Health and Human Services, Office of Science and Research.
Store data in a protected location, with limited access
A high level of protection for this type of data is mandated by these regulations. Establishing data protection protocols that are in-line with appropriate regulatory authorities is essential. Storage of protected information on an appropriately secure server is crucial for privacy protection [ 19 , 20 ]. The MER registry includes educational data protected under The Family Educational Rights and Privacy Act of 1974 (FERPA) [ 21 , 22 , 23 , 24 ].
Develop a standardized processes for registry data requests
Registry leadership needs to establish a process for making decisions about requests for data. A simple, well designed data request form that assess the degree of fit to the goals and regulations of the registry serves as an efficient way to begin the approval process and also serves to communicate those goals and regulations to potentially interested researchers. The registry consent applies only to routinely collected educational information as part of the required curriculum. This can cause confusion since researchers are often seeking to evaluate the impact of a curricular intervention. We often need to clarify that an intervention that is not a routine part of the curriculum - not available to all learners - would not meet registry criteria. In the case of an experimental design where only some students have access to the intervention, investigators need to approach the IRB directly for review. Once it is established that a request is appropriate, there needs to be a transparent, documented decision-making process, and timely feedback given to requestors.
The DREAM data request process is standardized (Table 4 , Fig. 2 ). Interested collaborators speak with registry representatives informally to review the scope of covered data and approval requirements. They then complete a data request survey, which is housed in REDCap, an IRB approved data program that collects essential study information (Table 4 ) [ 18 ]. PrMEIR’s internal team (authors SZ, LA, CG, JW, AK) reviews and discusses each proposal, follows-up to request required additional information, and provides a final decision. A registry data request is often an iterative, conversation, consultation and negotiation between the researcher and registry leadership. During the approval process, registry officials and applicants discuss study design, assessment strategy, and research questions. As noted earlier, this process helps develop applicants as education researchers, helps share information and knowledge about data, and serves to build collaboration among education researchers and synergies in education research projects. The decision of all registry requests is recorded in a request log available for audit by the IRB.
Maintain transparency around data usage & research
There are many concerns around use of education data for research. Some believe that learners are becoming more reluctant to allow their educational data to be used for research [ 13 ]. In our experience, curricular leaders often argue that they have ownership over the data produced during the conduct of formal curriculum they direct. In the era of “big data”, the public has had reason to become increasingly concerned about data use and sharing happening without their knowledge or consent. Public surveys show large variation in trust over use of personal data. Concerns have heightened in the wake of recent privacy breaches on social media platforms and in workplace information systems [ 25 , 26 ]. Medical Education researchers along with partners in the research regulation community must consciously and constantly monitor the protection of rights of research subjects. Pragmatically, this means that data usage plans should be outlined in detail, both verbally and in writing, throughout the research process and researchers must plan to communicate timely results to collaborators and stakeholders.
DREAM documentation outlines data use terms during consenting periods and shares updates with the PrMEIR/ ROMEO community regularly through annual email reminders. Registry personnel provide documentation of the terms of DREAM data usage as part of research training workshops and master’s programs for our community. The registry adheres to FERPA mandates by seeking explicit, plain-language consent to use learner data and by maintaining a record of all uses of those data. This process routinely evolves with the changing needs of registry users and within the context of the global data community. We continue to uphold that each learner’s data belongs to them as individuals and therefore they must give explicit consent for the collection, pooling, and analysis of their data.
Engage in continuous quality improvement
Internal quality improvement processes are vital to making a MER registry a dynamic engine within a vibrant and productive MER community of practice rather than simply a bureaucratic burden. The review process must fall in line with standard IRB continuing review requirements, including updating enrollment numbers, adding and deleting team members, and approving updated consent forms and procedures. However, we recommend going beyond this and ensuring that critical team members discuss, document, and troubleshoot any issues that have developed during the previous year of implementation in light of the goals of and vision for the registry. The PrMEIR team meets regularly to discuss research, consenting of trainees, and dissemination updates as well as routinely reviews the goals for DREAM.

Principle 3: a MER registry should add value to your institution or collaboration by creating a community of practice
Ensure the registry is trustworthy.
Trust is established by maintaining the integrity of the process and is vital in moments where risk or uncertainty exists [ 27 ]. In instances where trust is threatened, registry representatives must work to maintain and re-establish lost trust through regular, clear communication and transparency.
DREAM personnel work to be transparent about data collection, management, sharing and usage during initial consenting of subjects. Personnel maintain transparency after work is shared publicly (i.e. presentation and publication). We regularly respond to informational requests, make formal and informal presentations about the registry, and have basic information on our work publicly available on our website.
Over our 12-year history with consenting trainees, there has been just one, single complaint from a consenting subject about the registry raised to the IRB. This triggered a detailed audit requiring a full investigation of registry practices and review of data. Responding to this audit, which was time consuming and challenging at the time, required us to further strengthen our policies and practices and correct a few clerical mistakes (e.g. we used out-of-date IRB approved consent forms for a consenting session) unrelated to the complaint. In retrospect, this was a critically important and highly valuable “stress test” for the registry, providing much needed pressure to maintain rigorous trustworthy processes.
Provide consultative services for approved registry researchers
To maximize the validity of DREAM based research and in the spirit of collaboration, PrMEIR and the larger ROMEO community offers mentorship, introduction to institutional resources (e.g. research librarians, database selection and use, consultative statisticians) and support (e.g. research assistance, transcription) pragmatically [ 28 ]. During the data request review process, study protocols and data analysis plans are refined. Registry researchers are routinely welcomed to registry management meetings, and to present at larger PrMEIR meetings for guidance and mentorship [ 28 ]. We have found that this enables researchers to hone their plans by refining research questions, identifying study appropriate conceptual and theoretical models, and crafting data analysis plans. When studies are underway, we provide assistance in abstract and manuscript preparation individually and in groups. Most commonly we find ourselves helping researchers put their work into the context of the existing literature and with articulating the implications of their research. Over time, this has allowed us to build a robust medical education research community in our institution.
Create a space for a community of practice
Communities of practice are groups of people who come together physically and/ or virtually to collaboratively learn and share in developing a joint enterprise through establishing an engaging social structure and sharing expertise and resources [ 29 ]. The ROMEO unit began in 2005, having originally been designed as an interprofessional, interdepartmental collaborative community aimed at conducting medical education scholarship to improve patient and population health. With weekly research meetings, ROMEO served to build a community of researchers with shared passions for contributing to the MER field. The output of this community reflects a wide range of research areas and a rich network of collaboration (Table 2 ).
The DREAM registries are key projects that tie the ROMEO community into a rich network of collaborators across health professions and clinical disciplines, including psychology, learning and library sciences, informatics and more. Further insight into the history can be seen when looking at how data collection and structuring evolved to meet new demands, all of this, in summation, created a vibrant community of practice.
Conclusions
MER registries have the potential to provide the much-needed infrastructure enabling the community to conduct programs of research that fill critical gaps in our understanding of the direct link between health professions education and the health of patients. This work has the potential to be transformational. We have built a community of practice within the NYU community through the building of DREAM and hope, by persisting in this work the full potential of this tool and the community will be realized. At present, researchers with access to the registry have focused primarily on curricular and program evaluation, learner competency assessment, and measure validation (Table 1 ). We hope to expand the output of the registry to include patient outcomes by linking learner educational and clinical performance across the UME-GME continuum and into independent practice. Future publications will reflect our efforts in reaching this goal and will highlight the long-term impact of our collaborative work.
We are also working toward making these de-identified education research data sets publicly available and in particular are working with other medical schools to implement similar registries in the hopes of being able to make comparable data from multiple institutions in order to explore the many contextual factors that are of interest to the medical education community. The advice outlined above, reflects our hard-earned learning about how to build and maintain a productive MER registry.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study. While data for DREAM participants is not currently publicly available, the authors are working to make them available in the future. In the meantime, the authors are collaborating in building additional research registries within external medical education communities.
Abbreviations
Bureau of Health Professions
Clinical Knowledge
Collaborative Institutional Training Initiative
Database for Research on Academic Medicine
DREAM Identification Number
The Family Educational Rights and Privacy Act of 1974
Full-time Equivalent
Grade Point Average
Graduate Medical Education
Health Insurance Portability and Accountability Act of 1996
Human Resource Services Administration
Information Technology
Institutional Review Board
Medical Center Information Technology
Medical College Admission Test
Medical Education Research
New York University
Objective Structured Clinical Examinations
Principal Investigator
Principal Investigator Development and Resources
Program for Medical Innovations and Research
Research on Medical Education Outcomes
Undergraduate Medical Education
Chahine S, Kulasegaram KM, Wright S, Monteiro S, Grierson LE, Barber C, et al. A call to investigate the relationship between education and health outcomes using big data. Acad Med. 2018;93(6):829–32.
Article Google Scholar
Triola MM, Campion N, McGee JB, et al. An XML standard for virtual patients: exchanging case-based simulations in medical education. AMIA Annu Symp Proc. Bethesda. 2007;2007:741–745. Published 2007 Oct 11.
Sarpel U, Hopkins M, More F, Yavner S, Pusic M, Nick M, et al. Medical students as human subjects in educational research. Med Educ Online. 2013;18:19524.
Cook DA, Andriole DA, Durning SJ, Roberts NK, Triola MM. Longitudinal research databases in medical education: facilitating the study of educational outcomes over time and across institutions. Acad Med. 2010;85(8):1340–6.
Arts DGT, de Keiser NF, Scheffer G-J. Defining and improving data quality in medical registries: a literature review, case study, and generic framework. J Am Med Inform Assoc. 2002;9(6):600–11.
Irgens L. The origin of registry-based medical research and care. Acta Neurol Scand Suppl. 2012;126:4–6.
Gonnella JS, Hojat M, Veloski JJ. Abstracts: Jefferson longitudinal study of medical education, [full volume]. Jefferson Longitudinal Study of Medical Education; 2005. p. 1.
Google Scholar
Gillespie C, Zabar S, Altshuler L, Fox J, Pusic M, Xu J, et al. The research on medical education outcomes (ROMEO) registry: addressing ethical and practical challenges of using “bigger,” longitudinal educational data. Acad Med. 2016;91(5):690–5.
Jongbloed B, Enders J, Salerno C. Higher education and its communities: interconnections, interdependencies and a research agenda. High Educ. 2008;56(3):303–24.
Ellaway RH, Pusic MV, Galbraith RM, Cameron T. Developing the role of big data and analytics in health professional education. Med Teacher. 2014;36:216–22.
Kimball R, Reeves L, Ross M, Thornthwaite W. The data warehouse lifecycle toolkit: expert methods for designing, developing, and deploying data warehouses: John Wiley & Sons; 1998.
Solomon DJ, Henry RC, Hogan JG, Van Amburg GH, Taylor J. Evaluation and implementation of public health registries. Public Health Rep. 1991;106(2):142.
Ellaway RH, Topps D, Pusic M. Data, Big and Small: Emerging Challenges to Medical Education Scholarship. Acad Med. 2019;94(1):31-36. https://doi.org/10.1097/ACM.0000000000002465 .
Choi HJ, Lee MJ, Choi C-M, Lee J, Shin S-Y, Lyu Y, et al. Establishing the role of honest broker: bridging the gap between protecting personal health data and clinical research efficiency. PeerJ. 2015;3:e1506.
El Emam K, Rodgers S, Malin B. Anonymising and sharing individual patient data. Bmj. 2015;350:h1139.
Dhir R, Patel AA, Winters S, Bisceglia M, Swanson D, Aamodt R, et al. A multidisciplinary approach to honest broker services for tissue banks and clinical data: a pragmatic and practical model. Cancer. 2008;113(7):1705–15.
Dokholyan RS, Muhlbaier LH, Falletta JM, Jacobs JP, Shahian D, Haan CK, et al. Regulatory and ethical considerations for linking clinical and administrative databases. Am Heart J. 2009;157(6):971–82.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Mercuri RT. The HIPAA-potamus in health care data security. Commun ACM. 2004;47(7):25–8.
Choi YB, Capitan KE, Krause JS, Streeper MM. Challenges associated with privacy in health care industry: implementation of HIPAA and the security rules. J Med Syst. 2006;30(1):57–64.
Armstrong D, Kline-Rogers E, Jani SM, Goldman EB, Fang J, Mukherjee D, et al. Potential impact of the HIPAA privacy rule on data collection in a registry of patients with acute coronary syndrome. Arch Intern Med. 2005;165(10):1125–9.
O'Donnell ML. FERPA: Only a piece of the privacy puzzle. JC & UL. 2002;29:679.
Rinehart-Thompson LA. Amendments to FERPA regulations: new changes attempt to balance safety and privacy in student records. J AHIMA. 2009;80(7):56–7.
Weinberger JA, Michael JA. Federal restrictions on educational research. Educ Res. 1976;5(11):3–8.
Liao S. New survey finds Americans’ trust in Facebook continues to decline The Verge. 2018 [Available from: https://www.theverge.com/2018/3/26/17163818/facebook-american-user-trust-data-survey .
Thielsch MT, Meeßen SM, Hertel G. Trust and distrust in information systems at the workplace. PeerJ. 2018;6:e5483.
Mayer RC, Davis JH, Schoorman FD. An integrative model of organizational trust. Acad Manag Rev. 1995;20(3):709–34.
Sambunjak D, Straus SE, Marusic A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med. 2010;25(1):72–8.
Wenger E. Communities of practice: a brief introduction; 2011.
Download references
Acknowledgements
The authors would like to acknowledge Amanda Mari, Khemraj Hardowar, Harriet Fisher, PrMEIR staff, various faculty, and the ROMEO community for their continued passion of our DREAM database for quality improvement and data, and for their meaningful contributions to our community of practice.
Declaration of interest
All authors declare that they have no conflicts of interest.
This work was funded by 3 consecutive grants from the Health Resources Services Administration Academic Administrative Unit HRSA# D54HP05446 PI Gourevitch 2011–2016, PI Zabar 2015–2017.
Author information
Authors and affiliations.
Department of Medicine, Division of General Internal Medicine and Clinical Innovation, NYU Robert I. Grossman School of Medicine, 462 1st Avenue, New York, NY, 10016, USA
Jeffrey A. Wilhite, Lisa Altshuler, Sondra Zabar, Colleen Gillespie & Adina Kalet
Institute for Innovations in Medical Education, Division of Education Quality, 550 First Avenue, Medical Science Building, Suite G107, New York, NY, 10016, USA
Colleen Gillespie
Robert D. and Patricia E. Kern Institute for the Transformation of Medical Education, Medical College of Wisconsin, 8701 W. Watertown Plank Road, Wauwatosa, WI, 53226, USA
Adina Kalet
You can also search for this author in PubMed Google Scholar
Contributions
Authors JW and AK conceptualized and outlined the rough manuscript. JW, AK, LA, SZ, and CG shared equal responsibility in contributing insight, writing, and revision following initial inception through final versions. All authors (JW, AK, LA, SZ, and CG) have read and approve the submitted manuscript for publication. All authors (JW, AK, LA, SZ, and CG) routinely interact with the DREAM.
Authors’ information
Adina Kalet, MD, MPH.
Adina is the Director of the Robert D. and Patricia E. Kern Institute for the Transformation of Medical Education at the Medical College of Wisconsin. Up until September 2019 she was a professor of medicine and surgery at the New York University School of Medicine and is the co-director of the Program on Medical Education Innovation and Research (PrMEIR), whose mission is to advance medical education scholarship and to institute best practices for patient centered, evidence-based medical education. Adina is a founder of the DREAM initiative.
Sondra Zabar, MD.
Sondra is director of the Division of General Internal Medicine and Clinical Innovation and a professor of medicine. Sondra serves as co-director of the Program on Medical Education Innovation and Research (PrMEIR) and co-founder of the DREAM initiative.
Colleen Gillespie, PhD.
Colleen is an associate professor of medicine and director of the Division of Education Quality at NYU’s Institute for Innovation in Medical Education. Colleen provides direct oversight on the DREAM project, enabling NYU Langone researchers to make use of longitudinal educational data.
Lisa Altshuler, PhD.
Lisa is the Associate Director of Evaluation and Assessment at Program on Medical Education Innovation and Research (PrMEIR) and an assistant professor at the School of Medicine. Lisa serves as a DREAM team member and provides consultative services to interested collaborators.
Jeffrey Wilhite, MPH.
Jeffrey is the Honest Broker of the DREAM registries. Jeffrey serves as a lead and point of contact for all things consenting, IRB, and data management for the medical education registry.
Corresponding author
Correspondence to Jeffrey A. Wilhite .
Ethics declarations
Ethics approval and consent to participate.
All participants in the DREAM registries consent to having their routinely collected educational data used for research purposes. NYU Robert I. Grossman School of Medicine’s Institutional Review Board (IRB) has approved this registry and appropriate documentation of study modifications and continuing review has been maintained since inception. This particular paper does not present any data aside from an aggregate, de-identified count of participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wilhite, J.A., Altshuler, L., Zabar, S. et al. Development and maintenance of a medical education research registry. BMC Med Educ 20 , 199 (2020). https://doi.org/10.1186/s12909-020-02113-5
Download citation
Received : 20 June 2019
Accepted : 15 June 2020
Published : 19 June 2020
DOI : https://doi.org/10.1186/s12909-020-02113-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Research registry
- Graduate medical education
- Undergraduate medical education
- Medical education research
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Research at Mayo Clinic

Scientists probe health risks of tiny plastic particles

Breast cancer screening recommendations for transgender people.

Explore options to join a clinical trial.
More than 90 articles from 25 countries featured i... Wednesday, April 10, 2024

Research highlights
- The Digital Innovation Lab promotes advances in machine learning and artificial intelligence through cloud-based computing technologies.
- The Women's Health Research Center supports projects to understand sex differences and how unique processes of the female body affect health.
- The Collaborative Lupus Initiative for New Glucocorticoid Strategies (CLING) focuses on creating evidence-based standards for steroid use.
Areas of Research
Discover research activities, initiatives and projects.
- Laboratories
- Core Resources
- Centers and Programs
- Departments and Divisions
Clinical Trials
Clinical trials testing the effects and safety of new drugs, devices and therapies.
Researchers
About research.
See how Mayo Clinic research advances the science of medicine and improves patient care.
Research Centers
- Cancer Center
- Center for Biomedical Discovery
- Center for Individualized Medicine
- Center for Regenerative Biotherapeutics
- Center for the Science of Health Care Delivery
- All research centers
Publications
See how our academic publishing disseminates the latest in innovative patient care and biomedical research in a variety of venues.
Research in Florida

Research in Arizona

Research in Minnesota

Explore research positions and career opportunities.
- Training grant positions - Careers Training grant positions
- Postdoctoral research opportunities - Careers Postdoctoral research opportunities
- Jobs at Mayo Clinic - Careers Jobs at Mayo Clinic
Institutional Review Board
Protecting the rights, privacy and welfare of research participants.
Research facts & funding
Learn about the vast resources that fuel discovery science at Mayo Clinic.
Philanthropy at Mayo Clinic
Your support accelerates powerful innovations in patient care, research and education.
- Give now - Philanthropy at Mayo Clinic Give now
- Giving to Mayo Clinic - Philanthropy at Mayo Clinic Giving to Mayo Clinic
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.

Medical Education Research
Innovations.
Medical education is a collaborative effort between instructors and students, with a specific emphasis at CWRU School of Medicine on student-directed learning. Research in medical education helps to inform curriculum modifications to improve student satisfaction, student performance, instructor competency, content delivery and content acquisition. The opportunity for the dissemination of the research findings in this area are numerous, both intra and extramurally. IRB-approved research is currently being conducted in the following areas:
- In collaboration with the Office of Information Technology Services, the Dept. of Neurology is a first adopter in integrating, professionally produced content-rich videos into the undergraduate medical curriculum.
- Researchers are exploring several video formats to identify the optimal format for both student satisfaction and content delivery.
- PGY3 residents in Neurology participate in medical education as both students and instructors. The added value that PGY3 residents bring to the undergraduate medical curriculum is being actively researched.
- Researchers are exploring the impact of content modifications in the pre-clinical curriculum to optimize integration of clinical and basic science principles.
Current Studies
Research in medical education involves collaboration among students, residents and faculty from many departments and disciplines. Current studies have generated numerous abstracts, some presented at national and international meetings. Two studies will be submitted for peer-reviewed publication. The current titles of these publications are “Neurology PGY3 Residents at the Nexus of Medical Education.” David D. Friel, Ph.D., Chanel M. Wood, MM, and Maureen W. McEnery, Ph.D., MAT and “Implementing the flipped classroom: development and evaluation of an online educational module” Chanel M. Wood, MM, Krishan Chandar, MBBS, MRCP and Maureen W. McEnery, Ph.D., MAT.
Medical Education Research Design
Affiliations.
- 1 Associate Chair of Education, Department of Radiology, Mayo Clinic Arizona, Phoenix, Arizona; Senior Reviewer, ABR Ongoing Learning Assessment-Ultrasound Committee; Member, ACR Ultrasound Commission; Member, ACR Appropriateness Criteria-Women's Imaging Panel; Chair, ACR Incidental Findings Committee-Adnexa; and Executive Committee Member, Society of Radiologists in Ultrasound.
- 2 Director of Undergraduate Medical Education and Chair, Diversity Inclusion and Equity Committee and Diversity Liaison, Department of Radiology, University of North Carolina School of Medicine, Chapel Hill, North Carolina; Deputy Chief Editor, ACR RadExam; Member, ACR Commission on Publications and Lifelong Learning; and Executive Committee Member, ACR North Carolina Radiological Society. Electronic address: [email protected].
- PMID: 35346617
- DOI: 10.1016/j.jacr.2022.01.019
As with clinical care, radiology education benefits when stakeholders collaborate to gather and analyze data to answer questions and solve issues. Just as importantly, radiology educators benefit academically and professionally when they demonstrate a portfolio of published scholarship to promotion committees and department leaders. The principles and techniques used in the design of medical education research are not well understood by many radiology educators because educational scholarship methodologies have received little attention in our literature. Lack of familiarity and inexperience with research methodologies, particularly qualitative research, are barriers that education researchers can address with knowledge acquisition and practice. This overview surveys the landscape and offers suggested medical education research resources to help researchers explore topics to increase understanding of quantitative, qualitative, mixed-methods, survey, and educational design methodologies.
Keywords: Medical education; qualitative research; quantitative research; radiology education; research design.
Copyright © 2022 American College of Radiology. Published by Elsevier Inc. All rights reserved.
- Biomedical Research*
- Education, Medical*
- Fellowships and Scholarships
- Qualitative Research
- Research Design
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Pak J Med Sci
- v.34(4); Jul-Aug 2018
Roles of medical education department: What are expectations of the faculty?
Saima batool.
1 Prof. Dr. Saima Batool, FCPS (Pediatrics), MHPE. Professor of Pediatrics, University College of Medicine, The University of Lahore, Lahore, Pakistan
Muhammad Ahsan Raza
2 Dr. Muhammad Ahsan Raza, MPhil, CHPE. Associate Professor of Biochemistry, M. Islam Medical College, Gujranwala, Pakistan
Rehan Ahmed Khan
3 Prof. Dr. Rehan Ahmed Khan, FCPS, FRCS, MHPE, Ph.D. (Scholar). Professor of Surgery, Assistant Director Medical Education Department, Riphah International University, Islamabad, Pakistan
Background & Objective:
Pakistan like many Asian countries is investing in medical education to address increased societal needs and to meet the requirement of national and international accrediting bodies. Establishing medical education departments is part of this investment. The research question was “What are the expectations of faculty from medical education department?” The objective of this study was to explore the Faculty’s perception about the roles of medical education department and their suggestions for its future endeavors.
A qualitative case study design was chosen for this study. Heterogeneous group of faculty members from basic and clinical sciences departments of University College of Medicine, Lahore were invited for this study. They represented a variety of disciplines, and seniority levels. They were queried about their perception of the roles of medical education department and were encouraged to give suggestions for better functioning of department. Data was collected by audio recording through focus group interviews. Data analysis was done using NVIVO 11 software.
Initially 55 nodes/codes emerged which were then condensed to 35 nodes. Out of these three main themes emerged. The three emergent themes were:
- Knowledge about the roles of medical education department.
- Interactions with the medical education department.
- Future Prospects of the medical education department.
Roles of medical education department identified by the faculty were mainly related to faculty development, curriculum planning and implementation, student support, policy making for student induction, improving teaching strategies, student assessment, quality assurance and accreditation of the medical college. Faculty development not only encompassed faculty training but also provision of opportunities for research and curriculum development. Student support was found to be a neglected role and faculty members suggested it to be an important area to be looked upon by medical education departments.
Conclusion:
Institutions must ensure consultation with faculty members and should take proactive measures to sustain change, including giving ownership and team building among the faculty members.
INTRODUCTION
In Pakistan, first Medical education department was established by the College of Physicians and Surgeons, Pakistan (CPSP) in 1979, with the objective to support the college in the development of Postgraduate training programs and examination system, as well as, to help training the faculties for these programs. In 2008 Pakistan Medical and Dental Council (PMDC) sent a directive to all Public and Private medical colleges in the country to set up Departments of Medical Education (DME).
Setting up a department of medical education can be seen as a major change in a medical school in response to various pressures, expectations and changes in society, education and medicine. 1
Benor (2000) predicted that, in the future, society is likely to impose a requirement for certification of medical teachers. 2 Taking the development of DME as a change, faculty members’ perceptions and expectations in this regard need to be understood in order to sustain this change. 3
A major function of medical education department is to help prepare the teaching staff with the necessary skills to undertake effectively their roles as medical teachers. 4 Other well-known functions are curriculum development, service provision, assessment and ensuring the accreditation of medical college. 5 The aim of this study was to explore faculty’s perspective about the roles of medical education department.
An exploratory case study approach was employed to identify the emerging concepts and relationships. A central question for the study was put forward and during the interviews, few more questions were asked. 6 Selective, axial and open coding techniques were applied. 7
The Constructivist ontology approach used helped in providing a wide range of opinions from the participants.
Constructivists have a world view (ontology) or a manner of understanding their own and others’ views about the nature of reality that is based on a belief that “human beings are active participants in the researched world” and that “social phenomena are more than the sum of their parts and can be understood only holistically” 7 . The epistemological basis of this study is the concept of `Constructivism`. The concept of constructivism as described by Creswell, came from Mannheim and from works such as Berger and Luekmann’s in 1967 and the Social Construction of Reality by Lincoln and Guba’s Naturalistic Inquiry in 1985 8 .
The questions asked from the focus group participants were:
- What are your perceptions about roles of medical education department?
- What are the good and bad experiences while working with medical education department?
- How the medical education department should function in future?
The study was conducted in University College of Medicine, the University of Lahore, between January to August 2016. The study population was faculty members, who were selected on the basis of their teaching experience. A purposive sampling technique was chosen and a total of sixteen faculty members were identified, four each, in four focus group interviews.
The data was collected through focus group interviews, audio recorded with two mobile phones and transcribed simultaneously, to avoid missing any information. A semi-structured interview approach was used and a uniform set of open-ended questions were asked to each focus group. 8 The questions were put forward according to the knowledge gap identified through the literature search. The assistant moderator also took hand written notes to ensure transparency. The transcriptions were sent back to the interviewees for member checking. 8
A thematic analysis of the data was completed using NVIVO 11 software and by manual analysis. Initially open coding generated nodes/codes, which were used to define themes. Axial codes were used to define correlation between themes. Merger of open and axial codes helped in making subthemes.
The credibility (internal validity) and conformability of the results was achieved by thick description, member checking and reflexivity. 9 The transcripts were sent back to the participants for member checking and they were allowed to edit their responses. 10 Inter-interviewee comparison and rich, thick description were two other methods employed in this context. 11 , 12
Thematic analysis identified three themes/categories. The emergent themes were:
- Knowledge of faculty about the roles of medical education department.
The hierarchy of themes and their relationships are shown in Fig.1 . The participants were of the view that medical education department has far more scope than what it is doing currently. Besides well-known roles of faculty development, student support, research and curriculum development, 5 policy making for student induction, provision of logistics and equipment and maintaining student portfolios were the new roles identified by the faculty. As participant A said “They should conduct aptitude test and interviews not just the merit alone and while devising this test should involve the concerned departments as well”.

Hierarchy of themes and subthemes.
Most of the respondents, especially the junior faculty members were dissatisfied with the current functioning of the DME. They thought that the concepts and terminologies that the medical educationists use are confusing for them. While the senior faculty noted lack of persuasion, poor strategic planning and abrupt implementation of its policies to be the worth mentioning deficiencies. Participant D talked about medical education concepts being confusing for her: “After attending so many programs by DME, I feel that these words like spiral curriculum, integration etc. are very new for me. I am still confused about medical Education”.
The participants were asked about their suggestions for better functioning of the department. Many of them believed that a systematic approach to identify the strengths and weaknesses of DME through faculty’s feedback would help plan its future endeavors.
Theme-1: Knowledge about the functions of medical education department
The department of medical education has a wide-ranging function that includes research, teaching, service provision including advice and support in curriculum development and assessment. Another well-known role is fostering the careers of the academic staff. 5
Twelve out of 16 members (75%) identified Faculty development workshops to be an effective learning experience. They categorically identified faculty development as the most important responsibility of medical education department. 13
Faculty perceives that the DME is ‘taking over the curriculum’ and that is threatening for them and in turn they may respond by ‘attacking’ the DME. 13 Similar findings have been identified by authors, as the participants find the DME ‘a sudden change’, which was being imposed on them and medical educationists use ‘difficult words’ which are confusing for them.
Provision of teaching rooms, IT facilities and other logistic support is the responsibility of the medical college’s management. 14 Surprisingly, the authors have found that the faculty looks forward to DME for this purpose. It seems to be an undue expectation from a department mainly concerned with educational and research activities.
Theme-2: Interactions with the medical education department
The junior staff members are more enthusiastic about faculty development workshops as compared to senior ones. Similar findings have been found by other researchers. 14
Unexpectedly no participant in this study talked about teaching and assessing professionalism at undergraduate level. Probably this is because of lack of awareness among faculty that Professionalism must be taught explicitly in the formal curriculum. 15
Remarks about unpleasant interactions are related to DME being a ‘sudden change’ for the faculty. Castillo (2014) claims that “Acceptance of change in an educational institute can only be achieved if the expectations of those involved in the change process are sought for and given weightage at every step of change management”. 16 That is why; the outcomes of change must meet the expectations of the participants.
Theme-3: Future Prospects of medical education department
Improvement in the faculty development activities is the most frequentlyrecommended activity by the interviewees. Inviting external speakers, increasing the frequency of activities to fortnightly and giving time and duty relaxations to those attending should are ensured by DME. These findings are similar to other studies. 17 Curriculum mapping, introduction of smart phone learning and conducting pilot projects with the faculty are other tasks identified by the participants. 18 , 19
A ‘new task’, the faculty has identified is provision of teaching space, logistics and equipment to the faculty. The authors haves not been able to find any other study which states this to be a function of DME, rather the researchers have clearly stated it to be responsibility of management of medical school. 13
Limitations of the study
Faculty members from only one medical college were included in this study so further research is warranted on this topic on a larger scale. Secondly, as only 5 out of 16 participants in this study had attended a formal program or are enrolled in master of Medical education (MME), the results can differ if the study is repeated on a sample of participants who have received formal training in medical education. Purposive sampling and a small sample size, used have imposed restrictions regarding any attempt to generalize these results.
Researchers can study other aspects like seeking Student’s or the management’s perspectives or Performing longitudinal study to see the effects of reforms in light of recommendations of this study.
Recommendations
The findings of this study point to following recommendations for addressing and improving the functioning of medical education department. DME should:
- Procure the support of the dean and other powerful advocates within the medical school.
- Ensure a non-threatening and non-judgmental approach to the school and faculty members.
- Employ appropriate staff for itself with an experience in developing integrated curriculum.
- Convince the management to provide funding for a few years until self-supporting.
- Establish contact with other groups/DME both nationally and internationally.
Medical Education is a specialized field that is becoming a necessity for any medical school in the World. In a qualitative case study the faculty members highlighted various roles that a medical education department is expected to perform. Most of the faculty members were dissatisfied with the department’s current functioning. The study concludes that the institution must ensure consultations with faculty members and should take proactive measures to sustain change including giving ownership and team building among the faculty members. As Dent (2017) recommended, that proactive measures against resistance or non-acceptance of an institutional change are better than addressing the resistance once it had happened, because it could be viewed as being reactionary. 14
Authors’ Contribution
SB conceived, designed and facilitated focus group discussion session. Final editing of manuscript was also done by her.
MAR , was the assistant facilitator in Focus Group discussion and manuscript writing.
RAK helped in editing of the manuscript and critically reviewed it as an expert Medical educationist.
SB takes the responsibility and is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of Interest: None.
Text Resize
Use the buttons below to increase or decrease the text size
Contrast switch
Use the toggle below to switch the contrast.
- Color Blind
- Green Weakness
SCREEN READER
Listen to the content of the page by clicking play on ReadSpeaker.
To discover more about accessibility, view our Accessibility Options here
- Our Leaders
- Customer Happiness Charter
- Projects and Initiatives
- Policies and Certificates
- Policies and Regulations
- Dubai Medical Registry
Medical Research
Dubai Health Authority is constantly working to improve the health care services provided in the emirate, by keeping abreast of developments and medical solutions, encouraging medical research, and studying methods of diagnosing and treating various diseases. Therefore, it provides the following services to support researchers while ensuring the rights and safety of the human subjects participating in these researches.
DHA Medical Research Service Catalogue
The Dubai Scientific Research Ethics Committee (DSREC) acts as the Central Ethics Committee for the emirate of Dubai. It takes the final decision on health research proposal requests after reviewing them thoroughly during periodic meetings. DSREC recognizes the establishment of Local Ethics Committee within the academic institution or private or government or semi government health institution or research center falling under the jurisdiction of the Emirate of Dubai.
You may click here for more information on the different types of studies that can be submitted to DSREC by the Local Ethics Committee for either In-depth Review/Approval or for Final Approval only.
Any research planned at DHA licensed facilities WITHOUT the review or approval of Local Ethics Committee must directly be submitted to the DSREC for review and approval.
Who can apply?
Researchers either health professionals or health university/college students who wish to obtain ethical approval on the research planned at the research sites that fall under the jurisdiction of the emirate of Dubai.
Submission Procedure
Submit following documents to (Email [email protected] ):
Note: If the attachments size exceeds 120 MB, please notify us through [email protected] so that we can share with you a secured link to upload the required documents.
1. Cover letter on headed paper (Addressed by Principal Investigator to DSREC):
- Please specify role of each investigator in the study.
- Index all documents submitted, with version if applicable.
2. DSREC Application Form (Click here) , duly signed and dated:
- All questions mentioned in the form must be answered. In case NOT APPLICABLE, mention NA.
- If there are more than one sites involved in the study, Principal Investigator (PI) must obtain the administrative site approval from Head Of Department (HOD) from each study site.
- If study involves 3 or more than 3 sites, please contact us for more information on the submission procedure.
- If PI is Head of Department, please obtain an administrative site approval from a higher authority.
- If a research is planned at a wider scale of the Emirate of Dubai (at sites such as all governmental hospitals and/or all private hospitals which are under jurisdiction of DHA and/or public places in Dubai and/or on the whole population (Emiratis/residents), then an administrative site approval from Head of Medical Research Section of DHA’s Medical Education and Research Department, must be obtained.
3. Study proposal/Synopsis
4. patient/ participant information sheet and informed consent form (click here) if applicable:.
- Informed consent form must be submitted in both Arabic and English.
- Attached template may be used as guidance to consider all of the required information for patient/participant enlightment during the recruitment process.
- Attached template may be used and customized according to study requirements.
5. Questionnaires: If applicable, to be submitted in both English and Arabic
6. confidentiality agreement patient information (click here) to be signed by principal investigator and co-investigators, 7. resume of principal investigator and co-investigators, 8. source of funding, if applicable, please submit supporting documents along with funding requirements, 9. device form (click here) if applicable, 10. clinical trial undertaking letter (click here ): applicable for clincial trials only, 11. all relevant enclosures such as data collection tool/case report form / proforma/ follow-up cards etc..
Payment Procedure
Payment is accepted through bank transfer to Dubai Health Authority’s Bank Account. For details, please click here.
Please send the transfer proof (receipt) to [email protected], then payment will be confirmed with the Finance Dept team who will then share the payment voucher.
An additional AED 20 will be charged as Knowledge and Innovation fees.
Download Free Structure
Download bank details.
Stranded Operating Procedure
Structure and Function of Dubai Scientific Research Ethics Committee
Submissions of new applications and opinions to dsrec, review of standard operating procedures and terms of reference, monitoring of clinical studies, handling of complaints, office location.
Dubai Health Authority Headquarters - First Floor - Medical Education & Research Department - Medical Research Section
7:30 AM to 15:00 PM - Monday to Thursday 7:30 AM to 12:00 PM - Friday
Mrs. Medha Mukund Kulkarni - 04 502 7518
This service aims at Ensuring researchers’ commitment to the highest standards of scientific research ethics throughout the implementation of procedures for managing violations related to research misconduct. Research participants, investigators, health professionals or any interested individuals can raise a complaint on research misconduct or if they suspect the integrity of published research by filling the (Report Research Misconduct Form) click here and sending it to [email protected].
This applies to all research activities that are conducted in health institutions, research centers, health universities or colleges in the Emirate of Dubai, whether by DHA employees or Non-DHA employees who are health professionals or students of health majors.
Please note that DHA doesn’t accept anonymous complaints.
Regulations and Documents
Medical Research Section at Dubai Health Authority provides the service of booking a free consultation session with one of the specialists in below areas:
Preparing a Research Proposal
Research Design
Sample Size Calculation
Statistical Analysis
Researchers can book the session by filling the electronic form in the link below:
Ms. Medha Mukund Kulkarni - 04 502 7518
Do you find this Content helpful?
This link may allow you to access a non - DHA website. Dubai Health Authority has no control over the linked website and is not liable for your use of it.
Dear customer, due to the expected weather conditions within the next few days, and to maintain your safety, you are encouraged to use our digital channels to obtain our services..
(Contact Center 800342, Website & social media channels)
This link will allow you to access a DHA website. Dubai Health Authority has full control over the linked website and you can browse it safely

IMAGES
VIDEO
COMMENTS
Maine Medical Center Department of Medical Education. Maine Medical Center (MMC) is Maine's only academic medical center conducting cutting edge biomedical research that provides the most advanced treatment options for our patients. Since 1874, MMC has maintained a proud tradition of high-quality medical education and training. We are ...
medical education research in the past 20 years, noted that MedEd research frequently explores the psychological impact of these factors on the individual student. Below is a list of the top themes in medical education research cited in the 20-year review. 1. Student assessment & evaluation
From Director's Desk. The Department of Medical Education and Research is contributing to the society not only by providing tertiary level health care services but also developing huge human resource in the form of doctors and paramedics; who are in future, going to strengthen the health care services in the state, country and worldwide.
How to Apply. Collect your letters of support, your personal statement, the description of your proposed research, and submit your application via the application form. Application Instructions. 333 Cedar Street. New Haven, CT 06510. This two-year degree program in the Medical Education track features an education research project and includes ...
Department of Medicine Medical Education Works-in-Progress. Presenter: Alec O'Connor, MD, MPH. Friday, March 29, 2024 Noon-12:50pm. ... Research, and Evaluation Committee and directed the AAMC's Medical Education Research Certificate program, where he teaches quantitative methods. Currently serving as the President-elect of the Society of ...
Medical Education and Research. The Department of Medical Education (MED) is responsible for provision of medical education, research and continuing professional development of healthcare experts in the United Arab Emirates. The Academic Affairs Centre (AAC) under the governance of MED established the Dubai Residency Training Program (DRTP) in ...
Dr. Wish-Baratz is deeply involved in both medical education innovation and its evaluation. Multiple studies of the efficacy of HoloAnatomy and HoloNeuroanatomy preceded their implementation and continue to be of great value as we learn new and different ways to teach and learn with these modalities. Additional studies have focused on ...
Explore education and research opportunities and resources at Mayo Clinic, where academic leaders, faculty members, and scientists work together to improve patient care.
Medical education researchers and clinician educators steer the future of health care through scholarship, refinement of educational techniques, and direct teaching. 1, 2 However, academic promotion has historically been tied to research productivity alone and not success in educating learners. Though medical education researchers discover new ...
The AAMC has been a leader in CBME for more than two decades and continues to support the development, implementation, and assessment of new competencies. With services and programs that span the transition from undergraduate to graduate medical education, the AAMC is partnering with stakeholders across the community to improve this critical ...
The medical education (Med Ed) research community characterises itself as drawing on the insights, methods, and knowledge from multiple disciplines and research domains (e.g. Sociology, Anthropology, Education, Humanities, Psychology). This common view of Med Ed research is echoed and reinforced by the narrative used by leading Med Ed departments and research centres to describe their ...
The Department of Research and Academic Affairs at Larkin Community Hospital oversees the scholarly activities and initiatives associated with Medical Education. The department provides strategic leadership and administrative coordination to deliver short and long-term support to promote critical thinking and academic excellence in our medical ...
Background Medical Education research suffers from several methodological limitations including too many single institution, small sample-sized studies, limited access to quality data, and insufficient institutional support. Increasing calls for medical education outcome data and quality improvement research have highlighted a critical need for uniformly clean and easily accessible data ...
The Department of Medical Education at the Texas A&M University College of Medicine was created in 2018 to bring together core faculty educators who are committed to, and passionate about, moving the overarching mission and vision of the College of Medicine forward as it pertains to medical education. ... Scholarship and research around medical ...
They discuss several key elements of education research labs: the importance of lab identity, the signaling effect of a lab designation, required infrastructure, and the training mission of a lab. The need for medical education researchers to be visionary and strategic when designing their labs is emphasized, start-up considerations and the ...
Research. Educational research initiatives at the Heersink School of Medicine create, implement, evaluate, and share projects to advance training locally, and subsequently improve outcomes in each of these areas. Ongoing projects in educational research explore trainee wellbeing, methods for trainee enrichment, grading validity and reliability ...
By ROBERT McDONALD May 12, 2021 Education. With the world demanding innovative and forward-thinking approaches to medical education, Harvard Medical School is using its convening power to bring advancements in medical education to the worldwide education community. In fall 2019, a group of senior leaders from international medical schools ...
Research highlights. The Digital Innovation Lab promotes advances in machine learning and artificial intelligence through cloud-based computing technologies. The Women's Health Research Center supports projects to understand sex differences and how unique processes of the female body affect health. The Collaborative Lupus Initiative for New ...
Medical education is a collaborative effort between instructors and students, with a specific emphasis at CWRU School of Medicine on student-directed learning. Research in medical education helps to inform curriculum modifications to improve student satisfaction, student performance, instructor competency, content delivery and content acquisition.
The Medical Education & Research Department (MERD) came into existence in 2001 with the purpose of providing innovative medical educational opportunities for the employees of the Dubai Health Authority (DHA) in order to improve the quality of healthcare to its customers using Medical Education Section, Medical Training Section and Medical ...
1 Associate Chair of Education, Department of Radiology, Mayo Clinic Arizona, Phoenix, Arizona; Senior Reviewer, ABR Ongoing Learning Assessment ... The principles and techniques used in the design of medical education research are not well understood by many radiology educators because educational scholarship methodologies have received little ...
The department of medical education has a wide-ranging function that includes research, teaching, service provision including advice and support in curriculum development and assessment. Another well-known role is fostering the careers of the academic staff. 5.
Dubai Health Authority Headquarters - First Floor - Medical Education & Research Department - Medical Research Section Timing. 7:30 AM to 15:00 PM - Monday to Thursday 7:30 AM to 12:00 PM - Friday. Phone. Mrs. Medha Mukund Kulkarni - 04 502 7518. This service aims at Ensuring researchers' commitment to the highest standards of scientific ...