- Find-a-Dentist

Lesson Plans
Talking with children about their oral health can be a rewarding activity for both you and you students. The ADA believes that it's never too early to begin oral health education and screening. By sharing these sample presentations and resources with your class, you can help educate students of all ages think about and discuss the importance of dental health. This section contains exercises ranging from learning and coloring the different parts of the tooth to more dynamic lessons that engage preteen students on why making smart choices can protect their teeth and health.
Remember: Teaching children good oral hygiene habits early can lead to a lifetime of healthy smiles.


- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Dental Health Education
Published by Katrina Ryan Modified over 4 years ago
Similar presentations
Presentation on theme: "Dental Health Education"— Presentation transcript:
Oral Health Fourth Grade
Medical Technologies Jr. Program
The Teeth © PDST Home Economics. Healthy Teeth & Gums Help us to digest food Help us to digest food Make us look better Make us look better Good health.
Dental Health by Abbey Flick.
Cleo Lacey, Savannah Spirov, Mara Maus P.2
UNCLASSIFIED//REL TO NATO/ISAF
Equine Dental Abnormalities & Dentistry Brendan Kraus, DVM Photos courtesy Leon Scrutchfield,DVM.
Veterinary dental nursing procedures
(Smiling and self esteem). The first teeth which are shed and replaced by permanent teeth. There are 20 primary teeth The primary teeth are replaced starting.
BASIC ORAL ANATOMY.

Dental Hygiene What You Need to Know About Taking Care of Your Teeth.
Digestion: Chewing & Dissolving
Tuesday Hand in and Review last nights Homework Notes – Teeth and Eye
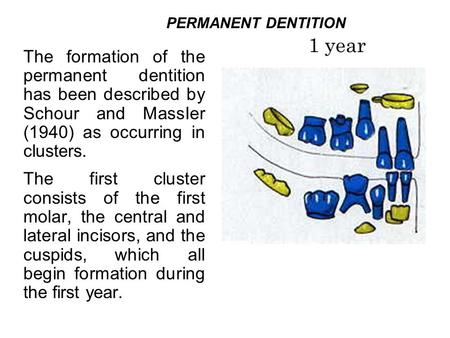
PERMANENT DENTITION 1 year
PRIMARY DENTITION It takes from 2 to 3 years for the primary dentition to be completed . Calcification of the primary teeth begins in utero 13 and 16 weeks.
HEALTHY CHOICES: Care of Your Teeth Ms. Mai Lawndale High School.
By: Breanna, Pamela, and Asia OawEg&feature=related.

Infant Oral Health Care
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Internet Explorer Alert
It appears you are using Internet Explorer as your web browser. Please note, Internet Explorer is no longer up-to-date and can cause problems in how this website functions This site functions best using the latest versions of any of the following browsers: Edge, Firefox, Chrome, Opera, or Safari . You can find the latest versions of these browsers at https://browsehappy.com
- Publications
- HealthyChildren.org
Shopping cart
Order Subtotal
Your cart is empty.
Looks like you haven't added anything to your cart.
- Career Resources
- Philanthropy
- About the AAP
- The Role of the Pediatrician in the Promotion of Healthy, Active Living
- How Can You Support Patients in Healthy, Active Living? Check Out Updated Report
- Helping Kids Build Healthy Active Lives: AAP Policy Explained
- Climate Change & Children’s Health: AAP Policy Explained
- News Releases
- Policy Collections
- The State of Children in 2020
- Healthy Children
- Secure Families
- Strong Communities
- A Leading Nation for Youth
- Transition Plan: Advancing Child Health in the Biden-Harris Administration
- Health Care Access & Coverage
- Immigrant Child Health
- Gun Violence Prevention
- Tobacco & E-Cigarettes
- Child Nutrition
- Assault Weapons Bans
- Childhood Immunizations
- E-Cigarette and Tobacco Products
- Children’s Health Care Coverage Fact Sheets
- Opioid Fact Sheets
- Advocacy Training Modules
- Subspecialty Advocacy Report
- AAP Washington Office Internship
- Online Courses
- Live and Virtual Activities
- National Conference and Exhibition
- Prep®- Pediatric Review and Education Programs
- Journals and Publications
- NRP LMS Login
- Patient Care
- Practice Management
- AAP Committees
- AAP Councils
- AAP Sections
- Volunteer Network
- Join a Chapter
- Chapter Websites
- Chapter Executive Directors
- District Map
- Create Account
- Early Relational Health
- Early Childhood Health & Development
- Safe Storage of Firearms
- Promoting Firearm Injury Prevention
- Mental Health Education & Training
- Practice Tools & Resources
- Policies on Mental Health
- Mental Health Resources for Families
Oral Health Education and Training
The information and resources below will help you to identify oral disease, provide caries prevention services, and establish referral relationships with dental professionals.
Smiles for Life National Oral Health Curriculum
Developed by the Society for Teachers of Family Medicine, the Smiles for Life National Oral Health Curriculum has 2 child-focused modules:
- Child Oral Health
- Caries Risk Assessment, Fluoride Varnish, and Counseling
These modules are endorsed by the AAP and approved for continuing medical education.
Bright Futures Oral Health Resources
The Bright Futures Guidelines for Health Supervision for Infants, Children, and Adolescents prioritizes oral health as a major health topic to be included in practice. View the Bright Futures: Oral Health Pocket Guide as well as practice guides and other Bright Futures resources .
Education and Quality Improvement in Pediatric Practice (EQIPP)
EQIPP features the Oral Health in Primary Care course that discusses the importance of dental home referral, caries risk assessment, anticipatory guidance, and fluoride varnish application. More information about this quality improvement resource can be found on the EQIPP website .
Pediatric Oral Health Flip Chart and Reference Guide
The Pediatric Guide to Children’s Oral Health Flip Chart and Reference Guide includes pictures and speaker’s notes to help you to counsel patients about oral health and apply fluoride varnish, and take action against oral injuries and disease. It is available for purchase through shopAAP .
PediaLink is the AAP's online learning center offering a variety of educational opportunities and resources, including the below focused on oral health. This video series is free for AAP members and others.
- Providing fluoride varnish in the medical setting (30 minutes)
- Providing preventative oral health services in practice (30 minutes)
Training Videos
Minnesota Oral Health Coalition (MOHC) Videos : MOHC has many helpful video resources focused on collaborating with communities and schools, improvements through innovation and integration, and the lifelong importance of oral health.
Smiles for Life Training Videos : Smiles for Life has several demonstration videos of patient care including knee-to-knee, fluoride varnish application, and palpation of the temporomandibular (TMJ) and the floor of the mouth.
How To Apply Fluoride Varnish (From the First Tooth) : From the First Tooth has instructional videos of how to apply fluoride varnish in a primary care setting for very young children.
Protecting All Children's Teeth (PACT): A Pediatric Oral Health Training Program
Educators can use the below oral health educational content (downloadable PowerPoint presentations) for medical students and pediatricians in training. The content is for educational purposes only. CME credit for presenting this content is not available from the AAP. This content is no longer available as an online module.
Each PowerPoint presentation includes an outline, learner objectives, speaker notes, references, and a question-and-answer series following the presentation.
Presentations may be downloaded and tailored to meet the needs of your learners. If you plan to significantly edit the content of your presentation, please contact us for permission to update the AAP copyrighted material. The content is for educational purposes only.
- Basic Oral Anatomy
- Oral Health Screening
- Oral Injury
- Dental Development
- Oral Pathology
- Preventive Care
- Oral Findings
- Special Needs
- Oral Habits
- Systemic Diseases
- Oral Health in Adolescents
PACT Post-Test – Learners can be directed to this link to complete a comprehensive post-test. If you require a hard copy of the post-test and answer key, please e-mail [email protected].
PACT Instructor Guide –This guide will help instructors implement the PACT materials within their educational settings.
Dental caries is the most common chronic disease in children. Pediatricians and other medical providers play an important role in improving children's oral health outcomes. Access issues prevent many children from visiting a dentist. If you are knowledgeable about oral health, you can discover problems, emphasize cavity prevention, and make life saving referrals.
Last Updated
American Academy of Pediatrics
Home Collections Education Oral Health Education PPT
Oral Health Education PPT Template and Google Slides
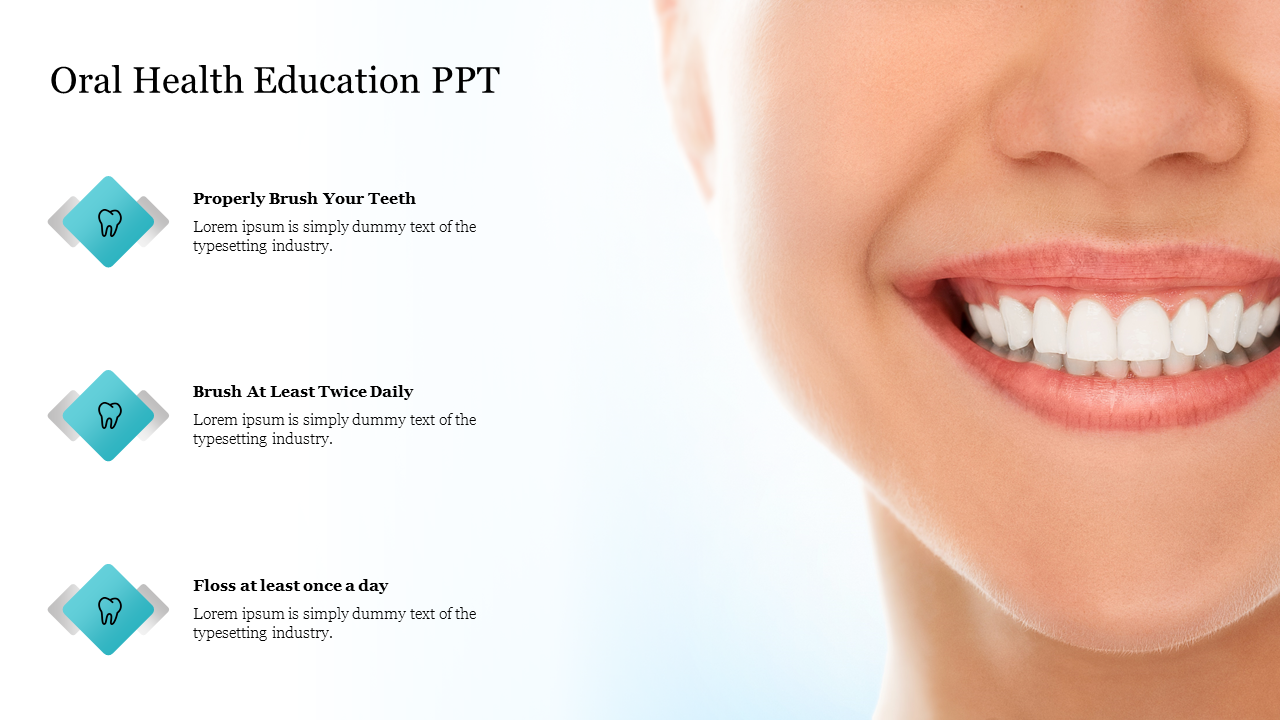
Best Oral Hygiene Education Slide For Presentation
About this template , feature of this template .
- Oral Health Education
- Oral Hygeine Instructions
- Oral Health Education And Health
- Dental Health Education
- School Oral Health Programme
49+ Templates
177+ Templates
1294+ Templates
Animals and birds
266+ Templates
Country Flags
46+ Templates

417+ Templates
179+ Templates

Galaxy or Space
124+ Templates

30+ Templates
You May Also Like These PowerPoint Templates

Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

solar eclipse
25 templates
academic writing
15 templates

8 templates

education technology
180 templates
32 templates
citizenship
14 templates
Oral Health: Periodontal Disease
Oral health: periodontal disease presentation, free google slides theme and powerpoint template.
Any periodontal disease is an oral health condition that affects the tissues supporting the teeth, including the gums, ligaments, and bone. These diseases can be caused by poor oral hygiene, smoking, genetic factors, and certain medical conditions. We hope you brush your teeth regularly, and we also hope you download this template to create informative or educational presentations about periodontal diseases. Make your own slides by using the simple-to-edit layouts included, use the editable map to indicate the prevalence of a certain disease, customize the infographics to enhance data visualization... To save time, there's no better choice than this template!
Features of this template
- 100% editable and easy to modify
- 20 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.
Premium template
Unlock this template and gain unlimited access

- Preferences

Oral Health Education - PowerPoint PPT Presentation
- Oral Health Education
... with a tooth brush and toothpaste and flossing) can ... Decay can be spread from parent to child. Brush your child's teeth after ... Tooth Decay is ... – PowerPoint PPT presentation
- for South Dakota Families
- Baby teeth are important.
- Keep them clean to
- prevent decay.
- Baby teeth help your child
- Grow and develop
- Speak clearly
- Hold space for permanent teeth
- Can occur shortly after teeth appear
- Caused by germs (acid producing bacteria) which can be spread from parents
- Caused by eating and drinking sugary foods and beverages
- If detected early in
- the process, decay
- can be stopped and
- even reversed
- Cavities can lead to
- Pain infection
- Hospitalization or surgery
- Poor performance in school
- Speech problems
- Poor nutrition
- Cause other medical problems
- Cavities are an infectious disease and bacteria can be passed from parents to infants and children.
- Keeping your teeth clean (by brushing with a tooth brush and toothpaste and flossing) can prevent decay and prevent the spread of the bacteria.
- DONT wet pacifier with saliva, share spoon, pre-chew infants food
- Baby teeth are important
- Babies should NOT be put to bed with a bottle
- Bottles should not be filled with sweet liquids
- Bottles should not be used as pacifiers
- Babies should never be given a pacifier dipped in sweet liquid
- Begin using a cup as soon as developmentally appropriate
- Babies mouths need to be cleaned
- Children should brush or have their teeth brushed after each meal and before bed!
- Use only a pea-sized amount of toothpaste with fluoride.
- Balanced diet is as important to oral health as general health
- Food and drink high in sugar cause
- the most cavities (pop and candy)
- Acid production is the greatest in first
- 20 minutes after eating or drinking
- Amount eaten is less important than how often and how long
- Healthy Snacks
- Raw fruits/veggies
- Unsweetened applesauce
- Limited Snacks
- Sticky foods (fruit chews/roll-ups, raisins)
- High sugar (soda pop, candy, pastries)
- Look in your childs mouth
- about once a month.
- Lift your childs lip to
- view the gum line.
- Look at the back side
- of the teeth and the
- biting surfaces.
- Dental Visits
- At age one, and regularly after that
- Do not to wait until a child is in pain.
- Treatment can often be done without shots or drills using new procedures
- Medical providers should look at the child's teeth at every well-child visit.
- Decay can be spread from parent to child
- Brush your childs teeth after meals and before bed
- Use only a pea-sized amount of tooth paste
- Take your child to the dentist at age one
- No bottle at bed time, or only water in the bottle
- Baby teeth are important !
PowerShow.com is a leading presentation sharing website. It has millions of presentations already uploaded and available with 1,000s more being uploaded by its users every day. Whatever your area of interest, here you’ll be able to find and view presentations you’ll love and possibly download. And, best of all, it is completely free and easy to use.
You might even have a presentation you’d like to share with others. If so, just upload it to PowerShow.com. We’ll convert it to an HTML5 slideshow that includes all the media types you’ve already added: audio, video, music, pictures, animations and transition effects. Then you can share it with your target audience as well as PowerShow.com’s millions of monthly visitors. And, again, it’s all free.
About the Developers
PowerShow.com is brought to you by CrystalGraphics , the award-winning developer and market-leading publisher of rich-media enhancement products for presentations. Our product offerings include millions of PowerPoint templates, diagrams, animated 3D characters and more.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Geriatr
- PMC10494401

The impact of health education interventions on oral health promotion among older people: a systematic review
Saeid bashirian.
1 Autism Spectrum Disorders Research Center, Hamadan University of Medical Sciences, Hamadan, Iran

Sahar Khoshravesh
2 Department of Community Health Nursing, School of Nursing and Midwifery, Hamadan University of Medical Sciences, Hamadan, Iran
3 Chronic Diseases (Home Care) Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
Erfan Ayubi
4 Cancer Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
5 Social Determinants of Health Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
Akram Karimi-Shahanjarini
Samane shirahmadi.
6 Department of Community Oral Health, School of Dentistry, Dental Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
Parshang Faghih Solaymani
Associated data.
All supporting data is available through the corresponding author.
One of the most common pathologic changes in older people is oral and dental problems. The oral health of older people is a public health concern. Promotion of good oral health for this cohort will have beneficial impacts on the longer-term quality of life. This study aimed to identify the types of health education interventions for the oral health of older people and to determine their effects on the oral and dental health of older people.
Potential articles were retrieved from four electronic databases (PubMed/Medline, Scopus, Web of Sciences, and Embase) up to 31 September 2022 in English without limit of time. Experimental and quasi-experimental interventional studies investigating the impact of educational interventions on oral and dental health among older people over 60 years old in both sexes were considered. The quality assessment tool was the Effective Public Health Practice Project (EPHPP).
In the initial search, 1104 articles were retrieved. Finally, according to the inclusion criteria, 23 studies (seventeen randomized controlled trials (RCT) and six quasi-experimental studies) were reviewed. In this review, educational interventions for older people and their caregivers are classified. Theoretical frameworks were used in only three interventions related to older people. Outcome measures were both self-reported and objective measures. Fifteen of the included studies were of moderate quality.
This review provides evidence that the use of oral and dental health educational interventions was effective in improving the oral health of older people. Educational interventions were carried out both among older people and among their caregivers. Although a variety of interventions were used in the reviewed studies, more lectures were used in the interventions related to older people. In the interventions related to caregivers, in addition to lectures, practical education was also used. It is recommended to perform higher quality studies for assessing the effectiveness of interventions in this field.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-023-04259-5.
Introduction
The improvement of living conditions and the increase in life expectancy have led to the phenomenon of aging in societies [ 1 ], in such a way that it has become one of the challenges of public health all over the world [ 2 ]. According to the report of the World Health Organization, between 2015 and 2050, the proportion of the population over 60 will almost double from 12 to 22% [ 3 ]. The aging process includes a natural course in which many physiological and psychological changes occur in the body [ 4 ]. Oral and dental problems are generally pathological processes that may also result from the aging process. These problems include tooth loss, dry mouth, gum disease, tooth decay, oral mucosa disorders, and chewing disorders [ 5 ]. These changes can affect the quality of life of older people [ 6 ].
One of the important concerns for public health is the improvement of older people's health, which can lead to an improved quality of life among them [ 7 ]. The evidence indicates that oral and dental health problems among older people have been given less attention compared to cardiovascular or neoplastic diseases [ 8 , 9 ]. Oral and dental health means the health of the oral cavity and its related tissues. Good oral health facilitates a person for eating, speaking and social interaction [ 10 ]. Oral health-related quality of life (OHRQOL) is a complex concept that consists of four dimensions: functional factors, psychological factors, social factors, and experience of pain or discomfort [ 11 ]. Patients with poor oral and dental health may have lower mood, more life stress and reduced quality of life [ 12 ]. Some older people have many oral and dental problems that can negatively affect their physical or psychosocial health. For example, it can lead to a reduction in fruit and vegetable consumption in older people [ 13 ]. This nutritional style can cause nutritional disorders in older people [ 14 , 15 ]. Often, older people with dentures complain of a wide range of problems including eating, social interaction, and communication, and these problems have a detrimental effect on their quality of life [ 16 ].
In recent years, in order to improve the oral health-related quality of life, attention has been focused on evaluating the effectiveness of oral health education programs. A number of systematic reviews have been conducted on the available evidence, the results of which have shown that oral health education can be effective in the short term in increasing knowledge and to some extent behaviors such as brushing teeth and healthy eating [ 17 ]. Considering the phenomenon of aging and the importance of the health and quality of life of older people, which is affected by various factors such as oral and dental hygiene, the importance of prevention and the need for appropriate interventions to improve the health of older people are felt. Therefore, this study aimed to identify the types of health education interventions and to determine their effects on oral and dental health in older people.
This study was performed based on the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines [ 18 ]. This systematic review as approved by the Research Ethics Committee of Hamadan University of Medical Sciences (No. IR.UMSHA.REC.1400. 829).
Search strategy
Potential articles were retrieved from four electronic databases (PubMed/Medline, Scopus, web of sciences, and Embase) up to 31 September 2022 in English without limit of time. The search strategy was developed using Medical Subject Headings (MeSH). We used the keywords of Wang et al.'s study as a basis [ 19 ]. The keywords were considered based on Population, Intervention, Comparison, Outcomes and Study design (PICOS) as a framework to formulate eligibility criteria in this study [ 20 ]. The search strategy for PubMed/Medline is described in Appendix 1 .
Older people over 60 years old in both sexes without cognitive impairment/dementia were considered.
Intervention
All interventional studies investigating the effect of educational interventions on oral and dental health were included in the study. These educational interventions could involve older people or their caregivers. The use of the theoretical framework in the reviewed studies was also investigated.
Interventional studies with all types of comparatives were included in this study.
Promoting oral and dental health in older people was the first outcome. The second outcome was the quality of life related to oral health.
Selection of studies
The results of initial searches were independently screened by two authors according to titles, abstracts, and full texts. Any disagreement among the researchers regarding the exclusion or inclusion of articles in the study was resolved with discussion. All searched articles in the initial search were entered into EndNote X8 software.
Study eligibility
Experimental and quasi-experimental interventional studies investigating the impact of educational interventions on oral and dental health among older people over 60 years old in both sexes were considered. Descriptive, qualitative, review studies, letters and correspondences, editorials, conference proceedings and studies that consider oral and dental health along with other interventions to perform other health behaviors were excluded.
Data extraction
Data was independently extracted by two authors (PF and SK). Any discrepancy was resolved through discussion. The extracted information included the following: first author (year), country, study design, study population (age, gender), study groups, description of intervention and control, and oral health main findings. In this study, the results of data extraction are independently presented based on the subjects of intervention (older people and caregivers). After completing the search in the mentioned databases, it was found that the educational interventions related to the oral and dental health of older people were carried out in two ways: directly (the target group was the older people themselves) and indirectly (the target group was the caregivers of older people). For this reason, the classification of studies was carried out by the research team in the current form in order to provide the possibility of comparison.
Quality assessment tool
The included studies were independently evaluated by two authors using the Effective Public Health Practice Project (EPHPP) quality assessment tool [ 21 ].
This tool has six subscales including selection bias, study design, confounding, blinding, data collection methods, and withdrawals/drop-outs. Any disagreement among the researchers regarding the scoring of the quality assessment tool was resolved by discussion or by a third author. Inter-rater reliability was approved by Cohen’s Kappa coefficient. Cohen suggested the Kappa result be interpreted as follows: values ≤ 0 as indicating no agreement and 0.01–0.20 as none to slight, 0.21–0.40 as fair, 0.41– 0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1.00 as almost perfect agreement [ 22 ]. None of the studies were excluded based on quality assessment results.
Results of the searched studies
1102 articles were retrieved from the four electronic databases; PubMed/Medline ( n = 122), Scopus ( n = 580), Web of Sciences ( n = 297), and Embase ( n = 103). To minimize retrieval bias, the inclusion criteria were manually checked for additional eligible documents that could have been missed during the mentioned database and grey literature search ( n = 2). Finally, 1104 articles were retrieved in the initial search. Duplicated items were identified using EndNote X8 software and manually removed from the articles file. After removing duplicates, 830 articles remained. Of these articles, 793 articles were excluded because they were not in line with the objectives of the study. Then, 37 articles were screened. Three articles were excluded from the screening stage. In the next step, the full texts of 34 eligible articles were assessed. Finally, 23 articles were reviewed in this systematic review (Fig. 1 ). Details of the included final studies are presented in Tables 1 and 2 based on the subjects of intervention (older people and caregivers).

PRISMA flow diagram of the systematic review and meta-analysis selection process
Effectiveness of intervention to oral health promotion among older people
Note: n Number, G Group, I Intervention, C Control or Comparison, RCT Randomized Controlled Trial
Effectiveness of interventions to oral health promotion of older people among their caregivers
Design of the studies
In 14 studies, interventions were related to older people [ 23 – 32 ]. The ten studies were randomized controlled trials (RCT) studies [ 23 – 32 ] and four studies had quasi-experimental design [ 33 – 36 ]. Of the 23 included studies, nine studies were related to the caregivers of older people [ 37 – 43 ], that seven studies had RCT design [ 37 – 43 ] and two studies were quasi-experimental studies [ 44 , 45 ]. Totally, there were 17 randomized controlled trials (RCT) studies [ 23 – 32 , 37 – 43 ] and six studies had quasi experimental design [ 33 – 36 , 44 , 45 ].
Study time and settings
Nine studies were published in 2018 or later [ 23 – 25 , 30 , 31 , 33 , 36 , 42 , 43 ]. Four studies were carried out in the UK [ 29 , 37 , 38 , 44 ], three studies in Thailand [ 23 , 28 , 35 ], three in South Korea [ 24 , 25 , 33 ], two in USA [ 27 , 31 ], two in Sweden [ 43 , 45 ], two in India [ 39 , 40 ], one in Japan [ 26 ], one in Australia [ 34 ], one in Taiwan [ 36 ], one in China [ 32 ], One in Iran [ 30 ], one in Germany [ 42 ], and one in Canada [ 41 ].
Participants and follow-up duration
Most studies had a sample size less than 200 [ 23 – 26 , 28 , 31 , 33 – 36 , 39 , 43 , 44 ]. Fifteen studies were conducted among older people [ 23 – 36 ]. Nine studies focused on caregivers of older people [ 37 – 45 ]. The follow-up duration for one study was 36 months [ 27 ], one study 18 months [ 44 ], three studies were 12 months [ 31 , 42 , 45 ], one study nine months [ 44 ], six studies six months [ 28 , 37 – 40 , 42 ], six studies three months [ 23 , 28 , 35 , 41 , 43 , 44 ], one study two months [ 29 ], three studies six weeks [ 24 , 25 , 33 ], four studies one month [ 30 ], and four studies without any follow-up [ 26 , 32 , 34 , 36 ]. In fact, one study had three follow-ups [ 44 ] and five studies had two follow-ups [ 23 , 28 , 37 , 38 , 42 ].
Theoretical framework usage
Theoretical frameworks have been used only in interventions related to older people. Of all the included studies, only 13% of them used theoretical framework. These studies include the Health Belief Model (HBM) in the study of Keyong et al., [ 23 ], adult learning theory in the study of Shokouhi et al., [ 30 ], and Social Cognitive Theory (SCL) in the study of Mariño et al. [ 34 ]. The Health Belief Model (HBM) as a conceptual framework in health education research was applied to improve self-management. The HBM can to predict behaviors according to constructs such as perceived susceptibility (person’s belief about chances of getting a disease or harmful situation), perceived severity (person’s belief about danger of a disease or harmful situation), perceived benefits (person’s belief regarding benefits to risk reduction of getting a disease or harmful situation), perceived barriers (person’s belief regarding costs of new behavior), cues to action (feel the necessity to take action), and self-efficacy (feel confident for the ability to perform a behavior) [ 46 ]. The adult learning theory refers to an organized process for raising the awareness, cognition, and skills of adults in order to be able to move towards excellence and evolution. The experience of people in the learning process and adults’ desire to learn without any compulsion are an important role in this theory [ 47 ]. The Social Cognitive Theory (SCL) helps to explain the interaction of the individual, environment, and behavior on behaviors [ 48 ]. The results of a review of eHealth intervention revealed that the majority of studies were based on SCT [ 47 ].
Types of intervention
In the included studies of this review, educational interventions have been used for changing behavior or improving attitudes and increase awareness of oral health. In this review, educational interventions were provided for both older people [ 23 – 36 ] and caregivers [ 37 – 45 ]. In the related interventions to older people, different educational methods have been used such as lectures [ 23 , 26 – 33 , 36 ], mobile apps [ 24 , 25 ], workbooks [ 25 , 33 ], web based [ 34 ], educational video [ 28 ], motivational interviewing [ 30 , 31 , 35 ], and sending educational messages [ 30 ].
Also, the related interventions to caregivers included lectures [ 37 – 45 ], a live demonstration of oral hygiene techniques on study models [ 39 ], to provide oral health education CD and manual to the respective institutions [ 39 ], a videotape about oral health [ 44 , 45 ], CD-ROM and full color pocket book about intensive training in mouth care [ 44 ], practical training with different types of prosthetic restoration by using typodonts [ 42 ], and hands-on guidance about oral hygiene procedures and discussions on oral care routines [ 43 ]. In one study, multifaceted programs including in-person training (individual training and group discussion) and non-attendance training (sending educational messages) were used [ 30 ].
Types of outcome measures
From the results of 23 reviewed studies, 20 studies used self-reports as one of the outcome measurement methods [ 23 – 26 , 28 – 40 , 42 , 43 , 45 ]. In the related interventions to older people, the self-report measured variables included attitude [ 34 , 35 ], knowledge [ 23 – 25 , 27 , 31 , 33 – 35 ], oral health perceptions [ 23 , 25 ], oral health recognition [ 33 ], self-efficacy [ 31 , 34 ], oral health related quality of life (OHRQoL) [ 30 , 31 ], oral health literacy [ 36 ], practices [ 34 , 35 ], and skills of oral health [ 23 – 25 , 27 , 33 – 35 ]. In the related interventions to caregivers, the self-report measured variables included attitude [ 37 , 38 , 43 , 45 ], knowledge [ 37 – 40 , 42 , 45 ], and performance of oral health [ 38 ].
Also, in the reviewed studies, objective measures were used to evaluate the effects of interventions. Objective measures are contained below:
1) In interventions related to older people, these items included tongue pressure, unstimulated salivary flow rate [ 24 ], resting salivation in the second and third cumulated Repetitive Saliva Swallowing Test times [ 26 ], plaque score [ 23 , 28 , 35 ], clinical attachment level (CAL) [ 35 ], gingival inflammation [ 23 ], clinical attachment loss [ 23 , 28 ], percentage of bleeding on probing (BOP) [ 35 ], probing depth [ 28 ], root surfaces with new caries [ 28 ], active root caries surfaces [ 28 ], subjective oral dryness [ 24 ], O’Leary index [ 25 , 33 ], tongue coating index [ 25 , 33 ], bitterness threshold [ 26 ], coronal caries events [ 27 ], root caries events [ 27 ], gingival index score [ 28 , 35 ], pocket depth [ 35 ], and glycemic indexes (glycosylated hemoglobin (HbA1c) and fasting plasma glucose (FPG)) [ 28 , 35 ].
2) In interventions related to the caregivers, the items of objective measures included oral health scores [ 38 , 45 ], denture hygiene [ 44 ], plaque control record [ 42 ], Denture Hygiene Index (DHI) [ 42 ], plaque levels [ 43 ], denture plaque score [ 38 , 40 ], denture stomatitis score [ 38 , 40 , 44 ], debris score [ 40 ], the number of residents wearing dentures overnight [ 44 ], oral mucosal disease [ 44 ], angular cheilitis [ 44 ], revised oral assessment guide gums and lips scores [ 43 ], gingival bleeding [ 43 ], and plaque score [ 40 ].
The effects of interventions
In the related interventions to older people, the self-report measured variables improved including attitude [ 34 , 35 ], knowledge [ 23 – 25 , 27 , 31 , 33 – 35 ], oral health perceptions [ 23 , 25 ], oral health recognition [ 33 ], self-efficacy [ 31 , 34 ], oral health related quality of life (OHRQoL) [ 30 , 31 ], oral health literacy [ 36 ], practices [ 34 , 35 ], and skills of oral health [ 23 – 25 , 27 , 33 – 35 ]. In the related interventions to caregivers, the self-report measured variables improved including attitude [ 37 , 38 , 43 , 45 ], knowledge [ 37 – 40 , 42 , 45 ], and performance of oral health [ 38 ].
The interventions in older people and caregivers have led to improvement or decreasing the below objective measures.
In the related interventions to older people, the improved objective measures included tongue pressure, unstimulated salivary flow rate [ 24 ], resting salivation in the second and third cumulated Repetitive Saliva Swallowing Test times [ 26 ] and decreased items included plaque score [ 23 , 28 , 35 ], clinical attachment level (CAL) [ 35 ], gingival inflammation [ 23 ], clinical attachment loss [ 23 , 28 ], percentage of bleeding on probing (BOP) [ 35 ], probing depth [ 28 ], root surfaces with new caries [ 28 ], a great number of active root caries surfaces [ 28 ], subjective oral dryness [ 24 ], O’Leary index [ 25 , 33 ], tongue coating index [ 25 , 33 ], bitterness threshold [ 26 ], coronal caries events [ 27 ], root caries events [ 27 ], gingival index score [ 28 , 35 ], pocket depth [ 35 ], and glycemic indexes (glycosylated hemoglobin (HbA1c), fasting plasma glucose (FPG)) [ 28 , 35 ].
In the related interventions to caregivers, the improved objective measures included the following: oral health scores [ 38 , 45 ], denture hygiene [ 44 ], plaque control record (PCR) [ 42 ], denture hygiene index (DHI) [ 42 ], and plaque levels [ 43 ], and the objective measures included reduction of items such as denture plaque score [ 38 , 40 ], denture stomatitis score [ 38 , 40 , 44 ], debris score [ 40 ], the number of residents wearing dentures overnight [ 44 ], oral mucosal disease [ 44 ], angular cheilitis [ 44 ], revised oral assessment guide gums and lips scores.
[ 43 ], gingival bleeding [ 43 ], and plaque score [ 40 ]. In one study, intervention group was not significantly different from baseline [ 41 ].
Risk of bias of the included studies
We did not exclude studies based on the results of the quality assessment. Inter-rater agreement varied across EPHPP components ratings. Overall, there was a good agreement between the two reviewers (Kappa coefficient = 0.80, p < 0.001). Fifteen studies of the included studies were of moderate quality and eight studies were weak quality (Table (Table3 3 ).
Quality assessment using EPHPP quality rating
To the best of our knowledge, there are no systematic reviews to identify the types of health education interventions and to determine their effects on oral and dental health among older people. As mentioned previously, older people have many oral and dental problems that can negatively affect their physical or psychosocial health [ 14 , 15 ]. This situation is exacerbated in some older people, such as older people with cognitive impairment/ dementia. Evidence shows that cognitive impairment and dementia influence oral-dental health and these disorders lead to the reduction of dental service use. According to the study of Jockusch et al., with increasing cognitive impairment/dementia among older people, there was a significant difference in the number of decayed teeth. Also, with increasing dementia, the degree.
of restoration decreased and oral/denture hygiene declined significantly [ 49 ]. So, studies that have done interventions for the oral and dental health of older people with cognitive impairment/ dementia disorders were excluded from this review. The results of the current study demonstrated that the majority of the included studies had randomized controlled trials design (17/23). Eight studies (34%) were categorized as low quality. As is clear, randomized clinical trials are the best method for controlling selection and confounding biases [ 50 , 51 ]. Quasi-experimental designs, due to the lack of random allocation, cannot express the effect of an intervention as clearly as experimental studies [ 52 ]. In this review, although 17 studies were randomized controlled trials, six of them were of low quality. It seems that in the future studies in the field of oral and dental health of older people, it is necessary to conduct more high-quality randomized clinical trial studies. In this review, it was found that theoretical frameworks had been used in only three interventions related to older people (13%). These studies include the Health Belief Model (HBM) in the study of Keyong et al., [ 23 ], adult learning theory in the study of Shokouhi et al., [ 30 ], and Social Cognitive Theory (SCL) in the study of Mariño et al. [ 34 ]. Evidence indicates that interventions aimed at changing or modifying behavior would be more effective if they are designed and implemented based on a suitable theoretical frameworks [ 53 , 54 ], because theoretical frameworks offer a systematic approach to a better understanding of phenomena by providing explanations related to why and under what conditions. In other words, for more effectiveness of educational programs, it is recommended to use theoretical frameworks of health education and health promotion [ 55 ]. Results demonstrated that using the mentioned theoretical frameworks led to improved oral health perception, behavior, and oral health status [ 23 ], improved oral health knowledge, attitudes, and self-efficacy [ 34 ], and improved oral health-related quality of life among older people [ 30 ]. In this review, we could not discuss in detail the quality and effectiveness of framework-based interventions for two reasons: a) Frameworks were used in only three studies. b) Due to the use of different frameworks in the design of interventions, the outcomes were not the same, so that we could compare them.
Also, the results of this review show that although a variety of interventions were used in the reviewed studies, more lectures were used in the interventions related to older people [ 23 , 26 – 33 , 36 ]. In the interventions related to caregivers, in addition to lectures [ 37 – 45 ], practical training was also used [ 39 , 42 – 44 ]. Some of the educational lectures in the interventions related to older people or caregivers were: oral hygiene instruction, facial and tongue muscle exercise, and salivary gland massage [ 26 ], and toothbrushing with fluoride toothpaste, cleaning dentures, and self-check oral health [ 28 ], and the importance of oral health, common oral health problems among older people (coronal and root dental caries, gingivitis, periodontitis, oral cancer), and oral hygiene self-care (flossing, brushing, rinsing, and denture care) [ 31 ]. Also, some of the practical education included a live demonstration of oral hygiene techniques on study models [ 39 ], brushing techniques for teeth/prostheses, and handling of interdental space brushes [ 42 ], and tooth brushing, denture care, and a variety of oral hygiene aids [ 44 ]. In fact, the majority of interventions used traditional methods for education, and only one study used web-based oral health presentations for the older people [ 34 ]. The finding of a review of interventional studies in Iran about investigating the effect of different educational methods in preventing disease in elderly people showed that no study had used electronical interventions using social networking software (Telegram, WhatsApp, etc.), web-based, or e-mail-based interventions. In other words, all studies had used traditional approaches for modifiying lifestyle and promoting health behaviors [ 56 ]. It seems that although the traditional methods of education are more pleasant and comfortable for older people and even caregivers, in the digital age, it is necessary to use new technologies in the education of older people. Indeed, the reduced use of new technologies by older people compared to other age groups has caused the digital divide. One of the effective ways to overcome this problem is to help older people accept new information and communication technologies [ 57 ]. The evidence shows that various theoretical frameworks have been used to accept technology in older people, such as diffusion of innovations [ 58 ], theory of reasoned action [ 59 ], and theory of planned behavior [ 56 , 60 ]. The use of new technologies not only provides support services such as remote care for older people, but also improves their quality of life and individual independence. Further studies are recommended in the area of educational methods and comparison of these methods [ 56 ].
From the results of 23 reviewed studies, 20 studies used self-reports as one of the outcome measurement methods [ 23 – 26 , 28 – 40 , 42 , 43 , 45 ]. In interventions related to older people, more self-report variables were measured than interventions related to caregivers. In the related interventions to caregivers, the self-report measured variables included attitude [ 37 , 38 , 43 , 45 ], knowledge [ 37 – 40 , 42 , 45 ], and performance of oral health [ 38 ], which all self-report measured variables were improved compared to before the intervention. In the interventions related to older people and caregivers, a wide variety of objective outcomes were measured, so it was practically impossible to compare the outcomes of the interventions. Only plaque score was measured both in interventions related to older people [ 23 , 28 , 35 ] and in interventions related to caregivers [ 40 ]. In the study of Khanagar et al., (2015) led to a significant reduction of mean plaque score from a baseline score of 3.17 ± 0.40 to 1.57 ± 0.35 post-intervention (six-month) [ 40 ]. Also, in the studies of keyong et al., (2019), Saengtipbovorn et al., (2015), and Saengtipbovorn et al., (2014) in older people led to a significant reduction of mean plaque score at baseline score compared to post-intervention (3.28 ± 1.03 Vs. 2.69 ± 0.56, 0.04 ± 0.07 Vs. 0.23 ± 0.07, and 0.59 ± 0.42 Vs. 0.26 ± 0.31, respectively). These results show that the reduction of the mean plaque score in the intervention related to caregivers was reported more than the interventions related to older people. It seems that considering this index in interventions related to caregivers will be more effective. Dental plaque is a biofilm of microorganisms on the tooth surface that plays an important role in the spread of caries and periodontal disease [ 61 ]. Gram-positive and gram-negative bacteria that are present on the surface of dental plaque can cause gingivitis and, if left untreated, can create periodontitis [ 62 ]. Some factors such as poor and insufficient oral health status and the use of prosthesis lead to promote the creation and accumulation of plaque in older people [ 63 ]. Plaque control is an effective way to treat and prevent gingivitis and is an essential part of all methods of treating and preventing periodontal diseases [ 64 ]. Although mechanical control of plaque is the most reliable method of oral hygiene, plaque control by brushing alone is not enough to control periodontal diseases [ 65 ]. The use of chemical substances such as mouthwashes, gel and antimicrobial toothpaste is of particular importance [ 66 , 67 ]. The results of a current scoping review demonstrated that mechanical, chemical and educational strategies are effective in dental plaque control in older people [ 68 ].
Strengths and limitations
The most important strength of this study was that the current study was the first systematic review in order to identify the types of health education interventions and to determine their effects on oral and dental health in older people. Considering the role of interventions in improving the oral and dental health of older people in the reviewed studies, it seems that interested researchers can use the experiences of these studies in the design and implementation of interventions according to the characteristics of their studied society. This review had some limitations. First of all, we included only studies in English. The second limitation was the lack of access to the full text of some articles. The third limitation was that although the current study includes numerous RCTs, many of them have very low sample size and imbalance in the sample size of the studied groups. It is possible that, despite being RCTs, the strength of evidence is less than ideal. Finally, the results may have a degree of selection bias because of ignoring gray literature, unpublished studies, and studies published in other databases.
Acknowledgements
The authors thank the Vice-chancellor for Research and Technology of Hamadan University of Medical Sciences for financial support.
Authors’ contributions
Study design: SB, EA, AK-S, SS, PFS, Data acquisition, analysis and interpretation: SK, EA, SS, PFS, Writing of the first draft: SB, EA, AK-S, SS, PFS, Revising first draft for important intellectual content: SK, AK-S, SS, PFS, All the authors have read and approved the final version of the manuscript.
This study was financially supported by Vice-chancellor for Research and Technology of Hamadan University of Medical Sciences (No. 140110138639).
Availability of data and materials
Declarations.
This study was approved by the Ethics Committee at Hamadan University of Medical Sciences (No. IR.UMSHA.REC.1401.829).
Not applicable.
The authors declare no competing interests.
The original online version of this article was revised: the affiliation details for the 3rd, 4th and 6th author were incorrect.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
A Correction to this paper has been published: 10.1186/s12877-023-04351-w

- Upload Ppt Presentation
- Upload Pdf Presentation
- Upload Infographics
- User Presentation
- Related Presentations

Brain tumors
By: JenniferDwayne Views: 1586

Training and Conditioning Techniques
By: JenniferDwayne Views: 1511

Infection Control
By: JenniferDwayne Views: 1667

Cardiorespiratory Fitness
By: JenniferDwayne Views: 1084
Protect Your Health
By: JenniferDwayne Views: 1262

Aphthous Stomatitis
By: archana Views: 1842
Traumatic Injuries To The Teeth
By: medhelp Views: 494

Dental Bridge
By: romaldodasneves Views: 1664

Anesthesia and Pain Control in Dentistry
By: yourdoctors Views: 454
Infant Oral Health Program
By: drdwayn Views: 742

- About : Professor, College of Nursing and Health Sciences
- Occupation : Medical Professional
- Specialty : MD
- Country : United States of America
HEALTH A TO Z
- Eye Disease
- Heart Attack
- Medications

IMAGES
COMMENTS
Lesson Plans. Talking with children about their oral health can be a rewarding activity for both you and you students. The ADA believes that it's never too early to begin oral health education and screening. By sharing these sample presentations and resources with your class, you can help educate students of all ages think about and discuss the ...
Downloads and Resources. As part of Dental Buddy, in association with teachers, educational authorities and oral health professionals, we have developed a range of specialised resources to help deliver better oral health to all. From Early Years' Education to Key Stage Two, these excellent resources are available for anybody to deliver oral ...
Part 1 Slide Presentation on Using Plain Language and Social Media Platforms to Ensure your Community Understands the Importance of Children's Oral Health. Topics: Kindergarten Oral Health Assessment, Messaging. Part 2 Slide Presentation on Sharing Strategies for Engaging Local News Media and Bloggers, Enhancing your Odds of Getting Media Coverage.
To address the gap between oral health and medicine literacy, the Harvard School of Dental Medicine and the Forsyth School of Dental Hygiene/Massachusetts College of Pharmacy and Health Science partnered to create evidence-based education modules- the Oral-Systemic Health Tool Kit (OSHTK) Project. This project aims to empower you to make ...
D. devda263. Economy & Finance Health & Medicine. 1 of 6. Download Now. Download to read offline. Oral Health Power Point Presentation - Download as a PDF or view online for free.
14. DEFINITION "the process of enabling people to increase control over, and to improve their health". -Ottawa Charter for Health Promotion, 1st International Conference on Health Promotion, Ottawa, 21-Nov-1986. 15. Five priority action areas for health promotion: 1. Building healthy public policy 2.
Download ppt "Dental Health Education". Impact of oral disease Dental decay (cavities) is one of the most common chronic illnesses among children. Although most dental diseases are preventable, many children unnecessarily suffer from dental disease because of: inadequate home care, and lack of access to dental services.
Protecting All Children's Teeth (PACT): A Pediatric Oral Health Training Program. Educators can use the below oral health educational content (downloadable PowerPoint presentations) for medical students and pediatricians in training. The content is for educational purposes only. CME credit for presenting this content is not available from the AAP.
Oral Health Education. Literature. Free literature for use in Missouri can be ordered by completing the following form: ... Full Playlist of narrated oral health presentations K-12. Spanish Version. Kindergarten Grade 1 Grade 2 Grade 3 Grade 4 Grade 5 Grades 6-8 Grades 9-12. e-Learning .
Prevention of periodontal disease includes includes self-care and professional oral care, saliva substitutes, and proper nutrition. Oral care includes utilizing an electric toothbrush, toothpaste with fluoride, interdental aids, therapeutic mouthrinses, and proper denture care. There is a relationship between cognitive function and oral health.
22 likes • 22,113 views. C. CHCBC. Importance of Oral Health. Health & Medicine. 1 of 10. Download Now. Download to read offline. Importance of Oral Health - Download as a PDF or view online for free.
Product Details. Educate your audience on the best practices to maintain the health of their mouth and teeth and overall oral hygiene in a captivating manner with the help of our Oral Health presentation template. Crafted to work best with MS PowerPoint and Google Slides, this versatile deck will make comprehension easy for your intended audience.
Free Google Slides theme and PowerPoint template. The mouth is the gateway to our digestive system and an integral part of our ability to speak, eat, and smile with confidence. Maintaining good oral hygiene is essential to prevent common dental problems such as cavities, gingivitis, and gum disease. So it's clear as day: brush your teeth and ...
1. The Slides are available in different nodes & colors. 2. This slide contains 16:9 and 4:3 formats. 3. It is easy to change the slide colors quickly. 4.It is a well-crafted template with an instant download facility. 5. The best PowerPoint theme template.
SLIDES 1-20: Provider-Patient Education. These slides are from the "Oral Health Care Patient Education" PowerPoint presentation prepared for the AIDS Education and Training Center National Resource Center by Diana Travieso Palow, MPH, MS, RN; Jeanne Adler, MSN, ARNP-C; Carol Stewart, DDS, MS; and Claudette Grant, MEd, CCRC, RN.
Download Free and Premium Oral Health Education PowerPoint Templates. Choose and download Oral Health Education PowerPoint templates, and Oral Health Education PowerPoint Backgrounds in just a few minutes.And with amazing ease of use, you can transform your "sleep-inducing" PowerPoint presentation into an aggressive, energetic, jaw-dropping presentation in nearly no time at all.
Any periodontal disease is an oral health condition that affects the tissues supporting the teeth, including the gums, ligaments, and bone. These diseases can be caused by poor oral hygiene, smoking, genetic factors, and certain medical conditions. We hope you brush your teeth regularly, and we also hope you download this template to create ...
Dec 23, 2012 •. 344 likes • 213,271 views. Manisha Saxena. ppt on dental hygiene and oral care for easy understanding for common people. 1 of 36. Download Now. Download to read offline. Dental hygiene and oral care - Download as a PDF or view online for free.
Abstract. In recent years, attention has been drawn toward assessing the effectiveness of oral health education programs. This is in line with demand for evidence based research and will help to inform policy makers on how to allocate resources. (1) Collect and collate all information on oral health education programs.
Title: Oral Health Education 1. Oral Health Education ; for South Dakota Families ; Funded by WellMark Foundation, Dental Dental, SD ... They'll give your presentations a professional, memorable appearance - the kind of sophisticated look that today's audiences expect. Boasting an impressive range of designs, they will support your ...
Baseline: The health educator gave a PowerPoint presentation on oral health to the caretakers and a live demonstration of oral hygiene techniques on study models. Also, a health education CD and manual were provided to the respective institutions ... Conclusion: oral health education program, offered to nursing personnel in special housing for ...
Slide 3-. Goals of Oral Health Program Treat pain, diagnose pathology, and eliminate sources of infection 2. Stabilize and preserve oral tissues 3. Restore oral function 4. Educate patient regarding maintenance 5. Facilitate maintenance of adequate nutrition 6. Contribute to self-esteem and quality of life. Slide 4-.
Designing an eyecatching presentation template is time-consuming. Download the following free and ready-to-use Oral health powerpoint templates and Google slides themes for the upcoming presentation. You only need to change text, logo or colors on the professional PPT templates.