The Importance of Global COVID-19 Vaccination
- Download PDF Copy

Since the World Health Organization (WHO) declared the COVID-19 outbreak a pandemic back in March 2020, the virus has claimed more than 2.5 million lives globally with upwards of 113 million cases being confirmed by laboratory tests (March 2021).

Image Credit: rangizzz / Shutterstock.com
The pandemic has impacted almost every corner of life, causing global economies to stall, changing the way we work and interact with our loved ones, and stretching healthcare systems to the limit. Governments around the world have been forced to implement harsh restrictions on human activity to curb the spread of the virus.
COVID-19 vaccination is now offering a way to transition out of this phase of the pandemic. Without them, many scientists believe that natural herd immunity would not have been sufficient to restore society to its normal status quo and that it would have resulted in extreme fatality. This is something that has been echoed by many health organizations including the WHO. In a scenario without access to vaccines, strict behavioral measures may have had to remain for the foreseeable future.
Fortunately, the beginning of 2021 saw numerous vaccines given emergency approval and begin their roll out in countries across the world. As of March 2021, just shy of 300 million vaccine doses had been administered worldwide. The figures give hope of a return to ‘normal’. However, global COVID-19 vaccination faces several challenges which may impact its success.

Efficacy of COVID-19 vaccination
Currently, a total of seven COVID-19 vaccines available across three platforms have been approved and are being rolled out across the globe. However, some question the efficacy of these vaccines, especially given the emergence of new strains of the virus. Vaccines must be effective at significantly reducing the spread of the virus for them to be successful.
Research has demonstrated that the Moderna and the mRNA-based Pfizer vaccines are 94-95% effective, and these figures have proven true even in trials studying those at high risk and the elderly.
It is a common misconception that this means 95% who get the vaccine are protected from the disease, leaving 5% unprotected. If this were true, in a population of 100,000 were vaccinated this would lead to 5,000 people contracting the virus and developing the disease over three months. This rate is similar to the current UK COVID-19 case rate.
The 95% effectiveness actually means that people with the vaccine have a 95% lower risk of COVID-19 when compared to a control group. Without the vaccine, we would expect roughly 1% of the population to get the disease, and with the vaccine, this reduces to 0.05%. At such low rates, the vaccines will allow society to get back to ‘normal’ and for restrictions to be permanently eased.
Evolution of SARS -CoV -2 virus
While the current vaccines have proven to be highly effective against the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) strain that has caused the pandemic, recent data has highlighted the emergence of several mutational strains. There has been uncertainty as to whether the current vaccines will protect against these variants.
Related Stories
- Study finds no clinically useful biomarkers for long COVID in routine lab tests
- SARS-CoV-2 evolves differently in the brain, revealing critical insights into viral tropism
- Prioritizing older individuals for COVID-19 boosters yields best public health outcomes, study finds
Recently, the WHO has eased concerns, stating that current vaccinations have at least some protection against new variants. They also stress that data is being collected and analyzed on new variants, and as our knowledge grows, as will our ability to modify the already approved vaccines to be more effective against emerging variants. As more data is collected, researchers will understand how to amend the current COVID-19 vaccinations so that in the future, to protect against the various strains, booster shots may be administered to maintain the level of protection required to curb the spread of the virus.
What is clear is that it is necessary to achieve herd immunity through vaccination globally in order to prevent SARS-CoV-2 from continuing to mutate, becoming more resistant to current vaccines and causing more periods of mass fatality.
Production, affordability, and allocation of COVID-19 vaccinations
One challenge that has been increasingly discussed is that of offering the vaccine to those who need it most and preventing disparities in vaccination access. Some research is showing that those in well-off regions are more likely to have access to vaccination, with those in poorer communities at greater risk of having less accessibility. For the vaccines to work to the highest of their ability, access should not be dictated by wealth. Ideally, those at high-risk should be vaccinated first, as they are doing in the UK, with less vulnerable groups receiving their vaccine last.
The world needs more doses of the COVID-19 vaccine than it ever has for any disease in history. This, therefore, requires significant production efforts to ensure that needs are met. While the vaccine itself is effective, its impact will be compromised if not enough doses can be produced in a timely fashion.
Fortunately, COVID-19 vaccinations have not suffered from underinvestment like so many others and this investment looks likely to continue to support the need for modified vaccines that address the newer COVID-19 variants.
Public opinion of COVID-19 vaccination
One major potential barrier to the success of COVID-19 vaccinations is a negative public opinion of the vaccine. A June 2020 survey found that 71.5% of people would be very or somewhat likely to take a COVID-19 vaccine, leaving almost a third less accepting of the vaccine. If significant portions of the population were to reject the vaccine, this could have a serious impact on the vaccine’s potential efficacy at controlling the spread of COVID-19. Some populations, in particular, have low acceptance rates; in Russia, for example, less than 55% of those surveyed would accept the vaccine.
This challenge can be overcome by educating the public about the importance of COVID-19 vaccination and being transparent about the development of the vaccine along with the prevalence of potential adverse events. Educating people helps to build trust in the decision to offer vaccinations, without which, the world will not be able to overcome the pandemic and return to ‘normal’ life.
- Annavajhala, M., Mohri, H., Zucker, J., Sheng, Z., Wang, P., Gomez-Simmonds, A., Ho, D. and Uhlemann, A., 2021. A Novel SARS-CoV-2 Variant of Concern, B.1.526, Identified in New York. https://www.medrxiv.org/content/10.1101/2021.02.23.21252259v1
- Lazarus, J., Ratzan, S., Palayew, A., Gostin, L., Larson, H., Rabin, K., Kimball, S. and El-Mohandes, A., 2020. A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine , 27(2), pp.225-228. https://www.nature.com/articles/s41591-020-1124-9
- Mahase, E., 2021. Covid-19: Where are we on vaccines and variants?. BMJ , p.n597. https://www.bmj.com/content/372/bmj.n597
- Olliaro, P., 2021. What does 95% COVID-19 vaccine efficacy really mean?. The Lancet Infectious Diseases ,. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(21)00075-X/fulltext
Further Reading
- All Coronavirus Disease COVID-19 Content
- The COVID-19 Pandemic: What have the experts learned?
- What Mutations of SARS-CoV-2 are Causing Concern?
- What Role has Social Media Played in COVID-19?
- Unlocking our clinical understanding of SARS-CoV-2 infection, Post-Acute COVID Syndrome (PACS), and systemic recovery
Last Updated: Jan 17, 2022
Sarah Moore
After studying Psychology and then Neuroscience, Sarah quickly found her enjoyment for researching and writing research papers; turning to a passion to connect ideas with people through writing.
Please use one of the following formats to cite this article in your essay, paper or report:
Moore, Sarah. (2022, January 17). The Importance of Global COVID-19 Vaccination. News-Medical. Retrieved on September 04, 2024 from https://www.news-medical.net/health/The-Importance-of-Global-COVID-19-Vaccination.aspx.
Moore, Sarah. "The Importance of Global COVID-19 Vaccination". News-Medical . 04 September 2024. <https://www.news-medical.net/health/The-Importance-of-Global-COVID-19-Vaccination.aspx>.
Moore, Sarah. "The Importance of Global COVID-19 Vaccination". News-Medical. https://www.news-medical.net/health/The-Importance-of-Global-COVID-19-Vaccination.aspx. (accessed September 04, 2024).
Moore, Sarah. 2022. The Importance of Global COVID-19 Vaccination . News-Medical, viewed 04 September 2024, https://www.news-medical.net/health/The-Importance-of-Global-COVID-19-Vaccination.aspx.
Suggested Reading

Cancel reply to comment
- Trending Stories
- Latest Interviews
- Top Health Articles

How can microdialysis benefit drug development
Ilona Vuist
In this interview, discover how Charles River uses the power of microdialysis for drug development as well as CNS therapeutics.

Global and Local Efforts to Take Action Against Hepatitis
Lindsey Hiebert and James Amugsi
In this interview, we explore global and local efforts to combat viral hepatitis with Lindsey Hiebert, Deputy Director of the Coalition for Global Hepatitis Elimination (CGHE), and James Amugsi, a Mandela Washington Fellow and Physician Assistant at Sandema Hospital in Ghana. Together, they provide valuable insights into the challenges, successes, and the importance of partnerships in the fight against hepatitis.

Addressing Important Cardiac Biology Questions with Shotgun Top-Down Proteomics
In this interview conducted at Pittcon 2024, we spoke to Professor John Yates about capturing cardiomyocyte cell-to-cell heterogeneity via shotgun top-down proteomics.

Latest News

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Impact of the COVID-19 pandemic on routine vaccine landscape: A global perspective
Affiliations.
- 1 Medical and Biological Computing Laboratory, School of Biosciences and Technology (SBST), Vellore Institute of Technology (VIT), Vellore, India.
- 2 Department of Biotechnology, SBST, VIT, Vellore, India.
- 3 Department of Biosciences, SBST, VIT, Vellore, India.
- 4 Department of Bio-medical sciences, SBST, VIT, Vellore, India.
- 5 School of Sports and Health Sciences, Cardiff Metropolitan University, Cardiff, UK.
- PMID: 37078597
- PMCID: PMC10294763
- DOI: 10.1080/21645515.2023.2199656
The coronavirus disease (COVID-19) threat is subsiding through extensive vaccination worldwide. However, the pandemic imposed major disruptions in global immunization programs and has aggravated the risks of vaccine-preventable disease (VPD) outbreaks. Particularly, lower-middle-income regions with minimal vaccine coverage and circulating vaccine-derived viral strains, such as polio, suffered additional burden of accumulated zero-dose children, further making them vulnerable to VPDs. However, there is no compilation of routine immunization disruptions and recovery prospects. There is a noticeable change in the routine vaccination coverage across different phases of the pandemic in six distinct global regions. We have summarized the impact of COVID-19 on routine global vaccination programs and also identified the prospects of routine immunization to combat COVID-like outbreaks.
Keywords: COVID-19; disruption; routine immunization; vaccines.
PubMed Disclaimer
Conflict of interest statement
No potential conflict of interest was reported by the author(s).
Global vaccine coverage (in percentage)…
Global vaccine coverage (in percentage) of routine vaccines in 2019 (pre-pandemic).
Global vaccine coverage (in percentage) of routine vaccines in 2020 (pandemic-peak phase).
Global vaccine coverage (in percentage) of routine vaccines in 2021 (pandemic-recovery phase).
Trends in global vaccine coverage…
Trends in global vaccine coverage between 2019 and 2021.
WHO-region-specific rise of some of…
WHO-region-specific rise of some of the VPDs during the course of the pandemic.
Similar articles
- Estimating global changes in routine childhood vaccination coverage during the COVID-19 pandemic, 2020-2021. Ghaznavi C, Eguchi A, Suu Lwin K, Yoneoka D, Tanoue Y, Kumar Rauniyar S, Horiuchi S, Hashizume M, Nomura S. Ghaznavi C, et al. Vaccine. 2023 Jun 23;41(28):4151-4157. doi: 10.1016/j.vaccine.2023.05.034. Epub 2023 May 22. Vaccine. 2023. PMID: 37246068 Free PMC article.
- Implementation of integrated supportive supervision in the context of coronavirus 19 pandemic: its effects on routine immunization and vaccine preventable surveillance diseases indicators in the East and Southern African countries. Bello IM, Lebo E, Shibeshi ME, Akpan GU, Chakauya J, Masresha BG, Daniel F. Bello IM, et al. Pan Afr Med J. 2021 Feb 12;38:164. doi: 10.11604/pamj.2021.38.164.27349. eCollection 2021. Pan Afr Med J. 2021. PMID: 33995771 Free PMC article.
- The impact of COVID-19 and catch-up strategies on routine childhood vaccine coverage trends in Latin America: A systematic literature review and database analysis. Castrejon MM, Leal I, de Jesus Pereira Pinto T, Guzmán-Holst A. Castrejon MM, et al. Hum Vaccin Immunother. 2022 Nov 30;18(6):2102353. doi: 10.1080/21645515.2022.2102353. Epub 2022 Sep 9. Hum Vaccin Immunother. 2022. PMID: 36084255 Free PMC article.
- Vaccines and routine immunization strategies during the COVID-19 pandemic. Dinleyici EC, Borrow R, Safadi MAP, van Damme P, Munoz FM. Dinleyici EC, et al. Hum Vaccin Immunother. 2021 Feb 1;17(2):400-407. doi: 10.1080/21645515.2020.1804776. Epub 2020 Aug 26. Hum Vaccin Immunother. 2021. PMID: 32845739 Free PMC article. Review.
- Risks of low vaccination coverage and strategies to prevent the resurgence of vaccine-preventable diseases in infants in the COVID-19 pandemic scenario: recommendations for Latin America and the Caribbean by the group of experts on infant immunization for Latin America. Avila Agüero ML, Castillo JBD, Falleiros-Arlant LH, Berezín E, de Moraes JC, Torres-Martínez C, Lopez EL, Castillo ME, Laris-Gonzalez A, Solorzano F, Gentile A, Torres Torretti JP, López-Medina E. Avila Agüero ML, et al. Expert Rev Vaccines. 2023 Jan-Dec;22(1):1091-1101. doi: 10.1080/14760584.2023.2271057. Epub 2023 Nov 8. Expert Rev Vaccines. 2023. PMID: 37843489 Review.
- Evaluating the impact of COVID-19 on routine childhood immunizations coverage in Zambia. Mwangilwa K, Chileshe C, Simwanza J, Chipoya M, Simwaba D, Kapata N, Mazaba ML, Mbewe N, Muzala K, Sinyange N, Fwemba I, Chilengi R. Mwangilwa K, et al. PLOS Glob Public Health. 2024 Jul 30;4(7):e0003407. doi: 10.1371/journal.pgph.0003407. eCollection 2024. PLOS Glob Public Health. 2024. PMID: 39078841 Free PMC article.
- Editorial: Vaccines and immunization services during the pandemic era and beyond. Amponsah-Dacosta E, Fulurija A, Afum-Adjei Awuah A, Mathema S, Wariri O. Amponsah-Dacosta E, et al. Front Health Serv. 2024 Mar 14;4:1394381. doi: 10.3389/frhs.2024.1394381. eCollection 2024. Front Health Serv. 2024. PMID: 38550921 Free PMC article. No abstract available.
- Knowledge, Attitudes, and Coverage of Recommended Vaccinations in Individuals with Chronic Medical Conditions: A Cross-Sectional Telephone Survey in Italy. Sansone V, Miraglia Del Giudice G, Della Polla G, Angelillo IF. Sansone V, et al. Vaccines (Basel). 2024 Mar 20;12(3):336. doi: 10.3390/vaccines12030336. Vaccines (Basel). 2024. PMID: 38543970 Free PMC article.
- Has COVID-19 Affected DTP3 Vaccination in the Americas? Aguinaga-Ontoso I, Guillén-Aguinaga S, Guillén-Aguinaga L, Alas-Brun R, Aguinaga-Ontoso E, Rayón-Valpuesta E, Guillén-Grima F. Aguinaga-Ontoso I, et al. Vaccines (Basel). 2024 Feb 25;12(3):238. doi: 10.3390/vaccines12030238. Vaccines (Basel). 2024. PMID: 38543872 Free PMC article.
- Assessing the impact of booster vaccination on diphtheria transmission: Mathematical modeling and risk zone mapping. Fauzi IS, Nuraini N, Sari AM, Wardani IB, Taurustiati D, Simanullang PM, Lestari BW. Fauzi IS, et al. Infect Dis Model. 2024 Jan 17;9(1):245-262. doi: 10.1016/j.idm.2024.01.004. eCollection 2024 Mar. Infect Dis Model. 2024. PMID: 38312350 Free PMC article.
- WHO Coronavirus (COVID-19) Dashboard [Internet] . World Health Organization; 2022. https://covid19.who.int/ .
- WHO . Immunization agenda 2030. A global strategy to leave no one behind. [Internet]. World Health Organization; 2022. http://www.immunizationagenda2030.org/ .
- Abbas K, Procter SR, van Zandvoort K, Clark A, Funk S, Mengistu T, Hogan D, Dansereau E, Jit M, Flasche S, et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit–risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob Health [Internet]. 2020;8:1–8. doi:10.1016/S2214-109X(20)30308-9. - DOI - PMC - PubMed
- Castilletti C, Capobianchi MR.. Polio is back? The risk of poliomyelitis recurrence globally, and the legacy of the severe acute respiratory syndrome coronavirus 2 pandemic. Clin Microbiol Infect [Internet]. 2022;29:414–6. http://www.ncbi.nlm.nih.gov/pubmed/36503117 . - PMC - PubMed
- Dinleyici EC, Borrow R, Safadi MAP, van Damme P, Munoz FM. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum Vaccines Immunother [Internet]. 2021;17:400–7. doi:10.1080/21645515.2020.1804776. - DOI - PMC - PubMed
Publication types
- Search in MeSH
Related information
Grants and funding, linkout - more resources, full text sources.
- Europe PubMed Central
- PubMed Central
- Taylor & Francis
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Loading metrics
Open Access
Peer-reviewed
Research Article
COVID-19 vaccine brand hesitancy and other challenges to vaccination in the Philippines
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation School of Medicine and Public Health, Ateneo de Manila University, Manila, Philippines
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing
Affiliations School of Medicine and Public Health, Ateneo de Manila University, Manila, Philippines, The Medical City, Manila, Philippines
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Supervision, Validation, Writing – review & editing
- Arianna Maever L. Amit,
- Veincent Christian F. Pepito,
- Lourdes Sumpaico-Tanchanco,
- Manuel M. Dayrit

- Published: January 13, 2022
- https://doi.org/10.1371/journal.pgph.0000165
- See the preprint
- Peer Review
- Reader Comments
Effective and safe COVID-19 vaccines have been developed at a rapid and unprecedented pace to control the spread of the virus, and prevent hospitalisations and deaths. However, COVID-19 vaccine uptake is challenged by vaccine hesitancy and anti-vaccination sentiments, a global shortage of vaccine supply, and inequitable vaccine distribution especially among low- and middle-income countries including the Philippines. In this paper, we explored vaccination narratives and challenges experienced and observed by Filipinos during the early vaccination period. We interviewed 35 individuals from a subsample of 1,599 survey respondents 18 years and older in the Philippines. The interviews were conducted in Filipino, Cebuano, and/or English via online platforms such as Zoom or via phone call. All interviews were recorded, transcribed verbatim, translated, and analysed using inductive content analysis. To highlight the complex reasons for delaying and/or refusing COVID-19 vaccines, we embedded our findings within the social ecological model. Our analysis showed that individual perceptions play a major role in the decision to vaccinate. Such perceptions are shaped by exposure to (mis)information amplified by the media, the community, and the health system. Social networks may either positively or negatively impact vaccination uptake, depending on their views on vaccines. Political issues contribute to vaccine brand hesitancy, resulting in vaccination delays and refusals. Perceptions about the inefficiency and inflexibility of the system also create additional barriers to the vaccine rollout in the country, especially among vulnerable and marginalised groups. Recognising and addressing concerns at all levels are needed to improve COVID-19 vaccination uptake and reach. Strengthening health literacy is a critical tool to combat misinformation that undermines vaccine confidence. Vaccination systems must also consider the needs of marginalised and vulnerable groups to ensure their access to vaccines. In all these efforts to improve vaccine uptake, governments will need to engage with communities to ‘co-create’ solutions.
Citation: Amit AML, Pepito VCF, Sumpaico-Tanchanco L, Dayrit MM (2022) COVID-19 vaccine brand hesitancy and other challenges to vaccination in the Philippines. PLOS Glob Public Health 2(1): e0000165. https://doi.org/10.1371/journal.pgph.0000165
Editor: Dione Benjumea-Bedoya, Corporacion Universitaria Remington, COLOMBIA
Received: October 27, 2021; Accepted: December 22, 2021; Published: January 13, 2022
Copyright: © 2022 Amit et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All data relevant to the study are included in the article.
Funding: AMLA/VCFP/LST/MMD are funded by the Ateneo de Manila University Research Council COVID-19 Research Grant (Grant No. COVID-URC 01 2021). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: We have read the journal’s policy and the authors of this manuscript have the following competing interests: VCFP owns shares of GMA Network, Inc., a Philippine Stock Exchange-listed company with interests in mass media. AMLA, VCFP, and MMD receive funding from Sanofi to conduct research on self-care.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic continues to burden health systems and communities globally, with millions of cases and deaths [ 1 ]. Because of the significant and continued impact of COVID-19, vaccines have been developed at a rapid and unprecedented pace to control the spread of the virus, and prevent hospitalisations and deaths [ 2 ]. Many vaccines have been shown to be safe and effective with high-income countries having vaccinated more than half of their population [ 3 ]. Despite the availability of these vaccines, countries are faced with various challenges including vaccine hesitancy and anti-vaccination sentiments, limited global supply, and inefficient vaccine deployment [ 4 , 5 ]. These issues in vaccine uptake, together with declining community acceptance of other public health interventions, will mean a delayed recovery and prolonged pandemic [ 6 ].
The World Health Organization (WHO) in 2019 identified vaccine hesitancy or the reluctance to vaccinate as one of the top ten threats to global health despite evidence of the important role of vaccines in improving population health outcomes [ 7 ]. Together with weak primary health care and other health challenges, countries especially low- and middle-income countries (LMICs) will struggle to meet the demands of the communities within their health system capacity. With the pandemic, countries are further burdened with many health systems overwhelmed throughout its course. The Philippines presently faces these challenges: vaccine hesitancy and increasing anti-vaccination sentiments, a weak primary health care system with efforts to strengthen it through the recently implemented Universal Health Care Law, and an overwhelmed health system because of the demands of COVID-19 and other public health problems [ 8 – 13 ]. These challenges are further compounded by a global shortage of vaccine supply with inequitable vaccine distributions [ 14 ].
Historically, the Philippines was one of the countries with generally high vaccine confidence rates [ 15 ]. Following the dengue vaccine controversy in 2017 however, confidence levels have dramatically dropped and have impacted succeeding vaccination efforts including the COVID-19 vaccination campaign [ 9 , 12 , 15 – 17 ]. Dengvaxia, the world’s first commercially available dengue vaccine developed by Sanofi Pasteur, was introduced as part of a national school-based immunization programme despite the lack of empirical data on the risks associated with administration of the vaccine among those not previously infected with dengue or seronegative children [ 9 , 12 , 15 – 17 ]. By the time reports were released that the vaccine may cause more severe disease among seronegatives, the Philippines had already inoculated more than 800,000 Filipino school-age children [ 9 ]. This was highly politicised, and damaged trust in vaccines and the health sector [ 9 , 12 , 15 – 17 ]. As a result, immunisation rates dropped and the country saw outbreaks of previously controlled vaccine-preventable diseases such as measles and polio [ 18 , 19 ]. In addition to vaccine hesitancy, the Philippine health system is not prepared for additional health care demands. As early as the first phase of the pandemic, critical care capacity was overwhelmed with the influx of patients in hospitals [ 10 , 11 ]. As of 16 September 2021, the Philippines ranks third among countries with the highest number of newly confirmed cases per one million population [ 1 , 20 ]. Globally, 42.9% of the world population have received one dose of a COVID-19 vaccine, with much lower rates in LMICs like the Philippines [ 20 , 21 ]. Only 55% of Filipinos have expressed willingness to be vaccinated against COVID-19, and as of 16 September 2021, only 30% of the population have been fully vaccinated[ 21 , 22 ].
To end this pandemic, it is critical to implement all possible public health interventions and strategies from face masks, physical distancing, to getting vaccinated [ 4 , 23 ]. However, there is a need to recognise that the adoption of all these interventions is influenced by individual risk perceptions, and these perceptions are shaped by various sources of information and experiences [ 24 ]. Additionally, there are interpersonal and structural factors that influence health decisions of individuals. Recognising the multiple dimensions in which behaviours and decisions occur, theories and models have been proposed to explain how individuals make decisions on their health based on factors that change over time and context [ 25 , 26 ]. The social ecological model provides a useful framework for investigating health behaviours and decisions by recognising that a multiplicity of factors interacts to influence health of individuals [ 26 ]. These include individual factors representing biological or behavioural characteristics, interpersonal factors representing networks and social capital operating within a defined boundary, and structural factors that include health systems and are mediated through laws and policies [ 26 ]. Published studies on vaccination that utilised this model reported that vaccine intentions and attitudes operate along multiple dimensions, with a series of events influencing decisions related to vaccination [ 17 , 27 , 28 ]. Improving adherence to interventions and vaccination rates therefore requires a better understanding of the different reasons behind vaccine mistrust and not just determining their individual beliefs, knowledge, and levels of trust [ 17 , 27 , 28 ]. A recently published scoping review supports the use of the social ecological model in understanding attitudes towards COVID-19 vaccination [ 29 ]. The review showed that influencing factors are embedded within the social ecological model and that multilevel interventions are needed to improve uptake of vaccines [ 29 ]. This scoping review of 50 articles had representation from various countries, but did not include data from the Philippines. We address this gap by exploring the vaccination narratives and challenges experienced and observed by Filipinos during the early COVID-19 vaccination period. We used qualitative data from a mixed-methods study conducted from June to August 2021 that aimed to understand how people in the Philippines view COVID-19 and what influences their behaviours. With these findings, we hope to provide insights to possible avenues of future research and directions for improving COVID-19 vaccine uptake and reach.
Material and methods
Design and setting.
We conducted an online survey among adults ages 18 and older in the Philippines (n = 1,599) from June to August 2021. A subsample participated in the semi-structured interviews (n = 35) with representation from the general population and health workforce from July to August 2021. Data from the interviews informed the findings of this paper.
Participants and recruitment
We aimed to interview participants from different regions in the Philippines, various age groups, socio-economic classes, and vaccination status and attitudes. This allowed us to ensure maximum variation sampling, which aims to capture as many population contexts as possible. We contacted a total of 115 individuals through the information they provided (i.e., mobile number, phone number, e-mail). Out of the 115, 35 participants completed the interviews. The remaining 80 either refused or could not be contacted after a maximum of three attempts. We classified participants according to their vaccination priority group based on the COVID-19 Vaccination Program’s prioritisation framework [ 30 ]. Those in the first priority group (A1) were frontline workers in health facilities; other priority groups (A2 to C) comprised and represented the general population ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0000165.t001
Data collection
We conducted the interviews in Filipino, Cebuano, and/or English via online platforms such as Zoom or via phone call. The interview guide included questions about their views on COVID-19, vaccines, and their risk perceptions and behaviours. We recruited interview participants until saturation was reached (i.e., no new information was being obtained from the interviews) [ 31 ]. The interviews lasted between 60 to 90 minutes with a token amounting to USD 6 provided to each participant. All participants consented to the interview being recorded.
Data analysis
The interviews were digitally recorded, transcribed verbatim, and translated from Filipino or Cebuano to English. The research team are native and/or fluent speakers of the three languages, and checked for linguistic and conceptual equivalence in the translated documents. We de-identified all participants and assigned pseudonyms. We analysed the data using inductive content analysis focusing on the experiences and views towards vaccination [ 32 ]. Our analysis was guided by principles of grounded theory. Transcripts of the interviews were read to identify themes and two investigators (AMLA, VCFP) independently coded the interviews according to emergent themes in Microsoft Excel [ 33 ]. We used coding language that was close to the participants’ terms and phrases to ensure that we were co-constructing accurate categories reflective of their responses [ 34 ]. The codes were reviewed, and areas of disagreement were resolved between the two investigators. Themes from the interviews were further explored through discussions with the other members of the team. We considered reflexivity throughout data collection and analysis, acknowledging that our preconceptions and experiences about vaccination as public health practitioners and health professionals may influence the way we analyse and interpret data. Our use of the grounded theory allowed us to explore the experiences of our participants and our own shared experiences, and avoided being limited by how we view COVID-19 vaccination [ 35 ]. To highlight the complex reasons for delaying and/or refusing COVID-19 vaccination, we embedded our findings within the social ecological model with three broad themes: individual factors (attitudes, beliefs, knowledge, behaviours), interpersonal factors (relationships and social networks), and structural factors (health systems and service delivery; media; and policies, regulations, and laws at the local, national, and global level) [ 26 ] ( Fig 1 ). The quotes presented in this paper are either in the original English or translated from Filipino or Cebuano.
This figure shows the three main tiers of factors influencing vaccination intention and uptake: individual (beliefs, attitudes, knowledge, health literacy), interpersonal (relationships, networks), and structural (health systems and service delivery, media, policies). These three dimensions are jointly or individually impacted by misinformation (white circles).
https://doi.org/10.1371/journal.pgph.0000165.g001
Patients and public involvement
The public were not directly involved in the design, recruitment, conduct, reporting, or dissemination plans of this research. Their only involvement was as research participants.
Ethics statement
This study was approved by the University Research Ethics Office of Ateneo de Manila University (Study No. SMPH CORISK 2021). All participants were informed about the aims and objectives of the study by including the written consent form in the email correspondence. Prior the interview, the research team thoroughly explained the study to them and provided them the opportunity to ask questions they may have. Written digital consent was taken from study participants before the interview.
We interviewed 35 participants with representation from different vaccination priority groups working in various parts of the country. Our participants also had different educational backgrounds, employment status, and vaccination attitude ( Table 2 ). There was an almost equal proportion of females and males (females: 19; males: 16) with a median age of 38 years old (range: 21 to 74 years old) in the overall study population.
https://doi.org/10.1371/journal.pgph.0000165.t002
Participant views on the barriers to COVID-19 vaccination are presented below, organised using the three tiers of the social ecological model. Individual barriers include perceptions; attitudes; and beliefs about the science, about vaccines, about the health system and government. Interpersonal barriers are the networks and social capital that influence health beliefs and decisions. Vaccine procurement, supply, and logistics, together with media- and policy-related issues, comprise the structural barriers. Where there are differences between the general population and health workers, these are highlighted in the text.
Individual barriers
Vaccine brand hesitancy and brand preferences..
Vaccine brand hesitancy or delay in getting the vaccine due to brand preferences was a common theme among the participants. The country’s first administered vaccine was Sinovac-CoronaVac, which is manufactured by a Chinese biopharmaceutical company. This was given to health workers despite lack of published data on effectiveness at the time and initial announcements that these were not recommended for high-risk individuals ( Quote I1, Table 3 ). In addition to concerns about the effectiveness of the vaccine, participants also read and heard information on how this vaccine was made. They believed this specific vaccine was using the same virus to ‘immunise’ an individual’s system, which may have unintended effects ( Quote I2, Table 3 ). Other participants cited that this specific brand was not recognised by other countries, and therefore wanted and waited for other vaccines. Meanwhile, others refused to receive mRNA vaccines due to beliefs about its safety and effectiveness.
https://doi.org/10.1371/journal.pgph.0000165.t003
Negative experiences with the health system as source of vaccine hesitancy and anti-vaccination sentiments.
The participants cited negative experiences in the past, whether these happened recently or decades ago, as causes of their negative attitude towards vaccines. Three participants who identified themselves as COVID-19 ‘anti-vaxxers’ or those opposed to vaccines, had different sources of anti-vaccination sentiments. These three participants belong to different priority groups. One belongs to the A1 or frontliner group and is working as a Barangay Health/Emergency Response Team (BHERT) member who responds to COVID-19 related health care needs in the community. The second is a retired professional (A2 or senior citizen group) while the third is an environmental protection officer who oversees implementation of public health standards in the community (B2 or other government workers). These participants experienced an undesired event related to vaccines and/or medical care from four years to more than three decades prior the pandemic ( Quotes I3-I5, Table 3 ). Except for one anti-vaxxer, no other health worker reported negative experiences that caused mistrust in the COVID-19 vaccines and vaccination campaign.
Vaccines are viewed as unsafe and deadly.
Perceptions on risk of getting infection with and dying from the virus varied among the participants. However, for those who were opposed to the vaccines, their fear of the COVID-19 vaccine and its effects was greater than their fear of the virus and outcomes ( Quote I6, Table 3 ). This fear and their view of vaccines being unsafe and deadly resulted to vaccine refusals or delays. According to them, the deaths observed after administration of the vaccine are caused by the vaccine; however, medical doctors and hospitals report the death as being caused by underlying conditions such as comorbidities ( Quotes I7-I8, Table 3 ). Some participants also believed the circulating theory that the life span of those who are vaccinated is shortened and they only have two to three years to live: “ you are healthy but because of the vaccine , you suddenly die ”. In addition to the belief that vaccines cause death or shorten an individual’s life span, participants also had doubts about the COVID-19 vaccines particularly the mRNA vaccines that use a relatively new technology ( Quote I9, Table 3 ). These concerns about the safety profile of vaccines either caused delays in vaccine acceptance and uptake or refusals. The reverse was reported among most of the health workers and other participants who viewed vaccines positively. They believed that the vaccine protects them from severe illness, hospitalisation, and death, and that vaccines only have minimal risk.
Vaccines are viewed as unnecessary and insufficient to prevent disease.
Vaccines were viewed as unnecessary by some participants, especially those in older age groups who are not allowed to go out ( Quote I10, Table 3 ). Those in lower priority groups felt that others needed the vaccine more than them. Younger participants shared that they were COVID-19 survivors even without the vaccine; but those at high risk especially the elderly and persons with comorbidities will need the vaccine to protect them ( Quote I11, Table 3 ) . The participants also viewed vaccines as insufficient–they expected that getting vaccinated means no longer needing other public health interventions but were disappointed to learn that vaccines are only one part of the solution. Participants therefore questioned the need for the vaccines given the information they have read and/or watched about still being at risk of getting infected despite being vaccinated ( Quote I12, Table 3 ). The lack of clarity in the role of the vaccines has negatively influenced people’s decisions on getting the vaccine.
Skepticism towards vaccine incentives.
Vaccine incentives in the country, such as promotions and offers for those vaccinated, created skepticism among some of the participants. These incentives ‘bothered’ participants and raised questions about the role of vaccines and the intentions of the government. As a result, these incentives ‘disincentivised’ participants from getting the vaccine as participants felt being forced to take it ( Quote I13, Table 3 ).
Use of vaccines not fully approved by the Food and Drug Administration (FDA).
Participants viewed decisions to vaccinate individuals as ‘rash’ and expressed concerns about vaccines not yet being fully approved by the Food and Drug Administration (FDA). Some also shared concerns about the rapid development of vaccines compared to other vaccines that took decades to develop ( Quote I14, Table 3 ). Participants felt that they were being experimented on using an unproven vaccine, relating this with the dengue vaccine controversy ( Quote I15, Table 3 ). This caused delay or refusal in getting the vaccines when it was offered to them.
Low health literacy and lack of critical skills to evaluate health information.
Health literacy or how people acquire, evaluate, and apply health information to inform their decisions, including getting the vaccine, is an important but underestimated tool to combat misinformation. Participants shared that Filipinos seemed to know a lot about vaccines, but only superficially. They shared that those among low-resource communities and older population groups were especially vulnerable to misinformation ( Quote I16, Table 3 ). This lack of awareness and critical skills to evaluate information, together with the rapid spread of misinformation, influences people’s decisions to get their first dose, to return to their second and get fully vaccinated ( Quote I17, Table 3 ). There were also several participants who shared that they were confused with the contradictory information they were reading and hearing ( Quotes I18, Table 3 ).
Religious beliefs do not support vaccines.
‘Antichrist’–this was how one participant described the vaccines against COVID-19. Another participant shared concerns about the vaccines and how they would replace antibodies created by God ( Quote I19, Table 3 ). She mentioned that these vaccines have active chemicals that are causing unintended side effects and deaths.
Interpersonal barriers
Family influence and opposition to vaccines..
Participants recognised the influence of their family on their health decisions including getting vaccinated. One participant who was opposed to COVID-19 vaccines shared that everyone in their family was unvaccinated because they believed her (A1, 51–60 years old, female, Misamis Oriental). Similarly, a mother who had a negative experience related to the dengue vaccine that was administered to her child, refused to have herself and her family vaccinated against COVID-19 (B2, 41–50 years old, female, National Capital Region).
Misinformation spread by networks.
Rumours and misinformation about COVID-19 vaccines are easily spread by networks, whether by word of mouth or through social media. A participant said her “ eyes have been opened only now because of YouTube ” (A2, 61–70 years old, female, Camarines Norte). Participants believed that this affected vaccine uptake, especially among individuals who do not have the opportunity to receive accurate information from official sources including the Department of Health ( Quote IC1, Table 4 ).
https://doi.org/10.1371/journal.pgph.0000165.t004
Perceived conflicts of interest of health professionals.
Participants viewed key figures in the response to the pandemic as having conflicts of interests. This perception of having ‘hidden agenda’ created mistrust in the information provided health professionals, health organisations, and other figures and institutions. These conflicts of interest, whether financial or non-financial, subject evidence and data to bias especially if there are undesired adverse effects to the treatment or vaccine ( Quote IC2, Table 4 ).
Structural barriers: Health systems and service delivery
Inadequate supply of vaccines..
Observations of participants regarding supply of vaccines varied according to location and membership to the vaccine priority groups. Participants, especially those from cities and provinces outside of metropolitan areas, reported that the supply of vaccines was insufficient to meet the demands and needs of the communities ( Quote S-HS1, Table 5 ). However, even within highly urbanised areas, participants shared that there were those who did not get their second doses on time because no vaccines arrived ( Quote S-HS2, Table 5 ). Health workers found that vaccines for them were easily accessible, however those in other groups had to wait longer before getting the vaccine ( Quote S-HS3, Table 5 ).
https://doi.org/10.1371/journal.pgph.0000165.t005
Perceived inefficiencies of the vaccination system.
Participants highlighted issues with the system including the slow rollout of vaccines, long waiting time, inefficient registration systems, and lack of a centralised system. Participants mentioned getting frustrated with the speed at which vaccines are being distributed and administered in the country ( Quote S-HS4, Table 5 ). Participants also mentioned issues with the waiting process to get a slot after registration and the waiting time at the day of the vaccination, with some being asked to stay at vaccination sites for two hours to watch a seminar on COVID-19 and vaccines ( Quotes S-HS5-6, Table 5 ). There was perceived risk of exposure, which could be lessened if the process was faster and more efficient. There were also glitches in the online registration systems used by local governments that caused additional delays in getting people vaccinated ( Quote S-HS7, Table 5 ). Local governments are responsible for the distribution and administration of vaccines among their constituents, and individuals may register with various local governments depending on their place of residence or work. This lack of a centralised system makes it difficult to track who have already been vaccinated and where they have been vaccinated such that those who are still waiting for a slot are unable to secure one ( Quote S-HS8, Table 5 ).
View that the vaccination system is inflexible and excludes vulnerable and marginalised populations.
The current vaccination system of some local governments is viewed as inflexible that excludes vulnerable and marginalised populations. There are individuals who lack access to technology and digital platforms. Especially in rural areas and among the elderly, their exclusion due to access issues is further compounded by their low digital health literacy. These individuals are then unable to register online and get the vaccine ( Quote S-HS9, Table 5 ). While registration is online, even those in older age groups who are part of highly prioritised groups because of their susceptibility to the virus are required to go to the vaccination centre ( Quote S-HS10, Table 5 ). Similarly, those belonging to marginalised groups and communities also encounter considerable challenges to getting the vaccine ( Quote S-HS11, Table 5 ).
Logistical challenges.
A participant recognised that there are also logistical constraints in the distribution of vaccines, in addition to problems with supply. The COVID-19 vaccines have different temperature requirements with some requiring special distribution systems ( S-HS12, Table 5 ). These logistical challenges influence the distribution of vaccine brands to areas that have the capability to store them and affect decisions to delay getting the vaccine especially among those who prefer other brands ( S-HS13, Table 5 ).
Health professionals seen as amplifiers of misinformation.
Misinformation on vaccines and treatment were not only observed within families and social networks, but also within the medical community reported by participants who are health professionals themselves. There have been debates about Ivermectin as treatment for COVID-19, as well as vaccines, which have created factions within the group ( S-HS14, Table 5 ). Some of these health professionals who are anti-vaxxers or opposed to vaccines publicly share their views in media and in their practice ( S-HS15, Table 5 ). Because of the stature and credibility of health professionals, their views, whether backed by science or not, get amplified in the media and communities.
Pandemic response deemed as ineffective affects trust in health institutions.
The response and messaging of health organisations, together with other key figures and institutions in the country, were viewed by participants as ineffective ( S-HS16, Table 5 ). As a result, there is declining trust in these organisations with participants doubting information provided, such that Filipinos no longer take the pandemic seriously ( S-HS17, S-HS18, Table 5 ). In turn, participants turn to other sources of information that they think are more credible and trustworthy.
Structural barriers: Media and policies
Traditional and digital media accelerating the infodemic..
Information on the virus and vaccines are easily and effectively amplified by the media. With the infodemic (portmanteau of information and epidemic) or the exponential production of information whether scientifically accurate or not, traditional media and digital media become drivers of (mis)information or fear towards vaccines ( Quotes S-MP1-S-MP2, Table 6 ). Information that participants were receiving from these sources influenced their health beliefs and vaccine decisions ( Quote S-MP3, Table 6 ).
https://doi.org/10.1371/journal.pgph.0000165.t006
Perceived poor policy implementation and lack of evidence-based policies contributing to loss of confidence in vaccines and health institutions.
The government developed the Philippine “National Deployment and Vaccination Plan for COVID-19 Vaccines” that identifies population groups to be prioritised ensure vaccine equity accounting for different risks and needs [ 36 ]. This plan also stated that only vaccines granted with emergency use authorisation (EUA) or certificate of product registration (CPR) by the Philippine FDA will be purchased by the government. However, this was reported by participants to be poorly implemented with others using connections also known as ‘ palakasan ’ system to get the vaccine ahead of those in the priority list ( Quote S-MP4, Table 6 ). Even within the government, the Presidential Security Group were given vaccines even without EUA and/or CPR registration from the FDA ( Quote S-MP5, Table 6 ). In addition, the government purchased vaccines that did not publish their results, and reportedly had lower efficacy rates but more expensive ( Quote S-MP6, Table 6 ). As a result, participants felt that the government was ‘settling for less’ and that Filipinos deserved better (A4, 21–30 years old, female, National Capital Region). These issues contributed to declining confidence in vaccines and health institutions, with Filipinos questioning the safety of such vaccines and the implementation of these prioritisation frameworks.
National and local political issues.
Past and current political issues contributed to refusals to specific vaccine brands. Together with reports of how the virus emerged from Wuhan, China, these triggered skepticism towards vaccines manufactured in their country. Participants mentioned the dispute of the Philippines and China regarding contested territory at the West Philippine Sea (South China Sea) as a reason for not preferring and/or refusing vaccines from their country, even when donations of Sinovac from China were the first vaccines to be available ( Quote S-MP7, Table 6 ). This dispute also influenced how participants thought about the origins of the virus and why other countries developed their own vaccines ( Quote S-MP8, Table 6 ). Locally, participants viewed politics to have influence on which cities or provinces receive preferred vaccine brands. They mentioned that these ‘favored hospitals and provinces’ were prioritised, which was perceived as unfair and causing further delays in the vaccination rollout ( Quote S-MP9, Table 6 ).
One of the most effective public health strategies, vaccination, has been the focus of false and inaccurate information with rapidly declining rates of acceptance. [ 37 ]. In the Philippines, vaccine confidence plummeted after the Dengue vaccine controversy [ 9 , 12 , 15 – 17 ]. While anti-vaccination views and vaccine hesitancy are not yet the main barrier to vaccination in the Philippines which still struggles with vaccine access and distribution, lessons from other countries indicate that these equally and urgently need to be addressed in addition to other challenges [ 38 ]. Our study supports the findings of other published research that report a host of individual, interpersonal, and structural barriers that work individually or collectively against vaccination uptake and reach [ 29 ]. Therefore, there is a need for a holistic approach to promote COVID-19 vaccination that not only addresses barriers at the individual level, but also at the interpersonal and structural levels [ 38 , 39 ].
Individual perceptions, beliefs, and experiences play a major role on the decision to vaccinate. These are shaped by exposure to (mis)information spread by networks, by key health figures and institutions, and through the media [ 40 – 43 ]. Misinformation regarding vaccines have been present since vaccines were first developed [ 44 – 46 ], but the advent of social media made its propagation much easier [ 43 , 45 , 47 ]. Unique to the Philippine context is vaccine brand hesitancy, specifically towards Chinese manufactured vaccines and mRNA vaccines. This is caused in part by lack of transparency and scientific information, and spread through networks and the media. Further aggravating the issue is how some people attempt to correct misconceptions in a way that alienates people instead of addressing misinformation. People involved in vaccine promotion activities, especially primary care providers, may need to be trained on how to engage with vocal vaccine deniers and promote vaccination. The World Health Organization document outlining how to respond to vaccine misinformation would be an important resource in such an endeavour [ 48 ]. Celebrities and social media influencers may also play a role in promoting vaccination [ 41 ], but it is essential that they disclose conflicts of interest to develop trust with their audience. The media also needs to be trained on how to present news regarding adverse effects following immunsation, and regarding COVID-19 in general, so as not to create unnecessary panic and dissuade people from getting vaccinated. A study reported that there may be a need to use first-person, people-centred narratives to prevent ‘psychic numbing’ and give faces to numbers [ 49 ]. In all these, it is vital to engage with the public, especially those who are vaccine hesitant, in order to promote vaccination using language that is inclusive and applicable to their context [ 48 ].
The health system and one’s interactions with it also contribute to one’s decision to get vaccinated. As in this study, trust in the health system has been found to be a major factor in getting COVID-19 vaccine [ 41 , 50 ]. The Philippine government has instituted several health system confidence-building policies. The recent COVID-19 Vaccination Program Act stipulates the provision of free COVID-19 vaccines to all Filipinos and the establishment of an indemnification fund for people who could possibly develop adverse effects following immunisation [ 51 ]. Perceptions of ‘ palakasan ’ (i.e., use of political connections), stemming from instances during the course of the pandemic where powerful individuals seem to be above the law [ 52 ], contribute to vaccine hesitancy and poor uptake of vaccines. These negative impacts are further compounded by the highly politicised Dengvaxia controversy where individuals, especially parents of school-age children, felt that health institutions and governments were experimenting on them [ 9 , 12 ] with our participants relating the COVID-19 vaccine ‘experiment’ with the dengue vaccine. In addition, inadequate supply, logistical challenges, and perceptions about the inefficiency and inflexibility of the system negatively impact vaccination rates in the country. As of 16 September 2021, only 3 in 10 Filipinos received one dose with significant differences between population groups: almost all frontline and health workers have been vaccinated while only 2 in 5 elderly Filipinos received their first dose [ 21 ]. Those in the third priority group have higher rates than the elderly population group, which were offered the vaccines earlier. Apart from individual reasons, marginalised and vulnerable groups such as the elderly have reported not being able to get their vaccine due to lack of home vaccination services and guidance in using online registration systems. The system will need to consider needs of all population groups to improve vaccination uptake. In all these, trust in the health system needs to be maintained, while disregarding regulations and policies in place can erode trust in the vaccination process.
In the Philippines, the national government has the responsibility to procure, allocate, and distribute the vaccines to the different provinces and municipalities, but it is the local government that is responsible for last-mile transport and actual inoculation. This results in wide variations in client registration and procedures between different localities. This underlines the need to identify best practices in vaccine rollout systems to implement a system that is efficient and inclusive to ensure that access to technology and mobility will not be barriers to vaccination.
There are a number of limitations that need to be considered when interpreting our findings. First, we were not able to have representation from the A5 priority group (indigent population). While we initially were able to get a participant from this group based on the survey response, we later found during the interview that this individual belonged to a different vaccination priority classification. This may point to issues with online data collection where researchers are unable to reach individuals from low-resource households. Second, there may be social desirability bias because we were unable to ensure if the respondent had other people with them that may have caused a change in their responses. Additionally, we did not disclose any political affiliations and interests, but participants may have been cautious in mentioning negative experiences related to vaccination. Participants may also have chosen more positive responses considering our background as health researchers. However, we emphasised that they will remain anonymous and their data treated with utmost confidentiality. Lastly, factors influencing COVID-19 vaccination uptake is context-specific, and this paper does not aim to represent all situations and circumstances.
Challenges to COVID-19 vaccination may be individual, interpersonal, and/or structural, which interact to influence decisions. Individual perceptions play a major role in the decision to vaccinate, and such perceptions are shaped by exposure to (mis)information amplified by the media, the community, and the health system. In the Philippines, vaccine brand hesitancy and misinformation are prevalent due to their rapid spread through social media and sensationalism in traditional media. Information on the effectiveness of safety of vaccines regardless of brand needs to be communicated to the public to increase COVID-19 vaccine confidence. At the interpersonal level, exposure to networks and health workers who are opposed to vaccines heightens public skepticism of vaccination. Structural barriers including political issues and poor implementation further contribute to vaccine refusals. The ongoing infodemic and anti-vaccination sentiments operating at all three levels (individual, interpersonal, structural) require empowering individuals to evaluate health information, and therefore health literacy becomes a critical tool to combat misinformation. Families and peers also need to be involved in these discussions as they influence vaccine uptake. Individuals engaged in vaccine promotion activities may need to be retrained on how to engage with vocal vaccine deniers in public. Given the involvement of traditional media, trainings on public health and science communication may be helpful in reporting vaccination-related news. Public figures need to disclose conflicts of interests and be transparent to the public, laying out the risks and benefits of vaccines. Laws should be well-implemented and equally implemented regardless of socioeconomic class or social position to encourage trust in the health care system and in vaccination initiatives. There is also a need to study best practices in vaccine rollout to implement systems that are efficient and inclusive so that we can vaccinate as many people against COVID-19 as quickly and as inclusively as possible: provide technological support particularly among older populations and allow flexible options for receiving the vaccine such as home vaccination. Given resource limitations, the vaccination rollout could also be improved by increasing the role of the private sector in the rollout and administration of the vaccine. The government and health organisations will need to connect with individuals, communities, and other institutions, including those who are against vaccines or hesitant towards vaccines, to co-create effective and sustainable solutions.
Acknowledgments
We would like to thank Michelle Edillon, Kriselle Abcede, Ryan Molen, and Josef Bondoc for their invaluable support to this project. We provide credit to BioRender.com for the figures illustrated in this paper. Finally, we are grateful to our participants who generously shared their stories with us.
- View Article
- Google Scholar
- PubMed/NCBI
- 34. Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London, Great Britain: SAGE Publications Ltd; 2006.
- 35. Strauss A, Corbin J. Grounded theory methodology. Handbook of qualitative research. New York: Sage; 1994. pp. 273–85.
- 51. Department of Health (Philippines). Implementing rules and regulations of Republic Act No. 11525 known as "An Act Establishing the COVID-19 Vaccination Program Expediting the Vaccine Procurement and Administration Process, Providing Funds Therefor, and For Other Purposes | Department of Health website. 2021 [Cited 16 Sep 2021]. Available from: https://doh.gov.ph/IRR-of-RA11525-An-Act-Establishing-the-COVID-19-Vaccination-Program-Expediting-the-Vaccine-Procurement-and-Administration-Process-Providing-Funds-Therefor-and-For-Other-Purposes
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

An overview of global epidemics and the challenges faced
Nizam uddin.
1 Department of Nutrition and Food Engineering, Faculty of Allied Health Science, Daffodil International University, Dhaka, Bangladesh
Thamina Acter
2 Department of Mathematical and Physical Sciences, East West University, Dhaka, Bangladesh
In this chapter, the global epidemiological events causing infections that ravaged humanity throughout its existence by bringing hardship to rich and poor nations alike are aggregated and presented. Among these, the largest known epidemics including the recent COVID-19 pandemic will be highlighted along with the analysis of the actual and common reason behind the occurring of all the epidemic scenarios. The epidemiological and nonepidemiological impacts of the most fatal pandemics recorded in history are also discussed. The vulnerable countries’ readiness for coping with epidemics is assessed in terms of different indices. Furthermore, the current and future challenges in fighting epidemiological events are on the frontline and a number of preparative measures and strategies have been suggested.
- • Global epidemic events, that is, plague, influenza, coronaviruses have been evolving from deadly human pathogens.
- • Most of the emerging pathogens are of “zoonotic” or animal origin.
- • Practicing nonpharmacological interventions is an effective weapon in fighting against an epidemic.
- • The 2019 Global Health Security Index indicated the weakness of global preparedness.
- • The next global pandemic is not so far away.
- • A number of preparative measures should be undertaken for tackling future epidemics.
1.1. Introduction to global epidemics
The disease of a living system is a mechanism of dysfunction that includes specific symptoms and signs that hinder the body’s normal homeostatic processes ( Wikipedia, 2020b ). Many external and internal factors may be responsible for a disease. Usually, there are four main types of diseases: infectious diseases, deficiency diseases, hereditary diseases, and physiological diseases. In terms of the transmission chance of any disease, it can either be communicable or noncommunicable. Communicable diseases are mostly infectious diseases, which introduced the epidemic phenomenon into the world a long time ago. A very rare disease that does not occur randomly in a population is usually categorized as an epidemic. The term epidemic originates from the two Greek words “epi,” meaning “upon,” and “demos,” meaning “population”. According to WHO, a regional outbreak of an illness that spreads unexpectedly is known as an epidemic ( Jha, 2020 ). The broad definition of epidemic disease delivered by the Centers for Disease Control and Prevention (CDC) is “the occurrence of large number cases of disease, injury, or other health condition than expected in a given community or region or among a specific group of persons during a particular period.”
There are three major components of an epidemiologic triad: external agent, susceptible host, and environment. The agent means an infectious pathogen such as a virus, bacterium, parasite, or other microbes that can attack the host in a favorable and balanced environment. All these three components work together to cause disease and other health events. The assessment of the interactions among these three components is required for developing effective interventions to control an epidemic ( CDC, 2006 ).
There are four phases of an epidemic: the emergence of a disease in a community, outbreak of the disease with localized transmission, sustained outbreak of the disease in the community, and reduced transmission by controlling the disease or acquiring immunity. The epidemic concept is different from the other related infectious disease terms like “endemic”, “outbreak,” and “pandemic” in terms of the spreading of the disease. Knowing the difference among these terms is important for understanding the baseline rate of incidence and public health updates and thus implementing appropriate health responses ( CDC, 2006 ). An endemic disease belongs to a particular geographic area. For example, malaria was an endemic disease in parts of Africa. An outbreak deals with an increase in the number of endemic cases and becomes an epidemic if not controlled quickly. The terms “epidemic” and “outbreak” are sometimes used interchangeably. While a disease-causing agent is different from current strains and much more infectious, the epidemic disease spreads over multiple countries by affecting a substantial number of people, and thus a situation, named a pandemic, arises ( CDC, 2006 ). In general, pandemics affect far more people than an epidemic in wider geographical areas in the entire world and cause impaired health and many more deaths than epidemics, which often creates enormous social disruption, economic loss, and hardship ( CDC, 2006 ).
1.2. List of epidemics
Until the 21 st century the world has faced several global pandemic and epidemic diseases including COVID-19, ( Fig. 1–1 and Table 1–1 ) ranging from asymptomatic to lethal and caused by different viruses and bacteria ( Wikipedia, 2020c ). All these pandemics posed a major challenge across the world and ultimately led to the death of thousands of people and the destruction of civilization as well as the economy.

Burden of epidemics: illustrations: epidemic events* globally, 2011–17**: a total of 1307 epidemic events in 172 countries.
Table 1–1
List of epidemics that occurred worldwide until the 21st century.
| Name of epidemic | Period | Type of disease | Place | Number of deaths | Reference |
|---|---|---|---|---|---|
| Athens Plague | 429–26 BCE | typhus, typhoid fever, or viral hemorrhagic fever | Greece, Libya, Egypt, Ethiopia | 75,000–100,000 | ( ) |
| Justinian Plague (1 plague) | 541–42 | Bubonic plague | Europe and West Asia | 30–50 million | ( ) |
| Black Death (2 plague) | 1346–53 | Bubonic plague | Europe, Asia, and North Africa | 75–200 million | ( ) |
| 1510 influenza | 1510 | Asia, North Africa, Europe | Influenza | Around 1% of those infected | ( ) |
| Naples Plague | 1656 | Bubonic plague | Italy | 240,000–1,250,000 | ( ) |
| 1 cholera | 1817–24 | Cholera | Asia and Europe | 100,000+ | ( ) |
| 2 cholera | 1826–37 | Cholera | Asia, Europe, and North America | 100,000+ | ( ) |
| 3 cholera | 1846–60 | Cholera | Russia | 1 million+ | ( ) |
| 3 plague | 1855–1960 | Bubonic plague | Worldwide | 12 million+ | ( ) |
| 4 cholera | 1863–75 | Cholera | Middle East | 600,000 | ( ) |
| 5 cholera | 1881–96 | Cholera | Asia, Africa, Europe, and South America | 298,600 | ( ) |
| 1889–90 flu | 1889–90 | Influenza or HCoV-OC43 | Worldwide | 1 million | ( ) |
| 6 cholera | 1899–1923 | Cholera | Europe, Asia, and Africa | 800,000+ | ( ) |
| Spanish flu | 1918–20 | Influenza A virus subtype H1N1 | Worldwide | 50 million+ | ( ) |
| Asian flu | 1957–58 | Influenza A virus subtype H2N2 | Worldwide | 1–4 million | ( ) |
| Hong Kong flu | 1968–70 | Influenza A virus subtype H3N2 | Worldwide (mainly in Hong Kong) | 1–4 million | ( ) |
| HIV/AIDS | 1981–present (data as of 2018) | Human immunodeficiency virus | Worldwide | 32 million+ | ( ) |
| Bangladesh cholera epidemic | 1991 | Cholera | Bangladesh | 8410–9432 | ( ) |
| SARS | 2002–04 | Severe acute respiratory syndrome (SARS) | Worldwide | 774 | ( ) |
| Swine flu | 2009–10 | Influenza A virus subtype H1N1 | Worldwide | Estimated death toll: 284,000 | ( ) |
| MERS | 2012–present | Middle East respiratory syndrome/MERS-CoV | Worldwide | 935 (as of 4 July 2020) | ( ) |
| West African Ebola | 2013–16 | Ebola virus virion | Worldwide, primarily concentrated in Guinea, Liberia, and Sierra Leone | 11,323+ | ( ) |
| Avian influenza | 2013–19 | Influenza A virus subtype H7N9 | China | 616 | ( ) |
| Zika virus | 2015–16 | Zika virus | Worldwide | 53 | ( ) |
| Dengue fever | 2019–present | Dengue fever | Asia-Pacific and Latin America | 3930 | ( ) |
| COVID-19 | 2019–present | SARS-CoV-2 virus | Worldwide | 1.3 million+ (as of December 2020) | ( ) |
1.3. Origin of epidemics hitting the globe
Usually, most of the epidemics may have a common origin ( CDC, 2006 ). Despite the fact that the etiology of the multitude of shimmered pandemics is at first dark, the origin of the continuously evolving epidemics hitting the globe seems to be natural and comprises a diverse species of bacteria, viruses, fungi, and parasites.
Since the ancient age of human ecology, any novel microbe or pathogen, either newly emerging or reemerging, has been considered an independent variable to which the immunologically susceptible population lacks significant degrees of procured invulnerability to avert the disease ( Morse, 2009 ). Until the 21st century, 70% of more than 1500 emerging human pathogens have been proven to be “zoonotic” or of animal origin, which indicates that the next pandemic would be a zoonosis. The major sources of zoonotic transmission are farmed animals (such as poultry), livestock production systems, wildlife reservoirs, unsafe storage of farmed animals in commercial places, consumption of wild species, and contact with wildlife such as wild animal trade ( Morse et al., 2012 ). Besides, certain animal disease vectors are responsible for animal-to-human transmission. Other nonanimal disease vectors contributing to the diffusion of epidemics in a region are contaminated drinking water, food, air, and surfaces, and human touch ( WHO, 2018 ).
Pandemic risk mainly depends on the survival and adaptation behavior of zoonotic pathogens. The adaptation behavior of pathogens can be spanned into five stages ( Table 1–2 ), ranging from animal reservoir transmission (stage 1) to human-to-human transmission (stage 5). In the case of stages 2–3, the geographical spread of pathogens is restricted by the territorial scope of an animal reservoir, and thus pathogens cannot adapt well to humans, causing only localized outbreaks. These stages subsequently increase the adaptability of pathogens within a human population. Over stage 3, the pathogens adapt well to humans, increasing the risk of pandemic ( Madhav et al., 2017 ).
Table 1–2
Pathogen adaptation and pandemic risk.
| Stages | Transmission to humans | Type of pathogen | Route of transmission |
|---|---|---|---|
| (1) Transmission to animal reservoir only | None | H3N8 influenza virus | |
| (2) Primary infection | Only from animals | Anthrax | |
| (3) Limited outbreaks | Limited human-to-human transmission chains | Marburg virus | |
| (4) Sustained outbreaks | Many human-to-human transmission chains | H1N1influenza virus | |
| (5) Predominant human transmission | Human-to-human | Smallpox virus |
For example, the origin of human plague may be the wild rodent fleas found in rural areas such as Southwestern United States ( Gage et al., 1995 ); infected animals such as guinea pigs in Peru and Ecuador ( Gabastou et al., 2000 ); infected camels in Central Asia and the Middle East ( Fedorov, 1960 ); or the handling of infected cats and the consumption of plague-infected rodents in Africa ( Isaäcson et al., 1973 ) or the United States ( Gage et al., 2000 ).
Fig. 1–2 represents the possible transmission pathways for the plague foci through rodent hosts and their associated fleas. When a commensal rodent consumes an infected flea, the cycle continues ( Fig. 1–2B ) until the commensal rodents die, and then their fleas move to alternative hosts, for example, humans. Finally, human-to-human transmission may occur depending on the favorable conditions if humans are infected by pneumonic plague through the transmission of respiratory droplets as well as the handling of infected animals such as rodents, cats, camels, mammal predators, and birds ( Fig. 1–2C ). The most likely sources of the Ebola virus are bats transmitting the virus to other animals, that is monkeys, apes, duikers, and humans ( WHO, 2016a ). A major reservoir host of the MERS-CoV infection is dromedary camels transmitted by bats. Since 1986, acquired immunodeficiency syndrome (AIDS) has emerged from different primate species and generated new pathogens through cross-species infections with lentiviruses named simian immunodeficiency viruses (SIVs). The species of human immunodeficiency virus type 1 (HIV-1), human immunodeficiency virus type 2 (HIV-2), and SIVs may have originated from the zoonotic transfers of viruses, ( Fig. 1–3 ) which infected mostly different primates such as African green monkeys, sooty mangabeys, mandrills, and chimpanzees found in sub-Saharan Africa ( Sharp and Hahn, 2011 ).

Possible transmission pathways for the plague agent Yersinia pestis .

Origins of human AIDS viruses.
The main causes behind triggering an epidemic are the recent introduction of a new strain of an infectious agent to a host population that is unknown to the hosts’ immune systems, sudden reduction of the host immunity to the agent below the endemic equilibrium, and the increment of virulence of the agent due to its exceeding threshold that leads to an enhanced mode of transmission. A number of strains of multidrug-resistant microorganisms can evolve due to the inappropriate use of antibiotics for treating viral infections. There are also some seasonal epidemics such as whooping cough, influenza, and measles ( Marcovitch, 2005 ).
The number of cases and usual frequency of disease during an epidemic can vary according to the time and place of occurrence and the size and type of population exposed to the disease in an area ( Cliff et al., 1998 ). The possible diverse epidemic drivers speeding up the pathogenic proliferation on a global scale are trade-induced pathogenic diffusion such as increased speed of trade and migration, advances in transportation technologies, qualitative changes in globalization processes, knowledge and fear diffusion via telecommunications media, burgeoning human population, increased speed of travel, and accelerated genetic mixing ( Morse, 2009 ).
1.4. Comparison of the magnitude of all epidemics
1.4.1. the plague epidemic.
One of the most ancient scourges in human history is the plague, which is an acute infectious disease caused by the bacillus Yersinia pestis ( Stenseth et al., 2008 , Gage and Kosoy, 2005 ). Different Y. pestis strains that have different phenotypic properties are of four types of biovars or geographic origins, namely Antiqua, Mediaevalis, Orientalis, and Microtus ( Zhou et al., 2004 ). Different biovars of Y. pestis caused three major world pandemics having different paths of spread, which resulted in devastating mortality among people. The first pandemic, occurring in the 6th century CE (i.e., 541), was called the Justinian Plague, which evolved in central Africa following spreading around the Mediterranean Sea. The second pandemic, occurring in the 14th century (i.e., 1347), was known as the Black Death, which started in Asia following spreading to Europe, and mainly affected the social, economic, cultural, religious, and political progression of the continents ( Twigg, 1984 ). The third pandemic, occurring in the middle of the 19th century (i.e., 1894), known as the pneumonic plague, evolved in Yunnan, China following spreading to Hong Kong and India, and then finally throughout the world as well ( Stenseth et al., 2008 ). Most of the plague epidemics were bubonic plague caused by the infection of lymph nodes. The other plague epidemics were of septicemic or pneumonic type ( Gage and Kosoy, 2005 ).
All the recorded plague pandemics greatly affected the social and economic statuses of various nations and continents. Fig. 1–4 represents the global epidemiology of plagues all over the world since 1954, where the increased number of cases reported in recent years indicates the plague as a reemerging as well as an endemic disease ( Schrag and Wiener, 1995 ) that presently exists in some parts of South and North America, Africa, and Central Asia ( Fig. 1–4A ). Ultimately, the bubonic and pneumonic plague disease has shifted from Asia to Africa since the 19th century, where most cases and deaths occur in the Democratic Republic of the Congo (DRC), Madagascar, Mozambique, Malawi, Tanzania, and Uganda ( Fig. 1–4B ). Between 1900 and 2015, the number of infected plague cases in the United States was 1036 with an average of 9 cases/year. Furthermore, the number of plague cases in the United States including rural California, northern Arizona, northern New Mexico, southern Colorado, southern Oregon, and far western Nevada in 2015 was 16 ( CDC, 2019b ).

Plague distribution worldwide: (A) Map showing countries with known presence of plague in wild reservoir species (red), (B) Annual number of human plague cases over different continents, reported to the WHO in the period of 1954–2005, (C) Cumulative number of countries that have reported plague to the WHO since 1954.
The total number of plague cases and deaths in the world was 3248 and 584, respectively, within the period of 2010–15, while the most affected countries were the DRC, Madagascar, and Peru ( Stenseth et al., 2008 ). The DRC was the most affected country for over a decade since 2001. In the DRC, the large pneumonic plague outbreak occurred in October and November, 2006 ( WHO, 2006 ). The host of regular plague epidemics has been Madagascar since 2012. In Madagascar, the major pneumonic and bubonic plague disease outbreak occurred in 2017, which led to more than 2417 infected plague cases and 209 deaths. As a result, the plague preparedness alert was imposed in nine countries and territories connected to Madagascar for trade and travel. As of July 2020, a bubonic plague case was reported in Bayannur, Inner Mongolia of China and Mongolia due to which a plague-prevention system has been activated throughout the year ( Stenseth et al., 2008 ).
1.4.2. Influenza pandemic (H1N1 virus)
In the last 140 years, there have been five severe epidemics of influenza A virus that have emerged as different variants such as the bird flu, dog flu, H1N1 flu, H3N2 flu, horse flu, human flu, and swine flu ( Fig. 1–5 ) ( CDC, 2019a ). Among these, the most deadly flu pandemic (category 5 influenza) was the 1918 flu (Spanish flu) caused by the H1N1-type influenza A virus that spread to the Arctic and remote Pacific islands ( Potter, 2001 ). The death toll of the 1918 influenza pandemic was more than 50 million worldwide, similar to that of the Black Death, due to the extremely high infection rate caused by cytokine storms and lung infection ( Patterson Kd Fau et al., 1991 ). As a result, the 1918 pandemic caused mental harm to numerous individuals, social disruption, and a sense of fear in the affected regions ( NationalAcademiesPress, 2005 ).

Types of influenza viruses evolved in humans causing recurring influenza pandemics since 1889.
The next influenza pandemic was the category 2 flu pandemic named the Asian flu, which emerged in Guizhou, China in 1956 and then spread to Singapore, Hong Kong, and the United States in 1957 ( Mittal and Medhi, 2007 ). The death toll of the Asian flu worldwide was in the range of 1 million to 4 million. In the period between 1968 and 1969, a strain of the H3N2 influenza virus caused the category 2 Hong Kong flu pandemic, killing 1 million people worldwide ( AssociatedPress, 2009 ).
The latest pandemic of the 21st century of the influenza A virus named swine flu was caused by a strain of H1N1 in 2009 ( CDC, 2019a ). According to the WHO, the number of infected cases and deaths during the influenza H1N1 pandemic were 482,300 and 18,000, respectively, in 199 countries. During the 2009 influenza pandemic, the main comorbidities were acute myocardial infarction and stroke, which significantly increased the number of deaths.
1.4.3. AIDS
One of the most annihilating diseases that has evolved in recent history is AIDS, an infection caused by a member of retroviruses called the human immunodeficiency virus (HIV) ( Sepkowitz, 2001 ). According to the CDC, AIDS is defined as a disease at least moderately predictive of a defect in cell-mediated immunity, occurring in a person with no known cause for diminished resistance to that disease. The symptoms of AIDS are degrading immune function and unintended weight loss along with developing opportunistic infections. The major routes of transmission of the virus are contaminated blood transfusions, contaminated and used needles, unprotected sex, and pregnant and breastfeeding mothers ( Cohen et al., 2011 ).
In 1981, the first five AIDS cases were reported in homosexual men due to a rare fungal infection caused by Pneumocystis carinii pneumonia, which was recognized by the CDC ( Sharp and Hahn, 2011 , Gallo, 2006 ). Since the first identification of AIDS cases in 1981, the number of HIV infections and the number of deaths has tremendiously increased worldwide ( Merson et al., 2008 ). Higher HIV/AIDS morbidity and mortality were observed in developing countries, while the highest prevalence rates were observed in sub-Saharan Africa ( UNAIDS, 2020 ). As of 2019, the number of infected HIV cases was 38 million with 690,000 deaths, among which 20.6 million were from eastern and southern Africa. Thus HIV/AIDS is still actively spreading and is considered a pandemic ( Kallings, 2008 ). The disease outbreak has caused large economic impacts, many controversies involving religion, and discrimination in society ( UNAIDS, 2006 ).
1.4.4. Coronavirus epidemics
1.4.4.1. severe acute respiratory syndrome coronavirus.
The first coronavirus causing disease was severe acute respiratory syndrome (SARS), which is a relatively rare viral respiratory infection ( CDC, 2017 ). The sign of SARS infection is similar to that of atypical pneumonia, and its symptoms are mainly breathing difficulties along with dry cough, fever, and headache. The SARS virus is readily transmissible and thus can spread directly through air like the influenza virus and indirectly via surfaces touched by infected persons.
The SARS outbreak first emerged in Guangdong province, southeastern China on 16 November, 2002, and then spread to 29 countries in North America, South America, Europe, and Asia within about 8 months, from November 2002 to July 2003 ( Routledge, 2003 ). According to the WHO, the total number of SARS infections was reported to be 8098, including 29 cases from the United States, while the total number of deaths was 774 ( Fig. 1–6 ) ( Routledge, 2003 ). The case fatality rate (CFR) of the SARS epidemic was 11% ( Chan-Yeung and Xu, 2003 ) and it depends on the patient’s age and gender ( Routledge, 2003 ). Patients that were 65 years old and male were most likely to die ( NationalAcademiesPress, 2004 ). The SARS outbreak mainly caused hospital-based as well as healthcare worker infections. Furthermore, the outbreak raised fear and economic instability across the world.

2003 Probable cases of SARS worldwide.
After the 2002–03 SARS outbreak, a few SARS infections were reported until May 2004 ( WHO, 2004 ). Since May 2004, there have not been any known cases of SARS reported worldwide. In December 2019, the SARS-related virus strain called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was detected, which caused the coronavirus disease 2019 (COVID-19) pandemic ( Morens and Fauci, 2020 ).
1.4.4.2. Middle East respiratory syndrome coronavirus
Another coronavirus that appeared in Saudi Arabia in the Middle East region in 2012 was responsible for causing an epidemic called Middle East respiratory syndrome (MERS) ( Parry, 2015 ). MERS is also a viral respiratory disease like SARS. The MERS coronavirus (MERS-CoV) originated from bats and then was transmitted to humans via infected camels ( Zumla et al., 2015 ).
The first MERS case was identified in June 2012 in Jeddah, Saudi Arabia, and Saudi Arabia was the most affected place in the Arabian Peninsula.” ( Zumla et al., 2015 ). In the period of 2012–13, the largest MERS epidemic spread fatally into Saudi Arabia, United Arab Emirates, and the Republic of Korea, while Saudi Arabia (approximately 80% of human cases) was the most affected country ( Fig. 1–7 ) ( Zumla et al., 2015 ). Since 2012, the countries that have reported MERS cases have been Algeria, Austria, Bahrain, China, Egypt, France, Germany, Greece, Islamic Republic of Iran, Italy, Jordan, Kuwait, Lebanon, Malaysia, Netherlands, Oman, Philippines, Qatar, Republic of Korea, Kingdom of Saudi Arabia, Thailand, Tunisia, Turkey, United Arab Emirates, United Kingdom, United States, and Yemen. Larger MERS outbreaks have been seen in South Korea and Saudi Arabia in 2015 and 2018, respectively ( WHO, 2017 ).

Confirmed cases of MERS-CoV worldwide in the period of 2012–15.
According to the WHO, the number of MERS cases as of January 2020 was about 2500, while the death rate was 35% of the reported cases ( Carmona et al., 2012 ). The spread of MERS-CoV mainly occurred in healthcare facilities among family members, patients, and healthcare workers before MERS-CoV was diagnosed and where infection prevention practices were inadequate. The patients with chronic lung disease, diabetes, immunodeficiency, and renal failure were at high risk of MERS severity. The impact of the MERS epidemic has been observed in the Republic of Korea in different aspects of life, such as travel, trade, and economies.( Al-Osail and Al-Wazzah, 2017 )
1.4.4.3. Severe acute respiratory syndrome coronavirus-2
The most recent outbreak of coronavirus disease 2019 (currently known as COVID-19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has been a potential threat to human health ( Acter et al., 2020 ). The origin of the disease was Huanan Seafood Wholesale Market, located in Wuhan, Hubei, China, and then it subsequently spread to Thailand, Japan, and then other regions in Asia, Europe, North America, South America, Africa, and Oceania, developing into the global 2019–20 coronavirus pandemic by March. WHO declared this massive global outbreak as the sixth Public Health Emergency of International Concern on January 30 and a pandemic on March 11, 2020 as the disease spread worldwide.
According to figures compiled by US-based Johns Hopkins University, as of January 04, 2021, there are 85,603,740 confirmed cases, 23,188,005 active cases, 60,562,667 recoveries, and 1,853,068 deaths in about 191 countries/territories and 26 cruise/naval ships. The current scenario of the ten most affected countries in the world is presented in Table 1–3 . As the number of confirmed COVID-19 infections is higher than the total number of suspected SARS cases, the SARS-CoV-2 virus is assumed to be more contagious than other coronaviruses, that is, SARS, MERS, and influenza. The natural reservoir of the SARS-CoV-2 virus is assumed to be bats. The human-to-human transmission of the virus mainly occurs via respiratory droplets produced from the coughs or sneezes of an infected person. The pandemic has caused global health impacts; social, economic, educational, and agricultural disruption; panic buying; widespread supply and food shortages; and postponement or cancellation of events ( Cave and May, 2020 , Horowitz, 2020 , Larson, 2020 , Litvinova et al., 2019 , Maxmen, 2020 ).
Table 1–3
COVID-19 pandemic by location for ten most affected countries.
| Country | Total COVID-19 cases | Total deaths due to COVID-19 | Total recovered from COVID-19 |
|---|---|---|---|
| United States | 21,113,528 | 360,078 | 12,436,958 |
| India | 10,341,291 | 149,686 | 9,946,867 |
| Brazil | 7,733,746 | 196,018 | 6,813,008 |
| Russia | 3,260,138 | 58,988 | 2,640,036 |
| Turkey | 2,241,912 | 21,488 | 2,136,534 |
| Colombia | 1,675,820 | 43,965 | 1,542,353 |
| Italy | 2,155,446 | 75,332 | 1,503,900 |
| Argentina | 1,640,718 | 43,482 | 1,452,960 |
| Germany | 1,783,896 | 35,105 | 1,401,200 |
| Mexico | 1,448,755 | 127,213 | 1,098,431 |
1.4.4.4. The ebola epidemic
One of the most severe, deadliest, and most fatal viral diseases is Ebola virus disease (EVD) or Ebola hemorrhagic fever caused by a group of ebolaviruses such as Ebola virus (species Zaire ebolavirus ), Sudan virus (species Sudan ebolavirus ), Taï Forest virus (species Taï Forest ebolavirus ), Bundibugyo virus (species Bundibugyo ebolavirus ), Reston virus (species Reston ebolavirus ), and Bombali virus (species Bombali ebolavirus ) in human and nonhuman primates (such as monkeys, gorillas, and chimpanzees), among which the human disease-causing ebolaviruses are Ebola, Sudan, Taï Forest, and Bundibugyo viruses ( WHO, 2016a ).
The most likely sources of the ebolavirus are infected wild animals such as fruit bats; porcupines; and nonhuman primates such as chimpanzees, apes, and monkeys. The spreading of the virus may take place through direct contact with the infected blood, body fluids, or secretions of infected people; mucous membranes in the eyes, nose, or mouth; tissues of infected animals; and contaminated objects or surfaces ( WHO, 2016a ). Besides, the virus may exist in the semen or breast milk of an EVD-recovered person ( WHO, 2015a ). The incubation period of the disease is from 2 days to 3 weeks, while its major signs and symptoms are fever, sore throat, muscular pain, headaches, vomiting, diarrhea, decreased liver and kidney functions, sometimes internal and external bleeding, and low blood pressure from fluid loss ( WHO, 2016a , Singh and Ruzek, 2013 ). The Ebola epidemic overwhelmed the healthcare systems and caused a lack of routine diagnosis and treatment for endemic diseases such as malaria, HIV/AIDS, and tuberculosis. As a result, the nonebola diseases contributed to an estimated 10,600 additional deaths during the Ebola epidemic in Guinea, Liberia, and Sierra Leone of West Africa ( Parpia et al., 2016 ). Besides, understaffing and fear of contracting the disease caused the closure of facilities that led to decreasing routine childhood immunization rates and routine healthcare in affected countries.
The Ebola virus first emerged with two simultaneous outbreaks in two tropical regions of sub-Saharan Africa named Sudan (in a village near Ebola river) and the DRC (formerly Zaire) in 1976, while the number of infections was 284 (with a mortality rate of 53%) and 318 (with a mortality rate of 88%) in the first and second outbreaks, respectively ( WHO, 2016a ). In the last 40 years, the Ebola virus has been mostly affecting several African countries with occasional outbreaks as well as a sparking alarm worldwide due to more than 25 deadly outbreaks ( Table 1–4 ). The most severe EVD epidemic since 1976 that caused a large number of deaths occurred in West Africa (Guinea, Liberia, and Sierra Leone) from December 2013 to January 2016, with 28,646 cases and 11,323 deaths ( WHO, 2016a ). According to the WHO, the numbers of confirmed Ebola cases and deaths due to this disease were 2387 and 1590, respectively, from 1976 through 2020. The emergency alert for EVD was withdrawn on 29 March 2016. Recently, EVD has been reemerged in the DRC, Africa from May 2017 ( K, 2017 ). The average CFR of EVD is about 50%, which indicates that the disease has a high risk of death ( WHO, 2016a ).

Table 1–4
Chronology of previous ebola virus disease outbreaks.
| Year | Country | EVD | Cases | Deaths | Case fatality |
|---|---|---|---|---|---|
| 2020 | Democratic Republic of the Congo | Zaire | Ongoing | ||
| 2018–20 | Democratic Republic of the Congo | Zaire | 3481 | 2299 | 66% |
| 2018 | Democratic Republic of the Congo | Zaire | 54 | 33 | 61% |
| 2017 | Democratic Republic of the Congo | Zaire | 8 | 4 | 50% |
| 2015 | Italy | Zaire | 1 | 0 | 0% |
| 2014 | Spain | Zaire | 1 | 0 | 0% |
| 2014 | United Kingdom | Zaire | 1 | 0 | 0% |
| 2014 | United States | Zaire | 4 | 1 | 25% |
| 2014 | Senegal | Zaire | 1 | 0 | 0% |
| 2014 | Mali | Zaire | 8 | 6 | 75% |
| 2014 | Nigeria | Zaire | 20 | 8 | 40% |
| 2014–16 | Sierra Leone | Zaire | 14,124* | 3956* | 28% |
| 2014–16 | Liberia | Zaire | 10,675* | 4809* | 45% |
| 2014–16 | Guinea | Zaire | 3811* | 2543* | 67% |
| 2014 | Democratic Republic of the Congo | ||||
| 2012 | Democratic Republic of the Congo | Bundibugyo | 57 | 29 | 51% |
| 2012 | Uganda | Sudan | 7 | 4 | 57% |
| 2012 | Uganda | Sudan | 24 | 17 | 71% |
| 2011 | Uganda | Sudan | 1 | 1 | 100% |
| 2008 | Democratic Republic of the Congo | Zaire | 32 | 14 | 44% |
| 2007 | Uganda | Bundibugyo | 149 | 37 | 25% |
| 2007 | Democratic Republic of the Congo | Zaire | 264 | 187 | 71% |
| 2005 | Democratic Republic of the Congo | Zaire | 12 | 10 | 83% |
| 2004 | Sudan | Sudan | 17 | 7 | 41% |
| 2003 (Nov-Dec) | Democratic Republic of the Congo | Zaire | 35 | 29 | 83% |
| 2003 (Jan-Apr) | Democratic Republic of the Congo | Zaire | 143 | 128 | 90% |
| 2001–02 | Democratic Republic of the Congo | Zaire | 59 | 44 | 75% |
| 2001–02 | Gabon | Zaire | 65 | 53 | 82% |
| 2000 | Uganda | Sudan | 425 | 224 | 53% |
| 1996 | South Africa (ex-Gabon) | Zaire | 1 | 1 | 100% |
| 1996 (Jul-Dec) | Gabon | Zaire | 60 | 45 | 75% |
| 1996 (Jan-Apr) | Gabon | Zaire | 31 | 21 | 68% |
| 1995 | Democratic Republic of the Congo | Zaire | 315 | 254 | 81% |
| 1994 | Côte d’Ivoire | Taï Forest | 1 | 0 | 0% |
| 1994 | Gabon | Zaire | 52 | 31 | 60% |
| 1979 | Sudan | Sudan | 34 | 22 | 65% |
| 1977 | Democratic Republic of the Congo | Zaire | 1 | 1 | 100% |
| 1976 | Sudan | Sudan | 284 | 151 | 53% |
| 1976 | Democratic Republic of the Congo | Zaire | 318 | 280 | 88% |
1.5. Assessing countries’ readiness for coping with epidemics
In order to cope with an epidemic, five crucial stages are required to be followed: prediction of the novel pathogen; faster pathogen detection in animal reservoirs and human populations; disease containment at the beginning phases of transmission; control of the epidemic during its amplification; and elimination of the outbreak risk ( CDC, 2006 ). Effective readiness of a country during an epidemic involves a disease surveillance system; early mitigation efforts; actual response measures such as case and contact tracing; identifying infected cases; and preventive measures in healthcare facilities and public health measures, such as clean water and handwashing etiquette ( Gates, 2015 ).
In order to flatten the epidemic curve, nonpharmacological interventions such as using personal protective equipment (PPE; i.e., masks, gloves, etc.) and social distancing have been exercised in the affected countries ( Stawicki et al., 2020 ). Vaccine production, as well as the purchasing capability, is variable from country to country. For example, according to the WHO, 19 countries manufactured the influenza vaccine, while only the United States and France were the suppliers of the H1N1 vaccine in 2009 ( CDC, 2019c ).
Until now, different effective ways have been followed in the countries for coping with the epidemics, resulting in various impacts in the affected regions. The indices for measuring and identifying countries’ preparedness and responses against the threats of epidemics worldwide are the Global Health Security (GHS) Index and the COVID-19 Safety, Risk and Treatment Efficiency framework and indices. There is a relationship between global health security and its ability to cope with pandemics. In this context, the GHS Index is an assessment index projected by the Nuclear Threat Initiative and the Johns Hopkins Center for Health Security (CHS) and developed with the Economist Intelligence Unit that benchmarks the capabilities of the health security of any nation affected by infectious disease outbreaks and thus encourages to upgrade the health facilities of the respective country. The GHS index usually is calculated based on 140 questions organized into six categories, namely the prevention of emerging diseases, the detection and reporting of confirmed cases and deaths, rapid response to the epidemic, the health system, the compliance with global norms, and the risk environment.
The 2019 GHS Index reported the rankings of 195 countries and territories, which finds that the average score is 40.2 out of 100, indicating the fundamental weakness of global healthcare systems and preparedness to face epidemics ( LePan, 2020 ). The pre-COVID-19 GHS report highlights the global health security problems of the current world due to the following reasons:
- • Worldwide weak national health security required for facing epidemic response
- • Few efforts taken by countries for testing the capacities of health securities
- • Inadequate funding for filling up the preparedness gaps of the countries
- • Inadequate coordination and training among health professionals.
As shown in Fig. 1–8 , 81% of the countries had a low score pertaining to the health security system in 2019, while 85% of countries did not exercise biological threat-focused simulation efforts along with the WHO. According to GHS, the score of the United States (98.2) was higher than that of Germany (84.6) and South Korea (92.1) in the case of detection, reporting, and infection control practices and availability of equipment, while the private sector of South Korea had sufficient protective equipment such as masks and developed and implemented test kits faster. Along with sufficient protective equipment, Germany had greater healthcare facilities such as hospital beds, intensive care beds, and ventilators ( Lafortune, 2020 ). One of the limitations of GHS methodology in testing and the adaptability of health systems is that the index may over or underestimate the preparedness level of certain countries. One of the effective measures to flatten the epidemic curve is imposing lockdowns of nonessential economic activities, especially implemented by most Asian countries, including South Korea, and some European countries, including France and Germany. However, these shutdown approaches are responsible for the economic impacts of the affected regions.

Global Health Security Index of countries with population of more than 5 million. ( GHSI, 2019 ).
Table 1–5 shows the ranking of the GSH index of the top ten countries that have adequate healthcare systems, which are best prepared to deal with a pandemic although there are still some gaps in their preparedness. Overall, the top 2019 GHS-ranked countries globally are the United States, the United Kingdom, and the Netherlands. In addition, Fig. 1–9 shows that numerous medical service frameworks have had their security tested with the episode of COVID-19 ( Lafortune, 2020 ). The highest number of deaths per capita was reported in countries like Belgium, France, Italy, Spain, United States, and United Kingdom during the COVID-19 pandemic. The countries near the origin of the COVID-19 outbreak, such as South Korea, have started to release the lockdown measures due to effective management of the disease outbreak.
Table 1–5
The top 10 highest-ranking countries in the Global Health Security index ( GHSI, 2019 ).
| Ranking | Name of country | GHS index score |
|---|---|---|
| 1 | United States | 83.5 |
| 2 | United Kingdom | 77.9 |
| 3 | Netherlands | 75.6 |
| 4 | Australia | 75.5 |
| 5 | Canada | 75.3 |
| 6 | Thailand | 73.2 |
| 7 | Sweden | 72.1 |
| 8 | Denmark | 70.4 |
| 9 | South Korea | 70.2 |
| 10 | Finland | 68.7 |

Confirmed COVID-19 cases versus Global Health Security score. ( GHSI, 2019 ).
The COVID-19 Safety, Risk and Treatment Efficiency framework and indices have been released by the Deep Knowledge Group (a consortium of profit and nonprofit organizations) in March 2020, which cover 150 countries. This “Safety” index was calculated based on 72 metrics grouped into 3 indices, namely Safety, Risk and Treatment Efficiency, and 12 underlying quadrants. The data was collected from the WHO, Johns Hopkins University, Worldometer, and the CDC. Overall, the top COVID-19 Safety Indexed countries of 2020 are Israel, Germany, and South Korea.
Countries like Australia and South Korea performed well on both the November 2019 GHS Index and COVID-19 Safety Index. The top-ranked GHS Indexed countries such as the United Kingdom and the United States and Other OECD (Organisation for Economic Co-operation and Development) countries such as France, Spain, and Sweden were not in the list of the top 40 COVID-19 Safety Indexed countries. On the other hand, better ranked COVID-19 Safety countries were observed to be Austria, China, Hungary, Israel, Japan, New Zealand, Singapore, and the United Arab Emirates according to their GHS ranks. Besides, Germany ranked 2 nd and 14 th on the COVID-19 Safety Index and GHS Index, respectively. Asian countries performed well in the effective management of the COVID-19 crisis, such as massive testing, intense reconnaissance frameworks, and quick detachment of tainted patients and the subsequent leveling of the epidemic curve ( Lafortune, 2020 ).
1.6. Challenges in battling with epidemics
Epidemics of any disease put the resources of the health systems of the affected countries under pressure due to the admission of a large number of patients to hospitals. The most recent COVID-19 pandemic shows that the health and nonhealth impacts of a pandemic could be devastating even with good public health surveillance systems ( Acter et al., 2020 ). All attention given to the emergency of medical supplies and supports may often be responsible for neglecting other regular health facilities. As a result, people with other diseases may not get healthcare services on time during an epidemic, and thus mortality rates get higher. The situation is worsening in poorer communities around the world and low-income countries, and countries facing severe epidemics faced mainly this type of difficulty. For example, the Ebola virus in West Africa spread rapidly in more than 2 months before diagnosis and thus caused the Ebola epidemics. Besides, the epidemic caused by any novel virus may generate fear among certain at-risk populations, which leads to the generation of inadequate decisions or inappropriate behaviors.
The rapidly evolving nature of known epidemic diseases, such as cholera, HIV infection, influenza, meningitis, malaria, and tuberculosis still remains a threat for the globe. It is sometimes difficult to effectively access public health measures even in cases of known epidemics. The major limitations of access to vaccines are inadequate production capacity for diseases, for example yellow fever and influenza; vaccines out of stock during explosive outbreaks (e.g., meningitis); and the absence of markets during emergencies (e.g., oral cholera vaccine). Unprepared health systems could be challenged during epidemics of infectious diseases. In the case of inadequately undertaken preventive measures such as triage and isolation, the hospitals could be a source of transmission for unknown and emerging pathogens (for instance, MERS) from infected patients. Healthcare workers are usually at high risk of infection, which results in shortages of them during emergencies of epidemics and thus further weakens the health workforce. Therefore training new healthcare workers is time consuming. The traditional containment measures like home quarantine are sometimes unacceptable, which should be reevaluated in the perception of people’s freedom of movement. The term “infodemics” is a new health risk among the population in the era of epidemics, which includes the rapid spreading of unauthentic, misleading, and unreliable information through social media nationally and internationally.
1.7. Concerns about future pandemics
The 21st century has been vigorously attacked by so many major epidemics ( Gates, 2015 ). People will always remember the West African Ebola outbreak in 2014. The coronaviruses, that is, MERS, are still active, and the recent COVID-19 pandemic is still ongoing. Viral hemorrhagic fevers, that is, Ebola and Marburg viruses, causing disease could become pandemics. The history of pandemics occurring every decade tells us that the recurrences between pandemics become more limited as seen with SARS in 2003, influenza A H1N5 (bird flu) in 2007, H1N1 (swine flu) in 2009, MERS in 2012, and Ebola in 2014 ( Morse and Schluederberg, 1990 , Jones et al., 2008 ).
Multidrug-resistant strains of tuberculosis (MDR-TB) are a major concern. Without dynamic reconnaissance and regulation measures, the possibility of avian influenza (H5N1) infection joining with human seasonal infections is a concern to researchers. The emergence and spread of multidrug-resistant strains of the plague virus would pose a major concern to human health ( Inglesby et al. ). As plague can originate in wildlife rodent reservoirs, it could not be eradicated. Africa is particularly at risk due to possibly favorable contact between plague reservoirs and peridomestic rodents in poor rural communities ( Stenseth et al., 2008 ). The plague is known to be affected by various environmental conditions such as hotter springs and wetter summers that may turn out to be more normal in the future ( Parmenter et al. , Enscore et al. ). Furthermore, plague bacillus may adapt to new ecological niches due to its genomic rearrangement capacity and antibiotic resistivity ( Parkhill et al. , Galimand et al., 1997 ).
As the current world remains vulnerable to epidemic events, the possibility of the next global pandemic could not be ignored. Although the advancement of medical science has been progressing rapidly in recent years, the natural immunity of humans to a newly mutated disease would not develop, and thus there are still concerns about global, sustained, and threatening public health emergencies in the future ( Ross et al., 2015 ). As diseases very rarely disappear, there is always space for new ones. There are some reasons behind emerging and reemerging new pathogens and the increasing transmissibility and severity of infectious diseases. The major potential factors that serve as the breeding grounds for concerns of the future transmission of respiratory and fecal-oral pathogens are overpopulation ( Alirol et al. ); weak populations along with malnourishment in low-to-middle-income countries (LMICs); quick and extreme mobility of individuals, with expanded vehicle offices; greater interconnectivity between megacities; poverty; globalization; relentless urbanization ( Alirol et al. ); swelling populations of city dwellers; global warming; environmental degradation; ecological changes; habitat destruction; close and rehashed interaction among individuals, animals, and livestock; domestic animals; drug resistance to entering pathogens and the existence of viral pathogens with high nucleotide substitution rate, poor mutation error-correction rate ability, and quick adaptation capacity to human hosts ( Jones et al., 2008 ). Given the abovementioned contributing factors, it is almost certain that the following arising infection will likewise spread quickly and far.
1.8. Preparative measures for tackling future pandemics
It is impossible to create a pandemic-free world. But meticulous preparation and rapid response can be helpful to prevent, detect, and respond effectively and rapidly to most episodes from gaining out of power at the very start of a disease outbreak that represents potential international threats. In order to make the world safer, the following pandemic preparation methods should be undertaken:
- • Addressing the root cause of health insecurity and strengthening health systems with a strong focus on surveillance systems.
- • Providing protected, compelling, and subjective wellbeing administrations prior to, during, and after scourges by long-term substantial investments.
- • Building and sustaining versatile limits at public, local, and worldwide levels.
- • Ensuring, improving, and implementing rapid accessibility of essential life-saving health services and interventions including medicines and vaccines and other countermeasures worldwide during crises.
- • Early recognition of a new microbe and the beginning of human-to-human transmission during emergence by detecting unusual clusters of severe cases.
- • Raising clinicians’ awareness by training them effectively as detectors and first-line responders.
- • Flexibility of preparedness to adapt to any novel agent.
- • Employing risk communication and sophisticated skills among health specialists, offices, doctors, and health experts to limit the social, political, and monetary effects of a scourge.
- • Permitting innovative work exercises in any event during pandemics to quickly track the accessibility of powerful tests, immunizations, and drugs.
- • Empowering and engaging anthropologist communities for better understanding human ecology as well as addressing fear and trust issues.
- • Empowering and engaging the health workforce community in creating and executing strong arrangements and techniques toward widespread health coverage.
- • Adequate clinical management and better supportive care for patients by involving skilled, qualified, and dedicated health personnel.
- • Recently, computational or artificial intelligence (AI) techniques have been playing a significant role in coping with global epidemics and addressing public health surveillance ( Zeng et al., 2021 , Dananjayan and Raj, 2020 , Bansal et al., 2020 ). AI can help researchers in predicting the magnitude and impact of future epidemics. However, there are still some challenges regarding AI techniques, that is, unawareness, data sparsity, lack of skilled operating manpower, high cost, software malfunction, noninvincibility, algorithm bias, data breach, etc. ( Harkut and Kasat, 2019 ). In order to explore AI techniques widely in the areas of global epidemics, some developments in AI techniques such as research on collaborative systems, fine-tuning of networks of neural network algorithms, generation of innovative ways to explore human intelligence, deep learning, development of neural biological networks, advent of reinforcement learning, limitations in the cost of high computational capacity, and wide availability of labeled data should be performed ( Harkut and Kasat, 2019 ).
Furthermore, a number of hygiene measures are recommended in order to maintain health and prevent the spread of disease outbreaks in the future.
- • Medical hygiene: The standard infection control precautions, that is, frequent handwashing; use and disinfection of PPE including masks, gowns, caps, eyewear, and gloves; prevention of sharp injury; disinfection of surgical equipment and environment; airborne and contact precautions; droplet precautions; isolation of infected patients; and safe removal of clinical waste, etc. should be practiced in medical care settings ( WHO 2007 ).
- • Home hygiene: Home hygiene may include frequent handwashing with soap and water, using hand sanitizer, food hygiene, water hygiene, cleaning common surfaces, care of domestic animals, using tissues or covering mouth during coughing, and disposal of used tissues after coughing ( Bloomfield et al., 2009 ).
- • Social hygiene: Social hygiene may include social distancing in public transport, educational institutions, workplaces, and markets; installment of handwashing set-ups; and frequent use of disinfectants in public places.
1.9. Review questions
- 1. What is the common origin of the continuously evolving epidemics hitting the globe and how does the transmission of any infectious disease take place?
- 2. How does a pathogen adapt to the human population?
- 3. How many times did the influenza viruses reemerge as variants until the 21st century?
- 4. Which coronavirus is the deadliest virus in history and why?
- 5. How many stages are essential for coping with an epidemic?
- 6. What are the popular nonpharmaceutical interventions that should be followed during an epidemic?
- 7. What is the relationship between countries’ preparedness measuring index and its ability to cope with pandemics?
- 8. How can the Global Health Security (GHS) index be calculated for measuring the preparedness of a vulnerable country?
- 9. Write about the current health security problems worldwide.
- 10. Why are the health systems of any country the most affected part during any epidemic?
- 11. What are the major challenges faced during an epidemic?
- 12. Which factors contribute most to evolving novel pathogens in the human population?
- 13. How can an epidemic be responded to in a short time?
- 14. How can the challenges of computational or artificial intelligence (AI) techniques be overcome?
- 15. How can different hygiene practices be maintained?
1.10. Problem statements for young researchers
- 1. The countries with a good 2019 GHS Index score and COVID-19 Safety Index score performed effective management of epidemics. The top-ranked GHS Indexed countries are not always the top-ranked COVID-19 Index countries. What is the reason behind this dissimilarity?
- 2. The number of cases and the usual frequency of any disease during an epidemic can vary according to the time and place of occurrence and the size and type of population exposed to the disease in an area. How is this statement true in terms of epidemic events that have occurred in history?
1.11. Discussion questions
- 1. All the epidemic events show the devastating health and nonhealth impacts even with good public health surveillance systems. The poorer communities are the main victims of this scenario. Besides, healthcare workers are at high infection risk even in developed countries. How can the resources of the health system be enriched in order to cope with an epidemic and reduce the infection risk of healthcare providers?
- 2. There have been many major epidemics since the early age of human evolution. The recent epidemics include the West African 2014 Ebola outbreak, 2012 MERS, and COVID-19. The history of pandemics occurring is a reflection of concern for future epidemics. What kind of key issues can be raised regarding the growing concerns of the future transmission of human pathogens?
- 3. Any novel microbe or pathogen, either newly emerging or reemerging, is considered an independent variable that causes disease in the susceptible human population. While most of the emerging human pathogens are of animal origin, discuss the main causes behind the triggering of an epidemic.
- Acter T., et al. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: a global health emergency. Sci. Total. Environ. 2020; 730 :138996. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ali M., et al. The global burden of cholera. Bull. World Health Organ. 2012; 90 :209–218A. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alirol, E., et al. Urbanisation and infectious diseases in a globalised world. [ PMC free article ] [ PubMed ]
- Al-Osail A.M., Al-Wazzah M.J. The history and epidemiology of Middle East respiratory syndrome corona virus. Multidiscip. Respiratory Med. 2017; 12 :20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Associated Press. 2009. World health group issues alert Mexican president tries to isolate those with swine flu [Online]. Associated Press.
- Bansal A., et al. Utility of artificial intelligence amidst the COVID 19 pandemic: a review. J. Med. Syst. 2020; 44 :156. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bloomfield S.F., et al. 2009. The global burden of hygiene-related diseases in relation to the home and community. < https://www.ifh-homehygiene.org/review/global-burden-hygiene-related-diseases-relation-home-and-community?OpenDocument= >.
- Burki T. Justinian’s flea: plague, empire and the birth of Europe. Lancet Infect. Dis. 2007; 7 :774. [ Google Scholar ]
- Carmona N.A., et al. Excited state intermolecular proton and energy transfer of 1-hydroxypyrene interacting with the human serum albumin protein. J. Photochemistry Photobiology A: Chem. 2012; 234 :3–11. [ Google Scholar ]
- Cave, D. & May, T. 2020. World feared china over coronavirus. Now the tables are turned [Online]. The New York Times.
- CDC . Principles of Epidemiology in Public Health Practice. Department of Health and Human Services; USA: 2006. [ Google Scholar ]
- CDC. 2017. SARS basics fact sheet [Online]. Centers for Disease Control and Prevention (CDC). < https://www.cdc.gov/sars/about/fs-sars.html > [Accessed].
- CDC. 2019a. 1918 Pandemic (H1N1 virus). < https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html >.
- CDC. 2019b. Map and statistics: plague in the United States [Online]. Centers for Disease Control and Prevention. < https://www.cdc.gov/plague/maps/index.html > [Accessed].
- CDC. 2019c. Ten years of gains: a look back at progress since the 2009 H1N1 pandemic [Online]. USA: Centers for Disease Control and Prevention. < https://www.cdc.gov/flu/spotlights/2018-2019/decade-since-h1n1-pandemic.html > [Accessed].
- Chan-Yeung M., Xu R.-H. SARS: epidemiology. Respirology. 2003; 8 :S9–S14. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cliff A., Haggett P., Smallman-Raynor M. Deciphering Global Epidemics. Cambridge University Press; 1998. C.S.i.H. Geography. [ Google Scholar ]
- Cohen M.S., et al. Acute HIV-1 Infection. N. Engl. J. Med. 2011; 364 :1943–1954. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dananjayan S., Raj G.M. Artificial Intelligence during a pandemic: The COVID-19 example. Int. J. Health Plan. Manag. 2020; 35 :1260–1262. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Desk, N. 2020. MERS coronavirus update: 61 cases reported in first half of 2020. Outbreak News Today.
- Enscore, R.E., et al. Modeling relationships between climate and the frequency of human plague cases in the southwestern United States, 1960-1997. [ PubMed ]
- FAO. 2019. FAO H7N9 situation update—avian influenza A(H7N9) virus [Online]. < http://www.fao.org/ag/againfo/programmes/en/empres/H7N9/situation_update.html > [Accessed].
- Fedorov V.N. Plague in camels and its prevention in the USSR. Bull. World Health Organ. 1960; 23 :275–281. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gabastou J.-M., et al. An outbreak of plague including cases with probable pneumonic infection, Ecuador, 1998. Trans. R. Soc. Tropical Med. Hyg. 2000; 94 :387–391. [ PubMed ] [ Google Scholar ]
- Gage K.L., Kosoy M.Y. Natural history of plague: perspectives from more than a century of research. Annu. Rev. Entomology. 2005; 50 :505–528. [ PubMed ] [ Google Scholar ]
- Gage K.L., et al. Cases of cat-associated human plague in the Western US, 1977-1998. Clin. Infect. Dis. 2000; 30 :830–900. [ PubMed ] [ Google Scholar ]
- Gage K.L., Ostfeld R.S., Olson J.G. Nonviral Vector-Borne Zoonoses Associated with Mammals in the United States. J. Mammalogy. 1995; 76 :695–715. [ Google Scholar ]
- Galimand M., et al. Multidrug Resistance in Yersinia pestis Mediated by a Transferable Plasmid. N. Engl. J. Med. 1997; 337 :677–681. [ PubMed ] [ Google Scholar ]
- Gallo R.C. A reflection on HIV/AIDS research after 25 years. Retrovirology. 2006; 3 :72. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gates B. The Next Epidemic — Lessons from Ebola. N. Engl. J. Med. 2015; 372 :1381–1384. [ PubMed ] [ Google Scholar ]
- GHSI. 2019. 2019 Global Health Security Index [Online]. < https://www.ghsindex.org/ >.
- Gordon M.S., et al. Fragmentation methods: a route to accurate calculations on large systems. Chem. Rev. 2012; 112 :632–672. [ PubMed ] [ Google Scholar ]
- Harkut D.G., Kasat K. In: Artificial Intelligence—Scope and Limitations. HARKUT D.G., editor. 2019. Introductory chapter: artificial intelligence—challenges and applications. [ Google Scholar ]
- Hays, J.N. 2005. Epidemics and Pandemics: Their Impacts on Human History.
- Horowitz, J. 2020. Italy announces restrictions over entire country in attempt to halt coronavirus [Online]. The New York Times. [Accessed].
- Inglesby, T.V., et al. Plague as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. [ PubMed ]
- Isaäcson M., Fau - Levy D., et al. Unusual cases of human plague in Southern Africa. South. Afr. Med. J. 1973 [ PubMed ] [ Google Scholar ]
- Jha, F. 2020. Pandemic, epidemic, endemic—what these mean and how they are different from each other. The Print.
- Jones K.E., et al. Global trends in emerging infectious diseases. Nature. 2008; 451 :990–993. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- K, H. 2017. Ebola outbreak declared in Democratic Republic of the Congo after three die. The Guardian.
- Kallings L.O. The first postmodern pandemic: 25 years of HIV/AIDS. J. Intern. Med. 2008; 263 :218–243. [ PubMed ] [ Google Scholar ]
- Lafortune, G. 2020. Respond to pandemics? Insights from two country-level indices [Online]. USA: Sustainable Development Solutions Network (SDSN). < https://www.unsdsn.org/how-much-do-we-know-about-countries-preparedness-to-respond-to-pandemics-insights-from-two-country-level-indices >.
- Larson H.J. Blocking information on COVID-19 can fuel the spread of misinformation. Nature. 2020 [ PubMed ] [ Google Scholar ]
- LePan, N. 2020. Ranked: Global Pandemic Preparedness by Country [Online]. Visual Capitalist. < https://www.visualcapitalist.com/global-pandemic-preparedness-ranked/ >.
- Litvinova M., et al. Reactive school closure weakens the network of social interactions and reduces the spread of influenza. Proc. Natl Acad. Sci. U S Am. 2019; 116 :13174. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Madhav N., et al. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd ed. The World Bank; 2017. Pandemics: Risks, Impacts, and Mitigation. [ Google Scholar ]
- Marcovitch D.H. Black’s Medical Dictionary. A & C Black Publishers Limited; 2005. [ Google Scholar ]
- Maxmen, A. 2020. How poorer countries are scrambling to prevent a coronavirus disaster [Online]. Nature, News. [Accessed]. [ PubMed ]
- Merson M.H., et al. The history and challenge of HIV prevention. Lancet. 2008; 372 :475–488. [ PubMed ] [ Google Scholar ]
- Mittal N., Medhi B. The bird flu: a new emerging pandemic threat and its pharmacological intervention. Int. J. Health Sci. 2007; 1 :277–283. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morens D.M., Fauci A.S. Emerging pandemic diseases: how we got to COVID-19. Cell. 2020; 182 :1077–1092. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morens D.M., North M., Taubenberger J.K. Eyewitness accounts of the 1510 influenza pandemic in Europe. Lancet (London, Engl.) 2010; 376 :1894–1895. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morse S.A. Contagion and chaos: disease, ecology, and national security in the era of globalization. Emerg. Infect. Dis. 2009; 15 :1881–1882. [ Google Scholar ]
- Morse S.S., Schluederberg A. Emerging viruses: the evolution of viruses and viral diseases. J. Infect. Dis. 1990; 162 :1–7. [ PubMed ] [ Google Scholar ]
- Morse S.S., et al. Prediction and prevention of the next pandemic zoonosis. Lancet. 2012; 380 :1956–1965. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- NationalAcademiesPress . Learning from SARS: Preparing for the Next Disease Outbreak: Workshop Summary. The National Academies Press; Washington, DC: 2004. [ PubMed ] [ Google Scholar ]
- NationalAcademiesPress . The Threat of Pandemic Influenza: Are We Ready? Workshop Summary. The National Academies Press; Washington, DC: 2005. [ PubMed ] [ Google Scholar ]
- Papagrigorakis, M.J., et al. DNA examination of ancient dental pulp incriminates typhoid fever as a probable cause of the Plague of Athens. [ PubMed ]
- Parkhill, J., et al. Genome sequence of Yersinia pestis, the causative agent of plague. [ PubMed ]
- Parmenter, R.R., et al. Incidence of plague associated with increased winter-spring precipitation in New Mexico. [ PubMed ]
- Parpia A.S., et al. Effects of response to 2014–2015 ebola outbreak on deaths from malaria, HIV/AIDS, and tuberculosis, West Africa. Emerg. Infect. Dis. 2016; 22 :433–441. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Parry, R.L. 2015. Travel alert after eighth camel flu death. The Times.
- Patterson Kd Fau -, Pyle G.F., Pyle G.F. The geography and mortality of the 1918 influenza pandemic. Bull. History Med. 1991; 65 :4–21. [ PubMed ] [ Google Scholar ]
- Paul W.E. Fundamental Immunology. Lippincott Williams & Wilkins; 2012. [ Google Scholar ]
- Potter C.W. A history of influenza. J. Appl. Microbiology. 2001; 91 :572–579. [ PubMed ] [ Google Scholar ]
- Robinson D.J. Review of A Pest in the Land: New World Epidemics in a Global Perspective. Am. 2004; 61 :274–275. [ Google Scholar ]
- Ross A.G.P., Crowe S.M., Tyndall M.W. Planning for the Next Global Pandemic. Int. J. Infect. Dis. 2015; 38 :89–94. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Routledge A Chronicle on the SARS Epidemic. Chin. Law & Gov. 2003; 36 :12–15. [ Google Scholar ]
- Scasciamacchia S., Fau - Serrecchia, L., et al. Plague epidemic in the Kingdom of Naples, 1656–1658. [ PMC free article ] [ PubMed ]
- Schrag S.J., Wiener P. Emerging infectious disease: what are the relative roles of ecology and evolution? Trends Ecol. Evolution. 1995; 10 :319–324. [ PubMed ] [ Google Scholar ]
- Sepkowitz K.A. AIDS—the first 20 years. N. Engl. J. Med. 2001; 344 :1764–1772. [ PubMed ] [ Google Scholar ]
- Sharp P.M., Hahn B.H. Origins of HIV and the AIDS pandemic. Cold Spring Harb. Perspect. Med. 2011; 1 :a006841. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Singh S.K., Ruzek D. Viral Hemorrhagic Fevers. 1st ed . CRC Press; 2013. [ Google Scholar ]
- Stawicki S.P., et al. The 2019-2020 novel coronavirus (severe acute respiratory syndrome coronavirus 2) pandemic: a joint american college of academic international medicine-world academic council of emergency medicine multidisciplinary COVID-19 working group consensus paper. J. Glob. Infect. Dis. 2020; 12 :47–93. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stenseth N.C., et al. Plague: past, present, and future. PLOS Med. 2008; 5 :e3. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Twigg G. Black Death: A Biological Reappraisal. Batsford Academic and Educational Press; London: 1984. [ Google Scholar ]
- UNAIDS. 2006. The impact of AIDS on people and societies. Report on the global AIDS epidemic 2006 [Online]. UNAIDS. < https://data.unaids.org/pub/globalreport/2006/2006_gr_ch04_en.pdf >.
- UNAIDS. 2010. UNAIDS Report on the global AIDS epidemic 2010 [Online]. UNAIDS. < https://www.unaids.org/globalreport/Global_report.htm >.
- UNAIDS. 2020. Global HIV & AIDS statistics—2020 fact sheet [Online]. UNAIDS. < https://www.unaids.org/en/resources/fact-sheet#:~:text=GLOBAL%20HIV%20STATISTICS&text=38.0%20million%20%5B31.6%20million%E2%80%9344.5,AIDS%2Drelated%20illnesses%20in%202019 >.
- WHO. 2004. China’s latest SARS outbreak has been contained, but biosafety concerns remain-Update 7 [Online]. World Health Organization (WHO). < https://www.who.int/csr/don/2004_05_18a/en/ >.
- WHO. 2006. Plague-Democratic Republic of the Congo [Online]. World Health Organization (WHO). < https://www.who.int/csr/don/23-july-2020-plague-drc/en/#:~:text=The%20health%20zone%20of%20Rethy,and%20an%20enlarged%20lymph%20node >.
- WHO. 2015a. Preliminary study finds that Ebola virus fragments can persist in the semen of some survivors for at least nine months [Online]. WHO Africa. < https://www.afro.who.int/news/preliminary-study-finds-ebola-virus-fragments-can-persist-semen-some-survivors-least-nine >.
- WHO. 2015b. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003 [Online]. World Health Organization (WHO). < https://www.who.int/publications/m/item/summary-of-probable-sars-cases-with-onset-of-illness-from-1-november-2002-to-31-july-2003 >.
- WHO. 2016a. Ebola (Ebola Virus Disease) [Online]. World Health Organization (WHO). < https://www.who.int/health-topics/ebola#tab=tab_1 >.
- WHO. 2016b. Ebola data and statistics: Situation summary. Latest available situation summary, 11 May 2016 [Online]. World Health Organization (WHO). < https://apps.who.int/gho/data/view.ebola-sitrep.ebola-summary-latest.%20Accessed%20on%20December%2030 >.
- WHO. 2017. Epidemic and pandemic-prone diseases: Emerging infectious disease outbreaks reported in the Eastern Mediterranean Region in 2017 [Online]. WHO | Regional Office for the Eastern Mediterranean. < http://www.emro.who.int/pandemic-epidemic-diseases/news/emerging-infectious-disease-outbreaks-reported-in-the-eastern-mediterranean-region-in-2017.html > (Accessed 02 January 2021).
- WHO. 2018. Managing epidemics [Online]. < https://www.who.int/emergencies/diseases/managing-epidemics-interactive.pdf >.
- WHO. 2020. Dengue and severe dengue [Online]. World Health Organization (WHO). < https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue >.
- WHO. 2007. WHO interim guidelines: infection prevention and control of epidemic- and pandemic-prone acute respiratory diseases in health care. [ PubMed ]
- Wikipedia. 2020a. 2015–2016 Zika virus epidemic [Online]. Wikipedia. < https://en.wikipedia.org/wiki/2015%E2%80%932016_Zika_virus_epidemic > (Accessed 22 December 2020).
- Wikipedia. 2020b. Disease [Online]. < https://en.wikipedia.org/wiki/Disease#cite_note-:1-1 .
- Wikipedia. 2020c. List of epidemics [Online]. https://en.wikipedia.org/wiki/List_of_epidemics > (Accessed 30 December, 2020).
- Zeng D., Cao Z., Neill D.B. Artificial intelligence–enabled public health surveillance—from local detection to global epidemic monitoring and control. Artif. Intell. Med. 2021:437–453. [ Google Scholar ]
- Zhou D., et al. Genetics of metabolic variations between Yersinia pestis biovars and the proposal of a new biovar, microtus. J. Bacteriol. 2004; 186 :5147. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zumla A., Hui D.S., Perlman S. Middle East respiratory syndrome. Lancet. 2015; 386 :995–1007. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Skip to Content
- Skip to Search
03 February 2021
GSK and CureVac to develop next generation mRNA COVID-19 vaccines
For media and investors only, issued: london, uk/ tübingen, germany/ boston, ma, usa.
- Companies aim to develop a multi-valent candidate vaccine to address emerging variants for pandemic and endemic use
- Development to begin immediately targeting vaccine availability in 2022, subject to regulatory approval
- GSK will also support manufacture of up to 100 million doses of CureVac’s first generation COVID-19 vaccine CVnCoV in 2021
GlaxoSmithKline plc (LSE/NYSE: GSK) and CureVac N.V. (Nasdaq: CVAC) today announced a new €150m collaboration, building on their existing relationship, to jointly develop next generation mRNA vaccines for COVID-19 with the potential for a multi-valent approach to address multiple emerging variants in one vaccine.
GSK will also support the manufacture of up to 100 million doses of CureVac’s first generation COVID-19 vaccine candidate CVnCoV in 2021.
Through this new exclusive co-development agreement, GSK and CureVac will contribute resources and expertise to research, develop, and manufacture a number of novel mRNA vaccine candidates, including multi-valent and monovalent approaches. The aim of this work is to offer broader protection against a variety of different SARS-CoV2 variants, and to enable a quick response to new variants potentially emerging in the future. The development programme will begin immediately, with the target of introducing the vaccine in 2022, subject to regulatory approval.
The increase in emerging variants with the potential to reduce the efficacy of first generation COVID-19 vaccines requires acceleration of efforts to develop vaccines against new variants to keep one step ahead of the pandemic. These next generation COVID-19 vaccines may either be used to protect people who have not been vaccinated before, or to serve as boosters in the event that COVID-19 immunity gained from an initial vaccination reduces over time. In addition, the collaboration will assess the development of novel mRNA vaccines to protect against multiple respiratory viruses, including COVID-19.
This collaboration will build on CureVac’s first generation COVID-19 vaccine candidate CVnCoV, which is currently in Phase 2b/3 clinical trial and on CureVac’s ability to optimise mRNA for a strong immune response, manufacturability, and stability at standard 2-8°C cold chain conditions for vaccines. CureVac’s platform is uniquely adapted to designing multi-valent vaccines with a balanced immune response and a low dose of mRNA.
Emma Walmsley, Chief Executive Officer, GSK, said: “We believe that next generation vaccines will be crucial in the continued fight against COVID-19. This new collaboration builds on our existing relationship with CureVac and means that together, we will combine our scientific expertise in mRNA and vaccine development to advance and accelerate the development of new COVID-19 vaccine candidates. At the same time, we will also support the production of CureVac’s first generation vaccines with the manufacture of 100 million doses in 2021.”
Franz-Werner Haas, Chief Executive Officer of CureVac , said: “We are very pleased to build on our existing relationship with GSK with a new agreement to jointly develop next generation mRNA-based vaccines, in addition to our current candidate CVnCoV. With the help of GSK’s proven vaccine expertise, we are equipping ourselves to tackle future health challenges with novel vaccines.”
As part of the new collaboration, GSK will also support manufacture of CureVac’s first-generation COVID-19 vaccine candidate CVnCoV which is currently in Phase 2b/3 trials. Using its established manufacturing network in Belgium, GSK aims to support manufacturing of up to 100 million doses of the vaccine in 2021.
Under the terms of the new collaboration agreement, GSK will be the marketing authorisation holder for the next generation vaccine, except in Switzerland, and will have exclusive rights to develop, manufacture, and commercialise the next generation COVID-19 vaccine in all countries with the exception of Germany, Austria and Switzerland. GSK will make an upfront payment of €75m and a further milestone payment of €75m, conditional on the achievement of specific milestones.
GSK is a science-led global healthcare company with a special purpose: to help people do more, feel better, live longer. For further information please visit www.gsk.com/about-us .
About CureVac
CureVac is a global biopharmaceutical company in the field of messenger RNA (mRNA) technology, with more than 20 years of expertise in developing and optimizing the versatile biological molecule for medical purposes. The principle of CureVac’s proprietary technology is the use of non-chemically modified mRNA as a data carrier to instruct the human body to produce its own proteins capable of fighting a broad range of diseases. Based on its proprietary technology, the company has built a deep clinical pipeline across the areas of prophylactic vaccines, cancer therapies, antibody therapies, and the treatment of rare diseases. CureVac had its initial public offering on the New York Nasdaq in August 2020. In January 2021 the company entered into a collaboration and services agreement with Bayer. CureVac is headquartered in Tübingen, Germany, and employs more than 500 people at its sites in Tübingen, Frankfurt, and Boston, USA. Further information can be found at www.curevac.com/ .
Cautionary statement regarding forward-looking statements
GSK cautions investors that any forward-looking statements or projections made by GSK, including those made in this announcement, are subject to risks and uncertainties that may cause actual results to differ materially from those projected. Such factors include, but are not limited to, those described under Item 3.D "Risk Factors" in the company's Annual Report on Form 20-F for 2019 and any impacts of the COVID-19 pandemic.
CureVac Forward-Looking Statements
This press release contains statements that constitute “forward looking statements” as that term is defined in the United States Private Securities Litigation Reform Act of 1995, including statements that express the opinions, expectations, beliefs, plans, objectives, assumptions or projections of CureVac (the “company”) regarding future events or future results, in contrast with statements that reflect historical facts. Examples include discussion of the potency efficacy of the company’s vaccine candidate and the company’s strategies, financing plans, growth opportunities and market growth. In some cases, you can identify such forward-looking statements by terminology such as “anticipate,” “intend,” “believe,” “estimate,” “plan,” “seek,” “project,” or “expect,” “may,” “will,” “would,” “could,” “potential,” “intend,” or “should,” the negative of these terms or similar expressions. Forward-looking statements are based on management’s current beliefs and assumptions and on information currently available to the company. However, these forward-looking statements are not a guarantee of the company’s performance, and you should not place undue reliance on such statements. Forward-looking statements are subject to many risks, uncertainties and other variable circumstances, including negative worldwide economic conditions and ongoing instability and volatility in the worldwide financial markets, ability to obtain funding, ability to conduct current and future preclinical studies and clinical trials, the timing, expense and uncertainty of regulatory approval, reliance on third parties and collaboration partners, ability to commercialize products, ability to manufacture any products, possible changes in current and proposed legislation, regulations and governmental policies, pressures from increasing competition and consolidation in the company’s industry, the effects of the COVID-19 pandemic on the company’s business and results of operations, ability to manage growth, reliance on key personnel, reliance on intellectual property protection, ability to provide for patient safety, and fluctuations of operating results due to the effect of exchange rates or other factors. Such risks and uncertainties may cause the statements to be inaccurate and readers are cautioned not to place undue reliance on such statements. Many of these risks are outside of the company’s control and could cause its actual results to differ materially from those it thought would occur. The forward-looking statements included in this press release are made only as of the date hereof. The company does not undertake, and specifically declines, any obligation to update any such statements or to publicly announce the results of any revisions to any such statements to reflect future events or developments, except as required by law.
For further information, please reference the company’s reports and documents filed with the U.S. Securities and Exchange Commission (SEC). You may get these documents by visiting EDGAR on the SEC website at www.sec.gov .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 20 November 2023
Outlook of pandemic preparedness in a post-COVID-19 world
- B. Adam Williams ORCID: orcid.org/0009-0001-1558-9562 1 ,
- Charles H. Jones ORCID: orcid.org/0009-0004-0368-6463 1 ,
- Verna Welch 1 &
- Jane M. True 1
npj Vaccines volume 8 , Article number: 178 ( 2023 ) Cite this article
13k Accesses
13 Citations
38 Altmetric
Metrics details
- Public health
- Viral infection
The COVID-19 pandemic was met with rapid, unprecedented global collaboration and action. Even still, the public health, societal, and economic impact may be felt for years to come. The risk of another pandemic occurring in the next few decades is ever-present and potentially increasing due to trends such as urbanization and climate change. While it is difficult to predict the next pandemic pathogen threat, making reasonable assumptions today and evaluating prior efforts to plan for and respond to disease outbreaks and pandemics may enable a more proactive, effective response in the future. Lessons from the COVID-19 response and pandemic influenza preparedness underscore the importance of strengthening surveillance systems, investing in early-stage research on pandemic pathogens and development of platform technologies, and diversifying response plans across a range of tactics to enable earlier access to safe and effective interventions in the next pandemic. Further, sustaining the robust vaccine manufacturing capacity built because of COVID-19 will keep it ready for rapid response in the future. These actions will not be successful without improved global coordination and collaboration. Everyone, including the biopharmaceutical industry, has a role to play in pandemic preparedness, and working together will ensure that the most lives are saved in the next pandemic.
Similar content being viewed by others

Promoting versatile vaccine development for emerging pandemics

Looking beyond COVID-19 vaccine phase 3 trials

The evolution and future of influenza pandemic preparedness
Introduction.
The substantial public health and societal costs of the COVID-19 pandemic are wide-ranging and have been observed across the world. As of August 2023, COVID-19 has infected over 770 million people and resulted in over 6.9 million reported deaths globally 1 , although the World Health Organization (WHO) estimates mortality could be much higher based on global excess mortality 2 . It has contributed to a reduction in global life expectancy; in the United States alone, life expectancy fell by an estimated 1.8 years, with a disproportionate drop among racial minorities. Many of those infected with COVID-19 still suffer from long-term COVID, with symptoms remaining months after the initial illness 3 .
More broadly, COVID-19 led to substantial indirect health effects. Mental health declined worldwide, with a 25% increase in the global prevalence of anxiety and depression in the first year of the pandemic 4 . Disruptions to routine immunization programs in at least 68 countries affected more than 80 million children worldwide, likely resulting in higher rates of vaccine-preventable diseases 5 , 6 . Delays and avoidance of medical care contributed to more severe observed health outcomes; for example, delayed cancer screening and treatment have resulted in increased cancer mortality rates 7 . Beyond direct and indirect health effects, the pandemic challenged conventions around how people learn, work, and play. For example, delivering quality education virtually posed a challenge in some parts of the world, while in other parts of the world, formal education stopped altogether, setting back learning and development for an entire generation of children 8 , 9 , 10 . The negative health and societal impacts of COVID-19 may be felt for years to come. Unfortunately, many of these statistics and estimates will likely increase in magnitude with post-pandemic analyses, and as of the date of this publication, the entirety and extent of the pandemic’s impact are still not known.
The resulting global economic impacts of the COVID-19 pandemic were also unprecedented and may continue for years. Across countries, gross domestic product (GDP) fell by 2–4% in 2020, and the US had the worst contraction in national GDP since World War II 11 , 12 . This decline pales in comparison to the global economic losses extending through to 2024 which are estimated to be $13.8 trillion 13 . The effect on productivity and livelihood left governments around the world juggling priorities to quickly implement response initiatives.
Despite major economic shocks, the economic burden of the pandemic may have been worse if not for at least some prior spending on pandemic preparedness and response tactics. For example, the US National Institutes of Health (NIH) spent $17.2 billion in vaccine technology research—more than $500 million toward mRNA, virus-like particle, and nanoparticle vaccines—before 2020 with specific attention to diseases with pandemic potential 14 . These early initiatives set some of the foundational work on which new COVID-19 vaccine candidates were based. However, even with these investments, a report by a WHO-established panel found that on the whole, investment in pandemic preparedness before COVID-19 was inadequate, prompting efforts to revisit how the world prepares for the next pandemic, an ongoing risk 15 .
The risk of another pandemic
Smaller-scale outbreaks or large-scale pandemics related to emerging infectious diseases have increased over the past century, and are projected to do so over time 16 . Evidence suggests the probability of another pandemic occurring within one’s lifetime is roughly 17% and may even grow to 44% within the next couple decades 17 . This means that in any given year, the chance of another pandemic occurring is over 2% 17 . Yet, it is difficult to determine exactly what pathogen will cause the next pandemic.
Most emerging infectious diseases with pandemic potential are initially transmitted from animals to humans—zoonotic spillover—and those that have or evolve the ability to move from human to human have the potential to become dangerous 18 . In fact, zoonotic spillover has likely been the trigger for most of the viral pandemics in the 20th century 19 . Meanwhile, societal trends are increasing the likelihood of zoonotic spillover. Urbanization and habitat destruction are placing humans and animals in closer contact, giving pathogens more opportunities to migrate to humans 20 . Climate change is also altering animal habitats and forcing them to migrate to new territories, causing many species to meet for the first time 20 . Pathogens may travel between several animal species before reaching humans; therefore, novel species interactions driven by climate change also increase the risk of zoonotic spillover 20 .
Under the right circumstances, a newly emerged pathogen can grow from a disease outbreak to pandemic proportions. The balance of a pathogen’s characteristics, including transmissibility, case fatality rate, replication rate, and mutability—among other factors—will influence the likelihood of becoming a widespread pandemic 21 . For example, pathogens with a higher case fatality rate and lower transmissibility, combined with pronounced symptomology (e.g., Ebola), are more likely to be more limited in geographic footprint. Meanwhile, SARS-CoV-2 had comparably moderate case fatality, and higher transmissibility through airborne transmission and asymptomatic spread, which led to an exponential growth in the number of infections. Additionally, societal trends that increase connectiveness between countries, like globalization and travel, can further accelerate the spread of high-risk pathogens 20 . Lastly, high pathogen mutation rates—as seen in particular with RNA viruses—also contribute to a greater risk because random mutations are a source of potential adaptations that benefit the virus. Altogether, given their high mutation rates and transmissibility, evidence suggests the next pandemic will likely be a respiratory RNA virus like a coronavirus or influenza (flu) virus, though the threat from other pathogen types remains 22 .
This perspective discusses the current state of preparations for the next pandemic considering key lessons learned from the COVID-19 response and pandemic influenza preparedness, with a particular focus on vaccines. While it is difficult to predict the type and magnitude of the next pandemic pathogen threat, making reasonable assumptions today may enable a more effective response in the future. As with COVID-19, the world may once again rely heavily on non-pharmaceutical interventions (NPIs) amid a disease outbreak, and it may need to deploy stockpiled medical countermeasures—or quickly develop and manufacture new interventions. Observations about past pandemic response and preparedness can guide proactive actions now, which may increase the world’s success in preventing or taming the next pandemic—an ongoing and potentially increasing threat.
What happened during COVID-19?
Although the health and economic impact of COVID-19 was immense, it could have been far worse had it not been for modern technology (Fig. 1 ). Historically, pandemics have, at times, reached extraordinary scales; 200 million people died during the bubonic plague between 1346 and 1353, and up to 50 million people died during the 1918 influenza pandemic 23 . While these pathogens differ from SARS-CoV-2 in virulence and transmissibility, they illustrate the potential scale of what can happen without the rapid availability of effective treatments and vaccines.
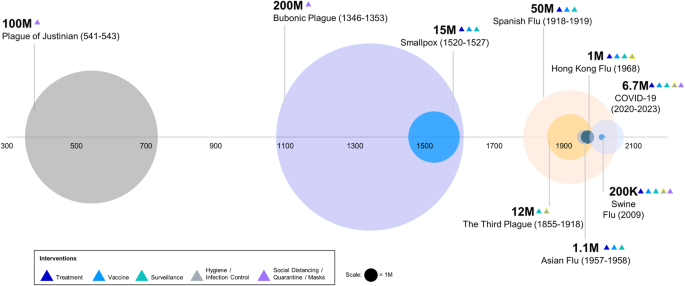
Death tolls of major epidemics or pandemics in the last millennia are signified by circle size. Different interventions (triangles) were used during each pandemic, and advancements in intervention strategies likely reduced death tolls significantly, especially during COVID-19.
Similar to some historic epidemics and pandemics, targeted vaccines and therapeutics were not available during the early days of the COVID-19 pandemic 24 . As such, NPIs including lockdowns, social-distancing measures, and mask mandates became priority measures in the early response. NPI implementation and severity differed across the globe but generally included public information campaigns, school and workplace closures, bans on public events, domestic and international travel restrictions, quarantines, and stay-at-home orders 25 . These interventions also played a critical role in reducing disease spread and preserving hospital capacity 25 , 26 , 27 .
In addition to NPIs, the development of new medical countermeasures, including vaccines, was critical to the COVID-19 pandemic response. Countries and multilateral organizations quickly took varying approaches to funding vaccine development, manufacturing, and procurement. Negotiations among manufacturers, governments, and multilaterals ensued even before COVID-19 vaccines were known to be successful. By mid-2020, the US government’s Operation Warp Speed had contracted numerous manufacturers to support research, development, and product procurement across a variety of technologies 28 . Similarly, the Coalition for Epidemic Preparedness Innovations (CEPI) invested in a diverse portfolio of vaccine technologies. The European Commission secured a number of advanced agreements for specific technologies, but it faced challenges to do so quickly given representation across 27 sovereign states with different budgets and risk tolerances 29 . Altogether, governments and multilateral organizations spent billions on medical countermeasures, though early investments represented just a fraction of spending on the COVID-19 pandemic. Indeed, government spending to shore up the US economy exceeded $5 trillion while vaccines and treatments made up about 2% of total spending 30 .
Fortunately, safe, and effective vaccines and treatments were quickly developed and given emergency authorization to begin addressing the burden of COVID-19. The first vaccines were developed in approximately nine months, and to date, more than 13 billion COVID-19 vaccines have been administered 1 , 31 . The speed of vaccine availability was thanks in-part to flexible strategies used across sectors, including the issuance of emergency approvals by regulatory authorities. For example, the UK’s Medicines and Healthcare products Regulatory Agency (MHRA)—the first stringent regulatory authority to issue an emergency approval of a COVID-19 vaccine—relied on a rolling review process, allowing for the evaluation of clinical data as it became available and thus reducing the time to vaccine roll-out 32 . In fact, this pandemic harbored the fastest response, regulatory emergency authorization, and rollout of a vaccine in history.
Thankfully, the rapid introduction of vaccines and treatments helped to reduce morbidity and mortality of SARS-CoV-2, while helping to alleviate costs. Estimates suggest that vaccinations prevented over 14 million deaths in 185 countries and territories just in the first year of deployment 33 . A recent study conducted in the US suggested that without COVID-19 vaccines, between December 2020 to November 2022, there would have been nearly 120 million more COVID-19 infections, 18.5 million hospitalizations, and 3.2 million deaths 34 . The recent development of antivirals and antibody treatments for use early after symptom onset and for mild to moderate COVID-19 have also begun to further reduce hospitalizations and deaths 34 , 35 , 36 .
Beyond reductions in infections and deaths, research suggests vaccination contributed to major economic benefits. Vaccination may have averted $1.15 trillion in medical costs in the US alone. A local study based in New York City estimated that every $1 invested in COVID-19 vaccine programs yielded a savings of approximately $10 in direct and indirect healthcare costs 37 . The benefits of vaccination continue to progress as ongoing surveillance and speedy manufacturing support the development of updated vaccines for evolving variants of SARS-CoV-2 38 .
While COVID-19 vaccines supported health and economic gains in some places, the pandemic also highlighted the need for strategies to improve rapid, equitable access to vaccines across the world. Higher-income countries had more immediate access to a range of vaccine technologies while lower-income countries faced delays due to additional challenges in financing and operations. The global initiative COVAX (COVID-19 Vaccines Global Access) was created in 2020 to address these issues, striving to provide rapid and equitable access to COVID-19 vaccines and treatments 39 . While admirable and justified, such a goal was also incredibly ambitious. As of the end of 2022, though COVAX had shipped over 1 billion vaccines to 144 countries, only about 22% of people in low-income countries had received at least one COVID-19 vaccine dose 40 , 41 .
Challenges to vaccine equity in-part underscored risks associated with relying more heavily on single-source suppliers. Despite COVAX’s goal of investments across a range of vaccine technologies, nearly three-quarters of COVAX’s initial supplies were from one supplier in India. When a massive COVID-19 wave hit India in March 2021, vaccine exports were banned, leaving COVAX short 90 million expected doses 42 . Similarly, Australia had limited access to vaccine doses throughout the first half of 2021, having initially counted on the success of a narrow range of vaccine technologies 43 . At-risk investments across multiple technologies and manufacturers aimed to account for significant uncertainties on if, or when, new vaccines would be available.
In sum, COVID-19 represented a novel global challenge, and governments and organizations took various pathways in their responses, including vaccine development and deployment, but extended to a range of other interventions (e.g., use of NPIs or development of new treatments). These experiences can translate into lessons learned and guide preparations for the next pandemic, but first, it is valuable to assess the state of pandemic preparedness before COVID-19.
The focus on influenza
Until the COVID-19 pandemic caused by the virus SARS-CoV-2, influenza was predicted to be the most likely pathogen to cause the next pandemic due to its high rate of mutation and transmission. In fact, many past pandemics were flu-related; the 1918 influenza pandemic was caused by an H1N1 virus, and smaller-scale influenza pandemics occurred in 1957, 1968, and 2009. Additionally, the World Bank had previously estimated that a moderate or severe flu pandemic could cost $570 billion annually (or 0.7% of global income) highlighting the ongoing threat to global health and economies 44 .
Prior to the COVID-19 pandemic, governments and public health organizations allocated billions of dollars each year for pandemic preparedness and medical countermeasures. Given the potential societal impact of pandemics, preparations for another flu pandemic have been underway for decades, including a focus on stockpiling vaccine products and therapeutics, forging advanced purchase agreements (APAs), research and development toward novel vaccine technologies, and strengthening manufacturing capacity.
Strategic stockpiles are a stopgap in a health emergency, offering critical medical countermeasures when market supplies may be short. The US Biomedical Advanced Research and Development Authority’s (BARDA) Pandemic Influenza Vaccine Stockpile Program stockpiles antivirals and pre-pandemic flu vaccines using egg- and cell-based technologies, as well as adjuvants 45 . BARDA has for example accumulated hundreds of millions of prepandemic H5N1 bulk vaccine doses, with multiple other countries having stockpiled H5N1 vaccines 45 . Stockpiles also extend beyond influenza; Gavi in partnership with UNICEF has routinely stockpiled Ebola vaccines 46 . Another example includes the stockpiling of smallpox vaccines, which were quickly distributed amid a 2022 outbreak of monkeypox 47 . If a pathogen with an outbreak or pandemic potential emerges that closely aligns with a stockpile, it can be quickly distributed to protect the population or provide some level of protection before more tailored interventions are developed if they are necessary. For that reason, stockpiles are one of a set of tools used for pandemic preparedness. One of the limitations of stockpiling is the short shelf life of some products leading to significant financial and material wastage. An additional consideration is that maintaining stockpiles requires stringent inventory management and replenishment. The rise of new SARS-CoV-2 variants every year demonstrates the speed at which pathogen evolution can occur, potentially making stockpiles outdated.
In the case where the next pathogen to cause an outbreak or pandemic is not adequately addressed with stockpiled products, new or updated vaccines will need to be quickly manufactured as was the case with the 2009 H1N1 pandemic. A limiting factor is that some current production processes for influenza vaccines require several time-consuming steps. As per current egg-based manufacturing practices, viral flu vaccines are developed by isolating a new virus strain, growing it in a seed stock, propagating it, and inactivating and purifying it—a process that may take 5–6 months—all before distribution 48 , 49 . Even still, as the 2009 pandemic showed, the H1N1 influenza virus did not grow well in egg-based medium, the most widely used influenza vaccine technology at the time, contributing to further delays 50 , 51 .
Given these limitations, research and development has focused on vaccine technology innovation for influenza. A more reliable vaccine technology would lessen the health and economic impact of a pandemic by virtue of an earlier, potentially more effective intervention to slow the spread and health burden of the virus. For example, BARDA supported the development of recombinant influenza vaccines with the goal of reducing the time to vaccine availability in the event of an influenza pandemic, while investments in adjuvants aimed to allow for lower antigen dosing and therefore potentially more supply 52 , 53 , 54 . Recombinant technology and adjuvants were leveraged amid the range of COVID-19 vaccine candidates that arose after the pandemic declaration 55 . In the future, having both existing stockpiles and a fast, reliable—but also flexible—vaccine development process would ensure a more comprehensive level of protection in the event of another pandemic.
Pandemic preparations also extend to the manufacturing and distribution of vaccines. Global manufacturing capacity at any point in time is finite, so it is important to create plans for adequate and thoughtful production and distribution. As previously mentioned, governments and organizations have forged APAs with vaccine manufacturers to prioritize available manufacturing capacity and ensure access once vaccines are available. APAs are agreements to purchase products not yet available, or reserve manufacturing capacity in the case of a disease outbreak, even if the products or capacity are no longer needed by the time they are produced. During the 2009 H1N1 pandemic, APAs were in place to ensure access to products once a pandemic was declared, while further sustaining manufacturing capacity for emergency use before the pandemic phase 56 .
APAs mitigate the risk manufacturers take on when they produce a new vaccine, increasing the likelihood that doses will be available early in a pandemic 56 . Unfortunately, manufacturers may still be limited by slow vaccine production processes. Additionally, APAs may not adequately address issues around vaccine equity. The reservation of supplies by high-income countries with APAs during the 2009 H1N1 pandemic limited initial vaccine orders for lower-income countries and countries without APAs 56 . These limitations underscore the need to reform the design of APAs to prioritize equitable access in a timely manner and invest in vaccine discovery platforms for more rapid vaccine manufacturing.
As an alternative to relying on de novo vaccine development and manufacturing, governments and multilateral organizations have explored the development of “universal” vaccines, though these technologies may be years away. A universal influenza vaccine is one that provides at least partial cross-protection against all influenza strains and variants, even ones that have yet to emerge, thereby potentially preventing severe disease and protecting health systems from being overwhelmed before more strain-specific vaccines become available. Vaccine candidates may target conserved epitopes of influenza viruses that may theoretically be able to provide universal protection against both seasonal and pandemic flu strains. Such a strategy could effectively prevent or mitigate influenza-caused pandemics. To date, no single approach has been successful in late-stage clinical trials. Clinical data for available universal vaccine candidates suggest that these vaccines may not achieve the levels of efficacy needed to control an influenza pandemic 49 . While pursuits toward a universal vaccine continue, a variety of pandemic preparedness and response tactics for influenza, as previously highlighted, must be considered.
Stockpiling, rapid manufacturing through new technologies, and APAs exemplify some of the central approaches to pandemic preparedness today, beyond conducting research and developing pandemic-focused products. These strategies have their individual advantages and limitations, but with robust investment and thoughtful planning, can be improved and leveraged in the next pandemic. Because pandemic preparedness largely focused on influenza before the COVID-19 pandemic, many available interventions were not relevant to the COVID-19 response. Moving forward, broader pathogen-inclusive thinking is warranted when considering relevant preparedness tactics, including stockpiled products and vaccine development and manufacturing technologies. Recognizing that a proactive approach will benefit future populations, it is essential to use lessons learned focused on influenza in the past—as well as the COVID-19 pandemic response—to enhance strategies for pandemic preparedness.
Lessons from COVID-19 and pandemic influenza
Pandemic preparedness requires comprehensive thinking, from the earliest stages of research to enable effective development of countermeasures, to monitoring pandemic threats, and to coordination of pandemic response efforts in real-time. The time for action is during non-pandemic times, enabling a more effective response in an emergency. While this article highlights lessons specific to pandemic preparedness, many of the recommendations may also apply to local, regional, and global responses to other health emergencies, from smaller-scale disease outbreaks and biosecurity threats to weather-related catastrophes (Table 1 ).
Lesson #1: Prioritize early-stage R&D and platform technologies
Early-stage research and platform technology approaches enable earlier access to vaccines and treatments. The biggest turning point during the COVID-19 crisis was the deployment of vaccines; and vaccines using novel platform technologies, like mRNA and adenovirus platforms, were among the fastest to be developed and authorized. Technology platforms are frameworks that allow the development of new vaccines without customizing the process, allowing for rapid production of multiple vaccines from a single system. The speed and flexibility of vaccine platforms contributed to reducing overall morbidity and mortality from COVID-19, which eventually lowered reliance on NPIs to slow disease spread 35 , 36 . The earlier a vaccine is made available in a pandemic, likely the more favorable the outcome 33 .
Thus, world leaders have set ambitious goals to respond more swiftly to the next pandemic. The US set goals to design, test, and review a new vaccine just 100 days after a pandemic declaration and to produce enough vaccines for the US and the world in 130 and 200 days, respectively 57 . Similarly, both CEPI and the G7 have initiatives that aim for new vaccines to be ready for authorization within 100 days after recognition of a pandemic pathogen 58 , 59 . Such speeds will require streamlining existing processes, like increasing collaboration and information sharing between government and industry and faster approval processes.
Crucially, the mRNA vaccines developed to combat SARS-CoV-2 were not an overnight success. Development of the COVID-19 mRNA vaccines was enabled by decades of research following the initial production of synthetic mRNA in the 1980s 60 , 61 . Equally important, advancements in carrier lipid nanoparticles enabled the delivery of mRNA to cells 62 . mRNA’s use as a therapeutic has been examined since the 1990s but was finally demonstrated at a global scale during the COVID-19 pandemic 61 . Importantly, research conducted by the US National Institute of Allergy and Infectious Diseases (NIAID) on both severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) revealed the spike protein as a target for vaccine development, allowing for rapid production of mRNA vaccines against SARS-CoV-2 49 , 58 . Further research discovered that the 2 P stabilization of the spike protein was a modification that helps to stabilize the S protein in its prefusion form, which is a target for the immune response and therefore crucial for vaccine efficacy 63 . The fundamental role of basic research cannot be overstated. The success of the COVID-19 mRNA vaccines relied on years of progress in basic and translational research on influenza and previous coronaviruses 60 . Therefore, continuing to invest in basic research, as well as flexible vaccine development platforms, could help to speed response to the next pandemic 58 , 64 .
Basic and translational research must continue following COVID-19 because the next pandemic pathogen may be even harder to target than SARS-CoV-2 60 . Ongoing research should be informed by surveillance systems that track pathogens with the potential to cause an outbreak or pandemic. Understanding vaccine targets and correlates of protection of these pathogens and generating data may provide the solid foundation of science needed for rapid vaccine development. This process requires continuous funding, yet typically, there are valleys in funding that follow high peaks during a disease outbreak or pandemic. This was highlighted by the lack of sustained, continuous investment in vaccine research following the SARS outbreak in the early 2000s, which affected the development of new vaccine technologies 49 . Commitments to maintain funding for vaccine research from both public and private funds—and an acceptance of funding research with a higher risk of failure, given difficult-to-target pathogens—may ensure rapid development of a vaccine when a new pathogen emerges.
Some initiatives are already committed to funding research with the aim of advancing our understanding of various virus families and developing effective vaccines. NIAID, for instance, focuses on studying potential pandemic-causing viruses, and CEPI is aiming to develop a comprehensive library of prototype vaccines against a range of viral pathogen families 65 , 66 , 67 . While these efforts could be complicated and slow given the range of pathogens of outbreak and pandemic potential, early-stage R&D initiatives such as these may provide enough learnings to jump-start future pandemic responses.
Further, agile vaccine technology will be critical for the response to any future pandemic due to the unpredictability of emerging pathogens. Existing mRNA vaccine platforms are highly suitable for a rapid response to an emerging pathogen given their proven manufacturing agility and scale, as demonstrated during the COVID-19 pandemic 68 . Typically, manufacturing can commence shortly after the antigen genetic sequence has been ascertained. This could result in both timely and effective responses to emerging threats from influenza, coronaviruses, or other pathogens with pandemic potential. Alongside an adaptable vaccine platform, research should also focus on addressing limitations in vaccine storage and distribution. For current mRNA vaccines, the requirement to keep doses frozen is a significant barrier to global distribution 69 . There exist goals to develop a more “ideal” vaccine, one which has a longer shelf life, extended durability, minimal dosing schedule, and wider breadth of coverage 70 .
Currently, efforts are also underway to apply mRNA technology to influenza following the proven success against SARS-CoV-2 71 , 72 , 73 . But this technology may also hold promise for other endemic pathogens for which vaccines have been difficult to develop or pathogens with significant outbreak or pandemic potential 74 . Efforts are needed to steer research funding toward a better understanding of pandemic pathogens and vaccine targets; projects such as the WHO’s recently launched process to update their list of pathogens with pandemic potential may begin to accomplish this 75 .
The benefit of vaccine technologies such as mRNA relies on their “plug and play” possibilities to allow for a flexible response in the next pandemic, enabled by research identifying the most effective vaccine targets for a range of pandemic pathogens. Unlocking the potential of platform technologies will require collaboration across governments, multilaterals, academia, and industry to prioritize it. In the future, mRNA vaccine technology will be an important tool among a suite of options to respond to pandemics, one that has already been proven as an effective platform on a global scale.
Lesson #2: Bolster pandemic pathogen intelligence
Detecting novel pathogens as they arise allows for the earliest possible response, so surveillance systems should be expanded and more extensively leveraged to better detect and respond to infectious disease outbreaks in real time. Sentinel surveillance systems for global influenza—e.g., the Global Influenza Surveillance and Response System (GISRS)—were leveraged during the COVID-19 pandemic and could continue to play an important role for SARS-CoV-2 and future pathogens. In partnership with WHO, GISRS was systematically expanded to include RSV in 2015 and SARS-CoV-2 in 2020, and vitally acting as early testing centers for SARS-CoV-2 76 . Strengthening systems like GISRS to include even more pathogens of outbreak or pandemic potential can improve future surveillance efforts. In parallel, there is a need to expand the number of surveillance sites globally; more than 70 countries still lack WHO-designated influenza surveillance centers, let alone broader systems 77 .
Excluding systems for West Nile virus and other arboviruses, no formal system exists to actively monitor a broad range of priority emerging and re-emerging infectious diseases, both in animals and humans 78 , 79 . For respiratory diseases, using existing influenza surveillance systems to monitor outliers of influenza-like illness (ILI) more extensively, which may encompass a range of pathogens, could also lead to earlier outbreak detection. One study speculated that if such a robust surveillance system were in use, the spread of COVID-19 could have been detected more than 13 weeks before the first reported infection peaks 80 . Earlier detection of SARS-CoV-2 could have led to an earlier response, potentially limiting its health and economic impact.
An expanded global surveillance system would also require investment in laboratory infrastructure, diagnostic capabilities, and workforce development at a local-, national-, and international level. Projects such as the Seattle Flu Study and the US Agency for International Development’s PREDICT may provide a roadmap. The Seattle Flu Study, launched in 2018 by the Brotman Baty Institute, University of Washington School of Medicine, Seattle Children’s Hospital, and the Fred Hutchinson Cancer Research Center, is a city-wide platform for the surveillance of respiratory pathogens, as well as pilot interventions 81 . This platform was used to identify the first documented U.S. case of COVID-19 community transmission in February 2020. PREDICT, which operated across more than 30 countries for a decade, worked from the ground up to strengthen surveillance for both known and newly discovered viral threats. Given lessons from COVID-19, it may also be time to experiment with new models of building surveillance systems at the local level 82 . Community-based surveillance, particularly in low- and middle-income countries, integrated with national and global surveillance hubs, such as WHO’s newly launched Hub for Pandemic and Epidemic Intelligence, could help drive earlier detection of emerging infectious diseases 83 , 84 .
With information on pathogens coming from surveillance systems, major public health authorities have evolved strategies to constantly evaluate pandemic risk. The CDC’s Influenza Risk Assessment Tool (IRAT) and WHO’s Tool for Influenza Pandemic Risk Assessment (TIPRA) evaluate the risk of viruses not currently circulating in humans and help to prioritize investments in pandemic preparedness 85 , 86 . For example, changes in the viral properties of a particular flu strain may signal the need to assess this strain for pandemic potential 86 . These tools may guide research and surveillance, while also serving as a forum to share information between scientists, public health authorities, and other stakeholders. They may also facilitate the development of pre-pandemic vaccines; this happened following the emergence of the pandemic flu strain H7N9 in 2013 48 . As in this example, disease intelligence must be translated into action.
Furthermore, to effectively respond to newly detected disease outbreaks, sharing pathogen data is essential. Originally established in 2011, the WHO’s Pandemic Influenza Preparedness (PIP) Framework allows for pathogen samples to be shared with companies to support vaccine development. In exchange, manufacturers agree to approaches that increase access to pandemic vaccines, thereby increasing equity in the event of a pandemic 87 . Efforts like these lay the groundwork for data sharing in a future pandemic, but must not require additional negotiation in the event of a crisis, leading to delays in the development of medical countermeasures. For example, varied national interpretation of the Nagoya Protocol—a supplemental agreement to the Convention on Biological Diversity (CBD) that came into effect in 2014—has led to delays in sharing virus samples and subsequent manufacturing for seasonal influenza vaccines 88 . During COVID-19, China’s sequencing and sharing of the SARS-CoV-2 genome just days after identifying it was pivotal to successful vaccine development 89 . Continuous genetic sequencing of the circulating virus then allowed the detection of variants as they emerged 90 . Sequencing combined with surveillance may uncover the next SARS-CoV-2 variant or novel pathogen before it escalates, as long as frameworks are in place to rapidly disperse this information to the world.
On top of detection and assessment, an optimal disease intelligence system would seek to predict the next pathogen with pandemic potential. Vast amounts of existing data can be used to inform decision-making on pandemic policy and response through, for example, predictive modeling 91 . Other efforts are underway to use artificial intelligence to predict the next pathogen spillover event 92 . There is an opportunity to test new approaches to predict emerging pathogens using a range of data sources while ensuring surveillance systems focus on threats of respiratory pathogens 93 . Above all, sharing disease intelligence and data—quickly, in the event of a disease outbreak—can speed response to the next pandemic.
Lastly, it is pertinent to assess how to ensure prompt reactions when surveillance systems ring the alarm. In January 2020, the WHO sounded the pandemic alarm for COVID-19, yet few countries responded immediately 94 . Many of the calls to action by WHO were ignored, such as suggestions to quickly begin testing and social distancing 95 , 96 . These delays occurred for many reasons and varied from country to country. Some governments exercised caution to not disrupt their people’s livelihood and economy, and others lacked an understanding of the pandemic signifier itself 94 .
One suggested approach to kick-starting earlier vaccine development is to have a gradient of warnings that separate dangerous pandemics from more manageable outbreaks. This system, akin to the early warning systems used in healthcare and weather-related scenarios 97 , 98 , 99 , 100 , could be employed for pandemic preparedness. For instance, in healthcare settings, an artificial intelligence platform could help prioritize patients based on their medical needs, effectively managing resources during triage situations 100 . Similarly, a gradient-based warning system for pandemics could initiate appropriate responses at different levels of threat, with each level tied to specific actions. An early warning or Level 1 may involve increased surveillance and information sharing, while higher levels could trigger more drastic measures like regional shutdowns or global travel restrictions. Low-grade alarms may also result in more active information sharing by governments since an innocuous signal would diminish fears of causing panic and disrupting economies 94 . However, the success of such a system hinges on complete adherence to the rules it prescribes. An incomplete application could potentially lead to inefficiencies or confusion, but despite this, even partial application of these systems could prompt earlier responses and slow down the spread of a pandemic.
Undeniably, the evolution of disease surveillance and intelligence systems is not simple. It requires major investment and coordination across global-, national-, and local levels. The inherent complexity requires cooperation across borders, and strong leadership from global health actors given the need to quickly act and share intelligence globally. Strengthening leadership and funding at the global level may help with coordination, but countries must also commit to sustained cooperation in the short- and long-term 15 .
Lesson #3: Optimize and de-risk earlier pandemic interventions
NPIs saved lives but are not without limitations and consequences. Persistent long-term reliance on NPIs can be challenging because people grow tired and apathetic toward them 101 . Another limitation is that there may not be, or necessarily should be, a universal strategy for NPIs. Differences in NPI timing, intensity, and adherence showed varying levels of success, demonstrating the importance of geographically specific and informed NPI policies 102 . Research from countries that imposed lockdowns showed that while NPIs were very effective at controlling spread, they resulted in significant economic, social, and health costs 26 , 102 , 103 . Some consequences were clearly visible, like increasing unemployment rates from business and school closures and the spike in non-COVID-19 deaths due to the unavailability or avoidance of medical care 7 , 26 . Others, like the effect of social distancing on the mental health of children and adolescents, continue to be difficult to measure.
Beyond NPIs, early action should aim to leverage all available interventions as soon as possible in pandemic response, which may require pre-planning strategies and stockpiling a broad range of essential supplies. While leaders were encouraging social distancing early during the COVID-19 pandemic, US hospitals were already reporting shortages in basic supplies and essential medicines 104 . Shortages were amplified by supply chain bottlenecks, which limited access to many basic supplies, including personal protective equipment (PPE) for frontline hospital staff 104 . The shortage of facilities and pharmaceutical glass, especially Type I glass vials used for vaccines, also strained fill-finish capacity 105 . The existing fill-finish capacity shortages were further intensified by the pandemic due to a shift from vials to syringes and cartridges, increasing the demand for syringe capacity 106 . In response, companies reprioritized their manufacturing networks to ensure adequate production of supplies such as sterile injectables and PPE. In preparation for the next pandemic, several improvements can be made to ensure adequate supplies of essential products for healthcare systems. Governments and health systems may pre-plan access to essential medicines, hospital supplies, and treatments in anticipation of growing needs. They may also discourage the use of medical supplies, like PPE, in nonmedical settings and redirect those supplies to the most overburdened areas 104 .
Beyond targeted medical countermeasures, NPIs and emergency supplies represent the need to think broadly about what is needed to respond most effectively in the earliest days of the next outbreak or pandemic. NPIs will continue to be an early mainstay of pandemic response, and research has suggested interventions such as physical distancing can be cost-effective 107 . Additional research may inform the most timely and locally acceptable ways to roll out NPIs in the future. Furthermore, scenario planning may help pre-plan NPI strategies, as well as contents of strategic stockpiles moving forward, employing lessons learned from COVID-19.
These actions along with NPIs may significantly curb the spread of a pandemic virus, but ultimately, the earlier availability of medical countermeasures like vaccines and treatments is needed. In the time before tailor-made solutions are available, governments may utilize all available “off the shelf” solutions, including stockpiled products, to blunt the impact of disease outbreaks. WHO, for example, recommends the stockpiling of influenza antiviral therapeutics to reduce mortality in a pandemic 87 .
The response to COVID-19 required a rapid end-to-end response, which may again be the case in the next outbreak or pandemic. COVID-19 demonstrated the importance of diverse interventions—including NPIs and medical countermeasures—across a range of preparedness tactics, manufacturers, and product technologies to help mitigate risks. While it is impossible to predict the efficacy of any single intervention in the next pandemic, planning to employ a range of responses can guard against the risk any single intervention will not work or be available in an emergency.
Lesson #4: Sustain and leverage manufacturing capacity
New vaccines rely on manufacturers to make them. Adequate vaccine manufacturing capacity—scalable and aimed at rapid deployment—is vital. At the start of the COVID-19 pandemic, early surge capacity was inadequate to meet demand, and prior research had already predicted this would be the case 108 . But since 2020, manufacturers have scaled up to unprecedented capacity. The International Federation of Pharmaceutical Manufacturers and Associations (IFPMA) estimated that worldwide vaccine manufacturing capacity would reach 12.5 billion by the end of 2021 109 . More recent data suggests this number will reach 20 billion by the end of 2022 110 .
Momentum is growing to create additional end-to-end vaccine manufacturing capacity in low- and middle-income countries 111 . Local manufacturing seeks to overcome barriers around unequal vaccine distribution and trade restrictions experienced during the COVID-19 pandemic. The largest barriers for new manufacturers appear to be cost and demand. Manufacturers building new facilities may need to price vaccines higher than global competitors to cover high start-up costs, and institutional buyers may need to be prepared to absorb the premium despite limited financing 112 . Furthermore, the sustainability of those facilities is directly tied to demand for vaccine production—if demand is limited, local production will be threatened. This has been the case for manufacturing COVID-19 vaccines in South Africa. Despite technology transfer to manufacturers for locally produced vaccines, health authorities reported limited purchasing by African countries given the availability of free doses elsewhere 113 .
One potential solution could be found with international organizations helping to guarantee demand for vaccines to support investments into new manufacturing. For example, the Pneumococcal Advance Market Commitment (AMC) has helped ensure access to pneumococcal vaccines in developing countries by guaranteeing a market for vaccines before development 114 . Another potential solution is to produce a range of routine immunizations beyond pandemic vaccines 112 . There are several vaccine markets that currently have high demand but a low number of suppliers, such as measles, rubella, cholera, and malaria 112 . The suitability of mRNA technology for vaccine development for these and many other pathogens remains unknown at this time. However, if new manufacturers produce vaccines that are needed on a routine basis worldwide, they may sustain their manufacturing capacities despite the potential for higher costs early on. But new manufacturers also need to ensure that there are buyers for these vaccines. Therefore, alone, this strategy is not enough, but with multilateral organizations like Gavi prepared to purchase from these new facilities at risk, along with other countries in the region, new manufacturers would be set up for greater success. International efforts to strengthen routine healthcare systems, including last-mile delivery of health products, and encouraging health-seeking behaviors, could help further build the demand needed to sustain local facilities.
Certain countries may also need to further develop and standardize regulatory systems surrounding medical products 115 . Additional regulatory expertize may be needed because many countries lack robust regulatory agencies, which may slow or limit the development of local manufacturing facilities and their approval or the acceptance of products from other countries. Multilateral organizations and governments are helping to address these challenges with the goal of ensuring biosecurity for lower-income countries before the next pandemic, though ensuring the sustainability of new manufacturing facilities is crucial.
Efforts to further localize manufacturing in low- and middle-income countries may take years to build up, so while these efforts continue to evolve, it is beneficial to sustain and use the capacity currently available. Existing facilities can be leveraged as a reliable source of production capacity in a future pandemic if it is sustained over time. Sustained capacity will require regular investments in infrastructure and operations and a trained workforce. Additionally, there will be a need for steady supplies of raw materials to support vaccine manufacturing in the event of a pandemic. Raw materials for mRNA vaccine production have been costly and scarce given the novelty of the platform. Harnessing the major benefits of an mRNA vaccine platform would therefore require careful management of raw material suppliers, at least in the near term. Establishing raw material stockpiles may prove useful in absorbing the initial need during a pandemic. With basic components in place, existing manufacturing facilities can be “warm”, primed, and ready to respond to a future pandemic. Global manufacturers have a role to play in ensuring capacity is allocated fairly, above the interests of any one country. Ultimately, international collaboration will be the key to ensuring everyone, everywhere, has access to life-saving vaccines.
Lesson #5: Troubleshoot trade, regulatory, and procurement barriers
Viruses do not have a nationality, yet vaccine nationalism—governments reserving vaccines for their own populations, leaving limited access for the rest of the world—was a pervasive problem during COVID-19. Vaccine nationalism and a lack of regulatory harmonization slowed the movement of vaccines, health products, and essential supplies across borders. Early decision-making in the COVID-19 pandemic was influenced by national interests, underscored by the uncertainty of a new outbreak. The resulting inequality of vaccine access posed a danger to all individuals as the virus spread across borders. Despite this, many high-income countries quickly developed procurement agreements for vaccines to cover their own populations. Meanwhile, COVAX, as a new organization representing many low- and lower-middle-income countries, faced challenges to begin operations 116 . Manufacturers honored commitments in the order of when contracts were forged, which ultimately meant many high-income countries had earlier access to vaccines than lower-income countries.
Trade and regulatory barriers further slowed the manufacture and distribution of essential products 117 . During the COVID-19 pandemic, countries repeatedly prioritized their own populations even though pandemics are, by definition, a global concern. In response to COVID-19, many countries imposed export restrictions on essential products. For example, in March 2021, Italy refused shipment of 250,000 vaccine doses to Australia 118 . When India halted vaccine exports, as previously discussed, it heavily affected the ability of COVAX to serve low- and lower-middle-income countries 119 . The US and EU also restricted the export of raw materials used for vaccine production 119 . These issues could potentially be overcome with pre-established agreements for the distribution of vaccines, health products, and raw materials coupled with efforts to ensure adequate manufacturing capacity is kept “warm.” These incidences reiterate a need to not only establish proactive mechanisms that foster a more robust response in the future but to do so in a fair, diplomatic, and equitable manner.
Preplanning supply agreements and determining in advance how manufacturing capacity is used in the event of a pandemic can enhance the safety of all countries before an emergency occurs. Establishing agreements (e.g., APAs) among national governments, multilateral organizations, and manufacturers with diverse vaccine technology platforms on how to respond in the event of a future pandemic could support the rapid delivery of new vaccines and treatments and help manufacturers reduce uncertainty around supply and demand. Furthermore, agreements should aim to achieve greater health equity by covering countries across income ranges. Tiered pricing of agreements and early considerations for vaccine donations, along with efforts to reserve capacity specifically for low- and lower-middle-income countries, are tools that may provide equitable access to a suite of necessary health interventions in the early days of a pandemic. This would ensure early access to pandemic vaccines and therapeutics in parallel across all countries.
To support preparedness, governments and multilateral organizations should establish sustainable and proactive global funding mechanisms, with clear policies and governance. Efforts are already underway to develop long-term funding mechanisms for low- and middle-income countries to invest in prevention, preparedness, and response. These tailor-made mechanisms may help ease and hasten the initial pandemic response and overcome bottlenecks to financing, as experienced for example by COVAX 120 .
Importantly, global financing and preparedness platforms can also further incentivize local investments and planning, including the development of integrated preparedness plans at the national level 121 . Experts recommend these country-level preparedness plans should include a focus on allocating emergency financing toward preparedness, in addition to surveillance and monitoring and connection to robust commodity supply chains, including therapeutics and vaccines, among other areas 122 . By prioritizing health equity goals and creating a mechanism through which high-income countries and multilateral organizations can collaborate on pandemic preparedness, these funding platforms may also further avoid vaccine nationalism felt during the COVID-19 pandemic.
Lastly, greater governance and regulatory cooperation, and harmonization would speed up access to new health technologies during a pandemic. Even with initiatives already in place, like the International Coalition of Medicines Regulatory Authorities (ICMRA), COVID-19 caused trade restrictions that led to imbalances in supply and demand across the globe. Countries, multilateral organizations, and manufacturers should commit to building harmonized frameworks across borders that prevent these issues in the future and consider flexibilities including rolling reviews and consensus on the use of real-world data, where appropriate. In addition, pre-existing regulatory approvals for components of vaccine platforms, such as the components of mRNA platforms, may mean only targeted, supplementary regulatory submissions would be necessary in the event of an emergency. The ideal future situation includes regulatory submissions whereby manufacturers could effectively disseminate a robust, standardized data package to support regulatory approvals across multiple markets at the same time. Moreover, thoughtful indemnification and liability schemes could be developed in advance to enable innovation in an emergency. Streamlined, widely adopted efforts like these would quicken global response.
Lesson #6: Leverage the power of partnerships to overcome health systems challenges
Strengthening health systems may be another lever through which the world may better prepare for the next pandemic. Essential healthcare infrastructure, from service delivery, health workforce, supply chain, financing, and consumer engagement provides the basis through which emergency response may operate. The response to COVID-19 showed the power of international, cross-sector collaboration, as well as partnership across governments, multilateral organizations, and the private sector to solve health systems challenges.
While partnerships across sectors are not new, the COVID-19 pandemic should provide more momentum to achieve even bigger goals, including new ways of working. For example, Pfizer and BioNTech partnered with Zipline to provide not only financial support but also technical assistance to enable the world’s first drone delivery of COVID-19 vaccines requiring ultra-cold chain in Ghana 123 . Pfizer also collaborated with the Global Environment and Technology Foundation to collaborate with Project Last Mile. The partnership focused on aligning the supply chain expertise and technical capabilities of Coca-Cola, a company whose supply chain is characterized as having one of the widest reaches in the world, with technical expertise from Pfizer on vaccine handling, storage, and administration to improve the availability of vaccines in developing countries. These and other examples show the biopharmaceutical industry can play a role in health systems strengthening beyond serving as only a manufacturer and transactional supplier of medicines and vaccines 124 .
One area ripe for cross-sector collaboration is tackling vaccine hesitancy. Given the wider global availability of COVID-19 vaccines, the primary roadblocks to vaccine uptake continue to include vaccine hesitancy 122 . In the United States, almost three years into the pandemic, nearly one-third of people are not fully vaccinated for COVID-19—and research shows that hesitancy is prevalent worldwide 125 , 126 . The challenge of vaccine hesitancy could continue to limit COVID-19 vaccine primary and booster uptake, but also the uptake of both routine immunizations and future pandemic vaccines.
As decision-makers for their own health and that of their children, adult consumers are a primary audience for efforts to increase vaccine uptake. Making routine adult vaccination a mainstay of every clinical visit, beginning with primary care as is done for pediatric vaccination, could potentially help address hesitancy. Public health leaders, governments, and manufacturers may integrate lessons learned from other therapeutic areas as well; for example, making HIV testing more routine in primary care visits has been shown to increase diagnosis and linkage to care. A better understanding of behaviors leading to vaccine hesitancy—and designing solutions to address them—could increase the success of vaccination campaigns in a future pandemic. Multiple stakeholders may all have a role to play, thus collaboration remains key 127 .
COVID-19 had an historic impact that will be felt for years to come, but the risk of another pandemic is ever-present even as the memory of COVID-19 fades. The swift response included an unprecedented collaboration and movement of resources to save lives, develop new systems, and forge partnerships (Fig. 2 ). These actions were important in alleviating the health and economic burdens of COVID-19, but it is also clear that improvements can be made to ensure readiness for the next pandemic—and these efforts may also aid broader response to other widespread health emergencies.
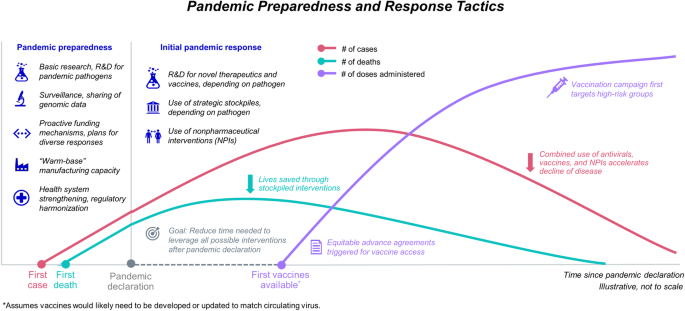
The number of cases (pink line), number of deaths (teal line), and number of vaccine doses administered (purple line) are all influenced by pandemic preparedness and response tactics. Decreasing the delay between responses and the point of pandemic declaration would lower the number of cases and deaths earlier in a pandemic. Vaccination is a key intervention for this result.
Advancements and refinements can be implemented throughout every point of the pandemic response, from sentinel surveillance systems to global vaccine distribution. Investing in innovative vaccine technologies and platforms, sustaining manufacturing capacity, facilitating local manufacturing where necessary, and forming regulatory agreements proactively, will be some of the first steps.
There should also be a focus on maintaining global momentum around preparedness and avoiding complacency. Despite the costs of responding to public health emergencies estimated in the billions and trillions of dollars, average spending for public health preparedness in higher-income countries has stayed relatively flat or decreased over time 128 . Bolstering proactive and dedicated financing for preparedness and working to pre-establish cross-border and cross-sector agreements may also help to achieve greater health equity in the next pandemic response.
Interlaced amongst all potential initiatives is an increased need for cooperation in the global community. Each player is part of a global ecosystem, and every type of organization—including the private sector—has a role to play. Protection against a global threat like a pandemic pathogen requires a united front that is built upon collaboration. The risk of another pandemic is ever-present and real, but there can be countless lives saved tomorrow if everyone comes together today.
Data availability
No datasets were generated or analyzed for this manuscript.
Johns Hopkins. COVID-19 Map Dashboard , https://coronavirus.jhu.edu/map.html (2022).
Msemburi, W. et al. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature 613 , 130–137 (2023).
Article CAS PubMed Google Scholar
Mantovani, A. et al. Long Covid: where we stand and challenges ahead. Cell Death Differ. 29 , 1891–1900 (2022).
PubMed PubMed Central Google Scholar
Brunier, A. & Drysdale, C. COVID-19 Pandemic Triggers 25% Increase in Prevalence of Anxiety and Depression Worldwide . https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide (2022).
SeyedAlinaghi, S. et al. Impact of COVID-19 pandemic on routine vaccination coverage of children and adolescents: A systematic review. Health Sci. Rep. 5 , e00516 (2022).
Article PubMed PubMed Central Google Scholar
Ingram, T. COVID-19 Pandemic Fuels Largest Continued Backslide in Vaccinations in Three Decades. https://www.who.int/news/item/15-07-2022-covid-19-pandemic-fuels-largest-continued-backslide-in-vaccinations-in-three-decades (2022).
Wenger, N. S. et al. The impact of COVID-19 on routine medical care and cancer screening. J. Gen. Intern. Med. 37 , 1450–1456 (2022).
Aburto, J. M. et al. Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: a population-level study of 29 countries. Int. J. Epidemiol. 51 , 63–74 (2022).
Article PubMed Google Scholar
Cullen, W., Gulati, G. & Kelly, B. D. Mental health in the COVID-19 pandemic. QJM 113 , 311–312 (2020).
Pokhrel, S. & Chhetri, R. A literature review on impact of COVID-19 pandemic on teaching and learning. High. Educ. Future 8 , 133–141 (2021).
Article Google Scholar
Maliszewska, M., Mattoo, A. & Van Der Mensbrugghe, D. The potential impact of COVID-19 on GDP and trade: a preliminary assessment. World Bank Policy Research Working Paper (World Bank Group, 2020).
CEPAL. United States Economic Outlook: 2020 in Review and Early 2021 Developments , https://www.cepal.org/en/notes/united-states-economic-outlook-2020-review-and-early-2021-developments (CEPAL, 2021).
Gopinath, G. A Disrupted Global Recovery , https://www.imf.org/en/Blogs/Articles/2022/01/25/blog-a-disrupted-global-recovery (2022).
Kiszewski, A. E., Cleary, E. G., Jackson, M. J. & Ledley, F. D. NIH funding for vaccine readiness before the COVID-19 pandemic. Vaccine 39 , 2458–2466 (2021).
Article CAS PubMed PubMed Central Google Scholar
Sirleaf, H. E. J. & Clark, R. H. H. Transforming or Tinkering? Inaction lAys the Groundwok for Another Pandemic . https://theindependentpanel.org/wp-content/uploads/2022/05/Transforming-or-tinkering_Report_Final.pdf (2022).
Jones, K. E. et al. Global trends in emerging infectious diseases. Nature 451 , 990–993 (2008).
Marani, M., Katul, G. G., Pan, W. K. & Parolari, A. J. Intensity and frequency of extreme novel epidemics. Proc. Natl Acad. Sci. USA 118 , e2105482118 (2021).
Ellwanger, J. H. & Chies, J. A. B. Zoonotic spillover: understanding basic aspects for better prevention. Genet. Mol. Biol. 44 , e20200355 (2021).
Vora, N. M. et al. Want to prevent pandemics? Stop spillovers. Nature 605 , 419–422 (2022).
Baker, R. E. et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 20 , 193–205 (2022).
Amesh, A., Watson, M., Toner, E., Cicero, A. & Inglesby, T. The Characteristics of Pandemic Pathogens , https://centerforhealthsecurity.org/sites/default/files/2022-12/180510-pandemic-pathogens-report.pdf (2018).
May, M. Tomorrow’s biggest microbial threats. Nat. Med. 27 , 358–359 (2021).
Piret, J. & Boivin, G. Pandemics throughout history. Front. Microbiol. 11 , 631736 (2021).
Thompson, J. & Wattam, S. Estimating the impact of interventions against COVID-19: From lockdown to vaccination. PLoS ONE 16 , e0261330 (2021).
Stokes, J., Turner, A. J., Anselmi, L., Morciano, M. & Hone, T. The relative effects of non-pharmaceutical interventions on wave one Covid-19 mortality: natural experiment in 130 countries. BMC Public Health 22 , 1113 (2022).
Hsiang, S. et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 584 , 262–267 (2020).
Gonzenbach, T. P., McGuinness, S. P., Parke, R. L. & Merz, T. M. Impact of Nonpharmaceutical interventions on ICU admissions during lockdown for Coronavirus Disease 2019 in New Zealand—a retrospective cohort study. Crit. Care Med 49 , 1749 (2021).
Slaoui, M. & Hepburn, M. Developing safe and effective Covid vaccines—Operation Warp Speed’s strategy and approach. N. Engl. J. Med. 383 , 1701–1703 (2020).
Deutsch, J. & Wheaton, S. How Europe fEll behind on Vaccines. https://www.politico.eu/article/europe-coronavirus-vaccine-struggle-pfizer-biontech-astrazeneca/ (2021).
Parlapiano, A., Solomon, D., Ngo, M. & Cowley, S. Where $5 Trillion in Pandemic Stimulus Money Went . https://www.nytimes.com/interactive/2022/03/11/us/how-covid-stimulus-money-was-spent.html#:~:text=Roughly%20%245%20trillion%20went%20to,blow%20inflicted%20by%20Covid%2D19 . (2022).
CEPI. CEPI Welcomes UK Approval of Pfizer/BioNtech Vaccine. https://cepi.net/news_cepi/cepi-welcomes-uk-approval-of-pfizer-biontech-vaccine/ (2020).
GOV.UK. UK Medicines Regulator Gives Approval for First UK COVID-19 Vaccine , https://www.gov.uk/government/news/uk-medicines-regulator-gives-approval-for-first-uk-covid-19-vaccine (2020).
Watson, O. J. et al. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect. Dis. 22 , 1293–1302 (2022).
Fitzpatrick, M. C., Moghadas, S., Pandey, A. & Galvani, A. P. Two Years of U.S. COVID-19 Vaccines Have Prevented Millions of Hospitalizations and Deaths . https://www.commonwealthfund.org/blog/2022/two-years-covid-vaccines-prevented-millions-deaths-hospitalizations (2022).
Beusekom, M. V. Paxlovid, Molnupiravir Benefit Older COVID-19 Patients, 2 Studies S how. https://www.cidrap.umn.edu/news-perspective/2022/08/paxlovid-molnupiravir-benefit-older-covid-19-patients-2-studies-show (2022).
FDA. Coronavirus (COVID-19) Update: FDA Authorizes New Monoclonal Antibody for Treatment of COVID-19 that Retains Activity Against Omicron Variant . https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-new-monoclonal-antibody-treatment-covid-19-retains (2022).
Sah, P. et al. Return on investment of the COVID-19 vaccination campaign in New York City. JAMA Netw. Open 5 , e2243127–e2243127 (2022).
FDA. Coronavirus (COVID-19) Update: FDA Authorizes Moderna, Pfizer-BioNTech Bivalent COVID-19 Vaccines for Use as a Booster Dose . https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-moderna-pfizer-biontech-bivalent-covid-19-vaccines-use (2022).
Berkley, S. COVAX Explained. https://www.gavi.org/vaccineswork/covax-explained?gclid=EAIaIQobChMI9u31qpr--QIV0dSzCh29hAKmEAAYASAAEgKR_PD_BwE (2020).
Our Wold in Data. Coronavirus (COVID-19) Vaccinations . https://ourworldindata.org/covid-vaccinations (2023).
GAVI. COVAX Has So Far Shipped Over 1 Billion COVID-19 Vaccines to 144 Participants . https://www.gavi.org/covax-vaccine-roll-out (2022).
Goldhill, O. ‘Naively Ambitious’: How COVAX Failed on Its Promise to Vaccinate the World , https://www.statnews.com/2021/10/08/how-covax-failed-on-its-promise-to-vaccinate-the-world (2021).
Stobart, A. & Duckett, S. Australia’s response to COVID-19. Health Econ Policy Law. 17 , 95–106 (2022).
Sands, P., et al. From Panic and Neglect to Investing in Health Security . https://documents1.worldbank.org/curated/en/979591495652724770/pdf/115271-REVISED-FINAL-IWG-Report-3-5-18.pdf (2017).
Medical Countermeasures. Influenza & Emerging Infectious Diseases Pandemic Vaccines and Adjuvants Program . https://www.medicalcountermeasures.gov/barda/influenza-and-emerging-infectious-diseases/pandemic-influenza-vaccine-stockpile-program/ (2005).
National Academies of Sciences, Engineering & Medicine. Globally Resilient Supply Chains for Seasonal and Pandemic Influenza Vaccines . https://nap.nationalacademies.org/catalog/26285/globally-resilient-supply-chains-for-seasonal-and-pandemic-influenza-vaccines (2021).
ASPR. JYNNEOS Vaccine Distribution by Jurisdiction. https://aspr.hhs.gov/SNS/Pages/JYNNEOS-Distribution.aspx (2022).
Harrington, W. N., Kackos, C. M. & Webby, R. J. The evolution and future of influenza pandemic preparedness. Exp. Mol. Med. 53 , 737–749 (2021).
National Academies of Sciences, Engineering & Medicine. Vaccine Research and Development to Advance Pandemic and Seasonal Influenza Preparedness and Response: Lessons from COVID-19 . https://pubmed.ncbi.nlm.nih.gov/35312264/ (2021).
Broadbent, A. J. & Subbarao, K. Influenza virus vaccines: lessons from the 2009 H1N1 pandemic. Curr. Opin. Virol. 1 , 254–262 (2011).
Borse, R. H. et al. Effects of vaccine program against pandemic influenza A(H1N1) virus, United States, 2009-2010. Emerg. Infect. Dis. 19 , 439–448 (2013).
GOVTRIBE. Advanced Development of Recombinant Influenza Virus Vaccines . https://govtribe.com/opportunity/federal-contract-opportunity/advanced-development-of-recombinant-influenza-virus-vaccines-dhhsbarda0706 (2007).
PHE. HHS Awards Contracts to Develop New Flu Vaccine Technology. https://www.phe.gov/Preparedness/news/Pages/fluvaccinetech-110228.aspx (2011).
Kis, Z. et al. Pandemic-response adenoviral vector and RNA vaccine manufacturing. npj Vaccines 7 , 29 (2022).
WHO. COVID-19 Vaccine Tracker and Landscape . https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (2023).
Thornton, I., Wilson, P. & Gandhi, G. “No Regrets” purchasing in a pandemic: making the most of advance purchase agreements. Glob. Health 18 , 1–14 (2022).
Lander, E. & Sullivan, J. American Pandemic Preparedness: Transforming Our Capabilities . https://www.whitehouse.gov/wp-content/uploads/2021/09/American-Pandemic-Preparedness-Transforming-Our-Capabilities-Final-For-Web.pdf (2021).
Saville, M. et al. Delivering pandemic vaccines in 100 days—what will it take?. N. Engl. J. Med. 387 , e3 (2022).
Vallance, P., Gates, M. 100 Days Mission to Respond to Future Pandemic Threats . https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/992762/100_Days_Mission_to_respond_to_future_pandemic_threats__3_.pdf (2021).
Cleve, M. What the lightning-fast quest for Covid vaccines means for other diseases. Nature 589 , 16–18 (2021).
Dolgin, E. The tangled history of mRNA vaccines. Nature 597 , 318–324 (2021).
Kiaie, S. H. et al. Recent advances in mRNA-LNP therapeutics: immunological and pharmacological aspects. J. Nanobiotechnol. 20 , 276 (2022).
Article CAS Google Scholar
Hsieh, C.-L. et al. Structure-based design of prefusion-stabilized SARS-CoV-2 spikes. Science 369 , 1501–1505 (2020).
Best, S. & Williams, S. J. What have we learnt about the sourcing of personal protective equipment during pandemics? Leadership and management in healthcare supply chain management: a scoping review. Public Health Front . 9 , 765501 (2021).
NIAID. Antiviral Program for Pandemics. https://www.niaid.nih.gov/research/antivirals (2022).
NIAID. NIAID Pandemic Preparedness Plan. https://www.niaid.nih.gov/sites/default/files/pandemic-preparedness-plan.pdf (2021).
Mooney, T. Preparing for the next “Disease X”. https://cepi.net/news_cepi/preparing-for-the-next-disease-x/ (2021).
Kumar, A. et al. The mRNA vaccine development landscape for infectious diseases. Nat. Rev. Drug Discov. 21 , 333–334 (2022).
Hogan, M. J. & Pardi, N. mRNA vaccines in the COVID-19 Pandemic and Beyond. Annu. Rev. Med. 73 , 17–39 (2022).
WHO. WHO tArget Product Profiles for COVID-19 Vaccines. Revised version April 2022. https://www.who.int/publications/m/item/who-target-product-profiles-for-covid-19-vaccines (2022)
Pitts, J. & Dunn, B. Pfizer Starts Study of mRNA-Based Next Generation Flu Vaccine Program . https://www.pfizer.com/news/press-release/press-release-detail/pfizer-starts-study-mrna-based-next-generation-flu-vaccine (2021).
Woodin, M. B. & Talukdar, L. Moderna Announces First Participants Dosed in Phase 3 Study of Seasonal Inuenza Vaccine Candidate (mRNA-1010). https://s29.q4cdn.com/435878511/files/doc_news/Moderna-Announces-First-Participants-Dosed-in-Phase-3-Study-of-Seasonal-Influenza-Vaccine-Candidate-mRNA-1010-2022.pdf (2022).
GlaxoSmithKline. A Study on the Safety, Reactogenicity and Immune Response of a Vaccine Against Influenza in Healthy Younger and Older Adults . https://clinicaltrials.gov/ct2/show/NCT05446740?term=curevac+and+mrna&cond=Influenza&draw=2&rank=1 (2022).
Sparrow, E. et al. Leveraging mRNA platform technology to accelerate development of vaccines for some emerging and neglected tropical diseases through local vaccine production. Front. Trop. Dis . 3 , https://doi.org/10.3389/fitd.2022.844039 (2022).
WHO. WHO to Identify Pathogens That Could Cause Future Outbreaks and Pandemics. https://www.who.int/news/item/21-11-2022-who-to-identify-pathogens-that-could-cause-future-outbreaks-and-pandemics (2022).
Hammond, A. et al. Leveraging global influenza surveillance and response system for the COVID-19 pandemic response and beyond. China CDC Wkly. 3 , 937 (2021).
Gupta, S., Gupta, T. & Gupta, N. Global respiratory virus surveillance: strengths, gaps, and way forward. Int. J. Infect. Dis. 121 , 184–189 (2022).
Carroll, D. et al. Preventing the next pandemic: the power of a global viral surveillance network. BMJ 372 , n485 (2021).
WHO. 2018 Annual Review of Diseases Prioritized under the Research and Development Blueprint . https://www.who.int/news-room/events/detail/2018/02/06/default-calendar/2018-annual-review-of-diseases-prioritized-under-the-research-anddevelopment-blueprint (2018).
Cobb, N. L. et al. Global influenza surveillance systems to detect the spread of influenza-negative influenza-like illness during the COVID-19 pandemic: Time series outlier analyses from 2015–2020. PLoS Med. 19 , e1004035 (2022).
Boeckh, M. et al. The Seattle Flu Study: when regulations hinder pandemic surveillance. Nat. Med. 28 , 7–8 (2022).
US AID. What is Predict? . https://p2.predict.global/predict-project (2020)
Guerra, J., Acharya, P. & Barnadas, C. Community-based surveillance: a scoping review. PLoS ONE 14 , e0215278 (2019).
WHO. WHO, Germany Open Hub for Pandemic and Epidemic Intelligence in Berlin. https://www.who.int/news/item/01-09-2021-who-germany-open-hub-for-pandemic-and-epidemic-intelligence-in-berlin#:~:text=The%20WHO%20Hub%20is%20currently,a%20wide%20range%20of%20disciplines . (2021).
CDC. Influenza Risk Assessment Tool (IRAT) . https://www.cdc.gov/flu/pandemic-resources/national-strategy/risk-assessment.htm (2020).
WHO. Tool for Influenza Pandemic Risk Assessment (TIPRA) . https://www.who.int/teams/global-influenza-programme/avian-influenza/tool-for-influenza-pandemic-risk-assessment-(tipra) (2020).
WHO. Pandemic Influenza Preparedness (PIP) Framework. https://www.who.int/initiatives/pandemic-influenza-preparedness-framework (2023)
Cueni, T. In an ‘Age of Pandemics,’ Pathogen-sharing Can’t Be Optional. https://www.japantimes.co.jp/opinion/2022/02/23/commentary/world-commentary/monetizing-covid-19/ (2022).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 382 , 727–733 (2020).
Nature Research Custom Media. Future Pandemic Preparedness, Powered by Genomics , https://www.nature.com/articles/d42473-020-00484-3 (2020).
Shaman, J. Pandemic preparedness and forecast. Nat. Microbiol. 3 , 265–267 (2018).
Cary Institute of Ecosystm Studies. Using AI to Predict & Preempt Epidemics , https://www.caryinstitute.org/news-insights/lecture-video/using-ai-predict-preempt-epidemics (2019).
Gray, G. C., Robie, E. R., Studstill, C. J. & Nunn, C. L. Mitigating future respiratory virus pandemics: new threats and approaches to consider. Viruses 13 , 637 (2021).
Maxmen, A. Why did the world’s pandemic warning system fail when COVID hit? Nature 589 , 499–501 (2021).
Maxmen, A. & Tollefson, J. Two decades of pandemic war games failed to account for Donald Trump. Nature 584 , 26–29 (2020).
Mallapaty, S. What the data say about border closures and COVID spread. Nature 589 , 185 (2021).
Linares, C., Martinez, G. S., Kendrovski, V. & Diaz, J. A new integrative perspective on early warning systems for health in the context of climate change. Environ. Res. 187 , 109623 (2020).
Gillies, C. E. et al. Demonstrating the consequences of learning missingness patterns in early warning systems for preventative health care: a novel simulation and solution. J. Biomed. Inform. 110 , 103528 (2020).
Au-Yeung, W.-T. M., Sahani, A. K., Isselbacher, E. M. & Armoundas, A. A. Reduction of false alarms in the intensive care unit using an optimized machine learning based approach. NPJ Digit. Med. 2 , 86 (2019).
Addai, N. Gradient Health, Inc: Equitable Healthcare A.I . https://solve.mit.edu/challenges/equitable-health-systems/solutions/57687 (2023).
Crane, M. A., Shermock, K. M., Omer, S. B. & Romley, J. A. Change in reported adherence to nonpharmaceutical interventions during the COVID-19 pandemic, April-November 2020. JAMA 325 , 883–885 (2021).
Pozo-Martin, F. et al. The impact of non-pharmaceutical interventions on COVID-19 epidemic growth in the 37 OECD member states. Eur. J. Epidemiol. 36 , 629–640 (2021).
Serra, M. et al. Optimal policies for mitigating pandemic costs: a tutorial model. Phys. Biol. 19 , 055001 (2022).
Ranney, M. L., Griffeth, V. & Jha, A. K. Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 382 , e41 (2020).
SGD Pharma. Glass Packaging Case Study , https://www.sgd-pharma.com/sites/default/files/mediacenter-file/sgd_pharma_-_customer_case_study.pdf .
Challener, C. A. Focus on Fill and Finish , https://www.biopharminternational.com/view/focus-on-fill-and-finish (2022).
Vardavas, C. et al. The cost of the COVID-19 pandemic vs the cost-effectiveness of mitigation strategies in the EU/UK/EEA and OECD countries: a systematic review. BMJ Open 13 , e077602 (2023).
Sell, T. K. et al. Building the global vaccine manufacturing capacity needed to respond to pandemics. Vaccine 39 , 1667 (2021).
Dunster, E. As COVID-19 Vaccine Output Estimated to Reach over 12 Billion by Year End and 24 Billion by Mid-2022, Innovative Vaccine Manufacturers Renew Commitment to Support G20 Efforts to Address Remaining Barriers to Equitable Access . https://www.ifpma.org/news/as-covid-19-vaccine-output-estimated-to-reach-over-12-billion-by-year-end-and-24-billion-by-mid-2022-innovative-vaccine-manufacturers-renew-commitment-to-support-g20-efforts-to-address-remaining-barr/ (2021).
Etten, M. V. New Data: COVID-19 Vaccine Global Production Capacity Projected to Exceed 20 Billion Doses This Year. https://catalyst.phrma.org/new-data-covid-19-vaccine-global-production-capacity-projected-to-exceed-20-billion-doses-this-year (2022).
Kessa, F. Call for the Sustainable Manufacturing of Covid-19 and Other mRNA Vaccines in the Americas. https://prais.paho.org/en/mrna/ (2021).
GAVI. A New Era of Vaccine Manufacturing in Africa. https://www.gavi.org/sites/default/files/white-paper/new-era-vaccine-manufacturing-in-africa-wp.pdf (2022).
Adepoju, P. Africa CDC warns COVID-19 vaccine production could cease. Lancet 399 , 1683 (2022).
GAVI. Pneumococcal AMC . https://www.gavi.org/investing-gavi/innovative-financing/pneumococcal-amc .
Shah, D. Africa Must Produce Its Own Vaccines—It’ll Need Investment in Regulation to Get There . https://wellcome.org/news/africa-must-produce-its-own-vaccines-need-investment-regulation (2022).
Taylor, A. Why Covax, the Best Hope for Vaccinating the World, Was Doomed to Fall Short . https://www.washingtonpost.com/world/2022/03/22/covax-problems-coronavirus-vaccines-next-pandemic/ (2022).
Etten, M. V. Ensuring Global Vaccine Equity Requires Eliminating Trade and Regulatory Barriers. https://phrma.org/blog/ensuring-global-vaccine-equity-requires-eliminating-trade-and-regulatory-barriers (2021).
Italy, EU Refuse AstraZeneca Request to Ship 250,000 Doses of Vaccine to Australia . https://www.abc.net.au/news/2021-03-05/italy-eu-block-250000-astrazeneca-doses-to-australia/13218348 (2021).
Peters, R. & Prabhakar, D. Export Restrictions Do Not Help Fight COVID-19. https://unctad.org/news/export-restrictions-do-not-help-fight-covid-19 (2021).
WHO. Supply Bottleneck, Financial Challenges Fuel Delays in Africa’s COVID-19 Vaccine rollout. https://www.afro.who.int/news/supply-bottleneck-financial-challenges-fuel-delays-africas-covid-19-vaccine-rollout (2021).
World Bank. The Pandemic Fund . https://www.worldbank.org/en/programs/financial-intermediary-fund-for-pandemic-prevention-preparedness-and-response-ppr-fif/overview (2022).
Sachs, J. D. et al. The Lancet Commission on lessons for the future from the COVID-19 pandemic. Lancet 400 , 1224–1280 (2022).
Pfizer. Zipline, Pfizer and BioNTech Collaboration Paves the Way for Automated, On-Demand Delivery of First mRNA COVID-19 Vaccines in Ghana . https://www.pfizer.com/news/press-release/press-release-detail/zipline-pfizer-and-biontech-collaboration-paves-way (2021).
Global Health Progress. Global Health Progress—Collaborating for a Sustainable Future. https://globalhealthprogress.org/ (2023).
NY Times. Coronavirus in the U.S.: Latest Map and Case Count . https://www.nytimes.com/interactive/2021/us/covid-cases.html (2023).
Hou, Z. et al. Assessing COVID-19 vaccine hesitancy, confidence, and public engagement: a global social listening study. J. Med. Internet Res. 23 , e27632 (2021).
Valdez, R. B. & Romero, K. S. Improving adult vaccination status in the United States. Healthcare 9 , 1411 (2021).
Glassman, A. & Smitham, E. Financing for Global Health Security and Pandemic Preparedness: Taking Stock and What’s Next. https://www.cgdev.org/blog/financing-global-health-security-and-pandemic-preparedness-taking-stock-whats-next (2021).
Download references
Acknowledgements
We thank Joyce Thuss, Jessica Adams, Angela Zhang, and Ruju Panjabi (Red Nucleus, Yardley, PA, USA) for their editorial support in preparing this article. We also thank Andrew Hill and Marie Beitelshees (Bulmore Technical Writing Consulting, Lockport, NY, USA) for their editorial review. This work was funded by Pfizer.
Author information
Authors and affiliations.
Pfizer, 66 Hudson Boulevard East, New York, NY, 10001, USA
B. Adam Williams, Charles H. Jones, Verna Welch & Jane M. True
You can also search for this author in PubMed Google Scholar
Contributions
B.A.W. developed an outline, researched sources, and drafted and edited the manuscript. C.H.J. and V.W. provided strategic input, as well as drafting and editing support. J.M.T. conceptualized the publication and provided strategic oversight and editing.
Corresponding authors
Correspondence to B. Adam Williams or Jane M. True .
Ethics declarations
Competing interests.
B.A.W., C.H.J., V.W. and J.M.T. report that they are employees of Pfizer Inc. and may hold stock or stock options in the company.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Williams, B.A., Jones, C.H., Welch, V. et al. Outlook of pandemic preparedness in a post-COVID-19 world. npj Vaccines 8 , 178 (2023). https://doi.org/10.1038/s41541-023-00773-0
Download citation
Received : 18 July 2023
Accepted : 02 November 2023
Published : 20 November 2023
DOI : https://doi.org/10.1038/s41541-023-00773-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- All topics »
- Fact sheets
Feature stories
Publications.
- Questions & answers
- Tools and toolkits
Coronavirus disease (COVID-19) pandemic
- Ukraine emergency
- Environment and health
Mpox (monkeypox)
- Calls for experts
- Initiatives
- European Programme of Work
- Sustainable Development Goals
- The Pan-European Mental Health Coalition
- Empowerment through Digital Health
- The European Immunization Agenda 2030
- Healthier behaviours: incorporating behavioural and cultural insights
- Moving towards UHC
- Protecting against health emergencies
- Promoting health and well-being
- News stories
- Media releases
Photo stories
- Questions and answers
- Media Contacts
Newsletters
- European Health Information Gateway
- European health report
- Core health indicators
- WHO Immunization Data portal
- Noncommunicable diseases (NCD) dashboard
- Events
- Teams »
- Data and digital health
- Policy & Governance f. Health through the Life Course
- Groups and networks »
- Health Evidence Network (HEN)
The European Health Report 2021 »

- Conflict in Israel and the occupied Palestinian territory
- Armenian refugee health response
- Climate crisis: extreme weather
- Türkiye and Syria earthquakes
- About health emergencies
- Health emergencies newsletter
- Health emergencies list

- Regional Director
- Executive Council
- Technical centres
- Faces of WHO
- Regional Committee for Europe
- Standing Committee
- Partnerships
- Groups and networks
- WHO collaborating centres
74th session of the WHO Regional Committee for Europe

- Situations /
Links and resources
The coronavirus disease 2019 (COVID-19) pandemic is a global outbreak of coronavirus – an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Cases of novel coronavirus (nCoV) were first detected in China in December 2019, with the virus spreading rapidly to other countries across the world. This led WHO to declare a Public Health Emergency of International Concern (PHEIC) on 30 January 2020 and to characterize the outbreak as a pandemic on 11 March 2020.
On 5 May 2023, more than three years into the pandemic, the WHO Emergency Committee on COVID-19 recommended to the Director-General, who accepted the recommendation, that given the disease was by now well established and ongoing, it no longer fit the definition of a PHEIC. This does not mean the pandemic itself is over, but the global emergency it caused is – for now. A review committee will be established to develop long-term, standing recommendations for countries on how to manage COVID-19 on an ongoing basis.
Since the COVID-19 pandemic started, over 2 million people in the European Region have died from the disease.
On 25 October 2023 WHO/Europe made several changes to its respiratory virus surveillance and data reporting systems. The COVID-19 Situation Dashboard played a pivotal role in providing essential information during the early stages of the pandemic. However, the landscape has now shifted, and so have data needs.
A new WHO/Europe COVID-19 Information Hub is replacing the previous COVID-19 Situation Dashboard to serve as a comprehensive resource, providing links to the most current health information, datasets and products concerning COVID-19.
Within the Hub, WHO/Europe and the European Centre for Disease Prevention and Control (ECDC)’s weekly European Respiratory Virus Surveillance Summary (ERVISS) displays integrated surveillance data for influenza, COVID-19, and respiratory syncytial virus (RSV) in the WHO European Region, including the European Union (EU)/European Economic Area (EEA).
- COVID-19 and related health topics
- Q&As on COVID-19 and related health topics
- Post COVID-19 condition (Long COVID) - fact sheet
- Coronavirus disease (COVID-19) pandemic: global resources
- COVID-19 chatbot: HealthBuddy+
- WHO European Region Operational Updates (archive)
- Global situation dashboard
- Global situation reports
- Surveillance reports (SARS-CoV-2 and mpox in animals)
- Dashboards and interactive platforms
- COVID-19 vaccination
- WHO/Europe COVID-19 vaccination monitor
- Country & Technical Guidance
- Regional publications and guidance on COVID-19
- Global publications and guidance on COVID-19
- Country information
- Public Health and Social Measures in Response to COVID-19
- COVID-19 Health System Response Monitor (HSRM)
- InfluenzaNet
- Emergency Medical Teams - Global EMT
- The Independent Panel for Pandemic Preparedness and Response (IPPR)
- Review Committee on the Functioning of the International Health Regulations (2005) during the COVID-19 Response
- Laboratories
Statement – Solidarity and partnership to save lives: how WHO/Europe worked with the European Union to respond to COVID-19
Amid a summer wave of COVID-19, a new WHO/Europe study confirms the lifesaving impact of vaccines
Half a million children in WHO European Region not fully vaccinated in their first year of life: New 2023 data reveal both gaps and gains in immunization coverage
Essential laboratory equipment arrives in Bulgaria as part of a broader project to protect the health of Ukrainian refugees
Honouring the health humanitarians working to create a safer world
Building trust in vaccination: 350 health workers trained in communication in Kyrgyzstan
Treat mental health as seriously as physical heath: interview with Inês Mália Sarmento, youth activist

Joint bimonthly surveillance report on SARS-CoV-2 and mpox in animals in the European Region, May and...
Strengthened surveillance using a One Health approach in at-risk animal populations and at the animal-human-environment interface is required to timely...

City leadership for age-friendly communities in the post-pandemic era: five lessons for building health...
The COVID-19 pandemic hit older people hardest. This policy brief, intended for planners, policy-makers and politicians, was produced by the 16 cities...

Influenza virus characterization: summary report, Europe, March 2024

Report on the impact of the COVID-19 pandemic on the daily routine and behaviours of school-aged children:...
The WHO Regional Office for Europe established the WHO European Childhood Obesity Surveillance Initiative (COSI) in 2007 in response to the need...

A timeline of WHO's COVID-19 Response in the WHO European Region: a living document...

A timeline of WHO’s response to COVID-19 in the WHO European Region: a living document (update to version...
This “living” document presents an update to the previous timeline covering from 31 December 2019 to 31 December 20201. It describes the continuation...

A timeline of WHO’s response to COVID-19 in the WHO European Region: a living document (Version 2.0...
2020 was a year that will be remembered for generations, for having put the lives and livelihoods of everyone into an unprecedented stress test. Health...
Republic of Moldova - Vaccination saves lives: Supporting the deployment of COVID-19 vaccines and routine vaccination systems in the Eastern Partnership Republic of Moldova - Vaccination saves lives: Supporting the deployment of COVID-19 vaccines and routine vaccination systems in the Eastern Partnership
Belarus - vaccination saves lives: supporting the deployment of covid-19 vaccines and routine vaccination systems in the eastern partnership belarus - vaccination saves lives: supporting the deployment of covid-19 vaccines and routine vaccination systems in the eastern partnership, ukraine - vaccination saves lives: supporting the deployment of covid-19 vaccines and routine vaccination systems in the eastern partnership ukraine - vaccination saves lives: supporting the deployment of covid-19 vaccines and routine vaccination systems in the eastern partnership.
Increasing Recognition, Research and Rehabilitation for Post COVID-19 Condition (long COVID)
WHO remains committed to learning more about long COVID and to finding ways to improve the medium- and long-term outcomes for people affected by it, as Dr Hans Henri P. Kluge ...
Taking stock of the health-related SDG during COVID-19
The European Health Report is produced every three years as a flagship publication by the WHO Regional Office for Europe. The aims of the 2021 edition are to provide insight into R ...
Considering physical activity and COVID-19
During the COVID-19 pandemic several public health measures were adopted, including lockdowns and limitations of access to public spaces for physical activity. These measures have ...
Partnering with the European Union to support and strengthen vaccination
The European Union (EU) and WHO/Europe together provide critical assistance to Member States and territories of the WHO European Region on effective vaccination against COVID-19 an ...

Faith Leaders Unite for Health Amid COVID 19

Keeping safe from influenza, COVID 19 and RSV this autumn and winter

From permacrisis to resilience: noncommunicable diseases in emergency preparedness and response

The CO-FLOW long COVID study at Erasmus MC, Rotterdam, Netherlands
Related health topic.
Coronavirus disease (COVID-19)
Coronavirus disease (COVID-19) - Global site

Coronavirus disease (COVID-19) pandemic (Global)
For COVID-19 enquiries contact (7 days a week): WHO/Europe Press Office Tel.: +49 228 815 0432 Email address: [email protected]
Peer Reviewed
GPT-fabricated scientific papers on Google Scholar: Key features, spread, and implications for preempting evidence manipulation
Article metrics.
CrossRef Citations
Altmetric Score
PDF Downloads
Academic journals, archives, and repositories are seeing an increasing number of questionable research papers clearly produced using generative AI. They are often created with widely available, general-purpose AI applications, most likely ChatGPT, and mimic scientific writing. Google Scholar easily locates and lists these questionable papers alongside reputable, quality-controlled research. Our analysis of a selection of questionable GPT-fabricated scientific papers found in Google Scholar shows that many are about applied, often controversial topics susceptible to disinformation: the environment, health, and computing. The resulting enhanced potential for malicious manipulation of society’s evidence base, particularly in politically divisive domains, is a growing concern.
Swedish School of Library and Information Science, University of Borås, Sweden
Department of Arts and Cultural Sciences, Lund University, Sweden
Division of Environmental Communication, Swedish University of Agricultural Sciences, Sweden

Research Questions
- Where are questionable publications produced with generative pre-trained transformers (GPTs) that can be found via Google Scholar published or deposited?
- What are the main characteristics of these publications in relation to predominant subject categories?
- How are these publications spread in the research infrastructure for scholarly communication?
- How is the role of the scholarly communication infrastructure challenged in maintaining public trust in science and evidence through inappropriate use of generative AI?
research note Summary
- A sample of scientific papers with signs of GPT-use found on Google Scholar was retrieved, downloaded, and analyzed using a combination of qualitative coding and descriptive statistics. All papers contained at least one of two common phrases returned by conversational agents that use large language models (LLM) like OpenAI’s ChatGPT. Google Search was then used to determine the extent to which copies of questionable, GPT-fabricated papers were available in various repositories, archives, citation databases, and social media platforms.
- Roughly two-thirds of the retrieved papers were found to have been produced, at least in part, through undisclosed, potentially deceptive use of GPT. The majority (57%) of these questionable papers dealt with policy-relevant subjects (i.e., environment, health, computing), susceptible to influence operations. Most were available in several copies on different domains (e.g., social media, archives, and repositories).
- Two main risks arise from the increasingly common use of GPT to (mass-)produce fake, scientific publications. First, the abundance of fabricated “studies” seeping into all areas of the research infrastructure threatens to overwhelm the scholarly communication system and jeopardize the integrity of the scientific record. A second risk lies in the increased possibility that convincingly scientific-looking content was in fact deceitfully created with AI tools and is also optimized to be retrieved by publicly available academic search engines, particularly Google Scholar. However small, this possibility and awareness of it risks undermining the basis for trust in scientific knowledge and poses serious societal risks.
Implications
The use of ChatGPT to generate text for academic papers has raised concerns about research integrity. Discussion of this phenomenon is ongoing in editorials, commentaries, opinion pieces, and on social media (Bom, 2023; Stokel-Walker, 2024; Thorp, 2023). There are now several lists of papers suspected of GPT misuse, and new papers are constantly being added. 1 See for example Academ-AI, https://www.academ-ai.info/ , and Retraction Watch, https://retractionwatch.com/papers-and-peer-reviews-with-evidence-of-chatgpt-writing/ . While many legitimate uses of GPT for research and academic writing exist (Huang & Tan, 2023; Kitamura, 2023; Lund et al., 2023), its undeclared use—beyond proofreading—has potentially far-reaching implications for both science and society, but especially for their relationship. It, therefore, seems important to extend the discussion to one of the most accessible and well-known intermediaries between science, but also certain types of misinformation, and the public, namely Google Scholar, also in response to the legitimate concerns that the discussion of generative AI and misinformation needs to be more nuanced and empirically substantiated (Simon et al., 2023).
Google Scholar, https://scholar.google.com , is an easy-to-use academic search engine. It is available for free, and its index is extensive (Gusenbauer & Haddaway, 2020). It is also often touted as a credible source for academic literature and even recommended in library guides, by media and information literacy initiatives, and fact checkers (Tripodi et al., 2023). However, Google Scholar lacks the transparency and adherence to standards that usually characterize citation databases. Instead, Google Scholar uses automated crawlers, like Google’s web search engine (Martín-Martín et al., 2021), and the inclusion criteria are based on primarily technical standards, allowing any individual author—with or without scientific affiliation—to upload papers to be indexed (Google Scholar Help, n.d.). It has been shown that Google Scholar is susceptible to manipulation through citation exploits (Antkare, 2020) and by providing access to fake scientific papers (Dadkhah et al., 2017). A large part of Google Scholar’s index consists of publications from established scientific journals or other forms of quality-controlled, scholarly literature. However, the index also contains a large amount of gray literature, including student papers, working papers, reports, preprint servers, and academic networking sites, as well as material from so-called “questionable” academic journals, including paper mills. The search interface does not offer the possibility to filter the results meaningfully by material type, publication status, or form of quality control, such as limiting the search to peer-reviewed material.
To understand the occurrence of ChatGPT (co-)authored work in Google Scholar’s index, we scraped it for publications, including one of two common ChatGPT responses (see Appendix A) that we encountered on social media and in media reports (DeGeurin, 2024). The results of our descriptive statistical analyses showed that around 62% did not declare the use of GPTs. Most of these GPT-fabricated papers were found in non-indexed journals and working papers, but some cases included research published in mainstream scientific journals and conference proceedings. 2 Indexed journals mean scholarly journals indexed by abstract and citation databases such as Scopus and Web of Science, where the indexation implies journals with high scientific quality. Non-indexed journals are journals that fall outside of this indexation. More than half (57%) of these GPT-fabricated papers concerned policy-relevant subject areas susceptible to influence operations. To avoid increasing the visibility of these publications, we abstained from referencing them in this research note. However, we have made the data available in the Harvard Dataverse repository.
The publications were related to three issue areas—health (14.5%), environment (19.5%) and computing (23%)—with key terms such “healthcare,” “COVID-19,” or “infection”for health-related papers, and “analysis,” “sustainable,” and “global” for environment-related papers. In several cases, the papers had titles that strung together general keywords and buzzwords, thus alluding to very broad and current research. These terms included “biology,” “telehealth,” “climate policy,” “diversity,” and “disrupting,” to name just a few. While the study’s scope and design did not include a detailed analysis of which parts of the articles included fabricated text, our dataset did contain the surrounding sentences for each occurrence of the suspicious phrases that formed the basis for our search and subsequent selection. Based on that, we can say that the phrases occurred in most sections typically found in scientific publications, including the literature review, methods, conceptual and theoretical frameworks, background, motivation or societal relevance, and even discussion. This was confirmed during the joint coding, where we read and discussed all articles. It became clear that not just the text related to the telltale phrases was created by GPT, but that almost all articles in our sample of questionable articles likely contained traces of GPT-fabricated text everywhere.
Evidence hacking and backfiring effects
Generative pre-trained transformers (GPTs) can be used to produce texts that mimic scientific writing. These texts, when made available online—as we demonstrate—leak into the databases of academic search engines and other parts of the research infrastructure for scholarly communication. This development exacerbates problems that were already present with less sophisticated text generators (Antkare, 2020; Cabanac & Labbé, 2021). Yet, the public release of ChatGPT in 2022, together with the way Google Scholar works, has increased the likelihood of lay people (e.g., media, politicians, patients, students) coming across questionable (or even entirely GPT-fabricated) papers and other problematic research findings. Previous research has emphasized that the ability to determine the value and status of scientific publications for lay people is at stake when misleading articles are passed off as reputable (Haider & Åström, 2017) and that systematic literature reviews risk being compromised (Dadkhah et al., 2017). It has also been highlighted that Google Scholar, in particular, can be and has been exploited for manipulating the evidence base for politically charged issues and to fuel conspiracy narratives (Tripodi et al., 2023). Both concerns are likely to be magnified in the future, increasing the risk of what we suggest calling evidence hacking —the strategic and coordinated malicious manipulation of society’s evidence base.
The authority of quality-controlled research as evidence to support legislation, policy, politics, and other forms of decision-making is undermined by the presence of undeclared GPT-fabricated content in publications professing to be scientific. Due to the large number of archives, repositories, mirror sites, and shadow libraries to which they spread, there is a clear risk that GPT-fabricated, questionable papers will reach audiences even after a possible retraction. There are considerable technical difficulties involved in identifying and tracing computer-fabricated papers (Cabanac & Labbé, 2021; Dadkhah et al., 2023; Jones, 2024), not to mention preventing and curbing their spread and uptake.
However, as the rise of the so-called anti-vaxx movement during the COVID-19 pandemic and the ongoing obstruction and denial of climate change show, retracting erroneous publications often fuels conspiracies and increases the following of these movements rather than stopping them. To illustrate this mechanism, climate deniers frequently question established scientific consensus by pointing to other, supposedly scientific, studies that support their claims. Usually, these are poorly executed, not peer-reviewed, based on obsolete data, or even fraudulent (Dunlap & Brulle, 2020). A similar strategy is successful in the alternative epistemic world of the global anti-vaccination movement (Carrion, 2018) and the persistence of flawed and questionable publications in the scientific record already poses significant problems for health research, policy, and lawmakers, and thus for society as a whole (Littell et al., 2024). Considering that a person’s support for “doing your own research” is associated with increased mistrust in scientific institutions (Chinn & Hasell, 2023), it will be of utmost importance to anticipate and consider such backfiring effects already when designing a technical solution, when suggesting industry or legal regulation, and in the planning of educational measures.
Recommendations
Solutions should be based on simultaneous considerations of technical, educational, and regulatory approaches, as well as incentives, including social ones, across the entire research infrastructure. Paying attention to how these approaches and incentives relate to each other can help identify points and mechanisms for disruption. Recognizing fraudulent academic papers must happen alongside understanding how they reach their audiences and what reasons there might be for some of these papers successfully “sticking around.” A possible way to mitigate some of the risks associated with GPT-fabricated scholarly texts finding their way into academic search engine results would be to provide filtering options for facets such as indexed journals, gray literature, peer-review, and similar on the interface of publicly available academic search engines. Furthermore, evaluation tools for indexed journals 3 Such as LiU Journal CheckUp, https://ep.liu.se/JournalCheckup/default.aspx?lang=eng . could be integrated into the graphical user interfaces and the crawlers of these academic search engines. To enable accountability, it is important that the index (database) of such a search engine is populated according to criteria that are transparent, open to scrutiny, and appropriate to the workings of science and other forms of academic research. Moreover, considering that Google Scholar has no real competitor, there is a strong case for establishing a freely accessible, non-specialized academic search engine that is not run for commercial reasons but for reasons of public interest. Such measures, together with educational initiatives aimed particularly at policymakers, science communicators, journalists, and other media workers, will be crucial to reducing the possibilities for and effects of malicious manipulation or evidence hacking. It is important not to present this as a technical problem that exists only because of AI text generators but to relate it to the wider concerns in which it is embedded. These range from a largely dysfunctional scholarly publishing system (Haider & Åström, 2017) and academia’s “publish or perish” paradigm to Google’s near-monopoly and ideological battles over the control of information and ultimately knowledge. Any intervention is likely to have systemic effects; these effects need to be considered and assessed in advance and, ideally, followed up on.
Our study focused on a selection of papers that were easily recognizable as fraudulent. We used this relatively small sample as a magnifying glass to examine, delineate, and understand a problem that goes beyond the scope of the sample itself, which however points towards larger concerns that require further investigation. The work of ongoing whistleblowing initiatives 4 Such as Academ-AI, https://www.academ-ai.info/ , and Retraction Watch, https://retractionwatch.com/papers-and-peer-reviews-with-evidence-of-chatgpt-writing/ . , recent media reports of journal closures (Subbaraman, 2024), or GPT-related changes in word use and writing style (Cabanac et al., 2021; Stokel-Walker, 2024) suggest that we only see the tip of the iceberg. There are already more sophisticated cases (Dadkhah et al., 2023) as well as cases involving fabricated images (Gu et al., 2022). Our analysis shows that questionable and potentially manipulative GPT-fabricated papers permeate the research infrastructure and are likely to become a widespread phenomenon. Our findings underline that the risk of fake scientific papers being used to maliciously manipulate evidence (see Dadkhah et al., 2017) must be taken seriously. Manipulation may involve undeclared automatic summaries of texts, inclusion in literature reviews, explicit scientific claims, or the concealment of errors in studies so that they are difficult to detect in peer review. However, the mere possibility of these things happening is a significant risk in its own right that can be strategically exploited and will have ramifications for trust in and perception of science. Society’s methods of evaluating sources and the foundations of media and information literacy are under threat and public trust in science is at risk of further erosion, with far-reaching consequences for society in dealing with information disorders. To address this multifaceted problem, we first need to understand why it exists and proliferates.
Finding 1: 139 GPT-fabricated, questionable papers were found and listed as regular results on the Google Scholar results page. Non-indexed journals dominate.
Most questionable papers we found were in non-indexed journals or were working papers, but we did also find some in established journals, publications, conferences, and repositories. We found a total of 139 papers with a suspected deceptive use of ChatGPT or similar LLM applications (see Table 1). Out of these, 19 were in indexed journals, 89 were in non-indexed journals, 19 were student papers found in university databases, and 12 were working papers (mostly in preprint databases). Table 1 divides these papers into categories. Health and environment papers made up around 34% (47) of the sample. Of these, 66% were present in non-indexed journals.
| Indexed journals* | 5 | 3 | 4 | 7 | 19 |
| Non-indexed journals | 18 | 18 | 13 | 40 | 89 |
| Student papers | 4 | 3 | 1 | 11 | 19 |
| Working papers | 5 | 3 | 2 | 2 | 12 |
| Total | 32 | 27 | 20 | 60 | 139 |
Finding 2: GPT-fabricated, questionable papers are disseminated online, permeating the research infrastructure for scholarly communication, often in multiple copies. Applied topics with practical implications dominate.
The 20 papers concerning health-related issues are distributed across 20 unique domains, accounting for 46 URLs. The 27 papers dealing with environmental issues can be found across 26 unique domains, accounting for 56 URLs. Most of the identified papers exist in multiple copies and have already spread to several archives, repositories, and social media. It would be difficult, or impossible, to remove them from the scientific record.
As apparent from Table 2, GPT-fabricated, questionable papers are seeping into most parts of the online research infrastructure for scholarly communication. Platforms on which identified papers have appeared include ResearchGate, ORCiD, Journal of Population Therapeutics and Clinical Pharmacology (JPTCP), Easychair, Frontiers, the Institute of Electrical and Electronics Engineer (IEEE), and X/Twitter. Thus, even if they are retracted from their original source, it will prove very difficult to track, remove, or even just mark them up on other platforms. Moreover, unless regulated, Google Scholar will enable their continued and most likely unlabeled discoverability.
| Environment | researchgate.net (13) | orcid.org (4) | easychair.org (3) | ijope.com* (3) | publikasiindonesia.id (3) |
| Health | researchgate.net (15) | ieee.org (4) | twitter.com (3) | jptcp.com** (2) | frontiersin.org (2) |
A word rain visualization (Centre for Digital Humanities Uppsala, 2023), which combines word prominences through TF-IDF 5 Term frequency–inverse document frequency , a method for measuring the significance of a word in a document compared to its frequency across all documents in a collection. scores with semantic similarity of the full texts of our sample of GPT-generated articles that fall into the “Environment” and “Health” categories, reflects the two categories in question. However, as can be seen in Figure 1, it also reveals overlap and sub-areas. The y-axis shows word prominences through word positions and font sizes, while the x-axis indicates semantic similarity. In addition to a certain amount of overlap, this reveals sub-areas, which are best described as two distinct events within the word rain. The event on the left bundles terms related to the development and management of health and healthcare with “challenges,” “impact,” and “potential of artificial intelligence”emerging as semantically related terms. Terms related to research infrastructures, environmental, epistemic, and technological concepts are arranged further down in the same event (e.g., “system,” “climate,” “understanding,” “knowledge,” “learning,” “education,” “sustainable”). A second distinct event further to the right bundles terms associated with fish farming and aquatic medicinal plants, highlighting the presence of an aquaculture cluster. Here, the prominence of groups of terms such as “used,” “model,” “-based,” and “traditional” suggests the presence of applied research on these topics. The two events making up the word rain visualization, are linked by a less dominant but overlapping cluster of terms related to “energy” and “water.”
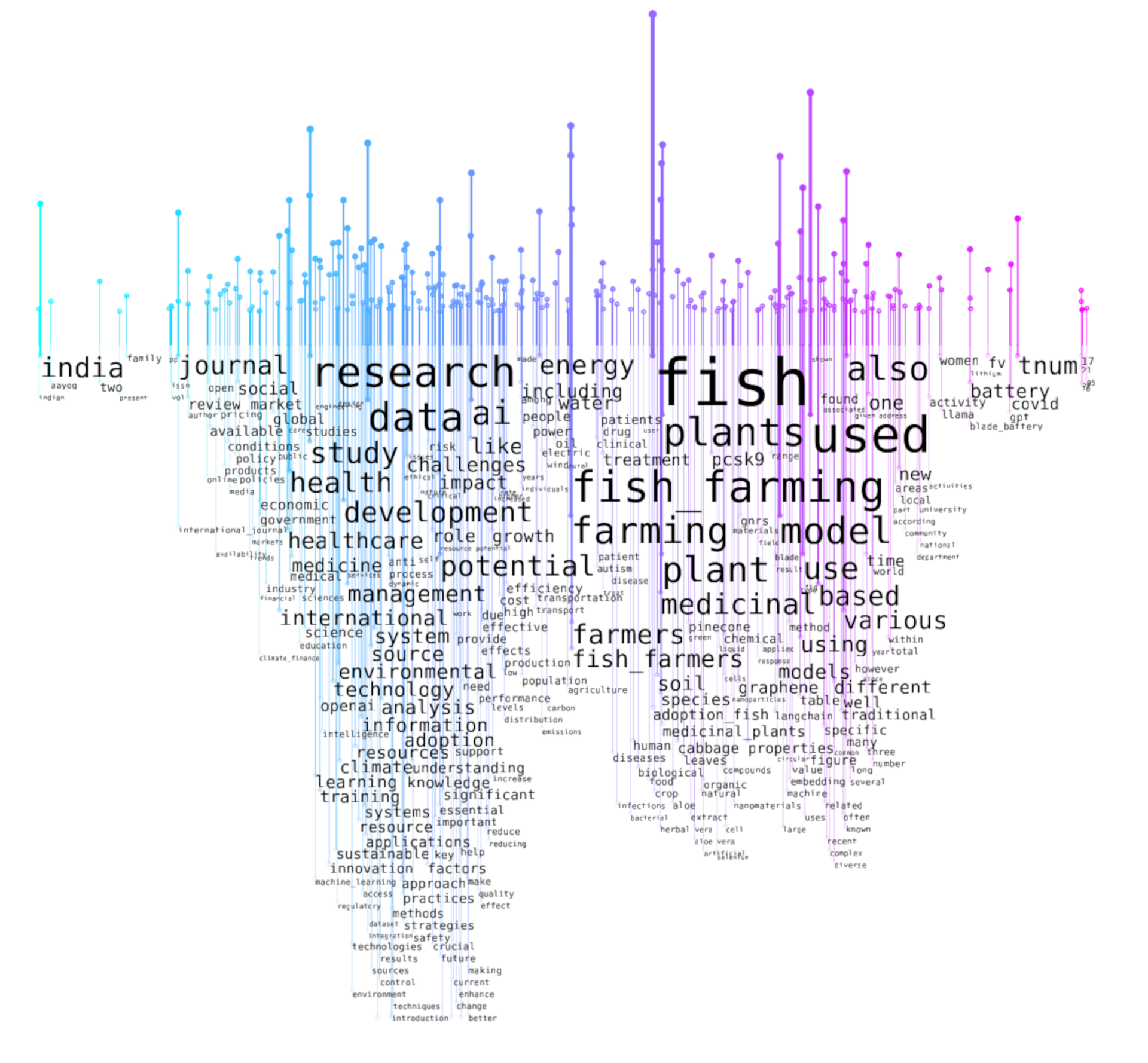
The bar chart of the terms in the paper subset (see Figure 2) complements the word rain visualization by depicting the most prominent terms in the full texts along the y-axis. Here, word prominences across health and environment papers are arranged descendingly, where values outside parentheses are TF-IDF values (relative frequencies) and values inside parentheses are raw term frequencies (absolute frequencies).
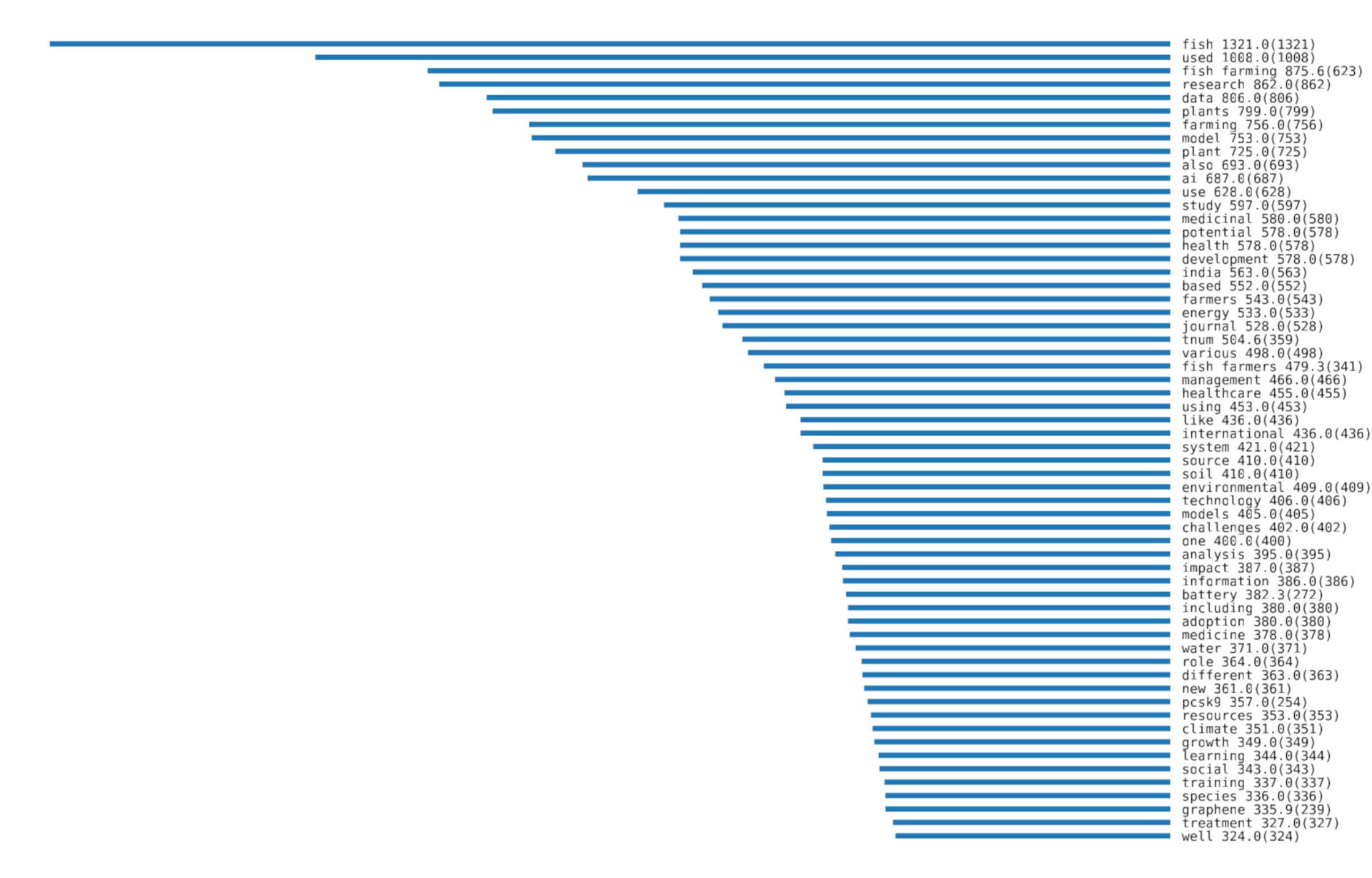
Finding 3: Google Scholar presents results from quality-controlled and non-controlled citation databases on the same interface, providing unfiltered access to GPT-fabricated questionable papers.
Google Scholar’s central position in the publicly accessible scholarly communication infrastructure, as well as its lack of standards, transparency, and accountability in terms of inclusion criteria, has potentially serious implications for public trust in science. This is likely to exacerbate the already-known potential to exploit Google Scholar for evidence hacking (Tripodi et al., 2023) and will have implications for any attempts to retract or remove fraudulent papers from their original publication venues. Any solution must consider the entirety of the research infrastructure for scholarly communication and the interplay of different actors, interests, and incentives.
We searched and scraped Google Scholar using the Python library Scholarly (Cholewiak et al., 2023) for papers that included specific phrases known to be common responses from ChatGPT and similar applications with the same underlying model (GPT3.5 or GPT4): “as of my last knowledge update” and/or “I don’t have access to real-time data” (see Appendix A). This facilitated the identification of papers that likely used generative AI to produce text, resulting in 227 retrieved papers. The papers’ bibliographic information was automatically added to a spreadsheet and downloaded into Zotero. 6 An open-source reference manager, https://zotero.org .
We employed multiple coding (Barbour, 2001) to classify the papers based on their content. First, we jointly assessed whether the paper was suspected of fraudulent use of ChatGPT (or similar) based on how the text was integrated into the papers and whether the paper was presented as original research output or the AI tool’s role was acknowledged. Second, in analyzing the content of the papers, we continued the multiple coding by classifying the fraudulent papers into four categories identified during an initial round of analysis—health, environment, computing, and others—and then determining which subjects were most affected by this issue (see Table 1). Out of the 227 retrieved papers, 88 papers were written with legitimate and/or declared use of GPTs (i.e., false positives, which were excluded from further analysis), and 139 papers were written with undeclared and/or fraudulent use (i.e., true positives, which were included in further analysis). The multiple coding was conducted jointly by all authors of the present article, who collaboratively coded and cross-checked each other’s interpretation of the data simultaneously in a shared spreadsheet file. This was done to single out coding discrepancies and settle coding disagreements, which in turn ensured methodological thoroughness and analytical consensus (see Barbour, 2001). Redoing the category coding later based on our established coding schedule, we achieved an intercoder reliability (Cohen’s kappa) of 0.806 after eradicating obvious differences.
The ranking algorithm of Google Scholar prioritizes highly cited and older publications (Martín-Martín et al., 2016). Therefore, the position of the articles on the search engine results pages was not particularly informative, considering the relatively small number of results in combination with the recency of the publications. Only the query “as of my last knowledge update” had more than two search engine result pages. On those, questionable articles with undeclared use of GPTs were evenly distributed across all result pages (min: 4, max: 9, mode: 8), with the proportion of undeclared use being slightly higher on average on later search result pages.
To understand how the papers making fraudulent use of generative AI were disseminated online, we programmatically searched for the paper titles (with exact string matching) in Google Search from our local IP address (see Appendix B) using the googlesearch – python library(Vikramaditya, 2020). We manually verified each search result to filter out false positives—results that were not related to the paper—and then compiled the most prominent URLs by field. This enabled the identification of other platforms through which the papers had been spread. We did not, however, investigate whether copies had spread into SciHub or other shadow libraries, or if they were referenced in Wikipedia.
We used descriptive statistics to count the prevalence of the number of GPT-fabricated papers across topics and venues and top domains by subject. The pandas software library for the Python programming language (The pandas development team, 2024) was used for this part of the analysis. Based on the multiple coding, paper occurrences were counted in relation to their categories, divided into indexed journals, non-indexed journals, student papers, and working papers. The schemes, subdomains, and subdirectories of the URL strings were filtered out while top-level domains and second-level domains were kept, which led to normalizing domain names. This, in turn, allowed the counting of domain frequencies in the environment and health categories. To distinguish word prominences and meanings in the environment and health-related GPT-fabricated questionable papers, a semantically-aware word cloud visualization was produced through the use of a word rain (Centre for Digital Humanities Uppsala, 2023) for full-text versions of the papers. Font size and y-axis positions indicate word prominences through TF-IDF scores for the environment and health papers (also visualized in a separate bar chart with raw term frequencies in parentheses), and words are positioned along the x-axis to reflect semantic similarity (Skeppstedt et al., 2024), with an English Word2vec skip gram model space (Fares et al., 2017). An English stop word list was used, along with a manually produced list including terms such as “https,” “volume,” or “years.”
- Artificial Intelligence
- / Search engines
Cite this Essay
Haider, J., Söderström, K. R., Ekström, B., & Rödl, M. (2024). GPT-fabricated scientific papers on Google Scholar: Key features, spread, and implications for preempting evidence manipulation. Harvard Kennedy School (HKS) Misinformation Review . https://doi.org/10.37016/mr-2020-156
- / Appendix B
Bibliography
Antkare, I. (2020). Ike Antkare, his publications, and those of his disciples. In M. Biagioli & A. Lippman (Eds.), Gaming the metrics (pp. 177–200). The MIT Press. https://doi.org/10.7551/mitpress/11087.003.0018
Barbour, R. S. (2001). Checklists for improving rigour in qualitative research: A case of the tail wagging the dog? BMJ , 322 (7294), 1115–1117. https://doi.org/10.1136/bmj.322.7294.1115
Bom, H.-S. H. (2023). Exploring the opportunities and challenges of ChatGPT in academic writing: A roundtable discussion. Nuclear Medicine and Molecular Imaging , 57 (4), 165–167. https://doi.org/10.1007/s13139-023-00809-2
Cabanac, G., & Labbé, C. (2021). Prevalence of nonsensical algorithmically generated papers in the scientific literature. Journal of the Association for Information Science and Technology , 72 (12), 1461–1476. https://doi.org/10.1002/asi.24495
Cabanac, G., Labbé, C., & Magazinov, A. (2021). Tortured phrases: A dubious writing style emerging in science. Evidence of critical issues affecting established journals . arXiv. https://doi.org/10.48550/arXiv.2107.06751
Carrion, M. L. (2018). “You need to do your research”: Vaccines, contestable science, and maternal epistemology. Public Understanding of Science , 27 (3), 310–324. https://doi.org/10.1177/0963662517728024
Centre for Digital Humanities Uppsala (2023). CDHUppsala/word-rain [Computer software]. https://github.com/CDHUppsala/word-rain
Chinn, S., & Hasell, A. (2023). Support for “doing your own research” is associated with COVID-19 misperceptions and scientific mistrust. Harvard Kennedy School (HSK) Misinformation Review, 4 (3). https://doi.org/10.37016/mr-2020-117
Cholewiak, S. A., Ipeirotis, P., Silva, V., & Kannawadi, A. (2023). SCHOLARLY: Simple access to Google Scholar authors and citation using Python (1.5.0) [Computer software]. https://doi.org/10.5281/zenodo.5764801
Dadkhah, M., Lagzian, M., & Borchardt, G. (2017). Questionable papers in citation databases as an issue for literature review. Journal of Cell Communication and Signaling , 11 (2), 181–185. https://doi.org/10.1007/s12079-016-0370-6
Dadkhah, M., Oermann, M. H., Hegedüs, M., Raman, R., & Dávid, L. D. (2023). Detection of fake papers in the era of artificial intelligence. Diagnosis , 10 (4), 390–397. https://doi.org/10.1515/dx-2023-0090
DeGeurin, M. (2024, March 19). AI-generated nonsense is leaking into scientific journals. Popular Science. https://www.popsci.com/technology/ai-generated-text-scientific-journals/
Dunlap, R. E., & Brulle, R. J. (2020). Sources and amplifiers of climate change denial. In D.C. Holmes & L. M. Richardson (Eds.), Research handbook on communicating climate change (pp. 49–61). Edward Elgar Publishing. https://doi.org/10.4337/9781789900408.00013
Fares, M., Kutuzov, A., Oepen, S., & Velldal, E. (2017). Word vectors, reuse, and replicability: Towards a community repository of large-text resources. In J. Tiedemann & N. Tahmasebi (Eds.), Proceedings of the 21st Nordic Conference on Computational Linguistics (pp. 271–276). Association for Computational Linguistics. https://aclanthology.org/W17-0237
Google Scholar Help. (n.d.). Inclusion guidelines for webmasters . https://scholar.google.com/intl/en/scholar/inclusion.html
Gu, J., Wang, X., Li, C., Zhao, J., Fu, W., Liang, G., & Qiu, J. (2022). AI-enabled image fraud in scientific publications. Patterns , 3 (7), 100511. https://doi.org/10.1016/j.patter.2022.100511
Gusenbauer, M., & Haddaway, N. R. (2020). Which academic search systems are suitable for systematic reviews or meta-analyses? Evaluating retrieval qualities of Google Scholar, PubMed, and 26 other resources. Research Synthesis Methods , 11 (2), 181–217. https://doi.org/10.1002/jrsm.1378
Haider, J., & Åström, F. (2017). Dimensions of trust in scholarly communication: Problematizing peer review in the aftermath of John Bohannon’s “Sting” in science. Journal of the Association for Information Science and Technology , 68 (2), 450–467. https://doi.org/10.1002/asi.23669
Huang, J., & Tan, M. (2023). The role of ChatGPT in scientific communication: Writing better scientific review articles. American Journal of Cancer Research , 13 (4), 1148–1154. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10164801/
Jones, N. (2024). How journals are fighting back against a wave of questionable images. Nature , 626 (8000), 697–698. https://doi.org/10.1038/d41586-024-00372-6
Kitamura, F. C. (2023). ChatGPT is shaping the future of medical writing but still requires human judgment. Radiology , 307 (2), e230171. https://doi.org/10.1148/radiol.230171
Littell, J. H., Abel, K. M., Biggs, M. A., Blum, R. W., Foster, D. G., Haddad, L. B., Major, B., Munk-Olsen, T., Polis, C. B., Robinson, G. E., Rocca, C. H., Russo, N. F., Steinberg, J. R., Stewart, D. E., Stotland, N. L., Upadhyay, U. D., & Ditzhuijzen, J. van. (2024). Correcting the scientific record on abortion and mental health outcomes. BMJ , 384 , e076518. https://doi.org/10.1136/bmj-2023-076518
Lund, B. D., Wang, T., Mannuru, N. R., Nie, B., Shimray, S., & Wang, Z. (2023). ChatGPT and a new academic reality: Artificial Intelligence-written research papers and the ethics of the large language models in scholarly publishing. Journal of the Association for Information Science and Technology, 74 (5), 570–581. https://doi.org/10.1002/asi.24750
Martín-Martín, A., Orduna-Malea, E., Ayllón, J. M., & Delgado López-Cózar, E. (2016). Back to the past: On the shoulders of an academic search engine giant. Scientometrics , 107 , 1477–1487. https://doi.org/10.1007/s11192-016-1917-2
Martín-Martín, A., Thelwall, M., Orduna-Malea, E., & Delgado López-Cózar, E. (2021). Google Scholar, Microsoft Academic, Scopus, Dimensions, Web of Science, and OpenCitations’ COCI: A multidisciplinary comparison of coverage via citations. Scientometrics , 126 (1), 871–906. https://doi.org/10.1007/s11192-020-03690-4
Simon, F. M., Altay, S., & Mercier, H. (2023). Misinformation reloaded? Fears about the impact of generative AI on misinformation are overblown. Harvard Kennedy School (HKS) Misinformation Review, 4 (5). https://doi.org/10.37016/mr-2020-127
Skeppstedt, M., Ahltorp, M., Kucher, K., & Lindström, M. (2024). From word clouds to Word Rain: Revisiting the classic word cloud to visualize climate change texts. Information Visualization , 23 (3), 217–238. https://doi.org/10.1177/14738716241236188
Swedish Research Council. (2017). Good research practice. Vetenskapsrådet.
Stokel-Walker, C. (2024, May 1.). AI Chatbots Have Thoroughly Infiltrated Scientific Publishing . Scientific American. https://www.scientificamerican.com/article/chatbots-have-thoroughly-infiltrated-scientific-publishing/
Subbaraman, N. (2024, May 14). Flood of fake science forces multiple journal closures: Wiley to shutter 19 more journals, some tainted by fraud. The Wall Street Journal . https://www.wsj.com/science/academic-studies-research-paper-mills-journals-publishing-f5a3d4bc
The pandas development team. (2024). pandas-dev/pandas: Pandas (v2.2.2) [Computer software]. Zenodo. https://doi.org/10.5281/zenodo.10957263
Thorp, H. H. (2023). ChatGPT is fun, but not an author. Science , 379 (6630), 313–313. https://doi.org/10.1126/science.adg7879
Tripodi, F. B., Garcia, L. C., & Marwick, A. E. (2023). ‘Do your own research’: Affordance activation and disinformation spread. Information, Communication & Society , 27 (6), 1212–1228. https://doi.org/10.1080/1369118X.2023.2245869
Vikramaditya, N. (2020). Nv7-GitHub/googlesearch [Computer software]. https://github.com/Nv7-GitHub/googlesearch
This research has been supported by Mistra, the Swedish Foundation for Strategic Environmental Research, through the research program Mistra Environmental Communication (Haider, Ekström, Rödl) and the Marcus and Amalia Wallenberg Foundation [2020.0004] (Söderström).
Competing Interests
The authors declare no competing interests.
The research described in this article was carried out under Swedish legislation. According to the relevant EU and Swedish legislation (2003:460) on the ethical review of research involving humans (“Ethical Review Act”), the research reported on here is not subject to authorization by the Swedish Ethical Review Authority (“etikprövningsmyndigheten”) (SRC, 2017).
This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided that the original author and source are properly credited.
Data Availability
All data needed to replicate this study are available at the Harvard Dataverse: https://doi.org/10.7910/DVN/WUVD8X
Acknowledgements
The authors wish to thank two anonymous reviewers for their valuable comments on the article manuscript as well as the editorial group of Harvard Kennedy School (HKS) Misinformation Review for their thoughtful feedback and input.

IMAGES
VIDEO
COMMENTS
The COVID-19 pandemic has led the world to undertake the largest vaccination campaign in human history. In record time, unprecedented scientific and governmental efforts have resulted in the acquisition of immunizers utilizing different technologies (nucleotide ...
COVID-19 vaccination has substantially altered the course of the pandemic, saving tens of millions of lives globally. However, inadequate access to vaccines in low-income countries has limited the impact in these settings, reinforcing the need for global vaccine equity and coverage.
The COVID-19 pandemic is unlikely to end until there is global roll-out of vaccines that protect against severe disease and preferably drive herd immunity. Regulators in numerous countries have authorised or approved COVID-19 vaccines for human use, with ...
The Covid pandemic has posed substantial challenges to societies and health systems globally. Many of these challenges have been technical, such as the development of effective vaccines and therapies.
As the world waits for a vaccine to defeat the COVID-19 pandemic, we look back to all that vaccines have achieved for humanity.
The Covid-19 pandemic—and its social and economic fallout—has thrust social and health-related inequalities into the spotlight. The pandemic, and our response to it, has induced new ...
The pandemic has likely increased deaths from other causes due to disruption to health service delivery and routine immunizations, fewer people seeking care, and shortages of funding for non-COVID-19 services.
Correlating globalization with the impact of the discovery of vaccines, it is stated that when facing a pandemic, humanity takes sustained efforts to accelerate the development of such products 15.
A Guide to Global COVID-19 Vaccine Efforts The swift development of effective vaccines against COVID-19 was an unprecedented scientific achievement. But production challenges, vaccine nationalism ...
In the context of the COVID-19 pandemic, global vaccine campaigns are a mass vaccination intervention conducted through routine service provision for individuals who have reached a specified age.
Vaccines are a major public health success story, but the COVID-19 pandemic underscores the many challenges involved in getting a vaccine to everyone who needs it.
COVID-19 vaccination is offering a way to end the COVID-19 pandemic if a response is coordinated globally.
pandemic. Following the approval of the first COVID-19 vaccine, several other COVID-19 vaccines were approved for emergency use by countries across the world. The approval of these vaccines led to the launch of a global campaign to vaccinate people to protect from COVID-19 infection.
The COVID-19 pandemic continues to pose a serious public health threat to nations around the world, as effective antiviral therapeutics or vaccines are yet to be developed.
Collaborative strategies are also needed to ensure equitable access to vaccines, medicines, and other essential supplies, including sharing the know-how and tools to expand global production capacities. Common standards, incentives, and enforcement mechanisms are needed to improve pandemic preparedness and response for the future.
Introduction The COVID-19 pandemic catalyzed unprecedented vaccine innovation, revealing critical shortcomings in achieving equitable vaccine access and underscoring the need for a focused review of the lessons learned to inform future pandemic preparedness, with emphasis on vaccine delivery, equity, and challenges in LMICs.
Vaccination is a simple, safe, and effective way of protecting people against harmful diseases, before they come into contact with them. It uses your body's natural defences to build resistance to specific infections and makes your immune system stronger.
Global change, including climate change, urbanization and global travel and trade, has affected the emergence and spread of infectious diseases. In the Review, Baker, Metcalf and colleagues ...
The coronavirus disease (COVID-19) threat is subsiding through extensive vaccination worldwide. However, the pandemic imposed major disruptions in global immunization programs and has aggravated the risks of vaccine-preventable disease (VPD) outbreaks. Particularly, lower-middle-income regions with minimal vaccine coverage and circulating ...
Effective and safe COVID-19 vaccines have been developed at a rapid and unprecedented pace to control the spread of the virus, and prevent hospitalisations and deaths. However, COVID-19 vaccine uptake is challenged by vaccine hesitancy and anti-vaccination sentiments, a global shortage of vaccine supply, and inequitable vaccine distribution especially among low- and middle-income countries ...
Abstract In this chapter, the global epidemiological events causing infections that ravaged humanity throughout its existence by bringing hardship to rich and poor nations alike are aggregated and presented. Among these, the largest known epidemics including the recent COVID-19 pandemic will be highlighted along with the analysis of the actual and common reason behind the occurring of all the ...
Introduction. The COVID-19 pandemic, which emerged out of Wuhan China at the end of 2019 (Spiteri et al., Citation 2020) had a profound impact on the world, triggering the largest global economic crisis in more than a century (Wade, Citation 2023).It saw health services throughout the world being overwhelmed, resulting in an estimated 18 million deaths by the end of 2021 (OECD, Citation 2023 ...
Companies aim to develop a multi-valent candidate vaccine to address emerging variants for pandemic and endemic use; Development to begin immediately targeting vaccine availability in 2022, subject to regulatory approval; GSK will also support manufacture of up to 100 million doses of CureVac's first generation COVID-19 vaccine CVnCoV in 2021
Lessons from the COVID-19 response and pandemic influenza preparedness underscore the importance of strengthening surveillance systems, investing in early-stage research on pandemic pathogens and ...
The coronavirus disease 2019 (COVID-19) pandemic is a global outbreak of coronavirus - an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Cases of novel coronavirus (nCoV) were first detected in China in December 2019, with the virus spreading rapidly to other countries across the world.
Wastewater surveillance holds great promise as a sensitive method to detect spillover of zoonotic infections and early pandemic emergence, thereby informing risk mitigation and public health response. Known viruses with pandemic potential are shed in human stool or urine, or both, and the experiences with SARS-CoV-2, monkeypox virus, and Zika virus highlight the feasibility of community-based ...
A similar strategy is successful in the alternative epistemic world of the global anti-vaccination movement (Carrion, 2018) and the persistence of flawed and questionable publications in the scientific record already poses significant problems for health research, policy, and lawmakers, and thus for society as a whole (Littell et al., 2024).