Essay on Coronavirus Prevention
500+ words essay on coronavirus prevention.
The best way of coronavirus prevention is not getting it in the first place. After extensive research, there are now COVID-19 vaccines available to the public. Everyone must consider getting it to lead healthy lives. Further, we will look at some ways in this essay in how one can lower their chances of getting the virus or stopping it from spreading.


The Spread of Coronavirus
The COVID-19 virus spreads mainly via droplets that are sent out by people while talking, sneezing, or coughing. However, they do not generally stay in the air for long. Similarly, they cannot go farther than 6 feet.
However, this virus can also travel via tiny aerosol particles that have the capacity to linger for around three hours. Likewise, they may also travel farther away. Therefore, it is essential to wear a face covering.
The face mask can prevent you from getting the virus as it helps you to avoid breathing it in. Further, one can also catch this virus if they touch something that an infected person has touched and then they touch their eyes, mouth, or nose.
Get the huge list of more than 500 Essay Topics and Ideas
How to Prevent Coronavirus
The first and foremost thing for coronavirus prevention is that everyone must do is get the vaccine as soon as it is their turn. It helps you avoid the virus or prevent you from falling seriously ill. Apart from this, we must not forget to take other steps as well to reduce the risk of getting the virus.
It includes avoiding close contact with people who are sick or are showing symptoms. Make sure you are at least 6 feet away from them. Similarly, you also remain at the same distance as others if you have contracted the virus.
What’s important to know is that you may have COVID-19 and spread it to others even if you are not showing any symptoms or aren’t aware that you have COVID-19. Moreover, we must avoid crowds and indoor places that are not well-ventilated.
Most importantly, keep washing your hands frequently with soap and water. If these are not present, carry an alcohol-based sanitiser with you. It must have a minimum amount of 60% alcohol.
In addition, wearing a face mask is of utmost importance in public spaces. Such places come with a higher risk of transmission of the virus. Thus, use surgical masks if they are available.
It is important to cover your mouth and nose when you are coughing or sneezing. If you don’t have a tissue, cover it with your elbow. Do not touch your eyes, nose and mouth. Likewise, do not share dishes, towels, glasses and other household items with a sick person.
Do not forget to clean and disinfect surfaces that people touch frequently like electronics, switchboards, counters, doorknobs, and more. Also, stay at home if you feel sick and do not take public transport as well.
To sum it up, coronavirus prevention can be done easily. We must work together to create a safe environment for everyone to live healthily. Make sure to do your bit so that everyone can stay safe and fit and things may return to normal like before.
FAQ of Essay on Coronavirus Prevention
Question 1: How long does it take for coronavirus symptoms to appear?
Answer 1: It may take around five to six days on average when someone gets infected with the virus. But, some people also take around 14 days.
Question 2: What are some coronavirus prevention tips?
Answer 2: One must get the vaccine as soon as possible. Further, always wear a mask properly and sanitize or wash your hands. Clean or disinfect areas that people touch frequently like door handles, electronics, and more. Always cover your mouth when sneezing or coughing and maintain physical distancing.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

The 12 Best COVID-19 Prevention Strategies
BY CARRIE MACMILLAN , JEREMY LEDGER October 12, 2020

Note: Information in this article was accurate at the time of original publication. Because information about COVID-19 changes rapidly, we encourage you to visit the websites of the Centers for Disease Control & Prevention (CDC), World Health Organization (WHO), and your state and local government for the latest information.
It’s been many months since COVID-19 upended our lives. We’ve adjusted to wearing masks, social distancing, constantly our washing hands , and working and learning remotely . But what do we really know about how to prevent COVID-19 infection ?
Scientists, doctors, and public health officials are still trying to fully understand how the virus spreads, what to do to prevent it, and the best ways to treat it. New findings sometimes lead to advice that conflicts with what we’ve been told previously—and it can be a challenge to keep track of it all. Fortunately, there is plenty of solid advice we can still follow.
“It can be really exhausting to be constantly vigilant and to take precautions, like wearing a mask and physically distancing, which may be physically and emotionally uncomfortable,” says Jaimie Meyer, MD, MS , a Yale Medicine infectious disease expert. “But sustaining these types of behaviors is really key to curbing this pandemic, especially before a vaccine is available.”
Plus, cooler weather is bringing more of us indoors, which is riskier than being outside because there is less airflow and it can be more difficult to keep people 6 feet apart. What’s more, says Dr. Meyer, there’s the possibility that SARS-CoV-2 , the virus that causes COVID-19, is airborne, making ventilation even more important.
The upcoming months also bring seasonal respiratory viruses, like cold and flu , leading to concern about the possibility of a “twindemic” that may overwhelm health care systems already spread thin by COVID-19. These other illnesses can bring confusion because symptoms are very similar to those of COVID-19.
Meanwhile, COVID-19 remains with us, resulting in more than 210,000 deaths in the U.S. to date. As we leave a chaotic spring and summer behind and head into fall, now is a good time to check in with Yale Medicine experts and review the standard—and most recent—advice on how to stay safe.
1. Wear your mask
Wearing a mask that covers your mouth and nose can prevent those who have COVID-19 from spreading the virus to others. Recent evidence suggests that masks may even benefit the wearer, offering some level of protection against infections.
The Centers for Disease Control and Prevention (CDC) recommends that everyone age 2 years and older wear masks in public settings and around people who don’t live in the same household—when you can’t stay 6 feet apart from others.
Masks should be made of two or more layers of washable, breathable fabric and fit snugly on your face. “A quick and easy test is to hold your mask up to the light. If light passes through, it’s too thin,” Dr. Meyer says. “Masks only work when they cover the nose and mouth because that is where infected droplets are expelled and because the virus infects people through the mucous membranes in their nose and throat.”
2. Stay socially distant
COVID-19 spreads mainly among people who are within 6 feet of one another (about two arms’ length) for a prolonged period (at least 15 minutes). Virus transmission can occur when an infected person coughs, sneezes, or talks, which releases droplets from the mouth or nose into the air.
People can be asymptomatic and spread the virus without knowing that they are sick, which makes it especially important to remain 6 feet away from others, whether you are inside or outside. Plus, the more people you interact with at a gathering and the longer time you spend interacting with each, the higher your risk of becoming infected with the virus by someone who has it.
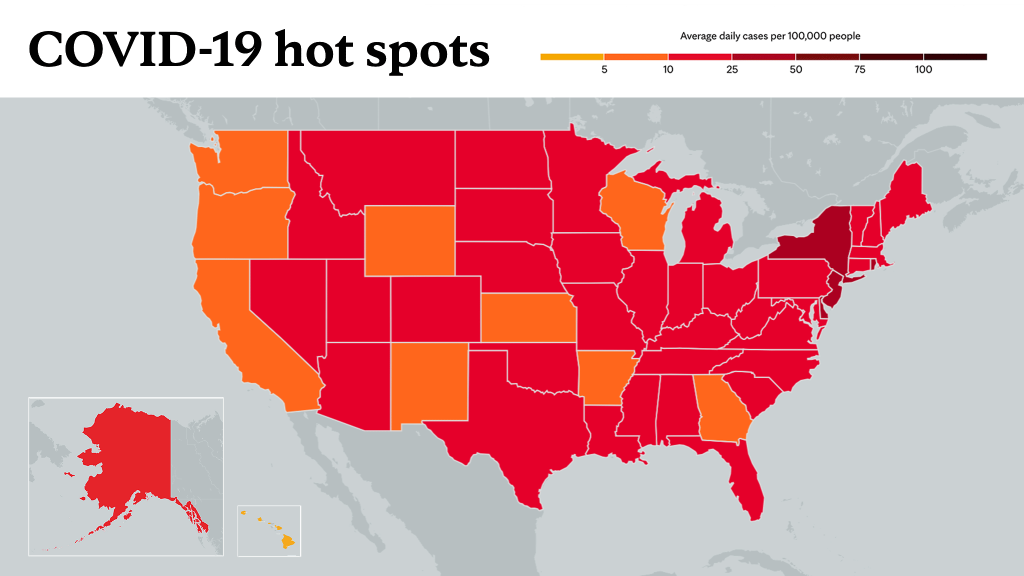
If you are attending an event or gathering of some kind, it’s also important to be aware of the level of community transmission. One method of estimating how high the risk may be is referred to as R 0.
“Pronounced ‘R naught,’ and also known as the reproduction number, this is a measure of how fast a disease is spreading,” explains Onyema Ogbuagu, MBBCh , a Yale Medicine infectious disease expert. “If the reproduction number is 5.0, that means one infected person will spread the virus to an average of five people. Therefore, the lower the rate, the safer it is.”
The R 0 for COVID-19 is believed to be in the range of 1.4 to 2.9. For comparison, measles, which has the highest reproduction number known among humans, ranges from 12 to 18. Seasonal influenza is around 0.9 and 2.1.
While R 0 refers to the basic, or initial, reproduction number, there is another measurement called R t, which is the current reproduction number and is the average number of people who become infected by an infectious person. If R t is above 1.0, it spreads quickly. If it’s below 1.0, it will eventually stop spreading. You can check the number for each state here .
3. Keep washing your hands
Washing your hands—and well—remains a key step to preventing COVID-19 infection. Wash your hands with soap often, and especially after you have been in a public place or have blown your nose, coughed, or sneezed, the CDC recommends.
You should wash your hands for at least 20 seconds and lather the back of your hands and scrub between all fingers, under all fingernails, and reach up to the wrist, the CDC advises. After washing, dry them completely (with an air dryer or paper towel) and avoid touching the sink, faucet, door handles, or other objects. If no soap is available, use a hand sanitizer with at least 60% alcohol content, and rub the sanitizer on your hands until they are dry.
Though the CDC states that the primary way the virus spreads is through close person-to-person contact, it may be possible to become infected with COVID-19 by touching a surface or object that has the virus on it and then touching your own mouth, nose, or eyes.
Therefore, you should also wash your hands after touching anything that may have been contaminated—such as a banister or door handle in a public place—and before you touch your face.
While the virus can survive for a short period on some surfaces, it is unlikely to be spread from mail or from products or packaging, the CDC says. Likewise, the risk of infection from food (that you cook, is prepared in a restaurant, or is ordered via takeout) is considered to be very low, as is the risk from food packaging or bags.
Still, there is much that is unknown about the virus, and it remains advisable to wash hands thoroughly after handling any food or products that come into your home.
4. Keep holiday gatherings small
Fall and winter also bring holidays, when many families get together. This can be especially tricky for those of us who live in parts of the country where it will no longer be easy to gather outside. “After months apart during this pandemic, families may be less willing to do a group Zoom call,” says Dr. Meyer. “This may be a year where we need to get creative and rethink how to celebrate together.”
That may simply mean more planning for the holidays, Dr. Meyer says. “Consider quarantining for 14 days prior to the event and/or having everyone get tested for COVID-19 if tests are available in your community,” she suggests. “If possible, limit gatherings to as few people as possible—perhaps just immediate family and close friends. When it is not possible to be outside, encourage your guests to wear masks indoors. Consider spreading out food and eating areas so people are distanced while eating with their masks down.”
Remember that your elderly family members and those with other medical conditions are most vulnerable to COVID-19, so take extra measures to protect them, says Dr. Meyer.
5. Dine out carefully
Although many restaurants offer outdoor dining, which experts say is the safer option, a recent CDC study showed that adults with COVID-19 infections were twice as likely to have visited a restaurant in the two weeks preceding their illness than those without an infection.
The study did not distinguish between indoor or outdoor dining, or consider adherence to social distancing and mask use. (Those with COVID-19 infections were more likely to report having dined out at places where few other people were wearing masks or socially distancing.)
“If you are meeting with others at a restaurant and sharing tables while eating, which does not allow for appropriate social distancing and mask use, it provides opportunities for the virus to spread from person to person,” Dr. Ogbuagu notes. “The probability of spreading infection is higher with each additional person you are in contact with, especially when people congregate.”
6. Travel safely
While you should avoid traveling if you can—as the CDC says staying home is the best way to avoid COVID-19—sometimes, it is necessary. But before you leave, you can check to see if the virus is spreading at your destination. More cases at your destination increases your risk of contracting the virus and spreading it to others. You can view each state’s weekly number of cases here on the CDC web site.
“Also, don’t forget to check the regulations for quarantining or testing at your destination or for when you return home,” says Dr. Meyer. Whether you are traveling by car, plane, bus, or train, there are precautions you can take along the way. The CDC has a detailed list of recommendations for each mode of transportation that mostly follows the advice listed above of practicing social distancing, wearing a mask, and washing hands, but also includes specific advice for various scenarios.
7. Get your flu shot
Health officials are concerned about an influx of flu and COVID-19 cases overwhelming hospitals. In the 2018-2019 flu season, 490,600 Americans were hospitalized for the flu, according to the CDC.
Public health experts say this is not the year to skip the flu vaccine. While measures to prevent COVID-19, including mask-wearing, washing hands, and social distancing, can also protect against the flu, the vaccine is especially important—and safe, doctors say.
Though many people claim that the flu shot “gave them the flu,” it is not possible to get infected with the influenza virus from the vaccine itself, Dr. Meyer says. “The vaccine is made up of inactivated virus and is designed to ‘tickle’ the immune system to respond to the real thing when it sees it,” she explains. “The most common side effect from the flu shot is soreness or redness at the site of the injection, which resolves within a day or two.”
The flu vaccine is recommended for everyone 6 months old and up. Talk to your doctor about finding a vaccine near you.
8. Differentiate between flu, colds, and COVID-19
Many people will likely struggle to differentiate between the flu, the common cold, and COVID-19, all of which have similar symptoms.
For example, both COVID-19 and the flu can cause fever, shortness of breath, fatigue, headache, cough, sore throat, runny nose, muscle pain, or body aches, as well as vomiting and diarrhea (though these last two are more common in children). Meanwhile, colds may be milder than the flu and are more likely to involve a runny or stuffy nose. One difference, however, is that COVID-19 is associated with a loss of taste and smell .
So, if you or someone in your family comes down with any of these symptoms, what should you do?
“First, you should stay away from others as much as possible and perform hand washing before you make contact with your face,” Dr. Ogbuagu says. “And certainly go see a doctor or to the hospital if you have serious symptoms, such as a high fever or shortness of breath. Otherwise, getting a COVID-19 test at a testing facility near you would help to define what type of respiratory illness you have and also how to advise people you had been in contact with.”
Parents, Dr. Meyer adds, will need to contact their children’s pediatricians about these symptoms because otherwise their children likely won’t be able to return to school.
“I would also add that people who are older and have underlying medical conditions should have a low threshold to seek care for any of these symptoms,” she says. “Earlier is better, especially for influenza, as we have antiviral medications that work if given within 72 hours of the onset of symptoms.”
9. Seek routine medical care
You should continue to seek any routine or emergency medical care or treatments you need. Many health centers and doctors are offering telehealth appointments (via video or phone) and most have protocols to minimize risk of exposure to the coronavirus.
Getting emergency care when you need it is especially important. Earlier in the pandemic, pediatric and adult physicians reported fewer emergency department visits, leading to a concern that patients were avoiding seeking care due to fears of contracting COVID-19.
“As important as it is to continue to engage in care for known medical issues, there is also a concern that people are falling behind on their preventive healthcare, like getting routine procedures including colonoscopies and pap smears, as well as vaccines,” Dr. Meyer says. “Those other health issues don’t go away just because there is a pandemic. Reach out to your primary care doctor if you’re unsure what you are due to receive.”
10. Be mindful of your mental health
Many people are experiencing anxiety, depression, and other mental health issues during the pandemic as it is a time of stress and uncertainty. All of this is normal, say mental health experts, who recommend that you allow yourself to embrace all emotions, including those that are unpleasant, in order to better manage them.
Experts advise limiting exposure to news if the events of the world are too much right now, practicing mindfulness (even just breathing exercises), eating healthy, and remaining physically active.
For kids, who are still adjusting to a lack of play dates, canceled activities, and different school schedules, parents can help by fully listening to their concerns and providing age-appropriate answers to their questions. By talking with kids about what they know and how they are doing, parents may be able to determine if further emotional support is needed.
11. Watch your weight
At a time when routines are disrupted and many people are working at home—where snacks are readily available—some may be gaining weight (the so-called quarantine 15). Now more than ever, Yale Medicine doctors recommend that you focus on eating a healthy diet, incorporating regular exercise, getting good sleep, and finding healthy ways to manage stress.
Meanwhile, obesity is emerging as an independent risk factor for severe COVID-19 illness—even among younger patients. One study, which examined hospitalized COVID-19 patients under age 60, found that those with obesity were twice as likely to require hospitalization and even more likely to need critical care than those who did not have it. Given that an estimated 42% of Americans have obesity (having a body mass index equal to or more than 30), this is important.
12. Keep up the good (safety) work
It is likely that COVID-19 will be with us for a while. “But with good efforts to continue to follow the public health measures to protect each other, and, hopefully, a successful vaccine in the future, there is a light at the end of the tunnel,” Dr. Ogbuagu says.
But even before a safe and effective vaccine is available, COVID-19 is a preventable disease, Dr. Meyer points out. “It just requires all of us to do the hard work of practicing the behaviors—described above—to keep our communities safe and healthy.”
Note: Information provided in Yale Medicine articles is for general informational purposes only. No content in the articles should ever be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider with any questions you have regarding a medical condition.
More news from Yale Medicine
The new covid-19 vaccine: answers to all the hard questions.

Ketamine for Depression: How It Works
The Updated COVID Vaccines Are Here: 9 Things to Know

- Português Br
- Journalist Pass
Importance of preventive health care during COVID-19 pandemic
Jason Howland
Share this:

Preventive health care helps you maintain your health. Screenings are important to avoid future health problems or catch them early when they are easier to treat. But the COVID-19 pandemic has led to a decrease in preventive screenings because some patients have been hesitant to see their health care provider.
"People are driven to seek medical care by pain. Pain is a strong driver to get relief. And since prevention is when you are without symptoms, people tend to put that on the back burner or they may feel unsafe to come in because of the uncertainty about COVID-19," says Dr. Cindy Kermott , a Mayo Clinic preventive medicine physician. "We know enough now about COVID-19, and we have personal protective equipment. We also have vaccines that have been available for health care workers now, and essentially all have been offered it. And it is safe to come in to get these preventive screens and vaccines done."
Watch: Dr. Cindy Kermott discusses the importance of preventive health care.
Journalists: Broadcast-quality sound bites with Dr. Kermott are available in the downloads at the end of the post. Please courtesy: "Cindy Kermott, M.D./Preventive Medicine/Mayo Clinic."
The U.S. Preventive Services Task Force recommends many evidence-based preventive screenings. The most common for older men are prostate cancer and abdominal aortic aneurysm screenings. Women should schedule Pap smears to check for cervical cancer and mammograms to detect breast cancer.
Other important preventive health measures for every adult include:
- Vaccinations
- Colorectal cancer screening
- Checking cholesterol levels
- Blood pressure screening
- Testing blood glucose levels for diabetes
The timing and frequency of these screenings depend on your age and risk factors, and most are covered by your insurance.
"A screen is just a tool to detect the disease earlier," says Dr. Kermott. "It could be a lab. It could be vital signs. It could be questions — a survey instrument for depression, for example. It could be taking a family history and finding clues for genetics because some genetic testing is covered as a screen. And sometimes we do imaging, such as bone density or colonoscopy and endoscopy to detect things."
Whether you're nervous about COVID-19 safety or simply putting off your next trip for care, don't delay in talking to your health care provider about scheduling your preventive health screenings.
"If we pick it up too late, then we don't have as good of a leg up on the situation. And we're hoping to intervene so that you can live longer and have more quality life years as a result of these screens," says Dr. Kermott.
_______________________________
For the safety of its patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was either recorded prior to COVID-19 or recorded in a nonpatient care area where social distancing and other safety protocols were followed.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org .
Learn more about tracking COVID-19 and COVID-19 trends .
- Consumer Health: Treating TB Expert alert: 5 tips for getting back into the game
Related Articles
Students’ Essays on Infectious Disease Prevention, COVID-19 Published Nationwide
As part of the BIO 173: Global Change and Infectious Disease course, Professor Fred Cohan assigns students to write an essay persuading others to prevent future and mitigate present infectious diseases. If students submit their essay to a news outlet—and it’s published—Cohan awards them with extra credit.
As a result of this assignment, more than 25 students have had their work published in newspapers across the United States. Many of these essays cite and applaud the University’s Keep Wes Safe campaign and its COVID-19 testing protocols.
Cohan, professor of biology and Huffington Foundation Professor in the College of the Environment (COE), began teaching the Global Change and Infectious Disease course in 2009, when the COE was established. “I wanted very much to contribute a course to what I saw as a real game-changer in Wesleyan’s interest in the environment. The course is about all the ways that human demands on the environment have brought us infectious diseases, over past millennia and in the present, and why our environmental disturbances will continue to bring us infections into the future.”
Over the years, Cohan learned that he can sustainably teach about 170 students every year without running out of interested students. This fall, he had 207. Although he didn’t change the overall structure of his course to accommodate COVID-19 topics, he did add material on the current pandemic to various sections of the course.
“I wouldn’t say that the population of the class increased tremendously as a result of COVID-19, but I think the enthusiasm of the students for the material has increased substantially,” he said.
To accommodate online learning, Cohan shaved off 15 minutes from his normal 80-minute lectures to allow for discussion sections, led by Cohan and teaching assistants. “While the lectures mostly dealt with biology, the discussions focused on how changes in behavior and policy can solve the infectious disease problems brought by human disturbance of the environment,” he said.
Based on student responses to an introspective exam question, Cohan learned that many students enjoyed a new hope that we could each contribute to fighting infectious disease. “They discovered that the solution to infectious disease is not entirely a waiting game for the right technologies to come along,” he said. “Many enjoyed learning about fighting infectious disease from a moral and social perspective. And especially, the students enjoyed learning about the ‘socialism of the microbe,’ how preventing and curing others’ infections will prevent others’ infections from becoming our own. The students enjoyed seeing how this idea can drive both domestic and international health policies.”
A sampling of the published student essays are below:
Alexander Giummo ’22 and Mike Dunderdale’s ’23 op-ed titled “ A National Testing Proposal: Let’s Fight Back Against COVID-19 ” was published in the Journal Inquirer in Manchester, Conn.
They wrote: “With an expansive and increased testing plan for U.S. citizens, those who are COVID-positive could limit the number of contacts they have, and this would also help to enable more effective contact tracing. Testing could also allow for the return of some ‘normal’ events, such as small social gatherings, sports, and in-person class and work schedules.
“We propose a national testing strategy in line with the one that has kept Wesleyan students safe this year. The plan would require a strong push by the federal government to fund the initiative, but it is vital to successful containment of the virus.
“Twice a week, all people living in the U.S. should report to a local testing site staffed with professionals where the anterior nasal swab Polymerase Chain Reaction (PCR) test, used by Wesleyan and supported by the Broad Institute, would be implemented.”
Kalyani Mohan ’22 and Kalli Jackson ’22 penned an essay titled “ Where Public Health Meets Politics: COVID-19 in the United States ,” which was published in Wesleyan’s Arcadia Political Review .
They wrote: “While the U.S. would certainly benefit from a strengthened pandemic response team and structural changes to public health systems, that alone isn’t enough, as American society is immensely stratified, socially and culturally. The politicization of the COVID-19 pandemic shows that individualism, libertarianism and capitalism are deeply ingrained in American culture, to the extent that Americans often blind to the fact community welfare can be equivalent to personal welfare. Pandemics are multifaceted, and preventing them requires not just a cultural shift but an emotional one amongst the American people, one guided by empathy—towards other people, different communities and the planet. Politics should be a tool, not a weapon against its people.”
Sydnee Goyer ’21 and Marcel Thompson’s ’22 essay “ This Flu Season Will Be Decisive in the Fight Against COVID-19 ” also was published in Arcadia Political Review .
“With winter approaching all around the Northern Hemisphere, people are preparing for what has already been named a “twindemic,” meaning the joint threat of the coronavirus and the seasonal flu,” they wrote. “While it is known that seasonal vaccinations reduce the risk of getting the flu by up to 60% and also reduce the severity of the illness after the contamination, additional research has been conducted in order to know whether or not flu shots could reduce the risk of people getting COVID-19. In addition to the flu shot, it is essential that people remain vigilant in maintaining proper social distancing, washing your hands thoroughly, and continuing to wear masks in public spaces.”
An op-ed titled “ The Pandemic Has Shown Us How Workplace Culture Needs to Change ,” written by Adam Hickey ’22 and George Fuss ’21, was published in Park City, Utah’s The Park Record .
They wrote: “One review of academic surveys (most of which were conducted in the United States) conducted in 2019 found that between 35% and 97% of respondents in those surveys reported having attended work while they were ill, often because of workplace culture or policy which generated pressure to do so. Choosing to ignore sickness and return to the workplace while one is ill puts colleagues at risk, regardless of the perceived severity of your own illness; COVID-19 is an overbearing reminder that a disease that may cause mild, even cold-like symptoms for some can still carry fatal consequences for others.
“A mandatory paid sick leave policy for every worker, ideally across the globe, would allow essential workers to return to work when necessary while still providing enough wiggle room for economically impoverished employees to take time off without going broke if they believe they’ve contracted an illness so as not to infect the rest of their workplace and the public at large.”

Women’s cross country team members and classmates Jane Hollander ’23 and Sara Greene ’23 wrote a sports-themed essay titled “ This Season, High School Winter Sports Aren’t Worth the Risk ,” which was published in Tap into Scotch Plains/Fanwood , based in Scotch Plains, N.J. Their essay focused on the risks high school sports pose on student-athletes, their families, and the greater community.
“We don’t propose cutting off sports entirely— rather, we need to be realistic about the levels at which athletes should be participating. There are ways to make practices safer,” they wrote. “At [Wesleyan], we began the season in ‘cohorts,’ so the amount of people exposed to one another would be smaller. For non-contact sports, social distancing can be easily implemented, and for others, teams can focus on drills, strength and conditioning workouts, and skill-building exercises. Racing sports such as swim and track can compete virtually, comparing times with other schools, and team sports can focus their competition on intra-team scrimmages. These changes can allow for the continuation of a sense of normalcy and team camaraderie without the exposure to students from different geographic areas in confined, indoor spaces.”
Brook Guiffre ’23 and Maddie Clarke’s ’22 op-ed titled “ On the Pandemic ” was published in Hometown Weekly, based in Medfield, Mass.
“The first case of COVID-19 in the United States was recorded on January 20th, 2020. For the next month and a half, the U.S. continued operating normally, while many other countries began their lockdown,” they wrote. “One month later, on February 29th, 2020, the federal government approved a national testing program, but it was too little too late. The U.S. was already in pandemic mode, and completely unprepared. Frontline workers lacked access to N-95 masks, infected patients struggled to get tested, and national leaders informed the public that COVID-19 was nothing more than the common flu. Ultimately, this unpreparedness led to thousands of avoidable deaths and long-term changes to daily life. With the risk of novel infectious diseases emerging in the future being high, it is imperative that the U.S. learn from its failure and better prepare for future pandemics now. By strengthening our public health response and re-establishing government organizations specialized in disease control, we have the ability to prevent more years spent masked and six feet apart.”
In addition, their other essay, “ On Mass Extinction ,” was also published by Hometown Weekly .
“The sixth mass extinction—which scientists have coined as the Holocene Extinction—is upon us. According to the United Nations, around one million plant and animal species are currently in danger of extinction, and many more within the next decade. While other extinctions have occurred in Earth’s history, none have occurred at such a rapid rate,” they wrote. “For the sake of both biodiversity and infectious diseases, it is in our best interest to stop pushing this Holocene Extinction further.”
An essay titled “ Learning from Our Mistakes: How to Protect Ourselves and Our Communities from Diseases ,” written by Nicole Veru ’21 and Zoe Darmon ’21, was published in My Hometown Bronxville, based in Bronxville, N.Y.
“We can protect ourselves and others from future infectious diseases by ensuring that we are vaccinated,” they wrote. “Vaccines have high levels of success if enough people get them. Due to vaccines, society is no longer ravaged by childhood diseases such as mumps, rubella, measles, and smallpox. We have been able to eradicate diseases through vaccines; smallpox, one of the world’s most consequential diseases, was eradicated from the world in the 1970s.
“In 2000, the U.S. was nearly free of measles, yet, due to hesitations by anti-vaxxers, there continues to be cases. From 2000–2015 there were over 18 measles outbreaks in the U.S. This is because unless a disease is completely eradicated, there will be a new generation susceptible.
“Although vaccines are not 100% effective at preventing infection, if we continue to get vaccinated, we protect ourselves and those around us. If enough people are vaccinated, societies can develop herd immunity. The amount of people vaccinated to obtain herd immunity depends on the disease, but if this fraction is obtained, the spread of disease is contained. Through herd immunity, we protect those who may not be able to get vaccinated, such as people who are immunocompromised and the tiny portion of people for whom the vaccine is not effective.”
Dhruvi Rana ’22 and Bryce Gillis ’22 co-authored an op-ed titled “ We Must Educate Those Who Remain Skeptical of the Dangers of COVID-19 ,” which was published in Rhode Island Central .
“As Rhode Island enters the winter season, temperatures are beginning to drop and many studies have demonstrated that colder weather and lower humidity are correlated with higher transmissibility of SARS-CoV-2, the virus that causes COVID-19,” they wrote. “By simply talking or breathing, we release respiratory droplets and aerosols (tiny fluid particles which could carry the coronavirus pathogen), which can remain in the air for minutes to hours.
“In order to establish herd immunity in the US, we must educate those who remain skeptical of the dangers of COVID-19. Whether community-driven or state-funded, educational campaigns are needed to ensure that everyone fully comprehends how severe COVID-19 is and the significance of airborne transmission. While we await a vaccine, it is necessary now more than ever that we social distance, avoid crowds, and wear masks, given that colder temperatures will likely yield increased transmission of the virus.”
Danielle Rinaldi ’21 and Verónica Matos Socorro ’21 published their op-ed titled “ Community Forum: How Mask-Wearing Demands a Cultural Reset ” in the Ewing Observer , based in Lawrence, N.J.
“In their own attempt to change personal behavior during the pandemic, Wesleyan University has mandated mask-wearing in almost every facet of campus life,” they wrote. “As members of our community, we must recognize that mask-wearing is something we are all responsible and accountable for, not only because it is a form of protection for us, but just as important for others as well. However, it seems as though both Covid fatigue and complacency are dominating the mindsets of Americans, leading to even more unwillingness to mask up. Ultimately, it is inevitable that this pandemic will not be the last in our lifespan due to global warming creating irreversible losses in biodiversity. As a result, it is imperative that we adopt the norm of mask-wearing now and undergo a culture shift of the abandonment of an individualistic mindset, and instead, create a society that prioritizes taking care of others for the benefit of all.”

Shayna Dollinger ’22 and Hayley Lipson ’21 wrote an essay titled “ My Pandemic Year in College Has Brought Pride and Purpose. ” Dollinger submitted the piece, rewritten in first person, to Jewish News of Northern California . Read more about Dollinger’s publication in this News @ Wesleyan article .
“I lay in the dead grass, a 6-by-6-foot square all to myself. I cheer for my best friend, who is on the stage constructed at the bottom of Foss hill, dancing with her Bollywood dance group. Masks cover their ordinarily smiling faces as their bodies move in sync. Looking around at friends and classmates, each in their own 6-by-6 world, I feel an overwhelming sense of normalcy.
“One of the ways in which Wesleyan has prevented outbreaks on campus is by holding safe, socially distanced events that students want to attend. By giving us places to be and things to do on the weekends, we are discouraged from breaking rules and causing outbreaks at ‘super-spreader’ events.”
An op-ed written by Luna Mac-Williams ’22 and Daëlle Coriolan ’24 titled “ Collectivist Practices to Combat COVID-19 ” was published in the Wesleyan Argus .
“We are embroiled in a global pandemic that disproportionately affects poor communities of color, and in the midst of a higher cultural consciousness of systemic inequities,” they wrote. “A cultural shift to center collectivist thought and action not only would prove helpful in disease prevention, but also belongs in conversation with the Black Lives Matter movement. Collectivist models of thinking effectively target the needs of vulnerable populations including the sick, the disenfranchised, the systematically marginalized. Collectivist systems provide care, decentering the capitalist, individualist system, and focusing on how communities can work to be self-sufficient and uplift our own neighbors.”
An essay written by Maria Noto ’21 , titled “ U.S. Individualism Has Deadly Consequences ,” is published in the Oneonta Daily Star , based in Oneonta, N.Y.
She wrote, “When analyzing the cultures of certain East Asian countries, several differences stand out. For instance, when people are sick and during the cold and flu season, many East Asian cultures, including South Korea, use mask-wearing. What is considered a threat to freedom by some Americans is a preventive action and community obligation in this example. This, along with many other cultural differences, is insightful in understanding their ability to contain the virus.
“These differences are deeply seeded in the values of a culture. However, there is hope for the U.S. and other individualistic cultures in recognizing and adopting these community-centered approaches. Our mindset needs to be revolutionized with the help of federal and local assistance: mandating masks, passing another stimulus package, contact tracing, etc… However, these measures will be unsuccessful unless everyone participates for the good of a community.”

A published op-ed by Madison Szabo ’23 , Caitlyn Ferrante ’23 ran in the Two Rivers Times . The piece is titled “ Anxiety and Aspiration: Analyzing the Politicization of the Pandemic .”
John Lee ’21 and Taylor Goodman-Leong ’21 have published their op-ed titled “ Reassessing the media’s approach to COVID-19 ” in Weekly Monday Cafe 24 (Page 2).
An essay by Eleanor Raab ’21 and Elizabeth Nefferdorf ’22 titled “ Preventing the Next Epidemic ” was published in The Almanac .
- Keep Wes Safe
- student publications
- Teaching during the pandemic
Related Articles
Hugo L. Black Lecturers Establish What’s at Stake When Free Expression on Campus is Imperiled
Art Comes to Life through Student Partnership with the Center for the Arts
True ‘Blue’: James Kaplan ’73 Documents a Key Collaboration in Jazz History
Previous matesan's new book explores political violence, islamist mobilization in egypt and indonesia, next students launch fun, interactive virtual program for school-aged kids.
- Open access
- Published: 23 November 2020
Global strategies and effectiveness for COVID-19 prevention through contact tracing, screening, quarantine, and isolation: a systematic review
- Tadele Girum 1 ,
- Kifle Lentiro 1 ,
- Mulugeta Geremew 2 ,
- Biru Migora 2 &
- Sisay Shewamare 3
Tropical Medicine and Health volume 48 , Article number: 91 ( 2020 ) Cite this article
44k Accesses
101 Citations
27 Altmetric
Metrics details
COVID-19 is an emerging disease caused by highly contagious virus called SARS-CoV-2. It caused an extensive health and economic burden around the globe. There is no proven effective treatment yet, except certain preventive mechanisms. Some studies assessing the effects of different preventive strategies have been published. However, there is no conclusive evidence. Therefore, this study aimed to review evidences related to COVID-19 prevention strategies achieved through contact tracing, screening, quarantine, and isolation to determine best practices.
We conducted a systematic review in accordance with the PRISMA and Cochrane guidelines by searching articles from major medical databases such as PubMed/Medline, Global Health Database, Embase, CINAHL, Google Scholar, and clinical trial registries. Non-randomized and modeling articles published to date in areas of COVID prevention with contact tracing, screening, quarantine, and isolation were included. Two experts screened the articles and assessed risk of bias with ROBINS-I tool and certainty of evidence with GRADE approach. The findings were presented narratively and in tabular form.
We included 22 (9 observational and 13 modeling) studies. The studies consistently reported the benefit of quarantine, contact tracing, screening, and isolation in different settings. Model estimates indicated that quarantine of exposed people averted 44 to 81% of incident cases and 31 to 63% of deaths. Quarantine along with others can also halve the reproductive number and reduce the incidence, thus, shortening the epidemic period effectively. Early initiation of quarantine, operating large-scale screenings, strong contact tracing systems, and isolation of cases can effectively reduce the epidemic. However, adhering only to screening and isolation with lower coverage can miss more than 75% of asymptomatic cases; hence, it is not effective.
Quarantine, contact tracing, screening, and isolation are effective measures of COVID-19 prevention, particularly when integrated together. In order to be more effective, quarantine should be implemented early and should cover a larger community.
Introduction
Coronavirus disease 2019 (COVID-19) is an emerging infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The novel coronavirus was first identified in December 2019 in Wuhan China, then spread globally within weeks and resulted in an ongoing pandemic [ 1 , 2 , 3 , 4 , 5 ]. Currently, coronavirus is affecting 213 countries and territories around the world. As of 27 May 2020, more than 5.7 million cases and 353,664 deaths were reported globally [ 2 , 3 ]. Thirteen percent of the closed cohorts and 2–5% of the total cohort reportedly died [ 2 , 3 , 4 , 5 ]. The USA, Brazil, Russia, Spain, Italy, France, and the UK are the most affected countries [ 3 , 4 , 5 , 6 , 7 ].
The full spectrum of COVID-19 infection ranges from subclinical self-limiting respiratory tract illness to severe progressive pneumonia with multi-organ failure and death. As evidenced from studies and reports, more than 80% of cases remained asymptomatic and 15% of cases appeared as mild cases with common symptoms like fever, cough, fatigue, and loss of smell and taste [ 2 , 3 , 4 , 5 , 6 ]. Severe disease onset that needs intensive care might result in death due to massive alveolar damage and progressive respiratory failure [ 1 , 4 , 5 , 6 , 7 , 8 ].
The virus transmits through direct and indirect contacts. Person-to-person transmissions primarily occur during close contact, droplets produced through coughing, sneezing, and talking. Indirect transmission occurs through touching contaminated surfaces or objects and then touching the face. It is more contagious during the first few days after the onset of symptoms, but asymptomatic cases can also spread the disease [ 5 , 6 , 7 , 8 ].
Recommended prevention measures was designed based on overcoming the mode of transmissions including frequent hand washing, maintaining physical distance, quarantine, covering the mouth and nose during coughs, and avoiding contamination of face with unwashed hands. In addition, use of mask is recommended particularly for suspected individuals and their caregivers. There is limited evidence against the community wide use of masks in healthy individuals. However, most of these preventive measures are recommended and were not researched well [ 4 , 5 , 6 , 7 , 8 ].
To the extent of our search, there is no systematic review on the preventive aspects and effectiveness of COVID-19 infection through contact tracing, screening, quarantine, and isolation. The findings were inconclusive; in some studies, certain preventive mechanisms were shown to have minimal effects, while in others different preventive mechanisms have better effect than expected. On the other hand, some studies have reported that integration of interventions is more effective than specific interventions [ 2 , 6 , 8 ].
Therefore, we aimed to conduct a comprehensive systematic review through reviewing globally published studies on the strategies and effectiveness of different preventive mechanisms (contact tracing, screening, quarantine, and isolation) developed to prevent and control COVID-19. This synthesized measure will be important to bring conclusive evidence, so that policy makers and other stakeholders could have clear evidence to rely on during decision making.
To support the existing local and national COVID-19 prevention program with tangible evidence, we conducted a systematic review on global strategies for COVID-19 prevention through contact tracing, screening, quarantine, and isolation. We aimed to answer issues related to alternative strategic implementation and effectiveness in the prevention of the disease or death. The following key questions were considered:
Is contact tracing, screening, quarantine, and isolation effective to control the COVID-19 outbreak?
Is there difference in the effectiveness of contact tracing, screening, quarantine, and isolation in different settings?
How and when these strategies should be applied to control the COVID-19 outbreak?
We conducted the review in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidance for reporting of systematic reviews and meta-analyses [ 9 ] and the Cochrane Handbook of Systematic Review [ 10 ] through systematic literature search of articles published to date (June 02/2020) containing information on COVID-19 prevention by contact tracing, screening, quarantine, and isolation. First, a working protocol was developed (but unpublished) and followed in the process.
Eligibility (inclusion and exclusion) criteria for the review
Based on the relevance of the reported evidence for decision making at local, national, and international levels, the papers were selected and prioritized for the review. The relevant outcomes observed in the review were reduction in incidence, transmission, adverse outcome, and cost-effectiveness of COVID-19 prevention through contact tracing, screening, quarantine, and isolation.
Types of studies
Due to the infancy of the epidemic, lack of researches, and ethical concerns, randomized controlled trials were not included. Therefore, we considered non-randomized observational studies and modeling (mathematical and/or epidemiological) studies to supplement the existing evidences.
We included cohort studies, case-control studies, time series, case series, and mathematical modeling studies conducted anywhere, in any area, and in any setting reported in the English language. Whereas, commentaries, letter to editor, case reports, and governmental reports were excluded.
Types of participants
Depending on the type of the research, for each preventive methods, different participants were included. These includes individuals who have had contacts with confirmed or suspected case of COVID-19, or individuals who lived in areas with COVID-19 outbreak, or individuals considered to be at high risk for COVID-19/suspected cases or cases of COVID-19 infection. The number of participants varies according to the individual researches. Individuals who have confirmed other symptomatic respiratory diseases were excluded.
Types of interventions
We included different types of interventions applied specifically or in combination, either voluntary or mandatory and in different settings (facility or community). In comparative studies, the interventions were compared with the non-applied groups or other comparison groups. We excluded interventions other than the aforementioned strategies.
Types of outcome measures
To identify the extent to which these interventions were applied globally and to measure their effectiveness in COVID-19 prevention, we used the following outcome measures: incidence of COVID-19, onward transmission, mortality or other adverse outcomes, and cost-effectiveness. We did not address secondary outcomes such as psychological impacts, economic impacts, and social impacts.
Literature search strategy
A systematic literature search of articles was done by information system professionals and the researchers. Articles published between January 1, 2020, and June 2, 2020, containing information on different prevention strategies such as contact tracing, screening, quarantine, and isolation, and studies assessing their effectiveness were retained for the review. Electronic bibliographic databases and libraries such as PubMed/Medline, Global Health Database, Embase, CINAHL (Cumulative Index to Nursing and Allied Health Literature; Ebsco), the Cochrane Library, and African Index Medicus were used.
In addition, we searched gray literatures, pre-prints, and resource centers of The Lancet , JAMA , and N Engl J Med . Lastly, we screened the reference lists of systematic reviews for additional source. Combination of the following search terms were used with (AND, OR, NOT) Boolean (Search) Operators.
Corona virus
Coronavirus Infections
Novel corona
Prevention/control
- Contact tracing
1 or 2 or 3 or 4 or 5 and 6 and 7 or 8 or 9 or 10
Data collection and analysis
Study selection process.
The team screened all the titles and abstracts based on predefined eligibility criteria. Two authors independently screened the titles and abstracts and reached consensus by discussion or by involving a third author. After that, the review author team retrieved the full texts of all included abstracts. Two review authors screened all the full-text publications independently, and disagreements were resolved with consensus or by a third person involvement.
Data extraction and management
Titles and abstracts found through primary electronic search were thoroughly assessed for the possibility of reporting the intended outcome and filtered for potential eligibility. One of the review authors who have experience extracted data from the included studies into standardized tables, and the second author checked completeness. From each eligible research, the following information was extracted based on the preformed format: author information, title, study participants, study design, study setting, type of intervention, length of intervention, year of publication, study duration, eligibility criteria, rate, and effect of intervention measures. For modeling studies, the data extraction items also included the type of model and the data source.
Assessment of risk of bias in included studies
Risk of bias was assessed through evaluating reliability and validity of data in included studies based on the Risk-Of-Bias In Non-randomized Studies - of Interventions (ROBINS-I) tool [ 11 ]. The first author rated the risk of bias, the second author checked the ratings, and the third author was involved in the disagreements. For each studies, the study design, participants, outcome, and presence of bias were assessed based on the eligibility criteria and quality assessment check list. Moreover, all studies with the same participants and outcome were measured using the same standard.
On the other hand, modeling studies were assessed by the International Society for Pharmaco-economics and Outcomes (ISPOR) and the Society for Medical Decision making (SMDM) for dynamic mathematical transmission model tools [ 12 ]. Modeling studies that fulfilled all the three criteria were rated as “no concerns to minor concerns, ” and if one or more categories were unclear, it is rated as “moderate concerns,” and if one or more categories were not fulfilled, we had it rated as “major concerns.”
Data synthesis and analysis
The qualitative data was systematically reviewed and presented in accordance with the Cochrane guide line. We synthesized results from quantitative measures narratively and reported in tabular form. Because of the heterogeneity of the primary studies, quantitative analyses (meta-analysis) were not conducted.
Assessment of the certainty of the evidence
By using the GRADE approach [ 13 ], we graded the certainty of evidence for the main outcomes, reported in standard terms using tables. One of the authors conducted the certainty assessment which consists of assessments of risk of bias, indirectness, inconsistency, imprecision, and publication bias, and then, classified to one of the four categories: a high certainty (estimated effect lies close to the true effect), a moderate certainty (estimated effect is probably close to the true effect), a low certainty (estimated effect might substantially differ), and very low certainty (estimated effect is probably markedly different) from the true effect.
Studies included
The PRISMA flow diagram for the selected studies in the search process and the eligibility assessment are summarized in (Fig. 1 ). The initial electronic database search led to 1542 potentially relevant citations in the form of a title, abstract, bibliography, and full-text research. After removal of duplicates and initial screening, 125 articles were selected for further evaluation via full-text articles. Of these full-text articles, 103 articles were excluded due to the following reasons: 38 studies reported the prevention of SARS other than COVID-19; 36 have measured prevention measures other than contact tracing, screening, quarantine, and isolation; 19 had inappropriate study designs (commentaries, letters and case reports); and 10 were reviews or protocols. Thus, 22 studies [ 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ] met the inclusion criteria and were included in the systematic review.
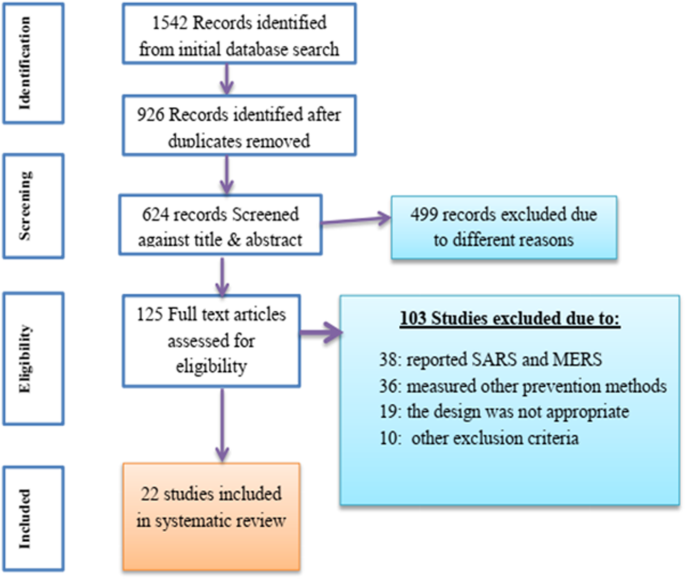
Flow chart for study search, selection, and screening for the review
Study characteristics
The 22 studies [ 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ] that were retained for the final analysis were published in the period from January 15, 2020, to June 02, 2020, based on participant populations in the following countries: China ( n = 10), UK ( n = 4), USA ( n = 2), Hong Kong ( n = 2), and Netherlands, Japan, France, and Taiwan ( n = 1 from each). The included studies comprised of 9 observational [ 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 ] and 13 modeling studies [ 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ]. With duplicates (repeated count), 3 of the studies assessed the overall prevention strategies [ 21 , 22 , 23 ], 5 assessed the effect of contact tracing [ 14 , 24 , 25 , 33 , 35 ], 2 assessed screening strategies [ 17 , 34 ], 12 assessed the effect of quarantine [ 15 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 ], and 6 assessed the effect of isolation [ 17 , 25 , 26 , 31 , 33 , 35 ]. The sample sizes in the studies varied from hundreds to millions. Four studies were investigated for effect at the health facility level, while the remaining 18 studies explored at the community or national level. Survey characteristics and summary results are described in Table 1 .
Quality (risk of bias) assessment within included studies
Summaries of the risk of bias assessment of non-randomized studies and quality rating of the modeling studies are presented in Tables 2 and 3 , respectively. Two studies [ 14 , 19 ] have low bias due to confounding, eight studies have low bias in selection of participants into the study, and all studies have low bias in classification of interventions. The overall risk of bias is moderate for eight studies and serious for one study. On the other hand, we have no concern for nine modeling studies, and two studies have major concerns.
COVID-19 prevention strategies and effectiveness
The summary result is presented in Table 1 . Among the nine observational studies, three of them assessed COVID-19 transmission with the existing prevention measures at a community level in Taiwan, China, and Hong Kong [ 18 , 19 , 20 ]. The other two studies assessed the effect of escalating prevention measures at health facilities in China and Hong Kong [ 21 , 22 ], and three studies [ 15 , 16 , 17 ] assessed national- and metropolitan-based quarantine strategies and the effect of laboratory-based quarantine in the prevention of COVID-19. The last study evaluated the effect of community-based contact tracing in UK [ 14 ].
The three studies [ 18 , 19 , 20 ] that assessed the overall prevention strategies found out that integration of interventions need to be applied instead of adhering to a single intervention. Cheng [ 18 ] reported that isolating symptomatic patients alone may not be sufficient enough to contain the epidemic. Wang [ 19 ] and Law [ 20 ] also concluded that in intimate contacts the transmission is 40–60%. Preventing contact through different strategies and integration is very important.
Studies conducted on the effect of quarantine [ 15 , 16 , 17 ] found that it can have a massive preventive effect. One of the studies [ 15 ] that assessed the effect of quarantine in different populations and quarantine strategies found that it should be integrated with input population reduction (travel restriction), and the other study [ 16 ] that assessed the effects of metropolitan-wide quarantine on the Spread of COVID-19 in China found that quarantine would prevent 79.27% (75.10–83.45%) of deaths and 87.08% (84.68–89.49%) of infections. Also, the other researcher [ 17 ] evidenced that laboratory-based screenings accomplished within hours can enhance the efficiency of quarantine.
Two studies described infection control preparedness measures in health care settings of Hong Kong and China [ 21 , 22 ]. One of these studies [ 21 ] reported that infection transmission is highly increased within a short period of time and multiplicity of infection prevention strategies were recommended for prevention in health care setups. The other study [ 22 ] also concluded that practicing working shift among professionals working in facilities can be used as strategy to prevent thetransmission of COVID infection.
A study conducted by Keeling et al. [ 14 ] assessed the efficacy of contact tracing for the containment of COVID-19 in the UK. The study evaluated the contact pattern of the community and concluded that rapid contact tracing to reduce the basic reproduction number ( R 0 ) from 3.11 to 0.21 enables the outbreak to be contained. Additionally, it was found that each new case requires an average of 36 individuals to be traced, with 8.7% of cases having more than 100 close traceable contacts.
In this review, we identified 13 modeling studies [ 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ] that assessed the effectiveness of contact tracing, screening, quarantine, and isolation for prevention of COVID-19 in different settings and groups. The simulation was done in individual or group basis and with different assumptions. Most of these studies used a model parameter from Chinese reports.
Three of these researches [ 25 , 26 , 27 ] particularly emphasized on the way how the R 0 can be reduced and the epidemic would be reduced. The simulation by Tang et al. [ 25 ] aimed to estimate the R 0 of SARS-CoV-2 and infer the required effectiveness of isolation and quarantine to contain the outbreak. Their susceptible-exposed-infected-recovered (SEIR) model estimated R 0 of 6.47 and generalized that 50% reduction of contact rate achieved by isolation and quarantine would decrease the confirmed cases by 44%; reducing contacts by 90% also can decrease the number of cases by 65%. The other researcher, Rocklov (27), by using data from the Diamond Princess Cruise ship, concluded that quarantine of passengers prevented 67% of cases and lowered the R 0 from 14.8 to 1.78. Similarly, the reduction of R 0 was achieved from quarantine [ 28 ].
In addition to these, five studies [ 24 , 28 , 30 , 31 , 35 ] which modeled the effectiveness of different public interventions consistently reported that integrated intervention is better than a single intervention. One of these research conducted in the UK [ 24 ] found that combined isolation and tracing strategies would reduce transmission more than mass testing or self-isolation alone (50–60% compared to 2–30%). The other study [ 28 ] also reported that with R 0 of 2.4, a combination of case isolation and voluntary quarantine for 3 months could prevent 31% of deaths. The others also concluded that quarantine should be strict and integrated with contact tracing, screening, and other interventions [ 30 , 31 , 35 ].
Five modeling studies also assessed the effect of quarantine [ 23 , 29 , 32 ], contact tracing [ 33 ], and screening [ 34 ]. All of the studies [ 23 , 29 , 32 ] reported that quarantine has reduced the incidence of infection and shortened the duration of the epidemic. However, the effectiveness depends on the level of integration with other strategies. Similarly, model simulations that assessed the effect of contact tracing and screening reported that the strategies are effective. However, as the report of Hellewell [ 33 ] stated, contact tracing and isolation might not contain outbreaks of COVID-19 unless very high levels of contact tracing are achieved. Similarly, the other researcher [ 34 ] reported that in a stable epidemic, under the assumption that 25% of cases are subclinical, it is estimated that arrival screening alone would detect roughly one-third of infected travelers.
This study aimed to assess the effectiveness of contact tracing, screening, and quarantine and isolation to prevent COVID-19 infection by reviewing existing literatures. The review identified and systematically synthesized the findings of 22 studies (9 observational and 13 modeling studies) [ 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ] to bring the best available evidence that policy makers and implementers can use in the process of infection prevention interventions.
The studies consistently reported the benefit of contact tracing, screening, quarantine, and isolation in the prevention of COVID-19. The effectiveness of quarantine in particular is very high. Compared to individuals without any intervention quarantined people exposed to a confirmed case highly averted infections and deaths [ 15 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 ]. Also, the effectiveness of quarantine increases whenever it is implemented along with other prevention measures such as isolation, contact tracing, and travel ban [ 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 ]. Although, screening and contact tracing are very important to control the epidemic, early initiation, larger coverage, and integration with other programs are very important. Unless the level of contact tracing and screening is high, prevention through isolation only is very limited, as the screening programs misses 75% of cases [ 3 , 24 ].
Quarantine measures applied alone or integrated with other measures were reported to be the most effective measures [ 25 , 26 , 27 , 28 , 29 , 30 , 31 ]. However, integration of quarantine with other public health measures increases the effectiveness and efficiency of the program [ 36 ]. Implementation of early quarantine measures makes the strategy a more cost effective one [ 28 , 30 ]. Quarantine implemented as self-quarantine and group quarantine is effective at varying levels once effectively implemented [ 28 , 32 ]. Total lockdown measures enhance the effectiveness of quarantine measures [ 15 , 16 , 17 , 18 , 19 ]. When laboratory tests are very fast, laboratory-based quarantine could be an effective in health care setups [ 17 ].
This evidence is in line with the finding of other reviews and modeling studies conducted to assess the effectiveness of these measures in the prevention of SARS, MERS, and COVID-19 [ 28 , 35 , 36 , 37 ]. As reported before, combination of case isolation and voluntary quarantine for 3 months could prevent 31% of deaths compared to any single intervention. And adding social distancing on the previous interventions on people aged 70 years or older for 4 months increases the prevention proportion of deaths to 49%. It can also reduce the reproductive number by half; hence, it can tremendously reduce the incidence of infection, reduce the period of epidemic, and enhance effectiveness of control [ 28 , 36 ].
Our findings also witnessed the effectiveness of contact tracing measures used for pandemic response efforts at multiple levels of health care systems. Isolation of suspected and confirmed patients and their contact is at the heart of the prevention strategy. However, for the contact tracing to be an effective measure, it has to be integrated with other measures such as quarantine and screening. Because larger shares of individuals are asymptomatic, contact tracing may be difficult in areas where contact recording is unachievable. According to world health organization, contact tracing is also one of the most essential and effective strategies to control the epidemic [ 14 , 24 , 25 , 33 , 35 ]. Other studies also evidenced the importance of contact tracing and isolation in different settings [ 36 , 37 ].
The finding of our review revealed that screening and isolation are important measures of disease prevention [ 17 , 25 , 26 , 31 , 33 , 35 ]. Most of the researches recommend high-risk group screening and contact cases screening in a resource-limited setting. However, these programs are effective when the screening capacity is higher and contact tracing is effective. Otherwise, screening and isolation programs miss more than half of cases and may not be implemented alone [ 25 , 33 , 35 ]. Also evidences from different countries indicated that screening and isolation measures are implemented along with other measures, yet their role in the prevention of the epidemic is high [ 2 , 3 , 8 , 36 , 37 ].
This review included a wide variety of study designs (observational and model studies); hence, it failed to include meta-analysis (statistical measures). Modeled studies also assume different scenarios, where it may not be true in the general cases. Also, the review has included only publications reported in the English language and open access resources.
Conclusion and recommendation
Quarantine, contact tracing, screening, and isolation are effective measures of COVID-19 prevention, particularly whenever integrated together. In order to be more effective, quarantine should be implemented early and covers larger community. Controlling population travel will enhance the effectiveness of quarantine. Screening, contact tracing, and isolation are effective particularly in areas where contact tracing is easily attainable. Although screening is the effective measure recommended by the WHO, since the disease is asymptomatic, it may miss a larger share of the population. Therefore, this should be integrated with other preventive measures. In order to control the COVID-19 epidemic, the health care system should consider high level of contact tracing, early initiation of nationwide quarantine measures, increasing coverage of screening service, and preparing effective isolation centers.
Availability of data and materials
Please contact author for data requests.
Abbreviations
Coronavirus disease 2019
Middle East respiratory syndrome
Severe acute respiratory syndrome
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Basic reproduction number
Susceptible-exposed-infected-recovered
World Health Organization
Guan W, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020.
World Health Organization. Novel coronavirus (2019-nCOV); 2020. Situation Report 51. [Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 .
Google Scholar
Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir– ritonavir in adults hospitalized with severe covid-19. N Engl J Med. 2020;382(19):1787.
Article PubMed Google Scholar
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
Article CAS PubMed PubMed Central Google Scholar
Chan JF, Yuan S, Kok K-H, To KK-W, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–23.
Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–2.
Baden LR, Rubin EJ. Covid-19—the search for effective therapy. N Engl J Med. 2020.
World Health Organization. Coronavirus disease (COVID-19) outbreak; 2020. Available from: https://www.who.int/emergencies/diseases/novelcoronavirus-2019 .
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Article PubMed PubMed Central Google Scholar
JPT H, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Cochrane; 2019.
Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919. https://doi.org/10.1136/bmj.i4919 .
Caro JJ, Briggs AH, Siebert U, Kuntz KM. ISPOR-SMDM modeling good research practices task force. Modeling good research practices--overview: a report of the ISPOR-SMDM modeling good research practices task Force-1. Med Decis Mak. 2012;32(5):667–77.
Article Google Scholar
Morgan RL, Thayer KA, Bero L, et al. GRADE: assessing the quality of evidence in environmental and occupational health. Environ Int. 2016;92-93:611–6 10.1016/j.envint.2016.01.004.
Keeling MJ, Hollingsworth TD, Read JM. The efficacy of contact tracing for the containment of the 2019 novel coronavirus (COVID-19). medRxiv. 2020;74(10):861. https://doi.org/10.1101/2020.02.14.2002303 .
Hu Z, Cui Q, Han J, Wang X, Sha WEI, Teng Z. Evaluation and prediction of the COVID-19 variations at different input population and quarantine strategies, a case study in Guangdong province, China. Int J Infect Dis. 2020;95:231–40. https://doi.org/10.1016/j.ijid.2020.04.010 .
Shen M, Peng Z, Guo Y, et al. Assessing the effects of metropolitan-wide quarantine on the spread of COVID-19 in public space and households [published online ahead of print, 2020 may 8]. Int J Infect Dis. 2020;S1201-9712(20):30326. https://doi.org/10.1016/j.ijid.2020.05.019 .
Article CAS Google Scholar
Lagier JC, Colson P, Tissot Dupont H, et al. Testing the repatriated for SARS-Cov2: should laboratory-based quarantine replace traditional quarantine? Travel Med Infect Dis. 2020;34:101624. https://doi.org/10.1016/j.tmaid.2020.101624 .
Cheng HY, Jian SW, Liu DP, et al. Contact tracing assessment of COVID-19 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020;180:e202020. https://doi.org/10.1001/jamainternmed.2020.2020 .
Wang G, Chen W, Jin X, Chen YP. Description of COVID-19 cases along with the measures taken on prevention and control in Zhejiang, China [published online ahead of print, 2020 Apr 20]. J Med Virol. 2020. https://doi.org/10.1002/jmv.25906 .
Law S. Leung aw, Xu C. severe acute respiratory syndrome (SARS) and coronavirus disease-2019 (COVID-19): from causes to preventions in Hong Kong. Int J Infect Dis. 2020;94:156–63.
Cheng VCC, Wong SC, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41(5):493–8. https://doi.org/10.1017/ice.2020.58 .
Article CAS PubMed Google Scholar
Bai Y, Wang X, Huang Q, et al. SARS-CoV-2 infection in health care workers: a retrospective analysis and a model study. medRxiv. 2020. https://doi.org/10.1101/2020.03.29.20047159 .
Xiuli L, Geoffrey H, Shouyang W, Minghui Q, Xin X, Shan Z, et al. Modelling the situation of COVID-19 and effects of different containment strategies in China with dynamic differential equations and parameters estimation. medRxiv. 2020. https://doi.org/10.1101/2020.03.09.20033498 .
Adam JK, Petra K, Andrew J, Conlan K, Stephen M, et al. Effectiveness of isolation, testing, contact tracing and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis. 2020;20(10):1151 CMMID repository. [Preprint]. Last accessed: July 02, 2020.
Tang B, Wang X, Li Q, et al. Estimation of the transmission risk of the 2019-nCoV and its implication for public health interventions. J Clin Med. 2020;9(2):462Published 2020 Feb 7. https://doi.org/10.3390/jcm9020462 .
Article PubMed Central Google Scholar
Rocklöv J, Sjödin H, Wilder-Smith A. COVID-19 outbreak on the diamond princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures. J Travel Med. 2020;27(3):taaa030. https://doi.org/10.1093/jtm/taaa030 .
Zhao S, Chen H. Modeling the epidemic dynamics and control of COVID-19 outbreak in China [published online ahead of print, 2020 mar 11]. Quant Biol. 2020;1:1–9. https://doi.org/10.1007/s40484-020-0199-0 .
Ferguson NM, Laydon D, Nedjati-Gilani G, Imai N, Ainslie K, Baguelin M, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. Available from www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf 2020 .
Yang Z, Zeng Z, Wang K, et al. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. J Thorac Dis. 2020;12(3):165–74. https://doi.org/10.21037/jtd.2020.02.64 .
Peak CM, Kahn R, Grad YH, et al. Individual quarantine versus active monitoring of contacts for the mitigation of COVID-19: a modelling study [published online ahead of print, 2020 may 20]. Lancet Infect Dis. 2020;20(9):1025. https://doi.org/10.1016/S1473-3099(20)30361-3 .
Tang B, Xia F, Tang S, et al. The effectiveness of quarantine and isolation determine the trend of the COVID-19 epidemics in the final phase of the current outbreak in China [published online ahead of print, 2020 Apr 17]. Int J Infect Dis. 2020;95:288–93. https://doi.org/10.1016/j.ijid.2020.03.018 .
Hou C, Chen J, Zhou Y, et al. The effectiveness of quarantine of Wuhan city against the corona virus disease 2019 (COVID-19): a well-mixed SEIR model analysis. J Med Virol. 2020;92(7):841–8. https://doi.org/10.1002/jmv.25827 .
Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts [published correction appears in lancet glob health. 2020 mar 5]. Lancet Glob Health. 2020;8(4):e488–96. https://doi.org/10.1016/S2214-109X(20)30074-7 .
Gostic K, Gomez AC, Mummah RO, Kucharski AJ, Lloyd-Smith JO. Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. Elife. 2020;9:e55570Published 2020 Feb 24. https://doi.org/10.7554/eLife.55570 .
Mirjam E. Kretzschmar, Ganna Rozhnova, Michiel van Boven. Isolation and contact tracing can tip the scale to containment of COVID-19 in populations with social distancing. doi: https://doi.org/10.1101/2020.03.10.20033738 .
Nussbaumer-Streit B, Mayr V, AIulia D, Chapman A, Persad E, Klerings I, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;1(Issue 4):CD013574. https://doi.org/10.1002/14651858.CD013574 .
Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis [published online ahead of print, 2020 Jun 1]. Lancet. 2020;395(10242):1973. https://doi.org/10.1016/S0140-6736(20)31142-9 .
Download references
Acknowledgements
All authors who provided us information whenever we contacted them.
Not applicable
Author information
Authors and affiliations.
Department of Public Health, College of Medicine and Health Sciences, Wolkite University, Wolkite, Ethiopia
Tadele Girum & Kifle Lentiro
Department of Statistics, College of natural and computational Sciences, Wolkite University, Wolkite, Ethiopia
Mulugeta Geremew & Biru Migora
Department of Physics, College of natural and computational Sciences, Wolkite University, Wolkite, Ethiopia
Sisay Shewamare
You can also search for this author in PubMed Google Scholar
Contributions
TG and MG conceived the project, took the primary role in the data acquisition, analysis, and interpretation; writing the manuscript; and the publication of the project. All others revised the project, were involved in the interpretation and manuscript preparation. All authors revised the final draft of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Tadele Girum .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing of interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Girum, T., Lentiro, K., Geremew, M. et al. Global strategies and effectiveness for COVID-19 prevention through contact tracing, screening, quarantine, and isolation: a systematic review. Trop Med Health 48 , 91 (2020). https://doi.org/10.1186/s41182-020-00285-w
Download citation
Received : 26 June 2020
Accepted : 16 November 2020
Published : 23 November 2020
DOI : https://doi.org/10.1186/s41182-020-00285-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Tropical Medicine and Health
ISSN: 1349-4147
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
COVID-19 Overview and Infection Prevention and Control Priorities in non-U.S. Healthcare Settings
Summary of changes: itf ipc covid-19 overview and infection prevention and control priorities in non-u.s. healthcare settings webpage.
- Updated transmission section to reflect CDC guidance
- Added information on certain activities that can increase risk of COVID-19 infection with references to ventilation guidance by CDC and WHO
- Updated and re-arranged list of symptoms on webpage to reflect current CDC guidance
- Removed section on Illness Severity
- Amended information and references in People at Higher Risk for Severe Illness, noting that these people should be prioritized for vaccination
- Revised COVID-19 Preventative actions section to reflect vaccination, masks, and additional preventative actions that should be continued
- Added additional references to preventative actions section
- Removed treatment section
- Added information on IPC in the context of vaccination delivery
- Revised list of Aerosol Generating Procedures based on updated guidance from WHO and updated references
- COVID-19 Background
Transmission
- People at Higher Risk
- Prevention and Treatment
- What is IPC?
COVID-19 Overview and Infection Prevention and Control Priorities in non-US Healthcare Settings [PPT – 5 MB]
This overview was created for healthcare workers in non-U.S. healthcare settings and government officials at ministries of health working on the Coronavirus Disease 2019 (COVID-19) response.
The information in this document draws from the Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) guidance documents and Infection Prevention and Control (IPC) priorities for the response to COVID-19 in healthcare settings and includes information that can be used in non-U.S. contexts.
Structure of the document
This overview is organized by first presenting a background on coronaviruses. It then briefly describes the emergence, transmission, symptoms, prevention, and treatment of COVID-19. The rest of the document reviews COVID-19 IPC priorities, in non-U.S. healthcare settings.
Coronavirus Background:
Coronaviruses are a large family of viruses that can cause illness in animals or humans. In humans there are several known coronaviruses that cause respiratory infections. These coronaviruses range from the common cold to more severe diseases such as severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and COVID-19.
Coronavirus Disease 2019:
COVID-19 was identified in Wuhan, China in December 2019. COVID-19 is caused by the virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a new virus in humans causing respiratory illness which can be spread from person-to-person. Early in the outbreak, many patients were reported to have a link to a large seafood and live animal market; however, later cases with no link to the market confirmed person-to-person transmission of the disease. Additionally, travel-related exportation of cases occurred.
There are three main ways that COVID-19 can spread:
- By breathing in air carrying droplets or aerosol particles that contain the SARS-CoV-2 virus when close to an infected person or in poorly ventilated spaces with infected persons
- By having droplets and particles that contain the SARS-CoV-2 virus land on the eyes, nose, or mouth – especially through splashes and sprays like a cough or sneeze
- By touching the eyes, nose, or mouth with hands that have the SARS-CoV-2 virus particles on them
The droplets that contain the SARS-CoV-2 virus are released when someone with COVID-19 sneezes, coughs, or talks. Infectious droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. A physical distance of at least 1 meter (3 ft) between persons is recommended by the WHO to avoid infection, 1 whereas CDC recommends maintaining a physical distance of at least 1.8 meters (6ft) between persons. Respiratory droplets can land on hands, objects, or surfaces around the person when they cough or talk, and people can then become infected with COVID-19 from touching hands, objects or surfaces with droplets and then touching their eyes, nose, or mouth. Additionally, transmission can occur from those with mild symptoms or from those who do not feel ill.
There are certain circumstances that can increase the risk of infection for COVID-19 such as poorly ventilated space. In indoor spaces with poor ventilation, the concentration of virus particles is often higher than outdoors. 2,3 Other factors that are associated with increased COVID-19 risk include prolonged exposure to those infected with COVID-19, close contact with infected persons, and any other activity that leads to exposure to a greater amount of respiratory droplets and particles.
A wide range of symptoms for COVID-19 have been reported. 4 These symptoms include:
- Fever or chills
- Muscle or body aches
- Sore throat
- Nasal congestion or runny nose
- Shortness of breath or difficulty breathing
- Loss of smell or taste
The estimated incubation period is between 2 and 14 days with a median of 5 days. It is important to note that some people become infected and do not develop any symptoms or feel ill.
People at Higher Risk for Severe Illness
COVID-19 is a relatively new disease; therefore, additional risk factors for severe COVID-19 may continue to be identified. In some cases, people who get COVID-19 can develop severe complications, including difficulty breathing, causing a need for hospitalization and intensive care. 5 These severe complications often lead to death. The risk of severe disease increases steadily as people age. Additionally, those of all ages with underlying medical conditions , including but not limited to heart disease, diabetes or lung disease, are at higher risk to develop severe COVID-19 compared to those without these conditions. 5 Those at higher risk for severe illness should be prioritized for vaccination. 6
COVID-19 Preventative Actions
COVID-19 can be prevented through pharmaceutical (i.e., vaccination) and non-pharmaceutical interventions (e.g., masking, physical distancing, hand hygiene). All of these preventative measures are important to protect individuals from acquiring and transmitting the SARS-CoV-2 virus and should be done in conjunction with one another.
Vaccination
Getting vaccinated is a preventative measure that people can take to avoid getting sick with COVID-19 and to avoid infecting others. While safe and effective vaccines are a great tool for prevention, it is important to continue other preventative actions such as wearing masks, performing hand hygiene, physically distancing from others, and avoiding crowded spaces and spaces with poor ventilation. 7 There are several vaccine candidates, and many have been listed under WHO’s emergency use.
Wearing masks is another important preventative action for COVID-19 that should continue to be performed. When selecting a mask, there are many factors to consider. 8 Masks should
- Have two or more layers of washable, breathable fabric
- Completely cover the nose and mouth
- Fit snug against the sides of the face and not have gaps
- Have a nose wire to prevent air from leaking out of the top of the mask
It is also important to choose and wear the proper type of mask based on your setting. For example, in a community setting, cloth masks should be worn, whereas during aerosol generating procedures in a healthcare setting, should be worn.
Other preventative actions
Even with the introduction of vaccinations as a tool for prevention against COVID-19 and the proper use of masks, CDC recommends the following key COVID-19 preventative activities: 7 — avoiding crowded spaces or spaces that have poor ventilation or wear a mask in these spaces; performing proper hand hygiene; keeping high touch surfaces clean; monitoring symptoms; and getting tested if ill.
IPC for COVID-19
Infection prevention and control (IPC) is the practice of preventing or stopping the spread of infections from the delivery of healthcare services in facilities like hospitals, outpatient clinics, dialysis centers, long-term care facilities, or traditional practitioners. IPC is a critical part of health system strengthening and must be a priority to protect patients and healthcare workers. In the context of COVID-19, the IPC goal is to support the maintenance of essential healthcare services by containing and preventing COVID-19 transmission within healthcare facilities to keep patients and healthcare workers healthy and safe.
COVID-19 IPC Priorities
- Rapid identification of suspect cases
- Screening/triage at initial healthcare facility encounter and rapid implementation of source control
- Limiting the entry of healthcare workers and/or visitors with suspected or confirmed COVID-19
- Immediate isolation and referral for testing
- Group patients with suspected or confirmed COVID-19 separately
- Test all suspected patients for COVID-19
- Safe clinical management
- Immediate identification of inpatients and healthcare workers with suspected COVID-19
- Adherence to IPC practices
- Appropriate use of personal protective equipment (PPE)
- Unvaccinated healthcare workers, patients, and visitors should be offered resources and counseled about the importance of vaccination.
COVID-19 IPC in the context of vaccination delivery
As safe and effective COVID-19 vaccines continue to be delivered, there are certain recommendations and principles that should be implemented and considered for vaccine administration. Consultations and consensus between WHO, the United Nations Children’s Fund (UNICEF), and the ad hoc WHO COVID-19 IPC Guidance Development Group have led to the development of a document that outlines key IPC principles and recommended proper precautions for safe administration of COVID-19 vaccines. Consult the Infection prevention and control (IPC) principles and procedures for COVID-19 vaccination activities document when preparing for vaccine deployment. 10
The key IPC principles for COVID-19 vaccine deployment set out in the document include:
- Applying standard precautions during any vaccination activity
- Performing additional IPC precautions like mask use in the context of the COVID-19 pandemic
- Providing healthcare workers with specific training and providing the public with targeted information regarding IPC measures for safe vaccine delivery
- Having a clean, hygienic, and well-ventilated environment with appropriate waste management, and adequate spaces that facilitate best IPC practices like physical distancing
- Ensuring consultation and adherence to national guidance and protocols for IPC measures, including those related to COVID-19
Standard and Transmission-Based Precautions
Standard precautions are a set of practices that apply to the care of patients in all healthcare settings at all times. Standard precautions remain the cornerstone of infection prevention and control. Application of these precautions depends on the nature of the healthcare worker-patient interaction and the anticipated exposure to a known infectious agent. Standard precautions include:
- Hand hygiene
- Personal protective equipment
- Respiratory hygiene and cough etiquette
- Cleaning and disinfection of devices and environmental surfaces
- Safe injection practices
- Medication storage and handling
Transmission-based precautions are a set of practices specific for patients with known or suspected infectious agents that require additional control measures to prevent transmission. These precautions are used in addition to standard precautions.
COVID-19 Transmission-Based Precautions:
Current WHO guidance for healthcare workers caring for suspected or confirmed COVID-19 patients recommends the use of contact and droplet precautions in addition to standard precautions unless an aerosol generated procedure is being performed, in which case airborne precautions are needed. 1 Disposable or dedicated patient care equipment, such as stethoscopes, blood pressure cuffs, should be used. If equipment needs to be shared among patients, it should be cleaned and disinfected between use for each patient using products containing ethyl alcohol of at least 70%.
Also, adequately ventilated single rooms or wards are suggested. For general ward rooms with natural ventilation, adequate ventilation for COVID-19 patients is considered to be 60 L/s per patient. When single rooms are not available, suspected COVID-19 patients should be grouped together with beds at least 1 meter (3ft) apart based on WHO’s recommendations, although some member states, including the United States, have recommended maintaining greater distances whenever possible. COVID-19 isolation rooms or wards should have dedicated bathrooms, which should be cleaned and disinfected at least twice daily.
Additionally, healthcare facilities can also consider designating healthcare workers to care for patients with COVID-19 and restricting the number of visitors allowed in the facility.
Transportation of patients with COVID-19 should be avoided unless medically necessary. If transportation is deemed medically necessary, a mask should be placed on the suspected or confirmed COVID-19 patient. Healthcare workers should also wear the appropriate PPE when transporting patients.
COVID-19 PPE
Contact and droplet precaution PPE are recommended for healthcare workers before entering the room of suspected or confirmed COVID-19 patients. Healthcare workers should be trained on the correct use of PPE, including how to put it on and remove it. Extended use and re-use of certain PPE items such as masks and gowns can be considered when there are supply shortages. Healthcare workers should:
- Use a medical mask (at least a surgical/medical mask)
- Wear eye protection (goggles) or facial protection (face shield)
- Wear a clean, non-sterile, long-sleeve gown
There is a higher risk of self-contamination when removing PPE. Please see instructions for putting on and removing PPE [2.9 MB, 3 pages] for guidance.
For healthcare workers performing any of the following aerosol generating procedures on patients with COVID-19, it is recommended that a fitted respirator mask (surgical N95 respirators, FFP2 or equivalent) is used as opposed to surgical/medical masks. In addition to wearing a fitted respirator mask, healthcare workers should also wear appropriate PPE, including gloves, a gown and eye protection.
Although there is a difference in determination on which procedures generate infectious aerosol, the current WHO list of Aerosol Generating Procedures includes: 1
- Endotracheal intubation
- Bronchoscopy
- Non-invasive ventilation
- Tracheotomy
- Manual ventilation before intubation
- Cardiopulmonary resuscitation
- Sputum induction
- Dentistry and autopsy procedures
Infection Prevention and Control Resources for COVID-19 in non-U.S. Healthcare Settings:
- Strategic Priority IPC Activities for Containment and Prevention
- Identification of Healthcare Workers and Inpatients with Suspected COVID-19
- WHO. Infection prevention and control during health care when novel coronavirus disease (COVID-19) is suspected or confirmed .29 June 2020.
- Kai-Wang To, K., Tak-Yin Tsang, O., Chik-Yan Yip, C., Chan, KH., Wu, TC., Man-Chun Chan, J…Yuen, KY. Consistent detection of 2019 novel coronavirus in saliva . Clinical Infectious Diseases . 12 February 2020. ciaa149.
- WHO. Transmission of SARS-CoV-2: implications for infection prevention precautions . 9 July 2020.
- WHO. Clinical management of severe acute respiratory infection when COVID-19 is suspected . 13 March 2020.
- The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) – China 2020 . CDCweekly . 17 February 2020. 10.46234/ccdcw2020.032
- Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus Disease 2019 Case Surveillance — United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:759–765. DOI: http://dx.doi.org/10.15585/mmwr.mm6924e2
- Chen, J., Lu, H., Melino, G. et al. COVID-19 infection: the China and Italy perspectives. Cell Death Dis 11, 438 (2020). https://doi.org/10.1038/s41419-020-2603-0
- WHO. Advise on the use of masks in the context of COVID-19 . 5 June 2020.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
ORIGINAL RESEARCH article
Intention and practice on personal preventive measures against covid-19 among older adults in the kingdom of saudi arabia: an epidemiological study using the theory of planned behaviour.

- 1 Department of Family and Community Medicine, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
- 2 College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
- 3 National Program for Community Development – Tanmiah, Riyadh, Saudi Arabia
Introduction: Older adults aged 65 years and above are among the most vulnerable to adverse outcomes and death following a COVID-19 infection. The weekly epidemiological updates by the World Health Organisation show that the continued emergence of concerning subtypes of the virus indicates that the pandemic remains a public health concern and the public should continue to comply with personal preventive measures (PPMs). This study applies the Theory of Planned Behaviour (TPB) which is rooted in the field of Public Health, Epidemiology, and Preventive Medicine to Saudi older adults to predict their health behaviour.
Methods: This behavioural epidemiological study recruited older adult participants aged 65 years of age and above. A tool which consisted of sociodemographic and health-related questions, as well as questions regarding the components of the TPB, namely, Attitude, Subjective Norm, Perceived Behavioural Control was used. Bivariate analyses, followed by unadjusted and adjusted multivariable logistic regression analyses were performed to derive odds ratios and 95% confidence intervals.
Results: The total number of participants was 502. The mean age was 70.34 years, with similar distributions between males and females. In total, 52.2% intended to practice PPMs, whereas only 48% had a good practice. Also, 56% had a favourable Attitude towards PPMs, 61.4% had a positive Subjective Norm and 39.8% had perceived they had a high control over their behaviour. Females, and high educational status were predictors for high intention to practice PPMs (OR = 1.59, 95% CI = 1.01–2.52 and OR = 2.72, 95% CI = 1.44–5.16 respectively). Further predictors included Attitudes, Subjective Norm and Perceived Behavioural Control. Results also show that intention to practice was significantly associated with a lower odd of practicing PPMs (OR = 0.06, 95% CI = 0.04–0.10).
Conclusion: Current findings highlight the need to continue with public health efforts targeting vulnerable older adults. Also, the fact that intention negatively predicted practice highlights the need for further behavioural epidemiological studies addressing the intention-behaviour gap.
Introduction
Disease prevention is crucial in various aspects of life and health. Ever since the emergence of the coronavirus disease – 2019 (COVID-19) in late December of 2019, and it being announced as a pandemic in March of 2020, over 770 million confirmed cases and almost 7 million deaths have been registered ( 1 , 2 ). This disease originates from a single-stranded RNA virus that is able to cause respiratory, gastrointestinal and central nervous system infections in its host ( 3 ). Due to the virus’s ability to rapidly spread and evolve, it remains a public health priority to this day.
Very early on, specific groups of people were understood to be at a higher risk of mortality after a COVID-19 infection. These groups include older adults aged 65 years of age and above, patients with comorbidities as well as immunocompromised patients ( 4 , 5 ). Therefore, preventive measures have been put in place, with the World Health Organisation (WHO) leading global efforts by setting up periodic bulletins with guidelines, as well as establishing the COVID-19 dashboard, and the United Nations supporting national preparedness and response plans to countries worldwide ( 1 , 6 ). During the early stages of the pandemic, and while vaccines were still under development, the primary focus was on non-pharmaceutical interventions ( 7 ). These were steps that could be taken to mitigate and control the spread of the disease, and consequently alleviate its burden and allow time to develop the much-needed vaccines and treatments.
The Kingdom of Saudi Arabia (KSA) was among the first countries to proactively implement preventive measures that were – in those early stages – considered unprecedented. For example, two months before the detection of any cases in the country, a national committee with members from different governmental agencies had been entrusted with overviewing global updates and providing recommendations in preparing for the possibility of cases locally ( 8 ). Upon the discovery of the first case, all entry points to the two holy cities of Makkah and Madinah were suspended and international flights were cancelled, shifting schools and other educational institutions to remote learning as well as nationwide curfews ( 8 , 9 ). Furthermore, health campaigns over official governmental social media accounts and text messages were streamed daily to raise public awareness and to remind everyone to abide by national preventative measures ( 8 , 10 ). These measures have greatly assisted in reducing and controlling the spread and potential further burden of the disease ( 9 ).
The Theory of Planned Behaviour (TPB) is a theory that attempts to draw the framework for predicting adherence and compliance to preventive measures ( 11 ). This theory is a conceptual model that was established in 1980 as an extension of the Theories of Reasoned Action to explain the effect of information and motivation on behaviours ( 12 ).
Even though this theory has been extensively studied in several countries, very few studies within the KSA are found, and none have studied older adults specifically and/or preventive measures in general. For example, it has been applied to dental healthcare workers to examine the factors associated with infection control behaviour ( 13 ), as well as among the general public to study their intent to receive the COVID-19 vaccine alone ( 13 , 14 ). Although on the 5th of March of 2022, all restrictions have been scraped, the continued emergence of concerning subtypes of COVID-19 and the fact that older adults remain at risk of complicated outcomes and death compounded by the lack of research on this specific vulnerable population has given rise to this research.
Therefore, this study will first provide a theoretical foundation for the TPB within the context of COVID-19, and subsequently apply the components of the theory to Saudi older adults to examine their intention to practice personal preventive measures (PPMs) as set out by the Saudi health authority guidelines. The study will also discuss the study’s findings and provide implications for public health policy.
Theoretical foundation
Several theories that attempt to predict health behaviours are available in the medical literature. These include – but are not limited to – the Health Belief Model, Technology Acceptance Model, and the TPB ( 11 , 15 , 16 ). The TPB argues that behaviour is driven by the intention to perform that particular behaviour forming what is known as the individual’s “belief structure” ( 11 ). In the case of COVID-19 preventive measures, this structure would be comprised of Attitude towards preventive measures (i.e., their perceived necessity), Subjective Norms (i.e., whether others support and perform these measures), and Perceived Behavioural Control (i.e., the extent of which the preventive measures are within the individual’s control).
The TPB is related to the science of behavioural epidemiology which has been emerging since the late 1970s ( 17 , 18 ). Behavioural epidemiology is under the umbrella of Public Health and consists mainly of two concepts, the first is to identify the epidemiological relationship between individual behaviour and disease occurrence, and the second is the epidemiological study of the actual behaviour itself ( 19 ). There is a vast literature supporting the application of this theory to predict health behaviour in general and for COVID-19 specifically ( 12 , 18 , 20 – 22 ).
Materials and methods
Study design, setting, and study participants.
This behavioural epidemiological study employed a cross-sectional design and was conducted in the Eastern region of the KSA. The study setting were community health centres where older adult participants attended routine physical examinations. Eligibility for inclusion included both male and female participants who were aged 65 years and above, and that they were clear from any neurocognitive disorders such Parkinson’s disease and dementia and were capable of communicating verbally.
Ethical considerations
The Imam Abdulrahman Bin Faisal University’s Institutional Review Board approved the study (IRB-2022-01-294). The participation was voluntary and there was no requirement to obtain personally identifiable information. Consent to participate was obtained from all participants. The study complied with the principles of the Declaration of Helsinki.
Sample size and sampling technique
The minimum required sample size was 383. This was based on a previous study in which the intention to practice PPMs was 52% ( 22 ), with a precision of 5% and at an alpha level of 0.05. The Epi info software version 7.0 was used for sample size calculations. Since the study targets a delicate population, a non-probability sampling technique was used to recruit participants.
Data collection tool and processes
The questionnaire was adapted from the WHO Survey tool and guidance and incorporated recent international literature that had also used the TPB within the context of COVID-19 ( 14 , 20 – 24 ). Since these studies were either on the general population or on specific health workers, the authors had to adapt the tool to better represent the older adults’ population who are the focus of this work. Three experts namely, a geriatrician, preventive medicine consultant and a public health consultant had reviewed the tool to check for its clarity and appropriateness. Then, a pilot study was performed on a sample of 10 participants aged 65 years and above, all questions were clear and the average time to complete the tool was 8 min.
The first set of variables in the tool included questions on sociodemographic and health-related characteristics. Also, the tool asked whether the participants knew of a previous COVID-19 infection, and if yes, the perceived severity level of that infection (mild, moderate or severe, i.e., hospitalised). The second set of variables were pertaining to the TPB. These included questions on the three main elements of the theory, namely, Attitude towards PPMs, Subjective Norm and Perceived Behavioural Control. Attitudes may be defined as the degree to which an individual holds a favourable or unfavourable assessment of a particular behaviour. Subjective Norm is the belief of whether other people within the community approve or disapprove of a particular behaviour, whereas Perceived Behavioural Control is the perceived difficulty or easiness of performing that behaviour ( 11 ). PPMs against COVID-19 may be defined as those measures that are known to protect and prevent infection and which included the following six preventive recommendations; handwashing with soap and water for a minimum of 20 s, avoid touching eyes, mouth, and nose when hands are not washed, staying at home if sick, covering mouth and nose when coughing and sneezing, physical distancing and self-isolation. Furthermore, the tool asked the participants on their intention to practice these PPMs and whether they already do so in the present time.
Data were collected through an online tool which allowed the team to share the link within themselves during the data collection period. In order to protect both the older adult participants and the team, guidelines were followed in terms of respiratory etiquette and distancing.
Measurements
The Attitude to practice PPMs was measured using the six main recommendations stated above on a five-point Likert’s scale. The mean score was computed for each participant, and those who score the overall mean and above were considered as having a good Attitude, whereas those who scored below the mean were considered to have a poor Attitude. As for Subjective Norm, it was based on two questions, namely, if you were infected with COVID-19, would you let people know? and how much do you trust the prevention information issued by the MoH? These were both measured on the five-point Likert’s scale. Similar to Attitude, participants scoring above the mean were considered to have a positive Subjective Norm and participants scoring below the mean were considered to have a negative Subjective Norm. The Perceived Behavioural Control construct was similarly computed and was based on three questions, namely, do you think COVID-19 would have a serious impact on you and your family? Are you still worried about COVID-19 and other large infectious diseases? And do you have the confidence to protect yourself and your family against COVID-19 and other large scale infectious diseases? ( 22 , 24 ).
Intention to practice PPMs was measured based on the above six PPM questions, and further questions were added that included the use of antibiotics to prevent and treat COVID-19. These were measured on a Likert’s scale and those who were intending had scored above the mean. The current practicing of PPMs was a simple yes/no response. This allowed us to differentiate between the intention and actual practicing of these measures.
Data analyses
Descriptive statistics were computed as frequencies and percentages for categorical variables and means ± standard deviations for continuous variables. The study had two outcomes, the first was intention to practice PPMs and the second was the current practice. Bivariate associations were performed to study the associations between these outcomes and all elements of the TPB as well as sociodemographic and health-related characteristics. Both unadjusted and adjusted binary logistic regression analyses were performed for the two outcomes of the study to compute the Odds Ratios (ORs) and their accompanying 95% confidence intervals (CIs). The level of significance was set at 0.05. All analyses were performed in Stata Statistical Software version 15.0 (Stata Corp) ( 25 ).
Sociodemographic and health characteristics of study participants
The study included 502 participants. The mean age was 70.34 years ±5.85 years. The distribution of males and females were very similar (49 and 51% respectively). The majority of participants (44.40%) had a high school degree and only 1.60% were postgraduates. Only 2.80% reported that they once were healthcare professionals. With regards to their health status, 75.30% reported the presence of a chronic disease condition. Also, 4.60% were living alone and 45.60 of the total sample reported a “good” financial status, compared to only 2% who had reported a bad financial status.
In total, 87.30% had known people who were previously infected with COVID-19, and 42.8% had known someone who had died from it. With regards to personal history, 47.60% reported a previous COVID-19 infection, of those sub-sample of participants, 15.5% were hospitalised due to the severity of the infection ( Table 1 ).
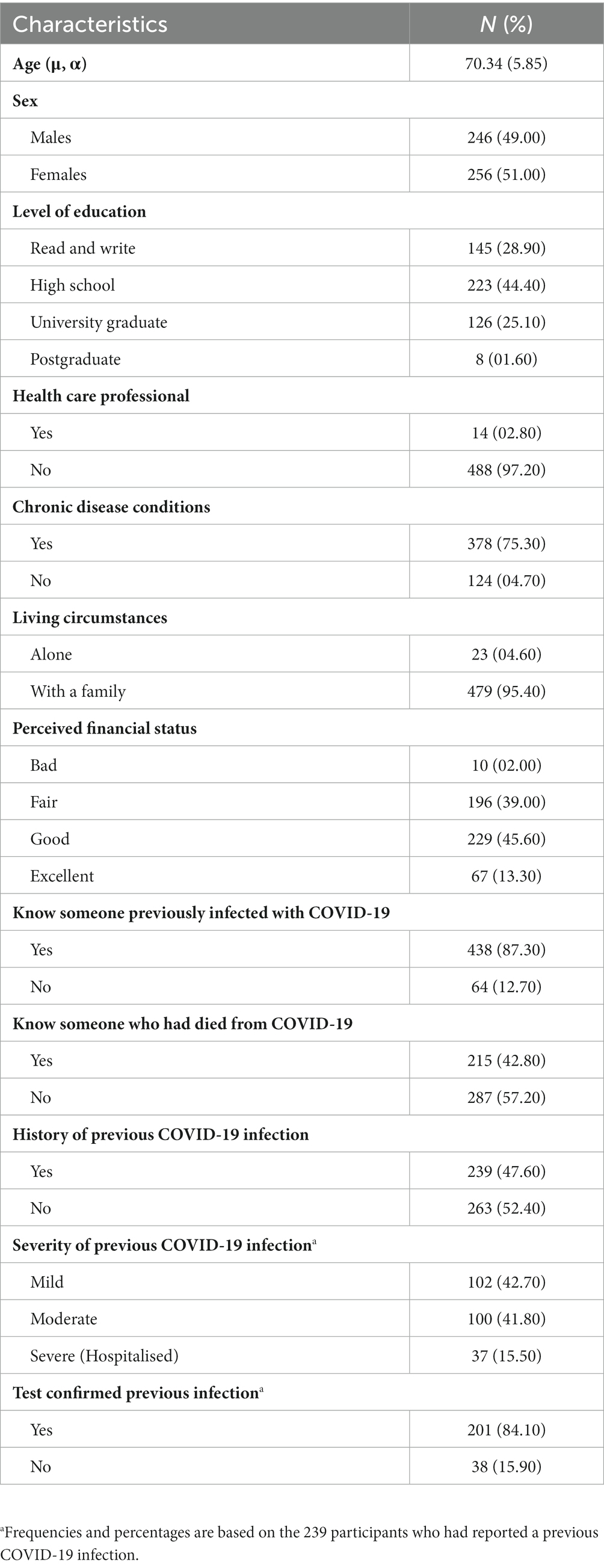
Table 1 . Sociodemographic and health characteristics of the older adult participants.
Subjective Norm and Perceived Behavioural Control and Attitude of the study participants
The mean score for the Subject Norm was 8.44 ± 1.68 (range 2–10). In total, 61.4% had a positive Subjective Norm. As for the Perceived Behavioural Control, the mean was 8.33 ± 2.01 (range 3–13) and 39.8% perceived that they had a higher control in their behaviour. Whereas for the Attitude, the median score was 25.51 ± 4.83 (range 6–30) and 56% were found to have a favourable Attitude ( Table 2 ).
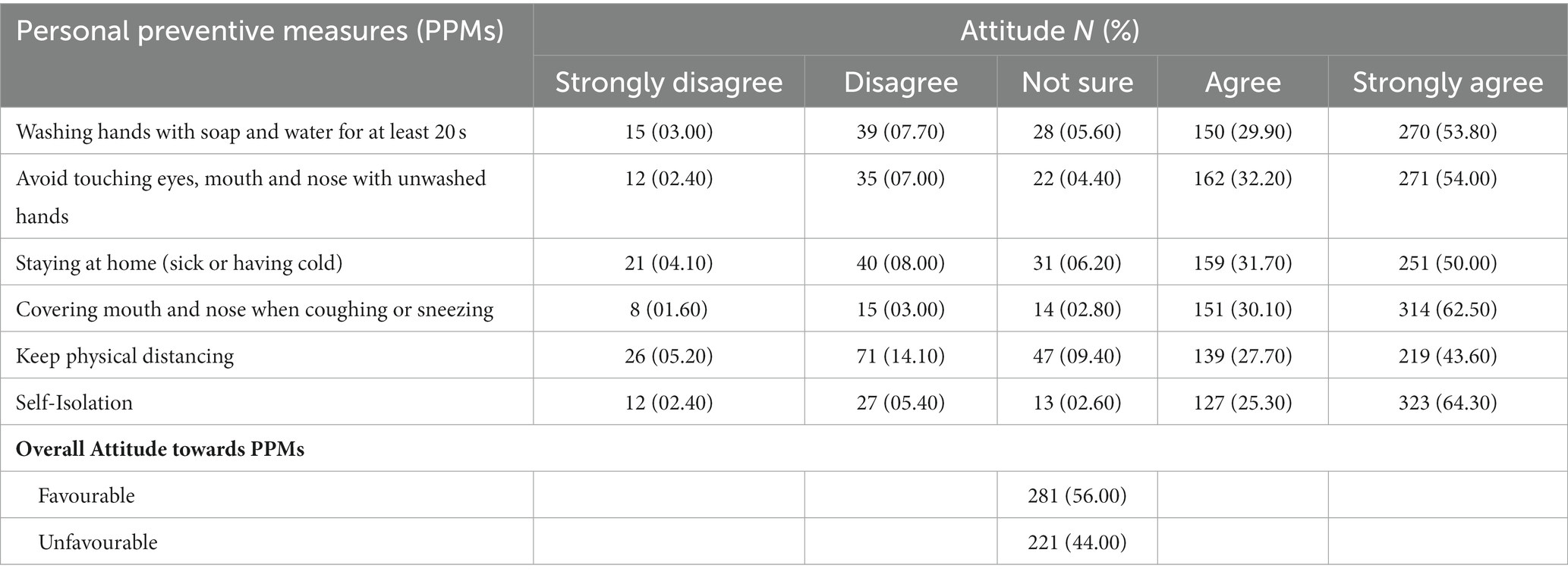
Table 2 . Attitude towards personal preventive measures against COVID-19 among older adult participants.
Likewise, along the range of the five degrees of Attitudes towards the PPMs, over half the participants (50.00 to 64.30%) strongly agreed to most of them, except for physical distancing which showed the least amount of agreement (43.60%). Physical distancing also showed a higher proportion of strong disagreement compared to other statements (05.20%).

Intention and practice on PPMs against COVID-19
The mean score for the intention to practice PPMs was 29.44 ± 8.56 (range 10–50). In total, 52.2% had intended on practicing the stated preventive measures. Along the range of the five degrees of intention, 50.8% had very likely intended to practice washing hands with soap and water for at least 20 s. Participants reported lesser percentages of being very likely intending to avoid touching eyes, mouth, and nose with unwashed hands (44.20%), as well as for using disinfectants to clean hands when soaps are unavailable (35.3%). A large proportion of participants exhibited being very unlikely to intend to use antibiotics to prevent or treat COVID-19 (62.70 and 59.40% respectively) ( Table 3 ).
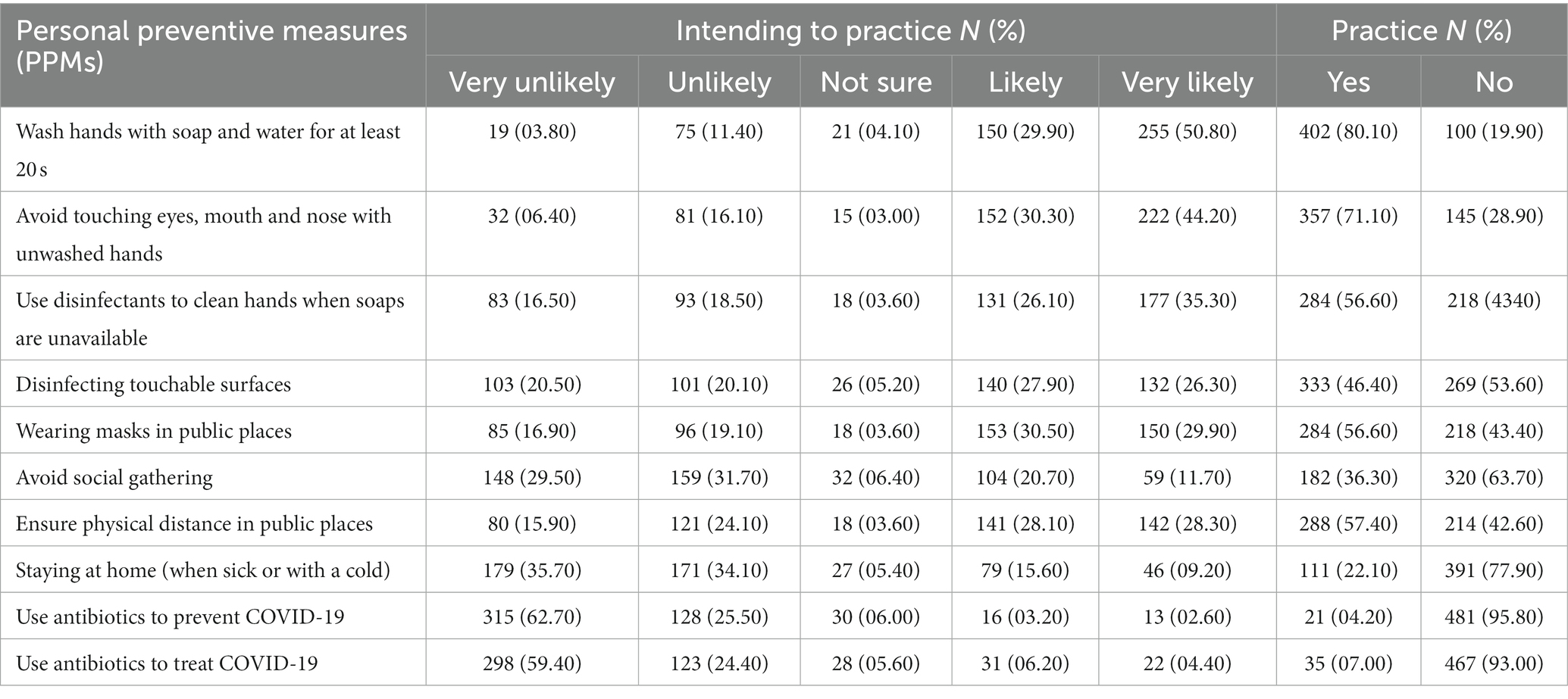
Table 3 . Intention and practice of personal preventive measures against COVID-19 among older adult participants.
With regards to the actual practice of PPMs, the analysis found that the mean practice score was 15.62 ± 2.58 (range 10–20) and the proportion of participants who had good practice were 48.0%. Hand washing with soap and water for at least 20 min was reported among 80.1%, avoid touching eyes, nose, and mouth with unwashed hands was stated among 71.1%. The least commonly reported practice was using antibiotics to prevent COVID-19 (7.0%).
Factors associated with the intention to practice PPMs against COVID-19 infection
Results shows statistically significant differences in the intention to practice PPMs in relation to age, level of education, Attitude towards PPMs, Subjective Norm, and Perceived Behavioural Control ( p < 0.05). Given these results, Table 4 shows unadjusted and adjusted logistic regression analyses of participants’ characteristics in relation to intention to practice PPMs. The odds of intention were significantly lower among the ≥70-year age group, although this was not significant in the adjusted model. Sex arose as a factor where females were 59% more likely to exhibit intention to practice PPMs (95% CI = 1.0–2.52). Also, the results show that the odds of intention increased with higher education. With respect to the studied four components of the TPB, it was observed that participants who had a favourable Attitude were 4.41 times more likely intending to practice PPMs (95% CI = 2.89–6.73). Also, higher odds were seen among participants who had a positive Subjective Norm (95% CI = 1.53–3.65). Similarly, the odds of intention were 72.3% times higher among those participants with a high Perceived Behavioural Control compared to their counterparts.
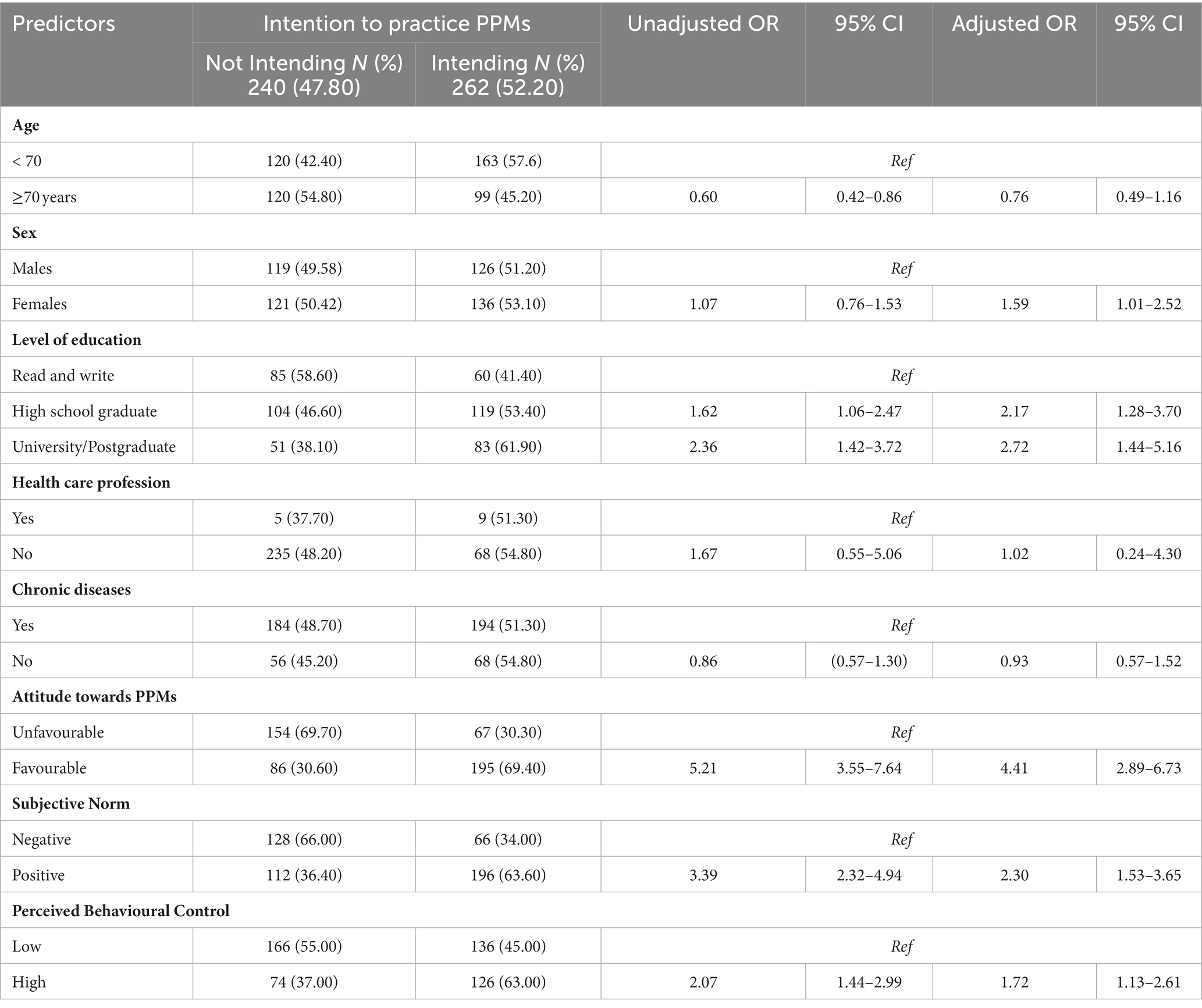
Table 4 . Unadjusted and adjusted binary logistic regression analyses of older adult participants predictors of the intention to practice personal preventive measures against COVID-19 infection.
Factors associated with current practicing of PPMs
Results show that there were statistically significant differences in the current practicing of PPMs in relation to the level of education, having been a healthcare professional, Attitude towards PPMs, Subjective Norm, and Perceived Behavioural Control and the intention to practicing PPMs ( p < 0.05).
Given these results, Table 5 shows unadjusted and adjusted logistic regression analyses of participants’ characteristics in relation to the current practicing of PPMs. In the adjusted model, only three of the four components of the TPB were statistically significant. Firstly, participants with a favourable Attitude were 62.10% less likely to report practicing PPMs (95% CI = 0.22–0.63). For Perceived Behavioural Control, participants who had reported a high Control were 40% less likely to practice PPMs (95% CI =0.36–0.98). As for the intention, participants who were intending to practice PPMs were 93.4% less likely to currently practice them (95% CI = 0.04–0.10).
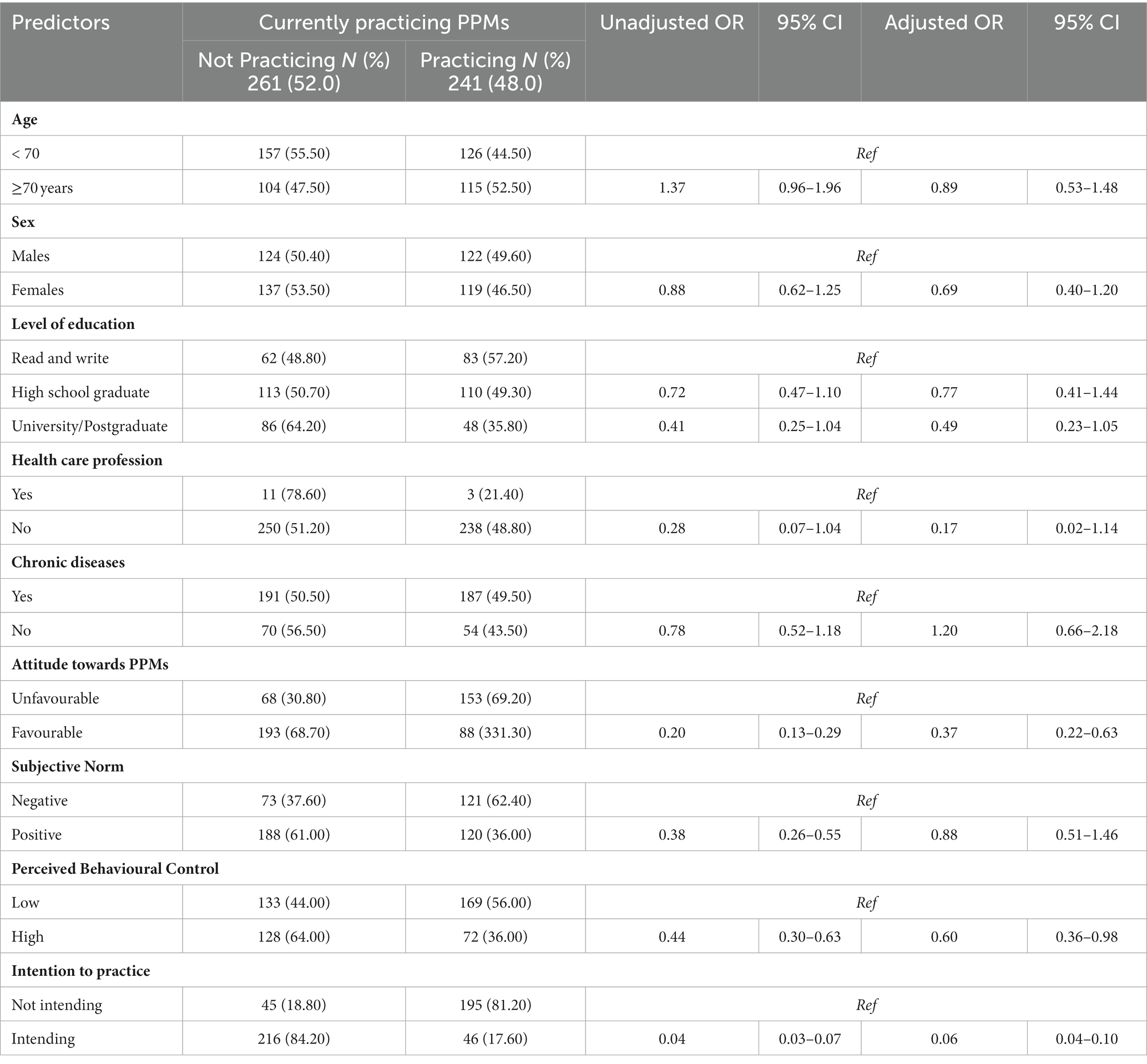
Table 5 . Unadjusted and adjusted binary logistic regression analyses of older adult participants predictors of the current practicing of personal preventive measures against the COVID-19 infection.
Despite all scientific evidence, epidemiologically or biologically, on the positive effects of preventive measures against COVID-19, compliance with these measures remains variable. Cultural and behavioural factors play an important role in this variability. To the best of our knowledge, this is the first study to apply the TPB to predict adherence to public health preventive measures against the COVID-19 infection in the older adults’ vulnerable population. We examined both the intention as well as the actual current practicing of PPMs. It is also important to note that the collection of the data was past the date at which the government had scraped all restrictions, hence the results presented here show the attitudes and beliefs of the participants long after the extensive health campaigns and the COVID-19 public concern. Several important findings have been found regarding the intention and practice towards PPMs among the older adult Saudi population.
In our study, we found that over half the participants had intended to practice PPMs. These figures are very similar to those of studies in parts of Africa ( 22 , 26 ), but are in stark contrast to those in the US where the national average intent to comply with four recommendations, namely, washing hands, social distancing, cough etiquette and stay at home was over 80% ( 27 ). These differences may be due to fatality differences between the two regions which may have played a role in the increased intention in the US.
Factors associated with the intention to practice PPMs against COVID-19
Our study analysed factors predicting older adults’ intention to practice PPMs. We found that females were more likely to intend to practice PPMs, and those with higher education had an even greater odd of intention. This aligns with another that showed that women, and those with higher educational attainment, were more likely to adopt preventive measures ( 28 ). Rooted within the TPB, our findings also revealed that participants with a favourable Attitude were more likely to intend to practice PPMs. This underlines the impact of personal Attitudes on health behaviours, as confirmed by multiple studies, which found that positive Attitudes towards preventive measures significantly increased their adoption ( 29 , 30 ). The role of social factors was also highlighted in our study. Participants with positive Subjective Norms were more likely to intend to practice PPMs against COVID-19, supporting the findings of a previous study which reported that positive social norms significantly influenced the uptake of preventive measures ( 31 ). Lastly, our study showed that older adults with high Perceived Behavioural Control were more likely to intend to practice PPMs against COVID-19, indicating the importance of individuals’ confidence in their ability to perform preventive behaviours. This complements the findings of a local study which found that perceived control significantly impacted the adoption of preventive measures ( 32 ). Overall, our findings confirm and expand upon existing literature, emphasizing the role of sex, education, Attitudes, social norms, and perceived control in influencing older adults’ intention to practice PPMs against COVID-19.
Factors associated with the current practice of PPMs against COVID-19
With regards to the current practicing of PPMs, we found that, among the study participants, those with a favourable Attitude towards PPMs were about two-thirds less likely to practice PPMs. This contradicts the findings of previous studies, which demonstrated a positive correlation between Attitudes towards PPMs and their adoption ( 28 , 31 ). We also found that participants who had a Perceived Behavioural Control were less likely to practice PPMs. This is in stark contrast to the findings of previous studies which highlighted that Perceived Behavioural Control was a significant predictive factor in the adoption of PPMs ( 30 , 33 ). These studies suggested that individuals who believe they have the skills and resources to perform PPMs are more likely to do so. Interestingly, our study showed that participants who reported intending to practice PPMs were almost two times less likely to actually practice PPMs against COVID-19. This divergence between intention and behaviour contradicts the findings of a Turkish study which found a strong positive correlation between intentions and subsequent behaviour, particularly around health-related actions ( 34 ). It is interesting to find that in an Ethiopian study, although those who intended to practice PPMs were more likely to actually practice it, this association was not significant in their adjusted model ( 22 ). It is important though to note that the mean age in the first study was only 38.76 years, and in the second study it was 42.67 years, whereas in our study the mean age was 70.36 years. Notably, this divergence between intention and practice is not unheard of, the intention-behaviour gap is a phrase that describes the failure of intentions to be translated into actions ( 26 ). It maybe that the older adult population as a defined group possess specific behavioural characteristics unique to all other age groups. Overall, our unexpected findings highlight a complex interaction between Attitudes, Perceived Behavioural Control, intentions, and actual behaviour in the practice of PPMs among older adults. These findings suggest that other factors might be influencing the adoption of PPMs and that further research especially in the intention-practice gap is needed to fully understand these dynamics.
Implications and future directions
Although literature focusing on the role of the TPB during the pandemic is flourishing, there is a lack of research focusing on the older adult population. The current finding in that intention does not necessarily mean practice is extremely important to investigate in further epidemiological studies for this particular vulnerable population. Public health agencies within the KSA should continue its efforts to raise awareness through communication plans regarding the importance of adopting these preventive measures even long after lifting all restrictions. These communication plans should incorporate the role of friends and family especially since social constructs have been found to be associated with adoption of preventive measures. Furthermore, epidemiologists should further conduct behavioural epidemiological studies that would further suggest practical recommendations for public health agencies and health authorities in the KSA. Funded national surveys managed by experienced epidemiologists would be particularly helpful in order to reach sample sizes of sufficient and generally representative quality. Also, given the current focus on the practice of Family and primary care physicians, particularly with the expansion in preventive clinics, the role of these healthcare practitioners is crucial in increasing both awareness and promoting the health of older adults and other vulnerable groups.
Strengths and limitations
This is the first study to apply the TPB to the older adult population in the KSA within the context of preventive measures against COVID-19. However, the cross-sectional nature and the fact that both the intention and the actual practice were taken at the same time does not allow for any temporal associations to be made. Furthermore, the non-probability sampling technique, albeit consciously chosen due to the sensitive nature of our population, limits the generalisability of our results.
This study has shown that long after lifting all restrictions against COVID-19 in the KSA, a little over half the older adult participants intend to practice PPMs. It also showed that females, participants with a higher education level, those with a favourable Attitude towards preventive measures, positive Subjective Norm and high Perceived Behavioural Control exhibited a higher odd of intending to practice PPMs. Most importantly, that intending to practice does not necessarily mean actual practicing. We recommend that public health agencies, health authorities and primary care physicians in the country to continue the efforts to raise awareness of proper preventive measures through customised communication plans. Also, the role of epidemiologists in terms of behavioural epidemiological studies should not be neglected.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional review board of Imam Abdulrahman Bin Faisal University (IRB-2022-01-294). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RA: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AmA: Conceptualization, Data curation, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. LA: Conceptualization, Data curation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. SA: Conceptualization, Data curation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. ZA: Conceptualization, Data curation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. HA: Conceptualization, Data curation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. FA: Conceptualization, Data curation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. MA-S: Conceptualization, Data curation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. NoA: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MS: Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. AsA: Conceptualization, Formal analysis, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NiA: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank all individuals who have kindly agreed to participate in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer OA declared a shared affiliation with the authors to the handling editor at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. WHO. WHO COVID-19 dashboard . Geneva: WHO (2020).
Google Scholar
2. Hu, B, Guo, H, Zhou, P, and Shi, Z-L. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol . (2021) 19:141–54. doi: 10.1038/s41579-020-00459-7
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Gupta, A, Madhavan, MV, Sehgal, K, Nair, N, Mahajan, S, Sehrawat, TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med . (2020) 26:1017–32. doi: 10.1038/s41591-020-0968-3
4. SeyedAlinaghi, S, Karimi, A, Barzegary, A, Mojdeganlou, H, Vahedi, F, Mirghaderi, SP, et al. COVID-19 mortality in patients with immunodeficiency and its predictors: a systematic review. Eur J Med Res . (2022) 27:195. doi: 10.1186/s40001-022-00824-7
5. Kowsar, R, Rahimi, AM, Sroka, M, Mansouri, A, Sadeghi, K, Bonakdar, E, et al. Risk of mortality in COVID-19 patients: a meta-and network analysis. Sci Rep . (2023) 13:2138. doi: 10.1038/s41598-023-29364-8
6. UN. United Nations Comprehensive Response to COVID-10. Saving lives, protecting societies, recovering better . New York: UN (2020).
7. Chow, EJ, Uyeki, TM, and Chu, HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol . (2023) 21:195–210. doi: 10.1038/s41579-022-00807-9
CrossRef Full Text | Google Scholar
8. Algaissi, AA, Alharbi, NK, Hassanain, M, and Hashem, AM. Preparedness and response to COVID-19 in Saudi Arabia: building on MERS experience. J Infect Public Health . (2020) 13:834–8. doi: 10.1016/j.jiph.2020.04.016
9. Alumran, A. Role of precautionary measures in containing the natural course of novel coronavirus disease. J Multidiscip Healthc . (2020) 13:615–20. doi: 10.2147/jmdh.S261643
10. Alhassan, FM, and AlDossary, SA. The Saudi Ministry of Health’s twitter communication strategies and public engagement during the COVID-19 pandemic: content analysis study. JMIR Public Health Surveill . (2021) 7:e27942. doi: 10.2196/27942
11. Ajzen, I. The theory of planned behavior. Organ Behav Hum Decis Process . (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
12. Armitage, CJ, and Conner, M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol . (2001) 40:471–99. doi: 10.1348/014466601164939
13. Shubayr, MA, Mashyakhy, M, Al Agili, DE, Albar, N, and Quadri, MF. Factors associated with infection-control behavior of dental health-care workers during the COVID-19 pandemic: a cross-sectional study applying the theory of planned behavior. J Multidiscip Healthc . (2020) 13:1527–35. doi: 10.2147/jmdh.S278078
14. Almoayad, F, Bin-Amer, LA, Althubyani, NT, Alajmi, SM, Alshammari, AA, and Alsuwayal, RA. The general public’s intent to receive a COVID-19 vaccine in Saudi Arabia. Int J Health Promot Educ . (2022):1–16. doi: 10.1080/14635240.2022.2047094
15. Anagaw, TF, Tiruneh, MG, and Fenta, ET. Application of behavioral change theory and models on COVID-19 preventive behaviors, worldwide: a systematic review. SAGE Open Med . (2023) 11:20503121231159750. doi: 10.1177/20503121231159750
16. Alsyouf, A, Lutfi, A, Alsubahi, N, Alhazmi, FN, Al-Mugheed, K, Anshasi, RJ, et al. The use of a technology acceptance model (TAM) to predict patients' usage of a personal health record system: the role of security, privacy, and usability. Int J Environ Res Public Health . (2023) 20:1347. doi: 10.3390/ijerph20021347
17. Bauch, C, D'Onofrio, A, and Manfredi, P. “Modeling the interplay between human behavior and the spread of infectious diseases,” in Behavioral epidemiology of infectious diseases: an overview (2013):1–19. Available at: https://link.springer.com/chapter/10.1007/978-1-4614-5474-8_1
18. Corace, KM, Srigley, JA, Hargadon, DP, Yu, D, MacDonald, TK, Fabrigar, LR, et al. Using behavior change frameworks to improve healthcare worker influenza vaccination rates: a systematic review. Vaccine . (2016) 34:3235–42. doi: 10.1016/j.vaccine.2016.04.071
19. Mason, JO, and Powell, KE. Physical activity, behavioral epidemiology, and public health. Public Health Rep . (1985) 100:113–5.
20. Adiyoso, W, and Wilopo,. Social distancing intentions to reduce the spread of COVID-19: the extended theory of planned behavior. BMC Public Health . (2021) 21:1836. doi: 10.1186/s12889-021-11884-5
21. Tran, QA, HTT, N, Bui, TV, Tran, NT, Nguyen, NT, Nguyen, TT, et al. Factors associated with the intention to participate in coronavirus disease 2019 frontline prevention activities among nursing students in Vietnam: an application of the theory of planned behavior. Front Public Health . (2021) 9:699079. doi: 10.3389/fpubh.2021.699079
22. Andarge, E, Fikadu, T, Temesgen, R, Shegaze, M, Feleke, T, Haile, F, et al. Intention and practice on personal preventive measures against the COVID-19 pandemic among adults with chronic conditions in southern Ethiopia: a survey using the theory of planned behavior. J Multidiscip Healthc . (2020) 13:1863–77. doi: 10.2147/jmdh.S284707
23. WHO. Survey tool and guidance. Rapid, simple, flexible behavioural insights on COVID-19. Monitoring knowledge, risk perceptions, preventive behaviours and trust to inform pandemic outbreak response . Geneva: World Health Organisation (2020).
24. Zhang, X, Wang, F, Zhu, C, and Wang, Z. Willingness to self-isolate when facing a pandemic risk: model, empirical test, and policy recommendations. Int J Environ Res Public Health . (2019) 17. doi: 10.3390/ijerph17010197
25. StataCorp. Stata statistical software: release 16 . College Station, TX: StataCorp LLC (2019).
26. Faries, MD. Why we don’t “just do it”: understanding the intention-behavior gap in lifestyle medicine. Am J Lifestyle Med . (2016) 10:322–9. doi: 10.1177/1559827616638017
27. Lennon, RP, Sakya, SM, Miller, EL, Snyder, B, Yaman, T, Zgierska, AE, et al. Public intent to comply with COVID-19 public health recommendations. Health Lit Res Pract . (2020) 4:e161–5. doi: 10.3928/24748307-20200708-01
28. Al-Hanawi, MK, Angawi, K, Alshareef, N, Qattan, AMN, Helmy, HZ, Abudawood, Y, et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Front Public Health . (2020) 8:217. doi: 10.3389/fpubh.2020.00217
29. Hao, F, Wang, B, Tan, W, Husain, SF, McIntyre, RS, Tang, X, et al. Attitudes toward COVID-19 vaccination and willingness to pay: comparison of people with and without mental disorders in China. BJPsych Open . (2021) 7:e146. doi: 10.1192/bjo.2021.979
30. Clark, C, Davila, A, Regis, M, and Kraus, S. Predictors of COVID-19 voluntary compliance behaviors: an international investigation. Glob Transit . (2020) 2:76–82. doi: 10.1016/j.glt.2020.06.003
31. Zhong, B-L, Luo, W, Li, H-M, Zhang, Q-Q, Liu, X-G, Li, W-T, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci . (2020) 16:1745–52. doi: 10.7150/ijbs.45221
32. Alqahtani, MMJ, Arnout, BA, Fadhel, FH, and Sufyan, NSS. Risk perceptions of COVID-19 and its impact on precautionary behavior: a qualitative study. Patient Educ Couns . (2021) 104:1860–7. doi: 10.1016/j.pec.2021.02.025
33. Bish, A, and Michie, S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol . (2010) 15:797–824. doi: 10.1348/135910710X485826
34. Yıldırım, M, and Güler, A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud . (2022) 46:979–86. doi: 10.1080/07481187.2020.1793434
Keywords: public health, epidemiology, Theory of Planned Behaviour, older adults, COVID-19
Citation: AlOmar RS, AlHarbi AS, Abu Abdullah LA, Almuqbil SM, Albahrani ZS, Aldar HM, Alzouri FS, Al-Shiban MA, AlShamlan NA, Shafey MM, AlAbdulKader AM and Alotaibi NS (2023) Intention and practice on personal preventive measures against COVID-19 among older adults in the Kingdom of Saudi Arabia: an epidemiological study using the Theory of Planned Behaviour. Front. Public Health . 11:1315443. doi: 10.3389/fpubh.2023.1315443
Received: 10 October 2023; Accepted: 20 November 2023; Published: 14 December 2023.
Reviewed by:
Copyright © 2023 AlOmar, AlHarbi, Abu Abdullah, Almuqbil, Albahrani, Aldar, Alzouri, Al-Shiban, AlShamlan, Shafey, AlAbdulKader and Alotaibi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Reem S. AlOmar, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Educ Health Promot
Understanding COVID-19 preventive behavior: An application of the health belief model in the Philippine setting
Engracia arceo.
Department of Medical Technology, College of Allied Medical Professions, Angeles University Foundation, Angeles City, Philippines
John Edlor Jurado
Leslee anne cortez.
1 Department of Education, Dasmarinas, Cavite, Philippines
Nestor Sibug
2 Department of Psychology, Holy Angel University, Angeles City Philippines
Gestrelle Lides Sarmiento
Amica coleen lawingco, carisse carbungco, raphael enrique tiongco, background:.
With the Philippines emerging as the hotspot in the Western Pacific Region for the COVID-19 cases, the study aimed to understand the COVID-19 preventive behavior of Filipinos using the health belief model (HBM).
MATERIALS AND METHODS:
The cross-sectional study included 304 respondents recruited for the whole month of July 2020 through various social media platforms. Participants were requested to answer an online questionnaire, and results were analyzed using SPSS software.
The majority of respondents were female (71.1%), with an average age of 29, college graduate (57.6%), and living in an area where modified general community quarantine is implemented (63.2%). Good preventive behavior was noted among the participants, and not shaking of hands with others and refraining from touching of surfaces were reported as the most practiced behavior. Spearman's correlation and Pearson's Chi-square showed that age and sex are significant predictors for the HBM constructs and preventive behavior. Furthermore, results showed that cues to action, self-efficacy, and perceived barrier have a significant association with COVID-19 preventive behavior.
CONCLUSION:
Findings prove that HBM is useful in understanding preventive behaviors in times of coronavirus pandemic. Strategies that promote a supportive environment and help overcome the perceived barriers can guide Filipinos to adopt the desired health behavior. Interventions to promote preventive behaviors should be focused on males and younger individuals.
Introduction
COVID-19 is a novel pandemic that has caused a tremendous negative impact on the health and economy of many countries around the world. Current evidence shows that SARS-CoV-2, the virus causing the disease, is transmitted between people through respiratory droplets and contact routes.[ 1 ] Efforts to minimize the spread of the infection focus on behavioral interventions and protective behaviors like home quarantine, frequent handwashing, and social distancing.
In the absence of vaccines, large-scale social distancing measures – workplace nonattendance, school closure, and lockdown – appear to be the most effective means of mitigation.[ 2 ] In the US, one study noted that 3–4 months of moderate distancing could actually save 1.7 million lives and lead to substantial economic benefits.[ 3 ] However, noncompliance to social distancing has been observed, and the behavior has been linked to several factors, including political reasons[ 4 ] and personal expectations like duration of self-isolation.[ 5 ]
Public health experts have used different theories and models to explain the various factors influencing health behavior. One of the most commonly used frameworks in public health research is the health belief model (HBM). The general acceptance and popularity of the theory are due to its reliability in predicting behavior. According to the HBM, the behavior is predicted by a person's perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and cues to action. The model is designed to explain the reasons why people are compliant or noncompliant to preventive health behaviors.
While there is one study that explored the COVID-19 preventive behavior in Iran,[ 6 ] cultural differences may influence the variables. Unlike other countries around the world, the Philippines has been in various forms of community quarantine and has the world's longest and strictest lockdown. Reports show that the end to this lockdown is still not in sight because of the failure in controlling the pandemic, thus making the country with the fastest rise in virus cases in the Western Pacific Region.[ 7 ] This situation raises a unique challenge for both public health practitioners and government authorities. There is a need to better understand the factors influencing COVID-19 preventive behaviors in order to ensure the public's compliance and cooperation. By obtaining the possible predictors of the said behavior using the HBM, this can serve as a pivotal point in the planning, promotion, and implementation of better health program protocols to prevent the further spread of the disease in the country.
Materials and Methods
Study population.
The cross-sectional study targeted participants who were currently living in the Philippines, at least 18 years old, and have access to the internet. Since this was an online survey study, participants were selected through convenience sampling technique. Eligible participants were recruited through Facebook, a popular social media platform in the country. The researchers posted the link of the online questionnaire on private accounts and shared in public pages and groups for the whole month of July 2020. Researchers requested the participation of their online friends through recruitment posts and personal messages with an included link to the online survey. To widen the coverage, they also asked their online friends to share the link. Furthermore, the link was also posted on public groups on Facebook and requested the administrators of organizations and institutions to post the questionnaire link on their respective pages. At the end of the online data collection period, the online survey was closed and data were then analyzed.
Research instrument
The research tool was adapted from one published study in Iran.[ 6 ] In order to fit the Philippine setting, the questionnaire was slightly modified, translated into the Filipino language, and pilot tested. To check for the internal consistency, Cronbach's alpha was calculated. A revision was done until the internal consistency for both English and Tagalog versions was within the acceptable range. The final English and Tagalog versions have an internal consistency of 0.776 and 0.644, respectively. Both were converted into Google Forms to facilitate the online survey.
The questionnaire included three sections – demographic profile, HBM constructs, and COVID-19 preventive behaviors. The demographic profile included age, birthdate, sex, educational background, and the lockdown category of the participants. The lockdown category was included because the government, through the interagency task force on emerging infectious diseases, classified each area in the country into various categories. They are the enhanced community quarantine (ECQ), modified ECQ (MECQ), general community quarantine (GCQ), and modified GCQ (MGCQ), which are enumerated based on decreasing restrictions in terms of social movement and business operations. ECQ is the strictest type of lockdown where most establishments were closed, only food businesses and health-care institutions were allowed to operate, and only one person per household was allowed to go out for essential errands.
The questionnaire also included 22 questions about HBM constructs and 7 questions on COVID-19 preventive behaviors. All were on 1–5 Likert scales, which range from strongly agree to strongly disagree. Participants were asked to click on the option that best describes their current status and their understanding of each statement. Once done, they only need to click the submit button and there was no incentive given for their participation.
Ethical consideration
Ethical clearance was obtained from an ethics review board prior to the conduct of the study. A voluntary informed consent form was included on the first page of Google forms. All participants who agreed were asked to click on the “I agree” box before proceeding to answer the rest of the questionnaire. All data obtained were treated with extreme confidentiality.
Statistical analysis
The Mann–Whitney U-test, Pearson's Chi-square, and Spearman's rank correlation analyses were run to determine the association between the participant's demographics (sex, lockdown category, and age) with both HBM constructs and their COVID-19 preventive behaviors. On the other hand, Spearman's rank correlation analysis was also used to investigate the effect of each HBM construct on the performance of COVID-19 preventive behavior. All P values were computed at a two-sided 5% level of significance.
A total of 304 responses from eligible participants were analyzed. The respondents of the online survey have an average age of 29.0 ± 10.4, mostly female (71.1%), college graduates (57.6%), and living in an area where MGCQ is implemented (63.2%). Of the different constructs in the study, Table 1 shows that the perceived benefits (4.7) and perceived self-efficacy (4.7) had the highest mean, followed by perceived severity (4.5), cues to action (4.4), preventive behavior (4.2), perceived susceptibility (3.6), and perceived barriers (3.5).
Demographic profile of the study participants
*Mean±SD. SD=Standard deviation, MGCQ=Modified general community quarantine, GCQ=General community quarantine, MECQ=Modified enhanced community quarantine, ECQ=Enhanced community quarantine
Table 2 summarizes the correlation result of the participant's demographic profile with the HBM constructs and preventive behavior. Based on the results, only age and sex have a significant association with the constructs under study. Age showed a significant positive relationship with perceived susceptibility ( P = 0.04), perceived barriers ( P < 0.001), and cues to action ( P < 0.001), which indicates that as age increases, the mean scores of these constructs also increase. Findings also revealed a significant association of the participant's sex on perceived self-efficacy ( P = 0.02), cues to action ( P = 0.01), and preventive behavior ( P = 0.001).
Association of the participants’ age, sex, educational attainment, and lockdown category with health belief model constructs
*Significant at P <0.05, **Spearman’s rank correlation, ***Pearson’s Chi-square
Further analysis of the association of sex with HBM constructs was done by comparing the mean scores among males and females using the Mann–Whitney U-test [ Table 3 ]. Based on our findings, mean scores for perceived severity, perceived self-efficacy, cues to action, and preventive behavior were significantly higher among females than in males.
Comparison of mean scores for the various health belief constructs and preventive behavior among males and females
*level of significance at < 0.05
In terms of COVID-19 preventive behavior, Table 4 shows that overall, there was a good practice among the participants of the study as represented by their mean score. Not shaking of hands with others and refraining from touching of surfaces was the most practiced behavior, and not touching the eyes, nose, or mouth and not taking of cellphone out from the pocket/bag was the least practiced.
Summary of the participant’s preventive behavior
Table 5 summarizes the result of Spearman's correlation of HBM constructs with the participants’ preventive behavior. Among the different constructs, only three showed a significant association. Both perceived self-efficacy and cues to action have a significant direct relationship with preventive behavior, whereas perceived barriers showed a significant indirect relationship.
Association of the health belief model constructs with COVID-19 preventive behavior
*Significant at P <0.05
COVID-19 is steadily increasing in the world, and in the Philippines, the cases continue to rise, necessitating a second round of stricter implementation of MECQ in the country's capital city and the continuous implementation of various types of community quarantine in different areas.[ 8 ] With the rising number of Filipinos infected with the novel disease, the researchers aimed to determine the COVID-19 preventive behaviors of Filipinos and the role of the HBM constructs to their adherence to health protocols.
Out of the demographic profile studied, age and sex were shown to be important variables affecting the HBM constructs. Participants have increasing perceived susceptibility as they age, and this is probably because age has always been considered as a predictor of fatal outcome in COVID-19 cases.[ 9 ] Older people are at higher risk of contracting COVID-19 due to the physiological body changes that come with aging as well as the potential underlying comorbidities and decreased immune function that they experience which can make them more susceptible to the complications of the disease. Furthermore, the elderly who have existing comorbidities are more likely to engage in health-promoting behaviors since they feel that noncompliance will render them more susceptible to the infection.[ 10 ]
It was also noted that female respondents have higher perceived severity, perceived self-efficacy, cues to action, and preventive behavior. When compared with a previous study involving hospital staff workers, females are also reported to have a higher score of perceived threat.[ 11 ] This result coincides with another published study which noted that men tend to have lower rates of handwashing, social distancing, wearing masks, and proactively seeking medical help.[ 12 ] The same result was noted in a large-scale international investigation that shows women are more likely to engage in health behaviors than men.[ 13 ] The result of the present and previous studies is interesting, considering that reports show that the number of men who died from COVID-19 is 2.4 times that of women.[ 14 ] This only shows the need to intensify public interventions that address the unique needs of men when it comes to COVID-19.
The results also showed that the participants have good COVID-19 preventive behavior. However, it is noted that when outside, taking out of cellphones from their pocket/bag is a common practice among the participants of the study. This result is not surprising given the fact that nowadays, most people use their cell phones when outside to communicate with their families and friends amid the pandemic. While there are no documented cases of COVID-19 transmission through cell phone use, Han et al . cited one study in China which reported that the virus has been isolated from door handles and cell phones[ 15 ] and that human coronaviruses can persist on inanimate surfaces for up to 9 days.[ 16 ] The evidence of transmitting various respiratory infections via contaminated hands and contaminated inanimate objects comes from several studies.[ 17 ] Therefore, individuals may have a higher risk of being infected with COVID-19 if they touch their nose, mouth, or eyes after contacting contaminated items.
Another area for improvement revealed in the study is the frequent touching of the nose, mouth, and eyes with hands. Face-touching behavior is a common practice and has been associated as a potential vector for self-inoculation and transmission of respiratory infections. As such, it is recommended that increasing awareness of face-touching behavior and improving the understanding of self-inoculation as a route for transmission can help break the transmission cycle of common respiratory diseases.[ 18 ] While the use of face mask has been mandatory in the country and many parts of the world, it has been noted that its use promotes face touching. In a study conducted in Mexico, patients with face mask touched their face 11.41 times on average and ranged up to 80 times. The study suggests that face-touching behavior has a role in COVID-19 transmission, and thus, mask use should be accompanied by proper hand hygiene and reminders not to touch one's face in order to be more effective in preventing COVID-19 infection.[ 19 ] These findings are consistent with what the WHO emphasizes on the importance of frequent hand hygiene, along with respiratory etiquette, environmental cleaning, and disinfection to prevent the transmission of COVID-19 infection.[ 1 ]
Of the HBM constructs, perceived self-efficacy and cues to action were noted to be positively correlated with the COVID-19 preventive behavior. Findings are congruent with the results conducted in Saudi Arabia and Iran, showing that participants with higher perceived self-efficacy and cues to action scores are more likely to adhere to the coronavirus preventive measures than those with lower scores. The researchers have emphasized the importance of the existence of high perceived self-efficacy as a way to overcome perceived barriers[ 6 , 20 ] .
Self-efficacy is an important construct considered to be a predictor of health behavior in various settings, and improvement of this can increase the likelihood of adopting a particular behavior.[ 21 , 22 , 23 ] Self-efficacy reflects people's confidence in their capacity to change behavior and deal with the problem. In the context of COVID-19, self-efficacy does not only lead to higher preventive behavior but also to better mental health status. Studies show that it is a mediating variable associated with lesser stress and anxiety. Individuals with higher self-efficacy scores have better mental health status. This is quite interesting, considering that the current pandemic has a strong negative impact on the lives of people.[ 11 , 24 , 25 ]
Cues to action is another construct found to be associated with the COVID-19 preventive behavior. This refers to the stimulus needed to trigger the decision-making process for a person to adopt a recommended health action. The theoretical construct is pivotal in influencing health behaviors.[ 26 , 27 ] In the present study, the stimulus includes external cues such as mass and social media information, government regulation, and the presence of supportive infrastructures. To help individuals take action, the Philippine government enforces mandatory use of face mask and compulsory infrastructure changes for businesses prior to re-opening like provision of barriers and foot markings, and adherence to several public health measures related to personal protection, environmental sanitation, physical and social distancing, and travel-related measures. Information as to COVID-19 is widely disseminated, and Filipinos identified traditional media such as television and radio as main sources of information about the virus.[ 28 ] It has been shown in various studies that when the environment is more supportive, people are more likely to adopt the desired behavior.[ 29 , 30 ] The existing laws and regulations in the country on COVID-19 prevention and the relatively conservative attitude of Filipinos may explain the higher preventive behavior observed in the study. In India, one study even mentioned that participants perceived the following government's protocols as an effective way to avoid infection.[ 10 ]
The last construct found that this time negatively associated with COVID-19 preventive behavior is the perceived barrier. This construct serves as a deterrent, and individuals must be able to overcome it to adopt the desired behavior. In the present study, the participants’ perceived barriers were hand hygiene, face touching, staying at home, social distancing, and non-readiness of businesses. These factors were strongly related to the scarcity of masks and disinfecting solutions, especially during the first part of the year, when the pandemic was just starting. In the country, it was this time when hoarding of face mask and alcohol, panic buying, establishments limiting the purchase of commodities, and price increase were very common.[ 31 ] In addition to the supply-related barriers, the mandatory home quarantine and social distancing were concepts new to people. Thus, they were perceived as barriers since many do not fully understand their benefits, and they have negative associations with it. Home quarantine is related to various psychological stresses such as fear, frustration, boredom, and financial loss.[ 32 ] During the H1N1 pandemic, researchers found that in order to increase compliance to home quarantine, clear, consistent, and simple information about it should be provided by authorities.[ 33 ]
Limitations
While the study offers a timely approach to understanding COVID-19 preventive behavior in a developing country like the Philippines, it has its own limitations. First, since it was conducted during community lockdown, the convenience sampling method and online survey were the only options available to the researchers. Thus, sample clustering may have limited the generalizability of the study. Second, the present work relied on the self-reported behaviors and responses of the participants, and thus, the actual behavior and responses may vary. The responses are also subject to recall bias as participants may be unable to report accurate estimates.
The study proved that the HBM is useful in understanding COVID-19 preventive behavior. Strategies that increase self-efficacy, promote cues to action, and overcome the perceived barriers can help Filipinos adopt the desired health behavior. This may include offering a more supportive environment like the availability of masks and hand sanitizers in public places, foot markings to remind social distancing measures, credible social media campaigns on promoting preventive behaviors, and intensified implementation of home quarantine measures for nonessential outdoor errands. In addition, dissemination of specific and actionable information through current media coverage (i.e., online and mobile platforms) may be impactful in delivering public health messages to increase positive attitude toward preventive behavior. It may also be important to leverage the influence of the community such as family and friends in inducing and sustaining behavior change. Finally, interventions to promote COVID-19 preventive behavior among Filipinos should be focused on males and younger individuals, and key health messages used to drive information must be contextualized in a manner that considers the culture and existing practices of local people in the country.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
COVID-19: Prevention and control measures in community
Affiliations.
- 1 Department of Infectious Diseases and Clinical Microbiology, Faculty of Medicine,Yıldırım Beyazıt University,Ankara City Hospital, Ankara,Turkey
- 2 COVID-19 Advisory Committee of the Ministry of Health of Turkey
- PMID: 32293835
- PMCID: PMC7195988
- DOI: 10.3906/sag-2004-146
On January 30, 2020, the WHO declared the COVID-19 outbreak a public health emergency of international concern and, in March 2020, began to characterize it as a pandemic in order to emphasize the gravity of the situation and urge all countries to take action in detecting infection and preventing spread. Unfortunately, there is no medication that has been approved by the FDA, gone through controlled studies and demonstrated an effect on the virus for this global pandemic. Although there are cures for illnesses and developments made by leaps and bounds in our day, the strongest and most effective weapon that society has against this virus that is affecting not just health but also economics, politics, and social order, is the prevention of its spread. The main points in preventing the spread in society are hand hygiene, social distancing and quarantine. With increased testing capacity, detecting more COVID-19 positive patients in the community will also enable the reduction of secondary cases with stricter quarantine rules.
Keywords: COVID-19; community; prevention; quarantine; social distancing; Turkey.
This work is licensed under a Creative Commons Attribution 4.0 International License.
Publication types
- Betacoronavirus
- Communicable Disease Control / methods*
- Coronavirus Infections / prevention & control*
- Disinfection
- Hand Hygiene
- Pandemics / prevention & control*
- Personal Protective Equipment
- Pneumonia, Viral / prevention & control*
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 25 March 2024
COVID-19 information sources, knowledge, attitude, control practices and the predictors among health workers during the pandemic in Ebonyi state, Nigeria
- Ugwu I. Omale 1 ,
- Ifeyinwa M. Okeke 1 ,
- Okechukwu O. Ukpabi 1 ,
- Richard L. Ewah 2 , 3 ,
- Osarhiemen Iyare 1 ,
- Chidinma I. Amuzie 4 ,
- Onyinyechukwu U. Oka 1 ,
- Azuka S. Adeke 1 ,
- Victor U. Uduma 5 ,
- Glory E. Nkwo 4 ,
- Cordis O. Ikegwuonu 1 ,
- Ugochi I. A. Nwali 1 &
- Olaedo O. Nnachi 1
Scientific Reports volume 14 , Article number: 7072 ( 2024 ) Cite this article
102 Accesses
Metrics details
- Epidemiology
- Infectious diseases
- Medical research
The COVID-19 pandemic has changed into an endemic COVID-19 disease and health workers continue to be at high risk. The situation requires continued use of COVID-19 control measures by health workers and this will likely depend on their sources of information/knowledge/attitude about COVID-19 and previous use of COVID-19 control measures. We explored the COVID-19 information sources, knowledge, attitude, control practices, and the predictors, among health workers in Ebonyi state, Nigeria. We implemented an online-offline analytical cross-sectional survey from March 12 to May 9, 2022 among all categories of health workers (clinical/non-clinical, public/private) working/living in Ebonyi state who gave consent and were selected via convenience/snowballing sampling. Data was collected with a structured self-administered/interviewer-administered questionnaire via WhatsApp/KoBoCollect. Descriptive/inferential analyses were done including multivariate generalized linear models. 1276 health workers were surveyed. The commonest individual source of information about COVID-19 was health workers (used by 83.8%), followed by radio (67.9%), television (59.6%), family members/relatives/friends (57.9%) etc. The main individual source of information for majority of the participants was health workers (for 35.0%) followed by radio (24.5%), television (14.4%) etc. The most trusted individual source of information for majority of the participants was health workers (for 39.4%) followed by radio (26.0%), television (14.3%) etc. Interpersonal sources were the main/most trusted source of information for the majority (48.0%/49.8%) followed by traditional media (39.4%/40.6%) and internet/social media/SMS (12.6%/9.6%). 42.3%, 81.3%, and 43.0% respectively had good knowledge, good attitude, and good control practice about COVID-19. The most important predictors of the main/most trusted sources of information about COVID-19 were place of work (public/private), level of place of work (primary-secondary/tertiary), age, and years of working experience. Good knowledge about COVID-19, good attitude towards COVID-19, strong COVID-19 experience/perception, working at a tertiary facility, tertiary education, and decrease in years of working experience were strong predictors of good control practice about COVID-19. This study’s evidence regarding the commonest/main/most trusted information sources and control practice about COVID-19 should be considered by later COVID-19/similar health emergencies’ policy actions to optimise emergency health information dissemination and use of control measures by health workers in Ebonyi state/Nigeria/other similar settings.
Similar content being viewed by others

COVID-19 awareness, knowledge and perception towards digital health in an urban multi-ethnic Asian population
Cong Ling Teo, Miao Li Chee, … Ching-Yu Cheng
How level of understanding and type of used sources relate to adherence to COVID-19 public health measures in Canada
Clémentine Courdi, Sahar Ramazan Ali, … Roxane de la Sablonnière

Knowledge and sources of information on COVID-19 among children in Ghana
Sylvester Kyei-Gyamfi & Zita Kyei-Gyamfi
Introduction
After the devastating global health and economic effects of the coronavirus disease 2019 (COVID-19) pandemic since the emergence of COVID-19 more than four years ago 1 , COVID-19 has been declared to no longer be a public health emergency of international concern 2 . However, as an endemic disease with persistence of new infections and re-infections and the risk of upsurge from new strains of the COVID-19 virus, COVID-19 still poses a real threat to the health and economies of populations around the world 1 . Notwithstanding the decrease in the testing and reporting rates (and the fact that testing and reporting have stopped in many countries) 1 , 3 , more than 503,000 COVID-19 cases and over 10,000 related deaths were confirmed between the 28-day period of 7 January and 4 February 2024 3 . The non-use or decline in the use of preventive public health measures have been contributing to the persistence of the threat from COVID-19 and it is thus global imperative to continue the use of COVID-19 control measures for the foreseeable future 1 .
Health workers were at higher risk of contracting COVID-19 compared to the general public because of their involvement in management of patients, including COVID-19 patients, and the risk persisted as new COVID-19 infections or re-infections continued to occur. Hence, the continued use of COVID-19 control measures by health workers was very essential and would very likely be influenced by not only their COVID-19 health information sources, level of knowledge, and level of attitude towards COVID-19 4 , 5 , 6 , but also by their level of use of these control measures during the COVID-19 pandemic.
The knowledge, attitude, and practices about COVID-19 among health workers during the pandemic were assessed by some studies around the world and in Nigeria 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 . Fewer studies assessed health workers’ sources of information about COVID-19 6 , 7 , 9 , 10 , 11 , 12 , 13 , 14 , 15 . However, most of these studies were only online studies among limited categories of health workers and carried out during the initial waves of the pandemic. We could not identify any studies that extensively assessed health workers’ use and trust for COVID-19 information sources and the determinants. To our knowledge, there was no study on health workers’ information sources, knowledge, attitude, and practices about COVID-19 during the pandemic in Ebonyi state.
Context-specific understanding of how the health workers in Ebonyi state, Nigeria, were getting information about COVID-19 and their knowledge, attitude, and control practices, including the predictors, would guide subsequent public health policy interventions to enhance the use of preventive public health measures for long-term control of COVID-19 and for the control of any similar infectious diseases/pandemics in the future. The misinformation/disinformation and conspiracy theories about COVID-19 in the social and conventional media was unprecedented. So, it would be particularly important to understand health workers’ use and confidence in the sources of information about COVID-19. In addition, as health opinion leaders and sources of health information for the general public, health workers’ use and confidence in COVID-19 information sources and their knowledge, attitude, and control practices about COVID-19 would most likely influence the general public’ confidence and use of COVID-19 information sources and control practices. An exploratory study of health workers’ use/confidence in COVID-19 information sources and their knowledge, attitude, and control practices was thus an imperative.
We conducted an extensive online and offline study to assess COVID-19 vaccination acceptance and the determinants among the health workers in Ebonyi state 18 . As part of the study, we also explored the COVID-19 information sources, knowledge, attitude, and control practices, and the predictors, among the health workers during the COVID-19 pandemic in Ebonyi state, Nigeria, and the findings are reported in this paper.
Study design and participants
The study was an analytical cross-sectional survey implemented between March 12 and May 9, 2022 among all categories of health workers, including clinical and non-clinical and public and private health workers, in Ebonyi state, southeast of Nigeria. The study protocol has been described elsewhere 18 . Health workers who were working or living in Ebonyi state and gave verbal consent were eligible to participate in the survey. Participants were selected via convenience and snowballing sampling methods. The investigators first contacted many health workers who were available and/or easily accessible physically or via phone calls and sought their consent. Afterwards, those who gave verbal consent were sent the web link for the self-administered electronic questionnaire through their private WhatsApp addresses. They were also asked to forward the web link to other eligible health workers. Health workers who were available and/or easily accessible but had no WhatsApp addresses responded to the electronic questionnaire in android devices after giving verbal consent (to the interviewers). A sample size of I880 was estimated for the parent study 18 and 1276 (67.9%) of health workers successfully participated in the survey.
Independent factors and outcome measures
Independent factors include sociodemographic characteristics (gender, age, marital status, educational level) and work-related attributes (work category, years of working experience, primary place of work, level of primary place of work). The outcome measures include the main and most trusted sources of information about COVID-19, level of knowledge of COVID-19, level of attitude towards COVID-19 (vaccination), and level of control practice about COVID-19. Regarding the evaluation of predictors of the level of control practice about COVID-19, additional independent factors include the main and most trusted sources of information about COVID-19, level of knowledge of COVID-19, level of attitude towards COVID-19 (vaccination), and extent of COVID-19 experience and perception.
The sources of information about COVID-19 as well as the main and most trusted sources of information were grouped into interpersonal information sources consisting of family members/relatives/friends, health workers, place of work, place of worship/religious forums; traditional media consisting of radio, television, and prints (newspaper and magazine); and internet/social media/SMS consisting of internet sites, WhatsApp, Facebook, and SMS/text messages.
The assessment of basic knowledge of COVID-19 involved participants responses to 44 knowledge items in the questionnaire. A score of “1” was assigned for each correct response and “0” for each incorrect response, giving a maximum score of 44 and a minimum of zero for each participant. For each participant, a total knowledge score of ≥ 75% of 44 was categorized as good knowledge and < 75% was poor knowledge. The assessment of attitude towards COVID-19 and COVID-19 vaccination involved participants responses to 16 attitude items in the questionnaire. Every attitude item had five options of strongly disagree, disagree, not sure, agree, and strongly agree and scores of “1” to “5” or “5” to “1” were respectively assigned to the items as appropriate, giving a maximum score of 80 and a minimum of 16 for each participant. For each participant, a total attitude score of ≥ 75% of 80 was categorized as good attitude and < 75% was poor attitude. The assessment of control practices about COVID-19 involved participants responses to 24 practice items in the questionnaire. A score of “1” was assigned for each correct response and “0” for each incorrect response, giving a maximum score of 24 and minimum of zero for each participant. For each participant, a total practice score of ≥ 75% of 24 was categorized as good control practice and < 75% was poor control practice.
Data collection
Data collection was through a structured self-administered and interviewer-administered questionnaire survey of the health workers 18 . The following sections were part of the questionnaire: sociodemographic characteristics; COVID-19 experiences and perceptions; basic knowledge of COVID-19; attitude towards COVID-19 and COVID-19 vaccination; and practices about COVID-19. The electronic version of the questionnaire was programmed using the KoBoToolbox software and was pre-tested among health workers who were not included in the survey. The web link for the electronic questionnaire was distributed to health workers via WhatsApp and they were also asked to forward the web link to other eligible health workers they know within the study area. Interviewer-administered questionnaire in KoBoCollect installed in android devices was used for the survey of health workers who had no WhatsApp addresses and those living in remote/rural areas with very poor or no internet access.
Statistical analyses
Statistical analyses were carried out using Stata/SE version 15.1 (Stata Corp, College Station, TX, USA). Data was described using frequencies with proportions/percentages and median with inter-quartile range as appropriate. Inferential analyses involved the use of generalized linear models (GLM) at 2.5% significance level to compensate for multiple comparisons. For dichotomous/categorical independent factors, prevalence difference in the outcomes with the corresponding 97.5% CI and p-values were computed using binomial identity GLM models with robust standard errors. For continuous independent factors, coefficients in the outcomes with the corresponding 97.5% CI and p-values were computed using the binomial identity GLM models. All the independent variables were simultaneously added to the GLM model in the adjusted analyses. Where binomial identity GLM models failed to achieve convergence, Gaussian identity GLM models were used instead 19 .
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Ebonyi State Health Research and Ethics Committee (EBSHREC/15/01/2022-02/01/2023) and Research and Ethics Committee of Alex Ekwueme Federal University Teaching Hospital Abakaliki (14/12/2021–17/02/2022). Verbal informed consent was obtained from the study participants during which the purpose the study, kind of participation, likely duration of participation, voluntary nature of participation, absence of potential harm, potential benefit, and confidential nature of the study were duly communicated to them. The research procedures were in compliance with the Declaration of Helsinky.
Sociodemographic and background characteristics
The sociodemographic and background (work-related) characteristics of the study participants are presented in Table 1 . The median age (IQR) was 33 years (26–43) and the median years of working experience was 5 years (2–13); 857 (67.2%) were females; 691 (54.2%) were married; 726 (56.9%) had a tertiary education; 1110 (87.0%) were clinical staff; 652 (51.1%) were working primarily in private health facilities; and 952 (74.6%) were working at primary health facilities.
Sources of information about COVID-19
The study participants’ sources of information about COVID-19, including their main and most trusted sources, are presented in Table 2 . For interpersonal sources, the commonest source of information was health workers (used by 1069 or 83.8% of participants) followed by family members/relatives/friends (used by 739 or 57.9%), place of work (used by 606 or 48.3%), and place of worship (used by 577 or 45.2%). For traditional media sources, the commonest source of information was radio (used by 867 or 67.9%) followed by television (used by 760 or 59.6%) and prints (used by 336 or 26.3%). For internet/social media/text message sources, the commonest source of information was WhatsApp (used by 412 or 32.3%) and text messages (used by 412 or 32.3%) followed by Facebook (used by 407 or 31.9%) and internet sites (used by 394 or 30.9%). Overall, the commonest source of information was health workers (used by 83.8%) followed by radio (used by 67.9%), television (used by 59.6%), family members/relatives/friends (used by 57.9%), etc. (Table 2 ).
The main sources of information for majority of the participants were interpersonal sources (for 613 or 48.0%) followed by traditional media (for 502 or 39.4%) and internet/social media/text messages (for 161 or 12.6%). The main individual source of information was health workers (for 447 or 35.0%) followed by radio (for 312 or 24.5%), television (for 184 or 14.4%) etc. (Table 2 ). The most trusted sources of information for majority of the participants were interpersonal sources (for 636 or 49.8%) followed by traditional media (for 518 or 40.6%) and internet/social media/text messages (for 122 or 9.6%) (Table 2 ). The most trusted individual source of information for majority of the participants was health workers (for 503 or 39.4%) followed by radio (for 332 or 26.0%), television (for 183 or 14.3%) etc. (Table 2 ).
Knowledge of COVID-19
The study participants’ knowledge of COVID-19 is presented in Table 3 . Most of the participants (1253 or 98.2%) knew people get COVID-19 by staying close to infected persons when they cough or sneezes. The most reported symptom of COVID-19 was cough (by 1112 or 87.2% of participants) followed by fever (by 1082 or 84.8%), tiredness (by 806 or 63.2%), difficulty in breathing (by 792 or 62.1%), sore throat (by 683 or 53.5%), body pains (by 644 or 50.5%), chest pain (by 563 or 44.1%), headache (by 553 or 43.3%), etc. (Table 3 ). Elderly people were said to be more at risk of having severe COVID-19 by 1097 or 86.0% of the participants, 592 (46.4%) said people with chronic illness, 379 (29.7%) said young adults, 324 (25.4%) said children, 257 (20.1%) said people who smoke, 202 (15.8%) said pregnant women etc. (Table 3 ). Regarding COVID-19 preventive measures: 1244 (97.5%) said by wearing of face mask, 1240 (97.2%) said by maintaining at least 1–2 m distance away from people coughing or sneezing, 1217 (95.4%) said by avoiding crowd, 1189 (93.2%) said by frequent washing of hands with soap and water, etc. (Table 3 ).
Attitude towards COVID-19 and COVID-19 vaccination
The study participants’ attitude towards COVID-19 and COVID-19 vaccination is presented in Table 4 . More of the participants (769 or 60.3%) strongly agreed that COVID-19 was real followed by those who agreed (277 or 21.7%); more of them (811 or 63.6%) strongly agreed the risk of getting COVID-19 could be reduced by avoiding crowd followed by those who agreed (325 or 25.5%); more of them (807 or 63.3%) strongly agreed the risk of getting COVID-19 could be reduced by wearing face mask followed by those who agreed (337 or 26.4%); more of them (385 or 30.2%) strongly disagreed the risk of getting COVID-19 could be reduced by taking chloroquine followed by those who were not sure (375 or 29.4%); more of them (414 or 32.4%) strongly disagreed the risk of getting COVID-19 could be reduced by the use of herbs/roots (native medicine) followed by those who were not sure (393 or 30.8%); etc. (Table 4 ).
Control practices about COVID-19
The study participants’ control practices about COVID-19 is presented in Table 5 . The most ever practiced preventive measure was the wearing of face mask (by 1176 or 92.2%) followed by maintaining at least 1–2 m distance away from people coughing or sneezing (by 1078 or 84.5%), frequent washing of hands with soap and water (by 1045 or 81.9%) and frequent cleaning of hands with alcoholic sanitisers (by 1045 or 81.9%), etc.; and the most currently practiced (in the two weeks preceding the survey) preventive measure was wearing of face mask (by 944 or 74.0%) followed by frequent washing of hands with soap and water (by 728 or 57.1%), frequent cleaning of hands with alcoholic sanitisers (by 654 or 51.3%), the maintaining at least 1–2 m distance away from people coughing or sneezing (by 397 or 31.1%), etc. (Table 5 ). Taking of chloroquine was the most ever practiced (by 106 or 8.3%) and currently practiced (by 80 or 6.3%) COVID-19 treatment/preventive measure followed by the use of ginger/garlic (by 92 or 7.2% and 51 or 4.0%), etc. Most of the participants (1084 or 85.0%) had never practiced and most of them (1147 or 89.9%) were not currently practicing these treatment/preventive measures (Table 5 ).
Level of knowledge, attitude, and control practice about COVID-19 and COVID-19 vaccination
Regarding the level of COVID-19 (vaccination) knowledge, attitude, and control practice among the 1276 study participants: 540 (42.3%) had good knowledge about COVID-19 while 736 (57.7%) had poor knowledge; 1037 (81.3%) had good attitude towards COVID-19 (vaccination) while 239 (18.7%) had poor attitude; 549 (43.0%) had good control practice about COVID-19 while 727 (57.0%) had poor practice.
Predictors of the main and most trusted sources of information about COVID-19
The associations between the main sources and most trusted sources of information about COVID-19 and sociodemographic and background factors are presented in Table 6 . As presented in Table 6 , the predictors of interpersonal sources as the main and most trusted source of information about COVID-19 is first presented, with the other sources (traditional media and internet/social media/text message) as reference. The predictors of traditional media as the main and most trusted source of information about COVID-19 is also presented, with the other sources (interpersonal and internet/social media/text message) as reference.
As shown by the adjusted results, the predictors of having an interpersonal source as the main source of information about COVID-19 were: being a health worker at a primary/secondary health facility (adjusted prevalence difference (aPD) 19.2%, 97.5% CI 10.2–28.2, p < 0.0001); being a health worker at a public health facility (aPD 11.6%, 3.2–19.9, p = 0.0019); age as one year increase in age increases the probability of having an interpersonal source as the main source of information about COVID-19 by 0.7% (adjusted coefficient (aCoef) 0.7%, 97.5% CI 0.2–1.2, p = 0.0017); and working experience as one year increase in working experience reduces the probability of having an interpersonal source as the main source of information about COVID-19 by 0.7% (aCoef − 0.7%, − 1.3–(− 0.1), p = 0.0127). The predictors of having an interpersonal source as the most trusted source of information about COVID-19 were: being a health worker at a public health facility (aPD 10.0%, 1.6–18.3, p = 0.0077) and age as one year increase in age increases the probability of having an interpersonal source as the most trusted source of information about COVID-19 by 0.7% (aCoef 0.7%, 0.2–1.2, p = 0.0010).
The predictors of having traditional media as the main source of information about COVID-19 was working experience as one year increase in working experience increases the probability of having traditional media as the main source of information about COVID-19 by 0.7% (aCoef 0.7%, 0.2–1.3, p = 0.0047). The predictors of having traditional media as the most trusted source of information about COVID-19 were: being a health worker at a primary/secondary health facility (aPD 14.5%, 6.1–22.9, p = 0.0001); working experience as one year increase in working experience increases the probability of having traditional media as the most trusted source of information about COVID-19 by 0.6% (aCoef 0.6%, 0.04–1.2, p = 0.0160); and age as one year increase in age reduces the probability of having traditional media as the most trusted source of information about COVID-19 by 0.5% (aCoef 0.5%, − 1.0–(− 0.03), p = 0.0180).
Predictors of the level of control practice about COVID-19
The associations between the level of control practice about COVID-19 and sociodemographic and background factors are presented in Table 7 . As shown by the adjusted results, the predictors of good control practice about COVID-19 were: good knowledge about COVID-19 (aPD 24.0%, 17.3–30.7, p < 0.0001); good attitude towards COVID-19 (vaccination) (aPD 11.9%, 4.1–19.7, p = 0.0006); strong COVID-19 experience and perception (aPD 17.1%, 10.0–24.2, p < 0.0001); being a health worker at a tertiary health facility (aPD 10.7%, 1.0–20.4, p = 0.0130); having a tertiary education (aPD 21.7%, 14.3–29.2, p < 0.0001); and working experience as one year increase in working experience reduces the probability of having good COVID-19 control practice by 1.2% (aCoef − 1.2%, − 1.7 to (− 0.7), p < 0.0001).
This study explored the COVID-19 information sources, knowledge, attitude, and control practices, and the predictors among health workers during the COVID-19 pandemic in Ebonyi state, Nigeria. The main study findings include: the overall commonest source of information was health workers followed by radio, television, and family members/relatives/friends; interpersonal sources like health workers was the main and most trusted source of information for majority of the participants followed by traditional media such as radio; 42.3% had good knowledge about COVID-19, 81.3% had good attitude towards COVID-19 (vaccination), and 43.0% had good control practice about COVID-19.
In this study: the predictors of having an interpersonal source as the main source of information about COVID-19 were being a health worker at a primary/secondary health facility, being a health worker at a public health facility, increase in age, and increase in years of working experience; the predictors of having an interpersonal source as the most trusted source of information about COVID-19 were being a health worker at a public health facility and increase in age; the predictors of having traditional media as the main source of information about COVID-19 was increase in years of working experience; the predictors of having traditional media as the most trusted source of information about COVID-19 were being a health worker at a primary/secondary health facility, increase in years of working experience, and decrease in age; and the predictors of good control practice about COVID-19 were good knowledge about COVID-19, good attitude towards COVID-19 (vaccination), strong COVID-19 experience and perception, being a health worker at a tertiary health facility, having a tertiary education, and decrease in years of working experience.
In our study, health workers was the commonest source of information about COVID-19 (and radio was the second commonest). In comparison, the commonest source of information about COVID-19 was ministry of health (website) in studies in Saudi 7 , 12 and scientific literature in Venezuela 14 . In our study, interpersonal sources like health workers was the main and most trusted source of information for majority of the participants (and traditional media such as radio was the second main and most trusted source). In comparison, the main information source was social media in a study in Nepal 9 and Yemen 11 ; ministry of health in Saudi 10 ; internet websites in Jordan 13 ; the World Health Organization 15 and radio/television 6 in Ethiopia.
In contrast to the other previous studies, the fact that interpersonal sources like health workers was the commonest, main, and most trusted source of information for majority of the participants has some important policy implications. Unlike the other studies, our study was not only online but also offline and among the entire populations/categories of health workers in the formal and informal health sectors and in both urban/semi-urban and rural areas. As a result, our study perhaps had relatively more proportion of lay/lower cadre health workers and/or health workers in rural/semi-urban who had no access or poor access to the internet and social media. This made interpersonal sources of information to be relatively very popular and this very much reflects the context of the study setting. This logic is supported by our study finding that being a health worker at a primary/secondary health facility (mostly found in remote rural areas) was a predictor of interpersonal source as the main source of information about COVID-19 compared to being a health worker at a tertiary health facility (found in the state capital). Our finding also indicate that health workers are not only health opinion leaders and important source of health information for the general public but also for other health workers especially in poor resource settings. In the study in Venezuela, colleagues/other health workers was the second commonest source of information after scientific literature even though the study was only online 14 . It is good to note that many of the previous studies did not measure/report on the use of health workers or interpersonal sources of information. Subsequent studies among health workers in poor resource settings should include the use of interpersonal sources of information (health workers etc.) in the evaluation of (health emergency) information sources.
The aforementioned explanation/reason can also be used to explain our findings that radio was the second commonest, main, and most trusted source of information for majority of the participants. Compared to the other modern/mass media, radio is more accessible and affordable with more geographical coverage including the remote rural areas. As a result, the fact that radio was the second most popular source of information was a reflection of the prevailing context of the study setting. Radio is a major channel that is always used by Ebonyi state government for information dissemination and it is very popular across the entire state. Perhaps the information from radio is more or less mainly from the state government. Thus, the fact that radio was the second commonest, main, and most trusted source of information about COVID-19 in our study, coupled with the fact that government sources (ministry of health) was the commonest and main source of information in the studies in Saudi 7 , 10 , 12 , emphasises the usefulness of government information channels during health emergencies and calls for government to take-charge of heath information disseminating during health emergencies especially when there is a lot of misinformation/disinformation and conspiracy theories as observed during the COVID-19 pandemic. Subsequent qualitative studies on the factors that influence health workers’ confidence in government as a source of health information during health emergencies are recommended.
In our study, 42.3% had good knowledge about COVID-19, 81.3% had good attitude towards COVID-19 (vaccination), and 43.0% had good control practice about COVID-19. In comparison, higher prevalence of: 83.7% had good knowledge and 77.6% had good preventive practice (although similar proportion of 78.9% had positive attitude) about COVID-19 4 and 88.6% had good knowledge and 81.4% had good preventive practice about COVID-19 8 in studies in Nigeria. However, another study in Nigeria reported lower prevalence of good attitude of 58.3% and good practice of 38.6% and higher prevalence of good knowledge of 59.1% 5 . Similarly, higher and lower prevalence were reported by foreign studies: higher prevalence of good knowledge of 48.2% and lower prevalence of good attitude of 33.8% in a study in Saudi 7 ; higher prevalence of adequate knowledge of 76.0% and appropriate preventive practice of 78.6% and lower prevalence of positive attitude of 54.7% in Nepal 9 ; higher prevalence of adequate knowledge of 67.8% and appropriate practice of 80.2% and lower prevalence of positive attitude of 72.2% in Saudi 10 ; higher prevalence of adequate knowledge of 69.8% and good practice of 87.7% and slightly higher prevalence of positive attitude of 85.1% in Yemen 11 ; and higher prevalence of good knowledge of 81.4%, good attitude of 87.1% and satisfactory practice of 77.9% in Jordan 13 . Higher prevalence (especially of good knowledge and good practice) and lower prevalence (especially of good/positive attitude) were also reported by other studies in Venezuela 14 , Ethiopia 6 , 15 , Sierra Leone 16 , and Pakistan 17 .
The comparatively higher/lower values in the other previous studies could perhaps be explained by contextual and timing differences between those studies and our study. Previous evidence has shown time and context-specific trends in COVID-19 risk perception 20 and COVID-19 knowledge, attitude, and preventive practice 21 , 22 . Unlike our study: most of the previous studies were only online among privileged heath workers who largely had good internet access; involved limited categories of health workers; were implemented during the initial waves of the pandemic when uncertainties, confusion, fear, and anxiety were more prevalent; and some of those studies were conducted in settings with higher burden of the pandemic. These contexts means the health workers in those studies were of different sociodemographic background and relatively had higher/more privileged professional attributes and socioeconomic/educational status which could have accounted for the higher prevalence of good knowledge and good practice in those studies. Higher socioeconomic and educational status have been associated with higher COVID-19 knowledge and preventive practice 22 .
The largely lower prevalence of good/positive attitude towards COVID-19 in those studies could also be explained by the more widespread negative perceptions during the initial waves of the pandemic when there were much uncertainties, confusion, fear, and anxiety amidst the unprecedented misinformation, disinformation, and conspiracy theories. In addition, there were fewer number of COVID-19 cases/related-deaths and limited or no actual COVID-19 vaccines/vaccination during the initial waves of the pandemic when most of the previous studies were conducted. As a result, perhaps fewer participants in those studies had direct/indirect experience of COVID-19 and more of the participants had limited or no real experiences of the importance, safety/side-effects, and effectiveness of COVID-19 vaccination/vaccines and were perhaps more prone to the adverse influence of the misinformation/disinformation which could have more adversely affected their perceptions regarding COVID-19 and COVID-19 vaccines/vaccination. Subsequent studies, especially qualitative studies, are needed to provide more insights on how interactions between misinformation/disinformation/conspiracy theories and real direct/indirect experiences influence perceptions and behaviours/practices regarding COVID-19/health emergencies.
We did not identify any relevant and comparable studies to appropriately compare our findings regarding the predictors of having an interpersonal source as the main/most trusted source of information about COVID-19 and of having traditional media as the main/most trusted source of information about COVID-19. However, our findings provide the evidence that professional/work-related attributes and sociodemographic characteristics were important determinants of the health workers’ use of and confidence in COVID-19 information sources. Considering the fact that interpersonal source (such as health workers) was the commonest, main, and most trusted source of information about COVID-19 (followed by traditional media (such as radio)) in our study, the identified predictors indicate professional and sociodemographic factors to be considered in designing and implementing subsequent COVID-19/health emergencies’ health information tailored to health workers in Ebonyi state/Nigeria and other similar settings. Subsequent studies on COVID-19/health emergencies should not only aim to describe the use of information sources but should extensively assess health workers’ use of and confidence in information sources and the predictors.
In our study, the predictors of good control practice about COVID-19 were good knowledge about COVID-19, good attitude towards COVID-19 (vaccination), strong COVID-19 experience and perception, being a health worker at a tertiary health facility, having a tertiary education, and decrease in years of working experience. It is worth noting that the main and most trusted source of information about COVID-19 were not predictors. Similarly, the predictor of COVID-19 preventive practice in other studies were: good knowledge of COVID-19 (two studies in Nigeria) 4 , 5 , higher educational level (Nepal, Saudi) 9 , 10 , male gender (Saudi) 10 and 5 or more years of working experience in Ethiopia 6 . Also, COVID-19 information sources were not predictors in a study in Nepal 9 . However, COVID-19 information source was a predictor in a study in Ethiopia 6 . Also, working in a primary health facility was a predictor in one of the studies in Nigeria 5 in contrast to being a health worker at a tertiary health facility in our study. In addition, good/positive attitude towards COVID-19 were not predictors in the studies in Nigeria 4 , 5 and adequate knowledge was not a predictor in Ethiopia 6 .
The contrasting findings regarding predictors could be due to the differences in timing of the studies and contextual factors and differences in the definitions, measurements, and categorization of predictor and outcome variables. Perhaps the higher confidence level of 97.5% that we used to correct for multiple comparisons reduced the number of predictors identified in our study. However, these predictors should be prioritised in the development of context-specific and tailored policy interventions to increase subsequent control practice about COVID-19 and similar health emergencies.
Reporting bias was a potential limitation in this study which was questionnaire-based study that relied on participants expressing their perceptions and control practices regarding COVID-19. The sensitive nature of the COVID-19 pandemic and the national/global response to control the pandemic perhaps increased the tendency for some respondents to exaggerate desirable perceptions and practices and underestimate undesirable perceptions and practices. To minimise this bias, the anonymous and confidential nature of the questionnaire survey were properly explained and emphasized to the participants. This study was also prone to selection bias because of the convenience and snowballing sampling techniques employed for the selection of study participants.
This study had many strengths. It was both online and offline and involved the entire populations and categories of health workers (in the formal and informal health sectors) in both rural and urban/semi-urban areas in Ebonyi state. Thus, the findings of this study are more generalisable to the general population of health workers in the state and other parts of Nigeria, including other less privileged settings with limited internet access. In addition, the outcome measures and the potential covariates were pre-specified in the study protocol which was prospectively registered and prospectively submitted to a peer-review journal before the implementation of this study started.
Conclusions
The commonest source of information about COVID-19 and the main and most trusted source of information for majority of the health workers during the COVID-19 pandemic in Ebonyi state, Nigeria was interpersonal sources such as health workers followed by traditional media such as radio. There was low knowledge as only less than half had good knowledge about COVID-19, satisfactory attitude as four-fifth had good attitude towards COVID-19 (vaccination), and poor practice as only less than half had good control practice about COVID-19. The most important predictors of the main and most trusted sources of information about COVID were primary place of work (public/private facility), level of primary place of work (primary/secondary versus tertiary facility), age, and years of working experience. Good knowledge about COVID-19, good attitude towards COVID-19 (vaccination), strong COVID-19 experience and perception, being a health worker at a tertiary health facility, having a tertiary education, and decrease in years of working experience were strong predictors of good control practice about COVID-19.
Subsequent policy actions regarding COVID-19 and similar health emergencies in Ebonyi state and Nigeria, and other similar settings, should prioritise the identified commonest, main, and most trusted information sources, their predictors, and the predictors of good control practice about COVID-19 in the strategies to optimise emergency health information dissemination and use of control measures by health workers respectively. Later studies should explore the extent of two-way communications, and the determinants, in the health emergency information dissemination process and the effects on the use of control measures by health workers.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
World Health Organization (WHO). From emergency response to long-term COVID-19 disease management: sustaining gains made during the COVID-19 pandemic. Geneva: WHO; 2023.
WHO. Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic [Internet]. 2023 [cited 2024 Jan 18]. https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic
WHO. COVID-19 Epidemiological Update: Edition 164. Geneva; 2024.
Tsiga-Ahmed, F. I. et al. COVID 19: Evaluating the knowledge, attitude and preventive practices of healthcare workers in Northern Nigeria. Int. J. Maternal Child Health AIDS (IJMA). 10 (1), 88–97 (2021).
Article Google Scholar
Adeoye, P., Oke, G., Fadele, K. & Awotunde, T. Knowledge, attitude, practice and predictors of preventive practices toward COVID-19 among healthcare workers in Ogbomoso, Nigeria: A cross-sectional study. Niger. J. Med. 30 (4), 452 (2021).
Ashebir, W. et al. Knowledge, attitude, practice, and factors associated with prevention practice towards COVID-19 among healthcare providers in Amhara region, northern Ethiopia: A multicenter cross-sectional study. PLOS Glob. Public Health. 2 (4), e0000171 (2022).
Article PubMed PubMed Central Google Scholar
Alduraywish, A. A. et al. A Countrywide Survey in Saudi Arabia regarding the knowledge and attitude of health care professionals about coronavirus disease (COVID-19). Int. J. Environ. Res. Public Health. 17 (20), 1–15 (2020).
Mbachu, C. N. P. et al. COVID-19 infection: Knowledge, attitude, practices, and impact among healthcare workers in a South-Eastern Nigerian State. J. Infect. Dev. Ctries. 14 (9), 943–952 (2020).
Article CAS PubMed Google Scholar
Tamang, N., Rai, P., Dhungana, S., Sherchan, B., Shah, B., Pyakurel, P., et al . COVID-19: A National Survey on perceived level of knowledge, attitude and practice among frontline healthcare Workers in Nepal. BMC Public Health . 20 (1), 1905 (2020).
Almohammed, O. A. et al. Knowledge, attitude, and practices associated with COVID-19 among healthcare workers in hospitals: A cross-sectional study in Saudi Arabia. Front. Public Health. 9 , 643053 (2021).
Alrubaiee, G.G., Al-Qalah, T.A.H., Al-Aawar, M.S.A. Knowledge, attitudes, anxiety, and preventive behaviours towards COVID-19 among health care providers in Yemen: An online cross-sectional survey. BMC Public Health . 20 (1), 1541 (2020).
Rabbani, U. & Al Saigul, A. M. Knowledge, attitude and practices of health care workers about corona virus disease 2019 in Saudi Arabia. J. Epidemiol. Glob. Health. 11 (1), 60–68 (2021).
Amro, F.M., Rayan, A.H., Eshah, N.F., ALBashtawy, M.S. Knowledge, attitude, and practices concerning COVID-19 preventive measures among healthcare providers in Jordan. SAGE Open Nurs . 8 , 1–8 (2022).
Mendoza Millán, D. L. et al. Knowledge, attitudes, and practices regarding COVID-19 among healthcare workers in Venezuela: An online cross-sectional survey. Front. Public Health. 9 , 633723 (2021).
Farah, A.M., Nour, T.Y., Obsiye, M., Aden, M.A., Ali, O.M., Hussein, M.A., et al . Knowledge, attitudes, and practices regarding COVID-19 among health care workers in public health facilities in Eastern Ethiopia: Cross-sectional survey study. JMIR Form Res . 5 (10), e26980 (2021).
Kanu, S. et al. Healthcare workers’ knowledge, attitude, practice and perceived health facility preparedness regarding COVID-19 in Sierra Leone. J. Multidiscip. Healthc. 14 , 67–80 (2021).
Hussain, I. et al. Knowledge, attitude, and practices toward COVID-19 in primary healthcare providers: A Cross-sectional study from three tertiary care hospitals of Peshawar, Pakistan. J. Community Health. 46 (3), 441–449 (2021).
Article PubMed Google Scholar
Omale, U.I., Iyare, O., Ewah, R.L., Amuzie, C.I., Oka, O.U., Uduma, V.U., et al . COVID-19 vaccination acceptance among community members and health workers in Ebonyi state, Nigeria: Study protocol for a concurrent-independent mixed method analyses of intention to receive, timeliness of the intention to receive, uptake and hesitancy to COVID-19 vaccination and the determinants. BMJ Open . 12 (12), e061732 (2022).
Pedroza, C., Thanh Truong, V.T. Performance of models for estimating absolute risk difference in multicenter trials with binary outcome. BMC Med. Res. Methodol . 16 (1), 113 (2016).
Liu, B. et al. Trends and factors associated with risk perception, anxiety, and behavior from the early outbreak period to the controlled period of COVID-19 epidemic: Four cross-sectional online surveys in China in 2020. Front. Public Health. 9 , 768867 (2022).
Rahman, M. M. et al. Knowledge, attitude and practices toward coronavirus disease (COVID- 19) in Southeast and South Asia: A mixed study design approach. Front. Public Health. 9 , 875727 (2022).
Siddiquea, B.N., Shetty, A., Bhattacharya, O., Afroz, A., Billah, B. Global epidemiology of COVID-19 knowledge, attitude and practice: A systematic review and meta-analysis. BMJ Open . 11 (9), e051447 (2021).
Download references
This study was funded by the authors.
Author information
Authors and affiliations.
Department of Community Medicine, Alex Ekwueme Federal University Teaching Hospital Abakaliki (AEFUTHA), Abakaliki, Ebonyi State, Nigeria
Ugwu I. Omale, Ifeyinwa M. Okeke, Okechukwu O. Ukpabi, Osarhiemen Iyare, Onyinyechukwu U. Oka, Azuka S. Adeke, Cordis O. Ikegwuonu, Ugochi I. A. Nwali & Olaedo O. Nnachi
Department of Anaesthesia, Alex Ekwueme Federal University Teaching Hospital Abakaliki (AEFUTHA), Abakaliki, Ebonyi State, Nigeria
Richard L. Ewah
Anaesthesia Unit, Department of Surgery, Ebonyi State University, Abakaliki, Ebonyi State, Nigeria
Department of Community Medicine, Federal Medical Centre Umuahia, Umuahia, Abia State, Nigeria
Chidinma I. Amuzie & Glory E. Nkwo
Department of Internal Medicine, Alex Ekwueme Federal University Teaching Hospital Abakaliki (AEFUTHA), Abakaliki, Ebonyi State, Nigeria
Victor U. Uduma
You can also search for this author in PubMed Google Scholar
Contributions
UIO conceptualised and designed the study, designed the data collection tool and programmed the software, wrote the protocol and directed the implementation of the study, oversaw data management, did the statistical analyses and interpretation, and wrote the manuscript. OI, RLE, CIA, OUO, VUU, ASA, COI, OON, OOU, and IMO contributed to the development of the study design, data collection tool, first and final versions of the protocol. GEN, UIAN contributed to the development of the study design, data collection tool, and final version of the protocol. OI, OUO, VUU, ASA, COI, OON, OOU, IMO, RLE, and UIAN contributed to the implementation and data management. All authors revised the manuscript, read, edited, and approved the final manuscript.
Corresponding author
Correspondence to Ugwu I. Omale .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Omale, U.I., Okeke, I.M., Ukpabi, O.O. et al. COVID-19 information sources, knowledge, attitude, control practices and the predictors among health workers during the pandemic in Ebonyi state, Nigeria. Sci Rep 14 , 7072 (2024). https://doi.org/10.1038/s41598-024-57647-1
Download citation
Received : 01 August 2023
Accepted : 20 March 2024
Published : 25 March 2024
DOI : https://doi.org/10.1038/s41598-024-57647-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Information sources
- Control practices
- Health workers
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 15 June 2022
A systematic review and meta-analysis on the preventive behaviors in response to the COVID-19 pandemic among children and adolescents
- Feifei Li 1 , 2 na1 ,
- Wei Liang 1 , 2 na1 ,
- Ryan E. Rhodes 3 ,
- Yanping Duan 1 , 2 ,
- Xiang Wang 4 ,
- Borui Shang 5 ,
- Yide Yang 6 ,
- Jiao Jiao 7 ,
- Min Yang 2 ,
- Rashmi Supriya 1 , 2 ,
- Julien S. Baker 1 , 2 &
- Longyan Yi 8
BMC Public Health volume 22 , Article number: 1201 ( 2022 ) Cite this article
2905 Accesses
8 Citations
2 Altmetric
Metrics details
The purpose of this review was to synthesize the empirical evidence of relevant studies related to preventive behaviors in response to the COVID-19 pandemic among children and adolescents. Further to this, we aimed to identify the demographic, psychological, and social and environmental correlates of such behaviors.
Following PRISMA guidelines, eligible literature was identified by searching seven databases (PsycINFO, PubMed, MEDLINE, EMBASE, Cochrane Library, PROSPERO registry platform, and ClinicalTrials.gov website) and reference list of included studies and relevant review papers from 1 st Jan 2020 to 28 th Feb 2021. The standardized mean difference and correlation coefficients r were extracted to estimate the effect sizes. Analyses were conducted using R software.
Of the 35,271 original papers, 23 eligible studies were included in the qualitative synthesis and all these studies were of moderate-to-high quality, of which 17 studies were further included into the quantitative analysis. Children and adolescents (6–20 yrs.) showed a poorer practice of COVID-19 preventive behaviors compared to younger adults (21–59 yrs.) with a small-to-medium effect size (SMD = -.25, 95%CI = -.41 to -.09). For the demographic correlates, children and adolescents’ COVID-19 preventive practice was found to be significantly associated with gender ( r = .14, 95%CI = .10 to .18), while not with age ( r = -.02, 95%CI = -.14 to .10). Narratively, knowledge was found to be consistently and significantly correlated. For the psychological correlates, small-to-medium overall effects were identified for the association with attitudes ( r = .26, 95%CI = .21 to .31) and perceived severity ( r = .16, 95%CI = .01 to .30). For the family and social correlates, a non-significant association was identified between family economic status and COVID-19 preventive behaviors ( r = .004, 95%CI = -.12 to .12).
Conclusions
Interventions and relevant policies of promoting children and adolescent’s preventive measures should be a priority. Further, empirical studies identifying the demographic, psychological, and family and social correlates of children and adolescents’ preventive behaviors are needed.
Peer Review reports
Introduction
The COVID-19 pandemic has continued for over two years, substantially influencing global societies. Up until the end of April 2022, there were more than 510 million confirmed cases and over 6.2 million deaths related to SARS-CoV-2 reported worldwide [ 1 ]. SARS-CoV-2 is primarily transmitted by respiratory droplets of infected or even asymptomatic people during direct contact with individuals and by contact routes [ 2 , 3 , 4 ]. Based on available evidence, WHO recommended droplet and contact precautions, which were consistent with national guidelines in most countries [ 5 ]. Preventive behaviors such as physical distancing, hand hygiene, and facemask wearing, have been advocated and proven to be effective in suppressing transmission of the virus and to flatten the pandemic curve [ 6 ]. Further, preventive behaviors are still needed following vaccination in order to enhance the suppressive effect (especially when transmission from one person to another following vaccination for COVID-19 is unknown) [ 7 ]. In addition, the omicron variant of SARS-CoV-2 is less responsive to two doses of vaccination, which results in substantial morbidity and mortality [ 8 ]. Therefore, preventive behaviors are still highly recommended to control the transmission of COVID-19.
Much research and public health messaging has been focused on adults and the role of children and adolescents in the prevalence and transmission of COVID-19 is still controversial. Children and adolescents were identified as being less susceptible to SARS-CoV-2 with mostly mild and asymptomatic cases compared with adults [ 9 ]. This might have underestimated the prevalence of COVID-19 among this population, as early routine testing and diagnosis was mainly restricted to symptomatic cases. The role of children and adolescents in the transmission of COVID-19 was also debated, particularly within the context of their threat to other vulnerable family populations [ 10 ]. In addition, children and adolescents were not the priority group to vaccinate in most countries.
Despite this early-stage lower focus, multisystem inflammatory syndrome in children, likely related to COVID-19 exposure or infection, has been increasingly reported and may lead to multi-organ failure [ 11 ]. Hence, practicing preventive behavior, as part of a comprehensive package of public health intervention, is important for children and adolescents.
A series of potential factors may determine and modify compliance with virus transmission preventive behaviors. Previous psychosocial theories, such as health belief model (HBM), the theory of planned behavior (TPB), health action process approach (HAPA), and ecological model, have proposed that individuals preventive behaviors could be affected by diverse demographic and psychosocial factors that should be targeted in the relevant behavioral promotion intervention and policy making [ 12 ]. For example, HBM suggested that individuals’ preventive behaviors are determined by their health beliefs (e.g., risk awareness, perceived susceptibility, and severity) [ 13 , 14 ]. Both TPB and HAPA highlighted the intention-behavior relationship which provided a more comprehensive understanding for the individuals’ behavioral change process. TPB emphasized the antecedents of behavioral intention (i.e., motivational factors), such as social norms, attitudes, and perceived behavioral control, suggesting these factors affected the formation of behavioral intention that subsequently facilitated the behavioral change [ 15 ]. HAPA model focused on both motivational (e.g., risk perception, outcome expectancies, and action self-efficacy) and volitional factors (e.g., planning and action control) of behavioral change, highlighting the continuous process from intention formation to behavioral initiation and maintenance [ 16 ]. In addition to the above intrapersonal/individual factors, the ecological model suggested including the social and environmental (e.g., peers, parents, community environmental, and social policy) influence into consideration with respect to the promotion of health behavior [ 17 ]. An increasing group of evidence has supported the important role of these factors in initiating preventive behaviors in various populations, including children and adolescents [ 9 ]. However, as the characteristics of behaviors differ prominently across different age groups, distinguishing the correlates targeting children and adolescents is also required to the design of behavioral interventions and health policy decision-making in the fight against COVID-19 and future pandemics [ 18 ].
At present, there is limited summary evidence on both child and adolescents’ practice of preventive behaviors and relevant correlates during the initial stage of the COVID-19 pandemic. Therefore, the present study aimed to synthesize relevant evidence to explore the practice of COVID-19 preventive behaviors in children and adolescents compared with adult populations, and to identify the potential correlates (demographic, psychological, and social and environmental) of preventive behaviors among children and adolescents during the initial stage of the COVID-19 pandemic.
The present systematic review and meta-analysis was undertaken following the Cochrane guidelines and GRADE approach [ 19 ], and the results were reported following the PRISMA statement and MOOSE guidelines [ 20 , 21 ]. The study protocol has been prospectively registered on PROSPERO (CRD42021242062).
Search strategy and study selection
Following the PICOS principles, the inclusion criteria were: (1) Population: studies including children and adolescents aged 6–20 yrs. were eligible according to the Colarusso’s recommendation (1992) [ 22 ]; (2) Intervention/exposure: studies targeting any preventive behaviors in response to the COVID-19 pandemic were included; (3) Comparison: not applicable for the observational studies. The baseline data of randomized controlled trials were used; (4) Outcomes of interest: the practice of preventive behaviors (e.g., physical distancing, face mask wearing, hand hygiene, and other preventive measures) in response to the COVID-19 pandemic, and the association of preventive practice with behavioral correlates (i.e., demographic, psychological, or family and social factors); and (5) Study types: cross-sectional, longitudinal cohort, randomized controlled trial, and experimental or quasi-experimental studies were eligible for inclusion, and commentaries. Pure qualitative assessments or case studies were not eligible. In addition, we only included full-text articles containing primary data that could be retrieved through online databases, library requests, or email correspondence with the authors.
According to a pre-defined literature search strategy (Additional file 1 : Appendix 1), the following databases were searched electronically: PsycINFO, PubMed, MEDLINE (EBSCOhost used), EMBASE (Ovid platform used), and Cochrane Library. In addition, two databases were searched by hand: PROSPERO registry platform (COVID-19 theme) and ClinicalTrials.gov website. Finally, a hand search of the references of included papers and relevant systematic reviews was conducted. Since the COVID-19 pandemic was first announced by the WHO on 31 Dec 2019 [ 1 ], the time of the literature search was limited from 1 st Jan 2020 to 28 th Feb 2021. The literature search was restricted to human participants with no special requirements for language.
The primary search was conducted by two reviewers (JJ, FL) independently using Mendeley software. Following de-duplication, titles and abstracts were initially screened to exclude irrelevant studies. Then, the full texts of the remaining articles after initial screening were assessed for eligibility. Any disagreements between the two reviewers were resolved by consensus or confirmed by a third reviewer (WL).
Study quality assessment
Two reviewers (WL/FL) independently evaluated the quality of the included studies using the National Institute of Health (NIH) quality assessment tool for observational cohort and cross-sectional studies (NIH, 2020) [ 23 ]. The NIH quality assessment tool used 14 measures of assessment, e.g. clarity of research questions, appropriateness of study population, sample size justification, quality of outcome measures, and accuracy of statistical analysis. The study quality was determined using four categories, “high = satisfying all assessed items”, “good = did not satisfy one item”, “moderate = did not satisfy two to four items”, and “poor = did not satisfy more than four items” [ 24 ]. Disagreement between the two reviewers were resolved by consensus or decided by a third reviewer (BS).
Data extraction
Information of all eligible studies were extracted, including authors, regions, study design, date of data collection, sample size, participants’ demographics, preventive behavior(s), and the correlate measured. Two reviewers (WL/MY) independently extracted data and checked for errors mutually. Disagreements were resolved by consensus or by discussion with a third reviewer (FL). In our study, the outcomes included either a single preventive behavior (e.g., physical distancing, hand hygiene, facemask wearing) or combined preventive behaviors (e.g., practice aspect of knowledge, attitude, and practice [KAP] towards COVID-19). The practice score and/or percentage of adopting the preventive measures was extracted. Physical distancing referred to staying at home and away from crowded places, avoiding mass gatherings, and keeping certain space with each other, refraining from physical contacts especially with individuals who may sick. Hand hygiene referred to washing hands with soap, water, or alcohol-based hand rub lasting for a specified time. Referring to the potential determinates to preventive behaviors among children and adolescents, demographic, psychosocial, and family and social correlates were identified and categorized accordingly.
Data synthesis and meta-analysis
Meta-analyses were implemented only if three studies at least provided effect sizes for the same parameter (only narrative analyses were conducted in case of not enough data). To compare the preventive practice across different age groups (study purpose 1), the sample size, mean score of preventive practice with standard deviation (SD), and number of adopting and non-adopting the preventive practice for each age group (6–20, 21–59, ≥ 60 yrs.) were extracted to calculate the standardized mean difference (SMD) and 95% confidence intervals (95%CI) [ 25 ]. For the investigation of behavioral correlates among children and adolescents (study purpose 2), the correlation coefficients ( r ) were extracted for the effect size estimates. Several studies used multivariate linear regression, the standardized regression coefficients ( β ) were converted to r values using a series of transformations [ 26 ]. Several studies only provided the OR, and the data was arithmetically converted to SMD or r using a spreadsheet where different formulas have been pre-inserted supporting for the automatic transformation of diverse effect sizes developed by DeCoster (2010) [ 27 , 28 ]. All the data were converted to normally distributed Fisher’s z to calculate the pooled effect size and 95%CI using random effect models.
The percentage of total variation across the studies due to heterogeneity (Cochran’s Q -statistic) was used to calculate the I 2 statistics, with 25%, 50%, and 75% indicating mild, moderate, and high degrees of heterogeneity, respectively [ 29 ]. Subgroup analyses were conducted if possible (e.g., the number of included effects is ≥ 10) to evaluate the robustness of the summary estimates to determine whether a particular study accounted for the heterogeneity [ 30 , 31 ]. Sensitivity tests were conducted on study quality and study design. The publication bias was identified using the funnel plot, Egger’s regression test, and Fail-safe N approach [ 32 ]. All the analyses were conducted in R (R Core Team, 2013) and a p value of < 0.05 was considered statistically significant.
Study characteristics
A total of 23 studies were identified and eligible for the present study as shown in Fig. 1 . Among them, 17 studies which reported enough statistical information were extracted to the meta-analysis. A summary of study characteristics is presented in Table 1 and details of each included study are summarized in Additional file 2 : Appendix 2. There were 11 studies that focused on the prevalence of preventive behavior containing children and adolescents (age 10–20 yrs.; n = 7,998) as a separate subgroup to compare with adults (age 21–59 and ≥ 60 yrs..; n = 62,172). Most of the studies were conducted in Asian countries (n = 10) and were observational studies with a cross-sectional design (n = 10). A total of four studies measured practice of KAP, six with multiple preventive behavior, and one focused only on each single behavior of physical distancing, hand hygiene, and facemask wearing. In addition, 12 studies that targeted only children and adolescents (age 6–20 yrs.; n = 19,663) to explore correlates of preventive behaviors during the COVID-19 pandemic. Five of the eligible studies were conducted in the Asian countries, with the remaining studies undertaken in countries of Europe (n = 4), North America (n = 2), and Africa (n = 1). All studies were observational studies, of which the majority used a cross-sectional design (n = 10). Multiple preventive behavior was the most frequently investigated outcomes (including practice of KAP; n = 8), and then physical distancing (n = 5).
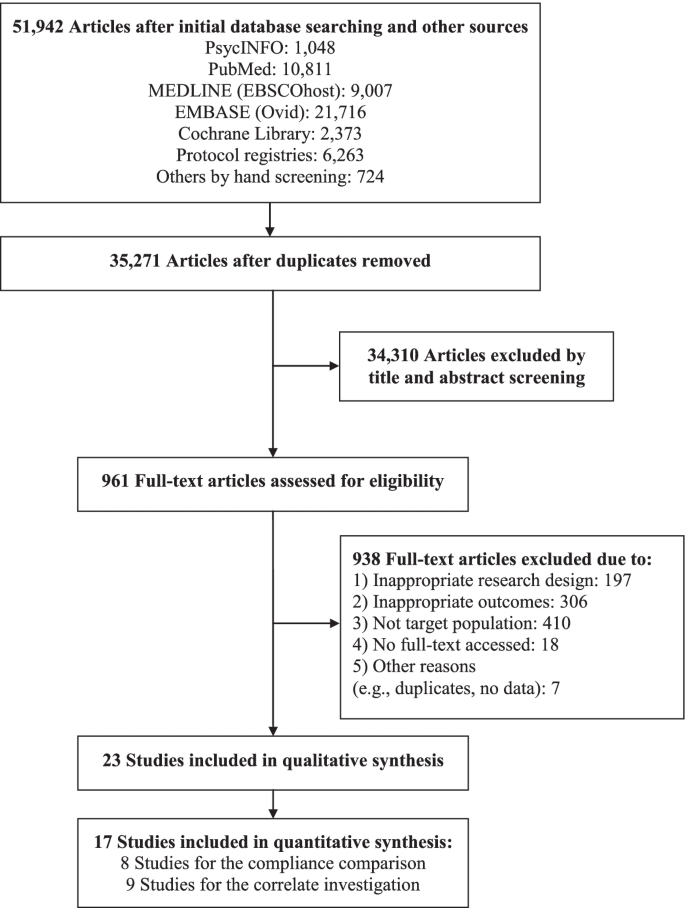
PRISMA flow chart outlining literature search process, inclusion and exclusion of studies
The quality of selected studies was assessed by two authors independently (inter-rater agreement = 96%). All studies were of moderate-to-high quality. Particularly, 30.4% of studies were rated as high quality ( k = 7), while 52.2% ( k = 12) and 17.4% ( k = 4) of studies were rated as good and moderate quality, respectively. Among studies with good and moderate quality, the major problem was the lack of reporting on sample size estimation ( k = 14; 77.8%). In addition, three studies did not explicitly indicate the inclusion criteria for participants and another three did not report the reliability and validity of relevant measures (see Additional file 3 : Appendix 3).
Practice of preventive behaviors among children and adolescents
The majority of the included studies (18/23, 78.3%) targeted the practice of multiple preventive behaviors (e.g., hand hygiene, facemask wearing, physical distancing, covering coughs, house disinfection, intake vitamin C), where the percentage of children and adolescents adopting the preventive practice in response to the COVID-19 pandemic ranged from 16 to 94%. Seven studies targeted the specific preventive behavior of children and adolescents, indicating compliance rates of 76–89%, 60–88%, 31–87% for hand hygiene, facemask wearing, and physical distancing respectively.
When comparing the practice of COVID-19 preventive behaviors across different age groups, a pooled analysis of eight studies revealed a significant difference in preventive behaviors between children/adolescents and younger adults (21–59 yrs.), with a small-to-medium effect size ( k = 8, n = 68,257, SMD = -0.25, p = 0.008; adults as reference) (Fig. 2 ). Heterogeneity was large between included studies ( Q = 57.0, I 2 = 88%, p < 0.001). Compared with older adults (≥ 60 yrs.), a non-significant difference in preventive behaviors was found in the meta-analysis ( k = 4, n = 7,548, SMD = -0.08, p = 0.33; adults as reference). The effect sizes were comparatively homogenous across studies ( Q = 5.52, I 2 = 45.7%, p = 0.14). Sensitivity tests indicated a consistent result when excluding one article which was rated as moderate quality [ 33 ]. Per the inspection of funnel plots, Egger’s regression (all p < 0.05), and Fail-safe-N analyses, a non-significant risk of publication bias was identified for both comparisons (Additional file 4 : Appendix 4).
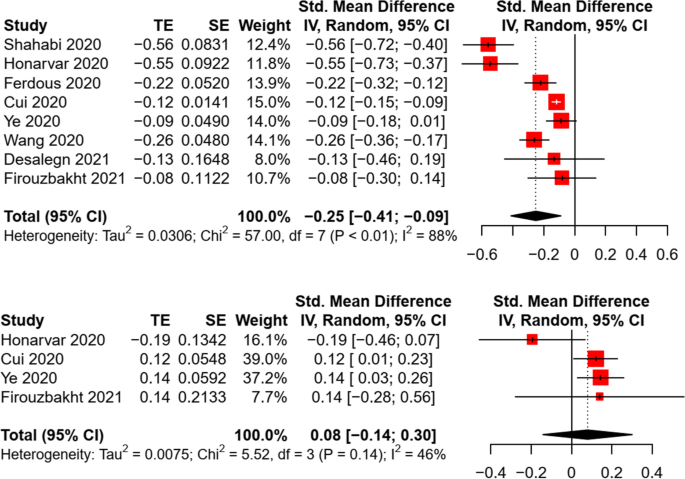
Random effect of the difference in preventive behaviors between children/adolescents and adults
Demographic correlates of preventive behaviors in children and adolescents
Age, gender, and education level were the most examined demographic factors. Of the 12 studies targeting only children and adolescents, seven studies examined the association of age with COVID-19 preventive behaviors. Three studies targeted multiple preventive behaviors and found no significant age-behavior correlation in children and adolescents [ 17 , 34 , 35 ], while similar results were also revealed in another four studies targeting hand hygiene or physical distancing [ 36 , 37 , 38 ]. A non-significant association between age and preventive practice was revealed in the meta-analysis ( k = 5, n = 3,182, r = -0.02, p = 0.72) (see Fig. 3 ), with a large heterogeneity between studies ( Q = 27.95, I 2 = 86%, P < 0.001). Sensitivity test revealed a consistent finding when excluding a cohort study [ 39 ]. The funnel plot, Egger’s regression ( b = 2.77, p = 0.68), and Fail-safe-N analyses indicated a non-significant publication bias (Additional file 4 : Appendix 4).
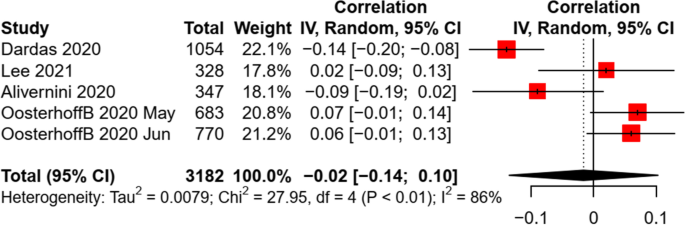
Random effect of age on preventive behaviors in children and adolescents
All the 12 studies examined the difference in COVID-19 preventive behaviors across gender, among which seven studies were eligible to be included into the meta-analysis. A small and significant effect size was identified by synthesizing the data ( k = 7, n = 13,791, r = 0.14, p < 0.001). A moderate heterogeneity of effect sizes was found between studies ( Q = 21.98, I 2 = 73%, P = 0.001) (Fig. 4 ). A sensitivity test revealed a consistent finding when excluding a cohort study [ 40 ]. The funnel plot, Egger’s regression ( b = -1.82, p = 0.21), and Fail-safe-N analyses indicated a non-significant publication bias of included studies (Additional file 4 : Appendix 4).

Random effect of gender on preventive behaviors in children and adolescents
For the association between education level and preventive behaviors, there was not enough data for the meta-analysis. Narratively, four studies indicated mixed results, particularly three reporting no significant difference in combined preventive behaviors [ 14 , 40 , 41 ], while one finding a positive association of education levels with both hand hygiene and facemask wearing [ 42 ]. In addition, two studies examined the contribution of ethnicity (white vs. non-white), indicating a significant negative association of white ethnicity with physical distancing, but the association was not statistically significant with disinfecting behaviors [ 36 , 37 ].
Psychological correlates of preventive behaviors in children and adolescents
A series of psychological factors were measured in the included studies, such as knowledge, attitude (perceived benefits, barriers), risk perception (perceived susceptibility, severity), social interaction (trust, social norms, moral factors), and psychological well-being (depression, anxiety). Four studies measured behavior-related knowledge [ 13 , 38 , 41 , 43 ], among which only two studies examined the association of knowledge with preventive behaviors, indicating a significant positive relationship [ 13 , 38 ]. In addition, several studies examined the association of diverse psychological factors, e.g. social trust [ 36 , 40 ], moral disengagement [ 39 , 40 ], social norms [ 36 , 37 , 40 ], and psychological well-being [ 37 , 41 ], with preventive behaviors in response to the pandemic, revealing mixed results.
Due to the limited data, the meta-analysis was conducted only for the association of preventive practice with attitude and risk perception (i.e., perceived severity). A significant association between attitude and preventive behaviors was revealed, with a small-to-medium effect size ( k = 4, n = 3,304, r = 0.26, p < 0.001). Similarly, a small and significant association was found between perceived severity and preventive behaviors in children and adolescents ( k = 3, n = 1,895, r = 0.16, p = 0.045). The heterogeneity of effect sizes was non-significant between studies (see Fig. 5 ). A non-significant risk of publication bias was identified by the funnel plots, Egger’s tests (all p < 0.05), and Fail-safe-N analyses (see Additional file 4 : Appendix 4).
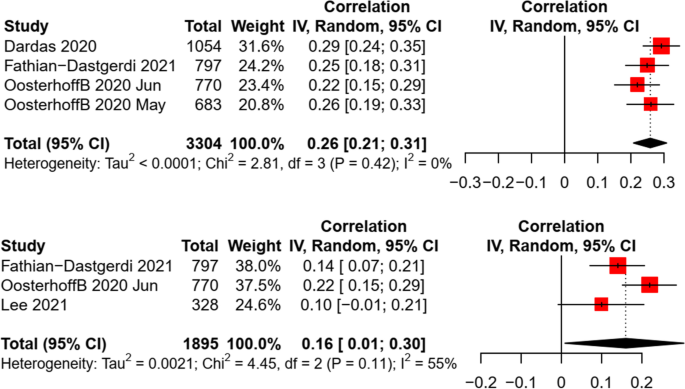
Random effect of attitude and perceived severity on preventive behaviors in children and adolescents
Social and environmental correlates of preventive behaviors in children and adolescents
Several studies examined the association of children and adolescents’ preventive practice with social and environmental factors, such as family residence (e.g., rural/urban), family economic status, parental education levels, and community/city sanitation levels. For the association between residence and preventive behaviors, inconsistent results were found in three studies [ 13 , 38 , 41 ]. Mixed findings were also revealed for the relationship between parental education levels and preventive behaviors in four studies [ 36 , 37 , 38 , 42 ]. The community/city sanitation levels (e.g., lockdown) was found to have a significant positive association with physical distancing [ 37 ], facemask wearing [ 42 ], and combined preventive behaviors [ 17 ], but negatively associated with hand hygiene [ 42 ]. For family economic status, a pooled analysis revealed a non-significant association with preventive behaviors in children and adolescents ( k = 4, n = 2,518, r = 0.004, p = 0.93). A moderate heterogeneity was found between studies (see Fig. 6 ). Sensitivity test revealed a consistent finding when excluding a cohort study [ 40 ]. The funnel plots, Egger’s tests ( b = 4.90, p = 0.53), and Fail-safe-N analyses indicated a non-significant publication bias (Additional file 4 : Appendix 4).
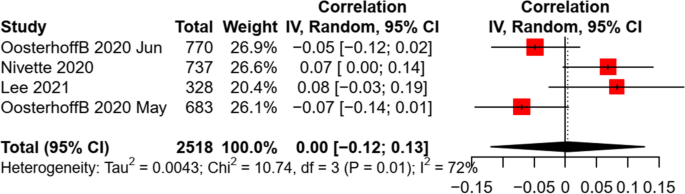
Random effect of family economic status on preventive behaviors in children and adolescents
The purpose of this paper was to synthesize and review the evidence for children and adolescent’s practice of COVID-19 preventive behaviors in comparison to adult samples. A secondary purpose was to review current evidence for the demographic, psychological, and social and environmental correlates of the preventive practice among children and adolescents during the pandemic (Table 2 ). The results are the first quantitative summary statistics for this age group and give new insights into designing effective interventions and making relevant policy-decisions to promote children and adolescents’ preventive behaviors in the fight against the COVID-19 and future pandemics.
Collectively, this review represents 23 studies with over 25,000 children and adolescents from diverse regions. The majority of studies included in the quantitative analysis were rated as good and high quality (16/17, 94.1%) and there was no statistically significant publication bias for all included studies. The majority of the included studies (18/23, 78.3%) measured the multiple preventive practice combining not only the three major preventive behaviors (i.e., hand hygiene, facemask wearing, physical distancing) but also other preventive measures (e.g., covering coughs, house disinfection, intake vitamin C). In addition to the combination of multiple preventive behaviors, seven studies provided examinations on certain specific behavior, including hand hygiene (n = 4), facemask wearing (n = 2), and physical distancing (n = 5).
For the prevalence of combined preventive behaviors, 16–94% of children and adolescents adopted relevant preventive measures in response to the COVID-19 pandemic. In terms of three major preventive measures, the compliance rate was 76–89%, 60–88%, and 31–87% for hand hygiene, facemask wearing, and physical distancing, respectively. When comparing the preventive practice across different age groups, we found a poorer preventive practice of children and adolescents compared with that of younger adults, while there were non-significant behavioral differences relative to the older adults. This highlights an urgent need of relevant interventions and policies for promoting preventive behaviors in children and adolescents during the pandemic. As the compulsory policy of school closure has been enacted in many countries, the contact pattern and activity of children and adolescents are mainly community and family interactions [ 44 ] and personal protection is more expected accordingly. The under expectation of precautionary practice rises the concern that children and adolescents may threaten other susceptible individuals within community and family with virus transmission.
For the demographic correlates of preventive behaviors, a significant association with small effect size was found between gender and preventive behaviors, where girls showed a higher behavioral compliance during the pandemic. Consistent findings were reported in previous studies, which indicated that girls were more inactive and cautious to decrease outdoor activities during other respiratory epidemics [ 45 ], while boys had a high risk-taking tendency [ 46 ]. Interestingly, previous review studies with adult populations also indicated a higher level of preventive behaviors [ 45 , 47 ] and utility of preventive care service [ 48 ] in females. Thus, there seems to be a robust gendered affect across all ages in terms of the pandemic preventive practice. One potential interpretation might be the personality difference that females tend to be higher in agreeableness [ 49 ]. Another explanation might be the difference in the general social position and social roles between males and females (e.g., females are more sanitary in general, who are more likely to be caregivers and thus take precautions more seriously; females spend more time at home and thus more social distance, etc.) [ 50 ]. This suggests that more targeted messaging for men and boys is likely needed and further examination on this assumption is needed. In contrast to gender, other demographics such as age, education levels, and ethnicity were not identified as significant correlates of preventive behaviors among children and adolescents, hinting that the same types of intervention approaches may be administered without targeting by these demographic factors. Nevertheless, these findings are concluded narratively due to the limited evidence and more empirical studies on this aspect are warranted.
For psychological correlates of preventive behaviors, only attitudes and perceived severity were identified as consistently significant correlates of COVID-19 preventive behaviors in children and adolescents. As suggested by various psychosocial theories, e.g. TPB and HBM [ 13 , 14 ], individuals’ health beliefs, cognitive and emotional appraisals for certain behaviors, and risk perception towards the diseases play a crucial role in initiating behaviors. The findings of this study are consistent with previous review articles investigating adult populations [ 51 ]. We also found that children and adolescents showed a comparatively lower level of knowledge and attitude than adults. The findings presented here to some extent may provide an explanation as to why children and adolescents demonstrate inferior behavioral compliance during the COVID-19 pandemic. However, it is worth noting that more than half of the included studies did not report the theoretical framework and there was limited data to quantitatively analyze the effect size of other psychosocial correlates (e.g., social norms, intention, self-efficacy). Based on relevant theories and evidence, these factors are important and deserve more research and attention, especially targeting children and adolescents [ 52 ]. The above findings particularly suggest the use of psychological theories in future interventions on promoting children and adolescents’ preventive behaviors in fight against the pandemics. For example, “threat” components or information about negative disease consequences could be used sparingly in the interventions. Further, a focus on causal explanation arguments of high positive expectancy benefits and appropriate persuasive peripheral cues (e.g., aiming to form positive attitudes) could be provided [ 53 ]. In addition, more research on the maintenance of preventive behaviors is needed by taking several factors other than cognitions (e.g., habit, social identity, self-regulation) into account.
For the family and social correlates of preventive behaviors, mixed results were revealed for a series of factors, such as parental education levels and family residence. It is notable that the community/city sanitation levels were narratively identified as an important correlate of preventive behaviors in children and adolescents and more empirical evidence is needed for quantitative synthesis. In addition, we found a non-significant relationship between family economic status and preventive behaviors among children and adolescents. The findings were inconsistent with previous studies in adult populations. The reason might be that adults determine family economic status rather than the children and adolescents, so the influence of economic status on children and adolescents’ behaviors is relatively weak [ 54 ]. This might be also attributed to measurement issues (i.e., implicit measures for family economic status, and diverse types of preventive behaviors).
Despite notable findings in this review, there are several limitations. First, due to the limited data, we were not able to conduct moderator analyses (e.g., cultural contexts, types of preventive behaviors, chronic health condition of children) and future research including testing of potential moderators is warranted. Next, despite our best efforts to implement a thorough literature search of the limited databases, we may have omitted suitable studies by not including key terms over the time span that was searched. The current review only summarized the evidence during the initial stage of the pandemic and further updates are needed, especially for the key correlates of behavioral maintenance. Moreover, a high degree of heterogeneity, and the small number of included studies could result in cautious interpretation of the synthesized results. As a result, any generalizations of the findings to different cultural contexts should be applied with caution and this point deserves further investigation. As the relevant evidence continues to increase, future research syntheses may be able to detect effects of more demographic, psychological, parental, social, and environmental factors of children’s preventive behaviors. Finally, this paper only targeted the general practice of preventive behaviors during the initial stage the COVID-19 pandemic while the synthesis for specific behavior has not been undertaken due to limited evidence. Further examination on the characteristics and distinction of different preventive behaviors is needed.
To the best of our knowledge, this was the first review and meta-analysis on the compliance and associated factors of preventive behaviors in children and adolescents during the initial stage of the COVID-19 pandemic. Our findings showed that the compliance with preventive behaviors in children and adolescents was significantly lower than younger adults. In addition, small-to-medium overall effects were identified for the associations of COVID-19 preventive behaviors with gender, attitudes, and perceived severity in children and adolescents. Interventions and relevant policy to promot children and adolescent’s compliance with preventive measures should be a priority in the battle against COVID-19 and future pandemics. More studies are warranted to examine the impacts of diverse demographic, psychosocial, and social environmental correlates of children and adolescents’ preventive behaviors during pandemics.
Implications and contribution
This study has made a better understanding of the practice of preventive behaviors among children and adolescents and its associated factors which is important in designing interventions and relevant policy changes in the battle against pandemics.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
WHO: Coronavirus disease (COVID-19) pandemic. http://www.whoint/emergencies/diseases/novel-coronavirus-2019 (Accessed 30 Mar 2021) 2020.
Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, Xing F, Liu J, Yip CC, Poon RW, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet (London, England). 2020;395(10223):514–23.
Article CAS Google Scholar
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, et al. Early Transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–207.
Zhou R, Li F, Chen F, Liu H, Zheng J, Lei C, Wu X. Viral dynamics in asymptomatic patients with COVID-19. Int J Infect Dis. 2020;96:288–90.
Stockmaier S, Stroeymeyt N, Shattuck EC, Hawley DM, Meyers LA, Bolnick DI. Infectious diseases and social distancing in nature. Science. 2021;371(6533):eabc8881.
Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, Wesolowski A, Santillana M, Zhang C, Du X, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585(7825):410–3.
Huang B, Wang J, Cai J, Yao S, Chan PKS, Tam TH, Hong YY, Ruktanonchai CW, Carioli A, Floyd JR, et al. Integrated vaccination and physical distancing interventions to prevent future COVID-19 waves in Chinese cities. Nat Human Behaviour. 2021;5:695–705.
Lauring AS, Tenforde MW, Chappell JD, Gaglani M, Ginde AA, McNeal T, Ghamande S, Douin DJ, Talbot HK, Casey JD, et al. Clinical severity of, and effectiveness of mRNA vaccines against, covid-19 from omicron, delta, and alpha SARS-CoV-2 variants in the United States: prospective observational study. BMJ (Clinical research ed). 2022;376: e069761.
Google Scholar
Siebach MK, Piedimonte G, Ley SH. COVID-19 in childhood: Transmission, clinical presentation, complications and risk factors. Pediat Pulmonol. 2021;56(6):1342–56.
Zhu Y, Bloxham CJ, Hulme KD, Sinclair JE, Tong ZWM, Steele LE, Noye EC, Lu J, Xia Y, Chew KY, et al. A meta-analysis on the role of children in severe acute respiratory syndrome coronavirus 2 in household transmission clusters. Clin Infect Dis. 2021;72(12):e1146–53.
Feldstein LR, Tenforde MW, Friedman KG, Newhams M, Rose EB, Dapul H, Soma VL, Maddux AB, Mourani PM, Bowens C, et al. Characteristics and outcomes of US children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. JAMA. 2021;325(11):1074–87.
Duan Y, Shang B, Liang W, Lin Z, Hu C, Baker JS, Wang Y, He J. Predicting hand washing, mask wearing and social distancing behaviors among older adults during the covid-19 pandemic: an integrated social cognition model. BMC Geriatr. 2022;22(1):91.
Dardas LA, Khalaf I, Nabolsi M, Nassar O, Halasa S. Developing an understanding of adolescents’ knowledge, attitudes, and practices toward COVID-19. J School Nurs. 2020;36(6):430–41.
Fathian-Dastgerdi Z, Khoshgoftar M, Tavakoli B, Jaleh M. Factors associated with preventive behaviors of COVID-19 among adolescents: Applying the health belief model. Res Soccial Adm Pharm. 2021;17(10):1786–90.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Article Google Scholar
Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl Psychol Int Rev. 2008;57(1):1–29.
Lee J, Allen J, Lim H, Choi G. Determinants of Behavioral Changes Since COVID-19 among Middle School Students. Healthcare (Basel, Switzerland). 2021;9(1):75.
Liu C, He Y, Liu L, Li F, Shi Y. Children with COVID-19 behaving milder may challenge the public policies: a systematic review and meta-analysis. BMC Pediatr. 2020;20(1):410.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed). 2008;336(7650):924–6.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097.
Colarusso C: Adolescence (Ages12-20). In: Child and Adult Development. Critical Issues in Psychiatry (An Educational Series for Residents and Clinicians). Boston: Springer; 1992
National Institute of Health. Quality assessment tool for observational cohort and cross-sectional studies. Bethesda: The National Heart, Lung, and Blodd Institute [ https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools ]
Okoli GN, Lam OLT, Racovitan F, Reddy VK, Righolt CH, Neilson C, Chit A, Thommes E, Abou-Setta AM, Mahmud SM. Seasonal influenza vaccination in older people: A systematic review and meta-analysis of the determining factors. PLoS ONE. 2020;15(6):e0234702.
Practical Meta-Analysis Effect Size Calculator [ https://www.campbellcollaboration.org/escalc/html/EffectSizeCalculator-SMD9.php ]
Peterson RA, Brown SP. On the use of beta coefficients in meta-analysis. J Appl Psychol. 2005;90(1):175–81.
Duan Y, Shang B, Liang W, Du G, Yang M, Rhodes RE. Effects of eHealth-based multiple health behavior change interventions on physical activity, healthy diet, and weight in people with noncommunicable diseases: systematic review and meta-analysis. J Med Internet Res. 2021;23(2):e23786.
DeCoster J: Converting effect sizes Microsoft Excel Spreadsheets. Stat-Help. http://www.stat-help.com/spreadsheets.html (Accessed 6 Feb 2021). 2012.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed). 2003;327(7414):557–60.
Higgins PG, Sally: Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0 (updated March 2011). London: The Cochrane Collaboration; 2011.
Fu R, Gartlehner G, Grant M, Shamliyan T, Sedrakyan A, Wilt TJ, Griffith L, Oremus M, Raina P, Ismaila A, et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the effective health care program. J Clin Epidemiol. 2011;64(11):1187–97.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed). 1997;315(7109):629–34.
Ferdous MZ, Islam MS, Sikder MT, Mosaddek ASM, Zegarra-Valdivia JA, Gozal D. Knowledge, attitude, and practice regarding COVID-19 outbreak in Bangladesh: an online-based cross-sectional study. PLoS ONE. 2020;15(10):e0239254.
Pinchoff J, Santhya KG, White C, Rampal S, Acharya R, Ngo TD. Gender specific differences in COVID-19 knowledge, behavior and health effects among adolescents and young adults in Uttar Pradesh and Bihar, India. PLoS ONE. 2020;15(12):e0244053.
Ogubuike C. Asolescents’ perception, practice and coping strategies during COVID-19 pandemic in Rivers State Nigeria. Int J Pathogen Res. 2021;6(2):17–27.
Oosterhoff B, Palmer CA. Attitudes and psychological factors associated with news monitoring, social distancing, disinfecting, and hoarding behaviors among US adolescents during the coronavirus disease 2019 pandemic. JAMA Pediatr. 2020;174(12):1184–90.
Oosterhoff B, Palmer CA, Wilson J, Shook N. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179–85.
Riiser K, Helseth S, Haraldstad K, Torbjørnsen A, Richardsen KR. Adolescents’ health literacy, health protective measures, and health-related quality of life during the Covid-19 pandemic. PLoS ONE. 2020;15(8): e0238161.
Alivernini F, Manganelli S, Girelli L, Cozzolino M, Lucidi F, Cavicchiolo E. Physical distancing behavior: the role of emotions, personality, motivations, and moral decision-making. J Pediatr Psychol. 2021;46(1):15–26.
Nivette A, Ribeaud D, Murray A, Steinhoff A, Bechtiger L, Hepp U, Shanahan L, Eisner M. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Soc Sci Med. 1982;2021(268): 113370.
Xue Q, Xie X, Liu Q, Zhou Y, Zhu K, Wu H, Wan Z, Feng Y, Meng H, Zhang J, et al. Knowledge, attitudes, and practices towards COVID-19 among primary school students in Hubei Province China. Children Youth Services Rev. 2021;120:105735.
Chen X, Ran L, Liu Q, Hu Q, Du X, Tan X. Hand Hygiene, Mask-Wearing Behaviors and Its Associated Factors during the COVID-19 Epidemic: A Cross-Sectional Study among Primary School Students in Wuhan, China. Int J Environ Res Public Health. 2020;17(8):2893.
Guzek D, Skolmowska D, Głąbska D. Analysis of Gender-Dependent Personal Protective Behaviors in a National Sample: Polish Adolescents' COVID-19 Experience (PLACE-19) Study. Int J Environ Res Public Health. 2020;17(16):5570.
Seale H, Dyer CEF, Abdi I, Rahman KM, Sun Y, Qureshi MO, Dowell-Day A, Sward J, Islam MS. Improving the impact of non-pharmaceutical interventions during COVID-19: examining the factors that influence engagement and the impact on individuals. BMC Infect Dis. 2020;20(1):607.
Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. 2010;15(Pt 4):797–824.
Auerbach RP, Tsai B, Abela JRZ. Temporal relationships among depressive symptoms, risky behavior engagement, perceived control, and gender in a sample of adolescents. J Res Adolescence. 2010;20(3):726–47.
Hiller J, Schatz K, Drexler H. Gender influence on health and risk behavior in primary prevention: a systematic review. Zeitschrift fur Gesundheitswissenschaften=J Public Health. 2017;25(4):339–49.
Vaidya V, Partha G, Karmakar M. Gender differences in utilization of preventive care services in the United States. J Women’s Health (2002). 2012;21(2):140–5.
Yu Y, Zhang Y. Personality and developmental characteristics of primary school students’ personality types. Front Psychol. 2021;12: 693329.
Eagly AH, Mitchell AA: Social role theory of sex differences and similarities: Implications for the sociopolitical attitudes of women and men. In: Praeger guide to the psychology of gender. Praeger Publishers/Greenwood Publishing Group; 2004: 183–206.
Urbán R, Király O, Demetrovics Z. Who complies with coronavirus disease 2019 precautions and who does not? Curr Opin Psychiatry. 2021;34(4):363–8.
Zirinsky E, Paintsil E, Oliveira CR. The clinical epidemiology of coronavirus disease 2019 in children and adolescents mirrors the widening gap in healthcare disparities. Curr Opin Pediatr. 2021;33(3):281–5.
Mosler HJ. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: a conceptual model, a review, and a guideline. Int J Environ Health Res. 2012;22(5):431–49.
Fitzgerald DA, Nunn K, Isaacs D. Consequences of physical distancing emanating from the COVID-19 pandemic: an Australian perspective. Paediatr Respir Rev. 2020;35:25–30.
PubMed PubMed Central Google Scholar
Download references
Acknowledgements
National Natural Science Foundation of China (81903336), the Hunan Provincial Natural Science Foundation of China (2019JJ50376), Scientific Research Project of Hunan Provincial Health Commission (202112031516).
Author information
Feifei Li and Wei Liang are shared first authorship.
Authors and Affiliations
Center for Health and Exercise Science Research, Hong Kong Baptist University, Kowloon Tong, Hong Kong, China
Feifei Li, Wei Liang, Yanping Duan, Rashmi Supriya & Julien S. Baker
Department of Sport, Physical Education and Health, Hong Kong Baptist University, Kowloon Tong, Hong Kong, China
Feifei Li, Wei Liang, Yanping Duan, Min Yang, Rashmi Supriya & Julien S. Baker
School of Exercise Science, Physical and Health Education, University of Victoria, Victoria, Canada
Ryan E. Rhodes
Department of Curriculum and Instruction, the Education University of Hong Kong, Ting Kok, Hong Kong, China
Department of Social Sciences, Hebei Sport University, Shijiazhuang, China
Borui Shang
Key Laboratory of Molecular Epidemiology of Hunan Province, School of Medicine, Hunan Normal University, Changsha, China
Dr. Stephen Hui Research Centre for Physical Recreation and Wellness, Hong Kong Baptist University, Kowloon Tong, Hong Kong, China
China Institute of Sport and Health Science, Beijing Sport University, Beijing, China
You can also search for this author in PubMed Google Scholar
Contributions
WL and FFL conceived and initiate the study. FFL and WL drafted the paper. RR and JSB polished the language. All authors revised, read, and approved the final manuscript.
Corresponding author
Correspondence to Longyan Yi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
All the authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search strategies.
Additional file 2.
Summary of included studies with their characteristics.
Additional file 3.
Study quality.
Additional file 4.
Funnel plots and Fail-safe-N analysis.
Additional file 5.
PRISMA 2020 checklist.
Additional file 6.
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Li, F., Liang, W., Rhodes, R.E. et al. A systematic review and meta-analysis on the preventive behaviors in response to the COVID-19 pandemic among children and adolescents. BMC Public Health 22 , 1201 (2022). https://doi.org/10.1186/s12889-022-13585-z
Download citation
Received : 02 November 2021
Accepted : 03 June 2022
Published : 15 June 2022
DOI : https://doi.org/10.1186/s12889-022-13585-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preventive behaviors
- Children and adolescents
- Demographics
- Psychosocial factors
- Social and environmental factors
- Review and meta-analysis
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Share full article

Opinion Guest Essay
Covid Precautions Are Still With Us. Just Look Down.
Supported by

Photographs and Text by Sara Barrett
A senior photo editor in Opinion
- March 16, 2024
In the early days of the Covid pandemic, public health experts announced that maintaining a distance of six feet between yourself and other people would help prevent the spread of the virus. Seemingly overnight, stickers began to appear on the floors of grocery stores, post offices, pharmacies, and other public spaces, as well as the sidewalks in front of them. Placed six feet apart, they helped us navigate the directive to distance ourselves, indicating where we should stand to be safe.

Many of the stickers were cheerfully colored and most bore words of instruction: Stand here. Maintain your distance. Stop the spread. Others were more polite, adding pleases and thank-yous. Some advertised products. Others simply said, “Stay safe.”
Some shop owners chose to forgo the stickers in favor of a customized approach. Sometimes this was just a big duct-taped X or a spray-painted pair of shoes in which you placed your feet like pieces in a jigsaw puzzle.
Whenever we ventured out of the house in those first dark months, we took our places on these dots with a mixture of annoyance and fear: Is the person in front of me going to get the last roll of paper towels? Am I being exposed? Is standing here worth the risk of dreadful sickness or worse?
Four years later, the need for social distancing has receded, but the markers — now tattered — serve as a reminder of that surreal time when we struggled to protect ourselves, collectively yet in isolation, from an invisible enemy.
Sara Barrett is a senior photo editor in Opinion.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Advertisement

IMAGES
COMMENTS
500+ Words Essay on Coronavirus Prevention. The best way of coronavirus prevention is not getting it in the first place. After extensive research, there are now COVID-19 vaccines available to the public. Everyone must consider getting it to lead healthy lives. Further, we will look at some ways in this essay in how one can lower their chances ...
While measures to prevent COVID-19, including mask-wearing, washing hands, and social distancing, can also protect against the flu, the vaccine is especially important—and safe, doctors say. Though many people claim that the flu shot "gave them the flu," it is not possible to get infected with the influenza virus from the vaccine itself ...
Table 1. COVID-19 prevention and control measures in community. The most important strategy for the population to undertake is to frequently wash their hands and use portable hand sanitizer and avoid contact with their face and mouth after interacting with a possibly contaminated environment.
The health resources have a significant effect on implementing and managing social and health measures against COVID-19, such as medical equipment, personnel, and financial dealings. ... We estimate the efficiency percent of confronting categorized case studies according to the number of published papers in the field of treatment, prevention ...
As we go into the winter months, WHO/Europe is urging people to take preventive measures, including getting vaccinated, to help stop the spread of COVID-19. Over recent weeks, the WHO European Region has seen a huge surge in case numbers. In the last week alone, there were more than 2.5 million new cases and 29 466 deaths from the disease. As Katie Smallwood, Incident Manager for COVID-19 ...
COVID-19 Prevention Actions. There are many ways your actions can help protect you, your household, and your community from severe illness from COVID-19. CDC's COVID-19 hospital admission levels provide information about the amount of severe illness in the community where you are located to help you decide when to take action to protect ...
We included the studies that investigated the effect of the implemented public health measures to prevent and control the outbreak of 2019 novel coronavirus disease (COVID-19). The database search using the predefined combinations of Mesh terms found 13,497 studies of which 3595 in PubMed, 7393 in Science Direct 2509 preprints in MedRxiv.
Keep physical distance of at least 1 metre from others, even if they don't appear to be sick. Avoid crowds and close contact. Wear a properly fitted mask when physical distancing is not possible and in poorly ventilated settings. Clean your hands frequently with alcohol-based hand rub or soap and water.
Jason Howland. March 23, 2021. Preventive health care helps you maintain your health. Screenings are important to avoid future health problems or catch them early when they are easier to treat. But the COVID-19 pandemic has led to a decrease in preventive screenings because some patients have been hesitant to see their health care provider.
Staying Safe from COVID-19. The coronavirus that causes COVID-19 spreads primarily from person to person through respiratory droplets. This can happen when someone with the virus coughs, sneezes, sings or talks when close to others. By closely following a few safety measures, you can help protect yourself and others from getting sick.
Background Novel coronavirus disease 2019 (COVID-19) has become a pandemic, and over 80 million cases and over 1.8 million deaths were reported in 2020. This highly contagious virus is spread primarily via respiratory droplets from face-to-face contact and contaminated surfaces as well as potential aerosol spread. Over half of transmissions occur from presymptomatic and asymptomatic carriers ...
Kalyani Mohan '22 and Kalli Jackson '22 penned an essay titled " Where Public Health Meets Politics: COVID-19 in the United States ," which was published in Wesleyan's Arcadia Political Review. They wrote: "While the U.S. would certainly benefit from a strengthened pandemic response team and structural changes to public health ...
Introduction: The coronavirus disease 2019 (COVID-19) pandemic has led to an increase in global awareness of relevant public health preventive measures. This awareness can be explored using online search trends from major search engines, such as Google Trends. We investigated the relationship between public awareness of preventative measures and progression of the COVID-19 pandemic.
Background COVID-19 is an emerging disease caused by highly contagious virus called SARS-CoV-2. It caused an extensive health and economic burden around the globe. There is no proven effective treatment yet, except certain preventive mechanisms. Some studies assessing the effects of different preventive strategies have been published. However, there is no conclusive evidence. Therefore, this ...
COVID-19 transmission. It can spread through small liquid particles. These particles range from larger respiratory droplets to smaller aerosols released when an infected person coughs, sneezes, speaks, sings or breathes. It spreads mainly between people who are in close contact with each other, typically within 1 metre.
COVID-19 Preventative Actions. COVID-19 can be prevented through pharmaceutical (i.e., vaccination) and non-pharmaceutical interventions (e.g., masking, physical distancing, hand hygiene). All of these preventative measures are important to protect individuals from acquiring and transmitting the SARS-CoV-2 virus and should be done in ...
Despite all scientific evidence, epidemiologically or biologically, on the positive effects of preventive measures against COVID-19, compliance with these measures remains variable. Cultural and behavioural factors play an important role in this variability. To the best of our knowledge, this is the first study to apply the TPB to predict ...
Primary prevention. Face masks reduce the risk of transmission of COVID-19 from 17.4% to 3.1% and physical distancing lowers the risk from 12.8% to 2.6%.[] Facial shield or eye protection reduces risk from 16% to 5.5%. Masks are proven to bring down the mortality risks associated with COVID-19[] and mandatory mask wearing regulations[] and universal masking[] are proven preventive measures ...
In terms of COVID-19 preventive behavior, Table 4 shows that overall, there was a good practice among the participants of the study as represented by their mean score. Not shaking of hands with others and refraining from touching of surfaces was the most practiced behavior, and not touching the eyes, nose, or mouth and not taking of cellphone ...
On January 30, 2020, the WHO declared the COVID-19 outbreak a public health emergency of international concern and, in March 2020, began to characterize it as a pandemic in order to emphasize the gravity of the situation and urge all countries to take action in detecting infection and preventing spread. Unfortunately, there is no medication ...
Many questions have been raised in the ongoing battle against COVID-19: How does the public perceive the COVID-19 prevention campaign as a member of the community?; ... Based on this, the final screening was conducted in consideration of some factors such as 'preventive measures for individuals and households,' 'hygiene and immunity, face ...
Protective measures. How to Protect yourself. As the number of people with COVID-19 continues to increase in the current pandemic, everyone has a role to play in taking care of ourselves and our loved ones, and slowing the spread of the new coronavirus.
The COVID-19 pandemic has changed into an endemic COVID-19 disease and health workers continue to be at high risk. The situation requires continued use of COVID-19 control measures by health ...
Interventions and relevant policy to promot children and adolescent's compliance with preventive measures should be a priority in the battle against COVID-19 and future pandemics. More studies are warranted to examine the impacts of diverse demographic, psychosocial, and social environmental correlates of children and adolescents ...
In the early days of the Covid pandemic, public health experts announced that maintaining a distance of six feet between yourself and other people would help prevent the spread of the virus.