- Search Menu
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Introduction, rationale for theory-comparison research, rationale for multiple-behavior research, common themes in theory-comparison and multiple-behavior research of the nih’s bcc.
- < Previous
Theory-comparison and multiple-behavior research: common themes advancing health behavior research
- Article contents
- Figures & tables
- Supplementary Data
Claudio R. Nigg, John P. Allegrante, Marcia Ory, Theory-comparison and multiple-behavior research: common themes advancing health behavior research, Health Education Research , Volume 17, Issue 5, October 2002, Pages 670–679, https://doi.org/10.1093/her/17.5.670
- Permissions Icon Permissions
Research that seeks to compare and contrast theories of behavior change and assess the utility of a particular theoretical model for changing two or more health-related behaviors is critical to advancing health behavior research. Theory-comparison can help us learn more about the processes by which people change and maintain health behaviors than does study of any single theory alone and thus has the potential to better guide the development of intervention. Multiple-behavior interventions promise to have much greater impact on public health than single-behavior interventions. However, theory-comparison and multiple-behavior research presents several emerging challenges. These include finding new ways to enhance recruitment and retention, especially among diverse populations; improving treatment fidelity; developing common metrics across behaviors that can be used to advance the measurement and assessment of behavioral change; and expanding the reach and translation of intervention approaches that have demonstrated efficacy. This paper discusses the rationale for conducting theory-comparison and multiple-behavior research and presents several common themes that have emerged from the work of the National Institutes of Health Behavior Change Consortium (BCC). The activities of each BCC workgroup and the potential contribution of each to these common themes to advance health behavior research are also described.
The Behavior Change Consortium (BCC), sponsored by the National Institutes of Health (NIH), the American Heart Association and the Robert Wood Johnson Foundation, was initiated to support a new generation of research on innovative approaches to disease prevention through behavior change ( Ory et al ., 2002a ). The goal of this initiative has been to stimulate the investigation of innovative strategies designed to initiate and maintain changes in health behaviors.
In addition to demonstrating the efficacy of a single theory or single behavior change program, the intervention studies of the BCC also provide a unique opportunity to compare theories of behavior change and assess the utility of a particular theoretical model for changing two or more health-related behaviors. The collective work of the BCC is oriented toward identifying common theoretical and methodologic themes of interest to advancing health behavior research. This paper discusses the rationale for conducting theory-comparison and multiple-behavior research, and presents several common themes that have emerged from the work of the BCC and its workgroups.
Research on theory-based intervention in changing health behavior has increased dramatically ( Smedley and Syme, 2000 ). Most of the research has focused on studying the explanatory and predictive validity of individual theories, including the Health Belief Model ( Rosenstock, 1966 ; Becker, 1974 ), Self-Determination Theory ( Deci and Ryan, 1980 ), Social Cognitive Theory ( Bandura, 1977 ), Theory of Reasoned Action/Planned Behavior ( Ajzen and Fishbein, 1980 ; Ajzen and Madden, 1986 ) and the Transtheoretical Model ( Prochaska et al ., 1992 ), among others. Indeed, these theories have formed the familiar dialectic of the theoretical perspective that has dominated the field of research in health behavior ( Allegrante and Roizen, 1998 ).
These theories can be categorized as belief-attitude theories, competence-based theories, control-based theories and decision-making theories [e.g. ( Biddle and Nigg, 2000 )]. The emphasis of most of these theories is on understanding the cognitive psychology of the individual, either alone or within the context of the individual’s social environment, and from the point of view of several key constructs (i.e. motivation, intentions and behavior). Such theories reflect a long-standing preoccupation with psychological and social-psychological factors that have been shown to be critically necessary although not sufficient ‘determinants’ of health behavior ( Sallis and Owen, 1999 ).
Broader approaches to understanding health behavior have emerged and are increasingly pursued in health promotion and health behavior change research. These include ecological models [e.g. ( McLeroy et al ., 1988 ; Green and Kreuter, 1999 )] and community models of intervention [e.g. ( Minkler and Wallerstein, 1997 )], where individual psychology comprises but one element of the broader social and environmental context in which health behavior is determined. For example, large-scale studies of population-wide cardiovascular risk reduction conducted at Minnesota ( Luepker et al ., 1995 ), Stanford ( Farquhar et al ., 1990 ) and Pawtucket ( Carleton et al ., 1995 ), supported by the National Heart, Lung and Blood Institute, were among the first generation of studies to synthesize these broader theoretical perspectives in the design of community intervention programs. While such perspectives have demonstrated differential utility in explaining modest percentages of variance across different behaviors and populations, they have proved useful in providing a more general understanding of the process of health behavior change at both individual and community levels.
Intervention approaches have since been expanded to include advocating for policy changes. Policy approaches have been applied to several studies of health behavior change, including those directed at smoking cessation, increasing physical activity, and improving diet and nutrition ( International Longevity Center, 1999 ); however, research with ecologic and community models of health behavior has sought to study the theories singly, not in comparison.
Comparing and contrasting theories can be fruitful for several reasons. First, as Maddux has suggested, it is counterproductive to hold statistical horse races to see what theory brings about more behavior change and discard the ‘loser’ ( Maddux, 1993 ). Theory-comparison research may help behavioral and social scientists engaged in health behavior research to avoid Marsh’s concept of the ‘jingle-jangle’ fallacy ( Marsh, 1994 ). Theory comparison can inform if the same constructs are being addressed but labeled differently (jingle) or if the theories operationalize the same construct differently (jangle). Moreover, studying multiple theories simultaneously allows for empirically driven integration of theories and may lead to the construction of a more complete or holistic theory of health behavior change than currently exists.
Second, theory comparison can help us learn more about the behavior change process than does study of any theory in isolation and thus better guide intervention development. While one theory may contribute to our understanding of how best to motivate an individual to adopt a new health behavior, another theory may contribute to our understanding of how an individual maintains that behavior change over time. In addition, moderators (e.g. minority status and age) may differentially influence the effectiveness of theories. Moreover, while a particular theory may be appropriate if the disease of interest is proximal, a different theory may prove useful to elicit the desired behavior if the disease to which it is relevant is temporally removed.
Finally, comparing and contrasting theories may help us to understand that some behavior change and the observed variance in change cannot be explained at all by existing theories, perhaps necessitating the development of entirely new theories, and the identification of new variables and novel measurement strategies.
Regardless of the aims, theory-based research will improve our understanding of the health behavior change process. Theory-based research allows for: (1) an understanding of the mechanism of behavior change involved, (2) an understanding of the underlying reasoning of why the mechanism worked or failed, (3) identification of what mediators of behavior an intervention should target and (4) the design of evaluations that can determine why an intervention was (or was not) successful (i.e. process to outcome analyses).
Smoking, high-fat diet and physical inactivity are three behaviors underlying the most preventable causes of disease and death in the US ( National Center for Health Statistics, 1997 ) and are three of the top five priorities of Healthy People 2010 ( US Department of Health and Human Services, 2000 ). In 1997, an international panel of cancer experts concluded that as many as 30–40% of all cancer cases worldwide could be avoided if people ate a healthy diet, avoided obesity and got enough exercise ( Hellmich, 1997 ). Although multiple risk factors are associated with a heightened risk of morbidity and mortality, the majority of health promotion interventions address risk factors as categorically separate entities, with the exception of obesity and diabetes interventions. Yet we know that health behaviors often cluster. For example, in a sample of 1559 manufacturing workers, 46% of smokers had two other risk factors (diet and inactivity) compared to 28% of non-smokers ( Emmons et al ., 1994 ). Further, the rate of heart attack increases from 46 per 1000 persons at risk with one risk factor (smoking) to 95 per 1000 persons at risk for a combination of three risk factors [smoking, hypertension and hyperlipidemia ( American Heart Association, 1997 )]. Thus, a potentially more effective paradigm may be to target multiple behaviors by developing intervention approaches that integrate what we have learned from modular approaches in order to focus on behavior-change issues common or generic to several risk behaviors. The critical questions of interest are: Is it valuable to work on multiple behaviors simultaneously or should one behavior be addressed at a time? What are the key behavioral constructs and processes common to these problem behaviors? How do multiple behaviors interact to increase or decrease health risks?
There is growing evidence that multiple-behavior interventions have the potential for much greater impact on public health than single-behavior interventions. The risk of cardiovascular disease can be lowered by 50–70% when people quit smoking and by 45% by maintaining a physically active lifestyle ( Manson et al ., 1993 ). If intervening on a single behavior can yield such significant improvements in public health, the natural extension of such a corollary is that intervening on multiple behaviors has the potential to greatly increase the impact of the intervention on public health across different diseases. Furthermore, changing multiple health behaviors should result in more favorable benefits measured in terms of quality of life outcomes and health care utilization. Given the growing interest in developing effective theory to both understand and intervene on multiple health behaviors, surprisingly little is known about what is the most effective way to intervene on multiple behaviors ( Smedley and Syme, 2000 ; Emmons, 2001 ).
For example, regular physical activity aids in decreasing both physiological and psychological responses to stress and helps reduce depression, which often accompanies smoking cessation ( Hughes, 1984 ; Holmes and Roth, 1988 ). Preliminary studies have demonstrated the utility of physical activity in enhancing quit rates and decreasing the likelihood of relapse following smoking cessation ( Marcus et al ., 1991 , 1995 ). Physical activity also results in increased caloric expenditure, which may lessen the post-smoking cessation weight gain that often leads to relapse ( Hall et al ., 1989 ; Klesges et al ., 1991 ). There is also some evidence that adopting physical activity leads to dietary changes ( Kano and Tucker, 1993 ). For example, physical activity is not only inversely related to fat intake, it seems to act as a mild appetite suppressant, at least for the first few hours following exercise training ( Wilmore and Costill, 1994 ). Finally, in a study of the cognitive-behavioral mediators of changing multiple behaviors in smokers, King et al . found significant relationships in decisional balance and self-efficacy between smoking and physical activity ( King et al ., 1996 ). This study provided preliminary cross-sectional data on how change in one risk behavior (smoking) may relate to change in another (physical inactivity).
Despite such intriguing evidence, it is currently unknown whether treating more behaviors is more or less effective than treating fewer behaviors and, if so, why. Treating multiple behaviors may have a positive effect due to the multiple exposures to the principles of behavior change. Conversely, treating multiple behaviors may be less effective due to the increased response burden produced by trying to change several behaviors at once. Moreover, there may be a maximum number or hierarchy of order of behaviors that individuals can better cope with trying to change at any given time and with different incentives. Understanding the best ways to change multiple risk behaviors and what motivates those changes is essential for designing effective intervention programs at both the individual and population levels.
The impact of an intervention is partly determined by the percent of the target population recruited and the efficacy of the intervention, i.e. intervention impact = recruitment×efficacy ( Abrams et al ., 1994 ). Recently, another dimension of intervention impact, retention , has been added to this equation, i.e. intervention impact = recruitment×retention×efficacy ( Marcus et al ., 2000 ). This equation could be expanded to assess the impact of multiple-behavior interventions, i.e. intervention impact = recruitment ×retention×mean efficacy×number of behaviors (the mean efficacy may be each behavior’s effect size multiplied by a coefficient derived from the contribution to all cause mortality, which is then averaged for behaviors addressed). In addition to evaluating a summary estimate of behavioral change, projected reductions in morbidity and mortality will inform public health impact and decision making ( Woolf, 1999 ).
Developing integrated intervention approaches that can take advantage of the data pointing to the synergy that exists between multiple health behaviors and what is known about the impact of intervention, however, will require a better understanding of what behaviors are the most difficult to change and maintain, why and how these behaviors can be best used as examples. In addition, further research is required to better understand the relationship of dose to response ( Steckler et al ., 1995 ), i.e. whether intervention dosing based on one theory is equivalent to intervention dosing based on another theory and, related, if intervention dosing based on one behavior is equivalent to dosing of a different behavior.
The BCC has endeavored to support cross-site collaborations that are designed to begin answering such questions by supporting theory-comparison and multiple-behavior research. BCC workgroups are engaged in activities on several common themes in theory-comparison and multiple-behavior research (Figure 1 ). These include recruitment and retention, treatment fidelity, measurement and assessment, and reach and translation.
Recruitment and retention
A critical issue in advancing the next generation of health behavior research is conducting representative recruitment and implementing strategic retention plans, especially among underserved populations. While there is a basic understanding that meeting recruitment goals is critical for the scientific integrity of the proposed research, until recently this has been seen as an administrative problem rather than as an area of scientific inquiry ( Ory et al ., 2002b ). Similarly, there is a lack of information on the factors associated with preventing attrition, particularly among underserved populations. There is an urgent need for systematic, empirical research that compares the effectiveness of different approaches to recruitment and retention; that examines the factors and conditions that maximize recruitment and retention; and that assesses various methods most sensitive to the needs of ethnic and racial minorities. Such studies need to consider the recruitment and retention complexities in the context of an increasingly urban, multi-ethnic and multi-racial society ( Levkoff et al ., 2000 ).
To evaluate the effectiveness of multiple-theory and multiple-behavior interventions in an unbiased and scientific manner, mechanisms to ensure that the maximum number of representative study participants are recruited and retained throughout the investigation need to be developed and refined. Recruitment and retention are paramount to ensure generalizability of results and may affect statistical power and an investigation’s effect size ( Altman et al ., 2001 ); however, recruitment and retention remains a challenge to investigators ( Wragg et al ., 2000 ). These challenges may be magnified in theory-comparison and multiple-behavior research where the number of assessments and the dose of the intervention increases, requiring more time from the participants, potentially influencing completion and adherence rates.
The BCC recruitment and retention workgroup is endeavoring to provide an open forum for the discussion of recruitment and retention issues, including representative recruitment, retention plan development, ongoing problem solving of compliance barriers, and evaluation of general and population-specific recruitment and retention techniques. In addition, this workgroup disseminates the most up-to-date recruitment and retention strategies, materials, resources and evaluation methods. This is in an effort to strengthen the validity and generalizability among BCC-funded research projects that study highly diverse groups with variable medical conditions and social environments, and to advance knowledge of recruitment and attrition biases in the social and behavioral sciences.
Treatment fidelity
To further ensure both internal and external validity of intervention research, treatment fidelity must be maximized. Treatment fidelity involves both treatment integrity (the degree to which a treatment condition is implemented as intended) and treatment differentiation (whether the treatment conditions differ from one another as intended) ( Moncher and Prinz, 1991 ). Verification of treatment fidelity is integral to both the interpretation and generalization of research findings. Treatment fidelity can inform whether a ‘type 3’ error is made, concluding that the intervention is ineffective, when in fact it was never implemented.
Elements underlying treatment fidelity, include:
Design: Is the study consistent with the underlying theory?
Training: Has the provider acquired and maintained the requisite skill?
Delivery: Was the intervention delivered as intended?
Receipt: Did the participant understand the intervention?
Enactment: To what extent are the behaviors, skills, and/or cognitive strategies implemented by participants in real life settings?
The BCC has established a treatment fidelity workgroup whose overall aim is to advance the definition and measurement of treatment fidelity and adherence in order to facilitate the interpretation of findings and increase our understanding of the relationship of treatment intensity and dosage to treatment outcome. The workgroup also provides BCC investigators with the information and resources needed to ensure that interventions are delivered as intended, and that the dose delivered and the dose received are measured in a quantifiable manner for use in treatment validity, treatment outcome and treatment cost-effectiveness analyses. Based on existing models of treatment fidelity ( Moncher and Prinz, 1991 ; Lichstein et al ., 1994 ), this workgroup is developing and will disseminate best practice guidelines to enhance treatment fidelity in behavioral interventions.
Measurement and assessment across multiple behaviors
Conducting multiple-behavior research requires identification and organization of common measurements and assessment criteria across constructs and behaviors. There are three key issues when identifying similarities in constructs and measures between behaviors to standardize assessment. First, the equivalence of change in different behaviors has not been investigated. For example, is the equivalence of a one-cigarette reduction or an increase in a serving of vegetables the same as being physically active for 30 min in reducing morbidity and mortality? Does a dichotomous or a continuous conceptualization hold greater utility in prediction? It is also important to consider effect size within this topic of inquiry. For example, BCC intervention studies include a comparison condition so effect sizes can be calculated for each study to express a standardized treatment difference. This will allow for an interpretation of the differential magnitude of behavioral change effects for the different theories and when interventions are applied to different behaviors. Of course, because effect sizes are expressed in standard deviation units, they can and do vary with different populations, and with different inclusionary/exclusionary criteria, so this must be accounted for in comparative analyses. Another notion of equivalence is as an input and assessment of the resources needed to effect a behavioral change. With this interpretation the issue is the meaningful quantification of the resources across behaviors.
Second, instead of metric comparisons, an evaluative perspective could be adopted to identify a consensus definition of a ‘successful’ outcome or criteria in each behavioral domain. For example, for smoking 7-day abstinence rates ( Fiore et al ., 2000 ), for diet interventions using a ‘5-a-day’ behavioral criteria ( Potter et al ., 2000 ) and for physical activity using the recommendations published by CDCP/ACSM ( Pate et al ., 1995 ) may be adopted.
The third key issue when identifying similarities in constructs and measures between theories is documenting and measuring progress in the treatment population. Do we focus on and measure progress towards achievement of individual behavioral goals or do we focus on a single criterion success? In either case, interpretation of progress needs to include the clinical and the public health significance of behavioral changes.
Resolving measurement issues in theorycomparison and multiple-behavior research can aid in advancing our capability to understand relative contributions and trade-offs, and provide evaluation criteria to apply to any health behavior. This presents the opportunity for comparing interventions to establish whether different treatments are more or less effective across health behaviors. However, with using a common metric across behaviors, the issue of similarity of criteria may need to be addressed. For example, is being physically active for 30 min or more on most days of the week on the same ‘difficulty level’ as quitting smoking, or eating five servings of fruits and vegetables a day?
Using the same metric across behaviors also facilitates the identification of gateway behaviors. A gateway behavior can be thought of as a behavior that, when intervened upon, has a positive influence on other behavior changes. Generally stated, it may be that only a few behaviors are related to general health of a specific population. There is preliminary evidence that points toward this possibility as a large number of behaviors are somewhat related ( Nigg et al ., 1999 ). Examining the effect of single behavior change interventions on other health behavior changes is a first step to further develop knowledge regarding potential gateway behaviors.
The BCC workgroup on transbehavioral outcomes assessment is working to further the science of health behavior change and maintenance through cross-project collaboration by working on these kinds of issues. The workgroup has been working to explore the development of transbehavioral indices or assessment methods (such as a behavior change index) to be used in behavior change research regardless of behavior being addressed.
Reach and translation
Despite considerable advances and increasing evidence supporting health behavior interventions, few programs that have been demonstrated efficacious have been adopted in practice settings. Among the major reasons for the failure to adopt effective programs include the concern about the ability to generalize from non-representative efficacy studies, barriers to adoption under constraints of limited time and resources, and difficulties with consistency of implementation.
In general, the next generation of health behavior research needs to more closely consider issues of external validity. The studies involved in the BCC and other recent intervention research [e.g. ( Glasgow et al ., 1996 ; Nigg et al ., 1997 ; Brug et al ., 1998 )] have paid greater attention to the representativeness of individual participants than have previous studies. Work such as this provides an important step in the effort to advance our understanding of health behavior change, and how this can be translated into behavioral and environmental changes that facilitate improvements in individual and population health. The representativeness of the settings in which multiple-theory and multiple-behavior research takes place, and the intervention agents conducting the treatment are equally important as the representativeness of individual participants, but have received less attention ( Glasgow et al ., 1999 , 2002 ).
Recommendations for ways in which to increase adoption by target organizations (e.g. worksites, health care settings and schools) and the likelihood that intervention activities will be maintained after the formal evaluation is completed, include: (1) involving such organizations in intervention design beginning at the earliest stages of program planning, (2) collaborative partnerships by investigators to disseminate successful programs to target organizations, (3) reducing barriers to participation requirements and exclusion criteria for organizations, and (4) paying attention to issues of feasibility and breadth of appeal when designing interventions and contact schedules. The increased understanding through multiple-theory investigations, and the increased impact and applicability of multiple-behavior programs, should facilitate translation efforts as organizations today are less interested in having to adopt a separate health promotion program for every separate target behavior or risk factor.
With funding from the Robert Wood Johnson Foundation, the BCC workgroup on reach and translation is attempting to systematically address reach and translation issues through a two-part project that is designed to develop, implement and evaluate a framework to measure intervention impact in its broadest sense (that takes into account issues of internal and external validity). This work is based on the earlier work of Glasgow et al . ( Glasgow et al ., 1999 ) who have suggested that multilevel interventions are evaluated based on their settings, goals and purpose. The RE-AIM framework for assessing such intervention includes the dimensions of reach, efficacy, adoption, implementation and maintenance. The reach and translation work group is further refining the RE-AIM framework, has surveyed the various BCC projects about how they are addressing these various issues and is serving as a coordinating resource for projects having the goal of translating their results into practice.
The mission of the BCC is to further the science of health behavior change by supporting individual projects and through cross-project collaboration that can shed further light on the processes by which people make and maintain changes in behaviors that can promote health or prevent disease in different populations and in different settings. By stimulating a wide range of cross-project collaborations, the BCC supports unique efforts for theory-comparison and multiple-behavior research that can better integrate empirical theory in our efforts to change human health behavior. Conducting theory-comparison and multiple-behavior research presents several emerging challenges but needs to be recognized as a priority research area. This includes finding new ways to enhance recruitment and retention, especially among diverse populations; improving treatment fidelity; developing common metrics across behaviors that can be used to advance the measurement and assessment of behavioral change; and expanding the reach and translation of effective intervention approaches. Such work promises to provide a stronger basis for advancing our knowledge of the processes by which people change and maintain health behaviors and how we can best facilitate those processes.

Common themes in theory-comparison and multiple-behavior research.
The authors would like to thank the NIH Behavior Change Consortium workgroups on recruitment and retention, treatment fidelity, transbehavioral outcomes, conceptual mediators, methodology and data, and reach and translation for their collective work, and for their valuable discussions and contributions. Specifically, we would like to acknowledge Drs Belinda Borelli, Mace Coday, Russell E. Glasgow and Lisa M. Klesges for their contributions to earlier drafts. We also thank Ms Janey Peterson, and Drs Patricia J. Jordan, Jay E. Maddock and Randi L. Wolf for their insightful comments.
Abrams, D. B., Orleans, C. T., Niaura, R. N., Goldstein, M. G., Velicer, W. F. and Prochaska, J. O. (1994) Smoking treatment issues: towards a stepped care approach. Tobacco Control , 2 , 517 –537.
Ajzen, I. and Fishbein, M. (1980) Understanding Attitudes and Predicting Social Behavior . Prentice-Hall, Englewood Cliffs, NJ.
Ajzen, I. and Madden, T. J. ( 1986 ) Prediction of goal-directed behavior: attitudes, intentions, and perceived behavioral control. Journal of Experimental Social Psychology , 22 , 453 –474.
Allegrante, J. P. and Roizen, M. F. ( 1998 ) Can net-present value economic theory be used to explain and change health-related behaviors? Health Education Research , 13 , i –iv.
Altman, D. G., Schulz, K. F., Moher, D., Egger, M., Davidoff, F., Elbourne, D., Gotzsche, P. C. and Lang, T. ( 2001 ) The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Annals of Internal Medicine , 134 , 663 –694.
American Heart Association (1997) Heart and Stroke Statistical Update . American Heart Association, Dallas, TX.
Bandura, A. (1977) Social Learning Theory . Prentice-Hall, Englewood Cliffs, NJ.
Biddle, S. J. H. and Nigg, C. R. ( 2000 ) Theories of exercise behavior. International Journal of Sport Psychology , 31 , 290 –304.
Becker, M. H. (1974) The Health Belief Model and Personal Health Behavior. Health Education Monographs , 2 (Entire Issue).
Brug, J., Glanz, K., Van Assema, P., Kok, G. and van Breukelen, G. J. ( 1998 ) The impact of computer-tailored feedback and iterative feedback on fat fruit and vegetable intake. Health Education and Behavior , 25 , 517 –531.
Carleton, R. A., Lasater, T. M., Assaf, A. R., Feldman, H. A. and McKinlay, S. ( 1995 ) The Pawtucket Heart Health Program: community changes in cardiovascular risk factors and projected disease risk. American Journal of Public Health , 85 , 777 –785.
Deci, E. and Ryan, R. ( 1980 ). Self-determination theory: when mind mediates behavior. Journal of Mind and Behavior , 1 , 33 –43.
Emmons, K. M., Marcus, B. H., Linnan, L., Rossi, J. S. and Abrams, D. B. ( 1994 ) Mechanisms in multiple risk factor interventions: smoking, physical activity, and dietary fat intake among manufacturing workers. Working Well Research Group. Preventive Medicine , 23 , 481 –489.
Emmons, K. M. (2001) Behavioral and social science contributions to the health of adults in the United States. In Smedley, B. D. and Syme, S. L. (eds), Promoting Health: Intervention Strategies from Social and Behavioral Research. Committee on Capitalizing on Social and Behavioral Research to Improve the Public’s Health. National Academy Press, Washington, DC., pp. 254–231.
Farquhar, J. W. Fortmann, S. P., Flora, J. A., Taylor, C. B., Haskell, W. L., Williams, P. T., Maccoby, N. and Wood, P. D. ( 1990 ) Effects of communitywide education on cardiovascular disease risk factors. The Stanford Five-City Project. Journal of the American Medical Association , 264 , 359 –365.
Fiore, M., Bailey, W., Bennett, G., Bennett, H., Cohen, S., Dorfman, S. F., Fox, B., Goldstein, M., Gritz, E., Hasselblad, V., et al . (2000) Treating Tobacco Use and Dependence. Clinical Practice Guideline . US Department of Health and Human Services, Public Health Service, Rockville, MD.
Glasgow, R. E., Eakin, E. G. and Toobert, D. J. ( 1996 ) How generalizable are the results of diabetes self-management results? The impact of participation and attrition. The Diabetes Educator , 22 , 573 –585.
Glasgow, R. E., Vogt, T. M. and Boles S. M. ( 1999 ) Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health , 89 , 1322 –1327.
Glasgow, R. E., Bull, S. S., Gillette, C., Klesges, L. M. and Dzewaltowski, D. A. (2002) Behavior change intervention research in health care settings: a review of recent reports, with emphasis on external validity. American Journal of Preventive Medicine , in press.
Green, L. W. and Kreuter, M. W. (1999) Health Promotion Planning: An Educational and Ecological Approach . Mayfield, Mountain View, CA.
Hall, S. M., McGee, R., Turnstall, C. D., Duffy, J. and Benowitz, N. ( 1989 ) Changes in food intake and activity after quitting smoking. Journal of Consulting Clinical Psychology , 57 , 81 –86.
Hellmich, N. (1997) Fighting cancer: diet and exercise. USA Today , October 1,
Holmes, D. S. and Roth, D. L. ( 1988 ) Effects of aerobic exercise training and relaxation training on cardiovascular activity during psychological stress. Journal of Psychosomatic Research , 32 , 469 –474.
Hughes, J. R. ( 1984 ) Psychological effects of habitual aerobic exercise: a critical review. Preventive Medicine , 13 , 66 –78.
International Longevity Center (1999) Maintaining Healthy Lifestyles: A Lifetime of Choices . A workshop co-sponsored by Canyon Ranch Resort and International Life Sciences Institute.
Kano, M. J. and Tucker, L. A. ( 1993 ) The relationship between aerobic fitness and dietary intake in adult females. Medicine, Exercise, Nutrition and Health , 2 , 155 –161.
King, T. K., Marcus, B. M., Pinto, B. M., Emmons, K. M. and Abrams, D. B. ( 1996 ) Cognitive-behavioral mediators of changing multiple behaviors: smoking and a sedentary lifestyle. Preventive Medicine , 25 , 648 –691.
Klesges, R. C., Benowitz, N. L. and Meyers, A. W. ( 1991 ) Behavioral and biobehavioral aspects of smoking and smoking cessation: the problem of post cessation weight gain. Behavioral Therapy , 22 , 179 –199.
Levkoff, S., Prohaska, T., Weitzman, P. F. and Ory, M. G. ( 2000 ) Recruitment and retention in minority populations: lessons learned in conducting research on health promotion and minority aging. Journal of Mental Health and Aging , 6 , 5 –8.
Lichstein, K. L., Riedel, B. W. and Grieve, R. ( 1994 ) Fair tests of clinical trials: a treatment implementation model. Advances in Behavioral Research and Therapy , 16 , 1 –29.
Luepker, R. V., Murray, D. M., Jacobs, D. R., Jr. Mittelmark, M. B., Bracht, N., Carlaw, R., Crow, R., Elmer, P., Finnegan, J., Folsom, A. R., Grimm, R., Hannan, P. J., Jeffrey, R., Lando, H., McGovern, P., Mullis, R., Perry, C. L., Pechacek, T., Pirie, P., Sprafka, M., Weisbrod, R. and Blackburn, H. ( 1995 ) Community education for cardiovascular disease prevention: risk factor changes in the Minnesota Heart Health Program. American Journal of Public Health , 83 , 1383 –1393.
Maddux, J. E. ( 1993 ) Social cognitive models of health and exercise behavior: an introduction and review of conceptual issues. Journal of Applied Sport Psychology , 5 , 116 –140.
Manson, J. E., Tosteson, H., Ridker, P. M., Satterfield, S., Hebert, P., O’Connor, G. T., Buring, J. E. and Hennekens, C. H. ( 1993 ) The primary prevention of myocardial infarction. New England Journal of Medicine , 326 , 1406 –1416.
Marcus, B. H., Albrecht, A. E., Niaura, R. S., Abrams, D. B. and Thompson, P. D. ( 1991 ) Usefulness of physical exercise for maintaining smoking cessation in women. American Journal of Cardiology , 68 , 406 –407.
Marcus, B. H., Albrecht, A. E., Niaura, R. S., Taylor, E. R., Simkin, L. R., Feder, S. I., Thompson, P. D. and Abrams, D. B. ( 1995 ) Exercise enhances the maintenance of smoking cessation in women. Addictive Behaviors , 20 , 87 –92.
Marcus, B. H., Nigg, C. R., Riebe, D. and Forsyth, L. H. ( 2000 ) Interactive communication strategies: implications for population-based physical-activity promotion. American Journal of Preventive Medicine , 19 , 121 –126.
Marsh, H. W. ( 1994 ) Sport motivation orientations: beware of jingle-jangle fallacies. Journal of Sport & Exercise Psychology , 16 , 365 –380.
McLeroy, K. R., Bibeau, D., Steckler, A. and Glanz, K. ( 1988 ) An ecological perspective on health promotion programs. Health Education Quarterly , 15 , 351 –377.
Minkler, M. and Wallerstein, N. (1997) Improving health through community organization and community building. In Glanz, K., Lewis, F. M. and Rimer, B. K. (eds), Health Behavior and Health Education: Theory, Research and Practice . Erlbaum, Mahwah, NJ, pp. 60–84.
Moncher, F. J. and Prinz, R. J. ( 1991 ) Treatment fidelity in outcome studies. Clinical Psychology Review , 11 , 247 –266.
National Center for Health Statistics. ( 1997 ) Top ten US population causes of death. Monthly Vital Statistics Report , 45 , 40 –43.
Nigg, C. R., Burbank, P., Padula, C., Dufresne, R., Rossi, J. S., Velicer, W. F., Laforge, R. G. and Prochaska, J. O. ( 1999 ) Stages of change across ten health risk behaviors for older adults. The Gerontologist , 39 , 473 –482.
Nigg, C. R., Courneya, K. S. and Estabrooks, P. A. ( 1997 ) Maintaining attendance at a fitness center: an application of the decision balance sheet. Behavioral Medicine , 23 , 130 –137.
Ory, M., Jordan, P. J. and Bazzarre T. ( 2002 ) The Behavior Change Consortium: setting the stage for a new century of health behavior-change research. Health Education Research , 17 , 500 –511.
Ory, M. G., Lipman, P. D., Karlen, P. L., Gerety, M. B., Stevens, V. J., Fiatarone, M. A., Buchner, D. M., Schechtman, K. B. and The FICSIT Group (2002b) Recruitment of older participants in frailty/injury prevention studies. Prevention Science , in press.
Pate, R. R., Pratt, M., Blair, S. N., Haskell, W. L. Macera, C. A., Bouchard, C., Buchner, D., Ettinger, W., Heath, G. W., King, A. C., Kriska, A., Leon, A. S., Marcus, B. H., Morris, J., Pfaffenbarger, R. S., Patrick, K., Pollock, M. L., Rippe, J. M., Sallis, J. and Whilmore, J. H. ( 1995 ) Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Journal of the American Medical Association , 273 , 402 –407.
Potter, J. D., Finnegan, J. R., Guinard, J. X., Huerta, E. E., Kelder, S. H., Kristal, A. R., Kumanyika, S., Lin, R., McAdams Motsinger, B., Prendergast, F. G., Sorensen, G. and Callahan, K. M. (2000) 5 A Day for Better Health Program Evaluation Report . NIH publ. 01-4904. National Institutes of Health, National Cancer Institute, Bethesda, MD.
Prochaska, J. O., DiClemente, C. C. and Norcross, J. C. ( 1992 ) In search of how people change: applications to the addictive behaviors. American Psychologist , 47 , 1102 –1114.
Rosenstock, I. M. ( 1966 ) Why people use health services. Milbank Memorial Fund Quarterly , 44 , 94 –124.
Sallis, J. F. and Owen, N. (1999) Physical Activity & Behavioral Medicine . Sage, Thousand Oaks, CA.
Smedley, B. D. and Syme, S. L. (eds) (2000) Promoting Health: Intervention Strategies from Social and Behavioral Research . National Academy Press, Washington, DC.
Steckler, A., Allegrante, J. P., Altman, D., Brown, R., Burdine, J. N., Goodman, R. M. and Jorgensen, C. ( 1995 ) Health education intervention strategies: recommendations for future research. Health Education Quarterly , 22 , 307 –328.
US Department of Health and Human Services (2000) Healthy People 2010 Fact Sheet [Online]. Office of Disease Prevention and Health Promotion. Available: http://www.health.gov/healthypeople . Accessed: 7 February 2000.
Wilmore, J. H. and Costill, D. L. (1994) Physiology of Sport and Exercise . Human Kinetics, Champaign, IL.
Woolf, S. H. ( 1999 ) The need for perspective in evidence-based medicine. Journal of the American Medical Association , 282 , 2358 –2365.
Wragg, J. A., Robinson, E. J. and Lilford, R. J. ( 2000 ) Information presentation and decisions to enter clinical trials: a hypothetical trial of hormone replacement therapy. Social Science & Medicine , 51 , 453 –462.
Author notes
Department of Public Health Sciences and Epidemiology, John A. Burns School of Medicine, University of Hawaii at Mãnoa, Honolulu, HI 96822, 1National Center for Health Education and Department of Health and Behavior Studies, Teachers College, Columbia University, New York, NY 10027, and 2School of Rural Public Health, Texas A & M University System, College Station, TX 77840, USA, and formerly National Institutes of Health, Bethesda, MD 20892, USA
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Research article
- Open access
- Published: 08 September 2010
The effectiveness of interventions to change six health behaviours: a review of reviews
- Ruth G Jepson 1 ,
- Fiona M Harris 2 ,
- Stephen Platt 3 &
- Carol Tannahill 4
BMC Public Health volume 10 , Article number: 538 ( 2010 ) Cite this article
82k Accesses
245 Citations
15 Altmetric
Metrics details
Several World Health Organisation reports over recent years have highlighted the high incidence of chronic diseases such as diabetes, coronary heart disease and cancer. Contributory factors include unhealthy diets, alcohol and tobacco use and sedentary lifestyles. This paper reports the findings of a review of reviews of behavioural change interventions to reduce unhealthy behaviours or promote healthy behaviours. We included six different health-related behaviours in the review: healthy eating, physical exercise, smoking, alcohol misuse, sexual risk taking (in young people) and illicit drug use. We excluded reviews which focussed on pharmacological treatments or those which required intensive treatments (e.g. for drug or alcohol dependency).
The Cochrane Library, Database of Abstracts of Reviews of Effectiveness (DARE) and several Ovid databases were searched for systematic reviews of interventions for the six behaviours (updated search 2008). Two reviewers applied the inclusion criteria, extracted data and assessed the quality of the reviews. The results were discussed in a narrative synthesis.
We included 103 reviews published between 1995 and 2008. The focus of interventions varied, but those targeting specific individuals were generally designed to change an existing behaviour (e.g. cigarette smoking, alcohol misuse), whilst those aimed at the general population or groups such as school children were designed to promote positive behaviours (e.g. healthy eating). Almost 50% (n = 48) of the reviews focussed on smoking (either prevention or cessation). Interventions that were most effective across a range of health behaviours included physician advice or individual counselling, and workplace- and school-based activities. Mass media campaigns and legislative interventions also showed small to moderate effects in changing health behaviours.
Generally, the evidence related to short-term effects rather than sustained/longer-term impact and there was a relative lack of evidence on how best to address inequalities.
Conclusions
Despite limitations of the review of reviews approach, it is encouraging that there are interventions that are effective in achieving behavioural change. Further emphasis in both primary studies and secondary analysis (e.g. systematic reviews) should be placed on assessing the differential effectiveness of interventions across different population subgroups to ensure that health inequalities are addressed.
Peer Review reports
Chronic diseases, such as cancers, cardiovascular diseases (CVD), diabetes, and respiratory diseases, account for 59% of the 57 million deaths annually and 46% of the global burden of disease [ 1 ]. In 2002, the World Health Report [ 2 ] identified a number of important lifestyle risk factors for such diseases, including physical inactivity; diet-related factors and obesity; and the use of addictive substances such as tobacco, alcohol and illicit drugs.
These lifestyle factors have significant effects on mortality and morbidity, particularly in industrialised countries. For example, data for the WHO European Region show that physical inactivity is a risk factor for diseases such as cardiovascular diseases, non-insulin- dependent diabetes, hypertension, some forms of cancer, musculoskeletal diseases and psychological disorders. These diseases are estimated to account for nearly 600,000 deaths per year [ 3 ]. Similarly, obesity and being overweight are risk factors for diseases such as type 2 diabetes, certain types of cancer and cardiovascular diseases, and affect between 30% and 80% of adults and up to one third of children [ 4 ]. Alcohol is also a significant cause of mortality: alcohol-related deaths increased by 15% between 2000 and 2002, and now represent 6.3% of all deaths in the European Region [ 5 ].
Sexual risk taking and drug misuse also significantly contribute to ill health and have negative effects on well being among young people. In 28 high income (OECD) nations at least 1.25 million teenagers become pregnant each year; of these, approximately 40% (half a million) will seek to terminate the pregnancy while the other 60% (three quarters of a million) will become teenage mothers [ 6 ]. The United States has the highest teenage birth rate in the developed world and the United Kingdom has the highest teenage birth rate in Europe [ 6 ]. Worldwide, young people (15-24 years) have the highest rate of sexually transmitted infections (STIs) of any age group. Up to 60% of the new infections and 50% of all people living with HIV globally are in this age group [ 7 ].
Most public health and health promotion interventions - whether they focus on the individual, community, whole populations or the environment - seek in some way to change health behaviour by changing health-related knowledge, attitudes and/or structural barriers and facilitators [ 8 ]. Social psychological theories such as social cognition theory are commonly used in the development of interventions [ 9 ]. Key elements of such theories include knowledge of health risks, perceived self efficacy, goals and motivations and barriers and facilitators [ 10 ]. Most health promotion interventions include one or more of the following components: education and knowledge building (around the health issue); motivation and goal setting (e.g. alcohol brief interventions and counselling); and community-based techniques to encourage a change in behaviour or reduce structural or cultural barriers. These interventions can be delivered at three different levels, which we explore below: individual, community and population level interventions. Individually targeted interventions are usually aimed at those with an existing 'risky' behaviour such as smoking or alcohol misuse. Community level interventions focus on particular population groups such as people in a particular workplace or young people in schools. Finally, population level interventions tend to rely on the use of mass media activities, policies or legislation.
All three levels of intervention are aimed at achieving changes in lifestyle, as well as improving knowledge and influencing attitudes towards positive healthy behaviours. However, there is a need to take into account the socio-economic and cultural contexts within which they are located. For instance, an intervention to promote healthy eating within an affluent locality might involve a rather different approach from one undertaken in an area of low income and high unemployment.
In light of the growing concern around the link between 'negative' health behaviours and ill health, we were commissioned by the Public Health section of the UK's National Institute of Health and Clinical Excellence (NICE) under the Behaviour Change Programme Development Group to review the relevant evidence in this area. This paper is an update of the findings of this 'review of reviews' of interventions to change health behaviours [ 11 ]. It was one type of evidence used to develop NICE public health programme guidance on behaviour change [ 12 ].
Our aim was systematically to collate, evaluate and synthesise review-level findings on the effectiveness of interventions to change unhealthy behaviours or promote healthy behaviours. This synthesis was intended to provide researchers, policy planners, decision-makers and practitioners with an accessible, good quality overview of the evidence in these topic areas. The review focused on six groups of behaviour change interventions:
Interventions to encourage people to quit tobacco use
Interventions to reduce heavy alcohol use
Interventions to encourage physical activity
Interventions to encourage healthy eating (excluding diets for weight loss)
Interventions to prevent or reduce illicit drug use (excluding drug dependency)
Interventions to prevent or reduce sexual risk taking in young people.
A subsidiary aim of the review was explore, where possible, the evidence of impact of interventions on health inequalities.
Inclusion criteria
1) types of reviews.
Systematic reviews and meta-analyses published between 1995 and 2008 (reviews published before this time are likely to be out of date)
English language reviews as we were constrained by time and resource issues. (However, many of the included English language reviews contained primary studies in languages other than English.)
Cochrane reviews and systematic reviews in the Database of Abstracts of Reviews of Effects (DARE), which encompasses reviews gathered from searching a wide range of OVID databases
Other good quality reviews which have a low risk of bias (see section on quality assessment)
Less robust systematic reviews in areas where no other evidence exists.
2) Content of the reviews
Two sets of inclusion and exclusion criteria were applied in the selection process: those that applied across all the health behaviours (see Table 1 ); and those that were specific to particular health behaviours (Table 2 ). For the six specific health behaviours of interest, interventions aimed at either preventing or delaying onset of the health behaviour were included, as well as those aimed at helping people to change an existing behaviour. However, interventions aimed at treating alcohol or drug dependency were not included as they were considered to require more intensive types of treatments, hence different forms of intervention. Healthy eating and physical activity were limited to outcomes related to changes in knowledge, attitudes or behaviour but did not include outcomes such as weight loss, weight reduction, nor programmes of obesity treatment or exercise specifically targeting high risk groups such as people with cardiovascular disease or cancer. Reviews of the following interventions were also excluded: health screening; psychiatric interventions as part of treatment for those with mental illness; interventions with only a clinical or pharmacological focus (e.g. reducing risk of heart disease); interventions carried out within secondary or tertiary care; drug interventions (including the use of vitamin supplements for healthy diets); and interventions aimed at treating alcohol or drug dependency.
Search strategy
Searches were initially conducted in February 2006 for Cochrane and other systematic reviews and updated in 2008, as detailed below. As a starting point to identify the highest quality review level evidence, the Cochrane Database of Systematic Reviews (CDSR) was searched to identify Cochrane Reviews and the Database of Reviews of Effectiveness (DARE) was used for non-Cochrane reviews. DARE includes published and unpublished systematic reviews that have been assessed according to strict quality criteria by the Centre for Reviews and Dissemination (CRD) in York, UK. DARE represents an excellent resource since it includes quality assessed systematic reviews sourced by monthly searches of a wide range of electronic databases. As a final check to reveal what more recent reviews might be missed through this strategy, we also ran searches for each of the six public health topics on a range of OVID databases: AMED, ERIC, Cinahl, EmBase, Medline and PsycINFO. These searches were restricted by terms to identify reviews only, including 'meta-analysis', 'evidence-based review' or 'systematic review'. Full search histories are available on request from the corresponding author.
These searches generated a total of 2709 potentially relevant reviews. The search was updated in November 2008 by searching The Cochrane Library and DARE for new and updated Cochrane reviews and other high quality systematic reviews published since February 2006. This yielded a further 16 new reviews (out of 30 identified through the search), and 12 Cochrane reviews which had been updated since the initial search.
Applying inclusion criteria
Titles and abstracts were independently screened by two reviewers. Any discrepancies in selections were discussed until consensus was reached. Another stage of screening consisted of a mapping exercise, where references were mapped into categories of evidence and two reviewers agreed to include or exclude further references based on the quality of the reviews and the date of publication. Since Cochrane reviews are usually the most comprehensive and of high quality, they were selected if there was more than one review in a particular topic area. Other reviews were selected on the basis of most recent publication date and quality of the review (see below for details of how we assessed quality of the reviews). The full review process is illustrated in the quorum statement (see Figure 1 ).
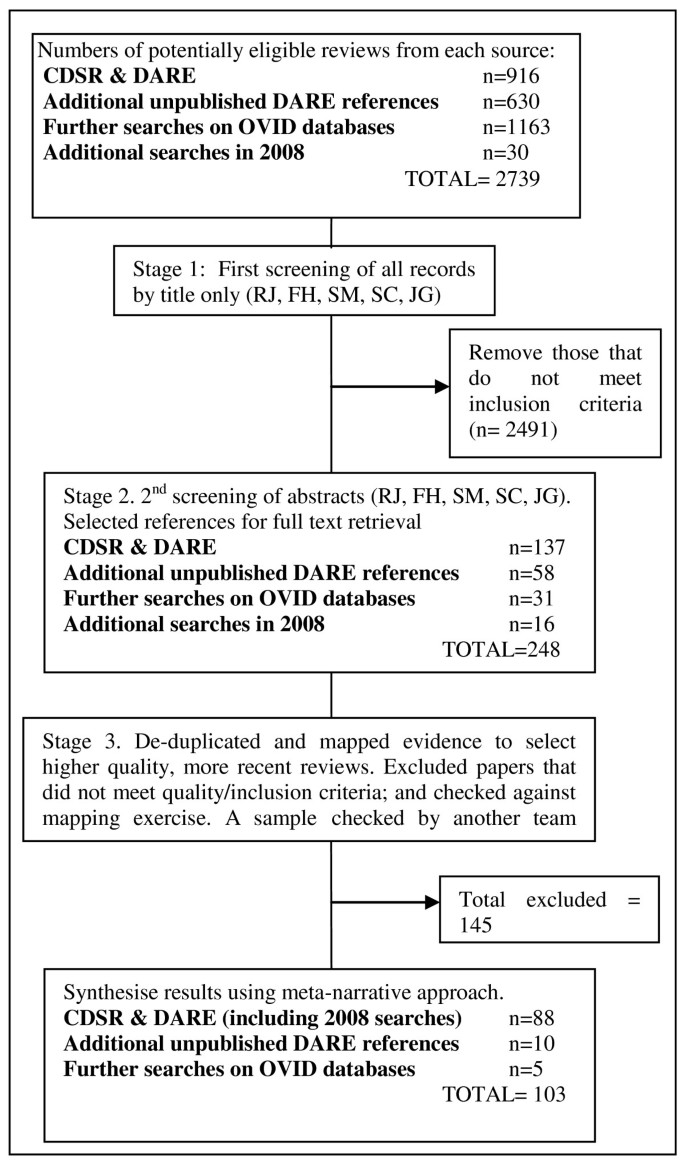
Quorum statement .
Quality assessment
Potentially relevant reviews were assessed for quality using a checklist adapted from the NICE 'Methods for the development of NICE public health guidance' [ 13 ]. We prioritised reviews that had a transparent and replicable data search methodology and analysis. We scored reviews as "++" if at least 10 specified criteria were met, "+" if at least seven criteria were met, and "-" if fewer than seven criteria were met (Table 3 ). We also scored reviews on the type of evidence they were reviewing, such as RCTs or non-RCTs (see Table 4 ). The classification of bias (e.g. ++) was then combined with the type of evidence (e.g. 1) to give a level of evidence. For example, high-quality meta-analyses or systematic reviews of RCTs were coded as 1++. All data extracted on quality were extracted by one reviewer and checked by a second member of the team. Any discrepancies in the data that were extracted (e.g. differences in scoring) were resolved by discussion
Data extraction
Data were extracted by one of four people, and a sample checked by another member of the team. No formal synthesis (such as meta-analysis) was undertaken: a narrative summary of the results was more appropriate for a review of reviews.
We identified 103 systematic reviews evaluating interventions aimed at changing health behaviour in one or more of the six areas. Some of these reviews covered several behaviours. The reviews included studies which targeted specific individuals or organisations (e.g. through counselling within education) or more generally (e.g. mass media interventions or legislation).
We synthesised the results under three research areas:
Evidence for the effectiveness of interventions to prevent, reduce or promote the six health behaviours
Evidence for the effectiveness of interventions across several health behaviours
Evidence for the effectiveness of interventions in targeting health inequalities.
Full consideration of such a large number of reviews would prove too lengthy for this paper, therefore we have chosen to highlight the main findings rather than provide details of individual interventions discussed within each paper. A fuller version of the original document is available from the authors on request. Table 5 summarises the quality of the included reviews and Table 6 provides a brief overview of the studies, grouped by level of intervention (population, community or individual).
1. Evidence for the effectiveness of interventions to prevent, reduce or promote each of the six health behaviours
The focus of interventions varied, depending on the target population. Interventions targeting individuals generally aimed to change an existing behaviour such as cigarette smoking or alcohol misuse, whilst interventions targeting workplaces, schools or the general population were often more focused on promoting positive behaviours (e.g. healthy eating or exercise).
1.1. Smoking and tobacco use
We identified 48 systematic reviews which evaluated interventions to aid smoking cessation, prevent relapse or prevent people taking up smoking [ 14 – 61 ]. One further review evaluated population-level tobacco control interventions and their effect on social inequalities [ 62 ]. This review is discussed in more detail in section 3.
Eleven reviews evaluated interventions aimed at the prevention of smoking, promoting smoking cessation or reducing smoking prevalence in young people [ 22 , 27 , 29 , 30 , 40 , 46 , 50 , 51 , 53 , 56 , 60 , 61 ]. There is some evidence that mass media interventions can be effective in preventing the uptake of smoking in young people, but overall the evidence is not strong. Information provision interventions alone are not effective and there is only limited evidence for the effects of interventions that mainly seek to develop social competence.
There is little evidence of effectiveness of other interventions, such as reducing tobacco sales to minors. Interventions with retailers can lead to large decreases in the number of outlets selling tobacco to youths but there is insufficient evidence to say whether this is linked to reduction or cessation of smoking in young people.
Twenty six of the 48 systematic reviews evaluated interventions aimed at achieving positive changes in tobacco use in adults known to use tobacco (i.e. targeting smokers). Of these, twenty-two of these evaluated interventions for adult cigarette smokers in general, two focussed specifically on pregnant and postpartum women [ 25 , 36 ], and two evaluated interventions for smokeless tobacco use [ 24 , 38 ]. The following sections describe the range of interventions to reduce tobacco consumption in individuals and are grouped by their effectiveness.
Interventions which show a positive effect include advice from health professionals, the rapid smoking form of aversion therapy, self help materials, telephone counselling (compared to less intensive interventions), nurse-delivered interventions, group counselling (which is also more effective than self help), and oral examination and feedback for reducing smokeless tobacco use. However, there is no evidence for the effectiveness of interventions targeting waterpipe smokers. Interventions to promote smoking cessation or smoking reduction with pregnant women are generally effective across the range of intervention types, indicating that pregnancy may be a point in the lifecourse when positive behaviour change can be achieved.
There is less clear or inconclusive evidence of effectiveness for social support interventions (e.g. buddy systems or friends and family support), relapse prevention, biomarker feedback or biomedical risk assessment, exercise, Internet and computer-based interventions and interventions by community pharmacy personnel or dentists. Currently there is not enough evidence to show which interventions are most effective for decreasing parental smoking and preventing exposure to tobacco smoke in childhood.
Interventions for which there is no evidence of effectiveness include hypnotherapy and interventions based on the transtheoretical model of change. The latter proposes that interventions designed to take into account an individual's current stage of change (or readinesss to change a health behaviour) will be more effective and efficient than "one size fits all" interventions [ 63 ]. The model assumes that people move through six changes of change, from 'pre-contemplation' through to 'termination' (when the behaviour has successfully been changed). However, this assumption does not sit comfortably within wider theories of social change, which posit that change rarely moves in a linear fashion. Additionally, a systematic review exploring a range of 'stage based' interventions for smoking cessation found little evidence of effectiveness [ 45 ].
Six studies evaluated smoking interventions that were undertaken in either workplace or community settings [ 19 , 26 , 33 , 49 , 64 , 65 ]. Interventions which show an effect in the workplace include those aimed at encouraging individuals to quit. The results are consistent with those found in other settings [ 64 ]. Particularly effective interventions include individual and group counselling and pharmacological treatment to overcome nicotine addiction. Self-help materials are less effective, and competitions and incentives, while increasing attempts to stop smoking, were not consistently found to increase the rate of quitting. Interventions aimed at the wider community included multi-component interventions and those which use multiple channels to provide reinforcement, support and norms for non-smoking. These show limited effectiveness.
Five systematic reviews evaluated interventions aimed at the general population to prevent the uptake of smoking or reduce smoking rates [ 15 , 16 , 28 , 47 , 66 ]. Mass media interventions show evidence of a small effect in preventing the uptake of smoking, but the evidence comes from a heterogeneous group of studies of variable methodological quality. Smoking cessation interventions that show some evidence of effectiveness include 'Quit and Win' contests and policies to reduce smoking in public places. However, policy interventions are normally evaluated using non-controlled designs (e.g. before and after studies), which makes it difficult to determine the extent to which the outcomes could be attributed to the intervention.
1.2. Physical activity
Twenty-four systematic reviews evaluated interventions to increase or promote the uptake of physical activity [ 23 , 39 , 58 , 67 – 85 ]. Six of these explored the effectiveness of interventions to increase physical activity in young people [ 70 , 78 , 83 , 85 – 87 ]. There is moderate evidence of effectiveness for curriculum-based activities in schools. The most effective school-based physical activity interventions include printed educational materials and curricula that promoted increased physical activity during the whole day (i.e., recess, lunch, class-time, and physical education classes). The most effective non-curricular school activities include education and provision of equipment for monitoring TV or video-game use; engaging parents in supporting and encouraging their children's physical activity; and those implemented during school breaks (painting school playgrounds, playground supervisors implementing a games curriculum, and taught playground games or introduced equipment). There is no evidence of an effect of other non-curricular activities, such as active travel to school, extra-curricular activities and summer schools or camps.
The most recent review reported strong evidence that school-based interventions with involvement of the family or community and multi-component interventions can increase physical activity in adolescents [ 85 ].
Ten systematic reviews evaluated targeted interventions aimed at increasing physical activity for adults. Eight of these evaluated interventions for adults over 18 years [ 23 , 39 , 71 , 72 , 74 , 75 , 88 , 89 ], while two evaluated interventions specifically for the older population [ 69 , 84 ]. The interventions included the use of pedometers, telephone counselling, and professional advice and guidance (with continued support). Most of the reviews found some evidence of moderate effectiveness in the short term (less than three months) in increasing physical activity, but effects are not necessarily sustained over a longer time period (e.g. twelve months). Many of the studies were limited by the recruitment of motivated volunteers, and no studies examined the effect of interventions on participants from varying socioeconomic or ethnic groups. In addition, even those interventions which are moderately effective in increasing exercise did not necessarily meet a predetermined threshold of physical activity. These findings were also supported by the findings from reviews of interventions for the older population, which found a small but short-lived effect of home-based, group-based and educational physical activity interventions on increasing physical activity.
Physical activity interventions for which there is inconclusive evidence include biomarker feedback and brief motivational interventions. In addition, there is no evidence that interventions based on the stages of change model increase levels of physical activity.
One systematic review evaluated physical activity programmes in the workplace [ 82 ], finding evidence of a moderate effect on increasing physical activity levels. Interventions comprised self-help or educational programmes, and exercise programmes involving aerobics, walking, jogging, swimming, cycling, muscle strengthening, endurance, flexibility and stretching.
Four systematic reviews evaluated interventions aimed at increasing physical activity in the general population. Two evaluated interventions to increase participation in sport [ 76 , 90 ], one evaluated interventions to promote walking and cycling [ 81 ], and one evaluated mass media interventions [ 73 ]. However, the first two reviews found that no studies had been undertaken to identify any intervention designed to increase active and/or non-active participation in sport (including policy interventions). There is evidence that targeted behaviour change programmes can be effective in changing the transport choices of motivated subgroups, but the social distribution of their effects and their effects on the health of local populations are unclear. Evidence of effectiveness of other types of intervention is inconsistent, of low validity, based on single, highly contextualised studies, or non-existent. There is evidence (with a higher risk of bias) that mass media interventions may increase physical activity, but the effects tend to be in small subgroups or for specific behaviours, such as walking.
1.3. Alcohol misuse
Fifteen reviews evaluated a range of interventions aimed at reducing alcohol consumption in problem drinkers, preventing or delaying the onset of alcohol use in young people, or reducing dangerous activities associated with drinking (e.g. drink-driving) [ 91 – 105 ]. No consistent definitions of what constitutes harmful alcohol consumption were available from existing guidelines or research; however, it is commonly held that behavioural interventions are appropriate for mild to moderate alcohol consumption or binge drinking, whereas more severe problems, such as alcohol dependency, may require specialist addiction treatment. Interventions for the latter were excluded from the review.
Two reviews evaluated interventions targeting school children [ 95 , 96 ]. There is evidence of a positive effect of school-based instructional programmes for reducing riding with drivers under the influence of alcohol. However, there is insufficient evidence to determine the effectiveness of these programmes for reducing drinking and driving. There is also insufficient evidence to determine the effectiveness of peer organisations (e.g. groups of students and/or staff who encourage others to refrain from drinking alcohol) and social norming campaigns (typically, public information programmes based on the assumption that children may overestimate the amount and frequency of their peers' alcohol consumption) to reduce alcohol use, due to the small number of available studies.
Several reviews evaluated interventions for adult problem drinkers. One review assessed home visits for pregnant women who were problem drinkers [ 93 ] and found insufficient evidence to recommend their routine use. Three reviews were of interventions aimed at reducing driving under the influence of alcohol [ 97 , 100 , 103 ]. For convicted drink drivers, there is evidence of an effect of alcohol interlock programmes (where the car ignition is locked until the driver provides an appropriate breath specimen), but the effect of other interventions is inconclusive due to the variable quality of the evidence. According to a Cochrane review [ 97 ] which evaluated the impact of increased police patrols for alcohol impaired drinking, most studies found that such patrols reduce traffic crashes and fatalities. However these conclusions were based on poor quality evidence.
Four further reviews evaluated interventions for problem drinkers in general [ 91 , 98 , 102 , 105 ]. There is evidence of a small positive effect of brief behavioural counselling interventions in reducing alcohol intake. The most recent Cochrane review [ 98 ] of brief interventions delivered to people attending primary care (1-4 sessions) found that, overall, such interventions lower alcohol consumption. When data were available by gender, the effect was clear in men at one year of follow up, but not in women. The authors concluded that longer duration of counselling probably has little additional effect.
Four systematic reviews evaluated mass media interventions [ 92 , 94 ] and legislative interventions [ 99 , 104 ] aimed at people who drink and drive. None of the reviews included evidence from RCTs, mainly because of the difficulty of conducting controlled trials in these areas. One well conducted review found insufficient evidence of effectiveness for mass media 'designated driver programmes' in increasing the number of designated drivers [ 92 ]. The other reviews reported that effective interventions for reducing alcohol and driving related outcomes included mass media campaigns [ 94 ]; low blood alcohol concentration laws for young drivers [ 104 ]; and a policy of a minimum legal drinking age (MLDA) of 21 years (which reduced traffic crashes and alcohol consumption) [ 99 ].
We did not identify any reviews which evaluated evidence relating to mass media interventions to promote 'safe' drinking levels or reduce 'risk drinking' (e.g. binge drinking).
1.4. Healthy eating
Thirteen systematic reviews evaluating behavioural or psychological interventions to promote healthy eating were identified [ 23 , 58 , 79 , 106 – 115 ]. Overall there is evidence that interventions can change eating habits, at least in the short term.
Four reviews evaluated interventions targeted at children or young people [ 79 , 112 – 114 ]. There is evidence of an effect of interventions aimed at increasing fruit and vegetable intake in children aged 4-10 years and interventions for youth aged 11-16 years. However, there is insufficient evidence of an effect of interventions in pre-school children.
Three reviews evaluated community based interventions. One review reported evidence of a small effect of community interventions for people aged 4 years and above on increasing fruit and vegetable intake [ 107 ]. There is also evidence that interventions based in supermarkets are effective for promoting positive changes in shopping habits, although effectiveness was found to be confined only to the period during which the intervention took place [ 110 ]. Lastly one review evaluated community-level interventions for older people [ 109 ] but found little or no effect of interventions to increase fruit and vegetable intake.
Six reviews evaluated a range of targeted interventions or interventions aimed at individuals. There is evidence of a positive effect of stage-based lifestyle interventions delivered to a primary care population [ 58 ], telephone based interventions [ 108 ] and nutritional counselling interventions [ 106 ]. A review of interventions using a Mediterranean diet showed positive results for a range of outcomes, but it is not clear how the interventions brought about behaviour change [ 111 ].
There is inconclusive evidence as to the effectiveness of motivational interviewing [ 23 ] for changing eating behaviours. There is also inconclusive evidence for interventions such as health education, counselling, changes in environment and changes in policy, to encourage pregnant women to eat healthily [ 115 ].
1.5. Illicit drug use
Only four reviews met our inclusion criteria for this section. There is more review level evidence relating to interventions aimed at treating drug users, which was specifically excluded under our search criteria.
All four reviews evaluated community-level interventions to prevent illicit drug use with young people [ 101 , 116 – 118 ]. The evidence base for this topic is limited and there are substantial gaps in knowledge. A positive effect of skill-based programmes in schools is demonstrated, but it is not possible to reach any conclusion about the effectiveness of non-school based programmes. There is also some evidence that the 11-13 age range may be a crucial period for intervention with vulnerable young people.
1.6. Sexual risk taking in young people
Eight systematic reviews evaluating community based interventions were identified in this area. Four reviews focused on the reduction or prevention of HIV or other sexually transmitted infections (STIs) [ 119 – 122 ], while four evaluated sexual health promotion and the reduction or prevention of teenage pregnancies [ 123 – 126 ]. The reviews were of variable quality and most commented on the poor quality of existing primary studies, which made the process of synthesising evidence difficult. However, two conclusions can be drawn. First, in the area of risk reduction and prevention programmes, interventions are most effective in promoting the uptake of condom use, with some success in reducing the number of sexual partners and the frequency of sex. Second, interventions seeking to promote the use of contraception are more effective than interventions that promote abstinence. There was a single study of counselling to prevent or reduce teenage pregnancies, but the authors found that the available evidence was of such poor quality that they were unable to reach any firm conclusions about effectiveness.
2. Evidence to suggest that some interventions are effective/ineffective across the range of health behaviours
Many of the interventions included in this review were behaviour specific - e.g. aversion therapy for smoking cessation, tobacco bans and drink driver-related interventions. However, there were a few interventions - such as counselling and physician advice, mass media and motivational interventions - that were used across a range of behaviours. Table 7 outlines the interventions and their effectiveness across different behaviours.
3. Evidence for the effectiveness of interventions in targeting health inequalities
Despite the widely acknowledged link between social and economic inequalities and health, our review of reviews found no evidence which helped to develop an understanding of the following:
Inequalities in levels of physical activity; alcohol misuse; healthy eating; illicit drug use; and sexual risk taking among young people.
Inequalities in access to interventions to promote change in behaviour
Inequalities in recruitment to interventions of 'hard to reach' groups
Differential effectiveness of health behaviour interventions, which may result in increased health inequalities.
One review evaluated potential role of moderators (e.g. race, gender age, and setting) in the effectiveness of interventions to change the environment which had the aim of improving diet and/or activity in persons aged 3 to 18 years [ 87 ]. The authors found that only 17% of the 41 included studies looked at the effect of modifiers (gender being the most commonly studied and tested). The authors concluded that, 'Rather than being an exception, it is argued that tests of effect modifiers should become common practice in behavioral nutrition and physical activity research to increase our understanding of mechanisms of behavior change and to optimize interventions.'
A further review explicitly explored the impact of population-level smoking cessation interventions on social inequalities [ 62 ]. It found that those in lower socio-economic groups, in manual occupations and those under the age of 25 years (particularly boys and 'non-white' young people) are more likely to be affected by increases in the price of tobacco products. However, it reported that there is also some evidence that price increases may be effective in people with a higher education. It also found that smoking restrictions in schools and restrictions on sales to minors may be more effective in girls than boys.
Most of the systematic reviews did not consider socio-economic differences or conduct sub-group analyses. Although some reviews may report socio-economic data, this does not reveal anything about inequalities unless there is an explicit attempt to explore data appropriately, for example whether there is differential take-up and/or effectiveness of the interventions according to variables such as gender, age and income.
A limitation of a review of reviews approach for knowledge synthesis might also be regarded as one of its strengths. Given the heterogeneity of interventions included within each review and the large number of papers across the six health behaviour areas, it has not been possible to report any particular area in great depth. While some readers might be frustrated by the lack of detail, one of the strengths of this review is its capacity to offer a broad overview of the evidence. We are able to bring to the attention of other researchers, policy makers and commissioners of research the areas where no systematic reviews have been conducted, and suggest potential research questions worthy of investigation at the review level. It was outside the scope of a review of reviews to determine whether this corresponded to gaps in primary data, or whether this reflected the research priorities/questions of systematic review authors.
Given the importance of socio-economic determinants of health and illness, and their impact on morbidity (as well as mortality), it is crucial that interventions designed to improve health take account of those very factors that may work against positive outcomes. As indicated above, this is one of the most significant gaps in the evidence base revealed by our study.
Until the mid 20 th century, infectious diseases were one of the main causes of mortality and morbidity in industrialised nations. Once these were largely brought under control, chronic diseases such as cancer and coronary heart disease assumed prominence. The 1970 s saw the emergence of a 'new' public health, highlighting the social and cultural factors which affect chronic diseases (e.g. lifestyle), and of new disciplines such as health promotion. Today the focus has shifted in line with the epidemiological transition, so there is increasing emphasis on social determinants of health rather than on infectious agents.
A series of reports on health inequalities been published in the UK (for instance, The Black Report [ 127 ], the Acheson Report [ 128 ] and the Wanless Report [ 129 ]). While the Black Report of 1980 focused primarily on material deprivation as a major explanatory factor in health inequalities, more recent research has explored the interplay between social position and the lifecourse in relation to the determinants of health [ 129 – 133 , 133 ]. The more recent change of focus from material deprivation towards a more multi-faceted understanding of determinants of health is important for interventions aimed at effecting changes in behaviour that may have an adverse affect on health. However, what is not clear is whether current health promotion initiatives have absorbed and embedded the 'determinants' approach in order to improve the health of those who might benefit most. It has been argued that the inverse care law is not always considered in relation to local provision of health promoting activities [ 134 ]. Indeed, it has been suggested that health promotion interventions frequently increase, rather than decrease, socioeconomic inequalities in health [ 128 ], since health promotion messages and interventions have a differential take-up across different social class groups. Those who are more affluent and have a higher level of formal education are more likely to modify their diets, give up smoking and increase levels of physical activity than are the less affluent with lower levels of formal education [ 135 ]. For instance, a mass media campaign to increase walking in Scotland ('Fitline') found that it had less appeal for those in the lower socioeconomic groups, despite higher awareness levels among these groups [ 136 ]. Furthermore, one-third of those who telephoned 'Fitline' to obtain further information were already regular exercisers, and may not have incurred any additional benefit.
In Tables 8 and 9 we have highlighted areas worthy of further synthesis. Despite the importance of socio-economic status as a determinant of health, few reviews explored socio-economic status or whether interventions had targeted those with the poorest health (e.g. those living in areas of disadvantage). Employment status, occupation, income level, gender, age, education, mobility and ethnicity are only some of the complex factors related to the determinants of health, and these do not include the more recent psychosocial [ 132 ] and lifecourse approaches [ 133 ]. Indeed, as Wilkinson argues, "The social consequences of people's differing circumstances in terms of stress, self-esteem and social relations may now be one of the most important influences on health" [ 137 ], pg 128]. We now understand how individuals become resilient to adverse circumstances (e.g. living in conditions of social deprivation) through, for instance, access to social support and strong social networks.
Studies that have explored the accumulation of risk of ill health over the lifecourse have highlighted the importance of social location and social capital. For instance, Schoon and Bynner [ 138 ], in a paper related to risk and resilience in young people, argue that interventions to improve health should aim to bolster incidences of positive adaptations to adverse circumstances rather than simply focusing on trying to put right negative behaviours. Linking into the health promotion agenda, they argue for the importance of primary prevention interventions, which take account of the context of the lives that an intervention seeks to improve, rather than simply taking a 'one size fits all' approach. However, there is little evidence at systematic review level that interventions to effect changes in behaviour are tackling the more complex interplay between health, illness and the wider determinants of health. As we noted above, this does not necessarily mean that the researchers in the primary studies themselves were unaware of a determinants approach. Nevertheless it is a significant finding that the systematic reviews covered here largely failed to take account of the inequalities agenda.
Research evidence clearly indicates that illness tends to cluster within lower socio-economic groups [ 139 , 140 ]. This means that it is even more crucial that those conducting systematic reviews (as well as those designing interventions) make health inequalities a central concern. As a recent WHO report states: "Together, the structural determinants and conditions of daily life constitute the social determinants of health and are responsible for a major part of health inequities between and within countries" [ 130 ].
The Cochrane Collaboration has a Cochrane Health Equity Field which aims to encourage reviewers to 'include explicit descriptions of the effect of the interventions not only on the whole population but to describe their effect upon the disadvantaged and/or their ability to reduce socioeconomic inequalities in health and to promote their use to the wider community.' To aid reviewers in this task, they have developed an 'Equity Tool' which is available from their website http://equity.cochrane.org/en/index.html . We would urge reviewers to access this tool and include data on inequities in future publications.
Another notable finding is that there were many more reviews evaluating individual-level interventions than those at community or population level, which again may reflect practical/methodological concerns. What we were not able to ascertain was whether the lack of such reviews reflected a lack of primary population based intervention studies. However, as the success of mass media advertising campaigns in marketing consumer goods clearly demonstrates, population-level interventions certainly hold promise, despite not lending themselves to evaluation by traditional means, such as the randomised controlled trial.
Whatever the level or target of the intervention, one of the most significant challenges is to bring about a change in behaviour that is sustained over time. In the smoking cessation field this is dealt with through relapse prevention schemes. However, sustained change is a difficulty also faced by healthy eating and physical activity programmes, where the intervention may be highly effective for the duration of contact with participants but then become less effective and even lead to a reversal of positive change in behaviour over time.
Interventions aiming to achieve long-term, sustained behaviour change will require a different approach to evaluation. Currently, the majority of studies have a relatively short period of follow-up, with the longest usually no more than two years. In order to determine long-term effectiveness, there is a need to develop longitudinal studies that can run alongside the intervention and revisit the participants at several time points, charting the challenges to sustaining the healthy behaviours and learning from those who have successfully maintained new, healthful habits. This would enable policy makers and those delivering the interventions to gain a deeper understanding of the strengths and weaknesses of the intervention, with a view to improving the effectiveness of future interventions. Participatory and ethnographic approaches may be particularly suited to this form of evaluation.
Limitations of the review methodology
Reviews are known as 'secondary' data sources because they collate and interpret original primary studies, and provide an interpretive overview of the collated findings. Reviews of reviews (such as the one reported here) bring together all of the systematic reviews in an area in order to provide an overview of the evidence. They involve a large body of high quality research literature, brought together in a systematic way, which can then be explored in more detail, if necessary, to answer particular research or clinical questions. Although 'reviews of reviews' are a useful endeavour for bringing together a large body of evidence and for investigating broad questions, several limitations should be acknowledged.
First, the evidence provided in such a review is 'twice removed' from the original primary data and the original primary research aims. Therefore, it is limited in its ability to provide detailed evidence of effectiveness for a particular intervention in a particular population group. Second, some of the high quality reviews might contain poor quality evidence (or very limited evidence), because that is all that is available. Third, even where no good quality reviews have been carried out in a particular area (e.g. mass media interventions for preventing illicit drug use), the absence of good primary evidence on that topic should not be assumed. There are many high quality primary studies that have not yet been synthesised into reviews. These primary studies cannot be included in a review of reviews, and often gaps in systematic review areas are thought to imply gaps in the primary evidence when this is not the case. Fourth, separate reviews may actually consider similar topic areas and therefore include a number of the same studies. Often the reviewers may have slightly different research questions, inclusion criteria and methods of analysis. Consequently, the results and conclusions may differ even though the included studies are very similar. Such differences are difficult to uncover and report within a review of reviews. Finally, when looking at the evidence in reviews, we were often limited by the questions that the authors of the reviews had decided are important and the outcomes that they included. These were often not the same questions that we have prioritised, even though the data might have been available in the primary research papers.
This review of reviews was also unable to identify the effectiveness of interventions which used comprehensive approaches (e.g. multi-component, working with a range of health behaviours). It is likely, however, that the effectiveness of the specific interventions reviewed would be enhanced through complementary supportive action. For example, behaviours are often interlinked (e.g. smoking and alcohol use; physical activity and healthy eating) and changing one behaviour may impact on one or more related behaviour.
Despite the limitations of a review of reviews, we have gathered together a wide body of evidence which illustrates that there are many interventions that have effectively achieved behaviour change across a range of health behaviours. The interventions that appear to be most successful include workplace interventions to support smoking cessation, physical activity and healthy eating; school based interventions across the health behaviours; individual-level interventions drawing on physician advice to promote healthy eating, smoking cessation and responsible/safe levels of alcohol use; and counselling for tobacco and alcohol use. Pregnancy may be a point in the lifecourse when women are especially amenable to making health improving changes (particularly in smoking cessation, and physical activity).
Mass media interventions are relatively effective in addressing the interconnectedness of knowledge, attitudes and behaviour within health promoting social marketing. Similarly, population-level legislative interventions (such as smoking bans and age limits for alcohol use) tend to be a part of much wider, more comprehensive campaigns to secure public support for the underlying health promoting message. Clearly, interventions at the individual and community levels should recognise the importance of changing knowledge and attitudes along with promoting healthy behaviour. Although many of the interventions currently include educational components, few explicitly attempt to evaluate their success.
Systematic reviews should explore data from the primary studies showing how effectiveness varies in relation to social and economic difference (including wider determinants of health, such as gender, ethnicity and geographic location). Further research is needed to synthesise primary studies of the effectiveness of interventions across all six health behaviours to target those of lower socio-economic status who may be at highest risk of ill-health and who may engage in a range of unhealthy behaviours. For this reason, it is likely that health promoting interventions might benefit from a more multi-faceted approach: the effectiveness of the specific interventions reviewed here is likely to be enhanced through complementary supportive action. The inter-relationship between activities, such as alcohol use and smoking, may lend itself to a two-pronged intervention.
While there is a good body of high quality evidence of effectiveness of interventions to promote healthy behaviours, longer term follow-up is required in order to determine whether positive change is sustained and for how long.
WHO: Chronic disease risk factors. 2003, WHO, Geneva
Google Scholar
WHO: The world health report 2002 - Reducing Risks, Promoting Healthy Life. 2002, WHO, Geneva
Cavill N, Kahlmeier S, Racioppi F: Physical activity and health in Europe: evidence for action. 2007, WHO, Geneva
WHO: The challenge of obesity in the WHO European Region and the strategies for response. 2007, WHO, Geneva
WHO: Framework for alcohol policy in the WHO European Region. 2006, WHO, Geneva
UNICEF: A league table of teenage births in rich nations'. 2001, Innocenti Research Centre, Florence
WHO: Sexually transmitted infections among adolescents: the need for adequate health services. 2005, WHO, Geneva
Halpern D, Bates C, Aldridge S: Personal responsibility and changing behaviour: the state of knowledge and its implications for public policy. 2004, Cabinet Office, Prime Minister's Strategy Unit Discussion Paper, London
Rutter D, Quine L: Social cognition models and changing health behaviour. Changing health behaviour. Edited by: Rutter D, Quine L. 2002, Philadelphia: Open University Press
Bandura A: Health Promotion by Social Cognitive Means. Health Educ Behav. 2004, 31: 143-164. 10.1177/1090198104263660.
PubMed Google Scholar
Jepson R, Harris F, MacGillivray S, Kearney N, Rowa-Dewar N: A Review of the effectiveness of interventions, approaches and models at individual, community and population level that are aimed at changing health outcomes through changing knowledge, attitudes and behaviour. 2006, NICE, London, [ http://www.nice.org.uk/nicemedia/live/11868/44521/44521.pdf ]
NICE: PH6 Behaviour change: guidance. 2007, NICE, London
NHS National Institute for Health and Clinical Excellence: Methods for development of NICE public health guidance. 2006, NICE, London
Abbot NC, Stead LF, White AR, Barnes J: Hypnotherapy for smoking cessation. Cochrane Database of Systematic Reviews. 1998
Bains N, Pickett W, Hoey J: The use and impact of incentives in population-based smoking cessation programs: a review. American Journal of Health Promotion. 1998, 12: 307-320.
CAS PubMed Google Scholar
Bala M, Strzeszynski L, Cahill K: Mass media interventions for smoking cessation in adults. Cochrane Database of Systematic Reviews. 2008
Bize R, Burnand B, Mueller Y, Cornuz J: Biomedical risk assessment as an aid for smoking cessation. Cochrane Database of Systematic Reviews. 2005
Brothwell DJ: Should the use of smoking cessation products be promoted by dental offices: an evidence-based report. Journal of the Canadian Dental Association. 2001, 67: 149-155.
Cahill K, Perera R: Competitions and incentives for smoking cessation. Cochrane Database of Systematic Reviews. 2008
Cahill K, Perera R: Quit and Win contests for smoking cessation. Cochrane Database of Systematic Reviews. 2008
Cahill K, Moher M, Hey K, Lancaster T: Workplace interventions for smoking cessation. The Cochrane Database of Systematic Reviews. 2008
Christakis DA, Garrison MM, Ebel BE, Wiehe SE, Rivara FP: Pediatric smoking prevention interventions delivered by care providers: a systematic review. American Journal of Preventive Medicine. 2003, 25: 358-362. 10.1016/S0749-3797(03)00214-9.
Dunn C, Deroo L, Rivara FP: The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001, 96: 1725-1742. 10.1046/j.1360-0443.2001.961217253.x.
Ebbert JO, Rowland LC, Montori V, Vickers KS, Erwin PC, Dale LC, Stead LF: Interventions for smokeless tobacco use cessation. Cochrane Database of Systematic Reviews. 2004
Edwards N, Aubin P, Morrison M: The effectiveness of postpartum smoking relapse prevention strategies. 2000, Hamilton, Ontario, Canada
Fichtenberg CM, Glantz SA: Effect of smoke-free workplaces on smoking behavior: systematic review. BMJ. 2002, 325: 188-191. 10.1136/bmj.325.7357.188.
PubMed PubMed Central Google Scholar
Fichtenberg CM, Glantz SA: Youth access interventions do not affect youth smoking. Pediatrics. 2002, 109: 1088-1092. 10.1542/peds.109.6.1088.
Friend K, Levy DT: Reductions in smoking prevalence and cigarette consumption associated with mass-media campaigns. Health Education Research. 2002, 17: 85-98. 10.1093/her/17.1.85.
Garrison MM, Christakis DA, Ebel BE, Wiehe SE, Rivara FP: Smoking cessation interventions for adolescents: a systematic review. American Journal of Preventive Medicine. 2003, 25: 363-367. 10.1016/S0749-3797(03)00213-7.
Grimshaw GM, Stanton A: Tobacco cessation interventions for young people. Cochrane Database of Systematic Reviews. 2008
Hajek P, Stead LF: Aversive smoking for smoking cessation. Cochrane Database of Systematic Reviews. 2001
Hajek P, Stead LF, West R, Jarvis M, Lancaster T: Relapse prevention interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2005
Hopkins DP, Briss PA, Ricard CJ, Husten CG, Carande K, Fielding JE, Alao MO, McKenna JW, Sharp DJ, Harris JR, Task Force on Community Preventive Services: Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. American Journal of Preventive Medicine. 2001, 20: 16-66. 10.1016/S0749-3797(00)00297-X.
Lancaster T, Stead LF: Individual behavioural counselling for smoking cessation. Cochrane Database of Systematic Reviews. 2008
Lancaster T, Stead LF: Self-help interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2005
Lumley J, Oliver SS, Chamberlain C, Oakley L: Interventions for promoting smoking cessation during pregnancy. Cochrane Database of Systematic Reviews. 2004
May S, West R: Do social support interventions ("buddy systems") aid smoking cessation: a review. Tobacco Control. 2000, 9: 415-422. 10.1136/tc.9.4.415.
CAS PubMed PubMed Central Google Scholar
Maziak W, Ward K, Eissenberg T: Interventions for waterpipe smoking cessation. Cochrane Database of Systematic Reviews. 2007
McClure JB: Are biomarkers useful treatment aids for promoting health behavior change? An empirical review. American Journal of Preventive Medicine. 2002, 22: 200-207. 10.1016/S0749-3797(01)00425-1.
Murphy-Hoefer R, Griffith R, Pederson LL, Crossett L, Iyer SR, Hiller MD: A review of interventions to reduce tobacco use in colleges and universities. American Journal of Preventive Medicine. 2005, 28: 188-200. 10.1016/j.amepre.2004.10.015.
Nishi N, Jenicek M, Tatara K: A meta-analytic review of the effect of exercise on smoking cessation. Journal of Epidemiology. 1998, 8: 79-84.
Park EW, Schultz JK, Tudiver F, Campbell T, Becker L: Enhancing partner support to improve smoking cessation. Cochrane Database of Systematic Reviews. 2004
Priest N, Roseby R, Waters E, Polnay A, Campbell R, Spencer N, Webster P, Ferguson-Thorne G: Family and carer smoking control programmes for reducing children's exposure to environmental tobacco smoke. Cochrane Database of Systematic Reviews. 2008
Rice VH, Stead LF: Nursing interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2004
Riemsma RP, Pattenden J, Bridle C, Sowden A, Mather L, Watt IS, Walker A: Systematic review of the effectiveness of stage based interventions to promote smoking cessation. BMJ. 2003, 1175-1177. 10.1136/bmj.326.7400.1175.
Secker-Walker RH, Gnich W, Platt S, Lancaster T: Community interventions for reducing smoking among adults. Cochrane Database of Systematic Reviews. 2002
Serra C, Bonfill X, Pladevall V, Cabezas P: Interventions for preventing tobacco smoking in public places. Cochrane Database of Systematic Reviews. 2008
Sinclair HK, Bond CM, Stead LF: Community pharmacy personnel interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2004
Smedslund G, Fisher KJ, Boles SM, Lichtenstein E: The effectiveness of workplace smoking cessation programmes: a meta-analysis of recent studies. Tobacco Control. 2004, 13: 197-204. 10.1136/tc.2002.002915.
Sowden A, Stead L: Community interventions for preventing smoking in young people. The Cochrane Database of Systematic Reviews Issue. 2003
Sowden AJ, Arblaster L: Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews. 1998
Stead LF, Lancaster T: Group behaviour therapy programmes for smoking cessation. Cochrane Database of Systematic Reviews. 2005
Stead LF, Lancaster T: Interventions for preventing tobacco sales to minors. Cochrane Database of Systematic Reviews. 2005
Stead LF, Bergson G, Lancaster T: Physician advice for smoking cessation. Cochrane Database of Systematic Reviews. 2008
Stead LF, Lancaster T, Perera R: Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews. 2003
Thomas R, Baker P, Lorenzetti D: Family-based programmes for preventing smoking by children and adolescents. Cochrane Database of Systematic Reviews. 2008
Ussher M: Exercise interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2005
van Sluijs EMF, van Poppel MNM, Van Mechelen W: Stage-based lifestyle interventions in primary care - Are they effective?. American Journal of Preventive Medicine. 2004, 26: 330-343.
Walters ST, Wright JA, Shegog R: A review of computer and Internet-based interventions for smoking behavior. Addictive Behaviors. 2006, 31: 264-277. 10.1016/j.addbeh.2005.05.002.
Wiehe SE, Garrison MM, Christakis DA, Ebel BE, Rivara FP: A systematic review of school-based smoking prevention trials with long-term follow-up. Journal of Adolescent Health. 2005, 36: 162-169. 10.1016/j.jadohealth.2004.12.003.
Thomas R: School-based programmes for preventing smoking. Cochrane Database of Systematic Reviews. 2002
Thomas S, Fayter D, Misso K, Ogilvie D, Petticrew M, Sowden A, Whitehead M, Worthy G: Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tobacco Control. 2008, 17: 230-237. 10.1136/tc.2007.023911.
Prochaska JO, DiClemente CC: Trans-theoretical therapy - toward a more integrative model of change. Psychotherapy: Theory, Research and Practice. 1982, 19: 276-288. 10.1037/h0088437.
Secker-Walker R, Gnich W, Platt S, Lancaster T: Community interventions for reducing smoking among adults. Cochrane Database of Systematic Reviews. 2008
Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, Stave CD, Olkin I, Sirard JR: Using Pedometers to Increase Physical Activity and Improve Health: A Systematic Review. JAMA. 2007, 298: 2296-2304. 10.1001/jama.298.19.2296.
Brunton G, Harden A, Rees R, Kavanagh J, Oliver S, Oakley A: Promoting physical activity amongst children outside of physical education classes: a systematic review integrating intervention and qualitative studies. 2003
Conn VS, Minor MA, Burks KJ, Rantz MJ, Pomeroy SH: Integrative review of physical activity intervention research with aging adults. Journal of the American Geriatrics Society. 2003, 51: 1159-1168. 10.1046/j.1532-5415.2003.51365.x.
Dobbins M, Lockett D, Michel I, Beyers J, Feldman L, Vohra J, Micucci S: The effectiveness of school-based interventions in promoting physical activity and fitness among children and youth: a systematic review. 2001, Hamilton, On, Canada
Eakin EG, Lawler SP, Vandelanotte C, Owen N: Telephone interventions for physical activity and dietary behavior change: a systematic review. American Journal of Preventive Medicine. 2007, 32: 419-434. 10.1016/j.amepre.2007.01.004.
Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM: Clinician counseling to promote physical activity. 2002, Rockville, MD, USA
Finlay SJ, Faulkner G: Physical activity promotion through the mass media: inception, production, transmission and consumption. Preventive Medicine. 2005, 40: 121-130. 10.1016/j.ypmed.2004.04.018.
Hillsdon M, Foster C, Thorogood M: Interventions for promoting physical activity. Cochrane Database of Systematic Reviews. 2005
Holtzman J, Schmitz K, Babes G, Kane RL, Duval S, Wilt TJ, MacDonald RM, Rutks I: Effectiveness of behavioral interventions to modify physical activity behaviors in general populations and cancer patients and survivors. 2004, Rockville, MD, USA
Jackson NW, Howes FS, Gupta S, Doyle JL, Waters E: Interventions implemented through sporting organisations for increasing participation in sport. Cochrane Database of Systematic Reviews. 2005
Jackson NW, Howes FS, Gupta S, Doyle JL, Waters E: Policy interventions implemented through sporting organisations for promoting healthy behaviour change. Cochrane Database of Systematic Reviews. 2006
Jago R, Baranowski T: Non-curricular approaches for increasing physical activity in youth: a review. Preventive Medicine. 2004, 39: 157-163. 10.1016/j.ypmed.2004.01.014.
Kremers SP, Droomers M, van Lenthe F, Brug J: Moderators of environmental intervention effects on diet and activity in youth. American Journal of Preventive Medicine. 2007, 32: 163-172. 10.1016/j.amepre.2006.10.006.
Kroeze W, Brug JA: A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviours. Annals of Behavioral Medicine. 2006, 31: 205-223. 10.1207/s15324796abm3103_2.
Ogilvie D, Egan M, Hamilton V, Petticrew M: Promoting walking and cycling as an alternative to using cars: systematic review. BMJ. 2004, 329: 760-
Proper K, Koning M, van-der-Beek AJ, Hildebrandt VH, Bosscher RJ, van MW: The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clinical Journal of Sport Medicine. 2003, 13: 106-117. 10.1097/00042752-200303000-00008.
Rees R, Harden A, Shepherd J, liver S, akley A: Young people and physical exercise: a systematic review of research on barriers and facilitators. 2001, London: EPPI Centre
van-der-Bij AK, Laurant MG, Wensing M: Effectiveness of physical activity interventions for older adults: a review. American Journal of Preventive Medicine. 2002, 22: 120-133. 10.1016/S0749-3797(01)00413-5.
van Sluijs EMF, McMinn AM, Griffin SJ: Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007, 335: 703-10.1136/bmj.39320.843947.BE.
Brunton G, Harden A, Rees R, Kavanagh J, Oliver S, Oakley A: Promoting physical activity amongst children outside of physical education classes: a systematic review integrating intervention and qualitative studies. 2003, London: EPPI Centre
Kremers SP, de Bruijn GJ, Droomers M, van Lenthe F, Brug J: Moderators of environmental intervention effects on diet and activity in youth. American Journal of Preventive Medicine. 2007, 32: 163-172. 10.1016/j.amepre.2006.10.006.
van Sluijs EMF, van Poppel MNM, Van Mechelen W: Stage-based lifestyle interventions in primary care - Are they effective? (Review). American Journal of Preventive Medicine. 2004, 26: 330-343.
Jackson NW, Howes FS, Gupta S, Doyle JL, Waters E: Policy interventions implemented through sporting organisations for promoting healthy behaviour change. Cochrane Database of Systematic Reviews. 2005
Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B: Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Archives of Internal Medicine. 2005, 165: 986-995. 10.1001/archinte.165.9.986.
Ditter SM, Elder RW, Shults RA, Sleet DA, Compton R, Nichols JL: Effectiveness of designated driver programs for reducing alcohol-impaired driving: a systematic review. American Journal of Preventive Medicine. 2005, 28: 280-287. 10.1016/j.amepre.2005.02.013.
Doggett C, Burrett SL, Osborn DA: Home visits during pregnancy and after birth for women with an alcohol or drug problem. The Cochrane Database of Systematic Reviews. 2005
Elder RW, Shults RA, Sleet DA, Nichols JL, Thompson RS, Rajab W: Effectiveness of mass media campaigns for reducing drinking and driving and alcohol-involved crashes: A systematic review. American Journal of Preventive Medicine. 2004, 27 (1): 57-65. 10.1016/j.amepre.2004.03.002.
Elder RW, Nichols JL, Shults RA, Sleet DA, Barrios LC, Compton R: Effectiveness of school-based programs for reducing drinking and driving and riding with drinking drivers: a systematic review. American Journal of Preventive Medicine. 2005, 28: 288-304. 10.1016/j.amepre.2005.02.015.
Foxcroft DR, Ireland D, Lowe G, Breen R: Primary prevention for alcohol misuse in young people. Cochrane Database of Systematic Reviews. 2002
Goss C, Van Bramer L, Gliner J, Porter T, Roberts I, DiGuiseppi C: Increased police patrols for preventing alcohol-impaired driving. Cochrane Database of Systematic Reviews. 2008
Kaner E, Dickinson H, Beyer F, Campbell F, Schlesinger C, Heather N, Saunders J, Burnand B, Pienaar E: Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of Systematic Reviews. 2008
Wagenaar AC, Toomey TL: Effects of minimum drinking age laws: a review and analyses of the literature from 1960 to 2000. Journal of Studies on Alcohol. 2002, 206-225. Supplement 14
Wells PE, Bangert DR, McMillen R, Williams M: Final results from a meta-analysis of remedial interventions with drink/drive offenders. Addiction. 1995, 90: 907-926. 10.1111/j.1360-0443.1995.tb03545.x.
Werch CE, Owen DM: Iatrogenic effects of alcohol and drug prevention programs. Journal of Studies on Alcohol. 2002, 63: 581-590.
Whitlock EP, Polen MR, Green CA, Orleans T, Klein J: Clinical guidelines. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2004, 140: 557-568.
Willis C, Lybrand S, Bellamy N: Alcohol ignition interlock programmes for reducing drink driving recidivism. The Cochrane Database of Systematic Reviews. 2004
Zwerling C, Jones MP: Evaluation of the effectiveness of low blood alcohol concentration laws for younger drivers. American Journal of Preventive Medicine. 1999, 16: 76-80. 10.1016/S0749-3797(98)00114-7.
Walters Glenn D: Behavioral self-control training for problem drinkers: A meta-analysis of randomized control studies. Behavior Therapy. 2000, 31: 135-149. 10.1016/S0005-7894(00)80008-8.
Ammerman A, Pignone M, Fernandez L, Lohr K, Driscoll JA, Nester C, Orleans T, Pender N, Woolf S, Sutton SF, Lux LJ, Whitener L: Counseling to promote a healthy diet. 2002, Rockville, USA
Ciliska D, Miles E, O'Brien MA, Turl C, Tomasik HH, Donovan U, Beyers J: The effectiveness of community interventions to increase fruit and vegetable consumption in people four years of age and older. 1999, Dundas, ON, Canada
Fletcher A, Rake C: Effectiveness of interventions to promote healthy eating in elderly people living in the community: a review. 1998, Health Education Authority, London
Roe L, Hunt P, Bradshaw H, Rayner M: Health promotion interventions to promote healthy eating in the general population: a review. 1997, Health Education Authority, London
Serra-Majem L, Roman B, Estruch R: Scientific evidence of interventions using the Mediterranean diet: a systematic review. Nutrition Reviews. 2006, 64: S27-S47. 10.1111/j.1753-4887.2006.tb00232.x.
Shepherd J, Harden A, Rees R, Brunton G, Garcia J, Oliver S, Oakley A: Young people and healthy eating: a systematic review of research on barriers and facilitators. 2002, EPPI centre, London
Tedstone A, Aviles M, Shetty P, Daniels L: Effectiveness of interventions to promote healthy eating in preschool children aged 1 to 5 years: a review. 1998, Health Education Authority, London
Thomas J, Sutcliffe K, Harden A, Oakley A, Oliver S, Rees R, Brunton G, Kavanagh J: Children and Healthy Eating: A systematic review of barriers and facilitators. 2003, EPPI-Centre, London
van Teijlingen E, Wilson B, Barry N, Ralph A, McNeill G, Graham W, Campbell D: Effectiveness of interventions to promote healthy eating in pregnant women and women of childbearing age: a review. 1998, Health Development Agency, London
Faggiano F, Vigna-Taglianti FD, Versino E, Zambon A, Borraccino A, Lemma P: School-based prevention for illicit drugs' use. Cochrane Database of Systematic Reviews. 2005
Gates S, McCambridge J, Smith LA, Foxcroft DR: Interventions for prevention of drug use by young people delivered in non-school settings. Cochrane Database of Systematic Reviews. 2006
Roe S, Becker J: Drug prevention with vulnerable young people: A review. Drugs: Education, Prevention and Policy. 2005, 12: 85-99. 10.1080/0968763042000322639.
Morrison-Beedy D, Nelson LE: HIV prevention interventions in adolescent girls: what is the state of the science?. Worldviews on Evidence-Based Nursing. 2004, 1: 165-175. 10.1111/j.1524-475X.2004.04047.x.
Mullen PD, Ramirez G, Strouse D, Hedges LV, Sogolow E: Meta-analysis of the effects of behavioral HIV prevention interventions on the sexual risk behavior of sexually experienced adolescents in controlled studies in the United States. Journal of Acquired Immune Deficiency Syndromes. 2002, 30: S94-S105.
Pedlow CT, Carey MP: HIV sexual risk-reduction interventions for youth: a review and methodological critique of randomized controlled trials. Behavior Modification. 2003, 27: 135-90. 10.1177/0145445503251562.
Yamada J, DiCenso A, Feldman L, Cormillott P, Wade K, Wignall R, Thomas H: A systematic review of the effectiveness of primary prevention programs to prevent sexually transmitted diseases in adolescents. 1999, Dundas, Canada
Bennett SE, Assefi NP: School-based teenage pregnancy prevention programs: a systematic review of randomized controlled trials. Journal of Adolescent Health. 2005, 36: 72-81. 10.1016/j.jadohealth.2003.11.097.
DiCenso A, Guyatt G, Willan A, Griffith L: Interventions to reduce unintended pregnancies among adolescents: systematic review of randomised controlled trials. BMJ. 2002, 324: 1426-1430. 10.1136/bmj.324.7351.1426.
Moos MK, Bartholomew NE, Lohr KN: Counseling in the clinical setting to prevent unintended pregnancy: an evidence-based research agenda. Contraception. 2003, 67: 115-132. 10.1016/S0010-7824(02)00472-9.
Robin L, Dittus P, Whitaker D, Crosby R, Ethier K, Mezoff J, Miller K, Pappas-Deluca K: Behavioral interventions to reduce incidence of HIV, STD, and pregnancy among adolescents: a decade in review. Journal of Adolescent Health. 2004, 34: 3-26. 10.1016/S1054-139X(03)00244-1.
Black D, Morris J, Smith C, Townsend P: Inequalities in health: report of a Research Working Group. 1980, D.H.S.S, London
Acheson D, Barker D, Chambers J, Graham H, Marmot M: Independent inquiry into inequalities in health report. 1998, HMSO, London
Wanless D: Securing Our Future Health: Taking a Long-Term View: Final Report. 2002, London: HM Treasury
CSDH: Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. 2008, WHO, Geneva
Department of Health: Variations in health: what can the Department of Health and NHS do?. 1995, Department of Health, London
Wilkinson R, Marmot M: Social determinants of health: the solid facts (2nd edition). 2003, WHO, Geneva
Davey Smith G: Health Inequalities: Lifecourse Approaches. 2003, Bristol: Policy Press
McIntyre S: The social patterning of exercise behaviours: the role of personal and local resources. British Journal of Sports Medicine. 2000, 34: 6-10.1136/bjsm.34.1.6.
Vetter N: Health promotion--quo vadis now?. J Public Health. 2005, 27: 239-240. 10.1093/pubmed/fdi039.
Wimbush E, MacGregor A, Fraser E: Impacts of a national mass media campaign on walking in Scotland. Health Promot Int. 1998, 13: 45-53. 10.1093/heapro/13.1.45.
Wilkinson R: Unhealthy societies: The afflictions of inequality. 1996, London: Routledge
Schoon I, Bynner J: Risk and Resilience in the Life Course: Implications for Interventions and Social Policies. Journal of Youth Studies. 2003, 6: 21-31. 10.1080/1367626032000068145.
Pickett KE, Pearl M: Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. Journal of Epidemiology and Community Health. 2001, 55: 111-122. 10.1136/jech.55.2.111.
Whitehead M: The concepts and principles of equity and health. 1990, WHO Copenhagen
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/10/538/prepub
Download references
Acknowledgements
The original review of reviews was funded by the National Institute for Health and Clinical Excellence (NICE) as part of the development of their guidance on behaviour change. However, the paper is the work of the authors and does not necessarily represent the views of NICE. We would like to acknowledge the contribution of members of staff at the Centre for Reviews and Dissemination in York, the Cancer Care Research Centre at the University of Stirling and the University of Abertay.
Author information
Authors and affiliations.
Department of Nursing and Midwifery, University of Stirling, Stirling, FK9 4LA, UK
Ruth G Jepson
Nursing Midwifery & Allied Health ProfessionsResearch Unit, University of Stirling, Stirling, UK
Fiona M Harris
Centre for Population Health Sciences, University of Edinburgh, Edinburgh, EH8 9AG, UK
Stephen Platt
Glasgow Centre for Population Health, 94 Elmbank Street, Glasgow, G2 4DL, UK
Carol Tannahill
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ruth G Jepson .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
RJ was the Principal Investigator on the project, conceived the design of the study, involved in data extraction, analysis and drafting the manuscript. FH was involved in data extraction and analysis and drafting the manuscript. SP and CT were involved in the study as advisors and were also involved in drafting and commenting on the manuscript. All authors read and approved the final manuscript.
Ruth G Jepson, Fiona M Harris, Stephen Platt and Carol Tannahill contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Jepson, R.G., Harris, F.M., Platt, S. et al. The effectiveness of interventions to change six health behaviours: a review of reviews. BMC Public Health 10 , 538 (2010). https://doi.org/10.1186/1471-2458-10-538
Download citation
Received : 20 January 2010
Accepted : 08 September 2010
Published : 08 September 2010
DOI : https://doi.org/10.1186/1471-2458-10-538
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Physical Activity
- Smoking Cessation
- Sexual Risk
- Healthy Eating
- Health Inequality
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Tools and Resources
- Customer Services
- Affective Science
- Biological Foundations of Psychology
- Clinical Psychology: Disorders and Therapies
- Cognitive Psychology/Neuroscience
- Developmental Psychology
- Educational/School Psychology
- Forensic Psychology
- Health Psychology
- History and Systems of Psychology
- Individual Differences
- Methods and Approaches in Psychology
- Neuropsychology
- Organizational and Institutional Psychology
- Personality
- Psychology and Other Disciplines
- Social Psychology
- Sports Psychology
- Share This Facebook LinkedIn Twitter
Article contents
Methods of health behavior change.
- Ildiko Tombor Ildiko Tombor Department Behavioural Science and Health, University College London
- and Susan Michie Susan Michie Department of Psychology, University College London
- https://doi.org/10.1093/acrefore/9780190236557.013.125
- Published online: 27 July 2017
People’s behavior influences health, for example, in the prevention, early detection, and treatment of disease, the management of illness, and the optimization of healthcare professionals’ behaviors. Behaviors are part of a system of behaviors within and between people in that any one behavior is influenced by others. Methods for changing behavior may be aimed at individuals, organizations, communities, and/or populations and at changing different influences on behavior, e.g., motivation, capability, and the environment. A framework that encapsulates these influences is the Behavior Change Wheel, which links an understanding of behavior in its context with methods to change behavior. Within this framework, methods are conceptualized at three levels: policies that represent high-level societal and organizational decisions, interventions that are more direct methods to change behavior, and behavior change techniques that are the smallest components that on their own have the potential to change behavior. In order to provide intervention designers with a systematic method to select the policies, interventions, and/or techniques relevant for their context, a set of criteria can be used to help select intervention methods that are likely to be implemented and effective. One such set is the “APEASE” criteria: affordability, practicability, effectiveness, acceptability, safety, and equity.
- health behaviors
- population health
- frameworks of behavior change
- Behavior Change Wheel
- methods to behavior change
- interventions
- behavior change techniques
- implementation
Health Behavior Change and Population Health
Health behaviors refer to any behaviors that impact on people’s physical and mental health and quality of life. “Behavior” can be defined as “anything a person does in response to internal or external events. Actions may be overt (motor or verbal) and directly measurable or, covert (activities not viewable but involving voluntary muscles) and indirectly measurable; behaviours are physical events that occur in the body and are controlled by the brain” (Davis, Campbell, Hildon, Hobbs, & Michie, 2015 , p. 327). Behaviors are part of a system in that any given behavior is influenced by other behaviors of the same or other individuals (Michie, Atkins, & West, 2014 ). Individual behaviors (e.g., lighting up a cigarette or eating an energy-dense snack) are often recurring and thus better described as “behavior patterns” (e.g., smoking, overeating) characterized by aggregated measures such as frequency, duration, intensity, or volume of consumption (Michie et al., 2014 ). Behaviors are dynamic in that not only do they interact (positively and negatively) with each other, but these relationships change over time. Three types of behavior are related to population health: behaviors that contribute to the prevention of disease, behaviors that involve care-seeking and adherence to treatment, and behaviors that relate to the delivery of healthcare. For behaviors to translate into population health, they must be maintained over the long run and factors influencing maintenance may differ from those influencing initiation of change. This important topic is beyond the scope of this article, but we refer you to publications in this area (Gardner, 2015 ; Verplanken & Wood, 2006 ; Wood & Rünger, 2016 ).
Tobacco smoking, excessive alcohol consumption, physical inactivity, and unhealthy eating are leading contributors to preventable premature death and ill health in high-income countries (AIHW, 2014 ; Department of Health, 2014 ; Johnson, Hayes, Brown, Hoo, & Ethier, 2014 ). Historically, the overall burden of disease in low-income countries was mainly attributed to infectious diseases as opposed to non-communicable diseases, such as cancer, stroke, heart disease, respiratory disease, and liver disease (World Health Organization, 2009 ). However, due to the increased prevalence of smoking, alcohol consumption, and obesity, low-income countries have begun to face a huge combined burden from both non-communicable and infectious diseases (World Health Organization, 2009 ). In addition to non-communicable diseases, the risks of infectious diseases such as HIV/AIDS can also be reduced or completely prevented by behavior change, such as by using condoms (Holmes, Levine, & Weaver, 2004 ).
Behaviors that involve care-seeking and adherence to treatment include taking part in vaccination programs. This can limit the spread of disease such as pandemic or seasonal influenza and childhood infectious diseases (e.g., diphtheria, polio, neonatal tetanus) (CDC, 2013 ; Hinman, 1999 ; Rubinstein, Marcu, Yardley, & Michie, 2015 ). Moreover, improving adherence to antibiotic therapy among patients (Llor et al., 2013 ) is important to minimize the development of antimicrobial-resistant infections that contribute to 700,000 deaths each year globally (O’Neill, 2014 ). If the onset of disease cannot be prevented, early diagnosis of (pre-clinical) conditions and adherence to treatment can improve prognosis. For example, participating in screening programs, such as the U.K. National Health Service bowel cancer screening program, can help identify cancer in the early stages when the prognosis of recovery is potentially much better (Logan et al., 2011 ). Similarly, engaging with regular monitoring of chronic health conditions (e.g., high blood pressure) and adhering to medications for long-term conditions (e.g., HIV, heart disease) can slow the progression of disease and improve patients’ quality of life (Ito et al., 2012 ; Ownby, Waldrop-Valverde, Jacobs, Acevedo, & Caballero, 2013 ).
The extent to which the delivery of healthcare is based on evidence is an important contributor to effectiveness and quality of care (Sackett, Rosenberg, Gray, Haynes, & Richardson, 1996 ). Changing healthcare professionals’ behaviors so that they implement evidence-based guidelines is likely to improve health (Michie et al., 2005 ). Examples of interventions designed to change healthcare professional behavior include feedback to improve hand-hygiene practices (Fuller et al., 2012 ), training and education to improve the management of mild brain injury in emergency departments (Tavender et al., 2015 ), and feedback to reduce unnecessary antibiotic prescribing (Hallsworth et al., 2016 ).
Effective interventions and policies are needed to tackle population health challenges globally. This will require systematic analyses of the behaviors of those who receive and those who deliver healthcare and a better understanding of potential mechanisms by which change is brought about. Frameworks of behavior and behavior change can be useful for this purpose.
Frameworks for Behavior Change
Behavior change can be aimed at different levels, including individual, organizational, community, and population levels, and any intervention delivered at one level can impact on other levels. The most effective interventions are those that target several levels simultaneously and consistently (NICE, 2007 , 2014 ). There are a variety of types of methods to bring about behavior change; a review of effective behavior change interventions and recommendations for practice at population, community, and individual levels identified evidence-based principles underlying effective behavior change (NICE, 2007 ). These are (Abraham, Kelly, West, & Michie, 2009 ):
Knowledge and outcome expectancies (improving people’s knowledge about the health consequences of their behaviors),
Personal relevance (drawing people’s attention to what health behavior change would mean for them),
Positive affective attitudes (promoting positive feelings about behavior change),
Descriptive norms (increasing the visibility of positive health behaviors in the social environment),
Subjective norms (improving social approval of positive health behaviors),
Personal and moral norms (promoting personal commitments to behavior change),
Self-efficacy (increasing people’s belief in their ability to change their behaviors),
Intention/goal setting and the formation of concrete plans (helping people set goals and form plans on how to achieve them),
Behavioral contracts (facilitating that people share their plans and goals with others),
Social relationships (drawing attention to the social influences on health behaviors), and
Relapse prevention (helping people develop skills to cope with difficult situations).
The updated review and recommendations for interventions aimed at individuals identified good evidence for the effectiveness of goals and planning, feedback and monitoring, and social support (NICE, 2014 ).
These evidence-based principles of behavior change can be conceptualized in terms of three high-level influences on behavior: capability, opportunity, and motivation. These are encapsulated in the COM-B (Capability, Opportunity, Motivation, Behavior) model (Michie, van Stralen, & West, 2011 ). Capability refers to people’s physical skills, strength, and physical stamina (e.g., having the strength to walk up stairs) and psychological capability such as knowledge, behavioral regulation, psychological skills, mental strength, and stamina (e.g., having knowledge about vaccination programs) to perform the behavior. Motivation involves automatic processes such as habits, emotional states (e.g., having an urge to smoke), and reflective processes such as self-conscious intentions, beliefs, and identity (e.g., having a strong motivation to become more athletic) that energize and direct behavior. Opportunity refers to the social environment involving the cultural milieu, social norms, social influences, and modeling (e.g., having a senior colleague as role model to aspire or imitate) and physical environmental in terms of resources, cues, locations, and time (e.g., being able to access stop-smoking support) that permit the behavior. The COM-B framework proposes that intrapersonal (capability and motivation) and environmental (opportunity) influences on behavior interact in that capability, opportunity, and motivation influence behavior, capability and opportunity influence motivation, and behavior influences all three components. Behavior change therefore requires change in one or more of capability, opportunity, and motivation, and these can serve as targets for behavior change interventions. Table 1 shows how evidence-based principles of behavior change (Abraham et al., 2009 ) can be conceptualized as one or more of the COM-B components.
Table 1. Linking Evidence-Based Principles of Behavior Change with Components of the COM-B Model
Three components of the COM-B model (capability, opportunity, and motivation) can be further elaborated by the Theoretical Domains Framework (Cane, O’Connor, & Michie, 2012 ; Michie et al., 2005 ). The Theoretical Domains Framework was originally developed to help intervention designers and policymakers develop theory-based implementation interventions to improve the implementation of research evidence into practice. It consists of 14 domains developed from synthesizing constructs identified in 33 theories (Cane et al., 2012 ; Michie et al., 2005 ):
Social/professional role and identity,
Beliefs about capabilities,
Beliefs about consequences,
Memory, attention, and decision processes,
Environmental context and resources,
Social influences,
Behavioral regulation,
Intentions, and
Reinforcement.
Components of COM-B map on domains of the Theoretical Domains Framework in that (1) physical capability includes skills; (2) psychological capability includes knowledge, skills, memory, attention, and decision processes and behavioral regulation; (3) social opportunity includes social influences; (4) physical opportunity includes environmental context and resources; (5) automatic motivation includes emotion and reinforcement; and (6) reflective motivation includes goals, intentions, beliefs about consequences, beliefs about capabilities, optimism, and social/professional role and identity (Francis, O’Connor, & Curran, 2012 ). Table 2 shows how domains of the Theoretical Domains Framework can be linked with evidence-based principles of behavior change and components of the COM-B model.
Table 2. Linking the Theoretical Domains Framework with Evidence-Based Principles of Behavior Change and the COM-B Model
The Theoretical Domains Framework provides a method for systematically investigating influences on behavior change (Francis et al., 2012 ). A large number of studies across various disciplines and settings have used the COM-B and/or the more elaborated Theoretical Domains Framework to identify barriers and enablers to behaviors in order to inform the design of behavior change interventions. Examples include studies focusing on healthcare professionals’ behavior in relation to prescribing medications (Duncan et al., 2012 ; Fleming, Bradley, Cullinan, & Byrne, 2014 ; Sinnott et al., 2015 ) and managing low back pain without unnecessary x-ray referrals (Bussieres, Patey, Francis, Sales, & Grimshaw, 2012 ; French et al., 2012 ). Another example is a study of being vaccinated and taking antiviral medicines, which found that the identity of being a healthy person (reflective motivation, social/professional role and identity) can be a barrier because it evoked feelings of invulnerability and beliefs about being able to fight disease without taking medications (Rubinstein et al., 2015 ). In terms of facilitators, recommendations from credible sources (social opportunity, social influences) in favor of vaccination was found to increase people’s motivation to seek prevention and treatment. These findings suggest that interventions to promote engagement with vaccination programs could include communications that challenge these identity beliefs and that explain how vaccination can boost immunity for everyone.
The “Nudge” Approach
A group of methods that has attracted wide attention over the last decade is summarized in the book Nudge: Improving Decisions About Health, Wealth and Happiness (Thaler & Sunstein, 2008 ). These “nudge” methods have been applied by national governments in the United Kingdom and the United States (Cabinet Office Behavioural Insights Team, 2010 ; Local Government Association, 2013 ; Matjasko, Cawley, Baker-Goering, & Yokum, 2016 ). They are defined as “any aspect of the ‘choice architecture’ that alters people’s behaviour in a predictable way without forbidding any options or significantly changing their economic incentives” (Thaler & Sunstein, 2008 , p. 5). They take a “libertarian paternalist” stance regarding human behavior, suggesting that the government can influence people in their best interests as long as the influence is non-intrusive and people’s freedom of choice is retained (Thaler & Sunstein, 2008 ). One of its key concepts, which is rooted in behavioral economics, is that it focuses on how people make decisions and how changes in the environment where the different choices are presented (e.g., healthy snacks versus chocolate bars in shops) can help them make choices that will improve their health (Matjasko et al., 2016 ; Thaler & Sunstein, 2008 ).
Typically, “nudge” interventions include environmental restructuring (e.g., placing healthy food closer to the counter), modeling (e.g., drawing attention to others’ behavior in the social group), and (non-financial) incentivization (e.g., provide collectable badges in digital interventions), all effective in influencing behavior in certain circumstances (Marteau, Ogilvie, Roland, Suhrcke, & Kelly, 2011 ; Matjasko et al., 2016 ; Michie & West, 2013 ). However, they do not include interventions, such as financial incentivization, restrictions, and coercion (e.g., fines for transgressions) or policies such as legislation, regulation and fiscal measures (House of Lords, 2011 ; Marteau et al., 2011 ; Michie & West, 2013 ).
Limiting interventions in this way restricts their effectiveness and cost-effectiveness for equitable public health (Marteau et al., 2011 ; Michie & West, 2013 ) and raises questions about the ideological reasons for these constraints (e.g., giving industry freedoms to make profits at the expense of public health) (Baldwin, 2014 ; Bonell, McKee, Fletcher, Wilkinson, & Haines, 2011 ). A national report on behavior change concluded that it also limited the usefulness of behavior change interventions for national government (House of Lords, 2011 ). For example, countries that introduced legislation to reduce the salt content in foods achieved five times higher reduction in adults’ daily salt consumption, a well-known contributor to high blood pressure, than the United Kingdom, where a different approach was taken involving negotiations with the food industry with only a threat of potential legislation (Cappuccino & Capewell, 2010 ).
Changing people’s behavior on a population scale requires intervention strategies that operate at many levels (individual, organizational, community, population) and use a variety of methods simultaneously in order to target different influences on behavior (BMA, 2012 ; House of Lords, 2011 ; Michie & West, 2013 ; NICE, 2007 , 2014 ). An integrative framework for intervention development that provides a comprehensive range of interventions and policies can inform decisions regarding the most appropriate methods to bring about behavior change.
An Integrative Framework for Designing Behavior Change Interventions: The Behavior Change Wheel
The Behavior Change Wheel is a synthesis of 19 frameworks of behavior change identified in a systematic literature review (Michie, van Stralen, & West, 2011 ). They include widely used frameworks such as “intervention mapping” (Bartholomew, Parcel, Kok, Gottlieb, & Fernandez, 2011 ) and “MINDSPACE” (Institute for Government, 2010 ); the full list and details of the synthesis process can be found in the supplementary files of Michie et al. ( 2011 ). These frameworks were evaluated against three criteria that were deemed to be essential characteristics of their usefulness to inform intervention development: conceptual coherence, comprehensive coverage of intervention types, and linkage to a model of behavior. A conceptually coherent framework includes categories of the same type and specificity of entity, and a comprehensive framework offers the full range of potential types of interventions for intervention designers to consider. The third criterion encapsulates the importance for a framework to provide a system whereby one can formally analyze the target behavior based on a theoretical model and systematically select intervention types depending on what influences need to be changed to achieve behavior change. Since none of the frameworks met all three criteria and there was overlap between them, an integrative framework was developed from the 19 frameworks (Michie, van Stralen, & West, 2011 ).
Figure 1. The Behavior Change Wheel
The Behavior Change Wheel (Figure 1 ) has the COM-B model at its hub surrounded by two rings of intervention strategies. The first ring has nine intervention functions that are direct methods for changing behavior, with the outer ring being seven policy categories which are high-level societal and organizational strategies for implementing and sustaining behavior change. Each intervention function reflects many different behavior change techniques; these are the smallest intervention components that on their own have the potential to change behavior (Michie et al., 2014 ; Michie & Johnston, 2013 ).
The Behavior Change Wheel provides a systematic guide for designing behavior change interventions (Michie et al., 2014 ; Michie, van Stralen, & West, 2011 ). It has been used widely across a range of behavioral domains, settings, and problems. Examples include interventions designed to increase engagement with face-to-face smoking cessation support among adults (Fulton, Brown, Kwah, & Wild, 2016 ), aid smoking cessation among pregnant women (Tombor et al., 2016 ), improve childhood weight management among parents (Curtis, Lahiri, & Brown, 2015 ), promote attentive eating among overweight and obese adults (Robinson et al., 2013 ), reduce cardiovascular disease risk among people with severe mental illness in primary care (Osborn et al., 2016 ), improve the implementation of upper limb exercise in stroke rehabilitation (Connell, McMahon, Redfern, Watkins, & Eng, 2015 ) and improve general practitioners’ management of long-term medications (Sinnott et al., 2015 ).
Selecting effective strategies for behavior change needs to be based on a clear understanding of which behaviors are likely to be most easy to change with greatest impact. This decision should be informed by a “behavioral diagnosis.” A behavioral diagnosis starts with defining the problem that the intervention aims to address (e.g., to reduce childhood obesity) in behavioral terms (e.g., improving children’s diet, increasing their physical activity etc.). For each key candidate behavior, one needs to define the behavior very precisely in terms of who needs to do what differently, when, where, with whom, and how. For example, in order to improve children’s diet, one may suggest that parents need to pack fruits and vegetables in children’s lunchbox every day instead of snacks, or that children need to cut down their daily sugary drink consumption, or that healthcare professionals need to support parents in managing their children’s diet, or that teachers need to include the topic of healthy eating in the school curriculum. Behaviors tackled at policy level include additional categories of people whose behavior is relevant to the target behavior. For example, for food consumption, relevant people would include those involved in the food industry, commissioners of health and social services, town planners, policymakers within local and national government, etc. Given that any behavior is influenced by other behaviors within and between people, both positive and negative “spillover” effects and the significance of these consequences need to be considered.
After specifying the target behavior and population in as much detail as possible (e.g., to help parents pack fruits and vegetables in children’s lunchbox every day instead of snacks), the next step in the behavioral diagnosis involves using the COM-B model or the Theoretical Domains Framework to investigate what needs to be changed in people and/or the environment to bring about behavior change (Francis et al., 2012 ; Michie et al., 2014 ; Michie, van Stralen, & West, 2011 ). A thorough assessment of behavior draws on different sources. This can include evidence from the scientific literature, findings from formal research, and less formal data gathering conducted with people from the target population, stakeholders, and experts in relevant fields by means of interviews, focus groups, and questionnaires (Francis et al., 2012 ). A behavioral diagnosis contributes to a better understanding of the nature of the target behavior in terms of the intrapersonal (e.g., parents’ knowledge and beliefs about what constitutes a “healthy lunchbox”) and environmental influences on its development (e.g., influences of what other parents in the social environment pack in their children’s lunchbox), maintenance, and predicted levers for future change. This can inform decision-making regarding the interventions and policies that are likely to be effective in a given context (Michie et al., 2014 ; Michie, van Stralen, & West, 2011 ).
Within the Behavior Change Wheel, each of the nine intervention functions refers to a general method by which an intervention can change behavior (Michie et al., 2014 ; Michie, van Stralen, & West, 2011 ), and these can be linked with evidence-based principles of behavior change (Table 3 ). The intervention functions are:
Education (e.g., increasing parents’ knowledge about the importance of a healthy diet),
Persuasion (e.g., inducing positive feelings to pack fruits and vegetables in children’s lunchbox),
Incentivization (e.g., creating expectation of financial or other rewards if one packed fruits and vegetables in the child’s lunchbox every day),
Coercion (e.g., increasing the cost of salty food and snacks),
Training (e.g., providing training to parents to improve their skills to cook with healthy ingredients),
Restriction (e.g., using rules to reduce purchasing of energy-dense food),
Environmental restructuring (e.g., using prompts in shops to increase the attractiveness of fruits and vegetables),
Modeling (e.g., providing an example for parents to aspire or imitate when managing their children’s diet), and
Enablement (e.g., providing behavior support for weight management).
For example, a behavioral diagnosis may indicate that increasing parents’ reflective motivation (e.g., their beliefs, intentions, and plans) is one of the important factors to be targeted in interventions aimed at increasing the fruit and vegetable content of children’s lunchbox. One can then draw on the Behavior Change Wheel to identify the intervention functions relevant to changing these: education, persuasion, incentivization, and modeling.
Table 3. Linking Intervention Functions in the Behavior Change Wheel with Evidence-Based Principles of Behavior Change
Depending on the intervention functions selected, the Behavior Change Wheel points to seven policy categories to enable or support the interventions (Michie et al., 2014 ; Michie, van Stralen, & West, 2011 ). These are:
Communication and marketing (e.g., distributing leaflets and organizing mass media campaigns to promote a healthy diet),
Guidelines (e.g., establishing protocols for what constitutes a healthy lunchbox for children),
Fiscal measures (e.g., implementing higher tax on snacks),
Regulation (e.g., prohibiting vending machines on school premises),
Legislation (e.g., introducing laws to ban added sugar in foods marketed for children),
Environmental and social planning (e.g., providing easy access to healthy food items in the localities), and
Service provision (e.g., establishing digital healthcare services to help parents keep track of their children’s diet).
For example, interventions focusing on modeling to change behavior may be supported by policies involving communication and marketing activities and service provision. Definitions of the intervention functions and policy categories are provided in Michie, van Stralen, & West ( 2011 ) and Michie et al. ( 2014 ).
Intervention functions can be put into practice by a large number of behavior change techniques; 93 have been identified and organized into a taxonomy in an international project (Michie et al., 2013 , 2015 ). For more information about these techniques, see Michie et al. ( 2014 , p. 145), online training , and a smartphone app that can be found by searching “BCT taxonomy” in the app stores. Intervention designers can use systematic methods to identify which behavior change techniques are likely to be the most appropriate given their target behavior/s, population, setting, and intervention constraints (Michie et al., 2014 ).
Behavior Change Techniques and Taxonomies
Behavior change interventions are complex, at least in part, because they include many interacting components (Craig et al., 2008 ). Specifying interventions by behavior change techniques improves the precise reporting of the content of complex interventions so that they can be evaluated, delivered with fidelity, replicated, and generalized to different contexts. Using a shared language when describing intervention content can facilitate this process, and taxonomies of behavior change techniques have been developed with agreed labels and definitions. For example, “action planning” must include detailed planning of performance of the behavior in terms of at least one of context, frequency, duration, or intensity (Michie et al., 2013 ).
Several taxonomies have been developed for specific behavioral domains including physical activity and healthy eating (Abraham & Michie, 2008 ; Michie, Ashford, et al., 2011 ), smoking cessation (Michie, Hyder, Walia, & West, 2011 ; West, Evans, & Michie, 2011 ), reducing excessive alcohol consumption (Michie et al., 2012 ), and increasing condom use (Abraham, Good, Huedo-Medina, Warren, & Johnson, 2012 ). Building on these taxonomies, the Behavior Change Techniques Taxonomy v1 (BCTTv1) was developed by an international consensus of 400 experts from 12 countries. It includes 93 distinct behavior change techniques that are hierarchically structured and clustered into 16 higher-order groups (Michie et al., 2013 , 2015 ).
An empirical approach, involving open-sort grouping tasks and hierarchical cluster analysis, was used to group behavior change techniques in the BCTTv1 (Michie et al., 2013 , 2015 ). The structure of each higher-order grouping containing similar behavior change techniques in terms of their mechanisms of change can aid easier recall of behavior change techniques and the practical use of the taxonomy. Behavior change techniques in the BCTTv1 can also be reliably linked to domains from the Theoretical Domains Framework. There is a moderate overlap between higher-order groups and theoretical domains. Both of these and the simpler COM-B model can aid the selection of behavior change techniques to inform theory-based intervention development, which is used by researchers appears to reflect personal preference and past practice. Higher-order groups with example behavior change techniques are:
Goals and planning (e.g., “goal setting”),
Feedback and monitoring (e.g., “self-monitoring of behavior”),
Social support (e.g., “social support, practical”),
Shaping knowledge (e.g., “instruction on how to perform a behavior”),
Natural consequences (e.g., “information about health consequences”),
Comparison of behavior (e.g., “social comparison”),
Associations (e.g., “prompts/cues”),
Repetition and substitution (e.g., “behavioral practice/rehearsal”),
Comparison of outcomes (e.g., “pros and cons”),
Reward and threat (e.g., “material reward, behavior”),
Regulation (e.g., “pharmacological support”),
Antecedents (e.g., “adding objects to the environment”),
Identity (e.g., “valued self-identity”),
Scheduled consequences (e.g., “behavior cost”),
Self-belief (e.g., “self-talk”), and
Covert learning (e.g., “imaginary reward”).
Evidence regarding the effectiveness of behavior change techniques is accumulating for different behaviors and populations, for example, to improve dietary behaviors (Lara et al., 2014 ), increase sedentary behavior (Gardner, Smith, Lorencatto, Hamer, & Biddle, 2016 ), and aid physical activity among healthy and overweight adults (Williams & French, 2011 ), obese adults (Olander et al., 2013 ), and older adults (French, Olander, Chisholm, & Sharry, 2014 ). There is some evidence to suggest that interventions that use more behavior change techniques are more effective than those that use fewer behavior change techniques (Gardner et al., 2016 ; Webb, Joseph, Yardley, & Michie, 2010 ).
Behavior change techniques may yield greater effects if they are delivered in theoretically informed groups rather than in isolation. An effective combination of behavior change techniques that work synergistically together is self-monitoring with goal-setting, action planning, and/or feedback on behavior (Dombrowski et al., 2012 ; Michie, Abraham, Whittington, McAteer, & Gupta, 2009 ). Also, problem-solving has been found to be more effective in combination with providing rewards for behavior (van Genugten, Dusseldorp, Webb, & van Empelen, 2016 ). A third example is that although using threatening communications about health risks has been advocated to change behavior, such as to aid smoking cessation (Borland et al., 2009 ), its effectiveness has been found to be greater if it is paired with increasing people’s confidence to change (“self-efficacy”) (Peters, Ruiter, & Kok, 2013 ).
Relevant research evidence is an important criterion for selecting behavior change techniques for a given behavior, population, and setting. However, there are other criteria to be considered when selecting behavior change techniques that are likely to increase the implementation of interventions.
Systematic Context-Based Decision-Making About Behavior Change Interventions: The APEASE Criteria
The process of intervention development is likely to generate a large number of possible intervention functions, behavior change techniques, and policy categories. However, it may not be possible or appropriate to implement all of these given the context and limitations such as the mode of delivery of the intervention and resources, and thus decisions have to be made as to which methods to include based on explicit reasons (Michie et al., 2014 ).
The APEASE (Affordability, Practicability, Effectiveness and cost-effectiveness, Acceptability, Safety and side effects, Equity) criteria have been developed to help intervention developers and policymakers follow a systematic decision-making process when designing behavior change interventions (Michie et al., 2014 ). “Affordability” refers to interventions being designed and delivered within a specified budget and accessed by people from the target population. “Practicability” refers to whether it is feasible to deliver the intervention as intended. “Effectiveness” refers to whether the intervention is effective in relevant real-world contexts. This should be judged based on evidence primarily from high-quality randomized controlled trials and experimental and observational studies. When considering the implementation of effective interventions, more weight should be given to the more cost-effective ones. “Acceptability” refers to whether the intervention is likely to be acceptable to relevant stakeholders, including people from the target population, policymakers, healthcare professionals, funding agencies, and national governments. The criterion of “safety and side effects” refers to the possible unwanted or unintended consequences of an effective intervention. A behavior change intervention meets the criterion of “equity” to the extent that it reduces the disparities between different groups of society and provides equal access to the intervention across the social spectrum.
Although APEASE provides a structured way of assessing intervention methods, intervention designers and policymakers need to draw on local knowledge and their own expertise when selecting the most appropriate intervention functions, behavior change techniques, and policies to be implemented in a given context. The criteria will be illustrated in relation to interventions to increase smoking cessation.
There is ample evidence that the most effective treatments for tobacco dependence are those that combine pharmacotherapy with behavioral support provided by smoking cessation specialist advisors (Kotz, Brown, & West, 2013 ; Stead & Lancaster, 2012 ). Although these are both effective and cost-effective interventions (APPG, 2010 ; West, May, West, Croghan, & McEwen, 2013 ), some of the more expensive smoking cessation medications (e.g., varenicline) and multi-session counseling may not be globally affordable, especially in low-income countries (West et al., 2015 ). On the other hand, brief opportunistic smoking cessation advice from healthcare professionals, proactive telephone support, text messaging interventions, printed self-help materials, and some forms of pharmacotherapy (e.g., cytisine) are also effective and appear to be globally affordable to aid cessation (West et al., 2015 ).
In terms of practicability, effective behavior change techniques, such as providing feedback on smokers’ expired carbon monoxide readings (Shahab, West, & McNeill, 2011 ), may be considered as more feasible if delivered face-to-face rather than via digital interventions (Tombor, Neale, Shahab, Ruiz, & West, 2015 ).
Providing financial incentives for smoking cessation in pregnancy has been found to be effective and highly cost-effective, and therefore it may be considered in high-income countries as a valuable addition to existing public health services (Boyd, Briggs, Bauld, Sinclair, & Tappin, 2015 ; Higgins et al., 2012 ; Lumley et al., 2009 ; Tappin et al., 2015 ).
In terms of acceptability, it has been found that a third of current smokers in England would support a total ban on sale of tobacco products (Shahab & West, 2010 ). However, if this is not aligned with national governmental objectives, the intervention is unlikely to be supported by relevant policies.
Providing financial incentives is effective in increasing smoking cessation rates among pregnant smokers (Tappin et al., 2015 ); however, unintended consequences have been identified including creating distrust between healthcare professionals and clients and increasing the negative public perception of pregnant smokers (Thomson et al., 2014 ). It is important to identify potential negative consequences, and it needs to be considered whether the expected benefits of a behavior change intervention would be likely to outweigh its potential risks.
Smokers from low-socioeconomic groups are less likely to stop smoking than smokers from high socioeconomic groups (Kotz & West, 2009 ). Even though they are motivated to quit (Kotz & West, 2009 ), smokers from disadvantaged backgrounds are less likely to attend face-to-face support and use pharmacotherapy for long enough to aid cessation (ASH, 2016 ; Hiscock & Bauld, 2013 ). Improving equity of access to, and use of, effective smoking cessation support requires interventions to meet the needs of smokers across the social spectrum and target deprived communities where smoking prevalence is the highest (ASH, 2016 ; Hiscock & Bauld, 2013 ).
The APEASE criteria have been used to inform the development and evaluation of behavior change interventions in various settings, such as to improve antibiotic prescribing in long-term care facilities (Fleming et al., 2014 ), improve the routine delivery of caries prevention and management in primary dental care (Templeton et al., 2015 ), optimize general practitioners’ medication management for patients with multiple chronic conditions (Sinnott et al., 2015 ), select modes of delivery for an intervention targeting multiple health behaviors among students (Tzelepis et al., 2015 ), and modify an existing evidence-based intervention for sepsis treatment in order to improve its implementation (Steinmo et al., 2016 ).
Future Directions
For policymakers, intervention designers and researchers, a key question is: What behavior change interventions work, how well, for whom, in what settings, for what behaviors and why? To assist in this, future work is building an “ontology” of behavior change interventions (Larsen et al., 2017 ). Ontologies provide systematic and efficient methods for generating organized structures of knowledge base. An ontological framework comprises clearly defined key concepts (“classes”) (e.g., intervention, mechanisms of action, intervention usage, context, and behavior) and the relationship between them. Classes and relationships are specified using controlled vocabularies (e.g., the BCTTv1 can be used to specify behavior change techniques) and codified in a computer-readable format (Larsen et al., 2017 ). The Human Behaviour-Change Project is a collaboration between behavioral scientists, information scientists and computer scientists. This multi-disciplinary team aims to build an artificial intelligence system that will continually scan the scientific literature on behavior change, identify key information using natural language processing and machine learning, and extract relevant information into the Behavior Change Intervention Ontology. Knowledge generated in this project through the evidence synthesis can provide a basis for a better understanding of human behavior and effective methods to achieve behavior change beyond the context of individual studies. The system will be accessible to researchers, intervention designers, and policymakers so that they can obtain up-to-date evidence of effective methods to change particular behaviors given the target population and context. The Human Behaviour-Change Project will accumulate evidence on behavior change more efficiently and rapidly and contribute to designing more effective interventions tailored to behaviors, populations, and contexts.
Further Reading
- The UCL Centre for Behaviour Change and further resources for topics mentioned in this article .
- Soundcloud is a source for podcasts about behavior change .
- BCT Taxonomy v1 online training .
- Jepson, R. G. , Harris, F. M. , Platt, S. , & Tannahill, C. (2010). The effectiveness of interventions to change six health behaviours: A review of reviews . BMC Public Health, 10 , 538.
- Kok, G. , Gottlieb, N. H. , Peters, G.-J. Y. , Dolan Mullen, P. , Parcel, G. S. , Ruiter, R. A. C. et al. (2016). A taxonomy of behaviour change methods: An intervention mapping approach . Health Psychology Review, 10 (3), 297–312.
- Peters, G. J. , de Bruin, M. , & Crutzen, R. (2015). Everything should be as simple as possible, but no simpler: Towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions . Health Psychology Review, 9 (1), 1–14.
- Presseau, J. , Johnston, M. , Heponiemi, T. , Elovainio, M. , Francis, J. J. , Eccles, M. P. et al. (2014). Reflective and automatic processes in health care professional behaviour: A dual process model tested across multiple behaviours . Annals of Behavior Medicine, 48 , 347–358.
- Riley, W. T. , & Rivera, D. E. (2014). Methodologies for optimizing behavioral interventions: Introduction to special section . Translational Behavioral Medicine: Practice, Policy and Research, 4 (3), 234–237.
- Spruijt-Metz, D. , Hekler, E. , Saranummi, N. , Intille, S. , Korhonen, I. , Nilsen, W. et al. (2015). Building new computational models to support health behavior change and maintenance: New opportunities in behavioral research . Translational Behavioral Medicine: Practice, Policy and Research, 5 (3), 335–346.
- Tate, D. F. , Lytle, L. A. , Sherwood, N. E. , Haire-Joshu, D. , Matheson, D. , Moore, S. M. et al. (2016). Deconstructing interventions: Approaches to studying behavior change techniques across obesity interventions . Translational Behavioral Medicine: Practice, Policy and Research, 6 (2), 236–243.
- Abraham, C. , Good, A. , Huedo-Medina, T. , Warren, M. , & Johnson, B. (2012). Reliability and utility of the SHARP Taxonomy of Behaviour Change Techniques. EHPS 2012 abstracts . Psychology & Health, 27 (Suppl. 1), 1–357.
- Abraham, C. , Kelly, M. P. , West, R. , & Michie, S. (2009). The UK National Institute for Health and Clinical Excellence Public Health Guidance on behaviour change: A brief introduction . Psychology, Health and Medicine, 14 (1), 1–8.
- Abraham, C. , & Michie, S. (2008). A taxonomy of behavior change techniques used in interventions . Health Psychology, 27 (3), 379–387.
- AIHW . (2014). Australia’s health 2014 . Canberra, Australia: Australian Institute of Health and Welfare.
- APPG . (2010). Inquiry into the effectiveness and cost-effectiveness of tobacco control: Submission to the 2010 Spending Review and Public Health White Paper Consultation process . London: All Party Parliamentary Group on Smoking and Health.
- ASH . (2016). Health inequalities and smoking. Action on Smoking and Health . Available at http://www.ash.org.uk/current-policy-issues/health-inequalities/smoking-and-health-inequalities .
- Baldwin, R. (2014). From regulation to behaviour change: giving nudge the third degree. The Modern Law Review, 77 (6), 831–857.
- Bartholomew, L. , Parcel, G. , Kok, G. , Gottlieb, N. , & Fernandez, M. E. (2011). Planning health promotion programmes: An intervention mapping approach (3d ed.). San Francisco: Jossey-Bass.
- BMA . (2012). Behaviour change, public health and the role of the state—BMA position statement . London: British Medical Association.
- Bonell, C. , McKee, M. , Fletcher, A. , Wilkinson, P. , & Haines, A. (2011). One nudge forward, two steps back . BMJ , 342 , d401.
- Borland, R. , Yong, H.-H. , Wilson, N. , Fong, G. T. , Hammond, D. , Cummings, K. M. , et al. (2009). How reactions to cigarette packet health warnings influence quitting: Findings from the ITC Four-Country survey . Addiction, 104 (4), 669–675.
- Boyd, K. A. , Briggs, A. H. , Bauld, L. , Sinclair, L. , & Tappin, D. (2015). Are financial incentives cost-effective to support smoking cessation during pregnancy? Addiction, 111 , 360–370.
- Bussieres, A. E. , Patey, A. M. , Francis, J. , Sales, A. E. , & Grimshaw, J. M. (2012). Identifying factors likely to influence compliance with diagnostic imaging guideline recommendations for spine disorders among chiropractors in North America: A focus group study using the Theoretical Domains Framework. Implementation Science, 7 (1), 82.
- Cabinet Office Behavioural Insights Team . (2010). Applying behavioural insight to health . London: Cabinet Office Behavioural Insights Team.
- Cane, J. , O’Connor, D. , & Michie, S. (2012). Validation of the Theoretical Domains framework for use in behaviour change and implementation research . Implementation Science, 7 (37).
- Cappuccino, F. P. , & Capewell, S. (2010). How to cut down salt intake in populations . Heart, 96 (23), 1863–1864.
- CDC . (2013). Ten great public health achievements in the 20th century. Centers for Disease Control . Available at http://www.cdc.gov/about/history/tengpha.htm .
- Connell, L. A. , McMahon, N. E. , Redfern, J. , Watkins, C. L. , & Eng, J. J. (2015). Development of a behaviour change intervention to increase upper limb exercise in stroke rehabilitation . Implementation Science, 10 , 34.
- Craig, P. , Dieppe, P. , Macintyre, S. , Michie, S. , Nazareth, I. , & Petticrew, M. (2008). Developing and evaluating complex interventions: The new Medical Research Council guidance . British Medical Journal, 337 (a1655).
- Curtis, K. E. , Lahiri, S. , & Brown, K. E. (2015). Targeting parents for childhood weight management: development of a theory-driven and user-centered healthy eating app. JMIR Mhealth Uhealth, 3 (2), e69.
- Davis, R. , Campbell, R. , Hildon, Z. , Hobbs, L. , & Michie, S. (2015). Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review . Health Psychology Review, 9 (3), 323–344.
- Department of Health . (2014). Living well for longer: National support for local action to reduce premature avoidable mortality . London: Department of Health.
- Dombrowski, S. U. , Sniehotta, F. F. , Avenell, A. , Johnston, M. , MacLennan, G. , & Araujo-Soares, V. (2012). Identifying active ingredients in complex behavioural interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: A systematic review . Health Psychology Review, 6 (1), 7–32.
- Duncan, E. M. , Francis, J. , Johnston, M. , Davey, P. , Maxwell, S. , McKay, G. A. , et al. (2012). Learning curves, taking instructions, and patient safety: Using a theoretical domains framework in an interview study to investigate prescribing errors among trainee doctors. Implementation Science, 7 (1), 86.
- Fleming, A. , Bradley, C. , Cullinan, S. , & Byrne, S. (2014). Antibiotic prescribing in long-term care facilities: A qualitative multidisciplinary investigation . BMJ OPen, 4 (11), e006442.
- Francis, J. , O’Connor, D. , & Curran, J. A. (2012). Theories of behaviour change synthesised into a set of theoretical groupings: Introducing a thematic series on the theoretical domains framework. Implementation Science, 7 (1), 35.
- French, D. P. , Olander, E. K. , Chisholm, A. , & Sharry, J. Mc . (2014). Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review . Annals of Behavioral Medicine, 48 , 225–234.
- French, S. D. , Green, S. E. , O’Connor, D. A. , McKenzie, J. E. , Francis, J. , Michie, S. , et al. (2012). Developing theory-informed behaviour change interventions to implement evidence into practice: A systematic approach using the Theoretical Domains Framework . Implementation Science, 7 , 38.
- Fuller, C. , Michie, S. , Savage, J. , McAteer, J. , Besser, S. , Charlett, A. , et al. (2012). The Feedback Intervention Trial (FIT)—Improving hand-hygiene compliance in UK healthcare workers: A stepped wedge cluster randomised controlled trial. PLoS One, 7 (10), e41617.
- Fulton, E. A. , Brown, K. , Kwah, K. , & Wild, S. (2016). Stop-app: Using the Behaviour Change Wheel to develop an app to increase uptake and attendance at NHS Stop Smoking Services . Healthcare 4 (2), 31.
- Gardner, B. (2015). A review and analysis of the use of “habit” in understanding, predicting and influencing health-related behaviour . Health Psychology Review, 9 (3), 277–295.
- Gardner, B. , Smith, L. , Lorencatto, F. , Hamer, M. , & Biddle, B. J. (2016). How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults . Health Psychology Review, 10 (1), 89–112.
- Hallsworth, M. , Chadborn, T. , Sallis, A. , Sanders, M. , Berry, D. , Greaves, F. , et al. (2016). Provision of social norm feedback to high prescribers of antibiotics in general practice: A pragmatic national randomised controlled trial . Lancet, 387 (10029), 1743–1752.
- Higgins, S. T. , Washio, Y. , Heil, S. H. , Solomon, L. J. , Gaalema, D. E. , Higgins, T. M. , et al. (2012). Financial incentives for smoking cessation among pregnant and newly postpartum women . Preventive Medicine, 55 (Suppl.), S33–S40.
- Hinman, A. (1999). Eradication of vaccine-preventable diseases . Annual Review of Public Health, 20 , 211–229.
- Hiscock, R. , & Bauld, L. (2013). Stop smoking services and health inequalities. In A. McEwen (Ed.), Stop smoking services and health inequalities, 10 , 1–7. London: National Centre for Smoking Cessation and Training.
- Holmes, K. K. , Levine, R. , & Weaver, M. (2004). Effectiveness of condoms in preventing sexually transmitted infections. Bulletin of the World Health Organization, 82 (6), 454–461.
- House of Lords . (2011). Behaviour change (2nd Report of Session 2010–2012). London: House of Lords, Science and Technology Select Committee.
- Institute for Government . (2010). MINDSPACE: Influencing behaviour through public policy . London: Institute for Government, the Cabinet Office.
- Ito, K. , Shrank, W. , Avron, J. , Patrick, A. R. , Brennan, T. A. , Antman, E. M. , et al. (2012). Comparative cost-effectiveness of interventions to improve medication adherence after myocardial infarction . Health Services Research, 47 (6), 2097–2117.
- Johnson, N. B. , Hayes, L. D. , Brown, K. , Hoo, E. C. , & Ethier, K. A. (2014). CDC National Health Report: Leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005–2013. Morbidity and Mortality Weekly Report , 63 (4), 3–27.
- Kotz, D. , Brown, J. , & West, R. (2013). “Real-world” effectiveness of smoking cessation treatments: a population study . Addiction, 109 (3), 491–499.
- Kotz, D. , & West, R. (2009). Explaining the social gradient in smoking cessation: It’s not in the trying, but in the succeeding . Tobacco Control, 18 , 43–46.
- Lara, J. , Evans, E. H. , O’Brien, N. , Moynihan, P. J. , Meyer, T. D. , Adamson, A. J. , et al. (2014). Associations of behaviour change techniques with effectiveness of dietary interventions among adults of retirement age: A systematic review and meta-analysis of randomised controlled trials . BMC Medicine, 12 (60), 177.
- Larsen, K. R. , Michie, S. , Hekler, E. B. , Gibson, B. , Spruijt-Metz, D. , Ahern, D. , et al. (2017). Behavior change interventions: The potential of ontologies for advancing science and practice . Journal of Behavioral Medicine, 40 (1), 6–22.
- Llor, C. , Hernandez, S. , Bayona, C. , Moragas, A. , Sierra, N. , Hernandez, M. , et al. (2013). A study of adherence to antibiotic treatment in ambulatory respiratory infections . International Journal of Infectious Diseases, 17 (3), e168–e172.
- Local Government Association . (2013). Changing behaviours in public health. To nudge or to shove? London: Local Government Association.
- Logan, R. F. A. , Patnick, J. , Nickerson, C. , Coleman, L. , Rutter, M. D. , & von Wagner, C. (2011). Outcomes of the Bowel Cancer Screening Programme (BCSP) in England after the first 1 million tests. . Gut, 61 (10), 1439–1446.
- Lumley, J. , Chamberlain, C. , Dowswell, T. , Oliver, S. , Oakley, L. , & Watson, L. (2009). Interventions for promoting smoking cessation during pregnancy . Cochrane Database of Systematic Reviews, 8 (3).
- Marteau, T. M. , Ogilvie, D. , Roland, M. , Suhrcke, M. , & Kelly, M. P. (2011). Judging nudging: Can nudging improve population health? BMJ, 342 , d228.
- Matjasko, J. L. , Cawley, J. H. , Baker-Goering, M. M. , & Yokum, D. V. (2016). Applying behavioral economics to public health policy: Illustrative examples and promising directions . American Journal of Preventive Medicine, 50 (5 Suppl. 1), S13–S19.
- Michie, S. , Abraham, C. , Whittington, C. , McAteer, J. , & Gupta, S. (2009). Effective techniques in healthy eating and physical activity interventions: A meta-regression . Health Psychology, 28 (6), 690–701.
- Michie, S. , Ashford, S. , Sniehotta, F. F. , Dombrowski, S. U. , Bishop, A. , & French, D. P. (2011). A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy . Psychology & Health, 26 (11), 1479–1498.
- Michie, S. , Atkins, L. , & West, R. (2014). The Behaviour Change Wheel: A guide to designing interventions . London: Silverback Publishing.
- Michie, S. , Hyder, N. , Walia, A. , & West, R. (2011). Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation . Addictive Behaviors, 36 (4), 315–319.
- Michie, S. , & Johnston, M. (2013). Behavior change techniques. In J. R. Turner (Ed.), Encyclopedia of behavioral medicine (pp. 182–187). New York: Springer.
- Michie, S. , Johnston, M. , Abraham, C. , Lawton, R. , Parker, D. , & Walker, A. (2005). Making psychological theory useful for implementing evidence based practice: A consensus approach . Quality & Safety in Health Care, 14 (1), 26–33.
- Michie, S. , Richardson, M. , Johnston, M. , Abraham, C. , Francis, J. , Hardeman, W. , et al. (2013). The Behavior Change Technique Taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions . Annals of Behavioral Medicine , 46 (1), 81–95.
- Michie, S. , van Stralen, M. M. , & West, R. (2011). The Behaviour Change Wheel: A new method for characterising and designing behaviour change interventions . Implementation Science, 6 (42).
- Michie, S. , & West, R. (2013). Behaviour change theory and evidence: A presentation to Government . Health Psychology Review, 7 (1), 1–22.
- Michie, S. , Whittington, C. , Hamoudi, Z. , Zarnani, F. , Tober, G. , & West, R. (2012). Identification of behaviour change techniques to reduce excessive alcohol consumption . Addiction, 107 (8), 1431–1440.
- Michie, S. , Wood, C. E. , Johnston, M. , Abraham, C. , Francis, J. J. , & Hardeman, W. (2015). Behaviour change techniques: The development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data) . Health Technology Assessment, 19 (99), 1–188.
- NICE . (2007). Behaviour change at population, community and individual levels . London: National Institute for Health and Clinical Excellence.
- NICE . (2014). Behaviour change: Individual approaches . London: National Institute for Health and Clinical Excellence.
- O’Neill, J. (2014). Antimicrobial resistance: Tackling a crisis for the health and wealth of nations . London: U.K. Government
- Olander, E. K. , Fletcher, H. , Williams, S. , Atkinson, L. , Turner, A. , & French, D. P. (2013). What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behaviour: A systematic review and meta-analysis. International Journal of Behavioural Nutrition and Physical Activity, 10 (1), 29.
- Osborn, D. , Burton, A. , Walters, K. , Nazareth, I. , Heinkel, S. , Atkins, L. , et al. (2016). Evaluating the clinical and cost effectiveness of a behaviour change intervention for lowering cardiovascular disease risk for people with severe mental illnesses in primary care (PRIMROSE study): Study protocol for a cluster randomised controlled trial . Trials, 17 , 80.
- Ownby, R. , Waldrop-Valverde, D. , Jacobs, R. J. , Acevedo, A. , & Caballero, J. (2013). Cost effectiveness of computer-delivered intervention to improve HIV medication adherence . BMC Medical Informatics and Decision Making, 13 , 29
- Peters, G.-J. Y. , Ruiter, R. A. C. , & Kok, G. (2013). Threatening communication: A critical re-analysis and a revised meta-analytic test of fear appeal theory . Health Psychology Review, 7 (Suppl 1), S8–S31.
- Robinson, E. , Higgs, S. , Daley, A. J. , Jolly, K. , Lycett, D. , Lewis, A. , et al. (2013). Development and feasibility testing of a smart phone based attentive eating intervention . BMC Public Health, 13 (1), 639.
- Rubinstein, H. , Marcu, A. , Yardley, L. , & Michie, S. (2015). Public preferences for vaccination and antiviral medicines under different pandemic flu outbreak scenarios . BMC Public Health, 15 , 190.
- Sackett, D. L. , Rosenberg, W. M. C. , Gray, J. A. M , Haynes, R. B. , & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t . BMJ, 312 , 71.
- Shahab, L. , & West, R. (2010). Public support in England for a total ban on the sale of tobacco products . Tobacco Control, 19 , 143–147.
- Shahab, L. , West, R. , & McNeill, A. (2011). A randomized, controlled trial of adding expired carbon monoxide feedback to brief stop smoking advice: Evaluation of cognitive and behavioral effects . Health Psychology, 30 (1), 49–57.
- Sinnott, C. , Mercer, S. W. , Payne, R. A. , Duerden, M. , Bradley, C. P. , & Byrne, M. (2015). Improving medication management in multimobidity: Development of the MultimorbiditY COllaborative Medication Review And DEcision Making (MY COMRADE) intervention using the Behaviour Change Wheel . Implementation Science, 10 , 132.
- Stead, L. F. , & Lancaster, T. (2012). Combined pharmacotherapy and behavioural interventions for smoking cessation . Cochrane Database of Systematic Reviews, 12 , CD008286.
- Steinmo, S. H. , Michie, S. , Fuller, C. , Stanley, S. , Stapleton, C. , & Stone, S. P. (2016). Bridging the gap between pragmatic intervention design and theory: Using behavioural science tools to modify an existing quality improvement programme to implement “Sepsis Six” . Implementation Science, 11 , 14.
- Tappin, D. , Bauld, L. , Purves, D. , Boyd, K. , Sinclair, L. , MacAskill, S. , et al. (2015). Financial incentives for smoking cessation in pregnancy: Randomised controlled trial . BMJ, 350 (h134).
- Tavender, E. J. , Bosch, M. , Gruen, R. L. , Green, S. E. , Michie, S. , Brennan, S. E. , et al. (2015). Developing a targeted, theory-informed implementation intervention using two theoretical frameworks to address health professional and organisational factors: A case study to improve the management of mild traumatic brain injury in the emergency department . Implementation Science, 10 (74).
- Templeton, A. R. , Young, L. , Bish, A. , Gnich, W. , Cassie, H. , Treweek, S. , et al. (2015). Patient-, organization-, and system-level barriers and facilitators to preventive oral health care: A convergent mixed-methods study in primary dental care . Implementation Science, 11 , 5.
- Thaler, R. , & Sunstein, C. (2008). Nudge: Improving decisions about health, wealth and happiness . New Haven, CT: Yale University Press.
- Thomson, G. , Morgan, H. , Crossland, N. , Bauld, L. , Dykes, F. , & Hoddinott, P. (2014). Unintended consequences of incentive provision for behaviour change and maintenance around childbirth . PLoS One, 9 (10), e111322.
- Tombor, I. , Neale, J. , Shahab, L. , Ruiz, M. , & West, R. (2015). Healthcare providers’ views on digital smoking cessation interventions for pregnant women . Journal of Smoking Cessation, 10 (2), 116–123.
- Tombor, I. , Shahab, L. , Brown, J. , Crane, D. , Michie, S. , & West, R. (2016). Development of SmokeFree Baby: A smoking cessation smartphone app for pregnant smokers . Translational Behavioral Medicine: Practice, Policy and Research, 6 (4), 533–545.
- Tzelepis, F. , Paul, C. L. , Wiggers, J. , Kypri, K. , Bonevski, B. , McElduff, P. , et al. (2015). Targeting multiple health risk behaviours among vocational education students using electronic feedback and online and telephone support: Protocol for a cluster randomised trial . BMC Public Health, 15 , 550.
- van Genugten, L. , Dusseldorp, E. , Webb, T. L. , & van Empelen, P. (2016). Which combinations of techniques and modes of delivery in Internet-based interventions effectively change health behavior? A meta-analysis . JMIR Mhealth Uhealth, 18 (6), e155.
- Verplanken, B. , & Wood, W. (2006). Interventions to break and create consumer habits. Journal of Public Policy and Marketing, 25 (1), 90–103.
- Webb, T. L. , Joseph, J. , Yardley, L. , & Michie, S. (2010). Using the Internet to promote health behaviour change: a systematic review and meta-analysis of the impact of theoretical basis, use of behaviour change techniques, and mode of delivery on efficacy . Journal of Medical Internet Research, 12 (1), e4.
- West, R. , Evans, A. , & Michie, S. (2011). Behavior change techniques used in group-based behavioral support by the English stop-smoking services and preliminary assessment of association with short-term quit outcomes . Nicotine & Tobacco Research, 13 (12), 1316–1320.
- West, R. , May, S. , West, M. , Croghan, E. , & McEwen, A. (2013). Performance of English stop smoking services in first 10 years: Analysis of service monitoring data . BMJ, 347 (f4921).
- West, R. , Raw, M. , McNeill, A. , Stead, L. , Aveyard, P. , Britton, J. , et al. (2015). Healthcare interventions to promote and assist tobacco cessation: A review of efficacy, effectiveness and affordability for use in national guideline development . Addiction, 110 (9), 1388–1403.
- Williams, S. L. , & French, D. P. (2011). What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour—and are they the same? Health Education Research, 26 (2), 308–322.
- Wood, W. , & Rünger, D. (2016). Psychology of habit . Annual Review of Psychology, 67 , 289–314.
- World Health Organization (WHO) . (2009). Global health risks: Mortality and burden of diseases attributable to selected major risks . Geneva: World Health Organization.
Related Articles
- Habit Formation and Behavior Change
- Psychological Aspects of Tobacco Control
- Internet-Based Methods in Managing Alcohol Misuse
- Illness-Related Cognition
- Loneliness and Health
- Exercise Psychology Considerations for Chronically Ill Patients
- Theoretical Approaches to Physical Activity Promotion
- Use of Wearable Activity Trackers for Physical Activity Promotion
Printed from Oxford Research Encyclopedias, Psychology. Under the terms of the licence agreement, an individual user may print out a single article for personal use (for details see Privacy Policy and Legal Notice).
date: 29 April 2024
- Cookie Policy
- Privacy Policy
- Legal Notice
- Accessibility
- [66.249.64.20|185.148.24.167]
- 185.148.24.167
Character limit 500 /500
The transtheoretical model of health behavior change
Affiliation.
- 1 Cancer Prevention Research Center, University of Rhode Island, Kingston 02881-0808, USA. [email protected]
- PMID: 10170434
- DOI: 10.4278/0890-1171-12.1.38
The transtheoretical model posits that health behavior change involves progress through six stages of change: precontemplation, contemplation, preparation, action, maintenance, and termination. Ten processes of change have been identified for producing progress along with decisional balance, self-efficacy, and temptations. Basic research has generated a rule of thumb for at-risk populations: 40% in precontemplation, 40% in contemplation, and 20% in preparation. Across 12 health behaviors, consistent patterns have been found between the pros and cons of changing and the stages of change. Applied research has demonstrated dramatic improvements in recruitment, retention, and progress using stage-matched interventions and proactive recruitment procedures. The most promising outcomes to data have been found with computer-based individualized and interactive interventions. The most promising enhancement to the computer-based programs are personalized counselors. One of the most striking results to date for stage-matched programs is the similarity between participants reactively recruited who reached us for help and those proactively recruited who we reached out to help. If results with stage-matched interventions continue to be replicated, health promotion programs will be able to produce unprecedented impacts on entire at-risk populations.
Publication types
- Research Support, U.S. Gov't, P.H.S.
- Decision Making, Computer-Assisted
- Expert Systems
- Health Behavior*
- Health Promotion / methods*
- Models, Psychological*
- Smoking Cessation / methods
- Treatment Outcome
Grants and funding
- CA 27821/CA/NCI NIH HHS/United States
- CA50087/CA/NCI NIH HHS/United States
- HC 48190/HC/NHLBI NIH HHS/United States

Using these brief interventions, you can help your patients make healthy behavior changes.
STEPHANIE A. HOOKER, PHD, MPH, ANJOLI PUNJABI, PHARMD, MPH, KACEY JUSTESEN, MD, LUCAS BOYLE, MD, AND MICHELLE D. SHERMAN, PHD, ABPP
Fam Pract Manag. 2018;25(2):31-36
Author disclosures: no relevant financial affiliations disclosed.

Effectively encouraging patients to change their health behavior is a critical skill for primary care physicians. Modifiable health behaviors contribute to an estimated 40 percent of deaths in the United States. 1 Tobacco use, poor diet, physical inactivity, poor sleep, poor adherence to medication, and similar behaviors are prevalent and can diminish the quality and length of patients' lives. Research has found an inverse relationship between the risk of all-cause mortality and the number of healthy lifestyle behaviors a patient follows. 2
Family physicians regularly encounter patients who engage in unhealthy behaviors; evidence-based interventions may help patients succeed in making lasting changes. This article will describe brief, evidence-based techniques that family physicians can use to help patients make selected health behavior changes. (See “ Brief evidence-based interventions for health behavior change .”)
Modifiable health behaviors, such as poor diet or smoking, are significant contributors to poor outcomes.
Family physicians can use brief, evidence-based techniques to encourage patients to change their unhealthy behaviors.
Working with patients to develop health goals, eliminate barriers, and track their own behavior can be beneficial.
Interventions that target specific behaviors, such as prescribing physical activity for patients who don't get enough exercise or providing patient education for better medication adherence, can help patients to improve their health.
CROSS-BEHAVIOR TECHNIQUES
Although many interventions target specific behaviors, three techniques can be useful across a variety of behavioral change endeavors.
“SMART” goal setting . Goal setting is a key intervention for patients looking to make behavioral changes. 3 Helping patients visualize what they need to do to reach their goals may make it more likely that they will succeed. The acronym SMART can be used to guide patients through the goal-setting process:
Specific. Encourage patients to get as specific as possible about their goals. If patients want to be more active or lose weight, how active do they want to be and how much weight do they want to lose?
Measurable. Ensure that the goal is measurable. For how many minutes will they exercise and how many times a week?
Attainable. Make sure patients can reasonably reach their goals. If patients commit to going to the gym daily, how realistic is this goal given their schedule? What would be a more attainable goal?
Relevant. Ensure that the goal is relevant to the patient. Why does the person want to make this change? How will this change improve his or her life?
Timely. Help patients define a specific timeline for the goal. When do they want to reach their goal? When will you follow-up with them? Proximal, rather than distal, goals are preferred. Helping patients set a goal to lose five pounds in the next month may feel less overwhelming than a goal of losing 50 pounds in the next year.
Problem-solving barriers . Physicians may eagerly talk with patients about making changes — only to become disillusioned when patients do not follow through. Both physicians and patients may grow frustrated and less motivated to work on the problem. One way to prevent this common phenomenon and set patients up for success is to brainstorm possible obstacles to behavior change during visits.
After offering a suggestion or co-creating a plan, physicians can ask simple, respectful questions such as, “What might get in the way of your [insert behavior change]?” or “What might make it hard to [insert specific step]?” Physicians may anticipate some common barriers raised by patients but be surprised by others. Once the barriers are defined, the physician and patient can develop potential solutions, or if a particular barrier cannot be overcome, reevaluate or change the goal. This approach can improve clinical outcomes for numerous medical conditions and for patients of various income levels. 4
For example, a patient wanting to lose weight may commit to regular short walks around the block. Upon further discussion, the patient shares that the cold Minnesota winters and the violence in her neighborhood make walking in her area difficult. The physician and patient may consider other options such as walking around a local mall or walking with a family member instead. Anticipating every barrier may be impossible, and the problem-solving process may unfold over several sessions; however, exploring potential challenges during the initial goal setting can be helpful.
Self-monitoring . Another effective strategy for facilitating a variety of behavioral changes involves self-monitoring, defined as regularly tracking some specific element of behavior (e.g., minutes of exercise, number of cigarettes smoked) or a more distal outcome (e.g., weight). Having patients keep diaries of their behavior over a short period rather than asking them to remember it at a visit can provide more accurate and valuable data, as well as provide a baseline from which to track change.
When patients agree to self-monitor their behavior, physicians can increase the chance of success by discussing the specifics of the plan. For example, at what time of day will the patient log his or her behavior? How will the patient remember to observe and record the behavior? What will the patient write on the log? Logging the behavior soon after it occurs will provide the most accurate data. Although patients may be tempted to omit unhealthy behaviors or exaggerate healthy ones, physicians should encourage patients to be completely honest to maximize their records' usefulness. For self-monitoring to be most effective, physicians should ask patients to bring their tracking forms to follow-up visits, review them together, celebrate successes, discuss challenges, and co-create plans for next steps. (Several diary forms are available in the Patient Handouts section of the FPM Toolbox .)
A variety of digital tracking tools exist, including online programs, smart-phone apps, and smart-watch functions. Physicians can help patients select which method is most convenient for daily use. Most online programs can present data in charts or graphs, allowing patients and physicians to easily track change over time. SuperTracker , a free online program created by the U.S. Department of Agriculture, helps patients track nutrition and physical activity plans, set goals, and work with a group leader or coach. Apps like Lose It! or MyFitnessPal can also help.
The process of consistently tracking one's behavior is sometimes an intervention itself, with patients often sharing that it created self-reflection and resulted in some changes. Research shows self-monitoring is effective across several health behaviors, especially using food intake monitoring to produce weight loss. 5
BEHAVIOR-SPECIFIC TECHNIQUES
The following evidence-based approaches can be useful in encouraging patients to adopt specific health behaviors.
Physical activity prescriptions . Many Americans do not engage in the recommended amounts of physical activity, which can affect their physical and psychological health. Physicians, however, rarely discuss physical activity with their patients. 6 Clinicians ought to act as guides and work with patients to develop personalized physical activity prescriptions, which have the potential to increase patients' activity levels. 7 These prescriptions should list creative options for exercise based on the patient's experiences, strengths, values, and goals and be adapted to a patient's condition and treatment goals over time. For example, a physician working with a patient who has asthma could prescribe tai chi to help the patient with breathing control as well as balance and anxiety.
In creating these prescriptions, physicians should help the patient recognize the personal benefits of physical activity; identify barriers to physical activity and how to overcome them; set small, achievable goals; and give patients the confidence to attempt their chosen activity. Physicians should also put the prescriptions in writing, give patients logs to track their activity, and ask them to bring those logs to follow-up appointments for further discussion and coaching. 8 More information about exercise prescriptions and sample forms are available online.
Healthy eating goals . Persuading patients to change their diets is daunting enough without unrealistic expectations and the constant bombardment of fad diets, cleanses, fasts, and other food trends that often leave both patients and physicians uncertain about which food options are actually healthy. Moreover, physicians in training receive little instruction on what constitutes sound eating advice and ideal nutrition. 9 This confusion can prevent physicians from broaching the topic with patients. Even if they identify healthy options, common setbacks can leave both patients and physicians less motivated to readdress the issue. However, physicians can help patients set realistic healthy eating goals using two simple methods:
Small steps. Studies have shown that one way to combat the inertia of unhealthy eating is to help patients commit to small, actionable, and measurable steps. 10 First, ask the patient what small change he or she would like to make — for example, decrease the number of desserts per week by one, eat one more fruit or vegetable serving per day, or swap one fast food meal per week with a homemade sandwich or salad. 11 Agree on these small changes to empower patients to take control of their diets.
The Plate Method. This model of meal design encourages patients to visualize their plates split into the following components: 50 percent fruits and non-starchy vegetables, 25 percent protein, and 25 percent grains or starchy foods. 12 Discuss healthy options that would fit in each of the categories, or combine this method with the small steps described above. By providing a standard approach that patients can adapt to many forms of cuisine, the model helps physicians empower their patients to assess their food options and adopt healthy eating behaviors.
Brief behavioral therapy for insomnia . Many adults struggle with insufficient or unrestful sleep, and approximately 18.8 percent of adults in the United States meet the criteria for an insomnia disorder. 13 The first-line treatment for insomnia is Cognitive Behavioral Therapy for Insomnia (CBT-I), which involves changing patients' behaviors and thoughts related to their sleep and is delivered by a trained mental health professional. A physician in a clinic visit can easily administer shorter versions of CBT-I, such as Brief Behavioral Therapy for Insomnia (BBT-I). 14 BBT-I is a structured therapy that includes restricting the amount of time spent in bed but not asleep and maintaining a regular sleep schedule from night to night. Here's how it works:
Sleep diary. Have patients maintain a sleep diary for two weeks before starting the treatment. Patients should track when they got in bed, how long it took to fall asleep, how frequently they woke up and for how long, what time they woke up for the day, and what time they got out of bed. Many different sleep diaries exist, but the American Academy of Sleep Medicine's version is especially user-friendly.
Education. In the next clinic appointment, briefly explain how the body regulates sleep. This includes the sleep drive (how the pressure to sleep is based on how long the person has been awake) and circadian rhythms (the 24-hour biological clock that regulates the sleep-wake cycle).
Set a wake-up time. Have patients pick a wake-up time that will work for them every day. Encourage them to set an alarm for that time and get up at that time every day, no matter how the previous night went.
Limit “total time in bed.” Review the patient's sleep diary and calculate the average number of hours per night the patient slept in the past two weeks. Add 30 minutes to that average and explain that the patient should be in bed only for that amount of time per night until your next appointment.
Set a target bedtime. Subtract the total time in bed from the chosen wake-up time, and encourage patients to go to bed at that “target” time only if they are sleepy and definitely not any earlier.
For example, if a patient brings in a sleep diary with an average of six hours of sleep per night for the past two weeks, her recommended total time in bed will be 6.5 hours. If she picks a wake-up time of 7 a.m., her target bedtime would be 12:30 a.m. It usually takes up to three weeks of regular sleep scheduling and sleep restriction for patients to start seeing improvements in their sleep. As patients' sleep routines become more solid (i.e., they are falling asleep quickly and sleeping more than 90 percent of the time they are in bed), slowly increase the total time in bed to possibly increase time asleep. Physicians should encourage patients to increase time in bed in increments of 15 to 30 minutes per week until the ideal amount of sleep is reached. This amount is different for each patient, but patients generally have reached their ideal amount of sleep when they are sleeping more than 85 percent of the time in bed and feel rested during the day.
Patient education to prevent medication nonadherence . Medication adherence can be challenging for many patients. In fact, approximately 20 percent to 30 percent of prescriptions are never picked up from the pharmacy, and 50 percent of medications for chronic diseases are not taken as prescribed. 15 Nonadherence is associated with poor therapeutic outcomes, further progression of disease, and decreased quality of life. To help patients improve medication adherence, physicians must determine the reason for nonadherence. The most common reasons are forgetfulness, fear of side effects, high drug costs, and a perceived lack of efficacy. To help patients change these beliefs, physicians can take several steps:
Educate patients on four key aspects of drug therapy — the reason for taking it (indication), what they should expect (efficacy), side effects and interactions (safety), and how it structurally and financially fits into their lifestyle (convenience). 16
Help patients make taking their medication a routine of their daily life. For example, if a patient needs to use a controller inhaler twice daily, recommend using the inhaler before brushing his or her teeth each morning and night. Ask patients to describe their day, including morning routines, work hours, and other responsibilities to find optimal opportunities to integrate this new behavior.
Ask patients, “Who can help you manage your medications?” Social networks, including family members or close friends, can help patients set up pillboxes or provide medication reminders.
The five Rs to quitting smoking . Despite the well-known consequences of smoking and nationwide efforts to reduce smoking rates, approximately 15 percent of U.S. adults still smoke cigarettes. 17 As with all kinds of behavioral change, patients present in different stages of readiness to quit smoking. Motivational interviewing techniques can be useful to explore a patient's ambivalence in a way that respects his or her autonomy and bolsters self-efficacy. Discussing the five Rs is a helpful approach for exploring ambivalence with patients: 18
Relevance. Explore why quitting smoking is personally relevant to the patient.
Risks. Advise the patient on negative consequences of continuing to smoke.
Rewards. Ask the patient to identify the benefits of quitting smoking.
Roadblocks. Help the patient determine obstacles he or she may face when quitting. Common barriers include weight gain, stress, fear of withdrawal, fear of failure, and having other smokers such as coworkers or family in close proximity.
Repeat. Incorporate these aspects into each clinical contact with the patient.
Many patients opt to cut back on the amount of tobacco they use before their quit date. However, research shows that cutting back on the number of cigarettes is no more effective than quitting abruptly, and setting a quit date is associated with greater long-term success. 19
Once the patient sets a quit date, repeated physician contact to reinforce smoking cessation messages is key. Physicians, care coordinators, or clinical staff should consider calling or seeing the patient within one to three days of the quit date to encourage continued efforts to quit, as this time period has the highest risk for relapse. Evidence shows that contacting the patient four or more times increases the success rate in staying abstinent. 18 Quitting for good may take multiple a empts, but continued encouragement and efforts such as setting new quit dates or offering other pharmacologic and behavioral therapies can be helpful.
GETTING STARTED
Family physicians are uniquely positioned to provide encouragement and evidence-based advice to patients to change unhealthy behaviors. The proven techniques described in this article are brief enough to attempt during clinic visits. They can be used to encourage physical activity, healthy eating, better sleep, medication adherence, and smoking cessation, and they can help patients adjust their lifestyle, improve their quality of life, and, ultimately, lower their risk of early mortality.
Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all-cause mortality: a systematic review and meta-analysis. Prev Med . 2012;55(3):163-170.
Bodenheimer T, Handley MA. Goal-setting for behavior change in primary care: an exploration and status report. Patient Educ Couns . 2009;76(2):174-180.
Lilly CL, Bryant LL, Leary JM, et al.; Evaluation of the effectiveness of a problem-solving intervention addressing barriers to cardiovascular disease prevention behaviors in three underserved populations: Colorado, North Carolina, West Virginia, 2009. Prev Chronic Dis . 2014;11:E32.
U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans (7th Ed). Washington, D.C: U.S. Government Printing Office; 2010.
Sreedhara M, Silfee VJ, Rosal MC, Waring ME, Lemon SC. Does provider advice to increase physical activity differ by activity level among U.S. adults with cardiovascular disease risk factors? Fam Pract . 2018;35(4):420-425.
Pinto BM, Lynn H, Marcus BH, DePue J, Goldstein MG. Physician-based activity counseling: intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med . 2001;23(1):2-10.
Hechanova RL, Wegler JL, Forest CP. Exercise: a vitally important prescription. JAAPA . 2017;30(4):17-22.
Guo H, Pavek M, Loth K. Management of childhood obesity and overweight in primary care visits: gaps between recommended care and typical practice. Curr Nutr Rep . 2017;6(4):307-314.
Perkins-Porras L, Cappuccio FP, Rink E, Hilton S, McKay C, Steptoe A. Does the effect of behavioral counseling on fruit and vegetable intake vary with stage of readiness to change?. Prev Med . 2005;40(3):314-320.
Kahan S, Manson JE. Nutrition counseling in clinical practice: how clinicians can do better. JAMA . 2017;318(12):1101-1102.
Choose My Plate. U.S. Department of Agriculture website. https://www.choosemyplate.gov/ . Updated January 31, 2018. Accessed February 1, 2018.
Ford ES, Cunningham TJ, Giles WH, Croff JB. Trends in insomnia and excessive daytime sleepiness among U.S. adults from 2002 to 2012. Sleep Med . 2015;16(3):372-378.
Edinger JD, Sampson WS. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep . 2003;26(2):177-182.
Viswanathan M, Golin CE, Jones CD, et al.; Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med . 2012;157(11):785-795.
Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice: the patient-centered approach to medication management services . 3rd ed. New York: McGraw-Hill; 2012.
Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults — United States, 2005–2015. MMWR Morb Mortal Wkly Rep . 2016;65(44):1205-1211.
Patients not ready to make a quit attempt now (the “5 Rs”). Agency for Healthcare Research and Quality website. http://bit.ly/2jVvpoY . Updated December 2012. Accessed February 2, 2018.
Larzelere MM, Williams DE. Promoting smoking cessation. Am Fam Physician . 2012;85(6):591-598.
Continue Reading
More in FPM
More in pubmed.
Copyright © 2018 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Advertisement
Using Health Chatbots for Behavior Change: A Mapping Study
- Mobile & Wireless Health
- Published: 04 April 2019
- Volume 43 , article number 135 , ( 2019 )
Cite this article

- Juanan Pereira ORCID: orcid.org/0000-0002-7935-3612 1 &
- Óscar Díaz 1
8360 Accesses
104 Citations
11 Altmetric
Explore all metrics
This study conducts a mapping study to survey the landscape of health chatbots along three research questions: What illnesses are chatbots tackling? What patient competences are chatbots aimed at? Which chatbot technical enablers are of most interest in the health domain? We identify 30 articles related to health chatbots from 2014 to 2018. We analyze the selected articles qualitatively and extract a triplet <technicalEnablers, competence, illness> for each of them. This data serves to provide a first overview of chatbot-mediated behavior change on the health domain. Main insights include: nutritional disorders and neurological disorders as the main illness areas being tackled; “affect” as the human competence most pursued by chatbots to attain change behavior; and “personalization” and “consumability” as the most appreciated technical enablers. On the other hand, main limitations include lack of adherence to good practices to case-study reporting, and a deeper look at the broader sociological implications brought by this technology.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
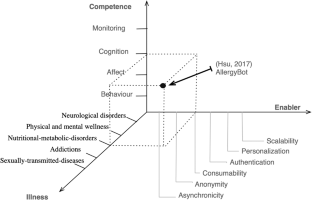
Similar content being viewed by others
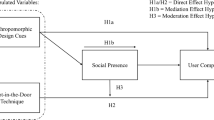
AI-based chatbots in customer service and their effects on user compliance


An Overview of Chatbot Technology

ChatGPT: towards AI subjectivity
Abashev, A., Grigoryev, R., Grigorian, K., and Boyko, V., Programming tools for messenger-based chatbot system organization: Implication for outpatient and translational medicines. BioNanoScience. 7(2):403–407, 2017. https://doi.org/10.1007/s12668-016-0376-9 .
Article Google Scholar
Andersson, G., and Cuijpers, P., Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cognit. Behav. Ther. 38(4):196–205, 2009. https://doi.org/10.1080/16506070903318960 .
Atay, C., Ireland, D., Liddle, J., Wiles, J., Vogel, A., Angus, D., Bradford, D., Campbell, A., Rushin, O., and Chenery, H. J., Can a smartphone-based chatbot engage older community group members? The impact of specialised content. Alzheimer’s Dement.: J. Alzheimer’s Assoc. 12(7):P1005–P1006, 2016. https://doi.org/10.1016/j.jalz.2016.06.2070 .
Beun, R.J., Brinkman, W.-P., Fitrianie, S., Griffioen-Both, F., Horsch, C., Lancee, J., and Spruit, S.: Improving adherence in automated e-coaching. In: International conference on persuasive technology. pp. 276–287. Springer, 2016).
Bickmore, T. W., Puskar, K., Schlenk, E. A., Pfeifer, L. M., and Sereika, S. M., Maintaining reality: Relational agents for antipsychotic medication adherence. Interact. Comput. 22(4):276–288, 2010. https://doi.org/10.1016/j.intcom.2010.02.001 .
Brinkman, P., Virtual health agents for behavior change: Research perspectives and directions. Proceedings of the workshop on graphical and robotic embodied agents for therapeutic systems (GREATS16) held during the international conference on intelligent virtual agents (IVA16), 2016.
Brixey, J., Hoegen, R., Lan, W., Rusow, J., Singla, K., Yin, X., Artstein, R., and Leuski, A., SHIHbot: A Facebook chatbot for sexual health information on HIV/AIDS. Proceedings of the 18th annual SIGdial meeting on discourse and dialogue. 370–373, 2017.
Callejas, Z., Griol, D., McTear, M.F., López-Cózar, R.: A virtual coach for active ageing based on sentient computing and m-health. International workshop on ambient assisted living: 59–66. Springer, 2014.
Cameron, G., Cameron, D., Megaw, G., Bond, R., Mulvenna, M., O’Neill, S., Armour, C., and McTear, M., Towards a chatbot for digital counselling. J. Med. Internet Res. 4(1):e3, 2017.
Google Scholar
Cheng, A., Raghavaraju, V., Kanugo, J., Handrianto, Y.P., and Shang, Y., Development and evaluation of a healthy coping voice interface application using the Google home for elderly patients with type 2 diabetes. Consumer Communications & Networking Conference (CCNC), 2018 15th IEEE annual. Pp. 1–5. IEEE, 2018.
Chung, K., and Park, R.C., Chatbot-based healthcare service with a knowledge base for cloud computing. Cluster Computing. 1–13,2018. doi: https://doi.org/10.1007/s10586-018-2334-5.
Crawford, E., Bots are awesome! Humans? Not so much, https://chatbotsmagazine.com/bots-are-awesome-humans-not-so-much-7b2d62630668 .
Cruz-Sandoval, D., and Favela, J., Semi-autonomous conversational robot to Deal with problematic behaviors from people with dementia. International conference on ubiquitous computing and ambient intelligence. 677–688. Springer, 2017.
Cruzes, D.S., and Dyba, T., Recommended steps for thematic synthesis in software engineering. In: 2011 international symposium on empirical software engineering and measurement. pp. 275–284. IEEE, 2011.
Dale, R., The return of the chatbots. Nat. Lang. Eng. 22(5):811–817, 2016. https://doi.org/10.1017/S1351324916000243 .
Dubosson, F., Schaer, R., Savioz, R., and Schumacher, M., Going beyond the relapse peak on social network smoking cessation programmes: ChatBot opportunities. Swiss Med. Inform. 33, 2017.
Elmasri, D., and Maeder, A., A conversational agent for an online mental health intervention. International conference on brain and health informatics. 243–251. Springer, 2016.
Eysenbach, G., and Group, C.-E., CONSORT-EHEALTH: Improving and standardizing evaluation reports of web-based and mobile health interventions. Journal of medical Internet research. 13(4), 2011. doi: https://doi.org/10.2196/jmir.1923 .
Fadhil, A., A conversational Interface to improve medication adherence: Towards AI support in Patient’s treatment. arXiv preprint arXiv:1803.09844. 2018.
Fadhil, A., and Gabrielli, S., Addressing challenges in promoting healthy lifestyles: The al-chatbot approach. Proceedings of the 11th EAI international conference on pervasive computing Technologies for Healthcare. 261–265. ACM, 2017.
Fadhil, A., Villafiorita, A.: An adaptive learning with gamification & conversational UIs: The rise of CiboPoliBot. Adjunct publication of the 25th conference on user modeling, adaptation and personalization: 408–412. ACM, 2017.
Fernandez-Luque, L., Lattab, A., Hors, S., and Ahmedna, M., Implementation and feasibility study of a tailored health education bot in telegram for mothers of children with obesity and overweight. Qatar Foundation annual research conference proceedings. p. HBPD506. HBKU press Qatar, 2018.
Fogg, B. J., Persuasive technology: Using computers to change what we think and do. Ubiquity. 2002(December):5, 2002. https://doi.org/10.1145/764008.763957 .
Gabrielli, S., Marie, K., and Corte, C.D., SLOWBot (Chatbot) lifestyle assistant. In: Proceedings of the 12th EAI international conference on pervasive computing Technologies for Healthcare. 367–370. ACM, New York, NY, USA, 2018.
Griol, D., and Molina, J.M., An ambient assisted living Mobile application for helping people with Alzheimer. International conference on practical applications of agents and multi-agent systems: 3–14. Springer, 2015.
Hsu, P., Zhao, J., Liao, K., Liu, T., Wang, C.: AllergyBot: A Chatbot technology intervention for young adults with food allergies dining out. In: Proceedings of the 2017 CHI conference extended abstracts on human factors in computing systems. pp. 74–79. ACM, 2017.
Huang, C., Yang, M., Huang, C., Chen, Y., Wu, M., Chen, K.: A Chatbot-supported smart wireless interactive healthcare system for weight control and health promotion. 2018 IEEE international conference on industrial engineering and engineering management (IEEM): 1791–1795, 2018.
Inkster, B., Sarda, S., and Subramanian, V., An empathy-driven, conversational artificial intelligence agent (Wysa) for digital mental well-being: Real-world data evaluation mixed-methods study. JMIR mHealth and uHealth. 6:e12106, 2018. https://doi.org/10.2196/mhealth.12106 .
Article PubMed PubMed Central Google Scholar
Isern, D., and Moreno, A., A systematic literature review of agents applied in healthcare. J. Med. Syst. 40(2):43, 2016. https://doi.org/10.1007/s10916-015-0376-2 .
Article PubMed Google Scholar
Ivarsson, M., and Gorschek, T., A method for evaluating rigor and industrial relevance of technology evaluations. Empiric. Softw. Eng. 16:365–395, 2011. https://doi.org/10.1007/s10664-010-9146-4 .
Jeong, S., and Breazeal, C., Toward robotic companions that enhance psychological wellbeing with smartphone technology. Proceedings of the companion of the 2017 ACM/IEEE international conference on human-robot interaction. pp. 345–346. ACM, 2017.
Kimani, E., Bickmore, T., Trinh, H., Ring, L., Paasche-Orlow, M.K., and Magnani, J.W., A smartphone-based virtual agent for atrial fibrillation education and counseling. International conference on intelligent virtual agents. 120–127. Springer, 2016.
Kitchenham, B.A., Budgen, D., and Brereton, P., Evidence-based software engineering and systematic reviews. CRC Press, 2015.
Klopfenstein, L.C., Delpriori, S., Malatini, S., and Bogliolo, A., The rise of bots: A survey of conversational interfaces, patterns, and paradigms. Proceedings of the 2017 conference on designing interactive systems. 555–565. ACM, New York, NY, USA, 2017.
Kobori, Y., Osaka, A., Soh, S., and Okada, H., Novel application for sexual transmitted infection screening with an ai chatbot. J. Urol. 199(4, Supplement):e189–e190, 2018. https://doi.org/10.1016/j.juro.2018.02.516 .
Kowatsch, T., Ni’s sen, M., Shih, C.-H.I., Rüegger, D., Volland, D., Filler, A., Künzler, F., Barata, F., Hung, S., and Büchter, D., Text-based healthcare Chatbots supporting patient and health professional teams: Preliminary results of a randomized controlled trial on childhood obesity. Persuasive embodied agents for behavior change (PEACH2017). ETH Zurich, 2017.
Kowatsch, T., Volland, D., Shih, I., Rüegger, D., Künzler, F., Barata, F., Filler, A., Büchter, D., Brogle, B., and Heldt, K., Design and evaluation of a Mobile chat app for the open source behavioral health intervention platform MobileCoach. International conference on design science research in information systems: 485–489. Springer, 2017.
Kozinakova, B., Analysis of chatbot systems focusing on the elderly as users. Master Thesis, Politecnico de Milano, 2017.
Lambert, A.O.C., Montañez, C.H.T., Martinez, M.B., and Funes-Gallanzi, M., A conversational agent for use in the identification of rare diseases. In: Applications for future internet. 128–139. Springer, 2017.
Laranjo, L., Dunn, A. G., Tong, H. L., Kocaballi, A. B., Chen, J., Bashir, R., Surian, D., Gallego, B., Magrabi, F., and Lau, A., Conversational agents in healthcare: A systematic review. J. Am. Med. Inform. Assoc. , 2018. https://doi.org/10.1093/jamia/ocy072 .
Lisetti, C., Amini, R., and Yasavur, U., Now all together: Overview of virtual health assistants emulating face-to-face health interview experience. KI-Künstliche Intelligenz. 29(2):161–172, 2015. https://doi.org/10.1007/s13218-015-0357-0 .
Ly, K. H., Ly, A.-M., and Andersson, G., A fully automated conversational agent for promoting mental well-being: A pilot RCT using mixed methods. Internet Interven. 10:39–46, 2017. https://doi.org/10.1016/j.invent.2017.10.002 .
Miner, A., Chow, A., Adler, S., Zaitsev, I., Tero, P., Darcy, A., and Paepcke, A., Conversational agents and mental health: Theory-informed assessment of language and affect. Proceedings of the fourth international conference on human agent interaction. 123–130. ACM, 2016.
Miner, A. S., Milstein, A., Schueller, S., Hegde, R., Mangurian, C., and Linos, E., Smartphone-based conversational agents and responses to questions about mental health, interpersonal violence, and physical health. JAMA Intern. Med. 176(5):619–625, 2016. https://doi.org/10.1001/jamainternmed.2016.0400 .
Oh, K.-J., Lee, D., Ko, B., and Choi, H.-J., A Chatbot for psychiatric counseling in mental healthcare service based on emotional dialogue analysis and sentence generation. Mobile data management (MDM), 2017 18th IEEE international conference on. 371–375. IEEE, 2017.
Pereira, J., Díaz, Ó.: Chatbot dimensions that matter: Lessons from the trenches. In: Web engineering, lecture notes in computer science, pp. 129–135. Springer, Cham (2018). doi: https://doi.org/10.1007/978-3-319-91662-0_9
Chapter Google Scholar
Petersen, K., Feldt, R., Mujtaba, S., and Mattsson, M., Systematic mapping studies in software engineering. Proceedings of the 12th International Conference on Evaluation and Assessment in Software Engineering. pp. 68–77. BCS Learning & Development Ltd., Swindon, UK, 2008.
Richards, D., and Caldwell, P., Improving health outcomes sooner rather than later via an interactive website virtual specialist. IEEE Journal of Biomedical and Health Informatics. 1–1, 2017. doi: https://doi.org/10.1109/JBHI.2017.2782210 .
Richards, D., Caldwell, P.H.: Gamification to improve adherence to clinical treatment advice. Health literacy: Breakthroughs in research and practice: Breakthroughs in research and practice. 80, 2017. doi: https://doi.org/10.4018/978-1-5225-1928-7.ch005 .
Roniotis, A., and Tsiknakis, M., Detecting depression using voice signal extracted by Chatbots: A feasibility study. In: Interactivity, game creation, design, learning, and innovation. Springer, 2017, 386–392.
Schueller, S. M., Tomasino, K. N., and Mohr, D. C., Integrating human support into behavioral intervention technologies: The efficiency model of support. Clin. Psychol.: Sci. Pract. 24(1):27–45, 2017. https://doi.org/10.1111/cpsp.12173 .
Stratou, G., Morency, L.P., DeVault, D., Hartholt, A., Fast, E., Lhommet, M., Lucas, G., Morbini, F., Georgila, K., Scherer, S., Gratch, J., Marsella, S., Traum, D., and Rizzo, A., A demonstration of the perception system in SimSensei, a virtual human application for healthcare interviews. 2015 international conference on affective computing and intelligent interaction (ACII). pp. 787–789, 2015.
van Heerden, A., Ntinga, X., and Vilakazi, K., The potential of conversational agents to provide a rapid HIV counseling and testing services. The Frontiers and advances in data science (FADS), 2017 international conference on. 80–85. IEEE, 2017.
Van Vuuren, S., and Cherney, L.R., A virtual therapist for speech and language therapy. International conference on intelligent virtual agents. 438–448. Springer, 2014.
Download references
Author information
Authors and affiliations.
ONEKIN Research Group, University of the Basque Country, UPV/EHU, Leioa, Spain
Juanan Pereira & Óscar Díaz
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Óscar Díaz .
Ethics declarations
Conflict of interest.
Juanan Pereira declares that he has no conflict of interest. Óscar Díaz declares that he has no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mobile & Wireless Health
Rights and permissions
Reprints and permissions
About this article
Pereira, J., Díaz, Ó. Using Health Chatbots for Behavior Change: A Mapping Study. J Med Syst 43 , 135 (2019). https://doi.org/10.1007/s10916-019-1237-1
Download citation
Received : 10 January 2019
Accepted : 06 March 2019
Published : 04 April 2019
DOI : https://doi.org/10.1007/s10916-019-1237-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mobile healthcare
- Instant messaging
- Software agents
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Taylor & Francis Open Select

Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review
Rachel davis.
a Department of Clinical, Educational and Health Psychology , University College London , London, UK
Rona Campbell
b School of Social and Community Medicine , University of Bristol , Bristol, UK
Lorna Hobbs
Susan michie.
Interventions to change health-related behaviours typically have modest effects and may be more effective if grounded in appropriate theory. Most theories applied to public health interventions tend to emphasise individual capabilities and motivation, with limited reference to context and social factors. Intervention effectiveness may be increased by drawing on a wider range of theories incorporating social, cultural and economic factors that influence behaviour. The primary aim of this paper is to identify theories of behaviour and behaviour change of potential relevance to public health interventions across four scientific disciplines: psychology, sociology, anthropology and economics. We report in detail the methodology of our scoping review used to identify these theories including which involved a systematic search of electronic databases, consultation with a multidisciplinary advisory group, web searching, searching of reference lists and hand searching of key behavioural science journals. Of secondary interest we developed a list of agreed criteria for judging the quality of the theories. We identified 82 theories and 9 criteria for assessing theory quality. The potential relevance of this wide-ranging number of theories to public health interventions and the ease and usefulness of evaluating the theories in terms of the quality criteria are however yet to be determined.
Introduction
Human behaviours, including tobacco and alcohol consumption, dietary behaviours, physical activity and sexual practices, play a key role in many of the leading causes of death in developing and developed countries (Aveyard & West, 2007 ; Danaei et al., 2009 ; Ezzati et al., 2002 ; Mokdad, Marks, Stroup, & Gerberding, 2004 ; Parkin, Boyd, & Walker, 2011 ; Solomon & Kington, 2002 ). Even small changes in such behaviours can have substantial effects on population health outcomes (Ezzati et al., 2002 ; Mokdad et al., 2004 ; National Institute for Health and Clinical Excellence (NICE), 2010 ; Solomon & Kington, 2002 ). Understanding these behaviours and the contexts in which they occur is essential for developing effective evidence-based health behaviour change interventions and policies and for reducing avoidable mobility and mortality (House of Lords, 2011 ; Office of Behavioural and Social Sciences Research, 2006 ).
Despite the relatively small investment in preventive health and behavioural science (Marteau, Dieppe, Foy, Kinmonth, & Schneiderman, 2006 ), there is evidence for the effectiveness of behaviour change interventions at individual, community and population levels (Abraham, Kelly, West, & Michie, 2009 ; Albarracin et al., 2005 ; Michie & West, 2013 ; National Institute for Health and Care Excellence, 2007 ; Nigg, Allegrante, & Ory, 2002 ). Interventions have been targeted at behavioural risk factors (e.g., smoking; Carr & Ebbert, 2012 ; Rice & Stead, 2008 ), encouraging protective behaviours (e.g., health screening; Brouwers et al., 2011 ; Everett et al., 2011 ), improving adaptation to chronic and acute illness (e.g., adherence to medical advice; Cutrona et al., 2010 ) and changing health professional behaviours to improve the quality and efficiency of services (e.g., hand hygiene compliance; Fuller et al., 2012 ). While there are many examples of successful interventions, there are also examples of ineffective interventions (e.g., Coleman, 2010 ; Summerbell et al., 2005 ); for those that are effective, the effects tend to be modest, with significant heterogeneity of short-term and long-term effects (Michie, Johnston, Francis, Hardeman, & Eccles, 2008 ).
To maximise the potential efficacy of interventions, it is necessary to understand behaviour and behaviour change: in other words, it is necessary to have a theoretical understanding of behaviour change. In this context, theory represents the accumulated knowledge of the mechanisms of action (mediators) and moderators of change as well as the a priori assumptions about what human behaviour is, and what the influences on it are. The application of theory is advocated as an integral step in intervention design and evaluation and in evidence synthesis, for example, by the UK Medical Research Council's guidance for developing and evaluating complex interventions (Campbell et al., 2000 , 2007 ; Craig et al., 2008 ; Glanz & Bishop, 2010 ). This is for several reasons. First, the antecedents of behaviour and the causal determinants of change can be appropriately identified and targeted by the intervention (Hardeman et al., 2005 ; Michie & Abraham, 2004 ; Michie et al., 2008 ) and component behaviour change techniques can be selected and/or refined and tailored (Michie & Prestwich, 2010 ; Michie et al., 2008 ; Rothman, 2004 ). Second, theoretically identified mechanisms of action (i.e., mediators) can be investigated to gain further understanding as to how the intervention brings about its effects (Michie & Abraham, 2004 ; Rothman, 2004 , 2009 ). This allows researchers to determine whether unsuccessful interventions have failed either because the intervention has had no effect upon the hypothesised mediator or because the hypothesised (and successfully influenced) mediator has had no effect upon behaviour (Michie & Abraham, 2004 ; Rothman, 2004 , 2009 ), thus facilitating more efficient refinement of the intervention. Third, theory summarises the cumulative knowledge of how to change behaviour across different populations, behaviours and contexts. Finally, theory-based interventions provide an opportunity in which theory can be tested. This aids development of more useful theories which, in turn, supports intervention optimisation (Michie et al., 2008 ; Rothman, 2004 ).
The question as to whether interventions that are explicitly based on theory are more effective that those that are not is a complex one. Some reviews have found a positive association (Albada, Ausems, Bensing, & van Dulmen, 2009 ; Albarracin et al., 2005 ; Glanz & Bishop, 2010 ; Noar, Benac, & Harris, 2007 ; Swann, Bowe, Kosmin, & McCormick, 2003 ; Taylor, Conner, & Lawton, 2011 ), but others have found no association, or, even a negative association (Gardner, Wardle, Poston, & Croker, 2011 ; Roe, Hunt, Bradshaw, & Rayner, 1997 ; Stephenson, Imrie, & Sutton, 2000 ). Some reviews have reported a mixture depending on the measure of effectiveness (Ammerman, Lindquist, Lohr, & Hersey, 2002 ; Bhattarai et al., 2013 ; Kim, Stanton, Li, Dickersin, & Galbraith, 1997 ).
There are several factors that may explain this mixed picture. Theory is often poorly applied. A review investigating application of theory using the 19-item ‘Theory Coding Scheme’ (Michie & Prestwich, 2010 ), found that only 10% of studies of theory-based interventions reported links between behaviour change techniques and theoretical constructs and only 9% reported that all the constructs had been targeted by behaviour change techniques. Another explanation may be that the choice of theory may not have been appropriate. For example, if a behaviour is heavily influenced by habit or emotional states then a theory that focuses on beliefs and reflective thought processes may not be appropriate when informing intervention design.
The importance of understanding the theoretical underpinnings of behavioural interventions has been highlighted in previous research suggesting theoretical bases for combining behaviour change techniques within interventions to allow synergistic effects and enhance their effectiveness (Dombrowski et al., 2012 ; Michie, Abraham, Whittington, McAteer, & Gupta, 2009 ; Taylor et al., 2011 ; Webb, Joseph, Yardley, & Michie, 2010 ). Despite the advantages of theory, behaviour change interventions are often designed without reference to theory (Davies, Walker, & Grimshaw, 2010 ; Prestwich et al., 2013 ). For instance, a recent meta-analysis found that only 22.5% of 235 implementation studies explicitly used theories of behaviour change (Davies et al., 2010 ). Where theory is used, it is often only loosely referred to rather than rigorously applied to intervention design and evaluation (Painter, Borba, Hynes, Mays, & Glanz, 2008 ; Prestwich et al., 2013 ). In those situations where interventions are based on ‘explicit theory’, theory is often used sub-optimally to develop or evaluate the intervention (e.g., only a few of the theoretical constructs may be targeted and/or theory is not used to appropriately tailor the intervention).
Choosing a relevant theory can be a challenging task for intervention designers, especially given the large number of theories, many of which have the same or overlapping constructs, to choose from (Michie et al., 2005 ). There is a lack of guidance on how to select an appropriate theory for a particular purpose (Michie, 2008 ), with a predominance in published intervention evaluations of a small number of theories that have already gained recognition in the field (Painter et al., 2008 ). By using a ‘common’ or ‘favourite’ theory, rather than one that may be more suited to the particular characteristics of the target population, behaviour and context, the potential benefit of using theory is limited.
One approach to addressing the plethora of different, overlapping theories and lack of guidance as to how to choose between them was the development of the Theoretical Domains Framework (TDF; Cane, O'Connor, & Michie, 2012 ; Michie et al., 2005 ). Developed by psychologists and implementation researchers, the TDF provides a framework of theoretical domains to explain barriers and facilitators of behaviour in any particular situation. Informed by 128 explanatory constructs from 33 theories of behaviour, the TDF has been used in many contexts to understand behaviour and design theoretically informed interventions (Francis, O'Connor, & Curran, 2012 ; French et al., 2012 ). Another resource for theory-informed research is the US National Institute of Health's ‘Grid Enabled Measures’ (GEM) web-based database. GEM provides the descriptions of theoretical constructs and behavioural and social measures to assess these constructs ( https://www.gem-beta.org/Public/Home.aspx ). While both these approaches are of value, neither specifies relationships between theoretical domains and constructs in terms of the effect that one domain or construct may have on another. They deal with theoretical domains and constructs, not theories per se. One previous consensus exercise did generate a list of eight constructs thought to influence HIV-related behaviours, with the resulting framework specifying links between the constructs and behaviour (Fishbein et al., 2001 ). However, it is not clear how this consensus was reached and how relevant the included constructs are to other behaviours, given the focus on HIV-related behaviours. Researchers or interventions designers may want to select specific theories either at the beginning of the intervention design process or after conducting some preliminary research to indicate which theories are likely to be relevant and useful. In these situations there is a need for an accessible source of potentially useful theories, as well as a method for selecting amongst them.
At present, theories used in public health and behaviour change interventions more generally tend to emphasise individual and sometimes interpersonal rather than broader social and environmental variables (Glanz & Bishop, 2010 ). Capabilities and motivation (individual factors) are often targeted, but context (social and environmental variables) is far less likely to be considered. NICE's ( 2007 ) behaviour change guidance concluded that interventions were more effective if they simultaneously targeted variables at different levels (e.g., individual, community and population; National Institute for Health and Care Excellence, 2007 ). Therefore, to maximise effectiveness, intervention designers are likely to benefit from drawing from a wider range of theories than currently used. Current resources on theories of behaviour change tend to reflect specific contexts and disciplines, and are thus inevitably limited in the range of theories considered (Agar, 2008 ; Conner & Norman, 2005 ; Glanz & Bishop, 2010 ; Glanz, Rimer, & Lewis, 2002 ).
To improve the selection and application of theory we need to consider, across relevant disciplines, those theories which may be of potential use in informing public health questions. By identifying a range of theories we can assess which theories may be of value given the behaviour, population and context in question. To this end, we conducted a scoping review and consensus exercise, informed by the disciplines of psychology, sociology, anthropology and economics. The scoping review and consensus exercise primarily aimed to address the question, ‘What theories exist across the disciplines of psychology, sociology, anthropology and economics that could be of value to guiding behaviour change interventions?’
To be as comprehensive as possible we focused on both theories of behaviour and behaviour change. Theories of behaviour tend to be linear, and explain the reasons why behaviour may occur by considering a number of predictors and their associations with one another and how these could influence the likelihood of a particular behaviour (Agar, 2008 ; Conner & Norman, 2005 ; Glanz & Rimer, 1997 ; Head & Noar, 2013 ). Theories of change tend to be more cyclical and identify interactional and dynamic behaviour change processes (Agar, 2008 ; Head & Noar, 2013 ). In practice, it is sometimes difficult to distinguish between the two and some theories could be viewed as both.
Of secondary interest we also addressed ‘What criteria should we consider when evaluating the quality and potential appropriateness of behaviour change theory?’ Finally, we assessed the extent to which the theories we identified had been applied within the behaviour change field.
The scope of the present paper is twofold: (i) to report in detail the methodology employed to identify relevant theories and to produce a compendium of these theories and (ii) to provide the list of agreed criteria for judging the quality of the theories. Ways in which some of the theories have been used to study behaviour change are also briefly summarised, though it is beyond the scope of this paper to discuss this in detail. Research examining how the theories have been operationalised and the quality of their empirical application (as measured by the quality criteria reported here) forms part of the future research programme.
Theories of behaviour and behaviour change were identified through five sources: expert consultation with a multidisciplinary project advisory group, electronic databases, web searching, forward and backward searching of reference lists and hand searching of key behavioural science journals. Empirical application of the theories was identified from electronic databases and searching the reference lists of retrieved articles. These, together with expert consultations with the advisory group, informed the development of the quality assessment criteria.
Expert advisory group
Twenty-four UK experts from the social and behavioural sciences and/or population health research formed the advisory group, which determined the scope, methods and conduct of the review. The group comprised four sociologists, five economists, five psychologists, four health service researchers, three anthropologists, two epidemiologists and one policy researcher.
Definition of key terms
One of the first tasks of the advisory group was to agree definitions of the terms ‘theory’ and ‘behaviour’. A shortlist of potentially relevant definitions of each term was compiled from peer-reviewed journals, reports and books, for example, the American Psychological Association Dictionary . In the first of two rounds of a Delphi process, advisory group members were asked to rate each definition and parts of the definition for potential use. When a definition (or a part of it) was rated as important by at least 50% of the group it was retained as relevant. In the second round, core concepts were extracted and synthesised by the authors and used to create working definitions which were then considered for refinement by the advisory group in order to create the final definitions:
The term theory was defined as: ‘a set of concepts and/or statements with specification of how phenomena relate to each other. Theory provides an organising description of a system that accounts for what is known, and explains and predicts phenomena’.
Behaviour was defined as: ‘anything a person does in response to internal or external events. Actions may be overt (motor or verbal) and directly measurable or, covert (activities not viewable but involving voluntary muscles) and indirectly measurable; behaviours are physical events that occur in the body and are controlled by the brain’.
Identification of relevant theories
To inform the literature search strategy, theories of behaviour and behaviour change were identified through expert consultation with the advisory group and an initial scoping of the literature using generic and discipline-specific terms related to behaviour and behaviour change theories. For example, the term ‘cultural change’ tended to be used by anthropologists, ‘action’ by sociologists and ‘behaviour’ by psychologists.
Literature search strategy
The literature search was conducted primarily to uncover theories of behaviour and behaviour change that were not identified through expert consultation with our advisory group. Secondary to this we identified the ways in which the theories we identified had been empirically applied. While we briefly report this, it was beyond the scope of the study to analyse this comprehensively and in detail. In order to retrieve relevant literature across different disciplines six databases were searched between 1 January 1960 and 11 September 2012: PsycINFO, Econlit, Cochrane Database of Systematic reviews, International Bibliography of Social Sciences, EMBASE and MEDLINE. Databases were chosen based on their coverage of discipline- and content-specific literature and on the volume of public health literature. Databases that did not allow the use of wildcards (to account for variations in spellings) or sets of search terms to be entered and combined through the use of Boolean operators, and/or databases that only retrieved titles of articles but not abstracts were not used (e.g., Anthropology Index Online). The final search was conducted on the 11 September 2012.
The search strategy included four sets of search terms: those that (i) apply theory to behaviour change (e.g., ‘behaviour change theory’); (ii) are relevant to behaviour change and also of relevance in understanding behaviour more generally [e.g., ‘Health Belief Model’ (HBM)]; (iii) are relevant to behaviour change but that do not mention theory (e.g., ‘behaviour modification’); and (iv) discipline-specific terms combined with the term behaviour change (e.g., ‘economics and behaviour change’). A list of the search terms together with how these terms were combined can be found in the online supplemental material ( Supplemental Figure 1 ).
The search strategy was customised to each database. Standard filters were used to capture systematic reviews where applicable. A sensitivity analysis was performed to ensure that the search results included key articles on theories relevant to behaviour change (identified through the initial scoping of the literature). Given the complex body of evidence, in terms of cross-cutting disciplines and sheer breadth and volume of literature, the search was restricted to titles and abstracts to tighten the search specificity.
Additional potentially relevant theories were identified through expert consultation and web searching for key documents from organisations known for their interest in behaviour change. This included, from the USA, the National Institute of Health's Behaviour Change Consortium and, from the UK, the NICE, Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI Centre), Government Social Research Unit, House of Lords Science and Technology Select Committee Report on Behaviour Change and National Institute of Health Research's Health Technology Assessment.
Forward and backward citation searching, and hand searching of key behavioural science journals were performed to minimise the likelihood of relevant theories being missed. The journals hand searched were: Annals of Behavioural Medicine , BMC Health Services Research , British Journal of Health Psychology , Health Psychology , Health Psychology Review , Implementation Science , International Journal of Clinical and Health Psychology , Journal of Applied Behavioural Science and Social Science & Medicine .
Inclusion criteria for theories
Theories were included if they: (i) met our definition of theory and behaviour and (ii) considered individual behaviour as an outcome or part of the process leading to the outcome. Theories that considered group behaviour (e.g., ‘organisational behaviour’), without reference to individual behaviour were excluded. While we acknowledge that such theories are of interest to intervention designers who want to change group behaviour we decided to limit the scope of the review to theories concerned with individual behaviour change to keep it manageable. The inclusion of each theory was considered independently by at least two of the four authors and by members of the advisory group. Inter-rater reliability was assessed.
Theories that focused purely on cognition were not included. Examples of such theories include Social Comparison Theory (Festinger, 1954 ), which aims to explain how people's opinions are influenced within social groups and Cognitive Adaptation Theory (Taylor, 1983 ), which aims to explain how people cognitively adapt to threatening events. While these theories contribute to our understanding of knowledge, beliefs and intentions about behaviour there are often significant gaps between these and behaviour (Sheeran, 2002 ) and this project was about theories of behaviour and behaviour change.
We distinguished frameworks, which provide an organising structure, from theories which, in addition, offer explanations of how phenomena relate to each other and permit outcomes to be predicted. Thus, conceptual frameworks such as the TDF (Cane et al., 2012 ; Michie et al., 2005 ), or the Ecological Model (McLeroy, Bibeau, Steckler, & Glanz, 1988 ) that are commonly used to guide the design, implementation or evaluation of interventions were not included. While these frameworks have value in implementation and in public health research, policy and practice, this review was of specific theories.
Inclusion criteria for articles
Screening of articles was in two stages. The first stage (title and abstract) was intentionally inclusive, retaining articles if they mentioned: (i) theory in relation to behaviour or behaviour change or (ii) changing behaviour but made no reference to theory (the full text of the article was then checked to see if theory was used to inform the research). We considered all behaviour to be of relevance, not just health-related behaviours. At the second stage of screening (full-text) tighter restrictions applied and articles were included if: (i) theory and behaviour was defined as per our study definitions and (ii) they fell into one of four categories of article: descriptive, intervention, evaluative or review:
- Descriptive articles were defined as those that contained the original description of a theory by the author/s who originally conceived of the theory (i.e., primary theory sources) or by an author/s who proposed advances in the theory by re-specification. Secondary theory sources (i.e., those that only provided an overview/description of the theory) were not included.
- Intervention articles were defined as those that stated in their methods that they used theory to inform the development and/or evaluation of an intervention aimed at changing behaviour and that included a measure of behaviour as an outcome. We focused on behaviour as the end-point rather than the consequence of the behaviour (e.g., weight loss) because there are a number of factors further along the causal chain that could affect the link between behaviour and outcome (Hardeman et al., 2005 ).
- Evaluative articles were defined as those reporting studies that empirically tested a theory longitudinally.
- Review articles were defined as those that systematically reviewed a theory in relation to a change in behavioural outcomes. Narrative reviews or selective overviews of the literature (i.e., those without a description of a search strategy and no clear methodology that could be reproduced independently) were not included.
Articles were excluded if they: focused on cognition (e.g., intention to change behaviour) rather than actual behaviour; were restricted to research participation behaviours, animal studies, scale development, measurement or programme development, cost-effectiveness or single case studies; focused on mental health including therapeutic interventions where cognitive or emotional variables were the primary outcome. Dissertations and doctoral theses, books and book reviews, conference posters and presentations, editorials and commentaries were excluded for practical reasons to limit the volume of material to be retrieved and reviewed to manageable proportions. Articles that used multiple theories to inform their methodology were excluded because our review was of the empirical application of individual theories to changing behaviour.
We did not exclude articles based on their quality, since the methodology of applying these criteria has yet to be developed.
Inter-rater reliability
Articles were screened for relevance at abstract and full-text stage by the lead author (Rachel Davis). At both screening stages, 30% of the abstracts were independently screened by two other researchers (each of which screened 15%) and inter-rater reliability (calculated using percentage agreement) was assessed. Since the data constitute unbalanced cells, we have used percentage agreement as it provides a more transparent and more readily interpretable parameter than Cohen's kappa. As kappa corrects for chance agreement among multiple coders, use of kappa is likely to underestimate reliability (Steinijans, Diletti, Bomches, Greis, & Solleder, 1997 ). Differences of views about inclusion were resolved through discussion and consensus with the other authors.
Data extraction
Data were extracted on: (i) country where the research took place, (ii) theory used, (iii) type of article (descriptive, intervention, evaluative or review), (iv) design (quantitative, qualitative or mixed methods), (v) target behaviour (e.g., smoking, physical activity), (vi) target direction of behaviour [i.e., increase (which also included maintaining behaviour) or decrease in uptake] and (vii) measurement of behaviour (self-report, objective or both). Dual data extraction was conducted independently on 60% of the included papers by two researchers and inconsistencies resolved through joint discussion.
Quality assessment criteria
We reviewed key literature which synthesised scientific and philosophical perspectives on what makes a theory scientific and useful for the purpose of effecting healthy behaviour change in a target population (e.g., Glanz & Rimer, 1997 ; West, 2006 ) and used this to draft an initial list of quality criteria. These were considered by the advisory group in both a face-to-face discussion and a subsequent electronic Delphi-like consultation aimed at achieving consensus.
We report the theories of behaviour and behaviour change identified in our review and the agreed criteria for assessing theory quality. A high-level summary of the key characteristics of the review articles is also provided.
A high level of agreement was observed for decisions on inclusion in relation to both the theories and the articles included in the review (>90%).
Theories identified
Eighty-two theories of behaviour and behaviour change were identified. These are listed in Table 1 along with the lead author, date of the paper that originally described the theory and the number of articles that reported using the theory. Fifty-nine (out of the 82 theories) were applied in the articles included in our review. The remaining theories ( N = 23) were identified by the advisory group and/or through abstracts of the articles retrieved in our literature search. In other words, these were theories that met our inclusion criteria but did not have relevant articles retrieved from our search strategy that met our article inclusion criteria, i.e., articles did not fall within one of our four categories (descriptive, intervention, evaluative, review). Theories identified through our search that were excluded, with reasons for exclusion, can be found in the online supplemental material ( Supplemental Table 1 ).
Note: Theories 30–32 were all reported in one paper.
It is important to note here that while our intention was to provide a list of potentially relevant theories across different disciplines, it was not possible to categorise the theories according to disciplines. Many of the theories had influences from more than one discipline and/or authors were from several disciplines or could not be categorised into any one discipline.
Nine defining features were identified as conceptually important for a good theory: (i) clarity of constructs – ‘Has the case been made for the independence of constructs from each other?’ (ii) clarity of relationships between constructs – ‘Are the relationships between constructs clearly specified?’ (iii) measurability – ‘Is an explicit methodology for measuring the constructs given?’ (iv) testability – ‘Has the theory been specified in such a way that it can be tested?’ (v) being explanatory – ‘Has the theory been used to explain/account for a set of observations? (statistically or logically)’; (vi) describing causality – ‘Has the theory been used to describe mechanisms of change?’ (vii) achieving parsimony – ‘Has the case for parsimony been made?’ (viii) generalisablity – ‘Have generalisations been investigated across’: (a) behaviours? (b) populations? (c) contexts?’ and (ix) having an evidence base.
Articles retrieved
In the results sections that follow we briefly summarise the main findings of the articles included in our review. Further examination of the empirical application of these theories using our quality assessment criteria is part of the future research programme.
Of 8680 articles retrieved through the database search, 6620 were excluded at the first stage of screening (title and abstract) and 1804 articles (out of the remaining 2060) were excluded after full-text screening, leaving 256 articles. To these a further 20 articles were added through searching the reference lists of the included articles, resulting in 276 articles. Figure 1 displays a flow chart of the search results.

Article characteristics
Articles were published between 1977 and 2012, with most of the research conducted in Europe and North America. Eighteen categories of behaviours were identified, with three accounting for 50% of the articles: increasing physical activity ( N = 72; 26%), safe sex practices ( N = 36; 13%) and smoking cessation ( N = 30; 11%). Fifty-two (19%) articles addressed multiple health-related behaviours, with 17 (6%) of these targeting healthy eating and physical activity together. The remaining categories comprised behaviours relating to: healthy eating ( N = 13), addictive behaviours including alcohol and drugs ( N = 12), health examinations and tests ( N = 11), environmental conservation ( N = 10), violence and delinquency ( N = 9), sun protection ( N = 9), drug adherence ( N = 5), job- or education-related activities ( N = 4), Internet- or other technology-related behaviours ( N = 4), health care professional adherence to health care guidelines ( N = 3), financial-related activities ( N = 2), speeding ( N = 2) and 2 ‘others’ which were behaviours that did not fall into any of the above categories including pet removal from domestic residence ( N = 1) and repairing mosquito nets ( N = 1).
The majority of articles used quantitative methods ( N = 243; 88%) and most reported interventions ( N = 168; 61%) or were evaluative ( N = 62; 35%). Thirty-one descriptive articles (either primary theory sources or extensions of a theory) were identified. Behaviour was most commonly measured by self-report methods ( N = 194; 70%). For a high-level summary of these key characteristics, please refer to Table 2 ; a more detailed account of each individual article can be found online in Supplemental Table 2 .
Papers published by the same first author and focused on the same theory were assessed to identify cases in which multiple articles based on the same intervention (i.e., intervention protocol and outcomes) or data-set had been published. This was found to be the case for 19 articles in total (covering 9 interventions/data-sets; see Tables 1 and and2 2 ).
Frequency of use
Of the 82 theories identified, just 4 theories accounted for 174 (63%) of articles: the Transtheoretical Model of Change (TTM; N = 91; 33%), the Theory of Planned Behaviour (TPB; N = 36; 13%), Social Cognitive Theory (SCT; N = 29; 11%) and the Information-Motivation-Behavioural-Skills Model (IMB; N = 18; 7%). A further four theories accounted for an additional 32 (12%) of the included articles: the HBM ( N = 9; 3%), Self-determination Theory (SDT; N = 9; 3%), Health Action Process Approach (HAPA; N = 8; 3%) and Social Learning Theory (SLT; N = 6; 2%; SLT is a precursor of SCT). The remaining theories ( N = 70) were applied fewer than 6 times each in the literature that met our inclusion criteria, with most only being applied once or twice (see Table 1 ).
This scoping review of theories of behaviour/behaviour change of potential relevance to designing and evaluating public health interventions was informed by the disciplines of psychology, sociology, anthropology and economics. Eighty-two theories were identified that spanned a myriad of behaviours and could be applied to designing and evaluating interventions to improve public health, as well as tackle other social issues such as environmental sustainability and public safety.
It is important to note that the literature identified in the scoping review reflects the search strategy that aimed to identify theories rather than exhaustively review theoretically informed empirical studies. Therefore, whilst the review identified articles that use the theories in relation to our inclusion criteria, it does not reflect the wider application of these theories to public health-related research.
Scoping reviews are used to map or configure a body of evidence. They therefore tend to focus on breadth, including studies that are representative of the variation within the evidence base, rather than focusing on depth and assembling all the eligible material. It can also mean that establishing what the boundaries of the review are, and therefore what should be included or excluded, may be refined during the course of the review (Shemilt et al., 2013 ). Consensus methods can help with this process. While we intended to conduct this review in a systematic and reproducible way, as it was the first attempt that we were aware of to review a bodies of theory in this way, its purpose seemed more akin to that of a scoping than a systematic review. As Gough, Thomas, and Oliver ( 2012 ) have suggested, there is a clear distinction between aggregative systematic reviews that are ‘about seeking evidence to inform decisions’ and configurative scoping reviews which are about ‘seeking concepts to provide enlightenment through new ways of understanding’. Arguably what we wanted to attempt was a combination of these two things but we have nevertheless labelled what we did a scoping review.
From the theories we identified, only a few were frequently applied in literature. While the purpose of our scoping review was not to uncover all the relevant literature on how these theories have been applied, the finding is of interest because it is consistent with other reviews and publications (e.g., Glanz & Bishop, 2010 ; Painter et al., 2008 ; Prestwich et al., 2013 ). Sixty-three per cent of the articles identified in the review related to just four theories: the TTM, TPB, SCT and the IMB Skills Model. While the literature we uncovered was limited by our inclusion criteria, and includes a small number cases in which authors have published more than one article applying the same theory to the same data-set or intervention, it indicates the very uneven distribution of frequency of theory use. This raises the question as to why many theories are so little used. One explanation may be that how often a theory is used, could in part, be confounded by the year in which the theory was introduced. Knowledge of a theory in terms of how much it is discussed in the public domain is also likely to play a role. Another explanation might be that those that are used more frequently are ‘better’ theories and selected for use because they have a stronger evidence base or meet other quality criteria. However, a couple of examples suggest that frequency does not necessarily follow quality. For example, the theory appearing most frequently in our review, the TTM, has been criticised on several grounds (West, 2005 ) and its empirical support has been questioned by systematic review findings (e.g., Cahill, Lancaster, & Green, 2010 ; Etter & Perneger, 1999 ; Littell & Girvin, 2002 ; Whitelaw, Baldwin, Bunton, & Flynn, 2000 ). On the other hand, recent meta-regression evidence has shown good support for Control Theory (Dombrowski et al., 2012 ; Ivers et al., 2012 ; Michie et al., 2009 ); however, this was identified in only one article in our review. Another explanation is that people are not aware of the full range of theories from which to choose and so instead opt for those most commonly applied in the literature. Frequency of use may not reflect perceived quality of the theory but instead, fashion, familiarity, prior training, exposure or incentivisation. We hope that this review will help to increase awareness among intervention designers and researchers about the range of theories available. We report nine criteria agreed as markers of theory quality that could aid selection of the most appropriate theory or theories.
Our decision to focus on theories of behaviour change at the level of the individual and exclude theories concerned with group behaviour is likely to be part of the explanation for the preponderance of psychological theories identified in the review, although even interventions at the community level tend to be informed by psychological or social–psychological theories (e.g., Bonell, Fletcher, et al., 2013 ; Bonell, Jamal, et al., 2013 ; Glanz & Bishop, 2010 ; National Institute for Health and Care Excellence, 2007 ). This, and the decision not to include books where sociological and anthropological theories are more likely to be found, may go some way to explaining why these types of theory are under-represented. In addition, Kelly et al. ( 2010 ) found that sociological theories were missed in electronic searches, particularly if they were more than 25 years old. Given that interventions may be improved by drawing on theories specifically targeting group behaviours, this would be a useful focus for a future literature review as we are not aware of there being such a review.
This review raised the issues as to what constitutes ‘a theory’ and ‘a behaviour’. Theories, as conceptualised here, ranged from quite specific (e.g., to a particular behavioural domain or type of intervention) to very general, including multiple levels of influence. The cut-offs at either end of this spectrum were agreed by consensus but were inevitably arbitrary. A general observation was that more general theories may have greater face validity but be less useable in guiding research than more specific theories; choice of theory will therefore be partly guided by the purpose it is to be put to. Another observation was that there appeared to be no generally accepted use of terms such as theory, model, framework and orientation, with different uses by different authors. Increasing the precision of, and consensus on, use of terminology would be helpful for the field.
‘Behaviour’ also varies in level of specificity: for example, physical activity includes sports which includes volleyball which includes running. Behaviours are also part of sequences, often dependent on previous behaviours (e.g., carrying gym kit) and sometimes on other people's behaviours (e.g., others turning up for a team game). Just as the relevance of a particular theory may vary across type of behaviour, so it may vary according to the level of specificity.
The review also suggests that there are a large number of theories that are of potential use in designing public health interventions. The cataloguing of 83 theories of behaviour change is an important resource for researchers wishing to draw on theories beyond the few that currently dominate the literature. However, few of these theories have been subjected to wide-scale rigorous empirical evaluation. There have been calls for more operationalization, application, testing and refining of theories over many years (e.g., Michie & Johnston, 2012 ; Noar & Zimmerman, 2005 ; Rothman, 2004 ; Weinstein, 2007 ; Weinstein & Rothman, 2005 ), but advances are slow. We need more investment into methodological and substantive research in this area, for example, the use of fractionated factorial (Collins et al., 2011 ) and n -of-1 (Johnston, Jones, Charles, McCann, & McKee, 2013 ) designs to tease apart complex interventions and the extent to which theories can be generalised across populations, behaviours and contexts.
Identifying the theories in this review is just the first step in a much larger and ongoing programme of work aimed at improving the use of appropriate theory and the scientific rigour with which it is applied. Future work will investigate the ways in which theories have been operationalised and the extent to which different theories share constructs and can be seen as ‘families’ of theory. Transforming the nine quality criteria into forms, such as reliable scales or response options that can be used in evaluating theories is a complex task, and a study in its own right. The evolution of theories over time, including the issue of when a theory is considered a new theory, will also be examined. Many theories contained similar constructs or the same constructs but with slightly different names. Understanding these similarities and working towards a common set of terminology would facilitate the building of a cumulative understanding of mechanisms of action from both primary research and evidence syntheses. It would also further our understanding of the evolution of theories and how theories have been revised and/or integrated with other theories over time. Having said this, it is also important to recognise that not only language varies across and within disciplines but so do epistemological and ontological assumptions and preoccupations.
The next phase of the current research is to (i) investigate the connectedness of theories with each other and (ii) operationalize and demonstrate the application of the agreed quality criteria. These will both inform the understanding of theory and its development, and help guide researchers, policy-makers and interventions on the appropriate selection and application behaviour change theories to developing public health and other behaviour change interventions.
Acknowledgements
We are grateful to the study's advisory group for developing the literature search strategy, key definitions and the quality criteria for evaluating theory: Robert Aunger, Mary Barker, Mick Bloor, Heather Brown, Richard Cookson, Cyrus Cooper, Peter Craig, Paul Dieppe, Anna Dixon, Rachel Gooberman-Hill, Simon Griffin, Graham Hart, Kate Hunt, Susan Jebb, Marie Johnston, Mike Kelly, Steve Morris, Mark Petticrew, Paschal Sheeran, Mark Suhreke, Ivo Vlaev, Robert West, Daniel Wight, Daniel Zizzo. We are also grateful to Kate Sheals for invaluable help in the latter stages of manuscript preparation.
Funding Statement
Funding : This project was funded by the Medical Research Council's Population Health Sciences Research Network [grant number PHSRN10 ]. The work was undertaken with the support of The Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UKCRC Public Health Research: Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council [ RES-590-28-0005 ], Medical Research Council, the Welsh Government and the Wellcome Trust [ WT087640MA ], under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged.
This project was funded by the Medical Research Council's Population Health Sciences Research Network [grant number PHSRN10]. The work was undertaken with the support of The Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UKCRC Public Health Research: Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council [RES-590-28-0005], Medical Research Council, the Welsh Government and the Wellcome Trust [WT087640MA], under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged.
Supplemental material
Supplemental material for this article can be accessed here: http://dx.doi.org/10.1080/17437199.2014.941722 .
- Abraham C., Kelly M. P., West R., Michie S. The UK National Institute for Health and Clinical Excellence public health guidance on behaviour change: A brief introduction. Psychology, Health and Medicine . 2009;(1):1–8. doi: 10.1080/13548500802537903. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Agar J. What happened in the sixties? British Journal for the History of Science . 2008:567–600. doi: 10.1017/S0007087408001179. [ CrossRef ] [ Google Scholar ]
- Albada A., Ausems M. G. E. M., Bensing J. M., van Dulmen S. Tailored information about cancer risk and screening: A systematic review. Patient Education and Counseling . 2009:155–171. doi: 10.1016/j.pec.2009.03.005. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Albarracin D., Gillette J. C., Earl A. N., Glasman L. R., Durantini M. R., Ho M. H. A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychological Bulletin . 2005:856–897. doi: 10.1037/0033-2909.131.6.856. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ammerman A. S., Lindquist C. H., Lohr K. N., Hersey J. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: A review of the evidence. Preventive Medicine . 2002;(1):25–41. doi: 10.1006/pmed.2002.1028. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aveyard P., West R. Managing smoking cessation. BMJ . 2007;(7609):37–41. doi: 10.1136/bmj.39252.591806.47. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bhattarai N., Prevost A., Wright A., Charlton J., Rudisill C., Gulliford M. Effectiveness of interventions to promote healthy diet in primary care: Systematic review and meta-analysis of randomised controlled trials. BMC Public Health . 2013;(1):1–14. doi: 10.1186/1471-2458-13-1203. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bonell C. P., Fletcher A., Jamal F., Wells H., Harden A., Murphy S., Thomas J. Theories of how the school environment impacts on student health: Systematic review and synthesis. Health & Place . 2013:242–249. doi: 10.1016/j.healthplace.2013.09.014. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bonell C., Jamal F., Harden A., Wells H., Parry W., Fletcher A., et al.Moore L. Systematic review of the effects of schools and school environment interventions on health: Evidence mapping and synthesis. Public Health Research . 2013;(1) Retrieved from http://www.journalslibrary.nihr.ac.uk/__data/assets/pdf_file/0016/71161/FullReport-phr01010.pdf . [ PubMed ] [ Google Scholar ]
- Brouwers M. C., De Vito C., Bahirathan L., Carol A., Carroll J. C., Cotterchio M., et al.Wathen N. What implementation interventions increase cancer screening rates? A systematic review. Implementation Science . 2011:111. doi: 10.1186/1748-5908-6-111. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cahill K., Lancaster T., Green N. Stage-based interventions for smoking cessation. Cochrane Database of Systematic Reviews . 2010;(11) doi: 10.1002/14651858.CD004492.pub4. CD004492. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Campbell M., Fitzpatrick R., Haines A., Kinmonth A. L., Sandercock P., Spiegelhalter D., Tyrer P. Framework for design and evaluation of complex interventions to improve health. BMJ . 2000:694–696. doi: 10.1136/bmj.321.7262.694. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Campbell N. C., Murray E., Darbyshire J., Emery J., Farmer A., Griffiths F., et al.Kinmonth A. L. Designing and evaluating complex interventions to improve health care. BMJ . 2007:455–459. doi: 10.1136/bmj.39108.379965.BE. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cane J., O'Connor D., Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Science . 2012:37. doi: 10.1186/1748-5908-7-37. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carr A. B., Ebbert J. Interventions for tobacco cessation in the dental setting. Cochrane Database of Systematic Reviews . 2012 doi: 10.1002/14651858.CD005084.pub3. CD005084. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coleman T. Do financial incentives for delivering health promotion counselling work? Analysis of smoking cessation activities stimulated by the quality and outcomes framework. BMC Public Health . 2010:167. doi: 10.1186/1471-2458-10-167. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Collins L. M., Baker T. B., Mermelstein R. J., Piper M. E., Jorenby D. E., Smith S. S., et al.Fiore M. C. The multiphase optimization strategy for engineering effective tobacco use interventions. Annals of Behavioral Medicine . 2011:208–226. doi: 10.1007/s12160-010-9253-x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Conner N., Norman P. Predicting health behaviour: Research and practice with social cognition models . Buckingham: Open University Press; 2005. 2nd ed. [ Google Scholar ]
- Craig P., Dieppe P., Macintyre S., Michie S., Nazareth I., Petticrew M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ . 2008:a1655. doi: 10.1136/bmj.a1655. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cutrona S. L., Choudhry N. K., Stedman M., Servi A., Liberman J. N., Brennan T., et al.Shrank W. H. Physician effectiveness in interventions to improve cardiovascular medication adherence: A systematic review. Journal of General Internal Medicine . 2010:1090–1096. doi: 10.1007/s11606-010-1387-9. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Danaei G., Ding E. L., Mozaffarian D., Taylor B., Rehm J., Murray C. J., Ezzati M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Medicine . 2009;(4):e1000058. doi: 10.1371/journal.pmed.1000058. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davies P., Walker A. E., Grimshaw J. M. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implementation Science . 2010:14. doi: 10.1186/1748-5908-5-14. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dombrowski S. U., Sniehotta F. F., Avenell A., Johnston M., MacLennan G., Araujo-Soares V. Identifying active ingredients in complex behavioural interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: A systematic review. Health Psychology Review . 2012:7–32. doi: 10.1080/17437199.2010.513298. [ CrossRef ] [ Google Scholar ]
- Etter J. F., Perneger T. V. A comparison of two measures of stage of change for smoking cessation. Addiction . 1999:1881–1889. doi: 10.1046/j.1360-0443.1999.9412188113.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Everett T., Bryant A., Griffin M. F., Martin-Hirsch P. P. L., Forbes C. A., Jepson R. G. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database of Systematic Reviews . 2011;(5):CD002834. doi: 10.1002/14651858.Cd002834.Pub2. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ezzati M., Lopez A. D., Rodgers A., Vander Hoorn S., Murray C. J. L., Coll C. R. A. Selected major risk factors and global and regional burden of disease. Lancet . 2002:1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Festinger L. A theory of social comparison processes. Human Relations . 1954:117–140. doi: 10.1177/001872675400700202. [ CrossRef ] [ Google Scholar ]
- Fishbein M., Triandis H. C., Kanfer F. H., Becker M., Middlestadt S. E., Eichler A. Factors influencing behaviour and behaviour change. In: Baum A., Revenson T. A., Singer J. E., editors. Handbook of health psychology . Mahwah, NJ: Lawrence Erlbaum Associates; 2001. pp. 3–17. [ Google Scholar ]
- Francis J. J., O'Connor D., Curran J. Theories of behaviour change synthesised into a set of theoretical groupings: Introducing a thematic series on the theoretical domains framework. Implementation Science . 2012:35. doi: 10.1186/1748-5908-7-35. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- French S. D., Green S. E., O'Connor D. A., McKenzie J. E., Francis J. J., Michie S., et al.Grimshaw J. M. Developing theory-informed behaviour change interventions to implement evidence into practice: A systematic approach using the theoretical domains framework. Implementation Science . 2012:38. doi: 10.1186/1748-5908-7-38. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fuller C., Michie S., Savage J., McAteer J., Besser S., Charlett A., et al.Stone S. The feedback intervention trial (FIT) – improving hand-hygiene compliance in UK healthcare workers: A stepped wedge cluster randomised controlled trial. PLoS One . 2012;(10):e41617. doi: 10.1371/journal.pone.0041617. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gardner B., Wardle J., Poston L., Croker H. Changing diet and physical activity to reduce gestational weight gain: A meta-analysis. Obesity Reviews . 2011:e602–e620. doi: 10.1111/j.1467-789X.2011.00884.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Glanz K., Bishop D. B. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health . 2010:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Glanz K., Rimer B. K. Theory at a glance: A guide for health promotion practice . Bethesda, MD: National Cancer Institute; 1997. [ Google Scholar ]
- Glanz K., Rimer B. K., Lewis F. M., editors. Health behavior and health education. Theory, research and practice . San Francisco, CA: Jossey-Bass; 2002. [ Google Scholar ]
- Gough D., Thomas J., Oliver S. Clarifying differences between review designs and methods. Systematic Reviews . 2012:28. doi: 10.1186/2046-4053-1-28. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hardeman W., Sutton S., Griffin S., Johnston M., White A., Wareham N. J., Kinmonth A. L. A causal modelling approach to the development of theory-based behaviour change programmes for trial evaluation. Health Education Research . 2005:676–687. doi: 10.1093/Her/Cyh022. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Head K., Noar S. M. Facilitating progress in health behaviour theory development and modification: The reasoned action approach as a case study. Health Psychology Review . 2013:34–52. [ PubMed ] [ Google Scholar ]
- House of Lords . Behaviour change. Science and technology select committee, 2nd Report of Session 2010 . London: The Stationery Office (on authority of the House of Lords); 2011. [ Google Scholar ]
- Ivers N., Jamtvedt G., Flottorp S., Young J. M., Odgaard-Jensen J., French S. D., et al.Oxman A. D. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews . 2012 doi: 10.1002/14651858.CD000259.pub3. CD000259. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnston D. W., Jones M. C., Charles K., McCann S. K., McKee L. Stress in nurses: Stress-related affect and its determinants examined over the nursing day. Annals of Behavioral Medicine . 2013:348–356. doi: 10.1007/s12160-012-9458-2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kelly M., Morgan A., Ellis S., Younger T., Huntley J., Swann C. Evidence based public health: A review of the experience of the National Institute of Health and Clinical Excellence (NICE) of developing public health guidance in England. Social Science and Medicine . 2010:1056–1062. doi: 10.1016/j.socscimed.2010.06.032. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kim N., Stanton B., Li X., Dickersin K., Galbraith J. Effectiveness of the 40 adolescent AIDS-risk reduction interventions: A quantitative review. Journal of Adolescent Health . 1997:204–215. doi: 10.1016/s1054-139x(96)00169-3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Littell J. H., Girvin H. Stages of change: A critique. Behavior Modification . 2002:223–273. doi: 10.1177/0145445502026002006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marteau T., Dieppe P., Foy R., Kinmonth A. L., Schneiderman N. Behavioural medicine: Changing our behaviour – A growing body of evidence shows how to make behavioural interventions effective. British Medical Journal . 2006:437–438. doi: 10.1136/bmj.332.7539.437. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McLeroy K. R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Education and Behavior . 1988:351–377. doi: 10.1177/109019818801500401. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michie S. Designing and implementing behaviour change interventions to improve population health. Journal of Health Services Research and Policy . 2008;(3):64–69. doi: 10.1258/jhsrp.2008.008014. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michie S., Abraham C. Interventions to change health behaviours: Evidence-based or evidence-inspired? Psychology & Health . 2004;(1):29–49. doi: 10.1080/0887044031000141199. [ CrossRef ] [ Google Scholar ]
- Michie S., Abraham C., Whittington C., McAteer J., Gupta S. Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychology . 2009:690–701. doi: 10.1037/a0016136. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michie S., Johnston M. Theories and techniques of behaviour change: Developing a cumulative science of behaviour change. Health Psychology Review . 2012:1–6. doi: 10.1080/17437199.2012.654964. [ CrossRef ] [ Google Scholar ]
- Michie S., Johnston M., Abraham C., Lawton R., Parker D., Walker A., Psychological Theory Group Making psychological theory useful for implementing evidence based practice: A consensus approach. Quality & Safety in Health Care . 2005;(1):26–33. doi: 10.1136/qshc.2004.011155. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michie S., Johnston M., Francis J., Hardeman W., Eccles M. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Applied Psychology . 2008:660–680. doi: 10.1111/j.1464-0597.2008.00341.x. [ CrossRef ] [ Google Scholar ]
- Michie S., Prestwich A. Are interventions theory-based? Development of a theory coding scheme. Health Psychology . 2010;(1):1–8. doi: 10.1037/a0016939. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michie S., West R. Behaviour change theory and evidence: A presentation to government. Health Psychology Review . 2013:1–22. doi: 10.1080/17437199.2011.649445. [ CrossRef ] [ Google Scholar ]
- Mokdad A. H., Marks J. S., Stroup D. F., Gerberding J. L. Actual causes of death in the United States, 2000. JAMA . 2004:1238–1245. doi: 10.1001/jama.291.10.1238. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Institute for Health and Care Excellence . Behaviour change at population, community and individual levels [NICE public health guidance 6] London: Author; 2007. [ Google Scholar ]
- National Institute for Health and Clinical Excellence . Health systems and health-related behaviour change – A review of primary and secondary evidence . London: Author; 2010. [ Google Scholar ]
- Nigg C. R., Allegrante J. P., Ory M. Theory-comparison and multiple-behavior research: Common themes advancing health behavior research. Health Education Research . 2002:670–679. doi: 10.1093/Her/17.5.670. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Noar S. M., Benac C. N., Harris M. S. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin . 2007:673–693. doi: 10.1037/0033-2909.133.4.673. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Noar S. M., Zimmerman R. S. Health behavior theory and cumulative knowledge regarding health behaviors: Are we moving in the right direction? Health Education Research . 2005:275–290. doi: 10.1093/her/cyg113. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Office of Behavioural and Social Sciences Research . Healthier lives through behavioral and social science research . Bethesda, MD: Author; 2006. [ Google Scholar ]
- Painter J. E., Borba C. P. C., Hynes M., Mays D., Glanz K. The use of theory in health behavior research from 2000 to 2005: A systematic review. Annals of Behavioral Medicine . 2008:358–362. doi: 10.1007/s12160-008-9042-y. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Parkin D. M., Boyd L., Walker L. C. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. British Journal of Cancer . 2011;(2):S77–S81. doi: 10.1038/bjc.2011.489. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prestwich A., Sniehotta F. F., Whittington C., Dombrowski S. U., Rogers L., Michie S. Does theory influence the effectiveness of health behavior interventions? Meta-analysis. Health Psychology . 2013:465–474. doi: 10.1037/a0032853. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rice V. H., Stead L. F. Nursing interventions for smoking cessation. Cochrane Database of Systematic Reviews . 2008;(8):CD001188. doi: 10.1002/14651858.Cd001188.Pub3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roe L., Hunt P., Bradshaw H., Rayner M. Health promotion interventions to promote healthy eating in the general population : A review . London: Health Education Authority; 1997. [ Google Scholar ]
- Rothman A. J. “Is there nothing more practical than a good theory?” Why innovations and advances in health behavior change will arise if interventions are used to test and refine theory. International Journal of Behavioral Nutrition and Physical Activity . 2004:11. doi: 10.1186/1479-5868-1-11. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rothman A. J. Capitalizing on opportunities to refine health behavior theories. Health Education & Behavior . 2009:150s–155s. doi: 10.1177/1090198109340514. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sheeran P. Intention-behaviour relations: A conceptual and empirical overview. European Review of Social Psychology . 2002;(1):1–36. doi: 10.1080/14792772143000003. [ CrossRef ] [ Google Scholar ]
- Shemilt I., Simon A., Hollands G. J., Marteau T. M., Ogilvie D., O'Mara-Eves A., et al.Thomas J. Pinpointing needles in giant haystacks: Use of text mining to reduce impractical screening workload in extremely large scoping reviews. Research Synthesis Methods . 2013;(1):31–49. doi: 10.1002/jrsm.1093. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Solomon S., Kington R. National efforts to promote behavior-change research: Views from the Office of Behavioral and Social Sciences Research. Health Education Research . 2002:495–499. doi: 10.1093/her/17.5.495. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Steinijans V. W., Diletti E., Bomches B., Greis C., Solleder P. Interobserver agreement: Cohen's kappa coefficient does not necessarily reflect the percentage of patients with congruent classifications. International Journal of Clinical Pharmacology and Therapeutics . 1997:93–95. [ PubMed ] [ Google Scholar ]
- Stephenson J. M., Imrie J., Sutton S. R. Rigorous trials of sexual behaviour interventions in STD/HIV prevention: What can we learn from them? AIDS . 2000;(3):S115–S124. [ PubMed ] [ Google Scholar ]
- Summerbell C. D., Waters E., Edmunds L. D., Kelly S., Brown T., Campbell K. J. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews . 2005;(12):CD001871. [ PubMed ] [ Google Scholar ]
- Swann C., Bowe K., Kosmin M., McCormick G. Teenage pregnancy and parenthood: A review of reviews. Evidence briefing . London: Health Development Agency; 2003. [ Google Scholar ]
- Taylor N., Conner M., Lawton R. The impact of theory on the effectiveness of worksite physical activity interventions: A meta-analysis and meta-regression. Health Psychology Review . 2011:33–73. doi: 10.1080/17437199.2010.533441. [ CrossRef ] [ Google Scholar ]
- Taylor S. E. Adjustment to threatening events: A theory of cognitive adaptation. American Psychologist . 1983:1161–1173. doi: 10.1037/0003-066X.38.11.1161. [ CrossRef ] [ Google Scholar ]
- Webb T. L., Joseph J., Yardley L., Michie S. Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research . 2010;(1):e4. doi: 10.2196/jmir.1376. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weinstein N. D. Misleading tests of health behavior theories. Annals of Behavioral Medicine . 2007;(1):1–10. doi: 10.1207/s15324796abm3301_1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weinstein N. D., Rothman A. J. Commentary: Revitalizing research on health behavior theories. Health Education Research . 2005:294–297. doi: 10.1093/her/cyg125. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- West R. Time for a change: Putting the Transtheoretical (Stages of Change) Model to rest. Addiction . 2005:1036–1039. doi: 10.1111/j.1360-0443.2004.00995.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- West R. Theory of addiction . Oxford: Blackwell; 2006. [ Google Scholar ]
- Whitelaw S., Baldwin S., Bunton R., Flynn D. The status of evidence and outcomes in stages of change research. Health Education Research . 2000:707–718. doi: 10.1093/her/15.6.707. [ PubMed ] [ CrossRef ] [ Google Scholar ]
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
- We're Hiring!
- Help Center
Health Behaviour Change
- Most Cited Papers
- Most Downloaded Papers
- Newest Papers
- Save to Library
- Last »
- Health Behaviors Follow Following
- Health Psychology Follow Following
- Health Promotion Follow Following
- Health Education Follow Following
- Health Communication Follow Following
- Public Health Follow Following
- Health Outcomes Follow Following
- Self-Management of Health Follow Following
- Implementation Intentions Follow Following
- Medication Adherence Follow Following
Enter the email address you signed up with and we'll email you a reset link.
- Academia.edu Publishing
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

NPP > JOURNALS > HBR
Health Behavior Research (HBR) is the official journal of the American Academy of Health Behavior (AAHB). Published four-times per year, HBR is a peer-reviewed open-access scholarly journal that publishes original research articles, current issues papers, commentaries, and abstracts from the annual meeting of the Academy.
- Test theoretical principles across a diverse array of settings and populations to enable investigators to better specify the scope of a theory;
- Further develop processes that shape primary constructs identified in health behavior theories to inform guidelines for strategies to target constructs in policy, planning, and practice;
- Address the causal processes invoked by mediators and moderators that inform theory refinement;
- Provide empirical evidence that informs researchers about the potential factors that lack predictive and explanatory health behaviors so as to refine and reduce the number of constructs within existing theories that predict and explain health behavior;
- Provide rationale for theory refinement based on application and rigorous testing.
- Address new and emerging concepts and theory used in health behavior research, conceptual frameworks, methods, and analyses.
For more information about AAHB, and becoming a member, please visit the academy’s website at www.aahb.org .
Current Issue: Volume 7, Number 2 (2024)
Sapere Aude — Dare to Be Wise: Robert J. McDermott Robert J. McDermott
Research Articles
Just Pin It: Understanding the Dynamics of Pinterest Use, Motivation, Self-Efficacy, and Health Behaviors Kathryn E. Dolphin, Rachel Char, and Summer Rogers
Electronic Nicotine Product (ENP) Graphic Warnings: Association between Exposure and Changes in Perceived Susceptibility and Severity of Explosion and Lung Injuries Erica Harp, Matthew E. Rossheim, Xiaoquan Zhao, Christian Seiter, Ogechikamma C. Emechebe, and Eric Soule
- Editorial Board
- Policies/Information for Authors
- Become a Reviewer for HBR
- Become an AAHB Member
- Support HBR by Donating to AAHB
- AAHB Annual Scientific Meeting
- Call for Special Issue on Mentoring
- Special Collections
- Submit Article
- Most Popular Papers
- Receive Email Notices or RSS
Advanced Search
ISSN: 2572-1836
NPP Home | About NPP | My Account | Accessibility Statement
Privacy Copyright
Loading metrics
Open Access
Decolonising global health research: Shifting power for transformative change
Roles Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations United Nations University-International Institute for Global Health, Kuala Lumpur, Malaysia, Department of Community and Family Medicine, Faculty of Medicine, University of Jaffna, Jaffna, Sri Lanka
Roles Conceptualization, Writing – review & editing
Affiliation United Nations University-International Institute for Global Health, Kuala Lumpur, Malaysia
Roles Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing
- Ramya Kumar,
- Rajat Khosla,
- David McCoy

Published: April 24, 2024
- https://doi.org/10.1371/journal.pgph.0003141
- Reader Comments
Recent debates on decolonizing global health have spurred interest in addressing the power asymmetries and knowledge hierarchies that sustain colonial ideas and relationships in global health research. This paper applies three intersecting dimensions of colonialism (colonialism within global health; colonisation of global health; and colonialism through global health) to develop a broader and more structural understanding of the policies and actions needed to decolonise global health research. It argues that existing guidelines and checklists designed to make global health research more equitable do not adequately address the underlying power asymmetries and biases that prevail across the global health research ecosystem. Beyond encouraging fairer partnerships within individual research projects, this paper calls for more emphasis on shifting the balance of decision-making power, redistributing resources, and holding research funders and other power-holders accountable to the places and peoples involved in and impacted by global health research.
Citation: Kumar R, Khosla R, McCoy D (2024) Decolonising global health research: Shifting power for transformative change. PLOS Glob Public Health 4(4): e0003141. https://doi.org/10.1371/journal.pgph.0003141
Editor: Ananya Banerjee, McGill University, CANADA
Copyright: © 2024 Kumar et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
1. Introduction
Inequity within international research partnerships has troubled the field of global health for decades. In particular, power asymmetries between actors from wealthier and historically-privileged countries and their counterparts in the Global South (GS) have led to paternalistic ways of working, unequal sharing of resources, skewed distribution of benefits, and limited commitments to capacity strengthening [ 1 ]. Recent debates on decolonizing global health have brought renewed attention to addressing these problems in global health research. In addition to highlighting equity concerns, these discussions draw attention to the epistemic injustice and “white saviour” mentalities that underpin research collaborations [ 2 – 8 ].
Recognising that power asymmetries in global health are produced by both historical and current exploitation and resource extraction, our approach to decolonizing global health involves three intersecting dimensions: 1) colonialism within global health; 2) colonisation of global health; and 3) colonialism through global health [ 9 ]. The first dimension speaks to power differentials and resource disparities between different actors within the field of global health. The second deals with the dominance of certain powerful actors and vested interests over the overall complex of global health structures, systems, policies and practices. The third dimension refers to exploitative and extractive practices that occur through the health sector [ 9 ].
This paper uses this framework of three dimensions to arrive at a broader understanding of the scope of policies and actions needed to decolonise global health research. We begin by briefly outlining persisting inequities within research partnerships- already addressed by a large body of literature. Next, we draw attention to issues that are underexplored, specifically who controls the agenda of global health research (i.e., colonisation of global health research), and who benefits from such research (i.e., colonialism through global health research) ( Fig 1 ). We then present a brief review of recent guidelines and checklists that seek to decolonize global health research and/or centre the needs and aspirations of the GS in research, revealing an emphasis on addressing inequity within research partnerships. We end by recommending policies and actions that would decolonize the field of global health research in an effective and comprehensive manner.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0003141.g001
This paper employs the terminology “Global North” (GN) and “Global South” (GS) to reflect asymmetries in power and access to resources between not just countries but also population groups. This terminology only partly corresponds to the classification of countries according to per capita gross national income, i.e., low-income, middle-income, and high-income countries (LIC, MIC, and HIC) [ 10 ]. However, where we quote from sources that explicitly refer to LICs, MICs or HICs, these terms are retained. We borrow from Garcia-Basteiro and Abimbola [ 11 ] to define global health research as research that seeks to address health inequity within and across countries, aiming to improve health in what they call “low-resource settings” described as regions weighed down by financial constraints, suboptimal service delivery, underdeveloped physical and knowledge infrastructure, historical, political and sociocultural contexts/specificities, and geographical, environmental and human resource limitations.
2. Colonialism within global health research: Who leads?
According to the World Health Organization (WHO), in 2020, of the USD 37 billion spent worldwide on ‘biomedical research’, 98.7% went to HICs [ 12 ]. Perhaps more reflective of the global health research landscape, in 2021, 82% of the Bill and Melinda Gates Foundation’s (BMGF) grant funding went to HIC recipients [ 13 ]. This unequal distribution of funding is striking when one considers that much global health research is carried out in GS settings.
The inequitable global health research funding patterns reflect not only the wider socio-economic disparity between GN and GS, but also the biases within the global health research system. For example, grant calls, either explicitly or through eligibility criteria or capacity requirements, favour GN-based institutions [ 14 ] with research funding agencies of key donor countries often requiring principal investigators (PI) to be based in their country or compel PIs from the GS to partner with a researcher based in the donor country [ 15 , 16 ]. Eligibility criteria based on geographic location and experience may further restrict applications from GS-based researchers [ 17 ]. GN-based researchers are also better able to navigate the funding terrain with their training, networks and resources [ 18 , 19 ].
Although most global health funding agencies require GN-based researchers to “collaborate” with local “partners,” the terms of collaboration are usually set by the former who typically conceptualise the research before inviting others onboard [ 20 ]. This gives GS-based researchers limited influence over the research, despite their expertise and familiarity with the context [ 7 , 21 , 22 ], thus supporting what has been called “parachute” research, where GN-based collaborators fly in for weeks at a time for onsite “supervision” [ 23 , 24 ]. As grant cycles are usually short, the urgency to meet deadlines results in lopsided decision-making, hasty administrative approvals and, at times, the undermining of local administrative and ethics procedures [ 8 ].
Much grant funding goes towards the salaries of GN-based researchers with substantially less dedicated to research systems and capacity strengthening in GS settings [ 2 , 14 ]. This lack of long-term commitment to the development of GS-based institutions sustains the status quo [ 25 ]. Meanwhile, extant capacity strengthening initiatives are often uni-directional and paternalistic, involving assumptions about what competencies GS collaborators may lack [ 26 ].
Inequity is further reinforced by authorship patterns that are biased towards GN-based researchers [ 27 , 28 ]. Authorship guidelines of prominent journals systematically exclude non-native English writers [ 29 ] by giving weight to written contributions over field work [ 30 ]. Representation at conferences and symposia is similarly unequal, although research collaborations do enable participation for some GS-based researchers. Even so, visa and other barriers challenge researchers from travelling to meeting destinations [ 31 ].
3. Colonisation of global health research: Who controls?
Global health funding agencies wield significant power in defining global health problems and the approaches taken to addressing them [ 7 , 32 ]. Under the current system, researchers based at universities and other research institutions respond to grant calls, crafting their research to fit with the agendas and ideologies of global health funders rather than vice versa [ 33 ].
Extreme wealth concentration under neoliberal globalization and the rise of ‘philanthrocapitalism’ by which global health problems are framed as market opportunities, has seen a shift from public to private financing in global health [ 34 , 35 ]. However, private actors have interests and priorities that may be at odds with the public interest or with achieving equity in health. For instance, the shift from publicly-funded to industry-funded research has distorted scientific evidence on infant formula with detrimental effects on infant and child health [ 36 ]. Moreover, the funding decisions of corporations and foundations are ultimately approved by a handful of largely GN-based board members, who are not subjected to any independent mechanisms of accountability for their funding decisions or their impact on people affected by these decisions [ 32 , 37 ]. Although some funders have recently instituted measures to address diversity within their leadership [ 13 , 38 ], such change will not be transformative without redistributing power and resources, and genuine efforts to improve accountability [ 39 ].
Research funders favour specific thematic areas, not always based on the health problems prevailing in specific GS settings [ 19 , 40 ]. They tend to promote technology-based solutions and favour innovation and entrepreneurship in projects that yield quick and quantifiable results [ 41 ]. The preference for short-term impact over longer-term improvements in health results in grant proposals that centre “magic bullets” (e.g., vaccines, medicines, bed nets, mobile apps) rather than systems building, local capacity strengthening and unblocking the social and political barriers to the scale up of proven and more sustainable alternatives [ 42 , 43 ].
Academic programmes in global health continue to be characterised by what has been called a “white saviour complex” or a depoliticized, patronizing and charity-based approach shaped, in part, by a wider aid industry [ 44 , 45 ]. Global health curricula remain largely disconnected from the many realities and locales of the GS, both in geography and lived experience. Dominant Eurocentric epistemologies, which are embraced and propagated by powerful global health institutions, are usually given primacy in research training, even as heterodox methodologies that interrogate power and inequality are marginalized [ 45 , 46 ].
The inability of countries of the GS to weigh in on the global health research agenda and define their own priorities is perpetuated by their minimal contributions to research funding [ 25 , 47 , 48 ]. While domestic investment is critical to shift the balance of power, debt-ridden governments of lower-income countries may have limited leeway with their health and R&D budgets owing to fiscal constraints [ 19 ]. For these countries, HIC-driven global health research collaborations may present a welcome source of foreign currency. Too often however, external funding for health research takes place with little coordination among granting agencies [ 49 , 50 ], facilitating duplication, and making impact assessment difficult.
4. Colonialism through global health research: Who benefits?
The asymmetric global health research funding structure also gives powerful states and private actors opportunities to craft research in the GS in ways that they benefit from financially or economically. These benefits are primarily driven by the commercialization of research and publishing, supported by imperatives to expand markets, unfair intellectual property rights (IPR) regimes, and predatory academic journals.
Arguably, the biggest profits are made by commercial entities that hold patents for global health technologies often tested through research carried out in GS settings. Such research aids market expansion for medicines, vaccines, diagnostic tests, mobile devices, etc. benefitting big pharma, biotechnology, and big tech companies, while doing little to strengthen public health infrastructure and services or reduce dependency [ 19 , 41 ]. Indeed, some private foundations are routing a growing proportion of their tax-subsidised grants to private for-profit organisations, in both GN and GS settings [ 37 , 51 ].
Current IPR regimes which provide private companies with extensive monopoly rights over new and modified technologies despite much basic research being funded publicly is one aspect of an R&D ecosystem biased in favour of private financial interests at the expense of public health. This was seen with the billions of dollars of private profits generated from COVID-19 vaccines despite vast amounts of public and charitable funds that went into their development [ 52 ].
The unequal benefits accrued through authorship in global health journals have been widely studied [ 27 , 28 ] but less is known about their commercial dimensions. The revenue of academic publishers is estimated to be about USD 19 billion annually, where about half the market share is controlled by five transnational companies, with Elsevier alone accounting for 16% of the market share, with profit margins in the order of 40 per cent [ 53 ]. These corporations are all headquartered in the GN and maximise profits through article processing charges (APCs), subscriptions, and the uncompensated labour of authors and peer-reviewers. Ever-increasing APCs are required to publish ‘open access’ in prestigious journals, implemented in the name of equity, but barring most GS-based researchers through stringent waiver criteria [ 54 ]. Global spending on APCs alone is estimated to exceed USD 2 billion annually [ 55 ]. Academic journals are, in turn, linked to bibliometric platforms that track the ‘impact’ of research communications, which feed into commercialised university ranking systems [ 56 ]. With research funding and citations in ‘high-impact’ journals being key elements of performance indices, the top-twenty universities, as ranked by Academic Ranking of World Universities and Time Higher Education, are all located in the GN [ 57 ].
The current system of global health education supports extraction of wealth and other resources from GS to GN. A recent analysis of masters in global health degrees revealed that 95% of them are based in HICs, costing on average USD 37,732 in tuition [ 58 ]. Given the location and cost of global health postgraduate programmes, their graduates, including those from GS settings, are likely to be drawn to work with global or GN-based institutions both to repay the debt incurred and because of the lack of well-remunerated positions back home [ 58 ]. Ultimately, career trajectories in global health are skewed towards the GN and not “low-resource settings” where global health work and resources are much needed [ 23 ].
In sum, whether in terms of leadership, control or benefits, GN-based actors and institutions are privileged within the broader global health research ecosystem, often to the detriment of researchers, institutions and ‘beneficiaries’ in GS settings. It appears that global health research supports a renewed form of extractivism, where resources in the GS, including funding, knowledge and researchers, are drawn to the GN. In the next section, we examine whether and to what extent recent guidelines on decolonising global health research address the three intersecting dimensions of colonialism in global health research.
5. Recent guidelines that aim to decolonise global health research
We searched the literature for tools that either explicitly or in their framing seek to decolonise global health research and/or centre the needs and aspirations of the GS in research. As searches on PubMed and Scopus [(“decol*” OR “colonial*”) AND “global health” AND “research” AND (manual OR guideline OR checklist)] yielded less than 10 publications, we also searched Google Scholar, Google, and pursued reference lists of identified publications. Criteria for inclusion were: addressing equity in global health research with reference to colonialism or explicit attention to making research fairer for peoples and institutions in the GS; including a set of standards or guidelines; targeting researchers, research institutions or funders; published within the five-year period of 2019 to 2023. We identified eight tools that fit our criteria as described below.
Hodson et al. [ 40 ] offer a set of “practical measures” for global health researchers, underpinned by four principles: “1) seek locally derived and relevant solutions to global health issues, 2) create paired collaborations between HIC and LMIC institutions at all levels of training, 3) provide funding for both HIC and LMIC team members, [and] 4) assign clear roles and responsibilities to value, leverage, and share the strengths of all team members.” This guideline addresses specific challenges experienced in GS settings by advocating for: educating all team members on global health history; early engagement of GN-based researchers with local administrations; capacity strengthening to support independent research in GS settings; protected research time for all team members; preventing GS-based researchers being drawn away from regular work; and ensuring knowledge translation to local communities, among other measures. Despite the commitment to long-term capacity strengthening, the guideline focuses primarily on research processes within partnerships.
Kumar et al. [ 26 ] propose a set of individual and institutional level actions to advance equity in global health research. Those at the individual level include questioning “notions of absolute scientific objectivity” (p.146), adopting a decolonial approach towards global health concepts and implicit hierarchies, cultivating respect and humility, promoting fairness at all levels (including at the level of global health leadership), and going beyond ‘equality’ to recognize ‘equity’ within collaborations. At the institutional level, they support decentring the GN in global health efforts (including the location of centres of knowledge), promoting solidarity, investing in researchers from LMICs, bi-directional capacity strengthening, evaluating partnerships by “measures of fairness” and “ethical and culturally responsive engagement,” and correcting “colonising and unethical practices” (p.146). While some of these actions aim to rectify power asymmetries well beyond research partnerships, they do not include specific guidance on implementation.
Embracing a feminist decolonial approach, Singh et al. [ 59 ] offer a guideline for researchers working in situations of forced displacement that centres participant agency, voice, and experience; it aims to address power hierarchies through a set of recommendations targeting various stages of research. The guideline demands: consideration to “political, social, economic, and historical contexts and power hierarchies of the research setting” (p.561); involving marginalised groups in the research design; reflecting on how coloniality and gendered power relations may be reinforced during data collection; an intersectional analysis of gendered power relations; collaboration in analysis and knowledge dissemination; and using research to “challenge unjust systems and policies and deliver gender transformative and equitable programmes” (p.561). Although the guideline aims to reconfigure power within individual research projects, it offers no direction on how to redistribute power.
Rashid [ 8 ] offers guidance for researchers in LICs to “[navigate] the violent process of decolonisation in global health research.” The guideline includes a list of dos and don’ts to help researchers in LICs contend with power asymmetries in international research collaborations. They recommend carefully reviewing agreements, clarifying systems of reporting and accountability, insisting on inclusion in communications with funders, meticulous documentation, boosting one’s profile, expanding networks, and building solidarity. However, this guideline focuses on change at the individual level on the part of researchers in GS settings rather than systemic change.
The TRUST Code–“A Global Code of Conduct for Equitable Research Partnerships” is based on the core values of fairness, respect, care, and honesty [ 60 ]. Compiled by a team with wide representation from the GS, the TRUST Code consists of 23 articles. Apart from conventional ethical standards, the tool emphasises: bona fide involvement of local communities in research, fairness in the transfer and ownership of data and biological materials, and fair compensation of local collaborators. It emphasises cultural acceptability, community assent, respect for local ethics review and giving consideration to the impact of research on local human resources, animal welfare, and the environment. It calls for clarity on roles, responsibilities, capacity strengthening, transparency, and integrity of the research process. Although broadly framed around justice for communities and researchers in the GS, the tool primarily concentrates on making individual research partnerships more equitable.
The Research for Health Justice Framework proposed by Pratt and colleagues [ 61 ] offers two sets of guidelines, one for health researchers and another for granting agencies. Developed through an iterative process and fine-tuned through case studies in GS settings, the guidelines emphasize equity, justice, and inclusion, with accompanying explanations on implementation. The guideline for researchers addresses: selection of the research population and research problem, research capacity development, delivery of ancillary care, and knowledge translation practices. With respect to granting agencies, it asks that they prioritise the health concerns of the worst-off, promote ownership of the research agenda by LMIC researchers and support projects that seek to advance equity within healthcare systems, atop measures to support equitable research practices. While this framework is comprehensive in scope, the guidelines are still largely limited to the research process and do not explicitly seek to transform the global health granting system and the power asymmetries within it.
Focusing specifically on global health research funding, Charani et al. [ 19 ] outline eight areas of action for funders: 1) developing situational awareness, including an understanding of institutional dynamics and who benefits from grants; 2) formulating a mission statement that pledges equity in research; 3) equitable allocation of funds to cover differential needs of HIC- and LMIC-based researchers; 4) funding structures that encourage local ownership and leadership; 5) bi-directional capacity strengthening that enables all partners to engage with funders; 6) diversity and inclusion across the grant cycle, including in design, knowledge dissemination, access to training etc.; 7) knowledge generation, including methodologies, frameworks, tools and clarity on data ownership; and 8) reflection and feedback involving HIC and LMIC researchers on equal terms. Encouraging funders to include specific requirements for grant recipients to comply with participatory approaches and fair sharing of resources and benefits, the guideline also speaks to what should be funded, who should be funded and how. Moreover, among its recommendations—albeit with no details provided—are “a transparent process for tracking the progress of funding” and “a code of ethics for global health funders”.
The Global Health Decolonisation Movement Africa [ 17 ], self-described as a collective of African citizens, has published a guideline called, Pragmatic Approaches to Decolonising Global Health in Africa . What is unique about this guideline is that it addresses multiple “stakeholders” in HICs, including individual practitioners, funding agencies, academic and training institutions, scientific publishers, and event conveners and organisers, among others. The guideline broadly seeks to address racism against Africans within global health, and promotes African leadership and self-determination. The section for funders calls for diversifying grant review panels, rejecting “parachute” proposals, and removing requirements for researchers based in Africa to collaborate with HIC-based institutions. For academic and training institutions, the guideline recommends diversifying leadership and recruitment practices, and addressing coloniality in global health curricula. And for scientific journals, it demands diversifying authorship and peer-review panels. While this guideline emphasises diversity, equity, and inclusion, it remains constrained by the limitations of the current system of global health research funding.
In sum, there is considerable variation in guidance on improving equity in research partnerships and decolonising global health research. All reviewed sources strive to make the research process fairer and rectify power asymmetries through diversity, equity and inclusion measures, but only some engage with historical imbalances in power, interrogate dominant knowledge paradigms, centre the concerns of marginalized groups, and create space for self-determination. The guidelines for funders go beyond research partnerships to address who and what is funded. However, for the most part, these guidelines neglect the wider contextual factors that shape agenda-setting in global health research, as well as the actors and institutions that control and benefit from them.
6. Shifting the balance of power in global health research: Going forward
In this section, we draw on the three intersecting dimensions of colonialism in global health research to present seven action areas that we call for to mitigate inequitable, exploitative and extractive arrangements in global health research ( Fig 2 ).
https://doi.org/10.1371/journal.pgph.0003141.g002
First, and most fundamentally, we call for a critical examination of the epistemological and ideological underpinnings of global health research. While current debates engage to some extent with the marginalization of indigenous perspectives, few question the dominance of positivist approaches and the biomedical paradigm. Guided by a biased hierarchy of evidence that favours quantitative assessments, global health research remains over-occupied with testing the efficacy of discrete, downstream and often clinical technologies and interventions, taking attention away from the social and structural determinants of health, which are more challenging to measure [ 41 , 43 , 62 ]. Shaped by neoliberal ideology, understandings of health and healthcare have evolved from collectivist to individualist interpretations, giving way to economistic evaluations based on assumptions that resource constraints in low-income settings are inevitable [ 63 ]. Global health education could challenge dominant paradigms and mainstream approaches that advance social justice and equity in health [ 64 ].
Second, we need a better and more detailed analysis of the overall pattern and performance of research funding: where it comes from, where it goes, how it is spent, and its impact. A few of the guidelines reviewed earlier do address the global health research funding system. For instance, Charani et al. [ 19 ] recommend that funding agencies self-monitor whom they fund and also call for a code of ethics for funders, while the Global Health Decolonisation Movement Africa [ 17 ] asks funders to remove requirements for researchers based in Africa to collaborate with GN-based institutions. Even so, these measures remain couched within the current structure and system of grant funding that lacks transparency and leaves power concentrated in the hands of largely GN-based donors. The problematic norm of donors funding favoured research areas over those that are identified locally remains largely unchallenged. At the very least, information should be available by funder, recipient, research area, and research setting, possibly through a centralized system that requires funders to provide information on their funding practices. Auditing such data should enable analysis of not only where research funding comes from and who receives it but also its impact.
Third, efforts to address power asymmetries in global health research must compel reform at the highest levels of global governance. By virtue of their funding contributions, powerful states, their bilateral agencies, private foundations, and corporate actors, among others, shape the global health research agenda. Bilateral agencies tend to push foreign policy and other domestic interests [ 65 , 66 ], while corporate actors are driven by profit, and many private foundations by the creed that the private sector can more effectively tackle intractable global health problems [ 67 ]. Bilateral and multilateral agencies should be held accountable for what they fund with taxpayer contributions, while private funders—who are primarily accountable to their boards—must be appropriately regulated and prevented from having undue influence on the shaping of research priorities [ 68 , 69 ].
A comprehensive guideline for research funders that promotes fairer distribution of resources and improved accountability is needed. Such a guideline could incorporate the measures proposed by Charani et al. [ 19 ], Pratt et al. [ 61 ] and the Global Health Decolonisation Movement Africa [ 17 ]. An international agreement, akin to the Declaration of Helsinki [ 70 ]—the World Medical Association’s ethical principles for medical research—could encourage and eventually normalise funding of equity-oriented research and local ownership. Decision-making on funding priorities must be shared with the GS, not just with governments but also with researchers, institutions, and the beneficiaries of research [ 26 ].
Fourth, national research systems should be supported and strengthened with in-built mechanisms of accountability. While there are calls for LMIC governments to invest more in R&D [ 25 ], the onus for change cannot be placed on these countries alone. Rather donors must also commit to investing in local research infrastructure, human resources, and higher education systems, all key to building research capacities. Meanwhile, government allocations for health research in GS settings should be guided by appropriate needs assessments and strategic plans to strengthen national research capacity [ 71 ] as once encouraged by the Commission on Health Research for Development (COHRED), an independent global initiative that supported research for heath and development in LMICs [ 72 ]. Systemic investments in research capacity strengthening with long-term budget commitments and harmonised mechanisms should be established [ 73 ] to replace the current piecemeal manner in which health research is conducted, often subject to the whims of external funders. Bi-directional scholarships for postgraduate training in research, with service requirements in GS settings, could target specific human resource gaps. Fifth, a global fund for research [ 74 ], guided by a multilateral framework that pools donor funds and channels them based on national health priorities may help to harmonise external funding, avoid duplication, and enable greater transparency and accountability.
Sixth, given acute human resource constraints in many GS countries, brain drain must be stemmed. The WHO Global Code of Practice on the International Recruitment of Health Personnel [ 75 ] provides a multilateral framework but fails to hold the GN to account for their unethical recruitment practices. Instead, the Code focuses on the rights of migrating health workers and places the onus on ‘developing countries’ to retain them. It does not recognize the vast amounts of (often public) resources invested in health worker training in GS settings, nor does it recommend compensation to source countries for this training. Academic global health programmes should re-orient their curricula [ 76 ] so that the primary career pathways for global health practitioners are viewed to be in GS settings.
Lastly, interventions to promote fairer distribution of benefits should look beyond authorship and academic credit, to address extractivist practices within the research industry that impede access to knowledge and technologies in the GS. The current IPR regime upholds patent protection, allowing big pharma to control product pricing and restrict market entry of generic manufacturers who could drive down the cost of medicines and other health products [ 77 , 78 ]. IPR regimes need to be revised to enhance fairness in the distribution of the benefits of science rather than support industry benefits and profit over public health.
In this paper, we applied three intersecting dimensions (colonialism within global health; colonisation of global health; and colonialism through global health) to develop a broader and more structural understanding of the policies and actions needed to decolonise global health research. We highlighted the tendency of existing guidelines that seek to make research partnerships more equitable and less colonial, to target the behaviour of researchers and research institutions within the boundaries of individual research projects. Following such guidance should result in better and more appropriate global health research. However, efforts to decolonise global health research should go beyond addressing equity within research partnerships to reconfiguring power arrangements within the global health research ecosystem. This means re-orienting research along social justice and equity lines, building research capacities in GS settings, and moving away from the existing donor-driven model.
Of critical concern is the prevailing system of research funding that functions with little transparency or downward accountability. Data should be made available to scrutinize and evaluate the funding processes of research funders and the appropriateness and impact of funding patterns and practices. It would be important to examine not just the specific outputs and outcomes of individual grant programmes and research projects, but also the impact of the entire global health research portfolio on the overall functioning of health research systems at global and national levels and, in particular, how research outputs contribute towards advancing health equity. Quick fixes and half-hearted measures would simply not work. Time is now for the global health community to come together and demand a complete overhaul of the competitive global health research funding system, and its replacement or accompaniment with a more strategic and publicly-driven pooling and harmonised allocation of resources aimed at correcting the many deep and structural inequalities across the global health research ecosystem. This would also require fostering equity-oriented research approaches, grounded in local ownership, with systems of accountability built in.
Acknowledgments
The authors thank Emer Breen, Tiffany Nassiri-Ansari, and Emma Rhule, for helpful feedback on earlier versions of the paper.
- View Article
- PubMed/NCBI
- Google Scholar
- 10. World Bank Group [Internet]. World Bank country and lending groups; n.d. [cited 2023 Sept 27]. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- 12. World Health Organization [Internet]. Investments on grants for biomedical research by funder, type of grant, health category and recipient; 2023 [cited 2023 Sept 27]. https://www.who.int/observatories/global-observatory-on-health-research-and-development/monitoring/investments-on-grants-for-biomedical-research-by-funder-type-of-grant-health-category-and-recipient
- 13. Bill and Melinda Gates Foundation [Internet]. DEI progress report 2021; n.d. [cited 2023 Sept 27]. https://docs.gatesfoundation.org/documents/bill_and_melinda_gates_foundation_2021_dei_progress_report.pdf
- 15. National Institutes of Health [Internet]. NIH global health funding; 2023 [cited 2023 Sept 27]. https://www.fic.nih.gov/Funding/Pages/NIH-funding-opportunities.aspx
- 16. National Institute for Health and Care Research [Internet]. Eligibility; 2023 [cited 2023 Sept 27]. https://www.nihr.ac.uk/researchers/i-need-help-funding-my-research/eligibility/
- 17. Global Health Decolonisation Movement Africa [Internet]. Pragmatic approaches to decolonizing global health in Africa; 2021 [cited 2023 Sept 27]. https://ghdmafrica.org/wp-content/uploads/2021/02/GHDM_brochure_web.pdf
- 30. International Committee of Medical Journal Editors ICJME. Defining the Role of Authors and Contributors; 2023 [cited 2023 Sept 27]. https://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html
- 32. Rushton S, Williams OD. Private actors in global health governance. In: Rushton S, Williams OD, editors. Partnerships and foundations in global health governance. Hampshire: Palgrave MacMillan; 2011. pp.1–25.
- 34. McCoy D, McGoey L. Global health and the Gates Foundation—in perspective. In: Rushton S, Williams OD, editors. Partnerships and foundations in global health governance. Hampshire: Palgrave MacMillan; 2011. pp.143–163.
- 35. Wilson J. Philanthrocapitalism and global health. In: Benatar S, Brock G, editors. Global health: ethical challenges. Cambridge: Cambridge University Press; 2021. pp.416–428.
- 38. Wellcome Trust [Internet]. Diversity and inclusion: helping more ideas thrive; n.d. [cited 2023 Sept 28]. https://wellcome.org/what-we-do/diversity-and-inclusion
- 51. Breen E, Kumar, R [Internet]. Private foundations and their global health grant-making patterns: a rapid analysis of the Rockefeller Foundation, Wellcome Trust, and Bill and Melinda Gates Foundation; 2023 [cited 2024 March 29]. https://www.globalpolicy.org/en/publication/private-foundations-and-their-global-health-grant-making-patterns
- 56. Chen G, Chan L. University rankings and governance by metrics and algorithms. In: Hazelkorn E, editor. Research handbook on university rankings: theory, methodology, influence and impact. Cheltenham: Edward Elgar; 2021. pp. 424–441.
- 57. Nassir-Ansari T, McCoy D. World-class universities? Interrogating the biases and coloniality of global university rankings [Internet]. Kuala Lumpur: United Nations University-International Institute for Global Health; 2023 [cited 2023 Sept 27]. https://collections.unu.edu/eserv/UNU:9082/UNI-Ranking-paper_February-2023.pdf
- 60. TRUST (2018). The TRUST Code–A global code of conduct for equitable research partnerships. https://www.globalcodeofconduct.org/the-code/
- 63. Adams V. Metrics: what counts in global health. Durham: Duke University Press; 2016.
- 65. Oxfam. Sick development: how rich-country government and World Bank funding to for-profit private hospitals causes harm, and why it should be stopped; 2023 [cited 2023 Sept 28]. https://oxfamilibrary.openrepository.com/bitstream/handle/10546/621529/bp-sick-development-funding-for-profit-private-hospitals-260623-en.pdf?sequence=14
- 72. Commission on Health Research for Development. Health research: essential link to equity in development; 1990 [cited 2023 Sept 28]. http://www.cohred.org/downloads/open_archive/ComReports_0.pdf
- 73. WHO Council on the Economics of Health for All [Internet]. Health for all: transforming economies to deliver what matters: Final report; 2023 [cited 2023 Sept 28]. https://cdn.who.int/media/docs/default-source/council-on-the-economics-of-health-for-all/council-eh4a_finalreport_web.pdf?sfvrsn=a6505c22_5&download=true
- 75. WHO. WHO Global Code of Practice on the International Recruitment of Health Personnel; 2010 [cited 2023 Sept 28]. https://cdn.who.int/media/docs/default-source/health-workforce/migration-code/code_en.pdf?sfvrsn=367f7d35_7&download=true
This paper is in the following e-collection/theme issue:
Published on 29.4.2024 in Vol 26 (2024)
Effectiveness of a Smartphone App–Based Intervention With Bluetooth-Connected Monitoring Devices and a Feedback System in Heart Failure (SMART-HF Trial): Randomized Controlled Trial
Authors of this article:

Original Paper
- Minjae Yoon 1 , MD ;
- Seonhwa Lee 2 , MD ;
- Jah Yeon Choi 3 , MD, PhD ;
- Mi-Hyang Jung 4 , MD, PhD ;
- Jong-Chan Youn 4 , MD, PhD ;
- Chi Young Shim 5 , MD, PhD ;
- Jin-Oh Choi 6 , MD, PhD ;
- Eung Ju Kim 3 , MD, PhD ;
- Hyungseop Kim 2 , MD, PhD ;
- Byung-Su Yoo 7 , MD, PhD ;
- Yeon Joo Son 8 , BS ;
- Dong-Ju Choi 1 , MD, PhD
1 Division of Cardiology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seognam, Republic of Korea
2 Division of Cardiology, Department of Internal Medicine, Keimyung University Dongsan Hospital, Daegu, Republic of Korea
3 Cardiovascular Center, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Republic of Korea
4 Division of Cardiology, Department of Internal Medicine, Seoul St. Mary's Hospital, Catholic Research Institute for Intractable Cardiovascular Disease, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
5 Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
6 Cardiac and Vascular Center, Samsung Medical Center, Sungkyunkwan University, Seoul, Republic of Korea
7 Department of Internal Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Woonju, Republic of Korea
8 Healthcare Business Department, AI/DX Convergence Business Group, KT, Seoul, Republic of Korea
Corresponding Author:
Dong-Ju Choi, MD, PhD
Division of Cardiology, Department of Internal Medicine
Seoul National University Bundang Hospital, Seoul National University College of Medicine
82, Gumi-ro 173 Beon-gil, Bundang-gu
Seognam, 13620
Republic of Korea
Phone: 82 317877007
Fax:82 317877041
Email: [email protected]
Background: Current heart failure (HF) guidelines recommend a multidisciplinary approach, discharge education, and self-management for HF. However, the recommendations are challenging to implement in real-world clinical settings.
Objective: We developed a mobile health (mHealth) platform for HF self-care to evaluate whether a smartphone app–based intervention with Bluetooth-connected monitoring devices and a feedback system can help improve HF symptoms.
Methods: In this prospective, randomized, multicenter study, we enrolled patients 20 years of age and older, hospitalized for acute HF, and who could use a smartphone from 7 tertiary hospitals in South Korea. In the intervention group (n=39), the apps were automatically paired with Bluetooth-connected monitoring devices. The patients could enter information on vital signs, HF symptoms, diet, medications, and exercise regimen into the app daily and receive feedback or alerts on their input. In the control group (n=38), patients could only enter their blood pressure, heart rate, and weight using conventional, non-Bluetooth devices and could not receive any feedback or alerts from the app. The primary end point was the change in dyspnea symptom scores from baseline to 4 weeks, assessed using a questionnaire.
Results: At 4 weeks, the change in dyspnea symptom score from baseline was significantly greater in the intervention group than in the control group (mean –1.3, SD 2.1 vs mean –0.3, SD 2.3; P =.048). A significant reduction was found in body water composition from baseline to the final measurement in the intervention group (baseline level mean 7.4, SD 2.5 vs final level mean 6.6, SD 2.5; P =.003). App adherence, which was assessed based on log-in or the percentage of days when symptoms were first observed, was higher in the intervention group than in the control group. Composite end points, including death, rehospitalization, and urgent HF visits, were not significantly different between the 2 groups.
Conclusions: The mobile-based health platform with Bluetooth-connected monitoring devices and a feedback system demonstrated improvement in dyspnea symptoms in patients with HF. This study provides evidence and rationale for implementing mobile app–based self-care strategies and feedback for patients with HF.
Trial Registration: ClinicalTrials.gov NCT05668000; https://clinicaltrials.gov/study/NCT05668000
Introduction
Heart failure (HF) is a rapidly growing public health problem, with an estimated prevalence of 64 million people globally [ 1 - 5 ]. Although outcomes of HF have recently improved with the development of medications, a high rate of readmission remains after initial hospitalization for acute HF [ 6 - 10 ]. Recent studies have shown that 18%-23% of patients with acute HF were readmitted within 1 month, and these numbers have not decreased recently [ 6 , 11 , 12 ]. Therefore, the postdischarge management of patients with HF is important. In particular, multidisciplinary interventions, in addition to pharmacotherapy and discharge education, are known to improve quality of life and reduce hospitalizations [ 13 - 16 ]. A recent meta-analysis has shown that self-management interventions, including symptom and sign monitoring, education, and enhancement of drug adherence, improve outcomes of HF-related hospitalization and all-cause death, despite heterogeneity in the interventions [ 17 ]. Thus, current HF guidelines recommend multidisciplinary management, specific discharge education, and support to facilitate HF self-care [ 18 - 20 ].
Although encouraging self-care and providing feedback from health care providers are the most effective means, they are difficult to implement in a real-world clinical setting. These are also associated with higher costs and require more infrastructure and manpower. Smartphones are currently available to most of the general population at an affordable cost. The advent of mobile health (mHealth) technology and advances in artificial intelligence (AI) have enabled patient self-care, symptom, and sign monitoring, as well as mobile-based feedback via smartphone apps. Recent studies using smartphone apps for the self-management of cardiovascular disease demonstrated that this intervention led to better outcomes than the control groups [ 21 - 23 ]. Additionally, some recent studies and meta-analyses regarding mHealth apps have supported self-care among patients with HF [ 24 - 30 ]. However, these previous studies had a small number of participants and limited app functionality. Self-monitoring and feedback are particularly important, and the lack of these critical features limits the interpretation of the effectiveness of HF apps. Furthermore, functions provided in previous mobile-based interventions for HF were heterogeneous and varied between studies, which may lead to inconsistent results.
Given the uncertainty regarding the benefits of mobile apps for HF and their diverse functionality, we developed a mHealth platform to provide self-management interventions for patients with HF. This study aimed to evaluate whether this smartphone app–based intervention with Bluetooth-connected monitoring devices and a feedback system could improve the symptoms and clinical outcomes of HF.
Study Design and Population
The self-monitoring using a mobile app to improve symptoms and reduce rehospitalization and mortality in heart failure (SMART-HF) study is a prospective, multicenter, randomized, open-label trial to evaluate the efficacy of smartphone apps in improving the symptoms and outcomes of HF. A total of 7 tertiary university hospitals in South Korea participated in this study. The study design was registered at ClinicalTrials.gov (NCT05668000).
We enrolled patients aged older than 20 years who were hospitalized for acute HF with obvious symptoms or signs of HF at admission. Patients with N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels ≥400 pg/mL or brain natriuretic peptide levels ≥100 pg/mL were enrolled. Since smartphone use was essential in this study, participants should be able to use Android smartphones well and be capable of following instructions on how to use apps. Patients with a baseline systolic blood pressure (BP) of <90 mm Hg or a resting heart rate (HR) of <50 beats per minute were excluded from this study. Additionally, patients were excluded if they had a cardiac [ 30 ] implantable electronic device that could interfere with body water analysis. Patients who were expected to have a prolonged hospital stay owing to medical problems other than HF were also excluded. The detailed inclusion and exclusion criteria are presented in Table S1 in Multimedia Appendix 1 .
Ethical Considerations
This clinical trial was approved by the institutional review boards of Seoul National University Bundang Hospital (B-2211-795-304) and other hospitals. The study was conducted in accordance with the Declaration of Helsinki, and all study data were deidentified. All patients provided written informed consent upon enrollment.
Patient Recruitment and Randomization
After a comprehensive interview, eligible participants were asked to provide written informed consent before being discharged from the hospital. At baseline (visit 1), all participants were assessed for sex, age, demographics, vital signs, comorbidities, laboratory data, and medication use. Eligible participants were randomized 1:1 to either the intervention group (app with Bluetooth-connected monitoring devices and feedback) or the control group (app only) using a web-based central randomization service ( Figure 1 A). Due to the nature of the intervention, the study participants and investigators interacting with the patients were not blinded to the group allocation.

Intervention and Follow-Up
We developed a mobile app and operating platform to improve the symptoms and outcomes of patients with HF. The app and platform comprised three parts: (1) a smartphone app for patients, (2) a dashboard system for physicians, and (3) a clinical decision support system (CDSS) on the platform ( Figure 1 B and Figures S1 and S2 in Multimedia Appendix 1 ).
The smartphone app comprised 4 menu screens ( Figure 2 ), and the detailed functions of the app are described in Table S2 in Multimedia Appendix 1 . In the “Today” menu, patients can enter their information, including body water, weight, BP, HR, symptom diary, medications, diet, and exercise. Patients can input their symptoms of HF, including dyspnea, fatigue, ankle edema, and palpitations, daily. Symptoms were scored as 0 (no symptoms), 1 (mild symptoms), 2 (moderate symptoms), and 3 (severe symptoms; Table S3 in Multimedia Appendix 1 ). Moreover, they could enter their daily diet or physical activity into the apps, and the amount of sodium in their diet was assessed through a camera image using AI (Figure S3 in Multimedia Appendix 1 ). Additionally, the BP, HR, weight, and body water could be entered into the app by the patients (intervention + control group) or automatically paired using Bluetooth-connected monitoring devices (intervention group only). In the “Records” menu, patients can access and review their historical data entered by date, as well as receive feedback regarding medication adherence, dietary habits, and exercise. Furthermore, the app can analyze and evaluate a patient’s symptom scores or measured vital signs and subsequently generate alerts based on a predefined algorithm (Tables S3 and S4 in Multimedia Appendix 1 ) using the CDSS. In the event of rapid changes in a patient’s symptoms or vital signs, the app prompts the patient to provide information regarding medication adherence, symptom severity, and any other concerns. Upon perceiving significant changes, it sends a message to the patients, advising them to contact their health care provider. In the “Contents” menu, the app can provide patients with information about HF, including symptoms, treatment, dietary guidelines, and exercise recommendations using chatbots.

The dashboard system was designed to present stored information to physicians (Figure S4 in Multimedia Appendix 1 ). This information included BP, HR, body weight, body water composition, HF symptom score, medications, diet, exercise, and any data entered by the patient. Physicians could easily observe the vital sign trends (daily, weekly, and monthly) of the participants. The CDSS analyzes the input data and generates recommendations for users using AI and algorithms. For example, it aggregates data and information from the patient and sends necessary messaging alerts to the patient’s app and, if needed, to the health care provider’s dashboard during office visits.
After randomization, both groups installed the study app on their Android smartphones, which the research nurse provided. Only the intervention group had full access to all functions of the app, and the apps were automatically paired with Bluetooth-connected monitoring devices, including a BP monitor, weight scale, and body water analyzer. The intervention group received feedback and alerts from the app. In the control group, patients could enter their BP, HR, and weight into the app using conventional non-Bluetooth devices only. Additionally, they received no feedback or alerts from the app. The “Contents” menu providing information about HF was available in both groups. The study aimed to evaluate the improvement in HF symptoms based on the functionality of the mobile app between the intervention and control groups, with a particular focus on Bluetooth-connected monitoring devices and the feedback function of the app.
We used a Bluetooth-enabled BP monitor BP170 (InBody Co). Bioimpedance analysis was performed using a portable multifrequency bioimpedance device (BWA ON; InBody Co) to analyze body water composition. Bioimpedance analysis has recently proven its efficacy in patients with acute HF with dyspnea [ 31 ], and the device can estimate body fluid status using extracellular water divided by total body water of the 4 limbs and trunk. The parameters of extracellular water divided by total body water <0.390, 0.390-0.400, and >0.400 were considered to be “normal,” “slightly over,” and “over,” respectively (Table S5 in Multimedia Appendix 1 ). The device classifies body water levels from levels 1 to 16.
Follow-up visits were scheduled at 2 (visit 2, optional) and 4 (visit 3) weeks after randomization. Both groups received standard care according to the current HF guidelines [ 20 , 32 ], and HF medication could be modified at the discretion of the treating physicians.
Study Outcomes
The primary end point of the study was the change in dyspnea symptom scores from baseline to 4 weeks, which was assessed using a questionnaire. We used a visual analog scale and a numerical rating scale for dyspnea ranging from 0 to 10 based on previous studies [ 33 , 34 ] (Figure S5 in Multimedia Appendix 1 ).
There were two secondary end points: (1) a composite outcome, including death, rehospitalization, and urgent visit for HF and (2) the change in body water composition from baseline to the last measurement in the intervention group. The exploratory clinical outcome was adherence to the app, which was calculated using either log-in access logs or the percentage of days when symptoms were entered into the app. App adherence was defined as follows:

We also compared app satisfaction scores at 4 weeks through a questionnaire, ranging from 0 to 10, between the intervention and control groups. If patients could not attend the scheduled study date, the outcome measures were assessed telephonically.
Sample Size and Statistical Analysis
Due to the absence of previous research and the pioneering nature of our intervention, our study adopts an exploratory approach. The primary objective was not to test a specific hypothesis regarding efficacy but rather to collect preliminary data and assess feasibility in preparation for a larger-scale study. Consequently, a sample size calculation was not conducted at this preliminary stage. Since this was a pilot study to explore the benefits of mobile apps for HF, we enrolled a total of 84 participants across 7 institutes, considering the duration of the study and the number of participating hospitals.
Categorical variables are reported as frequencies (percentages), and continuous variables are expressed as means (SD) or medians with IQR. Categorical variables were compared using the Pearson chi-square test or Fisher exact test, and continuous variables were compared using the Student t test or the Mann-Whitney U test. The change in body water composition from baseline to the last measurement after randomization was analyzed using the paired t test.
The intention-to-treat analysis included all randomized patients. The efficacy end points were primarily analyzed using the full analysis set, which included randomized participants who used the mobile app at least once. We also performed a per-protocol sensitivity analysis, including patients who completed the study protocol. For patients who dropped out before the end of the trial or had missing data, we used the latest available records for analysis, namely, the last observation carried forward method.
All tests were 2-tailed, and a P value <.05 was considered statistically significant. Statistical analyses were performed by using R (version 4.2.0; R Core Team).
Patient Enrollment and Clinical Characteristics
From October 2022 to January 2023, 132 patients from 7 centers were screened for eligibility, and 84 were randomly assigned to the intervention (n=43) or control (n=41) group ( Figure 3 and CONSORT [Consolidated Standards of Reporting Trials] checklist in Multimedia Appendix 2 ). After allocation, 7 patients (4 and 3 in the intervention and control groups, respectively) were excluded because they did not use the app at least once; thus, 77 patients (39 and 38 in the intervention and control groups, respectively) were included in the full analysis set.

The baseline characteristics of the groups are presented in Table 1 . The mean age of the total population was 62.1 (SD 14.7) years; 62% were male, 61% had de novo HF, and 30% had HF of an ischemic etiology. The median left ventricular ejection fraction was 38.7% (IQR 28%-58%) and the median NT-proBN P value was 2572 (IQR 1211-6651) pg/mL. The baseline characteristics, including age, sex, demographic data, laboratory values, and comorbidities, were well balanced between the 2 groups, except for diastolic BP. Additionally, the medication use at discharge was not significantly different between the 2 groups.
a HF: heart failure.
b NYHA: New York Heart Association.
c LVEF: left ventricular ejection fraction.
d eGFR: estimated glomerular filtration rate.
e NT-proBNP: N-terminal pro-B-type natriuretic peptide.
f RAS: renin-angiotensin system.
g SGLT2: sodium-glucose cotransporter 2.
Dyspnea Symptom Score
The dyspnea symptom scores assessed using the questionnaire are presented in Table 2 and Figure 4 . The baseline dyspnea symptom scores were not significantly different between the 2 groups (intervention vs control: mean 2.4, SD 2.8 vs mean 2.0, SD 2.0; P =.46). Regarding the primary end point, change in dyspnea symptom score from baseline to 4 weeks was significantly greater in the intervention group than in the control group (mean –1.3, SD 2.1 vs mean –0.3, SD 2.3; P =.048).

Secondary End Points
Secondary composite end points, including death, rehospitalization, and urgent visit for HF, were not significantly different between the 2 groups (3/39 vs 3/38; P >.99). A significant reduction was found in the level of body water composition from baseline to the last measurement in the intervention group (baseline level mean 7.4, SD 2.5 vs final level mean 6.6, SD 2.5; P =.003; Figure 5 ).

App Adherence and Patient Satisfaction
The distribution of app adherence among the treatment and control groups is presented in Figure 6 . App adherence, which was assessed based on log-in access logs was higher in the intervention group than in the control group (80.0%, IQR 45.0%-96.8% vs 39.3%, IQR 20.6%-77.4%; P =.003). Additionally, the app adherence evaluated based on the percentage of days when symptom was entered into the app was significantly higher in the intervention group than in the control group (58.6%, IQR 19.2%-79.5% vs 30.6%, IQR 9.1%-64.3%; P =.046).

We also analyzed differences in app adherence according to age. Patients aged 65 years and older showed lower app adherence, as indicated by log-in access logs than those aged younger than 65 years in the overall population (45.9%, IQR 8.9%-79.2% vs 74.9%, IQR 35.7%-95.5%; P =.02). The intervention group showed similar results (61.4%, IQR 13.5%-89.5% vs 92.9%, IQR 64.2%-98.5%; P =.04); however, in the control group, no significant difference was found in app adherence according to the age cutoff of 65 years (39.4%, IQR 5.7%-76.7% vs 39.3%, IQR 27.8%-74.6%; P =.40).
App satisfaction scores at 4 weeks tended to be higher in the intervention group than in the control group; however, the difference was not statistically significant (mean 7.1, SD 2.6 vs mean 6.2, SD 2.9; P =.15).
Sensitivity Analysis
Overall, 74 patients (37 in the intervention group and 37 in the control group) completed the trial over 4 weeks (per-protocol analysis; Figure 3 ). Table S6 and Figure S6 in Multimedia Appendix 1 show the results of sensitivity analyses of the per-protocol population. There was a trend toward a greater reduction in dyspnea symptom scores from baseline to 4 weeks in the intervention group than in the control group, similar to the primary analyses (mean –1.4, SD 2.1 vs mean –0.5, SD 2.1; P =.08). Regarding body water composition, the intervention group showed a greater reduction in the level of body water composition from baseline to last measurement, consistent with the main analysis (baseline level mean 7.4, SD 2.5 vs final level mean 6.6, SD 2.6; P =.006).
Principal Results
We developed a smartphone app and mHealth platform for patients with HF. The main findings of this study are (1) a mobile-based health platform with Bluetooth-connected monitoring devices and feedback improved dyspnea symptoms compared with the control group and (2) this app-based intervention led to an improvement in the level of body water composition and higher adherence to the app. We believe that the findings of this prospective, randomized study will help in formulating public health strategies to improve HF outcomes using smartphones.
Support for facilitating self-care is crucial for patients with HF [ 18 - 20 ]. However, proper patient self-care and delivery of health care provider feedback are challenging to implement in a real-world clinical setting because of the required time, financial, and human resources. It is challenging for patients to know how to respond to changes in their symptoms or vital signs. It is also impossible for medical staff to quickly check patient information or provide feedback 24 hours a day, 7 days a week. These disadvantages can be overcome by self-management interventions via smartphones, including self-care, symptom and sign monitoring, and mobile-based feedback, which are easily accessible anytime, anywhere. Considering these advantages of a smartphone app–based intervention, including cost-effective and accessible methods, our group has previously developed mobile app platforms for patients with atrial fibrillation [ 35 , 36 ] or hypertension [ 37 ]. Therefore, we planned to develop an app for patients with HF.
Our mobile app for HF provides diverse functions using the concept of mHealth platforms for personalized interventions. Vital signs and body water can be paired with Bluetooth-connected devices, and patients can enter their HF symptoms into the apps. Patients can also receive feedback or alerts from the app based on the information they have entered. Additionally, patients can obtain information about HF using chatbots. Although direct interaction between patients and health care providers may be an ideal situation, it may not be feasible owing to rising costs and a shortage of medical staff. Our app-based monitoring and feedback system had the advantage of being accessible and quick for patients to receive feedback promptly on their changes without high personnel or cost. Although patients in the control group had access to the smartphone app for HF self-care, the improvement in dyspnea symptoms was more pronounced in the intervention group than in the control group. Patients in the control group could only use the limited functionality of the app, were unable to use Bluetooth devices, and could not receive any feedback or alerts. Therefore, our study suggests that the comprehensive functionality of apps, especially in the monitoring and feedback system, is particularly important for their role.
Comparison With Prior Work
Some previous studies have focused on mHealth apps for HF [ 24 - 30 ]. However, these studies were limited by the small number of participants and limited app functionality. Additionally, previous mobile apps have heterogeneous functions and platforms [ 24 , 25 ], and this diversity might have influenced the benefits of mobile apps in HF. Considering the inconsistent benefits of mobile apps in HF [ 25 ], we developed a mobile app with multiple functions in collaboration with 1 of the largest high-tech information technology companies in Korea (KT). In our opinion, this app has a considerably wider range of features and is more efficiently organized than other existing apps [ 28 - 30 ]. Our app has the advantage of keeping patients engaged in their condition and self-management after leaving the hospital. Not only does this provide psychological reassurance, but it also serves the patient’s best interests by keeping a close eye on any changes in their clinical presentation or symptoms. Patients can assess their symptoms more frequently, make lifestyle changes, or contact health care providers earlier. The dashboard system also enables health care professionals to identify changes in a patient’s condition quickly. Furthermore, the app contains elements that may be of interest to patients, including sodium analysis in food using AI and various HF information. Overall, we assumed that the monitoring and feedback function and app adherence are especially important for the mobile app’s role in HF and believe that the benefits of our app could improve the symptoms of HF.
Increasing app adherence has been a common challenge in many studies. For example, a recent study showed that only approximately 30% of patients actively used the HF app, underscoring the importance of caution regarding the enrollment of critically ill, postacute, and older patients [ 30 ]. In our study, median adherence to apps based on log-in access logs was 80% and 39% in the intervention and control groups, respectively, which we believe should be further improved. In the intervention group, we believe that a more comprehensive functionality of apps, including Bluetooth-connected monitoring devices and a feedback system, may lead to higher adherence to apps than in the control group. Additionally, this disparity in app functionality may be associated with a higher trend in app satisfaction scores within the intervention group.
Particularly, as a large proportion of patients with HF tend to be older and app adherence appears to decline in those aged 65 years and older in our study, increasing adherence to apps for HF is crucial; this can be achieved by improving the platform to make it more user-friendly for older patients. Interestingly, at the cutoff age of 65 years, a difference was observed in app adherence according to age category in the intervention group but not in the control group, probably due to overall higher app adherence in the intervention group. In the subgroup analysis, no difference was found in the change of dyspnea symptom scores between the intervention and control groups according to an app adherence cutoff of 50%. This is probably due to the small sample size. Therefore, further research with larger study populations is warranted to confirm whether the frequency of app usage directly affects the outcomes.
Limitations and Strengths
This study had some limitations. First, our results are limited by the small sample size of the study. Second, we only enrolled patients who had smartphones and could use them; therefore, the results of our trial may not be applicable to patients who cannot use smartphones, such as very old adults. Since a large proportion of patients with HF are older and have difficulty using smartphones, excluding them from participation may lead to bias and study limitations. Third, the true engagement and use frequency of the apps and the real responses of participants to feedback could not be analyzed. There is a lack of clarity on exactly how the frequency of app use affects clinical outcomes. Additionally, there was a relatively large number of older patients, and adherence to the app declined toward the end of the study. These limitations are commonly observed in studies that use mobile apps. Fourth, we evaluated the dyspnea symptom score using a visual analog scale and a numerical rating scale ranging from 0 to 10. However, at baseline, the average of these scores was <3 points, suggesting that this study was conducted on patients who already had achieved significant improvement in their dyspnea, which limits surveying on a scale of 0-10 over 4 weeks. Fifth, the HF medications could be modified at the discretion of each physician, which could be a confounding factor. Sixth, baseline diastolic BP was higher in the intervention group than in the control group, while patients in the intervention group tended to be younger. This difference in baseline characteristics may limit the generalizability of our conclusions. Seventh, the follow-up period in our studies was only 4 weeks, which was shorter than that in a similar study [ 29 ]; therefore, the effect of mobile apps on patients’ symptoms for a long-term follow-up period was unknown. Furthermore, secondary clinical outcomes, including death, rehospitalization, and urgent visits for HF, were not significantly different between the 2 groups in this study, although a similar study using apps [ 28 ] for HF showed reduced hospitalization for HF by mobile app. Finally, we tested a single app, and our results may not be generalizable to other smartphone-based apps for patients with HF.
Despite these limitations, the major strength of this study is the use of a mobile app with various functions developed in collaboration with a cutting-edge technology company. We believe that the features of our app can be effective solutions for improving self-care in patients with HF.
Conclusions
The smartphone app–based intervention with Bluetooth-connected monitoring devices and feedback improved dyspnea symptoms among patients with HF compared with the control group. Considering the high cost of classical patient-provider interventions, self-care, and feedback through mobile apps are promising alternatives. Therefore, our study provides evidence and rationale for mobile app–based self-care and feedback for patients with HF.
Acknowledgments
The app used in this study was developed in collaboration between the Digital Health Council (DHC) from the Korean Society of Heart Failure and KT Corporation. This research was supported by KT’s Internalization of Digital Therapeutics Business project. This research was supported by a grant from the Korea Health Technology Research & Development Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI21C1074).
Data Availability
The data sets generated and analyzed during this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
None declared.
App characteristics and functionalities, and participants’ clinical characteristics and outcomes.
CONSORT-EHEALTH checklist.
- Shahim B, Kapelios CJ, Savarese G, Lund LH. Global public health burden of heart failure: an updated review. Card Fail Rev. 2023;9:e11. [ FREE Full text ] [ CrossRef ] [ Medline ]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-1858. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Park JJ, Lee CJ, Park SJ, Choi JO, Choi S, Park SM, et al. Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021;3(4):224-236. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet. 2018;391(10120):572-580. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cho JY, Cho DH, Youn JC, Kim D, Park SM, Jung MH, et al. Korean Society of Heart Failure guidelines for the management of heart failure: definition and diagnosis. Int J Heart Fail. 2023;5(2):51-65. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kimmoun A, Takagi K, Gall E, Ishihara S, Hammoum P, El Bèze N, et al. Temporal trends in mortality and readmission after acute heart failure: a systematic review and meta-regression in the past four decades. Eur J Heart Fail. 2021;23(3):420-431. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, Normand SLT, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA. 2010;303(21):2141-2147. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bozkurt B, Savarese G, Eryd SA, Bodegård J, Cleland JGF, Khordoc C, et al. Mortality, outcomes, costs, and use of medicines following a first heart failure hospitalization: EVOLUTION HF. JACC Heart Fail. 2023;11(10):1320-1332. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Maggioni AP, Dahlström U, Filippatos G, Chioncel O, Leiro MC, Drozdz J, et al. EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail. 2013;15(7):808-817. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, Choi JO, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF). Korean Circ J. 2017;47(3):341-353. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Khan MS, Sreenivasan J, Lateef N, Abougergi MS, Greene SJ, Ahmad T, et al. Trends in 30- and 90-day readmission rates for heart failure. Circ Heart Fail. 2021;14(4):e008335. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29-322. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333(18):1190-1195. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111(2):179-185. [ FREE Full text ] [ CrossRef ] [ Medline ]
- McAlister FA, Stewart S, Ferrua S, McMurray JJJV. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44(4):810-819. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bhatia A, Maddox TM. Remote patient monitoring in heart failure: factors for clinical efficacy. Int J Heart Fail. 2021;3(1):31-50. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jonkman NH, Westland H, Groenwold RHH, Ågren S, Atienza F, Blue L, et al. Do self-management interventions work in patients with heart failure? An individual patient data meta-analysis. Circulation. 2016;133(12):1189-1198. [ FREE Full text ] [ CrossRef ] [ Medline ]
- McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. Corrigendum to: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42(48):4901. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol. 2022;79(17):e263-e421. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Youn JC, Kim D, Cho JY, Cho DH, Park SM, Jung MH, et al. Korean Society of Heart Failure guidelines for the management of heart failure: treatment. Int J Heart Fail. 2023;5(2):66-81. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cruz-Ramos NA, Alor-Hernández G, Colombo-Mendoza LO, Sánchez-Cervantes JL, Rodríguez-Mazahua L, Guarneros-Nolasco LR. mHealth apps for self-management of cardiovascular diseases: a scoping review. Healthcare (Basel). 2022;10(2):322. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kalagara R, Chennareddy S, Scaggiante J, Matsoukas S, Bhimani A, Smith C, et al. Blood pressure management through application-based telehealth platforms: a systematic review and meta-analysis. J Hypertens. 2022;40(7):1249-1256. [ CrossRef ] [ Medline ]
- Alessa T, Abdi S, Hawley MS, de Witte L. Mobile apps to support the self-management of hypertension: systematic review of effectiveness, usability, and user satisfaction. JMIR Mhealth Uhealth. 2018;6(7):e10723. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wali S, Demers C, Shah H, Wali H, Lim D, Naik N, et al. Evaluation of heart failure apps to promote self-care: systematic app search. JMIR Mhealth Uhealth. 2019;7(11):e13173. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Athilingam P, Jenkins B. Mobile phone apps to support heart failure self-care management: integrative review. JMIR Cardio. 2018;2(1):e10057. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mortara A, Vaira L, Palmieri V, Iacoviello M, Battistoni I, Iacovoni A, et al. Would you prescribe mobile health apps for heart failure self-care? An integrated review of commercially available mobile technology for heart failure patients. Card Fail Rev. 2020;6:e13. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Giordan LB, Tong HL, Atherton JJ, Ronto R, Chau J, Kaye D, et al. The use of mobile apps for heart failure self-management: systematic review of experimental and qualitative studies. JMIR Cardio. 2022;6(1):e33839. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sahlin D, Rezanezad B, Edvinsson ML, Bachus E, Melander O, Gerward S. Self-care management intervention in heart failure (SMART-HF): a multicenter randomized controlled trial. J Card Fail. 2022;28(1):3-12. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dorsch MP, Farris KB, Rowell BE, Hummel SL, Koelling TM. The effects of the ManageHF4Life mobile app on patients with chronic heart failure: randomized controlled trial. JMIR Mhealth Uhealth. 2021;9(12):e26185. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zisis G, Carrington MJ, Oldenburg B, Whitmore K, Lay M, Huynh Q, et al. An m-Health intervention to improve education, self-management, and outcomes in patients admitted for acute decompensated heart failure: barriers to effective implementation. Eur Heart J Digit Health. 2021;2(4):649-657. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Park CS, Lee SE, Cho HJ, Kim YJ, Kang HJ, Oh BH, et al. Body fluid status assessment by bio-impedance analysis in patients presenting to the emergency department with dyspnea. Korean J Intern Med. 2018;33(5):911-921. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Park SM, Lee SY, Jung MH, Youn JC, Kim D, Cho JY, et al. Korean Society of Heart Failure guidelines for the management of heart failure: management of the underlying etiologies and comorbidities of heart failure. Korean Circ J. 2023;53(7):425-451. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zhang X, Zhao C, Zhang H, Liu W, Zhang J, Chen Z, et al. Dyspnea measurement in acute heart failure: a systematic review and evidence map of randomized controlled trials. Front Med (Lausanne). 2021;8:728772. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Placido R, Gigaud C, Gayat E, Ferry A, Cohen-Solal A, Plaisance P, et al. Assessment of dyspnoea in the emergency department by numeric and visual scales: a pilot study. Anaesth Crit Care Pain Med. 2015;34(2):95-99. [ CrossRef ] [ Medline ]
- Kim IC, Lee JH, Choi DJ, Park SJ, Lee JH, Park SM, et al. Rationale design and efficacy of a smartphone application for improving self-awareness of adherence to edoxaban treatment: study protocol for a randomised controlled trial (adhere app). BMJ Open. 2022;12(4):e048777. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Yoon M, Park JJ, Hur T, Hua CH, Shim CY, Yoo BS, et al. The ReInforcement of adherence via self-monitoring app orchestrating biosignals and medication of RivaroXaban in patients with atrial fibrillation and co-morbidities: a study protocol for a randomized controlled trial (RIVOX-AF). Front Cardiovasc Med. 2023;10:1130216. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Choi DJ, Park JJ, Yoon M, Park SJ, Jo SH, Kim EJ, et al. Self-monitoring of blood pressure and feed-back using APP in TReatment of UnconTrolled Hypertension (SMART-BP): a randomized clinical trial. Korean Circ J. 2022;52(10):785-794. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 22.08.23; peer-reviewed by O El-Gayar, P Athilingam; comments to author 18.10.23; revised version received 07.11.23; accepted 12.03.24; published 29.04.24.
©Minjae Yoon, Seonhwa Lee, Jah Yeon Choi, Mi-Hyang Jung, Jong-Chan Youn, Chi Young Shim, Jin-Oh Choi, Eung Ju Kim, Hyungseop Kim, Byung-Su Yoo, Yeon Joo Son, Dong-Ju Choi. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 29.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

IMAGES
VIDEO
COMMENTS
Research on health behaviour change examines how to help people engage in healthy behaviours to prevent the development or worsening of chronic disease and early mortality and to improve mental health and well-being. ... A key step in advancing the science of behavior change. Health Psychology Review. doi: 10.1080/17437199.2020.1719183.
INTRODUCTION. The primary practical purpose of research into behavior change is the development of interventions that will be effective, subject to other constraints such as affordability [1, 2].In doing so, one wants to be able to draw on research findings that identify behavior change techniques (BCTs) that, if enacted appropriately, are most likely to effect the desired change.
Yet, knowledge gaps limit understanding of how to use habit to support lasting behaviour change. This paper sets out research questions that emerged from discussions at the 'Synergy Expert Meeting' at the 2019 European Health Psychology Society (EHPS) conference, held in Dubrovnik, Croatia. ... Health Psychology and Behavioral Medicine, 5, ...
Transtheoretical model (TTM) is one of the most commonly used methods in behavioral change modeling. The aim of this study was to conduct a systematic review (SR) to determine research gaps with regard to this template with an emphasis on intervention for patients with chronic diseases (CDs).
Abstract. The transtheoretical model posits that health behavior change involves progress through six stages of change: precontemplation, contemplation, preparation, action, maintenance, and termination. Ten processes of change have been identified for producing progress along with decisional balance, self-efficacy, and temptations.
Interests: her main areas of research are health psychology and behavioral medicine with interests in health behavior motivation, self-regulation, and change; she is particularly interested in understanding the multiple effects of motivational, volitional, and automatic processes on health behavior and the translation of research findings into ...
Introduction. The Behavior Change Consortium (BCC), sponsored by the National Institutes of Health (NIH), the American Heart Association and the Robert Wood Johnson Foundation, was initiated to support a new generation of research on innovative approaches to disease prevention through behavior change (Ory et al., 2002a).The goal of this initiative has been to stimulate the investigation of ...
Abstract. The transtheoretical model posits that health behavior change involves progress through six stages of change: precontemplation, contemplation, preparation, action, maintenance, and ...
What Are Habits and Habitual Behaviors?. Everyday behaviors shape human health. Many of the dominant causes of death, including heart disease, diabetes, cancer, chronic lower respiratory diseases, and stroke, are preventable (World Health Organization, 2017).Adopting health-promoting behaviors such as eating more healthily or increasing physical activity may improve quality of life, physical ...
Several World Health Organisation reports over recent years have highlighted the high incidence of chronic diseases such as diabetes, coronary heart disease and cancer. Contributory factors include unhealthy diets, alcohol and tobacco use and sedentary lifestyles. This paper reports the findings of a review of reviews of behavioural change interventions to reduce unhealthy behaviours or ...
Abstract. In 2002, the Society of Behavioral Medicine's special interest group on Multiple Health Behavior Change was formed. The group focuses on the interrelationships among health behaviors and interventions designed to promote change in more than one health behavior at a time. Growing evidence suggests the potential for multiple-behavior ...
1. Knowledge and outcome expectancies (improving people's knowledge about the health consequences of their behaviors), 2. Personal relevance (drawing people's attention to what health behavior change would mean for them), 3. Positive affective attitudes (promoting positive feelings about behavior change), 4.
The thousands of research papers that exist on patient adherence and health behavior change can leave professionals overwhelmed. This book synthesizes the results from more than 50 years of empirical research, resulting in simple, powerful, and practical guidance for health professionals who want to know the most effective strategies for ...
Behavior change for effective self-management can improve health outcomes and quality of life in people living with such chronic illnesses. The science of developing behavior change interventions with impact for patients aims to optimize the reach, effectiveness, adoption, implementation, and maintenance of interventions and rigorous evaluation ...
A total of 1070 papers were identified out of 530,358 records in ACM digital library. The first author screened the records from the paper title. 354 records were screened out because of duplication (N=15), not being relevant to health behavior change (N=337), or being the workshop introduction (N=2).
Abstract. The transtheoretical model posits that health behavior change involves progress through six stages of change: precontemplation, contemplation, preparation, action, maintenance, and termination. Ten processes of change have been identified for producing progress along with decisional balance, self-efficacy, and temptations.
As much as behavior change is a process, it may not be easy to some people thus the challenge to health communication. However, the following a re stimuli that influence peo ple to change behavior.
Effectively encouraging patients to change their health behavior is a critical skill for primary care physicians. Modifiable health behaviors contribute to an estimated 40 percent of deaths in the ...
encouraging health behavior change. As Bandura ( 1997) ... This review paper concludes that for a more nuanced understanding of environmental activism and pro-environmental behaviours at large ...
In [ 22 ], the chatbot explicitly requests users about message appropriateness, and change its behavior accordingly. In addition, personalization techniques can also help simulate affect. Discussing about addictions or at-risk behaviors can be emotional engaging (e.g. shame, discouragement, fear, anger) [ 41, 17 ].
Webb T. L., Joseph J., Yardley L., Michie S. Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research. 2010;(1):e4. doi: 10.2196/jmir.1376.
In this paper we (a) synthesize literature in the areas of trans-positive care and clinical behavior change according to predisposing, reinforcing, and enabling factors, factors to be addressed as a part of the Precede-Proceed model, a model to develop and evaluate behavior change interventions, and (b) discuss future directions for research ...
Health Behavior Research (HBR) is the official journal of the American Academy of Health Behavior (AAHB). Published four-times per year, HBR is a peer-reviewed open-access scholarly journal that publishes original research articles, current issues papers, commentaries, and abstracts from the annual meeting of the Academy. Health Behavior Research is dedicated to the translation of research to ...
Recent debates on decolonizing global health have spurred interest in addressing the power asymmetries and knowledge hierarchies that sustain colonial ideas and relationships in global health research. This paper applies three intersecting dimensions of colonialism (colonialism within global health; colonisation of global health; and colonialism through global health) to develop a broader and ...
Innovating and supporting large-scale observational studies, mechanistic investigations, and translational research to better understand how social and behavioral factors shape biological aging, well-being, and health. We hope you will stay informed about NIA's BSR-focused research and join us on that journey by signing up for the BSR ...
Background: Current heart failure (HF) guidelines recommend a multidisciplinary approach, discharge education, and self-management for HF. However, the recommendations are challenging to implement in real-world clinical settings. Objective: We developed a mobile health (mHealth) platform for HF self-care to evaluate whether a smartphone app-based intervention with Bluetooth-connected ...