

Tracking your heart rate? 5 questions answered about what that number really means
Associate Professor of Health and Sport Science, University of Dayton
Disclosure statement
Anne R. Crecelius does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
University of Dayton provides funding as a member of The Conversation US.
View all partners
The rise of wearable fitness trackers has increased the number of people monitoring their heart rate, both throughout the day and during exercise.
Whether you’re an athlete trying to gain the competitive edge , a weekend warrior tracking progress or someone who is just trying to improve your health, consider heart rate a valuable tool in understanding the work of your amazing body as it achieves those first steps, that next 5K or even Olympic gold.
Heart rate is one of your body’s most basic vital signs, yet many people have questions about what heart rate really tells them. What should your target heart rate be during exercise? Does it even matter?
1. What is your heart rate?
First, the basics: Your heart rate , also sometimes called your pulse rate, is the number of times your heart contracts per minute.
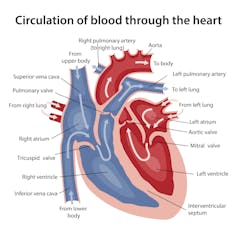
Physiologists like me focus on the contractions of the left ventricle, the chamber of the heart that generates pressure to drive blood out through the aorta and on to the entire body. The heart’s pumping capacity directly relates to its ability to deliver oxygen to the body’s organs.
If you’re running up the stairs or hauling something heavy, your muscles and organs are going to need more oxygen to help power your actions. And so your heart beats faster.
2. How do you measure heart rate?
The easiest way to measure heart rate is to find your pulse and count the number of pulses felt over the course of one minute.
In adults, the best places to feel for a pulse are large arteries that are near the surface of the skin, such as the carotid at the side of your neck or the radial on the underside of your wrist. If feeling for the carotid pulse, don’t press hard enough to disrupt blood flow to and from the head.
More recently, watches and other wrist-based fitness monitors have incorporated optical sensors to track heart rate. These wearable devices use technology called photoplethysmography , which has been around since the mid-1970s . Each beat of your heart sends a little surge of blood through your veins. The monitor detects this by shining green light onto your skin and then analyzing the light that gets refracted back by the red blood flowing underneath .
This kind of heart-rate monitoring is popular, but it has shortcomings for people with dark skin .
Some exercisers rely on chest straps that measure electrical activity and then transmit that signal to a watch or other display device. This technique depends on picking up the electrical signals within your body that direct your heart to beat.
For the most part, the two techniques are about equally accurate .
3. What controls your heart rate?
Your autonomic nervous system is mostly in charge of your heart rate. That’s the portion of the nervous system that runs without your even thinking about it.
In healthy hearts , as someone begins to exercise, the autonomic nervous system does two things. First, it removes the “brake” that keeps your heart beating slowly and steadily under normal conditions. And then it “hits the gas” to actively stimulate the heart to beat faster.
In addition, the amount of blood ejected from the left ventricle with each heart beat – called the stroke volume – increases, particularly during the initial stages of exercise.
Together, higher stroke volume and more beats per minute mean the amount of blood delivered by the heart increases to match the increased oxygen demand of exercising muscles.

4. How does heart rate relate to exercise intensity?
As your exercise session becomes more intense and more work is done, your heart beats faster and faster. This relationship means you can use heart rate as a surrogate measure for the intensity of exertion, relative to one’s maximal heart rate.
Your maximum heart rate is the fastest your heart can functionally beat. So how do you know what your number actually is?
In order to determine your maximum heart rate, you could do increasingly difficult exercise, like walking on a treadmill and increasing the grade each minute, until you can no longer keep up. But it’s much more common (and often safer!) to estimate it. Many studies have identified that maximal heart rate goes down with age , and thus age is included in all estimation equations.
The most common and simplest prediction equation is: Maximal heart rate is equal to 220 minus your age. From that number, you can calculate a percentage of maximum to provide target heart rate ranges in the moderate (50%-70%) or vigorous (70%-85%) categories of exercise, important in terms of meeting the recommended levels of exercise for overall health benefits.
Interestingly, this equation, while perhaps most common, wasn’t based upon empirical research and is not as accurate as others you can try, like your age multiplied by 0.7 and then subtracted from 208 .
As with any prediction equation, there is always some individual variability. To accurately know your max heart rate at your current age, you’d need to measure it during maximal exercise.
5. Why is exercise intensity important?
In addition to helping you to know whether you’re meeting general recommendations for exercise, knowing the intensity of a given workout session can be of benefit in other ways.
First, the body uses different primary sources of energy to fuel exercise of different relative intensities. During lower-intensity exercise, a greater proportion of the energy you’re using comes from fat sources in your body. During higher-intensity exercise, more of the energy utilized comes from carbohydrate sources.
But don’t slow that treadmill down just yet if you’re hoping to drop pounds of fat. Lower-intensity exercise also requires less energy overall. So, to burn the same amount of calories with lower-intensity exercise, you’ll need to exercise for longer than you would at a higher intensity.
Secondly, the intensity of a set amount of work – like a particular speed/grade combo on the treadmill, or a certain wattage on a rowing ergometer – reflects your overall fitness. Once you can complete the same amount of work at a lower relative intensity – like if you can run a mile in the same amount of time but with your heart beating slower than it did in the past – you know you’ve gained fitness. And increased fitness is associated with a decrease in death from any cause .
- Exercise physiology
- Heart rate monitors
- Resting heart rate
- Maximum heart rate
- Exercise intensity
- Wearable technology

Faculty of Law - Academic Appointment Opportunities

Operations Manager

Senior Education Technologist

Audience Development Coordinator (fixed-term maternity cover)

Lecturer (Hindi-Urdu)
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 27 July 2023
High blood pressure with elevated resting heart rate: a high risk “Sympathetic” clinical phenotype
- Guido Grassi 1 na1 ,
- Raffaella Dell’Oro 1 na1 ,
- Michele Bombelli 1 ,
- Cesare Cuspidi 1 &
- Fosca Quarti-Trevano 1
Hypertension Research volume 46 , pages 2318–2325 ( 2023 ) Cite this article
383 Accesses
2 Altmetric
Metrics details
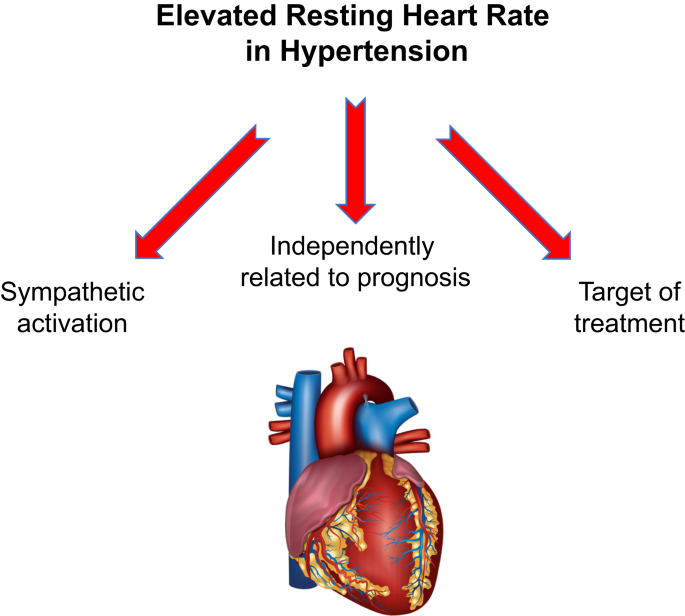
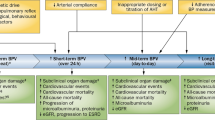
Epidemiological studies have unequivocally shown that elevated heart rate values measured at rest have an adverse prognostic impact in the hypertensive patient, being associated with an increased risk of cardiovascular events and complications. In recent years new data have been collected on this issue, strengthening the clinical relevance of elevated heart rate as a specific hypertensive phenotype. The present paper will review old and new data on the prognostic importance of resting tachycardia in the hypertensive patient. It will also examine the role of the sympathetic nervous system in the development of this alteration as well as its therapeutic implications. The different approaches to dynamically assess heart rate values in the clinical setting will be finally discussed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Blood pressure variability: its relevance for cardiovascular homeostasis and cardiovascular diseases
Gianfranco Parati, Camilla Torlasco, … Juan Eugenio Ochoa

Reduced heart-rate variability and increased risk of hypertension—a prospective study of the ELSA-Brasil
Rosangela A. Hoshi, Itamar S. Santos, … Isabela Bensenor
Central hemodynamic characteristics of young adults with isolated systolic hypertension: an ambulatory blood pressure monitoring-based study of real-world clinical patients
Sunwon Kim, Jong-Seok Lee, … Woo-Hyuk Song
Gillman MW, Kannel WB, Belanger A, D’Agostino RB. Influence of heart rate on mortality among persons with hypertension: the Framingham study. Am Heart J. 1993;125:1148–54.
Article CAS PubMed Google Scholar
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Eur Heart J. 2018;39:3021–104.
Article PubMed Google Scholar
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. 2023. https://doi.org/10.1097/HJH.0000000000003480 . Online ahead of print.
Grassi G, Vailati S, Bertinieri G, Seravalle G, Stella ML, Dell’Oro R, et al. Heart rate as marker of sympathetic activity. J Hypertens. 1998;16:1635–9.
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, et al. Plasma norepinephrine as a guide to prognosis in patients with congestive heart failure. N. Engl J Med. 1984;311:819–23.
Tage-Jensen U, Henriksen JH, Christensen E, Widding A, Ring-Larsen H, Christensen NJ. Plasma catecholamine level and portal venous pressure as guides to prognosis in patients with cirrhosis. J Hepatol. 1988;6:350–8.
Rouleau J, Packer M, Moye L, De Champlain M, Bichet D, Klein M, et al. Prognostic value of neurohumoral activation in patients with an acute myocardial infarction: effect of Captopril. J Am Coll Cardiol. 1994;24:583–91.
Benedict CR, Shelton B, Johnstone DE, Francis G, Greenberg B, Konstam M, et al. Prognostic significance of plasma norepinephrine in patients with asymptomatic left ventricular dysfunction. SOLVD Investigators. Circulation. 1996;94:690–7.
Reuben DB, Talvi SLA, Rowe JW, Seeman TE. High urinary catecholamine excretion predicts mortality and functional decline in high functioning, community dwelling older persons: MacArthur studies of successful aging. J Gerontol. 2000;55:M618–M625.
Article CAS Google Scholar
Sander D, Winbeck K, Klingelhofer J, Etgen T, Conrad B. Prognostic relevance of pathological sympathetic activation after acute thromboembolic stroke. Neurology. 2001;57:833–8.
Zoccali C, Mallamaci F, Parlongo S, Cutrupi S, Benedetto FA, Tripepi G, et al. Plasma norepinephrine predicts survival and incident cardiovascular events in patients with end-stage renal disease. Circulation. 2002;105:1354–9.
Vesalainen RK, Kantola IM, Airaksinen KEJ, Tahynainen KUO, Kaila TJ. Vagal cardiac activity in essential hypertension: the effects of metoprolol and ramipril. Am J Hypertens. 1998;11:649–58.
Petkovich BW, Vega J, Thomas S. Vagal modulation in hypertension. Curr Hypertens Rep. 2015;17:532.
Mancia G, Grassi G. The autonomic nervous system in hypertension. Circ Res. 2014;114:1804–14.
Grassi G, Esler M. How to assess sympathetic activity in humans. J Hypertens. 1999;17:719–34.
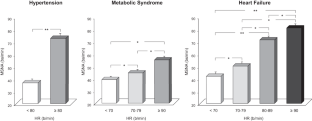
Grassi G, Quarti-Trevano F, Seravalle G, Dell’Oro R, Facchetti R, Mancia G. Association between the European Society of Cardiology/European Society of Hypertension heart rate thresholds for cardiovascular risk and neuroadrenergic markers. Hypertension. 2020;76:577–82.
Grassi G, Seravalle G, Vanoli J, Facchetti R, Spaziani D, Mancia G. Relationships between sympathetic markers and heart rate thresholds for cardiovascular risk in chronic heart failure. Clin Res Cardiol. 2023;112:59–67.
Seravalle G, Vanoli J, Molisano C, Merati V, Grassi G. Heart rate thresholds for cardiovascular risk and sympathetic activation in the metabolic syndrome. Acta Diabetol. 2022;59:1429–35.
Article CAS PubMed PubMed Central Google Scholar
Seravalle G, Facchetti R, Cappellini C, Annaloro A, Gelfi E, Grassi G. Elevated heart rate as sympathetic biomarker in human obesity. Nutr Metab Cardiovasc Dis. 2022;32:2367–74.
Grassi G, Fowler B, Scali B, Rossi F, Motto E, Pieruzzi F, et al. Sympathetic activation and heart rate tresholds for cardiovascular risk in chronic kidney disease. J Hypertens. 2022;40:1530–6.
Ho JE, Larson MG, Ghorbani A, Cheng S, Coglianese EE, Vasan RS, et al. Long-term cardiovascular risks associated with an elevated heart rate: the Framingham Heart Study. J Am Heart Assoc. 2014;3:e000668.
Article PubMed PubMed Central Google Scholar
Benetos A, Rudnichi A, Thomas F, Safar M, Guize L. Influence of heart rate on mortality in a French population: role of age, gender, and blood pressure. Hypertension. 1999;33:44–52.
Wang A, Chen S, Wang C, Zhou Y, Wu Y, Xing A, et al. Resting heart rate and risk of cardiovascular diseases and all-cause death: the Kailuan study. PLoS One. 2014;9:e110985.
Jensen MT, Marott JL, Allin KH, Nordestgaard BG, Jensen GB. Resting heart rate is associated with cardiovascular and all-cause mortality after adjusting for inflammatory markers: the Copenhagen City Heart Study. Eur J Prev Cardiol. 2012;19:102–8.
Castagno D, Skali H, Takeuchi M, Swedberg K, Yusuf S, Granger CB, et al. Association of heart rate and outcomes in a broad spectrum of patients with chronic heart failure: results from the CHARM (Candesartan in Heart Failure: Assessment of Reduction in Mortality and morbidity) program. J Am Coll Cardiol. 2012;59:1785–95.
Bohm M, Schumacher H, Teo KK, Lonn EM, Mahfoud F, Ukena C, et al. Resting heart rate and cardiovascular outcomes in diabetic and nondiabetic individuals at high cardiovascular risk analysis from the ONTARGET/ TRANSCEND trials. Eur Heart J. 2020;41:231–8.
Hillis GS, Woodward M, Rodgers A, Chow CK, Li Q, Zoungas S, et al. Resting heart rate and the risk of death and cardiovascular complications in patients with type 2 diabetes mellitus. Diabetologia. 2012;55:1283–90.
Palatini P. Resting heart rate as a cardiovascular risk factor in hypertension. Am J Hypertens. 2012;34:307–17.
Article Google Scholar
Palatini P, Parati G, Virdis A, Reboldi G, Masi S, Mengozzi A, et al. High heart rate amplifies the risk of cardiovascular mortality associated with elevated uric acid. Eur Prev Cardiol. 2021;14:zwab023.
Google Scholar
Mancia G, Masi S, Palatini P, Tsioufis C, Grassi G. Elevated heart rate and cardiovascular risk in hypertension. J Hypertens. 2021;39:1060–9.
Cuspidi C, Sala C, Casati A, Bombelli M, Grassi G, Mancia G. Clinical and prognostic value of hypertensive cardiac damage in the PAMELA study. Hypertens Res. 2017;40:329–35.
Vaz M, Jennings G, Turner A, Cox H, Lambert G, Esler M. Regional sympathetic nervous activity and oxygen consumption in obese normotensive human subjects. Circulation. 1997;96:3423–9.
Grassi G. Sympathetic overdrive and cardiovascular risk in the metabolic syndrome. Hypertens Res. 2006;29:839–47.
Mancia G, Kjeldsen SE, Kreutz R, Pathak A, Grassi G, Esler MD. Individualized beta-blocker treatment for high blood pressure dictated by medical comorbidities. Indications beyond the 2018 European Society of Cardiology/European Society of Hypertension guidelines. Hypertension. 2022;79:1153–66.
Flannery G, Gehrig-Mills R, Billah B, Krum H. Analysis of randomised controlled trials on the effect of magnitude of heart rate reduction on clinical outcomes in patients with systolic chronic heart failure receiving beta-blockers. Am J Cardiol. 2008;101:865–9.
Herman M, Donovan J, Tran M, McKenna B, Gore JM, Goldberg RJ, et al. Use of beta blockers and effects on heart rate and blood pressure post-acute coronary syndromes:are we on target? Am Heart J. 2009;158:784–94.
Kolloch R, Legler UF, Champion A, Cooper-Dehoff RM, Handberg E, Zhou Q, et al. Impact of resting heart rate on outcomes in hypertensive patients with coronary artery disease: findings from the International VErapamil-SR/trandolapril STudy (INVEST). Eur Heart J. 2008;29:1327–34.
Lonn EM, Rambihar S, Gao P, Custodis FF, Sliwa K, Teo KK, et al. Heart rate is associated with increased risk of major cardiovascular events, cardiovascular and all-cause death in patients with stable chronic cardiovascular disease: an analysis of ONTARGET/TRANSCEND. Clin Res Cardiol. 2014;103:149–59.
Palatini P, Thijs L, Staessen JA, Fagard RH, Bulpitt CJ, Clement DL, et al. Predictive value of clinic and ambulatory heart rate for mortality in elderly subjects with systolic hypertension. Arch Intern Med. 2002;162:2313–21.
Julius S, Palatini P, Kjeldsen SE, Zanchetti A, Weber MA, McInnes GT, et al. Usefulness of heart rate to predict cardiac events in treated patients with high-risk systemic hypertension. Am J Cardiol. 2012;109:685–92.
Grassi G, Turri C, Vailati S, Dell’Oro R, Mancia G. Muscle and skin sympathetic nerve traffic during the "white-coat" effect. Circulation. 1999;100:222–5.
Palatini P, Winnicki M, Santonastaso M, De Venuto G, Zanata G, Bertolo O, et al. Reproducibility of heart rate measured in the clinic and with 24-hour intermittent recorders. Am J Hypertens. 2000;13:92–98.
Palatini P, Reboldi G, Beilin LJ, Eguchi K, Imai Y, Kario K, et al. Predictive value of night-time heart rate for cardiovascular events in hypertension. The ABP-International study. Int J Cardiol. 2012;168:1490–5.
Download references
Author information
These authors contributed equally: Guido Grassi, Raffaella Dell’Oro
Authors and Affiliations
Clinica Medica, Department of Medicine and Surgery, University of Milano-Bicocca, Milan, Italy
Guido Grassi, Raffaella Dell’Oro, Michele Bombelli, Cesare Cuspidi & Fosca Quarti-Trevano
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Guido Grassi .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Grassi, G., Dell’Oro, R., Bombelli, M. et al. High blood pressure with elevated resting heart rate: a high risk “Sympathetic” clinical phenotype. Hypertens Res 46 , 2318–2325 (2023). https://doi.org/10.1038/s41440-023-01394-9
Download citation
Received : 18 May 2023
Revised : 04 July 2023
Accepted : 08 July 2023
Published : 27 July 2023
Issue Date : October 2023
DOI : https://doi.org/10.1038/s41440-023-01394-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sympathetic nervous system
- Hypertension
- Cardiovascular
Study Links E-Cigarette Use with Higher Risk of Heart Failure
Large study adds to growing body of evidence that vaping may harm the heart.
Apr 02, 2024
Contact: Nicole Napoli , [email protected], 202-669-1465
WASHINGTON (Apr 02, 2024) -
People who use e-cigarettes are significantly more likely to develop heart failure compared with those who have never used them, according to one of the largest prospective studies to date investigating possible links between vaping and heart failure. The findings are being presented at the American College of Cardiology’s Annual Scientific Session.
Heart failure is a condition affecting more than 6 million U.S. adults in which the heart becomes too stiff or too weak to pump blood as effectively as it should. It can often lead to debilitating symptoms and frequent hospitalizations as people age. Electronic nicotine products, which include e-cigarettes, vape pens, hookah pens, personal vaporizers and mods, e-cigars, e-pipes and e-hookahs, deliver nicotine in aerosol form without combustion. Since they were first introduced in the U.S. in the late 2000s, electronic nicotine products have often been portrayed as a safer alternative to smoking, but a growing body of research has led to increased concern about potential negative health effects.
“More and more studies are linking e-cigarettes to harmful effects and finding that it might not be as safe as previously thought,” said Yakubu Bene-Alhasan, MD, a resident physician at MedStar Health in Baltimore and the study’s lead author. “The difference we saw was substantial. It’s worth considering the consequences to your health, especially with regard to heart health.”
For the study, researchers used data from surveys and electronic health records in All of Us, a large national study of U.S. adults run by the National Institutes of Health, to analyze associations between e-cigarette use and new diagnoses of heart failure in 175,667 study participants (an average age of 52 years and 60.5% female). Of this sample, 3,242 participants developed heart failure within a median follow-up time of 45 months.
The results showed that people who used e-cigarettes at any point were 19% more likely to develop heart failure compared with people who had never used e-cigarettes. In calculating this difference, researchers accounted for a variety of demographic and socioeconomic factors, other heart disease risk factors and participants’ past and current use of other substances, including alcohol and tobacco products. The researchers also found no evidence that participants’ age, sex or smoking status modified the relationship between e-cigarettes and heart failure.
Breaking the data down by type of heart failure, the increased risk associated with e-cigarette use was statistically significant for heart failure with preserved ejection fraction (HFpEF)—in which the heart muscle becomes stiff and does not properly fill with blood between contractions. However, this association was not significant for heart failure with reduced ejection fraction (HFrEF)—in which the heart muscle becomes weak and the left ventricle does not squeeze as hard as it should during contractions. Rates of HFpEF have risen in recent decades, which has led to an increased focus on determining risk factors and improving treatment options for this type of heart failure.
The findings align with previous studies conducted in animals, which signaled e-cigarette use can affect the heart in ways that are relevant to the heart changes involved in heart failure. Other studies in humans have also shown links between e-cigarette use and some risk factors associated with developing heart failure. However, previous studies attempting to assess the direct connection between e-cigarette use and heart failure have been inconclusive, which Bene-Alhasan said is due to the inherent limitations of the cross-sectional study designs, smaller sample sizes and the smaller number of heart failure events seen in previous research.
Researchers said the new study findings point to a need for additional investigations of the potential impacts of vaping on heart health, especially considering the prevalence of e-cigarette use among younger people. Surveys indicate that about 5% to 10% of U.S. teens and adults use e-cigarettes. In 2018, the U.S. Surgeon General called youth e-cigarette use an epidemic and warned about the health risks associated with nicotine addiction.
“I think this research is long overdue, especially considering how much e-cigarettes have gained traction,” Bene-Alhasan said. “We don’t want to wait too long to find out eventually that it might be harmful, and by that time a lot of harm might already have been done. With more research, we will get to uncover a lot more about the potential health consequences and improve the information out to the public.”
Bene-Alhasan also said e-cigarettes are not recommended as a tool to quit smoking, since many people may continue vaping long after they quit smoking. The U.S. Centers for Disease Control and Prevention recommends a combination of counseling and medications as the best strategy for quitting smoking.
Researchers said that the study’s prospective observational design allows them to infer, but not conclusively determine, a causal relationship between e-cigarette use and heart failure. However, with its large sample size and detailed data on substance use and health information, Bene-Alhasan said the study is one of the most comprehensive studies to assess this relationship to date.
For more information about the health effects of e-cigarettes, visit CardioSmart.org/StopSmoking .
Bene-Alhasan will present the study, “Electronic Nicotine Product Use Is Associated with Incident Heart Failure - The All of Us Research Program,” on Sunday, April 7, 2024, at 3:15 p.m. ET / 19:15 UTC in Hall B4-5.
ACC.24 will take place April 6-8, 2024, in Atlanta, bringing together cardiologists and cardiovascular specialists from around the world to share the newest discoveries in treatment and prevention. Follow @ACCinTouch , @ACCMediaCenter and #ACC24 for the latest news from the meeting.
The American College of Cardiology (ACC) is the global leader in transforming cardiovascular care and improving heart health for all. As the preeminent source of professional medical education for the entire cardiovascular care team since 1949, ACC credentials cardiovascular professionals in over 140 countries who meet stringent qualifications and leads in the formation of health policy, standards and guidelines. Through its world-renowned family of JACC Journals, NCDR registries, ACC Accreditation Services, global network of Member Sections, CardioSmart patient resources and more, the College is committed to ensuring a world where science, knowledge and innovation optimize patient care and outcomes. Learn more at ACC.org .
< Back to Listings
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
- Frontiers in Sports and Active Living
- Exercise Physiology
- Research Topics
New Perspectives and Insights on Heart Rate Variability in Exercise and Sports
Total Downloads
Total Views and Downloads
About this Research Topic
During the current decade, sports science has been actively seeking innovative tools and strategies for effectively monitoring the training load and physiological responses of athletes and physical practitioners. In this domain, achieving proper recovery after training, guided by physiological markers, is ...
Keywords : Heart rate variability, HRV, exercise, sports, recovery, response
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines, participating journals.
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Science & Research
- Science and Research Special Topics
- Advancing Regulatory Science
Adapting a Measure of Heart Failure to an Adolescent Population
CERSI Collaborators: Stanford University: Christopher Almond, MD, MPH; Chiu-Yu Chen, MD, PhD; Korey Hood, PhD; Molly Tanenbaum, PhD
FDA Collaborators: Center for Devices and Radiological Health: Fraser Bocell, PhD; Vasum Peiris, MD, MPH; Anindita Saha; Brittany Caldwell, PhD; Michelle Tarver, MD, PhD
CERSI Subcontractors: Mayo Clinic: Jonathan Johnson, MD; Jennifer Ridgeway, PhD; Emma Behnken
CERSI In-Kind Collaborators: OptumLabs - William Crown, PhD; University of San Francisco - Sanket Dhruva, MD
Non-Federal Entity Collaborators: Johnson and Johnson- Karla Childers, MSJ, Paul Coplan, ScD, MBA, Stephen Johnston, MSc
Project Start Date: December 2018

Regulatory Science Challenge
The evaluation and approval of medical devices in pediatric populations lags far behind adult populations. Many devices, including life-saving devices, are adapted and used in children without the benefit of first going through a well-controlled study to evaluate their safety and effectiveness. One way to encourage studies of devices in pediatric populations is to provide additional measures to facilitate efficient evidence generation, such as Patient-Reported Outcomes Measures (PROMs). PROMs are questionnaires about health status that are answered by the patient. PROMs have become an important method to include the patient voice in clinical studies and can help provide evidence of the safety and effectiveness of a device and evaluate the impact a treatment on a patient’s life. However, PROMs must be developed to fit the clinical research in which they will be used, and companies within the medical device industry do not always have the resources necessary to develop new PROMs for new areas of research. Thus, this project was conceived to provide an example of how to efficiently and cost-effectively adapt an existing PROM, making changes to the questions, to fit a new population; in this case, pediatric heart failure patients.
The adaptation of a PROM for appropriate use in this population will provide an additional method for collecting evidence to support the use of devices in pediatric heart failure. Additionally, it provides an example of methods other stakeholders can use to adapt other PROMs for use in device studies.
Project Description and Goals
The aim of this project is to understand how adolescents perceive the symptoms and impact of their heart failure, while adapting existing adult PROMs to capture and quantify this perception for use in clinical care and regulatory decision making. The development of a PROM is a multi-step undertaking where each subsequent step is informed by the prior. The major steps include a literature review of existing publications and evidence, a short survey to capture clinician input, focus groups and interviews to confirm the question selection and inform adaptation, the completion of the adapted PROM, and a study to evaluate the PROM’s properties in a larger sample. The final PROM will be available for further testing and potential use in pediatric cardiology device submissions.
Research Outcomes/Results
An analysis of interview transcripts found common and consistent themes from patient interviews, which included:
- Symptoms of fatigue, shortness of breath, and chest discomfort.
- Limitations in ability to perform ordinary tasks, participate in extracurricular activities, and keep up with peers.
- Social and emotional impacts from being treated differently by others.
- Burden of medical care.
Caregivers reported similar symptoms and impacts on patient function, and further described social exclusion by peers and caregiver anxiety about illness burden in the future such as college and career limitations, ability to have children, etc.
Research Impacts
Incorporating patient preference information into decisions that FDA makes about regulating devices is one of the major goals of FDA’s Center for Devices and Radiological Health (CDRH). Study findings show that patients prefer specific outcomes related to prostate ablation therapies like HIFU. The study results may help inform the design and regulation of current and future prostate tissue ablation devices by providing information about outcomes that patients most desire.
Publications
- PMID: 34677594; Citation: Wallach JD, Deng Y, McCoy RG, Dhruva SS, Herrin J, Berkowitz A, Polley EC, Quinto K, Gandotra C, Crown W, Noseworthy P, Yao X, Shah ND, Ross JS, Lyon TD. Real-world Cardiovascular Outcomes Associated With Degarelix vs Leuprolide for Prostate Cancer Treatment. JAMA Netw Open. 2021;4(10):e2130587. doi:10.1001/jamanetworkopen.2021.30587 .
- PMID: 36191949; Citation: Deng Y, Polley EC, Wallach JD, Dhruva SS, Herrin J, Quinto K, Gandotra C, Crown W, Noseworthy P, Yao X, Lyon TD, Shah ND, Ross JS, McCoy RG. Emulating the GRADE trial using real world data: retrospective comparative effectiveness study. BMJ . 2022 Oct 3;379:e070717. doi: 10.1136/bmj-2022-070717 .
More than half a million global stroke deaths may be tied to climate change
Stroke-related deaths on rise in regions with high temperatures.
A changing climate may be linked to growing death and disability from stroke in regions around the world, according to a study published in the April 10, 2024, online issue of Neurology ® , the medical journal of the American Academy of Neurology. Researchers found over three decades that non-optimal temperatures, those above or below temperatures associated with the lowest death rates, were increasingly linked to death and disability due to stroke. The study does not prove that climate change causes stroke. It only shows an association. The study also did not examine other risk factors such as high blood pressure and high cholesterol levels.
Researchers found that the majority of these strokes were due to lower than optimal temperatures, however they also found an increase in strokes tied to higher than optimal temperatures. With lower temperatures, a person's blood vessels can constrict, increasing blood pressure. High blood pressure is a risk factor for stroke. Higher temperatures may cause dehydration, affecting cholesterol levels and resulting in slower blood flow, factors that can also lead to stroke.
"Dramatic temperature changes in recent years have affected human health and caused widespread concern," said study author Quan Cheng, PhD, of Xiangya Hospital Central South University in Changsha, China. "Our study found that these changing temperatures may increase the burden of stroke worldwide, especially in older populations and areas with more health care disparities.
For the study, researchers looked at 30 years of health records for more than 200 countries and territories. They examined the number of stroke deaths and burden of stroke-related disability due to non-optimal temperatures.
They then divided the data to look at different regions, countries and territories. They also looked at age groups and genders.
In 2019, there were 521,031 stroke deaths linked to non-optimal temperatures. There were also 9.4 million disability-adjusted life years due to stroke linked to non-optimal temperatures. Disability-adjusted life years are the number of years of life lost due to premature death and years lived with illness.
When looking at low temperatures compared to high temperatures, they found that 474,002 of the total deaths were linked to low temperatures.
Researchers found that the rate of death from stroke from temperature changes for male participants was 7.7 per 100,000 compared to 5.9 per 100,000 for female participants.
When looking at regions, central Asia had the highest death rate for stroke linked to non-optimal temperatures with 18 per 100,000. At the national level, North Macedonia had the highest death rate with 33 per 100,000.
"More research is needed to determine the impact of temperature change on stroke and to target solutions to address health inequalities," Cheng said. "Future research should aim to reduce this threat by finding effective health policies that address potential causes of climate change, such as the burning of fossil fuels, deforestation and industrial processes."
The study was supported by Hunan Youth Science and Technology Talent Project.
- Heart Disease
- Stroke Prevention
- Brain Injury
- Global Warming
- Cholesterol
- Sudden infant death syndrome
- Attribution of recent climate change
- Hypercholesterolemia
- Temperature record of the past 1000 years
- Global warming controversy
- Low density lipoprotein
Story Source:
Materials provided by American Academy of Neurology . Note: Content may be edited for style and length.
Journal Reference :
- Chunrun Qu, Yu Chen, Chen Liu, Zhiwen Hu, Jingwei Zhang, Luzhe Yan, Hao Zhang, Yifan Liu, Wanyao Liu, Quan Cheng, Peng Luo, Zhixiong Liu. Burden of Stroke Attributable to Nonoptimal Temperature in 204 Countries and Territories . Neurology , 2024; 102 (9) DOI: 10.1212/WNL.0000000000209299
Cite This Page :
Explore More
- Quantum Effects in Electron Waves
- Star Trek's Holodeck Recreated Using ChatGPT
- Cloud Engineering to Mitigate Global Warming
- Detecting Delayed Concussion Recovery
- Genes for Strong Muscles: Healthy Long Life
- Brightest Gamma-Ray Burst
- Stellar Winds of Three Sun-Like Stars Detected
- Fences Causing Genetic Problems for Mammals
- Ozone Removes Mating Barriers Between Fly ...
- Parkinson's: New Theory On Origins and Spread
Trending Topics
Strange & offbeat.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
A “Growth-at-All-Costs” Mindset Can Stall Your Company

If leaders don’t consider employees in their growth strategies, then disengagement, burnout, and lack of innovation will persist.
The strength of any organization depends on its people. Research has found a strong positive relationship between employee well-being and firm performance. When people feel healthy and engaged, their work performance improves, their relationships are stronger, and they’re better motivated to impact change. This is what’s at the heart of “human sustainability”— a concept introduced in Deloitte’s “2023 Global Human Capital Trends” report. It’s about creating value in people’s lives — from their physical and mental well-being to their career skills and overall sense of purpose. It starts with individuals, but ultimately has a ripple effect to the people they encounter and the organizations they’re part of. Research shows that a focus on human sustainability drives stronger business results. All organizations need a business growth strategy where people feel they’re prioritized. Before you launch your next growth initiative, make sure you’re not sabotaging your employees, and your company in turn. This article offers five questions to ask yourself as you’re setting your own growth strategy.
Sustainable growth can be elusive. Research has shown that only about 15% of the companies in the top growth quartile in 1985 were able to sustain their top-quartile performance for at least 30 years. While factors such as operating systems, financial health, and internal processes are all critical in determining whether growth can continue, studies show that of all the resources a company has, human capital is the most important. In other words, consistent and profitable growth is never easy, but it’s nearly impossible without “the quality, talent, and mindset of its people.”
- Jenn Lim is a global workplace expert , one of the World’s Top 50 Keynote Speakers, the bestselling author of Beyond Happiness , and CEO/Cofounder of Delivering Happiness .
- Jen Fisher is Deloitte’s Human Sustainability leader in the United States. She’s also the bestselling author of the book, Work Better Together , a TEDx speaker , the Human Sustainability Editor-At-Large for Thrive Global , and the host of the WorkWell podcast series .
Partner Center
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Eur Rev Aging Phys Act

Effects of different exercise interventions on heart rate variability and cardiovascular health factors in older adults: a systematic review
Bernhard grässler.
1 Department of Sport Science, Faculty of Humanities, Otto von Guericke University, 39104 Magdeburg, Germany
Beatrice Thielmann
2 Department of Occupational Medicine, Faculty of Medicine, Otto von Guericke University, Magdeburg, Germany
Irina Böckelmann
Anita hökelmann, associated data.
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Aging impairs physiological processes in the autonomic nervous, endocrine, and cardiovascular systems which are associated with increased risk of cardiovascular disease. Heart rate variability (HRV), the beat-to-beat variations of successive heartbeats, is an indicator of cardiac autonomic control and cardiovascular health. Physical activity has beneficial effects on cardiovascular health. However, no review has been conducted to summarize the effects of different exercise modalities on HRV in older adults. Therefore, the aim of this systematic review was to summarize the effects of endurance, resistance, coordinative, and multimodal exercise interventions on resting HRV and secondary health factors in healthy older adults aged 60 years in average and over.
Five databases (PubMed, Scopus, SPORTDiscus, Ovid, and Cochrane Library) were searched for eligible studies published between 2005 and September 8th, 2020. Two reviewers independently assessed the studies for potential inclusion. Outcome measures were changes in resting HRV indices, baroreflex sensitivity, blood pressure, body fat, body mass, body mass index, cardiac output, distance in the six-minute walking test, stroke volume, total peripheral resistance, and VO 2 max or VO 2 peak from pre to post intervention. The methodological quality of the final data set was assessed using two scales (TESTEX and STARD HRV ). This review was registered in PROSPERO: CRD42020206606.
The literature search retrieved 3991 articles, of which 13 were included in the review. Five studies used multimodal, three studies endurance, two studies resistance, two studies coordinative, and one study used an endurance and a resistance training intervention. The majority of the studies revealed significant positive effects on cardiac autonomic control, except for the resistance training interventions. All exercise modalities improved secondary health factors. The methodological quality assessment revealed a few criteria to improve the quality of and comparability between studies.
This systematic review revealed beneficial effects on cardiac autonomic control in healthy older adults through endurance, coordinative, and multimodal training but not through resistance training. Secondary health factors improved after all types of physical interventions. Future investigations should more thoroughly adhere to methodological standards of exercise interventions and ECG recording for the assessment of autonomic regulation.
Supplementary Information
The online version contains supplementary material available at 10.1186/s11556-021-00278-6.
Introduction
People aged 65 or over make up the world’s fastest growing age group. In 2019, approximately 9% belong to this age group [ 1 ]. In particular Western societies have experienced a demographic expansion of older adults’ population due to improved medical care and declining birth rates in recent decades. For example, the proportion of people aged 65 or over in Europe and North America is as high as 18% and could rise to 25% by 2100 [ 1 ]. As longer lives are accompanied by cardiovascular and other diseases of aging, our society is facing enormous medical challenges. As a result, the burden on the healthcare system is increasing due to a growing number of patients and a greater need for therapeutic interventions and treatment of diseases. For example, global expenditures for health care increased by 3.9% annually between 2000 and 2017, reaching US$7.8 trillion in 2017 [ 2 ]. To reduce health care costs while ensuring a high quality of life, the focus should be on prevention rather than treatment [ 3 ].
Normal aging processes cause impairment of cardiac autonomic control and manifest as reduced parasympathetic modulation of the cardiovascular system [ 4 , 5 ]. This parasympathetic modulation can be indexed as heart rate variability (HRV), a non-invasive measure describing beat-to-beat variations of the time intervals between successive heart beats [ 6 – 8 ]. These fluctuations are the result of heart-brain interactions and dynamic non-linear autonomic nervous system (ANS) processes [ 9 ]. HRV can be described with time-domain, frequency-domain, and non-linear metrics [ 9 ]. In general, good cardiac autonomic control, indexed as relatively high HRV, is related to better mental and physical health, whereas lower values are related to reduced regulatory capacity, disturbances in the cardiovascular system, and impaired adaptability to internal and external changes [ 8 , 10 ]. Reduced cardiac autonomic control is associated with a number of pathological conditions, including coronary heart disease and mortality [ 11 – 13 ], future functional decline [ 14 ], chronic heart failure [ 15 ], sarcopenia [ 16 ], and hypertension [ 17 ]. This contributes to increased risk for cardiovascular diseases [ 18 – 20 ], decreased physical fitness [ 21 ], and quality of life in older adults [ 22 ].
Age-related decline in HRV has been reported in several studies [ 13 , 23 , 24 ], but is also the result of lifestyle factors and not aging processes alone [ 25 , 26 ]. In this context, cross-sectional studies reported a positive relationship between long-term sportive lifestyle and HRV in older adults [ 25 – 28 ]. Moreover, HRV has also been proven to predict longevity in very old persons better than an annual health examination [ 29 ].
Apart from changes in cardiac autonomic control, aging is also associated with a progressive impairment of cardiovascular functioning. Among the affected functions are a reduced arterial baroreflex control of heart rate and increased vascular resistance favoring hypertension [ 30 – 32 ]. Furthermore, resting metabolic rate [ 33 ] and daily physical activity decline as a consequence of the aging process [ 19 ]. In women, estrogen production is reduced after menopause, leading to an increase in sympathetic activity and a decrease in endothelial function. These alterations increase blood pressure and favor hypertension in older women, and may account for the higher cardiovascular mortality among older women compared to older men [ 34 ].
Despite these age-related alterations in the cardiovascular system and impairments in physical performance, sedentary behavior becomes more prevalent and participation in structured exercise programs declines with increasing age [ 35 , 36 ]. Indeed, previous reviews demonstrated the positive effects of physical interventions on HRV in children [ 37 ], young adults [ 38 ], and diseased individuals [ 39 – 41 ], and in studies using aerobic [ 42 , 43 ], resistance [ 44 ], or interval training interventions [ 45 ]. However, in the older adults, the effects of physical training on HRV are scarcer and more controversial. Type, intensity, and duration of intervention are possible reasons for these discrepancies [ 5 ]. In addition, there is limited research on the effects of combined endurance and resistance training interventions [ 46 ]. Finally, we are not aware of any review considering the effects of physical interventions on cardiac autonomic control and secondary health factors in older adults. Looking at factors determining cardiovascular health, such as blood pressure, body fat, or aerobic capacity, provides a more comprehensive view of cardiovascular health than only assessing HRV. For these reasons, there is a need for a systematic review of current studies with physical interventions focusing on the effects on cardiac autonomic control in older adults. In addition to HRV as an indicator of parasympathetic modulation, we intended to consider other physiological parameters related to cardiovascular health to gain a more comprehensive picture of the effects of physical interventions on the autonomic and cardiovascular health of older adults. These secondary outcomes were extracted from the eligible studies focusing on changes in cardiac autonomic control.
The aim of this systematic review was to summarize the existing literature on the effects of exercise interventions on cardiac autonomic control and secondary health factors in healthy adults aged 60 years in average and over. Given the above described positive influence of physical training on cardiac autonomic control and cardiovascular health, we hypothesized positive effects of any type of physical intervention on resting cardiac autonomic control and cardiovascular health.
A systematic review, investigating the effects of different exercise interventions on resting cardiac autonomic control and secondary health factors in healthy older adults, based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement was conducted [ 47 ]. We also performed a methodological and reporting quality assessment by using the tools TESTEX [ 48 ] and STARD HRV [ 49 ].
This review follows in its structure a previous review conducted by the same authors on young adults [ 38 ]. HRV variables were chosen as indicator of cardiac autonomic control because HRV is sensitive to exercise training-induced adaptations and convenient for the investigation of the effects of exercise training on the state of the ANS [ 7 , 50 ]. For that purpose, the traditional exercise activities, endurance and resistance training, were included. Additionally, coordinative training, intended to improve specific motor skills, and multimodal exercise interventions, comprising at least two types of modalities, were included as well. This procedure follows our previous review with young adults [ 38 ]. Secondary to HRV indices, some cardiovascular health factors, that were evaluated in the intervention studies, were considered in this review as well. These were the following variables: baroreflex sensitivity (BR), body fat (BF), body mass (BM), body mass index (BMI), blood pressure (BP), cardiac output (CO), stroke volume (SV), total peripheral resistance (TPR), VO 2 max or VO 2 peak, and distance in the six-minute walking test (6-MWT). Further, methodological and reporting quality of the eligible studies were evaluated via two quality assessment tools (TESTEX and STARD HRV ).
Data sources and search strategy
A comprehensive, systematic search using the databases PubMed, Scopus (Elsevir), SPORTDiscus, Ovid, and Cochrane Library was conducted. The search was restricted to manuscripts published between January 1st, 2005, and September 8th, 2020. The following terms were used: (resistance training OR resistance exercise OR strength training OR strength exercise OR aerobic training OR aerobic exercise OR physical training OR physical exercise OR multimodal training OR multimodal exercise OR coordinative training OR coordinative exercise) AND (heart rate variability OR HRV OR cardiac autonomic control OR autonomic function OR parasympathetic activity OR parasympathetic nervous system OR cardiac vagal tone OR autonomic cardiac modulation OR vagus nerve OR vagal tone OR vagal activity).
Inclusion and exclusion criteria
The inclusion criteria for relevant studies were: (1) involving at least ten healthy participants aged 60 years in average or over without diseases relevant for HRV analysis in the training group (please see for a detailed description of diseases relevant for HRV analysis: Sammito & Böckelmann [ 51 ]); (2) physical training intervention (including the following exercise modalities: endurance, resistance, coordinative, or multimodal training) with a minimum of four weeks and eight training sessions; (3) randomized controlled trials, quasi-experimental trials, cross-over controlled trials, or controlled trials without randomization; (4) measurement of at least one HRV parameter at resting position before (pre) and after (post) the intervention through Holter ECG or chest belt; (5) studies with 24-h ECG measurement when a short-term recording segment at resting position was analyzed; (6) full-text in English or German language; and (7) human participants. The exclusion criteria consisted of: (1) studies with participants with diagnosis of dementia, mental diseases, neurological diseases, endocrine diseases (diabetes, thyroid gland disease), cardiac diseases, hypertension (systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg [ 52 ]), or other health-related diseases; (2) measuring acute exercise effects or HRV during exercise; (3) single-case studies, review articles, short communications, letters with insufficient information to analyze the results, guidelines, theses, dissertations, qualitative studies, scientific conference abstracts, or studies on animals; (4) 24-h ECG recording without short-term analysis at resting position; (5) HRV assessment through recording the pulse rate manually or through photoplethysmography; and (6) studies with professional athletes. 24-h ECG recordings were excluded as they do not provide standardized conditions for interindividual comparisons. In addition, comparisons between pre- and postintervention are limited because behavior and daily activities would have to be identical at both measurements. Therefore, in this review, we restricted to standardized short-term measurements under laboratory conditions to assess cardiac autonomic control.
Data collection and analysis
Selection of studies.
The search was applied to each electronic database and all retrieved articles were transferred to the Citavi 6 reference manager (Swiss Academic Software, Wädenswil, Switzerland). After removing duplicates, two authors (B.G. and B.T.) independently screened all titles and abstracts for retrieving relevant articles. Further, based on the criteria for inclusion and exclusion, the full-text of each relevant article was screened by the same two authors independently. Finally, the references of the eligible articles were screened for further articles. When necessary, the opinion of a third author (I.B.) was considered at any stage of the search process.
Data extraction
Data of the final studies sample were extracted based on the PICOS approach [ 53 ] and conducted by two authors (B.G. and B.T.) independently. The following data were extracted: sample characteristics (sample size, age, gender), HRV protocol (method [ECG or chest belt], respiration [paced or spontaneous], position [supine, sitting, standing], sampling frequency), analyzed HRV parameters, secondary outcomes (BF, BM, BMI, BP, BR, CO, SV, TPR, VO 2 max or peak, and 6-MWT), recording length, characteristics of intervention (type, duration of intervention, sessions per week), and control group. Regarding physical training interventions, studies were considered that utilized long-term physical exercises, performed regularly in a planned, structured, and purposive manner with the objective to improve or at least maintain individual capabilities [ 54 ]. Therefore any form of endurance (aerobic), resistance, multimodal, and coordinative exercise modalities intended to improve physical performance were considered. There were no further restrictions regarding type of exercise. Therefore, any form of endurance training (e.g., continuous or interval training) and resistance training (e.g., isometric or dynamic training) was included. Likewise, forms of coordinative training were included as long as they were described as “physical activity” that contributed to the increase in energy expenditure [ 54 ]. The extracted HRV parameters with their physiological meaning are displayed in Table 1 . All extracted information of the studies is summarized in Table 2 . More details on physiological background of the HRV parameters can be found in the referenced literature [ 6 , 9 , 63 ]. Additionally, resting heart rate (RHR) and mean RR interval (mRR) were also extracted.
Description of extracted HRV parameters
HF (nu), power in high frequency range (in normalized units); Hz, Hertz; LF (nu), power in low frequency range (in normalized units); ms, millisecond; NN50, number of pairs of adjacent NN intervals differing by more than 50 ms in the entire recording; pNN50, number of pairs of adjacent NN intervals differing by more than 50 ms in the entire recording divided by the total number of all NN intervals; RMSSD, square root of the mean of the sum of the squares of differences between adjacent NN intervals; SD1, standard deviation of instantaneous beat-to-beat variability, extracted from Poincaré Plot; SD2, standard deviation of the long-term variability, extracted from Poincaré Plot; SDNN, standard deviation of NN intervals. Modified Sammito & Böckelmann [ 55 ].
Characteristics of the studies included and TESTEX and STARD HRV score
BF, body fat; BM, body mass; BMI, body mass index; BP, blood pressure; BR, baroreflex sensitivity; CO, cardiac output; DG, dancing group; ECG, electrocardiography; HF (nu), power in high frequency range (in normalized units); HF%, relative power in high frequency range; LF (nu), power in low frequency range (in normalized units); LF%, relative power in low frequency range; ln, natural logarithm; MG, memory training group; mRR, mean RR interval; n.r., not reported; pNN50, number of pairs of adjacent NN intervals differing by more than 50 ms in the entire recording divided by the total number of all NN intervals; RHR, resting heart rate; RMSSD, square root of the mean of the sum of the squares of differences between adjacent NN intervals; SD1, standard deviation of instantaneous beat-to-beat variability, extracted from Poincaré Plot; SD2, standard deviation of the long-term variability, extracted from Poincaré Plot; SDNN, standard deviation of NN intervals; SV, stroke volume; TG, treadmill walking group; TP, total power; TPR, total peripheral resistance; TV, total variance; VO 2 max, maximum oxygen consumption; VO 2 peak, peak oxygen consumption; 6-MWT, six minute walking test
Quality assessment
Two assessment tools were applied for evaluation of the methodological and reporting quality of the selected studies: “Tool for the Assessment of Study Quality and reporting in Exercise (TESTEX) scale” [ 48 ] and “STARD HRV ” [ 49 ]. The first tool is designed to evaluate the quality of exercise training studies by using twelve items with a maximum score of 15 points. The second tool focuses on the quality of ECG recording, processing, and analyzing of HRV parameters. It includes 25 items and has a maximum score of 25 points. Two authors (B.G. and B.T.) evaluated the quality of the included studies independently. Again, any conflicts were resolved in consultation with a third author (I.B.). We used slightly modified versions of the tools, which were already used in a previous review [ 38 ] and are described in the additional files 1 and 2 .
Data synthesis and analysis
The changes in HRV measures and secondary outcomes of the intervention groups from pre to post measurement of the included interventions were collected and summarized in Table 3 . Upward pointing arrows indicate a significant increase, downward pointing arrows a significant decrease. Horizontal arrows indicate no change.
Outcome of selected heart rate related variables and secondary health factors
BF, body fat; BM, body mass; BMI, body mass index; BR, baroreflex sensitivity; CO, cardiac output; DBP, diastolic blood pressure; DG, dancing group; HF (nu), power in high frequency range (in normalized units); LF (nu), power in low frequency range (in normalized units); ln, natural logarithm; MBP, mean blood pressure; MG, memory training group; mRR, mean RR interval; RHR, resting heart rate; RMSSD, square root of the mean of the sum of the squares of differences between adjacent NN intervals; SBP, systolic blood pressure; SD1, standard deviation of instantaneous beat-to-beat variability, extracted from Poincaré Plot; SD2, standard deviation of the long-term variability, extracted from Poincaré Plot; SDNN, standard deviation of NN intervals; SV, stroke volume; TG, treadmill walking group; TP, total power; TPR, total peripheral resistance; VO 2 max, maximum oxygen consumption; VO 2 peak, peak oxygen consumption; 6-MWT, six minute walking test; 2TG: training group exercising two times per week; 3TG: training group exercising three times per week. ↑ indicates significant increase ( p < 0.05); ↓ indicates significant decrease; ↔ indicates no significant change
Study selection
The database search initially identified 5068 records. After removing 1078 duplicates and adding one article through other sources, the titles and abstracts of 3991 articles were screened. 96 articles remained for full-text analysis. Finally, 13 studies fulfilled all inclusion and exclusion criteria. The selection process is shown in the PRISMA flow diagram in Fig. 1 .

PRISMA flow diagram showing identified, included, and excluded studies
Study characteristics
The characteristics of the 13 eligible studies and scores in TESTEX and STARD HRV are outlined in Table Table2. 2 . The outcome of the most frequently used heart rate related parameters and secondary outcomes can be found in Table Table3. 3 . A detailed description of the characteristics of the included studies and the results of all heart rate related variables are available in the additional files 3 and 4 , respectively.
Participants characteristics
In total, 422 participants were included, of which 289 were allocated to training groups and 133 to control groups. 300 participants were women and 122 were men. Three studies did not include a control group [ 46 , 57 , 59 ]. Three studies included two or three training groups [ 22 , 46 , 59 ]. In the study of Audette et al. [ 21 ], the effects of practicing Tai Chi and brisk walking was compared. The walking group was not included as training group in this review since the sample size was < 10. Sample sizes ranged from ten [ 57 ] to 70 participants [ 59 ]. The mean age of the collated sample was 67.8 ± 5.4 years and ranged from 59.2 [ 60 ] to 78.8 years [ 59 ]. We still included the intervention of Rezende Barbosa et al. [ 60 ] because the mean age of the training group was 60.0 years, which was one of our inclusion criteria. The mean age of the training groups of the final sample was 69.3 ± 6.00 years and the mean age of the control groups was 67.3 ± 6.3 years. Regarding training groups, the mean age ranged from 60.0 [ 60 ] to 80.7 years [ 59 ]. Regarding control groups, the mean age ranged from 58.5 [ 60 , 61 ] to 78.8 years [ 22 ]. Eight trials comprised female and male participants [ 5 , 18 , 20 , 22 , 46 , 56 , 59 , 60 ]. Four trials considered only female [ 21 , 58 , 60 , 61 ] and one study included only male participants [ 62 ]. All participants were in a general healthy physical and mental condition without diseases affecting cardiac autonomic control [ 51 ], but they were sedentary or in an untrained physical state. In one investigation, 28% of the participants had an BMI > 30 kg/m 2 [ 22 ].
HRV and secondary health factors measurement
Four of 13 studies used ECG to record the heart rate [ 18 , 21 , 57 , 62 ]. The remaining nine studies used chest belts. Six studies reported their breathing protocol [ 21 , 22 , 57 , 58 , 61 , 62 ]. While in five studies a spontaneous breathing protocol was applied [ 21 , 22 , 58 , 61 , 62 ], a spontaneous and a paced breathing protocol was applied in one study [ 57 ]. The participants` position during the ECG recording varied between the studies. One study [ 22 ] recorded in supine and standing position. Six studies recorded while the participants were sitting [ 5 , 18 , 46 , 56 , 58 , 59 ]. A supine position was chosen in five studies [ 20 , 22 , 57 , 60 , 61 ] and one study did not provide any information about the position during the recording [ 21 ]. Eight studies recorded NN intervals for a fixed time range. Six studies recorded for five minutes [ 18 , 20 – 22 , 58 , 59 ], one study for six minutes during both breathing modes [ 57 ], and one study recorded for ten minutes [ 62 ]. Three studies analyzed 256 NN intervals [ 5 , 56 , 61 ], one study 300 NN intervals [ 46 ], and one study analyzed 1000 NN intervals [ 60 ]. Only five studies provided any information about the sampling frequency. Four studies recorded ECG with 1000 Hz [ 20 , 57 , 59 , 62 ] and one study recorded with 500 Hz [ 18 ]. All 13 studies analyzed frequency-domain parameters. All studies except one [ 21 ] analyzed time-domain parameters and only one study used non-linear parameters [ 58 ], namely SD1 and SD2. All studies used the HRV parameter HF (ms 2 , nu, ln, or %). LF (ms 2 , nu, ln, or %) was used in ten studies. Only three studies did not apply LF [ 20 , 22 , 59 ]. Total power was reported in two studies [ 46 , 62 ]. RMSSD was the most frequently used time-domain parameter. Eight studies used it [ 5 , 20 , 46 , 56 , 58 – 61 ]. Seven studies analyzed SDNN [ 5 , 22 , 57 – 61 ]. pNN50 [ 20 ] and the unusual parameter total variance [ 18 ] were used in one trial each. RHR were reported in eight studies [ 18 , 22 , 46 , 57 , 58 , 60 – 62 ] and mRR in four studies [ 58 , 60 – 62 ].
Three studies did not report any secondary health factor [ 5 , 59 , 61 ]. Six studies analyzed resting BP [ 18 , 22 , 46 , 58 , 60 , 62 ]. Four studies analyzed VO 2 max or VO 2 peak [ 20 , 21 , 56 , 62 ] and four studies recorded BM and BMI [ 22 , 46 , 58 , 62 ]. The 6-MWT was applied in three studies [ 20 , 22 , 46 ]. Only two studies measured BF [ 22 , 58 ] and two studies evaluated BR [ 18 , 57 ].
Physical training protocols
Five studies applied multimodal exercise interventions. Two of them used a combination of endurance and resistance training [ 61 , 62 ]. One study [ 46 ] included balance, endurance, and resistance training. The participants in another study [ 60 ] trained their strength, coordination, balance, and agility as well as their aerobic capacity through a walking program. Three training groups exercised in the final study [ 59 ]. All groups performed strength and balance exercises. In addition, one group also performed a virtual reality dance program (DG, dance group), another group a treadmill walking program with simultaneous verbal memory training (MG, memory group), and the final group a treadmill walking program without memory training (TG, treadmill group). Endurance training only was used in four studies [ 5 , 22 , 56 , 57 ]. One study [ 22 ] included an endurance and a resistance training group. A form of resistance training was used in two studies [ 18 , 58 ]. Finally, coordinative exercises were performed by the participants in two studies. Participants in one study [ 20 ] had to dance and participants in another study [ 21 ] practiced Tai Chi. The duration of the interventions varied between six weeks [ 20 ] and one year [ 57 , 62 ] and lasted in average 20.4 weeks. In all studies, participants exercised for two or three sessions per week. However, in the first two weeks of one intervention [ 20 ], participants had to dance five times per week, in the next two weeks three times per week, and in the last two weeks two times per week.
Heart rate related variables
Endurance training.
Four studies with types of endurance training were retrieved from the literature search. The interventions included aquaerobics and swimming [ 56 ], walking, circuit-training, stepping, and running [ 5 ], walking, running, swimming, and cycling [ 57 ], and walking, stepping, and dancing [ 22 ]. All four interventions included men and women. Within-group or between-group analysis demonstrated significant improvements following training interventions for HF and RMSSD [ 5 , 56 ], SDNN [ 5 , 57 ], and HF/(LF + HF) [ 56 ]. RHR significantly decreased after one intervention [ 22 ]. Interestingly, another intervention [ 57 ] showed an increase of HRV in sedentary older participants after the intervention with similar HRV values to those of master athletes and sedentary younger adults who were studied before the intervention but did not undergo the intervention.
Resistance training
Three studies examined the effects of whole-body resistance training on cardiac autonomic control [ 18 , 22 , 58 ]. One study examined only women [ 58 ] and two studies examined men and women [ 18 , 22 ]. No study found significant changes in HRV, mRR, or RHR.
Coordinative training
Literature search retrieved two studies using coordinative exercise interventions. In one study, female participants practiced Tai Chi [ 21 ] and in the other study men and women practiced an exergaming-based dance program [ 20 ]. After the interventions, HF nu [ 20 , 21 ] and RMSSD [ 20 ] improved significantly, and LF nu decreased significantly [ 21 ].
Multimodal training
Significant within-group or between-group increases were detected for RMSSD [ 59 – 61 ], HF [ 59 ], HF nu [ 61 ], and mRR [ 60 , 61 ]. Significant decreases were found in RHR [ 60 , 61 ], LF nu, and LF/HF [ 61 ]. In one study [ 59 ], the pre-post comparisons within groups were estimated from the graphs because no statistical significance was provided. The graphs showed a clear improvement of HF, RMSSD, and SDNN in the group performing the multimodal training with dancing as main component of the training. In the same study, the two combined cognitive-motor training groups (DG and MG) were compared with the exclusively physical training group (TG). A significant increase in SDNN for the first groups, but no change in the TG were detected. Furthermore, HF, RMSSD, and SDNN significantly increased in the DG while it remained unchanged in the TG. In contrast to the previous results, significant reductions of ln HF, ln LF, RMSSD, and total power (TP) were detected in the study of McKune et al. [ 46 ] in the training group exercising three times per week. The training group exercising only two times per week showed no significant changes in any of the HRV parameters.
Secondary health factors
All studies except one [ 5 ] evaluated health factors secondary to HRV and found positive improvements. VO 2 max [ 56 , 57 ], 6-MWT [ 22 ], and SV [ 57 ] significantly increased, while BM, TPR [ 57 ], BF [ 22 ], and BP [ 22 , 57 ] significantly decreased.
All three studies using resistance training evaluated secondary health factors [ 18 , 22 , 58 ]. A significant reduction of systolic BP was reported in one study [ 58 ]. BF was significantly reduced after another intervention [ 22 ].
Secondary health factors were measured in two interventions [ 20 , 21 ]. Both interventions lead to significant improvements in VO 2 max. In addition, 6-MWT distance increased in the study of Varas-Diaz et al. [ 20 ].
Three of five studies assessed secondary health factors [ 46 , 60 , 62 ]. Multimodal training interventions were able to reduce diastolic BP [ 46 , 60 ] and improve VO 2 peak [ 62 ]. Interestingly, while participants exercising two times per week significantly improved diastolic and systolic BP, participants exercising three times per week significantly improved only diastolic BP.
The methodological and reporting quality of the studies was assessed via the tools TESTEX and STARD HRV . The total scores are shown in Table Table3. 3 . A detailed summary is displayed in the additional file 5 for TESTEX and in the additional file 6 for STARD HRV .
The average score of the TESTEX was 8.88 ± 2.47 and ranged from 4.5 [ 57 , 61 ] to 12.5 points [ 58 ]. However, Okazaki et al. [ 57 ] did not include a control group and was therefore limited to a maximum score of eight points. Nearly all studies specified eligibility criteria in sufficient detail except one [ 46 ]. All but one study allocated their participants randomly to the groups. Participants in the control group of the study of Audette et al. [ 21 ] were not randomly allocated to the control group. No study concealed the allocation of the participants and performed an intention-to-treat analysis. In only two studies [ 21 , 58 ], assessors were blinded to group allocation.
The score of the STARD HRV ranged from 18 [ 61 ] to 23 points [ 18 ]. The average score was 20.00 ± 1.56 points. All studies fulfilled the items 1, 2, 14, 18, 20, and 24. Only half a point was deducted in the items 3 [ 22 ] and 9 [ 21 ]. Twelve of 13 points were awarded in the items 4, 7, and 8. Furthermore, 11.5 points were awarded in the items 5 and 19. Contrarily, only five studies calculated their intended sample size [ 18 , 21 , 58 – 60 ]. Finally, acknowledgement of breathing [ 18 , 21 , 57 , 58 , 61 , 62 ], reasons for missing data, along with percentage of missing data [ 5 , 21 , 22 , 46 , 56 , 59 , 60 ], and artefact cleaning methods with percentage of corrected beats were further items, that were fulfilled by only a small number of studies. The last item was fulfilled in sufficient detail only in three studies [ 5 , 18 , 59 ].
Purpose and main findings
The present systematic review was conducted to summarize the existing literature on the effects of different exercise interventions on heart rate related variables including HRV parameters, reflecting cardiac autonomic control in older adults aged 60 years in average and over. In addition, we also considered health-related secondary variables that were assessed in these studies to look for possible interactions between changes in HRV and these secondary health factors. 13 endurance, resistance, coordinative, or multimodal training interventions, lasting for at least four weeks, were considered as eligible. Literature review revealed endurance, multimodal, and forms of coordinative training as appropriate modalities to improve cardiac autonomic control and secondary health factors in sedentary, healthy older adults. Ten of the 13 studies evaluated at least one secondary health factor. All but one study [ 18 ] demonstrated a significant improvement in at least one parameter. Furthermore, we evaluated the methodological and study reporting quality of the eligible studies through two assessment tools: TESTEX and STARD HRV . The evaluation showed quite good quality in reporting the methods and results of the studies. A few limitations concern the processing and analysis of HRV.
Three of four studies applying endurance training interventions demonstrated significant improvements in HRV parameters [ 5 , 56 , 57 ]. No significant changes in HRV were reported in the study of Wanderley et al. [ 22 ], despite the second longest intervention period of the four endurance interventions was applied in this study and no obvious major differences were identifiable between the studies regarding their training protocols. However, the authors stated that participants with greater subclinical inflammation at baseline showed higher HRV improvements after the intervention. In fact, exercise and training variables, as well as training principles must be taken into account when planning physical training [ 54 ]. Concerning older adults, vigorous intensity of ~ 75% HRmax for ~ 200 min/week for at least 6 to 12 months are recommended to improve health state [ 57 ]. This must be countered by the fact that participants in two studies [ 5 , 56 ] could increase their HRV even with lower intensities and shorter intervention periods.
RHR decreased in one study [ 22 ] and may be explained by a decreased sympathetic outflow and decreased intrinsic heart rate [ 64 ]. The positive effects on cardiac autonomic control in the remaining studies could be attributed to the individualization of the training programs and the gradual increase of the training intensities [ 5 , 56 , 57 ]. Interestingly, significant effects on HRV were detected only for global and parasympathetic components of HRV (SDNN, RMSSD, and HF), while LF, which reflects a mix of sympathetic and parasympathetic activity [ 9 ], did not change significantly in none of these three studies. In conclusion, the studies demonstrated positive effects on parasympathetic modulation in older adults. Endurance training seems to be equally effective in improving cardiac autonomic control in older as in younger adults [ 38 , 65 ].
Regarding resistance training, literature revealed controversial effects on HRV in older adults [ 18 ]. Similarly, our systematic review did not find any positive effects of resistance training on HRV, irrespective of the training intensities applied in the interventions. One explanation for the missing HRV changes in the present review may be the dynamic nature of the resistance training since isometric training lead to positive effects on parasympathetic modulation in a previous study [ 66 ]. Furthermore, the small sample sizes in all training groups have to be mentioned as limitation. Finally, aging is supposed to reduce HRV sensitivity to training [ 42 , 67 ] since studies with young participants showed beneficial effects of resistance training on HRV [ 38 , 68 ]. Resistance training is supposed to decrease blood flow in the presence of increased vascular stiffness due to normal aging processes [ 69 ]. This might be the reason why resistance training interventions do not improve cardiac autonomic control in older adults. In conclusion, resistance training seems to be less effective in improving cardiac autonomic control in older adults. Given the positive effects of endurance training on HRV as stated above and in a previous review [ 70 ], it is recommended to include aerobic elements when planning exercise training programs for older adults.
Two coordinative training interventions demonstrated beneficial effects on cardiac autonomic control [ 20 , 21 ]. The beneficial effects of Tai Chi has already been demonstrated in previous studies showing acute HRV increases after a single session of Tai Chi [ 71 , 72 ]. We suggest that long-term practice of Tai Chi could lead to manifest adaptations of cardiac autonomic control and increase HRV. Despite the short intervention period of six weeks in the study of Varas-Diaz et al. [ 20 ] significant improvements were produced, that might be the result of the high training frequency in the first two weeks of the intervention. The number of training sessions per week decreased from five in the first two weeks to two sessions in the last two weeks. The results indicate dancing for older adults as a suitable training modality to improve cardiac autonomic control. In addition, compared to traditional, conditioning-oriented training modalities, it is a well-tolerated aerobic exercise, it increases motivation, and there are no safety concerns [ 73 ].
In conclusion, dancing and Tai Chi are suggested as proper training modalities to improve cardiac autonomic control in older adults. However, further studies are required to investigate the required intensity and volume to stimulate the ANS since no information were given about the intensity in the interventions. Given the small number of participants in both studies, interventions with bigger sample sizes are necessary for more powerful conclusions.
While significant improvements in cardiac autonomic control were reported [ 59 – 61 ], no changes [ 62 ] and even significant reductions [ 46 ] were reported after multimodal training interventions as well. The results of the study of McKune et al. [ 46 ] with two training groups are inconclusive. On the one hand, the training group exercising two times per week showed no significant changes in HRV parameters. On the other hand, the group exercising three times per week showed significant reductions in HF, LF, RMSSD, and TP [ 46 ]. This result contradicts Raffin et al. [ 43 ] recommending higher training frequency for better improvements in cardiac autonomic control. These findings could be the result of differing levels of baseline vagal activity between the training groups [ 42 ]. Participants of the study of McKune et al. [ 46 ] had to rate their perceived exertion during each exercise session to ensure that the prescribed intensity was maintained. On a scale from 0 to 10, exercise intensity was set at 2 to 4 indicating an intensity from “easy” to “sort of hard”. This relatively low intensity may be another explanation for the absence of significant improvements in this study.
Although the participants exercised two to three times per week for one year, no significant effects on cardiac autonomic control were detected in the study of Verheyden et al. [ 62 ]. This finding contradicts other study results showing positive effects with even shorter intervention periods and a similar number of training sessions per week [ 59 – 61 ]. However, the authors speculated that small training effects overlapped with larger interindividual differences in HRV [ 62 ]. Furthermore, physical training interventions involving low intensity resistance training (i.e., low weights and high number of repetitions) might have no effects on cardiac autonomic control [ 62 ]. Instead, other authors recommend strenuous endurance training to improve autonomic functioning [ 74 , 75 ].
In conclusion, the effects of multimodal training interventions on cardiac autonomic control are somewhat vague. Although a recording length of at least five minutes is recommended for short-term measurements [ 63 ], two studies used a specific number of NN intervals, namely 256 [ 61 ] and 300 NN intervals [ 46 ]. Finally, as resistance training interventions did not show significant positive effects on resting autonomic control but endurance training interventions did, resistance training within multimodal interventions could exert negative influences on cardiac autonomic control.
Endurance training interventions lead to significant improvements in certain secondary health factors, including VO 2 max [ 56 , 57 ], 6-MWT [ 22 ], and BP [ 22 , 57 ]. Although improvements in several secondary health variables were observed in the study of Wanderley et al. [ 22 ], no improvements were observed in autonomic measures. In contrast, Albinet et al. [ 56 ] and Okazaki et al. [ 57 ] observed improvements in HRV as well as in secondary factors. Decreased arterial compliance leads to age-related impairment of cardiovagal BR [ 30 ]. Although physical activity is supposed to attenuate this process and preserve BR [ 76 ], BR was not improved, even with higher exercise intensities and remained lower than that of master athletes and young controls at baseline in the study of Okazaki et al. [ 57 ]. However, BR might be improved by a prolonged training intervention combined with other therapies designed to improve arterial stiffness. Interestingly, both groups in one intervention [ 56 ], swimming and stretching group, equally improved VO 2 max. This unexpected finding may be the result of the pedestrian nature of the test. According to the authors, a water-based test could have resulted in stronger improvements in the swimming group. On the other hand, the lower VO 2 max of the stretching group at baseline could have biased the results. Therefore, this group had a higher ability to improve aerobic power.
In light of the increased cardiovascular risk in older adults due to an age-related increase in vascular stiffness contributing to systolic hypertension [ 77 ], increase in cardiac sympathetic modulation [ 31 ], changes in the endocrine system [ 78 ], as well as attenuated autonomic modulation [ 79 , 80 ], the beneficial effects of endurance interventions are of great importance. In summary, as it was expected, endurance training is an adequate type of intervention to reduce the cardiovascular risk in older adults.
Resistance training showed contradicting results regarding BP with no [ 18 , 22 ] or positive effects [ 58 ]. The absence of BP changes are in line with the small but non-significant reductions in HRV [ 18 , 22 ]. High-intensity resistance training is supposed to increase heart rate and BP acutely through increased arterial stiffness [ 81 , 82 ] and sympathetic modulation [ 4 ]. Indeed, increased arterial stiffness could be harmful to the cardiovascular system [ 18 ]. Therefore, resistance training should be used carefully in older adults and the risk of hypertension should be clarified before beginning any training intervention. Furthermore, in contrast to the resistance training group, the endurance training group was able to reduce BP significantly indicating that endurance training is better able to reduce BP than resistance training [ 22 ]. Since both groups did not significantly improve HRV, it may be speculated that the two training modalities address different physiological mechanisms.
The results regarding the change in body composition are likewise inconclusive. A reduction in BF was demonstrated in one study [ 22 ] but not in another [ 58 ]. This reduction was already shown in a previous study [ 83 ]. In both studies [ 22 , 58 ], BM and BMI remained unchanged. The intervention of the study of Gerage et al. [ 58 ] lasted for only 12 weeks. This may be an explanation for the absence of BF reduction compared to the study of Wanderley et al. [ 22 ] applying an intervention period of 8 months. Furthermore, Wanderley et al. [ 22 ] mentioned the high drop-out rate in the resistance training group as one limitation. These results are noteworthy in that a recent review demonstrated that resistance training has beneficial effects on body composition in older individuals [ 84 ]. However, two studies are not enough to draw final conclusions regarding change in body composition after resistance training. In conclusion, the baseline level of the participants regarding body composition, the objective of the intervention, and the training protocol play an important role in the change of body composition. For example, high-intensity resistance training with strong hypertrophic character will not be suitable to reduce BM or BMI. However, it potentially reduces BF equally well as endurance training.
Both coordinative training interventions lead to positive effects on cardiovascular fitness [ 20 , 21 ], which is in line with the HRV improvements. Dancing as proper training modality to improve aerobic capacity and cardiovascular health has been shown in previous studies [ 85 ]. Dancing is supposed to keep BP constant and therefore ensuring adequate perfusion to vital organs [ 20 , 86 , 87 ]. Finally, dancing has been shown to improve quality of life, psychological well-being, oxygen uptake, metabolic parameters, and positively affects brain volumes in older adults [ 85 , 88 , 89 ]. Therefore, dancing seems to be a physical activity affecting the physical state positively through other mechanisms, namely social aspects. Based on the promising results of the present investigations, more studies should be conducted to investigate the effects of different kinds of coordinative training modalities on various secondary health factors. Additionally, other cardiovascular factors, such as BP and BR, should be assessed in order to evaluate the effects on cardiovascular health and potentially link it to the evaluation of cardiac autonomic control. However, the training load should be monitored carefully for optimally tailoring the training program individually and comparing the effects on ardiovascular health with other training modalities.
While BP decreased in two studies with relatively short intervention periods of twelve [ 46 ] and 18 weeks [ 60 ], participants in another study [ 62 ] showed no BP changes after one year of training, despite participants of this and another intervention [ 46 ] showed similar baseline BP levels. Given the increased BP of the training group compared to the control group [ 60 ], the decrease after the combined intervention in the training group is not surprising and supported by a further study [ 90 ]. In summary, multimodal training interventions seem to be moderately appropriate to decrease BP.
Despite no improvement in BP, aerobic capacity increased after one intervention [ 62 ]. This finding could be the consequence of the strong aerobic character of this intervention because participants had to perform seven exercises with two sets and 20 to 30 repetitions. Contrarily, McKune et al. [ 46 ] assessed aerobic capacity with the 6-MWT but did not detect significant changes. This could be the result of the low training volume and intensity, which was insufficient to induce effects on the cardiorespiratory system, as participants rated their perceived exertion and should stay at a score of 2 to 4 out of a maximum of 10.
The diverging results regarding secondary factors are in line with the HRV results showing improvements [ 60 ], no changes [ 62 ], or contradicting results [ 46 ]. In conclusion, more studies investigating secondary health factors like BP and body composition are necessary to elucidate the exact effects of multimodal interventions. Furthermore, concurrent training of two or more conditional skills requires a sophisticated interpretation of the effects. One possibility to address this issue is to have several training groups in parallel in order to study the isolated and combined effects on cardiovascular variables.
Possible mechanisms behind autonomic and cardiovascular adaptations
Although the exact mechanisms behind the autonomic adaptations through physical activity are not completely understood and remains to be fully elucidated [ 91 ], several possible mechanisms have been identified.
Mechanisms leading to HRV improvements through aerobic training involve the decrease in plasma norepinephrine concentration [ 92 , 93 ], suppression of angiotensin II expression [ 94 ], and reduction of oxidative stress by lowering the expression of nicotinamide adenine dinucleotide phosphate oxidase [ 95 ]. Those mechanisms lead to a decrease of sympathetic influences on heart rate at rest lowering resting heart rate [ 93 , 96 ]. Normalization of excitatory glutamatergic and angiotensinergic mechanisms within the paraventricular nucleus also contributes to the reduction in sympathetic outflow [ 97 ]. Stimulation of nitric oxide syntheses [ 91 , 94 , 98 – 100 ] and anti-inflammatory processes after aerobic training [ 99 , 101 , 102 ] may be also involved in increasing cardiac autonomic control. Finally, it is also suggested that changes in body composition and enhanced lactate tolerance as a result of long-term aerobic training positively affects cardiac autonomic control [ 44 ].
Concerning resistance training, it is proposed that reductions in the concentration of metabolites and pro-inflammatory cytokines as well as the decrease in plasma concentration of norepinephrine positively influences autonomic functioning [ 103 ]. In addition, improved baroreflex sensitivity, vascular adaptations, and increased nitric oxide synthesis could contribute to improved autonomic functioning after resistance training with low [ 104 ] or moderate [ 105 ] intensities.
The effects of coordinative training on HRV depend substantially on the intensity of the intervention and are the result of the sum of acyclic movements in the coordinative program. Pal et al. [ 106 ] proposed increased levels of serotonin and dopamine, and decreased levels of epinephrine and norepinephrine as underlying reasons for improved HRV after a coordinative exercise program with yoga. Another intervention involving capoeira indicated the decreased psychological stress and anxiety as well as socialization, friendship, and relaxation as possible contributors to improved parasympathetic modulation [ 107 ].
Since previous reviews with younger populations have found stronger positive effects of physical training on HRV than this review [ 38 , 65 ], it may be speculated that ageing impairs the ability to improve HRV [ 67 ]. For example, resistance training interventions did not lead to significant improvements in HRV [ 18 , 22 , 58 ]. This is supported by studies that found a reduced adaptive capacity of the cardiovascular system of older adults [ 108 , 109 ]. One possible reason could be the loss of cardiac neural network function with ageing [ 110 ]. However, other studies showed similar improvements in young and older adults in HRV after aerobic training [ 57 , 74 , 111 ].
The mechanisms that contribute to the improvement of autonomic and cardiovascular function partially overlap. For example, a decrease in inflammatory markers leads to a decrease in BP and increase in HRV [ 22 ]. The improved blood flow after resistance training enhances BR [ 105 ] and decreases BP through reduced peripheral vascular resistance [ 112 ]. It has been proposed that preserved BR sensitivity in fit older adults is related to preserved mechanical transduction by an improved arterial compliance and neural transduction [ 30 , 76 ]. BR adaptations might also occur as a result of high BP peaks during resistance training lowering peripheral vascular resistance and finally reduce BP after resistance training [ 112 ]. Furthermore, vasodilation in metabolically active muscles through nitric oxide and other endothelium-dependent and independent mediators is another explanation for reduced BP after resistance training [ 113 ]. Improved blood flow after endurance training also improves cardiorespiratory fitness (i.e., VO 2 max) [ 114 ].
The methodological and reporting quality of the included studies was analyzed by using the tool TESTEX. Based on our assessment, the studies scored between 4.5 [ 57 , 61 ] and 12.5 points [ 58 ]. Since one investigation [ 57 ] did not include a control group, the maximum score in this trial was limited to eight points. The mean score of all 13 studies was 8.9 ± 2.5 points. This is higher than the studies achieved in our previous review with young adults [ 38 ]. However, 8.9 out of 15 possible points means that less than 60% of the criteria were met. Two criteria, namely allocation concealment and intention-to-treat-analysis, were fulfilled by none of the studies. Additionally, in only two studies [ 21 , 58 ], the assessors were blinded to group allocation and activity was sufficiently monitored in only three studies [ 5 , 56 , 58 ]. Despite these shortcomings, there were some points that were fully met by almost all studies: specification of eligibility criteria (12 of 13), specification of randomization (12 of 13), and keeping relative exercise intensity constant (11 of 13).
The quality score of NN interval recording, processing, and analyzing assessed by the tool STARD HRV , ranged between 18 [ 61 ] and 23 points [ 18 ], with an average score of 20.0 ± 1.6 points. As for the TESTEX, this is a higher score than achieved in our previous review with young adults [ 38 ], where the mean was 18.44 points. Six criteria where fully met by all interventions: 1, 2, 14, 18, 20, and 24. However, a few criteria were fulfilled only by a small number of studies: intended sample size and how it was determined (5 of 13), acknowledgement of breathing (5 of 13), and artefact cleaning methods with percentage of corrected beats (3 of 13). Especially the last two criteria are crucial for a good quality of study reporting in HRV research. Therefore, we recommend to follow the prescribed criteria to improve the quality of and comparability between studies.
Practical implications and future directions
The literature showed beneficial effects of different kinds of exercise training on cardiac autonomic control in healthy older adults. However, the research also showed that there is still a need for some research. As most of the studies did not compare the effects on cardiac autonomic control between women and men, no gender-specific effects could be assessed. Therefore, we recommend to investigate the differences in HRV changes in women and men in more detail since the decrease in estrogen production in older women increases the cardiovascular risk of postmenopausal compared to premenopausal women [ 115 ]. This review identified only one study measuring non-linear parameters [ 58 ]. Therefore, future studies should not only consider the traditional time- and frequency-domain parameters, namely SDNN, RMSSD, and HF, but non-linear parameters should be analyzed as well. These parameters provide a different view on heart rate regulation, namely heart rate complexity, and they could be used as “a reliable marker of complications and mortality in patients with cardiovascular disease” [ 116 ]. Heart rate fragmentation could serve as an additional biomarker in the assessment of cardiovascular risk [ 117 ]. Hence, this relatively new marker could be measured as well when assessing the risk for adverse cardiovascular events in healthy adults without clinical cardiovascular disease. Furthermore, analyzing cardiac autonomic control at several time points during the intervention would provide a more accurate reflection of the effectiveness of the intervention. Exercise-induced adaptations of cardiac autonomic control can be well detected by weekly averaging the parameter RMSSD [ 118 , 119 ] because single measurements reduce the sensitivity to identify changes in HRV [ 118 ]. In addition to resting state measurements, HRV measurements during the orthostatic test [ 120 , 121 ] or during walking [ 118 ] are practical alternatives for evaluating cardiac autonomic control. Follow-up analysis would give an estimation of how long the effects of a physical intervention remain. Finally, we also recommend to include a passive control group and compare the effects on autonomic functioning with this group.
The quality assessment revealed some important aspects regarding ECG recording and processing, and study reporting. Based on the results of TESTEX and STARD HRV , we recommend to follow the criteria of these two tools. Regarding ECG measurement and HRV analysis, we recommend to follow the criteria stated in recent reviews [ 122 , 123 ]. Furthermore, we recommend to state training adherence rate and ensure a minimum of 48 h between the last training session and ECG measurement to avoid acute training effects on parasympathetic modulation [ 124 ]. Regarding ECG recording, a high sampling frequency of 1000 Hz is recommended [ 55 ] to avoid errors in the recognition of the QRS complex [ 125 ].
Strengths and limitations
This systematic review has a few limitations. First, we did not conduct a meta-analysis, which could provide a quantitative view on the effects of physical training on HRV. Instead, we performed a qualitative analysis with the main focus on providing a comprehensive summary of the effects of different exercise modalities on resting HRV and secondary health factors in healthy older adults. We decided to refrain from a quantitative analysis due to the high heterogeneity of the studies in relation to the intervention modality, exercise protocol, and HRV analysis. The literature search was limited to English and German articles. Therefore, it is possible that we missed studies in other languages. Another limitation concerns the age criterion. Since we used an average sample-based value, namely 60 years as lower limit, participants in the retrieved studies could also be under 60 years. Thus, the results are generally not applicable to people over 60 years of age. Furthermore, we included only short-term ECG measurements. 24-h ECG recordings would provide additional information about the ANS during daily activities. Future studies should also look at 24-h recordings. It should also be considered that HRV is an indirect measure of ANS activity [ 126 , 127 ] and HRV improvements after exercise interventions might be due to sinus node and heart remodeling itself rather than increases of parasympathetic control [ 128 ]. Finally, it should also be mentioned that when using data editing software of heart rate monitors, the HF band of women over 60 years of age demonstrates limited agreement with traditional ECG [ 129 ]. Therefore, traditional ECG systems and manual editing of NN intervals should be used whenever possible [ 129 ].
However, this review also has several strengths. To the best of our knowledge, it is the first review summarizing the effects of different exercise modalities on cardiac autonomic control and cardiovascular health in healthy older adults. Thus, it provides a comprehensive overview of the current literature regarding physical interventions to improve autonomic control of heart rate in healthy older adults. We described the exercise protocols, NN interval recording, HRV analyzing processes, and the outcomes of the studies thoroughly. Furthermore, we analyzed the methodological and reporting quality of the studies via two assessment tools, namely TESTEX and STARD HRV . Finally, we described strengths and limitations of the studies, as well as possible mechanisms for HRV improvements or non-improvements with a focus on the older population.
This systematic review showed that endurance, multimodal, and coordinative training interventions are appropriate modalities to improve cardiac autonomic control in healthy older adults aged 60 years in average and over, indexed as HRV. These results indicate that these exercise modalities are equally effective in older adults as in younger adults. However, isolated resistance training without including aerobic training do not significantly improve cardiac autonomic control. In this review, the effects on secondary health factors were evaluated as well, providing additional information about the effects of exercise training on cardiovascular health status. All exercise modalities contribute to the reduction of risk factors, namely a reduction in blood pressure, body fat, body mass, total peripheral resistance, and an increase in VO 2 max, stroke volume, distance covered in the 6-MWT, and VO 2 peak. It should be noted that these health factors were collected as secondary outcomes and considered only in studies assessing HRV as a primary outcome. Therefore, the significance of these secondary outcomes is limited. The physiological mechanisms responsible for these adaptations are not yet fully understood. Further studies are needed to reveal the underlying physiological background leading to improved parasympathetic autonomic control and reduction of the risk for adverse cardiovascular events.
Apart from analyzing the effects of the training interventions, the methodological quality of the studies was also assessed using the tools TESTEX and STARD HRV . The quality assessment revealed a few deficits in the reporting of the methodologies and HRV processing. For better comparability between studies, we recommend to adhere to the criteria of these two tools. Based on the qualitative analysis in this review, we recommend the combination of different exercise modalities to improve autonomic control and reduce cardiovascular risk. A certain amount of exercise intensity and volume is necessary to stimulate the ANS and cardiovascular system. Leisure-time recreational exercises seems to be insufficient to induce positive effects on cardiac autonomic control. Dancing seems to be a very good exercise modality for older adults. It combines coordinative and conditional skills and counteracts the detrimental effects on the aging brain. We also recommend to assess not only the autonomic and cardiovascular systems but also other physiological systems such as the endocrine system as it is involved in the development of frailty. When planning training interventions, programs should be individually tailored and a gradual increase in training intensity should be ensured for optimal adaptation. Finally, aerobic interventions with at least two training sessions per week has been proved to positively influence cardiac autonomic control in healthy older adults. Contrarily, resistance training, especially high-intensity resistance training, is inappropriate to improve cardiac autonomic control.
Acknowledgements
Not applicable.
Abbreviations
Authors’ contributions.
BG developed the concept for this review and designed the review process. BG and BT performed the literature search and analysis. BG wrote and edited the manuscript. BT, IB and AH reviewed the drafted versions. All authors have read and approved the submitted version.
Authors’ information
BG was financed by the European Regional Development Fund (grant number: ZS/2018/08/94206). The funder has no role in the design or conduct of this review.
Availability of data and materials
Declarations.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bernhard Grässler, Email: [email protected] .
Beatrice Thielmann, Email: [email protected] .
Irina Böckelmann, Email: [email protected] .
Anita Hökelmann, Email: [email protected] .

IMAGES
VIDEO
COMMENTS
A total of 66,788 Health eHeart Study participants contributed 3,144,332 HR-PPG measurements. The mean real-world HR was 79.1 bpm ± 14.5. The 95th percentile of real-world HR was ≤110 in individuals aged 18-45, ≤100 in those aged 45-60 and ≤95 bpm in individuals older than 60 years old. In multivariable linear regression, the number ...
1 answer. May 29, 2023. " During REM sleep, a person's brain activity, breathing, heart rate, and blood pressure increase, and the eyes move rapidly while closed. The muscles in the arms and legs ...
Evolution of cardiovascular topics—trends and 'hot' topics. We identified 175 topics, listed alphabetically in Supplementary material online, Table S2. This list groups specific topics within areas such as atherosclerosis, coronary artery disease, arrhythmias, heart failure, and their evolution over time.
Substantial evidence has established the value of high levels of physical activity, exercise training (ET), and overall cardiorespiratory fitness in the prevention and treatment of cardiovascular diseases. This article reviews some basics of exercise physiology and the acute and chronic responses of ET, as well as the effect of physical ...
Introduction. Previous epidemiological studies generated evidence for a correlation between heart rate and risk of cardiovascular disease and hence life expectancy in the general population and in patients with coronary heart disease (CHD) [1-4].Most of coronary perfusion takes place in diastole, a phase characterized by a reduced wall tension compared to systole.
Heart rate variability (HRV) represents fluctuations in the time intervals between successive heartbeats, which are termed interbeat intervals. ... Four major questions regarding resonance frequency assessment require further research. These questions include whether resonance frequency training is more effective than 6-bpm slow paced breathing ...
A: Fortunately, numerous studies now provide reassurance to individuals with cardiac conditions who have such concerns. Sexual activity is associated with a very light- to moderate-energy expenditure, 2 to 3 metabolic equivalents or METs, and associated transient increases in heart rate and blood pressure ( 11 ).
Heart Rate Recovery. In the current issue of Circulation Research, McCrory et al 1 report on the association of heart rate recovery after simple orthostatic challenge—otherwise known as standing up—with all-cause mortality. The authors measured heart rate changes in the first 110 seconds after standing up in 4475 participants of an Irish ...
The most common and simplest prediction equation is: Maximal heart rate is equal to 220 minus your age. From that number, you can calculate a percentage of maximum to provide target heart rate ...
The development of a new tool, analytic device, or approach frequently facilitates rapid growth in scientific understanding, although the process is seldom linear. The study of heart rate variability (HRV) defined as the extent to which beat-to-beat variation in heart rate varies, is a rapidly maturing paradigm that integrates health and wellness observations across a wide variety of ...
In current clinical pratice assessment of office heart rate (HR) values in resting hypertensive patients represents a procedure of routine performance which may allow to obtain important ...
Explore the latest questions and answers in Heart Rate Variability, and find Heart Rate Variability experts. Questions (182) ... This is a little outside my usual research area, so I want to be ...
In addition to heart rate (HR) responses to exercise, research has recently focused more on heart rate variability (HRV). Increased HRV has been associated with lower mortality rate and is ...
Furthermore, a decrease in heart rate at quiet condition was found after tai chi exercise in healthy adults as shown in the meta-analysis of Zheng, Li, Huang, Liu, Tao and Chen . However, to the best of our knowledge, a comprehensive review and meta-analysis of the effects of regular physical exercise on the RHR in various sports and exercise ...
Learn more about our cardiovascular research topics. Skip Navigation. Advisory for Baltimore-Area Patients . Baltimore Region: Due to the recent collapse of the Francis Scott Key Bridge, please anticipate delays when travelling to appointments. ... Heart Rhythm and Arrhythmias. HIV and Heart Disease. Hypertension. Imaging. Interventional ...
The goal is to measure your heart rate several times throughout the day. Take your pulse first thing in the morning, before you've even gotten out of bed. This is your resting heart rate. Record the data in a table, like the one below, in your lab notebook. Take your pulse within the first 5 minutes of waking up.
Your heart rate, or pulse, is the number of times your heart beats per minute. Normal heart rate varies from person to person. Knowing yours can be an important heart-health gauge. As you age, changes in the rate and regularity of your pulse can change and may signify a heart condition or other condition that needs to be addressed.
Over the last decades, assessment of heart rate variability (HRV) has increased in various fields of research. HRV describes changes in heartbeat intervals, which are caused by autonomic neural regulation, i.e. by the interplay of the sympathetic and the parasympathetic nervous systems. The most frequent application of HRV is connected to cardiological issues, most importantly to the ...
The autonomic nervous system (ANS) regulates the body's physiology, including cardiovascular function. As the ANS develops during the second to third trimester, fetal heart rate variability (HRV) increases while fetal heart rate (HR) decreases. In this way, fetal HR and HRV provide an index of fetal autonomic nervous system development and future neurobehavioral regulation. Fetal HR and HRV ...
Unfavorable social factors may raise heart disease risk factors in Asian American adults. ScienceDaily . Retrieved April 13, 2024 from www.sciencedaily.com / releases / 2024 / 04 / 240403130632.htm
The findings align with previous studies conducted in animals, which signaled e-cigarette use can affect the heart in ways that are relevant to the heart changes involved in heart failure. Other studies in humans have also shown links between e-cigarette use and some risk factors associated with developing heart failure.
Keywords: Heart rate variability, HRV, exercise, sports, recovery, response . Important Note: All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable ...
The aim of this project is to understand how adolescents perceive the symptoms and impact of their heart failure, while adapting existing adult Patient Reported Outcome Measures (PROMs) to capture ...
Table 2 shows the correlation between RHR and SBP, DBP and PP. Considering the relationship between heart rate and SBP and DBP, for each increased heartbeat there is a .090-mmHg increase in SBP of boys and a 0.063 mmHg increase in SBP of girls. Regarding DBP, the increase is 0.179 mmHg in boys and 0.161 mmHg in girls.
In a new book, Nobel Prize-winning molecular biologist Venki Ramakrishnan raises critical questions about the societal, political and ethical costs of attempts to live forever.
Researchers found that the rate of death from stroke from temperature changes for male participants was 7.7 per 100,000 compared to 5.9 per 100,000 for female participants.
Sustainable growth can be elusive. Research has shown that only about 15% of the companies in the top growth quartile in 1985 were able to sustain their top-quartile performance for at least 30 ...
The outcome of the most frequently used heart rate related parameters and secondary outcomes can be found in Table Table3. 3. A detailed description of the characteristics of the included studies and the results of all heart rate related variables are available in the additional files 3 and 4, respectively.
(SACRAMENTO) Falcon-eye viewers have been noticing the peregrine eggs disappearing over the last week, with the final egg now lying on the concrete as of Wednesday morning.. As we've reported since last month, a pair of peregrine falcons are back to their nest atop UC Davis Medical Center for the sixth season.
(SACRAMENTO) The UC Davis Department of Psychiatry and Behavioral Sciences opened its new Advanced Psychiatric Therapeutics (APT) Clinic this week. Located at the Ambulatory Care Center on the Sacramento campus, the facility is dedicated to treating patients with treatment-resistant depression.