Overview of Alcohol Use Disorder
Information & authors, metrics & citations, view options, current u.s. rates of alcohol consumption, binge drinking, heavy drinking, and aud, adverse consequences of aud, neurobiology of aud, etiology of aud.

Current Treatments for AUD
Psychosocial treatments, pharmacological treatments, fda-approved medications, disulfiram., naltrexone., acamprosate., off-label medications, topiramate., gabapentin., promising medications that require further study, psychedelic drugs., phosphodiesterase-4 inhibitors., precision treatments, conclusions, information, published in.
- Substance-Related and Addictive Disorders
- Psychopharmacology
Competing Interests
Funding information, export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - American Journal of Psychiatry
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Alcohol use
Alcohol use is a major risk factor for death and disability worldwide. In some countries, it is the number one risk factor for men.
Photo by Chuttersnap, Unsplash.
On this page:
How much alcohol is safe to drink.
The risks of drinking alcohol depend on age, local disease patterns, and underlying health conditions:
- For young adults ages 15–39 , there are no health benefits to drinking alcohol, only health risks.
- For people over age 40 , drinking a small amount of alcohol may provide some health benefits.
Young people tend to experience a higher rate of injuries as a result of alcohol use, leading to an increase in death and disability for that age group.
For older adults without underlying health issues, having 1-2 standard drinks per day may reduce the risk of cardiovascular disease, stroke, and diabetes. However, overconsuming alcohol can lead to additional health problems, like liver cirrhosis and some cancers.
On a global scale, the impact of drinking alcohol varies by age
Relative proportions of global disability-adjusted life years (DALYs) for causes associated with alcohol use, by cause and age (2020)

IHME & The Lancet infographic: Drinking alcohol has significant health risks for young people, small amounts may be beneficial for some older adults

Dr. Emmanuela Gakidou, Professor of Health Metrics Science
“Our message is simple: young people should not drink, but older people may benefit from drinking small amounts. While it may not be realistic to think young adults will abstain from drinking, we do think it’s important to communicate the latest evidence so that everyone can make informed decisions about their health.”
Why isn’t there a scientific consensus about safe levels of alcohol use?
The patterns for alcohol use and its health impacts are specific to each region of the world and vary depending on the age of the consumer and their overall health status. This results in different recommendations for alcohol consumption. For example:
- In central sub-Saharan Africa, 15% of alcohol-related health risks for those aged 55+ were due to tuberculosis, leading to a recommendation of less than half a standard drink per day.
- By contrast, in North Africa and the Middle East, around 1% of alcohol-related health risks were due to tuberculosis, reflected in a recommendation of about 1 standard drink per day.
There is also some disagreement in the scientific community about the effects of alcohol on cardiovascular disease in individuals over 65. Some studies suggest that small amounts of alcohol may offer protection from cardiovascular disease, while other studies show that alcohol may contribute to it.
Always be sure to consult a health care professional for individual recommendations based on your personal health risks.
Alcohol use is a prominent health risk.

What is the disease burden of alcohol use?
In 1990, high alcohol use was the 15th most relevant risk factor for deaths worldwide; in 2021, it has risen to the 10th most relevant risk factor , responsible for over 1.8 million deaths from various alcohol-attributable causes.
Men are disproportionately prone to health problems stemming from alcohol use, and Eastern Europe in particular is disproportionately affected by alcohol use disorders. Excessive alcohol consumption can lead to several serious health conditions, including:
- Cirrhosis of the liver
- Fetal alcohol syndrome
- Chronic illnesses such as heart disease, stroke, and some cancers
- Interpersonal violence, self-harm (suicide), drunk driving – related injuries, and other unintentional injuries

Researchers Dr. Emmanuela Gakidou, Dana Bryzaka, and Marissa Reitsma discuss key findings from an analysis published in The Lancet and what alcohol consumption recommendations should be made based on age and location.
News and events
The curious case of japan's alcohol contest.

Is alcohol good for your heart? It’s complicated, despite new insights
Urgent action is needed on alcohol harm in nigeria, 9/14/2022: nfl, us open, mlb, gakidou, usfs.

Subscribe to our newsletter

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Volume 40 Issue 3 November 12, 2020
Epidemiology of Recovery From Alcohol Use Disorder
Part of the Topic Series: Recovery From Alcohol Use Disorder
Jalie A. Tucker, 1 Susan D. Chandler, 1 and Katie Witkiewitz 2
1 Department of Health Education and Behavior and the Center for Behavioral Economic Health Research, University of Florida, Gainesville, Florida
2 Department of Psychology and the Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico, Albuquerque, New Mexico
Almost one-third of the U.S. population meets alcohol use disorder (AUD) criteria on a lifetime basis. This review provides an overview of recent research on the prevalence and patterns of alcohol-related improvement and selectively reviews nationally representative surveys and studies that followed risk groups longitudinally with a goal of informing patients with AUD and AUD researchers, clinicians, and policy-makers about patterns of improvement in the population. Based on the research, alcohol use increases during adolescence and early adulthood and then decreases beginning in the mid-20s across the adult life span. Approximately 70% of persons with AUD and alcohol problems improve without interventions (natural recovery), and fewer than 25% utilize alcohol-focused services. Low-risk drinking is a more common outcome in untreated samples, in part because seeking treatment is associated with higher problem severity. Sex differences are more apparent in help-seeking than recovery patterns, and women have lower help-seeking rates than men. Whites are proportionately more likely to utilize services than are Blacks and Hispanics. Improving recovery rates will likely require offering interventions outside of the health care sector to affected communities and utilizing social networks and public health tools to close the longstanding gap between need and utilization of AUD-focused services.
Introduction
Substance use disorder (SUD) is among the most prevalent mental health disorders in the United States and in general clinical practice, with 7% of the U.S. population age 12 and older (19.7 million people) having an SUD of some kind in 2018. 1 Alcohol use disorder (AUD) is the most prevalent SUD, with 5% of persons age 12 and older reporting AUD in 2018. 1 Of persons with an SUD in 2018, and excluding those with a tobacco use disorder, 60% had AUD, 27% had an illicit drug use disorder, and 13% had disorders involving alcohol and illicit drugs. 1 On a lifetime basis, almost one-third of persons in the United States meet criteria for AUD. 2 In addition to the high AUD prevalence, many more individuals engage in risky drinking or experience alcohol-related negative consequences that fall short of meeting clinical diagnostic criteria for AUD. 3 Thus, harmful alcohol use is a major public health problem, costing the United States approximately $250 billion per year, and it is the third leading cause of preventable death. 4
Most individuals who develop an AUD or have subclinical alcohol-related problems will reduce or resolve their problem on their own or with assistance from professional alcohol treatment or mutual help groups. 5-9 The epidemiology of this robust phenomenon is the focus of this article. After initial consideration of complexities involved in defining improvement in alcohol-related problems, which is discussed in depth by Witkiewitz et al., 10 this article describes the prevalence and heterogeneity of pathways to recovery and examines relationships between patterns of seeking help for and improvements in alcohol-related problems. Then, the topic is examined from a life span developmental perspective, which is less well-researched and involves relationships among age-related rates of problem onset, reduction, and persistence. The final section discusses differences in the overall patterns previously discussed as a function of gender and race/ethnicity. Emphasis is placed on illustrative recent findings. Earlier work is covered in prior literature. 11,12
Defining Improvement in Alcohol-Related Problems
As discussed by Witkiewitz et al., 10 the conceptualization and measurement of improvements among persons with AUD and the constellation of improvements that define “recovery” have been debated for decades and continue to evolve. Clinical diagnostic criteria for AUD are offered by the American Psychiatric Association’s fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 3 and the World Health Organization, 13 with the former predominating in the United States. Numerous reputable organizations offer definitions of low- and high-risk drinking practices 4,14 as well as AUD recovery or remission. 15 These various criteria have been revised over time as research evidence has accumulated, generally in the direction of recognizing that alcohol consumption and AUD occur on severity continua. Furthermore, most individuals who engage in harmful alcohol use either do not meet AUD criteria or meet criteria for a mild disorder characterized by lower levels of symptomology. 16
Characterizations of improvement in alcohol-related problems have correspondingly become more nuanced over time in recognition of the heterogeneity of pathways, processes, and outcomes relevant to understanding how people reduce or resolve alcohol-related problems. 10 The term “recovery” is generally reserved for broad-based, sustained improvements in drinking practices and other areas of functioning adversely affected by drinking. Therefore, this article uses the term “recovery” to refer to a broadly conceived process resulting in sustained improvements in multiple domains, and uses the term “remission” to refer to more limited improvements in specific symptoms or problem behaviors (e.g., drinking practices). This is in line with the National Institute on Alcohol Abuse and Alcoholism’s (NIAAA) recent definition of recovery from AUD as distinct from remission from AUD, defined symptomatically based on DSM‑5 criteria, or cessation of heavy drinking without characterizing the presence or absence of other symptoms or improvements. It also is consistent with other recovery definitions, including those from the recovery community or patient perspectives, that encompass improved well-being and functioning and are not limited to attainment of abstinence or stable low-risk drinking. 8,17
It is also important to acknowledge the association of the term “recovery” with Alcoholics Anonymous (AA) and other mutual support groups. Even though the term is widely used in the clinical literature, many persons attempting to resolve their alcohol problems do not identify with being in recovery 8 and reject clinical labels indicative of AUD, especially those individuals attempting to resolve a drinking problem on their own. 9 Moreover, salutary improvements can occur in circumscribed areas of alcohol-related dysfunction, and reductions in drinking can contribute to improved health and well-being even if ongoing drinking falls short of traditional definitions of recovery that emphasize abstinence as a required element. 18
As discussed by Witkiewitz and Tucker, 16 a core issue debated for decades is the extent to which drinking practices should be central to defining improvement or recovery. Early writings regarded sustained abstinence as the hallmark of recovery among persons with severe alcohol problems who had repeatedly been unable to limit their drinking or abstain. 19 Newer clinical diagnostic systems such as DSM‑5 emphasize development of tolerance and physical dependence and drinking in harmful ways and under conditions that increase risk for adverse consequences. 3 Drinking practices are not a criterion in accepted diagnostic systems for AUD, including DSM‑5, and most schemes define recovery based on symptom reduction, improved functioning, and well-being and are not heavily focused on drinking practices per se. Yet, the large treatment outcome literature concerned with promoting recovery has relied heavily on drinking practices as the major outcome metric, typically by using quantity-frequency criteria considered indicative of higher-risk drinking practices (any occasions of more than 14 drinks weekly or more than five drinks daily for men; more than seven drinks weekly or more than four drinks daily for women in the past year). 4,14
Recent work, however, has shown that such consumption-based thresholds lack sensitivity and specificity for predicting problems related to drinking and do not differentiate individuals based on measures of health, functioning, and well-being. 20,21 Improvements in functioning and life circumstances are considered central features of recovery in many models, including AA, but assessment of these domains is a relatively recent development, primarily evident in clinical research. 18,21 It is generally lacking in survey research that has provided the bulk of epidemiological data on population patterns of alcohol-related improvement, so this body of work only partially addresses the multiple domains considered important for investigating recovery, broadly defined.
A second core issue is that improvement in alcohol-related problems, including recovery from AUD, is a dynamic process of behavior change. Thus, longitudinal studies provide superior information to cross-sectional studies with retrospective assessments of drinking status, although the latter are common in the literature. Cross-sectional surveys have utility if they employ sound retrospective measures of past drinking status, but this is another qualification of the current epidemiological database on alcohol-related improvement and recovery. Longitudinal research has become more common in recent years. However, the intervals over which repeated measures are obtained rarely exceed 3 to 5 years, although there are notable exceptions with follow-ups of 8 to 10 years or more. 22-24 Following large nationally representative samples for decades would be ideal, but the inevitable limitations on research resources have resulted in a collective body of work that generally comprises large representative studies that are cross-sectional or have short-term (e.g., 1 year) follow-ups. Studies with longer-term follow-ups tend to employ smaller, less representative samples. These core issues should be kept in mind when considering the epidemiology of improvements in alcohol-related problems, including recovery from AUD, as discussed next.
Recovery Pathways and Relationships Between Help-Seeking and Drinking-Related Outcomes
Population-based survey research conducted over many decades has consistently revealed the following patterns with respect to improvements in alcohol-related problems:
- The majority of individuals who develop AUD reduce or resolve their problem over time. 7,8,25 Rates of improvement vary widely depending on features of the research, such as the intervals over which drinking status was assessed (e.g., lifetime basis, shorter-term assessment based on a year or more); demographic characteristics, problem severity, and help-seeking status of respondents; and how improvement or recovery/remission was measured. But improvement over time is a reliable pattern and one that argues against a view of AUD as an inevitably progressive disease process.
- Seeking help for drinking problems from professional treatment or community and peer resources such as mutual help groups is uncommon, 1,26 and a large gap persists between population need and service utilization. Most surveys indicate that less than 25% of persons in need utilize alcohol-focused helping resources.
- The great majority of persons who resolve their drinking problems do so without interventions, and such “natural recoveries” are the dominant pathway to problem resolution. Survey research has typically found that more than 70% of problem resolutions occur outside the context of treatment. 7,9
- Stable low-risk drinking (moderation) is a relatively more common outcome in untreated samples, in part because seeking treatment is associated with higher problem severity, 7,12 and most treatment programs emphasize abstinence.
For example, Fan and colleagues 7 reported on the past-year prevalence of AUD recovery in the United States by using data from the NIAAA-funded 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III) 2 and DSM‑5 diagnostic criteria. 3 Survey respondents who met AUD criteria prior to the past year ( n = 7,785) were assessed with respect to their current (past-year) AUD and risk drinking status. Drinking status was determined based on quantity-frequency criteria considered indicative of higher-risk drinking practices and DSM‑5 AUD symptom counts. Measures of functioning and well-being were not collected.
Only 34% of respondents had persistent AUD, and most respondents had some degree of problem reduction; 16% achieved abstinence without symptoms, and 18% achieved low-risk drinking without symptoms. In addition, only 23% of the Fan et al. sample reported having ever received alcohol treatment, and those who did tended to fall into the persistent AUD (26%) or abstinent without symptoms (43%) outcome groups that generally are associated with higher problem severity. 7 In contrast, among the subset of respondents who reported abstinence or low-risk drinking without symptoms, 87% of those who reported low-risk drinking without symptoms were never treated, and only 12% were treated. An additional 15% of the sample reported low-risk drinking with symptoms, and 15% reported high-risk drinking without symptoms. 7 This is a refinement in outcome measurement compared to earlier surveys and illustrates the heterogeneity of recovery-relevant outcomes even in the absence of assessment of functioning and well-being.
This illustrative representative sample survey, among others, 8,9 reveals a more optimistic and variable view of recovery pathways and outcomes than suggested by early research using treatment samples, which emphasized the chronic, relapsing nature of alcohol problems and the difficulty of maintaining remission. Population data indicate that, even though alcohol problems are prevalent, most affected individuals have less serious problems than the minority who seek treatment, and many improve on their own, including achieving stable abstinence or low-risk drinking without problems.
In contrast to these encouraging findings concerning rates of improvement, population research on the prevalence and patterns of help-seeking for alcohol-related problems indicates that the gap between need and service utilization is large and chronic. This is the case even though alcohol-related services have improved and expanded considerably over the past several decades 27,28 and reliably yield benefits for a majority of recipients. Among the 25% or fewer who seek care, sources of care span the professional, community, and peer-helping sectors. Within the professional sector, care is diffused through mental health, medical, and community services systems, and only a minority receive alcohol-focused services from qualified programs or professionals. 8,27
Prevalence estimates for utilization of different types of alcohol services are not reliably available for several reasons. For example, specialty treatment programs are often addiction-oriented and not alcohol-specific, most include mutual help group participation as a program requirement, and the anonymity principle of mutual help groups deters determination of utilization rates apart from treatment. Nevertheless, membership estimates for AA (2.1 million members worldwide, including 1.3 million U.S. residents; https:// www.aa.org ) suggest that AA participation is relatively widespread. Comparable membership data are not available for other mutual help groups such as Self-Management and Recovery Training (SMART Recovery), which holds more than 3,000 meetings per week worldwide ( https://www.smartrecovery.org/ ), and LifeRing Secular Recovery, which offers more than 140 face-to-face meetings in the United States as well as online meetings and other electronic supports ( https://www.lifering.org/ ). Regarding professional treatment, the 2016 National Survey on Drug Use and Health estimated that about 3.8 million U.S. residents age 12 and older received any type of substance use treatment in the past year, 27 but these numbers are not specific to alcohol treatment. Also missing are data on relative remission rates as a function of type of care-seeking.
Higher problem severity predicts help-seeking, with higher severity reflected in greater alcohol dependence levels and alcohol-related impairment in areas of life functioning such as intimate, family, and social relationships; employment and finances; and legal affairs. 29 Perceived need also predicts help-seeking; however, even among those who perceive a need, only 15% to 30% receive help, 30 and problem recognition often precedes seeking care by a decade. 28 Thus, although most individuals who develop AUD will eventually resolve their problem, treatment utilization remains less used as a pathway to recovery. This pattern has persisted for decades despite recent expansion in the spectrum of services beyond clinical treatment to offer less costly and less intensive services that often can be accessed outside of the health care system and are suitable for those with less severe problems. 28 In addition, provisions of the Patient Protection and Affordable Care Act expanded access to and coverage of services for SUD.
Recovery Across the Life Span
Studies that followed risk groups and people with drinking problems longitudinally—typically using smaller samples than survey research—provide information on patterns of improvement and recovery across the life span. Some studies assessed functioning and life circumstances, in addition to drinking practices, and revealed the following age-related patterns with respect to the onset of and improvements in alcohol-related problems:
- Drinking to intoxication, binge drinking, and alcohol-related problems increase during adolescence and early adulthood, generally peaking between ages 18 and 22. Prevalence of past-year binge drinking (45%) and AUD (19%) is highest in the early 20s 31 and then decreases beginning in the mid-20s and continuing well after early adulthood. This nonlinear trajectory for the majority of adolescents and young adults, often termed “maturing out,” has been found in cross-sectional and longitudinal research using large national samples 2,32,33 and by the annual cross-sectional National Survey on Drug Use and Health. 1
- Adult role transitions (e.g., employment, marriage, parenthood) and personal maturation (e.g., decreased impulsivity) are associated with remission or recovery in early adulthood. 31,34-36 As is the case for the general adult population with AUD, only about a quarter of adolescents and young adults in need of treatment receive it. 1
- A subset of young adults who engage in harmful alcohol use and develop AUD in early adulthood show persistent or escalating problems in later life. Alcohol use before age 21 predicts persistence and severity of harmful use throughout the life span; 37 however, reductions in problem drinking in early adulthood are more likely to occur among individuals who had the most severe problems at earlier ages. 34
- Development of AUD is less common after age 25, and reductions in problem drinking, including recovery from AUD, continue past early adulthood and across the adult life span, including through late middle and old age (ages 60 to 80 and older). 22,34 Reductions in problem drinking at older ages are predicted by relatively heavier alcohol use in early old age that prompted complaints from concerned others. 22
These trends favoring increased remission rates over the life span are generally representative of the population, but can mask important nuances about age-related associations between problem onset, remission, and recurrence rates. 31,34-36 For example, Vergés and colleagues 35,36 used NESARC data from Waves 1 and 2 (from 2001–2002 to 2004–2005) to “deconstruct” age-related patterns of three different dynamic changes that contributed to overall age-related trends in the prevalence of DSM‑IV alcohol dependence at each wave. Although rates of new alcohol problem onset and recurrence of or relapse to earlier problems declined with age, rates of persistence of alcohol problems over time were relatively stable across ages 18 to 50 and older. These different processes that contributed to the overall trend of decreased alcohol-related problems with increasing age suggest that “maturing out”—as young people assume adult roles—is not a sufficiently complete account of remission rates across the life span.
In related research that also used NESARC data from Waves 1 and 2, Lee and colleagues examined how rates of remission, which they termed “desistance,” from mild, moderate, or severe levels of AUD varied across age groups ranging between ages 20 to 24 and 48 to 55. 34 Using Markov models to characterize patterns of longitudinal transitions in drinking status, they found differences in rates of AUD desistance from young adulthood to middle age as a function of AUD severity levels. Desistance rates from severe AUD, defined as six or more DSM‑IV symptoms, were considerably higher in earlier age groups (ages 25 to 29 and 30 to 34) relative to older age groups (ages 35 to 39, 40 to 47, and 48 to 55) as compared to rates found in surveys that aggregated data across AUD severity levels. Desistance rates from moderate AUD showed a similar, but less dramatic pattern across age groups, whereas desistance rates from mild AUD were relatively stable across age groups. When considered with the work of Vergés and colleagues, 35,36 these studies (1) show that resolution of severe AUD contributes heavily and distinctively to early adulthood remission prevalence, and (2) highlight the importance of deconstructing overall AUD prevalence curves by taking into account onset, remission, and recurrence of different levels of AUD severity over the life span.
Finally, a few studies observed increased binge drinking among middle-aged and older adults, 33 suggesting dynamic changes may occur in binge drinking in midlife; these changes are not well researched. Similarly, most natural recovery research comprises samples showing that midlife recovery from AUD is normative. 9,38 Middle age is also when treatment entry tends to occur. 5 Recovery in midlife and later ages is associated with an accumulation of alcohol-related problems coupled with life contexts that support and reinforce maintenance of drinking reductions and involve post-resolution improvements in functioning and well-being. 38,39
Role of Gender and Race/Ethnicity
In addition to age, rates of recovery or remission of AUD symptoms vary by gender and race/ethnicity. Using NESARC Wave 1 data, Dawson et al. found that older age and female gender predicted abstinence, but not low-risk drinking, in both treated and untreated respondents who had alcohol dependence prior to the past year. 5 Compared to non-Hispanic Whites, non-Hispanic Blacks had proportionately higher rates of abstinence than low-risk drinking. In the Fan et al. 7 replication of Dawson et al. 5 using NESARC-III data, female gender predicted both abstinence and low-risk drinking.
Also using NESARC-III data, Vasilenko et al. examined AUD prevalence by age and race/ethnicity (White, Black, Hispanic). 40 Although AUD prevalence generally peaked in the 20s and declined steadily with age, prevalence was higher for Whites at younger ages and higher for Blacks at older ages. This cross-over pattern typically occurred around age 60. In midlife, prevalence was similar for Blacks and Whites. Also, Whites reported higher AUD rates than Hispanic respondents at all ages, and men reported higher AUD rates than women until older age, when women were more likely than men to report AUD in their 70s. However, the number of participants older than age 70 was very small.
The study by Lee et al. that investigated age-related patterns of AUD desistance as a function of AUD severity also found gender and race/ethnicity differences. 34 Desistance patterns for males were generally consistent with the full sample findings—namely, elevated desistance rates for severe AUD in early adulthood and relatively stable rates for mild and moderate AUD. In contrast, females showed markedly higher rates of desistance from moderate AUD in early adulthood compared to older ages and attenuated rates of desistance from severe AUD compared to males during ages 30 to 34 only. With respect to race/ethnicity, results for Whites were generally consistent with the full sample, but findings differed for Hispanics and Blacks. For Hispanics, the early adulthood spike in rates of desistance from severe AUD was more time-limited, occurring only during ages 30 to 34 with much lower rates during ages 25 to 29. For Blacks, desistance rates for mild AUD also were relatively stable but were elevated for both moderate AUD (ages 25 to 29 and 30 to 34) and severe AUD (ages 25 to 29). For severe AUD, desistance rates among Blacks were very low during ages 30 to 34.
Patrick and colleagues analyzed age and gender relations with binge drinking using data from 27 cohorts of the annual Monitoring the Future surveys (1976 to 2004). 41 Participants were followed from 12th grade (modal age 18) through modal age 29/30. Across cohorts, the age of peak binge drinking prevalence increased from age 20 in 1976–1985 to age 22 in 1996–2004 for women, and from age 21 in 1976–1985 to age 23 in 1996–2004 for men. Similar to the typical population life span trajectory for AUD remission, for men the high prevalence of binge drinking persisted through ages 25 to 26, followed by reductions during the late 20s. For women ages 21 to 30, more recent cohorts reported significantly higher binge drinking prevalence than in earlier cohorts, with risk remaining high throughout the 20s. These shifts toward older age of peak binge drinking prevalence indicate an extension of risks associated with harmful alcohol consumption in young adulthood, especially for women.
Taken together, these studies on rates of improvement by gender and race/ethnicity suggest that many of the differences observed involve variations in the timing and extent of reductions in binge drinking and AUD during either young adulthood or older age, even though all groups tended to show overall patterns similar to the population as a whole. Differences during midlife were less extensive, although this developmental period has not been the focus of much research.
Help-Seeking
Help-seeking patterns and preferences also vary by gender and race/ethnicity. The gap between need and receipt of treatment is larger for women than for men, even after controlling for the higher prevalence of AUD and greater problem severity among men. 42,43 For example, using NESARC data from Waves 1 and 2, Gilbert et al. found that women identified as having DSM‑IV alcohol abuse or dependence at Wave 1 had significantly lower odds than men at Wave 2 of having used any alcohol service, specialty treatment, or mutual help groups. 42 These utilization differences occurred even though women and men reported similar low perceived need for help and similar numbers of treatment barriers. Women were more likely to report expecting that their problem would improve without intervention, whereas men were more likely to report prior help-seeking that was unhelpful. No differences in service utilization or perceived need were found for race/ethnicity among White, Black, and Hispanic respondents. Consistent with the larger literature, greater alcohol problem severity was associated with higher odds of service utilization.
Studies using pooled data from multiple waves of the national probability samples collected in the National Alcohol Surveys found differences in service utilization as a function of gender and race/ethnicity. 44,45 Zemore et al. used pooled data from three waves (1995–2005) to investigate lifetime alcohol treatment utilization and perceived barriers among Latinx respondents ( N = 4,204). 44 Among respondents, 3.4%, 2.7%, and 2.1% reported any lifetime treatment, AA participation, and institutional treatment, respectively. Men were significantly more likely than women to report receipt of any treatment services (5.6% vs. 1.1%), AA (4.7% vs. 0.6%), or institutional treatment (3.2% vs. 1.0%). Completion of the study interview in English (4.3%) versus Spanish (2.3%) also predicted higher utilization. These patterns were similar among the subsample of respondents who reported lifetime alcohol dependence, among whom rates of service utilization were much higher (20.4% for men and 15.3% for women). The authors suggested that underutilization of treatment by women and Spanish speakers may be due to cultural stigma against women with an alcohol problem, concerns about racial/ethnic stereotyping or stigmatization when seeking treatment, and additional barriers faced by individuals who are uncomfortable speaking English.
A later study using pooled data from the 2000–2010 National Alcohol Surveys included Whites, Blacks, and Latinx participants and found lower service utilization among Latinx, Blacks (vs. Whites), and women (vs. men). 45 Racial/ethnic differences in utilization were moderated by gender. Among women, only 2.5% of Latinas and 3.4% of Blacks with lifetime AUD used specialty treatment compared to 6.7% of Whites; among men, the corresponding figures were 6.8% for Latinos, 12.2% for Blacks, and 10.1% for Whites. 45 Higher utilization among Whites than among Blacks and Hispanics also was found using the 2014 cohort from the National Survey on Drug Use and Health. 46
Overall, research on race/ethnicity and help-seeking is not extensive, and groups other than Whites, Blacks, and Hispanics/Latinx have not been well studied. 47 Available research suggests that the gap between need and service utilization common among those with an alcohol problem is accentuated among ethnic and racial minority groups; however, research is in its infancy on why this is the case and how to address it.
Research on the epidemiology of recovery from AUD is somewhat uneven in scope and methods, and gaps remain in the knowledge base. Nonetheless, the bulk of evidence converges in showing that (1) improvements in alcohol-related problems, including recovery from AUD, are commonplace; (2) natural recovery is the dominant pathway; (3) greater problem severity is associated with treatment utilization; and (4) low-risk drinking outcomes are more common among untreated samples. Problem prevalence and rates of remission of AUD symptoms in the U.S. population peak during the 20s and are followed by a slow, steady decline over the adult life span. The specific ages when these characteristic dynamics in the temporal patterning of harmful alcohol use and remission of symptoms occur vary somewhat as a function of gender and race/ethnicity, but the overall general pattern is well established.
These findings provide a rich foundation concerning population patterns and dynamics of recovery, remission, and help-seeking. Future research aimed at disaggregating these complex associations at the population level should be a priority and can inform approaches to promoting remission and recovery in two general ways. 48 First, longitudinal studies of the onset of and improvements in alcohol-related problems 31,34-36 exemplify how epidemiological risk factors are reliably associated with the course of alcohol problem development and improvement and can be used to target at-risk individuals for preventive interventions. Second, “upstream” population-level interventions can be applied to prevent or reduce the determinants of risk (e.g., through changes in policy, taxation, and health and community infrastructure). The latter approach, although less common, takes advantage of the well-established prevention paradox—small reductions in harmful alcohol use by risky drinkers with less serious problems result in far greater health improvements at the population level than do changes in harmful alcohol use by the minority of persons with AUD.
This body of research qualifies the usual characterization of AUD as a chronic, relapsing/remitting disorder for which intensive intervention is essential for recovery. That characterization may be representative for a small minority of persons with more severe AUD, but it is inaccurate for the large majority of persons with mild to moderate problems, many of whom resolve their problems the first time they attempt to quit and often without interventions. 9,49 Whether this qualification applies to SUD other than AUD is not established.
The recovery literature is characterized by a mix of cross-sectional population surveys with short-term retrospective assessments (1 year is typical) and prospective follow-ups of smaller-sized samples of risk groups that, with some notable exceptions, 22-24 also had relatively short follow-ups. Use of data from the multiple waves of the NESARC dominates this research literature. Although the NESARC obtained data from a very large nationally representative sample of the U.S. population age 18 and older (e.g., N = 36,309 in NESARC‑III), it shares limitations inherent to most survey research—namely, assessments must be relatively brief, meaning that the domains of inquiry must be limited and selected carefully and cannot be probed to obtain the detail typically useful in clinical applications.
These design characteristics have contributed to gaps in the literature due to overreliance on drinking practices as the major outcome metric and less common measurement of functioning, well-being, and life circumstances, which are central features of recovery and can occur with or without reductions in drinking. Correlates of remission rates are being reported with increasing frequency in survey research, but tend to be limited to demographic characteristics, problem severity variables related to drinking practices, help-seeking history, and, in some cases, psychiatric comorbidity. Other than the seminal research program of Moos and colleagues, 22,39 assessment of functioning, context, and well-being surrounding drinking behavior change is a relatively recent development, primarily evident in clinical research 18,21 and process-oriented research on natural recovery. 38 Connecting these research literatures in meaningful ways in future investigations is essential for broadening scientific knowledge about how affected individuals reduce and resolve their alcohol-related problems and for guiding improvements in alcohol services that are responsive to heterogeneity in recovery-related outcomes and pathways.
Another issue in need of further research involves deconstruction of separable processes that contribute to overall problem prevalence and remission rates across the life span. As highlighted in the research of Vergés, Lee, Sher, and colleagues, 31,34-36 overall population rates are influenced by age-related associations between problem onset, remission, and recurrence rates, which raises questions about whether remission patterns reflect a simple “maturing out” of harmful alcohol use that began in early adulthood. Based on the available data, Lee and Sher 31 concluded: “[T]he continual declines in AUD rates observed throughout the life span . . . appear mainly attributable to reductions in new onsets . . . whereas potential for desistance from an existing AUD may peak in young adulthood . . . [especially] for those with a severe AUD” (p. 37).
The timing and targeting of prevention and treatment programs could be refined to enhance intervention effectiveness if these age-related associations between problem onset, remission, and recurrence rates were firmly established and used to guide intervention delivery. Conducting this kind of research is challenging because it requires collecting data on all three processes over the life span, and there are additional complexities in studying the tails of the age distribution. For example, clinical diagnostic systems may overdiagnose AUD in adolescence, which would inflate estimates of remission rates in early adulthood. 50 Attrition biases are of concern with advancing age as poor health and death may remove proportionately more older adults with AUD from population samples, thereby inflating estimates of remission rates in old age particularly from severe AUD. 5,34
A final generalization from this research concerns the limited contribution of alcohol treatment or other alcohol-focused services to recovery prevalence in the population. Low rates of service utilization have persisted despite improvements in AUD treatment and lower threshold options 28 and the expansion of access and coverage of services for SUD provided by the Affordable Care Act. The enduring gap between population need and service utilization despite these advances strongly suggests that alternative avenues are needed to increase intervention diffusion and uptake. It has proven insufficient to offer improved treatment predominately through the health care sector, and priority needs to be given to reaching broader segments of the at-risk population of drinkers who contribute most of the alcohol-related harm and cost. Nevertheless, a sizable subset of individuals with AUD improve or recover without interventions, and recent evidence suggests that individuals with more severe AUD exercise some degree of appropriate self-selection into treatment. 29 Empirical questions warranting further investigation are how to distinguish among individuals or risk groups for whom natural recovery is a high probability outcome and how to segment the market so that treatment services are targeted and available for those in need who are not likely to achieve recovery without treatment.
Further improvements in reducing the prevalence of AUD and increasing the prevalence of recovery likely depend on dissolving the silos that have long existed between clinical and epidemiological research and applications 11 and finding novel ways to disseminate evidence-based services to the large underserved at-risk population of drinkers who will not use professional services, at least in their present form. It is also important to consider a broader public health approach to dispel long-held beliefs that alcohol is a problem only for those with severe AUD and that those with AUD can resolve their problem only through abstinence. Perpetuation of these myths over many decades has stigmatized the disorder and deterred help-seeking among the millions of people who would benefit from drinking reductions.
In conclusion, recovery from AUD and alcohol-related problems is the most common outcome among those with problem alcohol use, and recovery without abstinence is possible, even among those with severe AUD. Changing the narrative to highlight the high likelihood of recovery could help engage more individuals in alcohol-related services and may encourage individuals to reduce their drinking in the absence of formal treatment.
Acknowledgments
Portions of the research reported were supported in part by National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism grant R01 AA022328.
Disclosures
The authors have no competing financial interests to disclose.
Publisher's note
Opinions expressed in contributed articles do not necessarily reflect the views of the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. The U.S. government does not endorse or favor any specific commercial product or commodity. Any trade or proprietary names appearing in Alcohol Research: Current Reviews are used only because they are considered essential in the context of the studies reported herein. Unless otherwise noted in the text, all material appearing in this journal is in the public domain and may be reproduced without permission. Citation of the source is appreciated.
- Substance Abuse and Mental Health Services Administration (SAMHSA). Key Substance Use and Mental Health Indicators in the United States: Results From the 2018 National Survey on Drug Use and Health . Rockville, MD: SAMHSA; 2019. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf . Accessed August 16, 2020.
- Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry . 2015;72(8):757-766. https://doi.org/10.1001/jamapsychiatry.2015.0584 .
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders . 5th ed. Washington, DC: APA; 2013. https://doi.org/10.1176/appi.books.9780890425596 .
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). Alcohol Facts and Statistics . Rockville, MD: NIAAA; 2019. https://www.niaaa.nih.gov/alcohol-facts-and-statistics . Accessed January 9, 2020.
- Dawson DA, Grant BF, Stinson FS, et al. Recovery from DSM-IV alcohol dependence: United States, 2001-2002. Addiction . 2005;100(3):281-292. https://doi.org/10.1111/j.1360-0443.2004.00964.x .
- Dawson DA, Goldstein RB, Grant BF. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: A 3-year follow-up. Alcohol Clin Exp Res . 2007;31(12):2036-2045. https://doi.org/10.1111/j.1530-0277.2007.00536.x .
- Fan AZ, Chou SP, Zhang H, et al. Prevalence and correlates of past-year recovery from DSM-5 alcohol use disorder: Results from National Epidemiologic Survey on Alcohol and Related Conditions-III. Alcohol Clin Exp Res . 2019;43(11):2406-2420. https://doi.org/10.1111/acer.14192 .
- Kelly JF, Bergman B, Hoeppner BB, et al. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug Alcohol Depend . 2017;181:162-169. https://doi.org/10.1016/j.drugalcdep.2017.09.028 .
- Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: Prevalence in two population studies. Am J Public Health . 1996;86(7):966-972. https://doi.org/2105/ajph.86.7.966 .
- Witkiewitz K, Montes K, Schwebel F, et al. What is recovery? Alcohol Res . 2020;40(3):1. https://doi.org/10.35946/arcr.v40.3.01 .
- Room R. Measurement and distribution of drinking patterns and problems in general populations. In: Edwards G, Gross MS, Keller M, et al., eds. Alcohol-Related Disabilities. Geneva, Switzerland: World Health Organization; 1977:61-87.
- Tucker JA. Natural resolution of alcohol-related problems. In: Galanter M, et al., eds. Recent Developments in Alcoholism. Volume 16: Research in Alcoholism Treatment. Boston, MA: Springer; 2002;77-90. https://doi.org/10.1007/0-306-47939-7_7 .
- World Health Organization (WHO). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines . Geneva, Switzerland: WHO;1992.
- Helping Patients Who Drink Too Much: A Clinician’s Guide . Rockville, MD: NIAAA; 2005. https://pubs.niaaa.nih.gov/publications/practitioner/cliniciansguide2005/guide.pdf . Accessed August 16, 2020.
- Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. J Subst Abuse Treat . 2007;33(3):221-228. https://doi.org/10.1016/j.jsat.2007.06.001 .
- Witkiewitz K, Tucker JA. Abstinence not required: Expanding the definition of recovery from alcohol use disorder. Alcohol Clin Exp Res . 2020;44(1)36-40. https://doi.org/10.1111/acer.14235 .
- Kaskutas LA, Borkman TJ, Laudet A, et al. Elements that define recovery: The experiential perspective. J Stud Alcohol Drugs . 2014;75(6): 999-1010. https://doi.org/10.15288/jsad.2014.75.999 .
- Witkiewitz K, Wilson AD, Pearson MR, et al. Profiles of recovery from alcohol use disorder at three years following treatment: Can the definition of recovery be extended to include high functioning heavy drinkers? Addiction . 2019;114(1):69-80. https://doi.org/10.1111/add.14403 .
- Jellinek EM. The Disease Concept of Alcoholism . New Haven, CT: Hillhouse Press; 1960.
- Pearson MR, Kirouac M, Witkiewitz K. Questioning the validity of the 4+/5+ binge or heavy drinking criterion in college and clinical populations. Addiction . 2016;111(10):1720-1726. https://doi.org/10.1111/add.13210 .
- Wilson AD, Bravo AJ, Pearson MR, et al. Finding success in failure: Using latent profile analysis to examine heterogeneity in psychosocial functioning among heavy drinkers following treatment. Addiction . 2016;111(12):2145-2154. https://doi.org/10.1111/add.13518 .
- Brennan PL, Schutte KK, Moos BS, et al. Twenty-year alcohol-consumption and drinking-problem trajectories of older men and women. J Stud Alcohol Drugs . 2011;72(2):308-321. https://doi.org/10.15288/jsad.2011.72.308 .
- Vaillant GE. The Natural History of Alcoholism Revisited . Cambridge, MA: Harvard University Press; 1995.
- Mattisson C, Bogren M, Horstmann V, et al. Remission from alcohol use disorder among males in the Lundby Cohort during 1947–1997. Psychiatry J . 2018;4829389. https://doi.org/10.1155/2018/4829389 .
- Sarich P, Canfell K, Banks E, et al. A prospective study of health conditions related to alcohol consumption cessation among 97,852 drinkers aged 45 and over in Australia. Alcohol Clin Exp Res . 2019;43(4):710‑721. https://doi.org/10.1111/acer.13981 .
- Grella CE, Stein JA. Remission from substance dependence: Differences between individuals in a general population longitudinal survey who do and do not seek help. Drug Alcohol Depend . 2013;133(1):146-153. https://doi.org/10.1016/j.drugalcdep.2013.05.019 .
- SAMHSA. National Survey of Substance Abuse Treatment Services (N-SSATS): 2016. Data on Substance Abuse Treatment Facilities . Rockville, MD: SAMHSA; 2017. https://www.samhsa.gov/data/sites/default/files/2016_NSSATS.pdf
- Tucker JA, Simpson CA. The recovery spectrum: From self-change to seeking treatment. Alcohol Res Health . 2011;33(4):371-379.
- Tuithof M, ten Have M, van den Brink W, et al. Treatment seeking for alcohol use disorders: Treatment gap or adequate self-selection? Eur Addict Res . 2016;22(5):277-285. https://doi.org/10.1159/000446822 .
- Schuler MS, Puttaiah S, Mojtabai R, et al. Perceived barriers to treatment for alcohol problems: A latent class analysis. Psychiatr Serv . 2015;66(11):1221-1228. https://doi.org/10.1176/appi.ps.201400160 .
- Lee MR, Sher KJ. “Maturing out” of binge and problem drinking. Alcohol Res . 2018;39(1):31-42.
- Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry . 2017;74(9):911-923. https://doi.org/10.1001/jamapsychiatry.2017.2161 .
- Grucza RA, Sher KJ, Kerr WC, et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: A meta-analysis of 6 national survey series. Alcohol Clin Exp Res . 2018;42(10):1939-1950. https://doi.org/10.1111/acer.13859 .
- Lee MR, Boness CL, McDowell YE, et al. Desistance and severity of alcohol use disorder: A lifespan-developmental investigation. Clin Psychol Sci . 2018;6(1):90-105. https://doi.org/10.1177/2167702617736852 .
- Vergés A, Jackson KM, Bucholz KK, et al. Deconstructing the age-prevalence curve of alcohol dependence: Why "maturing out" is only a small piece of the puzzle. J Abnorm Psychol . 2012;121(2):511-523. https://doi.org/10.1037/a0026027 .
- Vergés A, Haeny AM, Jackson KM, et al. Refining the notion of maturing out: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Public Health . 2013;103(12):e67-e73. https://doi.org/10.2105/ajph.2013.301358 .
- Hingson RW, Hereen T, Winter MR. Age at drinking onset and alcohol dependence: Age at onset, duration, and severity. Arch Pediatr Adolesc Med . 2006;160(7):739-746. https://doi.org/10.1001/archpedi.160.7.739 .
- Tucker JA, Cheong J, James TG, et al. Preresolution drinking problem severity profiles associated with stable moderation outcomes of natural recovery attempts. Alcohol Clin Exp Res . 2020;44(3):738-745. https://doi.org/1111/acer.14287 .
- Moos RH, Finney JW, Cronkite RC. Alcoholism Treatment: Context, Process, and Outcome . New York, NY: Oxford University Press; 1990.
- Vasilenko SA, Evans-Polce RJ, Lanza ST. Age trends in rates of substance use disorders across ages 18-90: Differences by gender and race/ethnicity. Drug Alcohol Depend . 2017;180:260-264. https://doi.org/10.1016/j.drugalcdep.2017.08.027 .
- Patrick ME, Terry-McElrath YM, Lanza ST, et al. Shifting age of peak binge drinking prevalence: Historical changes in normative trajectories among young adults aged 18 to 30. Alcohol Clin Exp Res . 2019;43(2):287-298. https://doi.org/10.1111/acer.13933 .
- Gilbert PA, Pro G, Zemore SE, et al. Gender differences in use of alcohol treatment services and reasons for nonuse in a national sample. Alcohol Clin Exp Res . 2019;43(4):722-31. https://doi.org/10.1111/acer.13965 .
- Greenfield SF, Black SE, Lawson K, et al. Substance abuse in women. Psychiatr Clin North Am . 2010;33(2):339-355. https://doi.org/10.1016/j.psc.2010.01.004 .
- Zemore SE, Mulia N, Ye Y, et al. Gender, acculturation, and other barriers to alcohol treatment utilization among Latinos in three National Alcohol Surveys. J Subst Abuse Treat . 2009;36(4):446-456. https://doi.org/10.1016/j.jsat.2008.09.005 .
- Zemore SE, Murphy RD, Mulia N, et al. A moderating role for gender in racial/ethnic disparities in alcohol services utilization: Results from the 2000 to 2010 National Alcohol Surveys. Alcohol Clin Exp Res . 2014;38(8):2286-2296. https://doi.org/10.1111/acer.12500 .
- SAMHSA. Behavioral Health Trends in the United States: Results From the 2014 National Survey on Drug Use and Health . Rockville, MD: SAMHSA; 2015. https://store.samhsa.gov/product/results-from-the-2014-national-survey-on-drug-and-use-and-health-summary-of-national-findings/sma15-4927 . Accessed August 16, 2020.
- Vaeth PAC, Wang-Schweig M, Caetano R. Drinking, alcohol use disorder, and treatment access and utilization among U.S. racial/ethnic groups. Alcohol Clin Exp Res . 2017;41(1):6-19. https://doi.org/10.1111/acer.13285 .
- Rose G. Sick individuals and sick populations. Int J Epidemiol . 2001;30(3):427-434. https://doi.org/10.1093/ije/30.3.427 .
- Kelly JF, Greene MC, Bergman BG, et al. How many recovery attempts does it take to successfully resolve an alcohol or drug problem? Estimates and correlates from a national study of recovering U.S. adults. Alcohol Clin Exp Res . 2019;43(7):1533-1544. https://doi.org/10.1111/acer.14067 .
- Caetano R, Babor TF. Diagnosis of alcohol dependence in epidemiological surveys: An epidemic of youthful alcohol dependence or a case of measurement error? Addiction . 2006;101(s1):111-114. https://doi.org/10.1111/j.1360-0443.2006.01599.x .
Cite this as: Alcohol Research. 2020;40(3):02. https://doi.org/10.35946/arcr.v40.3.02
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
- Alcohol or alcoholic beverages contain ethanol, a psychoactive and toxic substance that can cause dependence.
- Worldwide, around 2.6 million deaths were caused by alcohol consumption in 2019. Of these, 1.6 million deaths were from noncommunicable diseases, 700 000 deaths from injuries and 300 000 deaths from communicable diseases.
- The alcohol-attributable mortality was heaviest among men, accounting for 2 million deaths compared to 600 000 deaths among women, in 2019.
- An estimated 400 million people, or 7% of the world’s population aged 15 years and older, lived with alcohol use disorders. Of this, 209 million people (3.7% of the adult world population) lived with alcohol dependence.
- Alcohol consumption, even at low levels can bring health risks, but most alcohol related harms come from heavy episodic or heavy continuous alcohol consumption.
- Effective alcohol control interventions exist and should be utilized more, at the same time it is important for people to know risks associated with alcohol consumption and take individual actions to protect from its harmful effects.
Alcohol and alcoholic beverages contain ethanol, which is a psychoactive and toxic substance with dependence-producing properties. Alcohol has been widely used in many cultures for centuries, but it is associated with significant health risks and harms.
Worldwide, 2.6 million deaths were attributable to alcohol consumption in 2019, of which 2 million were among men and 0.6 million among women. The highest levels of alcohol-related deaths per 100 000 persons are observed in the WHO European and African Regions with 52.9 deaths and 52.2 deaths per 100 000 people, respectively.
People of younger age (20–39 years) are disproportionately affected by alcohol consumption with the highest proportion (13%) of alcohol-attributable deaths occurring within this age group in 2019.
The data on global alcohol consumption in 2019 shows that an estimated 400 million people aged 15 years and older live with alcohol use disorders, and an estimated 209 million live with alcohol dependence.
There has been some progress; from 2010 to 2019, the number of alcohol-attributable deaths per 100 000 people decreased by 20.2% globally.
There has been a steady increase in the number of countries developing national alcohol policies. Almost all countries implement alcohol excise taxes. However, countries report continued interference from the alcohol industry in policy development.
Based on 2019 data, about 54% out of 145 reporting countries had national guidelines/standards for specialized treatment services for alcohol use disorders, but only 46% of countries had legal regulations to protect the confidentiality of people in treatment.
Access to screening, brief intervention and treatment for people with hazardous alcohol use and alcohol use disorder remains very low, as well as access to medications for treatment of alcohol use disorders. Overall, the proportion of people with alcohol use disorders in contact with treatment services varies from less than 1% to no more than 14% in all countries where such data are available.
Health risks of alcohol use
Alcohol consumption is found to play a causal role in more than 200 diseases, injuries and other health conditions. However, the global burden of disease and injuries caused by alcohol consumption can be quantified for only 31 health conditions on the basis of the available scientific evidence for the role of alcohol use in their development, occurrence and outcomes.
Drinking alcohol is associated with risks of developing noncommunicable diseases such as liver diseases, heart diseases, and different types of cancers, as well as mental health and behavioural conditions such as depression, anxiety and alcohol use disorders.
An estimated 474 000 deaths from cardiovascular diseases were caused by alcohol consumption in 2019.
Alcohol is an established carcinogen and alcohol consumption increases the risk of several cancers, including breast, liver, head and neck, oesophageal and colorectal cancers. In 2019, 4.4% of cancers diagnosed globally and 401 000 cancer deaths were attributed to alcohol consumption.
Alcohol consumption also causes significant harm to others, not just to the person consuming alcohol. A significant part of alcohol-attributable disease burden arises from injuries such as road traffic accidents. In 2019, of a total of 298 000 deaths from alcohol-related road crashes, 156 000 deaths were caused by someone else’s drinking.
Other injuries, intentional or unintentional, include falls, drowning, burns, sexual assault, intimate partner violence and suicide.
A causal relationship has been established between alcohol use and the incidence or outcomes of infectious diseases such as tuberculosis and HIV.
Alcohol consumption during pregnancy increases the risk of having a child with fetal alcohol spectrum disorders (FASDs), the most severe form of which is fetal alcohol syndrome (FAS), which is associated with developmental disabilities and birth defects. Alcohol consumption during pregnancy can also increase the risk of pre-term birth complications including miscarriage, stillbirth and premature delivery.
Younger people are disproportionately negatively affected by alcohol consumption, with the highest proportion (13%) of alcohol-attributable deaths in 2019 occurring among people aged between 20 and 39 years.
In the long term, harmful and hazardous levels of alcohol consumption can lead to social problems including family problems, issues at work, financial problems, and unemployment.
Factors affecting alcohol consumption and alcohol-related harm
There is no form of alcohol consumption that is risk-free. Even low levels of alcohol consumption carry some risks and can cause harm.
The level of risk depends on several factors, including the amount consumed, frequency of drinking, the health status of the individual, age, sex, and other personal characteristics, as well as the context in which alcohol consumption occurs.
Some groups and individuals who are vulnerable or at risk may have a higher susceptibility to the toxic, psychoactive and dependence-inducing properties of alcohol. On the other hand, individuals who adopt lower-risk patterns of alcohol consumption may not necessarily face a significantly increased likelihood of negative health and social consequences.
Societal factors which affect the levels and patterns of alcohol consumption and related problems include cultural and social norms, availability of alcohol, level of economic development, and implementation and enforcement of alcohol policies.
The impact of alcohol consumption on chronic and acute health outcomes is largely determined by the total volume of alcohol consumed and the pattern of drinking, particularly those patterns which are associated with the frequency of drinking and episodes of heavy drinking. Most alcohol related harms come from heavy episodic or heavy continuous alcohol consumption.
The context plays an important role in the occurrence of alcohol-related harm, particularly as a result of alcohol intoxication. Alcohol consumption can have an impact not only on the incidence of diseases, injuries and other health conditions, but also on their outcomes and how these evolve over time.
There are gender differences in both alcohol consumption and alcohol-related mortality and morbidity. In 2019, 52% of men were current drinkers, while only 35% of women had been drinking alcohol in the last 12 months. Alcohol per capita consumption was, on average, 8.2 litres for men compared to 2.2 litres for women. In 2019, alcohol use was responsible for 6.7% of all deaths among men and 2.4% of all deaths among women.
WHO response
The Global alcohol action plan 2022–2030, endorsed by WHO Member States, aims to reduce the harmful use of alcohol through effective, evidence-based strategies at national, regional and global levels. The plan outlines six key areas for action: high-impact strategies and interventions, advocacy and awareness, partnership and coordination, technical support and capacity-building, knowledge production and information systems, and resource mobilization.
Implementation of global strategy and action plan will accelerate global progress towards attaining alcohol-related targets under the Sustainable Development Goal 3.5 on strengthening the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
Achieving this will require global, regional and national actions on the levels, patterns and contexts of alcohol consumption and the wider social determinants of health, with a particular focus on implementing high-impact cost effective interventions.
It is vital to address the determinants that drive the acceptability, availability and affordability of alcohol consumption through cross-sectoral, comprehensive and integrated policy measures. It is also of critical importance to achieve universal health coverage for people living with alcohol use disorders and other health conditions due to alcohol use by strengthening health system responses and developing comprehensive and accessible systems of treatment and care that for those in need.
The SAFER initiative, launched in 2018 by WHO and partners, supports countries to implement the high-impact, cost-effective interventions proven to reduce the harm caused by alcohol consumption.
The WHO Global Information System on Alcohol and Health (GISAH) presents data on levels and patterns of alcohol consumption, alcohol-attributable health and social consequences and policy responses across the world.
Achieving a reduction in the harmful use of alcohol in line with the targets included in the Global alcohol action plan, the SDG 2030 agenda and the WHO Global monitoring framework for noncommunicable diseases, requires concerted action by countries and effective global governance.
Public policies and interventions to prevent and reduce alcohol-related harm should be guided and formulated by public health interests and based on clear public health goals and the best available evidence.
Engaging all relevant stakeholders is essential but the potential conflicts of interest, particularly with the alcohol industry, must be carefully assessed before engagement. Economic operators should refrain from activities that might prevent, delay or stop the development, enactment, implementation and enforcement of high-impact strategies and interventions to reduce the harmful use of alcohol.
By working together, with due diligence and protection from conflicts of interest, the negative health and social consequences of alcohol can be effectively reduced.
Global status report on alcohol and health and treatment of substance use disorders
Global strategy to reduce the harmful use of alcohol
Global Alcohol Action Plan 2022–2030
SAFER Alcohol Control Initiative
More on alcohol
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Trend of alcohol use disorder as a percentage of all-cause mortality in North America
Affiliations.
- 1 Institute for Mental Health Policy Research, Centre for Addiction and Mental Health (CAMH), 33 Ursula Franklin Street, Toronto, ON, M5S 2S1, Canada. [email protected].
- 2 Campbell Family Mental Health Research Institute, CAMH, 250 College Street, Toronto, ON, M5T 1R8, Canada. [email protected].
- 3 Institute for Mental Health Policy Research, Centre for Addiction and Mental Health (CAMH), 33 Ursula Franklin Street, Toronto, ON, M5S 2S1, Canada.
- 4 Campbell Family Mental Health Research Institute, CAMH, 250 College Street, Toronto, ON, M5T 1R8, Canada.
- 5 Dalla Lana School of Public Health, University of Toronto, 155 College Street, 6th Floor, Toronto, ON, M5T 3M7, Canada.
- 6 Department of Psychiatry, University of Toronto, 250 College Street, 8th Floor, Toronto, ON, M5T 1R8, Canada.
- 7 Institute of Medical Science (IMS), University of Toronto, Medical Sciences Building, 1 King's College Circle, Room 2374, Toronto, ON, M5S 1A8, Canada.
- 8 Center for Interdisciplinary Addiction Research (ZIS), Department of Psychiatry and Psychotherapy, University Medical Center Hamburg-Eppendorf (UKE), Martinistraße 52, 20246, Hamburg, Germany.
- 9 Program on Substance Abuse & WHO CC, Public Health Agency of Catalonia, 81-95 Roc Boronat St, Barcelona, 08005, Spain.
- PMID: 39210466
- PMCID: PMC11360856
- DOI: 10.1186/s13104-024-06882-w
Objective: To evaluate the trend of alcohol use disorder (AUD) mortality as a percentage of all-cause mortality in Canada and the United States (US) between 2000 and 2019, by age group.
Results: Joinpoint regression showed that AUD mortality as a percentage of all-cause mortality significantly increased between 2000 and 2019 in both countries, and across all age groups (i.e., young adults (20-34 years), middle-aged adults (35-49 years), and older adults (50 + years)). The trend has been levelling off, and even reversing in some cases, in recent years. The average annual percentage change differed across countries and between age groups, with a greater increase among Canadian adults aged 35-49 years and among adults aged 50 + years in the US. Over the past two decades, AUD mortality as a percentage of all-cause mortality has been increasing among all adults in both Canada and the US.
Keywords: AUD; Alcohol-attributable harm; Disease trends; Joinpoint regression.
© 2024. The Author(s).
PubMed Disclaimer
Conflict of interest statement
The authors declare no competing interests.
Joinpoint regression analysis of percentage…
Joinpoint regression analysis of percentage AUD of all-causes of mortality, raw data (black…
- Spillane S, Shiels MS, Best AF, Haozous EA, Withrow DR, Chen Y, et al. Trends in alcohol-induced deaths in the United States, 2000–2016. JAMA Netw open. 2020;3(2):e1921451–e. 10.1001/jamanetworkopen.2019.21451 - DOI - PMC - PubMed
- Lee E, Navadurong H, Liangpunsakul S. Epidemiology and trends of alcohol use disorder and alcohol-associated liver disease. Clin Liver Disease. 2023;22(3):99–102. - PMC - PubMed
- Doycheva I, Watt KD, Rifai G, Abou Mrad R, Lopez R, Zein NN, et al. Increasing burden of chronic liver disease among adolescents and young adults in the USA: a silent epidemic. Dig Dis Sci. 2017;62:1373–80. 10.1007/s10620-017-4492-3 - DOI - PubMed
- Flemming JA, Dewit Y, Mah JM, Saperia J, Groome PA, Booth CM. Incidence of cirrhosis in young birth cohorts in Canada from 1997 to 2016: a retrospective population-based study. Lancet Gastroenterol Hepatol. 2019;4(3):217–26. 10.1016/S2468-1253(18)30339-X - DOI - PubMed
- Rehm J, Dawson D, Frick U, Gmel G, Roerecke M, Shield KD et al. Burden of disease associated with alcohol use disorders in the United States. Alcoholism: Clinical and Experimental Research. 2014;38(4):1068-77. - PMC - PubMed
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- BioMed Central
- PubMed Central
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Alcohol Use and Your Health
- Preventing Alcohol-Related Harms
- Underage Drinking
- Data on Excessive Alcohol Use
- U.S. Deaths from Excessive Alcohol Use
- Publications
- About Surveys on Alcohol Use
- About Standard Drink Sizes
- CDC Alcohol Program
- Alcohol Outlet Density Measurement Tools
- Resources to Prevent Excessive Alcohol Use
- Online Alcohol Tools and Apps
- Funding to Prevent Excessive Alcohol Use
Related Topics:
- View All Home
- Alcohol-Related Disease Impact (ARDI) Application
- Check Your Drinking. Make a Plan to Drink Less.
- Controle su forma de beber. Haga un plan para beber menos.
- Addressing Excessive Alcohol Use: State Fact Sheets
- Excessive alcohol use can have immediate and long-term effects.
- Excessive drinking includes binge drinking, heavy drinking, and any drinking during pregnancy or by people younger than 21.
- Drinking less is better for your health than drinking more.
- You can lower your health risks by drinking less or choosing not to drink.

Why it's important
- The rest of the alcohol can harm your liver and other organs as it moves through the body.
- Using alcohol excessively on occasion or over time can have immediate and long-term health risks.
- By drinking less alcohol, you can improve your health and well-being.
Deaths from excessive alcohol use
Understanding alcohol use, excessive alcohol use.
Excessive alcohol use is a term used to describe four ways that people drink alcohol that can negatively impact health. Excessive drinking can also be deadly.
Excessive alcohol use includes:
- Binge drinking—Four or more drinks for women, or five or more drinks for men during an occasion.
- Heavy drinking—Eight or more drinks for women, or 15 or more drinks for men during a week.
- Underage drinking —any alcohol use by people younger than 21.
- Drinking while pregnant—any alcohol use during pregnancy .
Moderate alcohol use
Moderate drinking is having one drink or less in a day for women, or two drinks or less in a day for men.
Keep in mind
Effects of short-term alcohol use.
Drinking excessively on an occasion can lead to these harmful health effects:
- Injuries— motor vehicle crashes , falls, drownings, and burns.
- Violence—homicide, suicide, sexual violence, and intimate partner violence.
- Alcohol poisoning—high blood alcohol levels that affect body functions like breathing and heart rate.
- Overdose—from alcohol use with other drugs , like opioids.
- Sexually transmitted infections or unplanned pregnancy—alcohol use can lead to sex without protection, which can cause these conditions.
- Miscarriage, stillbirth, or fetal alcohol spectrum disorder (FASD) —from any alcohol use during pregnancy.
Effects of long-term alcohol use
Over time, drinking alcohol can have these effects:
- The risk of some cancers increases with any amount of alcohol use. 2 This includes breast cancer (in women). 2 A
- More than 20,000 people die from alcohol-related cancers each year in the United States. 3
Other chronic diseases
Excessive alcohol use can lead to:
- High blood pressure.
- Heart disease.
- Liver disease.
- Alcohol use disorder—this affects both physical and mental health. B
- Digestive problems.
- Weaker immune system—increasing your chances of getting sick.
Social and wellness issues
- Mental health conditions, including depression and anxiety.
- Learning problems, and issues at school or work.
- Memory problems, including dementia.
- Relationship problems with family and friends.
You can take steps to lower your risk of alcohol-related harms.
The less alcohol you drink, the lower your risk for these health effects, including several types of cancer.
Check your drinking
- The risk of alcohol use leading to breast cancer in men has not been established.
- Most people who drink excessively do not have alcohol use disorder (also known as "alcohol dependence" or "alcoholism"). Many people who drink excessively can lower their alcohol use without specialized medical treatment. Facts about alcohol use disorder are available at: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder .
- Esser MB, Sherk A, Liu Y, Naimi TS. Deaths from excessive alcohol use — United States, 2016-2021. MMWR Morb Mortal Wkly Rep . 2024;73:154–161. doi: http://dx.doi.org/10.15585/mmwr.mm7308a1
- Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer . 2015;112(3):580-593. doi: 10.1038/bjc.2014.579
- Esser MB, Sherk A, Liu Y, Henley SJ, Naimi TS. Reducing alcohol use to prevent cancer deaths: estimated effects among U.S. adults. Am J Prev Med . 2024;66(4):725–729. doi: 10.1016/j.amepre.2023.12.003
Alcohol Use
Excessive alcohol use can harm people who drink and those around them. You and your community can take steps to improve everyone’s health and quality of life.

For Everyone
Public health.

Understanding alcohol use disorders and their treatment
People with alcohol use disorders drink to excess, endangering both themselves and others. This question-and-answer fact sheet explains alcohol problems and how psychologists can help people recover.
- Substance Use, Abuse, and Addiction

For many people, drinking alcohol is nothing more than a pleasant way to relax. People with alcohol use disorders, however, drink to excess, endangering both themselves and others. This question-and-answer fact sheet explains alcohol problems and how psychologists can help people recover.
When does drinking become a problem?
For most adults, moderate alcohol use — no more than two drinks a day for men and one for women and older people — is relatively harmless. (A "drink" means 1.5 ounces of spirits, 5 ounces of wine, or 12 ounces of beer, all of which contain 0.5 ounces of alcohol.
Moderate use, however, lies at one end of a range that moves through alcohol abuse to alcohol dependence:
Alcohol abuse is a drinking pattern that results in significant and recurrent adverse consequences. Alcohol abusers may fail to fulfill major school, work, or family obligations. They may have drinking-related legal problems, such as repeated arrests for driving while intoxicated. They may have relationship problems related to their drinking.
People with alcoholism — technically known as alcohol dependence — have lost reliable control of their alcohol use. It doesn't matter what kind of alcohol someone drinks or even how much: Alcohol-dependent people are often unable to stop drinking once they start. Alcohol dependence is characterized by tolerance (the need to drink more to achieve the same "high") and withdrawal symptoms if drinking is suddenly stopped. Withdrawal symptoms may include nausea, sweating, restlessness, irritability, tremors, hallucinations and convulsions.
Although severe alcohol problems get the most public attention, even mild to moderate problems cause substantial damage to individuals, their families and the community.
According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA) , 6.2 percent of adults in the United States aged 18 and older had alcohol use disorder. 1 For example, a government survey revealed that about one in five individuals aged 12 to 20 were current alcohol users and about two in five young adults, aged 18 to 25, were binge alcohol users and about one in 10 were heavy alcohol users. 2
What causes alcohol-related disorders?
Problem drinking has multiple causes, with genetic, physiological, psychological,and social factors all playing a role. Not every individual is equally affected by each cause. For some alcohol abusers, psychological traits such as impulsiveness, low self-esteem and a need for approval prompt inappropriate drinking. Some individuals drink to cope with or "medicate" emotional problems. Social and environmental factors such as peer pressure and the easy availability of alcohol can play key roles. Poverty and physical or sexual abuse also increase the odds of developing alcohol dependence.
Genetic factors make some people especially vulnerable to alcohol dependence. Contrary to myth, being able to "hold your liquor" means you're probably more at risk — not less — for alcohol problems. Yet a family history of alcohol problems doesn't mean that children will automatically grow up to have the same problems. Nor does the absence of family drinking problems necessarily protect children from developing these problems.
Once people begin drinking excessively, the problem can perpetuate itself. Heavy drinking can cause physiological changes that make more drinking the only way to avoid discomfort. Individuals with alcohol dependence may drink partly to reduce or avoid withdrawal symptoms.
How do alcohol use disorders affect people?
While some research suggests that small amounts of alcohol may have beneficial cardiovascular effects, there is widespread agreement that heavier drinking can lead to health problems.
Short-term effects include memory loss, hangovers, and blackouts. Long-term problems associated with heavy drinking include stomach ailments, heart problems, cancer, brain damage, serious memory loss and liver cirrhosis. Heavy drinkers also markedly increase their chances of dying from automobile accidents, homicide, and suicide. Although men are much more likely than women to develop alcoholism, women's health suffers more, even at lower levels of consumption.
Drinking problems also have a very negative impact on mental health. Alcohol abuse and alcoholism can worsen existing conditions such as depression or induce new problems such as serious memory loss, depression or anxiety.
Alcohol problems don't just hurt the drinker. Spouses and children of heavy drinkers may face family violence; children may suffer physical and sexual abuse and neglect and develop psychological problems. Women who drink during pregnancy run a serious risk of damaging their fetuses. Relatives, friends and strangers can be injured or killed in alcohol-related accidents and assaults.
When should someone seek help?
Individuals often hide their drinking or deny they have a problem. How can you tell if you or someone you know is in trouble? Signs of a possible problem include having friends or relatives express concern, being annoyed when people criticize your drinking, feeling guilty about your drinking and thinking that you should cut down but finding yourself unable to do so, or needing a morning drink to steady your nerves or relieve a hangover.
Some people with drinking problems work hard to resolve them. With the support of family members or friends, these individuals are often able to recover on their own. However, those with alcohol dependence usually can't stop drinking through willpower alone. Many need outside help. They may need medically supervised detoxification to avoid potentially life-threatening withdrawal symptoms, such as seizures. Once people are stabilized, they may need help resolving psychological issues associated with problem drinking.
There are several approaches available for treating alcohol problems. No one approach is best for all individuals.
How can a psychologist help?
Psychologists who are trained and experienced in treating alcohol problems can be helpful in many ways. Before the drinker seeks assistance, a psychologist can guide the family or others in helping to increase the drinker's motivation to change.
A psychologist can begin with the drinker by assessing the types and degrees of problems the drinker has experienced. The results of the assessment can offer initial guidance to the drinker about what treatment to seek and help motivate the problem drinker to get treatment. Individuals with drinking problems improve their chances of recovery by seeking help early.
Using one or more of several types of psychological therapies, psychologists can help people address psychological issues involved in their problem drinking. A number of these therapies, including cognitive-behavioral coping skills treatment and motivational enhancement therapy, were developed by psychologists. Additional therapies include 12-Step facilitation approaches that assist those with drinking problems in using self-help programs such as Alcoholics Anonymous (AA).
These therapies can help people boost their motivation to stop drinking, identify circumstances that trigger drinking, learn new methods to cope with high-risk drinking situations, and develop social support systems within their own communities.
All three of these therapies have demonstrated their effectiveness. One analysis of cognitive-behavioral approaches, for instance, found that 58 percent of patients receiving cognitive-behavioral treatment fared better than those in comparison groups. 3 In another study , motivational interventions reduced how often and how much adolescents drank following alcohol-related emergency room treatment. 4 And an intervention called Making Alcoholics Anonymous Easier significantly increased participants' odds of abstaining from alcohol. 5 Many individuals with alcohol problems suffer from other mental health conditions, such as severe anxiety and depression, at the same time. Psychologists can also diagnose and treat these "co-occurring" psychological conditions. Further, a psychologist may play an important role in coordinating the services a drinker in treatment receives from various health professionals.
Psychologists can also provide marital, family, and group therapies, which often are helpful for repairing interpersonal relationships and for resolving problem drinking over the long term. Family relationships influence drinking behavior, and these relationships often change during an individual's recovery. The psychologist can help the drinker and significant others navigate these complex transitions, help families understand problem drinking and learn how to support family members in recovery, and refer family members to self-help groups such as Al-Anon and Alateen.
Because a person may experience one or more relapses and return to problem drinking, it can be crucial to have a trusted psychologist or other health professional with whom that person can discuss and learn from these events. If the drinker is unable to resolve alcohol problems fully, a psychologist can help with reducing alcohol use and minimizing problems.
Psychologists can also provide referrals to self-help groups. Even after formal treatment ends, many people seek additional support through continued involvement in such groups.
Alcohol-related disorders severely impair functioning and health. But the prospects for successful long-term problem resolution are good for people who seek help from appropriate sources.
The American Psychological Association gratefully acknowledge the assistance of Peter E. Nathan, PhD, John Wallace, PhD, Joan Zweben, PhD, and A. Thomas Horvath, PhD, in developing this fact sheet .
1 National Institute on Alcohol Abuse and Alcoholism. (2018). "Alcohol Use Disorder."
2 Substance Abuse and Mental Health Services Administration. (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/
3 Magill, M., & Ray, L.A. (2009). "Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials." Journal of Studies on Alcohol and Drugs, 70 (4): 516-527.
4 Spirito, A., Sindelar-Manning, H., Colby, S.M., Barnett, N.P., Lewander, W., Rohsenow, D.J., & et al. (2011). "Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department." Archives of Pediatrics and Adolescent Medicine, 165 (3): 269-274.
5 Kaskutas, L.A., Subbaraman, M.S., Witbrodt, J., & Zemore, S.E. (2009). "Effectiveness of Making Alcoholics Anonymous Easier: A group format 12-step facilitation approach." Journal of Substance Abuse Treatment, 37 (3): 228-239.
Updated Sept. 2018
Recommended Reading

Related Reading
- Overcoming opioid abuse: How psychologists help people with opioid dependence and addiction
- Understanding anger: How psychologists help with anger problems
- Managing traumatic stress: After the hurricanes
You may also like
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 06 September 2024
Bariatric Surgery
Alcohol use disorders after bariatric surgery: a study using linked health claims and survey data
- Oliver Riedel ORCID: orcid.org/0000-0002-1721-502X 1 ,
- Malte Braitmaier ORCID: orcid.org/0000-0001-7534-4068 1 ,
- Mark Dankhoff ORCID: orcid.org/0009-0004-9988-4930 2 ,
- Ulrike Haug 1 , 3 ,
- Melanie Klein ORCID: orcid.org/0009-0009-7651-0641 4 ,
- Wiebke Zachariassen ORCID: orcid.org/0009-0005-3471-0910 4 &
- Jana Hoyer ORCID: orcid.org/0000-0001-9872-4813 5
International Journal of Obesity ( 2024 ) Cite this article
Metrics details
- Lifestyle modification
Previous studies have repeatedly reported alcohol use disorders (AUDs) in patients after bariatric surgery (BS). This research field can benefit from studies combining health claims data with survey data.
Based on a combined retrospective cohort and cross-sectional study, 2151 patients with BS identified in a large health claims database received a questionnaire, by which we assessed the presence of AUDs based on a validated instrument (AUDIT) as well as by ICD-10 codes from the health claims data. We described patients with vs. without AUDs regarding sex, time since surgery, satisfaction with weight loss and health care resource utilization (HCRU).
The majority of patients were female (80.7%) with a median time since surgery of 6 years (Interquartile range: 4–9 years). For the majority of patients, the bariatric intervention was either a RYGB-Bypass (50%) or sleeve gastrectomy (43%). Overall, 3% had at least one AUD diagnosis code in the claims data (men: 5.5%, women: 2.5%). Among men, 43.6% of diagnoses were coded after but not before the surgery (women: 52%). According to AUDIT (completed by 1496 patients), 9.4% of all patients showed at least hazardous/harmful alcohol consumption. Higher scores were associated with sex of the person, longer time since surgery, dissatisfaction with the weight loss and higher HCRU, with contradicting results regarding psychotherapeutic care.
Conclusions
The proportion with AUDs in the study population gives rise to concern as alcohol consumption should be restricted after BS. The results suggest the necessity for close monitoring and post-surgical care.
Similar content being viewed by others
Associations of semaglutide with incidence and recurrence of alcohol use disorder in real-world population

Association of alcohol use and multimorbidity among adults aged 40 years and above in rural South Africa
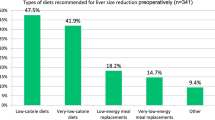
Global variations in preoperative practices concerning patients seeking primary bariatric and metabolic surgery (PACT Study): A survey of 634 bariatric healthcare professionals
There is evidence that severe obesity and addictive disorders are potentially connected or even causally related [ 1 , 2 ], partly with inconsistent findings between men and women [ 3 ]. The relationship between obesity and alcohol disorders is especially relevant for patients living with severe overweight. Bariatric surgery (BS) —indicated in patients with a body mass index (BMI) of more than 40 kg/m² after unsuccessful conventional therapy—permanently modifies the anatomy of the gastrointestinal tract by bypassing the digestive tract. This also affects the digestion of alcohol: it is absorbed more rapidly, higher maximum concentrations are reached, and the elimination time is prolonged, increasing the risk of addiction and alcohol-related harm [ 4 , 5 , 6 ]. Therefore, alcohol use disorders (AUDs) are a contraindication for BS [ 7 ]. Data suggest that patients undergoing BS are subsequently at increased risk of developing substance use disorders, particularly AUDs [ 8 ] but also abuse of other drugs [ 9 , 10 ]. Despite variations in the frequencies of AUDs in patients after BS reported in the literature, the review by Linlin and Wu [ 11 ] summarized a prevalence in the range of 8–18% shortly after surgery and up to 35% as a lifetime prevalence. Up to 43% of all patients with post-surgical AUDs did not show any signs of pre-surgical AUDs [ 12 ].
In recent years, an increasing number of findings on AUDs in patients with BS have been published, although the results were sometimes inconclusive due to heterogeneous methodological quality [ 13 ]. Flaws of some of the previous studies comprise their limitations regarding the available follow-up times or their sample sizes, which did not allow sufficiently stratified analyses of subgroups of patients (e.g. by sex or by type of bariatric intervention). The repeated calls for studies [ 14 , 15 ] with a longer observation period and larger sample sizes were addressed by a recently published, high-quality study using on health claims data [ 16 ]. Based on a follow-up time of more than 8 years and more than 400 000 patients with bariatric interventions, the authors reported an increased post-surgical risk for AUDs according to coded ICD-diagnoses. This research field can further benefit from studies that combine these advantages of health claims data with the advantages of survey data, which can provide a more detailed picture on AUDs by using standardized questionnaires.
Therefore, the present study aims at describing the presence of alcohol-related disorders in 2151 persons with BS before and up to 12 years after surgery, based upon a linked data set comprising health claims data and survey data.
Study design
The design of the underlying “ABARO” study has been presented previously in more detail [ 17 ]. Briefly, we linked longitudinal health claims data (cohort analyses) with cross-sectional survey data from patients after BS using a multistep approach. First, we used data from one statutory health insurance (SHI) provider included in the German Pharmacoepidemiological Research Database (12 million persons who have been insured at this SHI since 2004 or later) [ 18 ] to identify patients with BS anytime between 2004 and 2018 and who were still alive at the end of 2018 ( n = 6913). After excluding n = 1691 patients who could not be contacted for various reasons (e.g. end of insurance with this SHI or objection to receiving mail), a questionnaire was sent to a total of n = 5222 patients in 2021 (see the next section for more details). Hereof, n = 2521 patients responded. As for the present analyses, only patients with at least three years of baseline prior to surgery were considered, n = 267 patients without sufficient baseline were excluded. For n = 103 patients, surveys could not be linked to the claims data due to lack of consent. Therefore, the analysis data set comprised n = 2151 patients with BS between 2007 and 2018, for whom both cross-sectional survey and longitudinal health claims data were available (see Supplementary Fig. S1 for further details). For the cohort analyses in this paper, the time prior to the BS was considered as “pre-surgery”, the time after surgery as “post-surgery”.
Assessment of AUDs
The study variables were derived from the health claims data and survey data.
Based on health claims data, AUDs were assessed by the existence of corresponding diagnostic ICD-10 codes (F10). To avoid overestimation, AUDs were only considered if they were documented by at least (a) one inpatient main or secondary discharge diagnosis, or (b) two (or more) identical outpatient diagnoses in subsequent quarters or (c) two (or more) outpatient diagnoses in the same quarter coded by different physicians. In sensitivity analyses, we only considered patients with at least one inpatient discharge diagnosis of AUDs (additional outpatient diagnoses were allowed) as inpatient diagnoses typically have the highest validity. Each patient was further categorized as to whether they had AUDs only pre-surgery, only post-surgery, pre- and post-surgery (“both”) or never.
In the survey, AUDs were measured with the Alcohol Use Disorders Identification Test (AUDIT), which consists of 10 items addressing aspects of alcohol consumption (e.g. frequency of consumption, loss of control). The value of each item ranges from 0 ( = unproblematic) to 4 ( = severe), thus constituting a possible total score between 0 and 40. Based on this total score, patients were categorized as having “low-risk consumption” (scores ≤7), “hazardous/harmful consumption” (scores 8–14) or a “moderate-severe alcohol use disorder” (scores ≥15) [ 19 , 20 ]. As these cut-off scores have not been validated in patients after BS before, we have additionally conducted three sensitivity analyses as presented in Suppl. Table S1 to avoid underestimations of AUDs in this population. In analysis A, we doubled the weighting of the consumption items 1–3; in analysis B, we increased the score of these items by one and in analysis C, we chose lower cut-offs for the total score categories as mentioned above (≤4, 5–11 and ≥12).
Further study variables
Comorbidities were assessed using the health claims data, implementing algorithms of high specificity by taking into account either inpatient codes or information on medication [ 21 ]. The anthropometrics were derived from the survey data. The BMI was calculated by dividing the body weight (in kilograms) by the square of height in meters, and was categorized as “normal weight” (18.5–24.9), “overweight” (25.0–29.9), “obesity class I” (30.0–34.9), “obesity class II” (35.0–39.9) and “obesity class III” (>40). The total weight loss (TWL, %) was calculated by dividing the number of kilograms lost by the number of kilograms in the patient’s pre-surgical body weight. The utilization of health care services (i.e. number of inpatient treatment days, hospitalizations, outpatient visits and psychosocial/psychotherapeutical interventions) was estimated by health claims data and survey data.
Statistical analyses
Summary statistics consisted of counts and percentages. Means and medians are presented with 95% confidence intervals (CI) and quartiles (Q1, Q3), where appropriate. Based on previous recommendations and debates [ 22 , 23 , 24 ], we did not perform significance tests. First, because this observational study was not based on specific hypotheses and secondly to avoid misinterpretation of p values due to the large sample size. Associations with categorical predictor variables were calculated by using odds ratios (OR) estimated from logistic regressions with 95% CI. All statistical analyses were conducted using R version 4.3.1 and SAS 9.4 (program codes available on request).
The study was approved by the Hamburg Medical Chamber Ethics Committee (October 11, 2021, No. 2021-10543-BO-ff) and was performed according to the 1964 Declaration of Helsinki. Written informed consent was obtained from each participant.
Study population
The n = 2151 included patients had a mean age of 54.6 years (95% CI: 54.1—55.0) when they filled the survey, and 80.7% were women. The median time since surgery was 6 years (Q1: 4; Q3: 9). The mean BMI at the conduction of the survey was 34.8 (95% CI: 34.4—35.1) and 51.9 (95% CI: 51.5—52.4) prior to surgery. The median TWL was 32.7% (Q1: 24.5; Q3: 40.7). For the vast majority of patients, the bariatric intervention was either a Roux-en-Y gastric bypass (RYGB, 50%) or sleeve gastrectomy (43%); 5.5% had a gastric band, 0.3% reported gastric balloons and 1.1% reported other procedures.
AUDs by ICD-10 diagnoses
Figure 1 displays the proportion of patients with pre-/post-surgical AUD diagnoses in the health claims data by considering in-/outpatient diagnoses (Fig. 1a ) or at least one inpatient diagnosis (Fig. 1b ). Overall, 3% of all patients were classified as having an AUD according to claims data (at least one inpatient diagnosis: 2%). AUD diagnoses were 2.2-times more common in men; this difference by sex increased if patients with at least one inpatient diagnosis codes were considered. For both sexes, more than 40% of diagnoses were coded after but not before the surgery. This proportion was 70% if considering only patients with at least one inpatient AUD diagnosis.

ICD-10 diagnoses of alcohol use disorders (F10) in the health claims data of the patients, considering patients ( a ) in- and/or outpatient diagnoses or ( b ) at least one inpatient diagnosis ( N = 2151).
AUDs by AUDIT screening test
For 655 patients, an AUDIT total score could not be computed due to missing of at least one item (predominantly regarding the amount of regular drinking, n = 626). Thus, a total score was available for n = 1496 patients. Patients with incomplete AUDITs were older than those with completed AUDITs (55.7 years, 95%-CI: 54.9—56.5 vs. 53.9 years, 95%-CI: 53.4—54.5) and more often male (20.5% vs. 16.8%). When considering the single AUDIT items, non-completers tended to respond more often with lower scores (i.e. “never or less than monthly”, “no”) than completers (see Suppl. Table S2 for more details). In a sensitivity analysis, we additionally compared the AUDIT score distributions after replacing the missing values of the item on the drinking amount by the highest scores (see Supplementary Table S3 ).
The mean AUDIT score was 3.4 (95% CI: 3.1—3.6) with higher scores in men (4.8, 95% CI: 4.2—5.4) than in women (3.4, 95% CI: 2.8—3.2). Regarding type of BS, the mean AUDIT scores were 3.5 (95% CI: 3.2—3.9, “gastric bypass”), 3.2 (95% CI: 2.8—3.5, “gastric sleeve”), 3.0 (95% CI: 3.2—3.0, “gastric band”) and 1.2 (95% CI: 0.2—2.6, “gastric balloon”). Table 1 shows the distribution of the AUDIT categories. Overall, 9.4% of all patients showed at least hazardous/harmful consumption. The proportion was higher in men than women (17.3% vs. 7.3%). In the sensitivity analyses, these proportions increased to up to 18.3% (see Supplementary Table S1 ), also with higher proportions for men (up to 33.7%) than for women (up to 14.4%). The AUDIT categories did not differ regarding age, time since and type of surgery or BMI (see Table 1 ). A lower TWL was associated with higher proportions of at least hazardous/harmful consumption. Figure 2 displays the associations between these parameters and an AUDIT score of ≥8, adjusted for sex. A higher likelihood for at least hazardous alcohol consumption was found for males as compared to females, a longer time since surgery and dissatisfaction with post-surgical weight loss. This association still remained stable after additionally adjusting for post-surgical TWL and BMI (OR = 1.74, 95% CI: 1.13–2.68). Post-surgical care of any duration and higher TWLs were associated with a lower likelihood of hazardous drinking.

Associations between patient characteristics and at least a “hazardous consumption of alcohol” (AUDIT score ≥8), estimated by separate logistic regression models and adjusted for sex ( N = 1496).
For patients with at least hazardous/harmful alcohol consumption according to the AUDIT, also higher numbers of inpatient treatment days and hospitalizations were observed (Table 2 ) as compared to patients with low-risk consumption. Regarding psychotherapy, the proportion of patients with at least one corresponding reimbursement code were similar across the AUDIT categories. More patients with moderate or severe AUDs reported psychotherapy consultations after surgery as compared to patients with less severe drinking patterns. The proportion of patients with comorbidities during baseline and follow-up is shown in Fig. 3 . While overall obesity-related comorbidities (e.g. hypertension, diabetes) decreased post-surgery, there were similar proportions of affected patients among those with higher and those with lower AUDIT-scores, respectively. The only exceptions were antidepressant treatment and smoking, both of which were pre- and post-surgically more common in patients with AUDIT scores >7 than lower scores.

Frequency of comorbidities as coded at least once during ( a ) baseline and ( b ) follow-up, stratified by AUDIT-Score (0–7: “no alcohol use disorder” vs. ≥8: at least “hazardous consumption”) ( N = 1496).
We investigated the frequency of AUDs in patients after BS based on a large patient sample with a post-bariatric history of up to twelve years by analyzing survey data as well as health claims data from the same patient population. This approach enabled us to at least partially compensate for the inherent disadvantages of one data source (health claims data: no information on lifestyle or subthreshold diseases; survey data: e.g. inherent potential recall bias, inaccuracy of medical information) with the strengths of the other data source (health claims data: e.g. accurate depiction of comorbidities and cross-sectoral health care resource utilization over a long observation period; survey data: e.g. documentation of lifestyle behaviors, trend in post-surgical body weight, evaluation of subthreshold mental disorders). This helped us to get a more complete picture of the research subject.
Based on health claims data, we found a proportion of 2–3% who had been diagnosed with AUDs at least once during the observation period. According to AUDIT, one in ten patients reported risky drinking, with almost six percent meeting the criteria for hazardous alcohol consumption and almost four percent meeting the criteria for alcohol dependence. Almost twice as higher proportions were found when increasing the weighting or the scoring of the AUDIT items that relate to the consumption patterns of alcohol, as well as decreasing the original cut-off scores of the instrument. According to these sensitivity analyses which have been introduced as to our knowledge the AUDIT has not been validated in post-bariatric patients before, one in three male patients and one in seven female patients revealed at least risky consumption patterns.
The performance of our study participants is comparable to previous findings reported from the general population and from patients attending to general practices [ 25 , 26 ]. Unlike the AUDIT screening, which was applied only once in our study after surgery, the use of health claims data allowed us to count the frequencies of AUDs pre-/post-surgery. Notably, up to 70% of patients with AUDs were diagnosed post-surgery but not before. This is in line with previous studies which reported an increased risk of incident AUDs after BS in patients without an AUD history, based on established psychometric instruments [ 8 , 12 , 27 , 28 ]. However, we wish to emphasize that the interpretation of AUDs based on health claims data warrants great caution, since miscodings cannot be fully excluded. While inpatient discharge diagnoses usually can be considered valid, the accuracy of single outpatient diagnoses can be questionable. We attempted to overcome this shortcoming by requiring outpatient diagnoses to be confirmed by at least another outpatient diagnosis (either consecutive or from different physicians). Nonetheless, we attribute a higher diagnostic validity to the group of patients with at least one inpatient diagnosis available in our data than to the group with outpatient diagnoses without the necessity of an inpatient diagnosis. However, it must be clearly stated that our results are of a purely descriptive nature and that a direct, causal relationship between bariatric surgery and the occurrence of AUDs cannot be assessed with our study design. The lack of an otherwise comparable control group but without bariatric intervention is a clear limitation of our study.
In essence, the frequencies we found for severe alcohol disorders are of the same order of magnitude as those reported for non-bariatric populations. In a German nationwide health study, Jacobi et al. [ 29 ] found a 12-month prevalence for alcohol dependence of 3%, based on a structured clinical interview (with men affected about four times more often than women). Similarly, in a re-analysis of several European epidemiology studies, Wittchen et al. [ 30 ] reported a 12-month prevalence of 3.4% for alcohol dependence. It should be considered, however, that these figures were derived from the general population. In contrast, our data refer to a population for whom AUDs are actually an exclusion criterion for BS and for whom reduced alcohol consumption (if not abstinence) is indicated after surgery [ 7 ]. Thus, these figures still give rise to concern. In this context, however, it is remarkable that, although the frequency of alcohol dependence is comparable, the proportion of those without manifest dependence yet with latent alcohol abuse is three times higher than in the general population [ 29 ]. That is, although patients in our sample were not more often alcohol dependent than the general population according to the AUDIT, the proportion of patients with “risky drinking” was substantially increased which might indicate that BS puts patients at risk of substance abuse (although, as mentioned before, this cannot be verified with our study design). The incorporation of our study results into the previously reported frequencies of post-bariatric AUDs is complicated due to the methodological heterogeneity of the studies. A recently published review which included 18 articles revealed inconclusive findings with studies reporting both worsening and improvement of drinking behaviors after surgery [ 31 ]. Svensson et al. [ 32 ] compared the development of AUDs in bariatric patients and in non-bariatric controls with obesity in a prospective cohort study. Almost seven percent of patients after bariatric interventions reported an alcohol consumption pattern beyond low risk, which is slightly lower than our estimates in the main analyses and corresponds to our estimates in the sensitivity analyses, which replaced missing values on the item regarding the quantity of drinks. However, while this work is among the few with a longer follow-up, these results have limited comparability with ours because they are derived exclusively from inpatient data and from patients without a pre-surgical history of AUDs, potentially limiting the generalizability of their findings. Suzuki et al. [ 33 ] reported AUDs two times more often (12%) in inpatients after BS, also using the AUDIT instrument for the detection of alcohol disorders, and they found no association between post-surgical weight loss and AUDs. However, patients with a history of AUDs and specific types of surgery were more likely to have post-surgical AUDs. The authors themselves acknowledge that the precision of their study is limited by the small number of patients included ( n = 51). The validity might have been compromised by a low response rate (11–22%), which potentially introduced bias to their study. According to structured clinical diagnostic interviews of 200 patients up to three years after a RYGB, eight percent developed an AUD and almost half of these patients had no pre-surgical history of AUDs [ 12 ]. Similar results were reported for other addictive disorders covered by the interviews. Also, when comparing pre- and post-surgical prevalence rates of high-risk drinking according to the AUDIT-C instrument, Wong et al. [ 28 ] reported an almost two times higher proportion of affected patients one year after surgery (23% vs. 13%). Another recently published study investigating AUDs in patients after bariatric surgery by using the AUDIT-C was conducted by White et al. [ 34 ]. Based upon a multicenter prospective cohort study on 217 adolescent patients (aged 13—19 years) undergoing BS, the authors concluded that nearly half of all patients screened positive for AUDs during the follow-up of up to eight years. While this study is among the few covering a longer observation period, these findings are difficult to align with ours due to the different age ranges under study. However, especially regarding the age range covered by White and colleagues, which is of high public health relevance, these findings are important and point out to further studies.
We found higher rates of AUDs in patients whose surgery had occurred a longer time ago compared with patients with a shorter post-surgical history. While this finding has to be treated with caution since longer observation periods per se allow a higher cumulative incidence, this result is consistent with several studies suggesting a slow rather than a rapid development of AUDs over several years after surgery, putting emphasis on the need for long-term follow-up and care. For instance, results from a previously published multicenter cohort study covering two thousand patients after BS and a maximum follow-up of seven years [ 9 ], prevalence of substance disorders, including AUDs, ranged between 7% at baseline and up to 16% seven years after surgery. Notably, the prevalence as well as the cumulative incidence of AUDs varied by type of bariatric intervention and AUDs were more than twice as high for patients with RYGB as for patients with gastric banding. Again, no data were available for patients with sleeve gastrectomy, as at the time of study conduction this intervention was less common than it is today. As more than 40% of our patients had this type of intervention, our study provides further insights.
However, while the aforementioned studies generally suggest a steady increase in AUDs after surgery, there is also evidence of a more uneven or even reversible course. Wee et al. [ 35 ] presented findings from a multicenter study on 375 patients with a post-surgical follow-up of two years. In addition to a proportion of 7% of patients with incident high-risk drinking, more than half of patients with pre-surgical high-risk drinking discontinued this behavior after surgery. Similarly, findings from a re-analysis of ten studies on the risk of post-surgical AUDs demonstrated an increased risk from the third year on but not during the first two years after surgery [ 13 ]. However, these findings warrant caution as the majority of the considered studies included comparably fewer participants (eight studies covered 800 patients or fewer), had shorter durations (three years or less in six studies) or offered cross-sectional data only (four studies). The authors emphasize the need for long-term investigations to determine if there is a true increase in AUD prevalence in the context of BS. Similarly, Sen et al. [ 36 ] investigated the post-bariatric risk of AUDs as estimated with AUDIT in 183 patients up to 6 years after sleeve gastrectomy and reported a reduction in AUDIT scores in the first 3-year follow-up and an increase in the 4–6-year follow-up. Therefore, regarding the sample size and the long-term follow-up in our study, our data might contribute to these findings. In this regard, it is a limitation that we used the AUDIT screening only once after surgery. Thus, we could not determine a change of drinking patterns with this instrument. However, with all due caution the results from the health claims data discussed earlier might hint at an increasing rather than a declining trend.
We found increased health care resource utilization in patients with risky drinking, even in those patients who showed hazardous consumption but not (yet) alcohol dependency. This held true for the number of hospitalizations as well as for the number of inpatient days. Interestingly, for both measures, these differences only emerged from the second year after surgery, but not during the first year or before. This supports the previously mentioned studies, which suggest a slow rather than an immediate development of AUDs. It is important to note that these differences in our data cannot be explained by higher comorbidities. Although some obesity-related comorbidities (e.g. hypertension, diabetes) were less frequent after surgery than before, the comorbidities between patients with low-risk consumption and hazardous alcohol consumption/AUDs were largely comparable at both points in time. This was true with the exception of smoking and treatment with antidepressants, which can be explained by a higher association of AUDs with depressive disorders and which has been reported in the literature [ 37 ]. Against this background, it is noteworthy that according to health claims data, patients with AUDs do not appear to receive or seek psychotherapy more often than patients without. Undertreatment of AUDs, although already a known problem [ 38 ], would be of particular concern in this patient population for whom close follow-up care is indicated. However, in the questionnaire, patients with AUDs reported being treated by psychiatrists or psychotherapists more often. This obvious contradiction in our data cannot be satisfactorily resolved. It is not unlikely that laypersons do not know the difference between psychiatrists and psychotherapists. However, since in Germany, the services of both professions can be reimbursed equally by statutory health insurance providers, this unawareness would not explain the difference.
This study was the first to investigate AUDs in patients after BS using survey data and health claims data from the same study population. In addition to the long post-surgical period of up to twelve years, the large sample size also facilitated stratification by sex, enabling us to investigate AUDs in male patients also. This is important, since on the one hand, women with BS surgery clearly outrank men in sample size in most studies, while on the other hand in most populations, alcohol-related disorders are more common in men. Moreover, the use of health claims data—available from each patient irrespective of survey response status—also allowed us to assess whether non-responders and responders differed in terms of sociodemographic and clinical parameters, which was not the case [ 17 ]. It can therefore be assumed that the problem of responder bias, which occurs very frequently in field studies, was considerably lower in this study. In addition to the need for caution in the interpretation of our health claims data, as already discussed, a further limitation is that only the F-diagnoses were used. We did not use diagnoses that indicate consequences of AUDs or severe drinking (e.g. fat liver, liver cirrhosis). Furthermore, it can generally be assumed that the extent of alcohol disorders is significantly underestimated in both data sources: only cases of diagnosed AUDs are documented in the health claims data, while clinically significant but not yet full-blown AUDs cannot be identified here. In the survey data, an underestimation can occur due to untrue statements about drinking behavior on the part of the participant and/or a lack of understanding of the “drinking units” as queried in the AUDIT. Against this background, the prevalences we found must be critically scrutinized. This also holds true as the standard cut-off score of the AUDIT might underestimate the true prevalence since it has not been validated for this specific population, which might require lower cut-off recommendations due to altered metabolism of alcohol. Another methodological limitation stems from the gap of at least three years between BS and the survey, as only patients with BS between 2004 and 2018 could be included, but the survey was conducted in 2021. Therefore, it is not possible to use the AUDIT to infer drinking patterns during the first two years after surgery. However, in the context of previous research, we estimate this limitation to be minor because, as discussed earlier, many studies already considered the early years after surgery.
In conclusion, the proportion of patients with BS and with alcohol disorders gives rise to concern as alcohol consumption should be restricted after BS. The results suggest the necessity for close monitoring and post-surgical care.
Data availability
As we are not the owners of the data we are not legally entitled to grant access to the data of the German Pharmacoepidemiological Research Database. In accordance with German data protection regulations, access to the data is granted only to employees of the Leibniz Institute for Prevention Research and Epidemiology—BIPS on the BIPS premises and in the context of approved research projects. Third parties may only access the data in cooperation with BIPS and after signing an agreement for guest researchers at BIPS.
Barry D, Clarke M, Petry NM. Obesity and its relationship to addictions: is overeating a form of addictive behavior? Am J Addict. 2009;18:439–51.
Article PubMed PubMed Central Google Scholar
Tomasi D, Volkow ND. Striatocortical pathway dysfunction in addiction and obesity: differences and similarities. Crit Revs Biochem Mol Biol. 2013;48:1–19.
Article CAS Google Scholar
White GE, Richardson GA, Mair C, Courcoulas AP, King WC. Do associations between alcohol use and alcohol use disorder vary by weight status? results from the national epidemiologic survey on alcohol and related conditions-III. Alcohol (NY). 2019;43:1498–509.
Article Google Scholar
Hagedorn JC, Encarnacion B, Brat GA, Morton JM. Does gastric bypass alter alcohol metabolism? Surg Obes Relat Dis. 2007;3:543–48.
Article PubMed Google Scholar
Pepino MY, Okunade AL, Eagon JC, Bartholow BD, Bucholz K, Klein SL. Effect of Roux-en-Y gastric bypass surgery: converting 2 alcoholic drinks to 4. JAMA Surg. 2015;150:1096–98.
Woodard GA, Downey J, Hernandez-Boussard T, Morton JM. Impaired alcohol metabolism after gastric bypass surgery: a case-crossover trial. J Am Coll Surg. 2011;212:209–14.
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures-2019 update: Cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis. 2020;16:175–247.
Heinberg LJ, Ashton K, Coughlin J. Alcohol and bariatric surgery: review and suggested recommendations for assessment and management. Surg Obes Relat Dis. 2012;8:357–63.
King WC, Chen JY, Courcoulas AP, Dakin GF, Engel SG, Flum DR, et al. Alcohol and other substance use after bariatric surgery: Prospective evidence from a US multicenter cohort study. Surg Obes Relat Dis. 2017;13:1392–404.
Svensson PA, Peltonen M, Andersson-Assarsson JC, Ahlin S, Brembeck P, Engström M, et al. Non-alcohol substance use disorder after bariatric surgery in the prospective, controlled Swedish Obese Subjects study. Obesity. 2023;31:2171–77.
Article CAS PubMed Google Scholar
Li LL, Wu LT. Substance use after bariatric surgery: a review. J Psychiatr Res. 2016;76:16–29.
Mitchell JE, Steffen K, Engel S, King WC, Chen JY, Winters K, et al. Addictive disorders after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2015;11:897–905.
Azam H, Shahrestani S, Phan K. Alcohol use disorders before and after bariatric surgery: a systematic review and meta-analysis. Ann Transl Med. 2018;6:148.
Spadola CE, Wagner EF, Dillon FR, Trepka MJ, De la Cruz-Munoz N, Messiah SE. Alcohol and drug use among postoperative bariatric patients: A systematic review of the emerging research and its implications. Alcohol (NY). 2015;39:1582–601.
Strommen M, Bakken IJ, Klockner C, Sandvik J, Kulseng B, Holen A. Diagnoses related to abuse of alcohol and addictive substances after gastric bypass and sleeve gastrectomy: A nation-wide registry study from Norway. Surg Obes Relat Dis. 2020;16:464–70.
Mellinger JL, Shedden K, Winder GS, Fernandez AC, Lee BP, Waljee J, et al. Bariatric surgery and the risk of alcohol-related cirrhosis and alcohol misuse. Liver Int. 2021;41:1012–19.
Article CAS PubMed PubMed Central Google Scholar
Riedel O, Braitmaier M, Dankhoff M, Hornschuch M, Klein M, Zachariassen W, et al. Quality of life in bariatric patients up to twelve years after surgery – Results from a nationwide retrospective cohort study. Obes Res Clin Pr. 2023;17:353–60.
Haug U, Schink T German Pharmacoepidemiological Research Database (GePaRD), in Databases for Pharmacoepidemiological Research. Edited by Sturkenboom M,Schink T Cham, Switzerland, Springer, 2021.
Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire - Choosing a cutoff score. Addiction. 1995;90:1349–56.
Rumpf HJ, Wohlert T, Freyer-Adam J, Grothues J, Bischof G. Screening questionnaires for problem drinking in adolescents: Performance of AUDIT, AUDIT-C, CRAFFT and POSIT. Eur Addict Res. 2013;19:121–7.
Schröder H, Brückner G, Schüssel K, Breitkreuz J, Schlotmann A & Günster C Monitor: Vorerkrankungen mit erhöhtem Risiko für schwere COVID-19-Verläufe. Verbreitung in der Bevölkerung Deutschlands und seinen Regionen, Berlin, 2020.
Greenland S, Senn SJ, Rothman KJ, Carlin JB, Poole C, Goodman SN, et al. Statistical tests, P values, confidence intervals, and power: A guide to misinterpretations. Eur J Epidemiol. 2016;31:337–50.
Lash T. The harm done to reproducibility by the culture of null hypothesis significance testing. Am J Epidemiol. 2017;186:627–35.
Ludwig DA. Use and misuse of p-values in designed and observational studies: guide for researchers and reviewers. Aviat Space Environ Med. 2005;76:675–80.
PubMed Google Scholar
Bischof G, Reinhardt S, Grothues J, Dybek I, Meyer C, Hapke U, et al. Effects of item sequence on the performance of the AUDIT in general practices. Drug Alcohol Depend. 2005;79:373–7.
Källmen H, Wennberg P, Leifman H, Bergman H, Berman AH. Alcohol habits in Sweden during 1997–2009 with particular focus on 2005 and 2009, assessed with the AUDIT: A repeated cross-sectional study. Eur Addict Res. 2011;17:90–6.
Mitchell JE, Lancaster KL, Burgard MA, Howell LM, Krahn DD, Crosby RD, et al. Long-term follow-up of patients’ status after gastric bypass. Obes Surg. 2001;11:464–8.
Wong E, Fleishman A, Brem A, Jones DB, Wee CC. High-risk alcohol use and disordered eating behavior before and 1 year after sleeve gastrectomy. Obes Surg. 2022;32:593–8.
Jacobi F, Hofler M, Siegert J, Mack S, Gerschler A, Scholl L, et al. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: The Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH). Int J Methods Psychiatr Res. 2014;23:304–19.
Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jonsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655–79.
Vides MC, Campello de Oliveira M, Lassi DLS, Malbergier A, Florio L, de Azevedo-Marques Périco C, et al. Bariatric surgery and its influence on alcohol consumption: Differences before and after surgery - A systematic review and meta-analysis. Int Rev Psychiatry. 2023;35:367–76.
Svensson PA, Anveden A, Romeo S, Peltonen M, Ahlin S, Burza MA, et al. Alcohol consumption and alcohol problems after bariatric surgery in the Swedish Obese Subjects study. Obesity. 2013;21:2444–51.
Suzuki J, Haimovici F, Chang G. Alcohol use disorders after bariatric surgery. Obes Surg. 2012;22:201–7.
White GE, Boles RE, Courcoulas AP, Yanovski SZ, Zeller MH, Jenkins TM, et al. A prospective cohort of alcohol use and alcohol-related problems before and after metabolic and bariatric surgery in adolescents. Ann Surg. 2023;278:E519–25.
Wee CC, Mukamal KJ, Huskey KW, Davis RB, Colten ME, Bolcic-Jankovic D, et al. High-risk alcohol use after weight loss surgery. Surg Obes Relat Dis. 2014;10:508–13.
Sen O, Unubol H, Turkcapar AG, Yerdel MA. Risk of alcohol use disorder after sleeve gastrectomy. J Laparoendosc Adv Surg Tech. 2021;31:24–8.
Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abus Treat. 2009;37:127–37.
Carvalho AF, Heilig M, Perez A, Probst C, Rehm J. Alcohol use disorders. Lancet. 2019;394:781–92.
Download references
Acknowledgements
We would like to thank the statutory health insurance provider DAK-Gesundheit which provided data for this study. The authors would also like to thank Dr. Heike Gerds for proof-reading the manuscript.
The underlying study (“ABARO”) was funded by the German Innovation Fund (grant number: 01VSF19045). The sponsor was neither involved in the design of the study nor in the collection, analysis or interpretation pf data, nor in the writing of the manuscript or in the decision to submit it for publication. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Leibniz Institute for Prevention Research and Epidemiology—BIPS, Bremen, Germany
Oliver Riedel, Malte Braitmaier & Ulrike Haug
Hamburg, Germany
Mark Dankhoff
University of Bremen, Faculty of Human and Health Sciences, Bremen, Germany
Ulrike Haug
DAK Gesundheit, Hamburg, Germany
Melanie Klein & Wiebke Zachariassen
Adipositas-Zentrum, Städtisches Klinikum Dresden, Dresden, Germany
You can also search for this author in PubMed Google Scholar
Contributions
OR and JH wrote the first draft of the manuscript and conceptualized the statistical analyses. MB conducted the statistical analyses including sensitivity analyses and reviewed the draft of the manuscript. MD, MK, UH and WZ reviewed the draft of the manuscript and provided critique.
Corresponding author
Correspondence to Oliver Riedel .
Ethics declarations
Competing interests.
OR, MB and UH are working at an independent, non-profit research institute, the Leibniz Institute for Prevention Research and Epidemiology—BIPS. Unrelated to this study, BIPS occasionally conducts studies financed by the pharmaceutical industry. Almost exclusively, these are post-authorization safety studies (PASS) requested by health authorities. The design and conduct of these studies as well as the interpretation and publication are not influenced by the pharmaceutical industry. The study presented was not funded by the pharmaceutical industry and was performed in line with the ENCePP Code of Conduct. All authors declare no conflict of interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, suppl table s1, suppl table s2, suppl table s3, suppl figure s1, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Riedel, O., Braitmaier, M., Dankhoff, M. et al. Alcohol use disorders after bariatric surgery: a study using linked health claims and survey data. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01606-3
Download citation
Received : 12 April 2024
Accepted : 07 August 2024
Published : 06 September 2024
DOI : https://doi.org/10.1038/s41366-024-01606-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Facts About Aging and Alcohol
On this page:
The effects of alcohol change as we age
How does drinking damage the body, cautions about mixing alcohol and medicines, how alcohol affects safety, what are signs of alcohol misuse or alcohol use disorder, getting the help you need for alcohol misuse or alcohol use disorder, strategies to help cut back or quit drinking, learn your patterns and plan ahead.
Many people enjoy an alcoholic beverage or two on occasion with friends or family, but alcohol can be addictive. As we age, alcohol consumption can also make existing health problems worse and have dangerous interactions with some medications. Anyone at any age can develop an unhealthy reliance on alcohol.

Sometimes, families, friends, and health care workers may overlook the concerns about older people drinking. This can be the case because the side effects of drinking in older adults are mistaken for other conditions related to aging, for example, a problem with balance. But how the body handles alcohol changes with age.
As you grow older, health problems or prescribed medicines may require that you drink less alcohol or avoid it completely. You may also notice that your body’s reaction to alcohol is different than before. Some older people feel the effects of alcohol more strongly without increasing the amount they drink. This can make them more likely to have accidents such as falls, fractures, and car crashes. Also, older women are more sensitive than men to the effects of alcohol.
Other people develop a harmful reliance on alcohol later in life. Sometimes this is a result of major life changes, such as the death of a spouse or other loved one, moving to a new home, or failing health. These kinds of changes can cause loneliness, boredom, anxiety, or depression. In fact, depression in older adults often aligns with drinking too much.
People who drink daily do not necessarily have alcohol use disorder . And not all who misuse alcohol or have alcohol use disorder drink every day. But heavy drinking, even occasionally, can have harmful effects.
Drinking too much at one time or on any given day, or having too many drinks over the course of a week, increases the risk of harmful consequences, including injuries and health problems. People who consistently misuse alcohol over time are also at greater risk of developing alcohol use disorder.
Drinking too much alcohol over a long time can:
- Lead to some kinds of cancer, liver damage, immune system disorders, and brain damage
- Worsen some health conditions such as osteoporosis, diabetes, high blood pressure, stroke, ulcers, memory loss, and mood disorders
- Make some medical conditions hard for doctors to accurately diagnose and treat. For example, alcohol causes changes in the heart and blood vessels. These changes can dull pain that might be a warning sign of a heart attack.
- Cause some older people to be forgetful and confused — symptoms that could be mistaken for signs of Alzheimer’s disease or a related dementia.
Many medicines — prescription, over the counter, or herbal remedies — can be dangerous or even deadly when mixed with alcohol. Many older people take medications every day, making this a particular concern.
Before taking any medicine, ask your doctor or pharmacist if you can safely drink alcohol. Here are some examples of potential dangers caused by mixing alcohol with some medicines:
- If you take aspirin and drink, your risk of stomach or intestinal bleeding increases.
- When combined with alcohol, cold and allergy medicines (antihistamines) may make you feel very sleepy.
- Alcohol used with large doses of acetaminophen, a common painkiller, may cause liver damage.
- Some medicines, such as cough syrups and laxatives, have a high alcohol content. If you simultaneously drink alcohol, that will add to the effects.
- Alcohol used with some sleeping pills, pain pills, or anxiety/anti-depression medicine can be deadly.
Learn more about mixing alcohol with medicines .
Drinking even a small amount of alcohol can lead to dangerous or even deadly situations because it can impair a person’s judgment, coordination, and reaction time. This increases the risk of falls, car crashes, and other accidents.
Alcohol is a factor in about 30% of suicides and fatal motor vehicle crashes, 40% of fatal burn injuries, 50% of fatal drownings and homicides, and 65% of fatal falls. People should not drink alcohol if they plan to drive, use machinery, or perform other activities that require attention, skill, or coordination.
In older adults, especially, too much alcohol can lead to balance problems and falls , which can result in hip or arm fractures and other injuries. Older people have thinner bones than younger people, so their bones break more easily. Studies show that the rate of various types of fractures in older adults increases with heavy alcohol use.
Adults of all ages who drink alcohol and drive are at higher risk of traffic accidents than those who do not drink. Drinking slows reaction times and coordination, and interferes with eye movement and information processing. People who drink even a moderate amount are at higher risk for traffic accidents, possibly resulting in injury or death to themselves and others. (Note that even without alcohol, the risk of a car accident goes up starting at age 55.) Also, older drivers tend to be more seriously hurt in crashes than younger drivers. Alcohol adds to these age-related risks.
In addition, alcohol misuse or alcohol use disorder can strain relationships with family members, friends, and others. At the extreme, heavy drinking can contribute to domestic violence and child abuse or neglect. Alcohol use is often involved when people become violent, as well as when they are violently attacked. If you feel that alcohol is endangering you or someone else, call 911 or obtain similar help right away.
Alcohol misuse or alcohol use disorder is a pattern of drinking that can cause harm to a person’s health and social relationships. Drinking too much at one time or on any given day or having too many drinks over the course of a week increases the risk of harmful consequences, including injuries and health problems. Men should not have more than two drinks a day and women only one. Drinking less alcohol is better for health than drinking more.
The definition of “one drink” means:
- One 12-ounce can or bottle of regular beer, ale, or hard seltzer
- One 8- or 9-ounce can or bottle of malt liquor
- One 5-ounce glass of red or white wine
- One 1.5-ounce shot glass of 80-proof distilled spirits like gin, rum, tequila, vodka, or whiskey.
Understanding these “standard” drink sizes can make it easier to follow health guidelines. Another thing to keep in mind is that drinks may be stronger than you think they are if the actual serving sizes are larger than the standard sizes. In addition, drinks within the same beverage category, such as beer, can contain different percentages of alcohol. It’s important to read the label to understand and be aware of how much you’re actually drinking.
Some people have no trouble cutting back on their drinking. But others will need to stop drinking completely. Alcohol problems can happen to people from all walks of life at any age, and, each year, millions of people seek help for alcohol problems.

If you or someone you love is thinking of changing their habits around alcohol, the “Rethinking Drinking” website , hosted by NIH’s National Institute on Alcohol Abuse and Alcoholism (NIAAA), provides information on signs of a problem and tools that can help lead to better health.
Making a change in your drinking habits can be hard. Don’t give up! If you don’t reach your goal the first time, try again. The good news is you’re not in this alone. Don’t be afraid to talk with a doctor and ask your family and friends for help. Here are some approaches to try to get started:
- Ask your doctor about advances in medication that might help you stick with alcohol abstinence longer or reduce cravings. Your health care professional may also be able to give you advice about treatment .
- Talk to a trained counselor who knows about alcohol problems in older people.
- Find a support group for older people with alcohol problems. Many people find group counseling sessions or meetings helpful.
- Choose individual, family, or group therapy, depending on what works for you.
- Check out an organization such as Alcoholics Anonymous that offers support and programs for people who want to stop drinking.
- Consider websites or mobile applications that can help you track your alcohol intake and offer positive support as you make progress toward your goals.
Many older adults decide to quit drinking in later life. You can do it, too. Here are some ways to cut back or stop drinking:
- Count how many ounces of alcohol you are getting in each drink.
- Keep track of the number of drinks you have each day.
- Decide how many days a week you want to drink. Plan some days that are free of alcohol.
- In place of alcohol, try drinking water, juice, or soda. You could also try nonalcoholic “mocktails” or low-alcohol beer.
- Remove alcohol from your home.
- Ask for support from your family and advice from your health care provider. Get the help you need to cut back or quit.
As you evaluate your alcohol use, you may find that you drink more often in particular settings or in reaction to certain emotions, such as stress or boredom. Take time to learn about your habits and plan ahead on ways to make a change. Here are some ideas:
- Develop interests that don’t involve alcohol.
- Avoid people, places, and situations that may trigger your drinking.
- Avoid drinking when you’re angry or upset or if you’ve had a bad day.
- Plan what you will do if you have an urge to drink.
- Learn to say “no, thanks” when you’re offered an alcoholic drink.
- Remember to stay healthy for the fun things in life, such as the birth of a grandchild, a long-anticipated trip, or a holiday party.
Your body changes as you get older and that can affect daily routines. Be alert to these changes and think about adjusting your alcohol use so you can enjoy your life to the fullest.
Learn more about available types of alcohol treatment .
To find alcohol treatment for yourself or a loved one, visit the NIAAA Alcohol Treatment Navigator .
You may also be interested in
- Finding out how to help someone you know who drinks too much
- Getting tips for talking with your doctor about sensitive issues
- Learning ways to take care of your cognitive health
Sign up for email updates on healthy aging
For more information about alcohol use and safety.
National Institute on Alcohol Abuse and Alcoholism National Institutes of Health 888-696-4222 [email protected] www.niaaa.nih.gov
Rethinking Drinking: Alcohol and Your Health www.rethinkingdrinking.niaaa.nih.gov
Substance Abuse and Mental Health Services Administration 877-726-4727 800-487-4889 (TTY) [email protected] www.samhsa.gov
Alcoholics Anonymous 212-870-3400 www.aa.org
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
Content reviewed: July 19, 2022
nia.nih.gov
An official website of the National Institutes of Health

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Cannabis and hallucinogen use among adults remained at historic highs in 2023
Vaping among younger adults and binge drinking among mid-life adults also maintained historically high levels, NIH-supported study shows

Past-year use of cannabis and hallucinogens stayed at historically high levels in 2023 among adults aged 19 to 30 and 35 to 50, according to the latest findings from the Monitoring the Future survey . In contrast, past-year use of cigarettes remained at historically low levels in both adult groups. Past-month and daily alcohol use continued a decade-long decline among those 19 to 30 years old, with binge drinking reaching all-time lows. However, among 35- to 50-year-olds, the prevalence of binge drinking in 2023 increased from five and 10 years ago. The Monitoring the Future study is conducted by scientists at the University of Michigan’s Institute for Social Research, Ann Arbor, and is funded by the National Institutes of Health.
Reports of vaping nicotine or vaping cannabis in the past year among adults 19 to 30 rose over five years, and both trends remained at record highs in 2023. Among adults 35 to 50, the prevalences of nicotine vaping and of cannabis vaping stayed steady from the year before, with long-term (five and 10 year) trends not yet observable in this age group as this question was added to the survey for this age group in 2019.
For the first time in 2023, 19- to 30-year-old female respondents reported a higher prevalence of past-year cannabis use than male respondents in the same age group, reflecting a reversal of the gap between sexes. Conversely, male respondents 35 to 50 years old maintained a higher prevalence of past-year cannabis use than female respondents of the same age group, consistent with what’s been observed for the past decade.
“We have seen that people at different stages of adulthood are trending toward use of drugs like cannabis and psychedelics and away from tobacco cigarettes,” said Nora D. Volkow, M.D., director of NIH’s National Institute on Drug Abuse (NIDA). “These findings underscore the urgent need for rigorous research on the potential risks and benefits of cannabis and hallucinogens – especially as new products continue to emerge.”
Since 1975, the Monitoring the Future study has annually surveyed substance use behaviors and attitudes among a nationally representative sample of teens. A longitudinal panel study component of Monitoring the Future conducts follow-up surveys on a subset of these participants (now totaling approximately 20,000 people per year), collecting data from individuals every other year from ages 19 to 30 and every five years after the participants turn 30 to track their drug use through adulthood. Participants self-report their drug use behaviors across various time periods, including lifetime, past year (12 months), past month (30 days), and other use frequencies depending on the substance type. Data for the 2023 panel study were collected via online and paper surveys from April 2023 through October 2023.
Full data summaries and data tables showing the trends below, including breakdowns by substance, are available in the report . Key findings include:
Cannabis use in the past year and past month remained at historically high levels for both adult age groups in 2023. Among adults 19 to 30 years old, approximately 42% reported cannabis use in the past year, 29% in the past month, and 10% daily use (use on 20 or more occasions in the past 30 days). Among adults 35 to 50, reports of use reached 29%, 19%, and 8%, respectively. While these 2023 estimates are not statistically different from those of 2022, they do reflect five- and 10-year increases for both age groups.
Cannabis vaping in the past year and past month was reported by 22% and 14% of adults 19 to 30, respectively, and by 9% and 6% of adults 35 to 50 in 2023. For the younger group, these numbers represent all-time study highs and an increase from five years ago.
Nicotine vaping among adults 19 to 30 maintained historic highs in 2023. Reports of past-year and past-month vaping of nicotine reached 25% and 19%, respectively. These percentages represent an increase from five years ago, but not from one year ago. For adults 35 to 50, the prevalence of vaping nicotine remained steady from the year before (2022), with 7% and 5% reporting past-year and past-month use.
Hallucinogen use in the past year continued a five-year steep incline for both adult groups, reaching 9% for adults 19 to 30 and 4% for adults 35 to 50 in 2023. Types of hallucinogens reported by participants included LSD, mescaline, peyote, shrooms or psilocybin, and PCP.
Alcohol remains the most used substance reported among adults in the study. Past-year alcohol use among adults 19 to 30 has showed a slight upward trend over the past five years, with 84% reporting use in 2023. However, past month drinking (65%), daily drinking (4%), and binge drinking (27%) all remained at study lows in 2023 among adults 19 to 30. These numbers have decreased from 10 years ago. Past-month drinking and binge drinking (having five or more drinks in a row in the past two week period) decreased significantly from the year before for this age group (down from 68% for past month and 31% for binge drinking reported in 2022).
Around 84% of adults 35 to 50 reported past-year alcohol use in 2023, which has not significantly changed from the year before or the past five or 10 years. Past-month alcohol use and binge drinking have slightly increased over the past 10 years for this age group; in 2023, past-month alcohol use was at 69% and binge drinking was at 27%. Daily drinking has decreased in this group over the past five years and was at its lowest level ever recorded in 2023 (8%).
Additional data: In 2023, past-month cigarette smoking, past-year nonmedical use of prescription drugs, and past-year use of opioid medications (surveyed as “narcotics other than heroin”) maintained five- and 10-year declines for both adult groups. Among adults 19 to 30 years old, past-year use of stimulants (surveyed as “amphetamines”) has decreased for the past decade, whereas for adults 35 to 50, past-year stimulant use has been modestly increasing over 10 years. Additional data include drug use reported by college/non-college young adults and among various demographic subgroups, including sex and gender and race and ethnicity.
The 2023 survey year was the first time a cohort from the Monitoring the Future study reached 65 years of age; therefore, trends for the 55- to 65-year-old age group are not yet available.
“The data from 2023 did not show us many significant changes from the year before, but the power of surveys such as Monitoring the Future is to see the ebb and flow of various substance use trends over the longer term,” said Megan Patrick, Ph.D., of the University of Michigan and principal investigator of the Monitoring the Future panel study. “As more and more of our original cohorts – first recruited as teens – now enter later adulthood, we will be able to examine the patterns and effects of drug use throughout the life course. In the coming years, this study will provide crucial data on substance use trends and health consequences among older populations, when people may be entering retirement and other new chapters of their lives.”
View more information on data collection methods for the Monitoring the Future panel study and how the survey adjusts for the effects of potential exclusions in the report . Results from the related 2023 Monitoring the Future study of substance use behaviors and related attitudes among teens in the United States were released in December 2023, and 2024 results are upcoming in December 2024.
If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat at 988lifeline.org . To learn how to get support for mental health, drug or alcohol conditions visit FindSupport.gov . If you are ready to locate a treatment facility or provider, you can go directly to FindTreatment.gov or call 800-662-HELP (4357) .
About the National Institute on Drug Abuse (NIDA): NIDA is a component of the National Institutes of Health, U.S. Department of Health and Human Services. NIDA supports most of the world’s research on the health aspects of drug use and addiction. The Institute carries out a large variety of programs to inform policy, improve practice, and advance addiction science. For more information about NIDA and its programs, visit www.nida.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
About substance use disorders: Substance use disorders are chronic, treatable conditions from which people can recover. In 2022, nearly 49 million people in the United States had at least one substance use disorder. Substance use disorders are defined in part by continued use of substances despite negative consequences. They are also relapsing conditions, in which periods of abstinence (not using substances) can be followed by a return to use. Stigma can make individuals with substance use disorders less likely to seek treatment. Using preferred language can help accurately report on substance use and addiction. View NIDA’s online guide .
NIH…Turning Discovery Into Health®
Related Articles

Doctors reluctant to treat addiction most commonly report “lack of institutional support” as barrier

Reported drug use among adolescents continued to hold below pre-pandemic levels in 2023

Heart medication shows potential as treatment for alcohol use disorder
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(10); 2022 Oct

Effects of Alcohol Consumption on Various Systems of the Human Body: A Systematic Review
Jerin varghese.
1 Medical School, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Sarika Dakhode
2 Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Prolonged alcohol intake for many years has been known to cause serious ailments in human beings since time memorial. Even after knowing that this dangerous addiction paves the way to one’s own grave, there isn’t much difference in the way the community sees this deadly habit. Time and again history has proven that this fatal addiction could make the life of those who consume it terrible. Also, the lives of the dear ones of alcoholic people are affected as alcohol not only affects those who consume them but also kin and friends. Various research studies conducted over many years clearly show the association of prolonged alcohol intake in the causation, aggravation, worsening, and deterioration of the health of its consumers. Moreover, chronic alcohol intake single-handedly is one of the major etiological factors in various serious diseases.
Introduction and background
Through the ages, alcoholism has been undisputedly maintaining its position in the list of risk factors for preventable diseases in the world. According to a WHO report, 5.3% of all deaths that occurred worldwide in the year 2016 were because of harmful alcohol use [ 1 ]. It is the main culprit behind the advancing nature of many chronic diseases. It drastically increases the severity of diseases and also makes the treatments less effective. Alcohol not only affects the person physiologically, but it has many adverse effects psychologically and socially too. Also, the habit of alcoholism leads to huge expenses [ 2 ]. Apart from systemic involvement, which causes various clinical manifestations, there are certain signs and symptoms that are most of the times non-specific and that as such don’t point out or say lead to a particular diagnosis, such as nausea, agitation, vomiting, anxiety, diaphoresis, tremors, headache, visual hallucinations, tachycardia, seizures, delirium, temperature elevation, etc. It is not always necessary that these mentioned signs and symptoms are compulsorily linked with disease conditions.
Alcohol clearly plays a very important role in making many other diseases progress to their advanced stages. It has been also noted that alcohol intake and its related disorders are often associated with many other manifestations; for example, patients with alcoholic neuropathy often have associated nutritional deficiencies. Recent studies have clearly proved that alcoholism is associated with many types of cancers too and this understanding of alcoholism has spurred research minds all over the globe to find out the exact pathophysiology behind the same. Alcohol is a very easily available source of addiction, which is one of the main reasons why it remains a serious threat to the community. There is a huge variety that is available as far as alcoholic drinks are concerned. Alcohol is also one of the cheaply accessible means of addiction; this explains why alcoholism is so prevalent. A person may initially start consuming alcohol in very low amounts most probably with just a desire to try it, but once he or she gets addicted, then getting rid of the habit becomes extremely difficult. Even if a person is mentally resolute enough to quit alcoholism, his or her body, which has been modified because of the chronic use of alcohol, won’t be up to the challenge anytime soon; he or she has to overcome many hurdles put forward by the body, which could in an umbrella term be referred to as alcohol withdrawal syndrome.
There are many social stigmas associated with alcohol intake. Most people get into this addiction by getting inspired by the people whom they admire, like actors, celebrities, role models, etc. Also, exposure to the sight of family members, relatives and friends drinking alcohol has a huge impact on one’s mindset as he or she may take it to be something that is normal. In the long run, most of the time, even without their realization, people get pathetically trapped in this dangerous fatal habit of alcoholism, which eventually makes their lives pitiful in almost all aspects. Studies have shown that alcohol is also a key player in many other domains too like accidents, suicide, depression, hallucinations, violence, memory disturbances, etc.
The main purpose of this review article is to enable any person reading this article to get a comprehensive insight into the effects of alcohol on the various systems of the human body, and for the same, many recognized research articles published in numerous well-acknowledged journals across the globe are reviewed. The article is written using very basic and simple terminologies so that even a layperson who reads it would be able to understand it. For the easy acceptability and understanding of the reader, the discussion is written in such a way that almost every major system is reviewed one by one and the effect of alcohol on these systems put forward in very simple language. The strategies used for the establishment of this review article are summarised in Figure Figure1; 1 ; these include considering research articles that have been published in journals with are indexed in reputed platforms, segregating articles according to the different systems, framing the review like a discussion section of an article where details are explained in simple and straight forward sentences, etc.

Impact of alcohol on the central nervous system (CNS)
Alcohol exerts various effects on our CNS in various ways, the common ones being depression of the CNS, destruction of the brain cells, contraction of the tissues of the brain, suppression of the excitatory nerve pathway activity, neuronal injury, etc [ 3 ]. Alcohol’s impact on the functioning of the brain ranges from mild and anxiolytic disinhibitory effects, motor incoordination, sedation, emesis, amnesia, hypnosis and ultimately unconsciousness [ 4 ]. The synaptic transmission is heavily disturbed and altered by ethanol, and the intrinsic excitability in various areas of the brain is also compromised. The effects of ethanol may be pre-synaptic, post-synaptic, and at times, non-synaptic too. Alcohol being a psychotropic depressant of the CNS exerts a deeply profound impact on the neurons, which alters the biological and behavioural well-being of the one who consumes it by the promotion of interference in various neuronal pathways [ 5 ]. The treatments of many disorders of the CNS are shown to be affected by the consumption of alcohol, and thus, it is generally advised to keep oneself away from alcohol if one is undergoing treatment for any CNS manifestations, like anxiety or mood disorders [ 6 ].
Alcohol use disorder (AUD) is chronic in nature and is characterized by uncontrolled drinking and also a preoccupation with alcohol. The severity of AUD is a crucial factor in how it is going to affect the human body. AUD can be mild, moderate, or severe according to the symptoms a person experiences. The clinical manifestations of AUD include signs and symptoms such as inability to control the amount of alcohol intake, spending a lot of time drinking, feeling an uncontrollable craving for alcohol, loss of interest in social activities, failure to fulfil tasks within the time provided, etc. Most of the time, along with the person who consumes alcohol, several other factors are also to be taken care of in order to effectively manage alcohol-related health conditions. These factors can be social, environmental, genetic, psychological, etc, which make a considerable impact on how alcohol affects the behaviour and body of those consuming it. Binge drinking, i.e., drinking to such an extent on a single occasion that the blood alcohol concentration level becomes 0.08% or more, is a very relevant aspect of alcohol intake, which has to be dealt with, with utmost urgency. Certain research studies suggest that mild to moderate alcohol intake provides a certain sort of protection against a few CNS disorders like dementia, ischemia of neurons, etc, but this in no way should encourage the community in promoting alcohol intake as in reality, it is very difficult to remain within the limits of mild to moderate alcohol intake, and thus, eventually, people do end up as full-time severe alcohol abusers. Epilepsy, a seizure disorder caused by disturbed nerve cell activity in the brain, aggravates on excessive alcohol intake as alcohol increases the frequency of seizures in patients of epilepsy [ 7 ]. The issue becomes more severe in those epileptic patients who have refractory forms of epilepsy. As far as comorbidities are concerned, a valid history of abuse of substances or alcohol dependence is believed to be strongly associated with a high risk of sudden unexpected death in epilepsy (SUDEP) [ 8 ]. Heavy alcohol drinking over a long period of time has been found to have an intensely negative undesirable effect on the autonomic nervous system too.
Impact of alcohol on the cardiovascular system (CVS)
Chronic alcohol intake is undoubtedly a very important risk factor as far as cardiovascular diseases are concerned and several clinical trials do point out this fact. The results of several research studies conducted in various settings clearly indicate that increased intake of alcohol has increased adverse effects on our heart and its vasculature. Alcohol exerts its action on the cardiovascular system both directly and indirectly. Blood pressure, a very vital player in the domain of cardiovascular diseases, is in turn itself affected by increased alcohol consumption. Blood pressure gets increased on regular consumption of alcohol in a manner which is dose-dependent, which in turn increases the risk of hypertension and eventually leads to various cardiovascular complications. How exactly alcohol causes hypertension is still unclear with many pathophysiological theories out there. Atrial fibrillation, one of the most common causes of arrhythmia, is associated with the high-volume chronic intake of alcohol and above 14 g alcohol/day, the relative risk dramatically increases by 10% for each extra standard drink (14 g ethanol) [ 9 ].
Cerebrovascular accidents are increased to a great extent at almost all levels of alcohol intake [ 10 ]. Alcohol intake leads to both acute (depresses the cardiac function and also alters the blood flow of the involved region) and chronic cardiovascular manifestations [ 11 ]. Alcohol abuse along with other associated factors is one of the leading causes of secondary cardiomyopathy [ 12 ]. Cardiac arrhythmias get precipitated by alcohol consumption, be it acute or chronic. Heavy alcohol drinking is shown to impact the cardiovascular system in many ways, one of the most important among them being rebound hypertension [ 13 ]. Apart from congenital disorders of the cardiovascular system, it indeed is a very well-evident fact, which could be understood from the history of most of the patients diagnosed with cardiovascular disorders, that they used to consume a lot of alcohol for many years.
Impact of alcohol on the digestive system
Chronic alcoholism is found to have a very strong relationship with both acute pancreatitis and chronic pancreatitis. Chronic alcohol intake impairs the repair ability of the structures of the exocrine pancreas, thereby leading to pancreatic dysfunctioning [ 14 ]. Most of the patients diagnosed with pancreatitis have a strong history of chronic intake of alcohol. Liver diseases related to alcohol intake are known to humankind from the very beginning and probably are one of the oldest known forms of injury to the liver [ 15 ]. In liver diseases linked with alcohol, liver cirrhosis is a major concern. Statistics show that liver cirrhosis is one of the top 10 causes of death worldwide and this in itself indicates the severity of the same [ 16 ]. The changing lifestyle and also many people turning to prolonged alcohol intake for many years are contributing to the increased number of liver cirrhosis patients in the modern world. In liver cirrhosis patients, there occurs an increased severity of fibrosis due to the loss of parenchyma and fibrous scar proliferation [ 17 ]. Alcoholic liver disease (ALD) is an umbrella term which incorporates a wide range of injuries of the liver, spanning from simple steatosis to cirrhosis, and this also includes alcohol-related fatty liver disease (AFLD) and also alcoholic hepatitis [ 18 ]. Advancements in the diagnostic modalities have helped to diagnose ALD at an early phase and there is no doubt that newer and better investigations that have helped to detect more cases have led to a surge in the number of ALD patients on whole. Alcohol intake has a prominently bigger impact on the mortality of liver cirrhosis when compared with the morbidity [ 19 ]. A systemic review and meta-analysis suggests that women might be at a higher risk as far as developing liver cirrhosis is concerned even with little consumption of alcohol, as compared to men [ 20 ].
Impact of alcohol on the causation of cancer
Alcohol has much to do with cancers too and continuous research studies are conducted in order to find out the relationship between the two in detail. In a meta-analysis, it was found that women consuming alcohol had a later menopause onset, which is found to be associated with reduced cardiovascular disease risk and also all-cause mortality, but unfortunately, the happiness of this advantage gets compromised by the ironic fact that it has an increased risk of cancer (including ovarian and breast cancers) [ 21 , 22 ]. Large cohort studies, many meta-analyses, experimental research studies, etc are suggestive of the fact that the chronic intake of alcohol clearly increases colon and gastric cancer risk [ 23 ]. A causal association is also found between alcohol intake and cancers of the rectum, colon, liver, oesophagus, larynx, pharynx and oral cavity [ 24 ]. There are various theories put forward so as to understand the role of the consumption of alcohol in the development of cancer; there is suspicion that the rise in the number of alcohol users worldwide may be one of the reasons why the number of cancer patients is increasing at a global level. Chronic intake of alcohol may promote the genesis of cancer in many ways, some of the most notable ones being acetaldehyde (weak mutagen and carcinogen) production, cytochrome P450 2E1 induction associated oxidative stress, S-adenosylmethionine depletion/ which leads to global DNA hypomethylation induction, iron induction associated oxidative stress, retinoic acid metabolism impairment, etc [ 25 ].
Impact of alcohol on other systems
Apart from the systemic manifestations which do affect a particular system of the body, there are various disorders in which alcohol indirectly provides its crucial contribution. It is a common finding that one could perceive that alcohol is most of the time in the list of risk factors for various diseases. Alcohol has been found to adversely affect our immune system and the matter of concern as far as this issue is concerned is that immune responses are influenced by even moderate amounts of alcohol intake [ 26 ]. Alcohol affects innate immunity and also interferes with almost all the various aspects of the adaptive immune response. Alcohol is a key player in impairing anti-inflammatory cytokines and also promotes proinflammatory immune responses. The gastrointestinal biome is severely manipulated by the use of alcohol over a long period of time, which in turn is found to have a link with the establishment of various complications [ 27 ]. Alcohol and its metabolites are found to promote inflammation in the intestines and they do so through varied pathways [ 28 ]. Alcohol being a teratogen is documented to cause abnormalities of the brain, limbs, etc [ 29 ]. Multiple studies have been conducted across the globe to understand the effect of alcohol on humans; implications from certain such studies are put forth in Table Table1 1 .
| Serial number | Objectives of the study | Type of study | Implications | Author, Country ( if applicable), Year [citations] |
| (1) | To provide a quantitative assessment of the association between the risk of cirrhosis of the liver and alcohol intake. | Systemic review and meta-analysis | Consumption of alcohol has a significantly large impact on the mortality of cirrhosis of the liver when compared with morbidity. | Rehm et al., July 2010 [ ]. |
| (2) | To systematically sum up the risk relationship between the incidence of liver cirrhosis and different alcohol consumption levels. | Systemic review and meta-analysis | Consuming about one drink per day in comparison to the long-term abstainers showed an increased risk in women for liver cirrhosis, but not in men. | Roerecke et al., October 2019 [ ]. |
| (3) | To analyse the impact of various drinking patterns in the causation of alcoholic cirrhosis of the liver. | A prospective cohort study | Recent alcohol consumption rather than earlier in life was found to be associated with a risk of alcoholic cirrhosis. | Askgaard et al., Denmark, May 2015 [ ]. |
| (4) | To investigate the relationship between the risk of colon and rectal cancer and the amount and type of alcohol. | Cohort study | Alcoholic intake significantly increases the risk of rectal cancer but this risk seems to be reduced with the inclusion of wine. | Pedersen et al., Denmark, June 2003 [ ]. |
| (5) | To examine the relationship between cancers of the upper digestive tract (oesophageal and oropharyngeal) and different types of alcoholic drinks. | Cohort study | A moderate wine intake does not probably increase the risk of cancer of the upper digestive tract, whereas a moderate intake of spirits or beers considerably increases the risk. | Grønbaek et al., Denmark, September 1998 [ ]. |
| (6) | To examine the relationship between death from all causes, coronary heart disease, and cancer and intake of different alcohol types. | Cohort study | Heavy drinkers who avoid wine are found to be at more high risk for death from all causes than heavy drinkers who do include wine in their alcohol intake. | Grønbaek et al., Denmark, September 2000 [ ]. |
| (7) | To investigate the long-term effects of the consumption of alcohol on morbidity and mortality. | Cohort study | The morbidity and mortality which is associated with different consumption levels of alcohol are associated with the same diseases, which suggests that alcohol might be one of the causative factors for these diseases. | Theobald et al., Sweden, November 2001 [ ]. |
| (8) | To provide updated quantification of association between the intake of alcohol intake and colorectal cancer. | Meta-analysis of the published observational studies | Showed evidence which strongly depicted an association between colorectal cancer risk and intake of alcohol. | Wang et al., May 2015 [ ]. |
| (9) | To investigate the association between atrial fibrillation risk in a prospective study of Swedish men and women and alcohol consumption. | Prospective study and a dose-response meta-analysis | Consumption of alcohol, even though at a moderate level, is one of the risk factors for atrial fibrillation. | Larsson et al., Sweden, July 2014 [ ]. |
| (10) | To examine the dose-response relationship between AF and consumption of alcohol. | Systemic review and meta-analysis | There is a causal impact of the consumption of alcohol on the onset of atrial fibrillation with a monotonic dose-response relationship. | Samokhvalov et al., December 2010 [ ]. |
| (11) | To investigate the effect of the consumption of alcohol on new-onset atrial fibrillation development in healthy individuals who are asymptomatic. | Multicenter study | In a healthy asymptomatic population, alcoholic drinking does increase the risk of new-onset atrial fibrillation in a dose-dependent manner which is regardless of the individual’s sex. | Cha et al., December 2020 [ ]. |
| (12) | To prospectively assess the association between incident atrial fibrillation (AF) among women and regular alcohol consumption. | Randomized control trial | Heavy consumption of two or more drinks per day was found to be associated with a small but statistically significant increased atrial fibrillation (AF) risk. | Conen et al., U.S., December 2008 [ ]. |
| (13) | To characterize the association between incident atrial fibrillation and chronic intake of alcohol. | Systemic review and meta-analysis | High intake of alcohol is associated with heightened atrial fibrillation (AF) risk across both genders. | Gallagher et al., November 2017 [ ]. |
Conclusions
Alcohol seldom leaves any system untouched as far as leaving its impression is concerned, spanning from single tissue involvement to complex organ system manifestations. Almost all the major organs that make up a human’s physiological being are dramatically affected by the overconsumption of alcohol. There is an enormous overall economic cost that is paid for alcohol abuse all over the world.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.

IMAGES
COMMENTS
Advances in the science and treatment of alcohol use ...
Alcohol Research Resource (R24 and R28) Awards. Resources include biological specimens, animals, data, materials, tools, or services made available to any qualified investigato r to accelerate alcohol-related research in a cost-effective manner. Current and potential alcohol research investigators and trainees are encouraged to subscribe to our ...
Alcohol | National Institute on Drug Abuse (NIDA)
ARCR Celebrates Its 50th Anniversary. 2024 marks the 50th anniversary of Alcohol Research: Current Reviews (ARCR), an open-access, peer-reviewed journal published by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) at the National Institutes of Health. View All News and Notes.
Alcohol is regularly consumed throughout most of the world, including by nearly half the U.S. population age 12 or older. Heavy drinking, which is also common, contributes to multiple adverse medical, psychiatric, and social outcomes and more than 140,000 deaths annually in the United States. It is the major risk factor for alcohol use disorder (AUD), whose current U.S. prevalence is 11% ...
Introduction. Alcohol use disorder (AUD) is one of the most common and costly public health problems in the United States and throughout the world[1, 2].A person with AUD consumes alcohol in quantities that might be injurious to themselves and to people around them[2, 3].Infect, the physical and mental health issues associated with excessive consumption of alcohol are known for centuries.
In this prospective longitudinal study of alcohol consumption and patterns in heavy drinking young adults, significant reductions in alcohol use quantity, frequency and problems were observed from ...
Research and analysis. Health risks and issues. Alcohol use. Alcohol use is a major risk factor for death and disability worldwide. In some countries, it is the number one risk factor for men. Photo by Chuttersnap, Unsplash. 1.34 billionpeople consumed harmful amounts of alcohol in 2020. 38%of deaths from cirrhosis and other liver diseases are ...
New research from the University of New Mexico, the University of Washington, and Syracuse University published in Psychology of Addictive Behaviors shows that assessing patients based on biological and psychological domains of addiction could be a good way to predict treatment outcomes.
Discussion. Research on the epidemiology of recovery from AUD is somewhat uneven in scope and methods, and gaps remain in the knowledge base. Nonetheless, the bulk of evidence converges in showing that (1) improvements in alcohol-related problems, including recovery from AUD, are commonplace; (2) natural recovery is the dominant pathway; (3 ...
Associations of common mental disorder with alcohol use ...
Alcohol - World Health Organization (WHO) ... Alcohol
NIAAA supports and conducts research on the impact of alcohol use on human health and well-being. Learn About Alcohol's Effects on Health. NIAAA is now on LinkedIn The Healthcare Professional's Core Resource on Alcohol from NIAAA Play it Safe This Summer - Be Mindful of Alcohol's Effects on the Body ...
During the COVID-19 pandemic, research revealed that alcohol consumption increased especially in adolescents and college students. 14,15 This was determined by factors such as stay-at-home policies, social isolation, and the relaxation of alcohol restrictions during the pandemic. 16,17 Personal effects of the pandemic such as becoming sick or experiencing the loss of close social contacts ...
Objective: To evaluate the trend of alcohol use disorder (AUD) mortality as a percentage of all-cause mortality in Canada and the United States (US) between 2000 and 2019, by age group. Results: Joinpoint regression showed that AUD mortality as a percentage of all-cause mortality significantly increased between 2000 and 2019 in both countries, and across all age groups (i.e., young adults (20 ...
Although research indicates that alcohol use and depression are related over time (Briere et al., 2014), relatively few studies have examined specific pathways linking the two, particularly using longitudinal data. In the current study we conducted secondary analyses to examine whether coping motives may serve to connect depression and alcohol ...
Alcohol Use and Your Health
Alcohol's Effects on Health
Understanding alcohol use disorders and their treatment
Background: The use of alcohol and illicit drugs during adolescence can lead to serious short- and long-term health related consequences. Despite a global trend of decreased substance use, in particular alcohol, among adolescents, evidence suggests excessive use of substances by young people in socioeconomically affluent areas. To prevent substance use-related harm, we need in-depth knowledge ...
"Alcohol is a carcinogen and contributes to about 50 different types of death," said Dr. Timothy Naimi, who directs the Canadian Institute for Substance Use Research at the University of ...
Alcohol Use Disorder - StatPearls
Previous studies have repeatedly reported alcohol use disorders (AUDs) in patients after bariatric surgery (BS). This research field can benefit from studies combining health claims data with ...
Alcohol Facts and Statistics
Facts About Aging and Alcohol | National Institute on Aging
The research reviewed here represents a wide spectrum of approaches to understanding the risks and benefits of alcohol consumption. These research findings can help shape the efforts of communities to reduce the negative consequences of alcohol consumption, assist health practitioners in advising consumers, and help individuals make informed ...
Alcohol remains the most used substance reported among adults in the study. Past-year alcohol use among adults 19 to 30 has showed a slight upward trend over the past five years, with 84% reporting use in 2023. However, past month drinking (65%), daily drinking (4%), and binge drinking (27%) all remained at study lows in 2023 among adults 19 to 30.
Effects of Alcohol Consumption on Various Systems of the ...