0800 118 2892
- +44 (0)203 151 1280


Teen Cocaine Addiction Case Study: Chloe's Story

This case study of drug addiction can affect anyone – it doesn’t discriminate on the basis of age, gender or background. At Serenity Addiction Centres, our drug detox clinic is open to everyone, and our friendly and welcoming approach is changing the way rehab clinics are helping clients recover from addiction.
We’ve asked former Serenity client, Chloe, to share her experience of drug rehab with Serenity Addiction Centre’s assistance.
Chloe’s Addiction
If you met Chloe today, you would never know about her past. This born and bred London girl is 20 years old, and a flourishing law student with a bright future in the City.
A few years ago though, it seemed as if this straight A student was about to throw away her life, thanks to a class A drug addiction .
Chloe had a great childhood. By her own admission, school was a breeze for her, with strong academic achievement and social skills making her as successful on the playground as she was in the classroom.
Age 7, Chloe started at a boarding school, and loved having friends around her all the time. With no parents about, Chloe and her friends found themselves invited to house parties. As soon as I could convince people they we 18, they moved on to London’s nightclubs.
It was here where Chloe first came across drugs, and it was a slippery slope to cocaine addiction. She explains: “At 15, I was taking poppers, graduated to MDMA at 16, and then I tried cocaine at our year 13 parties. I got separated from my friends, and found them taking cocaine in a back room. I didn’t want to be left out, so I tried it.”
Chloe scored straight As in her A levels, and accepted a place at Kings College London to study law. She was introduced to new people, and it seemed that cocaine was available at every place they went. Parties, clubs, and even her new friends were all good sources of a line of cocaine. As a self confessed wild child by this point, Chloe didn’t want to miss out.
The demands of a law degree were high, but so was Chloe’s desire for more cocaine.
Going out almost every night to snort coke, she started to wonder if she was becoming an addict. She spent every penny of the generous allowance from her parents. Chloe spent every penny available on credit cards, and even took on a £2000 bank loan to support her habit.
Chloe estimated that at one point, her addiction had saddled her with more than £13,000 of debt.
Coming out of Addiction Denial
Chloe’s light bulb moment finally came when her best friend, who she shared a flat with, sat her down and asked why they were drifting apart.
Chloe realised that cocaine had become more important to her than her friends, family, and studies. It had to stop. Chloe found the details for Serenity Addiction Centres, and called the same day to ask for help with her addiction.
One thing Chloe particularly appreciated about Serenity Addiction Centres was the flexible approach of the counsellors . They got to know Chloe, listening to her worries, and working out a non-residential rehab plan for her. This allowed her to continue with her studies.
Chloe’s treatment was organised at a clinic not far from her university, allowing her to keep her studies on track, and keeping her life as normal as possible.
Chloe says: “Talking about how I was using cocaine, along with contributing problems from earlier in my life, were a massive help. I didn’t want to be known just as a party girl”.
“If I’d not found Serenity Addiction Centres, there would probably have been a long wait for NHS treatment. Serenity Addiction Centres got the right treatment. Everything was organised with privacy and discretion. I only shared what was happening with my flatmate.”
This level of discretion was really helpful, and the rapid results of her treatment meant that after just three months Chloe felt able to tell her parents what had been happening.
Life after rehab
It’s amazing that Chloe has now had nearly a year where not taken cocaine, and faced her debts by working part time to repay what she owes. Even better, thanks to Serenity’s fast intervention. Chloe is on course for a 2:1 in her law degree.
If you’re ready to detox? Serenity Addiction Centre’s addiction support team are here to help you find the rehab programme which works for you. Serenity can help you beat your addiction. Gaining control over drugs, allowing you to move on and take back control of your life.
This Drug Addiction Case Study is here so others may identify. Contact us today , and begin your detox journey with Serenity Addiction Centres.
FREE CONSULTATION
Get a no-obligation confidential advice from our medical experts today
Request a call back
We provide a healthy environment uniquely suited to support your growth and healing.
- Rehab Clinic - Serenity Rehabilitation LTD. Arquen House,4-6 Spicer Street, St Albans, Hertfordshire AL3 4PQ
- 0800 118 2892 +44(0)203 151 1280

- Testimonials
- Case Studies
Popular Pages
- Alcohol Addiction
- How To Home Detox From Alcohol
- Alcohol Rehab Centres
- Methadone addiction
Top Locations
- Leicestershire
Module 9: Substance-Related and Addictive Disorders
Case studies: substance-abuse disorders, learning objectives.
- Identify substance abuse disorders in case studies
Case Study: Benny
The following story comes from Benny, a 28-year-old living in the Metro Detroit area, USA. Read through the interview as he recounts his experiences dealing with addiction and recovery.
Q : How long have you been in recovery?
Benny : I have been in recovery for nine years. My sobriety date is April 21, 2010.
Q: What can you tell us about the last months/years of your drinking before you gave up?
Benny : To sum it up, it was a living hell. Every day I would wake up and promise myself I would not drink that day and by the evening I was intoxicated once again. I was a hardcore drug user and excessively taking ADHD medication such as Adderall, Vyvance, and Ritalin. I would abuse pills throughout the day and take sedatives at night, whether it was alcohol or a benzodiazepine. During the last month of my drinking, I was detached from reality, friends, and family, but also myself. I was isolated in my dark, cold, dorm room and suffered from extreme paranoia for weeks. I gave up going to school and the only person I was in contact with was my drug dealer.
Q : What was the final straw that led you to get sober?
Benny : I had been to drug rehab before and always relapsed afterwards. There were many situations that I can consider the final straw that led me to sobriety. However, the most notable was on an overcast, chilly October day. I was on an Adderall bender. I didn’t rest or sleep for five days. One morning I took a handful of Adderall in an effort to take the pain of addiction away. I knew it wouldn’t, but I was seeking any sort of relief. The damage this dosage caused to my brain led to a drug-induced psychosis. I was having small hallucinations here and there from the chemicals and a lack of sleep, but this time was different. I was in my own reality and my heart was racing. I had an awful reaction. The hallucinations got so real and my heart rate was beyond thumping. That day I ended up in the psych ward with very little recollection of how I ended up there. I had never been so afraid in my life. I could have died and that was enough for me to want to change.
Q : How was it for you in the early days? What was most difficult?
Benny : I had a different experience than most do in early sobriety. I was stuck in a drug-induced psychosis for the first four months of sobriety. My life was consumed by Alcoholics Anonymous meetings every day and sometimes two a day. I found guidance, friendship, and strength through these meetings. To say early sobriety was fun and easy would be a lie. However, I did learn it was possible to live a life without the use of drugs and alcohol. I also learned how to have fun once again. The most difficult part about early sobriety was dealing with my emotions. Since I started using drugs and alcohol that is what I used to deal with my emotions. If I was happy I used, if I was sad I used, if I was anxious I used, and if I couldn’t handle a situation I used. Now that the drinking and drugs were out of my life, I had to find new ways to cope with my emotions. It was also very hard leaving my old friends in the past.
Q : What reaction did you get from family and friends when you started getting sober?
Benny : My family and close friends were very supportive of me while getting sober. Everyone close to me knew I had a problem and were more than grateful when I started recovery. At first they were very skeptical because of my history of relapsing after treatment. But once they realized I was serious this time around, I received nothing but loving support from everyone close to me. My mother was especially helpful as she stopped enabling my behavior and sought help through Alcoholics Anonymous. I have amazing relationships with everyone close to me in my life today.
Q : Have you ever experienced a relapse?
Benny : I experienced many relapses before actually surrendering. I was constantly in trouble as a teenager and tried quitting many times on my own. This always resulted in me going back to the drugs or alcohol. My first experience with trying to become sober, I was 15 years old. I failed and did not get sober until I was 19. Each time I relapsed my addiction got worse and worse. Each time I gave away my sobriety, the alcohol refunded my misery.
Q : How long did it take for things to start to calm down for you emotionally and physically?
Benny : Getting over the physical pain was less of a challenge. It only lasted a few weeks. The emotional pain took a long time to heal from. It wasn’t until at least six months into my sobriety that my emotions calmed down. I was so used to being numb all the time that when I was confronted by my emotions, I often freaked out and didn’t know how to handle it. However, after working through the 12 steps of AA, I quickly learned how to deal with my emotions without the aid of drugs or alcohol.
Q : How hard was it getting used to socializing sober?
Benny : It was very hard in the beginning. I had very low self-esteem and had an extremely hard time looking anyone in the eyes. But after practice, building up my self-esteem and going to AA meetings, I quickly learned how to socialize. I have always been a social person, so after building some confidence I had no issue at all. I went back to school right after I left drug rehab and got a degree in communications. Upon taking many communication classes, I became very comfortable socializing in any situation.
Q : Was there anything surprising that you learned about yourself when you stopped drinking?
Benny : There are surprises all the time. At first it was simple things, such as the ability to make people smile. Simple gifts in life such as cracking a joke to make someone laugh when they are having a bad day. I was surprised at the fact that people actually liked me when I wasn’t intoxicated. I used to think people only liked being around me because I was the life of the party or someone they could go to and score drugs from. But after gaining experience in sobriety, I learned that people actually enjoyed my company and I wasn’t the “prick” I thought I was. The most surprising thing I learned about myself is that I can do anything as long as I am sober and I have sufficient reason to do it.
Q : How did your life change?
Benny : I could write a book to fully answer this question. My life is 100 times different than it was nine years ago. I went from being a lonely drug addict with virtually no goals, no aspirations, no friends, and no family to a productive member of society. When I was using drugs, I honestly didn’t think I would make it past the age of 21. Now, I am 28, working a dream job sharing my experience to inspire others, and constantly growing. Nine years ago I was a hopeless, miserable human being. Now, I consider myself an inspiration to others who are struggling with addiction.
Q : What are the main benefits that emerged for you from getting sober?
Benny : There are so many benefits of being sober. The most important one is the fact that no matter what happens, I am experiencing everything with a clear mind. I live every day to the fullest and understand that every day I am sober is a miracle. The benefits of sobriety are endless. People respect me today and can count on me today. I grew up in sobriety and learned a level of maturity that I would have never experienced while using. I don’t have to rely on anyone or anything to make me happy. One of the greatest benefits from sobriety is that I no longer live in fear.
Case Study: Lorrie

Figure 1. Lorrie.
Lorrie Wiley grew up in a neighborhood on the west side of Baltimore, surrounded by family and friends struggling with drug issues. She started using marijuana and “popping pills” at the age of 13, and within the following decade, someone introduced her to cocaine and heroin. She lived with family and occasional boyfriends, and as she puts it, “I had no real home or belongings of my own.”
Before the age of 30, she was trying to survive as a heroin addict. She roamed from job to job, using whatever money she made to buy drugs. She occasionally tried support groups, but they did not work for her. By the time she was in her mid-forties, she was severely depressed and felt trapped and hopeless. “I was really tired.” About that time, she fell in love with a man who also struggled with drugs.
They both knew they needed help, but weren’t sure what to do. Her boyfriend was a military veteran so he courageously sought help with the VA. It was a stroke of luck that then connected Lorrie to friends who showed her an ad in the city paper, highlighting a research study at the National Institute of Drug Abuse (NIDA), part of the National Institutes of Health (NIH.) Lorrie made the call, visited the treatment intake center adjacent to the Johns Hopkins Bayview Medical Center, and qualified for the study.
“On the first day, they gave me some medication. I went home and did what addicts do—I tried to find a bag of heroin. I took it, but felt no effect.” The medication had stopped her from feeling it. “I thought—well that was a waste of money.” Lorrie says she has never taken another drug since. Drug treatment, of course is not quite that simple, but for Lorrie, the medication helped her resist drugs during a nine-month treatment cycle that included weekly counseling as well as small cash incentives for clean urine samples.
To help with heroin cravings, every day Lorrie was given the medication buprenorphine in addition to a new drug. The experimental part of the study was to test if a medication called clonidine, sometimes prescribed to help withdrawal symptoms, would also help prevent stress-induced relapse. Half of the patients received daily buprenorphine plus daily clonidine, and half received daily buprenorphine plus a daily placebo. To this day, Lorrie does not know which one she received, but she is deeply grateful that her involvement in the study worked for her.
The study results? Clonidine worked as the NIDA investigators had hoped.
“Before I was clean, I was so uncertain of myself and I was always depressed about things. Now I am confident in life, I speak my opinion, and I am productive. I cry tears of joy, not tears of sadness,” she says. Lorrie is now eight years drug free. And her boyfriend? His treatment at the VA was also effective, and they are now married. “I now feel joy at little things, like spending time with my husband or my niece, or I look around and see that I have my own apartment, my own car, even my own pots and pans. Sounds silly, but I never thought that would be possible. I feel so happy and so blessed, thanks to the wonderful research team at NIDA.”
- Liquor store. Authored by : Fletcher6. Located at : https://commons.wikimedia.org/wiki/File:The_Bunghole_Liquor_Store.jpg . License : CC BY-SA: Attribution-ShareAlike
- Benny Story. Provided by : Living Sober. Located at : https://livingsober.org.nz/sober-story-benny/ . License : CC BY: Attribution
- One patientu2019s story: NIDA clinical trials bring a new life to a woman struggling with opioid addiction. Provided by : NIH. Located at : https://www.drugabuse.gov/drug-topics/treatment/one-patients-story-nida-clinical-trials-bring-new-life-to-woman-struggling-opioid-addiction . License : Public Domain: No Known Copyright

Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
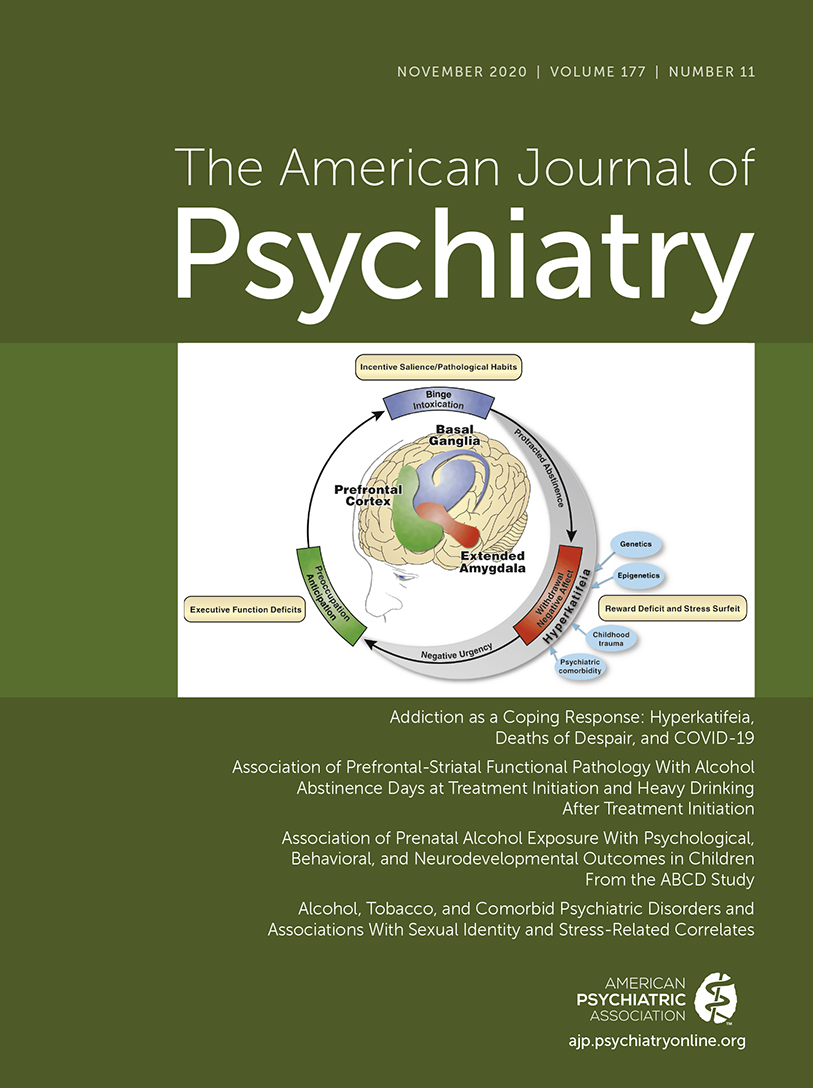
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Abstract , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
March 1, 2017
Case Study: When Chronic Pain Leads to a Dangerous Addiction
How did an educated, elderly engineer wind up with a heroin habit?
By Daniel Barron

It was 4 P.M., and Andrew
* had just bought 10 bags of heroin. In his kitchen, he tugged one credit-card-sized bag from the rubber-banded bundle and laid it on the counter with sacramental reverence. Pain shot through his body as he pulled a cutting board from the cabinet. Slowly, deliberately, he tapped the bag's white contents onto the board and crushed it with the flat edge of a butter knife, forming a line of fine white powder. He snorted it in one pass and shuffled back to his armchair. It was bitter, but snorting heroin was safer than injecting, and he was desperate: his prescription pain medication was gone.
I met Andrew the next day in the emergency room, where he told me about the previous day's act of desperation. I admitted him to control his swelling legs and joint pain. He was also detoxing from opioids.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Andrew looked older than his 69 years. His face was wrinkled with exhaustion. A frayed, tangled mop of grizzled hair fell to his shoulders. Andrew had been a satellite network engineer, first for the military, more recently for a major telecommunications company. An articulate, soft-spoken fellow, he summed up his (rather impressive) career modestly: “Well, I'd just find where a problem was and then find a way to fix it.”
Yet there was one problem he couldn't fix. “Doctor, I'm always in the most terrible pain,” he said, with closed eyes. “I had no other options. I started using heroin, bought it from my neighbor to help with the pain. I'm scared stiff.”
For two decades Andrew had suffered serial joint failures from a combination of arthritis, obesity and other factors. Each began as an achy pain and ended in a joint replacement. His right shoulder was the first to go, followed by both hips, a knee and an ankle. Pain always ensued. The new joints kept getting infected: more surgery, more pain. To make things worse, a bathtub mishap broke his right femur. That led to an operation to insert a full-length titanium rod. A perfect storm of complications had left Andrew barely able to hobble around the small apartment he shared with his adult son. (Andrew's wife had left him shortly after he broke his femur, and his son took him in.) Pain became Andrew's all-consuming nemesis, devouring most of his waking hours.
Andrew was first prescribed an opioid after one of his many surgeries. This was in the late 1990s, around the time when prescriptions for these painkillers began to take off nationally. His doctor began him on Vicodin, a commonly used opioid that combines hydrocodone with acetaminophen (Tylenol).
Pain, like vision, touch or taste, is a sensory signal. The brain has an elaborate network of receptors, neurons and centers dedicated to pain. Opioids exert their effects by binding to mu-opioid receptors, which are densely concentrated in brain regions that regulate pain perception and reward. Activating mu receptors blocks pain signals in the spinal cord and the response to this signal in the brain. Mu receptors also cause the release of dopamine in reward pathways, which is why opioids cause both analgesia and euphoria.
Surgery after surgery, opioids became Andrew's vitamins, as vital to his pain control as blood pressure drugs are for hypertension. Yet in 2005 Andrew noticed he was feeling anxious about his pill supply. “You start out with a bottle of 30 pills, then there's only 20, then only 10. It's scary when you run out.”

Credit: Chris Gash
Months after his surgeries, after his scars were healed, he still struggled with deep, biting pain. It had spread throughout his body and required more pills to tame. Andrew had transitioned from what is called acute pain (pain from his surgical wounds) to chronic pain (pain in the absence of an obvious cause). He had also developed a tolerance to the opioids. On a cellular level, this means that his neurons expressed fewer mu receptors, so he needed to flood his system with higher doses to get the same effect as before. (Andrew, ever the engineer, appreciated the irony of wrangling yet another network, this time with drugs.)
Possibly, the opioids had contributed to Andrew's spreading pain. Some patients on these drugs have been known to develop increased pain sensitivity known as opioid-induced hyperalgesia.
From Prescription Meds to Street Drugs
As his tolerance for opioids grew, Andrew found that even 15 milligrams of oxycodone no longer worked for him. After he relocated to his son's apartment, he no longer had a primary care provider familiar with his history and could not refill his medications.
With nowhere to turn, Andrew mentioned his situation to his neighbor, who sold him diverted opioids—prescription medications hawked on the street. When these ran out, his neighbor sold him heroin. Andrew's dependence on heroin terrified him, and at $100 a day, it threatened to bankrupt him as well.
This trajectory is by no means unusual, according to Andrew's lead doctor, William Becker, an addiction medicine specialist and assistant professor at the Yale School of Medicine: “Chronic pain is the new initiation to heroin. We're finding that it's older and older patients, who start on the path to chronic pain, then on to opioids, then on to heroin.” Andrew's case is a “classic example,” he said. “The numbers are controversial, but as tens of millions of people taking opioids for pain age, we think 10 percent and maybe more will develop at least a mild opioid use disorder. And their pain isn't going away. We have to become more fluent in managing the co-occurrence of chronic pain and addiction.”
His words and recent warnings from U.S. surgeon general Vivek H. Murthy about the “urgent health crisis” caused by our lax approach to opioids now come to mind every time I consider writing a prescription for one of these painkillers. I also think of Andrew standing at his kitchen counter, hands trembling as he forms a line of heroin.
Relief and Release
Luckily for Andrew, Becker runs the Opioid Reassessment Clinic, which is pioneering strategies to taper patients with chronic pain from high-dose opioid use to Suboxone, a clever sublingual tablet that combines buprenorphine and naloxone. Buprenorphine activates the mu-opioid receptor. When taken under the tongue, it provides pain relief and prevents withdrawal. Naloxone is added as a safeguard to keep abusers from injecting the drug. When taken sublingually, naloxone has no effect. When injected, it blocks the mu receptor and causes acute withdrawal, a physiological inducement to use Suboxone in the prescribed manner.
At a dollar a day, Suboxone is affordable. In combination with intensive psychosocial therapy, it is a safe and highly efficacious treatment for opioid use disorders. And, as Andrew attested, it actually controls pain better than heroin. Instead of being strung out on heroin, Suboxone allowed Andrew to meaningfully interact with our medical team. He undertook a program of proved therapies for chronic pain that included physical therapy, mindfulness training and psychosocial therapy. Andrew left the hospital after nearly three weeks with a clear plan: weekly check-ins at Becker's Suboxone clinic and continued physical and psychosocial therapy tailored for pain. The last time I saw him in his hospital room, he was excited at the prospects: “The plan is to continue with Suboxone and to stay with it. And hopefully I won't have any more surgeries. It's been a rough decade, a long haul, but I'm making slow progress.”
Andrew will be managing pain and addiction for the rest of his life, but now he has a variety of tools for doing so that are safe, legal and effective.
Daniel Barron is director of the Pain Intervention and Digital Research Program, a National Institutes of Health–funded research clinic devoted to developing better tools to define chronic pain and psychiatric conditions, at Brigham and Women's Hospital and Spaulding Rehabilitation Hospital. He completed his medical training and psychiatry residency at Yale University, his graduate work at the University of Texas and his fellowship in interventional pain medicine at the University of Washington. He is author of Reading Our Minds: The Rise of Big Data Psychiatry . Follow him on X (formerly Twitter) @daniel__barron or visit his website at danielsbarron.com
- Open Access
- By Publication (A-Z)
- Case Reports
- Publication Ethics
- Publishing Policies
- Editorial Policies
- Submit Manuscript
- About Graphy

New to Graphy Publications? Create an account to get started today.
Registered Users
Have an account? Sign in now.

- Full-Text HTML
- Full-Text PDF
- About This Journal
- Aims & Scope
- Editorial Board
- Editorial Process
- Author Guidelines
- Special Issues
- Articles in Press

Jo-Hanna Ivers 1* and Kevin Ducray 2
In October 2012, 83 front-line Irish service providers working in the addiction treatment field received accreditation as trained practitioners in the delivery of a number of evidence-based positive reinforcement approaches that address substance use: 52 received accreditation in the Community Reinforcement Approach (CRA), 19 in the Adolescent Community Reinforcement Approach (ACRA) and 12 in Community Reinforcement and Family Training (CRAFT). This case study presents the treatment of a 17-year-old white male engaging in high-risk substance use. He presented for treatment as part of a court order. Treatment of the substance use involved 20 treatment sessions and was conducted per Adolescent Community Reinforcement Approach (A-CRA). This was a pilot of A-CRA a promising treatment approach adapted from the United States that had never been tried in an Irish context. A post-treatment assessment at 12-week follow-up revealed significant improvements. At both assessment and following treatment, clinician severity ratings on the Maudsley Addiction Profile (MAP) and the Alcohol Smoking and Substance Involvement Screening Test (ASSIST) found decreased score for substance use was the most clinically relevant and suggests that he had made significant changes. Also his MAP scores for parental conflict and drug dealing suggest that he had made significant changes in the relevant domains of personal and social functioning as well as in diminished engagement in criminal behaviour. Results from this case study were quite promising and suggested that A-CRA was culturally sensitive and applicable in an Irish context.
1. Theoretical and Research Basis for Treatment
Substance use disorders (SUDs) are distinct conditions characterized by recurrent maladaptive use of psychoactive substances associated with significant distress. These disorders are highly common with lifetime rates of substance use or dependence estimated at over 30% for alcohol and over 10% for other substances [1 , 2] . Changing substance use patterns and evolving psychosocial and pharmacologic treatments modalities have necessitated the need to substantiate both the efficacy and cost effectiveness of these interventions.
Evidence for the clinical application of cognitive behavioural therapy (CBT) for substance use disorders has grown significantly [3 - 8] . Moreover, CBT for substance use disorders has demonstrated efficacy both as a monotherapy and as part of combination treatment [7] . CBT is a time-limited, problem-focused, intervention that seeks to reduce emotional distress through the modification of maladaptive beliefs, assumptions, attitudes, and behaviours [9] . The underlying assumption of CBT is that learning processes play an imperative function in the development and maintenance of substance misuse. These same learning processes can be used to help patients modify and reduce their drug use [3] .
Drug misuse is viewed by CBT practitioners as learned behaviours acquired through experience [10] . If an individual uses alcohol or a substance to elicit (positively or negatively reinforced) desired states (e.g. euphorigenic, soothing, calming, tension reducing) on a recurrent basis, it may become the preferred way of achieving those effects, particularly in the absence of alternative ways of attaining those desired results. A primary task of treatment for problem substance users is to (1) identify the specific needs that alcohol and substances are being used to meet and (2) develop and reinforce skills that provide alternative ways of meeting those needs [10 , 11] .
CRA is a broad-spectrum cognitive behavioural programme for treating substance use and related problems by identifying the specific needs that alcohol and or other substances are satisfying or meeting. The goal is then to develop and reinforce skills that provide alternative ways of meeting those needs. Consistent with traditional CBT, CRA through exploration, allows the patient to identify negative thoughts, behaviours and beliefs that maintain addiction. By getting the patient to identify, positive non-drug using behaviours, interests, and activities, CRA attempts to provide alternatives to drug use. As therapy progresses the objective is to prevent relapse, increase wellness, and develop skills to promote and sustain well-being. The ultimate aim of CRA, as with CBT is to assist the patient to master a specific set of skills necessary to achieve their goals. Treatment is not complete until those skills are mastered and a reasonable degree of progress has been made toward attaining identified therapy goals. CRA sessions are highly collaborative, requiring the patient to engage in ‘between session tasks’ or homework designed reinforce learning, improve coping skills and enhance self efficacy in relevant domains.
The use of the Community Reinforcement Approach is empirically supported with inpatients [12 , 13] , outpatients [14 - 16] and homeless populations (Smith et al., 1998). In addition, three recent metaanalytic reviews cited CRA as one of the most cost-effective treatment programmes currently available [17 , 18] .
A-CRA is a evidenced based behavioural intervention that is an adapted version of the adult CRA programme [19] . Garner et al [19] modified several of the CRA procedures and accompanying treatment resources to make them more developmentally appropriate for adolescents. The main distinguishing aspect of A-CRA is that it involves caregivers—namely parents or guardians who are ultimately responsible for the adolescent and with whom the adolescent is living.
A-CRA has been tested and found effective in the context of outpatient continuing care following residential treatment [20 - 22] and without the caregiver components as an intervention for drug using, homeless adolescents [23] . More recently, Garner et al [19] collected data from 399 adolescents who participated in one of four randomly controlled trials of the A-CRA intervention, the purpose of which was to examine the extent to which exposure to A-CRA procedures mediated the relationship between treatment retention and outcomes. The authors found adolescents who were exposed to 12 or more A-CRA procedures were significantly more likely to be in recovery at follow-up.
Combining A-CRA with relapse prevention strategies receives strong support as an evidence based, best practice model and is widely employed in addiction treatment programmes. Providing a CBT-ACRA therapeutic approach is imperative as it develops alternative ways of meeting needs and thus altering dependence.
2. Case Introduction
Alan is a 17 year-old male currently living in County Dublin. Alan presented to the agency involuntarily and as a requisite of his Juvenile Liaison Officer who was seeing him on foot of prior drugs arrest for ‘possession with intent to supply’; a more serious charge than a simple ‘drugs possession’ charge. As Alan had no previous charges he was placed on probation for one year. This was Alan’s first contact with the treatment services. A diagnostic assessment was completed upon entry to treatment and included completion of a battery of instruments comprising the Maudsley Addiction Profile (MAP), The World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and the Beck Youth Inventory (BYI) (see appendices for full description of outcome measures) (Table 1).

3. Diagnostic Criteria
The apparent symptoms of substance dependency were: (1) Loss of Control - Alan had made several attempts at controlling the amounts of cannabis he consumed, but those times when he was able to abstain from cannabis use were when he substituted alcohol and/or other drugs. (2) Family History of Alcohol/Drug Usage - Alan’s eldest sister who is now 23 years old is in recovery from opiate abuse. She was a chronic heroin user during her early adult years [17 - 21] . During this period, which corresponds to Alan’s early adolescent years [12 - 15] she lived in the family home (3) Changes in Tolerance - Alan began per day. At presentation he was smoking six to eight cannabis joints daily through the week, and eight to twelve joints daily on weekends.
4. Psychosocial, Medical and Family History
At time of intake Alan was living with both of his parents and a sister, two years his senior, in the family home. Alan was the youngest and the only boy in his family. He had two other older sisters, 5 and 7 years his senior. He was enrolled in his 5th year of secondary school but at the time of assessment was expelled from all classes. Alan had superior sporting abilities. He played for the junior team of a first division football team and had the prospect of a professional career in football. He reported a family history positive for substance use disorders. An older sister was in recovery for opiate dependence. Apart from his substance use Alan reported no significant psychological difficulties or medical problems. His motives for substance use were cited as boredom, curiosity, peer pressure, and pleasure seeking. His triggers for use were relationship difficulties at home, boredom and peer pressure. Pre-morbid personality traits included thrill seeking and impulsivity (Table 2).

5. Case Conceptualisation
A CBT case formulation is based on the cognitive model, which hypothesizes that "a person’s feelings and emotions are influenced by their perception of events" . It is not the actual event that determines how the person feels, but rather how they construe the event (Beck, 1995 p14). Moreover, cognitive theory posits that the “child learns to construe reality through his or her early experiences with the environment, especially with significant others” and that “sometimes these early experiences lead children to accept attitudes and beliefs that will later prove maladaptive” [24] . A CBT formulation (or case conceptualisation) is one of the key underpinnings of Cognitive Behavioural Therapy (CBT). It is the ‘blueprint’ which aids the therapist to understand and explain the patient’s’ problems.
Formulation driven CBT enables the therapist to develop an individualised understanding of the patient and can help to predict the difficulties that a patient may encounter during therapy. In Alan’s case, exploring his existing negative automatic thoughts about regarding school and his academic competences highlighted the difficulties he could experience with CBT homework completion. Whilst Alan was good at between session therapy assignments, an exploration of what is meant by ‘homework’ in a CBT context was crucial.
A collaborative CBT formulation was done diagrammatically together with Alan (Figure 1). This formulation aimed to describe his presenting problems and using CBT theory, to explore explanatory inferences about the initiating and maintaining factors of his drug use which could practically inform meaningful interventions.

Simmons and Griffiths et al. make the insightful observation that particular group differences need to be specifically considered and suggest that the therapist should be cognizant of the role of both society and culture when developing a formulation. They firstly suggest that the impact played by gender, sexuality and socio-cultural roles in the genesis of a psychological disorder, namely the contribution that being a member of a group may have on predisposing and precipitating factors, be carefully considered. An example they offer is the role of poverty on the development of psychological problems, such as the link evidenced between socio economic group and onset of schizophrenia. This was clearly evident in the case of Alan, who being a member of a deprived socioeconomic group, growing up and living in an area with a high level of economic deprivation, perceived that his choices for success were limited. His thinking, as an adolescent boy, was dichotomous in that he saw himself as having only two fixed and limited choices (a) being good at sport he either pursue a career as a professional sportsman or alternatively (b) he engage in crime and work his way up through the ranks as a ‘career criminal’. Simmons & Griffiths secondly suggest that being a member of a particular group can heavily influence a person’s understanding of the causality of their psychological disorder. A third consideration when developing a formulation is the degree to which being a member of a particular group may influence the acceptance or rejection of a member experiencing a psychological illness. Again this is pertinent in Alan’s case as he was part of a sub-group, a gang engaged in crime. For this cohort, crime and drug use were synonymous. Using drugs was viewed as a rite of passage for Alan.
Drug use, according to CBT models, are socially learned behaviours initiated, maintained and altered through the dynamic interaction of triggers, cues, reinforcers, cognitions and environmental factors. The application of a such a formulation, sensitive to Simmons and Griffiths (2009) aforementioned observations, proved useful in affording insights into the contextual and maintaining factors of Alan’s drug use which was heavily influenced by the availability of drugs ,his peer group (with whom he spent long periods of time) and their petty drug dealing and criminality. Similarly, engaging with his football team mates during the lead up to an important match significantly reduced his drug use and at certain times of the year even lead to abstinence. Sharing this formulation allowed him to note how his drug use patterns were driven, as per the CBT paradigm, by modifiable external, transient, and specific factors (e.g. cues, reinforcements, social networks and related expectations and social pressures).
Employing the A-CRA model allowed for this tailored fit as A-CRA specifically encourages the patient to identify their own need and desire for change. Alan identified the specific needs that were met by using substances and he developed and reinforced skills that provided him with alternative ways of meeting those needs. This model worked extremely well for Alan as he had identified and had ready access to a pro- social ‘alternative group’ or community. As he had had access to an alternative positive peer group and another activity (sport) which he was ‘really good at’, he simply needed to see the evidence of how his context could radically affect his substance use; more specifically how his beliefs, thinking and actions in certain circumstances produced very different drug use consequences and outcomes.
6. Course of Treatment and Assessment of Progress
One focus of CBT treatment is on teaching and practising specific helpful behaviours, whilst trying to limit cognitive demands on clients. Repetition is central to the learning process in order to develop proficiency and to ensure that newly acquired behaviours will be available when needed. Therefore, behavioural using rehearsal will emphasize varied, realistic case examples to enhance generalization to real life settings. During practice periods and exercises, patients are asked to identify signals that indicate high-risk situations, demonstrating their understanding of when to use newly acquired coping skills. CBT is designed to remedy possible deficits in coping skills by better managing those identified antecedents to substance use. Individuals who rely primarily on substances to cope have little choice but to resort to substance use when the need to cope arises. Understanding, anticipating and avoiding high risk drug use scenarios or the “early warning signals” of imminent drug use is a key CBT clinical activity.
A major goal of a CBT/A-CRA therapeutic approach is to provide a range of basic alternative skills to cope with situations that might otherwise lead to substance use. As ‘skill deficits’ are viewed as fundamental to the drug use trajectory or relapse process, an emphasis is placed on the development and practice of coping skills. A-CRA was manualised in 2001 as part of the Cannabis Youth Treatment Series (CYT) and was tested in that study [21] and more recently with homeless youth [23] . It was also adapted for use in a manual for Assertive Continuing Care following residential treatment [20] .
There are twelve standard and three optional procedures proposed in the A-CRA model. The delivery of the intervention is flexible and based on individual adolescent needs, though the manual provides some general guidelines regarding the general order of procedures. Optional procedures are ‘Dealing with Failure to Attend’, ‘Job-Seeking Skills’, and ‘Anger Management’. Standard procedures are included in table 3 below. For a more detailed description of sessions and procedures please see appendices.

Smith and Myers describe the theoretical underpinnings of CRA as a comprehensive behavioural program for treating substance-abuse problems. It is based on the belief that environmental contingencies can play a powerful role in encouraging or discouraging drinking or drug use. Consequently, it utilizes social, recreational, familial, and vocational reinforcers to assist consumers in the recovery process. Its goal is to essentially make a sober lifestyle more rewarding than the use of substances. Interestingly the authors note: ‘Oddly enough, however, while virtually every review of alcohol and drug treatment outcome research lists CRA among approaches with the strongest scientific evidence of efficacy, very few clinicians who treat consumers with addictions are familiar with it’. ‘The overall philosophy is to promote community based rewarding of non drug-using behaviour so that the patient makes healthy lifestyle changes’ p.3 [25] .
A-CRA procedures use ‘operant techniques and skills training activities’ to educate patients and present alternative ways of dealing with challenges without substances. Traditionally, CRA is provided in an individual, context-specific approach that focuses on the interaction between individuals and those in their environments. A-CRA therapists teach adolescents when and where to use the techniques, given the reality of each individual’s social environment. This tailored approach is facilitated by conducting a ‘functional analysis’ of the adolescent’s behaviour at the beginning of therapy so they can better understand and interrupt the links in the behavioural chain typically leading to episodes of drug use. A-CRA therapists then teach individuals how to improve communication and other skills, build on their reinforcers for abstinence and use existing community resources that will support positive change and constructive support systems.
A-CRA emphasises lapse and relapse prevention. Relapseprevention cognitive behavioural therapy (RP-CBT) is derived from a cognitive model of drug misuse. The emphasis is on identifying and modifying irrational thoughts, managing negative mood and intervening after a lapse to prevent a full-blown relapse [26] . The emphasis is on development of skills to (a) recognize High Risk Situations (HRS) or states where clients are most vulnerable to drug use, (b) avoidance of HRS, and (C) to use a variety of cognitive and behavioural strategies to cope effectively with these situations. RPCBT differs from typical CBT in that the accent is on training people who misuse drugs to develop skills to identify and anticipate situations or states where they are most vulnerable to drug use and to use a range of cognitive and behavioural strategies to cope effectively with these situations [26] .
7. Access and Barriers to Care
Alan engaged with the service for eight months. During this time he received twenty sessions, three of which were assessment focused, the remaining seventeen sessions were A-CRA focused; two of the seventeen involved his mother, the remaining fifteen were individual. As Alan was referred by the probation services, he was initially somewhat ambivalent about drug use focussed interventions. His early motivation for engagement was primarily to avoid the possibility of a custodial sentence.
8. Treatment
My sessions with Alan were guided by the principles of A-CRA [27] which focuses on coping skills training and relapse prevention approaches to the treatment of addictive disorders. Prior to engaging with Alan, I had completed the training course and commenced the A-CRA accreditation process, both under the stewardship of Dr Bob Meyers, whose training and publication offers detailed guidelines on skills training and relapse prevention with young people in a similar context [27] .
During the early part of each session I focused on getting a clear understanding of Alan’s current concerns, his general level of functioning, his substance abuse and pattern of craving during the past week. His experiences with therapy homework, the primary focus being on what insight he gained by completing such exercises was also explored. I spent considerable time engaged in a detailed review of Alan’s experience with the implementation of homework tasks during which the following themes were reviewed:
-Gauging whether drug use cessation was easier or harder than he anticipated? -Which, if any, of the coping strategies worked best? -Which strategies did not work as well as expected. Did he develop any new strategies? -Conveying the importance of skills practice, emphasising how we both gained greater insights into how cognitions influenced his behaviour. After developing a clear sense of Alan’s general functioning, current concerns and progress with homework implementation, I initiated the session topic for that week. I linked the relevance of the session topic to Alan’s current cannabis-related concerns and introduced the topic by using concrete examples from Alan’s recent experience. While reviewing the material, I repeatedly ensured that Alan understood the topic by asking for concrete examples, while also eliciting Alan’s views on how he might use these particular skills in the future.
Godley & Meyers [21] propose a homework exercise to accompany each session. An advantage of using these homework sheets is that they also summarise key points about each topic and therefore serve as a useful reminder to the patient of the material discussed each week. Meyers, et al. (2011) suggests that rather than being bound by the suggested exercises in the manualised approach, they may be used as a starting point for discussing the best way to implement the required skill and to develop individualised variations for new assignments [27] . The final part of each session focused on Alan’s plan for the week ahead and any anticipated high-risk situations. I endeavoured to model the idea that patients can literally ‘plan themselves out of using’ cannabis or other drugs. For each anticipated high-risk situation, we identified appropriate and viable coping skills. Better understanding, anticipating and planning for high-risk situations was difficult in the beginning of treatment as Alan was not particularly used to planning or thinking through his activities. For a patient like Alan, whose home life is often chaotic, this helped promote a growing sense of self efficacy. Similarly, as Alan had been heavily involved with drug use for a long time, he discovered through this process that he had few meaningful activities to fill his time or serve as alternatives to drug use. This provided me with an opportunity to discuss strategies to rebuild an activity schedule and a social network.
During our sessions, several skill topics were covered. I carefully selected skills to match Alan’s needs. I selected coping skills that he has used in the past and introduced one or two more that were consistent with his cognitive style. Alan’s cognitive score indicated a cognitive approach reflecting poor problem solving or planning. Sessions focused on generic skills including interpersonal skills, goal setting, coping with criticism or anger, problem solving and planning. The goal was to teach Alan how to build on his pro- social reinforcers, how to use existing community resources supportive of positive change and how to develop a positive support system.
The sequence in which these topics were presented was based on (a) patient needs and (b) clinician judgment (a full description of individual sessions may be found in appendices).
A-CRA procedures use ‘operant techniques and skills training activities’ to educate patients and present alternative ways of dealing with challenges without substances. Traditionally, CRA is provided in an individual, context-specific approach that focuses on the interaction between individuals and those in their environments. A-CRA therapists teach adolescents when and where to use the techniques, given the reality of each individual’s social environment.
9. Assessment of Treatment Outcome
A baseline diagnostic assessment of outcomes was completed upon treatment entry. This assessment consisted of a battery of psychological instruments including (see appendices for full a description of assessment measures):
-The Maudsley Addiction Profile (MAP). -The Beck Youth Inventories. -The World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST).
In addition to the above, objective feedback on Alan’s clinical and drug use status through urine toxicology screens was an important part of his drug treatment. Urine specimens were collected before each session and available for the following session. The use of toxicology reports throughout treatment are considered a valuable clinical tool. This part of the session presents a good opportunity to review the results of the most recent urine toxicology screen and promote meaningful therapeutic activities in the context of the patient’s treatment goals [28] .
In reporting on substance use since the last session, patients are likely to reveal a great deal about their general level of functioning and the types of issues and problems of most current concern. This allows the clinician to gauge if the patient has made progress in reducing drug use, his current level of motivation, whether there is a reasonable level of support available in efforts to remain abstinent and what is currently bothering him. Functional analyses are opportunistically used throughout treatment as needed. For example, if cannabis use occurs, patients are encouraged to analyse antecedent events so as to determine how to avoid using in similar situations in the future. The purpose is to help the patient understand the trajectory and modifiable contextual factors associated with drug use, challenge unhelpful positive drug use expectancies, identify possible skills deficiencies as well as seeking functionally equivalent non- drug using behaviours so as to reduce the probability of future drug use. The approach I used is based on the work of [28] .
The Functional Analysis was used to identify a number of factors occurring within a relatively brief time frame that influenced the occurrence of problem behaviours. It was used as an initial screening tool as part of a comprehensive functional assessment or analysis of problem behaviour. The results of the functional analysis then served as a basis for conducting direct observations in a number of different contexts to attest to likely behavioural functions, clarify ambiguous functions, and identify other relevant factors that are maintaining the behaviour.
The Happiness Scale rates the adolescent’s feelings about several critical areas of life. It helps therapists and adolescents identify areas of life that adolescents feel happy about and alternatively areas in which they have problems or challenges. Most importantly it identifies potential treatment goals subjectively meaningful to the patient, facilitates positive behaviour change in a range of life domains as well as help clients track their progress during treatment.
Alan’s BYI score (Table 4) indicates that at the time of assessment he was within the average scoring range on ‘self-concept’, and moderately elevated in the areas of ‘depression’, ‘anxiety’, and ‘disruptive behaviour’. His score for ‘anger’ suggested that his anger fell within the extremely elevated range. When this was discussed with Alan he agreed that this was quite accurate. Anger, and in particular controlling his anger, was subjectively identified as a treatment goal.

10. Follow-up
Given that follow-up occurred by telephone it was not feasible to administer the full battery of tests. With Alan’s treatment goals in mind it was decided to administer the MAP and ASSIST. Table 5 below illustrates Alan’s score at baseline and follow-up for the MAP and ASSIST. For summary purposes I have taken areas for concern at baseline for both instruments.

Alan’s score for cannabis was the most clinically relevant as it placed him in the 'high risk’ domain while his alcohol score indicated that he had engaged in binge drinking (6+ drinks) at T1. However, at T2 Alan’s score suggests that he had made considerable reductions in the use of both substances. Also his MAP scores for parental conflict and drug dealing suggest that he had also made major positive changes in the relevant domains of personal and social functioning as well as ceasing criminal behaviour.
At 3 months post-discharge I contacted Alan by phone. He had maintained and continued to further his progress. His drug use was at a minimal level (1 or 2 shared joints per month). He was no longer engaged in crime and his probationary period with the judicial system had passed. He had received a caution for his earlier drugs charge. At the time of follow-up he was enjoying participating in a Sports Coaching course and was excelling with his study assignments. Relationships had improved considerably with his mother and sister and he had re-engaged with a previous, positive, peer group linked to his involvement with the GAA . Overall he felt he was doing extremely well.
11. Complicating Factors with A-CRA Model
There are many challenges that may arise in the treatment of substance use disorders that can serve as barriers to successful treatment. These include acute or chronic cognitive deficits, health problems, social stressors and a lack of social resources [7] . Among individuals presenting with substance use there are often other significant life challenges including early school leaving, family conflicts, legal issues, poor or deviant social networks, etc. A particular challenge with Alan’s case was the social and environmental milieu which he shared with his drug using peers. For Alan, who initially had few skills and resources, engaging in treatment meant not only being asked to change his overall way of life but also to renounce some of those components in which he enjoyed a sense of belonging, particularly as he had invested significantly in these friendships. A sense of ‘belonging to the substance use culture’ can increase ambivalence for change [7] . Alan’s mother strongly disapproved of his drug using peer group and failed to acknowledge Alan’s perceived loss. This resulted in mother- son conflict. The use of the caregiver session allowed an exploration of perceived ‘losses’ relative to the ‘gains’ associated with Alan’s abstinence. It was moreover seen to be critical to establish alternatives for achieving a sense of belonging, including both his social connection and his social effectiveness. Alan’s sports ability allowed for this to be fostered. He is a talented sportsman which often meant his acceptance within a team or group is a given.
Despite the positive effects of A-CRA it is not without its shortcomings. The approach is at times quite American- oriented, particularly around identifying local resources and its focus on culturally specific outlets in promoting social engagement as alternatives to substance use. While this is supported in the literature, it may not necessarily be transferable to certain Irish adolescent contexts or subcultures.
12. Treatment Implications of the Case
A-CRA captures a broad range of behavioural treatments including those targeting operant learning processes, motivational barriers to improvement and other more traditional elements of cognitivebehavioural interventions. Overall, this intervention has demonstrated efficacy. Despite this heterogeneity, core elements emerge based in a conceptual model of SUDs as disorders characterized by learning processes and driven by the strongly reinforcing effects of the substances of abuse. There is rich evidence in the substance use disorders literature that improvement achieved by CBT (7) and indeed A-CRA (Godley et al. and Garner et al. [22 , 20] ) generalizes to all areas of functioning, including social, work, family and marital adjustment domains. The present study’s finding that a reduction in substance-related symptoms was accompanied by improved levels of functioning, social adjustment and enhanced quality of life, provides further support for this point.
In conclusion, there is some preliminary evidence that A-CRA is a promising treatment in the rehabilitation of adolescent substance users in Ireland and culturally similar societies. Clearly, results from a case study have limited generalisability and there is need for larger controlled studies providing robust outcomes to confirm the efficacy of A-CRA in an Irish context. A more systematic study of this issue is in the interest of adolescent substance users and the health services providers faced with the challenge of providing affordable, evidencebased mental health and addiction care to young people.
13. Recommendations to Clinicians and Students
The ACRA model is a structured assemblage of a range of cognitive and behavioural activities (e.g. a rationale and overview of the paradigm, sobriety sampling, functional analyses, communication skills, problem solving skills, refusal skills, jobs counselling, anger management and relapse prevention) which are shared in varying degrees with other CBT approaches. The ACRA model has the advantage of established effectiveness. A foundation in empirical research together with its manual- supported approach results in it being an appropriate “off the shelf ” intervention, highly applicable to many adolescent substance misusers. Such a focussed approach also has the advantage of limiting therapist “drift”. Notwithstanding the accessible manual and other resources available on- line, clinicians and students are strongly encouraged to undergo accredited ACRA training and supervision.
Unfortunately such a structured model, despite its many advantages, does have limitations. This model may not meet the sum of all drug misusing adolescent service user treatment needs, nor is it applicable to all adolescent drug users, particularly highly chaotic individuals with high levels of co- morbidities or multi-morbidities as often found in this population [29 , 30] . Whilst focussing on specifically on drug use, ACRA does not directly address co-existing problem behaviours or challenges such as depression, anxiety, personality disorder, or post traumatic stress disorder (PTSD) synergistically linked to drug use. It is possible that given the high levels of dual diagnoses encountered in this population as well as the compounding effect that drug use exerts on multiple systems, clinicians and practitioners may find a strict application of the ACRA model limiting, necessitating the application of an additional range or layer of psychotherapeutic competencies? Additionally the ACRA model does not focus explicitly on other psychological activities useful in the treatment of drug misuse such as the control and management of unhelpful cognitive styles or habits; breathing or progressive relaxation skills; anger management; imagery, visualisation and mindfulness. That is, as a manual based approach comprising a number of fixed components, a major potential challenge facing clinicians and students is the tension they may experience between maintaining strict fidelity to a pure ACRA approach, versus the flexibility l approved by more formulation driven CBT approaches?
The advantages of a skilled application of a formulation driven approach which are cited and summarised in are multiple and include the collaborative nature of goal setting, the facilitation of problem prioritisation in a meaningful and useful manner; a more immediate direction and structuring of the course of treatment; the provision of a rationale for the most fitting intervention point or spotlight for the treatment; an integration of seemingly unrelated or dissimilar difficulties in a meaningful yet parsimonious fashion; an influence on the choice of procedures and “homework” exercises; theory based mechanisms to understand the dynamics of the therapeutic relationship and a sense of targeted and ‘extra-therapeutic’ issues and how they could be best explained and managed, especially in terms of precipitators or triggers, core beliefs, assumptions and automatic thoughts.
Thus given the above observations and together with the importance placed on engagement and retention, the high variability in the cognitive, emotional, social and developmental domains [4] differences in roles (e.g. teenagers who are also parents) and levels of autonomy as well as high degrees of dual diagnosis or co- morbidities found in this group [29 , 30] practitioners are encouraged to also develop competencies in allied psychological treatment models such as Motivational Interviewing [31] ; familiarity with the core principles of CBT, disorder specific and problem-specific CBT competences, the generic and meta- competences of CBT as well as an advanced knowledge and understanding of mental health problems that will provide practitioners with the confidence and capacity to implement treatment models in a more flexible yet coherent manner,. In addition to seeking supervision and mentorship students and practitioners are directed, as a starting point, to University College London’s excellent resources outlining the competencies required to provide a more comprehensive interventions [11] .
Both authors reported no conflict of interest in the content of this paper.
Author Contributions
Conceived and designed the experiments: JI. Recruitment & assessment and on going treatment t of patient JI. On going supervision of case KD. Contributed reagents/materials/analysis tools: JI, & KD. Wrote the paper: JI. Contributed to final draft paper KD.
Acknowledgments
We thank Adolescent Addiction Services, Health Service Executive.
- Compton WM, Thomas YF, Stinson FS, Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry 64: 566-576. View
- Hasin DS, Stinson FS, Ogburn E, Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 64: 830-842. View
- Carroll KM, Nich C, Ball SA, McCance E, Frankforter TL, et al. (2000) Oneyear follow-up of disulfiram and psychotherapy for cocaine-alcohol users: sustained effects of treatment. Addiction 95: 1335-1349. View
- Stetler CB, Ritchie J, Rycroft-Malone J, Schultz A, Charns M (2007) Improving quality of care through routine, successful implementation of evidence-based practice at the bedside: an organizational case study protocol using the Pettigrew and Whipp model of strategic change. Imp Sci 2: 1-13. View
- Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, et al. (2004) Efficacy of disulfiram and cognitive behavior therapy in cocaine-dependent outpatients: a randomized placebo-controlled trial. Arch Gen Psychiatry 61: 264-272. View
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, et al. (2008) Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. Am J Psychiatry 165: 881-888. View
- McHugh RK, Hearon BA, Otto MW (2010) Cognitive behavioral therapy for substance use disorders. Psychiatr Clin North Am 33: 511-525. View
- Waldron HB, Kaminer Y (2004) On the learning curve: the emerging evidence supporting cognitive-behavioral therapies for adolescent substance abuse. Addiction 99 Suppl 2: 93-105. View
- Freeman A, Reinecke MA (1995) Cognitive therapy. New York: Guilford Press.
- Stephens RS, Babor TF, Kadden R, Miller M; Marijuana Treatment Project Research Group (2002) The Marijuana Treatment Project: rationale, design and participant characteristics. Addiction 97 Suppl 1: 109-124. View
- Pilling S, Hesketh K, Mitcheson L (2009) Psychosocial interventions in drug misuse: a framework and toolkit for implementing NICE-recommended treatment interventions. London: British Psychological Society, Centre for Outcomes, Research and Effectiveness (CORE) Research Department of Clinical, Educational and Health Psychology, University College. View
- Azrin NH (1976) Improvements in the community-reinforcement approach to alcoholism. Behav Res Ther 14: 339-348. View
- Hunt GM, Azrin NH (1973) A community-reinforcement approach to alcoholism. Behav Res Ther 11: 91-104. View
- Azrin NH, Sisson RW, Meyers R, Godley M (1982) Alcoholism treatment by disulfiram and community reinforcement therapy. J Behav Ther Exp Psychiatry 13: 105-112. View
- Meyers RJ, Miller WR (2001) A community reinforcement approach to addiction treatment: (International Research Monographs in the Addictions) Cambridge Univ Press.
- Mallams JH, Godley MD, Hall GM, Meyers RJ (1982) A social-systems approach to resocializing alcoholics in the community. J Stud Alcohol 43: 1115-1123.
- Finney JW, Monahan SC (1996) The cost-effectiveness of treatment for alcoholism: a second approximation. J Stud Alcohol 57: 229-243. View
- Rollnick S, Miller WR (1999) What is motivational interviewing? Behav Cogn Psychotherapy. 23: 325-334. View
- Garner BR, Barnes B, Godley SH (2009) Monitoring fidelity in the Adolescent Community Reinforcement Approach (A-CRA): the training process for A-CRA raters. J Behav Anal Health Fit Med 2: 43-54. View
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, et al. (2004) The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat 27: 197-213. View
- Garner BR, Godley MD, Funk RR, Dennis ML, Godley SH (2007) The impact of continuing care adherence on environmental risks, substance use, and substance-related problems following adolescent residential treatment. Psychol Addict Behav. 21: 488-497. View
- Slesnick N, Prestopnik JL, Meyers RJ, Glassman M (2007) Treatment outcome for street-living, homeless youth. Addict Behav 32: 1237-1251. View
- Beck AT, Hollon SD, Young JE, Bedrosian RC, Budenz D (1985) Treatment of depression with cognitive therapy and amitriptyline. Arch Gen Psychiatry 42: 142-148. View
- Smith C (1998) Assessing health needs in women's prisons. PSJ 224.
- Maude-Griffin PM1, Hohenstein JM, Humfleet GL, Reilly PM, Tusel DJ, et al. (1998) Superior efficacy of cognitive-behavioral therapy for urban crack cocaine abusers: main and matching effects. J Consult Clin Psychol 66: 832-837. View
- Godley SH, Meyers RJ, Smith JE, Karvinen T, Titus JC, et al. (2001) The adolescent community reinforcement approach for adolescent cannabis users: US Department of Health and Human Services. View
- Carroll KM (1998) A cognitive-behavioral approach: Treating cocaine addiction. National Institute on Drug Abuse. View
- Bukstein OG, Glancy LJ, Kaminer Y (1992) Pattern of affective comorbidity in a clinical population of dually diagonised adolescent substance abusers. J Ame Aca Child Adol Psychiat 31: 1041-1045. View
- Kaminer Y, Burleson JA, Goldberger R (2002) Psychotherapies for adolescent substance abusers: Short- and long-term outcomes. J Nerv Ment Dis 190: 737-745.
- Miller WR, Rollnick S (2002) Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press. View
- Open access
- Published: 14 April 2011
A Research Strategy Case Study of Alcohol and Drug Prevention by Non-Governmental Organizations in Sweden 2003-2009
- Charli Eriksson 1 ,
- Susanna Geidne 1 ,
- Madelene Larsson 1 &
- Camilla Pettersson 1
Substance Abuse Treatment, Prevention, and Policy volume 6 , Article number: 8 ( 2011 ) Cite this article
29k Accesses
10 Citations
Metrics details
Alcohol and drug prevention is high on the public health agenda in many countries. An increasing trend is the call for evidence-based practice. In Sweden in 2002 an innovative project portfolio including an integrated research and competence-building strategy for non-governmental organisations (NGOs) was designed by the National Board of Health and Welfare (NBHW). This research strategy case study is based on this initiative.
The embedded case study includes 135 projects in 69 organisations and 14 in-depth process or effect studies. The data in the case study has been compiled using multiple methods - administrative data; interviews and questionnaires to project leaders; focus group discussions and seminars; direct and participatory observations, interviews, and documentation of implementation; consultations with the NBHW and the NGOs; and a literature review. Annual reports have been submitted each year and three bi-national conferences Reflections on preventions have been held.
A broad range of organisations have been included in the NBHW project portfolio. A minority of the project were run by Alcohol or drug organisations, while a majority has children or adolescents as target groups. In order to develop a trustful partnership between practitioners, national agencies and researchers a series of measures were developed and implemented: meeting with project leaders, project dialogues and consultations, competence strengthening, support to documentation, in-depth studies and national conferences. A common element was that the projects were program-driven and not research-driven interventions. The role of researchers-as-technical advisors was suitable for the fostering of a trustful partnership for research and development. The independence of the NGOs was regarded as important for the momentum in the project implementation. The research strategy also includes elements of participatory research.
Conclusions
This research strategy case study shows that it is possible to integrate research into alcohol and drug prevention programs run by NGOs, and thereby contribute to a more evidence-based practice. A core element is developing a trustful partnership between the researchers and the organisations. Moreover, the funding agency must acknowledge the importance of knowledge development and allocating resources to research groups that is capable of cooperating with practitioners and NGOs.
Introduction
Alcohol and drug prevention is high on the public health agenda in most countries. The national initiatives differ, although action plans have been proposed by international organizations such as WHO [ 1 ]. Moreover, there is an increasing demand for evidence-based alcohol and drug prevention, causing an increased emphasis on research for prevention, an emphasis that this field shares with health promotion, prevention in general, and social work [ 2 – 8 ]. This means that prevention research needs to move "from basic to more and more applied research; from descriptive hypothesis-generating pilot studies to full-fledged, methodologically sophisticated, hypothesis-testing studies; from smaller to larger samples for testing; from greater to lesser control of experimental conditions; from more artificial 'laboratory' environments to real-world geographically defined communities; from testing the effects of single intervention strategies into more complex studies of multiple strategies integrated into intervention systems; and from research-driven outcome studies to 'demonstration' projects that evaluate the capacity of various types of communities to implement prevention programs based on prior evaluations" [[ 9 ], p 183]. It has also been more than 10 years since Nutbeam [ 10 , 11 ] noted the gap between the need for knowledge and the priorities among researchers.
Many years have passed since these recommendations, but still the gap between evidence and practice has not been bridged despite important achievements in implementation research [ 12 ], designs for effectiveness and translation research [ 13 ], and a series of initiatives regarding the evidence-practice gaps [ 14 – 22 ]. The call for more practice-based evidence is a challenge for policy-makers, practitioners, researchers, and funding agencies [ 17 , 23 ]. In several countries research on alcohol and drug issues has been incorporated into addiction research centres [ 24 – 28 ]. For many years much addiction research has been the product of specialized research centres rather than the contribution of standalone scientists. Moreover it is the specialist centres, in collaboration with the national funding agencies, which today assert leadership, set agendas, and help determine standards [ 24 ]. However, a common element in the missions of these centres is monitoring the substance use in the population, its causes, and courses, while prevention research is not high on the agendas. Furthermore, the establishment of national centres demonstrates the political administration's emphasis on scientific, evidence-based policies, but at the same time demonstrates the view that credible research is best performed within independent scientific bodies [ 26 ].
In Sweden in 2002 an innovative project portfolio for non-governmental organisations (NGOs) was designed by the National Board of Health and Welfare (NBHW). This included an integrated research and competence-building strategy to strengthen alcohol and drug prevention. This case study aims to describe and analyse this initiative.
AD prevention in Sweden - legislation, national action plans, resources, and actors
Sweden has a long tradition of a restrictive alcohol policy [ 29 ]. The temperance movement became a powerful actor in the Swedish alcoholic beverage policy [ 30 ]. Moreover, Sweden is one of the few countries in Europe with a narcotics policy that aims to create a society entirely free of illicit drugs [ 31 ].
The overall goal of the Swedish action plan on alcohol and narcotics is to promote public health by reducing the medical and social harm caused by alcohol and to create a drug-free society. The strategy for achieving this goal with regard to alcohol is to reduce the total consumption and prevent harmful drinking, taking into account differences in living conditions among boys, girls, men, and women. Six priority sub-goals have been adopted: alcohol should not be consumed in transport contexts, at workplaces, or during pregnancy; children should grow up in an alcohol-free environment; the age of alcohol debut should be postponed; drinking to point of intoxication should be reduced; there should be more alcohol-free environments; and illicit alcohol should be eliminated. The sub-goals in the action plan on narcotics are to reduce recruitment to drug abuse, induce people with substance abuse problems to give up their abuse, and to reduce the supply of drugs. Interventions targeting children, adolescents, and parents are of high priority [ 32 ].
Swedish alcohol policy is based on a combination of taxed-based price controls and the alcohol retail monopoly in order to limit the availability and accessibility of alcohol [ 32 ]. There is strong evidence for the preventive effects of an alcohol retail monopoly [ 33 , 34 ] and high prices on alcohol are regarded as one of the most effective ways of reducing total alcohol consumption and alcohol-related problems [ 35 ]. When Sweden entered the EU in 1995, the conditions changed and Sweden could no longer have an independent alcohol policy. For example, the availability of alcohol increased as a result of changed rules for private import, and alcohol taxes had to be adjusted. The numbers of alcohol shops as well as their opening hours have also increased remarkably since 1995 [ 29 ]. The increased movements across borders have also had an influence on the illicit drugs market. Almost all narcotics that are consumed in Sweden have been produced outside the country. A well-developed international collaboration is therefore of high importance for the limitation of illicit drugs in Sweden [ 32 ].
An effective alcohol and drug policy also requires national coordination. The Swedish government has established a national council for alcohol, narcotics, doping, and tobacco. The council consists of members of public authorities, civil society, and researchers, and is led by the State Secretary of the Ministry of Health and Social Affairs. The council is commissioned to advise the government on issues about alcohol, drugs, doping, and tobacco and to present information about research results [ 36 ].
There is a need for the different sectors in society to increase and deepen their cooperation for an effective prevention of the use of alcohol, tobacco, and drugs. In the Swedish action plan on alcohol and illicit drugs as well as in the government bill for public health the importance of the voluntary sector is emphasized [ 36 , 37 ]. In the latter document, A renewed public health policy , it is stated that cooperation between the state and the voluntary sector should be expanded and that the conditions for the voluntary sector's work should improve [ 37 ]. An agreement about the relations between the government, the voluntary sector in the social setting, and the Swedish Association of Local Authorities and Regions has recently been developed through a dialogue between the parties. The dialogue is another way for the government to call attention to the voluntary sector and to its ambition to strengthen the sector and improve its conditions. The goal of the agreement was to strengthen the independence of the voluntary sector as moulders of public opinion and to support the development of public medical service carried out by the voluntary sector [ 38 ]. The Swedish voluntary sector has a long tradition of alcohol prevention, especially the temperance movements [ 39 ].
NGOs in Sweden
The Swedish voluntary sector is both different and similar to those in other countries. A major difference lies in its history in that, for instance, as early as in the 16th century the responsibility for health and care was organized under the state instead of in the regime of the church. In parts of Europe the church still is an active actor in health and care [ 40 , 41 ]. Also, popular mass movements have played an important role in the development of Swedish society [ 41 , 42 ]. The Swedish voluntary sector is as large as in other industrialized countries, although quite different in character. It is dominated by organizations in the cultural and recreational field, mainly sports organizations. Since the early 1990s the Swedish voluntary sector has expanded, particularly in the two areas of culture and recreation, as well as in the area of social care [ 43 ]. It can also be called membership-based; almost everyone in Sweden is a member of some organization. Because of these differences in history and structure in different societies, the voluntary sector plays different roles. In Sweden, NGOs are more of a complement then a substitute for state programs, and have an important role as forerunners and innovators [ 44 ].
Previous research has shown that the Swedish voluntary sector was highly dependent on public financing, which is partly correct. Looking at the entire sector together, about 30 percent of its financing comes from government funding. However, within the health care and social service sector, public financing stands for more than 70 percent. That is quite high in comparison with other European countries, but not the highest [ 45 ].
Support to NGOs today
Organizational grants.
The National Board of Health and Welfare (NBHW) has a government commission to administer the grants to national organizations for the disabled, the elderly, and relatives of elderly persons; to national organizations in the social setting; and to national and local organizations. For the moment this amounts to about 300 million SEK to about 100 organizations. Also the Swedish National Institute of Public Health has funds to distribute to NGOs or to other organizations working together with NGOs. The Swedish State Inheritance Fund is also a possible source of funding for NGOs. They administer over 300 million SEK a year to provide grants to NGOs working with children, youth, and the disabled. In addition other governmental agencies such as the Swedish National Board for Youth Affairs also support NGOs.
Project grants
In the late 1990s a new system of awarding grants to NGOs in the arenas of alcohol and narcotics, vulnerable children and their families, and violence against women was prepared. The previous systems were from the late 1970s and early 1980s, and during the 1990s many investigations recommended a better, more structured follow-up and evaluation of the NGOs' work. One new idea that emerged during the 1990s was increased performance management, that is, the need to point out achieved results and effects of different activities. It was emphasized that the government should not interfere with the running of the organizations but does have the duty to monitor the use of the grants. There was also a desire that renewal efforts and collaborations should be encouraged and supported.
In the late 20th century grants were awarded through the Swedish National Institute of Public Health (with money from the Swedish State Inheritance Fund) to a number of alcohol and drug prevention projects. A final report and an internal evaluation were required from the applicants. There was also an external evaluator, who conducted an evaluation of 11 projects focusing on their working processes [ 46 ]. Among the lessons learned from this evaluation were that the way of working should be characterized by frequent contacts and dialogue between the funding agency and the project, and also by supervision. The evaluation report also suggested that the support to the project leaders should be reviewed with regard to the possibility of different types of need-based support. Moreover, the short-term thinking in the funding of these kinds of projects was not in line with the needed time-frame.
Setting the Scene: NGO strategy for alcohol and drug prevention
Non-governmental organizations have received grants from the NBHW to conduct alcohol and drug preventive work in a special venture since 2003 [ 47 ]. This initiative is part of the national plan of action to prevent alcohol-related harm and the national plan of action against narcotics and comes from the Ministry of Health and Social Affairs. The working committee, which decides who will get funding, consists of members of the NBHW, the Swedish National Institute of Public Health, and the Swedish National Board for Youth Affairs (previously members of the Swedish Alcohol Committee and the Swedish National Drug Policy Coordinator were included). The working committee, after consulting the research team at Örebro University, also decides which projects will be studied in-depth. NBHW's initiative represented a new way of thinking. One point of departure was to create a project portfolio with a broad combination of organizations to mobilize many forces in the alcohol and drug preventive work. The initiative also contains supervision for the project leaders, competence support through regular meetings for project leaders, and an integrated Research & Development (R&D) investment (Figure 1 ).
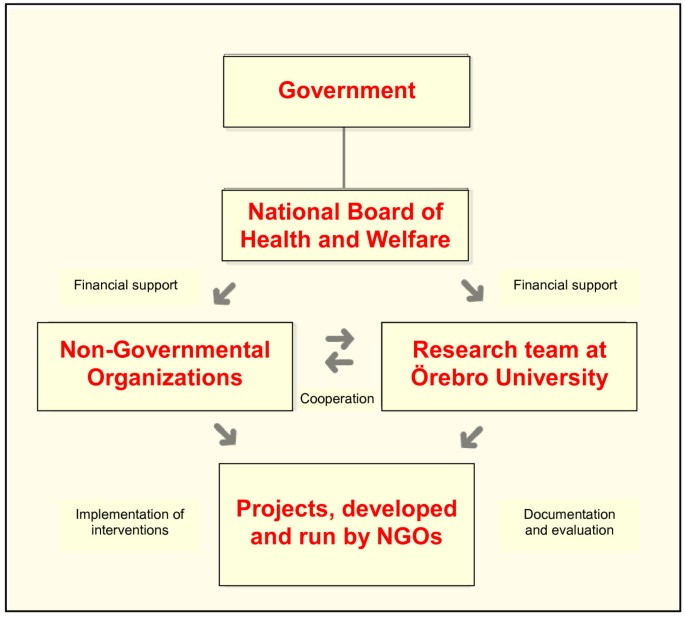
Integrated research and development for NGO alcohol and drug prevention .
Need for knowledge building and learning
There is an increasing trend towards promoting evidence-based public health initiatives. International expert committees have presented the state of science with regard to alcohol prevention: Alcohol Control Policies in Public Health Perspectives [ 48 ]; Alcohol Policy and the Public Good [ 49 ]; and Alcohol: No Ordinary Commodity -Research and Public Policy [ 33 , 50 ]. National authorities have presented reviews presenting evidence for practitioners and politicians [ 51 – 53 ]. However, there are important knowledge gaps to be filled. Among these is the lack of effectiveness studies where the external validity is high. If we want to see more evidence-based practice we need more practice-based evidence [ 54 ]. This means an improved emphasis on cooperation between researchers and practitioners [ 10 ].
A comprehensive perspective on the concept of knowledge, including scientific and practical knowledge as well as practical wisdom, is needed. Scientific knowledge about alcohol and drug issues needs to be complemented with knowledge about methods for alcohol and drug prevention. As in other public health fields, ethical issues and practical wisdom are important [ 55 ]. Moreover, the science, craft, and art of implementation are of utmost importance. There are many reasons besides practicalities that are significant for the implementation of programs [ 7 , 56 ]. In a recent review, 23 different factors were found that were of importance for the degree of the implementation [ 12 ] and that also have a great impact on the program effects.
Research on alcohol and drugs has often been organized in special research institutes, which often focus on basic research on alcohol and drugs [ 24 – 28 ]. This basic research is related both to basic biomedicine as well as social and behavioural studies. Another activity, which has been accorded great prominence, is the monitoring of alcohol and drug use in the population in general as well in different groups. Intervention research has been given less prominence in these often national research institutes. However, the national agencies, such as the Swedish Institute of Public Health, have been involved in the evaluation of different intervention projects. So far research on NGO-driven alcohol and drug prevention has been almost completely lacking. Research has been a more or less exclusive activity for the university. However, this has been based on the trust in the impartiality and objectivity of the university-based researchers. The downside of this position is that this type of research may lack the necessary cultural awareness and insights necessary for a proper understanding of basic factors for successfully planning intervention programs as well as evaluating research efforts. In other words the roles of the researcher in intervention studies need to be addressed. In a recent study, Holmila et al. [ 57 ] outlined three different positions for researchers in community intervention studies. The researcher can be an external observer, not taking part in the preventive activities - acting as an unobtrusive observer . The researcher assumes no responsibility for the design or implementation of the projects but acts as an independent conductor of process evaluation and observer of project outcomes. Another position is to be a researcher-as-technical advisor . In this role the researcher has responsibility for evaluation but also takes the responsibility for providing scientific advice on effective preventive strategies if asked for [ 58 – 60 ]. This could include training and technical assistance to the projects. Progress reports on findings as well as results from different on-going studies can be presented to the practitioners, which may use this information as they desire. A third type is researcher-as-designer , where the project is designed by the research team in partnership with the practitioner. The researcher is an active participant in project planning as well as the process of carrying it out and evaluating the effects. This approach is particularly useful when the goal is to test one or more designed prevention strategies under as close to optimal conditions as possible. Examples of such in Sweden are the STAD Project in Stockholm [ 61 ] and the Trelleborg Project [ 62 ]. The Örebro Prevention Program is an example of a program where all parts of the process were in the hands of the researchers [ 63 ].
The present paper aims to describe and analyse alcohol and drug prevention supported by the NBHW and implemented by NGOs in Sweden during 2003-2009 with a special emphasis on research and development for an evidence-based practice. The case study analyses also the integrated research strategy and its main components.
Three research questions will be addressed:
Which types of organizations and projects have received grants from the NBHW for AD prevention?
What types of research and development activities for an evidence-based practice have been included?
How can a trustful partnership develop between practitioners, national agencies, and researchers?
Methods and materials, case study approach.
A case study method was chosen as the intention was to understand a real-life phenomenon in depth and the contextual factors were highly pertinent to the study [ 64 ]. This method investigates according to Yin contemporary phenomenon in depth and within its real-life context, especially when the boundary between the phenomenon and context are not clearly evident. Moreover, the case study approach copes with the situation such as in this case in which there will be more variables of interest than data, which leads to the need for multiple sources of evidence, with data needing to converge in a triangulating fashion. Furthermore, benefits from the prior development of theoretical propositions to guide data collection and analysis [ 64 ]. The present research strategy case study is on an organisational level. It studies a social process in a situation in which we have little knowledge of the phenomenon, integration of research in alcohol and drug prevention run by NGOs. Case studies as a main research strategy are selected as this is a unique case in Sweden, the impossibility to isolate the process and the intention is to combine research and action [ 65 ].
An embedded single-case design was chosen for the study. All the projects run by the NGOs are seen as embedded units of analysis in the study with special emphasis on the fourteen in-depth studies.
Participants
The embedded case study includes 135 projects in 69 organisations and 14 in-depth process or effect studies. The participants in this research strategy case study are the NGOs applying for funding to the NBHW and especially those NGOs that have received funding during 2003-2009. The project leaders and managers in the NGOs as well as the members of the different target groups are also participants in this study. Moreover, staff at the NBHW as well as other stakeholders is included.
Case study questions
When the research program started a set of overall research questions were developed. In this paper the focus is in one of these, how can a trustful partnership for practice-based research be developed? Additional questions concerns: the role as a project leader in NGOs, the impact of competence development, methods for documentation of project development, and the added value of running projects in NGOs.
Case study protocol
A plan for the research and development activities was developed the first year and amended each year after the completion of the annual report to the NBHW. This plan consisted of several parts relating to the overall activities as well as the different in-depth studies. Notes were taken at meetings and as part of the strategy a series of presentations as progress reports were given to, project leaders, NGOs and the NBHW.
Development of a Case Study Database
In the present study a broad range of methods was used in the data collection. This includes six types of data.
Administrative data
The applications from the NGOs to the NBHW as well as the funding decisions were the initial data, which was complemented by bi-annual as well as annual progress reports from all funded projects. These reports, which were submitted following a format developed by the research team, gave information on implementation and goal achievement as well as reflections on barriers and facilitating factors. The research team introduced this approach at a meeting with the project leaders, and this reporting resulted in an annual report to the NBHW on the progress of the alcohol and drug prevention projects run by the NGOs.
Interviews and questionnaires to project leaders
Data was collected from project leaders and their organizations in the years when funding was received from the NBHW. In 2003, 2005, 2007, and 2009 all project leaders were invited to respond to a questionnaire containing questions on being a project leader in a non-governmental organization. If the same project leaders were responsible for a project for more than one year they responded to more than one questionnaire. Most of those who answered the 2003 questionnaire also answered the 2005 questionnaire, due to the fact that many of those projects receiving funding in 2003 also were being funded in 2005. In total, 84 persons participated in the questionnaire study over the years. Of these, 38 project leaders answered the questions more than one year.
Focus group discussions and seminars
Thematic discussions were held as a part of the meetings with the project leaders. These highlighted special issues related to the practice of alcohol and drug prevention. Moreover, a series of joint seminars with NGOs and the research team have been held at national and organizational conferences focusing on different projects.
Direct observations, participatory observations, interviews, and documentation of implementation of the in-depth studies
The research team collected information by a variety of methods during the planning, implementation, and evaluation of the in-depth studies. Part of this data has been used in the analysis, resulting in separate reports and scientific publications. However, in this context more process-related data will be used to give insights into the development of the partnerships between researchers and practitioners.
Consultation with the NBHW and the NGOs
In the present paper information retrieved during the management of the NBHW support to the NGOs will be an additional source of information. Regular meetings have taken place with the steering committee and the senior administrative officer, who have been the same persons during all years. The consultations with the NGOs were more intense for those organizations selected for in-depth studies, but several meetings have also taken place with other organizations. Apart of the in-depth studies was feedback on preliminary results from different studies; this never radically changed the interpretation of results but did add valuable information.
Literature review
A systematic review of the research strategies for alcohol and drug prevention has been carried out as an integral part of the research program. A number of publications related to collaboration between researchers and practitioners were found. Special thematic sections and series have been looked for. Among the key words are addiction research centre, alcohol and drug research, preventive research, practice-based research, and evidence-practice gaps.
Analytical methods
The analytical approach in this case study follows a common strategy used in research programs: to start with the ordinary preventive activities and then study what is happening [ 66 , 67 ]. Using a naturalistic approach, which is always practice-based, it has been important to let different actors and stakeholders into the knowledge-building program. This also has implications for the selection of research and evaluation methods, given a need for mixed-method approaches [ 68 – 70 ]. In studies of effects, quantitative approaches are essential, but important contributions can be achieved if qualitative studies are also included [ 71 , 72 ]. The mixed-methods approaches have been developed for some of the more extensively studied programs, which also will be included in doctoral dissertations [ 73 , 74 ].
The analysis starts with a quantitative description of the investment in NGOs by agencies awarding grants and an analysis of which organizations and projects that were supported. The types of organizations are analysed with regard to their main focus or mission. Then the investment in research is described including an overview of the participants in different empirical studies using a range of data collection methods. This includes a description of how the embedded units, the project in the NBHW portfolio, have been documented and presented in annual reports using a format for the written reports based on questions and answers in the case study database [ 64 ]. The two types of in-depth studies are briefly presented: effect studies and studies of process and implementation.
An analysis of the experiences of cross-project comparisons as well as using the multiple sources of evidence in the case study database follows. The different measures in the research program was developed in order to foster a trustful partnership is then presented. These measures were assessed by all project leaders in the annuals reporting to the research team, which reviewed the content of the research strategy each year in the annual report to the NBHW. The implementation of the research strategy with regard to evaluation initiatives together with the NGOs as well as in-depth studies was carefully documented over the years and used as indicator for developing a research partnership with the NGOs. In this case study the focus is on the implementation of the research and evaluation efforts and not on the outcome of the alcohol and drug prevention program. This has been reported in other publications [ 47 ]. The different types of data and perspectives included in the case study database are used for triangulation and finding key elements and mechanisms in the research strategy. In this case study a mixed-methods approach means parallel mixed data analysis, i.e. parallel analysis of qualitative and quantitative data from different sources. Moreover, integrated mixed data analysis also occurs in the analysis of the project portfolio and subsequent development of research initiatives. To grasp the complexity and inclusiveness of integrated methods the term inference has been proposed as the last and most important stage of research [ 70 ]. The inference process consists of a dynamic journey from ideas to results in an effort to make sense of data. In our case study the regular project leader meetings as well as the preparation of the annual evaluation and reporting to the NBHW are key activities in this process of drawing inferences. Key concepts in an integrative framework are inference quality, which is related to design quality, interpretative rigour, and inference transferability.
The results will be presented according to the three research questions. The calls for applications resulted in many proposals from many different organizations for a variety of projects engaging many project leaders.
Investing in the NGOs - Allocation of Grants 2003-2009
Since 2003 10-15 million SEK per year have been administered to this special venture (Table 1 ). The government's decisions have over the years differed somewhat according to which target groups are being specially addressed in the calls for grant applications. For the first period, which was a two-year period, the call was broad. For the second period, 2005, the main part of the grants went to projects from the earlier period. From 2006 to 2009 the target groups have been children, youth, young adults, and the workplace according to the national action plans. It has also been emphasized that the projects would be new or in the process of expanding existing activities.
About one in four applications were awarded a grant. The amount of funds provided to NGOs varies. The minimum amount of funding for one year was 40,000 SEK and the largest amount was 1,200,000 SEK. Many organizations have been funded for several years. Over the years 2003-2009 the NBHW has in total apportioned about 80,000,000 SEK to the NGOs. In addition a yearly grant has been awarded to an integrated Research & Development (R&D) program as well as funds for administration and information activities. The total allocation from the NBHW has been 95,000,000 SEK, covering 135 projects in 69 organizations funded during these years.
The projects differed in size. Table 2 presents these 219 project grants over the years 2003-2009. The reason for this lower number of project (135) is that 50 projects have been funded over more than one year, 26 projects over two years, 17 projects over three years, and two projects over four and five years each. The first period, which covered two years, had the highest number of large projects. Moreover, the number of funded project has increased between 2005 and 2008 and the number of large projects has remained relatively stable since 2005.
Organizations and projects
The strategy to involve a broad range of organizations has been successful. In Figure 2 the 69 organizations and the 135 projects are presented according to type of organization. The largest number of projects were run by the nine alcohol and drug organizations. More than half of these projects were run by the Swedish temperance organisation IOGT-NTO (24 of 38 projects) amounting to 15 million SEK. The majority of these were small one-year projects, except for two programs where effect studies were conducted by the research team and the organization jointly. Between 15 and 20 projects were run by organizations focusing on social work, assistance, and ethnic groups. About 10 projects were run by sports, adult education, and religious organizations respectively. Furthermore, 14 projects were set up by two umbrella organizations each consisting of a number of member organizations.
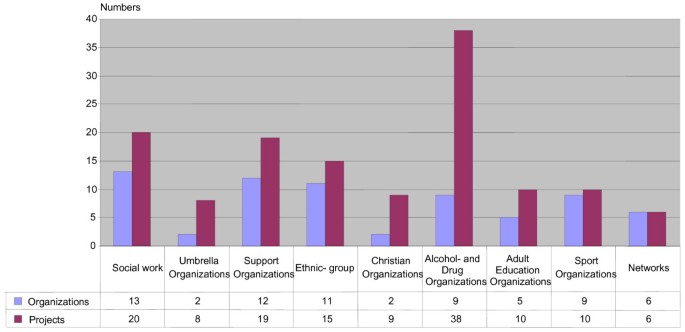
Organizations and projects in different types of organizations according to main objectives .
The projects have different primary target groups for their activities. A majority of the projects have children or adolescents as target groups. Some of these projects are focused on young girls with the aim of promoting self confidence and a positive self image. Sports organizations have been developing alcohol and drug policies including anti-doping initiatives. Projects run by ethnic groups have as their target group members of their organizations including children, adolescents, and parents. A few projects have the workplace as the arena for intervention.
During the first years, three community-based projects were funded. These aimed to reduce drugs in two parts of Stockholm and the island Gotland. The strategy included a range of activities and collaboration with different actors. A broad membership in the organizations seems to be important for the sustainability of the community-based prevention.
Only one project has reduction of availability as its focus. This project focused on following up the alcohol legislation concerning the sale of beer to minors in Sweden [ 75 ] and the effect of different strategies to influence shops to comply with the law [ 74 ].
Internet has a great potential in promotion and preventive work [ 76 ]. The majority of the organizations have their own website on the Internet and about one third have a project-specific site. The organizations used information technology as a source of health information in three projects, as an intervention medium in four, for professional development in two, and as a research instrument in one project. The use of e-screening as a tool for drug prevention is studied by researchers at Karolinska Institute. There are still very few scientific evaluations of the use of Internet in drug prevention [ 77 ].
Basic characteristics of the project leaders in the alcohol and drug prevention projects are given in Table 3 . All four years the proportion of women was larger than men; about two of three project leaders were women. Most of the project leaders belonged to the age group 41-50 years in the early periods (2003/2005) while in the later periods (2007/2009) an increased proportion of the project leaders were 50 years or older. Moreover, nearly one in ten project leaders was 30 years or younger. Many of the project leaders in volunteer work were members of the organization before being appointed project leaders (Table 3 ). In 2003 eight of ten project leaders were members compared with four of ten in 2007 and 2009. Nearly half of the project leaders were also doing volunteer or non-paid work in the organization. No gender differences were found in the prevalence of non-paid work.
Investing in Research and Development
A research and evaluation strategy was developed by the research team at the School of Health and Medical Sciences, Örebro University. This strategy rests on collaboration with the NGOs through regular meetings with all project leaders, development of systematic documentation of project objectives, activities, and results, annual reports to the NBHW, and biannual national conferences Reflections on prevention (2006, 2008, and 2010). The role of the researchers can most closely be characterized as researchers as technical advisors . In some projects the researcher had the position of an unobtrusive observer -for instance in following up some projects in which no longitudinal data collection was included. In addition, in no project did the researcher have the position of researcher as designer . Moreover, separate competence development and discussion of evaluation studies were conducted with a smaller number of organizations. The steering committee at the NBHW also decided, after consulting the research team, on a number of in-depth studies. Fourteen such studies were included in the funding from the NBHW (Table 4 ). The research team was also involved in three additional studies funded by other sources. These studies focused on policy development in the Swedish Football Confederation, evaluation of regional collaboration against illegal alcohol, and alcohol prevention in Novgorod, Russia.
This set of studies included systematic collection of data from children, parents, and actors in projects. A description of the empirical studies carried out between autumn 2003 and spring 2009 is given in Table 5 . Different methods, including questionnaires, personal interviews, telephone interviews, and focus group interviews, have been used depending on the purpose of the study. The main research questions have been related to the process or effect evaluations of these projects. The majority of the studies have been carried out with adolescents, as many of the projects receiving grants from the NBHW are targeting adolescents for the purpose of preventing alcohol and tobacco use. In three studies, data have been collected from both adolescents and parents, and two of these are longitudinal studies with adolescents and their parents. Dyads of adolescents and parents are identified and have been followed over the three years of secondary school. All youth surveys have been carried out in a school environment while the questionnaires to the parents have been sent by mail. Municipalities, schools, and organizations across Sweden have participated in the studies. There are many advantages with the partnerships that have been developed between the research team and the project leaders within the NGOs. For example, the large scale of the studies that have been carried out during the six years could not been managed without this cooperation. The project leaders have done much of the practical work locally, such as the dialogue with participating schools and organizations, distribution of questionnaires, and sometimes also feedback to participants.
What types of research and development have been included?
All projects in the project portfolio had to submit semi-annual and annual reports. These reports were analysis and synthesized into an annual report to the NBHW. This was based on a reporting format using questions for different important elements in the projects as well as key aspects of project management. The preparation of the annual reports included cross-project comparisons with regard to the case study questions, which resulted in some amendments and changes over the years in the research and development activities.
After the decision on potential projects for in-depth studies, planning meetings were convened with the project leaders and managers in the NGOs. Based on the project proposals and joint planning between the project leaders and the researchers, a plan for the in-depth studies was developed. Depending on the evaluation and research questions and available resources the focus, design, process, and outcome measures were set (Table 6 ). The overall results were positive; ten of the fourteen in-depth studies were completed. One project did not succeed in recruiting high-risk parents to a parental support program (IOGT-NTO Centro). Three projects were only partially completed: one started before the research team was organized, making the evaluation impossible (IOGT-NTO: Dare/Young and King); one was cancelled after a decision by the municipality (SMART Västernorrland); and in one it was impossible to follow up information from policy-makers due to a low response rate (Makalösa föräldrar). Eleven of the in-depth studies started during the first period (Table 4 ). There were some common research questions such as the effects of the projects. The NGOs wanted their approach to be studied in such a way that, in the event of positive results, the program could be regarded as evidence-based.
Effect Studies
Seven projects were considered for evaluation with effect studies, which were planned for all seven projects. However, one project was unsuccessful and two only partially completed due to overly limited implementation. One project was already implemented when the research group was appointed. It was nevertheless possible to plan and successfully complete effect studies even with short-term yearly funding.
KSAN "About small things"
The aim of this project was to develop and test an early intervention targeting pregnant women to prevent alcohol injuries in unborn children. The project was developed by the KSAN, an umbrella organization for women's organizations concerned with alcohol and drug issues, and the Swedish Association of Midwives. It was implemented in a maternal health centre in Stockholm. A randomized controlled study was completed with 454 mothers randomly assigned to either receiving an information folder with the message "Pregnancy is not a time for risk-taking" sent to their home after the telephone contact for booking the first visit to the midwife, or getting the folder during their first visit to the midwife. The effects of the intervention were measured by a questionnaire that the pregnant women answered at the maternal health centre before they met with the midwife.
IOGT-NTO: Strong and Clear
Strong and Clear is a parental support program targeting parents with children aged 13-16 years. It is a universal program aiming to prevent drinking among adolescents and to maintain parents' restrictive attitudes concerning adolescents and alcohol. The program is manual based and includes thirteen activities during the three years of secondary school. The parents can sign up for the program during the whole period the program is carried out. There are both group and self-administered activities divided into four types: parent meetings, family dialogues, friend meetings, and family meetings. The program was implemented in six schools.
The research program includes the effect study, which was designed as a longitudinal quasi-experimental study, and studies of parental attitudes and behaviour with regard to adolescents and alcohol [ 78 ] as well as reasons for non-participation [ 73 ]. In the longitudinal study, 706 children and 613 parents participated in the baseline questionnaire, which was followed by repeated data collection in the two following school years.
IOGT-NTO: Parents Together
The program Parents Together consists of three parents' meetings during three years in secondary schools. The intention is to motivate the class parents to come to an agreement on the following issues: "We enforce the 18-year limit for alcohol; We will not provide each other's children alcohol; We will get in touch with each other if we see a child we know who is not sober, is behaving badly, or is out at times and places where we would not want our own children to be."This agreement is used to strengthen the cooperation among parents. The idea is that this will make a difference with respect to the children's alcohol use. A parent-teachers meeting is held each year to update the agreement.
The design of the study is a cluster randomized controlled study in Swedish secondary schools with seven intervention and six control school. The study included almost 2000 pupils and their parents. The program Parents Together was carried out over three years in the seven intervention schools with a start in both school years 7 and 8 (Figure 3 ). The six control schools have been offered the program for parents whose children are in year 7 in the spring 2009 and the program will follow in the years 2010 and 2011. To reveal effects of the program the evaluation also includes a questionnaire about the prevention work in schools and implementation reports. The non-governmental organization IOGT-NTO is responsible for the program and the implementation in the seven intervention schools. To maintain the cooperation between the thirteen schools, the NGO, and the research team, an agreement has been signed. The agreement includes information about the responsibilities of each party such as that the researchers should the results of surveys, within six months after the data collection, are published on the website.
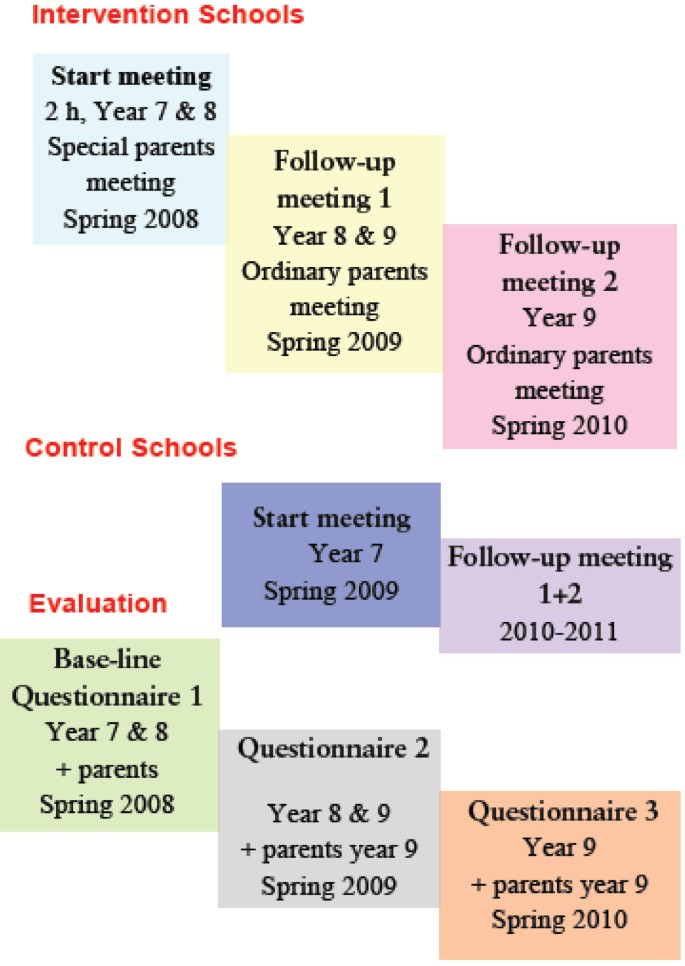
Design of the intervention and evaluation of the program Parents Together .
IOGT-NTO Centro: Parental Support
This project was planned to include before and after questionnaires to high risk parents. However, the project did not succeed in attracting this type of parents to the program.
Hassela solidaritet: Peer Support in School
This NGO works with training and assisting school children to be peer supporters in their own school. The aims of the project are to prevent social exclusion by reducing teenage alcohol consumption, experimentation with drugs, and bullying through peer support in schools, and to promote a school that is a positive, creative, and stimulating workplace for all. The program was first implemented in one part of the school, and was planned to be extended to the whole school. Subsequent implementation in a second school was planned. However, this extended implementation was only partly carried out due to limited resources. The evaluation included focus group interviews with peer supporters and repeated cross-sectional questionnaires to schoolchildren in school years 7-9 in the two schools.
National Federation SMART: SMART Västernorrland
The main objective of this NGO is to prevent or postpone alcohol, tobacco, and other drug use among children through positive reinforcement and signing of contracts. The parents sign the contract together with their child. The content of these contracts varies between local organizations. The membership gives the child positive benefits reinforcing positive behaviours. The program was implemented in a Swedish county, Västernorrland. The evaluation plan included an effect study among schoolchildren in Kramfors, a study of parents, and an interview of stakeholders in the county. The program was cancelled by the municipality of Kramfors with negative consequences for the effect study, which had been planned as a repeated cross-sectional study of schoolchildren in years 4-9. Data was collected with questionnaires and during the three years, 2,052 children answered the questionnaire. The research team decided to implement the evaluation as planned even if there was no intervention the third year.
The Swedish Youth Temperance Movement (UNF): Folk Beer Project
The Non-governmental organization UNF is a politically and religiously independent organization. They are a sister organization to IOGT-NTO (The Swedish Temperance organization), which is a part of the International Organization of Good Templars. All members are between 13 and 25 years of age. To be a member you have to be a teetotaller. The activities are of different kinds, for example arranging theatrical performances, discos, cafés, study circles, and a large number of courses. Besides dealing with alcohol regulations and politics regarding alcohol, they also work with international exchange and democracy issues. Their vision is a democratic and socially responsible world free from drugs. Although they are politically independent, their task is to act politically in letting the politicians know which issues are important to them. UNF has an almost 40-year history of conducting underage alcohol purchase attempts.
In 2003 UNF applied for funding for a new idea. They wanted to compare two different strategies that included underage purchase attempts. The first was an elaboration of their earlier method, which meant confronting the media with the results of the purchase attempts, reporting the check-out clerks who sold them beer to the police, and informing the municipalities of which stores that sold beer to minors. The other method was based on the idea to actively seek cooperation with the retail grocery sector, the municipality's alcohol administrator or drug coordinator (the municipalities are organized differently), the police, and the labour unions. The evaluation program was designed as a quasi-experimental study and as a follow up of the alcohol legislation concerning the sale of beer to minors in Sweden [ 75 ] and of the effect of different strategies to influence the shops to comply with the law [ 74 ].
Studies of Process and Implementation
Seven of the in-depth studies focussed on the working process in the projects. Three projects were community-based and had a clear geographical area where the programs were implemented. Motgift Gotland was an alliance for preventing the use of narcotics on the island of Gotland. Söder mot Narkotika was also an alliance against narcotics in a central district (Södermalm) of the capital Stockholm. A broad range of agencies and organizations collaborated in these efforts. A third community-based project was run by Verdandi Tensta Rinkeby. The three community-based projects were studied during 2005-2006 and included interviews with stakeholders and actors in the projects. A lesson learned is that community-based prevention needs to have broad support and cannot depend heavily on individual project leaders.
Verdandi: Get safe in Tensta - Rinkeby. Meet us!
An in-depth analysis was made of the third project in order to uncover their successful strategy. Verdandi, founded in 1896, is a Swedish workers' organization striving for social justice and a society free from alcohol-related injuries. From the very beginning, Verdandi - as an independent organization within the workers' movement - has aimed to improve people's social and financial situations. Today's aim is to analyse the development of society through the experiences and voices of those who are not heard otherwise. People of all ages, in all parts of the country, may participate in Verdandi's activities, which are quite different from place to place since they are based on local needs. According to Verdandi, without a local angle, the organization would soon lose touch with reality as well as lose credibility and members.
Verdandi runs activities for youth. The project includes support for children both in school and after. The youth in the organization can use a facility in the neighbourhood in their leisure time. Youth activities have focused on "the young leading the young" and the project has demonstrated young people's ability to organize and run a rewarding activity in the evenings and on weekends. The aim of this prevention program is to empower young people in their daily lives and help them empower their friends. This, according to the organization, contributes to young people avoiding drugs, and the neighbourhood has become calmer and safer. The activity has a bottom-up nature and the youth are involved in the planning. They have the opportunity to develop activities and thereby affect their daily lives. Among the success factors, according to the in-depth study, are: confidence in the organization, equality, youth involvement and power, memberships, support from the parents, training of leaders, common norms and roles, volunteer work, easily accessible premises, and a leadership that facilitates democratic processes.
IOGT-NTO: Dare/Young and King
This program is a redesigned version of the American program DARE [ 79 ], which was implemented before the research group was appointed. However, an adult education component, Young and King, aiming to strengthen parents was implemented and a follow-up study was completed of this component of the program.

IOGT-NTO:s Juniorförbund: Junis sisters
In this project, groups of schoolgirls in years 5 and 6 are organized with the objective to strengthen their self-esteem and promote meaningful leisure activities and thereby delay the onset of alcohol consumption by the girls. The evaluation focused on the group leaders, who were interviewed in focus groups. A lesson learned is that special effort must be put into recruiting and assisting group leaders to achieve sustainable programs.
Makalösa föräldrar: Single Parent with Teenagers
The project consisted of two main parts. One part focused on improving the knowledge about how it is to be a single parent with a teenager in the family. A survey of single parents was done in a part of Stockholm and a small newsletter was produced. The other part included self-help groups for single parents and summer camps. The evaluation of the self-help groups consisted of follow-up questionnaires to participants. An unsuccessful part of the evaluation was the follow-up of the newsletter, which was well planned and properly designed. It was not possible to get feedback from policy-makers on the publication, which may be due to lack of awareness of the publication and its contents.
The Swedish Ice Hockey Association: School Ambassadors
The project aimed to train top athletes to become school ambassadors in order to influence the attitudes of schoolchildren and give them the opportunity to try out ice hockey. Moreover, the project was also an attempt to improve the collaboration between schools and top ice hockey clubs. In the second year the specialized ice hockey secondary schools were included in the program. The evaluation consisted of following up the training of the athletes and studying the work of the secondary school ice hockey players by means of a questionnaire to schoolchildren.
In order to promote the development of a partnership a series of measures were implemented (Table 7 ). All project leaders were invited to regular meetings, which were held in Örebro as well as in Stockholm, Gothenburg, and Malmö. The agenda included presentation of project plans, information from the NBHW, and the research and development activities by the research team. Thematic lectures and discussion on issues such as the art of project management, measures to reach target groups, media advocacy, Internet as a tool for prevention, and planned communication were held at different meetings. The main objective of these meetings was to promote exchange of experiences and learning in order to strengthening the quality of the implementation of the projects as well as networking. Moreover, the systematic bi-annual and annual reports were introduced and discussed.
Depending on the needs of the different projects special project dialogues and consultations were held between individual projects, or a small group of similar projects, and the research teams. The results of these meetings ranged from refinement of project ideas to long-term collaborations. All in-depth studies started with such meetings. The competence development took different forms. In the first period an academic training program in alcohol and drug prevention was offered to the project leaders, of whom about 10 participated. Supervision in groups was implemented in three groups during the first two years, and thereafter one or two groups were run by independent supervisors annually. During 2009 the research team arranged more project leader meeting including training in project management as an alternative to supervision.
The in-depth studies were also an important measure to foster the partnership between the NGOs and the research team. Due to available resources, more extensive process and effect evaluation activities could only be implemented in a limited number of projects. Many more projects asked to be the focus of in-depth studies than the fourteen that were initiated.
The research team together with the NBHW arranged a national conference Reflections on prevention - Collaboration for better alcohol and drug prevention. Conferences were arranged in the spring of 2006, 2008, and 2010. Among the key issues discussed at the first conference were the role of parents in prevention, adolescents, community-based approaches, and supply-reducing initiatives. The second conference also discussed the role of civil society and how to promote more effective cooperation among the different stakeholders. The third conference focussed on evidence and evidence-based practice, which have received increased attention in Sweden in many sectors of society. A main emphasis has been setting the context for reflection and sharing of experiences among the participants at the conferences; therefore a series of seminars with project presentations and panel discussions have been part of the conferences. Moreover, plenary sessions as well as theatrical performances further set the stage for professional dialogues on alcohol and drug prevention. The conferences have been well received and have attracted actors from different sectors of society as well as national agencies and NGOs.
In the annual reports the project leaders also assess the implemented measures by the researchers. These have guided the future efforts of the research team. As an example, the assessments made in January 2005 are presented in Figure 4 . The financial support was very important, followed by the support from the NBHW, the project leader meetings, and the supervision. One third of the project leaders regarded the support for the documentation as very important. The academic training in alcohol and drug prevention was regarded as very important by one fifth of the project leaders, which is a high proportion given that only a small group participated in the distance education course. Only eight projects were at that time included in the in-depth studies, nevertheless one third of the project leaders reported this measure as very important. The case study data bank includes information for questionnaires, interview and other data sources for the assessment of the implementation of the research strategy.
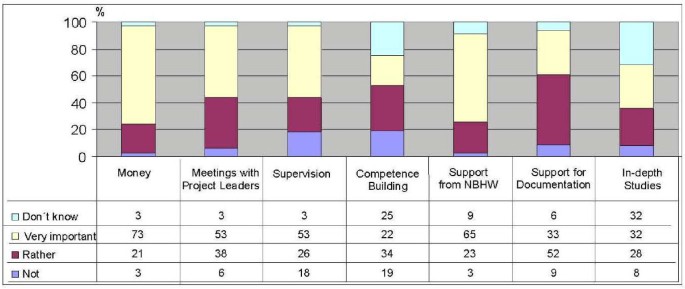
Assessment by project leaders of measures to improve collaboration between NGO and research in 2006 .
The research strategy has been successfully implemented despite the fact that only some projects were running more than one year while new projects and project leaders are included every year. The first two years a focus in the meetings with the project leaders was on the in-depth studies which were presented by the organisations and the researchers. Then the focus changed to addressing common concerns among the project leaders such as how to reach target groups, use of Internet, different type of prevention projects and mass communication skills. The presentations from the research teams were more concentrated to the national conferences that were organized bi-annually. The networking between the projects also resulted in new applications jointly by two organisations.
An important element was the relationship between the NBHW and the research team at Örebro University. During this period the NGO portfolio was managed at the NBHW by the same senior official. However, the department director changed three times during this period. The members of the working committee also changes over the years. The chairman was the same during all years. The support to the research and development activities was nevertheless maintained and also renewed for another year. The continuity with regard to persons seems to be very important for such an endeavour as included in this case study.
Discussion - towards practice-based research for alcohol and drug prevention
The integration of the research and development component into the support from the NBHW resulted in a unique possibility to do comparative studies involving, among other things, project management and implementation as well as project results. The measures to promote a partnership for practice-based research also improved the quality and success of the different projects. A few of the in-depth studies were unsuccessful due to factors hindering the implementation, and in several cases these factors were related to a lack of resources on the part of collaborating partners in the municipalities or other organizations.
The research strategy has been based on the overall aim to contribute to the evidence base for alcohol and drug prevention, an emphasis that this field shares with health promotion, prevention in general, and social work [ 2 – 8 ]. The current development of practice-based research will give more relevant knowledge and our research program attempts to be a part of this trend. Moreover, the utilization of research results may also be improved if studies on efficacy, effectiveness, and dissemination are promoted [ 18 ]. The strategy that the NBHW developed in this program of governmental support to NGOs was an attempt to bridge this gap as described by Nutbeam [ 10 , 11 ]. This challenge for agencies to respond to the push from the funders and pull from the communities has been noted by Green and Mercier [ 23 ] and the public health researcher also needs to leave the university campus to get involved in more practice-based research. Our research program has developed along such lines.
The research strategy includes the use of qualitative, quantitative, and mixed methods. This means that data collection and data analysis are done using guidelines for these three traditions. The challenge is most apparent with regard to inference and integration. In the stages of inference in a study, quality issues such as internal and external validity in the quantitative approach and aspects of credibility, confirmability, and transferability in the qualitative approach are pertinent. Integration is the mixed-methods approach of working across strands and using meta-inferential issues related to the integration of findings and inferences from the two strands. Here design quality, interpretative rigour, and inference transferability have been proposed as indicators of quality [ 70 ]. In this research strategy case study, the set of research entities changed each year due to the funding of applications from NGOs by the NBHW. The present study covered a six-year period, and the stages of inference and integration were completed yearly in the preparation of the annual reports to the NBHW.
The research strategy also includes elements of participatory research. The organizations were involved in developing the main research questions in the in-depth studies. Sometimes the organizations also assisted in collecting questionnaires from school children; in making participatory observations, as in the studies of beer purchasing by minors; or in providing feedback to school staff and target groups, as in the parental support programs. Moreover, the organizations also played a role in discussing preliminary results as part of a validating process for the empirical studies. These discussions never changed the interpretations of the findings but often gave more insight into the noble art of implementation of preventive programs. Nevertheless, as in other research programs, a number of methodological challenges had to be dealt with. The resources were limited, which gave room for only a small number of in-depth studies. Therefore the research strategy included additional elements such as support to documentation as well as support to the project leaders in meetings and management training. The selection of these studies was mainly done by the steering committee at the NBHW. The research team developed a proper design for these studies based on the assessed potential for a successful implementation and possible options given the resources available for effect or process studies. Then the choice of methods for data collections was reviewed and target groups for the evaluation research selected. In this process the best choice from an academic point of view was often not possible due to limited staff and other resources. Nevertheless, the research program resulted in data collected from 9,568 children, 4,832 parents and 327 actors or stakeholders. Moreover, it was possible to carry out two large longitudinal studies of children and their parents in this research program. Even if the funding was granted annually, it was possible to think and plan on more long-term basis.
A broad range of organizations received project funding from the NBHW. Although the largest number of projects was run by the nine alcohol and drug organizations, the alcohol and drug prevention was successfully integrated into a range of organizations with other main objectives. Moreover, the project leaders also came from different societal sectors. This was an intended effect of the governmental initiative to strengthen the alcohol and drug prevention in Sweden. This led to another methodological challenge caused by the fact that the programs were so different. The research team developed questionnaires with common modules that could be used in different evaluations thus giving them access to data from schoolchildren and parents in different contexts and programs. This made it possible, for instance, to study the reasons for non-participation in parental support programs [ 73 ]. Another added value related to this was the possibility to organize a study of project management through a special study of the project leaders, which was integrated into the overall design of the support from the NBHW.
A challenge for the research team was that the funding for the research as well as for the alcohol and drug projects was decided annually by the NBHW. However, the research was planned with a longer time period in mind, which has actually led to a research program that has been running more than six years. A more long-term grant would have been beneficial for the development of a partnership between the NGOs and the research team. In order to overcome this barrier a multi-year agreement has been signed for the newer in-depth studies, but it was still signed on the condition of renewed funding the following year. Nevertheless, a trustful partnership was developed between all three partners: the practitioners in the NGOs, the national agencies, and the researchers. In many cases the planning and implementation were done jointly, dividing the responsibilities according to skills and keeping the roles clear and feasible to complete successfully. The validity of the results was also a major concern as well as an emphasis on a participatory approach to the research process.
Ethical concerns were very important, as stipulated by Swedish law. The effect studies were assessed by the regional research ethics boards. However, it is also important to analyse if the NGOs have vested interests in the research process. Government agencies as well as NGOs can also have a vested interest in scientific research, such as when science is misused to benefit a particular political agenda, ideology, or favoured interest group [ 80 ]. However, the problem of vested interests is more dangerous when key parts of the government sector are in conflict over their public health responsibilities; for instance health sector engagement in partnership arrangements with addictive consumption industries (particularly alcohol, tobacco, and gambling) entails too many risks [ 81 ]. In our case there have been shared visions and objectives between the government agency and the NGOs, which guided the developmental activities as well as the research work. Moreover, the division of responsibilities between the NGOs and the researcher was important. The NGOs had the responsibility for developing the proposals, conducting the interventions, and implementing the preventive programs or initiatives. The researchers had the responsibility for planning the effect evaluations after consulting with representatives of the NGOs, as well as for implementing the research components, analysis, and reporting of results, including dialogues about the outcomes, and presenting the findings for the NGOs.
The organization of the research program under the auspices of public health science at Örebro University was natural as the principal investigator holds a professorial chair in public health there. During the first two years, other members of the research group were formally employed by an NGO but worked at the university campus in Örebro. All members of the research team were subsequently offered employment at the university, giving the research team a formal independence from all NGOs.
The addiction research centres have mandates that are broader than the present research program. The centre in Michigan has the mission to develop new knowledge about the cause, course, and consequences of substance use disorder and to train the next generation of researchers [ 28 ]; and the Canadian centre in British Columbia to create an internationally recognized centre distributed across BC that is dedicated to research and knowledge exchange on substance use, harm reduction, and addiction [ 27 ]. The Swiss institute is primarily involved in collecting alcohol-related information and making it available to professionals and the general public. The Swiss Institute will continue to monitor substance use, while stepping up its prevention research activities and ensuring that it is able to react promptly to emerging phenomena [ 25 ]. Our small research team is attempting to fill a gap in knowledge about the NGO alcohol and drug prevention efforts as these offer unique opportunities [ 82 ].
The research strategy was successful in establishing prevention research for alcohol and drug prevention by NGOs, which previously had been lacking in Sweden. Moreover, added value came from having meetings for project leaders, and the capacity building led to new innovative collaboration between different NGOs, which resulted in new applications for funding and successful implementation of new initiatives. The administrative support for improving the documentation of the implementation and progress of the projects was also recognized as beneficial for the practitioners and the national agency as well as the researchers. The best approach is always transparency and discussion, disclosure and debate [ 83 , 84 ].
A weakness in the research strategy was that the funding was not sufficient for more than a limited number of in-depth studies. The role of researchers-as-technical advisors was suitable for the fostering of a trustful partnership for research and development. The independence of the NGOs was regarded as important for the momentum in the project implementation. It was beneficial because it gave the research team opportunities to address other issues. From a strictly research point of view it would have been of interest to see what could be achieved by researchers-as-designer , but this would have been very costly and all funds allocated to the integrated research activities would have been consumed by just one project. In other words, the present research strategy can be regarded as cost-effective.
The overall strategy for research and development includes capacity building for both the practitioners in the NGOs and the research team, and two doctoral dissertations will be finalized during the coming year. The NBHW has also noted that, given the limited duration of funding, this organization of knowledge development - as an integral part of the support to NGOs - is beneficial, which is indicated by the annual renewal of the contract with Örebro University. Moreover, the much more extensively funded projects in municipalities, regions, and counties still lack this strategic element. At present there is a trend that some larger governmental grants are given to such parties, but a mandatory linkage to universities for research is included in the call for proposals. This could lead to similar forms of trustful partnerships as found in the present research strategy case study.
The in-depth studies in this research strategy varied in content, design, and size. A common element was that they were program-driven and not research-driven interventions [ 9 ]. This may give the studies improved external validity [ 54 ]. The research strategy aimed at improving the evidence-base for alcohol and drug prevention. In our case this has meant using qualitative, quantitative, and mixed methods, as well a variety of designs to answer questions in practice-based settings. Including feedback and dialogue with the NGOs has further contributed to sustainable AD prevention in different settings. The missions of the NGOs differ, but the AD prevention has been included as an essential part of their activities, which in many cases meant that AD prevention has received increased priority. Moreover, the integrated research program has also been seen as beneficial and important for the organizations, which often wanted their programs to be recognized as evidence-based. Therefore, the demand for research by the NGOs is larger than what we can supply at present. This is a challenge to the funding agencies as well as research bodies. The addiction research centres seem to nurture creativity but often lack the networks and priorities for preventive research. It is important to go beyond the notion that a lack of evidence for a program is necessarily a sign of a lack of effectiveness. Therefore, practice-based research and collaboration between decision-makers, national agencies, NGOs, local authorities and researchers is needed. Using a combination of different and interactive measures it was possible to over the years built a trustful partnership between these parts. This research strategy case study shows that it is possible even in such a dynamic field as alcohol and drug prevention in NGOs where the organisations are competing for grants from the NBHW. There are added values in supporting a research group assigned to a project portfolio instead of having a series of smaller independent evaluations.
This research strategy case study shows that it is possible to integrate research into alcohol and drug prevention programs run by NGOs, and thereby contribute to a more evidence-based practice. A core element is developing a trustful partnership between the researchers and the organizations. Competence development is necessary for developing evidence for policy and practice. Given research groups assignments to address the knowledge development issues is better than having minor evaluation in individual projects. Moreover, the funding agency must acknowledge the importance of knowledge development and allocating resources to research groups that is capable of cooperating with practitioners and NGOs.
WHO: Handbook for action to reduce alcohol-related harm. 2009, Copenhagen: World Health Organization
Google Scholar
Davies JK, Macdonald G, (Eds): Quality, Evidence and Effectiveness in Health Promotion. 1998, London: Routledge
Eriksson C: Learning and knowledge-production for public health - a review of approaches to evidence-based public health. Scandinavian Journal of Public Health. 2000, 28: 298-308.
Article CAS PubMed Google Scholar
Gomm R, Davies C, (Eds): Using Evidence in Health and Social Care. 2000, London: Sage
Oakley A: Experiment in Knowing. Gender and method in the social sciences. 2000, Cambridge: Polity Press
National Board of Health and Welfare: Nationellt stöd för kunskapsutveckling inom socialtjänsten. 2000, Stockholm: National Board of Health and Welfare, SoS Rapport, 12-[National support to knowledge development in social work].
Green LW, Kreuter MW: Health Program Planning. An Educational and Ecological Approach. 2005, Boston: McGraw Hill
Baum F: The New Public Health. 2002, Victoria, Australia: Oxford University Press
Holder H, Flay B, Howard J, Boyd G, Voss R, Grossman M: Phases of alcohol problem prevention research. Alcoholism: Clinical and Experimental Research. 1999, 23 (1): 183-194. 10.1111/j.1530-0277.1999.tb04043.x.
Article CAS Google Scholar
Nutbeam D: Achieving best practice in health promotion: Improving the fitbetween research and practice. Health Education Research, Theory and Practice. 1996, 11 (3): 317-326.
Nutbeam D: Evaluating health promotion - progress, problems and solutions. Health Promotion International. 1998, 13 (1): 27-44. 10.1093/heapro/13.1.27.
Article Google Scholar
Durlak JA, DuPre EP: Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. American Journal of Community Psychology. 2008, 41: 327-350. 10.1007/s10464-008-9165-0.
Article PubMed Google Scholar
Mercer SL, De Vinney BJ, Fine LJ, Green LW, Dougherty D: Study designs for effectiveness and translation research. Identifying trade-offs. American Journal of Preventive Medicine. 2007, 33 (2): 139-154. 10.1016/j.amepre.2007.04.005.
Cook WK: Integrating research and action: A systematic review of community-based participatory research to address health disparities in environmental and occupational health in the United States. Journal of Epidemiology and Community Health. 2008, 62 (8): 668-676. 10.1136/jech.2007.067645.
Article PubMed Central CAS PubMed Google Scholar
Evensen AE, Sanson-Fisher R, D'Este C, Fitzgerald M: Trends in publications regarding evidence-practice gaps: A literature review. Implementation Science. 2010, 5: 11-10.1186/1748-5908-5-11.
Article PubMed Central PubMed Google Scholar
Chaloupka FJ, Johnston LD: Bridging the gap. Research informing practice and policy for healthy youth behavior. American Journal of Preventive Medicine. 2007, 33 (4S): 147-161. 10.1016/j.amepre.2007.07.016.
Emshoff JG: Researchers, practitioners, and funders: Using the framework to get us on the same page. American Journal of Community Psychology. 2008, 41: 393-403. 10.1007/s10464-008-9168-x.
Flay BR, Biglan A, Boruch RF, Castro FG, Gottfredson D, Kellam S, Mo'scicki EK, Schinke S, Valenntine JC, Ji P: Standards of evidence: Criteria for efficacy, effectiveness and dissemination. Prevention Science. 2005, 6 (3): 151-175. 10.1007/s11121-005-5553-y.
Green LW: "Public Health Asks of Systems Science: To Advance Our Evidence-Based Practice, Can You Help Us Get More Practice-Based Evidence?". American Journal of Public Health. 2006, 96 (3): 406-409. 10.2105/AJPH.2005.066035. 2006
Green LW: Translation 2 research. The roadmap less travelled. American Journal of Preventive Medicine. 2007, 33 (2): 147-8. 10.1016/j.amepre.2007.04.023.
Straus S, Tetroe J, Graham ID: Knowledge Translation in Health Care. 2009, Oxford: Wiley-Blackwell, BMJ Books
Book Google Scholar
Tapp H, Dulin M: The science of primary health-care improvement: potential and use of community-based participatory research by practice-based research networks for translation of research into practice. Experimental Biology and Medicine. 2010, 235: 290-299. 10.1258/ebm.2009.009265.
Green LW, Mercer SL: "Can Public Health Researchers and Agencies Reconcile the Push From Funding Bodies and the Pull From Communities?". American Journal of Public Health. 2001, 91 (12): 1926-1929. 10.2105/AJPH.91.12.1926.
Edwards G: Addiction research centres and the nurturing of creativity. Addiction. 2009, 104: 687-10.1111/j.1360-0443.2009.02597.x.
Kuntsche E, Maffli E, Kuntsche S, Jordan MD: Addiction research centres and the nurturing of creativity: The Swiss Institute for the Prevention of Alcohol and Drug problems. Past, present and future. Addiction. 2009, 104: 699704-10.1111/j.1360-0443.2009.02556.x.
Stenius K, Ramstedt M, Olsson B: Addiction research centres and the nurturing of creativity: Centre for Social Research on Alcohol and Drugs (SoRAD), Stockholm University, Sweden. Addiction. 2010, 105: 402-407. 10.1111/j.1360-0443.2009.02838.x.
Stockwell T, Reist D, Macdonald S, Benoit C, Jansson M: Addiction research centres and the nurturing of creativity: The Centre for Addictions Research of British Columbia, Canada. Addiction. 2010, 105: 207-215. 10.1111/j.1360-0443.2009.02789.x.
Zucker RA: Addiction research centres and the nurturing of creativity: University of Michigan Addiction Research Center (UMARC): development, evolution, and direction. Addiction. 2010, 105: 966-97. 10.1111/j.1360-0443.2010.02904.x.
Norström T, Ramstedt M: "Sweden - is alcohol becoming an ordinary commodity?". Addiction. 2006, 101: 1543-1545.
Karlsson T, Österberg E: Sweden. Alcohol Policies in EU Member States and Norway A Collection of Country Reports. Edited by: Österberg E, Karlsson T. 2002, Helsinki: European Commission and STAKES
Chatwin C: Drug Policy Developments within the European Union. The Destabilizing Effects of Dutch and Swedish Drug Policies. British Journal of Criminology. 2003, 43: 567-582.
Swedish Government Bill 2005/06:30: Nationella alkohol- och narkotikahandlingsplaner. [National plan of actions for alcohol and drugs]. Stockholm
Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K: Alcohol: no ordinary commodity- research and public policy. 2003, Oxford: Oxford University Press
Holder H, (Ed.): Alcohol Monopoly and Public Health: Potential effects of privatization of the Swedish alcohol retail monopoly. 2008, Stockholm: Swedish National Institute of Public Health, R, 27-
Howat P, Sleet D, Maycock B, Elder R: Effectiveness of Health Promotion in Preventing Alcohol Related Harm. Global Perspectives on Health Promotion Effectiveness. Edited by: McQueen D, Jones C. 2006, Springer
Government Office of Sweden: Förebygga för framtiden. En presentation av regeringens politik på alkohol-, narkotika-, dopning-, och tobaksområdet. 2008, Stockholm: Ministry of Health and Social Affairs
Swedish Government: En förnyad folkhälsopolitik. 2007, Stockholm: Ministry of Health and Social Affairs, [A renewed public health policy]
Swedish Government White Paper, 2008/09:207: Överenskommelsen mellan regeringen, idéburna organisationer inom det sociala området och Sveriges Kommuner och Landsting. Stockholm: Ministry of Integration and Gender Equality, [The agreement between the government, idea-driven organizations in the field of social welfare, and Sweden's municipalities and county councils]
Andréasson S, Göransson B, Lindberg J, Nycander S, Romanus G, Westerholm B: Solidarisk alkoholpolitik. 2007, Stockholm: Hjalmarson & Högberg och Alkoholpolitiskt forum, [Socially responsible alcohol policy]
Wijkström F, Lundström T: Den ideella sektorn: organisationerna i det civila samhället. 2002, Stockholm: Sober, [The voluntary sector: the organisations in the civil society].
Wijkström F: Different Faces of Civil Society. 1998, Dissertation, Stockholm School of Economics
Gougoulakis P: Studiecirkeln: Livslångt lärande...på svenska!: en icke-formell mötesplats för samtal och bildning för alla. 2001, Dissertation, Stockholm: HLS Förlag, Studies in Educational Sciences, 40-[The Study Circle: Lifelong learning ... in swedish!]
Wijkström F, Einarsson T: Från nationalstat till näringsliv? Det civila samhällets organisationsliv i förändring. 2006, Stockholm School of Economics, [From nation state to business sector? The changing organizational community of civil society]
Lundström T, Svedberg L: The Voluntary Sector in a Social Democratic Welfare State - The Case of Sweden. Journal of Social Policy. 2003, 32 (2): 217-238.
Wijkström F: The Swedish nonprofit sector in international comparison. Annals of Public and Cooperative Economics. 1997, 68 (4): 625-663.
Nygren S: Identitet och nätverk - en utvärdering av elva alkohol- och drogförebyggande projekt. 2000, Stockholm: Folkhälsoinstitutet, 2-[Indentity and Network - an evaluation of eleven alcohol and drug preventive projects]
Eriksson C, Geidne S, Larsson M, Pettersson C: Med kraft och vilja. Alkohol- och drogförebyggande arbete inom Socialstyrelsens stöd till frivilligorganisationer 2003-2009. 2010, Örebro: Örebro University; Studies in Public Health Sciences, 1-[With strength and will. Alcohol and drug prevention efforts within the National Board of Health and Welfare's support for voluntary organizations 2003-2009].
Bruun K, Edwards G, Lumio M, Mäkelä K, Pan L, Popham RE, Room R, Schmidt W, Skog OJ, Sulkunen P, Österberg E: Alcohol control policies in public health perspective. 1975, Helsinki: The Finnish Foundation for Alcohol Studies
Edwards G, Andersson P, Babor TF, Casswell S, Ferrence R, Giesbrecht N: Alcohol Policy and the Public Good. 1994, Oxford: Oxford University Press
Babor TF, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, Grube JW, Hill L, Holder H, Homel R: Alcohol: No Ordinary Commodity. Research and Public Policy. 2010, Oxford: Oxford Univesity Press, second
Andréasson S, (Ed.): Den svenska supen i det nya Europa - Nya villkor för alkoholprevention: en kunskapsöversikt. 2002, Stockholm: Förlagshuset Gothia, [Swedish Alcohol Culture in the new Europe - new challenges for alcohol prevention: a review].
Andréasson S, (Ed.): Narkotika i Sverige. Metoder för förebyggande arbete. 2008, Östersund: Statens folkhälsoinstitut, Rapport R, 23-[Illicit Drugs in Sweden. Methods for prevention].
Ferrer-Wreder L, Stattin H, Lorente CC, Tubman JG, Adamson L: Successful Prevention and Youth Development Programs: Across Borders. 2004, New York:Kluwer Academic/Plenum Publishers
Green LW, Glasgow RE: Evaluating the Relevance, Generalization, and Applicability of Research. Issues in External Validation and Translation Methodology. Evaluation & the Health Profession. 2006, 29 (1): 126-153.
Tones K, Green J: Health Promotion. Planning and Strategies. 2004, London: SAGE Publications
Birkeland S, Murphy-Graham E, Weiss C: Good reasons for ignoring good evaluation: The case of the drug abuse resistance education (D.A.R.E.) program. Evaluation and Program Planning. 2005, 28: 247-256. 10.1016/j.evalprogplan.2005.04.001.
Holmila M, Holder H, Andreasson S, Baklien B, Rossow I: Roles for researchers in community action projects to prevent alcohol and other drug problems: Methodological choices. Drugs: education, prevention and policy. 2008, 15 (4): 410-423. 10.1080/09687630701839149.
Wagenaar AC, Murray DM, Toomey TL: Community mobilizing for change on alcohol (CMCA): Effects of a randomized trial on arrests and traffic crashes. Addiction. 2000, 95: 209-217. 10.1046/j.1360-0443.2000.9522097.x.
Holmila M: The evaluation of the metropolitan project: Process and causality. NAT. Nordic Studies on Alcohol and Drugs. English Supplement. 2003, 22: 350-357.
Wallin E, Norström T, Andréasson S: Alcohol prevention targeting licensed premises: A study of effects of violence. Journal of Studies on Alcohol. 2003, 64: 270-277.
Andréasson S, Sjöström E, Bränström R: A six community prevention trial to reduce alcohol and drugs related problems in Sweden. Substance Use & Abuse. 2007, 42 (12-13): 2017-27. (2007)
Stafström M, Östergren PO, Larsson S, Lindgren B, Lundborg P: A community action programme for reducing harmful drinking behaviour among adolescents: The Trelleborg project. Addiction. 2006, 101: 813-823.
Koutakis N, Stattin H, Kerr M: Reducing youth alcohol drinking through a parent-targeted intervention: the Örebro Prevention Program. Addiction. 2008, 103: 1629-1637. 10.1111/j.1360-0443.2008.02326.x.
Yin RK: Case Study Research. Design and Methods. 2009, Los Angeles: Sage, Fourth
Swanborn P: Case Study Research. What, why and how?. 2010, Los Angeles: SAGE
Kazi MAF: Realist Evaluation in Practice. Health and Social Work. 2003, London: SAGE Publications
Reason P, Bradbury H, (Eds): Handbook of Action Research. Participative Inquiry & Practice. 2001, London: SAGE Publications
Creswell JW, Piano CVL: Designing and Conducting Mixed Methods Research. 2007, Thousand Oaks: Sage Publications
Saks M, Allsop J: Researching Health. Qualitative, Quantitative and Mixed Methods. 2007, Los Angelse: Sage
Teddlie C, Tashakkori A: Foundations of Mixed Methods Research. Integrating Quantitative and Qualitative Approaches in the Social and BehavioralSciences. 2009, Los Angeles: SAGE
Bonnie K, Schensul SL: Contribution of qualitative research to the validityof intervention research. Journal of School Psychology. 2005, 43: 177-195. 10.1016/j.jsp.2005.04.003.
Jack SM: Utility of Qualitative Research Findings in Evidence-based Public Health Practice . Public Health Nursing. 2006, 23 (3): 277-283. 10.1111/j.1525-1446.2006.230311.x.
Pettersson C, Lindén-Boström M, Eriksson C: Reasons for nonparticipation in a parental program concerning underage drinking: A mixed-method study. BMC Public Health. 2009, 9: 478-10.1186/1471-2458-9-478.
Geidne S, Eriksson C: Working with or against the stores? A nongovernmental organization working with purchase attempts. Health Education. 2009, 109: 259-278. 10.1108/09654280910955584.
Geidne S, Eriksson C: How do minors succeed in buying beer in Sweden?. Nordic Studies on Alcohol and Drugs. 2008, 25: 115-127.
Lintonen TP, Konu AI, Seedhouse D: Information technology in health promotion. Health Education Research. 2007, 23 (2): 560-566.
PubMed Google Scholar
Bewick BM, Trusler K, Barkman M, Hill AJ, Cahill J, Mulhern B: The effectiveness of web-based interventions designed to decrease alcohol consumption - A systematic review. Preventive Medicine. 2008, 47: 17-26. 10.1016/j.ypmed.2008.01.005. (2008)
Pettersson C, Lindén-Boström M, Eriksson C: Parental Attitudes and Behaviour Concerning Youth Alcohol Consumption - do socio-demographic factors matter?. Scandinavian Journal of Public Health. 2009, 37: 509-517. 10.1177/1403494809105790.
Lindström P, Svensson R: Skolungdomars attityder till droger - En utvärdering av VÅGA-programmet. 1998, Nordisk Alkohol & Narkotikatidskrift, 15: 5-19. (1998).[Attitudes to drugs among school children - An evaluation of DARE program].
Babor T, Miller P, Edwards G: Vested interests, addiction research and public policy. Addiction. 2010, 104: 4-5. 10.1111/j.1360-0443.2009.02664.x.
Adams PJ, Buetow A, Rossen F: Vested interests in Addiction Research and Policy: Poisonous partnerships: health sector buy-in to arrangements with government and addictive consumption industries. Addiction. 2010, 105: 585-590. 10.1111/j.1360-0443.2009.02815.x.
Nathan S, Rotem A, Ritchie J: Closing the gap: building the capacity of non-government organizations as advocates for health equity. Health Promotion International. 2002, 17 (1): 69-78. 10.1093/heapro/17.1.69.
Holder HD, Reynolds R: Science and alcohol policy at the local level: a respectful partnership. Addiction. 1998, 93 (10): 1467-1473. 10.1046/j.1360-0443.1998.931014673.x. (1998).
Holder H: Prevention programs in the 21 st century: what we do not discuss in public. Addiction. 2009, 105: 578-581. 10.1111/j.1360-0443.2009.02752.x. (2009).
Download references
Acknowledgements
The authors are very grateful to all the NGOs that have shared their efforts and experiences with the research team. We would also like to acknowledge Åke Setréus for his support and encouragement during the whole period. The Swedish National Board of Health and Welfare supported the study.
Author information
Authors and affiliations.
School of Health and Medical Sciences, Örebro University, S-701 82, Örebro, Sweden
Charli Eriksson, Susanna Geidne, Madelene Larsson & Camilla Pettersson
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Charli Eriksson .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
The four authors of the manuscript are presented in alphabetical order and their shares of the responsibility for the paper are equal. CE is the principal investigator for the research program integrated in the NBHW support to NGOs for alcohol and drug prevention. CE, ML, and CP were involved in all aspects of the program as well as this study. SG was involved in the planning, project implementation, and writing of the section on NGOs. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Eriksson, C., Geidne, S., Larsson, M. et al. A Research Strategy Case Study of Alcohol and Drug Prevention by Non-Governmental Organizations in Sweden 2003-2009. Subst Abuse Treat Prev Policy 6 , 8 (2011). https://doi.org/10.1186/1747-597X-6-8
Download citation
Received : 28 September 2010
Accepted : 14 April 2011
Published : 14 April 2011
DOI : https://doi.org/10.1186/1747-597X-6-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Project Leader
- Drug Prevention
- Voluntary Sector
- Project Portfolio
- Alcohol Policy
Substance Abuse Treatment, Prevention, and Policy
ISSN: 1747-597X
- General enquiries: [email protected]

An official website of the United States government, Department of Justice.
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
NCJRS Virtual Library
Case studies of drug abuse and criminal behavior, additional details.
1640 5th Street , Santa Monica , CA 90401 , United States
No download available
Availability, related topics.
- Case report
- Open access
- Published: 06 April 2024
Patients' perspectives on buprenorphine subcutaneous implant: a case series
- Claudio Pierlorenzi 1 ,
- Marco Nunzi 1 ,
- Sabino Cirulli 1 ,
- Giovanni Francesco Maria Direnzo 2 ,
- Lucia Curatella 1 ,
- Sandra Liberatori 2 ,
- Annalisa Pascucci 2 ,
- Edoardo Petrone 3 ,
- Generoso Ventre 2 ,
- Concettina Varango 4 ,
- Maria Luisa Pulito 4 ,
- Antonella Varango 4 ,
- Cosimo Dandolo 4 ,
- Brunella Occupati 5 ,
- Roberta Marenzi 6 &
- Claudio Leonardi 7
Journal of Medical Case Reports volume 18 , Article number: 202 ( 2024 ) Cite this article
184 Accesses
1 Altmetric
Metrics details
Considering the enormous burden represented by the opioid use disorder (OUD), it is important to always consider, when implementing opioid agonist therapy (OAT), the potential impact on patient’s adherence, quality of life, and detoxification. Thus, the purpose of the study is to evaluate how the introduction of a novel OAT approach influences these key factors in the management of OUD.
Case presentation
This article marks the pioneering use of OAT through buprenorphine implant in Europe and delves into the experience of six patients diagnosed with OUD at a relatively young age. The patients, comprising both males and a female, are of Caucasian Italian and African Italian ancestry (case 4) and exhibit an age range from 23 to 63, with an average drug abuse history of 19 ± 12 years. All patients were on stable traditional OAT before transitioning to buprenorphine implants. Despite the heterogeneity in social and educational backgrounds, health status, and drug abuse initiation histories, the case series reveals consistent positive treatment outcomes such as detoxification, absence of withdrawal symptoms and of side effects. Notably, all patients reported experiencing a newfound sense of freedom and improved quality of life.
Conclusions
These results emphasise the promising impact of OAT via buprenorphine implants in enhancing the well-being and quality of life in the context of OUD.
Peer Review reports
Introduction
Opioid use disorder (OUD) is a chronic, relapsing condition accounting for over 16 million people worldwide [ 1 , 2 ]. International guidelines recommend opioid agonist therapy (OAT) with sublingual buprenorphine or methadone as first-line treatments of opioid dependence [ 3 ]. However, the rates of oral OAT misuse, abuse, and diversion are of public concern due to their social, sanitary, and economic repercussions [ 4 , 5 ]. Additionally, patient adherence to oral OAT remains a challenge nowadays.
Little research has been carried out about strategies to support long-term remission from opioid dependence [ 6 , 7 ]. An implantable formulation of buprenorphine has been developed to address problems with adherence, diversion, and non-medical use [ 6 ]. The rod-shaped implant consists of a mixture of a polymeric ethylene vinyl acetate matrix and buprenorphine that, following an initial pulse release, delivers a constant and stable medication level over 6 months after a single procedure [ 8 ].
Buprenorphine implant has shown its effectiveness in placebo-controlled studies [ 6 , 8 , 9 ] displaying a significant reduction of the opioid abuse (percentage of opioid-negative urine samples: 36% in implant group vs. 14.4% in placebo) and percentage of participants who completed the study [ 8 ]. As compared with standard sublingual buprenorphine or buprenorphine/naloxone tablets, the implant showed comparable efficacy and adverse event rate [ 6 , 8 ]. A systematic benefit-risk assessment, based on a semiquantitative analysis of the available data, found a favourable profile for buprenorphine implant in comparison to sublingual buprenorphine [ 10 ]. The main benefits identified for buprenorphine implant included: improved compliance and convenience, reduced risk of illicit opioid abuse, quality of life, and risk of misuse/diversion. On the other hand, risks were mostly associated with the insertion and removal procedure. The benefits mentioned so far outweighed the risks [ 10 ]and long-acting buprenorphine implants appears to sustain the long-term remission of patients suffering from OUD [ 10 ].
This article describes a series of patients with OUD who received OAT through buprenorphine implant, marking the pioneering cases at the European level. Each case report provides a comprehensive narrative, encompassing the patients' history and clinical progression, starting from the initiation of drug abuse to the subsequent outcomes (in terms of detoxification, absence of withdrawal symptoms, side effects and improved quality of life) achieved with buprenorphine implant.
Case report 1
Clinical case description.
The patient is a 54-year-old male of Caucasian Italian ancestry with lower secondary education. The patient, the youngest child of 5, experienced the tragic loss of a brother at the age of 17 due to an accident, and the father passed away 38 years ago from gastric haemorrhage. The mother, who is still alive and in fair health, works from home as a seamstress. The patient lives with his mother, but often sleeps away from home because of work. He engaged in a romantic relationship, including cohabitation, which lasted for a few years. Ultimately, at the conclusion of this period, he returned to live with his mother and stated: “ I was not in the right state of mind… Who wants to be with me? I'm never at home… and then I'm fine like this ”. He worked as a welder for a brief period. At the age of 18, he started working as a courier and then as a truck driver for third parties, constantly moving around Italy. Currently, he continues to work as a truck driver, but on his own account.
Medical history
The patient reports having contracted common childhood exanthems and undergoing a splenectomy due to a car accident in his 20s, followed by hemotransfusions. In 1986, he was diagnosed with chronic HCV hepatitis (it is unclear whether it was related to drug addiction), classified as G4, F2-related, and was treated with glecaprevir/pibrentasvir.
Toxicological history
At the age of 23, the patient began his journey with drugs by abusing intravenous heroin, cocaine, and alcohol (in the latter case, moderately). He was referred in April 1991, based on Article 75, to the Addiction Service of Lodi by the Prefecture of Piacenza. Two months later, the patient started OAT with a daily dose of 50 mg of methadone. From the age of 23 to 27, the patient exhibited very oppositional behaviour: he was lying, provocative, sometimes aggressive and threatening. During that period, the patient began and interrupted several therapeutic programmes.
Traditional opioid agonist therapy
In July 2004, the first contact with our Addiction Service occurred. The patient began therapy with sublingual buprenorphine at 8 mg/day in increments, but he never completed the scaling. In this regard, in 2013, we read in the clinical diary: “He is not able to disengage from buprenorphine despite remaining abstinent from drugs for some months” . The patient continued with sublingual buprenorphine 2 mg/day until May 2018, at which point he transitioned to a dosage of 2 mg every other day. The patient maintained this regimen until June 2022.
- Buprenorphine implant
In May 2022 we proposed the subcutaneous buprenorphine implant treatment to the patient, as he appeared to align with the characteristics of the ideal patient. He showed immediate interest and accepted. The selection was based on his consistent use of 2 mg sublingual buprenorphine every other day over the years, prolonged negative drug tests, frequent business-related travel as a lorry driver, and the logistical challenge of attending the Addiction Service every weekend (which also involved transfers to various Services). Furthermore, the patient expressed a desire to avoid encounters with other users at the Addiction Service with whom he no longer wished to share experiences.
In August 2022, the implant surgery was conducted for the patient.
Follow up visits
Throughout the six months of treatment, the patient underwent several visits, including monthly and sometimes fortnightly follow-ups. A urine toxicology check was performed every two weeks, consistently yielding negative results. The patient did not encounter any issues with the implanted arm site, finding it easy to use. He reported a notable absence of the fluctuations ("spikes") experienced with tablet intake, a diminished taste for cigarettes, and a complete lack of cravings for drugs. He expressed satisfaction with his choice but recommended the buprenorphine implant primarily for individuals aiming to cease the use of drugs of abuse. In his perspective, the implant may seem "a bit light" and more suitable for those seeking complete abstinence rather than those intending to remain on agonist therapy. The patient did not have interviews with the psychologist due to work-related commitments.
The organisation and management of the patient’s surgery proceeded smoothly. The patient was consistently monitored through visits, urine tests, and phone calls, especially during his business travels. The psychophysical condition of the patient has always been good, and the patient also observed a stabilisation in his nightly rest. In February 2023, the patient removed the device after the 6-month period, expressing great satisfaction with the experience. Subsequently, the patient did not encounter any issues and did not require buprenorphine/naloxone. In fact, the patient conveyed the intention to abstain from a second implant and forgo further OAT because he felt well. During the months with the implant, he successfully distanced himself from addiction after many years.
Case report 2
The patient is a 63-year-old man of Caucasian Italian ancestry who underwent treatment at the Medical Toxicology Department in Florence. He is a former addict, having maintained abstinence for over 30 years from heroin and methadone. After an extended period of traditional OAT with sublingual buprenorphine, he consistently expressed his desire to discontinue this treatment. Subsequently, the patient was presented with the option of a buprenorphine implant, which he accepted with the goal of achieving detoxification as the dosage in the subcutaneous implant is depleted by the end of the 6th month.
The patient's family history includes a hypertensive mother who died in 2010at the age of 86, a father who died at the age of 89, and an older sister in apparent good health. Throughout his life, the patient has experienced chronic hypoxia, maintained a low body mass index (BMI), and displayed regular diuresis and bowel function. Employed as an office worker, he grapples with insomnia and smokes approximately 15 cigarettes daily. Since the 1990s, the patient has tested positive for Hepatitis C (HCV). In 2008, he was diagnosed with renal heteroplasia on the right side, necessitating surgical exeresis. In 2010, a fracture of the right distal condyle of the femur occurred, prompting surgical intervention. From 2017 onward, the patient has been under the surveillance of the Systemic Manifestations of Hepatitis Virus Centre (MASVE), where he was diagnosed with cryoglobulinemia. Successful HCV eradication measures were undertaken.
The patient began illicit drug abuse in 1978 at the age of 19, with heroin being the primary substance of abuse. Of note, around the age of 30, the patient underwent a period of community day care. Concomitantly, he has consistently used and continues to use cannabinoids. Currently, the patient has been abstinent from heroin use for about 30 years.
From 1982 to 2007, the patient received treatment at the Medical Toxicology Department of the regional reference centre with methadone for heroin use disorder. Subsequently, he underwent OAT with sublingual buprenorphine until October 2022 (Table 1 ), at which point he transitioned to buprenorphine implant therapy.
Psychological aspects prior to buprenorphine implant
The patient exhibits compensated histrionic traits without psychosocial relapse. He is also characterised by an anxious temperament but maintains an on-axis mood [ 8 ]. The acceptance of this treatment stems from the desire for increased freedom, as it eliminates the need for frequent visits to the facility for sublingual buprenorphine, with the ultimate goal of achieving definitive detoxification.
At the time of implantation, the patient was on 8 mg sublingual buprenorphine agonist therapy. The patient underwent subcutaneous implant surgery in October 2022. The implantation was performed at the Vascular Access Centre Unit, Department of Anaesthesia and Resuscitation AOUC (for a comprehensive outline of the procedure, please refer to Additional file 1 : Appendix SI). Except for the initial days when the patient experienced mild withdrawal symptoms and a minor infection at the implant site, promptly addressed with antibiotics, the patient expressed overall satisfaction and happiness with the decision made.
Follow-up visits
The patient engaged in numerous follow-up visits, during which evaluations were performed to assess both physical and psychological outcomes. The Clinical Opiate Withdrawal Scale (COWS) score was employed throughout these visits to monitor the patient's withdrawal symptoms and general well-being (Table 2 ). The COWS categorical score ranges are defined as follows: no withdrawal (0–4), mild (5–12), moderate (13–24), moderately severe (25–36), and severe withdrawal (> 36) [ 11 , 12 ].
The removal of the implant, initially planned at the latest after 7 months from insertion, was delayed by a few months at the patient's request. The patient underwent monitoring of buprenorphine blood levels, which showed a slow decline in values, maintaining excellent toxicological compensation. The removal procedure was scheduled for the July 17, 2023, at the Vascular Access Centre Unit of the AOUC, but it was unsuccessful. After 2 h, the removal intervention was interrupted, and the patient was directed to ultrasound and MRI examination, which allowed visualization of the implants in the subfascial space in the brachial biceps muscle of the left arm instead of subcutaneous space. Following a thorough orthopaedic consultation, it was decided to forgo surgical intervention due to the patient's asymptomatic clinical presentation. Instead, the plan is to monitor the progress through semi-annual follow-ups. As of now, no complications have been identified.
The patient consistently reported minimal withdrawal symptoms and no significant cravings throughout the follow-up period with an excellent toxicological compensation. Furthermore, the patient expressed overall satisfaction with the subcutaneous implant, emphasizing its positive impact on mood, anxiety levels, and sleep patterns. Despite the initial challenges in the removal procedure, the patient's clinical presentation remains asymptomatic, contributing to the overall success of the buprenorphine implant treatment.
Case report 3
The patient, a 55-year-old woman of Caucasian Italian ancestry, was admitted to a psychiatric clinic in 2012 with a diagnosis of “depressive syndrome in a patient suffering from bipolar disorder, diffuse polyarthralgias and resumption of alcoholism”. She has been consistently under the care of a trusted psychiatrist since then.
Her primary substance of abuse was heroin until the late 1990s, followed by the development of alcohol use disorder. Alcohol consumption persisted over the years with long periods of remission and brief relapses mainly in a binge-like manner. Due to her history, the patient had been actively engaging with the Alcohol Centre and participating in self-help groups. She has been abstinent from alcohol consumption since 2021 and from heroin for over 20 years.
Since 2004, the patient has been undergoing OAT with buprenorphine (Table 3 ), and during this period, she has also been consistently receiving stable and concurrent psychopharmacological therapy. The patient had repeatedly expressed interest in discontinuing OAT, thus at the end of 2022 she was offered the option of using a buprenorphine implant. The proposed plan involved utilizing the implant for a duration of either 6 or 12 months, contingent on the patient's decision to pursue or decline a second implant at the conclusion of the initial period. This approach aimed to facilitate the detoxification process. At the time of the decision, the patient was in good compensation from a psychiatric and toxicological point of view.
The patient underwent subcutaneous implant surgery in February 2023. For the detailed procedure, please refer to Additional file 1 : Appendix SII. The patient did not show any signs of withdrawal or overdose in the days following implantation.
Psychological aspects following the buprenorphine implant
Generally, the patient considers herself satisfied and happy with the choice made. Moreover, the World Health Organization Quality of Life – BREF (WHOQOL-BREF), a self-report questionnaire assessing quality of life [ 13 ], was administered to the patient. Her assessment yielded the following scores: physical health = 21 (scale range: 7–35), psychological health = 23 (scale range: 6–30), social relationships = 10 (scale range: 3–15), and environment = 27 (scale range: 8–40).
During the follow-up visits, the patient’s physical and psychological state were assessed, and the COWS score was employed to evaluate withdrawal symptoms and general well-being (Table 4 ).
Throughout the observation period, the patient displayed overall well-being. However, as the removal procedure approached, she experienced mild anxiety, which was successfully managed with low doses of sublingual buprenorphine. The clinician notes that the patient's overall progress indicates a positive response to the buprenorphine implant treatment, showcasing effective control over withdrawal symptoms and cravings. The patient herself expresses satisfaction with her experience.
Case report 4
The patient, a 53-year-old male of African Italian ancestry, reported that his initial exposure to drugs, particularly THC, occurred around the age of 12. Subsequently, following the dissolution of his marriage, he had encounters with cocaine and later opioids, leading to the development of addiction.
After a period spent abroad, the patient returned to Italy in 2002 and sought treatment from various Addiction Services, where he began treatment with methadone. Approximately four years ago he transitioned to OAT with sublingual buprenorphine. Upon admission to our Service in May 2022, his therapy consisted of sublingual buprenorphine 6 mg + sublingual naloxone 1.5 mg per day.
During the meetings, the patient consistently demonstrated willingness and motivation. While his language was partially fluent, there were occasional interruptions attributed to difficulties in recalling certain phases of his life history. He showed spontaneity and did not need to be triggered to express himself, showing reflexivity and ability to contextualise. Adequate introspection and the absence of emotional blocks related to traumatic experiences were evident. The patient exhibited an internal locus of control and a sense of self-efficacy overall. From the behavioural point of view, within the service and with the clinical staff, we can highlight a good adherence to the indications given and to the scheduled appointments, and a good general compliance.
Due to pharmacological stability for over 5 years and restricted drug use limited to cannabinoids, the patient was deemed eligible for the buprenorphine implant, meeting the psychosocial inclusion criteria. Following the proposal, he exhibited heightened curiosity about the implant, experiencing a sense of "euphoria" in anticipation of this novel experience. His interest increased during the presentation of the implant procedure, which he quickly accepted. The impetus to accept the proposal stemmed from some of the patient's reflections, especially regarding the potential for a lifestyle change and the reclamation of "his time," envisioning more opportunities for hobbies, family, and travel. Moreover, he imagined the recovery and achievement of life goals linked both to everyday life and to the possibility of planning without “personal” constraints of time and organisation. Eventually, some reflections "almost of tiredness" emerged, referencing both to the regular visits to the Addiction Service and to the interactions with other service users. This weariness stemmed from the perceived hindrance of traditional OAT, seen as a substantial impediment to daily freedom due to the commitment required for therapy. Additionally, it extended to the challenges in achieving personal and life goals.
Since this was the first buprenorphine implant carried out at our facility, it was necessary to draw up a procedure, and have it approved by the Health Management. This protocol encompassed the establishment of a dedicated outpatient file and the provision of a specialized room, serving both for the surgical procedure and for consultations with prospective candidates, some of whom were referred from other Addiction Services.
The patient exhibited a comprehensive shift in mood, a heightened inclination toward openness with others, and a rejuvenated approach to life planning. Following the implant procedure, the patient demonstrated improved speech fluency attributed to heightened introspective abilities. He identified the socio-affective dimension as the most significant element in the initiated change, leading to increased stability on the affective level. This translated into a newfound capacity to navigate relationships with more meaningful and secure emotional grounding. Moreover, the initial days following the implant marked a shift in self-perception and how the patient was perceived by others. The awareness of the significant impact of the intervention on his life became apparent, bringing about a rediscovery of energy, an enhanced "esprit de vivre", and a transformation in interpersonal relations with the Addiction Service staff. Overall, a newfound optimism and fortitude was evident.
During the post-implant interviews, the patient was subjected to a patient-reported outcome (PRO) measure using a visual analog scale (VAS) to capture the severity or other aspects of craving. A VAS measure usually requires participants to indicate their response by marking a point on a 100-mm line, with the extremities represented by 0 as "no craving for heroin" and 100 as "absolute craving for heroin" [ 12 , 14 ]. At the follow-up the patient reported a “lack of craving” in terms of intensity and frequency, and he also denied the possibility of starting drug use in the event of experiencing craving. Throughout the course of treatment, the patient underwent weekly visits during the first month, followed by fortnightly visits in the second month, and eventually transitioning to monthly visits. Toxicological tests were conducted during these visits to monitor the patient's progress. No additional sublingual buprenorphine tablets or other drugs were necessary. Out of 11 toxicological tests carried out on urine samples, 2 were negative for all the substances sought. All other tests showed positivity for cannabinoids; this was consistent with the patient’s reported reduced daily use of THC before going to sleep.
From the outset, the patient expressed a reluctance to pursue a second implant, although he did not entirely rule out the possibility. As a result, the decision was made to defer the removal of the implant, allowing for close follow-up to monitor any changes. If needed, oral therapy could be resumed while awaiting a potential second implant to be grafted. In line with the patient's preferences and the agreement with healthcare providers, the implant remained in place beyond the initially planned sixth month. This extension allowed the patient additional time to contemplate the option of a second implant while ongoing urine buprenorphine screening, toxicological monitoring, and regular interviews were conducted. The removal was originally scheduled for the end of the seventh month. However, due to the patient's unavailability, primarily driven by severe personal reasons, the removal was subsequently postponed by two weeks. As of today, the removal procedure has been successfully performed and the patient exhibits a complete absence of craving and no desire to use substances. During the last interview the patient reported: “Every day I feel better!” .
Overall, the patient has experienced significant improvements in mood, interpersonal openness, and life planning. Additionally, there appears to be a reduction in THC use. Remarkably, even after the removal of the implant, the patient has not reported any cravings related to substance use.
Case report 5
The patient, a 40-year-old male of Caucasian Italian ancestry university graduate currently in permanent employment, initiated drug experimentation around the age of 20. In this period, he became fascinated with and started attending rave parties, leading to gradual experimentation (reported as "controlled") with illicit drugs including Afghan opium, eventually resulting in the development of an addiction disorder.
The patient’s toxicological history indicated a pattern of polyaddiction, involving the use of cannabinoids, particularly hashish, since the age of 18. At the age of 21, he began attending rave parties, engaging in simultaneous and occasional consumption of various drugs such as cocaine, MDMA, amphetamines, LSD, and Ketamine. Subsequently, the patient transitioned from regular opium use to heroin after approximately two years.
He continued his substance use until the age of 25, at which point he initiated treatment with sublingual buprenorphine at an Addiction Service. Upon admission, he had a diagnosis of OUD in protracted remission under treatment with partial OAT (buprenorphine in combination with naloxone), and concomitant depression. Throughout the course of treatment, the patient maintained a steady intake of buprenorphine/naloxone sublingual tablets at a fixed dosage of 2 mg/0.5 mg per day. Since his initial admission, he consistently reported challenges in discontinuing OAT. Specifically, he mentioned being able to refrain from the medication for a few days (up to a maximum of 4 days). However, with the onset of anxiety and intensified cravings for buprenorphine, the patient resumed his daily intake of 2 mg. Since initiating OAT, the patient reported abstinence from opium or heroin use. Despite maintaining a stable clinical picture, the presence of recurrent unsuccessful attempts to discontinue OAT prompted consideration for transitioning from sublingual to subcutaneous therapy. In August 2022, during a toxicology interview, the possibility of buprenorphine implant therapy was proposed to the patient.
In conjunction with the pharmacological aspect of the new therapy, the patient concurrently received treatment with specific antidepressants. Additionally, he has actively participated in individual psychotherapy for a duration of two years and is presently engaged in group psychotherapy. The patient promptly made himself available and demonstrated willing adherence to the instructions provided by the medical staff, consistently attending his scheduled appointments. Notably, he exhibited overall good mentalisation and fair self-esteem.
The patient initially exhibited moderate curiosity during the first interview introducing the buprenorphine implant. However, his interest in the proposed treatment escalated swiftly. This interest and curiosity stimulated thoughts about the prospect of embarking on a new lifestyle. Throughout the interviews, he conveyed that he embraced the proposal due to tiredness from the constant mood swings induced by traditional OAT, which required daily visits to the facility. These factors, coupled with other personal considerations, amplified his discomfort with commitment, hindering the overall pursuit of life goals.
After establishing a dedicated room at our facility, the patient was directed to the Addiction Service, where an external doctor from the hospital conducted the implant surgery. Following the surgery, we maintained continuous monitoring through both group psychotherapy and individual therapy sessions.
Throughout the course of treatment, the patient initially underwent weekly visits during the first month, followed by fortnightly visits in the second and third month, and eventually transitioning to monthly visits. During these regular check-ups, the patient underwent toxicological controls, and notably, no additional sublingual buprenorphine tablets were required.
After the implant procedure, the patient experienced mood stabilization, which he described as surprisingly positive. This positive change was openly shared by the patient within the therapy group. He demonstrated introspective ability, albeit stereotyped, aligning with the ideological and social models of his peer group. Following the implant there appeared to be a recognition of subjective aspects that he had not previously explored, potentially serving as a foundation for renewed self-awareness. Moreover, the patient exhibited rich and articulate language, along with good introspective and self-reflective ability, fair insight, and a proficient recall of his life history. Shortly after the implant, he conveyed his sense of liberation in an email, stating: "…I am a free man…" . In a group session, he elaborated on this feeling, expressing that he now perceives himself as "like everyone else," no longer dependent on the daily tablet, and experiencing mood fluctuations akin to any other individual.
The patient has been undergoing treatment for several months and reported only experiencing a headache in the initial days following the implant. Toxicological controls indicate positivity only for THC, as the patient has consistently used cannabinoids by smoking a "joint" in the evening to relax before going to sleep, with no intention of discontinuing this habit.
In post-implant interviews, the patient underwent the VAS test and reported a "lack of craving" both in terms of intensity and frequency. Furthermore, he expressed no inclination to initiate drug use in the event of experiencing cravings.
From the outset, the patient has made it clear that he had no intention of pursuing a second implant. Although he does not rule out the possibility entirely, his hope is to attain complete liberation from OAT and, more broadly, from drugs. This suggests a reasonably sound capacity for judgment on his part. Hence, the decision was made to defer the removal of the initial implant, utilizing the gradual reduction of the drug, and assessing how best to support the patient on his journey towards detoxification.
The patient appears to be progressing well on the detoxification path, as evidenced by his expressed intention to refrain from further OAT after the removal of the implant. The patient's determination is a crucial factor in the success of the detoxification process. The absence of craving after the removal of the implant, along with the noted mood stabilization and positive treatment perception reported by the patient, are significant indicators contributing to the success of the patient's detoxification journey.
Case report 6
Filippo (fictitious name), a 23-year-old male of Caucasian Italian ancestry, reflects on his childhood, describing it as “normal”. His father is portrayed as a diligent worker, while his mother is characterized as a pragmatic and less sentimental woman. As an intelligent child, Filippo sensed the weight of the expectations his mother had placed on him. During the transition to middle school, he experienced a loss in friendships, became apathetic, distracted, and spent most of his time playing video games, rarely venturing outside. However, there was an improvement in his social life and academic performance during high school, which led Filippo to enrol in university, where he also initiated a romantic relationship with a girl.
In the summer of 2018, following his first year of university, Filippo started experiencing anxiety disorders, making it challenging for him to cope with his exams. Simultaneously, he found out that his girlfriend was using heroin and cocaine. In response, he decided to experiment with these substances. Initially, his usage was occasional and seemed "manageable", but Filippo rapidly developed both physical and mental addiction. Furthermore, he began using cocaine to counteract the effects of heroin. His drug abuse progressively escalated from occasional to daily, extending beyond social contexts to solitary moments. Filippo found himself trapped in a vicious cycle, marked by a constant need to soothe himself and promptly reactivate. His academic performance suffered, and financial resources were increasingly diverted towards substance abuse. Recognizing the severity of the situation, Filippo sought help from a psychiatrist-psychotherapist, who advised him to approach an Addiction Service. Although Filippo was not fully convinced, he perceived that seeking help was his only viable option. When he shared his predicament with his family, their initial response was a mix of anger and concern. However, that single conversation remained an isolated instance, and subsequently, they seemed to adopt an approach of denial, choosing not to acknowledge the reality of Filippo's struggles.
Filippo initiated his treatment at the Addiction Service in January 2020 with a dosage of 2 mg of sublingual buprenorphine. This regimen was subsequently increased to 4 mg after a few weeks. Notably, Filippo demonstrated commendable adherence to the treatment regimen, attending interviews regularly and concurrently engaging in private psychotherapy. He ceased his heroin use immediately after commencing OAT, and he also managed to discontinue cocaine, with only a few relapses in October 2020. Subsequently, Filippo experienced improvements in mood, school performance, and social interactions. However, his main concern revolved around the prospect of discontinuing the daily tablet intake.
In January 2022, after Filippo's previous doctor departed from the service, I had a clinical interview with Filippo. During this meeting, I suggested a questionnaire to assess the current state of his therapy and his interest in transitioning to newly available drug formulations. Filippo embraced the idea of transitioning to a subcutaneous buprenorphine implant with enthusiasm. Despite considering the possibility of balancing his personal life with regular visits to the Addiction Service, he expressed a keen interest in the new treatment. At that point, he had been on a 4 mg sublingual buprenorphine tablet regimen for approximately two years, and his toxicological tests consistently showed negative results for illicit drugs.
Filippo's excitement stemmed from several profound considerations: the weariness of identifying himself as an addict, a label that he felt no longer accurately portrayed his current state; the conscious desire to disengage from the daily ritual of medication, which he defined as a "substitute" for his previous heroin use, and thus corresponded to him as if still "getting high" every day; and the wish to regain control over his daily routine without being tethered to the demands of therapy, envisioning a future where he could plan vacations and travel abroad without the constraints of regular visits. Lastly, Filippo held a hopeful anticipation of achieving a definitive conclusion to his therapy, marking a significant milestone in his journey towards recovery. Despite receiving comprehensive information from the data sheet, Filippo's determination to pursue the subcutaneous buprenorphine implant treatment remained unwavering. He maintained a steadfast commitment to this choice, eagerly anticipating further details about the practicality and feasibility of undergoing the implant procedure. The Addiction Service practitioners collaborated closely with the hospital pharmacy and the Palliative Care operating unit to efficiently organize the day of the surgery. On the morning of the surgery, Filippo exhibited no signs of agitation. He adhered to the given directions and refrained from taking the morning sublingual buprenorphine tablet. Without experiencing any withdrawal symptoms, he maintained focus on the day's objective. The surgical procedure proceeded smoothly, lasting approximately an hour, after which Filippo proceeded to attend his university activities.
In the days following the surgery, Filippo reported a sustained, almost heightened sense of well-being, exceptional concentration (especially in his studies), and an energy level he had not experienced before. While there may have been a brief, two-day period resembling a hypomanic phase, Filippo soon returned to a stable and regular state of well-being, seamlessly resuming his daily activities. Despite being aware of the option to supplement the implant with buprenorphine tablets, Filippo never felt the necessity to do so. In agreement with the department director, we limited Filippo's visits to the Ser.D to the bare minimum needed to perform the monitoring required by the implant protocol. These included urine tests at various intervals post-intervention: 1 week, 2 weeks, 1.5 months, 3 months, 4.5 months, 6 months, and 7 months. During these visits, we assessed his overall health, general well-being, reactions at the implantation site, degree of patient satisfaction, and any withdrawal or craving symptoms, along with potential drug abuse.
In our regular phone interviews with Filippo, he would describe positive events that were taking place in his life. Approximately four months post-intervention, during an in-person interview, we delved into the impact of the implant on Filippo's lifestyle. A significant transformation was evident: his self-perception had undergone a complete shift. During the six-month period of the implant, Filippo encountered an emotional reconnection with his mother when he shared his experience with the subcutaneous treatment. Until then, his addiction had only been briefly mentioned within the family context, resulting in a negative outcome. This revelation left his mother surprised, astonished, and moved, but also visibly proud.
On a separate occasion, Filippo attended a party and unexpectedly spent the night away from home. He emphasized that he only realized the next day that such spontaneity would not have been possible without the implant. Without the need for daily tablets, he could participate freely without the fear of experiencing withdrawal symptoms the following morning. He no longer needed the “daily heroin substitute” and he no longer needed heroin. These and other episodes strengthened his conviction to “get rid” of therapy and of the fear of not being able to “walk without that crutch”. His determination grew, accompanied by the belief that the removal of the implant would mark the conclusion of his therapy. Filippo explicitly requested the removal of the implant not at the initially specified deadline but at a later time, and he duly signed a written request expressing this desire.
The implant removal occurred in mid-November 2022, precisely 7 months and 9 days after its initial placement. Despite Filippo was at the time a little tense, the removal proceeded smoothly. The urine test conducted at this time still showed a positive result for buprenorphine. In the subsequent days, Filippo experienced symptoms including chills, tearing, arthralgia, and asthenia. Initially attributing these symptoms to a form of flu without strong conviction, he persevered. After 20 days, despite lingering discomfort, his determination to discontinue oral OAT prevailed. The subsequent urine test confirmed the absence of buprenorphine, marking the achievement of Filippo's goal.
General discussion
The buprenorphine implant represents an innovative formulation for OAT, specifically designed for individuals with OUD who have achieved stabilization through prior oral therapy. Notably, the implant demonstrates equivalent therapeutic effectiveness and similar rates of adverse effects when compared to standard sublingual buprenorphine or buprenorphine/naloxone tablets [ 6 , 8 ]. Nonetheless, a comprehensive risk–benefit evaluation has revealed several advantages associated with the subcutaneous buprenorphine implant in comparison to conventional OAT [ 10 ]. These benefits include enhanced treatment adherence, improved quality of life for patients, decreased likelihood of engaging in illicit opioid abuse, and a reduced risk of misuse or diversion [ 10 ]. These findings have been validated through the experiences of the first six patients in Europe who underwent the buprenorphine implant, as outlined in this case series. The report provides insights into the tangible effects of the buprenorphine implant on patients' quality of life and the achievement of therapeutic objectives, specifically focusing on abstinence from illicit drug abuse and the detoxification process.
Eligible patients were carefully assessed by the medical equipe in terms of clinical, psychological, and pharmacological status. All patients had refrained from using illicit drugs, were receiving low-dose sublingual buprenorphine (≤ 8 mg), demonstrated adherence to OAT and regular visits to the Addiction Service, and exhibited psychological stability. The heterogeneity observed in this group of patients stemmed from variations in sociocultural background, gender, age, duration of substance abuse history, length of the period of drug abstinence, and the specifics of their medical and pharmacological history, including the duration, dosage, and any prior OAT before transitioning to buprenorphine (Table 5 ).
Buprenorphine implant emerges as a viable treatment alternative for diverse patient profiles, contingent upon achieving a certain level of pharmacological stability (≤ 8 mg), psychological well-being, and a documented recent history of drug withdrawal.
The reaction of the patients to the implant proposal ranged from moderate interest in some cases to genuine enthusiasm in others as delineated in Table 6 (Buprenorphine implant proposal). All patients embraced the buprenorphine implant to enhance their quality of life, eliminating the need for regular visits to the Addiction Service for the administration of tablets and moving closer to complete detoxification.
To assess the impact of both traditional OAT and buprenorphine implant, a semi-quantitative narrative analysis was conducted [ 15 , 16 , 17 , 18 ]. Every quote pertaining to patients' experiences with either treatment was considered in the analysis and subsequently categorised into one or more of the following topics: commitment to achieving complete detoxification, disengagement from therapy, smoothness of therapy, emotional impact, and improved quality of life in terms of free-time, finances, work, and interpersonal relationships (Fig. 1 ). Subsequently, the positive or negative valence associated with each statement was recorded. The implant was viewed as a valuable means to achieve abstinence from both drugs and medications, as evidenced by a total of 22 positive statements (Fig. 1 A), compared to 6 for traditional OAT (Fig. 1 B). The regular attendance at the Addiction Service was seen as a “constraint that disrupted daily routines” and “contributed to social stigma”, undermining patients' commitment to therapy and overall quality of life (7 out of 9 negative statements). The desire to break free from the daily tablet intake, perceived as a “substitute for heroin” and a source of mood swings, was a common sentiment. In contrast to the peaks associated with oral intake, the subcutaneous implant offered a stable release of buprenorphine, as evidenced by the 22 positive statements (Fig. 1 A) compared to 7 (Fig. 1 B) associated with traditional oral intake. This consistency helped in mitigating both physical and emotional fluctuations experienced by the patients.

A narrative analysis of patients' reported experiences was conducted for both traditional OAT ( A ) and buprenorphine implant ( B ). The analysis was conducted by categorizing the statements related to each treatment into the five identified topics positioned at the vertices of the pentagon. The number of positive (blue line) and negative (red line) statements per topic were plotted along the direction of the corresponding vertex and connected by a 5-pointed closed line. The distance from the centre indicates the frequency of iterations. Notably, the scale of the pentagon differs between the two graphs
In terms of surgical procedure, the buprenorphine implant insertion was carried out in a specialised facility, by a professional surgeon, and no significant issues were encountered for any of the patients (Table 6 , Surgery outcome). Solely one patient developed a minor infection at the implant site, which was promptly addressed with antibiotics. He also reported a subjective feeling of overdose in the initial days post-insertion, followed by mild withdrawal symptoms, that were stabilised by a 3-day course of 1 mg sublingual buprenorphine. Consistent with findings from a previous study [ 19 ], the buprenorphine implant insertion procedure and the subsequent adaptation to treatment appear to be overall safe and well-tolerated.
During 6 months of follow-up, as outlined in Table 6 (Follow-up visits), the potential onset of withdrawal symptoms was closely monitored through regular assessments for most patients. Psychometric tests were also conducted to evaluate various aspects. Importantly, no patient reported experiencing cravings throughout the course of treatment, and all toxicological tests yielded negative results for the detection of illegal opioid abuse. All the patients expressed satisfaction with the buprenorphine implant treatment, and most of them reported being content with their decision, as indicated in Fig. 1 and Table 6 (End of therapy). On an emotional level, all patients reported a sense of well-being, with 18 positive statements compared to 3 positive statements for traditional OAT (Fig. 1 A, B), and no instances of relapse were noted. Half of the patients experienced increased lucidity, improved introspective ability, and greater stability on the affective level (Table 6 , End of therapy). The majority showed an on-axis mood (4 out of 6), absence of anxiety, hypnic pattern within limits, and restful sleep. Two out of six patients explicitly described a marked improvement in self-perception during the 6-month buprenorphine implant treatment. Overall, buprenorphine implant was perceived as a step closer to complete detoxification with 13 positive statements (Fig. 1 A) vs. 5 positive statements for traditional OAT (Fig. 1 B).
The removal procedure was successful for most of the patients, and none of them opted for a second implant. Solely one patient reintroduced sublingual buprenorphine at low dosages, although this decision was not prompted by any withdrawal symptom. Most importantly, none of the patients experienced craving episodes, indicating the potential for them to continue living without any OAT and ultimately achieve complete detoxification.
In summary, this case series explores the pioneering use of buprenorphine implant as a treatment option for OUD in a small European cohort of eligible patients. The findings suggest positive outcomes, including improved patient satisfaction and quality of life, reduced stigma associated with regular clinic attendance, and perceived advantages in achieving opioid abstinence. However, certain limitations must be acknowledged, including the small sample size, the relatively short follow-up period, and the reliance on self-reported questionnaires to evaluate patients’ perspective and experiences. The relatively small yet heterogenous sample size, while providing valuable insights into how various patient profiles might respond to this treatment approach, could affect the generalizability of the findings to a broader population. Moreover, the variability in the frequency and duration of follow-up visits, while enabling to capture the moderate-to-long term effects of the treatment, limits the ability to assess longer-term outcomes. Furthermore, the study's reliance on self-reported questionnaires while focusing on patients’ perspective, might introduce the possibility of response bias. This could include an inclination to offer responses that align with social expectations or recall biases. Therefore, in future studies the adoption of standardized assessment tools will ensure consistency and facilitate more robust cross-study comparisons. Future research should prioritise larger cohorts, encompassing comparative analyses with traditional OAT, and long-term investigations to assess sustained efficacy and diverse dynamics of patient profiles. Collaborative efforts to standardize assessment protocols across facilities would further strengthen the reproducibility of research findings in this evolving field.
Final conclusions
This case series outlines the therapeutic journey of the first six European patients who underwent buprenorphine implant therapy. The results demonstrate favourable outcomes, including successful opioid abstention, alleviation of withdrawal symptoms, and enhanced quality of life and psychological well-being. Importantly, the treatment exhibited a high level of safety and tolerability, with no significant adverse events reported during the peri-operative period. The smooth insertion procedure and subsequent adaptation highlight the consistent benefits of the implant, with most patients achieving complete abstention, a milestone that might have been challenging with traditional approaches. Overall, the patients' satisfaction with the buprenorphine implant underscores its potential as a viable treatment option for pharmacologically stable individuals seeking to transition from traditional OAT. Nevertheless, further research into patient profiles, craving dynamics, and patient-centred outcomes is essential for optimizing personalized interventions in the field of addiction medicine.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Opioid use disorder
- Opioid agonist therapy
Hepatitis C Virus
Centro Manifestazioni Sistemiche Virus Epatitici, Systemic Manifestations of Hepatitis Virus Centre
World Health Organization Quality of Life-BREF
Tetrahydrocannabinol
Visual analog scale
Methylenedioxymethamphetamine
Lysergic acid diethylamide
Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2023 Jul 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK553166/ .
Strang J, Volkow ND, Degenhardt L, Hickman M, Johnson K, Koob GF, et al . Opioid use disorder. Nat Rev Dis Primers. 2020;6(1):3.
Article PubMed Google Scholar
Overview | Drug misuse in over 16s: opioid detoxification | Guidance | NICE [Internet]. NICE; https://www.nice.org.uk/guidance/cg52 . Accessed 1 Dec 2022.
Bell J, Strang J. Medication treatment of opioid use disorder. Biol Psychiatry. 2020;87(1):82–8.
Article CAS PubMed Google Scholar
Mannaioni G, Lugoboni F. Precautions in the management of opioid agonist therapy: from target population characteristics to new formulations and post-marketing monitoring—a focus on the Italian system. Drugs Context. 2023;12.
Rosenthal RN, Lofwall MR, Kim S, Chen M, Beebe KL, Vocci FJ, et al . Effect of buprenorphine implants on illicit opioid use among abstinent adults with opioid dependence treated with sublingual buprenorphine: a randomized clinical trial. JAMA. 2016;316(3):282–90.
Lagios K. Buprenorphine: extended‐release formulations “a game changer”! Med J Aust. 2021;214(11):534.
Rosenthal RN, Ling W, Casadonte P, Vocci F, Bailey GL, Kampman K, et al . Buprenorphine implants for treatment of opioid dependence: randomized comparison to placebo and sublingual buprenorphine/naloxone. Addiction (Abingdon, England). 2013;108(12):2141–9.
Ling W, Casadonte P, Bigelow G, Kampman KM, Patkar A, Bailey GL, et al . Buprenorphine implants for treatment of opioid dependence: a randomized controlled trial. JAMA. 2010;304(14):1576–83.
Osborne V, Davies M, Roy D, Tescione F, Shakir SAW. Systematic benefit-risk assessment for buprenorphine implant: a semiquantitative method to support risk management. BMJ Evid Based Med. 2020;25(6):199–205.
Article PubMed PubMed Central Google Scholar
Wesson DR, Ling W. The clinical opiate withdrawal scale (COWS). J Psychoactive Drugs. 2003;35(2):253–9.
Boyett B, Wiest K, McLeod LD, Nelson LM, Bickel WK, Learned SM, et al . Assessment of craving in opioid use disorder: psychometric evaluation and predictive validity of the opioid craving VAS. Drug Alcohol Depend. 2021;229: 109057.
World Health Organization. WHOQOL: Measuring Quality of Life [Internet]. 2012. https://www.who.int/tools/whoqol . Accessed 26 Jan 2024.
Goodyear K, Haass-Koffler CL. Opioid craving in human laboratory settings: a review of the challenges and limitations. Neurotherapeutics. 2020;17(1):100–4.
Nolte K, Drew AL, Friedmann PD, Romo E, Kinney LM, Stopka TJ. Opioid initiation and injection transition in rural northern New England: a mixed-methods approach. Drug Alcohol Depend. 2020;217: 108256.
Article CAS PubMed PubMed Central Google Scholar
Lai J, Goldfine C, Chapman B, Taylor M, Rosen R, Carreiro S, et al. Nobody wants to be narcan’d: a pilot qualitative analysis of drug users’ perspectives on naloxone. Western J Emerg Med. 2021;22(2).
Meyer M, Rist B, Strasser J, Lang UE, Vogel M, Dürsteler KM, et al . Exploring why patients in heroin-assisted treatment are getting incarcerated—a qualitative study. BMC Psychiatry. 2022;22(1):169.
Scurti P, Nunzi M, Leonardi C, Pierlorenzi C, Marenzi R, Lamartora V. The experience of buprenorphine implant in patients with opioid use disorder: a series of narrative interviews. Front Psychiatry. 2023;31:14.
Google Scholar
Frost M, Bailey GL, Lintzeris N, Strang J, Dunlop A, Nunes EV, et al . Long-term safety of a weekly and monthly subcutaneous buprenorphine depot (CAM2038) in the treatment of adult out-patients with opioid use disorder. Addiction. 2019;114(8):1416–26.
Download references
Acknowledgements
Realized with the unconditional support of L. Molteni & C. dei F.lli Alitti Società di Esercizio S.p.A.
Not applicable.
Author information
Authors and affiliations.
UOS Patologie da Dipendenza D9 ASL Roma 2, Rome, Italy
Claudio Pierlorenzi, Marco Nunzi, Sabino Cirulli & Lucia Curatella
UOC Patologie da Dipendenza D8 ASL Roma 2, Rome, Italy
Giovanni Francesco Maria Direnzo, Sandra Liberatori, Annalisa Pascucci & Generoso Ventre
UOS Terapia del Dolore ASL Roma 2 Ospedale S. Eugenio, Rome, Italy
Edoardo Petrone
Servizio Dipendenze Casalpusterlengo, ASST Lodi, Lodi, Italy
Concettina Varango, Maria Luisa Pulito, Antonella Varango & Cosimo Dandolo
Tossicologia Medica, Azienda Ospedaliero Universitaria Careggi, Florence, Italy
Brunella Occupati
ASST Papa Giovanni XXII, Ospedale Di Bergamo, Bergamo, Italy
Roberta Marenzi
Dipartimento Tutela Delle Fragilità ASL Roma 2, Rome, Italy
Claudio Leonardi
You can also search for this author in PubMed Google Scholar
Contributions
CV, MLP, AV, and CD collected, analysed, and interpreted the patient data regarding the Case n.1. BO collected, analysed, and interpreted the patient data regarding Case reports 2 and 3. CL, SB, GFMD, LC, SL, MN, AP, EP, CP, and GV collected, analysed, and interpreted the patient data regarding Case reports 4 and 5. RM collected, analysed, and interpreted the patient data regarding the Case report 6. All authors participated in the writing process, reviewed, and approved the final version of the manuscript.
Corresponding author
Correspondence to Claudio Leonardi .
Ethics declarations
Ethics approval and consent to participate.
The study was performed according to the Declaration of Helsinki. Informed consent was obtained from patients prior their participation to the study.
Consent for publication
Written informed consent was obtained from the patients for publication of these case reports and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: case report 1..
Buprenorphine implant procedure.
Additional file 2: Case report 2.
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pierlorenzi, C., Nunzi, M., Cirulli, S. et al. Patients' perspectives on buprenorphine subcutaneous implant: a case series. J Med Case Reports 18 , 202 (2024). https://doi.org/10.1186/s13256-024-04483-6
Download citation
Received : 24 May 2023
Accepted : 01 March 2024
Published : 06 April 2024
DOI : https://doi.org/10.1186/s13256-024-04483-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sublingual buprenorphine
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Robert’s story
Robert was living with an alcohol addiction and was homeless for over 25 years. He was well known in the local community and was identified as one of the top 100 A&E attendees at the Local General Hospital.
He drank all day every day until he would pass out and this was either in the town centre or just by the roadside. In addition, Robert was also incontinent and really struggled with any meaningful communication or positive decision making due to his alcohol usage. This often resulted in local services such as police, ambulance being called in to help. He had no independent living skills and was unable to function without alcohol.
In addition, and due to his lifestyle and presenting behaviours, Robert had a hostile relationship with his family and had become estranged from them for a long period of time.
Robert needed ongoing support and it was identified at the General Hospital that if he was to carry on “living” the way he currently was, then he wouldn’t survive another winter.
On the back of this, Robert was referred to Calico who organised a multi-disciplinary support package for him, which included support with housing as part of the Making Every Adult Matter programme.
After some initial challenges, Robert soon started to make some positive changes.
The intensive, multidisciplinary support package taught him new skills to support him to live independently, sustain his tenancy and make some positive lifestyle changes which in turn would improve his health and wellbeing.
This included providing daily visits in the morning to see Robert and to support him with some basic activities on a daily/weekly basis. This included getting up and dressed; support with shopping and taking to appointments; guidance to help make positive decisions around his associates; support about his benefits and managing his money. In addition, he was given critical support via accessing local groups such as RAMP (reduction and motivational programme) and Acorn (drugs and alcohol service), as well as 1 to 1 sessions with drugs workers and counsellors to address his alcohol addiction.
After six months Robert continued to do well and was leading a more positive lifestyle where he had greatly reduced his A&E attendance. He had significantly reduced his alcohol intake with long periods of abstinence and was now able to communicate and make positive decisions around his lifestyle.
Critically he had maintained his tenancy and continued to regularly attend local groups and other support for his alcohol addiction and had reconnected with some of his family members.
By being able to access these community resources and reduce his isolation he is now engaged in meaningful activities throughout the day and has been able to address some of his critical issues. A small but significant example is that Robert is now wearing his hearing aids which means that he can now interact and communicate more effectively.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Psychiatry
- PMC10273571

Challenges in addiction-affected families: a systematic review of qualitative studies
Mostafa mardani.
1 Department of Social Work, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Fardin Alipour
2 Department of Social Work, Social Welfare Management Research Center, Social Health Institute, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Hassan Rafiey
3 Social Welfare Management Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Masoud Fallahi-Khoshknab
4 Department of Nursing, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Maliheh Arshi
Associated data.
All data generated or analyzed during this study are included in this published article.
The relative paucity of research on Addiction-Affected Families’ (AAF) issues and the lack of attention given to their difficulties and treatment in interventions and clinical practices indicate that the primary focus consistently revolves around individuals with addictive disorders, even when the treatment process involves their families. However, it is believed that family members endure significant pressures that result in extensive negative consequences on the personal, familial, and social aspects of their lives. Aiming for a better understanding of the challenges and issues that AAF’s experience, this systematic review explored qualitative studies with a focus on the impact of addiction on different aspects of families.
We searched Research Gate, Scopus, Web of Science, ProQuest, Elsevier, and Google Scholar Databases. We included studies of qualitative design which have investigated the effects of addiction on families. Non-English language studies, medical views, and quantitative approaches were excluded. Participants in the selected studies included parents, children, couples, sisters/brothers, relatives, drug users and specialists. The data from the selected studies were extracted using a standard format for the systematic review of qualitative research (the National Institute of Health and Care Excellence [NICE] 2102a).
A thematic analysis of the findings of the studies identified 5 main themes: 1) initial shock (family encounter, searching for why), 2) family in the fog (social isolation, stigma and label), 3) sequence of disorders (emotional decline, negative behavioral experiences, mental disturbance, physical degeneration, family burden), 4) internal family chaos (instability of relationships, shadow people, erosive confrontation with the drug-using member, a newly emerging member, collapsing system, financial collapse), and 5) self-protection (attracting information, support, and protective sources, coping and adjusting the effects, the emergence of spirituality).
This systematic review of qualitative research highlights the various and complex issues which addiction-affected families go through in terms of financial, social, cultural, mental and physical health problems, as a result of which experts of the field are needed to investigate and take measures. The findings can inform policy and practice and the development of interventions aimed to lighten the burdens which addiction-affected families carry.
Today, due to the expansion of societies, the emergence of various social groups, and the diversity of needs, countries and the general public have faced a new world of needs, interests, progress, and even various problems. These issues and problems have penetrated the spirit of societies and have influenced individuals’ social world. In addition to the effects on the individuals, such problems have also had widespread effects on larger levels, such as the family and society levels.
When a family member enters the cycle of problems, the family, as the first group and institution, starts its support services for the individual, and since, in most cases, the family and its members do not have sufficient and specialized knowledge about the individual’s problem, they are under too much pressure. Maintenance, care, and support of a member with an injury and problem put a heavy burden on the shoulders of families, and since some families are not able to adapt to the problem and react appropriately to it, the family’s normal system and functioning are disturbed, and the family deviates from its normal path due to the severity of the problem [ 1 , 2 ]. Addiction is one of the biggest social problems that the current world is facing. It is a problem that does not only involve the drug user but also affects several individuals and social environments around the person [ 3 , 4 ]. Studies have shown that the impacts of drug and alcohol use on families are undeniable [ 5 – 7 ] and exposes family members to a wide range of issues such as: socio-economic and mental health problems, abuse, conflicts, dysfunctional family structure, various issues in community life, and several problems related to married life [ 8 ]. It is noteworthy that in the absence of sufficient social and governmental support, the burden of addiction or any other problem will be quite heavy and stressful for families, which, in addition to affecting the structure as well as the function and role of the family, makes family members face various and severe pressures and stresses [ 9 – 11 ]. Of course, it is essential to mention that the various effects of addiction in different cultures and also the drug user’s role in the family (wife, parent, or child) are not to be ignored [ 12 ]. Although such families suffer from the same pain, the severity of the challenges they face vary in different cultures [ 13 ].
Despite the abundance of research on addiction and its implications for individuals, there is a dearth of comprehensive understanding regarding the distinctive challenges faced by families affected by addiction. Although studies have provided valuable insights into the personal experiences of individuals grappling with addiction, a substantial gap still exists in the current literature when it comes to exploring the specific challenges, dynamics, and coping mechanisms within families affected by addiction [ 14 , 15 ]. In other words, such studies fail to notice the other side of addiction, which is addiction-affected families [ 16 ].
In addition, those other studies which do in fact investigate the challenges faced by addiction-affected families, have not comprehensively examined them and have targeted only limited parts of AAF’s experiences. For instance, in one study, only certain single challenges in isolation was considered [ 17 ], and in another paper, the effect of relationship, social and cultural factors on the AAF’s experiences were investigated [ 13 ]. Furthermore, the only existing qualitative review in this field reviews the qualitative studies on addiction-affected families until the year 2010 [ 18 ]. This is while the challenges faced by such families in recent years are beyond the ones investigated in these studies, and a comprehensive view on the problems faced by this group of people in all dimensions is still missing.
For these reasons, further research is needed in the field of AAF, so that they can ultimately lead to a change in the perspective of therapeutic measures and theoretical models in this field. By conducting comprehensive and detailed investigations a deeper understanding of AAF can be attained, which in turn has the capacity to reshape current perspectives and contribute to the advancement of this field [ 19 ]. The purpose of the present systematic review is to identify and gain a comprehensive view of qualitative studies and gain insights into the similarities and differences existing in the shared human experience of the same phenomenon through evaluation, critical analysis, and synthesis of qualitative results based on observations and main concepts in order to use the obtained data to make it possible to provide services and interventions in the area of ‘rehabilitation of addiction-affected families’. Since families play a significant role in the treatment process and a comprehensive study on the challenges that families face and the interventions and treatment processes which are most effective for them has not yet been carried out, the present study can pave the way to respond to the above-mentioned conditions.
The present study
What distinguishes qualitative research from quantitative research is their ways of looking at various phenomena and searching methods. In other words, qualitative research seeks to investigate the experiences of addiction-affected families regarding the addiction of one of their family members and subsequently gain deep insight into the phenomenon in question. In this way, qualitative research provides understanding and insight regarding the effects of addiction on families by examining the thoughts and feelings of the participants and analyzing the extracted themes [ 20 ]. The main goal is to provide a comprehensive understanding of the differences in human experiences regarding a phenomenon by analyzing and reviewing texts, images, and interviews. Qualitative research provides valuable insight into phenomena, policies, and practices, although such research traditionally had no place in systematic reviews [ 21 ]. The importance of developing a client-based policy was internationally accepted and recognized by clients themselves. Paying attention to the voice of clients means giving them enough power to express their issues and problems (having a voice) [ 22 ]. Addiction-affected families are often isolated and are somehow service receivers due to the many challenges and problems they face, and this makes them choose different ways to reach a solution, and on this path, they come across multiple issues and difficulties; as a result, if we want to achieve a correct and integrated understanding of the problems of addiction-affected families, it is necessary to conduct qualitative research. The main focus of this systematic review is to provide a general and comprehensive view of addiction-affected families and the issues and problems this group have when confronting the drug-using member. In particular, the present study aims to identify the gaps and analyze the issues and themes from different types of qualitative research to be aware of the services and actions needed for addiction-affected families in different dimensions.
Search strategy and criteria
The search strategy was restricted to studies published in English regarding the effects of addiction on families published between 1990 and 2022. In the search strategy, Research Gate, Scopus, Web of Science, ProQuest, Elsevier, and Google Scholar databases were used and analyzed from 1990 to January 2022. The keywords selected for international databases included: Addiction-affected family, the impact of addiction, addiction and drug abusers, Impact of addiction on families, negative consequence of addiction on families, addiction and family. The papers were first reviewed based on the titles and abstracts. In order to identify relevant studies for the present systematic review, inclusion and exclusion criteria were considered. For this review, a three-stage selection process was used to apply the inclusion and exclusion criteria [ 23 ]: 1- Looking at the title, 2- examining the abstract to identify its association with the research question and method, and 3- reviewing the entire paper.
Based on titles and abstracts, papers were excluded if they did not explore the experiences of addiction affected families or the effects of addiction on family members; exploration of AAF’s experiences and the effects of addiction on family members was required to be either an aim of the study or a substantial finding in the results. To ensure an in-depth understanding and a rich description of experiences, only studies presenting primary data using qualitative methods were included. Mixed-method studies were included if qualitative findings were presented separately. Searches were limited to publications in the English language. Studies were excluded, if papers were restricted to individuals with/suffering from addictive disorders, and if papers were related to family factors of addiction. These exclusion criteria were introduced in order to ensure that experiences and views were current and related to the target group’s (AAF) experience. Any book chapters, Interventions, commentaries, letters, reviews, first-person accounts, and abstracts were excluded. In addition to the mentioned cases, the reference lists of the obtained studies were also examined to identify the studies that were not obtained using the above methods.
In cases where the researcher was not certain about the inclusion criteria of an article, the intended article was kept for the next screening stage. Based on the search strategy of the texts, 518 studies were initially identified. An additional manual Google search was performed at this stage, and 14 more studies were identified. After removing duplicate cases and reviewing the titles and abstracts of these studies, 479 cases were removed and 53 cases were assigned to determine the inclusion criteria. After a removal process, a total of 25 studies were selected as eligible studies (Table (Table1). 1 ). An overview of the search steps can be observed in the PRISMA flowchart (Fig. 1 ). The 25 studies include two studies with a combined method, and one International report of a research project whose results of the qualitative thematic analysis contain valuable data in the research process.
Summary of included studies

PRISMA flow diagram
Data extraction
The data of the determined studies were extracted using a standard format for the systematic review of qualitative research (the National Institute of Health and Care Excellence [NICE] 2102a) [ 48 ]. The characteristics identified from each study included research questions, methods, sample size, and quality assessment. The desired data were carefully extracted and organized in relevant tables. In order to synthesize and analyze the findings of the studies, the desired data from the studies were extracted and categorized into specific thematic categories. Subsequently, the patterns present in the findings of the studies were searched and scrutinized to achieve a better and more comprehensive understanding of the issues and problems caused by addiction toward families.
Quality assessment
The quality assessment of the articles extracted from the journals was performed using the NICE quality assessment checklist for qualitative research (NICE 2012b) [ 49 ]. By following this guideline, the conducted assessment investigates the research questions and the robustness of the method concerning the key findings and a valid conclusion. Six main areas are considered and assessed in this guideline: Theoretical approach, study design, data collection, data reliability and validity, analysis method, and ethical considerations. The seventh overall assessment deals with the relevance of the study and provides an overall rating: “ + + ” in cases where all or most of the checklist criteria have been met and in cases where they have not been met but the conclusion has not been affected; “ + ” where some of the checklist criteria have been met and the conclusion is unlikely to change; and “-” where few or no criteria are met.
Two studies have been included in this systematic study using a combined method, and the quality assessment was performed only on the results of the qualitative data methodology of these studies. Regarding the quality assessment of the present study, a reviewer-researcher initially assessed the quality of the included studies, and the quality assessment was subsequently confirmed by another reviewer. Each search process in the different databases, the initial review of the found documents, matching with the inclusion and exclusion criteria of the findings, and quality assessment were conducted by two researchers independently to increase validity. In this study, the researchers were committed to being sufficiently accurate and honest in using the different sources in all stages of the work, including data collection, data analysis, and the report of the findings. The intellectual rights of all individuals related to the research are fully respected.
This study identified 99 abstracts screened for relevance to qualitative studies on addiction-affected families. Fifty-three full-text articles were studied and assessed, and 25 studies were finally identified as suitable for this review study. The obtained results were organized in relevant tables and classified into specific groups.
Characteristics of target studies
Of the 25 studies in the systematic review, only one analyzed the transcripts of online interviews, and the other 24 studies were results of direct contact with the target groups. The total number of participants in the studies included in this systematic review was 728 people, among whom parents ( n = 288, 39.56%), couples ( n = 222, 30.495%), sisters/brothers ( n = 65, 8. 92%), relatives ( n = 63, 8.65%), drug users ( n = 39, 5.35%), children ( n = 21, 2.88%), specialists ( n = 20, 2.74%), and female heads of households ( n = 10, 1.37%) accounted for the largest percentage of participants in the target studies of this research respectively. Also, the number of samples in the studies shows a great variety, from the smallest number of samples in a case study ( n = 1) [ 35 ] to the largest number of samples in a study ( n = 113) [ 46 ].
Geographical characteristics
In terms of the geographical distribution and information of the studies included in this systematic review, there are 8 studies conducted in Australia (32%), 4 studies from England (16%), 3 studies from South Africa (12%), 2 studies from Canada (8%), 1 study as a result of collaboration between England and Mexico (4%), and 1 study each for Scotland, Indonesia, Finland, Brazil, Iceland, India, and Italy (4% each).
The quality assessment carried out according to the NICE guidelines among the studies identified for the present research showed that 16 studies were of high quality (64%) and 9 were of medium quality (36%).
Qualitative methods
The most common qualitative methods used in the target studies reviewed in the present study included 7 studies using ethnographic and phenomenological methods (28%), 6 studies using the grounded theory method (24%), 3 studies using the thematic analysis method (12%), the use of the descriptive-exploratory method in 2 studies (8%), and 2 studies using the content analysis method (8%). In the remaining 5 studies (20%), various qualitative methods have been used, including 1 case using deviant case analysis in a study in Scotland with 74 samples of relatives, parents, and experts of the drug abuser [ 27 ], 1 case using the qualitative-analytical-exploratory method [ 30 ], 1 case study of 10 female heads of families [ 8 ], 1 case study of a mother with a child with drug abuse that has been analyzed using the interpretive phenomenological method [ 35 ], and 1 case using the framework analysis approach [ 40 ].
Thematic analysis of results
In order to analyze primary qualitative data, the thematic analysis approach is often used [ 50 ]. This approach is also an applicable method which can be used to synthesis the findings of multiple qualitative studies [ 51 ]. The synthesis will surpass the content of the original studies and generate further conceptions or understandings through developing the analytical themes [ 51 , 52 ]. The following three stages of thematic synthesis, planned by Thomas and Harden [ 51 ], were used: (1) Free line-by-line coding of the findings of the primary studies, (2) the organization of ‘free codes’ into related areas to construct descriptive themes and (3), finally, the development of analytical themes. In this synthesis, the published results from each of the included studies were coded. A thematic analysis of the findings of the studies identified 5 main themes: 1) Initial shock (family encounter, searching for why), 2) family in the fog (social isolation, stigma and label), 3) sequence of disorders (emotional decline, negative behavioral experiences, mental disturbance, physical degeneration, family burden), 4) internal family chaos (instability of relationships, shadow people, erosive confrontation with the drug-using member, a newly emerging member, collapsing system, financial collapse), and 5) self-protection (attracting information, support, and protective sources, coping and adjusting the effects, the emergence of spirituality). The visual outline of the identified themes can be seen in Fig. 2 . The frequent themes identified in the articles include the sequence of disorders in 22 studies, internal chaos in 18 studies, self-protection in 13 studies, family in the fog in 13 studies, and initial shock in 7 studies (Fig. 2 ).

Diagram of identified themes
The first theme (initial shock) is one of the themes identified from analyzing the findings of the studies consisting of themes such as family encounter and searching for why. Confusion, anger, inability, and dysfunction due to the family’s initial effort to respond to the raised problem are among the things that are mentioned in Barnard’s study [ 27 ], which uses the deviant case analysis method. Also, in a study to investigate the experiences of parents, Hoeck [ 29 ] investigated how parents are informed of their children’s addiction (being informed by a third party (police or hospital)/ by the drug user and the parents themselves) and showed that the families’ knowledge about addiction was very little at first or they had no information about it and there was no free discussion to express such problems in the home environment. Another study by Salter et al. [ 34 ], using the grounded theory method in England, showed that families suffered from difficulties such as confusion in the initial encounter with a problem and experienced problems like lack of awareness, the gradual process of awareness, drug user’s deceptive behavior, denial, self-contradictions, and the effects of external factors in the initial encounter with the addiction problem of one of their members. Investigating the process of parents’ adaptation and coping with a drug-abusing teenager was one of the goals that Choate [ 36 ] sought in a study using the grounded theory method. The results of the mentioned study indicate that the family first faces the way of becoming aware of their child’s drug addiction and perceives it as an intensified and progressive problem and then tries to find a logical answer for the cause and reasons for such a problem. At the same time, many parents proceed with examining their own behavioral records, and some parents consider their drug use experiences as a trigger and factor for their child’s drug addiction. In a study conducted using Ritchie and Spencer’s framework approach, Bulter et al. [ 40 ] viewed the family’s way of dealing with the addiction of one of its members as being one of the following cases: A person’s voluntary confession of drug use, observing abnormal behavior or changes in their normal behavior, denial of their drug use, difficulty recognizing, family devastation because their child is using drugs, experiencing it as a very shocking and traumatic event, experiencing it as the greatest fear, feeling defeated, self-blame, and the feeling of great shame at the beginning of facing the addiction problem. It is worth mentioning that the determination of factors and reasons such as mental health problems or learning problems as triggers and factors of drug dependence were among the explanations and mechanisms mentioned by the participants of Choate’s study [ 41 ] about the initial encounter with the addiction problem. The analysis of Jackson and Mannix’s [ 45 ] findings showed that one of the themes about which the addiction-affected families expressed their experiences was initial exposure and awareness. In this descriptive-exploratory study, the participants described their initial awareness of their child’s addiction with the sentence, “I could not deny that this had happened.” Generally speaking, the initial exposure and the way of awareness and then trying to respond to the addiction problem are among the negative experiences to which addiction-affected families frequently pay attention.
The second theme (family in the fog), with themes such as social isolation and stigma and label, is among other themes identified by qualitative analysis of the findings of the target studies. Regarding the stigma and label theme, in a study conducted via the phenomenological method to investigate the experiences of families with drug-using children, Wiarsih et al. [ 24 ] considered the family’s labeling one of the results of having a drug-abusing child. The findings of the mentioned study show that society’s attitude and feedback, self-view, and social discrimination are among the things that families perceive under the title of stigma. In this regard, in a qualitative-analytical and exploratory study on addiction-affected families, Rodrigues [ 30 ] has viewed society’s prejudice and society’s experience of stigma by the families to be of the factors that change the lives of families with drug-using members. The experience of stigma as one of the stressful factors at the level of families’ extended interactions is one of the findings of a study by Salter [ 34 ] in England using the grounded theory method. Among other themes identified in the present study is the social isolation of addiction-affected families. One of the negative experiences of addiction-affected family members is inhibiting social activities and, in some way, being away from the society and being isolated. Limited activities and social roles, especially for those with the most supportive contact with the drug user, were one of the findings of McCann’s study [ 28 ] conducted in Australia. In addition, in another study carried out to investigate the experiences of families regarding dealing with social isolation, McCann [ 25 ] showed that one of the families’ measures in dealing with the addiction of their family members was to minimize contact with others and consequently face things such as shame and embarrassment, fear of being judged by others, self-quarantine, and unwillingness to access informal and official support. In this regard, in a study carried out by the thematic analysis of 100 transcripts of online interviews with couples, Wilson [ 32 ] presented the impact on the family social network and the challenges of families in this area as one of the main themes of his research. In another work of research by Arlappa et al. [ 8 ], which was conducted in India as a case study, the effects of a drug-using member on a family’s social life were presented as one of the results of the study, according to which families prefer to limit their social interactions following the addiction of one of their members. In a study to examine the effects of addiction on family from the parents’ perspectives, Salter [ 34 ] analyzed the data obtained from semi-structured interviews using the grounded theory method. The findings of the mentioned study show that addiction-affected families are disturbed in the broad and essential levels of their interactions, which will result in the disassociation of such families from the social world and lack of active participation by those families. Also, many families will face the challenge of getting help because they try to hide the addiction problem of one of their members and thus limit their communication and experience serious challenges regarding asking for help and support [ 36 ]. It should be mentioned that the challenge of asking for help and the weak support of addiction-affected families are due to hiding the problem from others and disassociating from others, which is also one of the findings of Arcidiacono’s study [ 46 ] in Australia. Isolation of the family is another finding in this section, to which Jackson [ 37 ] refers in the findings of his study in Australia as the main theme of isolated, disgraced, and humiliated as if the family is only with the drug user and has no other social connection. This concept is also expressed in the results from Ahuja’s study [ 47 ] under the title of social isolation and also in the results of Bulter’s study [ 40 ]. The results from Bulter’s study indicated that self-imposed experiences, the family’s feelings of embarrassment or shame due to drug use by one of their members, and worrying about others’ opinions played a significant role in the isolation of family members and parents.
The third theme (sequence of disorders) is completed with themes such as emotional decline, negative behavioral experiences, mental disturbance, physical degeneration, and family burden. The findings of the present study showed that family’s emotional dimension is severely affected due to the abuse of one of its members, and families experience a wide range of emotionally distressing situations. The feelings of disbelief, non-acceptance, disappointment, shame, shock, anger, and regret in the family are mentioned in the findings by Wiarsih et al. [ 24 ]. Furthermore, the findings of Incerti’s study [ 26 ] have indicated feelings of sadness, hopelessness, and distrust as the fundamental challenges against addiction-affected families. Fatigue and emotional exhaustion, as well as fear and despair about the future in addiction-affected families, were mentioned in the results of an interpretive phenomenological analysis of 31 semi-structured interviews in McCann’s study [ 28 ] in Australia. Feelings of helplessness and despair, desperate cries for help, and living with guilt are feeling which are typical examples of the emotional distress experiences of addiction-affected families, which were found by various studies [ 29 , 35 , 38 , 41 , 44 ]. Families naturally experience a wide range of emotions, a significant part of which are positive emotions. However, in his study to investigate the experiences of addiction-affected families in Iceland with 16 participants, Ólafsdóttir [ 33 ] showed that one of the negative experiences of addiction-affected families was the transformation of their positive feelings, such as worry and care, over time to negative emotions, such as anger, shame, and sadness. Also, the increase in negative feelings toward the drug user, the increase in negative feelings caused by the drug user, and the increase in negative feelings in general (confusion, etc.) in Salter’s study [ 34 ], emotional distress and the use of pills to moderate stress in Groenewald’s study [ 35 ], and variable emotions shifting from positive components (love, admiration, and care) to negative components (desire for separation, etc.) in Velleman’s study [ 43 ] are among other findings in this regard. By analyzing the findings of the target studies, it was found that negative emotional experiences in families with addiction problems were widespread. In addition to the mentioned cases, there were cases such as worry and uncertainty about the individual’s situation, the family’s status, the family’s future, the effects of the individual on the family [ 34 , 43 , 46 ], loss of trust and feeling of mistrust [ 37 , 46 ], feelings of blame and shame [ 37 , 38 , 41 , 44 , 46 ], feelings of fear and trembling of family members [ 44 , 45 ], feeling of sadness due to the drug user’s negative and unexpected path [ 38 ], the emergence of destructive emotions such as inferiority, anger, division, and separation [ 39 ], negative effects on individuals’ emotional health, and the emergence of a wide range of negative emotions from continuous crying to the feeling of separation and leaving the family [ 40 ]. Negative behavioral experience is one of the other themes identified in the present study. Experiencing aggression and verbal or physical violence [ 25 , 27 , 29 , 33 , 37 , 46 , 53 ], theft [ 27 , 30 , 41 ], tension and controversy at home [ 34 ], and experiencing domestic violence towards household members and items [ 47 ] are among the cases mentioned by addiction-affected families in the target studies. Additionally, in the psychological dimension, the families reported negative experiences under the title of mental disturbance. Things like different levels of stress and anxiety [ 27 , 29 , 33 , 53 ], the experience of mental and psychological violence [ 33 ], different effects on mental health [ 34 ], and suicidal ideation and attempt [ 35 ] are among the cases identified from the analysis of the findings of the target studies. The findings from Orford’s study [ 39 ], which was carried out in order to investigate the experiences of stress and pressure in addiction-affected families, indicated that the physical health of families was also affected by the addiction of one of their members, and family members sometimes reported cases such as the emergence of physical weakness, specific physical symptoms, excessive fatigue, lack of sleep, and anorexia. The incidence of physical degeneration was also identified and investigated in the findings of other studies [ 34 , 40 ]. In addition to the mentioned cases, families also have an unpleasant experience under the title of family pressure and burden as a result of the drug abuse process of one of their members. The analysis of the findings of the studies showed that physical, psychological, social, and economic burdens [ 24 ], high levels of tension and pressure during the treatment of the drug-using member [ 34 ], and long-term processes of treatment and rehabilitation [ 36 ] were among the things experienced by addiction-affected families in this regard.
The fourth theme (internal family chaos) was another identified theme completed with the following themes: Instability of relationships, shadow people, erosive confrontation with the drug-using member, a newly emerging member, collapsing system, and financial collapse. The internal relations of families are among the first things which are affected by the newly created conditions, and families experience a wide range of disorders in this area, from problems and differences between parents and extensive marital differences [ 8 , 29 , 47 ] to the disturbance of the general structure of interpersonal relationships at home [ 27 , 30 , 32 , 34 , 40 ]. Also, the occurrence of chaos and failure in family communication and family conflicts are other things mentioned in the findings of the studies [ 41 ]. “Shadow people” refers to family members who have been neglected by others, especially parents, due to the addiction of another member, and the needs and psychological conditions of these individuals are somehow not paid attention to. Being neglected [ 34 ] and being ignored and not approved [ 26 ], being exposed to drugs and the possibility of entering the use process and dealing with public reactions [ 27 ], experiencing negative psychosocial effects, being isolated [ 33 ], suppressed anger and rage [ 37 ], lack of affection and attention, as well as reluctance towards social interactions and bringing friends to the home environment [ 47 ] are among the issues mentioned in various studies. In dealing with the drug user, the families also tried different ways, and the analysis of the findings showed that a significant part of the families’ energy is spent on these efforts. Rejection of the drug user was one of these ways that Barnard [ 27 ] found in his study in Scotland, and Orford [ 39 ] referred to it in his study as “an unpleasant life with the drug user.” Controlling the person and setting various limits for the drug-using person were other ways used by the families to deal with their drug-abusing member. Worrying about the person, trying to protect the person, and maintaining the relationship with love and friendship were other actions by the families in this area [ 38 , 45 ]. Also, the participants of Arcidiacono’s study [ 46 ] stated that the person was good but had terrible abuse, and with this view, they confronted their drug-abusing member as if a new person had emerged who had nothing in common with the previous one. The new person was a person whom the family did not trust, had not been at home in general as if he/she was missing, had left the house without any notice and the time of their return was not known, did not take any family rituals and gatherings (birthdays, Nowruz, etc.) seriously and was absent in them, had a noticeable inability to respond to the family’s expectations [ 43 ], their friends had changed in general, and they suffered a sharp drop in education, as well as a decrease in personal hygiene and physical health [ 44 ]. It is worth mentioning that due to these issues, families tend to have serious problems in family economy and financial capability and experience a kind of financial collapse [ 8 , 28 , 30 , 33 , 34 , 39 – 41 , 46 , 53 ]. Facing harmful family dynamics [ 28 ], threatening family functioning [ 29 ], jeopardizing the family system’s health[ 8 , 33 , 40 , 44 – 46 , 53 ], and moving from cohesion to confusion and collapse [ 46 ] are other threats that put the family on the path to internal chaos.
The fifth theme (self-protection) is related to the actions that families have taken to deal with new conditions. Themes such as attracting support sources, coping and adjusting the effects, and the emergence of spirituality are included in this category. In his study, Wiarsih [ 24 ] showed that the families tried to cope with the problem by attracting moral, financial, informational, and social support. In order to attract support sources, the findings of various other studies were also considered in this research. These findings showed that the attraction of support, informational, and therapeutic sources had been one of the dominant methods of encountering the addiction problem in the addiction-affected families studied [ 26 , 29 , 34 , 40 , 44 , 46 ]. Among other actions of addiction-affected families to protect themselves are coping and adjusting the effects, such as problem-solving methods [ 24 ], dealing with violence [ 25 ], adjusting the effects of stigma [ 31 ], and various coping strategies to reduce the consequences of the addiction of a family member [ 29 , 34 , 38 , 41 , 44 , 46 ]. Also, Rodrigues [ 30 ] showed in his study that faith and trust in God was one of the methods used by families to manage the effects of the problem and deal with it.
Although qualitative research on the issues and problems of addiction-affected families are limited and carried out in minority, these studies have been necessary to improve the understanding and insight of policymakers in this field, social service providers, professionals, and addiction-affected families. Effective and specialized support for this group is possible only when their voices are heard, and services are tailored to their conditions, and needs are noticed and provided for. For this purpose, this systematic review was conducted to identify and review those studies which have investigated the effects of addiction on addiction-affected families using qualitative research methods. The findings of the studies showed consistent themes among the research methods and the studied populations. Twenty-five high-quality and medium-quality articles with diverse contents which were suitable for the purposes of the current research were identified and reviewed. The analysis of the findings of the studies showed 5 main themes related to the fundamental challenges of addiction-affected families. The identified themes were the initial shock, family in the fog, sequence of disorders, internal family chaos, and self-protection. The initial encounter with addiction was one of the first themes of the present study. Families are initially confused and shocked due to lack of knowledge and experience [ 27 , 29 , 34 , 40 ] and are somehow unsure of their next steps to take. Some families start self-prescription and take actions that they consider appropriate, which creates the background for future problems for family members. At this stage, the family puts itself in a deep, long, and recurring mourning process [ 24 ]. This concept is very specific and has been mentioned in very few studies. In other words, encountering a family member’s addiction for the first time is so painful that families refer to it as their hardest experience in the addiction process [ 54 ]. Generally, Placing families on educational grounds and introducing support groups can play a significant role in getting families out of this vicious cycle. These groups play a significant role in modulating the effects of the initial shock in addiction-affected families by providing information about addiction and treatment, strengthening the morale of addiction-affected families, providing support, understanding their needs, providing a learning contexts, teaching family members to distance themselves from problematic situations, helping them overcome feelings of guilt, shame, and failure, teaching them to deal with risks and fears, and teaching coping strategies (physical and emotional distance of the family from the drug-abusing person). Furthermore, the key sentence of support groups for families is: Learn to live with anxiety and fear [ 29 ].
The analysis of the findings showed that families opt for social isolation to avoid social stigma and being labeled. These two processes have been described in the present study with the second theme, i.e., family in the fog. The most important challenge that these families experience at this stage is the challenge of getting help [ 36 ], because they generally pose an unwillingness to access formal and informal support available in the society [ 31 ]. This action of the families is taken due to the defense mechanism of secrecy. Families somehow prefer to respond to the problem on their own in any way possible in order to avoid the possibility of judgment [ 31 ], stigma [ 34 ], and being labeled, so that they can avoid social discrimination against the family [ 24 ]. In this regard, some families move toward social isolation and some try to manage the effects of this problem by adopting measures such as adjusting the effects of stigma, challenging the misconceptions of the people around them about drug abuse, or choosing specific individuals and communicating with them [ 31 ]. Furthermore, the experiences of shame, stigma, and social isolation are among the results which Di Sarno et al. [ 17 ] found in their study, which was conducted via the scoping review aiming to investigate the mental and physical problems faced by addiction-affected families. In their study, in addition to quantitative studies, they also aimed at those qualitative studies which specifically focused on the mental and physical challenges against addiction-affected families and found the three above-mentioned challenges to be common among all the investigated qualitative studies. What is expected to be noticed by policymakers and service providers is to eliminate the misconceptions about addiction-affected families. Support groups should compile and implement effective measures to adjust and finally remove the effects of social stigma. Also, the development of effective interventions at the individual and social levels by researchers in this field aiming at removing the social barriers against addiction-affected families can play a significant role in preventing the social isolation of this at-risk group.
The third and fourth themes identified in this study indicate the extent of harm in the family, both at the family health level and the family system and functioning level. Concerning the various aspects of the health of addiction-affected families, studies focusing on this area provide insights into the consequences of damages to emotional, mental, physical, and behavioral health of families with a drug-abusing member, showing the sequence of damages for addiction-affected families. The concept above is among the concepts which have been mentioned in various studies. In other words, addiction deeply affects family members on the psychological, emotional, physical, and behavioral levels [ 55 – 57 ].
Furthermore, concerning the fourth theme, i.e., internal chaos, this study determined that the family system and functioning might face serious threats at the levels of relationships, as well as in the family health system. Conflicts within the families affected by addition are among the challenges which all family members have mentioned and considered to be an indispensable part of addiction. It is to be noted that improper construct and function of a family and morbid relations between family members cause them to face more severe challenges and pressures [ 13 ]. Since different levels of family health and function are influenced in the third and fourth themes and all of the reviewed studies have taken them into account, it seems necessary to take measures in order to alleviate their effects.
Specialists consider family a source and support for its members, who fulfill their duties with all their limitations [ 27 ]. The results of the investigations showed various interventions around the world with different goals for addiction-affected families, and their implementation can play a key role in helping families exit this Bermuda process. Increasing social support, coping skills, modulating stress and pressure [ 58 ], reducing the symptoms of mental disorders and improving family functioning [ 59 ], improving family functioning at the system, structure, and strategy levels [ 60 ], training families in the areas of emotional support, social acceptance, reduction of problems caused by addiction [ 61 ], awareness of family needs, environmental and interpersonal changes, organization of family structure, use of social strengthening and family education models (craft) [ 62 ] and Matrix [ 63 ], participating in Naranan meetings for addiction-affected families, and participation in meetings are only part of the existing interventions for promoting and improving addiction-affected families. It is worth mentioning that one of the things that the experts in this area emphasize is the necessity to pay attention to those individuals who are at home under the shadow of the drug-using person. In other words, families, especially parents, neglect others due to the problems caused by the addiction of one of their members and spend all the energy and internal resources of the family (financial, mental and psychological, social, and cultural) on the mentioned person. This issue creates severe problems in the long run for other family members due to daily encounters with these issues and facing addiction to such an extent that may cause these individuals to suffer from severe psychosocial problems and isolation [ 53 ] or enter the path of drug use [ 27 ]. Since this systematic review has targeted all the qualitative studies conducted in the field of addiction-affected families and has identified valuable and comprehensive themes, the need to develop a comprehensive intervention according to the data of the present study, taking all dimensions of families into account, has become ever more evident.
As the final theme identified, self-protection is the main key to starting the recovery process in addiction-affected families. Seeking help, moral support, financial support, informational support, and social support [ 24 ] and trying to deal with the problem and reduce its negative effects are parts of the process that addiction-affected families embark on for self-protection. It is to be noted that lack of social support exposes families to serious problems [ 13 ]. The final concept in this section is the recovery process of addiction-affected families, which starts when they face the addiction of one of their members and are somehow involved in its maze. Intervening in the levels of compatibility with the drug user’s behavior, financial compliance with conditions, hidden interventions, formal and informal support, religious and spiritual support [ 12 ], and preparing for changes in family members and family functioning and increasing coping skills [ 64 ] all play an effective role in providing a context for families to protect themselves and ultimately lead to the recovery of families.
In general, the point revealed in this study and mentioned in all reviewed studies was that when the families expressed the challenges caused by addiction, they also expressed their efforts to overcome the problems and called it the challenge that addiction had created for them. In other words, the families tried to survive and keep their family members alive while they were frustrated and exhausted and provided the basis for the family’s recovery. Moreover, it is to be taken into account that the experience of addiction varies for different families based on social and cultural conditions, and provided that there is proper social support and healthy family functioning, family members will face less serious challenges when having to deal with the addition of one of the members [ 13 ]. However, they had doubts about how to do it, and they were prone to confusion and ambiguity. Investigating the recovery process of families is not one of the goals of this study, but it is a topic that can be considered for future research and used as a guide, reference, and path for the recovery of addiction-affected families.
The method for the present study is the systematic review of qualitative studies in the area of experiences and challenges faced by family members affected by addiction. In order to analyze the data, a thematic analysis was used. This study was designed in such a way to analyze only those qualitative studies which comprehensively address the challenges which addiction-affected families face and possess the required standard in accordance with NICE quality assessment checklist for qualitative research. Among those studies which can be compared with the present study, one can mention the valuable study conducted by Di Sarno et al. [ 17 ], in which the researchers implemented the scoping method in order to investigate the mental and physical challenges faced by addiction-affected families. In that study, with respect to the aim of the study, all qualitative and quantitative studies which only focus on the mental and physical challenges against families affected by addiction are analyzed. However, the present study has adopted a more comprehensive approach in order to present, in addition to the concepts above, all the other dimensions of addiction-affected families and to use thematic analysis in order to put forward family challenges comprehensively in 5 different conceptual categories. The present study has taken a step beyond Orford’s review study [ 18 ]. Orford has presented a summary of qualitative studies conducted in the area of addiction-affected families until 2010 and reported the results in the four categories of stress, strain, coping, and social support. The present study, however, has analyzed all the research conducted until 2022 on the challenges faced by addiction-affected families and has presented 18 sub-themes in addition to its main 5 themes.
Limitations and future directions of research
The present study was conducted using a protocol-oriented process and all the reliable scientific databases in the world. While, the concept of addiction includes a wide range of addictive behaviors, addiction in this research meant using any drug and alcohol. There are many limitations to the studies used in this research.
In the present study, the level at which a family member in engaged in substance use (low-risk drug users or occasional users compared to those users classified as harmful or dependent users) has not been considered, while this level can affect the challenges and difficulties faced by addiction-affected families. Three of the studies included in this review were published by the same authors and used the same group. However, each study addressed slightly different aspects of AAF’ experiences with living with a member with addiction problems [ 25 , 28 , 31 ]. It is important to mention that this study has not examined the families’ cultural, religious, and belief differences in dealing with addiction, and the lack of data and studies among different cultures and beliefs in this field is challenging for researchers. As a result, future studies should be able to show a better understanding of the psychosocial effects of addiction on families with more emphasis and sensitivity toward culture, ethnicity, and religion. Moreover, lack of attention to the role of the drug-using member in the family in the current study, can be effective regarding the type of its effects on other family members and other cases that can generally limit the conclusions that can be obtained from this study. For this reason, to produce more reliable results, future systematic studies should limit their search terms and phrases according to the role of the drug user in the family so that they can provide more reliable recommendations and suggestions to support addiction-affected families. Evidence shows that some studies, for various reasons, have more chances to be published in valid journals in the shortest time, and it is somehow easier to access and find such articles, while these articles may be poor in terms of both methodology and work processes. Therefore, in the current study, conclusions solely based on published studies can be misleading. The terms used in the field of addiction-affected families are diverse, and special titles and unique literature might have been used for some papers, as a result of which, we may have missed a number of relevant but inaccessible studies and future systematic studies should include a broader range of relevant terms to provide a more general insight and perspective regarding this group’s challenges and health status. However, in the present study, it is believed that the use of reliable and diverse scientific databases, double screening of the studies, and a strong search strategy have allowed us to identify all eligible articles. While this study has focused on the effects of drug addiction on families, it has also revealed the existence of a big gap in the knowledge of families affected by other addictive behaviors (Internet, gambling, etc.). It is, therefore, essential to compare and draw existing debates and narratives and their evolution over time to understand addiction-affected families’ challenges better.
In addition to the limitations outlined in Table Table1 1 regarding the examined studies, there are other important considerations that warrant attention. Firstly, since the reviewed studies were qualitative in nature, the common limitation of "limited generalizability" applies to all the studies under investigation. In other words, the findings of the reviewed studies cannot be easily generalized. Furthermore, as most studies relied on help-seeking or service-receiving samples, and the selection of participants was based either on snowball sampling or purposive sampling, their experiences may have been influenced by the type of services they received, making them inadequate representatives for all families affected by addiction.
Implications for research and practice
This is the first systematic review of qualitative research on the challenges of addiction-affected families, which has targeted studies over the past 30 years. Qualitative research provides an opportunity to hear the voices of research participants in order to provide valid empirical and perceptual evidence, which can be used to inform and influence policies and provide mental health services using an evidence-based perspective. This systematic review provides a reference of evidence-based knowledge obtained from qualitative research by drawing the themes and findings of qualitative studies on the challenges of addiction-affected families. The first outcome of the present study in practice can be to pay attention to wider dimensions (social, cultural, economic, and individual) of families. In other words, a drug-using person consciously or unconsciously faces their family with fundamental challenges, and these challenges provide the basis for future problems. For example, while societies try to accept this group, social stigmatization and labeling is an issue that this group constantly faces, and it plays a special role in concealment and self-censorship by families, which subsequently causes more severe problems to arise for them. The second outcome of this study for practice and action is the need to train social, educational, and health service providers in order for them to try to accept addiction-affected family members and provide psychosocial, educational, and preventive services in case of encountering any members of this group. Also, this review study has provided the basis for studies and interventions in this field, and, by providing a visual diagram of the identified themes, it has provided the framework for interventions needed by addiction-affected families for researchers in this field. It is worth mentioning that with access to these rich qualitative data, which were the results of the experiences of addiction-affected families, it is possible to design and implement more effective support and educational mechanisms for families that have just entered this long process.
Conclusions
The analysis of the data obtained from the present research identified 5 main themes in this process: Initial shock, family in the fog, sequence of disorders, internal family chaos, and self-protection. The findings of the present study clearly state that any types of intervention to be carried out within addiction-affected families need to consider all problems and challenges created by addiction. These 5 themes were identified in different studies with different qualitative methods and different target populations. The implications of the present study at the levels of policymaking, practice, and research have also been clearly stated. Addiction-affected families want a space that is far from any judgment and labeling so that they can control their mental, psychological, and social conditions and the society can prevent the initial shock of this group when encountering the addiction of one of its members by arriving on time and providing the right educational services. The voices of addiction-affected families revealed the need for educational, informational, and therapeutic support to improve their coping skills in order to face and moderate the effects of addiction. The results of the present study provide a rich source of evidence-based information to provide the best services and policymaking for addiction-affected families. It is also important to mention that in developing countries and in countries where the governments play a small role in providing welfare for their citizens, individuals and families are intertwined elements, and any problem for each member can significantly impact the whole system. Therefore, paying attention to addiction-affected families in these areas is only in its initial stages, and the need to pay attention to this group has become apparent more than ever.
Acknowledgements
The authors would like to appreciate the researchers of the presented articles for their hard work in applying qualitative research methods to examine the challenges of addiction-affected families.
Abbreviations
Authors’ contributions.
MM contributed to the design of study, conceptualization, data curation, formal analysis, investigation, methodology, resources and visualization. FA contributed to the design of study, conceptualization, formal analysis, and revised the manuscript. HR contributed to the design of the study, screening and revised the manuscript and was the Academic Supervisor. MF was the Academic Supervisor. MA advised and revised the manuscript. All authors read and approved the final manuscript.
Not applicable.
Availability of data and materials
Declarations.
The authors declare that they have no competing interests.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mostafa Mardani, Email: moc.oohay@inadramafatsom .
Fardin Alipour, Email: moc.liamg@ruopiladobrab .

More Changes to Addiction Terminology
New suggested wording for when someone takes fentanyl..
Posted April 8, 2024 | Reviewed by Monica Vilhauer
- What Is Addiction?
- Find counselling to overcome addiction
- Language related to addiction seems to be ever-changing.
- Not everyone agrees with some changes.
- Parents, especially, seem to want a say "poisoned" when their child dies from fentanyl, specifically.
In a previous post, “ The New Definition of Sober ,” I noted that some of the terminology used to refer to people with alcohol or substance use disorder has changed. (The two phrases, “alcohol use disorder” and “substance use disorder” are examples of the changes.) The purpose of the new terms is to focus on the disease rather than on a label for a person—such as alcoholic or drug addict , which can be considered derogatory—and hopefully help to remove the stigma around addiction .
“Poisoned” Vs. “Overdosed”
Currently, some parents of individuals who have unknowingly taken fentanyl when they thought they were taking a different substance are asking for yet another word or phrase to be changed. As a March 11, 2024 New York Times article explains, these parents would like it to be said that their loved one “was poisoned,” rather than that they “overdosed.”
It would change the perception of what really happened in each case, the writer says. “…[O]verdose suggests that their loved ones were addicted and responsible for their own deaths, whereas “poisoning shows they were victims.” Or, as one parent says, “It [saying my child was poisoned] keeps the door open. But ‘overdose’ is a closed door.”
A Sample Case and a Helpful Non-Profit
In 2022, Ryan Bagwell, 19, from Texas, took what he thought was Percocet, a pain reliever that he had bought in Mexico from a friend. He died after taking it; it was not Percocet, it contained “lethal quantities of fentanyl.” When his mother saw the death certificate, it said that Ryan had died from a fentanyl overdose. Ryan’s mother would like the record to read that he had been poisoned, and she explains why in the New York Times article.
A non-profit group related to these parents, Texas Against Fentanyl, has succeeded in getting Texas Governor Abbott to support statewide awareness campaigns to educate the public about such fentanyl poisonings. This group and other family members in a similar situation as Ryan’s mother are making strides in having politicians and documents reflect the new terminology, and other states have taken up the cause with bills and resolutions.
Why This Language Is Important
One expert interviewed—Leo Beletsky, an expert on drug policy enforcement at Northeastern University School of Law—praised the suggested change. “Language is really important because it shapes policy and other responses,” he says. However, the article provides several views to consider and points out that addiction is complicated and nuanced. Perhaps addiction experts on this site will weigh in and explain further. For people like me, a journalist and sibling who watched and worried about someone with substance use disorder, the changing language is fascinating.
A Relevant Commercial
The poisoning of people who don’t know they’re taking fentanyl and die as a result is a whole new ballgame. If you watched the Super Bowl on TV in February, perhaps you saw the commercial that featured the New York parents whose daughter, a freshman home from college for Thanksgiving, went to a friend’s house. She took what she thought was Percocet, and the implication was that it was to “party” with friends. It was fentanyl, and as with Ryan Bagwell in Texas, it killed her.
The second photo in the internet article about the commercial identifies her as a “local overdose victim.” But if you click on the link in the paragraph beneath the photo, there’s a headline on another photo on that page with a different title: “Poison pill: How one pill lead [led] to a local teen ’s death.”
The commercial uses both terms, “overdose” and “poisoned,” but perhaps the news about the suggested language change wasn’t as widespread when the commercial was written. We can’t know why the commercial used both. In any event, the group responsible for sponsoring the commercial—the New York State Office of Addiction Service—is to be commended for spreading awareness of this horrible drug that’s killing so many of our unsuspecting youth.

I noticed that this public service commercial now appears on my local TV station as well.

Pat Olsen is a journalist, author and ghostwriter. She coauthored a book with an addiction expert, Sober Siblings: How to Help Your Alcoholic Brother and Sister ― and Not Lose Yourself.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

IMAGES
VIDEO
COMMENTS
This case study of drug addiction can affect anyone - it doesn't discriminate on the basis of age, gender or background. At Serenity Addiction Centres, our drug detox clinic is open to everyone, and our friendly and welcoming approach is changing the way rehab clinics are helping clients recover from addiction.. We've asked former Serenity client, Chloe, to share her experience of drug ...
Abstract. In this article, a case-based format is used to address complex clinical issues in addiction medicine. The cases were developed from the authors' practice experience, and were presented at the American College of Medical Toxicology Addiction Academy in 2015. Section I: Drug and Alcohol Dependence and Pain explores cases of patients ...
Summary of case. W.R is a 30 years old man. Client was referred by psychiatrist, from Drug Rehabilitation Center, Fountain House Lahore, Pakistan for psychological assessment and management of the problem of client. The client was presented with the complaints of stealing habit, drug addiction, poor problem solving, poor abstract reasoning, and ...
Case Study: Lorrie. Figure 1. Lorrie. Lorrie Wiley grew up in a neighborhood on the west side of Baltimore, surrounded by family and friends struggling with drug issues. She started using marijuana and "popping pills" at the age of 13, and within the following decade, someone introduced her to cocaine and heroin.
Weiss RD, Potter JS, Griffin ML, et al. Long-term outcomes from the National Drug Abuse Treatment Clinical Trials Network Prescription Opioid Addiction Treatment Study. Drug Alcohol Depend 2015 ...
Dr. George Eng: An immunoassay panel that is used to screen for drugs of abuse, including opioids, was performed on a urine sample that had been obtained 16 hours after the patient presented to ...
Case Study: Counseling a Substance Abuse Treatment . Client With AD/HD . John R., a 29-year-old African-American man, is seeking treatment. He has been in several treatment programs but always dropped out after the first 4 weeks. He tells the counselor he dropped out because he would get cravings and that he just could
A CASE STUDY TO EXPLORE THE PERCEPTION OF A WOMAN ... Addiction to drugs is a complex, chronic, and multi-faceted disease that often involves cycles of relapse and remission. The lifetime prevalence of alcohol and drug ... for example, Hepatitis C and human immunodeficiency virus (HIV) rates have increased
This case is first of the kind depicting clinical features as well as withdrawal of combined volatile and moderate alcohol abuse. The feature of combined intoxication of the two abused substances makes it difficult for the clinician to reach a diagnosis. Our case report thus puts forward the scenario of increasing combined alcohol and volatile ...
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
It was 4 P.M., and Andrew. * had just bought 10 bags of heroin. In his kitchen, he tugged one credit-card-sized bag from the rubber-banded bundle and laid it on the counter with sacramental ...
Methamphetamine Case Study presents with new-onset heart failure associated with significant hypertension. Refusal to participate in clinical addictions recovery and counseling programs is common in drug-addicted persons. Several studies have documented adverse effects of beta-blockade in patients with ongoing cocaine or amphetamine use.
Case Studies "Jessie and her mom were able to repair their mother-daughter relationship, Jessie successfully completed criminal drug court, and past hurts were addressed and allowed the family to move forward in a cohesive and loving way." ... Drug and alcohol addiction, depression, school failure. Joy had just flunked out of her first year ...
Alcohol use was reported in 5.02%, tobacco in 3. 21% and sedative- hy pnotics in 0.04% respondents. Th e study also r eveals. increasing u se o f substan ces among females: substance abuse was ...
Specific Guidance for Writing Case Reports in Addiction Medicine. 1. Obtain consent and state clearly in the report what was obtained (eg, written consent was obtained from the patient to report their case in the medical literature). Accepted standards of consent, such as those supported by the International Committee of Medical Journal Editors ...
Cocaine addiction remains a high-morbidity chronic-relapsing illness with few treatment options. A review of the literature shows that late-life cocaine use is sparsely recognized. Of particular interest are the clinical presentations in which a higher index for detection is warranted. The high rate of medical comorbidity associated with ...
Addiction. Detox alone has limited utility long term Opiate use disorder is chronic and relapse is frequent (85% in 6 months) Neuronal adaptations take place in the CNS creating tolerance, dependence and craving, some of which may be permanent. 42. Methadone maintenance.
2. Case Introduction. Alan is a 17 year-old male currently living in County Dublin. Alan presented to the agency involuntarily and as a requisite of his Juvenile Liaison Officer who was seeing him on foot of prior drugs arrest for 'possession with intent to supply'; a more serious charge than a simple 'drugs possession' charge.
Background Alcohol and drug prevention is high on the public health agenda in many countries. An increasing trend is the call for evidence-based practice. In Sweden in 2002 an innovative project portfolio including an integrated research and competence-building strategy for non-governmental organisations (NGOs) was designed by the National Board of Health and Welfare (NBHW). This research ...
QUESTIONS AT THE END OF EACH CASE OFFER GUIDELINES FOR ACHIEVING A BETTER UNDERSTANDING OF THE LIFE STYLE AND BEHAVIOR OF THE PEOPLE DEPICTED. MANY JUVENILE CASES ARE INCLUDED. (AUTHOR ABSTRACT) Additional Details. Sale Source. Goodyear Publishing Co. 1640 5th Street, Santa Monica, CA 90401, United States. Publication Type.
Opioid use disorder (OUD) is a chronic, relapsing condition accounting for over 16 million people worldwide [1, 2].International guidelines recommend opioid agonist therapy (OAT) with sublingual buprenorphine or methadone as first-line treatments of opioid dependence [].However, the rates of oral OAT misuse, abuse, and diversion are of public concern due to their social, sanitary, and economic ...
Case studies; Robert's story; Robert's story. Robert was living with an alcohol addiction and was homeless for over 25 years. He was well known in the local community and was identified as one of the top 100 A&E attendees at the Local General Hospital. ... (drugs and alcohol service), as well as 1 to 1 sessions with drugs workers and ...
In the remaining 5 studies (20%), various qualitative methods have been used, including 1 case using deviant case analysis in a study in Scotland with 74 samples of relatives, parents, and experts of the drug abuser , 1 case using the qualitative-analytical-exploratory method , 1 case study of 10 female heads of families , 1 case study of a ...
current issue. current issue; browse recently published; browse full issue index; learning/cme
One expert interviewed—Leo Beletsky, an expert on drug policy enforcement at Northeastern University School of Law—praised the suggested change. "Language is really important because it ...