Writing about COVID-19 in a college admission essay
by: Venkates Swaminathan | Updated: September 14, 2020
Print article

For students applying to college using the CommonApp, there are several different places where students and counselors can address the pandemic’s impact. The different sections have differing goals. You must understand how to use each section for its appropriate use.

The CommonApp COVID-19 question
First, the CommonApp this year has an additional question specifically about COVID-19 :
Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts. If you need it, this space is yours to describe those impacts. Colleges care about the effects on your health and well-being, safety, family circumstances, future plans, and education, including access to reliable technology and quiet study spaces. Please use this space to describe how these events have impacted you.
This question seeks to understand the adversity that students may have had to face due to the pandemic, the move to online education, or the shelter-in-place rules. You don’t have to answer this question if the impact on you wasn’t particularly severe. Some examples of things students should discuss include:
- The student or a family member had COVID-19 or suffered other illnesses due to confinement during the pandemic.
- The candidate had to deal with personal or family issues, such as abusive living situations or other safety concerns
- The student suffered from a lack of internet access and other online learning challenges.
- Students who dealt with problems registering for or taking standardized tests and AP exams.
Jeff Schiffman of the Tulane University admissions office has a blog about this section. He recommends students ask themselves several questions as they go about answering this section:
- Are my experiences different from others’?
- Are there noticeable changes on my transcript?
- Am I aware of my privilege?
- Am I specific? Am I explaining rather than complaining?
- Is this information being included elsewhere on my application?
If you do answer this section, be brief and to-the-point.
Counselor recommendations and school profiles
Second, counselors will, in their counselor forms and school profiles on the CommonApp, address how the school handled the pandemic and how it might have affected students, specifically as it relates to:
- Grading scales and policies
- Graduation requirements
- Instructional methods
- Schedules and course offerings
- Testing requirements
- Your academic calendar
- Other extenuating circumstances
Students don’t have to mention these matters in their application unless something unusual happened.
Writing about COVID-19 in your main essay
Write about your experiences during the pandemic in your main college essay if your experience is personal, relevant, and the most important thing to discuss in your college admission essay. That you had to stay home and study online isn’t sufficient, as millions of other students faced the same situation. But sometimes, it can be appropriate and helpful to write about something related to the pandemic in your essay. For example:
- One student developed a website for a local comic book store. The store might not have survived without the ability for people to order comic books online. The student had a long-standing relationship with the store, and it was an institution that created a community for students who otherwise felt left out.
- One student started a YouTube channel to help other students with academic subjects he was very familiar with and began tutoring others.
- Some students used their extra time that was the result of the stay-at-home orders to take online courses pursuing topics they are genuinely interested in or developing new interests, like a foreign language or music.
Experiences like this can be good topics for the CommonApp essay as long as they reflect something genuinely important about the student. For many students whose lives have been shaped by this pandemic, it can be a critical part of their college application.
Want more? Read 6 ways to improve a college essay , What the &%$! should I write about in my college essay , and Just how important is a college admissions essay? .

Homes Nearby
Homes for rent and sale near schools

How our schools are (and aren't) addressing race

The truth about homework in America

What should I write my college essay about?
What the #%@!& should I write about in my college essay?
Yes! Sign me up for updates relevant to my child's grade.
Please enter a valid email address
Thank you for signing up!
Server Issue: Please try again later. Sorry for the inconvenience
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Newsletters
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Balance transfer cards
- Cash back cards
- Rewards cards
- Travel cards
- Online checking
- High-yield savings
- Money market
- Home equity loan
- Personal loans
- Student loans
- Options pit
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
New on Yahoo
- Privacy Dashboard
How to Write About the Impact of the Coronavirus in a College Essay
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many -- a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
[ Read: How to Write a College Essay. ]
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.
Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
[ Read: What Colleges Look for: 6 Ways to Stand Out. ]
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them -- and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
[ Read: The Common App: Everything You Need to Know. ]
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic -- and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
Special Issue: COVID-19
This essay was published as part of a Special Issue on Misinformation and COVID-19, guest-edited by Dr. Meghan McGinty (Director of Emergency Management, NYC Health + Hospitals) and Nat Gyenes (Director, Meedan Digital Health Lab).
Peer Reviewed
The causes and consequences of COVID-19 misperceptions: Understanding the role of news and social media
Article metrics.
CrossRef Citations
Altmetric Score
PDF Downloads
We investigate the relationship between media consumption, misinformation, and important attitudes and behaviours during the coronavirus disease 2019 (COVID-19) pandemic. We find that comparatively more misinformation circulates on Twitter, while news media tends to reinforce public health recommendations like social distancing. We find that exposure to social media is associated with misperceptions regarding basic facts about COVID-19 while the inverse is true for news media. These misperceptions are in turn associated with lower compliance with social distancing measures. We thus draw a clear link from misinformation circulating on social media, notably Twitter, to behaviours and attitudes that potentially magnify the scale and lethality of COVID-19.
Department of Political Science, McGill University, Canada
Munk School of Global Affairs and Public Policy, University of Toronto, Canada
Max Bell School of Public Policy, McGill University, Canada
School of Computer Science, McGill University, Canada
Department of Languages, Literatures, and Cultures, McGill University, Canada
Computer Science Program, McGill University, Canada
Research Questions
- How prevalent is misinformation surrounding COVID-19 on Twitter, and how does this compare to Canadian news media?
- Does the type of media one is exposed to influence social distancing behaviours and beliefs about COVID-19?
- Is there a link between COVID-19 misinformation and perceptions of the pandemic’s severity and compliance with social distancing recommendations?
Essay Summary
- We evaluate the presence of misinformation and public health recommendations regarding COVID-19 in a massive corpus of tweets as well as all articles published on nineteen Canadian news sites. Using these data, we show that preventative measures are more encouraged and covered on traditional news media, while misinformation appears more frequently on Twitter.
- To evaluate the impact of this greater level of misinformation, we conducted a nationally representative survey that included questions about common misperceptions regarding COVID-19, risk perceptions, social distancing compliance, and exposure to traditional news and social media. We find that being exposed to news media is associated with fewer misperceptions and more social distancing compliance while conversely, social media exposure is associated with more misperceptions and less social distancing compliance.
- Misperceptions regarding the virus are in turn associated with less compliance with social distancing measures, even when controlling for a broad range of other attitudes and characteristics.
- Association between social media exposure and social distancing non-compliance is eliminated when accounting for effect of misperceptions, providing evidence that social media is associated with non-compliance through increasing misperceptions about the virus.
Implications
The COVID-19 pandemic has been accompanied by a so-called “infodemic”—a global spread of misinformation that poses a serious problem for public health. Infodemics are concerning because the spread of false or misleading information has the capacity to change transmission patterns (Kim et al., 2019) and consequently the scale and lethality of a pandemic. This information can be shared by any media, but there is reason to be particularly concerned about the role that social media, such as Facebook and Twitter, play in incidentally boosting misperceptions. These platforms are increasingly relied upon as primary sources of news (Mitchell et al., 2016) and misinformation has been heavily documented on them (Garrett, 2019; Vicario et al., 2016). Scholars have found medical and health misinformation on the platforms, including that related to vaccines (Radzikowski et al., 2016) and other virus epidemics such as Ebola (Fung et al., 2016) and Zika (Sharma et al., 2017).
However, misinformation content typically makes up a low percentage of overall discussion of a topic (e.g. Fung et al., 2016) and mere exposure to misinformation does not guarantee belief in that misinformation. More research is thus needed to understand the extent and consequences of misinformation surrounding COVID-19 on social media. During the COVID-19 pandemic, Twitter, Facebook and other platforms have engaged in efforts to combat misinformation but they have continued to receive widespread criticism that misinformation is still appearing on prominent pages and groups (Kouzy et al., 2020; NewsGuard, 2020). The extent to which misinformation continues to circulate on these platforms and influence people’s attitudes and behaviours is still very much an open question.
Here, we draw on three data sets and a sequential mixed method approach to better understand the consequences of online misinformation for important behaviours and attitudes. First, we collected nearly 2.5 million tweets explicitly referring to COVID-19 in the Canadian context. Second, we collected just over 9 thousand articles from nineteen Canadian English-language news sites from the same time period. We coded both of these media sets for misinformation and public health recommendations. Third, we conducted a nationally representative survey that included questions related to media consumption habits, COVID-19 perceptions and misperceptions, and social distancing compliance. As our outcome variables are continuous, we use Ordinary Least Squares (OLS) regression to identify relationships between news and social media exposure, misperceptions, compliance with social distancing measures, and risk perceptions. We use these data to illustrate: 1) the relative prevalence of misinformation on Twitter; and 2) a powerful association between social media usage and misperceptions, on the one hand, and social distancing non-compliance on the other.
Misinformation and compliance with social distancing
We first compare the presence of misinformation on Twitter with that on news media and find, consistent with the other country cases (Chadwick & Vaccari, 2019; Vicario et al., 2016), comparatively higher levels of misinformation circulating on the social media platform. We also found that recommendations for safe practices during the pandemic (e.g. washing hands, social distancing) appeared much more frequently in the Canadian news media. These findings are in line with literature examining fake news which finds a large difference in information quality across media (Al-Rawi, 2019; Guess & Nyhan, 2018).
Spending time in a media environment that contains misinformation is likely to change attitudes and behaviours. Even if users are not nested in networks that propagate misinformation, they are likely to be incidentally exposed to information from a variety of perspectives (Feezell, 2018; Fletcher & Nielsen, 2018; Weeks et al., 2017). Even a highly curated social media feed is thus still likely to contain misinformation. As cumulative exposure to misinformation increases, users are likely to experience a reinforcement effect whereby familiarity leads to stronger belief (Dechêne et al., 2010).
To evaluate this empirically, we conducted a national survey that included questions on information consumption habits and a battery of COVID-19 misperceptions that could be the result of exposure to misinformation. We find that those who self-report exposure to the misinformation-rich social media environment do tend to have more misperceptions regarding COVID-19. These findings are consistent with others that link exposure to misinformation and misperceptions (Garrett et al., 2016; Jamieson & Albarracín, 2020). Social media users also self-report less compliance with social distancing.
Misperceptions are most meaningful when they impact behaviors in dangerous ways. During a pandemic, misperceptions can be fatal. In this case, we find that misperceptions are associated with reduced COVID-19 risk perceptions and with lower compliance with social distancing measures. We continue to find strong effects after controlling for socio-economic characteristics as well as scientific literacy. After accounting for the effect of misperceptions on social distancing non-compliance, social media usage no longer has a significant association with non-compliance, providing evidence that social media may lead to less social distancing compliance through its effect on COVID-19 misperceptions.
While some social media companies have made efforts to suppress misinformation on their platforms, there continues to be a high level of misinformation relative to news media. Highly polarized political environments and media ecosystems can lead to the spread of misinformation, such as in the United States during the COVID-19 pandemic (Allcott et al., 2020; Motta et al., 2020). But even in healthy media ecosystems with less partisan news (Owen et al., 2020), social media can continue to facilitate the spread of misinformation. There is a real danger that without concerted efforts to reduce the amount of misinformation shared on social media, the large-scale social efforts required to combat COVID-19 will be undermined.
We contribute to a growing base of evidence that misinformation circulating on social media poses public health risks and join others in calling for social media companies to put greater focus on flattening the curve of misinformation (Donovan, 2020). These findings also provide governments with stronger evidence that the misinformation circulating on social media can be directly linked to misperceptions and public health risks. Such evidence is essential for them to chart an effective policy course. Finally, the methods and approach developed in this paper can be fruitfully applied to study other waves of misinformation and the research community can build upon the link clearly drawn between misinformation exposure, misperceptions, and downstream attitudes and behaviours.
We found use of social media platforms broadly contributes to misperceptions but were unable to precise the overall level of misinformation circulating on non-Twitter social media. Data access for researchers to platforms such as Facebook, YouTube, and Instagram is limited and virtually non-existent for SnapChat, WhatsApp, and WeChat. Cross-platform content comparisons are an important ingredient for a rich understand of the social media environment and these social media companies must better open their platforms to research in the public interest.
Finding 1: Misinformation about COVID-19 is circulated more on Twitter as compared to traditional media.
We find large differences between the quality of information shared about COVID-19 on traditional news and Twitter. Figure 1 shows the percentage of COVID-19 related content that contains information linked to a particular theme. The plot reports the prevalence of information on both social and news media for: 1) three specific pieces of misinformation; 2) a general set of content that describes the pandemic itself as a conspiracy or a hoax; and 3) advice about hygiene and social distancing during the pandemic. We differentiate content that shared misinformation (red in the plot) from content that debunked misinformation (green in the plot).
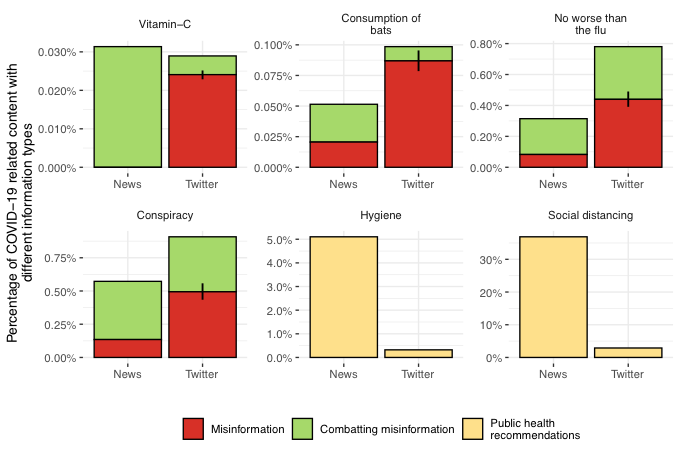
There are large differences between the levels of misinformation on Twitter and news media. Misinformation was comparatively more common on Twitter across all four categories, while debunking was relatively more common in traditional news. Meanwhile, advice on hygiene and social distancing appeared much more frequently in news media. Note that higher percentages are to be expected for longer format news articles since we rely on keyword searches for identification. This makes the misinformation findings even starker – despite much higher average word counts, far fewer news articles propagate misinformation.
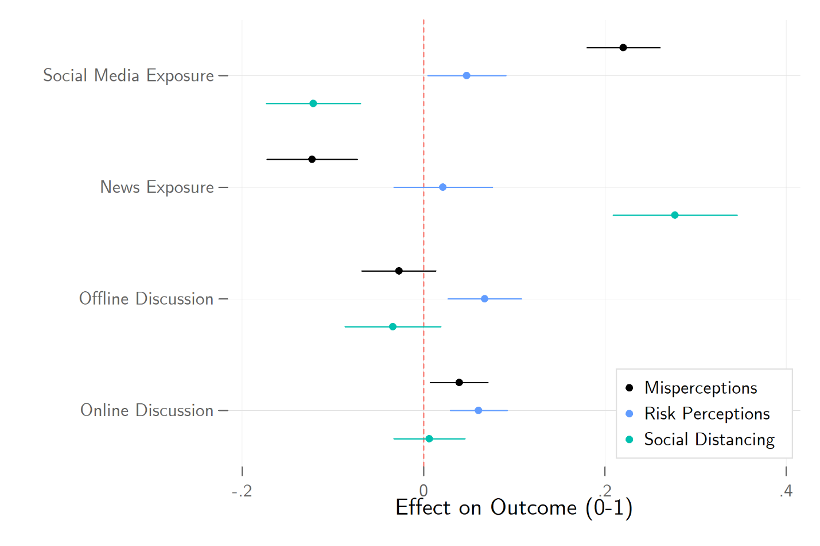
Finding 2: There is a strong association between social media exposure and misperceptions about COVID-19. The inverse is true for exposure to traditional news.
Among our survey respondents we find a corresponding strong association between social media exposure and misperceptions about COVID-19. These results are plotted in Figure 2, with controls included for both socioeconomic characteristics and demographics. Moving from no social media exposure to its maximum is expected to increase one’s misperceptions of COVID-19 by 0.22 on the 0-1 scale and decreased self-reported social distancing compliance by 0.12 on that same scale.
This result stands in stark contrast with the observed relationship between traditional news exposure and our outcome measures. Traditional news exposure is positively associated with correct perceptions regarding COVID-19. Moving from no news exposure to its highest level is expected to reduce misperceptions by 0.12 on the 0-1 scale and to increase social distancing compliance by 0.28 on that same scale. The effects are plotted in Figure 2. Social media usage appears to be correlated with COVID-19 misperceptions, suggesting these misperceptions are partially a result of misinformation on social media. The same cannot be said of traditional news exposure.
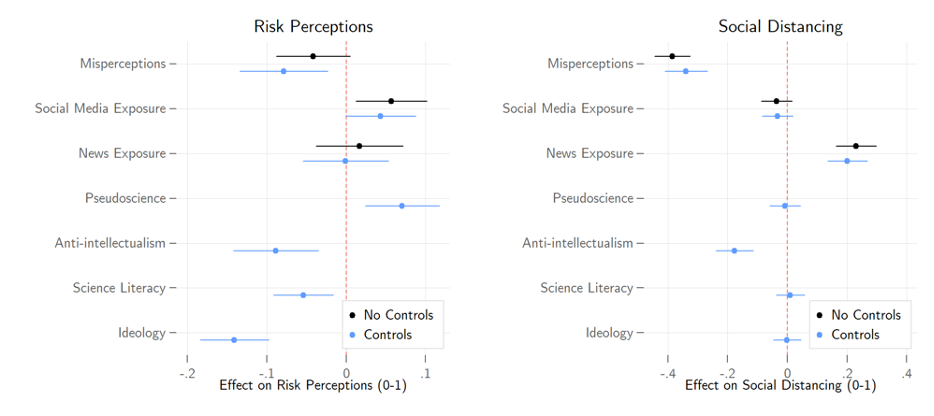
Finding 3: Misperceptions about the pandemic are associated with lower levels of risk perceptions and social distancing compliance.
COVID-19 misperceptions are also powerfully associated with lower levels of social distancing compliance. Moving from the lowest level of COVID-19 misperceptions to its maximum is associated with a reduction of one’s social distancing by 0.39 on the 0-1 scale. The previously observed relationship between social media exposure and misperceptions disappears, suggestive of a mediated relationship. That is, social media exposure increases misperceptions, which in turn reduces social distancing compliance. Misperceptions is also weakly associated with lower COVID-19 risk perceptions. Estimates from our models using COVID-19 concern as the outcome can be found in the left panel of Figure 3, while social distancing can be found in the right panel.
Finally, we also see that the relationship between misinformation and both social distancing compliance and COVID-19 concern hold when including controls for science literacy and a number of fundamental predispositions that are likely associated with both misperceptions and following the advice of scientific experts, such as anti-intellectualism, pseudoscientific beliefs, and left-right ideology. These estimates can similarly be found in Figure 3.
Canadian Twitter and news data were collected from March 26 th to April 6 th , 2020. We collected all English-language tweets from a set of 620,000 users that have been determined to be likely Canadians. For inclusion, a given user must self-identify as Canadian-based, follow a large number of Canadian political elite accounts, or frequently use Canadian-specific hashtags. News media was collected from nineteen prominent Canadian news sites with active RSS feeds. These tweets and news articles were searched for “covid” or “coronavirus”, leaving a sample of 2.25 million tweets and 8,857 news articles.
Of the COVID-19 related content, we searched for terms associated with four instances of misinformation that circulated during the COVID-19 pandemic: that COVID-19 was no more serious than the flu, that vitamin C or other supplements will prevent contraction of the virus, that the initial animal-to-human transfer of the virus was the direct result of eating bats, or that COVID-19 was a hoax or conspiracy. Given that we used keyword searches to identify content, we manually reviewed a random sample of 500 tweets from each instance of misinformation. Each tweet was coded as one of four categories: propagating misinformation, combatting misinformation, content with the relevant keywords but unrelated to misinformation, or content that refers to the misinformation but does not offer comment.
We then calculated the overall level of misinformation for that instance on Twitter by multiplying the overall volume of tweets by the proportion of hand-coded content where misinformation was identified. Each news article that included relevant keywords was similarly coded. The volume of the news mentioning these terms was sufficiently low that all news articles were hand coded. To identify health recommendations, we used a similar keyword search for terms associated with particular recommendations: 1) social distancing including staying at home, staying at least 6 feet or 2 meters away and avoiding gatherings; and 2) washing hands and not touching any part of your face. 1 Further details on the media collection strategy and hand-coding schema are available in the supporting materials.
For survey data, we used a sample of nearly 2,500 Canadian citizens 18 years or older drawn from a probability-based online national panel fielded from April 2-6, 2020. Quotas we set on age, gender, region, and language to ensure sample representativeness, and data was further weighted within region by gender and age based on the 2016 Canadian census.
We measure levels of COVID-19 misperceptions by asking respondents to rate the truthfulness of a series of nine false claims, such as the coronavirus being no worse than the seasonal flu or that it can be warded off with Vitamin C. Each was asked on a scale from definitely false (0) to definitely true (5). We use Cronbach’s Alpha as an indicator of scale reliability. Cronbach’s Alpha ranges from 0-1, with scores above 0.8 indicating the reliability is “good.” These items score 0.88, so we can safely construct a 0-1 scale of misperceptions from them.
We evaluate COVID-19 risk perceptions with a pair of questions asking respondents how serious of a threat they believe the pandemic to be for themselves and for Canadians, respectively. Each question was asked on a scale from not at all (0) to very (4). We construct a continuous index with these items.
We quantify social distancing by asking respondents to indicate which of a series of behaviours they had undertaken in response to the pandemic, such as working from home or avoiding in-person contact with friends, family, and acquaintances. We use principal component analysis (PCA) to reduce the number of dimensions in these data while minimizing information loss. The analysis revealed 2 distinct dimensions in our questions. One dimension includes factors strongly determined by occupation, such as working from home and switching to online meetings. The other dimension contains more inclusive behaviours such as avoiding contact, travel, and crowded places. We generate predictions from the PCA for this latter dimension to use in our analyses. The factor loadings can be found in Table A1 of the supporting materials.
We gauge news and social media consumption by asking respondents to identify news outlets and social media platforms they have used over the past week for political news. The list of news outlets included 17 organizations such as mainstream sources like CBC and Global, and partisan outlets like Rebel Media and National Observer. The list of social media platforms included 10 options such as Facebook, Twitter, YouTube, and Instagram. We sum the total number of outlets/platforms respondents report using and take the log to adjust for extreme values. We measure offline political discussion with an index based on questions asking how often respondents have discussed politics with family, friends, and acquaintances over the past week. Descriptions of our primary variables can be found in Table A2 of the supporting materials.
We evaluate our hypotheses using a standard design that evaluates the association between our explanatory and outcome variables controlling for other observable factors we measured. In practice, randomly assigning social media exposure is impractical, while randomly assigning misinformation is unethical. This approach allows us to describe these relationships, though we cannot make definite claims to causality.
We hypothesize that social media exposure is associated with misinformation on COVID-19. Figure 2 presents the coefficients of models predicting the effects of news exposure, social media exposure, and political discussion on COVID-19 misinformation, risk perceptions, and social distancing. Socio-economic and demographic control estimates are not displayed. Full estimation results can be found in the Table A3 of the supporting materials.
We further hypothesize that COVID-19 misinformation is associated with lower COVID-19 risk perceptions and less social distancing compliance. Figure 3 presents the coefficients for models predicting the effects of misinformation, news exposure, and social media exposure on severity perceptions and social distancing. We show models with and without controls for science literacy and other predispositions. Full estimation results can be found in the Table A4 of the supporting materials.
Limitations and robustness
A study such as this comes with clear limitations. First, we have evaluated information coming from only a section of the overall media ecosystem and during a specific time-period. The level of misinformation differs across platforms and online news sites and a more granular investigation into these dynamics would be valuable. Our analysis suggests that similar dynamics exist across social media platforms, however. In the supplementary materials we show that associations between misperceptions and social media usage are even higher for other social media platforms, suggesting that our analysis of Twitter content may underrepresent the prevalence of misinformation on social media writ large. As noted above, existing limitations on data access make such cross-platform research difficult.
Second, our data is drawn from a single country and language case study and other countries may have different media environments and levels of misinformation circulating on social media. We anticipate the underlying dynamics found in this paper to hold across these contexts, however. Those who consume information from platforms where misinformation is more prevalent will have greater misperceptions and that these misperceptions will be linked to lower compliance with social distancing and lower risk perceptions. Third, an ecological problem is present wherein we do not link survey respondents directly to their social media consumption (and evaluation of the misinformation they are exposed to) and lack the ability to randomly assign social media exposure to make a strong causal argument. We cannot and do not make a causal argument here but argue instead that there is strong evidence for a misinformation to misperceptions to lower social distancing compliance link.
- / Fake News
- / Mainstream Media
- / Public Health
- / Social Media
- / Twitter/X
Cite this Essay
Bridgman, A., Merkley, E., Loewen, P. J., Owen, T., Ruths, D., Teichmann, L., & Zhilin, O. (2020). The causes and consequences of COVID-19 misperceptions: Understanding the role of news and social media. Harvard Kennedy School (HKS) Misinformation Review . https://doi.org/10.37016/mr-2020-028
Bibliography
Allcott, H., Boxell, L., Conway, J. C., Gentzkow, M., Thaler, M., & Yang, D. Y. (2020). Polarization and Public Health: Partisan Differences in Social Distancing during the Coronavirus Pandemic (Working Paper No. 26946; Working Paper Series). National Bureau of Economic Research. https://doi.org/10.3386/w26946
Al-Rawi, A. (2019). Gatekeeping Fake News Discourses on Mainstream Media Versus Social Media. Social Science Computer Review , 37 (6), 687–704. https://doi.org/10.1177/0894439318795849
Chadwick, A., & Vaccari, C. (2019). News sharing on UK social media: Misinformation, disinformation, and correction [Report]. Loughborough University. https://repository.lboro.ac.uk/articles/News_sharing_on_UK_social_media_misinformation_disinformation_and_correction/9471269
Dechêne, A., Stahl, C., Hansen, J., & Wänke, M. (2010). The Truth About the Truth: A Meta-Analytic Review of the Truth Effect. Personality and Social Psychology Review , 14 (2), 238–257. https://doi.org/10.1177/1088868309352251
Donovan, J. (2020). Social-media companies must flatten the curve of misinformation. Nature . https://doi.org/10.1038/d41586-020-01107-z
Feezell, J. T. (2018). Agenda Setting through Social Media: The Importance of Incidental News Exposure and Social Filtering in the Digital Era. Political Research Quarterly , 71 (2), 482–494. https://doi.org/10.1177/1065912917744895
Fletcher, R., & Nielsen, R. K. (2018). Are people incidentally exposed to news on social media? A comparative analysis. New Media & Society , 20 (7), 2450–2468. https://doi.org/10.1177/1461444817724170
Fung, I. C.-H., Fu, K.-W., Chan, C.-H., Chan, B. S. B., Cheung, C.-N., Abraham, T., & Tse, Z. T. H. (2016). Social Media’s Initial Reaction to Information and Misinformation on Ebola, August 2014: Facts and Rumors. Public Health Reports , 131 (3), 461–473. https://doi.org/10.1177/003335491613100312
Garrett, R. K. (2019). Social media’s contribution to political misperceptions in U.S. Presidential elections. PLoS ONE , 14 (3). https://doi.org/10.1371/journal.pone.0213500
Garrett, R. K., Weeks, B. E., & Neo, R. L. (2016). Driving a Wedge Between Evidence and Beliefs: How Online Ideological News Exposure Promotes Political Misperceptions. Journal of Computer-Mediated Communication , 21 (5), 331–348. https://doi.org/10.1111/jcc4.12164
Guess, A., & Nyhan, B. (2018). Selective Exposure to Misinformation: Evidence from the consumption of fake news during the 2016 U.S. presidential campaign. European Research Council , 49.
Jamieson, K. H., & Albarracín, D. (2020). The Relation between Media Consumption and Misinformation at the Outset of the SARS-CoV-2 Pandemic in the US. Harvard Kennedy School Misinformation Review , 2 . https://doi.org/10.37016/mr-2020-012
Kim, L., Fast, S. M., & Markuzon, N. (2019). Incorporating media data into a model of infectious disease transmission. PLOS ONE , 14 (2), e0197646. https://doi.org/10.1371/journal.pone.0197646
Kouzy, R., Abi Jaoude, J., Kraitem, A., El Alam, M. B., Karam, B., Adib, E., Zarka, J., Traboulsi, C., Akl, E. W., & Baddour, K. (2020). Coronavirus Goes Viral: Quantifying the COVID-19 Misinformation Epidemic on Twitter. Cureus , 12 (3). https://doi.org/10.7759/cureus.7255
Mitchell, A., Gottfried, J., Barthel, M., & Shearer, E. (2016, July 7). The Modern News Consumer. Pew Research Center’s Journalism Project . https://www.journalism.org/2016/07/07/the-modern-news-consumer/
Motta, M., Stecula, D., & Farhart, C. E. (2020). How Right-Leaning Media Coverage of COVID-19 Facilitated the Spread of Misinformation in the Early Stages of the Pandemic [Preprint]. SocArXiv. https://doi.org/10.31235/osf.io/a8r3p
NewsGuard. (2020). Superspreaders . https://www.newsguardtech.com/superspreaders/
Owen, T., Loewen, P., Ruths, D., Bridgman, A., Gorwa, R., MacLellan, S., Merkley, E., & Zhilin, O. (2020). Lessons in Resilience: Canada’s Digital Media Ecosystem and the 2019 Election . Public Policy Forum. https://ppforum.ca/articles/lessons-in-resilience-canadas-digital-media-ecosystem-and-the-2019-election/
Radzikowski, J., Stefanidis, A., Jacobsen, K. H., Croitoru, A., Crooks, A., & Delamater, P. L. (2016). The Measles Vaccination Narrative in Twitter: A Quantitative Analysis. JMIR Public Health and Surveillance , 2 (1), e1. https://doi.org/10.2196/publichealth.5059
Sharma, M., Yadav, K., Yadav, N., & Ferdinand, K. C. (2017). Zika virus pandemic—Analysis of Facebook as a social media health information platform. American Journal of Infection Control , 45 (3), 301–302. https://doi.org/10.1016/j.ajic.2016.08.022
Shin, J., Jian, L., Driscoll, K., & Bar, F. (2018). The diffusion of misinformation on social media: Temporal pattern, message, and source. Computers in Human Behavior , 83 , 278–287. https://doi.org/10.1016/j.chb.2018.02.008
Vicario, M. D., Bessi, A., Zollo, F., Petroni, F., Scala, A., Caldarelli, G., Stanley, H. E., & Quattrociocchi, W. (2016). The spreading of misinformation online. Proceedings of the National Academy of Sciences , 113 (3), 554–559. https://doi.org/10.1073/pnas.1517441113
Weeks, B. E., Lane, D. S., Kim, D. H., Lee, S. S., & Kwak, N. (2017). Incidental Exposure, Selective Exposure, and Political Information Sharing: Integrating Online Exposure Patterns and Expression on Social Media. Journal of Computer-Mediated Communication , 22 (6), 363–379. https://doi.org/10.1111/jcc4.12199
The project was funded through the Department of Canadian Heritage’s Digital Citizens Initiative.
Competing Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The research protocol was approved by the institutional review board at University of Toronto. Human subjects gave informed consent before participating and were debriefed at the end of the study.
This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided that the original author and source are properly credited.
Data Availability
All materials needed to replicate this study are available via the Harvard Dataverse: https://doi.org/10.7910/DVN/5QS2XP .

- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- Games & Quizzes
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction
Horrific history
The early days, health and medicine.

What was the impact of COVID-19?
Our editors will review what you’ve submitted and determine whether to revise the article.
- Table Of Contents

On February 25, 2020, a top official at the Centers for Disease Control and Prevention decided it was time to level with the U.S. public about the COVID-19 outbreak. At the time, there were just 57 people in the country confirmed to have the infection, all but 14 having been repatriated from Hubei province in China and the Diamond Princess cruise ship , docked off Yokohama , Japan .
The infected were in quarantine. But Nancy Messonnier, then head of the CDC’s National Center for Immunization and Respiratory Diseases, knew what was coming. “It’s not so much a question of if this will happen anymore but rather more a question of exactly when this will happen and how many people in this country will have severe illness,” Messonnier said at a news briefing.
“I understand this whole situation may seem overwhelming and that disruption to everyday life may be severe,” she continued. “But these are things that people need to start thinking about now.”
Looking back, the COVID-19 pandemic stands as arguably the most disruptive event of the 21st century, surpassing wars, the September 11, 2001, terrorist attacks , the effects of climate change , and the Great Recession . It has killed more than seven million people to date and reshaped the world economy, public health , education, work, social interaction, family life, medicine, and mental health—leaving no corner of the globe untouched in some way. Now endemic in many societies, the consistently mutating virus remains one of the leading annual causes of death, especially among people older than 65 and the immunosuppressed.
“The coronavirus outbreak, historically, beyond a doubt, has been the most devastating pandemic of an infectious disease that global society has experienced in well over 100 years, since the 1918 influenza pandemic ,” Anthony Fauci , who helped lead the U.S. government’s health response to the pandemic under Pres. Donald Trump and became Pres. Joe Biden ’s chief medical adviser, told Encyclopædia Britannica in 2024.
“I think the impact of this outbreak on the world in general, on the United States, is really historic. Fifty years from now, 100 years from now, when they talk about the history of what we’ve been through, this is going to go down equally with the 1918 influenza pandemic , with the stock market crash of 1929 , with World War II —all the things that were profoundly disruptive of the social order.”
What few could imagine in the first days of the pandemic was the extent of the disruption the disease would bring to the everyday lives of just about everyone around the globe.
Within weeks, schools and child-care centers began shuttering, businesses sent their workforces home, public gatherings were canceled, stores and restaurants closed, and cruise ships were barred from sailing. On March 11, actor Tom Hanks announced that he had COVID-19, and the NBA suspended its season. (It was ultimately completed in a closed “bubble” at Walt Disney World .) On March 12, as college basketball players left courts mid-game during conference tournaments, the NCAA announced that it would not hold its wildly popular season-ending national competition, known as March Madness , for the first time since 1939. Three days later, the New York City public school system, the country’s largest, with 1.1 million students, closed. On March 19, all 40 million Californians were placed under a stay-at-home order.

By mid-April, with hospital beds and ventilators in critically short supply, workers were burying the coffins of COVID-19 victims in mass graves on Hart Island, off the Bronx . At first, the public embraced caregivers. New Yorkers applauded them from windows and balconies, and individuals sewed masks for them. But that spirit soon gave way to the crushing long-term reality of the pandemic and the national division that followed.
Around the world, it was worse. On the day Messonnier spoke, the virus had spread from its origin point in Wuhan , China, to at least two dozen countries, sickening thousands and killing dozens. By April 4, more than one million cases had been confirmed worldwide. Some countries, including China and Italy, imposed strict lockdowns on their citizens. Paris restricted movement, with certain exceptions, including an hour a day for exercise, within 1 km (0.62 mile) of home.
In the United States , the threat posed by the virus did not keep large crowds from gathering to protest the May 25 slaying of George Floyd , a 46-year-old Black man, by a white police officer, Derek Chauvin. The murder, taped by a bystander in Minneapolis , Minnesota , sparked raucous and sometimes violent street protests for racial justice around the world that contributed to an overall sense of societal instability.
The official World Health Organization total of more than seven million deaths as of March 2024 is widely considered a serious undercount of the actual toll. In some countries there was limited testing for the virus and difficulty attributing fatalities to it. Others suppressed total counts or were not able to devote resources to compiling their totals. In May 2021, a panel of experts consulted by The New York Times estimated that India ’s actual COVID-19 death toll was likely 1.6 million, more than five times the reported total of 307,231.
An average of 3,100 people—one every 28 seconds—died of COVID-19 every day in the United States in January 2021.
When “ excess mortality”—COVID and non-COVID deaths that likely would not have occurred under normal, pre-outbreak conditions—are included in the worldwide tally, the number of pandemic victims was about 15 million by the end of 2021, WHO estimated.
Not long after the pandemic took hold, the United States, which spends more per capita on medical care than any other country, became the epicenter of COVID-19 fatalities. The country fell victim to a fractured health care system that is inequitable to poor and rural patients and people of color, as well as a deep ideological divide over its political leadership and public health policies, such as wearing protective face masks. By early 2024, the U.S. had recorded nearly 1.2 million COVID-19 deaths.
Life expectancy at birth plunged from 78.8 years in 2019 to 76.4 in 2021, a staggering decline in a barometer of a country’s health that typically changes by only a tenth or two annually. An average of 3,100 people—one every 28 seconds—died of COVID-19 every day in the United States in January 2021, before vaccines for the virus became widely available, The Washington Post reported.
The impact on those caring for the sick and dying was profound. “The second week of December [2020] was probably the worst week of my career,” said Brad Butcher, director of the medical-surgical intensive care unit at UPMC Mercy hospital in Pittsburgh , Pennsylvania. “The first day I was on service, five patients died in a shift. And then I came back the next day, and three patients died. And I came back the next day, and three more patients died. And it was completely defeating,” he told The Washington Post on January 11, 2021.
“We can’t get the graves dug fast enough,” a Maryland funeral home operator told The Washington Post that same day.
As the pandemic surged in waves around the world, country after country was plunged into economic recession , the inevitable damage caused by layoffs, business closures, lockdowns, deaths, reduced trade, debt repayment moratoriums , the cost to governments of responding to the crisis, and other factors. Overall, the virus triggered the greatest economic calamity in more than a century, according to a 2022 report by the World Bank .
“Economic activity contracted in 2020 in about 90 percent of countries, exceeding the number of countries seeing such declines during two world wars, the Great Depression of the 1930s, the emerging economy debt crises of the 1980s, and the 2007–09 global financial crisis,” the report noted. “In 2020, the first year of the COVID-19 pandemic, the global economy shrank by approximately 3 percent, and global poverty increased for the first time in a generation.”
A 2020 study that attempted to aggregate the costs of lost gross domestic product (GDP) estimated that premature deaths and health-related losses in the United States totaled more than $16 trillion, or roughly “90% of the annual GDP of the United States. For a family of 4, the estimated loss would be nearly $200,000.”
In April 2020, the U.S. unemployment rate stood at 14.7 percent, higher than at any point since the Great Depression. There were 23.1 million people out of work. The hospitality, leisure, and health care industries were especially hard hit. Consumer spending, which accounts for about two-thirds of the U.S. economy, plunged.
With workers at home, many businesses turned to telework, a development that would persist beyond the pandemic and radically change working conditions for millions. In 2023, 12.7 percent of full-time U.S. employees worked from home and 28.2 percent worked a hybrid office-home schedule, according to Forbes Advisor . Urban centers accustomed to large daily influxes of workers have suffered. Office vacancies are up, and small businesses have closed. The national office vacancy rate rose to a record 19.6 percent in the fourth quarter of 2023, according to Moody’s Analytics , which has been tracking the statistic since 1979.
Many hospitals were overwhelmed during COVID-19 surges, with too few beds for the flood of patients. But many also demonstrated their resilience and “surge capacity,” dramatically expanding bed counts in very short periods of time and finding other ways to treat patients in swamped medical centers. Triage units and COVID-19 wards were hastily erected in temporary structures on hospital grounds.
Still, U.S. hospitals suffered severe shortages of nurses and found themselves lacking basic necessities such as N95 masks and personal protective garb for the doctors, nurses, and other workers who risked their lives against the new pathogen at the start of the outbreak. Mortuaries and first responders were overwhelmed as well. The dead were kept in refrigerated trucks outside hospitals.
The country’s fragmented public health system proved inadequate to the task of coping with the outbreak, sparking calls for major reform of the CDC and other agencies. The CDC botched its initial attempt to create tests for the virus, leaving the United States almost blind to its spread during the early stages of the pandemic.
Beyond the physical dangers, mental health became a serious issue for overburdened health care personnel, other “essential” workers who continued to labor in crucial jobs, and many millions of isolated, stressed, fearful, locked-down people in the United States and elsewhere. Parents struggled to care for children kept at home by the pandemic while also attending to their jobs.
In a June 2020 survey, the CDC found that 41 percent of respondents said they were struggling with mental health and 11 percent had seriously considered suicide recently. Essential workers, unpaid caregivers , young adults, and members of racial and ethnic minority groups were found to be at a higher risk for experiencing mental health struggles, with 31 percent of unpaid caregivers reporting that they were considering suicide. WHO reported two years later that the pandemic had caused a 25 percent increase in anxiety and depression worldwide, young people and women being at the highest risk.
The rate of homicides by firearm in the United States rose by 35 percent during the pandemic to the highest rate in more than a quarter century.
A silver lining in the chaos of the pandemic’s opening year was the development in just 11 months of highly effective vaccines for the virus, a process that normally had taken 7–10 years. The U.S. government’s bet on unproven messenger RNA technology under the Trump administration’s Operation Warp Speed paid off, and the result validated the billions of dollars that the government pours into basic research every year.
On December 14, 2020, New York nurse Sandra Lindsay capped the tumultuous year by receiving the first shot of the vaccine that eventually would help end the public health crisis caused by COVID-19 pandemic.
- Share full article
Advertisement
Supported by
student opinion
How Is the Coronavirus Outbreak Affecting Your Life?
How are you staying connected and sane in a time of social distancing?

By Jeremy Engle
Find all our Student Opinion questions here.
Note: The Times Opinion section is working on an article about how the coronavirus outbreak has disrupted the lives of high school students. To share your story, fill out this form .
The coronavirus has changed how we work , play and learn : Schools are closing, sports leagues have been canceled, and many people have been asked to work from home.
On March 16, the Trump administration released new guidelines to slow the spread of the coronavirus, including closing schools and avoiding groups of more than 10 people, discretionary travel, bars, restaurants and food courts.
How are you dealing with these sudden and dramatic changes to how we live? Are you practicing social distancing — and are you even sure what that really means?
In “ Wondering About Social Distancing? ” Apoorva Mandavilli explains the term and offers practical guidance from experts:
What is social distancing? Put simply, the idea is to maintain a distance between you and other people — in this case, at least six feet. That also means minimizing contact with people. Avoid public transportation whenever possible, limit nonessential travel, work from home and skip social gatherings — and definitely do not go to crowded bars and sporting arenas. “Every single reduction in the number of contacts you have per day with relatives, with friends, co-workers, in school will have a significant impact on the ability of the virus to spread in the population,” said Dr. Gerardo Chowell, chair of population health sciences at Georgia State University. This strategy saved thousands of lives both during the Spanish flu pandemic of 1918 and, more recently, in Mexico City during the 2009 flu pandemic.
The article continues with expert responses to some common questions about social distancing. Here are excerpts from three:
I’m young and don’t have any risk factors. Can I continue to socialize? Please don’t. There is no question that older people and those with underlying health conditions are most vulnerable to the virus, but young people are by no means immune. And there is a greater public health imperative. Even people who show only mild symptoms may pass the virus to many, many others — particularly in the early course of the infection, before they even realize they are sick. So you might keep the chain of infection going right to your own older or high-risk relatives. You may also contribute to the number of people infected, causing the pandemic to grow rapidly and overwhelm the health care system. If you ignore the guidance on social distancing, you will essentially put yourself and everyone else at much higher risk. Experts acknowledged that social distancing is tough, especially for young people who are used to gathering in groups. But even cutting down the number of gatherings, and the number of people in any group, will help. Can I leave my house? Absolutely. The experts were unanimous in their answer to this question. It’s O.K. to go outdoors for fresh air and exercise — to walk your dog, go for a hike or ride your bicycle, for example. The point is not to remain indoors, but to avoid being in close contact with people. You may also need to leave the house for medicines or other essential resources. But there are things you can do to keep yourself and others safe during and after these excursions. When you do leave your home, wipe down any surfaces you come into contact with, disinfect your hands with an alcohol-based sanitizer and avoid touching your face. Above all, frequently wash your hands — especially whenever you come in from outside, before you eat or before you’re in contact with the very old or very young. How long will we need to practice social distancing? That is a big unknown, experts said. A lot will depend on how well the social distancing measures in place work and how much we can slow the pandemic down. But prepare to hunker down for at least a month, and possibly much longer. In Seattle, the recommendations on social distancing have continued to escalate with the number of infections and deaths, and as the health system has become increasingly strained. “For now, it’s probably indefinite,” Dr. Marrazzo said. “We’re in uncharted territory.”
Abdullah Shihipar writes in an Opinion essay, “ Coronavirus and the Isolation Paradox ,” that while social distancing is required to prevent infection, loneliness can make us sick:
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Volume 76, Issue 2
- COVID-19 pandemic and its impact on social relationships and health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1512-4471 Emily Long 1 ,
- Susan Patterson 1 ,
- Karen Maxwell 1 ,
- Carolyn Blake 1 ,
- http://orcid.org/0000-0001-7342-4566 Raquel Bosó Pérez 1 ,
- Ruth Lewis 1 ,
- Mark McCann 1 ,
- Julie Riddell 1 ,
- Kathryn Skivington 1 ,
- Rachel Wilson-Lowe 1 ,
- http://orcid.org/0000-0002-4409-6601 Kirstin R Mitchell 2
- 1 MRC/CSO Social and Public Health Sciences Unit , University of Glasgow , Glasgow , UK
- 2 MRC/CSO Social and Public Health Sciences Unit, Institute of Health & Wellbeing , University of Glasgow , Glasgow , UK
- Correspondence to Dr Emily Long, MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, Glasgow G3 7HR, UK; emily.long{at}glasgow.ac.uk
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the nature of the public health response. We then introduce four distinct domains of social relationships: social networks, social support, social interaction and intimacy, highlighting the mechanisms through which the pandemic and associated public health response drastically altered social interactions in each domain. Throughout the essay, the lens of health inequalities, and perspective of relationships as interconnecting elements in a broader system, is used to explore the varying impact of these disruptions. The essay concludes by providing recommendations for longer term recovery ensuring that the social relational cost of COVID-19 is adequately considered in efforts to rebuild.
- inequalities
Data availability statement
Data sharing not applicable as no data sets generated and/or analysed for this study. Data sharing not applicable as no data sets generated or analysed for this essay.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/jech-2021-216690
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Infectious disease pandemics, including SARS and COVID-19, demand intrapersonal behaviour change and present highly complex challenges for public health. 1 A pandemic of an airborne infection, spread easily through social contact, assails human relationships by drastically altering the ways through which humans interact. In this essay, we draw on theories of social relationships to examine specific ways in which relational mechanisms key to health and well-being were disrupted by the COVID-19 pandemic. Relational mechanisms refer to the processes between people that lead to change in health outcomes.
At the time of writing, the future surrounding COVID-19 was uncertain. Vaccine programmes were being rolled out in countries that could afford them, but new and more contagious variants of the virus were also being discovered. The recovery journey looked long, with continued disruption to social relationships. The social cost of COVID-19 was only just beginning to emerge, but the mental health impact was already considerable, 2 3 and the inequality of the health burden stark. 4 Knowledge of the epidemiology of COVID-19 accrued rapidly, but evidence of the most effective policy responses remained uncertain.
The initial response to COVID-19 in the UK was reactive and aimed at reducing mortality, with little time to consider the social implications, including for interpersonal and community relationships. The terminology of ‘social distancing’ quickly became entrenched both in public and policy discourse. This equation of physical distance with social distance was regrettable, since only physical proximity causes viral transmission, whereas many forms of social proximity (eg, conversations while walking outdoors) are minimal risk, and are crucial to maintaining relationships supportive of health and well-being.
The aim of this essay is to explore four key relational mechanisms that were impacted by the pandemic and associated restrictions: social networks, social support, social interaction and intimacy. We use relational theories and emerging research on the effects of the COVID-19 pandemic response to make three key recommendations: one regarding public health responses; and two regarding social recovery. Our understanding of these mechanisms stems from a ‘systems’ perspective which casts social relationships as interdependent elements within a connected whole. 5
Social networks
Social networks characterise the individuals and social connections that compose a system (such as a workplace, community or society). Social relationships range from spouses and partners, to coworkers, friends and acquaintances. They vary across many dimensions, including, for example, frequency of contact and emotional closeness. Social networks can be understood both in terms of the individuals and relationships that compose the network, as well as the overall network structure (eg, how many of your friends know each other).
Social networks show a tendency towards homophily, or a phenomenon of associating with individuals who are similar to self. 6 This is particularly true for ‘core’ network ties (eg, close friends), while more distant, sometimes called ‘weak’ ties tend to show more diversity. During the height of COVID-19 restrictions, face-to-face interactions were often reduced to core network members, such as partners, family members or, potentially, live-in roommates; some ‘weak’ ties were lost, and interactions became more limited to those closest. Given that peripheral, weaker social ties provide a diversity of resources, opinions and support, 7 COVID-19 likely resulted in networks that were smaller and more homogenous.
Such changes were not inevitable nor necessarily enduring, since social networks are also adaptive and responsive to change, in that a disruption to usual ways of interacting can be replaced by new ways of engaging (eg, Zoom). Yet, important inequalities exist, wherein networks and individual relationships within networks are not equally able to adapt to such changes. For example, individuals with a large number of newly established relationships (eg, university students) may have struggled to transfer these relationships online, resulting in lost contacts and a heightened risk of social isolation. This is consistent with research suggesting that young adults were the most likely to report a worsening of relationships during COVID-19, whereas older adults were the least likely to report a change. 8
Lastly, social connections give rise to emergent properties of social systems, 9 where a community-level phenomenon develops that cannot be attributed to any one member or portion of the network. For example, local area-based networks emerged due to geographic restrictions (eg, stay-at-home orders), resulting in increases in neighbourly support and local volunteering. 10 In fact, research suggests that relationships with neighbours displayed the largest net gain in ratings of relationship quality compared with a range of relationship types (eg, partner, colleague, friend). 8 Much of this was built from spontaneous individual interactions within local communities, which together contributed to the ‘community spirit’ that many experienced. 11 COVID-19 restrictions thus impacted the personal social networks and the structure of the larger networks within the society.
Social support
Social support, referring to the psychological and material resources provided through social interaction, is a critical mechanism through which social relationships benefit health. In fact, social support has been shown to be one of the most important resilience factors in the aftermath of stressful events. 12 In the context of COVID-19, the usual ways in which individuals interact and obtain social support have been severely disrupted.
One such disruption has been to opportunities for spontaneous social interactions. For example, conversations with colleagues in a break room offer an opportunity for socialising beyond one’s core social network, and these peripheral conversations can provide a form of social support. 13 14 A chance conversation may lead to advice helpful to coping with situations or seeking formal help. Thus, the absence of these spontaneous interactions may mean the reduction of indirect support-seeking opportunities. While direct support-seeking behaviour is more effective at eliciting support, it also requires significantly more effort and may be perceived as forceful and burdensome. 15 The shift to homeworking and closure of community venues reduced the number of opportunities for these spontaneous interactions to occur, and has, second, focused them locally. Consequently, individuals whose core networks are located elsewhere, or who live in communities where spontaneous interaction is less likely, have less opportunity to benefit from spontaneous in-person supportive interactions.
However, alongside this disruption, new opportunities to interact and obtain social support have arisen. The surge in community social support during the initial lockdown mirrored that often seen in response to adverse events (eg, natural disasters 16 ). COVID-19 restrictions that confined individuals to their local area also compelled them to focus their in-person efforts locally. Commentators on the initial lockdown in the UK remarked on extraordinary acts of generosity between individuals who belonged to the same community but were unknown to each other. However, research on adverse events also tells us that such community support is not necessarily maintained in the longer term. 16
Meanwhile, online forms of social support are not bound by geography, thus enabling interactions and social support to be received from a wider network of people. Formal online social support spaces (eg, support groups) existed well before COVID-19, but have vastly increased since. While online interactions can increase perceived social support, it is unclear whether remote communication technologies provide an effective substitute from in-person interaction during periods of social distancing. 17 18 It makes intuitive sense that the usefulness of online social support will vary by the type of support offered, degree of social interaction and ‘online communication skills’ of those taking part. Youth workers, for instance, have struggled to keep vulnerable youth engaged in online youth clubs, 19 despite others finding a positive association between amount of digital technology used by individuals during lockdown and perceived social support. 20 Other research has found that more frequent face-to-face contact and phone/video contact both related to lower levels of depression during the time period of March to August 2020, but the negative effect of a lack of contact was greater for those with higher levels of usual sociability. 21 Relatedly, important inequalities in social support exist, such that individuals who occupy more socially disadvantaged positions in society (eg, low socioeconomic status, older people) tend to have less access to social support, 22 potentially exacerbated by COVID-19.
Social and interactional norms
Interactional norms are key relational mechanisms which build trust, belonging and identity within and across groups in a system. Individuals in groups and societies apply meaning by ‘approving, arranging and redefining’ symbols of interaction. 23 A handshake, for instance, is a powerful symbol of trust and equality. Depending on context, not shaking hands may symbolise a failure to extend friendship, or a failure to reach agreement. The norms governing these symbols represent shared values and identity; and mutual understanding of these symbols enables individuals to achieve orderly interactions, establish supportive relationship accountability and connect socially. 24 25
Physical distancing measures to contain the spread of COVID-19 radically altered these norms of interaction, particularly those used to convey trust, affinity, empathy and respect (eg, hugging, physical comforting). 26 As epidemic waves rose and fell, the work to negotiate these norms required intense cognitive effort; previously taken-for-granted interactions were re-examined, factoring in current restriction levels, own and (assumed) others’ vulnerability and tolerance of risk. This created awkwardness, and uncertainty, for example, around how to bring closure to an in-person interaction or convey warmth. The instability in scripted ways of interacting created particular strain for individuals who already struggled to encode and decode interactions with others (eg, those who are deaf or have autism spectrum disorder); difficulties often intensified by mask wearing. 27
Large social gatherings—for example, weddings, school assemblies, sporting events—also present key opportunities for affirming and assimilating interactional norms, building cohesion and shared identity and facilitating cooperation across social groups. 28 Online ‘equivalents’ do not easily support ‘social-bonding’ activities such as singing and dancing, and rarely enable chance/spontaneous one-on-one conversations with peripheral/weaker network ties (see the Social networks section) which can help strengthen bonds across a larger network. The loss of large gatherings to celebrate rites of passage (eg, bar mitzvah, weddings) has additional relational costs since these events are performed by and for communities to reinforce belonging, and to assist in transitioning to new phases of life. 29 The loss of interaction with diverse others via community and large group gatherings also reduces intergroup contact, which may then tend towards more prejudiced outgroup attitudes. While online interaction can go some way to mimicking these interaction norms, there are key differences. A sense of anonymity, and lack of in-person emotional cues, tends to support norms of polarisation and aggression in expressing differences of opinion online. And while online platforms have potential to provide intergroup contact, the tendency of much social media to form homogeneous ‘echo chambers’ can serve to further reduce intergroup contact. 30 31
Intimacy relates to the feeling of emotional connection and closeness with other human beings. Emotional connection, through romantic, friendship or familial relationships, fulfils a basic human need 32 and strongly benefits health, including reduced stress levels, improved mental health, lowered blood pressure and reduced risk of heart disease. 32 33 Intimacy can be fostered through familiarity, feeling understood and feeling accepted by close others. 34
Intimacy via companionship and closeness is fundamental to mental well-being. Positively, the COVID-19 pandemic has offered opportunities for individuals to (re)connect and (re)strengthen close relationships within their household via quality time together, following closure of many usual external social activities. Research suggests that the first full UK lockdown period led to a net gain in the quality of steady relationships at a population level, 35 but amplified existing inequalities in relationship quality. 35 36 For some in single-person households, the absence of a companion became more conspicuous, leading to feelings of loneliness and lower mental well-being. 37 38 Additional pandemic-related relational strain 39 40 resulted, for some, in the initiation or intensification of domestic abuse. 41 42
Physical touch is another key aspect of intimacy, a fundamental human need crucial in maintaining and developing intimacy within close relationships. 34 Restrictions on social interactions severely restricted the number and range of people with whom physical affection was possible. The reduction in opportunity to give and receive affectionate physical touch was not experienced equally. Many of those living alone found themselves completely without physical contact for extended periods. The deprivation of physical touch is evidenced to take a heavy emotional toll. 43 Even in future, once physical expressions of affection can resume, new levels of anxiety over germs may introduce hesitancy into previously fluent blending of physical and verbal intimate social connections. 44
The pandemic also led to shifts in practices and norms around sexual relationship building and maintenance, as individuals adapted and sought alternative ways of enacting sexual intimacy. This too is important, given that intimate sexual activity has known benefits for health. 45 46 Given that social restrictions hinged on reducing household mixing, possibilities for partnered sexual activity were primarily guided by living arrangements. While those in cohabiting relationships could potentially continue as before, those who were single or in non-cohabiting relationships generally had restricted opportunities to maintain their sexual relationships. Pornography consumption and digital partners were reported to increase since lockdown. 47 However, online interactions are qualitatively different from in-person interactions and do not provide the same opportunities for physical intimacy.
Recommendations and conclusions
In the sections above we have outlined the ways in which COVID-19 has impacted social relationships, showing how relational mechanisms key to health have been undermined. While some of the damage might well self-repair after the pandemic, there are opportunities inherent in deliberative efforts to build back in ways that facilitate greater resilience in social and community relationships. We conclude by making three recommendations: one regarding public health responses to the pandemic; and two regarding social recovery.
Recommendation 1: explicitly count the relational cost of public health policies to control the pandemic
Effective handling of a pandemic recognises that social, economic and health concerns are intricately interwoven. It is clear that future research and policy attention must focus on the social consequences. As described above, policies which restrict physical mixing across households carry heavy and unequal relational costs. These include for individuals (eg, loss of intimate touch), dyads (eg, loss of warmth, comfort), networks (eg, restricted access to support) and communities (eg, loss of cohesion and identity). Such costs—and their unequal impact—should not be ignored in short-term efforts to control an epidemic. Some public health responses—restrictions on international holiday travel and highly efficient test and trace systems—have relatively small relational costs and should be prioritised. At a national level, an earlier move to proportionate restrictions, and investment in effective test and trace systems, may help prevent escalation of spread to the point where a national lockdown or tight restrictions became an inevitability. Where policies with relational costs are unavoidable, close attention should be paid to the unequal relational impact for those whose personal circumstances differ from normative assumptions of two adult families. This includes consideration of whether expectations are fair (eg, for those who live alone), whether restrictions on social events are equitable across age group, religious/ethnic groupings and social class, and also to ensure that the language promoted by such policies (eg, households; families) is not exclusionary. 48 49 Forethought to unequal impacts on social relationships should thus be integral to the work of epidemic preparedness teams.
Recommendation 2: intelligently balance online and offline ways of relating
A key ingredient for well-being is ‘getting together’ in a physical sense. This is fundamental to a human need for intimate touch, physical comfort, reinforcing interactional norms and providing practical support. Emerging evidence suggests that online ways of relating cannot simply replace physical interactions. But online interaction has many benefits and for some it offers connections that did not exist previously. In particular, online platforms provide new forms of support for those unable to access offline services because of mobility issues (eg, older people) or because they are geographically isolated from their support community (eg, lesbian, gay, bisexual, transgender and queer (LGBTQ) youth). Ultimately, multiple forms of online and offline social interactions are required to meet the needs of varying groups of people (eg, LGBTQ, older people). Future research and practice should aim to establish ways of using offline and online support in complementary and even synergistic ways, rather than veering between them as social restrictions expand and contract. Intelligent balancing of online and offline ways of relating also pertains to future policies on home and flexible working. A decision to switch to wholesale or obligatory homeworking should consider the risk to relational ‘group properties’ of the workplace community and their impact on employees’ well-being, focusing in particular on unequal impacts (eg, new vs established employees). Intelligent blending of online and in-person working is required to achieve flexibility while also nurturing supportive networks at work. Intelligent balance also implies strategies to build digital literacy and minimise digital exclusion, as well as coproducing solutions with intended beneficiaries.
Recommendation 3: build stronger and sustainable localised communities
In balancing offline and online ways of interacting, there is opportunity to capitalise on the potential for more localised, coherent communities due to scaled-down travel, homeworking and local focus that will ideally continue after restrictions end. There are potential economic benefits after the pandemic, such as increased trade as home workers use local resources (eg, coffee shops), but also relational benefits from stronger relationships around the orbit of the home and neighbourhood. Experience from previous crises shows that community volunteer efforts generated early on will wane over time in the absence of deliberate work to maintain them. Adequately funded partnerships between local government, third sector and community groups are required to sustain community assets that began as a direct response to the pandemic. Such partnerships could work to secure green spaces and indoor (non-commercial) meeting spaces that promote community interaction. Green spaces in particular provide a triple benefit in encouraging physical activity and mental health, as well as facilitating social bonding. 50 In building local communities, small community networks—that allow for diversity and break down ingroup/outgroup views—may be more helpful than the concept of ‘support bubbles’, which are exclusionary and less sustainable in the longer term. Rigorously designed intervention and evaluation—taking a systems approach—will be crucial in ensuring scale-up and sustainability.
The dramatic change to social interaction necessitated by efforts to control the spread of COVID-19 created stark challenges but also opportunities. Our essay highlights opportunities for learning, both to ensure the equity and humanity of physical restrictions, and to sustain the salutogenic effects of social relationships going forward. The starting point for capitalising on this learning is recognition of the disruption to relational mechanisms as a key part of the socioeconomic and health impact of the pandemic. In recovery planning, a general rule is that what is good for decreasing health inequalities (such as expanding social protection and public services and pursuing green inclusive growth strategies) 4 will also benefit relationships and safeguard relational mechanisms for future generations. Putting this into action will require political will.
Ethics statements
Patient consent for publication.
Not required.
- Office for National Statistics (ONS)
- Ford T , et al
- Riordan R ,
- Ford J , et al
- Glonti K , et al
- McPherson JM ,
- Smith-Lovin L
- Granovetter MS
- Fancourt D et al
- Stadtfeld C
- Office for Civil Society
- Cook J et al
- Rodriguez-Llanes JM ,
- Guha-Sapir D
- Patulny R et al
- Granovetter M
- Winkeler M ,
- Filipp S-H ,
- Kaniasty K ,
- de Terte I ,
- Guilaran J , et al
- Wright KB ,
- Martin J et al
- Gabbiadini A ,
- Baldissarri C ,
- Durante F , et al
- Sommerlad A ,
- Marston L ,
- Huntley J , et al
- Turner RJ ,
- Bicchieri C
- Brennan G et al
- Watson-Jones RE ,
- Amichai-Hamburger Y ,
- McKenna KYA
- Page-Gould E ,
- Aron A , et al
- Pietromonaco PR ,
- Timmerman GM
- Bradbury-Jones C ,
- Mikocka-Walus A ,
- Klas A , et al
- Marshall L ,
- Steptoe A ,
- Stanley SM ,
- Campbell AM
- ↵ (ONS), O.f.N.S., Domestic abuse during the coronavirus (COVID-19) pandemic, England and Wales . Available: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/domesticabuseduringthecoronaviruscovid19pandemicenglandandwales/november2020
- Rosenberg M ,
- Hensel D , et al
- Banerjee D ,
- Bruner DW , et al
- Bavel JJV ,
- Baicker K ,
- Boggio PS , et al
- van Barneveld K ,
- Quinlan M ,
- Kriesler P , et al
- Mitchell R ,
- de Vries S , et al
Twitter @karenmaxSPHSU, @Mark_McCann, @Rwilsonlowe, @KMitchinGlasgow
Contributors EL and KM led on the manuscript conceptualisation, review and editing. SP, KM, CB, RBP, RL, MM, JR, KS and RW-L contributed to drafting and revising the article. All authors assisted in revising the final draft.
Funding The research reported in this publication was supported by the Medical Research Council (MC_UU_00022/1, MC_UU_00022/3) and the Chief Scientist Office (SPHSU11, SPHSU14). EL is also supported by MRC Skills Development Fellowship Award (MR/S015078/1). KS and MM are also supported by a Medical Research Council Strategic Award (MC_PC_13027).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Paragraph Writing
- Paragraph Writing On Covid 19
Paragraph Writing on Covid 19 - Check Samples for Various Word Limits
The Covid-19 pandemic has been a deadly pandemic that has affected the whole world. It was a viral infection that affected almost everyone in some way or the other. However, the effects have been felt differently depending on various factors. As it is a virus, it will change with time, and different variants might keep coming. The virus has affected the lifestyle of human beings. The pandemic has affected the education system and the economy of the world as well. Many people have lost their lives, jobs, near and dear, etc.
Table of Contents
Paragraph writing on covid-19 in 100 words, paragraph writing on covid-19 in 150 words, paragraph writing on covid-19 in 200 words, paragraph writing on covid-19 in 250 words, frequently asked questions on covid-19.
Check the samples provided below before you write a paragraph on Covid-19.
Coronavirus is an infectious disease and is commonly called Covid-19. It affects the human respiratory system causing difficulty in breathing. It is a contagious disease and has been spreading across the world like wildfire. The virus was first identified in 2019 in Wuhan, China. In March, WHO declared Covid-19 as a pandemic that has been affecting the world. The virus was spreading from an infected person through coughing, sneezing, etc. Therefore, the affected people were isolated from everyone. The affected people were even isolated from their own family members and their dear ones. Other symptoms noticed in Covid – 19 patients include weariness, sore throat, muscle soreness, and loss of taste and smell.
Coronavirus, often known as Covid-19, is an infectious disease. It affects the human respiratory system, making breathing difficult. It’s a contagious disease that has been spreading like wildfire over the world. The virus was initially discovered in Wuhan, China, in 2019. Covid-19 was declared a global pandemic by the World Health Organization in March. The virus was transferred by coughing, sneezing, and other means from an infected person. As a result, the people who were affected were isolated from the rest of society. The folks who were afflicted were even separated from their own family members and loved ones. Weariness, sore throat, muscle stiffness, and loss of taste and smell are among the other complaints reported by Covid-19 individuals. Almost every individual has been affected by the virus. A lot of people have lost their lives due to the severity of the infections. The dropping of oxygen levels and the unavailability of oxygen cylinders were the primary concerns during the pandemic.
The Covid-19 pandemic was caused due to a man-made virus called coronavirus. It is an infectious disease that has affected millions of people’s lives. The pandemic has affected the entire world differently. It was initially diagnosed in 2019 in Wuhan, China but later, in March 2020, WHO declared that it was a pandemic that was affecting the whole world like wildfire. Covid-19 is a contagious disease. Since it is a viral disease, the virus spreads rapidly in various forms. The main symptoms of this disease were loss of smell and taste, loss of energy, pale skin, sneezing, coughing, reduction of oxygen level, etc. Therefore, all the affected people were asked to isolate themselves from the unaffected ones. The affected people were isolated from their family members in a separate room. The government has taken significant steps to ensure the safety of the people. The frontline workers were like superheroes who worked selflessly for the safety of the people. A lot of doctors had to stay away from their families and their babies for the safety of their patients and their close ones. The government has taken significant steps, and various protocols were imposed for the safety of the people. The government imposed a lockdown and shut down throughout the country.
The coronavirus was responsible for the Covid-19 pandemic. It is an infectious disease that has affected millions of people’s lives. The pandemic has impacted people all across the world in diverse ways. It was first discovered in Wuhan, China, in 2019. However, the World Health Organization (WHO) proclaimed it a pandemic in March 2020, claiming that it has spread throughout the globe like wildfire. The pandemic has claimed the lives of millions of people. The virus had negative consequences for those who were infected, including the development of a variety of chronic disorders. The main symptoms of this disease were loss of smell and taste, fatigue, pale skin, sneezing, coughing, oxygen deficiency, etc. Because Covid-19 was an infectious disease, all those who were infected were instructed to segregate themselves from those who were not. The folks who were affected were separated from their families and locked in a room. The government has prioritised people’s safety. The frontline personnel were like superheroes, working tirelessly to ensure the public’s safety. For the sake of their patients’ and close relatives’ safety, many doctors had to stay away from their families and babies. The government had also taken significant steps and implemented different protocols for the protection of people.
What is meant by the Covid-19 pandemic?
The Covid-19 pandemic was a deadly pandemic that affected the lives of millions of people. A lot of people lost their lives, and some people lost their jobs and lost their entire families due to the pandemic. Many covid warriors, like doctors, nurses, frontline workers, etc., lost their lives due to the pandemic.
From where did the Covid-19 pandemic start?
The Covid-19 pandemic was initially found in Wuhan, China and later in the whole world.
What are the symptoms of Covid-19?
The symptoms of Covid-19 have been identified as sore throat, loss of smell and taste, cough, sneezing, reduction of oxygen level, etc.
| ENGLISH Related Links | |
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Request OTP on Voice Call
Post My Comment
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.
How is COVID-19 affecting student learning?
Subscribe to the brown center on education policy newsletter, initial findings from fall 2020, megan kuhfeld , megan kuhfeld senior research scientist - nwea jim soland , jim soland assistant professor, school of education and human development - university of virginia, affiliated research fellow - nwea beth tarasawa , bt beth tarasawa executive vice president of research - nwea angela johnson , aj angela johnson research scientist - nwea erik ruzek , and er erik ruzek research assistant professor, curry school of education - university of virginia karyn lewis karyn lewis director, center for school and student progress - nwea.
December 3, 2020
The COVID-19 pandemic has introduced uncertainty into major aspects of national and global society, including for schools. For example, there is uncertainty about how school closures last spring impacted student achievement, as well as how the rapid conversion of most instruction to an online platform this academic year will continue to affect achievement. Without data on how the virus impacts student learning, making informed decisions about whether and when to return to in-person instruction remains difficult. Even now, education leaders must grapple with seemingly impossible choices that balance health risks associated with in-person learning against the educational needs of children, which may be better served when kids are in their physical schools.
Amidst all this uncertainty, there is growing consensus that school closures in spring 2020 likely had negative effects on student learning. For example, in an earlier post for this blog , we presented our research forecasting the possible impact of school closures on achievement. Based on historical learning trends and prior research on how out-of-school-time affects learning, we estimated that students would potentially begin fall 2020 with roughly 70% of the learning gains in reading relative to a typical school year. In mathematics, students were predicted to show even smaller learning gains from the previous year, returning with less than 50% of typical gains. While these and other similar forecasts presented a grim portrait of the challenges facing students and educators this fall, they were nonetheless projections. The question remained: What would learning trends in actual data from the 2020-21 school year really look like?
With fall 2020 data now in hand , we can move beyond forecasting and begin to describe what did happen. While the closures last spring left most schools without assessment data from that time, thousands of schools began testing this fall, making it possible to compare learning gains in a typical, pre-COVID-19 year to those same gains during the COVID-19 pandemic. Using data from nearly 4.4 million students in grades 3-8 who took MAP ® Growth™ reading and math assessments in fall 2020, we examined two primary research questions:
- How did students perform in fall 2020 relative to a typical school year (specifically, fall 2019)?
- Have students made learning gains since schools physically closed in March 2020?
To answer these questions, we compared students’ academic achievement and growth during the COVID-19 pandemic to the achievement and growth patterns observed in 2019. We report student achievement as a percentile rank, which is a normative measure of a student’s achievement in a given grade/subject relative to the MAP Growth national norms (reflecting pre-COVID-19 achievement levels).
To make sure the students who took the tests before and after COVID-19 school closures were demographically similar, all analyses were limited to a sample of 8,000 schools that tested students in both fall 2019 and fall 2020. Compared to all public schools in the nation, schools in the sample had slightly larger total enrollment, a lower percentage of low-income students, and a higher percentage of white students. Since our sample includes both in-person and remote testers in fall 2020, we conducted an initial comparability study of remote and in-person testing in fall 2020. We found consistent psychometric characteristics and trends in test scores for remote and in-person tests for students in grades 3-8, but caution that remote testing conditions may be qualitatively different for K-2 students. For more details on the sample and methodology, please see the technical report accompanying this study.
In some cases, our results tell a more optimistic story than what we feared. In others, the results are as deeply concerning as we expected based on our projections.
Question 1: How did students perform in fall 2020 relative to a typical school year?
When comparing students’ median percentile rank for fall 2020 to those for fall 2019, there is good news to share: Students in grades 3-8 performed similarly in reading to same-grade students in fall 2019. While the reason for the stability of these achievement results cannot be easily pinned down, possible explanations are that students read more on their own, and parents are better equipped to support learning in reading compared to other subjects that require more formal instruction.
The news in math, however, is more worrying. The figure below shows the median percentile rank in math by grade level in fall 2019 and fall 2020. As the figure indicates, the math achievement of students in 2020 was about 5 to 10 percentile points lower compared to same-grade students the prior year.
Figure 1: MAP Growth Percentiles in Math by Grade Level in Fall 2019 and Fall 2020
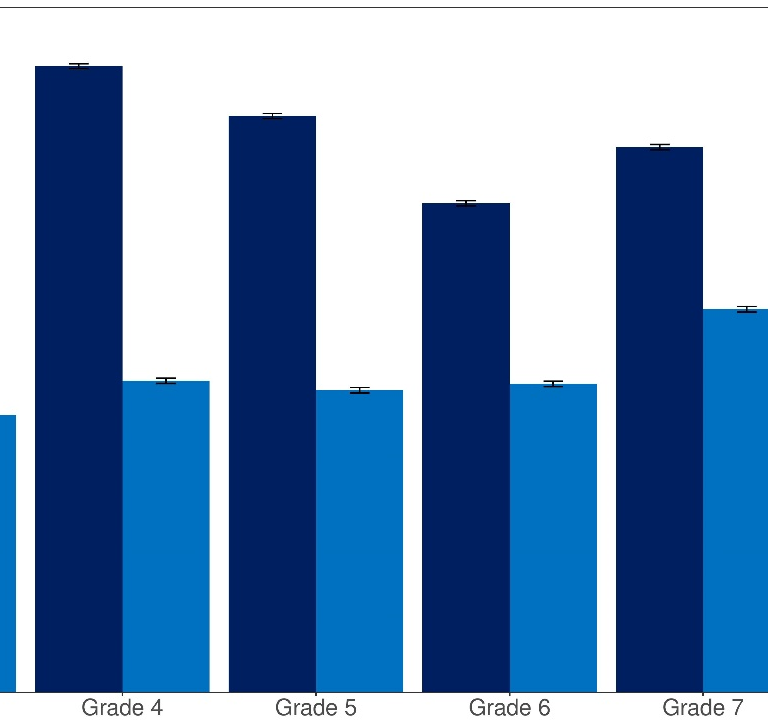
Source: Author calculations with MAP Growth data. Notes: Each bar represents the median percentile rank in a given grade/term.
Question 2: Have students made learning gains since schools physically closed, and how do these gains compare to gains in a more typical year?
To answer this question, we examined learning gains/losses between winter 2020 (January through early March) and fall 2020 relative to those same gains in a pre-COVID-19 period (between winter 2019 and fall 2019). We did not examine spring-to-fall changes because so few students tested in spring 2020 (after the pandemic began). In almost all grades, the majority of students made some learning gains in both reading and math since the COVID-19 pandemic started, though gains were smaller in math in 2020 relative to the gains students in the same grades made in the winter 2019-fall 2019 period.
Figure 2 shows the distribution of change in reading scores by grade for the winter 2020 to fall 2020 period (light blue) as compared to same-grade students in the pre-pandemic span of winter 2019 to fall 2019 (dark blue). The 2019 and 2020 distributions largely overlapped, suggesting similar amounts of within-student change from one grade to the next.
Figure 2: Distribution of Within-student Change from Winter 2019-Fall 2019 vs Winter 2020-Fall 2020 in Reading

Source: Author calculations with MAP Growth data. Notes: The dashed line represents zero growth (e.g., winter and fall test scores were equivalent). A positive value indicates that a student scored higher in the fall than their prior winter score; a negative value indicates a student scored lower in the fall than their prior winter score.
Meanwhile, Figure 3 shows the distribution of change for students in different grade levels for the winter 2020 to fall 2020 period in math. In contrast to reading, these results show a downward shift: A smaller proportion of students demonstrated positive math growth in the 2020 period than in the 2019 period for all grades. For example, 79% of students switching from 3 rd to 4 th grade made academic gains between winter 2019 and fall 2019, relative to 57% of students in the same grade range in 2020.
Figure 3: Distribution of Within-student Change from Winter 2019-Fall 2019 vs. Winter 2020-Fall 2020 in Math

It was widely speculated that the COVID-19 pandemic would lead to very unequal opportunities for learning depending on whether students had access to technology and parental support during the school closures, which would result in greater heterogeneity in terms of learning gains/losses in 2020. Notably, however, we do not see evidence that within-student change is more spread out this year relative to the pre-pandemic 2019 distribution.
The long-term effects of COVID-19 are still unknown
In some ways, our findings show an optimistic picture: In reading, on average, the achievement percentiles of students in fall 2020 were similar to those of same-grade students in fall 2019, and in almost all grades, most students made some learning gains since the COVID-19 pandemic started. In math, however, the results tell a less rosy story: Student achievement was lower than the pre-COVID-19 performance by same-grade students in fall 2019, and students showed lower growth in math across grades 3 to 8 relative to peers in the previous, more typical year. Schools will need clear local data to understand if these national trends are reflective of their students. Additional resources and supports should be deployed in math specifically to get students back on track.
In this study, we limited our analyses to a consistent set of schools between fall 2019 and fall 2020. However, approximately one in four students who tested within these schools in fall 2019 are no longer in our sample in fall 2020. This is a sizeable increase from the 15% attrition from fall 2018 to fall 2019. One possible explanation is that some students lacked reliable technology. A second is that they disengaged from school due to economic, health, or other factors. More coordinated efforts are required to establish communication with students who are not attending school or disengaging from instruction to get them back on track, especially our most vulnerable students.
Finally, we are only scratching the surface in quantifying the short-term and long-term academic and non-academic impacts of COVID-19. While more students are back in schools now and educators have more experience with remote instruction than when the pandemic forced schools to close in spring 2020, the collective shock we are experiencing is ongoing. We will continue to examine students’ academic progress throughout the 2020-21 school year to understand how recovery and growth unfold amid an ongoing pandemic.
Thankfully, we know much more about the impact the pandemic has had on student learning than we did even a few months ago. However, that knowledge makes clear that there is work to be done to help many students get back on track in math, and that the long-term ramifications of COVID-19 for student learning—especially among underserved communities—remain unknown.
Related Content
Jim Soland, Megan Kuhfeld, Beth Tarasawa, Angela Johnson, Erik Ruzek, Jing Liu
May 27, 2020
Amie Rapaport, Anna Saavedra, Dan Silver, Morgan Polikoff
November 18, 2020
Education Access & Equity K-12 Education
Governance Studies
Brown Center on Education Policy
Andrew J. Seligsohn, Rebecca Silliman
August 19, 2024
Online only
9:30 am - 11:00 am EDT
Douglas N. Harris
August 13, 2024

45,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Essay On Covid-19: 100, 200 and 300 Words

- Updated on
- Apr 30, 2024

COVID-19, also known as the Coronavirus, is a global pandemic that has affected people all around the world. It first emerged in a lab in Wuhan, China, in late 2019 and quickly spread to countries around the world. This virus was reportedly caused by SARS-CoV-2. Since then, it has spread rapidly to many countries, causing widespread illness and impacting our lives in numerous ways. This blog talks about the details of this virus and also drafts an essay on COVID-19 in 100, 200 and 300 words for students and professionals.
Table of Contents
- 1 Essay On COVID-19 in English 100 Words
- 2 Essay On COVID-19 in 200 Words
- 3 Essay On COVID-19 in 300 Words
- 4 Short Essay on Covid-19
Essay On COVID-19 in English 100 Words
COVID-19, also known as the coronavirus, is a global pandemic. It started in late 2019 and has affected people all around the world. The virus spreads very quickly through someone’s sneeze and respiratory issues.
COVID-19 has had a significant impact on our lives, with lockdowns, travel restrictions, and changes in daily routines. To prevent the spread of COVID-19, we should wear masks, practice social distancing, and wash our hands frequently.
People should follow social distancing and other safety guidelines and also learn the tricks to be safe stay healthy and work the whole challenging time.
Also Read: National Safe Motherhood Day 2023
Essay On COVID-19 in 200 Words
COVID-19 also known as coronavirus, became a global health crisis in early 2020 and impacted mankind around the world. This virus is said to have originated in Wuhan, China in late 2019. It belongs to the coronavirus family and causes flu-like symptoms. It impacted the healthcare systems, economies and the daily lives of people all over the world.
The most crucial aspect of COVID-19 is its highly spreadable nature. It is a communicable disease that spreads through various means such as coughs from infected persons, sneezes and communication. Due to its easy transmission leading to its outbreaks, there were many measures taken by the government from all over the world such as Lockdowns, Social Distancing, and wearing masks.
There are many changes throughout the economic systems, and also in daily routines. Other measures such as schools opting for Online schooling, Remote work options available and restrictions on travel throughout the country and internationally. Subsequently, to cure and top its outbreak, the government started its vaccine campaigns, and other preventive measures.
In conclusion, COVID-19 tested the patience and resilience of the mankind. This pandemic has taught people the importance of patience, effort and humbleness.
Also Read : Essay on My Best Friend
Essay On COVID-19 in 300 Words
COVID-19, also known as the coronavirus, is a serious and contagious disease that has affected people worldwide. It was first discovered in late 2019 in Cina and then got spread in the whole world. It had a major impact on people’s life, their school, work and daily lives.
COVID-19 is primarily transmitted from person to person through respiratory droplets produced and through sneezes, and coughs of an infected person. It can spread to thousands of people because of its highly contagious nature. To cure the widespread of this virus, there are thousands of steps taken by the people and the government.
Wearing masks is one of the essential precautions to prevent the virus from spreading. Social distancing is another vital practice, which involves maintaining a safe distance from others to minimize close contact.
Very frequent handwashing is also very important to stop the spread of this virus. Proper hand hygiene can help remove any potential virus particles from our hands, reducing the risk of infection.
In conclusion, the Coronavirus has changed people’s perspective on living. It has also changed people’s way of interacting and how to live. To deal with this virus, it is very important to follow the important guidelines such as masks, social distancing and techniques to wash your hands. Getting vaccinated is also very important to go back to normal life and cure this virus completely.
Also Read: Essay on Abortion in English in 650 Words
Short Essay on Covid-19
Please find below a sample of a short essay on Covid-19 for school students:
Also Read: Essay on Women’s Day in 200 and 500 words
to write an essay on COVID-19, understand your word limit and make sure to cover all the stages and symptoms of this disease. You need to highlight all the challenges and impacts of COVID-19. Do not forget to conclude your essay with positive precautionary measures.
Writing an essay on COVID-19 in 200 words requires you to cover all the challenges, impacts and precautions of this disease. You don’t need to describe all of these factors in brief, but make sure to add as many options as your word limit allows.
The full form for COVID-19 is Corona Virus Disease of 2019.
Related Reads
Hence, we hope that this blog has assisted you in comprehending with an essay on COVID-19. For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Simran Popli
An avid writer and a creative person. With an experience of 1.5 years content writing, Simran has worked with different areas. From medical to working in a marketing agency with different clients to Ed-tech company, the journey has been diverse. Creative, vivacious and patient are the words that describe her personality.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
45,000+ students realised their study abroad dream with us. take the first step today..

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Feature stories /
The impact of COVID-19 on mental health cannot be made light of

One of the biggest global crises in generations, the COVID-19 pandemic has had severe and far-reaching repercussions for health systems, economies and societies. Countless people have died, or lost their livelihoods. Families and communities have been strained and separated. Children and young people have missed out on learning and socializing. Businesses have gone bankrupt. Millions people have fallen below the poverty line.
As people grapple with these health, social and economic impacts, mental health has been widely affected. Plenty of us became more anxious; but for some COVID-19 has sparked or amplified much more serious mental health problems. A great number of people have reported psychological distress and symptoms of depression, anxiety or post-traumatic stress. And there have been worrying signs of more widespread suicidal thoughts and behaviours, including among health care workers.
Some groups of people have been affected much more than others. Faced with extended school and university closures young people have been left vulnerable to social isolation and disconnectedness which can fuel feelings of anxiety, uncertainty and loneliness and lead to affective and behavioural problems. For some children and adolescents being made to stay at home may have increased the risk of family stress or abuse, which are risk factors for mental health problems. Women have similarly faced greater stress in homes, with one rapid assessment reporting that 45% of women had experienced some form of violence, either directly or indirectly during the first year of the pandemic.
While mental health needs have risen, mental health services have been severely disrupted. This was especially true early on in the pandemic when staff and infrastructure were often redeployed to COVID-19 relief. Social measures also prevented people from accessing care at that time. And in many cases, poor knowledge and misinformation about the virus fuelled fears and worries that stopped people from seeking help.
Fear factor
Esenam Abra Drah lives with bipolar disorder in Ghana, where fear of the virus has been an unprecedented stressor to the mental health of many individuals. “I have many friends who had relapses in their mental health because of the increased levels of fear and panic,” says Esenam. “It was almost as if fear was contagious.”
Esenam explains that most people are afraid to seek help because they think that if they visit the hospital, they might end up getting infected with COVID-19. “I myself did not go to the clinic for therapy for an entire year partly because of this fear,” she says.
At that time Esenam, like so many others, was unemployed and did not have the funds for treatment. Even before the pandemic, cost of care was known to be a major barrier to people with mental health conditions seeking help.
“I have been privileged to have a good system of support,” says Esenam. “My pensioner parents managed to make sure my medications were always refilled.”
“But it is not the same for others,” she adds. “Some people could not afford treatment. It was and still is a very difficult time for a lot of people.”
Recommendations for response
Since the start of the pandemic, mental health service providers have tried to mitigate service disruptions, for example by delivering care via alternative routes when public health and social measures were in place. Community-based initiatives were often faster to adapt, finding innovative ways to provide psychosocial support, including through digital technologies and informal supports. And international organizations have also provided guidance, tools and resources to help responders, public health planners and the general public.
WHO recommends integrating Mental Health and Psychosocial Support (MHPSS) within all aspects of preparedness and response for all public health emergencies. To minimize the mental health consequences of the COVID-19 pandemic, WHO also recommends that countries:
- Apply a whole of society approach to promote, protect and care for mental health, including through social and financial protection to safeguard people from domestic violence or impoverishment, and by communicating widely about COVID-19 to counter misinformation and promote mental health.
- Ensure widespread availability of mental health and psychosocial support, including by scaling up access to self-help and supporting community initiatives.
- Support recovery from COVID-19 by building mental health services for the future.
The COVID-19 pandemic, like other ongoing crises, has made strengthening mental health systems more urgent all over the world. “The impact of COVID-19 on mental health cannot be underestimated. It cannot be made light of,” says Esenam. Change is possible.

- The Covid-19 Pandemic Impact on the Family Dynamic Words: 1623
- How the COVID-19 Pandemic Is Changing the Economy Words: 912
- The COVID-19 Pandemic’s Social Impact Words: 1648
- The COVID-19 Pandemic: Human Response Words: 1541
- The COVID-19 Pandemic Impacts on the US Words: 2569
- The Effectiveness of the US in Response COVID-19 Pandemic Words: 575
- COVID-19 Pandemic’s Impact on the Environment Words: 695
- Impact of the COVID-19 Pandemic on Human Well-Being Words: 552
- The Impact of the COVID-19 Pandemic on Intimate Partner Violence in the US Words: 874
- COVID-19: The Effects on Humankind Words: 858
- The COVID-19 Pandemic: Economic Impacts Words: 4159
The Impact of COVID-19 Pandemic
The year 2019 will forever be engraved in many people’s hearts and minds as the time when a deadly virus known as the coronavirus disease 2019 (COVID-19) invaded almost all the sectors, thereby disrupting daily activities. It is described as a communicable respiratory illness which is triggered by a new strain of coronavirus which leads to various ailments in human beings. There is currently no known cure or vaccine for the virus as scientists worldwide are still trying to learn about the illness to respond appropriately through research (Goodell, 2020). This paper aims at exploring the effects that the pandemic has had on society regarding the economy, social life, education, religion, and family.
The emergence of the pandemic, which began in China-2019, quickly spread to other nations across the world with devastating effects on their economies As a way of containing the disease, many countries instituted strict measures, such as curfews, the mandatory wearing of masks, and social distancing of 1 meter apart (Goodell, 2020). Covid-19 has significantly changed the way these preventive methods relate with each concerning trade matters. The majority of the states affected opted to close their borders as fear among the citizens increased. The implementation of the strict rules interfered with the business operations of many nations. It became difficult for international trade to continue as a result of the closed borders. Most businesses have also had to close due to financial constraints.
When it comes to socialization, people have been forced to use other means to meet their friends and families across the world. Social media platforms have seen an increased usage during this difficult time as people try to find new ways of socializing. It has happened especially in such countries as Australia, where the restrictions were extreme as it enforced a lockdown for close to a hundred days (Goodell, 2020). The use of masks is also quickly becoming the new norm across numerous states. Unlike in developed countries where the governments have offered their citizens some aid mostly in terms of cash transfers, developing countries have struggled to balance between the people’s livelihood and the containment of the Covid-19. As such, most people have turned to social media platforms as a medium of communication and socialization due to lockdowns.
Learning institutions have also not been spared by the Covid-19 pandemic. Most countries affected by the spread of the virus were forced to suspend their educational curriculum calendar to allow children and university students to stay home until the time when the disease is finally neutralized (Goodell, 2020). However, students and parents have been pushing the governments to resume schools with clear protocols which ensure that both the students and the teachers follow the rules, including the mandatory wearing of masks. Religion has also been significantly affected as it has become difficult for people to seek for spiritual nourishment (Goodell, 2020). Many religious leaders have had to devise other ways of reaching out to the congregates. For example, many churches now have to move their services online by using such platforms as YouTube, Facebook, Zoom, among others to convey essential teachings.
Covid-19 has also directly affected many families across the world, as the majority have succumbed to the disease. The United States of America and Italy are some of the pandemic’s worst casualties, where many people were killed by the lethal virus (Goodell, 2020). Some people have in the end lost more than one member of the family because of the disease, and in some worse case scenarios, the illness has claimed a whole family.
In conclusion, this paper has highlighted the impacts of the Covid-19 pandemic on the economy, social life, education, religion, and family units. Many countries and businesses had underestimated the disease’s impact before they later suffered from the consequences. Therefore, international bodies, such as the World Health Organization, need to help developing countries establish critical management healthcare systems, which can help to deal with the future pandemics.
Goodell, J. W. (2020). COVID-19 and finance: Agendas for future research. Finance Research Letters , 35 , 101512. Web.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, March 19). The Impact of COVID-19 Pandemic. https://studycorgi.com/the-impact-of-covid-19-pandemic/
"The Impact of COVID-19 Pandemic." StudyCorgi , 19 Mar. 2022, studycorgi.com/the-impact-of-covid-19-pandemic/.
StudyCorgi . (2022) 'The Impact of COVID-19 Pandemic'. 19 March.
1. StudyCorgi . "The Impact of COVID-19 Pandemic." March 19, 2022. https://studycorgi.com/the-impact-of-covid-19-pandemic/.
Bibliography
StudyCorgi . "The Impact of COVID-19 Pandemic." March 19, 2022. https://studycorgi.com/the-impact-of-covid-19-pandemic/.
StudyCorgi . 2022. "The Impact of COVID-19 Pandemic." March 19, 2022. https://studycorgi.com/the-impact-of-covid-19-pandemic/.
This paper, “The Impact of COVID-19 Pandemic”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: March 19, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Editor in Chief's Introduction to Essays on the Impact of COVID-19 on Work and Workers
On March 11, 2020, the World Health Organization declared that COVID-19 was a global pandemic, indicating significant global spread of an infectious disease ( World Health Organization, 2020 ). At that point, there were 118,000 confirmed cases of the coronavirus in 110 countries. China had been the first country with a widespread outbreak in January, and South Korea, Iran and Italy following in February with their own outbreaks. Soon, the virus was in all continents and over 177 countries, and as of this writing, the United States has the highest number of confirmed cases and, sadly, the most deaths. The virus was extremely contagious and led to death in the most vulnerable, particularly those older than 60 and those with underlying conditions. The most critical cases led to an overwhelming number being admitted into the intensive care units of hospitals, leading to a concern that the virus would overwhelm local health care systems. Today, in early May 2020, there have been nearly 250,000 deaths worldwide, with over 3,500,000 confirmed cases ( Hopkins, 2020 ). The human toll is staggering, and experts are predicting a second wave in summer or fall.
As the deaths rose from the virus that had no known treatment or vaccine countries shut their borders, banned travel to other countries and began to issue orders for their citizens to stay at home, with no gatherings of more than 10 individuals. Schools and universities closed their physical locations and moved education online. Sporting events were canceled, airlines cut flights, tourism evaporated, restaurants, movie theaters and bars closed, theater productions canceled, manufacturing facilities, services, and retail stores closed. In some businesses and industries, employees have been able to work remotely from home, but in others, workers have been laid off, furloughed, or had their hours cut. The International Labor Organization (ILO) estimates that there was a 4.5% reduction in hours in the first quarter of 2020, and 10.5% reduction is expected in the second quarter ( ILO, 2020a ). The latter is equivalent to 305 million jobs ( ILO, 2020a ).
Globally, over 430 million enterprises are at risk of disruption, with about half of those in the wholesale and retail trades ( ILO, 2020a ). Much focus in the press has been on the impact in Europe and North America, but the effect on developing countries is even more critical. An example of the latter is the Bangladeshi ready-made-garment sector ( Leitheiser et al., 2020 ), a global industry that depends on a supply chain of raw material from a few countries and produces those garments for retail stores throughout North America and Europe. But, in January 2020, raw material from China was delayed by the shutdown in China, creating delays and work stoppages in Bangladesh. By the time Bangladeshi factories had the material to make garments, in March, retailers in Europe and North American began to cancel orders or put them on hold, canceling or delaying payment. Factories shut down and workers were laid off without pay. Nearly a million people lost their jobs. Overall, since February 2020, the factories in Bangladesh have lost nearly 3 billion dollars in revenue. And, the retail stores that would have sold the garments have also closed. This demonstrates the ripple effect of the disruption of one industry that affects multiple countries and sets of workers, because consider that, in turn, there will be less raw material needed from China, and fewer workers needed there. One need only multiply this example by hundreds to consider the global impact of COVID-19 across the world of work.
The ILO (2020b) notes that it is difficult to collect employment statistics from different countries, so a total global unemployment rate is unavailable at this time. However, they predict significant increase in unemployment, and the number of individuals filing for unemployment benefits in the United States may be an indicator of the magnitude of those unemployed. In the United States, over 30 million filed for unemployment between March 11 and April 30 ( Bureau of Labor Statistics, 2020 ), effectively this is an unemployment rate of 18%. By contrast, in February 2020, the US unemployment rate was 3.5% ( Bureau of Labor Statistics, 2020 ).
Clearly, COVID-19 has had an enormous disruption on work and workers, most critically for those who have lost their employment. But, even for those continuing to work, there have been disruptions in where people work, with whom they work, what they do, and how much they earn. And, as of this writing, it is also a time of great uncertainty, as countries are slowly trying to ease restrictions to allow people to go back to work--- in a “new normal”, without the ability to predict if they can prevent further infectious “spikes”. The anxieties about not knowing what is coming, when it will end, or what work will entail led us to develop this set of essays about future research on COVID-19 and its impact on work and workers.
These essays began with an idea by Associate Editor Jos Akkermans, who noted to me that the global pandemic was creating a set of career shocks for workers. He suggested writing an essay for the Journal . The Journal of Vocational Behavior has not traditionally published essays, but these are such unusual times, and COVID-19 is so relevant to our collective research on work that I thought it was a good idea. I issued an invitation to the Associate Editors to submit a brief (3000 word) essay on the implications of COVID-19 on work and/or workers with an emphasis on research in the area. At the same time, a group of international scholars was coming together to consider the effects of COVID-19 on unemployment in several countries, and I invited that group to contribute an essay, as well ( Blustein et al., 2020 ).
The following are a set of nine thoughtful set of papers on how the COVID-19 could (and perhaps will) affect vocational behavior; they all provide suggestions for future research. Akkermans, Richardson, and Kraimer (2020) explore how the pandemic may be a career shock for many, but also how that may not necessarily be a negative experience. Blustein et al. (2020) focus on global unemployment, also acknowledging the privileged status they have as professors studying these phenomena. Cho examines the effect of the pandemic on micro-boundaries (across domains) as well as across national (macro) boundaries ( Cho, 2020 ). Guan, Deng, and Zhou (2020) drawing from cultural psychology, discuss how cultural orientations shape an individual's response to COVID-19, but also how a national cultural perspective influences collective actions. Kantamneni (2020) emphasized the effects on marginalized populations in the United States, as well as the very real effects of racism for Asians and Asian-Americans in the US. Kramer and Kramer (2020) discuss the impact of the pandemic in the perceptions of various occupations, whether perceptions of “good” and “bad” jobs will change and whether working remotely will permanently change where people will want to work. Restubog, Ocampo, and Wang (2020) also focused on individual's responses to the global crisis, concentrating on emotional regulation as a challenge, with suggestions for better managing the stress surrounding the anxiety of uncertainty. Rudolph and Zacher (2020) cautioned against using a generational lens in research, advocating for a lifespan developmental approach. Spurk and Straub (2020) also review issues related to unemployment, but focus on the impact of COVID-19 specifically on “gig” or flexible work arrangements.
I am grateful for the contributions of these groups of scholars, and proud of their ability to write these. They were able to write constructive essays in a short time frame when they were, themselves, dealing with disruptions at work. Some were home-schooling children, some were worried about an absent partner or a vulnerable loved one, some were struggling with the challenges that Restubog et al. (2020) outlined. I hope the thoughts, suggestions, and recommendations in these essays will help to stimulate productive thought on the effect of COVID-19 on work and workers. And, while, I hope this research spurs to better understand the effects of such shocks on work, I really hope we do not have to cope with such a shock again.
- Akkermans J., Richardson J., Kraimer M. The Covid-19 crisis as a career shock: Implications for careers and vocational behavior. Journal of Vocational Behavior. 2020; 119 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blustein D.L., Duffy R., Ferreira J.A., Cohen-Scali V., Cinamon R.G., Allan B.A. Unemployment in the time of COVID-19: A research agenda. Journal of Vocational Behavior. 2020; 119 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bureau of Labor Statistics (2020). Labor Force Statistics from the Current Population Survey. Retrieved May 6, 2020 from https://data.bls.gov/cgi-bin/surveymost .
- Cho E. Examining boundaries to understand the impact of COVID-19 on vocational behaviors. Journal of Vocational Behavior. 2020; 119 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Guan Y., Deng H., Zhou X. Understanding the impact of the COVID-19 pandemic on career development: Insights from cultural psychology. Journal of Vocational Behavior. 2020; 119 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Johns Hopkins (2020) Coronavirus Outbreak Mapped: Retrieved May 5, 2020 from https://coronavirus.jhu.edu/map.html .
- International Labor Organization ILO monitor: COVID-19 and the world of work. Third edition updated estimates and analysis. 2020. https://www.ilo.org/wcmsp5/groups/public/@dgreports/@dcomm/documents/briefingnote/wcms_743146.pdf Retrieved May 5, 2020 from:
- International Labor Organization (2020b) COVID-19 impact on the collection of labour market statistics. Retrieved May 6, 2020 from: https://ilostat.ilo.org .
- Kantamneni, N. (2020). The impact of the COVID-19 pandemic on marginalized populations in the United States: A research agenda. Journal of Vocational Behavior, 119 . [ PMC free article ] [ PubMed ]
- Kramer A., Kramer K.Z. The potential impact of the Covid-19 pandemic on occupational status, work from home, and occupational mobility. Journal of Vocational Behavior. 2020; 119 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Leitheiser, E., Hossain, S.N., Shuvro, S., Tasnim, G., Moon, J., Knudsen, J.S., & Rahman, S. (2020). Early impacts of coronavirus on Bangladesh apparel supply chains. https://www.cbs.dk/files/cbs.dk/risc_report_-_impacts_of_coronavirus_on_bangladesh_rmg_1.pdf .
- Restubog S.L.D., Ocampo A.C., Wang L. Taking control amidst the Chaos: Emotion regulation during the COVID-19 pandemic. Journal of Vocational Behavior. 2020; 119 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rudolph C.W., Zacher H. COVID-19 and careers: On the futility of generational explanations. Journal of Vocational Behavior. 2020; 119 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Spurk D., Straub C. Flexible employment relationships and careers in times of the COVID-19 pandemic. Journal of Vocational Behavior. 2020; 119 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- World Health Organization (2020). World Health Organization Coronavirus Update. Retrieved May 5, 2020 from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 .
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The impact of the COVID-19 pandemic on higher education: Assessment of student performance in computer science
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Department of Computer Science, Lublin University of Technology, Lublin, Poland, Systems Research Institute, Polish Academy of Sciences, Warsaw, Poland
Roles Conceptualization, Formal analysis, Software, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Computer Science, Lublin University of Technology, Lublin, Poland
Roles Data curation, Software
- Małgorzata Charytanowicz,
- Magdalena Zoła,
- Waldemar Suszyński

- Published: August 14, 2024
- https://doi.org/10.1371/journal.pone.0305763
- Reader Comments
The COVID-19 pandemic had radically changed higher education. The sudden transition to online teaching and learning exposed, however, some benefits by enhancing educational flexibility and digitization. The long-term effects of these changes are currently unknown, but a key question concerns their effect on student learning outcomes. This study aims to analyze the impact of the emergence of new models and teaching approaches on the academic performance of Computer Science students in the years 2019–2023. The COVID-19 pandemic created a natural experiment for comparisons in performance during in-person versus synchronous online and hybrid learning mode. We tracked changes in student achievements across the first two years of their engineering studies, using both basic (descriptive statistics, t-Student tests, Mann-Whitney test) and advanced statistical methods (Analysis of variance). The inquiry was conducted on 787 students of the Lublin University of Technology (Poland). Our findings indicated that first semester student scores were significantly higher when taught through online (13.77±2.77) and hybrid (13.7±2.86) approaches than through traditional in-person means as practiced before the pandemic (11.37±3.9, p-value < 0.05). Conversely, third semester student scores were significantly lower when taught through online (12.01±3.14) and hybrid (12.04±3.19) approaches than through traditional in-person means, after the pandemic (13.23±3.01, p-value < 0.05). However, the difference did not exceed 10% of a total score of 20 points. With regard to the statistical data, most of the questions were assessed as being difficult or appropriate, with adequate discrimination index, regardless of the learning mode. Based on the results, we conclude that we did not find clear evidence that pandemic disruption and online learning caused knowledge deficiencies. This critical situation increased students’ academic motivation. Moreover, we conclude that we have developed an effective digital platform for teaching and learning, as well as for a secure and fair student learning outcomes assessment.
Citation: Charytanowicz M, Zoła M, Suszyński W (2024) The impact of the COVID-19 pandemic on higher education: Assessment of student performance in computer science. PLoS ONE 19(8): e0305763. https://doi.org/10.1371/journal.pone.0305763
Editor: Prabhat Mittal, Satyawati College (Eve.), University of Delhi, INDIA
Received: October 15, 2023; Accepted: June 4, 2024; Published: August 14, 2024
Copyright: © 2024 Charytanowicz et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are available at the following link: https://zenodo.org/records/11583297 .
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
1. Introduction
The COVID-19 pandemic brought with it a number of health, economic and social consequences. Indeed, the spread of the SARS-CoV-2 virus turned out to be so dangerous that many countries implemented new regulations in the educational field to limit physical contact. The pandemic-induced school shutdowns and sudden transition to remote teaching and learning at all levels of education. This change-over generated a number of technical and social problems [ 1 – 6 ]. These problems had also affected the academic community, although online or blended learning methods were implemented before the COVID-19 pandemic [ 7 ].
On March 12, 2020, a state of epidemic emergency was declared in Poland, and a week later–a state of pandemic. In consequence, the Minister of Science and Higher Education issued a regulation on the temporary suspension of the functioning of education institutes, lasting from March 12 till 25 2020 [ 8 , 9 ]. On March 25, 2020, the education system, including higher education, was switched to online teaching and learning, as necessitated by the need to maintain social distancing measures. Universities had to adapt to the circumstances almost overnight. However, many universities were not fully prepared with regard to technical capabilities, educational resources and the skills of the teaching staff in organizing distance education [ 10 – 12 ]. Before the COVID-19 pandemic, the applicable regulations of the Ministry of Science and Higher Education did not encourage the authorities of most universities to invest in technologies for conducting fully remote studies. Poland was, however, not an exception in this respect. Many old, prestigious universities in Europe were also reserved about remote learning, and the virtual learning environment was mainly used as a teaching aid.
Fortunately, the information revolution had by this time developed more flexible approaches to learning with the form of Information and Communication Technology (ICT). Indeed, it is one of the leading factors that affect current teaching methodology [ 13 – 18 ]. E-learning systems, their accessibility and functionality, have provided new possibilities to acquire knowledge and to ease the burden of learning. As an outcome, remote teaching and learning are often seen as promising solutions that offer high flexibility and a learner-centered approach that enables students to learn at their own pace [ 19 , 20 ]. Thus, the role of the teacher in the classroom has transformed from that of being the font of knowledge, to an instructional manager identifying relevant resources and creating collaborative learning opportunities. Moreover, online assessments have become increasingly important and now represent one of the most critical aspects of the educational process. Unfortunately, the role of ICT in higher education is still somewhat controversial.
The extreme situation caused by the COVID-19 pandemic provided an opportunity to revise our approach both to traditional and online learning, yet also posing challenges for the future of education systems. The main question of our research was whether the sudden transition to online teaching and learning caused by the COVID-19 pandemic had a negative impact on students academic performance and upon the reliability of the assessment process. We believe that our study can help to reduce the controversies related to remote learning and teaching.
2. Related works
Before the year 2020, the principal recipients of remote education were adults participating in professional development courses [ 21 ]. The COVID-19 pandemic outbreak, however, resulted in increased interest in methods of education that do not require physical meeting between students and teachers. The closure of educational institutions to mitigate the spread of COVID-19 compelled schools and universities to find alternative ways of continuing their operations. This led to the widespread adoption of online learning (e-learning).
The use of e-learning platforms has enabled the transformation of the traditional model of education in which the lecturer transmitted knowledge, into a model of supervised self-education. A separate line of research has been dedicated to the impact of remote education on university students, who are predominantly young adults, and, as such, are less subject to parental supervision. Topics under study include student attitudes towards distance learning [ 22 , 23 ], the technologies and learning platforms utilized [ 24 – 26 ], and the impact of network quality on the smoothness of classes [ 22 , 27 ].
A relatively well researched aspect of e-learning is the analysis of its advantages and disadvantages in comparison to traditional learning [ 28 – 30 ], including its application during the COVID-19 pandemic [ 31 – 34 ]. Undoubtedly, remote education has its benefits, among others, flexibility, speed, time savings [ 35 , 36 ], as well as better use of the infrastructure and organizational savings for the institution [ 37 ]. Distance learning in the form of e-learning also comes with drawbacks, for example, limited interpersonal contacts [ 38 ], lack of immediate feedback [ 39 , 40 ], and problems with self-discipline and adaptability [ 41 – 43 ]. Considering its strengths and weaknesses, e-learning can be viewed as either a replacement or augmentation of traditional approaches to education.
An integral part of remote education is the verification of its results. The topic was covered in literature in the pre-COVID era [ 44 – 46 ], but much less so during the pandemic [ 47 , 48 ]. Our work focuses on the analysis of student performance under the e-learning setup during COVID-19 related confinement and afterwards. The differentiating characteristic of this paper is the fact that it covers a longer period of time, unlike some other research focusing only on a single academic semester [ 49 ].
The COVID-19 pandemic has provided the opportunity to advance usage of online platforms and digital media, as well as to create new education strategies. It should be noted that most students (and instructors) adapted successfully to online teaching and learning [ 50 , 51 ]. However, certain studies [ 52 – 54 ] have indicated negative student feedback. In the year 2023, education has returned to more traditional teaching/learning approaches after more than two years of online learning.
The outbreak of COVID-19 presented a serious challenge to academic education by enforcing a drastic change in the teaching methods. For this reason, we formulated the following research questions:
- How had the COVID-19 pandemic change applied teaching and learning strategies?
- Did the COVID-19 pandemic have a disruptive effect on the academic performance of students resulting in knowledge deficiency?
- How did the change from in-person to online learning affect the reliability of student assessment?
The rest of the paper is structured as follows. Section 3 presents the context of the study, materials and methods. Section 4 explains the results obtained. Sections 5 and 6 conclude our work and describe limitations and future scope.
3. Materials and methods
3.1. design and context.
The research was conducted in the Department of Computer Science of the Lublin University of Technology in Poland, the largest public technical university in the Lublin voivodship. This was a cross-sectional study carried out among students who were enrolled in the first semester of engineering studies in the academic years 2019/2020, 2020/2021 and 2021/2022 (from October to July). Because of the COVID-19 pandemic, the courses of interest in this study were conducted in different delivery formats (in-person, synchronous online and hybrid).
Traditional in-person course delivery format included lectures and laboratories. The former involved, primarily, oral presentations given to a group of students. A teacher-centered approach to learning was applied with discussion and multimedia presentation, as well as whiteboard or chalkboard visual aids to emphasize important points in the lecture. Moreover, a Learning Management System (Moodle LMS) was incorporated within the lectures to develop, organize, deliver and manage didactic materials and assess the effectiveness of education via tests, surveys or assignments. This tool was also employed to provide discussion forums. The faculty used the activity Quiz as a student self-assessment tool, as well as to determine knowledge and skills.
With regard to laboratory work, practical classes were conducted in programming laboratories for the selected courses. In such a teaching/learning format, we found that most students preferred working alone or conducting discussions with their partners or their neighbors.
All students used online manuals or didactic materials delivered by Moodle LMS. Final exams were held at the University via Moodle LMS through in-person proctoring, as this approach allowed the introduction of a live person to monitor the activity of students in a testing environment.
In the synchronous online course format, students obtained theoretical and practical education entirely online via Microsoft Teams by way of video meetings and Moodle LMS. Meetings in Teams include audio, video and screen sharing. All lectures were delivered synchronously using MS Teams. Practical sessions were conducted through online synchronous video meetings in small student groups. Interaction occurred via the discussion board, while MS Teams was also employed to enable scheduled online consultations. Supporting materials (videos, presentations, tasks to do, quizzes, and other didactic materials) were provided to the students through the Moodle LMS. Final exams were conducted under controlled conditions via Moodle LMS through online live proctoring by accepting screen, video and audio sharing.
The hybrid course delivery format combined in-person and online strategies. Students obtained theoretical education entirely online as synchronous sessions by way of MS Teams and Moodle LMS, whilst practical education was obtained through the traditional in-person format, in small student groups. Final exams were held at the University via Moodle LMS through in-person proctoring.
We analyzed exam scores across the first two years of the engineering studies using anonymous data from the Moodle. The Research Ethics Committee of Lublin University of Technology approved the study (Ethical Approval Reference: 3/2023).
3.2. Course selection
The following criteria were used to select the courses:
- the courses covered algorithms and programming,
- the courses had unchanged objectives and learning outcomes during the investigated period,
- the courses were conducted by the same instructors using to the same tools and methods.
Two compulsory courses met these criteria: 1 –Introduction to Computer Science and 2 –Numerical Analysis Algorithms. Both courses were conducted in the Polish language and they provided fundamental knowledge for all areas of Computer Science learning and skills development. Enrolled students were obligated to complete 30 lesson hours of theory and 30 lesson hours of practical experience within a course length of 15 weeks. In the full-time option, four hours of classes were given each course week, and were distributed into two two-hour sessions. Herein, the first consisted of a master class lecture and the second consisted of an interactive problem-based learning laboratory. In the part-time option, the number of in-person teaching hours was reduced to half and classes were held, on average, twice a month, on Saturday and Sunday.
The Introduction to Computer Science course is taught in the first year and is covered in the first semester. Students who successfully completed the course gained five credits, according to the European Credit Transfer and Accumulation System (ECTS). The intention of the offered course is to provide students with knowledge of standard algorithms and data structures, and to provide them with the skills to analyze both the theoretical complexity of algorithms and their practical behaviors. The course covers the following topics:
- Introduction to algorithms and problem-solving techniques.
- Basic programming concepts, types, sequential data structures.
- Programming in Python.
- Searching and sorting algorithms.
- Examples of algorithms, algorithmic strategies.
- Testing and documenting programming code.
- Asymptotic notation and complexity analysis.
- Analyzing program code for correctness, efficiency, and errors.
- Automata theory and formal languages. Turing machine.
- Classes P and NP.
The knowledge and skills to implement and solve algorithmic problems using the mentioned algorithms are developed using Python.
The Numerical Analysis Algorithms course is taught in the second year and is covered in the third semester. Successful completion awards students with five credits, according to ECTS. The primary objective of the course is to develop basic understanding of numerical algorithms, as well as the skills to implement algorithms to solve computer-based mathematical problems. The course covers the following topics:
- Basic numerics, floating-point representation, convergence.
- Horner’s scheme.
- The theory of interpolation: Lagrange polynomial, Hermite interpolation, Neville’s iterative formula.
- Least square approximation.
- Numerical integration: Newton-Cotes formulas, Gaussian quadrature.
- Direct methods for solving systems of linear equations: Gaussian elimination, LU factorization, Cholesky decomposition.
- Householder method.
- Solving nonlinear equations and systems of nonlinear equations: Bisection method, fixed-point iteration, Newton’s method.
- Runge-Kutta methods for ordinary differential equations.
- Characteristic polynomial and eigenvalues.
The knowledge and skills to implement and solve algorithmic problems using the mentioned algorithms were developed using C++ due to its object-oriented programming with high performance, efficient memory management, low-level access to hardware and a rich standard library, including mathematical functions commonly used in numerical algorithms. These allow students to write efficient and customizable numerical algorithms. Objective C++ was one of the courses of the first year of studies.
3.3. The study participants
Study participants were selected from Computer Science students who were enrolled in the two mentioned compulsory courses: Introduction to Computer Science (ICS) (first semester) and Numerical Analysis Algorithms (NAA) (third semester). The first group of students began their studies in the academic year 2019/2020 in a traditional in-person course delivery format that was interrupted because of the confinement. They then continued their studies utilizing the synchronous online format. The second group consisted of students who began their studies in academic year 2020/2021 in the synchronous online format and continued these activities in a hybrid format. The third group of students began their studies in academic year 2021/2022 in a hybrid format that returned to an in-person format in the year 2022/2023. Online learning was supported by Moodle and MS Teams.
Only students enrolled in either the ICS and NAA courses participated in our research. Students who interrupted their studies and did not complete the courses were excluded. Thus, the study group included students who were enrolled in both courses and took both final exams. A total of 787 participants were selected. Table 1 summarizes the study participant groups according to education strategy.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0305763.t001
Males constituted 87.5% of the total study participants, while females constituted 12.5%. Regarding nationality, the majority, i.e. 85.5%, came from Poland, while 14.5% came from other countries, mainly Ukraine.
3.4. Online exam quizzes
In this study, the Moodle platform provided by the Computer Science Department from the Lublin University of Technology was applied to conduct the final exam process. Comparative analysis of student academic performance was anchored on the results obtained in their final exams. Final exams were carried through the Moodle platform using Quiz activity . All exams comprised questions of various types, including Multiple Choice , Short Answer , Numerical and Essay as follows:
- Multiple choice questions were employed for evaluating both theoretical and practical contents. For our purpose, the option Multiple answers are allowed was used. Multiple answers questions enable one or more answers to be chosen by providing check boxes next to the answers. We used a negative grade percentage for wrong answers, so that simply ticking all choices did not necessarily generate a full grade. If the sum of partial grades was negative, then the total grade for this question would be zero [ 55 ].
- Short answer or numerical questions were used to evaluate theoretical and practical contents. In a short answer question, the student types in a word or phrase in response to a question. This must exactly match one of the acceptable answers. Numerical questions resembled short-answer questions. Here, the difference was that numerical answers were allowed to have an accepted error for number.
- Essay questions were used to evaluate practical contents, mainly programming and coding skills. We employed essay-type questions to provide the option of answering by entering text online. The option Require the student to enter text was chosen. The Response format option was set to Plain text , monospaced font to improve the readability of code by ensuring consistent and clear alignment. This is particularly helpful for maintaining an organized layout. The essay questions had to be marked manually by the course instructor.
The number of multiple choice questions and short answer / numerical questions was comparable. One question was an essay question. Questions were created and stored separately in a Question bank and were organized into 10 categories according to the implemented curricula and learning outcomes. Each category consisted of at least 50 questions. Quiz settings were as follows:
- Quizzes included 20 questions worth 20 points. There were two categories of questions: theoretical and practical.
- Students were allowed to have one attempt at each quiz. The time limit option was set to 60 minutes.
- Students were not allowed to open other windows or programs while taking these quizzes.
- A password was required. The option Block concurrent connections was checked.
- The Choose Sequential navigation method was employed to compel the student to progress through the questions in order and not return to a previous question or skip to a later one.
- The timeframe when the students were able to see feedback was set to the option After the quiz is closed and the option Whether correct was checked.
- Employed questions were assessed for quality and modified for re-use in the next academic year.
Students were tested using the same evaluation methods and types of questions in in-person, synchronous online and hybrid groups. The Moodle platform collected assessment data and generated report statistics. The data containing students’ exam results (points) were collected and exported from the Moodle platform as.xlsx files.
3.5. Quiz report statistics
Quiz statistics provided test statistics and quiz structure analysis. The test statistics gave information on how students performed on a quiz, and employed descriptive statistics: average grade, median grade, standard deviation of grades, skewness and kurtosis. A detailed analysis of each question was given in quiz structure analysis, and applied the following measures: facility index, discrimination index and discriminative efficiency. Discriminative efficiency is a measure similar to discrimination index [ 55 ].
Facility index.
In this work, facility index of a question was determined by the average score divided by the maximum score and represented as a percentage. A higher value indicated an easier question. The interpretation of its values is given in Table 2 [ 55 ].
https://doi.org/10.1371/journal.pone.0305763.t002
Discrimination index.
Discrimination index is the correlation between the score for this question and the score for the whole quiz represented as a percentage. If the score for the question and the score for the test are well correlated, the question can be categorized as a question with good discrimination. The maximum discrimination requires a facility index in the range 30%–70%, although this is not tantamount to high discrimination index. Discrimination index values should be interpreted according to Table 3 [ 55 ].
https://doi.org/10.1371/journal.pone.0305763.t003
A negative value of a discrimination index would mean that the best students got this question wrong more often than the worst students. A discrimination index of zero would mean it was a poor discriminator between good and bad students. Discrimination index is considered excellent when the value is higher than 40%, and considered good when it ranges from 20% to 40%.
Discriminative efficiency.
The discriminative efficiency estimates how good the discrimination index is relative to the difficulty of the question. This attempts to discriminate between students of different ability, and the higher the value, the better is the question at discriminating between students of different abilities [ 55 ]. Values between 30%–50% provide adequate discrimination, while those above 50% provide very good discrimination.

3.6. Statistical analysis
Data collected was tabulated, and analysis was carried out by applying simple percentage analysis, as well as descriptive analysis, using mean, standard deviation and inferential analysis such as t-Student tests and ANOVA [ 56 , 57 ]. We performed non-parametric alternatives such as a Mann-Whitney U test and the Kruskal-Wallis test to compare samples that cannot be assumed to be normally distributed [ 58 , 59 ]. Statistical significance was set at p<0.05. Data analysis was performed using the Statistica Package, Version 13 (TIBCO Software Inc.).
Participants’ profile
Our study included 787 Computer Science students, aged 18 to 22 years. The participant background characteristics revealed that most students were male (87.5%) and native (Polish; 85.5%). Furthermore, most of the students were enrolled in full-time studies (85.5%) ( Table 4 ).
https://doi.org/10.1371/journal.pone.0305763.t004
The percentages of the students who began their studies in the academic years 2019/2020, 2020/2021 and 2021/2022 were comparable, around 30%. An important aspect of the analysis was the availability of data from the pre-pandemic period that was relevant for our investigations.
Comparison of in-person, synchronous online and hybrid learning
The comparison of in-person, synchronous online, and hybrid teaching methods in student learning outcomes based on background characteristics is presented in Tables 5 and 6 .
https://doi.org/10.1371/journal.pone.0305763.t005
https://doi.org/10.1371/journal.pone.0305763.t006
The findings indicated that for the first semester course Introduction to Computer Science, the relation between learning outcomes and student gender was insignificant (p = 0.427). Moreover, the relation between learning outcomes and study option was also insignificant (p = 0.223). However, there was statistically significant difference between learning outcomes and residency status (p < 0.001). The findings indicated that during in-person and online studies, native students had significantly higher learning outcomes than did non-native students (p < 0.001). In addition, full-time students of online studies had significantly higher learning outcomes (p = 0.002) than did part-time students.
Regarding the learning outcomes of the students as obtained in the third semester course Numerical Analysis Algorithms, gender and study options were also insignificant (p = 0.834; p = 0.157) in relation to learning outcomes. In contrast, residency status was significant (p < 0.001). The findings indicate that native students had significantly higher learning outcomes than did non-native students (p < 0.001). Moreover, full-time students of online studies had significantly higher learning outcomes as compared to part-time students (p = 0.011).
The comparison of teaching methods in participant performance based on different semesters (courses) is presented in Table 7 .
https://doi.org/10.1371/journal.pone.0305763.t007
The differences in mean scores related to the first semester course Introduction to Computer Science, during online and hybrid studies, were significantly higher compared to in-person studies (LSD post-hoc, p < 0.001). However, mean scores related to the third semester course Numerical Analysis Algorithms, during online and hybrid studies, were significantly lower in comparison to in-person studies (LSD post-hoc, p < 0.001). Switching to traditional in-person studies in the academic year 2022/2023 did not degrade student performance.
Quiz quality assessment
Tables 8 and 9 reveal the facility index, discrimination index and discriminative efficiency values from the final exams held from 2019/2020 to 2022/2023.
https://doi.org/10.1371/journal.pone.0305763.t008
https://doi.org/10.1371/journal.pone.0305763.t009
The lowest mean facility index was 47% ± 25%, while the highest mean facility index was 59% ± 20%. Moreover, the mean discrimination index was located within the range between 31% and 37% and the mean discriminative efficiency was found within the range between 43% and 54%. The results indicate, with regard to facility index, that most of the questions were moderately difficult, yet about right for the average student, and demonstrated adequate discrimination—regardless of the course delivery format.
5. Discussion and conclusions
In our study, we compared the learning outcomes of Computer Science students who were taught through synchronous online and hybrid systems, to those who learned in the traditional in-person system, and this revealed significantly higher learning outcomes when taught through online and hybrid systems versus in-person. It is worth noting that student scores showed an increasing trend in the years 2019–2023. Despite this, the significant difference in the results of the students’ final examination was not too large–as it did not exceed 10% of the maximal score.
A comparison between the student groups demonstrates that utilizing synchronous online learning can result in more enhanced educational opportunities for students. However, our findings indicated that native students had significantly higher learning outcomes than did non-native students. The reason could be that the study courses were held in Polish, which is a difficult language for non-native students to learn and utilize.
Several research studies have shown that online learning and the combination of online and in-person learning systems have positive and powerful roles in enhancing the effectiveness of education [ 19 , 29 , 41 , 47 , 60 ]. However, along with enhanced accessibility and flexibility, pure online learning also has several disadvantages, notably, the lack of interpersonal contacts and student satisfaction. In the hybrid form, however, flexibility and accessibility are enhanced, while human connection occurs.
Our results indicated that synchronous online learning could be appreciated as a successful method of conducting Computer Science education and can be used as a tool supporting traditional in-person methods. Although this approach is a little less flexible for teachers and students, and requires reliable technology, in comparison to asynchronous learning, this allows for more real time engagement and feedback [ 61 ].
As the effective measurement of knowledge acquired is an important component of Computer Science education, the use of the Moodle quizzes activity as a continuous assessment of students was analyzed according to statistical data such as the facility index, discrimination index and discriminative efficiency. Out of the exam tests conducted from the academic year 2019/2020 to 2022/2023, the mean facility index scores ranged from 47% to 59% and the mean discrimination index ranged from 31% to 37%. The statistic results indicated that, regarding facility index, most of the questions were moderately difficult and about right for the average student regardless of the course delivery format, and that a consistent and adequate level of discrimination indices was maintained. In addition, the similar results obtained in our study no matter the year, with three different groups of students, also confirmed the validity and reliability of the designed exam tests.
Although online learning requires extensive self-discipline, it allows universities to integrate new technologies into their offer, and hence, effectively facilitate the student learning process. After the COVID-19 pandemic, there has been a quick transition back to in-person teaching, but still there are many proffered activities being in an online format. At present, many students state that they prefer to learn through hybrid learning methods. Furthermore, several studies have shown that e-learning methods are used widely by students outside of their formal curricula for continuing their professional education [ 62 ]. This indicates that students and professionals appreciate and take advantage of self-paced learning environments in which they control their learning pace, information flow, selection of learning activities, as well as their time management. Thus, the digital transformation of the educational process has become a necessity to meet shifting student demands and seems to be one of the leading factors that affect current teaching methodology.
It is worth noting that the extreme situation caused by the COVID-19 pandemic provided an opportunity to revise our approach, both to traditional and online learning, but also posed challenges for the future of education systems. In conclusion, the results of the analysis allow us to answer the questions formulated before in the following way.
- The COVID-19 confinement caused online education, which previously was mainly used as an addition to traditional learning methods, to become the mainstream, in particular, in Computer Science.
- The COVID-19 pandemic did not have a disruptive effect that resulted in knowledge deficiency with regard to the academic performance of Computer Science students. In contrast, this situation increased student academic motivation. Indeed, students demonstrated higher exam scores during subsequent two academic years.
- Despite the change from in-person to online learning, the reliability of student assessment remained at similar levels.
6. Limitations and future works
Our context is algorithms and programming in the first two years of the engineering studies program. While we believe that the long period under study is an advantage of this work, its limitation is the fact that it focuses only on the students of Computer Science. We based our research on the data comprising the performance of students in only two courses. Moreover, only the exam scores from the 1 st and 3 rd semesters were included in the study. The courses of other semesters were not assessed because they did not meet the required assumptions regarding the course selection. Another limitation of our study was that students could share information about the content of the exam. However, we randomly assigned students to subcategory sets to avoid sharing information. In the future it is worth considering extending the analysis to students of other fields, as well as take into account student performance in more courses.
Acknowledgments
The authors thank Mr Jack Dunster for linguistic improvement of the text.
- View Article
- PubMed/NCBI
- Google Scholar
- 4. Salguero A, Alvarado C, Griswold WG, Porter L. Understanding Sources of Student Struggle in Early Computer Science Courses. In: Proceedings of the 17th ACM Conference on International Computing Education Research. 2021;319–333.
- 8. Poland, Ordinance of the Council of Ministers on establishing certain limitations, orders and prohibitions with respect to the occurrence of the state of epidemic, 31 March 2020, § 14–15.
- 9. Poland, Ordinance of the Council of Ministers on establishing certain limitations, orders and prohibitions with respect to the occurrence of the state of epidemic, 7 August 2020, version as of 29 August 2020, § 25.
- 12. European Union Agency for Fundamental Rights, Coronavirus pandemic in the EU–Fundamental rights implications. Bulletin #2, 21 March-30 April 2020, Publications Office, 2020. https://data.europa.eu/doi/10.2811/441998 .
- 13. Charytanowicz M. E-learning technologies in lifelong learning: opportunities and challenges. In ICERI’2019 Proceedings: 12th International Conference of Education, Research and Innovation. 2019;43,9414–9421.
- 14. Charytanowicz M, Miłosz E, Suszyński W, Stęgierski R, Łukasik E. Internet of things as a challenge for higher education. In INTED 2021: 15th International Technology, Education and Development Conference. 2021;5120–5129.
- 16. Miłosz M, Charytanowicz M, Skublewska-Paszkowska M. Analysis of trends in ICT and its implication in higher education curricula. In INTED 2020: 14th International Technology, Education and Development Conference, 2020;500–509.
- 18. Suszyński W, Stęgierski R, Charytanowicz M. Remote access to networking laboratory, secure and scalable solutions. In The 2020 International Conference on Computational Intelligence, Information Technology and Systems Research. 2020;22–23.
- 19. Makarova E. Effectiveness of traditional and online learning: comparative analysis from the student perspective. In: SHS Web of Conferences 2021;99, 01019.
- 31. Amarneh BM, Alshurideh MT, Al Kurdi BH, Obeidat Z. The Impact of COVID-19 on E-learning: Advantages and Challenges. In The international conference on artificial intelligence and computer vision, 2021;75–89. Cham: Springer International Publishing.
- 38. Singh AK, Yusoff MA, Oo N. A comparative study between traditional learning and e-learning. In Proceedings of Teaching and Learning Open Forum 2009. 2009:1–7. CSM, Sarawak.
- 55. docs.moodle.org [Internet]. Moodle Documentation; c2023 [cited 2023 Sep 26]. https://docs.moodle.org/ .
- 56. Boddy R, Smith G. Statistical methods in practice: For scientists and Technologists. Chichester, U.K: Wiley 2009.
- 57. Doncaster CP, Davey AJH. Analysis of variance and covariance: How to choose and construct models for the Life Sciences. Cambridge: Cambridge University Press 2007.
- 58. Freund RJ, Wilson WJ, Mohr DL. Statistical methods. London, United Kingdom: Academic Press, Amsterdam, Elsevier 2022.
- 59. Sprent P, Smeeton NC. Applied Nonparametric Statistical Methods. Boca Raton: Chapman et Hall/CRC 2007.
- 62. Charytanowicz M. E-learning technologies in lifelong learning: opportunities and challenges. ICERI2019 Proceedings. 2019:9414–21.

- Conferences
- Publications
Long-term effects of COVID-19 on the ocular surface

(Image Credit: AdobeStock/REC Stock Footage)

A team of Turkish investigators lead by Oğuzhan Kılıçarslan, FEBO, FICO, MD, reported that COVID-19 affected thecorneal endothelial cell morphology in patients with ocular symptoms. 1 Kılıçarslan is from the Department of Ophthalmology, Ayancık State Hospital, Sinop, Turkey.
They conducted a study in which they investigated the long-term effects of the virus on corneal endothelial cell morphology in patients with ocular symptoms to assess possible corneal involvement in patients who recovered from the disease.
The study was comprised of 2 groups, the COVID-19 group of patients who had been diagnosed and treated at Istanbul University Cerrahpasa Medical Faculty with confirmed SARS-CoV-2 infection and ocular irritation symptoms and the control group with no ocular pathologies that included age- and sex-matched individuals.
The investigators performed noncontact specular microscopy using the center method 156 days after COVID-19 had been diagnosed to analyze the endothelial cell density (ECD), hexagonality (HEX), coefficient of variation, and central corneal thickness.
Microscopy results
A total of 54 patients who had COVID-19 and had ocular irritation and 72 controls were included.
Specular microscopy showed that the ocular symptoms in the patients who had had COVID-19 included conjunctival hyperemia, foreign body sensation, tearing, ocular secretion, and chemosis. The mean ECDs were 2,770 cells/mm2 in the COVID-19 group and 2,897 cells/mm2 in the control group; the mean HEX was 46.52 in the COVID-19 group and 58.22 ± 13.94 in the control group.
The patients who had had COVID-19 had significantly lower endothelial ECD and HEX levels than controls ( p = 0.003 and p < 0.001, respectively).
Kılıçarslan and colleagues concluded, “COVID-19 can cause long-term alterations in the corneal endothelial cells, leading to decreased ECD and HEX. Future research should focus on the long-term implications of COVID-19 on the corneal health and visual outcomes.”
Kılıçarslan O, Yılmaz Çebi A, Doğan C, Arslan OS. Long-term corneal endothelial parameters of covid-19 patients with ocular surface symptoms. Cornea 2024;43:1124-1127; DOI: 10.1097/ICO.0000000000003552

Study identifies apolipoprotein E as key biomarker for corneal involvement in infectious conjunctivitis

Evaluating safety, efficacy of TP03 for Demodex blepharitis treatment

Study examines the impact of the COVID-19 pandemic on ophthalmology residency and fellowship training

Reflecting on life during a pandemnic

Brazilian retrospective study finds frequency of ocular metastases relatively low

Study: Virus that causes COVID-19 can penetrate blood-retinal barrier and may damage vision
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

- Open access
- Published: 13 August 2024
Natural and socio-environmental factors in the transmission of COVID-19: a comprehensive analysis of epidemiology and mechanisms
- Zhaoyuan Gong 1 na1 ,
- Tian Song 1 na1 ,
- Mingzhi Hu 1 na1 ,
- Qianzi Che 1 ,
- Jing Guo 1 ,
- Haili Zhang 1 ,
- Huizhen Li 1 ,
- Yanping Wang 1 ,
- Bin Liu 1 &
- Nannan Shi 1
BMC Public Health volume 24 , Article number: 2196 ( 2024 ) Cite this article
388 Accesses
18 Altmetric
Metrics details
Purpose of review
There are significant differences in the transmission rate and mortality rate of COVID-19 under environmental conditions such as seasons and climates. However, the impact of environmental factors on the role of the COVID-19 pandemic and the transmission mechanism of the SARS-CoV-2 is unclear. Therefore, a comprehensive understanding of the impact of environmental factors on COVID-19 can provide innovative insights for global epidemic prevention and control policies and COVID-19 related research. This review summarizes the evidence of the impact of different natural and social environmental factors on the transmission of COVID-19 through a comprehensive analysis of epidemiology and mechanism research. This will provide innovative inspiration for global epidemic prevention and control policies and provide reference for similar infectious diseases that may emerge in the future.
Recent findings
Evidence reveals mechanisms by which natural environmental factors influence the transmission of COVID-19, including (i) virus survival and transport, (ii) immune system damage, (iii) inflammation, oxidative stress, and cell death, and (iiii) increasing risk of complications. All of these measures appear to be effective in controlling the spread or mortality of COVID-19: (1) reducing air pollution levels, (2) rational use of ozone disinfection and medical ozone therapy, (3) rational exposure to sunlight, (4) scientific ventilation and maintenance of indoor temperature and humidity, (5) control of population density, and (6) control of population movement. Our review indicates that with the continuous mutation of SARS-CoV-2, high temperature, high humidity, low air pollution levels, and low population density more likely to slow down the spread of the virus.
Peer Review reports
Introduction
Coronavirus disease 2019 (COVID-19) is defined as a disease caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), which is an emerging respiratory infection. COVID-19 can occur through close contact with an infected person. The disease is characterized by high transmission rate, long incubation period, and global spread. On 11 March 2020, this disease was declared a global pandemic by the World Health Organization (WHO) [ 1 ]. The outbreak of COVID-19 has caused many threats and dangers to human health, including increased mortality and morbidity globally [ 2 , 3 ]. The COVID-19 pandemic is challenging the world economy and health systems and demonstrates the extent of global interdependence and the need to address global health threats [ 4 ].
Current research on COVID-19 mainly focuses on vaccines, viruses, hosts and drugs [ 5 ]. In contrast, research on the impact of environmental factors on COVID-19 needs to be further carried out. The incidence of many similar infectious diseases showed seasonal patterns, including human coronaviruses [ 6 ]. COVID-19 is no exception and may have seasonal epidemic peaks. Therefore, understanding which environmental factors influence COVID-19 can allow planning and implementing public health interventions and capacities to reduce the impact of the disease. It will provide innovative inspiration for global epidemic prevention and control policies and provide reference for similar infectious diseases that may emerge in the future.
Although SARS-CoV-2 transmission has been recorded in almost all countries, there is significant spatial and temporal heterogeneity in transmission dynamics, morbidity and mortality across countries, regions and even communities [ 7 ]. Many studies have investigated the correlation between this spatial and temporal heterogeneity and environmental factors, including natural environmental factors and social environmental factors [ 8 ]. Direct or indirect evidence shows that these environmental factors have an impact on the spread and development of COVID-19 [ 9 ].
This research is used in Scopus, ISI scientific network and PubMed database ("climate" OR "climate change" OR "temperature" OR "precipitation" OR "relative humidity" OR "wind speed" OR "sunlight" OR "wind speed" OR “water resources” OR “solar radiation” OR “social environment factor” OR “air pollution” OR “PM2.5” OR “PM10” OR “ozone” OR “NO 2 ” OR “CO” OR “wastewater” OR “heavy metal pollution” OR “sociodemographic characteristics” OR “local policies” OR “socioeconomic activity”) and ("COVID" OR "Coronavirus disease 2019" OR "COVID-19" OR "SARS-CoV-2" OR "Novel Coronavirus" OR "COVID-19 transmission" OR " Novel Coronavirus transmission" OR "COVID-19 confirm case"). Inclusion criteria are all relevant manuscripts that assess the impact of environmental factors on the number of cases and incidence rate of COVID-19. Exclusion criteria include comments, letters, editorials, conference abstracts, and low-quality research.
This review summarizes the impact of environmental factors on the transmission of COVID-19 and summarizes studies from epidemiological evidence to mechanisms. We divide environmental factors into natural environmental factors and social environmental factors. Natural environmental factors include air pollution, temperature, humidity, wind speed, rainfall, solar radiation, soil and water resources. Social environmental factors include sociodemographic characteristics, local policies and socioeconomic activity. Finally, there is a discussion of the potential future directions in this field. Critical assessments of these relationships can enhance estimates of the risk of similar infectious diseases from environmental exposures and guide the design of interventions to slow the spread of the virus and protect vulnerable populations from infection. This will provide innovative inspiration for global epidemic prevention and control policies and provide reference for similar infectious diseases that may emerge in the future.
Natural environment factors and transmission of COVID-19
Native environment factor, temperature and humidity.
The relationship between viral infections and meteorological conditions has been of concern in the past. Researchers from China looked at the link between temperature and humidity in more than 3750,000 confirmed COVID-19 cases from 185 countries. It found that 60.0% of confirmed COVID-19 cases occurred in places with temperatures between 5℃ and 15℃, with a peak of 11.54℃. In addition, about 73.8% of confirmed cases are concentrated in areas with absolute humidity of 3 g/m 3 to 10 g/m 3 [ 10 ]. In Japan, researchers conducted a longitudinal cohort study of 6,529 confirmed COVID-19 cases across 28 geographical areas. The results showed that the increase of the COVID-19 epidemic was significantly correlated with the increase of daily temperature or sunshine duration [ 11 ]. Haque and Rahman found that high temperature and high humidity significantly reduced the spread of COVID-19, respectively. In Bangladesh, more than four-fifths (84.2%) of the total cases were clustered within the average temperature range (26–28℃) [ 12 ]. This is consistent with the results of a previous ecological study, which found that the optimal ambient temperature associated with SARS cases was between 16℃ and 28℃, based on data from Hong Kong, Guangzhou, Beijing and Taiyuan [ 13 ]. The seasonal cycle of respiratory viral diseases has been widely recognized for thousands of years. The temporal trends of COVID-19 transmission presented a periodic fluctuation and reflected the seasonal changes. In terms of time series, in line with the seasons in Brazil, the average temperature and relative humidity from March to May (autumn) had a significant positive effect on new cases, while the months from June to August (winter) and September to November (spring) had a negative effect [ 14 ].
In a systematic review of 17 studies has found that climate parameters may be an important factor in the spread of COVID-19. Cold and dry conditions enhance the spread of the virus [ 15 ]. A systematic review of 62 publications were published between December 2019 and February 2021 on the association between climate factors and the spread of COVID-19, found consistent results that high temperatures may have significantly influenced the spread of COVID-19 and suppressed the pandemic [ 16 ]. Yuan et al. found that they may be negatively associated with daily new cases of COVID-19 in 127 countries when temperature, relative humidity, and wind speed are lower than 20 °C, 70%, and 7 m/s, respectively. In a follow-up study, it found to be inversely associated with daily new cases of COVID-19 in 188 countries when temperatures and relative humidity below 21 °C and 64%, respectively. And in these two studies, the researchers found that temperature and humidity were negatively correlated with the daily number of new COVID-19 cases and deaths [ 17 , 18 ]. In India, researchers found that most COVID-19 cases had surface temperatures between 24 and 30℃ and relative humidity between 50 and 80 percent, which is highly dependent on relative humidity at certain temperatures [ 19 ]. However, some studies [ 20 ] report that SARS-CoV-2 transmission is ineffective with increasing temperature. For the role of meteorological parameters, this contradictory discovery is mainly due to the difference in analysis methods and limitation in data availability of each study.
Solar radiation, sunlight exposure, and wind speed
Other climatological factors can also affect the spread of SARS-CoV-2, previous evidence shows that solar radiation and wind speed also affect the spread of infectious diseases [ 21 , 22 ]. For example, in the tropical state of Rio de Janeiro in Brazil, studies have found that high solar radiation can be shown to be a major climatic factor in curbing the spread of COVID-19. Solar radiation was positively correlated with the infection of COVID-19. There was a significant negative correlation between higher wind speed and lower incidence of COVID-19 [ 23 ]. Researchers in Iran found that areas with low wind speeds and exposure to solar radiation had higher rates of infection, which helped the virus survive [ 24 ]. In a descriptive observational cross-sectional study conducted in France, a significant negative association between sun exposure and COVID-19 mortality was observed [ 25 ]. Another study analyzed the correlation between the meteorological parameters and the transmission of COVID-19 in Baghdad, the capital of Iraq. The results show that temperature, wind speed and solar radiation are the primary meteorological parameters leading to the spread of COVID-19 in Baghdad and are related to the confirmed cases and deaths of COVID-19 [ 26 ]. But a study on the correlation between solar radiation exposure and the COVID-19 pandemic in Jakarta, Indonesia, found different results. The study found no significant correlation between sun exposure and morbidity and death in patients with COVID-19. Sunlight was significantly associated with recovery from COVID-19 [ 27 ]. In the latest study, Al-Khateeb et al. compared the association between multiple regional weather conditions in the Northern hemispheres, Southern hemispheres, and Irbid, Jordan and COVID-19 transmission, found that the relationship between wind speed and spread of COVID-19 was oscillatory and insignificant on a worldwide [ 28 ]. Statistical results may not confirm a specific causal relationship between exposure to solar UV radiation and disease variables such as morbidity and mortality [ 29 ].
Water resource
SARS-CoV-2 deposited on the surface of objects can be washed into the surface runoff by rainfall. Although the waterborne transmission of COVID-19 has not been confirmed, the potential risk cannot be ignored. Research therefore needs to answer whether hydrological conditions (such as river length, lake area, precipitation and volume of water resources) are related to COVID-19 outbreaks. For example, the researchers investigated the associations between hydrological factors such as lake area, river length, precipitation and volume of water resources in 30 regions of China and the incidence of COVID-19. The results showed that the number of confirmed COVID-19 cases was moderately correlated with river length and precipitation, but weakly correlated with water resources [ 30 ]. Precipitation had been analyzed in studies in Indonesia, the United States and Brazil, had not been found to be associated with COVID-19 [ 31 , 32 , 33 ]. However, other studies had also found that precipitation is positively correlated with the spread of COVID-19. Countries with higher rainfall showed an increase in disease transmission. On average, there were 56.01 additional cases per inch/day [ 33 ].
Environmental pollution factor and transmission of COVID-19
Air pollution.
Epidemiologic evidence shows a strong link between air pollution and COVID-19, contributing significantly to the transmission and severity of COVID-19 [ 34 , 35 ]. In the United States, researchers used ecological regression analysis to examine the relationship between long-term (2000–2016) average PM2.5 concentrations and COVID-19 mortality over 3,089 counties. After accounting for many county-level confounders, researchers found that a 1 μg per m 3 increase in PM2.5 was associated with an 11% increase in county-level COVID-19 mortality rate [ 36 ]. The same results were found in another study, in which researchers found a significant positive correlation between 2016 average PM2.5 concentrations in 3,110 US counties and COVID-19 mortality [ 37 ]. An ecological study in Italy found a positive correlation between PM2.5 concentrations and excess mortality associated with COVID-19 in Northern Italy. A one-unit increase in PM2.5 concentration (µg/m 3 ) is associated with a 9% increase in COVID-19 related mortality [ 38 ]. Several ecological studies in other countries such as China, UK and Netherlands had found the same results, with areas with poorer air quality are more likely to have elevated COVID-19 incidence and mortality [ 39 , 40 , 41 ].
Short-term exposure to air pollution may also affect COVID-19, with multiple studies finding that air pollution may affect recovery time, mortality, morbidity, and emergency department visits [ 42 ]. For example, researchers conducted a case-crossover study of 78,255 emergency department visits for COVID-19 in two Canadian provinces. The study found a significant correlation between PM2.5 and emergency department visits for COVID-19 [ 43 ]. In Changsha, China, Liu et al. found that long recovery duration among COVID-19 patients was positively correlated with short-term exposure to PM2.5, NO 2 , and CO [ 44 ]. The researchers also found that COVID-19 patients with both Delta and Omicron had an increased chance of developing early respiratory COVID‐19 manifestations after short-term exposure to air pollution [ 45 ].
In addition to particulate matter (PM), which has been widely studied, a number of studies have also involved carbon monoxide (CO), nitrogen dioxide (NO 2 ), ozone (O 3 ) and other air pollutants [ 46 ]. In a comparative study of the impact of air pollution on COVID-19 in multiple countries, a correlation between pollutant gases and COVID-19 risk was found in the United States, Italy and Spain, while in China the relationship was negative. Factors in air pollution have different associations with COVID-19 risk [ 47 ]. Another study looked at 446,440 COVID-19 cases, covering 4,609 census tracts in southern California. The pooled RR (95%CI) for the incidence of COVID-19 associated with 1-year exposure to NO 2 and O 3 were 1.09 (1.02, 1.17) per 3.2 ppb and 1.06 (1.00, 1.12) per 5.5 ppb respectively [ 48 ]. In Los Angeles, long-term exposure to NO 2 has been associated with an increased risk of COVID-19 cases and mortality. The researchers found that an 8.7 ppb increase in annual mean NO 2 concentrations was associated with a 16–31% increase in the rate of COVID-19 cases and a 35–60% increase in mortality [ 49 ].
The waterborne transmission of COVID-19 has not been confirmed. Early in the SARS-CoV-2 outbreak, it was reported that live SARS-CoV-2 could be isolated from the feces and urine of COVID-19 patients [ 50 ]. And according to the experience accumulated during the SARS epidemic, sewage systems could also be contaminated by the virus [ 51 ]. Different concentrations of SARS-CoV-2 have been detected in wastewater in the Netherlands, Belgium, Australia, and the United States [ 52 , 53 , 54 ]. To date, there have been no studies in the public domain on the persistence and survivability of SARS-CoV-2 in water or wastewater. But a link between the virus and persistence and survival can be found from previous studies of coronaviruses. For example, human coronavirus 229E can survive for 7 days in water at 23 °C [ 55 ]. Researchers performed SARS-CoV-2 RNA detection by real-time RT-PCR and infectivity test on culture cells on three river samples in Milan, Italy. Real-time RT-PCR results showed positive, but infectivity was not effective [ 56 ].
Through the secondary utilization of wastewater and the disposal of medical waste, SARS-CoV-2 can enter the soil environment [ 57 , 58 ]. In China, 20% of soil samples taken near hospitals receiving COVID-19 subjects and Wuhan sewage treatment plants recently tested positive for SARS-CoV-2 RNA, with abundance ranging from 205 to 550 copies/g [ 59 ]. Similar to the research status of viruses in water resources, the activity and infectivity of viruses in soil resources have not been widely studied and confirmed [ 60 ]. But there is no denying that the virus can seriously affect soil health, and improper handling will pose a threat to human and animal health.
Heavy metal pollution
Hydrosphere and pedosphere are essential natural environment factors. Since heavy metals are not biodegradable, heavy metal ions in water and in soil be biologically accumulated via the food chain towards the human body. Most heavy metals, such as arsenic (As), lead (Pb), mercury (Hg), and cadmium (Cd) are considered environmental pollutants [ 61 ]. Previous evidence suggested that heavy metal exposure is associated with higher mortality from influenza or pneumonia [ 62 ]. In the laboratory, heavy metal exposure has been found to play a role in impaired mucociliary clearance, reduced barrier function, airway inflammation, oxidative stress, and apoptosis [ 63 ]. Exposure to these heavy metals after COVID-19 infection may increase the risk of severe COVID-19 through these abnormal or exaggerated immune responses [ 64 ]. Studies had found that exaggerated immune responses are associated with multiple organ system failure, COVID-19 hospitalization, and death [ 65 ].
Chronic exposure to As, Cd, Hg, and Pb has been associated with respiratory dysfunction and respiratory diseases [ 66 ]. Solenkova et al. reviewed English-speaking medical literature to find that Hg, Pb, Cd, and as are associated with cardiovascular disease of atherosclerotic origin [ 67 ]. In additional, epidemiologic studies have found that cumulative exposure to heavy metal mixtures is associated with obesity and its associated chronic diseases, such as hypertension and type 2 diabetes [ 68 ]. These diseases have a significant impact on COVID-19. For example, the most common comorbidities found in COVID-19 cases in clinical studies are hypertension, followed by diabetes. More comorbidities were associated with poorer clinical outcomes. Obesity and type 2 diabetes are risk factors for poor COVID-19 prognosis [ 69 ].
While it is true that heavy metals have impact on COVID-19 patients, there is a lack of direct data linking exposure to heavy metals to the risk and/or severity of COVID-19. In a retrospective analysis of 306 patients confirmed COVID-19 in China, researchers analyzed levels of essential and/or toxic metals (classes) in whole blood, depending on the severity and outcome of the disease. The results found that among severely ill patients, the death group had higher levels of chromium and cadmium and lower levels of arsenic compared to the recovery group [ 70 ]. One study found that COVID-19 patients with elevated levels of chromium, cadmium, mercury and lead in their urine had a poorer prognosis (severe and non-severe) [ 71 ].
Social environment factor and transmission of COVID-19
Evidence linking sociodemographic characteristics to transmission of covid-19.
Droplet or airborne transmission is the main route of SARS-CoV-2 transmission, and higher population density often leads to the long-term spread of COVID-19 [ 72 ]. In Malaysia, areas with a high number of residents and high population density have a greater number of cases in proportion to the population of the area. The correlation between COVID-19 cases and population density was strongest in the central region [ 73 ]. Another study using long-term data on the relationship between external demographic parameters such as total population, population density and weighted population density and the spread of COVID-19 in Malaysia found different results. The results showed that there was a strong and significant positive correlation between total population and COVID-19 cases. However, a weak positive relationship was found between density variables (population density and weighted population density) and the spread of COVID-19 [ 74 ]. But most studies show that increasing population density in turn leads to an increase in COVID-19 cases and deaths [ 75 ]. Population density is thought to have a more significant impact on COVID-19 than meteorological factors. For example, the researchers investigated the correlation of spread and decay durations of the COVID-19 pandemic in China, the United Kingdom, Germany, and Japan with temperature, humidity, and population density. The results showed that propagation duration and decay durations were significantly correlated with population density, and the effect of population density was more significant than that of meteorological factors [ 76 ]. The characteristics of the built environment at different spatial scales caused by different population parameters will also affect the prevention and spread of infectious diseases. Poor housing conditions and high building density can lead to problems with inadequate sanitation facilities, which will create an environment conducive to disease transmission [ 77 ]. In Hong Kong, China, for example, research had shown that high transport accessibility, dense high-rise buildings, higher density of commercial land, and a higher land use mix are associated with a higher risk of being visited by confirmed cases. More green space, higher median household income, and lower commercial land density were associated with a higher risk of housing with confirmed cases [ 78 ].
There are race-related health disparities in the COVID-19 pandemic, with higher morbidity and mortality rates among ethnic minorities. Black workers most affected by the outbreak are more likely to be employed in key industries, in occupations that involve frequent exposure to infections and close relationships with others [ 79 ]. But other studies had found little evidence that occupation affects infection rates. For example, infection rates among frontline healthcare workers have not been shown to be higher than those non frontline healthcare workers. The strongest risk factors associated with COVID-19 infection among health care workers were neighborhood infection rates and ethnicity [ 80 ]. In addition, risk factors for developing COVID-19 in adults include age and gender [ 81 ]. For example, Increased mortality from COVID-19 was significantly associated with higher rates of obesity in women and higher rates of smoking in men [ 82 ]. There is growing evidence that COVID-19 produces more severe symptoms and higher mortality in men than in women [ 83 ]. As a vulnerable group with reduced immune system effectiveness, the elderly are often at a higher risk of infectious diseases [ 84 ]. Susceptibility to SARS-CoV-2 infection increases with age [ 85 , 86 ].
Evidence linking local policies and socioeconomic activity to transmission of COVID-19
Person-to-person transmission is the main way of transmission of COVID-19. In response to the threat of the epidemic, many countries have introduced measures to restrict the movement of people. In Wuhan, China, for example, there was a significant decrease in new cases during the four-day lockdown. During that time, the increase in new cases dropped by about 50%, with the number of cases fluctuating on the fifth day and then rapidly decreasing [ 87 ]. The researchers investigated the movement of people and government restrictions as a function during successive waves of SARS-CoV-2 mutation in Canada. The results showed that in the first two years, government restrictions were high, and turnover was low, characterizing a ‘seek-and-destroy’ approach. After this phase, the highly transmissible Omicron (B.1.1.529) variant began circulating in NS at the end of the following year, leading to an increase in cases, hospitalizations, and deaths. During Omicron, although the transmissibility (26.41 times) and lethality (9.62 times) of the new variant increased, unsustainable government restrictions and declining public compliance led to increased population mobility [ 88 ]. In another cross-sectional study, containment and confinement were found to be significantly associated with overall mobility and were associated with a reduction in SARS-CoV-2 infection [ 89 ]. Lockdowns also reduce air pollution, and NO 2 concentrations can be used as environmental indicators to evaluate the effectiveness of lockdowns. In the United Kingdom, researchers found that exposure to NO 2 dropped significantly during lockdowns, while exposure to PM2.5 dropped relatively little [ 90 ]. In a Cochrane systematic review, 84 studies were analyzed and found that isolation or microbiological testing, or a combination of both, prevented further cases. These interventions may have a positive shift in the development of the epidemic, and case detection may improve [ 91 ]. It has also been reported that 100% use of masks combined with lockdown is a measure that can reduce the risk of additional waves [ 92 ]. Masks could be one of the main pillars in the fight against the virus [ 93 ]. Finally, with lockdown measures in place, maintaining adequate indoor air quality levels is critical to slowing airborne viruses [ 94 ].
Socioeconomic activity has also been the focus of many studies investigating the factors affecting COVID-19 [ 95 ]. Epidemics may accelerate during periods of economic activity, possibly because of an increase in the number of people traveling, followed by an increase in human contact. For example, studies had proved that international trade exceeded other common parameters used to prove the spread of COVID-19 due to economic, demographic, environmental and climatic factors [ 96 ]. The sum of international data on import and export trade can be a complex but appropriate indicator for measuring the underlying socioeconomic dynamics of geo-economic areas [ 96 ]. Another study examined the role of trade in the dynamics of epidemic spread within and between countries in three large European countries: Italy, France, and Spain. The findings suggest that the association between trade and outbreak severity appears to be supported by empirical evidence, potentially introducing new hypotheses to explain the dynamics of COVID-19 transmission within and between countries [ 97 ].
Mechanism of nature environmental factors influencing the SARS-CoV-2
As noted above, there is growing epidemiologic evidence that the risk of transmission of SARS-CoV-2 was influenced by temperature and humidity. Many studies at the molecular level may further confirm this idea. Temperature can promote changes in the molecular structure of biomacromolecules (i.e., nucleic acids, proteins, lipids) until affecting their function. In the case of proteins, temperature is known to induce changes in secondary and tertiary structures, resulting in structural alterations that alter their stability and their role in regulating cellular processes, signal transduction, and intrinsic enzyme properties [ 98 ]. For example, the researchers used molecular dynamics simulation (MD) to reveal the molecular basis of the effect of temperature on the SARS-CoV-2 spike glycoprotein. The results showed that temperature induced conformational change of S1 subunit of SARS-CoV-2 spike glycoprotein that remodel the internal hydrogen bonding structure and especially affected secondary structure of the main region of interaction (RBD) of the spike glycoprotein of SARS-CoV-2 with the human ACE2 receptor [ 99 ]. Relative humidity (RH) can be considered an extrinsic factor for viral stability, as it controls evaporation, which affects the size of viral droplets, their physical fate, and their chemical microenvironment [ 100 ]. Table 1 summarizes some key studies of the effects of temperature and humidity on SARS-CoV-2 survival on different substrates. We found that the virus can survive on many substrates, and the lower the temperature and humidity, the longer the half-life of the virus. In one study, the half-life of the SARS-CoV-2 virus at 4 ℃ was three times that at 22 ℃. One of the studies in the table confirms that the virus is least active at 40% relative humidity. It was also found that temperature seemed to have a greater effect on viral activity than relative humidity. However, neither temperature nor humidity can instantly inactivate the virus under normal conditions (Table 1 ). Some controlled studies of human nasal mucus and sputum, as well as viral aerosols, have shown that SARS-CoV-2 decayed faster at higher relative humidity [ 101 ]. This is consistent with evidence of influenza virus survival that influenza is best transmitted at low absolute humidity [ 102 , 103 ].
Some innate immune responses are suppressed at low temperatures. The human upper respiratory tract is the first contact site of inhaled respiratory viruses and the body's first line of defense against these foreign pathogens. Once bacteria are detected in the front of the nose, the epithelial cells of the anterior nasal mucosa increase the release of extracellular vesicles (EVs) several times. These EVs enter the nasal mucus and have a direct antibacterial effect. At the same time, EVs can arm the more rear epithelial cells with immunoprotective proteins, inducing a four-fold increase in the production of nitric oxide in epithelial cells [ 112 ]. In a subsequent study, Huang et al. further explored the EVs biological mechanism, but found that the EVs-mediated potent antiviral immune defense function was impaired by cold exposure. At ambient conditions of 4.4 ℃, the number of EVs decreased by nearly 42%, while EVS-mediated functional delivery and the ability to neutralize viruses were weakened [ 113 ]. In addition, there is some research suggesting that cellular immune responses may also be affected by temperature and humidity. Mice airway epithelial cells initiated a stronger antiviral response at higher temperatures compared to lower temperatures [ 114 ], and mice exposed to low humidity conditions were more susceptible to influenza infection [ 115 ]. However, the effects of seasonal fluctuations in immune response on COVID-19 susceptibility and severity are still largely unknown. When the temperature is low, the human immune response is suppressed and the activity of the virus is increased, which promotes the spread of the COVID-19. When the temperature is high, it will change the conformation of SARS-CoV-2 spike glycoprotein S1 and reduce the activity of the virus, thus inhibiting the transmission of COVID-19. At 40% RH, the activity of the virus is lowest, thus inhibiting the spread of the novel coronavirus (Fig. 1 A).

Schematic diagram of the influence mechanism of natural environmental factors on the transmission of COVID-19. A Temperature. B Solar radiation. Promoting (upward arrow) or suppressing (downward arrow) the associated mechanism
Solar radiation
Among the different climatological factors, sunlight has been found to play an important role in determining the spread of SARS-CoV-2. Sunlight contains a spectrum of ultraviolet A (UVA), UVB, and UVC. UV germicidal is a commonly used disinfection method, and it has previously been reported that UV can inactivate aerosolized coronaviruses [ 116 ]. Lorca-Oro et al. used UV-C (100-280 nm wavelength) to inactivate SARS-CoV-2 in a laboratory simulating hospital intensive care unit conditions. The results showed that after 12 min or more of UV-C exposure, the titer was reduced by ≥ 99.91% to ≥ 99.99%, and the minimum distance between the UV-C device and the SARS-CoV-2 dry sample was 100 cm [ 117 ]. Under simulated sunlight conditions in the laboratory, the researchers found that 90% of SARS-CoV-2 was inactivated after 19 min of exposure under simulated winter and autumn UV conditions, while some degree of inactivation was achieved after just 8 min under simulated summer conditions [ 118 ]. Several other studies have found similar results, inactivating 90% of SARS-CoV-2 every 6.8 min in simulated saliva and every 14.3 min in culture medium when exposed to simulated sunlight at the summer solstice (ultraviolet (UV) range: 280–400 nm) [ 119 ]. In the United States and most cities around the world, 90% or more of SARS-CoV-2 will be inactivated after 11–34 min of exposure to midday sunlight in the summer [ 120 ]. Observation of the above studies found that SARS-CoV-2 is inherently sensitive to UV. However, UVC can be absorbed by atmospheric ozone, and sunlight reaching the Earth's surface cannot directly eradicate SARS-CoV-2 through virus-killing activity [ 121 ].
UVB exposure is closely related to vitamin D synthesis. The body relies primarily on sun exposure to meet its vitamin D needs. UVB is absorbed by the 7-dehydrogenated cholesterol in the skin, causing it to be converted to pre-vitamin D3, which is quickly converted to vitamin D3 [ 122 ]. Significant increases in vitamin D can be achieved at very low UVB doses [ 123 ]. Solar radiation is highest in summer and at lower altitudes. Studies have found that in northern Europe, adequate vitamin D status can be achieved through summer sun exposure. In winter, however, the UVB radiation in the environment is too low to produce any vitamin D [ 124 ]. Regardless of skin type and ethnicity, there is almost no vitamin D synthesis in winter and spring at latitudes > 50°. Vitamin D deficiency is associated with the severity of COVID-19. In a meta-analysis, vitamin D deficiency was found to be more severe in severe cases compared to mild cases. Insufficient vitamin D levels increase hospitalization rates and COVID-19 mortality [ 125 ]. Vitamin D can reduce the risk of COVID-19 in the following ways (Fig. 1 B): (1) Vitamin D helps immune cells produce antimicrobial peptides, which play an antibacterial and antiviral role [ 126 ]; (2) Vitamin D can inhibit T cell proliferation and the NF-κB pathway of B cells, and reduce the level of pro-inflammatory cytokines [ 127 ]; (3) Vitamin D can prevent the constriction response of pulmonary blood vessels in COVID-19 [ 128 ]; (4) Vitamin D alleviates lung injury by stimulating endothelial cell proliferation and migration, reducing epithelial cell apoptosis, and inhibiting TGF-β-induced epithelial-mesenchymal transformation [ 129 ]. More research is required to evaluate the mechanisms whereby vitamin D might reduce the risk of COVID-19 [ 130 ].
There is strong evidence to support airborne transmission of SARS-CoV-2 [ 131 , 132 ]. The World Health Organization (WHO) has identified inhalation of virus-carrying aerosols as the primary mode of transmission of SARS-CoV-2 over short and long distances. Airborne transmission is defined as less than 5 μm with > 1 to 2 m from an infected person [ 133 ]. Wind speed can strongly influence the transport of virus-carrying aerosols [ 134 ]. Aerosols tend to rise because they are warmer than ambient air and are confined indoors by surrounding walls and ceilings [ 135 ]. In open spaces, particles or droplets produced by normal breathing can only be transferred over short distances, and when sneezing or coughing, particles carry nearly the same distance, with differences only within a certain range. The greater the air flow outside, the greater the dispersion. One study found that the distance of breathing particles is 0.65m, the distance of coughing is 1.63m and the distance of sneezing is 2.86m [ 136 ]. In addition, studies have assessed the risk of spreading infectious particulate matter while chamber musicians play their instruments. It turns out that no matter the volume, pitch, or content of the play, it did not extend the range of the air flow [ 137 ]. While wind speed cannot completely remove the spread of the virus, ventilation helps remove aerosols that carry the virus to reduce airborne transmission. For example, studies using simulations to track infected aerosol plumes in real time have found that a stable state of the atmosphere with low wind speeds, low-level turbulence, and cool, moist ground conditions facilitates the spread of disease. The trajectory model found that the virus can travel in the air for up to 30 min, covering a radius of 200 m at a time, 1–2 km away from the original source [ 138 ]. A study used computational fluid dynamics to simulate viral air flow in an office while investigating the effects of different ventilation strategies on viral transmission. The results showed that the ventilation strategy of single ventilation had the highest infection probability [ 139 ]. Another study found that ambient winds (wind velocities range from 0 to 16 km/h) increase the complexity of secondary flows. Even at 3.05 m, the droplets flow well along the air stream and deposit on the human body and head area. Due to wind convection, the remaining droplets can travel above 3.05 m in the air, posing a potential health risk to people nearby [ 140 ]. The study also found that a reduction in ventilation rates or room capacity per person, or an increase in the ratio of infected people to susceptible people, would increase the distance of transmission. Effective environmental prevention strategies for respiratory infections require an appropriate increase in ventilation rates while maintaining sufficiently low occupancy rates [ 141 ]. Therefore, different ventilation strategies must be developed according to the actual indoor conditions to reduce the transmission of viruses in the air.
Environmental pollution factors
Particulate matter.
The relationship between air pollution and COVID-19 is well-established. Further research has found that air pollution can modify host susceptibility to infection and modify the severity of disease [ 142 ]. Table 2 summarizes some key in vivo studies of air pollution on COVID-19 related targets, immune cells, and oxidative stress. PM is the main component of air pollutants. Many studies have demonstrated that PM can increase the expression of angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine type 2 (TMPRSS2). SARS-CoV-2 can use ACE2 as an entry receptor and TMPRSS2 to activate S protein [ 143 ]. Cell studies have shown that ACE2 expression has become a risk factor for the development of COVID-19 [ 144 ]. Another study found that the expression of ACE2 and TMPRSS2 increased the infection rate of SARS-CoV-2 [ 145 ]. Therefore, PM can increase the expression of ACE2 and TMPRSS2 and affect the severity and incidence of COVID-19.
Severe COVID-19 is associated with high inflammation and elevated levels of inflammatory cytokines. Exposure to air pollutants increases the number of pro-inflammatory cytokines and immune cells that infiltrate the lungs, leading to systemic inflammation and immune disorders that reduce resistance to viruses (Fig. 2 ). Even low doses of PM2.5 induce lung inflammation, oxidative stress, and worsening lung impedance and histology in mice [ 153 ]. Once pathogens establish themselves, inflammation of respiratory mucous membranes caused by exposure to air pollution may lead to a higher risk of severe COVID-19 outcomes through compound inflammation [ 155 ]. For example, studies in mouse models exposed to PM2.5 have found that PM2.5 may increase IL-1β secretion through the TLR4/MyD88 and NLRP3 inflammasome pathways, leading to airway inflammation in mice [ 149 ]. Intranasal transfer of pulmonary microbiota in PM2.5 exposed mice has been found to influence PM2.5 induced lung inflammation and oxidative stress, such as increased levels of pro-inflammatory cytokines and dysregulation of biomarkers associated with oxidative damage [ 154 ]. PM exposure may promote the development of cytokine storms in SARS-CoV-2 infection.

Schematic diagram of the influence of particulate matter on the transmission of COVID-19. Promote (up arrow, color red) related mechanisms
PM2.5 not only damages the lungs directly exposed to air, but also causes pathological changes in other organ systems through excessive oxidative stress generated by mitochondria [ 156 ]. Inflammation, oxidative stress, and cell death in alveolar epithelial cells caused increased mitochondrial division and decreased mitochondrial fusion when exposed to PM2.5 [ 157 ]. The enzymes NOX2 (produce reactive oxygen species) and Toll-like receptor 4 (TLR), have been shown to be critical for PM-induced NADPH oxidase activation. PM2.5 triggers an increase in phospholipid oxidation in the lungs, which then mediates systemic cellular inflammation through TLR4/NADPH oxidation-dependent mechanisms [ 152 ]. In the case of influenza A virus infection, activation of NOX2 oxidase can promote the production of reactive oxygen species to inhibit antiviral and humoral signaling networks [ 158 ]. Therefore, PM can increase the infection rate of SARS-CoV-2 by activating NOX2 to promote reactive oxygen species. Contaminant-induced oxidative stress and cell damage may worsen prognosis [ 159 , 160 ]. Exposure to air pollution-induced oxidative stress is a key mechanism leading to cardiovascular morbidity and mortality [ 161 ].
Ozone is also a common air pollution in cities. It is a gaseous component that is produced by the interaction of air pollution components such as nitrogen oxides and organic compounds caused by sunlight. Inhaling ozone is very toxic to the lungs. Table 3 summarizes the mechanisms by which ozone may be associated with COVID-19. After inhalation, ozone does not enter cells, but comes into direct contact with the first layer of cells on the surface of the airway, such as airway and alveolar epithelial cells and airway macrophages [ 162 ]. These cells release reactive oxygen species and various other inflammatory mediators, including cytokines and lipids, from oxidative damage to the airway epithelium [ 163 ]. Oxidative stress is a major pathogenic factor of COVID-19. For example, it has been found that ozone stimulated macrophages to secrete pro-inflammatory cytokines (IL-1α, IL-1β and IL-18), and IL-1α stimulated epithelial cells to secrete CXCL1 and CCL2, thereby driving neutrophil influx [ 164 ]. Another study found that canonical transient receptor potential 6 (TRPC6) regulates NF-κB activation and intercellular adhesion molecule-1 (ICAM-1) expression after exposure to ozone. TRPC6 deficiency attenuates O3-induced recruitment of neutrophils to airway epithelial cells and ICAM-1 expression [ 165 ]. In addition, ozone can lead to loss of antioxidant Nrf2 and SOD activity in the body, enhanced intracellular oxidative stress and increased HIF-1α signaling, resulting in a persistent chronic inflammatory environment in the lungs [ 166 ]. Ozone can induce the expression of MAPK, NF-κB and AP-1 proteins through TLR4/MyD88 pathway, resulting in inflammatory response. Heat shock protein 70 (HSP70) was identified as a downstream mediator with ozone mediated TLR4 effects [ 167 ]. Ozone also induced apoptosis markers (lysed caspase 9) and autophagy markers (beclin-1) in alveolar macrophages and enhanced the expression of MMP-2 and MMP-9 [ 168 ]. However, the effects of ozone on different cell death pathways such as necrosis, apoptosis, ferroptosis, and autophagy have not been resolved [ 169 ]. These cell death pathways may be responsible for the emphysema process induced by oxidants. Just as ozone can make asthma worse, ozone may increase the incidence and severity of COVID-19 by inducing inflammation, oxidative stress, and airway remodeling (Fig. 3 ).

Schematic diagram of the influence of ozone on the transmission of COVID-19. Promote (up arrow, color red) or suppressing (downward arrow, color green) related mechanisms
Ozone is an excellent biocidal agent due to its strong oxidation, and its effectiveness against bacteria, fungi and viruses has been proven [ 173 ]. Ozone can be easily applied to large and small areas for disinfection and is broken down back into safe oxygen after treatment. Ozone is particularly deadly to viruses through peroxidation of lipid surface and subsequent damage to lipid envelopes and proteins, and enveloped viruses such as SARS-CoV-2 are more vulnerable to ozone attack [ 174 ]. Ozone has been shown to inactivate the SARS-CoV-2 virus on surfaces (such as plastic, glass, stainless steel, gauze, wood, wool, copper, and coupons in ambulance seats and floors) or in suspended fluids [ 175 ]. During the pandemic, ozone has been widely used to purify many enclosed spaces.
Ozone also has medical uses. Medical ozone is administered in the form of a balanced O2/O3 mixture by autologous blood therapy or rectal blow or also as a peritoneal injection in laboratory animals [ 176 ]. Medical ozone can interfere with the replication phase of the virus to play an antiviral role. Medical ozone's effects include the oxidation and inactivation of specific viral receptors used to form cell-membrane binding structures, thereby inhibiting the level of its first stage: cellular penetration [ 177 ]. Medical ozone can directly act on Nrf2, an important nuclear message transmitter, regulating and blocking the activity of ACE2 receptors. Thus, preventing SARS-CoV-2 from replicating [ 178 ]. SARS-CoV2 can cause oxidative stress and inflammation, further tissue damage and widespread triggering of the clotting cascade, culminating in the formation of blood clots [ 179 ]. Medical ozone, when administered in appropriate pathways and at small doses, may induce adaptive responses that reduce endogenous oxidative stress [ 180 ]. In addition, some studies have found that ozone can activate the cellular and humoral immune system and can reduce inflammation/apoptosis processes [ 177 ]. Clinical studies have further confirmed that ozone therapy can be used as a comprehensive treatment for COVID-19 with low cost and improve the health status of patients [ 181 ].
Since the outbreak, extensive research has investigated the factors that influence the spread of COVID-19. Representative studies on the impact of natural environmental factors and social environmental factors on COVID-19 are discussed in this review. The mechanisms and results of natural environmental factors affecting COVID-19 are shown in Fig. 4 . As can be seen from the epidemiological studies included in this paper, the current study covered multiple regions, multiple confounding factors, and long or short-term exposure times. The mechanism study also covers multiple pathways and targets in vivo and in vitro.

Schematic diagram of nature and social environment factors affects the transmission of COVID-19
Both mechanism and epidemiological studies have shown that air pollution, especially PM2.5 and ozone, greatly accelerates the spread of COVID-19. Some of the differences in air pollution effectiveness in transmitting the virus may be caused by differences in composition between different locations. However, there are important limitations to the available evidence, such as (1) methodological limitations, (2) incomplete coverage of the original data, and (3) large uncertainties in the analysis [ 182 , 183 ]. Studies on the mechanism of air pollution affecting the spread of COVID-19 have confirmed that air pollution can (1) increase the expression of key proteins in the entry pathway of SARS-CoV-2, (2) promote inflammation and release of pro-inflammatory cytokines, (3) causes pathological changes in organ systems, and (4) increase the risk of respiratory complications. This further provides evidence for COVID-19 prevention and control measures to reduce air pollution, rational use of ozone disinfection, and medical ozone therapy. To date, no study has accurately demonstrated seasonal changes in the global prevalence of COVID-19. Research on climate conditions is subject to similar challenges and limitations as air pollution [ 184 ]. But a growing body of evidence supports a statistically significant correlation between climatic conditions and morbidity, mortality, recovery cases, etc. [ 185 ]. In vitro experiments were conducted to study the activity of the virus under different climatic conditions and substrate conditions. Studies have shown that the SARS-CoV-2 has the longest half-life at lower temperatures, which promotes SARS-CoV-2 transmission. This also provides evidence for COVID-19 prevention and control measures to maintain indoor temperature and humidity. SARS-CoV-2 rots faster at higher relative humidity, inhibiting the spread of the virus. Solar radiation has a better inactivation effect on SARS-CoV-2, but UVC in the environment cannot directly eradicate SARS-CoV-2. Solar radiation (UVB) inhibits the spread and development of COVID-19 through the synthesis of vitamin D. Therefore, there is scientific evidence for COVID-19 prevention and control measures based on rational exposure to sunlight. For other climatic conditions (such as wind speed, water resource), no clear conclusions have been found.
Social environmental factors are also significantly related to the spread of COVID-19. The mechanisms and results of social environmental factors affecting COVID-19 are shown in Fig. 4 . People vary greatly in their daily routines, traveling from home, work, school, and public and commercial spaces can exhibit high personal exposure to pathogens [ 186 ]. Epidemiologic studies have shown that population density, built environment, occupation, age, gender, local policies and socioeconomic activity have an impact on COVID-19 [ 187 ]. This is also the scientific basis for the country to take measures such as control of population movement, control of population density, wearing masks, and disinfecting dense places [ 188 ]. Among them, population density is considered to have a more significant impact on COVID-19 than meteorological factors, and the increase in population density will in turn lead to an increase in COVID-19 cases and deaths [ 73 ]. In addition, socio-economic activities such as international trade are also key factors affecting the spread of COVID-19. The total import and export volume is highly positively correlated with confirmed cases [ 97 ]. Although there are differences between the results of the studies, this may be due to the limitations of the studies introducing bias. Like the limitations described earlier, single factor studies can be biased due to confounding factors at the individual level.
Future prospects
Now, as vaccination coverage increases and strains mutate, COVID-19 may be transitioning to an epidemic seasonal disease, such as influenza [ 189 ]. Climate may play a bigger role in determining COVID-19 infection. In the near term, as public health measures are reduced, the link between COVID-19 and natural environmental factors will become clearer. Future studies are needed to determine the effects of climate change on the spatiotemporal distribution of different strains of viruses. In addition, future research could focus on disease outcomes caused by climatic conditions in animal models of COVID-19, and further improve the range of environmental conditions used in laboratory studies to better simulate real-world environmental conditions (indoor and outdoor). A meta-analysis of climate-related epidemiologic should be attempted to provide more conclusive evidence.
In addition, it is worth studying whether long-term environmental changes and short-term climate changes have the same effect on the human body. The impact of environmental exposure changes throughout life [ 190 ]. We do not know how the duration of exposure will affect the susceptibility and severity of COVID-19. Existing mechanism research is focused on animal experiments, and ethical clinical trials are needed. Existing mechanism studies have found that both temperature and humidity, as well as air pollution, can have an impact on immunity. Future research should address the interaction between climate and immunity. Explore the specific mechanism of climate on immunity through clinical research.
Conclusions
The impact of COVID-19 on human health is significantly negative. The constant change of the current environment increases the probability of infectious diseases. Sorting out the key factors affecting infectious diseases for scientific prevention and control, personalized and precise treatment is critical, although there is still a lot of work to be done. Our review indicates that with the continuous mutation of SARS-CoV-2, high temperature, high humidity, low air pollution levels, and low population density may be more likely to slow down the spread of the virus. All of these measures appear to be effective in controlling the spread or mortality of COVID-19: (1) reducing air pollution levels, (2) rational use of ozone disinfection and medical ozone therapy, (3) rational exposure to sunlight, (4) scientific ventilation and maintenance of indoor temperature and humidity, (5) control of population density, and (6) control of population movement. They could play a vital role in the future face of infectious diseases. The arrival of new pathogens is inevitable. While focusing on the research and development of vaccines, diagnostic reagents, and drugs for infectious diseases, we use interdisciplinary methods to break through existing limitations and clarify the impact of environment on biology, disease and evolution from the molecular level with the development of methodology. It is an urgent need to safeguard people's health. This will provide innovative inspiration for global epidemic prevention and control policies and provide reference for similar infectious diseases that may emerge in the future.
Availability of data and materials
Not applicable.
Data availability
No datasets were generated or analysed during the current study.
Kamacooko O, Kitonsa J, Bahemuka UM, Kibengo FM, Wajja A, Basajja V, et al. Knowledge, attitudes, and practices regarding covid-19 among healthcare workers in uganda: a cross-sectional survey. Int J Environ Res Public Health. 2021;18:7004.
Article CAS PubMed PubMed Central Google Scholar
Sarhan RM, Madney YM, Abou Warda AE, Boshra MS. Therapeutic efficacy, mechanical ventilation, length of hospital stay, and mortality rate in severe COVID-19 patients treated with tocilizumab. Int J Clin Pract. 2021;75:e14079.
Article CAS PubMed Google Scholar
Sarhan RM, Mohammad MF, Boshra MS. Differential clinical diagnosis and prevalence rate of allergic rhinitis, asthma and chronic obstructive pulmonary disease among COVID-19 patients. Int J Clin Pract. 2021;75:4–6.
Article Google Scholar
Barouki R, Kogevinas M, Audouze K, Belesova K, Bergman A, Birnbaum L, et al. The COVID-19 pandemic and global environmental change: emerging research needs. Environ Int. 2021;146:106272.
Li M, Wang H, Tian L, Pang Z, Yang Q, Huang T, et al. COVID-19 vaccine development: milestones, lessons and prospects. Signal Transduction and Targeted Therapy. 2022;7(1):146.
Xiao S, Qi H, Ward MP, Wang W, Zhang J, Chen Y, et al. Meteorological conditions are heterogeneous factors for COVID-19 risk in China. Environ Res. 2020;2021(198):111182.
Google Scholar
Scannell Bryan M, Sun J, Jagai J, Horton DE, Montgomery A, Sargis R, et al. Coronavirus disease 2019 (COVID-19) mortality and neighborhood characteristics in Chicago. Ann Epidemiol. 2021;56:47-54.e5.
Article PubMed Google Scholar
Weaver AK, Head JR, Gould CF, Carlton EJ, Remais JV. Environmental Factors Influencing COVID-19 Incidence and Severity. Annu Rev Public Health. 2022;43:271–91.
Article PubMed PubMed Central Google Scholar
Weaver AK, Head JR, Gould CF, Carlton EJ, Remais J V. Environmental factors influencing COVID-19 incidence and severity. 2022. https://doi.org/10.1146/annurev-publhealth .
Huang Z, Huang J, Gu Q, Du P, Liang H, Dong Q. Optimal temperature zone for the dispersal of COVID-19. Sci Total Environ. 2020;736:139487.
Azuma K, Kagi N, Kim H, Hayashi M. Impact of climate and ambient air pollution on the epidemic growth during COVID-19 outbreak in Japan. Environ Res. 2020;190:110042.
Haque SE, Rahman M. Association between temperature, humidity, and COVID-19 outbreaks in Bangladesh. Environ Sci Policy. 2020;114:253–5.
Tan J, Mu L, Huang J, Yu S, Chen B, Yin J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J Epidemiol Community Health. 1978;2005(59):186–92.
Yin C, Zhao W, Pereira P. Meteorological factors’ effects on COVID-19 show seasonality and spatiality in Brazil. Environ Res. 2021;2022(208):112690.
Mecenas P, da Rosa Moreira Bastos RT, Rosário Vallinoto AC, Normando D. Effects of temperature and humidity on the spread of COVID-19: a systematic review. PLoS One. 2020;15(9):e0238339.
Zheng HL, Guo ZL, Wang ML, Yang C, An SY, Wu W. Effects of climate variables on the transmission of COVID-19: a systematic review of 62 ecological studies. Environ Sci Pollut Res. 2021;28:54299–316.
Article CAS Google Scholar
Yuan J, Wu Y, Jing W, Liu J, Du M, Wang Y, et al. Association between meteorological factors and daily new cases of COVID-19 in 188 countries: A time series analysis. Sci Total Environ. 2021;780:146538.
Yuan J, Wu Y, Jing W, Liu J, Du M, Wang Y, et al. Non-linear correlation between daily new cases of COVID-19 and meteorological factors in 127 countries. Environ Res. 2021;193:110521.
Mehta SK, Ananthavel A, Reddy TVR, Ali S, Mehta SB, Kakkanattu SP, et al. Indirect Response of the Temperature, Humidity, and Rainfall on the Spread of COVID-19 over the Indian Monsoon Region. Pure Appl Geophys. 2023;180:383–404.
Gupta A, Banerjee S, Das S. Significance of geographical factors to the COVID-19 outbreak in India. Model Earth Syst Environ. 2020;6:2645–53.
Cai QC, Lu J, Xu QF, Guo Q, Xu DZ, Sun QW, et al. Influence of meteorological factors and air pollution on the outbreak of severe acute respiratory syndrome. Public Health. 2007;121:258–65.
Berendt RF, Dorsey EL. Effect of simulated solar radiation and sodium fluorescein on the recovery of Venezuelan equine encephalomyelitis virus from aerosols. Appl Microbiol. 1971;21:447–50.
Rosario DKA, Mutz YS, Bernardes PC, Conte-Junior CA. Relationship between COVID-19 and weather: case study in a tropical country. Int J Hyg Environ Health. 2020;229:113587.
Ahmadi M, Sharifi A, Dorosti S, Jafarzadeh Ghoushchi S, Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci Total Environ. 2020;729:138705.
Lansiaux É, Pébaÿ PP, Picard JL, Forget J. Covid-19 and vit-d: disease mortality negatively correlates with sunlight exposure. Spat Spatiotemporal Epidemiol. 2020;35:100362.
Hashim BM, Al-Naseri SK, Hamadi AM, Mahmood TA, Halder B, Shahid S, et al. Seasonal correlation of meteorological parameters and PM2.5 with the COVID-19 confirmed cases and deaths in Baghdad, Iraq. Int J Disaster Risk Reduct. 2023;94:103799.
Asyary A, Veruswati M. Sunlight exposure increased Covid-19 recovery rates: a study in the central pandemic area of Indonesia. Sci Total Environ. 2020;729:139016.
Al-Khateeb MS, Abdulla FA, Al-Delaimy WK. Long-term spatiotemporal analysis of the climate related impact on the transmission rate of COVID-19. Environ Res. 2023;236:116741.
Sharun K, Tiwari R, Dhama K. COVID-19 and sunlight: Impact on SARS-CoV-2 transmissibility, morbidity, and mortality. Ann Med Surg. 2021;66:17–20.
Wang J, Li W, Yang B, Cheng X, Tian Z, Guo H. Impact of hydrological factors on the dynamic of COVID-19 epidemic: a multi-region study in China. Environ Res. 2021;198:110474.
Tosepu R, Gunawan J, Effendy DS, Ahmad LOAI, Lestari H, Bahar H, et al. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci Total Environ. 2020;725:138436.
Bashir MF, Ma B, Bilal, Komal B, Bashir MA, Tan D, et al. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci Total Environ. 2020;728:138835.
Auler AC, Cássaro FAM, da Silva VO, Pires LF. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: a case study for the most affected Brazilian cities. Sci Total Environ. 2020;729:139090.
Domingo JL, Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ Res. 2020;187:109650.
Copat C, Cristaldi A, Fiore M, Grasso A, Zuccarello P, Signorelli SS, et al. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ Res. 2020;191:110129.
Wu X, Nethery RC, Sabath MB, Braun D, Dominici F. Air pollution and COVID-19 mortality in the United States: strengths and limitations of an ecological regression analysis. Sci Adv. 2020;6:1–7.
Bossak BH, Andritsch S. COVID-19 and Air pollution: a spatial analysis of particulate matter concentration and pandemic-associated mortality in the US. Int J Environ Res Public Health. 2022;19:592.
Coker ES, Cavalli L, Fabrizi E, Guastella G, Lippo E, Parisi ML, et al. The effects of air pollution on COVID-19 related mortality in Northern Italy. Environ Resour Econ (Dordr). 2020;76:611–34.
Cole MA, Ozgen C, Strobl E. Air pollution exposure and Covid-19 in Dutch Municipalities. Environ Resour Econ (Dordr). 2020;76:581–610.
Travaglio M, Yu Y, Popovic R, Selley L, Leal NS, Martins LM. Links between air pollution and COVID-19 in England. Environ Pollut. 2021;268:115859.
Zhang X, Tang M, Guo F, Wei F, Yu Z, Gao K, et al. Associations between air pollution and COVID-19 epidemic during quarantine period in China. Environ Pollut. 2021;268:115897.
Zhou X, Josey K, Kamareddine L, Caine MC, Liu T, Mickley LJ, et al. Excess of COVID-19 cases and deaths due to fine particulate matter exposure during the 2020 wildfires in the United States. Sci Adv. 2021;7:1–12.
Lavigne E, Ryti N, Gasparrini A, Sera F, Weichenthal S, Chen H, et al. Short-term exposure to ambient air pollution and individual emergency department visits for COVID-19: A case-crossover study in Canada. Thorax. 2023;78:459–66.
Liu Z, Liang Q, Liao H, Yang W, Lu C. Effects of short-term and long-term exposure to ambient air pollution and temperature on long recovery duration in COVID-19 patients. Environ Res. 2023;216:114781.
Poniedziałek B, Rzymski P, Zarębska-Michaluk D, Rogalska M, Rorat M, Czupryna P, et al. Short-term exposure to ambient air pollution and COVID-19 severity during SARS-CoV-2 delta and omicron waves: a multicenter study. J Med Virol. 2023;95:e28962.
Vos S, De Waele E, Goeminne P, Bijnens EM, Bongaerts E, Martens DS, et al. Pre-admission ambient air pollution and blood soot particles predict hospitalisation outcomes in COVID-19 patients. Eur Respir J. 2023;62:2300309.
Alaniz AJ, Carvajal MA, Carvajal JG, Vergara PM. Effects of air pollution and weather on the initial COVID-19 outbreaks in United States, Italy, Spain, and China: a comparative study. Risk Anal. 2023;43:8–18.
Sidell MA, Chen Z, Huang BZ, Chow T, Eckel SP, Martinez MP, et al. Ambient air pollution and COVID-19 incidence during four 2020–2021 case surges. Environ Res. 2022;208:112758.
Lipsitt J, Chan-Golston AM, Liu J, Su J, Zhu Y, Jerrett M. Spatial analysis of COVID-19 and traffic-related air pollution in Los Angeles. Environ Int. D 2020;2021(153):106531.
Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382:929–36.
Peiris JSM, Chu CM, Cheng VCC, Chan KS, Hung IFN, Poon LLM, et al. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361:1767–72.
Izquierdo-Lara R, Elsinga G, Heijnen L, Oude Munnink BB, Schapendonk CME, Nieuwenhuijse D, et al. Monitoring SARS-CoV-2 circulation and diversity through community wastewater sequencing, the Netherlands and Belgium. Emerg Infect Dis. 2021;27:1405–15.
Ahmed W, Angel N, Edson J, Bibby K, Bivins A, O’Brien JW, et al. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci Total Environ. 2020;728:138764.
Wu F, Zhang J, Xiao A, Gu X, Lee L, Armas F, et al. SARS-CoV-2 titers in wastewater are higher than expected. mSystems. 2020;5:1–9.
Carraturo F, Del Giudice C, Morelli M, Cerullo V, Libralato G, Galdiero E, et al. Persistence of SARS-CoV-2 in the environment and COVID-19 transmission risk from environmental matrices and surfaces. Environ Pollut. 2020;265:115010.
Rimoldi SG, Stefani F, Gigantiello A, Polesello S, Comandatore F, Mileto D, et al. Presence and infectivity of SARS-CoV-2 virus in wastewaters and rivers. Sci Total Environ. 2020;744:140911.
Rahman MM, Bodrud-Doza M, Griffiths MD, Mamun MA. Biomedical waste amid COVID-19: perspectives from Bangladesh. Lancet Glob Health. 2020;8:e1262.
Martínez-Puchol S, Rusiñol M, Fernández-Cassi X, Timoneda N, Itarte M, Andrés C, et al. Characterisation of the sewage virome: comparison of NGS tools and occurrence of significant pathogens. Sci Total Environ. 2020;713:136604.
Wiktorczyk-Kapischke N, Grudlewska-Buda K, Wałecka-Zacharska E, Kwiecińska-Piróg J, Radtke L, Gospodarek-Komkowska E, et al. SARS-CoV-2 in the environment—non-droplet spreading routes. Sci Total Environ. 2021;770:85–94.
Anand U, Bianco F, Suresh S, Tripathi V, Núñez-Delgado A, Race M. SARS-CoV-2 and other viruses in soil: an environmental outlook. Environ Res. 2021;198:111297.
Gong Z, Chan HT, Chen Q, Chen H. Application of nanotechnology in analysis and removal of heavy metals in food and water resources. Nanomaterials. 2021;11:1–32.
Park SK, Sack C, Sirén MJ, Hu H. Environmental cadmium and mortality from influenza and pneumonia in U.S. adults. Environ Health Perspect. 2020;128:127004-1-127004–8.
Skalny AV, Lima TRR, Ke T, Zhou JC, Bornhorst J, Alekseenko SI, et al. Toxic metal exposure as a possible risk factor for COVID-19 and other respiratory infectious diseases. Food Chem Toxicol. 2020;146:111809.
Hu X, Kim KH, Lee Y, Fernandes J, Smith MR, Jung YJ, et al. Environmental cadmium enhances lung injury by respiratory syncytial virus infection. Am J Pathol. 2019;189:1513–25.
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4.
Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. 2022;399:2227–42.
Solenkova NV, Newman JD, Berger JS, Thurston G, Hochman JS, Lamas GA. Metal pollutants and cardiovascular disease: mechanisms and consequences of exposure. Am Heart J. 2014;168:812–22.
Wang X, Mukherjee B, Park SK. Associations of cumulative exposure to heavy metal mixtures with obesity and its comorbidities among U.S. adults in NHANES 2003–2014. Environ Int. 2018;121:683–94.
Sattar N, McInnes IB, McMurray JJV. Obesity Is a Risk Factor for Severe COVID-19 Infection: Multiple Potential Mechanisms. Circulation. 2020;142:4–6.
Zeng HL, Yang Q, Yuan P, Wang X, Cheng L. Associations of essential and toxic metals/metalloids in whole blood with both disease severity and mortality in patients with COVID-19. FASEB J. 2021;35:e21392.
Zeng HL, Zhang B, Wang X, Yang Q, Cheng L. Urinary trace elements in association with disease severity and outcome in patients with COVID-19. Environ Res. D 2020;2021(194):110670.
Zhang X, Maggioni V, Houser P, Xue Y, Mei Y. The impact of weather condition and social activity on COVID-19 transmission in the United States. J Environ Manage. 2022;302(Pt B):114085.
Ganasegeran K, Jamil MFA, Ch’ng ASH, Looi I, Peariasamy KM. Influence of population density for COVID-19 spread in Malaysia: an ecological study. Int J Environ Res Public Health. 2021;18:9866.
Wong HS, Hasan MZ, Sharif O, Rahman A. Effect of total population, population density and weighted population density on the spread of Covid-19 in Malaysia. PLoS One. 2023;18(4):1–15.
Md Iderus NH, Lakha Singh SS, Mohd Ghazali S, Yoon Ling C, Cia Vei T, Md Zamri ASS, et al. Correlation between population density and COVID-19 cases during the third wave in Malaysia: effect of the delta variant. Int J Environ Res Public Health. 2022;19:7439.
Diao Y, Kodera S, Anzai D, Gomez-Tames J, Rashed EA, Hirata A. Influence of population density, temperature, and absolute humidity on spread and decay durations of COVID-19: a comparative study of scenarios in China, England, Germany, and Japan. One Health. D 2020;2021(12):100203.
Pinter-Wollman N, Jelic A, Wells NM. The impact of the built environment on health behaviours and disease transmission in social systems. Biological Sciences: Philosophical Transactions of the Royal Society B; 2018. p. 373.
Kan Z, Kwan MP, Wong MS, Huang J, Liu D. Identifying the space-time patterns of COVID-19 risk and their associations with different built environment features in Hong Kong. Sci Total Environ. 2019;2021(772):145379.
Hawkins D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am J Ind Med. 2020;63:817–20.
Lan FY, Filler R, Mathew S, Buley J, Iliaki E, Bruno-Murtha LA, et al. Sociodemographic risk factors for coronavirus disease 2019 (COVID-19) infection among Massachusetts healthcare workers: A retrospective cohort study. Infect Control Hosp Epidemiol. 2021;42:1473–8.
Fauci AS, Lane HC, Redfield RR. Covid-19 — Navigating the Uncharted. N Engl J Med. 2020;382:1268–9.
Lamichhane DK, Shrestha S, Kim HC. District-level risk factors for COVID-19 incidence and mortality in Nepal. Int J Environ Res Public Health. 2022;19:2659.
Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588:315–20.
Flook M, Jackson C, Vasileiou E, Simpson CR, Muckian MD, Agrawal U, et al. Informing the public health response to COVID-19: a systematic review of risk factors for disease, severity, and mortality. BMC Infect Dis. 2021;21:1–23.
Ayoub HH, Chemaitelly H, Mumtaz GR, Seedat S, Awad SF, Makhoul M, et al. Characterizing key attributes of COVID-19 transmission dynamics in China’s original outbreak: model-based estimations. Glob Epidemiol. 2020;2:100042.
Hu S, Wang W, Wang Y, Litvinova M, Luo K, Ren L, et al. Infectivity, susceptibility, and risk factors associated with SARS-CoV-2 transmission under intensive contact tracing in Hunan, China. Nat Commun. 2021;12:1–11.
Yang X. Does city lockdown prevent the spread of COVID-19? New evidence from the synthetic control method. Glob Health Res Policy. 2021;6:20.
Sganzerla Martinez G, Hewins B, LeBlanc JJ, Ndishimye P, Toloue Ostadgavahi A, Kelvin DJ. Evaluating the effectiveness of lockdowns and restrictions during SARS-CoV-2 variant waves in the Canadian province of Nova Scotia. Front Public Health. 2023;11:1142602.
Erim DO, Oke GA, Adisa AO, Odukoya O, Ayo-Yusuf OA, Erim TN, et al. Associations of government-mandated closures and restrictions with aggregate mobility trends and SARS-CoV-2 infections in Nigeria. JAMA Netw Open. 2021;4:1–11.
Kazakos V, Taylor J, Luo Z. Impact of COVID-19 lockdown on NO2 and PM2.5 exposure inequalities in London, UK. Environ Res. 2021;198:111236.
Hohlfeld ASJ, Abdullahi L, Abou-Setta AM, Engel ME. International air travel-related control measures to contain the Covid-19 pandemic: a companion review to a Cochrane rapid review. New Microbes New Infect. 2022;49–50:101054.
Article PubMed Central Google Scholar
Stutt ROJH, Retkute R, Bradley M, Gilligan CA, Colvin J. A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down’ in managing the covid-19 pandemic. Proc R Soc A: Math, Phys Eng Sci. 2020;476:20200376.
Anand U, Cabreros C, Mal J, Ballesteros F, Sillanpää M, Tripathi V, et al. Novel coronavirus disease 2019 (COVID-19) pandemic: from transmission to control with an interdisciplinary vision. Environ Res. 2021;197:111126.
Nair AN, Anand P, George A, Mondal N. A review of strategies and their effectiveness in reducing indoor airborne transmission and improving indoor air quality. Environ Res. 2022;213:113579.
Bontempi E. Commercial exchanges instead of air pollution as possible origin of COVID-19 initial diffusion phase in Italy: more efforts are necessary to address interdisciplinary research. Environ Res. 2020;188:109775.
Bontempi E, Coccia M. International trade as critical parameter of COVID-19 spread that outclasses demographic, economic, environmental, and pollution factors. Environ Res. 2021;201:111514.
Bontempi E, Coccia M, Vergalli S, Zanoletti A. Can commercial trade represent the main indicator of the COVID-19 diffusion due to human-to-human interactions? A comparative analysis between Italy, France, and Spain. Environ Res. 2021;201:111529.
Dong YW, Liao ML, Meng XL, Somero GN. Structural flexibility and protein adaptation to temperature: molecular dynamics analysis of malate dehydrogenases of marine molluscs. Proc Natl Acad Sci U S A. 2018;115:1274–9.
Martí D, Torras J, Bertran O, Turon P, Alemán C. Temperature effect on the SARS-CoV-2: a molecular dynamics study of the spike homotrimeric glycoprotein. Comput Struct Biotechnol J. 2021;19:1848–62.
Marr LC, Tang JW, Van Mullekom J, Lakdawala SS. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J R Soc Interface. 2019;16:20180298.
Schuit M, Biryukov J, Beck K, Yolitz J, Bohannon J, Weaver W, et al. The stability of an isolate of the SARS-CoV-2 B.1.1.7 lineage in aerosols is similar to 3 earlier isolates. J Infect Dis. 2021;224:1641–8.
CAS PubMed Google Scholar
Shaman J, Kohn M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc Natl Acad Sci U S A. 2009;106:3243–8.
Shaman J, Pitzer VE, Viboud C, Grenfell BT, Lipsitch M. Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol. 2010;8:e1000316.
Kwon T, Gaudreault NN, Richt JA. Seasonal Stability of SARS-CoV-2 in Biological Fluids. Pathogens. 2021;10:540.
Kwon T, Gaudreault NN, Richt JA. Environmental stability of sars-cov-2 on different types of surfaces under indoor and seasonal climate conditions. Pathogens. 2021;10:1–8.
Pottage T, Onianwa O, Atkinson B, Spencer A, Bennett AM. Stability of SARS-CoV-2 variants of concern (Delta and Omicron) on surfaces at room temperature. Virology. 2023;583:27–8.
Guang Y, Hui L. Determining half-life of SARS-CoV-2 antigen in respiratory secretion. Environ Sci Pollut Res. 2023;30:69697–702.
Riddell S, Goldie S, Hill A, Eagles D, Drew TW. The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol J. 2020;17:1–7.
Matson MJ, Yinda CK, Seifert SN, Bushmaker T, Fischer RJ, van Doremalen N, et al. Effect of environmental conditions on SARS-CoV-2 stability in human nasal mucus and sputum. Emerg Infect Dis. 2020;26:2276–8.
Kwon T, Gaudreault NN, Cool K, McDowell CD, Morozov I, Richt JA. Stability of SARS-CoV-2 in biological fluids of animals. Viruses. 2023;15:761.
Morris DH, Yinda KC, Gamble A, Rossine FW, Huang Q, Bushmaker T, et al. Mechanistic theory predicts the effects of temperature and humidity on inactivation of sars-cov-2 and other enveloped viruses. Elife. 2021;10:1–59.
Nocera AL, Mueller SK, Stephan JR, Hing L, Seifert P, Han X, et al. Exosome swarms eliminate airway pathogens and provide passive epithelial immunoprotection through nitric oxide. J Allergy Clin Immunol. 2019;143:1525-1535.e1.
Huang D, Taha MS, Nocera AL, Workman AD, Amiji MM, Bleier BS. Cold exposure impairs extracellular vesicle swarm–mediated nasal antiviral immunity. J Allergy Clin Immunol. 2023;151:509-525.e8.
Foxman EF, Storer JA, Fitzgerald ME, Wasik BR, Hou L, Zhao H, et al. Temperature-dependent innate defense against the common cold virus limits viral replication at warm temperature in mouse airway cells. Proc Natl Acad Sci U S A. 2015;112:827–32.
Kudo E, Song E, Yockey LJ, Rakib T, Wong PW, Homer RJ, et al. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc Natl Acad Sci U S A. 2019;166:10905–10.
Walker CM, Ko G. Effect of ultraviolet germicidal irradiation on viral aerosols. Environ Sci Technol. 2007;41:5460–5.
Lorca-Oró C, Vila J, Pleguezuelos P, Vergara-Alert J, Rodon J, Majó N, et al. Rapid SARS-CoV-2 Inactivation in a simulated hospital room using a mobile and autonomous robot emitting ultraviolet-c light. J Infect Dis. 2022;225:587–92.
Schuit M, Ratnesar-Shumate S, Yolitz J, Williams G, Weaver W, Green B, et al. Airborne SARS-CoV-2 is rapidly inactivated by simulated sunlight. J Infect Dis. 2020;222:564–71.
Ratnesar-Shumate S, Williams G, Green B, Krause M, Holland B, Wood S, et al. Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces. J Infect Dis. 2020;222:214–22.
Sagripanti JL, Lytle CD. Estimated inactivation of coronaviruses by solar radiation with special reference to COVID-19. Photochem Photobiol. 2020;96:731–7.
O’Connor C, Courtney C, Murphy M. Shedding light on the myths of ultraviolet radiation in the COVID-19 pandemic. Clin Exp Dermatol. 2021;46:187–8.
Saraff V, Shaw N. Sunshine and vitamin D. Arch Dis Child. 2016;101:190–2.
Bogh MKB, Schmedes AV, Philipsen PA, Thieden E, Wulf HC. Vitamin D production depends on ultraviolet-B dose but not on dose rate: a randomized controlled trial. Exp Dermatol. 2011;20:14–8.
Bogh MKB. Vitamin D production after UVB: aspects of UV-related and personal factors. Scand J Clin Lab Invest. 2012;72(SUPPL. 243):24–31.
CAS Google Scholar
Pereira M, Dantas Damascena A, Galvão Azevedo LM, de Almeida OT, da Mota SJ. Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2022;62:1308–16.
Cannell JJ, Vieth R, Umhau JC, Holick MF, Grant WB, Madronich S, et al. Epidemic influenza and vitamin D. Epidemiol Infect. 2006;134:1129–40.
Mohan M, Cherian JJ, Sharma A. Exploring links between vitamin D deficiency and covid-19. PLoS Pathog. 2020;16(9):e1008874.
Kumar D, Gupta P, Banerjee D. Letter: does vitamin D have a potential role against COVID-19? Aliment Pharmacol Ther. 2020;52:409–11.
Zheng SX, Yang JX, Hu X, Li M, Wang Q, Dancer RCA, et al. Vitamin D attenuates lung injury via stimulating epithelial repair, reducing epithelial cell apoptosis and inhibits TGF-β induced epithelial to mesenchymal transition. Biochem Pharmacol. 2020;177:113955.
Mercola J, Grant WB, Wagner CL. Evidence regarding vitamin d and risk of covid-19 and its severity. Nutrients. 2020;12:1–24.
Lednicky JA, Lauzard M, Fan ZH, Jutla A, Tilly TB, Gangwar M, et al. Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patients. Int J Infect Dis. 2020;100:476–82.
Kutter JS, de Meulder D, Bestebroer TM, Lexmond P, Mulders A, Richard M, et al. SARS-CoV and SARS-CoV-2 are transmitted through the air between ferrets over more than one meter distance. Nat Commun. 2021;12:1653.
Wang CC, Prather KA, Sznitman J, Jimenez JL, Lakdawala SS, Tufekci Z, et al. Airborne transmission of respiratory viruses. Science. 2021;373:eabd9149.
Wei J, Li Y. Airborne spread of infectious agents in the indoor environment. Am J Infect Control. 2016;44:S102–8.
Chen W, Zhang N, Wei J, Yen HL, Li Y. Short-range airborne route dominates exposure of respiratory infection during close contact. Build Environ. 2020;176:106859.
Issakhov A, Omarova P, Abylkassymova A. Numerical simulation of social distancing of preventing airborne transmission in open space with lateral wind direction, taking into account temperature of human body and floor surface. Environ Sci Pollut Res. 2023;30:33206–28.
Spahn C, Hipp AM, Schubert B, Axt MR, Stratmann M, Schmölder C, et al. Airflow and Air velocity measurements while playing wind instruments, with respect to risk assessment of a SARS-CoV-2 infection. Public Health. 2021;18:5413.
Bhaganagar K, Bhimireddy S. Local atmospheric factors that enhance air-borne dispersion of coronavirus - high-fidelity numerical simulation of COVID19 case study in real-time. Environ Res. 2020;191:110170.
Motamedi H, Shirzadi M, Tominaga Y, Mirzaei PA. CFD modeling of airborne pathogen transmission of COVID-19 in confined spaces under different ventilation strategies. Sustain Cities Soc. 2022;76:103397.
Feng Y, Marchal T, Sperry T, Yi H. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: a numerical study. J Aerosol Sci. 2020;147:105585.
Chen W, Qian H, Zhang N, Liu F, Liu L, Li Y. Extended short-range airborne transmission of respiratory infections. J Hazard Mater. 2022;422:126837.
Bourdrel T, Annesi-Maesano I, Alahmad B, Maesano CN, Bind MA. The impact of outdoor air pollution on covid-19: a review of evidence from in vitro, animal, and human studies. Eur Respir Rev. 2021;30:1–18.
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271-280.e8.
Zhuang MW, Cheng Y, Zhang J, Jiang XM, Wang L, Deng J, et al. Increasing host cellular receptor—angiotensin-converting enzyme 2 expression by coronavirus may facilitate 2019-nCoV (or SARS-CoV-2) infection. J Med Virol. 2020;92:2693–701.
Zhou L, Xu Z, Castiglione GM, Soiberman US, Eberhart CG, Duh EJ. ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection. Ocular Surface. 2020;18:537–44.
Li HH, Liu CC, Hsu TW, Lin JH, Hsu JW, Li AFY, et al. Upregulation of ACE2 and TMPRSS2 by particulate matter and idiopathic pulmonary fibrosis: a potential role in severe COVID-19. Part Fibre Toxicol. 2021;18:1–13.
Sagawa T, Tsujikawa T, Honda A, Miyasaka N, Tanaka M, Kida T, et al. Exposure to particulate matter upregulates ACE2 and TMPRSS2 expression in the murine lung. Environ Res. 2020;2021(195):110722.
Chuang HC, Chen YY, Hsiao TC, Chou HC, Kuo HP, Feng PH, et al. Alteration in angiotensin-converting enzyme 2 by pm1 during the development of emphysema in rats. ERJ Open Res. 2020;6:1–8.
Wang H, Song L, Ju W, Wang X, Dong L, Zhang Y, et al. The acute airway inflammation induced by PM 2.5 exposure and the treatment of essential oils in Balb/c mice. Sci Rep. 2017;7:44256.
Deng L, Ma M, Li S, Zhou L, Ye S, Wang J, et al. Protective effect and mechanism of baicalin on lung inflammatory injury in BALB/cJ mice induced by PM2.5. Ecotoxicol Environ Saf. 2022;248:114329.
Du X, Jiang S, Zeng X, Zhang J, Pan K, Song L, et al. Fine particulate matter-induced cardiovascular injury is associated with NLRP3 inflammasome activation in Apo E -/- mice. Ecotoxicol Environ Saf. J 2018;2019(174):92–9.
Kampfrath T, Maiseyeu A, Ying Z, Shah Z, Deiuliis JA, Xu X, et al. Chronic fine particulate matter exposure induces systemic vascular dysfunction via NADPH oxidase and TLR4 pathways. Circ Res. 2011;108:716–26.
Riva DR, Magalhães CB, Lopes AA, Lanças T, Mauad T, Malm O, et al. Low dose of fine particulate matter (PM2.5) can induce acute oxidative stress, inflammation and pulmonary impairment in healthy mice. Inhal Toxicol. 2011;23:257–67.
Wang S, Zhou Q, Tian Y, Hu X. The lung microbiota affects pulmonary inflammation and oxidative stress induced by PM2.5 exposure. Environ Sci Technol. 2022;56:12368–79.
Martin PJ, Billet S, Landkocz Y, Fougère B. Inflammation at the crossroads: the combined effects of COVID-19, ageing, and air pollution. J Frailty Aging. 2021;10:281–5.
CAS PubMed PubMed Central Google Scholar
Wang B, Chen H, Yik X, Chan L, Oliver BG. Is there an association between the level of ambient air pollution and COVID-19? J Physiol Lung Cell Mol Physiol. 2020;319:416–21.
Liu Q, Weng J, Li C, Feng Y, Xie M, Wang X, et al. Attenuation of PM2.5-induced alveolar epithelial cells and lung injury through regulation of mitochondrial fission and fusion. Part Fibre Toxicol. 2023;20:28.
To EE, Vlahos R, Luong R, Halls ML, Reading PC, King PT, et al. Endosomal NOX2 oxidase exacerbates virus pathogenicity and is a target for antiviral therapy. Nat Commun. 2017;8:69.
Sciomer S, Moscucci F, Magrì D, Badagliacca R, Piccirillo G, Agostoni P. SARS-CoV-2 spread in Northern Italy: what about the pollution role? Environ Monit Assess. 2020;192:2–4.
Conticini E, Frediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut. 2020;261:114465.
Miller MR. Oxidative stress and the cardiovascular effects of air pollution. Free Radical Biol Med. 2020;151:69–87.
Bromberg PA. Mechanisms of the acute effects of inhaled ozone in humans. Biochim Biophys Acta Gen Subj. 2016;1860:2771–81.
Wiegman CH, Li F, Ryffel B, Togbe D, Chung KF. Oxidative stress in ozone-induced chronic lung inflammation and emphysema: a facet of chronic obstructive pulmonary disease. Front Immunol. 2020;11:1957.
Manzer R, Dinarello CA, McConville G, Mason RJ. Ozone exposure of macrophages induces an alveolar epithelial chemokine response through IL-1α. Am J Respir Cell Mol Biol. 2008;38:318–23.
Chen QZ, Zhou YB, Zhou LF, Fu ZD, Wu YS, Chen Y, et al. TRPC6 modulates adhesion of neutrophils to airway epithelial cells via NF-κB activation and ICAM-1 expression with ozone exposure. Exp Cell Res. 2019;377:56–66.
Wiegman CH, Li F, Clarke CJ, Jazrawi E, Kirkham P, Barnes PJ, et al. A comprehensive analysis of oxidative stress in: the ozone-induced lung inflammation mouse: model. Clin Sci. 2014;126:425–40.
Bauer AK, Rondini EA, Hummel KA, Degraff LM, Walker C, Jedlicka AE, et al. Identification of candidate genes downstream of TLR4 signaling after ozone exposure in mice: A role for heat-shock protein 70. Environ Health Perspect. 2011;119:1091–7.
Mumby S, Chung KF, Adcock IM. Transcriptional effects of ozone and impact on airway inflammation. Front Immunol. 2019;10:1610.
Paludan SR, Reinert LS, Hornung V. DNA-stimulated cell death: implications for host defence, inflammatory diseases and cancer. Nat Rev Immunol. 2019;19:141–53.
Zhang JH, Yang X, Chen YP, Zhang JF, Li CQ. Nrf2 activator RTA-408 Protects against ozone-induced acute asthma exacerbation by suppressing ROS and γδT17 cells. Inflammation. 2019;42:1843–56.
Fry RC, Rager JE, Zhou H, Zou B, Brickey JW, Ting J, et al. Individuals with increased inflammatory response to ozone demonstrate muted signaling of immune cell trafficking pathways. Respir Res. 2012;13:89.
Bao A, Yang H, Ji J, Chen Y, Bao W, Li F, et al. Involvements of p38 MAPK and oxidative stress in the ozone-induced enhancement of AHR and pulmonary inflammation in an allergic asthma model. Respir Res. 2017;18:216.
Mazur-Panasiuk N, Botwina P, Kutaj A, Woszczyna D, Pyrc K. Ozone treatment is insufficient to inactivate sars-cov-2 surrogate under field conditions. Antioxidants. 2021;10:1480.
Tizaoui C. Ozone: A Potential Oxidant for COVID-19 Virus (SARS-CoV-2). Ozone Sci Eng. 2020;42:378–85.
Tizaoui C, Stanton R, Statkute E, Rubina A, Lester-Card E, Lewis A, et al. Ozone for SARS-CoV-2 inactivation on surfaces and in liquid cell culture media. J Hazard Mater. 2022;428:128251.
Elvis AM, Ekta JS. Ozone therapy: a clinical review. J Nat Sci Biol Med. 2011;2:66–70.
Cattel F, Giordano S, Bertiond C, Lupia T, Corcione S, Scaldaferri M, et al. Ozone therapy in COVID-19: a narrative review. Virus Res. 2021;291:198207.
Sagai M, Bocci V. Mechanisms of action involved in ozone therapy: is healing induced via a mild oxidative stress? Med Gas Res. 2011;1:29.
Amor S, Fernández Blanco L, Baker D. Innate immunity during SARS-CoV-2: evasion strategies and activation trigger hypoxia and vascular damage. Clin Exp Immunol. 2020;202:193–209.
Bocci V, Borrelli E, Travagli V, Zanardi I. The ozone paradox: Ozone is a strong oxidant as well as a medical drug. Med Res Rev. 2009;29:646–82.
Serra MEG, Baeza-Noci J, Abdala CVM, Luvisotto MM, Bertol CD, Anzolin AP. Clinical effectiveness of medical ozone therapy in COVID-19: the evidence and gaps map. Med Gas Res. 2023;13:172–80.
Villeneuve PJ, Goldberg MS. Methodological considerations for epidemiological studies of air pollution and the sars and COVID-19 coronavirus outbreaks. Environ Health Perspect. 2020;128:95001.
Benmarhnia T. Linkages between air pollution and the health burden from covid-19: methodological challenges and opportunities. Am J Epidemiol. 2020;189:1238–43.
Shakil MH, Munim ZH, Tasnia M, Sarowar S. COVID-19 and the environment: a critical review and research agenda. Sci Total Environ. 2020;745:141022.
D’Amico F, Marmiere M, Righetti B, Scquizzato T, Zangrillo A, Puglisi R, et al. COVID-19 seasonality in temperate countries. Environ Res. 2021;2022(206):112614.
Jiang C, Wang X, Li X, Inlora J, Wang T, Liu Q, et al. Dynamic human environmental exposome revealed by longitudinal personal monitoring. Cell. 2018;175:277-291.e31.
Beltran RM, Holloway IW, Hong C, Miyashita A, Cordero L, Wu E, et al. Social determinants of disease: HIV and COVID-19 experiences. Curr HIV/AIDS Rep. 2022;19:101–12.
Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA - J Am Med Asso. 2020;323:1915–23.
Telenti A, Arvin A, Corey L, Corti D, Diamond MS, García-Sastre A, et al. After the pandemic: perspectives on the future trajectory of COVID-19. Nature. 2021;596:495–504.
Kurt OK, Zhang J, Pinkerton KE. Pulmonary health effects of air pollution. Curr Opin Pulm Med. 2016;22:138–43.
Download references
Acknowledgements
We thank BioRender (Gallery (biorender.com)) for its online mapping services provided during the writing of this manuscript.
This work was supported by the China Academy of Chinese Medical Sciences key collaborative project of Innovation Fund, Analysis of Dynamic Temporal and Spatial Characteristics of TCM Syndrome of COVID-19 and Research on Its Biological Connotation, (No.CI2022C004-01), National Key R&D Program of China (2023YFC3503400), the 2023 Agency/National Special Fund Project of National Administration of Traditional Chinese Medicine (F0212), and 2022 Qi Huang Young Scholar programme of the National Administration of Traditional Chinese Medicine (Nannan Shi) (Z0841, Z0865).
Author information
Zhaoyuan Gong, Tian Song and Mingzhi Hu contributed equally to this work.
Authors and Affiliations
Institute of Basic Research in Clinical Medicine, China Academy of Chinese Medical Sciences, Beijing, 100700, China
Zhaoyuan Gong, Tian Song, Mingzhi Hu, Qianzi Che, Jing Guo, Haili Zhang, Huizhen Li, Yanping Wang, Bin Liu & Nannan Shi
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: Yanping Wang, Bin Liu, and Nannan Shi; original draft preparation, Zhaoyuan Gong, Tian Song, and Mingzhi Hu; writing-review & editing, Qianzi Che, Jing Guo; and project administration, Haili Zhang and Huizhen Li. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Yanping Wang , Bin Liu or Nannan Shi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Gong, Z., Song, T., Hu, M. et al. Natural and socio-environmental factors in the transmission of COVID-19: a comprehensive analysis of epidemiology and mechanisms. BMC Public Health 24 , 2196 (2024). https://doi.org/10.1186/s12889-024-19749-3
Download citation
Received : 22 January 2024
Accepted : 09 August 2024
Published : 13 August 2024
DOI : https://doi.org/10.1186/s12889-024-19749-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nature environmental factor
- Social environmental factor
- Epidemiology
- Mechanism research
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Appointments at Mayo Clinic
- COVID-19 in babies and children
Anyone can get COVID-19 , also called coronavirus disease 2019, including children. Find out about the symptoms, testing and medical issues linked to COVID-19 in children. And learn how to help prevent COVID-19, especially in children at high risk of serious illness.
How likely is it for a child to become sick with coronavirus disease 2019 (COVID-19)?
Data tracking between 2020 and 2023 found that children made up about 18% of all people with reported COVID-19 in the United States.
While children are as likely as adults to catch the virus that causes COVID-19, kids are less likely to become seriously ill. From 2020 to the end of March 2024, children up to age 17 accounted for about 1.5% of people who needed to be treated for COVID-19 in the hospital.
But some children with COVID-19 need to be hospitalized, treated in the intensive care unit or placed on a machine to help them breathe, called a ventilator. Very rarely, COVID-19 can cause death.
Some health issues might raise a child's risk of serious illness with COVID-19, such as:
- Having more than one chronic disease, including those of the heart, lung or nervous system.
- Not being up to date with COVID-19 vaccination.
- Having a weakened immune system.
- Being born before the due date, called prematurity.
- Having obesity.
- Having type 1 or type 2 diabetes.
This is not a complete list. Other health issues, such as sickle cell disease, may be linked to more-serious COVID-19.
Having more than one risk factor raises the chance of serious COVID-19. Age younger than 1 year or older than 12 also raises the risk. And if a medical condition isn't under control, that can raise the risk of serious COVID-19.
A COVID-19 vaccine might prevent your child from getting the virus that causes COVID-19. It also may prevent your child from becoming seriously ill, having to stay in the hospital or dying of COVID-19.
How are babies affected by COVID-19?
Babies under age 1 might be at higher risk of serious illness with COVID-19 than are older children. This may be mostly due to the fact that babies born prematurely have the highest risk.
In general, the virus that causes COVID-19 doesn't spread from the pregnant person to the unborn baby. Infants typically get COVID-19 from a sick caregiver after delivery.
Pregnant people can help lower an infant's risk by getting the COVID-19 vaccine during pregnancy. Some evidence suggests protection can pass to the unborn baby and continue after birth.
What are the symptoms of COVID-19 in children?
Children with COVID-19 may have serious or mild symptoms or no symptoms at all. Symptoms may show up from 2 to 14 days after contact with the virus that causes COVID-19.
The most common symptoms are fever and a cough, including a barking cough linked to croup. For many children, symptoms are like those of other lung and breathing illnesses, called respiratory illnesses, and may include:
- Sore throat.
- Stuffy or runny nose.
- Feeling very tired, called fatigue.
- Nausea, vomiting or loose stools, called diarrhea.
- Muscle aches and pain.
Testing can help figure out if the virus that causes COVID-19 is the cause.
COVID-19 symptoms also may include problems breathing or shortness of breath, as well as new loss of taste or smell.
Breathing trouble
Get emergency help right away if your child is working hard to breathe. Symptoms of breathing trouble include grunting, flaring the nostrils, or having the chest pull at the collarbone and rib with a breath. Other symptoms of trouble breathing are shortness of breath at rest; rapid breathing; or wheezy, noisy or raspy breathing. In babies, this may show as not being able to cry or feed.
Get emergency help for other symptoms of serious illness, such as:
- Fever higher than 100.4 degrees Fahrenheit (38 degrees Celsius) in a child younger than 3 months old.
- Problems swallowing, for example, drooling in children younger than age 3 and in older children, not being able to swallow or open the mouth fully.
- Skin, lips or nail beds that are gray or blue.
- New confusion.
- Trouble staying awake or waking up.
- Chest pain or pressure that is constant.
- Vomiting or diarrhea that doesn't stop.
- Dehydration, which in babies younger than 3 month means fewer than three wet diapers in 24 hours.
This list doesn't include every emergency symptom. If the child you're taking care of has symptoms that worry you, get help. Let the healthcare team know about a positive test for COVID-19 or symptoms of the illness.
Testing for COVID-19
Testing for COVID-19 can help you quickly figure out if the COVID-19 virus is the cause of your child's illness. Testing helps you act quickly to prevent serious illness in kids who are at higher than average risk. It also helps protect others who may be at high risk.
Test for COVID-19 if you know you or your child was exposed to the virus or if you have symptoms. Testing during times when many people in your area have COVID-19 can help stop the spread of the virus that causes the illness.
Supporting Your Child During COVID-19 Nasal Swab Testing
The purpose of this video is to help children get ready for a COVID-19 nasal swab test. Knowing what to expect may help ease any fears they may have. When children know about the medical test they're about to take, the test is easier for them to take. Children as young as 4 years old can watch this video.
Jennifer Rodemeyer, Child Life Program Manager, Mayo Clinic: Hi, I'm Jennifer and I am a child life specialist at Mayo Clinic. My job is to help kids like you prepare for medical tests.
You may have heard there is a virus going around that can make people feel sick. A virus is a germ and it is so tiny you can't even see it.
Some people who get this virus can have a fever or a cough and may feel achy and tired, while some people can have this virus and not feel sick at all. People may get this virus from touching things. That's why it's important to wash your hands often with soap and water. The virus also can spread through a cough or a sneeze. So it's important to always cover your cough or sneeze.
Today, even though you may or may not be feeling sick, we will need to give you a test so we know how to best proceed with your medical care. This medical test will tell us if you have the virus.
When you go to take your test, the health care provider will wear special protective clothing. They wear this clothing to keep themselves and you safe from getting germs. They will wear a mask to cover their nose and mouth and a clear plastic shield to protect their eyes.
The most important thing you can do during your test is to sit perfectly still like a statue. To help make sure you don't move, your parent or caregiver will help keep you still and calm during your test. The health care provider needs to touch the inside of the back of your nose with a long, skinny Q-tip. To do this, you need to hold your chin up, then the health care provider will put the Q-tip in your nose for a short time to collect a sample.
While this happens you may feel like you want to push the Q-tip away, but it's really important to stay as still as possible so the health care provider can finish the test. The Q-tip will be in and out of your nose in a few seconds.
Some kids tell me that counting to 3 or taking a deep breath relaxes them before the test happens, and some tell me they like to hold on to their favorite stuffed animal or blanket. Maybe you have your own way to relax.
Remember that during the test, the most important thing to do is to keep your body perfectly still.
You may have many feelings seeing the health care provider wearing different clothing, but know this person is caring and wants to help you.
Thank you for helping us get this test done, so we know how to proceed with your medical care.
What is multisystem inflammatory syndrome in children (MIS-C)?
Multisystem inflammatory syndrome in children (MIS-C) is a serious condition linked to infection with the virus that causes COVID-19.
With MIS-C, children have fever, blood markers of inflammation and serious disease throughout the body. Organs such as the brain, eyes, heart, lungs, kidneys, digestive system and skin may become inflamed. MIS-C symptoms are treated in the hospital as the illness runs its course.
MIS-C is rare. In 2023, the U.S. Centers for Disease Control and Prevention received 117 reports of MIS-C. Most of these children had no medical issues before getting MIS-C.
Symptoms usually show up in about 2 to 6 weeks after infection with the virus that causes COVID-19.
Symptoms of MIS-C include a fever that doesn't go away, along with other symptoms:
- Belly pain.
- Bloodshot eyes.
- Dizziness or lightheadedness.
Emergency warning signs of MIS-C include:
- Difficulty breathing.
- Gray or blue skin, lips or nail beds.
- Terrible belly pain.
If your child shows any emergency warning signs or is severely sick with other symptoms, take your child to the nearest emergency department or call 911 or your local emergency number. If your child isn't seriously ill but shows other symptoms of MIS-C, contact your child's healthcare professional right away for advice.
Most children get better quickly and don't have any medical issues caused by MIS-C.
Staying up to date with COVID-19 vaccination offers protection against MIS-C. And most children who have had MIS-C can get a COVID-19 vaccine on schedule.
Can children who get COVID-19 experience long-term effects?
Anyone who has had COVID-19 can develop a post-COVID-19 syndrome. New symptoms or conditions that develop after infection with the virus that causes COVID-19 is more often linked to serious COVID-19 illness. But anyone who catches the COVID-19 virus can develop a post-COVID-19 syndrome.
Symptoms often include a high level of tiredness that affects day-to-day life. And some symptoms may get worse after certain activities.
Symptoms may relate to trouble with:
- Trouble with thinking.
- Fast heartbeat.
- Sleep problems
- Digestive issues.
- Pain in the joints or muscles.
Depending on their age, children may have trouble explaining some of these issues, which may be difficult for healthcare teams to diagnose.
These symptoms could affect your child's ability to attend school or do typical activities. If your child has post-COVID-19 symptoms that aren't getting better, talk with your healthcare professional. Working with your child's school, it may be possible to compensate for these symptoms.
Staying up to date with COVID-19 vaccines offers protection against post-COVID-19 syndrome.
What COVID-19 vaccines are available to kids in the U.S.?
The COVID-19 vaccines available in the United States are:
- 2023-2024 Pfizer-BioNTech COVID-19 vaccine, available for people age 6 months and older.
- 2023-2024 Moderna COVID-19 vaccine, available for people age 6 months and older.
- 2023-2024 Novavax COVID-19 vaccine, available for people age 12 years and older.
In general, people older than age 4 with typical immune systems can get any vaccine that is approved or authorized for their age. And people usually don't need to get vaccines from the same vaccine maker each time.
Some people should get all their vaccine doses from the same vaccine maker, including:
- Children age 6 months to 4 years.
- People age 5 years and older with weakened immune systems.
- People age 12 and older who have had one shot of the Novavax vaccine. They should get the second Novavax shot in the two-dose series.
Talk with your healthcare professional if you have any questions about the vaccines for you or your child. Your healthcare team can help you if:
- The vaccine you or your child got earlier isn't available.
- You don't know which vaccine you or your child received.
- You or your child started a vaccine series but couldn't finish it due to side effects.
What can I do to prevent my child from getting COVID-19?
There are many steps you can take to prevent your child from getting the COVID-19 virus and spreading it to others.
- Get vaccinated. If the timing works out, a COVID-19 vaccine can be given to eligible children on the same day as other vaccines.
- Keep hands clean. Encourage frequent hand-washing with soap and water for at least 20 seconds. Teach your kids to keep washing their hands until they have sung the entire "Happy Birthday" song twice, which takes about 20 seconds. Or use an alcohol-based hand sanitizer that contains at least 60% alcohol. Have your child cover the mouth and nose with an elbow or a tissue when coughing or sneezing. Remind your child to avoid touching the eyes, nose and mouth.
- Clean and disinfect your home. Clean high-touch surfaces and objects regularly and after you have visitors in your home. Also, regularly clean areas that easily get dirty, such as a baby's changing table, and surfaces and items that your child often touches.
- Get the air flowing. Use fans, open windows or doors, and use filters to keep air and germs moving out of your indoor space.
- Keep some distance. If possible, avoid close contact with anyone who is sick or has symptoms. Spread out in crowded indoor places, especially in places with poor airflow.
- Wear face masks. If you are in an area with a high number of people in the hospital with COVID-19, the CDC recommends wearing a well-fitted mask indoors in public. Don't place a face mask on a child younger than age 2 or a child with a disability who can't safely wear a mask.
Keep up with well-child visits and your child's other vaccines. COVID-19 is just one of many illnesses that can be prevented with vaccination. Vaccines for children are timed carefully. Vaccines are given when protection inherited from the mother fades and the child's immune system is ready, but before kids are likely to come in contact with the germs that cause real infections.
Following guidelines to protect against the COVID-19 virus can be difficult for kids. Stay patient. Be a good role model and your child will be more likely to follow your lead.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Children and COVID-19: State data report. American Academy of Pediatrics. https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/. Accessed April 3, 2024.
- Information for pediatric healthcare providers. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html. Accessed April 3, 2024.
- COVID data tracker. Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#pediatric-data. Accessed April 3, 2024.
- Willis ZI, et al. Guidance for prevention and management of COVID-19 in children and adolescents: A consensus statement from the Pediatric Infectious Diseases Society Pediatric COVID-19 Therapies Taskforce. Journal of the Pediatric Infectious Diseases Society. 2024; doi:10.1093/jpids/piad116.
- Stay up to date with your vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed April 4, 2024.
- Hughes BL, et al. COVID-19: Antepartum care of pregnant patients with symptomatic infection. https://www.uptodate.com/contents/search. Accessed April 4, 2024.
- AskMayoExpert. COVID-19: Pregnancy. Mayo Clinic; 2024.
- Halasa NB, et al. Effectiveness of maternal vaccination with mRNA COVID-19 vaccine during pregnancy against COVID-19-associated hospitalization in infants aged <6 months — 17 states, July 2021-January 2022. MMWR Morbidity and Mortality Weekly Report. 2022; doi:10.15585/mmwr.mm7107e3.
- AskMayoExpert. COVID-19: Outpatient and inpatient management (child). Mayo Clinic; 2024.
- Symptoms of COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed April 4, 2024.
- Testing and respiratory viruses. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/testing.html. Accessed April 4, 2024.
- Information for healthcare providers about multisystem inflammatory syndrome in children (MIS-C). Centers for Disease Control and Prevention. https://www.cdc.gov/mis/mis-c/hcp_cstecdc/index.html. Accessed April 4, 2024.
- Notes from the field: Surveillance for multisystem inflammatory syndrome in children, United States, 2023. MMWR Morbidity and Mortality Weekly Report. 2024; doi:10.15585/mmwr.mm7310a2.
- For parents: Multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/mis/mis-c.html. Accessed April 4, 2024.
- Long COVID or post-COVID conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html. Accessed April 3, 2024.
- Caring for people with long COVID. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/care-post-covid.html. Accessed April 4, 2024.
- Interim clinical considerations for use of COVID-19 vaccines currently approved or authorized in the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html. Accessed April 3, 2024.
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed April 4, 2024.
- When and how to wash your hands. Centers for Disease Control and Prevention. https://www.cdc.gov/handwashing/when-how-handwashing.html. Accessed April 4, 2024.
- Everyday cleaning. Centers for Disease Control and Prevention. https://www.cdc.gov/hygiene/cleaning/index.html. Accessed April 4, 2024.
- Taking steps for cleaner air for respiratory virus prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/air-quality.html. Accessed April 4, 2024.
- Masks and respiratory viruses prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/masks.html. Accessed April 4, 2024.
- Timing and spacing of immunobiologics. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/timing.html. Accessed April 4, 2024.
- Infants and children birth through age 6. U.S. Department of Health and Human Services. https://www.hhs.gov/immunization/who-and-when/index.html. Accessed April 4, 2024.
- Your child's first vaccines. Centers for Disease Control and Prevention. http://www.cdc.gov/vaccines/hcp/vis/vis-statements/multi.html. Accessed April 4, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- COVID-19 vaccines for kids: What you need to know - Related information COVID-19 vaccines for kids: What you need to know
- Coronavirus disease 2019 (COVID-19) - Related information Coronavirus disease 2019 (COVID-19)
- Multisystem inflammatory syndrome in children (MIS-C) and COVID-19 - Related information Multisystem inflammatory syndrome in children (MIS-C) and COVID-19
- Resilience: Build skills to endure hardship - Related information Resilience: Build skills to endure hardship
- 31 - Related information 31
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.
- Introduction
- Conclusions
- Article Information
eFigure. Cardiac magnetic resonance image for a patient with myocarditis.
- JAMA Network Journals’ Articles of the Year 2021 JAMA Medical News & Perspectives December 28, 2021 This Medical News article is our fifth-annual roundup of the top-viewed articles from each of the JAMA Network Journals. Jennifer Abbasi
- Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021 JAMA Original Investigation January 25, 2022 This descriptive study compares the effect of mRNA-based COVID-19 vaccination with BNT162b2 (Pfizer-BioNTech) vs mRNA-1273 (Moderna) on the reported cases of myocarditis in the US after each vaccination dose. Matthew E. Oster, MD, MPH; David K. Shay, MD, MPH; John R. Su, MD, PhD, MPH; Julianne Gee, MPH; C. Buddy Creech, MD, MPH; Karen R. Broder, MD; Kathryn Edwards, MD; Jonathan H. Soslow, MD, MSCI; Jeffrey M. Dendy, MD; Elizabeth Schlaudecker, MD, MPH; Sean M. Lang, MD; Elizabeth D. Barnett, MD; Frederick L. Ruberg, MD; Michael J. Smith, MD, MSCE; M. Jay Campbell, MD, MHA; Renato D. Lopes, MD, PhD, MHS; Laurence S. Sperling, MD; Jane A. Baumblatt, MD; Deborah L. Thompson, MD, MSPH; Paige L. Marquez, MSPH; Penelope Strid, MPH; Jared Woo, MPH; River Pugsley, PhD, MPH; Sarah Reagan-Steiner, MD, MPH; Frank DeStefano, MD, MPH; Tom T. Shimabukuro, MD, MPH, MBA
- Myocarditis Following a Third BNT162b2 Vaccination Dose in Military Recruits in Israel JAMA Research Letter April 26, 2022 This study assessed whether a third vaccine dose was associated with the risk of myocarditis among military personnel in Israel. Limor Friedensohn, MD; Dan Levin, MD; Maggie Fadlon-Derai, MHA; Liron Gershovitz, MD; Noam Fink, MD; Elon Glassberg, MD; Barak Gordon, MD
- JAMA Network Articles of the Year 2022 JAMA Medical News & Perspectives December 27, 2022 This Medical News article is our annual roundup of the top-viewed articles from all JAMA Network journals. Melissa Suran, PhD, MSJ
- Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination JAMA Cardiology Brief Report October 1, 2021 This study describes 4 patients who presented with acute myocarditis after mRNA COVID-19 vaccination. Han W. Kim, MD; Elizabeth R. Jenista, PhD; David C. Wendell, PhD; Clerio F. Azevedo, MD; Michael J. Campbell, MD; Stephen N. Darty, BS; Michele A. Parker, MS; Raymond J. Kim, MD
- Temporal Associations Between Immunization With the COVID-19 mRNA Vaccines and Myocarditis JAMA Cardiology Editorial October 1, 2021 Ann Marie Navar, MD, PhD; Elizabeth McNally, MD, PhD; Clyde W. Yancy, MD, MSc; Patrick T. O’Gara, MD; Robert O. Bonow, MD, MS
- Myocarditis Occurring After Immunization With mRNA-Based COVID-19 Vaccines JAMA Cardiology Editorial October 1, 2021 David K. Shay, MD, MPH; Tom T. Shimabukuro, MD, MPH, MBA; Frank DeStefano, MD, MPH
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Montgomery J , Ryan M , Engler R, et al. Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol. 2021;6(10):1202–1206. doi:10.1001/jamacardio.2021.2833
Manage citations:
© 2024
- Permissions
Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military
- 1 Immunization Healthcare Division, Defense Health Agency, Falls Church, Virginia
- 2 Walter Reed National Military Medical Center, Bethesda, Maryland
- 3 Naval Medical Center, San Diego, California
- 4 Uniformed Services University of the Health Sciences, Bethesda, Maryland
- 5 Womack Army Medical Center, Fort Bragg, North Carolina
- 6 Wilford Hall Ambulatory Surgical Center, Lackland Air Force Base, San Antonio, Texas
- 7 Naval Hospital Bremerton, Bremerton, Washington
- 8 Marine Expeditionary Forces, Okinawa, Japan
- 9 Mayo Clinic, Jacksonville, Florida
- Editorial Temporal Associations Between Immunization With the COVID-19 mRNA Vaccines and Myocarditis Ann Marie Navar, MD, PhD; Elizabeth McNally, MD, PhD; Clyde W. Yancy, MD, MSc; Patrick T. O’Gara, MD; Robert O. Bonow, MD, MS JAMA Cardiology
- Editorial Myocarditis Occurring After Immunization With mRNA-Based COVID-19 Vaccines David K. Shay, MD, MPH; Tom T. Shimabukuro, MD, MPH, MBA; Frank DeStefano, MD, MPH JAMA Cardiology
- Medical News & Perspectives JAMA Network Journals’ Articles of the Year 2021 Jennifer Abbasi JAMA
- Original Investigation Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021 Matthew E. Oster, MD, MPH; David K. Shay, MD, MPH; John R. Su, MD, PhD, MPH; Julianne Gee, MPH; C. Buddy Creech, MD, MPH; Karen R. Broder, MD; Kathryn Edwards, MD; Jonathan H. Soslow, MD, MSCI; Jeffrey M. Dendy, MD; Elizabeth Schlaudecker, MD, MPH; Sean M. Lang, MD; Elizabeth D. Barnett, MD; Frederick L. Ruberg, MD; Michael J. Smith, MD, MSCE; M. Jay Campbell, MD, MHA; Renato D. Lopes, MD, PhD, MHS; Laurence S. Sperling, MD; Jane A. Baumblatt, MD; Deborah L. Thompson, MD, MSPH; Paige L. Marquez, MSPH; Penelope Strid, MPH; Jared Woo, MPH; River Pugsley, PhD, MPH; Sarah Reagan-Steiner, MD, MPH; Frank DeStefano, MD, MPH; Tom T. Shimabukuro, MD, MPH, MBA JAMA
- Research Letter Myocarditis Following a Third BNT162b2 Vaccination Dose in Military Recruits in Israel Limor Friedensohn, MD; Dan Levin, MD; Maggie Fadlon-Derai, MHA; Liron Gershovitz, MD; Noam Fink, MD; Elon Glassberg, MD; Barak Gordon, MD JAMA
- Medical News & Perspectives JAMA Network Articles of the Year 2022 Melissa Suran, PhD, MSJ JAMA
- Brief Report Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination Han W. Kim, MD; Elizabeth R. Jenista, PhD; David C. Wendell, PhD; Clerio F. Azevedo, MD; Michael J. Campbell, MD; Stephen N. Darty, BS; Michele A. Parker, MS; Raymond J. Kim, MD JAMA Cardiology
Question Should myocarditis be considered a potential adverse event following immunization with messenger RNA (mRNA) COVID-19 vaccines?
Findings In this case series of 23 male patients, including 22 previously healthy military members, myocarditis was identified within 4 days of receipt of a COVID-19 vaccine. For most patients (n = 20), the diagnosis was made after the second dose of mRNA COVID-19 vaccine; these episodes occurred against the backdrop of 2.8 million doses of mRNA COVID-19 vaccines administered.
Meaning Vigilance for rare adverse events, including myocarditis, after COVID-19 vaccination is warranted but should not diminish overall confidence in vaccination during the current pandemic.
Importance Myocarditis has been reported with COVID-19 but is not clearly recognized as a possible adverse event following COVID-19 vaccination.
Objective To describe myocarditis presenting after COVID-19 vaccination within the Military Health System.
Design, Setting, and Participants This retrospective case series studied patients within the US Military Health System who experienced myocarditis after COVID-19 vaccination between January and April 2021. Patients who sought care for chest pain following COVID-19 vaccination and were subsequently diagnosed with clinical myocarditis were included.
Exposure Receipt of a messenger RNA (mRNA) COVID-19 vaccine between January 1 and April 30, 2021.
Main Outcomes and Measures Clinical diagnosis of myocarditis after COVID-19 vaccination in the absence of other identified causes.
Results A total of 23 male patients (22 currently serving in the military and 1 retiree; median [range] age, 25 [20-51] years) presented with acute onset of marked chest pain within 4 days after receipt of an mRNA COVID-19 vaccine. All military members were previously healthy with a high level of fitness. Seven received the BNT162b2-mRNA vaccine and 16 received the mRNA-1273 vaccine. A total of 20 patients had symptom onset following the second dose of an appropriately spaced 2-dose series. All patients had significantly elevated cardiac troponin levels. Among 8 patients who underwent cardiac magnetic resonance imaging within the acute phase of illness, all had findings consistent with the clinical diagnosis of myocarditis. Additional testing did not identify other etiologies for myocarditis, including acute COVID-19 and other infections, ischemic injury, or underlying autoimmune conditions. All patients received brief supportive care and were recovered or recovering at the time of this report. The military administered more than 2.8 million doses of mRNA COVID-19 vaccine in this period. While the observed number of myocarditis cases was small, the number was higher than expected among male military members after a second vaccine dose.
Conclusions and Relevance In this case series, myocarditis occurred in previously healthy military patients with similar clinical presentations following receipt of an mRNA COVID-19 vaccine. Further surveillance and evaluation of this adverse event following immunization is warranted. Potential for rare vaccine-related adverse events must be considered in the context of the well-established risk of morbidity, including cardiac injury, following COVID-19 infection.
Myocarditis is a heterogeneous disease with diverse clinical patterns, etiologies, and therapeutic responses, reflecting inflammatory injury to myocardial tissue in the absence of ischemia. 1 While viral infections, now including SARS-CoV-2, are the most common triggers of the disease, some myocarditis cases are associated with certain drugs and vaccine exposures. 1 With the exception of cases following live-attenuated smallpox vaccine in the military population, 2 myocarditis as an adverse event following immunization is described in rare published case reports and infrequent submissions to the Vaccine Adverse Events Reporting System (VAERS). 3 , 4
Serious adverse events associated with receipt of new vaccines targeting COVID-19 are of high interest to the public and to public health vaccine safety surveillance. We describe a series of 23 individuals who developed probable hypersensitivity myocarditis in temporal association with COVID-19 messenger RNA (mRNA) vaccination.
The US military initiated COVID-19 vaccination following US Centers for Disease Control and Prevention (CDC)–defined phased distribution in December 2020. Adverse events following immunizations were identified from referrals to Defense Health Agency clinical specialists and through review of VAERS reports. Retrospective review of cases was conducted in accordance with the Walter Reed National Military Medical Center Institutional Review Board–approved protocol, “Adverse Events Following Immunization: Case Definitions and Outcomes Retrospective Review,” and exempt from formal consent procedures.
A total of 23 male patients (22 currently serving in the military and 1 retiree; median [range] age, 25 [20-51] years) were evaluated between January and April 2021 for acute-onset chest pain following mRNA COVID-19 vaccination. Care was provided in 15 distinct geographic locations globally with varying diagnostic evaluations. Each patient had a final diagnosis of myocarditis without infectious, ischemic, or autoimmune etiologies identified. Diagnoses were reviewed by an adjudication process and met the CDC case definition criteria for probable myocarditis ( Table 1 ). A total of 8 patients had cardiac magnetic resonance imaging (cMRI) with T2 weighting showing subepicardial late gadolinium enhancement and/or focal myocardial edema, consistent with Lake Louise criteria for myocarditis. 1 The eFigure in the Supplement exemplifies cMRI findings for one of these patients.
The demographic and clinical characteristics of patients are summarized in Table 2 . All military service members were physically fit by military standards and lacking any known history of cardiac disease, significant cardiac risk factors, or exposure to cardiotoxic agents. All patients presented with acute chest pain and significantly elevated cardiac troponin levels (10-fold to 400-fold the upper limits of their respective reference ranges). Their symptoms began within 12 to 96 hours following immunization with an mRNA COVID-19 vaccine. Sixteen had received the mRNA-1273 vaccine (Moderna), and 7 had received the BNT162b2-mRNA vaccine (Pfizer-BioNTech). For all but 3 patients, the second dose of vaccine preceded their myocarditis presentations. Among the 3 patients presenting after an initial vaccine dose, all had confirmed COVID-19 infection more than 2 months prior to vaccination.
All patients underwent electrocardiography and echocardiography ( Table 2 ). Abnormal electrocardiography findings were recorded in 19 patients (83%); findings included ST-segment elevations, T-wave inversions, and nonspecific ST changes. Echocardiography in 4 patients (17%) demonstrated reduced left ventricular ejection fractions (40% to 50%). No structural abnormalities were noted on any echocardiograms. A total of 16 patients underwent coronary artery imaging (11 had cardiac catheterization and 5 had coronary computed tomography angiography); none showed evidence of coronary artery disease.
Nineteen patients had respiratory specimens tested for SARS-CoV-2 by polymerase chain reaction at the time of presentation; none had evidence of acute SARS-CoV-2 infection. There were no positive findings among 13 patients who were tested for other infections, nor among 9 patients who were tested for autoimmune diseases.
Cardiac symptoms resolved within 1 week of onset for 16 patients. Seven patients continued to have chest discomfort at the time of this report; follow-up is ongoing.
The number of doses of mRNA COVID-19 vaccine administered by the Military Health System through April 30, 2021, is shown in Table 3 . Overall, 2 810 000 doses were administered; 1 065 000 second doses were administered; 544 000 second doses were administered to military service members; and 436 000 second doses were administered to male military service members. The expected number of myocarditis cases occurring in a 30-day period after vaccination may be estimated using an international incidence of 22 cases per 100 000 person-years 5 or a US incidence of 1 to 10 cases per 100 000 person-years. 6 Observed numbers of myocarditis in the Military Health System were higher than some estimates of expected numbers, especially when considering the subset of the population who were military service members who received second doses of an mRNA COVID-19 vaccine ( Table 3 ).
In this case series, we describe 23 patients with clinical evidence of myocarditis following mRNA COVID-19 vaccination and meeting the CDC case definition for probable myocarditis. Eight patients had cMRI findings consistent with myocarditis. All patients in this series reflect substantial similarities in demographic characteristics, proximate vaccine dose, onset interval, and character of vaccine-associated myocarditis. The consistent pattern of clinical presentation, rapid recovery, and absence of evidence of other causes support the diagnosis of hypersensitivity myocarditis. Without myocardial biopsy, histology cannot be defined, but the clinical course suggests eosinophilic hypersensitivity myocarditis as described in the context of other drug-associated and vaccine-associated myocarditis. 1 - 3 Presentation after second vaccine dose or, in 3 patients, when vaccination followed SARS-CoV-2 infection, suggests that prior exposure was relevant in the hypersensitivity response.
With the exception of the smallpox vaccine, immunizations are rarely associated with hypersensitivity myocarditis. The spectrum of clinical presentation and reliance on patients seeking health care and on health care professionals recognizing a rare vaccine-associated adverse event limits determination of the true incidence of this condition. 7 In contrast to passive case finding, Engler et al 2 reported a significantly higher incidence of myocarditis and pericarditis after smallpox vaccination through active prospective follow-up of vaccinated participants. They noted that 60% of these patients would not have sought medical care for symptoms outside of the study protocol. 2 Recognition of vaccine-associated myocarditis is clinically important since diagnosis impacts management, recommendations for exercise, and monitoring for cardiomyopathy. 8
Notably, myocarditis cases were not reported following vaccination in clinical trials of current COVID-19 vaccines. 9 , 10 Adverse cardiac events of any kind were reported in less than 0.1% of trial participants, and rates were not higher in recipients of vaccine compared with placebo. The inability to identify rare adverse events is understandable in preauthorization testing since fewer than 20 000 participants received a vaccine in each trial.
Background rates of myocarditis in the general population are variable and may be challenging to determine. As noted, a global estimate of incidence is 22 cases per 100 000 person-years. 5 More recent estimates of US incidence are lower (1 to 10 cases per 100 000 person-years) and may be more appropriate for estimating expected rates of diagnoses in evaluations of immunization safety. 6 Applying both the US and global background incidence to the population vaccinated by the US military yields a range of expected numbers of cases of myocarditis in this period ( Table 3 ). The observed number of male military members who experienced myocarditis after their second dose of mRNA vaccine, while relatively small, is substantially higher than the expected number.
Finally, it is important to frame concerns about potential vaccine-associated myocarditis within the context of the current pandemic. Infection with SARS-CoV-2 is a clear cause of serious cardiac injury in many patients. 11 The mechanism of injury may be direct infection, an immune-mediated response, or a combination of direct or indirect effects. Prevalence of cardiac injury may be as high as 60% in seriously ill patients. Notably, nearly 1% of highly fit athletes with mild COVID-19 infection have evidence of myocarditis on cMRI. 12 , 13 Given that COVID-19 vaccines are remarkably effective at preventing infection, any risk of rare adverse events following immunization must be carefully weighed against the very substantial benefit of vaccination.
Important limitations to this case series should be considered. Passive surveillance, even when stimulated by global attention on vaccine safety, may not identify all cases. The patients described in this report were identified in a brief period of observation after vaccine implementation from a cohort of essential workers who are not necessarily representative of the general population. Clinical evaluations varied and did not include complete testing in some patients who received care in different hospitals and in different countries. In particular, consistent application of cMRI and thorough viral testing would have strengthened clinical conclusions. This early report is also unable to describe longer-term outcomes among these patients. Despite limitations of this review, it is notable that the clinical presentations of these 23 patients appear consistent with other recent case reports of myocarditis after second doses of mRNA COVID-19 vaccines. 14 , 15
We report a case series of probable hypersensitivity myocarditis with consistent temporal association to receipt of an mRNA COVID-19 vaccine. While the true incidence of this adverse event is unknown at this time, the presentation pattern and clinical course suggest an association with an inflammatory response to vaccination. Increased attention to myocarditis as a potential adverse event following immunization is warranted. Recognition of the substantial morbidity associated with COVID-19 infection, including risk of cardiac injury, and the strong effectiveness of immunization in preventing infection provide important context for this topic. Concerns about rare adverse events following immunization should not diminish overall confidence in the value of vaccination.
Accepted for Publication: June 1, 2021.
Published Online: June 29, 2021. doi:10.1001/jamacardio.2021.2833
Corresponding Author: Jay Montgomery, MD, Walter Reed National Military Medical Center, 4954 N Palmer Rd, Bldg 19, Room 4026, Bethesda, MD 20889 ( [email protected] ); Margaret Ryan, MD, MPH, Naval Medical Center San Diego, 34800 Bob Wilson Dr, Bldg 6, Room 4V7C1, San Diego, CA 92134 ( [email protected] ).
Author Contributions: Drs Montgomery and Ryan had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design : Montgomery, Ryan, McClenathan, Collins, Hrncir, Herring.
Acquisition, analysis, or interpretation of data : Montgomery, Ryan, Engler, Hoffman, McClenathan, Loran, Hrncir, Herring, Platzer, Adams, Sanou, Cooper.
Drafting of the manuscript : Montgomery, Ryan, Engler, Cooper.
Critical revision of the manuscript for important intellectual content : All authors.
Statistical analysis : Ryan, McClenathan.
Administrative, technical, or material support : Montgomery, Ryan, Engler, Hoffman, McClenathan, Collins, Loran, Hrncir, Herring, Platzer, Adams, Sanou.
Study supervision : Montgomery, Ryan, Cooper.
Conflict of Interest Disclosures: Dr Cooper has received personal fees from Bristol Myers Squibb, Cantargia, CardioPath, Kiniksa Pharmaceuticals, and Cardiol Therapeutics. No other disclosures were reported.
Disclaimer: The views expressed are those of the authors and do not necessarily reflect official policy of the Department of Defense or the US government.
Additional Contributions: We thank the eldest patient for granting permission to publish identifiable information. We appreciate the contributions of the many clinicians who provided care or consultation for these patients worldwide, including, but not limited to, Todd Looney, MD; Matthew Needleman, MD; J. Edwin Atwood, MD; Carlie Cerne, MD; P. Gabriel Peterson, MD; Benjamin St. Clair, MD; and Nathan Boggs, MD (Walter Reed National Military Medical Center, Bethesda, Maryland); and Michael Romero, HM1, USN. We appreciate the support of Col Tonya Rans, USAF, MC; Laurie Duran, MSN; Laurie Housel, MSN; Ann Morse, MSN; Catherine Skerrett, MSN (Immunization Healthcare Division, Defense Health Agency, Falls Church, Virginia); and the Clinical Immunization Safety Assessment professionals at the US Centers for Disease Control and Prevention.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Revisiting the covid-19 pandemic: mortality and predictors of death in adult patients in the intensive care unit.

1. Introduction
2.1. type of study and data collection, 2.2. data recoding, 2.3. statistical analysis, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest.
- Alizadehsani, R.; Alizadeh Sani, Z.; Behjati, M.; Roshanzamir, Z.; Hussain, S.; Abedini, N.; Hasanzadeh, F.; Khosravi, A.; Shoeibi, A.; Roshanzamir, M.; et al. Risk Factors Prediction, Clinical Outcomes, and Mortality in COVID-19 Patients. J. Med. Virol. 2021 , 93 , 2307–2320. [ Google Scholar ] [ CrossRef ]
- WHO World Health Organization. COVID-19 Epidemiological Update, Edition 165 Published 15 March 2024. Available online: https://www.who.int/publications/m/item/covid-19-epidemiological-update-15-march-2024 (accessed on 2 April 2024).
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk Factors Associated With Mortality among Patients With COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020 , 180 , 1345–1355. [ Google Scholar ] [ CrossRef ]
- Rezaei, F.; Ghelichi -Ghojogh, M.; Hemmati, A.; Ghaem, H.; Mirahmadizadeh, A. Risk Factors for COVID-19 Severity and Mortality among Inpatients in Southern Iran. J. Prev. Med. Hyg. 2021 , 62 , E808. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zanella, A. Time Course of Risk Factors Associated with Mortality of 1260 Critically Ill Patients with COVID-19 Admitted to 24 Italian Intensive Care Units. Intensive Care Med. 2021 , 47 , 995–1008. [ Google Scholar ]
- Iacovelli, A.; Oliva, A.; Siccardi, G.; Tramontano, A.; Pellegrino, D.; Mastroianni, C.M.; Venditti, M.; Palange, P. Risk Factors and Effect on Mortality of Superinfections in a Newly Established COVID-19 Respiratory Sub-Intensive Care Unit at University Hospital in Rome. BMC Pulm. Med. 2023 , 23 , 30. [ Google Scholar ] [ CrossRef ]
- Osme, S.F.; Almeida, A.P.S.; Lemes, M.F.; Barbosa, W.O.; Arantes, A.; Mendes-Rodrigues, C.; Filho, P.P.G.; Ribas, R.M. Costs of Healthcare-Associated Infections to the Brazilian Public Unified Health System in a Tertiary-Care Teaching Hospital: A Matched Case–Control Study. J. Hosp. Infect. 2020 , 106 , 303–310. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Osme, S.F.; Souza, J.M.; Osme, I.T.; Almeida, A.P.S.; Arantes, A.; Mendes-Rodrigues, C.; Filho, P.P.G.; Ribas, R.M. Financial Impact of Healthcare-Associated Infections on Intensive Care Units Estimated for Fifty Brazilian University Hospitals Affiliated to the Unified Health System. J. Hosp. Infect. 2021 , 117 , 96–102. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sousa-Neto, A.; Mendes-Rodrigues, C.; Pedroso, R.; Brito Röder, D. Aspergillosis and COVID-19 in an Intensive Care Unit in Brazil: A Series of Cases. Divers. J. 2023 , 8 , 1349–1361. [ Google Scholar ] [ CrossRef ]
- Neto, A.L.d.S.; Campos, T.; Mendes-Rodrigues, C.; dos Pedroso, R.S.; de Röder, D.V.D.B. Factors Influencing Central Venous Catheter-Associated Bloodstream Infections in COVID-19 Patients. Microbiol. Res. 2024 , 15 , 1134–1143. [ Google Scholar ] [ CrossRef ]
- Ferreira, G.M.; Claro, I.M.; Grosche, V.R.; Cândido, D.; José, D.P.; Rocha, E.C.; de Moura Coletti, T.; Manuli, E.R.; Gaburo, N.; Faria, N.R.; et al. Molecular Characterization and Sequecing Analysis of SARS-CoV-2 Genome in Minas Gerais, Brazil. Biologicals 2022 , 80 , 43–52. [ Google Scholar ] [ CrossRef ]
- de Brito, V.P.; Carrijo, A.M.M.; Martins, M.V.T.; de Oliveira, S.V. Epidemiological Monitoring of COVID-19 in a Brazilian City: The Interface between the Economic Policies, Commercial Behavior, and Pandemic Control. World 2022 , 3 , 344–356. [ Google Scholar ] [ CrossRef ]
- Asaduzzaman, M.; Bhuia, M.R.; Bari, M.Z.J.; Alam, Z.N.; Rahman, K.; Hossain, E.; Alam, M.M.J. Predictors of Mortality and ICU Requirement in Hospitalized COVID-19 Patients with Diabetes: A Multicentre Study. Nurs. Open 2023 , 10 , 3178. [ Google Scholar ] [ CrossRef ]
- Dermikol, M.E.; Kaya, M.; Kocadag, D.; Özdan, E. Prognostic Value of Complete Blood Count Parameters in COVID-19 Patients. Northwestern Med. J. 2022 , 2 , 94–102. [ Google Scholar ]
- López-Escobar, A.; Madurga, R.; Castellano, J.M.; Ruiz de Aguiar, S.; Velázquez, S.; Bucar, M.; Jimeno, S.; Ventura, P.S. Hemogram as Marker of In-Hospital Mortality in COVID-19. J. Investig. Med. 2021 , 69 , 962–969. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Agresti, A. Frontmatter. In Categorical Data Analysis , 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2002; 734p, Available online: https://onlinelibrary.wiley.com/doi/epdf/10.1002/0471249688.fmatter (accessed on 2 June 2024).
- Armstrong, R.A.; Kane, A.D.; Cook, T.M. Outcomes from Intensive Care in Patients with COVID-19: A Systematic Review and Meta-Analysis of Observational Studies. Anaesthesia 2020 , 75 , 1340–1349. [ Google Scholar ] [ CrossRef ]
- Taxbro, K.; Hammarskjöld, F.; Nilsson, M.; Persson, M.; Chew, M.S.; Sunnergren, O. Factors Related to COVID-19 Mortality among Three Swedish Intensive Care Units—A Retrospective Study. Acta Anaesthesiol. Scand. 2023 , 67 , 788–796. [ Google Scholar ] [ CrossRef ]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and Efficacy of the ChAdOx1 NCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK. Lancet 2021 , 10269 , 99–111. [ Google Scholar ] [ CrossRef ]
- Kurtz, P.; Bastos, L.S.L.; Salluh, J.I.F.; Bozza, F.A.; Soares, M. SAPS-3 Performance for Hospital Mortality Prediction in 30,571 Patients with COVID-19 Admitted to ICUs in Brazil. Intensive Care Med 2021 , 47 , 1047–1049. [ Google Scholar ] [ CrossRef ]
- Lázaro, A.P.P.; Albuquerque, P.L.M.M.; Meneses, G.C.; Zaranza, M.D.S.; Batista, A.B.; Aragão, N.L.P.; Beliero, A.M.; Guimarães, Á.R.; Aragão, N.L.; Leitão, A.M.M.; et al. Critically Ill COVID-19 Patients in Northeast Brazil: Mortality Predictors during the First and Second Waves Including SAPS 3. Trans. R. Soc. Trop. Med. Hyg. 2022 , 116 , 1054–1062. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Aziz, F.; Reisinger, A.C.; Aberer, F.; Sourij, C.; Tripolt, N.; Siller-Matula, J.M.; von-Lewinski, D.; Eller, P.; Kaser, S.; Sourij, H.; et al. Simplified Acute Physiology Score 3 Performance in Austrian COVID-19 Patients Admitted to Intensive Care Units with and without Diabetes. Viruses 2022 , 14 , 777. [ Google Scholar ] [ CrossRef ]
- Bonanad, C.; García-Blas, S.; Tarazona-Santabalbina, F.; Sanchis, J.; Bertomeu-González, V.; Fácila, L.; Ariza, A.; Núñez, J.; Cordero, A. The Effect of Age on Mortality in Patients With COVID-19: A Meta-Analysis with 611,583 Subjects. J. Am. Med. Dir. Assoc. 2020 , 21 , 915–918. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Silva, G.A.; Jardim, B.C.; Lotufo, P.A. Mortalidade por COVID-19 padronizada por idade nas capitais das diferentes regiões do Brasil. Cad. Saúde Pública 2021 , 37 , e00039221. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Geldsetzer, P.; Mukama, T.; Jawad, N.K.; Riffe, T.; Rogers, A.; Sudharsanan, N. Sex Differences in the Mortality Rate for Coronavirus Disease 2019 Compared to Other Causes of Death: An Analysis of Population-Wide Data from 63 Countries. Eur. J. Epidemiol. 2022 , 37 , 797–806. [ Google Scholar ] [ CrossRef ]
- Yang, Y.; Zhong, W.; Tian, Y.; Xie, C.; Fu, X.; Zhou, H. The Effect of Diabetes on Mortality of COVID-19. Medicine 2020 , 99 , e20913. [ Google Scholar ] [ CrossRef ]
- Govender, N.; Khaliq, O.P.; Moodley, J.; Naicker, T. Insulin Resistance in COVID-19 and Diabetes. Prim. Care Diabetes 2021 , 15 , 629–634. [ Google Scholar ] [ CrossRef ]
- Lim, S.; Bae, J.H.; Kwon, H.-S.; Nauck, M.A. COVID-19 and Diabetes Mellitus: From Pathophysiology to Clinical Management. Nat. Rev. Endocrinol. 2021 , 17 , 11–30. [ Google Scholar ] [ CrossRef ]
- Steenblock, C.; Richter, S.; Berger, I.; Barovic, M.; Schmid, J.; Schubert, U.; Jarzebska, N.; von Mässenhausen, A.; Linkermann, A.; Schürmann, A.; et al. Viral Infiltration of Pancreatic Islets in Patients with COVID-19. Nat. Commun. 2021 , 12 , 3534. [ Google Scholar ] [ CrossRef ]
- Kastora, S.; Patel, M.; Carter, B.; Delibegovic, M.; Myint, P.K. Impact of Diabetes on COVID-19 Mortality and Hospital Outcomes from a Global Perspective: An Umbrella Systematic Review and Meta-Analysis. Endocrinol. Diabetes Metab. 2022 , 5 , e00338. [ Google Scholar ] [ CrossRef ]
- Russell, C.D.; Lone, N.I.; Baillie, J.K. Comorbidities, Multimorbidity and COVID-19. Nat. Med. 2023 , 29 , 334–343. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gosangi, B.; Rubinowitz, A.N.; Irugu, D.; Gange, C.; Bader, A.; Cortopassi, I. COVID-19 ARDS: A Review of Imaging Features and Overview of Mechanical Ventilation and Its Complications. Emerg. Radiol. 2022 , 29 , 23–34. [ Google Scholar ] [ CrossRef ]
- Green, A.; Rachoin, J.-S.; Schorr, C.; Dellinger, P.; Casey, J.D.; Park, I.; Gupta, S.; Baron, R.M.; Shaefi, S.; Hunter, K.; et al. Timing of Invasive Mechanical Ventilation and Death in Critically Ill Adults with COVID-19: A Multicenter Cohort Study. PLoS ONE 2023 , 18 , e0285748. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J.; et al. Epidemiology, Clinical Course, and Outcomes of Critically Ill Adults with COVID-19 in New York City: A Prospective Cohort Study. Lancet 2020 , 395 , 1763–1770. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Castro, A.A.M.; Calil, S.R.; Freitas, S.A.; Oliveira, A.B.; Porto, E.F. Chest Physiotherapy Effectiveness to Reduce Hospitalization and Mechanical Ventilation Length of Stay, Pulmonary Infection Rate and Mortality in ICU Patients. Respir. Med. 2013 , 107 , 68–74. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Goldfarb, M.J.; Bibas, L.; Bartlett, V.; Jones, H.; Khan, N. Outcomes of Patient- and Family-Centered Care Interventions in the ICU: A Systematic Review and Meta-Analysis. Crit. Care Med. 2017 , 45 , 1751. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shryane, N.; Pampaka, M.; Aparicio-Castro, A.; Ahmad, S.; Elliot, M.J.; Kim, J.; Murphy, J.; Olsen, W.; Ruiz, D.P.; Wiśniowski, A. Length of Stay in ICU of Covid-19 Patients in England, March–May 2020. Int. J. Popul. Data Sci. 2021 , 5 , 1411. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- García-Macías, M.; Verónica-Pérez, X.S.; Godínez-García, F. Mortalidad En Pacientes Con COVID-19 y Lesión Renal Aguda En Hemodiálisis. Rev. Med. Inst. Mex. Seguro Soc. 2023 , 61 (Suppl. S2), S207–S212. [ Google Scholar ] [ PubMed ]
- Leisman, D.E.; Mehta, A.; Li, Y.; Kays, K.R.; Li, J.Z.; Filbin, M.R.; Goldberg, M.B. Vasopressin Infusion in COVID-19 Critical Illness Is Not Associated with Impaired Viral Clearance: A Pilot Study. Br. J. Anaesth. 2021 , 127 , e146–e148. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hafeez, Z.; Zeeshan, A.; Shahid, S. Hyponatremia Secondary to Vasopressin in an ECMO Dependent Patient with Severe ARDS due to COVID-19. Chest 2021 , 160 (Suppl. S4), A669. [ Google Scholar ] [ CrossRef ]
- The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Association between Administration of Systemic Corticosteroids and Mortality among Critically Ill Patients with COVID-19: A Meta-Analysis. JAMA 2020 , 324 , 1330–1341. [ Google Scholar ] [ CrossRef ]
- Guillon, A.; Jouan, Y.; Kassa-Sombo, A.; Paget, C.; Dequin, P.-F. Hydrocortisone Rapidly and Significantly Reduces the IL-6 Level in Blood and Lungs of Patients with COVID-19-Related ARDS. Crit Care 2024 , 28 , 101. [ Google Scholar ] [ CrossRef ]
- Barbalho, I.M.P.; Fernandes, F.; Barros, D.M.S.; Paiva, J.C.; Henriques, J.; Morais, A.H.F.; Coutinho, K.D.; Coelho Neto, G.C.; Chioro, A.; Valentim, R.A.M. Electronic Health Records in Brazil: Prospects and Technological Challenges. Front. Public Health 2022 , 10 , 963841. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jung, F.; Connes, P. Morphology and Function of Red Blood Cells in COVID-19 Patients: Current Overview 2023. Life 2024 , 14 , 460. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Umadevi, K.; Rajarikam, N.; Lavanya, M.; Ali, M.I.; Begum, F.; Vadana, S.P.S. Red Cell Distribution Width, Platelet Distribution Width, and Plateletcrit as Indicators of Prognosis in COVID-19 Patients—A Single-Center Study. Asian J. Med. Sci. 2023 , 14 , 13–17. [ Google Scholar ] [ CrossRef ]
- Ozdin, M.; Cokluk, E.; Yaylaci, S.; Koroglu, M.; Genc, A.C.; Cekic, D.; Aydemir, Y.; Karacan, A.; Erdem, A.F.; Karabay, O. Evaluation of Coagulation Parameters: Coronavirus Disease 2019 (COVID-19) between Survivors and Nonsurvivors. Rev. Assoc. Med. Bras. 2021 , 67 (Suppl. S1), 74–79. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Teimury, A.; Khameneh, M.T.; Khaledi, E.M. Major Coagulation Disorders and Parameters in COVID-19 Patients. Eur. J. Med. Res. 2022 , 27 , 25. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Conway, E.M.; Mackman, N.; Warren, R.Q.; Wolberg, A.S.; Mosnier, L.O.; Campbell, R.A.; Gralinski, L.E.; Rondina, M.T.; van de Veerdonk, F.L.; Hoffmeister, K.M.; et al. Understanding COVID-19-Associated Coagulopathy. Nat. Rev. Immunol. 2022 , 22 , 639–649. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Terra, P.O.C.; Donadel, C.D.; Oliveira, L.C.; Menegueti, M.G.; Auxiliadora-Martins, M.; Calado, R.T.; De Santis, G.C. Neutrophil-to-Lymphocyte Ratio and D-Dimer Are Biomarkers of Death Risk in Severe COVID-19: A Retrospective Observational Study. Health Sci. Rep. 2022 , 5 , e514. [ Google Scholar ] [ CrossRef ]
- Henry, B.M.; Aggarwal, G.; Wong, J.; Benoit, S.; Vikse, J.; Plebani, M.; Lippi, G. Lactate Dehydrogenase Levels Predict Coronavirus Disease 2019 (COVID-19) Severity and Mortality: A Pooled Analysis. Am. J. Emerg. Med. 2020 , 38 , 1722–1726. [ Google Scholar ] [ CrossRef ]
- Bartziokas, K.; Kostikas, K. Lactate Dehydrogenase, COVID-19 and Mortality. Med. Clin. 2021 , 156 , 37. [ Google Scholar ] [ CrossRef ]
- Aditianingsih, D.; Soenarto, R.F.; Puiantana, A.M.; Pranata, R.; Lim, M.A.; Raharja, P.A.R.; Birowo, P.; Meyer, M. Dose Response Relationship between D-Dimer Level and Mortality in Critically Ill COVID-19 Patients: A Retrospective Observational Study. F1000Research 2022 , 11 , 269. [ Google Scholar ] [ CrossRef ]
- Simadibrata, D.M.; Lubis, A.M. D-Dimer Levels on Admission and All-Cause Mortality Risk in COVID-19 Patients: A Meta-Analysis. Epidemiol. Infect. 2020 , 148 , e202. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Russo, A.; Pisaturo, M.; Monari, C.; Ciminelli, F.; Maggi, P.; Allegorico, E.; Gentile, I.; Sangiovanni, V.; Esposito, V.; Gentile, V.; et al. Prognostic Value of Creatinine Levels at Admission on Disease Progression and Mortality in Patients with COVID-19—An Observational Retrospective Study. Pathogens 2023 , 12 , 973. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Todor, S.-B.; Bîrluțiu, V.; Topîrcean, D.; Mihăilă, R.-G. Role of Biological Markers and CT Severity Score in Predicting Mortality in Patients with COVID-19: An Observational Retrospective Study. Exp. Ther. Med. 2022 , 24 , 698. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- de Paula Nunes, E.; Leite, E.S.; de Carvalho, W.R.G. Rastreamento Geográfico da COVID-19 Segundo Fatores Socioeconômicos e Demográficos no Município de Uberlândia, Minas Gerais. J. Health Biol. Sci. 2020 , 8 , 1–6. [ Google Scholar ] [ CrossRef ]
- Policarpo, D.A.; Lourenzatto, E.C.A.; Brito, T.C.e.S.; Rossi, D.A.; de Melo, R.T. Epidemiological Aspects of the Initial Evolution of COVID-19 in Microregion of Uberlândia, Minas Gerais (MG), Brazil. Int. J. Environ. Res. Public Health 2021 , 18 , 5245. [ Google Scholar ] [ CrossRef ]
| % Yes (95% Confidence Interval) [n] | p-Value | Unadjusted Odds-Ratio (95% Confidence Interval) | ||
|---|---|---|---|---|
| Trait | Survivor (n = 263) | Non-Survivor (n = 325) | ||
| Admitted from another service | 67.30 (61.63–72.97) [177] | 63.38 (58.15–68.62) [206] | 0.321 | 0.84 (0.60–1.19) |
| Female sex | 45.25 (39.23–51.26) [119] | 33.85 (28.70–38.99) [110] | 0.005 | 0.62 (0.44–0.87) |
| Obesity presence | 35.74 (29.95–41.53) [94] | 32.62 (27.52–37.71) [106] | 0.427 | 0.87 (0.62–1.23) |
| Systemic arterial hypertension presence | 48.29 (42.25–54.33) [127] | 53.23 (47.81–58.66) [173] | 0.233 | 1.22 (0.88–1.69) |
| Diabetes mellitus presence | 19.01 (14.27–23.75) [50] | 32.92 (27.81–38.03) [107] | <0.001 | 2.09 (1.42–3.07) |
| Cardiovascular disease presence | 10.65 (6.92–14.37) [28] | 12.92 (9.28–16.57) [42] | 0.395 | 1.25 (0.75–2.07) |
| Asthma presence | 1.90 (0.25–3.55) [5] | 1.54 (0.20–2.88) [5] | 0.736 | 0.81 (0.23–2.82) |
| Chronic obstructive pulmonary disease presence | 7.60 (4.40–10.81) [20] | 11.38 (7.93–14.84) [37] | 0.120 | 1.56 (0.88–2.76) |
| Chronic kidney disease presence | 7.22 (4.10–10.35) [19] | 10.15 (6.87–13.44) [33] | 0.210 | 1.45 (0.81–2.62) |
| Etilism habit presence | 4.94 (2.32–7.56) [13] | 8.00 (5.05–10.95) [26] | 0.134 | 1.67 (0.84–3.32) |
| Smoking habit presence | 18.63 (13.93–23.34) [49] | 23.08 (18.5–27.66) [75] | 0.187 | 1.31 (0.88–1.96) |
| COVID-19 vaccine previous hospital admission | 17.11 (12.56–21.66) [45] | 20.31 (15.93–24.68) [66] | 0.323 | 1.23 (0.81–1.88) |
| Invasive mechanical ventilation use | 39.54 (33.63–45.45) [104] | 98.46 (97.12–99.80) [320] | <0.001 | 97.85 (39.1–244.86) |
| Median (Quartile 1–Quartile 2) [n] | p-value | Odds-Ratio (95% Confidence interval) | ||
| Trait | Survivor (n = 263) | Non-survivor (n = 325) | ||
| Age in years | 53 (40.5–65.5) [263] | 65 (52–73) [325] | <0.001 | 1.03 (1.02–1.04) |
| Total number of comorbidities | 1 (0–2) [263] | 1 (1–2) [325] | 0.007 | 1.19 (1.03–1.36) |
| Time in days from symptom to ICU admission | 11 (8–14) [245] | 11 (7–14) [285] | 0.229 | 0.99 (0.96–1.02) |
| Simplified Acute Physiology Score 3 score | 49 (38–58) [263] | 61 (49–71) [325] | <0.001 | 1.05 (1.04–1.06) |
| Simplified Acute Physiology Score in % | 15.9 (6–31.5) [263] | 39.8 (19–58.5) [325] | <0.001 | 1.04 (1.03–1.05) |
| Length of stay at the ICU in days | 8 (4–17) [263] | 11 (6–22) [325] | <0.001 | 1.02 (1.00–1.03) |
| Length of stay at the Hospital in days | 19 (11–31) [263] | 15 (7–27) [325] | <0.001 | |
| % Yes (95% Confidence Interval) [n] | p-Value | Unadjusted Odds-Ratio (95% Confidence Interval) | ||
|---|---|---|---|---|
| Trait | Survivor | Non-Survivor | ||
| Admitted from another service | 74.04 (65.61–82.46) [77] | 62.81 (57.52–68.11) [201] | 0.033 | 0.59 (0.36–0.97) |
| Female sex | 57.69 (48.2–67.19) [60] | 32.81 (27.67–37.96) [105] | <0.001 | 0.36 (0.23–0.56) |
| Obesity presence | 38.46 (29.11–47.81) [40] | 33.13 (27.97–38.28) [106] | 0.322 | 0.79 (0.5–1.25) |
| Systemic arterial hypertension presence | 45.19 (35.63–54.76) [47] | 53.13 (47.66–58.59) [170] | 0.160 | 1.37 (0.88–2.14) |
| Diabetes mellitus presence | 20.19 (12.48–27.91) [21] | 33.13 (27.97–38.28) [106] | 0.010 | 1.96 (1.15–3.33) |
| Cardiovascular disease presence | 7.69 (2.57–12.81) [8] | 12.81 (9.15–16.47) [41] | 0.140 | 1.76 (0.8–3.89) |
| Asthma presence | 0 (0–0) [0] | 1.56 (0.2–2.92) [5] | 0.092 | |
| Chronic obstructive pulmonary disease presence | 4.81 (0.70–8.92) [5] | 11.56 (8.06–15.07) [37] | 0.032 | 2.59 (0.99–6.77) |
| Chronic kidney disease presence | 2.88 (0–6.1) [3] | 10.31 (6.98–13.64) [33] | 0.009 | 3.87 (1.16–12.9) |
| Etilism habit presence | 5.77 (1.29–10.25) [6] | 8.13 (5.13–11.12) [26] | 0.417 | 1.44 (0.58–3.61) |
| Smoking habit presence | 11.54 (5.40–17.68) [12] | 23.44 (18.8–28.08) [75] | 0.006 | 2.35 (1.22–4.52) |
| COVID-19 vaccine previous admission | 13.46 (6.90–20.02) [14] | 20.31 (15.9–24.72) [65] | 0.109 | 1.64 (0.88–3.06) |
| Blood transfusion | 26.92 (18.40–35.45) [28] | 31.56 (26.47–36.65) [101] | 0.368 | 1.25 (0.76–2.05) |
| Use of noradrenaline | 90.38 (84.72–96.05) [94] | 99.38 (98.51–100.00) [318] | <0.001 | 16.92 (3.64–78.55) |
| Use of vasopressin | 17.31 (10.04–24.58) [18] | 70.94 (65.96–75.91) [227] | <0.001 | 11.66 (6.65–20.47) |
| Use of hydrocortisone | 29.81 (21.02–38.6) [31] | 71.56 (66.62–76.51) [229] | <0.001 | 5.93 (3.65–9.63) |
| Use of neuroblocker | 71.15 (62.45–79.86) [74] | 68.13 (63.02–73.23) [218] | 0.560 | 0.87 (0.53–1.41) |
| Use of midazolam | 94.23 (89.75–98.71) [98] | 91.25 (88.15–94.35) [292] | 0.315 | 0.64 (0.26–1.59) |
| Use of fentanyl | 98.08 (95.44–100.72) [102] | 93.44 (90.72–96.15) [299] | 0.045 | 0.28 (0.06–1.21) |
| Use of propofol | 59.62 (50.19–69.05) [62] | 51.25 (45.77–56.73) [164] | 0.136 | 0.71 (0.46–1.12) |
| Use of ketamine | 37.5 (28.20–46.8) [39] | 44.06 (38.62–49.5) [141] | 0.238 | 1.31 (0.83–2.07) |
| Use of non-invasive ventilation | 62.5 (53.20–71.8) [65] | 61.56 (56.23–66.89) [197] | 0.864 | 0.96 (0.61–1.52) |
| Use of indwelling bladder catheter | 100 (100–100) [104] | 97.19 (95.38–99.00) [311] | 0.024 | |
| Use of tracheostomy | 40.38 (30.95–49.81) [42] | 13.75 (9.98–17.52) [44] | <0.001 | 0.24 (0.14–0.39) |
| Use of central venous catheter | 100 (100–100) [104] | 98.75 (97.53–99.97) [316] | 0.132 | |
| Renal replacement therapy | 18.27 (10.84–25.7) [19] | 58.44 (53.04–63.84) [187] | <0.001 | 6.29 (3.65–10.85) |
| Haematocrit abnormal | 33.65 (24.57–42.74) [35] | 48.28 (42.79–53.76) [154] | 0.009 | 1.84 (1.16–2.82) |
| Red cell distribution width >15 | 13.46 (6.9–20.02] [14] | 27.59 (22.68–32.49] [88] | 0.002 | 2.45 (1.32–4.53) |
| Neutrophil to platelet ratio abnormal | 17.48 (10.14–24.81] [18] | 33.54 (28.34–38.75] [106] | 0.001 | 2.38 (1.36–4.17) |
| Prototombin activation time abnormal | 6.12 (1.38–10.87] [6] | 19.02 (14.61–23.42] [58] | 0.001 | 3.60 (1.50–8.63) |
| International Normalized Ratio abnormal | 5.1 (0.75–9.46] [5] | 15.84 (11.73–19.95] [48] | 0.003 | 3.50 (1.35–9.06) |
| Median (Quartile 1–Quartile 2) [n] | p-Value | Unadjusted Odds-Ratio (95% Confidence Interval) | ||
|---|---|---|---|---|
| Trait | Survivor | Non-Survivor | ||
| Age in years | 49.50 (38–61) [104] | 64.00 (51–72) [320] | <0.001 | 1.05 (1.03–1.06) |
| Total number of comorbidities | 1 (0–2) [104] | 1 (1–2) [320] | 0.003 | 1.31 (1.08–1.6) |
| Time in days from symptom to ICU admission | 11 (8–13.75) [98] | 11 (7–14) [282] | 0.676 | 0.99 (0.95–1.03) |
| Length of stay at the ICU in days | 21.5 (13–33.5) [104] | 12 (6–22) [320] | <0.001 | 0.97 (0.96–0.98) |
| Simplified Acute Physiology Score 3 score | 51 (37.75–62) [104] | 61 (49–71) [320] | <0.001 | 1.04 (1.02–1.05) |
| Simplified Acute Physiology Score in % | 20.25 (6–39.8) [104] | 39.8 (19–58.5) [320] | <0.001 | 1.03 (1.02–1.04) |
| Days of mechanical ventilation use | 15.5 (9–27.25) [104] | 11.5 (5–19) [312] | <0.001 | 0.98 (0.97–1.00) |
| Hemoglobin in g/dL | 12.6 (11.18–14.13) [104] | 12.4 (10.8–14.05) [319] | 0.641 | 0.97 (0.88; 1.06) |
| Leukocytes in 1000/mm | 11.3 (7.58–13.7) [104] | 11.9 (8.4–17.05) [319] | 0.056 | 1.05 (1.01–1.09) |
| Haematocrit in % | 37.65 (34.18–41.58) [104] | 37.3 (32.7–41.55) [319] | 0.631 | 0.99 (0.96–1.02) |
| Mean Corpuscular Volume in fL | 88.9 (85.35–91.2) [104] | 88.9 (85.1–93.2) [319] | 0.275 | 1.02 (0.99–1.05) |
| Mean Corpuscular Hemoglobin in pg | 29.65 (28.8–30.6) [104] | 29.9 (28.6–31.1) [319] | 0.219 | 1.06 (0.97–1.16) |
| Mean Corpuscular Hemoglobin Concentration in g/dL | 33.5 (32.2–34.63) [104] | 33.6 (32.45–34.6) [319] | 0.873 | 0.98 (0.86–1.13) |
| Red cell distribution width in % | 13.9 (13.2–14.6) [104] | 14.1 (13.2–15.2) [319] | 0.097 | 1.16 (1.00–1.34) |
| Mean platelet volume in fL | 10.5 (10–11.1) [103] | 10.7 (10–11.4) [314] | 0.405 | 1.05 (0.84–1.32) |
| Myelocytes in units by mm | 0 (0–0) [104] | 0 (0–0) [319] | 0.590 | 1.00 (1.00–1.00) |
| Rods in units by mm | 601 (298–1349) [104] | 755 (377.5–1444.5) [319] | 0.177 | 1.00 (1.00–1.00) |
| Segmented in units by mm | 8406 (5901.5–11,436.25) [104] | 9480 (6335.5–13,751) [319] | 0.044 | 1.00005 (1.00001–1.0001) |
| Lymphocytes in units by mm | 810.5 (483.5–1120.5) [104] | 687 (385–1150) [319] | 0.256 | 1.00 (1.00–1.00) |
| Monocytes in units by mm | 380 (271–633) [102] | 426 (282–750) [317] | 0.215 | 1.00 (1.00–1.00) |
| Neutrophils in units by mm | 9400 (6499–12,578.25) [104] | 10250 (7138–15,178) [319] | 0.057 | 1.00 (1.00–1.00) |
| Platelet in units/1000 by mm | 234 (190.5–299) [103] | 215 (167.25–292) [316] | 0.040 | 0.998 (0.996–1.00) |
| Neutrophils Lymphocytes Ratio | 11.63 (7.86–17.65) [104] | 14.67 (8.96–23.5) [319] | 0.017 | 0.999 (0.996–1.002) |
| Platelet Lymphocytes Ratio | 299.43 (209.61–477.12) [104] | 308.97 (191.26–483.73) [318] | 0.798 | 1.00 (1.00–1.00) |
| Creatinine in mg/dL | 0.81 (0.61–1.09) [104] | 1.22 (0.85–2.24) [318] | <0.001 | 1.52 (1.21–1.91) |
| Albumin in mg/dl | 3.23 (2.85–3.56) [84] | 3.13 (2.65–3.44) [265] | 0.060 | 1.01 (0.97–1.05) |
| Glutamic-oxaloacetic transaminase in U/L | 50.1 (37.98–73.18) [100] | 52.9 (33.8–85.6) [283] | 0.845 | 1.00 (1.00–1.01) |
| Glutamic-pyruvic transaminase in U/L | 45.05 (28.45–74.7) [100] | 37.15 (22.4–59.68) [282] | 0.061 | 1.00 (1.00–1.00) |
| Lactic dehydrogenase in U/L | 562 (432.5–670) [87] | 615 (453–856) [233] | 0.016 | 1.00 (1.00–1.01) |
| C-reactive protein in mg/dL | 12.64 (7.41–19.1) [102] | 13.4 (6.95–21.69) [300] | 0.499 | 1.01 (0.99–1.04) |
| D-dimer in ng/mL | 1135 (628.5–4063) [91] | 2381 (826.2–6545) [263] | 0.009 | 1.0003 (0.999–1.0001) |
| Interleukin 6 in pg/mL | 48.7 (26.57–142.68) [76] | 89.37 (40.86–178.4) [219] | 0.024 | 0.9999 (0.9995–1.0003) |
| Prototombin activation time in % | 100.00 (96.5–100) [98] | 96.00 (75–100) [305] | <0.001 | 0.97 (0.96–0.99) |
| International Normalized Ratio | 1.00 (1.00–1.02) [98] | 1.01 (1.00–1.12) [303] | <0.001 | 5.32 (1.07–26.51) |
| Neutrophils Lymphocytes derivate Ratio | 7.33 (5.25–10.11) [104] | 7.33 (5.25–11.5) [319] | 0.180 | 1.04 (1.00–1.08) |
| Monocytes Lymphocytes Ratio | 0.60 (0.33–0.8) [102] | 0.67 (0.33–1.18) [317] | 0.049 | 1.48 (1.07–2.06) |
| Neutrophils Platelet Ratio | 38.80 (28.52–51.39) [103] | 47.35 (33.09–67.27) [316] | 0.001 | 1.02 (1.01–1.03) |
| Systemic immune-inflammation index | 2.86 (1.63–4.54) [104] | 3.31 (1.70–5.39) [319] | 0.187 | 0.99 (0.98–1.01) |
| Length of stay at the Hospital in days | 31.5 (22.75–48.50) [104] | 15.50 (7.00–27) [320] | <0.001 | |
| Model Applied to All Patients | ||||
|---|---|---|---|---|
| Full Multiple Model | Reduced Multiple Model | |||
| Traits Included | p-Value | Adjusted Odds Ratio (95% Confidence Interval) | p-Value | Adjusted Odds Ratio (95% Confidence Interval) |
| Invasive mechanical ventilation use | <0.001 | 351.70 (95.94–1289.22) | <0.001 | 306.74 (87.47–1075.71) |
| Age in years | <0.001 | 1.05 (1.03–1.07) | <0.001 | 1.04 (1.03–1.06) |
| Simplified Acute Physiology Score 3 score | 0.001 | 1.03 (1.01–1.05) | 0.001 | 1.03 (1.01–1.04) |
| Length of stay at the ICU in days | <0.001 | 0.96 (0.95–0.98) | <0.001 | 0.96 (0.95–0.98) |
| Asthma presence | 0.299 | 6.13 (0.20–187.18) | ||
| Chronic kidney disease presence | 0.331 | 1.80 (0.55–5.93) | ||
| Diabetes mellitus presence | 0.288 | 1.44 (0.74–2.80) | ||
| COVID-19 vaccine previous hospital admission | 0.491 | 1.29 (0.62–2.68) | ||
| Obesity presence | 0.415 | 1.26 (0.72–2.22) | ||
| Smoking habit presence | 0.728 | 1.16 (0.51–2.61) | ||
| Time in days from symptom to ICU admission | 0.701 | 1.01 (0.96–1.06) | ||
| Etilism habit presence | 0.995 | 1.00 (0.27–3.61) | ||
| Cardiovascular disease presence | 0.791 | 0.87 (0.32–2.36) | ||
| Chronic obstructive pulmonary disease presence | 0.616 | 0.75 (0.24–2.33) | ||
| Admitted from another service | 0.118 | 0.64 (0.36–1.12) | ||
| Systemic arterial hypertension presence | 0.095 | 0.59 (0.32–1.10) | ||
| Model applied to patients in invasive mechanical ventilation | ||||
| Full Multiple model | Reduced multiple model | |||
| Traits included | p-value | Adjusted Odds Ratio (95% Confidence Interval) | p-value | Ajusted Odds Ratio (95% Confidence Interval) |
| Use of vasopressin | <0.001 | 7.49 (3.29–17.05) | <0.001 | 7.87 (3.54–17.46) |
| Renal replacement therapy | <0.001 | 5.19 (2.23–12.09) | <0.001 | 5.42 (2.55–11.51) |
| Red cell distribution width >15 | 0.011 | 3.52 (1.34–9.26) | 0.003 | 3.84 (1.60–9.21) |
| Use of hydrocortisone | 0.030 | 2.57 (1.10–6.03) | 0.038 | 2.33 (1.05–5.16) |
| Age in years | 0.041 | 1.03 (1.00–1.05) | 0.006 | 1.03 (1.01–1.05) |
| Days of invasive mechanical ventilation use | <0.001 | 0.94 (0.92–0.96) | <0.001 | 0.95 (0.93–0.97) |
| Admitted from another service | 0.026 | 0.43 (0.21–0.90) | 0.020 | 0.43 (0.21–0.87) |
| Female sex | 0.035 | 0.47 (0.23–0.95) | 0.010 | 0.42 (0.22–0.82) |
| Use of noradrenaline | 0.060 | 15.67 (0.90–274.17) | ||
| Neutrophil to platelet ratio abnormal | 0.088 | 2.18 (0.89–5.32) | ||
| Diabetes mellitus presence | 0.492 | 1.54 (0.45–5.22) | ||
| Haematocrit abnormal | 0.478 | 1.30 (0.63–2.67) | ||
| Smoking habit presence | 0.733 | 1.19 (0.44–3.18) | ||
| Time from symptom to ICU admission | 0.510 | 1.02 (0.96–1.09) | ||
| Simplified Acute Physiology Score 3 score | 0.527 | 1.01 (0.98–1.03) | ||
| Total number of comorbidities | 0.712 | 0.91 (0.55–1.50) | ||
| Chronic kidney disease presence | 0.862 | 0.84 (0.13–5.68) | ||
| Chronic obstructive pulmonary disease presence | 0.675 | 0.72 (0.16–3.29) | ||
| Use of Fentanyl | 0.050 | 0.13 (0.02–1.00) | ||
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Sousa Neto, A.L.d.; Mendes-Rodrigues, C.; Pedroso, R.d.S.; Röder, D.V.D.d.B. Revisiting the COVID-19 Pandemic: Mortality and Predictors of Death in Adult Patients in the Intensive Care Unit. Life 2024 , 14 , 1027. https://doi.org/10.3390/life14081027
Sousa Neto ALd, Mendes-Rodrigues C, Pedroso RdS, Röder DVDdB. Revisiting the COVID-19 Pandemic: Mortality and Predictors of Death in Adult Patients in the Intensive Care Unit. Life . 2024; 14(8):1027. https://doi.org/10.3390/life14081027
Sousa Neto, Adriana Lemos de, Clesnan Mendes-Rodrigues, Reginaldo dos Santos Pedroso, and Denise Von Dolinger de Brito Röder. 2024. "Revisiting the COVID-19 Pandemic: Mortality and Predictors of Death in Adult Patients in the Intensive Care Unit" Life 14, no. 8: 1027. https://doi.org/10.3390/life14081027
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
COVID-19 drops to 10th leading cause of death as U.S. mortality rates fall in 2023
- Download PDF Copy

In a recent Morbidity and Mortality Weekly Report , researchers used provisional data on deaths to examine mortality trends that can inform public health interventions and policies. Provisional data provide an early estimate of deaths before the final annual data is available, but these figures may be revised as more information is received.
Their results indicate that mortality from coronavirus disease 2019 (COVID-19) is now the tenth leading cause of death in the U.S. and that across causes of death, the overall mortality rate is highest among African American or non-Hispanic Black individuals.

Provisional* number of COVID-19–associated deaths† and other deaths and percentage of deaths associated with COVID-19, by week of death — National Vital Statistics System, United States, 2023
The National Center for Health Statistics (NCHS) collects and publishes yearly death statistics using data from certificates of death issued in the U.S. Final figures for each year are usually available 11 months later due to the time needed for thorough investigation and review.
However, provisional data, such as those used in this report, offer an early signal about shifts in mortality trends. These estimates help track changes in death trends and shape public health strategies aimed at reducing deaths, especially in high-mortality groups.
About the study
The National Vital Statistics System (NVSS) regularly releases provisional death data, including COVID-19 deaths. This report covers provisional data on mortality in the U.S. for 2023 and compares it to 2022. NCHS provided statistics on total deaths, including deaths attributed to COVID-19, breaking them down by race/ethnicity, age, and sex.
Researchers followed the International Classification of Diseases to identify the causes of mortality. Deaths with COVID-19 as a contributing or underlying cause were included in COVID-19 counts. They then ranked the most common causes of mortality based on these figures, excluding deaths abroad and in American territories.
Weekly death counts and rates were analyzed, with rates adjusted for age and calculated for overall deaths and by specific groups. Population estimates for these calculations came from the Census Bureau of the U.S.
In 2023, there were 3,090,582 deaths in the U.S., with an age-adjusted mortality rate of 750.4 for every 100,000 people, a 6.1% decrease from 2022. The highest death counts were in the weeks that ended January 7, during which time 68,965 died, and December 30, during which time 65,257 people died.

Related Stories
- Mucosal COVID-19 vaccine prevents airborne transmission of SARS-CoV-2
- Urinary metals linked to higher cardiovascular disease risk and mortality
- Study finds long-term cognitive and psychiatric issues persist in COVID-19 patients two to three years post-infection
Leading underlying causes of death* — National Vital Statistics System, United States, 2023
People between the ages of 5 and 14 had the lowest death rate (14.7 per 100,000) and highest for those aged 85 and older (14,286 per 100,000). Death rates fell across every age group in 2023 compared to 2022, though not significantly among children aged up to four. The death rate adjusted for age was higher for males at 884.2 compared to females at 632.8, and both decreased from 2022.
Death rates varied by ethnicity and race, with multiracial individuals having the lowest rate (352.1 per 100,000) and Black individuals the highest (924.3 per 100,000). The most common causes of death included cancer, unintentional injuries, and heart disease. COVID-19, which was the fourth leading cause of death in 2022, became the 10th in 2023, accounting for 1.6% of deaths.
COVID-19 was implicated in 76,446 deaths in 2023, accounting for a death rate of 18.2 among every 100,000, representing a decrease of 68.9% from 2022. The death rate due to COVID-19 dropped across every age group and racial/ethnic group, with males (22.1 for every 100,000 individuals) having a higher rate than females, who had a death rate of 15.4 for every 100,000 individuals.
Conclusions
This report offers an initial overview of provisional mortality data for 2023, providing early insights into mortality trends. Such data are crucial for offering timely and actionable information, which can guide public health policies and interventions aimed at reducing mortality rates, particularly in populations experiencing higher mortality. These preliminary estimates are valuable for researchers and policymakers as they can signal shifts in mortality patterns sooner than final data.
However, the provisional nature of these data means they are subject to change. The estimates may be underrepresentative due to potential delays in death certificate submissions, which can vary by jurisdiction. Such delays, especially from jurisdictions with large populations, could skew the overall death rates and alter the national distribution of mortality data. Additionally, there is a risk of misclassification in racial and ethnic categories on death certificates, which could result in inaccuracies in reported death rates for some groups.
These limitations underscore the need for a cautious interpretation of the data and highlight the importance of final mortality figures for a more accurate and comprehensive understanding of mortality trends in the U.S.
- Ahmad, F.B., Cisewski, J.A., Anderson, R.N. Mortality in the United States – Provisional Data, 2023. Morbidity and Mortality Weekly Report (2024). DOI: 10.15585/mmwr.mm7331a1, https://www.cdc.gov/mmwr/volumes/73/wr/mm7331a1.htm?s_cid=mm7331a1_w
Posted in: Business / Finance | Medical Research News | Medical Condition News
Tags: Cancer , Children , Coronavirus , covid-19 , Heart , Heart Disease , International Classification of Diseases , Mortality , Public Health

Priyanjana Pramanik
Priyanjana Pramanik is a writer based in Kolkata, India, with an academic background in Wildlife Biology and economics. She has experience in teaching, science writing, and mangrove ecology. Priyanjana holds Masters in Wildlife Biology and Conservation (National Centre of Biological Sciences, 2022) and Economics (Tufts University, 2018). In between master's degrees, she was a researcher in the field of public health policy, focusing on improving maternal and child health outcomes in South Asia. She is passionate about science communication and enabling biodiversity to thrive alongside people. The fieldwork for her second master's was in the mangrove forests of Eastern India, where she studied the complex relationships between humans, mangrove fauna, and seedling growth.
Please use one of the following formats to cite this article in your essay, paper or report:
Pramanik, Priyanjana. (2024, August 11). COVID-19 drops to 10th leading cause of death as U.S. mortality rates fall in 2023. News-Medical. Retrieved on August 20, 2024 from https://www.news-medical.net/news/20240811/COVID-19-drops-to-10th-leading-cause-of-death-as-US-mortality-rates-fall-in-2023.aspx.
Pramanik, Priyanjana. "COVID-19 drops to 10th leading cause of death as U.S. mortality rates fall in 2023". News-Medical . 20 August 2024. <https://www.news-medical.net/news/20240811/COVID-19-drops-to-10th-leading-cause-of-death-as-US-mortality-rates-fall-in-2023.aspx>.
Pramanik, Priyanjana. "COVID-19 drops to 10th leading cause of death as U.S. mortality rates fall in 2023". News-Medical. https://www.news-medical.net/news/20240811/COVID-19-drops-to-10th-leading-cause-of-death-as-US-mortality-rates-fall-in-2023.aspx. (accessed August 20, 2024).
Pramanik, Priyanjana. 2024. COVID-19 drops to 10th leading cause of death as U.S. mortality rates fall in 2023 . News-Medical, viewed 20 August 2024, https://www.news-medical.net/news/20240811/COVID-19-drops-to-10th-leading-cause-of-death-as-US-mortality-rates-fall-in-2023.aspx.
Suggested Reading

Cancel reply to comment
- Trending Stories
- Latest Interviews
- Top Health Articles

Addressing Important Cardiac Biology Questions with Shotgun Top-Down Proteomics
In this interview conducted at Pittcon 2024, we spoke to Professor John Yates about capturing cardiomyocyte cell-to-cell heterogeneity via shotgun top-down proteomics.

A Discussion with Hologic’s Tim Simpson on the Future of Cervical Cancer Screening
Tim Simpson
Hologic’s Tim Simpson Discusses the Future of Cervical Cancer Screening.

From Waste to Taste: The Transformative Power of Fermented Foods
Maria Marco
In this interview conducted at Pittcon 2024 in San Diego, Maria Marco discusses her research on the health benefits, safety, and waste reduction potential of fermented foods, and the microbial processes involved in their production.

Latest News

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback

- Israel-Gaza War
- War in Ukraine
- US Election
- US & Canada
- UK Politics
- N. Ireland Politics
- Scotland Politics
- Wales Politics
- Latin America
- Middle East
- In Pictures
- Executive Lounge
- Technology of Business
- Women at the Helm
- Future of Business
- Science & Health
- Artificial Intelligence
- AI v the Mind
- Film & TV
- Art & Design
- Entertainment News
- Destinations
- Australia and Pacific
- Caribbean & Bermuda
- Central America
- North America
- South America
- World’s Table
- Culture & Experiences
- The SpeciaList
- Natural Wonders
- Weather & Science
- Climate Solutions
- Sustainable Business
- Green Living
WHO declares mpox global health emergency

The World Health Organization (WHO) has declared the mpox outbreak in parts of Africa a public health emergency of international concern.
The highly contagious disease - formerly known as monkeypox - has killed at least 450 people during an initial outbreak in the Democratic Republic of Congo.
It has now spread across parts of central and east Africa, and scientists are concerned about how fast a new variant of the disease is spreading and its high fatality rate.
WHO chief Tedros Adhanom Ghebreyesus said the potential for further spread within Africa and beyond "is very worrying".
"A co-ordinated international response is essential to stop this outbreak and save lives," he said.
Mpox is transmitted through close contact, such as sex, skin-to-skin contact and talking or breathing close to another person.
It causes flu-like symptoms, skin lesions and can be fatal, with four in 100 cases leading to death.
Outbreaks can be controlled by preventing infections with vaccines, though these are usually only available for people at risk or those who have been in close contact with an infected person.
- Explained: What is mpox and how is it spread?
- Podcast: What does the new mpox strain mean for you?
There are two main types of mpox - Clade 1 and Clade 2.
A previous mpox public health emergency, declared in 2022, was caused by the relatively mild Clade 2. However, this time it is the far more deadly Clade 1 - which has killed up to 10% of those getting sick in previous outbreaks - that is surging.
There was a change in the virus around September last year. Mutations led to an offshoot - called Clade 1b - that has since spread rapidly. This new variant has been labelled “the most dangerous yet” by one scientist.
Since the start of the year, there have been more than 13,700 cases of mpox in the DR Congo, with at least 450 deaths.
It has since been detected in other African countries - including Burundi, the Central African Republic, Kenya and Rwanda.
It is hoped the declaration of mpox as a public health emergency will lead to research, funding, and the introduction of other international public health measures being accelerated.
Dr Josie Golding, from the Wellcome Trust, said it was a "strong signal", while Emory University's Dr Boghuma Titanji said the move "underscores the gravity of the crisis".
Prof Trudie Lang, the director of the Global Health Network at the University of Oxford, said it was "important and timely", but added that the emergence of a new strain meant there were "many unknowns that need to be addressed".
In July 2022 the milder Clade 2 strain of mpox spread to nearly 100 countries , including some in Europe and Asia.
It spread rapidly, and there were more than 87,000 cases and 140 deaths reported during that outbreak, according to a WHO count.
Although anyone can catch monkeypox, the outbreak was largely concentrated among men who had sex with men.
That outbreak was brought under control by vaccinating vulnerable groups.
On Tuesday, scientists from the Africa Centres for Disease Control and Prevention declared a public health emergency.
The head of the organisation, Jean Kaseya, warned that this current outbreak could spiral out of control if immediate steps were not taken to contain it.
"We must be proactive and aggressive in our efforts to contain and eliminate this threat," he said.
Additional reporting by Alex Smith

IMAGES
COMMENTS
COVID-19 is a social action, and it can also be considered a great social problem on the basis of Richard Puller's definition. When looked at generally, COVID-19 is a disease spreading through close human contacts in day-to-day social relationships. ... This may cause some effects in supply chain networks in Sri Lanka as well as South Asian ...
Writing About COVID-19 in College Essays. Experts say students should be honest and not limit themselves to merely their experiences with the pandemic. The global impact of COVID-19, the disease ...
From lifestyle changes to better eating habits, people are using this time to get healthier in many areas. Since the pandemic started, nearly two-thirds of the survey's participants (62%) say ...
COVID-19 (Coronavirus) has affected day to day life and is slowing down the global economy. This pandemic has affected thousands of peoples, who are either sick or are being killed due to the spread of this disease. The most common symptoms of this viral infection are fever, cold, cough, bone pain and breathing problems, and ultimately leading ...
COVID-19 is characterized by a variety of symptoms, including fever, cough, congestion, fatigue, shortness of breath, headache, sore throat, nausea or vomiting, loss of smell or taste, and body aches. COVID-19 may progress to severe respiratory illness, with symptoms of chest pain and extreme difficulty in breathing, requiring hospitalization.
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
The student or a family member had COVID-19 or suffered other illnesses due to confinement during the pandemic. The student suffered from a lack of internet access and other online learning challenges. Students who dealt with problems registering for or taking standardized tests and AP exams. Jeff Schiffman of the Tulane University admissions ...
However, we do find that the effects of the COVID-19 pandemic are mixed, and that while some trends, such as opioid overdose deaths, worsened in 2020 compared to 2019, others, such as in some ...
October 21, 2020 · 7 min read. The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no ...
We investigate the relationship between media consumption, misinformation, and important attitudes and behaviours during the coronavirus disease 2019 (COVID-19) pandemic. We find that comparatively more misinformation circulates on Twitter, while news media tends to reinforce public health recommendations like social distancing. We find that exposure to social media is associated with ...
Horrific history. Looking back, the COVID-19 pandemic stands as arguably the most disruptive event of the 21st century, surpassing wars, the September 11, 2001, terrorist attacks, the effects of climate change, and the Great Recession. It has killed more than seven million people to date and reshaped the world economy, public health, education ...
So while physical isolation will be required for many Americans who have Covid-19 or have been exposed to it, it's important that we don't let such measures cause social and emotional ...
100 Words Essay on Covid 19. COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very ...
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the ...
The COVID-19 pandemic has had a profound impact on individuals, societies, and economies worldwide. Its multifaceted nature presents a wealth of topics suitable for academic exploration. This essay provides guidance on developing engaging and insightful essay topics related to COVID-19, offering a comprehensive range of perspectives to choose from.
Paragraph Writing on Covid-19 in 100 Words. Coronavirus is an infectious disease and is commonly called Covid-19. It affects the human respiratory system causing difficulty in breathing. It is a contagious disease and has been spreading across the world like wildfire. The virus was first identified in 2019 in Wuhan, China.
The long-term effects of COVID-19 are still unknown. In some ways, our findings show an optimistic picture: In reading, on average, the achievement percentiles of students in fall 2020 were ...
Essay On Covid-19: 100, 200 and 300 Words. COVID-19, also known as the Coronavirus, is a global pandemic that has affected people all around the world. It first emerged in a lab in Wuhan, China, in late 2019 and quickly spread to countries around the world. This virus was reportedly caused by SARS-CoV-2. Since then, it has spread rapidly to ...
Other infections, such as the flu and polio, can lead to long-term illness. But the virus that causes COVID-19 has only been studied since it began to spread in 2019. So, research into the specific effects of long-term COVID-19 symptoms continues. Researchers do think that post-COVID-19 syndrome can happen after an illness of any severity.
As people grapple with these health, social and economic impacts, mental health has been widely affected. Plenty of us became more anxious; but for some COVID-19 has sparked or amplified much more serious mental health problems. A great number of people have reported psychological distress and symptoms of depression, anxiety or post-traumatic ...
In conclusion, this paper has highlighted the impacts of the Covid-19 pandemic on the economy, social life, education, religion, and family units. Many countries and businesses had underestimated the disease's impact before they later suffered from the consequences. Therefore, international bodies, such as the World Health Organization, need ...
Editor in Chief's Introduction to Essays on the Impact of COVID-19 on Work and Workers. On March 11, 2020, the World Health Organization declared that COVID-19 was a global pandemic, indicating significant global spread of an infectious disease ( World Health Organization, 2020 ). At that point, there were 118,000 confirmed cases of the ...
The COVID-19 pandemic had radically changed higher education. The sudden transition to online teaching and learning exposed, however, some benefits by enhancing educational flexibility and digitization. The long-term effects of these changes are currently unknown, but a key question concerns their effect on student learning outcomes. This study aims to analyze the impact of the emergence of ...
The mean ECDs were 2,770 cells/mm2 in the COVID-19 group and 2,897 cells/mm2 in the control group; the mean HEX was 46.52 in the COVID-19 group and 58.22 ± 13.94 in the control group. The patients who had had COVID-19 had significantly lower endothelial ECD and HEX levels than controls (p = 0.003 and p< 0.001, respectively).
Purpose of review There are significant differences in the transmission rate and mortality rate of COVID-19 under environmental conditions such as seasons and climates. However, the impact of environmental factors on the role of the COVID-19 pandemic and the transmission mechanism of the SARS-CoV-2 is unclear. Therefore, a comprehensive understanding of the impact of environmental factors on ...
Children with COVID-19 may have serious or mild symptoms or no symptoms at all. Symptoms may show up from 2 to 14 days after contact with the virus that causes COVID-19. The most common symptoms are fever and a cough, including a barking cough linked to croup.
This descriptive study compares the effect of mRNA-based COVID-19 vaccination with BNT162b2 (Pfizer-BioNTech) vs mRNA-1273 (Moderna) on the reported cases of myocarditis in the US after each vaccination dose. ... Infection with SARS-CoV-2 is a clear cause of serious cardiac injury in many patients. 11 The mechanism of injury may be direct ...
COVID-19 has generated a global impact due to its contagiousness and high lethality rates, with a large number of deaths occurring in intensive care units (ICUs). This study aimed to verify the occurrence of and understand the factors related to mortality in adult patients with COVID-19 admitted to the ICU in a tertiary hospital. This is a retrospective cohort study, which included COVID-19 ...
Please use one of the following formats to cite this article in your essay, paper or report: APA. Pramanik, Priyanjana. (2024, August 11). COVID-19 drops to 10th leading cause of death as U.S ...
It causes flu-like symptoms, skin lesions and can be fatal, with four in 100 cases leading to death. Outbreaks can be controlled by preventing infections with vaccines, though these are usually ...