Clinical Trials
Kidney transplant.
Displaying 94 studies
The purpose of this study is to better understand how the immune system reacts to kidney transplantation in individuals who are potentially at higher risk for rejection.
The purpose of this study is to evaluate how advancing stages of chronic kidney disease (CKD) may impact the hypothalamic-pituitary-gonadal axis,and how alterations in sex hormones and menstrual cycles correlate with changes in endothelial health and sexual function before and after transplant.
The objectives of this study are to retrospectively assess detailed post-transplant outcomes in a large cohort of patients across 3 sites with a specific emphasis on the outcomes of Hispanics and American Indians compared to non-white Hispanics, to develop and implement a questionnaire to assess socioeconomic risk factors in transplant patients (including a cohort of Hispanics and American Indians), and to perform genetic studies (high-resolution HLA typing and whole genome sequencing studies) to identify genes associated with transplant outcomes (diabetes, rejection and graft loss) in Hispanics and American Indians.
The purpose of this study is to evaluate how treatment and self-care after kidney transplant impacts people’s lives, relationships, and finances.
The purpose of this study is to test whether a dosing regimen of eculizumab in addition to standard posttransplant care in positive crossmatch deceased donor kidney transplant recipients will reduce the incidence of acute humoral rejection (AHR).
Patients included in this study will be those who have demonstrable anti-human leukocyte antigen (HLA) antibody specific for their deceased donor. It is our hypothesis that blockade of terminal complement activation with eculizumab at the time of transplant in combination with our current protocols will reduce the incidence of AHR in recipients of deceased donor kidney transplants who have anti-donor HLA antibody
The purpose of this study is to see if treating patients who have high levels of donor specific alloantibodies post-transplant with bortezomib might prevent the development of transplant glomerulopathy and preserve allograft function.
To evaluate the efficacy of Cinryze® given for the treatment of acute antibody-mediated rejection (of renal allograft) (AMR) in kidney transplant recipients as measured by the proportion of subjects with new or worsening transplant glomerulopathy (TG) at 6 months after treatment initiation.
The objectives of this study are to establish the dynamic changes in iron metabolism and circulating iron-regulatory immune cells in kidney transplant infection, and to determine quantitative changes in tissue levels of hepcidin and iron-regulatory macrophages in transplant biopsy and compare pyelonephritis case with control.
The purpose of this study is to test the hypothesis that pregnancy post-transplant will increase the risk of adverse renal events (defined as acute rejection, reduction in GFR by 30%, new or worsening proteinuria, or graft-loss). The risk will be increased in women with complications in pregnancy, such as preeclampsia or pre-term delivery.
The purpose of this pilot study is to investigate whether contrast-enhanced ultrasound (CEUS) may help evaluate segmental differences in renal perfusion better than doppler ultrasound and thus help direct a biopsy to the most abnormal part of the renal cortex.
The purpose of this study is to determine the effectiveness of ultrasound elastography in prediction of renal allograft fibrosis.
The investigators will evaluate a technology-enabled strategy designed to promote medication adherence, routinely monitor regimen use, and mobilize appropriate transplant center resources to respond early to kidney transplant recipients demonstrating inadequate adherence.
Thirteen APOLLO Clinical Centers (CCs), or Networks, will prospectively enroll eligible living kidney donors and recipients of kidneys from eligible living and deceased kidney donors transplanted at all transplant programs in the continental United States including Puerto Rico. The APOLLO Scientific and Data Research Center (SDRC or Coordinating Center) will support and participate in studies determining the impact of donor and recipient APOL1 genotypes on kidney transplant outcomes in recipients of a kidney transplant from a donor with recent African ancestry, and follow African ancestry living kidney donors for changes in vital status, kidney function and proteinuria. APOLLO’s Study Chair ...
The purpose of this study is to investigate whether clazakizumab (an anti-interleukin (IL)-6 monoclonal antibody (mAb)) may be beneficial for the treatment of CABMR in recipients of a kidney transplant by inhibiting the production of Donor Specific Antibodies (DSA) and re-shaping T cell alloimmune responses.
The purpose of this study is to assess the benefits and risks of changing from Cyclosporine or Tacrolimus to Belatacept for maintenance rejection suppression after kidney transplant.
The purpose of this study is to develop a digital droplet PCR-based method to quantitate ccfDNA., and to establish ranges of donor ccfDNA that correspond to rejection status.
The purpose of this study is to assess the safety and effectiveness of eculizumab for the prevention of antibody-caused rejection in patients who are having a kidney transplant from a living donor with a different blood type than their own.
The primary purpose of this study is to assess the benefits and risks of changing from Cyclosporine or Tacrolimus to Belatacept between 6-60 months after kidney transplant.
The purpose of this study is to obtain knowledge of the viscoelastic material properties of the kidney in healthy individuals, patients with chronic kidney disease, and patients who have received a kidney transplant. The aim of the study is to evaluate if these properties are unique indicators of renal health.
The main purpose of this study is to investigate pre-transplant risk factors and beliefs regarding weight gain in patients with a diagnosis of type 2 diabetes mellitus (T2DM) who have undergone a kidney transplant. The aim is to guide an understanding of the rationale behind weight gain and an exploration of potential preventative measures, ultimately resulting in recommendations for future patient-centered interventions at a Midwestern tertiary healthcare center. The research question follows the PICOT format: population, intervention, comparison, outcome, and time. The question of interest is: In adult patients ≥ 18 years of age with T2DM who received a kidney transplant ...
This study aims to understand the pharmacogenomics of Native American patients compared to Caucasians who are undergoing kidney transplant for treatment of kidney disease.
The purpose of this study is to determine the usefulness of a pharmacist-led motivational interview intervention for transplant recipients, and to determine the acceptance and satisfaction of transplant patients with a pharmacist-led motivational interview intervention.
The purpose of this study is to compare the rate of progression from prediabetes at 4 months to frank diabetes at 12 months (as defined by increase in HbA1C or fasting BS to diabetic range based on the ADA criteria) after transplantation in kidney transplant recipients on Exenatide SR + SOC vs. standard-of-care alone.
The aim of this study is to determine the validity of two tests on bone marrow of sensitized kidney transplant recipients in order to better understand why these patients with antibodies against their donors are at a greater risk of rejection of their transplanted organs.
This study aims to measure the percentage of time spent in hyperglycemia in patients on insulin therapy and evaluate diabetes related patient reported outcomes in kidney transplant recipients with type 2 diabetes. It also aimes to evaluate immunosuppression related patient reported outcomes in kidney transplant recipients with type 2 diabetes.
The purpose of this study is to use renal and kidney plus pancreas transplant patient samples to validate both the clinical utility of the CMV scoring algorithm and develop a clinically useful scoring guide for the BK virus immune competence assay.
The purpose of this study of posoleucel ALVR105 is to assess the safety and tolerability of posoleucel ALVR105 in kidney transplant recipients. The key secondary objective is to test the hypothesis that the administration of posoleucel ALVR105 to kidney transplant recipients with BK viremia will demonstrate superiority in suppressing BK viral load compared with placebo.
The purpose of this study to collect blood samples and data to assess the diagnostic capability of an updated version of the Prospera™ test. The current standard of care for detection of rejection in renal allograft recipients is serum creatinine, often used in combination with other blood tests such as proteinuria. Natera has developed an assay called Prospera™ to detect the amount of donor-derived cell-free DNA (dd-cfDNA), which is a marker of kidney rejection.
There is a need to develop blood and/or urine tests that will help to detect early signs of rejection in people who have had kidney transplant. Researchers will examine blood, urine, and tissue samples and try to identify genetic markers for certain conditions like rejection, response to therapy, and scarring of the kidney. By studying gene patterns, researchers hope to be able to diagnose these conditions earlier and improve kidney survival.
The purpose of this study is to evaluate the safety and effectiveness of the VERIS CMV Assay as an aid in the management of anti-CMV treatment for solid organ transplant patients by showing that virus levels are in agreement with the observed clinical status.
The purpose of this study is to collect and share detailed clinical data from all kidney transplant recipients from 7 kidney transplant centers (Mayo Clinic, Rochester, MN; Mayo Clinic, Scottsdale, AZ; Mayo Clinic, Jacksonville, FL; Cornell University, New York, NY; University of Michigan, Ann Arbor, MI; Henry Ford, Detroit, MI; University of Pittsburgh Medical Center, Pittsburg, PA) to retrospectively and prospectively study kidney transplant recipients.
The purpose of this study is to to determine the safety and effectivness of a single dose of autologous polyTregs or darTregs in renal transplant recipients with subclinical inflammation (SCI) in the 6 month post‐transplant allograft protocol biopsy compared to control patients treated with CNI‐based immunosuppression.
The purpose of this study is to determine if Eculizumab is safe and could be used to prevent delayed graft function following kidney transplantation.
This study aims to determine the potential barriers that contribute to fewer patients with Chronic Kidney Disease (CKD) being placed on the waiting list for a kidney transplant and that accomplished through evaluating:
American Indians (AI) have cultural, emotional, physical and religious variables that influence the patient’s perception about kidney transplantation and dialysis, some of which may lead to delays in completion of kidney transplant evaluation and kidney transplantation. The purpose of this study is to asses the patient's perceptions about the kidney transplant evaluation process at Mayo Clinic Arizona, assess the patient's attitudes and feelings about the process of kidney transplantation and how that influences their emotional, physical, cultural and religious well-being and determine the patient's attitude and experience with their dialysis.
The purpose of this study is to understand differences in quality of life across multiple domains in three distinct older populations: those on dialysis in the community setting, those wait-listed for kidney transplantation, and those who have successfully undergone kidney transplantation.
This is a double-blind, randomized-withdrawal, placebo-controlled study consisting of 2 treatment periods, and a post-treatment Follow-up Period during which retreatment is permitted if needed.
The purpose of this trial is to determine the safety and efficacy of eculizumab in the prevention of antibody mediated rejection (AMR) in living donor kidney recipients requiring desensitization therapy.
The purpose of this study is to assess the effectiveness and safety of NPC-21 when administered prophylactically to cytomegalovirus (CMV) seronegative patients receiving a first kidney transplant from a CMV seropositive donor.
The aims of this study are to identify frailty trajectories and biomarkers of frailty after kidney transplantation. Subjects will be followed beginning immediately prior to kidney transplantation until 1 year after kidney transplantation. Frailty will be prospectively assessed using performance-based measures (Fried criteria and Short Physical Impairment Battery). The relationship between frailty measures and blood levels of promising candidate biomarkers will be analyzed.
The primary purpose of this study in Phase 1 is to characterize the safety and tolerability of isatuximab in kidney transplant candidates. The primary purpose of this study in Phase 2 is to evaluate the effectiveness of isatuximab in desensitization of patients awaiting kidney transplantation.
The purpose of this study is to evaluate the efficacy of ASP0113 compared to placebo in reducing the incidence of cytomegalovirus (CMV) viremia in CMV-seronegative subjects receiving a kidney from a CMV-seropositive donor. This study will also evaluate the safety of ASP0113 in this patient population.
The purpose of this study is to measure and characterize specific immune cell abnormalities found in patients who have type 1 diabetes and may or may not be on the waiting list for either a pancreas alone or a pancreas and kidney transplant.
This current study aims to evaluate the efficacy of engagement modules in assisting patients who are candidates for renal and liver transplantation make significant lifestyle modifications. With the help of the Center for Innovation (CFI), a smartphone app (Android and iOS compatible) has been created to assist in both educating and engaging patients to develop and maintain healthy lifestyle modifications. Our goal is to create a cost-effective, smartphone-based platform that serves to not only efficiently educate but to also verify competence and keep our patients engaged.
The purpose of this study is to (i)assess glucose variability at pre specified time points after Pancreas Transplantation (ii) collect pre-specified serious adverse events after PT and in appropriate control groups (iii) assess mixed meal dynamics after pancreas transplantation.
The purpose of this study is to see if certain pre-transplant markers are able to predict how the kidney will respond after a liver transplant.
The purpose of this trial is to evaluate the reduction in incidence and severity of delayed graft function when using QPI-1002 with kidney transplants from donors older than 45 years who have brain death.
The purpose of this study is to determine if “booster” revaccination with the Janssen Ad26.CoV2.S vaccine (JNJ-78436735, aka the J&J vaccine, a viral vector vaccine) increases anti-COVID spike protein antibody levels in solid organ transplant recipients who did not form acceptable levels of anti-COVID spike protein antibody after receiving two doses of a mRNA vaccine: Pfizer-BioNTech (BNT162b2 vaccine) or Modena (mRNA-1273).
The purpose of this study is to compare tacrolimus formulations (Envarsus XR® versus twice a day tacrolimus) with the hypothesis that Envarsus XR® improves transplant- and tacrolimus- associated symptoms when compared to a twice a day tacrolimus regimen.
The purpose of this study is to validate the use of an RNA-seq based peripheral blood assay in renal transplant recipients in adult kidney transplant recipients.
The purpose of this research is to to determine whether home-based cardiac rehabilitation (CR) is an effective intervention to improve decreased physical function in patients with varying levels of kidney function. We will determine if home-based CR improves frailty parameters and SPPB scores. We will also determine if home-based CR improves health-related quality of life (HRQOL), body composition, physical activity, and adverse outcomes, including hospitalizations and death.
The purpose of this study is to compare the efficacy of brincidofovir (BCV) to valganciclovir (vGCV) for the prevention of CMV disease in kidney transplant recipients who are CMV seropositive pretransplant and received antilymphocyte induction therapy.
A Multicenter, Prospective, Double-Blind, Randomized, Placebo-Controlled, Phase 3 Study of ANG-3777 (formerly BB3) to Improve Graft Function and Reduce the Severity of Kidney Dysfunction or Delayed Graft Function Following Kidney Transplantation in Recipients of a Deceased Donor Kidney
The purpose of this study is to determine if patient satisfaction with a pharmacist-video visit is non-inferior to a face-to-face, in-clinic pharmacist visit.
The purpose of this study is to validate an MRI method to detect renal fibrosis in patients after kidney transplantation (KT).
This trial studies whether the nonavalent human papillomavirus vaccine given to adult women prior to kidney transplantation can help the body build and maintain an effective immune response during the post-transplant period when they receive immunosuppressive drugs to prevent transplant rejection. This study will help inform our scientific understanding about vaccine-induced immune responses among immunosuppressed individuals.
The purpose of this study is to to determine whether or not prior living kidney donors have an increased risk of bone fractures. The study will also determine bone structure and health in prior living donors as compared to matched controls.
We will determine if living kidney donors are at increased risk of bone disease and fractures following kidney donation. This information will be valuable in informing future kidney donors of the risks of donation and in devising treatments, such as administration of vitamin D analogs like calcitriol, to ...
The purpose of this study is to create a group of blood and urine samples from Mayo Clinic patients being screened for the kidney donor program as well as to collect risk factor data through a questionnaire. The data, blood and urine samples will be used for future research of kidney diseases at Mayo Clinic and future research at Mayo Clinic to learn about, prevent, or treat other health problems.
Frailty is a condition characterized by slowness, weakness, low physical activity, wasting, and exhaustion. Frailty increases the risk for adverse outcomes following transplant such as increased length of stay in the hospital, mortality, or graft function. No interventions for frailty are known for patients with renal disease, but exercise programs like pulmonary rehabilitation have been effective in improving frailty in patients with other diseases, such as lung disease. The goal of this study is to test whether exercise will also improve frailty among patients who are waiting for a kidney transplant and who are considered frail or pre-frail.
Hypothesis: we hypothesize that the abundance and functions of Breg subsets in kidney transplant patients could be associated with transplant tolerance and rejection, including DSA-mediated kidney transplant rejection. In addition, oral corticosteroid treatment significantly alters the frequency and function of Breg subsets, which could lead altered clinical outcomes. Aims, purpose, or objectives: 1. Investigate the frequency Bregs and their ability to express IL-10 along with other immune cells in the context of tolerance/rejection in kidney transplant patients. we hypothesize that the abundance and functions of Breg subsets in kidney transplant patients could be associated with transplant tolerance and rejection, ...
To compare the efficacy of brincidofovir (BCV) to valganciclovir (vGCV) for the prevention of cytomegalovirus (CMV) disease in kidney transplant allograft recipients who are CMV seronegative pretransplant and received a kidney from a CMV seropositive donor.
The purpose of this study is to conduct a clinical trial examining the preliminary effectiveness, feasibility, and acceptability of an exercise intervention on frailty after kidney transplantation (KT).
The purpose of this study is to investigate how efficiently the study medication imlifidase reduces the amount of donor specific antibodies (DSA) in comparison with plasma exchange (PE) therapy, in patients who have an active antibody mediated rejection (AMR) after recently been kidney transplanted. The purpose is also to investigate and compare safety for these two treatments. 20 patients will be treated with imlifidase and 10 with PE.
The purpose of this study of obinutuzumab administered as intravenous (IV) infusion in adults with end stage renal disease is to assess the safety and tolerability of the regimen at week 24 of the desensitization phase and at week 28 post kidney transplantation. All participants will be monitored for a minimum of 12 months following the last obinutuzumab infusion.
Patients that need reconstruction or re-building of their urinary bladder are often limited to having a segment of their intestine used for that purpose. Using intestine is less than ideal as it is an absorptive, mucous producing tissue and placing this in constant contact with urine creates significant long term problems. In patients that require a kidney transplant and bladder reconstruction, this study seeks to use a bladder graft from a deceased donor rather than intestine.
The purpose of this study is to connect the findings of TruGraf (a peripheral blood RNA signature that has been shown to correlate with rejection in kidney transplants) with rejection episodes in kidney transplant patients that are managed using standard of care clinical protocols at the three Mayo transplant sites.
The purpose of this study is to attempt to improve outcomes after kidney transplantation and to improve the safety of living kidney donation based upon variation in the apolipoprotein L1 gene (APOL1). Genes control what is inherited from a family, such as eye color or blood type. Variation in APOL1 can cause kidney disease. African Americans, Afro-Caribbeans, Hispanic Blacks, and Africans are more likely to have the APOL1 gene variants that cause kidney disease. APOLLO will test DNA from kidney donors and recipients of kidney transplants for APOL1 to determine effects on kidney transplant-related outcomes.
The purpose of this study will be to evaluate the effect of the US Health Resources and Services Administration (HRSA) program to reimburse lost wages on the decision of individuals to initiate evaluation for living organ donation.
The purpose of this study is to evaluate the utility of using anti-HLA antibody titer to measure the effectiveness of antibody lowering therapy (i.e., desensitization) in highly-sensitized kidney transplant candidates.
The purpose of this study is to use urinary exosomes to non-invasively identify (protein biomarkers) various conditions affecting the renal transplant.
The purpose of this study is to obtain valuable knowledge to rapidly promote the Hispanic Kidney Transplant Program (HKTP) as a novel approach for increasing living donor kidney transplants(LDKT) nationally in the Hispanic community.
The purpose of this study is to attempt to improve outcomes after kidney transplantation and to improve the safety of living kidney donation based upon variation in the apolipoprotein L1 gene (APOL1). Genes control what is inherited from a family, such as eye color or blood type. Variation in APOL1 can cause kidney disease. African Americans, Afro-Caribbeans, Hispanic Blacks, and Africans are more likely to have the APOL1 gene variants that cause kidney disease. APOLLO will test DNA from kidney donors and recipients of kidney transplants for APOL1 to determine effects on kidney transplant-related outcomes.
The specific purpose of this study is to compare the characteristics of patients at Mayo Clinic Rochester who received a living donor kidney transplant here preemptively versus those who dialyzed either less than 1 year or more than 1 year.
The purpose of this study is to determine the safety of the SARS-CoV-2 vaccination in patients listed for solid organ transplantation, including heart, lung, liver, kidney, and pancreas.
The purpose of this study is to evaluate post-transplant clinical outcomes in receipients of kidney transplants who are undergoing TruGraf® and TRAC™ monitoring.
The purpose of this study is to determine if the Living Donor Assessment Tool (LDAT) is an effective tool to improve the psychosocial evaluation of potential live kidney and liver donors. The LDAT was developed by the living donation team at the Zweig Family Center for Living Donation at the Mount Sinai Recanati/Miller Transplantation Institute. It assesses important areas of the evaluation process such as motivation (reason) for donation, knowledge of living donation, support, relationship to organ recipient, feelings about donation, stability in life and psychiatric and addiction history and provides a score that can be used to measure the ...
The purpose of this study is to evaluate KidneyCare (AlloSure, AlloMap kidney and iBox) in patients with negative c4d microvascular inflammation (MVI) with or without Donor-Specific Antibodies (DSA) as compared to cohort with normal biopsies without DSA.
The purpose of this study is to create a detailed immune profile of transplant patients and donors to determine what characteristics are associated with response to COVID vaccination.
Transplant recipients and donors who respond to immunization to COVID vaccine will have a different immunologic profile at basline than those who do not repspond.
We woudl like to create a detailed immune profile of Transplant patients and donors to determne what characteristics are associated with response to the COVID vaccination.
The purpose of this study is to find out if the size of a donor's remaining kidney or the microscopic appearance of a tissue biopsy from the donated kidney is predictive of long-term kidney function and overall health.
The study will prospectively determine the clinical utility of CMV cell-mediated immunity using the Quantiferon test. The investigators will use the assay results to tailor the duration of CMV prophylaxis in solid organ transplant patients.
The purpose of this study is to analyze the effect of parity, menopause and reproductive lifespan on kidney structure and function.
The primary purpose of this study is to implement the Hispanic Kidney Transplant Program (HKTP) at two transplant centers by conducting a needs assessment of barriers and using a “learning collaborative” model to deliver HKTP protocols, scripts, and materials.
This study will compare the incidence of a two-part composite endpoint consisting of de novo donor specific antibody (DSA) formation or a designation of "immune activation" (IA) on peripheral blood molecular profiling in patients maintained on twice daily, immediate-release tacrolimus versus those maintained on Astagraf XL in the first two years post-transplant.
The objectives of this study are to determine whether adequate blood volumes can be obtained with the Tasso+ device for anti-HLA antibody testing, to compare MFI levels from at-home collected capillary blood to venous blood, and to obtain user feedback and experiences from patients.
The purpose of this study is to assess the safety, effectiveness, and overall benefit of FCR001 cell therapy in de novo living donor renal transplantation.
The primary objective of this study is to demonstrate the safety and efficacy of cellular immunotherapy with MDR-101 for induction of functional immune tolerance in recipients of human leukocyte antigen (HLA)-matched, living donor kidney transplants.
The purpose of this study is to evaluate safety and efficacy outcomes in renal transplant recipients in whom post-transplant care is managed using AlloSure®. AlloSure® is a non-invasive test to measure donor-derived cell-free DNA (dd-cfDNA). The AlloSure test is intended to assess the probability of allograft rejection in kidney transplant recipients with clinical suspicion of rejection and to inform clinical decision-making regarding the necessity of renal biopsy in such patients at least 2 weeks post-transplant in conjunction with standard clinical assessment. Amendment 1 (A1): Is an observational study to develop and validate the clinical use of KidneyCare®.
The purpose of this study is to evaluate the clinical performance of the Aptima CMV Quant assay on the Panther system in ethylenediaminetetraacetic acid (EDTA) plasma samples from solid organ transplantation recipients (SOTR) and hematopoietic stem cell transplant recipients (HSCTR).
The purpose of this study is to determine the change in exercise capacity by comparing VO2 max results pre & post renal transplant.
The purpose of this study is to assess the feasibility and safety of delivering adipose mesenchymal stem cells (AMSCs) to kidney allografts.
The purpose of this study is to determine the incidence of biopsy proven acute rejections detected due to elevated dd-cfDNA independent of change in serum creatinine, to determine incidence of DeNovo Donor specific antibody (DSA) or increase in preexisting DSA’s in presence of elevated dd-cfDNA, and to determine the association of elevated dd-cfDNA with progression of chronic changes in surveillance biopsies.
The purpose of this study is to decrease the waiting time on the transplant list for patients who have high level of anti-HLA antibodies with ESRD and improve the patients and allograft survival after transplant.
The overall goal of this study is to determine the safety and feasibility of infusing adipose-derived mesenchymal stem cells directly into the artery of renal allografts with biopsy-proven rejection in order to reduce inflammation detected in the graft. We contend that future studies will show that administering immunomodulatory cells directly into the allograft will be more effective and safer than the current approaches of delivering massive doses of systemic immunosuppression.
Study participation involves receiving mesenchymal stem cells (MSC), created from the adipose tissue (body fat) of a donor, and infused into the main artery of a transplanted ...
The purpose of this study is to determine the prevalence of genetic mutations of cancer in kidney transplant patients receiving care at Mayo Clinic Arizona.

Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.

Popular Services
- Patient & Visitor Guide
Committed to improving health and wellness in our Ohio communities.
Health equity, healthy community, classes and events, the world is changing. medicine is changing. we're leading the way., featured initiatives, helpful resources.
- Refer a Patient
Kidney Transplantation
The ohio state university wexner medical center’s comprehensive transplant center is home to one of the largest kidney transplant programs in the country., why choose ohio state for kidney transplant.
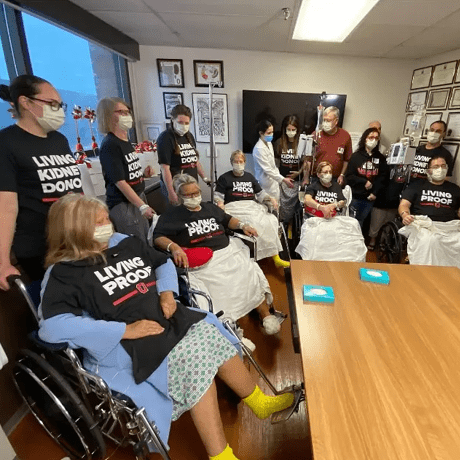
Expertise: We perform nearly 300 kidney transplants a year, including adult living donor transplants , making us one of the top 20 transplant programs by volume in the United States. A kidney transplant from a living donor is the best option for a patient with end-stage kidney disease. Our program is focused on expanding access to living kidney donation by overcoming blood type incompatibility through our kidney donor exchange program. In early 2020, we completed an 8-way kidney donor exchange consisting of 8 living donors and 8 recipients. This bested our previous chain, a 6-way , performed in 2011. Our 8-way is the largest, single-institution living kidney donor exchange to date in Ohio, and one of only a handful in the country.
Experience: Our Comprehensive Transplant Center has one of the largest organ transplant programs in the nation and is a preferred provider for all major insurance companies. Each year we perform nearly 600 kidney, liver, pancreas, combined kidney-pancreas, heart and lung transplants. Since our program started in 1967, we have performed 12,500 lifesaving organ transplants including 8,350 kidney transplants.
Kidney transplant research: We participate in clinical trials of new immunosuppressive drugs and antirejection therapies including novel cell therapy to prevent kidney transplant failure.
Kidney Transplant Candidates
Patient process, treatment team, frequently asked questions.
- Diabetes mellitus
- Hypertension
- Autoimmune disease: Your body's immune system protects you from disease and infection. But if you have an autoimmune disease, your immune system attacks healthy cells in your body by mistake. Autoimmune diseases can affect many parts of the body.
- Congenital abnormalities: A birth defect is a problem that happens while a baby is developing in the mother's body. Most birth defects happen during the first three months of pregnancy. One out of every 33 babies in the United States is born with a birth defect. A birth defect may affect how the body looks, works or both. Some birth defects like cleft lip or neural tube defects are structural problems that can be easy to see. To find others, like heart defects, doctors use special tests. Birth defects can vary from mild to severe.
Kidney Transplant Process
Referral phase.
- The referring party is responsible for providing the coordinator with all applicable medical information according to the transplant referral protocol provided at time of referral
- You will need to notify your insurance company before making your initial evaluation appointment. Our pre-transplant office and hospital business office will work with you to determine insurance availability and precertification requirements
- Pre-transplant coordinators and business office staff then work together to meet insurance company requirements for evaluation and transplant procedure approval
Clinic Evaluation Phase
Candidacy phase, active wait list phase, transplant phase, post-transplant phase.
- Lab Tests: You will visit a lab for testing two times a week for the first three months post-transplant . Your lab results are evaluated by a transplant coordinator and a transplant surgeon.
- Outpatient Clinic Visits: you will be seen in our outpatient clinic weekly for the first month, then again at 6 weeks, 9 weeks, 12 weeks, 4 months, 6 months, and one year post-transplant (and at any other time in between if warranted). You will be seen annually thereafter, unless more frequent visits are required. After you are released by your surgeon, you will be seen by the Transplant Medicine Service. Lab frequency is reduced as you progress.
We will communicate with your referring physician at the beginning and end of each hospitalization, as well as with each outpatient clinic visit. Because of the many interactions of other medications with immunosuppressives, please check with the post-transplant office prior to filling any prescription.
Once your kidney function stabilizes, you may be eligible to transition back to a nephrologist closer to home. This transition is dependent on your kidney function and overall health at that time. Please discuss this option with your post-transplant coordinator.
Financial Assistance
Kidney transplant team, transplant nephrologist.
This doctor specializes in kidney transplants and will follow you before, during and after your transplant. They will complete a physical exam and discuss what additional testing is needed to prepare you for your transplant.
Transplant Surgeon
Infectious disease physician.
These doctors, who specialize in infectious diseases, will follow you before and after your transplant (if needed) to reduce risk of infection.
Advanced Practice Provider
The advanced practice providers include physician assistants and nurse practitioners who work closely with your physician to ensure continuity of care throughout your stay at the hospital and your transition to outpatient care. He or she orders and monitors diagnostic tests and treatments, responds to urgent needs, diagnoses and treats problems if they arise and provides the educational tools and resources necessary to continue success with your transplant once you are discharged.
Transplant Coordinator
These are nurses who will be your primary contact from the time you are referred for a transplant evaluation throughout your care here. They will help answer any questions you may have and assist you throughout your transplant experience.
Social Worker and Psychologist
These professionals meet with you to evaluate your psychological readiness for transplantation.
Transplant Pharmacist
Pharmacy patient assistance coordinator.
The pharmacy patient assistance coordinator offers assessment, linkage and referrals for assistance to patients who need certain medications and have high co-pays or no prescription drug coverage.
Contact: 800-626-2538
Kidney Transplant Frequently Asked Questions
Which health insurance are accepted.
The list of accepted insurances for kidney transplant can often change. Please contact your health care insurance provider to confirm your coverage for transplant at Ohio State’s Comprehensive Transplant Center.
What is tissue typing?
Are there any support groups to join.
Organ transplant affects a person’s body, spirit and life in numerous ways. Adjusting to these changes can often be easier with the assistance of others with similar experiences.
Open to all Ohio State’s abdominal transplant recipients AND waitlisted kidney, pancreas and liver patients, Ohio State’s Abdominal Transplant Support Group offers an emotionally supportive community before and after the transplant journey and is one of many additional, optional resources offered to benefit our transplant patients.
- What: Ohio State's Abdominal Transplant Support Group
- Who: Transplant recipients (liver, kidney and/or pancreas) and patients waitlisted for transplant
- Date: 3rd Thursday of each month
- Time: 5:30 – 6:30 p.m.
- Location: Virtual - click HERE to join meeting
For any questions or concerns, please call the transplant social work office at 614-366-3273.
Why kidney transplant from a living donor is the best option?
There are currently three options for treatment of end-stage kidney disease: 1. dialysis, 2. kidney transplant from a deceased donor, or 3. kidney transplant from a living donor .
With dialysis, a machine is used to artificially clean the blood, doing the work of a healthy kidney. It’s time-consuming and exhausting, as frequent as three times a week for up to four hours each session. While a patient can remain on dialysis for many years, it’s not a cure for kidney disease. In fact, ten percent of patients on dialysis die each year while waiting for a kidney transplant. For some groups, such as elderly patients and patients with diabetes, there is an even greater risk of dying.
A kidney transplant is the preferred treatment option for patients with end-stage kidney disease. But the demand for kidneys from deceased donors is greater than the number available – which means patients can wait years for a kidney transplant, often growing weaker while waiting.
The best and fastest option for kidney transplant is to receive a kidney from a living donor .
What are the advantages of a living kidney donor transplant?
- Wait times for recipients are reduced from years to months , potentially avoiding dialysis.
- Outcomes are better , as surgery can be scheduled when you are your healthiest.
- Risk of rejection is low .
- And because the complete health history of the living donor is known, kidneys from living donors are the healthiest, lasting longer than kidneys from deceased donors . (At Ohio State, we have patients nearing their 40 th transplant anniversary with a kidney from a living donor.)
About a third of the transplants performed at Ohio State are performed with kidneys from living donors. Often living donors are family members, but a growing number are friends or co-workers. There are also people who choose to donate a kidney without having a specific recipient in mind. These extraordinary people are called non-directed or altruistic donors.
Where to learn more about living kidney donation?
Anyone interested in being a living kidney donor can complete an online health history questionnaire to start the process, or visit Ohio State's living kidney donation webpage for more information about the donor surgery, risks and criteria.
Who can be a living kidney donor?
Anyone meeting the following basic criteria can be evaluated to be a living kidney donor at Ohio State:
- Between the ages of 18 and 75 years old.
- Good overall physical and mental health.
- Don’t have uncontrolled high blood pressure.
- Don't have diabetes, cancer, HIV/AIDS, hepatitis or organ disease.
Who pays for the living donation surgery?
The recipient’s medical insurance pays the cost of the living donor’s evaluation, testing and surgery, and therefore, the donor should not incur any medical expenses. However, time off work and travel expenses need to be considered. The usual recovery time for a donor is four to six weeks. Some donors may be eligible to receive financial assistance for donation expenses like transportation, parking and hotels. There is no financial assistance available for lost wages. A new Ohio law gives state employees paid time off work for donating.
How to ask for a living kidney donation?
Receiving a kidney transplant from a living donor is the best and fastest option to restoring your health. However, finding a living donor is easier said than done.
The truth is there is an enormous physical and emotional toll of living with end-stage kidney disease, not to mention the exhaustion of dialysis treatment. So it is not a surprise that finding a living donor can be overwhelming. In fact, the conversation is so difficult more than half of all people in need of a kidney transplant don't even ask one person to donate !
For help starting the conversation , our donor toolkit can help.
Donor Conversation Toolkit
And though you may not want to ask, often friends and family members are eager to be your donor champion and spread the word for you to help identify potential living donors.
Donor Champion Information
Patient Success Stories

Kidney donation from one brother to another, half a country apart

Mother and son donate kidneys to ailing husband and father, 21 years apart
Transplant surgeon Amer Rajab, MD, PhD , performed both procedures across the decades for ‘blessed’ patient.
Read their amazing story here.

Kidney Recipient 30+ Years After Transplantation
After more than 30 years of living with a kidney transplant, Rick has come away with a very important life lesson: don’t take anything for granted.

Nicaraguan Travels to OSU for Kidney Transplant

Kidney Transplant Recipient Has Baby After 10 Year Wait
After a decade battle with kidney disease, Bethany is finally able to start her family, thanks to a living kidney donation transplanted at Ohio State's Wexner Medical Center.

One of the longest living patients with a transplanted organ at the Ohio State Comprehensive Transplant Center shares his story
Our latest kidney transplant news.
5-way kidney transplant chain saves lives at Ohio State

Living donor gives kidney to former colleague
Additional Information
- Comprehensive Transplant Center
- Buckeye for Life
- Transplant Fellowships
- COPPER Laboratory
- Lifeline of Ohio
Subscribe. Get just the right amount of health and wellness in your inbox.
Kidney Transplant Program
One of north carolina’s best kidney transplant centers.
If you need kidney transplant surgery, you can feel confident choosing Duke for your care. Our team has performed thousands of complex kidney transplants that have improved the quality of life for our patients and their loved ones.
Please check your filter options and try again.
Why Choose Duke
Fast Evaluation We offer a comprehensive, one-day evaluation . You’ll be seen by all the necessary specialists -- a nephrologist, transplant surgeon, dietitian, social worker, financial counselor, and possibly a psychologist -- during one visit, at one clinic location. We conduct these evaluations three times a week and often have appointments available within a few weeks. You’ll get from a referral by your doctor to a decision by our team faster than any other center in the state.
We’re Good (Organ) Matchmakers We get to know you, your medical conditions, and what kind of kidney transplant you need, and we stay up-to-date on your status. When we get offers for available kidneys, we use a systematic approach to consider each one carefully, to ensure it is the offer that will fit your needs the best. During the process , we make every effort to find you a kidney, and we make sure you’re ready when the right one becomes available.
We Allow Multiple Listings to Reduce Wait Time Adding your name to the waitlist at more than one transplant center – called multiple listing -- may increase your chances of finding a matched donor kidney sooner. Multiple listing does not affect your wait time at your current center. If you want to designate Duke as your “home” transplant center and are receiving your care elsewhere, you can transfer the time you have accrued at that center to Duke. Our team can often use previous test results and other medical information from your current center to speed up the evaluation process.
We Have Extensive Experience The Duke kidney transplant program has been performing kidney transplants for more than 50 years. It is one of the highest volume programs in North Carolina.
We Achieve Excellent Results Our outcomes are consistently excellent -- a notable accomplishment considering that we often perform transplants for people who have multiple, complex medical problems.
Kidney transplant surgery is performed at Duke University Hospital. Pre- and post-transplant appointments take place at our nephrology clinics in Durham.
You Have Options if You and Your Donor Don't Match If a loved one offers to donate a kidney and it’s medically safe for that person to do so, there are multiple routes for you to take. The simplest is for you to receive your donor’s kidney if blood and tissue tests show that you’re a match. If you and your donor aren’t a match, you may be eligible for another option such as:
- ABO-incompatible transplantation: You receive medical treatments before and after transplant that allows you to receive a kidney from a donor with a different blood type.
- Paired exchange: You receive a kidney from someone else’s donor, and another recipient receives your donor’s kidney.
We Prepare You for Transplant Quickly If you are considered a candidate for a kidney transplant but do not have a potential living donor, you will be waitlisted in a national database maintained and administered by the United Network of Organ Sharing (UNOS ). While our wait times are on par with national averages, we prepare you to be transplanted quickly. We have one of the largest active waiting lists in the region, meaning more of our patients are ready to get a kidney when a kidney is offered.
You'll Stay in a Dedicated Hospital Unit for Transplant Patients Our solid organ transplant unit is dedicated to caring for people throughout their organ transplant journey, whether they are waiting for a transplant, recovering from surgery, or are returning to the hospital. The unit is staffed by a dedicated team of providers experienced in caring for people undergoing liver , kidney, small bowel, pancreas, or intestinal transplants. These include doctors, nurses, pharmacists, social workers, patient coordinators, and more. Patients and their families can establish relationships with our providers and staff and feel secure in the hospital environment.
If you are interested in making an appointment for an evaluation, please ask your nephrologist to submit a referral.
HIV-Positive Kidney Transplants The HOPE Act made it possible for HIV-positive donors to offer their organs to HIV-positive recipients. Duke is the only transplant center in North Carolina, and one of just a few in the nation currently approved to perform HOPE Act living donor kidney transplants. In 2019, our kidney transplant surgeons performed the first live kidney donation under the HOPE Act in North Carolina and the Southeast region, and the second in the United States.
Options if You've Had a Prior Transplant If you’ve had a prior transplant, we offer multiple anti-rejection regimens. These options can make it more likely you’ll find a match among potential living donors and more likely we can waitlist you for a deceased donor transplant . If your immune system is highly sensitized, our innovative, newly available approaches are proving better at overcoming this problem.
We Perform Multi-Organ Transplants Our colleagues in the other Duke organ transplant teams share our commitment to providing you the life-changing transplant you need with the best possible outcome. We regularly partner with them to help you and your caregivers throughout each step of the process.
Related Conditions
- Hypertension
- Kidney Failure Treatment
Duke University Hospital is proud of our team and the exceptional care they provide. They are why we are once again recognized as the best hospital in North Carolina, and nationally ranked in 11 adult and 9 pediatric specialties by U.S. News & World Report for 2023–2024.
Laboratories
Murakami Lab

Kasinath Lab
Congratulations to Xiaofei Li on being promoted to Instructor!
Congratulations to Sungwook Jung on being promoted to Instructor!

Happy Holidays from the Transplant Research Center!
JAMIL AND REZA FROM THE TRANSPLANTATION RESEARCH CENTER RECEIVING THE BRIGHAM IGNITE AWARD

FEATURED EVENTS
March 17, 2022, transplantation as the center of the universe.
In this inaugural lecture of the Virtual Transplantation Seminar Series hosted by the Transplantation Research Center at BWH, Dr. Allan D. Kirk provides a broad overview of transplant research as an example of broadly applicable, multidisciplinary science. In reviewing the challenges and accomplishments of the transplant community, Dr. Kirk presents transplantation biology as an effective vehicle for young investigators to take into innumerable domains of contemporary scientific investigation.
November 19, 2021
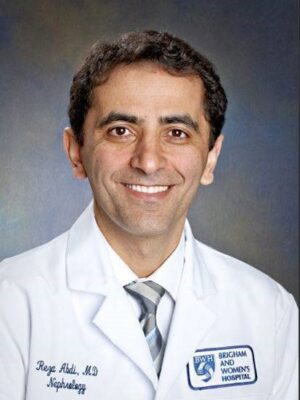
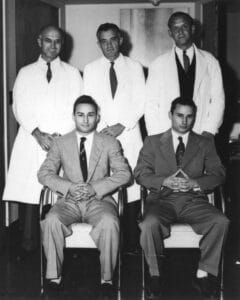
A second chance to live: a historical perspective on the first successful kidney transplant, june 15, 2021, from the discovery of the first angiogenesis inhibitors to the development of controlled drug delivery systems and the foundation of tissue engineering, reza abdi, md, professor of medicine, harvard medical school director, transplantation research center staff physician, renal division, brigham & women’s hospital.

Dr. Robert Langer, Sc.D.
Institute professor at mit.
MERRILL ARCHIVE
Archival images courtesy of Brigham and Women’s Hospital Archives and the Harvard Medical Library in the Countway Library of Medicine
Emergency Department Construction To Begin 2/19/2024 — Patients To Be Rerouted To Fountain Circle Entrance
- Our Mission, Vision & Values
- Diversity, Equity & Inclusion
- Academic Medical Center
- Academics & Research
- Excellence & Achievements
- Find a Location
- Parking & Directions
- Visiting Hours
- Patient Portal
- Insurance & Billing
- Medical Records
- Onsite Amenities & Dining Options
- Clinical Trials
- University Pharmacy
- Events Calendar
- Health Information Center
- Make An Appointment
- Pastoral Care
- Patient Experience
- Plan Your Visit
- Treatments & Procedures
- Primary Care
- Specialty Care
- Urgent Care
- Main Campus
- Regional Health Centers
- Centers of Excellence
- Ways to Give
Kidney Transplant

Kidney transplant is a surgical procedure that removes one healthy kidney from one person and places it in another person who suffers from kidney disease or failure, allowing the transplanted kidney to perform the duties that the patient’s two failed kidneys cannot do.
- Living donor (donates kidney): While the patient is unconscious and pain-free (general anesthesia), an incision is made in the side of the abdomen (flank). The kidney is removed and the incision is closed.
- Kidney recipient (receives kidney): While the patient is unconscious and pain-free (general anesthesia), an incision is made in the lower abdomen. The new kidney is stitched into place within the pelvis and the incision is closed.
The kidney is placed inside the patient’s body between the upper thigh and abdomen. The surgeon connects the artery and vein of the new kidney to the patient’s artery and vein. The new kidney may start working right away or take a few weeks to create urine.
The kidney transplant surgery can take anywhere from three to six hours, with the average hospital stay lasting from five to seven days. After leaving the hospital, the patient requires regular follow-up visits. If a relative or close friend donates the kidney, the donor probably will stay in the hospital for less than a week, providing there are no complications.
Types of Donors
- Living-Related Donor: A live family member who donates a kidney.
- Cadaver Donor: A donor who recently has died but did not suffer from kidney disease or injury.
- Living-Unrelated Donor: A spouse or friend who donates a kidney.
A donor’s blood and tissues must closely match the patient’s to help prevent the body’s immune system from rejecting the new kidney. Tests on blood cells will be conducted to find out if the body will accept the new kidney.
The time it takes to get a kidney varies. The patient must be placed on a waiting list to receive a cadaver donor kidney. However, if a relative donates a kidney, the transplant operation can be done sooner.
Related Conditions & Treatments
- Kidney Cancer
Treatment Locations

Center for Transplant Services
1924 Alcoa Highway Knoxville, TN 37920
Phone: 865-305-9236
Our Experts

Karen Hensley, NP
Specialties: Transplant Surgery
Clinical Focus: Kidney Transplant

Wala Abusalah, MD
Transplant Nephrologist
Specialties: Transplant Surgery, Nephrology
Clinical Focus: Transplant medicine, immunosuppression, chronic kidney disease
Patient Story - Mary Bell & Dr. Joe Bailey
Becky - life-saving kidney transplant.

Nurse Donates Her Kidney to Her Co-Worker
A nurse at East Tennessee Children’s Hospital’s neonatal intensive care unit said she felt led to help her co-worker after she found out she was in need of a kidney.

The Gift of Life – The Impact of Living Donation
The two leading causes of chronic kidney disease are high blood pressure and diabetes. Our program offers patients with type I diabetes the opportunity for pancreas transplant.

Kidney Transplant at University of Minnesota Medical Center
Celebrating 46 years of transplant success, University of Minnesota Medical Center has more than 7,000 kidney transplants to our credit. Our program is one of the two largest and oldest kidney transplant programs in the world. We performed the world’s first kidney-pancreas transplant in 1966.
Why choose us?
We utilize more living donors than any other kidney transplant program in the world.
In April 2009, we performed our 50th non-directed kidney donor transplant. A non-directed donor is someone who decides they want to donate their kidney to anyone who might need it. Click the link to learn more about our Living Kidney Donor Program.
Kidney transplantation is the treatment of choice for patients with end-stage kidney disease. Compared to dialysis, a transplant provides increased longevity and a markedly better quality of life. More transplant patients than patients on dialysis are able to return to an active lifestyle in their community, school, or the workforce. In some situations, the improvement in survival with transplantation vs. dialysis is dramatic. This is true, for example, in patients with diabetes. In others, there are specific reasons why a transplant is preferred over dialysis -- such as improved growth in children.
The first successful kidney transplant was done between identical twins in 1954. It was almost a decade later before development of immunosuppressive drugs allowed non-twin transplants. Since then, there has been incremental improvement in both patient survival and transplant graft survival. Currently, one-year patient and graft survival rates are more than 90%. Click on the link for more information on kidney transplant success rates at University of Minnesota Medical Center.
Coronavirus (COVID-19): Latest Updates | Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies | COVID-19 Testing | Vaccine Information Vaccine Information Vaccine Information
Kidney Transplant
Our philosophy of care.
At the University of Rochester Medical Center, we believe a kidney transplant is a lifelong commitment for you and for us. We will stay involved with you and your family through the entire transplant process. We get to know you very well and recognize that preparing for and living with a transplant will affect your lifestyle in many ways. We will help you maintain and resume many of your activities and even become involved in new ones.
We are committed to the time, effort, and resources required to make your transplant a success. Our definition of success extends far beyond the operating room. We will work with you to make your life after the transplant as successful as possible.
What is a Kidney Transplant?
A kidney transplant is when a patient whose kidneys are no longer working gets a healthy kidney from another person. A transplant surgeon opens the patient’s abdomen and places the healthy kidney in the patient’s body. With kidney transplants, the donor can be living or deceased.
The Kidney Transplant Process
- Evaluation - You will need to be evaluated to determine if you are eligible for a transplant. The evaluation includes a variety of tests, including a physical exam, X-rays and CT scans, blood tests and any other tests your providers feel necessary.
- Finding an kidney - If you qualify for a kidney transplant, you will be placed on a waiting list to receive an organ. Or, if you have a family member who is a compatible match and is willing to donate their kidney, living donor transplantation may be an option for you.
- Getting a kidney - If you are on the waitlist and a kidney becomes available, you will need to get to the hospital immediately for the procedure.
- Surgery - During the surgery, the surgeon makes an incision and places the new kidney in your lower abdomen.
- Recovery - After your surgery, you will need to stay in the hospital for about a week. You will then need several checkups in the weeks after you leave the hospital. During the years following your surgery, you will need to receive follow-up care from your transplant team.
You’ll be contacted when a kidney is available. If your new kidney is from a living donor, both you and the donor will be in surgery at the same time. One team of surgeons will do the nephrectomy (removing the kidney from the donor), while another prepares you to receive the donated kidney.
If your new kidney is from a person who has recently died, your surgery starts when it arrives at the hospital and the results of the cross-match test, described above, are negative (satisfactory).
The surgery can take from 3 to 4 hours or more. You will be given general anesthesia. Your surgeon makes an incision in your lower abdomen and puts the new kidney in place. Then the surgeon connects the artery and vein of the new kidney to your own artery and vein. Your blood will then flow through the new kidney. The ureter from the new kidney will be connected to your bladder. Often, the new kidney will start making urine as soon as your blood starts flowing through it, but sometimes a few weeks pass before it starts working. Unless they are causing infection or high blood pressure, your own kidneys are left in place.
Home / Care & Treatment / Nephrology & Hypertension
Kidney Transplant
Long history of excellence for capital region residents.
Albany Medical Center's transplant program has a long history of experience and expertise at every level, with physicians who specialize in kidney transplants. Since 1969, our kidney transplant program has received numerous accolades and is among the top-ranking programs in the nation. We take a collaborative multidisciplinary approach to caring for transplant recipients to achieve successful outcomes for our patients and provide support, before, during and after a transplant.
We have performed close to 3,000 kidney transplants.
In addition to our long history of expertise, we offer:
- Cooperative efforts between surgical, anesthesiology, nephrology, endocrinology, and infectious disease specialists
- Excellent outcomes in recipients of organ transplants
- Dedicated transplant unit and staff
To learn more about joining the kidney transplant program at Albany Medical Center, call 518-262-5614. Before a formal evaluation appointment, you must complete any necessary tests and attend an educational seminar. Test results can be forwarded via fax at 518-262-5571.
Patients being considered for a kidney transplant must complete a comprehensive medical and psychosocial evaluation. Patients must be healthy enough for transplant surgery and follow-up.
Patients eligible for transplant are placed on a donor list for our region. When a match comes from a donor who has died, patients are called on short notice for a transplant.
A match can also come from someone who chooses to donate a healthy kidney, called a living donor. More than 500 family members and friends have donated a kidney to a loved one at Albany Medical Center in the past 40 years.
A successful kidney transplant may allow you to live a longer and more normal life. In most cases, patients will remain on immunosuppressant drugs which take strict monitoring.
View our transplant surgery educational videos .
Donating a kidney to someone you care for is one of the greatest gifts. We view living donation with the utmost respect and have a strong commitment to the safety and wellbeing of every potential donor in our program.
What are some of the advantages of living donors vs. cadaveric donor transplants?
- Decreased incidence of kidney rejection due to similar genetic backgrounds.
- Immunosuppressive drug doses may be lowered sooner and thus possibly lessen the side effects of the medications.
- Convenient scheduling. This may permit the recipient to shorten their time on dialysis or avoid dialysis completely. The wait for a cadaveric kidney usually takes several years.
- Immediate function of the transplanted kidney. Occasionally, a cadaveric kidney may not function for days or weeks after being transplanted and the recipient will require dialysis in the interim.
- The possibility exists of obtaining a perfectly matched kidney from a sibling which has proven to be the best for longterm success.
Chief of Transplant Surgery

Dr. Shahbazov completed a fellowship in transplant surgery at the University of Virginia Medical Center in Charlottesville, Va., a transplant research fellowship at Baylor Transplant Institute in Dallas, and a transplant surgery fellowship at Baskent University in Ankara, Turkey. He completed general surgery residencies at King Faisal Hospital in Al-Taif, Kingdom of Saudi Arabia, and Clinical Hospital #5 in Baku, Azerbaijan. He received his medical degree from Azerbaijan Medical University, also in Baku.
Dr. Shahbazov is a fellow of the American College of Surgeons and European Board of Surgery as well as a member of numerous professional societies, including the American Society of Transplant Surgeons and the American Medical Association. He has authored or co-authored dozens of publications in professional journals and authored a chapter on Living Donor Liver Transplantation in the book Transplantation Surgery. He is fluent in English, Azerbaijani, Russian, and Turkish, and is proficient in Arabic.

Center for Donation and Transplant
Learn more about donation at the Center for Donation and Transplant and register to be an organ, eye, or tissue donor. CDT offers hope and healing to donor families in upstate New York and western Vermont, empowering our community to restore the health of those needing an organ or tissue transplant.
Related News

Not a patient? Find information for:
- Search Menu
- Advance Articles
- Editor's Choice
- Cover Archive
- Author videos
- Supplements
- Cover Images
- Author Guidelines
- Submission Site
- Open Access Options
- Why publish with NDT?
- About the ERA
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Terms and Conditions
- Editorial Fellowship
- The ERA Journals
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Importance and complexity of medical research funding, scientific societies: at the interface between investigators and funding bodies, conflict of interest statement.
- < Previous
Funding kidney research as a public health priority: challenges and opportunities
- Article contents
- Figures & tables
- Supplementary Data
Carmine Zoccali, Raymond Vanholder, Carsten A Wagner, Hans-Joachim Anders, Peter J Blankestijn, Annette Bruchfeld, Giovambattista Capasso, Mario Cozzolino, Friedo W Dekker, Danilo Fliser, Denis Fouque, Ron T Gansevoort, Dimitrios Goumenos, Kitty J Jager, Ziad A Massy, Tom A J Oostrom, Ivan Rychlık, Maria Jose Soler, Kate Stevens, Goce Spasovski, Christoph Wanner, Funding kidney research as a public health priority: challenges and opportunities, Nephrology Dialysis Transplantation , Volume 37, Issue 1, January 2022, Pages 21–28, https://doi.org/10.1093/ndt/gfaa163
- Permissions Icon Permissions
Medical societies have a social responsibility to disseminate knowledge and inform health authorities on threats to public health posed by various diseases. Advocacy for health protection programmes and for medical research funding is now embedded into the missions of most scientific societies. To promote kidney research funding in Europe, the European Renal Association – European Dialysis and Transplant Association (ERA-EDTA), rather than acting as an individual society advocating for the fight against kidney disease, has actively helped to create an alliance of national associations centred on kidney diseases, the European Kidney Health Alliance (EKHA), and joined the Biomedical Alliance (BMA). The ERA-EDTA is fully committed to supporting its working groups (WGs) and consortia of its members to allow them to produce valuable kidney research. The framing and formalization of projects, and the regulatory issues related to submission to the European Commission, are complex. To help WGs to gain expert advice from agencies with specific know-how, the ERA-EDTA has adopted a competitive approach. The best research projects proposed by WGs and consortia of other European investigators will receive seed funding to cover the costs of consultancy by expert agencies. Via its broader platforms, the EKHA and the BMA, the ERA-EDTA will strive towards broader recognition of kidney disease and related clusters of non-communicable diseases, by European and national agencies, as major threats to the qualities of life of their populations and their economies.
Historically, the advancement of science has been supported by affluent individuals or families, and investigators have rarely been self-sustaining. Galileo’s discoveries were funded mainly by wealthy individuals while Darwin’s voyage to the Galapagos islands was, in part, paid for out of his own pocket. Today, over $1 trillion per year are spent worldwide on sustaining research [ 1 ] and medicine is one of the most financially demanding research areas. In 2014, health research absorbed about 45% of the US government’s total investment in research and development [ 2 ]. In general, health projects of public interest are mainly sustained by governments and foundations, while research into treatment is conducted almost exclusively by industry. In 2018, drug companies spent $44.2 billion on funding for clinical trials [ 3 ], which was about one-third of the whole health budget of the National Health Service in the UK in the same year [ 4 ].
On a worldwide scale, the prevalence of chronic kidney disease (CKD) is 9.1% ( Figure 1 ) [ 5 , 6 ]. In 2017, 1.2 million deaths from CKD were registered and mortality increased by 41.5% between 1990 and 2017 in the face of a stable background mortality rate [ 5 ]. CKD is one of the most rapidly advancing diseases on the list of the world’s most deadly conditions, and mortality associated with it is expected to rise by a factor of two, advancing CKD from number 16 in 2016 to number 5 by 2040 [ 7 ]. Over the last 27 years, the prevalence of CKD worldwide has hardly declined, in contrast to many other important non-communicable diseases (NCDs) [ 5 ]. Unfortunately, the global burden of kidney disease has long been overlooked by the World Health Organization (WHO) and no specific goals to limit the CKD epidemic have been established by this organization so far [ 8 ]. NCDs as a whole are health conditions with the largest imbalances between disability-adjusted life years and research investment [ 9 ]. Among NCDs, scientific advancements in biotechnology and in ‘omic’ sciences have produced breakthroughs in oncology and cardiology, but basic and clinical research on kidney disease has lagged behind over the last decade [ 10 ]. Nephrology is probably the specialty that produces the lowest number of randomized clinical trials and quality concerns have been expressed regarding trials focusing on kidney diseases [ 11 ]. Europe lacks Clinical Trial Service Units (CTSUs) that could coordinate network-based clinical studies and support clinicians. Such CTSUs exist in other parts of the world such as Australia, Canada and the USA, and have already contributed to our understanding of treatments for NCDs. Clearly, at this time juncture, there is a need to maximize efforts aimed at promoting effective collaborations between kidney investigators involved in clinical and translational research to sustain the growth of the specialty ( Box 1 ). Gaps in therapeutic advancements in nephrology have been made clear in analyses made by CenterWatch [ 10 ]. In 2019, investment in research from the National Institutes of Health (NIH) in the USA amounted to $11.1 billion for cancer, $3.0 billion for Human Immunodeficiency Virus and $5.2 billion for cardiovascular disease, but only $680 million for kidney diseases [ 12 ]. Solving the problem of adequately funding kidney research is crucial if we are to effectively counter the CKD epidemic, as well as acute kidney injury, which is a frequent cause of CKD [ 13 ] and is considered by some to represent a continuum with CKD [ 14 ]. The coronavirus disease 2019 (COVID-19) pandemic has painfully exposed a number of weaknesses in our current medical research funding models. While allotting adequate funding for the development of a vaccine against the group of coronaviruses would have had a high cost, it would have prevented the present financial crisis, which will cost much more. Of course, the financial impact of CKD is less dramatic, but it is still costly, and is continuous rather than temporary.
Multicentre interventional studies with better trial design, and therefore a higher probability that the measured outcomes will aligned with measurable differences to patient care:
Development of novel tests and technologies for improved patient care, e.g. artificial intelligence.
Ability to achieve translation from ‘bench to bedside’ more quickly.
Expansion of the nephrology workforce with better training.

Key numbers relating to CKD and CKD research.
Scientific discoveries are a product of the intellectual capital of society. Funding is fundamental to nurture such capital. For medicine, decisions about research funding are extraordinarily complex because financially demanding resources need to be allocated for the production of knowledge related to human health at all levels, from basic science to clinical science and prevention ( Box 2 ). In 2012, $119 billion was spent on medical research in the USA and $82 billion in European countries, and most of this investment came from industry, 59% in the USA and 65% in Europe [ 15 ]. To effectively support scientific advancements in biomedicine, medical research funding should have adequate time projections and should be prioritized on the basis of the present and future (predicted) epidemiological impacts of diseases on human health, at national or international levels, and the potential impacts of the resulting products on outcomes, quality of life and societal costs. Indeed, whereas almost all other research products are subject to liberal rules of price-setting regulated by supply and demand, for therapies a third party, i.e. social security, and as a consequence society at large, is often involved. The actual investment in research and its distribution over time should be calibrated against the complexity of the research goals. These factors (robustness of the investment, duration of funding and complexity of the questions being investigated) will dictate the organization of the research and the sizes of the networks needed. For example, nanotechnology is needed to produce nanostructured materials for drug delivery and therefore clinicians, pharmacologists in particular, need to establish strong collaborations with nanotechnology experts. Bioartificial organ development, which is now being actively pursued to find more efficient alternatives to traditional dialysis treatment, necessitates close collaboration between cell biologists and polymer chemists to generate the scaffolds on which cells will be seeded [ 16 ].
Decisions about research funding in medicine are difficult because financially demanding resources need to be allocated for the production of knowledge related to human health at all levels, from basic science to clinical science and prevention.
Public research funding should have adequate time projections and be prioritized on the basis of the present and future (predicted) epidemiological impact of diseases on human health, at a national or international level.
The actual investment in research and its distribution over time should be calibrated against the complexity of the research goals.
Public research funding
Society should be prepared to face threats to human health (e.g. environmental pollution and epidemics) by funding appropriate research programmes for the prediction and prevention of epidemics, for timely responses to health disasters and to mitigate environmental pollution.
Public models of research funding, like those provided by the US NIH or by the European Commission and the various corresponding national agencies, supply most of the funding needed to tackle major health threats.
The public model, which is based on periodic research calls, depends on economic cycles, with funding being increased during periods of economic growth and vice versa.
Cushioning the effect of economic cycles on medical research is essential to ensure the continuity of scientific advancement.
In European countries, healthcare systems are funded by national governments, while the medical research is funded both by national governments and, increasingly so, by the European Commission. Over the last 6 years, the European Union (EU) has provided almost €80 billion in funding for the Horizon 2020 research programme (2014–20). Such European framework programmes have grown to over four times the amount provided in 2006 [ 19 ], and are planned to grow further in the eighth programme, called Horizon Europe [ 20 ]. Over the same period of time, the amount of internal research funding committed by national governments has either remained stable or dwindled. For example in Italy, global medical research funding (including private funding) in 2016 totalled just €2.6 billion [ 21 ].
Private research funding
The development of a basic understanding of a disease or of biochemical pathways that are disrupted in disease states is a prerequisite to drug development. In addition to investigations conducted in academic institutes, many such studies in research laboratories are funded by industry. Furthermore, pharmaceutical companies fund the bulk of clinical trials. This kind of industrial funding is fundamental to provide the evidence upon which medical practice is based, but has the inherent problem of conflict of interest. Understandably, the main interest of the pharmaceutical industry is the ability to achieve financial returns, a goal that may not always coincide with the of provision of robust scientific underpinning. At least 40 primary studies, and a variety of systematic reviews and meta-analyses, have documented the fact that industry-favouring results are more likely in trials funded by pharmaceutical companies [ 22 ]. The problem is in the public domain and is openly discussed in the media. Safeguards like adaptations in the training of ethics committees, and improved scrutiny by regulatory bodies like the US Food and Drug Administration or the European Medicines Agency, regarding the ethical implications of clinical trials being sponsored by industry are increasingly applied. On the other hand, it should be recognized that investigator-initiated clinical trials are not immune to problems such as adequate funding, regulatory issues and trial oversight, and suboptimal expertise in statistics and data management [ 23 ]. In addition, in recent years, we have seen a rise in the availability of overly expensive drugs for orphan diseases [ 24 ], for which (for obvious reasons) it is difficult to provide a solid evidence base. This practice imposes increasing pressure on regulators, forcing them to withdraw resources from sometimes more justified interventions. If not reimbursed, an additional risk of inequity is imposed, whereby some people may be able to gain access to a therapy and while others may not (for example, because of better income or a better social network allowing crowdfunding).
Thus, there is a need for independent (i.e. not industry-sponsored) health economic research to be conducted on every drug entering the market that stringently assesses societal benefit and cost-effectiveness. Furthermore, regulators, supported by ethicists and health economists, need to open up conversations with industry to provide a sound ethical framework.
Foundations
With the exception of large charitable institutions like the Bill and Melinda Gates Foundation, support to research by foundations tends to focus on the domains of organ-specific institutions. In the area of kidney disease, foundations like the US National Kidney Foundation [ 25 ] represent an independent source of research funding in the USA. Such foundations are sparse in Europe and, in general, pursue limited goals. In this respect, The Netherlands is a notable exception. Indeed, since 1968 the Dutch Kidney Foundation (DKF) (Nierstichting Nederland) has achieved effective funding of selected research programmes conceived by kidney disease investigators in its country [ 26 ]. In 2018, the DKF launched Beating Kidney Disease (Nierziekte de Baas), involving a variety of stakeholders that included kidney patients, to develop an ambitious national strategic agenda to the improve outcomes and quality of life of kidney patients [ 27 ]. Based on four main pillars (prevention, patient quality of life, personalized medicine and regenerative medicine), it is now being considered for presentation to the Directorate-General for Health of the European Commission, to be rolled out, after adjustment, in the coming years throughout the EU.
Medical societies have the social responsibility of disseminating knowledge regarding the threats to public health posed by the various diseases and informing health authorities of the risks posed by them.
Advocacy for health protection programmes and for medical research funding is now embedded into the mission of most scientific societies.
In the USA, kidney research funding reached an all-time low in 2013 [ 29 ]. About 20 years ago, the American Society of Nephrology (ASN) initiated advocacy activities to promote kidney research and public funding for CKD in the USA. From 2010 onwards, the costs of these activities by the ASN gradually increased to $200 000 in 2019 [ 30 ]. Thanks to the ASN’s actions, in March 2018 Congress approved an increase in funding of over $2 billion for kidney research [ 31 ], and last July President Trump signed an executive order to reform the US End-Stage Kidney Disease treatment industry. This order is expected to create new payment models and facilitate kidney transplantation and home dialysis [ 32 ]. Furthermore, in 2012, the US Food and Drug Administration (FDA) and the ASN created the Kidney Health Initiative (KHI), a public–private partnership that aims to stimulate innovative approaches to the optimization of drugs and devices to improve the future of kidney patients, including their safety [ 33 ], by bringing together regulators, patients, academic and non-academic nephrologists, and other governmental agencies [ 10 ]. The KHI now includes five government partners—the Centers for Disease Control, the FDA, the NIH, Veterans Affairs and the Center for Medicare—11 foundations and patient associations, 31 drug companies, 19 device manufacturers, 7 dialysis providers, 10 research organizations, and 4 not-for-profit, digital health and artificial intelligence companies. In 2018, the KHI launched a technology roadmap for innovative approaches to renal replacement therapy to stimulate an internationally oriented, multidisciplinary approach to solution development for kidney patients. The KHI aims to realize the possibility of a portable/wearable and ultimately regenerated kidney [ 34 ].
The European Renal Association – European Dialysis and Transplant Association
The European Renal Association – European Dialysis and Transplant Association (ERA-EDTA) operates in the geopolitically complex EU, which includes 27 member states, but also serves non-EU countries in Europe or bordering Europe and the Mediterranean. While in the USA—a true federation of states—the Federal Government has access to a broad array of tax revenues, the EU is largely dependent on what the member states contribute, which is only about 1% of their Gross Domestic Product. As a consequence, the EU’s yearly budget is only a fraction of that of the USA. Thus, the potential for the EU to fund research is inherently limited compared with the situation in the USA. In Europe, public research largely relies on funding provided at country level. Mainly due to the negative economic cycle that started in 2007, government budget allocations for research and development as percentages of state expenditures declined quite substantially from 2000 to 2014 in the Netherlands (−0.9%), Belgium (−1.1%), France (−1.3%), the UK (−3.7%), Italy (−5.2%) and Spain (−5.3%) [ 35 ].
In this difficult environment, since 2005 the ERA-EDTA has invested over €3 million in seven research projects selected via a competitive process, some of which are still ongoing. Among these projects, the Validation of the Oxford classification of IgA (VALIGA) study [ 36 ] has had a major impact on the way the most common form of glomerulonephritis, IgA nephropathy, is diagnosed histologically and has provided unique information on the prognostic value of kidney histology for kidney outcomes. The Cardiovascular Morbidity in Children with Chronic Kidney Disease (4C) study [ 37 ], a project focusing on cardiovascular disease in children based on data from 54 academic institutions, has generated unique information on this fundamental issue and published over 30 papers in major nephrology and internal medicine journals. However, due to the current financial climate, no additional investments of this kind are likely to be made by the society in the foreseeable future. Therefore, to promote kidney research funding in Europe, the ERA-EDTA has explored alternative possibilities ( Figure 2 ). Rather than acting as an individual society to advocate for the fight against kidney disease, it is actively helping to create an alliance between national and international associations focused on kidney diseases, the European Kidney Health Alliance (EKHA), and has joined the Biomedical Alliance (BMA). These alliances are key for advocacy at the level of the European Commission and the European Parliament on the urgency of funding kidney research. Furthermore, the ERA-EDTA, via its Scientific Advisory Board (SAB), offers competitive fellowships to stimulate its working groups (WGs) to develop research networks that will initiate valuable projects focusing on priority themes that can be submitted for funding by the European Commission and other funding bodies.

The ERA-EDTA and research organization and funding.
The EKHA, created in 2007, is an association that includes as full members the ERA-EDTA and three other international and national societies focusing on kidney diseases, namely the European Kidney Patients’ Federation (EKPF), the European Dialysis and Transplant Nurses Association/European Renal Care Association (EDTNA/ERCA) and the DKF, in addition to a number of affiliated members, which are national stakeholder organizations representing not only nephrologists but also patients and foundations [ 38 ]. The EKHA works on the principle that the prevention and treatment of kidney diseases should be based on a shared vision at European level, and strives to achieve optimal quality of care and patient quality of life at affordable societal cost, with outreach to all valid candidates. The EKHA has established links with 19 Members of the European Parliament (MEP) that form the MEP Group for Kidney Health, a group of European politicians from 10 countries that is committed to improving policy responses to the growing burden of kidney disease in Europe. Interaction with the European Commission and the European Parliament has been quite successful and, starting from 2015, in early spring of each year the EKHA has organized ‘the European Kidney Forum’ event held at the European Parliament. At this event, EKHA members, the MEP Group for Kidney Health, other MEPs, European and national administrators, and other stakeholders openly discuss priority kidney care issues. The EKHA has published recommendations that aim to help European and national policy makers understand and design kidney health policies [ 39 ], including prevention and early detection, choice of treatment, access to transplantation and treatment, and reimbursement strategies [ 38 ]. The EKHA has also contributed to several publications on policy and regulatory measures related to kidney disease [ 40–42 ]. A proposal by the EKHA, the ‘Effect of Differing Kidney Disease Treatment Modalities and Organ Donation and Transplantation Practices on Health Expenditure and Patient Outcomes (EDITH)’, a project including 15 European countries, has been awarded €1 million [ 43 ] and is approaching its conclusion together with the disclosure of its first results. The project is assessing disparities in access to renal replacement therapy throughout Europe and the reasons for them. Finally, the EKHA was commissioned by the EU to convene a Thematic Network of stakeholders to offer recommendations to the European Commission on how to improve organ donation and transplantation throughout the EU, which resulted in a Joint Statement on the issue [ 44 ]. To provide information to the EKHA Board on perceived research needs regarding CKD in Europe, the ERA-EDTA has created a Nephrology and Public Health Committee, and this Committee recently formulated a series of proposals to stimulate research collaboration on CKD in adults and children in Europe [ 45 ]. The EKHA is also a member and currently holds the chair of the European Chronic Diseases Alliance (ECDA), an EU advocacy platform of 11 societies involved with the broad spectrum of interrelated NCDs, which affect about 75% of the adult European population [ 46 ]. the ECDA’s focus is essentially on prevention and lifestyle measures.
In 2019 the ERA-EDTA joined the BMA. This is a large alliance of over 30 leading European medical societies covering almost the full range of medical specialties, and aggregating >400 000 investigators and clinicians [ 47 ]. The mission of this association is to speak with a common voice to help the growth of biomedical research in Europe. The BMA facilitates the training and mobility of investigators and clinicians in Europe, and aims to improve public understanding of medical research in Europe. The alliance is a strong advocate for increased funding in favour of biomedical research to promote excellence and improve health in European countries. The BMA calls on the European Institutions to increase the total Horizon Europe budget to at least €120–125 billion, and to dedicate 25–30% of the Horizon Europe budget to biomedical and health-related research. The alliance also aims to develop a long-term vision and strategy through the creation of a European Council for Health Research. Furthermore, the BMA is a European Medicine Stakeholder and, as such, it is consulted by the European Medicines Agency on themes related to the specific expertise of its member societies. The richness of competencies and knowledge among BMA medical societies is vast and includes the European Society of Cardiology, the European Association for the Study of Diabetes, the European Association for the Study of Obesity, the European Society of Endocrinology, the European Federation of Immunology societies, the European Respiratory Society and other societies that may share a proximate interest in kidney diseases with the ERA-EDTA. Thus, within the BMA, unique opportunities for large-scale collaborations and ambitious projects exist for investigators of various origins that are interested in kidney research.
The ERA-EDTA WGs and seed funding
To stimulate scientific collaboration among its members, in 2009 the ERA-EDTA created WGs in various areas of kidney research, from glomerulonephritis to diabetes, nutrition, metabolic bone disorders and cardiovascular risk in CKD. These WGs are transnational networks overseen by the SAB that share common interests in themes related to kidney diseases, and that pursue common research and educational activities in their area of expertise. There are currently eight WGs [ 48 ] that have produced a continuous flow of publications in major journals including The Lancet , Nature Reviews Nephrology , the Journal of the American Society of Nephrology , Kidney International , Nephrology Dialysis Transplantation [ 49–52 ] and other nephrology journals. The ERA-EDTA is fully committed at supporting its WGs and consortia of European kidney disease investigators to allow them to produce valuable research on these diseases. To facilitate interaction, in October 2019 a special event was organized in Vienna, the Scientific Educational and Interaction Day, where the WGs had the opportunity to discuss issues related to the development of shared research projects and set the basis for the creation of effective research consortia. The framing and formalization of projects, and the regulatory issues related to submission to the European Commission are complex. Therefore, WGs need expert advice from agencies with specific know-how on how to frame project-related administrative issues. With this in mind, the ERA-EDTA council has decided to provide seed funding to cover the costs of consultancy from expert agencies. This novel approach has facilitated the creation of two large research consortia composed of institutions and investigators with diverse expertise. The first is a project that aims investigating the complex links between the kidneys and the brain. Understanding these links is a priority if we are to reduce cognitive problems related to CKD. Consequently, in March 2020 the European Commission decided to fund the project as a Cooperation in Science & Technology (COST) Action. COST funding enables researchers to set up interdisciplinary research networks, thereby enabling the establishment of synergies with EU-funded research projects. The second consortium aims to improve the identification and clinical management of CKD using real-world data from European healthcare agencies, registries and cohorts. Using a comparative health systems approach, it is using machine learning algorithms and artificial intelligence programmes to investigate the patient trajectory from primary to specialist care in different settings. Thus, the provision of seed funding to WGs and consortia of European investigators has the potential to stimulate research on kidney diseases and maximize the channelling of funds towards kidney research. Within the budgetary limits fixed by the ERA-EDTA Council, a yearly, competitive call will be made for investigators to submit research projects that are potentially fundable by the European Commission to the SAB. The SAB will evaluate these projects and the most meritorious will be awarded the seed money needed for expert consultancy on submission-related issues to the European Commission by the Council.
Funding patterns and mechanisms of funding by major health organizations remain poorly defined. Transparency and prioritization issues need to be addressed. Raising the awareness of governmental bodies and agencies responsible for health research funding about the burdens of various diseases is of paramount importance for improvement of the allocation of funding. In this respect, kidney research remains largely underfunded in Europe, as it was in the USA until 2 years ago. Scientific societies can play an important role in interacting with funding bodies in order to optimize the allocation of research funding in Europe. In this respect, initiatives based on solid epidemiological data about the burdens of diseases via large multispecialty alliances are more likely to be successful than efforts by single scientific or patient associations. In addition, societies dealing with NCDs including CKD should join forces in advocacy and research planning when their aims overlap. In the case of kidney disease, diabetes, hypertension and cardiovascular disease traditionally come to mind, but cancer, liver disease and even pulmonary disorders are also linked to kidney disease [ 35 ]. Efforts should not be restricted to traditional basic and clinical research topics, but also to health economics, patient quality of life and prevention. The ERA-EDTA has already adopted this approach to help increase the funding of kidney research in Europe. In addition, the ERA-EDTA will support meritorious proposals with the initial seed funding needed to optimize how projects are framed prior their submission to the European Commission.
Via its broader platforms, the EKHA and the BMA, the ERA-EDTA will also strive to achieve broader recognition by the EU and national agencies that kidney disease, and a related clusters of NCDs, are major threats to the qualities of life of their populations and economies. Whereas acute problems, like the current COVID-19 epidemic, necessitated immediate and transnational action, it should be noted that those most severely affected by COVID-19 have been those with comorbid conditions, namely NCDs as a whole [ 53 ], but also more specifically patients with CKD [ 54 ]. Thus, for the reasons explained in this article, it is essential that these diseases gain the attention that they deserve.
None declared. All authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Costs of scientific research/Dr.M on Science, Research, & Scientists [Internet] [cited 3 March 2020 ]. https://dr-monsrs.net/tag/costs-of-scientific-research/
R&D in the FY 2014 Omnibus: The Big Picture/American Association for the Advancement of Science [Internet] [cited 3 March 2020 ]. https://www.aaas.org/news/rd-fy-2014-omnibus-big-picture
Clinical Trials Market Size & Share/Industry Trends Report, 2019–2026 [Internet] [cited 31 January 2020 ]. https://www.grandviewresearch.com/industry-analysis/global-clinical-trials-market
NHS Finance. The NHS budget and how it has changed/The King’s Fund [Internet]. Department of health budget , 2017 [cited 2 February 2020 ]. https://www.kingsfund.org.uk/projects/nhs-in-a-nutshell/nhs-budget
Bikbov B , Purcell CA , Levey AS et al. . Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017 . Lancet 2020 ; 395 : 709 – 733
Google Scholar
Jager KJ , Kovesdy C , Langham R et al. . A single number for advocacy and communication-worldwide more than 850 million individuals have kidney diseases . Nephrol Dial Transplant 2019 ; 34 : 1803 – 1805
Foreman KJ , Marquez N , Dolgert A et al. . Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories . Lancet 2018 ; 392 : 2052 – 2090
Luyckx VA , Tonelli M , Stanifer JW. The global burden of kidney disease and the sustainable development goals . Bull World Health Organ 2018 ; 96 : 414 – 422C
Allen L. Non-communicable disease funding . Lancet Diabetes Endocrinol 2017 ; 5 : 92
Archdeacon P , Shaffer RN , Winkelmayer WC et al. . Fostering innovation, advancing patient safety: the Kidney Health Initiative . Clin J Am Soc Nephrol 2013 ; 8 : 1609 – 1617
Chatzimanouil MKT , Wilkens L , Anders HJ. Quantity and reporting quality of kidney research . J Am Soc Nephrol 2019 ; 30 : 13 – 22
NIH Categorical Spending -NIH Research Portfolio Online Reporting Tools (RePORT) [Internet] [cited 21 April 2020 ]. https://report.nih.gov/categorical_spending.aspx
Hsu RK , Hsu C-Y. The role of acute kidney injury in chronic kidney disease . Semin Nephrol 2016 ; 36 : 283 – 292
Vanmassenhove J , Vanholder R , Lameire N. Points of concern in post acute kidney injury management . Nephron 2018 ; 138 : 92 – 103
Medical Research - Wikipedia [Internet] [cited 31 January 2020 ]. https://en.wikipedia.org/wiki/Medical_research
Schophuizen CMS , De Napoli IE , Jansen J et al. . Development of a living membrane comprising a functional human renal proximal tubule cell monolayer on polyethersulfone polymeric membrane . Acta Biomater 2015 ; 14 : 22 – 32
Klein R. A new paradigm for funding medical research . Stem Cells Transl Med 2012 ; 1 : 3 – 5
United States. Congress. Senate. Committee on Appropriations. Subcommittee on Departments of Labor, Health and Human Services, Education, and Related Agencies. Clinical Research: Hearing Before a Subcommittee of the Committee On Appropriations, United States Senate. One Hundred Fourth Congress, Second Session, Special Hearing. [Corr. print.] Washington: U.S. G.P.O., 1996 .
Hines P. Why fund research? , 2017 . http://sciencebusiness.net/OurReports/DownloadFree
Horizon Europe - the next research and innovation framework programme/European Commission [Internet] [cited 31 March 2020 ]. https://ec.europa.eu/info/horizon-europe-next-research-and-innovation-framework-programme_en
La ricerca di punta è senza lucro/Scienza in Rete [Internet] [cited 31 January 2020 ]. https://www.scienzainrete.it/articolo/ricerca-di-punta-è-senza-lucro/luca-carra-sergio-cima/2019-03-18
Doucet M , Sismondo S. Evaluating solutions to sponsorship bias . J Med Ethics 2008 ; 34 : 627 – 630
Konwar M , Bose D , Gogtay NJ et al. Investigator-initiated studies: challenges and solutions . Perspect Clin Res 2018 ; 9 : 179 – 183
Phillips MI. Big Pharma’s new model in orphan drugs and rare diseases . Expert Opin Orphan Drugs 2013 ; 1 : 1 – 3
Research Grants/National Kidney Foundation [Internet] [cited 2 March 2020 ]. https://www.kidney.org/professionals/research/awards
Dutch Kidney Foundation ( www.narcis.nl ) [Internet] [cited 2 March 2020 ]. https://www.narcis.nl/organisation/RecordID/ORG1238896/Language/en
Beating kidney disease A joint agenda for research and innovation. https://www.nierstichting.nl/media/filer_public/4d/6d/4d6d6b4e-ce56-4a4b-8ba2-f5ac957d0df8/beating_kidney_disease_-_joint_agenda_for_ri_june_2018.pdf
Viergever RF , Hendriks T. The 10 largest public and philanthropic funders of health research in the world: what they fund and how they distribute their funds . Health Res Policy Sys 2016 ; 14 : 12
Bryan L , Ibrahim T , Zent R et al. . The kidney research predicament . J Am Soc Nephrol 2014 ; 25 : 898 – 903
American Society of Nephrology Lobbying Profile • OpenSecrets [Internet] [cited 3 February 2020 ]. https://www.opensecrets.org/federal-lobbying/clients/summary? id=F200220
Budget Boosts Funds for Kidney Disease Research, Prevention/Kidney News [Internet] [cited 3 February 2020 ]. https://www.kidneynews.org/kidney-news/current-issue/budget-boosts-funds-for-kidney-disease-research-prevention
Jost TS , Lazarus S. Trump’s executive order on health care—can it undermine the ACA if congress fails to act? N Engl J Med 2017 ; 376 : 1201 – 1203
Wieringa FP , Sheldon M. The Kidney Health Initiative innovation roadmap for renal replacement therapies: building the yellow brick road, while updating the map . Artif Organs 2020 ; 44 : 111 – 122
Bonventre JV , Hurst FP , West M et al. . A technology roadmap for innovative approaches to kidney replacement therapies a catalyst for change . Clin J Am Soc Nephrol 2019 ; 14 : 1539 – 1547
Reale E. The PREF study – Analysis of national public research funding - European Commission [Internet] [cited 4 February 2020 ]. https://rio.jrc.ec.europa.eu/en/library/pref-study-–-analysis-national-public-research-funding
European Validation Study of the Oxford Classification of Iga Nephropathy (VALIGA) [Internet] [cited 31 March 2020 ]. http://web.era-edta.org/uploads/valiga-report-2018.pdf
The Cardiovascular Morbidity in Children with Chronic Kidney Disease (4C) Study [Internet] [cited 2020 Mar 31]. http://web.era-edta.org/uploads/4c-study-report(1).pdf
Home/EKHA - European Kidney Health Alliance [Internet] [cited 2 March 2020 ]. http://ekha.eu/
Recommendations for Sustainable Kidney Care/EKHA - European Kidney Health Alliance [Internet] [cited 31 March 2020 ]. http://ekha.eu/accomplishments/recommendations-sustainable-kidney-care/
Vanholder R , Annemans L , Brown E et al. ; on behalf of the European Kidney Health Alliance. Reducing the costs of chronic kidney disease while delivering quality health care: a call to action . Nat Rev Nephrol 2017 ; 13 : 393 – 409
How to Increase Kidney Transplant Activity Throughout Europe-an Advocacy Review by the European Kidney Health Alliance [Internet] [cited 31 March 2020 ]. https://pubmed.ncbi.nlm.nih.gov/30629203/?from_single_result=Vanholder%2C+NDT%2C+34%2C+1254-1261%2C+2019
van der Tol A , Stel VS , Jager KJ et al. . A call for harmonization of European kidney care: dialysis reimbursement and distribution of kidney replacement therapies . Nephrol Dial Transplant 2020 ; 35 : 979 – 978
Jager KJ , Stel VS , Branger P et al. . The effect of differing kidney disease treatment modalities and organ donation and transplantation practices on health expenditure and patient outcomes . Nephrol Dial Transplant 2018 ; 33 : 560 – 562
Updated final version of the Joint Statement on Organ Donation and Transplantation now available!/EKHA - European Kidney Health Alliance [Internet] [cited 31 March 2020 ]. http://ekha.eu/blog/updated-final-version-of-the-joint-statement-on-organ-donation-and-transplantation-now-available/
Massy ZA , Caskey FJ , Finne P et al. . Nephrology and Public Policy Committee propositions to stimulate research collaboration in adults and children in Europe . Nephrol Dial Transplant 2019 ; 34 : 1616 – 1616 .
European chronic disease alliance – European chronic disease alliance [Internet] [cited 31 March 2020 ]. https://alliancechronicdiseases.org/
BioMed Alliance - Home [Internet] [cited 6 March 2020 ]. https://www.biomedeurope.org/
ERA-EDTA Scientific Working Groups - Homepage [Internet] [cited 6 March 2020 ]. http://www.era-edtaworkinggroups.org/en-US/homepage
Coppo R , D’Arrigo G , Tripepi G et al. . Is there long-term value of pathology scoring in immunoglobulin A nephropathy? A validation study of the Oxford Classification for IgA Nephropathy (VALIGA) update . Nephrol Dial Transplant 2018 ; 32 : 1002 – 1009
Bellur SS , Roberts ISD , Troyanov S et al. . Reproducibility of the Oxford classification of immunoglobulin A nephropathy, impact of biopsy scoring on treatment allocation and clinical relevance of disagreements: evidence from the VALidation of IGA study cohort . Nephrol Dial Transplant 2019 ; 34 : 1681 – 1690
Lerch C , Shroff R , Wan M et al. . Effects of nutritional vitamin D supplementation on markers of bone and mineral metabolism in children with chronic kidney disease . Nephrol Dial Transplant 2018 ; 33 : 2208 – 2217
Wuttke M , Wong CS , Wühl E et al. . Genetic loci associated with renal function measures and chronic kidney disease in children: the Pediatric Investigation for Genetic Factors Linked with Renal Progression Consortium . Nephrol Dial Transplant 2016 ; 31 : 262 – 269
Wu Z , McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 Cases from the Chinese Center for Disease Control and Prevention . JAMA 2020 ; 323 : 1239 – 1242
Henry BM , Lippi G. Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection . Int Urol Nephrol 2020 ; 52 : 1193 – 1194
- hemodialysis
- kidney diseases
- kidney failure, chronic
- edetic acid
- societies, scientific
- dialysis procedure
- public health medicine
- transplantation
- edetate disodium
- medical research
- research funding
- whole genome sequencing
Email alerts
Citing articles via.
- ndt Twitter
- ERA Twitter
- ERA Facebook
- ERA Instagram
- ERA LinkedIn
- Recommend to Your Librarian
Affiliations

- Online ISSN 1460-2385
- Print ISSN 0931-0509
- Copyright © 2024 European Renal Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Utility Menu
Request an Appointment
Popular Searches
- Adult Primary Care
- Orthopedic Surgery
Kidney Transplant Surgery
Hours of Operation: Monday-Friday 8:00 AM - 4:00 PM
Existing Patients
New patients, refer a patient.
Refer a patient
Fax: 617.638.8427
Phone: 617.638.8430
The Kidney Transplant Referral Form is required for all patients prior to undergoing evaluation.
E-Mail: [email protected]
Fax: 617-638-8427
Select your language:
COVID-19 Information for Transplant Patients
For 45 years, the Kidney Transplant Program at Boston Medical Center (BMC) has provided compassionate, expert care. Our experienced transplant surgeons are supported by a multidisciplinary clinical team, devoted to improving our patients’ quality of life through organ transplantation. The transplant team carefully guides patients and loved ones every step of the way throughout the process.
Why Choose BMC’s Kidney Transplant Program?
- Unlike other transplant programs, we focus only on kidney transplantation. This means all of our team members are trained to provide you with highly specialized care.
- With more than 55 years of combined transplant experience, our accomplished kidney transplant surgeons have performed more than 1,000 kidney transplant surgeries—a number that continues to grow every year.
- Our living kidney donor program has successfully performed more than 350 living donor transplants and actively works to reduce racial disparities in living donor kidney donation .
- Our transplant nurse coordinators have a combined 40 years of experience. They will be with you every step of the way to guide you through any clinical or social situation.
- In addition to your transplant surgeon and transplant nurse coordinator, your care team includes a transplant pharmacist, a transplant social worker, and a transplant dietician. Your team will give you all the tools and education you need to manage the transplant process, both before and after transplant surgery.
- Our financial services team works closely with you and your family to maximize insurance coverage for your kidney transplant and to make sure you fully understand the financial aspects of the transplant process.
- Our patients come from a wide range of backgrounds. Our diverse, multilingual staff is on hand to support all of them.
- The BMC Kidney Transplant Program follows all transplanted patients for life–with frequent blood draws, testing, and follow-up visits.
- BMC maintains strong relationships with local dialysis centers and nephrologists to ensure we receive all of the necessary information to provide the best possible outcomes for our patients.
- Our team is fully committed to providing every patient with exceptional care, without exception.
- As the #1 most racially inclusive hospital in Massachusetts , we are proud to be recognized for our commitment to serving the people of color in our community.
Interested in becoming a kidney donor?
Take the first step by filling out the Living Kidney Donor Questionnaire .
Monday-Friday 8:00 AM - 4:00 PM

Become A Kidney Donor
Living kidney donation program, contact kidney transplant surgery, kidney transplant surgeons, jeffrey cooper, md.

Aman Kumar, MD

Sayeed K Malek, MBBS

Stefan G Tullius, MD

Kidney Transplant Nephrologists
Jean m francis, md, sandeep ghai, md.

Kidney Transplant Donor Surgeon
David s wang, md.

Organ Transplant Psychiatrist
Barbara j horner, md.

Kidney Transplant Coordinators
Karen a curreri, rn, cctc.

Vladimir Doxy, RN

Anne M Hutchinson, RN

Clinical Pharmacy Specialist
Justine dickson, pharmd, bcacp.

Patient Education & Resources
Living donor evaluation process, living donor forms and donor advocate information, kidney transplant patient education, helpful links, faqs for living kidney donors, organ transplant patient stories, mary jane and michelle.
Good Neighbors

Life-changing Call

Ferdison and Melissa
Sisterly Love

Questions and Prayers Answered
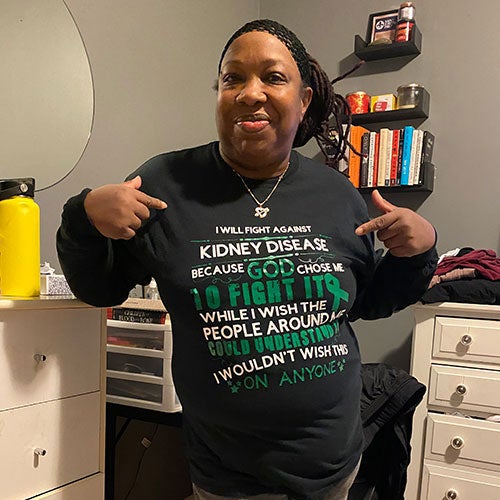
Patience and Positivity

Barbara and Lisa
Age Appropriate

Department News
Cops and partners — a kidney donation made them something else: bonded for life.
Two local cops who once worked together became a team again when Peter Petrides donated his kidney to Mark Kalinowski. They share their incredible story of organ donation with The Boston Globe.

Why Minority Organ Donors Matter
August is National Minority Donor Awareness Month, a time dedicated to promoting organ and tissue donation and bridging the gaps between donations and need in minority populations.

Instagram Takeover
Meet BMC’s Transplant Surgery team members and check out some behind-the-scenes of their day to day. They also walk through the transplant process and answer questions from BMC social media followers!
Latest from HealthCity
Why is there a gap in kidney donation among people of color.
Black Americans make up the largest group in need of organ transplants but only 8% of living kidney donors.
Reducing Racial Disparities in Living Donor Kidney Donation
How BMC is addressing the gap of living donor kidney transplantation amongst Black Americans.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clin J Am Soc Nephrol
- v.17(9); 2022 Sep

Transplant Nephrology
Michel chonchol.
1 Division of Renal Diseases and Hypertension, University of Colorado Denver Anschutz Medical Center, Aurora, Colorado
Orlando M. Gutierrez
2 Division of Nephrology, University of Alabama at Birmingham, Birmingham, Alabama
Mahboob Rahman
3 Division of Nephrology and Hypertension, University Hospital Cleveland Medical Center, Cleveland, Ohio
David M. Charytan
4 Division of Nephrology at New York University Grossman School of Medicine, New York, New York
Mitchell Rosner
5 Nephrology Division, Department of Medicine, University of Virginia, Charlottesville, Virginia
Kidney transplant, a life-changing procedure, provides better patient outcomes and lower costs than dialysis; as a result, there has been significant growth in the number of patients with kidney transplants in the United States ( 1 ). Increasing access to kidney transplantation is critical to improving outcomes and extending the lives of patients with kidney failure. Through the 2019 Advancing American Kidney Health Initiative, the US government called to double the number of kidney transplants over 10 years ( 2 ).
To achieve the goals of the Advancing American Kidney Health Initiative ( 2 ), all aspects of the provision of nephrology and transplant care must function seamlessly ( 3 ). In this issue of CJASN , the American Society of Nephrology Task Force on Academic Nephrologist Compensation and Productivity presents two Perspectives that review the roles and responsibilities of transplant nephrology as well as existing transplant nephrology compensation models ( 4 , 5 ). In addition, Singh et al. ( 6 ) present a survey of salaries and job satisfaction of transplant nephrologists in the United States. These articles discuss transplant nephrology's challenges related to clinical role, compensation, and reporting structure ( 3 ).
Moe et al. ( 4 ) review the importance of the transplant nephrologist to a successful kidney transplant program. As a transplant team member, the transplant nephrologist plays a vital role in managing the complex medical needs of patients receiving transplants, spanning from pretransplant referral to long-term post-transplant management. In collaboration with their surgical colleagues, transplant nephrologists manage delayed graft function, immunosuppression, and antimicrobial prophylaxis and assess the risk of recurrent disease. Some of these responsibilities are not that different from the role of the general nephrologist: monitoring the progression of kidney disease in patients with CKD, managing long-term immunosuppression of patients with glomerular disorders, and mitigating cardiovascular risk factors in patients with advanced kidney disease. Thus, the clinical care provided by transplant and general nephrologists is similarly complex ( Figure 1 ).

Transplant nephrologists have similar duties and responsibilities as general nephrologists .
Although many transplant nephrologists feel privileged to work in the field, the subspecialty of transplant nephrology faces challenges related to its workforce and training ( 7 , 8 ). Given that transplant care is often uniquely structured in different health systems, solutions will have to be local but should address critical issues such as transparent compensation models, incentivization of positive outcomes, practice support to offload administrative burdens, efficient use of advanced practitioners in post-transplant care, and protection of work-life balance to avoid burnout. Moreover, if health systems and the United States are to meet the goals of the Advancing American Kidney Health Initiative, then general and transplant nephrologists must work together in a model that stresses the goal of transplantation for all eligible patients.
Another key challenge for transplant nephrology is compensation, which, if left unaddressed, may threaten transplant care and create a deep divide between transplant nephrologists and their colleagues in general nephrology. In this issue of CJASN , Singh et al. ( 6 ) present the results of a web-based survey to gather data on productivity, compensation, and job satisfaction measures. The survey was sent to 809 nephrologist members of the American Society of Transplantation, but only 260 respondents (32%) were included for analysis. Most respondents were men, 50% were White, and up to 45% of respondents had a major administrative title, such as medical director. Clinical productivity was measured by individual work relative value units (wRVUs) in over 60% of the respondents, and at least 50% of the medical directors reported protected time from clinical services for administrative work. The average yearly wRVU target for respondents aware of an established wRVU target was a mean of 4765. The mean total compensation was $274,460±$91,509, and higher compensation was associated with higher job satisfaction; however, 43% of respondents reported some or complete burnout in their current position.
The study by Singh et al. ( 6 ) is the first public effort to report the clinical productivity, compensation, job satisfaction, and burnout of US transplant nephrologists. However, it has significant limitations, including the sample size, response rate, and sampling bias, with a wide range of reported values. Of interest was the low proportion of respondents who indicated that they understood compensation structures, the high proportions of transplant nephrologists whose compensation is not driven by wRVUs, and the high proportion of burnout among transplant nephrologists. In its 2019 Physician Compensation and Productivity Survey, SullivanCotter—a consulting group that helps health care entities establish compensation and benefit plans—reported that the median total compensations for staff physicians in the nephrology and transplant nephrology specialties were $271,800 and $273,600, respectively ( 9 ). Hence, the compensation reported by Singh et al. ( 6 ) is in line with what has been previously reported. Nonetheless, local markets drive salaries more so than nationally reported data. In some instances, health care systems dictate market rates, sometimes creating salary inflation and inequities among nephrologists. It is not unusual for transplant centers to subsidize transplant nephrologist salaries, sometimes from revenue generated from general nephrology activities, or use local compensation models or incentives to compensate for transplant-related metrics. However, these subsidies or models rarely exist for general nephrologists, creating a further divide in compensation plans within the nephrology community.
The different compensation models between transplant and general nephrologists can be a source of conflict that needs urgent attention. In specific markets, a general nephrology practice may even subsidize the salaries of transplant nephrologists who lack dialysis billing or medical directorships ( 3 ). It is critical that health systems and transplant centers cover the lion’s share of costs associated with transplant nephrology to minimize the subsidy required from clinical revenue derived from general nephrology activities, which otherwise will serve to divide practices and create tensions. More broadly, the underlying financial models that fail to recognize or reimburse nephrologists (both transplant and general) for work contributing to health systems’ bottom line despite not directly generating relative value units for individual nephrologists should be reconsidered.
Josephson et al. ( 5 ) also reviewed transplant nephrology models of care and how they affect funds flow, compensation, and reporting structures. The Perspective describes the advantages and disadvantages of three models, which include ( 1 ) the division/department model, ( 2 ) the transplant institute model, and ( 3 ) the community model. Independent of the model, there was consensus among the transplant nephrologists on the task force that transplant nephrology wRVU clinical activity does not generate enough revenue to cover transplant nephrologist salaries and that supplemental support from a third party is needed. In our opinion, this supplemental support should be largely provided by the health care system as it would not be sustainable to continue to expect all of these costs to be covered solely by academic divisions or private practices. There was also agreement among members of the task force that the division model is likely the best of all of the models as it is the one that is more aligned with the academic mission. In our opinion, this model will protect transplant nephrologists from the competing goals. Scholarly activity remains the key criteria for academic promotion and is critical to moving the field of kidney transplantation forward, and these goals, in some cases, do not align with the mission of clinical service lines often embodied by transplant institutes or affiliated health care systems. We acknowledge that transplant nephrology should be recognized for the additional training and exceptional services provided to patients undergoing kidney transplants and be adequately compensated. However, general nephrologists must also be recognized for becoming more subspecialized and providing medical care to complex medical cases.
Disclosures
D.M. Charytan reports consultancy agreements with Allena Pharmaceuticals (Data Safety Monitoring Board [DSMB]), Amgen, AstraZeneca, CSL Behring, Eli Lilly/Boehringer Ingelheim, Fresenius, Gilead, GSK, Janssen (steering committee), Medtronic, Merck, Novo Nordisk, PLC Medical (clinical events committee), Renalytix, and Zogenix; reports research funding from Amgen, Bioporto (clinical trial support), Gilead, Medtronic (clinical trial support), and Novo Nordisk; serves as an associate editor of CJASN ; and reports expert witness fees related to proton pump inhibitors. M. Chonchol reports consultancy agreements with Amgen, Corvidia, Otsuka, Reata, Tricidia, and Vifor; research funding from Corvidia, the National Institutes of Health, OTSUKA, Reata, and Sanofi; honoraria from Amgen, Corvidia, Reata, Tricidia, and Vifor; and serving as a deputy editor of CJASN . O.M. Gutierrez reports consultancy agreements with QED; research funding from Amgen and GlaxoSmithKline; honoraria from Akebia, Amgen, Ardelyx, AstraZeneca, and Reata; and serving as an associate editor of CJASN . M. Rahman reports consultancy agreements with Barologics; research funding from Bayer Pharmaceuticals and the Duke Clinical Research Institute; honoraria from Bayer, Reata, and Relypsa; and serving as an editorial board member of American Journal of Nephrology and an associate editor of CJASN . M. Rosner reports consultancy agreements with Baxter; honoraria from the American Society of Nephrology and Baxter; serving in an advisory or leadership role for the American Society of Nephrology and as an Editor-at-Large, Clinical Practice for CJASN ; and serving on data safety monitoring boards for Reata and Retrophin.
Acknowledgments
The content of this article reflects the personal experience and views of the author and should not be considered medical advice or recommendations. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or CJASN . Responsibility for the information and views expressed herein lies entirely with the author(s).
Because Dr. David M. Charytan, Dr. Michel Chonchol, Dr. Orlando M. Gutierrez, Dr. Mahboob Rahman, and Dr. Mitchell Rosner serve on the Editorial Team of CJASN , they were not involved in the peer review process for this manuscript. Another editor oversaw the peer review and decision-making process for this manuscript.
Published online ahead of print. Publication date available at www.cjasn.org .
See related article, “Survey of Salary and Job Satisfaction of Transplant Nephrologists in the United States,” on pages 1372–1381 , and Perspectives, “The Importance of Transplant Nephrology to a Successful Kidney Transplant Program,” on pages 1403–1406 , and “Existing Transplant Nephrology Compensation Models and Opportunities for Equitable Pay,” on pages 1407–1409 .
Author Contributions
M. Chonchol wrote the original draft, and D.M. Charytan, M. Chonchol, O.M. Gutierrez, M. Rahman, and M. Rosner reviewed and edited the manuscript.
COLUMBIA UNIVERSITY IN THE CITY OF NEW YORK

Clinical Coordinator III NP
- Columbia University Medical Center
- Opening on: Apr 9 2024
- Job Type: Officer of Administration
- Bargaining Unit:
- Regular/Temporary: Regular
- End Date if Temporary:
- Hours Per Week: 35
- Standard Work Schedule:
- Salary Range: 135,000.00 - $145,000.00
Position Summary
The Clinical Coordinator III will function in the outpatient setting of the Kidney/Pancreas Transplant Program in collaboration with the Kidney/Pancreas Transplant multidisciplinary team to care for and manage post-transplant kidney and pancreas recipients, post-operative kidney living donors, and patients who underwent surgical or invasive procedures by the Kidney/Pancreas transplant surgeons.
Responsibilities
- Coordinators surgical and medical management of kidney and pancreas transplant patients in the outpatient setting.
- Manage living donor follow up in collaboration with living donor coordinators.
- Coordinate care of surgical patients that undergo hernia repairs, dialysis catheters, and other elective surgical procedures conducted by our kidney and pancreas surgeons.
- Assisting transplant surgeons and nephrologists in the outpatient clinic to perform comprehensive history and physical exams, develop differential diagnoses, implement plan of care and document patient’s response to care.
- Conduct pre-operative history and physical exams, as well as obtain transplant and other surgical consents.
- Provide direct patient care by evaluating patients awaiting transplant, as well as post- transplant recipients, and kidney donors.
- Collect, order and interpret lab work and diagnostic studies under agreed upon protocols.
- Order and obtain medication prior authorizations for kidney transplant recipients.
- Develop practice protocols, standard of care, and patient education material for kidney/pancreas transplant recipients.
- In conjunction with the research team, monitor and provide care to patients participating in research studies.
- In partnership with Quality, Research and Education group, help develop and manage detail clinical databases to evaluate and improve patient outcomes.
Minimum Qualifications
Minimum education:
- Master of Science in Nursing
Minimum related experience:
- 3 years nursing or related experience.
Minimum licensing/certifications required upon start date:
- NYS RN and NP Licenses and ANCC Board Certification..
- BLS, ACLS, PALS (if applicable) Certification
- DEA Certification
Minimum computer skills:
- Intermediate to advanced level MS Office skills.
Preferred Qualifications
- Proficiency with technology and social media platforms.
- Effective interpersonal and communication skills required.
Equal Opportunity Employer / Disability / Veteran
Columbia University is committed to the hiring of qualified local residents.
Commitment to Diversity
Columbia university is dedicated to increasing diversity in its workforce, its student body, and its educational programs. achieving continued academic excellence and creating a vibrant university community require nothing less. in fulfilling its mission to advance diversity at the university, columbia seeks to hire, retain, and promote exceptionally talented individuals from diverse backgrounds. , share this job.
Thank you - we'll send an email shortly.
Other Recently Posted Jobs
Executive Director of Communication
Finance and operations manager, student administrative worker.
Refer someone to this job

- ©2022 Columbia University
- Accessibility
- Administrator Log in
Wait! Before you go, are you interested in a career at Columbia University? Sign up here!
Thank you, for sharing your information. A member of our team will reach out to you soon!
This website uses cookies as well as similar tools and technologies to understand visitors' experiences. By continuing to use this website, you consent to Columbia University's usage of cookies and similar technologies, in accordance with the Columbia University Website Cookie Notice .

IMAGES
VIDEO
COMMENTS
Kidney transplant services in Kansas City. The Transplant Institute at the Research Medical Center has a nationally recognized kidney transplant program. We are the only institution to offer the greater Kansas City a simultaneous pancreas/kidney transplant procedure, where both organs are replaced at the same time, resulting in even better ...
The Transplant Institute at the Research Medical Center is fortunate to have a large team of experienced transplant surgeons who are devoted to providing you with expert surgical services. In addition, we are proud to have a nationally recognized kidney transplant program, as well as being the only institution in the greater Kansas City area ...
The Johns Hopkins Comprehensive Transplant Center developed methods to make a donated kidney more compatible. Our Incompatible Kidney Transplant Program (InKTP), founded in 1998, is a world leader in this kind of transplant, and has shown dramatic outcomes. At Johns Hopkins, we also participate in kidney swaps and exchanges, where donor ...
In fact, approximately 20% to 25% of kidney transplants are lost because of disease recurrence. To address this problem, Mayo Clinic researchers have taken several steps. First, researchers identified diseases that are most likely to recur in the transplanted kidney. Second, with the use of protocol biopsies, researchers identified the earliest ...
The APOLLO Scientific and Data Research Center (SDRC or Coordinating Center) will support and participate in studies determining the impact of donor and recipient APOL1 genotypes on kidney transplant outcomes in recipients of a kidney transplant from a donor with recent African ancestry, and follow African ancestry living kidney donors for ...
Abstract. Recent advances in surgical, immunosuppressive and monitoring protocols have led to the significant improvement of overall one-year kidney allograft outcomes. Nonetheless, there has not been a significant change in long-term kidney allograft outcomes. In fact, chronic and acute antibody-mediated rejection (ABMR) and non-immunological ...
Over the past 65 years, kidney transplantation has evolved into the optimal treatment for patients with kidney failure, dramatically reducing suffering through improved survival and quality of life. However, access to transplant is still limited by organ supply, opportunities for transplant are inequitably distributed, and lifelong transplant survival remains elusive. To address these ...
In 2019, a record 24,273 kidney transplants were performed in the United States ( Figure 1) ( 4 ). Approximately 72% of these transplants were from a deceased donor. Transplant recipients were 61% men, and half had either diabetes mellitus (30%) or hypertension (20%) as the listed cause of ESKD, whereas GN (18%) and cystic kidney disease (13% ...
The T100 are published in 15 journals (Table. . 1 ). The New England Journal of Medicine has published the highest number of articles (n = 26; 15,642 citations), followed by Transplantation (n = 24; 12,883 citations). Half of the T100 are published in the 2 aforementioned journals.
Kidney transplant research: We participate in clinical trials of new immunosuppressive drugs and antirejection therapies including novel cell therapy to prevent kidney transplant failure. ... It is preferred that these tests be completed at Ohio State's Wexner Medical Center, but depending on your geographic location or payer preference, they ...
Our team can often use previous test results and other medical information from your current center to speed up the evaluation process. We Have Extensive Experience. The Duke kidney transplant program has been performing kidney transplants for more than 50 years. It is one of the highest volume programs in North Carolina.
In this inaugural lecture of the Virtual Transplantation Seminar Series hosted by the Transplantation Research Center at BWH, Dr. Allan D. Kirk provides a broad overview of transplant research as an example of broadly applicable, multidisciplinary science. In reviewing the challenges and accomplishments of the transplant community, Dr. Kirk ...
Overview. Kidney transplant is a surgical procedure that removes one healthy kidney from one person and places it in another person who suffers from kidney disease or failure, allowing the transplanted kidney to perform the duties that the patient's two failed kidneys cannot do. Living donor (donates kidney): While the patient is unconscious ...
Celebrating 46 years of transplant success, University of Minnesota Medical Center has more than 7,000 kidney transplants to our credit. Our program is one of the two largest and oldest kidney transplant programs in the world. We performed the world's first kidney-pancreas transplant in 1966.
With kidney transplants, the donor can be living or deceased. The Kidney Transplant Process. Evaluation - You will need to be evaluated to determine if you are eligible for a transplant. The evaluation includes a variety of tests, including a physical exam, X-rays and CT scans, blood tests and any other tests your providers feel necessary ...
This Special Issue in renal transplantation covers a variety of clinical and research areas in kidney transplantation. The recent decade is associated with an ongoing shortage of organs for transplantation with efforts to increase the organ pool with DCDs and extended criteria donors. However, with the increasing success rate of kidney ...
WRNMMC Organ Transplant department is eager and excited to offer kidney transplant services to our active duty, dependents, and veterans. To learn more, visit the WRNMMC's Kidney Transplant Program's website; or call 301-295-4331 to speak with a transplant coordinator. For more information about kidney disease, visit the CDC website. The ...
To learn more about joining the kidney transplant program at Albany Medical Center, call 518-262-5614. Before a formal evaluation appointment, you must complete any necessary tests and attend an educational seminar. Test results can be forwarded via fax at 518-262-5571. Receiving a Kidney.
In the USA, kidney research funding reached an all-time low in 2013 . About 20 years ago, the American Society of Nephrology (ASN) initiated advocacy activities to promote kidney research and public funding for CKD in the USA. From 2010 onwards, the costs of these activities by the ASN gradually increased to $200 000 in 2019 .
Español. COVID-19 Information for Transplant Patients. For 45 years, the Kidney Transplant Program at Boston Medical Center (BMC) has provided compassionate, expert care. Our experienced transplant surgeons are supported by a multidisciplinary clinical team, devoted to improving our patients' quality of life through organ transplantation.
These articles discuss transplant nephrology's challenges related to clinical role, compensation, and reporting structure . Moe et al. review the importance of the transplant nephrologist to a successful kidney transplant program. As a transplant team member, the transplant nephrologist plays a vital role in managing the complex medical needs ...
These sessions are scheduled weekly at Cooperman Barnabas Medical Center. Transplant Recipient Referral Form. If you are interested in more information, or would like to schedule an appointment to be evaluated for kidney transplant, please call us at 1-888.409.4707. "I've always had a good feeling about the hospital, and when I spoke to the ...
Principal Investigator: Jonathan Orens, M.D. Research in the Jonathan Orens Lab examines topics such as clinical outcomes of lung transplantation, chronic allograft rejection and ischemic reperfusion injury, also known as primary graft dysfunction. Research Areas: ischemia-reperfusion injury, chronic allograft rejection, pulmonary medicine ...
Position Summary. The Clinical Coordinator III will function in the outpatient setting of the Kidney/Pancreas Transplant Program in collaboration with the Kidney/Pancreas Transplant multidisciplinary team to care for and manage post-transplant kidney and pancreas recipients, post-operative kidney living donors, and patients who underwent ...