Organization Menu
Additional organization links, search and explore, primary menu, vaccine timeline before jenner and after covid-19.
The history of vaccines did not begin with Jenner's smallpox vaccine. It will not end with the recent vaccines against the novel coronavirus, which caused the COVID-19 pandemic. The history of vaccines begins before the first vaccine, with an immunizing procedure called "inoculation" by some and "variolation" by others. According to researchers, inoculation with materials from smallpox lesions to trigger immunity against smallpox dates back to antiquity in China. And the first written account of the procedure was written in 1549.

Variolation
Versions of an earlier time of practicing inoculation were more oral histories than written records. , "In this version [of inoculation in China before it was written] (inoculation) was invented by a Taoist or Buddhist monk, or possibly a nun, about 1000 AD and practiced by Taoists as a mixture of medicine, technique, magic, and spells which were transmitted orally and which were covered by a taboo so that they were never written down. Needham can give no firmer evidence for this version than the fact that it was a widely accepted tradition. An editorial commentator wonders whether it is realistic to believe that something with the importance of inoculation would have remained completely secret for over 500 years."
Secret or not, the practice of inoculation traveled west toward the Ottoman Empire in the 1500s, reaching Constantinople (modern day Istanbul, Turkey) in the mid-1600s. From there, inoculation traveled to Europe and Northern Africa. From Northern Africa, . He told Reverend Cotton Mather -- -- about being inoculated by enslavers to resist smallpox and get better pay for his enslavement. Cotton Mather, together with a local doctor in Boston, adopted and promoted inoculation as .
Around the same time, , a British socialite living in Constantinople with her diplomat husband, had her son inoculated by a local physician. She then asked her daughter -- back home in Scotland -- to be inoculated. By 1723, the evidence was clear that inoculation in a controlled setting and under the supervision of a physician was preferable to catching smallpox "the natural way."
After his son died from smallpox in 1736, . He wrote several introductions to written works of the time about the procedure. In one such document written in 1759, Benjamin Franklin even included some numbers on the death rates of those who were inoculated (also known as "variolated"). The numbers gave even more proof that the risk of death was lower in those who were inoculated, cementing the practice in Europe and North America. Such was the adoption of variolation that .
Vaccination
By the late 1700s, observed that milkmaids and others previously infected with cowpox were immune to smallpox. Cowpox caused lesions similar to smallpox, but the lesions were localized, and the disease was much milder and not considered deadly. Building on the world and observations of other physicians at the time, . The gambit paid off. The subjects of these experiments showed a mild reaction to cowpox, and no reaction nor disease to smallpox inoculation. The first vaccine was born.
For almost eighty years, cowpox vaccination against smallpox remained the only vaccine in use around the world. Science and technology were not yet there to create vaccines against other disease-causing organisms, though many tried. One such person was , a French biochemist who enjoyed experimenting with microorganisms and kept detailed records of all his laboratory procedures. In Pasteur's time, . Rabid animals from the forest would bite and infect street dogs or cattle. People who would then be bitten by the dogs or exposed through their cattle would succumb to rabies.
Attenuation
Pasteur theorized that something in the saliva of the rabid animals was causing rabies. Though he could not see the rabies virus, Pasteur proved the disease was communicable, and he got to work on a vaccine. The work involved exposing animals to small doses of rabies, much like the variolation had been done in the past. This did not work, however. The rabies virus was too infectious, too virulent. As a result, Pasteur approached the problem differently: weaken the infectious agent somehow before giving it to a person.
One version of smallpox variolation involved drying the material extracted from smallpox lesions before giving it to someone. It was believed the drying caused the material to be less virulent, so . By this time, it was understood that the virus attacked the central nervous system of infected animals. Even if the virus could not be seen, the damage was visible. Pasteur took the dried brain and spinal cord from one rabbit, and gave it to another. He would wait for that rabbit to develop rabies, euthanize it, and repeat the process with a third, then a fourth, etc. Late down the chain, rabbits exposed to the dried brain and spinal cord were not getting sick. Furthermore, they were resisting any attempts at infection through fresh specimens of saliva from rabid animals.
Before going public with his findings, Louis Pasteur -- like Edward Jenner -- took a gamble and exposed human subjects to the dried material in reverse. He started with dried brain and spinal cord from the last rabbit to be inoculated, and worked toward the material from the first rabbit, delivering stronger and stronger doses of the rabies virus. The most well-known human subject was , a young man bitten by a rabid animal. To save Joseph's life, physicians allowed Pasteur to practice his procedure on Joseph. After all, without a cure, Joseph would likely suffer a painful death from rabies. Attempting something was better than nothing.
After the expected incubation period of rabies of about 21 days, Joseph did not develop any signs or symptoms of the disease. Pasteur's vaccine was a success. The next leap in vaccination technology had occurred. Scientists used an analogue to the infectious agent -- cowpox for smallpox -- to use the infectious agent in a less virulent ("attenuated") way. Other vaccines developed at, or in collaboration with, the Pasteur Institute in Paris, France, were based on the same principle of weakening the pathogen before giving it as an inoculation.
Toxoid Vaccines
Later in the 1800s, scientists studying the immune response of humans and other animals discovered antibodies. These proteins were created some time after infection, and they would bind to the pathogen and inactivate it. That "some time after infection" was critical, however. Without antibodies, the person could develop the disease and perish. Scientists then worked on safe ways to create those antibodies in large batches and give them to people as a sort of immune patch, while people developed their own antibodies. Thus was born the era of anti-toxins.
While not true vaccinations, anti-toxins were created when a toxin from tetanus or was given to a large mammal, like a horse. The mammal would develop antibodies against the toxin, and the antibodies were harvested, purified, and given to people showing signs of the disease. In 1902, contamination of one such anti-toxin with actual tetanus toxin led to several injuries. . It was the first step toward regulation of medicines and therapies, something we still see today.
Later, in the 1920s, scientists discovered that an antitoxin combined with a toxin would inactivate the toxin, but leave it intact enough for the human immune system to react against it. Antitoxin-toxin vaccines for diphtheria and tetanus were developed. However, a problem persists in a large segment of the population receiving antitoxin (alone or in combination with a toxin). They were developing an allergic reaction to the proteins from the animals used to create the antitoxin. To solve this problem, scientists found a way to inactivate the toxin before giving it as a vaccine. The age of toxoid vaccines was born, giving us such vaccines as the diphtheria and tetanus vaccines. Protection against those diseases became safer after not having to rely on large mammals to produce them.
Electron Microscopy
In the 1930s, scientists developed the electron microscope. Unlike traditional light microscopes, electrons were used as the "probe" to visualize structures smaller than those seen under light microscopes. This brought about a revolution in virology, as individual viral particles were first seen and classified according to their shapes and sizes. It was no longer necessary to wait and see what kind of infection would be caused by inoculating cell cultures or laboratory animals. Now, a specimen could be placed under an electron microscope, and the causative agent identified.
Electron microscopy led to an explosion in viral research. Samples from the 1918 Spanish Flu pandemic were analyzed, and the influenza virus was observed and classified. Samples from nerve tissue of polio victims showed the poliovirus. Based on their size and shape, where they were isolated from in a body, and what type of infection and disease they were producing, viruses were being catalogued quickly. Vaccines against them arrived almost as fast.
In the 1940s, scientists worked on vaccines against influenza, polio, measles, and other viruses deemed critical national security importance. That decade brought vaccines against influenza, which was then understood to be not just one virus, but several types of influenza virus for which different vaccines would be needed. Similarly, polio was understood to be three types of virus in the same group, so a vaccine against one type did not protect against the others.
Armed with the knowledge of different virus types of the same virus group, scientists worked on vaccines against all types to prevent all disease. By 1954, after decades of well-funded research, . It was a vaccine against polio, and it went against the dogmas established at the time: the vaccine had to contain live/attenuated virus, and that a dead virus could not cause an immune response. The work of , and other women helped lead the way to a vaccine that saved thousands of children's lives.
The 1960s brought the oral polio vaccine as a replacement to Salk's vaccine, after the eroded the public's trust in vaccines. The oral vaccine, developed by Albert Sabin, was tested in the Soviet Union and Latin America, and then brought to the United States with much success. By the 1990s, polio was eliminated from the United States and much of Europe. By the early 2000s, polio was eliminated from the Americas, Europe, and most of Asia. By the 2010s, polio had receded to local outbreaks in Africa and Central Asia. By the 2020s, types 2 and 3 of polio are eradicated, and type 1 is only present in Central Asia.
Eradication
The 1950s and 60s also brought great cooperation among the nations in eliminating and then . That old adversary, the one that got the whole science of vaccination started, was on the retreat through programs in developed nations to vaccinate every individual starting at a young age, not allowing for any exceptions except medical ones. Those who did not want to be vaccinated , or even in certain jobs. Through a worldwide effort to vaccinate every person alive, smallpox became the first human virus to be eradicated when the . Since its eradication, the smallpox vaccine is only used in personnel working with the smallpox virus and in military members as part of readiness against an intentional release of the virus.
Scientific Leaps
More advances in scientific understanding of microorganisms and immunity brought leaps in vaccine technology. When it was understood that the pathogen could be killed and still elicit an immune response, the question was asked whether the whole pathogen was needed or just a protein on its surface. The answer was that some pathogens' surface proteins were enough to trigger an immune response against future infection. The era of subunit vaccines was born.
Later, scientists discovered that the genetic material of pathogens could be used in the laboratory to create the proteins. This did away with the need to grow pathogens in hazardous settings, reducing the risk of accidental exposures for laboratorians working on vaccines. The proteins created could then be "glued" onto another material and delivered to the body via a vaccine, triggering an immune response. The era of recombinant vaccines was born.
In late 2019, . By early 2020, the cluster had grown into the COVID-19 pandemic that continues into mid-2022. The novel coronavirus causing COVID-19 was a relative of the coronavirus that caused an outbreak in several countries in 2003-2004, and another that caused another multinational outbreak in 2013-2014. Because of the urgency of the COVID-19 pandemic, governments around the world invested heavily in vaccine development.
China announced the in June 2020. Sinovac used killed virus to trigger an immune response. Russia announced its in August 2020, after only two months of clinical trials. Sputnik V used a "hollowed out" adenovirus to deliver the messenger RNA of the coronavirus into the recipient's immune cells. That same month, two companies in the United States, Pfizer and Moderna, , which used lipid nanoparticles instead of a viral vector to deliver the genetic material to immune cells. By December 2020, the FDA approved the two mRNA vaccines for emergency use in the United States in people at risk for infection and complications.
Once in the immune cells, the messenger RNA tells the cells' protein-producing machinery to create proteins similar to those on the coronavirus' surface. The immune cells then present these proteins to other cells: T cells and B cells. The T cells then destroy any virus or virus-infected cells, while the B cells produce antibodies to deactivate viruses and give long-term immunity.
The History So Far
That is where we are as of mid-2022. We now have several types of vaccines: inactivated; live-attenuated; subunit, recombinant, polysaccharide, and conjugate; toxoid; viral vector; and mRNA. However, there is much more to the history of vaccines than what was covered in this overview. There are stories from outside the United States (and "The West" in general) that need to be told. The well-known "pioneers" in vaccination were not alone in their work and discoveries. Most vaccine advancements were a group effort.
So, please look at the timeline and all the events we have researched and posted there for you. We will continue to update the timeline as needed, expanding it to include events in other parts of the world where advances in vaccine science happened but were overlooked. We will also add accomplishments from people you may have never hard from. If you have any questions, please contact us. We would be happy to discuss the science and history of vaccines with you.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- 28 September 2020
The origins of vaccination
- Alexandra Flemming 0
Nature Reviews Immunology
You can also search for this author in PubMed Google Scholar
Credit: Chronicle / Alamy Stock Photo
You have full access to this article via your institution.
Edward Jenner (1749–1823), a physician from Gloucestershire in England, is widely regarded as the ‘father of vaccination’ ( Milestone 2 ). However, the origins of vaccination lie further back in time and also further afield. In fact, at the time Jenner reported his famous story about inoculating young James Phipps with cowpox and then demonstrating immunity to smallpox, the procedure of ‘variolation’ (referred to then as ‘inoculation’), by which pus is taken from a smallpox blister and introduced into a scratch in the skin of an uninfected person to confer protection, was already well established.
Variolation had been popularized in Europe by the writer and poet Lady Mary Wortley Montagu, best known for her ‘letters from the Ottoman Empire’. As wife of the British ambassador to Turkey, she had first witnessed variolation in Constantinople in 1717, which she mentioned in her famous ‘letter to a friend’. The following year, her son was variolated in Turkey, and her daughter received variolation in England in 1721. The procedure was initially met with much resistance — so much so that the first experimental variolation in England (including subsequent smallpox challenge) was carried out on condemned prisoners, who were promised freedom if they survived (they did). Nevertheless, the procedure was not without danger and subsequent prominent English variolators devised different techniques (often kept secret) to improve variolation, before it was replaced by the much safer cowpox ‘vaccination’ as described by Jenner.
But how did variolation emerge in the Ottoman Empire? It turns out that at the time of Lady Montagu’s letter to her friend, variolation, or rather inoculation, was practised in a number of different places around the world. In 1714, Dr Emmanuel Timmonius, resident in Constantinople, had described the procedure of inoculation in a letter that was eventually published by the Philosophical Transactions of the Royal Society (London). He claimed that “the Circassians, Georgians, and other Asiatics” had introduced this practice “among the Turks and others at Constantinople”. His letter triggered a reply from Cotton Maher, a minister in Boston, USA, who reported that his servant Onesimus had undergone the procedure as a child in what is now southern Liberia, Africa. Moreover, two Welsh doctors, Perrot Williams and Richard Wright, reported that inoculation was well known in Wales and had been practised there since at least 1600.
Patrick Russell, an English doctor living in Aleppo (then part of the Ottoman Empire), described his investigations into the origins of inoculation in a letter written in 1786. He had sought the help of historians and doctors, who agreed that the practice was very old but was completely missing from written records. Nevertheless, it appears that at the time, inoculation was practised independently in several parts of Europe, Africa and Asia. The use of the needle (and often pinpricks in a circular pattern) was a common feature, but some places had other techniques: for example, in Scotland, smallpox-contaminated wool (a ‘pocky thread’) was wrapped around a child’s wrist, and in other places, smallpox scabs were placed into the hand of a child in order to confer protection. Despite the different techniques used, the procedure was referred to by the same name — ‘buying the pocks’ — which implies that inoculation may have had a single origin.
Two places in particular have been suggested as the original ‘birthplace of inoculation’: India and China. In China, written accounts of the practice of ‘insufflation’ (blowing smallpox material into the nose) date to the mid-1500s. However, there are claims that inoculation was invented around 1000 ad by a Taoist or Buddhist monk or nun and practised as a mixture of medicine, magic and spells, covered by a taboo, so it was never written down.
Meanwhile, in India, 18th century accounts of the practice of inoculation (using a needle) trace it back to Bengal, where it had apparently been used for many hundreds of years. There are also claims that inoculation had in fact been practised in India for thousands of years and is described in ancient Sanscrit texts, although this has been contested.
Given the similarities between inoculation as practised in India and in the Ottoman Empire, it may be more likely that variolation, as described by Lady Montagu, had its roots in India, and it may have emerged in China independently. However, given that the ancient accounts of inoculation in India are contested, it is also possible that the procedure was invented in the Ottoman Empire and spread along the trade routes to Africa and the Middle East to reach India.
Regardless of geographical origin, the story of inoculation eventually led to one of the greatest medical achievements of humankind: the eradication of smallpox in 1980. And of course, it inspired the development of vaccines for many more infectious diseases, turning this planet into a much safer place.
Further reading
Boylston, A. The origins of inoculation. J. R. Soc. Med . 105 , 309–313 (2012).
Related Articles

ATLAS - Joint PhD Program from BioNTech and TRON with a focus on translational medicine
5 PhD positions for ATLAS, the joint PhD Program from BioNTech and TRON with a focus on translational medicine.
Mainz, Rheinland-Pfalz (DE)
Translational Oncology (TRON) Mainz
Alzheimer's Disease (AD) Researcher/Associate Researcher
Xiaoliang Sunney XIE’s Group is recruiting researchers specializing in Alzheimer's disease (AD).
Beijing, China
Changping Laboratory
Supervisory Bioinformatics Specialist CTG Program Head
The National Library of Medicine (NLM) is a global leader in biomedical informatics and computational health data science and the world’s largest b...
Bethesda, Maryland (US)
National Library of Medicine, National Center for Biotechnology Information
Post Doctoral Research Scientist
Post-Doctoral Research Scientist Position in Human Transplant Immunology at the Columbia Center for Translational Immunology in New York, NY
New York City, New York (US)
Columbia Center for Translational Immunoogy
Postdoctoral Associate- Neuromodulation and Computational Psychiatry
Houston, Texas (US)
Baylor College of Medicine (BCM)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- Games & Quizzes
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction & Top Questions
The first vaccines
Vaccine effectiveness, vaccine types, table of vaccine-preventable diseases.
- Benefits of vaccination
- Adverse reactions

How are vaccines made?
- What did Louis Pasteur discover?
- What did Louis Pasteur invent?
- What was Louis Pasteur’s family like?

Our editors will review what you’ve submitted and determine whether to revise the article.
- LiveScience - How Do Vaccines Work?
- National Library of Medicine - MedlinePlus - Vaccine
- National Center for Biotechnology Information - PubMed Central - Vaccine Development Throughout History
- Better Health Channel - Vaccines
- Smithsonian National Museum of American History - History of Vaccines
- Biology LibreTexts - Vaccines
- vaccine - Children's Encyclopedia (Ages 8-11)
- vaccine - Student Encyclopedia (Ages 11 and up)
- Table Of Contents

What is a vaccine?
A vaccine is a suspension of weakened, killed, or fragmented microorganisms or toxins or other biological preparation, such as those consisting of antibodies , lymphocytes , or mRNA , that is administered primarily to prevent disease.
A vaccine is made by first generating the antigen that will induce a desired immune response. The antigen can take various forms, such as an inactivated virus or bacterium, an isolated subunit of the infectious agent, or a recombinant protein made from the agent. The antigen is then isolated and purified, and substances are added to it to enhance activity and ensure stable shelf life. The final vaccine is manufactured in large quantities and packaged for widespread distribution. Learn more about mRNA vaccine creation.
What is a vaccine delivery system?
A vaccine delivery system is the means by which the immune-stimulating agent constituting the vaccine is packaged and administered into the human body to ensure that the vaccine reaches the desired tissue. Examples of vaccine delivery systems include liposomes , emulsions , and microparticles.
How do vaccines work?
A vaccine imitates infection so as to encourage the body to produce antibodies against infectious agents. When a vaccinated person later encounters the same infectious agent, their immune system recognizes it and can fight it off. Learn more.
Recent News
vaccine , suspension of weakened, killed, or fragmented microorganisms or toxins or other biological preparation, such as those consisting of antibodies , lymphocytes , or messenger RNA (mRNA), that is administered primarily to prevent disease .

A vaccine can confer active immunity against a specific harmful agent by stimulating the immune system to attack the agent. Once stimulated by a vaccine, the antibody-producing cells, called B cells (or B lymphocytes ), remain sensitized and ready to respond to the agent should it ever gain entry to the body. A vaccine may also confer passive immunity by providing antibodies or lymphocytes already made by an animal or human donor. Vaccines are usually administered by injection (parenteral administration), but some are given orally or even nasally (in the case of flu vaccine). Vaccines applied to mucosal surfaces, such as those lining the gut or nasal passages, seem to stimulate a greater antibody response and may be the most effective route of administration. (For further information, see immunization .)

The first vaccine was introduced by British physician Edward Jenner , who in 1796 used the cowpox virus (vaccinia) to confer protection against smallpox , a related virus, in humans. Prior to that use, however, the principle of vaccination was applied by Asian physicians who gave children dried crusts from the lesions of people suffering from smallpox to protect against the disease. While some developed immunity, others developed the disease. Jenner’s contribution was to use a substance similar to, but safer than, smallpox to confer immunity. He thus exploited the relatively rare situation in which immunity to one virus confers protection against another viral disease . In 1881 French microbiologist Louis Pasteur demonstrated immunization against anthrax by injecting sheep with a preparation containing attenuated forms of the bacillus that causes the disease. Four years later he developed a protective suspension against rabies .

After Pasteur’s time, a widespread and intensive search for new vaccines was conducted, and vaccines against both bacteria and viruses were produced, as well as vaccines against venoms and other toxins. Through vaccination, smallpox was eradicated worldwide by 1980, and polio cases declined by 99 percent. Other examples of diseases for which vaccines have been developed include mumps , measles , typhoid fever , cholera , plague , tuberculosis , tularemia , pneumococcal infection, tetanus , influenza , yellow fever , hepatitis A, hepatitis B , some types of encephalitis , and typhus —although some of those vaccines are less than 100 percent effective or are used only in populations at high risk. Vaccines against viruses provide especially important immune protection, since, unlike bacterial infections, viral infections do not respond to antibiotics .

The challenge in vaccine development consists in devising a vaccine strong enough to ward off infection without making the individual seriously ill. To that end, researchers have devised different types of vaccines. Weakened, or attenuated , vaccines consist of microorganisms that have lost the ability to cause serious illness but retain the ability to stimulate immunity. They may produce a mild or subclinical form of the disease. Attenuated vaccines include those for measles, mumps, polio (the Sabin vaccine ), rubella , and tuberculosis. Inactivated vaccines are those that contain organisms that have been killed or inactivated with heat or chemicals. Inactivated vaccines elicit an immune response, but the response often is less complete than with attenuated vaccines. Because inactivated vaccines are not as effective at fighting infection as those made from attenuated microorganisms, greater quantities of inactivated vaccines are administered. Vaccines against rabies , polio (the Salk vaccine ), some forms of influenza , and cholera are made from inactivated microorganisms. Another type of vaccine is a subunit vaccine, which is made from proteins found on the surface of infectious agents. Vaccines for influenza and hepatitis B are of that type. When toxins, the metabolic by-products of infectious organisms, are inactivated to form toxoids , they can be used to stimulate immunity against tetanus , diphtheria , and whooping cough (pertussis).

In the late 20th century, advances in laboratory techniques allowed approaches to vaccine development to be refined. Medical researchers could identify the genes of a pathogen (disease-causing microorganism) that encode the protein or proteins that stimulate the immune response to that organism. That allowed the immunity-stimulating proteins (called antigens ) to be mass-produced and used in vaccines. It also made it possible to alter pathogens genetically and produce weakened strains of viruses . In that way, harmful proteins from pathogens can be deleted or modified, thus providing a safer and more-effective method by which to manufacture attenuated vaccines.

Recombinant DNA technology has also proven useful in developing vaccines to viruses that cannot be grown successfully or that are inherently dangerous. Genetic material that codes for a desired antigen is inserted into the attenuated form of a large virus, such as the vaccinia virus, which carries the foreign genes “piggyback.” The altered virus is injected into an individual to stimulate antibody production to the foreign proteins and thus confer immunity. The approach potentially enables the vaccinia virus to function as a live vaccine against several diseases, once it has received genes derived from the relevant disease-causing microorganisms. A similar procedure can be followed using a modified bacterium, such as Salmonella typhimurium , as the carrier of a foreign gene.

Vaccines against human papillomavirus (HPV) are made from viruslike particles (VLPs), which are prepared via recombinant technology . The vaccines do not contain live HPV biological or genetic material and therefore are incapable of causing infection. Two types of HPV vaccines have been developed, including a bivalent HPV vaccine, made using VLPs of HPV types 16 and 18, and a tetravalent vaccine, made with VLPs of HPV types 6, 11, 16, and 18.
Another approach, called naked DNA therapy, involves injecting DNA that encodes a foreign protein into muscle cells. The cells produce the foreign antigen, which stimulates an immune response.
Vaccines based on RNA have been of particular interest as a means of preventing diseases such as influenza , cytomegalovirus infection, and rabies . Messenger RNA (mRNA) vaccines are advantageous because the way in which they are made allows them to be developed more quickly than vaccines made via other methods. In addition, their production can be standardized, enabling rapid scale-up for the manufacture of large quantities of vaccine. Novel mRNA vaccines are safe and effective; they do not contain live virus, nor does the RNA interact with human DNA.
Vaccine-preventable diseases in the United States , presented by year of vaccine development or licensure.
| disease | year |
|---|---|
| Vaccine recommended for universal use in U.S. children. For smallpox, routine vaccination was ended in 1971. | |
| Vaccine developed (i.e., first published results of vaccine usage). | |
| Vaccine licensed for use in United States. | |
| smallpox | 1798 |
| rabies | 1885 |
| typhoid | 1896 |
| cholera | 1896 |
| plague | 1897 |
| diphtheria | 1923 |
| pertussis | 1926 |
| tetanus | 1927 |
| tuberculosis | 1927 |
| influenza | 1945 |
| yellow fever | 1953 |
| poliomyelitis | 1955 |
| measles | 1963 |
| mumps | 1967 |
| rubella | 1969 |
| anthrax | 1970 |
| meningitis | 1975 |
| pneumonia | 1977 |
| adenovirus | 1980 |
| hepatitis B | 1981 |
| Haemophilus influenzae type b | 1985 |
| Japanese encephalitis | 1992 |
| hepatitis A | 1995 |
| 1995 | |
| 1998 | |
| rotavirus | 1998 |
| human papillomavirus | 2006 |
| 2019 | |
- Skip to main content
- Keyboard shortcuts for audio player
Planet Money

- LISTEN & FOLLOW
- Apple Podcasts
- Amazon Music
Your support helps make our show possible and unlocks access to our sponsor-free feed.
The Very First Vaccine

Sarah Gonzalez

A vaccine is just exposing yourself to a little bit of the bad thing that can kill you.
But when did we first get the idea to inject ourselves with something that can kill us, in order to save us?
On today's show we trace the 2000-year history of the very first vaccine. We go from Ancient Greece to Imperial China to Britain. And we learn how this led to an achievement we'd love to repeat again now with the coronavirus — completely eradicating a deadly disease.
Music: " Love Is Hard ," " Seismic Encounters ," and " Time Traveler's Checks "
Find us: Twitter / Facebook / Instagram / TikTok
Subscribe to our show on Apple Podcasts , Pocket Casts and NPR One .
Inoculate yourself with a weekly dose of economics and subscribe to the Planet Money's Newsletter .
REVIEW article
Vaccines through centuries: major cornerstones of global health.

- 1 Department of Biomedical Sciences, Oakland University William Beaumont School of Medicine, Rochester, MI, USA
- 2 Department of Anatomy, Cell Biology and Physiology, Faculty of Medicine, American University of Beirut, Beirut, Lebanon
- 3 Lebanese Health Society, Beirut, Lebanon
- 4 Department of Experimental and Clinical Neurosciences, University of Palermo, Palermo, Italy
Multiple cornerstones have shaped the history of vaccines, which may contain live-attenuated viruses, inactivated organisms/viruses, inactivated toxins, or merely segments of the pathogen that could elicit an immune response. The story began with Hippocrates 400 B.C. with his description of mumps and diphtheria. No further discoveries were recorded until 1100 A.D. when the smallpox vaccine was described. During the eighteenth century, vaccines for cholera and yellow fever were reported and Edward Jenner, the father of vaccination and immunology, published his work on smallpox. The nineteenth century was a major landmark, with the “Germ Theory of disease” of Louis Pasteur, the discovery of the germ tubercle bacillus for tuberculosis by Robert Koch, and the isolation of pneumococcus organism by George Miller Sternberg. Another landmark was the discovery of diphtheria toxin by Emile Roux and its serological treatment by Emil Von Behring and Paul Ehrlih. In addition, Pasteur was able to generate the first live-attenuated viral vaccine against rabies. Typhoid vaccines were then developed, followed by the plague vaccine of Yersin. At the beginning of World War I, the tetanus toxoid was introduced, followed in 1915 by the pertussis vaccine. In 1974, The Expanded Program of Immunization was established within the WHO for bacille Calmette–Guerin, Polio, DTP, measles, yellow fever, and hepatitis B. The year 1996 witnessed the launching of the International AIDS Vaccine Initiative. In 1988, the WHO passed a resolution to eradicate polio by the year 2000 and in 2006; the first vaccine to prevent cervical cancer was developed. In 2010, “The Decade of vaccines” was launched, and on April 1st 2012, the United Nations launched the “shot@Life” campaign. In brief, the armamentarium of vaccines continues to grow with more emphasis on safety, availability, and accessibility. This mini review highlights the major historical events and pioneers in the course of development of vaccines, which have eradicated so many life-threatening diseases, despite the vaccination attitudes and waves appearing through history.
Introduction
Vaccines constitute one of the greatest success stories within the health sector. They form part of a multifaceted public health response to the emergence of pandemics. This review is general in nature. It highlights the major historical cornerstones in the development and progress of various types of vaccines since the beginning and through the ages until today.
It recognizes the major pioneers whose work has made a difference in the advancement of this vital health field, despite all the anti-vaccination movements that appeared through the ages. Multiple reviews were encountered during our literature search; however, each of those reviews dealt with a specific aspect of vaccination like effectiveness of a particular vaccine, or side effects of another or even attitudes toward vaccines. Consequently, this work tried to put together the major achievements through history stressing the importance, continuous vital role, and the need for immunization for health prevention and protection as well as its impact on human experience.
The physiological mechanisms behind vaccination are well established. Vaccination activates the immune system and induces both innate and adaptive immune responses thus leading to the production of antibodies, in the case of a humoral response, or to the generation of memory cells that will recognize the same antigen, if there is a later exposure. Periodic repeat injections can improve the efficacy and effectiveness of inoculations ( 1 ).
The approval of a vaccine abides by a set of well-established international rules and regulations. Prior to their approval by the respective health authorities, scientists test vaccines extensively in order to ensure their efficacy, safety, and effectiveness. Next to antibiotics, vaccines are the best defense that we have to date against infectious diseases; however, no vaccine is actually 100% safe or effective for everyone. This is attributed to the fact that each body reacts to vaccines differently ( 2 – 4 ). Significant progress has been made over the years to monitor side effects and conduct research relevant to vaccine safety. In addition, vaccine licensing is a lengthy process that may take 10 years or longer. The Food and Drug Administration (FDA) and the National Institute of Health (NIH) require that vaccines undergo the required phases of clinical trials on human subjects prior to any use in the general public. This process is becoming more complex as more caution and care is being allocated to the quality of the market product.
Furthermore, vaccines can be divided into different categories depending on the way that they are prepared including live-attenuated vaccines, inactivated vaccines, subunit vaccines, conjugate vaccines, and toxoids.
Live-Attenuated Vaccines
Live-attenuated vaccines are used more frequently for viruses rather than bacteria, since the former contain a lesser amount of genes and can be controlled more easily ( 5 ). The most common method in formulating live-attenuated vaccines involves passing the virus through successions of cell cultures to weaken it. This will produce a form of the virus that is no longer able to replicate in human cells. However, it will still be recognized by the human immune system, hence protecting the body from future invasions. Examples of such vaccines are measles, rubella, mumps, varicella (more commonly known as chickenpox), and influenza. The disadvantage of using this technique is that the virus may transform into a more virulent form due to a certain mutation and cause illness once injected into the body. Although this rarely occurs, it must always be taken into consideration ( 6 ).
Inactivated Vaccines
By using heat, radiation, or certain chemicals, one can inactivate a microbe. The microbe will no longer cause illness but can still be recognized by the immune system. Poliovirus and Hepatitis A are common examples of inactivated vaccines. This type of vaccine has the disadvantage of being effective for a shorter period of time than live-attenuated vaccines. Multiple boosters of the vaccine are sometimes required to improve effectiveness and sustainability ( 6 ).
Subunit Vaccines
A subunit vaccine contains only portions of the microbe that can be presented as antigens to the human immune system instead of the microbe as a whole. The antigens or the microbe portions that best activate the immune response are usually selected. An influenza vaccine in the form of shots is an example. In addition, a recombinant subunit vaccine has been made for the hepatitis B virus. Hepatitis B genes are injected into maker cells in culture. Once these cells reproduce, the desired antigens of the virus are produced as well, and these can be purified for use in vaccines ( 6 ).
Conjugate Vaccines
Conjugate vaccines are designed from parts of the bacterial coat. However, these parts may not produce an effective immune response when presented alone. Hence, they are combined with a carrier protein. These carrier proteins are chemically linked to the bacterial coat derivatives. Together, they generate a more potent response and can protect the body against future infections. Vaccines against pneumococcal bacteria used in children are an example of conjugate vaccines ( 6 ).
Some bacteria release harmful toxins that cause illness in infected individuals. Vaccinations against such types of bacteria are prepared by inactivating or weakening the toxin using heat or certain chemicals. This will help prepare the immune system against future invasion. The vaccine against tetanus caused by the neurotoxin of Clostridium tetani is a good example of a toxoid ( 6 ).
Vaccination: Its Determinants and Modulation with Age
The generation of vaccine-mediated protection is a complex challenge. Effective early protection is conferred primarily by the induction of antigen-specific antibodies. The quality of such antibody responses has been identified as a determining factor of efficacy. Efficacy requires long-term protection, namely, the persistence of vaccine antibodies and/or the generation of immune memory cells capable of rapid and effective reactivation upon subsequent microbial exposure ( 7 ).
The exponential development of new vaccines raises many questions about their impact on the immune system. Such questions related to immunological safety of vaccines as well as triggering conditions such as allergy, autoimmunity, or even premature death ( 7 ). Such issues were always looked for and monitored and some vaccines were even stopped because of these issues.
Recent vaccine models rely on both a cell-mediated response and a humoral immune response with highly specific antibodies and have shown an adequate amount of success. This, however, has not been the case for a few diseases such as tuberculosis where the humoral immunity mounted by the bacille Calmette–Guerin (BCG), the only currently used human vaccine, is inefficient in conferring proper immunization ( 8 ). However, T cells do take part indirectly in the production of antibodies and of secreted biological molecules (e.g., Interferon) for protection. It seems that a proper mounted immunity is better achieved by vaccine-induced antibodies, whereas a T cell immune response is needed for disease attenuation. Hence, a robust understanding of B and T cell function is needed for proper immunization ( 9 ).
Multiple determinants modulate the primary vaccine antibody response in healthy individuals; they include the vaccine type, live versus inactivated, protein versus polysaccharide, and use of adjuvants ( 10 ). They also include the nature of the antigen and its intrinsic immunogenicity ( 11 ), the dose of the antigen, the route of administration, the vaccine schedule, and the age at administration ( 12 ). In addition, genes play a direct role in the body’s response to vaccination even in healthy individuals ( 13 , 14 ). For each of the above determinants, there might be a particular mechanism involved and is further influenced by other factors including extremes of life, acute or chronic diseases, immunosuppression, and nutrition status ( 12 ).
Early life immune responses are limited by (1) limited magnitude of antibody responses to polysaccharides and proteins, (2) short persistence of antibody responses to protein, (3) influence of maternal antibodies, and (4) limited CD8+ T cell and interferon-gamma responses. Such factors are difficult to study in human infants due to neonatal immune immaturity and the inhibitory influence of maternal antibodies, which increase with gestational age and wane a few months post-natal ( 7 ).
On the other hand, in elderly persons, the immune system undergoes characteristic changes, termed immunosenescence, which leads to increased incidence and severity of infectious diseases and to insufficient protection following vaccination ( 15 ). Vaccines induce both innate (non-specific) and adaptive (specific) immune responses, which decline substantially with age thus leading to the decreased efficacy of vaccines in elderly persons. In the elderly, the innate immune response will witness a reduced phagocytic capacity of neutrophils and macrophages, a decrease in their oxidative burst, and impairment in the up-regulation of MHC class II expression among other parameters ( 16 ). In addition, persistent inflammatory processes occur with increasing age and may reduce the capacity to recognize stimuli induced by pathogens or vaccines. For the elderly, improved special antigen delivery systems are needed to overcome these limitations ( 12 ).
Furthermore, the adaptive immune response is functionally defective in the elderly. The involution of the thymus with aging leads to a decrease in content and in output of mature naïve T cells into the periphery, which hampers the induction of adaptive immune responses to neoantigens. In the context of primary vaccination, this causes reduced response rate ( 7 – 12 ). B cells also undergo age-related changes that aggravate the functionality of B cells colonies. As effector B cells accumulate, naïve B cells decrease in number and this leads to a reduction in the diversity of antibody responses. In brief, vaccines tailored to the needs of the elderly will have to be developed, taking into consideration these limitations in order to improve protection in this population.
Vaccine Efficacy and Effectiveness in the Context of the Translational Research Map
In 2010, Weinberg and Szilagyl eloquently approached the issues of efficacy and effectiveness clarifying the road to correctly answer the relevant but complex question: “How well does the candidate vaccine prevent the disease for which it was developed?” They highlighted clearly the distinction between efficacy (individual level) and effectiveness (population level), which are often confused terms that fit well into the new paradigm of translational research ( 15 ). At about the same time, Curns et al. elaborated on the distinction between the epidemiologic concepts of vaccine efficacy and effectiveness within the context of translational research ( 17 ). Such concepts were also addressed earlier, but slightly differently, by Clemens and co-workers in two separate publications in 1984 and 1996, and also by Orenstein et al. in 1989 ( 18 – 20 ).
Accordingly, vaccine efficacy is measured as the proportionate reduction in disease attack rate when comparing vaccinated and unvaccinated populations. Vaccine efficacy studies always have rigorous control for biases through randomized prospective studies and vigilant monitoring for attack rates ( 15 ). In addition to proportionate reduction in attack rates, these studies can furthermore assess outcomes through hospitalization rates, medical visits, and costs. Despite the complexity and expenses that arise from the initial trials, they are needed to establish vaccine efficacy ( 15 ).
On the other hand, the related but distinct concept of vaccine effectiveness has always been compared to a “real world” view of how a vaccine reduces disease in a population. As such, it can evaluate risks versus benefits behind a vaccination program under more natural field conditions rather than in a controlled clinical trial. Vaccination program efficiency is proportional to vaccine potency or efficacy in addition to the degree and success of immunization of the target groups in the population. In brief, it is influenced by other non-vaccine-related factors that could influence the outcome. The “real world” picture provided by vaccine effectiveness data is desirable in planning public health initiatives, an advantage that makes these studies attractive. Translating research data into real public health application are a process that has been reengineered by the NIH as part of a road map for future research. Consequently, a new expanded definition of translational research, consisting of four steps was proposed, which fits nicely within the continuum of vaccine research ( 21 ). In this new process of phase I to phase IV clinical trials, safety, immunogenicity, efficacy, and post-licensure effectiveness of a particular vaccine are assessed ending up in phase IV with the burden of the disease ( 15 ).
Vaccines stood the test of time and many techniques have been introduced into the world of vaccination. Practitioners used to write articles about their vaccinating instruments and techniques. According to John Kirkup, vaccinators and physicians used various instruments and techniques to inject the vaccinating material into the human body. More than 45 different vaccinating instruments have been recorded in British, American, German, and French catalogs between the years 1866 and 1920; most of them are out of use nowadays ( 22 ).
Beginning of Vaccines
There are multiple major landmarks in the history of vaccines. It was reported that the origin goes as far back as Hippocrates, the father of modern medicine, 400 B.C. He described mumps, diphtheria, and epidemic jaundice among other conditions ( 23 ). The earliest methods of immunization and protection against smallpox date back to about 1000 A.D., and are attributed to the Chinese. It has been said that the son of a Chinese statesman was inoculated against smallpox by blowing powdered smallpox sores into his nostrils ( 24 ). Another method used for inoculation was the removal of fluid from the pustules of an infected individual and subsequently rubbing it into a skin scratch of a healthy individual. This procedure was later introduced into Turkey around 1672, long before reaching Europe ( 25 ). It took six centuries for variolation to be introduced to Great Britain, in 1721 ( 26 ).
Through the Eighteenth Century
The eighteenth century was marked by several major events that started with the spread of variolation from Turkey and China to England and America, followed, in the late eighteenth century, by Edward Jenner’s breakthrough of vaccination.
Variolation from Turkey to England
Variolation, derived from the Latin word varus , meaning “mark on the skin,” or inoculation, derived from the Latin word inoculare , meaning “to graft,” are two words that were used interchangeably in describing the aforementioned immunization process. By 1715, variolation was introduced to England after the pursuit of an English aristocrat, Lady Mary Wortley Montague, who had been personally inflicted with an episode of smallpox. After being informed of the method of variolation, she made the embassy surgeon, Charles Maitland, perform the procedure on her 5-year-old son in 1718 in Turkey. In 1721, Dr. Charles Maitland performed the first English variolation on Lady Montague’s 4-year-old daughter after their return to London ( 27 ).
Lady Montague became a great proponent of the procedure and worked thoroughly on advocating this process for its ability to protect against the spread of smallpox.
Data from the U.S. National Library of Medicine and the NIH showed that 1–2% of those variolated died as compared to 30% of those who contracted the disease naturally. Correspondingly, Rev. Cotton Mather and Dr. Zabdiel Boylston introduced variolation in America and were also great advocates of this procedure especially since, in the same year, there was a smallpox epidemic in Boston that killed hundreds ( 28 ). However, Lady Montague, Rev. Mather, and Dr. Boylston faced great opposition regarding their promotion of variolation even with the presentation of the comparative analysis of fatality rates, which reached 2% for those variolated compared to 14% for the naturally occurring disease ( 27 ).
Spreading the Word
Despite some variolation-related deaths, the word of inoculation kept spreading along with data suggesting that variolation was still the safeguard against the spread of smallpox. In addition, Benjamin Franklin, who lost his son in 1736, wrote: “I long regretted that I had not given it to him by inoculation, which I mention for the sake of parents who omit that operation on the supposition that they should never forgive themselves if a child died under it; my example showing that the regret may be the same either way, and that therefore the safer should be chosen” ( 24 ). In 1759, Dr. William Heberden, at his own expense and with the support of Benjamin Franklin, wrote a pamphlet entitled “Some Account of the Success of Inoculation for the Small-Pox in England and America: together with plain instructions by which any person may be enabled to perform the operation and conduct the patient through the distemper” ( 29 ).
Edward Jenner’s Breakthrough
Toward the late eighteenth century came Jenner’s breakthrough in finding a safer immunizing technique than variolation, which is vaccination.
The method of variolation had low yet significant death rates; therefore, physicians were on the quest of finding a new and more secure method of immunization with minimal or no death rates. On this basis, an English physician named Edward Jenner (1748–1823) searched for a cure for smallpox, a debilitating disease that rendered the world helpless. Jenner became interested in certain individuals who were immune to smallpox because they had contracted cowpox in the past. He personally witnessed this when he learned of a dairymaid that was immune to smallpox due to her previous infection with the cowpox virus, usually transmitted from infected cattle. During that time, an English farmer named Benjamin Jesty personally took charge of inoculating his wife and children with fresh matter from a cowpox lesion in one of his cows out of fear of having his wife and children become victims of the smallpox epidemic. He applied this method after having contracted cowpox himself and believing he was immune to smallpox. He never published his results even though his wife and children did not show symptoms after being exposed to smallpox ( 27 ). During these years, there were still outbreaks of smallpox. George Washington, after surviving smallpox, ordered mandatory inoculation for his troops in 1777 ( 27 ).
After many speculations on the role of cowpox and its immunizing effect against smallpox, Jenner, in 1796, inoculated an 8-year-old boy named James Phipps using matter from a fresh cowpox lesion on the hands of a dairymaid named Sarah Nelms who caught them from her infected cattle. After several days, Jenner inoculated the boy again but this time with fresh matter from a smallpox lesion and noted that the boy did not acquire the disease proving that he was completely protected ( 27 ). A few years later, word of his success circulated among the public, and Jenner wrote “ An Inquiry into the Causes and Effects of the Variolae Vaccinae, a Disease Discovered in some of the Western Counties of England, particularly Gloucestershire and Known by the Name of CowPox ,” after adding several cases to his initial achievement with the boy Phipps. At first, his publication and achievement did not stir any interest in his community, but with time, word of Jenner’s breakthrough began spreading ( 27 ).
The late eighteenth century was characterized by the implementation of the new process of immunization, vaccination, which required the inoculation of fresh matter from cowpox lesions into the skin of healthy individuals.

Through the Nineteenth Century
The nineteenth century was a major landmark in the history of vaccines since it witnessed discoveries made by Louis Pasteur, the father of microbiology, and Robert Koch, the scientist who discovered the germ responsible for tuberculosis ( 26 ).
Vaccination Versus Variolation
In the beginning of the nineteenth century, the term “Vaccination” was introduced by Richard Dunning from the Latin word for cow “Vacca.” After becoming aware of the fact that vaccination was more secure than variolation, several physicians initiated movements against the use of variolation and advocated for its eradication. Dr. Jean de Carro, for example, aided in the elimination of variolation and its substitution with vaccination. Some of the major efforts implemented in America were initiated by Dr. Benjamin Waterhouse, who received the vaccine from Edward Jenner and vaccinated his own family. He later proved that they acquired immunity when they remained asymptomatic after he infected them with smallpox. Waterhouse worked effectively on making vaccination universal in the U.S. Unfortunately, like any other medical breakthrough, problems arose both because Waterhouse aimed at making profit and the public was not ready to implement these procedures. However, after breaking his initial monopoly, Waterhouse accepted to share his vaccines and made the supplies available to other physicians ( 24 ). Despite all these efforts, smallpox epidemics continued to occur and Jenner stated in a pamphlet that he wrote, “The annihilation of the small pox, the most dreadful scourge of the human species, must be the final result of this practice.” Eradication was finally achieved 176 years later. The time it took could be attributed to the fact that Jenner did not think of the necessity of revaccination nor of the instability of vaccines, which made them unable to handle different environmental conditions, including countries other than England ( 30 ).
The late nineteenth century was distinguished by Pasteur’s achievements that made him the father of vaccines after creating the first laboratory vaccine. Louis Pasteur (1822–1895), a French chemist and microbiologist, was the first to propose the “Germ Theory” of disease in addition to discovering the foundations of vaccination ( 26 ). He studied chicken cholera and received strains of bacteria causing anthrax and septic Vibrio . Pasteur started his experiments by intentionally infecting chickens by feeding them cholera-polluted meals and then recording the fatal progression of the illness. At first, Pasteur was using fresh cultures of the bacteria to inoculate the chickens, most of which did not survive. During that time, Pasteur had to go on a holiday, so he placed his assistant in charge of injecting the chickens with fresh cultures. However, his assistant accidentally forgot to perform the injections, and the bacterial cultures were left in a medium that was exposed to room air for about a month. Later, the attendant injected the chickens with the now “attenuated” strain of bacteria resulting in mild, non-fatal symptoms. Pasteur later re-injected these chickens, but this time with fresh bacteria. To his surprise, they did not get ill. Ultimately, Pasteur reasoned that what made the bacteria less deadly was exposure to air, mainly oxygen. Pasteur used the French verb “vacciner” during the years 1879 and 1880 to describe how he was able to provide total body immunity through vaccination by inoculation of an attenuated virulence which was the first vaccine made by a human in the laboratory ( 31 ).
Pasteur also developed the anthrax vaccine in his laboratory, not long after performing his studies on chicken cholera. In 1881, Pasteur used his own anthrax vaccine, which contained attenuated live bacterial cultures in addition to carbolic acid, and demonstrated that all vaccinated animals survived while the control group died ( 32 ). During the same year, Louis Pasteur in France and George Miller Sternberg in the U.S. almost simultaneously and independently isolated and grew the pneumococcus organism. Later in 1884, Pasteur successfully fought rabies that was endangering the European livestock by using his attenuated rabies vaccine obtained from desiccated brain tissue inactivated with formaldehyde, which provided immunity to dogs against rabies in his experiments ( 26 ). He reported his success to the Academy of Sciences in France, and a year later, he applied his original vaccine 60 h after a 9-year-old boy was bitten several times by a rabid dog. The boy survived after being first inoculated with the most attenuated organisms, then subsequently with less attenuated organisms each day for 10 days ( 33 ). In 1888, the Pasteur Institute was established as a rabies treatment center as well as an infectious diseases research and training institute.
From Live Vaccines to Killed Vaccines
After Pasteur’s successful live vaccines, a new type of vaccine was introduced in the last few years of the nineteenth century. These were killed vaccines, which were directed against three chief bacterial causes of human morbidity: cholera, typhoid, and the plague. The first cholera vaccine used to immunize humans was actually a live vaccine developed by Jaime Ferran (1852–1929), which provided a high level of protection during the 1884 epidemic in Spain. However, the first killed vaccine for cholera was developed in 1896 by Wilhelm Kolle (1868–1935) and was used in Japan in 1902 with over 80% efficiency. The credit for developing the killed typhoid vaccine during the 1890s goes to both Richard Pfeiffer and Almroth Wright who made great contributions. Wright was later credited for carrying out the “first large-scale vaccination using a killed typhoid vaccine” ( 34 ). Finally, the killed vaccine for plague was first developed in 1896 by Haffkine, who was one of Pasteur’s followers, when an epidemic struck Bombay.
Late Nineteenth and Twentieth Century
During this period, vaccine production was taken over by factory-type laboratories, which formed the precursors of the biological products supply houses. Many types were produced.
Paul Ehrlich (1854–1915), a German physician and scientist who worked under a contractual collaboration with Behring, noted the existence of toxoids in the late 1890s. He also promoted enrichment and standardization protocols. These protocols enabled the exact determination of quality of the diphtheria antitoxins. In 1907, it was demonstrated that toxoids could be used to durably immunize guinea pigs. It is crucial to briefly address the historical background of the bacterial infections that led to some of the earliest and most successful use of toxoids, inactivated forms of bacterial toxins, for the purpose of immunization. Until the twentieth century, diphtheria, tetanus, and pertussis proved to be significant causes of illness and death with no effective treatments or prevention in sight. Fortunately, advances in 1890 improved the prognosis of numerous future patients ( 35 ). At the end of the nineteenth century, especially in 1896 and 1897, the cholera and typhoid vaccines were developed, followed by the introduction of the plague vaccine. The latter was preceded by the preparation of anti plague horse serum at the Pasteur Institute by Alexandre Yersin.
Yersin demonstrated disease protection in animals. Later, he went to China to try his vaccine on humans during a plague epidemic ( 26 ).
Diphtheria is a potentially fatal disease that primarily involves tissues of the upper respiratory tract and kills its victims slowly by suffocation. In 1884, a German physician, Edwin Klebs (1834–1913), was able to successfully isolate the bacteria that proved to be the etiological agent of the disease. It was later proved that toxin production is initiated only after the bacteria are themselves infected by a specific virus or a bacteriophage carrying the toxin’s genetic instructions ( 35 ).
In France, during the year 1888, Emile Roux discovered the diphtheria toxin. His discovery led to the development of passive serum therapies through the scientific contributions of many, including Emil Von Behring and Paul Ehrlich ( 26 ). Similarly, the etiological agent of Pertussis, commonly known as the “whooping cough,” was found to be a bacterium isolated from infected patient tissues in 1906 ( 36 ). Tetanus was similarly a significant cause of mortality usually resulting from dysfunction of the autonomic nervous system or the respiratory muscles ( 37 ). In 1884, another German scientist, Arthur Nicolaier (1862–1942), correlated tetanus with an anaerobic soil bacterium found in wounds. A few years later, the Japanese investigator Shibasaburo Kitasato (1853–1931) was able to isolate this bacterium ( 35 ). At the beginning of World War I in 1914, the tetanus toxoid was introduced following the development of an effective therapeutic serum against tetanus by Emil Von Behring and Shibasaburo Kitasato. The rabies and typhoid vaccines were then licensed in the U.S. as the etiology of these destructive diseases was slowly being uncovered, by Shibasaburo Kitasato along with Emil von Behring ( 26 ). They discovered that the serum of animals that had been exposed to sub-lethal doses of the bacteria involved in tetanus and diphtheria was protective against the lethal effects associated with these pathogens by having an antitoxin effect when injected into another animal. Additionally, this discovery, which earned Behring the inaugural Nobel Prize for Physiology and Medicine in 1901, was the concept of passive transfer in addition to serum therapy. He proved that serum could be acquired from immune animals and transferred to others as protection ( 38 ). Once this concept made its way to clinical practice in 1891, technical problems were faced while developing the right antitoxin concentration and potency. As a result, in the early twentieth century, the U.S. Congress enacted the Biologics Control Act legislation “to regulate the sale of viruses, serums, toxins, and similar products” to ensure medication quality control. Nevertheless, with the increasing use and popularity of antitoxins derived from animal serum, scientists began to observe a syndrome now called serum sickness, or a reaction to immune-complexes formed from combining high concentrations of antigens with antibodies. This eventually led to the use of human rather than animal serum in order to decrease the frequency of adverse events; still, serum therapy was not perfect in preventing disease due to the frequency of adverse events and its brief duration of action. Later on, combining diphtheria toxin and antitoxin in the same syringe proved much more effective in decreasing mortality rate. This combination became commercially available in 1897. This was the first step in the shift from passive to active immunization ( 35 ). In 1923, Gaston Ramon (1886–1963), a French veterinarian working at the Pasteur Institute, used a diphtheria toxoid produced by formalin and heat inactivation without the use of antitoxin to safely induce active immunity in humans. This product, termed anatoxine, was the basis for the novel and clinically effective toxoid vaccine against diphtheria. Experiments followed to improve the durability of the protective response of the vaccine, and in 1926, the importance of aluminum salts as an adjuvant added to the vaccine to augment the immune response to the antigen, became apparent ( 38 ). This was discovered by Alexander Thomas Glenny (1882–1965) who proved that toxoid alone produced a lower level of antibody and immunity than desired, whereas better immunity was achieved when an inflammatory reaction was triggered. With these significant improvements, tetanus and diphtheria toxoids became routinely used across America and Europe in the 1930s and 1940s ( 35 ).
Since then, refinements have been made to these vaccines to yield higher purity and reduce the number of booster doses. Nowadays, widespread childhood vaccination is reducing the burden of these diseases. While this is a huge advantage, vaccines may potentially produce adverse effects that can discourage their acceptance by some populations. This has led to numerous safety movements which culminated in the congressionally legislated National Childhood Vaccine Injury Act in the 1980s created to compensate families for selected adverse events potentially related to mandatory childhood vaccinations ( 37 ). Nevertheless, global recommendations continue to call for routine immunization of children against diphtheria, tetanus, and pertussis with the combined DTP vaccine to sustain immunity in childhood and adolescence. DTP has, therefore, become one of the most widely used vaccines to achieve widespread immunity across age groups ( 35 ).
Tuberculosis and BCG
Tuberculosis, otherwise known as the “Great White Plague,” is another disease that started spreading as an epidemic once industrialization began. This disease caused approximately 15% of deaths in the eighteenth and nineteenth centuries across all socioeconomic groups ( 39 ).
A French physician named Jean Antoine Villemin (1827–1892) demonstrated that the mode of transmission of disease is through the respiratory system. Robert Koch (1843–1910), known as the founder of modern bacteriology, revealed in 1882 that the causative agent of the disease is Mycobacterium tuberculosis , which later became known as Koch’s bacillus ( 40 ). Following this discovery, Koch created what later came to be known as Koch’s postulates, which listed the criteria necessary for proof of bacterial causality: “the organism must be present in diseased tissues; it must be isolated and grown in pure culture; and the cultured organisms must induce the disease when inoculated into healthy experimental animals” ( 39 ).
In 1908, two bacteriologists working in the Pasteur Institute in Lille, Albert Calmette (1863–1933) and Camile Guerin (1872–1961), announced their discovery of Mycobacterium bovis , which is a strain of tubercle bacilli that could be used to create a vaccine against tuberculosis. This occurred after it became evident that different forms of the bacterium were required to prevent or treat tuberculosis, including non-pathogenic, attenuated, or killed tubercle bacilli from different sources, including human, bovine, and equine. This strain had an attenuated virulence while maintaining its antigenicity and became known as BCG ( 40 ).
Bacille Calmette–Guerin vaccinations proved to be successful in animal studies in 1921 and were soon used as an oral vaccine to immunize humans against tuberculosis. In 1927, the BCG vaccine, constituted by the live-attenuated M. bovis , was first used in newborns. It has become the most widely administered of all vaccines in the WHO Expanded Program for Immunization, but has been estimated to prevent only 5% of all potentially vaccine-preventable deaths due to tuberculosis ( 26 ). Despite its imperfections, BCG remains the only effective vaccination for protection against human tuberculosis ( 39 ).
Yellow Fever
Yellow fever is a highly fatal infection caused by a small, enveloped, single-stranded RNA virus and results in renal, hepatic, and myocardial injury, along with hemorrhage and shock ( 41 ). Unlike previously mentioned diseases, the history of yellow fever is highly uncertain and filled with misconceptions. Early work on immunization against the disease began with Carlos Finlay (1833–1915) in the 1870s and 1880s when Koch’s postulates were becoming increasingly accepted. Finlay proposed that mosquitos carried the yellow fever “germ.” He attempted to prove it by feeding mosquitos that had fed on yellow fever patients. However, it was later revealed that his process failed due to the lack of an incubation period within the mosquito, which is a transmission requirement that Finlay was unaware of ( 42 ).
Since 1900, significant advances have been made in creating a vaccine by the Yellow Fever Commission, which was originally led by Walter Reed (1851–1902) along with Jesse Lazear, Aristedes Agramonte, and James Carroll. Reed’s experiments took Finlay’s discovery one step further by adding an incubation period of approximately 2 weeks and achieved the same positive results. When mosquitos bite non-immune individuals after feeding on individuals who had yellow fever, none of the non-immune subjects died and very few suffered disease. This led the Commission of investigators to a major discovery, namely, the identification of the Asibi strain, which is the parent strain of the present 17D vaccine, obtained via continuous indirect passage through the Aegypti mosquitos and direct passage through monkeys. In addition to identifying the etiological agent of the disease, the Commission also identified rhesus monkeys as susceptible hosts, hence providing a means for testing future vaccine attempts. This paved the way for Max Theiler and other Rockefeller Foundation scientists to develop a successful live-attenuated vaccine for yellow fever in 1937. “The most important experimental passage series – designated 17D – used a virus that had been subcultured eighteen times in whole mouse embryos, followed by 58 passages in whole-minced chick embryo cultures, after which the virus was passed in minced chick embryo depleted of nervous tissue.” Theiler himself was actually one of the first individuals to be successfully vaccinated. The vaccine was quickly implemented, and alternative vaccines shown to be more dangerous were discontinued ( 42 ).
Influenza has proved to be very difficult to trace back in history due to its non-specific symptoms and features. It was not until the early twentieth century that influenza outbreaks began to be systematically studied due to well-documented clinical descriptions and epidemiological data. In 1918, the “Spanish flu” influenza pandemic was responsible for 25–50 million deaths worldwide and more than one-half million in the U.S. This virus was unusual because it spread so quickly, was so deadly ( 26 ). Richard E. Shope (1901–1966), a physician who conducted his research in the Department of Animal Pathology at The Rockefeller Institute in Princeton, was the first to isolate influenza virus; a member of the orthomyxovirus family, from a mammalian host in 1931 ( 43 ). He was able to induce the syndrome of swine influenza in pigs by applying respiratory secretions intranasally. He also isolated a bacterium from the respiratory tract of infected pigs called Haemophilus influenzae suis . When this bacterium was combined with a filterable agent and inoculated, the pigs developed the clinical manifestations of swine influenza. These two agents seemed to act synergistically with the virus to damage the respiratory tract hence creating the suitable environment needed for the virus to exercise its pathological effects. In 1933, scientists from the British National Institute for Medical Research including Christopher Andrews, Wilson Smith, and Patrick Laidlaw successfully isolated and transmitted the influenza virus from humans. Throughout this year, “Burnet has successfully cultivated the organism in chick embryos; other influenza types had been recognized; neutralizing antibodies had been identified and quantitated; and viral surface glycoproteins, H and N had been described” ( 43 ).
These discoveries led scientists to introduce the inactivated vaccine in the mid-1940s that is still used to this day ( 44 ). The influenza A/B vaccine was initially presented to the Armed Forces Epidemiological Board in 1942. It was licensed following the war and used for civilians in 1945 in the U.S. Starting 1985, a series of vaccines were licensed for Haemophilus influenza type b (Hib) polysaccharide vaccines. These vaccines are recommended routinely for children at 15 and 24 months of age. The vaccine was, however, not consistently immunogenic in children <18 months of age. In 1987, the protein-conjugated Hib vaccine was licensed and in the next 2 years, it became available. During 1996, a combined vaccine Hib conjugate and Hepatitis B was licensed. Later on, in 2003, the first nasally administered influenza vaccine was licensed. This live influenza A and B virus vaccine was indicated for healthy, non-pregnant persons ages 5–49 years. The contracts to develop vaccine against the H5N1 avian influenza virus were awarded to Aventis Pasteur and to Chiron in 2004. During the following year, an inactivated, injectable influenza vaccine was licensed. It was indicated for adults 18 years of age and older.
During the same year, the FDA approved Afluria, a new inactivated influenza vaccine, for use in people aged 18 years and older. Two years later in 2009, the Department of Health and Human Services, supported the building of a facility to manufacture cell-based influenza vaccine. It also directed toward development of a vaccine for novel influenza A (H1N1). During the same year, the FDA approved four vaccines against the H1N1 influenza virus high-dose inactivated influenza vaccine (Fluzone High-Dose) for people aged 65 years and older. In 2012, the FDA approved several vaccines: HibMenCY a new combination of meningococcal and Hib vaccine for infants; Flucelvax, which is the first seasonal influenza vaccine, manufactured using cell culture technology and a quadrivalent formulation of Fluarix ( 26 ).
Unfortunately, one of the difficulties in dealing with influenza is the continuous mutability of the viral genome necessitating annual reassessments and reformulations of the vaccine. This has led to a suboptimal effectiveness of influenza vaccines, which are only successful against strains included in the vaccine formulation or strains of homogenous subtype. Several pandemics were caused by the influenza virus: during the years 1957–1958, The “Asian” influenza pandemic caused by H2N2 influenza virus resulted in an estimated 70,000 deaths in the U.S. alone and in the years 1968–1969, the “Hong Kong” influenza pandemic caused by an H3N2 influenza virus induced roughly 34,000 deaths in the U.S. ( 26 ). Future studies should focus on producing vaccines protective against variant strains and creating surveillance systems to detect novel strains in time to formulate the proper vaccines.
Poliomyelitis
Poliomyelitis, or Polio, is an intestinal infection spread between humans through the fecal–oral route. It is a disease of the developed nations striking younger individuals most frequently in warmer weather. One of the most famous polio victims, President Franklin D. Roosevelt, founded the National Foundation for Infantile Paralysis in 1938, later known as the March of Dimes ( 26 ). It is well established that better hygiene decreases childhood exposure to the disease, when infection would usually be milder since protective maternal antibodies are present ( 45 ). In 1954, the Nobel Prize in Medicine was awarded to John Enders, Thomas Weller, and Fredrick Robbins for their discovery of the ability of poliomyelitis viruses to grow in tissue cultures ( 26 ). Two major lifelong competitors were involved in the race for the Polio vaccine, Jonas Salk (1914–1995) and Albert Sabin (1906–1993). Salk took a more traditional route using a killed-virus approach, which did not involve natural infection in acquiring immunity. Instead, his approach involved a fully inactivated virus that still had the ability to induce protective antibodies. Sabin, on the other hand, set out to create a live-virus vaccine based on the belief that this would trigger natural immunity and provide a lasting protection. Salk had speed, simplicity, and safety on his side since a killed-virus did not have the ability to revert to virulence, whereas the live-virus vaccine could be given orally, establish longer lasting immunity, and offer passive vaccination through the excreted weakened virus potentially immunizing a large portion of non-vaccinated communities ( 46 ).
Not surprisingly, Salk’s vaccine was the first to make it to the population. Following successful clinical trials in 1954, six companies began mass production of the vaccine. Unfortunately, Salk’s vaccines were soon suspended and recalled when contaminated samples were found in the market due to poor monitoring and control in some laboratories leading to serious health consequences and national panic. The first Cutter polio vaccine incident was reported on April 25, 1955 with 5 more cases reported just a day later with the number eventually rising to 94 of those vaccinated and in 166 of their close contacts. On April 27, the Laboratory of Biologics Control requested that Cutter Laboratories recall all vaccines and the company did so immediately. On May 7, the Surgeon General recommended that all polio vaccinations be suspended pending inspection of each manufacturing facility and thorough review of the procedures for testing vaccine safety. The investigation found that live polio virus had survived in two batches of vaccines produced by Cutter Laboratories. Large-scale polio vaccinations resumed in the fall of 1955 ( 26 ). At the same time, Sabin had been making great advances with his live-virus vaccine since 1951. After successful clinical trials conducted in the Soviet Union that left polio virtually wiped out with no safety issues, it soon became the vaccine of choice in the West. The Polio Vaccination Assistance Act was enacted by Congress and was the first federal involvement in immunization activities. It allowed Congress to appropriate funds to the Communicable Diseases Center [later the Centers for Disease Control and Prevention (CDC)] to help states and local communities acquire and administer vaccines. At the beginning of the 1960s, the oral polio vaccine types 1, 2, and 3 as well as the trivalent product were licensed in the U.S. The first 2 were developed by Sabin and grown in monkey kidney cell culture, while the trivalent oral polio was developed to improve upon the killed Salk vaccine ( 26 ). As a result, in the late 1990s, the CDC recommended switching back to Salk’s killed-virus polio vaccine, while the WHO also advocated the switch for polio-free nations and the continued use of the favored live-virus vaccine for routine immunization ( 45 ).
The last two cases of wild type polio were reported in an unvaccinated Amish in 1979 and in a 5-year-old boy from Peru in 1991 ( 26 ). In 1990, the enhanced-potency inactivated poliovirus vaccine was licensed.
Measles, Mumps, and Rubella
Following successful developments in the polio vaccine, attention soon shifted to three other common viral diseases of childhood: measles, mumps, and rubella.
The measles virus is an RNA virus from the genus Morbillivirus belonging to the Paramyxooviridae family. It causes an acute illness that includes fever, cough, malaise, coryza, and conjunctivitis, in addition to a maculopapular rash. In general, measles is a mild disease but, like many others, has the potential to cause serious complications. In addition, measles is known to be one of the most contagious human diseases causing major outbreaks to occur very often. Until the year 2000, measles was still the leading cause of vaccine-preventable childhood deaths worldwide ( 47 ).
John Enders (1897–1985), known as the “Father of Modern Vaccines” had a particular interest in revealing the virus responsible for measles. He isolated the Edmonston strain of the virus in 1954, which was named after the child from whom it was isolated. A formalin-inactivated measles virus vaccine derived from this strain was subsequently licensed in the U.S. in 1963. However, following the discontinuation of this vaccine in 1967 due to short-lived and incomplete immunity, over 20 further attenuated vaccines were developed and used throughout the world, most of which were also derived from the Edmonston strain ( 48 ). The first live-virus measles vaccine, Rubeovax, was licensed in 1963. Other live-attenuated virus measles vaccines were eventually licensed in the U.S. in 1965. The recommended age for routine administration was changed from 9 to 12 months of age.
The first national measles vaccine campaign was launched in 1966. The world recorded a 90% decreased incidence compared to the pre-vaccination years. In 1968, a second live, further attenuated measles virus vaccine was also licensed. In 1989, both the Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) issued recommendations for a routine second dose of the measles vaccine. During the mid-to-late 1980s, a high proportion of reported measles cases were in school-aged children (5–19 years) who had been appropriately vaccinated. These vaccine failures led to new national recommendations of a second dose of measles-containing vaccine ( 26 ).
Mumps is another acute viral illness. It is the only virus known to cause epidemic parotiditis in humans accompanied by fever, anorexia, headache, and malaise. K. Habel and John Enders isolated the virus in 1945 ( 26 ), and trials of formalin-inactivated mumps vaccine in humans began the same year by Joseph Stokes and colleagues and by Enders. This approach was abandoned in the 1950s due to short-lived immunity, and work began to develop live-attenuated mumps vaccines in 1959 by the vaccinologist Maurice Hilleman (1919–2005) and colleagues ( 48 ). Hilleman isolated the wild type virus from his daughter, Jeryl Lynn, who contracted the virus at the age of 5 and was recovering from it. It became known as the Jeryl Lynn strain of mumps virus. The mumps live-virus vaccine was licensed in December 28, 1967 ( 26 ). Trials with this attenuated virus resulted in 100% protective efficacy and the vaccine was licensed in the U.S. in 1967. This strain is still used to produce mumps vaccines until this day. It is given as part of the measles, mumps, and rubella (MMR) vaccine ( 49 ).
Rubella is a rash disease in children and adolescents caused by a filterable virus. It poses a severe threat to pregnant women and their children by potentially causing congenital deafness and cataracts. In 1964, a rubella epidemic swept the U.S. resulting in 12.5 million cases of rubella infection, with an estimated 20,000 newborns having congenital rubella syndrome (CRS), along with fetal and neonatal deaths in the thousands ( 26 ). The rubella virus was detected and isolated by two groups of scientists, Thomas Weller and Franklin Neva at Harvard Medical School, in addition to Paul Parkman and colleagues at the Walter Reed Army Institute of Research (WRAIR). Similar to measles and mumps, inactivated whole virus vaccines proved ineffective, so efforts turned to discovering a live-attenuated vaccine ( 26 ).
In 1963, Paul Parkman left WRAIR and joined Harry Meyer Jr. at the NIH Division of Biological Standards, and the pair developed the first live-attenuated rubella vaccine in 1966, HPV-77, which was subsequently included in the initial MMR vaccine used in the U.S. in the 1970s ( 26 ). Maurice Hilleman discovered the superior RA 27/3 vaccine that became the only vaccine used outside of Japan starting in the late 1970s. This vaccine maintained its preference due to many factors including increased durability and harmlessness to fetuses of inadvertently vaccinated pregnant women ( 47 ). In 1969, three rubella virus strains were licensed in the U.S.: HPV-77 strain grown in dog-kidney culture, HPV-77 grown in duck-embryo culture, and Cendehill strain grown in rabbit-kidney culture. A decade later, in 1979, the RA 27/3 (human diploid fibroblast) strain of rubella vaccine (Meruvax II) by Merck was licensed. All other strains were discontinued. Merck’s combined trivalent MMR as well as the combined measles and rubella vaccine (M-RVax) developed by Maurice Hilleman and colleagues, was licensed by the U.S. government in 1971 ( 26 ), and is still in use today. Moreover, the age for routine vaccination with MMR vaccine was changed from 12 to 15 months in the year of 1976. The next vaccine that combined measles, mumps, rubella, and varicella antigens (Proquad) was licensed in 2005. It was indicated for use in children 12 months to 12 years. In response to the association of this vaccine with autism, in 2004, the eighth and final report of the Immunization Safety Review Committee was issued by the Institute of Medicine concluded that the body of epidemiological evidence favors rejection of a causal relationship between the MMR vaccine and autism ( 26 ). Combination vaccines hold many advantages including reduced need for several injections, therefore, reducing the incidence of vaccination site reaction ( 48 ).
The etiological agent of clinical hepatitis, identified by its distinguishing yellow jaundice, was found to be infectious in the early 1900s. The different hepatitis strains, A and B, were first differentiated in 1942 ( 26 ). In the mid-1960s, Blumberg and co-workers and Prince discovered hepatitis B surface antigen in the circulating blood of carriers of the infection. Deinhardt et al. soon followed this discovery with that of the hepatitis A virus ( 49 ). Provost et al. successfully prepared a killed hepatitis A vaccine in 1986, which proved to be safe and highly effective in extensive clinical trials. The first inactivated hepatitis A vaccine (Havrix) was licensed in 1995. The following year, a second inactivated vaccine (Vaqta) also became available ( 50 ).
Hepatitis B, on the other hand, rarely causes any severe risk as a primary infection. However, those who develop a chronic persistent infection may continue to have severe disease for the rest of their lives. This may even lead to cirrhotic destruction of the liver due to host immune response to the virus. The discovery of the surface antigen particles of the hepatitis B virus by Blumberg and colleagues in the plasma of human carriers was followed by attempts to create a vaccine. In 1968, a killed hepatitis B vaccine was developed and clinical trials began in 1975 proving the safety and efficacy of the vaccine. Merck and Pasteur Institute subsequently independently licensed the plasma-derived vaccine in 1981 ( 50 ). On July 23rd 1986, the recombinant hepatitis B vaccine (Recombivax HB) was licensed. Using recombinant DNA technology, Merck scientists developed a hepatitis B surface antigen subunit vaccine. Three years later, on August 28th 1989, the recombinant hepatitis B vaccine (Engerix-B) was licensed. A decade later in 1999, the FDA approved a two-dose schedule of hepatitis B vaccination for adolescents 11–15 years of age using Recombivax HB (by Merck) with the 10-μg (adult) dose at 0 and 4–6 months later. At the beginning of the new millennium, in 2001, a combined hepatitis A inactivated and hepatitis B (recombinant) vaccine, Twinrix was licensed. The following year, a vaccine combining diphtheria, tetanus, acellular pertussis, inactivated polio, and hepatitis B antigens (Pediarix) was licensed ( 26 ). In conclusion, fortunately, both hepatitis A and B are now preventable due to the discovery of these highly effective vaccines that proved to maintain long-term immunity in vaccinated individuals ( 50 ).
MID Twentieth and Twenty-First Century
In 1966, the World Health Assembly called for global smallpox eradication, which was launched the following year. During the first year of the program 217,218 cases of polio were reported in 31 countries that were endemic to smallpox. Four years later, the CDC recommended discontinuation of routine vaccination for smallpox in the U.S. following a greatly reduced risk of disease ( 26 ).
During the 70s, especially in 1974, the Expanded Program on Immunization was created within WHO, in response to poor immunization levels in developing countries (<5% of children in 1974). The following vaccines were used by the Expanded Program on Immunization: BCG, Polio, DTP, measles (often MMR vaccine), yellow fever (in endemic countries), and hepatitis B. Three years later, in October 1977, the last case of naturally acquired smallpox occurred in the Merca District of Somalia. In the same year, the first pneumococcal vaccine was licensed, containing 14 serotypes (of the 83 known serological groups) that composed 80% of all bacteremic pneumococcal infections in the U.S. ( 26 ).
On May 8 1980, the World Health Assembly declared the world free of naturally occurring smallpox. On the other hand, in July 1983, two enhanced pneumococcal polysaccharide vaccines (Pneumovax 23 and Pnu-imune 23) were certified. These vaccines included 23 purified capsular polysaccharide antigens of Streptococcus pneumoniae and replaced the 14-valent polysaccharide vaccine licensed in 1977. A few years later, in 1988, the World Health Assembly passed a resolution to eradicate polio by the year 2000 ( 26 ). Later on, in 1992, the Japanese encephalitis (JE) inactivated virus vaccine (JE-Vax) was licensed.
During the year 1994, The Expanded Program for Vaccine Development and the Vaccine Supply and Quality Program were merged creating the Global Program for Vaccines and Immunization. During the same year, the Western Hemisphere was finally labeled as “polio-free” by the International Commission for the Certification of Polio-Eradication.
The 1996 was another monumental year with the launching of the International AIDS Vaccine Initiative (IAVI) that called for the speedy development of a human immunodeficiency virus (HIV) vaccine for use worldwide. This in turn led to the introduction of the Scientific Blueprint for AIDS Vaccine Development. IAVI was funded by several NGOs and foundations. It is a Collaborating Center of the Joint United Nations Program on HIV/AIDS (UNAIDS) whose efforts led finally lead to the first possible vaccine against HIV (Aidsvax) which reached Phase III trials, the largest recorded human HIV vaccine trial at that time. The trial involved 5400 volunteers from the U.S., Canada, and the Netherlands, the majority of whom were men who have sex with men ( 26 ). Preliminary results from the trial of AIDS VAX (VaxGen) vaccine were reported in early 2003. While the vaccine was shown to be protective amongst non-Caucasian populations, especially African-Americans, the same effect was not reproducible in Caucasians ( 26 ).
During the same year, the Children’s Vaccine Program was established at WHO’s Program for Appropriate Technology in Health (PATH). The program’s goal was to provide vaccines to children in the developing world and to accelerate research and development of new vaccines. The first vaccines purchased were Hib, Hepatitis B, Rotavirus, and Pneumococcal, which were not commonly used in the developing world ( 26 ).
At the beginning of the new millennium, the Western Pacific Region of the world was certified as polio-free. During the next 2 years, the European Region also became certified as polio-free. In 2006, the FDA licensed the first vaccine developed to prevent cervical cancer (Gardesil), precancerous genital lesions and genital warts due to human papillomavirus (HPV) types 6, 11, 16, and 18. The first smallpox vaccine for certain immune-compromised populations was delivered under Project BioShield on July 10th 2010. The following year 2010, the WHO declared the “Decade of Vaccines” and in 2012, the United Nations Foundation launched Shot@Life campaign ( 26 ).
Varicella Zoster: Herpes Virus
Varicella (“chickenpox”) is caused by the varicella zoster virus (VZV). Michiaki Takahashi, Professor of Virology at the Research Institute for Microbial Diseases at Osaka University, successfully produced the Oka vaccine strain of live, attenuated varicella vaccine in the 1970s. Takahashi was able to make this remarkable advance at a time when very few viruses had been attenuated to produce efficacious live-virus vaccines including yellow fever, polio, measles, mumps, and rubella as previously mentioned. The VZV vaccine is the first and only licensed live, attenuated herpesvirus vaccine in the world. Numerous trials in the early 1970s continued to prove the safety and efficacy of the vaccine in both healthy and immunocompromised, high-risk individuals. As a result of these successful trials, the live varicella virus vaccine (Varivax) was licensed in 1995 for the active immunization of persons 12 months of age and older ( 51 ). About 10 years later, in 2006, VariZIG, a new immune globulin product for post-exposure prophylaxis of varicella, became available under an Investigational New Drug Application Expanded Access Protocol ( 26 ).
As a herpesvirus, VZV possesses the unique ability to establish latent infection subsequent to primary infection. Zoster results from reactivation of latent VZV that spreads through nerves to the skin. Therefore, one fear associated with this vaccination was the possibility that it could increase the incidence and/or severity of zoster when compared to natural disease. Conversely, it was actually shown that following vaccination, zoster is less common than after natural infection ( 51 ). In 2006, the FDA licensed a new vaccine to reduce the risk of shingles in the elderly. The vaccine, Zostavax was approved for use in people aged 60 years of age and older ( 26 ).
Rotavirus is the leading cause of severe diarrhea and vomiting (severe acute gastroenteritis) among young infants and children worldwide. No significant difference was found in the incidence of rotavirus in industrialized and developing countries, suggesting that vaccination may be the only way to control the impact of this severe disease. Dr. Ruth Bishop and colleagues were the first to describe rotavirus in humans in 1973. It was clear, early on, that a naturally acquired first infection, whether symptomatic or asymptomatic, was the most effective defense against severe reinfection, and subsequent infections progressively created greater protection. Therefore, the goal was to create a vaccination that mimicked the effectiveness of naturally acquired immunity following infection. The development of live, attenuated, oral, safe, and effective rotavirus vaccines was then attempted starting in the mid-1970s. Dr. Albert Kapikian and colleagues, at the NIH, developed the RRV strain that was subsequently used to develop the RRV-TV, or the RotaShield, live oral, and tetravalent vaccine licensed in 1998 to be used in infants at 2, 4, and 6 months of age ( 26 ). However, due to several reported cases of vaccine-associated intestinal intussusception, RotaShield was pulled off the market in the U.S. 14 months after its introduction on the 16th of October, 1999. In 2004, the National Institute of Allergy and Infectious Diseases (NIAID), part of the NIH, awarded a new license agreement for RotaShield to BIOVIRx, Inc. of Minneapolis, MN, USA, which planned its global commercialization. In 2011, history of intussusception was added as a contraindication for rotavirus vaccination ( 26 ). Clark, Offit, and Plotkin then produced the RotaTeq vaccine by Merck based on their bovine strain WC3 in 1992, which was licensed in 2006 by the U.S. FDA. This vaccine, live oral and pentavalent, is destined for use in infants ages 6–32 weeks ( 26 ). Another vaccine, Rotarix, was also licensed in 2008. It is a liquid given in a two-dose series to infants from 6 to 24 weeks of age. Before being licensed, both vaccines were shown to be safe and effective in rigorous clinical trials ( 52 ).
Response to Emerging Diseases in the Twenty-First Century
During the past two decades, improvements in environmental health have contributed tremendously to disease vector control. However, substantial challenges remain in dealing with the newly emerging diseases such as severe acute respiratory syndrome (SARS), H1N1, H7N9, and H5N1 influenza, middle east respiratory syndrome (MERS-CoV), rotavirus, Ebola virus, and a variety of other viral, bacterial, and protozoal diseases ( 53 ).
The role of vaccines in the control and protection from the above mentioned emerging diseases cannot be overemphasized. Actually, the importance of inducing protective immunity through vaccination came out to be the most powerful tool and effective strategy to prevent the spread of emerging viruses among populations, in particular, among people that are immunologically naïve and susceptible hosts. Such emerging diseases represent a major public health concern; they affect livestock and humans thus threatening the world’s economy and public health. Vaccine strategies for emerging pathologies are limited by sudden appearance of the pathogen and the delayed time consuming traditional vaccine development process. Novel methods to rapidly develop vaccine are being experimented, whereby investigators are working to achieve a better understanding of the nature of the interactions between the immune system and a panel of novel harmful microbes. On this basis several novel strategies have been developed and applied. Such strategies included the use of (1) recombinant proteins, or nanoparticles like in SARS-CoV and MERS-CoV, (2) synthetic peptides like the case of influenza virus, (3) virus-like particles, (4) multimeric presentation of viral antigens like the case of Hepatitis, (5) replication of competent viral vectors like in the Rift Valley Fever virus or the EBOLA viruses, (6) recombinant bacteria for Listeria and Salmonella among others, and (7) nucleic acid vaccines for EBOLA or Dengue or Rift Valley Fever viruses ( 54 ).
In managing or even in preventing the emergence of new infectious diseases, a plan should be developed to strengthen surveillance and promote a multi-partners response within local, national, and global programs.
With the high burden of emerging infectious diseases (EID) it becomes an essential part to find an effective method of either preventing or controlling their spread, that is where the role of vaccines prevails. It is significant to mention that the average case fatality rate for Ebola is around 50% and outbreaks are affecting both developed and developing countries. Another emerging disease, MERS-CoV, has caused the death of around 36% of people reported to have contracted the disease. Another disease with high health and economic burden would be rotavirus which was estimated to have annual direct and indirect costs of around $1 billion with “more than 400,000 physician visits, more than 200,000 emergency department (ED) visits, 55,000 to 70,000 hospitalizations, and 20 to 60 deaths each year in children younger than 5 years” (CDC, 2015). These are few of the facts regarding the affliction of EID most of which have no approved vaccine yet. On the other hand, the influenza virus which was estimated to cause an average of 23,607 deaths annually with a $12 billion cost of an epidemic, showed that with the introduction of its vaccine, studies proved it to be 80% effective in preventing death ( 55 ). These figures have managed to influence many governmental and non-profit organizations to intervene either through governmental funding of vaccines where the congress provides yearly international EID funding to several U.S. governmental agencies or through international non-profit organizations which are the leaders in global health innovation ( 56 ).
Disease Burden: Different Influential Aspects
Vaccines remain among the most reliable and effective medical interventions in providing the means to fight debilitating and preventable diseases thus ensuring the continuity of mankind and saving lives. Through reviewing the factsheets provided by the World Health Organization, which provide statistical data on the mortality and morbidity percentages before and after the introduction of the vaccines, one can comprehend the vital role vaccines have played up till this day. Some of the figures that depict the impact of vaccines in decreasing mortality and morbidity include more than 99% decrease in Polio cases since 1988, with cases reaching 350,000 from over 125 endemic countries down to 359 cases as reported in 2014 with only 2 endemic countries, measles vaccine has prevented the death of around 15.6 million children during 2000–2013, in general vaccines prevent around 6 million deaths annually worldwide ( 57 ). This success in providing better public health does not negate the economic burden of vaccination. Vaccination programs require excessive funding to ensure proper handling and maintenance of vaccines, adequate staffing and ongoing provision over efficacy and safety of vaccines and the development of newer vaccines ( 58 ). Nevertheless, the economic and social burden related to the expenses in hospitalizing affected unvaccinated people still outweighs the aforementioned burden. Moreover, better health in the society would promote economic growth and productivity. Consequently, public awareness and public efforts agree on the importance of vaccination and the implementation of policies regarding mandatory vaccinations as a way to decrease outbreaks of preventable diseases and improve global health and prosperity.
Turning Point: Vaccine Controversies
As early as the introduction of vaccines, campaigns against vaccination were raging. As with any new medical intervention there are safety concerns that arise which might be deleterious to the public health. Concerns regarding vaccines often follow a path that starts with the hypothesis of a potential adverse event that is impulsively announced to the public without having reproducible studies to confirm this hypothesis, and thus it would take the public several years to regain trust in the vaccine. A notable example in the recent history would be of the paper published by Andrew Wakefield in the British medical journal the Lancet in 1998, linking the MMR vaccine to autism. However, his research was discredited and the paper was retracted from the journal after it was proven that actually there is no link between MMR vaccine and autism as per the systemic review by the Cochrane library ( 59 ). The battle against vaccines did not reach a halt, and there are still ongoing campaigns that come from religious, political, community-based, and even individual-based grounds raising even ethical issues regarding the mandatory vaccinations proposed by the government. According to the CDC, this year 95% of the children were vaccinated in the U.S., leaving 5% unvaccinated due to religious and philosophical exemptions or even parental refusal due to the fear of vaccine’s side effects and concerns regarding autism from vaccines ( 60 ); this is still a critical number since the unvaccinated would pose risk of outbreaks even among the immunized, which necessitates the need for additional awareness campaigns regarding the importance of vaccination since vaccines remain the only plausible measure of protection against preventable diseases. Actually, a trend was reported in the health news lately, in the U.S., that pediatricians refuse to offer medical care for children whose parents declined their vaccination.
Vaccination has been of great importance throughout centuries (Tables 1 and 2 ). People started with inoculation techniques dating back to 1000 A.D. with the Chinese, Turks, and Asians. With every century and with every curious physician, inoculation techniques improved gradually giving rise to newer vaccination techniques with Edward Jenner and later on, Louis Pasteur and others. However, there is still plenty of room for improvement with the presence of ongoing epidemics and the spread of newly emerging diseases. One important goal is to strengthen the science base for vaccine development and for public health action and disease prevention. Despite the common belief that infectious diseases were virtually eliminated by the middle of the twentieth century, new and reemerging infections are appearing along with drug resistant infections in the past two decades in the various parts of the world and whose incidence threatens to increase in the near future, due to changes in human demographics and behavior, immigration, and speed of international travel among other things ( 61 – 63 ). The importance of vaccine safety continued to grow throughout the twenty-first century, with the development and licensure of new vaccines added to the already robust immunization armamentarium. Scientists also perfected new ways of administering immunizations including edible vaccines and needleless injections. However, formulated or delivered, vaccines will remain the most effective tool we possess for preventing disease and improving public health in the future. Despite the anti-vaccination campaign and the association of vaccines with some side effects, vaccines continue to remain a cornerstone in global health.
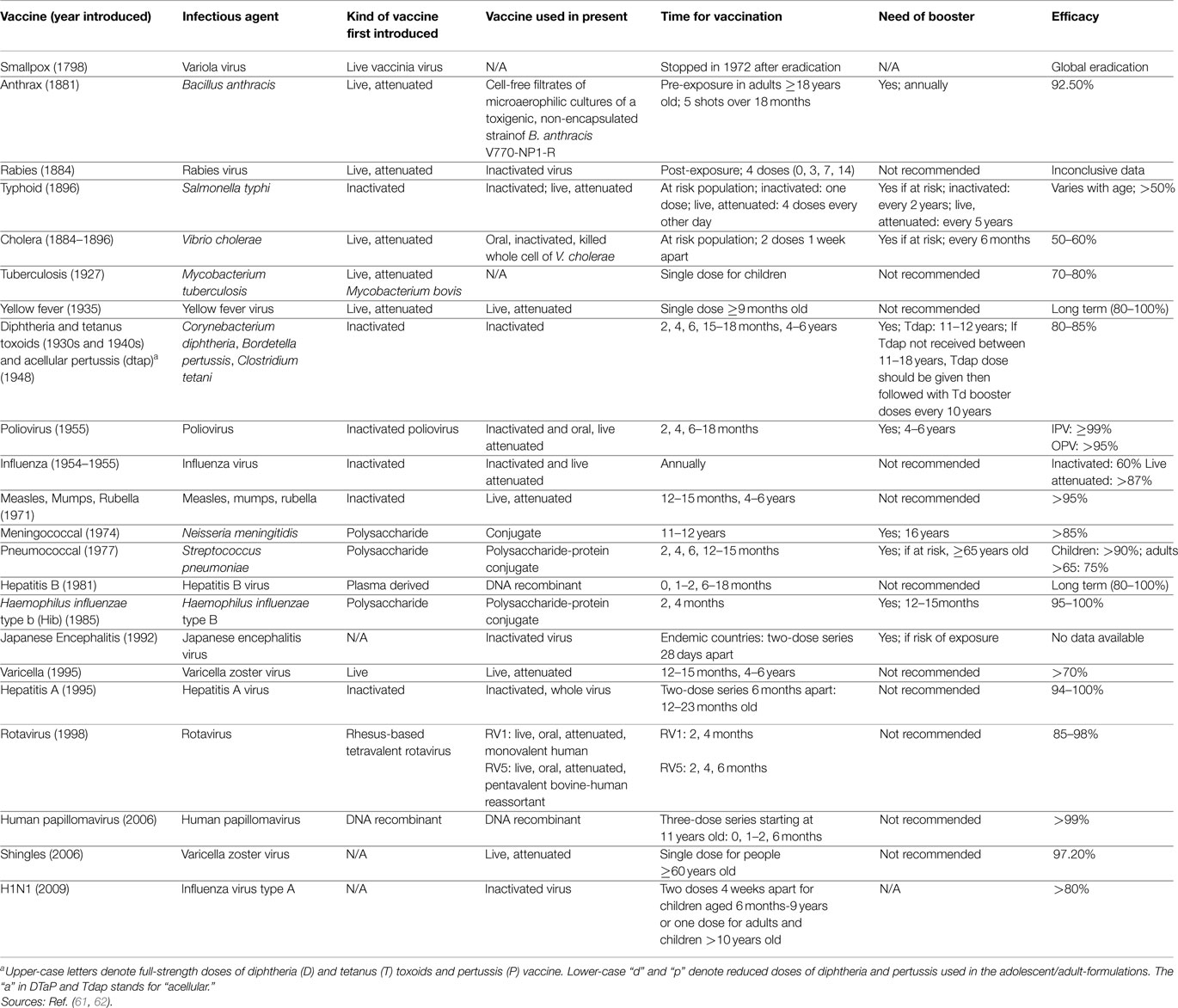
Table 1. Development, introduction, infectious agent, schedule, and efficacy of vaccines .
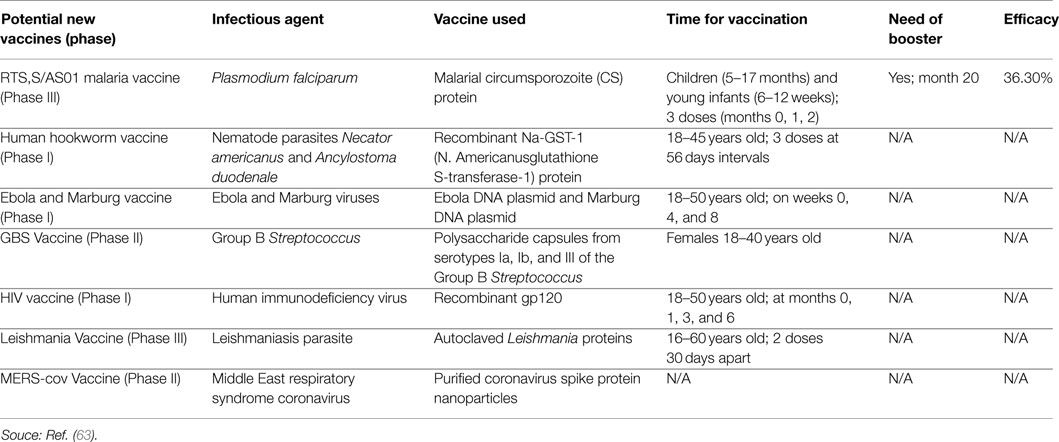
Table 2. Development, introduction, infectious agent, schedule, and efficacy of potential new vaccines .
The distinctions between national and international health problems are losing ground and could be misleading, the “world is a village.” Clinicians and public health workers need to interact on regular basis with veterinarians and veterinary public health. Actually, good examples of the necessity of such collaboration is the emergence of SARS-CoV and MERS-CoV, it shows clearly how coronaviruses can spillover from animals into humans at any time, causing lethal diseases. Foodborne diseases could lead to regional and international outbreaks which might constitute a threat to national and global security.
Author Contributions
IH is the first author. She provided the idea and followed along with AJ the execution of the work and final editing. NC and SC did the literature search for the eighteenth and nineteenth century and the respective preliminary writing about this period. SS and RB did the literature search for the twenty-first century, and about general aspects of vaccination and the respective preliminary writing about this period. MR did the literature search regarding vaccine efficacy and effectiveness in the context of the transnational research map and regarding vaccination instruments and inoculating techniques. AG did the literature search and the preliminary writing for the early history of vaccination and wrote a draft of a manuscript about this period. AL edited thoroughly and commented on the final manuscript. AJ supervised the whole process from inception to the final submission and edited the whole manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Centers for Disease Control and Prevention. Vaccines and Immunizations: The Basics . Washington, DC: Government Printing Office (2012).
Google Scholar
2. CDC.gov . Pinkbook. Epidemiology of VPDs, Vaccine Safety . (2015). Available from: http://www.cdc.gov/vaccines/pubs/pinkbook/safety.html
3. Ellenberg S, Chen RT. The complicated task of monitoring vaccine safety. Public Health Rep (1997) 112 (1):10–20.
PubMed Abstract | Google Scholar
4. Chen RT, Hibbs B. Vaccine safety: current and future challenges. Pediatr Ann (1998) 27 (7):445–55. doi:10.3928/0090-4481-19980701-11
CrossRef Full Text | Google Scholar
5. NIAID. Topics: Vaccines (2012). Available from: http://www.niaid.nih.gov/topics/vaccines/documents/undvacc.pdf
6. The College of Physicians of Philadelphia. Articles – Different Types of Vaccines (2014). Available from: http://www.historyofvaccines.org/content/articles/different-types-vaccines
7. Siegrist CA. General aspects of vaccination. 6th ed. In: Plotkin SA, Orenstein WA, Offit PA, editors. Vaccines . Philadelphia, PA: Elseiver Inc (2008). p. 17–36.
8. Hanekom WA. The immune response to BCG vaccination of newborns. Ann N Y Acad Sci (2005) 1062 :69–78. doi:10.1196/annals.1358.010
PubMed Abstract | CrossRef Full Text | Google Scholar
9. Casadevall A. The methodology for determining the efficacy of antibody-mediated immunity. J Immunol Methods (2004) 291 :1–10. doi:10.1016/j.jim.2004.04.027
10. Rimaniol AC, Gras G, Verdier F, Capel F, Grigoriev VB, Porcheray F, et al. Aluminum hydroxide adjuvant induces macrophage differentiation towards a specialized antigen presenting cell type. Vaccine (2004) 22 :3127–35. doi:10.1016/j.vaccine.2004.01.061
11. Tan PL, Jacobson RM, Poland GA, Jacobsen SJ, Pankratz VS. Twin studies of immunogenicity–determining the genetic contribution to vaccine failure. Vaccine (2001) 19 :2434–9. doi:10.1016/S0264-410X(00)00468-0
12. Weinberger B, Herndler-Brandstetter D, Schwanninger A, Weiskopf D, Grubeck-Loebenstein B. Biology of immune responses to vaccines in elderly persons. Clin Infect Dis (2008) 46 (7):1078–84. doi:10.1086/529197
13. Konradsen HB, Henrichsen J, Wachmann H, Holm N. The influence of genetic factors on the immune response as judged by pneumococcal vaccination of mono- and dizygotic Caucasian twins. Clin Exp Immunol (1993) 92 :532–6. doi:10.1111/j.1365-2249.1993.tb03433.x
14. Newport MJ, Goetghebuer T, Weiss HA, Whittle H, Siegrist CA, Marchant A, et al. Genetic regulation of immune responses to vaccines in early life. Genes Immun (2004) 5 :122–9. doi:10.1038/sj.gene.6364051
15. Weinberg GA, Szilagyi PG. Vaccine epidemiology: efficacy, effectiveness, and the translational research roadmap. J Infect Dis (2010) 201 (11):1607–10. doi:10.1086/652404
16. Gomez CR, Boehmer ED, Kovacs EJ. The aging innate immune system. Curr Opin Immunol (2005) 17 :457–62. doi:10.1016/j.coi.2005.07.013
17. Curns AT, Steiner CA, Barrett M, Hunter K, Wilson E, Parashar UD. Reduction in acute gastroenteritis hospitalizations among us children after introduction of rotavirus vaccine: analysis of hospital discharge data from 18 US states. J Infect Dis (2010) 201 (10):1617–24. doi:10.1086/652403
18. Clemens JD, Shapiro E. Resolving the pneumococcal vaccine controversy: are there alternatives to randomized clinical trials? Rev Infect Dis (1984) 6 :589–600. doi:10.1093/clinids/6.5.589
19. Clemens J, Brenner R, Rao M, Tafari N, Lowe C. Evaluating new vaccines for developing countries. Efficacy or effectiveness? JAMA (1996) 275 :390–7. doi:10.1001/jama.275.5.390
20. Orenstein WA, Bernier RH, Hinman AR. Assessing vaccine efficacy in the field. Further observations. Epidemiol Rev (1988) 10 :212–41.
21. Szilagyi PG. Translational research and pediatrics. Acad Pediatr (2009) 9 :71–80. doi:10.1016/j.acap.2008.11.002
22. Kirkup J. The Evolution of Surgical Instruments . Novato, CA: Historyofscience.com (2006).
23. Stanford S. The history of pediatric infectious diseases. Pediatr Res (2004) 55 :163–76. doi:10.1203/01.PDR.0000101756.93542.09
24. The College of Physicians of Philadelphia. History of Vaccines Timelines . The College of Physicians of Philadelphia (1885). Available from: http://www.historyofvaccines.org/content/timelines/all
25. Marble A. Surgeons, Smallpox, and the Poor: A History of Medicine and Social Conditions in Nova Scotia, 1749-1799 . Montreal, QC: McGill-Queen’s University Press (1993).
26. The Immunization Action Coalition. Vaccine Timeline . The Immunization Action Coalition (2013). Available from: http://www.immunize.org/timeline/
27. Riedel S. Edward Jenner and the history of smallpox and vaccination. Proc (Bayl Univ Med Cent) (2005) 18 (1):21–5.
28. Henry EH. Experience in Massachusetts and a few other places with smallpox and vaccination. Boston Med Surg J (1921) 185 :221–8. doi:10.1056/NEJM192108251850802
29. Pepper W. The Medical Side of Benjamin Franklin . Philadelphia, PA: W.J. Campbell (1911).
30. Fenner F. History of Vaccine Development (Smallpox Eradication: The Vindication of Jenner’s Prophesy Chapter) . New York, NY: Springer Science & Business Media (2011). p. 27–32.
31. Bazin H. History of Vaccine Development. (Pasteur and the Birth of Vaccines Made in the Laboratory Chapter) . New York, NY: Springer Science & Business Media (2011). p. 33–45.
32. Sternbach G. The history of anthrax. J Emerg Med (2003) 24 (4):463–7. doi:10.1016/S0736-4679(03)00079-9
33. Bourhy H, Perrot A, Cavaillon J. Vaccines: A Biography (Rabies) . New York, NY: Springer Science & Business Media (2010). p. 73–85.
34. Carpenter C, Hornick R. Vaccines: A Biography (Killed Vaccines: Cholera, Typhoid, and Plague) . New York, NY: Springer Science & Business Media (2010). p. 87–103.
35. Grabenstein JD. Vaccines: A Biography (Toxoid Vaccines) . New York, NY: Springer Science & Business Media (2010). p. 105–24.
36. Cherry JD. Historical review of pertussis and the classical vaccine. J Infect Dis (1996) 174 :59–63. doi:10.1093/infdis/174.Supplement_3.S259
37. CDC.gov . Preventing tetanus, diphtheria, and pertussis among adolescents: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccines recommendations of the advisory committee on immunization practices (ACIP). (2015). Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5503a1.htm
38. Lombard M, Pastoret PP, Moulin AM. A brief history of vaccines and vaccination. Rev Sci Tech (2007) 26 (1):29–48.
39. Gheorghiu M, Lagranderie M, Balazuc AM. Vaccines: A Biography (Tuberculosis and BCG Chapter) . New York, NY: Springer Science & Business Media (2010). p. 125–40.
40. Daniel TM. The history of tuberculosis. Respir Med (2006) 100 (11):1862–70. doi:10.1016/j.rmed.2006.08.006
41. Barrett ADT, Higgs S. Yellow fever: a disease that has yet to be conquered. Annu Rev Entomol (2007) 52 :209–29. doi:10.1146/annurev.ento.52.110405.091454
42. Monath TP. Vaccines: A Biography (Yellow Fever Chapter) . New York, NY: Springer Science & Business Media (2010). p. 159–89.
43. Potter CW. A history of influenza. J Appl Microbiol (2001) 91 :572–9. doi:10.1046/j.1365-2672.2001.01492.x
44. Artenstein AW. Vaccines: A Biography (Influenza Chapter) . New York, NY: Springer Science & Business Media (2010). p. 191–205.
45. Oshinsky D. Vaccines: A Biography (Polio Chapter) . New York, NY: Springer Science & Business Media (2010). p. 207–21.
46. Blume S, Geesink I. A brief history of polio vaccines. Science (2000) 288 (5471):1593–4. doi:10.1126/science.288.5471.1593
47. Gallagher KM, Plotkin SA, Katz SL, Orenstein WA. Vaccines: A Biography (Measles, Mumps, and Rubella Chapter) . New York, NY: Springer Science & Business Media (2010). p. 223–47.
48. Stern AM, Markel H. The history of vaccines and immunization: familiar patterns, new challenges. Health Aff (2005) 24 (3):611–21. doi:10.1377/hlthaff.24.3.611
49. Hilleman MR. Vaccines in historic evolution and perspective: a narrative of vaccine discoveries. Vaccine (2000) 18 :1436–47. doi:10.1016/S0264-410X(99)00434-X
50. Hilleman MR. History of Vaccine Development (Three Decades of Hepatitis Vaccinology in Historic Perspective. A Paradigm of Successful Pursuits Chapter) . New York, NY: Springer Science & Business Media (2011). p. 233–46.
51. Gershon AA. Vaccines: A Biography (Varicella and Zoster Chapter) . New York, NY: Springer Science & Business Media (2010). p. 265–77.
52. Dennehy PH. Vaccines: A Biography (Rotavirus Chapter) . New York, NY: Springer Science & Business Media (2010). p. 347–60.
53. Fineberg HV. Pandemic preparedness and response – lessons from the H1N1 influenza of 2009. N Engl J Med (2014) 370 :1335–42. doi:10.1056/NEJMra1208802
54. Hughes JM. Emerging infectious diseases: a CDC perspective. Emerg Infect Dis (2001) 7 (3):494–6. doi:10.3201/eid0707.017702
55. World Health Organization. Fact Sheets . World Health Organization (2015). Available from: http://www.who.int/mediacentre/factsheets/en/
56. KFF.org . The U.S. Government & Global Emerging Infectious Disease Preparedness and Response (2015). Available from: http://kff.org/global-health-policy/fact-sheet/the-u-s-government-global-emerging-infectious-disease-preparedness-and-response/
57. Andre F, Booy R, Bock H, Clemens J, Datta S, John T, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ (2008) 86 (2):140–6. doi:10.2471/BLT.07.040089
58. Roush S. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA (2007) 298 (18):2155. doi:10.1001/jama.298.18.2155
59. Demicheli V, Rivetti A, Debalini M, Di Pietrantonj C. Vaccines for measles, mumps and rubella in children. Cochrane Database Syst Rev (2012) 19 (4):CD004407. doi:10.1002/14651858.CD004407.pub3
60. CDC.gov . Vaccination Coverage Among Children in Kindergarten – United States, 2013–14 School Year (2015). Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6341a1.htm
61. Immunize.org . Historic Dates and Events Related to Vaccines and Immunization (2015). Available from: http://www.immunize.org/timeline/
62. CDC.gov . Morbidity and Mortality Weekly Report (MMWR) | MMWR (2015). Available from: http://www.cdc.gov/mmwr/index.html
63. Clinicaltrials.gov . Home – ClinicalTrials.gov (2015). Available from: https://clinicaltrials.gov/ct2/home
Keywords: vaccines, immunization, history of vaccines, global health
Citation: Hajj Hussein I, Chams N, Chams S, El Sayegh S, Badran R, Raad M, Gerges-Geagea A, Leone A and Jurjus A (2015) Vaccines Through Centuries: Major Cornerstones of Global Health. Front. Public Health 3:269. doi: 10.3389/fpubh.2015.00269
Received: 07 September 2015; Accepted: 11 November 2015; Published: 26 November 2015
Reviewed by:
Copyright: © 2015 Hajj Hussein, Chams, Chams, El Sayegh, Badran, Raad, Gerges-Geagea, Leone and Jurjus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Inaya Hajj Hussein, hajjhuss@oakland.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- University Libraries
- Research Guides
- History of Vaccines
History of Vaccines: Home
Introduction.
Welcome to our History of Vaccine's guide! This guide serves as an introduction to the history of vaccines while highlighting various sources. The pages that follow cover the history of the Smallpox, Polio, Measles, and Covid-19 vaccines with some additional sources.
We hope this page can serve as a starting point for anyone wishing to conduct their own research into the history of vaccines.

General Research Division, The New York Public Library. (1879-04-19). Sanitary Precautions against a Smallpox Edpidemic - An Inspector of the Board of Health Vaccinating Tramps in a Station House Retrieved from https://digitalcollections.nypl.org/items/89149e23-e0a5-0582-e040-e00a18064625
- The History of Vaccines. By the College of Physicians of Philadelphia. An education resource including articles and an interactive timeline on the history of vaccines.
- History of Medicine IndexCat Scroll down to "Search IndexCat" and enter a keyword to begin searching. Advanced search options are available once a search is made.
- National Library of Medicine: History of Medicine Division Scroll down to search the National Library of Medicine catalog by keyword or select a category of material types to begin a search.
Stanley Plotkin "History of Vaccines" In The Biomedical & Life Sciences Collection, Henry Stewart Talks.
Note: The link provided is a preview for the talk. In order to watch the entire talk, you must be logged in through your UB account. Click here to go to the catalog page for this video and click the link (make sure you are logged in).
Engraving of vaccination during smallpox scare in Jersey City, NJ

Source: The National Library of Medicine Image License: The National Library of Medicine believes this item to be in the public domain.
- HathiTrust Digital Library This link opens in a new window A digital repository of online books and other scholarly materials. More Info Partial Full-Text PUBLIC
- JSTOR This link opens in a new window Full-text of the most important journals in the social sciences, humanities, general sciences as well as in the fields of mathematics, botany & ecology. More Info Full-Text UB ONLY
- Project Muse This link opens in a new window Full-text journals in the humanities & social sciences. More Info Full-Text UB ONLY
- PubMed This link opens in a new window Provides free of charge access to all MEDLINE citations. Supported browsers are Chrome, Firefox, and Safari. PubMed is an NCBI resource and NCBI no longer supports Internet Explorer. More Info Partial Full-Text PUBLIC
- Eighteenth Century Collections Online This link opens in a new window This collection contains every significant English-language and foreign-language title printed in the United Kingdom between the years 1701 and 1800. More Info Full-Text UB ONLY
Curator, Robert L. Brown History of Medicine Collection

Guide Created by Matthew Gadziala May 2021
- Next: Smallpox >>
- Chikungunya
- Hepatitis A
- Hepatitis B
- Hib ( Haemophilus Influenzae type b)
- HPV (Human Papillomavirus)
- Japanese Encephalitis
- Meningococcal ACWY
- Meningococcal B
- Pneumococcal
- RSV (Respiratory Syncytial Virus)
- TBE (Tick-borne Encephalitis)
- Varicella (Chickenpox)
- Yellow Fever
- Zoster (Shingles)
- VISs Overview
- Translations
- DTaP (Diphtheria, Tetanus, Pertussis)
- Influenza (Inactivated or Recombinant)
- Influenza (Live Intranasal)
- MMR (Measles, Mumps, Rubella)
- MMRV (Measles, Mumps, Rubella, Varicella)
- Multi-Vaccine
- PCV (Pneumococcal Conjugate)
- PPSV (Pneumococcal Polysaccharide)
- RSV Preventive Antibody – IIS
- Smallpox/Monkeypox
- Td (Tetanus, Diphtheria)
- Tdap (Tetanus, Diphtheria, Pertussis)
- VIS Translations Vaccine-specific VISs translated into dozens of languages
- Vaccine History Timeline Notable milestones in immunization going back to 400 BC
- CDC Recommended Schedules Current immunization schedules from CDC
- ACIP Vaccine Recommendations As endorsed and published by CDC
- Search All Clinical Resources
- All Patient Handouts
- All Resources for Staff & Providers
- Addressing Vaccination Anxiety
- Administering Vaccines
- Adolescent Vaccination
- Adult Vaccination
- Contraindications & Precautions
- Documenting Vaccination
- Healthcare Personnel
- Managing Vaccine Reactions
- Parent Handouts
- Pregnancy and Vaccines
- Q&As by Diseases and Vaccines
- Schedules for Patients
- Screening Checklists
- Standing Orders Templates
- Storage & Handling
- Strategies & Policies
- Vaccine Confidence
- Vaccine Recommendations
- Vaccine Confidence Overview
- Alternative Medicine
- Alternative Schedules
- Importance of Vaccines
- Improving the Vaccination Experience
- MMR Vaccine
- Religious Concerns
- Responding to Parents
- Unprotected People Stories
- Vaccine Hesitancy
- Vaccine Safety
- Image Library Overview
- Meningococcal
- Vaccination
- Vaccine Manufacturers
- Vaccine Apps
- Email News Services
- Immunize.org Partners
- Webinars & Videos Our library of educational videos and webinar recordings
- Ask the Experts Overview
- View All Questions
- View All Video Questions
Vaccine Topics
- MMR (Measles, Mumps, and Rubella)
General Topics
- Billing & Reimbursement
- Combination Vaccines
- Scheduling Vaccines
- Travel Vaccines
- CDC Recommended Schedules
- ACIP Vaccine Recommendations
- Additional CDC Resources
- Package Inserts & EUAs
- Additional FDA Resources
- Vaccine-Specific Requirements
- State Exemptions
- State Immunization Websites
- Additional State Resources
- WHO Position papers on vaccines and other vaccine-related resources from the World Health Organization
- About IZ Express
- Current Issue
- Browse All Issues
- Website Updates
- Press Releases
- Official Release Repository Chronological listing of vaccine-related announcements from FDA, CDC, and ACIP
- Calendar of Events Immunization-related events, including national conferences and training programs, plus Immunize.org webinars
- Publication Archives Repository of our publications since 1994, including IAC Express (now IZ Express), Needle Tips, and more
- Board of Directors
- Recognition
- Our Founder
- Publication Archives
- Our History Through Film
- Corporate Membership Program
Patient Safety Honor Rolls
- Influenza Vaccination Honor Roll
- Hepatitis B Birth Dose Honor Roll
- MenB Vaccination Honor Roll
- Honor Rolls Honorees
- The Immunize.org Becky Payne Award
- Immunize.org In the News
Home / Vaccines & VISs / Vaccine History Timeline
Vaccine History Timeline

Not long ago we celebrated the 225th anniversary of Edward Jenner’s first smallpox vaccination in 1796 . The development of vaccines continued at a fairly slow rate until the last several decades when new scientific discoveries and technologies led to rapid advances in virology, molecular biology, and vaccinology. Here we present a timeline of the vaccine- and immunization-related events that have occurred since Jenner’s critical discovery. This list is by no means exhaustive. If you know of an event that you would like us to add, contact us at [email protected] .
Related Resources
Vaccine Timeline Before Jenner and After COVID-19
An interactive website from the College of Physicians of Philadelphia.
History of Medicine
The National Library of Medicine collects, preserves, makes available, and interprets for diverse audiences one of the world’s richest collections of historical material related to human health and disease.
CDC approves ACIP recommendations for RSV for adults, DTaP-IPV-Hib-HepB (Vaxelis®️), COVID-19, Influenza, and Pneumococcal Vaccines. June 28, 2024
CDC Recommends Updated 2024-2025 COVID-19 and Flu Vaccines for Fall/Winter Virus Season. June 27, 2024
CDC Updates RSV Vaccination Recommendation for Adults. June 26, 2024
CDC HAN Health Advisory “Increased Risk of Dengue Virus Infections in the United States.” June 25, 2024
FDA approves PCV21 (Capvaxive, Merck) in individuals 18 years of age and older. June 17, 2024
FDA updates advice to manufacturers of COVID-19 Vaccines (2024-2025 Formula): If feasible Use KP.2 Strain of JN.1-Lineage. June 13, 2024
FDA approves expanded age indication for Arexvy (GSK) the first respiratory syncytial virus (RSV) vaccine for adults aged 50-59 at increased risk. June 10, 2024
FDA approves Mrsevia (mRNA-1345), an mRNA respiratory syncytial virus (RSV) vaccine, to protect adults aged 60 years and older. May 31, 2024
CDC HAN Health Advisory “Meningococcal Disease Cases Linked to Travel to the Kingdom of Saudi Arabia (KSA): Ensure Pilgrims are Current on Meningococcal Vaccination.” May 20, 2024
ACIP recommends use of an additional updated 2023–2024 COVID-19 vaccine dose for adults aged 65 Years and older. April 25, 2024
ACIP recommendations for use of pentavalent meningococcal vaccine (Pfizer) for persons 10 years and older. April 18, 2024
CDC HAN Health Advisory “Highly Pathogenic Avian Influenza A(H5N1) Virus: Identification of Human Infection and Recommendations for Investigations and Response.” April 5, 2024
CDC HAN Health Advisory “Increase in Invasive Serogroup Y Meningococcal Disease in the United States.” March 28, 2024
CDC HAN Health Advisory “Increase in Global and Domestic Measles Cases and Outbreaks: Ensure Children in the United States and Those Traveling Internationally 6 Months and Older are Current on MMR Vaccination.” March 18, 2024
CDC posts guidance for constrained U.S. Td supply, 2024. March 6, 2024
CDC updates and simplifies respiratory virus recommendations. March 1, 2024
CDC endorses ACIP recommendations for additional dose 2023-24 COVID-19 vaccine for adults ages 65 years and older and Chikungunya vaccine for travelers and lab workers. February 28, 2024
CDC urges mpox vaccination for those eligible given continued U.S. mpox cases. February 12, 2024
CDC COCA Now – Stay alert for measles cases. January 25, 2024
CDC’s guidance on using Td for infants and children who should not receive acellular pertussis-containing vaccines. January 23, 2024
CDC COCA Now – Information on respiratory syncytial virus (RSV) vaccine administration errors in young children and pregnant people. January 22, 2024
MMWR – ACIP Recommended Immunization Schedule for Children and Adolescents Aged 18 Years or Younger — US, 2024. January 11, 2024
MMWR – ACIP Recommended Immunization Schedule for Adults Aged 19 Years or Older — US, 2024. January 11, 2024
CDC COCA Now – Updated guidance for healthcare providers on increased supply of nirsevimab to protect young children from severe respiratory syncytial virus (RSV) during the 2023–2024 season. January 5, 2024
ACIP recommends Inactivated Polio Vaccine (IPV) for all adults 18 years and older known or suspected to be unvaccinated or incompletely vaccinated against polio. December 8, 2023
2024 U.S. Recommended Immunization Schedule for Adults Aged 19 years or older posted. November 16, 2023
2024 U.S. Recommended Immunization Schedule for Children and Adolescents Aged 18 years or younger posted. November 16, 2023
ACIP recommends use of Tick-Borne Encephalitis (TBE) vaccine for certain travelers and any laboratory workers who work with the virus. November 10, 2023
FDA approves the first chikungunya vaccine (IXCHIQ, Valneva), approved for individuals 18 years of age and older who are at increased risk of exposure to chikungunya virus. November 9, 2023
CDC approves ACIP recommendations for meningococcal and mpox vaccines, approves the 2024 US Recommended Child and Adolescent Immunization Schedule and Recommended Adult Immunization Schedule, including addenda for new and updated vaccine recommendations. October 26, 2023
CDC HAN- Limited Availability of Nirsevimab in the United States—Interim CDC Recommendations to Protect Infants from Respiratory Syncytial Virus (RSV) during the 2023–2024 Respiratory Virus Season. October 23, 2023
FDA approves Penbraya (PFR) for ages 10 through 25 years, a pentavalent vaccine protects against five meningococcal bacteria groups – A, B, C, W and Y – which are known to commonly cause the disease. October 20, 2023
ACIP recommends use of updated COVID-19 vaccines for persons 6 months of age and older. October 10, 2023
ACIP recommends RSV vaccine (Abrysvo, Pfizer) for pregnant persons at 32–36 weeks’ gestation using seasonal administration (September–January in most of the United States) to prevent RSV-associated lower respiratory infections in infants less than 6 months of age. October 6, 2023
FDA amends EUA to include Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula), now authorized for use in individuals 12 years of age and older. Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) is no longer authorized for use in the United States. October 3, 2023
ACIP recommendations on the use of PCV20 (Pfizer) for children. September 29, 2023
CDC recommends new vaccine to help protect babies against severe respiratory syncytial virus (RSV) illness after birth. September 22, 2023
CDC recommends everyone 6 months and older get an updated COVID-19 vaccine. Updated COVID-19 vaccines from Pfizer-BioNTech and Moderna will be available later this week. September 12, 2023
FDA approves and authorizes emergency use of updated mRNA vaccines (Moderna, Pfizer) for 2023-24. The updated mRNA vaccines are each approved for individuals 12 years of age and older and are authorized under emergency use for individuals 6 months through 11 years of age. Bivalent Moderna and Pfizer-BioNTech COVID-19 vaccines are no longer authorized for use in the United States. September 11, 2023
ACIP recommendations for using pneumococcal vaccine in adults 19 and older. September 8, 2023
ACIP recommendations for using nirsevimab (Beyfortus, Sanofi) in infants under 8 months old born during or entering their first RSV season and for infants and children 8–19 months old who are at increased risk of severe RSV disease entering their second RSV season. August 25, 2023
ACIP recommendations for the prevention and control of seasonal influenza with vaccines for the 2023–24 influenza season. August 25, 2023
FDA approves the first vaccine (Abrysvo, Pfizer) for pregnant individuals at 32–36 weeks gestational age, to prevent RSV in infants up to 6 months old. August 21, 2023
CDC adopts ACIP recommendation for using nirsevimab (Beyfortus, Sanofi), a long-acting monoclonal antibody product shown to reduce the risk of both hospitalizations and healthcare visits for RSV in infants by about 80 percent. August 3, 2023
FDA approved Ebola vaccine (Ervebo, Merck) to include individuals 12 months and older. July 27, 2023
ACIP recommendations for using RSV (respiratory syncytial virus) vaccine (Pfizer Abrysvo and GSK Arexvy) in older adults. July 21, 2023
FDA approved Cyfendus (Emergent BioSolutions) (Anthrax Vaccine Adsorbed, Adjuvanted) a two-dose anthrax vaccine for post-exposure prophylaxis use for adults aged 18–65. July 20, 2023
CDC adopted 2023–24 ACIP flu vaccination recommendations, to be published in the summer. June 29, 2023
CDC adopted ACIP recommendations for using RSV vaccine in adults 60 and older using shared clinical decision-making. June 29, 2023
ACIP interim recommendations for using bivalent mRNA COVID-19 vaccine in children aged 6 months to 5 years, adults 65 and older, and those with immunocompromising conditions. June 16, 2023
FDA approved Abrysvo (Pfizer) RSV (respiratory syncytial virus) vaccine, approved for individuals 60 and older. May 31, 2023
End of COVID-19 Public Health Emergency. May 11, 2023
FDA approved the first RSV (respiratory syncytial virus) vaccine. Arexvy (GSK) was approved for individuals 60 and older. May 3, 2023
FDA authorized additional doses of Pfizer-BioNTech COVID-19 vaccine, bivalent for ages 6 months through 4 years with immunocompromise who had previously received three 0.2 mL doses (Pfizer-BioNTech COVID-19 vaccine or Pfizer-BioNTech COVID-19 vaccine, bivalent). April 28, 2023
FDA approves Prevnar 20 (Pfizer) for infants and children, now approved for 6 weeks and older. April 27, 2023
CDC simplified COVID-19 vaccine recommendations to allow older and immunocompromised adults to get a second dose of the bivalent vaccine. April 19, 2023
FDA amended EUAs of Moderna and Pfizer-BioNTech COVID-19 bivalent mRNA vaccines. Bivalent vaccines were to be used for all doses given to individuals 6 months and older. Monovalent COVID-19 vaccines were no longer authorized for use in the United States. April 18, 2023
FDA authorized bivalent Pfizer-BioNTech COVID-19 vaccine as a booster dose for certain children 6 months through 4 years old. March 14, 2023
CDC released the 2023 recommended immunization schedule for children, adolescents, and adults. February 10, 2023
CDC expanded updated COVID-19 vaccines to include children 6 months through 5 years old. December 9, 2022
FDA authorized updated (bivalent) COVID-19 vaccines for children as young as 6 months old. December 8, 2022
ACIP recommended Priorix (GSK) as an additional option to prevent MMR according to existing vaccine recommendations and off-label uses. November 18, 2022
ACIP interim recommendations for using bivalent booster doses of COVID-19 vaccines. November 11, 2022
CDC allowed 18-year-olds and older the option to receive a Novavax monovalent booster instead of an updated (bivalent) Pfizer-BioNTech or Moderna booster if they have completed primary series vaccination but have not previously received a COVID-19 booster. October 19, 2022
FDA issued an EUA for the Novavax COVID-19 vaccine to provide a first booster dose to individuals 18 and older for whom an FDA-authorized mRNA bivalent COVID-19 booster vaccine was not accessible or clinically appropriate and to individuals 18 and older who elect to receive the Novavax COVID-19 vaccine. October 19, 2022
CDC recommended expanding the use of updated (bivalent) COVID-19 vaccines (Pfizer-BioNTech for children 5–11 years old, Moderna for children and adolescents 6–11 years old) to children 5–11 years old. October 12, 2022
FDA amended EUAs to authorize bivalent formulations of COVID-19 vaccines (Pfizer-BioNTech for children 5–11 years old, Moderna for children and adolescents 6–17 years old) for use as a single booster dose two months after a primary series or booster dose. October 12, 2022
FDA approved previously licensed Boostrix (GSK) as the first vaccine specifically for use during the third trimester of pregnancy to prevent pertussis (whooping cough) in infants younger than 2 months old. October 7, 2022
ACIP recommendation for using the cholera (Vaxchora, Emergent Biosolutions) vaccine. September 30, 2022
ACIP recommended the use of PCV15 as an option for pneumococcal vaccination for children under 19 years old, using current PCV13 dosing and schedules. September 16, 2022
The United States joined a list of 30 countries that meet WHO criteria for circulating vaccine-derived poliovirus (cVDPV). September 13, 2022
CDC recommended the first updated bivalent COVID-19 booster. September 1, 2022
FDA amended EUAs of Moderna and Pfizer-BioNTech COVID-19 vaccines to authorize bivalent formulations for use as a single booster dose at least two months following primary or booster vaccination. August 31, 2022
CDC released ACIP recommendations for using influenza vaccines for the 2022-23 influenza season. August 26, 2022
CDC recommended Novavax COVID-19 vaccine for adolescents 12–17 years old as a primary series option. August 22, 2022
FDA expanded age indication of Novavax COVID-19 vaccine, adjuvanted EUA to include individuals 12 years and older. August 19, 2022
FDA issued EUA of JYNNEOS (Bavarian Nordic A/S) allows subcutaneous administration to those under 18 and intradermal administration of vaccine to 18-year-olds and older to increase vaccine supply. August 9, 2022
FDA issued EUA for Novavax, COVID-19 vaccine adjuvanted to provide a two-dose primary series to individuals 18 and older. August 9, 2022
ACIP interim recommendation for using Novavax COVID-19 vaccine in adults 18 and older. July 13, 2022
FDA expanded age indication of Comirnaty (Pfizer-BioNTech) vaccine to include adolescents 12–15 years old for a two-dose primary series (the EUA remained in effect for additional doses for immunocompromised for 12 years and older and for booster doses). July 8, 2022
ACIP published interim recommendations for using Moderna and Pfizer-BioNTech COVID-19 vaccines in children 6 months to 5 years old. June 28, 2022
CDC endorsed ACIPʼs recommendation of Modernaʼs COVID-19 vaccine for those 6-17 years old, in addition to its already recommended use in children 6 months through 5 years old and adults 18 and older. June 24, 2022
CDC endorsed the ACIP recommendation that all children 6 months through 5 years old should receive a Moderna or Pfizer-BioNTech COVID-19 vaccine. All children, including children who have already had COVID-19, should get vaccinated. June 18, 2022
FDA amended Moderna COVID-19 EUA to include the use of the vaccine in individuals 6 months through 17 years old. June 17, 2022
FDA amended Pfizer-BioNTech COVID-19 EUA to include the use of the vaccine in individuals 6 months through 4 years old. June 17, 2022
FDA approved expanded age recommendation for Vaxneuvance (PCV15, Merck) pneumococcal vaccine to individuals 6 weeks and older. June 17, 2022
FDA approved the Priorix (GSK) (Measles, Mumps, and Rubella vaccine, Live) vaccine for the prevention of measles, mumps, and rubella in individuals 12 months and older. June 3, 2022
ACIP published recommendations for using Jynneos (smallpox and monkeypox, now known as Mpox) vaccine, live, nonreplicating) for preexposure vaccination of persons at risk for occupational exposure to orthopoxviruses. May 27, 2022
CDC recommended that children 5–11 years old should receive a booster shot five months after their initial Pfizer-BioNTech vaccination series, strengthens its recommendation that those 12 and older who are immunocompromised and those 50 and older should receive a second booster dose at least four months after their first. May 19, 2022
FDA amended the EUA and expanded eligibility for Pfizer-BioNTech COVID-19 vaccine booster dose to children 5–11 years old. May 17, 2022
ACIP updated rabies recommendations: use of modified preexposure prophylaxis vaccination schedule to prevent human rabies. May 6, 2022
ACIP recommended universal hepatitis B vaccination in adults 19–59 years old. April 1, 2022
FDA authorized and CDC recommended a second COVID-19 vaccine booster for certain individuals. March 29, 2022
FDA amended EUA and authorizes additional presentation of Moderna COVID-19 vaccine for booster vaccination doses (dark blue caps with purple border labels). March 29, 2022
ACIP recommended using the Moderna COVID-19 vaccine in adults 18 and older, with considerations for extended intervals for primary series doses of mRNA COVID-19 vaccines. March 18, 2022
ACIP recommended two additional groups for the use of the Ebola vaccine. February 22, 2022
CDC released the 2022 recommended immunization schedules for children and adolescents, as well as for adults, on its website. February 18, 2022
FDA approved COVID-19 vaccine Spikevax (Moderna) for individuals 18 and older. (The EUA remained in effect for the third primary series dose and booster dose.) January 31, 2022
CDC published ACIP updated recommendations for adults to use PCV15 and PCV20 pneumococcal vaccines. January 28, 2022
CDC published ACIP recommendations for using recombinant zoster (shingles) vaccine in immunocompromised adults. January 21, 2022
CDC published ACIP updated interim recommendations for using the Janssen (Johnson & Johnson) COVID-19 vaccine. January 21, 2022
FDA shortened the interval to a booster dose of Moderna COVID-19 vaccine to five months. January 7, 2022
CDC endorsed ACIPʼs recommendation to expand eligibility of booster doses to those 12–15 years old. CDC recommends that all adolescents 12–17 years old should receive a booster shot five months after their initial Pfizer-BioNTech vaccination series. January 5, 2022
CDC recommended Pfizer-BioNTech booster five months after completing the primary series. CDC recommends moderately or severely immunocompromised children 5–11 years old receive an additional primary dose of the Pfizer-BioNTech COVID-19 vaccine 28 days after their second shot. January 4, 2022
FDA amended EUA Pfizer-BioNTech vaccine (COVID-19); expanded use of a single booster dose to include 12–15-year-olds, shortened time to booster dose to at least five months, and allowed for third primary dose for certain immunocompromised children 5–11 years old. January 3, 2022
CDC published ACIP recommendations for using the dengue vaccine. December 17, 2021
FDA revised Janssen fact sheets to include contraindications and risks of TTS (thrombosis and thrombocytopenia syndrome). December 14, 2021
FDA and CDC expanded Pfizer-BioNTech booster recommendations to 16–17-year-olds. December 9, 2021
FDA approved PreHevbrio (VBI Vaccines) for adults 18 and older. November 30, 2021
CDC recommended that all 18-year-olds and older get a COVID-19 booster. November 29, 2021
FDA amended EUAs for COVID-19 mRNA vaccines for using booster doses for 18-year-olds and older. November 19, 2021
CDC published ACIP interim recommendations for using Pfizer-BioNTech COVID-19 vaccine in children 5–11 years old. November 5, 2021
FDA authorized EUA for Pfizer-BioNTech COVID-19 vaccine for children 5–11 years old. October 29, 2021
CDC published ACIP recommendations for COVID-19 additional primary and booster doses. October 29, 2021
FDA amended EUAs of all COVID-19 vaccines, allowing for booster doses, and mix-and-match doses in eligible individuals. October 20, 2021
FDA approved expanded age indication for Flucelvax Quad (Seqirus), licensed for 6-month-olds and older. October 14, 2021
FDA authorized booster dose of Pfizer-BioNTech COVID-19 vaccine for 65-year-olds and older, 18–64-year-olds at high risk of severe COVID-19, and 18–64-year-olds who have institutional or occupational exposure to SARS-CoV-2. September 22, 2021
CDC released ACIP recommendations on using influenza vaccines for the 2021–22 influenza season. August 27, 2021
FDA approved the first COVID-19 vaccine Comirnaty (Pfizer-BioNTech) for individuals 16 and older. (The EUA remains in effect for individuals 12 and older and for the third dose for immunocompromised individuals 12 and older). August 23, 2021
FDA approved Ticovac (Pfizer), a vaccine to prevent tick-borne encephalitis (TBE) vaccine in individuals 1 year old and older. August 13, 2021
FDA amended the emergency use authorizations (EUAs) for Pfizer-BioNTech and Moderna COVID-19 vaccines to allow the use of an additional dose in certain immunocompromised individuals. August 12, 2021
FDA expanded the indication of the Shingrix vaccine to include adults 18 and older who are or will be at increased risk of zoster (shingles) due to immunodeficiency or immunosuppression caused by known disease or therapy. July 23, 2021
FDA approved Vaxneuvance (Merck & Co.) pneumococcal 15-valent conjugate vaccine for adults 18 and older. July 16, 2021
FDA revised fact sheets for Janssen COVID-19 vaccine (Johnson & Johnson), adding Guillain-Barré syndrome (GBS) warning and revising thrombocytopenia warning. July 8, 2021
Update from ACIP: Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients. July 6, 2021
FDA revised EUA mRNA (Pfizer and Moderna) patient and provider fact sheets regarding the suggested increased risks of myocarditis and pericarditis following vaccination. June 25, 2021
FDA approved Prevnar 20 (Pfizer) pneumococcal 20-valent conjugate vaccine for adults 18 and older. June 9, 2021
ACIP interim recommendations for the Pfizer-BioNTech COVID-19 vaccine in adolescents 12–15 years old. May 14, 2021
FDA expanded the EUA of the Pfizer-BioNTech COVID-19 vaccine to include adolescents 12–15 years old. May 10, 2021
Updated recommendation from ACIP for the Janssen (Johnson & Johnson) COVID-19 vaccine after reports of thrombosis with thrombocytopenia syndrome (TTS) among vaccine recipients. April 27, 2021
CDC and FDA lifted the recommended pause of use of the Johnson & Johnson (Janssen) COVID-19 vaccine in the United States after a review by ACIP. The use of the Janssen vaccine should resume. EUA fact sheets for Johnson & Johnson (Janssen) COVID-19 vaccine revised. April 23, 2021
CDC and FDA recommended a pause in the use of the Janssen (Johnson & Johnson) COVID-19 vaccine in the United States out of an abundance of caution. A CDC Health Alert Network (HAN) was issued with recommendations. April 13, 2021
CDC published ACIP interim recommendations for the Janssen (Johnson & Johnson) COVID-19 vaccine. March 2, 2021
FDA issued emergency use authorization (EUA) for Janssen (Johnson & Johnson) COVID-19 vaccine. February 27, 2021
CDC released the 2021 recommended immunization schedules for children and adolescents, as well as for adults, on its website. February 12, 2021
CDC published ACIP recommendations for the Ebola vaccine. January 8, 2021
CDC published ACIP interim recommendations for the Moderna COVID-19 vaccine. December 20, 2020
FDA issues emergency use authorization (EUA) for the Moderna COVID-19 vaccine. December 18, 2020
CDC published ACIP interim recommendations for the Pfizer-BioNTech COVID-19 vaccine. December 13, 2020
FDA issued emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine. December 11, 2020
CDC published ACIP recommendations for meningococcal vaccines. September 25, 2020
CDC released ACIP recommendations for influenza vaccines for the 2020–21 influenza season. August 21, 2020
CDC published updated ACIP recommendations for hepatitis A vaccines. July 3, 2020
FDA expanded the license for Gardasil 9 to include preventing oropharyngeal and other head-and-neck cancers caused by relevant HPV types. June 24, 2020
FDA approved MenQuadfi (MenACWY) conjugate vaccine for the prevention of invasive meningococcal disease caused by serogroups A, C, W, and Y in individuals aged 2 and older. April 23, 2020
Declaration of COVID-19 Public Health Emergency. March 13, 2020
FDA approved the Fluad Quadrivalent (influenza vaccine, adjuvanted; Seqirus) for adults 65 and older. February 21, 2020
CDC released the 2020 recommended immunization schedules for children and adolescents, as well as for adults, on its website. February 3, 2020
CDC (January 30, 2020) and WHO (February 1, 2020) declared public health emergencies regarding the 2019 novel coronavirus. February 1, 2020
CDC published updated ACIP recommendations for Td and Tdap vaccines. January 24, 2020
FDA approved Ervebo (Ebola Zaire vaccine, live; Merck), the first U.S.-licensed vaccine for the prevention of Ebola virus disease. December 19, 2019
CDC published ACIP recommendations for the BioThrax (Emergent BioSolutions) anthrax vaccine, adsorbed. December 13, 2019
CDC published updated ACIP recommendations for PCV13 and PPSV23 pneumococcal vaccines for adults 65 and older. November 22, 2019
FDA approved the Fluzone High-Dose Quadrivalent (Sanofi Pasteur) for adults 65 and older—which will be available for the 2020-21 influenza season. November 4, 2019
CDC released ACIP recommendations for influenza vaccines for the 2019–20 influenza season. August 28, 2019
CDC published updated ACIP recommendations for HPV (human papillomavirus) vaccines in adults. August 16, 2019
AAFP, AAP, ACHA, ACOG, APhA, SAHM, and IAC released a ” Dear Colleague ” letter stressing the importance of 16-year-old immunization visits . August 1, 2019
CDC published ACIP recommendations for Japanese encephalitis vaccines. July 19, 2019
CDC published ACIP recommendations for the hepatitis A vaccine in persons experiencing homelessness. February 15, 2019
CDC released the 2019 U.S. recommended immunization schedules for children and adolescents, as well as for adults, on its website. February 5, 2019
FDA approved using the 0.5 mL dose of Sanofiʼs Fluzone Quadrivalent influenza vaccine to include children 6-35 months old. January 23, 2019
FDA approved the expanded use of Sanofiʼs Adacel Tdap vaccine for a second dose in people 10-64 years old. January 14, 2019
FDA approved Vaxelis (MCM Vaccine Co), a new combination DTaP-IPV-Hib-HepB vaccine for children 6 weeks to 4 years old. December 21, 2018
ACIP published updated recommendations for the hepatitis A vaccine for pre- and post-exposure prophylaxis for international travel. November 7, 2018
The American Dental Association adopted a policy to support the use and administration of the HPV vaccine for the prevention of oral HPV infection. October 25, 2018
FDA approved expanded age indication for the Seqirus Afluria influenza vaccine to include children 6 months through 59 months old. October 8, 2018
FDA announced the approval of the expanded use of the Merck Gardasil 9 (HPV9, HPV) vaccine to include adults 27-45 years old. October 5, 2018
CDC published ACIPʼs 2018–19 influenza vaccination recommendations. August 24, 2018
CDC published ACIPʼs recommendations for using quadrivalent live attenuated influenza vaccine (LAIV4) in the 2018–19 influenza season. June 8, 2018
The American College of Obstetricians and Gynecologists issued a committee opinion on maternal immunization. June 2018
CDC released information about a new rapid rabies test that could save lives and lead to fewer unnecessary rabies shots. May 16, 2018
CDC published a comprehensive summary of previously published ACIP recommendations for the prevention of tetanus, diphtheria, and pertussis in the United States. April 27, 2018
CDC published ACIP recommendations for the hepatitis B vaccine with a novel adjuvant (Heplisav-B). April 20, 2018
The American College of Obstetricians and Gynecologists released a committee opinion on influenza vaccination in pregnancy. April 2018
CDC published the 2018 U.S. recommended immunization schedule for 0-to-18-year-olds. February 6, 2018
CDC published the 2018 U.S. recommended adult immunization schedule. February 6, 2018
CDC published ACIP recommendations for herpes zoster (shingles) vaccines. January 26, 2018
CDC published updated ACIP recommendations for the prevention of hepatitis B virus infection. January 12, 2018
CDC published ACIP recommendations for a third dose of MMR during a mumps outbreak. January 12, 2018
FDA approved expanded pediatric age indication for the Fluarix Quadrivalent influenza vaccine. January 11, 2018
FDA licensed Heplisav-B, the new hepatitis B vaccine from Dynavax, for adults 18 and older. November 9, 2017
FDA licensed Shingrix, the new zoster (shingles) vaccine from GlaxoSmithKline, for adults 50 and older. October 20, 2017
CDC published updated dosing instructions for hepatitis A prophylaxis with immune globulin. September 15, 2017
FDA expanded the licensure of the Afluria quadrivalent (Seqirus) influenza vaccine to include individuals aged 5 and older. August 31, 2017
CDC published ACIP 2017-18 influenza vaccination recommendations. August 25, 2017
AAP issued a policy stating that newborns should routinely receive the hepatitis B vaccine within 24 hours of birth. August 2017
CDC published a vaccine information statement (VIS) for cholera. July 6, 2017
CDC and FDA announced a new Vaccine Adverse Event Reporting System (VAERS) website and reporting form. June 30, 2017
CDC published ACIPʼs updated recommendations for the Trumenba meningococcal serogroup B vaccine. May 19, 2017
CDC published ACIP recommendations for the cholera vaccine. May 12, 2017
CDC published ACIP recommendations titled “General Best Practice Guidelines for Immunization” to replace the 2011 “General Recommendations on Immunization.” April 20, 2017
CDC published the 2017 U.S. recommended immunization schedules for 0 to 18-year-olds; including the new “16-year-old vaccination” column. February 7, 2017
CDC published the 2017 U.S. recommended adult immunization schedule. February 7, 2017
CDC published ACIPʼs recommendations on the 2-dose HPV vaccine series for younger adolescents. December 16, 2016
FDA approved extending the age range for the FluLaval Quadrivalent influenza vaccine to include children 6–35 months old. November 18, 2016
CDC published ACIP recommendations for meningococcal conjugate vaccines in HIV-infected persons. November 4, 2016
PAHO and WHO announced measles elimination in the Americas. September 27, 2016
CDC published 2016-17 influenza vaccination recommendations. August 26, 2016
AAP released a new policy statement urging states to eliminate all non-medical exemptions to vaccine requirements. August 2016
FDA extended the age indication for the PCV13 (Prevnar 13) pneumococcal vaccine to include adults 18-49 years old. July 11, 2016
ACIP voted that live attenuated influenza vaccine (LAIV) should not be used during the 2016-17 flu season. June 22, 2016
FDA approved revisions in the package insert for YF-Vax (yellow fever) to reflect changes to International Health Regulations and WHO/ACIP recommendations. June 15, 2016
FDA approved Vaxchora for the prevention of cholera. June 10, 2016
FDA approved changes to the vaccine administration schedule for the Trumenba (meningococcal) vaccine. April 14, 2016
The National Vaccine Program Office releases a National Adult Immunization Plan. February 5, 2016
2016 U.S. recommended immunization schedules for 0-to-18-year-olds and “catch up” published in MMWR . February 5, 2016
FDA approved Hiberix for the full Hib vaccine series. January 14, 2016
FDA expanded Gardasil 9 (HPV) licensure to include males 16-26 years old. December 14, 2015
FDA approved a new injectable influenza vaccine, Fluad, for people 65 and older. November 24, 2015
ACIP published recommendations for serogroup B meningococcal vaccines in adolescents and young adults. October 23, 2015
CDC published updated ACIP recommendations regarding the intervals between PCV13 and PPSV23 pneumococcal vaccines for immunocompetent adults 65 and older. September 4, 2015
WHO published “Recommendations on Vaccine Hesitancy” in a special issue of the journal Vaccine . August 14, 2015
ACIP published recommendations for yellow fever booster doses. June 19, 2015
ACIP published recommendations for serogroup B meningococcal vaccines in people 10 and older at increased risk for serogroup B meningococcal disease. June 12, 2015
American Medical Association adopted a new policy supporting ending non-medical vaccine exemptions, including those for healthcare professionals. June 8, 2015
The Pan American Health Organization declared rubella eliminated in the Americas. April 29, 2015
CDC published ACIP recommendations for a 9-valent HPV vaccine. March 27, 2015
CDC published new ACIP recommendations for typhoid vaccination. March 27, 2015
FDA approved Quadracel, a new combination DTaP+IPV vaccine for children 4-6 years old. March 24, 2015
CDCʼs Health Alert Network issued a health advisory about a multi-state outbreak of measles linked to Disneyland. January 23, 2015
FDA approved Bexsero, the second vaccine licensed in the United States to prevent serogroup B meningococcal disease. January 23, 2015
FDA approved Rapivab to treat influenza infection. December 19, 2014
FDA approved quadrivalent formulation of Fluzone Intradermal inactivated influenza vaccine. December 11, 2014
FDA approved the Gardasil 9 (Merck) 9-valent HPV vaccine in the United States. December 10, 2014
FDA approved Trumenba in the United States to prevent serogroup B meningococcal disease. October 29, 2014
CDC published ACIP recommendations for PCV13 and PPSV23 pneumococcal vaccines in adults 65 and older. September 19, 2014
CDC published ACIPʼs recommendations for the MenACWY-CRM vaccine in children 2–23 months old at increased risk for meningococcal disease. June 20, 2014
WHO director-general declared the 2014 international spread of wild poliovirus a Public Health Emergency of International Concern. May 5, 2014
CDC report showed a 20-year U.S. immunization program spares millions of children from diseases. April 25, 2014
FDA lowered the age of licensure for Adacel (Tdap) vaccine administration from age 11 to 10 years old. March 24, 2014
CDC published ACIP recommendations for the prevention and control of Hib ( Haemophilus influenzae type b) disease. February 28, 2014
CDC published guidance for hepatitis B virus protection and postexposure management of healthcare personnel. December 20, 2013
CDC published new recommendations for the Japanese encephalitis vaccine in children. November 15, 2013
The National Vaccine Advisory Committee released the revised ”Standards for Adult Immunization Practice.” September 10, 2013
FDA extended the FluLaval IIV (GlaxoSmithKline) age range to include children and teens 3–17 years old; licenses quadrivalent FluLaval influenza vaccine product. August 16, 2013
FDA expanded the age indication for the Menveo (Novartis) meningococcal vaccine to include infants and toddlers 2–23 months old. August 1, 2013
CDC issued updated recommendations for VariZIG immune globulin for varicella (chicken pox) postexposure prophylaxis. July 19, 2013
CDC issued recommendations for PCV and PPSV pneumococcal vaccination of children with immunocompromising conditions. June 28, 2013
ACIP voted to recommend the FluBlok influenza vaccine for people 18–49 years old with an egg allergy. June 20, 2013
CDC published recommendations for preventing measles, rubella, congenital rubella syndrome, and mumps. June 14, 2013
FDA approved Fluzone (Sanofi Pasteur) as the third quadrivalent influenza vaccine licensed for U.S. use. June 7, 2013
A booster dose of the yellow fever vaccine is not needed, according to WHO. A single dose of the vaccine provides long-term protection from yellow fever. May 17, 2013
ACIP recommended a dose of the Tdap vaccine during each pregnancy. February 22, 2013
UNICEF and WHO condemned attacks on polio vaccination workers in Nigeria. February 8, 2013
FDA approved the Prevnar 13 pneumococcal vaccine in older children and teens 6-17 years old. January 25, 2013
The Institute for Safe Medication Practices (ISMP) launched a new Vaccine Error Reporting Program . December 18, 2012
FDA approved quadrivalent formulation of the Fluarix (GlaxoSmithKline) inactivated influenza vaccine. December 12, 2012
FDA approved the first seasonal influenza vaccine manufactured using cell culture technology (Flucelvax, Novartis). November 20, 2012
ACIP voted to recommend HibMenCY (Menhibrix, GlaxoSmithKline), a new combination (meningococcal and Hib) vaccine, in infants at increased risk for meningococcal disease. October 24, 2012
ACIP voted to recommend that pregnant women receive a dose of Tdap during each pregnancy irrespective of the patient’s prior Tdap history. October 24, 2012
FDA approved HibMenCY (Menhibrix, GlaxoSmithKline), a new combination (meningococcal and Hib) vaccine for infants. June 24, 2012
FDA expanded licensure of PCV13 (pneumococcal conjugate vaccine) to include adults 50 and older. June 7, 2012
The U.S. Department of Health and Human Services (HHS) Office of the Inspector General (OIG) released a report titled “Vaccines for Children (VFC) Program: Vulnerabilities in Vaccine Management.” June 5, 2012
The United Nations Foundation launched the Shot@Life campaign. April 1, 2012
FDA expanded the use of the Prevnar 13 (PCV13, Pfizer) pneumococcal vaccine to include people 50 and older. December 30, 2011
ACIP recommended all 11-to-12-year-old males get vaccinated against HPV. October 25, 2011
Addition of history of intussusception as a contraindication for rotavirus vaccination. October 21, 2011
A national survey indicated HPV vaccine rates trail other teen vaccines. August 25, 2011
The Institute of Medicine issued a report titled “Review of Adverse Effects of Vaccines.” Overall, the committee concludes that few health problems are caused by or clearly associated with vaccines. August 25, 2011
FDA approved Boostrix (Tdap, GlaxoSmithKline) to prevent tetanus, diphtheria, and pertussis in older people. July 8, 2011
CDC hailed vaccinations as one of 10 public health achievements of the first decade of the 21st century in the Morbidity and Mortality Weekly Report (MMWR) . May 19, 2011
FDA approved the first vaccine (Menactra, meningococcal conjugate vaccine, Sanofi Pasteur) to prevent meningococcal disease in infants and toddlers. April 22, 2011
HHS released the U.S. National Vaccine Plan, which covers activities, goals, and priorities for 2010-15. February 15, 2011
FDA approved the Gardasil HPV vaccine to include the indication for the prevention of anal cancer. December 22, 2010
WHO declared an end to the 2009 H1N1 influenza pandemic. August 11, 2010
The first smallpox vaccine for certain immune-compromised populations was delivered under Project BioShield. July 10, 2010
ACIP recommended a reduced (4-dose) vaccine schedule for PEP to prevent human rabies. March 19, 2010
FDA approved licensure of the pneumococcal 13-valent conjugate vaccine (PCV13), which offers broader protections against Streptococcus pneumoniae infections. February 24, 2010
FDA approved licensure of Menveo (Novartis), a meningococcal conjugate vaccine for people 11-55 years old. February 19, 2010
WHO hailed the new Gates Foundation support ($10 billion) as the “Decade of Vaccines.” January 29, 2010
ACIP recommended universal influenza vaccination for those 6 months and older. February 24, 2010
FDA approved the pneumococcal 13-valent conjugate vaccine (Prevnar 13), which offers broader protection against Streptococcus pneumoniae . February 24, 2010
FDA approved the high-dose inactivated influenza vaccine (Fluzone High-Dose) for people 65 and older. December 23, 2009
CDC issued Health Advisory 2009 H1N1 Pandemic Update: Pneumococcal vaccination recommended to help prevent secondary infections. November 16, 2009
Merck announced that the company will not resume production of monovalent measles, mumps, and rubella vaccines. October 21, 2009
FDA approved the new HPV vaccine (Cervarix, GlaxoSmithKline) for the prevention of cervical cancer. October 16, 2009
FDA approved a new indication for Gardasil to prevent genital warts in men and boys. October 16, 2009
FDA approved four vaccines against the 2009 H1N1 Influenza virus. September 15, 2009
WHO and ACIP issued recommendations for H1N1 influenza vaccines. July 1, 2009
HHS announced an advanced development contract for a new way to make influenza vaccine. June 23, 2009
Dr. Margaret Chan, director-general of WHO, declared the world was now at the start of the 2009 influenza pandemic. June 11, 2009
HHS directed $1 billion toward the development of a vaccine for novel influenza A (H1N1). May 22, 2009
ACIP voted to recommend hepatitis A vaccination for close contact with international adoptees from countries with high and intermediate endemicity. March 16, 2009
Vaccine Court ruled that the MMR vaccine, when administered with thimerosal-containing vaccines, does not cause autism. February 12, 2009
HHS awarded a $487 million contract to Novartis Vaccines and Diagnostics to build a facility to manufacture cell-based influenza vaccine. January 15, 2009
FDA approved changes in the schedule for administering the BioThrax (Emergent BioSolutions) anthrax vaccine and its route of administration. December 11, 2008
FDA approved an expanded indication for the Boostrix Tdap vaccine in people 10-64 years old. December 4, 2008
The National Quality Forum included the hepatitis B birth dose among its consensus standards for improving health care for mothers and newborns. October 27, 2008
FDA approved a new DTaP-IPV vaccine (Kinrix) for children 4-6 years old. June 24, 2008
FDA approved Pentacel (Sanofi Pasteur), a new combination DTaP-IPV-Hib vaccine for children 6 weeks to 4 years old. June 20, 2008
FDA approved Sanofi Pasteurʼs Tenivac tetanus and diphtheria toxoids adsorbed for adults 60 and older. In the original licensure, the age indication was for persons 7-59 years old. June 5, 2008
FDA approved a new rotavirus vaccine (Rotarix) in the United States. Rotarix was a liquid given in a two-dose series to infants at 6–24 weeks old. April 3, 2008
CDC issued a Health Advisory in response to widespread measles outbreaks in the United States. April 2, 2008
CDC updated its recommendations for administering a combination MMRV vaccine. March 14, 2008
CDC announced it has begun distributing the new-generation smallpox vaccine, ACAM2000 (Acambis, Cambridge, MA), to civilian laboratory personnel, the military, and state public health preparedness programs. February 29, 2008
ACIP voted to expand influenza recommendations to include vaccination for children 6 months to 18 years old. February 27, 2008
CDC published an updated recommendation for meningococcal vaccination for at-risk children 2-10 years old in MMWR . December 7, 2007
ACIP voted to recommend using FluMist, the live attenuated influenza vaccine (LAIV; nasal-spray formulation), to include children 2-5 years old. October 26, 2007
CDC published updated recommendations for the prevention of hepatitis A virus infection after exposure and before international travel in MMWR . October 19, 2007
FDA approved the use of Menactra, a bacterial meningitis vaccine, in children 2-10 years old. October 18, 2007
FDA approved Afluria, a new inactivated influenza vaccine for people 18 and older. September 28, 2007
FDA approved the FluMist nasal-spray influenza vaccine in children 2-5 years old. September 19, 2007
CDC notified MMWR readers of revised recommendations to vaccinate all persons 11-18 years old with MCV4 (meningococcal conjugate vaccines, quadrivalent) at the earliest opportunity. August 10, 2007
MMWR notified readers that revised International Health Regulations are now in effect for the United States. July 20, 2007
HHS announced a plan to provide $175 million to assist states in pandemic influenza preparedness efforts. July 17, 2007
ACIP voted to recommend routine use of meningococcal conjugate vaccine in adolescents 11-18 years old. June 27-28, 2007
HHS awarded $132.5 million to Sanofi Pasteur and MedImmune over five years to retrofit existing domestic vaccine manufacturing facilities on a cost-sharing basis and to provide warm-base operations for manufacturing pandemic influenza vaccines. June 15, 2007
FDA approved an accelerated dosing schedule for Twinrix (hepatitis A and hepatitis B vaccine). The schedule consists of three doses given within three weeks followed by a booster dose at 12 months old (0, 7, 21-30 days, 12 months). March 28, 2007
FDA approved the first U.S. vaccine for humans against the avian influenza virus H5N1. April 17, 2007
FDA licensed the refrigerator formulation of FluMist influenza vaccine. January 7, 2007
ACIP recommended a second dose of varicella (chickenpox) vaccine for children. June 29, 2006
FDA licensed the first vaccine developed to prevent cervical cancer (Gardasil by Merck & Co.), precancerous genital lesions, and genital warts due to human papillomavirus (HPV) types 6, 11, 16, and 18. June 8, 2006
FDA licensed a new vaccine to reduce the risk of shingles (herpes zoster) in the elderly. The vaccine (Zostavax by Merck & Co.) was approved for people 60 and older. May 25, 2006
VariZIG, a new immune globulin product for postexposure prophylaxis of varicella (chickenpox), was available under an Investigational New Drug Application Expanded Access Protocol. February 24, 2006
The rotavirus vaccine, live, oral, pentavalent (RotaTeq by Merck) was licensed for infants 6–32 weeks old. February 3, 2006
A final order on the anthrax vaccine was issued by the FDA, stating that the licensed anthrax vaccine is safe and effective for the prevention of anthrax disease, regardless of the route of exposure. December 19, 2005
FDA approved lowering the age limit to 12 months old for the remaining U.S.-licensed hepatitis A vaccines in the United States (Havrix by GlaxoSmithKline). October 18, 2005
A new Federal Medicare rule became effective requiring all long-term care facilities to offer annual vaccination for influenza and one-time vaccination for pneumococcal disease to all residents as a condition of participation in Medicare. October 7, 2005
A vaccine that combined the measles, mumps, rubella, and varicella (chickenpox) antigens (Proquad by Merck) was licensed. The vaccine was indicated for children 12 months to 12 years old. September 6, 2005
An inactivated, injectable influenza vaccine (Fluarix by GlaxoSmithKline) was licensed. The vaccine was indicated for adults 18 and older. August 31, 2005
FDA approved lowering the age limit to 12 months old for one of the two licensed hepatitis A vaccines (Vaqta by Merck). August 11, 2005
FDA licensed a second Tdap vaccine (Adacel by Sanofi Pasteur) for persons 11-64 years old. June 10, 2005
An acellular pertussis vaccine combined with the adult formulation of tetanus and diphtheria (Tdap: Boostrix by GSK) was licensed for use as an active booster in persons 10-18 years old. This product became the first licensed acellular pertussis-containing vaccine with an indication for adolescents. May 3, 2005
DHHS awards a contract for $97 million to Sanofi Pasteur to develop cell culture-based influenza vaccines for the United States. April 3, 2005
CDC announced that rubella was no longer endemic in the United States. March 21, 2005
The first meningococcal polysaccharide (Serogroups A, C, Y, and W-135) diphtheria toxoid conjugate vaccine (Menactra by Sanofi Pasteur) was licensed. This marked the first meningococcal vaccine that was immunogenic and indicated for children younger than 2 years old. January 14, 2005
A significant shortage of influenza vaccines occurred in the United States. August-October 2004
History: On August 25, 2004, as a result of routine testing required by the FDA, Chiron Corporation, located in the U.K. and one of two suppliers of inactivated influenza vaccine for the United States, identified bacterial contamination in a limited number of lots (approx 4.5 million doses) of its influenza vaccine. Chiron was expected to produce between 46 million and 48 million doses of vaccine for the United States as part of a total vaccine supply of about 100 million doses. On Oct 4, 2004, authorities in the U.K. suspended the company’s license for 3 months. On Oct 16, 2004, FDA announced that none of the influenza vaccines manufactured by Chiron for the U.S. market was safe for use. U.S. authorities recommended the allocation of vaccines to those at highest risk of complications from influenza.
The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institute of Health (NIH), awarded a new license agreement for RotaShield, an oral rotavirus vaccine created by NIAID scientists in the 1980s. The license was awarded to BIOVIRx of Minneapolis, which planned the global commercialization of RotaShield. May 4, 2004
Contracts were awarded to Aventis Pasteur and to Chiron to develop a vaccine against the H5N1 avian influenza virus. May 2004
The eighth and final report of the Immunization Safety Review Committee was issued by the Institute of Medicine. The report concluded that the body of epidemiological evidence favors the rejection of a causal relationship between the MMR vaccine (and thimerosal-containing vaccines) and autism. 2004
Tetanus and diphtheria toxoids adsorbed for adult use (Decavac by Aventis Pasteur), preservative-free, were licensed. March 24, 2004
ACIP voted to recommend that children 6–23 months old be vaccinated annually against influenza, with implementation scheduled for the fall of 2004. October 15, 2003
$81 million was awarded by NIAID through four new contracts to support the development of candidate HIV vaccines. The awards are part of NIAID’s HIV Vaccine Design and Development Teams program, a public-private partnership seeking to accelerate HIV vaccine development. The contract recipients are AlphaVAx Human Vaccines (Durham, NC), Epimmune (San Diego, CA), Novavax (Columbia, MD), and Progenics Pharmaceuticals (Tarrytown, NY). 2003
The Project Bioshield Act of 2003 was enacted. It authorized more than $5 billion over 10 years to pay for the development of vaccines, drugs, and other biomedical countermeasures for biological, chemical, nuclear, and radiological weapons. The Act also empowered the Secretary of Health and Human Services to authorize the use of drugs and vaccines not licensed by the FDA in the event of an act of bioterrorism or other public health emergencies. 2003
The first nasally administered influenza vaccine (FluMist by MedImmune) was licensed. This live influenza A and B virus vaccine was indicated for healthy, non-pregnant persons 5-49 years old. June 17, 2003
A vaccine that combines diphtheria, tetanus, acellular pertussis, inactivated polio, and hepatitis B antigens (Pediarix by GlaxoSmithKline) was licensed. December 13, 2002
The European Region of the world was certified as polio-free. June 21, 2002
Diphtheria and tetanus toxoids and acellular pertussis vaccine (Daptacel by Aventis Pasteur) were licensed. May 14, 2002
GlaxoSmithKline announced that the company will no longer manufacture or distribute its Lyme disease vaccine, LYMErix, because of insufficient sales. February 25, 2002
President Bush announced a major smallpox vaccination program to protect the nation against the threat of potential biological warfare. The first phase of the program was targeted to 450,000 public health and healthcare personnel, however, the program stalls, with fewer than 40,000 healthcare workers and emergency responders vaccinated. December 13, 2002
The Bill and Melinda Gates Foundation earmarked $70 million to develop and produce meningococcal vaccines tailored for children and adults living in Africa. 2001
Following the events of September 11, 2001, IOM again called for the creation of a national vaccine authority “to advance the development, production, and procurement of new and improved vaccines of limited commercial potential but of global public health need.” 2001
A combined hepatitis A inactivated and hepatitis B (recombinant) vaccine (Twinrix by SmithKline Beecham) was licensed. May 11, 2001
A 7-valent pneumococcal conjugate vaccine (Prevnar by Wyeth Pharmaceuticals) was licensed for infants at 2, 4, 6, and 12-15 months of age to prevent invasive pneumococcal disease. Feb 17, 2000
Measles was declared no longer endemic in the United States following eradication campaigns that began in 1967. 2000
The Western Pacific Region of the world was certified as polio-free. 2000
Diphtheria and tetanus toxoids and acellular pertussis vaccine (Tripedia by Connaught) were licensed. Dec 9, 1999
ACIP voted to withdraw its recommendation for the rotavirus vaccine after investigating reports of intussusception (a type of bowel obstruction that occurs when one part of the intestine folds into an immediately adjoining part) in infants within the first two weeks of receipt of the vaccine. Intussusception was found to occur at a rate of approximately one case for every 5,000 children vaccinated. Oct 22, 1999
Wyeth Lederle Vaccines voluntarily withdrew Rotashield (rotavirus) from the market. Oct 16, 1999
A meningococcal group C conjugate vaccine was introduced into the routine schedule in the U.K. for infants, adolescents (15-17 years old), and college entrants. A second phase was planned to begin in January 2000, subject to the availability of the vaccine. Fall 1999
FDA approved a 2-dose schedule of hepatitis B vaccination for adolescents 11-15 years old using Recombivax HB (Merck) with the 10 µg (adult) dose at 0 and 4-6 months later. Sept 1999
ACIP recommended exclusive use of inactivated poliovirus vaccine (IPV) for infants and children. June 17, 1999
The Dale and Betty Bumpers Vaccine Research Center (VRC) was established at the National Institutes of Health to facilitate research in vaccine development. The primary focus of VRC research was to be the development of vaccines for AIDS. 1999
ACIP recommended DTaP vaccines for all five doses in the vaccination schedule, because local reactions, fever, and other systemic events are found to occur substantially less often after DTaP administration than after administration of whole-cell DTP. 1998
The Childrenʼs Vaccine Program was established at WHOʼs Program for Appropriate Technology in Health (PATH) with a $125 million gift from the Bill and Melinda Gates Foundation. The programʼs goal was to provide vaccines to children in the developing world and to accelerate the research and development of new vaccines. The first vaccines purchased were Hib, hepatitis B, rotavirus, and pneumococcal, which are not commonly used in the developing world. Aug 26, 1998
Lyme Disease Vaccine (Recombinant OspA), (LYMErix by SmithKline Beecham) was licensed for persons 15-70 years old. ACIP recommended that decisions on the use of the vaccine be made based on an assessment of individual risk, which includes the extent of both person-tick contact and geographic risk. Just 3+ years later, on February 25, 2002, GlaxoSmithKline announced they would no longer manufacture or distribute LYMErix because of insufficient sales. Dec 21, 1998
Rotavirus vaccine, live, oral, tetravalent (RotaShield by Wyeth) was licensed for infants at 2, 4, and 6 months old. Aug 31, 1998
Diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (Certiva by North American Vaccine) were licensed for primary and booster immunization of infants and children (except as a fifth dose in children who previously received four doses of DTaP). July 29, 1998
The first vaccine for the prevention of HIV/AIDS (Aidsvax) enters Phase III trial, the first large-scale human trial of an HIV vaccine. The trial involved more than 5,400 volunteers from the United States, Canada, and the Netherlands, the majority of whom were men who have sex with men. Preliminary results from the trial AIDS VAX (VaxGen) vaccine in early 2003 showed the HIV vaccine appeared to show a protective effect among non-Caucasian populations, especially African Americans, although sample sizes are small. However, for the majority of the participants, who are Caucasians, the effect of the vaccine was minimal. 1998
The FDA Modernization Act (FDAMA) was signed into law, amending the Food, Drug, and Cosmetic Act and the Public Health Service Act to modernize the regulation of food, medical products, and cosmetics. FDAMA initiatives include measures to modernize the regulation of biological products. Specifically, changes include eliminating the need for the establishment of license applications, streamlining the approval processes for manufacturing changes, and reducing the need for environmental assessment as part of a product application. Nov 21, 1997
ACIP recommends booster doses of the pneumococcal polysaccharide vaccine after five years for persons at the highest risk of disease. 1997
The rabies vaccine (RabAvert by Chiron Behring) was licensed. Oct 20, 1997
Diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (Infanrix by SmithKline Beecham) are licensed for the first four doses of the series. Jan 29, 1997
ACIP recommends adopting a sequential series of two doses of IPV followed by two doses of OPV for all infants and children to decrease the rare occurrences of vaccine-associated paralytic poliomyelitis (VAPP) that were noted following the administration of the live oral poliovirus vaccine. Jan 1997
Diphtheria and tetanus toxoids and acellular pertussis vaccine (Acel-Imune by Lederle) are licensed for use as the first through fifth doses in the series. Dec 30, 1996
A combined Haemophilus influenzae type b conjugate and hepatitis B vaccine (Comvax by Merck) was licensed. Oct 2, 1996
A combination DTaP and Hib vaccine (TriHIBit by Aventis Pasteur) was licensed for the fourth dose in the DTaP and Hib series. Sept 27, 1996
Diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (Tripedia by Aventis Pasteur) were licensed for primary and booster immunization of infants. July 31, 1996
A second inactivated hepatitis A vaccine (Vaqta by Merck) was licensed. Mar 29, 1996
The International AIDS Vaccine Initiative (IAVI) was launched, calling for the speedy development of a human immunodeficiency virus (HIV) vaccine for use worldwide. The initiative created the Scientific Blueprint for AIDS Vaccine Development. Since 1996, IAVI invested nearly $20 million in the research and development of HIV vaccines by companies and research institutes worldwide. IAVI received major financial support from the Bill and Melinda Gates Foundation; the World Bank; the Rockefeller, Sloan, and Starr foundations; Becton, Dickinson & Co.; and eight national governments, among other donors. IAVI is a Collaborating Centre of the Joint United Nations Programme on HIV/AIDS (UNAIDS). 1996
The first inactivated hepatitis A vaccine (Havrix by SmithKline Beecham) was licensed. Feb 22, 1995
Varicella virus vaccine, live (Varivax by Merck), was licensed for the active immunization of persons 12 months and older. Mar 17, 1995
ACIP, the American Academy of Pediatrics, and the American Association of Family Physicians issued the first “harmonized” childhood immunization schedule, combining the recommendations of all three national groups. 1995
Typhoid Vi polysaccharide inactivated injectable polysaccharide vaccine (Typhim Vi by Aventis Pasteur) was licensed. Nov 28, 1994
The Global Programme for Vaccines and Immunization was created, merging two WHO programs—the Expanded Programme for Immunization and the former Programme for Vaccine Development and adding a new unit for Vaccine Supply and Quality. 1994
The entire Western Hemisphere was certified as polio-free by the International Commission for the Certification of Polio Eradication, WHO. 1994
The Institute of Medicine publishes “The Childrenʼs Vaccine Initiative: Achieving the Vision.” Later, following the events of September 11, 2001, the Institute of Medicine again called for the creation of a national vaccine authority “to advance the development, production, and procurement of new and improved vaccines of limited commercial potential but of global public health need.” 1993
The National Immunization Program (NIP) was created as a separate program reporting directly to the Office of the Director at CDC. NIP was established to provide federal leadership and services to all local and state public health departments involved in immunization activities (e.g., disease surveillance for vaccine-preventable diseases, and development of vaccine information management systems). 1993
The costs of the influenza vaccine and its administration become a covered benefit under Medicare Part B. May 1, 1993
Conjugated Haemophilus influenzae type b vaccines (ActHIB by Connaught/Mérieux and OmniHib by SmithKline Beecham) are licensed. March 1993
A combined Haemophilus influenzae type b vaccine and whole-cell DTP vaccine (Tetramune by Lederle/Praxis) was licensed. March 1993
The development of immunization registries was promoted at the national level. A national health goal for 2010 was subsequently established to increase participation in population-based immunization registries to 95 percent. 1993
The Vaccines for Children Program was established after the passage of the Omnibus Budget Reconciliation Act of 1993. Federally purchased vaccines under this program are made available to children from birth through 18 years old who meet one of the following requirements: Medicaid-enrolled, without health insurance, and American Indian or Alaskan native. Also, children with health insurance that does not cover the costs of immunization are eligible to receive vaccines at a federally qualified health center or a rural health clinic. All ACIP-recommended vaccines receive funding, which includes new vaccines, new vaccine combinations, and revised recommendations for vaccine use. 1993
Japanese encephalitis (JE) virus vaccine inactivated (JE-Vax by Research Foundation for Microbial Diseases of Osaka University [BIKEN]) was licensed. JE is the leading cause of viral encephalitis in Asia. WHO acts as a facilitator for the development of new JE vaccines that are safer, require fewer doses, and are more suitable for public health use, in particular, in disease-endemic developing countries. Dec 10, 1992
Diphtheria and tetanus toxoids and acellular pertussis vaccine (Tripedia by Connaught) are licensed for use as the fourth and fifth doses in the series. Sept 20, 1992
Diphtheria and tetanus toxoids and acellular pertussis vaccine (Acel-Imune by Lederle) are licensed for use as the fourth and fifth doses in the series. Dec 17, 1991
ACIP recommendations for routine hepatitis B vaccination for all infants are published in MMWR . Nov 22, 1991
The last case of indigenous polio in the Western Hemisphere occurred in a 5-year-old boy, Luis Fermin Tenorio, in Pichanaqui, Peru. August 1991
Recommendations of ACIP for routine Hib vaccination for infants beginning at 2 months old are published in MMWR . Jan 11, 1991
An enhanced-potency inactivated poliovirus vaccine (Ipol by Pasteur Mérieux Vaccines et Serums) was licensed. Dec 21, 1990
ACIP recommendations for the use of any of the three licensed Hib conjugate vaccines (ProHIBIT, HibTITER, and PedvaxHIB) for children as young as 15 months old are published in MMWR . April 13, 1990
Conjugated Hib ( Haemophilus influenzae type b) vaccine (PedvaxHIB by Merck) was licensed. Dec 20, 1989
A live, oral typhoid vaccine (Ty21a, Vivotif Berna by Swiss Serum Institute) was licensed. Dec 15, 1989
A recombinant hepatitis B vaccine (Engerix-B by SmithKline Beecham) was licensed. Aug 28, 1989
Recommendations for routine second doses of measles-containing vaccine were issued by both ACIP and the AAP. During the mid-to-late-1980s, a high proportion of reported measles cases were found in school-aged children (5-19 years old) who had been appropriately vaccinated. These vaccine failures led to national recommendations for a second dose of measles-containing vaccine. 1989
Conjugated Haemophilus influenzae type b vaccine (HibTITER by Wyeth-Lederle) was licensed. Dec 21, 1988
The Center for Biologics Evaluation and Research (CBER) was created within the FDA to regulate biological products, including blood, vaccines, tissue, allergenic, and biological therapeutics. 1988
The World Health Assembly (the ministers of health of all member states of the WHO) passed a resolution to eradicate polio by the year 2000. 1988
The National Vaccine Injury Compensation Program (NVICP) was established to provide compensation following a vaccine-related adverse event that resulted in injury or death. NVICP was intended to serve as an alternative to civil litigation. The law established a Vaccine Injury Table providing a list of compensable vaccination events and, for each, an associated time requirement. 1988
ACIP recommendations to administer Hib conjugate vaccine in all children at 18 months old are published in MMWR . Jan 22, 1988
Protein-conjugated Haemophilus influenzae type b vaccine (PRP-D, ProHibit by Connaught) was licensed. Dec 22, 1987
The recombinant hepatitis B vaccine (Recombivax HB by Merck) was licensed. Using recombinant DNA technology, Merck scientists developed a hepatitis B surface antigen subunit vaccine. July 23, 1986
Congress created the National Vaccine Program (NVP) to coordinate the vaccine research and development programs of AID (Agency for International Development, now known as USAID), NIH, CDC, the DOD, and the FDA. 1986
The National Childhood Vaccine Injury Act of 1986 was enacted by Congress. The HHS established the Vaccine Adverse Event Reporting System (VAERS) , co-administered by the FDA and CDC, to accept all reports of suspected adverse events in all age groups after administration of any U.S.-licensed vaccine. The Act requires healthcare providers and vaccine manufacturers to report specific adverse events following the administration of measles, mumps, rubella, polio, pertussis, diphtheria, or tetanus vaccines, and any combinations thereof to the HHS. 1986
Hib ( Haemophilus influenzae type b) polysaccharide vaccines (b-CAPSA 1 by Praxis Biologics, Hib-VAX by Connaught, and Hib-IMUNE by Lederle) were licensed. For children enrolled in childcare, the vaccine was recommended at 15 months and for all children at 24 months old. The vaccine was not consistently immunogenic in children under 18 months old. Apr 12, 1985
The costs of the hepatitis B vaccine and its administration became a covered benefit under Medicare Part B. Sept 1, 1984
Two enhanced pneumococcal polysaccharide vaccines were licensed (Pneumovax 23 by Merck on July 11 and Pnu-Imune 23 by Lederle on July 21). These vaccines included 23 purified capsular polysaccharide antigens of Streptococcus pneumoniae and replaced the 14-valent polysaccharide vaccine licensed in 1977. July 1983
The first hepatitis B viral vaccines, developed by Merck and the Pasteur Institute, were licensed. Both had independently developed plasma-based hepatitis B viral vaccines. 1981
Quadrivalent groups A, C, Y, and W-135 (Menomune A/C/Y/W-135 by Connaught) meningococcal vaccine was licensed. Because of the finding that this and other polysaccharide meningococcal vaccines can induce a relatively poor immune response in children younger than 2 years old and unable to elicit long-term immunologic memory, use had to be limited to individuals 2 years old and older. Nov 23, 1981
The costs of the pneumococcal vaccine and its administration became a covered benefit under Medicare Part B. July 1, 1981
The World Health Assembly certified the world free of naturally occurring smallpox. May 8, 1980
Rabies human diploid-cell vaccine (Imovax Rabies by Mérieux and Wyvac by Wyeth) was licensed. 1980
The RA 27/3 (human diploid fibroblast) strain of the rubella vaccine (Meruvax II by Merck) was licensed; all other strains were discontinued. 1979
The last cases of wild type 1 poliovirus occurred in the United States among unvaccinated Amish persons and members of other religious groups who did not accept vaccination. The source of the outbreak was determined to have been brought over to the United States from the Netherlands by members of an unvaccinated religious group. 1979
The yellow fever vaccine (YF-Vax by Connaught) was licensed in the United States. Jan 3, 1978
Monovalent group A (Menomune-A by Connaught), group C (Menomune-C by Connaught) meningococcal vaccines, and a bivalent vaccine for both groups A and C (Menomune-A/C by Connaught) were licensed. Jan 3, 1978
The first pneumococcal vaccine was licensed, containing 14 serotypes (of the 83 known serological groups) that comprised 80% of all bacteremic pneumococcal infections in the United States. Nov 21, 1977
The last case of naturally acquired smallpox occurred in the Merca District of Somalia. Oct 26, 1977
Joseph A. Califano Jr., Secretary of the Department of Health, Education, and Welfare (later Health and Human Services) launched the National Childhood Immunization Initiative intending to achieve 90% vaccination levels among all children. 1977
The age for routine vaccination with the MMR vaccine was changed from 12 months to 15 months old. 1976
The first monovalent (group C) meningococcal polysaccharide vaccine (Merck) was licensed. Apr 2, 1974
The Expanded Programme on Immunization was created by WHO in response to poor immunization levels in developing countries (less than 5% of children in 1974). The following vaccines are used by the program: BCG, polio, DTP, measles (often MMR), yellow fever (in endemic countries), and hepatitis B. 1974
The measles and mumps virus vaccine, live (M-M-Vax by Merck) was licensed. July 18, 1973
The Division of Biologics Standards was transferred from NIH to FDA and renamed the Bureau of Biologics. It was responsible for the regulation of all biologics, including serums, vaccines, and blood products. 1972
The combined measles, mumps, and rubella vaccine (MMR by Merck), as well as the combined measles and rubella vaccine (M-R-Vax by Merck), were licensed; the vaccine was developed by Maurice Hilleman and colleagues at Merck. Apr 22, 1971
CDC recommended the discontinuation of routine vaccination for smallpox in the United States following a greatly reduced risk of disease. 1971
Three rubella virus strains were licensed in the United States: HPV-77 strain grown in dog-kidney culture (Rubelogen by Parke-Davis); HPV-77 grown in duck-embryo culture (Meruvax by Merck); and Cendehill strain grown in rabbit-kidney culture (Cendevax by RIT-SKF, and Lirubel and Lirutrin by Dow). 1969
The “Hong Kong” influenza pandemic, caused by an H3N2 influenza virus, resulted in roughly 34,000 deaths in the United States. 1968-69
A second live, further attenuated measles virus vaccine (Attenuvax by Merck, based on the Moraten strain, derived from the Edmonston strain) was licensed. 1968
The Global Smallpox Eradication Program was launched by WHO. During the first year of the program, 44 countries, 31 of which had endemic smallpox, reported 217,218 cases. 1967
Mumps virus vaccine live (MumpsVax by Merck) was licensed. The vaccine was developed by Maurice Hilleman who isolated a wild-type virus from his daughter, Jeryl Lynn, who was recovering from mumps. It became known as the Jeryl Lynn strain of mumps virus. Dec 28, 1967
The World Health Assembly called for global smallpox eradication. 1966
CDC announced the first national measles eradication campaign. Within two years, measles incidence had decreased by more than 90% compared with prevaccine-era levels. 1966
The rubella virus was attenuated by Paul Parkman and Harry Meyer Jr. 1966
Bifurcated needles for the smallpox vaccine were introduced. 1965
Live, further attenuated measles virus vaccine (Lirugen by Pitman Moore-Dow based on the Schwarz strain, derived from the Edmonston strain) was licensed in the United States. The recommended age for routine administration was changed from 9 months to 12 months old. 1965
A rubella epidemic swept the United States resulting in 12.5 million cases of rubella infection, an estimated 20,000 newborns with congenital rubella syndrome (CRS), and excess fetal and neonatal deaths in the thousands. 1964
The Immunization Practices Advisory Committee (ACIP) to the U.S. Public Health Service was formed to review the recommended childhood immunization schedule and note changes in manufacturer vaccine formulations, revise recommendations for the use of licensed vaccines, and make recommendations for newly licensed vaccines. 1964
The trivalent oral polio vaccine was licensed. The vaccine development began in 1957 by Albert Sabin to improve upon the killed Salk vaccine. June 25, 1963
The Federal Immunization Grant Program was established. The grants, authorized under section 317 of the Public Health Service Act, were made to states to provide funds to purchase vaccines and to support the basic functions of an immunization program. The only vaccines available at the time were DTP, polio, and smallpox. 1963
The first live virus measles vaccine (Rubeovax by Merck) was licensed. Other live virus measles vaccines were eventually licensed (M-Vac by Lederle, Pfizer-vax Measles-L by Pfizer, and generic vaccines by Lilly, Parke Davis, and Philips Roxane). Mar 21, 1963
The inactivated measles vaccine (Pfizer-vax Measles-K by Pfizer and a generic vaccine by Lilly) was licensed in the United States. These vaccines were eventually withdrawn from the U.S. market in 1967. 1963
President John F. Kennedy signed the Vaccination Assistance Act into law. It allowed the CDC to support mass immunization campaigns and to initiate maintenance programs. 1962
Oral polio vaccine type 3 was licensed in the United States, as well as the trivalent product. Mar 27, 1962
Oral polio vaccine types 1 and 2, developed by Dr. Albert Sabin and grown in monkey kidney cell culture, were licensed for use in the United States. 1961
The “Asian” influenza pandemic, caused by an H2N2 influenza virus, resulted in an estimated 70,000 deaths in the United States alone. 1957-58
The Polio Vaccination Assistance Act was enacted by Congress, the first federal involvement in immunization activities. It allowed Congress to allocate funds to the Communicable Disease Center (later the Centers for Disease Control and Prevention) to help states and local communities acquire and administer vaccines. 1955
The Cutter polio vaccine incident began on April 25, 1955, when polio was reported in a vaccine recipient. One day later, five more cases were reported. All cases had received vaccines produced by Cutter Laboratories. Polio was reported in 94 vaccinees and 166 close contacts of vaccinees. On April 27, the Laboratory of Biologics Control requested that Cutter Laboratories recall all vaccines and the company did so immediately. On May 7, the surgeon general recommended that all polio vaccinations be suspended pending inspection of each manufacturing facility and a thorough review of the procedures for testing vaccine safety. The investigation found that the live polio virus had survived in two batches of vaccine produced by Cutter Laboratories. In 1955, as a result of the Cutter Incident, the Laboratory of Biologics Control was raised to division status within NIH, to strengthen and expand its biologics control function. Large-scale polio vaccinations resumed in the fall of 1955. 1955
The first polio vaccine was licensed—an inactivated poliovirus vaccine (IPV) pioneered by Dr. Jonas Salk. Apr 12, 1955
The Nobel Prize in Medicine was awarded to John Enders, Thomas Weller, and Fredrick Robbins for their discovery of the ability of poliomyelitis viruses to grow in tissue cultures. 1954
John Enders and Thomas Peebles isolated the measles virus in cell culture. 1954
Tetanus and diphtheria toxoids (adult formulation) were first licensed in the United States after the concentration of diphtheria toxoids was reduced. 1953
The yellow fever vaccine (Merrell National Labs) was first licensed in the United States. May 22, 1953
Heat-phenol inactivated typhoid vaccine by Wyeth was licensed. July 16, 1952
The worst recorded polio epidemic in U.S. history occurred with 57,628 reported cases. 1952
Diphtheria and tetanus toxoids and pertussis (DTP) were licensed. 1949
The last case of smallpox in the United States was reported; however, it took another two decades before the disease was eradicated globally. 1949
The combination of diphtheria and tetanus toxoids for pediatric use was first licensed in the United States. 1947
The inactivated influenza vaccine was first licensed in the United States. 1945
Karl Habel and John Enders isolated the mumps virus. 1945
The Public Health Services Act of 1944 was enacted, consolidating all legislation affecting the functions of the Public Health Service. 1944
Penicillin first became mass-produced. This medical miracle, rediscovered by Alexander Fleming in 1928, was capable of attacking many types of disease-causing bacteria. It played a vital role in treating infected wounds during World War II. 1943
The influenza A/B vaccine was introduced to the Armed Forces Epidemiological Board. The influenza vaccine was licensed in 1945 and, following the war, was also used for civilians. 1942
Hepatitis A and hepatitis B viruses were first differentiated. 1942
President Franklin D. Roosevelt, a victim of polio, founded the National Foundation for Infantile Paralysis, later known as the March of Dimes. 1938
An adsorbed form of tetanus toxoid was first licensed in the United States. 1937
The Division of Biologics Control was formed within the National Institute of Health. Much later, in 1972, the Division was transferred to the FDA. 1937
A live yellow fever vaccine (17D) was first licensed. The development of the chorioallantoic membrane for culturing viruses led to its development. 1935
The Hygienic Laboratory changed its name to the National Institute (singular) of Health and authorized the establishment of fellowships for biological and medical research. 1930
Cell culture was developed and shown to be able to grow virus, thus paving the way for the subsequent production of viral vaccines. 1930
The first iron lung was used to preserve breathing function in patients with acute polio . 1928
BCG (Bacille Calmette-Guérin) vaccine was first used in newborns, having been developed by Albert Calmette and Camille Guérin in 1921. BCG (live-attenuated Mycobacterium bovis BCG) represented the only vaccine against tuberculosis. It has become the most widely administered of all vaccines in the WHO Expanded Programme for Immunization, but has been estimated to prevent only 5% of all potentially vaccine-preventable deaths due to tuberculosis. 1927
Diphtheria toxoid was licensed; and prepared from the inactivated bacterial toxin that has lost its toxicity but retains its antitoxin-producing properties. In 1924, Gaston Ramon discovered diphtheria toxoid. Along with the discovery of antitoxins, Ramon uncovered the role of adjuvant substances in immunity. 1923
The “Spanish flu” influenza pandemic was responsible for at least 50 million deaths worldwide, with about 675,000 deaths in the United States. This virus was unusual because it spread so quickly, was so deadly, and exacted its worst toll on the young and healthy. About one-third of the world’s population (~500 million people) were infected. 1918
The pertussis vaccine, a suspension of inactivated Bordetella pertussis cells, was licensed. Inactivated vaccines were prepared with a microorganism or virus that had been killed, usually with a chemical such as formaldehyde. 1915
The typhoid vaccine was first licensed in the United States. 1914
Rabies vaccine was first licensed in the United States. 1914
Tetanus toxoid was introduced following the development of an effective therapeutic serum against tetanus by Emil Von Behring and Shibasaburo Kitasato. 1914
The first county health departments in the United States were formed. 1908
The Pure Food and Drugs Act was formed, prohibiting interstate commerce in misbranded and adulterated foods, drinks, and drugs. 1906
The Biologics Control Act was formed. It included the regulation of vaccine and antitoxin producers and required both licensing and inspections of manufacturers. The standards imposed by the 1902 Act resulted in bankruptcy for one-third of the companies manufacturing antitoxins and vaccines while benefiting the manufacturers already in compliance. In total, 10 firms held licenses with the Laboratory of Hygiene following the 1902 Act. April 5, 1902
In St. Louis, 13 children died of tetanus-contaminated diphtheria antitoxin. In the autumn of 1901, nine children in Camden, New Jersey, died from the tainted smallpox vaccine. Efforts to ensure the purity of biological treatments by government oversight followed the Biologics Control Act of 1902. 1901
The first Nobel Prize for Physiology and Medicine was awarded to Emil von Behring for his work on the development of a diphtheria antitoxin (later known as antiserum). 1901
The plague vaccine was introduced, following the preparation of anti-plague horse serum at the Pasteur Institute by Alexandre Yersin. After demonstrating protection from disease in immunized animals, Yersin went to China with the vaccine to protect humans during a plague epidemic. 1897
Cholera and typhoid vaccines were first developed. 1896
City and state public health departments began mass production of diphtheria antitoxin, following its introduction in European laboratories. 1893
The Pasteur Institute was established as a rabies treatment center as well as an infectious diseases research and training institute. 1888
The diphtheria toxin was discovered by Emile Roux. Passive serum therapies were developed through the scientific contributions of many, including Emil Von Behring who developed the first effective therapeutic serum against diphtheria, and Paul Ehrlich who developed enrichment and standardization protocol, which allowed for an exact determination of the quality of the diphtheria antitoxins. 1888
Joseph Kinyoun established one of the country’s first bacteriological laboratories in the Marine Health Service Hospital on Staten Island, NY. He was director of the Laboratory of Hygiene, which moved to Washington, D.C., in 1891. Kinyoun brought the latest techniques such as the procedure for preparing diphtheria antitoxin back from his visits to Europe. 1887
Louis Pasteur first used rabies vaccine in humans. 1885
The first live attenuated viral vaccine (rabies) was developed by Louis Pasteur, using desiccated brain tissue inactivated with formaldehyde. 1884
Robert Koch identified the tubercle bacillus as the cause of tuberculosis, subsequently called Koch’s bacillus. 1882
Louis Pasteur and George Miller Sternberg almost simultaneously isolated and grew the pneumococcus organism. 1881
Louis Pasteur created the first live attenuated bacterial vaccine (chicken cholera). 1879
Louis Pasteur proposed the germ theory of disease. 1877
Edward Jenner published his work on the development of a vaccination that would protect against smallpox. Two years earlier, in 1796, he had first speculated that protection from smallpox disease could be obtained through inoculation with a related virus, vaccinia or cowpox. He tested his theory by inoculating 8-year-old James Phipps with cowpox pustule liquid recovered from the hand of a milkmaid, Sarah Nelmes. 1798
The Marine Health Service was established in 1798 as the nation’s first public health agency. It provided hospital care for merchant seamen and protected port cities against diseases such as smallpox, cholera, and yellow fever. 1798
Variolation was introduced to Great Britain. 1721
The variolation technique was developed, involving the inoculation of children and adults with dried scab material recovered from smallpox patients. Variations of variolation have been noted in Turkey, Africa, China, and Europe. 1100s
Hippocrates described mumps, diphtheria, epidemic jaundice, and other conditions. 400 BC
This page was updated on July 5, 2024 .
Our Affiliated Sites
Ohio State nav bar
The Ohio State University website
- BuckeyeLink
- Find People
- Search Ohio State

The History of Vaccination: Top 10 Things to Know
- Chris Otter
Australian scientists have been successful in growing the Wuham virus in a lab, increasing the possible development of a vaccine for the Corona virus. Just what do we know about the history behind the creation of vaccines?
Written by Dr. Christopher Otter. Narration by Dr. Nicholas Breyfogle.
Video production by Laura Seeger and Dr. Nicholas B. Breyfogle. Audio production by Paul Kotheimer, College of Arts & Sciences Academic Technology Services.The Origins ' editorial team includes Editors Nicholas Breyfogle, Steven Conn and David Steigerwald; Managing Editors Lauren Henry, Sarah Paxton, and Renae Sullivan; Associate Editors: Mina Park and Kristin Osborne
We thank the Stanton Foundation for their funding of this and other Origins projects.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Research Council (US) Division of Health Promotion and Disease Prevention. Vaccine Supply and Innovation. Washington (DC): National Academies Press (US); 1985.
Vaccine Supply and Innovation.
- Hardcopy Version at National Academies Press
2 Vaccines: Past, Present, and Future
- Types of Immunization
Immunization involves the induction (or administration) of antibodies and other natural defense mechanisms to protect against specific pathogens. There are two types of immunization, active and passive.
Active immunization is the major focus of this report. It involves the administration of a modified pathogenic agent, or a component of a pathogen, to stimulate the recipient's immune mechanisms to produce long-lasting protection without causing the clinical manifestations or other consequences of disease.
Three major types of preparations are employed to produce active immunity. The first consists of vaccines made from whole, inactivated (killed) pathogens or components of a pathogen. 1 Examples of whole, inactivated vaccines include currently licensed pertussis vaccines, influenza vaccines, and the Salk poliovirus vaccine. The pneumococcal, meningococcal, and hepatitis B vaccines are among those that contain the immunity-producing fraction of the pathogen.
Toxoids are the second type of active immunogen. The diphtheria and tetanus vaccines are good examples. Toxoids are toxins that have been treated by physical or chemical means until they no longer produce clinical disease, but retain the capacity to induce immunity.
Attenuated infectious vaccines are the third type. Virus vaccines in this group are derived from the offending organism after it has undergone repeated passages in the laboratory in culture; it remains infectious for man but loses the ability to induce clinical disease. Examples include the oral (Sabin) poliovirus vaccine, and the measles, mumps, rubella, and yellow fever vaccines. Other examples of this type of vaccine contain live organisms or agents that are related to but different from the species that causes the disease. These vaccines produce "cross-reacting" immunity. Examples include the vaccinia virus vaccine used to prevent smallpox and BCG (Bacillus Calmette-Guerin), which is used in some countries for immunization against tuberculosis, but only rarely administered for this purpose in the United States.
Passive immunization is accomplished by transferring antibodies against a given disease from an immune person or animal to a nonimmune individual, usually by injection of serum (antisera) or some partially purified serum extract. Examples are diphtheria and tetanus antitoxins, and immune serum globulin for the prevention of hepatitis. In some diseases, such as diphtheria, passive immunization is effective not only as a preventive measure, but also as a treatment. Immunity acquired in this way is transient, however; it usually requires recognition or anticipation of exposure, and is not infrequently associated with untoward side effects such as serum sickness, manifested by transient fever and arthritis resulting from hypersensitivity to animal sera.
- History of Immunization
Active immunization began with smallpox and was based on the observation that immunity could be conferred by rubbing smallpox scabs against the skin, which usually resulted in a mild case of the disease. 2 Inoculation of susceptibles with infectious material from individuals with mild smallpox was practiced in China and Africa many centuries ago. It was introduced in Britain and the American colonies early in the eighteenth century. It is interesting to note that these inoculations caused an occasional death, resulting even then in controversy about the benefits and risks of the procedure. These concerns led to the search for a "better vaccine."
This search eventually focused on the fact that a vesicular eruption of cow udders, known as cowpox, often led to the development of small blisters or "milkers' nodes" on the hands of milkmaids. 2 By the middle of the eighteenth century, physicians recognized that persons infected with cowpox appeared to be protected from later exposure to smallpox, resulting in Edward Jenner's classic experiment in 1796.
Use of the smallpox vaccine spread quickly in the united States. In fact, the vaccine was the subject of the nation's first law regulating the distribution of drugs, the Vaccine Act of 1813. 3 This act authorized the President to appoint a federal agent to "preserve the genuine vaccine matter, and to furnish the same to any citizen" who requested it. It was repealed in 1822, after Congress decided that vaccine regulation should be left to local authorities.
The apparent success of early smallpox vaccination efforts and the developing science of microbiology led to other attempts to control feared infectious diseases in the late nineteenth century. Among these was the Pasteur method of active immunization against rabies, first tested in a child in 1885. 4
Serum therapy, later called antitoxin therapy, began in the early 1890s with the discovery that animals inoculated with heat-killed broth cultures of diphtheria or tetanus bacilli were able to survive subsequent (otherwise fatal) inoculations with those organisms. Early researchers did not realize at first that the (cell-free) supernatant of the broth culture, not the killed bacteria, was responsible for the development of immunity. 5 It also was shown that protection derived from immunization could be transferred to other animals by inoculating them with body fluids, such as serum, obtained from those that had been immunized. The first child with diphtheria treated with antitoxin was in Berlin in 1891. 5 By the mid-1890s, diphtheria antitoxin was produced for widespread use in both Britain and Germany. 6 The antitoxin was first produced and tested in the United States in 1895 by the Mulford Company of Philadelphia, later absorbed by Merck Sharp & Dohme.
The effectiveness of diphtheria antitoxin in the prevention and treatment of diphtheria (although not 100 percent) led a number of competing companies, both in the United States and abroad, to begin to manufacture it for commercial purposes. In the absence of regulations for testing and certification, substandard, ineffective, or dangerous preparations were sometimes produced and sold, occasionally by charlatans. At first, warnings by responsible authorities went essentially unheeded. 6
Concerns about uncontrolled production of smallpox vaccine and diphtheria antitoxin were expressed in editorials in the Journal of the American Medical Association late in 1894. 7 , 8 The potential role of state governments in supervising the propagation of vaccine virus was discussed at the National Conference of State Boards of Health held that December. 7 The recognized variability in the efficacy of different smallpox vaccines was attributed, at least in part, to defective preparations.
On December 5, 1894, the New York City Board of Health instructed the Health Department to develop a plan that would assure the potency and purity of diphtheria antitoxin preparations sold in New York City. 8 Although antitoxin shipped in small amounts from two German manufacturers appeared to exhibit acceptable purity and efficacy, some antitoxins from the United States were never subjected to testing and at least one that was tested was inert. Profiteering by manufacturers of presumably effective antitoxins also was lamented by the authorities.
When the concern reached the Congress, an Illinois member recommended that Congress create a national commission for the investigation of the antitoxin treatment of diphtheria. 8 Unfortunately, no definitive action was taken until 1902. This action followed the deaths from tetanus of 13 children in St. Louis who received diphtheria antitoxin prepared from a horse that shortly thereafter died of tetanus. 6 (The antitoxin, incidentally, was prepared by the St. Louis City Health Department, not by a commercial firm.)
This tragedy and the furor it caused in the public press resulted in the passage of the virus-toxin act by Congress in 1902. 6 This act established a board under the Department of the Treasury to develop licensing regulations for the producers of vaccines and antitoxins for interstate or foreign commerce. Under the direction of this board, the Hygienic Laboratory of the Public Health Service was authorized to inspect manufacturing establishments, issue and revoke licenses, and in other ways ensure, insofar as possible, the safety and efficacy of these biologics. By 1904, licenses had been issued to 13 manufacturers of biologics, primarily smallpox vaccine and diphtheria antitoxin. The number of producers licensed reached 41 by 1921. Standards for potency were developed at the Hygienic Laboratory. Manufacturers failing to meet acceptable standards had their licenses revoked or refused.
These responsibilities were later transferred to the National Microbiological Institute of the National Institutes of Health (NIH) The 1902 act subsequently was incorporated into the Public Health Service Act of 1944. In the 1950s, the Public Health Service Hygienic Laboratory was reconstituted as the Division of Biologics Standards at the NIH, and in 1972 these responsibilities were transferred to the Food and Drug Administration (FDA) with the establishment of the Bureau of Biologics. By 1971, regulations had been established for more than 80 generic biological products employed for passive and active immunization. More recently, the Bureau of Biologics (as the Office of Biologics Research and Review [OBRR]) was combined with the Bureau of Drugs in the FDA to form the Center for Drugs and Biologics.
Following the transfer of the Division of Biologics Standards to the FDA in 1972, procedures were developed for the review of safety, effectiveness, and labeling of biologics. The Bureau of Biologics established outside consultant panels, three of which were concerned with vaccines and antitoxins. These panels reviewed vaccines, toxoids, and products used for passive immunization against bacterial diseases; viral and rickettsial vaccines and products used for passive immunization against viral diseases; and bacterial preparations ''without U.S. standards of potency'' (e.g., older products such as "mixed respiratory vaccines"). The panels were charged with evaluating the generic safety and efficacy of all vaccines, immunoglobulins, and antitoxins, and with assessing the individual products. After evaluating the safety and efficacy of a manufacturer's preparation, the panels' options were to recommend maintenance of licensure, maintenance of licensure for a limited number of years until further evidence of efficacy could be obtained (only for products deemed to be safe), or revocation of licensure. The final reports of these panels were submitted to the Commissioner of the FDA by 1979.
In creasing evidence in the early 1900s of the effectiveness of diphtheria antitoxin and smallpox vaccination led to the idea that many or all infectious diseases might be amenable to immunologic prevention and therapy. Tetanus antitoxin, prepared in horses, came into general use in the military during World War I. For the first few months of the war, antitoxin was not employed by the British, and monthly rates of tetanus per 1,000 wounded reached the extraordinary figure of 32. 9 With the advent of antitoxin, the British rate was reduced to 1.2. For U.S. wounded during World War I, to whom tetanus antitoxin was given universally, the rate was 0.16 per 1,000. 9 Between the two world wars, tetanus toxoid was developed; by 1940, it was obligatory in the French army, 9 and its mandated use for U.S. military during World War II kept the number of cases of tetanus in the U.S. Armed Forces to 12. 10 By the late 1940s, tetanus toxoid was recommended as a routine public health measure for all children in the United States and usually was administered in combination with diphtheria toxoid and pertussis vaccine.
The ability to induce immunity to diphtheria in animals with diphtheria toxin suggested that the same could be applied to man. The first preparation for active immunization against diphtheria was a mixture of toxin and antitoxin, and was introduced in 1913. 11 Although effective, this product was not entirely satisfactory because of instability of the mixture and allergic reaction of some recipients to horse serum. Diphtheria toxoid (toxin inactivated by formalin) was developed in the early 1920s, and it has been used, with minor modifications, since the mid 1930s.
The first definitive experiments with pertussis vaccine were conducted in the 1920s. 12 Because the portions of the pertussis organism responsible for clinical immunity to whooping cough had not been identified, the vaccine was composed of whole, killed organisms. Progress in improving the vaccine was slow, and it was still considered experimental in the early 1940s; 13 by the late 1940s, however, several studies had demonstrated its efficacy. 14 , 15 The pertussis bacterium has been unusually slow in yielding its biological secrets, and as a consequence current U.S. vaccines, though better standardized, still contain the whole, killed organism. Some progress has been made recently, however, in improving our understanding of this organism and its relationship to human disease and immunity. 16
After World War II, remarkable advances were made in the development of vaccines for other diseases. Such developments were made possible by better understanding of the microorganisms involved, advances in immunology, and the use of cell culture techniques for the propagation of viruses. In rapid succession, viral vaccines were developed for the control of poliomyelitis, measles, rubella, and mumps. Safe, effective vaccines were developed for use under special circumstances in individuals in jeopardy from rabies (replacing older vaccines made from central nervous system tissues of animals), adenovirus infections, meningococcal disease, and others.
It is clear that vaccines widely employed as public health measures in the United States and other industrialized countries have had an enormous impact on morbidity and mortality. Major achievements include the following: 17 , 18
- The last confirmed cases of smallpox were reported in 1977; in May 1980, the World Health Organization announced global eradication of smallpox. 17
- Reported U.S. rubella cases dropped from 57,686 cases with 29 deaths in 1969 to 2,325 cases and 4 deaths in 1982.
- The incidence of measles in the United States decreased from 894,134 reported cases with more than 2,250 deaths in 1941 to 1,497 reported cases and 2 deaths in 1983.
- The incidence of mumps in the United States dropped from 150,000 reported cases in 1968 to fewer than 3,500 reported cases in 1983.
- The average incidence of diphtheria in the United States between 1980 and 1984 was 3 cases per year with 1 or no deaths. In contrast, in the late 1950s the number of reported cases averaged more than 1,000 per year with about 75 deaths per year.
- Reported U.S. tetanus cases and deaths dropped steadily from a high of 601 cases in 1948 to fewer than 95 cases in 1983.
- Paralytic poliomyelitis, which afflicted more than 57,000 persons in the U.S. in 1952, is now a rarity; fewer than 4 cases were reported in 1984.
- The incidence of pertussis in the United States dropped from a high of 265,269 reported cases with more than 7,500 deaths in 1934, to fewer than 2,000 cases with only 4 deaths in 1982. 18
Much of the success in the United States can be attributed to the high levels of vaccination among young children that result from the school immunization laws. In the developing world, only about 30 percent of children are vaccinated.
- The Present
Twelve commercial manufacturers (five of which only produce vaccines abroad), two state laboratories, and one university are licensed to produce one or more vaccines for use in the United States. Vaccines against 20 different infectious diseases are marketed, several in various combinations. Three are licensed for use in the military only. Seven vaccines (pertussis; poliomyelitis viruses 1, 2, and 3; measles virus; mumps virus; and rubella virus; and the diphtheria and tetanus toxoids) are recommended for routine administration to all children. The other vaccines are intended primarily for use in groups of individuals who are at special risk because of circumstances such as age, exposure, life-style, or underlying health problems. Often, these vaccines have very limited use; an example is anthrax vaccine, which is recommended only for persons who work with animal hides and a few laboratory personnel who come into contact with the organism.
Many other infections should be amenable to control by immunization, and a variety of potential vaccines are in different stages of development. 19 Vaccines for varicella (chicken pox) and rotavirus diarrhea are being evaluated and probably will be licensed soon. * Studies of vaccines for hepatitis A, both types of herpes simplex infections, cytomegalovirus, gonorrhea, and group B streptococci are in progress. Prospects for vaccines against various vital respiratory and intestinal illnesses are good. The whole field of immunization against parasitic scourges, such as malaria and schistosomiasis, is only beginning to develop.
In contrast to the trial-and-error fashion in which the earliest vaccines, such as those for smallpox and diphtheria, were developed, most current vaccine innovation is based on increasing knowledge of microbiology, mechanisms of infection and immunity, and the cellular biology of the infecting organisms, including basic biochemical structures and molecular genetics. These developments offer promise of immunologic prevention of many widespread infectious diseases that hitherto have not been amenable to control, and will help meet new needs for vaccines. Changes in life-style, hygiene, and the environment cause shifts in the patterns of infectious diseases. Advances in medicine also produce new target populations, e.g., transplant patients and others whose immune systems have been suppressed for therapeutic reasons.
Development of Vaccines and Recommendations for Vaccine Use
The development of a new vaccine to the point of application for licensure is a complex, arduous, and expensive process involving both public-and private-sector participants. The initial steps in the process include assessments of the impact of the infectious disease (measured by rates of mortality, acute morbidity, and permanent sequelae in the population); of the estimated cost of the disease and the projected costs of development, production, and administration of the vaccine; and of the vaccine's ranking among other health care priorities. Of major importance to commercial manufacturers is the likely utilization, i.e., the market, which is dependent both on acceptance of the vaccine by the public and the enthusiasm of physicians and other health care providers. Assuming that the health and economic impacts of the disease appear to warrant pursuit of a vaccine, many problems of a technical and practical nature must be identified and solved.
Identification of the causative organism is only the first step. The pathogenesis of the infection (how the organism produces the disease), what components of the organism are responsible for the manifestations of the disease (infectivity, virulence, pathogenicity) and which determine subsequent immunity, and whether current techniques can be anticipated to produce a safe and effective immunizing agent all represent crucial questions. The basic research necessary to answer these questions, which is often extremely time-consuming and expensive, usually is performed by investigators exploring the natural history of the disease. Commercial manufacturers rarely consider the possibility of a specific vaccine until the groundwork has been laid, typically by academic or government researchers.
The most basic technical requirement is the ability to consistently produce the organism (maintaining its immunogenicity) in the laboratory in sufficient quantities for study and, ultimately, for vaccine production. A reliable means must be found to measure immunity without exposure to disease. Researchers also must determine if the organism exists as more than one immunologically distinct type. For example, there are more than 80 immunologically distinct types of pneumococci, and infection or immunization with one type generally produces strong immunity only to that specific type.
Many questions depend on the nature of the organism. For example, in the case of an anticipated bacterial vaccine, can the immunity-producing component(s) be separated from irrelevant, potentially toxic moieties? Can the immunogenic antigen of a virus be extracted or, employing techniques of genetic engineering, be incorporated into another organism? In the case of a potential live vaccine, can the virulence of the pathogen be attenuated in the laboratory, and can reversion to the more virulent form be avoided with certainty?
The development of an animal model to evaluate toxicity, potency, and, if possible, clinical protection usually is desired. In addition, laboratory tests must be established, insofar as possible, to assess the toxicity and potency of the vaccine in a manner that correlates with test results in man.
These steps to understanding an infectious disease and developing preventive measures such as vaccines are conducted with continuing formal and informal consultations among agencies of the federal government, concerned scientists, and manufacturers. Conferences, often sponsored by federal agencies and professional societies and sometimes by manufacturers, provide useful opportunities to exchange advice, counsel, and ideas, and to coordinate efforts in the development of a vaccine.
After the extensive and complex background work outlined above has been completed and it appears that the proposed vaccine offers promise of safety and efficacy, permission may be sought from the OBRR for studies in humans. 20 By regulation, this involves filing a permit referred to as an IND (Notice of Claimed Exemption for Investigational New Drug). To obtain an IND, the responsible investigators must meet appropriate specifications that cover everything from evidence of sterility of the product to the qualifications of the investigators and the approaches to testing in humans. Full background data in support of the proposed vaccine and its use must be provided.
Three sequential phases of evaluation must be described in an IND. Phase 1 constitutes initial testing of the vaccine in a small number of persons to determine first its safety and then its immunogenicity at various dose levels and for different routes of administration. Phase 2 studies include administration of the vaccine to a larger number of persons to obtain further data on adverse effects and the immune response, and, perhaps, limited evidence of disease prevention.
Phase 1 and 2 studies often overlap, and the results provide the basis for Phase 3 studies, which are controlled field trials with sufficient study subjects to develop reasonable estimates of safety and efficacy. Efficacy usually is measured in terms of protection against clinical disease. Situations in which controlled field trials are not possible or ethical include the testing of an improved, presumably more efficacious vaccine for an otherwise fatal disease, such as rabies, for which there is already a vaccine that protects many or most persons. In these and other cases, it may be necessary to employ serologic or other methods to ascertain the development of immunity. The use of such surrogate methods requires firm evidence of a direct correlation between the results of the method and clinical protection in humans.
By federal regulation, any Phase 1, 2, or 3 study conducted on a population by an institution, such as a university, must be approved by that institution's review committee for protection of human subjects. Strict regulations exist for the institutional review mechanism, and include monitoring of all studies at least once a year. Progress reports by the investigator also must be submitted at least annually to the FDA.
It is generally desirable for Phase 3 studies to be conducted at more than one institution and by different investigators. The number of study subjects required varies with the disease and the vaccine, but usually is in the hundreds or thousands. It is important to ensure that there is adequate representation of all population groups for whom the vaccine may be recommended. The license application process includes review of all records of production, testing, and clinical evaluation by the OBRR. The product itself is submitted to laboratory testing by appropriate scientists at the OBRR, who also conduct on-site inspection of the production facilities. Customarily, although not by regulation, the OBRR convenes one or more meetings of the Vaccines and Related Biological Products Advisory Committee for full discussion and review of the product, its projected uses, and its labeling. When the OBRR is satisfied that the product is safe and effective, a license may be granted. Each marketed vaccine requires such a license, as does each vaccine manufacturer.
Although hundreds or thousands of individuals may have received a vaccine prior to licensure, these numbers are insufficient to identify rare untoward events resulting from the vaccine. (A classic example of an unexpected, rare reaction was the Guillain-Barré syndrome that occurred at a very low rate in persons who received the swine flu vaccine in 1976 [ Chapter 5 ].) Therefore, the OBRR encourages continuing surveillance of recipients as a vaccine becomes widely used. Any reports of untoward events must be made available by the manufacturer for review by the OBRR.
After licensure, the manufacturer must submit data on each new production lot and samples of vaccine to the OBRR for testing. The OBRR also periodically reinspects manufacturing facilities.
Recommendations for vaccine use in the United States are made by a number of advisory groups, most notably the Immunization Practices Advisory Committee (ACIP) of the U.S. Public Health Service, the American Academy of Pediatrics, through its Committee on Infectious Diseases, and the Committee on Immunization of the Council of Medical Societies, American College of Physicians (ACP). These committees maintain close liaison with each other and with the OBRR, thus assuring reasonable consistency between manufacturers' labeling and recommendations by the advisory bodies.
The Department of the Army oversees efforts to develop vaccines needed to protect military personnel (and others at risk) from a range of pathogens not generally encountered by the U.S. civilian population. 21 These include tropical disease pathogens and potential biological warfare agents. Research conducted for these purposes is often valuable in a broader context, e.g., contributions to the development of a vaccine for malaria. Recommendations for the use of these vaccines for military personnel are developed by the Armed Forces Epidemiological Board. As with vaccines for general public use, the ultimate availability of these vaccines depends on the willingness of a commercial manufacturer to undertake final development and production.
These mechanisms for developing new vaccines, for pursuing licensure, and for establishing recommendations for use are complex and time-consuming, but are clearly necessary to ensure to the extent possible that marketed vaccines are acceptably safe and effective. Further, it is to be expected that the nascent technology for the production of vaccines by genetic engineering will increase the responsibilities and activities of the OBRR and public advisory groups concerned with recommendations for vaccine use.
New technologies and better understanding of the immune process have launched a new era in the field of immunization. On the horizon are effective vaccines for a wide spectrum of human ailments, the vital diarrheal diseases, malaria, and other parasitic diseases responsible for enormous morbidity and mortality. Many current vaccines (especially the killed viral and bacterial vaccines) contain superfluous materials (some derived from the production substrates) that could contribute to reactivity and that are irrelevant to the production of immunity. Through further research, we may soon have the capability to replace existing vaccines with specific antigens that are more efficacious, safer, and possibly less expensive.
It is hoped that these vaccines with improved immunogenicity and stability will lead to greater utilization of immunization throughout the world. Millions of children in less-developed countries are disabled or die from diseases that are preventable. Also, no country can be considered safe from a disease as long as it persists in other populations—geographic isolation from disease threats is an unrealistic concept in the current age of extensive travel.
Prospects for new vaccines stem primarily from advances in genetic engineering and the ability to define the antigens responsible for inducing clinical immunity. Current laboratory goals are to determine the precise biochemical structures of these antigens and to synthesize them.
The greatest advances have occurred in the area of vital vaccines, but it is expected that these techniques also will be applicable to the production of bacterial vaccines and, ultimately, parasitic vaccines. Among the approaches available are: 22
Recombinant DNA Techniques In this approach, the genetic material responsible for production of the immunity-inducing antigen is incorporated into the genetic apparatus of another replicating virus, bacterium, yeast, or animal cell. The result is a hybrid organism that replicates and produces the antigen desired, often in large amounts. A vaccine is made from the purified antigen. The production of a potential new hepatitis B vaccine illustrates this process: the DNA sequence coding for hepatitis B surface antigen is incorporated into yeast and activated to synthesize the antigen, which is then purified. Preliminary tests indicate that the product is effective in humans. 23 A variant of the same approach that shows promise involves incorporation of the gene for a desired immunizing antigen into a virus that produces a generally benign infection in man, such as the vaccinia virus (smallpox vaccine). Preliminary experiments in nonhuman primates indicate that this approach may be efficacious. These recombinant DNA vaccines offer promise of effective products that are less reactive and less expensive.
Polypeptide Synthesis The ability to define the amino acid sequence of protein subunits (peptides) has allowed researchers to characterize the structures of some immunogenic peptides. Based on this knowledge, several viral antigens have been synthesized. These early man-made antigens are less immunogenic than natural viral antigens, but researchers believe that this situation will improve with further study. In some cases, adjuvants may be required to boost immunogenicity. The synthetic antigens, because of their purity, are expected to be less reactogenic and safer than their natural counterparts. Also, the cost of large-scale production of these antigens probably will be relatively low.
Specific Attenuation of Pathogens The third type consists of modified or attenuated live pathogens, usually viruses. The live, attenuated oral poliovirus vaccine is one example of how this approach can be used. The principal disadvantage of these vaccines is that they contain viruses that have the potential to revert to a virulent, disease-producing form. Fortunately, increasing knowledge of molecular biology is providing a better understanding of many of the changes or mutations that occur in the process of attenuation. Comparing the nucleotide sequences of fully attenuated viruses with those of partially attenuated or fully virulent forms ultimately may provide a mechanism for early recognition of potential mutation of a live vaccine to the more virulent, disease-producing form. Methods of manipulation that result in an attenuated virus incapable of reversion would be even more desirable. Two possible approaches are being studied. One involves gene reassortment, segregation of genes responsible for protection from those responsible for disease manifestations, to produce a nonvirulent but still infectious variant of the same virus. The second approach is "deletion mutation," which would result in the production of a mutant that is incapable of reversion to virulence because it lacks a specific gene.
Anti-Idiotype Antibodies Most remarkable are prospects for the development of anti-idiotype antibodies. The idiotype of an antibody molecule is a recognition site located at or near its antigen-binding site; 22 the idiotype acts as an antigenic site when the body makes anti-antibody molecules (a natural immune system mechanism used to control the level of antibodies in the blood). In some cases, the anti-idiotype antibody appears to resemble the antigenic site of the original antigen and can induce a similar immune response. For example, anti-idiotype antibodies directed against antibody to the hepatitis antigen HBsAg may induce protection against hepatitis. Theoretically, this approach could produce a vaccine that contained no vital components whatsoever, but a variety of technical and safety questions must be resolved before its full potential is known.
Based on these and possibly other techniques, prospects for new and better vaccines are considerable. Their development, however, may be impeded by the same problems (discussed in subsequent chapters) that deter development of vaccines by traditional methods. These problems must be resolved before the full public health benefits of new approaches to vaccine development can be achieved.
- References and Notes
- 7. Editorial. 1894. A timely topic . JAMA 23:919-920.
A vaccine against Hemophilus influenzae type b, the most frequent cause of meningitis in young children, was licensed April 12, 1985.
- Cite this Page National Research Council (US) Division of Health Promotion and Disease Prevention. Vaccine Supply and Innovation. Washington (DC): National Academies Press (US); 1985. 2, Vaccines: Past, Present, and Future.
- PDF version of this title (3.9M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Vaccines: Past, Present, and Future - Vaccine Supply and Innovation Vaccines: Past, Present, and Future - Vaccine Supply and Innovation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Spotlight /
- History of Vaccination /
- History of smallpox vaccination
The only human disease to be eradicated so far
One of the deadliest diseases known to humans, smallpox remains the only human disease to have been eradicated. Many believe this achievement to be the most significant milestone in global public health.
Key components of the worldwide smallpox eradication effort included universal childhood immunization programmes in some countries, mass vaccination in others, and targeted surveillance-containment strategies during the end-game.
Over thousands of years, smallpox killed hundreds of millions of people. The rich, the poor, the young, the old. It was a disease that didn’t discriminate, killing at least 1 in 3 people infected, often more in the most severe forms of disease.
The symptoms of smallpox were gruesome: high fever, vomiting and mouth sores, followed by fluid-filled lesions on the whole body. Death would come suddenly, often within 2 weeks, and survivors could be left with permanent harms such as blindness and infertility. in the most severe forms of disease.
Mozart was infected, as was Abraham Lincoln.

Smallpox was highly infectious, with no known cure. It began as early as 1350 BCE, with cases being found in the study of Egyptian mummies.
The ancient practice of variolation (named for smallpox, also known as variola or ‘la variole’) was widely used in Asia and some parts of Africa.
This consisted of transferring to healthy people small amounts of material from smallpox sores, resulting in milder forms of illness and much lower mortality than natural infection. Some sources suggest practices of variolation were taking place as early as 200 BCE.
Written accounts from the mid-1500s describe a form of variolation used in China known as insufflation, where smallpox scabs were dried, ground and blown into the nostril using a pipe.
In India, similar practices were carried out through inoculation, using a lancet or needle to transfer material from smallpox pustules to the skin of healthy children. Accounts from the 18th century suggest this technique dates back hundreds of years.

Variolation (in the form of inoculation) was introduced in Europe by Lady Mary Wortley Montagu 300 years ago in 1721, after she had observed the practice in the Ottoman Empire, where her husband was stationed as ambassador to Turkey.
Around the same time, it came to public attention in the American colonies. Enslaved West Africans had long practised the technique, and after his slave Onesimus told him about how it worked in 1716, Cotton Mather publicized it and argued for its use in response to a 1721 outbreak of smallpox in Massachusetts.
It wasn’t until May 1796 that the world’s first vaccine was demonstrated, using the same principle as variolation but with a less dangerous viral source, cowpox. Having heard of local beliefs and practices in rural communities that cowpox protected against smallpox, Dr Edward Jenner inoculated 8-year-old James Phipps with matter from a cowpox sore on the hand of Sarah Nelmes, a local milkmaid.
Phipps reacted to the cowpox matter and felt unwell for several days but made a full recovery. Two months later, in July 1796, Jenner took matter from a human smallpox sore and inoculated Phipps with it to test his resistance.
Phipps remained in perfect health, the first person to be vaccinated against smallpox.

Not everyone was on board with Jenner and his vaccine. Rumours circulated at the time that it would turn people into cows. But by 1801, through extensive testing, it was shown to effectively protect against smallpox.
The vaccine was soon in use on other continents, where vaccine continued to be inoculated from arm to arm until vaccination programmes were established. Mandatory smallpox vaccination came into effect in Britain and parts of the United States of America in the 1840s and 1850s, as well as in other parts of the world, leading to the establishment of the smallpox vaccination certificates required for travel.
While some European regions eliminated the disease by 1900, smallpox was still ravaging continents and areas under colonial rule, with over 2 million people dying every year. It took another 50 years to achieve global solidarity in the fight against the disease.

Vaccine research and studies in vaccine delivery were carried out around the world in the search for more resilient and effective vaccines.
By the 1950s, advances in production techniques meant that heat-stable, freeze-dried smallpox vaccines could be stored without refrigeration.
Vaccination led to smallpox elimination in western Europe, North America and Japan. In the absence of a large-scale coordinated international programme, the disease persisted in other areas.
In 1958, the World Health Assembly called for the global eradication of smallpox – the permanent reduction to zero cases – without risk of reintroduction.
As the World Health Organization launched the Smallpox Eradication Programme in 1959, WHO Member States enhanced their support and cooperation. Good progress was made in many countries with the support of technical assistance and vaccine provision coordinated by WHO.
Efforts were redoubled with the launch of the Intensified Smallpox Eradication Programme in 1967. The Soviet Union provided freeze-dried vaccine, which became the basis for elimination of smallpox from eastern Europe, China and India.
With renewed political commitment and the contributions of hundreds of thousands of local surveillance officers and health workers, even regions with nascent health systems and tremendous logistical challenges made remarkable progress.

Throughout this period WHO played a critical role, with international workers supporting legions of national personnel. Epidemiologists from the Soviet Union and the United States of America worked side by side in the middle of a cold war.
For example, in 1970, an outbreak in south-west India led to over 1300 cases and 123 deaths. In response, all available national and international health personnel were dispatched on a week-long house-by-house search of the area, vaccinating everyone identified as a contact of a recent case.
With this strategy they were able to eliminate highly contagious smallpox from the district within weeks.
In higher-risk countries, laboratories began to produce higher-quality freeze-dried vaccines , and mass production of the innovative and easy-to-use bifurcated needle to administer doses contributed to vaccination efforts.
Thanks to the combined efforts of national health agencies, WHO and scientists around the world, smallpox was eliminated from South America in 1971, Asia in 1975 and Africa in 1977.
The cost of the Intensified Smallpox Eradication Programme was approximately US$300 million, two thirds of which came from endemic countries for their own eradication efforts. British, Canadian, Cuban, French, Soviet, and US vaccines were given freely to WHO and distributed onwards, sometimes with the strategic financial support of Sweden.
Also important in the 1970s were vaccine technology transfers allowing countries to become producers of their own freeze-dried vaccine and suppliers within their region.
Through all this, the United States and the Soviet Union worked in rare solidarity. It was an unprecedented demonstration of global unity in the face of a common threat. As a major contributor to the programme, the United States reportedly recoups their investment every 26 days in money not spent on administering further vaccinations and treating new cases.

In 1980, WHO declared smallpox officially eradicated :
The world and all its people have won freedom from smallpox, which was the most devastating disease sweeping in epidemic form through many countries since earliest times, leaving death, blindness and disfigurement in its wake.
WHO preserves the Archives of the Smallpox Eradication Programme at its headquarters in Switzerland. WHO also maintains a stockpile of vaccines as an emergency reserve in Switzerland and in several other countries.
A cure was never found for smallpox before eradication, with those infected being treated only by cleaning wounds and lessening pain.
Instead, following the discovery of Dr Jenner’s vaccine, eradication was achieved through prevention, as he himself predicted. Bolstered by efforts united around the world, Jenner’s concept survived to defeat a historic scourge.
After 3000 years of suffering and death from the disease, there hasn’t been a recorded case of smallpox in almost half a century.

Smallpox eradication: science, solutions, solidarity
Related history of vaccination stories

A brief history of vaccination

History of the polio vaccine

History of the measles vaccine

History of the influenza vaccine

IMAGES
VIDEO
COMMENTS
For centuries, humans have looked for ways to protect each other against deadly diseases. From experiments and taking chances to a global vaccine roll-out in the midst of an unprecedented pandemic, immunization has a long history.. Vaccine research can raise challenging ethical questions, and some of the experiments carried out for the development of vaccines in the past would not be ethically ...
Member of the World Health Organization's Vaccine Safety Net. Featured Content. Explore Resources For. Educators. Explore, a prolific vaccine developer. Explore. The History of . Home. The College of Physicians of Philadelphia 19 S 22nd Street Philadelphia, PA 19103. 215.563.3737 [email protected]. Footer Social Links. Instagram ...
Scientific advances in the first half of the 20th Century led to an explosion of vaccines that protected against whooping cough (1914), diphtheria (1926), tetanus (1938), influenza (1945) and mumps (1948). Thanks to new manufacturing techniques, vaccine production could be scaled up by the late 1940s, setting global vaccination and disease ...
The history of vaccines begins before the first vaccine, with an immunizing procedure called "inoculation" by some and "variolation" by others. According to researchers, inoculation with materials from smallpox lesions to trigger immunity against smallpox dates back to antiquity in China. And the first written account of the procedure was ...
Introduction and background. Although inoculation practices were started more than 500 years ago, the term vaccine was first described in the 18th century by Edward Jenner. It is derived from Vacca, a Latin word for cow. Jenner inoculated an eight-year-old boy with cowpox lesions from the hands of milkmaids in 1796.
The origins of vaccination. Edward Jenner (1749-1823), a physician from Gloucestershire in England, is widely regarded as the 'father of vaccination' ( Milestone 2 ). However, the origins of ...
A vaccine can confer active immunity against a specific harmful agent by stimulating the immune system to attack the agent. Once stimulated by a vaccine, the antibody-producing cells, called B cells (or B lymphocytes), remain sensitized and ready to respond to the agent should it ever gain entry to the body.A vaccine may also confer passive immunity by providing antibodies or lymphocytes ...
Vaccines have a history that started late in the 18th century. From the late 19th century, vaccines could be developed in the laboratory. However, in the 20th century, it became possible to develop vaccines based on immunologic markers. In the 21st century, molecular biology permits vaccine development that was not possible before.
On today's show we trace the 2000-year history of the very first vaccine. We go from Ancient Greece to Imperial China to Britain. And we learn how this led to an achievement we'd love to repeat ...
Vaccines have a history that started late in the 18th century. From the late 19th century, vaccines could be developed in the laboratory. However, in the 20th century, it became possible to develop vaccines based on immunologic markers. In the 21st century, molecular biology permits vaccine development that was not possible before.
This paper explores the history of vaccines and immunization, beginning with Edward Jenner's creation of the world's first vaccine for smallpox in the 1790s. We then demonstrate that many of ...
Smallpox used to kill millions. But a chance discovery led to the first vaccine, and a transformation in human health. Smallpox was a terrible disease. "Your body would ache, you'd have high ...
Multiple cornerstones have shaped the history of vaccines, which may contain live-attenuated viruses, inactivated organisms/viruses, inactivated toxins, or merely segments of the pathogen that could elicit an immune response. The story began with Hippocrates 400 B.C. with his description of mumps and diphtheria.
The Vaccine Controversy by Kurt Link While millions of Americans receive vaccinations each year, a vocal segment of the population is opposed to all immunizations_some even refusing to get mandated vaccinations for their children. In The Vaccine Controversy, Dr. Kurt Link_a specialist in internal medicine_explores that paradox and provides a history of vaccine development, including such ...
Introduction. Vaccination has been relatively successful in preventing many childhood-related infections and saving millions of lives. Well in excess of 10 million lives were saved between mid-1960s and 2015 with viral vaccines 1, 2 such as measles, mumps, rubella, chickenpox and hepatitis A, produced from acceptable cell culture substrates. However, approximately 1.5 million children under 5 ...
Amid the staggering amount of suffering and death during this historic pandemic of COVID-19, a remarkable success story stands out. The development of several highly efficacious vaccines against a previously unknown viral pathogen, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), in less than 1 year from the identification of the virus is unprecedented in the history of vaccinology.
Vaccination began as a traditional therapy over a thousand years ago. Vaccines are often seen as a marvel of modern medicine. Surprisingly, the history of vaccination extends back centuries. This ...
Vaccine History Timeline. Not long ago we celebrated the 225th anniversary of Edward Jenner's first smallpox vaccination in 1796. The development of vaccines continued at a fairly slow rate until the last several decades when new scientific discoveries and technologies led to rapid advances in virology, molecular biology, and vaccinology ...
The origins of vaccination lie in the practice of variolation, which was used to protect against smallpox. By. Chris Otter. Australian scientists have been successful in growing the Wuham virus in a lab, increasing the possible development of a vaccine for the Corona virus. Just what do we know about the history behind the creation of vaccines?
1385 Words. 6 Pages. Open Document. The Matter of Vaccine. When children are born and for the first two years of their lives, they receive multiple shots and drops of vaccines. These vaccines protect them from getting diseases that were deadly and common in children many decades ago. Vaccine is one of the greatest achievement in medicine history.
The History of Vaccines 1921 Tuberculosis Vaccine 1923 Tetanus & Diphtheria Vaccine 1935 Yellow Fever Vaccine 1952 Polio Vaccine 1954 Anthrax Vaccine 1963 Measles Vaccine 1967 Partitis (Mumps) Vaccine 1969 ... Vaccine 2020 COVID-19 Vaccine Source: Centers for Disease Control and Prevention,
Immunization involves the induction (or administration) of antibodies and other natural defense mechanisms to protect against specific pathogens. There are two types of immunization, active and passive. Active immunization is the major focus of this report. It involves the administration of a modified pathogenic agent, or a component of a ...
Mandatory smallpox vaccination came into effect in Britain and parts of the United States of America in the 1840s and 1850s, as well as in other parts of the world, leading to the establishment of the smallpox vaccination certificates required for travel. While some European regions eliminated the disease by 1900, smallpox was still ravaging ...