Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
A 26-year-old female arrives with a companion to an urgent care at 0845 by personal vehicle for treatment of suspected foot infection. The patient’s companion (a female roommate) reports to the triage nurse that the patient cut her foot while wading in the ocean over the weekend. They did not initially notice the cut but discovered it while removing tar from the bottom of the right foot. Approximately 24 hours later, her foot became too painful for ambulation, and a “thick, yellowish” discharge began to drain from the cut. Vitals upon arrival at urgent care showed a temperature of 101.5F, heart rate of 130, respiratory rate of 24, and blood pressure of 86/40. Her pain was 9/10 in her right foot and described as throbbing. During a HTT assessment by the PA, the patient is reported to be arousable to voice, oriented to person and place only, and complaining of nausea. The patient reports she took Tylenol that morning to relieve pain and fever. Her skin is pale, diaphoretic, and hot.
The urgent care calls 911, and medics are dispatched to the center for transfer to the local hospital to treat the patient for suspected sepsis. Upon arrival, medics find the patient is still tachycardic, and that her blood pressure has dropped to 80/40. Her respiratory rate has increased to 30. During transport, medics insert a 20 gauge peripheral IVs in the patient’s left antecubital. They infuse a fluid bolus of 500 mL of normal saline to manage her patient’s hypotension, and administer oxygen by simple mask at 4L/min. During the primary assessment, the patient’s right foot reveals a two-inch laceration with no active bleeding that is erythematous, edematous (non-pitting), and radiating heat. Edema is covering the entire bottom of the right foot and extends to the patient’s ankle.
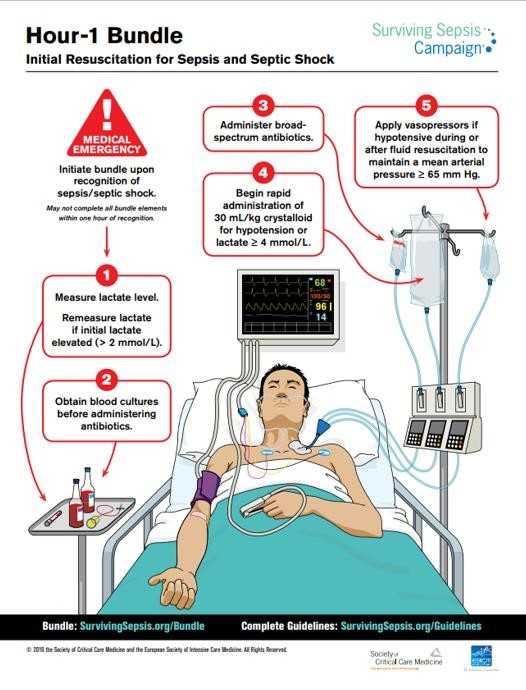
The patient arrives to the emergency room within 15 minutes and is admitted for treatment at 1000. On the unit, Code Sepsis is called, and the agency’s sepsis protocol based on the Surviving Sepsis campaign is implemented. The patient’s vitals are now a temperature of 102F, heart rate of 140, respiratory rate of 34, and blood pressure of 96/42. Lactate levels are immediately measured. A second 20 gauge peripheral IV is inserted into the right antecubital, blood cultures are drawn, and a swab sample is taken of the cut and submitted to the laboratory for a culture and sensitivity test. Broad spectrum antibiotic ceftriaxone (Rocephin) is administered, and patient is given Ibuprofen to manage her fever. The patient is diagnosed with septic shock, and because she is still hypotensive, 30mL/kg of normal saline is infused. The patient’s lactate levels come back as 2.4 mmol/L. Norepinephrine (Levophed) is also hung, and the patient is further monitored. With careful titration and vital monitoring, the use of vasopressors restores the patient’s blood pressure to 101/52. Although fluid resuscitation helps to bring the patient’s heart rate down to 104, Nicardipine (Cardene) was ordered in anticipation of further needs to manage tachycardia. The patient is transferred to the ICU at 1300 for further monitoring and management of her hemodynamic status.
In the ICU, the patient’s vitals stabilize. Her tachypneic state reduces, and respiratory rate is now 18. She no longer requires oxygen supplementation. Her pain is being managed with IV morphine and she rates the pain in her as 3/10. Her IV pump is running 125 mL an hour of normal saline along with piggybacked ceftriaxone (Rocephin), and labs return a lactate level of 1.5 mmol/L. The patient’s roommate arrives. She is tearful and explains to the ICU nurse that she wanted to tell the patient’s parents what happened, but the patient refused. The ICU nurse calls for the case manager and a social service consult to inquire further. The patient’s roommate explains to the interdisciplinary team that the patient does not have insurance because she is 26 and has been removed from her parents’ medical plan. The parents are also currently engaged in a divorce, do not speak to each other, and use their daughter to communicate. The patient is aware of their financial situation and her lack of medical coverage and does not want to worry her parents in spite of her critical medical state.
- What are the priority nursing interventions for this patient in the ICU setting?
- What signs and symptoms in this patient would indicate the need for mechanical ventilation?
- What is the nurse’s role in addressing the patient’s financial concerns?
References:
Gordon, A.C., Mason, A.J., Thirunavukkarasu, N., et al. (2016). Effect of early vasopressin vs norepinephrine on kidney failure in patient with septic shock: The VANISH randomized clinical trial. JAMA, 316 (5), 509–518. doi:10.1001/jama.2016.10485
Hinkle, J. L., & Cheever, K. H. (2014). Brunner & Suddarth’s textbook of medical-surgical nursing. Philadelphia: Lippincott Williams & Wilkins. PulmCCM. (2019, January 14). From the Surviving Sepsis Guidelines: Criteria for diagnosis of sepsis. Retrieved from https://pulmccm.org/review-articles/surviving-sepsis-guidelines-criteria-diagnosis-sepsis/
Schmidt, G.A., & Mandel, J. (2019, March). Evaluation and management of suspected sepsis and septic shock in adults. Retrieved from https://www.uptodate.com/contents/evaluation-and-management-of-suspected-sepsis-and-septic-shock-in-adults?search=sepsis treatmentadult&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H465649907
Society of Critical Care Medicine. (2019). Hour-1 bundle: Initial resuscitation for sepsis and septic shock. Retrieved from http://www.survivingsepsis.org/SiteCollectionDocuments/Surviving-Sepsis-Campaign-Hour-1-Bundle.pdf
Zhang, M., Zheng, Z., & Ma, Y. (2014). Albumin versus other fluids for fluid resuscitation in patients with sepsis: A meta-analysis. PloS one , 9 (12), e114666.
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.

Share This Book
Case-based learning: recognising sepsis
Sepsis can lead to organ failure and death. However, early diagnosis and recognition may help prevent these potentially fatal consequences.

JL / Science Photo Library / Shutterstock.com
Several personal stories of sepsis survivors and deaths from sepsis have been published in the media, highlighting the importance of sepsis as a major cause of preventable deaths in the UK. This article will provide an overview of sepsis with particular focus on the role of pharmacy professionals in recognition and referral.
Pathophysiology
Sepsis is characterised by a systemic inflammatory response to an invasive infection that has become unregulated [1] . White blood cells and pro-inflammatory cytokines are released causing widespread vasodilation and an increase in capillary permeability, resulting in the loss of fluid from circulation. This results in hypovolaemia and a fall in systemic vascular resistance, which in turn leads to a fall in blood pressure and a decrease in organ perfusion, culminating in tissue hypoxia and organ failure [1] .
There are around 250,000 cases of sepsis annually in the UK, 20% of which are fatal [1], [2] . The UK Sepsis Trust estimates that early diagnosis of sepsis and the application of evidence-based treatment could save 14,000 lives per year [2] . Therefore, the timely identification of sepsis can lead to rapid treatment and potential mortality reduction.
Initial recognition of sepsis relies on identifying symptoms, which presents challenges for healthcare professionals as the common symptoms are not specific to sepsis and could be caused by non-infective pathology (e.g. trauma, pancreatitis, burns ) [3] .
The inflammatory-response-induced hypovolaemia affects the brain and can cause confusion, slurred speech and loss of consciousness. Similarly, as the kidneys are affected, there is a reduction in glomerular filtration resulting in a drop in urine output and development of acute kidney injury [1] , [3] .
Gas exchange across the alveoli is compromised as fluid and proteins leak into the lungs, causing a drop in systemic oxygen saturation and a rise in carbon dioxide levels. The body attempts to compensate by increasing its respiratory rate, but the problem is ultimately compounded as the drop in organ perfusion affects the lungs, meaning that even if oxygen-rich air is present, there is little blood flow with which gas exchange can take place [1] , [3] .
Initially, the heart rate increases in an attempt to compensate for the drop in blood pressure. However, the reduction in circulating volume and the fall in systemic vascular resistance ultimately undermine this action. This is because a reduction in venous return prevents the ventricles from properly filling before they contract, reducing the cardiac output [1] .
The typical signs and symptoms of sepsis may vary across different age groups, be general or may not all be present. Examples of moderate- and high-risk symptoms include:
- Reduced urine output (e.g. dry nappies in babies and toddlers);
- Feeling cold with shivering or chills;
- Rapid breathing (increased resting breaths per minute);
- Rapid heart rate (increased resting heart rate per minute);
- Mottled (see Photoguide A) or ashen appearance;
- Cyanosis (blue tint) of skin, lips or tongue (see Photoguide B);
- Non-blanching rash (see Photoguide C) [1] , [4] , [5] .
Additional signs in babies and young children (aged under five years)
- Not responding normally to social cues (e.g. does not smile);
- Visibly unwell (e.g. floppy or overly passive);
- Wakes only with prolonged stimulation or, if roused, does not stay awake;
- Weak high-pitched or continuous cry;
- Parent or carer is concerned that the child is behaving differently from normal;
- Has a seizure or convulsion;
- Pallor of the skin, lips or tongue;
- Cold extremities, but head and torso may be hot to the touch;
- Change in temperature (e.g. red flag temperatures are over 38 o C in those aged under 3 months, 39 o C in those aged 3–6 months and less than 36 o C for any age) [1] , [4] , [5] .
Additional signs that can affect patients aged over five years
- Evidence of new-onset confusion (history may be from a parent, carer, relative or friend);
- Slurred speech;
- Signs of potential infection (e.g. redness, swelling or discharge at surgical site, breakdown of the wound);
- Tympanic temperature less than 36 o C;
- New onset arrhythmia [1] , [4] , [5] .
If sepsis is suspected, the patient should be immediately referred for emergency medical assessment.
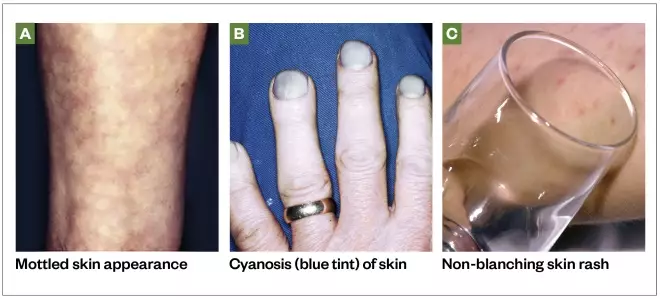
Photoguide: symptoms of sepsis
Source: Science Photo Library / Shutterstock.com
At-risk groups
Sepsis can affect anyone, but there are some patient groups that should be considered to be more susceptible to the development of sepsis, including:
- Very young children (aged under 1 year);
- Frail or older people (aged over 75 years);
- Immunocompromised people (e.g. those being treated for cancer with or without chemotherapy, post-splenectomy, taking long-term steroids or other immunosuppressant drugs);
- People who have had surgery or other invasive procedures in the past six weeks;
- People with any breach of skin integrity (e.g. cuts, burns, blisters or skin infections);
- People who misuse drugs intravenously;
- People with indwelling lines or catheters;
- Pregnant women;
- Women who have given birth or who have had a termination of pregnancy or miscarriage in the past six weeks [4] .
Understanding the patient risk factors may help improve timely diagnosis of suspected sepsis.
Sepsis can occur in response to a wide range of infections, but is most commonly associated with bacterial infection of the lungs, urinary tract, abdomen, central nervous system, or skin and soft tissues [1] . It is primarily diagnosed by a clinical assessment. Any number or combination of signs and symptoms may be present on diagnosis.
The National Institute of Health and Care Excellence (NICE) and the UK Sepsis Trust have published risk stratification tools to facilitate appropriate recognition of sepsis and the level of risk to the patient. Most NHS organisations use these tools or a locally approved variation of them [1] , [4] . These tools cater to a wide range of patients of different ages and the recommended action differs depending on whether patients’ symptoms are recognised in the primary or secondary care setting.
Patients who meet the high-risk criteria (see Box for the criteria for children aged under five years) should be sent urgently for emergency care (at a setting with resuscitation facilities). These patients should receive intravenous antibiotics with an appropriate level of cover within one hour of recognition of sepsis, along with other treatments and investigations [1] , [4] .
Box: high-risk criteria for children aged under five years outside of the hospital setting
- No response to social cues;
- Appears ill to a healthcare professional;
- Does not wake, or if roused, does not stay awake;
- Weak high-pitched or continuous cry.
- Aged under one year: 160 beats per minute or more;
- Aged one to two years: 150 beats per minute or more;
- Aged three to four years: 140 beats per minute or more;
- Heart rate less than 60 beats per minute at any age.
Respiratory rate
- Aged under one year: 60 breaths per minute or more;
- Aged one to two years: 50 breaths per minute or more;
- Aged three to four years: 40 breaths per minute or more;
- Oxygen saturation of less than 90% in air or increased oxygen requirement over baseline.
Temperature
- Aged under three months: 38°C or more;
- Any age: less than 36°C.
To see examples of mottled skin or ashen appearance, non-blanching rash of the skin, and cyanosis of the skin, lips or tongue, see the Photoguide.
Source: National Institute for Health and Care Excellence [8]
Initial blood tests should be requested to aid diagnosis and further inform on the likelihood of infection and prognosis. These should include:
- C-reactive protein — to detect inflammatory response;
- Full blood count — to detect immune response;
- Lactate — to detect tissue hypoxia.
Other investigations, such as a chest X-ray or lumbar puncture, may also be indicated depending on the likely focus of the suspected infection.
Point-of-care testing and future diagnostics
In the future, point-of-care testing facilities for key biomarkers may have a greater role in both primary care and hospital emergency departments, aiding healthcare professionals in diagnosing infection and sepsis. Recently published research into the use of sensor technologies designed to rapidly report on raised levels of biomarkers closely associated with sepsis (notably interleukin-6) may have the potential to aid sepsis diagnosis in the future [6] , [7] .
Case studies
Case study 1: a 12-month-old baby with suspected sepsis.
A mother brings her 12-month-old daughter Alice* into the pharmacy and asks to speak to the pharmacist. The mother clearly appears concerned and expresses that Alice seems very poorly and is not her usual self.
Consultation
The mother explains that her daughter attended nursery today and the nursery staff phoned in the afternoon to report that Alice was not feeling well. As she had a temperature of 39 o C, they administered a dose of paracetamol. The nursery staff also said that Alice had not been eating or drinking well and her nappies were dry all day.
Alice takes no regular medicine and has no ongoing health problems. She seems withdrawn and is not smiling or engaging with anyone, which the mother insists is unusual behaviour.
When assessing the patient, Alice’s hands feel cold despite her body and head feeling hot. During the interaction with Alice, she is noticeably very passive and inactive, and seems floppy in her mother’s arms. Alice does not appear to have a rash, though her skin appears pale.
Alice’s breathing appears very rapid.
Information given in the consultation suggests that Alice may have sepsis. Use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for children aged under five years out of hospital and compare it to the information obtained during the consultation [8] . By doing so, it is apparent that the following moderate-to-high risk criteria were demonstrated by the patient:
- Behaviour: parent or carer concern that the child is behaving differently than usual; not responding normally to social cues; no smile; and decreased activity;
- Cold hands or feet;
- Reduced urine output;
- Between 40 and 49 breaths per minute (normal resting respiratory rate for a 12-month-old is typically 20–40 breaths per minute);
- Pallor of skin, lips or tongue.
Although her temperature was high (39 o C), this would only be a moderate-risk criterion if Alice was aged between 3–6 months of age outside the hospital setting.
Advice and recommendations
Alice’s symptoms clearly indicate moderate-to-high risk of sepsis. According to the risk stratification tool, Alice should be referred either for a definitive diagnosis for treatment outside the hospital (i.e. to the patient’s GP), or to hospital for further review.
Considering the risk of sepsis and the importance of timely management, referral to hospital is the best choice for this patient. Calmly and clearly explain to the mother that Alice may have a serious infection and that the best course is for her to go to the hospital immediately.
Case study 2: an 11-year-old child with a viral infection
An 11-year-old boy called Liam* is brought into the pharmacy by his parents. They explain that he has not been feeling well for the past few days. The parents want to know if Liam’s symptoms can be treated with an over-the-counter (OTC) product or whether they should take him to the GP.
Liam has been unwell for the past three or four days and his condition does not seem to be improving. He has not yet taken any medicine for this illness. His temperature was 37.8 o C when most recently checked using an ear thermometer at home.
Liam says that he has a sore throat, a cough and a blocked nose. Liam describes the severity of his throat pain as three out of ten. Liam has been eating and drinking normally, has no long-term medical conditions and takes no regular medicine.
Liam and his parents agree that his behaviour and function are normal and he appears alert and coherent through the consultation. Liam’s breathing rate does not appear to be raised and his skin and lips appear normal, with no signs of a rash.
Liam may have an infection, which is likely to be viral, but does not require medical attention at present. However, to rule out sepsis, use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for children aged 5–11 years out of hospital and compare this to the information obtained during the consultation [8] . By doing so, it is apparent that no moderate-to-high risk criteria were demonstrated by the patient.
Liam can be treated with OTC analgesics to alleviate his throat pain and his raised temperature. Liam’s parents should ensure he is taking plenty of fluids and continue to monitor his temperature. If they become concerned about his condition, his behaviour or general functional ability, they should return to or call the pharmacy. Particular symptoms you advise them to look out for include development of a rash, if his skin becomes pale or mottled, his urine output drops, his breathing rate increases, or any general concern that mental state or activity is not normal.
Case study 3: an adult with red flag sepsis
Rahul*, a 28-year-old man, comes into the pharmacy and asks to see the pharmacist as he has begun to feel very unwell.
Rahul works as a driver, and he fell and scraped his leg while getting out of his van the previous day. Rahul explains that at the time he did not think much about the cut, so he did not clean or dress the wound and has not yet taken any medicine for it. Although the wound began to swell and weep overnight, Rahul went into work this morning, but left when he suddenly started to feel seriously unwell — around an hour ago.
Rahul says the wound now looks much worse than it previously did. On examination you find the wound is very red and swollen, the tissue around the wound is blistering and weeping, and there are red track marks extending further up Rahul’s leg. It is clear that this wound is infected.
Rahul uses inhalers for mild asthma, but otherwise takes no regular medicine.
Rahul says he is feeling hot and sluggish, and is clearly struggling to maintain his train of thought. His condition appears to be worsening by the minute. He needs to be referred for further help, but more information is required to decide whether he is referred to his GP or to a hospital emergency department.
Rahul’s temperature is 35.8 o C. His breathing appears to be rapid. His blood pressure is 92/58mmHg and his heart rate is 140 beats per minute. Rahul does not appear to have a skin rash, although his lips seem to have a blue tint.
Rahul is likely to have a serious infection, which requires urgent attention. Use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for people aged 18 years and over outside of the hospital setting and compare this to the information obtained during the consultation [8] . The patient has moderate- to high-risk criteria, such as tympanic temperature less than 36 o C and signs of potential infection. He also has several high-risk criteria that require urgent referral to emergency care:
- Altered behaviour or mental state;
- Respiratory rate over 25 breaths per minute;
- Heart rate more than 130 beats per minute;
- Cyanosis of skin, lips or tongue.
Tell Rahul that it is likely that he has a serious infection, and ask him to sit and wait in the pharmacy while an ambulance is called. It is not safe for him to drive to hospital. Share his information with the 999 operator and make another note of the details gathered during the consultation to hand over to the ambulance team upon arrival.
*All cases are fictional
Useful additional resources
- The UK Sepsis Trust. The Sepsis Manual. 2017–2018: Available at: https://sepsistrust.org/wp-content/uploads/2018/06/Sepsis_Manual_2017_web_download.pdf
- National Institute for Health and Care Excellence. Sepsis: risk stratification tools. Available at: https://www.nice.org.uk/guidance/ng51/resources/algorithms-and-risk-stratification-tables-compiled-version-2551488301
- For patients who are interested in finding out more about sepsis you can direct them to the NHS website. Available at: https://www.nhs.uk/conditions/sepsis/
[1] The UK Sepsis Trust. The Sepsis Manual. 2017–2018. 2017. Available at: https://sepsistrust.org/wp-content/uploads/2018/06/Sepsis_Manual_2017_web_download.pdf (accessed October 2019)
[2] The UK Sepsis Trust. Professional Resources. Available at: https://sepsistrust.org/professional-resources/ (accessed October 2019)
[3] Gotts JE & Matthay MA. Sepsis: pathophysiology and clinical management. BMJ 2016;353:i1585. doi: 10.1136/bmj.i1585
[4] National Institute for Health and Care Excellence. Sepsis: recognition, diagnosis and early management. NICE guideline [NG51]. 2016. Available at: https://www.nice.org.uk/Guidance/NG51 (accessed October 2019)
[5] National Health Service: Overview — Sepsis. 2019. Available at: https://www.nhs.uk/conditions/sepsis/ (accessed October 2019)
[6] Russell C, Ward AC, Vezza V et al . Development of a needle shaped microelectrode for electrochemical detection of the sepsis biomarker interleukin-6 (IL-6) in real time. Biosens Bioelectron 2019;126:806–814. doi: 10.1016/j.bios.2018.11.053
[7] Dolin H, Papadimos T, Stepkowski S et al. A novel combination of biomarkers to herald the onset of sepsis prior to the manifestation of symptoms. Shock 2018;49(4):364–370. doi: 10.1097/SHK.0000000000001010
[8] National Institute for Health and Care Excellence. Sepsis: Risk stratification tools. 2017. Available at: https://www.nice.org.uk/guidance/ng51/resources/algorithms-and-risk-stratification-tables-compiled-version-2551488301 (accessed October 2019)
You might also be interested in…

How the London Ambulance Service is working to transform medicines management

All emergency departments must have dedicated pharmacist, royal college and UKCPA say

Hyponatraemia: clinical presentation, diagnosis and treatment
Case Study: A Systematic Approach to Early Recognition and Treatment of Sepsis
Submitted by Madeleine Augier RN BSN
Tags: assessment Case Study emergency department guidelines mortality prevention risk factors sepsis standard of care treatment

Share Article:
Sepsis is a serious medical condition that affects 30 million people annually, with a mortality rate of approximately 16 percent worldwide (Reinhart, 2017). The severity of this disease process is not well known to the public or health care workers. Often, health care providers find sepsis difficult to diagnose with certainty. Deaths related to sepsis can be prevented with accurate assessments and timely treatment. Sepsis must be considered an immediate life-threatening condition and needs to be treated as a true emergency.
Relevance and Significance
Sepsis is defined as “the life-threatening organ dysfunction resulting from a dysregulated host response to infection” (Kleinpell, Schorr, & Balk, 2016, p. 459). Jones (2017) study of managing sepsis affirms that the presence of sepsis requires a suspected source of infection plus two or more of the following: hyperthermia (>38.1 degrees Celsius) or hypothermia (<36 degrees Celsius), tachycardia (>91 beats per minute), leukocytosis or leukopenia, altered mental status, tachypnea (>21 breaths per minute), or no urine output for 12 hours. If the infection persists, acute organ dysfunction or failure occurs from widespread inflammation, eventually leading to septic shock (Palleschi, Sirianni, O’Connor, Dunn, & Hasenau, 2013). Palleschi et al. (2013) states that during septic shock, “the cardiovascular system fails, resulting in hypotension, depriving vitals organs of an adequate supply of oxygenated blood” (p. 23). Ultimately the body can go into multiple organ dysfunction syndrome (MODS), leading to death if there is inaccurate assessment and inadequate treatment.
The purpose of this case study is to make the nurse practitioner aware of the severity sepsis, and how to accurately diagnose and treat using evidence-based data. Sepsis can affect everyone, despite his or her age or comorbidity. Center for Medicare and Medicaid Services (CMS) has diagnosed this problem as a priority and uses sepsis management in determining payment to providers (Tedesco, Whiteman, Heuston, Swanson-Biearman, & Stephens, 2017). This medical diagnosis is unpredictable and presents a challenge to nurse practitioners worldwide. Early recognition and treatment of sepsis by the nurse practitioner is critical to decrease morbidity and mortality.
After completing this case study, the reader should be able to:
- Identify the risk factors of sepsis
- Identify the signs and symptoms of sepsis
- Identify the treatment course of sepsis
Case Presentation
A 65-year-old Asian female presented to the emergency department accompanied by her husband with a chief complaint of altered mental status. Upon assessment, the patient was lethargic, and alert and oriented to person only. The patient’s heart rate was 136, blood pressure 104/50, oral temperature 99 degrees Fahrenheit, oxygen saturation 97% on 4 liters nasal cannula, and respirations 26 per minute. The patient’s blood glucose was obtained with a result 454.
Further orders, such as labs and imaging were made by the provider to rule out potential diagnoses. A rectal temperature was obtained revealing a fever of 103.7 degrees Fahrenheit. The patient remained restless on the stretcher. After one hour in the emergency department, her heart rate spiked to 203 beats per minute, respirations became more rapid and shallow, and she became more lethargic. The patient’s altered mental status, increasing heart rate and respirations caused the providers to act rapidly.
Medical History
The patient’s husband reports that she is a type one diabetic, he denies any other medical conditions. In addition, the patient’s husband states that she has not been exposed to any sick individuals in the past few weeks. The husband reports a family history of diabetes, other wise no significant familial history. No history of smoking, drinking, or illicit drug use was to be noted.
Physical Assessment Findings
The patient appeared lethargic and confused with a Glasgow Coma Scale of 12. She appeared tachypnic, with shallow respirations, and a rate of 28 breaths per minute. Upon auscultation, breath sounds were coarse. Her abdomen was soft and non-tender, no nausea or vomiting noted. The patient appeared diaphoretic, and her legs were mottled.
Laboratory and Diagnostic Testing and Results
During the initial assessment, a complete blood count (CBC), basic metabolic panel (BMP), and lactic acid level were ordered for blood work. A STAT electrocardiogram (EKG), urinalysis, and a chest X-ray were ordered to differentiate possible diagnoses. The CBC revealed leukocytosis with a white blood cell count of 23,000 and an increased lactic acid level of 4.3. The anion gap and potassium level remained within a normal limit, ruling out the possibility of diabetic ketoacidosis (DKA). The patient’s EKG showed supraventricular tachycardia (SVT). The chest X-ray revealed infiltrates to the right lung. The urinalysis was free from leukocytes or nitrites. Blood cultures were ordered to confirm their hypothesized diagnosis, septicemia.
Pharmacology
The provider initiated intravenous (IV) fluid treatment with Lactated Ringers at a bolus of 30 mL/kg. Because the patient’s heart rate was elevated, 6 mg of adenosine was ordered to combat the SVT. Additionally, broad-spectrum IV antibiotics were initiated. One gram of vancomycin and 3.375 grams of piperacillin-tazobactam were the preferred antibiotics of choice.
Final Diagnosis
Upon arrival, the providers were ruling out DKA and sepsis, given the patient’s history.
The patient’s elevated white blood cell counts, temperature, lactic acid level, heart/respiratory rate, and altered mental status were all clinical indicators of sepsis. The chest X-ray revealed a right lung infiltrate, persuading the providers to diagnose the patient with sepsis secondary to pneumonia.
Patient Management
After sepsis was ruled as the patient’s diagnosis, rapid antibiotic administration and IV fluid treatment became priority after the patient’s heart rate was controlled. A cooling blanket and a temperature sensing urinary catheter was placed to continuously monitor and control the patient’s fever. Later, the patient was transferred to a critical care unit for further treatment. Shortly after being transferred, the patient went into respiratory failure and was placed on a ventilator. After two days in the ICU, the patient remained in septic shock, and died from multisystem organ failure.
When the patient initially presented to the emergency department, accurate and rapid diagnosis of sepsis was critical in order to stabilize the patient and prevent mortality. A challenge was presented to the provider regarding a rapid diagnosis due to the patient’s history and her presenting signs and symptoms. Increased awareness and interprofessional education regarding sepsis and its’ treatment is vital to decrease mortality. Health care providers need to be competent in recognizing and accurately treating sepsis in a rapid manner.
Research shows that outcomes in sepsis are improved with timely recognition and early resuscitation (Javed et al., 2017). It is important for the provider to identify certain risk factors and symptoms to easily diagnose sepsis. A research study by Henriksen et al. (2015) proved that age, and comorbidities including psychotic disorders, immunosuppression, diabetes, and alcohol abuse served as top risk factors for sepsis.
Once the diagnosis of sepsis is determined, rapid treatment must be initiated. The golden standard of treatment consists of a bundle of care that includes blood cultures, broad-spectrum antibiotic agents, and lactate measurement completed within 3 hours as described by Henriksen et al. (2015). A study by Seymour et al. (2017) showed that the more rapid administration of the bundle of care is correlated with a decreased mortality rate. In addition, The Survival of Sepsis Campaign formed a guideline to sepsis treatment; Rhodes et al. (2016) suggests giving a 30 mL/kg of IV crystalloid fluid for hypoperfusion. If hypotension persists (mean arterial pressure <65), vasopressors, preferably norepinephrine, should be initiated (Rhodes et al., 2016). Prompt recognition of sepsis and implementation of the bundle of care can help reduce avoidable deaths.
To increase awareness, interprofessional education regarding sepsis and its’ common signs and symptoms needs to be established. Evidence-based protocols should be utilized in hospital care settings that provide nurse practitioners with a guideline to follow to ensure rapid and accurate treatment is given. Increased awareness and education helps providers and other healthcare workers to properly identify and accurately treat sepsis.
The public and health care providers must become more aware and educated on the severity of sepsis. It is crucial to be able to recognize signs and symptoms of sepsis to prevent further complications such as septic shock and multi-organ failure. Increased awareness, interprofessional education, accurate assessment, and rapid treatment can help reduce incidence and mortality. Sepsis management must focus upon early goal-directed therapy (antibiotic administration, fluid resuscitation, blood cultures, lactate level) and individualized management pertaining to the patient’s history and assessment (Head & Coopersmith, 2016). Misdiagnosis and delay in emergency treatment can result in missed opportunities to save lives.
- Head, L. W., & Coopersmith, C. M. (2016). Evolution of sepsis management:from early goal-directed therapy personalized care. Advances in Surgery, 50 (1), 221-234. doi:10.1016/j.yasu.2016.04.002
- Henriksen, D. P., Pottegard, A., Laursen, C. B., Jensen, T. G., Hallas, J., Pedersen, C., & Lassen, A. T. (2015). Risk factors for hospitalization due to community-acquired sepsis-a population-based case-control study. PLOS ONE, 10 (4), 1-12. doi:10.1371/journal.pone.0124838
- Javed, A., Guirgis, F. W., Sterling, S. A., Puskarich, M. A., Bowman, J., Robinson, T., & Jones, A. E. (2017). Clinical predictors of early death from sepsis. Journal of Critical Care, 42 , 30-34. doi:10.1016/j.jcrc.2017.06.024
- Jones, J. (2017). Managing sepsis effectively with national early warning scores and screening tools. British Journal of Community Nursing, 22 (6), 278-281. doi:10.12968/bjcn.2017.22.6.278
- Kleinpell, R. M., Schorr, C. A., & Balk, R. A. (2016). The new sepsis definitions: Implications for critical care. American Journal of Critical Care, 25 (5), 457-464. doi:10.4037/ajcc2016574
- Palleschi, M. T., Sirianni, S., O'Connor, N., Dunn, D., & Hasenau, S. M. (2013). An interprofessioal process to improve early identification and treatment for sepsis. Journal for Healthcare quality, 36 (4), 23-31. doi:10.1111/jhq.12006
- Reinhart, K., Daniels, R., Kissoon, N., Machado, F. R., Schachter, R. D., & Finfer, S. (2017). Recognizing sepsis as a global health priority-A WHO resolution. The New England Journal of Medicine, 377 (5), 414-417. doi:10.1056/NEJMp1707170
- Rhodes, A., Evans, L. E., Alhazzani, W., Levy, M. M., Anotnelli, M., Ferrer, R.,...Beale, R. (2017). Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Medicine, 43 (3), 304-377. doi:10.1007/s00134-017-4683-6
- Seymour, C. W., Gesten, F., Prescott, H. C., Friedrich, M. E., Iwashyna, T. J., Phillips, G. S.,...Levy, M. M. (2017). Time to treatment and mortality during mandated emergency care for sepsis. The New England Journal of Medicine, 376 (23), 2235-2244. doi:10.1056/NEJMoal1703058
- Tedesco, E. R., Whiteman, K., Heuston, M., Swanson-Biearman, B., & Stephens, K. (2017). Interprofessional collaboration to improve sepsis care and survival within a tertiary care emergency department. Journal of Emergency Nursing, 43 (6), 532-538. doi:10.1016/j.jen.2017.04.014
Career Opportunities

More Like This

Septic Shock (Sepsis) Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
What initial nursing assessments need to be performed for Mr. McMillan?
- Full set vital signs (T, P, RR, BP, SpO 2 )
- OLDCARTS or PQRST assessment of symptoms (urinary burning)
- LOC/orientation assessment
- Heart and lung sounds
Upon further assessment, Mr. McMillan is weak, his face is flushed, his skin is warm and dry. He is oriented to person and place, but states the year is 1952. His vital signs were as follows:
BP 99/60 mmHg Ht 170.2 cm
HR 92 bpm and regular Wt 60 kg
RR 28 bpm SpO 2 93% on Room Air
Temp 38.9°C
What diagnostic tests should be ordered for Mr. McMillan?
- Blood Tests – CBC, BMP, ABG, Lactic Acid, Blood Cultures x 2
- Urine Tests – Urinalysis, Urine Culture
- X-rays – Chest, Kidneys/Ureters/Bladder
What nursing actions would you take at this time for Mr. McMillan? Why?
- Elevate the HOB to improve breathing and oxygenation
- Apply cardiac monitor
- Notify provider of elevated temp and low SpO 2
- Apply cool washcloth to forehead and/or behind neck for comfort
- Possibly get ice packs to axillae and groin and remove any blankets to help bring the patient’s temperature closer to normal.
The ED provider orders the following:
- Bloodwork – CBC, BMP, ABG, Lactic Acid, Blood Cultures x 2
- Diagnostics – CXR (chest x-ray), KUB (x-ray of kidneys, ureters, and bladder)
- Nasal Cannula to keep SpO 2 > 92%
- Meds – 1L Normal Saline bolus IV x 1, now. 1,500 mg Vancomycin IVPB x 1 dose, now
Which order should you implement first? Why?
- Blood and urine cultures must be drawn before any antibiotics are administered.
- Blood work – urine tests – fluids – antibiotics
- IF the patient’s SpO 2 is below 92%, apply oxygen via nasal cannula – at this time, there is no indication of that, yet.
All blood and urine tests are completed and you initiate the fluid bolus for Mr. McMillan. You are still waiting for the Vancomycin to arrive from the pharmacy. You notice he is more drowsy. He is now only oriented to self and feels warmer. You take another set of vital signs to find the following:
BP 86/50 mmHg MAP 62 mmHg
HR 108 bpm Temp 39.3°C
RR 36 bpm SpO 2 88% on Room Air
Mr. McMillan’s lab results have also resulted, the following abnormal values were reported:
WBC 22,000 / mcL Lactic Acid 3.6 mmol/L
pH 7.22 pCO 2 30 mmHg
HCO 3 16 mEq/L pO 2 64 mmHg
Urine Cloudy with sediment
What action(s) should you take at this time? Why?
- #1 – apply oxygen via nasal cannula – ensure HOB elevated for easy breathing
- Notify provider of decreasing blood pressure and elevated WBC, lactic acid ANSWER
What orders do you anticipate for Mr. McMillan? (procedures, meds, transfer, etc?)
- Mr. McMillan may need another liter of IV fluids. The guidelines are for patients to receive 30 mL/kg of body weight in the first 6 hours. That means he would need to receive at least 1,800 mL of IV fluid bonuses.
- Mr. McMillan may need vasopressors to improve his blood pressure – in which case he will also need a central line for administration of those medications as well as an arterial line to monitor his MAP.
- Mr. McMillan will need to be transferred to the ICU for close monitoring and management of his drips
Mr. McMillan responds well to the first liter of fluids, and antibiotics are initiated within an hour of arrival. The ED physicians place an arterial line and central line to initiate vasopressors. They order a Norepinephrine infusion to be titrated to keep MAP > 65 mmHg. The Critical Care team asks you to prepare the patient for transfer to the ICU.
Art. Line BP 82/48 mmHg MAP 58 mmHg
HR 122 bpm CVP 4 mmHg
RR 32 bpm SVR 640 dynes/sec/m -5 SpO 2 90% on Room Air
What, physiologically, is going on with Mr. McMillan?
- Mr. McMillan has an infection, likely urinary, and it has created a systemic inflammatory response. That inflammatory response is causing massive peripheral vasodilation so his vital organs are not receiving adequate blood flow
- He is showing signs of decreased perfusion to his brain (↓ LOC) and decreased cardiac output (↓ BP).
- His skin is warm and flushed and his temperature is elevated because of the vasodilation in the non-vital organs.
What does it mean to titrate an infusion to keep MAP >65?
- Titration means achieving the desired result with the least amount of drug possible. Therefore we would adjust the infusion up or down to maintain the MAP above, but not too far above, 65 mmHg
After 2 days in the ICU, a norepinephrine infusion and a total of two liters of normal saline, Mr. McMillan’s blood pressure is stable, his MAP is 67 mmHg. He is becoming more alert and is now oriented to person, place, and time. His blood and urine cultures were positive for bacterial growth. He has received multiple doses of Vancomycin as well as antibiotics targeted to his specific bacterial infection. He is being weaned off of the vasopressors, and the providers hope he can transfer out of the ICU tomorrow.
What explanation or education topics would you want to provide to the patient and his caregiver before discharge?
- Sepsis and septic shock are a result of a severe infection that has gotten into the bloodstream and affected the patient’s ability to pump blood to the body. This is what makes their blood pressure drop so low. We treat this condition by getting the infection under control and supporting the patient’s blood pressure.
- Signs and symptoms of infection – in elderly people, one of the first signs of infection is altered mental status. If the patient seems ‘off’ or ‘not themselves’, it is worth notifying a healthcare provider to prevent a worse situation.
- The patient will need to ensure he is drinking plenty of fluids and practicing good hygiene to prevent urinary tract infections. He may also consider cranberry juice.
- If receiving a PO course of antibiotics – be sure to take the full course and notify HCP of any adverse reactions.
Happy Nursing!
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Sepsis Patient Case Study

Executive Summary
The percentage of sepsis patient cases meeting bundle requirements was below benchmark and there was opportunity to improve both mortality and length of stay (LOS).
Key Stakeholders
Medical Staff, nursing, performance improvement, virtual sepsis unit (VSU), healthcare informatics, laboratory personnel, pharmacy and patients.
People, Process and Technology
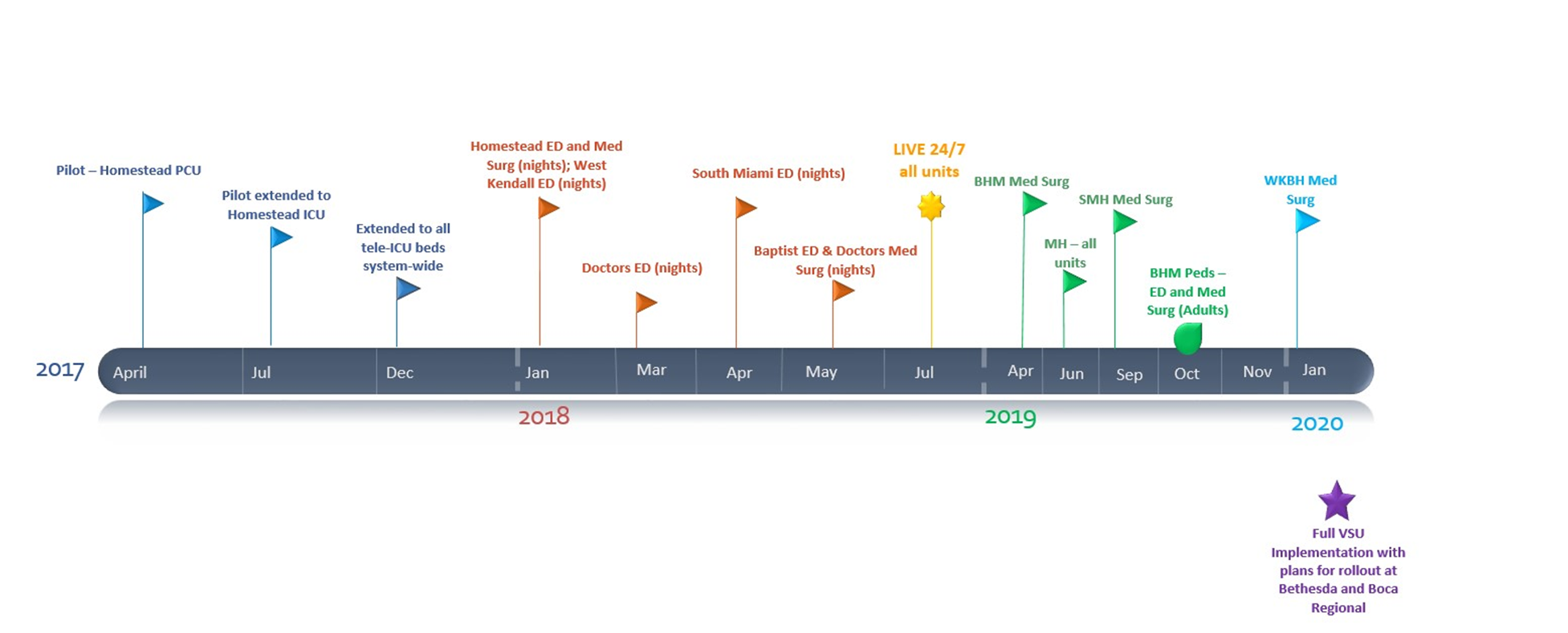
- Interdisciplinary Committee, established December 2017
- Assign patient champions
- Ongoing Physician Education (Team Health EDP group onboard)
- VSU/eICU (PCU/ICU and Med-Surg Units) April 2017; January 2018
- Sepsis Handoff Tool – May 2019
- Sepsis Bundles
- Device integration
- Bedside specimen collection and scanning
- Clinical decision support (CDS)–Alerts
- Care team communication
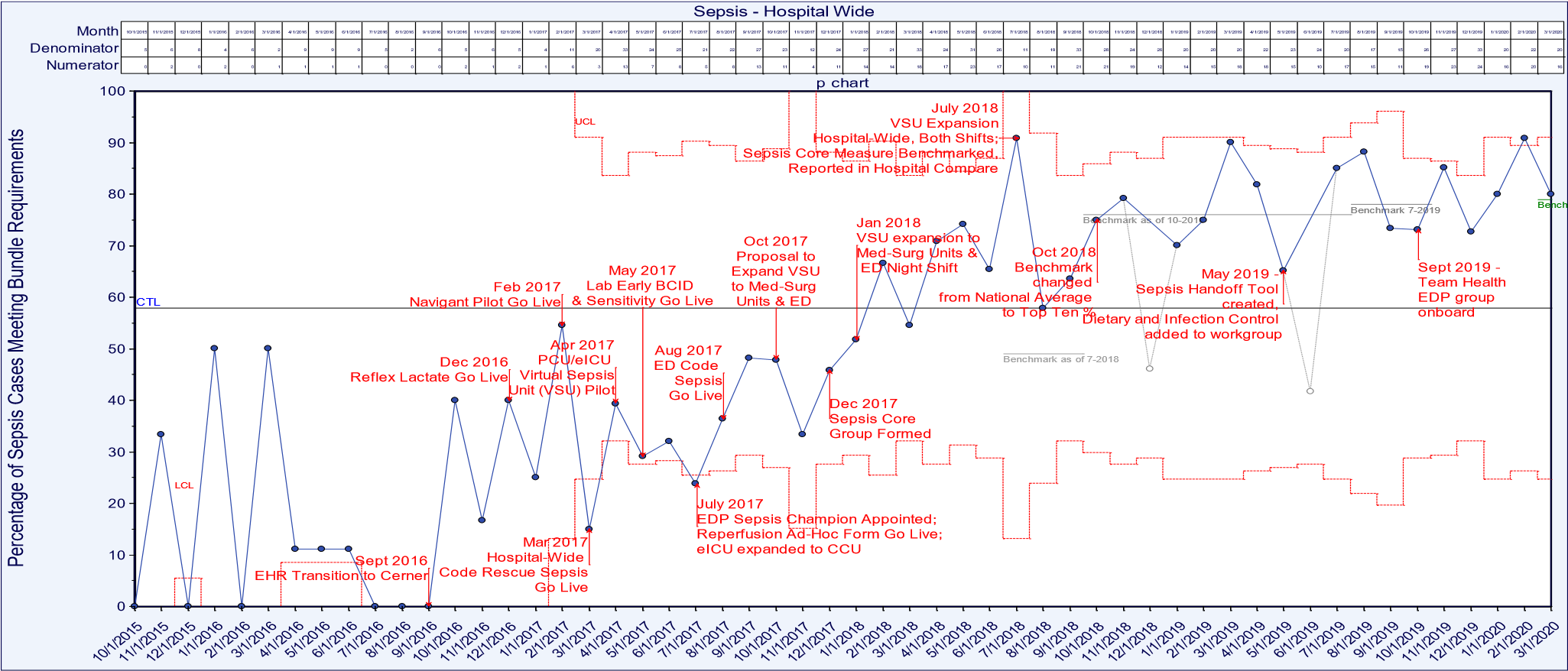
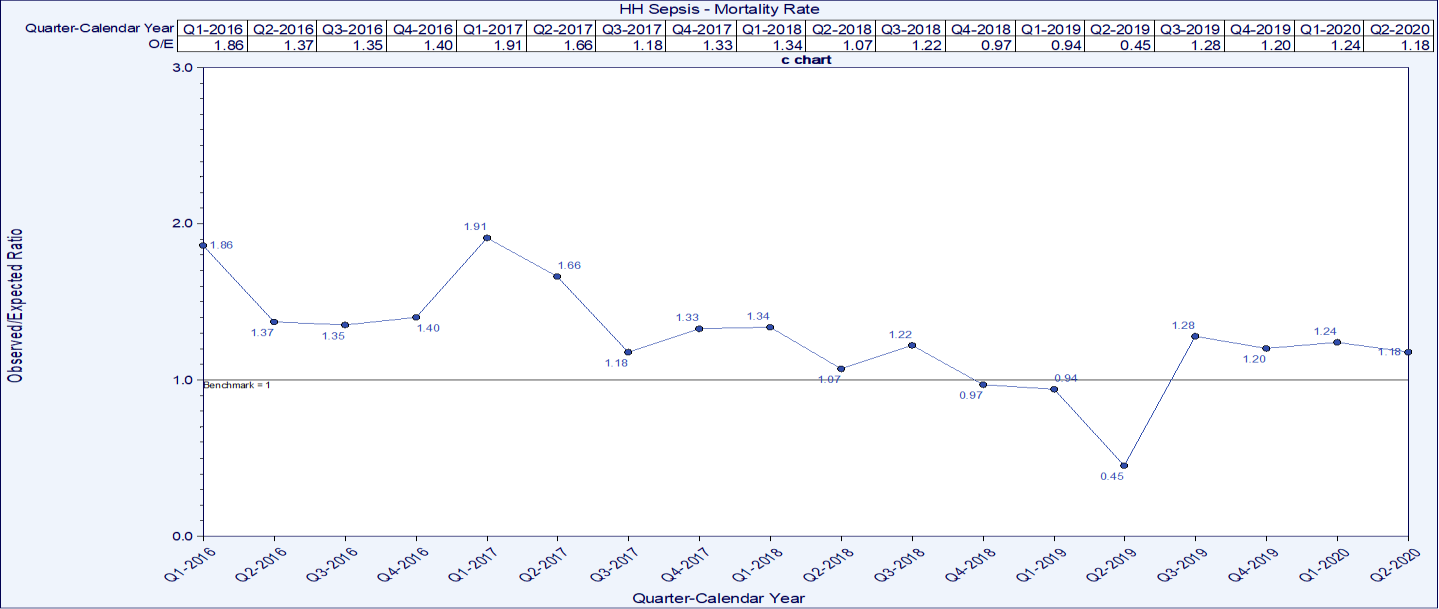
The sepsis patient mortality rate decreased from as high as 1.91 in Q1 2017 to as low as 0.45 in 2019. Cases meeting the bundle compliance increased from as low as 52% in Jan 2018 to as high as 88% in August 2019. LOS also decreased from a high of 6.83 days on average in January of 2017 to as low as 3.88 days on average in August of 2019.
Lesson Learned
- Teamwork and collaboration were instrumental in the success of bundle build and increasing bundle compliance. Accountability and the ability to measure outcomes and compliance are critical
- Assign a patient champion who is an expert in sepsis management
- Utilization of a VSU such as an eICU provides another layer of surveillance.
- CDS, alerts, dashboards and direct communication with the care teams are part of the direct communication in place to improve care.
Define the Clinical Problem and Pre-Implementation Performance
Local problem.
Our goal was to reduce clinical variation in the care of sepsis patients at Homestead Hospital and throughout the system at Baptist Health South Florida (BHSF). We engaged the care team in improving processes related to the treatment of patients presenting to respective Emergency Departments (ED), via direct admission, or who become septic during their stay.
Sepsis affects over 26 million people worldwide every year, and the organization treats over 3,000 patients annually with sepsis, severe sepsis or septic shock. Sepsis is the body’s response to an infection that has become overwhelming and can lead to tissue damage, organ failure, amputations and death. Mortality increases 8% for every hour that treatment is delayed and as many as 80% of sepsis deaths could have been prevented with rapid diagnosis and treatment. Sepsis patients have the largest cost of hospitalizations in the United States consuming more than $24 billion dollars each year. Sepsis patients also have almost double the average cost per stay at around $18,400 per admission.
Previous work to improve bundle compliance was achieved through the BHSF Accelerated Change Team (ACT), which developed system wide order sets. The reflex lactate was also implemented through the BHSF ACT enabling lab to automatically order a timed lactate to achieve follow-up lactate compliance.
Homestead Hospital has a robust sepsis patient committee that meets monthly, reviewing outcome measures and providing education, mock codes, as well as reviewing cases month to month. The organization partnered with Navigant on the T2020 initiative which includes redesigning care for select DRGs. Navigant and the organization decided upon a structure of a Sepsis Steering Committee as well as two design groups: An ED team and an inpatient and ICU team. These teams collaborated on creating clinical specification to ensure sepsis patients got the same care every patient, every time. BHSF facilities such as Homestead Hospital had varied levels of success in completing the Centers for Medicare and Medicaid Services (CMS) 3-hour and 6-hour bundles for patients identified as septic. The inconsistency of implementing the two bundles in a timely manner led to significant LOS and improved mortality opportunities. Earlier identification and implementation of the interventions described in the bundles led to better outcomes for sepsis patients and a decrease in the LOS.
The mortality rate decreased from as high as 1.91 in Q1 2017 to as low as 0.45 in 2019. Sepsis patient cases meeting bundle compliance increased from as low as 52% in Jan 2018 to as high as 88% in August 2019. LOS also decreased from a high of 6.83 days on average in January of 2017 to as low as 3.88 days on average in August of 2019.
All patients >18 years of age are screened for sepsis, the numerator is the total count of patients treated in compliance with the bundle and the denominator includes all patients with the MS-DRG of sepsis (positive screen). Mortality rates are based on severity adjusted benchmarks and LOS is based on the average LOS against the benchmark of CMS and Premier.
Targeted performance
To meet and/or exceed the benchmark.
Benchmark data
BHSF benchmarks sepsis patient data against CMS, the Acute Physiology And Chronic Health Evaluation (APACHE) IV severity of disease classification system (ICU/PCU), Premier, and internal goals.
Technology initiatives
Electronic health record (EHR) data, CDS such as the St. Johns Sepsis Alert, clinical dashboards, Ascom phones for communication, the eICU for virtual care management, bedside specimen collection scanning, device integration for clinical data and bundle management via PowerPlans™.
People and Process
The evidence-based clinical care (EBCC) committee oversees the organizational structure for process waves which identify areas for improvement. The VSU is a component that enhances people, process and technology. The sepsis patient champions help to optimize infection management and emphasize the importance of early recognition and timely treatment, they also facilitate sepsis patient care and optimize patient outcomes. Ongoing physician and team education are available via lunch and learns with classroom time, elbow to elbow support, web-based learning, online formats on the EBCC website via the intranet and on the Baptist Health South website which is available in the public domain. The continuing education is a vital component to the hospital-wide code rescue response team.
Design and Implementation Model Practices and Governance
Baptist Health South Florida’s EBCC initiative is a strategic system-wide standardization effort to reduce variation and unnecessary costs while focusing on evidence-based, quality care. The process is driven by key stakeholders and is supported by real-time, statistically supported benchmarked data. The charter was signed in 2016 and provides the foundation for a methodical approach to improve patient outcomes (Figure 1).
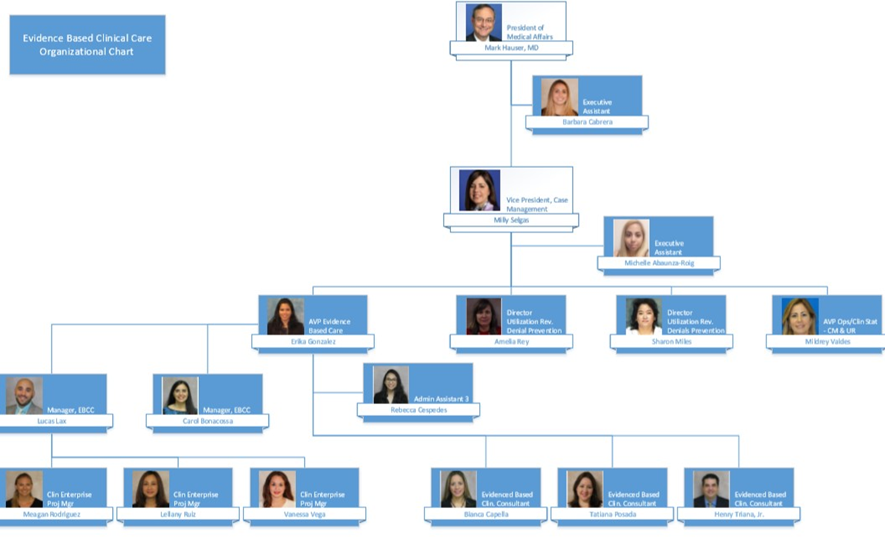
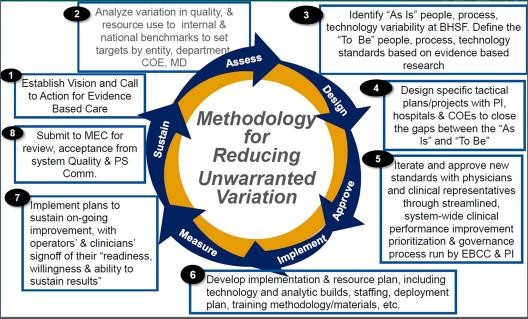
The methodology begins with a call to action to for an evidenced based care assessment of current and future state, design plan, team approval, development of an implementation plan, measurement and sustainment plans (Figure 2).
Each specific project is supported by a sub-group who are experts in on the focus topic. The Service Line Collaborative includes:
- Cardiac and Vascular
- Critical Care
- Emergency Department
- Gastrointestinal
- Infectious Disease
- Neonatology
- Neuroscience
- Orthopedics
- Surgery/PEI/ERAS/NSQIP
Navigant and BHSF decided upon a structure for a Sepsis Steering Committee to reduce variation in the management of sepsis to improve the sepsis patient mortality rate.
Education was completed via lunch and learns with classroom time, online formats on the EBCC website via the intranet and on the organization’s website which is available in the public domain.
PowerPlan™ education is a consistent part of physician education and CME education is available with every MS-DRG or pathway as it rolls out. The pilot for the sepsis patient go-live began in February 2017 and the hospital wide go-live was April 2017. The iterations over time have continued based on new benchmarks and evidence as it becomes available.
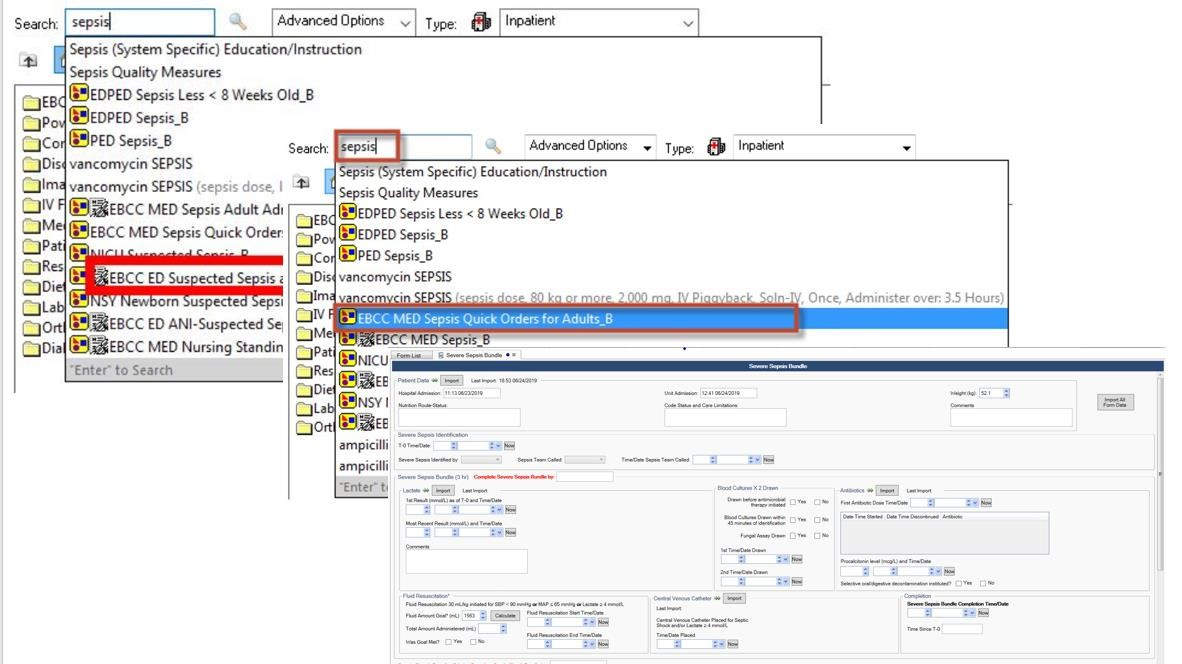
Technologies include: the physiologic data within the EHR, device integration, CDS, bedside specimen collection, sepsis algorithm, support from the eICU/VSU, dashboards and PowerPlans™ for the care bundle.
Clinical Transformation enabled through Information and Technology
To reduce clinical variation in the care of sepsis patients throughout the health system at BHSF, we engaged the care teams to improve processes related to the treatment of patients presenting to respective EDs, via direct admission, or who become septic during their stay. The workflows are geared to meet the care requirements as outlined by the industry in evidenced based research such as CMS and the Society of Critical Care Medicine’s Surviving Sepsis Campaign (Figure 3). While the overarching goal is the same throughout the venues of care, the workflows are created to meet clinical specification to ensure sepsis patients get the same care—every patient, every time. The utilization of the bundle is the foundation for minimizing the variation in care, and the people, process and technology as overseen by the EBCC committee provides the balance to drive action.
The workflows for the ED begin at triage and lead to the engagement of the VSU (Figure 4). The VSU is “air traffic control” for compliance and workflows are also designed for the ICU/PCU and med/surg areas (Figures 5 and 6). The VSU is operated out of the eICU and the virtual team streamlines the workflows to improve compliance to CMS guidelines, improving outcomes and reducing reimbursement penalties.
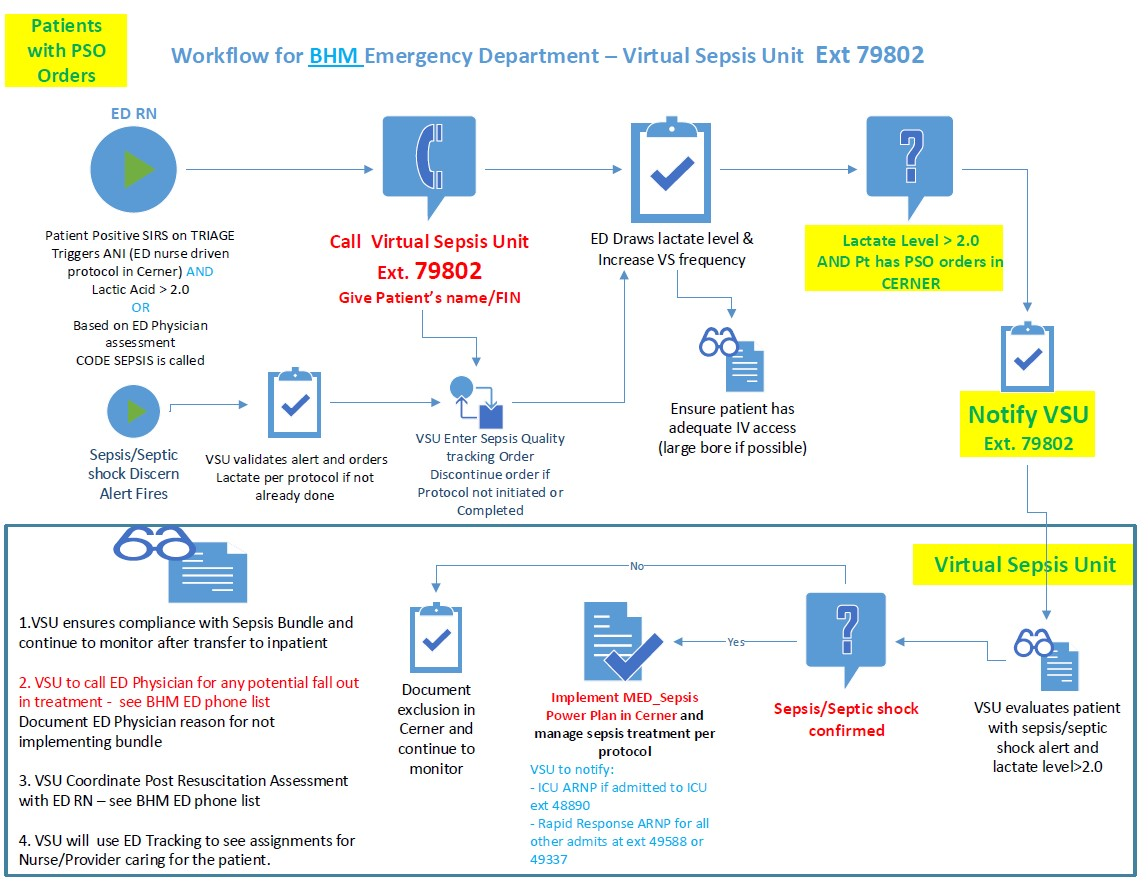
The algorithm that drives the alert is embedded into the EHR (Figure 7). The EHR supplies the clinical data required for the alert by integrating technologies such as vital sign devices, bedside specimen collection and scanning and lab values. Dashboards are available in the VSU, ED and nursing units to enhance access to the alerts, as well as alerting within the EHR.
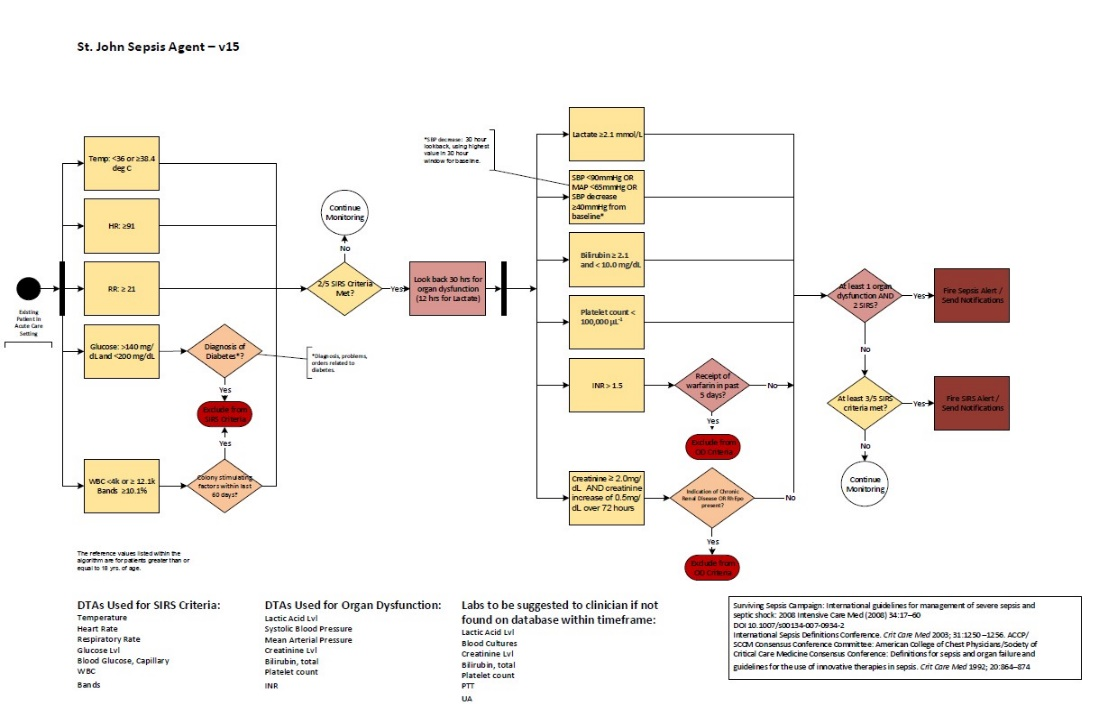
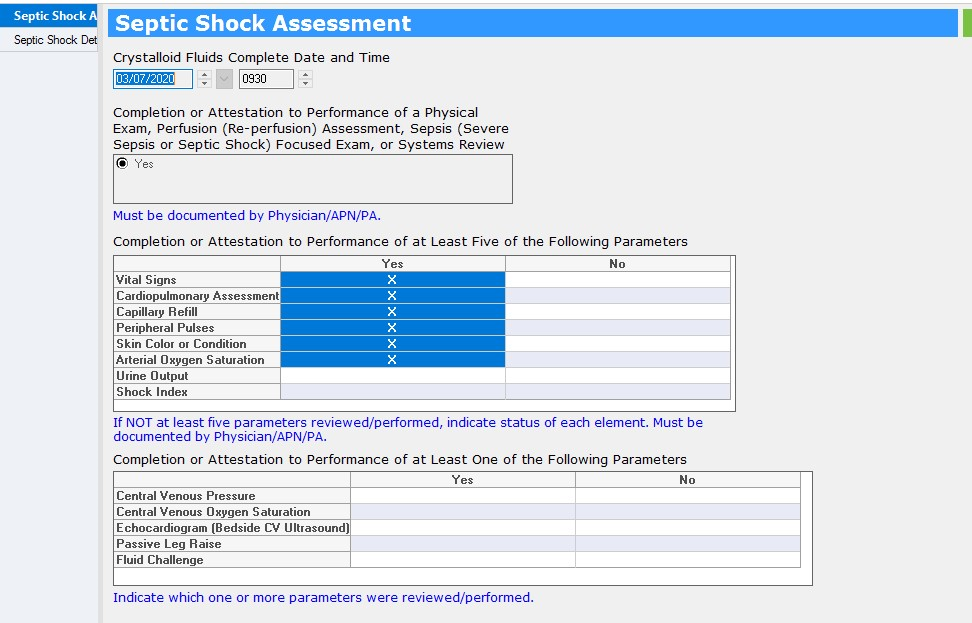
Documentation of care takes place in the EHR and the CDS for the algorithm generates the alert (Figure 8).
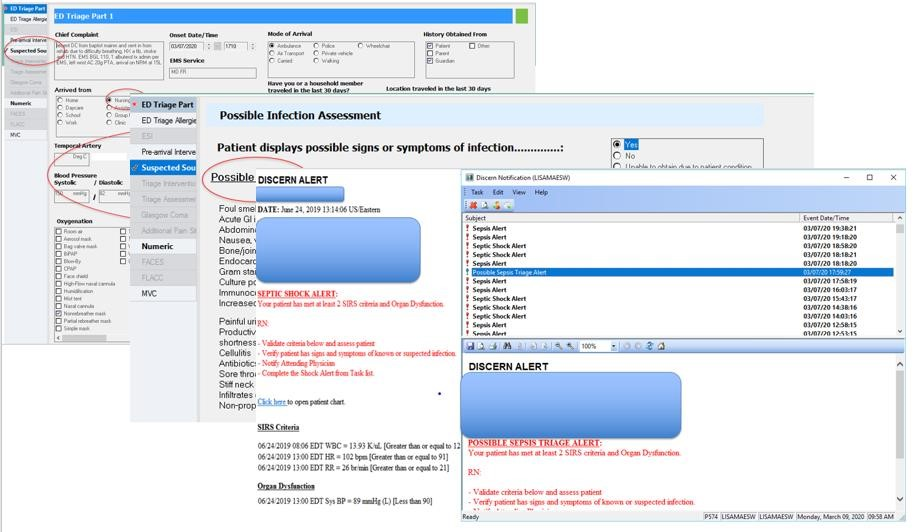
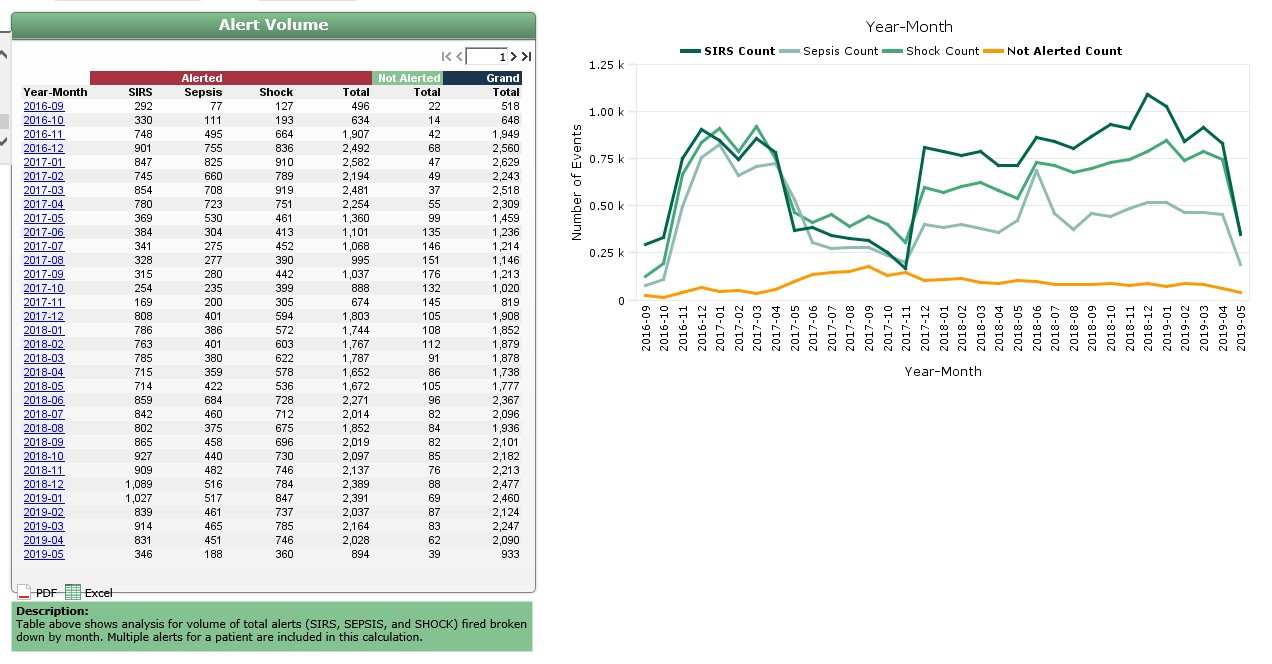
Managing the alert volume to prevent alert fatigue is a key responsibility of the VSU. The VSU reduces the number of non-actionable alerts going to physicians and nurses. Fewer alerts help to improve the specificity of the alert and provides clinical validation. (Figure 9).
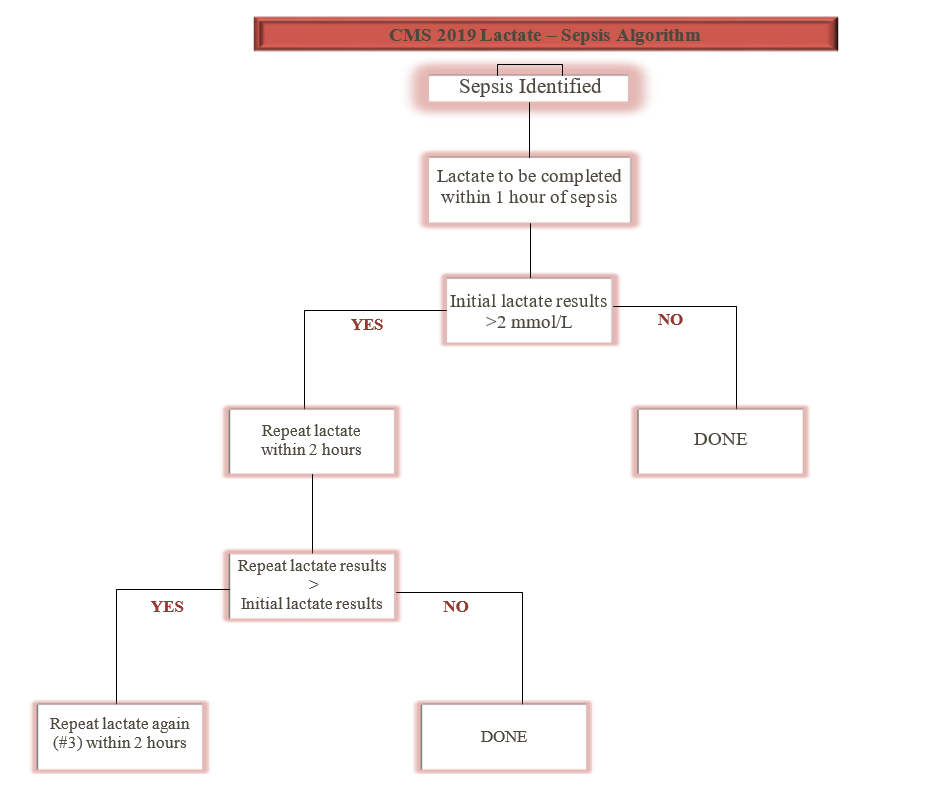
In 2019, new guidelines were released for the recommendation of lactate measures and these recommendations were built into the bundle and the workflows (Figure 10).
Examples of documentation for the bundle includes suspected sepsis patient and a quick bundle (Figure 9). Education for all care is available in the electronic version of ‘what I need to know’ (eWINK), a BHSF online education tool in the public domain which also offers CMEs/CEUs. Education for staff also includes lunch and learns with classroom time, elbow to elbow support and online formats on the EBCC website via the intranet. PowerPlan™ education is a consistent part of physician education and WINK collateral, CME education is available with every MS-DRG or pathway as it rolls out (Figure 11).
Using existing infrastructure of the eICU, virtual sepsis management was incorporated into exiting workflows. PowerPlans™ are used for bundle documentation, integration of clinical data within the EHR is supported by device integration and specimen collection and the EBCC drives pushing the current evidence to the point of care and keeps the educational material up to date.
Improving Adherence to the Standard of Care
All patients >18 years of age are screened for sepsis upon triage in the ED and all inpatients >18 years of age are monitored via CDS surveillance with the sepsis alert running within the EHR. The numerator is the total count of patients treated in compliance with the bundle and the denominator includes all patients with the MS-DRG of sepsis (positive screen). The organization transitioned to the current EHR in September of 2016 and implemented the bundle PowerPlans™ and sepsis initiative in 2017. Prior data indicated the facilities had varied levels of success in completing the bundles for patients identified as septic and the inconsistency led to opportunities to improve LOS and mortality rate.
Over time, at Homestead Hospital the compliance rate for the CMS 3-hour sepsis bundle increased from ~35% in 2015 to >90% in February 2020, with the data steward being CMS (Figure 12).
Homestead Hospital followed the standard process of change management and care redesign as outlined in the EBCC methodology. The EBCC is the governing body driving the utilization of evidence-based care focused on eliminating variation in care delivery.
Improving Patient Outcomes
The sepsis severity adjusted mortality rate decreased from as high as 1.91 in Q1 2017 to as low as 0.45 in 2019 (Figure 13). Average LOS also decreased from a high of 6.83 days on average in January of 2017 to as low as 3.88 days on average in August of 2019 (Figure 14). The risk adjusted mortality and O:E ratio are generated from Premier data.
Accountability and Driving Resilient Care Redesign
BHSF and Homestead Hospital rely on a data driven and evidence based clinical care approach to guide the design and implementation of sepsis patient care bundles. The goals of the organization’s EBCC are to decrease variation across the clinical areas and provide predictable, data-driven high quality, affordable care. Having the tools to collect as close to real-time as possible compliance data and report on that data in near-real-time reflects the ability of the organization to target and successfully improve care delivery, and ultimately improve the clinical outcomes.
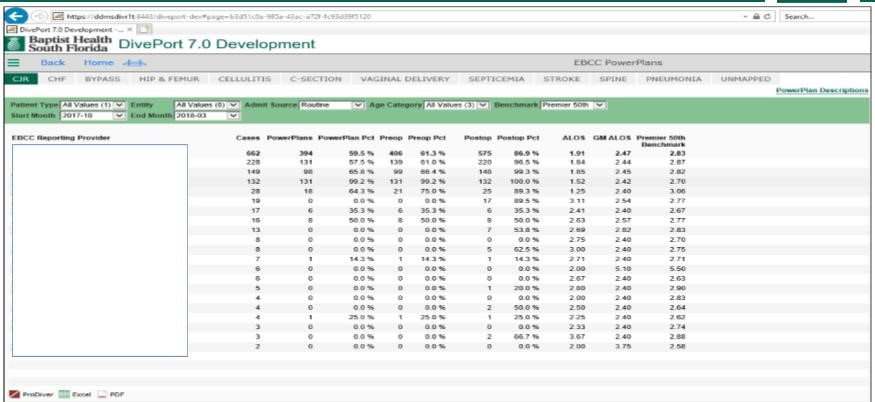
In near-real-time, the clinical team document the compliance of bundle utilization and the data is then accessible in their DivePort analytics dashboard (Figures 15 and 16). The dashboard is designed to provide statistical analysis, benchmark information and severity adjusted data with the capability to drill in multiple layers.
PowerPlans™ and bundle utilization is also available in DivePort, lending to the capability of measuring and reporting not only on the outcomes, but also to the compliance of the guidelines (Figure 17).
Using analytics to find variation
- APR-DRG Population Group is identified based on cost opportunity when compared to HCUP 40th percentile (Total Cost Per Case and ALOS).
- EBCC and Analytics Integrity Committee members review MS-DRG specific groupings that correspond with APR-DRG grouping.
- Premier benchmark levels of 50th and 75th percentile variable cost opportunities are used to further validate the data.
- MS-DRGs are recommended for EBCC team redesign based on variable cost opportunity, average LOS and volume.
- EBCC DivePort 7.0 Portal reporting is updated as DRGs waves are defined for tracking outcomes.
The rollout of the VSU is an example of using data to further refine the care redesign to complement the people, process and technology to enhance care delivery (Figure 18).
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award showcases the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.
Begin Your Path to a Davies Award

- View All Courses
- Courses by Topic
- Live Webinars
- CE Enduring Activities
- Sponsor Courses
- Virtual Conferences
- Virtual Symposia
- Discussions
- Log In / Home
- Cart (0 items)
- Contact Sepsis Alliance

Sepsis Case Studies
Product not yet rated
Recorded On: 03/18/2020
- CE Information
- Course Contents

Description:
Delve into sepsis case studies that illustrate common assessments and tools used to care for sepsis. This presentation details case studies that cover three different healthcare areas, as well as the team members involved in the assessment, diagnosis, and treatment of patients with sepsis. These cases highlight the need for all members of the healthcare team to be aware of acute changes, and the need to communicate them to the appropriate provider. It is also a reminder that patients need to be assessed at every shift for early identification and early treatment.
Learning Objectives:
At the end of the activity, the learner should be able to:
- Identify SIRS and qSOFA criteria;
- Restate the importance of early identification and treatment of sepsis across the continuum of care;
- List clinical pearls from sepsis case studies across different healthcare settings.
Target Audience:
Nurses, advanced practice providers, physicians, emergency responders, pharmacists, medical technologists, respiratory therapists, physical/occupational therapists, infection prevention specialists, data/quality specialists, and more.
Webinar Supporter:
Sepsis Alliance gratefully acknowledges the support provided for this webinar by bioMérieux.
Lori Muhr, DNP, MHSM/MHA
Sepsis program coordinator, jps health network.
Lori brings over 30 years of clinical, managerial, and educational experience to this project. She has a Doctorate Degree in Nursing Practice, a dual Master’s Degree in Management and Administration, is certified Adult Clinical Nurse Specialist, and works as an Advance Practice Nurse. She has experience in ED, Critical Care, and Community Health. Lori has experience working in rural hospitals, Level 1 Trauma centers, For-Profit and Not-for-profit organizations, all of which bring a unique perspective in her ability to reach all levels of healthcare providers. She has recently led JPS Hospital to achieve Joint Commission - Disease Specific Certification in Sepsis and has led them to be the first community safety net hospital to receive this designation. Her ability to simplify complex issues and passion for teaching comes through in her energetic and motivational style.
Provider approved by the California Board of Registered Nursing, Provider Number CEP17068 for 1.6 contact hours.
Other healthcare professionals will receive a certificate of attendance for 1.25 contact hours.
- Medical Disclaimer
The information on or available through this site is intended for educational purposes only. Sepsis Alliance does not represent or guarantee that information on or available through this site is applicable to any specific patient’s care or treatment. The educational content on or available through this site does not constitute medical advice from a physician and is not to be used as a substitute for treatment or advice from a practicing physician or other healthcare professional. Sepsis Alliance recommends users consult their physician or healthcare professional regarding any questions about whether the information on or available through this site might apply to their individual treatment or care.
Please Log In
Find sepsis education.
- Sepsis Program Overviews and Performance Improvement
- Sepsis Core Measure and Surviving Sepsis Campaign Guidelines
- Sepsis and Technology
- Infection Prevention and Sepsis Prevention
- Sepsis Recognition, Diagnosis, Treatment, and Monitoring
- Sepsis Populations and Comorbidities
- Pre-Hospital and Post-Acute Sepsis
- Specialty Topics
- Sepsis Stories (Patients, Family, and Caregivers)
- CE Enduring Courses
- Courses by Speaker
- Privacy Policy
- Funding and Sponsorship Policy
Copyright ©2024 Sepsis Alliance. All rights reserved.
Sepsis Alliance is a tax-exempt organization under Sections 501(c)(3) of the Internal Revenue Code. Contributions are deductible for computing income estate taxes. Sepsis Alliance tax ID 38-3110993

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

7: Case Study #6- Sepsis
- Last updated
- Save as PDF
- Page ID 9901
- 7.1: Learning Objectives
- 7.2: Patient- George Thomas
- 7.3: Sleepy Hollow Care Facility
- 7.4: Emergency Room
- 7.5: Day 1- Medical Ward
- 7.6: Day 2- Medical Ward
Your Browser is Out of Date
To provide you with the best experience, our websites uses features that are not supported by your current browser. For the best experience on Childrenshospitals.org, please open this site in a different browser such as Google Chrome
Pediatric Sepsis: Nathan's Story
In November 2012, 17-year-old Nathan came home from school and told his parents he wasn’t feeling well. He was still recovering from a virus he had the week before that caused him to miss four days of school. With a history of respiratory infections, Nathan’s mother, Sherry, was vigilant about monitoring his symptoms. She called the pediatrician who said that Nathan should come in in the morning if he wasn’t feeling better.

By 4 a.m., Nathan was struggling to breathe and experiencing severe pain in his back and chest. His parents rushed him to the nearest emergency room, and they transported him to Nationwide Children’s Hospital in an ambulance. Sherry was terrified—she didn’t know what was wrong with her son. But with at least 10 doctors and nurses taking care of Nathan at once, she knew they were doing everything they could.
That first day, the family had a meeting with the lead physician. They had just met, but he gave them hugs at the end of the meeting, giving a small measure of comfort to Sherry and her husband. Nathan’s white blood cell count was through the roof. While doctors waited for the cultures to grow, Nathan was intubated and put on a ventilator. Sherry recalled, "I’ve never seen so many machines and tubes coming out of a person."
Each morning, when the doctors and nurses conducted their rounds, they would invite Sherry to join the discussion about Nathan’s care. Being part of the daily rounds, Sherry said, made a huge difference. "Being right there, as a part of the conversation, made it easier to understand. Not once did we feel like we were in the way. They never asked us to leave the room, and we were included in decision-making. It gave me a sense of control."
Then, Nathan was diagnosed with sepsis. The doctors told Sherry he had an infection running through his blood system that could shut down his organs. "I had heard the word, but had no clue what sepsis was,” Sherry said. “I asked the doctors if he could die, and they told me it was a possibility."
But after three and a half days in the ICU, Nathan began to recover and was transferred to another unit. He was diagnosed with double pneumonia in both lungs, but went home after a week in the hospital.
Sherry wasn’t aware that lung infections are one of the top four infections most often associated with sepsis, or that children with compromised immune systems are more susceptible. Since she wasn’t familiar with sepsis, she didn’t know the signs or to ask the doctors if that’s what he might have had.
"He just went downhill," Sherry said. "We were surprised at how fast it happened. If I had taken him to the emergency room even a few hours earlier, things might not have been as severe."
Four years later, Nathan is healthy. His family takes preventive measures if he experiences respiratory symptoms, and they know to trust their instincts.
Pediatric experts estimate that about 55 percent of patients develop sepsis before they get to the hospital. Even for pediatric clinicians, it can be difficult to recognize in children, as symptoms vary and awareness of the condition is low.
Sherry is grateful for the care Nathan received at Nationwide Children’s. "We’re lucky Nathan was taken to Children’s, otherwise I don’t think he would have survived."
Sepsis is a leading cause of death in hospitalized children, killing almost 5,000 children annually in the U.S.
Sharing these sepsis patient stories is part of the Improving Pediatric Sepsis Outcomes collaborative, a multi-year quality initiative to significantly reduce sepsis-related mortality and morbidity across children’s hospitals.
For more information, connect with us.
About Sepsis
Sepsis is a leading cause of death in hospitalized children, and children’s hospitals are dedicated to improving outcomes through collaboration, early identification and timely treatment.
Related Content

Bringing People and Data Together

Defining, Developing and Understanding Pediatric Sepsis Outcomes

Investigating MIS-C, Differentiating It From Sepsis
3 scenarios to train for diagnosis, treatment of sepsis
Use simulation education to teach ems providers to recognize and treat sepsis.

BLS providers practice capnography monitoring with a high-fidelity patient simulator.
Photo/Aaron Dix

By Aaron Dix
EMS is dispatched to a local residence for a 20-year-old female with foot pain. Medics find the patient sitting in a recliner with her left foot supported by a pillow.
She spent the weekend at the beach and cut her foot on a piece of glass while walking in the ocean. Over the past several days her foot has become increasingly painful, and this morning she developed a fever that hasn’t responded to acetaminophen. She is conscious and alert but weak. Skin is pale, dry and hot. Heart rate 110, respiratory rate 24, blood pressure 100/60. An oral thermometer is not available.
Focused assessment of the patient’s foot reveals a one-inch laceration with no active bleeding that is red, swollen and painful. Swelling is present throughout the bottom of her foot and ankle. Since the patient does not appear to be in any acute distress, the medics suggest that she go to the local urgent care center in the morning and a refusal is obtained.
The next morning, medics are dispatched to the urgent care center for a transfer to the local hospital for hypotension. Upon arrival, the same medics find the above-mentioned patient with a blood pressure of 86/40 and a heart rate of 140. Tympanic temperature of 101.5 was obtained by the urgent care staff. The patient is urgently transported to the local emergency department. During transport, medics infuse 500 mL of normal saline per protocol for the management of medical hypotension.
At the emergency department, blood cultures are drawn, ibuprofen is administered for her fever, and she is admitted to the hospitalist service. Antibiotics for cellulitis from an infected wound are started once she is admitted. Her blood pressure continues to worsen throughout the night, and she is intubated and moved to the ICU. Despite blood pressure support and aggressive antibiotic treatment, the patient dies 24 hours after arriving at the hospital. The young patient in the above description died from septic shock secondary to her foot wound.
Sepsis is manageable with early diagnosis and treatment
A leading cause of death in the United States, sepsis carries a significantly higher mortality rate than both stroke and STEMI [1]. But when identified and treated with antibiotics at the onset of symptoms, sepsis is manageable and survivable.
Early antibiotic treatment is associated with drastically improved outcomes, yet many EMS providers lack the training to readily recognize sepsis and septic shock. Mortality increases an estimated nine percent per hour when antibiotics are delayed after hypotension [2].
Unlike STEMI and stroke, sepsis recognition does not require a specific exam or new equipment. As a recent study demonstrated, effective EMS sepsis recognition only requires the provider to evaluate respiratory rate, heart rate, temperature and the possibility of an infection [3]. Measuring lactate, while useful in determining the severity of sepsis, is not necessary in the recognition phase.
Simulation education for sepsis recognition
Simulation education can be useful in educating EMS providers, both basic and advanced, in both sepsis recognition and treatment. Here are four learning objectives to use or modify for an EMS sepsis training:
1. Discuss the SIRS criteria and how it relates to sepsis recognition. 2. Demonstrate an appropriate sepsis assessment. 3. Identify patients who have a high probability of being septic. 4. Differentiate between the flu and pneumonia.
Simulation tip: Some simulators have limitations and certain vital signs such as temperature and glucose will not be obtainable utilizing standard EMS equipment. The facilitator will need to provide the correct information when promoted by the participant’s actions, either verbally or through the simulator’s patient monitor. However, all high-fidelity simulators have the ability to provide respiratory rate, heart rate, blood pressure and lung sounds. Providers should be prompted to assess the simulator as a real patient and gather vital signs and history in real time.
Here are three simulation scenarios to use or modify for your EMS training program.
Scenario 1: Standard Sepsis
Facilitators should begin with a non-complicated scenario that easily demonstrates the signs and symptoms of sepsis. The debriefing should concentrate on ensuring that a proper assessment will yield all the necessary information a provider needs to determine sepsis: two or more SIRS criteria and a known or suspected infection. Two common causes of sepsis EMS providers are likely to encounter are pneumonia and urinary tract infections.
Overview: Crew arrives to find a 68-year-old male complaining of shortness of breath. His shortness of breath began after waking six hours earlier and is progressively getting worse. Since lunch he has been unable to ambulate without becoming significantly short of breath. He hasn’t been feeling great over the past several days and has had a productive cough that has occasionally awoken him from sleep.
History: HTN, previous MI (2002), hypothyroid
Allergies: none
Medications: lisinopril, levothyroxine, warfarin
Patient weight/height: 180 pounds/5 feet, 11 inches
Vitals: HR is 130, BP is 106/60, RR is 26/min, SpO2 is 90 percent, glucose 250 mg/dl, temp 101.3 F, ETCO2 30 mm Hg with a normal waveform, and lung sounds are bilateral rhonchi.
Treatment should include oxygenation administration, fluid replacement, sepsis alert and antibiotic therapy if available.
Scenario 2: Differentiating sepsis/pneumonia from the flu
EMS providers must be capable of maintaining a high sensitivity for sepsis patients while limiting false positives. The flu can easily mimic pneumonia, making sepsis recognition more difficult. In this case, the rapid onset, non-productive cough and clear lung sounds make the argument for a flu diagnosis over pneumonia.
Overview: Crew arrives to find a 56-year-old female with sudden onset of high fever, general malaise and a non-productive cough. She woke this morning feeling normal. Her symptoms began suddenly right after lunch and worsened rapidly. She has a frequent non-productive cough, and her fever has not responded to acetaminophen.
History: hyperlipidemia and type 2 diabetes
Allergies: penicillin and naproxen
Medications: simvastatin and metformin
Patient weight/height: 120 pounds/5 feet, 6 inches
Vitals: HR is 100, BP is 118/70, RR is 20/min, SpO2 is 98 percent, glucose 140 mg/dl, temp 103.5 F, ETCO2 40 mm Hg with a normal waveform, and lung sounds are clear.
Scenario 3: Septic shock
Septic shock has a mortality rate near 50 percent and requires aggressive treatment. This case has two main objectives: aggressively treating septic shock and understanding that sepsis can occur in the presence of hypothermia. While approximately 80 percent of septic patients will show hyperthermia, temperature dysregulation, not fever, is the hallmark sign.
ETCO2 can also be discussed as an identifier of severe sepsis or septic shock . Decreases in ETCO2 correlate with elevated levels of lactate and increases in mortality.
Overview: EMS responds to a local nursing home for altered mental status. Patient is a 72-year-old male who was admitted to a skilled nursing facility for rehabilitation following a total hip replacement. Staff states he became altered this afternoon and was unable to ambulate this evening. He was admitted to the facility last night, and very little information is known.
History: hypertension, atrial-fibrillation, and type 2 diabetes
Medications: metformin, lisinopril, amiodarone and warfarin
Patient weight/height: 220 pounds and 5ft 9in
Vitals: HR is 150, BP is 84/50, RR is 22/min, O2 is 96 percent, glucose 280 mg/dl, temp 94.8 F, ETCO2 20 mm Hg with a normal waveform, and lung sounds are clear.
Additional info: Swollen and red surgical incision site on the right hip covered by the gown visible only if inspected.
Treatment: High volumes of normal saline, pressor support (norepinephrine preferred), sepsis alert and antibiotic therapy if available.
In conclusion, simulation training can improve the ability of both advanced and basic providers to diagnose and treat sepsis. Facilitators should concentrate on ensuring a comprehensive patient assessment to identify and treat patients who have a high probability of sepsis. Assess respiratory rate, heart rate, temperature and the possibility of an infection to make an accurate determination of sepsis. Faster recognition and treatment by EMS providers will lead to improved patient outcomes.
1. Cronshaw, 2011. Impact of surviving sepsis campaign on the recognition and management of severe sepsis in the emergency department: Are we failing? EMJ, Volume 12, pp. 296-327.
2. Kumar et al, 2006. Duration of hypotension before initiation of effective antimicrobial therapy is the determinant of survival in human septic shock. Critical Care Medicine, Volume 34, pp. 589-596.
3. Walchok et al, 2016. Paramedic-Initiated CMS Sepsis Core Measure Bundle Prior to Hospital Arrival: A Stepwise Approach, Prehospital Emergency Care, DOI: 10.1080/10903127.2016.1254694
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Sepsis assessment and management in critically Ill adults: A systematic review
Contributed equally to this work with: Mohammad Rababa, Dania Bani Hamad, Audai A. Hayajneh
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Adult Health Nursing Department, Faculty of Nursing, Jordan University of Science and Technology, Irbid, Jordan
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing
- Mohammad Rababa,
- Dania Bani Hamad,
- Audai A. Hayajneh

- Published: July 1, 2022
- https://doi.org/10.1371/journal.pone.0270711
- Reader Comments
Early assessment and management of patients with sepsis can significantly reduce its high mortality rates and improve patient outcomes and quality of life.
The purposes of this review are to: (1) explore nurses’ knowledge, attitude, practice, and perceived barriers and facilitators related to early recognition and management of sepsis, (2) explore different interventions directed at nurses to improve sepsis management.
A systematic review method according to the PRISMA guidelines was used. An electronic search was conducted in March 2021 on several databases using combinations of keywords. Two researchers independently selected and screened the articles according to the eligibility criteria.
Nurses reported an adequate of knowledge in certain areas of sepsis assessment and management in critically ill adult patients. Also, nurses’ attitudes toward sepsis assessment and management were positive in general, but they reported some misconceptions regarding antibiotic use for patients with sepsis, and that sepsis was inevitable for critically ill adult patients. Furthermore, nurses reported they either were not well-prepared or confident enough to effectively recognize and promptly manage sepsis. Also, there are different kinds of nurses’ perceived barriers and facilitators related to sepsis assessment and management: nurse, patient, physician, and system-related. There are different interventions directed at nurses to help in improving nurses’ knowledge, attitudes, and practice of sepsis assessment and management. These interventions include education sessions, simulation, decision support or screening tools for sepsis, and evidence-based treatment protocols/guidelines.
Our findings could help hospital managers in developing continuous education and staff development training programs on assessing and managing sepsis in critical care patients.
Nurses have poor to good knowledge, practices, and attitudes toward sepsis as well as report many barriers related to sepsis management in adult critically ill patients. Despite all education interventions, no study has collectively targeted critical care nurses’ knowledge, attitudes, and practice of sepsis management.
Citation: Rababa M, Bani Hamad D, Hayajneh AA (2022) Sepsis assessment and management in critically Ill adults: A systematic review. PLoS ONE 17(7): e0270711. https://doi.org/10.1371/journal.pone.0270711
Editor: Paavani Atluri, Bay Area Hospital, North Bend Medical Center, UNITED STATES
Received: December 1, 2021; Accepted: June 14, 2022; Published: July 1, 2022
Copyright: © 2022 Rababa et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the article and its files.
Funding: This study was funded by The deanship of research at Jordan University of Science and Technology (grant number 20200668).
Competing interests: The authors have declared that no competing interests exist.
Introduction
Sepsis is a global health problem that increases morbidity and mortality rates worldwide and which is one of the most common complications documented in intensive care units (ICUs) [ 1 ]. About 48.9 million cases of sepsis and 11 million sepsis-related deaths were documented in 2017 worldwide [ 2 ]. Sepsis is an emergency condition leading to several life-threatening complications, such as septic shock and multiple organ dysfunction and failure [ 3 ]. Sepsis has negative physiological, psychological, and economic consequences. Untreated sepsis can lead to septic shock; multiple organ failure, such as acute renal failure [ 4 ]; respiratory distress syndrome [ 5 ]; cardiac arrhythmia (e.g. Atrial Fibrillation) [ 6 ]; and disseminated intravascular coagulation (DIC) [ 7 ]. Also, sepsis is associated with anxiety, depression, and post-traumatic stress disorder [ 8 ]. As for the financial burden of sepsis on the healthcare system, the cost of healthcare services and supplies for ICU critical care patients with sepsis is high [ 1 ]. In 2017, the estimated annual cost of sepsis in the United States (US) was over $24 billion [ 2 ].
Previous studies have shown that among nurses, misunderstanding and misinterpretation of the early clinical manifestations of sepsis, poor knowledge, attitudes, and practices related to sepsis, and inadequate training might lead to delayed assessment and management of sepsis [ 9 – 11 ]. Moreover, the limited numbers of specific and sensitive assessment tools and standard protocols for the early identification and assessment of sepsis in critical care patients leads to delayed management, therefore increasing sepsis-related mortality rates [ 10 ].
Critical care nurses, as frontline providers of patient care, play a vital role in the decision-making process for the early identification and prompt management of sepsis [ 11 ]. Therefore, improving nurses’ knowledge, attitudes, and practices related to the early identification and management of sepsis is associated with improved patient outcomes [ 12 , 13 ]. To date, there remains a wide gap between the findings of previous research and sepsis-related clinical practice in critical care units (CCUs). Furthermore, there is no evidence in the nursing literature regarding nurses’ knowledge, attitudes, and practices related to the early identification and management of sepsis in adult critical care patients and the association of these factors with patient health outcomes. Therefore, summarizing and synthesizing the existing research on sepsis assessment and management among adult critical care patients is needed to guide future directions of sepsis-related clinical practice and research. Accordingly, this review aims to identify nurses’ knowledge, and attitudes, practices related to the early identification and management of sepsis in adult critical care patients.
Materials and methods
The present review used a systematic review design guided by structured questions constructed after reviewing the nursing literature relevant to sepsis assessment and management in adult critical care patients. The authors (MR, DB, AH) carefully reviewed and evaluated the selected articles and synthesized and analyzed their findings to reach a consensus. This review was guided by the following questions: (a) what are nurses’ knowledge, attitudes, and practices related to sepsis assessment and management in adult critical care patients?, (b) what are the perceived facilitators of and barriers to the early identification and effective management of sepsis in adult critical care units?, and (c) what are the interventions directed at improving nurses’ sepsis assessment and management?
Eligibility criteria
The review questions were developed according to the PICOS (Participants, Interventions, Comparisons, Outcome, and Study Design) framework, as displayed in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0270711.t001
Inclusion criteria.
The articles were retrieved and assessed independently by two researchers (MR, DB) according to the following inclusion criteria: (1) being written in English, (2) having an abstract and reference list, (3) having been published during the past 10 years, (4) focusing on critical care nurses as a target population, (5) examining knowledge, attitudes, and practices related to the assessment and management of sepsis, and (6) having been conducted in adult critical care units.
Exclusion criteria.
Studies were excluded if they were (1) written in languages other than English, and (2) conducted in pediatric critical care units or non-ICU. Dissertations, reports, reviews, editorials, and brief communications were also excluded.
Search strategy.
An electronic search of the databases CINAHL, MEDLINE/PubMed, EBSCO, Embase, Cochrane, Scopus, Web of Science, and Google Scholar was conducted using combinations of the following keywords: critical care, intensive care, critically ill, critical illness, knowledge, awareness, perception, understanding, attitudes, opinion, beliefs, thoughts, views, practice, skills, strategies, approaches, barriers, obstacles, challenges, difficulties, issues, problems, limitations, facilitators, motivators, enablers, sepsis, septic, septic shock, and septicemia. The search terms used in this review were described in S1 File . The search was initially conducted in March 2021, and a search re-run was conducted in April 2022. The search was conducted in the selected databases from inception to 4/2022. The initial search, using the keywords independently, resulted in 1579 articles, and after using the keyword combinations, this number was reduced to 241 articles. Then, after applying the inclusion and exclusion criteria, the number of articles was reduced to 92. A manual search of the reference lists of the 92 articles was carried out to identify any relevant publications not identified through the search. The researcher (MR) used the function “cited by” on Google Scholar to explore these publications in more depth. The researchers (MR, DB) then screened the identified citations of these publications, applying the eligibility criteria. In case of discrepancies, the researchers (MR, DB) discussed their conflicting points of view until a consensus was reached. Then, after careful reading of the article abstracts, 61 irrelevant articles were excluded, and a total of 31 articles were included in this review. Fig 1 below shows the Preferred Reporting Items for Meta-Analysis (PRISMA) checklist and flow chart used as a method of screening and selecting the eligible studies.
https://doi.org/10.1371/journal.pone.0270711.g001
Data extraction
The following data were extracted from each of the selected studies: (1) the general features of the article, including the authors and publication year; (2) the characteristics of the study setting (e.g., single vs. multisite); (3) the sociodemographic and clinical characteristics of the target population, including mean age, and medical diagnosis (e.g., sepsis, septic shock, and SIRS); (4) the name of the sepsis protocol used, if any; (5) the characteristics of the study methodology (e.g., sample size and measurements); (7) the main significant findings of the study; and (8) the study strengths and limitations. All extracted data were summarized in an evidence-based table ( Table 2 ). Data extraction was performed by two researchers (MR, DB). An expert third researcher (AH) was consulted to reach a consensus between the two researchers throughout the process of data extraction.
https://doi.org/10.1371/journal.pone.0270711.t002
Ethical considerations
There was no need to obtain ethical approval to conduct this systematic review since no human subjects were involved.
Quality assessment and data synthesis
A quality assessment of the selected studies was performed independently by two researchers based on the guidelines of Melnyk and Fineout-Overholt [ 14 ]. Disagreements between the two researchers (MR, DB) were identified and resolved through a detailed discussion held during a face-to-face meeting. For complicated cases, the researchers (MR, DB) requested a second opinion from a third researcher (AH). According to the guidelines of Melnyk and Fineout-Overholt [ 14 ], twelve of the studies were at level 3 in terms of quality, four studies at level 5, and nine studies at level 6.
A qualitative synthesis was performed to synthesize the findings of the reviewed studies. The following steps were applied throughout the process of data synthesis:
- The data in the selected studies were assessed, evaluated, contrasted, compared, and summarized in a table ( Table 2 ). This data included the design, purpose, sample, main findings, strengths/limitations, and level of evidence for each of the studies.
- The similarities and differences between the main findings of the selected studies were highlighted.
- The strengths and limitations of the reviewed studies were discussed.
Description of the selected studies
Most of the reviewed studies were conducted in Western countries [ 9 , 11 , 12 ], with only one study conducted in Eastern countries [ 1 ], and two in Middle-Eastern countries [ 15 , 16 ]. The detailed geographical distribution of the studies and other characteristics are described in Table 2 .
Nurses’ knowledge, attitudes, and practices
Nine of the selected studies assessed nurses’ knowledge and attitudes related to sepsis assessment and management in critically ill adult patients [ 1 , 9 , 12 , 15 , 17 – 21 ] ( Table 3 ) . Nucera et al. [ 18 ] found that ICU nurses had poor attitudes towards blood culture collection techniques and timing and poor levels of knowledge related to the early identification, diagnosis, and management of sepsis. For example, the majority of nurses reported that there is no need to sterilize the tops of culture bottles, and there is no specific time for specimen collection [ 18 ]. However, the participating nurses reported good levels of knowledge related to blood culture procedures and the risk factors for sepsis. Similarly, R. J. Roberts et al. [ 19 ] found the participating nurses to have good knowledge of septic shock and good attitudes toward the initiation of antibiotics for critically ill adult patients with sepsis. Only two studies assessed nurses’ practices related to sepsis assessment and management [ 15 , 19 ]. For example, in the study of R. J. Roberts et al. [ 19 ], 40% of the nurse participants reported that they were aware of the importance of initiating antibiotics and IV fluid within one hour of septic shock recognition [ 20 ]. Also, Yousefi et al. [ 15 ] found the participating nurses to have good practices related to sepsis assessment and management.
https://doi.org/10.1371/journal.pone.0270711.t003
Barriers to and facilitators of sepsis assessment and management
The reviewed studies identified three types of barriers to the early identification and management of sepsis, namely patient-, nurse-, and system-related barriers ( Table 4 ). Meanwhile, only nurse- and system-related facilitators were reported in the reviewed studies. The most-reported barriers and facilitators were system-related. The reported barriers included (a) the lack of written sepsis treatment protocols or guidelines adopted as hospital policy [ 22 , 23 ]; (b) the complexity and atypical presentation of the early symptoms of sepsis [ 19 ]; (c) nurses’ poor level of education and clinical experience [ 1 , 12 ]; (d) the lack of sepsis educational programs or training workshops for nurses [ 22 , 23 ]; (e) the high comorbid burden among patients with sepsis, which complicates the critical thinking process of sepsis management [ 19 ]; (f) nurses’ deficits in knowledge related to sepsis treatment protocols and guidelines [ 22 – 24 ]; (g) the lack of mentorship programs in which junior nurses’ actions/activities are strictly supervised by experienced nurses [ 17 , 23 ]; (h) heavy workloads or high patient-nurse ratios [ 22 ]; (i) the shortage of well-trained and experienced physicians, particularly in EDs [ 19 , 22 , 23 ]; (j) the lack of awareness related to antibiotic use for patients with sepsis [ 19 , 22 ]; (k) the lack of IV access and unavailability of ICU beds [ 25 ]; (l) the non-use of drug combinations for the treatment of sepsis [ 22 , 26 , 27 ], and (m) poor teamwork and communication skills among healthcare professionals [ 22 , 26 ]. Only three facilitators of sepsis assessment and management were identified in the reviewed studies. These facilitators were (1) nurses’ improved confidence in caring for patients with sepsis, (2) increased consistency in sepsis treatment, and (3) positive enforcement of successful stories of sepsis management [ 22 , 27 ].
https://doi.org/10.1371/journal.pone.0270711.t004
Measurement tools of sepsis-related knowledge, attitudes, and practices
One of the reviewed studies used a Knowledge, Attitudes, and Practice (KAP) questionnaire developed according to the Surviving Sepsis Campaign (SSC) guidelines [ 15 ] to measure nurses’ knowledge, attitudes, and practices related to sepsis assessment and management. Meanwhile, eight studies [ 1 , 9 , 12 , 17 – 21 ] used self-developed questionnaires based on the literature and SSC guidelines and validated by expert panels. Details of these measurement tools and their psychometric properties are summarized in Table 5 .
https://doi.org/10.1371/journal.pone.0270711.t005
Interventions directed at improving nurses’ sepsis assessment and management
Educational programs..
Only four of the selected studies examined the impact of educational programs on nurses’ knowledge, attitudes, and practices related to sepsis management and found significant improvements in nurses’ posttest scores ( Table 6 ) [ 11 , 15 , 28 , 29 ]. For example, Drahnak’s study [ 28 ] implemented an educational program developed by the authors and integrated with patients’ health electronic records (HER) and found significant improvements in nurses’ post-test nursing knowledge scores. Another educational program developed by the authors was implemented to improve ICU nurses’ knowledge, attitudes, and practices related to sepsis and found a significant improvement in posttest scores among the intervention group [ 15 ]. Another study was designed to examine the effectiveness of the Taming Sepsis Educational Program® (TSEP™) in improving nurses’ knowledge of sepsis [ 11 ]. A 15-minute structured educational session was developed to decrease the mean time needed to order a sepsis order set for critically ill patients through improving ER nurses’ knowledge about SSC guidelines and found that the mean time was reduced by 33 minutes among the intervention group [ 29 ].
https://doi.org/10.1371/journal.pone.0270711.t006
Simulation.
Only two studies examined the effect of using simulation in improving the early recognition and prompt treatment of sepsis by critical care nurses ( Table 6 ) [ 30 , 31 ]. Vanderzwan et al. [ 30 ] assessed the effect of a medium-fidelity simulation incorporated into a multimodel nursing pedagogy on nurses’ knowledge of sepsis and showed significant improvements in six of the nine questionnaire items. While Giuliano et al. examined the difference in mean times required for sepsis recognition and treatment initiation between nurses exposed to two different monitor displays in response to simulated case scenarios of sepsis and showed a significant reduction in the mean times required for sepsis recognition and treatment initiation by those nurses who were exposed to enhanced bedside monitor (EBM) display [ 31 ].
Decision support tools.
Four of the selected studies examined the effectiveness of decision support tools, adapted based on the SSC guidelines and the “sepsis alert protocol”, on the early identification and management of sepsis and confirmed the effectiveness of these tools ( Table 7 ) [ 32 – 35 ]. The decision support tools used in three of the studies guided the nurses throughout their decision-making processes to reach effective assessment, high quality and timely management of sepsis, and, in turn, optimal patient outcomes [ 32 , 33 , 35 ]. However, no significant differences in the time of blood culture collection and antibiotic administration were reported between the intervention and control groups in the study of Delawder et al. [ 34 ].
https://doi.org/10.1371/journal.pone.0270711.t007
Sepsis protocols.
Eight of the selected studies examined the effectiveness of sepsis protocols [ 24 , 36 – 38 ] and sepsis screening tools [ 16 , 39 – 41 ] for the early assessment and management of sepsis ( Table 7 ). All of these articles revealed that the implementation of sepsis screening tools or protocols based on the SSC guidelines leads to the early identification and timely management of sepsis, as well as the improvement in nurses’ compliance to the SSC guidelines for the detection and management of sepsis. For example, in one study, patients who received Early Goal-Directed Therapy (EGDT) had a lower mortality rate as compared to patients who received usual care [ 16 ]. The sepsis screening tools and guidelines were also tested to examine their impact on some patient outcomes, and variabilities were identified. For example, the use of the Modified Early Warning Score (MEW-S) tool revealed no significant improvement in patient mortality rate [ 41 ]. In contrast, mortality rates were decreased by using the Nurse Driven Sepsis Protocol (NDS) [ 40 ], Quality Improvement (QI) initiative [ 38 ], and a computerized protocol [ 37 ]. In addition, nurses in the computerized protocol group had better compliance with the SSC guidelines than did nurses in the paper-based group [ 37 ]. One of the selected studies compared between a paper-based sepsis protocol and a computer-based protocol and found that antibiotic administration, blood cultures, and lactate level checks were conducted more often and sooner by nurses in the computerized protocol group [ 37 ]. Two of the selected studies used the EGDT as a screening tool for sepsis and found no significant differences in times of diagnosis, blood culture collection, or lactate measurements between the control and intervention groups [ 16 , 24 ]. However, significant differences were found in the time of antibiotic administration in the study of Oliver et al. [ 24 ]. Although El-khuri et al. [ 16 ] revealed no significant differences in the time of antibiotic administration, the mortality rate among patients in the intervention group declined significantly.
Most of the reviewed studies focused on assessing critical care nurses’ knowledge, attitudes, and practices related to sepsis assessment and management, revealing poor levels of knowledge, moderate attitude levels, and good practices. Also, this review revealed that the three most common barriers to effective sepsis assessment and management were nursing staff shortages, delayed initiation of antibiotics, and poor teamwork skills. Meanwhile, the three most common facilitators of sepsis assessment and management were the presence of standard sepsis management protocols, professional training and staff development, and positive enforcement of successful stories of sepsis treatment. Moreover, this review reported on a wide variety of interventions directed at improving sepsis management among nurses, including educational sessions, simulations, screening or decision support tools, and intervention protocols. The impacts of these interventions on patient outcomes were also explored.
The findings of our review are consistent with the findings of previous studies which have explored critical care nurses’ knowledge related to sepsis assessment and management [ 42 ]. Also, recent studies conducted in different clinical settings support the findings of our review regarding nurses’ knowledge of sepsis. For example, a recent study conducted in a medical-surgical unit revealed that nurses had good knowledge of early sepsis identification in non-ICU adult patients [ 43 ]. The variations in nurses’ levels of knowledge related to sepsis assessment were attributed to variations in educational level and work environment (i.e., ICU vs. non-ICU).
The evidence indicates that the successful treatment of critically ill patients with suspected or actual sepsis requires early identification or assessment [ 44 , 45 ]. Early assessment is a critical step for the initiation of antibiotics for patients with sepsis, leading to improved patient outcomes and a decline in mortality rates [ 44 ]. The current review also revealed the significant role of educational programs in improving nurses’ knowledge, attitudes, and practices related to the early recognition and management of sepsis. These findings are in line with the findings of another study, which tested the impact of e-learning educational modules on pediatric nurses’ retention of knowledge about sepsis [ 45 ]. The study revealed that the educational modules improved the nurses’ knowledge acquisition and retention and clinical performance related to sepsis management [ 45 ]. The findings of our review related to sepsis screening and decision support tools are in congruence with the findings of a previous clinical trial which assessed the impact of a prompt telephone call from a microbiologist upon a positive blood culture test on sepsis management [ 46 ]. The study revealed that this screening tool contributed to the prompt diagnosis of sepsis and antibiotic administration, improved patient outcomes, and reduced healthcare costs [ 46 ]. The findings of our review related to the effectiveness of educational programs in improving the assessment and management of sepsis were consistent with the findings of a recent quasi-experimental study. The study found that incorporating sepsis-related case scenarios in ongoing educational and professional training programs improved nurses’ self-efficacy and led to a prompt and accurate assessment of sepsis [ 47 ]. One of the interventions explored in this review was a simulation that facilitated decision-making related to sepsis management. The simulation was found to be effective in mimicking the real stories of patients with sepsis and proved to be a safe learning environment for inexperienced nurses before encountering real patients, increasing nurses’ competency, self-confidence, and critical thinking skills [ 48 ]. Also, a recent study showed that the combination of different interventions aimed at targeting sepsis assessment and management, including educational programs and simulation, may lead to optimal nurse and patient outcomes [ 49 ].
Limitations
The present review has several limitations. There is limited variability in the findings of the reviewed studies in terms of the main variable, sepsis. Moreover, the review excluded studies written in languages other than English and conducted among populations other than critical care nurses. However, there may be studies written in other languages which may have significant findings not considered in this review. Further, only eight databases were used to search for articles related to the topic of interest, which may have limited the number of retrieved studies. Finally, due to the heterogeneity between the selected studies, a meta-analysis was not performed.
Relevance to clinical practice
Our findings could help hospital managers in developing continuous education and staff development training programs on assessing and managing sepsis for critical care patients. Establishing continuous education, workshops, professional developmental lectures focusing on sepsis assessment and management for critical care nurses, as well as training courses on how to use evidence-based sepsis protocol and decision support and screening tools for sepsis, especially for critical care patients are highly recommended. Also, our findings could be used to development of an evidence-based standard sepsis management protocol tailored to the unmet healthcare need of patients with sepsis.
To date, nurses remain to have poor to good knowledge of and attitudes towards sepsis and report many barriers related to the early recognition and management of sepsis in adult critically ill patients. The most-reported barriers were system-related, pertaining to the implementation of evidence-based sepsis treatment protocols or guidelines. Our review indicated that despite all educational interventions, no study has collectively targeted nurses’ knowledge, attitudes, and practices related to the assessment and treatment of sepsis using a multicomponent interactive teaching method. Such a method would aim to guide nurses’ decision-making and critical thinking step by step until a prompt and effective treatment of sepsis is delivered. Also, despite all available protocols and guidelines, no study has used a multicomponent intervention to improve health outcomes in adult critically ill patients. Future research should focus on sepsis-related nurse and patient outcomes using a multilevel approach, which may include the provision of ongoing education and professional training for nurses and the implementation of a multidisciplinary sepsis treatment protocol.
Supporting information
S1 checklist. prisma 2020 checklist..
https://doi.org/10.1371/journal.pone.0270711.s001
S1 File. Search strategies.
https://doi.org/10.1371/journal.pone.0270711.s002
Acknowledgments
The authors want to thank the Liberian of Jordan University of Science and Technology for his help in conducting this review.
- View Article
- PubMed/NCBI
- Google Scholar
- 14. Melnyk BM, Fineout-Overholt E, editors. Evidence-based practice in nursing & healthcare: A guide to best practice. Lippincott Williams & Wilkins; 2011.
Early diagnosis and management of neonatal sepsis: a perspective
- Published: 31 March 2024
Cite this article
- Li-Zhong Du 1
Avoid common mistakes on your manuscript.
Neonatal sepsis is an illness caused by bloodstream bacteria or fungal infections that affect newborn infants under 28 days of age. It stands as a significant contributor to morbidity and mortality in neonatal intensive care units (NICUs). With the improved survival rates of very low-birth-weight or extremely premature infants, a growing number of these vulnerable infants are receiving intensive care and undergoing invasive procedures, making nosocomial infections a persistent challenge in NICUs. The mortality rate associated with neonatal sepsis varies depending on factors such as birth weight, gestational age, and other co-morbidities. It can also lead to a range of long-term health consequences, including neurodevelopmental disabilities like cerebral palsy, visual or hearing impairments, and cognitive problems. Furthermore, neonatal sepsis is linked to various adverse outcomes, including respiratory complications, bronchopulmonary dysplasia, nutritional and growth issues, and immunological dysfunction [ 1 ]. Due to its atypical clinical presentation and the low rate of specific diagnostic indicators, such as a positive blood culture, accurately diagnosing neonatal sepsis is challenging. Consequently, the appropriateness of antibiotic treatment is often a matter of controversy.
Disease burden and epidemiology
The incidence of sepsis is most prevalent in neonates. Both bacterial early-onset sepsis (EOS) and late-onset sepsis (LOS) continue to pose serious complications in NICUs, resulting in high morbidity and mortality rates. In the USA, the overall incidence of EOS has remained relatively stable at about 0.8 cases per 1000 live births (LBs) over the past two decades [ 2 ]. However, the incidence of EOS among inborn infants of < 34 weeks’ gestation in 18 Chinese perinatal centers was notably higher at 9.7 cases per 1000 LBs [ 3 ].
The lack of standardization in diagnostic criteria and the definition of sepsis across available studies present obstacles to accurately estimating the global burden. A comprehensive study reviewed evidence from observational epidemiological studies to gauge the global burden and mortality of sepsis in neonates and children. The population-level estimate for neonatal sepsis was 2202 per 1,00,000 LBs, with mortality rates ranging from 11% to 19%. This would translate to an annual incidence of 3.0 million cases of neonatal sepsis globally [ 4 ]. In China, birth population-based surveys conducted in one region, which approximated national average levels, estimated the incidence of neonatal sepsis at 25.6 per 1000 LBs [ 5 ]. The case fatality rate of EOS in China was 19% (61 out of 321) [ 3 ].
As a middle-income country, China has limited population-based data on neonatal sepsis available in the literature. However, the recently launched national neonatal network, the Chinese Neonatal Network (CHNN), systematically collected multicenter qualified data from very low-birth-weight or very preterm infants in Chinese NICUs. Through the standardization of diagnostic criteria and the definition of sepsis, the incidence of LOS sepsis in very low-birth-weight infants in Chinese NICUs was determined to be 9.4% [ 6 ].
Screening and diagnosis
Clinical signs of neonatal sepsis encompass a spectrum from sub-clinical infection to severe manifestations of focal or systemic disease. Given that the clinical presentations of neonatal sepsis are non-specific, precise diagnosis is extremely important. Underdiagnosis may lead to the development of overwhelming infection or central nervous system involvement, while overdiagnosis can result in inappropriate antibiotic use. Various predictive models and scoring systems for neonatal sepsis have been developed and applied in diagnostic settings and retrospective studies. [ 7 , 8 , 9 ]. The clinical perinatal risk assessment program and the development guidelines for EOS, such as the National Institute for Health and Care Excellence (NICE) sepsis guideline [ 10 ], and Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics (AAP) guidelines for EOS risk assessment [ 11 ], play crucial roles in this regard. In 2019, China developed guidelines for the screening and diagnosis of neonatal sepsis in those at risk [ 12 ]. Both the NICE and the US sepsis guidelines emphasize clinical presentation and risk factor assessment, whereas the Chinese guideline incorporates laboratory non-specific markers such as C-reactive protein (CRP) or complete blood cell count (CBC) to a greater extent. Nevertheless, countries need to adapt these guidelines or screening procedures according to the local disease spectrum and health policy context. Whether these differences result in increased sensitivity for sepsis diagnosis or contribute to overdiagnosis requires further validation through study.
The American College of Obstetricians and Gynecologists (ACOG) recommends universal maternal screening through vaginal-rectal culture between 36 and 38 weeks of gestation as an effective measure to prevent Group B Streptococcus (GBS) EOS [ 13 ]. However, no standard guidelines currently exist for maternal GBS screening and neonatal GBS disease prevention in China. GBS is one of the leading causes of neonatal sepsis and maternal disease globally. Neonatal GBS infections have been increasingly reported in Chinese literature since the early twenty-first century. Recent studies, such as one in Shanghai involving 12,132 women in late pregnancy, revealed a GBS colonization rate of 6.52% [ 14 ]. A systematic review indicated that the maternal GBS colonization rate in mainland China ranged from 3.70% to 14.52%, with an incidence of invasive GBS disease in infants ranging from 0.55% to 1.79% per 1000 LBs and a case fatality risk between 6.45% and 7.10% [ 15 ]. Presently, universal prenatal screening for GBS carriage has not been implemented in China [ 16 ].
Surveillance and prevention of LOS are crucial issues. Advances in neonatal intensive care, coupled with an increased number of very to extremely preterm infants receiving care and undergoing invasive procedures or indwelling catheter use, contribute to a higher rate of nosocomial infections or LOS. Clinical management is further complicated by an increasing proportion of bacterial pathogens displaying in vitro resistance to commonly used first and second-line antibiotics for LOS treatment.
Neonatal sepsis work-up is essential for timely diagnosis and preventing adverse outcomes before the development of overwhelming sepsis or septic shock. Although a positive blood culture has traditionally been considered the gold standard, its yield is relatively low and can be influenced by factors such as sample volume, culture technique, and antibiotic usage prior to sampling [ 17 ]. Polymerase chain reaction and reverse hybridization of the 16S rRNA gene offer a fast and sensitive means of detecting the presence of bacteria and differentiating between Gram-positive and Gram-negative bacteria in clinical specimens [ 18 ]. Recently, metagenomic techniques using next-generation sequencing have enabled rapid, accurate, and unbiased identification of multiple microorganisms, particularly in cases with negative cultures or when identifying unusual microorganisms that are challenging to grow in culture, such as viruses, fungi, and parasites. However, current investigations using this technology are limited, and studies carry a high risk of bias. Further research employing this technique could enhance the rational use of antibiotics. One limitation is the difficulty in distinguishing between pathogens and commensals typical of each anatomical site [ 19 ].
In culture-independent sepsis work-up, non-specific biomarkers such as procalcitonin, CRP, white blood cell count, and absolute neutrophil count are commonly included. Some institutes also utilize serum cytokines to aid in the diagnosis [ 20 ]. However, these biomarkers are generally more reliable for negative predictivities than positive predictivities and should be used in conjunction with clinical presentations such as poor perfusion, heart rate variation, apnea, and poor feeding. It is noteworthy that in China, some institutes tend to over-rely on a CRP level of ≥ 8–10 mg/L as a cutoff for a positive predictive value, diagnosing sepsis even in the absence of significant clinical symptoms or signs, and initiating antibiotic treatment. Given the complexity of neonatal sepsis diagnosis, sepsis work-up should never replace clinical judgment and risk assessment.
Prevention and treatment
To prevent sepsis, several measures can be implemented to reduce infection rates, particularly for LOS. Practices such as hand hygiene, promoting enteral breastfeeding, minimizing the duration of central lines, and implementing care bundles for infection control have proven effective in sepsis prevention. Quality improvement programs introducing evidence-based practice have shown promise in reducing infections in Chinese neonatal intensive care units [ 21 ].
Empirical treatment of neonatal sepsis should be initiated promptly upon suspicion. However, challenges arise in finding the right balance, as both undertreating due to ineffective diagnosis and overtreating from overdiagnosis are concerns, with the latter being more pronounced in neonatal sepsis management. A recent multicenter study analyzed antibiotic prescription patterns for 2674 neonates from 15 hospitals in China, using the World Health Organization’s (WHO) Essential Medicines List Access, Watch, and Reserve (AWaRe), and the Management of Antibiotic Classification (MAC) Guidelines. The study revealed that meropenem was the most commonly prescribed antibiotic (11.8%), and broad-spectrum antibiotics, including those in the Watch and Special groups, were likely overused in Chinese neonates [ 22 ]. To address this issue, the Chinese Neonatal Society has developed regulations standardizing the application of meropenem in newborns, aiming to reduce inappropriate usage [ 23 ]. Implementation of the Smart Use of Antibiotics Program has also proven effective in reducing antibiotic exposure without compromising the quality of care [ 24 ].
A quality improvement program highlighted that among infants without infection, early antibiotic use was associated with an increased risk of developing bronchopulmonary dysplasia and late (after 7 days of age) antibiotic use [ 25 ]. These findings underscore the importance of careful consideration in antibiotic administration to neonates, emphasizing the need for judicious use to avoid potential adverse outcomes.
In summary, sepsis remains a significant challenge in NICUs. The increased survival of vulnerable very or extremely preterm infants who require intensive care complicates efforts in sepsis control. Advances in sepsis prevention, screening, diagnosis, and treatment have facilitated early recognition and intervention for neonates at risk. The development of neonatal quality improvement programs for sepsis control has shown promise.
Jiang S, Yang C, Yang C, Yan W, Shah V, Shah PS, REIN-EPIQ Study Group, et al. Epidemiology and microbiology of late-onset sepsis among preterm infants in China, 2015–2018: a cohort study. Int J Infect Dis. 2020;96:1–9.
Article CAS PubMed Google Scholar
Schrag SJ, Farley MM, Petit S, Reingold A, Weston EJ, Pondo T, et al. Epidemiology of invasive early-onset neonatal sepsis, 2005 to 2014. Pediatrics. 2016;138: e20162013.
Article PubMed Google Scholar
Jiang S, Hong L, Gai J, Shi J, Yang Y, Lee SK, REIN-EPIQ Study Group, et al. Early-onset sepsis among preterm neonates in China, 2015 to 2018. Pediatr Infect Dis J. 2019;38:1236–41.
Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, Schlapbach LJ, Reinhart K, Kissoon N. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med. 2018;6:223–30.
Wang H, Yue H, Sun B, Zhu X, Niu H, Qi T, et al. Birth population survey in Huai’an in 2015: perinatal-neonatal mortality and preterm birth rate in emerging regions in China. J Matern Fetal Neonatal Med. 2020;33:838–46.
Cao Y, Jiang S, Sun J, Hei M, Wang L, Zhang H, et al. Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Netw Open. 2021;4:e2118904.
Article PubMed PubMed Central Google Scholar
Sahu P, Raj Stanly EA, Simon Lewis LE, Prabhu K, Rao M, Kunhikatta V. Prediction modelling in the early detection of neonatal sepsis. World J Pediatr. 2022;18:160–75.
Kopec G, Collin M, Das A. Application of Kaiser Sepsis Calculator in culture positive infants with early onset sepsis. World J Pediatr. 2021;17:429–33.
Zhao C, Xin MY, Li J, Zhao JF, Wang YJ, Wang W, et al. Comparing the precision of the pSOFA and SIRS scores in predicting sepsis-related deaths among hospitalized children: a multi-center retrospective cohort study. World J Emerg Med. 2022;13:259–65.
NICE guideline. Neonatal infection: antibiotics for prevention and treatment. https://www.nice.org.uk/guidance/ng195 . Accessed 18 Feb 2024.
Brady MT, Polin RA. Prevention and management of infants with suspected or proven neonatal sepsis. Pediatrics. 2013;132:166–8.
Subspecialty Group of Neonatology, the Society of Pediatric, Chinese Medical Association; Professional Committee of Infectious Diseases, Neonatology Society, Chinese Medical Doctor Association. Expert consensus on the diagnosis and management of neonatal sepsis (version 2019). Zhonghua Er Ke Za Zhi. 2019;57:252–7 ( in Chinese ).
Google Scholar
Prevention of group B streptococcal early-Onset disease in newborns: ACOG committee opinion, number 797. Obstet Gynecol. 2020;135:e51–e72.
Ma H, Xu J, Zhang Y, Zhang R, Wu J. The current status of Group B Streptococcus infection in the reproductive tract of late-pregnancy women and its impact on pregnancy outcomes. Arch Gynecol Obstet. 2024. https://doi.org/10.1007/s00404-023-07343-8 .
Huang J, Lin XZ, Zhu Y, Chen C. Epidemiology of group B streptococcal infection in pregnant women and diseased infants in mainland China. Pediatr Neonatol. 2019;60:487–95.
Chen X, Cao S, Fu X, Ni Y, Huang B, Wu J, et al. The risk factors for Group B Streptococcus colonization during pregnancy and influences of intrapartum antibiotic prophylaxis on maternal and neonatal outcomes. BMC Pregnancy Child birth. 2023;23:207.
Article Google Scholar
Yaacobi N, Bar-Meir M, Shchors I, Bromiker R. A prospective controlled trial of the optimal volume for neonatal blood cultures. Pediatr Infect Dis J. 2015;34:351–4.
Shang S, Chen Z, Yu X. Detection of bacterial DNA by PCR and reverse hybridization in the 16S rRNA gene with particular reference to neonatal septicemia. Acta Paediatr. 2001;90:179–83.
Agudelo-Pérez S, Fernández-Sarmiento J, León DR, Peláez RG. Metagenomics by next-generation sequencing (mNGS) in the etiological characterization of neonatal and pediatric sepsis: a systematic review. Front Pediatr. 2023;11:1011723.
Genel F, Atlihan F, Gulez N, Kazanci E, Vergin C, Terek DT, et al. Evaluation of adhesion molecules CD64, CD11b and CD62L in neutrophils and monocytes of peripheral blood for early diagnosis of neonatal infection. World J Pediatr. 2012;8:72–5.
Cao Y, Jiang S, Zhou Q. Introducing evidence-based practice improvement in Chinese neonatal intensive care units. Transl Pediatr. 2019;8:257–61.
Zhang J, Lin L, Lu G, Wu K, Tian D, Tang L, et al. Patterns of antibiotic administration in Chinese neonates: results from a multi-center, point prevalence survey. BMC Infect Dis. 2024;24:186.
Guideline Development Group of Clinical Practice Guidelines for Meropenem Therapy in Neonatal Sepsis. Clinical Practice guidelines for meropenem therapy in neonatal sepsis. Zhongguo Dang Dai Er Ke Za Zhi. 2024;26:107–17.
Lu C, Liu Q, Yuan H, Wang L. Implementation of the smart use of antibiotics program to reduce unnecessary antibiotic use in a neonatal ICU: a prospective interrupted time-series study in a developing country. Crit Care Med. 2019;47:e1–7.
Yu W, Zhang L, Li S, Yan W, Bai R, Yang Z, et al. Early antibiotic use and neonatal outcomes among preterm infants without infections. Pediatrics. 2023;151:e2022059427.
Download references
Acknowledgements
The author thanks WJP editorial office for editing this manuscript.
This work was financially supported by National Natural Science Foundation of China (82241017).
Author information
Authors and affiliations.
Neonatal Intensive Care Unit, Children’s Hospital Zhejiang University School of Medicine, National Clinical Research Center for Child Health, 3333 Binsheng Road, Hangzhou, 310052, China
Li-Zhong Du
You can also search for this author in PubMed Google Scholar
Contributions
DLZ wrote, revised, and approved the final version of the manuscript.
Corresponding author
Correspondence to Li-Zhong Du .
Ethics declarations
Conflict of interest.
The author declare that he has no financial or non-financial conflict of interest. Author Li-Zhong Du is a member of the Editorial Board for World Journal of Pediatrics . The paper was handled by the other Editor and has undergone a rigorous peer review process. Author Li-Zhong Du was not involved in the journal's review of, or decisions related to, this manuscript. Other authors have no conflict of interest to disclose.
Ethical approval
Not needed.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Du, LZ. Early diagnosis and management of neonatal sepsis: a perspective. World J Pediatr (2024). https://doi.org/10.1007/s12519-024-00803-4
Download citation
Published : 31 March 2024
DOI : https://doi.org/10.1007/s12519-024-00803-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research

1 in 3 Americans who die in hospital had sepsis–and that’s just one of the many areas where AI can improve early diagnosis
W hile much of the public conversation around the rise of artificial intelligence has centered on its potential harms , academic and health care researchers have been quietly but aggressively finding ways to use AI to advance the practice of medicine.
Many of those projects will be years in the pipeline, owing in part to the medical research community’s rigorous standards of testing and interpreting results. Already, though, we’re beginning to see glimpses of how future AI might be used to the good–and a recent study suggests one very promising result.
In a prospective, pre-post study, published in Nature’s npj digital medicine , researchers found that an AI algorithm they’d developed can more quickly and accurately identify patients at risk for the serious blood infection sepsis than do existing protocols. The algorithm, called COMPOSER, also saves lives: a 1.9% absolute decrease in mortality corresponding to a 17% relative decrease across the two hospital emergency departments where it was used, the researchers found.
“That’s what I think people get excited about,” says Gabriel Wardi, the chief of critical care in emergency medicine at University of California San Diego Heath and senior author of the study. “Just the burden of sepsis coming down in the United States by 1.9% is huge.”
Improvements in sepsis detection
Although there’s more work to be done, the implications are significant. Sepsis, where infection triggers a chain reaction in the body that can lead to tissue damage, organ failure, and death, develops in about 1.7 million Americans each year and is linked to 350,000 deaths annually . The World Health Organization puts the global count at nearly 50 million cases and 11 million dead each year.
More to the point, one in three people who die in a U.S. hospital had sepsis during that hospitalization, according to the Centers for Disease Control and Prevention. Until now, this was largely a condition that was recognized only after its effects were beginning to be seen and felt.
“Early sepsis detection is on everyone’s mind,” says Shamim Nemati, director of predictive health analytics at UCSD and a co-author of the study. While there are some existing rule-based alerts for the infection, he says, most of them not only are slower, but suffer from a high rate of false alarms. In busy emergency departments with multiple alerts, that’s a fair concern.
The algorithm was constructed to address that. The deep-learning AI model that continuously monitors more than 150 patient variables–things like vital signs, lab results, current medications, and medical history–once that patient has been checked in. Using multiple layers of artificial neural networks, it identifies patients at high risk for sepsis while limiting false positives. “It works silently and safely behind the scenes, continuously surveilling every patient for signs of possible sepsis,” Wardi told me.
A high-risk detection triggers a notification to the ED nursing staff through the hospital’s electronic health record, and nurses can then relay the information to physicians. No alert is sent if the detected pattern can be explained by other conditions with higher confidence.
“When the algorithm sees a complex case that is unlike anything it has seen before, it says ‘I don’t know’ instead of making an ill-informed recommendation,” says researcher Aaron Boussina, a Ph.D. student in biomedical informatics at UCSD and co-author of the paper. “That is important since false alarms erode trust in the AI (model) and contribute to alarm fatigue, in which true alerts may be ignored.”
The researchers analyzed the results of more than 6,000 patient admissions before and after COMPOSER was activated at the two EDs–what is known as a pre-post study. The 1.9% absolute reduction in mortality, Wardi says, worked out to about 60 lives saved per year at the hospitals. (The system went live in December 2022.) Nationally, a nearly 2% reduction in sepsis mortality would translate to many thousands of saved lives.
The study was limited to the two San Diego facilities, and it was a non-randomized trial. Andre Holder, a physician researcher with expertise in prediction modeling using machine learning, who was not involved with the study, told me he had no major concerns with the methodology. “The authors note the limitations of the study,” Holder says, “but the study design is most fit to identify the real-world benefit of their tool.”
One concern in studies like this is what researchers call surveillance bias–looking more for something like sepsis, can find milder cases. This can make the death rates seem lower. The researchers say that during the study period, their hospitals did not experience changes in billing coding or screening practices, nor did they observe a significant increase in overall sepsis cases or the case mix, once COMPOSER was implemented.
Much more than sepsis
The use of AI in medicine is certainly not new . The National Institutes of Health sponsored the first AI in Medicine workshop at Rutgers University in 1975, and two years ago the FDA authorized the use of 91 AI-enabled medical devices, including an algorithm that helps clinicians identify collapsed lungs on imaging.
The decades in between have been punctuated by aggressive advances in AI technology in medicine. Investigators at Cedars-Sinai developed an AI tool that may help predict who will develop the most common type of pancreatic cancer , a notoriously difficult disease to forecast. They’re also using AI in brain cell modeling and Alzheimer’s research , among many other facets of medicine.
Several experts, including some at the respected New England Journal of Medicine wrote last year that they’ve been inundated by research manuscript submissions that reference some aspect of AI, adding that there is “virtually no area in medicine and care delivery that is not already being touched by AI.” Potential uses include easing administrative workflow, reducing dosage errors when patients self-administer certain medications, helping detect and track infectious diseases and estimating the 10-year cardiovascular risk in patients from a chest x-ray–it’s a nearly endless list of possibilities.
Still, a majority of Americans remain wary of AI’s inclusion in their own health care cases, its implementation in most areas is deliberate, and not all AI tools can yet be considered "medical grade." But some AI tools have already changed the way researchers do their work, and they may aid in such critical everyday tasks as early detection of breast cancer and self-supervised learning on retinal images , which may help detect not only eye-related but other systemic ailments, such as heart failure and Parkinson’s disease.
The Biden administration has called for careful monitoring of AI’s development in medicine, but also embraced its greater possibilities. A White House memo late last year said that by one estimate , “AI’s broader adoption could help doctors and health care workers deliver higher-quality, more empathetic care to patients in communities across the country while cutting healthcare costs by hundreds of billions of dollars annually.”
Perhaps unsurprisingly, other machine-learning algorithms to test for sepsis already exist. “But only a handful of people have actually put the algorithms into clinical practice,” Wardi says–one reason why people in the field are excited about the UCSD study’s results. The authors reported that this was the first study to show improvement in patient outcomes using an AI deep-learning sepsis prediction model.
More broadly, the notion of AI as not only helpful but essential to the future practice of medicine is beginning to take root. In a world in which artificial intelligence is often associated with darker themes, this may well prove to be part of its higher use.
“I’m cautiously optimistic,” says Nemati, “that future generations will look back at this period as the miracle years of AI in Medicine.”
Carolyn Barber, M.D ., is an internationally published science and medical writer and a 25-year emergency physician. She is the author of the book Runaway Medicine: What You Don’t Know May Kill You , and the co-founder of the California-based homeless work program Wheels of Change .
More must-read commentary published by Fortune :
- Glassdoor CEO : ‘Anonymous posts will always stay anonymous’
- We analyzed 46 years of consumer sentiment data–and found that today’s ‘vibecession’ is just men starting to feel as bad about the economy as women historically have
- Housing market data suggests the most optimistic buyers during the pandemic are more likely to stop paying their mortgages
- Intel CEO : ‘Our goal is to have at least 50% of the world’s advanced semiconductors produced in the U.S. and Europe by the end of the decade’
The opinions expressed in Fortune.com commentary pieces are solely the views of their authors and do not necessarily reflect the opinions and beliefs of Fortune .
This story was originally featured on Fortune.com

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Med (Lausanne)
Case report: An unusual presentation of puerperal sepsis
Doron kabiri.
1 Department of Obstetrics and Gynecology, Hadassah Medical Center, Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel
2 Department of Pathology, Hadassah Medical Center, Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel
Gali Gordon
Yossef ezra, associated data.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Group A Streptococcus (GAS; Streptococcus pyogenes ) is a facultative gram-positive coccus, uncommonly colonizing parturient genitalia, where its presence can potentially lead to a life-threatening invasive infection after delivery. GAS infection typically occurs within the first 4 days post-partum and is characterized by high fever, chills, flashing, abdominal pain, and uterine tenderness. Nonetheless, patients with GAS puerperal sepsis may have an unusual presentation, when fever is absent, and the symptoms and signs can be mild, non-specific, and not indicative of the severity of infection. This unusual presentation may lead to a delayed diagnosis and increase the risk for severe puerperal sepsis. Therefore, in these cases, a high index of suspicion and prompt early antibiotic and surgical treatment is crucial to saving the parturient’s life.
A 38-year-old woman, gravida 6 para 5, with an unremarkable past medical history presented to labor and delivery in active labor at 39 weeks of gestation and delivered vaginally shortly thereafter. Delivery was uneventful, without regional anesthesia and without perineal tears nor other complications. Twenty-four hours after delivery, the patient developed isolated left lower quadrant pain. Physical examination, abdominal ultrasound, and laboratory tests including complete blood count and basic metabolic panel were unremarkable, and the pain subsided after a bowel movement. On the following day, abdominal pain worsened, while the patient remained afebrile and was hemodynamically stable. Clinical assessment and physical examination of the pelvis and abdomen by the gynecological and surgical teams were unremarkable and revealed no acute distress; the abdomen was soft and non-tender on palpation, and bowel sounds were normal in all four quadrants. Notably, there was a significant discrepancy between the symptoms (referred abdominal pain) and the objective clinical findings. An abdominal and pelvic CT scan demonstrated normal post-partum uterus, endometrium and pelvic organs without signs of acute pathology. A large fecal burden throughout the colon was seen, suggesting possible constipation. Subsequently, 60 h after birth, her clinical condition deteriorated as the patient developed tachycardia with 130 beats per minute, tachypnea with 20 breaths per minute, and blood pressure of 103/65 mmHg. Laboratory values included a white blood cell count of 1.5 × 10 9 /L and C-Reactive Protein (CRP) of 27.1 mg/dl and Lactic acid of 4.05 mmol/L. Creatinine, liver-function tests, and electrolytes were within the normal range. Due to a high clinical suspicion of puerperal sepsis at this point, a wide-spectrum antibiotic regime of ampicillin, clindamycin and gentamicin was initiated, and the patient was transferred to the intensive care unit (ICU). Shortly afterward, the patient became hemodynamically and respiratorily unstable and required sedation, mechanical ventilation, and the use of inotropes to maintain adequate blood pressure. Laboratory results revealed worsening leukopenia, thrombocytopenia, and lactic acidosis. A post-contrast computed tomography scan showed an enlarged uterus with abundant periovarian and peritoneal fluid. Since the presence of pus in the abdomen was suspected and due to the severe clinical deterioration, an emergency exploratory laparotomy was executed, during which 600 ml of thick yellowish-white abdominal fluid was aspirated. The uterus and both ovaries were swollen, necrotic, and covered with fibrin, therefore a total abdominal hysterectomy and bilateral salpingo-oophorectomy were performed. Ovarian preservation was not possible because of severe necrosis. Gross findings of the post-operative pathological specimen showed an ischemic and partially necrotic uterus ( Figure 1 ), while microscopic examination of the uterus revealed a severe acute inflammatory process with necrotic myometrium and bacterial colonies ( Figures 2A,B ), confirmed later to be Streptococcus pyogenes on blood-agar medium culture. Post-operatively, the patient underwent a prolonged recovery period and was discharged without any further obstetrical or gynecological complications.

Macroscopic examination of the uterus: Hypertrophic post-partum uterus with necrotic tissue (white arrows), following severe Streptococcus pyogenes puerperal sepsis.

Histological specimens of the uterus. Microscopic examination of the uterus showing: (A) Hypertrophic post-partum uterus with acute inflammatory process characterized by extensive areas of recent hemorrhage and dilated congested vessels of the placental site. Black arrows indicate the focus of necrotic myometrium with bacterial colonies (hematoxylin and eosin staining, X1.25); (B) Acute inflammation with necrotic myometrium. Black arrows indicate bacterial colonies (hematoxylin and eosin staining, X60).
Maternal sepsis or puerperal sepsis is the third leading cause of maternal death in the United States and worldwide ( 1 – 4 ). Maternal sepsis is a life-threatening condition defined as organ dysfunction resulting from infection during pregnancy, childbirth, post-abortion, or post-partum period ( 5 ). Streptococcus pyogenes , Escherichia coli , Staphylococcus aureus , Group B Streptococcus, Streptococcus pneumoniae , Methicillin-resistant Staphylococcus aureus (MRSA), Clostridium septicum , and Morganella morganii are the predominant pathogens in maternal sepsis. The incidence of maternal sepsis ranges between 0.0001 and 0.004% and maternal mortality due to puerperal sepsis occurs in 9–14% ( 6 – 8 ). It is assumed that about 40% of maternal sepsis cases are preventable if early recognition, early escalation of care, and appropriate antibiotic treatment are applied ( 9 , 10 ). Risk factors for maternal sepsis include advanced maternal age, preterm premature rupture of the membranes (PPROM) and preterm delivery, multiple gestation pregnancies, cesarean delivery, retained products of conception, post-partum hemorrhage, and maternal comorbidities although maternal sepsis often occurred in patients without risk factors ( 6 ).
Group A Streptococcus (GAS; S. pyogenes ) is a facultative gram-positive coccus, uncommonly colonizing parturient genitalia, where its presence can potentially lead to a life-threatening invasive infection after delivery ( 11 – 14 ). GAS infection typically occurs within the first 4 days post-partum and is characterized by high fever, chills, flushing, abdominal pain, and uterine tenderness. Nonetheless, patients with GAS puerperal sepsis may have an unusual presentation, where fever is absent, signs and symptoms can be mild, non-specific, and not indicative of the severity of infection. This unusual presentation may lead to a delayed diagnosis and increase the risk of severe puerperal sepsis. Therefore, in these cases, a high index of suspicion, early escalation of care, and prompt early antibiotic and surgical treatment are crucial to saving the parturient’s life ( 15 – 21 ).
Data availability statement
Author contributions.
DK, RA, GG, SP, and YE conceived and designed the case report. DP helped with data acquisition. DK wrote the draft manuscript. All authors read the draft manuscript and made significant intellectual contributions to the final version and were responsible for the integrity of the data and accuracy of the analysis, and approved the final version of the manuscript for submission.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.

IMAGES
COMMENTS
Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med 2017;45:486-552. Crossref
The patient arrives to the emergency room within 15 minutes and is admitted for treatment at 1000. On the unit, Code Sepsis is called, and the agency's sepsis protocol based on the Surviving Sepsis campaign is implemented. The patient's vitals are now a temperature of 102F, heart rate of 140, respiratory rate of 34, and blood pressure of 96/42.
Case study 1: a 12-month-old baby with suspected sepsis. A mother brings her 12-month-old daughter Alice* into the pharmacy and asks to speak to the pharmacist. The mother clearly appears concerned and expresses that Alice seems very poorly and is not her usual self.
A study by Seymour et al. (2017) showed that the more rapid administration of the bundle of care is correlated with a decreased mortality rate. In addition, The Survival of Sepsis Campaign formed a guideline to sepsis treatment; Rhodes et al. (2016) suggests giving a 30 mL/kg of IV crystalloid fluid for hypoperfusion.
Soares MO, Welton NJ, Harrison DA, et al. An evaluation of the feasibility, cost and value of information of a multicentre randomised controlled trial of intravenous immunoglobulin for sepsis ...
This septic shock case study is designed to help the nursing student better understand nursing care for a patient with sepsis. Mr. McMillan, a 92-year old male, presents to the Emergency Department (ED) with urinary hesitancy and burning and a fever at home of 101.6°F. His caregiver states "he just doesn't seem like himself".
The study found that incorporating sepsis-related case scenarios in ongoing educational and professional training programs improved nurses' self-efficacy and led to a prompt and accurate assessment of sepsis . One of the interventions explored in this review was a simulation that facilitated decision-making related to sepsis management.
The sepsis patient mortality rate decreased from as high as 1.91 in Q1 2017 to as low as 0.45 in 2019. Cases meeting the bundle compliance increased from as low as 52% in Jan 2018 to as high as 88% in August 2019. LOS also decreased from a high of 6.83 days on average in January of 2017 to as low as 3.88 days on average in August of 2019.
This case study explores the importance of adequate assessment of patients on their initial presentation to the emergency department, during hospitalization, and before discharge. The clinical evaluation, recognition, and management of sepsis continue to be essential for patient survival to prevent and decrease the mortality rate.
Sepsis is a life-threatening and debilitating sickness in the elderly. This case study explores the importance of adequate assessment of patients on their initial presentation to the emergency department, during hospitalization, and before discharge. The clinical evaluation, recognition, and management of sepsis continue to be essential for ...
More than 1.5 million cases of sepsis occur in the United States annually, and many patients with sepsis present to the emergency department. 1 International clinical practice guidelines and the ...
Description: Delve into sepsis case studies that illustrate common assessments and tools used to care for sepsis. This presentation details case studies that cover three different healthcare areas, as well as the team members involved in the assessment, diagnosis, and treatment of patients with sepsis. These cases highlight the need for all ...
The following is a case of an eight months old, female infant, admitted in to the clinic for fever (39.7 C), with an onset five days before the admission, following trauma to the inferior lip and gum. ... Gerlach H. et al. An international sepsis survey: a study of doctor's knowledge and perception about sepsis. Crit Care. 2004; 8:R409-13 ...
Sepsis incidence rates are up to 535 cases per 100,000 person-years and rising. In-hospital mortality remains high at 25-30%. The majority of these are in low- and middle-income countries (LMICs) . In a multicentre study, it was revealed that sepsis in Southeast Asia has a high mortality . There is paucity of data regarding sepsis in Sri Lanka.
This page titled 7: Case Study #6- Sepsis is shared under a CC BY-SA 4.0 license and was authored, remixed, and/or curated by Glynda Rees, Rob Kruger, and Janet Morrison via source content that was edited to the style and standards of the LibreTexts platform; a detailed edit history is available upon request.
Sepsis is a leading cause of death in hospitalized children, killing almost 5,000 children annually in the U.S. Sharing these sepsis patient stories is part of the Improving Pediatric Sepsis Outcomes collaborative, a multi-year quality initiative to significantly reduce sepsis-related mortality and morbidity across children's hospitals.
Skin is pale, dry and hot. Heart rate 110, respiratory rate 24, blood pressure 100/60. An oral thermometer is not available. Focused assessment of the patient's foot reveals a one-inch ...
CASE STUDY: Failure to Identify Sepsis and Initiate Treatment Leads to Patient Death. Jeanne E. Mapes, JD, CPCU, CPHRM. Case Details. The patient in this case was a 49-year-old female who had a significant medical history, including chronic obstructive pulmonary disease (COPD), coronary artery disease, hypertension, and hyperlipidemia. ...
The study found that incorporating sepsis-related case scenarios in ongoing educational and professional training programs improved nurses' self-efficacy and led to a prompt and accurate assessment of sepsis . One of the interventions explored in this review was a simulation that facilitated decision-making related to sepsis management.
A recent study of the "National Reference Center for Pneumococci" at the Austrian Agency for Health and Food Safety (AGES) depicting infections with S. pneumoniae in 2009 revealed that 303 invasive illnesses and 19 deaths occurred due to S. pneumoniae in Austria. Extrapolated to the population, Austria had 3.62 invasive diseases/100,000 ...
The mortality rate for patients with SARS-CoV-2-associated sepsis was initially high: 33 percent over the first three months of the pandemic. However, the rate declined over time and eventually became similar to the mortality rate for presumed bacterial sepsis: about 14.5 percent. That rate then remained stable throughout the study period.
The reviewers identified 50 observational studies with highly diverse improvement programs and study designs. Despite this heterogeneity, the meta-analysis showed that sepsis performance improvement programs were consistently associated with increased compliance with 6-h (OR 4.12, 95% CI 2.95-5.76) and 24-h (OR 2.57, 95%-CI 1.74-3.77 ...
A comprehensive study reviewed evidence from observational epidemiological studies to gauge the global burden and mortality of sepsis in neonates and children. The population-level estimate for neonatal sepsis was 2202 per 1,00,000 LBs, with mortality rates ranging from 11% to 19%.
Sepsis education plays a significant role throughout the health care continuum, from onboarding of new hires to discharging patients from the hospital. Education should include physicians, health care staff, patients, families and caregivers. From onboarding and yearly training to real-time feedback on cases, providing sepsis education is key ...
Sepsis, where infection triggers a chain reaction in the body that can lead to tissue damage, organ failure, and death, develops in about 1.7 million Americans each year and is linked to 350,000 ...
Individual case study We chose to investigate individuals in our test set who suffered from a history of congestive heart failure (CHF), a condition known to present challenges in sepsis fluids administration, as over-administration of fluids can worsen their condition, and lead to adverse outcomes such as pulmonary edema. We modelled the ...
The incidence of maternal sepsis ranges between 0.0001 and 0.004% and maternal mortality due to puerperal sepsis occurs in 9-14% (6-8). It is assumed that about 40% of maternal sepsis cases are preventable if early recognition, early escalation of care, and appropriate antibiotic treatment are applied (9, 10).