- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram

Among teens, sleep deprivation an epidemic
Sleep deprivation increases the likelihood teens will suffer myriad negative consequences, including an inability to concentrate, poor grades, drowsy-driving incidents, anxiety, depression, thoughts of suicide and even suicide attempts.
October 8, 2015 - By Ruthann Richter

The most recent national poll shows that more than 87 percent of U.S. high school students get far less than the recommended eight to 10 hours of sleep each night. Christopher Silas Neal
Carolyn Walworth, 17, often reaches a breaking point around 11 p.m., when she collapses in tears. For 10 minutes or so, she just sits at her desk and cries, overwhelmed by unrelenting school demands. She is desperately tired and longs for sleep. But she knows she must move through it, because more assignments in physics, calculus or French await her. She finally crawls into bed around midnight or 12:30 a.m.
The next morning, she fights to stay awake in her first-period U.S. history class, which begins at 8:15. She is unable to focus on what’s being taught, and her mind drifts. “You feel tired and exhausted, but you think you just need to get through the day so you can go home and sleep,” said the Palo Alto, California, teen. But that night, she will have to try to catch up on what she missed in class. And the cycle begins again.
“It’s an insane system. … The whole essence of learning is lost,” she said.
Walworth is among a generation of teens growing up chronically sleep-deprived. According to a 2006 National Sleep Foundation poll, the organization’s most recent survey of teen sleep, more than 87 percent of high school students in the United States get far less than the recommended eight to 10 hours, and the amount of time they sleep is decreasing — a serious threat to their health, safety and academic success. Sleep deprivation increases the likelihood teens will suffer myriad negative consequences, including an inability to concentrate, poor grades, drowsy-driving incidents, anxiety, depression, thoughts of suicide and even suicide attempts. It’s a problem that knows no economic boundaries.
While studies show that both adults and teens in industrialized nations are becoming more sleep deprived, the problem is most acute among teens, said Nanci Yuan , MD, director of the Stanford Children’s Health Sleep Center . In a detailed 2014 report, the American Academy of Pediatrics called the problem of tired teens a public health epidemic.
“I think high school is the real danger spot in terms of sleep deprivation,” said William Dement , MD, PhD, founder of the Stanford Sleep Disorders Clinic , the first of its kind in the world. “It’s a huge problem. What it means is that nobody performs at the level they could perform,” whether it’s in school, on the roadways, on the sports field or in terms of physical and emotional health.
Social and cultural factors, as well as the advent of technology, all have collided with the biology of the adolescent to prevent teens from getting enough rest. Since the early 1990s, it’s been established that teens have a biologic tendency to go to sleep later — as much as two hours later — than their younger counterparts.
Yet when they enter their high school years, they find themselves at schools that typically start the day at a relatively early hour. So their time for sleep is compressed, and many are jolted out of bed before they are physically or mentally ready. In the process, they not only lose precious hours of rest, but their natural rhythm is disrupted, as they are being robbed of the dream-rich, rapid-eye-movement stage of sleep, some of the deepest, most productive sleep time, said pediatric sleep specialist Rafael Pelayo , MD, with the Stanford Sleep Disorders Clinic.
“When teens wake up earlier, it cuts off their dreams,” said Pelayo, a clinical professor of psychiatry and behavioral sciences. “We’re not giving them a chance to dream.”

Teens have a biologic tendency to go to sleep later, yet many high schools start the day at a relatively early hour, disrupting their natural rhythym. Monkey Business/Fotolia
Understanding teen sleep
On a sunny June afternoon, Dement maneuvered his golf cart, nicknamed the Sleep and Dreams Shuttle, through the Stanford University campus to Jerry House, a sprawling, Mediterranean-style dormitory where he and his colleagues conducted some of the early, seminal work on sleep, including teen sleep.
Beginning in 1975, the researchers recruited a few dozen local youngsters between the ages of 10 and 12 who were willing to participate in a unique sleep camp. During the day, the young volunteers would play volleyball in the backyard, which faces a now-barren Lake Lagunita, all the while sporting a nest of electrodes on their heads.
At night, they dozed in a dorm while researchers in a nearby room monitored their brain waves on 6-foot electroencephalogram machines, old-fashioned polygraphs that spit out wave patterns of their sleep.
One of Dement’s colleagues at the time was Mary Carskadon, PhD, then a graduate student at Stanford. They studied the youngsters over the course of several summers, observing their sleep habits as they entered puberty and beyond.
Dement and Carskadon had expected to find that as the participants grew older, they would need less sleep. But to their surprise, their sleep needs remained the same — roughly nine hours a night — through their teen years. “We thought, ‘Oh, wow, this is interesting,’” said Carskadon, now a professor of psychiatry and human behavior at Brown University and a nationally recognized expert on teen sleep.
Moreover, the researchers made a number of other key observations that would plant the seed for what is now accepted dogma in the sleep field. For one, they noticed that when older adolescents were restricted to just five hours of sleep a night, they would become progressively sleepier during the course of the week. The loss was cumulative, accounting for what is now commonly known as sleep debt.
“The concept of sleep debt had yet to be developed,” said Dement, the Lowell W. and Josephine Q. Berry Professor in the Department of Psychiatry and Behavioral Sciences. It’s since become the basis for his ongoing campaign against drowsy driving among adults and teens. “That’s why you have these terrible accidents on the road,” he said. “People carry a large sleep debt, which they don’t understand and cannot evaluate.”
The researchers also noticed that as the kids got older, they were naturally inclined to go to bed later. By the early 1990s, Carskadon established what has become a widely recognized phenomenon — that teens experience a so-called sleep-phase delay. Their circadian rhythm — their internal biological clock — shifts to a later time, making it more difficult for them to fall asleep before 11 p.m.
Teens are also biologically disposed to a later sleep time because of a shift in the system that governs the natural sleep-wake cycle. Among older teens, the push to fall asleep builds more slowly during the day, signaling them to be more alert in the evening.
“It’s as if the brain is giving them permission, or making it easier, to stay awake longer,” Carskadon said. “So you add that to the phase delay, and it’s hard to fight against it.”
Pressures not to sleep
After an evening with four or five hours of homework, Walworth turns to her cellphone for relief. She texts or talks to friends and surfs the Web. “It’s nice to stay up and talk to your friends or watch a funny YouTube video,” she said. “There are plenty of online distractions.”
While teens are biologically programmed to stay up late, many social and cultural forces further limit their time for sleep. For one, the pressure on teens to succeed is intense, and they must compete with a growing number of peers for college slots that have largely remained constant. In high-achieving communities like Palo Alto, that translates into students who are overwhelmed by additional homework for Advanced Placement classes, outside activities such as sports or social service projects, and in some cases, part-time jobs, as well as peer, parental and community pressures to excel.

William Dement
At the same time, today’s teens are maturing in an era of ubiquitous electronic media, and they are fervent participants. Some 92 percent of U.S. teens have smartphones, and 24 percent report being online “constantly,” according to a 2015 report by the Pew Research Center. Teens have access to multiple electronic devices they use simultaneously, often at night. Some 72 percent bring cellphones into their bedrooms and use them when they are trying to go to sleep, and 28 percent leave their phones on while sleeping, only to be awakened at night by texts, calls or emails, according to a 2011 National Sleep Foundation poll on electronic use. In addition, some 64 percent use electronic music devices, 60 percent use laptops and 23 percent play video games in the hour before they went to sleep, the poll found. More than half reported texting in the hour before they went to sleep, and these media fans were less likely to report getting a good night’s sleep and feeling refreshed in the morning. They were also more likely to drive when drowsy, the poll found.
The problem of sleep-phase delay is exacerbated when teens are exposed late at night to lit screens, which send a message via the retina to the portion of the brain that controls the body’s circadian clock. The message: It’s not nighttime yet.
Yuan, a clinical associate professor of pediatrics, said she routinely sees young patients in her clinic who fall asleep at night with cellphones in hand.
“With academic demands and extracurricular activities, the kids are going nonstop until they fall asleep exhausted at night. There is not an emphasis on the importance of sleep, as there is with nutrition and exercise,” she said. “They say they are tired, but they don’t realize they are actually sleep-deprived. And if you ask kids to remove an activity, they would rather not. They would rather give up sleep than an activity.”
The role of parents
Adolescents are also entering a period in which they are striving for autonomy and want to make their own decisions, including when to go to sleep. But studies suggest adolescents do better in terms of mood and fatigue levels if parents set the bedtime — and choose a time that is realistic for the child’s needs. According to a 2010 study published in the journal Sleep , children are more likely to be depressed and to entertain thoughts of suicide if a parent sets a late bedtime of midnight or beyond.
In families where parents set the time for sleep, the teens’ happier, better-rested state “may be a sign of an organized family life, not simply a matter of bedtime,” Carskadon said. “On the other hand, the growing child and growing teens still benefit from someone who will help set the structure for their lives. And they aren’t good at making good decisions.”
They say they are tired, but they don’t realize they are actually sleep-deprived. And if you ask kids to remove an activity, they would rather not. They would rather give up sleep than an activity.
According to the 2011 sleep poll, by the time U.S. students reach their senior year in high school, they are sleeping an average of 6.9 hours a night, down from an average of 8.4 hours in the sixth grade. The poll included teens from across the country from diverse ethnic backgrounds.
American teens aren’t the worst off when it comes to sleep, however; South Korean adolescents have that distinction, sleeping on average 4.9 hours a night, according to a 2012 study in Sleep by South Korean researchers. These Asian teens routinely begin school between 7 and 8:30 a.m., and most sign up for additional evening classes that may keep them up as late as midnight. South Korean adolescents also have relatively high suicide rates (10.7 per 100,000 a year), and the researchers speculate that chronic sleep deprivation is a contributor to this disturbing phenomenon.
By contrast, Australian teens are among those who do particularly well when it comes to sleep time, averaging about nine hours a night, possibly because schools there usually start later.
Regardless of where they live, most teens follow a pattern of sleeping less during the week and sleeping in on the weekends to compensate. But many accumulate such a backlog of sleep debt that they don’t sufficiently recover on the weekend and still wake up fatigued when Monday comes around.
Moreover, the shifting sleep patterns on the weekend — late nights with friends, followed by late mornings in bed — are out of sync with their weekday rhythm. Carskadon refers to this as “social jet lag.”
“Every day we teach our internal circadian timing system what time it is — is it day or night? — and if that message is substantially different every day, then the clock isn’t able to set things appropriately in motion,” she said. “In the last few years, we have learned there is a master clock in the brain, but there are other clocks in other organs, like liver or kidneys or lungs, so the master clock is the coxswain, trying to get everybody to work together to improve efficiency and health. So if the coxswain is changing the pace, all the crew become disorganized and don’t function well.”
This disrupted rhythm, as well as the shortage of sleep, can have far-reaching effects on adolescent health and well-being, she said.
“It certainly plays into learning and memory. It plays into appetite and metabolism and weight gain. It plays into mood and emotion, which are already heightened at that age. It also plays into risk behaviors — taking risks while driving, taking risks with substances, taking risks maybe with sexual activity. So the more we look outside, the more we’re learning about the core role that sleep plays,” Carskadon said.
Many studies show students who sleep less suffer academically, as chronic sleep loss impairs the ability to remember, concentrate, think abstractly and solve problems. In one of many studies on sleep and academic performance, Carskadon and her colleagues surveyed 3,000 high school students and found that those with higher grades reported sleeping more, going to bed earlier on school nights and sleeping in less on weekends than students who had lower grades.
Sleep is believed to reinforce learning and memory, with studies showing that people perform better on mental tasks when they are well-rested. “We hypothesize that when teens sleep, the brain is going through processes of consolidation — learning of experiences or making memories,” Yuan said. “It’s like your brain is filtering itself — consolidating the important things and filtering out those unimportant things.” When the brain is deprived of that opportunity, cognitive function suffers, along with the capacity to learn.
“It impacts academic performance. It’s harder to take tests and answer questions if you are sleep-deprived,” she said.
That’s why cramming, at the expense of sleep, is counterproductive, said Pelayo, who advises students: Don’t lose sleep to study, or you’ll lose out in the end.
The panic attack
Chloe Mauvais, 16, hit her breaking point at the end of a very challenging sophomore year when she reached “the depths of frustration and anxiety.” After months of late nights spent studying to keep up with academic demands, she suffered a panic attack one evening at home.
“I sat in the living room in our house on the ground, crying and having horrible breathing problems,” said the senior at Menlo-Atherton High School. “It was so scary. I think it was from the accumulated stress, the fear over my grades, the lack of sleep and the crushing sense of responsibility. High school is a very hard place to be.”
We hypothesize that when teens sleep, the brain is going through processes of consolidation — learning of experiences or making memories. It’s like your brain is filtering itself.
Where she once had good sleep habits, she had drifted into an unhealthy pattern of staying up late, sometimes until 3 a.m., researching and writing papers for her AP European history class and prepping for tests.
“I have difficulty remembering events of that year, and I think it’s because I didn’t get enough sleep,” she said. “The lack of sleep rendered me emotionally useless. I couldn’t address the stress because I had no coherent thoughts. I couldn’t step back and have perspective. … You could probably talk to any teen and find they reach their breaking point. You’ve pushed yourself so much and not slept enough and you just lose it.”
The experience was a kind of wake-up call, as she recognized the need to return to a more balanced life and a better sleep pattern, she said. But for some teens, this toxic mix of sleep deprivation, stress and anxiety, together with other external pressures, can tip their thinking toward dire solutions.
Research has shown that sleep problems among adolescents are a major risk factor for suicidal thoughts and death by suicide, which ranks as the third-leading cause of fatalities among 15- to 24-year-olds. And this link between sleep and suicidal thoughts remains strong, independent of whether the teen is depressed or has drug and alcohol issues, according to some studies.
“Sleep, especially deep sleep, is like a balm for the brain,” said Shashank Joshi, MD, associate professor of psychiatry and behavioral sciences at Stanford. “The better your sleep, the more clearly you can think while awake, and it may enable you to seek help when a problem arises. You have your faculties with you. You may think, ‘I have 16 things to do, but I know where to start.’ Sleep deprivation can make it hard to remember what you need to do for your busy teen life. It takes away the support, the infrastructure.”
Sleep is believed to help regulate emotions, and its deprivation is an underlying component of many mood disorders, such as anxiety, depression and bipolar disorder. For students who are prone to these disorders, better sleep can help serve as a buffer and help prevent a downhill slide, Joshi said.
Rebecca Bernert, PhD, who directs the Suicide Prevention Research Lab at Stanford, said sleep may affect the way in which teens process emotions. Her work with civilians and military veterans indicates that lack of sleep can make people more receptive to negative emotional information, which they might shrug off if they were fully rested, she said.
“Based on prior research, we have theorized that sleep disturbances may result in difficulty regulating emotional information, and this may lower the threshold for suicidal behaviors among at-risk individuals,” said Bernert, an instructor of psychiatry and behavioral sciences. Now she’s studying whether a brief nondrug treatment for insomnia reduces depression and risk for suicide.
Sleep deprivation also has been shown to lower inhibitions among both adults and teens. In the teen brain, the frontal lobe, which helps restrain impulsivity, isn’t fully developed, so teens are naturally prone to impulsive behavior. “When you throw into the mix sleep deprivation, which can also be disinhibiting, mood problems and the normal impulsivity of adolescence, then you have a potentially dangerous situation,” Joshi said.
Some schools shift
Given the health risks associated with sleep problems, school districts around the country have been looking at one issue over which they have some control: when school starts in the morning. The trend was set by the town of Edina, Minnesota, a well-to-do suburb of Minneapolis, which conducted a landmark experiment in student sleep in the late 1990s. It shifted the high school’s start time from 7:20 a.m. to 8:30 a.m. and then asked University of Minnesota researchers to look at the impact of the change. The researchers found some surprising results: Students reported feeling less depressed and less sleepy during the day and more empowered to succeed. There was no comparable improvement in student well-being in surrounding school districts where start times remained the same.
With these findings in hand, the entire Minneapolis Public School District shifted start times for 57,000 students at all of its schools in 1997 and found similarly positive results. Attendance rates rose, and students reported getting an hour’s more sleep each school night — or a total of five more hours of sleep a week — countering skeptics who argued that the students would respond by just going to bed later.
For the health and well-being of the nation, we should all be taking better care of our sleep, and we certainly should be taking better care of the sleep of our youth.
Other studies have reinforced the link between later start times and positive health benefits. One 2010 study at an independent high school in Rhode Island found that after delaying the start time by just 30 minutes, students slept more and showed significant improvements in alertness and mood. And a 2014 study in two counties in Virginia found that teens were much less likely to be involved in car crashes in a county where start times were later, compared with a county with an earlier start time.
Bolstered by the evidence, the American Academy of Pediatrics in 2014 issued a strong policy statement encouraging middle and high school districts across the country to start school no earlier than 8:30 a.m. to help preserve the health of the nation’s youth. Some districts have heeded the call, though the decisions have been hugely contentious, as many consider school schedules sacrosanct and cite practical issues, such as bus schedules, as obstacles.
In Fairfax County, Virginia, it took a decade of debate before the school board voted in 2014 to push back the opening school bell for its 57,000 students. And in Palo Alto, where a recent cluster of suicides has caused much communitywide soul-searching, the district superintendent issued a decision in the spring, over the strenuous objections of some teachers, students and administrators, to eliminate “zero period” for academic classes — an optional period that begins at 7:20 a.m. and is generally offered for advanced studies.
Certainly, changing school start times is only part of the solution, experts say. More widespread education about sleep and more resources for students are needed. Parents and teachers need to trim back their expectations and minimize pressures that interfere with teen sleep. And there needs to be a cultural shift, including a move to discourage late-night use of electronic devices, to help youngsters gain much-needed rest.
“At some point, we are going to have to confront this as a society,” Carskadon said. “For the health and well-being of the nation, we should all be taking better care of our sleep, and we certainly should be taking better care of the sleep of our youth.”

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Hope amid crisis
Psychiatry’s new frontiers

Save 45% on a Home Sleep Test – Shop Now
How Lack of Sleep Impacts Cognitive Performance and Focus

Staff Writer
Eric Suni has over a decade of experience as a science writer and was previously an information specialist for the National Cancer Institute.
Want to read more about all our experts in the field?

Dr. Nilong Vyas
Pediatrician
Dr. Vyas is a pediatrician and founder of Sleepless in NOLA. She specializes in helping parents establish healthy sleep habits for children.
Sleep Foundation
Fact-Checking: Our Process
The Sleep Foundation editorial team is dedicated to providing content that meets the highest standards for accuracy and objectivity. Our editors and medical experts rigorously evaluate every article and guide to ensure the information is factual, up-to-date, and free of bias.
The Sleep Foundation fact-checking guidelines are as follows:
- We only cite reputable sources when researching our guides and articles. These include peer-reviewed journals, government reports, academic and medical associations, and interviews with credentialed medical experts and practitioners.
- All scientific data and information must be backed up by at least one reputable source. Each guide and article includes a comprehensive bibliography with full citations and links to the original sources.
- Some guides and articles feature links to other relevant Sleep Foundation pages. These internal links are intended to improve ease of navigation across the site, and are never used as original sources for scientific data or information.
- A member of our medical expert team provides a final review of the content and sources cited for every guide, article, and product review concerning medical- and health-related topics. Inaccurate or unverifiable information will be removed prior to publication.
- Plagiarism is never tolerated. Writers and editors caught stealing content or improperly citing sources are immediately terminated, and we will work to rectify the situation with the original publisher(s)
- Although Sleep Foundation maintains affiliate partnerships with brands and e-commerce portals, these relationships never have any bearing on our product reviews or recommendations. Read our full Advertising Disclosure for more information.
Table of Contents
How Poor Sleep Affects the Brain
How does poor sleep affect creativity and other cognitive processes, are the cognitive impacts of poor sleep the same for everyone, can sleep disorders affect cognition, does too much sleep affect cognition, will improving sleep quality benefit cognition.
Getting enough hours of high-quality sleep fosters attention and concentration, which are prerequisites for most learning. Sleep also supports numerous other aspects of cognition, including memory, problem-solving, creativity, emotional processing, and judgment. Levels of brain activity fluctuate during each stage of sleep — including both rapid eye movement (REM) and non-REM (NREM) sleep — and evidence increasingly suggests that sleep enhances most types of cognitive function.
For people with sleep deprivation, insomnia, sleep apnea, or other conditions that prevent them from getting adequate rest, short-term daytime cognitive impairment is common. Improving sleep quality can boost cognitive performance, promote sharper thinking, and may reduce the likelihood of age-related cognitive decline.
During a typical night of sleep, an individual cycles through the three stages of NREM sleep, followed by a period of REM sleep every 90 to 120 minutes, several times per night. Both the brain and body experience distinct changes during these cycles that correspond to individual stages of sleep . During each part of this process, different chemicals in the brain become activated or deactivated to coordinate rest and recovery.
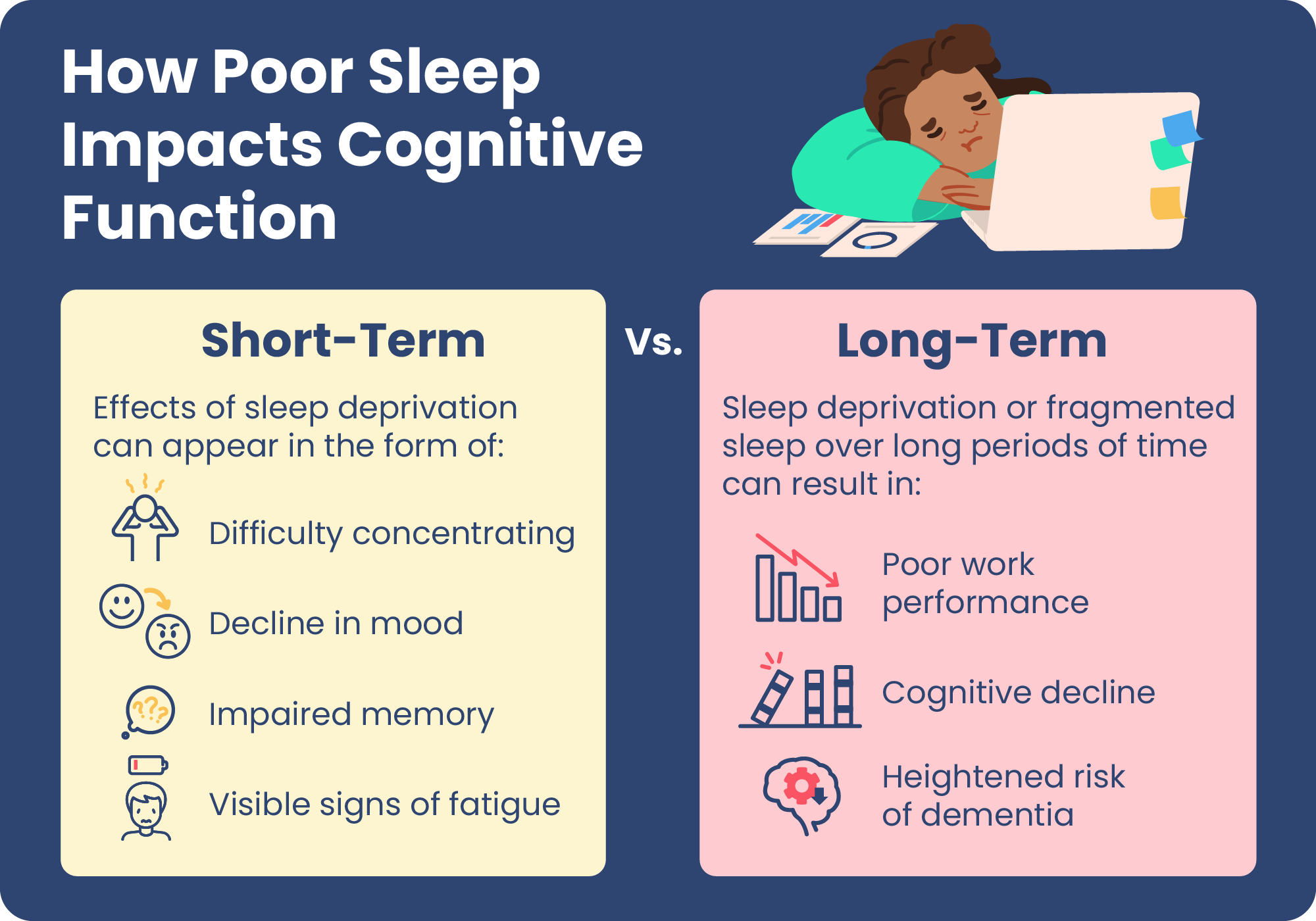
Poor sleep can take many forms, including short sleep duration or fragmented sleep. Without adequate sleep, the brain struggles to function properly. Because they do not have time to recuperate, neurons in the brain become overworked and less capable of optimal performance in various types of thinking.
The short-term detriments of poor sleep on the brain and cognition can be the result of pulling an occasional all-nighter, while those with chronic sleep problems may see a continuous negative effect on day-to-day tasks. Over the long-term, poor sleep may put someone at a higher risk of cognitive decline and dementia.
What Are the Short-Term Cognitive Impacts of Poor Sleep?
Poor sleep can harm intellectual performance, academic achievement, creative pursuits, and productivity at work. The cognitive impacts of poor sleep can also create safety risks, including drowsy driving . Motor skills, keeping rhythm, and even some types of speech can decline without proper sleep. The potential short-term impacts of poor sleep are wide-ranging:
- Excessive Sleepiness: Drowsiness and fatigue are common daytime effects of a night of poor sleep. In response to excessive fatigue, a person may inadvertently nod off for a few seconds, which is known as a microsleep .
- Poor Attention Span: Poor sleep reduces a person’s attention, as well as their learning and processing. A lack of sleep has also been found to induce effects that are similar to being drunk Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source , which slows down thinking and reaction time . Poor sleep also diminishes placekeeping Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source , which includes the ability to carry out instructions.
- Reduced Adaptability: Some studies have found lack of sleep to hinder cognitive flexibility, reducing the ability to adapt and thrive in uncertain or changing circumstances. A major reason this occurs is rigid thinking and “feedback blunting” Trusted Source Oxford Academic Journals (OUP) OUP publishes the highest quality journals and delivers this research to the widest possible audience. View Source , in which the capacity to learn and improve on-the-fly is diminished.
- Reduced Emotional Capacity: Poor sleep can also alter how emotional information is understood Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source . When learning something new, analyzing a problem, or making a decision, recognizing the emotional context is often important. However, insufficient sleep impedes the ability to properly process the emotional component of information.
- Impaired Judgment: In some cases, this dysregulated emotional response impairs judgment. People who do not get sufficient sleep are more likely to make risky choices Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source and may focus on a potential reward rather than downsides. It can be difficult to learn from these mistakes, since the normal method of processing and consolidating emotional memory is compromised due to lack of sleep.
What Are the Long-Term Cognitive Impacts of Poor Sleep?
Insufficient sleep and sleep fragmentation are frequently associated with cognitive decline and dementia. Furthermore, in people already diagnosed with dementia, poor sleep has been linked to a worse disease prognosis. Some cognitive effects of poor sleep can be felt immediately, but mounting evidence shows that sleep influences your long-term risk of cognition issues:
- Impaired Memory: Both NREM and REM sleep appear to be important for broader memory consolidation Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source , which helps reinforce information in the brain so that it can be recalled when needed. NREM sleep has been linked with declarative memory, which includes things like basic facts or statistics, and REM sleep is believed to boost procedural memory such as remembering a sequence of steps. Poor sleep impairs memory consolidation by disrupting the normal process that draws on both NREM and REM sleep for building and retaining memories. Studies have even found that people who are sleep deprived are at risk of forming false memories Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source .
- Alzheimer’s Disease: Research shows that sleep helps the brain conduct important housekeeping, such as clearing out potentially dangerous beta amyloid proteins. In Alzheimer’s disease, beta amyloid forms in clusters, called plaques, that worsen cognitive function. Studies have found that even one night of sleep deprivation can increase the amount of beta amyloid in the brain Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source . One analysis found a considerably higher risk of Alzheimer’s disease Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source in people with sleep problems, estimating as many as 15% of cases of Alzheimer’s disease were attributable to poor sleep.
Creativity is another aspect of cognition that is hindered by sleeping problems. Connecting loosely associated ideas is a hallmark of creativity, and this ability is strengthened by good sleep. NREM sleep provides an opportunity for information to be restructured and reorganized Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source in the brain, while new ideas and links between thoughts often emerge during REM sleep. These processes enable insight, a core element of innovation and creative problem-solving.
Limited or restless sleep can also indirectly affect cognition. For example, migraine sufferers are more likely to have morning headache attacks Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source when they do not get enough sleep, and lack of sleep can increase the risk of infections Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source like the common cold. Sleep deprivation may worsen symptoms of mental health conditions like anxiety and depression. These and numerous other physical and mental health issues are shaped by sleep quality, and may affect a person’s attention and concentration.
Not everyone is affected by poor sleep in the same way. Studies have found that some individuals may be more susceptible to cognitive impairment from sleep deprivation, and this may be influenced by genetics.
Research has discovered that adults are better at overcoming the effects of sleep deprivation than younger people. Teens are considered to be at a heightened risk for detrimental effects of poor sleep on thinking, decision-making, and academic performance because of the ongoing brain development that occurs during teen years .
Some studies have also found that women are more adept at coping with the effects of sleep deprivation than men, although it is not yet clear if this is related to biological factors, social and cultural influences, or a combination of both.
Sleep disorders, like insomnia, frequently involve insufficient or fragmented sleep, so it comes as little surprise that they can be linked to cognitive impairment.
Obstructive sleep apnea (OSA) is among the most common sleep disorders. It occurs when the airway gets blocked, which then leads to lapses in breathing during sleep and reduced oxygen in the blood. OSA has been associated with daytime sleepiness as well as notable cognitive problems related to attention, thinking, memory, and communication. Studies have also found that people with sleep apnea have a higher risk of developing dementia .
Many studies examining the effects of sleep on thinking have found that an excess of sleep can also be problematic for brain health. In many cases, research has discovered that both too little and too much sleep Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source are associated with cognitive decline.
The explanation for this association remains unclear. It is not known if excess sleep is caused by a coexisting health condition that may also predispose someone to cognitive problems. Overall, these research findings are an important reminder to get the right amount of sleep each night.
For people with sleeping problems, improving sleep quality offers a practical way to enhance cognitive performance. Getting the recommended amount of uninterrupted sleep can help the brain recuperate and avoid many of the negative consequences of poor sleep on diverse aspects of thinking.
Researchers and public health experts increasingly view good sleep as a potential form of prevention against dementia and Alzheimer’s disease Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source . Although more studies are needed to conclusively determine sleep’s role in preventing cognitive decline, early research suggests that taking steps to improve sleep may reduce the longer-term likelihood of developing Alzheimer’s disease.
Tips To Improve Sleep and Cognitive Performance
Anyone who feels that they are experiencing cognitive impairment or excessive daytime sleepiness should first speak with their doctor. A physician can help identify or rule out any other conditions, including sleep disorders, that may be causing these symptoms. They can also discuss strategies to get better sleep.
Many approaches to improving sleep start with healthy sleep hygiene . By optimizing your bedroom environment and everyday habits and routines, you can eliminate many common barriers to sleep. Setting a regular bedtime and sleep schedule, avoiding alcohol and caffeine in the evening, and minimizing electronics in the bedroom are a few examples of sleep hygiene tips that can make it easier to rest well each night.
About Our Editorial Team

Eric Suni, Staff Writer

Medically Reviewed by
Dr. Nilong Vyas, Pediatrician MD
References 14 sources.
Dawson, D., & Reid, K. (1997). Fatigue, alcohol and performance impairment. Nature, 388(6639), 235.
Stepan, M. E., Altmann, E. M., & Fenn, K. M. (2020). Effects of total sleep deprivation on procedural placekeeping: More than just lapses of attention. Journal of experimental psychology. General, 149(4), 800–806.
Whitney, P., Hinson, J. M., Jackson, M. L., & Van Dongen, H. P. (2015). Feedback Blunting: Total Sleep Deprivation Impairs Decision Making that Requires Updating Based on Feedback. Sleep, 38(5), 745–754.
Killgore, W. D. (2010). Effects of sleep deprivation on cognition. Progress in Brain Research, 185, 105–129.
Van Someren, E. J., Cirelli, C., Dijk, D. J., Van Cauter, E., Schwartz, S., & Chee, M. W. (2015). Disrupted sleep: From molecules to cognition. The Journal of Neuroscience, 35(41), 13889–13895.
Maquet P. (2000). Sleep on it!. Nature neuroscience, 3(12), 1235–1236.
Lo, J. C., Chong, P. L., Ganesan, S., Leong, R. L., & Chee, M. W. (2016). Sleep deprivation increases formation of false memory. Journal of sleep research, 25(6), 673–682.
Shokri-Kojori, E., Wang, G. J., Wiers, C. E., Demiral, S. B., Guo, M., Kim, S. W., Lindgren, E., Ramirez, V., Zehra, A., Freeman, C., Miller, G., Manza, P., Srivastava, T., De Santi, S., Tomasi, D., Benveniste, H., & Volkow, N. D. (2018). β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proceedings of the National Academy of Sciences of the United States of America, 115(17), 4483–4488.
Bubu, O. M., Brannick, M., Mortimer, J., Umasabor-Bubu, O., Sebastião, Y. V., Wen, Y., Schwartz, S., Borenstein, A. R., Wu, Y., Morgan, D., & Anderson, W. M. (2017). Sleep, Cognitive impairment, and Alzheimer’s disease: A Systematic Review and Meta-Analysis. Sleep, 40(1), 10.1093/sleep/zsw032.
Yordanova, J., Kolev, V., Wagner, U., & Verleger, R. (2010). Differential associations of early- and late-night sleep with functional brain states promoting insight to abstract task regularity. PloS one, 5(2), e9442.
Lin, Y. K., Lin, G. Y., Lee, J. T., Lee, M. S., Tsai, C. K., Hsu, Y. W., Lin, Y. Z., Tsai, Y. C., & Yang, F. C. (2016). Associations Between Sleep Quality and Migraine Frequency: A Cross-Sectional Case-Control Study. Medicine, 95(17), e3554.
Prather, A. A., Janicki-Deverts, D., Hall, M. H., & Cohen, S. (2015). Behaviorally Assessed Sleep and Susceptibility to the Common Cold. Sleep, 38(9), 1353–1359.
Ma, Y., Liang, L., Zheng, F., Shi, L., Zhong, B., & Xie, W. (2020). Association Between Sleep Duration and Cognitive Decline. JAMA network open, 3(9), e2013573.
Spira, A. P., Chen-Edinboro, L. P., Wu, M. N., & Yaffe, K. (2014). Impact of sleep on the risk of cognitive decline and dementia. Current Opinion in Psychiatry, 27(6):478-83.
Learn More About Sleep Deprivation

Can a Lack of Sleep Cause Headaches?

How Sleep Deprivation Affects Your Heart

Interrupted Sleep: Causes & Helpful Tips

Sleep Deprivation: Symptoms, Treatment, & Effects

Lack of Sleep May Increase Calorie Consumption

Sleepless Nights: How to Function on No Sleep

What All-Nighters Do To Your Cognition

Sleep Deprivation and Reaction Time

Understanding Sleep Deprivation and New Parenthood

Effects of Sleep Deprivation
Other articles of interest, sleep solutions, sleep hygiene, sleep apnea.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
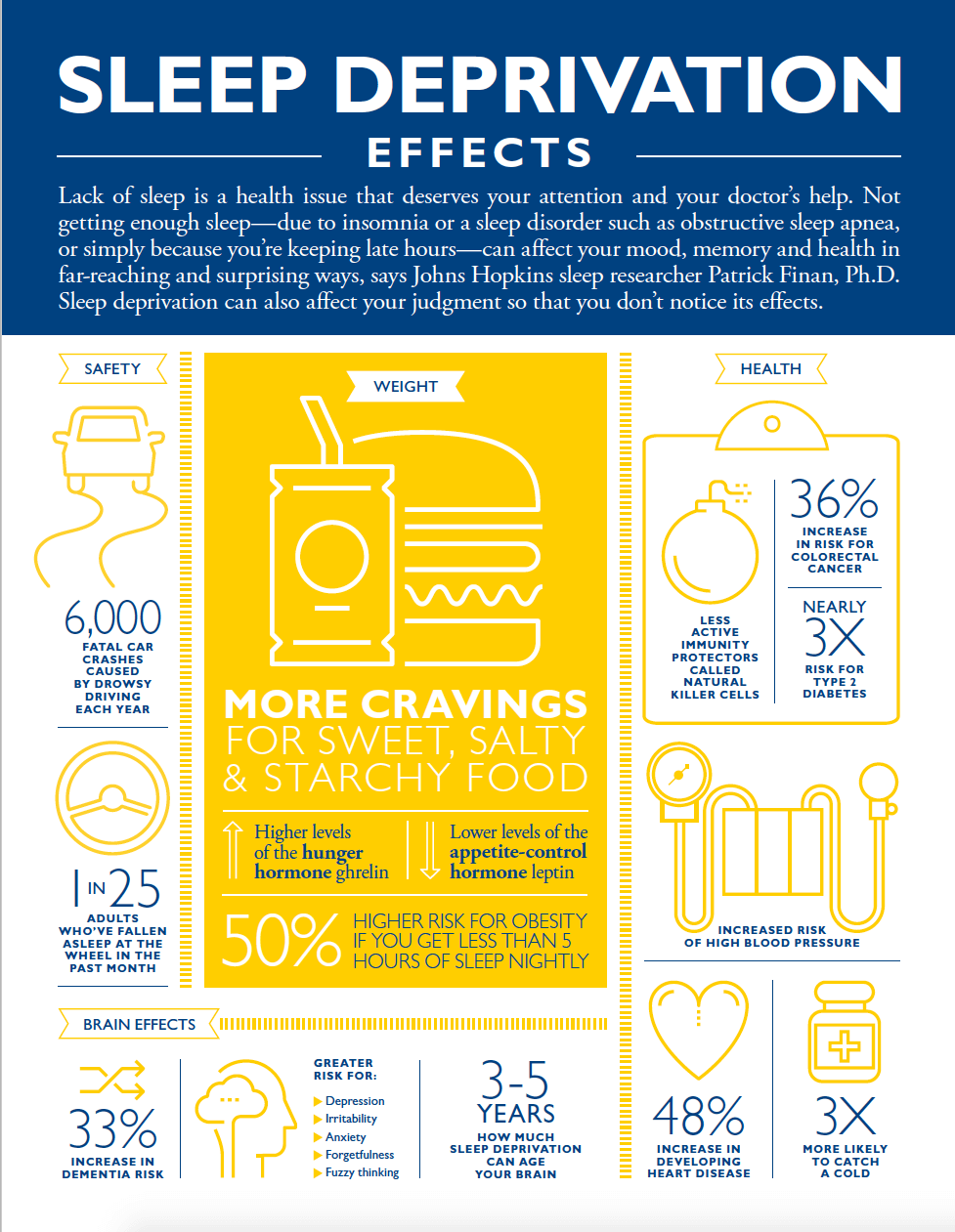
The Effects of Sleep Deprivation
Not getting enough sleep can affect your mood, memory and health in far-reaching and surprising ways, says Johns Hopkins sleep researcher Patrick Finan, Ph.D. Learn more about the effects of sleep deprivation. Download the infographic as a PDF .
Find a Doctor
Specializing In:
- Sleep Disorders
- Snoring Disorders
- Circadian Rhythm Disorders
Find a Treatment Center
- Pediatric Sleep Center (Johns Hopkins Children's Center)
- Center for Sleep and Wellness
Find Additional Treatment Centers at:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Request an Appointment
Do You Need Sleep Help?

4 Signs You Might Have Sleep Apnea
The Dangers of Uncontrolled Sleep Apnea
Related Topics
- Health Risks of Poor Sleep
- Sleep Conditions

Why sleep is important

Sleep is essential for a person’s health and wellbeing, according to the National Sleep Foundation (NSF). Yet millions of people do not get enough sleep and many suffer from lack of sleep. For example, surveys conducted by the NSF (1999-2004) reveal that at least 40 million Americans suffer from over 70 different sleep disorders and 60 percent of adults report having sleep problems a few nights a week or more. Most of those with these problems go undiagnosed and untreated. In addition, more than 40 percent of adults experience daytime sleepiness severe enough to interfere with their daily activities at least a few days each month — with 20 percent reporting problem sleepiness a few days a week or more. Furthermore, 69 percent of children experience one or more sleep problems a few nights or more during a week.
According to psychologist and sleep expert David F. Dinges, Ph.D., of the Division of Sleep and Chronobiology and Department of Psychiatry at the University of Pennsylvania School of Medicine, irritability, moodiness and disinhibition are some of the first signs a person experiences from lack of sleep . If a sleep-deprived person doesn’t sleep after the initial signs, said Dinges, the person may then start to experience apathy, slowed speech and flattened emotional responses, impaired memory and an inability to be novel or multitask. As a person gets to the point of falling asleep, he or she will fall into micro sleeps (5-10 seconds) that cause lapses in attention, nod off while doing an activity like driving or reading and then finally experience hypnagogic hallucinations, the beginning of REM sleep. (Dinges, Sleep, Sleepiness and Performance , 1991)
Everyone’s individual sleep needs vary. In general, most healthy adults are built for 16 hours of wakefulness and need an average of eight hours of sleep a night. However, some individuals are able to function without sleepiness or drowsiness after as little as six hours of sleep. Others can't perform at their peak unless they've slept ten hours. And, contrary to common myth, the need for sleep doesn't decline with age but the ability to sleep for six to eight hours at one time may be reduced. (Van Dongen & Dinges, Principles & Practice of Sleep Medicine , 2000)
Psychologists and other scientists who study the causes of sleep disorders have shown that such problems can directly or indirectly be tied to abnormalities in the following systems:
Physiological systems
Brain and nervous system
Cardiovascular system
Metabolic functions
Immune system
Furthermore, unhealthy conditions, disorders and diseases can also cause sleep problems, including:
Pathological sleepiness, insomnia and accidents
Hypertension and elevated cardiovascular risks (MI, stroke)
Emotional disorders (depression, bipolar disorder)
Obesity; metabolic syndrome and diabetes
Alcohol and drug abuse (Dinges, 2004)
Groups that are at particular risk for sleep deprivation include night shift workers, physicians (average sleep = 6.5 hours a day; residents = 5 hours a day), truck drivers, parents and teenagers. (American Academy of Sleep Medicine and National Heart, Lung, and Blood Institute Working Group on Problem Sleepiness. 1997).
Stress is the number one cause of short-term sleeping difficulties , according to sleep experts. Common triggers include school- or job-related pressures, a family or marriage problem and a serious illness or death in the family. Usually the sleep problem disappears when the stressful situation passes. However, if short-term sleep problems such as insomnia aren't managed properly from the beginning, they can persist long after the original stress has passed.
Drinking alcohol or beverages containing caffeine in the afternoon or evening, exercising close to bedtime, following an irregular morning and nighttime schedule, and working or doing other mentally intense activities right before or after getting into bed can disrupt sleep.
If you are among the 20 percent of employees in the United States who are shift workers, sleep may be particularly elusive. Shift work forces you to try to sleep when activities around you — and your own "biological rhythms" — signal you to be awake. One study shows that shift workers are two to five times more likely than employees with regular, daytime hours to fall asleep on the job.
Traveling also disrupts sleep, especially jet lag and traveling across several time zones. This can upset your biological or “circadian” rhythms.
Environmental factors such as a room that's too hot or cold, too noisy or too brightly lit can be a barrier to sound sleep. And interruptions from children or other family members can also disrupt sleep. Other influences to pay attention to are the comfort and size of your bed and the habits of your sleep partner. If you have to lie beside someone who has different sleep preferences, snores, can't fall or stay asleep, or has other sleep difficulties, it often becomes your problem too!
Having a 24/7 lifestyle can also interrupt regular sleep patterns: the global economy that includes round the clock industries working to beat the competition; widespread use of nonstop automated systems to communicate and an increase in shift work makes for sleeping at regular times difficult.
A number of physical problems can interfere with your ability to fall or stay asleep. For example, arthritis and other conditions that cause pain, backache, or discomfort can make it difficult to sleep well.
Epidemiological studies suggest self-reported sleep complaints are associated with an increased relative risk of cardiovascular morbidity and mortality. For women, pregnancy and hormonal shifts including those that cause premenstrual syndrome (PMS) or menopause and its accompanying hot flashes can also intrude on sleep.
Finally, certain medications such as decongestants, steroids and some medicines for high blood pressure, asthma, or depression can cause sleeping difficulties as a side effect.
It is a good idea to talk to a physician or mental health provider about any sleeping problem that recurs or persists for longer than a few weeks.
According to the DSM, some psychiatric disorders have fatigue as a major symptom. Included are: major depressive disorder (includes postpartum blues), minor depression , dysthymia, mixed anxiety-depression, seasonal affective disorder and bipolar disorder .
According to a long-term study published in the 2004 April issue of Alcoholism: Clinical and Experimental Research , young teenagers whose preschool sleep habits were poor were more than twice as likely to use drugs, tobacco or alcohol. This finding was made by the University of Michigan Health System as part of a family health study that followed 257 boys and their parents for 10 years. The study found a significant connection between sleep problems in children and later drug use, even when other issues such as depression, aggression, attention problems and parental alcoholism were taken into account. Long-term data on girls isn't available yet. The researchers suggest that early sleep problems may be a "marker" for predicting later risk of early adolescent substance abuse — and that there may be a common biological factor underlying both traits. Although the relationship between sleep problems and the abuse of alcohol in adults is well known, this is the first study to look at the issue in children.
Nightmares are dreams with vivid and disturbing content. They are common in children during REM sleep. They usually involve an immediate awakening and good recall of the dream content.
Sleep terrors are often described as extreme nightmares. Like nightmares, they most often occur during childhood, however they typically take place during non-REM (NREM) sleep. Characteristics of a sleep terror include arousal, agitation, large pupils, sweating, and increased blood pressure. The child appears terrified, screams and is usually inconsolable for several minutes, after which he or she relaxes and returns to sleep. Sleep terrors usually take place early in the night and may be combined with sleepwalking. The child typically does not remember or has only a vague memory of the terrifying events.
In the August 2004 issue of the journal Sleep , Dr. Timothy Roehrs, the Director of research at the Sleep Disorders and Research Center at Henry Ford Hospital in Detroit published one of the first studies to measure the effect of sleepiness on decision making and risk taking. He found that sleepiness does take a toll on effective decision making.
Cited in the October 12, New York Times Science section, Dr. Roehrs and his colleagues paid sleepy and fully alert subjects to complete a series of computer tasks. At random times, they were given a choice to take their money and stop. Or they could forge ahead with the potential of either earning more money or losing it all if their work was not completed within an unknown remainder of time.
Dr. Roehrs found that the alert people were very sensitive to the amount of work they needed to do to finish the tasks and understood the risk of losing their money if they didn't. But the sleepy subjects chose to quit the tasks prematurely or they risked losing everything by trying to finish the task for more money even when it was 100 percent likely that they would be unable to finish, said Dr. Roehrs.
According to the National Commission on Sleep Disorders Research (1998) and reports from the National Highway Safety Administration (NHSA)(2002), high-profile accidents can partly be attributed to people suffering from a severe lack of sleep.
Each year the cost of sleep disorders, sleep deprivation and sleepiness, according to the NCSDR, is estimated to be $15.9 million in direct costs and $50 to $100 billion a year in indirect and related costs. And according to the NHSA, falling asleep while driving is responsible for at least 100,000 crashes, 71,000 injuries and 1,550 deaths each year in the United States. Young people in their teens and twenties, who are particularly susceptible to the effects of chronic sleep loss, are involved in more than half of the fall-asleep crashes on the nation's highways each year. Sleep loss also interferes with the learning of young people in our nation's schools, with 60 percent of grade school and high school children reporting that they are tired during the daytime and 15 percent of them admitting to falling asleep in class.
According to the Department of Transportation (DOT), one to four percent of all highway crashes are due to sleepiness, especially in rural areas and four percent of these crashes are fatal.
Risk factors for drowsy driving crashes:
Late night/early morning driving
Patients with untreated excessive sleepiness
People who obtain six or fewer hours of sleep per day
Young adult males
Commercial truck drivers
Night shift workers
Medical residents after their shift
According to sleep researchers, a night's sleep is divided into five continually shifting stages, defined by types of brain waves that reflect either lighter or deeper sleep. Toward morning, there is an increase in rapid eye movement, or REM sleep, when the muscles are relaxed and dreaming occurs, and recent memories may be consolidated in the brain. The experts say that hitting a snooze alarm over and over again to wake up is not the best way to feel rested. “The restorative value of rest is diminished, especially when the increments are short,” said psychologist Edward Stepanski, PhD who has studied sleep fragmentation at the Rush University Medical Center in Chicago. This on and off again effect of dozing and waking causes shifts in the brain-wave patterns. Sleep-deprived snooze-button addicts are likely to shorten their quota of REM sleep, impairing their mental functioning during the day. ( New York Times , October 12, 2004)
Certain therapies, like cognitive behavioral therapy teach people how to recognize and change patterns of thought and behavior to solve their problems. Recently this type of therapy has been shown to be very effective in getting people to fall asleep and conquer insomnia.
According to a study published in the October 2004 issue of The Archives of Internal Medicine , cognitive behavior therapy is more effective and lasts longer than a widely used sleeping pill, Ambien, in reducing insomnia. The study involved 63 healthy people with insomnia who were randomly assigned to receive Ambien, the cognitive behavior therapy, both or a placebo. The patients in the therapy group received five 30-minute sessions over six weeks. They were given daily exercises to “recognize, challenge and change stress-inducing” thoughts and were taught techniques, like delaying bedtime or getting up to read if they were unable to fall asleep after 20 minutes. The patients taking Ambien were on a full dose for a month and then were weaned off the drug. At three weeks, 44 percent of the patients receiving the therapy and those receiving the combination therapy and pills fell asleep faster compared to 29 percent of the patients taking only the sleeping pills. Two weeks after all the treatment was over, the patients receiving the therapy fell asleep in half the time it took before the study and only 17 percent of the patients taking the sleeping pills fell asleep in half the time. (New York Times, October 5, 2004)
According to leading sleep researchers, there are techniques to combat common sleep problems:
Keep a regular sleep/wake schedule
Don’t drink or eat caffeine four to six hours before bed and minimize daytime use
Don’t smoke, especially near bedtime or if you awake in the night
Avoid alcohol and heavy meals before sleep
Get regular exercise
Minimize noise, light and excessive hot and cold temperatures where you sleep
Develop a regular bed time and go to bed at the same time each night
Try and wake up without an alarm clock
Attempt to go to bed earlier every night for certain period; this will ensure that you’re getting enough sleep
In clinical settings, cognitive-behavior therapy (CBT) has a 70-80 percent success rate for helping those who suffer from chronic insomnia. Almost one third of people with insomnia achieve normal sleep and most reduce their symptoms by 50 percent and sleep an extra 45-60 minutes a night. When insomnia exists along with other psychological disorders like depression, say the experts, the initial treatment should address the underlying condition.
But sometimes even after resolving the underlying condition, the insomnia still exists, says psychologist Jack Edinger, PhD, of the VA Medical Center in Durham, North Carolina and Professor of Psychiatry and Behavioral Sciences at Duke University and cautions that treating the depression usually doesn’t resolve the sleep difficulties. From his clinical experience, he has found that most patients with insomnia should be examined for specific behaviors and thoughts that may perpetuate the sleep problems. When people develop insomnia, they try to compensate by engaging in activities to help them get more sleep. They sleep later in the mornings or spend excessive times in bed. These efforts usually backfire, said Edinger.
From his clinical work and research on sleep, psychologist Charles M. Morin, PhD, a Professor in the Psychology Department and Director of the Sleep Disorders Center at University Laval in Quebec, Canada says that ten percent of adults suffer from chronic insomnia. In a study released in the recent issue of Sleep Medicine Alert published by the NSF, Morin outlines how CBT helps people overcome insomnia. Clinicians use sleep diaries to get an accurate picture of someone’s sleep patterns. Bedtime, waking time, time to fall asleep, number and durations of awakening, actual sleep time and quality of sleep are documented by the person suffering from insomnia.
A person can develop poor sleep habits (i.e. watching TV in bed or eating too much before bedtime), irregular sleep patterns (sleeping too late, taking long naps during the day) to compensate for lost sleep at night. Some patients also develop a fear of not sleeping and a pattern of worrying about the consequences of not sleeping, said Morin. “Treatments that address the poor sleep habits and the faulty beliefs and attitudes about sleep work but sometimes,” said Morin, “medication may play a role in breaking the cycle of insomnia. But behavioral therapies are essential for patients to alter the conditions that perpetuate it.”
CBT attempts to change a patient’s dysfunctional beliefs and attitudes about sleep. “It restructure thoughts — like, ‘I’ve got to sleep eight hours tonight’ or ‘I’ve got to take medication to sleep’ or ‘I just can’t function or I’ll get sick if I don’t sleep.’ These thoughts focus too much on sleep, which can become something like performance anxiety — sleep will come around to you when you’re not chasing it,” said Edinger.
What works in many cases, said Morin and Edinger, is to standardize or restrict a person’s sleep to give a person more control over his or her sleep. A person can keep a sleep diary for a couple of weeks and a clinician can monitor the amount of time spent in bed to the actual amount of time sleeping. Then the clinician can instruct the patient to either go to bed later and get up earlier or visa versa. This procedure improves the length of sleeping time by imposing a mild sleep deprivation situation, which has the result of reducing the anxiety surrounding sleep. To keep from falling asleep during the day, patients are told not to restrict sleep to less than five hours.
Standardizing sleep actually helps a person adjust his or her homeostatic mechanism that balances sleep, said Edinger. “Therefore, if you lose sleep, your homeostatic mechanism will kick in and will work to increase the likelihood of sleeping longer and deeper to promote sleep recovery. This helps a person come back to their baseline and works for the majority.”
A person can also establish more stimulus control over his or her bedroom environment, said Morin. This could include: going to bed only when sleepy, getting out of bed when unable to sleep, prohibiting non-sleep activities in the bedroom, getting up at the same time every morning (including weekends) and avoiding daytime naps.
Finally, a person can incorporate relaxation techniques as part of his or her treatment. For example, a person can give herself or himself an extra hour before bed to relax and unwind and time to write down worries and plans for the following day.
In CBT, said Morin, breaking the thought process and anxiety over sleep is the goal. “After identifying the dysfunctional thought patterns, a clinician can offer alternative interpretations of what is getting the person anxious so a person can think about his or her insomnia in a different way.” Morin offers some techniques to restructure a person’s cognitions. “Keep realistic expectations, don’t blame insomnia for all daytime impairments, do not feel that losing a night’s sleep will bring horrible consequences, do not give too much importance to sleep and finally develop some tolerance to the effects of lost sleep.
According to Edinger, aging weakens a person’s homeostatic sleep drive after age 50. Interestingly, the length of the circadian cycle stays roughly the same over the lifespan but the amplitude of the circadian rhythm may decline somewhat with aging.
National Sleep Foundation http://www.thensf.org
American Academy of Sleep Medicine http://www.aasmnet.org/
American Insomnia Association http://www.americaninsomniaassociation.org/
Sleep Research Society http://www.sleepresearchsociety.org/
NIH National Center for Sleep Disorders Research http://www.nhlbi.nih.gov/sleep
The MayoClinic.com Sleep Center
(Blake, et al, Psychological Reports, 1998; National Heart, Lung and Blood Institute Working Group on Insomnia, 1998)
David F. Dinges, PhD , Professor of Psychology in Psychiatry, Chief, Division of Sleep and Chronobiology, University of Pennsylvania School of Medicine
Jack Edinger, PhD , of the VA Medical Center in Durham, North Carolina and Professor of Psychiatry and Behavioral Sciences at Duke University
Charles M. Morin, PhD , a Professor in the Psychology Department and Director of the Sleep Disorders Center at University Laval in Quebec, Canada
Timothy Roehrs, PhD , the Director of Research, Sleep Disorders and Research Center at Henry Ford Hospital
Edward Stepanski, PhD , who has studied sleep fragmentation at the Rush University Medical Center in Chicago
Related Reading
- Getting a good night’s sleep: How psychologists help with insomnia
- What to Do When You Dread Your Bed
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

A Systematic Review of Sleep Deprivation and Neurobehavioral Function in Young Adults
Stephanie griggs.
Case Western Reserve University, Frances Payne Bolton School of Nursing, Cleveland, Ohio, USA 44106
Alison Harper
Case Western Reserve University, Frances Payne Bolton School of Nursing, Department of Anthropology, Cleveland, Ohio, USA 44106

Ronald L. Hickman, Jr
Ruth M. Anderson Endowed Professor of Nursing and Associate Dean for Research Case Western Reserve University, Frances Payne Bolton School of Nursing, Cleveland, OH, USA 44106
To examine the effect of sleep deprivation (total and partial) on neurobehavioral function compared to a healthy sleep opportunity (7–9 hours) in young adults 18–30 years.
Background:
More than one-third of young adults are sleep deprived, which negatively affects a range of neurobehavioral functions, including psychomotor vigilance performance (cognitive), affect, and daytime sleepiness.
A systematic review of randomized controlled trials (RCTs) on sleep deprivation and neurobehavioral function. Multiple electronic databases (Cochrane Central Registry of Controlled Trials [CENTRAL], PubMed, PsycINFO, CINAHL, and Web of Science) were searched for relevant RCTs published in English from the establishment of each database to December 31, 2020.
Nineteen RCTs were selected (N = 766, mean age = 23.7 ± 3.1 years; 44.8% female). Seven were between-person (5 were parallel-group designs and 2 had multiple arms), and 12 were within-person designs (9 were cross over and 3 used a Latin square approach). Total sleep deprivation had the strongest detrimental effect on psychomotor vigilance performance, with the largest effects on vigilance tasks in young adults in the included studies.
Conclusion:
Acute sleep deprivation degrades multiple dimensions of neurobehavioral function including psychomotor vigilance performance, affect, and daytime sleepiness in young adults. The effect of chronic sleep deprivation on the developing brain and associated neurobehavioral functions in young adults remains unclear.
1. Introduction
Sleep loss has a negative effect on multiple neurobehavioral functions, such as psychomotor vigilance performance (cognitive), daytime sleepiness, and affect ( Franzen et al., 2011 ; Van Dongen et al., 2003 ). Degradation of vigilance following sleep deprivation is one of the most robust alterations in healthy young adults aged 18–30 years ( Lim & Dinges, 2010 ). Multiple dimensions of neurobehavioral impairment are differentially affected by sleep deprivation ( Van Dongen et al., 2004 ). Sleep deprivation affects regions of the prefrontal cortex ( Chee & Choo, 2004 ), which continues to mature up to the late ‘20s ( Johnson et al., 2009 ), leading to executive dysfunctions with the prefrontal cortex ( Dinges et al., 1997 ; Nilsson et al., 2005 ). The prefrontal cortex is most vulnerable to the effects between states of sleep and wake due to the metabolic change associated with sleep deprivation ( Muzur et al., 2002 ).
Biological, social, and environmental factors converge, resulting in sleep deprivation in more than one-third (32.3%) of young adults ( Peltzer & Pengpid, 2016 ). Sleep deprivation contributes to a negative interaction between homeostatic and circadian processes. In young adulthood, there is reduced homeostatic sleep pressure (adenosine) accumulation during wakefulness, a delay in sleep timing, and a delay in releasing the onset of melatonin that peaks in the mid-’20s ( Crowley & Carskadon, 2010 ; Fischer et al., 2017 ). Motor vehicular accident risk increases at the circadian cycle nadir following total sleep deprivation which, correlates with slowing of psychomotor vigilance performance ( Patanaik, Zagorodnov, Kwoh, et al., 2014 ).
The broad effect of sleep manipulation (sleep deprivation, sleep restriction, and sleep improvement) on cognitive functioning in adolescents aged 10 – 19 years was addressed in one previous systematic review ( de Bruin et al., 2017 ). In the systematic review, the effect of total sleep deprivation was examined in 4 studies, partial sleep deprivation in 10 studies, sleep extension in one study, and cognitive behavioral therapy for insomnia in one study and 45 unique cognitive tests were reported where a vast array of cognition was assessed ( de Bruin et al., 2017 ). In the review, partial sleep deprivation had a small or no effect on cognitive functioning, total sleep deprivation negatively affected psychomotor vigilance performance, and sleep extension improved working memory in the adolescents studied ( de Bruin et al., 2017 ). However, conclusions could not be made about the specific domains affected by sleep manipulation due to the differences and quantity of tests ( de Bruin et al., 2017 ). The extent of the associations between total and partial sleep deprivation and neurobehavioral impairment (e.g., decrements in psychomotor vigilance performance – cognitive performance impairment, affect, and daytime sleepiness) remains unclear.
The primary aim of this research was to determine the effect of sleep deprivation compared to healthy sleep opportunity (sleep duration 7–9 hours) on psychomotor vigilance performance as measured by psychomotor vigilance testing (PVT) only. PVT-related outcomes may include mean and median response time, reciprocal response time slowest 10%, mean reaction time fastest 10%, number of lapses (No. of times RT is > 500 ms lapses). The secondary aim of this research was to determine the effect of sleep deprivation on affect or daytime sleepiness compared to a healthy sleep opportunity. Secondary outcomes were change in affect or daytime sleepiness outcomes measured by diagnostic criteria or self-reported questionnaires.
Our focus is on young adults aged 18 to 30 years who are at a key developmental stage at a great risk of sleep deprivation and sleep deprivation-related neurobehavioral impairment. This focus addresses a significant gap in the existing literature. Additionally, the focus on sleep deprivation with a primary outcome of psychomotor vigilance performance to assess cognitive performance via psychomotor vigilance testing, a proven assay for evaluating vigilance ( Dinges et al., 2004 ), will allow a common outcome to be synthesized across studies.
2.1. Design
The Preferred Reporting Items for Systematic Reviews and Meta-analyses Statement guidelines were followed for this systematic review ( Nagendrababu et al., 2019 ). We registered our protocol with the PROSPERO registry before implementing the search in the International Prospective Register of Systematic Reviews (Prospero; registration number CRD42021225200).
2.2. Search methods
Studies with participants between the ages of 18 to 30 years were included. Sampling adults across the lifespan has a great potential to underestimate the effects of sleep deprivation in young adults. The following studies were included in this systematic review: (1) randomized controlled trials (RCTs) of young adults published in English; (2) data collected for both the intervention and control group(s); (3) sample mean age from 18 to 30 years; and (4) one or more objectively measured neurobehavioral-related outcomes (e.g., mean reaction time, median reaction time, reciprocal response time slowest 10%, mean reaction time fastest 10%, number of lapses (No. of times RT is > 500 ms lapses) by psychomotor vigilance testing only. Additionally, affect or daytime sleepiness outcomes were also extracted if available. We excluded studies of people with: (1) known sleep disorders; (2) chronic medical; (3) severe psychiatric illness (e.g., bipolar disorder, schizophrenia); (4) Body Mass Index (BMI) > 35 kg/m 2 in addition to (5) night shift workers.
The following databases were searched with controlled vocabulary and keywords: Cochrane Central Registry of Controlled Trials (CENTRAL), PubMed, PsycINFO, CINAHL, and Web of Science. Articles published in English from the establishment of each database to December 13, 2020 were searched. We provide the PubMed search terms in Table 1 . We adjusted the syntax for the search strategies for each database as appropriate.
Database: PubMed ALL Search Strategy
| 1 | exp sleep deprivation |
| 2 | “total sleep deprivation”.mp. |
| 3 | “partial sleep deprivation”.mp. |
| 4 | 1 or 2 or 3 |
| 5 | “vigilance”.nip. |
| 6 | “cognitive”.mp. |
| 7 | 5 or 6 |
| 8 | 4 and 7 |
| 9 | limit 8 to “young adult” (19 to 44 years) |
| 10 | 10 and 11 |
The search was conducted under the guidance of a health science librarian with input from the primary and senior investigator. Also, an ancestry/bibliographic search was conducted to identify additional articles until the end of December 2020.
2.3. Search outcome
All 4,149 references were imported to Covidence ™ (Veritas Health Information) and duplicates were removed. A total of 3,110 were screened through Covidence ™ . Two reviewers independently screened all titles and abstracts with 93% agreement. Next, the two reviewers independently assessed full texts. A third reviewer resolved any disagreements regarding eligibility when consensus was not reached among the first two reviewers. The largest study was included when more than one article included the same trial and/or participants.
2.4. Quality appraisal
The risk of bias in the included studies was assessed independently by two reviewers using the Cochrane risk of bias tool through Covidence ™ ( Jørgensen et al., 2016 ). Sequence generation, concealment of allocation, blinding of outcome assessment blinding, >80% incomplete outcome data (< 80%), selective reporting of outcomes, and ‘other issues’ were the components of the risk of bias tool. The blinding domain was omitted as the intervention was sleep deprivation, and thus it would not be possible to blind participants.
2.5. Data abstraction and synthesis
A customized spreadsheet was used to extract and record data from the papers. Study characteristics, total or partial sleep deprivation with hours and length of time, age, measures used, the sample size (intervention and control groups), along with means and standard deviations of data were extracted. We contacted corresponding authors when insufficient or unclear data were reported. Extracted data were compared between the two reviewers, and disagreements were resolved by consultation with data in original papers and discussion.
We followed guidance on the conduct of a narrative synthesis described by Popay et al. (2006) . Three standardized data tables were used to organize the data which included (1) all studies, (2) between-persons designs, and (3) within-person designs. We started with a preliminary synthesis to organize findings from the studies to describe patterns along with direction and size of the effect when effects were reported. Next, we explored relationships considering factors that might explain any differences in significance or direction/size of the effect if applicable. Lastly, we assessed the robustness of the synthesis to draw conclusions and assess generalizability/reproducibility of the findings. Significant PVT outcomes and the effect size if applicable are presented in Table 2 . The between-person and within-person designs were considered and described separately as within-person comparisons have the advantage of a smaller within-person variation and possibility of a carryover effect ( Jones & Kenward, 2014 ).
Characteristics of studies
| Authors, reference | Country | Sample | Age in years mean (SD) | % female | Sleep Measure/Setting | Sleep deprivation condition | Design | PVT Outcome, (Effect Size) |
|---|---|---|---|---|---|---|---|---|
| US | N=12 | 27.5 (5.4) | 41.7 | PSG/Lab | 24-h TSD | Latin square | Mean RT (NR) | |
| Italy | N = 50 | 22 (2.1) | 62 | ACT/Lab | 24-h TSD | 1:1 | Mean RT, Slowest 10% RT, Lapses, (NR) | |
| US | N = 29 | 24.4 (2.8) | 51.7 | PSG/Lab | 24-h TSD | 1:1 | MeanRT ( = 0.17), Lapses = 0.22) | |
| Finland | N = 20 | 23.8 (2.3) | 0 | PSG Lab | 120-hPSD (4h/night) | 1:1 | Lapses (NR) | |
| US | N = 56 | 27.2 (4.6) | 50.8 | PSG/Lab | 38-hTSD | Latin square | Fastest 10%, Median RT, Slowest 10% Sig NR | |
| US | N = 26 | 25.9 (4) | 38.5 | PSG/Lab | 62-h TSD | Latin square | Fastest 10%, Median RT, Slowest 10% Sig NR | |
| US | N = 61 | 18–30 | NR | NR/Lab | 24-h TSD | Multi-arm | Median RT, Slowest 10%, Median RT (NR) | |
| Japan | N = 16 | 21.4 (1.6) | 0 | ACT/Home | 36-h TSD | Cross-over | Median RT (NR) | |
| South China | N = 24 | 21.4 (2.1) | 66.7 | PSG/Lab | 24-h TSD | Cross-over | 1/RT (d=−0.98) Lapses (d=1.34) | |
| Singapor e | N = 135 | 21.9 (1.7) | 51.1 | ACT/Lab | 24-h TSD | Cross-over | Mean RT, Median RT, Lapses (NR) | |
| Canada | N = 13 | 25 (2.7) | 46.2 | PSG/Lab | 25-h TSD | Cross-over | Mean RT (NR) | |
| . | Australia | N = 19 | 20.2 (2.1) | 63.2 | ACTVHome | PSD (4h/1night) | Cross-over | Mean RT ( = .24) |
| Schwartz et al. 2016 | Germany | N = 47 | 26 (6.8) | 72.3 | ACTVHome | PSD (4h/1night) | Cross-over | 1/RT, Lapses (d=0.77) |
| Schwartz et al. 2013 | Germany | N = 33 | 21.6 (2.7) | 84.8 | ACT/Home | PSD (4h/1night) | Cross-over | Mean RT ( =0.21) |
| Italy | N = 25 | 23.8 (2.4) | 56 | NR/Lab | 24-h TSD | Cross-over | NS (NR) | |
| US | N = 84 | 25 (3.7) | 26.2 | ACT/Lab | 54-h TSD | 1:1 | Interaction TSD and Mean RT (NR) | |
| US | N = 22 | 26 (3.6) | 9 | PSG/Lab | 72-h TSD | Multi-arm | Mean RT, Lapses (NR) | |
| US | N = 26 | 26.6 (4.4) | 38.5 | PSG/Lab | 62-h TSD | 1:1 | Lapses ( =0.53) | |
| Singapore | N = 68 | 22 (2.5) | 47.1 | ACT/Lab | 24-h TSD | Cross-over | Mean RT (NR) |
Note: ACT, actigraphy; PSG, polysomnography; TSD, total sleep deprivation; PSD, partial sleep deprivation; Lab, controlled setting; 1:1 parallel group design; multi-arm, more than two experimental conditions - only the TSD condition is listed on the table when the study has multiple arms; NR: not reported. All studies were randomized controlled trials. Data from two studies are presented in one article.
3.1. Study selection
We identified 19 RCTs and present results below. We contacted seven corresponding authors; two responded, one shared additional data, and one provided additional clarification on their data. The study selection process is illustrated in Figure 1 .

PRISMA Flow Diagram
3.2. Characteristics of the included studies
A summary of the details of the 19 RCTs included in this systematic review is presented in Table 2 . A total of 766 young adults with mean ages ranging from 20.2 to 27.5 years (mean age, 23.7 ± 3.09 years; 55.2% male) were included in these RCTs. BMI was only reported in one trial, and the mean was 20.0 ± 1.9 kg/m 2 . Seven were between-person (5 were parallel-group designs and 2 had multiple arms), and 12 were within-person designs (9 were cross over and 3 used a Latin square approach).
Sleep was measured via polysomnography in 9 studies and with actigraphy in eight studies ( Table 2 ). The setting for a majority of these studies was a controlled laboratory (e.g., temperature, sound, avoidance of alcohol and caffeine) except for four studies ( Kaida & Niki, 2014 ; Rossa et al., 2014 ; Schwarz et al., 2016 ; Schwarz et al., 2013 ). The RCTs were conducted in the following countries: the United States (8), Italy (2), Finland (1), Australia (1), Japan (1), South China (1), Singapore (2), Canada (1), and Germany (2). All RCTs had a sleep deprivation experimental condition (15 were total sleep deprivation ranging from 24 hours to 72 hours and four were partial sleep deprivation of 4-hours per night ranging from one night to four nights) and a healthy sleep opportunity (duration of 7–9 hours) comparison condition.
The dose-response effect of total and partial sleep deprivation on psychomotor vigilance performance was examined in three different RCTs ( Drake et al., 2001 ; Jewett et al., 1999 ; Van Dongen et al., 2004 ). Acute sleep deprivation was assessed in two trials ( Drake et al., 2001 ; Jewett et al., 1999 ) and chronic sleep deprivation in the other trial ( Van Dongen et al., 2004 ). All trials had one 8-hour condition and one total sleep deprivation condition, but total sleep deprivation varied in each of the trials and was for one night in one trial ( Jewett et al., 1999 ), two nights in the second trial ( Drake et al., 2001 ), and three nights in the third trial ( Van Dongen et al., 2004 ). The comparison groups also varied in dose and length with 8-hours, 5-hours, or 2-hours for one night ( Jewett et al., 1999 ); 8-hours for four nights, 6-hours for four nights, and 4-hours for two nights ( Drake et al., 2001 ); and 8-hours, 6-hours, or 4-hours per night for 14 nights ( Van Dongen et al., 2004 ).
The daytime sleepiness measures used in the trials included a 9-item self-report Karolinska Sleepiness Scale ( Akerstedt & Gillberg, 1990 ), 7-item self-report Stanford Sleepiness Scale ( Babkoff et al., 1991 ), a visual analogue scale ( Monk, 1989 ), and objective pupillography as a physiological daytime sleepiness indicator ( Lüdtke et al., 1998 ). The affect measures included the 10-item positive and negative affect schedule (PANAS) ( Watson et al., 1988 ), 100mm visual analogue profile of mood states (POMS) ( McNair et al., 1971 ), and visual analogue scale ( Tempesta et al., 2014 ).
3.3. Risk of bias
A graph summarizing the risk of bias of the included studies is presented in Table 3 and Figure 2 . We determined that a majority of the studies were of high quality, with an overall low risk of bias ( n = 8). Sequence generation was judged six times to be both low and high risk, as allocation of the participants was low risk, but the time in between the sleep deprivation trial and the control condition for cross-over studies was only a week; therefore, there was a high likelihood of carryover effects from sleep deprivation. Incomplete outcome data was unclear in 6 trials, and selective outcome reporting was unclear in one. Selective outcome reporting was determined to be both low risk and high risk as it was low risk for objective measures but high risk for self-reported measures like affect and daytime sleepiness. Other source of bias was high risk in four studies due to the trials being held outside of a controlled laboratory setting.

Cochrane Risk of Bias Assessment Across Studies (Higgins et al., 2011)
Cochrane Risk of Bias Assessment
| Authors, reference | Sequence generatio n | Allocation concealme nt | Blinding of outcome assessment | Incomplete outcome data (< 80%) | Selective outcome reporting | Other source of bias | ||
|---|---|---|---|---|---|---|---|---|
| + | − | + | + | + | + | + | ||
| + | + | + | + | + | + | |||
| + | + | + | + | + | + | |||
| + | + | + | + | + | + | |||
| + | + | + | + | + | + | |||
| + | + | + | + | + | + | |||
| + | + | + | + | + | + | |||
| + | − | + | + | + | + | − | ||
| + | + | + | ? | + | + | |||
| + | − | + | + | ? | + | − | + | |
| + | + | + | ? | + | + | |||
| . | + | − | + | + | + | + | − | |
| + | + | + | + | + | − | |||
| + | − | + | + | ? | + | − | ||
| + | − | + | + | + | + | − | + | |
| + | + | + | + | + | + | |||
| + | + | + | + | + | + | |||
| + | + | + | ? | + | + | |||
| + | + | + | ? | + | − | + | ||
| − | ||||||||
3.4. Effect of sleep deprivation by outcome
3.4.1. effect of sleep deprivation on cognitive performance.
The effect of total sleep deprivation on cognitive performance was tested in 6 RCT’s using a between-person comparison ( n = 272); four were parallel-group ( Esposito et al., 2015 ; Franzen et al., 2008 ; Tucker et al., 2009 ; Whitney et al., 2015 ) and two had multiple-arms ( Jewett et al., 1999 ; Van Dongen et al., 2004 ). In these RCTs, the total sleep deprivation condition ranged from 24 hours to 72 hours, and all trials had a healthy sleep opportunity condition for comparison. Significant declines in psychomotor vigilance performance were observed in all trials using a between-person comparison with a slower mean reaction time in three trials ( Drake et al., 2001 ; Esposito et al., 2015 ; Tucker et al., 2009 ; Van Dongen et al., 2004 ), increased slowest 10% in one trial ( Esposito et al., 2015 ), and a higher number of lapses in four trials ( Esposito et al., 2015 ; Franzen et al., 2008 ; Haavisto et al., 2010 ; Whitney et al., 2015 ). The effect sizes ranged from small ( Franzen et al., 2008 ) to medium ( Whitney et al., 2015 ) and were not reported in four between-person comparison trials ( Esposito et al., 2015 ; Haavisto et al., 2010 ; Jewett et al., 1999 ; Tucker et al., 2009 ). In Haavisto’s trial of 20 young adults comparing 4 hours of partial sleep deprivation ( n = 13) to healthy sleep opportunity ( n = 7), lapses increased significantly for the partial sleep deprivation group compared to the healthy sleep opportunity group (0.92 ± 0.73 to 3.54 ± 0.73 vs. 0.62 ± 1.00 to 0.90 ± 1.00, p = .0321, respectively) and there was a tendency that the slowest 10% of all responses were slower in the partial sleep deprivation group, but the group difference was not significant ( p = .16) ( Haavisto et al., 2010 ).
The effect of total sleep deprivation on psychomotor vigilance performance was tested in nine RCT’s using a within-person comparison ( n = 375) ( Kaida & Niki, 2014 ; Lin et al., 2020 ; Patanaik, Zagorodnov, Kwoh, et al., 2014 ; Robillard et al., 2011 ; Rossa et al., 2014 ; Schwarz et al., 2016 ; Schwarz et al., 2013 ; Tempesta et al., 2014 ; Yeo et al., 2015 ), three of which used a Latin square approach ( Drake et al., 2001 ; Honn et al., 2020 ). Total sleep deprivation ranged from 32 to 62 hours, and the cross-over between the sleep deprivation and healthy sleep opportunity conditions ranged from one week to one month. One night of total sleep deprivation resulted in significant decrements in psychomotor vigilance performance in four of the cross-over trials ( Drake et al., 2001 ; Kaida & Niki, 2014 ; Patanaik, Zagorodnov, Kwoh, et al., 2014 ; Robillard et al., 2011 ) with a slower mean reaction time in four trials ( Adler et al., 2017 ; Drake et al., 2001 ; Kaida & Niki, 2014 ; Patanaik, Zagorodnov, Kwoh, et al., 2014 ; Robillard et al., 2011 ), slower median reaction time in two of the trials ( Kaida & Niki, 2014 ; Patanaik, Zagorodnov, Kwoh, et al., 2014 ), and a higher number of lapses in two of the trials ( Lin et al., 2020 ; Patanaik, Zagorodnov, Kwoh, et al., 2014 ).
The difference was not significant between the total sleep deprivation and healthy sleep opportunity condition in Tempesta et al. 2014 ’s cross-over trial of 25 young adults (mean age 23.8 ± 2.4 years). In this trial, a 5-minute PVT on a computer was used when a 10-minute PVT was used in most studies which may have affected these outcomes ( Tempesta et al., 2014 ). The reaction time was slower in the sleep deprivation condition in one trial; however, whether the difference between the two conditions was significant was not reported as the focus of the analysis was not on change in PVT performance ( Honn et al., 2020 ). In the cross-over trials where significant decrements in psychomotor vigilance performance from total sleep deprivation were reported, effect sizes ranged from medium ( Rossa et al., 2014 ) to large ( Lin et al., 2020 ). The effect size was not reported in four trials ( Drake et al., 2001 ; Kaida & Niki, 2014 ; Patanaik, Zagorodnov, Kwoh, et al., 2014 ; Robillard et al., 2011 ). Differences in age and sex were not discussed in all but two studies reported in one paper ( Honn et al., 2020 ), where no significant group differences in age or sex were found (p = 0.24 and 0.26 respectively).
3.4.2. Dose-response effects on cognitive performance from sleep deprivation
The dose-response effect of sleep deprivation on psychomotor vigilance performance was tested in 3 RCTs ( n = 121) ( Drake et al., 2001 ; Jewett et al., 1999 ; Van Dongen et al., 2004 ). Greater psychomotor vigilance performance impairment was observed in all three trials with larger doses of sleep deprivation ( Drake et al., 2001 ; Jewett et al., 1999 ). In Jewett’s trial of 61 young adults (0-hours, 2-hours, 5-hours, or 8-hours for one night), all PVT metrics improved as sleep duration increased ( p < .0002), particularly between the 0-hour and 2-hour sleep conditions; however, only a slight improvement was observed between the 5-hour and 8-hour sleep conditions with a 2.14-hour decay mean rate for all PVT metrics. Chronic sleep deprivation (8-hours, 6-hours, 4-hours – time in bed (TIB) per night for 14 nights) resulted in cumulative dose-dependent deficits in psychomotor vigilance performance, and daytime sleepiness showed an acute response but did not differentiate between the 6-hour and 4-hour conditions in Van Dongen’s trial of 48 young adults (mean age 26 ± 3.6 y). In this same trial, deficits in cognitive performance were equivalent between the chronic sleep deprivation of sleep to 6-hours or less per night over 10 nights and up to 2-nights of total sleep deprivation conditions ( Van Dongen et al., 2004 ). In Drake’s trial of 12 young adults using a Latin square design (no sleep loss-8 hours TIB for 4-nights; slow: 6-hours TIB hours for 4 nights; intermediate: 4-hours TIB for two nights; and rapid: 0-hours TIB for one night), higher impairment of cognitive performance impairment with rapid loss of sleep loss as opposed to when loss of sleep occurred or accumulated over time ( Drake et al., 2001 ). Also, alertness levels were lower in the 6-hour per night condition relative to the 8-hour condition in the same trial ( Drake et al., 2001 ). We present a dose response graph comparing pooled baseline to partial sleep deprivation conditions (6- and 4-hour sleep duration) and total sleep deprivation (0-hour sleep duration) mean reaction time as measured by the PVT over the days of monitoring in Figure 3 .

Dose Response graph Note: 1 day = 24 hours; 0-hour time in bed is total sleep deprivation; 4 and 6-hour time in bed is partial sleep deprivation; and 8-hour time in bed is a healthy sleep opportunity.
3.4.3. Effect of sleep deprivation on daytime sleepiness
The effect of sleep deprivation on self-reported daytime sleepiness was assessed in 5 trials ( n = 135) using a between-person comparison ( Esposito et al., 2015 ; Franzen et al., 2008 ; Haavisto et al., 2010 ; Jewett et al., 1999 ; Van Dongen et al., 2004 ) and objective daytime sleepiness was additionally assessed in one of the trials ( Franzen et al., 2008 ). Trials of total sleep deprivation ( Esposito et al., 2015 ; Franzen et al., 2008 ; Jewett et al., 1999 ; Van Dongen et al., 2004 ) and partial sleep deprivation ( Haavisto et al., 2010 ) resulted in significantly higher daytime sleepiness ratings in the sleep deprivation as opposed to the healthy sleep opportunity conditions. In comparison to the PVT, the largest magnitude of effects were seen in all measures of daytime sleepiness (2 objective and 1 self-report) in Franzen et al. 2008 ’s trial of 29 young adults following one night of total sleep deprivation ( n = 15) compared to a healthy sleep opportunity condition ( n = 14) (mean sleep latency test F = 25.08, p < .001, n 2 = 0.501, pupillary unrest test F = 11.58, p = .002, n 2 = 0.317, visual analogue scale F = 42.80, p <.001, n 2 = 0.631).
The effect of total sleep deprivation on self-reported daytime sleepiness was assessed in 4 cross-over trials ( Lin et al., 2020 ; Patanaik, Zagorodnov, Kwoh, et al., 2014 ; Tempesta et al., 2014 ; Yeo et al., 2015 ). Results were not reported in 3 trials ( Patanaik, Zagorodnov, & Kwoh, 2014 ; Tempesta et al., 2014 ; Yeo et al., 2015 ). The effect of one night of total sleep deprivation on self-reported daytime sleepiness was only significant in one of the cross-over trials (F 1,28.95 = 103.09; p < 0.01) ( Tempesta et al., 2014 ); whereas a marginal increase in daytime sleepiness was noted in the other cross-over trial, but the effect was not significant ( t = −1.890, p = 0.071, Cohen’s d = −0.39) ( Lin et al., 2020 ). On the other hand, the effect of partial sleep deprivation (4-hours for one night) on self-reported daytime sleepiness relative to healthy sleep opportunity was significant in 3 cross-over trials with a medium effect size ( Rossa et al., 2014 ; Schwarz et al., 2016 ; Schwarz et al., 2013 ). Also, the partial sleep deprivation as opposed to the healthy sleep opportunity condition displayed higher objective daytime sleepiness via the pupillary unrest test (5.7 ± 2.1 vs. 4.5 ± 2.1 mm/min, p = .002) with a medium effect size (Cohen’s d = 0.55) ( Schwarz et al., 2016 ).
3.4.4. Effect of sleep deprivation on affect
The effect of sleep deprivation on affect was only assessed in one trial using a between persons comparison ( Franzen et al., 2008 ). Those in the total sleep deprivation condition (n = 14) as opposed to the healthy sleep opportunity condition (n = 15) had a higher negative mood ( F = 4.76, p = .039), lower positive affect ( F = 4.78, p = .038), but the change in negative affect was not significant ( F = 1.74, p = .20) ( Franzen et al., 2008 ).
The effect of sleep deprivation on affect was assessed in 5 RCTs using a within-person comparison ( n = 178) ( Drake et al., 2001 ; Kaida & Niki, 2014 ; Lin et al., 2020 ; Rossa et al., 2014 ; Tempesta et al., 2014 ). The effect of one night of total sleep deprivation resulted in a significant negative effect on affect in 3 trials relative to the healthy sleep opportunity condition ( Drake et al., 2001 ; Kaida & Niki, 2014 ; Lin et al., 2020 ). Compared to a healthy sleep opportunity, both positive affect and negative affect were significantly reduced when participants were totally sleep deprived in one cross-over trial ( Lin et al., 2020 ) and partially sleep-deprived (4-hours one night) in another cross over trial ( Rossa et al., 2014 ). The effect size was small in the partial-sleep deprivation cross over trial ( Rossa et al., 2014 ), medium in one of the total sleep deprivation cross-over trials (Cohen’s d = 0.51) ( Lin et al., 2020 ), and not reported in the other two trials ( Drake et al., 2001 ; Kaida & Niki, 2014 ). Lastly, there was a significant interaction between sleep loss and negative affect in working memory performance, but not with PVT performance in Tempesta et al. (2014) ‘s cross-over trial of 25 young adults.
4. Discussion
In this systematic review, the effect of sleep deprivation on neurobehavioral functioning (psychomotor vigilance performance, affect, and daytime sleepiness) in young adults was examined. The primary aim of this study was to examine the effect of sleep deprivation on psychomotor vigilance performance. The largest effects with significant decrements on the most PVT metrics were found in total sleep deprivation studies ( Drake et al., 2001 ; Esposito et al., 2015 ; Franzen et al., 2008 ; Honn et al., 2020 ; Jewett et al., 1999 ; Kaida & Niki, 2014 ; Lin et al., 2020 ; Patanaik, Zagorodnov, Kwoh, et al., 2014 ; Robillard et al., 2011 ; Tempesta et al., 2014 ; Tucker et al., 2009 ; Van Dongen et al., 2004 ). There was a dose-response relationship between the rate of sleep loss and psychomotor vigilance performance measured via PVT. Also, adaptation occurred with a slower accumulation of sleep loss ( Drake et al., 2001 ; Jewett et al., 1999 ; Van Dongen et al., 2004 ). The short time constant that was observed in one of the trials (0h to 2h conditions) ( Jewett et al., 1999 ) indicates that the first few hours of sleep may serve to restore psychomotor vigilance decrements following sleep deprivation. This may partially explain why a nap affords recovery disproportionate to its duration ( Jewett et al., 1999 ).
The second aim of this systematic review was to determine how sleep deprivation affected daytime sleepiness. Daytime sleepiness was measured via self-report in a majority of the trials with the Karolinska Sleepiness Test or Stanford Sleepiness Test and objectively with the Multiple Sleep Latency Test and Pupillary Unrest Index ( Lüdtke et al., 1998 ) in two trials ( Franzen et al., 2008 ; Schwarz et al., 2016 ). Most of the trials included acute sleep deprivation, however in the trial where partial sleep deprivation was examined over 14-days ( Van Dongen et al., 2004 ), chronic partial sleep deprivation of 4 – 6 hours resulted in an initial elevation of self-report ratings on both the Stanford Sleepiness Scale and Karolinska Sleepiness Scale, but as the study progressed only minor further increases in self-report daytime sleepiness that did not mirror the decrements in PVT performance were observed. Even at the end of the 14 days, participants only reported feeling slightly sleepy ( Van Dongen et al., 2004 ). This suggests that there is an adaptation to chronic partial sleep deprivation especially considering the chronic partial sleep deprivation condition was compared to a total sleep deprivation condition ruling out the potential for a ceiling effect as the total sleep deprivation condition showed considerably greater levels of daytime sleepiness after two nights ( Van Dongen et al., 2004 ). Another consideration when assessing daytime sleepiness is that it might be intertwined with affect and related to the same latent construct making it difficult to differentiate perceptions of daytime sleepiness from mood; therefore, it is warranted to include physiologic measures more sensitive than self-report measures as suggested by Franzen et al, 2008 .
Regarding our final aim to determine the effect of sleep deprivation on affect, it must be highlighted that affect was only assessed in one-third of the studies. Also, the designs and instruments to measure affect varied, making it difficult to draw conclusions. Nonetheless, both partial and total sleep deprivation conditions resulted in worsened affect in the young adults in the selected studies, which is consistent with other young adult and adolescent studies ( Baum et al., 2014 ; Franzen et al., 2008 ; Haavisto et al., 2010 ). Studies where objective physiological and/or neural measures of affect were assessed provide additional verification of the emotional dysregulation following sleep deprivation. This was demonstrated in two of the trials in the current review with additional measures of pupillary affective response ( Franzen et al., 2008 ; Schwarz et al., 2016 ). In previous research, a 60% amplification in reactivity of the amygdala assessed using functional MRI (fMRI) was observed following one night of total sleep deprivation (n = 14) in response to negative pictures triggering emotions, when compared to a healthy sleep opportunity condition ( n = 12) ( Yoo et al., 2007 ).
Limitations
There are some limitations of this systematic review that should be considered. First, regarding sample characteristics, we included individuals free of medical, psychiatric, and sleep disorders with previous healthy weight and sleep schedules, limiting the generalizability of these findings. Second, although psychomotor vigilance performance was a common outcome across studies, only 6 used a parallel-group design, and with a lack of baseline and outcome data reporting, we could not conduct a meta-analysis. Baseline and some post-intervention values were not available to calculate mean change in these studies, so our results are fully based on a narrative review. Third, although outcomes were common via the PVT, the heterogeneity across designs, analyses, and objectives made the synthesis and analysis difficult. We recommend more transparent data reporting in the future, particularly through the inclusion of baseline data. This would allow for meta-analyses to be performed in the future, allowing the effects to be pooled to advance the science. Also, because of the different designs and analyses, a determination about reproducibility could not be made.
Objective assessments and physiologic measures (e.g., the Multiple Sleep Latency test and Pupillary Unrest Index) were more precise and sensitive, which may have affected the self-reported daytime sleepiness and affective outcomes. A larger effect size was reported for the physiologic measures (daytime sleepiness and affect regulation) as opposed to the self-report mood and PVT outcomes in one of the trials ( Franzen et al., 2008 ).
5. Conclusions
We determined that sleep deprivation degrades young adults’ neurobehavioral functioning. These results are congruent with adult and adolescent studies, where total sleep deprivation (as opposed to partial sleep deprivation) has a substantial detrimental effect on psychomotor vigilance performance, with the largest effects for vigilance tasks ( de Bruin et al., 2017 ; Lim & Dinges, 2010 ). The studies were all based on acute sleep deprivation, so it was not possible to determine if psychomotor vigilance deficits accumulate over time during chronic sleep deprivation, which is most consistent with real-world settings ( Goel et al., 2009 ). This is important as young adult brains are sensitive to sleep loss, as indicated by imaging studies examining the prefrontal cortex ( Chee & Choo, 2004 ). There is considerable evidence that the prefrontal cortex continues to develop into early adulthood which may affect speed of performance on psychomotor vigilance tasks, although this association has not been examined longitudinally ( Chee & Choo, 2004 ; Gied et al., 1999; Muzur et al., 2002 ). Thus, the effects of chronic sleep deprivation on the psychomotor vigilance performance of the developing brain remain unclear. Also, though our primary intention was to assess the effect of sleep deprivation on psychomotor vigilance performance via PVT, daytime sleepiness was only assessed in 10 and affect in 6 of the studies limiting the ability to comprehensively assess neurobehavioral function among young adults in the included studies.
The findings presented underscore the importance of measuring different neurobehavioral function metrics (e.g., psychomotor vigilance - cognitive performance via PVT, daytime sleepiness via self-report and objective measures, and affect) when studying their response to sleep and wakefulness. Larger RCTs that include an objective to examine the effect of sleep deprivation on neurobehavioral function under controlled conditions are needed to reveal predictors and negative effects of acute and chronic sleep deprivation in this high-risk group. Researchers should also consider including moderators (e.g., age, sex, dose) when these larger studies are available for meta-analysis. Nurses working across tertiary care and the community are well-positioned to take the lead on advocating for policies and practices promoting a healthy sleep opportunity and sleep education to optimize brain development in this age group.
- Total and partial sleep deprivation lead to significant decrements in neurobehavioral function (cognitive performance, affect, and sleepiness) in young adults.
- Adaptation to sleep loss can occur when it accumulates over time.
- The focus of the current literature is on short term sleep loss limiting the ability to draw inference to real world settings where sleep loss occurs at a more stable state over time (e.g., chronic partial sleep deprivation).
- The prefrontal cortex continues to develop until the late 20’s, thus the effects of sleep loss over time in the developing brain remain unclear.
Acknowledgements:
The authors would like to acknowledge the contributions of DG in screening for inclusion and assisting with quality assessment.
Funding Statement:
This work was supported by American Academy of Sleep Medicine Foundation (AASM), 220-BS-19 and the National Institute for Nursing Research (NINR), K99NR018886. Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the authors and do not necessarily reflect the views of the AASM Foundation or NIH.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CRediT authorship contribution statement: Stephanie Griggs: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data Curation, Writing – original draft, Project administration, Funding acquisition. Alison Harper: Validation, Formal analysis, Investigation, Data Curation, Writing – original draft. Ronald L. Hickman: Supervision, Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing – review and editing, Project administration.
Declaration of competing interests: No conflict of interest has been declared by the authors.
Contributor Information
Stephanie Griggs, Case Western Reserve University, Frances Payne Bolton School of Nursing, Cleveland, Ohio, USA 44106.
Alison Harper, Case Western Reserve University, Frances Payne Bolton School of Nursing, Department of Anthropology, Cleveland, Ohio, USA 44106.
Ronald L. Hickman, Jr, Ruth M. Anderson Endowed Professor of Nursing and Associate Dean for Research Case Western Reserve University, Frances Payne Bolton School of Nursing, Cleveland, OH, USA 44106.
- Adler A, Gavan MY, Tauman R, Phillip M, & Shalitin S (2017). Do children, adolescents, and young adults with type 1 diabetes have increased prevalence of sleep disorders? Pediatric Diabetes , 18 ( 6 ), 450–458. 10.1111/pedi.12419 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Akerstedt T, & Gillberg M (1990). Subjective and objective sleepiness in the active individual . International Journal of Neuroscience , 52 ( 1–2 ), 29–37. 10.3109/00207459008994241 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Babkoff H, Caspy T, & Mikulincer M (1991). Subjective sleepiness ratings: the effects of sleep deprivation, circadian rhythmicity and cognitive performance . Sleep , 14 ( 6 ), 534–539. 10.1093/sleep/14.6.534 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baum KT, Desai A, Field J, Miller LE, Rausch J, & Beebe DW (2014). Sleep restriction worsens mood and emotion regulation in adolescents . The Journal of Child Psychology and Psychiatry , 55 ( 2 ), 180–190. 10.1111/jcpp.12125 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chee MWL, & Choo WC (2004). Functional imaging of working memory after 24 hr of total sleep deprivation . Journal of Neuroscience , 24 ( 19 ), 4560–4567. 10.1523/jneurosci.0007-04.2004 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crowley SJ, & Carskadon MA (2010). Modifications to weekend recovery sleep delay circadian phase in older adolescents . Chronobiology International , 27 ( 7 ), 1469–1492. https://dx.doi.org/10.3109%2F07420528.2010.503293 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- de Bruin EJ, van Run C, Staaks J, & Meijer AM (2017). Effects of sleep manipulation on cognitive functioning of adolescents: A systematic review . Sleep Medicine Reviews , 32 , 45–57. 10.1016/j.smrv.2016.02.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dinges DF, Pack F, Williams K, Gillen KA, Powell JW, Ott GE, Aptowicz C, & Pack AI (1997). Cumulative sleepiness, mood disturbance and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night . Sleep: Journal of Sleep Research & Sleep Medicine , 20 ( 4 ), 267–277. [ PubMed ] [ Google Scholar ]
- Dinges DF, Rogers NL, & Dorrian J (2004). Psychomotor vigilance performance: Neurocognitive assay sensitive to sleep loss. In Sleep deprivation (pp. 67–98). CRC Press. [ Google Scholar ]
- Drake CL, Roehrs TA, Burduvali E, Bonahoom A, Rosekind M, & Roth T (2001). Effects of rapid versus slow accumulation of eight hours of sleep loss . Psychophysiology , 38 ( 6 ), 979–987. 10.1111/1469-8986.3860979 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Esposito MJ, Occhionero M, & Cicogna P (2015). Sleep deprivation and time-based prospective memory . Sleep , 38 ( 11 ), 1823–1826. 10.5665/sleep.5172 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fischer D, Lombardi DA, Marucci-Wellman H, & Roenneberg T (2017). Chronotypes in the US–influence of age and sex . PLoS One , 12 ( 6 ), e0178782. 10.1371/journal.pone.0178782 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Franzen PL, Gianaros PJ, Marsland AL, Hall MH, Siegle GJ, Dahl RE, & Buysse DJ (2011). Cardiovascular reactivity to acute psychological stress following sleep deprivation . Psychosomatic Medicine , 73 ( 8 ), 679–682. 10.1097/PSY.0b013e31822ff440 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Franzen PL, Siegle GJ, & Buysse DJ (2008). Relationships between affect, vigilance, and sleepiness following sleep deprivation . Journal of Sleep Research , 17 ( 1 ), 34–41. 10.1111/j.1365-2869.2008.00635.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Giedd JN, Snell J, Lange N, Rajapakse J Casey BJ, Kozuch P, et al. (1996). Quantitative magnetic imaging of human brain development: Ages 4–18 . Cerebral Cortex , 6 , 551–560. 10.1093/cercor/6.4.551 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goel N, Rao H, Durmer JS, & Dinges DF (2009). Neurocognitive consequences of sleep deprivation . Seminars in Neurology , 29 ( 4 ), 320–339. 10.1055/s-0029-1237117 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haavisto ML, Porkka-Heiskanen T, Hublin C, Härmä M, Mutanen P, Müller K, Virkkala J, & Sallinen M (2010). Sleep restriction for the duration of a work week impairs multitasking performance . Journal of Sleep Research , 19 ( 3 ), 444–454. 10.1111/j.1365-2869.2010.00823.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Honn KA, Halverson T, Jackson ML, Krusmark M, Chavali VP, Gunzelmann G, & Van Dongen HPA (2020). New insights into the cognitive effects of sleep deprivation by decomposition of a cognitive throughput task . Sleep: Journal of Sleep and Sleep Disorders Research , 43 ( 7 ), 1–14. 10.1093/sleep/zsz319 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jewett ME, Dijk D-J, Kronauer RE, & Dinges DF (1999). Dose-response relationship between sleep duration and human psychomotor vigilance and subjective alertness . Sleep: Journal of Sleep Research & Sleep Medicine , 22 ( 2 ), 171–179. 10.1093/sleep/22.2.171 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnson SB, Blum RW, & Giedd JN (2009). Adolescent maturity and the brain: the promise and pitfalls of neuroscience research in adolescent health policy . Journal of Adolescent Health , 45 ( 3 ), 216–221. 10.1016/j.jadohealth.2009.05.016 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jones B, & Kenward MG (2014). Design and analysis of cross-over trials (Third edition. ed.). CRC Press/Taylor & Francis. [ Google Scholar ]
- Jørgensen L, Paludan-Müller AS, Laursen DR, Savović J, Boutron I, Sterne JA, Higgins JP, & Hróbjartsson A (2016). Evaluation of the Cochrane tool for assessing risk of bias in randomized clinical trials: overview of published comments and analysis of user practice in Cochrane and non-Cochrane reviews . Systematic Reviews , 5 , 80. 10.1186/s13643-016-0259-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaida K, & Niki K (2014). Total sleep deprivation decreases flow experience and mood status . Neuropsychiatric Disease and Treatment , 10 , 19–25. 10.2147/ndt.s53633 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lim J, & Dinges DF (2010). A meta-analysis of the impact of short-term sleep deprivation on cognitive variables . Psychological Bulletin , 136 ( 3 ), 375–389. 10.1037/a0018883 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lin Y, Hu P, Mai ZF, Jiang TX, Mo L, & Ma N (2020). Sleep deprivation impairs cooperative behavior selectively: Evidence from prisoner’s and chicken dilemmas . Nature and Science of Sleep , 12 , 29–37. 10.2147/nss.s237402 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lüdtke H, Wilhelm B, Adler M, Schaeffel F, & Wilhelm H (1998). Mathematical procedures in data recording and processing of pupillary fatigue waves . Vision Research , 38 ( 19 ), 2889–2896. 10.1016/s0042-6989(98)00081-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McNair D, Lorr M, & Droppleman L (1971). Manual for the profile of mood states (POMS) . San Diego: Educational and Industrial Testing Service. [ Google Scholar ]
- Monk TH (1989). A Visual Analogue Scale technique to measure global vigor and affect . Psychiatry Research , 27 ( 1 ), 89–99. 10.1016/0165-1781(89)90013-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Muzur A, Pace-Schott EF, & Hobson JA (2002). The prefrontal cortex in sleep . Trends in Cognitive Sciences , 6 ( 11 ), 475–481. 10.1016/s1364-6613(02)01992-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nagendrababu V, Duncan H, Tsesis I, Sathorn C, Pulikkotil S, Dharmarajan L, & Dummer P (2019). Preferred reporting items for systematic reviews and meta- analyses for abstracts: best practice for reporting abstracts of systematic reviews in Endodontology . International Endodontic Journal , 52 ( 8 ), 1096–1107. https://onlinelibrary.wiley.com/doi/pdf/ 10.1111/iej.13118 [ PubMed ] [ Google Scholar ]
- Nilsson JP, Söderström M, Karlsson AU, Lekander M, Akerstedt T, Lindroth NE, & Axelsson J (2005). Less effective executive functioning after one night’s sleep deprivation . Journal of Sleep Research , 14 ( 1 ), 1–6. 10.1111/j.1365-2869.2005.00442.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Patanaik A, Zagorodnov V, & Kwoh C (2014). Parameter estimation and simulation for one-choice Ratcliff diffusion model. Proceedings of the 29th Annual ACM Symposium on Applied Computing . [ Google Scholar ]
- Patanaik A, Zagorodnov V, Kwoh CK, & Chee MWL (2014). Predicting vulnerability to sleep deprivation using diffusion model parameters . Journal of Sleep Research , 23 ( 5 ), 576–584. 10.1111/jsr.12166 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peltzer K, & Pengpid S (2016). Sleep duration and health correlates among university students in 26 countries . Psychology, Health, and Medicine , 21 ( 2 ), 208–220. 10.1080/13548506.2014.998687 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, … & Duffy S (2006). Guidance on the conduct of narrative synthesis in systematic reviews . A Product from the ESRC Methods Programme Version , 1 , b92 [ Google Scholar ]
- Robillard R, Prince F, Boissonneault M, Filipini D, & Carrier J (2011). Effects of increased homeostatic sleep pressure on postural control and their modulation by attentional resources . Clinical Neurophysiology , 122 ( 9 ), 1771–1778. 10.1016/j.clinph.2011.02.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rossa KR, Smith SS, Allan AC, & Sullivan KA (2014). The effects of sleep restriction on executive inhibitory control and affect in young adults . Journal of Adolescent Health , 55 ( 2 ), 287–292. 10.1016/j.jadohealth.2013.12.034 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwarz JFA, Geisler P, Hajak G, Zulley J, Rupprecht R, Wetter TC, & Popp RFJ (2016). The effect of partial sleep deprivation on computer-based measures of fitness to drive . Sleep and Breathing , 20 ( 1 ), 285–292. 10.1007/s11325-015-1220-0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwarz JFA, Popp R, Haas J, Zulley J, Geisler P, Alpers GW, Osterheider M, & Eisenbarth H (2013). Shortened night sleep impairs facial responsiveness to emotional stimuli . Biological Psychology , 93 ( 1 ), 41–44. 10.1016/j.biopsycho.2013.01.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tempesta D, De Gennaro L, Presaghi F, & Ferrara M (2014). Emotional working memory during sustained wakefulness . Journal of Sleep Research , 23 ( 6 ), 646–656. 10.1111/jsr.12170 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tucker AM, Basner RC, Stern Y, & Rakitin BC (2009). The variable response-stimulus interval effect and sleep deprivation: An unexplored aspect of psychomotor vigilance task performance . Sleep: Journal of Sleep and Sleep Disorders Research , 32 ( 10 ), 1393–1395. 10.1093/sleep/32.10.1393 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van Dongen HPA, Baynard MD, Maislin G, & Dinges DF (2004). Systematic interindividual differences in neurobehavioral impairment from sleep loss: Evidence of trait-like differential vulnerability . Sleep , 27 ( 3 ), 423–433. [ PubMed ] [ Google Scholar ]
- Van Dongen HPA, Maislin G, Mullington JM, & Dinges DF (2003). The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation . Sleep , 26 ( 2 ), 117–126. 10.1093/sleep/26.2.117 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales . Journal of Personality and Social Psychology , 54 ( 6 ), 1063–1070. 10.1037//0022-3514.54.6.1063 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Whitney P, Hinson JM, Jackson ML, & Van Dongen HPA (2015). Feedback blunting: Total sleep deprivation impairs decision making that requires updating based on feedback . Sleep: Journal of Sleep and Sleep Disorders Research , 38 ( 5 ), 745–754. 10.5665/sleep.4668 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yeo BTT, Tandi J, & Chee MWL (2015). Functional connectivity during rested wakefulness predicts vulnerability to sleep deprivation . Neuroimage , 111 , 147–158. 10.1016/j.neuroimage.2015.02.018 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yoo SS, Gujar N, Hu P, Jolesz FA, & Walker MP (2007). The human emotional brain without sleep--a prefrontal amygdala disconnect . Current Biology , 17 ( 20 ), R877–878. 10.1016/j.cub.2007.08.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]

How Sleep Deprivation Affects Your Metabolic Health
By Nicole Molumphy

Do you ever get those late-night cravings or feel like your hunger is never satiated? Research shows that consistent short sleep duration (less than 7 hours per night) can influence metabolic health, affect the function of appetite hormones, increase food cravings, and lead to a 38 percent increase in obesity in adults.
Consistent sleep deprivation can lead to altered functioning of the appetite hormones ghrelin and leptin . Ghrelin increases our appetite and is released by cells in the stomach lining. When your stomach is “growling,” that is the ghrelin hormone talking. Conversely, the hormone leptin, made by our fat cells, lowers our appetite. Studies have revealed that sleep deprivation can lead to increased ghrelin and decreased leptin, resulting in an overall experience of constantly being hungry.
“There are so many health conditions associated with poor sleep,” says Rob Oh, MD, family physician at the Veterans Affairs Health Care System in Palo Alto. “With chronic sleep deprivation, your metabolism becomes dysregulated, leading to cravings for processed foods. Also, you’re less likely to exercise, you feel more stressed, and you’re more likely to think poorly. The combination of these factors can lead to metabolic health problems like obesity and type 2 diabetes.”
Sleep Deprivation Increases Stress Hormones
Our cortisol levels are typically lowest near midnight and then increase towards waking hours, ultimately peaking around 9 a.m. Studies demonstrate that reoccurring poor sleep is associated with an altered cortisol secretion pattern .
For example, delaying your bedtime could lead to high cortisol levels in the middle of the day, rather than just in the morning. Sustained high levels of cortisol can lead to an increased amount of insulin in the blood , which promotes the accumulation of belly fat and has the potential to lead to prediabetes, type 2 diabetes, and other metabolic disorders. An increase in cortisol levels during the day may induce prolonged feelings of stress, increased food cravings, and further insomnia—promoting a recurrent, cyclical pattern.
“Inadequate sleep disrupts hormone levels, which dysregulates one’s metabolism and makes individuals hungrier,” says Dr. Oh. ” When we are hungrier, we eat more, which leads to weight gain and potentially metabolic disease.”
If that’s not bad enough, cravings for ultra-processed foods, sugars, and alcohol become more of a tease with sleep deprivation. A possible mechanism for this added hunger is an increased activation of the endocannabinoid system , which is found throughout the body and controls several biological systems, including sleep, mood, and appetite.
Sleep Deprivation and Increased Risk of Diabetes
Research shows that a lack of sleep may also result in insulin resistance , a driving factor in prediabetes and type 2 diabetes . Insulin is a hormone made by the pancreas that regulates blood glucose levels. Insulin resistance occurs when cells in the liver, fat, and muscles do not respond well to insulin, and in turn, glucose is not taken up into the blood.
The exact mechanism behind the causal relationship between insufficient sleep and insulin resistance is still being studied, however, some studies note that increased inflammatory markers, like C-reactive protein and hormone dysregulation, such as cortisol may be involved.
Currently, prediabetes affects one in three adults in the US. While many mechanisms contribute to the development of prediabetes and type 2 diabetes, some of the more prominent ones include impaired cellular insulin sensitivity, modified gut microbiota, and overly-sensitive sympathetic nervous system (fight-or-flight) activation. When the sympathetic nervous system is activated, it signals the liver to release more glucose into the bloodstream, leading to higher blood sugar levels.
What Can We Do About It?
Unfortunately, research finds that “weekend recovery sleep” is not enough to bring your metabolism back into balance after a lack of sufficient sleep throughout the week. Instead, Dr. Oh recommends taking a holistic approach and examining not only your sleep habits but also your nutritional choices and workout routines to support the restoration of metabolic health.
For those with pre-diabetes and type 2 diabetes, a diet focused on whole foods and low refined carbohydrates is critical for weight loss and glucose control.
Specifically, Dr. Oh recommends a low carbohydrate diet, such as consuming 75 to 100 grams of carbohydrates per day, to control and balance blood sugar levels. He also recommends quick, 20-minute, high intensity workouts for time-efficient and effective exercises that promote metabolic health. Regarding supplements, Dr. Oh recommends magnesium to promote muscle recovery and relaxation before bedtime.
“Optimal sleep is so intertwined with athletic and exercise performance, brain health, and metabolic health,” says Dr. Oh. “Sleep really is a keystone area where many of us can do better and hence reducing our risk for metabolic diseases and lengthening our healthspan.”
You might also like

- Lifestyle Medicine Blog
- In the News
- Research Publications
- Movement & Exercise
- Healthful Nutrition
- Restorative Sleep
- Stress Management
- Social Engagement
- Cognitive Enhancement
- Gratitude & Reflection
Email (required) *
Example: Yes, I would like to receive emails from Lifestyle Medicine. (You can unsubscribe anytime)

Sleep Deprivation and Learning at University Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Brief information about the issue, arguments in support of the idea, counterargument.
Nowadays, sleep deprivation is considered one of the most common problems among students of different educational establishments. In fact, it frequently results in poor academic performance and physical health issues. In terms of learning, sleep plays a prominent role, as this process consolidates memory and improves concentration. Therefore, despite the belief that sleeping several hours per night is a useful strategy for achieving positive goals in education, this process should occupy up to a third of the human lifespan.
It is a widely known fact that numerous people face the problem of lack of sleep. For instance, approximately 37% of people ages 20-39 report this issue (Patrick et al., 2017). However, the percentage of students struggling with this problem is even higher. It is estimated that over 70% of them do not sleep the appropriate amount of time (Schlarb et al., 2017). As for the causes of such a global problem, it is essential to note several factors, such as part-time jobs, stress, alcohol, and addiction to social media platforms. Moreover, a vast number of students include energy drinks and caffeine in their nutrition, thereby, contributing to the problem of sleep deprivation. At the same time, some individuals are not aware of the fact that they are sleep-deprived. In fact, the person struggling with this issue is likely to experience fatigue, moodiness, depression, and forgetfulness. In turn, if these factors correspond to the symptoms faced by the student, the basic recommendations should be followed. Usually, it is recommended to exercise, limit daytime naps, as well as avoid drinking alcohol.
First, an adequate amount of sleep is associated with improved grades. It can be explained by the ability of the brain to stay more focused on the process of learning. For example, the overall course grades for students getting at least 7 hours of sleep were 50 percent better compared to the students who were getting one hour less sleep (Maheshwari & Shaukat, 2019). Second, sleeping is essential for increasing the productivity of students in the context of learning. For instance, if the student goes to bed at 10, they are expected to be more productive than students who go to bed at 2 (Alotaibi et al., 2020). Thus, sleeping can be used in order to boost productivity and improve overall academic performance at university.
Today, there are a variety of supporters of the idea that considerable goals can only be achieved if the person dedicates to sleep no more than 4 hours per night. This belief can be considered inaccurate, as the human brains are not able to function at their best with such a limited time for the rest. The average adult should dedicate 7-9 hours to sleep in order to learn new information and develop essential professional skills (Barahona-Correa et al., 2018). If this basic human need is ignored, students will most likely suffer from a lowered ability to focus, impairment of brain development, and mental health issues.
In conclusion, sleeping is an integral part of human life, which can either enhance its quality or worsen it. In terms of learning at university, this process can improve grades, boost productivity, and facilitate the perception of new information. Simultaneously, if the students do not get adequate sleep, they can struggle with poor coordination, lack of motivation, and lowered ability to use critical thinking skills.
Alotaibi, A. D., Alosaimi, F. M., Alajlan, A. A., & Abdulrahman, K. A. B. (2020). The relationship between sleep quality, stress, and academic performance among medical students. Journal of Family Community Medicine , 27 (1), 23−28. Web.
Barahona-Correa, J. E., Aristizabal-Mayor, J. D., Lasalvia, P., Ruiz, Á. J., & Hidalgo-Martínez, P. (2018). Sleep disturbances, academic performance, depressive symptoms and substance use among medical students in Bogota, Colombia. Sleep Science , 11 (4), 260−268. Web.
Maheshwari, G., & Shaukat, F. (2019). Impact of poor sleep quality on the academic performance of medical students. Cureus , 11 (4), e4357. Web.
Patrick, Y., Lee, A., Raha, O., Pillai, K., Gupta, S., Sethi, S., Mukeshimana, F., Gerard, L., Moghal, M. U., Saleh, S. N., Smith, S. F., Morrell, M. J., & Moss, J. (2017). Effects of sleep deprivation on cognitive and physical performance in university students . Sleep and Biological Rhythms , 15 (3), 217−225. Web.
Schlarb, A. A., Friedrich, A., & Claben, M. (2017). Sleep problems in university students: An intervention . Neuropsychiatric Disease and Treatment , 13 (2), 1989−2001. Web.
- Psychological Health and Social Environment Correlation
- Application of Public Health Concepts for the Uninsured
- Sleep Deprivation Impacts on College Students
- Effects of Sleeping Disorders on Human
- Sleep Deprivation: Biopsychology and Health Psychology
- Human Trafficking: Solution to Treat Survivors And A Public Health Issues
- Rwandan Healthcare: A Transformational Leadership
- Amplifiers of the COVID-19 Pandemic Hiding in Plain Sight
- Health Communication Issue and Modernization in Africa
- Defibrillators in All the Schools of Indiana
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, February 22). Sleep Deprivation and Learning at University. https://ivypanda.com/essays/sleep-deprivation-and-learning-at-university/
"Sleep Deprivation and Learning at University." IvyPanda , 22 Feb. 2022, ivypanda.com/essays/sleep-deprivation-and-learning-at-university/.
IvyPanda . (2022) 'Sleep Deprivation and Learning at University'. 22 February.
IvyPanda . 2022. "Sleep Deprivation and Learning at University." February 22, 2022. https://ivypanda.com/essays/sleep-deprivation-and-learning-at-university/.
1. IvyPanda . "Sleep Deprivation and Learning at University." February 22, 2022. https://ivypanda.com/essays/sleep-deprivation-and-learning-at-university/.
Bibliography
IvyPanda . "Sleep Deprivation and Learning at University." February 22, 2022. https://ivypanda.com/essays/sleep-deprivation-and-learning-at-university/.
Home — Essay Samples — Sociology — Effects of Social Media — Impact Social Media on Sleep Deprivation
Sleeping Habits and Social Media Usage
- Categories: Effects of Social Media Social Media
About this sample

Words: 1546 |
Published: Mar 19, 2020
Words: 1546 | Pages: 4 | 8 min read
Table of contents
Introduction.
- Tandon, A., Kaur, P., Dhir, A., & Mäntymäki, M. (2020). Sleepless due to social media? Investigating problematic sleep due to social media and social media sleep hygiene. https://www.sciencedirect.com/science/article/pii/S0747563220302399 Computers in human behavior, 113, 106487.
- Alonzo, R., Hussain, J., Stranges, S., & Anderson, K. K. (2021). Interplay between social media use, sleep quality, and mental health in youth: A systematic review. Sleep medicine reviews, 56, 101414. (https://www.sciencedirect.com/science/article/abs/pii/S108707922030157X)
- Kolhar, M., Kazi, R. N. A., & Alameen, A. (2021). Effect of social media use on learning, social interactions , and sleep duration among university students. https://pubmed.ncbi.nlm.nih.gov/33911938/ Saudi Journal of Biological Sciences, 28(4), 2216-2222.
- Shimoga, S. V., Erlyana, E., & Rebello, V. (2019). Associations of social media use with physical activity and sleep adequacy among adolescents: Cross-sectional survey. Journal of medical Internet research, 21(6), e14290. (https://www.jmir.org/2019/6/e14290/)
- Abi-Jaoude, E., Naylor, K. T., & Pignatiello, A. (2020). Smartphones, social media use and youth mental health. Cmaj, 192(6), E136-E141. (https://www.cmaj.ca/content/192/6/E136.short)
Should follow an “upside down” triangle format, meaning, the writer should start off broad and introduce the text and author or topic being discussed, and then get more specific to the thesis statement.
Provides a foundational overview, outlining the historical context and introducing key information that will be further explored in the essay, setting the stage for the argument to follow.
Cornerstone of the essay, presenting the central argument that will be elaborated upon and supported with evidence and analysis throughout the rest of the paper.
The topic sentence serves as the main point or focus of a paragraph in an essay, summarizing the key idea that will be discussed in that paragraph.
The body of each paragraph builds an argument in support of the topic sentence, citing information from sources as evidence.
After each piece of evidence is provided, the author should explain HOW and WHY the evidence supports the claim.
Should follow a right side up triangle format, meaning, specifics should be mentioned first such as restating the thesis, and then get more broad about the topic at hand. Lastly, leave the reader with something to think about and ponder once they are done reading.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Heisenberg
Verified writer
- Expert in: Sociology

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 917 words
3 pages / 1166 words
2 pages / 983 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Effects of Social Media
There are many ways in which humans can choose to live healthier. Two key behaviors of a healthy lifestyle are getting enough sleep and adequately exercising (Voelker, 2016). Our bodies need rest to rejuvenate and if an [...]
The prevalence of technology and social media in modern society The potential harm of social media on mental health Statistics on social media usage among young adults Operant conditioning theory and its [...]
Social media life right now has incredible effect on how information is acquired and traded. Therefore, organizations need to grow new methodologies in hierarchical correspondence, while social media life can wind up noteworthy [...]
“A profound and heart-rending study of personality, class and culture” To what extent do you agree with this assessment of the novel? Throughout “The Remains of the Day”, Mr Stevens, the protagonist, not only explores the [...]
Wole Soyinka once said, “History teaches us to beware of the excitation of the liberated and the injustices that often accompany their righteous thirst for justice”.A Nigerian playwright, Soyinka, was born into a Yoruba [...]
A key to any revolution, in any time period, is spreading the keypoints within the ideology of the revolution in an efficient and effective manner. The Protestant Reformation, which is accredited chiefly to the efforts of the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

IMAGES
COMMENTS
This sleep deprivation essay explores how the functioning of the human body is influenced by various factors, primarily determined by an individual's health status. While most people do not understand the implications of sleep, human effectiveness solely depends on the amount of time dedicated to sleeping. However, for various reasons, people ...
INTRODUCTION. Sleep is vital for health and well-being in children, adolescents, and adults. 1-3 Healthy sleep is important for cognitive functioning, mood, mental health, and cardiovascular, cerebrovascular, and metabolic health. 4 Adequate quantity and quality of sleep also play a role in reducing the risk of accidents and injuries caused by sleepiness and fatigue, including workplace ...
Sleep deprivation leads to poor performance in the workplace and in schools. Children need 10-12 hours of sleep per day, while adults need 7-8 hours minimum (Blass et al. 28). Lack of sleep among school-going children can result in bad grades, while adults may underperform at work. The body needs sleep to enhance thinking and learning, and a ...
Reductions in attention make a sleep-deprived person more prone to mistakes, increasing the risk of a workplace or motor vehicle accident. Mood changes: Sleep loss can lead to mood changes and make a person feel more anxious or depressed. Without enough sleep, people may feel irritable, frustrated, and unmotivated.
In a detailed 2014 report, the American Academy of Pediatrics called the problem of tired teens a public health epidemic. "I think high school is the real danger spot in terms of sleep deprivation," said William Dement, MD, PhD, founder of the Stanford Sleep Disorders Clinic, the first of its kind in the world. "It's a huge problem.
Sleep deprivation can also cause neurological disturbances like: Blurred vision. Memory lapse. Poor reaction time. "Deep sleep allows our brains to clear the toxins that accumulate during our ...
In the long-term, this lack of sleep can come with steep consequences, including an increased risk of car crashes, workplace error, heart problems, reduced immune function, obesity, a lower quality of life, and an earlier death. We explore symptoms of sleep deprivation, the process of being diagnosed, and tips for treating and preventing this ...
Sleep deprivation is a significant issue that affects millions of people worldwide. It can have profound effects on physical health, mental well-being, and overall quality of life.Understanding the causes, effects, and potential solutions to sleep deprivation is crucial for individuals' well-being and society as a whole. This essay will explore the various factors leading to sleep deprivation ...
The short-term detriments of poor sleep on the brain and cognition can be the result of pulling an occasional all-nighter, while those with chronic sleep problems may see a continuous negative effect on day-to-day tasks. Over the long-term, poor sleep may put someone at a higher risk of cognitive decline and dementia.
The Effects of Sleep Deprivation. Sleep Health Risks of Poor Sleep Sleep Conditions. Not getting enough sleep can affect your mood, memory and health in far-reaching and surprising ways, says Johns Hopkins sleep researcher Patrick Finan, Ph.D. Learn more about the effects of sleep deprivation. Download the infographic as a PDF.
Problem of Sleep Deprivation. This is due to disruption of the sleep cycle. Based on the negative effects of sleep deprivation, there is need to manage this disorder among Americans. The Issue of Chronic Sleep Deprivation. The quality of sleep significantly impacts the health and performance of the human body.
This essay will argue just how dangerous driving under the influence of sleep deprivation really is. This essays argument will be supported by two major papers the first one is "Impairment of Driving Performance Caused by Sleep Deprivation or Alcohol: A Comparative Study" which was. 1427 Words; 6 Pages;
Each year the cost of sleep disorders, sleep deprivation and sleepiness, according to the NCSDR, is estimated to be $15.9 million in direct costs and $50 to $100 billion a year in indirect and related costs. And according to the NHSA, falling asleep while driving is responsible for at least 100,000 crashes, 71,000 injuries and 1,550 deaths each ...
Insufficient sleep is a pervasive and prominent problem in the modern 24-h society. A considerable body of evidence suggests that insufficient sleep causes hosts of adverse medical and mental dysfunctions. An extensive literature search was done in all the major databases for "insufficient sleep" and "public health implications" in this ...
1. Introduction. Sleep loss has a negative effect on multiple neurobehavioral functions, such as psychomotor vigilance performance (cognitive), daytime sleepiness, and affect (Franzen et al., 2011; Van Dongen et al., 2003).Degradation of vigilance following sleep deprivation is one of the most robust alterations in healthy young adults aged 18-30 years (Lim & Dinges, 2010).
Research shows that consistent short sleep duration (less than 7 hours per night) can influence metabolic health, affect the function of appetite hormones, increase food cravings, and lead to a 38 percent increase in obesity in adults. Consistent sleep deprivation can lead to altered functioning of the appetite hormones ghrelin and leptin ...
However, going without adequate sleep carries with it both short- and long-term consequences. In the short term, a lack of adequate sleep can affect judgment, mood, ability to learn and retain information, and may increase the risk of serious accidents and injury. In the long term, chronic sleep deprivation may lead to a host of health problems ...
Lack of sleep resulted in inadequate psychomotor performance and poor brain function. In order to combat the effects of sleep deprivation on one's physiological health, napping for a. short period of time and early in the day can be used to maintain optimal brain function. In.
What Makes a Good Sleep Deprivation Essay Topics. When it comes to writing an essay on sleep deprivation, choosing the right topic is crucial. A good essay topic should be thought-provoking, engaging, and relevant to the subject matter. In order to come up with a strong essay topic on sleep deprivation, it is important to consider various ...
This essay views sleep and sleep deprivation from five different motivational perspectives in order to gain a holistic understanding of the phenomena. From evolutionary, psychodynamic, behaviourist, cognitive, and hierarchy of needs perspectives, it is inferred that the cognitive and behaviourist perspectives uphold the most merit for gaining ...
Arguments in Support of the Idea. First, an adequate amount of sleep is associated with improved grades. It can be explained by the ability of the brain to stay more focused on the process of learning. For example, the overall course grades for students getting at least 7 hours of sleep were 50 percent better compared to the students who were ...
Sleep Deprivation Essay. Sleep is one of the most crucial functions of the human body. While a person's body sleeps, many essential processes are completed, such as the rest for one's body, the drainage of excess fluid and growth, amongst others. Regardless of the fact that sleep is such an essential process for the body, it is commonly ...
How sleep deprivation can harm your physical and mental health — or even turn fatal A YouTuber streamed his attempt to stay awake for 11 days straight, but sleep experts that spoke to the Star ...
Evidence & citing: First, the time young people spend on social media may actually encroach on the time that is available to sleep, this is the time displacement hyphothesis. Second, social media use is known to increase arousal. Third, when adolescents engage in social media use they are exposed to bright screen lights, which can disrupt the ...