- Technical Support
- Find My Rep

You are here
Statistical Methods in Medical Research
Preview this book.
- Description
- Aims and Scope
- Editorial Board
- Abstracting / Indexing
- Submission Guidelines
Statistical Methods in Medical Research is a highly ranked, peer reviewed scholarly journal and is the leading vehicle for articles in all the main areas of medical statistics and therefore an essential reference for all medical statisticians. It is particularly useful for medical researchers dealing with data and provides a key resource for medical and statistical libraries, as well as pharmaceutical companies.
This unique journal is devoted solely to statistics and medicine and aims to keep professionals abreast of the many powerful statistical methods now available to the medical profession. As new methods are constantly adopted by statisticians working both inside and outside the medical environment, this review journal aims to satisfy the increasing demand for accurate and up-to-the-minute information.
Why choose Statistical Methods in Medical Research?
- Contains both reviews and original papers of the latest statistical developments relevant to medical research
- Covers all areas of medical statistics
- Full of well-written papers by leading experts in the field
- Accessible to a wide audience of medical statisticians and statistically minded medical researchers
- An indispensable reference for medical statisticians, statistical libraries and pharmaceutical companies.
Books available to review from the US Book Review Editor
Books available to review from the UK Book Review Editor
Click here for the full list of Statistical Methods in Medical Research back issues
This journal is a member of the Committee on Publication Ethics (COPE).
Sign up for the latest table of content alerts.
Statistical Methods in Medical Research is a highly ranked, peer reviewed scholarly journal and is the leading vehicle for review and non-review articles in all the main areas of medical statistics. It is therefore an essential reference for all medical statisticians. It is particularly useful for medical researchers dealing with data and it provides a key resource for medical and statistical libraries, as well as pharmaceutical companies.
This unique journal is devoted solely to statistics and medicine and aims to keep professionals abreast of the many powerful statistical techniques now available to the medical profession. As techniques are constantly adopted by statisticians working both inside and outside the medical environment, this review journal aims to satisfy the increasing demand for accurate and up-to-the-minute information.
- Full of statistics and statistical techniques
- Contains the latest, accurate information
- Academic Search Premier
- Applied Social Sciences Index & Abstracts (ASSIA)
- Current Contents / Clinical Medicine
- Current Index To Statistics
- Current Mathmatical Publications
- EMBASE/Excerpta Medica
- Elsevier BIOBASE/Current Awareness in Biological Sciences
- ISI Discovery Agent
- Index Medicus
- Index Medicus (Ceased 2004)
- Journal Contents in Quantitative Methods
- Mathematical Reviews Database
- Science Citation Index
- Science Citation Index Expanded
- Zentralblatt MATH
Manuscript Submission Guidelines: Statistical Methods in Medical Research
This Journal is a member of the Committee on Publication Ethics .
This Journal recommends that authors follow the Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals formulated by the International Committee of Medical Journal Editors (ICMJE).
Please read the guidelines below then visit the Journal’s submission site http://mc.manuscriptcentral.com/smmr to upload your manuscript. Please note that manuscripts not conforming to these guidelines may be returned.
Only manuscripts of sufficient quality that meet the aims and scope of Statistical Methods in Medical Research (SMMR) will be reviewed.
There are no fees payable to submit or publish in this Journal. Open Access options are available - see section 3.3 below.
As part of the submission process you will be required to warrant that you are submitting your original work, that you have the rights in the work, and that you have obtained and can supply all necessary permissions for the reproduction of any copyright works not owned by you, that you are submitting the work for first publication in the Journal and that it is not being considered for publication elsewhere and has not already been published elsewhere. Please see our guidelines on prior publication and note that Statistical Methods in Medical Research may accept submissions of papers that have been posted on pre-print servers; please alert the Editorial Office when submitting (contact details are at the end of these guidelines) and include the DOI for the preprint in the designated field in the manuscript submission system. Authors should not post an updated version of their paper on the preprint server while it is being peer reviewed for possible publication in the journal. If the article is accepted for publication, the author may re-use their work according to the journal's author archiving policy.
- What do we publish? 1.1 Aims & Scope 1.2 Article types 1.3 Writing your paper
- Editorial policies 2.1 Peer review policy 2.2 Authorship 2.3 Acknowledgements 2.4 Funding 2.5 Declaration of conflicting interests 2.6 Research ethics and patient consent 2.7 Clinical trials 2.8 Reporting guidelines 2.9 Research Data
- Publishing policies 3.1 Publication ethics 3.2 Contributor's publishing agreement 3.3 Open access and author archiving
- Preparing your manuscript 4.1 Formatting 4.2 Artwork, figures and other graphics 4.3 Supplemental material 4.4 Reference style 4.5 Journal layout 4.6 English language editing services
- Submitting your manuscript 5.1 ORCID 5.2 Information required for completing your submission 5.3 Permissions
- On acceptance and publication 6.1 SAGE Production 6.2 Online First publication 6.3 Access to your published article 6.4 Promoting your article
- Further information
1. What do we publish?
1.1 Aims & Scope
Before submitting your manuscript to Statistical Methods in Medical Research , please ensure you have read the Aims & Scope .
1.2 Article Types
The aim of the journal is to publish both review types detailing the way particular statistical methods are (and could be) employed within medical research, and, accounts of innovative methodological developments or applications. The latter, although not review papers per se, should include an introduction that acts as a brief overview of the area to be discussed.
Both types of paper should include a motivating example or, in some cases, several examples and should be written to be accessible to a broad audience. This implies that material of a very technical nature should be relegated to an appendix.
The following papers, which have appeared in previous issues, might be taken as good examples of what the journal is aiming for:
Hudgens MG, Gilbert PB and Self SG. 2004; 13: 89-114 ( http://smm.sagepub.com/content/13/2/89.full.pdf+html ). Zhou H. 2006; 15: 181-194. ( http://smm.sagepub.com/content/15/2/181.full.pdf+html )
Authors should include their name and initials, their affiliations, and their address for correspondence with telephone and fax numbers or email address.
Papers should be around 8,000 words. Any diagrams or tables should be counted as equivalent to around 200 words or half a page of text. The editor should be informed if this is likely to be a problem.
An abstract of up to 200 words and a selection of keywords should precede the text. Any acknowledgements or conflicts of interest will be printed at the end of the text.
All authors need to follow the Statistical Methods in Medical Research reference style, authors that do not will find their paper returned to them. For more information please see 4.4 Reference Style .
Electronic versions: Microsoft Word is the preferred format, but files can be accepted from any common word processing program. PDF files should only be supplied in addition to source files. PDF files alone are not acceptable.
1.3 Writing your paper
The SAGE Author Gateway has some general advice and on how to get published , plus links to further resources. SAGE Author Services also offers authors a variety of ways to improve and enhance their article including English language editing, plagiarism detection, and video abstract and infographic preparation.
1.3.1 Make your article discoverable
When writing up your paper, think about how you can make it discoverable. The title, keywords and abstract are key to ensuring readers find your article through search engines such as Google. For information and guidance on how best to title your article, write your abstract and select your keywords, have a look at this page on the Gateway: How to Help Readers Find Your Article Online .
Back to top
2. Editorial policies
2.1 Peer review policy
The journal's policy is to obtain at least two independent reviews of each article. It operates a double blind peer reviewing policy in which the reviewer’s name is withheld from the author and, the author’s name from the reviewer. Referees will be encouraged to provide substantive, constructive reviews that provide suggestions for improving the work and distinguish between mandatory and non-mandatory recommendations.
2.2 Authorship
Papers should only be submitted for consideration once consent is given by all contributing authors. Those submitting papers should carefully check that all those whose work contributed to the paper are acknowledged as contributing authors.
The list of authors should include all those who can legitimately claim authorship. This is all those who:
- Made a substantial contribution to the concept or design of the work; or acquisition, analysis or interpretation of data,
- Drafted the article or revised it critically for important intellectual content,
- Approved the version to be published,
- Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Authors should meet the conditions of all of the points above. When a large, multicentre group has conducted the work, the group should identify the individuals who accept direct responsibility for the manuscript. These individuals should fully meet the criteria for authorship.
Acquisition of funding, collection of data, or general supervision of the research group alone does not constitute authorship, although all contributors who do not meet the criteria for authorship should be listed in the Acknowledgments section. Please refer to the International Committee of Medical Journal Editors (ICMJE) authorship guidelines for more information on authorship.
Please note that AI chatbots, for example ChatGPT, should not be listed as authors. For more information see the policy on Use of ChatGPT and generative AI tools .
2.3 Acknowledgements
All contributors who do not meet the criteria for authorship should be listed in an Acknowledgements section. Examples of those who might be acknowledged include a person who provided purely technical help, or a department chair who provided only general support.
Please supply any personal acknowledgements separately to the main text to facilitate anonymous peer review.
2.3.1 Third party submissions
Where an individual who is not listed as an author submits a manuscript on behalf of the author(s), a statement must be included in the Acknowledgements section of the manuscript and in the accompanying cover letter. The statements must:
- Disclose this type of editorial assistance – including the individual’s name, company and level of input
- Identify any entities that paid for this assistance
- Confirm that the listed authors have authorized the submission of their manuscript via third party and approved any statements or declarations, e.g. conflicting interests, funding, etc.
Where appropriate, SAGE reserves the right to deny consideration to manuscripts submitted by a third party rather than by the authors themselves .
2.3.2 Writing assistance
Individuals who provided writing assistance, e.g. from a specialist communications company, do not qualify as authors and so should be included in the Acknowledgements section. Authors must disclose any writing assistance – including the individual’s name, company and level of input – and identify the entity that paid for this assistance. It is not necessary to disclose use of language polishing services.
2.4 Funding
Statistical Methods in Medical Research requires all authors to acknowledge their funding in a consistent fashion under a separate heading. Please visit the Funding Acknowledgements page on the SAGE Journal Author Gateway to confirm the format of the acknowledgment text in the event of funding, or state that: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
2.5 Declaration of conflicting interests
It is the policy of Statistical Methods in Medical Research to require a declaration of conflicting interests from all authors enabling a statement to be carried within the paginated pages of all published articles.
Please ensure that a ‘Declaration of Conflicting Interests’ statement is included at the end of your manuscript, after any acknowledgements and prior to the references. If no conflict exists, please state that ‘The Author(s) declare(s) that there is no conflict of interest’. For guidance on conflict of interest statements, please see the ICMJE recommendations here .
2.6 Research ethics and patient consent
Medical research involving human subjects must be conducted according to the World Medical Association Declaration of Helsinki .
Submitted manuscripts should conform to the ICMJE Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals , and all papers reporting animal and/or human studies must state in the methods section that the relevant Ethics Committee or Institutional Review Board provided (or waived) approval. Please ensure that you have provided the full name and institution of the review committee, in addition to the approval number.
For research articles, authors are also required to state in the methods section whether participants provided informed consent and whether the consent was written or verbal.
Information on informed consent to report individual cases or case series should be included in the manuscript text. A statement is required regarding whether written informed consent for patient information and images to be published was provided by the patient(s) or a legally authorized representative. Please do not submit the patient’s actual written informed consent with your article, as this in itself breaches the patient’s confidentiality. The Journal requests that you confirm to us, in writing, that you have obtained written informed consent but the written consent itself should be held by the authors/investigators themselves, for example in a patient’s hospital record. The confirmatory letter may be uploaded with your submission as a separate file.
Please also refer to the ICMJE Recommendations for the Protection of Research Participants .
2.7 Clinical trials
Statistical Methods in Medical Research conforms to the ICMJE requirement that clinical trials are registered in a WHO-approved public trials registry at or before the time of first patient enrolment as a condition of consideration for publication. The trial registry name and URL, and registration number must be included at the end of the abstract.
2.8 Reporting guidelines
The relevant EQUATOR Network reporting guidelines should be followed depending on the type of study. For example, all randomized controlled trials submitted for publication should include a completed CONSORT flow chart as a cited figure and the completed CONSORT checklist should be uploaded with your submission as a supplementary file. Systematic reviews and meta-analyses should include the completed PRISMA flow chart as a cited figure and the completed PRISMA checklist should be uploaded with your submission as a supplementary file. The EQUATOR wizard can help you identify the appropriate guideline.
Other resources can be found at NLM’s Research Reporting Guidelines and Initiatives .
The journal is committed to facilitating openness, transparency and reproducibility of research, and has the following research data sharing policy. For more information, including FAQs please visit the SAGE Research Data policy pages .
Subject to appropriate ethical and legal considerations, authors are encouraged to:
- share your research data in a relevant public data repository
- include a data availability statement linking to your data. If it is not possible to share your data, we encourage you to consider using the statement to explain why it cannot be shared.
- cite this data in your research
Statistical Methods in Medical Research requests all authors submitting any primary data used in their research articles [“alongside their article submissions” or “if the articles are accepted”] to be published in the online version of the journal, or provide detailed information in their articles on how the data can be obtained. This information should include links to third-party data repositories or detailed contact information for third-party data sources. Data available only on an author-maintained website will need to be loaded onto either the journal’s platform or a third-party platform to ensure continuing accessibility. Examples of data types include but are not limited to statistical data files, replication code, text files, audio files, images, videos, appendices, and additional charts and graphs necessary to understand the original research. The editor can also grant exceptions for data that cannot legally or ethically be released. All data submitted should comply with Institutional or Ethical Review Board requirements and applicable government regulations.
3. Publishing Policies
3.1 Publication ethics
SAGE is committed to upholding the integrity of the academic record. We encourage authors to refer to the Committee on Publication Ethics’ International Standards for Authors and view the Publication Ethics page on the SAGE Author Gateway .
3.1.1 Plagiarism
Statistical Methods in Medical Research and SAGE take issues of copyright infringement, plagiarism or other breaches of best practice in publication very seriously. We seek to protect the rights of our authors and we always investigate claims of plagiarism or misuse of published articles. Equally, we seek to protect the reputation of the journal against malpractice. Submitted articles may be checked with duplication-checking software. Where an article, for example, is found to have plagiarised other work or included third-party copyright material without permission or with insufficient acknowledgement, or where the authorship of the article is contested, we reserve the right to take action including, but not limited to: publishing an erratum or corrigendum (correction); retracting the article; taking up the matter with the head of department or dean of the author's institution and/or relevant academic bodies or societies; or taking appropriate legal action.
3.1.2 Prior publication
If material has been previously published it is not generally acceptable for publication in a SAGE journal. However, there are certain circumstances where previously published material can be considered for publication. Please refer to the guidance on the SAGE Author Gateway or if in doubt, contact the Editor at the address given below.
3.2 Contributor's publishing agreement
Before publication, SAGE requires the author as the rights holder to sign a Journal Contributor’s Publishing Agreement. SAGE’s Journal Contributor’s Publishing Agreement is an exclusive licence agreement which means that the author retains copyright in the work but grants SAGE the sole and exclusive right and licence to publish for the full legal term of copyright. Exceptions may exist where an assignment of copyright is required or preferred by a proprietor other than SAGE. In this case copyright in the work will be assigned from the author to the society. For more information please visit the SAGE Author Gateway
3.3 Open access and author archiving
Statistical Methods in Medical Research offers optional open access publishing via the Sage Choice programme and Open Access agreements, where authors can publish open access either discounted or free of charge depending on the agreement with Sage. Find out if your institution is participating by visiting Open Access Agreements at Sage . For more information on Open Access publishing options at Sage please visit Sage Open Access . For information on funding body compliance, and depositing your article in repositories, please visit Sage’s Author Archiving and Re-Use Guidelines and Publishing Policies .
4. Preparing your manuscript for submission
4.1 Formatting
The preferred format for your manuscript is Word. LaTeX files are also accepted. The text should be double-spaced throughout and with a minimum of 3cm for left and right hand margins and 5cm at head and foot. Text should be standard 10 or 12 point.Word and (La)Tex templates are available on the Manuscript Submission Guidelines page of our Author Gateway.We recommend using Bibitem rather than Bibtex for reference formatting.
4.2 Artwork, figures and other graphics
For guidance on the preparation of illustrations, pictures and graphs in electronic format, please visit SAGE’s Manuscript Submission Guidelines .
Images should be supplied as bitmap based files (i.e. with .tiff or .jpeg extension) with a resolution of at least 300 dpi (dots per inch). Line art should be supplied as vector-based, separate .eps files (not as .tiff files, and not only inserted in the Word or pdf file), with a resolution of 600 dpi. Images should be clear, in focus, free of pixilation and not too light or dark.
In text: tables and figures are either inserted as part of a sentence, for example table 1 or in parentheses for example (figure 1). Each table should carry a descriptive heading. Each figure should be submitted electronically.
Line drawings should be black and white. Figures should ideally be produced for a reduction of one third i.e. 3:2 or 150:100 mm.
Figures supplied in colour will appear in colour online regardless of whether or not these illustrations are reproduced in colour in the printed version. For specifically requested colour reproduction in print, you will receive information regarding the costs from SAGE after receipt of your accepted article.
4.3 Supplemental material
This journal is able to host additional materials online (e.g. datasets, podcasts, videos, images etc) alongside the full-text of the article. For more information please refer to our guidelines on submitting supplemental files
4.4 Reference style
Statistical Methods in Medical Research adheres to the SAGE Vancouver reference style. View the SAGE Vancouver guidelines to ensure your manuscript conforms to this reference style. Manuscripts with references not in this style will be returned.
If you use EndNote to manage references, you can download the SAGE Vancouver EndNote output file .
4.5 Journal Layout
When preparing your paper: - Use the minimum formatting. - Roman, bold and italic type can be used, but use only one typeface and size. - Capitals should be used only where they are to appear in the finished text. - The text should be ranged left and unjustified, with hyphenation cancelled. - Indents, underlining and tabs should be avoided unless absolutely necessary. - Headings and paragraphs should be separated by two carriage returns. - There should be only one space between words and only one space after any punctuation.
Abbreviations should be spelled out when first used in the text. Full stops should be used in lower case abbreviations (e.g., i.e.) but not for capitals (SAS, ANOVA). Spelling should follow the Oxford Dictionary.
Mathematical: All vectors and matrices should be shown in bold type. Numbers below 10 should be written out in the text unless used in conjunction with units (e.g. three apples, 4 kg).
Full points (not commas) should be used for decimals. For numbers less than one, a nought should be inserted before the decimal point. Use spaces (not commas) within numbers (e.g. 10 000, 0.125 275).
4.6 English language editing services
Authors seeking assistance with English language editing, translation, or figure and manuscript formatting to fit the journal’s specifications should consider using SAGE Language Services. Visit SAGE Language Services on our Journal Author Gateway for further information.
5. Submitting your manuscript
Statistical Methods in Medical Research is hosted on SAGE Track, a web based online submission and peer review system powered by ScholarOne™ Manuscripts. Visit https://mc.manuscriptcentral.com/smmr to login and submit your article online.
IMPORTANT: Please check whether you already have an account in the system before trying to create a new one. If you have reviewed or authored for the journal in the past year it is likely that you will have had an account created. For further guidance on submitting your manuscript online please visit ScholarOne Online Help .
As part of our commitment to ensuring an ethical, transparent and fair peer review process SAGE has become a supporting member of ORCID, the Open Researcher and Contributor ID . ORCID provides a persistent digital identifier that distinguishes researchers from every other researcher and, through integration in key research workflows such as manuscript and grant submission, supports automated linkages between researchers and their professional activities ensuring that their work is recognized.
The collection of ORCID iDs from corresponding authors is now part of the submission process of this journal. If you already have an ORCID iD you will be asked to associate that to your submission during the online submission process. We also strongly encourage all co-authors to link their ORCID ID to their accounts in our online peer review platforms. It takes seconds to do: click the link when prompted, sign into your ORCID account and our systems are automatically updated. Your ORCID iD will become part of your accepted publication’s metadata, making your work attributable to you and only you. Your ORCID iD is published with your article so that fellow researchers reading your work can link to your ORCID profile and from there link to your other publications.
If you do not already have an ORCID iD please follow this link to create one or visit our ORCID homepage to learn more.
5.2 Information required for completing your submission
You will be asked to provide contact details and academic affiliations for all co-authors via the submission system and identify who is to be the corresponding author. These details must match what appears on your manuscript. The affiliation listed in the manuscript should be the institution where the research was conducted. If an author has moved to a new institution since completing the research, the new affiliation can be included in a manuscript note at the end of the paper. At this stage please ensure you have included all the required statements and declarations and uploaded any additional supplementary files (including reporting guidelines where relevant).
5.3 Permissions
Please also ensure that you have obtained any necessary permission from copyright holders for reproducing any illustrations, tables, figures or lengthy quotations previously published elsewhere. For further information including guidance on fair dealing for criticism and review, please see the Copyright and Permissions page on the SAGE Author Gateway .
6. On acceptance and publication
6.1 SAGE Production
Your SAGE Production Editor will keep you informed as to your article’s progress throughout the production process. Proofs will be made available to the corresponding author via our editing portal SAGE Edit or by email, and corrections should be made directly or notified to us promptly. Authors are reminded to check their proofs carefully to confirm that all author information, including names, affiliations, sequence and contact details are correct, and that Funding and Conflict of Interest statements, if any, are accurate.
6.2 Online First publication
Online First allows final articles (completed and approved articles awaiting assignment to a future issue) to be published online prior to their inclusion in a journal issue, which significantly reduces the lead time between submission and publication. Visit the SAGE Journals help page for more details, including how to cite Online First articles.
6.3 Access to your published article
SAGE provides authors with online access to their final article.
6.4 Promoting your article
Publication is not the end of the process! You can help disseminate your paper and ensure it is as widely read and cited as possible. The SAGE Author Gateway has numerous resources to help you promote your work. Visit the Promote Your Article page on the Gateway for tips and advice.
7. Further information
Any correspondence, queries or additional requests for information on the manuscript submission process should be sent to the Statistical Methods in Medical Research editorial office at [email protected] .
- Read Online
- Sample Issues
- Current Issue
- Email Alert
- Permissions
- Foreign rights
- Reprints and sponsorship
- Advertising
Member Subscription, Combined (Print & E-access)
Individual Subscription, Combined (Print & E-access)
Institutional Backfile Purchase, E-access (Content through 1998)
Institutional Subscription, E-access
Institutional Subscription & Backfile Lease, E-access Plus Backfile (All Online Content)
Institutional Subscription, Print Only
Institutional Subscription, Combined (Print & E-access)
Institutional Subscription & Backfile Lease, Combined Plus Backfile (Current Volume Print & All Online Content)
Individual, Single Print Issue
Institutional, Single Print Issue
To order single issues of this journal, please contact SAGE Customer Services at 1-800-818-7243 / 1-805-583-9774 with details of the volume and issue you would like to purchase.
The Use of Statistics in Health Sciences: Situation Analysis and Perspective
- Published: 06 January 2016
- Volume 8 , pages 204–219, ( 2016 )
Cite this article

- Ricardo Ocaña-Riola 1 , 2
1079 Accesses
5 Citations
7 Altmetric
Explore all metrics
Statistics plays a crucial role in research, planning and decision-making in the health sciences. Progress in technologies and continued research in computational statistics has enabled us to implement sophisticated mathematical models within software that are handled by non-statistician researchers. As a result, over the last decades, medical journals have published a host of papers that use some novel statistical method. The aim of this paper is to present a review on how the statistical methods are being applied in the construction of scientific knowledge in health sciences, as well as, to propose some improvement actions. From the early twentieth century, there has been a remarkable surge in scientific evidence alerting on the errors that many non-statistician researchers were making in applying statistical methods. Today, several studies continue showing that a large percentage of articles published in high-impact factor journals contain errors in data analysis or interpretation of results, with the ensuing repercussions on the validity and efficiency of the research conducted. Scientific community should reflect on the causes that have led to this situation, the consequences to the advancement of scientific knowledge and the solutions to this problem.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

What is Qualitative in Qualitative Research
Patrik Aspers & Ugo Corte
Criteria for Good Qualitative Research: A Comprehensive Review
Drishti Yadav

Sampling Techniques for Quantitative Research
Ahmed M (2011) Meeting report: ISOSS Lahore conference. IMS Bull 40(5):11
Google Scholar
Altman DG (1994) The scandal of poor medical research. Br Med J 308:283–284
Article Google Scholar
Altman DG (1998) Statistical reviewing for medical journals. Stat Med 17:2661–2674
Altman DG (2002) Poor-quality medical research: what can journals do? J Am Med Assoc 287:2765–2767
Altman DG, Goodman SN, Schroter S (2002) How statistical expertise is used in medical research. J Am Med Assoc 287(21):2817–2820
Armitage P, Berry G, Matthews JNS (2002) Statistical methods in medical research, 4th edn. Blackwell Scientific, Oxford
Book Google Scholar
Azoulay P, Zivin JSG, Manso G (2011) Incentives and creativity: evidence from the academic life sciences. RAND J Econ 42(3):527–554
Basskin L (2003) Statistical interpretation can also bias research evidence. Br Med J 327(7417):752
Block WM, Morrison ML (2007) Tread lightly or carry a big stick? J Wildl Manage 71(2):301–302
Bornmann L, Daniel HD (2008) What do citation counts measure? A review of studies on citing behaviour. J Doc 64(1):45–80
Breen KJ (2003) Misconduct in medical research: whose responsibility? Intern Med J 33:186–191
Buchan IE (2000) StatsDirect-statistical software for medical research in the 21st century. Br Med J 321:7275
Buyse M, George SL, Evans S, Geller NL, Ranstam J, Scherrer B et al (1999) The role of biostatistics in the prevention, detection and treatment of fraud in clinical trials. Stat Med 18:3435–3451
Cartera RL, Scheafferb RL, Marksa RG (1986) The role of consulting units in statistics departments. Am Stat 40(4):260–264
Committee on Professional Ethics (1999) Ethical guidelines for statistical practice. American Statistical Association. www.amstat.org/about/ethicalguidelines.cfm . Accessed 17 Dec 2015
De Jonge B, Louwaars N (2009) Valorizing science: whose values? EMBO Rep 10(6):535–539
Dormolen JV (1991) Metaphors mediating the teaching and understanding of mathematics. In: Bishop AJ, Mellin-Olsen S, Dormolen JV (eds) Mathematical knowledge: its growts through teaching. Kluwer Academic Publishers, The Netherlands, pp 89–106
Dufault B, Klar N (2011) The quality of modern cross-sectional ecologic studies: a bibliometric review. Am J Epidemiol 174(10):1101–1107
Ercan I, Yaz \(\imath \) c \(\imath \) B, Yang Y, Özkaya G, Cangur S, Ediz B, Kan I (2007) Misusage of statistics in medical research. Eur J Gen Med 4(3):128–134
Fang FC, Steen RG, Casadevall A (2012) Misconduct accounts for the majority of retracted scientific publications. Proc Natl Acad Sci USA 109(42):17028–17033
Felson DT, Cupples LA, Meenan RF (1984) Misuse of statistical methods in arthritis and rheumatism. Arthritis Rheum 27(9):1018–1022
Fernandes-Taylor S, Hyun JK, Reeder RN, Harris AHS (2011) Common statistical and research design problems in manuscripts submitted to high-impact medical journals. BMC Res Notes 4:304
Fisher R (1955) Statistical methods and scientific induction. J R Stat Soc B 17(1):69–78
MathSciNet MATH Google Scholar
Gal I (2002) Adults’ statistical literacy: meanings, components, responsibilities. Int Stat Rev 70(1):1–51
Article MATH Google Scholar
García E, Alcaraz C (2004) Incongruence between test statistics and P values in medical papers. BMC Med Res Methodol 4:13
Gardner MJ, Machin D, Campbell MJ (1986) Use of check lists in assessing the statistical content of medical studies. Br Med J 292(22):810–812
Gelles RJ (1993) From yellow pads, to typewriters, to wordprocessors: confessions of a. writer?, author?, scholar? Marriage Fam Rev 18(1–2):81–92
Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S (2007) Helping doctors and patients make sense of health statistics. Psychol Sci Public Interest 8(2):53–96
Hall HR, Roussel LA (2012) Evidence-based practice: an integrative approach to research, administration and practice. Jones & Bartlett Learning, Burlington
Health & Medicine Week (2004) Published research contains high level of statistical errors. 21 June, p 887
Herman A, Notzer N, Libman Z, Braunstein R, Steinberg DM (2007) Statistical education for medical students: concepts are what remain when the details are forgotten. Stat Med 26(23):4344–4351
Article MathSciNet Google Scholar
ISI Council (2010) Declaration on professional ethics. International Statistical Institute, Reykjavik
Judson HF (2004) The great betrayal: fraud in science. Harcourt, New York
Lewis JA (1999) Statistical principles for clinical trials (ICH E9): an introductory note on an international guideline. Stat Med 18:1903–1904
Lipworth WL, Kerridge IH, Carter SM, Little M (2011) Journal peer review in context: a qualitative study of the social and subjective dimensions of manuscript review in biomedical publishing. Soc Sci Med 72:1056–1063
Marks RG, Dawson-Saunders EK, Bailar JC, Dan BB, Verran JA (1988) Interactions between statisticians and biomedical journal editors. Stat Med 7(10):1003–1011
Matcham J, Julious S, Pyke S, O’Kelly M, Todd S, Seldrup J, Day S (2011) Proposed best practice for statisticians in the reporting and publication of pharmaceutical industry-sponsored clinical trials. Pharm Stat 10:70–73
Michel MC (2014) How significant are your data? The need for a culture shift. Naunyn Schmiedebergs Arch Pharmakol 387:1015–1016
Micheel CM, Nass SJ, Omenn GS (eds) (2012) Evolution of translational omics: lessons learned and the path forward. The National Acadamies Press, Washington, DC
Monmonier M (1996) How to lie with maps, 2nd edn. University of Chicago Press, London
Book MATH Google Scholar
Moriguti S, Diggle PJ, Gower JC, Wallman KK, Ren WS (1992) The role of statisticians: report of the Ad Hoc Committee. Int Stat Rev 60(3):227–246
Nicholls D (1999) Statistics into the 21st century (with discussion). Aust N Z J Stat 41(2):127
Article MathSciNet MATH Google Scholar
Ocaña-Riola R (2007) The misuse of count data aggregated over time for disease mapping. Stat Med 26(24):4489–4504
Ocaña-Riola R (2010) Common errors in disease mapping. Geospat Health 4(2):139–154
OECD (2010) PISA 2009 assessment framework: key competencies in reading, mathematics and science. OECD, Paris
Pike MC, Berstein L (1985) Statistical errors invalidate conclusions in “caffeine and unsaturated fat diet significantly promotes DMBA-induced breast cancer in rats”. Cancer 55(8):1855–1857
Russell L (2011) The spread of evidence-poor medicine via flawed social-network analysis. Stat Politics Policy 2(1)
Salsburg DS (1985) The religion of statistics as practiced in medical journals. Am Stat 39(3):220–223
Schafer A (2004) Biomedical conflicts of interest: a defence of the sequestration thesis learning from the cases of Nancy Olivieri and David Healy. J Med Ethics 30:8–24
Schroter S, Black N, Evans S, Godlee F, Osorio L, Smith R (2008) What errors do peer reviewers detect, and does training improve their ability to detect them? J R Soc Med 101:507–514
Schurz G (2014) Philosophy of science: a unified approach. Routledge, New York
Shatz D (2004) Peer review: a critical inquiry. Rowman & Littlefield Publishers, Maryland
Shulman LS (1986) Those who understand: knowledge growth in teaching. Educ Res 15:4–14
Siegfried T (2010) Odds are, it’s wrong: science fails to face the shortcomings of statistics. Sci News 177(7):1–13
Smith D, Neutra RR (1993) Approaches to disease cluster investigations in a state health department. Stat Med 12:1757–1762
Smith R (2001) Medical editor lambasts journals and editors. Br Med J 323:651
Smith RW (2009) In search of an optimal peer review system. J Particip Med 1(1):e13
Snee R (1990) Statistical thinking and its contribution to quality. Am Stat 44:116–121
Sokal A, Bricmont J (1997) Impostures intellectuelles. Odile Jacob, Paris
Starbuck WH (2005) How much better are the most-prestigious journals? The statistics of academic publication. Organ Sci 16(2):180–200
Stephen LG (1985) Statistics in medical journals: a survey of current policies and proposals for editors. Med Pediatr Oncol 13(2):109–112
Stuart TE, Ding WW (2006) When do scientists become entrepreneurs? The social structural antecedents of commercial activity in the academic life sciences. Am J Sociol 112(1):97–144
Wang Q, Zhang B (1998) Research design and statistical methods in Chinese medical journals. J Am Med Assoc 280(3):283–285
Ware JH (2005) Statistical review for medical journals. In: Armitage P, Colton T (eds) Encyclopedia of biostatistics. Harvard School of Public Health, Boston
White KL (1967) Improved medical care statistics and the health services system. Public Health Rep 82(10):847–854
White KL (1973) Priorities for health services information. Health Serv Rep 88(2):106–112
White SJ (1979) Statistical errors in papers in the British Journal of Psychiatry. Br J Psychiatry 135:336–342
Wild CJ, Pfannkuch M (1999) Statistical thinking in empirical enquiry. Int Stat Rev 67(3):223–265
Zeger SL, Diggle PJ, Liang KY (2004) A Cox model for biostatistics of the future [Department of Biostatistics working paper]. Johns Hopkins University, Berkeley
Download references
Author information
Authors and affiliations.
Escuela Andaluza de Salud Pública, Campus Universitario de Cartuja, Cuesta del Observatorio 4, Apdo. 2070, 18011, Granada, Spain
Ricardo Ocaña-Riola
Instituto de Investigación Biosanitaria de Granada, Granada, Spain
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ricardo Ocaña-Riola .
Rights and permissions
Reprints and permissions
About this article
Ocaña-Riola, R. The Use of Statistics in Health Sciences: Situation Analysis and Perspective. Stat Biosci 8 , 204–219 (2016). https://doi.org/10.1007/s12561-015-9138-4
Download citation
Received : 16 November 2015
Revised : 17 December 2015
Accepted : 22 December 2015
Published : 06 January 2016
Issue Date : October 2016
DOI : https://doi.org/10.1007/s12561-015-9138-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health Sciences
- Medical research
- Statistical methods
- Statistical errors
- Find a journal
- Publish with us
- Track your research
Statistics in medicine
Affiliation.
- 1 Stanford, Calif. From the Department of Surgery, Stanford University School of Medicine.
- PMID: 21200241
- DOI: 10.1097/PRS.0b013e3181f95dd2
The scope of biomedical research has expanded rapidly during the past several decades, and statistical analysis has become increasingly necessary to understand the meaning of large and diverse quantities of raw data. As such, a familiarity with this lexicon is essential for critical appraisal of medical literature. This article attempts to provide a practical overview of medical statistics, with an emphasis on the selection, application, and interpretation of specific tests. This includes a brief review of statistical theory and its nomenclature, particularly with regard to the classification of variables. A discussion of descriptive methods for data presentation is then provided, followed by an overview of statistical inference and significance analysis, and detailed treatment of specific statistical tests and guidelines for their interpretation.
Publication types
- Statistics as Topic*
- Terminology as Topic
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Research: More People Use Mental Health Benefits When They Hear That Colleagues Use Them Too
- Laura M. Giurge,
- Lauren C. Howe,
- Zsofia Belovai,
- Guusje Lindemann,
- Sharon O’Connor

A study of 2,400 Novartis employees around the world found that simply hearing about others’ struggles can normalize accessing support at work.
Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager for the training, uptake of the program remains low. To understand why, a team of researchers conducted a randomized controlled trial with 2,400 Novartis employees who worked in the UK, Ireland, India, and Malaysia. Employees were shown one of six framings that were designed to overcome two key barriers: privacy concerns and usage concerns. They found that employees who read a story about their colleague using the service were more likely to sign up to learn more about the program, and that emphasizing the anonymity of the program did not seem to have an impact. Their findings suggest that one way to encourage employees to make use of existing mental health resources is by creating a supportive culture that embraces sharing about mental health challenges at work.
“I almost scheduled an appointment about a dozen times. But no, in the end I never went. I just wasn’t sure if my problems were big enough to warrant help and I didn’t want to take up someone else’s time unnecessarily.”
- Laura M. Giurge is an assistant professor at the London School of Economics, and a faculty affiliate at London Business School. Her research focuses on time and boundaries in organizations, workplace well-being, and the future of work. She is also passionate about translating research to the broader public through interactive and creative keynote talks, workshops, and coaching. Follow her on LinkedIn here .
- Lauren C. Howe is an assistant professor in management at the University of Zurich. As head of research at the Center for Leadership in the Future of Work , she focuses on how human aspects, such as mindsets, socioemotional skills, and leadership, play a role in the changing world of work.
- Zsofia Belovai is a behavioral science lead for the organizational performance research practice at MoreThanNow, focusing on exploring how employee welfare can drive KPIs.
- Guusje Lindemann is a senior behavioral scientist at MoreThanNow, in the social impact and organizational performance practices, working on making the workplace better for all.
- Sharon O’Connor is the global employee wellbeing lead at Novartis. She is a founding member of the Wellbeing Executives Council of The Conference Board, and a guest lecturer on the Workplace Wellness postgraduate certificate at Trinity College Dublin.
Partner Center
- Open access
- Published: 22 April 2024
The effect of peer mentoring program on clinical academic progress and psychological characteristics of operating room students: a parallel randomized controlled trial
- Amin Sedigh 1 ,
- Sara Bagheri 2 ,
- Pariya Naeimi 3 ,
- Vahid Rahmanian 4 &
- Nader Sharifi 5
BMC Medical Education volume 24 , Article number: 438 ( 2024 ) Cite this article
Metrics details
One of the new educational systems is the mentorship method. This study aimed to investigate the effect of peer mentoring program on clinical academic progress and psychological characteristics of operating room students.
This research was a randomized controlled trial that was conducted on undergraduate students in the operating room department of Khomein Faculty of Medical Sciences, Markazi Province in Iran. The number of operating room students were 70 that were divided into intervention and control groups by random allocation using Permuted Block Randomization. Inclusion criteria included all operating room students who were in internship, and exclusion criteria included failure to complete the questionnaires. The data collection tools were the demographic questionnaire, Depression Anxiety Stress Scale, Rosenberg Self-Esteem Scale and Situational Motivational Scale. In the control group, clinical training was done in the traditional way. In the intervention group, training was done by peer mentoring method. The obtained data were analyzed using descriptive statistics, independent t-test, paired t-test, chi-square test, ANCOVA, univariable and multivariable linear regression.
The study revealed significant differences between the intervention and control groups. Post-intervention, the intervention group demonstrated substantial increases in self-confidence (mean difference = 5.97, p < 0.001) and significant reductions in stress levels (mean difference = -3.22, p < 0.001). Conversely, minimal changes were noted in the control group for both self-confidence (mean difference = 0.057, p = 0.934) and stress levels (mean difference = 0.142, p = 0.656). Although both groups experienced decreases in anxiety and depression levels, these changes were not statistically significant ( p > 0.05). Furthermore, the intervention significantly enhanced academic progress in the intervention group compared to the control group (mean difference = 20.31, p < 0.001).
The results showed that the implementation of the peer mentoring program was effective in improving academic progress, self-confidence, and reducing the stress of operating room students. Therefore, this educational method can be used in addition to the usual methods to improve the education of operating room students.
Peer Review reports
Introduction
Using effective training methods can increase people's motivation and commitment, increase productivity and reduce mistakes [ 1 ]. Clinical training is an important part of training in medical sciences, which plays an essential role in shaping the basic skills and professional abilities of students, including students of the operating room [ 2 , 3 ]. Learning and mastering work roles and tasks in the operating room environment is challenging; In addition, operating room students should be trained in many interventions in the surgical process before, during and after surgery [ 4 ].
Operating room students are affected by various stresses during the course of clinical training, and various contextual and environmental factors play a role in creating this stress [ 5 ]. The results of a study among nursing students showed the prevalence of depression, anxiety and stress symptoms to be 28.7%, 41.7% and 20.2%, respectively [ 6 ]. Also, studies have shown students' self-efficacy at an average level [ 7 ]. The experience of stress in the clinical environment can affect students' learning and acquisition of clinical skills and lead to a drop in their academic performance [ 8 , 9 ]. Considering the high level of stress and the fact that mistakes have no place in the operating room, it is important to pay attention to the quality of training of operating room students and to strengthen the knowledge and skills of future operating room personnel [ 10 ].
Learners and students prefer new educational methods to traditional and passive methods. Active approach is a form of teacher-learner interaction in which learners are no longer passive listeners, but active participants in the learning process [ 11 , 12 ]. The basis of active and comprehensive learning methods is that learning is based on experience and learners actively create knowledge based on their personal experience [ 13 , 14 , 15 ]. The importance of active learning has led professional associations and accreditation organizations, as well as organizations such as UNESCO, to recommend active learning methods in education [ 16 ].
One of the new educational systems is the mentorship method. In this educational method, the mentor and mentee establish a long-term relationship based on friendship with each other. Positive attitude, experience and volunteering are characteristics of mentorship [ 17 , 18 ]. For the first time, Whitman and Fife examined the peer teaching strategy in university education. In this method, higher year students teach practical and theoretical lessons to lower year students [ 19 , 20 ]. The implementation of the mentorship program increases self-confidence, emotional support, and increases students' interactions [ 21 , 22 ]. When students, despite having knowledge and ability in clinical practice, lack sufficient competence, the reason may be a lack of self-confidence, confidence in their own ability, or understanding of the necessary self-efficacy [ 23 , 24 ]. This study was conducted with the aim of investigating the effect of peer mentoring program on clinical academic progress and psychological characteristics of operating room students.
Study design
This research was a parallel randomized controlled trial that was conducted on undergraduate students in the operating room department of Khomein Faculty of Medical Sciences, Markazi Province in Iran from September 2022 to April 2023.
Participants
The number of operating room students were 70, who were included in the study by census method. Inclusion criteria included all operating room students who were in internship, and exclusion criteria included failure to complete the questionnaires.
Randomization and blindness
First, the students completed the written consent to participate in the study, and then they were divided into intervention and control groups by random allocation using Permuted Block Randomization [ 25 ]. Therefore, 35 participants were placed in each group. Then the participants of the intervention and control groups completed the questionnaires before the beginning of the internship. Due to the nature of the intervention in the present study, it was not possible to blind the subjects under the study. Therefore, blinding was performed on those who collected and recorded the data and those who performed the analysis. This research was designed and implemented according to the CONSORT guidelines (Fig. 1 ).
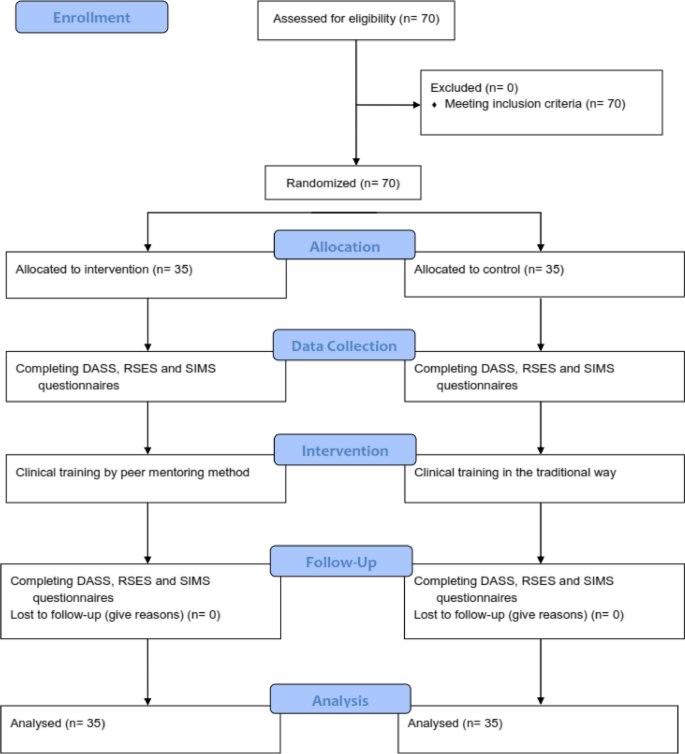
Consort -flow- diagram
Instrument and data collection
The demographic questionnaire included gender, age, marital status, economic status of the family, education level of parents and occupation of parents.
Depression Anxiety Stress Scale (DASS) consists of three subscales including 7 questions for each. Each question is scored from 0 (does not apply to me at all) to 3 (completely applies to me). Each of the areas of stress, anxiety and depression has 7 questions and the minimum score for each area is 0 and the maximum score is 21. The score of each area is obtained from the sum of the scores of the answers given to the questions of that area. Antony et al. analyzed the mentioned scale; The results of the correlation calculation indicated a correlation coefficient of 0.48 between the two factors of depression and stress, a correlation coefficient of 0.53 between anxiety and stress, and a correlation coefficient of 0.28 between anxiety and depression [ 26 ]. The reliability of this scale in Iran in a sample of 400 participants was reported as 0.7 for depression, 0.66 for anxiety and 0.76 for stress [ 27 ]. Also, in the validation study of this questionnaire in Iran by Sahebi et al. the reliability of this scale was investigated through internal consistency and its validity using factor analysis and criterion validity with the simultaneous implementation of Beck depression, Zang anxiety and perceived stress tests. In general, the obtained reliability and validity coefficients were very satisfactory and significant at the p < 0.001 level. The correlations between DASS depression subscale with Beck depression test were 0.70, DASS anxiety subscale with Zang anxiety test was 0.67, and DASS stress subscale with perceived stress test was 0.49. The internal consistency of DASS scales was also calculated using Cronbach's alpha and these results were obtained: depression 0.77, anxiety 0.79 and stress 0.78 [ 28 ].
Rosenberg Self-Esteem Scale (RSES) consists of 10 two-choice questions. Every statement that applies to the person receives the answer "I agree" and every statement that does not apply to the person receives the answer "I disagree". A positive answer to each of statements 1 to 5 will receive a positive score of one, a negative response to statements 1 to 5 will receive a negative score of one, a positive response to statements 6 to 10 will receive a negative score of one, and a negative response to statements 6 to 10 will receive a positive score of one. Then the total score is calculated. A positive score of 10 indicates the highest level of self-esteem, and a negative score of 10 indicates very low self-esteem. The retest correlation is in the range of 0.82–0.88 and the internal consistency coefficient or Cronbach's alpha is in the range of 0.77–0.88, this scale has satisfactory validity (0.77). It also has a high correlation with the New York and Guttman National Questionnaire in measuring self-esteem, so its content validity is also confirmed [ 29 ]. In Iran, Cronbach's alpha coefficients of 0.84 to 0.92 have been reported for this scale. Also, the reliability and validity of this tool has been checked by factor analysis, dichotomization and re-sampling methods, and the results show that this scale can be used in Iran as well [ 30 ].
The Situational Motivational Scale (SIMS): After confirming the content validity of the tool in Iran, its reliability has been confirmed by retest method (73.76) and Cronbach's alpha has been reported as 74–88%. The short form of this questionnaire was made by Bahrani in Shiraz. This questionnaire has 49 statements that are arranged on a Likert scale from completely disagree [ 1 ] to completely agree [ 5 ]. Reliability of the 49-question questionnaire used in this research was measured by Bahrani by retesting and calculating Cronbach's alpha. In the retest method, the reliability coefficient of the whole test was 0.95. Also, the internal consistency of the questionnaire was calculated as 0.77 [ 31 , 32 ].
Intervention program
In the control group, clinical training was done in the traditional way with the help of a trainer. In the intervention group, training was done by peer mentoring method with the help of fourth year operating room students and under the supervision of the instructor. Based on the overall GPA criteria, the first to sixth ranked students were selected as mentor students. Before using the students as mentors in the internship, 3 training sessions were held for them by the professors of the operating room.
In these meetings, the lesson plan of the internship course was fully explained based on the last chapter of the operating room field, and the necessary points regarding training and how to deal with students were explained.
Then, these students participated in three tests and the first to third students of each test were selected as mentors. Therefore, a total of nine students were selected as mentors. In the intervention group, internship training was carried out with the implementation of peer mentoring program during one academic semester. Students of the intervention group (35 participants) were placed in five groups of seven according to the internship program. The total training sessions of each group were 18 sessions, nine of which were conducted by the method of peer mentoring program. A total of 45 peer mentoring sessions were conducted for all groups. Each of the mentors mentored a seven-person group of mentees during nine sessions. At the beginning of each session, the mentor briefly explained the topics to the mentees according to the educational topics and guided them practically during the session. It should be noted that all the meetings were held under the supervision of the main teacher of the course and if necessary, this person provided the necessary guidance.
At the end of the academic semester, the Depression Anxiety Stress Scale, Rosenberg Self-Esteem Scale (RSES) and Situational Motivational Scale (SIMS) were completed again by the students of the intervention and control groups.
Statistical analysis
Stata software version 14 was used for the data analysis process. Initially, the data's normality was verified using the Kolmogorov–Smirnov test. The results were presented as mean, standard deviation, frequency, and percentage in the section on descriptive statistics.
The means of the study variable between the intervention and control groups were compared using an independent t-test, and the means before and after the intervention were compared using a paired t-test in the analytical statistics section. The Chi-square test was used to compare the associations between qualitative variables in the various groups.
The ANCOVA test was conducted after the intervention to control for any baseline differences in scores of self-confidence, stress, perceived anxiety, depression and academic progress between the two groups before the intervention (pre-test). This adjustment was made to account for any potential confounding factors that may have influenced the outcomes.
Univariable and multivariable linear regression by the backward method was applied to examine the association between self-confidence, stress, perceived anxiety, depression, gender, mother's education, father's education, family economic, and academic progress. A significance threshold of less than 0.05 was used.
The mean age of participants was 22.31 ± 2.59. Thirty-six individuals (51.4%) were female, and 50 individuals (71.4%) were single. Regarding education, 22 participants (31.4%) held diplomas from their fathers, and 21 participants (30%) held diplomas from their mothers. In terms of mothers' occupations, 35 individuals (52.9%) were housewives, and 31 individuals (44.3%) reported their family's economic status as medium (Table 1 ). On the other hand, there were no significant differences in age, gender, marital status, mothers' education, fathers' education, fathers' occupation, mothers' occupation, and family economic status between the intervention and control groups( p > 0.05) (Table 1 ). Also, in terms of variables of self-confidence, stress, anxiety, depression and academic progress between the intervention and control groups, no significant difference was observed before the intervention ( p > 0.05) (Table 2 ).
Before the intervention, high levels of stress (12.65; 12.25), anxiety (11.34; 11.02) and depression (10.08; 10.42) and low levels of self-confidence (1.31; 1.22) were observed in the intervention and control groups.
The results indicated a significant difference in the mean scores of self-confidence ( p < 0.001), stress ( p < 0.001), and academic progress ( p < 0.001), between the intervention and control groups after the educational intervention. Furthermore, this difference was also statistically significant in the intervention group before and after the educational intervention ( p < 0.05). However, there was no significant difference in the mean scores of anxiety and depression before and after the intervention, as well as in comparison with the control group ( p > 0.05) (Table 2 ).
The results showed significant differences between the intervention and control groups. Post-intervention, the intervention group showed substantial increases in self-confidence (mean difference = 5.97, p < 0.001) and significant reductions in stress levels (mean difference = -3.22, p < 0.001). In contrast, minimal changes were observed in the control group for both self-confidence (mean difference = 0.057, p = 0.934) and stress levels (mean difference = 0.142, p = 0.656). While both groups exhibited decreases in anxiety and depression levels, these changes were not statistically significant ( p > 0.05). Moreover, the intervention significantly improved academic progress in the intervention group compared to the control group (mean difference = 20.31, p < 0.001) (Table 2 ).
The ANCOVA test was used to compare the means of self-confidence, stress, anxiety, depression and academic progress in the two groups after adjusting the Pre-test as a covariate. Results showed there was a significant difference between the means in the self-confidence, stress and academic progress before and after intervention with adjusted pre- test score (before intervention) (Table 3 ).
The results of the univariate linear regression analysis showed that self-confidence and stress are associated with academic progress ( p < 0.05) (Table 4 ). Additionally, the results of the multiple regression analysis revealed that for a one-unit increase in the stress score, the mean academic progress score decreases by 0.520 (B = -0.520, P < 0.001). Furthermore, for a one-unit increase in age, the mean academic progress score increases by 0.220(B = 0.220, P = 0.029). Moreover, students whose fathers have university education have, on mean, a higher academic progress score compared to students whose fathers are illiterate, with an increase of 0.212 for each unit difference in paternal education level (B = 0.212, P = 0.036). According to the multiple regression model, 33.4% of the variations in academic progress can be predicted by stress, age, and father’s education (Table 4 ).
This research was conducted to determine the effect of peer mentoring program on clinical academic progress and psychological characteristics of operating room students.
The results showed that before the educational intervention, there was no significant difference between the control and intervention groups in demographic variables, academic progress, self-confidence, stress, anxiety and depression. It is noteworthy that according to the regression analysis, students whose fathers had a university education had a higher academic progress score compared to students whose fathers were illiterate.
The results of the study before the intervention show a high level of stress, anxiety and depression and a low level of self-confidence in students. Mohammadi's study showed the mean situational anxiety scores of the operating room students to be at a medium–high level [ 33 ]. Of course, according to Findik's study, the stress level of nursing students was low on the first day of operating room practice. It was found that students use the self-confidence approach in dealing with stress [ 34 ]. According to Norouzi's study, insufficient skills of students in communicating with staff, discrimination between paramedical students and assistants, lack of practical prerequisite skills, weak supportive performance of instructors and psychological needs are among the stressful factors of operating room students [ 3 ]. According to the students, practice with the support of staff and instructors in clinical training leads to better training. Improper interaction between staff and students negatively affects the clinical education process [ 35 , 36 ]. The results of Mohibi's research report the existence of discrimination as one of the main complaints of students in the clinical environment [ 37 ].
The results showed that training using the peer mentor method improved the mean scores of self-confidence, stress and academic progress variables in the intervention group after the educational intervention. Also, compared to the control group, the intervention group had achieved a significant improvement in the mentioned variables. In addition, the results showed that self-confidence and stress are related to academic progress, and as the stress score increases, the mean academic progress decreases. The results of Raymond's study showed that the implementation of the mentorship program was effective in reducing the stress and loneliness of first-year nursing students. In addition, an increase in their sense of self-efficacy and sense of psychological belonging was also reported [ 38 ]. According to Yoon's study, peer mentoring program increased students' self-confidence in basic nursing skills and critical thinking skills [ 39 ]. Considering that clinical educators play a fundamental role in controlling stress, creating a supportive environment and promoting students' self-confidence in the clinical learning environment [ 40 ], it seems that the use of students in the role of peer mentoring has been able to act as an important factor in increasing self-confidence, reducing stress and enjoying clinical experiences and thus improving their academic progress.
While in Walker's study, a significant reduction in the anxiety of a specific clinical situation was observed among nursing students who were guided by their peers [ 41 ], in the present study, no significant improvement was observed in the students' anxiety. It can be said that the special conditions of the operating room distinguish it from other clinical skills training departments, therefore peer training alone cannot be effective in reducing the anxiety of operating room students. Also, depression did not decrease significantly in any of the intervention and control groups. It should be said that anxiety and depression are more complex than stress and their reduction in operating room students requires the use of psychological interventions along with peer mentoring program.
Due to the limitation of the statistical population, sampling was not possible and the students were selected by census method. On the other hand, due to the special considerations of the operating room space, the implementation of the peer mentoring program faced limitations. Although the main teacher of the course was present in all the implementation sessions of the mentorship program, physicians and other clinical personnel did not trust the mentors to some extent.
Of course, the use of this training method could not be effective in reducing anxiety and depression, which can be aggravated as a result of working in the tense environment of the operating room, and it seems necessary to conduct more investigations in this field.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available because they contain raw data from study participants, and sharing these data requires participants' permission. But are available from the corresponding author on reasonable request.
Erfani Khanghahi M, Ebadi Fard Azar F, Ebadi Fard Azar G. A Model of Effective Factors on Educational Transfer among Health Deputy Staff of Iran University of Medical Sciences. J Heal. 2020;11(2):203–12.
Article Google Scholar
Tazakori Z, Mehri S, Mobaraki N, Dadashi L, Ahmadi Y, Shokri F, et al. Factors affecting on quality of clinical education from perspectives of operating room students. J Heal Care. 2015;17(2):128–36.
Google Scholar
Norouzi N, Imani B. Clinical education stressors in operating room students: a qualitative study. Investig y Educ en Enfermería. 2021;39(1):e08.
Chevillotte J. Operating room nursing diploma soon to be accessible through competence validation. Rev Infirm. 2014;199:10.
Geraghty S, Speelman C, Bayes S. Fighting a losing battle: Midwives experiences of workplace stress. Women and Birth. 2019;32(3):e297-306.
Zeng Y, Wang G, Xie C, Hu X, Reinhardt JD. Prevalence and correlates of depression, anxiety and symptoms of stress in vocational college nursing students from Sichuan, China: a cross-sectional study. Psychol Health Med. 2019;24(7):798–811.
Abdal M, Alavi NM, Adib-Hajbaghery M. Clinical self-efficacy in senior nursing students: A mixed-methods study. Nurs midwifery Stud. 2015;4(3):e29143.
Mussi FC, da S Pires CG, da Silva RM, de Macedo TTS, de ST Santos CA. Stress level among undergraduate nursing students related to the training phase and sociodemographic factors. Rev Lat Am Enfermagem. 2020;28:e3209.
Hasson F, Slater PF, Guo XJ. Resilience, stress and well-being in undergraduate nursing students in China and the UK. Int J Res Nurs. 2021;12(1):11–20.
Mirbagher Ajorpaz N, Zagheri Tafreshi M, Mohtashami J, Zayeri F. Mentoring in training of operating room students: A systematic review. J Nurs Educ. 2016;5(3):47–54.
Nguyen T, Netto CLM, Wilkins JF, Bröker P, Vargas EE, Sealfon CD, et al. Insights into students’ experiences and perceptions of remote learning methods: From the COVID-19 pandemic to best practice for the future. In: Frontiers in Education. Frontiers; 2021. p. 91.
Kurganovna KD, Abdusalamovna AS, Sabirovna AN, Gafurovna AS. The Use Of Interactive Methods And Literary Lessons And High School Education. J Posit Sch Psychol. 2022;6(10):4328–32.
Hartikainen S, Rintala H, Pylväs L, Nokelainen P. The concept of active learning and the measurement of learning outcomes: A review of research in engineering higher education. Educ Sci. 2019;9(4):276.
Cho HJ, Zhao K, Lee CR, Runshe D, Krousgrill C. Active learning through flipped classroom in mechanical engineering: improving students’ perception of learning and performance. Int J Stem Educ. 2021;8:1–3.
Tudevdagva U, Heller A, Hardt W. An implementation and evaluation report of the active learning method eduscrum in flipped class. Int J Inf Educ Technol. 2020;10(9):649–54.
Lima RM, Andersson PH, Saalman E. Active Learning in Engineering Education: a (re) introduction. Eur J Eng Educ. 2017;2;42(1):1–4.
Fard ZR, Azadi A, Khorshidi A, Mozafari M, O’Connor T, Budri AMV, et al. A comparison of faculty led, mentorship program and peer mentoring on nursing students wound dressing clinical skills. Nurse Educ Today. 2020;89: 104378.
Mullen CA, Klimaitis CC. Defining mentoring: a literature review of issues, types, and applications. Ann N Y Acad Sci. 2021;1483(1):19–35.
Safari M, Yazdanpanah B, Islam-Nik PS. Comparison of midwifery students satisfaction with the teaching of gynecology and infertility by lecture and peer education. Armaghane Danesh. 2019;23(6):722–36.
Messerer DAC, Kraft SF, Horneffer A, Messerer LAS, Böckers TM, Böckers A. What factors motivate male and female Generation Z students to become engaged as peer teachers? A mixed-method study among medical and dental students in the gross anatomy course. Anat Sci Educ. 2022;15(4):650–62.
Ahmed M, Muldoon TJ, Elsaadany M. Employing faculty, peer mentoring, and coaching to increase the self-confidence and belongingness of first-generation college students in biomedical engineering. J Biomech Eng. 2021;143(12): 121001.
Davey Z, Jackson D, Henshall C. The value of nurse mentoring relationships: Lessons learnt from a work-based resilience enhancement programme for nurses working in the forensic setting. Int J Ment Health Nurs. 2020;29(5):992–1001.
Sadeghi A, Oshvandi K, Moradi Y. Explaining the inhibitory characteristics of clinical instructors in the process of developing clinical competence of nursing students: a qualitative study. J Fam Med Prim care. 2019;8(5):1664.
Gemuhay HM, Kalolo A, Mirisho R, Chipwaza B, Nyangena E. Factors affecting performance in clinical practice among preservice diploma nursing students in Northern Tanzania. Nurs Res Pract. 2019;2019:3453085.
Zarrabi M, Imanieh M, Zarrabi K, Masjedi M, Kojuri J, Amini M, et al. Designing and organizing mentoring at shiraz medical school and reinforcing deep knowledge–based education using mentoring. J Med Spirit Cultiv. 2017;26(3):228–36.
Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176.
Maleki A, Asghari M, Salari R. Credit terms of scale, depression, anxiety Vastrs DASS-21 in the Iranian populatio1. Maleki A, Asghari M, Salari R. Credit terms of scale, depression, anxiety Vastrs DASS-21 in the Iranian population. J Iran Psychol. 2005;1(4):9–12.
Sahebi A, Asghari MJ, Salari RS. Validation of depression anxiety and stress scale (DASS-21) for an Iranian population. J Iran Psychol. 2005;1(4):36–54.
Martín-Albo J, Núñez JL, Navarro JG, Grijalvo F. The Rosenberg Self-Esteem Scale: translation and validation in university students. Span J Psychol. 2007;10(2):458–67.
Amini Manesh S, Nazari AM, Moradi A, Farzad V. Youth online gaming addiction: the role of self esteem, anxiety and depression. Strateg Stud Youth Sport. 2014;13(25):97–112.
Bahrani M. The study of validity and reliability of Harter’s scale of educational motivation. J Psychol Stud. 2009;5(1):51–72.
Østerlie O, Løhre A, Haugan G. The Situational Motivational Scale (SIMS) in physical education: A validation study among Norwegian adolescents. Cogent Educ. 2019;6(1):1603613.
Mohammadi G, Tourdeh M, Ebrahimian A. Effect of simulation-based training method on the psychological health promotion in operating room students during the educational internship. J Educ Health Promot. 2019;8:172.
Findik UY, Ozbas A, Cavdar I, Topcu SY, Onler E. Assessment of nursing students’ stress levels and coping strategies in operating room practice. Nurse Educ Pract. 2015;15(3):192–5.
Al-Zayyat AS, Al-Gamal E. Perceived stress and coping strategies among J ordanian nursing students during clinical practice in psychiatric/mental health courses. Int J Ment Health Nurs. 2014;23(4):326–35.
Bazrafkan L, Najafi Kalyani M. Nursing students’ experiences of clinical education: A qualitative study. Investig y Educ en Enferm. 2018;36(3):e04.
Mohebbi Z, Rambod M, Hashemi F, Mohammadi HR, Setoudeh G, Najafi DS. View point of the nursing students on challenges in clinical training, Shiraz. Iran Hormozgan Med J. 2012;16(5):415–21.
Raymond JM, Sheppard K. Effects of peer mentoring on nursing students’ perceived stress, sense of belonging, self-efficacy and loneliness. J Nurs Educ Pr. 2017;8(1):16.
Yoon MO, Ju YS. The effects of peer mentoring learnings-based preclinical OSCE program on self-confidence on core basic nursing skills and critical thinking disposition for nursing student. J Digit Converg. 2017;15(7):285–95.
Arkan B, Ordin Y, Yılmaz D. Undergraduate nursing students’ experience related to their clinical learning environment and factors affecting to their clinical learning process. Nurse Educ Pract. 2018;29:127–32.
Walker D, Verklan T. Peer mentoring during practicum to reduce anxiety in first-semester nursing students. J Nurs Educ. 2016;55(11):651–4.
Download references
Acknowledgements
The authors of this study wish to express their gratitude to all the students, especially Miss Azadeh Nasiri and the officials of Khomein University of Medical Sciences.
Informed consent
All participants provided written informed consent.
This research was supported by Khomain University of Medical Sciences (No: 400000009).
Author information
Authors and affiliations.
Molecular and Medicine Research Center, Khomein University of Medical Sciences, Khomein, Iran
Amin Sedigh
Department of Medical Education, School of Medical Education and Learning Technologies, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Sara Bagheri
Student Research Committee, Khomein University of Medical Sciences, Khomein, Iran
Pariya Naeimi
Department of Public Health, Torbat Jam Faculty of Medical Sciences, Torbat Jam, Iran
Vahid Rahmanian
Department of Public Health, Khomein University of Medical Sciences, Khomein, Iran
Nader Sharifi
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: A S, S B; Data curation: A S, P N; Formal analysis: N SH, V R; Methodology: A S, S B, N SH; Project administration: A S, P N, N SH; Writing–original draft: N SH, V R; Writing–review & editing: all authors.

Corresponding author
Correspondence to Nader Sharifi .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Human Research Ethics Committee at the Khomain University of Medical Sciences (Code IR.KHOMEIN.REC.1400.010). All study participants provided written informed consent. Confidentiality and anonymity were ensured. All procedures performed in studies involving human participants were by the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sedigh, A., Bagheri, S., Naeimi, P. et al. The effect of peer mentoring program on clinical academic progress and psychological characteristics of operating room students: a parallel randomized controlled trial. BMC Med Educ 24 , 438 (2024). https://doi.org/10.1186/s12909-024-05424-z
Download citation
Received : 29 December 2023
Accepted : 12 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s12909-024-05424-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Operating Room
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
10 facts about today’s college graduates

Having a bachelor’s degree remains an important advantage in many sectors of the U.S. labor market. College graduates generally out-earn those who have not attended college, and they are more likely to be employed in the first place. At the same time, many Americans say they cannot afford to get a four-year degree – or that they just don’t want to.
Here are key facts about American college graduates.
This Pew Research Center analysis about U.S. college graduates relies on data from sources including the Census Bureau, the Bureau of Labor Statistics, the National Center for Education Statistics, the National Student Clearinghouse and the Federal Reserve Bank, as well as surveys conducted by the Center.
Everyone who took the Pew Research Center surveys cited is a member of the Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Nearly four-in-ten Americans ages 25 and older have a bachelor’s degree, a share that has grown over the last decade. As of 2021, 37.9% of adults in this age group held a bachelor’s degree, including 14.3% who also obtained a graduate or professional degree, according to data from the Census Bureau’s Current Population Survey. That share is up 7.5 percentage points from 30.4% in 2011.
An additional 10.5% had an associate degree in 2021. About four-in-ten Americans ages 25 and older had a high school diploma with no further education (25.3%) or completed some college but didn’t have a degree (14.9%).
In a reversal, women are now more likely than men to graduate from college, according to the Current Population Survey . In 2021, 39% of women ages 25 and older had a bachelor’s degree or more education, compared with 37% of men in the same age range. The gap in college completion is even wider among adults ages 25 to 34: 46% of women in this age group have at least a bachelor’s degree, compared with 36% of men.
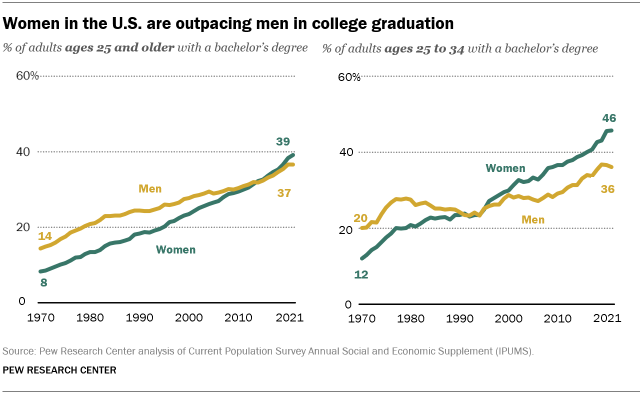
In an October 2021 Pew Research Center survey of Americans without a degree, 34% of men said a major reason why they have not received a four-year college degree is that they just didn’t want to. Only one-in-four women said the same. Men were also more likely to say a major reason they didn’t have a four-year degree is that they didn’t need more education for the job or career they wanted (26% of men said this vs. 20% of women).
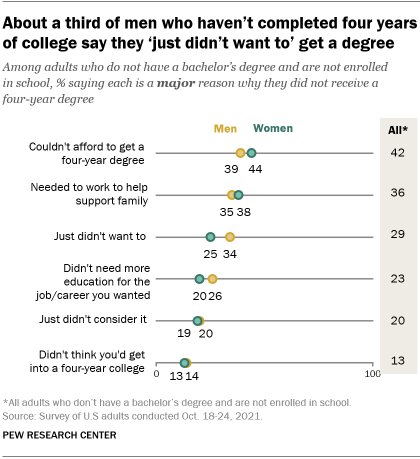
Women (44%) were more likely than men (39%) to say not being able to afford college was a major reason they don’t have a bachelor’s degree. Men and women were about equally likely to say a major impediment was needing to work to help support their family.
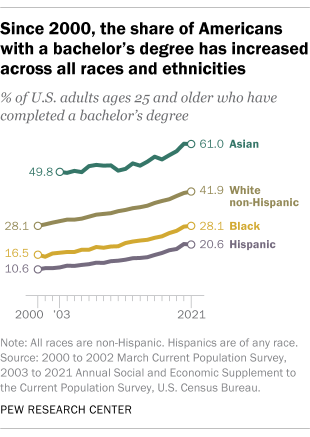
There are racial and ethnic differences in college graduation patterns, as well as in the reasons for not completing a degree. Among adults ages 25 and older, 61% of Asian Americans have a bachelor’s degree or more education, along with 42% of White adults, 28% of Black adults and 21% of Hispanic adults, according to 2021 Current Population Survey data. The share of bachelor’s degree holders in each group has increased since 2010. That year, 52% of Asian Americans had a four-year degree or more, compared with a third of White adults, 20% of Black adults and 14% of Hispanic adults.
The October 2021 Center survey found that among adults without a bachelor’s degree, Hispanic adults (52%) were more likely than those who are White (39%) or Black (41%) to say a major reason they didn’t graduate from a four-year college is that they couldn’t afford it. Hispanic and Black adults were more likely than their White counterparts to say needing to work to support their family was a major reason.
While a third of White adults said not wanting to go to school was a major reason they didn’t complete a four-year degree, smaller shares of Black (22%) and Hispanic (23%) adults said the same. White adults were also more likely to cite not needing more education for the job or career they wanted. (There weren’t enough Asian adults without a bachelor’s degree in the sample to analyze separately.)
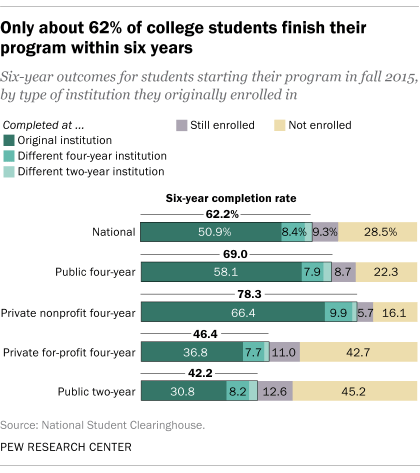
Only 62% of students who start a degree or certificate program finish their program within six years, according to the most recent data from the National Student Clearinghouse , a nonprofit verification and research organization that tracked first-time college students who enrolled in fall 2015 with the intent of pursuing a degree or certificate. The degree completion rate for this group was highest among students who started at four-year, private, nonprofit schools (78.3%), and lowest among those who started at two-year public institutions (42.2%).
Business is the most commonly held bachelor’s degree, followed by health professions. According to the National Center for Education Statistics , about a fifth (19%) of the roughly 2 million bachelor’s degrees conferred in 2019-20 were in business. Health professions and related programs were the second most-popular field, making up 12.6% of degrees conferred that year. Business has been the single most common major since 1980-81; before that, education led the way.
The least common bachelor’s degrees in 2019-20 were in military technologies and applied sciences (1,156 degrees conferred in 2019-20), library science (118), and precision production (39).
There is a growing earnings gap between young college graduates and their counterparts without degrees. In 2021, full-time workers ages 22 to 27 who held a bachelor’s degree, but no further education, made a median annual wage of $52,000, compared with $30,000 for full-time workers of the same age with a high school diploma and no degree, according to data from the Bureau of Labor Statistics. This gap has widened over time. Young bachelor’s degree holders earned a median annual wage of $48,481 in 1990, compared with $35,257 for full-time workers ages 22 to 27 with a high school diploma.
The unemployment rate is lower for college graduates than for workers without a bachelor’s degree, and that gap widened as a result of the coronavirus pandemic. In February 2020, just before the COVID-19 outbreak began in the U.S., only 1.9% of college graduates ages 25 and older were unemployed, compared with 3.1% of workers who completed some college but not a four-year degree, and 3.7% of workers with only a high school diploma. By June 2020, after the pandemic hit, 6.8% of college grads, 10.8% of workers with some college, and 12.2% of high school grads were unemployed.
By March 2022, the unemployment rate had nearly returned to pre-pandemic levels for college graduates (2%) while dropping to 3% among those with some college education but no four-year degree, and 4% among those with only a high school diploma.
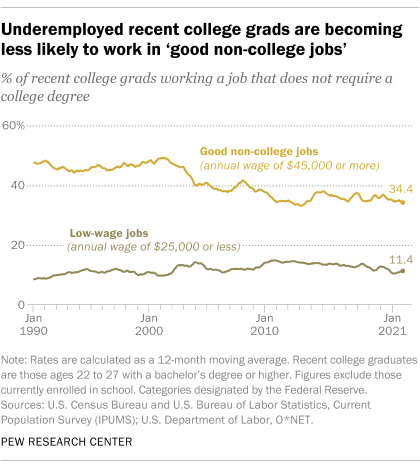
Recent college graduates are more likely than graduates overall to be underemployed – that is, working in jobs that typically do not require a college degree, according to an analysis of Census Bureau and BLS data by the Federal Reserve Bank of New York . As of December 2021, 41% of college graduates ages 22 to 27 were underemployed, compared with 34% among all college graduates. The underemployment rates for recent college grads rose in 2020 as the COVID-19 outbreak strained the job market, but have since returned to pre-pandemic levels.
As of the end of 2021, only 34% of underemployed graduates ages 22 to 27 worked what the Fed defines as “good non-college jobs” – those paying at least $45,000 a year – down from around half in the 1990s. The share of underemployed graduates ages 22 to 27 in low-wage jobs – those earning less than $25,000 annually – rose from about 9% in 1990 to 11% last year.
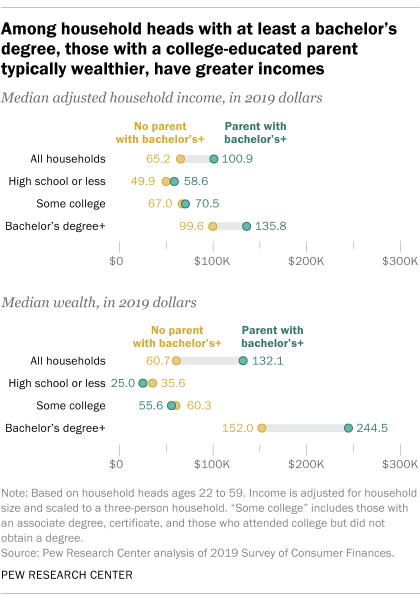
When it comes to income and wealth accumulation, first-generation college graduates lag substantially behind those with college-educated parents, according to a May 2021 Pew Research Center analysis . Households headed by a first-generation college graduate – that is, someone who has completed at least a bachelor’s degree but does not have a parent with a college degree – had a median annual income of $99,600 in 2019, compared with $135,800 for households headed by those with at least one parent who graduated from college. The median wealth of households headed by first-generation college graduates ($152,000) also trailed that of households headed by someone with a parent who graduated from college ($244,500). The higher household income of the latter facilitates saving and wealth accumulation.
The gap also reflects differences in how individuals finance their education. Second-generation college graduates tend to come from more affluent families , while first-generation college graduates are more likely to incur education debt than those with a college-educated parent.
Most Americans with college degrees see value in their experience. In the Center’s October 2021 survey , majorities of graduates said their college education was extremely or very useful when it came to helping them grow personally and intellectually (79%), opening doors to job opportunities (70%) and developing specific skills and knowledge that could be used in the workplace (65%).
Younger college graduates were less likely than older ones to see value in their college education. For example, only a third of college graduates younger than 50 said their college experience was extremely useful in helping them develop skills and knowledge that could be used in the workplace. Among college graduates ages 50 and older, 45% said this.
- Higher Education

Katherine Schaeffer is a research analyst at Pew Research Center
About 1 in 4 U.S. teachers say their school went into a gun-related lockdown in the last school year
About half of americans say public k-12 education is going in the wrong direction, what public k-12 teachers want americans to know about teaching, what’s it like to be a teacher in america today, race and lgbtq issues in k-12 schools, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Card Anaesth
- v.18(1); Jan-Mar 2015
Statistics in clinical research: Important considerations
Howard barkan.
Affiliated Researcher and Consulting Statistician, School of Public Health, University of California Berkeley, Berkeley, CA 94704-7380, Saybrook University, Oakland, CA 94612, USA
Statistical analysis is one of the foundations of evidence-based clinical practice, a key in conducting new clinical research and in evaluating and applying prior research. In this paper, we review the choice of statistical procedures, analyses of the associations among variables and techniques used when the clinical processes being examined are still in process. We discuss methods for building predictive models in clinical situations, and ways to assess the stability of these models and other quantitative conclusions. Techniques for comparing independent events are distinguished from those used with events in a causal chain or otherwise linked. Attention then turns to study design, to the determination of the sample size needed to make a given comparison, and to statistically negative studies.
INTRODUCTION
Clinicians examine and intervene with individual patients. The understandings of the clinical challenges they will need to address, of the likely past and future courses of the clinical conditions they are seeing, and evaluations of the effectiveness and risks of their clinical actions and strategies are all based on consideration of the characteristics and histories of clients similar to the one they’re now seeing and with whom they may be about to intervene. Statistics is a key tool linking the multiplicity of potential observations of every client with the more abstract concepts of clinical entities, natural histories, clinical response and risks. These more abstract constructs are the foundation on which clinical decisions rest. On a more applied level, clinicians need to understand statistics well enough to follow and evaluate the empirical studies that provide an evidence base for clinical practices. Studies conducted decades ago found major lacunae in physicians’ knowledge of statistics.[ 1 , 2 , 3 ] This is a problem more recent studies have found to be only somewhat reduced in magnitude.[ 4 , 5 , 6 ] It leads clinicians to mistrust, misunderstand and ignore the statistics in journal articles.[ 7 ]
There are several aspects of statistical concepts, methods and their application which are key to their understanding and interpretation. These have been presented for practitioners in major clinical journals by excellent clinicians and statisticians (for initial papers in such series, cf. e.g.[ 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ]). We will present these concepts and methods with goals of strengthening clinicians’ comprehension of statistical aspects of the clinical literature, their evaluation of the strengths and weaknesses of the analyses presented, and their active participation in research. The presentation in this paper is rooted in experience gained from studies conducted by the author[ 18 , 19 , 20 ] and the clinical literature. We hope to help make these inherently abstract statistical concepts and techniques more intelligible in the applied world of clinical practice. We will begin by discussing aspects of measurement, sampling, and analytic goal that guide the choice of statistical techniques. The discussion will then turn to aspects of analytic design and conduct, which impact important finer details of the project's conduct and of the interpretation of its results. The reader is referred to the paper series referenced above[ 8 , 9 , 10 , 11 , 13 , 14 , 15 , 16 , 17 ] for more detailed discussions of particular statistical techniques.
Clinical processes are real world. Statistics is abstract. Two-way translation is important
Biological and clinical entities are complex and changing, multi-dimensional structures and processes, which evolve over time. All research works begin by selecting particular features of physical objects and segments of processes, which will be used in the research to represent those structures and processes.[ 11 ] These selected observations operationalize the abstract concept of a clinical entity or process into specified measurements. Statistics works with these operationalizations, modeling and analyzing properties and processes which are shared among groups of observations. Note that, the external validity of the results of statistical analyses, while key to the value of those results, is importantly a function of measurement and sampling - that is, what was measured how, in which subjects, at which times, and how well those selected measurements represent the clinical entities and processes which the research is investigating.[ 21 ] A perfectly chosen and executed analysis will be at best misleading if it is conducted of the wrong data or data collected using an inaccurate measurement technique, or at the wrong time, and so on. To quote the frequent aphorism from introductory statistics courses, “Garbage in, garbage out.” We will discuss the analysis of appropriately selected and measured data. Evaluations of the validity of the measures collected as representations, of the modeling of causal processes, and of the generalizability of the results are all important to the value of statistical analyses but beyond the scope of this paper.
Measurement scaling
Certain aspects of measurement and sampling are key to which statistical techniques are appropriate. The first attribute, which indicates the appropriateness of and hence guides the choice among statistical procedures, is the scaling of the measurements being treated as variables in the analysis. Statistics represents measurements as scales. In terms of the appropriateness of statistical techniques, the key differentiation among scaling techniques is mathematical: What each number represents and which mathematical analyses of those numbers are valid.[ 9 , 11 , 14 , 23 , 24 ]
Measurements can be classified as using nominal, ordinal, and interval scalings. Nominal scalings use distinct and mutually-exclusive numbers are used to name each category of observation. Nominal scalings only classify observations. The numbers assigned in a nominal scale carry no further information about magnitude. Set theory, which deals with which observations belong in which groups and with how groups overlay, is the only mathematics appropriate for nominal scales. Clinical examples of nominal scalings include any notation that a disease is (simply) present or absent, a the binary classification used in calculating incidence and prevalence rates and the sensitivity and specificity of diagnostic tests, demographic measures (such as gender and ethnic group), and disease classification systems such as the International Classification of Disease (ICD)-10 and the Diagnostic and Statistical Manual of Mental Disorders-5. Sensitivity and specificity, key indices of the strength of diagnostic findings as evidence of a disease, both begin by treating the finding and the disease as binomial nominal variables. Binomials are attributes that are either present or absent.[ 25 , 26 , 27 ]
Ordinal scalings are mathematically the next more complex. Ordinal scalings place observations in order-say from least to most-but are not able to specify or compare the differences between pairs of measurements. Many clinical measurements and indices and many psychological and attitude measurements are ordinally scaled: e.g. tumor grade, pain scales, and Likert attitude scales. Disease stage is an example of an ordinal scaling. Stage 4 cancers are “worse” than stage 3 cancers which are in turn worse than stage 2 cancers, but the ordinal scaling of staging does not indicate how much worse. It is impossible to say whether the difference between stage 4 and stage 3 is more or less than the difference between stage 3 and stage 2 based on the assigned stage alone. That is, the statement that one stage is “worse” than another derives from the association of stage differences with other factors such as duration of survival rather than on the measurement of stage itself. Ordinal scalings add the mathematics of inequalities to set theory as permissible mathematical operations.
Interval scalings are mathematically the most complex of the measurement scales used. Interval scales place observations in order and specify both the magnitude of individual measurements and the distance between pairs of measurements. Interval scalings permit all of the basic arithmetic operations and the calculations based on those operations. Many widely used clinical observations are intervally scaled: e.g. anthropometric measurements of height and weight, blood pressure, and duration of time intervals.
Two other scaling options considerations are frequently mentioned for interval scales. The first is whether the source measurements are discreet (e.g. number of children in the household) or continuous (e.g. blood pressure). This distinction bears on the source measurement and may influence how collected data are displayed graphically, but has no influence on the choice or calculation of statistical analyses. The second difference among interval scales is whether or not the scale has a true “0” point. Those with a true “0” points are sometimes called ratio scales because the presence of a true “0” point makes division and hence the calculation of ratios possible. Consider, for example, temperature. The Kelvin scale has a true zero point at absolute zero and hence is a ratio scale. The Centigrade and Fahrenheit scales have a zero point that's mathematically arbitrary and hence are interval scales. This difference bears on which conclusions regarding these measurements are meaningful. For example, it is meaningful to say that the temperature of 30°K is half a temperature of 60°K while it is not valid to make the same statement regarding 30°F versus 60°F. This difference has no bearing on the choice of statistical procedures to analyze these data.
This mathematical type of scaling is one of the principal determinants of the appropriateness of a particular statistical analysis for a particular dataset.[ 28 ] In general, statistical analyses which can be conducted of mathematically simpler scales, say nominal scales, can also be conducted of more complex scales. For example, the mode, i.e. identification of the most frequent observation, which is the principal statistic describing central tendency for nominally scaled variables, can also be used to describe distributions of ordinally and intervally scaled variables. On the other hand, statistical analyses designed for more complex scales often cannot be applied to mathematically simpler scales. For example, calculation of an average depends on the ability to add and divide the observed measurements. These mathematical operations are not valid with ordinal and nominal scalings, making invalid the operations involved in calculating the average of such a scaling in a sample. Note that the greater power of the analyses available for interval scalings leads to a frequent temptation to treat measurements such as tumor stage which are appropriately scaled ordinally as though they were scaled intervally.
Descriptive statistics and measurement scaling: Single variables
Examinations of single variables use descriptive statistics to characterize the central tendency, the single best description of the sample of measurements, and variability. Descriptive statistics for single variables play important roles in research. Descriptive statistics summarize characteristics of the study and control groups in randomized trials.[ 18 ] To evaluate the baseline comparability of the an investigation's study and control groups, the proportions are examined when comparing nominally scaled variable such as gender. The median is can also be examined when comparing the ordinally scaled urgency. While Averages are can be examined when comparing intervally scaled characteristics: e.g. groups members’ age, serum albumin, and platelet count and other key hematologic indices. They are at the core of clinically relevant indices of prevalence and incidence, and of the evaluation of the sensitivity and specificity of diagnostic findings as evidence of particular conditions. The median is can also be examined when comparing the ordinally scaled urgency. While Averages are can be examined when comparing intervally scaled characteristics: e.g. groups members' age, serum albumin, and platelet count and other key hematologic indices.
In most general terms, a form of descriptive statistical analysis which is valid for simpler mathematical scalings can be used with mathematically more complex scalings. For example, the category containing the highest proportion of a nominal variable is termed the mode. The mode is a valid analysis of nominally scaled variables. We can count the number of patients assigned each ICD-9 coded diagnosis. We can then compare these counts to evaluate which diagnosis was most frequent that is, the mode. The mode can also be used to describe variables that are ordinally scaled - e.g. which stage of lung cancer is most frequent - and intervally scaled - e.g. what number of children/family is most frequent. In contrast, statistics designed specifically for more complex scalings may be invalid for measurements using mathematically simpler scalings. For example, it is valid to calculate the mean and standard deviation of the number of distant metastases/patient because our count of the number of distant metastases is intervally scaled: The difference between 0 and 1 distant metastases equals the difference between 3 and 4 distant metastases which equals one.[ 22 ] In contrast, we cannot calculate the average lung cancer stage because we cannot add or divide stage measurements: Is it at all meaningful to say that stage 2 lung cancer is twice stage 1 lung cancer? The situation is even more clouded with nominally scaled variables. The numbers used as codes in the ICD-9 carry no direct implication of magnitude. It is not meaningful to say that the diagnosis of reticulosarcoma is twice the diagnosis of leptospirosis icterohemorrhagica because reticulosarcoma's ICD-9 code of 200.0 is twice, the leptospirosis ICD-9 code of 100.0.[ 23 , 29 ]
Descriptive statistics and measurement scaling: Multiple variables
Let us now turn our attention to the associations among variables, first paying attention to how we describe that association. The strength of the association between two variables is described by correlation coefficients.[ 30 , 31 ] Correlation coefficients describe the strength of association between two variables of the same mathematical type. Correlation coefficients typically range from “0” indicating no association to “−1” and “1”, indicating perfect association. The square of the correlation coefficient can be interpreted as the proportion of the variance of one variable that is predicted by the other variable. The square of “1” equals the square of “−1” equals “1,” indicating perfect association. The most frequently used correlation coefficients are phi and Cramer's V for nominal variables, Spearman's rho (or rank-order) correlation for ordinal variables, and Pearson's r (or product-moment) correlation for interval variables. Kappa is also often used for binomial nominal variables. Binomial variables are nominal variables with only two values: e.g. gender and the presence versus absence of a characteristic or disease. Kappa adjusts in its calculation for the agreement expected by chance alone.[ 32 ] This has made kappa a useful index in investigations of inter-observer agreement among radiologists and other clinicians (there has been some argument about this interpretation of kappa, cf.[ 33 ]). Note that agreement does not imply accuracy. Accuracy, assessed for binary classifications by sensitivity, specificity, and receiver operating characteristic curves, will not be discussed further in this paper.[ 25 , 26 , 27 , 34 , 35 ]
For all but nominal variables, the sign of the correlation coefficient indicates the direction of the association. Positive correlation coefficients describe situations in which increases in value of one of the variables are associated with increases in the other variable, while negative coefficients describe situations in which increases in one of the variables are associated with decreases in the other. Correlation-based analyses using techniques such as factor analysis can be used to examine the associations among multiple measures used to investigate single events or conditions.[ 36 , 37 ] This technique can identify groupings and key measures, potentially reducing the length and increasing the efficiency of diagnostic evaluations.[ 38 , 39 ] Patterns found in factor analysis can be helpful in exploring biological interactions and indicate particular groupings which may have clinical implication.[ 40 , 41 , 42 ]
Measurement timing
The discussion so far has carried the implicit assumption that we are able to measure the entire course of the events we are studying. That may be true for many of the acute clinical events and processes in which cardiac anesthesiology plays a major role. However, this is clearly true neither for all long term processes in cardiac anesthesia nor for those iatrogenic effects whose appearance is delayed, nor for cardiology, nor for clinical processes generally. Clinical and research data are often gathered within a limited time frame while the processes to which clinical attention is being given, and those which are being studied continue beyond that time frame's boundaries. The techniques of survival analysis and life-table statistics have been developed to address these challenges presented by what is termed “right censoring.”[ 43 , 44 , 45 , 46 ] Right censoring exists when a study is investigating a process that has reached a conclusion in some, but not all of the subjects when the study ends hence censoring information about that outcome. In situations such as this, the sample size of those at risk for a study's terminal event varies over the course of the study because that size is reduced by “1” every time one of the study's terminal those events (say tumor recurrence or mortality) occurs, removing the person experiencing the event from the group at risk for it. Life-table analyses typically examine median time to the target event to avoid being biased by the long times to event of those in the sample who have not experienced the event by the time the study concludes and whose experience is right-censored. Life-table experience is typically depicted using Kaplan-Meier survival curves, where “survival time” is taken to signify time to the process designated's final effect (e.g. re-infection, tumor recurrence or mortality). Appropriate evaluation of statistical significance also uses techniques discussed below which take this right-censorship into account. It is important that studies whose samples are right-censored use such life-table based techniques. Studies in that situation that calculate survival time by averaging time to the terminal events which have occurred will produce biased estimates unless all of those terminal events have occurred because right-censorship will be excluding those with the potentially longest survival times.
Modeling associations and prediction
Correlations measure the strength and, for all types except nominal variables, the direction of associations between variables. Regression modeling provides the tools for making those predictions from one or more independent variables to the dependent variable.[ 30 , 31 , 47 , 48 , 49 , 50 ] The measurement and the completeness of the measurement of the dependent variable indicate which form of regression modeling is appropriate. If the dependent variable is a binomial, that is, a nominal variable with only two values, and it is known whether or not each member of the sample experienced that outcome, multiple logistic regression is used to model the effects of the independent variables on the odds ratio of experiencing that outcome.[ 51 , 52 ] When the outcome condition is relatively rare and with some other constraints, these odds ratios can be treated as estimates of the relative risk each independent variable carries for the outcome. This model is appropriate for outcomes in, say, a study of surgical intervention in which the outcome of interest is short term and can be predicted to have occurred before discharge from hospital. In contrast, the Cox proportional hazards model and regression is are used when the outcome data are right censored., that is, when the outcome status of all subjects is not known (often because insufficient time has passed for the outcome to have occurred in all subjects in whom it may eventually occur). This is likely to be the case, for example, if the study is investigating delayed effects after therapeutic interventions such as postsurgical survival in cancer patients. Cox regression models the risk of the target outcome as a hazard function which is a function of time and of the independent variables included in the model. The final principal form of regression modeling is (multiple) linear regression, which predicts a dependent variable measured on an interval scale based on the values of one or more predictors. For example, linear regression can be used to model the association of the natural log of urea with age[ 30 ] (taking the natural log of urea made the relationship of urea with age a straight line). Linear regressions predict straight lines (or planes or their multi-dimensional analogs). There are constraints on the type of distribution and on the associations among variables suitable for linear regression analysis.[ 30 ] Many clinical variables have exponential or other nonlinear associations. Discussion of the regression modeling of these processes and of their associations is beyond the scope of this paper.[ 53 ]
Result likelihood and stability
Clinical decisions and research need to move beyond the initial sample of measurements (of say the initial patient or group of patients) to reach more generalized conclusions. Say a change is noted in laboratory measurement following an operative procedure. How likely is it that other patients undergoing that procedure will experience the same change? Is that change other than the difference that would be seen in patients with the same clinical condition who are measured twice, but who do not undergo that procedure? What is the range of change in that laboratory measurement, which can be expected in future patients who do and who do not undergo that procedure?
These questions explore the extent to which we can generalize from our particular clinical observations and the trustworthiness of those generalizations. These questions are in the arena of statistical inference. There have been many presentations of the general logic underlying statistical inference (cf. e.g.[ 54 , 55 , 56 , 57 ]). The reader is referred to those sources, and to any classical statistics or biostatistics text for the logic underlying classical tests of statistical significance. We will now first discuss alternatives to the point comparison represented by classical significance testing. Then, given the widespread use of classical significance testing, we will discuss several modifications necessary for its appropriate use in clinical studies.
Classical tests of significance assess the likelihood of the study's actual results given a set of assumptions about the sources of the measures being compared. The tests are designed to support a point judgment about the likelihood of those source groups being identical. The statistical significance test result evaluates the likelihood of the results obtained were the data drawn from identical groups, saying nothing about the magnitude or stability of any differences that were actually found. Further, these tests refer to an arbitrary cut-point (usually P < 0.05) to support conclusions about similarity versus difference. There is a long-standing argument that analyses should estimate the range of inter-group differences consistent with the collected data rather than ending with a single statement regarding statistical significance.[ 58 , 59 , 60 , 61 , 62 , 63 ] Given that significance tests provide a point statement, while confidence intervals express a range of estimation, some advocate reporting both (e.g.[ 60 , 61 ]). Confidence intervals can also be calculated using what are termed “Bayesian” techniques. These techniques initially presented by Thomas Bayes (1702–1761) treat probability as a statement of degree of belief in a statement rather than as an estimate of the frequency. In clinical practice, Bayesian techniques are used to calculate the predictive value (positive) of a diagnostic finding given prior beliefs about the finding's sensitivity and specificity and about the prevalence of the diseases being considered.[ 27 ] In the context of statistical inference, Bayesian techniques take into account prior beliefs about the statistics being compared by the test of significance. This is in contrast to classical tests of statistical significance and calculations of confidence intervals that are based only on the sets of actual measurements and assumptions about the underlying population distributions.[ 63 , 64 , 65 ] The continual reassessment method, first proposed by O’Quigley in 1990, applies Bayesean techniques to toxicity data from dose-finding trials.[ 66 ] Bayesian techniques are used to reapply new trial data cyclically to prior toxicity estimates (from the trial or initially from elsewhere) to re-estimate dose-toxicity curves and estimate the optimal dose in Phase 1 clinical trials.[ 67 , 68 , 69 , 70 , 71 ]
The above paragraph noted that confidence intervals can be used to evaluate a likelihood of inter-group differences. These confidence intervals estimating the magnitude of the inter-group difference go beyond traditional point computations of statistical significance which only refer to the likelihood of the particular difference tested to estimate the magnitude of the inter-group difference. They also estimate the expected stability of associations between variables. Please note that confidence intervals can also be calculated around other statistics, ranging from the proportions and means calculated as descriptive statistics through correlation coefficients to regression coefficients. In each case, the confidence interval predicts the stability of the point statistic calculated using a defined sample. The confidence interval estimates the boundaries likely to include (desired target) proportions (often 95%) of future similar measurements made from that statistical population.
Independent versus paired measurement
While there is serious discussion about alternatives to classical tests of statistical significance as evaluations of the generalizability of findings as noted above, these classical tests continue to be widely used.[ 72 , 73 , 74 ] Several issues regarding the conduct of these tests and the interpretation of their findings recur repeatedly. The first issue is whether or not the measures being compared are independent.[ 54 , 75 , 76 ] Tests of the statistical significance of differences in paired measurements differ from tests of independent measurements because in paired observations the first set of measurements is a precise prediction against which the second measurement is compared. Any difference or any difference in a specified direction is potentially of interest when comparing independent samples. The sets of measurements in repeat measurement of the same subjects are obviously related, with the second measurements being departures from first measurements that are already in the sample study. Paired analyses are also needed when the selection of samples is matched. Matching is often used in epidemiological studies to maximize comparability of the samples on all factors other than the factor whose influence is being compared (i.e. a risk factor in a cohort study or clinical outcome in a study using a case–control design).
Adjustment for multiple outcomes
Classical tests of statistical significance assume there has been only a single examination of the relationship being investigated. This assumption is often violated. It is violated when there are a series of separate examinations of the association of a single dependent variable with multiple potential independent variables, or of a single independent variable with multiple potential effects.[ 77 , 78 ] This can also happen by design in randomized controlled trials, when the Data Safety Monitoring Committee by protocol reviews the data at prespecified intervals. Associations can also be examined during the study's initial design phase then reexamined in the full study. This is problematic because each analysis in multiple comparison which uses a P < 0.05 threshold has a 1 in 20 chance of producing a false positive result. In essence, this means that if 20 tests are performed there's a virtual certainty that at least one will yield a false positive result.[ 79 ] This risk of a false positive can be mitigated in the design by adjusting the threshold for declaring statistical significance. The simplest but most conservative approach, the Bonferroni adjustment, divides the target P value by the number of comparisons made. Equally rigorous but less stringent techniques such as the false detection rate are now in use.[ 80 ] All these techniques adjust individual comparison thresholds so the final statistical significance for all comparisons combined is P < 0.05.
Statistical power and negative studies
Clinical studies can only be effective if the sample size is large enough to give the study a reasonable chance of finding the association as hypothesized by the study's designers which it is investigating. The chance of a study yielding a statistically significant result if its hypothesis is supported is termed its statistical power. There are established methods for calculating statistical power for studies given the planned analysis, sample size, and assumptions about the population from which the sample will be drawn.[ 81 , 82 ]
If studies achieve statistically significant results, the question of statistical power is moot. The power was de facto adequate. The real challenge is when study results fail to reach statistical significance. Over a period of decades, examinations of studies with statistically nonsignificant results have found the studies to have been underpowered.[ 83 , 84 , 85 ] Paralleling Freiman's et al .[ 85 ] earlier study, Moher et al .[ 84 ] reviewed 383 randomized trials published in three major journals, finding 102 which had failed to reach statistical significance. Of the 70 of these negative trials which examined binary or intervally scaled primary outcomes, only 16 (22.9%) had 80% power to detect a 25% difference in outcome rates, and only 36 (51.4%) had 80% power to detect the easier to find 50% difference in outcome rates. This problem continues. In a recent study examining papers published in British orthopedic journals, Sexton et al .[ 83 ] found 49 papers reporting findings that failed to reach statistical significance. Only three (6.1%) of those papers reported a statistical power analysis and had a sample size large enough to give the study adequate statistical power.
Clinicians practice with individual patients, while conclusions about care practices almost always involve considerations of aspects of the clinical courses followed by many. Statistics is one of the important tools to help bridge this gap. This paper has reviewed certain selected key aspects of the statistical approach to clinical events and care. Please note that many of the studies used as examples are clinically illuminating and methodologically sound. However, there are also aspects of the design and execution which were the subject to recurring methodological weaknesses. These include statistical power analysis and sample size planning and the selection and conduct of appropriate analyses in light of the sampling and measurements used. Routine conduct of pilot studies before full studies are initiated could help strengthen study designs and lessen the threat of such methodological weaknesses.
Hopefully the clinical reader will use these tools to understand the strengths and weaknesses of past work. One central goal in conducting methodologically robust studies is to build a sound evidence base for clinical care. These quantitative tools can contribute to building such a solid foundation.
ACKNOWLEDGMENTS
The authors acknowledge the sincere efforts of Dr. Dave Nicholas in reviewing and developing the manuscript.
Source of Support: Nil
Conflict of Interest: None declared.
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Fatal Traffic Risks With a Total Solar Eclipse in the US
- 1 Department of Medicine, University of Toronto, Toronto, Ontario, Canada
- 2 Evaluative Clinical Science Platform, Sunnybrook Research Institute, Toronto, Ontario, Canada
- 3 Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada
- 4 Division of General Internal Medicine, Sunnybrook Health Sciences Centre, Toronto, Ontario, Canada
- 5 Center for Leading Injury Prevention Practice Education & Research, Toronto, Ontario, Canada
- 6 Department of Medicine, University of British Columbia, Vancouver, British Columbia, Canada
- 7 Centre for Clinical Epidemiology & Evaluation, University of British Columbia, Vancouver, British Columbia, Canada
A total solar eclipse occurs when the moon temporarily obscures the sun and casts a dark shadow across the earth. This astronomical spectacle has been described for more than 3 millennia and can be predicted with high precision. Eclipse-related solar retinopathy (vision loss from staring at the sun) is an established medical complication; however, other medical outcomes have received little attention. 1
Read More About
Redelmeier DA , Staples JA. Fatal Traffic Risks With a Total Solar Eclipse in the US. JAMA Intern Med. Published online March 25, 2024. doi:10.1001/jamainternmed.2023.5234
Manage citations:
© 2024
Artificial Intelligence Resource Center
Best of JAMA Network 2022
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
How to Thrive as You Age
Got tinnitus a device that tickles the tongue helps this musician find relief.

Allison Aubrey

After using the Lenire device for an hour each day for 12 weeks, Victoria Banks says her tinnitus is "barely noticeable." David Petrelli/Victoria Banks hide caption
After using the Lenire device for an hour each day for 12 weeks, Victoria Banks says her tinnitus is "barely noticeable."
Imagine if every moment is filled with a high-pitched buzz or ring that you can't turn off.
More than 25 million adults in the U.S., have a condition called tinnitus, according to the American Tinnitus Association. It can be stressful, even panic-inducing and difficult to manage. Dozens of factors can contribute to the onset of tinnitus, including hearing loss, exposure to loud noise or a viral illness.
There's no cure, but there are a range of strategies to reduce the symptoms and make it less bothersome, including hearing aids, mindfulness therapy , and one newer option – a device approved by the FDA to treat tinnitus using electrical stimulation of the tongue.
The device has helped Victoria Banks, a singer and songwriter in Nashville, Tenn., who developed tinnitus about three years ago.
"The noise in my head felt like a bunch of cicadas," Banks says. "It was terrifying." The buzz made it difficult for her to sing and listen to music. "It can be absolutely debilitating," she says.

Shots - Health News
Tinnitus bothers millions of americans. here's how to turn down the noise.
Banks tried taking dietary supplements , but those didn't help. She also stepped up exercise, but that didn't bring relief either. Then she read about a device called Lenire, which was approved by the FDA in March 2023. It includes a plastic mouthpiece with stainless steel electrodes that electrically stimulate the tongue. It is the first device of its kind to be approved for tinnitus.
"This had worked for other people, and I thought I'm willing to try anything at this point," Banks recalls.
She sought out audiologist Brian Fligor, who treats severe cases of tinnitus in the Boston area. Fligor was impressed by the results of a clinical trial that found 84% of participants who tried Lenire experienced a significant reduction in symptoms. He became one of the first providers in the U.S. to use the device with his patients. Fligor also served on an advisory panel assembled by the company who developed it.
"A good candidate for this device is somebody who's had tinnitus for at least three months," Fligor says, emphasizing that people should be evaluated first to make sure there's not an underlying medical issue.
Tinnitus often accompanies hearing loss, but Victoria Banks' hearing was fine and she had no other medical issue, so she was a good candidate.
Banks used the device for an hour each day for 12 weeks. During the hour-long sessions, the electrical stimulation "tickles" the tongue, she says. In addition, the device includes a set of headphones that play a series of tones and ocean-wave sounds.
The device works, in part, by shifting the brain's attention away from the buzz. We're wired to focus on important information coming into our brains, Fligor says. Think of it as a spotlight at a show pointed at the most important thing on the stage. "When you have tinnitus and you're frustrated or angry or scared by it, that spotlight gets really strong and focused on the tinnitus," Fligor says.
"It's the combination of what you're feeling through the nerves in your tongue and what you're hearing through your ears happening in synchrony that causes the spotlight in your brain to not be so stuck on the tinnitus," Fligor explains.

A clinical trial found 84% of people who used the device experienced a significant reduction in symptoms. Brian Fligor hide caption
A clinical trial found 84% of people who used the device experienced a significant reduction in symptoms.
"It unsticks your spotlight" and helps desensitize people to the perceived noise that their tinnitus creates, he says.
Banks says the ringing in her ears did not completely disappear, but now it's barely noticeable on most days.
"It's kind of like if I lived near a waterfall and the waterfall was constantly going," she says. Over time, the waterfall sound fades out of consciousness.
"My brain is now focusing on other things," and the buzz is no longer so distracting. She's back to listening to music, writing music, and performing music." I'm doing all of those things," she says.
When the buzz comes back into focus, Banks says a refresher session with the device helps.
A clinical trial found that 84% of people who tried Lenire , saw significant improvements in their condition. To measure changes, the participants took a questionnaire that asked them to rate how much tinnitus was impacting their sleep, sense of control, feelings of well-being and quality of life. After 12 weeks of using the device, participants improved by an average of 14 points.
"Where this device fits into the big picture, is that it's not a cure-all, but it's quickly become my go-to," for people who do not respond to other ways of managing tinnitus, Fligor says.
One down-side is the cost. Banks paid about $4,000 for the Lenire device, and insurance doesn't cover it. She put the expense on her credit card and paid it off gradually.
Fligor hopes that as the evidence of its effectiveness accumulates, insurers will begin to cover it. Despite the cost, more than 80% of participants in the clinical trial said they would recommend the device to a friend with tinnitus.
But, it's unclear how long the benefits last. Clinical trials have only evaluated Lenire over a 1-year period. "How durable are the effects? We don't really know yet," says audiologist Marc Fagelson, the scientific advisory committee chair of the American Tinnitus Association. He says research is promising but there's still more to learn.
Fagelson says the first step he takes with his patients is an evaluation for hearing loss. Research shows that hearing aids can be an effective treatment for tinnitus among people who have both tinnitus and hearing loss, which is much more common among older adults. An estimated one-third of adults 65 years of age and older who have hearing loss, also have tinnitus.
"We do see a lot of patients, even with very mild loss, who benefit from hearing aids," Fagelson says, but in his experience it's about 50-50 in terms of improving tinnitus. Often, he says people with tinnitus need to explore options beyond hearing aids.
Bruce Freeman , a scientist at the University of Pittsburgh Medical Center, says he's benefitted from both hearing aids and Lenire. He was fitted for the device in Ireland where it was developed, before it was available in the U.S.
Freeman agrees that the ringing never truly disappears, but the device has helped him manage the condition. He describes the sounds that play through the device headphones as very calming and "almost hypnotic" and combined with the tongue vibration, it's helped desensitize him to the ring.
Freeman – who is a research scientist – says he's impressed with the results of research, including a study published in Nature, Scientific Reports that points to significant improvements among clinical trial participants with tinnitus.
Freeman experienced a return of his symptoms when he stopped using the device. "Without it the tinnitus got worse," he says. Then, when he resumed use, it improved.
Freeman believes his long-term exposure to noisy instruments in his research laboratory may have played a role in his condition, and also a neck injury from a bicycle accident that fractured his vertebra. "All of those things converged," he says.
Freeman has developed several habits that help keep the high-pitched ring out of his consciousness and maintain good health. "One thing that does wonders is swimming," he says, pointing to the swooshing sound of water in his ears. "That's a form of mindfulness," he explains.
When it comes to the ring of tinnitus, "it comes and goes," Freeman says. For now, it has subsided into the background, he told me with a sense of relief. "The last two years have been great," he says – a combination of the device, hearing aids and the mindfulness that comes from a swim.
This story was edited by Jane Greenhalgh
- ringing in ears
- hearing loss

IMAGES
VIDEO
COMMENTS
Statistical Methods in Medical Research is a highly ranked, peer reviewed scholarly journal and is the leading vehicle for articles in all the main areas of medical statistics and therefore an essential reference for all medical statisticians. It is particularly useful for medical researchers dealing with data and provides a key resource for medical and statistical libraries, as well as ...
Introduction. This two-part series will present basic statistical principles for the practicing physician to use in his or her review of the literature and to the physician engaged in clinical research. The purpose of this series is threefold: (1) to provide an overview of common epidemiological and statistical terms and concepts that can be ...
The following are the general steps for statistical analysis: (1) formulate a hypothesis, (2) select an appropriate statistical test, (3) conduct a power analysis, (4) prepare data for analysis, (5) start with descriptive statistics, (6) check assumptions of tests, (7) run the analysis, (8) examine the statistical model, (9) report the results ...
The 2017 NIS contained 7,159,694 admissions that, when weighted, represent a national estimate of 35,798,453 hospitalizations. There was a total of 11,034 (1.6%) hospitalizations for emergency general surgery (EGS), representing an estimated 555,170 ± 5,969 (1.6% ± 0.01) nationally in 2017. Go to:
Seong Hoon Yoon. Alain Vandal. Claudia Rivera-Rodriguez. Preview abstract. Open Access Research article First published March 6, 2024 pp. 728-742. xml PDF / EPUB. Table of contents for Statistical Methods in Medical Research, 33, 4, Apr 01, 2024.
Statistical Methods in Medical Research is a highly ranked, peer reviewed scholarly journal and is the leading vehicle for review and non-review articles in all the main areas of medical statistics. It is therefore an essential reference for all medical statisticians. It is particularly useful for medical researchers dealing with data and it provides a key resource for medical and statistical ...
Statistical Methods in Medical Research is a highly ranked, peer reviewed scholarly journal and is the leading vehicle for articles in all the main areas of medical statistics and therefore an essential reference for all medical statisticians. It is particularly useful for medical researchers dealing with data and provides a key resource for medical and statistical libraries, as well as ...
An important requirement for validity of medical research is sound methodology and statistics, yet this is still often overlooked by medical researchers.1,2 Based on the experience of reviewing statistics in more than 1000 manuscripts submitted to The Lancet Group of journals over the past 3 years, this Correspondence provides guidance to commonly encountered statistical deficiencies in ...
The misuse of statistics in medical research has therefore been widely discussed, and it has been pointed out that it is both unethical and can have serious clinical conse quences (Altman 1981; Gardenier and Resnik 2002). As a re sult, there was respectable effort from many medical journals
Statistics in Medicine Welcomes New Tutorials Editor Statistics in Me dicine is pleased to welcome Paul Albert as the newest member of our editorial team. Dr Albert joins Lisa McShane, Robert Platt, and Nigel Stallard and Ben Van Calster as the Tutorials Editor on the journal. Dr Albert has 35 years of experience at the National Institutes of Health holding scientific and leadership positions ...
Introduction. An understanding of elementary statistics is both a UK generic graduate skill and a fundamental of medical practice. The correct interpretation of data for research, its limitations and its application are the foundations for a sound and evidence-based approach to healthcare.
It is very important for medical researchers and health science learners to be literate in biostatistics, as biostatistics is frequently used to assist in the design of medical research studies and to summarize, analyze, and report on data obtained from these studies. In recent years, results obtained from statistical analyses have been ...
Statistics plays a crucial role in research, planning and decision-making in the health sciences. Progress in technologies and continued research in computational statistics has enabled us to implement sophisticated mathematical models within software that are handled by non-statistician researchers. As a result, over the last decades, medical journals have published a host of papers that use ...
Statistical methods are essential in medical research. They are used for data analysis and drawing appropriate conclusions. Clarity and accuracy of statistical reporting in medical journals can enhance readers' understanding of the research conducted and the results obtained. In this manuscript, we provide guidelines for statistical reporting in medical journals for authors to consider, with ...
Statistics as Topic*. Terminology as Topic. The scope of biomedical research has expanded rapidly during the past several decades, and statistical analysis has become increasingly necessary to understand the meaning of large and diverse quantities of raw data. As such, a familiarity with this lexicon is essential for critical appraisal of med ….
Statistical content and complexity of medical research has increased steadily over recent decades. 1-3 Although there is considerable evidence that methodological errors are common in articles in medical journals, 4-6 much published research does not have substantive contribution from a statistician. Anecdote suggests that many physicians have difficulty getting expert advice or involvement in ...
The 4th edition of Statistics in Medicine continues to be a great biostatistics textbook. The book is designed for graduate students, clinical researchers, and health care professionals as a first course in statistics with emphasis on applications in medical, clinical, and public health research. This 4th edition reorganizes the structure and ...
hypothesis. Thus, the main aims of descriptive. statistics are to explore the research data, identify. data distribution, detect errors, and reveal unusual. values (outliers). Descriptive ...
This requires statistical literacy. From the aforesaid, it should be amply clear that statistical literacy is as important a skill for medical professionals, as is the ability to obtain a clinical history, percuss, palpate and auscultate. To this end, the proposal of Annals of Cardiac Anaesthesia to publish a series on "Statistical methods ...
The choice of the most appropriate summary statistic depends on the type and distribution of data. The following data types are distinguished: 2. Nominal data have 2 (eg, sex) or more (eg, blood type) nonordered categories. Ordinal data have categories with a logical order (eg, American Society of Anesthesiologists [ASA] physical status score).
While the potential for AI to be used in surgical education is high, current infrastructure and practices on data capture, storage, labeling, and analysis leave much to be desired to allow rigorous research using AI methods. 1 This practical guide provides an overview of important considerations in using AI techniques and tools in surgical ...
The term PRO encompasses a broad range of measures that may include health-related quality of life measures, symptoms and their affects, patient satisfaction, and the patient's experience with care.
Three years into the COVID-19 outbreak in the United States, Pew Research Center published this collection of survey findings about Americans' challenges with mental health during the pandemic.All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
A woman receives medication to terminate her pregnancy at a reproductive health clinic in Albuquerque, New Mexico, on June 23, 2022, the day before the Supreme Court overturned Roe v. ... This analysis primarily draws from two Pew Research Center surveys, one surveying 10,441 U.S. adults conducted March 7-13, 2022, and another surveying 6,174 U ...
A study of 2,400 Novartis employees around the world found that simply hearing about others' struggles can normalize accessing support at work. Novartis has trained more than 1,000 employees as ...
One of the new educational systems is the mentorship method. This study aimed to investigate the effect of peer mentoring program on clinical academic progress and psychological characteristics of operating room students. This research was a randomized controlled trial that was conducted on undergraduate students in the operating room department of Khomein Faculty of Medical Sciences, Markazi ...
Business is the most commonly held bachelor's degree, followed by health professions. According to the National Center for Education Statistics, about a fifth (19%) of the roughly 2 million bachelor's degrees conferred in 2019-20 were in business. Health professions and related programs were the second most-popular field, making up 12.6% of ...
Abstract. Statistical analysis is one of the foundations of evidence-based clinical practice, a key in conducting new clinical research and in evaluating and applying prior research. In this paper, we review the choice of statistical procedures, analyses of the associations among variables and techniques used when the clinical processes being ...
Public Health Research, Methods, Statistics Retinal Disorders Medical Devices and Equipment Ophthalmology Orthopedics Ethics Guidelines Substance Use and Addiction Medicine Alcohol. Download PDF Full Text. Cite This. Citation. Redelmeier DA, Staples JA. Fatal Traffic Risks With a Total Solar Eclipse in the US.
More than 25 million adults in the U.S. have tinnitus, a condition that causes ringing or buzzing in the ears. An FDA approved device that stimulates the tongue, helped 84% of people who tried it.