- Research article
- Open access
- Published: 04 June 2021

Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews
- Israel Júnior Borges do Nascimento 1 , 2 ,
- Dónal P. O’Mathúna 3 , 4 ,
- Thilo Caspar von Groote 5 ,
- Hebatullah Mohamed Abdulazeem 6 ,
- Ishanka Weerasekara 7 , 8 ,
- Ana Marusic 9 ,
- Livia Puljak ORCID: orcid.org/0000-0002-8467-6061 10 ,
- Vinicius Tassoni Civile 11 ,
- Irena Zakarija-Grkovic 9 ,
- Tina Poklepovic Pericic 9 ,
- Alvaro Nagib Atallah 11 ,
- Santino Filoso 12 ,
- Nicola Luigi Bragazzi 13 &
- Milena Soriano Marcolino 1
On behalf of the International Network of Coronavirus Disease 2019 (InterNetCOVID-19)
BMC Infectious Diseases volume 21 , Article number: 525 ( 2021 ) Cite this article
16k Accesses
28 Citations
13 Altmetric
Metrics details
Navigating the rapidly growing body of scientific literature on the SARS-CoV-2 pandemic is challenging, and ongoing critical appraisal of this output is essential. We aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Nine databases (Medline, EMBASE, Cochrane Library, CINAHL, Web of Sciences, PDQ-Evidence, WHO’s Global Research, LILACS, and Epistemonikos) were searched from December 1, 2019, to March 24, 2020. Systematic reviews analyzing primary studies of COVID-19 were included. Two authors independently undertook screening, selection, extraction (data on clinical symptoms, prevalence, pharmacological and non-pharmacological interventions, diagnostic test assessment, laboratory, and radiological findings), and quality assessment (AMSTAR 2). A meta-analysis was performed of the prevalence of clinical outcomes.
Eighteen systematic reviews were included; one was empty (did not identify any relevant study). Using AMSTAR 2, confidence in the results of all 18 reviews was rated as “critically low”. Identified symptoms of COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%) and gastrointestinal complaints (5–9%). Severe symptoms were more common in men. Elevated C-reactive protein and lactate dehydrogenase, and slightly elevated aspartate and alanine aminotransferase, were commonly described. Thrombocytopenia and elevated levels of procalcitonin and cardiac troponin I were associated with severe disease. A frequent finding on chest imaging was uni- or bilateral multilobar ground-glass opacity. A single review investigated the impact of medication (chloroquine) but found no verifiable clinical data. All-cause mortality ranged from 0.3 to 13.9%.
Conclusions
In this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic were of questionable usefulness. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards.
Peer Review reports
The spread of the “Severe Acute Respiratory Coronavirus 2” (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [ 1 ]. The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [ 2 ], causing massive economic strain, and escalating healthcare and public health expenses [ 3 , 4 ].
The research community has responded by publishing an impressive number of scientific reports related to COVID-19. The world was alerted to the new disease at the beginning of 2020 [ 1 ], and by mid-March 2020, more than 2000 articles had been published on COVID-19 in scholarly journals, with 25% of them containing original data [ 5 ]. The living map of COVID-19 evidence, curated by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), contained more than 40,000 records by February 2021 [ 6 ]. More than 100,000 records on PubMed were labeled as “SARS-CoV-2 literature, sequence, and clinical content” by February 2021 [ 7 ].
Due to publication speed, the research community has voiced concerns regarding the quality and reproducibility of evidence produced during the COVID-19 pandemic, warning of the potential damaging approach of “publish first, retract later” [ 8 ]. It appears that these concerns are not unfounded, as it has been reported that COVID-19 articles were overrepresented in the pool of retracted articles in 2020 [ 9 ]. These concerns about inadequate evidence are of major importance because they can lead to poor clinical practice and inappropriate policies [ 10 ].
Systematic reviews are a cornerstone of today’s evidence-informed decision-making. By synthesizing all relevant evidence regarding a particular topic, systematic reviews reflect the current scientific knowledge. Systematic reviews are considered to be at the highest level in the hierarchy of evidence and should be used to make informed decisions. However, with high numbers of systematic reviews of different scope and methodological quality being published, overviews of multiple systematic reviews that assess their methodological quality are essential [ 11 , 12 , 13 ]. An overview of systematic reviews helps identify and organize the literature and highlights areas of priority in decision-making.
In this overview of systematic reviews, we aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Methodology
Research question.
This overview’s primary objective was to summarize and critically appraise systematic reviews that assessed any type of primary clinical data from patients infected with SARS-CoV-2. Our research question was purposefully broad because we wanted to analyze as many systematic reviews as possible that were available early following the COVID-19 outbreak.
Study design
We conducted an overview of systematic reviews. The idea for this overview originated in a protocol for a systematic review submitted to PROSPERO (CRD42020170623), which indicated a plan to conduct an overview.
Overviews of systematic reviews use explicit and systematic methods for searching and identifying multiple systematic reviews addressing related research questions in the same field to extract and analyze evidence across important outcomes. Overviews of systematic reviews are in principle similar to systematic reviews of interventions, but the unit of analysis is a systematic review [ 14 , 15 , 16 ].
We used the overview methodology instead of other evidence synthesis methods to allow us to collate and appraise multiple systematic reviews on this topic, and to extract and analyze their results across relevant topics [ 17 ]. The overview and meta-analysis of systematic reviews allowed us to investigate the methodological quality of included studies, summarize results, and identify specific areas of available or limited evidence, thereby strengthening the current understanding of this novel disease and guiding future research [ 13 ].
A reporting guideline for overviews of reviews is currently under development, i.e., Preferred Reporting Items for Overviews of Reviews (PRIOR) [ 18 ]. As the PRIOR checklist is still not published, this study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement [ 19 ]. The methodology used in this review was adapted from the Cochrane Handbook for Systematic Reviews of Interventions and also followed established methodological considerations for analyzing existing systematic reviews [ 14 ].
Approval of a research ethics committee was not necessary as the study analyzed only publicly available articles.
Eligibility criteria
Systematic reviews were included if they analyzed primary data from patients infected with SARS-CoV-2 as confirmed by RT-PCR or another pre-specified diagnostic technique. Eligible reviews covered all topics related to COVID-19 including, but not limited to, those that reported clinical symptoms, diagnostic methods, therapeutic interventions, laboratory findings, or radiological results. Both full manuscripts and abbreviated versions, such as letters, were eligible.
No restrictions were imposed on the design of the primary studies included within the systematic reviews, the last search date, whether the review included meta-analyses or language. Reviews related to SARS-CoV-2 and other coronaviruses were eligible, but from those reviews, we analyzed only data related to SARS-CoV-2.
No consensus definition exists for a systematic review [ 20 ], and debates continue about the defining characteristics of a systematic review [ 21 ]. Cochrane’s guidance for overviews of reviews recommends setting pre-established criteria for making decisions around inclusion [ 14 ]. That is supported by a recent scoping review about guidance for overviews of systematic reviews [ 22 ].
Thus, for this study, we defined a systematic review as a research report which searched for primary research studies on a specific topic using an explicit search strategy, had a detailed description of the methods with explicit inclusion criteria provided, and provided a summary of the included studies either in narrative or quantitative format (such as a meta-analysis). Cochrane and non-Cochrane systematic reviews were considered eligible for inclusion, with or without meta-analysis, and regardless of the study design, language restriction and methodology of the included primary studies. To be eligible for inclusion, reviews had to be clearly analyzing data related to SARS-CoV-2 (associated or not with other viruses). We excluded narrative reviews without those characteristics as these are less likely to be replicable and are more prone to bias.
Scoping reviews and rapid reviews were eligible for inclusion in this overview if they met our pre-defined inclusion criteria noted above. We included reviews that addressed SARS-CoV-2 and other coronaviruses if they reported separate data regarding SARS-CoV-2.
Information sources
Nine databases were searched for eligible records published between December 1, 2019, and March 24, 2020: Cochrane Database of Systematic Reviews via Cochrane Library, PubMed, EMBASE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Web of Sciences, LILACS (Latin American and Caribbean Health Sciences Literature), PDQ-Evidence, WHO’s Global Research on Coronavirus Disease (COVID-19), and Epistemonikos.
The comprehensive search strategy for each database is provided in Additional file 1 and was designed and conducted in collaboration with an information specialist. All retrieved records were primarily processed in EndNote, where duplicates were removed, and records were then imported into the Covidence platform [ 23 ]. In addition to database searches, we screened reference lists of reviews included after screening records retrieved via databases.
Study selection
All searches, screening of titles and abstracts, and record selection, were performed independently by two investigators using the Covidence platform [ 23 ]. Articles deemed potentially eligible were retrieved for full-text screening carried out independently by two investigators. Discrepancies at all stages were resolved by consensus. During the screening, records published in languages other than English were translated by a native/fluent speaker.
Data collection process
We custom designed a data extraction table for this study, which was piloted by two authors independently. Data extraction was performed independently by two authors. Conflicts were resolved by consensus or by consulting a third researcher.
We extracted the following data: article identification data (authors’ name and journal of publication), search period, number of databases searched, population or settings considered, main results and outcomes observed, and number of participants. From Web of Science (Clarivate Analytics, Philadelphia, PA, USA), we extracted journal rank (quartile) and Journal Impact Factor (JIF).
We categorized the following as primary outcomes: all-cause mortality, need for and length of mechanical ventilation, length of hospitalization (in days), admission to intensive care unit (yes/no), and length of stay in the intensive care unit.
The following outcomes were categorized as exploratory: diagnostic methods used for detection of the virus, male to female ratio, clinical symptoms, pharmacological and non-pharmacological interventions, laboratory findings (full blood count, liver enzymes, C-reactive protein, d-dimer, albumin, lipid profile, serum electrolytes, blood vitamin levels, glucose levels, and any other important biomarkers), and radiological findings (using radiography, computed tomography, magnetic resonance imaging or ultrasound).
We also collected data on reporting guidelines and requirements for the publication of systematic reviews and meta-analyses from journal websites where included reviews were published.
Quality assessment in individual reviews
Two researchers independently assessed the reviews’ quality using the “A MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR 2)”. We acknowledge that the AMSTAR 2 was created as “a critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both” [ 24 ]. However, since AMSTAR 2 was designed for systematic reviews of intervention trials, and we included additional types of systematic reviews, we adjusted some AMSTAR 2 ratings and reported these in Additional file 2 .
Adherence to each item was rated as follows: yes, partial yes, no, or not applicable (such as when a meta-analysis was not conducted). The overall confidence in the results of the review is rated as “critically low”, “low”, “moderate” or “high”, according to the AMSTAR 2 guidance based on seven critical domains, which are items 2, 4, 7, 9, 11, 13, 15 as defined by AMSTAR 2 authors [ 24 ]. We reported our adherence ratings for transparency of our decision with accompanying explanations, for each item, in each included review.
One of the included systematic reviews was conducted by some members of this author team [ 25 ]. This review was initially assessed independently by two authors who were not co-authors of that review to prevent the risk of bias in assessing this study.
Synthesis of results
For data synthesis, we prepared a table summarizing each systematic review. Graphs illustrating the mortality rate and clinical symptoms were created. We then prepared a narrative summary of the methods, findings, study strengths, and limitations.
For analysis of the prevalence of clinical outcomes, we extracted data on the number of events and the total number of patients to perform proportional meta-analysis using RStudio© software, with the “meta” package (version 4.9–6), using the “metaprop” function for reviews that did not perform a meta-analysis, excluding case studies because of the absence of variance. For reviews that did not perform a meta-analysis, we presented pooled results of proportions with their respective confidence intervals (95%) by the inverse variance method with a random-effects model, using the DerSimonian-Laird estimator for τ 2 . We adjusted data using Freeman-Tukey double arcosen transformation. Confidence intervals were calculated using the Clopper-Pearson method for individual studies. We created forest plots using the RStudio© software, with the “metafor” package (version 2.1–0) and “forest” function.
Managing overlapping systematic reviews
Some of the included systematic reviews that address the same or similar research questions may include the same primary studies in overviews. Including such overlapping reviews may introduce bias when outcome data from the same primary study are included in the analyses of an overview multiple times. Thus, in summaries of evidence, multiple-counting of the same outcome data will give data from some primary studies too much influence [ 14 ]. In this overview, we did not exclude overlapping systematic reviews because, according to Cochrane’s guidance, it may be appropriate to include all relevant reviews’ results if the purpose of the overview is to present and describe the current body of evidence on a topic [ 14 ]. To avoid any bias in summary estimates associated with overlapping reviews, we generated forest plots showing data from individual systematic reviews, but the results were not pooled because some primary studies were included in multiple reviews.
Our search retrieved 1063 publications, of which 175 were duplicates. Most publications were excluded after the title and abstract analysis ( n = 860). Among the 28 studies selected for full-text screening, 10 were excluded for the reasons described in Additional file 3 , and 18 were included in the final analysis (Fig. 1 ) [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Reference list screening did not retrieve any additional systematic reviews.

PRISMA flow diagram
Characteristics of included reviews
Summary features of 18 systematic reviews are presented in Table 1 . They were published in 14 different journals. Only four of these journals had specific requirements for systematic reviews (with or without meta-analysis): European Journal of Internal Medicine, Journal of Clinical Medicine, Ultrasound in Obstetrics and Gynecology, and Clinical Research in Cardiology . Two journals reported that they published only invited reviews ( Journal of Medical Virology and Clinica Chimica Acta ). Three systematic reviews in our study were published as letters; one was labeled as a scoping review and another as a rapid review (Table 2 ).
All reviews were published in English, in first quartile (Q1) journals, with JIF ranging from 1.692 to 6.062. One review was empty, meaning that its search did not identify any relevant studies; i.e., no primary studies were included [ 36 ]. The remaining 17 reviews included 269 unique studies; the majority ( N = 211; 78%) were included in only a single review included in our study (range: 1 to 12). Primary studies included in the reviews were published between December 2019 and March 18, 2020, and comprised case reports, case series, cohorts, and other observational studies. We found only one review that included randomized clinical trials [ 38 ]. In the included reviews, systematic literature searches were performed from 2019 (entire year) up to March 9, 2020. Ten systematic reviews included meta-analyses. The list of primary studies found in the included systematic reviews is shown in Additional file 4 , as well as the number of reviews in which each primary study was included.
Population and study designs
Most of the reviews analyzed data from patients with COVID-19 who developed pneumonia, acute respiratory distress syndrome (ARDS), or any other correlated complication. One review aimed to evaluate the effectiveness of using surgical masks on preventing transmission of the virus [ 36 ], one review was focused on pediatric patients [ 34 ], and one review investigated COVID-19 in pregnant women [ 37 ]. Most reviews assessed clinical symptoms, laboratory findings, or radiological results.
Systematic review findings
The summary of findings from individual reviews is shown in Table 2 . Overall, all-cause mortality ranged from 0.3 to 13.9% (Fig. 2 ).

A meta-analysis of the prevalence of mortality
Clinical symptoms
Seven reviews described the main clinical manifestations of COVID-19 [ 26 , 28 , 29 , 34 , 35 , 39 , 41 ]. Three of them provided only a narrative discussion of symptoms [ 26 , 34 , 35 ]. In the reviews that performed a statistical analysis of the incidence of different clinical symptoms, symptoms in patients with COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%), gastrointestinal disorders, such as diarrhea, nausea or vomiting (5.0–9.0%), and others (including, in one study only: dizziness 12.1%) (Figs. 3 , 4 , 5 , 6 , 7 , 8 and 9 ). Three reviews assessed cough with and without sputum together; only one review assessed sputum production itself (28.5%).

A meta-analysis of the prevalence of fever

A meta-analysis of the prevalence of cough

A meta-analysis of the prevalence of dyspnea

A meta-analysis of the prevalence of fatigue or myalgia

A meta-analysis of the prevalence of headache

A meta-analysis of the prevalence of gastrointestinal disorders

A meta-analysis of the prevalence of sore throat
Diagnostic aspects
Three reviews described methodologies, protocols, and tools used for establishing the diagnosis of COVID-19 [ 26 , 34 , 38 ]. The use of respiratory swabs (nasal or pharyngeal) or blood specimens to assess the presence of SARS-CoV-2 nucleic acid using RT-PCR assays was the most commonly used diagnostic method mentioned in the included studies. These diagnostic tests have been widely used, but their precise sensitivity and specificity remain unknown. One review included a Chinese study with clinical diagnosis with no confirmation of SARS-CoV-2 infection (patients were diagnosed with COVID-19 if they presented with at least two symptoms suggestive of COVID-19, together with laboratory and chest radiography abnormalities) [ 34 ].
Therapeutic possibilities
Pharmacological and non-pharmacological interventions (supportive therapies) used in treating patients with COVID-19 were reported in five reviews [ 25 , 27 , 34 , 35 , 38 ]. Antivirals used empirically for COVID-19 treatment were reported in seven reviews [ 25 , 27 , 34 , 35 , 37 , 38 , 41 ]; most commonly used were protease inhibitors (lopinavir, ritonavir, darunavir), nucleoside reverse transcriptase inhibitor (tenofovir), nucleotide analogs (remdesivir, galidesivir, ganciclovir), and neuraminidase inhibitors (oseltamivir). Umifenovir, a membrane fusion inhibitor, was investigated in two studies [ 25 , 35 ]. Possible supportive interventions analyzed were different types of oxygen supplementation and breathing support (invasive or non-invasive ventilation) [ 25 ]. The use of antibiotics, both empirically and to treat secondary pneumonia, was reported in six studies [ 25 , 26 , 27 , 34 , 35 , 38 ]. One review specifically assessed evidence on the efficacy and safety of the anti-malaria drug chloroquine [ 27 ]. It identified 23 ongoing trials investigating the potential of chloroquine as a therapeutic option for COVID-19, but no verifiable clinical outcomes data. The use of mesenchymal stem cells, antifungals, and glucocorticoids were described in four reviews [ 25 , 34 , 35 , 38 ].
Laboratory and radiological findings
Of the 18 reviews included in this overview, eight analyzed laboratory parameters in patients with COVID-19 [ 25 , 29 , 30 , 32 , 33 , 34 , 35 , 39 ]; elevated C-reactive protein levels, associated with lymphocytopenia, elevated lactate dehydrogenase, as well as slightly elevated aspartate and alanine aminotransferase (AST, ALT) were commonly described in those eight reviews. Lippi et al. assessed cardiac troponin I (cTnI) [ 25 ], procalcitonin [ 32 ], and platelet count [ 33 ] in COVID-19 patients. Elevated levels of procalcitonin [ 32 ] and cTnI [ 30 ] were more likely to be associated with a severe disease course (requiring intensive care unit admission and intubation). Furthermore, thrombocytopenia was frequently observed in patients with complicated COVID-19 infections [ 33 ].
Chest imaging (chest radiography and/or computed tomography) features were assessed in six reviews, all of which described a frequent pattern of local or bilateral multilobar ground-glass opacity [ 25 , 34 , 35 , 39 , 40 , 41 ]. Those six reviews showed that septal thickening, bronchiectasis, pleural and cardiac effusions, halo signs, and pneumothorax were observed in patients suffering from COVID-19.
Quality of evidence in individual systematic reviews
Table 3 shows the detailed results of the quality assessment of 18 systematic reviews, including the assessment of individual items and summary assessment. A detailed explanation for each decision in each review is available in Additional file 5 .
Using AMSTAR 2 criteria, confidence in the results of all 18 reviews was rated as “critically low” (Table 3 ). Common methodological drawbacks were: omission of prospective protocol submission or publication; use of inappropriate search strategy: lack of independent and dual literature screening and data-extraction (or methodology unclear); absence of an explanation for heterogeneity among the studies included; lack of reasons for study exclusion (or rationale unclear).
Risk of bias assessment, based on a reported methodological tool, and quality of evidence appraisal, in line with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method, were reported only in one review [ 25 ]. Five reviews presented a table summarizing bias, using various risk of bias tools [ 25 , 29 , 39 , 40 , 41 ]. One review analyzed “study quality” [ 37 ]. One review mentioned the risk of bias assessment in the methodology but did not provide any related analysis [ 28 ].
This overview of systematic reviews analyzed the first 18 systematic reviews published after the onset of the COVID-19 pandemic, up to March 24, 2020, with primary studies involving more than 60,000 patients. Using AMSTAR-2, we judged that our confidence in all those reviews was “critically low”. Ten reviews included meta-analyses. The reviews presented data on clinical manifestations, laboratory and radiological findings, and interventions. We found no systematic reviews on the utility of diagnostic tests.
Symptoms were reported in seven reviews; most of the patients had a fever, cough, dyspnea, myalgia or muscle fatigue, and gastrointestinal disorders such as diarrhea, nausea, or vomiting. Olfactory dysfunction (anosmia or dysosmia) has been described in patients infected with COVID-19 [ 43 ]; however, this was not reported in any of the reviews included in this overview. During the SARS outbreak in 2002, there were reports of impairment of the sense of smell associated with the disease [ 44 , 45 ].
The reported mortality rates ranged from 0.3 to 14% in the included reviews. Mortality estimates are influenced by the transmissibility rate (basic reproduction number), availability of diagnostic tools, notification policies, asymptomatic presentations of the disease, resources for disease prevention and control, and treatment facilities; variability in the mortality rate fits the pattern of emerging infectious diseases [ 46 ]. Furthermore, the reported cases did not consider asymptomatic cases, mild cases where individuals have not sought medical treatment, and the fact that many countries had limited access to diagnostic tests or have implemented testing policies later than the others. Considering the lack of reviews assessing diagnostic testing (sensitivity, specificity, and predictive values of RT-PCT or immunoglobulin tests), and the preponderance of studies that assessed only symptomatic individuals, considerable imprecision around the calculated mortality rates existed in the early stage of the COVID-19 pandemic.
Few reviews included treatment data. Those reviews described studies considered to be at a very low level of evidence: usually small, retrospective studies with very heterogeneous populations. Seven reviews analyzed laboratory parameters; those reviews could have been useful for clinicians who attend patients suspected of COVID-19 in emergency services worldwide, such as assessing which patients need to be reassessed more frequently.
All systematic reviews scored poorly on the AMSTAR 2 critical appraisal tool for systematic reviews. Most of the original studies included in the reviews were case series and case reports, impacting the quality of evidence. Such evidence has major implications for clinical practice and the use of these reviews in evidence-based practice and policy. Clinicians, patients, and policymakers can only have the highest confidence in systematic review findings if high-quality systematic review methodologies are employed. The urgent need for information during a pandemic does not justify poor quality reporting.
We acknowledge that there are numerous challenges associated with analyzing COVID-19 data during a pandemic [ 47 ]. High-quality evidence syntheses are needed for decision-making, but each type of evidence syntheses is associated with its inherent challenges.
The creation of classic systematic reviews requires considerable time and effort; with massive research output, they quickly become outdated, and preparing updated versions also requires considerable time. A recent study showed that updates of non-Cochrane systematic reviews are published a median of 5 years after the publication of the previous version [ 48 ].
Authors may register a review and then abandon it [ 49 ], but the existence of a public record that is not updated may lead other authors to believe that the review is still ongoing. A quarter of Cochrane review protocols remains unpublished as completed systematic reviews 8 years after protocol publication [ 50 ].
Rapid reviews can be used to summarize the evidence, but they involve methodological sacrifices and simplifications to produce information promptly, with inconsistent methodological approaches [ 51 ]. However, rapid reviews are justified in times of public health emergencies, and even Cochrane has resorted to publishing rapid reviews in response to the COVID-19 crisis [ 52 ]. Rapid reviews were eligible for inclusion in this overview, but only one of the 18 reviews included in this study was labeled as a rapid review.
Ideally, COVID-19 evidence would be continually summarized in a series of high-quality living systematic reviews, types of evidence synthesis defined as “ a systematic review which is continually updated, incorporating relevant new evidence as it becomes available ” [ 53 ]. However, conducting living systematic reviews requires considerable resources, calling into question the sustainability of such evidence synthesis over long periods [ 54 ].
Research reports about COVID-19 will contribute to research waste if they are poorly designed, poorly reported, or simply not necessary. In principle, systematic reviews should help reduce research waste as they usually provide recommendations for further research that is needed or may advise that sufficient evidence exists on a particular topic [ 55 ]. However, systematic reviews can also contribute to growing research waste when they are not needed, or poorly conducted and reported. Our present study clearly shows that most of the systematic reviews that were published early on in the COVID-19 pandemic could be categorized as research waste, as our confidence in their results is critically low.
Our study has some limitations. One is that for AMSTAR 2 assessment we relied on information available in publications; we did not attempt to contact study authors for clarifications or additional data. In three reviews, the methodological quality appraisal was challenging because they were published as letters, or labeled as rapid communications. As a result, various details about their review process were not included, leading to AMSTAR 2 questions being answered as “not reported”, resulting in low confidence scores. Full manuscripts might have provided additional information that could have led to higher confidence in the results. In other words, low scores could reflect incomplete reporting, not necessarily low-quality review methods. To make their review available more rapidly and more concisely, the authors may have omitted methodological details. A general issue during a crisis is that speed and completeness must be balanced. However, maintaining high standards requires proper resourcing and commitment to ensure that the users of systematic reviews can have high confidence in the results.
Furthermore, we used adjusted AMSTAR 2 scoring, as the tool was designed for critical appraisal of reviews of interventions. Some reviews may have received lower scores than actually warranted in spite of these adjustments.
Another limitation of our study may be the inclusion of multiple overlapping reviews, as some included reviews included the same primary studies. According to the Cochrane Handbook, including overlapping reviews may be appropriate when the review’s aim is “ to present and describe the current body of systematic review evidence on a topic ” [ 12 ], which was our aim. To avoid bias with summarizing evidence from overlapping reviews, we presented the forest plots without summary estimates. The forest plots serve to inform readers about the effect sizes for outcomes that were reported in each review.
Several authors from this study have contributed to one of the reviews identified [ 25 ]. To reduce the risk of any bias, two authors who did not co-author the review in question initially assessed its quality and limitations.
Finally, we note that the systematic reviews included in our overview may have had issues that our analysis did not identify because we did not analyze their primary studies to verify the accuracy of the data and information they presented. We give two examples to substantiate this possibility. Lovato et al. wrote a commentary on the review of Sun et al. [ 41 ], in which they criticized the authors’ conclusion that sore throat is rare in COVID-19 patients [ 56 ]. Lovato et al. highlighted that multiple studies included in Sun et al. did not accurately describe participants’ clinical presentations, warning that only three studies clearly reported data on sore throat [ 56 ].
In another example, Leung [ 57 ] warned about the review of Li, L.Q. et al. [ 29 ]: “ it is possible that this statistic was computed using overlapped samples, therefore some patients were double counted ”. Li et al. responded to Leung that it is uncertain whether the data overlapped, as they used data from published articles and did not have access to the original data; they also reported that they requested original data and that they plan to re-do their analyses once they receive them; they also urged readers to treat the data with caution [ 58 ]. This points to the evolving nature of evidence during a crisis.
Our study’s strength is that this overview adds to the current knowledge by providing a comprehensive summary of all the evidence synthesis about COVID-19 available early after the onset of the pandemic. This overview followed strict methodological criteria, including a comprehensive and sensitive search strategy and a standard tool for methodological appraisal of systematic reviews.
In conclusion, in this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all the reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic could be categorized as research waste. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards to provide patients, clinicians, and decision-makers trustworthy evidence.
Availability of data and materials
All data collected and analyzed within this study are available from the corresponding author on reasonable request.
World Health Organization. Timeline - COVID-19: Available at: https://www.who.int/news/item/29-06-2020-covidtimeline . Accessed 1 June 2021.
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu/map.html . Accessed 1 June 2021.
Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A, et al. Assessing the Impact of Reduced Travel on Exportation Dynamics of Novel Coronavirus Infection (COVID-19). J Clin Med. 2020;9(2):601.
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. https://doi.org/10.1126/science.aba9757 .
Article CAS PubMed PubMed Central Google Scholar
Fidahic M, Nujic D, Runjic R, Civljak M, Markotic F, Lovric Makaric Z, et al. Research methodology and characteristics of journal articles with original data, preprint articles and registered clinical trial protocols about COVID-19. BMC Med Res Methodol. 2020;20(1):161. https://doi.org/10.1186/s12874-020-01047-2 .
EPPI Centre . COVID-19: a living systematic map of the evidence. Available at: http://eppi.ioe.ac.uk/cms/Projects/DepartmentofHealthandSocialCare/Publishedreviews/COVID-19Livingsystematicmapoftheevidence/tabid/3765/Default.aspx . Accessed 1 June 2021.
NCBI SARS-CoV-2 Resources. Available at: https://www.ncbi.nlm.nih.gov/sars-cov-2/ . Accessed 1 June 2021.
Gustot T. Quality and reproducibility during the COVID-19 pandemic. JHEP Rep. 2020;2(4):100141. https://doi.org/10.1016/j.jhepr.2020.100141 .
Article PubMed PubMed Central Google Scholar
Kodvanj, I., et al., Publishing of COVID-19 Preprints in Peer-reviewed Journals, Preprinting Trends, Public Discussion and Quality Issues. Preprint article. bioRxiv 2020.11.23.394577; doi: https://doi.org/10.1101/2020.11.23.394577 .
Dobler CC. Poor quality research and clinical practice during COVID-19. Breathe (Sheff). 2020;16(2):200112. https://doi.org/10.1183/20734735.0112-2020 .
Article Google Scholar
Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7(9):e1000326. https://doi.org/10.1371/journal.pmed.1000326 .
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231. https://doi.org/10.1186/s13643-017-0617-1 .
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane. 2020. Available from www.training.cochrane.org/handbook .
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. 2020; Available from www.training.cochrane.org/handbook .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18. https://doi.org/10.1186/s13643-018-0914-3 .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):29. https://doi.org/10.1186/s13643-018-0768-8 .
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39. https://doi.org/10.1186/s13643-018-0695-8 .
Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335. https://doi.org/10.1186/s13643-019-1252-9 .
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3(3):e123–30.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203. https://doi.org/10.1186/s12874-019-0855-0 .
Puljak L. If there is only one author or only one database was searched, a study should not be called a systematic review. J Clin Epidemiol. 2017;91:4–5. https://doi.org/10.1016/j.jclinepi.2017.08.002 .
Article PubMed Google Scholar
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254. https://doi.org/10.1186/s13643-020-01509-0 .
Covidence - systematic review software. Available at: https://www.covidence.org/ . Accessed 1 June 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Borges do Nascimento IJ, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9(4):941.
Article PubMed Central Google Scholar
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. https://doi.org/10.1186/s40249-020-00646-x .
Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279–83. https://doi.org/10.1016/j.jcrc.2020.03.005 .
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8. https://doi.org/10.1007/s00392-020-01626-9 .
Article CAS PubMed Google Scholar
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577–83. https://doi.org/10.1002/jmv.25757 .
Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390–1. https://doi.org/10.1016/j.pcad.2020.03.001 .
Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med. 2020;75:107–8. https://doi.org/10.1016/j.ejim.2020.03.014 .
Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–1. https://doi.org/10.1016/j.cca.2020.03.004 .
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8. https://doi.org/10.1016/j.cca.2020.03.022 .
Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–95. https://doi.org/10.1111/apa.15270 .
Lupia T, Scabini S, Mornese Pinna S, di Perri G, de Rosa FG, Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J Glob Antimicrob Resist. 2020;21:22–7. https://doi.org/10.1016/j.jgar.2020.02.021 .
Marasinghe, K.M., A systematic review investigating the effectiveness of face mask use in limiting the spread of COVID-19 among medically not diagnosed individuals: shedding light on current recommendations provided to individuals not medically diagnosed with COVID-19. Research Square. Preprint article. doi : https://doi.org/10.21203/rs.3.rs-16701/v1 . 2020 .
Mullins E, Evans D, Viner RM, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586–92. https://doi.org/10.1002/uog.22014 .
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JIP, et al. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel coronavirus (2019-nCoV): a systematic review. J Clin Med. 2020;9(3):623.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. https://doi.org/10.1016/j.tmaid.2020.101623 .
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. https://doi.org/10.2214/AJR.20.23034 .
Sun P, Qie S, Liu Z, Ren J, Li K, Xi J. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J Med Virol. 2020;92(6):612–7. https://doi.org/10.1002/jmv.25735 .
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017 .
Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Investig. 2020;50(3):e13209. https://doi.org/10.1111/eci.13209 .
Article CAS Google Scholar
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwanica. 2006;15(1):26–8.
Google Scholar
Suzuki M, Saito K, Min WP, Vladau C, Toida K, Itoh H, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117(2):272–7. https://doi.org/10.1097/01.mlg.0000249922.37381.1e .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7. https://doi.org/10.1016/S1473-3099(20)30244-9 .
Wolkewitz M, Puljak L. Methodological challenges of analysing COVID-19 data during the pandemic. BMC Med Res Methodol. 2020;20(1):81. https://doi.org/10.1186/s12874-020-00972-6 .
Rombey T, Lochner V, Puljak L, Könsgen N, Mathes T, Pieper D. Epidemiology and reporting characteristics of non-Cochrane updates of systematic reviews: a cross-sectional study. Res Synth Methods. 2020;11(3):471–83. https://doi.org/10.1002/jrsm.1409 .
Runjic E, Rombey T, Pieper D, Puljak L. Half of systematic reviews about pain registered in PROSPERO were not published and the majority had inaccurate status. J Clin Epidemiol. 2019;116:114–21. https://doi.org/10.1016/j.jclinepi.2019.08.010 .
Runjic E, Behmen D, Pieper D, Mathes T, Tricco AC, Moher D, et al. Following Cochrane review protocols to completion 10 years later: a retrospective cohort study and author survey. J Clin Epidemiol. 2019;111:41–8. https://doi.org/10.1016/j.jclinepi.2019.03.006 .
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1):224. https://doi.org/10.1186/s12916-015-0465-6 .
COVID-19 Rapid Reviews: Cochrane’s response so far. Available at: https://training.cochrane.org/resource/covid-19-rapid-reviews-cochrane-response-so-far . Accessed 1 June 2021.
Cochrane. Living systematic reviews. Available at: https://community.cochrane.org/review-production/production-resources/living-systematic-reviews . Accessed 1 June 2021.
Millard T, Synnot A, Elliott J, Green S, McDonald S, Turner T. Feasibility and acceptability of living systematic reviews: results from a mixed-methods evaluation. Syst Rev. 2019;8(1):325. https://doi.org/10.1186/s13643-019-1248-5 .
Babic A, Poklepovic Pericic T, Pieper D, Puljak L. How to decide whether a systematic review is stable and not in need of updating: analysis of Cochrane reviews. Res Synth Methods. 2020;11(6):884–90. https://doi.org/10.1002/jrsm.1451 .
Lovato A, Rossettini G, de Filippis C. Sore throat in COVID-19: comment on “clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis”. J Med Virol. 2020;92(7):714–5. https://doi.org/10.1002/jmv.25815 .
Leung C. Comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1431–2. https://doi.org/10.1002/jmv.25912 .
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. Response to Char’s comment: comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1433. https://doi.org/10.1002/jmv.25924 .
Download references
Acknowledgments
We thank Catherine Henderson DPhil from Swanscoe Communications for pro bono medical writing and editing support. We acknowledge support from the Covidence Team, specifically Anneliese Arno. We thank the whole International Network of Coronavirus Disease 2019 (InterNetCOVID-19) for their commitment and involvement. Members of the InterNetCOVID-19 are listed in Additional file 6 . We thank Pavel Cerny and Roger Crosthwaite for guiding the team supervisor (IJBN) on human resources management.
This research received no external funding.
Author information
Authors and affiliations.
University Hospital and School of Medicine, Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
Israel Júnior Borges do Nascimento & Milena Soriano Marcolino
Medical College of Wisconsin, Milwaukee, WI, USA
Israel Júnior Borges do Nascimento
Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare, College of Nursing, The Ohio State University, Columbus, OH, USA
Dónal P. O’Mathúna
School of Nursing, Psychotherapy and Community Health, Dublin City University, Dublin, Ireland
Department of Anesthesiology, Intensive Care and Pain Medicine, University of Münster, Münster, Germany
Thilo Caspar von Groote
Department of Sport and Health Science, Technische Universität München, Munich, Germany
Hebatullah Mohamed Abdulazeem
School of Health Sciences, Faculty of Health and Medicine, The University of Newcastle, Callaghan, Australia
Ishanka Weerasekara
Department of Physiotherapy, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka
Cochrane Croatia, University of Split, School of Medicine, Split, Croatia
Ana Marusic, Irena Zakarija-Grkovic & Tina Poklepovic Pericic
Center for Evidence-Based Medicine and Health Care, Catholic University of Croatia, Ilica 242, 10000, Zagreb, Croatia
Livia Puljak
Cochrane Brazil, Evidence-Based Health Program, Universidade Federal de São Paulo, São Paulo, Brazil
Vinicius Tassoni Civile & Alvaro Nagib Atallah
Yorkville University, Fredericton, New Brunswick, Canada
Santino Filoso
Laboratory for Industrial and Applied Mathematics (LIAM), Department of Mathematics and Statistics, York University, Toronto, Ontario, Canada
Nicola Luigi Bragazzi
You can also search for this author in PubMed Google Scholar
Contributions
IJBN conceived the research idea and worked as a project coordinator. DPOM, TCVG, HMA, IW, AM, LP, VTC, IZG, TPP, ANA, SF, NLB and MSM were involved in data curation, formal analysis, investigation, methodology, and initial draft writing. All authors revised the manuscript critically for the content. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Livia Puljak .
Ethics declarations
Ethics approval and consent to participate.
Not required as data was based on published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Search strategies used in the study.
Additional file 2: Appendix 2.
Adjusted scoring of AMSTAR 2 used in this study for systematic reviews of studies that did not analyze interventions.
Additional file 3: Appendix 3.
List of excluded studies, with reasons.
Additional file 4: Appendix 4.
Table of overlapping studies, containing the list of primary studies included, their visual overlap in individual systematic reviews, and the number in how many reviews each primary study was included.
Additional file 5: Appendix 5.
A detailed explanation of AMSTAR scoring for each item in each review.
Additional file 6: Appendix 6.
List of members and affiliates of International Network of Coronavirus Disease 2019 (InterNetCOVID-19).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Borges do Nascimento, I.J., O’Mathúna, D.P., von Groote, T.C. et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect Dis 21 , 525 (2021). https://doi.org/10.1186/s12879-021-06214-4
Download citation
Received : 12 April 2020
Accepted : 19 May 2021
Published : 04 June 2021
DOI : https://doi.org/10.1186/s12879-021-06214-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronavirus
- Evidence-based medicine
- Infectious diseases
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Population-based prevalence surveys during the Covid-19 pandemic: A systematic review
Affiliations.
- 1 Graduate Program in Cell and Molecular Biology (PPGBCM), Center of Biotechnology, Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, Rio Grande do Sul, Brazil.
- 2 Undergraduate Program in Biomedicine, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, Rio Grande do Sul, Brazil.
- 3 Graduate Program in Pathology, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, Rio Grande do Sul, Brazil.
- 4 Graduate Program in Epidemiology, Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, Rio Grande do Sul, Brazil.
- 5 Graduate Program in Health Sciences, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, Rio Grande do Sul, Brazil.
- 6 Undergraduate Program in Biomedical Informatics, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, Rio Grande do Sul, Brazil.
- 7 Department of Internal Medicine, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, Rio Grande do Sul, Brazil.
- 8 Department of Statistics, Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, Rio Grande do Sul, Brazil.
- 9 Department of Exact and Social Applied Sciences, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, Rio Grande do Sul, Brazil.
- 10 Department of Diagnostic Methods, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, Rio Grande do Sul, Brazil.
- 11 Department of Pharmacosciences, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, Rio Grande do Sul, Brazil.
- PMID: 34260777
- PMCID: PMC7883186
- DOI: 10.1002/rmv.2200
Population-based prevalence surveys of Covid-19 contribute to establish the burden of infection, the role of asymptomatic and mild infections in transmission, and allow more precise decisions about reopen policies. We performed a systematic review to evaluate qualitative aspects of these studies, assessing their reliability and compiling practices that can influence the methodological quality. We searched MEDLINE, EMBASE, bioRxiv and medRxiv, and included cross-sectional studies using molecular and/or serological tests to estimate the prevalence of Covid-19 in the general population. Survey quality was assessed using the Joanna Briggs Institute Critical Appraisal Checklist for Prevalence Studies. A correspondence analysis correlated methodological parameters of each study to identify patterns related to higher, intermediate and lower risks of bias. The available data described 37 surveys from 19 countries. The majority were from Europe and America, used antibody testing, and reached highly heterogeneous sample sizes and prevalence estimates. Minority communities were disproportionately affected by Covid-19. Important risk of bias was detected in four domains: sample size, data analysis with sufficient coverage, measurements in standard way and response rate. The correspondence analysis showed few consistent patterns for high risk of bias. Intermediate risk of bias was related to American and European studies, municipal and regional initiatives, blood samples and prevalence >1%. Low risk of bias was related to Asian studies, nationwide initiatives, reverse-transcriptase polymerase chain reaction tests and prevalence <1%. We identified methodological standards applied worldwide in Covid-19 prevalence surveys, which may assist researchers with the planning, execution and reporting of future population-based surveys.
Keywords: Covid-19; SARS-CoV-2; cross-sectional studies; epidemiology; infectious diseases; prevalence; severe acute respiratory syndrome coronavirus 2.
© 2020 John Wiley & Sons Ltd.
Publication types
- Research Support, Non-U.S. Gov't
- Systematic Review
- COVID-19 / diagnosis
- COVID-19 / epidemiology*
- COVID-19 Testing / methods
- Mass Screening / methods
- Population Surveillance* / methods
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Effectiveness of...
Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis
Linked editorial.
Public health measures for covid-19
- Related content
- Peer review
- Stella Talic , lecturer in clinical epidemiology and public health 1 2 ,
- Shivangi Shah , honours student 1 ,
- Holly Wild , lecturer and honours student 1 3 ,
- Danijela Gasevic , senior lecturer in epidemiology and chronic disease prevention 1 4 ,
- Ashika Maharaj , lecturer quality and safety and cancer epidemiology 1 ,
- Zanfina Ademi , associate professor of medical outcomes and health economics 1 2 ,
- Xue Li , assistant professor 4 6 ,
- Wei Xu , research student 4 ,
- Ines Mesa-Eguiagaray , statistical geneticist 4 ,
- Jasmin Rostron , research student 4 ,
- Evropi Theodoratou , professor of cancer epidemiology and global health 4 5 ,
- Xiaomeng Zhang , research student 4 ,
- Ashmika Motee , research student 4 ,
- Danny Liew , professor of medical outcomes and health economics 1 2 ,
- Dragan Ilic , professor of medical education and public health 1
- 1 School of Public Health and Preventive Medicine, Monash University, Melbourne, 3004 VIC, Australia
- 2 Monash Outcomes Research and health Economics (MORE) Unit, Monash University, VIC, Australia
- 3 Torrens University, VIC, Australia
- 4 Centre for Global Health, The Usher Institute, University of Edinburgh, Edinburgh, UK
- 5 Cancer Research UK Edinburgh Centre, MRC Institute of Genetics and Molecular Medicine, University of Edinburgh, Edinburgh, UK
- 6 School of Public Health and The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
- Correspondence to: S Talic stella.talic{at}monash.edu
- Accepted 21 October 2021
Objective To review the evidence on the effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality.
Design Systematic review and meta-analysis.
Data sources Medline, Embase, CINAHL, Biosis, Joanna Briggs, Global Health, and World Health Organization COVID-19 database (preprints).
Eligibility criteria for study selection Observational and interventional studies that assessed the effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality.
Main outcome measures The main outcome measure was incidence of covid-19. Secondary outcomes included SARS-CoV-2 transmission and covid-19 mortality.
Data synthesis DerSimonian Laird random effects meta-analysis was performed to investigate the effect of mask wearing, handwashing, and physical distancing measures on incidence of covid-19. Pooled effect estimates with corresponding 95% confidence intervals were computed, and heterogeneity among studies was assessed using Cochran’s Q test and the I 2 metrics, with two tailed P values.
Results 72 studies met the inclusion criteria, of which 35 evaluated individual public health measures and 37 assessed multiple public health measures as a “package of interventions.” Eight of 35 studies were included in the meta-analysis, which indicated a reduction in incidence of covid-19 associated with handwashing (relative risk 0.47, 95% confidence interval 0.19 to 1.12, I 2 =12%), mask wearing (0.47, 0.29 to 0.75, I 2 =84%), and physical distancing (0.75, 0.59 to 0.95, I 2 =87%). Owing to heterogeneity of the studies, meta-analysis was not possible for the outcomes of quarantine and isolation, universal lockdowns, and closures of borders, schools, and workplaces. The effects of these interventions were synthesised descriptively.
Conclusions This systematic review and meta-analysis suggests that several personal protective and social measures, including handwashing, mask wearing, and physical distancing are associated with reductions in the incidence covid-19. Public health efforts to implement public health measures should consider community health and sociocultural needs, and future research is needed to better understand the effectiveness of public health measures in the context of covid-19 vaccination.
Systematic review registration PROSPERO CRD42020178692.

- Download figure
- Open in new tab
- Download powerpoint
Introduction
The impact of SARS-CoV-2 on global public health and economies has been profound. 1 As of 14 October 2021, there were 239 007 759 million cases of confirmed covid-19 and 4 871 841 million deaths with covid-19 worldwide. 2
A variety of containment and mitigation strategies have been adopted to adequately respond to covid-19, with the intention of deferring major surges of patients in hospitals and protecting the most vulnerable people from infection, including elderly people and those with comorbidities. 3 Strategies to achieve these goals are diverse, commonly based on national risk assessments that include estimation of numbers of patients requiring hospital admission and availability of hospital beds and ventilation support.
Globally, vaccination programmes have proved to be safe and effective and save lives. 4 5 Yet most vaccines do not confer 100% protection, and it is not known how vaccines will prevent future transmission of SARS-CoV-2, 6 given emerging variants. 7 8 9 The proportion of the population that must be vaccinated against covid-19 to reach herd immunity depends greatly on current and future variants. 10 This vaccination threshold varies according to the country and population’s response, types of vaccines, groups prioritised for vaccination, and viral mutations, among other factors. 6 Until herd immunity to covid-19 is reached, regardless of the already proven high vaccination rates, 11 public health preventive strategies are likely to remain as first choice measures in disease prevention, 12 particularly in places with a low uptake of covid-19 vaccination. Measures such as lockdown (local and national variant), physical distancing, mandatory use of face masks, and hand hygiene have been implemented as primary preventive strategies to curb the covid-19 pandemic. 13
Public health (or non-pharmaceutical) interventions have been shown to be beneficial in fighting respiratory infections transmitted through contact, droplets, and aerosols. 14 15 Given that SARS-CoV-2 is highly transmissible, it is a challenge to determine which measures might be more effective and sustainable for further prevention.
Substantial benefits in reducing mortality were observed in countries with universal lockdowns in place, such as Australia, New Zealand, Singapore, and China. Universal lockdowns are not, however, sustainable, and more tailored interventions need to be considered; the ones that maintain social lives and keep economies functional while protecting high risk individuals. 16 17 Substantial variation exists in how different countries and governments have applied public health measures, 18 and it has proved a challenge for assessing the effectiveness of individual public health measures, particularly in policy decision making. 19
Previous systematic reviews on the effectiveness of public health measures to treat covid-19 lacked the inclusion of analytical studies, 20 a comprehensive approach to data synthesis (focusing only on one measure), 21 a rigorous assessment of effectiveness of public health measures, 22 an assessment of the certainty of the evidence, 23 and robust methods for comparative analysis. 24 To tackle these gaps, we performed a systematic review of the evidence on the effectiveness of both individual and multiple public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality. When feasible we also did a critical appraisal of the evidence and meta-analysis.
This systematic review and meta-analysis were conducted in accordance with PRISMA 25 (supplementary material 1, table 1) and with PROSPERO (supplementary material 1, table 2).
Eligibility criteria
Articles that met the population, intervention, comparison, outcome, and study design criteria were eligible for inclusion in this systematic review (supplementary material 1, table 3). Specifically, preventive public health measures that were tested independently were included in the main analysis. Multiple measures, which generally contain a “package of interventions”, were included as supplementary material owing to the inability to report on the individual effectiveness of measures and comparisons on which package led to enhanced outcomes. The public health measures were identified from published World Health Organization sources that reported on the effectiveness of such measures on a range of communicable diseases, mostly respiratory infections, such as influenza.
Given that the scientific community is concerned about the ability of the numerous mathematical models, which are based on assumptions, to predict the course of virus transmission or effectiveness of interventions, 26 this review focused only on empirical studies. We excluded case reports and case studies, modelling and simulation studies, studies that provided a graphical summary of measures without clear statistical assessments or outputs, ecological studies that provided a descriptive summary of the measures without assessing linearity or having comparators, non‐empirical studies (eg, commentaries, editorials, government reports), other reviews, articles involving only individuals exposed to other pathogens that can cause respiratory infections, such as severe acute respiratory syndrome or Middle East respiratory syndrome, and articles in a language other than English.
Information sources
We carried out electronic searches of Medline, Embase, CINAHL (Cumulative Index to Nursing and Allied Health Literature, Ebsco), Global Health, Biosis, Joanna Briggs, and the WHO COVID-19 database (for preprints). A clinical epidemiologist (ST) developed the initial search strategy, which was validated by two senior medical librarians (LR and MD) (supplementary material 1, table 4). The updated search strategy was last performed on 7 June 2021. All citations identified from the database searches were uploaded to Covidence, an online software designed for managing systematic reviews, 27 for study selection.
Study selection
Authors ST, DG, SS, AM, ET, JR, XL, WX, IME, and XZ independently screened the titles and abstracts and excluded studies that did not match the inclusion criteria. Discrepancies were resolved in discussion with the main author (ST). The same authors retrieved full text articles and determined whether to include or exclude studies on the basis of predetermined selection criteria. Using a pilot tested data extraction form, authors ST, SS, AM, JR, XL, WX, AM, IME, and XZ independently extracted data on study design, intervention, effect measures, outcomes, results, and limitations. ST, SS, AM, and HW verified the extracted data. Table 5 in supplementary material 1 provides the specific criteria used to assess study designs. Given the heterogeneity and diversity in how studies defined public health measures, we took a common approach to summarise evidence of these interventions (supplementary material 1, table 6).
Risk of bias within individual studies
SS, JR, XL, WX, IME, and XZ independently assessed risk of bias for each study, which was cross checked by ST and HW. For non-interventional observational studies, a ROBINS-I (risk of bias in non-randomised studies of interventions) risk of bias tool was used. 28 For interventional studies, a revised tool for assessing risk of bias in randomised trials (RoB 2) tool was used. 29 Reviewers rated each domain for overall risk of bias as low, moderate, high, or serious/critical.
Data synthesis
The DerSimonian and Laird method was used for random effects meta-analysis, in which the standard error of the study specific estimates was adjusted to incorporate a measure of the extent of variation, or heterogeneity, among the effects observed for public health measures across different studies. It was assumed that the differences between studies are a result of different, yet related, intervention effects being estimated. If fewer than five studies were included in meta-analysis, we applied a recommended modified Hartung-Knapp-Sidik-Jonkman method. 30
Statistical analysis
Because of the differences in the effect metrics reported by the included studies, we could only perform quantitative data synthesis for three interventions: handwashing, face mask wearing, and physical distancing. Odds ratios or relative risks with corresponding 95% confidence intervals were reported for the associations between the public health measures and incidence of covid-19. When necessary, we transformed effect metrics derived from different studies to allow pooled analysis. We used the Dersimonian Laird random effects model to estimate pooled effect estimates along with corresponding 95% confidence intervals for each measure. Heterogeneity among individual studies was assessed using the Cochran Q test and the I 2 test. 31 All statistical analyses were conducted in R (version 4.0.3) and all P values were two tailed, with P=0.05 considered to be significant. For the remaining studies, when meta-analysis was not feasible, we reported the results in a narrative synthesis.
Public and patient involvement
No patients or members of the public were directly involved in this study as no primary data were collected. A member of the public was, however, asked to read the manuscript after submission.
A total of 36 729 studies were initially screened, of which 36 079 were considered irrelevent. After exclusions, 650 studies were eligible for full text review and 72 met the inclusion criteria. Of these studies, 35 assessed individual interventions and were included in the final synthesis of results ( fig 1 ) and 37 assessed multiple interventions as a package and are included in supplementary material 3, tables 2 and 3. The included studies comprised 34 observational studies and one interventional study, eight of which were included in the meta-analysis.

Flow of articles through the review. WHO=World Health Organization
Risk of bias
According to the ROBINS-I tool, 28 the risk of bias was rated as low in three studies, 32 33 34 moderate in 24 studies, 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 and high to serious in seven studies. 59 60 61 62 63 64 65 One important source of serious or critical risk of bias in most of the included studies was major confounding, which was difficult to control for because of the novel nature of the pandemic (ie, natural settings in which multiple interventions might have been enforced at once, different levels of enforcement across regions, and uncaptured individual level interventions such as increased personal hygiene). Variations in testing capacity and coverage, changes to diagnostic criteria, and access to accurate and reliable outcome data on covid-19 incidence and covid-19 mortality, was a source of measurement bias for numerous studies ( fig 2 ). These limitations were particularly prominent early in the pandemic, and in low income environments. 47 52 62 63 65 The randomised controlled trial 66 was rated as moderate risk of bias according to the ROB-2 tool. Missing data, losses to follow-up, lack of blinding, and low adherence to intervention all contributed to the reported moderate risk. Tables 1 and 2 in supplementary material 2 summarise the risk of bias assessment for each study assessing individual measures.

Summary of risk of bias across studies assessing individual measures using risk of bias in non-randomised studies of interventions (ROBINS-I) tool
Study characteristics
Studies assessing individual measures.
Thirty five studies provided estimates on the effectiveness of an individual public health measures. The studies were conducted in Asia (n=11), the United States (n=9), Europe (n=7), the Middle East (n=3), Africa (n=3), South America (n=1), and Australia (n=1). Thirty four of the studies were observational and one was a randomised controlled trial. The study designs of the observational studies comprised natural experiments (n=11), quasi-experiments (n=3), a prospective cohort (n=1), retrospective cohorts (n=8), case-control (n=2), and cross sectional (n=9). Twenty six studies assessed social measures, 32 34 35 37 38 39 40 41 42 44 46 47 48 52 53 55 56 57 58 59 60 61 63 64 65 67 12 studies assessed personal protective measures, 36 43 45 49 50 57 58 60 63 66 68 three studies assessed travel related measures, 54 58 62 and one study assessed environmental measures 57 (some interventions overlapped across studies). The most commonly measured outcome was incidence of covid-19 (n=18), followed by SARS-CoV-2 transmission, measured as reproductive number, growth number, or epidemic doubling time (n=13), and covid-19 mortality (n=8). Table 1 in supplementary material 3 provides detailed information on each study.
Effects of interventions
Personal protective measures.
Handwashing and covid-19 incidence —Three studies with a total of 292 people infected with SARS-CoV-2 and 10 345 participants were included in the analysis of the effect of handwashing on incidence of covid-19. 36 60 63 Overall pooled analysis suggested an estimated 53% non-statistically significant reduction in covid-19 incidence (relative risk 0.47, 95% confidence interval 0.19 to 1.12, I 2 =12%) ( fig 3 ). A sensitivity analysis without adjustment showed a significant reduction in covid-19 incidence (0.49, 0.33 to 0.72, I 2 =12%) ( fig 4 ). Risk of bias across the three studies ranged from moderate 36 60 to serious or critical 63 ( fig 2 ).

Meta-analysis of evidence on association between handwashing and incidence of covid-19 using modified Hartung-Knapp-Sidik-Jonkman adjusted random effect model

Meta-analysis of evidence on association between handwashing and incidence of covid-19 using unadjusted random effect model
Mask wearing and covid-19 incidence —Six studies with a total of 2627 people with covid-19 and 389 228 participants were included in the analysis examining the effect of mask wearing on incidence of covid-19 ( table 1 ). 36 43 57 60 63 66 Overall pooled analysis showed a 53% reduction in covid-19 incidence (0.47, 0.29 to 0.75), although heterogeneity between studies was substantial (I 2 =84%) ( fig 5 ). Risk of bias across the six studies ranged from moderate 36 57 60 66 to serious or critical 43 63 ( fig 2 ).
Study characteristics and main results from studies that assessed individual personal protective and environmental measures
- View inline

Meta-analysis of evidence on association between mask wearing and incidence of covid-19 using unadjusted random effect model
Mask wearing and transmission of SARS-CoV-2, covid-19 incidence, and covid-19 mortality —The results of additional studies that assessed mask wearing (not included in the meta-analysis because of substantial differences in the assessed outcomes) indicate a reduction in covid-19 incidence, SARS-CoV-2 transmission, and covid-19 mortality. Specifically, a natural experiment across 200 countries showed 45.7% fewer covid-19 related mortality in countries where mask wearing was mandatory ( table 1 ). 49 Another natural experiment study in the US reported a 29% reduction in SARS-CoV-2 transmission (measured as the time varying reproductive number Rt) (risk ratio 0.71, 95% confidence interval 0.58 to 0.75) in states where mask wearing was mandatory. 58
A comparative study in the Hong Kong Special Administrative Region reported a statistically significant lower cumulative incidence of covid-19 associated with mask wearing than in selected countries where mask wearing was not mandatory ( table 1 ). 68 Similarly, another natural experiment involving 15 US states reported a 2% statistically significant daily decrease in covid-19 transmission (measured as case growth rate) at ≥21 days after mask wearing became mandatory, 50 whereas a cross sectional study reported that a 10% increase in self-reported mask wearing was associated with greater odds for control of SARS-CoV-2 transmission (adjusted odds ratio 3.53, 95% confidence interval 2.03 to 6.43). 45 The five studies were rated at moderate risk of bias ( fig 2 ).
Environmental measures
Disinfection in household and covid-19 incidence.
Only one study, from China, reported the association between disinfection of surfaces and risk of secondary transmission of SARS-CoV-2 within households ( table 1 ). 57 The study assessed disinfection retrospectively by asking participants about their “daily use of chlorine or ethanol-based disinfectant in households,” and observed that use of disinfectant was 77% effective at reducing SARS-CoV-2 transmission (odds ratio 0.23, 95% confidence interval 0.07 to 0.84). The study did not collect data on the concentration of the disinfectant used by participants and was rated at moderate risk of bias ( fig 2 ).
Social measures
Physical distancing and covid-19 incidence.
Five studies with a total of 2727 people with SARS-CoV-2 and 108 933 participants were included in the analysis that examined the effect of physical distancing on the incidence of covid-19. 37 53 57 60 63 Overall pooled analysis indicated a 25% reduction in incidence of covid-19 (relative risk 0.75, 95% confidence interval 0.59 to 0.95, I 2 =87%) ( fig 6 ). Heterogeneity among studies was substantial, and risk of bias ranged from moderate 37 53 57 60 to serious or critical 63 ( fig 2 ).

Meta-analysis of evidence on association between physical distancing and incidence of covid-19 using unadjusted random effect model
Physical distancing and transmission of SARS-CoV-2 and covid-19 mortality
Studies that assessed physical distancing but were not included in the meta-analysis because of substantial differences in outcomes assessed, generally reported a positive effect of physical distancing ( table 2 ). A natural experiment from the US reported a 12% decrease in SARS-CoV-2 transmission (relative risk 0.88, 95% confidence interval 0.86 to 0.89), 40 and a quasi-experimental study from Iran reported a reduction in covid-19 related mortality (β −0.07, 95% confidence interval −0.05 to −0.10; P<0.001). 47 Another comparative study in Kenya also reported a reduction in transmission of SARS-CoV-2 after physical distancing was implemented, reporting 62% reduction in overall physical contacts (reproductive number pre-intervention was 2.64 and post-intervention was 0.60 (interquartile range 0.50 to 0.68)). 61 These three studies were rated at moderate risk of bias 40 61 to serious or critical risk of bias 47 ( fig 2 ).
Study characteristics and main results from studies assessing individual social measures
Stay at home or isolation and transmission of SARS-CoV-2
All the studies that assessed stay at home or isolation measures reported reductions in transmission of SARS-CoV-2 ( table 2 ). A retrospective cohort study from the US reported a significant reduction in the odds of having a positive reproductive number (R0) result (odds ratio 0.07, 95% confidence interval 0.01 to 0.37), 41 and a natural experiment reported a 51% reduction in time varying reproductive number (Rt) (risk ratio 0.49, 95% confidence interval 0.43 to 0.54). 58
A study from the UK reported a 74% reduction in the average daily number of contacts observed for each participant and estimated a decrease in reproductive number: the reproductive number pre-intervention was 3.6 and post-intervention was 0.60 (95% confidence interval 0.37 to 0.89). 65 Similarly, an Iranian study projected the reproductive number using serial interval distribution and the number of incidence cases and found a significant decrease: the reproductive number pre-intervention was 2.70 and post-intervention was 1.13 (95% confidence interval 1.03 to 1.25). 55 Three of the studies were rated at moderate to serious or critical risk of bias, 55 58 65 and one study was rated at low risk of bias 41 ( fig 2 ).
Quarantine and incidence and transmission of SARS-CoV-2
Quarantine was assessed in two studies ( table 2 ). 34 59 A prospective cohort study from Saudi Arabia reported a 4.9% decrease in the incidence of covid-19 at eight weeks after the implementation of quarantine. 34 This study was rated at low risk of bias ( fig 2 ). A retrospective cohort study from India reported a 14 times higher risk of SARS-CoV-2 transmission associated with no quarantine compared with strict quarantine (odds ratio 14.44, 95% confidence interval 2.42 to 86.17). 59 This study was rated at moderate risk of bias ( fig 2 ).
School closures and covid-19 incidence and covid-19 mortality
Two studies assessed the effectiveness of school closures on transmission of SARS-CoV-2, incidence of covid-19, or covid-19 mortality ( table 2 ). 44 48 A US population based longitudinal study reported on the effectiveness of state-wide closure of primary and secondary schools and observed a 62% decrease (95% confidence interval −49% to −71%) in incidence of covid-19 and a 58% decrease (−46% to−68%) in covid-19 mortality. 48 Conversely, a natural experiment from Japan reported no effect of school closures on incidence of covid-19 (α coefficient 0.08, 95% confidence interval −0.36 to 0.65). 44 Both studies were rated at moderate risk of bias ( fig 2 ).
School closures and transmission of SARS-CoV-2
Two natural experiments from the US reported a reduction in transmission (ie, reproductive number); with one study reporting a reduction of 13% (relative risk 0.87, 95% confidence interval 0.86 to 0.89) 40 and another reporting a 10% (0.90, 0.86 to 0.93) reduction ( table 2 ). 58 A Swedish study reported an association between school closures and a small increase in confirmed SARS-CoV-2 infections in parents (odds ratio 1.17, 95% confidence interval 1.03 to 1.32), but observed that teachers in lower secondary schools were twice as likely to become infected than teachers in upper secondary schools (2.01, 1.52 to 2.67). 32 All three studies were rated at moderate risk of bias ( fig 2 ).
Business closures and transmission of SARS-CoV-2
Two natural experiment studies assessed business closures across 50 US states and reported reductions in transmission of SARS-CoV-2 ( table 2 ). 40 58 One of the studies observed a significant reduction in transmission of 12% (relative risk 0.88, 95% confidence interval 0.86 to 0.89) 40 and the other reported a significant 16% (risk ratio 0.84, 0.79 to 0.90) reduction. 58 Both studies were rated at moderate risk of bias ( fig 2 ).
Lockdown and incidence of covid-19
A natural experiment involving 202 countries suggested that countries that implemented universal lockdown had fewer new cases of covid-19 than countries that did not (β coefficient −235.8 (standard error −11.04), P<0.01) ( table 2 ). 52 An Indian quasi-experimental study reported a 10.8% reduction in incidence of covid-19 post-lockdown, 56 whereas a South African retrospective cohort study observed a 14.1% reduction in risk after implementation of universal lockdown ( table 2 ). 46 These studies were rated at high risk of bias 52 and moderate risk of bias 46 56 ( fig 2 ).
Lockdown and covid-19 mortality
The three studies that assessed universal lockdown and covid-19 mortality generally reported a decrease in mortality ( table 2 ). 35 38 42 A natural experiment study involving 45 US states reported a decrease in covid-19 related mortality of 2.0% (95% confidence interval −3.0% to 0.9%) daily after lockdown had been made mandatory. 35 A Brazilian quasi-experimental study reported a 27.4% average difference in covid-19 related mortality rates in the first 25 days of lockdown. 42 In addition, a natural experiment study reported about 30% and 60% reductions in covid-19 related mortality post-lockdown in Italy and Spain over four weeks post-intervention, respectively. 38 All three studies were rated at moderate risk of bias ( fig 2 ).
Lockdown and transmission of SARS-CoV-2
Four studies assessed universal lockdown and transmission of SARS-CoV-2 during the first few months of the pandemic ( table 2 ). The decrease in reproductive number (R0) ranged from 1.27 in Italy (pre-intervention 2.03, post-intervention 0.76) 39 to 2.09 in India (pre-intervention 3.36, post-intervention 1.27), 64 and 3.97 in China (pre-intervention 4.95, post-intervention 0.98). 33 A natural experiment from the US reported that lockdown was associated with an 11% reduction in transmission of SARS-CoV-2 (relative risk 0.89, 95% confidence interval 0.88 to 0.91). 40 All the studies were rated at low risk of bias 33 39 to moderate risk 40 64 ( fig 2 ).
Travel related measures
Restricted travel and border closures.
Border closure was assessed in one natural experiment study involving nine African countries ( table 3 ). 62 Overall, the countries recorded an increase in the incidence of covid-19 after border closure. These studies concluded that the implementation of border closures within African countries had minimal effect on the incidence of covid-19. The study had important limitations and was rated at serious or critical risk of bias. In the US, a natural experiment study reported that restrictions on travel between states contributed about 11% to a reduction in SARS-CoV-2 transmission ( table 3 ). 36 The study was rated at moderate risk of bias ( fig 2 ).
Study characteristics and main results from studies that assessed individual travel measures
Entry and exit screening (virus or symptom screening)
One retrospective cohort study assessed screening of symptoms, which involved testing 65 000 people for fever ( table 3 ). 54 The study found that screening for fever lacked sensitivity (ranging from 18% to 24%) in detecting people with SARS-CoV-2 infection. This translated to 86% of the population with SARS-CoV-2 remaining undetected when screening for fever. The study was rated at moderate risk of bias ( fig 2 ).
Multiple public health measures
Overall, 37 studies provided estimates on the effectiveness of multiple public health measures, assessed as a collective group. Studies were mostly conducted in Asia (n=15), the US (n=11), Europe (n=6), Africa (n=4), and South America (n=1). All the studies were observational. The most commonly measured outcome was transmission of disease (ie, measured as reproductive number, growth number, or epidemic doubling time) (n=23), followed by covid-19 incidence (n=19) and covid-19 mortality (n=8). This review attempted to assess the overall effectiveness of the public health intervention packages by reporting the percentage difference in outcome before and after implementation of measures or between regions or countries studied. Eleven of the 37 included studies noted a difference of between 26% and 50% in transmission of SARS-CoV-2 and incidence of covid-19, 70 71 72 73 74 75 76 77 78 79 80 nine noted a difference of between 51% and 75% in SARS-CoV-2 transmission, covid-19 incidence, and covid-19 mortality, 81 82 83 84 85 86 87 88 89 and 14 noted a difference of more than 75% in transmission of SARS-CoV-2, covid-19 incidence and covid-19 mortality. 79 80 89 90 91 92 93 94 95 96 97 98 99 100 For the remaining studies, the overall effectiveness was not assessed owing to a lack of comparators (see supplementary material 3, table 3). Two studies that assessed universal lockdown and physical distancing reported a decrease of between 0% and 25% in SARS-CoV-2 transmission and covid-19 incidence. 79 101 Studies that included school and workplace closures, 91 95 96 isolation or stay at home measures, 80 94 or a combination of both 79 89 93 97 98 99 reported decreases of more than 75% in SARS-CoV-2 transmission. Supplementary material 3, table 2 provides detailed information on each study.
Worldwide, government and public health organisations are mitigating the spread of SARS-CoV-2 by implementing various public health measures. This systematic review identified a statistically significant reduction in the incidence of covid-19 through the implementation of mask wearing and physical distancing. Handwashing interventions also indicated a substantial reduction in covid-19 incidence, albeit not statistically significant in the adjusted model. As the random effects model tends to underestimate confidence intervals when a meta-analysis includes a small number of individual studies (<5), the adjusted model for handwashing showed a statistically non-significant association in reducing the incidence of covid-19 compared with the unadjusted model.
Overall effectiveness of these interventions was affected by clinical heterogeneity and methodological limitations, such as confounding and measurement bias. It was not possible to evaluate the impact of type of face maks (eg, surgical, fabric, N95 respirators) and compliance and frequency of wearing masks owing to a lack of data. Similarly, it was not feasible to assess the differences in effect that different recommendations for physical distancing (ie, 1.5 m, 2m, or 3 m) have as preventive strategies.
The effectiveness of measures such as universal lockdowns and closures of businesses and schools for the containment of covid-19 have largely been effective, but depended on early implementation when incidence rates of covid-19 were still low. 42 52 58 Only Japan reported no decrease in covid-19 incidence after school closures, 44 and other studies found that different public health measures were sometimes implemented simultaneously or soon after one another, thus the results should be interpreted with caution. 32 46 56
Isolation or stay at home was an effective measure in reducing the transmission of SARS-CoV-2, but the included studies used results for mobility to assess stay at home or isolation and therefore could have been limited by potential flaws in publicly available phone data, 41 58 102 and variations in the enforcement of public health measures in different states or regions were not assessed. 55 58 102 Quarantine was found to be as effective in reducing the incidence of covid-19 and transmission of SARS-CoV-2, yet variation in testing and case detection in low income environments was substantial. 59 96 98 Another study reported that quarantine was effective in reducing the transmission of SARS-CoV-2 in a cohort with a low prevalence of the virus, yet it is unknown if the same effect would be observed with higher prevalence. 34
It was not possible to draw conclusions about the effectiveness of restricted travel and full border closures because the number of empirical studies was insufficient. Single studies identified that border closure in Africa had a minimal effect in reducing SARS-CoV-2 transmission, but the study was assessed as being at high risk of bias. 62 Screening for fever was also identified to be ineffective, with only 24% of positive cases being captured by screening. 54
Comparison with other studies
Previous literature reviews have identified mask wearing as an effective measure for the containment of SARS-CoV-2 103 ; the caveat being that more high level evidence is required to provide unequivocal support for the effectiveness of the universal use of face masks. 104 105 Additional empirical evidence from a recent randomised controlled trial (originally published as a preprint) indicates that mask wearing achieved a 9.3% reduction in seroprevalence of symptomatic SARS-CoV-2 infection and an 11.9% reduction in the prevalence of covid-19-like symptoms. 106 Another systematic review showed stronger effectiveness with the use of N95, or similar, respirators than disposable surgical masks, 107 and a study evaluating the protection offered by 18 different types of fabric masks found substantial heterogeneity in protection, with the most effective mask being multilayered and tight fitting. 108 However, transmission of SARS-CoV-2 largely arises in hospital settings in which full personal protective measures are in place, which suggests that when viral load is at its highest, even the best performing face masks might not provide adequate protection. 51 Additionally, most studies that assessed mask wearing were prone to important confounding bias, which might have altered the conclusions drawn from this review (ie, effect estimates might have been underestimated or overestimated or can be related to other measures that were in place at the time the studies were conducted). Thus, the extent of such limitations on the conclusions drawn remain unknown.
A 2020 rapid review concluded that quarantine is largely effective in reducing the incidence of covid-19 and covid-19 mortality. However, uncertainty over the magnitude of such an effect still remains, 109 with enhanced management of quality quarantine facilities for improved effective control of the epidemics urgently needed. 110 In addition, findings on the application of school and workplace closures are still inconclusive. Policy makers should be aware of the ambiguous evidence when considering school closures, as other potentially less disruptive physical distancing interventions might be more appropriate. 21 Numerous findings from studies on the efficacy of school closures showed that the risk of transmission within the educational environment often strongly depends on the incidence of covid-19 in the community, and that school closures are most successfully associated with control of SARS-CoV-2 transmission when other mitigation strategies are in place in the community. 111 112 113 114 115 116 117 School closures have been reported to be disruptive to students globally and are likely to impair children’s social, psychological, and educational development 118 119 and to result in loss of income and productivity in adults who cannot work because of childcare responsibilities. 120
Speculation remains as how best to implement physical distancing measures. 121 Studies that assess physical distancing measures might interchangeably study physical distancing with lockdown 35 52 56 64 and other measures and thus direct associations are difficult to assess.
Empirical evidence from restricted travel and full border closures is also limited, as it is almost impossible to study these strategies as single measures. Current evidence from a recent narrative literature review suggested that control of movement, along with mandated quarantine, travel restrictions, and restricting nationals from entering areas of high infection, are effective measures, but only with good compliance. 122 A narrative literature review of travel bans, partial lockdowns, and quarantine also suggested effectiveness of these measures, 123 and another rapid review further supported travel restrictions and cross border restrictions to stop the spread of SARS-CoV-2. 124 It was impossible to make such observations in the current review because of limited evidence. A German review, however, suggested that entry, exit, and symptom screening measures to prevent transmission of SARS-CoV-2 are not effective at detecting a meaningful proportion of cases, 125 and another review using real world data from multiple countries found that border closures had minimal impact on the control of covid-19. 126
Although universal lockdowns have shown a protective effect in lowering the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality, these measures are also disruptive to the psychosocial and mental health of children and adolescents, 127 global economies, 128 and societies. 129 Partial lockdowns could be an alternative, as the associated effectiveness can be high, 125 especially when implemented early in an outbreak, 85 and such measures would be less disruptive to the general population.
It is important to also consider numerous sociopolitical and socioeconomic factors that have been shown to increase SARS-CoV-2 infection 130 131 and covid-19 mortality. 132 Immigration status, 82 economic status, 81 101 and poverty and rurality 98 can influence individual and community compliance with public health measures. Poverty can impact the ability of communities to physically distance, 133 especially in crowded living environments, 134 135 as well as reduce access to personal protective measures. 134 135 A recent study highlights that “a one size fits all” approach to public health measures might not be effective at reducing the spread of SARS-CoV-2 in vulnerable communities 136 and could exacerbate social and economic inequalities. 135 137 As such, a more nuanced and community specific approach might be required. Even though screening is highly recommended by WHO 138 because a proportion of patients with covid-19 can be asymptomatic, 138 screening for symptoms might miss a larger proportion of the population with covid-19. Hence, temperature screening technologies might need to be reconsidered and evaluated for cost effectiveness, given such measures are largely depended on symptomatic fever cases.
Strengths and limitations of this review
The main strength of this systematic review was the use of a comprehensive search strategy to identify and select studies for review and thereby minimise selection bias. A clinical epidemiologist developed the search strategy, which was validated by two senior medical librarians. This review followed a comprehensive appraisal process that is recommended by the Cochrane Collaboration 31 to assess the effectiveness of public health measures, with specifically validated tools used to independently and individually assess the risk of bias in each study by study design.
This review has some limitations. Firstly, high quality evidence on SARS CoV-2 and the effectiveness of public health measures is still limited, with most studies having different underlying target variables. Secondly, information provided in this review is based on current evidence, so will be modified as additional data become available, especially from more prospective and randomised studies. Also, we excluded studies that did not provide certainty over the effect measure, which might have introduced selection bias and limited the interpretation of effectiveness. Thirdly, numerous studies measured interventions only once and others multiple times over short time frames (days v month, or no timeframe). Additionally, the meta-analytical portion of this study was limited by significant heterogeneity observed across studies, which could neither be explored nor explained by subgroup analyses or meta-regression. Finally, we quantitatively assessed only publications that reported individual measures; studies that assessed multiple measures simultaneously were narratively analysed with a broader level of effectiveness (see supplementary material 3, table 3). Also, we excluded studies in languages other than English.
Methodological limitations of studies included in the review
Several studies failed to define and assess for potential confounders, which made it difficult for our review to draw a one directional or causal conclusion. This problem was mainly because we were unable to study only one intervention, given that many countries implemented several public health measures simultaneously; thus it is a challenge to disentangle the impact of individual interventions (ie, physical distancing when other interventions could be contributing to the effect). Additionally, studies measured different primary outcomes and in varied ways, which limited the ability to statistically analyse other measures and compare effectiveness.
Further pragmatic randomised controlled trials and natural experiment studies are needed to better inform the evidence and guide the future implementation of public health measures. Given that most measures depend on a population’s adherence and compliance, it is important to understand and consider how these might be affected by factors. A lack of data in the assessed studies meant it was not possible to understand or determine the level of compliance and adherence to any of the measures.
Conclusions and policy implications
Current evidence from quantitative analyses indicates a benefit associated with handwashing, mask wearing, and physical distancing in reducing the incidence of covid-19. The narrative results of this review indicate an effectiveness of both individual or packages of public health measures on the transmission of SARS-CoV-2 and incidence of covid-19. Some of the public health measures seem to be more stringent than others and have a greater impact on economies and the health of populations. When implementing public health measures, it is important to consider specific health and sociocultural needs of the communities and to weigh the potential negative effects of the public health measures against the positive effects for general populations. Further research is needed to assess the effectiveness of public health measures after adequate vaccination coverage has been achieved. It is likely that further control of the covid-19 pandemic depends not only on high vaccination coverage and its effectiveness but also on ongoing adherence to effective and sustainable public health measures.
What is already known on this topic
Public health measures have been identified as a preventive strategy for influenza pandemics
The effectiveness of such interventions in reducing the transmission of SARS-CoV-2 is unknown
What this study adds
The findings of this review suggest that personal and social measures, including handwashing, mask wearing, and physical distancing are effective at reducing the incidence of covid-19
More stringent measures, such as lockdowns and closures of borders, schools, and workplaces need to be carefully assessed by weighing the potential negative effects of these measures on general populations
Further research is needed to assess the effectiveness of public health measures after adequate vaccination coverage
Ethics statements
Ethical approval.
Not required.
Data availability statement
No additional data available.
Acknowledgments
We thank medical subject librarians Lorena Romero (LR) and Marshall Dozier (MD) for their expert advice and assistance with the study search strategy.
Contributors: ST, DG, DI, DL, and ZA conceived and designed the study. ST, DG, SS, AM, HW, WX, JR, ET, AM, XL, XZ, and IME collected and screened the data. ST, DG, and DI acquired, analysed, or interpreted the data. ST, HW, and SS drafted the manuscript. All authors critically revised the manuscript for important intellectual content.. XL and ST did the statistical analysis. NA obtained funding. LR and MD provided administrative, technical, or material support. ST and DI supervised the study. ST and DI had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. ST is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: No funding was available for this research. ET is supported by a Cancer Research UK Career Development Fellowship (grant No C31250/A22804). XZ is supported by The Darwin Trust of Edinburgh.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: ET is supported by a Cancer Research UK Career Development Fellowship and XZ is supported by The Darwin Trust of Edinburgh; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; and no other relationships or activities that could appear to have influenced the submitted work.
The lead author (ST) affirms that the manuscript is an honest, accurate, and transparent account of the study reported; no important aspects of the study have been omitted. Dissemination to participants and related patient and public communities: It is anticipated to disseminate the results of this research to wider community via press release and social media platforms.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- ↵ World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2021. https://covid19.who.int/
- Parodi SM ,
- Bernal JL ,
- Andrews N ,
- Chodick G ,
- Patalon T ,
- Anderson RM ,
- Vegvari C ,
- Truscott J ,
- Khateeb J ,
- McArthur AG ,
- Banerjee A ,
- Sanyaolu A ,
- Marinkovic A ,
- ↵ World Health Organization. Coronavirus disease (COVID-19): Herd immunity, lockdowns and COVID-19. 2020. www.who.int/news-room/q-a-detail/herd-immunity-lockdowns-and-covid-19
- Stehlik P ,
- Glasziou PP
- ↵ World Health Organization. COVID-19 strategy update. 2020. www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba0_19
- Hollingsworth TD ,
- Klinkenberg D ,
- Heesterbeek H ,
- Anderson RM
- Aledort JE ,
- Wasserman J ,
- Bozzette SA
- ↵ World Health Organization. Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza 2019. 2019. https://apps.who.int/iris/bitstream/handle/10665/329438/9789241516839-eng.pdf?ua=1 .
- Yang Chan EY ,
- Shahzada TS ,
- Hellewell J ,
- Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group
- Mendez-Brito A ,
- El Bcheraoui C ,
- Pozo-Martin F
- Russell SJ ,
- Craig KJT ,
- Maatoug J ,
- Liberati A ,
- Tetzlaff J ,
- Altman DG ,
- PRISMA Group
- Holmdahl I ,
- ↵ Covidence Systematic Review Software. Veritas Health Innovation, Melbourne Australia. www.covidence.org
- Sterne JA ,
- Hernán MA ,
- Reeves BC ,
- Sterne JAC ,
- Savović J ,
- ↵ Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ. Welch VA, ed. Cochrane Handbook for Systematic Reviews of Interventions. : Chichester, UK: Wiley; 2019. 2nd edn. https://training.cochrane.org/handbook .
- Vlachos J ,
- Hertegård E ,
- B Svaleryd H
- Al-Tawfiq JA ,
- Al-Khadra H ,
- Siedner MJ ,
- Harling G ,
- Reynolds Z ,
- Cheong HH ,
- Van den Berg P ,
- Schechter-Perkins EM ,
- Guzzetta G ,
- Riccardo F ,
- Marziano V ,
- COVID-19 Working Group,2
- McAuley FM ,
- Figueiredo Filho D ,
- Fernandes A
- Krishnamachari B ,
- Zastrow D ,
- Santella AJ
- Miyakoshi C
- Motloba P ,
- Motaung KSC ,
- Alimohamadi Y ,
- Holakouie-Naieni K ,
- Sepandi M ,
- Richardson T ,
- Leffler CT ,
- Lykins JD ,
- McKeown CA ,
- Grzybowski A
- Luckhoff C ,
- Mitchell RD ,
- O’Reilly GM ,
- Khosravi A ,
- Rohani-Rasaf M ,
- Mehravaran S ,
- Thayer WM ,
- Sankhla P ,
- Valamparampil MJ ,
- Varghese B ,
- van Zandvoort K ,
- CMMID COVID-19 Working Group
- Ilesanmi OS
- Doung-Ngern P ,
- Suphanchaimat R ,
- Panjangampatthana A ,
- Salvatore M ,
- Jarvis CI ,
- Van Zandvoort K ,
- CMMID COVID-19 working group
- Bundgaard H ,
- Bundgaard JS ,
- Raaschou-Pedersen DET ,
- Cheng VC-C ,
- Chuang VW-M ,
- Malheiro R ,
- Figueiredo AL ,
- Magalhães JP ,
- Dasgupta S ,
- Kassem AM ,
- Sunshine G ,
- Bendavid E ,
- Bhattacharya J ,
- Ioannidis JPA
- Rothenbühler M ,
- Fisher BT ,
- Khosrawipour V ,
- Kocbach P ,
- Athotra A ,
- Vaisakh TP ,
- NCDC COVID Incident Management Team
- Courtemanche C ,
- Garuccio J ,
- Pinkston J ,
- Al Wahaibi A ,
- Al Manji A ,
- Al Maani A ,
- Timelli L ,
- Undurraga EA ,
- Laborde CC ,
- Bhattacharyya R ,
- Castillo RC ,
- Staguhn ED ,
- Weston-Farber E
- Cruz-Cano R ,
- Venkataramani A ,
- Gilbert RF ,
- Tchole AIM ,
- Cheeloo EcoHealth Consortium (CLEC)
- McCreesh N ,
- Dlamini V ,
- Edwards A ,
- Haapanen M ,
- McGrail DJ ,
- McAndrews KM ,
- Clipman SJ ,
- Wesolowski AP ,
- Gibson DG ,
- Brainard J ,
- Camargo MC ,
- Martinez-Silveira MS ,
- ↵ Abaluck J, Kwong LH, Styczynskyi A, et al. The Impact of Community Masking on COVID-19: A Cluster-Randomized Trial in Bangladesh. 2021. www.poverty-action.org/sites/default/files/publications/Mask_RCT____Symptomatic_Seropositivity_083121.pdf
- MacDougall CC ,
- Johnstone J ,
- Schwartz B ,
- O’Kelly E ,
- Nussbaumer-Streit B ,
- Dobrescu AI ,
- ↵ Nafees M, Khan F. Pakistan’s response to COVID-19 pandemic and efficacy of quarantine and partial lockdown: A review. Electronic Journal of General Medicine 2020;17:em240.
- Macartney K ,
- Pillsbury AJ ,
- NSW COVID-19 Schools Study Team
- Link-Gelles R ,
- DellaGrotta AL ,
- Fontanet A ,
- Tondeur L ,
- ↵ National Centre for Immunisation Research and Surveliance. COVID-19 in schools and early childhood education and care services – the Term 3 experience in NSW. 2020, NSW government. www.ncirsorgau/sites/default/files/2020-10/COVID-19%20Transmission%20in%20educational%20settings%20in%20NSW%20Term%203%20report_0pdf
- ↵ National Centre for Immunisation Research and Surveliance. COVID-19 in schools and early childhood education and care services – the Term 1 experience in NSW. 2020, NSW government. www.ncirsorgau/sites/default/files/2020-08/COVID-19%20Transmission%20in%20educational%20settings%20in%20NSW%20Term%201%20report_0pdf
- ↵ National Centre for Immunisation Research and Surveliance. COVID-19 in schools and early childhood education and care services – the Term 2 experience in NSW. 2020, NSW government. www.ncirsorgau/sites/default/files/2020-08/COVID-19%20Transmission%20in%20educational%20settings%20in%20NSW%20Term%202%20report_0pdf
- Chatterjee S ,
- Fenichel EP
- Bhattacharya S ,
- Chakraborty A
- Stephen S ,
- Movsisyan A ,
- Stratil JM ,
- Geyrhofer L ,
- Patiño-Lugo DF ,
- Velásquez Salazar P ,
- Parveen S ,
- ↵ Felsenthal M. COVID-19 to plunge global economy into worst recession since World War II 2020. www.worldbank.org/en/news/press-release/2020/06/08/covid-19-to-plunge-global-economy-into-worst-recession-since-world-war-ii .
- Brodeur A ,
- Powdthavee N
- Niedzwiedz CL ,
- O’Donnell CA ,
- Chadeau-Hyam M ,
- Bodinier B ,
- Elliott J ,
- Williamson E ,
- Walker AJ ,
- Bhaskaran K ,
- Garnier R ,
- Benetka JR ,
- Kraemer J ,
- Brasher C ,
- Chikumba E ,
- McDougall R ,
- Mellin-Olsen J ,
- Corburn J ,
- Cooney RE ,
- ↵ World Health Organization. Transmission of COVID-19 by asymptomatic cases. 2020. www.emro.who.int/health-topics/corona-virus/transmission-of-covid-19-by-asymptomatic-cases.html
- Contact Tracing
- Pandemic Data Initiative
- Webcasts & Videos
- 30-Minute COVID-19 Briefing
Research Papers
Jhu has stopped collecting data as of.
After three years of around-the-clock tracking of COVID-19 data from...
The Johns Hopkins Coronavirus Resource Center has collected, verified, and published local, regional, national, and international pandemic data since it launched in March 2020. From the beginning, the information has been freely available to all — researchers, institutions, the media, the public, and policymakers. As a result, the CRC and its data have been cited in many published research papers and reports. Here we have gathered publications authored by CRC team members that focus on the CRC or its data.
July 14, 2022
Misaligned Federal and State Covid data limits demographic insights
CDC underreports cases and deaths among African American and Hispanic or Latino individuals.
February 17, 2022
Experts Call for Open Public Health Data
Johns Hopkins team highlighted the urgent need for better COVID data collection.
Unifying Epidemiologists and Economists
Researchers from disparate fields join to chart a new path for formulating policies in response to future pandemics.
Mobility Data Supported Social Distancing
Study found that physical distancing was an effective COVID mitigation strategy.
Johns Hopkins Engineers Build COVID Dashboard
Lancet Infectious Diseases published first paper detailing how the global map was built.
Researchers Identify Disparities in COVID Testing
Johns Hopkins team conducted an analysis of state-published demographic data
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
A statistical analysis of the novel coronavirus (COVID-19) in Italy and Spain
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation School of Statistics, Renmin University of China, Beijing, China
- Jeffrey Chu

- Published: March 25, 2021
- https://doi.org/10.1371/journal.pone.0249037
- Reader Comments
The novel coronavirus (COVID-19) that was first reported at the end of 2019 has impacted almost every aspect of life as we know it. This paper focuses on the incidence of the disease in Italy and Spain—two of the first and most affected European countries. Using two simple mathematical epidemiological models—the Susceptible-Infectious-Recovered model and the log-linear regression model, we model the daily and cumulative incidence of COVID-19 in the two countries during the early stage of the outbreak, and compute estimates for basic measures of the infectiousness of the disease including the basic reproduction number, growth rate, and doubling time. Estimates of the basic reproduction number were found to be larger than 1 in both countries, with values being between 2 and 3 for Italy, and 2.5 and 4 for Spain. Estimates were also computed for the more dynamic effective reproduction number, which showed that since the first cases were confirmed in the respective countries the severity has generally been decreasing. The predictive ability of the log-linear regression model was found to give a better fit and simple estimates of the daily incidence for both countries were computed.
Citation: Chu J (2021) A statistical analysis of the novel coronavirus (COVID-19) in Italy and Spain. PLoS ONE 16(3): e0249037. https://doi.org/10.1371/journal.pone.0249037
Editor: Abdallah M. Samy, Faculty of Science, Ain Shams University (ASU), EGYPT
Received: July 14, 2020; Accepted: March 9, 2021; Published: March 25, 2021
Copyright: © 2021 Jeffrey Chu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The raw data files for the incidence of COVID-19 in Italy and Spain are available from the following links: https://github.com/pcm-dpc/COVID-19 https://github.com/datadista/datasets/tree/master/COVID%2019 .
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The novel coronavirus (COVID-19) was widely reported to have first been detected in Wuhan (Hebei province, China) in December 2019. After the initial outbreak, COVID-19 continued to spread to all provinces in China and very quickly spread to other countries within and outside of Asia. At present, over 45 million cases of infected individuals have been confirmed in over 180 countries with in excess of 1 million deaths [ 1 ]. Although the foundations of this disease are very similar to the severe acute respiratory syndrome (SARS) virus that took hold of Asia in 2003, it is shown to spread much more easily and there currently exists no vaccine.
Since the first confirmed cases were reported in China, much of the literature has focused on the outbreak in China including the transmission of the disease, the risk factors of infection, and the biological properties of the virus—see for example key literature such as [ 2 – 6 ]. However, more recent literature has started to cover an increasing number of regions outside of China.
For example, studies covering the wider Asia region include: investigations into the outbreak on board the Diamond Princess cruise ship in Japan, using a Bayesian framework with a Hamiltonian Monte Carlo algorithm [ 7 ]; estimation of the ascertainment rate in Japan using a Poisson process [ 8 ]; modelling the evolution of the basic and effective reproduction numbers in South Korea using Susceptible-Infected-Susceptible models [ 9 ] and generalised growth models with varying growth rates [ 10 ]; modelling the basic reproduction number in India with a classical Susceptible-Exposed-Infectious-Recovered-type compartmental model [ 11 ]; forecasting numbers of cases in Indian states using deep learning-based models [ 12 ].
Analyses on North and South America have also used similar classical methods, for example [ 13 ] model the progression of the outbreak in the United States until the end of 2021 with the simple Susceptible-Infected-Recovered model, and [ 14 ] predict epidemic trends in Brazil and Peru using a logistic growth model and machine learning techniques. However, other studies include: analysis of the spatial variability of the incidence in the United States using spatial lag and error models, and geographically weighted regression [ 15 ]; estimation of the number of deaths in the United States using a modified logistic fault-dependent detection model [ 16 ]; estimating prevalence and infection rates across different states in the United States using a sample selection model [ 17 ]; investigating the relationship between social media communication and the incidence in Colombia using non-linear regression models.
Focusing on Africa, [ 18 ] simulate and predict the spread of the disease in South Africa, Egypt, Algeria, Nigeria, Senegal, and Kenya, using a modified Susceptible-Exposed-Infectious-Recovered model; [ 19 ] apply a six-compartmental model to model the transmission in South Africa; [ 20 ] predict the spread of the disease in West Africa using a deterministic Susceptible-Exposed-Infectious-Recovered model; [ 21 ] implement Autoregressive Integrated Moving Average models to forecast the prevalence of COVID-19 in East Africa; [ 22 ] predict the spread of the disease using travel history and personal contact in Nigeria through ordinary least squares regression; [ 23 ] use logistic growth and Susceptible-Infected-Recovered models to generate real-time forecasts of daily confirmed cases in Saudi Arabia.
Aside from many of the classical models mentioned above, recent developments in the econometrics and statistics literature have led to a number of new models that could potentially be applied in the modelling of infectious diseases. These include (but are not limited to) mixed frequency analysis, model selection and combination, and dynamic time warping. Mixed frequency analysis is an iterative approach proposed for dealing with the joint dynamics of time series data which are sampled at different frequencies [ 24 ]. In the economic literature, the common example is quarterly gross domestic product (GDP) and monthly inflation. [ 25 ] notes that studying the co-movements between mixed frequency data usually involves analysing the joint process sampled at a common low frequency, however, this can mis-specify the relationship. [ 24 , 25 ] propose vector autoregressive models for mixed frequency analysis that operate at the highest sampling frequency of all the time series in the model. These models allow for the modelling of the joint dynamics of the dependent and independent variables using time disaggregation, where the low frequency variables are interpolated and time-aggregated into a higher frequency. In the context of infectious diseases, such models could be beneficial for modelling the relationship between higher frequency data such as the number of daily cases or deaths and lower frequency data relating to, say, weekly cases or deaths, news and information about health prevention measures, etc. [ 26 , 27 ] propose the use of Bayesian Predictive Synthesis (BPS) for model selection and combination. They note that there are many scenarios that generate multiple, interrelated time series, where the dependence has a significant impact on decisions, policies, and their outcomes. In addition, methods need to learn and integrate information about forecasters and models, bias, etc. and how they change over time, to improve their accuracy [ 26 ]. Decision and policy makers often use multiple sources, models, and forecasters to generate forecasts, in particular, probabilistic density forecasts. However, although complex estimation methods may have useful properties for policy makers, large standard deviations may be a result of the complexity of the data, model, etc., and it may be difficult to know the source. The aim is to use the dependencies between time series to improve forecasts over multiple horizons for policy decisions [ 27 ]. For example, in the economic literature, setting interest rates based on utility or loss that account for inflation, real economy measures, employment, etc. BPS relates to a decision maker that accounts for multiple models as providers of “forecast data” to be used for prior-posterior updating. The decision maker learns over time about relationships between agents, forecasts, and dependencies, which are incorporated into the model, and dynamically calibrate, learn, and update weights for ranges of forecasts from dynamic models, with multiple lags and predictors [ 26 ]. In epidemiology, BPS could potentially be used in a similar context to analyse the dependency between various interrelated time series such as daily cases and deaths, hospital capacity, number vaccinations, etc. Different models and sources of data could then be combined and characterised in one single model improving the accuracy of forecasts. Dynamic time warping as noted by [ 28 , 29 ] is a technique that has not been widely used outside of speech and gesture recognition. It can be used to identify the relation structure between two time series by describing their non-linear alignment with warping paths [ 28 ]. The procedure involves a local cost measure characterising the sum of the differences between pairs of realisations of data at each time point, where an optimal warping path gives the lowest total cost. The optimal path is found under a variable lead-lag structure, where the most suitable lag can then be found [ 28 ]. This then reveals and identifies the lead-lag effects between the time series data. Indeed, dynamic time warping has recently been used in the modelling of COVID-19 by [ 30 ]. [ 30 ] use the method to determine the lead-lag relation between the cumulative number of daily cases of COVID-19 in various countries, in addition to forecasting the future incidence in selected countries. This allows for the classification of countries as being in the early, middle, and late stages of an outbreak.
Controlling an infectious disease such as COVID-19 is an important, time-critical but difficult issue. The health of the global population is, perhaps, the most important factor as research is directed towards vaccines and governments scramble to implement public health measures to reduce the spread of the disease. In most countries around the world, these measures have come in the form of local or national lockdowns where individuals are advised or required to remain at home unless they have good reason not to—e.g. for educational or medical purposes, or if they are unable to work from home. However, the implications of trying to control COVID-19 are being felt not only by the health sector, but also in areas such as the economy, environment, and society.
As the number of cases of infected individuals has risen rapidly, there has been an increase in pressure on medical services as healthcare providers seek to test and diagnose infected individuals, in addition to the normal load of medical services that are offered in general. In many cases, trying to control COVID-19 has led to a backlog for and deprivation of other medical procedures [ 31 ], with healthcare providers needing to find a balance between the two. [ 32 ] note that this conflict may change the nature of healthcare with public and private health sectors working together more often. The implementation of restrictions on the movement of individuals has also led to many suggesting that anxiety and distress may lead to increased psychiatric disorders. These may be related to suicidal behaviour and morbidity and may have a long-term negative impact on the mental health of individuals [ 33 , 34 ].
In addition to restrictions on the movement of individuals, governments have required most non-essential businesses to close. This has negatively impacted national economies with many businesses permanently closing leading to a significant increase in unemployment. Limits on travel have severely affected the tourism and travel industries, and countries and economies that are dependent on these for income. Whilst many of the implications of controlling COVID-19 on the economy are negative, there have been some positive changes as businesses adapt to the ‘new normal’. For example, the banking industry is dealing with increased credit risks, while the insurance industry is developing more digital products and pandemic-focused solutions [ 32 ]. The automotive industry is expected to see profits reduced by approximately $100 billion, which may be offset by the development of software subscription services of modern vehicles [ 32 ]. Some traditional office-based businesses have been able to reduce costs by shifting to remote working, while the restaurant industry has shifted towards takeaway and delivery services [ 32 ].
In terms of the environment, the limitations on businesses that have been able to continue operating throughout the epidemic has led to possible improvements in the environment—mainly from the reduction in pollution [ 35 ]. However, societal issues have been exacerbated. [ 32 ] note that the reduction in the labour force that has resulted from controlling for COVID-19 has affected ethnic minorities and women most significantly. Furthermore, in many countries health services employ more women than men creating a dilemma for working mothers—either leave the labour force and provide childcare for their families or remain in employment and pay extra costs for childcare.
In Europe, Italy and Spain were two of the first European countries to be significantly affected by COVID-19. However, the majority of the literature covering the two countries focuses on the clinical aspects of the disease, [ 36 – 40 ], with only a limited number exploring the prevalence of the disease, [ 41 – 43 ].
As as a result of this on going pandemic, new results and reports are being produced and published daily. Thus, our motivation stems from wanting to contribute to the statistical analysis of the incidence of COVID-19 in Italy and Spain, where the literature is limited. The main contributions of this paper are: i) to model the incidence of COVID-19 in Italy and Spain using simple mathematical models in epidemiology; ii) to provide estimates of basic measures of the infectiousness and severity of COVID-19 in Italy and Spain; iii) to investigate the predictive ability of simple mathematical models and provide simple forecasts for the future incidence of COVID-19 in Italy and Spain.
The contents of this paper are organised as follows. In the data section, we describe the incidence data used in the main analysis and provide a brief summary analysis. The method section outlines the Susceptible-Infectious-Recovered model and the log-linear model used to model the incidence of COVID-19, and introduces the basic reproduction number and effective reproduction number as measures of the infectiousness of diseases. In the results section, we present the main results for the fitted models and estimates of the measures of infectiousness, in addition to simple predictions for the future incidence of COVID-19. Some concluding remarks are given in the conclusion.
The data used in this analysis consists of the daily and cumulative incidence (confirmed cases) of COVID-19 for Italy and Spain (nationally), and their respective regions or autonomous provinces. For Italy, this data covers 21 regions for 37 days from 21st February 2020 to 28th March 2020, inclusive; for Spain, this data covers 19 regions for 34 days from 27th February to 31st March 2020, inclusive. The data for Italy was obtained from [ 44 ] where the raw data was sourced from the Italian Department of Civil Protection; the data for Spain was obtained from [ 45 ] where the raw data was sourced from the Spanish Ministry of Health. The starting dates for both sets of data indicate the dates on which the first cases were confirmed in each country, however, it should be noted that in some regions cases were not confirmed until after these dates. These particular time periods were chosen as they cover over one month since the initial outbreaks in both countries and were the most up to date data available at the time of writing. In the remainder of this section, we provide a simple exploratory analysis of the incidence data.
Fig 1 plots the daily cumulative incidence for Italy and its 21 regions over the whole sample period. All cumulative incidence appears to show an exponential trend, increasing slowly for the first 14 days after the first cases are confirmed before growing rapidly. Checking the same plot on a log-linear scale, shown in Fig 2 , we find that the logarithm of cumulative incidence in some regions exhibits an approximate linear trend suggesting that cumulative incidence is growing exponentially. However, in the majority of regions (and nationally) this trend is not exactly linear, suggesting a slightly sub-exponential growth in cumulative incidence.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0249037.g001
https://doi.org/10.1371/journal.pone.0249037.g002
Of all the regions in Italy, the northern region of Lombardy is one of the worst affected and Fig 3 plots the daily incremental incidence for both Lombardy and Italy, respectively. In terms of the number of new cases confirmed each day, the trends are very similar and, again, possibly exponential until peaking around 21st March 2020 before levelling off. Comparing the trends for the other regions in Fig 4 , it can be seen that other significantly affected northern regions such as Piedmont and Emilia-Romagna exhibit similarities to Lombardy—growing, peaking, and levelling around the same times. However, many other regions show some slight differences such as peaking at earlier or later dates, and even exhibiting an erratic trend.
https://doi.org/10.1371/journal.pone.0249037.g003
https://doi.org/10.1371/journal.pone.0249037.g004
In Fig 5 , things are put in perspective when the cumulative incidence of all Italian regions are plotted on the same scale. It is clear that Lombardy is the most affected region contributing to the largest share of national cumulative incidence, and indeed it is the epicentre of the outbreak in Italy.
https://doi.org/10.1371/journal.pone.0249037.g005
In the case of Spain, Fig 6 plots the daily cumulative incidence nationally and for all 19 Spanish regions over the whole sample period. The trend appears to be exponential and is similar between regions, but is also similar to that of the daily cumulative incidence in Italy. On a log-linear scale, in Fig 7 , the growth of the daily cumulative incidence appears to be closer to an exponential trend compared with Italy, due to the plots arguably exhibiting a more linear trend. It can be seen that there is a slight difference with Italy in that it appears as though most Spanish regions were affected at approximately the same time—when the country’s first cases were confirmed. This is reflected by the majority of plots starting from the very left of the x-axis, with the exception of the plots for a few regions such as Ceuta and Melilla. In Italy only a small number of regions were affected when the country’s first cases were confirmed, with the growth in cumulative incidence for the majority of the other regions coming later on.
https://doi.org/10.1371/journal.pone.0249037.g006
https://doi.org/10.1371/journal.pone.0249037.g007
The worst affected regions in Spain are Madrid and Catalonia, and Fig 8 plots the daily incremental incidence for both regions and the national trend. The growth in daily incidence, in all three cases, could be classed as being approximately exponential, however, daily incidence appears to peak on 26th March 2020 before falling and peaking again on 31st March 2020. It is confirmed that the true peak daily incidence does indeed occur on 31st March 2020 and we return to this point later on in the analysis. In comparison to other Spanish regions, it seems that Madrid and Catalonia are the exceptions as the majority of regions exhibit an exponential rise in daily incidence and peak around 26th and 27th March 2020 before falling.
https://doi.org/10.1371/journal.pone.0249037.g008
Plotting the daily incidence of all regions on the same scale in Fig 9 , it is clear that Madrid and Catalonia are the most affected regions contributing the largest share of the national cumulative incidence. Whilst Madrid and Catalonia are the main epicentres of the outbreak in Spain, many coastal regions also show significant numbers of confirmed cases, although not quite on the same scale.
https://doi.org/10.1371/journal.pone.0249037.g009
The SIR (Susceptible-Infectious-Recovered) model
In the mathematical modelling of infectious diseases, there exist many compartmental models that can be used to describe the spread of a disease within a population. One of the simplest models is the SIR (Susceptible-Infectious-Recovered) model proposed by [ 46 ], in which the population is split into three groups or compartments: those who are susceptible ( S ) but not yet infected with the disease; those who are infectious ( I ); those who have recovered ( R ) and are immune to the disease or who have deceased.
The SIR model has been extensively researched and applied in practice, thus it would not be practical to mention and cover all of the literature. However, some of the most prominent literature covers areas such as the stability and optimality of the simple SIR model ([ 47 – 51 ]); pulse vaccination strategy in the SIR model ([ 52 – 55 ]); applications of the SIR in the modelling of infectious diseases ([ 56 – 64 ]).
With regards to COVID-19, many have applied the basic SIR model (or slightly modified versions) to model the outbreak. Some particular examples include (but are not limited to): [ 2 ] who estimate the overall symptomatic case fatality risk of COVID-19 in Wuhan and use the SIR model to generate simulations of the COVID-19 outbreak in Wuhan; [ 65 ] who apply a modified SIR model to identify contagion, recovery, and death rates of COVID-19 in Italy; [ 66 ] who combine the SIR model with probabilistic and statistical methods to estimate the true number of infected individuals in France; [ 67 ] who use a number of methods including the SIR model to estimate the basic and controlled reproduction numbers for the COVID-19 outbreak in Wuhan, China; [ 68 ] who show that the basic SIR model performs better than extended versions in modelling confirmed cases of COVID-19 and present predictions for cases after the lockdown of Wuhan, China; [ 69 ] who model the temporal dynamics of COVID-19 in China, Italy, and France, and find that although the rate of recovery appears to be similar in the three countries, infection and death rates are more variable; [ 70 ] who simulate the outbreak in Wuhan, China, using an extended SIR model and investigate the age distribution of cases; [ 71 ] who study the number of infections and deaths from COVID-19 in Sweden using the SIR model; [ 72 ] who use the SIR model, with an additional parameter for social distancing, to model and forecast the early stages of the COVID-19 outbreak in Brazil.
In reference to the SIR model, [ 74 ] note that it “examines only the temporal dynamics of the infection cycle and should thus be appropriate for the description of a well-localised epidemic outburst”, therefore, it would appear to be reasonable for use in analysis at city, province, or country level. In the form above, the dynamics of the model are controlled by the parameters β and γ , representing the rates of transition from S to I (susceptibility to infection), and I to R (infection to recovery or death), respectively.
To fit the model and find the optimal parameter values of β and γ , we use the optim function in R [ 75 ] to solve the minimisation problem. The system of differential equations, Eqs ( 1 ) to ( 3 ), are set up as a single function. The model is then initialised with starting values for S , I , and R , with parameters β and γ unknown. We obtain the daily cumulative incidence for the sample period, total population ( N ), and the susceptible population ( S ) as the total population minus the number of currently infected individuals. This is defined as the cumulative number of infected individuals minus the number of recovered or dead, however, these exact values are difficult to obtain. Thus, the cumulative number of infected individuals at the start date of the sample period is used as a proxy—since at the start date of the disease, this is likely to be close to the true value, as the number of recovered or dead should be very small (if not zero).
The residual sum of squares is then defined and set up as a function of β and γ . The optim package is used for general purpose optimisation problems, and in this case it is used to minimise the function RSS with respect to the sample of cumulative incidence. More specifically, we use the limited memory Broyden-Fletcher-Goldfarb-Shanno (L-BFGS-B) algorithm for the minimisation, which allows us to specify box constraints (lower and upper bounds) for the unknown parameters β and γ . The lower and upper bounds of zero and one, respectively, were selected for both parameters. The optim function then searches for the β and γ that minimise the RSS function, given starting values of 0.5 for both parameters. The optimal solution is found via the gradient method by repeatedly improving the estimates of RSS to try and find a solution with a lower value. The function makes small changes to the parameters in the direction of where RSS changes the fastest, where in this direction the lowest value of RSS is. This is repeated until no further improvement can be made or the improvement is below a threshold.
We consider convergence as the main criteria for finding an optimal solution in the minimisation of RSS —when the lowest RSS has been found, and no further improvement can be found or the improvement is below a threshold. In the case where convergence is not achieved, or there is some related error, then we use the parscale function in the optimisation. As the true values of β and γ are unknown, in the default case, the parameters are adjusted by a fixed step starting from their initial values. Most common issues were addressed using the parscale function to rescale—alter the sensitivity/magnitude of the parameters on the objective function. In other words, it allows the algorithm to compute the gradient at a finer scale (similar to the ndeps parameter—used to adjust step sizes for the finite-difference approximation to the gradient). In most cases, issues were solved by using a step size of 10 −4 . Of course, smaller step sizes could be used, but there is a risk that selecting too small a step size will lead to the optimal values of β and γ being found at their starting values. However, the results should be interpreted with caution. It is possible that estimates will vary with different population sizes N and the starting values specified for β and γ , which may also cause the optimisation process to be unstable.
It should be noted that the application of the basic SIR model to COVID-19 simplifies the analysis and makes the strong assumption that individuals who become infected but recover are immune to COVID-19. This is assumed purely for the simplification of modelling and we do not claim this to be true in reality. At present, it remains unclear whether those who recover from infection are immune [ 76 ]. Indeed, there have been studies and unconfirmed reports of individuals who have possibly recovered but then subsequently tested positive for the virus again, see for example [ 77 – 79 ].
The basic reproduction number R 0
Whilst the fitted model and optimal parameters allow us to make a simple prediction about how the trajectory of the number of susceptible, infectious, and recovered individuals evolves over time, a more useful statistic or parameter that can be computed from the fitted model is the basic reproduction number R 0 . Originally developed for the study of demographics in the early 20th century, it was adapted for use in the study of infectious diseases in the 1950’s [ 80 ]. It is defined as the “expected number of secondary infections arising from a single individual during his or her entire infectious period, in a population of susceptibles” [ 80 ], and is widely considered to be a fundamental concept in the study of epidemiology. In other words, it is the estimated number of people that an individual will go on to infect after becoming infected.
The R 0 value can provide an indication of the severity of the outbreak of an infectious disease: if R 0 < 1, each infected individual will go on to infect less than one individual (on average) and the disease will die out; if R 0 = 1, each infected individual will go on to infect one individual (on average) and the disease will continue to spread but will be stable; if R 0 > 1, each infected individual will go on to infect more than one individual (on average) and the disease will continue to spread and grow, with the possibility of becoming a pandemic ([ 80 , 81 ]).
Log-linear model
https://doi.org/10.1371/journal.pone.0249037.g010
To fit the log-linear model, we use the incidence package [ 82 ] in R [ 75 ] to obtain the optimal values of the parameters. Using the estimated parameters, the fitted model can be used to predict the trajectory of the incidence up until the peak incidence in the growth phase. However, although the log-linear model allows for the modelling and prediction of the incidence, compared with the SIR model it does not provide any indication about the number of susceptible or recovered individuals.
We are able to use the epitrix R package [ 84 ] to implement the method by [ 83 ] for empirical distributions to estimate R 0 from the growth rate r . However, [ 83 ] note that an “epidemic model implicitly specifies a generation interval distribution” (also known as the serial interval distribution), which is defined as “the time between the onset of symptoms in a primary case and the onset of symptoms in secondary cases” [ 85 ]. As we do not have access to more detailed COVID-19 patient data, we are not able to compute the parameters of the serial interval distribution directly. However, a number of existing analyses of COVID-19 patient data report some preliminary estimates of the best fitting serial interval distributions and their corresponding model parameters. These are: i) gamma distribution with mean μ = 7.5 and standard deviation σ = 3.4 [ 81 ]; ii) gamma distribution with mean μ = 7 and standard deviation σ = 4.5 [ 2 ]; iii) gamma distribution with mean μ = 6.3 and standard deviation σ = 4.2 [ 86 ]. By using these three serial intervals in conjunction with the above method, we are able to obtain estimates of R 0 from estimates of the growth rate r . It should be noted that serial interval distributions are not only restricted to the gamma distribution—other common distributions used include the Weibull and log-normal distributions, and that the parameters are dependent on a number of factors including the time to isolation [ 86 ].
The effective reproduction number R e
As mentioned above, the estimation of the R 0 value is not always ideal, due to it being a single fixed value reflecting a specific period of growth (in the log-linear model) or requiring assumptions that only hold true in specific time periods (in the basic SIR model). In other words, it is “time and situation specific” [ 85 ]. In reality, the reproduction number will vary over time but it will also be influenced by governments and health authorities implementing measures in order to reduce the impact of the disease. Therefore, a more useful approach for measuring the severity of an infectious disease is to track the reproduction number over time. The effective reproduction number R e is one way to achieve this, and thus allows us to see how the reproduction number changes over time in response to the development of the disease itself but also effectiveness of interventions. Although there are numerous methods that can be used to analyse the severity of a disease over time, the majority are not straightforward to implement (especially in software) [ 85 ].
One popular method for estimating R e is that proposed by [ 85 ]. The basic premise of this method is that “once infected, individuals have an infectivity profile given by a probability distribution w s , dependent on time since infection of the case, s , but independent of calendar time, t . For example, an individual will be most infectious at time s when w s is the largest. The distribution w s typically depends on individual biological factors such as pathogen shedding or symptom severity” [ 85 ].
The function models the transmissibility of a disease with a Poisson process, such that an individual infected at time t − s will generate new infections at time t at a rate of R t w s , where R t is the instantaneous (effective) reproduction number at time t . Thus, the incidence at time t is defined to be Poisson distributed with mean equal to the average daily incidence (number of new cases) at time t . This value is just for a single time period t , however, estimates for a single time period can be highly variable meaning that it is not easy to interpret, especially for making policy decisions. Therefore, we consider longer time periods of one week (seven days)—assuming that within a rolling window the instantaneous reproduction number remains constant. Note that there is a potential trade off, as using longer rolling windows gives more precise estimates of R t but this means fewer estimates can be computed (requires more incidence values to start with) and a more delayed trend reducing the ability to detect changes in transmissibility. Whereas shorter rolling windows lead to more rapid detection in changes but with more noise. Using this method, it is recommended that a minimum cumulative daily incidence of 12 cases have been observed before attempting to estimate R e . For the data sets used, this does not pose a problem as a cumulative total of 16 and 17 cases, respectively, exist on the first day of the sample at the country level, and by the seventh day the totals are around 200 and 650 for Spain and Italy, respectively.
From the posterior distribution, the posterior mean R t , τ can be computed at time t for the rolling window of [ t − τ , t ] by the ratio of the gamma distribution parameters. We refer the readers to the supplementary information of [ 85 ] for further details regarding the Bayesian framework. As noted by [ 85 ], this method works best when times of infection are known and the infectivity profile or distribution can be estimated from patient level data. However, as mentioned above, we do not have access to this level of data, and instead utilise three different serial intervals from the literature that have been estimated from real data.
In practice, the transmission of a disease will vary over time especially when health prevention measures are implemented. However, this method is the only reproduction number that can be easily computed in real-time, and in comparison to similar methods, it captures the effect of control measures since it will cause sudden decreases in estimates compared with other methods.
In this analysis, we use the most basic version of this method and estimate the effective reproduction number over a rolling window of seven days. This appears to be sufficient and in line with our results, as we do not suffer from the problem of small sample sizes as the samples are sufficiently large and we start computing the effective reproduction number after one mean serial interval. It should be noted that estimates of this reproduction number are dependent on the distribution of the infectiousness profile w s . In addition, it is known that this distribution may not always be well documented, especially in the early parts of an epidemic. However, here we assume that the serial interval is defined for our sample period and the use of the three serial intervals from the literature appears to give satisfactory results.
If problems did arise, or to account for uncertainty in the serial interval distribution, an alternative method is to implement a modified procedure by [ 85 ], which allows for uncertainty in the serial interval distribution. This modified method assumes that the serial interval is gamma distributed but the mean and standard deviation are allowed to vary according to a standard normal distribution. Some N * pairs of means and standard deviations are simulated—mean first and standard deviation second, with the constraint that the mean is less than the standard deviation to ensure that for each pair the probability density function of the serial interval distribution is null at time t = 0. Then, for each rolling window 1000 realisations are sampled of the instantaneous reproduction number using the posterior distribution conditional on the pair of parameters.
The SIR model and R 0
For both Italy and Spain, we set up and solve the minimisation problem for the SIR model described in Section for region-level and national-level COVID-19 incidence for the first 14 days after the first cases were confirmed in each respective country and region. The first 14 days after the first cases are detected can be considered to be the early stage of an outbreak, and it is reasonable to assume that there are few, if no, infected or immune individuals prior to this. However, it is a rather strong assumption as it is possible that individuals may be infected but do not display any symptoms. Tables 1 and 2 show the output corresponding to each region/country including the date that the first cases were confirmed, the population size (obtained from [ 88 ]), the cumulative number of cases at the 14th day after the first cases were confirmed, the fitted estimates for the parameters β and γ , and estimates for R 0 .
https://doi.org/10.1371/journal.pone.0249037.t001
https://doi.org/10.1371/journal.pone.0249037.t002
From Tables 1 and 2 , we observe that many of the first regions to be affected in both countries are those with the largest population sizes, however, the cumulative number of cases (after the first 14 days) in these regions are not always the highest among all regions. The estimates of the parameters β and γ also do not show any particular trends and this is reflected in the estimated R 0 values. It can be seen that for all regions in both Italy and Spain, the estimated R 0 values fall between one and three. This suggests that, according to the thresholds described above, the disease is spreading and growing in all Italian and Spanish regions during the 14 days after the first localised cases were confirmed. At a national level, the estimated values of R 0 are greater than two for both countries, again, suggesting a spreading and growing disease. This is perhaps not surprising since this time period reflects the early stages of the spread of the disease, thus we would expect it to be growing and spreading quickly before any preventative action is taken.
We note that in Tables 1 and 2 , there are some cases where the estimated value of β is very close to or at the upper limit of 1.000—e.g. Lombardy (Italy) and Madrid (Spain). This leads to the consequence that the parameter estimates appear to be bound by the upper limit. However, all parameter estimates are dependent on the starting values defined for β and γ , and the upper and lower bounds specified. For all cases of estimating the parameters in Tables 1 and 2 , we used the same optimisation procedure and criteria for determining a satisfactory estimate that is the convergence in the minimisation of the RSS ( Eq (4) ). In all cases, convergence was achieved but this is still slightly problematic. For cases where the estimated value of β is 1.000, although convergence was achieved, this indicates only that it generates the lowest RSS within the upper and lower limits defined. Therefore, there may or may not exist values of the parameter outside of this range that may be more optimal. Indeed, the results may vary depending on the upper and lower bounds, and the starting values that are selected. Thus, there is also the question of how to change the starting values and bounds appropriately (instead of, say, simply increasing them). Furthermore, as the R 0 value in the SIR model is computed as β / γ , another consequence of the estimated value of β being 1.000 is that the true value of β may actually be larger than this, and so the true value of R 0 may be larger than the estimated value.
Using the estimated parameters for the best fitted models, the predicted trajectories of the numbers in each of the compartments of the model can be generated. For brevity, in the remainder of the analysis, we show only the results for Italy, Spain, and their worst affected regions. Fig 11 plots the observed and predicted cumulative incidence for the 14 days immediately following the first confirmed cases in Lombardy and Italy, respectively. It can be seen that the model appears to under predict the true total number of cases in both cases during the early part of the outbreak before over estimating towards the end of the 14 days. In Fig 12 the SIR model trajectories are plotted along with the observed cumulative incidence on a logarithmic scale for Lombardy and Italy. The under prediction of the cumulative incidence in the first 14 days (to the left of the vertical dashed black line) is indicated by the solid red line (predicted cumulative incidence) lying below the black points (observed cumulative incidence) however, after the initial 14 days and after the implementation of a nationwide lock down (vertical dashed red line), the observed cumulative incidence grows at a slower rate than predicted by the fitted model. Indeed, this reflects the fact that the model is based only on the initial 14 days and does not account for any interventions.
https://doi.org/10.1371/journal.pone.0249037.g011
https://doi.org/10.1371/journal.pone.0249037.g012
In Fig 13 , the observed and predicted cumulative incidence for the 14 days immediately following the first confirmed cases in Catalonia, Madrid, and Italy, respectively, are shown. In contrast to the results for Italy, the fitted model for all three appears to predict the true total number of cases across the whole of the first 14 days reasonably well. Fig 14 plots the SIR model trajectories and the observed cumulative incidence on a logarithmic scale for Catalonia, Madrid, and Spain. Here, the more accurate predictions of the cumulative incidence are reflected in the area to the left of the vertical dashed black line. However, it can be seen that at the time when the nationwide lock down came into force (vertical dashed red line) the growth of the true total number of cases slowed down. It is likely that this is coincidental, since it is known that the effect on the incidence of infectious diseases from health interventions is not immediate, but instead lags behind.
https://doi.org/10.1371/journal.pone.0249037.g013
https://doi.org/10.1371/journal.pone.0249037.g014
Log-linear model and R 0
Following the SIR model, we implemented the log-linear model as described above for region-level and national-level COVID-19 daily incidence for the entire growth phase (from the time of the first confirmed cases until the time at which daily incidence peaks). The estimated parameters of the fitted log-linear models for the daily incidence of Lombardy and Italy, respectively, are shown in Table 3 . It can be seen that the peak daily incidence in both Lombardy and at country level occurred on the same day (21st March 2020), however, the growth rate (doubling time) is found to be slightly greater (shorter) at country level (0.18 and 3.88) compared with the Lombardy region (0.16 and 4.34). In comparison to the SIR model and modelling the cumulative incidence, the log-linear model modelling the daily incidence in the growth phase (as shown in Fig 15 ) appears to be slightly more accurate.
Upper and lower limits of the 95% confidence intervals are indicated by the dashed red lines.
https://doi.org/10.1371/journal.pone.0249037.g015
https://doi.org/10.1371/journal.pone.0249037.t003
In Table 4 , the estimated parameters of the fitted log-linear models for the daily incidence of Madrid, Catalonia, and Spain, respectively, are given. Similarly, the peak daily incidence occurs on the same day (31st March 2020) for Madrid, Catalonia, and Spain, although this is later than that for Italy. Interestingly, the growth rate (doubling time) is greatest (shortest) for Catalonia (0.24 and 3.85), whilst Madrid and Spain share similar growth rates and doubling times (0.21/0.22 and 3.24/3.21). It should be noted that there appears to be a slight difference in the observed daily incidence compared with the case of Italy and its regions. In Fig 16 , it can be seen that the observed daily incidence appears to initially peak in the last few days of March in all cases before falling, but then increases to a higher peak at the end of the growth phase. This seems to throw off the fitted log-linear model, as after the initial (approximate) 14 days the fitted model under predicts and then over predicts the daily incidence.
https://doi.org/10.1371/journal.pone.0249037.g016
https://doi.org/10.1371/journal.pone.0249037.t004
As with the SIR model, we are also able to use the fitted log-linear models in conjunction with the three serial intervals mentioned above to compute estimates of the R 0 value. Table 5 shows the mean estimates of the R 0 value for Italy, Spain, and their most affected regions, computed from the fitted log-linear models and the three serial intervals. In each case, the mean estimates are computed from 10,000 samples of R 0 values generated from the log-linear regression of the incidence data in the growth phase, and the distributions of these samples are plotted in S1 Fig . Compared with the estimates from the SIR model, we find that in all but the case of Italy, the estimates of R 0 from the log-linear model are greater than that from the SIR model—in these cases, the lowest estimates of R 0 from the log-linear models are larger by between 0.5 to 1. In the case of Italy, we find that the estimate of R 0 computed from the SIR model is approximately the same as that computed from the log-linear model using a serial interval using a gamma distribution with mean μ = 7 and standard deviation σ = 4.5 [ 2 ]. Using the log-linear models, the largest R 0 values computed are for Catalonia, whereas the smallest values are for Lombardy. It can also be seen that serial distributions with a lower mean appear to correspond with lower R 0 values. A possible explanation for the difference between the estimated R 0 values computed from the SIR models and the log-linear models is that the only incidence data from the first 14 days was used in the former, whereas incidence data from the whole growth phase was used in the latter—almost double the data. Therefore, it is arguable that the R 0 estimates from the log-linear models could be considered to be more accurate.
https://doi.org/10.1371/journal.pone.0249037.t005
Effective reproductive number R e .
Turning towards the more dynamic measure of the infectiousness of diseases, Figs 17 and 18 plot the estimated reproductive numbers computed for Lombardy, Italy, Madrid, Catalonia, and Spain, over the entire sample period. Using the method proposed by [ 85 ], in each case estimates were computed using rolling windows of the daily incidence over the previous 7 days and the same three serial distributions as for the log-linear models. As a result, no estimates are computed for the first 7 days of each respective sample period. In all cases, we analyse and compute the R e values over the whole sample period available allowing us to see how the infectiousness of COVID-19 varies during the initial outbreak stages and the effect of any interventions implemented by the respective governments. In Fig 17 , we observe that for both Lombardy and Italy, R e is generally decreasing over the time (under any of the three serial distributions), and although it is initially larger for Italy, after approximately the first 7 days the R e values are similar. However, the trend of R e both to the left and right (before and after) of the nationwide lockdown (indicated by the dotted line) shows some differences. Prior to the nationwide lockdown, R e decreases rapidly towards a value of between three and four, which could be attributed to the fact that northern Italy (including Lombardy) was the most affected area in the early stages of the outbreak and lockdowns local to the area were already being enforced from 21st February 2020. Thus, this is likely to have contributed (in part) to the initial reduction in the R e value. After the nationwide lockdown came into force on 9th March 2020, R e continues to decrease but at a slower pace and appears to level off approximately 14 days later—this coincides with the peak in daily incidence on 21st March 2020. After this point, it is likely that the effects of the nationwide lockdown are starting to appear with R e appearing to decrease again more rapidly towards the critical value of one (solid horizontal line)—suggesting that the disease is still spreading but stabilising.
Upper and lower limits of the 95% confidence intervals for the mean are indicated by the red dashed lines, and the grey dotted line indicates the date at which the national lock down becomes effective.
https://doi.org/10.1371/journal.pone.0249037.g017
https://doi.org/10.1371/journal.pone.0249037.g018
In Fig 18 , we observe a different trend in the R e value for Madrid, Catalonia, and Spain, compared with Lombardy and Italy. Whilst R e exhibits a decrease over the sample time period (under any of the three serial distributions), the initial values are actually larger for Madrid and Catalonia, however, the values for all three are similar after the initial 7 days. The trend in the estimated R e values before and after the nationwide lockdown again show some differences, but also differ to those for the cases of Lombardy and Italy. Prior to the nationwide lockdown (indicated by the dotted line), the trend of the estimated R e values is very erratic: decreasing, increasing, and then decreasing again. This could be due to the daily incidence for Madrid, Catalonia, and Spain, showing greater variation compared with that for Italy before the respective lockdowns. It is found that in the period before the lockdowns, Spanish daily incidence appears to show more alternation between increases and decreases compared with the previous day’s incidence, whilst Italian daily incidence shows much less. After the nationwide lockdown on 14th March 2020, for all three cases the estimated R e decreases significantly towards a value of two. More specifically, in mid-March 2020 daily incidence for Madrid, Catalonia, and Spain, levels off corresponding to the reduction in R e , but in the run up to 23rd March 2020 daily incidence again becomes more variable and alternates between significantly larger and smaller daily incidence, with R e levelling off. After 23rd March 2020, this levelling off is more sustained for Madrid and Spain compared with Catalonia. This may be attributed to the daily incidence initially peaking and then decreasing much more significantly for Catalonia, leading to a more significant decrease in R e at the latter end of the sample period. In general, the estimated R e values are larger for Spain than Italy, since Spain is lagging behind in terms of the start of the outbreak, however, it is found that the estimated R e is larger for Italy than Spain, but larger for Madrid and Catalonia than Lombardy.
Predictive ability of models.
Whilst the results regarding the estimated reproduction values ( R 0 and R e ) provide useful indicators about the infectiousness of COVID-19 and the variability over time, the predictive ability of models is also key—especially in the decay phase of an outbreak after the daily incidence has peaked and is in decline. Predictions about the daily incidence in the decay phase can contribute to determining whether health interventions are working, but can additionally provide time frames for when daily incidence may reach certain thresholds—e.g. below which the disease may be considered under control. To compare the predictive ability of the SIR and log-linear models, we use the projections package [ 89 ] in R [ 75 ]. As this section acts to provide only a brief analysis of the predictive ability of the models, we refer the readers to [ 89 ] for in-depth documentation regarding the finer details of the computations. The initial step is to consider which of the two models provides the best predictive ability in the growth phase of the COVID-19 outbreak and for simplicity, we analyse only Italy and Spain at country level. Using the estimated R 0 values for Italy and Spain from the SIR and log-linear models above, we combine these with the three serial distributions mentioned earlier. We then use the projections package [ 89 ] to forecast and predict the daily incidence for Italy and Spain from the 14th day (since the first cases in each location) until the day of peak incidence.
Plots of the true daily incidence in Italy and Spain during their respective growth phases and the predicted values using the SIR and log-linear models are shown in Figs 19 and 20 . In each figure, the first row plots the predictions using the SIR model; the second row plots the predictions using the log-linear model. For the case of Italy, the plots in Fig 19 appear to show that the predictions using the R 0 value estimated from the SIR model and the serial interval of a gamma distribution with mean μ = 7.5 and standard deviation σ = 3.4 [ 81 ] provide the most accurate general predictions. However, although using the R 0 value estimated from the log-linear model generates predictions which are accurate up until the last 7 days of the growth phase (where all three cases show over prediction), these results are more consistent compared with those using the SIR model. For the case of Spain, the plots in Fig 20 show that the predictions using the R 0 value estimated from the SIR model are consistent but significantly under predicting the observed daily incidence. In contrast, predictions using the R 0 value estimated from the log-linear model are consistent and accurate up until the initial peak in daily incidence a few days before the true peak at the end of the growth phase. Based on these results for the growth phase of the outbreak, we propose to use the log-linear model to compute basic predictions for the decay phase.
95% confidence intervals for the predicted incidence are indicated by the shaded light purple regions.
https://doi.org/10.1371/journal.pone.0249037.g019
https://doi.org/10.1371/journal.pone.0249037.g020
At the time of conducting this part of the analysis, approximately one month of daily incidence data was available for the decay phase (following peak daily incidence) of both Italy and Spain. Similarly, we follow the methodology for fitting the log-linear model but now apply it to the decay phase daily incidence. The model is fitted to the decay phase daily incidence in the same way, and model parameters can be computed. Note that for the decay phase, the values and interpretation of the estimated parameters change—the growth rate takes a negative value and the doubling time becomes the halving time (both reflecting the decay and decrease in daily incidence). The fitted log-linear regressions for Italy and Spain are shown in the left hand plots of Figs 21 and 22 , respectively. The fitted models appear to provide reasonable fits to the observed decay phase daily incidence much like the case for the growth phase.
Plots of the observed (dot-dashed black line) and projected daily incidence for the next 180 days using the log-linear model and serial interval distributions SI 1 (green line), SI 2 (blue line), and SI 3 (red line) (right).
https://doi.org/10.1371/journal.pone.0249037.g021
https://doi.org/10.1371/journal.pone.0249037.g022
Also, as in the growth phase, the R 0 value can still be computed for the log-linear model during the decay phase, and for consistency we obtain mean estimates of R 0 from 10,000 samples of R 0 generated from the log-linear regressions of the daily incidence during the decay phase in conjunction with the three serial distributions. Distributions of these estimates are plotted in S2 Fig and it can be seen that (in contrast to the growth phase) the mean estimates of R 0 for Italy and Spain, individually, are very similar (under the three serial distributions)—between 0.85 and 0.87 for Italy, and 0.77 and 0.83 for Spain. Using the mean estimated R 0 values and the three serial distributions, we computed projections of the daily incidence for the 180 days immediately following the end of the decay phase sample period on 22nd April 2020. The paths of these projections for Italy and Spain are shown in the right hand plots of Figs 21 and 22 , respectively.
A simple comparison of the projected daily incidence for both countries is given in Table 6 , at one and two months following the end of the decay phase sample period. Observed daily incidence for the remainder of the decay phase was obtained from [ 44 , 90 , 91 ]. In general, it appears that the predictions for future daily incidence (under all three serial distributions) in both Italy and Spain are significantly greater than the observed daily incidence. At the one month time point (21st May 2020) projections of daily incidence for Italy are approximately twice as large as the true incidence; projections of daily incidence for Spain are approximately two to three times as large as the true incidence. Moving forward to the two month time point (21st June 2020) projections of the daily incidence for Italy are approximately two to three times as large as the true incidence; projections of the daily incidence for Spain are up to twice as large as the true incidence. However, the projection of Spanish daily incidence using the serial interval of a gamma distribution with mean μ = 6.3 and standard deviation σ = 4.2 [ 86 ] is almost identical to the true incidence.
https://doi.org/10.1371/journal.pone.0249037.t006
Whilst the results of the projections generally show significant over estimation of future daily incidence in both Italy and Spain, they do provide some additional information to the reproduction values regarding the trends of daily incidence. However, such forecasts should be not be taken directly at face value as there are a number of pitfalls that will influence the predictions. Limited decay phase incidence data was available at the time of the original analysis, which is likely to have led to less accurate estimates of R 0 and thus predictions. On a related note, the predictions are conditional on the data up until the end of the sample decay phase data and thus do not account for any health policies or interventions implemented after this, likely leading to the over estimation.
In this paper, we have provided a simple statistical analysis of the novel Coronavirus (COVID-19) outbreak in Italy and Spain—two of the worst affected countries in Europe. Using data of the daily and cumulative incidence in both countries over approximately the first month after the first cases were confirmed in each respective country, we have analysed the trends and modelled the incidence and estimated the basic reproduction value using two common approaches in epidemiology—the SIR model and a log-linear model.
Results from the SIR model showed an adequate fit to the cumulative incidence of Spain and its most affected regions in the early stages of the outbreak, however, it showed significant under estimation in the case of Italy and its most affected regions. Estimates of the basic reproduction number in the early stage of the outbreak from the model were found to be greater than one in all cases, suggesting a growing infectiousness of COVID-19—in line with expectations. Applying the log-linear regression model to the daily incidence, results for the growth phase of the outbreak in Italy and Spain revealed a greater growth rate for Spain compared with Italy (and their most affected regions)—approximately between 0.21 to 0.24 for the former and 0.15 to 0.18 for the latter. The time for the daily incidence to double for Spain was also found to be shorter than Italy (approximately three days compared to four days).
With the lack of detailed clinical COVID-19 data for the two countries, we utilised existing results regarding the serial interval distribution of COVID-19 from the literature to estimate the basic reproduction number via the log-linear model. Estimates of this value were found to be between 2.1 and 3 for Italy and its most affected region Lombardy, and between 2.5 and approximately 4 for Spain and its most affected regions of Madrid and Catalonia. Further analysis of the effective reproduction number (based on the incidence over the previous seven days) indicated that in both countries the infectious of COVID-19 was decreasing and reflecting the positive impact of health interventions such as nationwide lock downs.
Basic predictions of future daily incidence in Italy and Spain were estimated using the log-linear regression model for the decay phase of the outbreak. Estimates of the projected daily incidence at various time points in the future were generally found to be between two to three times larger than the true levels of daily incidence. These results highlight the fact that the estimates may only give reasonable indications in the short term, since they are based on past data which may or may not account for factors which change in the short term—e.g. new health interventions, public policy, etc.
Despite the simplicity of our results, we believe that they provide an interesting insight into the statistics of the COVID-19 outbreak in two of the worst affected countries in Europe. Our results appear to indicate that the log-linear model may be more suitable in modelling the incidence of COVID-19 and other infectious diseases in both the growth and decay phases, and for short term predictions of the growth (or decay) of the number of new cases when no intervention measures have recently been implemented. In addition, the results could be useful in contributing to health policy decisions or government interventions—especially in the case of a significant second wave of COVID-19. However, these results should be used in conjunction with the results from other more complex mathematical and epidemiological models.
Supporting information
S1 fig. plots of the distributions of samples of r 0 values computed from the fitted log-linear regressions of growth phase incidence..
i) Lombardy (top left); ii) Italy (top right); iii) Madrid (middle left); iv) Catalonia (middle right); v) Spain (bottom). a) SI 1 (blue); b) SI 2 (red) c) SI 3 (green).
https://doi.org/10.1371/journal.pone.0249037.s001
S2 Fig. Plots of the distributions of samples of R 0 values computed from the fitted log-linear regressions of decay phase incidence.
i) Italy (left); ii) Spain (right). a) SI 1 (green); b) SI 2 (red) c) SI 3 (blue).
https://doi.org/10.1371/journal.pone.0249037.s002
- 1. Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU), 2020. Coronavirus COVID-19 (2019-nCoV). Available at: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 .
- View Article
- Google Scholar
- PubMed/NCBI
- 13. Atkeson, A., 2020. What Will Be the Economic Impact of COVID-19 in the US? Rough Estimates of Disease Scenarios. National Bureau of Economic Research, Working Paper 26867.
- 17. Benatia, D., Godefroy, R. and Lewis, J., 2020. Estimating COVID-19 Prevalence in the United States: A Sample Selection Model Approach. Available at: https://ssrn.com/abstract=3578760 .
- 32. McKinsey & Company, 2020. COVID-19: Implications for business. Available at: https://www.mckinsey.com/business-functions/risk/our-insights/covid-19-implications-for-business .
- 44. GitHub, 2020a. pcm-dpc/COVID-19: COVID-19 Italia—Monitoraggio situazione. Available at: https://github.com/pcm-dpc/COVID-19 .
- 45. GitHub, 2020b. datasets/COVID 19 at master ⋅ datadista/datasets. Available at: https://github.com/datadista/datasets/tree/master/COVID%2019 .
- 64. Correia A.M., Mena F.C., Soares A.J., 2011. An Application of the SIR Model to the Evolution of Epidemics in Portugal. In: M. Peixoto, A. Pinto and D. Rand eds. Dynamics, Games and Science II. Springer Proceedings in Mathematics, vol 2. Berlin: Springer. pp. 247-250.
- 65. Calafiore, G.C., Novara, C. and Possieri, C., 2020. A Modified SIR Model for the COVID-19 Contagion in Italy. arXiv:2003.14391v1.
- 66. Roques, L., Klein, E., Papax, J., Sar, A. and Soubeyrand, S., 2020. Using early data to estimate the actual infection fatality ratio from COVID-19 in France (Running title: Infection fatality ratio from COVID-19). arXiv:2003.10720v3.
- 67. You, C., Deng, Y., Hu, Y., Sun, J., Lin, Q., Zhou, F., et al. Estimation of the Time-Varying Reproduction Number of COVID-19 Outbreak in China. Available at SSRN: https://ssrn.com/abstract=3539694 .
- 71. Qi, C., Karlsson, D., Sallmen, K. and Wyss, R., 2020. Model studies on the COVID-19 pandemic in Sweden. arXiv:2004.01575v1.
- 72. Bastos, S.B. and Cajuero, D.O., 2020. Modeling and forecasting the early evolution of the Covid-19 pandemic in Brazil. arXiv:2003.14288v2.
- 75. R Development Core Team, 2020. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria (2020).
- 76. World Health Organization, 2020. “‘Immunity passports” in the context of COVID-19’. Available at: https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19 .
- 79. Reuters, 2020. “Explainer: Coronavirus reappears in discharged patients, raising questions in containment fight”. Available at: https://uk.reuters.com/article/us-china-health-reinfection-explainer/explainer-coronavirus-reappears-in-discharged-patients-raising-questions-in-containment-fight-idUKKCN20M124 .
- 82. Jombart, T., Kamvar, Z.N., FitzJohn, R., Cai, J., Bhatia, S., Schumacher, J, et al. 2020. incidence: Compute, Handle, Plot and Model Incidence of Dated Events. R package version 1.7.1. https://CRAN.R-project.org/package=incidence .
- 84. Jombart, T., Cori, A., Kamvar, Z.N. and Schumacher, D., 2019. epitrix: Small Helpers and Tricks for Epidemics Analysis. R package version 0.2.2. https://CRAN.R-project.org/package=epitrix .
- 87. Cori, A., Cauchemez, S., Ferguson, N.M., Fraser, C., Dahlqwist, E., Demarsh, P.A., et al. 2019. EpiEstim: Estimate Time Varying Reproduction Numbers from Epidemic Curves. R package version 2.2-1 https://cran.r-project.org/package=EpiEstim .
- 88. Eurostat, 2019. Population: demography, population projections, census, asylum & migration—Overview. Available at: https://ec.europa.eu/eurostat/web/population/overview .
- 89. Jombart, T., Nouvellat, P., Bhatia, S. and Kamvar, Z.N., 2018. projections: Project Future Case Incidence. R package version 0.3.1. https://CRAN.R-project.org/package=projections .
- 90. Worldometer, 2020. Worldometer—real time world statistics. Available at: https://www.worldometers.info/ .
- 91. Ministerio de Sanidad, Consumo y Bienestar Social. Enfermedad por nuevo coronavirus, COVID-19. Available at: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/ .
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 12, Issue 10
- Studies of prevalence: how a basic epidemiology concept has gained recognition in the COVID-19 pandemic
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-9761-206X Diana Buitrago-Garcia 1 , 2 ,
- http://orcid.org/0000-0002-3830-8508 Georgia Salanti 1 ,
- http://orcid.org/0000-0003-4817-8986 Nicola Low 1
- 1 Institute of Social and Preventive Medicine , University of Bern Faculty of Medicine , Bern , Switzerland
- 2 Graduate School of Health Sciences , University of Bern , Bern , Switzerland
- Correspondence to Professor Nicola Low; nicola.low{at}ispm.unibe.ch
Background Prevalence measures the occurrence of any health condition, exposure or other factors related to health. The experience of COVID-19, a new disease caused by SARS-CoV-2, has highlighted the importance of prevalence studies, for which issues of reporting and methodology have traditionally been neglected.
Objective This communication highlights key issues about risks of bias in the design and conduct of prevalence studies and in reporting them, using examples about SARS-CoV-2 and COVID-19.
Summary The two main domains of bias in prevalence studies are those related to the study population (selection bias) and the condition or risk factor being assessed (information bias). Sources of selection bias should be considered both at the time of the invitation to take part in a study and when assessing who participates and provides valid data (respondents and non-respondents). Information bias appears when there are systematic errors affecting the accuracy and reproducibility of the measurement of the condition or risk factor. Types of information bias include misclassification, observer and recall bias. When reporting prevalence studies, clear descriptions of the target population, study population, study setting and context, and clear definitions of the condition or risk factor and its measurement are essential. Without clear reporting, the risks of bias cannot be assessed properly. Bias in the findings of prevalence studies can, however, impact decision-making and the spread of disease. The concepts discussed here can be applied to the assessment of prevalence for many other conditions.
Conclusions Efforts to strengthen methodological research and improve assessment of the risk of bias and the quality of reporting of studies of prevalence in all fields of research should continue beyond this pandemic.
- EPIDEMIOLOGY
- STATISTICS & RESEARCH METHODS
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/bmjopen-2022-061497

Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
In introductory epidemiology, students learn about prevalence, an easy to understand concept, defined as ‘a proportion that measures disease occurrence of any type of health condition, exposure, or other factor related to health’, 1 or ‘the proportion of persons in a population who have a particular disease or attribute at a specified point in time or over a specified period.’ 2 Prevalence is an important measure for assessing the magnitude of health-related conditions, and studies of prevalence are an important source of information for estimating the burden of disease, injuries and risk factors. 3 Accurate information about prevalence enables health authorities to assess the health needs of a population, to develop prevention programmes and prioritise resources to improve public health. 4 Perhaps, owing to the apparent simplicity of the concept of prevalence, methodological developments to assess the quality of reporting, the potential for bias and the synthesis of prevalence estimates in meta-analysis have been neglected, 5 when compared with the attention paid to methods relevant to evidence from randomised controlled trials and comparative observational studies. 6 7
The COVID-19 pandemic has shown the need for epidemiological studies to describe and understand a new disease quickly but accurately. 8 Studies reporting on prevalence have been an important source of evidence to describe the prevalence of active SARS-CoV-2 infection and antibodies to SARS-CoV-2, the spectrum of SARS-CoV-2-related morbidity and helped to understand factors related to infection and disease to inform national decisions about containment measures. 9–11 Accurate estimates of prevalence of SARS-CoV-2 are crucial because they are used as an input for the estimation of other quantities, such as infection fatality ratios, which can be calculated indirectly using seroprevalence estimates. 12 Assessments of published studies have, however, highlighted methodological issues that affect study design, conduct, analysis, interpretation and reporting. 13–15 In addition, some questions about prevalence need to be addressed through systematic reviews and meta-epidemiological studies. A high proportion of published systematic reviews of prevalence, however, also have flaws in reporting and methodological quality. 5 16 Confidence in the results of systematic reviews is determined by the credibility of the primary studies and the methods used to synthesise them.
The objective of this communication is to highlight key issues about the risk of bias in studies that measure prevalence and about the quality of reporting, using examples about SARS-CoV-2 and COVID-19. We refer to prevalence at the level of a population, and not as a prediction at an individual level. The estimand is, therefore, ‘what proportion of the population is positive’ and not ‘what is the probability this person is positive.’ Although incidence and prevalence are related epidemiologically, we do not discuss incidence in this article because the study designs for measurement of the quantities differ. Bias is a systematic deviation of results or inferences from the underlying (unobserved) true values. 1 The risk of bias is a judgement about the degree to which the methods or findings of a study might underestimate or overestimate the true value in the target population, 7 in this case, the prevalence of a condition or risk factor. Quality of reporting refers to the completeness and transparency of the presentation of a research publication. 17 Risk of bias and quality of reporting are separate, but closely related, because it is only possible to assess the strengths and weaknesses of a study report if the methods and results are described adequately.
Bias in prevalence studies
The two main domains of bias in prevalence studies are those related to the study population (selection bias) and the condition being assessed (information bias) ( figure 1 ). Biases involved in the design, conduct and analysis of a study affect its internal validity. Selection bias also affects external validity, the extent to which findings from a specific study can be generalised to a wider, target population in time and space. There are many names given to different biases, often addressing the same concept. For this communication, we use the names and definitions published in the Dictionary of Epidemiology. 1
- Download figure
- Open in new tab
- Download powerpoint
Potential for selection bias and information bias in prevalence studies. Coloured lines relate to the coloured boxes, showing at which stage of study procedures selection bias (blue line) and information bias (purple line) can occur.
Selection bias
Selection bias relates to the representativeness of the sample used to estimate the prevalence in relation to the target population. The target population is the group of individuals to whom the findings, conclusions or inferences from a study can be generalised. 1 There are two steps in a prevalence study at which selection bias might occur: at the invitation to take part in the study and, among those invited, who takes part ( figure 1 ).
Selection bias in the invitation to take part in the study
The probability of being invited to take part in a study should be the same for every person in the target population. Evaluation of selection bias at this stage should, therefore, account for the complexity of the strategy for identification of participants. For example, if participants are invited from people who have previously agreed to participate in a registry or cohort, each level of invitation that has contributed to the final setting should be judged for the increasing risk of self-selection. Those who are invited to take part might be defined by demographic characteristics, for example, children below 10 years or study setting (eg, hospitalised patients), or a random sample of the general population. The least biased method to select participants in a prevalence study is to sample at random from the target population. For example, the Real-time Assessment of Community Transmission (REACT) Studies to assess the prevalence of the virus, using molecular diagnostic tests (REACT-1) and antibodies (REACT-2), invite random samples of people, stratified by area, from the National Health Service patient list in England. 9 Those invited are close to a truly random sample because almost everyone in England is registered with a general practitioner. In some cases, criteria applied to the selection of a random sample might still result in considerable bias. For example, a seroprevalence study conducted in Spain did not include care home addresses, which could have excluded around 6% of the Spanish older population. 18 Excluding people in care homes facilities might underestimate SARS-CoV-2 seroprevalence in older adults, if their risk of exposure was higher than the average in the general population. 13 Other methods of sampling are at risk of selection bias. For example, asking for volunteers through advertisements are liable to selection bias because not everyone has the same probability of seeing or replying to the advert. For example, the use of social media to invite people to a drive-in test centre to estimate the population prevalence of antibodies to SARS-CoV-2, 19 or online adverts to assess mental health symptoms during the pandemic, excludes those without an internet connection or who do not use social media, such as older people. 20
Selection bias related to who takes part in the study
Non-response bias occurs when people who have been invited, but do not take part in a study differ systematically from those who take part in ways that are associated with the condition of interest. 21 In the REACT-1 study, 22 for example, across four survey rounds, the investigators invited 2.4 million people; 596 000 swabs that were returned had a valid result (25%). The proportion of participants responding was lower in later than in earlier rounds, in men than women and in younger than older age groups. If the sociodemographic characteristics of the target population are known, the observed results could be weighted statistically to represent the overall population but might still be biased by unmeasurable characteristics that drive willingness to take part.
The direction of non-response bias is often not predictable (can result in over-or underestimation of the true prevalence) because information about the motivation to take part in a study, or not, is not usually collected. 13 In a multicentre cross-sectional survey of the prevalence of PCR-determined SARS-CoV-2 in hospitals in England, the authors suggested that different selection biases could have had opposing effects. 23 For example, staff might have volunteered to take part if they were concerned that they might have been exposed to COVID-19. If such people were more likely than unexposed people to be tested, prevalence might be overestimated. Alternatively, workers in lower-paid jobs, without financial support might have been less likely to take part than those at higher grades because of the consequences for themselves or their contacts if found to be infected. If the less-well paid jobs are also associated with a higher risk of exposure to SARS-CoV-2, the prevalence in the study population would be underestimated. Accorsi et al suggest that the risk of non-response bias in seroprevalence studies might be reduced by sampling from established and well-characterised cohorts with high levels of participation, in whom the characteristics of non-respondents are known. 13
As the proportion of invited people that do not take part in a study (non-respondents) increases, the probability of non-response bias might also increase if the topic of the study influences the probability and the composition of the study population. 24 Empirical evidence of bias was found in a systematic review of sexually transmitted Chlamydia trachomatis infection; prevalence surveys with the lowest proportion of respondents found the highest prevalence of infection, suggesting selective participation by those with a high risk of being infected. 25 Whether or not there is a dose–response relationship between the proportion of non-respondents and the likelihood of SARS-CoV-2 infection is unclear. The risks of selection bias at the stages of invitation and participation can be interrelated and might oppose each other. In the REACT-1 study, 22 it is not clear whether the reduction in selection bias through random sampling outweighed the potential for selection bias owing to the high and increasing proportion of non-respondents over time or vice versa.
Information bias
Information bias occurs when there are systematic errors affecting the completeness or accuracy of the measurement of the condition or risk factor of interest. There are different types of information bias.
Misclassification bias
This bias refers to the incorrect classification of a participant as having, or not having, the condition of interest. Misclassification is an important source of measurement bias in prevalence studies because diagnostic tests are imperfect and might not distinguish clearly among those with and without the condition. 26 For diagnostic tests, the predictive values will also be influenced by the prevalence of the condition in the study population. Seroprevalence studies are essential for determining the proportion of a population that has been exposed to SARS-CoV-2 up to a given time point. Detection of antibodies is affected by the test type and manufacturer, sample type such as serum, dried blood spots, saliva, urine or others, 27 28 and the time of sampling after infection. Different diagnostic tests might also be used in participants in the same study population, but adjustment for test performance is not always appropriate because the characteristics derived from studies in which the tests were validated might differ from the study population. 13 Accorsi et al have described in detail this issue and other biases in the ascertainment of SARS-CoV-2 seroprevalence studies. 13 Test accuracy can also change across populations, owing to the inherent characteristics of tests when clinical variability is present, 29 for example, when tests for SARS-CoV-2 detection are applied to people with or without symptoms.
In a new disease, such as COVID-19, diagnostic criteria might not be standardised or might change over time. For example, accurate assessment of the prevalence of persistent asymptomatic SARS-CoV-2 infection requires a complete list of symptoms and follow-up for a sufficiently long duration to ensure that symptoms did not develop later. 15 30 In a prevalence study conducted in a care home in March 2020, patients were asked about typical and non-typical symptoms of COVID-19. However, symptoms such as anosmia or ageusia had not been reported in association with SARS-CoV-2 at that time, so patients with these as isolated symptoms could have been wrongly classified as asymptomatic. 15 31 Poor quality of data collection has also been found in studies estimating the prevalence of mental health problems during the pandemic. 32 The use of non-validated scales, or dichotomisation to define the cases using inappropriate or unclear thresholds, will bias the estimated prevalence of the condition. Misclassification may also occur in calculations of the prevalence of SARS-CoV-2 in contacts of diagnosed cases if not all contacts are tested, and it is assumed that individuals that were not tested were also uninfected. 13
Recall bias
This bias results in misclassification when the condition has been measured through surveys or questionnaires that rely on memory. A study that aimed to describe the characteristics and symptom profile of individuals with SARS-CoV-2 infection in the USA collected information about symptoms before, and for 14 days after, being enrolled in the study. 33 The authors discuss the potential for recall bias when collecting symptoms retrospectively and if different people recollect different symptoms.
Observer bias
This bias occurs when an observer provides a wrong measurement due to lack of training or subjectivity. 21 For example, a study in the USA found variation between 14 universities in the prevalence of clinical and subclinical myocarditis in competitive athletes with SARS-CoV-2 infection. 34 One of the diagnostic tools was cardiac magnetic resonance imaging and authors attributed some of the variability to differences in the protocols and the expertise among assessors. To reduce the risk of observer bias, researchers should aim to use tools that minimise subjectivity and standardise training procedures.
Reporting studies of prevalence
There is no agreed list of preferred items for reporting studies of prevalence. The published article or a preprint are usually the only available record of a study to which most people, other than the investigators themselves, have access. The written report, therefore, needs to contain the information required to understand the possible biases and assess internal and external validity. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement is a widely used guideline, which includes recommendations for cross-sectional studies that examine associations between an exposure and outcome. 35 Table 1 shows selected items from the STROBE statement and recommendations for cross-sectional studies that are particularly relevant to the complete and transparent description of methods for studies of prevalence.
- View inline
Items from the STROBE checklist for cross-sectional studies that are relevant for prevalence studies
First, clear definitions of the target population, study setting and eligibility criteria to select the study population are required (STROBE items 5, 6a). These issues affect assessment of external validity 36 because estimates of prevalence in a specific population and setting are often generalised more widely. 1 14 Second, the denominator used to calculate the prevalence should be clearly stated, with a description of each stage of the study showing the numbers of individuals eligible, included and analysed (STROBE item 13a, b). Accurate reports of the numbers and characteristics of those who take part (responders) or do not take part (non-responders) in the study are needed for the assessment of selection bias, but this information is not always available. 24 37 Poor reporting about the proportion of responders has been described as one of the main limitations of studies in systematic reviews of prevalence. 38 As with reports of studies of any design, the statistical methods applied to provide prevalence estimates, including methods used to address missing data (STROBE item 12c) and to account for the sampling strategy (STROBE item 12d) need to be reported clearly. 35 The setting, location and periods of enrolment and data collection (STROBE item 5) are particularly important for studies of SARS-CoV-2; the stage of the pandemic, preventive measures in place and virus variants in circulation should all be described because these affect the interpretation of estimates of prevalence. Third, it is crucial to provide a clear definition of the condition or risk factor of interest (STROBE item 7) and how it was measured (STROBE item 8), so that the risk of information bias can be assessed. The definition may be straightforward if there are objective criteria for ascertainment. For example, studies of the prevalence of active SARS-CoV-2 infection should report the diagnostic test, manufacturer, sample type and criteria for a positive result. 39 40 For new conditions that have not been fully characterised, such as post-COVID-19 condition, also known as ‘long COVID-19’, reporting of prevalence can be challenging. 41 42 The WHO produced a case definition 43 in October 2021, but this might take time to be adopted widely.
The COVID-19 pandemic has produced an enormous amount of research about a single disease, published over a short time period. 44 45 Authors who have assessed the body of research on COVID-19 have highlighted concerns about the risks of bias in different study designs, including studies of prevalence. 13 44 In systematic reviews of a single topic, the occurrence of asymptomatic SARS-CoV-2 infection, we observed high between-study heterogeneity, serious risks of bias and poor reporting in the measurement of prevalence. 30 Biased results from prevalence studies can have a direct impact at the levels of the individual, community, global health and policy-making. This communication describes concepts about risks of bias and provides examples that authors can apply to the assessment of prevalence for many other conditions. Future research should be conducted to investigate sources of bias in studies of prevalence and empirical evidence of their influence on estimates of prevalence. The development of a tool that can be adapted to assess the risk of bias in studies of prevalence, and an extension to the STROBE reporting guideline, specifically for studies of prevalence, would help to improve the quality of published studies of prevalence in all fields of research beyond this pandemic.
Acknowledgments
We would like to thank Yuly Barón, who created figure 1.
- Rothman KJ ,
- Greenland S ,
- Institute for Health Metrics and Evaluation (IHME)
- GBD 2019 Diseases and Injuries Collaborators
- Hoffmann F ,
- Pieper D , et al
- Davey-Smith G ,
- Higgins JPT ,
- Lipsitch M ,
- Swerdlow DL ,
- Atchison C ,
- Ashby D , et al
- World Health Organization
- Siegler AJ ,
- Sullivan PS ,
- Sanchez T , et al
- Hanage WP ,
- Owusu-Boaitey N , et al
- Accorsi EK ,
- Rumpler E , et al
- Griffith GJ ,
- Morris TT ,
- Tudball MJ , et al
- Meyerowitz EA ,
- Richterman A ,
- Bogoch II , et al
- McKenzie JE ,
- Kirkham J , et al
- Hirst A , et al
- Pérez-Gómez B ,
- Pastor-Barriuso R , et al
- Bendavid E ,
- Mulaney B ,
- Sood N , et al
- Kalimullah NA ,
- Osuagwu UL , et al
- Catalogue of Bias Collaboration
- Chand M , et al
- Groves RM ,
- Peytcheva E
- Redmond SM ,
- Alexander-Kisslig K ,
- Woodhall SC , et al
- Bossuyt PMM , et al
- Kim H-S , et al
- Niedrig M ,
- El Wahed AA , et al
- Leeflang MMG ,
- Bossuyt PMM ,
- Buitrago-Garcia D ,
- Ipekci AM ,
- Heron L , et al
- Kimball A ,
- Hatfield KM ,
- Arons M , et al
- Yousaf AR ,
- Chu V , et al
- Daniels CJ ,
- Greenshields JT , et al
- Vandenbroucke JP ,
- von Elm E ,
- Altman DG , et al
- Baumann L ,
- Egli-Gany D , et al
- Cheng SMS , et al
- Corman VM ,
- Kaiser M , et al
- Whitaker M ,
- Elliott J ,
- Chadeau-Hyam M
- Michelen M ,
- Manoharan L ,
- Elkheir N , et al
- Raynaud M ,
- Louis K , et al
Twitter @dianacarbg, @Geointheworld, @nicolamlow
Contributors DB-G, GS and NL conceptualised the project. DB-G and NL wrote the manuscript. GS and NL provided feedback. GS and NL supervised the research. All authors edited the manuscript and approved the final manuscript.
Funding This work received support from the Swiss government excellence scholarship (grant number 2019.0774), the SSPH+ Global PhD Fellowship Programme in Public Health Sciences of the Swiss School of Public Health, and the Swiss National Science Foundation (project number 176233, and National Research Programme 78 COVID-19, project number 198418).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Open access
- Published: 11 April 2023
Effects of the COVID-19 pandemic on mental health, anxiety, and depression
- Ida Kupcova 1 ,
- Lubos Danisovic 1 ,
- Martin Klein 2 &
- Stefan Harsanyi 1
BMC Psychology volume 11 , Article number: 108 ( 2023 ) Cite this article
7900 Accesses
11 Citations
38 Altmetric
Metrics details
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact. According to the World Health Organization (WHO), anxiety and depression prevalence increased by 25% globally. In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population.
A cross-sectional study using an anonymous online-based 45-question online survey was conducted at Comenius University in Bratislava. The questionnaire comprised five general questions and two assessment tools the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS). The results of the Self-Rating Scales were statistically examined in association with sex, age, and level of education.
A total of 205 anonymous subjects participated in this study, and no responses were excluded. In the study group, 78 (38.05%) participants were male, and 127 (61.69%) were female. A higher tendency to anxiety was exhibited by female participants (p = 0.012) and the age group under 30 years of age (p = 0.042). The level of education has been identified as a significant factor for changes in mental state, as participants with higher levels of education tended to be in a worse mental state (p = 0.006).
Conclusions
Summarizing two years of the COVID-19 pandemic, the mental state of people with higher levels of education tended to feel worse, while females and younger adults felt more anxiety.
Peer Review reports
Introduction
The first mention of the novel coronavirus came in 2019, when this variant was discovered in the city of Wuhan, China, and became the first ever documented coronavirus pandemic [ 1 , 2 , 3 ]. At this time there was only a sliver of fear rising all over the globe. However, in March 2020, after the declaration of a global pandemic by the World Health Organization (WHO), the situation changed dramatically [ 4 ]. Answering this, yet an unknown threat thrust many countries into a psycho-socio-economic whirlwind [ 5 , 6 ]. Various measures taken by governments to control the spread of the virus presented the worldwide population with a series of new challenges to which it had to adjust [ 7 , 8 ]. Lockdowns, closed schools, losing employment or businesses, and rising deaths not only in nursing homes came to be a new reality [ 9 , 10 , 11 ]. Lack of scientific information on the novel coronavirus and its effects on the human body, its fast spread, the absence of effective causal treatment, and the restrictions which harmed people´s social life, financial situation and other areas of everyday life lead to long-term living conditions with increased stress levels and low predictability over which people had little control [ 12 ].
Risks of changes in the mental state of the population came mainly from external risk factors, including prolonged lockdowns, social isolation, inadequate or misinterpreted information, loss of income, and acute relationship with the rising death toll. According to the World Health Organization (WHO), since the outbreak of the COVID-19 pandemic, anxiety and depression prevalence increased by 25% globally [ 13 ]. Unemployment specifically has been proven to be also a predictor of suicidal behavior [ 14 , 15 , 16 , 17 , 18 ]. These risk factors then interact with individual psychological factors leading to psychopathologies such as threat appraisal, attentional bias to threat stimuli over neutral stimuli, avoidance, fear learning, impaired safety learning, impaired fear extinction due to habituation, intolerance of uncertainty, and psychological inflexibility. The threat responses are mediated by the limbic system and insula and mitigated by the pre-frontal cortex, which has also been reported in neuroimaging studies, with reduced insula thickness corresponding to more severe anxiety and amygdala volume correlated to anhedonia as a symptom of depression [ 19 , 20 , 21 , 22 , 23 ]. Speaking in psychological terms, the pandemic disturbed our core belief, that we are safe in our communities, cities, countries, or even the world. The lost sense of agency and confidence regarding our future diminished the sense of worth, identity, and meaningfulness of our lives and eroded security-enhancing relationships [ 24 ].
Slovakia introduced harsh public health measures in the first wave of the pandemic, but relaxed these measures during the summer, accompanied by a failure to develop effective find, test, trace, isolate and support systems. Due to this, the country experienced a steep growth in new COVID-19 cases in September 2020, which lead to the erosion of public´s trust in the government´s management of the situation [ 25 ]. As a means to control the second wave of the pandemic, the Slovak government decided to perform nationwide antigen testing over two weekends in November 2020, which was internationally perceived as a very controversial step, moreover, it failed to prevent further lockdowns [ 26 ]. In addition, there was a sharp rise in the unemployment rate since 2020, which continued until July 2020, when it gradually eased [ 27 ]. Pre-pandemic, every 9th citizen of Slovakia suffered from a mental health disorder, according to National Statistics Office in 2017, the majority being affective and anxiety disorders. A group of authors created a web questionnaire aimed at psychiatrists, psychologists, and their patients after the first wave of the COVID-19 pandemic in Slovakia. The results showed that 86.6% of respondents perceived the pathological effect of the pandemic on their mental status, 54.1% of whom were already treated for affective or anxiety disorders [ 28 ].
In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population. This study aimed to assess the symptoms of anxiety and depression in the general public of Slovakia. After the end of epidemiologic restrictive measures (from March to May 2022), we introduced an anonymous online questionnaire using adapted versions of Zung Self-Rating Anxiety Scale (SAS) and Zung Self-Rating Depression Scale (SDS) [ 29 , 30 ]. We focused on the general public because only a portion of people who experience psychological distress seek professional help. We sought to establish, whether during the pandemic the population showed a tendency to adapt to the situation or whether the anxiety and depression symptoms tended to be present even after months of better epidemiologic situation, vaccine availability, and studies putting its effects under review [ 31 , 32 , 33 , 34 ].
Materials and Methods
This study utilized a voluntary and anonymous online self-administered questionnaire, where the collected data cannot be linked to a specific respondent. This study did not process any personal data. The questionnaire consisted of 45 questions. The first three were open-ended questions about participants’ sex, age (date of birth was not recorded), and education. Followed by 2 questions aimed at mental health and changes in the will to live. Further 20 and 20 questions consisted of the Zung SAS and Zung SDS, respectively. Every question in SAS and SDS is scored from 1 to 4 points on a Likert-style scale. The scoring system is introduced in Fig. 1 . Questions were presented in the Slovak language, with emphasis on maintaining test integrity, so, if possible, literal translations were made from English to Slovak. The questionnaire was created and designed in Google Forms®. Data collection was carried out from March 2022 to May 2022. The study was aimed at the general population of Slovakia in times of difficult epidemiologic and social situations due to the high prevalence and incidence of COVID-19 cases during lockdowns and social distancing measures. Because of the character of this web-based study, the optimal distribution of respondents could not be achieved.
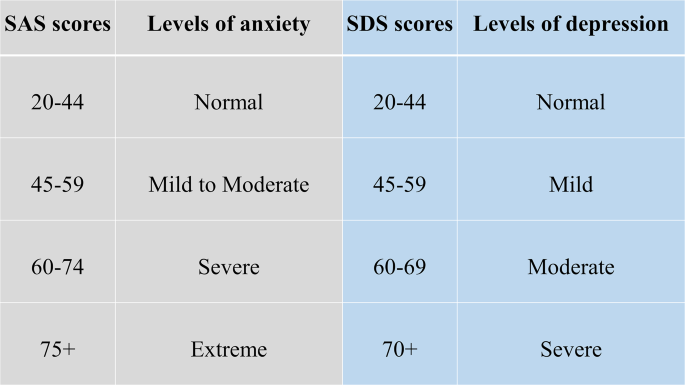
Categories of Zung SAS and SDS scores with clinical interpretation
During the course of this study, 205 respondents answered the anonymous questionnaire in full and were included in the study. All respondents were over 18 years of age. The data was later exported from Google Forms® as an Excel spreadsheet. Coding and analysis were carried out using IBM SPSS Statistics version 26 (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY, USA). Subject groups were created based on sex, age, and education level. First, sex due to differences in emotional expression. Second, age was a risk factor due to perceived stress and fear of the disease. Last, education due to different approaches to information. In these groups four factors were studied: (1) changes in mental state; (2) affected will to live, or frequent thoughts about death; (3) result of SAS; (4) result of SDS. For SAS, no subject in the study group scored anxiety levels of “severe” or “extreme”. Similarly for SDS, no subject depression levels reached “moderate” or “severe”. Pearson’s chi-squared test(χ2) was used to analyze the association between the subject groups and studied factors. The results were considered significant if the p-value was less than 0.05.
Ethical permission was obtained from the local ethics committee (Reference number: ULBGaKG-02/2022). This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines. Due to the anonymous design of the study and by the institutional requirements, written informed consent for participation was not required for this study.
In the study, out of 205 subjects in the study group, 127 (62%) were female and 78 (38%) were male. The average age in the study group was 35.78 years of age (range 19–71 years), with a median of 34 years. In the age group under 30 years of age were 34 (16.6%) subjects, while 162 (79%) were in the range from 31 to 49 and 9 (0.4%) were over 50 years old. 48 (23.4%) participants achieved an education level of lower or higher secondary and 157 (76.6%) finished university or higher. All answers of study participants were included in the study, nothing was excluded.
In Tables 1 and 2 , we can see the distribution of changes in mental state and will to live as stated in the questionnaire. In Table 1 we can see a disproportion in education level and mental state, where participants with higher education tended to feel worse much more than those with lower levels of education. Changes based on sex and age did not show any statistically significant results.
In Table 2 . we can see, that decreased will to live and frequent thoughts about death were only marginally present in the study group, which suggests that coping mechanisms play a huge role in adaptation to such events (e.g. the global pandemic). There is also a possibility that living in times of better epidemiologic situations makes people more likely to forget about the bad past.
Anxiety and depression levels as seen in Tables 3 and 4 were different, where female participants and the age group under 30 years of age tended to feel more anxiety than other groups. No significant changes in depression levels based on sex, age, and education were found.
Compared to the estimated global prevalence of depression in 2017 (3.44%), in 2021 it was approximately 7 times higher (25%) [ 14 ]. Our study did not prove an increase in depression, while anxiety levels and changes in the mental state did prove elevated. No significant changes in depression levels go in hand with the unaffected will to live and infrequent thoughts about death, which were important findings, that did not supplement our primary hypothesis that the fear of death caused by COVID-19 or accompanying infections would enhance personal distress and depression, leading to decreases in studied factors. These results are drawn from our limited sample size and uneven demographic distribution. Suicide ideations rose from 5% pre-pandemic to 10.81% during the pandemic [ 35 ]. In our study, 9.3% of participants experienced thoughts about death and since we did not specifically ask if they thought about suicide, our results only partially correlate with suicidal ideations. However, as these subjects exhibited only moderate levels of anxiety and mild levels of depression, the rise of suicide ideations seems unlikely. The rise in suicidal ideations seemed to be especially true for the general population with no pre-existing psychiatric conditions in the first months of the pandemic [ 36 ]. The policies implemented by countries to contain the pandemic also took a toll on the population´s mental health, as it was reported, that more stringent policies, mainly the social distancing and perceived government´s handling of the pandemic, were related to worse psychological outcomes [ 37 ]. The effects of lockdowns are far-fetched and the increases in mental health challenges, well-being, and quality of life will require a long time to be understood, as Onyeaka et al. conclude [ 10 ]. These effects are not unforeseen, as the global population suffered from life-altering changes in the structure and accessibility of education or healthcare, fluctuations in prices and food insecurity, as well as the inevitable depression of the global economy [ 38 ].
The loneliness associated with enforced social distancing leads to an increase in depression, anxiety, and posttraumatic stress in children in adolescents, with possible long-term sequelae [ 39 ]. The increase in adolescent self-injury was 27.6% during the pandemic [ 40 ]. Similar findings were described in the middle-aged and elderly population, in which both depression and anxiety prevalence rose at the beginning of the pandemic, during the pandemic, with depression persisting later in the pandemic, while the anxiety-related disorders tended to subside [ 41 ]. Medical professionals represented another specific at-risk group, with reported anxiety and depression rates of 24.94% and 24.83% respectively [ 42 ]. The dynamic of psychopathology related to the COVID-19 pandemic is not clear, with studies reporting a return to normal later in 2020, while others describe increased distress later in the pandemic [ 20 , 43 ].
Concerning the general population, authors from Spain reported that lockdowns and COVID-19 were associated with depression and anxiety [ 44 ]. In January 2022 Zhao et al., reported an elevation in hoarding behavior due to fear of COVID-19, while this process was moderated by education and income levels, however, less in the general population if compared to students [ 45 ]. Higher education levels and better access to information could improve persons’ fear of the unknown, however, this fact was not consistent with our expectations in this study, as participants with university education tended to feel worse than participants with lower education. A study on adolescents and their perceived stress in the Czech Republic concluded that girls are more affected by lockdowns. The strongest predictor was loneliness, while having someone to talk to, scored the lowest [ 46 ]. Garbóczy et al. reported elevated perceived stress levels and health anxiety in 1289 Hungarian and international students, also affected by disengagement from home and inadequate coping strategies [ 47 ]. Wathelet et al. conducted a study on French University students confined during the pandemic with alarming results of a high prevalence of mental health issues in the study group [ 48 ]. Our study indicated similar results, as participants in the age group under 30 years of age tended to feel more anxious than others.
In conclusion, we can say that this pandemic changed the lives of many. Many of us, our family members, friends, and colleagues, experienced life-altering events and complicated situations unseen for decades. Our decisions and actions fueled the progress in medicine, while they also continue to impact society on all levels. The long-term effects on adolescents are yet to be seen, while effects of pain, fear, and isolation on the general population are already presenting themselves.
The limitations of this study were numerous and as this was a web-based study, the optimal distribution of respondents could not be achieved, due to the snowball sampling strategy. The main limitation was the small sample size and uneven demographic distribution of respondents, which could impact the representativeness of the studied population and increase the margin of error. Similarly, the limited number of older participants could significantly impact the reported results, as age was an important risk factor and thus an important stressor. The questionnaire omitted the presence of COVID-19-unrelated life-changing events or stressors, and also did not account for any preexisting condition or risk factor that may have affected the outcome of the used assessment scales.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to compliance with institutional guidelines but they are available from the corresponding author (SH) on a reasonable request.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Article PubMed PubMed Central Google Scholar
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Liu Y-C, Kuo R-L, Shih S-R. COVID-19: the first documented coronavirus pandemic in history. Biomed J. 2020;43:328–33.
Advice for the public on COVID-19 – World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . Accessed 13 Nov 2022.
Osterrieder A, Cuman G, Pan-Ngum W, Cheah PK, Cheah P-K, Peerawaranun P, et al. Economic and social impacts of COVID-19 and public health measures: results from an anonymous online survey in Thailand, Malaysia, the UK, Italy and Slovenia. BMJ Open. 2021;11:e046863.
Article PubMed Google Scholar
Mofijur M, Fattah IMR, Alam MA, Islam ABMS, Ong HC, Rahman SMA, et al. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustainable Prod Consum. 2021;26:343–59.
Article Google Scholar
Vlachos J, Hertegård E, Svaleryd B. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A. 2021;118:e2020834118.
Ludvigsson JF, Engerström L, Nordenhäll C, Larsson E, Open Schools. Covid-19, and child and teacher morbidity in Sweden. N Engl J Med. 2021;384:669–71.
Miralles O, Sanchez-Rodriguez D, Marco E, Annweiler C, Baztan A, Betancor É, et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six european countries. Eur Geriatr Med. 2021;12:193–204.
Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: a review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104:368504211019854.
The Lancet null. India under COVID-19 lockdown. Lancet. 2020;395:1315.
Lo Coco G, Gentile A, Bosnar K, Milovanović I, Bianco A, Drid P, et al. A cross-country examination on the fear of COVID-19 and the sense of loneliness during the First Wave of COVID-19 outbreak. Int J Environ Res Public Health. 2021;18:2586.
COVID-19 pandemic. triggers 25% increase in prevalence of anxiety and depression worldwide. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide . Accessed 14 Nov 2022.
Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int J Clin Health Psychol. 2021;21:100196.
Hajek A, Sabat I, Neumann-Böhme S, Schreyögg J, Barros PP, Stargardt T, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the european COvid Survey (ECOS). J Affect Disord. 2022;299:517–24.
Piumatti G, Levati S, Amati R, Crivelli L, Albanese E. Trajectories of depression, anxiety and stress among adults during the COVID-19 pandemic in Southern Switzerland: the Corona Immunitas Ticino cohort study. Public Health. 2022;206:63–9.
Korkmaz H, Güloğlu B. The role of uncertainty tolerance and meaning in life on depression and anxiety throughout Covid-19 pandemic. Pers Indiv Differ. 2021;179:110952.
McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290:113104.
Funkhouser CJ, Klemballa DM, Shankman SA. Using what we know about threat reactivity models to understand mental health during the COVID-19 pandemic. Behav Res Ther. 2022;153:104082.
Landi G, Pakenham KI, Crocetti E, Tossani E, Grandi S. The trajectories of anxiety and depression during the COVID-19 pandemic and the protective role of psychological flexibility: a four-wave longitudinal study. J Affect Disord. 2022;307:69–78.
Holt-Gosselin B, Tozzi L, Ramirez CA, Gotlib IH, Williams LM. Coping strategies, neural structure, and depression and anxiety during the COVID-19 pandemic: a longitudinal study in a naturalistic sample spanning clinical diagnoses and subclinical symptoms. Biol Psychiatry Global Open Sci. 2021;1:261–71.
McCracken LM, Badinlou F, Buhrman M, Brocki KC. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. J Context Behav Sci. 2021;19:28–35.
Talkovsky AM, Norton PJ. Negative affect and intolerance of uncertainty as potential mediators of change in comorbid depression in transdiagnostic CBT for anxiety. J Affect Disord. 2018;236:259–65.
Milman E, Lee SA, Neimeyer RA, Mathis AA, Jobe MC. Modeling pandemic depression and anxiety: the mediational role of core beliefs and meaning making. J Affect Disorders Rep. 2020;2:100023.
Sagan A, Bryndova L, Kowalska-Bobko I, Smatana M, Spranger A, Szerencses V, et al. A reversal of fortune: comparison of health system responses to COVID-19 in the Visegrad group during the early phases of the pandemic. Health Policy. 2022;126:446–55.
Holt E. COVID-19 testing in Slovakia. Lancet Infect Dis. 2021;21:32.
Stalmachova K, Strenitzerova M. Impact of the COVID-19 pandemic on employment in transport and telecommunications sectors. Transp Res Procedia. 2021;55:87–94.
Izakova L, Breznoscakova D, Jandova K, Valkucakova V, Bezakova G, Suvada J. What mental health experts in Slovakia are learning from COVID-19 pandemic? Indian J Psychiatry. 2020;62(Suppl 3):459–66.
Rabinčák M, Tkáčová Ľ, VYUŽÍVANIE PSYCHOMETRICKÝCH KONŠTRUKTOV PRE, HODNOTENIE PORÚCH NÁLADY V OŠETROVATEĽSKEJ PRAXI. Zdravotnícke Listy. 2019;7:7.
Google Scholar
Sekot M, Gürlich R, Maruna P, Páv M, Uhlíková P. Hodnocení úzkosti a deprese u pacientů se zhoubnými nádory trávicího traktu. Čes a slov Psychiat. 2005;101:252–7.
Lipsitch M, Krammer F, Regev-Yochay G, Lustig Y, Balicer RD. SARS-CoV-2 breakthrough infections in vaccinated individuals: measurement, causes and impact. Nat Rev Immunol. 2022;22:57–65.
Accorsi EK, Britton A, Fleming-Dutra KE, Smith ZR, Shang N, Derado G, et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta Variants. JAMA. 2022;327:639–51.
Barda N, Dagan N, Cohen C, Hernán MA, Lipsitch M, Kohane IS, et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. 2021;398:2093–100.
Magen O, Waxman JG, Makov-Assif M, Vered R, Dicker D, Hernán MA, et al. Fourth dose of BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2022;386:1603–14.
Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301:113998.
Kok AAL, Pan K-Y, Rius-Ottenheim N, Jörg F, Eikelenboom M, Horsfall M, et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in dutch case-control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J Affect Disord. 2022;305:85–93.
Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve J-E, et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. The Lancet Public Health. 2022;7:e417–26.
Prochazka J, Scheel T, Pirozek P, Kratochvil T, Civilotti C, Bollo M, et al. Data on work-related consequences of COVID-19 pandemic for employees across Europe. Data Brief. 2020;32:106174.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239e3.
Zetterqvist M, Jonsson LS, Landberg Ã, Svedin CG. A potential increase in adolescent nonsuicidal self-injury during covid-19: a comparison of data from three different time points during 2011–2021. Psychiatry Res. 2021;305:114208.
Mooldijk SS, Dommershuijsen LJ, de Feijter M, Luik AI. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. 2022;149:274–80.
Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110247.
Stephenson E, O’Neill B, Kalia S, Ji C, Crampton N, Butt DA, et al. Effects of COVID-19 pandemic on anxiety and depression in primary care: a retrospective cohort study. J Affect Disord. 2022;303:216–22.
Goldberg X, Castaño-Vinyals G, Espinosa A, Carreras A, Liutsko L, Sicuri E et al. Mental health and COVID-19 in a general population cohort in Spain (COVICAT study).Soc Psychiatry Psychiatr Epidemiol. 2022;:1–12.
Zhao Y, Yu Y, Zhao R, Cai Y, Gao S, Liu Y, et al. Association between fear of COVID-19 and hoarding behavior during the outbreak of the COVID-19 pandemic: the mediating role of mental health status. Front Psychol. 2022;13:996486.
Furstova J, Kascakova N, Sigmundova D, Zidkova R, Tavel P, Badura P. Perceived stress of adolescents during the COVID-19 lockdown: bayesian multilevel modeling of the Czech HBSC lockdown survey. Front Psychol. 2022;13:964313.
Garbóczy S, Szemán-Nagy A, Ahmad MS, Harsányi S, Ocsenás D, Rekenyi V, et al. Health anxiety, perceived stress, and coping styles in the shadow of the COVID-19. BMC Psychol. 2021;9:53.
Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors Associated with Mental Health Disorders among University students in France Confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2025591.
Download references
Acknowledgements
We would like to provide our appreciation and thanks to all the respondents in this study.
This research project received no external funding.
Author information
Authors and affiliations.
Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Ida Kupcova, Lubos Danisovic & Stefan Harsanyi
Institute of Histology and Embryology, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Martin Klein
You can also search for this author in PubMed Google Scholar
Contributions
IK and SH have produced the study design. All authors contributed to the manuscript writing, revising, and editing. LD and MK have done data management and extraction, SH did the data analysis. Drafting and interpretation of the manuscript were made by all authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Stefan Harsanyi .
Ethics declarations
Ethics approval and consent to participate.
Ethical permission was obtained from the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava (Reference number: ULBGaKG-02/2022). The need for informed consent was waived by the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava due to the anonymous design of the study. This study did not process any personal data and the dataset does not contain any direct or indirect identifiers of participants. This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kupcova, I., Danisovic, L., Klein, M. et al. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol 11 , 108 (2023). https://doi.org/10.1186/s40359-023-01130-5
Download citation
Received : 14 November 2022
Accepted : 20 March 2023
Published : 11 April 2023
DOI : https://doi.org/10.1186/s40359-023-01130-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Evidence Review of the Adverse Effects of COVID-19 Vaccination and Intramuscular Vaccine Administration
Vaccines are a public health success story, as they have prevented or lessened the effects of many infectious diseases. To address concerns around potential vaccine injuries, the Health Resources and Services Administration (HRSA) administers the Vaccine Injury Compensation Program (VICP) and the Countermeasures Injury Compensation Program (CICP), which provide compensation to those who assert that they were injured by routine vaccines or medical countermeasures, respectively. The National Academies of Sciences, Engineering, and Medicine have contributed to the scientific basis for VICP compensation decisions for decades.
HRSA asked the National Academies to convene an expert committee to review the epidemiological, clinical, and biological evidence about the relationship between COVID-19 vaccines and specific adverse events, as well as intramuscular administration of vaccines and shoulder injuries. This report outlines the committee findings and conclusions.
Read Full Description
- Digital Resource: Evidence Review of the Adverse Effects of COVID-19 Vaccination
- Digital Resource: Evidence Review of Shoulder Injuries from Intramuscular Administration of Vaccines
- Press Release
Recent News
NAS Launches Science and Innovation Fund for Ukraine
Science Academies Issue Statements to Inform G7 Talks
Supporting Family Caregivers in STEMM
A Vision for High-Quality Preschool for All
- Load More...
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Some gender disparities widened in the U.S. workforce during the pandemic

The COVID-19 recession resulted in a steep but transitory contraction in employment, with greater job losses among women than men. The recovery began in April 2020 and is not complete. As of the third quarter of 2021, the labor force ages 25 and older remains nearly 2 million below its level in the same quarter of 2019.
The pandemic is associated with an increase in some gender disparities in the labor market. Among adults 25 and older who have no education beyond high school, more women have left the labor force than men. Other disparities have stayed the same or even narrowed: The gender pay gap has remained steady, for example, and the difference in the average hours worked by men and women has slightly diminished.
The COVID-19 recession differed from prior recent recessions in that it disproportionately eliminated jobs employing women. Media accounts often referred to it as a “ shecession .” As the economy and labor market have been recovering for more than 21 months, Pew Research Center conducted this analysis to investigate if there are lingering impacts on the labor market opportunities of women.
Labor force estimates and average hours worked are derived from the monthly Current Population Survey (CPS), sponsored jointly by the U.S. Census Bureau and the U.S. Bureau of Labor Statistics. The CPS is the nation’s premier labor force survey and is the basis for the monthly national unemployment rate released on the first Friday of each month. The CPS is based on a sample survey of about 70,000 households . The estimates are not seasonally adjusted.
For a quarter of the sample each month, the CPS also records data on usual hourly earnings for workers paid by the hour and usual weekly earnings and hours worked for other workers.
The CPS microdata files analyzed were provided by the Integrated Public Use Microdata Series (IPUMS) at the University of Minnesota .
The COVID-19 outbreak has affected data collection efforts by the U.S. government in its surveys, especially limiting in-person data collection. This resulted in about an 8 percentage point dec rease in the response rate for the CPS in September 2021. It is possible that some measures of labor market activity and its demographic composition are affected by these changes in data collection.
Overall, the number of women ages 25 and older in the labor force has fallen 1.3% since the third quarter of 2019, similar to the 1.1% decline of men in the labor force.
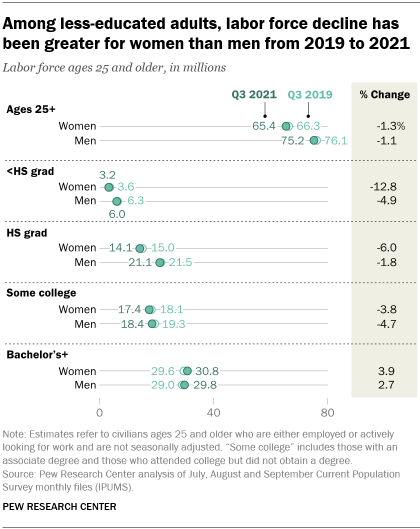
But this modest overall change obscures divergent outcomes for labor force members with different levels of education. Women who have no education beyond high school exited the labor force in greater numbers than similarly educated men. However, the pandemic has not interrupted the long-running gains of women among the college-educated labor force.
From the third quarter of 2019 to the same quarter of 2021, the number of women in the labor force who are not high school graduates decreased 12.8%, dwarfing the 4.9% contraction among comparably educated men. The pandemic also disproportionately affected women with a high school diploma. The ranks of women in the high-school-educated labor force have declined 6.0% since the third quarter of 2019. The labor force of similarly educated men has fallen only 1.8%.
Among the labor force with at least some amount of education beyond high school, women have fared at least as well as men. The number of men and women in the labor force who have some college experience but not a bachelor’s degree has contracted for both groups, with no strong disparities between the two. Both men and women with at least a bachelor’s degree saw positive gains in the labor force (2.7% and 3.9%, respectively) from 2019 to 2021.
What accounts for the larger labor force withdrawals among less-educated women than men during the pandemic? It is complex but there seems to be a consensus that it partly reflects how women are overrepresented in certain health care, food preparation and personal service occupations that were sharply curtailed at the start of the pandemic. Although women overall are more likely than men to be able to work remotely, they are disproportionately employed in occupations that require them to work on-site and in close proximity to others.
It is less clear whether women’s parental roles and limited child care and schooling options have played a large role in forcing them to exit the labor market. The number of mothers and fathers in the labor force has declined in similar fashion over the past two years.
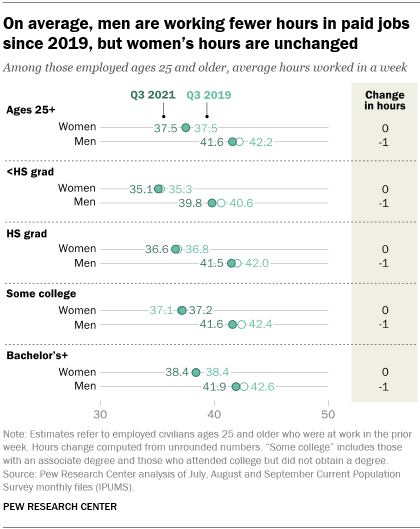
Turning to the number of hours employees work per week, on average, there have been small changes associated with the pandemic and they have occurred among men. In the third quarter of 2021, women ages 25 and older worked 37.5 hours on average in paid employment, unchanged from how much they worked two years earlier. Men ages 25 and older worked 41.6 hours on average in the third quarter of 2021. That is 0.7 fewer hours than they worked pre-pandemic (42.2). So, the disparity in hours of paid employment between women and men workers has somewhat narrowed.
The pandemic is also not associated with a widening of the gender pay gap . Among full- and part-time workers ages 25 and older, women earned 86% of what men earned based on median hourly earnings in the third quarter of 2021. Two years ago, the estimated gender pay gap was 85%.
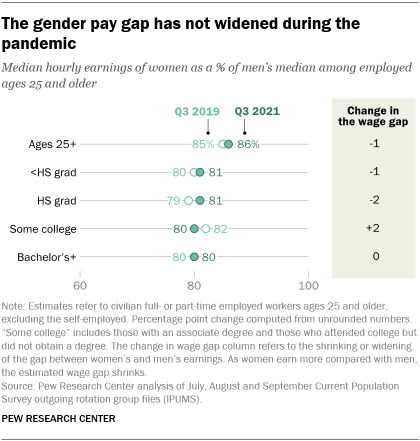
The overall pay gap partly reflects that employed women have higher levels of education than employed men. In 2021, 48% of women workers ages 25 and older had completed at least a bachelor’s degree compared with 40% of men. Workers with at least a bachelor’s degree tend to earn more and thus women’s earnings are boosted by their greater educational attainment. The gender pay gap is greater when you look at groups of women and men with equal levels of education. The gap depends on the education level, but in 2021 women ages 25 and older earned closer to 80 cents on the dollar compared with equally educated men.
- Coronavirus (COVID-19)
- COVID-19 & the Economy
- Economics, Work & Gender
- Gender & Work
- Gender Pay Gap
- Unemployment

How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, mental health and the pandemic: what u.s. surveys have found, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 13 January 2023
Long COVID: major findings, mechanisms and recommendations
- Hannah E. Davis ORCID: orcid.org/0000-0002-1245-2034 1 ,
- Lisa McCorkell ORCID: orcid.org/0000-0002-3261-6737 2 ,
- Julia Moore Vogel ORCID: orcid.org/0000-0002-4902-3540 3 &
- Eric J. Topol ORCID: orcid.org/0000-0002-1478-4729 3
Nature Reviews Microbiology volume 21 , pages 133–146 ( 2023 ) Cite this article
1.36m Accesses
982 Citations
16696 Altmetric
Metrics details
- Research data
- Viral infection
An Author Correction to this article was published on 17 April 2023
This article has been updated
Long COVID is an often debilitating illness that occurs in at least 10% of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections. More than 200 symptoms have been identified with impacts on multiple organ systems. At least 65 million individuals worldwide are estimated to have long COVID, with cases increasing daily. Biomedical research has made substantial progress in identifying various pathophysiological changes and risk factors and in characterizing the illness; further, similarities with other viral-onset illnesses such as myalgic encephalomyelitis/chronic fatigue syndrome and postural orthostatic tachycardia syndrome have laid the groundwork for research in the field. In this Review, we explore the current literature and highlight key findings, the overlap with other conditions, the variable onset of symptoms, long COVID in children and the impact of vaccinations. Although these key findings are critical to understanding long COVID, current diagnostic and treatment options are insufficient, and clinical trials must be prioritized that address leading hypotheses. Additionally, to strengthen long COVID research, future studies must account for biases and SARS-CoV-2 testing issues, build on viral-onset research, be inclusive of marginalized populations and meaningfully engage patients throughout the research process.
Similar content being viewed by others
The long-term health outcomes, pathophysiological mechanisms and multidisciplinary management of long COVID
Jingwei Li, Yun Zhou, … Chengdi Wang

Epidemiology, clinical presentation, pathophysiology, and management of long COVID: an update
Sizhen Su, Yimiao Zhao, … Lin Lu
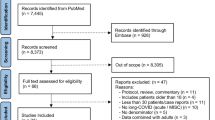
Long-COVID in children and adolescents: a systematic review and meta-analyses
Sandra Lopez-Leon, Talia Wegman-Ostrosky, … Sonia Villapol
Introduction
Long COVID (sometimes referred to as ‘post-acute sequelae of COVID-19’) is a multisystemic condition comprising often severe symptoms that follow a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. At least 65 million individuals around the world have long COVID, based on a conservative estimated incidence of 10% of infected people and more than 651 million documented COVID-19 cases worldwide 1 ; the number is likely much higher due to many undocumented cases. The incidence is estimated at 10–30% of non-hospitalized cases, 50–70% of hospitalized cases 2 , 3 and 10–12% of vaccinated cases 4 , 5 . Long COVID is associated with all ages and acute phase disease severities, with the highest percentage of diagnoses between the ages of 36 and 50 years, and most long COVID cases are in non-hospitalized patients with a mild acute illness 6 , as this population represents the majority of overall COVID-19 cases. There are many research challenges, as outlined in this Review, and many open questions, particularly relating to pathophysiology, effective treatments and risk factors.
Hundreds of biomedical findings have been documented, with many patients experiencing dozens of symptoms across multiple organ systems 7 (Fig. 1 ). Long COVID encompasses multiple adverse outcomes, with common new-onset conditions including cardiovascular, thrombotic and cerebrovascular disease 8 , type 2 diabetes 9 , myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) 10 , 11 and dysautonomia, especially postural orthostatic tachycardia syndrome (POTS) 12 (Fig. 2 ). Symptoms can last for years 13 , and particularly in cases of new-onset ME/CFS and dysautonomia are expected to be lifelong 14 . With significant proportions of individuals with long COVID unable to return to work 7 , the scale of newly disabled individuals is contributing to labour shortages 15 . There are currently no validated effective treatments.
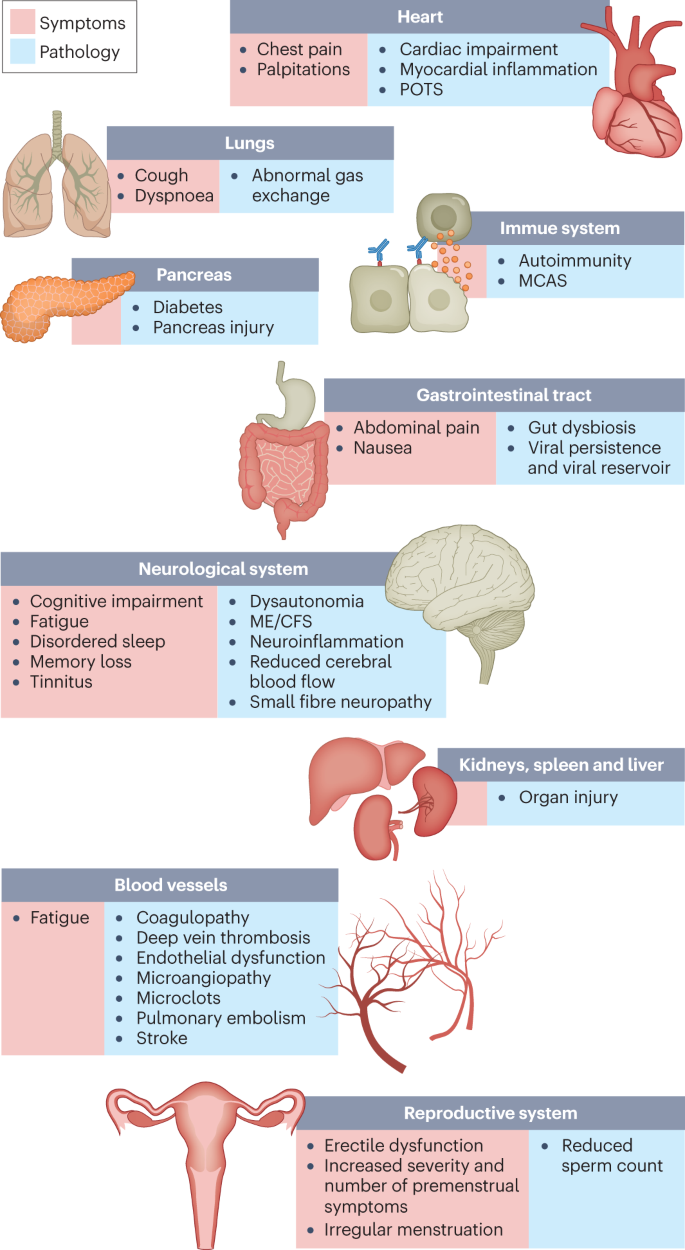
The impacts of long COVID on numerous organs with a wide variety of pathology are shown. The presentation of pathologies is often overlapping, which can exacerbate management challenges. MCAS, mast cell activation syndrome; ME/CFS, myalgic encephalomyelitis/chronic fatigue syndrome; POTS, postural orthostatic tachycardia syndrome.
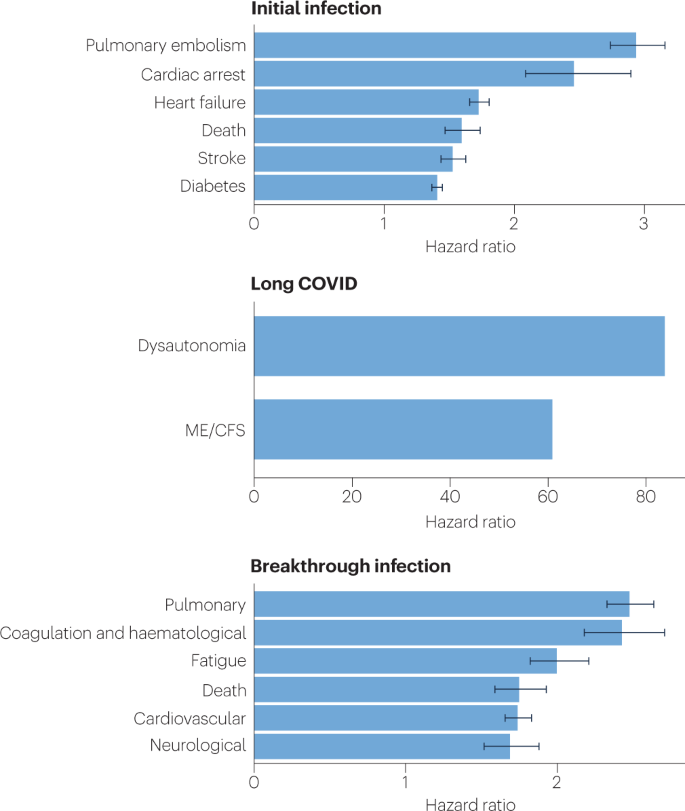
Because diagnosis-specific data on large populations with long COVID are sparse, outcomes from general infections are included and a large proportion of medical conditions are expected to result from long COVID, although the precise proportion cannot be determined. One year after the initial infection, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections increased the risk of cardiac arrest, death, diabetes, heart failure, pulmonary embolism and stroke, as studied with use of US Department of Veterans Affairs databases. Additionally, there is clear increased risk of developing myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia. Six months after breakthrough infection, increased risks were observed for cardiovascular conditions, coagulation and haematological conditions, death, fatigue, neurological conditions and pulmonary conditions in the same cohort. The hazard ratio is the ratio of how often an event occurs in one group relative to another; in this case people who have had COVID-19 compared with those who have not. Data sources are as follows: diabetes 9 , cardiovascular outcomes 8 , dysautonomia 12 , 201 , ME/CFS 10 , 202 and breakthrough infections 4 .
There are likely multiple, potentially overlapping, causes of long COVID. Several hypotheses for its pathogenesis have been suggested, including persisting reservoirs of SARS-CoV-2 in tissues 16 , 17 ; immune dysregulation 17 , 18 , 19 , 20 with or without reactivation of underlying pathogens, including herpesviruses such as Epstein–Barr virus (EBV) and human herpesvirus 6 (HHV-6) among others 17 , 18 , 21 , 22 ; impacts of SARS-CoV-2 on the microbiota, including the virome 17 , 23 , 24 , 25 ; autoimmunity 17 , 26 , 27 , 28 and priming of the immune system from molecular mimicry 17 ; microvascular blood clotting with endothelial dysfunction 17 , 29 , 30 , 31 ; and dysfunctional signalling in the brainstem and/or vagus nerve 17 , 32 (Fig. 3 ). Mechanistic studies are generally at an early stage, and although work that builds on existing research from postviral illnesses such as ME/CFS has advanced some theories, many questions remain and are a priority to address. Risk factors potentially include female sex, type 2 diabetes, EBV reactivation, the presence of specific autoantibodies 27 , connective tissue disorders 33 , attention deficit hyperactivity disorder, chronic urticaria and allergic rhinitis 34 , although a third of people with long COVID have no identified pre-existing conditions 6 . A higher prevalence of long Covid has been reported in certain ethnicities, including people with Hispanic or Latino heritage 35 . Socio-economic risk factors include lower income and an inability to adequately rest in the early weeks after developing COVID-19 (refs. 36 , 37 ). Before the emergence of SARS-CoV-2, multiple viral and bacterial infections were known to cause postinfectious illnesses such as ME/CFS 17 , 38 , and there are indications that long COVID shares their mechanistic and phenotypic characteristics 17 , 39 . Further, dysautonomia has been observed in other postviral illnesses and is frequently observed in long COVID 7 .
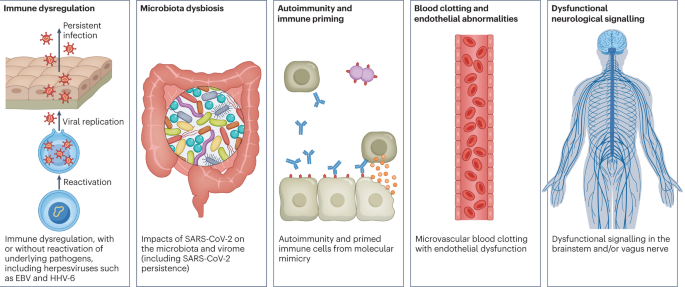
There are several hypothesized mechanisms for long COVID pathogenesis, including immune dysregulation, microbiota disruption, autoimmunity, clotting and endothelial abnormality, and dysfunctional neurological signalling. EBV, Epstein–Barr virus; HHV-6, human herpesvirus 6; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
In this Review, we explore the current knowledge base of long COVID as well as misconceptions surrounding long COVID and areas where additional research is needed. Because most patients with long COVID were not hospitalized for their initial SARS-CoV-2 infection 6 , we focus on research that includes patients with mild acute COVID-19 (meaning not hospitalized and without evidence of respiratory disease). Most of the studies we discuss refer to adults, except for those in Box 1 .
Box 1 Long COVID in children
Long COVID impacts children of all ages. One study found that fatigue, headache, dizziness, dyspnoea, chest pain, dysosmia, dysgeusia, reduced appetite, concentration difficulties, memory issues, mental exhaustion, physical exhaustion and sleep issues were more common in individuals with long COVID aged 15–19 years compared with controls of the same age 203 . A nationwide study in Denmark comparing children with a positive PCR test result with control individuals found that the former had a higher chance of reporting at least one symptom lasting more than 2 months 204 . Similarly to adults with long COVID, children with long COVID experience fatigue, postexertional malaise, cognitive dysfunction, memory loss, headaches, orthostatic intolerance, sleep difficulty and shortness of breath 204 , 205 . Liver injury has been recorded in children who were not hospitalized during acute severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections 206 , and although rare, children who had COVID-19 have increased risks of acute pulmonary embolism, myocarditis and cardiomyopathy, venous thromboembolic events, acute and unspecified renal failure, and type 1 diabetes 207 . Infants born to women who had COVID-19 during pregnancy were more likely to receive a neurodevelopmental diagnosis in the first year after delivery 208 . A paediatric long COVID centre’s experience treating patients suggests that adolescents with a moderate to severe form of long COVID have features consistent with myalgic encephalomyelitis/chronic fatigue syndrome 205 . Children experiencing long COVID have hypometabolism in the brain similar to the patterns found in adults with long COVID 209 . Long-term pulmonary dysfunction is found in children with long COVID and those who have recovered from COVID-19 (ref. 210 ). Children with long COVID were more likely to have had attention deficit hyperactivity disorder, chronic urticaria and allergic rhinitis before being infected 34 .
More research on long COVID in children is needed, although there are difficulties in ensuring a proper control group due to testing issues. Several studies have found that children infected with SARS-CoV-2 are considerably less likely to have a positive PCR test result than adults despite seroconverting weeks later, with up to 90% of cases being missed 189 , 190 . Additionally, children are much less likely to seroconvert and, if they develop antibodies, are more likely to have a waning response months after infection compared with adults 193 .
Major findings
Immunology and virology.
Studies looking at immune dysregulation in individuals with long COVID who had mild acute COVID-19 have found T cell alterations, including exhausted T cells 18 , reduced CD4 + and CD8 + effector memory cell numbers 18 , 19 and elevated PD1 expression on central memory cells, persisting for at least 13 months 19 . Studies have also reported highly activated innate immune cells, a lack of naive T and B cells and elevated expression of type I and type III interferons (interferon-β (IFNβ) and IFNλ1), persisting for at least 8 months 20 . A comprehensive study comparing patients with long COVID with uninfected individuals and infected individuals without long COVID found increases in the numbers of non-classical monocytes, activated B cells, double-negative B cells, and IL-4- and IL-6-secreting CD4 + T cells and decreases in the numbers of conventional dendritic cells and exhausted T cells and low cortisol levels in individuals with long COVID at a median of 14 months after infection 18 . The expansion of cytotoxic T cells has been found to be associated with the gastrointestinal presentation of long COVID 27 . Additional studies have found elevated levels of cytokines, particularly IL-1β, IL-6, TNF and IP10 (refs. 40 , 41 ), and a recent preprint has reported persistent elevation of the level of CCL11, which is associated with cognitive dysfunction 42 . It remains to be seen whether the pattern of cytokines in ME/CFS, where the levels of certain cytokines are elevated in the first 2–3 years of illness but decrease over time without a corresponding decrease in symptoms 43 , is similar in long COVID.
Multiple studies have found elevated levels of autoantibodies in long COVID 27 , including autoantibodies to ACE2 (ref. 28 ) (the receptor for SARS-CoV-2 entry), β 2 -adrenoceptor, muscarinic M2 receptor, angiotensin II AT 1 receptor and the angiotensin 1–7 MAS receptor 26 . High levels of other autoantibodies have been found in some patients with COVID-19 more generally, including autoantibodies that target the tissue (such as connective tissue, extracellular matrix components, vascular endothelium, coagulation factors and platelets), organ systems (including the lung, central nervous system, skin and gastrointestinal tract), immunomodulatory proteins (cytokines, chemokines, complement components and cell-surface proteins) 44 . A major comprehensive study, however, did not find autoantibodies to be a major component of long COVID 18 .
Reactivated viruses, including EBV and HHV-6, have been found in patients with long COVID 18 , 21 , 22 , 27 (and have been identified in ME/CFS 45 ), and lead to mitochondrial fragmentation and severely affect energy metabolism 46 . A recent preprint has reported that EBV reactivation is associated with fatigue and neurocognitive dysfunction in patients with long COVID 22 .
Several studies have shown low or no SARS-CoV-2 antibody production and other insufficient immune responses in the acute stage of COVID-19 to be predictive of long COVID at 6–7 months, in both hospitalized patients and non-hospitalized patients 47 , 48 . These insufficient immune responses include a low baseline level of IgG 48 , low levels of receptor-binding domain and spike-specific memory B cells, low levels of nucleocapsid IgG 49 and low peaks of spike-specific IgG 47 . In a recent preprint, low or absent CD4 + T cell and CD8 + T cell responses were noted in patients with severe long COVID 49 , and a separate study found lower levels of CD8 + T cells expressing CD107a and a decline in nucleocapsid-specific interferon-γ-producing CD8 + T cells in patients with long COVID compared with infected controls without long COVID 50 . High levels of autoantibodies in long COVID have been found to be inversely correlated with protective COVID-19 antibodies, suggesting that patients with high autoantibody levels may be more likely to have breakthrough infections 27 . SARS-CoV-2 viral rebound in the gut, possibly resulting from viral persistence, has also been associated with lower levels and slower production of receptor-binding domain IgA and IgG antibodies 51 . There are major differences in antibody creation, seroreversion and antibody titre levels across the sexes, with women being less likely to seroconvert, being more likely to serorevert and having lower antibody levels overall 52 , 53 , even affecting antibody waning after vaccination 54 .
Several reports have pointed towards possible viral persistence as a driver of long COVID symptoms; viral proteins and/or RNA has been found in the reproductive system, cardiovascular system, brain, muscles, eyes, lymph nodes, appendix, breast tissue, hepatic tissue, lung tissue, plasma, stool and urine 55 , 56 , 57 , 58 , 59 , 60 . In one study, circulating SARS-CoV-2 spike antigen was found in 60% of a cohort of 37 patients with long COVID up to 12 months after diagnosis compared with 0% of 26 SARS-CoV-2-infected individuals, likely implying a reservoir of active virus or components of the virus 16 . Indeed, multiple reports following gastrointestinal biopsies have indicated the presence of virus, suggestive of a persistent reservoir in some patients 58 , 61 .
Vascular issues and organ damage
Although COVID-19 was initially recognized as a respiratory illness, SARS-CoV-2 has capability to damage many organ systems. The damage that has been demonstrated across diverse tissues has predominantly been attributed to immune-mediated response and inflammation, rather than direct infection of cells by the virus. Circulatory system disruption includes endothelial dysfunction and subsequent downstream effects, and increased risks of deep vein thrombosis, pulmonary embolism and bleeding events 29 , 30 , 62 . Microclots detected in both acute COVID-19 and long COVID contribute to thrombosis 63 and are an attractive diagnostic and therapeutic target. Long-term changes to the size and stiffness of blood cells have also been found in long COVID, with the potential to affect oxygen delivery 64 . A long-lasting reduction in vascular density, specifically affecting small capillaries, was found in patients with long COVID compared with controls, 18 months after infection 65 . A study finding elevated levels of vascular transformation blood biomarkers in long COVID also found that the angiogenesis markers ANG1 and P-selectin both had high sensitivity and specificity for predicting long COVID status 66 .
An analysis of the US Department of Veterans Affairs databases (VA data) including more than 150,000 individuals 1 year after SARS-CoV-2 infection indicated a significantly increased risk of a variety of cardiovascular diseases, including heart failure, dysrhythmias and stroke, independent of the severity of initial COVID-19 presentation 8 (Fig. 2 ). Cardiac MRI studies revealed cardiac impairment in 78% of 100 individuals who had a prior COVID-19 episode (investigated an average of 71 days after infection 67 ) and in 58% of participants with long COVID (studied 12 months after infection 68 ), reinforcing the durability of cardiac abnormalities.
Multiple studies have revealed multi-organ damage associated with COVID-19. One prospective study of low-risk individuals, looking at the heart, lungs, liver, kidneys, pancreas and spleen, noted that 70% of 201 patients had damage to at least one organ and 29% had multi-organ damage 69 . In a 1-year follow-up study, conducted by the same research group with 536 participants, the study authors found that 59% had single-organ damage and 27% multi-organ damage 70 . A dedicated kidney study of VA data including more than 89,000 individuals who had COVID-19 noted an increased risk of numerous adverse kidney outcomes 71 . Another VA data analysis, including more than 181,000 individuals who had COVID-19, found that infection also increases the risk of type 2 diabetes 9 (Fig. 2 ). The organ damage experienced by patients with long COVID appears durable, and long-term effects remain unknown.
Neurological and cognitive systems
Neurological and cognitive symptoms are a major feature of long COVID, including sensorimotor symptoms, memory loss, cognitive impairment, paresthesia, dizziness and balance issues, sensitivity to light and noise, loss of (or phantom) smell or taste, and autonomic dysfunction, often impacting activities of daily living 7 , 32 . Audiovestibular manifestations of long COVID include tinnitus, hearing loss and vertigo 7 , 72 .
In a meta-analysis, fatigue was found in 32% and cognitive impairment was found in 22% of patients with COVID-19 at 12 weeks after infection 3 . Cognitive impairments in long COVID are debilitating, at the same magnitude as intoxication at the UK drink driving limit or 10 years of cognitive ageing 73 , and may increase over time, with one study finding occurrence in 16% of patients at 2 months after infection and 26% of patients at 12 months after infection 74 . Activation of the kynurenine pathway, particularly the presence of the metabolites quinolinic acid, 3-hydroxyanthranilic acid and kynurenine, has been identified in long COVID, and is associated with cognitive impairment 74 . Cognitive impairment has also been found in individuals who recovered from COVID-19 (ref. 75 ), and at higher rates when objective versus subjective measures were used 3 , suggesting that a subset of those with cognitive impairment may not recognize and/or report their impairment. Cognitive impairment is a feature that manifests itself independently of mental health conditions such as anxiety and depression 74 , 76 , and occurs at similar rates in hospitalized and non-hospitalized patients 74 , 76 . A report of more than 1.3 million people who had COVID-19 showed mental health conditions such as anxiety and depression returned to normal over time, but increased risks of cognitive impairment (brain fog), seizures, dementia, psychosis and other neurocognitive conditions persisted for at least 2 years 77 .
Possible mechanisms for these neuropathologies include neuroinflammation, damage to blood vessels by coagulopathy and endothelial dysfunction, and injury to neurons 32 . Studies have found Alzheimer disease-like signalling in patients with long COVID 78 , peptides that self-assemble into amyloid clumps which are toxic to neurons 79 , widespread neuroinflammation 80 , brain and brainstem hypometabolism correlated with specific symptoms 81 , 82 and abnormal cerebrospinal fluid findings in non-hospitalized individuals with long COVID along with an association between younger age and a delayed onset of neurological symptoms 83 . Multilineage cellular dysregulation and myelin loss were reported in a recent preprint in patients with long COVID who had mild infections, with microglial reactivity similar to that seen in chemotherapy, known as ‘chemo-brain’ 42 . A study from the UK Biobank, including brain imaging in the same patients before and after COVID-19 as well as control individuals, showed a reduction in grey matter thickness in the orbitofrontal cortex and parahippocampal gyrus (markers of tissue damage in areas connected to the primary olfactory cortex), an overall reduction in brain size and greater cognitive decline in patients after COVID-19 compared with controls, even in non-hospitalized patients. Although that study looked at individuals with COVID-19 compared with controls, not specifically long COVID, it may have an implication for the cognitive component of long COVID 84 . Abnormal levels of mitochondrial proteins as well as SARS-CoV-2 spike and nucleocapsid proteins have been found in the central nervous system 85 . Tetrahydrobiopterin deficiencies and oxidative stress are found in long COVID as well 86 .
In the eyes, corneal small nerve fibre loss and increased dendritic cell density have been found in long COVID 87 , 88 , as well as significantly altered pupillary light responses 89 and impaired retinal microcirculation 90 . SARS-CoV-2 can infect and replicate in retinal 59 and brain 91 organoids. Other manifestations of long COVID include retinal haemorrhages, cotton wool spots and retinal vein occlusion 92 .
Mouse models of mild SARS-CoV-2 infection demonstrated microglial reactivity and elevated levels of CCL11, which is associated with cognitive dysfunction and impaired neurogenesis 42 . Hamster models exhibited an ongoing inflammatory state, involving T cell and myeloid activation, production of pro-inflammatory cytokines and an interferon response that was correlated with anxiety and depression-like behaviours in the hamsters, with similar transcriptional signatures found in the tissue of humans who had recovered from COVID-19 (ref. 93 ). Infected non-human primates with mild illness showed neuroinflammation, neuronal injury and apoptosis, brain microhaemorrhages, and chronic hypoxaemia and brain hypoxia 94 .
Recent reports indicate low blood cortisol levels in patients with long COVID as compared with control individuals, more than 1 year into symptom duration 18 , 27 . Low cortisol production by the adrenal gland should be compensated by an increase in adrenocorticotropic hormone (ACTH) production by the pituitary gland, but this was not the case, supporting hypothalamus–pituitary–adrenal axis dysfunction 18 . This may also reflect an underlying neuroinflammatory process. Low cortisol levels have previously been documented in individuals with ME/CFS.
ME/CFS, dysautonomia and related conditions
ME/CFS is a multisystem neuroimmune illness with onset often following a viral or bacterial infection. Criteria include a “substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities” for at least 6 months, accompanied by a profound fatigue that is not alleviated by rest, along with postexertional malaise, unrefreshing sleep and cognitive impairment or orthostatic intolerance (or both) 95 . Up to 75% of people with ME/CFS cannot work full-time and 25% have severe ME/CFS, which often means they are bed-bound, have extreme sensitivity to sensory input and are dependent on others for care 96 . There is a vast collection of biomedical findings in ME/CFS 97 , 98 , although these are not well known to researchers and clinicians in other fields.
Many researchers have commented on the similarity between ME/CFS and long COVID 99 ; around half of individuals with long COVID are estimated to meet the criteria for ME/CFS 10 , 11 , 29 , 100 , and in studies where the cardinal ME/CFS symptom of postexertional malaise is measured, a majority of individuals with long COVID report experiencing postexertional malaise 7 , 100 . A study of orthostatic stress in individuals with long COVID and individuals with ME/CFS found similar haemodynamic, symptomatic and cognitive abnormalities in both groups compared with healthy individuals 101 . Importantly, it is not surprising that ME/CFS should stem from SARS-CoV-2 infection as 27.1% of SARS-CoV infection survivors in one study met the criteria for ME/CFS diagnosis 4 years after onset 102 . A wide range of pathogens cause ME/CFS onset, including EBV, Coxiella burnetii (which causes Q fever), Ross River virus and West Nile virus 38 .
Consistent abnormal findings in ME/CFS include diminished natural killer cell function, T cell exhaustion and other T cell abnormalities, mitochondrial dysfunction, and vascular and endothelial abnormalities, including deformed red blood cells and reduced blood volume. Other abnormalities include exercise intolerance, impaired oxygen consumption and a reduced anaerobic threshold, and abnormal metabolic profiles, including altered usage of fatty acids and amino acids. Altered neurological functions have also been observed, including neuroinflammation, reduced cerebral blood flow, brainstem abnormalities and elevated ventricular lactate level, as well as abnormal eye and vision findings. Reactivated herpesviruses (including EBV, HHV-6, HHV-7 and human cytomegalovirus) are also associated with ME/CFS 97 , 98 , 103 , 104 .
Many of these findings have been observed in long COVID studies in both adults and children (Box 1 ). Long COVID research has found mitochondrial dysfunction including loss of mitochondrial membrane potential 105 and possible dysfunctional mitochondrial metabolism 106 , altered fatty acid metabolism and dysfunctional mitochondrion-dependent lipid catabolism consistent with mitochondrial dysfunction in exercise intolerance 107 , redox imbalance 108 , and exercise intolerance and impaired oxygen extraction 100 , 109 , 110 . Studies have also found endothelial dysfunction 29 , cerebral blood flow abnormalities and metabolic changes 81 , 111 , 112 , 113 (even in individuals with long COVID whose POTS symptoms abate 114 ), extensive neuroinflammation 42 , 80 , reactivated herpesviruses 18 , 21 , 27 , deformed red blood cells 64 and many findings discussed elsewhere. Microclots and hyperactivated platelets are found not only in individuals with long COVID but also in individuals with ME/CFS 115 .
Dysautonomia, particularly POTS, is commonly comorbid with ME/CFS 116 and also often has a viral onset 117 . POTS is associated with G protein-coupled adrenergic receptor and muscarinic acetylcholine receptor autoantibodies, platelet storage pool deficiency, small fibre neuropathy and other neuropathologies 118 . Both POTS and small fibre neuropathy are commonly found in long COVID 111 , 119 , with one study finding POTS in 67% of a cohort with long COVID 120 .
Mast cell activation syndrome is also commonly comorbid with ME/CFS. The number and severity of mast cell activation syndrome symptoms substantially increased in patients with long COVID compared with pre-COVID and control individuals 121 , with histamine receptor antagonists resulting in improvements in the majority of patients 19 .
Other conditions that are commonly comorbid with ME/CFS include connective tissue disorders including Ehlers–Danlos syndrome and hypermobility, neuro-orthopaedic spinal and skull conditions, and endometriosis 33 , 122 , 123 . Evidence is indicating these conditions may be comorbid with long COVID as well. The overlap of postviral conditions with these conditions should be explored further.
Reproductive system
Impacts on the reproductive system are often reported in long COVID, although little research has been done to document the extent of the impact and sex-specific pathophysiology. Menstrual alterations are more likely to occur in women and people who menstruate with long COVID than in women and people who menstruate with no history of COVID and those who had COVID-19 but not long COVID 124 . Menstruation and the week before menstruation have been identified by patients as triggers for relapses of long COVID symptoms 7 . Declined ovarian reserve and reproductive endocrine disorder have been observed in people with COVID-19 (ref. 125 ), and initial theories suggest that SARS-CoV-2 infection affects ovary hormone production and/or the endometrial response due to the abundance of ACE2 receptors on ovarian and endometrial tissue 126 . Individuals with both COVID-19 and menstrual changes were more likely to experience fatigue, headache, body ache and pain, and shortness of breath than those who did not have menstrual changes, and the most common menstrual changes were irregular menstruation, increased premenstrual symptoms and infrequent menstruation 127 .
Research on ME/CFS shows associations between ME/CFS and premenstrual dysphoric disorder, polycystic ovarian syndrome, menstrual cycle abnormalities, ovarian cysts, early menopause and endometriosis 128 , 129 , 130 . Pregnancy, postpartum changes, perimenopause and menstrual cycle fluctuations affect ME/CFS and influence metabolic and immune system changes 129 . Long COVID research should focus on these relationships to better understand the pathophysiology.
Viral persistence in the penile tissue has been documented, as has an increased risk of erectile dysfunction, likely resulting from endothelial dysfunction 131 . In one study, impairments to sperm count, semen volume, motility, sperm morphology and sperm concentration were reported in individuals with long COVID compared with control individuals, and were correlated with elevated levels of cytokines and the presence of caspase 8, caspase 9 and caspase 3 in seminal fluid 132 .
Respiratory system
Respiratory conditions are a common phenotype in long COVID, and in one study occurred twice as often in COVID-19 survivors as in the general population 2 . Shortness of breath and cough are the most common respiratory symptoms, and persisted for at least 7 months in 40% and 20% of patients with long COVID, respectively 7 . Several imaging studies that included non-hospitalized individuals with long COVID demonstrated pulmonary abnormalities including in air trapping and lung perfusion 133 , 134 . An immunological and proteomic study of patients 3–6 months after infection indicated apoptosis and epithelial damage in the airway but not in blood samples 135 . Further immunological characterization comparing individuals with long COVID with individuals who had recovered from COVID-19 noted a correlation between decreased lung function, systemic inflammation and SARS-CoV-2-specific T cells 136 .
Gastrointestinal system
Long COVID gastrointestinal symptoms include nausea, abdominal pain, loss of appetite, heartburn and constipation 137 . The gut microbiota composition is significantly altered in patients with COVID-19 (ref. 23 ), and gut microbiota dysbiosis is also a key component of ME/CFS 138 . Higher levels of Ruminococcus gnavus and Bacteroides vulgatus and lower levels of Faecalibacterium prausnitzii have been found in people with long COVID compared with non-COVID-19 controls (from before the pandemic), with gut dysbiosis lasting at least 14 months; low levels of butyrate-producing bacteria are strongly correlated with long COVID at 6 months 24 . Persisting respiratory and neurological symptoms are each associated with specific gut pathogens 24 . Additionally, SARS-CoV-2 RNA is present in stool samples of patients with COVID-19 (ref. 139 ), with one study indicating persistence in the faeces of 12.7% of participants 4 months after diagnosis of COVID-19 and in 3.8% of participants at 7 months after diagnosis 61 . Most patients with long COVID symptoms and inflammatory bowel disease 7 months after infection had antigen persistence in the gut mucosa 140 . Higher levels of fungal translocation, from the gut and/or lung epithelium, have been found in the plasma of patients with long COVID compared with those without long COVID or SARS-CoV-2-negative controls, possibly inducing cytokine production 141 . Transferring gut bacteria from patients with long COVID to healthy mice resulted in lost cognitive functioning and impaired lung defences in the mice, who were partially treated with the commensal probiotic bacterium Bifidobacterium longum 25 .
The onset and time course of symptoms differ across individuals and by symptom type. Neurological symptoms often have a delayed onset of weeks to months: among participants with cognitive symptoms, 43% reported a delayed onset of cognitive symptoms at least 1 month after COVID-19, with the delay associated with younger age 83 . Several neurocognitive symptoms worsen over time and tend to persist longer, whereas gastrointestinal and respiratory symptoms are more likely to resolve 7 , 74 , 142 . Additionally, pain in joints, bones, ears, neck and back are more common at 1 year than at 2 months, as is paresthesia, hair loss, blurry vision and swelling of the legs, hands and feet 143 . Parosmia has an average onset of 3 months after the initial infection 144 ; unlike other neurocognitive symptoms, it often decreases over time 143 .
Few people with long COVID demonstrate full recovery, with one study finding that 85% of patients who had symptoms 2 months after the initial infection reported symptoms 1 year after symptom onset 143 . Future prognosis is uncertain, although diagnoses of ME/CFS and dysautonomia are generally lifelong.
Diagnostic tools and treatments
Although diagnostic tools exist for some components of long COVID (for example, tilt table tests for POTS 145 and MRI scans to detect cardiovascular impairment 68 ), diagnostic tools for long COVID are mostly in development, including imaging to detect microclots 63 , corneal microscopy to identify small fibre neuropathy 87 , new fragmentation of QRS complex on electrocardiograms as indicative of cardiac injury 146 and use of hyperpolarized MRI to detect pulmonary gas exchange abnormalities 147 . On the basis of the tests that are offered as standard care, the results for patients with long COVID are often normal; many providers are unaware of the symptom-specific testing and diagnostic recommendations from the ME/CFS community 148 . Early research into biomarkers suggests that levels of extracellular vesicles 85 and/or immune markers indicating high cytotoxicity 149 could be indicative of long COVID. Intriguingly, dogs can identify individuals with long COVID on the basis of sweat samples 150 . Biomarker research in ME/CFS may also be applicable to long COVID, including electrical impedance blood tests, saliva tests, erythrocyte deformation, sex-specific plasma lipid profiles and variables related to isocapnic buffering 151 , 152 , 153 , 154 . The importance of developing and validating biomarkers that can be used for the diagnosis of long COVID cannot be adequately emphasized — they will not only be helpful in establishing the diagnosis but will also be helpful for objectively defining treatment responses.
Although there are currently no broadly effective treatments for long COVID, treatments for certain components have been effective for subsets of populations (Table 1 ). Many strategies for ME/CFS are effective for individuals with long COVID, including pacing 7 , 37 and symptom-specific pharmacological options (for example, β-blockers for POTS, low-dose naltrexone for neuroinflammation 155 and intravenous immunoglobulin for immune dysfunction) and non-pharmacological options (including increasing salt intake for POTS, cognitive pacing for cognitive dysfunction and elimination diets for gastrointestinal symptoms) 96 . Low-dose naltrexone has been used in many diseases, including ME/CFS 155 , and has also shown promise in treating long COVID 156 . H 1 and H 2 antihistamines, often following protocols for mast cell activation syndrome and particularly involving famotidine, are used to alleviate a wide range of symptoms 19 , 157 , although they are not a cure. Another drug, BC007, potentially addresses autoimmunity by neutralizing G protein-coupled receptor autoantibody levels 158 . Anticoagulant regimens are a promising way to address abnormal clotting 159 ; in one study, resolution of symptoms was seen in all 24 patients receiving triple anticoagulant therapy 31 . Apheresis has also shown promise to alleviate long COVID symptoms; it has been theorized to help remove microclots 160 and has been shown to reduce autoantibodies in ME/CFS 161 . However, it is quite expensive, and its benefits are uncertain. Some supplements have shown promise in treating both long COVID and ME/CFS, including coenzyme Q 10 and d -ribose 162 , and may deserve further study.
Of note, exercise is harmful for patients with long COVID who have ME/CFS or postexertional malaise 110 , 163 and should not be used as a treatment 164 , 165 , 166 ; one study of people with long COVID noted that physical activity worsened the condition of 75% of patients, and less than 1% saw improvement 109 .
Pilot studies and case reports have revealed additional treatment options worth exploring. A case report noted resolution of long COVID following treatment with the antiviral Paxlovid 167 , and a study investigating the treatment of acute COVID-19 with Paxlovid showed a 25% reduction in the incidence of long COVID 168 ; Paxlovid should be investigated further for prevention and treatment of long COVID. A small trial of sulodexide in individuals with endothelial dysfunction saw a reduction in symptom severity 169 . Pilot studies of probiotics indicated potential in alleviating gastrointestinal and non-gastrointestinal symptoms 170 , 171 . Two patients with long COVID experienced substantial alleviation of dysautonomia symptoms following stellate ganglion block 172 . An early study noted that Pycnogenol statistically significantly improved physiological measurements (for example, reduction in oxidative stress) and quality of life (indicated by higher Karnofsky Performance Scale Index scores) 173 , 174 , as hypothesized on the basis of success in other clinical studies.
Taken together, the current treatment options are based on small-scale pilot studies in long COVID or what has been effective in other diseases; several additional trials are in progress 175 . There is a wide range of possible treatment options from ME/CFS covering various mechanisms, including improving natural killer cell function, removing autoantibodies, immunosuppressants, antivirals for reactivated herpesviruses, antioxidants, mitochondrial support and mitochondrial energy generation 176 , 177 ; most need to be clinically trialled, which should happen urgently. Many newer treatment options remain underexplored, including anticoagulants and SARS-CoV-2-specific antivirals, and a lack of funding is a significant limitation to robust trials.
Impact of vaccines, variants and reinfections
The impact of vaccination on the incidence of long COVID differs across studies, in part because of differing study methods, time since vaccination and definitions of long COVID. One study indicated no significant difference in the development of long COVID between vaccinated individuals and unvaccinated individuals 178 ; other studies indicate that vaccines provide partial protection, with a reduced risk of long COVID between 15% and 41% 4 , 5 , with long COVID continuing to impact 9% of people with COVID-19.
The different SARS-CoV-2 variants and level of (and time since) vaccination may impact the development of long COVID. The UK’s Office for National Statistics found that long COVID was 50% less common in double-vaccinated participants with Omicron BA.1 than in double-vaccinated participants Delta, but that there was no significant difference between triple-vaccinated participants; it also found long COVID was more common after Omicron BA.2 infection than after BA.1 infection in triple-vaccinated participants, with 9.3% developing long COVID from infection with the BA.2 variant 179 .
The impact of vaccination on long COVID symptoms in people who had already developed long COVID differs among patients, with 16.7% of patients experiencing a relief of symptoms, 21.4% experiencing a worsening of symptoms and the remainder experiencing unchanged symptoms 180 .
Reinfections are increasingly common 181 . The impact of multiple instances of COVID-19, including the rate of long COVID in those who recovered from a first infection but developed long COVID following reinfection, and the impact of reinfection on those with pre-existing long COVID is crucial to understand to inform future policy decisions. Early research shows an increasing risk of long COVID sequelae after the second and third infection, even in double-vaccinated and triple-vaccinated people 182 . Existing literature suggests multiple infections may cause additional harm or susceptibility to the ME/CFS-type presentation 33 , 183 .
There is also early evidence that certain immune responses in people with long COVID, including low levels of protective antibodies and elevated levels of autoantibodies, may suggest an increased susceptibility to reinfection 27 .
Challenges and recommendations
Issues with PCR and antibody testing throughout the pandemic, inaccurate pandemic narratives and widespread lack of postviral knowledge have caused downstream issues and biases in long COVID research and care.
Testing issues
Most patients with COVID-19 from the first waves did not have laboratory-confirmed infection, with PCR tests being difficult to access unless individuals were hospitalized. Only 1–3% of cases to March 2020 were likely detected 184 , and the CDC estimates that only 25% of cases in the USA were reported from February 2020 to September 2021 (ref. 185 ); that percentage has likely decreased with the rise in use of at-home rapid tests.
Although PCR tests are our best tool for detecting SARS-CoV-2 infections, their false negative rates are still high 186 . Further bias is caused by false negative rates being higher in women and adults younger than 40 years 187 , those with a low viral load 188 and children (Box 1 ), with several studies showing 52–90% of cases in children missed by PCR tests 189 , 190 . The high false negative PCR rate results in symptomatic patients with COVID-19, who seek a COVID-19 test but receive a false negative result, being included as a control in many studies. Those who have a positive PCR test result (who are more likely to be included in research) are more likely to be male or have a higher viral load. Additionally, the lack of test accessibility as well as the false negative rates has created a significant barrier to care, as many long COVID clinics require PCR tests for admission.
Similarly, there is a broad misconception that everyone makes and retains SARS-CoV-2 antibodies, and many clinicians and researchers are unaware of the limited utility of antibody tests to determine prior infection. Between 22% and 36% of people infected with SARS-CoV-2 do not seroconvert, and many others lose their antibodies over the first few months, with both non-seroconversion and seroreversion being more likely in women, children and individuals with mild infections 52 , 53 , 191 , 192 , 193 . At 4 and 8 months after infection, 19% and 61% of patients, respectively, who had mild infections and developed antibodies were found to have seroreverted, compared with 2% and 29% of patients, respectively who had severe infections 191 . Still, many clinicians and researchers use antibody tests to include or exclude patients with COVID-19 from control groups.
Furthermore, during periods of test inaccessibility, tests were given on the basis of patients having COVID-19-specific symptoms such as loss of smell and taste, fever, and respiratory symptoms, resulting in a bias towards people with those symptoms.
Misinformation on PCR and antibody tests has resulted in the categorization of patients with long COVID into non-COVID-19 control groups, biasing the research output. Because low or no antibody levels and viral load may be related to long COVID pathophysiology, including a clinically diagnosed cohort will strengthen the research.
Important miscues
The narrative that COVID-19 had only respiratory sequelae led to a delayed realization of the neurological, cardiovascular and other multisystem impacts of COVID-19. Many long COVID clinics and providers still disproportionately focus on respiratory rehabilitation, which results in skewed electronic health record data. Electronic health record data are also more comprehensive for those who were hospitalized with COVID-19 than for those who were in community care, leading to a bias towards the more traditional severe respiratory presentation and less focus on non-hospitalized patients, who tend to have neurological and/or ME/CFS-type presentations.
The narrative that initially mild COVID-19 cases, generally defined as not requiring hospitalization in the acute phase, would not have long-term consequences has also had downstream effects on research. These so-called mild cases that result in long COVID often have an underlying biology different from acute severe cases, but the same types of tests are being used to evaluate patients. This is despite basic tests such as D-dimer, C-reactive protein (CRP) and antinuclear antibody tests and complete blood count being known to often return normal results in patients with long COVID. Tests that return abnormal results in patients with ME/CFS and dysautonomia, such as total immunoglobulin tests, natural killer cell function tests, the tilt table or NASA lean test, the four-point salivary cortisol test, reactivated herpesvirus panels, small fibre neuropathy biopsy, and tests looking for abnormal brain perfusion 96 , should instead be prioritized. Other recurring issues include studies failing to include the full range of symptoms, particularly neurological and reproductive system symptoms, and not asking patients about symptom frequency, severity and disability. Cardinal symptoms such as postexertional malaise are not widely known, and therefore are rarely included in study designs.
Widespread lack of postviral knowledge and misinformation
The widespread lack of knowledge of viral-onset illnesses, especially ME/CFS and dysautonomia, as well as often imperfect coding, prevents these conditions from being identified and documented by clinicians; this means that they are frequently absent from electronic health record data. Further, because ME/CFS and dysautonomia research is not widely known or comprehensively taught in medical schools 194 , long COVID research is often not built on past findings, and tends to repeat old hypotheses. Additionally, long COVID research studies and medical histories tend to document only the risk factors for severe acute COVID-19, which are different from the risk factors for conditions that overlap with long COVID such as ME/CFS and dysautonomia (for example, connective tissue disorders such as Ehlers–Danlos syndrome, prior illnesses such as infectious mononucleosis and mast cell involvement) 33 , 195 , 196 .
Clinicians who are not familiar with ME/CFS and dysautonomia often misdiagnose mental health disorders in patients; four in five patients with POTS receive a diagnosis with a psychiatric or psychological condition before receiving a POTS diagnosis, with only 37% continuing to have the psychiatric or psychological diagnosis once they have received their POTS diagnosis 117 . Researchers who are unfamiliar with ME/CFS and dysautonomia often do not know to use specific validated tools when conducting mental health testing, as anxiety scales often include autonomic symptoms such as tachycardia, and depression scales often include symptoms such as fatigue, both of which overestimate mental health disorder prevalence in these conditions 197 , 198 .
Recommendations
Although research into long COVID has been expansive and has accelerated, the existing research is not enough to improve outcomes for people with long COVID. To ensure an adequate response to the long COVID crisis, we need research that builds on existing knowledge and is inclusive of the patient experience, training and education for the health-care and research workforce, a public communication campaign, and robust policies and funding to support research and care in long COVID.
We need a comprehensive long COVID research agenda that builds on the existing knowledge from ME/CFS, dysautonomia and other viral-onset conditions, including but not limited to brain and brainstem inflammation, appropriate neuroimaging techniques, neuroimmunology, metabolic profiling, impaired endothelial function, mitochondrial fragmentation, antiviral and metabolic phenotypes, hypoperfusion/cerebral blood flow, nanoneedle diagnostic testing, overlaps with connective tissue disorders, autoimmunity and autoantibodies, viral/microbial persistence, intracranial hypertension, hypermobility, craniocervical obstructions, altered T and B cells, metabolomics and proteomics, elevated blood lactate level, herpesvirus reactivations, immune changes in the early versus late postviral years, and changes to the gut microbiota. The mechanisms of and overlaps between long COVID and connective tissue involvement, mast cells and inflammatory conditions such as endometriosis are particularly understudied and should be focused on. Because of the high prevalence of ME/CFS, POTS and other postinfectious illnesses in patients with long COVID, long COVID research should include people who developed ME/CFS and other postinfectious illnesses from a trigger other than SARS-CoV-2 in comparator groups to improve understanding of the onset and pathophysiology of these illnesses 113 . Additionally, there is a known immune exhaustion process that occurs between the second and third year of illness in ME/CFS, with test results for cytokines being different between patients who have been sick for shorter durations (less than 2 years) than for those who have been sick for longer durations 43 . Because of this, studies should implement subanalyses based on the length of time participants have been ill. Because ME/CFS and dysautonomia research is not widely known across the biomedical field, long COVID research should be led by experts from these areas to build on existing research and create new diagnostic and imaging tools.
Robust clinical trials must be a priority moving forward as patients currently have few treatment options. In the absence of validated treatment options, patients and physicians conduct individual experiments, which result in the duplication of efforts without generalizable knowledge and pose undue risks to patients. Robust study design and knowledge sharing must be prioritized by both funding institutions and clinician-researchers.
It is critical that research on long COVID be representative of (or oversample) the populations who had COVID-19 and are developing long COVID at high rates, which is disproportionately people of colour 35 . Medical research has historically under-represented these populations, and over-representation of white and socio-economically privileged patients has been common in long COVID research. Researchers must work within communities of colour, LGBTQ+ communities and low-income communities to build trust and conduct culturally competent studies that will provide insights and treatments for long COVID for marginalized populations.
As a subset of patients will improve over time, and others will have episodic symptoms, care should be taken to incorporate the possibility of alleviation of symptoms into the study design, and care should be taken not to ascribe improvement to a particular cause without proper modelling.
Finally, it is critical that communities of patients with long COVID and associated conditions are meaningfully engaged in long COVID research and clinical trials. The knowledge of those who experience an illness is crucial in identifying proper study design and key research questions and solutions, improving the speed and direction of research.
Training and education of the health-care and research workforce
To prepare the next generation of health-care providers and researchers, medical schools must improve their education on pandemics, viruses and infection-initiated illnesses such as long COVID and ME/CFS, and competency evaluations should include these illnesses. As of 2013, only 6% of medical schools fully cover ME/CFS across the domains of treatment, research and curricula, which has created obstacles to care, accurate diagnosis, research and treatment 194 . To ensure people with long COVID and associated conditions can receive adequate care now, professional societies and government agencies must educate the health-care and research workforce on these illnesses, including the history of and current best practices for ME/CFS to not repeat mistakes of the past, which have worsened patients’ prognoses. The research community has made a misstep in its efforts to treat ME/CFS 199 , and some physicians, poorly educated in the aetiology and pathophysiology of the disorder, still advise patients to pursue harmful interventions such as graded exercise therapy and cognitive behavioural therapy, despite the injury that these interventions cause 200 and the fact that they are explicitly not advised as treatments 163 , 164 , 166 .
Public communications campaign
In addition to providing education on long COVID to the biomedical community, we need a public communications campaign that informs the public about the risks and outcomes of long COVID.
Policies and funding
Finally, we need policies and funding that will sustain long COVID research and enable people with long COVID to receive adequate care and support. For instance, in the USA, the creation of a national institute for complex chronic conditions within the NIH would go a long way in providing a durable funding mechanism and a robust research agenda. Further, we need to create and fund centres of excellence, which would provide inclusive, historically informed and culturally competent care, as well as conduct research and provide medical education to primary care providers. Additionally, research and clinical care do not exist in silos. It is critical to push forward policies that address both the social determinants of health and the social support that is needed for disabled people.
Conclusions
Long COVID is a multisystemic illness encompassing ME/CFS, dysautonomia, impacts on multiple organ systems, and vascular and clotting abnormalities. It has already debilitated millions of individuals worldwide, and that number is continuing to grow. On the basis of more than 2 years of research on long COVID and decades of research on conditions such as ME/CFS, a significant proportion of individuals with long COVID may have lifelong disabilities if no action is taken. Diagnostic and treatment options are currently insufficient, and many clinical trials are urgently needed to rigorously test treatments that address hypothesized underlying biological mechanisms, including viral persistence, neuroinflammation, excessive blood clotting and autoimmunity.
Acknowledgements
We would like to thank the long COVID and associated conditions patient and research community and the entire team at Patient-Led Research Collaborative. E.J.T. was supported by National Center for Advancing Translational Sciences (NCATS) grant UL1TR002550.
Author information
Authors and affiliations.
Patient-Led Research Collaborative, New York, NY, USA
Hannah E. Davis
Patient-Led Research Collaborative, Oakland, CA, USA
Lisa McCorkell
Scripps Research Translational Institute, Scripps Research, La Jolla, CA, USA
Julia Moore Vogel & Eric J. Topol
You can also search for this author in PubMed Google Scholar
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Correspondence to Eric J. Topol .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Reviews Microbiology thanks Akiko Iwasaki, Ziyad Al-Aly and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Davis, H.E., McCorkell, L., Vogel, J.M. et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol 21 , 133–146 (2023). https://doi.org/10.1038/s41579-022-00846-2
Download citation
Accepted : 05 December 2022
Published : 13 January 2023
Issue Date : March 2023
DOI : https://doi.org/10.1038/s41579-022-00846-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Variations in respiratory and functional symptoms at four months after hospitalisation due to covid-19: a cross-sectional study.
- Monika Fagevik Olsén
- Louise Lannefors
- Hanna C. Persson
BMC Pulmonary Medicine (2024)
Post-recovery health domain scores among outpatients by SARS-CoV-2 testing status during the pre-Delta period
- Jennifer P. King
- Jessie R. Chung
- Edward A. Belongia
BMC Infectious Diseases (2024)
Transforming health care systems towards high-performance organizations: qualitative study based on learning from COVID-19 pandemic in the Basque Country (Spain)
- Ane Fullaondo
- Irati Erreguerena
- Esteban de Manuel Keenoy
BMC Health Services Research (2024)
Psychometric properties of the COVID-19 Yorkshire Rehabilitation Scale: Post-Covid-19 syndrome in Iranian elderly population
- Negar Tamadoni
- Afsaneh Bakhtiari
- Hossein-Ali Nikbakht
Evaluation of disease severity and prediction of severe cases in children hospitalized with influenza A (H1N1) infection during the post-COVID-19 era: a multicenter retrospective study
- Hai-Feng Liu
- Xiao-Zhong Hu
- Hong-Min Fu
BMC Pediatrics (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis
- • Fever and cough are the most common symptoms in patients with COVID-19.
- • The most prevalent comorbidities are hypertension and diabetes which are associated with the severity of COVID-19.
- • ARDS and ACI may be the main obstacles to treatment recovery for patients.
- • The case severe rate and mortality is lower than that of SARS and MERS.
Since being first reported in Wuhan, China, in December 8, 2019, the outbreak of the novel coronavirus, now known as COVID-19, has spread globally. Some case studies regarding the characteristics and outcome of patients with COVID-19 have been published recently. We conducted a meta-analysis to evaluate the risk factors of COVID-19.
Medline, SinoMed, EMBASE, and Cochrane Library were searched for clinical and epidemiological studies on confirmed cases of COVID-19.
The incidence of fever, cough, fatigue, and dyspnea symptoms were 85.6 % (95CI 81.3–89.9 %), 65.7 % (95CI 60.1–71.4 %), 42.4 % (95CI 32.2–52.6 %) and 21.4 % (95CI 15.3–27.5 %). The prevalence of diabetes was 7.7 % (95CI 6.1–9.3 %), hypertension was 15.6 % (95CI 12.6–18.6 %), cardiovascular disease was 4.7 % (95CI 3.1–6.2 %), and malignancy was 1.2 % (95CI 0.5–1.8 %). The complications, including ARDS risk, ranged from 5.6–13.2 %, with the pooled estimate of ARDS risk at 9.4 %, ACI at 5.8 % (95CI 0.7–10.8 %), AKI at 2.1 % (95CI 0.6–3.7 %), and shock at 4.7 % (95CI 0.9–8.6 %). The risks of severity and mortality ranged from 12.6 to 23.5% and from 2.0 to 4.4 %, with pooled estimates at 18.0 and 3.2 %, respectively. The percentage of critical cases in diabetes and hypertension was 44.5 % (95CI 27.0–61.9 %) and 41.7 % (95CI 26.4–56.9 %), respectively.
Fever is the most common symptom in patients with COVID-19. The most prevalent comorbidities are hypertension and diabetes which are associated with the severity of COVID-19. ARDS and ACI may be the main obstacles for patients to treatment recovery. The case severe rate and mortality is lower than that of SARS and MERS.
1. Introduction
The ongoing outbreak of the corona virus disease 2019 (COVID-19) infection has posed significant threats to international health and the economy [ [1] , [2] , [3] ]. On 30 January, 2020, the World Health Organization (WHO) declared it to be a Public Health Emergency of International Concern. As of 10 March, 2020, more than 105 countries, 114,253 cases of COVID-19 and 4000 deaths have been reported all over the world, of which the number of confirmed patients in China has gradually decreased, but is increasing rapidly in other countries, especially in Italy, South Korea, and Iran, and there are lots of doctors engaged in combating it [ 4 , 5 ]. The SARS-CoV-2 was first reported in samples of bronchoalveolar lavage fluid from three patients in Wuhan Jinyintan hospital and was confirmed as the cause of COVID-19 on January 24, 2020 [ 6 ]. After deep examining the full-length genome, we found that the virus belongs to the beta-coronavirus 2b lineage in the phylogenetic tree [ 7 ] and is a new human-infecting beta-coronavirus which had previously not been detected in humans or animals. It is named COVID-19 by the WHO and SARS-CoV-2 by the International Committee on Taxonomy of Viruses as it is similar to the coronavirus responsible for severe acute respiratory syndrome (SARS-CoV) [ 8 ]; it shares more than 87.99 % identity sequencing with the Bat SARS-like coronavirus, and it shares more than 80 % identity nucleotide with the original SARS epidemic virus [ [9] , [10] , [11] ]. Coronavirus spike (S) glycoproteins promote entry into cells. They are the main target of antibodies and bind with high affinity to the angiotensin-converting enzyme 2 (ACE2) receptor in humans in a manner similar to SARS-CoV [ [12] , [13] , [14] ]. However, the SARS-CoV-2 S glycoprotein harbors a furin cleavage site at the boundary between the S1/S2 subunits, which is processed during biogenesis and sets this virus apart from SARS-CoV and SARS-related CoVs [ 15 , 16 ]. At present, research reports that the incubation period in most people range from 1 to 14 days with a median of 5–6 days, but the incubation period may even be as long as 24 days [ 17 ]. The reproductive number (R0) for SARS-CoV-2, although still preliminary, is estimated between 2 and 3, suggesting a higher pandemic potential than SARS [ 18 ]. Fever or cough may be the major symptom, but asymptomatic individuals have also been identified as potential sources of infection [ 19 ]. At present, we think that the new coronavirus is mainly transmitted through respiratory droplets and close contact, but transmission from an asymptomatic carrier appears to be possible [ 20 ]. A report of 9 pregnant patients suggests that perinatal transmission is unlikely but larger studies are needed to confirm this finding [ 21 ]. Although viral RNA is found in stool, whether it can be transmitted through the fecal-oral route still needs to be confirmed by subsequent investigations [ 22 , 23 ]. Recently, some patients were found to be re-positive after being treated with negative nucleic acid tests twice and symptoms disappeared. It is difficult for us to decrease the severity of COVID-19 owing to the complex structure and unclear physiological mechanism. With the increasing number of confirmed cases, the clinical investigation of patients and antiviral treatment solution has been insufficient, and there is an urgent need to find alternative methods to control the spread of disease. In order to prove more accurate conclusions on the prevalence of comorbidity and relation of clinical characteristics and mortality of patients with COVID-19, we searched the relevant literatures and carried out single arm meta-analysis to describe epidemiological, clinical characteristics, complications, and outcomes of patients confirmed to have 2019-nCoV infection, and to compare the severity between diabetes or hypertension and non-diabetes or non-hypertension patients. Our findings provide vital guidance for current clinical work on the prevention and treatment of 2019-nCoV infection.
Ethical approval or patient consent was not required because the present study was a review of previously published articles.
2.1. Search strategy and study selection criteria
A computerized search spanning January1, 1980 to March 10, 2020 was conducted in Medline, Sino Med, EMBASE, and Cochrane Library databases. The following search terms were used in all possible combinations: ("Corona Virus Disease-2019 "[Mesh] OR “2019 novel coronavirus "[Mesh] OR" SARS-CoV-2 "[Mesh] OR "COVID-19 "[Mesh] OR" 2019-nCoV "[Mesh] The search was limited to human subjects. There was no language limitation. The titles and abstracts of potentially relevant studies identified by the computerized search were reviewed. Full-text articles were obtained for detailed evaluation, and eligible studies were included in the systematic review. The inclusion criteria were the following: randomized controlled trial, clinical trials, and series cases; patients who were of either sex and had been diagnosed with COVID-19; all patients with laboratory-identified SARS-CoV-2 infection who had had both real-time reverse-transcriptase polymerase-chain-reaction detection of SARS-CoV-2 nucleic acid positive in throat swabs or lower respiratory tract, and CT scanning of the lung; inclusion of the epidemiological, clinical characteristics, laboratory and radiological characteristics, and treatment and outcome; clear description of the clinical characteristics such as comorbidities including hypertension, diabetes, cardiovascular disease, and malignancy and the signs and symptoms such as fever, cough, fatigue, and dyspnea; clear description of the outcomes including the major complications such as acute respiratory distress syndrome (ARDS), acute cardiac injury(ACI), acute kidney injury(AKI), shock, and incidence of severity and mortality.
The exclusion criteria were the following: absence of clinical characteristics, treatment outcome, clinical experience, and case reports.
2.2. Data collection and extraction
Two authors independently extracted data by reviewing all titles and abstracts of the searched papers. If any disagreement on the choice of the literature exists, a third evaluator will join in to make the decision. The following information was recorded from the included trials: first author, year of publication, number of participants, and residence of patients. Basic data about gender, age, and diagnosis were extracted and analyzed. To evaluate the proportion of comorbidity such as diabetes, hypertension, cardiovascular disease, and malignancy, the proportion of symptoms such as fever, cough, fatigue, and dyspnea, the proportion of clinical complications including ARDS, ACI, AKI, and shock, and the severity and mortality.
2.3. Quality assessment and risk of bias
Two readers independently extracted and reviewed the data from the enrolled studies to ensure consistency. The quality of the included studies was assessed by the Newcastle–Ottawa Scale. In order to objectively evaluate the publication bias of the included studies, the Egger test with P < 0.05 as the existence of publication bias was performed, and those with larger values were considered as having no publication bias.
2.4. Statistical methods
The single arm meta-analysis of proportions (and 95 %CI) was calculated for the clinical symptoms, complication, outcome, and for each of the selected comorbidities using STATA 15.0. The presence of heterogeneity among the identified studies (Cochran’s Q) and the extent of heterogeneity (I 2 index) were examined, as described previously. All original data included in the literature were first transformed by double arcsine method to make them conform to normal distribution and then analyzed in Stata. The initial conclusion obtained by Meta-analysis was then restored using formula (P=(sin(tp/2)) 2) to reach final conclusion.
2.5. Sensitivity analyses
We performed sensitivity analysis to assess the stability of the results and investigate the influence of each study by omitting a single study sequentially. Using the Egger test, we found no evidence of bias in any of the lag periods.
3.1. Included trial characteristics and quality assessment
The initial 1057 citations were identified based on a study of the subject and a summary of the literature, of which 694 articles were thereafter excluded because of duplication. After reviewing the title and abstract of the remaining 81 studies, only 34 full-text studies were evaluated for further assessment, and 13 obviously irrelevant records were excluded. Eventually, 21 clinical studies [ 6 , 17 , [24] , [25] , [26] , [27] , [28] , [29] , [30] , [31] , [32] , [33] , [34] , [35] , [36] , [37] , [38] , [39] , [40] , [41] , [42] ] were consistent with the inclusion requirements. A detailed study flow-diagram is shown in Fig. 1 . The basic characteristics and quality of the included studies were illustrated in Table 1 .

Flow diagram for selection of studies for inclusion in this meta-analysis.
Main characteristics and quality of the included studies.
3.2. Details of the trial process
Twenty-one studies were selected, with a total of 47,344 patients (24,419 male and 22,925 females), representing approximately 40 % of the WHO confirmed. One clinical trial investigated the characteristics of patients in Singapore and all others came from China, mainly in Wuhan. Systematic analysis of the studies describing the epidemiological, demographic, and clinical features of COVID-19 cases and reporting of the prevalence of a number of chronic diseases in the infectious disease was undertaken. The number of cases in the selected studies varied by approximately 3722-fold and ranged from 12 to 44,672 cases. The sex ratio (male to female) was 1.06 and the overall average age of the subjects was greater than 40 years. Forty-one cases reported in Jinyintan hospital are the earliest confirmed cases, patients treated in Wenzhou hospital almost are mild, but Xiaobo Yang et al. reported 52 cases with COVID-19 that were all critical patients. All studies detailed the pre-treatment biochemical characteristics and subsequent treatment.
3.3. Meta-analysis results
Eighteen studies reported the comorbidity of diabetes, only 7 of them introduced the proportion of severity, 14 studies reported hypertension and 6 of them introduced the proportion of severity, 13 studies reported malignant, and 12 studies reported CAD; with regard to symptoms, 20 studies recorded fever and cough, 12 studies reported fatigue and 15 studies reported dyspnea. Seven studies recorded the complication of ARDS and ACI, and shock was recorded in 4 and 5 studies respectively. Fifteen studies showed critical patients, and 12 research reported mortality. All studies provided incidence data of at least one kind of comorbidity, symptom, or complication. Sixteen forest plots were used to illustrate the prevalence of comorbidities in COVID-19 from the selected studies and to inspect the heterogeneity of the individual findings. Meta-analysis of the identified studies showed that the most prevalent clinical symptoms were fever 85.6 % (95CI 81.3–89.9 %) and cough 65.7 % (95CI 60.1–71.4 %), followed by fatigue 42.4 % (95CI 32.2–52.6 %) and shortness of breath 21.4 % (95CI 15.3–27.5 %) ( Fig. 2 ). There was significant heterogeneity (Cochran’s Q) in the estimates of clinical symptoms among the examined studies (p < 0.001) with an I 2 index varying from 87.4 % to 95.1 %. The prevalence of diabetes and hypertension comorbidities was 7.7 % (95CI 6.1–9.3 %) and 15.6 % (95CI 12.6–18.6 %), respectively. The incidence of cardiovascular disease and malignancy was 4.7 % (95CI 3.1–6.2 %) and 1.2 % (95CI 0.5–1.8 %), respectively ( Fig. 3 ). The case complications including ARDS risk ranged from 5.6 to 13.2 %, with the pooled estimate at 9.4 %. Acute cardiac injury 5.8 % (95CI 0.7–10.8 %), Acute kidney injury 2.1 % (95CI 0.6–3.7 %), and shock 4.7 % (95CI 0.9–8.6 %) were also present ( Fig. 4 ). The risks of severity and mortality rate ranged from 12.6 to 23.5 % and from 2.0 to 4.4 %, with pooled estimates at 18.0 and 3.2 %, respectively. The percentage of severe cases in diabetes and hypertension cases was 44.5 % (95CI 27.0–61.9 %) and 41.7 % (95CI 26.4–56.9 %), respectively ( Fig. 5 ).

Forest plot of the prevalence of symptoms in patients with COVID-19. Weights were calculated from binary random-effects model analysis. (a. fever. b. cough. c. fatigue. d. dyspnea). CI = confidence interval, COVID-19=Corona Virus Disease 2019.

Meta-analysis of the proportion of comorbidities in COVID-19 cases. Weights were calculated from binary random-effects model analysis. Values represent proportions of diabetes (a), hypertension (b), CAD (c), and malignancy (d). CAD = coronary artery disease, COVID-19=Corona Virus Disease 2019.

Forest plot of the incidence of complications in patients with COVID-19. (a. ARDS. b. ACI. c. AKI. d. shock), CI = confidence interval. ARDS = acute respiratory distress syndrome, ACI = acute cardiac injury, AKI = acute kidney injury, COVID-19=Corona Virus Disease 2019.

Forest plot of the incidence of severity and mortality in patients with COVID-19. (a. severe rate. b. mortality), meta-analysis of the severe rate of COVID-19 patients with diabetes (c), or hypertension (d). CI = confidence interval, COVID-19=Corona Virus Disease 2019.
3.4. Sensitivity analysis and publication bias
Sensitivity analysis was performed to assess the stability of pooled results. Among the 21 studies, the significant results were not obviously altered after sequentially omitting each study. In the pooled results, comparing the incidence of mortality after excluding the report by Chaolin Huang et al., the heterogeneity decreased significantly (OR = 0.719, 95 % CI = 0.277–1.865, P = 0.497, I² = 28 %) and showed that there was no significant difference in preventing the ARDS rate between the two groups; hence, it was regarded as a result of heterogeneity. Likewise, the other studies were considered as the source of heterogeneity because the heterogeneity significantly changed and showed that there was no significant difference in preventing ARDS between the two groups when each of these studies were excluded from the pooled results comparing the incidence of ARDS. A sensitivity analysis was conducted to determine whether the exclusion of this study would alter the result, and exclusion of this study from the meta-analysis did not substantially influence the results.
In this part of the study, ARDS was used to assess publication bias. Egger test results showed Pr > jzj = 1.00. Therefore, we believe that the risk of publication bias is low in this meta-analysis.
4. Discussion
4.1. summary of the main results.
The outbreak of COVID-19 has been declared a Public Health Emergency of International Concern by WHO. By March 10, 2020, the epidemic had spread to 25 countries around the world. In accordance with the experience of China, surgical masks are in widespread use which is beneficial to prevent the acquisition of COVID-19. In addition, Italy started taking measures to block traffic and lockdown villages. With the rising incidence of COVID-19 all over the world, feasible and effective messaging about the clinical characteristics of COVID-19 is greatly needed. Therefore, the focus of this analysis was to evaluate the prevalence of symptoms, comorbidity, complications, and different outcomes in China and Singapore. The meta-analysis identified 21 published studies that assessed this proportion. There are few published RCTs because of the rapid development of the epidemic and there are limited medical resources in addition to the presence of uncontrollable risk during treatment. Much of the evidence of effects cannot be adequately studied in randomized trials, such as long-term and rare outcomes. Therefore, we analyzed all retrospective studies in this study. For the main results, we found that the cases reported to date suggest that most are older adults, and there is no difference in susceptibility between male and female. Fever is the most common symptom in patients with 2019-nCoV infection. The most prevalent comorbidities are hypertension and diabetes which are associated with the rapid development of severe illness. ARDS and ACI may be the main obstacles for patients to treatment recovery. The severity and mortality of patients with 2019-nCoV infection is lower than that of Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), but the prevalence of COVID-19 is much higher than SARS and the MERS.
4.2. Comparison with previous studies
Two coronaviruses have previously caused significant outbreaks associated with more critical disease: the SARS coronavirus in 2002–2003 and the Middle East respiratory syndrome coronavirus that emerged in 2012 [ [43] , [44] , [45] ]. A lot of studies have reported the clinical characteristics of patients with COVID-19, but there is a lack of studies on the relation of severity and mortality with comorbidity. Similarly, there is no meta-analysis published on complications for patients COVID-19 infected. Therefore, this is a novel systematic review and meta-analysis. Due to the inadequate evidence, we present this meta-analysis by consolidating multiple studies to enable enhanced clinical decision making in the future. We report here a cohort of patients with laboratory-confirmed 2019-nCoV infection. Patients had serious, sometimes fatal, complications and were admitted to the designated hospital. Clinical presentations greatly resemble SARS-CoV. Patients with severe illness developed ARDS, AKI, ACI, or shock and required ICU admission and oxygen therapy.
4.3. Limitations of the study
However, despite a comprehensive analysis, there are also many limitations that should be taken into consideration in our meta-analysis. First, the studies included in the meta-analysis were not all RCTs. Second, in the literature-included studies, the treatment of every hospital is not completely similar. Third, owing to the treatment by grading of mild, ordinary, and critical, the severity of patients in different hospitals varies greatly. In addition, as the cause and physio pathological mechanism was unknown at the onset of emerging infections, the treatment in Wuhan was only based on clinical experience, leading to a higher complication and mortality. Fourth, partial missing information in a few articles may lead to biased results. We have attempted to contact investigators or study sponsors to verify key study characteristics and obtain missing numerical outcome data. Moreover, clinical and methodological heterogeneities were observed in several parameters in the meta-analysis given the variation in intervention techniques, patient composition, and preferences among different cities. True heterogeneity and poor methodological quality could also lead to an asymmetric plot. In the future, larger, higher quality clinical trials should be conducted, and we will conduct a more detailed subgroup analysis to explore the sources of heterogeneity to obtain a more reliable conclusion and more effort should be made to answer these questions in future studies.
5. Conclusion
COVID-19 is an emerging infectious disease of global public health concern. Our results note the similarity of clinical symptoms and complications between COVID-19 and previous beta-coronavirus infections. The incidence of severity and mortality of COVID-19 is much higher than that of ordinary influenza, and the prevalence of chronic diseases including diabetes and hypertension is rising as populations age and lifestyle and dietary habits change. In addition, we found that diabetes and hypertension are closely related to severity and mortality. Improving the protection against COVID-19 in persons with chronic disorders is essential. Last, but not least, there is a need to limit human-to-human transmission, including reducing secondary infections among close contacts and health-care workers, thus preventing transmission amplification events and preventing further international spread.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.

IMAGES
COMMENTS
Overall, this paper introduces new methods for analysing COVID-19 prevalence and mortality on a country-by-country and worldwide basis and chronicles the natural history of COVID-19 during 2020. On a global scale, we reveal broad trends in case and death counts as well as mortality trajectories, which present a coherent picture of the changing ...
The spread of the "Severe Acute Respiratory Coronavirus 2" (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [].The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [], causing massive economic strain ...
2.1. Basic statistics. COVID‐19 has currently spread to 181 countries and most national authorities have failed to keep its rapid spread contained. 13 WHO reports that it began in Wuhan city, located in Hubei province of China, first reported on 21st January. 14 COVID‐19 categorizes in three distinctions concerning it is infected host's severity of disease. 15, 16 To date, the statistics ...
Abstract. In early December 2019, an outbreak of coronavirus disease 2019 (COVID-19), caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), occurred in Wuhan City, Hubei Province, China. On January 30, 2020 the World Health Organization declared the outbreak as a Public Health Emergency of International Concern.
During 2020, the United States documented more COVID-19 cases and deaths than any other country in the world 1.The first US COVID-19 case was identified in Washington state on 20 January 2020 2 ...
Abstract. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a zoonotic infection, is responsible for COVID-19 pandemic and also is known as a public health concern. However, so far, the origin of the causative virus and its intermediate hosts is yet to be fully determined. SARS-CoV-2 contains nearly 30,000 letters of RNA that ...
Research Paper | Volume 29, 100630, December 2020. Download Full Issue. Download started. Ok. PDF [1 MB] PDF [1 MB] Figures. Figure Viewer; Download Figures (PPT) ... Socio-demographic heterogeneity in the prevalence of COVID-19 during lockdown is associated with ethnicity and household size: results from an observational cohort study ...
COVID-19 has already had a staggering impact on the world up to the beginning of the omicron (B.1.1.529) wave, with over 40% of the global population infected at least once by Nov 14, 2021. The vast differences in cumulative proportion of the population infected across locations could help policy makers identify the transmission-prevention strategies that have been most effective, as well as ...
Abstract. Population-based prevalence surveys of Covid-19 contribute to establish the burden of infection, the role of asymptomatic and mild infections in transmission, and allow more precise decisions about reopen policies. We performed a systematic review to evaluate qualitative aspects of these studies, assessing their reliability and ...
The COVID-19 Infection Survey Group of the COVID-19 Genomics UK (COG-UK) Consortium was supported by funding from the Medical Research Council part of UK Research & Innovation, the National ...
Our work shows that 45% of COVID-19 survivors, regardless of hospitalisation status, were experiencing a range of unresolved symptoms at ∼ 4 months. Current understanding is limited by heterogeneous study design, follow-up durations, and measurement methods. Definition of subtypes of Long Covid is unclear, subsequently hampering effective treatment/management strategies.
Introduction. The impact of SARS-CoV-2 on global public health and economies has been profound.1 As of 14 October 2021, there were 239 007 759 million cases of confirmed covid-19 and 4 871 841 million deaths with covid-19 worldwide.2 A variety of containment and mitigation strategies have been adopted to adequately respond to covid-19, with the intention of deferring major surges of patients ...
The Johns Hopkins Coronavirus Resource Center has collected, verified, and published local, regional, national and international pandemic data since it launched in March 2020. From the beginning, the information has been freely available to all — researchers, institutions, the media, the public, and policymakers. As a result, the CRC and its data have been cited in many published research ...
Introduction. SARS-CoV-2 infection was first reported in 2019, and has since spread throughout the world causing more than 208,470,375 COVID-19 cases and 4,377,979 deaths globally, as of August 18, 2021 [].Indonesia confirmed the first positive COVID-19 case on March 2, 2020 [].Within 40 days, COVID-19 cases were reported by all provinces [].As of August, 2021, Indonesia had 3,892,479 ...
COVID-19 can involve persistence, sequelae, and other medical complications that last weeks to months after initial recovery. This systematic review and meta-analysis aims to identify studies ...
Download MP3. In the final Coronapod of 2020, we dive into the scientific literature to reflect on the COVID-19 pandemic. Researchers have discovered so much about SARS-CoV-2 - information that ...
The novel coronavirus (COVID-19) that was first reported at the end of 2019 has impacted almost every aspect of life as we know it. This paper focuses on the incidence of the disease in Italy and Spain—two of the first and most affected European countries. Using two simple mathematical epidemiological models—the Susceptible-Infectious-Recovered model and the log-linear regression model, we ...
The WHO Covid-19 Research Database is a resource created in response to the Public Health Emergency of International Concern (PHEIC). Its content remains searchable and spans the time period March 2020 to June 2023. Since June 2023, manual updates to the database have been discontinued. The WHO evidence retrieval sub-group has begun ...
The COVID-19 pandemic has produced an enormous amount of research about a single disease, published over a short time period.44 45 Authors who have assessed the body of research on COVID-19 have highlighted concerns about the risks of bias in different study designs, including studies of prevalence.13 44 In systematic reviews of a single topic ...
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact.
WASHINGTON — A new report from the National Academies of Sciences, Engineering, and Medicine reviews evidence for 19 potential harms of the COVID-19 vaccines, and for nine potential shoulder injuries from intramuscular administration of vaccines more broadly. The committee that conducted the review identified sufficient evidence to draw 20 conclusions about whether these vaccines could cause ...
This analysis explores U.S. high school students' self-reported mental health challenges during the COVID-19 pandemic. It expands on Pew Research Center surveys that have explored U.S. adults' mental health difficulties during this time. Not all of the survey questions asked specifically about mental health during the pandemic.
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022. Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this ...
The Pfizer and Moderna COVID-19 vaccines can cause myocarditis, but do not appear to cause infertility, Guillain-Barré syndrome, Bell's palsy, thrombosis with thrombocytopenia syndrome (TTS) or heart attack, according to a new National Academies of Sciences, Engineering, and Medicine report examining whether COVID-19 vaccines can cause certain harms.
Some of the main new themes that were detected in faculty interviews during the Fall 2020 semester and which reflect faculty perceptions are represented as follow: COVID-19 impact on student and faculty motivation, COVID-19 impacts on labs and experiential learning, COVID-19 impact on mental health, COVID-19 impact on STEM students' involvement ...
The full impact of the pandemic has been much greater than what is indicated by reported deaths due to COVID-19 alone. Strengthening death registration systems around the world, long understood to be crucial to global public health strategy, is necessary for improved monitoring of this pandemic and future pandemics. In addition, further research is warranted to help distinguish the proportion ...
In a setting where most cases of COVID-19 were ascertained and followed, ... Research paper | Volume 12, 100193, July 2021. Download Full Issue. Download started. Ok. PDF [1 MB ... The UK Office for National Statistics has surveyed over 8000 people who tested positive for COVID-19 and reported that 21% were symptomatic at 5 weeks post-infection ...
The COVID-19 recession differed from prior recent recessions in that it disproportionately eliminated jobs employing women. Media accounts often referred to it as a "shecession."As the economy and labor market have been recovering for more than 21 months, Pew Research Center conducted this analysis to investigate if there are lingering impacts on the labor market opportunities of women.
Long COVID is an often debilitating illness that occurs in at least 10% of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections. More than 200 symptoms have been identified with ...
A lot of studies have reported the clinical characteristics of patients with COVID-19, but there is a lack of studies on the relation of severity and mortality with comorbidity. Similarly, there is no meta-analysis published on complications for patients COVID-19 infected. Therefore, this is a novel systematic review and meta-analysis.