81 Impressive Free Presentation Backgrounds for Outstanding Presentations
- Share on Facebook
- Share on Twitter
By Lyudmil Enchev
in Freebies
4 years ago
Viewed 57,321 times
Spread the word about this article:
Update: May 19, 2022
A collection of free presentation backgrounds for any topic.
Nowadays, presentations need to look modern and eye-catchy in order to keep the audience’s attention from beginning to end. Believe it or not, the visual factor plays a huge role in engaging your viewers. In this collection of free presentation backgrounds , we’ve gathered high-quality graphics – ready to import into your PowerPoint, Google Slides, or Keynote presentations and resize according to your needs.
In this article you will find: Free Business Presentation Backgrounds Free Minimalist & Geometric Presentation Backgrounds Colorful Gradients & Artistic Free Presentation Backgrounds Free Technology Presentation Backgrounds Free Liquid Presentation Backgrounds Free Cute Presentation Backgrounds Free Vintage Presentation Backgrounds Free Paper Presentation Backgrounds Free Holiday Presentation Backgrounds Bonus Backgrounds
Do you want to check out The Best Presentation Software Options on The Market ?

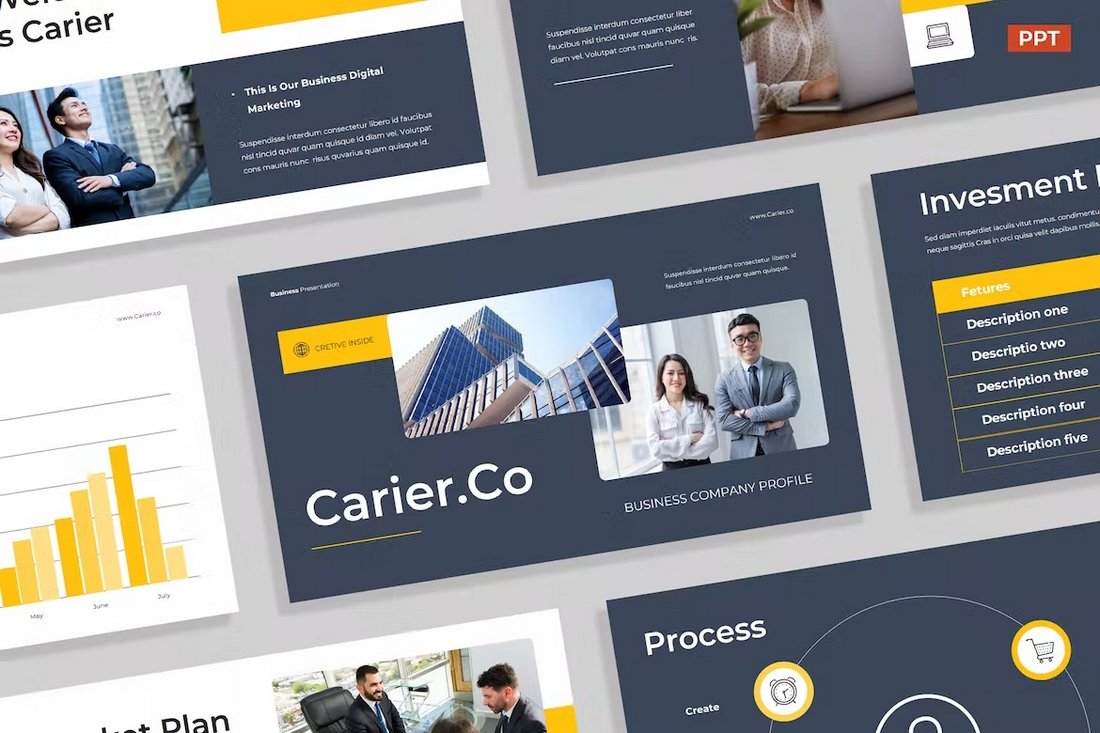
Free Business Presentation Backgrounds
Business presentation backgrounds are slightly different than other types of backgrounds. Unlike more casual presentations, business presentations usually consist of a business-related stock photo – office space, formally dressed people, whiteboards, etc. Take a look at the backgrounds we’ve collected for your company presentation:

1. Blurred Office Interior Background
Blurred light photographs are great for business presentations where they can fit in any slide.

2. Light Corporate Interior Background
This blurred hallway interior image can ideally match a professional presentation.

3. Person Writing on Laptop Background
Workstation backgrounds complete your idea if they don’t distract. In this case, the person working on a laptop is positioned in the corner of the frame.

4. Modern Business Building Background
This background might be an amazing first slide. But even if used somewhere else, it will still do a great job, unless used in all slides.

5. Business Handshake Network Creation Background
An amazing background for corporate presentations that is perfect for teamwork, business communication, partners, or proposals slides.

6. Businessman in Office Modern Skyscraper Landscape Background
This background, although made as a photograph, can actually help you achieve the formal vibe you are looking for.
Free Minimalist & Geometric Presentation Backgrounds
Suitable for literally any kind of presentation, these minimalist presentation background designs come with attractive geometric shapes and pleasant color combinations. The graphics are highly modern right now, so your presentation will certainly impress with good taste and professionalism. The resources are also available in fully editable and resizable vector file formats.
7. Modern Geometric Background
Shapes are very pleasant for the eye. This background uses very “soft” colors, making it quite feminine and good-looking.

8. Black and White Geometry Background
Playing with black and white backgrounds is the best way to proceed if you want to accent the text. This one looks stylish and modern, and it will add a premium feel to your slides.

9. Simple Dark Geometry Background
Using two dominant colors in one background is a great combination. It shows great power and even a bit of provocation.

10. Fresh Squares and Circles Background
Utilizing different shapes and a few variants of blue is a good mix. A non-intrusive design for presentations.

11. Abstract Blue Lines Background
This abstract blue lines background fits the standard business practices of non-aggressive design.

12. Colorful Memphis Style Background
This Memphis-style background shines with its combination of minimalistic design combined with shapes all around the place.

13. Cool Modern Colors Background
If you had to pick one image to explain the term “technology”, that would probably be it.
14. Trendy Outline Shapes Background
A casual style background with simple shapes with playful colors plus trendy black strokes.

15. Neon Modern Shapes Background
Abstract geometry definitely has its place under the sun and is becoming a hot trend – your younger audience will love it!

16. Colorful Geometry Shapes Background
This colorful background is an amazing option for presentation design that aims to get more creative.
17. Modern Lines and Dots Background
This background with blue/purple colors and linear shapes is perfect for more creative presentations.
18. Minimalist Shapes Background with Pastel Gradients
The minimalist signature is easily recognizable and the use of pastel gradients “softens” the shapes.

19. Simplistic White-Grey Background
Light, neutral background with dots and lines that can be used in any presentation.
20. 4 Simple Style Backgrounds
Four simple backgrounds can be used for any purpose. You will find an orange, purple, red, and cyan background for your presentations.
21. Seamless Patterns Mega Bundle with 15 Free Geometric Pattern Backgrounds
A huge pattern designs bundle with over 1000 premium. Still, you have 15 free seamless patterns that you can use as backgrounds to lit up your presentations.
Colorful Gradients & Artistic Free Presentation Backgrounds
The delicate play with colors is very important when it comes to presentation background – it should be easy on the eyes and feel… right. This collection is everything you need if you are looking for a vibrant, colorful background for your presentation. Free gradient presentation backgrounds, watercolor backgrounds, and more artistic suggestions for your colorful slides.

22. Blue Tone Gradient Background
Gradient backgrounds make flat colors look more vibrant. The blue tones are quite relaxing and trustworthy.

23. 4 Artistic Texture Backgrounds
Textures can be attention-grabbing. Picking such background can create a more professional feeling.
24. Nice Warm Colors Gradient Background
Warm colors are typically better for cheerful presentations, as they “uplift” the mood.

25. Cool Cold Colors Gradient Background
If you have to come up with a presentation related to a marine topic, that’s your perfect choice.

26. Modern Blue Gradient Background
Blue and purple are two solid colors. Using this background gradient is perfect for business presentations.

27. Energetic Orange Gradient Background
A clean background with a vivid orange color gradient. Perfect for different energetic presentations.

28. Colorful Rainbow Gradient Background
Using a rainbow gradient is an amazing option for presentations dedicated to kids, or teenage audience.

29. Elegant Blury Bokeh Background
Stolen from photographers, the “bokeh” effect background makes presentations stand out.
You may also be interested in The Best Color Combinations to Try Now
Free Technology Presentation Backgrounds
Presentation background designs suitable for technology and business presentations. These backgrounds look high-tech and modern but still won’t steal away the attention of the viewer. Available in vector file formats which makes them fully editable and resizeable depending on your presentation style and dimensions.

30. Modern Technology Background
This high-tech background design is perfect for innovation and digital presentations.

31. Abstract Modern Tech Background
Abstract design with modern simple squares – an amazing option for high-tech presentations.

32. Abstract Futuristic Background with Honeycomb
This abstract and futuristic dark background is perfectly suitable for technical presentations.

33. Futuristic Technology Interface Background
Great technology background with minimalist, clean design that will fit any high-tech presentation.
Free Liquid Presentation Backgrounds
A selection of free presentation backgrounds with liquids and bubbles. Flat or 3D, these backgrounds are super immersive and certainly impressive. They will be the perfect addition to a wide array of presentation topics. You can get them completely for free as fully editable and resizable vector file formats .

34. Blue Liquid Background
The combination of dark blue and light blue is an amazing option for a presentation. An amazing option, especially for financial services.
35. Yellow Liquid Background
These cheeky shapes and colors are an amazing way to present something that can be qualified as everything but boring. Great for uprising sales, or summer theme for example.

36. Purple Liquid Background
Purple is a royal color and combined with a liquid design background it becomes even better for a modern-day classy presentation.

37. Monochrome Liquid Background
A perfect blend between using 3D forms and gradient colors. The blur effect and reflections are also attributed to the exquisite look of this background.
38. Modern Blue-Green Liquid Background
It’s an interesting, yet impressive background design. You can definitely stand out with this modern, blue-green liquid background.

39. Watercolor Background with White Blue and Purple
This background, in particular, doesn’t have a practical use in business presentations but it fits perfectly in artistic ones.

40. Liquid Shapes Monochrome Background
You’ll rarely come across a better realistic 3D background for medical presentations.

41. Modern Dark Liquid Background
Compared to a couple of the previous backgrounds, this dark liquid background is pretty standard and it can fit multiple presentation themes.
Free Cute Presentation Backgrounds
Cute backgrounds are often used for educational projects – especially when presenting in front of kids. Smile-bringing designs will always win you emotional points, and it’s always a good idea to have a themed background or two just in case.

42. Cute Animal Background
In this background, you can find cute 2D animals all around the frame. At the same time, the central part is filled with white space, so you can add text there.

43. Colorful Pastel Color Pattern Background
These beautiful rounded shapes add the feeling of watercolor art and we can definitely catch the pattern design.

44. Space Rocket Child Background
If you’re about to teach a science class – that might be perfect. Well, unless you have university students.

45. Blue Pastel Sky and Clouds Background
It’s a simple blue background with white clouds. It can be used as a theme for a whole educational presentation.

46. Cute Doodle Frame Background
This beautiful cute doodles frame is also matched with a rainbow border vector and free text space in the center.
47. Green Park Illustration Landscape Background
There is nothing more suitable for educational presentation than a simple landscape illustration with trees, clouds and sun.
Free Vintage Presentation Backgrounds
Retro and vintage looks are quite modern right now, so no wonder people are choosing vintage looks for their presentations, as well. In this selection of free presentation backgrounds, you will find ornamental backgrounds, grudge backgrounds, worn-out materials, old paper effects, antique looks, damasks, etc. All are free to download in vector file formats – fully editable and scalable.
48. Ornamental Vintage Floral Background
Vintage backgrounds, especially floral are a very strong point if you’re coming with flower-related topics.
49. Vintage Frame Background
Frames are typically used in photography, so go for it if you have lots of pictures in your presentations.
50. Damask Pattern Vintage Background
Damask pattern is a specific vintage style which will not only look good, but also grab attention by being unique.
51. Grunge Texture Background
This grunge background focuses on the main picture, so it’s great for quizzes or presentations where there is one central topic.

52. Retro Grunge Texture Background
If you have a presentation related to Ancient times (especially Egypt), that’s your background.
53. Vintage Shapes Pattern Background
These vintage shapes are quite peculiar but you can use them for boring topics to give “life”.
54. Grunge Hearts Background
Another cool background design is the grunge hearts. It can be used for many presentations.
55. Old Paper Antique Texture Background
Old Paper can perfectly fit any slide related to the Middle centuries.
56. Blue Grunge Background
Another amazing grunge background that can be the greatest companion of any history-related presentation.

57. Vintage Paper Retro Background
Vintage paper can be an amazing background for any presentation for hand-made products.
Free Paper Presentation Backgrounds
Paper and cardboard textures give presentations a homey and hand-made feel. In this selection of free presentation backgrounds, you will see different paper textures. Adaptable for any presentation theme, these designs can be downloaded in vector file formats and edited in vector-based software.
58. White Paper Texture Background
Paper texture can be great for teachers who want a neutral background.
59. Package Paper Background
Package paper is great for presentations related to delivery services.

60. Simple White Paper Background
A simple white paper background that can fit any need.
61. Brown Paper Background
Another great background for delivery services presentations.

62. Paper Note Memphis Style Background
The combination of blank space and surrounding in Memphis Style makes this colorful background perfect to give a modern look to your presentation.
Free Holiday Presentation Backgrounds
Holiday backgrounds should not be used every day but they can be powerful triggers. Holiday presentations spark emotions which can be a good way to convey your message during festive periods. Let’s see some of the best free holiday backgrounds you can use for the occasion.

63. Christmas Decoration Photo Background
A marvelous Christmas concept background where you can add text on the left part of the slide and the Christmas elements are on the right.

64. White Simple Christmas Background
If you’re into texture and white backgrounds, this free Christmas photo is for you.

65. Cartoon Snowy Christmas Vector Background
This free vector background gives you the chance to edit details or add some more Christmas decorations.

66. Cute Christmas Background with Illustrations
The Christmas decorations are placed at the top and bottom of the background, so you have free space right in the middle.

67. Halloween Spider Web Background
A great combination of orange (the color associated with Hallowen) and spider web makes this vector background very straight to the point.

68. Flat Hallowen Vector Background With House
A flat illustration background with Halloween’s color palette and some standard “scary” motives.

69. Easter Egg Photo Frame Background
You can easily “catch” the Easter topic with the dyed eggs and the basket. The M&Ms are also an original idea to add flat shapes.

70. Watercolor Light Easter Vector Background
Watercolor Easter backgrounds look natural and beautiful. They can be a great addition to any Easter-related presentation.

71. Beautiful Landscape Thanksgiving Autumn Illustration Background
This illustration has the color palette of autumn which is also associated with Thanksgiving day.
72. Hand Drawn Thanksgiving Illustration Background
In the hand drawn thanksgiving illustration we can find the typical colors of autumn, plus the pumpkin and, of course, the Thanksgiving turkey.

73. Watercolor Thanksgiving Background
Watercolor art is very distinctive and for the “Thanksgiving” topic, it can create some beautiful results.

74. Thanksgiving Decoration Photo Background
The combination of a white background with green and brown leaves, plus pines and pumpkins enriches the image and adds contrast.
Bonus Presentation Backgrounds
A collection of high-resolution photos that impress with super high quality. These images show attention to detail but are still humble enough to keep the audience focused on your content. Attribution for using these images is not required, although it’s appreciated.

75. Clean Package Boxes Background
It’s a lovely background that is good for Christmas topics or any gift-related presentations.

76. Elegant Decoration Background Image
If you’re looking for a background for your wedding agency, you’re in the right place.

77. Pencils and Office Items Background
The elements in the background suggest you it is a perfect match for teachers and lecturers.

78. Simple Clean Background with a Book
Books are symbol of liberty and education. The background is great for science presentations.

79. Bridge Landscape Photography Background
Golden Gate bridge stands tall. So is the background which can be used for all kinds of presentations.

80. Sunset Background Image
Sunsets are proven to be stress-relieving, making this background suitable for meditation business presentations.

81. Monochrome Landscape Background
Skyscrapers, shady pinks, and overall – the perfect cosmetics presentation.
That’s it!
We hope this collection of free presentation backgrounds was useful to you. We hope it helps you make your next presentation super impressive and successful. If you’d like to see even more freebies, go ahead and have a look at these awesome suggestions:
- 39 Free Google Slides Templates For Your Next Presentation
- The Best Free PowerPoint Templates to Download in 2022
- How to Start and End a Presentation: 10 Practical Tips to Grab Attention

Add some character to your visuals
Cartoon Characters, Design Bundles, Illustrations, Backgrounds and more...
Like us on Facebook
Subscribe to our newsletter
Be the first to know what’s new in the world of graphic design and illustrations.
- [email protected]
Browse High Quality Vector Graphics
E.g.: businessman, lion, girl…
Related Articles
100+ adorable free baby cartoon vectors, clipart, and illustrations, 20 snackable cartoon flyer templates that can be grabbed for free, 99+ free responsive html email templates to grab in 2022, great free animal clipart for your next cartoon design, 60 free medical background resources with modern design, complete your designs with graphicmama’s design bundles:, enjoyed this article.
Don’t forget to share!
- Comments (0)

Lyudmil Enchev
Lyudmil is an avid movie fan which influences his passion for video editing. You will often see him making animations and video tutorials for GraphicMama. Lyudmil is also passionate for photography, video making, and writing scripts.

Thousands of vector graphics for your projects.
Complete your designs with GraphicMama's Design Bundles:
Hey you made it all the way to the bottom.
Here are some other articles we think you may like:

150+ Free Pattern Designs: Seamless & Fully Editable
by Lyudmil Enchev

Free Vectors
Free medical infographic maker by graphicmama.
by Al Boicheva

Free Facebook Cover Templates: 6 Sources to Check Out
by Iveta Pavlova
Looking for Design Bundles or Cartoon Characters?
A source of high-quality vector graphics offering a huge variety of premade character designs, graphic design bundles, Adobe Character Animator puppets, and more.
We use essential cookies to make Venngage work. By clicking “Accept All Cookies”, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts.
Manage Cookies
Cookies and similar technologies collect certain information about how you’re using our website. Some of them are essential, and without them you wouldn’t be able to use Venngage. But others are optional, and you get to choose whether we use them or not.
Strictly Necessary Cookies
These cookies are always on, as they’re essential for making Venngage work, and making it safe. Without these cookies, services you’ve asked for can’t be provided.
Show cookie providers
- Google Login
Functionality Cookies
These cookies help us provide enhanced functionality and personalisation, and remember your settings. They may be set by us or by third party providers.
Performance Cookies
These cookies help us analyze how many people are using Venngage, where they come from and how they're using it. If you opt out of these cookies, we can’t get feedback to make Venngage better for you and all our users.
- Google Analytics
Targeting Cookies
These cookies are set by our advertising partners to track your activity and show you relevant Venngage ads on other sites as you browse the internet.
- Google Tag Manager
- Infographics
- Daily Infographics
- Template Lists
- Graphic Design
- Graphs and Charts
- Data Visualization
- Human Resources
- Beginner Guides
Blog Business
25+ Business Background Images, Templates and Design Tips
By Jennifer Gaskin , Sep 27, 2022

There’s a time and place for a blank white background in your business communications. But if you’re trying to create an eye-catching presentation or even just a fun background for your Zoom meetings, at some point, you’ll need a supply of business background images.
If today’s that day, you’ve come to the right place!
Keep reading for a roundup of business background images you can quickly and easily apply to a whole host of content — from business cards to LinkedIn backgrounds, PowerPoints and more.
Click to jump ahead:
Business card background images, business linkedin background images, zoom business background images, powerpoint business background images, business presentation background images, professional business background images, business photo background images, design tips for business backgrounds.
Business cards might be small, but their impact can be major. A cool business card background can help you stand out in the minds of new connections.
Since most business cards contain very little content, the image can really be the star of the show, like in the following examples:
Real estate business background image

This image would be ideal for a business card for professionals in real estate, retail, architecture or construction. Be sure to think about the content you’ll place on the card.
In the case of the business card below, the designer chose to place the smallest type that appears on the image on a shaded box, which helps it pop against the darker parts of the photo.

Just so you know, some of our templates are free to use and some require a small monthly fee. Sign up is always free, as is access to Venngage’s online drag-and-drop editor.
Corporate business background image

Consider this business card background image if you’re working in a corporate environment (or want to be). If your firm is in the finance, real estate or legal industries, this image would be especially appropriate.
Create drama by cutting off part of the image, as this business card does, or use the full image, depending on your content.

Illustrated business background

An illustrated business card background image like this one can play many roles. Basically, any type of urban professional could use this background and make it their own.
In the business card example below, it works beautifully for a real estate agent. But again, an illustration like this is very versatile and hints at a creative personality!

Photography business background

Make a statement with a moody photograph. This type of business background would work for anyone in the environmental space or creatives, like photographers and artists.
Try turning the traditional business card on its head by creating one that’s vertical instead of horizontal, as the card below. This is a particularly good idea for people, like photographers, who need to emphasize that they have a unique perspective.

Return to Table of Contents
Adding a background image to your personal or company LinkedIn page gives you another way to showcase your personality and brand to your network.
As with other platforms, LinkedIn offers image recommendations , namely that banner background images should be 1,584 by 396 pixels. That means you need an image that’ll look good at a highly horizontal crop. You should also take into account what your profile picture looks like and how it will lay over the top of the background image.
Minimal LinkedIn banner

If you want to strike a serene vibe and showcase your minimalist sensibilities, use this LinkedIn business background image as your banner on the platform.
The designer below used the image, along with his name in red, to make it stick in viewers’ minds.

Office desk LinkedIn banner

An image like this can let potential employers know you’re accustomed to working in an office and are eager to pitch in and see how you can help.
When using an image that doesn’t really have any dead spaces, as in the banner below, think about where you’ll place your name and any other copy. And, of course, don’t forget about where your profile photo will overlay the image.

Research LinkedIn banner

This banner image for LinkedIn is a little more abstract, but evokes synergy, research and critical thinking. The different wires branching out could symbolize connection, or even, a system.
This would be a good pick if you’re in the research, marketing or design fields… or all of the above, like in the example below:

Educator LinkedIn Banner

If you’re looking for something simple yet eye-catching, try this zig zag illustration in vibrant colors. The lines here suggest someone who thinks in a non-linear manner — perfect for showcasing the unique points of view you bring to the table.
Whether you’re in education (like the example below), in a creative field or in a more laid-back business field, this versatile LinkedIn background would do the trick.

When thinking about a business background image for your Zoom meetings, it’s important to keep a few things in mind. First off, an aspect ratio of 16:9 is best for these images. And like with LinkedIn, you’ll want to think about the other thing people on the call will see: you.
Where will you sit within the frame? You’ll be centered, most likely, depending on how your camera is set up, so consider this when choosing your image. (Here are a few more tips for a great Zoom setup.)
Let’s look at some examples:
Cozy Zoom background

With more and more people working from home even after the pandemic , you may not want people to see into your actual space. So, why not give Zoom meeting attendants the illusion you live and work in a cozy space like this one?
This image comes from the following presentation template, but you could easily customize it to work as a Zoom background.

Modern kitchen Zoom background

Don’t want to show folks a fake living room? What about a fake kitchen? If you’re anything like me, the last thing you want people to see is your real-life messy kitchen, so think about an image like this as your Zoom virtual background.
Again, I found this option in a presentation template — it contains a few other images that could work as your Zoom background too.

Nature Zoom background

Go artistic (and botanical) with your Zoom meeting background and try an image like this one. Maybe mix up a piña colada with an umbrella if you really want to create a tropical vibe (but only after 5 p.m., right?).
Inspired by the following green-forward presentation, this Zoom background is an easy, soothing option:

Office Zoom background

You can also keep things corporate with a background image like this one. The benefit of using an image like this, as opposed to showing your actual office, is that you can control what people see… rather than leaving that up to the whims of your co-workers.
I found this beautiful loft-like office image in the following presentation. The image on the first slide would be a good choice, too.

By default (unless you installed special templates), PowerPoint’s slide sizes are 4:3 (standard) and 16:9 (widescreen). So, the first thing you need to decide is what size to use for your presentation.
Standard slides are closer to square, while widescreen slides are much more horizontal. But the following images will work for just about any PowerPoint size you go with, depending on the content for each slide:
Corporation PowerPoint background

Choose an image like this for your PowerPoint if you want to give your company an edgy, urban vibe. As you can see in the presentation below, this background can serve as the only big image in a presentation, or it can work as a series of city-based photos.
By dialing the opacity down on the image and underlaying a gray background, the designer of this presentation achieved a cooler, monochromatic look. Bonus: the image distracts less from the content this way.

(Want to know more about how to make stock images play well with your content? Here are our 10 best tips for incorporating stock photos into your designs .)
Finance PowerPoint background

Keep it corporate with this PowerPoint background image that looks toward the sky (and skyscrapers). Use it on its own as the only image in a presentation. Or, further curate the vibe by adding simple aesthetic images to the rest of the slides, as the presentation below does.
To achieve the softer tone of the main image, the designer reduced the opacity and added an orange-colored background in this instance.

Team-themed PowerPoint background

Emphasize the team-focused nature of your company with this all-hands-on-deck business background image for your next PowerPoint presentation. Keep the theme going by adding additional images of people’s hands or groups, as this presentation does.
Again, the designer here added a gray background behind the image and reduced the opacity to create a grayed out effect.

Creative PowerPoint background

You may think you’ll have a captive audience with a PowerPoint presentation, but this isn’t always the case. And in any event, it’s still important to create a beautiful, eye-catching design. If your PowerPoint presentation slides are more vertical than horizontal, consider this image as the first slide.
As you can see in the report below, it can work well with more understated images on other slides.

Looking for more options? Explore over 35 simple background images here .
As we’ve seen, business presentation backgrounds don’t come in just one form. Nor do you have to stick with one style. The perfect business presentation background image will depend on your goals and content, which is why it’s useful to have many to choose from.
Here are a few more of my favorite options:
Minimalist presentation background

This business presentation background image has a clear minimalist vibe — perfect for giving your presentation an understated but authoritative air.
See the slides below if you’re not convinced!

Bold power presentation background

Alternatively, you could also take a maximalist approach. Try using a high-energy image that will (ideally) leave your audience charged up.
You can see this image in use in the presentation below, but it could work for any other business presentation that needs to have a similar, energetic vibe.

Light wood presentation background

Sometimes you want a business presentation background to feel more like, well, a background element. When that’s the case, consider something like this image. The gray woodgrain floor provides some texture and visual interest, without overpowering the content.
In the example below, the designer adjusted the hue of the wood image to match the teal elements by adding a background of that color and reducing the opacity a smidge.

Not quite what you’re after? Here are over 15 more presentation background examples that are sure to engage your audience.
Professional business background images can run the gamut from simple artwork to complex, high-contrast photos. The right one depends on your needs in the moment, so it’s a good idea to have a supply of them on hand for different purposes.
Here are some more options to suit a variety of needs:
Abstract colorful background

The low-poly art style used in this image could work for a variety of business communication needs, including a presentation (as seen below). But it could easily slot into a social media template or even a business card, too.

New York background

Especially for firms actually based in the city, New York is a popular option for photography-based business background images because it’s so iconic. Whether you’re adding it to your business card, as seen below, or a presentation, few cities are as immediately recognizable.
As you can see in this example, the designer added a reddish background and dropped the opacity on the image to achieve a cohesive look and feel with the front of the card.

Geometric photography background

While this image appears in a business card below, it would work for just about any professional business need. The urban vibe it gives off can skew more corporate or more indie, depending on the elements surrounding it, which makes it incredibly versatile.
Versatility is important, as one key to making a lot of visual content is using similar (or the same) assets over and over again in new ways. For example, you could repurpose any of these versatile flyer background images , too.

Business photo backgrounds for your presentations, LinkedIn pages or Zoom calls can be just about anything!
You can go literal and have a picture of yourself or the front of your business. Or, you can get a little “thinky” and abstract with things.
Here are some examples:
Strategy business background

How can you get abstract? Creating a presentation to go over a new strategy you’ve come up with? Use an image like this one, as chess is the ultimate game of strategy.
While the presentation below has nothing to do with chess in a literal sense, using the photo immediately calls strategy to mind.

Technology business background

If your presentation is about a specific product or technology, it can be helpful to showcase what you’re talking about. For example, using an image of a person wearing a VR headset is a natural pairing for a presentation about tech trends, like the one below. But this image would also be perfect for a company in the VR space.
You know the drill: the designer tinted this image pink to match the rest of the presentation with the help of a background and opacity drop.

Desktop business background

Some business photo backgrounds create fun design opportunities, like this one. Super-impose whatever you want on the computer screen, as in the presentation below. You could showcase a series of icons, an image of your new store, a computer program… the sky’s the limit!

Of course, if you want something truly unique, you might have to make your own background. Don’t worry, it’s easier than it seems. Check out these free background generators .
There you have it! Hopefully, at this point, you’ve found the right business background for your needs or at least some inspiration.
If you’re getting ready to dive into your project, here are a few quick business background design tips to keep in mind:
- Set the right tone: an overly whimsical background image is probably not the right note to strike in your annual corporate presentation. But by the same token, it’s perfectly appropriate to use images with lighthearted themes for certain needs. So be sure the vibe created by the background image matches what you’re going for.
- Think about your content: depending on what’s in your background image, you might end up with spaces on the image that are darker or lighter or where there’s little if any visual content. Use these as opportunities for displaying content. If you find you have to move elements around too much in order to make them legible, then that’s probably not the right image for you.
- Don’t always take things literally: getting a bit abstract can be an excellent way to create a subtle connection between your background image and your content. Say, you’re putting together a monthly presentation during December and you want to use a wintry theme. Instead of an image with snow, consider one that’s an icy blue instead.
- Consider your platform: keep in mind, some of the business background images we talked about today have specific technical needs. For example, as I mentioned earlier, Zoom, recommends users upload images for virtual backgrounds at an aspect ratio of 16:9 , which is 1,920 by 1,080 pixels. But for an annual report that’s going to be printed on an office printer, you’ll need images that fit better into a letter or A4-sized presentation.
Showcase your professionalism with these business background images
There are so many options for business backgrounds. Hopefully, you found a few you love in this post.
Whether you’re looking to showcase your professionalism, highlight your team’s strengths or just dazzle your audience, you can get started today by signing for a free Venngage account — access all the business background images in this roundup and thousands more.
Happy designing!
80+ Modern Professional PowerPoint Templates 2024
In today’s collection, we’re bringing you a set of fresh new modern, professional PowerPoint templates for creating presentations that stand out from the crowd. Give your presentation a modern edge, and convey your message in a professional way.
We handpicked a collection of unique and modern PowerPoint templates that you can use for crafting slideshows for all kinds of presentations, including startup pitch decks to business projections, photography, marketing, design, and more.
We’re also sharing our tips for creating a modern presentation , to help you get started fast.
How Does Unlimited PowerPoint Templates Sound?
Download thousands of PowerPoint templates, and many other design elements, with a monthly Envato Elements membership. It starts at $16 per month, and gives you unlimited access to a growing library of over 2,000,000 presentation templates, fonts, photos, graphics, and more.
BeMind Minimal Template
Business PPT Templates
Corporate & pro.

Animated PPT Templates
Fully animated.
Explore PowerPoint Templates
Bore – Minimal Modern PowerPoint Template
This modern and creative PowerPoint template includes all the right elements of professional presentation design. It has a beautifully minimalist design, an attractive color palette, and a stylish content layout.
The template itself includes more than 30 unique slide designs you can easily customize to change colors and the fonts however you like. It also includes lots of editable vector graphics and shapes as well.
Why This Is A Top Pick
Since this template features a modern and universal design, you’ll be able to use it to design slideshows for all kinds of business, agency, and creative presentations.
Akbar – Modern Business PowerPoint Template

This PowerPoint template is perfect for diverse presentation needs including corporate and business profiles, creative agencies, portfolios, start-ups, pitch decks, and personal portfolios. It features 39 editable and resizable slides designed with free web fonts, based on master slides.
Osmar – Modern Business PowerPoint Template

Osmar is a business PowerPoint template that is perfect for crafting professional business presentations. Whether you’re a creative agency, startup, or looking to present a company profile, this template can be tailored to suit a variety of needs. With 39 editable and resizable slides, you can drag-and-drop content in an easily editable 16:9 widescreen ratio format.
Malaiz – Professional Business PowerPoint Template

A modern, dynamic PowerPoint template for all your professional presentations. Perfect for a range of contexts from startup pitches to photography portfolios, this easily editable 39-slide template incorporates free web fonts and resizable graphics based on master slides.
Meerotie – Professional PowerPoint Template
Meerotie is a dynamic, modern PowerPoint template perfect for both business and personal use. Features include 120 clean and creative slides with a bold design, a handmade infographic, a 16:9 ratio and easily editable images, fonts, and layouts. This fully adaptable template makes presenting your next project hassle-free and effective.
Enativing – Creative Agency PowerPoint Template

This is a versatile and modern tool for a multitude of fields, from advertising to startups. It features 30 unique slides that are fully editable and resizable, complete with over 500 icons and a drag-and-drop interface.
Black White – Professional Agency PowerPoint Template

A contemporary PowerPoint template perfect for enhancing your agency presentations. It features 20 unique, easily customizable slides with bold and elegant designs. The template offers drag-and-drop picture placeholders with auto-adjustment and comes complete with device mockups as well.
Professional Consulting PowerPoint Presentation
This is a modern, engaging template perfect for business presentations, project pitches, and lookbooks. Offering a variety of editable graphics and drag-and-drop picture placeholders in a widescreen format, the package includes PowerPoint and XML files along with fully editable layouts.
Hermoso – Modern Business PowerPoint Template

The Hermoso is a versatile PowerPoint template with a modern design. Ideal for contemporary businesses, this template can be used to present a variety of content including company profiles, portfolios, and startup pitches. With over 30 editable slides featuring resizable graphics, it provides convenience and flexibility.
Amin – Modern Business PowerPoint Template

A modern, easy-to-edit PowerPoint template ideal for various purposes, such as business presentations, corporate profiles, start-ups, creative agencies, or personal portfolios. It includes 39 slides, editable graphics, recommended free web fonts, and a 16:9 widescreen ratio.
Professional Portfolio PowerPoint Template

This is a modern, multipurpose PowerPoint Template ideal for presentations related to business, creative agencies, brand guidelines, and more. Offering 30 high-resolution slides in a 16:9 aspect ratio, this template is carefully designed for easy customization.
Alpha – Business PowerPoint Template
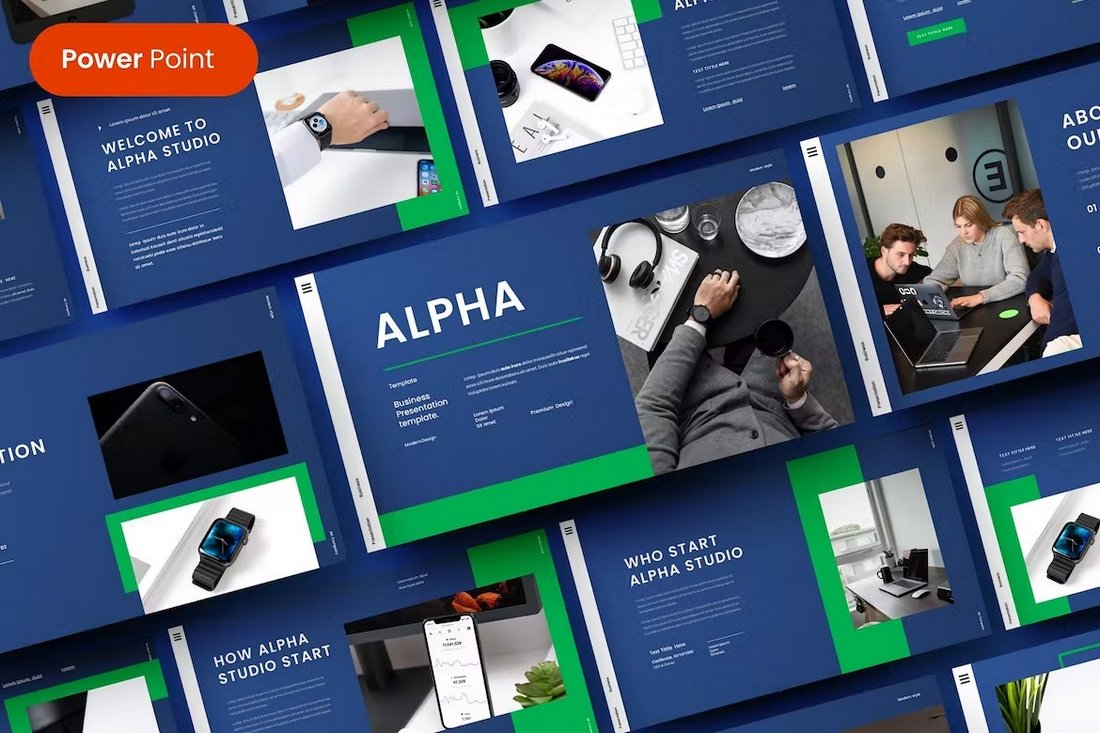
This PowerPoint template is made with modern businesses in mind. It’s ideal for crafting professional presentations for business meetings, company profiles, and pitch deck slideshows. The template includes 39 unique slides for you to choose from.
Stanbiz – Startup Business Plan PowerPoint Template

Design the perfect slideshow to showcase your startup and business plans with this professional PowerPoint template. There are 36 different slide layouts included in this template with fully customizable designs.
Gray Gold Company Profile Presentation Template
The dark gray and gold design of this PowerPoint template gives it a very stylish look and feel. The template is ideal for making slideshows for various marketing and product showcase presentations. It includes 26 unique slides.
Minimal Portfolio PowerPoint Presentation Template
The modern and minimal design of this PowerPoint template offers a beautiful canvas for crafting bold and beautiful presentations for your professional projects. There are 24 slides in the template that are especially suitable for portfolio presentations.

Aqua – Free Marketing Plan PowerPoint Template

This free PowerPoint template comes with a colorful watercolor-themed design. It’s perfect for professional marketing presentations and slideshows. The template has 32 unique slide layouts.
Minimal PowerPoint Presentation Template
Craft minimal presentations with an aesthetic feel using this PowerPoint template. It’s made with various business and agency portfolio presentations in mind. There are 21 different slide layouts to choose from.
Cell – Creative Professional PowerPoint Template

The bold and dark design of this PowerPoint template will allow you to make professional slideshows for presenting your projects and portfolio in style. The template includes fully customizable slides with image placeholders, device mockups, and much more.
Media-Press Kit – Professional PowerPoint Template

Just as the name suggests, this PowerPoint template is designed to help you craft a professional-looking media kit or a press kit for a brand. It includes 16 carefully crafted slides with all the important sections for promoting your brand and business.
Crowdfunding – PowerPoint Infographics Slides
If you’re planning on launching a crowdfunding campaign to raise funds for your business or product launch, this PowerPoint template will come in handy. It includes 17 different crowdfunding-themed infographic slides in 12 different color variations.
Photographer Portfolio – Free Professional PowerPoint Template
This free PowerPoint template is a great choice for crafting a simple portfolio slideshow for a photographer. There are 29 unique slides in the template with different styles of layouts for showcasing your work more effectively.
Gosamp – Urban Professional PowerPoint Template
Gosamp is a modern PowerPoint template that features a trendy and attractive design. It comes with more than 30 unique slide layouts you can use to create presentations for digital marketing and fashion brands. Each slide in the template also includes image placeholders, editable graphics, and much more.
Logica – IT Consultant PowerPoint Template

This template is designed with consulting agencies in mind. The template includes 30 different slide layouts with clean and professional designs. You can also customize it using PowerPoint, Keynote, and Google Slides.
Business Plan – Professional PowerPoint Template

If you’re looking for a PowerPoint template to create a killer business plan slide deck, this template is perfect for you. It includes 25 carefully crafted slides that can be used to make a professional presentation to showcase your business and company plans.
Tradents – Brand Guidelines Presentation Template

Use this PowerPoint template to make attractive brand guideline slide decks. You can choose from 30 unique slides, which include slides for detailing everything from font choices to color schemes and everything in between. You can easily edit and customize each slide to your preference as well.
Free Growth Business Plan PowerPoint Template

This free PowerPoint template is ideal for making simple and professional presentations for describing your business growth plans. There are 39 different slide layouts included in the template. Along with editable graphs, charts, and vector graphics.
Roline – Professional PowerPoint Template

This PowerPoint template combines elements from both professional and modern worlds to offer a set of beautiful slide layouts. It’s perfect for creating everything from business presentations to pitch decks and more. The template includes 50 unique slides with editable designs.
Koman – Modern Business PowerPoint Template

Presentations with dark designs are great for highlighting content more effectively. This PowerPoint template is designed to help achieve that goal. It includes a total of 39 slides with fully customizable layouts. And it features editable shapes and graphics as well.
Marketing Pitch – Modern PowerPoint Template

This PowerPoint template includes many different infographic slides you can use to visualize data in your marketing meetings. It features a clean and professional design. The template comes with 30 unique slides.
Wicka – Business PowerPoint Template

You can use this PPT to create professional presentations to promote creative brands and agencies. The template lets you choose from 39 different slides. It includes master slide layouts, editable vector graphics, image placeholders, and much more as well.
Free Business Profile PowerPoint Template
This is a free PowerPoint template for designing business presentations with professional slides. It comes with 23 unique slides. Each slide can be easily customized to change colors, fonts, and images to your preference.
Social Humanity – Modern PowerPoint Template
This professional PowerPoint template features a minimalist slide design. It’s perfect for making presentations for non-profit organizations and many other businesses. The template includes 30 unique slides.
Business & Corporate PowerPoint Template
Use this template to design a modern and creative presentation for your corporate business. It includes a total of 420 slides featuring 40 unique slides in 8 pre-made color schemes. The template also has transition animations as well.
Lonux – Professional PowerPoint Template

Lonux is a PowerPoint template you can use to design presentations to showcase your professional services. The template includes 39 unique slides filled with editable shapes, master slide layouts, image placeholders, and more.
Aserlla – Clean Business PowerPoint Template

Looking for a PowerPoint template with a clean and professional layout? Then this template is for you. It includes slides in both dark and light color themes as well as in 3 pre-made color schemes.
Business & Consulting Toolkit Free PPT

This creative PowerPoint template not only comes with a set of modern slides but also features multipurpose designs you can use to create many different types of presentations. It includes 50 unique slides with graphs, maps, infographics, and more.
Reendinguz – Modern PowerPoint Template
If you’re looking for a minimal PowerPoint template with a modern design to create clean and effective presentations, this template is perfect for you. It includes 30 unique slide designs featuring 5 different color schemes to choose from. The layouts made with vector shapes are easily editable as well.
Galerino – Professional PowerPoint Template

Galerino is another modern PowerPoint template that comes with a total of 150 slides. It features image placeholders for easily placing your images in the slides as well as master slide layouts, illustrations, and editable vector graphics.
Best Business – Modern PowerPoint Template
This is a great PowerPoint template you can use to design an elegant and attractive slideshow for a professional presentation. It includes 30 slides that you can choose from 5 different color schemes. It also comes with an infographic, gallery slide, illustrations, and much more.
Browney – Contemporary PowerPoint Template
If you are looking for an elegantly designed, professional PowerPoint template for modern businesses, Browney is an ideal choice. This collection of five templates, each having 30 slides, is a great option for making an impression on potential investors or clients.
Sparrow – Creative Agency PowerPoint Template

Exclusively designed for creative industries, Sparrow features a modern, uncluttered design with a splash of bright colors that instantly draws the attention of your audience. There is a smorgasbord of slides for you to customize to your heart’s content, and easy-to-use features that make the dreadful task of making a presentation look like a piece of cake.
Poolest – Simple PowerPoint Template

The best presentations are often the ones without any bells and whistles. Poolest is a minimal yet eye-catching option, making it one of the best professional PowerPoint templates on our list. We wholeheartedly recommend you try out Poolest for your upcoming presentation.
Modela – Free Creative PowerPoint Template
With a stylish, modern, and striking design, Modela is an effective presentation template with multi-purpose slides, data infographics, and a 16:9 widescreen ratio. It’s one of the best free modern PowerPoint templates available on the web and can be fully customized to reflect your own branding.
Arina – Free Business PowerPoint Template
Arina, a modern and sophisticated PowerPoint template is a great choice for businesses looking to make an impact. It features an elegant layout, easy-to-edit slides, and a range of amazing features that really should be seen to be fully appreciated.
Round – Clean Business PowerPoint Template
Round also comes with a set of modern and professional slide designs. Each slide in this PowerPoint template is available in 5 different colors. It also includes master slide layouts, image placeholders, editable vector graphics, and more.
Voodoo – Free Professional PowerPoint Template
VooDoo is a free PowerPoint template that features a set of highly professional slides, including ones with infographics. The free version of the template includes 5 free presentation slides and 5 infographic slides.
Kirkland – Business PowerPoint Template
This PowerPoint template is a great choice for making all types of professional and business presentations. It comes with a set of beautiful slides made with a minimal content layout full of colorful shapes and images. The template includes 30 unique slides with 5 different colors to choose from.
Twenty Five – Modern Professional PowerPoint Template
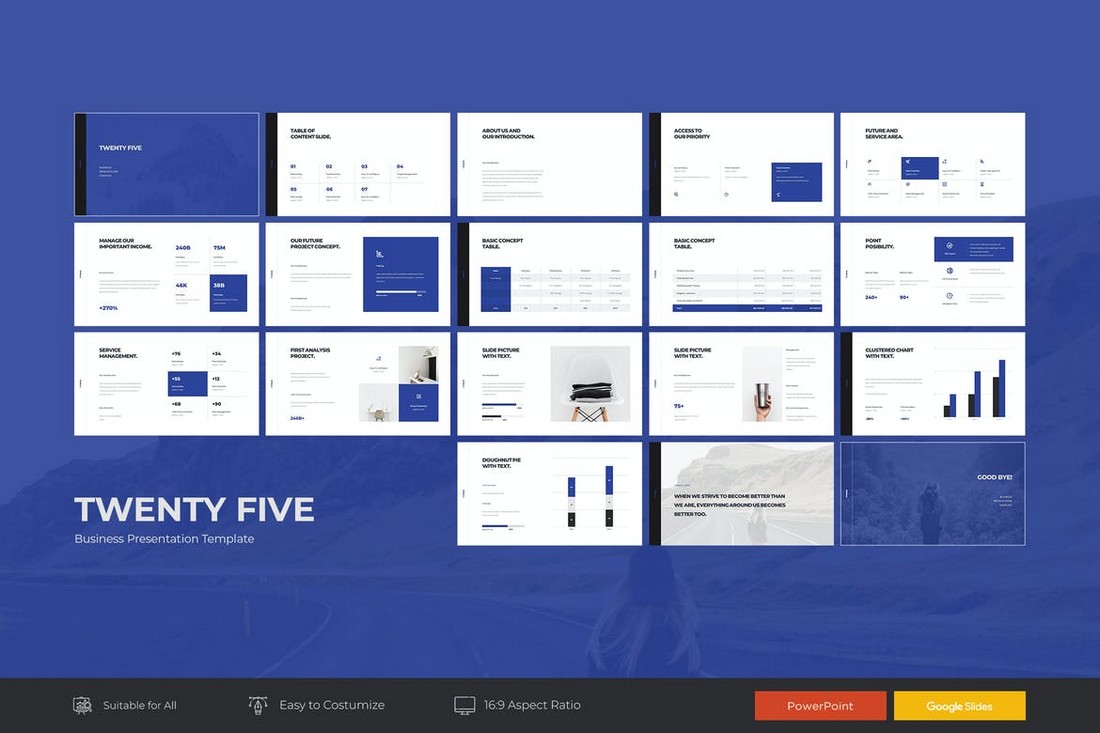
Minimalism takes a key role in every modern and professional presentation design. This template will allow you to leverage both those factors to your advantage by crafting a set of slides full of clarity and creativity. It includes 25 unique slides for you to choose from. And comes in Google Slides version as well.
Quizy – Quiz Themed Powerpoint Template
A very unique PowerPoint template designed specifically for quiz and questionnaire-based presentations. This template comes with 30 slides featuring colorful quiz-themed designs and layouts. It’s perfect for making your presentations more entertaining for events and conferences.
Rexse – Pitch Deck Powerpoint Template
Rexse is a pitch deck PowerPoint template you can use for all sorts of business and startup investor presentations. The template comes with 40 unique master slide layouts with modern designs. Each slide features editable graphics, icons, shapes, and image placeholders for easy customization.
Original – Free Modern PowerPoint Template
This beautiful PowerPoint template is completely free to download and use with your personal projects. It’s ideal for making a simple slideshow for design and lifestyle-themed presentations.
LEARN – Education Powerpoint Template

Just as the name suggests, this PowerPoint template is designed for all sorts of educational presentations. It’s ideal for making presentations for educating the audiences of your products and services. The template includes 30 unique slides.
Atea – Clean Professional Presentation Template

The clean and creative design of this presentation template gives it a truly unique look and feel. This PowerPoint template features 30 unique slides that are available in 5 different pre-made color schemes. It also comes in Keynote and Google Slides versions as well.
Accasia – Creative Business PowerPoint Template

This PowerPoint template comes with a slide design filled with creative and abstract shapes. This gives the entire presentation a very uncommon look and feel. The template includes 30 unique slides. You can easily customize the design using its pre-made color schemes and image placeholders.
Aquos – Minimal Professional PowerPoint Template

If you’re working on a presentation for a corporate brand or a modern business, this PowerPoint template will come in handy. It comes with 30 minimalist slides that feature plenty of visuals and shapes. The template includes gallery slides, portfolio slides, history slides, and lots more.
Hexxos – Free Modern PowerPoint Template
The vivid and colorful slides in this template give it a truly modern and trendy look. This PowerPoint template is perfect for making a presentation for modern fashion and lifestyle brands. It’s free to use with your personal projects.
Classy – Modern PowerPoint Template

Classy is a modern PowerPoint template that features a set of 30 unique slides that are available in 5 different color schemes, making it a total of 150 slides. It also includes image placeholders, editable vector graphics, and free fonts as well.
Sneaky – Fashion PowerPoint Template

Sneaky is a modern PowerPoint template that comes with a stylish visual slide design, which makes it perfect for creating fashion and apparel related presentations. The template includes 45 unique slides with drag and drop customization features.
Visionare – Modern PowerPoint Presentation
Visionare is a beautiful PowerPoint template you can use to design professional presentations for business and agency meetings and events. The template comes with 50 unique slides in HD resolution and features image placeholders, world maps, icons, and much more.
Zero – Creative PowerPoint Template

Zero is a modern and creative PowerPoint template featuring a colorful design. This template is most suitable for making marketing and sales related presentations. It includes 30 unique slides in 5 different color schemes, making a total of over 150 slides.
Yoon – Business PowerPoint Template

Yoon comes with a simple and clean design which allows you to effectively highlight your images and content. The template is perfect for making business profile and product showcase presentation slideshows.
Ashtray – Professional PowerPoint Template

Ashtray PowerPoint template features a creative slide design filled with lots of shapes, colors, and images. The template lets you choose from a total of 150 slides to craft unique business and professional presentations that stand out from the crowd.
Free Portfolio PowerPoint Template

This modern free PowerPoint template is designed specifically for creating professional portfolio presentations. It includes 12 unique slides filled with lots of icons and shapes.
Free Minimal PowerPoint Presentation
If you’re looking for a minimal PowerPoint template for making a portfolio showcase or an agency presentation, this free template is for you. It features 20 unique slides with image placeholders and icons.
Chroma – Modern PowerPoint Template

Chroma features a design unlike any other PowerPoint template in this collection. The template has a modern design featuring vibrant gradient colors. It includes 50 unique slides that are most suitable for modern startup and small businesses.
Molex – Dark PowerPoint Template

Molex is a stylish PowerPoint template that comes with a dark color theme, which effectively highlights text and other content in the design. The template is also available in 5 different color schemes and comes with 30 unique slides.
PRADIC – Creative PowerPoint Template

Pradic is a creative PowerPoint template you can use to design business and corporate presentations. It comes with slides full of colorful shapes, charts, graphs, image placeholders, and much more.
Gholem – Minimal PowerPoint Template

Gholem PowerPoint template features 30 unique slides that can be easily customized to your preference. The slides are also available in 5 different color variations and include a handcrafted infographic and gallery slides as well as image placeholders.
Rekxa – Clean PowerPoint Template
Rekxa is a clean and minimalist PowerPoint template most suitable for designing startup and business-related presentations. The template includes 150 slides with editable designs and 5 color schemes to choose from.
Pop – Free Colorful PowerPoint Template

This is a free demo of a premium PowerPoint template. It features a set of modern and colorful slide designs you can use to create a stylish slideshow to showcase your personal designs, artworks, and portfolios.
GMTRY – Free Geometric Presentation Template

This modern PowerPoint template features a unique style of design filled with creative geometric shapes. You can use it for free with personal projects.
Hanobi – Modern Professional PowerPoint Template

Hanobi is a modern and elegant PowerPoint template that features a professional design for making slideshows for business and creative presentations. It includes a total of 150 slide designs that are also available in 5 different color schemes.
Anada – Agency Modern Professional PowerPoint Template

Anada is a PowerPoint template most suitable for making marketing and sales related presentations. It comes with 30 unique slides featuring infographics, charts, graphs, and icons. The template s also available in 3 different colors as well as light and dark themes.
Space – Modern Professional PowerPoint Template

Space is a minimalist and professional PowerPoint template that includes a set of gorgeously designed slides featuring portfolio slides, infographics, vector graphics, image placeholders, and much more.
Laforest – Modern Professional PowerPoint Template

Laforest PowerPoint template comes with 12 different files featuring the slideshow in 3 premade color schemes and in light and dark themes. It includes 30 professionally designed slides featuring timelines, mockups, image placeholders, and more.
Pastel – Free PowerPoint Template

Pastel is another great free PowerPoint template you can use to design a colorful and attractive presentation to showcase your portfolio. It’s free to use with personal projects.
Free Corporate Powerpoint Template
This free PowerPoint template comes with 15 unique slide designs you can use to design various business and corporate presentations. It includes lots of shapes, infographics, and illustrations as well.
Mochica – Modern Professional PowerPoint Template

Mochica features a minimalist design with lots of clean and white space. The PowerPoint template lets you choose from 5 color schemes and a total of 150 slides to design professional presentations.
Project Proposal – Modern Professional PowerPoint Template

With this professional PowerPoint template, you’ll be able to create attractive presentations for project proposals and meetings. The template is available in 4 different color themes and it features lots of unique slides for describing pricing, project scope, budget, and more.
Cella PitchDeck Modern Professional PowerPoint Template

This PowerPoint template will definitely come in handy for startups and businesses for making powerful pitch decks to promote and present their ideas and startups to investors. The template includes a total of 120 slides.
MINIMAL PROPOSAL – Modern Professional PowerPoint Template
Another modern and professionally designed PowerPoint template for making attractive proposal presentations. This template comes with 50 unique slides that feature 3D infographics, icons, vector illustrations, and more.
Yellow Bussiness – Modern Professional PowerPoint Template

Create unique and persuasive marketing and sales presentations using this PowerPoint template. It features 50 unique slides you can easily edit to change colors, text, images, and shapes.
Free Fashion PowerPoint Presentation Template
Another great free PowerPoint template for crafting slideshows related to photography and fashion design. The template includes 10 unique slides you can customize to your preference.
Motagua – Free Multipurpose PowerPoint Template
Motagua is a modern and attractive free PowerPoint template that can be used to design all kinds of design, business, and creative presentations. It comes with 12 unique slides based on master slide layouts.
Latte PowerPoint Presentation Template

Latte is a professional PowerPoint template that comes with a minimal and a modern design. The template features lots of space for showing off images with a beautiful color scheme. It includes over 50 unique slides based on master slides with vector graphics and portfolio slides.
Marketing Plan 2.0 PowerPoint Template

This is a PowerPoint template designed specifically for creating marketing-related presentations. It includes 30 unique slides that come in 10 different color schemes. The slides are also available in white and dark background versions. The slideshow is also fully animated and print-ready as well.
Modev Professional PowerPoint Template

This professional PowerPoint template is most suitable for creating slideshows for design agency and freelancer presentations. It features an elegant color design, which is available in Green, Blue, and Pink versions. Each template consists of 30 unique slides.
Minimal Presentation PowerPoint Template

Just as the title suggests, this is a minimalist PowerPoint template that comes with a total of over 300 slides. The template features a modern design that makes it ideal for SaaS and small business related presentations. It’s also available in 10 different color schemes as well.
Visionary – Attractive PowerPoint Design

Visionary is a professionally designed PowerPoint template that includes 80 unique multipurpose slides with vibrant colors. The template is available in 30 different color schemes and it comes with 98 master slide layouts for creating your own unique slides.
MUNINE PowerPoint Template
Munine is a PowerPoint slideshow template with a feminine design. It’s perfect for designing slideshows for fashion and clothing brand related presentations. The template features 60 unique slides in 50 different premade color schemes. Each template is also available in dark and light color versions as well.
iDea – Creative Company PowerPoint Template

Idea is a PowerPoint template designed specifically for marketing related presentations. It’s also perfect for making presentations for creative and design agencies as well. It includes 30 unique slides in 3 different color schemes.
Kalium Corporate PowerPoint Presentation
Featuring a professional design, Kalium PowerPoint template is most suitable for creating presentations for corporate businesses, brands, and agencies. It includes 50 unique slides that are easily customizable and featuring lots of vector graphics and elements. The slides also come equipped with animations as well.
SPLASH – PowerPoint Template
This PowerPoint template is ideal for design agencies and other creative businesses. It features slides with a modern design for easily highlighting your portfolio, case studies, team, and galleries. The template includes 32 unique slides that are available in 5 premade color schemes.
SIMPLY – PowerPoint Template
Simply is a creatively designed PowerPoint presentation template that includes 32 unique slides. It’s also available in 5 different color variations and features plenty of vector elements, such as infographics, charts, graphs, and more. You can easily edit it to customize the slides to your preference.
Oxygen PowerPoint Presentation

Oxygen is the perfect PowerPoint template for creating marketing and creative presentations. It comes with an attractive slide design and a drag and drop editing environment. The template includes 50 unique slides featuring infographics, maps, charts, and graphs.
SKETCH 1 PowerPoint Template
This creative template includes 40 unique slides that feature lots of sketch-based illustrations and icons. The template is also available in 50 different color variations and with hundreds of vector graphics, icons, and shapes.
Exotic Project Presentation Template
Featuring a minimal and a modern design, this PowerPoint template is best for showcasing your projects and products in your presentations. It’s also great for making presentations for corporate and small business presentations as well. The template includes 62 multipurpose slides in 20 different color schemes.
NEXT PowerPoint Template
Next is a highly visual PowerPoint template that comes with a set of slides with a modern design. It includes 20 unique slides in 50 different color styles, including dark and light themes. The slides are also filled with lots of vector graphics and icons as well.
Rising Sun PowerPoint Template
If you’re working on a presentation for a creative agency or a small business, this PowerPoint template will come in handy. This template includes 20 master slides featuring lots of vector elements, gradient colors, and icons.
Real Estate PowerPoint Template
This is a PowerPoint template designed specifically for making presentations related to real-estate agencies. The template features 20 unique slides with plenty of space for highlighting properties with large images. It also includes charts, diagrams, graphs, and vector icons as well.
Lean PowerPoint Template

Lean is a professionally designed PowerPoint template that’s ideal for creating business and corporate presentation slideshows. The template includes 20 master slides featuring lots of vector graphics, icons, and shapes.
Add Color PowerPoint Template

This colorful PowerPoint template is perfect for creating presentation slideshows for all types of occasions, including schools, colleges, marketing, fashion, and more. The template comes packed with vector charts and graphs as well.
Mapped PowerPoint Template

Mapped is a PowerPoint template with a modern design. It’s best for making slideshows for eCommerce businesses and startups. The template includes slides based on 20 master slides and animations.
Ruby PowerPoint Template

Featuring a set of 50 unique slides, this PowerPoint template is made specifically for creating presentations for business and corporate projects. It includes resizable vector graphics and gallery slides as well.
Express – Freestyle PowerPoint Template

Express is a unique PowerPoint template with a modern and a creative design that will certainly make your presentations stand out. It includes 30 slides featuring attractive brush-strokes, vectors, icons, and graphics. The template is also available in 3 different color schemes.
Modern Real Estate PowerPoint Template

Another PowerPoint slideshow template for creating presentations for real-estate businesses. The template includes 30 clean and modern slides that are available in 5 premade color schemes. It comes with resizable graphics, vector illustrations, portfolio slides, and lots more.
Timeline 2.0 for PowerPoint

This is a massive bundle of PowerPoint templates that includes 50 unique templates of timeline slides. You can use them to create business projections charts, product-related graphs, and more. The templates are also available in 10 different premade color schemes.
Tidama – Modern Business PowerPoint Template

This is one of the most elegant PowerPoint templates in this collection. If you’re looking for a theme to design a presentation for a luxury brand or high-end product, this template is perfect for you. It includes 39 slide layouts with fully editable designs.
Bakooh PowerPoint Template

With a confident look and clean, creative slides, this is a versatile, flat design PowerPoint template. It’s got a modern style that blends plenty of colorful graphics, powerful charts, and minimal design elements.
Doros PowerPoint Template
Need a PowerPoint presentation design template with a modern style? One that’s easy to customize? And comes packed with the right slide designs to communicate your message effectively? Look no further than Doros.
Mokka PowerPoint Template
If you like minimal PowerPoint design templates, check this out. This is a minimal PowerPoint presentation design with plenty of template options built-in. If you’ve got important information to present, this set delivers. It’s perfect for personal or corporate use. And comes with a ton of easy-to-edit features that are 100% customizable.
Rising PowerPoint Template
Think big and get ready to go bold with this modern PowerPoint design theme. It’s got a powerful set of unique PPT slide designs that’ll help your message stand out. It mixes striking images with compelling layouts and a confident type. It also includes quick to work with components that pack a creative punch.
5 Tips for Creating a Modern PowerPoint Presentation
If you’re new to designing PowerPoint presentations, these tips will help you create a more professional looking slideshow to win your audience.
1. Use Minimal and Professional Slide Designs
Let’s face it, all of the default templates included in PowerPoint are terrible and have outdated designs. They’ll never help make your presentation stand out from the crowd.

So start your process by finding a better and professionally designed PowerPoint template to make your slideshow look more creative and original. You’d be surprised to see the amazing designs on some of the templates you can download from third-party websites. They’ll make your old presentations look like something from the 1980s.
2. Find and Use Better Custom Fonts
Fonts take a major role in presentation slideshows as they help attract attention to each of your slides. Consider using custom fonts in your presentations.

With the right combination of a big bold title font and a body font with an easy to read design, you can create presentations to deliver a great user experience that shows off professionalism.
3. Write Shorter Sentences
In most cases, a PowerPoint presentation should focus on highlighting the key points of a speech and to visualize data. And you should keep it that way and avoid making your presentation look like a novel filled with long paragraphs.
You can achieve this goal by creating a content layout for including shorter sentences and paragraphs. Use bullet points and icons as well.
4. Add Shapes, Images, Charts, and Graphs
Modern PowerPoint presentations are usually very visually appealing and it’s beautiful to look at. You can make similar presentations by including lots of shapes and large images to make each slide look more creative.
You can also use charts and infographics to visualize data from studies, show projections, summarize reports, and even make strong statements.
5. Use a Modern Color Palette
While using minimal designs is always a great approach to designing professional PowerPoint slideshows, many modern presentations feature colorful designs as well.

Create a color palette that matches your brand and your industry. Use it to add a stylish look to each of the slides in your presentations while maintaining a persistent design.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
49 templates
18 templates

32 templates
42 templates
40 templates
16 templates
Professional Business Meeting
Professional business meeting presentation, free google slides theme, powerpoint template, and canva presentation template.
A perfect speech, convincing data, and an amazing design are the perfect ingredients for a successful business meeting. There are lot of meetings happening in Slidesgo, that’s why we know that a good design is a key factor if you want your audience to pay attention for you. With this elegant design your data is guaranteed to stand out! The cream background and the minimal lines give your presentation a modern touch and the assortment of resources we’ve included will help you explain your data in a clear way. In addition, it is fully editable so feel free to adapt it to your company’s esthetics.
Features of this template
- 100% editable and easy to modify
- 27 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the free resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

We’re sorry, but Freepik doesn’t work properly without JavaScript enabled. FAQ Contact
- Notifications
- Go back Remove
- No notifications to show yet You’ll see useful information here soon. Stay tuned!
- Downloads 0/60 What is this?
- My collections
- My subscription
Find out what’s new on Freepik and get notified about the latest content updates and feature releases.
- Business wallpaper
- Businessman cartoon
- Businessman drawing
- Business woman cartoon
- Ceo business card
- Happy boss's day
- Office background
- Work background
- Leadership background
Business Background Images
Boost your professional image with these business backgrounds, designed for LinkedIn, PowerPoint, and Zoom. Whether you're making a strong impression in the boardroom, delivering impactful presentations, or participating in virtual meetings, these backgrounds are your key to an influential presence.

- Add to collection
- Save to Pinterest
- three dimensional
- cube background

- geometric background
- polygon shape
- geometric wallpaper

- abstract liquid
- blue modern

- paper wallpaper

- white wallpaper
- white abstract

- glass building
- business center
- modern architecture

- modern building
- business building
- office building

- layout background

- futuristic pattern
- digital pattern

- minimal background

- canvas background
- paper pattern

- connection background
- network background

- flat geometric
- flat background
- flat design

- abstract layout
- blue layout
- background cover

- abstract lights
- glow background

- formal background
- business frame
- blue border

- black background
- background themes
- abstract background

- technology geometric
- connecting lines

- white geometric

- abstract halftone
- halftone background

- business pattern
- line graphic

- commercial building

- corporate building

- 3d geometry
- 3d geometric

- natural paper
- page background

- blue square
- blue geometric

Home Blog Business Business Presentation: The Ultimate Guide to Making Powerful Presentations (+ Examples)
Business Presentation: The Ultimate Guide to Making Powerful Presentations (+ Examples)
A business presentation is a purpose-led summary of key information about your company’s plans, products, or practices, designed for either internal or external audiences. Project proposals, HR policy presentations, investors briefings are among the few common types of presentations.
Compelling business presentations are key to communicating important ideas, persuading others, and introducing new offerings to the world. Hence, why business presentation design is one of the most universal skills for any professional.
This guide teaches you how to design and deliver excellent business presentations. Plus, breaks down some best practices from business presentation examples by popular companies like Google, Pinterest, and Amazon among others!
3 General Types of Business Presentations
A business presentation can be given for a number of reasons. Respectively, they differ a lot in terms of content and purpose.
But overall, all types of business presentations can be classified as:
- Informative
- Persuasive
- Supporting
Informative Business Presentation
As the name suggests, the purpose of an informative presentation is to discern the knowledge you have — explain what you know. It’s the most common type of business presentation out there. So you have probably prepared such at least several times.
Examples of informative presentations:
- Team briefings presentation
- Annual stakeholder report
- Quarterly business reviews
- Business portfolio presentation
- Business plan presentation
- Project presentation
Helpful templates from SlideModel:
- Business plan PowerPoint template
- Business review PowerPoint template
- Project proposal PowerPoint template
- Corporate annual report template
Persuasive Business Presentation
The goal of this type of presentation is to persuade your audience of your point of view — convince them of what you believe is right. Developing business presentations of this caliber requires a bit more copywriting mastery, as well as expertise in public speaking . Unlike an informative business presentation, your goal here is to sway the audience’s opinions and prompt them towards the desired action.
Examples of persuasive presentations:
- Pitch deck/investor presentations
- Sales presentation
- Business case presentation
- Free business proposal presentation
- Business proposal PowerPoint template
- Pitch deck PowerPoint template
- Account Plan PowerPoint template
Supporting Business Presentation
This category of business PowerPoint presentations is meant to facilitate decision-making — explain how we can get something done. The underlying purpose here is to communicate the general “action plan”. Then break down the necessary next steps for bringing it to life.
Examples of supporting presentations:
- Roadmap presentation
- Project vision presentation
- After Action Review presentation
- Standard operating procedure (SOP) PowerPoint template
- Strategy map PowerPoint template
- After action review (ARR) PowerPoint template
What Should Be Included in a Business Presentation?
Overall, the content of your business presentation will differ depending on its purpose and type. However, at the very minimum, all business presentations should include:
- Introductory slide
- Agenda/purpose slide
- Main information or Content slides
- Key Takeaways slides
- Call-to-action/next steps slides
We further distill business presentation design and writing best practices in the next section (plus, provide several actionable business PowerPoint presentation examples!).
How to Make a Business Presentation: Actionable Tips
A business presentation consists of two parts — a slide deck and a verbal speech. In this section, we provide tips and strategies for nailing your deck design.
1. Get Your Presentation Opening Right
The first slides of your presentation make or break your success. Why? By failing to frame the narrative and set the scene for the audience from the very beginning, you will struggle to keep their interest throughout the presentation.
You have several ways of how to start a business presentation:
- Use a general informative opening — a summative slide, sharing the agenda and main points of the discussion.
- Go for a story opening — a more creative, personal opening, aimed at pulling the audience into your story.
- Try a dramatic opening — a less apparent and attention-grabbing opening technique, meant to pique the audience’s interest.
Standard Informative Opening
Most business presentation examples you see start with a general, informative slide such as an Agenda, Problem Statement, or Company Introduction. That’s the “classic” approach.
To manage the audience’s expectations and prepare them for what’s coming next, you can open your presentation with one or two slides stating:
- The topic of your presentation — a one-sentence overview is enough.
- Persuasive hook, suggesting what’s in it for the audience and why they should pay attention.
- Your authority — the best technique to establish your credibility in a business presentation is to share your qualifications and experience upfront to highlight why you are worth listening to.
Opening best suited for: Formal business presentations such as annual reports and supporting presentations to your team/business stakeholders.
Story Opening
Did you ever notice that most TED talks start with a quick personal story? The benefit of this presenting technique is that it enables speakers to establish quick rapport and hold the listener’s attention.
Here’s how Nancy Duarte, author of “Slide:ology: The Art and Science of Creating Great Presentations” book and TED presenter, recommends opening a presentation:
You know, here’s the status quo, here’s what’s going on. And then you need to compare that to what could be. You need to make that gap as big as possible, because there is this commonplace of the status quo, and you need to contrast that with the loftiness of your idea.
Storytelling , like no other tool, helps transpose the audience into the right mindset and get concentrated on the subject you are about to discuss. A story also elicits emotions, which can be a powerful ally when giving persuasive presentations. In the article how to start a presentation , we explore this in more detail.
Opening best suited for: Personal and business pitches, sales presentations, other types of persuasive presentations.
Dramatic Opening
Another common technique is opening your presentation with a major statement, sometimes of controversial nature. This can be a shocking statistic, complex rhetoric question, or even a provocative, contrarian statement, challenging the audience’s beliefs.
Using a dramatic opening helps secure the people’s attention and capture their interest. You can then use storytelling to further drill down your main ideas.
If you are an experienced public speaker, you can also strengthen your speech with some unexpected actions. That’s what Bill Gates does when giving presentations. In a now-iconic 2009 TED talk about malaria, mid-presentation Gates suddenly reveals that he actually brought a bunch of mosquitoes with him. He cracks open a jar with non-malaria-infected critters to the audience’s surprise. His dramatic actions, paired with a passionate speech made a mighty impression.
Opening best suited for: Marketing presentations, customer demos, training presentations, public speeches.
Further reading: How to start a presentation: tips and examples.
2. Get Your PowerPoint Design Right
Surely, using professional business PowerPoint templates already helps immensely with presentation deck design since you don’t need to fuss over slide layout, font selection, or iconography.
Even so, you’ll still need to customize your template(s) to make them on brand and better suited to the presentation you’re about to deliver. Below are our best presentation design tips to give your deck an extra oomph.
Use Images, Instead of Bullet Points
If you have ever watched Steve Jobs’s presentations, you may have noticed that he never used bullet-point lists. Weird right? Because using bullet points is the most universal advice in presentation design.
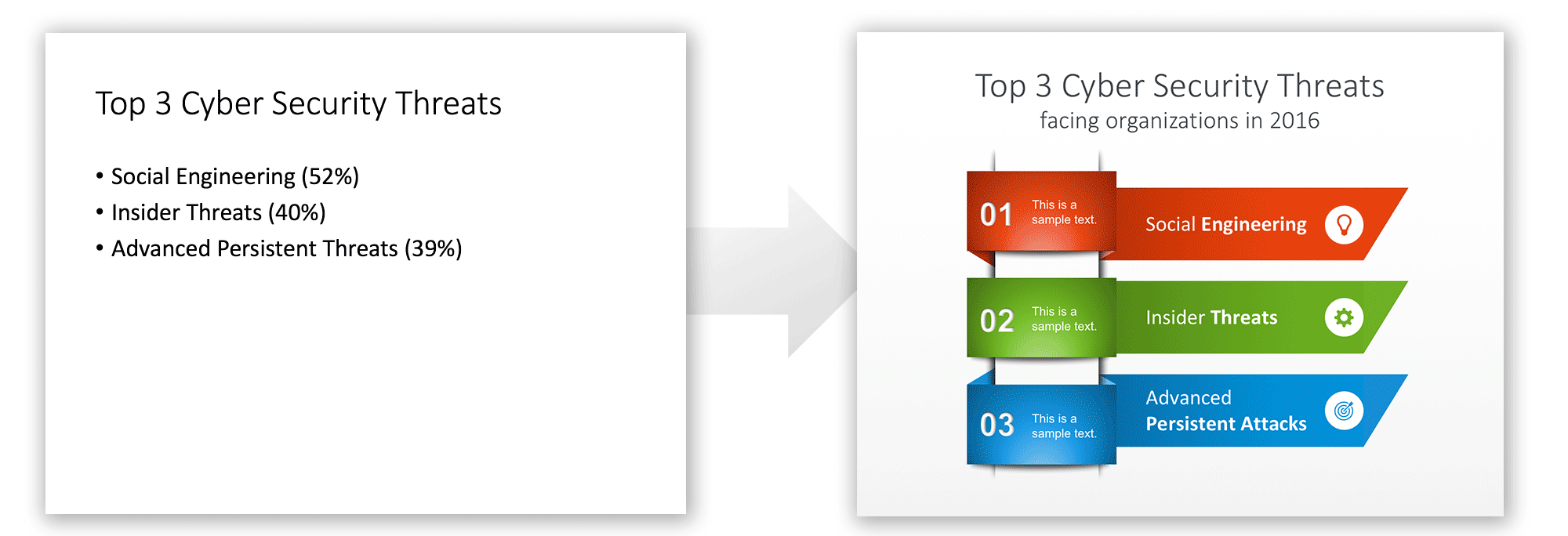
But there’s a valid scientific reason why Jobs favored images over bullet-point texts. Researchers found that information delivered in visuals is better retained than words alone. This is called the “ pictorial superiority effect ”. As John Medina, a molecular biologist, further explains :
“Hear a piece of information, and three days later you’ll remember 10% of it. Add a picture and you’ll remember 65%.”
So if your goal is to improve the memorability of your presentation, always replace texts with images and visualizations when it makes sense.
Fewer Slides is Better
No matter the value, a long PowerPoint presentation becomes tiring at some point. People lose focus and stop retaining the information. Thus, always take some extra time to trim the fluff and consolidate some repetitive ideas within your presentation.
For instance, at McKinsey new management consultants are trained to cut down the number of slides in client presentations. In fact, one senior partner insists on replacing every 20 slides with only two slides . Doing so prompts you to focus on the gist — the main business presentation ideas you need to communicate and drop filler statements.
Here are several quick tips to shorten your slides:
- Use a three-arc structure featuring a clear beginning (setup), main narrative (confrontation), ending (resolution). Drop the ideas that don’t fit into either of these.
- Write as you tweet. Create short, on-point text blurbs of under 156 symbols, similar to what you’d share on Twitter.
- Contextualize your numbers. Present any relevant statistics in a context, relevant to the listeners. Turn longer stats into data visualizations for easier cognition.
Consistency is Key
In a solid business presentation, each slide feels like part of the connecting story. To achieve such consistency apply the same visual style and retain the same underlying message throughout your entire presentation.
Use the same typography, color scheme, and visual styles across the deck. But when you need to accentuate a transition to a new topic (e.g. move from a setup to articulating the main ideas), add some new visual element to signify the slight change in the narrative.
Further reading: 23 PowerPoint Presentation Tips for Creating Engaging and Interactive Presentations
3. Make Your Closure Memorable
We best remember the information shared last. So make those business presentation takeaways stick in the audience’s memory. We have three strategies for that.
Use the Rule of Three
The Rule of Three is a literary concept, suggesting that we best remember and like ideas and concepts when they are presented in threes.
Many famous authors and speakers use this technique:
- “Duty – Honor – Country. Those three hallowed words reverently dictate what you ought to be, what you can be, and what you will be” . Gen. Douglas MacArthur.
- “Life, Liberty, and the Pursuit of Happiness” are the unalienable rights of all humans that governments are meant to protect.” Thomas Jefferson
The Rule of Three works because three is the maximum number of items most people can remember on their first attempt. Likewise, such pairings create a short, familiar structure that is easy to remember for our brains.
Try the Title Close Technique
Another popular presentation closing technique is “Title Close” — going back to the beginning of your narrative and reiterating your main idea (title) in a form of a takeaway. Doing so helps the audience better retain your core message since it’s repeated at least two times. Plus, it brings a sense of closure — a feel-good state our brains love. Also, a brief one-line closure is more memorable than a lengthy summary and thus better retained.
Ask a Question
If you want to keep the conversation going once you are done presenting, you can conclude your presentation with a general question you’d like the audience to answer.
Alternatively, you can also encourage the members to pose questions to you. The latter is better suited for informational presentations where you’d like to further discuss some of the matters and secure immediate feedback.
Try adding an interactive element like a QR code closing your presentation with a QR code and having a clear CTA helps you leverage the power of sharing anything you would like to share with your clients. QR codes can be customized to look alike your brand.
If you are looking for a smoother experience creating presentations on the fly, check out the AI PowerPoint maker —it offers everything you can ask forfrom presentation design in a couple of clicks.
12 Business Presentation Examples and What Makes Them Great
Now that we equipped you with the general knowledge on how to make a presentation for business, let’s take a look at how other presenters are coping with this job and what lessons you can take away from them.
1. N26 Digital Bank Pitch Deck
This is a fine business pitch presentation example, hitting all the best practices. The deck opens with a big shocking statement that most Millennials would rather go to the dentist than step into a bank branch.
Then it proceeds to discuss the company’s solution to the above — a fully digital bank with a paperless account opening process, done in 8 minutes. After communicating the main product features and value proposition, the deck further conceptualizes what traction the product got so far using data visualizations. The only thing it lacks is a solid call-to-action for closing slides as the current ending feels a bit abrupt.
2. WeWork Pitch Deck

For a Series D round, WeWork went with a more formal business presentation. It starts with laying down the general company information and then transitions to explaining their business model, current market conditions, and the company’s position on the market.
The good thing about this deck is that they quantify their business growth prospects and value proposition. The likely gains for investors are shown in concrete numbers. However, those charts go one after another in a row, so it gets a bit challenging to retain all data points.
The last part of their presentation is focused on a new offering, “We Live”. It explains why the team seeks funds to bring it to life. Likewise, they back their reasoning with market size statistics, sample projects, and a five-year revenue forecast.
3. Redfin Investor Presentation
If you are looking for a “text-light” business presentation example, Redfin’s investor deck is up to your alley. This simple deck expertly uses iconography, charts, and graphs to break down the company’s business model, value proposition, market share, and competitive advantages over similar startups. For number-oriented investors, this is a great deck design to use.
4. Google Ready Together Presentation
This isn’t quite the standard business presentation example per se. But rather an innovative way to create engaging, interactive presentations of customer case studies .
The short deck features a short video clip from a Google client, 7-11, explaining how they used the company’s marketing technology to digitally transform their operations and introduce a greater degree of marketing automation . The narrated video parts are interrupted by slides featuring catchy stats, contextualizing issues other businesses are facing. Then transitions to explaining through the words of 7-11 CMO, how Google’s technology is helping them overcome the stated shortcomings.
5. Salesforce Business Presentation Example
This is a great example of an informational presentation, made by the Salesforce team to share their research on customer experience (CX) with prospects and existing customers.
The slide deck errs on the lengthier side with 58 slides total. But bigger topics are broken down and reinforced through bite-sized statistics and quotes from the company leadership. They are also packaging the main tips into memorable formulas, itemized lists, and tables. Overall, this deck is a great example of how you can build a compelling narrative using different statistics.
6. Mastercard Business Presentation
This slide deck from Mastercard instantly captures the audience’s attention with unusual background images and major data points on the growth of populations, POS systems, and payment methods used in the upcoming decade.
Perhaps to offset the complexity of the subject, Mastercard chose to sprinkle in some humor in presentation texts and used comic-style visuals to supplement that. However, all their animations are made in a similar style, creating a good sense of continuity in design. They are also using colors to signify the transition from one part of the presentation to another.
In the second part, the slide deck focuses on distilling the core message of what businesses need to do to remain competitive in the new payments landscape. The team presents what they have been working on to expand the payment ecosystem. Then concludes with a “title close” styled call-to-action, mirroring the presentation title.
7. McKinsey Diversity & Inclusion Presentation
This fresh business slide deck from McKinsey is a great reference point for making persuasive business presentations on complex topics such as D&I. First, it recaps the main definitions of the discussed concepts — diversity, equity, and inclusion — to ensure alignment with the audience members.
Next, the business presentation deck focuses on the severity and importance of the issue for businesses, represented through a series of graphs and charts. After articulating the “why”, the narrative switches to “how” — how leaders can benefit from investment in D&I. The main points are further backed with data and illustrated via examples.
8. Accenture Presentation for the Energy Sector
Similar to McKinsey, Accenture keeps its slide deck on a short. Yet the team packs a punch within each slide through using a mix of fonts, graphical elements, and color for highlighting the core information. The presentation copy is on a longer side, prompting the audience to dwell on reading the slides. But perhaps this was meant by design as the presentation was also distributed online — via the company blog and social media.
The last several slides of the presentation deck focus on articulating the value Accenture can deliver for their clients in the Energy sector. They expertly break down their main value proposition and key service lines, plus quantify the benefits.
9. Amazon Web Services (AWS) Technical Presentation
Giving an engaging technical presentation isn’t an easy task. You have to balance the number of details you reveal on your slides to prevent overwhelm, while also making sure that you don’t leave out any crucial deets. This technical presentation from AWS does great in both departments.
First, you get entertained with a quick overview of Amazon’s progress in machine learning (ML) forecasting capabilities over the last decade. Then introduced to the main tech offering. The deck further explains what you need to get started with Amazon Forecast — e.g. dataset requirements, supported forecasting scenarios, available forecasting models, etc.
The second half of the presentation provides a quick training snippet on configuring Amazon SageMaker to start your first project. The step-by-step instructions are coherent and well-organized, making the reader excited to test-drive the product.
10. Snapchat Company Presentation
Snapchat’s business model presentation is on a funkier, more casual side, reflective of the company’s overall brand and positioning. After briefly recapping what they do, the slide deck switches to discussing the company’s financials and revenue streams.

This business slide deck by Snap Inc. itself is rather simplistic and lacks fancy design elements. But it has a strong unified theme of showing the audience Snapchat’s position on the market and projected vector of business development.
11. Visa Business Acquisition Presentation
If you are working on a business plan or M&A presentation for stakeholders of your own, this example from Visa will be helpful. The presentation deck expertly breaks down the company’s rationale for purchasing Plaid and subsequent plans for integrating the startup into their business ecosystem.
The business deck recaps why the Plaid acquisition is a solid strategic decision by highlighting the total addressable market they could dive into post-deal. Then it details Plaid’s competitive strengths. The slide deck then sums up all the monetary and indirect gains Visa could reap as an acquirer.
12. Pinterest Earnings Report Presentation

Annual reports and especially earnings presentations might not be the most exciting types of documents to work on, but they have immense strategic value. Hence, there’s little room for ambiguities or mistakes.
In twelve slides, this business presentation from Pinterest clearly communicates the big picture of the company’s finance in 2021. All the key numbers are represented as featured quotes in the sidebar with diagrams further showcasing the earning and spending dynamics. Overall, the data is easy to interpret even for non-finance folks.
To Conclude
With these business presentation design tips, presentation templates , and examples, you can go from overwhelmed to confident about your next presentation design in a matter of hours. Focus on creating a rough draft first using a template. Then work on nailing your opening slide sequence and shortening the texts in the main part of your presentation when needed. Make sure that each slide serves a clear purpose and communicates important details. To make your business presentation deck more concise, remove anything that does not pertain to the topic.
Finally, once you are done, share your business presentation with other team members to get their feedback and reiterate the final design.
Like this article? Please share
Business Presentations, Corporate Presentations, Design, Design Inspiration, Examples, Executive Reports, Inspiration, Presentation Ideas Filed under Business
Related Articles

Filed under Presentation Ideas • February 15th, 2024
How to Create a 5 Minutes Presentation
Master the art of short-format speeches like the 5 minutes presentation with this article. Insights on content structure, audience engagement and more.
Filed under Business • February 7th, 2024
How to Create & Present a Competitive Landscape Slide for Your Pitch Deck
Get to know how to properly create a winning competitive landscape slide for your pitch deck. Boost your pitch performance now.

Filed under Business • February 2nd, 2024
Business Plan Presentations: A Guide
Learn all that’s required to produce a high-quality business plan presentation in this guide. Suggested templates and examples are included.
Leave a Reply

- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
How to Make a “Good” Presentation “Great”
- Guy Kawasaki

Remember: Less is more.
A strong presentation is so much more than information pasted onto a series of slides with fancy backgrounds. Whether you’re pitching an idea, reporting market research, or sharing something else, a great presentation can give you a competitive advantage, and be a powerful tool when aiming to persuade, educate, or inspire others. Here are some unique elements that make a presentation stand out.
- Fonts: Sans Serif fonts such as Helvetica or Arial are preferred for their clean lines, which make them easy to digest at various sizes and distances. Limit the number of font styles to two: one for headings and another for body text, to avoid visual confusion or distractions.
- Colors: Colors can evoke emotions and highlight critical points, but their overuse can lead to a cluttered and confusing presentation. A limited palette of two to three main colors, complemented by a simple background, can help you draw attention to key elements without overwhelming the audience.
- Pictures: Pictures can communicate complex ideas quickly and memorably but choosing the right images is key. Images or pictures should be big (perhaps 20-25% of the page), bold, and have a clear purpose that complements the slide’s text.
- Layout: Don’t overcrowd your slides with too much information. When in doubt, adhere to the principle of simplicity, and aim for a clean and uncluttered layout with plenty of white space around text and images. Think phrases and bullets, not sentences.
As an intern or early career professional, chances are that you’ll be tasked with making or giving a presentation in the near future. Whether you’re pitching an idea, reporting market research, or sharing something else, a great presentation can give you a competitive advantage, and be a powerful tool when aiming to persuade, educate, or inspire others.
- Guy Kawasaki is the chief evangelist at Canva and was the former chief evangelist at Apple. Guy is the author of 16 books including Think Remarkable : 9 Paths to Transform Your Life and Make a Difference.
Partner Center

IMAGES
VIDEO
COMMENTS
7,063 templates. Create a blank Business Presentation. Beige Brown Minimal Organic Creative Project Presentation. Presentation by Equipo de Pronoia Studio. Blue Dark Professional Geometric Business Project Presentation. Presentation by Olmos Carlos. Brown Minimalist Casual Fashion Collection Presentation.
4,627 templates. Create a blank Professional Presentation. Pink Rose Watercolor Organic Creative Project Presentation. Presentation by Equipo de Pronoia Studio. Purple & white business profile presentation. Presentation by ARP Creation. Orange and white modern creative marketing plan Presentation.
Download the "Contrasted Grayscale Business Plan" presentation for PowerPoint or Google Slides. Conveying your business plan accurately and effectively is the cornerstone of any successful venture. This template allows you to pinpoint essential elements of your operation while your audience will appreciate the clear and concise presentation ...
Download the "Post Merger Integration" presentation for PowerPoint or Google Slides and take your marketing projects to the next level. This template is the perfect ally for your advertising strategies, launch campaigns or report presentations. Customize your content with ease, highlight your ideas and captivate your audience with a professional...
Download your presentation as a PowerPoint template or use it online as a Google Slides theme. 100% free, no registration or download limits. Create captivating presentations with these business slideshow templates that will leave a lasting impression. No Download Limits Free for Any Use No Signups.
These templates can also be used in Google Slides and Canva, so you can work in the platform you're most comfortable with. Designed for business professionals, students, and teachers, these templates are perfect for presenting data, making a sales pitch, or delivering a lecture. Make your professional presentations stand out with these templates.
5 Quick Tips to Make Any Business Presentation More Professional. When building a professional PowerPoint presentation, you need more than slide designs. ... 22+ Best Free Dark PowerPoint Background Templates for 2024 PPT Presentations. Barni Rajah. 09 Dec 2023. Common PowerPoint Business Presentation Questions Answered (FAQ)
Zeiro - Business Template for PowerPoint. This modern professional PowerPoint background is designed for businesses. The business template for PowerPoint has 15 slides, documentation, editable content, and plenty of visualization elements. Maleo - Professional PowerPoint Template.
Futuristic Background. When you need to impress everybody and stay relevant, you must look ahead and aim to be the first. Take a peek into the future with this new template Slidesgo has just designed. It's free and perfect for techie topics or just for giving your presentation a futuristic vibe! Multi-purpose. 16:9.
Captivate your audience with our collection of professionally-designed PowerPoint and Google Slides templates. Boost your presentations and make a lasting impression!
PowerPoint background templates are created with PowerPoint vector graphics, allowing the user to fully customize its appearance and effects. You can include the backgrounds in your existing presentations without any issues and keep the visual quality of the shapes. Our backgrounds can be adjusted to different aspect ratios and presentation ...
1 Pattern Background With a Color Overlay. There are lots of photographable objects and sections of architecture that can resemble patterns. For example, concrete slabs with holes, corrugated iron, or paneling. Add a strong color overlay with a little transparency and you've got a versatile presentation background.
But even if used somewhere else, it will still do a great job, unless used in all slides. FREE DOWNLOAD. 5. Business Handshake Network Creation Background. An amazing background for corporate presentations that is perfect for teamwork, business communication, partners, or proposals slides. FREE DOWNLOAD. 6.
The Business Tag gallery contains Professional Business PowerPoint Templates which range from 8 to 41 slides. Each template provides unique designs targeted for business applications. With these, you can prepare your business presentations using the appropriate tool, framework, diagram or content. The master design of the business templates ...
Business LinkedIn background images. Adding a background image to your personal or company LinkedIn page gives you another way to showcase your personality and brand to your network. As with other platforms, LinkedIn offers image recommendations, namely that banner background images should be 1,584 by 396 pixels.
The Professional Business Presentation Template is a company profile presentation slide deck. It will help present business information such as products and services, skills, expertise, growth success, etc. It is a collection of 16 creative slide layouts with blue, gray, and white color themes. This is a commonly used business theme for ...
Express - Freestyle PowerPoint Template. Express is a unique PowerPoint template with a modern and a creative design that will certainly make your presentations stand out. It includes 30 slides featuring attractive brush-strokes, vectors, icons, and graphics. The template is also available in 3 different color schemes.
Business Presentation Background Images. Images 100k Collections 370. ADS. ADS. ADS. Page 1 of 100. Find & Download Free Graphic Resources for Business Presentation Background. 100,000+ Vectors, Stock Photos & PSD files. Free for commercial use High Quality Images.
Free Google Slides theme, PowerPoint template, and Canva presentation template. A perfect speech, convincing data, and an amazing design are the perfect ingredients for a successful business meeting. There are lot of meetings happening in Slidesgo, that's why we know that a good design is a key factor if you want your audience to pay ...
396,272 Free images of Presentation Background. Presentation background images for free download. Browse or use the filters to find your next picture for your project. Find images of Presentation Background Royalty-free No attribution required High quality images.
Business Background Images. Boost your professional image with these business backgrounds, designed for LinkedIn, PowerPoint, and Zoom. Whether you're making a strong impression in the boardroom, delivering impactful presentations, or participating in virtual meetings, these backgrounds are your key to an influential presence.
Compelling business presentations are key to communicating important ideas, persuading others, and introducing new offerings to the world. Hence, why business presentation design is one of the most universal skills for any professional. This guide teaches you how to design and deliver excellent business presentations.
Read more on Business communication or related topics Power and influence, Presentation skills and Public speaking Carmine Gallo is a Harvard University instructor, keynote speaker, and author of ...
When in doubt, adhere to the principle of simplicity, and aim for a clean and uncluttered layout with plenty of white space around text and images. Think phrases and bullets, not sentences. As an ...