Stem Cell Research: Some Pros and Cons Essay
Introduction, works cited.
The benefits to society by the introduction of new medical technologies have been considerable. For example, the introduction of vaccines and antibiotics has significantly improved the well-being of people all over the globe. The science of stem cell treatments, potentially as or more significant than these other innovations, is beginning a new stage of exploration and growth that could be the forerunner of unprecedented cures and therapies. The present enthusiasm over prospective stem cell-produced remedies radiates from the new innovations of genetic biology.
Though one cannot forecast the results from basic research, there is enough information available to suggest that a good deal of this enthusiasm is justified.
The moral dilemma that surrounds the prohibition of aborted fetuses is the idea of abortion itself. Why would pro-lifers want to witness what they believe is a living being tossed away in vain? At least its ‘life’ could have meant something to humanity in a very real way. In 1999 alone, more than 850,000 abortions were performed in the U.S. (Elam-Evans et al, 2002). Whatever moral or political position, the fact is, all these fetuses could have served advance scientific and medical knowledge in immeasurable ways. Abortion laws vary state by state but the vast majority allow for abortions to be performed at least through the second trimester, 24 weeks into the pregnancy. This limitation was derived from the neurological point of view, which conforms to our society’s distinctness for the death as the absence of a cerebral EEG (electroencephalogram) pattern. This same definition must therefore also define life as there are no alternatives to these two options. The presence of the EEG pattern of a fetus can be detected approximately 27 weeks into the pregnancy. An embryo is referred to as a fetus at about seven to eight weeks following fertilization. At about four to five weeks, embryonic germ cells, about 2 mm long, are developing (Morowitz & Trefil, 1992).
More than half of European countries and others around the world such as Japan allow for embryonic stem cell research in various degrees. Australia followed the UK in allowing the use of tissue from aborted fetuses, with the parent’s consent, for scientific experimentation. “Here in Australia we would be allowed to use it [aborted fetus for embryonic research]. There would be no impediment to that” (Robotham & Smith, 2002). According to Health-Day, a daily news service reporting on consumer health, Swiss physicians at the University of Lausanne discovered that a two-and-a-half-inch piece of skin from a fetus, which was aborted at 14 weeks, provided several million grafts that were used to treat burn victims. The study also found that skin cells from an aborted fetus healed burns faster than standard grafts. Patrick Hohlfeld, the prime author of the study said “the use of fetal skin has tremendous potential because taking just one skin graft gives you the potential to treat thousands of people” (Strode, 2005).
Scientists provide the valid argument that embryos cannot be considered humans because of their stage of development. Embryonic stem cells are collected from embryos that are four to five days old. In this stage of development, they are called blastocysts and are smaller in diameter than a human hair. When viewed by a microscope, the blastocyst contains fewer than 200 cells and had no features that are recognizable as human nor has the capacity to feel any sensations including pain. An embryo only four or five days old does not yet contain any cells that are dedicated to making up bodily tissues. “Stem cells have traditionally been defined as not fully differentiated yet to be any particular type of cell or tissue” (Irving, 1999). An embryo this young in a woman’s body would not have as yet attached to the uterine wall. Therefore, the viability of the embryo is certainly not assured and is, in fact, unlikely. It can be argued that it could not possess a soul as well, at least not an individual soul.
Political, not prudent considerations are the cause of the stifling of embryonic stem cell research. Other countries will be much further advanced in this science and therefore reap the financial benefits. However, despite the human health and economic advantages of embryonic stem cell research, the ‘moralists’ of the right-wing refuse to give up their flawed reasoning. This is likely the result of refusing to become educated on the issue while employing a neutral, unbiased frame of mind. Inevitably, stem cell research will be commonplace and hopefully sooner than later but until then many people will continue to suffer from debilitating diseases and paralysis. Where is the morality in that? Who are these people that consider the life of a living human being less important than a four or five-day-old embryo?
Elam-Evans, Laurie D.; Strauss, Lilo T.; Herndon, Joy; Parker, Wilda Y.; Whitehead, Sara; & Berg, Cynthia J. “Abortion Surveillance – United States, 1999.” Morbidity and Mortality Weekly Report. Atlanta, GA: Center for Disease Control. (2002).
Irving, Dianne N.
“Stem Cell Research: Some Pros and Cons.” Written on request of Fr. Thomas King, S.J., Ph.D., Department of Theology, Georgetown University; President, University Faculty For Life, for their newsletter, UFL Pro-Vita. (1999).
Morowitz, H. J. & Trefil, J. S. The Facts of Life: Science and the Abortion Controversy. New York: Oxford University Press. (1992).
Robotham, Julie & Smith, Deborah. “Abortions Set to Fuel Stem Cell Research.” The Sydney Morning Herald. (2002).
Strode, Tom. “Life Digest: New Stem Cell Research Encouraging but Problematic; Researchers Find New Use for Aborted Babies.” Baptist Press News. (2005).
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, September 22). Stem Cell Research: Some Pros and Cons. https://ivypanda.com/essays/stem-cell-research-some-pros-and-cons/
"Stem Cell Research: Some Pros and Cons." IvyPanda , 22 Sept. 2021, ivypanda.com/essays/stem-cell-research-some-pros-and-cons/.
IvyPanda . (2021) 'Stem Cell Research: Some Pros and Cons'. 22 September.
IvyPanda . 2021. "Stem Cell Research: Some Pros and Cons." September 22, 2021. https://ivypanda.com/essays/stem-cell-research-some-pros-and-cons/.
1. IvyPanda . "Stem Cell Research: Some Pros and Cons." September 22, 2021. https://ivypanda.com/essays/stem-cell-research-some-pros-and-cons/.
Bibliography
IvyPanda . "Stem Cell Research: Some Pros and Cons." September 22, 2021. https://ivypanda.com/essays/stem-cell-research-some-pros-and-cons/.
- Chiropractic Treatment in Electroencephalography
- Uses of EEG Waves to Control MIDI
- Incidence of Pain Following Anterior Cruciate Ligament Reconstruction
- Aborted Take-Off of a Large Twin-Engine Commercial Aircraft
- Ethics of Stem Cell Research Creating Superhumans
- Using Embryonic Stem Cells to Grow Body Parts
- Wound Care and Skin Graft
- Epilepsy Prediction Using Machine Learning Method
- Tissue Engineering: Anterior Cruciate Ligament Reconstruction
- Embryonic Stem Cells and Nuclear Transfer
- Small Medical Business in Third World Countries
- "Drug Makers Tighten Their Belts Again" by Loftus and Berton
- Maraviroc: FDA Approved Drug
- Psychoactive Drugs and Their Effect on the Brain
- Pharmacist's Role During Opioid Crisis in the USA

- Foundations
- Write Paper

Search form
- Experiments
- Anthropology
- Self-Esteem
- Social Anxiety
- Foundations >
Stem Cell Research
Pros and cons in research.
The debate of the pros and cons of stem cell research clearly illustrate the difficult ethics evaluations researchers sometimes must do.
This article is a part of the guide:
- Ethics in Research
- Tuskegee Syphilis Study
- Privacy for Participants
- Scientific Misconduct
Browse Full Outline
- 1 Ethics in Research
- 2.1.1 Tuskegee Syphilis Study
- 3 Privacy for Participants
- 4 Animals in Research
- 5 Stem Cells
- 6.1 Scientific Misconduct
- 6.2.1 Subliminal Messages - An Example of Fraud
- 6.2.2 Scientific Falsification
- 6.3 Grant Funding
- 7.1 Academic Plagiarism
- 7.2 Sham Peer Review
- 8 Whistleblowers
All scientists must consider whether the positive effects from their research are likely to be significantly higher than the negative effects.
What are Stem Cells?
Stem Cells are crucial to develop organisms. They are nonspecialized cells which have the potential to create other types of specific cells, such as blood-, brain-, tissue- or muscle-cells.
Stem cells are in all of our body and lives, but are far more potent in a fetus (also spelled foetus, fœtus, faetus, or fætus) than in an adult body.
Some types of stem cells may be able to create all other cells in the body. Others have the potential to repair or replace damaged tissue or cells.
Embryonic Stem Cells are developed from a female egg after it is fertilized by sperm. The process takes 4-5 days.

What is Stem Cell Research?
Stem cell research is used for investigation of basic cells which develop organisms. The cells are grown in laboratories where tests are carried out to investigate fundamental properties of the cells.
The controversy surrounding stem cell research led to an intense debate about ethics. Up until the recent years, the research method mainly focused on Embryonic Stem Cells, which involves taking tissue from an aborted embryo to get proper material to study. This is typically done just days after conception or between the 5th and 9th week.
Since then, researchers have moved on to more ethical study methods, such as Induced Pluripotent Stem Cells (iPS). iPS are artificially derived from a non-pluripotent cell, such as adult somatic cells.
This is probably an important advancement in stem cell research, since it allows researchers to obtain pluripotent stem cells, which are important in research, without the controversial use of embryos.
There were two main issues concerning stem cell research with both pros and cons:
- How the knowledge will be used
- Concerns about the methods
The first issue is really not just about stem cell research, as it may be applied to most research about human health.
Since 2007, the second point, concerns about the methods involved, has been less debated, because of scientific developments such as iPS.
1) Stem Cell Research - Arguments Regarding the Usage of the Knowledge
As you will most probably notice, the following arguments are not exclusively in use when talking about stem cell research.
Stem cell research can potentially help treat a range of medical problems. It could lead humanity closer to better treatment and possibly cure a number of diseases:
- Parkinson’s Disease
- Alzheimer’s Disease
- Heart Diseases, Stroke and Diabetes (Type 1)
- Birth Defects
- Spinal Cord Injuries
- Replace or Repair Damaged Organs
- Reduced Risk of Transplantation (You could possibly get a copy of your own heart in a heart-transplantation in the future
- Stem cells may play a major role in cancer
Better treatment of these diseases could also give significant social benefits for individuals and economic gains for society
- "We should not mess with human life."
- "Humans should not be trying to play God"
- Some argue that stem cell research in the far future can lead to knowledge on how to clone humans. It is hard to say whether this is true, but we have seen devastating consequences of other research-programs, even with good intentions, such as nuclear research.
2) Stem Cell Research - Pros and Cons About the Methods Involved
The controversy regarding the method involved was much tenser when researchers used Embryonic Stem Cells as their main method for stem cell research.
DISCLAIMER: These points are based on the old debate about the methods of stem cells research, from before 2007. Since then, scientists have moved on to use more ethical methods for stem cell research, such as iPS. This section serves as an illustration of the difficult evaluations researchers may have to analyze.
Pros Before 2007
- "The benefits of stem cell research have such a great outcome that they outweigh the ethical issues." (Cost-benefit-analysis)
- "If someone is going to have an abortion, isn’t it better that we use it for something useful?"
- Adult stem cells would not be that interesting because they do not have the same properties as stem cells from a fetus.
- The research would give great insights about the basics of the body.
Cons Before 2007
- Critics against stem cell research argued that the ethical issues of scientific work on aborted fetuses did not justify the possible benefits.
- "A life is a life and that should never be compromised. A fertilized egg should be valued as a human life even if it is in its very first weeks. Destroying human life in the hopes of saving human life is not ethical."
- We should (and will) develop more ethical methods (such as using adult stem cells) which will enable us to research ethically. We should wait until those methods are available.
- The scientific value has been overstated or has flaws. E.g. we do not know for sure that we can use stem cells to clone transplantable organs.
The stem cell-research is an example of the, sometimes difficult, cost-benefit analysis in ethics which scientists need to do. Even though many issues regarding the ethics of stem cell research have now been solved, it serves as a valuable example of ethical cost-benefit analysis.
The previously heated debate seems to have lead to new solutions which makes both sides happier.
Stem Cell pros and cons had to be valued carefully, for a number of reasons.
When you are planning a research project, ethics must always be considered. If you cannot defend a study ethically, you should not and will not be allowed to conduct it. You cannot defend a study ethically unless the presumed cost is lower than expected benefits. The analysis needs to include human/animal discomfort/risks, environmental issues, material costs/benefits, economy etc.
Why was the debate regarding the stem cell research so intense?
First, it was a matter of life - something impossible to measure. And in this case, researchers had to do exactly that: measure life against life.
Both an abortion and someone dying, suffering from a possible curable disease, is a tragedy. Which have the highest value? Does a big breakthrough in the research justify the use of the method in the present?
Would the benefits of studying abortions outweigh the costs? The choice was subjective: Nobody knows all the risks or all the possible outcomes, so we had to value it with our perception of the outcome. Perception is influenced by our individual feelings, morals and knowledge about the issue.
Second, at the time we did not know whether the research was necessary and sufficient to give us the mentioned health benefits.
Third, other consequences of the research are uncertain. Could the research be misused in the future or not? We simply do not know. All knowledge acquired, within research or other arenas, may be used for evil causes in the future - it is impossible to know.
The Stem cell research-debate is an example on how people value various aspects differently. It is also an example of how critics and debate can lead to significant improvements for both sides.
- Psychology 101
- Flags and Countries
- Capitals and Countries
Explorable.com (Mar 20, 2008). Stem Cell Research. Retrieved May 04, 2024 from Explorable.com: https://explorable.com/stem-cell-pros-and-cons
You Are Allowed To Copy The Text
The text in this article is licensed under the Creative Commons-License Attribution 4.0 International (CC BY 4.0) .
This means you're free to copy, share and adapt any parts (or all) of the text in the article, as long as you give appropriate credit and provide a link/reference to this page.
That is it. You don't need our permission to copy the article; just include a link/reference back to this page. You can use it freely (with some kind of link), and we're also okay with people reprinting in publications like books, blogs, newsletters, course-material, papers, wikipedia and presentations (with clear attribution).
Related articles
Embryonic Stems Cells - Nobel Prize Medicine 2007
Want to stay up to date? Follow us!
Save this course for later.
Don't have time for it all now? No problem, save it as a course and come back to it later.
Footer bottom
- Privacy Policy
- Subscribe to our RSS Feed
- Like us on Facebook
- Follow us on Twitter

- Types of Stem Cell
- History of Stem Cell Use
- Importance of Stem Cells
- Pros and Cons
- Stem Cell FAQs
- Stem Cells at UNMC
Pros and Cons of Using Various Stem Cells
- Abundant somatic cells of donor can be used
- Issues of histocompatibility with donor/recipient transplants can be avoided
- Very useful for drug development and developmental studies

11 Stem Cell Research Pros and Cons
Stem cell research can be classified into two specific areas: embryonic stem cells and non-embryonic stem cells. Amniotic, induced pluripotent, and adult stem cells do not involve the creation or destruction of a human embryo to have them collected.
Even embryonic stem cells can be collected, to some extent, without the destruction of an embryo. Modern collection techniques include using stem cells that are found in the umbilical cord, in breast milk, or even in bone marrow.
The primary benefit of stem cell research is its clear potential. Since 1868, the idea of using stem cells as a medical treatment has been contemplated in one way or another, especially as we began to understand their full potential. With stem cell therapies, we have the potential to treat injuries, degenerative conditions, or even a genetic disease or disorder.
As for the primary disadvantage of stem cell research, the ethics of collecting embryonic stem cells tends to dominate the conversation. To some people, the idea of destroying an embryo to harvest cells equates to murder. For others, they see the hundreds of thousands of frozen embryos, many of which are simply thrown away after being stored for too long, as wasted potential.
Here are some additional stem cell research pros and cons to review.
List of the Pros of Stem Cell Research
1. It could treat several conditions that are virtually untreatable right now. Stem cell research opens numerous avenues for treatments or a cure to be found for several conditions that are either untreatable or without a cure today. Everything from Alzheimer’s disease to Parkinson’s disease to ALS could be improved. People who have a spinal cord injury could receive an injection of stem cells and potentially start the recovery process. Even mental health issues, such as schizophrenia, could one day be treated with stem cell applications.
2. It provides us with greater knowledge. By researching stem cells, we understand more about the growth process of humans. We learn more about how cells form and interact with one another. We can examine pluripotent cells, both induced and embryonic, to see what information is required for them to turn into a specific tissue cell. With a greater understanding of this micro-environment, we can learn more about who we are at our very core.
3. It offers new methods of testing. When new medical treatments are proposed, they must go through multiple stages of testing. This includes animal trials and human trials, which may or may not be successful. As our knowledge of stem cells grows, we could transition testing methods so that only cell populations are examined for a response instead of an innocent animal or a paid human research contributor. That may improve safety, reduce fatalities, and even speed up the approval process.
4. It reduces the risk of rejection. Many stem cell therapies today use the cells that are collected from a patient’s body. Because the cells are their own, the risk of rejection is reduced or even eliminated. If stem cells could be induced to form into organ tissues, such as a kidney, then the science of organ transplantation could be forever changed. Imagine growing a kidney that is a genetic match instead of trying to find a donor organ that could be rejected, even if a direct match is found. That is the potential of this medical research.
5. It could stop birth defects and mutations before they happen. By understanding the process of stem cell development, it could be possible to change the embryonic development process. Chromosomal concerns, birth defects, and other errors in development could be corrected before birth, giving more newborns a real chance to experience the gift of life. At the same time, the risks of pregnancy loss and health risks to new mothers could be decreased.
List of the Cons of Stem Cell Research
1. We have no idea about long-term side effect issues. According to the Canadian Cancer Society, there are several common short-term side effects that are associated with stem cell therapies. They may include infection, bleeding, skin or hair problems, unexplained pain, organ problems, or even the development of a secondary cancer. Every medical treatment provides some risk of a side effect, but this medical technology is so new that we have no idea what the long-term health effects might be.
2. It provides a health risk to everyone involved. Collecting stem cells from an adult carries a medical risk with it. Something could go wrong during the collection process that may reduce the quality of life for the patient. Their life could even be placed at-risk. For embryonic collection, the destruction of the blastocytes that are formed during egg fertilization is required. Since the embryo is technically a different form of human life, there will always be the chance of rejection occurring since the cells are not one’s own.
3. Adult stem cells offer limited potential. Our current stem cell research findings indicate that adult stem cells that have already transitioned into specific tissues or formats because of their body location will stay that way. That means stem cells taken from muscle tissue would only be able to create additional muscle tissues. Even if they are induced to be pluripotent, the end result tends to be duplication instead of identification because they have a determined type.
4. It is still an unproven medical technology. There is a lot of hope for stem cell treatments. Hematopoietic stem cell transplantation is performed about 50,000 times annually around the world and the success rate for the treatment is climbing above 90%. Because some forms of stem cell research are classified as illegal or immoral in the United States, however, progress to improve treatments or prove the effectiveness of this medical technology are not as advanced as their potential.
5. It isn’t cheap. Stem cell therapies are far from affordable. Because most health insurers classify this type of treatment as “experimental,” it is rarely a covered procedure. Most treatments that are approved for use in the US cost more than $10,000 per procedure. Some treatment options are six figures. Even the cost of harvesting stem cells from an embryo is a couple thousand dollars. Access to this technology is restricted to socioeconomic means globally and to almost everyone in the United States.
6. Opportunities are limited. Although stem cell research isn’t technically forbidden in the US, there are just 19 stem cell lines available for government grants and funding thanks to legislative restrictions that are enacted in 2001. Certain states have begun to draft legislation to completely ban stem cell research, or at least embryonic stem cell research, or at least place major restrictions on the process.
We should examine the ethics of embryonic stem cell research, but we should also examine the benefits it may provide. Adult stem cells, collected from consenting parties, should have no criticism whatsoever. As we move forward in this research, new pros and cons may also require additional contemplation. One thing is for certain: these stem cell research pros and cons show us that humanity is complex, beautiful, and wonderful in many ways.
Pros & Cons of Embryonic Stem Cell Research
- Liberal Voices and Events
- The U. S. Government
- U.S. Foreign Policy
- U.S. Conservative Politics
- Women's Issues
- Civil Liberties
- The Middle East
- Race Relations
- Immigration
- Crime & Punishment
- Canadian Government
- Understanding Types of Government
- M.B.A., California State University, Long Beach
- B.A., Journalism and Nonfiction Writing, University of California, Los Angeles
On March 9, 2009, President Barack Obama lifted, by Executive Order , the Bush administration's eight-year ban on federal funding of embryonic stem cell research .
Remarked the President, "Today... we will bring the change that so many scientists and researchers, doctors and innovators, patients and loved ones have hoped for, and fought for, these past eight years."
In Obama's Remarks on Lifting the Embryonic Stem Cell Research Ban, he also signed a Presidential Memorandum directing the development of a strategy for restoring scientific integrity to government decision-making.
Bush Vetoes
In 2005, H.R. 810, the Stem Cell Research Enhancement Act of 2005, was passed by the Republican-led House in May 2005 by a vote of 238 to 194. The Senate passed the bill in July 2006 by a bipartisan vote of 63 to 37.
President Bush opposed embryonic stem cell research on ideological grounds. He exercised his first presidential veto on July 19, 2006, when he refused to allow H.R. 810 to become law. Congress was unable to muster enough votes to override the veto.
In April 2007, the Democratic-led Senate passed the Stem Cell Research Enhancement Act of 2007 by a vote of 63 to 34. In June 2007, the House passed the legislation by a vote of 247 to 176.
President Bush vetoed the bill on June 20, 2007.
Public Support for Embryonic Stem Cell Research
For years, all polls report that the American public STRONGLY supports federal funding of embryonic stem cell research.
Reported the Washington Post in March 2009 : "In a January Washington Post-ABC News poll, 59 percent of Americans said they supported loosening the current restrictions, with support topping 60 percent among both Democrats and independents. Most Republicans, however, stood in opposition (55 percent opposed; 40 percent in support)."
Despite public perceptions, embryonic stem cell research was legal in the U.S. during the Bush administration: the President had banned the use of federal funds for research. He did not ban private and state research funding, much of which was being conducted by pharmaceutical mega-corporations.
In Fall 2004, California voters approved a $3 billion bond to fund embryonic stem cell research. In contrast, embryonic stem cell research is prohibited in Arkansas, Iowa, North and South Dakota and Michigan.
Developments in Stem Cell Research
In August 2005, Harvard University scientists announced a breakthrough discovery that fuses "blank" embryonic stem cells with adult skin cells, rather than with fertilized embryos, to create all-purpose stem cells viable to treat diseases and disabilities.
This discovery doesn't result in the death of fertilized human embryos and thus would effectively respond to pro-life objections to embryonic stem cell research and therapy.
Harvard researchers warned that it could take up to ten years to perfect this highly promising process.
As South Korea, Great Britain, Japan, Germany, India and other countries rapidly pioneer this new technological frontier, the US is being left farther and farther behind in medical technology. The US is also losing out on billions in new economic opportunities at a time when the country sorely needs new sources of revenues.
Therapeutic cloning is a method to produce stem cell lines that were genetic matches for adults and children.
Steps in therapeutic cloning are:
- An egg is obtained from a human donor.
- The nucleus (DNA) is removed from the egg.
- Skin cells are taken from the patient.
- The nucleus (DNA) is removed from a skin cell.
- A skin cell nucleus is implanted in the egg.
- The reconstructed egg, called a blastocyst, is stimulated with chemicals or electric current.
- In 3 to 5 days, the embryonic stem cells are removed.
- The blastocyst is destroyed.
- Stem cells can be used to generate an organ or tissue that is a genetic match to the skin cell donor.
The first 6 steps are same for reproductive cloning . However, instead of removing stem cells, the blastocyst is implanted in a woman and allowed to gestate to birth. Reproductive cloning is outlawed in most countries.
Before Bush stopped federal research in 2001, a minor amount of embryonic stem cell research was performed by US scientists using embryos created at fertility clinics and donated by couples who no longer needed them. The pending bipartisan Congressional bills all propose using excess fertility clinic embryos.
Stem cells are found in limited quantities in every human body and can be extracted from adult tissue with great effort but without harm. The consensus among researchers has been that adult stem cells are limited in usefulness because they can be used to produce only a few of the 220 types of cells found in the human body. However, evidence has recently emerged that adult cells may be more flexible than previously believed.
Embryonic stem cells are blank cells that have not yet been categorized or programmed by the body and can be prompted to generate any of the 220 human cell types. Embryonic stem cells are extremely flexible.
Embryonic stem cells are thought by most scientists and researchers to hold potential cures for spinal cord injuries, multiple sclerosis, diabetes, Parkinson's disease, cancer, Alzheimer's disease, heart disease, hundreds of rare immune system and genetic disorders and much more.
Scientists see almost infinite value in the use of embryonic stem cell research to understand human development and the growth and treatment of diseases.
Actual cures are many years away, though, since research has not progressed to the point where even one cure has yet been generated by embryonic stem cell research.
Over 100 million Americans suffer from diseases that eventually may be treated more effectively or even cured with embryonic stem cell therapy. Some researchers regard this as the greatest potential for the alleviation of human suffering since the advent of antibiotics.
Many pro-lifers believe that the proper moral and religious course of action is to save existing life through embryonic stem cell therapy.
Some staunch pro-lifers and most pro-life organizations regard the destruction of the blastocyst, which is a laboratory-fertilized human egg, to be the murder of human life. They believe that life begins at conception, and that destruction of this pre-born life is morally unacceptable.
They believe that it is immoral to destroy a few-days-old human embryo, even to save or reduce suffering in existing human life.
Many also believe that insufficient attention been given to explore the potential of adult stem cells, which have already been used to successfully cure many diseases. They also argue that too little attention has been paid to the potential of umbilical cord blood for stem cell research. They also point out that no cures have yet been produced by embryonic stem cell therapy.
At every step of the embryonic stem cell therapy process, decisions are made by scientists, researchers, medical professionals and women who donate eggs...decisions that are fraught with serious ethical and moral implications. Those against embryonic stem cell research argue that funding should be used to greatly expand adult stem research, to circumvent the many moral issues involving the use of human embryos.
Lifting the Ban
Now that President Obama has lifted the federal funding ban for embryonic stem cell research, financial support will soon flow to federal and state agencies to commence the necessary scientific research. The timeline for therapeutic solutions available to all Americans could be years away.
President Obama observed on March 9, 2009, when he lifted the ban:
"Medical miracles do not happen simply by accident. They result from painstaking and costly research, from years of lonely trial and error, much of which never bears fruit, and from a government willing to support that work...
"Ultimately, I cannot guarantee that we will find the treatments and cures we seek. No President can promise that.
"But I can promise that we will seek them -- actively, responsibly, and with the urgency required to make up for lost ground."
- The Obama Administration's Animal Protection Record, 2010-2011
- President Obama's Domestic Agenda
- Pros and Cons of Government Healthcare
- History of the North American Free Trade Agreements
- 5 Reasons Why Obama Won the 2008 U.S. Presidential Election
- Pros & Cons of the Death Penalty
- Biography of Joe Biden, 46th President of the United States
- Biography of Julián Castro, 2020 Presidential Candidate
- What Are U.S. Farm Subsidies?
- Biography of Elizabeth Warren, Senator and Scholar
- Biography of Ross Perot, Third-Party Presidential Candidate
- Congress Members Who Voted Against the 2002 Iraq War
- The Top 3 Arguments for Gun Control
- Top 10 Must-Reads for Liberals
- New Challenges to the Death Penalty
- Overview of Teddy Roosevelt's Bull Moose Party Beliefs
Pros and Cons of Stem Cell Research
Introduction.
There are no other cells in the human body that can generate more different cells than stem cells. Research scientists have developed an interest in stem cells’ composition and applicability in the medical field (Wang et al., 2017). Cell division of the stem cells can generally occur in the body or laboratories to create more different cells. The newly formed stem cells either become specialized for other functions or become new stem cells. Stem cells are of three different types (1) embryonic stem cells (ESCs), (2) adult stem cells, (3) induced pluripotent stem cells (iPSCs). The ECSs are generated from the blastocyst-stage embryos’ interior cell mass, iPSCs emanate from the somatic cells through genetic reprogramming, and adult stem cells are derived from fully developed tissues. Stem cells can renew and differentiate themselves on their own into many cell lines.
The ability of stem cells to undergo differentiation into different forms makes them admissible in treating many chronic diseases. The iPSCs and ESCs are pluripotent cells that undergo differentiation to form cells meant for different adult heredities such as the endoderms, ectoderms, and mesoderms (Wang et al., 2017). The adult stem cells are in two forms, namely, unipotent and multipotent stem cells. The multipotent stem cells also undergo differentiation to form different cell types under a single lineage. For instance, mesenchymal stem cells can undergo differentiation to form fat cells, osteoblasts, and chondrocytes. Unipotent stem cells undergo differentiation into only one cell type, such as the epidermal or satellite stem cells. However, it is worth noting that stem cell research application faces criticism from fatalities resulting from the protracted time of suppressed immunity after transplants; the ability to self-renew and differentiate into different lineages makes stem cell admissible in tissue engineering and treatment of diseases related to the central nervous system (CNS), heart, and brain in human beings.
Pros of Stem Cells Research
Following advancements in medical field research, MSCs have become frequently used in tissue engineering and regenerative treatment. MSCs were first discovered in the bone marrow. Still, science has proven that they are usually situated around the sinusoidal endothelium, whereby they are closely associated with neighborhood hematopoietic stem cells (Fitzsimmons et al., 2018). Besides the bone marrow, MSCs are also localized in various adult tissues such as the tendons, cartilages, lungs, skin, hearts, brain, kidneys, adipose tissues, and pancreas. The MSCs are obtained from many tissues such as the umbilical cords, bone marrow, and adipose tissue. The MSCs can also be cultured before their medical application. The MSC suspensions are introduced through injections or intravenously depending on the desired therapeutical purpose. When aiming to engineer specific tissues, the MSCs are first facilitated to differentiate towards a particular desired cell type. Then after that, they are implanted surgically, usually together with the scaffold materials. MCSs are used in the treatment of autoimmune ailments or stimulation of local tissue maintenance.
The relentless effort from stem cell researchers has yearned to introduce medical practices that are less aggressive and more efficient in treating diseases. The pluripotent stem cells have been reported to be suitable in therapeutical methods since they easily distinguish into different cell types (Rikhtegar et al., 2019). Researchers have given the identification of fully developed CSCs and their capability to repair the body tissues emphasis. Research scientists have shown that iPSCs are broadly applicable in constructing disease models and the formulation of treatment transplants. Additionally, iPSC derivatives have also been significantly proposed for the experimental treatments of neurological diseases. It is worth noting that stem cell research scientists have brought about substantial knowledge about how tissue regeneration can help repair damaged parts of the human body. Treatments on heart and brain diseases have been made possible by applying stem cell research findings (Song et al., 2018). The inception of stem cell application in the medical field has proposed various medical practices that are more effective in treating chronic diseases.
Tissue Regeneration
Stem cells are self-renewing and undergo differentiation into several lineages. The stem cells have been proven to maintain, generate and replace the incurably differentiated cells in their particular tissues resulting from tissue injuries (Fitzsimmons et al., 2018; Song et al., 2018). Tissue engineering encompasses three fundamental parts, namely
- the source or cells must have the suitable genetic composition and phenotype to successfully retain the particular functioning of the tissue
- the scaffolds housing the cells serve as the substitutes for the injured tissues
- bioreactive components or signals that trigger cells into functioning. The sources of the stem cells used in tissue engineering comprise adult stem cells or embryonic stem cells.
Downstream strategies have been embraced recently in tissue engineering and making the whole venture more promising. The downstream process entails implanting the precultured cells into the damaged part of the body and their synthetic scaffold complexes (Fitzsimmons et al., 2018; Song et al., 2018). The sources or cells taken away from the host’s target tissues are then expanded into vitro. They are then preseeded to the scaffold to offer a porous 3D component that provides accommodation to the seeded cells, forming an extracellular matrix. After that, various approaches such as cell printing, sheeting, aggregation, and micro-fabrication are employed in the generation of modular tissues. The abovementioned modular tissues are then accumulated randomly or cell sheets stacked into engineered tissues with a particular micro-architectural characteristic. Later, the tissues are transplanted into the damaged part of the human body. The method enables scientists to change the nanostructure of the components by regulating polymer degradation rates with the extracellular matrix generation and cellular infiltrations, increasing cell binding sequences.
The upstream alternative makes tissue engineering a promising venture through the combination of cells and biomaterial scaffolds. The upstream method encompasses two strategies of manufacturing the engineered tissues (1) culturing and consolidating biomaterial scaffolds and cells is carried out till the cells fill up the supportive structure, thus forming the engineered tissue. (2) The delivery of the integrated biomolecules and acellular scaffolds occurs following an injury. It can optionally incorporate progenitor cells within the defective area and facilitate differentiation and differentiation, making the injured tissue repaired (Fitzsimmons et al., 2018; Song et al., 2018). The upstream approach entails the combination and culturing of biomaterial scaffolds and cells into engineered tissue.
Treatment of Neurological Disorders
Neurological disorders are generally irreversible owing to insufficient production in the central nervous system. The central nervous system is deemed the most intricate and least understood system in a human being (Song et al., 2018). Diseases related to the central nervous system usually result in permanent damage to the nervous tissue structures and functioning. Through the research on stem cells’ rationale and admissibility, stem therapy is applicable in treating neurological complications. Neural stem cells have been proven to be significant in transplantation therapy in treating central nervous complications due to their ability to self-renew and produce different neural cell types. Apart from neural stem cells, other types of stem cells such as ESCs, iPSCs, and MSCs have also been found to be acceptable alternatives in central nervous system implantations.
Parkinson’s disease causes inflexibility and slowed physical movements in patients. Conventionally, Parkinson’s disease was being treated mainly using pharmacological therapies and brain stimulation whereby electrodes were implanted surgically into the host (Song et al., 2018). However, the above methods were not effective in alleviating the symptoms resulting from the disorder. Dopaminergic cells, gotten from different stem cell sources, have been found to survive in the host. They are used in triggering behavioral improvement and motor recovery. The transplanted cells enhance recovery based on two approaches. Firstly, each cell usually transplanted stays alive, expresses tyrosine hydroxylase, releases and uptakes dopamine, thus replacing the lost function neurons. Secondly, the transplanted cells can amount to asymptomatic relief using the protective and neurotrophic aspects. Dopaminergic cells have been found to alleviate Parkinson’s disease symptoms.
Indeed, transplants of neuro stem cells can result in neuroprotection by controlling the host niche using the local astrocytes’ facilitation, taking part in de-differentiation, and promoting the expression of the host-derived growth parameters. Research has shown that the use of the iPSCs has eased the process of obtaining cells from the somatic cells of a patient, thus averting the issues of immune refusal (Song et al., 2018). From the research on stem cells, it has been found that there are no tumor cases reported within the first 10-36 months following iPSCs administration. After successfully implanting the stem cells and their derivatives, there are improvements in the patients who have Parkinson’s disease. The patients usually show a decrease in tremors, inflexibility, and freezing attacks. Research has made it possible to use stem cells in the treatment of Parkinson’s disease.
Alzheimer’s disease is a progressive neurodegenerative condition in human beings in which research has availed its treatment using stem cells. According to Song et al. (2018), more than 48.6 million people are affected by the disorder globally. Studies have found that stem cells offer treatment through the utilization of iPSCs, NSCs, and ESCs together with their respective derivatives. The stem cells and their products transplanted can move into the nervous system and then integrated into the local neural circuits to augment synaptogenesis and improve synaptic transmissions. The iPSCs are proven by research in modeling Alzheimer’s disease, thus reducing the challenge resulting from the species-specific discrepancies and making it possible to stratify drug responses during the personalized medication period. The models also help to offer novel ground for drug screening and toxicological researches. The iPSC Alzheimer’s disease models are a practical approach to understanding Alzheimer’s disease syndrome’s underlying genetic information.
Cardiovascular Disease Treatment
Mesenchymal stem cells help treat heart diseases by improving cardiac functioning and reducing scar size. According to Rikhtegar et al. (2018), heart diseases damage the heart and result in heart failures by stimulating myocyte death and generating fibrosis and ventricular remodelings. During stem cell therapy, progenitor cells and stem cells are usually segregated from allogeneic or autologous source tissue components. The transplanted stem cells resuscitate the cardiac function and commence the myocardial repair directly or indirectly. The pluripotent stem cells effectively treat heart diseases due to their capacity to differentiate into different cell types, such as cardiomyocytes. The pluripotent stem cells are applicable in the treatment of heart diseases since they trivially determine into cardiomyocytes.
Cardiac diseases are treated by the replacement of the faulty muscles with the stem cells. Cardiac therapy is based on stem cells’ application to overcome the challenges posed by gene therapeutical operations through the adoptive dislocation of healthy cells instead of the isolated genes (Rikhtegar et al., 2018). The stem cells function directly through the replacement of the damaged cells in the damaged cardiac tissue. The cells can also work by secreting molecules that trigger endogenous processes for cardiac regeneration and immune control. The cells meant for the transplants are gotten from fully grown tissues such as skeletal, cardiac, and bone marrow tissues. By directly replacing the cardiac tissues, there is a stimulation of endogenous repairment by triggering endogenous heart precursors and cardiomyocyte proliferation, resulting in immunity modulation. The cardiac therapies involve replacing the faulty cardiac muscles with the stem cells from cardiac, bone, or skeletal muscle tissues.
Brain Disease Treatment
The advancement in research has yielded to the application of stem cell implantation in the human brain. Damages on the human brain from abrupt accelerations, blast waves, or penetration wounds usually result in hampered psychological, physical, and cognition functionality (Song et al., 2018). After a transplant, a biobridge is formed between the injured cortex and the neurogenic SVZ. Though it is formerly constituted of the transplanted stem cells, the newly created host’s cells overgrow it. The implanted cells form biobridge between the damaged brain location and the neurogenic site. Then the implanted cells disappear and relinquish their responsibilities to the host’s neurogenic cells. Transplantation of MSCs recruits the host’s cells and enhances endogenous neurogenesis and repair using the stem cell biobridges.
MSCs derived from the bone marrow are effective and safe in treating patients suffering from traumatic brain injuries. Research has shown that patients suffering from motor disorders show improvement after MSCs implantations (Song et al., 2018). Additionally, in a different experiment, patients with visual impairments due to cortical injuries were subjected to treatment. The sample received an intracerebroventricular grafting of human NSCs progenitor cells. The patients then showed improvement in their visual abilities. Another research, whereby a group of patients was subjected to four MSC transplants derived from umbilical cords through lumbar punctures, showed neurological function improvement. The abovementioned patients showed enhanced lower and upper extremity motor abilities, sensation, social cognition, self-care, and balance.
Research on stem cells has also provided a basis for glioblastoma therapy. According to Song et al. (2018), glioblastoma refers to the prevalent primary brain tumor type. The condition is highly malignant and deadly to the patients. The glioblastoma condition is generally aggressive and entails attacks and infiltrations. Surgical operations have been proven not to eradicate glioblastoma foci effectively. This condition’s intricacy is evident whereby patients die within less than a year in case of a reoccurrence of the tumor near the resected region. The tumors make chemical therapeutic remedies difficult because of their intricate locations within the brain.
However, stem cell research has made it possible to treat the dreadful glioblastoma conditions. Song et al. (2018) report that various anti-glioblastoma substances are usually incorporated into the NSCs as loads and help kill the tumor cells. Cytokines oncolytic viruses and the enzymes help in the eradicating of the tumor cells too. The cytokines belonging to the interleukin lineage, comprising the IL-23, IL-7, and IL-4, have been found to exhibit antitumor abilities that enhance immune responses. Additionally, the stem cells can transport enzymes that transfer the inactive pro-drugs into poisonous and active substances, helping fight against glioblastoma. Cytosine deaminase, a pro-drug activating enzyme, transmits 5-fluorocytosine into the poisonous 5-fluorouracil. The newly formed 5-fluorouracil kills the glioblastoma cells. Studies on stem cells have resulted in the invention of anti-glioblastoma substances.
The use of oncolytic viruses and herpes simplex viruses has been proven to fight against the human body’s glioblastoma cells. According to Song et al. (2018), the oncolytic virus approach entails the viruses that are cable of infecting, replicating within, and later on lysing the glioblastoma cells. NSCs containing replicating oncolytic adenovirus migrate around the tumor margins then attack the glioblastoma cells. Also, cells containing myxoma viruses and herpes simplex virus are proven to possess the ability to repress tumor growths. Oncolytic, myxoma and herpes simplex viruses are have portrayed efficacy in the fight against brain tumors.
Cons of Stem Cells Research
Though stem cell application in the medical field has been on the rise, there have been pertinent concerns from critics. According to Lukomska et al. (2019), the application of MSCs in treating different diseases has resulted in criticism. The treatment of various diseases using MSCs has been proven to be quite efficient. However, there are other potential risks during the transplant based on long-lasting observations. The authors opine that though there are no reports on the negative impacts of stem cell application in the medical field, there are many concerns worth noting. For instance, it was documented that a patient was reported to have a big tumor-like mass in the spinal cord after eight years of olfactory mucosal grafting. In as much as research on stem cells has yielded to the application of stem cells in the treatment of diseases, it is worth noting that many underlying risks are unreported.
Stem cells have been very admissible in treating heart diseases, whereby MSCs are a promising therapeutic cell. More than 17.3 million lives were lost to cardiac-related diseases in 2008 (Lukomska et al., 2019). Though adult stem cells have been unanimously proposed for myocardial repair by medical researchers, there is a potential risk of patients suffering from other infections. For instance, MSC grafting can increase relapse, pneumonia, fungal, bacterial, and viral infections. Graftings are also reported to fail in some cases. Though the MSC grafts help prevent and treat graft versus host diseases in patients who are not sensitive to steroids, infections are eminent. The acute and chronic graft versus host diseases in patients after an MSC transplant has been proven to be more than those who do not have the MSC. The infection-related deaths are high even after the graft versus host diseases have been determined. The instances are highly associated with the long immunosuppressive impacts of the MSCs. Stem cell implants are significantly associated with high mortality in patients than individuals who do not have the MCS implants.
Stem cell implantation is detrimental in patients. The MSCs facilitate tumor growth by modulating the tumor microenvironment (Lukomska et al., 2019). The stem cell implantation increases the risk of patients suffering from protumorigenic effects. This risk is augmented by the fact that MSCs are immunosuppressive. Different stem cell transplant types’ risk remains high until the bone marrow makes the white blood cells independently. However, during allogeneic transplants, the risk is highest since patients take drugs that lower their body’s immunity to prevent graft-versus-host diseases from taking place. Graft versus host diseases arises when the recipient’s immunity starts fighting the donor’s cells as foreign bodies, thus permanently destroying the organ. The stem cell is also associated with tumor stroma’s modulation and changes itself into fatal malignant cells. It is worth noting that the infections related to the MSCs remain a concern in medical-related researches.
The recovery time after a stem cell implant varies and can fatal to a patient. The suppression of the host’s body immunity following an implant can last for a while, rendering the patient susceptible to other diseases (Lukomska et al., 2019). Following stem cell grafting, it can take between six to twelve months or more to normalize the patient’s blood composition and immunity. A patient has a challenge of having low blood cell counts following a stem cell grafting since it takes some time for the stem cells to be transported to the bone marrow to start the process of synthesizing new blood cells. For instance, a patient with a low white blood cell count is highly prone to infections. Low blood cell count causes dizziness, fatigue, and malaise. Low platelet count makes the patient have a high risk of prolonged bleeding. It is not guaranteed that the patient’s immunity will quickly be improved since it varies from one individual to another. Kidney problems might also arise when chemotherapy drugs, meant to suppress immunity, are given to a patient before the transplant. The process of stem cell implantation can result in health complications owing to low immunity.
Stem cell research plays a significant role in tissue generation, treatment of neurological disorders, cardiovascular disease treatment, and brain disease treatment due to stem cells’ ability of self-renewing and differentiation into different lineages. However, stem cell application has faced criticism due to the increased fatalities caused by the suppressed immunity during the transplant period, which leaves the patient prone to other infections. Stem cell research has identified MSCs to be vital in tissue engineering. During the treatment exercises, the MSCs undergo differentiation into the desired cell then implanted into the target organ. However, suppressing the host’s body immunity prevents graft-versus-host diseases with fatal results, such as organ damage. Parkinson’s disease and Alzheimer’s disease, affecting many people globally, are now treatable through stem cell research.
MSCs are also admissible in the treatment of cardiac diseases, whereby they replace worn-out tissues. The transplantation of MSCs during brain disease treatment incorporates the host’s cells to facilitate the endogenous neurogenesis and repair using stem cell biobridges. Stem cell research has made it possible to treat the deadly glioblastoma diseases by incorporating anti-glioblastoma components in NSCs that are then used to kill the tumor cells. Occasionally, MSC transplants have also been reported to cause tumors that are sometimes fatal. Though stem cell has some disadvantages in its application, the many applications of stem cell research in the medical field give more hope that it can be admissible in treating many chronic diseases.
Fitzsimmons, R. E., Mazurek, M. S., Soos, A., & Simmons, C. A. (2018). Mesenchymal stromal/stem cells in regenerative medicine and tissue engineering . Stem Cells International , 1-16. Web.
Lukomska, B., Stanaszek, L., Zuba-Surma, E., Legosz, P., Sarzynska, S., & Drela, K. (2019). Challenges and controversies in human mesenchymal stem cell therapy . Stem Cells International . Web.
Rikhtegar, R., Pezeshkian, M., Dolati, S., Safaie, N., Rad, A. A., Mahdipour, M., Nouri, M., Jodat, A. R., & Yousefi, M. (2019). Stem cells as therapy for heart disease: iPSCs, ESCs, CSCs, and skeletal myoblasts. Biomedicine & Pharmacotherapy , 109 , 304-313. Web.
Song, C. G., Zhang, Y. Z., Wu, H. N., Cao, X. L., Guo, C. J., Li, Y. Q., Zheng, M. H., & Han, H. (2018). Stem cells: A promising candidate to treat neurological disorders. Neural Regeneration Research , 13 (7), 1294. Web.
Wang, M., Yuan, Z., Ma, N., Hao, C., Guo, W., Zou, G., Zhang, Y., Chen, M., Gao, S., Peng, J., Wang, Y., Sui, X., Xu, W., Lu, S., Liu, S., & Guo, Q. (2017). Advances and prospects in stem cells for cartilage regeneration. Stem Cells International , 1-16. Web.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, August 19). Pros and Cons of Stem Cell Research. https://studycorgi.com/pros-and-cons-of-stem-cell-research/
"Pros and Cons of Stem Cell Research." StudyCorgi , 19 Aug. 2022, studycorgi.com/pros-and-cons-of-stem-cell-research/.
StudyCorgi . (2022) 'Pros and Cons of Stem Cell Research'. 19 August.
1. StudyCorgi . "Pros and Cons of Stem Cell Research." August 19, 2022. https://studycorgi.com/pros-and-cons-of-stem-cell-research/.
Bibliography
StudyCorgi . "Pros and Cons of Stem Cell Research." August 19, 2022. https://studycorgi.com/pros-and-cons-of-stem-cell-research/.
StudyCorgi . 2022. "Pros and Cons of Stem Cell Research." August 19, 2022. https://studycorgi.com/pros-and-cons-of-stem-cell-research/.
This paper, “Pros and Cons of Stem Cell Research”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: August 19, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
- Utility Menu

GA4 tracking code

Examining the ethics of embryonic stem cell research

Following the recent passage by both houses of Congress of the Stem Cell Research Enhancement Act of 2007, which would permit federal funding of research using donated surplus embryonic stem cells from fertility clinics, the president has once again threatened a veto.
Because neither the House nor the Senate had sufficient votes to override a presidential veto, it appears unlikely this new bill will be enacted into law, further stalling the pace of this research. “This bill crosses a moral line that I and others find troubling,” stated Bush, following the Senate’s vote.
SCL : What are th e main arguments for and against embryonic stem cell research? MS : Proponents argue that embryonic stem cell research holds great promise for understanding and curing diabetes, Parkinson’s disease, spinal cord injury, and other debilitating conditions. Opponents argue that the research is unethical, because deriving the stem cells destroys the blastocyst, an unimplanted human embryo at the sixth to eighth day of development. As Bush declared when he vetoed last year’s stem cell bill, the federal government should not support “the taking of innocent human life.”
It is surprising that, despite the extensive public debate—in Congress, during the 2004 and 2006 election campaigns, and on the Sunday morning talk shows—relatively little attention has been paid to the moral issue at the heart of the controversy: Are the opponents of stem cell research correct in their claim that the unimplanted human embryo is already a human being, morally equivalent to a person?

“It is important to be clear about the embryo from which stem cells are extracted. It is not implanted and growing in a woman’s uterus. It is not a fetus. It has no recognizable human features or form. It is, rather, a blastocyst, a cluster of 180 to 200 cells, growing in a petri dish, barely visible to the naked eye.”
SCL : What are the contradictions in Bush’s stance? MS : Before we address that, it is important to be clear about the embryo from which stem cells are extracted. It is not implanted and growing in a woman’s uterus. It is not a fetus. It has no recognizable human features or form.
It is, rather, a blastocyst, a cluster of 180 to 200 cells, growing in a petri dish, barely visible to the naked eye. Such blastocysts are either cloned in the lab or created in fertility clinics. The bill recently passed by Congress would fund stem cell research only on excess blastocysts left over from infertility treatments.
The blastocyst represents such an early stage of embryonic development that the cells it contains have not yet differentiated, or taken on the properties of particular organs or tissues—kidneys, muscles, spinal cord, and so on. This is why the stem cells that are extracted from the blastocyst hold the promise of developing, with proper coaxing in the lab, into any kind of cell the researcher wants to study or repair.
The moral and political controversy arises from the fact that extracting the stem cells destroys the blastocyst. It is important to grasp the full force of the claim that the embryo is morally equivalent to a person, a fully developed human being.
For those who hold this view, extracting stem cells from a blastocyst is as morally abhorrent as harvesting organs from a baby to save other people’s lives. This is the position of Senator Sam Brownback, Republican of Kansas, a leading advocate of the right-to-life position. In Brownback’s view, “a human embryo . . . is a human being just like you and me; and it deserves the same respect that our laws give to us all.
If Brownback is right, then embryonic stem cell research is immoral because it amounts to killing a person to treat other people’s diseases.
SCL : What is the basis for the belief that personhood begins at conception? MS : Some base this belief on the religious conviction that the soul enters the body at the moment of conception. Others defend it without recourse to religion, by the following line of reasoning: Human beings are not things. Their lives must not be sacrificed against their will, even for the sake of good ends, like saving other people’s lives. The reason human beings must not be treated as things is that they are inviolable. At what point do humans acquire this inviolability? The answer cannot depend on the age or developmental stage of a particular human life. Infants are inviolable, and few people would countenance harvesting organs for transplantation even from a fetus.
Every human being—each one of us—began life as an embryo. Unless we can point to a definitive moment in the passage from conception to birth that marks the emergence of the human person, we must regard embryos as possessing the same inviolability as fully developed human beings.
SCL : By this line of reasoning, human embryos are inviolable and should not be used for research, even if that research might save many lives. MS : Yes, but this argument can be challenged on a number of grounds. First, it is undeniable that a human embryo is “human life” in the biological sense that it is living rather than dead, and human rather than, say, bovine.
But this biological fact does not establish that the blastocyst is a human being, or a person. Any living human cell (a skin cell, for example) is “human life” in the sense of being human rather than bovine and living rather than dead. But no one would consider a skin cell a person, or deem it inviolable. Showing that a blastocyst is a human being, or a person, requires further argument.
Some try to base such an argument on the fact that human beings develop from embryo to fetus to child. Every person was once an embryo, the argument goes, and there is no clear, non-arbitrary line between conception and adulthood that can tell us when personhood begins. Given the lack of such a line, we should regard the blastocyst as a person, as morally equivalent to a fully developed human being.
SCL : What is the flaw in this argument? MS : Consider an analogy: although every oak tree was once an acorn, it does not follow that acorns are oak trees, or that I should treat the loss of an acorn eaten by a squirrel in my front yard as the same kind of loss as the death of an oak tree felled by a storm. Despite their developmental continuity, acorns and oak trees differ. So do human embryos and human beings, and in the same way. Just as acorns are potential oaks, human embryos are potential human beings.
The distinction between a potential person and an actual one makes a moral difference. Sentient creatures make claims on us that nonsentient ones do not; beings capable of experience and consciousness make higher claims still. Human life develops by degrees.
SCL : Yet there are people who disagree that life develops by degrees, and believe that a blastocyst is a person and, therefore, morally equivalent to a fully developed human being. MS : Certainly some people hold this belief. But a reason to be skeptical of the notion that blastocysts are persons is to notice that many who invoke it do not embrace its full implications.
President Bush is a case in point. In 2001, he announced a policy that restricted federal funding to already existing stem cell lines, so that no taxpayer funds would encourage or support the destruction of embryos. And in 2006, he vetoed a bill that would have funded new embryonic stem cell research, saying that he did not want to support “the taking of innocent human life.”
“The distinction between a potential person and an actual one makes a moral difference. Sentient creatures make claims on us that nonsentient ones do not; beings capable of experience and consciousness make higher claims still. Human life develops by degrees.”
But it is a striking feature of the president’s position that, while restricting the funding of embryonic stem cell research, he has made no effort to ban it. To adapt a slogan from the Clinton administration, the Bush policy might be summarized as “don’t fund, don’t ban.” But this policy is at odds with the notion that embryos are human beings.
SCL : If Bush’s policy were consistent with his stated beliefs, how, in your opinion, would it differ from his current “don’t fund, don’t ban” policy? MS : If harvesting stem cells from a blastocyst were truly on a par with harvesting organs from a baby, then the morally responsible policy would be to ban it, not merely deny it federal funding.
If some doctors made a practice of killing children to get organs for transplantation, no one would take the position that the infanticide should be ineligible for federal funding but allowed to continue in the private sector. In fact, if we were persuaded that embryonic stem cell research were tantamount to infanticide, we would not only ban it but treat it as a grisly form of murder and subject scientists who performed it to criminal punishment.
SCL : Couldn’t it be argued, in defense of the president’s policy, that Congress would be unlikely to enact an outright ban on embryonic stem cell research? MS : Perhaps. But this does not explain why, if the president really considers embryos to be human beings, he has not at least called for such a ban, nor even called upon scientists to stop doing stem cell research that involves the destruction of embryos. In fact, Bush has cited the fact that “there is no ban on embryonic stem cell research” in touting the virtues of his “balanced approach.”
The moral oddness of the Bush “don’t fund, don’t ban” position confused even his spokesman, Tony Snow. Last year, Snow told the White House press corps that the president vetoed the stem cell bill because he considered embryonic stem cell research to be “murder,” something the federal government should not support. When the comment drew a flurry of critical press attention, the White House retreated. No, the president did not believe that destroying an embryo was murder. The press secretary retracted his statement, and apologized for having “overstated the president’s position.”
How exactly the spokesman had overstated the president’s position is unclear. If embryonic stem cell research does constitute the deliberate taking of innocent human life, it is hard to see how it differs from murder. The chastened press secretary made no attempt to parse the distinction. His errant statement that the president considered embryo destruction to be “murder” simply followed the moral logic of the notion that embryos are human beings. It was a gaffe only because the Bush policy does not follow that logic.
SCL : You have stated that the president’s refusal to ban privately funded embryonic stem cell research is not the only way in which his policies betray the principle that embryos are persons. How so? MS : In the course of treating infertility, American fertility clinics routinely discard thousands of human embryos. The bill that recently passed in the Senate would fund stem cell research only on these excess embryos, which are already bound for destruction. (This is also the position taken by former governor Mitt Romney, who supports stem cell research on embryos left over from fertility clinics.) Although Bush would ban the use of such embryos in federally funded research, he has not called for legislation to ban the creation and destruction of embryos by fertility clinics.
SCL : If embryos are morally equivalent to fully developed human beings, doesn’t it then follow that allowing fertility clinics to discard thousands of embryos is condoning mass murder? MS : It does. If embryos are human beings, to allow fertility clinics to discard them is to countenance, in effect, the widespread creation and destruction of surplus children. Those who believe that a blastocyst is morally equivalent to a baby must believe that the 400,000 excess embryos languishing in freezers in U.S. fertility clinics are like newborns left to die by exposure on a mountainside. But those who view embryos in this way should not only be opposing embryonic stem cell research; they should also be leading a campaign to shut down what they must regard as rampant infanticide in fertility clinics.
Some principled right-to-life opponents of stem cell research meet this test of moral consistency. Bush’s “don’t fund, don’t ban” policy does not. Those who fail to take seriously the belief that embryos are persons miss this point. Rather than simply complain that the president’s stem cell policy allows religion to trump science, critics should ask why the president does not pursue the full implications of the principle he invokes.
If he does not want to ban embryonic stem cell research, or prosecute stem cell scientists for murder, or ban fertility clinics from creating and discarding excess embryos, this must mean that he does not really consider human embryos as morally equivalent to fully developed human beings after all.
But if he doesn’t believe that embryos are persons, then why ban federally funded embryonic stem cell research that holds promise for curing diseases and saving lives?

- Table of Contents
- Random Entry
- Chronological
- Editorial Information
- About the SEP
- Editorial Board
- How to Cite the SEP
- Special Characters
- Advanced Tools
- Support the SEP
- PDFs for SEP Friends
- Make a Donation
- SEPIA for Libraries
- Entry Contents
Bibliography
Academic tools.
- Friends PDF Preview
- Author and Citation Info
- Back to Top
Ethics of Stem Cell Research
Human embryonic stem cell (HESC) research offers much hope for alleviating the human suffering brought on by the ravages of disease and injury. HESCs are characterized by their capacity for self-renewal and their ability to differentiate into all types of cells of the body. The main goal of HESC research is to identify the mechanisms that govern cell differentiation and to turn HESCs into specific cell types that can be used for treating debilitating and life-threatening diseases and injuries.
Despite the tremendous therapeutic promise of HESC research, the research has met with heated opposition because the harvesting of HESCs involves the destruction of the human embryo. HESCs are derived in vitro around the fifth day of the embryo’s development (Thomson et al . 1998). A typical day-5 human embryo consists of 200–250 cells, most of which comprise the trophoblast, which is the outermost layer of the blastocyst. HESCs are harvested from the inner cell mass of the blastocyst, which consists of 30–34 cells. The derivation of HESC cultures requires the removal of the trophoblast. This process of disaggregating the blastocyst’s cells eliminates its potential for further development. Opponents of HESC research argue that the research is morally impermissible because it involves the unjust killing of innocent human beings.
Scientists recently succeeded in converting adult human skin cells into cells that appear to have the properties of HESCs by activating four genes in the adult cells (Takahashi et al . 2007; Yu et al . 2007). The reprogrammed cells—“induced pluripotent stem cells” (iPSCs)—could ultimately eliminate the need for HESCs. However, at present, the consensus in the scientific community is that both HESC and iPSC research should be pursued, as we do not yet know whether iPSCs have the same potential as HESCs or whether it is safe to transplant them into humans. Thus, the controversies around HESC research will continue, at least in the near-term.
While the principal source of the controversy surrounding HESC research lies in competing views about the value of human embryonic life, the scope of ethical issues in HESC research is broader than the question of the ethics of destroying human embryos. It also encompasses questions about, among other things, whether researchers who use but do not derive HESCs are complicit in the destruction of embryos, whether there is a moral distinction between creating embryos for research purposes and creating them for reproductive ends, the permissibility of cloning human embryos to harvest HESCs, and the ethics of creating human/non-human chimeras. This entry provides an overview of all but the last two issues just listed; cloning and human-non-human chimeras are addressed in separate entries.
1.1 When does a human being begin to exist?
1.2 the moral status of human embryos, 1.3 the case of “doomed embryos”, 2. the ethics of using human embryonic stem cells in research, 3. the ethics of creating embryos for stem cell research and therapy, 4. stem cell-derived gametes, 5. stem cell-derived organoids, gastruloids, and synthetic embryos, cited resources, other resources, related entries, 1. the ethics of destroying human embryos for research.
The potential therapeutic benefits of HESC research provide strong grounds in favor of the research. If looked at from a strictly consequentialist perspective, it’s almost certainly the case that the potential health benefits from the research outweigh the loss of embryos involved and whatever suffering results from that loss for persons who want to protect embryos. However, most of those who oppose the research argue that the constraints against killing innocent persons to promote social utility apply to human embryos. Thus, as long as we accept non-consequentialist constraints on killing persons, those supporting HESC research must respond to the claim that those constraints apply to human embryos.
In its most basic form, the central argument supporting the claim that it is unethical to destroy human embryos goes as follows: It is morally impermissible to intentionally kill innocent human beings; the human embryo is an innocent human being; therefore it is morally impermissible to intentionally kill the human embryo. It is worth noting that this argument, if sound, would not suffice to show that all or even most HESC research is impermissible, since most investigators engaged in HESC research do not participate in the derivation of HESCs but instead use cell lines that researchers who performed the derivation have made available. To show that researchers who use but do not derive HESCs participate in an immoral activity, one would further need to establish their complicity in the destruction of embryos. We will consider this issue in section 2. But for the moment, let us address the argument that it is unethical to destroy human embryos.
A premise of the argument against killing embryos is that human embryos are human beings. The issue of when a human being begins to exist is, however, a contested one. The standard view of those who oppose HESC research is that a human being begins to exist with the emergence of the one-cell zygote at fertilization. At this stage, human embryos are said to be “whole living member[s] of the species homo sapiens … [which] possess the epigenetic primordia for self-directed growth into adulthood, with their determinateness and identity fully intact” (George & Gomez-Lobo 2002, 258). This view is sometimes challenged on the grounds that monozygotic twinning is possible until around days 14–15 of an embryo’s development (Smith & Brogaard 2003). An individual who is an identical twin cannot be numerically identical to the one-cell zygote, since both twins bear the same relationship to the zygote, and numerical identity must satisfy transitivity. That is, if the zygote, A, divides into two genetically identical cell groups that give rise to identical twins B and C, B and C cannot be the same individual as A because they are not numerically identical with each other. This shows that not all persons can correctly assert that they began their life as a zygote. However, it does not follow that the zygote is not a human being, or that it has not individuated. This would follow only if one held that a condition of an entity’s status as an individual human being is that it be impossible for it to cease to exist by dividing into two or more entities. But this seems implausible. Consider cases in which we imagine adult humans undergoing fission (for example, along the lines of Parfit’s thought experiments, where each half of the brain is implanted into a different body) (Parfit 1984). The prospect of our going out of existence through fission does not pose a threat to our current status as distinct human persons. Likewise, one might argue, the fact that a zygote may divide does not create problems for the view that the zygote is a distinct human being.
There are, however, other grounds on which some have sought to reject that the early human embryo is a human being. According to one view, the cells that comprise the early embryo are a bundle of homogeneous cells that exist in the same membrane but do not form a human organism because the cells do not function in a coordinated way to regulate and preserve a single life (Smith & Brogaard 2003, McMahan 2002). While each of the cells is alive, they only become parts of a human organism when there is substantial cell differentiation and coordination, which occurs around day-16 after fertilization. Thus, on this account, disaggregating the cells of the 5-day embryo to derive HESCs does not entail the destruction of a human being.
This account is subject to dispute on empirical grounds. That there is some intercellular coordination in the zygote is revealed by the fact that the development of the early embryo requires that some cells become part of the trophoblast while others become part of the inner cell mass. Without some coordination between the cells, there would be nothing to prevent all cells from differentiating in the same direction (Damschen, Gomez-Lobo and Schonecker 2006). The question remains, though, whether this degree of cellular interaction is sufficient to render the early human embryo a human being. Just how much intercellular coordination must exist for a group of cells to constitute a human organism cannot be resolved by scientific facts about the embryo, but is instead an open metaphysical question (McMahan 2007a).
Suppose that the 5-day human embryo is a human being. On the standard argument against HESC research, membership in the species Homo sapiens confers on the embryo a right not to be killed. This view is grounded in the assumption that human beings have the same moral status (at least with respect to possessing this right) at all stages of their lives.
Some accept that the human embryo is a human being but argue that the human embryo does not have the moral status requisite for a right to life. There is reason to think that species membership is not the property that determines a being’s moral status. We have all been presented with the relevant thought experiments, courtesy of Disney, Orwell, Kafka, and countless science fiction works. The results seem clear: we regard mice, pigs, insects, aliens, and so on, as having the moral status of persons in those possible worlds in which they exhibit the psychological and cognitive traits that we normally associate with mature human beings. This suggests that it is some higher-order mental capacity (or capacities) that grounds the right to life. While there is no consensus about the capacities that are necessary for the right to life, some of the capacities that have been proposed include reasoning, self-awareness, and agency (Kuhse & Singer 1992, Tooley 1983, Warren 1973).
The main difficulty for those who appeal to such mental capacities as the touchstone for the right to life is that early human infants lack these capacities, and do so to a greater degree than many of the nonhuman animals that most deem it acceptable to kill (Marquis 2002). This presents a challenge for those who hold that the non-consequentialist constraints on killing human children and adults apply to early human infants. Some reject that these constraints apply to infants, and allow that there may be circumstances where it is permissible to sacrifice infants for the greater good (McMahan 2007b). Others argue that, while infants do not have the intrinsic properties that ground a right to life, we should nonetheless treat them as if they have a right to life in order to promote love and concern towards them, as these attitudes have good consequences for the persons they will become (Benn 1973, Strong 1997).
Some claim that we can reconcile the ascription of a right to life to all humans with the view that higher order mental capacities ground the right to life by distinguishing between two senses of mental capacities: “immediately exercisable” capacities and “basic natural” capacities. (George and Gomez-Lobo 2002, 260). According to this view, an individual’s immediately exercisable capacity for higher mental functions is the actualization of natural capacities for higher mental functions that exist at the embryonic stage of life. Human embryos have a “rational nature,” but that nature is not fully realized until individuals are able to exercise their capacity to reason. The difference between these types of capacity is said to be a difference between degrees of development along a continuum. There is merely a quantitative difference between the mental capacities of embryos, fetuses, infants, children, and adults (as well as among infants, children, and adults). And this difference, so the argument runs, cannot justify treating some of these individuals with moral respect while denying it to others.
Given that a human embryo cannot reason at all, the claim that it has a rational nature has struck some as tantamount to asserting that it has the potential to become an individual that can engage in reasoning (Sagan & Singer 2007). But an entity’s having this potential does not logically entail that it has the same status as beings that have realized some or all of their potential (Feinberg 1986). Moreover, with the advent of cloning technologies, the range of entities that we can now identify as potential persons arguably creates problems for those who place great moral weight on the embryo’s potential. A single somatic cell or HESC can in principle (though not yet in practice) develop into a mature human being under the right conditions—that is, where the cell’s nucleus is transferred into an enucleated egg, the new egg is electrically stimulated to create an embryo, and the embryo is transferred to a woman’s uterus and brought to term. If the basis for protecting embryos is that they have the potential to become reasoning beings, then, some argue, we have reason to ascribe a high moral status to the trillions of cells that share this potential and to assist as many of these cells as we reasonably can to realize their potential (Sagan & Singer 2007, Savulescu 1999). Because this is a stance that we can expect nearly everyone to reject, it’s not clear that opponents of HESC research can effectively ground their position in the human embryo’s potential.
One response to this line of argument has been to claim that embryos possess a kind of potential that somatic cells and HESCs lack. An embryo has potential in the sense of having an “active disposition” and “intrinsic power” to develop into a mature human being (Lee & George 2006). An embryo can mature on its own in the absence of interference with its development. A somatic cell, on the other hand, does not have the inherent capacity or disposition to grow into a mature human being. However, some question whether this distinction is viable, especially in the HESC research context. While it is true that somatic cells can realize their potential only with the assistance of outside interventions, an embryo’s development also requires that numerous conditions external to it are satisfied. In the case of embryos that are naturally conceived, they must implant, receive nourishment, and avoid exposure to dangerous substances in utero . In the case of spare embryos created through in vitro fertilization—which are presently the source of HESCs for research—the embryos must be thawed and transferred to a willing woman’s uterus. Given the role that external factors—including technological interventions—play in an embryo’s realizing its potential, one can question whether there is a morally relevant distinction between an embryo’s and somatic cell’s potential and thus raise doubts about potentiality as a foundation for the right to life (Devolder & Harris 2007).
Some grant that human embryos lack the properties essential to a right to life, but hold that they possess an intrinsic value that calls for a measure of respect and places at least some moral constraints on their use: “The life of a single human organism commands respect and protection … no matter in what form or shape, because of the complex creative investment it represents and because of our wonder at the divine or evolutionary processes that produce new lives from old ones.” (Dworkin l992, 84). There are, however, divergent views about the level of respect embryos command and what limits exist on their use. Some opponents of HESC research hold that the treatment of human embryos as mere research tools always fails to manifest proper respect for them. Other opponents take a less absolutist view. Some, for example, deem embryos less valuable than more mature human beings but argue that the benefits of HESC research are too speculative to warrant the destruction of embryos, and that the benefits might, in any case, be achieved through the use of noncontroversial sources of stem cells (e.g., adult stem cells) (Holm 2003).
Many, if not most, who support the use of human embryos for HESC research would likely agree with opponents of the research that there are some circumstances where the use of human embryos would display a lack of appropriate respect for human life, for example, were they to be offered for consumption to contestants in a reality TV competition or destroyed for the production of cosmetics. But proponents of the research hold that the value of human embryos is not great enough to constrain the pursuit of research that may yield significant therapeutic benefits. Supporters of the research also frequently question whether most opponents of the research are consistent in their ascription of a high value to human embryos, as opponents generally display little concern about the fact that many embryos created for fertility treatment are discarded.
When spare embryos exist after fertility treatment, the individuals for whom the embryos were created typically have the option of storing for them for future reproductive use, donating them to other infertile couples, donating them to research, or discarding them. Some argue that as long as the decision to donate embryos for research is made after the decision to discard them, it is morally permissible to use them in HESC research even if we assume that they have the moral status of persons. The claim takes two different forms. One is that it is morally permissible to kill an individual who is about to be killed by someone else where killing that individual will help others (Curzer, H. 2004). The other is that researchers who derive HESCs from embryos that were slated for destruction do not cause their death. Instead, the decision to discard the embryos causes their death; research just causes the manner of their death (Green 2002).
Both versions of the argument presume that the decision to discard spare embryos prior to the decision to donate them to research entails that donated embryos are doomed to destruction when researchers receive them. There are two arguments one might marshal against this presumption. First, one who wants to donate embryos to research might first elect to discard them only because doing so is a precondition for donating them. There could be cases in which one who chooses the discard option would have donated the embryos to other couples were the research donation option not available. The fact that a decision to discard embryos is made prior to the decision to donate the embryos thus does not establish that the embryos were doomed to destruction before the decision to donate them to research was made. Second, a researcher who receives embryos could choose to rescue them, whether by continuing to store them or by donating them to infertile couples. While this would violate the law, the fact that it is within a researcher’s power to prevent the destruction of the embryos he or she receives poses problems for the claim that the decision to discard the embryos dooms them or causes their destruction.
Assume for the sake of argument that it is morally impermissible to destroy human embryos. It does not follow that all research with HESCs is impermissible, as it is sometimes permissible to benefit from moral wrongs. For example, there is nothing objectionable about transplant surgeons and patients benefiting from the organs of murder and drunken driving victims (Robertson 1988). If there are conditions under which a researcher may use HESCs without being complicit in the destruction of embryos, then those who oppose the destruction of embryos could support research with HESCs under certain circumstances.
Researchers using HESCs are clearly implicated in the destruction of embryos where they derive the cells themselves or enlist others to derive the cells. However, most investigators who conduct research with HESCs obtain them from an existing pool of cell lines and play no role in their derivation. One view is that we cannot assign causal or moral responsibility to investigators for the destruction of embryos from which the HESCs they use are derived where their “research plans had no effect on whether the original immoral derivation occurred.” (Robertson 1999). This view requires qualification. There may be cases in which HESCs are derived for the express purpose of making them widely available to HESC investigators. In such instances, it may be that no individual researcher’s plans motivated the derivation of the cells. Nonetheless, one might argue that investigators who use these cells are complicit in the destruction of the embryos from which the cells were derived because they are participants in a research enterprise that creates a demand for HESCs. For these investigators to avoid the charge of complicity in the destruction of embryos, it must be the case that the researchers who derived the HESCs would have performed the derivation in the absence of external demand for the cells (Siegel 2004).
The issue about complicity goes beyond the question of an HESC researcher’s role in the destruction of the particular human embryo(s) from which the cells he or she uses are derived. There is a further concern that research with existing HESCs will result in the future destruction of embryos: “[I]f this research leads to possible treatments, private investment in such efforts will increase greatly and the demand for many thousands of cell lines with different genetic profiles will be difficult to resist.” (U.S. Conference of Catholic Bishops 2001). This objection faces two difficulties. First, it appears to be too sweeping: research with adult stem cells and non-human animal stem cells, as well as general research in genetics, embryology, and cell biology could be implicated, since all of this research might advance our understanding of HESCs and result in increased demand for them. Yet, no one, including those who oppose HESC research, argues that we should not support these areas of research. Second, the claim about future demand for HESCs is speculative. Indeed, current HESC research could ultimately reduce or eliminate demand for the cells by providing insights into cell biology that enable the use of alternative sources of cells (Siegel 2004).
While it might thus be possible for a researcher to use HESCs without being morally responsible for the destruction of human embryos, that does not end the inquiry into complicity. Some argue that agents can be complicit in wrongful acts for which they are not morally responsible. One such form of complicity arises from an association with wrongdoing that symbolizes acquiescence in the wrongdoing (Burtchaell 1989). The failure to take appropriate measures to distance oneself from moral wrongs may give rise to “metaphysical guilt,” which produces a moral taint and for which shame is the appropriate response (May 1992). The following question thus arises: Assuming it is morally wrongful to destroy human embryos, are HESC researchers who are not morally responsible for the destruction of embryos complicit in the sense of symbolically aligning themselves with a wrongful act?
One response is that a researcher who benefits from the destruction of embryos need not sanction the act any more than the transplant surgeon who uses the organs of a murder or drunken driving victim sanctions the homicidal act (Curzer 2004). But this response is unlikely to be satisfactory to opponents of HESC research. There is arguably an important difference between the transplant case and HESC research insofar as the moral wrong associated with the latter (a) systematically devalues a particular class of human beings and (b) is largely socially accepted and legally permitted. Opponents of HESC research might suggest that the HESC research case is more analogous to the following kind of case: Imagine a society in which the practice of killing members of a particular racial or ethnic group is legally permitted and generally accepted. Suppose that biological materials obtained from these individuals subsequent to their deaths are made available for research uses. Could researchers use these materials while appropriately distancing themselves from the wrongful practice? Arguably, they could not. There is a heightened need to protest moral wrongs where those wrongs are socially and legally accepted. Attempts to benefit from the moral wrong in these circumstances may be incompatible with mounting a proper protest (Siegel 2003).
But even if we assume that HESC researchers cannot avoid the taint of metaphysical guilt, it is not clear that researchers who bear no moral responsibility for the destruction of embryos are morally obligated not to use HESCs. One might argue that there is a prima facie duty to avoid moral taint, but that this duty may be overridden for the sake of a noble cause.
Most HESCs are derived from embryos that were created for infertility treatment but that were in excess of what the infertile individual(s) ultimately needed to achieve a pregnancy. The HESCs derived from these leftover embryos offer investigators a powerful tool for understanding the mechanisms controlling cell differentiation. However, there are scientific and therapeutic reasons not to rely entirely on leftover embryos. From a research standpoint, creating embryos through cloning technologies with cells that are known to have particular genetic mutations would allow researchers to study the underpinnings of genetic diseases in vitro . From a therapeutic standpoint, the HESCs obtained from leftover IVF embryos are not genetically diverse enough to address the problem of immune rejection by recipients of stem cell transplants. (Induced pluripotent stem cells may ultimately prove sufficient for these research and therapeutic ends, since the cells can (a) be selected for specific genetic mutations and (b) provide an exact genetic match for stem cell recipients.) At present, the best way to address the therapeutic problem is through the creation of a public stem cell bank that represents a genetically diverse pool of stem cell lines (Faden et al . 2003, Lott & Savulescu 2007). This kind of stem cell bank would require the creation of embryos from gamete donors who share the same HLA-types (i.e., similar versions of the genes that mediate immune recognition and rejection).
Each of these enterprises has its own set of ethical issues. In the case of research cloning, some raise concerns, for example, that the perfection of cloning techniques for research purposes will enable the pursuit of reproductive cloning, and that efforts to obtain the thousands of eggs required for the production of cloned embryos will result in the exploitation of women who provide the eggs (President’s Council on Bioethics 2002, Norsigian 2005). With respect to stem cell banks, it is not practically possible to create a bank of HESCs that will provide a close immunological match for all recipients. This gives rise to the challenge of determining who will have biological access to stem cell therapies. We might construct the bank so that it provides matches for the greatest number of people in the population, gives everyone an equal chance of finding a match, or ensures that all ancestral/ethnic groups are fairly represented in the bank (Faden et al . 2003, Bok, Schill, & Faden 2004, Greene 2006).
There are, however, more general challenges to the creation of embryos for research and therapeutic purposes. Some argue that the creation of embryos for non-reproductive ends is morally problematic, regardless of whether they are created through cloning or in vitro fertilization. There are two related arguments that have been advanced to morally distinguish the creation of embryos for reproductive purposes from the creation of embryos for research and therapeutic purposes. First, each embryo created for procreative purposes is originally viewed as a potential child in the sense that each is a candidate for implantation and development into a mature human. In contrast, embryos created for research or therapies are viewed as mere tools from the outset (Annas, Caplan & Elias 1996, President’s Council on Bioethics 2002). Second, while embryos created for research and therapy are produced with the intent to destroy them, the destruction of embryos created for reproduction is a foreseeable but unintended consequence of their creation (FitzPatrick 2003).
One response to the first argument has been to suggest that we could, under certain conditions, view all research embryos as potential children in the relevant sense. If all research embryos were included in a lottery in which some of them were donated to individuals for reproductive purposes, all research embryos would have a chance at developing into mature humans (Devander 2005). Since those who oppose creating embryos for research would likely maintain their opposition in the research embryo lottery case, it is arguably irrelevant whether embryos are viewed as potential children when they are created. Of course, research embryos in the lottery case would be viewed as both potential children and potential research tools. But this is also true in the case of embryos created for reproductive purposes where patients are open to donating spare embryos to research.
As to the second argument, the distinction between intending and merely foreseeing harms is one to which many people attach moral significance, and it is central to the Doctrine of Double Effect. But even if one holds that this is a morally significant distinction, it is not clear that it is felicitous to characterize the destruction of spare embryos as an unintended but foreseeable side-effect of creating embryos for fertility treatment. Fertility clinics do not merely foresee that some embryos will be destroyed, as they choose to offer patients the option of discarding embryos and carry out the disposal of embryos when patients request it. Patients who elect that their embryos be discarded also do not merely foresee the embryos’ destruction; their election of that option manifests their intention that the embryos be destroyed. There is thus reason to doubt that there is a moral distinction between creating embryos for research and creating them for reproductive purposes, at least given current fertility clinic practices.
Recent scientific work suggests it is possible to derive gametes from human pluripotent stem cells. Researchers have generated sperm and eggs from mouse ESCs and iPSCs and have used these stem cell-derived gametes to produce offspring (Hayashi 2011; Hayashi 2012). While it may take several years before researchers succeed in deriving gametes from human stem cells, the research holds much promise for basic science and clinical application. For example, the research could provide important insights into the fundamental processes of gamete biology, assist in the understanding of genetic disorders, and provide otherwise infertile individuals a means of creating genetically related children. The ability to derive gametes from human stem cells could also reduce or eliminate the need for egg donors and thus help overcome concerns about exploitation of donors and the risks involved in egg retrieval. Nonetheless, the research gives rise to some controversial issues related to embryos, genetics, and assisted reproductive technologies (D. Mathews et al . 2009).
One issue arises from the fact that some research on stem cell-derived gametes requires the creation of embryos, regardless of whether one is using ESCs or iPSCs. To establish that a particular technique for deriving human gametes from stem cells produces functional sperm and eggs, it is necessary to demonstrate that the cells can produce an embryo. This entails the creation of embryos through in vitro fertilization. Since it would not be safe to implant embryos created during the early stages of the research, the likely disposition of the embryos is that they would be destroyed. In such instances, the research would implicate all of the moral issues surrounding the creation and destruction of embryos for research. However, the creation of embryos for research in this situation would not necessitate the destruction of the embryos, as it does when embryos are created to derive stem cell lines. One could in principle store them indefinitely rather than destroy them. This would still leave one subject to the objection that life is being created for instrumental purposes. But the force of the objection is questionable since it is not clear that this instrumental use is any more objectionable than the routine and widely accepted practice of creating excess IVF embryos in the reproductive context to increase the probability of generating a sufficient number of viable ones to produce a pregnancy.
Further issues emerge with the prospect of being able to produce large quantities of eggs from stem cells. As the capacity to identify disease and non-disease related alleles through preimplantation genetic diagnosis (PGD) expands, the ability to create large numbers of embryos would substantially increase the chances of finding an embryo that possesses most or all of the traits one wishes to select. This would be beneficial in preventing the birth of children with genetic diseases. But matters would become morally contentious if it were possible to select for non-disease characteristics, such as sexual orientation, height, superior intelligence, memory, and musical ability. One common argument against using PGD in this way is that it could devalue the lives of those who do not exhibit the chosen characteristics. Another concern is that employing PGD to select for non-disease traits would fail to acknowledge the “giftedness of life” by treating children as “objects of our design or products of our will or instruments of our ambition” rather accepting them as they are given to us (Sandel 2004, 56). There is additionally a concern about advances in genetics heightening inequalities where certain traits confer social and economic advantages and only the well-off have the resources to access the technology (Buchanan 1995). Of course, one can question whether the selection of non-disease traits would in fact lead to devaluing other characteristics, whether it would alter the nature of parental love, or whether it is distinct enough from currently permitted methods of gaining social and economic advantage to justify regulating the practice. Nonetheless, the capacity to produce human stem cell-derived gametes would make these issues more pressing.
There have been a number of recent scientific studies in which stem cells have, under certain in vitro culture conditions, self-organized into three-dimensional structures that resemble and recapitulate some of the functions of human organs (Lancaster & Knoblich 2014; Clevers 2016). These “organoids” have been established with human stem cells for a variety of organs, including, among others, the kidney, liver, gut, pancreas, retina, and brain. In addition to organoids, stem cells have been shown to self-organize into embryo-like structures in vitro . Human embryonic stem cells have formed structures – referred to as “gastruloids” – that bear some resemblance to embryos during gastrulation, which is the stage several days after implantation where the body plan and some tissues tissue types, including the central nervous system, start to develop (Warmflash et al. 2014; Deglincerti et al . 2016; Shahbazi 2016). Researchers have also combined mouse embryonic stem cells and trophoblast stem cells to create “synthetic embryos,” which have a structure akin to pre-implantation embryos (Rivron et al . 2018). Synthetic embryos have been shown to implant into the mouse uterus, though their potential to develop to term has not been demonstrated.
While these scientific advances offer promising avenues for better understanding human development and disease, they also raise some novel and challenging ethical issues. In the case of organoids, cerebral organoids raise the most vexing issues. Researchers have produced cerebral organoids with a degree of development similar to that of a few-months-old embryo, and have already used them to study how the Zika virus causes microcephaly in fetuses (Garcez et al . 2016). At present, there is some evidence that cerebral organoids may be able to receive afferent stimulations that produce simple sensations (Quadrato et al . 2017). However, they currently lack the kind of mature neural networks and sensory inputs and outputs essential to the development of cognition. If, through bioengineering, human cerebral organoids were to develop the capacity for cognition, that would provide grounds for ascribing an elevated moral status to them, and it would raise concomitant issues about our moral obligations towards them. In the nearer term, it is more likely that cerebral organoids will develop some degree of consciousness Assuming we have a shared understanding of consciousness (e.g., phenomenal consciousness), one challenge is to identify means of measuring the presence of consciousness, since a cerebral organoid cannot communicate its internal states (Lavazza & Massimini 2018). But even if we can verify that an organoid is conscious, there remains the question of the moral significance of consciousness (Shepherd 2018). There is debate over whether consciousness has intrinsic value (Lee 2018), and whether in some cases it is better for a conscious being to not possess it (Kahane & Savulescu 2009). Those who reject the intrinsic value and moral significance of consciousness might find the case of a conscious entity that has led a solely disembodied existence, emerges and persists in the absence of any social or cultural nexus, and lacks beliefs and desires, to be a paradigmatic case where the value of consciousness is doubtful.
With respect to gastruloids and synthetic embryos (if the latter are successfully produced with human stem cells), the central question is whether these entities are sufficiently like human embryos in their structure and functions to give rise to moral concerns about their use in research. Gastruloids do not possess all the characteristics of an embryo, as they do not form all of the embryonic tissues (e.g., they do not have the trophectoderm, which mediates the attachment to the uterus). At the same time, gastruloids may, with extra-embryonic tissues, achieve a developmental stage in which they manifest a whole body plan. Recall that one argument (discussed in Section 1.1 above) for rejecting that human embryos are human beings is that the cells that comprise the early embryo do not function in a coordinated way to regulate and preserve a single organism. Gastruloids can in principle operate with this higher level of coordination. While one may still reject that this characteristic of gastruloids confers human rights on them, their more advanced stage of development might ground reasonable claims for according them greater respect than embryos at an earlier stage. In the case of both gastruloids and human synthetic embryos, the possibility that they ultimately lack the potential to develop into mature human beings may be of significance in morally distinguishing them from normal human embryos. As noted previously (in section 1.2 above), one argument for ascribing a high moral status to human embryos and for distinguishing the potential of human embryos from the potential of somatic cells and embryonic stem cells is that embryos have an “active disposition” and “intrinsic power” to develop into mature humans on their own. If synthetic embryos and gastruloids do not possess this disposition and power, then those who oppose some forms of human embryo research might not object to the creation and use of human gastruloids and synthetic embryos for research.
- Annas, G., Caplan, A., and Elias, S., 1996, “The Politics of Human-Embryo Research—Avoiding Ethical Gridlock,” New England Journal of Medicine , 334: 1329–32.
- Benn, S.I., 1973, “Abortion, Infanticide, and Respect for Persons,” in The Problem of Abortion , Joel Feinberg (ed.), Belmont, CA: Wadsworth: 92–103.
- Bok H., Schill K.E., and Faden R.R., 2004, “Justice, Ethnicity, and Stem-Cell Banks,” Lancet , 364(9429): 118–21.
- Buchanan, A., 1995, “Equal Opportunity and Genetic Intervention,” Social Philosophy and Policy , 12(2): 105–35.
- Burtchaell, J.T., 1989, “The Use of Aborted Fetal Tissue in Research: A Rebuttal,” IRB: A Review of Human Subjects Research , 11(2): 9–12.
- Curzer, H., 2004, “The Ethics of Embryonic Stem Cell Research,” Journal of Medicine and Philosophy , 29(5): 533–562.
- Damschen, G., Gomez-Lobo, A., and Schonecker, D., 2006, “Sixteen Days? A reply to B. Smith and B. Brogaard on the Beginning of Human Individuals,” Journal of Medicine and Philosophy , 31: 165–175.
- Clevers, H., 2016, “Modeling Development and Disease with Organoids,” Cell , 165: 1586–1597.
- Deglincerti, A., et al ., 2016, “Self-Organization of the Attached In Vitro Human Embryo,” Nature , 533: 251–54.
- Devolder, K., 2005, “Human Embryonic Stem Cell Research: Why the Discarded-Created Distinction Cannot Be Based on the Potentiality Argument,” Bioethics , 19(2): 167–86.
- Devolder, K., and Harris, J., 2007, “The Ambiguity of the Embryo: Ethical Inconsistency in the Human Embryonic Stem Cell Debate,” Metaphilosophy , 38(2–3): 153–169.
- Dworkin, R., 1992, Life’s Dominion , New York: Vintage.
- Faden, R.R., et al ., 2003, Public Stem Cell Banks: Considerations of Justice in Stem Cell Therapy, Hastings Center Report , 33: 13–27.
- Feinberg, J., 1986, “Abortion,” in Matters of Life and Death , T. Regan (ed.), New York: Random House.
- FitzPatrick, W., 2003, “Surplus Embryos, Nonreproductive Cloning, and the Intend/Foresee Distinction,” Hastings Center Report , 33: 29–36.
- Garzes, P.P., et al ., 2016, “Zika Virus Impairs Growth in Human Neurospheres and Brain Organoids,” Science , 352: 816–18.
- George, R.P., and Gomez-Lobo, A., 2002, “Statement of Professor George (Joined by Dr. Gomez-Lobo),” in Human Cloning and Human Dignity: An Ethical Inquiry , report by the President’s Council on Bioethics: 258–266.
- Green, R., 2002, “Benefiting from ‘Evil’; An Incipient Moral Problem in Human Stem Cell Research,” Bioethics , 16(6): 544–556.
- Greene, M., 2006, “To Restore Faith and Trust: Justice and Biological Access to Cellular Therapies,” Hastings Center Report , 36(1): 57–63.
- Hayashi, K., et al ., 2011, “Reconstitution of the Mouse Germ Cell Specification Pathway in Culture by Pluripotent Stem Cells,” Cell , 146(4): 519–532.
- Hayashi, K., et al ., 2012, “Offspring from Oocytes Derived from In Vitro Primordial Germ Cell-Like Cells in Mice,” Science , 338(6109): 971–975.
- Holm, S., 2003, “The Ethical Case Against Stem Cell Research,” Cambridge Quarterly of Healthcare Ethics , 12: 372–83.
- Kahane, G. and Savulescu, J., 2009, “Brain Damage and the Moral Significance of Consciousness,” Journal of Medicine and Philosophy , 34: 6–26.
- Kuhse, H., and Singer, P., 1992, “Individuals, Human, and Persons: The Issue of Moral Status,” in Embryo Experimentation: Ethical, Legal, and Social Issues , P. Singer, et al. (eds.), Cambridge: Cambridge University Press, 65–75
- Lancaster, M.A., and Knoblich, J.A., 2014, “Organogenesis in a Dish: Modeling Development and Disease Using Organoid Technologies,” Science , 345(6194): 1247125.
- Lavazza, A. and Massimini, M., 2018, “Cerebral Organoids: Ethical Issues and Consciousness Assessment,” Journal of Medical Ethics , 44: 606–10.
- Lee, A.Y., 2018, “Is Consciousness Intrinsically Valuable,” Philosophical Studies , 20: 1–17.
- Lee, P., and George R., 2006, “Human-Embryo Liberation: A Reply to Peter Singer,” National Review Online (25 January). [ Available online ]
- Lott, J.P., and Savulescu, J., 2007, “Towards a Global Human Embryonic Stem Cell Bank,” American Journal of Bioethics , 7(8): 37–44.
- Marquis, D., 2002, “Stem Cell Research: The Failure of Bioethics,” Free Inquiry , 23(1): 40–44.
- Mathews, D., et al ., 2009, “Pluripotent Stem Cell-Derived Gametes: Truth and (Potential) Consequences,” Cell: Stem Cell , 5: 11–14.
- May, L., 1992, Sharing Responsibility , Chicago: University of Chicago Press.
- McMahan, J., 2002, The Ethics of Killing: Problems at the Margins of Life , New York: Oxford University Press.
- McMahan, J., 2007a, “Killing Embryos for Stem Cell Research,” Metaphilosophy , 38(2–3): 170–189.
- –––, 2007b, “Infanticide,” Utilitas , 19: 131–159.
- Norsigian, J., 2005, “Risks to Women in Embryo Cloning,” Boston Globe , February 25.
- Parfit, D., 1984, Reasons and Persons , Oxford: Clarendon Press.
- Quadrato, G., et al ., 2017, “Cell Diversity and Network Dynamics in Photosensitive Human Brain Organoids,” Nature , 545: 48–53.
- Rivron, N.C., et al ., 2018, “Blastocyst-Like Structures Generated Solely from Stem Cells,” Nature , 557: 106–11.
- Robertson, J., 1988, “Fetal Tissue Transplant Research is Ethical,” IRB: A Review of Human Subjects Research , 6(10): 5–8.
- –––, 1999, “Ethics and Policy In Embryonic Stem Cell Research,” Kennedy Institute of Ethics Journal , 2(9): 109–36.
- Sagan, A., and Singer, P., 2007, “The Moral Status of Stem Cells,” Metaphilosophy , 38(2–3): 264–284
- Sandel, M., 2004, “The Case Against Human Perfection,” Atlantic Monthly , 293(3): 51–62.
- Savulescu, J., 1999, “Should We Clone Human Beings?” Journal of Medical Ethics , 25(2): 87–98.
- Shahbazi, M.N., et al ., 2016, “Self-Organization of the Human Embryo in the Absence of Maternal Tissues,” Nature Cell Biology , 18: 700–08.
- Shepherd, J., 2018, “Ethical (and Epistemological) Issues Regarding Consciousness in Cerebral Organoids,” Journal of Medical Ethics , 44: 611–12.
- Smith, B., and Brogaard, B., 2003, “Sixteen Days,” Journal of Medicine and Philosophy , 28: 45–78.
- Siegel, A., 2003, “Locating Convergence: Ethics, Public Policy, and Human Stem Cell Research,” in The Stem Cell Controversy , M. Ruse and C. Pynes (eds.), Amherst, NY: Prometheus Books.
- –––, 2004, “Temporal Restrictions and the Impasse on Human Embryonic Stem Cell Research,” The Lancet , 364(9429): 215–18.
- Strong, C., 1997, “The Moral Status of Preembryos, Embryos, Fetuses, and Infants,” Journal of Medicine and Philosophy , 22(5): 457–78
- Takahashi, K., et al ., 2007, “Induction of Pluripotent Stem Cells from Adult Human Fibroblasts by Defined Factors,” Cell , 131: 861–872.
- Thomson, J.A., et al ., 1998, “Embryonic Stem Cell Lines Derived from Human Blastocysts,” Science , 282: 1145–47.
- Tooley, M., 1983, Abortion and Infanticide , New York: Oxford University Press.
- Warmflash, A., et al ., 2014, “A Method to Recapitulate Early Embryonic Spatial Patterning in Human Embryonic Stem Cells,” Nature Methods , 11: 847–854.
- Warren, M.A., 1973, “On the Moral and Legal Status of Abortion,” Monist , 57: 43–61.
- Yu, J., et al ., 2007, “Induced Pluripotent Stem Cell Lines Derived from Human Somatic Cells,” Science , 318: 1917–1920.
How to cite this entry . Preview the PDF version of this entry at the Friends of the SEP Society . Look up topics and thinkers related to this entry at the Internet Philosophy Ontology Project (InPhO). Enhanced bibliography for this entry at PhilPapers , with links to its database.
Other Internet Resources
- President’s Council on Bioethics, 2002, Human Cloning and Human Dignity: An Ethical Inquiry
- U.S. Conference of Catholic Bishops, 2001, Fact Sheet: President Bush’s Stem Cell Decision
- International Society for Stem Cell Research
- Stem Cell Resources from the American Association for the Advancement of Science
- Stem Cell Research and Applications , recommendations and findings from the AAAS and the Institute for Civil Society.
- Medline Plus: Stem Cells
- The Pew Forum on Religion and Public Life: Bioethics
- The Hinxton Group: An International Consortium on Stem Cell, Ethics, and Law
-->abortion, ethics of --> | cloning | double effect, doctrine of | ethics, biomedical: chimeras, human/non-human | parenthood and procreation | systems and synthetic biology, philosophy of
Copyright © 2018 by Andrew Siegel < asiegel @ jhu . edu >
- Accessibility
Support SEP
Mirror sites.
View this site from another server:
- Info about mirror sites
The Stanford Encyclopedia of Philosophy is copyright © 2023 by The Metaphysics Research Lab , Department of Philosophy, Stanford University
Library of Congress Catalog Data: ISSN 1095-5054
- Writing services
- Proofreading
- Math/Science
- Copywriting
- Dissertation services
- Admission services
- Our Writers
Stem Cell Research Persuasive Essay
Table of contents:
- General idea
- Introduction
Stem cell research is one of the most controversial topics of our day. As you think about writing a persuasive essay, consider the importance of this topic and how emotive it can be to discuss both the arguments for and against.
Any embryonic stem cell research essay needs to carefully weigh up the pros and cons, as well as the ethics involved. In a lot of ways, where you fall on stem cell research will be indicative of what you think about many different topics such as when you feel life begins, the justice and morality of using human cells to cure diseases, and how you interpret your own religious beliefs. Your audience, you may find, could have very different views from you on these issues, so be sure you’re not just in an echo chamber and ignoring those who differ from you.
Begin your introduction with a hook that captures your reader and sets expectations for who you want your audience to ideally be. Do you want to persuade people who might be misinformed on the subject, or do you want to sway people to your side with an emotive anecdote? Then go on to set up your thesis statement, which is the single most important sentence in a persuasive essay, and the foundation of everything you will be writing.
Introduction examples
Pro: Barack Obama says of stem cell research that “…we have been given the capacity and will to pursue this research and the humanity and conscience to do so responsibly.” He’s not the only one who feels that stem cell research holds vital importance for curing diseases and ensuring that children are born into a safer, healthier world.
Con: Stem cells harvested from foetuses are just not necessary to have the medical research we need to move forward in curing disease and human ailments. Umbilical cord blood, plus research from adult stem cells, provide all the useful information we could require for research.
Moving forward into the body of your essay, it might be relevant to touch on similar debates for comparison, like the one around cloning, or provide a sample of a debate between the two opposing sides. Your argument for or against could probably use some quotes from experts, or perhaps relevant verses from the holy book of your choice. Take the time to draw up an outline, as this will help you set the structure up.
Your conclusion is the summation of everything you’ve argued in the body of your essay, so make sure you briefly give a summary of your most important points. Then move on to call your readers to action. Don’t let the persuasive essay end without doing this, as this what the whole essay has been building up to.
Conclusion examples
Pro: Pluripotent stem cells, such as those found in embryonic stem cells, hold the key to so much. When future generations look back on what we’re accomplishing here, they will definitely feel the use of embryonic stem cells were worth it. Give your children and grandchildren a future by supporting stem cell research today!
Con: When it comes to ethics, we can’t compromise, and using embryonic stem cells is a step too far. Every disease cured due to stem cell research is bought with blood as surely as the research done during the Holocaust was. Don’t let this nightmare go on any longer! Write to your representative today!
- Essay samples
- Infographics
- Essay writing
- Crafting a Powerful Essay on Political Polarization
- Oral Health Overview Essay: Preventing Tooth Decay in Australia
- How to Write a Good Expository Essay About Macbeth
- How to Write An Expository Essay About Love
- How to Write a Great Expository Essay About Life
Price per page
Total price:
Limitless Amendments
Bibliography
Plagiarism Report
Get all these features for A$93.12 FREE
If you don't know exactly what type of paper you need or can't find the necessary one on the website - don't worry! Contact us and we'll help you out!
- Terms of Use
- Money Back Guarantee
- Cookie Policy
- Privacy Policy
- Write My Essay
- Custom Essay
- Essay Writer
- Do My Essay
- Type My Essay
- Pay For Essay
- Cheap Essay
- Write My Paper
- Write My Assignment
- Assignment Writer
- Buy Assignment
- Assignment Help
- Do My Assignment
- Nursing Essay Writing Service
- Management Essay
- Business Essay
- Law Essay Writing Service
- Education Essay Service
- Marketing Essay
- Accounting Essay
- Sociology Essay
Before continuing to use our service please make sure you got acquainted with our Cookie Policy and accepted it by clicking OK
What is Stem Cell Research and Pros and Cons about
Learn about stem cell research, including the benefits and drawbacks, as well as the numerous types of stem cells accessible.
Stem Cell Therapy enhances the body’s natural healing processes, and is one of the most exciting breakthroughs in recent regenerative medicine. It offers incredible treatment for a wide range of illnesses for which doctors previously had no acceptable treatments.
In this Mind The Graph article, you will learn about stem cell research: pros and cons , what is it, and the various types of stem cells available. This article will also provide you with successful stories to better understand the topic.
What are stem cells?
The body has original raw material in the form of stem cells. These stem cells are responsible for the development of all other cells with specific roles. When given the right conditions, either in the body or in a laboratory, stem cells divide to produce new cells known as daughter cells.
The daughter cells have the ability to transform into more stem cells or cells with a specific function, such as blood cells, brain cells, heart muscle cells, or bone cells. There is no other cell in the body that can naturally generate new cell types like a stem cell.
Types of stem cells
Embryonic stem cells.
Embryonic stem cells are extracted from the blastocyst, a mostly empty ball of cells that develops three to five days after an egg cell is fertilized by a sperm in humans. Embryonic stem cells are pluripotent, which means they can give rise to all cell types in a fully developed organism, save the placenta and umbilical cord.
These cells that have been separated from the inner cell mass will evolve into more specialized cells, which will give rise to all of the body’s tissues and organs. When scientists remove the inner cell mass and cultivate it in a particular laboratory environment, the cells maintain the qualities of embryonic stem cells.
These cells are extremely significant because they provide a sustainable supply for researching normal development and illness, as well as evaluating medicines and other treatments.
Tissue-specific stem cells
Tissue-specific stem cells (most known as adult stem cells) have a higher level of specialization than embryonic stem cells. Typically, these stem cells may produce a wide range of cell types for the tissue or organ in which they dwell.
Tissue-specific stem cells are rare to detect in the human body, and they do not appear to self-renew in culture as easily as embryonic stem cells. However, research on these cells has expanded our overall understanding of normal development, how aging affects us, and what occurs in the event of an injury and disease.
Mesenchymal stem cells
Cells derived from stroma, the connective tissue that surrounds other tissues and organs, are referred to as “mesenchymal stem cells” or MSC. Many scientists refer to cells with this designation as “stromal cells.”
These cells were initially found in the bone marrow and were demonstrated to be capable of producing bone, cartilage, and fat cells. They have now been produced from various tissues such as fat and cord blood. Various MSCs are assumed to have stem cell and even immunomodulatory qualities, and they are being explored as therapies for a wide range of illnesses, although there is no evidence that they are useful yet. Scientists do not know for certain if these cells are stem cells or what sorts of cells they can generate. They do agree that not all MSCs are the same and that their properties vary depending on where they come from in the body and how they are separated and produced.
Induced pluripotent stem cells
Induced pluripotent stem (iPS) cells are lab-engineered cells that have been transformed from tissue-specific cells, such as skin cells and into cells that act like embryonic stem cells. IPS cells are important tools for scientists to understand more about developmental stages, illness initiation, and progression, as well as create and test new medications and treatments.
While iPS cells possess a lot of the same properties as embryonic stem cells, such as the potential to give birth to all cell types in the body, they are not identical. Scientists are trying to figure out what these distinctions are and what they represent. For one thing, the first iPS cells were created by inserting additional copies of genes into tissue-specific cells using viruses. Researchers are exploring a variety of methods for creating iPS cells, to eventually use them as a source of cells or tissues for medicinal therapies.
Development in Stem Cell Research: successful stories
Before delving into the pros and cons of stem cell research , a few successful tales must be mentioned in this article.
Multiple Sclerosis
Reema Sandhu’s stem cell success story began in 2014 when she was diagnosed with multiple sclerosis, according to DailyMail. The disease can affect the brain and spinal cord, causing a variety of life-altering symptoms such as severe disabilities, muscular spasms, and memory issues. She got an autologous stem cell transplant after years of frustration, in which her own stem cells were extracted from her blood and infused back into her body through intravenous infusion. Major improvements in Reema’s brain function were immediately evident. Her vision recovered two months after the transplant, and she went back to work. These encouraging results indicate that Reema’s MS has slowed as a result of her stem cell transplant.
Heart attack
According to DailyMail, Dave Randle was left with serious heart failure and a grim warning from specialists after suffering a heart attack in 2016. However, after learning that stem cells may be used to heal damaged hearts, Dave enrolled in therapy and received shots for 5 days in a row that pushed his bone marrow to allow stem cells to enter his circulation. These cells were then extracted and reintroduced into his heart. Dave’s stem cell success story had a happy ending weeks after the transplant – he began to feel stronger and physicians detected significant changes.
In 2013, a woman was diagnosed with HIV. According to the Journal, she was also diagnosed with acute myeloid leukemia in March 2017, making her a candidate for a stem cell transplant. She had a stem cell transplant via two blood transfusions: one from an older relative and the other from an unrelated baby. The baby, a partially matched donor, has a mutation in the CCR5 gene, which inhibits HIV’s capacity to infiltrate host cells. The woman stopped taking her HIV medication in 2020, and she hasn’t shown any measurable indications of the infection ever since. She has also been in remission from leukemia for almost four years.
Stem Cell Research: Pros and Cons
- Improve understanding of illness etiology: Researchers may gain a better understanding of how illnesses and ailments emerge by monitoring stem cells grow into cells in bones, heart muscle, neurons, and other organs and tissue.
- Generate healthy cells to replace diseased cells (regenerative medicine): Stem cells can be manipulated to become particular cells that can be employed in humans to regenerate and heal tissues that have been damaged or impaired by illness.
- Test novel pharmaceuticals for safety and efficacy: Before administering investigational drugs to humans, researchers can utilize certain types of stem cells to assess the drugs’ effectiveness and safety.
- Minimal rejection risk: Adult stem cells are less likely to be rejected in transplants and can be reprogrammed. Adult stem cell success has also been established in a variety of therapeutic applications.
- Hard to grow: Adult stem cells are difficult to cultivate for an extended length of time and there is currently no technique available to create large amounts of adult stem cells.
- Embryonic stem cells are generally rejected: When employed in transplants, embryonic stem cells may not be accepted.
- New technology: Stem cell treatment is still being researched, and there are a lot of things that need to be established. The therapy’s long-term adverse effects are yet unknown.
- Concerns about ethics: stem cell treatment uses embryonic stem cells from a human embryo. Many conservatives argue that “human life begins at conception” and that stem cell research results in the death of living babies.
Make scientifically accurate infographics in minutes
Use the power of infographics to help your scientific job succeed. Mind The Graph tool can assist you by giving amazing templates and allowing you to browse through 40 000+ scientifically accurate images in 80+ popular fields.
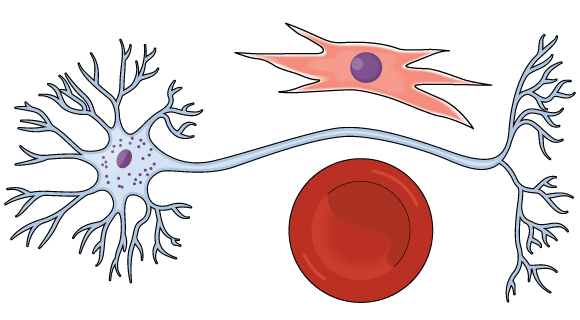
Subscribe to our newsletter
Exclusive high quality content about effective visual communication in science.
Unlock Your Creativity
Create infographics, presentations and other scientifically-accurate designs without hassle — absolutely free for 7 days!
About Jessica Abbadia
Jessica Abbadia is a lawyer that has been working in Digital Marketing since 2020, improving organic performance for apps and websites in various regions through ASO and SEO. Currently developing scientific and intellectual knowledge for the community's benefit. Jessica is an animal rights activist who enjoys reading and drinking strong coffee.
Content tags

Embryonic Stem Cell Research An Ethical Dilemma
Article sidebar.
Main Article Content
Introduction
In November 1998, two teams of U.S. scientists confirmed successful isolation and growth of stems cells obtained from human fetuses and embryos. Since then, research that utilizes human embryonic cells has been a widely debated, controversial ethical issue. Human embryonic cells possess the ability to become stem cells, which are used in medical research due to two significant features. First, they are unspecialized cells, meaning they can undergo cell division and renew themselves even with long periods of inactivity. Secondly, stem cells are pluripotent, with the propensity to be induced to become specified tissue or any “organ-specific cells with special functions” depending on exposure to experimental or physiologic conditions, as well as undergo cell division and become cell tissue for different organs.
The origin of stem cells themselves encapsulates the controversy: embryonic stem cells, originate from the inner cell mass of a blastocyst, a 5-day pre-implantation embryo. The principal argument for embryonic stem cell research is the potential benefit of using human embryonic cells to examine or treat diseases as opposed to somatic (adult) stem cells. Thus, advocates believe embryonic stem cell research may aid in developing new, more efficient treatments for severe diseases and ease the pain and suffering of numerous people. However, those that are against embryonic stem cell research believe that the possibility of scientific benefits of research do not outweigh the immoral action of tampering with the natural progression of a fetal development and interfering with the human embryo’s right to live. In light of these two opposing views, should embryonic stem cells be used in research? It is not ethically permissible to destroy human embryonic life for medical progress.
Personhood and the Scientific Questionability of Embryonic Stem Cell Research
The ethics behind embryonic stem cell research are controversial because the criteria of ‘personhood’ is “notoriously unclear.” Personhood is defined as the status of being a person, entitled to “moral rights and legal protections” that are higher than living things that are not classified as persons. Thus, this issue touches on existential questions such as: When does life begin? and What is the moral status that an embryo possesses? There is a debate on when exactly life begins in embryonic development and when the individual receives moral status. For example, some may ascribe life starting from the moment of fertilization, others may do so after implantation or the beginning of organ function. However, since the “zygote is genetically identical to the embryo,” which is also genetically identical to the fetus, and, by extension, identical to the baby, inquiring the beginning of personhood can lead to an occurrence of the Sorites paradox, also acknowledged as “the paradox of the heap.”
The paradox of the heap arises from vague predicates in philosophy. If there is a heap of sand and a grain is taken away from that heap one by one, at what point will it no longer be considered a heap – what classifies it as a heap? The definition of life is similarly arbitrary. When, in the development of a human being, is an embryo considered a person with moral standing? The complexity of the ethics of embryonic stem cell research, like the Sorites paradox, demonstrates there is no single, correct way to approach a problem; thus, there may be multiple different solutions that are acceptable. Whereas the definition of personhood cannot be completely resolved on a scientific basis, it serves a central role in the religious, political, and ethical differences within the field of embryonic stem cell research. Some ethicists attempt to determine what or who is a person by “setting boundaries” (Baldwin & Capstick, 2007).
Utilizing a functionalist approach, supporters of embryonic stem cell research argue that to qualify as a person, the individual must possess several indicators of personhood, including capacity, self-awareness, a sense of time, curiosity, and neo-cortical function. Proponents argue that a human embryo lacks these criteria, thereby is not considered a person and thus, does not have life and cannot have a moral status. Supporters of stem cell research believe a fertilized egg is just a part of another person’s body until the cell mass can survive on its own as a viable human. They further support their argument by noting that stem cell research uses embryonic tissue before its implantation into the uterine wall. Researchers invent the term “pre-embryo” to distinguish a pre-implantation state in which the developing cell mass does not have the full respects of an embryo in later stages of embryogenesis to further support embryonic stem cell research. Based on this reductionist view of life and personhood, utilitarian advocates argue that the result of the destruction of human embryos to harvest stem cells does not extinguish a life. Further, scientists state that any harm done is outweighed by the potential alleviation of the suffering enduring by tremendous numbers of people with varying diseases. This type of reasoning, known as Bentham’s Hedonic (moral) calculus, suggests that the potential good of treating or researching new cures for ailments such as Alzheimer’s disease, Parkinson’s disease, certain cancers, etc. outweighs any costs and alleviate the suffering of persons with those aliments. Thus, the end goal of stem cell use justifies sacrificing human embryos to produce stem cells, even though expending life is tantamount to murder. Opponents of embryonic stem cell research would equate the actions done to destroy the embryos as killing. Killing, defined as depriving their victims of life, will therefore reduce their victims to mere means to their own ends. Therefore, this argument touches on the question: if through the actions of embryotic stem cell research is “morally indistinguishable from murder?” (Outka, 2013). The prohibition of murder extends to human fetuses and embryos considering they are potential human beings. And, because both are innocent, a fetus being aborted and an embryo being disaggregated are direct actions with the intention of killing. Violating the prohibition of murder is considered an intolerable end. We should not justify this evil even if it achieves good. Under the deontological approach, “whether a situation is good or bad depends on whether the action that brought it about was right or wrong,” hence the ends do not justify the means. Therefore, under this feeble utilitarian approach, stem cell research proceeds at the expense of human life than at the expense of personhood.
One can reject the asserted utilitarian approach to stem cell research as a reductionist view of life because the argument fails to raise ethical concerns regarding the destruction embryonic life for the possibility of developing treatments to end certain diseases. The utilitarian approach chooses potential benefits of stem cell research over the physical lives of embryos without regard to the rights an embryo possesses. Advocates of embryonic stem cell research claim this will cure diseases but there is a gap in literature that confirms how many diseases these cells can actually cure or treat, what diseases, and how many people will actually benefit. Thus, killing human embryos for the potentiality of benefiting sick people is not ethically not ethically permissible.
Where the argument of personhood is concerned, the development from a fertilized egg (embryo) to a baby is a continuous process. Any effort to determine when personhood begins is arbitrary. If a newborn baby is a human, then surely a fetus just before birth is a human; and, if we extend a few moments before that point, we would still have a human, and so on all the way back to the embryo and finally to the zygote. Although an embryo does not possess the physiognomies of a person, it will nonetheless become a person and must be granted the respect and dignity of a person. Thus, embryotic stem cell research violates the Principle of “Full Human Potential,” which states: “Every human being […] deserves to be valued according to the full level of human development, not according to the level of development currently achieved.” As technology advances, viability outside the womb inches ever closer to the point of inception, making the efforts to identify where life begins after fertilization ineffectual. To complicate matters, as each technological innovation arrives, stem-cell scientists will have to re-define the start of life as many times as there are new technological developments, an exhausting and never-ending process that would ultimately lead us back to moment of fertilization. Because an embryo possesses all the necessary genetic information to develop into a human being, we must categorically state that life begins at the moment of conception. There is a gap in literature that deters the formation of a clear, non-arbitrary indication of personhood between conception and adulthood. Considering the lack of a general consensus of when personhood begins, an embryo should be referred to as a person and as morally equivalent to a fully developed human being.
Having concluded that a human embryo has the moral equivalent of a fully-fledged human being, this field of research clearly violates the amiable rights of personhood, and in doing so discriminates against pre-born persons. Dr. Eckman asserts that “every human being has a right to be protected from discrimination.” Thus, every human, and by extension every embryo, has the right to life and should not be discriminated against their for “developmental immaturity.” Therefore, the field of embryonic stem cell research infringes upon the rights and moral status of human embryos.
Principle of Beneficence in Embryonic Stem Cell Research
The destruction of human embryos for research is not ethically permissible because the practice violates the principle of beneficence depicted in the Belmont Report, which outlines the basic ethical principles and guidelines owed to human subjects involved in research. Stem cell researchers demonstrate a lack of respect for the autonomy and welfare of the human embryos sacrificed in stem cell research.
While supporters of embryonic stem cell research under the utilitarian approach argue the potential benefits of the research, the utilitarian argument however violates the autonomy of the embryo and its human rights, as well as the autonomy of the embryo donors and those that are Pro-Life. Though utilitarian supporters argue on the basis of rights, they exclusively refer to the rights of sick individuals. However, they categorically ignore the rights of embryos that they destroy to obtain potential disease curing stem cells. Since an embryo is regarded as a human being with morally obligated rights, the Principle of Beneficence is violated, and the autonomy and welfare of the embryo is not respected due to the destruction of an embryo in stem cell research. Killing embryos to obtain stem cells for research fails to treat embryos as ends in an of themselves. Yet, every human ought to be regarded as autonomous with rights that are equal to every other human being. Thus, the welfare of the embryo is sacrificed due to lack of consent from the subject.
The Principle of Beneficence is violated when protecting the reproductive interests of women in infertility treatment, who are dependent on the donations of embryos to end their infertility. Due to embryonic stem cell research, these patients’ “prospects of reproductive success may be compromised” because there are fewer embryos accessible for reproductive purposes. The number of embryos necessary to become fully developed and undergo embryonic stem cell research will immensely surpass the number of available frozen embryos in fertility clinic, which also contributes to the lack of embryos available for women struggling with infertility. Therefore, the basis of this research violates women’s reproductive autonomy, thus violating the Principle of Beneficence.
It is also significant to consider the autonomy and welfare of the persons involved. The autonomous choice to donate embryos to research necessitates a fully informed, voluntary sanction of the patient(s), which poses difficulty due to the complexity of the human embryonic stem cell research. To use embryos in research, there must be a consensus of agreement from the mother and father whose egg and sperm produced the embryo. Thus, there has to be a clear indication between the partners who has the authority or custody of the embryos, as well as any “third party donors” of gametes that could have been used to produce the embryo because these parties’ intentions for those gametes may solely have been for reproductive measures only. Because the researchers holding “dispositional authority” over the embryos may exchange cell lines and its derivatives (i.e., genetic material and information) with other researchers, they may misalign interests with the persons whose gametes are encompassed within the embryo. This mismatch of intent raises complications in confidentiality and autonomy.
Lastly, more ethical complications arise in the research of embryonic stem cells because of the existence viable alternatives that to not destroy human embryos. Embryonic stem cells themselves pose as a higher health risk than adult stem cells. Embryonic stem cells have a higher risk of causing tumor development in the patient’s body once the cells are implanted due to their abilities to proliferate and differentiate. Embryonic stem cells also have a high risk of immunorejection, where a patient’s immune system rejects the stem cells. Since the embryonic stem cells are derived from embryos that underwent in vitro fertilization, when implanted in the body, the stem cell’s marker molecules will not be recognized by the patient’s body, resulting in the destruction of the stem cells as a defensive response to protect the body (Cahill, 2002). With knowledge of embryonic stem cells having higher complications than the viable adult stem cells continued use of embryonic stem cells violates the Principle of Beneficence not only for the embryos but for the health and safety of the patients treated with stem cells. Several adult stem cell lines (“undifferentiated cells found throughout the body”) exist and are widely used cell research. The use of adult stem cells represents research that does not treat human beings as means to themselves, thus, complying with the Principle of Beneficence. This preferable alternative considers the moral obligation to discover treatments, and cures for life threating diseases while avoiding embryo destruction.
It is not ethically permissible to destroy human embryonic life for medical progress due to the violations of personhood and human research tenets outlined in the Belmont Report. It is significant to understand the ethical implications of this research in order to respect the autonomy, welfare, beneficence, and basic humanity afforded to all parties involved. Although embryonic stem cell research can potentially provide new medical advancements to those in need, the harms outweigh the potential, yet ill-defined benefits. There are adult stem cell alternatives with equivalent viability that avoid sacrificing embryos. As society further progresses, humans must be cautious of compromising moral principles that human beings are naturally entitled to for scientific advancements. There are ethical boundaries that are crossed when natural processes of life are altered or manipulated. Though there are potential benefits to stem cell research, these actions are morally and ethically questionable. Thus, it is significant to uphold ethical standards when practicing research to protect the value of human life.
Shamblott, M. J., J. Axelman, S. Wang, E. M. Bugg, J. W. Littlefield, P. J. Donovan, P. D. Blumenthal, G. R. Huggins, and J. D. Gearhart. “Derivation of Pluripotent Stem Cells from Cultured Human Primordial Germ Cells.” Proceedings of the National Academy of Sciences 95, no. 23 (November 10, 1998): 13726–31. doi:10.1073/pnas.95.23.13726.
National Institutes of Health, U.S. Department of Health and Human Services. “Stem Cell Basics I.” Stem Cell Information , 2016. https://stemcells.nih.gov/info/basics/1.htm .
Kitwood, Thomas Marris., Clive Baldwin, and Andrea Capstick. Tom Kitwood on Dementia: A Reader and Critical Commentary . Maidenhead, Berkshire: McGraw-Hill/Open University Press, 2007.
University of Michigan. “Stem Cell Research: Frequently Asked Questions,” 2013. http://www.stemcellresearch.umich.edu/overview/faq.html#section2 .
EuroStemCell. “Origins, Ethics and Embryos: The Sources of Human Embryonic Stem Cells,” 2016. https://www.eurostemcell.org/origins-ethics-and-embryos-sources-human-embryonic-stem-cells .
Perry, David L. “Some Issues in Contemporary Neurological Science and Technology,” 2011. https://www.scu.edu/ethics/focus-areas/bioethics/resources/ethics-and-personhood/ .
Swirsky, E. “Week Fourteen Unit: Minute Paper 5 [Blackboard Assignment],” 2018.
O’Mathúna, DP. “Personhood in Bioethics and Biomedical Research.” Research Practitioner 7 (2006): 167–74.
Grobstein, C. “External Human Fertilization.” Scientific American 240, no. 6 (June 1979): 57–67.
Mastin, L. “Deontology,” 2009. https://www.philosophybasics.com/branch_deontology.html .
Spitzer, Robert. “Introduction and Principles of Ethics.” In Ten Universal Principles: A Brief Philosophy of the Life Issues , xi–xii, 1-3, 20-29. San Fransisco, CA: Ignatius Press, 2011. https://www.catholiceducation.org/en/religion-and-philosophy/philosophy/introduction-amp-principles-of-ethics.html .
Eckman, Jim. “Human Embryonic Stem Cell Research.” Issues In Perspective , 2011. https://graceuniversity.edu/iip/2011/05/14-2/ .; Eckman, Jim. “The Devaluing of Life in America.” Issues In Perspective , 2015. https://graceuniversity.edu/iip/2015/09/the-devaluing-of-life-in-america/ .
Outka, Gene (2009) "The Ethics of Embryonic Stem Cell Research and the Principle of "Nothing is Lost"," Yale Journal of Health Policy, Law, and Ethics : Vol. 9 : Iss. 3 , Article 7.
Curzer, Howard. “The Ethics Of Embryonic Stem Cell Research.” The Journal of Medicine and Philosophy 29, no. 5 (October 1, 2004): 533–62. doi:10.1080/03605310490514225.
Lo, Bernard, and Lindsay Parham. “Ethical Issues in Stem Cell Research.” Endocrine Reviews 30, no. 3 (May 2009): 204–13. doi:10.1210/er.2008-0031.
Hubbard, James. “Embryonic Stem-Cell Research: Experts Debate Pros and Cons.” The Survival Doctor , 2013. http://thesurvivaldoctor.com/2013/02/14/doctors-debate-embryonic-stem-cell-research-pros-and-cons/ .
Koch, Valerie Gutmann, Beth E. Roxland, Barbara Pohl, and Sarah K. Keech. “Contemporary Ethical Issues in Stem Cell Research.” In Stem Cells Handbook , 29–37. New York, NY: Springer New York, 2013. doi:10.1007/978-1-4614-7696-2_2.
Cahill, Lisa Sowle. "Holland, Suzanne, Karen Lebacqz, and Laurie Zoloth, Eds. The Human Embryonic Stem Cell Debate: Science, Ethics, and Public Policy." The National Catholic Bioethics Quarterly 2, no. 3 (2002): 559-62. doi:10.5840/ncbq20022344.
Devolder, Katrien. The Ethics of Embryonic Stem Cell Research . Oxford University Press, 2015. doi:10.1093/acprof:oso/9780199547999.001.0001.
ScienceDaily. “Adult Stem Cell,” 2018. https://www.sciencedaily.com/terms/adult_stem_cell.htm .
Article Details
Stem Cell Research: Pros and Cons
After researching about cloning and finding out what it is exactly and how it works, I understood that cloning is a process. It is used to create an exact genetic copy of another cell, tissue or an organism by taking the genetic information from one living thing and creating exact copies of it (Cloning: MedlinePlus). Researchers have found many interesting and amazing ways of cloning a variety of biological materials, yes even entire organisms! Cloning happens naturally via asexual reproduction. This happens in some plants an also on some single-celled organisms, prokaryotes, like bacteria.
We could also say that identical twins are clones that happen naturally because since they are produced when a fertilized egg splits, they carry almost identical DNA. But cloning also happens artificially, and the three types of it are reproductive cloning, gene cloning, and therapeutic cloning. How cloning is done currently Gene cloning Gene cloning is what creates exact copies of the segments of DNA. Researchers use this to make copies of genes that they wish to examine.
They insert the gene from one organism into the genetic material of a vector, which are carriers such as bacteria or virus, that are then placed under lab conditions that cause it to multiply and end up in the gene being copied several times.
Reproductive cloning Animals are cloned through reproductive cloning which is able to produce copies of entire animals. What researchers do is that they remove a mature somatic cell, body cells such as skin, nerve or blood cell from the animal they want to copy and then transfer its DNA and place it into an egg cell that had its own nucleus, containing its DNA, removed.

Proficient in: Stem Cell Research
“ Very organized ,I enjoyed and Loved every bit of our professional interaction ”
The egg later becomes a just developing embryo in the test tube and is later implanted into the womb of the animal. This results a female adult animal giving birth to an animal that has the exact same genetic make up as the animal that donated the somatic cell. The first mammal that was successfully cloned was a sheep named Dolly (Cloning Fact Sheet). Therapeutic cloning Finally, therapeutic cloning is used to substitute bad or injured tissues through the production of embryonic stem cells. Embryonic stem cells, the ones that are used in therapeutic cloning, are stem cells that come from embryos that are between three to five days old. These stem cells are pluripotent which is what I described earlier, they can renew themselves and divide into more stem cells or they also have the ability to become any type of cell that is found in the body (Mayo Clinic 2019). They are important in cloning because they have many functions and they have the ability to repair organs and bad tissues. Stem cells are important because they could help understand how diseases happen, test a drug’s effectiveness and safety, generate and replace cells with new healthy ones.
Five uses of cloning to humans There are several uses of cloning to humans and each of them has its own unique benefits. There are medicinal benefits in cloning that have the potential to benefit everyone. Cloning could help have an extensive amount of animals for study and that way decrease the time needed to make a transgenic animal model. Animal models are genetically engineered to carry mutations in their genes that carry diseases. Genetic engineering works with genes in order to make different versions of a specific organism. Genetic engineering alters the genes in a living organism to produce a genetically modified organisms with a new genotype. GMOs are any organisms such as animal, plant or microorganism whose genetic makeup have been changed or modified using genetic engineering or other types of technology (What is a GMO?). Genetic modification happens in many of the products we consume regularly. This could help researchers learn more and faster about diseases by experimenting on more animals. This has the potential to save human lives because if researchers now more about diseases and have the opportunity to experiment on more animals, they could help prevent human diseases. What could also help treat or stop diseases in humans is gene therapy.
Gene therapy is when the genes inside the body’s cells are altered in an effort to treat or stop a disease. Genes that do not work properly could cause a disease. Gene therapy could help replace a bad gene or add a new gene in order to try to cure a diseases or help fight it. Another use of cloning to humans is to make stem cells. Stem cells function as a repair system for the body. Stem cells generate all other cells that have specialized functions. They are able to divide and form daughter cells if they are under the necessary conditions. The daughter cells can then renew themselves and become new stem cells or become cells with specific functions, such as brain cells, bone cells, heart muscle cells, blood cells etc. Stem cells are crucial in our lives because they maintain, build and repair the body. This could help people that burned their skin, people that have brain damage etc. What stem cells do is a natural process, so this process can be manipulated for reparation. Transferring stem cells from person to person can have negative effects, and this is where cloning becomes beneficial because this could help create genetically identical stem cells of a particular individual (Why Clone?). This could really be an advance in medicine because they could even be used in the creation of whole body organs and be used when a person may need an organ transplant. Stems cells also have a benefit when it comes to diseases. Stem cells from a sick person could be cloned and that way be further examined to learn more about the particular sickness and find a treatment.
Cloning could also be used by humans and benefit them by reproducing a sick pet. The clone may have the same genes, but that does not necessarily mean that it will behave the same and do everything just like the original pet. It is more than just their genes, it is also their environment that shapes an animal or a person’s personality. On December 22, 2001 a kitten named CC was the first domestic pet ever to be cloned. But the one that was cloned did not end up having the same color as the original cat. This problem has to do with the X chromosome, the gene that helps a cat determine their color, that was shut off, this is called X-inactivation (Why Clone). Another use of cloning to humans will be that it could help couples with infertility. People who are not able to produce children in a natural way could create their own kids through human cloning and that way have the same genes (20 Advantages and Disadvantages of Cloning Humans 2019). Infertility has the potential to not be a problem anymore because a fetus would be able to grow outside of the woman’s body through cloning.
Another interesting use of cloning to humans is cloning livestock, such as pigs or cows, the animals that produce milk and meat. This is used to produce copies of the best animals in the farm and breed them. This does not only benefit the farmer, but humans too. Cloning livestock process in detail The process of cloning livestock is more advanced than all of the other techniques farmers use to reproduce their cattle and very beneficial. If a farmer has, for example, a dairy cow that is just perfect because she gets pregnant really easily, does not get sick often like all the others, gets perfectly suited with her environment, has no complications when giving birth, and produce millions of gallons of the best quality milk and then suddenly that cow is about to die or is at the end of her reproductive life the farmer could just clone it and that way have that cow forever! It would not only be beneficial for the farmers, but also to all of those people that are consuming the cows’ milk. The farmer could just stay with that cow’s offsprings and keep breeding those and getting milk from them; but they will not get the same results that their best cow gave them. So in order to guarantee that they will be just like the best cow, the only option they have is to copy that specific cow. This would be a lot quicker than just breeding and waiting for a cow to have all of those amazing qualities.
Farmers could also clone this animals to produce and be able to sell high quality lean meat faster than if just having a couple of animals. If a farmer only has one animal that produces meat that is very lean and tender, by cloning it they could have all of that same quality meat in a faster and more efficient way. This would provoke them to sell more and grow their business. This would benefit humans by having more meat that is high quality and this will allow meat markets and supermarkets to have more supply. When cloning animals, they are still born just like any other regular animal, they do not just appear, think of it like identical twins that were not born at the same time. They still share the same genes as the original animal. Cloning serves as a type of control for farmers, it gives them the ability to choose which traits they want their clone to have. This type of cloning uses a process called somatic cell nuclear transfer. What scientists do is that they take an immature egg from the female animal and remove the nucleus from it. The nucleus is what contains the eggs genes, and by removing it, necessary materials for the beginning stages of embryo development are left behind. The nucleus or cell from the animal that has the traits the farmer wants to copy is then added. Later on, the nucleus combines with the ooplast, which are the eggs whose nucleus are removed and starts dividing and an embryo begins to form.
The embryo is then implanted in the uterus of a female animal and the clone is then born just like any regular animal (Medicine). What could go wrong with this is that the embryo could fail to develop correctly and may be flushed out of the uterus, it could also not implant properly, or the placenta may not form correctly causing the animal that is developing to not get the nutrients it needs. Other cons of this cloning are the amount of money that is required to do this. Not every cloning is successful and actually most of the time animal cloning is usually unsuccessful; and when it is successful it reduces genetic diversity for that type of animal. Cloned animals could experience health complications later in their life and have consequences on them and on humans that consume from them (Chief, 2018).
Another con is the growing concern on the similarities between stem cells and cancer cells because stem cells that are used during cloning could develop mutations that may lead to cancer. Ethically it could break up the idea of having an individual identity; since it may help with infertility, produce more meat or milk, and for business there is a debate on whether this should happen or not. One of the pros of cloning livestock is its ability to ease future food supply shortages. According to the United Nations, the planet may need food to support 20 billion people, which means cloning livestock animals will be very useful and very beneficial for our planet. A good thing about this is that according to The Food and Drug Administration, it is safe to eat food from cloned animals such as beef, or drinking milk and this could help improve human nutrition and offer more high quality meat or milk.
- 20 Advantages and Disadvantages of Cloning Humans. FutureofWorking.com. (2019, December 23).
- https://futureofworking.com/9-advantages-and-disadvantages-of-cloning-humans/.
- Chief, E. in. (2018, November 26). 24 Animal Cloning Pros and Cons. ConnectUS.
- https:// connectusfund.org/24-animal-cloning-pros-and-cons. Cloning Fact Sheet. Genome.gov.
- https://www.genome.gov/about-genomics/fact-sheets/Cloning- Fact-Sheet. Cloning: MedlinePlus.
- https://medlineplus.gov/cloning.html.
- Mayo Foundation for Medical Education and Research. (2019, June 8). Frequently asked questions about stem cell research. Mayo Clinic.
- https://www.mayoclinic.org/tests- procedures/bone-marrow-transplant/in-depth/stem-cells/art-20048117.
- Medicine, C. for V. A Primer on Cloning and Its Use in Livestock Operations. U.S. Food and Drug Administration.
- https://www.fda.gov/animal-veterinary/animal-cloning/primer- cloning-and-its-use-livestock-operations. What is a GMO? Non.
- https://www.nongmoproject.org/gmo-facts/what-is-gmo/. Why Clone? https://learn.genetics.utah.edu/content/cloning/whyclone/.
Cite this page
Stem Cell Research: Pros and Cons. (2022, Apr 22). Retrieved from https://paperap.com/stem-cell-research-pros-and-cons/
"Stem Cell Research: Pros and Cons." PaperAp.com , 22 Apr 2022, https://paperap.com/stem-cell-research-pros-and-cons/
PaperAp.com. (2022). Stem Cell Research: Pros and Cons . [Online]. Available at: https://paperap.com/stem-cell-research-pros-and-cons/ [Accessed: 4 May. 2024]
"Stem Cell Research: Pros and Cons." PaperAp.com, Apr 22, 2022. Accessed May 4, 2024. https://paperap.com/stem-cell-research-pros-and-cons/
"Stem Cell Research: Pros and Cons," PaperAp.com , 22-Apr-2022. [Online]. Available: https://paperap.com/stem-cell-research-pros-and-cons/. [Accessed: 4-May-2024]
PaperAp.com. (2022). Stem Cell Research: Pros and Cons . [Online]. Available at: https://paperap.com/stem-cell-research-pros-and-cons/ [Accessed: 4-May-2024]
- A Rundown of How Stem Cell Research and Treatment Works Pages: 2 (574 words)
- Stem Cell Research Outline Pages: 1 (208 words)
- Ivan Has Decided To Give His Persuasive Speech On Stem Cell Research Pages: 3 (653 words)
- History of Stem Cell Research Pages: 6 (1672 words)
- Cloning and Stem Cell Technology Pages: 3 (853 words)
- Is Stem Cell Reasearch and Treatmetn Ethical Pages: 4 (1034 words)
- A Review on Stem Cell Therapy For Facial Neuropathic Pain Pages: 4 (959 words)
- Stem Cell Policy Changes Pages: 4 (928 words)
- McDonalds Research Paper Pros and Cons Pages: 5 (1496 words)
- Pros and Cons of Natural Convection and Radiation Pages: 5 (1220 words)

IMAGES
VIDEO
COMMENTS
Abstract. The potential impact of stem cell technology on medical and dental practice is vast. Stem cell research will not only provide the foundation for future therapies, but also reveal unique insights into basic disease mechanisms. Therefore, an understanding of stem cell technology will be necessary for clinicians in the future.
Abstract. The ethical implications of stem cell research are often described in terms of risks, side effects, safety, and therapeutic value, which are examples of so-called hard impacts. Hard impacts are typically measurable and quantifiable. To understand the broader spectrum of ethical implications of stem cell research on science and society ...
The benefits to society by the introduction of new medical technologies have been considerable. For example, the introduction of vaccines and antibiotics has significantly improved the well-being of people all over the globe. The science of stem cell treatments, potentially as or more significant than these other innovations, is beginning a new ...
Pros. Stem cell research can potentially help treat a range of medical problems. It could lead humanity closer to better treatment and possibly cure a number of diseases: Parkinson's Disease. Alzheimer's Disease. Heart Diseases, Stroke and Diabetes (Type 1) Birth Defects. Spinal Cord Injuries.
Pros and Cons. Pros and Cons of Using Various Stem Cells. Limitations on ASC ability to differentiate are still uncertain; currently thought to be multi or unipotent. Unsure whether they would be rejected if used in transplants. Methods for ensured reproducibility and maintenance, as differentiated tissues are not certain.
11 Stem Cell Research Pros and Cons. November 5, 2017 by Louise Gaille. Stem cell research can be classified into two specific areas: embryonic stem cells and non-embryonic stem cells. Amniotic, induced pluripotent, and adult stem cells do not involve the creation or destruction of a human embryo to have them collected.
Millman hopes that these stem cell-derived beta cells could be ready for research in humans within 3-5 years. Stem cells could also have vast potential in developing other new therapies. Using ...
While embryonic stem cells develop from pre-implantation embryos and are pluripotent, adult stem cells occur in fetal and adult stages [3]. In the human body, adult stem cells function in the repair and replacement of worn-out tissues. This stem cell research argumentative essay will analyze stem cell research ethics' pros and cons and ...
Therapeutic cloning is a method to produce stem cell lines that were genetic matches for adults and children. Steps in therapeutic cloning are: An egg is obtained from a human donor. The nucleus (DNA) is removed from the egg. Skin cells are taken from the patient. The nucleus (DNA) is removed from a skin cell.
Stem cells are of three different types (1) embryonic stem cells (ESCs), (2) adult stem cells, (3) induced pluripotent stem cells (iPSCs). The ECSs are generated from the blastocyst-stage embryos' interior cell mass, iPSCs emanate from the somatic cells through genetic reprogramming, and adult stem cells are derived from fully developed tissues.
MS: Proponents argue that embryonic stem cell research holds great promise for understanding and curing diabetes, Parkinson's disease, spinal cord injury, and other debilitating conditions. Opponents argue that the research is unethical, because deriving the stem cells destroys the blastocyst, an unimplanted human embryo at the sixth to ...
Ethics of Stem Cell Research. First published Fri Apr 25, 2008; substantive revision Wed Dec 19, 2018. Human embryonic stem cell (HESC) research offers much hope for alleviating the human suffering brought on by the ravages of disease and injury. HESCs are characterized by their capacity for self-renewal and their ability to differentiate into ...
Stem cell research is one of the most controversial topics of our day. As you think about writing a persuasive essay, consider the importance of this topic and how emotive it can be to discuss both the arguments for and against. Any embryonic stem cell research essay needs to carefully weigh up the pros and cons, as well as the ethics involved.
Before delving into the pros and cons of stem cell research, a few successful tales must be mentioned in this article. Multiple Sclerosis. Reema Sandhu's stem cell success story began in 2014 when she was diagnosed with multiple sclerosis, according to DailyMail. The disease can affect the brain and spinal cord, causing a variety of life ...
The Pros and Cons of Stem Cell Research The pros of stem cell research are unlimited potential for possible cures to diseases such as Alzheimer's disease, Parkinson's disease, diabetes, stroke, bone diseases, and screening drugs for pharmaceutical companies, instead of using animals to test drugs. ... From simple essay plans, through to ...
Stem Cell Research Pros And Cons. 2398 Words10 Pages. Stem cell research has been a huge controversial topic for many years and will most likely remain controversial for many more. There are two main sides of this argument; one group believes that the medical benefits of stem cell research outweigh the moral cost and the other group believes ...
Introduction In November 1998, two teams of U.S. scientists confirmed successful isolation and growth of stems cells obtained from human fetuses and embryos. Since then, research that utilizes human embryonic cells has been a widely debated, controversial ethical issue. Human embryonic cells possess the ability to become stem cells, which are used in medical research due to two significant ...
Stem Cell Research Pros And Cons. Stem cell research is a huge controversial subject due to where stem cells are found and obtained. Stem cells an undifferentiated cell of a multicellular organism that is capable of giving rise to indefinitely more cells of the same type, and from which certain other kinds of cell arise by differentiation.
A Rundown of How Stem Cell Research and Treatment Works Pages: 2 (574 words) Stem Cell Research Outline Pages: 1 (208 words) Ivan Has Decided To Give His Persuasive Speech On Stem Cell Research Pages: 3 (653 words) History of Stem Cell Research Pages: 6 (1672 words) Cloning and Stem Cell Technology Pages: 3 (853 words)
I. Introduction. STEM CELL RESEARCH offers great promise for understanding basic mechanisms of human development and differentiation, as well as the hope for new treatments for diseases such as diabetes, spinal cord injury, Parkinson's disease, and myocardial infarction ().Pluripotent stem cells perpetuate themselves in culture and can differentiate into all types of specialized cells.