- Second Opinion

What Do You Know About HIV/AIDS?
According to the CDC, more than 1.1 million Americans are infected with HIV, the virus that causes AIDS. One in 8 of these people doesn't know he or she is infected. Find out more about HIV and AIDS by taking this quiz, based on information from the CDC.
Currently, no vaccine is available for HIV. Protect yourself by:
- Not having sex
- Staying in a sexual relationship with just one person (monogamous)
- Using a latex condom when you do have sex
- Taking PEP (post-exposure prophylaxis) or PrEP (pre-exposure prophylaxis) if you are having unprotected sex with someone with HIV whose virus may not be under control with medicine. Or if you are having unprotected sex with someone whose HIV status you don't know.
- Getting checked for and treated for any other sexually transmitted infections (STIs) you might have. STIs are also called sexually transmitted diseases (STDs).
- If you are having sex with someone who is living with HIV, making sure that they are taking their HIV medicines and their virus is "undetectable" for at least 6 months straight
Drug users must not share needles and syringes. They should not expose themselves to the blood of others. Remember, a person can be HIV-positive and not have symptoms. Have yourself tested to learn your status. Before you have sex with a new partner, ask the person about his or her HIV status. Ask when the person was last tested. Birth control pills and spermicides don’t protect you from getting HIV.
- Pediatric Cardiology
- Our Services
- Chiari Malformation Center at Stanford Medicine Children's Health
Related Topics
HIV/AIDS and Seniors Quiz
HIV/AIDS Quiz
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health
Coronavirus (COVID-19): Latest Updates | Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies | COVID-19 Testing | Vaccine Information Vaccine Information Vaccine Information
Health Encyclopedia
What do you know about hiv/aids.
According to the CDC, more than 1.1 million Americans are infected with HIV, the virus that causes AIDS. One in 8 of these people doesn't know they are infected. Find out more about HIV and AIDS by taking this quiz, based on information from the CDC.
Currently, no vaccine is available for HIV. Protect yourself by:
- Not having sex
- Staying in a sexual relationship with just one person (monogamous)
- Using a latex condom when you do have sex
- Taking PEP (post-exposure prophylaxis) or PrEP (pre-exposure prophylaxis) if you had unprotected sex with someone with HIV at high risk for HIV.
- Getting checked for and treated for any other STIs you might have. STIs are also called sexually transmitted diseases (STDs).
- If you are having sex with someone who is living with HIV, making sure that they are taking their HIV medicines and their virus is "undetectable" for at least 6 months straight
Drug users must not share needles and syringes. They should not expose themselves to the blood of others. Remember, a person can be HIV-positive and not have symptoms. Have yourself tested to learn your status. Before you have sex with a new partner, ask the person about his or her HIV status. Ask when the person was last tested. Birth control pills and spermicides don’t protect you from getting HIV.
Medical Reviewers:
- Felson, Sabrina MD
- Sather, Rita RN
- Wojcik, Stacey, MBS, BSN, RN
- Ask a Medical Librarian Make an Appointment Physicians & Services Physicians who treat Infectious Diseases
- Online Student Edition
- Study-to-Go
- Health Skills Activity: Create Your Own Dialog
- Glencoe's Health Podcast Activities
Chapter Activities
- Audio Chapter Summaries - English
- Audio Chapter Summaries - Spanish
- Crossword Puzzles/eFlashcards
- Eye on the Media
- Health Inventories
- Online Quizzes
- Interactive Study Guides
- Inclusion Strategies for Teachers
- Human Sexuality Module/Spanish
- Puzzlemaker
- Lesson Plans
- National Organizations
- Professional Development Articles
- Conference/Grant Links
- ExamView Assessment Suite Instructions
- Student Web Activities - Teacher Content
- Parent Letters-English/Spanish/Haitian Creole
- State Standards and Correlations
- Parent Letters - English
- Parent Letters - Spanish
- Parent Letters - Haitian Creole
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Overview of Sexually Transmitted Infections (STIs)
, MD, MPH, University of California San Diego
Screening for STIs
More information.
- 3D Models (0)
- Calculators (0)

- Lab Test (0)
Sexually transmitted infection (STI) refers to an infection that is passed through blood, semen, vaginal fluids, or other body fluids during oral, anal, or genital sex with an infected partner. Sexually transmitted disease (STD) refers to a disease that has developed from an STI.
Sexually transmitted infections may be caused by bacteria, viruses, or parasites.
Some infections can spread to other parts of the body, sometimes with serious consequences.
Most sexually transmitted infections can be effectively treated with medications.
Using condoms during genital sex can help prevent passing these infections from one person to another.
Sexual contact, including oral, anal, or genital sex, provides an opportunity for organisms to spread (be transmitted) from one person to another because it involves transfer of body fluids. Some infections that are spread through sexual contact can also be spread through kissing or close body contact.
STIs are relatively common. In the United States, over 25 million new cases of STIs occur each year; about half of the new cases occur in people ages 15 to 24 years (see also Centers for Disease Control and Prevention [CDC]: Sexually Transmitted Disease Surveillance 2020 ).
Several factors make prevention of transmission of STIs difficult. They include the following:
Unprotected sexual activity with one or more partners
Lack of education about safer sex practices
Reluctance to talk about safer sex practices with a partner
Reluctance to talk about sexual issues with a health care practitioner
Lack of access to health care
Infections that do not cause symptoms, so people do not know they need to be tested or treated
The need to treat both sex partners simultaneously to avoid transmitting the infection between partners again
Incomplete treatment, which can lead to development of organisms that are resistant to medications
Causes of STIs
Transmission
Although STIs usually result from having vaginal, oral, or anal sex with an infected partner, genital penetration is not necessary to spread an infection. Some STIs can also be spread in other ways, including

Breastfeeding—for HIV infection
Contaminated medical instruments—for HIV infection
Symptoms of STIs
Symptoms of STIs vary greatly, but the first symptoms usually involve the area where the organisms entered the body. For example, sores may form in the genital area or mouth. There may be a discharge from the penis or the vagina, or urination may be painful.
Complications
When STIs are not diagnosed and treated promptly, some organisms can spread through the bloodstream and infect internal organs, sometimes causing serious, even life-threatening problems. Such problems include
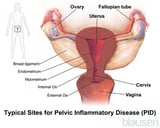
Pathway From the Vagina to the Ovaries
In men, organisms that enter through the penis may infect the tube that carries urine from the bladder through the penis (urethra). Complications are uncommon if infections are treated quickly, but chronic infection of the urethra can cause the following:
Tightening of the foreskin, so that it cannot be pulled over the head of the penis
Narrowing of the urethra, blocking the flow of urine
Development of an abnormal channel (fistula) between the urethra and the skin of the penis
Occasionally in men, organisms spread up the urethra and travel through the tube that carries sperm from the testis (ejaculatory duct and vas deferens) to infect the epididymis (the coiled tube on top of each testis).
Pathway From the Penis to the Epididymis
In both men and women, some STIs can cause persistent swelling of the genital tissues or infection of the urethra or rectum (proctitis).
Diagnosis of STIs
A doctor's evaluation
Examination of a sample of blood, urine, or discharge
Doctors often suspect an STI based on symptoms or a history of sexual contact with an infected partner.
To identify the organism involved and thus confirm the diagnosis, doctors may take a sample of blood, urine, or discharge from the vagina, cervix, or penis and examine it. The sample is usually sent to a laboratory for the organisms to be detected and identified; some tests for STIs can be done in the clinic.
Some tests for STIs are designed to identify the organism’s unique genetic material (DNA or RNA). Other tests check for the presence of antibodies that are produced by the immune system in response to the specific organism that is causing the infection. Doctors choose the type of test based on the most likely infection(s).

The disease being screened for is relatively common
People have a higher than average risk of having a disease (such as people with more than one sex partner), or in whom a disease is particularly dangerous (such as pregnant women)
The screening test is easy and relatively inexpensive
There is effective treatment for the disease
Treatment of STIs
Antibiotics or antiviral medications depending on the STI
Treatment of complications, if present
If possible, simultaneous treatment of sex partners
Most STIs can be effectively treated with medications (antibiotics for bacterial infections and antiviral medications for viral infections). However, some new strains of bacteria and viruses have become resistant to some medications, making treatment more difficult. Resistance to medications Antibiotic resistance Bacteria are microscopic, single-celled organisms. They are among the earliest known life forms on earth. There are thousands of different kinds of bacteria, and they live in every conceivable... read more is likely to increase because medications are sometimes misused.
People who are being treated for a bacterial STI should abstain from sexual intercourse until the infection has been eliminated from them and their sex partners. Thus, sex partners should be tested and treated simultaneously.

Prevention of STIs
The following can help prevent STIs:

Decreased risk of exposure to STIs by reducing the number of sex partners, not having high-risk sex partners (people with many sex partners or who do not practice safer sex), or practicing mutual monogamy or abstinence
Vaccination, available for some STIs
Circumcision (which can also reduce the spread of HIV to men)
Prompt diagnosis and treatment of STIs (to prevent spread to other people)
Identification of the sexual contacts of infected people, followed by counseling or treatment of these contacts
Vaccines are available for HPV infection Human Papillomavirus (HPV) Vaccine The human papillomavirus (HPV) vaccine helps protect against infection by the strains of HPV that are most likely to cause the following: Cervical cancer, vaginal cancer, and vulvar cancer in... read more , hepatitis A Hepatitis A Vaccine The hepatitis A vaccine helps protect against hepatitis A. Typically, hepatitis A is less serious than hepatitis B. Hepatitis A often causes no symptoms, although it can cause fever, nausea... read more , and hepatitis B Hepatitis B Vaccine The hepatitis B vaccine helps protect against hepatitis B and its complications ( chronic hepatitis, cirrhosis, and liver cancer). Generally, hepatitis B is more serious than hepatitis A and... read more .

Condoms must be used correctly to be effective. Condoms should be applied before penetration. Correct use involves the following:
Use a new condom for each act of sexual intercourse.
Use the correct size condom.
Carefully handle the condom to avoid damaging it with fingernails, teeth, or other sharp objects.
Put the condom on after the penis is erect and before any genital contact with the partner.
Determine which way the condom is rolled by placing it on the index finger and gently trying to unroll it, but only a little bit. If it resists, turn it over, and try the other way. Then reroll it.
Place the rolled condom over the tip of the erect penis.
Leave 1/2 inch at the tip of the condom to collect semen.
With one hand, squeeze trapped air out of the tip of the condom.
If uncircumcised, pull the foreskin back before unrolling the condom.
With the other hand, roll the condom over the penis to its base and smooth out any air bubbles.
Make sure that lubrication is adequate during intercourse.
With latex condoms, use only water-based lubricants. Oil-based lubricants (such as petroleum jelly, shortening, mineral oil , massage oils, body lotions, and cooking oil) can weaken latex and cause the condom to break.
Hold the condom firmly against the base of the penis during withdrawal, and withdraw the penis while it is still erect to prevent slippage.
The following English-language resource may be useful. Please note that THE MANUAL is not responsible for the content of this resource.
Centers for Disease Control and Prevention: Sexually Transmitted Diseases
Drugs Mentioned In This Article

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada)—dedicated to using leading-edge science to save and improve lives around the world. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge .
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Edition

- IN THIS TOPIC
STDs and HIV – CDC Basic Fact Sheet

If you have a sexually transmitted diseases (STD) , you are more likely to get HIV or transmit it to others. This fact sheet answers basic questions about STDs and HIV.
Are some stds associated with hiv.
Yes. In the United States, people who get syphilis, gonorrhea, and herpes often also have HIV, or are more likely to get HIV in the future.
Why does having an STD put me more at risk for getting HIV?
If you get an STD, you are more likely to get HIV than someone who is STD-free. This is because the same behaviors and circumstances that may put you at risk for getting an STD also can put you at greater risk for getting HIV. In addition, having a sore or break in the skin from an STD may allow HIV to more easily enter your body. If you are sexually active, get tested for STDs and HIV regularly, even if you don’t have symptoms.
What activities can put me at risk for both STDs and HIV?
- Having anal, vaginal, or oral sex without a condom;
- Having multiple sex partners;
- Having anonymous sex partners;
- Having sex while under the influence of drugs or alcohol can lower inhibitions and result in greater sexual risk-taking.
What can I do to prevent getting STDs and HIV?
The only 100% effective way to avoid STDs is to not have vaginal, anal, or oral sex. If you are sexually active, you can do the following things to lower your chances of getting STDs and HIV:
- Choose less risky sex activities;
- Use a new condom, consistently and correctly , for every act of vaginal, anal, and oral sex throughout the entire sex act (from start to finish);
- Reduce the number of people with whom you have sex;
- Limit or eliminate drug and alcohol use before and during sex;
- Have an honest and open talk with your healthcare provider and ask whether you should be tested for STDs and HIV;
- Talk to your healthcare provider and find out if either pre-exposure prophylaxis, or PrEP , or post-exposure prophylaxis, or PEP , is a good option for you to prevent HIV infection.
If I already have HIV, and then I get an STD, does that put my sex partner(s) at an increased risk for getting HIV?
It can. If you already have HIV, and then get another STD, it can put your HIV-negative partners at greater risk of getting HIV from you.
Your sex partners are less likely to get HIV from you if you
- Get on and stay on treatment called antiretroviral therapy (ART) . Taking HIV medicine as prescribed can make your viral load very low by reducing the amount of virus in your blood and body fluids. HIV medicine can make your viral load so low that a test can’t detect it (an undetectable viral load). If your viral load stays undetectable, you have effectively no risk of sexually transmitting HIV to HIV-negative partners, even if you have other STDs.
- Choose less risky sex activities.
- Use a new condom, consistently and correctly, for every act of vaginal, anal, and oral sex throughout the entire sex act (from start to finish).
The risk of getting HIV also may be reduced if your partner takes PrEP medications, as prescribed, after discussing this option with his or her healthcare provider and determining whether it is appropriate. When taken as prescribed, PrEP medications are highly effective for preventing HIV from sex. PrEP is much less effective if it is not taken consistently. Since PrEP does not protect against other STDs, use condoms the right way every time you have sex.
Will treating STDs prevent me from getting HIV?
No. It’s not enough.
If you get treated for an STD, this will help to prevent its complications, and prevent spreading STDs to your sex partners. Treatment for an STD other than HIV does not prevent the spread of HIV.
If you are diagnosed with an STD, talk to your doctor about ways to protect yourself and your partner(s) from getting reinfected with the same STD, or getting HIV.
You can add this content to your website by syndicating .
Detailed fact sheets are intended for physicians and individuals with specific questions about sexually transmitted diseases. Detailed fact sheets include specific testing and treatment recommendations as well as citations so the reader can research the topic more in depth.
STD Fact Sheet
STD Prevention
STD Treatment Guidelines
Need Help Printing this Page?
Consider adjusting the scale or “shrink to fit” in your browser settings, or consult the printing instructions applicable to your browser. Alternatively, consider using the STD facts brochures or ordering materials through CDC-INFO on Demand (please note: stock is limited). Chrome external icon | Safari external icon | Edge external icon | Firefox external icon | IE external icon
Additional Information
CDC-INFO In English , en Español
CDC National Prevention Information Network (NPIN)
American Sexual Health Association (ASHA) external icon
- STDs Home Page
- Bacterial Vaginosis (BV)
- Genital Herpes
- HIV/AIDS & STDs
- Human Papillomavirus (HPV)
- Mycoplasma genitalium (Mgen)
- Pelvic Inflammatory Disease (PID)
- STDs & Infertility
- STDs during Pregnancy
- Trichomoniasis
Enter your ZIP code to find an STI testing site near you.
- STD on Twitter
- STD on Facebook

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
If you're seeing this message, it means we're having trouble loading external resources on our website.
If you're behind a web filter, please make sure that the domains *.kastatic.org and *.kasandbox.org are unblocked.
To log in and use all the features of Khan Academy, please enable JavaScript in your browser.
Course: NCLEX-RN > Unit 1
- NCLEX-RN questions on tachycardias 1
- NCLEX-RN questions on tachycardias 2
- NCLEX-RN questions on acyanotic heart diseases 1
- NCLEX-RN questions on acyanotic heart diseases 2
- NCLEX-RN questions on vasculitis 1
- NCLEX-RN questions on vasculitis 2
- NCLEX-RN questions on pulmonary conditions 1
- NCLEX-RN questions on emphysema 1
- NCLEX-RN questions on emphysema 2
- NCLEX-RN questions on chronic bronchitis 1
- NCLEX-RN questions on chronic bronchitis 2
- NCLEX-RN questions on lung cancer 1
- NCLEX-RN questions on lung cancer 2
- NCLEX-RN questions on pneumonia 1
- NCLEX-RN questions on pneumonia 2
- NCLEX-RN questions on pleural effusion 1
- NCLEX-RN questions on pleural effusion 2
- Bleeding and impaired hemostasis quiz 1
- Bleeding and impaired hemostasis quiz 2
- Bleeding and impaired hemostasis quiz 3
- NCLEX-RN questions on anemia 1
- NCLEX-RN questions on anemia 2
- NCLEX-RN questions on leukemia 1
- NCLEX-RN questions on leukemia 2
- NCLEX-RN questions on bronchiolitis 1
- NCLEX-RN questions on bronchiolitis 2
- NCLEX-RN questions on shock 1
- NCLEX-RN questions on shock 2
- NCLEX-RN questions on stroke 1
- NCLEX-RN questions on stroke 2
- NCLEX-RN questions on asthma 1
- NCLEX-RN questions on asthma 2
- NCLEX-RN questions on asthma 3
- NCLEX-RN questions on asthma 4
- NCLEX-RN questions on heart-valve disease 1
- NCLEX-RN questions on heart-valve disease 2
- NCLEX-RN questions on Parkinson's disease 2
- NCLEX-RN questions on iron-deficiency anemia 1
- NCLEX-RN questions on iron-deficiency anemia 2
- NCLEX-RN questions on pneumothorax, hemothorax and chylothorax 1
- NCLEX-RN questions on pneumothorax, hemothorax and chylothorax 2
- NCLEX-RN questions on tuberculosis 1
- NCLEX-RN questions on tuberculosis 2
- NCLEX-RN questions on HIV/AIDS 1
- NCLEX-RN questions on abdominal aortic aneurysm 1
- NCLEX-RN questions on pregnancy 1
- NCLEX-RN questions on pregnancy 2
- NCLEX-RN questions on pertussis 1
- NCLEX-RN questions on pertussis 2
- NCLEX-RN questions on diabetes 1
- NCLEX-RN questions on stroke
- NCLEX-RN questions on hypertension 1
- NCLEX-RN questions on inflammatory bowel disease 1
NCLEX-RN questions on sexually transmitted infections 1
- NCLEX-RN questions on sexually transmitted infections 2
- NCLEX.RN questions on heart failure 1
- NCLEX-RN questions on heart failure 2
- NCLEX-RN questions on psychotic disorders 1
- NCLEX-RN questions on psychotic disorders 2
- NCLEX-RN questions on multiple sclerosis 1
- NCLEX-RN questions on multiple sclerosis 2
- NCLEX-RN questions on mood disorders 1
- NCLEX-RN questions on mood disorders 2
- NCLEX-RN questions on neurodevelopment disorders 1
- NCELX-RN questions on neurodevelopment disorders 2
- NCLEX-RN questions on delirium and dementia 1
- NCLEX-RN questions on delirium and dementia 2
- NCLEX-RN questions on anxiety disorders 1
- NCLEX-RN questions on anxiety disorders 2
- NCLEX-RN questions on drug abuse and addiction 1
- NCLEX-RN questions on drug abuse and addiction 2
- NCLEX-RN questions on gastroenteritis 1
- NCLEX-RN questions on gastroenteritis 2
- NCLEX-RN questions on polio 1
- NCLEX-RN questions on polio 2
- NCLEX-RN questions on heart block 1
- NCLEX-RN questions on heart block 2
- NCLEX-RN questions on hepatitis 1
- NCLEX-RN questions on hepatitis 2
- NCLEX-RN questions on malaria 1
- NCLEX-RN questions on malaria 2
- NCLEX-RN alcohol use and abuse
- NCLEX-RN questions on celiac Disease 1
- NCLEX-RN questions on celiac disease 2
- NCLEX-RN questions on arthritis 1
- NCLEX-RN questions on arthritis 2
- (Choice A) Reddish rash on the palms of the hands A Reddish rash on the palms of the hands
- (Choice B) Firm and painless genital ulcers B Firm and painless genital ulcers
- (Choice C) Sore throat and swollen lymph glands C Sore throat and swollen lymph glands
- (Choice D) Muscle weakness and visual changes D Muscle weakness and visual changes
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Sexually transmitted infections.
Michael Ray Garcia ; Stephen W. Leslie ; Anton A. Wray .
Affiliations
Last Update: May 30, 2023 .
- Continuing Education Activity
Sexually transmitted infections are disease processes from close physical contact between males and females by transmission through sexual contact. Sexually transmitted infections, previously known as sexually transmitted diseases, involve the transmission of an organism between sexual partners through different routes of sexual contact, either oral, anal, or vaginal. Sexually transmitted infections affect all people and can be prevented with proper education and barrier control. STIs are more frequently underrecognized and have a higher incidence in medically underserved populations. This activity outlines the evaluation and management of sexually transmitted infections and reviews the role of the interprofessional team in managing patients with this condition.
- Describe the evaluation of sexually transmitted infections.
- Outline the complications of a sexually transmitted infection.
- Identify the management of patients with sexually transmitted infections.
- Identify potential complications of treating and non-compliance of treatment of sexually transmitted infections.
- Introduction
What are sexually transmitted infections (STIs), and why are they important? This review will detail important points and reference important articles for physicians and other healthcare professionals to use in evaluating and treating patients with signs and symptoms suggestive of sexually transmitted infections. Physicians should use this article as a guide to further enhance their knowledge and help provide a better outcome for their patients.
Sexually transmitted infections, previously known as sexually transmitted diseases, involve the transmission of an organism between sexual partners through different routes of sexual contact, either oral, anal, or vaginal. [1] STIs become a concern and burden on healthcare systems, as many infections go untreated and lead to potentially serious complications. The natural history and patterns of spread of the most common sexually transmitted infections will be discussed as well as disease prevention, evaluation, diagnosis, and treatment. [2]
Sexually transmitted infections (STIs) are a worldwide health problem and should be recognized by all public health agencies. The etiology of the most common STIs, including symptoms, physical findings, complications, and the burden they place on infected persons and their families, will be reviewed. STIs are more frequently underrecognized and have a higher incidence in medically underserved populations.
The presenting condition or disease depends on the specific organism, route, signs, and symptoms of the disease. Risk factors that increase the transmission of STIs include having unprotected sexual contact with multiple partners, having a history of STIs, sexual assault, use of alcohol, prostitution, having a sexual partner who has additional concurrent sexual contacts or a prior history of an STI, use of recreational drugs, and intravenous drug use. Specific causative organisms are outlined below.
Male circumcision appears to significantly reduce the likelihood of acquiring several STIs, including human papillomavirus, genital herpes, and especially HIV, where the infective risk decreases by 50% to 60%. [3] [4]
The eight most common STDs include four curable infections (chlamydia, gonorrhea, syphilis, and trichomonas) and four that are treatable but incurable (hepatitis B, herpes simplex virus, HIV, and HPV). Hepatitis B is reviewed separately. (See our companion reference Statpearls article on "Hepatitis B.") [5]
The most common and relevant STIs include the following:
Chancroid [6]
- Haemophilus ducreyi is the causative organism of chancroid.
- It is a fastidious Gram-negative coccobacillus (very short rod) that requires special media and environmental conditions to grow in culture.
- Microscopically, the organism will tend to form long strands forming a pattern described as "railroad tracks" or "a school of fish."
- Significantly increases the risk and transmissibility of HIV.
- It is exceedingly rare in the US and developed countries globally.
Chlamydia [7]
- Gram-negative obligate, nonmotile intracellular bacteria known as Chlamydia trachomatis . [8]
- Typically serotypes D-K.
- The most common curable sexually transmitted infection in the United States, according to the CDC and WHO.
- Two infectious forms exist, the elementary body (EB) and the reticulate body (RB).
- The EB form invades the cell, and the RB form will produce other infectious EB that will infect other non-infectious forms. [7]
Genital Herpes [9] [10]
- Genital herpes is caused by the herpes simplex virus 1(HSV-1) or herpes simplex virus 2 (HSV-2). [11]
- HSV-1/HSV-2 is a double-stranded DNA virus coated by a lipoglycoprotein with an affinity to infect target cells. [9]
- HSV-1 is usually associated with orolabial infections, but according to CDC, HSV-1 is now leading in the cause of genital herpes in young and homosexual patients. [11]
- It is estimated that 50 million people in the US are infected with HSV.
Gonorrhea [12]
- Gram-negative diplococci bacteria are known as Neisseria gonorrhoeae.
- The second most common sexually transmitted infection compared to Chlamydia trachomatis . [11]
- Gonorrhea uses glucose to invade mucus epithelial cells.
- Gonorrhea modifies cellular proteins that allow further penetration of other organisms.
- The proliferation of gonorrhea leads to a localized inflammatory reaction leading to signs and symptoms of a sexually transmitted infection. [13]
Granuloma inguinale [14]
- Caused by Gram-negative intracellular Klebsiella granulomatis, formerly known as Calymmatobacterium granulomatis .
- Rarely found in the United States, it is seen mostly in developing countries, especially in the tropics.
- It is most commonly found in the Caribbean, southern Africa, South America, New Guinea, and India.
Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) [15]
- Enveloped retrovirus encapsulated with two single-stranded RNA.
- Primary HIV signs and symptoms are described as flu-like and often diagnosed as an acute viral syndrome. [15]
- The duration of onset of symptoms ranges from 4 to 10 weeks.
- Most HIV infections in the US are HIV1.
- AIDS is described as the late stage of HIV disease. [16]
- The median time to progression from HIV to AIDS is about 11 years but is highly variable.
- The risk of syphilis in patients infected with HIV is 77 times greater than in the general population. [17]
Human Papillomavirus (HPV) [18]
- HPV is a double-stranded DNA virus that replicates in the basal cell layer of the stratified squamous epithelial cells. This replication cycle induces hyperplasia and possible conversion carcinoma.
- HPV types 16 and 18 are oncogenic strains that induce malignant transformation. [18]
- HPV types 6 and 11 are common strains that induce anogenital warts, commonly known as condyloma acuminata. [1]
- By far, HPV is the most common sexually transmitted infectious organism in the US and worldwide.
Lymphogranuloma venereum [19]
- Caused by Chlamydia trachomatis, a Gram-negative obligate, nonmotile intracellular bacteria but a different serotype from the more common chlamydial infections.
- The bacteria are, specifically, serotypes or serovars L1, L2, and L3.
- Very rare in the US but common in tropical and subtropical regions.
- Transmissible through anal, oral, or vaginal sexual contact.
- Most frequently found in men who have sex with other men.
- Closely associated with HIV infections.
Mycoplasma genitalium [20]
- Mycoplasma genitalium is the second most common cause of nongonococcal urethritis after chlamydia and a common cause of female cervicitis.
- It is a common cause of resistant or recurrent urethritis.
- Mycoplasma is very slow growing in a culture which can take up to 6 months.
- Since it lacks a cell wall, it can't be Gram-stained.
- Risk factors include young age (<25 years), smoking, frequent sexual contacts, and a larger number of sexual partners.
Syphilis [21]
- Caused by a tiny spirochete bacterium, Treponema pallidum .
- T. pallidum is very slow growing and cannot be cultured nor seen on standard light microscopy.
- The initial immune response is muted because T. pallidum has few exposed proteins, and its outer membrane lacks lipopolysaccharides.
- Syphilis infections are increasing compared to previous reports, according to the CDC. [11]
- Syphilis is far more common in the developing world, particularly among the poorest populations with the most limited access to healthcare. [22]
- Syphilis presents with a painless chancre, which is a well-demarcated lesion at the site of inoculation. [21]
- Syphilis presents in various forms, depending on the duration, known as Primary, Secondary, or Tertiary. [11]
- It affects about 12% of all gay men (men having sex with men) globally.
Trichomoniasis [23]
- Caused by single-celled flagellated anaerobic protozoa known as Trichomonas vaginalis .
- Trichomoniasis causes direct damage to the epithelium. The injuries lead to microulcerations primarily in the vagina, cervix, urethra, and paraurethral glands. [24]
- Epidemiology
The most common STI in the United States by far is the human papillomavirus or HPV. At any given time, it is estimated that 80% of sexually active people are infected, including 42% of adults 18 to 59 years, while 7% will have oral HPV, and roughly 14 million new cases will be reported yearly. It is so common that the CDC estimates that virtually all sexually active persons who are not vaccinated will become infected at some point. HPV is often asymptomatic, especially in men, but it may cause venereal and anogenital warts. HPV is a known cause of cervical and oropharyngeal cancer, but it has also been linked to other, relatively uncommon malignancies such as cancer of the anus, penis, vagina, and vulva. HPV types 6 and 11 are very common and are most closely associated with the formation of anogenital warts, while HPV types 16 and 18 are linked to the development of malignancy. Worldwide, at least 291 million women have been infected with HPV.
The Centers for Disease Control (CDC) has determined that roughly 2.4 million non-HPV-related STIs were reported in the US in 2020. Chlamydia was the most common of these at 1.6 million cases, down 1.2% from 2016. Next, 677,769 cases of gonorrhea were reported in 2020, up 45% from 2016, and 133,945 cases of primary and secondary syphilis, up 52% over the same period. In 2020, congenital syphilis was identified in 2,148 infants, up 235% from 2016.
The majority of the reported cases of primary and secondary syphilis, over 80%, are found in men. Gay and bisexual men account for almost half (47%) of the reported cases in males. The CDC also estimates that 44% of gay and bisexual men who test positive for syphilis will also have HIV.
In general, the overall rate of STIs is increasing in the US, with 2.5 million STD cases or more expected when the final data is reported for 2022.
According to the World Health Organization (WHO), global epidemiological data for STIs indicates:
- Worldwide, over 1 million new potentially curable STIs are acquired daily, most of which are asymptomatic.
- It is estimated that there are 376 million new infections annually, with one of the four curable STIs (chlamydia, gonorrhea, syphilis, and trichomoniasis).
- Of these, trichomonas is the most common, with 156 million new cases yearly, followed by chlamydia at 127 million, gonorrhea at 87 million, and syphilis at 6.3 million.
- The overall incidence is rising. There was close to a 30% increase in reportable STIs in the US between 2015 and 2019.
- In the United States, about 12% of the population between 14 and 49 years is estimated to be infected with herpes.
- Herpes simplex virus type 2 has a global prevalence estimated at over 500 million people. [25]
- About one million pregnant women were estimated to have an STI in 2016, causing over 350,000 birthing and/or neonatal complications.
- HPV infections have been linked to over 310,000 cervical cancer deaths annually. [26]
- Syphilis is the second leading cause of stillbirths worldwide.
- HIV/AIDS affected about 37 million people worldwide in 2016. [15]
- It is estimated that 15% of HIV-infected individuals in the US are unaware they have the infection and are responsible for 40% of all new HIV infections. [27]
- According to the CDC, there are approximately 35,000 new cases of HIV in the US annually.
- Mycoplasma genitalium causes 15% - 20% of all non-gonococcal urethritis (NGU), 20% - 25% of all non-chlamydial NGU cases, and about 40% of all recurrent or persistent urethritis infections.
In an ideal world, physicians, public health officials, political leaders, international and regional healthcare organizations, and other healthcare professionals would have a centralized data collection system to be able to analyze and fully assess the incidence, distribution, progression, and treatment of all sexually transmitted infections. As health professionals, the best available sources include various published studies and official government agencies or healthcare organizations to assess STI's statistical importance, such as geographic areas of increasing incidence or particular demographics of affected populations and similar data. [28]
Sexually transmitted diseases (STDs) have a high incidence in most countries, especially between the ages of 15 to 50 years of age, including infants. [29] Undiagnosed STIs are responsible for an estimated 20,000 cases of female infertility annually in the US. The use of this data and information helps clinicians and other healthcare professionals better trend, identify and treat STIs by increasing awareness and allocating scarce resources to where they are most needed and beneficial.
- Pathophysiology
This review is intended to serve as a general presentation of sexually transmitted diseases, including the most common infections such as human immunodeficiency virus, gonorrhea, chlamydia, genital herpes, human papillomavirus, trichomoniasis, and syphilis. Sexually transmitted infections can be bacterial, viral, or parasites, transmitted through sexual activity with the exchange of bodily fluids from the infected partner. STIs invade the human body through microscopic abrasions within the mucosal membranes of the penis, vagina, anus, or any other mucosal surfaces. Transmission of STIs can include using intravenous drugs, exposure through the vagina during childbirth, or breastfeeding. [16] Organisms invade normal cells and overburden the immune system creating typical signs and symptoms of the disease.
Basic symptomatology, including genital, extragenital, or disseminated, with the use of a history and physical exam to assist with differential diagnosis and recommended treatments, will be reviewed. Updated treatment guidelines by the Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) will be presented as well as a general overview of all common sexually transmitted infections.
Physicians and other healthcare professionals must understand curable versus incurable sexually transmitted infections. Untreated STIs can lead to severe, lifelong health disorders, including infertility, scarring, chronic pain, sexual dysfunction, HIV, and cancer.
- History and Physical
Medical professionals are trained to communicate with patients, partners, and families to understand their chief complaints and formulate an effective and useful differential diagnosis. At the same time, taking a detailed history is mandatory, whether it occurs in a primary clinic or the Emergency Department. The clinician's role is to effectively communicate with the patient who presents with signs and symptoms suggestive of a previously undiagnosed sexually transmitted infection. Physicians should be aware that all adolescents under 18 have the right to an STI screening and treatment without parental consent in the US. [6]
Physicians should recognize that STIs closely correlate with patient behavior which should be addressed kindly, diplomatically, and non-judgmentally during the clinical evaluation. [30] The role of physicians is to help, treat, and educate patients about their illnesses as well as to promote and suggest healthy behaviors that will minimize re-infections.
Further details should be investigated with individual state health care systems or reference the "Sexually transmitted disease treatment guidelines 2021" published by the CDC. [31]
While performing the sexual history collection, an easy mnemonic that can help guide clinical questions can be remembered as the "other 5 Ps". [32]
- History of sexually transmitted infections
- Practices
- Prevention against pregnancy
- Protection against sexually transmitted infections
The physical exam should be guided by the presenting chief complaint and symptoms collected in the review of systems. [7] It should be conducted in a private setting with a chaperone at the bedside whose name can then be documented in the patient's medical record. The physical exam, along with the history, will provide a concise differential diagnosis and guide the evaluation, treatment, and management plan of the suspected disease process. [8] At the end of the exam, present the patient with an open-ended question to ensure that there is an open dialogue and to determine if the patient has any other details about their sexual practice not previously discussed.[18]
The physical exam will be broken down by the most common signs and symptoms, physical exam findings, and diagnosis.
Chancroid
- Signs and symptoms: Often occurs in the 20 to 30-year-old age group, frequently among sex workers and their clients. The areas most often affected include the distal portion of the penis in men, while in women, the vagina, labia, and perianal regions are involved. The most significant symptom is the extremely high pain level noted when the lesion reaches the ulcerative stage. [6]
- Physical Exam: The lesion starts as a reddish papule which rapidly progresses to a pustule followed by an extremely painful ulcer. The ulcer sometimes called a "soft chancre," will have soft and irregular margins with a friable base and a grayish-yellowish exudate. It tends to bleed easily. The ulcers are typically 1 cm to 2 cm in diameter and usually resolve spontaneously within three months, even if left untreated. Close to half of the affected individuals will develop regional lymphadenopathy, which may be tender. A minority (about 25%) of these patients will progress to infected bulla or abscesses, which can rupture and become superinfected leading to significant tissue destruction and damage to the genitalia. It is estimated that 10% of affected individuals will also have syphilis or genital herpes as well.
Chlamydia
- Signs and symptoms: Most infections can be asymptomatic but may present with vaginal discharge, abnormal vaginal bleeding, lower pelvic pain, urinary frequency, or dysuria. [33] If systemic infection is present, the patient may be febrile, with abdominal pain, nausea, vomiting, fatigue, and malaise. [7]
- Physical exam: inflammation of the cervix with mucopurulent discharge, ectropion, vaginal discharge, increased sensitivity of the cervix, tenderness of the adnexal regions and abdomen. [33] If systemic infection or Fitz-Hugh-Curtis syndrome is being considered in the differential, there may be right upper quadrant tenderness secondary to perihepatitis. [7]
- Males:
- Signs and symptoms: The most common presenting symptoms are dysuria, testicular pain, and pain with defecation secondary to inflammation of the rectal area and/or prostate. [7] It is a common cause of male urethral discharge which would typically be beige or yellowish.
- Physical Exam: Tenderness to the testicles (specifically over the epididymis) and/or discomfort with palpation to the prostate or rectum. [7]
Genital Herpes
- Females and males:
- Signs and symptoms: Primary infections tend to induce systemic symptoms, including painful vesicular lesions over affected areas, pruritus, dysuria, fever, headaches, malaise, and lymphadenopathy. Initial infections typically resolve spontaneously, starting at about two weeks. Reactivation usually presents with a prodromal phase, including tingling, itching, and rash consistent with vesicular lesions. [9] [10] Recurrent infections tend to be less intense with a shorter duration. [34]
- Physical Exam: The affected area may be localized or systemic. A primary herpes infection tends to be worse with diffuse symptomatically involving various systems, possibly resulting in pneumonitis, hepatitis, meningitis, and encephalitis. Females may have diffuse vesicular lesions in the internal and external vaginal areas. [34] Males may have diffuse vesicular lesions to the glans of the penis, penile shaft, scrotum, perineal/perianal area, and rectum, both internally and externally. Recurrent herpes infections may cause isolated vesicular lesions over a neuronal tract where the virus is dormant. [35]
Gonorrhea
- Genitourinary exam: This may include inflammation of the external vagina, causing excoriations from pruritus, mucopurulent discharge, and friable inflamed mucosal tissue of the cervix. [12] [36]
- Signs and symptoms: Patients may present with dysuria, urgency, urinary frequency, lower pelvic pain, and abnormal vaginal bleeding. [7]
- Physical Exam: If suspecting systemic infection, a thorough physical exam should be performed. [13]
- Signs and symptoms: Patients may present with testicular pain, dysuria, purulent discharge from the meatus, and pain with defecation secondary to inflammation of the rectum and/or prostate. [32] The physician should also observe carefully for systemic signs and symptoms consistent with disseminated gonococcal infection, i.e., sore throat, redness of the eyes, joint pain, and cutaneous lesions. [13]
- Physical Exam: There may be palpable tenderness over the epididymis, purulent discharge from the meatus, or palpable tenderness to the prostate or rectum. [32] A thorough general physical examination is required due to concerns about disseminated gonococcal infections. [13]
Granuloma Inguinale
- Signs and symptoms: Patients will present with highly vascularized lesions over the genitals and perineum that tend to be painless. [37] [38] It can cause severe scarring.
- Physical Exam: Typical findings include ulcer-like lesions that are beefy red, consistent with high vascularization that bleeds easily with manipulation. Subcutaneous granulomas may be present, but lymphadenopathy is uncommon. The lesions tend to be relatively large and irregular. It is often found to be associated with secondary infections.
- 1. Ulcerovegetative: large painless ulcer on the patient's physical exam.
- 2. Nodular: soft and erythematous that tend to ulcerate throughout the infectious process.
- 3. Cicatricial: dry ulcerations that tend to transition into plaques.
- 4. Hypertrophic: lesions are thick and painless. [37] [39]
HIV
- Signs and symptoms: Patients may be asymptomatic or present with an acute viral syndrome, including systemic symptoms: malaise, fatigue, anorexia, fever, chills, arthralgias, myalgias, or cutaneous presentations. [16] Signs of a more advanced infection include fever, diarrhea, shortness of breath, cough, and oral candidiasis. Acute retroviral syndrome may occur with a constellation of non-specific symptoms, including fatigue, muscle pain, skin rash, headache, sore throat, swollen lymph nodes, arthralgia, night sweats, and diarrhea. Acute retroviral syndrome will occur early in 50% to 90% of new HIV-infected individuals, usually before their antibody tests turn positive. [15]
- Physical Exam: The chief complaint will guide the physical exam. The patient should have a thorough history and physical exam to rule out a broad differential diagnosis. [15] Secondary and opportunistic infections are common, especially with AIDS.
HPV and Genital Warts
- Females and males:
- Signs and symptoms: Most complaints are cosmetic or incidental findings due to the asymptomatic nature of common HPV types 6 and 11. These are usually asymptomatic but are responsible for most (90%) venereal and anogenital warts. Patients may also present with ulcerative lesions secondary to oncogenic HPV types 16 and 18, which can progress to malignancies when triggered or stimulated by folate deficiency, UV light exposure, pregnancy, immunosuppression, or smoking. Lack of HPV vaccination is a risk factor. [18]
- Physical Exam: On exam, there may be an exophytic lesion described as a cauliflower-like growth known as condylomata acuminata. [18] Lesions can be observed over the external genital region, perineum, and/or perianal area. An examination for females includes a speculum exam with screening to rule out cervical cancer. [40]
Lymphogranuloma venereum (LGV)
- Signs and symptoms: Patients will present with painful lymphadenopathy localized to the inguinal area. Patients may note the initial presentation of a pustule that gradually progresses to large painful ulceration. [41] Men tend to present with early or acute stages, while women typically present much later. [19]
- Physical Exam: Lymphogranuloma venereum presents with two stages: Primary phase is a small painless papule/pustule that will ulcerate and can be visualized throughout the affected genital area. During the secondary phase, patients present with unilateral lymphadenopathy that is fluctuant with palpation or may be suppurative in a presentation known as buboes. [38] Buboes tend to rupture in the acute phase and progress to a thickened mass. [42]
Mycoplasma genitalium
- Signs and symptoms: Patients may present with pelvic pain, dysuria, and similar type symptoms to gonorrhea or chlamydia infection, including vaginal irritation, discharge, foul odor, or even pelvic inflammatory disease. [43] [20] [43]
- Physical Exam: Common findings would be irritation of the external and internal vagina, vaginal discharge, cervical tenderness, cervicitis, adnexal tenderness, or abnormal vaginal spotting. [44]
- Signs and symptoms: Patients may present with suprapubic pain, dysuria, urinary frequency, urgency, or testicular pain. A common cause (40%) of persistent or recurrent urethritis. [20]
- Physical exam: The examination may be painless and benign, or there may be tenderness to the epididymis with palpation or discomfort from the prostate on the rectal exam. [45]
Pelvic Inflammatory Disease (Females)
- Pelvic inflammatory disease is a sexually transmitted infection that involves the upper female genital tract. It can affect future fertility, and the infections can be serious. [37]
- Risk factors include multiple sexual partners, prior episodes of pelvic inflammatory disease, IUD implants, history of tubal ligation, and younger age.
- The most common causative organisms are chlamydia and gonorrhea, but Mycoplasma genitalium can also cause PID. There is no specific test for pelvic inflammatory disease, as the diagnosis is primarily clinical.
- The typical physical finding is tenderness on cervical motion and/or pain on palpation of the pelvic area.
- Other findings include cervical friability or discharge and increased WBCs on wet prep.
- Abdominal tenderness
- Adnexal tenderness
- Cervical motion tenderness
- Fever (>38 C or >100.4 F)
- Increased vaginal discharge
- Irregular menstrual bleeding
- Lower abdominal pain
- Mild pelvic pain
- Pain with intercourse
- Painful and frequent urination
- Pelvic organ tenderness
- Uterine tenderness
Syphilis
- Primary: Presents with a painless well-demarcated lesion/ulcer known as a chancre at the site of inoculation. [21] This is typically within three months of the inoculating event. If untreated, the lesions will heal on their own in 3 to 8 weeks, but 30% will progress to tertiary syphilis. [21]
- Secondary: Presents with systemic symptoms involving a cutaneous lesion and characteristic maculopapular rash. Cutaneous wart-like lesions known as condylomata lata may present and resolve during this phase. The rash does not itch and specifically includes mucus membranes as well as the palmar regions of the hands and soles of the feet, which are generally spared in other disorders. [21]
- Latent: No clinical signs or symptoms are present, but serological tests are positive. [21]
- Tertiary: Presentation can be within months or years from the original inoculation. Systemic symptoms can range from cardiovascular and neurologic to cutaneous gummatous lesions. Neurosyphilis can present with stroke-like symptoms, cranial nerve deficits, a change in mental status, general paresis, or tabes dorsalis. [46] (See our companion reference StatPearls articles on "Neurosyphilis" and "Tabes dorsalis." [47] [48]
- Signs and symptoms: Presenting symptoms of a syphilis infection depends on the phase of the infection at the time of evaluation. Symptoms can be broken down into primary, secondary, latent, and tertiary phases, which are best detailed and discussed in our reference companion StatPearls article on "Syphilis." [21]
- Physical Exam: The physical exam is dependent on the presenting phase of the syphilis infection.
Trichomoniasis
- Signs and symptoms: Females can remain asymptomatic with trichomonas vaginalis infections but, at times, may present with a complaint of foul-smelling discharge, pruritus, dyspareunia, dysuria, and vaginal spotting. [23]
- Physical Exam: The exam will show irritation of the external and internal vagina, including classic physical findings of "strawberry cervix," known as colpitis macularis. A foul frothy vaginal discharge may be present on exam. [49]
- Signs and symptoms: Males can remain asymptomatic with a trichomonas vaginalis infection but can also present with testicular pain, dysuria, or rectal pain.
- Physical Exam: Tenderness will be present with palpation to the epididymis and prostate on rectal exam. No overlying skin lesions or inflammatory processes will be seen. [49]
This is a brief overview of the most common signs and symptoms, physical exam findings, and diagnosis of sexually transmitted infections that can be evaluated in an acute setting such as the emergency department or a routine visit with the patient's primary care physician. The information and references cited should be used for a more in-depth approach to the signs and symptoms of a sexually transmitted infection.
Screening recommendations can be found in a detailed presentation through "Sexually Transmitted Disease Treatment Guidelines 2021," published by the CDC. [31] The information provided will be extrapolated from the guidelines and should be used at the physician's discretion in conjunction with the patient.
Depending on the clinical presentation of the patient and the severity of symptoms, a patient with a primary complaint concerning a possible sexually transmitted infection should involve ruling out localized and systemic STIs. Initial diagnostic testing will be guided by the presenting sexually transmitted infection as described in the CDC Sexually Transmitted Disease Treatment Guidelines that were updated in 2021. [31]
Most common laboratory testing performed includes:
- Nucleic Acid Amplification Test (NAAT)
- Cerebrospinal Fluid (CSF)
- Fluorescent Treponemal Antibody Absorption Test (FTA-ABS)
- Rapid Plasma Reagin (RPR)
- Treponema pallidum Particle Agglutination (TP-PA)
- Venereal Disease Research Laboratory (VDRL)
Chancroid
- Female/Male: Diagnosis is by clinical history and examination, together with the exclusion of alternative ulcerative infections such as herpes and syphilis. One or more deep, relatively large, painful ulcers on the genitalia associated with inguinal adenopathy that is tender and suppurative are highly suggestive of chancroid. (Herpetic ulcers are usually smaller and chancres from syphilis are typically painless.) [6]
- Gram stain may show a typical "school of fish" pattern, but this is only 80% reliable. The definitive diagnosis requires the growing of Haemophilus ducreyi in a culture which is difficult and requires the use of specially enriched media grown under conditions of high humidity and high CO2, not generally available to most clinical laboratories. There is currently no FDA-approved PCR serological test available for H. ducreyi . [50] Patients with chancroid should also be tested for HIV.
- One or more painful genital ulcers
- Clinical findings, such as the appearance of genital ulcers and regional lymphadenopathy consistent with chancroid
- No evidence of Treponema pallidum infection by darkfield microscopy of the exudate or by serologic testing within one week after the onset of ulcers
- A negative Herpes simplex virus culture or PCR test was performed on the exudate
Chlamydia :
- Female: Diagnosis is made by using a NAAT on a vaginal swab, first-catch urine sample, or self-endocervical swab.
- Male: Diagnosis is made using NAAT of a first-catch urine sample or urethral sample. [7] [51]
Genital Herpes
- Female/Male: Diagnosis is by clinical examination, NAAT from genital ulceration, or viral culture.
- Fluorescein-labeled monoclonal antibodies are used in a direct, immunofluorescence assay for herpes simplex virus antibodies, but it is not currently recommended due to its relative insensitivity.
- Cellular changes on cytologic examination associated with herpes simplex virus infections are also not recommended for diagnosis. It is considered too non-specific and insensitive.
- HIV testing is recommended in all patients who test positive for genital herpes. [9] [10] [34]
- Female: Diagnosis is made using a NAAT vulvovaginal or endocervical swab.
- Male: Diagnosis is made using NAAT of a first-catch urine sample or urethral sample. [12] [13]
Granuloma inguinale
- Female/Male: Diagnosis is primarily clinical, based on the gross appearance of the lesions and microscopic findings of intracellular Donovan bodies on a scraping, tissue crush, or biopsy specimen.
- Donovan bodies are rod or oval-shaped intracellular inclusions in the cytoplasm of histiocytes and/or mononuclear phagocytes of infected patients.
- Donovan bodies stain dark purple with Wright's stain.
- The infecting organism is very difficult to culture, and no FDA-approved molecular diagnostic laboratory test is currently available. [37]
- Female/Male: Diagnosis involves using a blood sample or saliva for antibodies as a preliminary test, followed up with more specific tests, including PCR or specific immunoassays. [15] [16]
- The CDC recommends at least one HIV test for all adults from 15 to 65 years.
- High-risk individuals (sexually active gays, bisexuals, and men who have sex with other men) should be tested at least annually.
- PCR testing is essentially diagnostic of an HIV infection.
- The CDC recommends HIV1/HIV2 antigen-antibody immunoassay.
- Patients who are unlikely to return for follow-up should be offered a rapid point-of-care HIV test. Results are available in <20 minutes but may be negative in early infections.
- An RT-PCR-based viral load test is also recommended.
- HIV RNA testing is best for acute HIV infections.
- An HIV1/HIV2 antibody differentiation assay would be confirmatory.
- HIV-infected individuals should be screened for chlamydia, gonorrhea, and syphilis when diagnosed and at least annually afterward.
- Individual assays to isolate specific antibodies or particular viral antigens can be used for confirmation. (See our companion reference StatPearls article on "HIV Testing.") [27]
- Female/Male: Diagnosis is primarily clinical, based on the gross appearance of any cutaneous or other lesions discovered on the physical examination.
- Immunocompromised patients (cancer risk is highest)
- Diagnosis is uncertain
- Atypical lesions
- Lesions that do not respond to standard therapy
- Female: Reflex HPV testing can be done on cervical cells from a Pap smear to identify HPV subtypes.
- Suspicious Pap smear results can be further evaluated by colposcopy using acetic acid to highlight specific white-colored areas that can be biopsied.
Lymphogranuloma venereum
- Female/Male: Initial diagnosis is primarily by clinical suspicion in regions where this infection is common and by eliminating other causes of genital ulcerations with inguinal lymphadenopathy.
- Ulcerative infections of the genitalia to exclude, which also cause inguinal lymphadenopathy, would be chancroid, herpes, granuloma inguinale, and syphilis.
- Lymphoma, penile cancer, and HIV are additional causes of lymphadenopathy.
- Serological testing with complement fixation, micro-immunofluorescence, or NAAT can confirm the diagnosis, but PVR-based genotyping is the most definitive.
- NAAT testing is usually preferred due to availability and is recommended for all patients who present with proctocolitis.
- Finding Chlamydia trachomatis in a genital, lymph node, or rectal specimens through culture, direct immunofluorescence, or nucleic acid amplification testing (NAAT) would be diagnostic and confirmatory.
- Men at high risk (men who have sex with men) and have proctocolitis should be tested for Chlamydia trachomatis .
- HIV testing is also recommended in this patient population. [19] [52] [53]
Pelvic Inflammatory Disease
- Female: Diagnosis is primarily clinical based on the presence of lower abdominal pain, pelvic discomfort, purulent vaginal discharge, abnormal vaginal bleeding, or dyspareunia.
- Fever >101 F (>38.3 C)
- Cervical friability
- Mucopurulent cervical discharge
- Saline microscopy of vaginal fluid shows abundant WBCs
- Elevated erythrocyte sedimentation rate (ESR) and/or C-reactive protein
- Laboratory confirmation of N. gonorrhea or C. trachomatis by NAAT or culture
- A diagnosis of pelvic inflammatory disease is unlikely if the cervical discharge is normal and no WBCs are seen on a wet prep of the vaginal fluid.
- NAAT testing for N.gonorrhoeae and C. trachomatis is recommended. Testing for M. genitalium is also recommended (if available).
- Serological testing for HIV and Treponema pallidum (syphilis) should also be performed.
- Pregnancy testing should be done, and pelvic ultrasonography should be considered if there is any suspicion of a tubo-ovarian abscess. [37]
Mycoplasma genitalium
- Female/Male: Initial diagnosis is primarily clinical based on symptoms and the exclusion of chlamydia and gonorrhea.
- NAAT assays for M. genitalium are now available and FDA-approved, with a sensitivity of 96% or better.
- Mycoplasma genitalium should be suspected in all patients with recurrent or persistent gonorrhea or chlamydia infections and intractable urethritis.
- Presumptive treatment can be initiated in suspected cases even without diagnostic confirmation. [20]
- Female/Male: Diagnosis is confirmed by a positive finding on serological tests to include at least one nontreponemal (VDRL, RPR) and one treponemal (FTA-ABS, TP-PA) assay.
- No NAAT tests are currently available. PCR tests for T. pallidum have been developed, but none are FDA-approved.
- A negative test would be non-reactive, while a positive test would demonstrate a titer ≥1:8.
- If the titer is <1:8, the test should be repeated, and a treponemal assay should be performed as well.
- Nontreponemal tests are simple, inexpensive, and are usually the initial screening tests for syphilis.
- They will identify roughly 80% of patients with primary syphilis and close to 100% with secondary syphilis.
- They typically turn positive only after the appearance of the primary chancre.
- When quantified, they can be used for disease tracking as a fourfold change in activity is generally considered significant.
- However, they are not specific for syphilis and can often give false-positive results, so they are inadequate for a definitive diagnosis alone without confirmation from a treponemal test.
- While specific treponemal antibodies appear early, their level does not correlate well with disease activity or stage.
- They typically remain positive for life even after successful treatment, making them useless for disease tracking.
- A positive result on at least one nontreponemal and one treponemal test is required to definitively confirm a syphilis diagnosis.
- Only quantifiable nontreponemal tests can be used for disease tracking.
- Darkfield microscopy can identify the infecting spirochete in 80% of cases even before serological testing but is rarely performed.
- VDRL testing of the cerebrospinal fluid is highly specific for neurosyphilis but not very sensitive.
- Treponemal testing of the cerebrospinal fluid is highly sensitive but less specific than the VDRL test for neurosyphilis.
- HIV testing should be performed on all patients testing positive for syphilis.
- For further details on diagnostic testing, see our companion reference StatPearls article on "Syphilis." [21]
- Female: Diagnosis using NAAT of the vagina, endocervical swab, urine analysis, or urethral sample.
- Alternatively, a wet mount will show motile flagellated protozoa.
- Patients diagnosed with trichomoniasis should also be tested for chlamydia, gonorrhea, HIV, and syphilis. [23] [54]
PREGNANCY - STI Screening Recommendations from the CDC 2021 Guidelines:
Sexually transmitted infections can seriously complicate pregnancy and potentially cause serious health consequences for the mother and her unborn child. [31] Therefore, the CDC currently recommends the following routine STI screenings in pregnancy:
- All pregnant women should be tested for HIV, Hepatitis B, Hepatitis C, and syphilis at their first prenatal visit.
- All pregnant women <25 years of age and older, pregnant women who are at increased risk for infection should be tested for chlamydia and gonorrhea.
- Pregnant women who test positive for chlamydia should be retested 3 to 4 weeks after treatment and again within three months.
- Rescreen women <25 years of age or at continued high risk and all those not previously tested for chlamydia, gonorrhea, and syphilis.
- Pregnant women with high-risk factors or who were not previously tested should be screened for HIV and hepatitis B.
- Those patients who tested positive for syphilis at the prenatal visit should be retested.
High-risk factors include:
- New or multiple sex partners
- Inconsistent use of condoms
- A sexual partner with concurrent or multiple partners
- A sexual partner who has a sexually transmitted infection (STI)
- History of illegal drug use or prostitution
- Living in an area with a high rate of STIs
- Incarcerated individuals
The CDC does not recommend routine testing in pregnancy for bacterial vaginosis, Herpes, HPV, or Trichomoniasis.
Treatment of STIs in Pregnancy
Curable STIs (chlamydia, gonorrhea, syphilis, and trichomonas) can be successfully treated with appropriate antibiotics deemed safe for administration during pregnancy. While viral STIs cannot be cured, they can generally be controlled with various antivirals and other preventive measures to minimize transmission to the baby and harm to the mother.
For detailed information on specific STI treatments in pregnancy, readers are referred to the 2021 WHO and CDC STI Guidelines. [31]
- Treatment / Management
The Centers for Disease Control and Prevention (CDC) published an update to their Sexually Transmitted Diseases Treatment Guidelines in 2021. There are sections in this treatment guideline that direct specific care for select populations such as pregnant women, adolescents, persons in correctional facilities, men who have sex with men, women who have sex with women, and transgender men/women. [6] [31] These topics should be explored and reviewed on a case by case issue.
The treatment and management of the patient should be supported by the history and physical exam, whether the patient is evaluated in the Emergency Department, primary care, or infectious disease office. Primary preferred treatments will be discussed, and further reference articles will be cited for different management options for physicians. [11] If the primary treatment is not tolerated or the patient is allergic, physicians should consult their pharmacy department or an infectious disease specialist for further recommendations.
The following recommendations are from the 2021 Centers for Disease Control (CDC) STD 2021 Treatment Guidelines. [31]
Acute Epididymitis :
- Ceftriaxone 500 mg IM one dose PLUS doxycycline 100 mg BID for 10 days.
- Levofloxacin 500 mg orally once daily for 10 days.
- Ceftriaxone 500 mg IM one dose PLUS levofloxacin 500 mg daily by mouth for 10 days
- For further details, see our companion reference StatPearls article on "Epididymitis." [55] [31] [55]
Chancroid : Subjective and objective improvement are typically noted within 1 to 2 weeks. Failure to respond suggests an incorrect initial diagnosis, a coinfection such as HIV, treatment non-compliance, or drug resistance. [6]
- Azithromycin 1 gm, orally as a single dose or
- Ceftriaxone 250 mg, intramuscularly (IM) as a single dose or
- Erythromycin 500 mg, orally 3 times per day for 7 days or
- Ciprofloxacin 500 mg, orally twice a day for 3 days
- (Azithromycin and ceftriaxone have the benefit of single-dose therapy.)
- Patients should be evaluated for treatment response 3 to 7 days after therapy.
- Some resistance to erythromycin and ciprofloxacin has been reported, but data on antimicrobial resistance is limited.
- For further details, see our companion reference StatPearls article on "Chancroid." [6]
Chlamydia : Primary treatment and management should be supported by the history, physical exam, and clinical presentation. Consideration of coinfections with the most common STIs should be considered and treated simultaneously. [7] [31]
- Doxycycline 100 mg twice daily to be taken by mouth for seven days is preferred. Alternative therapy would be one dose of azithromycin 1 gram or levofloxacin 500 mg daily for seven days. In pregnancy, azithromycin 1 gram orally or amoxicillin 500 mg TID for seven days is recommended. Other formulations can be taken but should be evaluated on a case-by-case presentation along with the concerns of the patient.
- For persistent or recurrent nonspecific urethritis, specific Mycoplasma genitalium testing is recommended. If that is not available, repeat the course of doxycycline 100 mg BID for seven days, followed by oral moxifloxacin 400 mg daily for seven days.
- After initial treatment, follow-up testing should be discussed with the patient.
- For further details on treatment, see our companion reference StatPearls article on "Chlamydia." [7]
Genital Herpes : Treatment and management of a primary infection should include systemic infection followed by symptomatic treatment and starting antiviral medications. The physician and patient should discuss medication options, including the financial strain that may hinder appropriate treatment. Treatment of reactivation herpes infection should be treated with whatever medication works best for the patient. [9] [10]
- Acyclovir 400 mg TID for 7-10 days OR
- Famciclovir 250 mg TID for 7-10 days OR
- Valacyclovir 1 gram BID for 7–10 days
- There are various formulations and treatment courses that should be started after the best management plan is discussed with the patient. [11]
- Acyclovir 400 mg BID OR
- Famciclovir 250 mg BID OR
- Valacyclovir 500 mg - 1 gram daily
- A higher dose schedule of these same agents is used for episodic outbreaks, and IV therapy is utilized for particularly severe cases.
- Topical antiviral therapy is not recommended due to its minimal proven clinical activity.
- Asymptomatic patients who test positive on serological testing do not need antiviral therapy.
- The efficacy of antiviral therapy in preventing viral transmission in asymptomatic individuals has not been adequately studied.
- Neonatal herpes is generally treated with systemic acyclovir at 20 mg/kg IV every 8 hours.
- For further details, see our companion reference StatPearls article on "Herpes Simplex." [9]
Gonorrhea : Primary treatment and management should be supported by the history, physical exam, and clinical presentation. Consideration of coinfections with the most common sexually transmitted infections should be considered and treated simultaneously. [12] [13]
- One dose of a 3rd generation of cephalosporin, specifically ceftriaxone 500 milligrams, must be given by intramuscular injection.
- Complicated or disseminated infections will need ceftriaxone 1 gram either once or every 24 hours, depending on the clinical presentation.
- If allergic to ceftriaxone or cephalosporins, the recommended alternative regimen would be a single dose of gentamicin 240 mg IM plus a single oral dose of 2 grams of azithromycin.
- If ceftriaxone is not available, the recommended alternative is a single oral dose of cefixime 800 mg.
- Doxycycline 100 mg BID for one week is recommended for chlamydial coinfections.
- After initial treatment, follow-up tests should be discussed with the patient.
- For further details on treatment, see our companion reference StatPearls article on "Gonorrhea." [12]
Granuloma inguinale : Treatment and management should be guided by the history, physical exam, and clinical presentation, as granuloma inguinale is not very common in the United States. [14] [37] [39]
- Azithromycin 1 gram weekly or 500 mg daily should be taken by mouth for at least three weeks or until the lesions resolve completely.
- Doxycycline 100 mg orally BID for at least three weeks or until all lesions resolve completely OR
- Erythromycin base 500 mg orally 4 times/day for at least three weeks or until all lesions resolve completely OR
- Trimethoprim-sulfamethoxazole one double-strength (160 mg/800 mg) tablet orally BID for at least three weeks or until all lesions resolve completely, whichever is longer.
- For further details on treatment, see our companion reference StatPearls article on "Granuloma Inguinale." [14]
HIV : Primary treatment and management consist of establishing viral load and CD4 count and starting a patient on highly active antiretroviral therapy (HAART). [56] Advice from an Infectious disease specialist experienced in HIV treatments is suggested to help determine whether antiretroviral therapy is necessary and the optimal regimen. If a patient is seen for an acute concern, such as sexual assault or exposure to an STI through high-risk sexual activity with a concern for HIV, a single combination medication should be started with close follow-up. [15] Antiviral therapy should be started as soon as possible. A viral load of <200 copies/mL is essentially non-transmissible. For further details on treatment, see our companion reference StatPearls article on "HIV Antiretroviral Therapy." [57]
- Pre-exposure prophylaxis (PrEP) is recommended for all high-risk, sexually active patients who test negative for HIV-1.
- Highly active antiretroviral therapy (HAART) includes the following classes.
- Nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs)
- NRTI fixed-dose combinations
- Integrase inhibitors
- Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
- CC chemokine receptor five inhibitors (CCR5 Inhibitor)
- Protease Inhibitors
HPV and Genital Warts :
- The CDC recommends HPV vaccinations for all children starting at age 12 and up to age 21 in men and 26 in women. [18]
- Treatment of genital warts depends on location, size, physician experience, and patient preference.
- The application of acetic acid will tend to make HPV-affected skin turn white.
- High-grade cervical dysplasia in older women or any persistent cervical dysplasia is treatable with cryotherapy, loop electrosurgical excision, or cold knife cone resection.
- If the lesion progresses to a malignancy, additional resection, surgery, chemotherapy, and/or radiation may be required.
- Accepted treatment methods for anogenital warts include surgical removal, cryotherapy (freezing the infected tissue), laser vaporization, and topical medications.
- Imiquimod is a topical immunomodulating therapy that stimulates local interferon and cytokine production, inducing an inflammatory reaction.
- Podofilox causes wart necrosis by interfering with cell mitosis.
- Sinecatechins work in an unknown fashion but appear effective as a topical therapy. They are not recommended in pregnant or immunocompromised patients.
- Irritant (podophyllin) based topical therapy is no longer recommended by the CDC as safer topical alternatives are available.
- HPV testing can also be done on tissue samples of various squamous cancers (head and neck, penis) to help determine susceptibility to various treatment options such as radiation therapy.
- For further details on treatment, see our companion reference StatPearls articles on "Human Papillomavirus," "Colposcopy," "Cervical Cancer," and "Genital Warts." [18] [58] [59] [60]
Lymphogranuloma venereum (LGV) : Treatment and management should be guided by the history, physical exam, and clinical presentation, as LGV is not very common in the United States. [19]
- Doxycycline 100 milligrams, taken by mouth twice daily for at least 21 days or until there is a complete resolution of the presenting symptoms, is the preferred treatment. [11]
- Alternative regimens would be azithromycin 1 gram orally per week for three weeks OR erythromycin base 500 mg 4 times daily for 21 days.
- Needle aspiration or incision and drainage may be needed from some buboes.
- For further details on treatment, see our companion reference StatPearls article on "Lymphogranuloma venereum." [19]
Mycoplasma genitalium : Concern for an M. genitalium infection should be entertained if a patient is suspected of resistant chlamydia or gonorrhea infection, especially if recurrent or persistent. [45] Specific testing for resistance is recommended, although Mycoplasma is notoriously slow growing in culture. Since M. genitalium lacks a cell wall, antibiotics that attack the cell wall (penicillins and cephalosporins) are ineffective. [31]
- Doxycycline 100 mg BID for seven days FOLLOWED BY azithromycin 1 gm orally on the first day, FOLLOWED BY azithromycin 500 mg orally 1x/day for 3 days.
- If macrolide resistance testing is unavailable or not performed, add oral moxifloxacin 400 mg daily for 7 days after completing the above.
- Increasing macrolide resistance is being reported. A NAAT test for M. genitalium and macrolide resistance is currently available only outside the US.
- Fluoroquinolones are still >90% effective. Moxifloxacin and Sitafloxacin (not available in the US) have been the most utilized agents.
- A test-of-cure should be performed 21 days after the completion of therapy.
- Start with doxycycline 100 mg BID for 14 days.
- If the NAAT test is positive for M. genitalium, add moxifloxacin 400 mg daily for 14 days. [31]
Pelvic Inflammatory Disease :
- Ceftriaxone 1 gm IV every 24 hours PLUS doxycycline 100 mg orally or IV every 12 hours PLUS metronidazole 500 mg orally or IV every 12 hours
- Cefotetan 2 gm by IV every 12 hours PLUS doxycycline 100 mg orally or by IV every 12 hours OR
- Cefoxitin 2 gm by IV every 6 hours PLUS doxycycline 100 mg orally or by IV every 12 hours OR
- Clindamycin (900 mg IV every 8 hours) plus gentamicin (3 to 5 mg/kg by IV once daily).
- Metronidazole 500 mg orally or by IV every 12 hours for 14 days should be added if there is any suspicion of trichomonas.
- Consider NAAT testing and initiating treatment for Mycoplasma genitalium if the above measures fail.
- For further details on treatment, see our companion reference StatPearls article on "Pelvic Inflammatory Disease." [37]
Syphilis : Treatment and management of secondary, latent, and tertiary syphilis should be independent of treatment of the primary syphilitic infection. [21]
- Primary, secondary, and early syphilis infection can be treated with benzathine penicillin G 2.4 million units to be given by a single intramuscular injection. [21]
- Treatment for infants and children is also benzathine penicillin G 50,000 units/kg body weight IM as a single dose up to a maximum of 2.4 million units.
- Tertiary syphilis (including latent syphilis, HIV patients, and in pregnancy) should be treated with benzathine penicillin G 2.4 million units IM once a week for a total of 3 weeks.
- Procaine penicillin G 2.4 million units IM once daily PLUS probenecid 500 mg orally four times/day for 10 to 14 days can be an acceptable alternative in highly reliable patients.
- After neurosyphilis treatment, normal RPR titers correlate well with negative CSF findings so that further lumbar punctures can be safely avoided in immunocompetent patients.
- Patients with a penicillin allergy should consider penicillin skin testing unless they have a history of anaphylaxis, hemolytic anemia, Stevens-Johnson syndrome, interstitial nephritis, or toxic epidermal necrolysis.
- If the skin testing is negative, this is usually followed by an oral penicillin challenge.
- Desensitization to penicillin can be considered in selected cases as penicillin remains the preferred antibiotic for syphilis, particularly during pregnancy and neurosyphilis, where no alternatives are recommended.
- Of these, doxycycline is usually preferred as it is inexpensive and easily administered. However, it cannot be used in pediatrics or during pregnancy.
- If azithromycin is used, the neonate would need treatment immediately after birth as azithromycin does not cross the placenta.
- Follow-up clinical examinations and serological testing is recommended at 6, 12, and 24 months after treatment or every three months for the first year and at 24 months in high-risk populations.
- A nontreponemal titer (VDRL or RPR) that has increased fourfold or more from previous levels suggests a reinfection or treatment failure.
- A high initial titer that does not fall fourfold by 24 months after therapy suggests a treatment failure, reinfection, and/or CNS involvement.
- For further details on treatment, see our companion reference StatPearls articles on "Syphilis", "Neurosyphilis", and "Congenital Syphilis". [21] [47] [61]
The Jarisch-Herxheimer reaction is an acute but self-limiting febrile syndrome characterized by headache, fever, chills, nausea, vomiting, muscle aches, tachycardia, flushing, hyperventilation, hypotension, exacerbation of skin lesions, and rigors that occur within the first 24 hours after initiation of antimicrobial therapy for syphilis. It may also occur with other infections caused by spirochetes, such as Lyme disease, leptospirosis, tick-borne relapsing fever, and certain other infections. The most common symptoms are fever and skin changes. [62]
It is caused by the sudden release of bacterial toxins, which induce an inflammatory cytokine response (interleukin-6. interleukin-8, and tumor necrosis factor-alpha) that is the immediate cause of the noted symptoms. The severity of the reaction is directly related to the patient's individual bacterial load. The reaction typically starts about 2 hours after the initial administration of an antimicrobial, lasts an average of about 9 hours, and generally resolves without treatment by 24 hours. It is most frequently seen when starting treatment of seropositive primary and secondary syphilis, most likely from the high bacterial loads. More than 50% of such high-risk patients are likely to experience a Jarisch-Herxheimer reaction. It is least likely in patients with latent syphilis. [62]
Patients should be informed of this possible reaction prior to initiating treatment, that it is a common, expected response to therapy and not a penicillin allergy. [62]
NSAIDs and acetaminophen have been used for symptomatic treatment, but they will not prevent the reaction. Anti-TNF-alpha antibodies and steroids have been used to help mitigate symptoms but have not been well studied. In rare cases, the Jarisch Herxheimer reaction can be life-threatening, usually due to prolonged hypotension. [62]
Early labor can be induced, and fetal distress has been reported when syphilis treatment is begun during pregnancy, and a Jarisch-Herxheimer reaction is precipitated. The incidence of the reaction in pregnancy has been estimated at 40%. Nevertheless, it is recommended that syphilis therapy not be delayed, although fetal monitoring is recommended in late pregnancy. [62] (See our companion reference StatPearls article on "Jarisch Herxheimer Reaction.") [62]
Trichomoniasis : Treatment and management should be established with that patient after diagnosis. [23] [49]
- For men, a single dose of metronidazole 2 grams is taken orally.
- For women, metronidazole 500 mg by mouth twice daily with food for seven days.
- Alternate therapy for both men and women is a single dose of tinidazole 2 grams to be taken by mouth.
- Desensitization therapy is recommended for patients who are allergic to nitroimidazoles (which includes both metronidazole and tinidazole.)
- Retesting all women (but not men) three months after therapy is recommended.
- For further details on treatment, see our companion reference StatPearls article on "Trichomoniasis." [23]
Evaluation and Treatment of Patients After a Sexual Assault
Victims of sexual assault may be exposed to unknown potential infections. They also tend to have poor follow-up, so prophylactic antibiotics for chlamydia, gonorrhea, and trichomoniasis are recommended. Emergency contraception, along with testing for hepatitis B, HIV, and HPV, is recommended by the CDC. [63] They should also be counseled regarding the need for follow-up testing and the possible signs of an STI. (See our companion reference article on "Sexual Assault Infectious Disease Prophylaxis.") [63]
For Patients with Urethral or Vaginal Discharge and Women with Lower Abdominal and/or Pelvic Pain Suspicious of Pelvic Inflammatory Disease:
- Perform nucleic-acid amplification tests (NAAT) to identify Neisseria gonorrhoeae and Chlamydia trachomatis whenever such infections or coinfections are likely.
- Start treatment the same day, based on test results, whenever possible.
- If test results are unavailable, the WHO recommends treating symptomatic patients for N. gonorrhoeae and C. trachomatis . Treatment of their sexual partners will depend on test results.
- If a urethral discharge is present, but test results for Neisseria and chlamydia are negative, treat for Mycoplasma genitalium and/or Trichomonas vaginalis.
- Patients with persistent or recurrent discharge after three weeks should have repeat NAAT testing to include N. gonorrhoeae, C. trachomatis, M. genitalium, and T. vaginalis.
- If the test for Neisseria gonorrhoeae is positive, check for antibiotic resistance.
- HIV and syphilis testing is generally recommended for all STI patients regardless of other findings.
For Patients with Genital Ulcerative Lesions
- Perform nucleic-acid amplification tests (NAAT) to identify the Herpes simplex virus and Treponema pallidum, as well as serological tests for syphilis.
- Start treatment the same day for syphilis and/or herpes if test results are available.
- If test results are not available, start treatment immediately based on the clinical impression and revise later when the information is forthcoming.
- Obtain similar molecular assays on anogenital lesions to identify lymphogranuloma venereum, where this is endemic.
- Treat for lymphogranuloma venereum only when the test results for this disease are positive.
- Treat for chancroid only in those regions where the disease has been identified.
- Differential Diagnosis
A broad differential should be approached when evaluating a patient, whether in an Emergency Department or a primary care setting. Sexually transmitted infections can be localized to the oropharynx, integumentary system, external and internal genitals depending on whether the patient is a male or female, perianal/perineal, and rectum. Physicians should initially establish a primary or preliminary diagnostic impression and differential diagnosis, then formulate a confirmatory plan. The history, physical exam, and clinical presentation should all support the definitive diagnosis and also rule out your differential diagnosis.
When approaching a differential diagnosis specifically for sexually transmitted infections, each system should be evaluated separately, i.e., cardiovascular, respiratory, gastrointestinal, genitourinary, central nervous system, musculoskeletal, and integumentary systems. Breaking the signs and symptoms down into systems specifically for each sexually transmitted infection will help differentiate a primary associated infectious process from a secondary, unrelated disorder or coinfection. [64]
Differential STIs should be assessed by system and symptomatology: Each of the following systems can be affected by STIs, leading to direct or indirect involvement.
- Cardiovascular: HIV, Syphilis, HSV-1/HSV-2
- Respiratory: HIV, chlamydia
- Gastrointestinal: HIV, HSV-1/HSV-2, chlamydia, gonorrhea, HPV
- Genitourinary: HIV, HSV-1/HSV-2, chlamydia, gonorrhea, HPV
- Central nervous system: HIV, syphilis, HSV-1/HSV-2, gonorrhea, HPV
- Musculoskeletal: HIV, HSV-1/HSV-2, chlamydia, gonorrhea, HPV
- Integumentary system:HIV, HSV-1/HSV-2, chlamydia, gonorrhea, HPV
The use of different resources, diagnostic methods, and laboratory tests should be individualized and optimized to quickly arrive at the proper diagnosis and better serve the patient population. [65]
The prognosis depends on the diagnosis of the specific disease, its extent and severity at the time of initial presentation, the general health and comorbidities of the patient, and their willingness to comply with necessary treatment, follow-up, and preventive measures. If the disease process is found in the acute phase and can be treated effectively with antivirals, antibiotics, or antifungals, the outcome is dependent on the treatment course and patient compliance. Medication adherence plays a primary role in treating an infection that is treatable or a chronic condition such as HIV, HSV-1/HSV-2, and partially treated or asymptomatic STIs. [2]
Worldwide, health services for diagnosing and treating STIs are generally underfunded, neglected, and inadequate.
Problems include the cultural stigmatization of STI patients, inadequate education of healthcare workers in this area, limited resources, overall poor quality of healthcare services, and the frequent need for patients to bear a significant financial burden for their own treatment, which many cannot afford.
Populations at the highest risk (workers in the sex trade, prostitutes, men who have sex with men, illegal drug users, prisoners, and young people in countries with high rates of STIs and HIV) often lack access to proper, affordable healthcare and STI treatment services.
In many parts of the world, STI services are not seen as significant or important, so they are underfunded and neglected. This only leads to higher numbers of infected but untreated patients, poorer training of healthcare workers, reduced laboratory testing ability, and inadequate supplies of appropriate medications.
- Complications
Sexually transmitted infections (STIs) that remain untreated lead to systemic infections leading to prolonged medical recovery, also include psychological, financial, and general health complications. STIs complications arise from partially treated or untreated infections. Medically underserved populations show an increase in undiagnosed untreated STIs because they have no attainable healthcare system. An increase in complications can be seen if resources are not allocated to the public sector, such as planned parenthood, to provide needed resources to educate people about safe sex practices, including prevention, treatment, and health promotion. [66]
There is a wide array of complications from STIs if left untreated. Females tend to be at higher risk for complications from STIs, including systemic infection from untreated pelvic inflammatory disease, sterility, and infertility from complicated gonorrhea/chlamydial infections. STIs in pregnant females will cause a higher percentage of preterm labor, premature rupture of membranes, newborns with low birth weight, chorioamnionitis, miscarriages, stillbirths, and early infant mortality. Newborns may become infected as the baby is exposed to various infections during passage through the birth canal. Newborns so exposed are at particular risk for lung and eye infections.
Infants born to mothers with untreated syphilis may develop problems in many organ systems, including bones, the brain, ears, eyes, the heart, skin, and teeth.
Females and males have a risk of neoplasm secondary to certain HPV strain types. [67] HIV infections, if not properly managed, can progress to AIDS, a fatal late complication secondary to a severely immunocompromised state.
- Consultations
For further information and details on specific infections, consult our companion reference StatPearls articles on the following:
- "Acquired Immune Deficiency Syndrome" [68]
- "Chancroid" [6]
- "Chlamydia" [7]
- "Congenital Syphilis" [61]
- "Epididymitis" [55]
- "Herpes Simplex Type 1" [9]
- "Herpes Simplex Type 2" [10]
- "Gonorrhea" [12]
- "Granuloma inguinale" [14]
- "HIV Disease Current Practice" [15]
- "Lypnhogranuloma venereum" [19]
- "Mycoplasma infections" [20]
- "Neurosyphilis" [47]
- "Pelvic Inflammatory Disease" [37]
- "Syphilis" [21]
- "Tabes dorsalis" [48]
- "Trichomoniasis" [23]
- Deterrence and Patient Education
Healthcare professionals should understand the most common sexually transmitted diseases in their area and should be comfortable with counseling patients on modifiable human behavior while providing a gold standard of care in line with the presenting disease. Patients should be provided information on prevention, counseling, and proper treatment for sexually transmitted infections. [66]
HPV Vaccine: There is a vaccine for HPV that is over 99% effective. It requires two dosages given 6 to 12 months apart. According to the CDC, these can be given starting at age 9, are optimal at ages 11 to 12, and are recommended for everyone not previously vaccinated up to age 26.
Between 27 and 45 years, the vaccination is not automatically recommended but may be reasonable for those at high-risk for HPV infections as the benefits of prophylactic vaccination decrease as people age.
Beyond age 45, vaccinations are not recommended as most adults of this age have already been exposed and will see minimal, if any, benefit.
HIV Pre-Exposure Prophylaxis: While not a vaccine, pre-exposure prophylaxis (PrEP) is 99% effective in preventing HIV infections in those taking the medication. Ideal candidates would be those at high-risk such as individuals with multiple sexual partners or open relationships. Patients must test negative for HIV-1 before starting this therapy and at least every three months while on prophylaxis (or every two months if receiving injections).
Of the 1.2 million individuals in the US who are considered at high-risk for HIV, where PrEP is recommended, only about 25% are taking the therapy. Strict compliance is essential to maintain the protective effects. The treatment is not considered adequate as the sole therapy for active HIV infections and will not prevent other STIs. Current recommended PrEP treatments include:
- Oral emtricitabine with tenofovir disoproxil fumarate is FDA-approved for PrEP.
- Oral emtricitabine with tenofovir alafenamide is FDA-approved for PrEP except for people born as females who engage in vaginal intercourse, as this group has not been adequately studied.
- Injectable cabotegravir is given every two months after the first two monthly administrations.
- Pearls and Other Issues
The key to managing sexually transmitted infections is to have an open dialogue with the patient regarding their sexual history, current practices, risk factors, and follow-up. Establishing a good relationship creates a neutral environment and optimizes the treatment course. Avoid shaming or judging a person's sexual history or practices because this can lead to patients' reservations about discussing their general and sexual health openly. It will also make it far less likely that they will return for necessary follow-up.
Whether a patient is seen in the emergency department or a primary care office, the patient's disposition should be determined solely by the clinical presentation. If the patient has a complicated systemic infection, admission is most likely warranted, but if they have a self-limiting complaint that can be easily treated with proper follow-up, the patient can be discharged home. Pitfalls a physician may encounter would most likely be limited education or familiarity with the newest guidelines on prevention and treatment, as well as limited local resources for their patient population.
- Enhancing Healthcare Team Outcomes
Sexually transmitted infections are a worldwide concern and issue. Untreated patients often suffer disastrous effects, including health issues, financial burdens, psychological disorders, and physical damage. Vaccines and prophylactic therapy (PrEP) should be recommended for all appropriate patients. Data collection for STIs is limited by country and geographical area. Access to a national and international data collection service can help identify the prevalence and incidence of certain STIs to better allocate limited community resources directed towards prevention and treatment.
Treatment will be headed by a clinician (MD, DO, NP, or PA), but depending on the disease and its progression, it may involve specialists in infectious disease or other organ systems affected. Nurses will assist in patient examinations and counseling and serve as liaisons for all interprofessional team members. Pharmacists can verify the appropriateness of antimicrobial therapy, check dosing, monitor for adverse events, counsel patients on their medications and compliance with the regimen, and answer patient questions; advanced cases may require an infectious disease specialty pharmacist. Psychological and mental health professionals may also need to weigh in on these cases. Open communication channels are essential in STI cases so that any team member can reach out to other practitioners on the case to voice concerns or report any issues. Meticulous record-keeping goes hand-in-hand with open communication so that every care team member can access the same updated patient information on which to base their decisions and interventions. The interprofessional model will lead to optimal patient care. [Level 5]
The World Health Organization and similar groups can help an interprofessional team and care coordinators to provide these services. [69] Patient-centered care should remain the priority whether patients are seen in the emergency department, their primary care office, or specialized regional STI clinics.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Michael Ray Garcia declares no relevant financial relationships with ineligible companies.
Disclosure: Stephen Leslie declares no relevant financial relationships with ineligible companies.
Disclosure: Anton Wray declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Garcia MR, Leslie SW, Wray AA. Sexually Transmitted Infections. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Sexual relationships, risk behaviour, and condom use in the spread of sexually transmitted infections to heterosexual men. [Genitourin Med. 1997] Sexual relationships, risk behaviour, and condom use in the spread of sexually transmitted infections to heterosexual men. Evans BA, Bond RA, MacRae KD. Genitourin Med. 1997 Oct; 73(5):368-72.
- Molecular Identification of Cervical Microbes in HIV-Negative and HIV-Positive Women in an African Setting Using a Customized Bacterial Vaginosis Microbial DNA Quantitative PCR (qPCR) Array. [Microbiol Spectr. 2022] Molecular Identification of Cervical Microbes in HIV-Negative and HIV-Positive Women in an African Setting Using a Customized Bacterial Vaginosis Microbial DNA Quantitative PCR (qPCR) Array. Taku O, Onywera H, Mbulawa ZZA, Businge CB, Meiring TL, Williamson AL. Microbiol Spectr. 2022 Jun 29; 10(3):e0222921. Epub 2022 Jun 1.
- Knowledge and attitude about sexually transmitted infections other than HIV among college students. [Indian J Sex Transm Dis AIDS. ...] Knowledge and attitude about sexually transmitted infections other than HIV among college students. Subbarao NT, Akhilesh A. Indian J Sex Transm Dis AIDS. 2017 Jan-Jun; 38(1):10-14.
- Review Avoiding sexually transmitted diseases. [Obstet Gynecol Clin North Am. ...] Review Avoiding sexually transmitted diseases. Stone KM. Obstet Gynecol Clin North Am. 1990 Dec; 17(4):789-99.
- Review The Presentation, Diagnosis, and Treatment of Sexually Transmitted Infections. [Dtsch Arztebl Int. 2016] Review The Presentation, Diagnosis, and Treatment of Sexually Transmitted Infections. Wagenlehner FM, Brockmeyer NH, Discher T, Friese K, Wichelhaus TA. Dtsch Arztebl Int. 2016 Jan 11; 113(1-02):11-22.
Recent Activity
- Sexually Transmitted Infections - StatPearls Sexually Transmitted Infections - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
With Gift Aid, your generous donation of £ 10 would be worth £ 12.50 at no extra cost to you.
I am a UK taxpayer and I understand that if I pay less Income and /or Capital Gains Tax than the amount of Gift Aid claimed on all my donations in the relevant tax year, it is my responsibility to pay any difference.
In our 35th year we’re asking people to donate £35 – that’s just £1 for every year we’ve been providing life-changing information. Any donation you make helps us continue our work towards a world where HIV is no longer a threat to health or happiness.
- £5 allows us to reach millions of people globally with accurate and reliable resources about HIV prevention and treatment.
- £10 helps us produce news and bulletins on the latest developments in HIV for healthcare staff around the world.
- £35 means we can empower more people living with HIV to challenge stigma with our information workshops, videos and broadcasts.
Sexually transmitted infections and HIV

- STIs don’t always have symptoms but can cause severe health problems, if left untreated.
- Regular sexual health checks are important if you are sexually active.
- All treatment at NHS sexual health clinics is confidential and free of charge for anyone.
Sexually transmitted infections (STIs) can be caused by bacteria, viruses or parasites. More common STIs include:
- genital and anal warts (caused by the human papillomavirus , or HPV )
- Lymphogranuloma venereum (LGV)
- mycoplasma genitalium, a bacterial infection
- hepatitis A, B and C
- herpes (caused by the herpes simplex virus, or HSV). This can cause both oral (on the mouth) and genital infection
- parasites such as pubic lice (sometimes called crabs) and scabies
- shigellosis , an illness caused by the bacteria Shigella , and other illnesses that cause diarrhoea
- trichomoniasis, an infection caused by a very small parasite.
Although STIs other than HIV can seem a minor issue, they can cause unpleasant symptoms. If left untreated, some can cause severe health problems. In the very long term, some can cause irreversible damage to your health or, in extreme cases, be fatal.
Some sexually transmitted viral infections, such as herpes simplex virus (HSV, normally just called herpes) and HPV, cannot be cured, although their symptoms can be reduced or treated.
Hepatitis A, B and C can all be passed on during sex (hepatitis B is especially infectious). They can all make you seriously ill if they are left untreated.
Sexual health check-ups
Vaccinations against stis, common symptoms, transmission and prevention of stis.
If you are sexually active, it is important to have regular sexual health check-ups. For people considered to be at high risk of STIs (because they have had sex without a condom with a new partner, have multiple partners, or been diagnosed with an STI), the recommendation is to have a check-up every three months.
Many HIV clinics share a building with a sexual health clinic and many HIV clinics include sexual health screening as part of their routine HIV care. You can choose which sexual health clinic you go to. It does not have to be the one nearest your home or the one linked to your HIV clinic.
Visits to sexual health clinics usually involve seeing a healthcare provider who will ask you about the kind of sex you are having and whether you have any symptoms of an STI before examining you. It is important to be honest about the types of sex you have had, so you can be given the appropriate tests. Sexual health clinics are very used to seeing all the communities affected by HIV in the UK. Most people are happy with their treatment at sexual health clinics, but if you are not treated in a professional and non-judgemental manner, you have a right to raise this or make a complaint.
Tests and examinations for STIs vary, often depending on whether you have symptoms. They might be done in the clinic. Or they may give you a kit and ask you to take your own swabs and samples which you then post to a laboratory for analysis.
Samples may be taken from the tip of your penis (only if you have symptoms) or from inside your vagina. If you have oral or anal sex, you will be asked for samples from the mouth, throat and anus. You may also be asked for a urine sample and a blood sample. These swabs and samples are then sent to a laboratory to look for evidence of infection and may be examined under a microscope for rapid detection.
Some results can be given to you at your visit, but it may be necessary to wait for a text message, a telephone call from the clinic, or to come back a week or so later for some other results.
All treatment at NHS sexual health clinics is confidential and free of charge (even if you are not normally entitled to free NHS care). The clinic will need a record of your postcode for administration purposes. Your GP will not be informed without your consent.
If it turns out that you have an STI, you may be offered the opportunity to see a sexual health adviser. Sexual health advisers can give you information about STIs and how to avoid them and can help you contact your sexual partners, if this is possible or practical, so they can also be tested and treated. This helps prevent infections from spreading in the wider community and can help reduce the chance of you becoming re-infected.
In the UK, some GPs or practice nurses offer sexual health screens. Free chlamydia testing and treatment is widely available for people under the age of 25. Many pharmacies also work with local sexual health clinics to provide screening and treatment.
STI postal testing kits that can be ordered online and used at home, with samples sent back to a laboratory for testing, may also be available in your area.
There are vaccines available for:
- hepatitis A
- hepatitis B
- human papillomavirus (HPV), which can cause genital and anal warts, as well as several types of cancer.
Your clinic can advise you on whether you need vaccination against hepatitis A. Unless you have natural immunity, the hepatitis B vaccine is recommended for all people with HIV.
The British HIV Association recommends that the following groups of people living with HIV should have the HPV vaccine: women up to the age of 40, gay and bisexual men up to the age of 40, and heterosexual men up to the age of 26.
There are some common symptoms of STIs. These include:

Basic information on health checks for people with HIV
- a discharge from your vagina, penis or anus. This may be discoloured – for example, milky, yellowish or like mucus – or may have blood in it
- pain or a burning feeling when you urinate (pee) or needing to urinate more often than usual
- pain while you are having sex
- abnormal stomach pains
- pain or swelling around your anus or testicles
- generally feeling unwell
- for herpes: numbness, itching and tingling, followed by bumps that become small, fluid-filled blisters
- for syphilis: small sores, spots or ulcers on the penis or around the mouth, vagina or anus at the site of infection; a rash on your torso, arms, palms or soles of feet
- for hepatitis A, B and C: symptoms can include jaundice (a yellowing of skin and eyes), nausea and vomiting, and tiredness
- for genital warts: lumps and bumps around the genital area and anus
- for parasites, especially scabies: itching around the genitals or in other concealed places, such as between the fingers or toes, or behind the knees
- diarrhoea with blood and rectal pain.
However, many people have no symptoms at all when they first get an STI, or their symptoms are so mild they don’t notice them. Regular sexual health checks are important because they can diagnose STIs even if you have no symptoms. Many STIs can go on to cause serious, long-term health problems if they are not diagnosed and treated, including causing infertility. Hepatitis B and C can become chronic (long-term) conditions and lead to serious liver damage while syphilis can affect organs such as the brain and heart.
Antibiotics can cure bacterial infections such as chlamydia, gonorrhoea and syphilis, and also the parasitical infection, trichomoniasis. Antibiotics may be given as tablets or by injections, depending on the STI you have.
Antiviral drugs can be used to treat (but not always cure) some viral infections. Herpes cannot be cured and the virus stays in nerve cells for life, although most of the time it may not cause symptoms. You may have episodes from time to time, especially if you have a weakened immune system. Your immune system may suppress HPV, the genital warts virus, but this may take a long time and for some people never happens. There are various treatment options to get rid of visible warts.
Drugs to treat hepatitis C can provide a cure, but they don’t protect you from being infected again.
sexually transmitted infections (STIs)
Although HIV can be sexually transmitted, the term is most often used to refer to chlamydia, gonorrhoea, syphilis, herpes, scabies, trichomonas vaginalis, etc.
Any perceptible, subjective change in the body or its functions that signals the presence of a disease or condition, as reported by the patient.
human papilloma virus (HPV)
Some strains of this virus cause warts, including genital and anal warts. Other strains are responsible for cervical cancer, anal cancer and some cancers of the penis, vagina, vulva, urethra, tongue and tonsils.
hepatitis A virus (HAV)
The hepatitis A virus is transmitted through contaminated food and water, as well as human faeces. It can be passed on during sex, particularly rimming (oral-anal contact). Symptoms usually last less than two months, although they continue in some people for up to six months. Drug treatment is not needed. A vaccine is available to prevent hepatitis A.
A sexually transmitted infection caused by the bacterium Treponema pallidum . Transmission can occur by direct contact with a syphilis sore during vaginal, anal, or oral sex. Sores may be found around the penis, vagina, or anus, or in the rectum, on the lips, or in the mouth, but syphilis is often asymptomatic. It can spread from an infected mother to her unborn baby.
Topical treatments, such as lotions, can clear infestations of parasites such as scabies or pubic lice. You should also wash clothing, towels and bedding at high temperatures.
It is important to finish the whole course of any drugs prescribed and to go to any follow-up appointments you are advised to have. You may be advised not to have sex (even with a condom) until any treatment is finished, and sometimes for a while after that. This will ensure you get the correct treatment and are completely cured of the STI, if that is possible.
Any sexual partners you have had since the time you may have been infected should also go for a sexual health check, as they may also need to be treated, even if they have no symptoms.
STIs can be transmitted through anal, oral and vaginal sex, and by sharing sex toys.
Some can also be passed on through rimming (mouth-to-anus contact), kissing or other close physical contact. Parasites can be passed on by sharing towels or bedding. Some STIs (including hepatitis A) and other infections (for example, gut infections such as giardia) can be caused by contact with infected faeces (excrement, shit), such as during rimming or fisting. Hepatitis A can also be transmitted through contact with infected faeces in contaminated food, for example, shellfish.
Hepatitis B is passed on by contact with the blood, semen, saliva, or vaginal fluids of a person with hepatitis B. It is easily passed on during sex without a condom and to a baby during childbirth. It is many times more infectious than HIV. Hepatitis C is normally passed on through blood-to-blood contact. It is also passed on through sex among gay men having anal sex without using condoms. Other factors that seem to be associated with sexual transmission of hepatitis C are group sex, fisting, sharing sex toys, injecting or snorting drugs, anal administration of drugs and the presence in either person of other STIs, especially syphilis or LGV infection.
Using condoms during anal or vaginal sex, using a condom or dental dam for oral sex, and not sharing sex toys can protect you against most STIs. If you are fisting, to protect yourself against hepatitis C, wear latex gloves and do not share pots of lubricant. With some STIs, using a condom or dental dam will reduce the risk of infection, but not protect you completely.
- Español (Spanish)
Webpage (HTML) Topic HIV-Related Conditions Sexually Transmitted Infections (STIs) Basic HIV and AIDS Information Fact Sheets Resource Link https://hivinfo.nih.gov/understanding-hiv/fact-sheets/hiv-and-sexually-transmit… Source HIVinfo.NIH.gov
An AI app claims it can detect sexually transmitted infections. Doctors say it’s a disaster
‘there are so many things wrong with this app that i don’t even know where to begin,’ one doctor said about calmara, which says it can identify sexually transmitted infections from photos of penises..
- Show more sharing options
- Copy Link URL Copied!
Late last month, the San Francisco-based startup HeHealth announced the launch of Calmara.ai , a cheerful, emoji-laden website the company describes as “your tech savvy BFF for STI checks.”
The concept is simple. A user concerned about their partner’s sexual health status just snaps a photo (with consent, the service notes) of the partner’s penis (the only part of the human body the software is trained to recognize) and uploads it to Calmara.
In seconds, the site scans the image and returns one of two messages: “Clear! No visible signs of STIs spotted for now” or “Hold!!! We spotted something sus.”
Calmara describes the free service as “the next best thing to a lab test for a quick check,” powered by artificial intelligence with “up to 94.4% accuracy rate” (though finer print on the site clarifies its actual performance is “65% to 96% across various conditions.”)
Since its debut, privacy and public health experts have pointed with alarm to a number of significant oversights in Calmara’s design, such as its flimsy consent verification , its potential to receive child pornography and an over-reliance on images to screen for conditions that are often invisible.
But even as a rudimentary screening tool for visual signs of sexually transmitted infections in one specific human organ, tests of Calmara showed the service to be inaccurate, unreliable and prone to the same kind of stigmatizing information its parent company says it wants to combat.
A Los Angeles Times reporter uploaded to Calmara a broad range of penis images taken from the Centers for Disease Control and Prevention’s Public Health Image Library , the STD Center NY and the Royal Australian College of General Practitioners.
Calmara issued a “Hold!!!” to multiple images of penile lesions and bumps caused by sexually transmitted conditions, including syphilis, chlamydia, herpes and human papillomavirus, the virus that causes genital warts .
But the site failed to recognize some textbook images of sexually transmitted infections, including a chancroid ulcer and a case of syphilis so pronounced the foreskin was no longer able to retract.
Calmara’s AI frequently inaccurately identified naturally occurring, non-pathological penile bumps as signs of infection, flagging multiple images of disease-free organs as “something sus.”
It also struggled to distinguish between inanimate objects and human genitals, issuing a cheery “Clear!” to images of both a novelty penis-shaped vase and a penis-shaped cake.
“There are so many things wrong with this app that I don’t even know where to begin,” said Dr. Ina Park , a UC San Francisco professor who serves as a medical consultant for the CDC’s Division of STD Prevention . “With any tests you’re doing for STIs, there is always the possibility of false negatives and false positives. The issue with this app is that it appears to be rife with both.”
Dr. Jeffrey Klausner, an infectious-disease specialist at USC’s Keck School of Medicine and a scientific adviser to HeHealth , acknowledged that Calmara “can’t be promoted as a screening test.”
“To get screened for STIs, you’ve got to get a blood test. You have to get a urine test,” he said. “Having someone look at a penis, or having a digital assistant look at a penis, is not going to be able to detect HIV, syphilis, chlamydia, gonorrhea. Even most cases of herpes are asymptomatic.”
Calmara, he said, is “a very different thing” from HeHealth’s signature product, a paid service that scans images a user submits of his own penis and flags anything that merits follow-up with a healthcare provider.
Klausner did not respond to requests for additional comment about the app’s accuracy.

STDs have been on the rise. Who should pick up the tab for testing?
The AIDS Healthcare Foundation has been resisting a push from L.A. County to ask people if they have insurance that can cover costs for STD tests.
Sept. 13, 2023
Both HeHealth and Calmara use the same underlying AI, though the two sites “may have differences at identifying issues of concern,” co-founder and CEO Dr. Yudara Kularathne said.
“Powered by patented HeHealth wizardry (think an AI so sharp you’d think it aced its SATs), our AI’s been battle-tested by over 40,000 users,” Calmara’s website reads, before noting that its accuracy ranges from 65% to 96%.
“It’s great that they disclose that, but 65% is terrible,” said Dr. Sean Young , a UCI professor of emergency medicine and executive director of the University of California Institute for Prediction Technology. “From a public health perspective, if you’re giving people 65% accuracy, why even tell anyone anything? That’s potentially more harmful than beneficial.”
Kularathne said the accuracy range “highlights the complexity of detecting STIs and other visible conditions on the penis, each with its unique characteristics and challenges.” He added: “It’s important to understand that this is just the starting point for Calmara. As we refine our AI with more insights, we expect these figures to improve.”
On HeHealth’s website , Kularathne says he was inspired to start the company after a friend became suicidal after “an STI scare magnified by online misinformation.”
“Numerous physiological conditions are often mistaken for STIs, and our technology can provide peace of mind in these situations,” Kularathne posted Tuesday on LinkedIn. “Our technology aims to bring clarity to young people, especially Gen Z.”
Calmara’s AI also mistook some physiological conditions for STIs.
The Times uploaded a number of images onto the site that were posted on a medical website as examples of non-communicable, non-pathological anatomical variations in the human penis that are sometimes confused with STIs, including skin tags, visible sebaceous glands and enlarged capillaries.
Calmara identified each one as “something sus.”
Such inaccurate information could have exactly the opposite effect on young users than the “clarity” its founders intend, said Dr. Joni Roberts , an assistant professor at Cal Poly San Luis Obispo who runs the campus’s Sexual and Reproductive Health Lab .
“If I am 18 years old, I take a picture of something that is a normal occurrence as part of the human body, [and] I get this that says that it’s ‘sus’? Now I’m stressing out,” Roberts said.
“We already know that mental health [issues are] extremely high in this population. Social media has run havoc on people’s self image, worth, depression, et cetera,” she said. “Saying something is ‘sus’ without providing any information is problematic.”
Kularathne defended the site’s choice of language. “The phrase ‘something sus’ is deliberately chosen to indicate ambiguity and suggest the need for further investigation,” he wrote in an email. “It’s a prompt for users to seek professional advice, fostering a culture of caution and responsibility.”
Still, “the misidentification of healthy anatomy as ‘something sus’ if that happens, is indeed not the outcome we aim for,” he wrote.
Users whose photos are issued a “Hold” notice are directed to HeHealth where, for a fee, they can submit additional photos of their penis for further scanning.
Those who get a “Clear” are told “No visible signs of STIs spotted for now . . . But this isn’t an all-clear for STIs,” noting, correctly, that many sexually transmitted conditions are asymptomatic and invisible. Users who click through Calmara’s FAQs will also find a disclaimer that a “Clear!” notification “doesn’t mean you can skimp on further checks.”

The first over-the-counter birth control pill becomes available. Where is it sold?
Health experts say the over-the-counter birth control pill gives contraception options to people who live in rural or remote areas.
March 19, 2024
Young raised concerns that some people might use the app to make immediate decisions about their sexual health.
“There’s more ethical obligations to be able to be transparent and clear about your data and practices, and to not use the typical startup approaches that a lot of other companies will use in non-health spaces,” he said.
In its current form, he said, Calmara “has the potential to further stigmatize not only STIs, but to further stigmatize digital health by giving inaccurate diagnoses and having people make claims that every digital health tool or app is just a big sham.”
HeHealth.ai has raised about $1.1 million since its founding in 2019, co-founder Mei-Ling Lu said. The company is currently seeking another $1.5 million from investors, according to PitchBook .
Medical experts interviewed for this article said that technology can and should be used to reduce barriers to sexual healthcare. Providers including Planned Parenthood and the Mayo Clinic are using AI tools to share vetted information with their patients, said Mara Decker , a UC San Francisco epidemiologist who studies sexual health education and digital technology.
But when it comes to Calmara’s approach, “I basically can see only negatives and no benefits,” Decker said. “They could just as easily replace their app with a sign that says, ‘If you have a rash or noticeable sore, go get tested.’”

Entertainment & Arts
Halle Berry’s perimenopause was misdiagnosed as ‘worst case of herpes’ her doc ever saw
Halle Berry says her doctor was convinced she had the ‘worst case of herpes’ he had ever seen when she described symptoms related to perimenopause.
March 27, 2024
More to Read

Laguna Beach High School investigates ‘inappropriate’ AI-generated images of students
April 2, 2024
Hollywood celebs are scared of deepfakes. This talent agency will use AI to fight them

Scandal over AI-generated nudes at Beverly Hills middle school exposes gaps in law
March 3, 2024

Corinne Purtill is a science and medicine reporter for the Los Angeles Times. Her writing on science and human behavior has appeared in the New Yorker, the New York Times, Time Magazine, the BBC, Quartz and elsewhere. Before joining The Times, she worked as the senior London correspondent for GlobalPost (now PRI) and as a reporter and assignment editor at the Cambodia Daily in Phnom Penh. She is a native of Southern California and a graduate of Stanford University.
More From the Los Angeles Times

Where Biden, Trump and Kennedy stand on housing and homelessness
RFK Jr. speaks candidly about his gravelly voice: ‘If I could sound better, I would’
April 8, 2024

9 lovely walks to explore L.A.’s most beautiful bridges
April 3, 2024

Jay Leno’s wife Mavis Leno sometimes ‘does not know’ him due to dementia, lawyer says

IMAGES
VIDEO
COMMENTS
Engaging in sexual contract while drinking or using drugs. What are possible long term effects of gonorrhea. Pelvic inflammatory disease. Infertility. Prostate issues. According to the data which group has the highest rate of chlamydia. Women aged 20-24. Those aged 15-19.
Answer: A man declines sex with his partner after being tempted many times. Sexually Transmitted Infections, HIV, and AIDS Pre Test. 4.7 (3 reviews) The pie chart shows the sources from which teens get information about sexual and reproductive health. Based on the graph, from which source is a teen most likely to get information about sexually ...
Find out more about HIV and AIDS by taking this quiz, based on information from the CDC. 1. When was HIV first recognized in the U.S.? A. 1970 B. 1975 C. 1981 D. 1986. 2. Which of these is a symptom of HIV infection? A. Swollen lymph nodes B. Fever C. Tiredness D. All of the above. 3.
A person has HIV for 5 years. 4. What does HIV-positive mean? A. Either antibodies against HIV or the virus particles themselves are present in the blood B. You have been tested for HIV C. Your white cell count is high D. You have been informed about HIV. 5. HIV attacks a certain kind of cell in the immune system.
When untreated, an STI can become a disease. HIV is a sexually transmitted infection, but it can progress to a disease called acquired immunodeficiency syndrome (AIDS) when HIV infection is untreated. Other examples of STDs are chlamydia , gonorrhea , human papillomavirus (HPV) infection, and syphilis. Having an STD can make it easier to get HIV.
Anyone who has sex is at risk, including people with HIV. STIs are also commonly referred to as sexually transmitted diseases (STDs). STIs are infections that are spread from person to person through sexual activity, including anal, vaginal, or oral sex. They are caused by bacteria, parasites, and viruses. HIV is an STI.
WHO fact sheet on sexually transmitted diseases (STIs), providing key facts, as a public health issue, infections and transmissions, STIs and women's health, adverse outcomes of pregnancy, HIV, STI syndromes, prevention, vaccination, mother-to-child transmission, WHO response. ... HIV and AIDS 13 July 2023. Human T-lymphotropic virus type 1 29 ...
Sexually transmitted infections (STIs) are caused by pathogenic microbes that are transmitted from one person to another by sexual intercourse. Some STIs, such as HIV, can also be caught in other ways, for example through contact with contaminated blood when infected drug users share needles, or from mother to baby during the birthing process.
The overall rate of new cases of HIV has risen since 1985. D) Teens have the fastest growing rates of HIV infection. 6. Which statement about HIV/AIDS is true? A) HIV is the same thing as AIDS. B) The HIV organism lives inside cells and body fluids. C) HIV organisms survive well in air and on surfaces. D) Babies never contract HIV from their ...
Breast milk. For transmission to occur, the HIV in these fluids must get into the bloodstream of an HIV-negative person through a mucous membrane (found in the rectum, vagina, mouth, or tip of the penis), through open cuts or sores, or by direct injection (from a needle or syringe). People with HIV who take HIV medicine as prescribed and get ...
More Information. Sexually transmitted infection (STI) refers to an infection that is passed through blood, semen, vaginal fluids, or other body fluids during oral, anal, or genital sex with an infected partner. Sexually transmitted disease (STD) refers to a disease that has developed from an STI.
AIDS is the late stage of HIV infection that occurs when the body's immune system is badly damaged because of the virus. In the U.S., most people with HIV do not develop AIDS because taking HIV medicine as prescribed stops the progression of the disease. A person with HIV is considered to have progressed to AIDS when: the number of their CD4 ...
This is because the same behaviors and circumstances that may put you at risk for getting an STD also can put you at greater risk for getting HIV. In addition, having a sore or break in the skin from an STD may allow HIV to more easily enter your body. If you are sexually active, get tested for STDs and HIV regularly, even if you don't have ...
Choose 1 answer: Reddish rash on the palms of the hands. A. Reddish rash on the palms of the hands. Firm and painless genital ulcers. B. Firm and painless genital ulcers. Sore throat and swollen lymph glands. C.
Sexually transmitted infections (STIs), or sexually transmitted diseases (STDs), are infections that are passed from one individual to another through sexual contact. Learn more about different STIs and HIV with the following resources. Page 1 of 1, showing results 1 - 19 of 19.
What are sexually transmitted infections (STIs), and why are they important? This review will detail important points and reference important articles for physicians and other healthcare professionals to use in evaluating and treating patients with signs and symptoms suggestive of sexually transmitted infections. Physicians should use this article as a guide to further enhance their knowledge ...
Sexually transmitted infections (STIs) can be caused by bacteria, viruses or parasites. More common STIs include: chlamydia. genital and anal warts (caused by the human papillomavirus, or HPV) gonorrhoea. Lymphogranuloma venereum (LGV) mycoplasma genitalium, a bacterial infection. hepatitis A, B and C. herpes (caused by the herpes simplex virus ...
Provide input on HIV research priorities until March 28: The NIH Office of AIDS Research seeks input to inform development of the next strategic plan for HIV research at NIH. Menu 1-800-448-0440 ... HIV and Sexually Transmitted Diseases (STDs) Fact Sheet Webpage (HTML) Topic. HIV-Related Conditions. Sexually Transmitted Infections (STIs)
An AI app claims it can detect sexually transmitted infections. Doctors say it's a disaster 'There are so many things wrong with this app that I don't even know where to begin,' one doctor ...