Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 10, Issue 11
- The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA study): a protocol study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5621-1833 Adrian I Espiritu 1 , 2 ,
- http://orcid.org/0000-0003-1135-6400 Marie Charmaine C Sy 1 ,
- http://orcid.org/0000-0002-1241-8805 Veeda Michelle M Anlacan 1 ,
- http://orcid.org/0000-0001-5317-7369 Roland Dominic G Jamora 1
- 1 Department of Neurosciences , College of Medicine and Philippine General Hospital, University of the Philippines Manila , Manila , Philippines
- 2 Department of Clinical Epidemiology, College of Medicine , University of the Philippines Manila , Manila , Philippines
- Correspondence to Dr Adrian I Espiritu; aiespiritu{at}up.edu.ph
Introduction The SARS-CoV-2, virus that caused the COVID-19 global pandemic, possesses a neuroinvasive potential. Patients with COVID-19 infection present with neurological signs and symptoms aside from the usual respiratory affectation. Moreover, COVID-19 is associated with several neurological diseases and complications, which may eventually affect clinical outcomes.
Objectives The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA) study investigators will conduct a nationwide, multicentre study involving 37 institutions that aims to determine the neurological manifestations and factors associated with clinical outcomes in COVID-19 infection.
Methodology and analysis This is a retrospective cohort study (comparative between patients with and without neurological manifestations) via medical chart review involving adult patients with COVID-19 infection. Sample size was determined at 1342 patients. Demographic, clinical and neurological profiles will be obtained and summarised using descriptive statistics. Student’s t-test for two independent samples and χ 2 test will be used to determine differences between distributions. HRs and 95% CI will be used as an outcome measure. Kaplan-Meier curves will be constructed to plot the time to onset of mortality (survival), respiratory failure, intensive care unit (ICU) admission, duration of ventilator dependence, length of ICU stay and length of hospital stay. The log-rank test will be employed to compare the Kaplan-Meier curves. Stratified analysis will be performed to identify confounders and effects modifiers. To compute for adjusted HR with 95% CI, crude HR of outcomes will be adjusted according to the prespecified possible confounders. Cox proportional regression models will be used to determine significant factors of outcomes. Testing for goodness of fit will also be done using Hosmer-Lemeshow test. Subgroup analysis will be performed for proven prespecified effect modifiers. The effects of missing data and outliers will also be evaluated in this study.
Ethics and dissemination This protocol was approved by the Single Joint Research Ethics Board of the Philippine Department of Health (SJREB-2020–24) and the institutional review board of the different study sites. The dissemination of results will be conducted through scientific/medical conferences and through journal publication. The lay versions of the results may be provided on request.
Trial registration number NCT04386083 .
- adult neurology
- epidemiology
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-040944
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms Study is a nationwide, multicentre, retrospective, cohort study with 37 Philippine sites.
Full spectrum of neurological manifestations of COVID-19 will be collected.
Retrospective gathering of data offers virtually no risk of COVID-19 infection to data collectors.
Data from COVID-19 patients who did not go to the hospital are unobtainable.
Recoding bias is inherent due to the retrospective nature of the study.
Introduction
The COVID-19 has been identified as the cause of an outbreak of respiratory illness in Wuhan, Hubei Province, China, in December 2019. 1 The COVID-19 pandemic has reached the Philippines with most of its cases found in the National Capital Region (NCR). 2 The major clinical features of COVID-19 include fever, cough, shortness of breath, myalgia, headache and diarrhoea. 3 The outcomes of this disease lead to prolonged hospital stay, intensive care unit (ICU) admission, dependence on invasive mechanical ventilation, respiratory failure and mortality. 4 The specific pathogen that causes this clinical syndrome has been named SARS-CoV-2, which is phylogenetically similar to SARS-CoV. 4 Like the SARS-CoV strain, SARS-CoV-2 may possess a similar neuroinvasive potential. 5
A study on cases with COVID-19 found that about 36.4% of patients displayed neurological manifestations of the central nervous system (CNS) and peripheral nervous system (PNS). 6 The associated spectrum of symptoms and signs were substantially broad such as altered mental status, headache, cognitive impairment, agitation, dysexecutive syndrome, seizures, corticospinal tract signs, dysgeusia, extraocular movement abnormalities and myalgia. 7–12 Several reports were published on neurological disorders associated with patients with COVID-19, including cerebrovascular disorders, encephalopathy, hypoxic brain injury, frequent convulsive seizures and inflammatory CNS syndromes like encephalitis, meningitis, acute disseminated encephalomyelitis and Guillain-Barre syndrome. 7–16 However, the estimates of the occurrences of these manifestations were based on studies with a relatively small sample size. Furthermore, the current description of COVID-19 neurological features are hampered to some extent by exceedingly variable reporting; thus, defining causality between this infection and certain neurological manifestations is crucial since this may lead to considerable complications. 17 An Italian observational study protocol on neurological manifestations has also been published to further document and corroborate these findings. 18
Epidemiological data on the proportions and spectrum of non-respiratory symptoms and complications may be essential to increase the recognition of clinicians of the possibility of COVID-19 infection in the presence of other symptoms, particularly neurological manifestations. With this information, the probabilities of diagnosing COVID-19 disease may be strengthened depending on the presence of certain neurological manifestations. Furthermore, knowledge of other unrecognised symptoms and complications may allow early diagnosis that may permit early institution of personal protective equipment and proper contact precautions. Lastly, the presence of neurological manifestations may be used for estimating the risk of certain important clinical outcomes for better and well-informed clinical decisions in patients with COVID-19 disease.
To address this lack of important information in the overall management of patients with COVID-19, we organised a research study entitled ‘The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA Study)’.
This quantitative, retrospective cohort, multicentre study aims: (1) to determine the demographic, clinical and neurological profile of patients with COVID-19 disease in the Philippines; (2) to determine the frequency of neurological symptoms and new-onset neurological disorders/complications in patients with COVID-19 disease; (3) to determine the neurological manifestations that are significant factors of mortality, respiratory failure, duration of ventilator dependence, ICU admission, length of ICU stay and length of hospital stay among patients with COVID-19 disease; (4) to determine if there is significant difference between COVID-19 patients with neurological manifestations compared with those COVID-19 patients without neurological manifestations in terms of mortality, respiratory failure, duration of ventilator dependence, ICU admission, length of ICU stay and length of hospital stay; and (5) to determine the likelihood of mortality, respiratory failure and ICU admission, including the likelihood of longer duration of ventilator dependence and length of ICU and hospital stay in COVID-19 patients with neurological manifestations compared with those without neurological manifestations.
Scope, limitations and delimitations
The study will include confirmed cases of COVID-19 from the 37 participating institutions in the Philippines. Every country has its own healthcare system, whose level of development and strategies ultimately affect patient outcomes. Thus, the results of this study cannot be accurately generalised to other settings. In addition, patients with ages ≤18 years will be excluded in from this study. These younger patients may have different characteristics and outcomes; therefore, yielded estimates for adults in this study may not be applicable to this population subgroup. Moreover, this study will collect data from the patient records of patients with COVID-19; thus, data from patients with mild symptoms who did not go to the hospital and those who had spontaneous resolution of symptoms despite true infection with COVID-19 are unobtainable.
Methodology
To improve the quality of reporting of this study, the guidelines issued by the Strengthening the Reporting of Observational Studies in Epidemiology Initiative will be followed. 19
Study design
The study will be conducted using a retrospective cohort (comparative) design (see figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Schematic diagram of the study flow.
Study sites and duration
We will conduct a nationwide, multicentre study involving 37 institutions in the Philippines (see figure 2 ). Most of these study sites can be found in the NCR, which remains to be the epicentre of the COVID-19 pandemic. 2 We will collect data for 6 months after institutional review board approval for every site.
Location of 37 study sites of the Philippine CORONA study.
Patient selection and cohort description
The cases will be identified using the designated COVID-19 censuses of all the participating centres. A total enumeration of patients with confirmed COVID-19 disease will be done in this study.
The cases identified should satisfy the following inclusion criteria: (A) adult patients at least 19 years of age; (B) cases confirmed by testing approved patient samples (ie, nasal swab, sputum and bronchoalveolar lavage fluid) employing real-time reverse transcription PCR (rRT-PCR) 20 from COVID-19 testing centres accredited by the Department of Health (DOH) of the Philippines, with clinical symptoms and signs attributable to COVID-19 disease (ie, respiratory as well as non-respiratory clinical signs and symptoms) 21 ; and (C) cases with disposition (ie, discharged stable/recovered, home/discharged against medical advice, transferred to other hospital or died) at the end of the study period. Cases with conditions or diseases caused by other organisms (ie, bacteria, other viruses, fungi and so on) or caused by other pathologies unrelated to COVID-19 disease (ie, trauma) will be excluded.
The first cohort will involve patients with confirmed COVID-19 infection who presented with any neurological manifestation/s (ie, symptoms or complications/disorder). The comparator cohort will compose of patients with confirmed COVID-19 infection without neurological manifestation/s.
Sample size calculation
We looked into the mortality outcome measure for the purposes of sample size computation. Following the cohort study of Khaledifar et al , 22 the sample size was calculated using the following parameters: two-sided 95% significance level (1 – α); 80% power (1 – β); unexposed/exposed ratio of 1; 5% of unexposed with outcome (case fatality rate from COVID19-Philippines Dashboard Tracker (PH) 23 as of 8 April 2020); and assumed risk ratio 2 (to see a two-fold increase in risk of mortality when neurological symptoms are present).
When these values were plugged in to the formula for cohort studies, 24 a minimum sample size of 1118 is required. To account for possible incomplete data, the sample was adjusted for 20% more. This means that the total sample size required is 1342 patients, which will be gathered from the participating centres.
Data collection
We formulated an electronic data collection form using Epi Info Software (V.7.2.2.16). The forms will be pilot-tested, and a formal data collection workshop will be conducted to ensure collection accuracy. The data will be obtained from the review of the medical records.
The following pertinent data will be obtained: (A) demographic data; (B) other clinical profile data/comorbidities; (C) neurological history; (D) date of illness onset; (E) respiratory and constitutional symptoms associated with COVID-19; (F) COVID-19 disease severity 25 at nadir; (G) data if neurological manifestation/s were present at onset prior to respiratory symptoms and the specific neurological manifestation/s present at onset; (H) neurological symptoms; (i) date of neurological symptom onset; (J) new-onset neurological disorders or complications; (K) date of new neurological disorder or complication onset; (L) imaging done; (M) cerebrospinal fluid analysis; (N) electrophysiological studies; (O) treatment given; (P) antibiotics given; (Q) neurological interventions given; (R) date of mortality and cause/s of mortality; (S) date of respiratory failure onset, date of mechanical ventilator cessation and cause/s of respiratory failure; (T) date of first day of ICU admission, date of discharge from ICU and indication/s for ICU admission; (U) other neurological outcomes at discharge; (V) date of hospital discharge; and (W) final disposition. See table 1 for the summary of the data to be collected for this study.
- View inline
Data to be collected in this study
Main outcomes considered
The following patient outcomes will be considered for this study:
Mortality (binary outcome): defined as the patients with confirmed COVID-19 who died.
Respiratory failure (binary outcome): defined as the patients with confirmed COVID-19 who experienced clinical symptoms and signs of respiratory insufficiency. Clinically, this condition may manifest as tachypnoea/sign of increased work of breathing (ie, respiratory rate of ≥22), abnormal blood gases (ie, hypoxaemia as evidenced by partial pressure of oxygen (PaO 2 ) <60 or hypercapnia by partial pressure of carbon dioxide of >45), or requiring oxygen supplementation (ie, PaO 2 <60 or ratio of PaO 2 /fraction of inspired oxygen (P/F ratio)) <300).
Duration of ventilator dependence (continuous outcome): defined as the number of days from initiation of assisted ventilation to cessation of mechanical ventilator use.
ICU admission (binary outcome): defined as the patients with confirmed COVID-19 admitted to an ICU or ICU-comparable setting.
Length of ICU stay (continuous outcome): defined as the number of days admitted in the ICU or ICU-comparable setting.
Length of hospital stay (continuous outcome): defined as the number of days from admission to discharge.
Data analysis plan
Statistical analysis will be performed using Stata V.7.2.2.16.
Demographic, clinical and neurological profiles will be summarised using descriptive statistics, in which categorical variables will be expressed as frequencies with corresponding percentages, and continuous variables will be pooled using means (SD).
Student’s t-test for two independent samples and χ 2 test will be used to determine differences between distributions.
HRs and 95% CI will be used as an outcome measure. Kaplan-Meier curves will be constructed to plot the time to onset of mortality (survival), respiratory failure, ICU admission, duration of ventilator dependence (recategorised binary form), length of ICU stay (recategorised binary form) and length of hospital stay (recategorised binary form). Log-rank test will be employed to compare the Kaplan-Meier curves. Stratified analysis will be performed to identify confounders and effects modifiers. To compute for adjusted HR with 95% CI, crude HR of outcomes at discrete time points will be adjusted for prespecified possible confounders such as age, history of cardiovascular or cerebrovascular disease, hypertension, diabetes mellitus, and respiratory disease, COVID-19 disease severity at nadir, and other significant confounding factors.
Cox proportional regression models will be used to determine significant factors of outcomes. Testing for goodness of fit will be done using Hosmer-Lemeshow test. Likelihood ratio tests and other information criteria (Akaike Information Criterion or Bayesian Information Criterion) will be used to refine the final model. Statistical significance will be considered if the 95% CI of HR or adjusted HR did not include the number one. A p value <0.05 (two tailed) is set for other analyses.
Subgroup analyses will be performed for proven prespecified effect modifiers. The following variables will be considered for subgroup analyses: age (19–64 years vs ≥65 years), sex, body mass index (<18.5 vs 18.5–22.9 vs ≥23 kg/m 2 ), with history of cardiovascular or cerebrovascular disease (presence or absence), hypertension (presence or absence), diabetes mellitus (presence or absence), respiratory disease (presence or absence), smoking status (smoker or non-smoker) and COVID-19 disease severity (mild, severe or critical disease).
The effects of missing data will be explored. All efforts will be exerted to minimise missing and spurious data. Validity of the submitted electronic data collection will be monitored and reviewed weekly to prevent missing or inaccurate input of data. Multiple imputations will be performed for missing data when possible. To check for robustness of results, analysis done for patients with complete data will be compared with the analysis with the imputed data.
The effects of outliers will also be assessed. Outliers will be assessed by z-score or boxplot. A cut-off of 3 SD from the mean can also be used. To check for robustness of results, analysis done with outliers will be compared with the analysis without the outliers.
Study organisational structure
A steering committee (AIE, MCCS, VMMA and RDGJ) was formed to direct and provide appropriate scientific, technical and methodological assistance to study site investigators and collaborators (see figure 3 ). Central administrative coordination, data management, administrative support, documentation of progress reports, data analyses and interpretation and journal publication are the main responsibilities of the steering committee. Study site investigators and collaborators are responsible for the proper collection and recording of data including the duty to maintain the confidentiality of information and the privacy of all identified patients for all the phases of the research processes.
Organisational structure of oversight of the Philippine CORONA Study.
This section is highlighted as part of the required formatting amendments by the Journal.
Ethics and dissemination
This research will adhere to the Philippine National Ethical Guidelines for Health and Health-related Research 2017. 26 This study is an observational, cohort study and will not allocate any type of intervention. The medical records of the identified patients will be reviewed retrospectively. To protect the privacy of the participant, the data collection forms will not contain any information (ie, names and institutional patient number) that could determine the identity of the patients. A sequential code will be recorded for each patient in the following format: AAA-BBB where AAA will pertain to the three-digit code randomly assigned to each study site; BBB will pertain to the sequential case number assigned by each study site. Each participating centre will designate a password-protected laptop for data collection; the password is known only to the study site.
This protocol was approved by the following institutional review boards: Single Joint Research Ethics Board of the DOH, Philippines (SJREB-2020-24); Asian Hospital and Medical Center, Muntinlupa City (2020- 010-A); Baguio General Hospital and Medical Center (BGHMC), Baguio City (BGHMC-ERC-2020-13); Cagayan Valley Medical Center (CVMC), Tuguegarao City; Capitol Medical Center, Quezon City; Cardinal Santos Medical Center (CSMC), San Juan City (CSMC REC 2020-020); Chong Hua Hospital, Cebu City (IRB 2420–04); De La Salle Medical and Health Sciences Institute (DLSMHSI), Cavite (2020-23-02-A); East Avenue Medical Center (EAMC), Quezon City (EAMC IERB 2020-38); Jose R. Reyes Memorial Medical Center, Manila; Jose B. Lingad Memorial Regional Hospital, San Fernando, Pampanga; Dr. Jose N. Rodriguez Memorial Hospital, Caloocan City; Lung Center of the Philippines (LCP), Quezon City (LCP-CT-010–2020); Manila Doctors Hospital, Manila (MDH IRB 2020-006); Makati Medical Center, Makati City (MMC IRB 2020–054); Manila Medical Center, Manila (MMERC 2020-09); Northern Mindanao Medical Center, Cagayan de Oro City (025-2020); Quirino Memorial Medical Center (QMMC), Quezon City (QMMC REB GCS 2020-28); Ospital ng Makati, Makati City; University of the Philippines – Philippine General Hospital (UP-PGH), Manila (2020-314-01 SJREB); Philippine Heart Center, Quezon City; Research Institute for Tropical Medicine, Muntinlupa City (RITM IRB 2020-16); San Lazaro Hospital, Manila; San Juan De Dios Educational Foundation Inc – Hospital, Pasay City (SJRIB 2020-0006); Southern Isabela Medical Center, Santiago City (2020-03); Southern Philippines Medical Center (SPMC), Davao City (P20062001); St. Luke’s Medical Center, Quezon City (SL-20116); St. Luke’s Medical Center, Bonifacio Global City, Taguig City (SL-20116); Southern Philippines Medical Center, Davao City; The Medical City, Pasig City; University of Santo Tomas Hospital, Manila (UST-REC-2020-04-071-MD); University of the East Ramon Magsaysay Memorial Medical Center, Inc, Quezon City (0835/E/2020/063); Veterans Memorial Medical Center (VMMC), Quezon City (VMMC-2020-025) and Vicente Sotto Memorial Medical Center, Cebu City (VSMMC-REC-O-2020–048).
The dissemination of results will be conducted through scientific/medical conferences and through journal publication. Only the aggregate results of the study shall be disseminated. The lay versions of the results may be provided on request.
Protocol registration and technical review approval
This protocol was registered in the ClinicalTrials.gov website. It has received technical review board approvals from the Department of Neurosciences, Philippine General Hospital and College of Medicine, University of the Philippines Manila, from the Cardinal Santos Medical Center (San Juan City) and from the Research Center for Clinical Epidemiology and Biostatistics, De La Salle Medical and Health Sciences Institute (Dasmariñas, Cavite).
Acknowledgments
We would like to thank Almira Abigail Doreen O Apor, MD, of the Department of Neurosciences, Philippine General Hospital, Philippines, for illustrating figure 2 for this publication.
- Adhikari SP ,
- Wu Y-J , et al
- Department of Health
- Philippine Society for Microbiology and Infectious Diseases
- Hu Y , et al
- Li Yan‐Chao ,
- Bai Wan‐Zhu ,
- Hashikawa T ,
- Wang M , et al
- Paterson RW ,
- Benjamin L , et al
- Hall JP , et al
- Varatharaj A ,
- Ellul MA , et al
- Mahammedi A ,
- Vagal A , et al
- Collantes MEV ,
- Espiritu AI ,
- Sy MCC , et al
- Merdji H , et al
- Sharifi Razavi A ,
- Poyiadji N ,
- Noujaim D , et al
- Zhou H , et al
- Moriguchi T ,
- Goto J , et al
- Nicholson TR , et al
- Ferrarese C ,
- Priori A , et al
- von Elm E ,
- Altman DG ,
- Egger M , et al
- Li J , et al
- Centers for Disease Control and Prevention
- Khaledifar A ,
- Hashemzadeh M ,
- Solati K , et al
- McGoogan JM
- Philippine Research Ethics Board
VMMA and RDGJ are joint senior authors.
AIE and MCCS are joint first authors.
Twitter @neuroaidz, @JamoraRoland
Collaborators The Philippine CORONA Study Group Collaborators: Maritoni C Abbariao, Joshua Emmanuel E Abejero, Ryndell G Alava, Robert A Barja, Dante P Bornales, Maria Teresa A Cañete, Ma. Alma E Carandang-Concepcion, Joseree-Ann S Catindig, Maria Epifania V Collantes, Evram V Corral, Ma. Lourdes P Corrales-Joson, Romulus Emmanuel H Cruz, Marita B Dantes, Ma. Caridad V Desquitado, Cid Czarina E Diesta, Carissa Paz C Dioquino, Maritzie R Eribal, Romulo U Esagunde, Rosalina B Espiritu-Picar, Valmarie S Estrada, Manolo Kristoffer C Flores, Dan Neftalie A Juangco, Muktader A Kalbi, Annabelle Y Lao-Reyes, Lina C Laxamana, Corina Maria Socorro A Macalintal, Maria Victoria G Manuel, Jennifer Justice F Manzano, Ma. Socorro C Martinez, Generaldo D Maylem, Marc Conrad C Molina, Marietta C Olaivar, Marissa T Ong, Arnold Angelo M Pineda, Joanne B Robles, Artemio A Roxas Jr, Jo Ann R Soliven, Arturo F Surdilla, Noreen Jhoanna C Tangcuangco-Trinidad, Rosalia A Teleg, Jarungchai Anton S Vatanagul and Maricar P Yumul.
Contributors All authors conceived the idea and wrote the initial drafts and revisions of the protocol. All authors made substantial contributions in this protocol for intellectual content.
Funding Philippine Neurological Association (Grant/Award Number: N/A). Expanded Hospital Research Office, Philippine General Hospital (Grant/Award Number: N/A).
Disclaimer Our funding sources had no role in the design of the protocol, and will not be involved during the methodological execution, data analyses and interpretation and decision to submit or to publish the study results.
Map disclaimer The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Extending health systems resilience into communities: a qualitative study with community-based actors providing health services during the COVID-19 pandemic in the Philippines
Affiliations.
- 1 Dalla Lana School of Public Health, University of Toronto, 155 College St, M5T 3M7, Toronto, ON, Canada.
- 2 School of Public Health Sciences, University of Waterloo, 200 University Ave West, N2L 3G1, Waterloo, ON, Canada.
- 3 International Care Ministries, Unit 1701, 17th Floor, West Tower, Philippine Stock Exchange Centre, Exchange Road, Metro Manila, 1605, Pasig City, Philippines.
- 4 Dalla Lana School of Public Health, University of Toronto, 155 College St, M5T 3M7, Toronto, ON, Canada. [email protected].
- 5 School of Public Health Sciences, University of Waterloo, 200 University Ave West, N2L 3G1, Waterloo, ON, Canada. [email protected].
- 6 International Care Ministries, Unit 1701, 17th Floor, West Tower, Philippine Stock Exchange Centre, Exchange Road, Metro Manila, 1605, Pasig City, Philippines. [email protected].
- 7 Dalla Lana School of Public Health, University of Toronto, 155 College St, M5T 3M7, Toronto, ON, Canada. [email protected].
- PMID: 36411439
- PMCID: PMC9677893
- DOI: 10.1186/s12913-022-08734-4
Background: Amidst ongoing calls for increased health systems resilience, gaps remain in our understanding of how health systems can reach further into communities to ensure resilient service delivery. Indeed, public health emergencies caused by infectious hazards reveal both the value and vulnerability of the workforce delivering health services in communities. This study explores ways in which a non-governmental organization (NGO) in the Philippines protected their frontline workforce during the first year of the COVID-19 pandemic.
Methods: Guided by a qualitative descriptive approach, 34 in-depth interviews were conducted with community-based health actors employed by the NGO between June 2020 and February 2021. Data analysis was guided by an iterative deductive and inductive approach.
Results: We identified four key activities that enabled the NGO and their staff to provide health and social services in communities in a safe and consistent manner as part of the organization's pandemic response. These include (1) ensuring adequate personal protective equipment (PPE) and hygiene supplies; (2) providing contextualized and role-specific infection prevention and control (IPC) training; (3) ensuring access to testing for all staff; and (4) providing support during quarantine or isolation.
Conclusion: Learning from the implementation of these activities offers a way forward toward health emergency preparedness and response that is crucially needed for NGOs to safely leverage their workforce during pandemics. Further, we describe how community-based health actors employed by NGOs can contribute to broader health systems resilience in the context of health emergency preparedness and response.
Keywords: COVID-19 pandemic; Community-based health services; Health workforce; Infection prevention and control; Non-governmental organizations; Public health emergencies; Southeast Asia.
© 2022. The Author(s).
- COVID-19* / epidemiology
- COVID-19* / prevention & control
- Community Health Services
- Health Workforce*
- Infection Control
- Organizations, Nonprofit
- Pandemics* / prevention & control
- Philippines / epidemiology
- Public Health
- Social Work
Grants and funding
- 439835/Canadian Institutes of Health Research (CIHR) and International Development Research Centre (IDRC)
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Study Protocol
Assessing the effect of the COVID-19 pandemic, shift to online learning, and social media use on the mental health of college students in the Philippines: A mixed-method study protocol
Roles Funding acquisition, Writing – original draft
Affiliation College of Medicine, University of the Philippines, Manila, Philippines
Roles Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing
Affiliations Department of Clinical Epidemiology, College of Medicine, University of the Philippines, Manila, Philippines, Institute of Clinical Epidemiology, National Institutes of Health, University of the Philippines, Manila, Philippines
Roles Methodology
Affiliation Department of Psychiatry, College of Medicine, University of the Philippines, Manila, Philippines
Roles Conceptualization, Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
- Leonard Thomas S. Lim,
- Zypher Jude G. Regencia,
- J. Rem C. Dela Cruz,
- Frances Dominique V. Ho,
- Marcela S. Rodolfo,
- Josefina Ly-Uson,
- Emmanuel S. Baja

- Published: May 3, 2022
- https://doi.org/10.1371/journal.pone.0267555
- Peer Review
- Reader Comments
Introduction
The COVID-19 pandemic declared by the WHO has affected many countries rendering everyday lives halted. In the Philippines, the lockdown quarantine protocols have shifted the traditional college classes to online. The abrupt transition to online classes may bring psychological effects to college students due to continuous isolation and lack of interaction with fellow students and teachers. Our study aims to assess Filipino college students’ mental health status and to estimate the effect of the COVID-19 pandemic, the shift to online learning, and social media use on mental health. In addition, facilitators or stressors that modified the mental health status of the college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning will be investigated.
Methods and analysis
Mixed-method study design will be used, which will involve: (1) an online survey to 2,100 college students across the Philippines; and (2) randomly selected 20–40 key informant interviews (KIIs). Online self-administered questionnaire (SAQ) including Depression, Anxiety, and Stress Scale (DASS-21) and Brief-COPE will be used. Moreover, socio-demographic factors, social media usage, shift to online learning factors, family history of mental health and COVID-19, and other factors that could affect mental health will also be included in the SAQ. KIIs will explore factors affecting the student’s mental health, behaviors, coping mechanism, current stressors, and other emotional reactions to these stressors. Associations between mental health outcomes and possible risk factors will be estimated using generalized linear models, while a thematic approach will be made for the findings from the KIIs. Results of the study will then be triangulated and summarized.
Ethics and dissemination
Our study has been approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2021-099-01). The results will be actively disseminated through conference presentations, peer-reviewed journals, social media, print and broadcast media, and various stakeholder activities.
Citation: Lim LTS, Regencia ZJG, Dela Cruz JRC, Ho FDV, Rodolfo MS, Ly-Uson J, et al. (2022) Assessing the effect of the COVID-19 pandemic, shift to online learning, and social media use on the mental health of college students in the Philippines: A mixed-method study protocol. PLoS ONE 17(5): e0267555. https://doi.org/10.1371/journal.pone.0267555
Editor: Elisa Panada, UNITED KINGDOM
Received: June 9, 2021; Accepted: April 11, 2022; Published: May 3, 2022
Copyright: © 2022 Lim et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: This project is being supported by the American Red Cross through the Philippine Red Cross and Red Cross Youth. The funder will not have a role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
The World Health Organization (WHO) declared the Coronavirus 2019 (COVID-19) outbreak as a global pandemic, and the Philippines is one of the 213 countries affected by the disease [ 1 ]. To reduce the virus’s transmission, the President imposed an enhanced community quarantine in Luzon, the country’s northern and most populous island, on March 16, 2020. This lockdown manifested as curfews, checkpoints, travel restrictions, and suspension of business and school activities [ 2 ]. However, as the virus is yet to be curbed, varying quarantine restrictions are implemented across the country. In addition, schools have shifted to online learning, despite financial and psychological concerns [ 3 ].
Previous outbreaks such as the swine flu crisis adversely influenced the well-being of affected populations, causing them to develop emotional problems and raising the importance of integrating mental health into medical preparedness for similar disasters [ 4 ]. In one study conducted on university students during the swine flu pandemic in 2009, 45% were worried about personally or a family member contracting swine flu, while 10.7% were panicking, feeling depressed, or emotionally disturbed. This study suggests that preventive measures to alleviate distress through health education and promotion are warranted [ 5 ].
During the COVID-19 pandemic, researchers worldwide have been churning out studies on its psychological effects on different populations [ 6 – 9 ]. The indirect effects of COVID-19, such as quarantine measures, the infection of family and friends, and the death of loved ones, could worsen the overall mental wellbeing of individuals [ 6 ]. Studies from 2020 to 2021 link the pandemic to emotional disturbances among those in quarantine, even going as far as giving vulnerable populations the inclination to commit suicide [ 7 , 8 ], persistent effect on mood and wellness [ 9 ], and depression and anxiety [ 10 ].
In the Philippines, a survey of 1,879 respondents measuring the psychological effects of COVID-19 during its early phase in 2020 was released. Results showed that one-fourth of respondents reported moderate-to-severe anxiety, while one-sixth reported moderate-to-severe depression [ 11 ]. In addition, other local studies in 2020 examined the mental health of frontline workers such as nurses and physicians—placing emphasis on the importance of psychological support in minimizing anxiety [ 12 , 13 ].
Since the first wave of the pandemic in 2020, risk factors that could affect specific populations’ psychological well-being have been studied [ 14 , 15 ]. A cohort study on 1,773 COVID-19 hospitalized patients in 2021 found that survivors were mainly troubled with fatigue, muscle weakness, sleep difficulties, and depression or anxiety [ 16 ]. Their results usually associate the crisis with fear, anxiety, depression, reduced sleep quality, and distress among the general population.
Moreover, the pandemic also exacerbated the condition of people with pre-existing psychiatric disorders, especially patients that live in high COVID-19 prevalence areas [ 17 ]. People suffering from mood and substance use disorders that have been infected with COVID-19 showed higher suicide risks [ 7 , 18 ]. Furthermore, a study in 2020 cited the following factors contributing to increased suicide risk: social isolation, fear of contagion, anxiety, uncertainty, chronic stress, and economic difficulties [ 19 ].
Globally, multiple studies have shown that mental health disorders among university student populations are prevalent [ 13 , 20 – 22 ]. In a 2007 survey of 2,843 undergraduate and graduate students at a large midwestern public university in the United States, the estimated prevalence of any depressive or anxiety disorder was 15.6% and 13.0% for undergraduate and graduate students, respectively [ 20 ]. Meanwhile, in a 2013 study of 506 students from 4 public universities in Malaysia, 27.5% and 9.7% had moderate and severe or extremely severe depression, respectively; 34% and 29% had moderate and severe or extremely severe anxiety, respectively [ 21 ]. In China, a 2016 meta-analysis aiming to establish the national prevalence of depression among university students analyzed 39 studies from 1995 to 2015; the meta-analysis found that the overall prevalence of depression was 23.8% across all studies that included 32,694 Chinese university students [ 23 ].
A college student’s mental status may be significantly affected by the successful fulfillment of a student’s role. A 2013 study found that acceptable teaching methods can enhance students’ satisfaction and academic performance, both linked to their mental health [ 24 ]. However, online learning poses multiple challenges to these methods [ 3 ]. Furthermore, a 2020 study found that students’ mental status is affected by their social support systems, which, in turn, may be jeopardized by the COVID-19 pandemic and the physical limitations it has imposed. Support accessible to a student through social ties to other individuals, groups, and the greater community is a form of social support; university students may draw social support from family, friends, classmates, teachers, and a significant other [ 25 , 26 ]. Among individuals undergoing social isolation and distancing during the COVID-19 pandemic in 2020, social support has been found to be inversely related to depression, anxiety, irritability, sleep quality, and loneliness, with higher levels of social support reducing the risk of depression and improving sleep quality [ 27 ]. Lastly, it has been shown in a 2020 study that social support builds resilience, a protective factor against depression, anxiety, and stress [ 28 ]. Therefore, given the protective effects of social support on psychological health, a supportive environment should be maintained in the classroom. Online learning must be perceived as an inclusive community and a safe space for peer-to-peer interactions [ 29 ]. This is echoed in another study in 2019 on depressed students who narrated their need to see themselves reflected on others [ 30 ]. Whether or not online learning currently implemented has successfully transitioned remains to be seen.
The effect of social media on students’ mental health has been a topic of interest even before the pandemic [ 31 , 32 ]. A systematic review published in 2020 found that social media use is responsible for aggravating mental health problems and that prominent risk factors for depression and anxiety include time spent, activity, and addiction to social media [ 31 ]. Another systematic review published in 2016 argues that the nature of online social networking use may be more important in influencing the symptoms of depression than the duration or frequency of the engagement—suggesting that social rumination and comparison are likely to be candidate mediators in the relationship between depression and social media [ 33 ]. However, their findings also suggest that the relationship between depression and online social networking is complex and necessitates further research to determine the impact of moderators and mediators that underly the positive and negative impact of online social networking on wellbeing [ 33 ].
Despite existing studies already painting a picture of the psychological effects of COVID-19 in the Philippines, to our knowledge, there are still no local studies contextualized to college students living in different regions of the country. Therefore, it is crucial to elicit the reasons and risk factors for depression, stress, and anxiety and determine the potential impact that online learning and social media use may have on the mental health of the said population. In turn, the findings would allow the creation of more context-specific and regionalized interventions that can promote mental wellness during the COVID-19 pandemic.
Materials and methods
The study’s general objective is to assess the mental health status of college students and determine the different factors that influenced them during the COVID-19 pandemic. Specifically, it aims:
- To describe the study population’s characteristics, categorized by their mental health status, which includes depression, anxiety, and stress.
- To determine the prevalence and risk factors of depression, anxiety, and stress among college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning.
- To estimate the effect of social media use on depression, anxiety, stress, and coping strategies towards stress among college students and examine whether participant characteristics modified these associations.
- To estimate the effect of online learning shift on depression, anxiety, stress, and coping strategies towards stress among college students and examine whether participant characteristics modified these associations.
- To determine the facilitators or stressors among college students that modified their mental health status during the COVID-19 pandemic, quarantine, and subsequent shift to online learning.
Study design
A mixed-method study design will be used to address the study’s objectives, which will include Key Informant Interviews (KIIs) and an online survey. During the quarantine period of the COVID-19 pandemic in the Philippines from April to November 2021, the study shall occur with the population amid community quarantine and an abrupt transition to online classes. Since this is the Philippines’ first study that will look at the prevalence of depression, anxiety, and stress among college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning, the online survey will be utilized for the quantitative part of the study design. For the qualitative component of the study design, KIIs will determine facilitators or stressors among college students that modified their mental health status during the quarantine period.
Study population
The Red Cross Youth (RCY), one of the Philippine Red Cross’s significant services, is a network of youth volunteers that spans the entire country, having active members in Luzon, Visayas, and Mindanao. The group is clustered into different age ranges, with the College Red Cross Youth (18–25 years old) being the study’s population of interest. The RCY has over 26,060 students spread across 20 chapters located all over the country’s three major island groups. The RCY is heterogeneously composed, with some members classified as college students and some as out-of-school youth. Given their nationwide scope, disseminating information from the national to the local level is already in place; this is done primarily through email, social media platforms, and text blasts. The research team will leverage these platforms to distribute the online survey questionnaire.
In addition, the online survey will also be open to non-members of the RCY. It will be disseminated through social media and engagements with different university administrators in the country. Stratified random sampling will be done for the KIIs. The KII participants will be equally coming from the country’s four (4) primary areas: 5–10 each from the national capital region (NCR), Luzon, Visayas, and Mindanao, including members and non-members of the RCY.
Inclusion and exclusion criteria
The inclusion criteria for the online survey will include those who are 18–25 years old, currently enrolled in a university, can provide consent for the study, and are proficient in English or Filipino. The exclusion criteria will consist of those enrolled in graduate-level programs (e.g., MD, JD, Master’s, Doctorate), out-of-school youth, and those whose current curricula involve going on duty (e.g., MDs, nursing students, allied medical professions, etc.). The inclusion criteria for the KIIs will include online survey participants who are 18–25 years old, can provide consent for the study, are proficient in English or Filipino, and have access to the internet.
Sample size
A continuity correction method developed by Fleiss et al. (2013) was used to calculate the sample size needed [ 34 ]. For a two-sided confidence level of 95%, with 80% power and the least extreme odds ratio to be detected at 1.4, the computed sample size was 1890. With an adjustment for an estimated response rate of 90%, the total sample size needed for the study was 2,100. To achieve saturation for the qualitative part of the study, 20 to 40 participants will be randomly sampled for the KIIs using the respondents who participated in the online survey [ 35 ].
Study procedure
Self-administered questionnaire..
The study will involve creating, testing, and distributing a self-administered questionnaire (SAQ). All eligible study participants will answer the SAQ on socio-demographic factors such as age, sex, gender, sexual orientation, residence, household income, socioeconomic status, smoking status, family history of mental health, and COVID-19 sickness of immediate family members or friends. The two validated survey tools, Depression, Anxiety, and Stress Scale (DASS-21) and Brief-COPE, will be used for the mental health outcome assessment [ 36 – 39 ]. The DASS-21 will measure the negative emotional states of depression, anxiety, and stress [ 40 ], while the Brief-COPE will measure the students’ coping strategies [ 41 ].
For the exposure assessment of the students to social media and shift to online learning, the total time spent on social media (TSSM) per day will be ascertained by querying the participants to provide an estimated time spent daily on social media during and after their online classes. In addition, students will be asked to report their use of the eight commonly used social media sites identified at the start of the study. These sites include Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, YouTube, and social messaging sites Viber/WhatsApp and Facebook Messenger with response choices coded as "(1) never," "(2) less often," "(3) every few weeks," "(4) a few times a week," and “(5) daily” [ 42 – 44 ]. Furthermore, a global frequency score will be calculated by adding the response scores from the eight social media sites. The global frequency score will be used as an additional exposure marker of students to social media [ 45 ]. The shift to online learning will be assessed using questions that will determine the participants’ satisfaction with online learning. This assessment is comprised of 8 items in which participants will be asked to respond on a 5-point Likert scale ranging from ‘strongly disagree’ to ‘strongly agree.’
The online survey will be virtually distributed in English using the Qualtrics XM™ platform. Informed consent detailing the purpose, risks, benefits, methods, psychological referrals, and other ethical considerations will be included before the participants are allowed to answer the survey. Before administering the online survey, the SAQ shall undergo pilot testing among twenty (20) college students not involved with the study. It aims to measure total test-taking time, respondent satisfaction, and understandability of questions. The survey shall be edited according to the pilot test participant’s responses. Moreover, according to the Philippines’ Data Privacy Act, all the answers will be accessible and used only for research purposes.
Key informant interviews.
The research team shall develop the KII concept note, focusing on the extraneous factors affecting the student’s mental health, behaviors, and coping mechanism. Some salient topics will include current stressors (e.g., personal, academic, social), emotional reactions to these stressors, and how they wish to receive support in response to these stressors. The KII will be facilitated by a certified psychologist/psychiatrist/social scientist and research assistants using various online video conferencing software such as Google Meet, Skype, or Zoom. All the KIIs will be recorded and transcribed for analysis. Furthermore, there will be a debriefing session post-KII to address the psychological needs of the participants. Fig 1 presents the diagrammatic flowchart of the study.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0267555.g001
Data analyses
Quantitative data..
Descriptive statistics will be calculated, including the prevalence of mental health outcomes such as depression, anxiety, stress, and coping strategies. In addition, correlation coefficients will be estimated to assess the relations among the different mental health outcomes, covariates, and possible risk factors.
Several study characteristics as effect modifiers will also be assessed, including sex, gender, sexual orientation, family income, smoking status, family history of mental health, and Covid-19. We will include interaction terms between the dichotomized modifier variable and markers of social media use (total TSSM and global frequency score) and shift to online learning in the models. The significance of the interaction terms will be evaluated using the likelihood ratio test. All the regression analyses will be done in R ( http://www.r-project.org ). P values ≤ 0.05 will be considered statistically significant.
Qualitative data.
After transcribing the interviews, the data transcripts will be analyzed using NVivo 1.4.1 software [ 50 ] by three research team members independently using the inductive logic approach in thematic analysis: familiarizing with the data, generating initial codes, searching for themes, reviewing the themes, defining and naming the themes, and producing the report [ 51 ]. Data familiarization will consist of reading and re-reading the data while noting initial ideas. Additionally, coding interesting features of the data will follow systematically across the entire dataset while collating data relevant to each code. Moreover, the open coding of the data will be performed to describe the data into concepts and themes, which will be further categorized to identify distinct concepts and themes [ 52 ].
The three researchers will discuss the results of their thematic analyses. They will compare and contrast the three analyses in order to come up with a thematic map. The final thematic map of the analysis will be generated after checking if the identified themes work in relation to the extracts and the entire dataset. In addition, the selection of clear, persuasive extract examples that will connect the analysis to the research question and literature will be reviewed before producing a scholarly report of the analysis. Additionally, the themes and sub-themes generated will be assessed and discussed in relevance to the study’s objectives. Furthermore, the gathering and analyzing of the data will continue until saturation is reached. Finally, pseudonyms will be used to present quotes from qualitative data.
Data triangulation.
Data triangulation using the two different data sources will be conducted to examine the various aspects of the research and will be compared for convergence. This part of the analysis will require listing all the relevant topics or findings from each component of the study and considering where each method’s results converge, offer complementary information on the same issue, or appear to contradict each other. It is crucial to explicitly look for disagreements between findings from different data collection methods because exploration of any apparent inter-method discrepancy may lead to a better understanding of the research question [ 53 , 54 ].
Data management plan.
The Project Leader will be responsible for overall quality assurance, with research associates and assistants undertaking specific activities to ensure quality control. Quality will be assured through routine monitoring by the Project Leader and periodic cross-checks against the protocols by the research assistants. Transcribed KIIs and the online survey questionnaire will be used for recording data for each participant in the study. The project leader will be responsible for ensuring the accuracy, completeness, legibility, and timeliness of the data captured in all the forms. Data captured from the online survey or KIIs should be consistent, clarified, and corrected. Each participant will have complete source documentation of records. Study staff will prepare appropriate source documents and make them available to the Project Leader upon request for review. In addition, study staff will extract all data collected in the KII notes or survey forms. These data will be secured and kept in a place accessible to the Project Leader. Data entry and cleaning will be conducted, and final data cleaning, data freezing, and data analysis will be performed. Key informant interviews will always involve two researchers. Where appropriate, quality control for the qualitative data collection will be assured through refresher KII training during research design workshops. The Project Leader will check through each transcript for consistency with agreed standards. Where translations are undertaken, the quality will be assured by one other researcher fluent in that language checking against the original recording or notes.
Ethics approval.
The study shall abide by the Principles of the Declaration of Helsinki (2013). It will be conducted along with the Guidelines of the International Conference on Harmonization-Good Clinical Practice (ICH-GCP), E6 (R2), and other ICH-GCP 6 (as amended); National Ethical Guidelines for Health and Health-Related Research (NEGHHRR) of 2017. This protocol has been approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2021-099-01 dated March 25, 2021).
The main concerns for ethics were consent, data privacy, and subject confidentiality. The risks, benefits, and conflicts of interest are discussed in this section from an ethical standpoint.
Recruitment.
The participants will be recruited to answer the online SAQ voluntarily. The recruitment of participants for the KIIs will be chosen through stratified random sampling using a list of those who answered the online SAQ; this will minimize the risk of sampling bias. In addition, none of the participants in the study will have prior contact or association with the researchers. Moreover, power dynamics will not be contacted to recruit respondents. The research objectives, methods, risks, benefits, voluntary participation, withdrawal, and respondents’ rights will be discussed with the respondents in the consent form before KII.
Informed consent will be signified by the potential respondent ticking a box in the online informed consent form and the voluntary participation of the potential respondent to the study after a thorough discussion of the research details. The participant’s consent is voluntary and may be recanted by the participant any time s/he chooses.
Data privacy.
All digital data will be stored in a cloud drive accessible only to the researchers. Subject confidentiality will be upheld through the assignment of control numbers and not requiring participants to divulge the name, address, and other identifying factors not necessary for analysis.
Compensation.
No monetary compensation will be given to the participants, but several tokens will be raffled to all the participants who answered the online survey and did the KIIs.
This research will pose risks to data privacy, as discussed and addressed above. In addition, there will be a risk of social exclusion should data leaks arise due to the stigma against mental health. This risk will be mitigated by properly executing the data collection and analysis plan, excluding personal details and tight data privacy measures. Moreover, there is a risk of psychological distress among the participants due to the sensitive information. This risk will be addressed by subjecting the SAQ and the KII guidelines to the project team’s psychiatrist’s approval, ensuring proper communication with the participants. The KII will also be facilitated by registered clinical psychologists/psychiatrists/social scientists to ensure the participants’ appropriate handling; there will be a briefing and debriefing of the participants before and after the KII proper.
Participation in this study will entail health education and a voluntary referral to a study-affiliated psychiatrist, discussed in previous sections. Moreover, this would contribute to modifications in targeted mental-health campaigns for the 18–25 age group. Summarized findings and recommendations will be channeled to stakeholders for their perusal.
Dissemination.
The results will be actively disseminated through conference presentations, peer-reviewed journals, social media, print and broadcast media, and various stakeholder activities.
This study protocol rationalizes the examination of the mental health of the college students in the Philippines during the COVID-19 pandemic as the traditional face-to-face classes transitioned to online and modular classes. The pandemic that started in March 2020 is now stretching for more than a year in which prolonged lockdown brings people to experience social isolation and disruption of everyday lifestyle. There is an urgent need to study the psychosocial aspects, particularly those populations that are vulnerable to mental health instability. In the Philippines, where community quarantine is still being imposed across the country, college students face several challenges amidst this pandemic. The pandemic continues to escalate, which may lead to fear and a spectrum of psychological consequences. Universities and colleges play an essential role in supporting college students in their academic, safety, and social needs. The courses of activities implemented by the different universities and colleges may significantly affect their mental well-being status. Our study is particularly interested in the effect of online classes on college students nationwide during the pandemic. The study will estimate this effect on their mental wellbeing since this abrupt transition can lead to depression, stress, or anxiety for some students due to insufficient time to adjust to the new learning environment. The role of social media is also an important exposure to some college students [ 55 , 56 ]. Social media exposure to COVID-19 may be considered a contributing factor to college students’ mental well-being, particularly their stress, depression, and anxiety [ 57 , 58 ]. Despite these known facts, little is known about the effect of transitioning to online learning and social media exposure on the mental health of college students during the COVID-19 pandemic in the Philippines. To our knowledge, this is the first study in the Philippines that will use a mixed-method study design to examine the mental health of college students in the entire country. The online survey is a powerful platform to employ our methods.
Additionally, our study will also utilize a qualitative assessment of the college students, which may give significant insights or findings of the experiences of the college students during these trying times that cannot be captured on our online survey. The thematic findings or narratives from the qualitative part of our study will be triangulated with the quantitative analysis for a more robust synthesis. The results will be used to draw conclusions about the mental health status among college students during the pandemic in the country, which will eventually be used to implement key interventions if deemed necessary. A cross-sectional study design for the online survey is one of our study’s limitations in which contrasts will be mainly between participants at a given point of time. In addition, bias arising from residual or unmeasured confounding factors cannot be ruled out.
The COVID-19 pandemic and its accompanying effects will persistently affect the mental wellbeing of college students. Mental health services must be delivered to combat mental instability. In addition, universities and colleges should create an environment that will foster mental health awareness among Filipino college students. The results of our study will tailor the possible coping strategies to meet the specific needs of college students nationwide, thereby promoting psychological resilience.
Nutrition in Times of Crisis: A Qualitative Study in Siargao Island, Philippines, during the COVID-19 Pandemic
- Gideon Lasco Department of Anthropology, University of the Philippines Diliman, Quezon City, Philippines; Development Studies Program, Ateneo de Manila University, Quezon City, Philippines
- Vincen Gregory Yu Development Studies Program, Ateneo de Manila University, Quezon City, Philippines; Social Medicine Unit, College of Medicine, University of the Philippines Manila
- Julie Madelo Compra Surigao State College of Technology – Del Carmen Campus, Siargao Island, Surigao del Norte, Philippines
- Phetdavanh Leuangvilay Equity Initiative, Bangkok, Thailand
- Rapeepong Suphanchaimat International Health Policy Program, Ministry of Public Health, Nonthaburi, Thailand; Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand
- Yunting Zhang Child Health Advocacy Institute, Shanghai Children’s Medical Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- Charina Javier Food and Nutrition Research Institute, Department of Science and Technology, Taguig, Philippines
Objectives. Despite the public-health significance of both malnutrition and crises, little has been done to explore the convergence of the two domains and develop ways to improve policies and practices, especially in rural communities. This article remedies that knowledge gap by focusing on nutrition-related changes, responses, and practices during crisis situations in Siargao Island, Philippines, using the COVID-19 pandemic as a backdrop. Methods. Forty-six (46) semi-structured interviews were conducted among parents, caregivers, local health workers, and local officials of Del Carmen, Siargao Island. Principles of thematic analysis were applied to data analysis using NVivo 12. Afterwards, the preliminary data were presented in a virtual validation session with the local community and stakeholders. Results. Despite the high prevalence of malnutrition amid a backdrop of economic and nutritional difficulties, the community members generally viewed their children as healthy. Rice remained (disproportionately) central to people’s diets; possible alternatives like root crops were considered emergency foods only and not culturally acceptable as staples, in spite of their cheap and ubiquitous nature. Lastly, the economic and financial repercussions of the COVID-19 pandemic have also negatively affected the community members’ overall nutrition and food sources.
Conclusion. More efforts should be directed toward encouraging the consumption of root vegetables and fruits as rice alternatives in everyday diet—a costeffective strategy that would also promote dietary diversification. More importantly, nutrition responses should consider local food systems in terms of specific local economies and geographies, while health promotion efforts should engage with local notions of ‘health’ and ‘nutrition’ and encourage community participation in (re)designing policy interventions.
Make a Submission
Information
- For Readers
- For Authors
- For Librarians
- For Peer Reviewers

Published by the University of the Philippines Manila Indexed in Scopus, Google Scholar, Asean Citation Index (ACI), Western Pacific Region Index Medicus (WPRIM) and Herdin Plus Publishing since 1939.
- Open access
- Published: 09 April 2024
A qualitative study of leaders’ experiences of handling challenges and changes induced by the COVID-19 pandemic in rural nursing homes and homecare services
- Malin Knutsen Glette 1 , 2 ,
- Tone Kringeland 2 ,
- Lipika Samal 3 , 4 ,
- David W. Bates 3 , 4 &
- Siri Wiig 1
BMC Health Services Research volume 24 , Article number: 442 ( 2024 ) Cite this article
Metrics details
The COVID-19 pandemic had a major impact on healthcare services globally. In care settings such as small rural nursing homes and homes care services leaders were forced to confront, and adapt to, both new and ongoing challenges to protect their employees and patients and maintain their organization's operation. The aim of this study was to assess how healthcare leaders, working in rural primary healthcare services, led nursing homes and homecare services during the COVID-19 pandemic. Moreover, the study sought to explore how adaptations to changes and challenges induced by the pandemic were handled by leaders in rural nursing homes and homecare services.
The study employed a qualitative explorative design with individual interviews. Nine leaders at different levels, working in small, rural nursing homes and homecare services in western Norway were included.
Three main themes emerged from the thematic analysis: “Navigating the role of a leader during the pandemic,” “The aftermath – management of COVID-19 in rural primary healthcare services”, and “The benefits and drawbacks of being small and rural during the pandemic.”
Conclusions
Leaders in rural nursing homes and homecare services handled a multitude of immediate challenges and used a variety of adaptive strategies during the COVID-19 pandemic. While handling their own uncertainty and rapidly changing roles, they also coped with organizational challenges and adopted strategies to maintain good working conditions for their employees, as well as maintain sound healthcare management. The study results establish the intricate nature of resilient leadership, encompassing individual resilience, personality, governance, resource availability, and the capability to adjust to organizational and employee requirements, and how the rural context may affect these aspects.
Peer Review reports
In 2021, essential healthcare services in 90% of the world’s countries were disrupted by the COVID-19 pandemic [ 1 ]. Healthcare services were heavily stressed and had to address unexpected issues and sudden changes, whilst still providing high quality care over a prolonged period [ 2 , 3 ]. Despite the intense focus on hospitals during this period, other parts of the healthcare system such as nursing homes and homecare services also faced extreme challenges. These included issues such as having to introduce and constantly adapt new infection control routines, as well as being given increased responsibility in caring for infected and seriously ill patients in facilities that were not built for such circumstances [ 4 , 5 , 6 , 7 ]. Mortality rates in nursing homes were especially high [ 8 ].
Resilience in healthcare is about a system’s ability to adapt to challenges and changes at different levels (e.g., organization, leaders, health personnel) to maintain high quality care [ 9 , 10 ]. During the COVID-19 pandemic, leaders and the front line were forced to rapidly adjust to keep healthcare services afloat. It has been demonstrated in previous research that effective leadership is crucial in navigating crises and building resilience within health systems [ 11 , 12 , 13 ]. Furthermore, leaders play key roles in facilitating health personnel resilience, for example, through promoting a positive outlook on change and by developing health personnels’ competencies and strengths [ 12 , 14 , 15 ]. During the COVID-19 pandemic, this role became intensified [ 16 , 17 , 18 ], and leaders’ roles in promoting resilient healthcare services were central, for example safeguarding resources, providing emotional support and organizing systems to cope with extreme stresses [ 3 , 19 ].
Smaller, rural nursing homes and home care services are geographically dispersed and typically remote from specialized healthcare services or other nursing home and homecare services. They also tend to have reduced access to personnel due to low population density, frequently leading to the need to make independent decisions, often in complex situations [ 20 ]. Overall, rural healthcare services face different challenges than their urban counterparts [ 21 , 22 , 23 ]. The COVID-19 pandemic intensified some of these issues and created new ones which needed to be managed [ 21 , 24 , 25 ].
The research base on COVID-19 has expanded extensively the past years [ 26 ], covering areas such as clinical risks and outcomes for healthcare workers [ 27 ] and patients [ 28 ], hospital admissions [ 29 ] and healthcare utilization during the pandemic [ 30 ]. Moreover, areas like healthcare leaders' [ 16 , 17 , 31 ] and healthcare professionals’ [ 2 , 32 ] strategies to handle the pandemic challenges, and COVID related strategies’ effect on quality of care [ 33 , 34 ]. And lastly, but not exhaustively, the COVID-19 pandemic in different healthcare settings such as hospitals [ 35 ], primary healthcare services and [ 36 ] mental healthcare services [ 37 ]. However, research on rural healthcare settings, particularly leaders in rural nursing homes and homecare services, have received less attention [ 38 , 39 , 40 ]. Despite the anticipated importance of primary healthcare services in future healthcare and the prevalence of rural healthcare options [ 41 , 42 ]. Overall, there are still lessons to be learned from the COVID-19 pandemic, specifically identifying resilience promoting and inhibiting factors in different health care settings during crisis, how leaders deal with crisis management, and furthermore, to understand and draw lessons from challenges that were overcome during the pandemic[ 43 , 44 ].
Aim and research question
The aim of this study was to assess how healthcare leaders in rural primary healthcare services managed nursing homes and homecare services during the COVID-19 pandemic. Moreover, the study aimed to explore how adaptations to changes and challenges induced by the pandemic were handled by these leaders.
The research question guiding the study was: How did primary healthcare leaders in rural areas experience their leadership during the COVID-19 pandemic, and how did they adapt to the rapid onset changes demanded by the COVID-19 outbreak?
The study employed a qualitative explorative design to study in-depth, how nursing home and homecare leaders in Norwegian rural primary healthcare services experienced and addressed the extreme challenges and needs for change induced by the COVID-19 pandemic [ 45 , 46 ]. Four rural municipalities of different sizes were included in the study. Nursing home and homecare leaders at different organizational levels participated in individual interviews (See Table 1 ).
Norway is divided into 356 municipalities. These municipalities have the autonomy to administer and manage their primary healthcare services, subject to certain laws and regulations (e.g., Act on municipal health and care services [ 47 ], Act on patient and user rights [ 48 ] and Regulation on quality in nursing and care services for service provision [ 49 ]). All municipalities are obligated to offer specified healthcare services independent of their size and inhabitant number (Se Fig. 1 for a brief overview of healthcare services provided by the Norwegian municipalities, comprising nursing homes and home care services, and included municipalities).
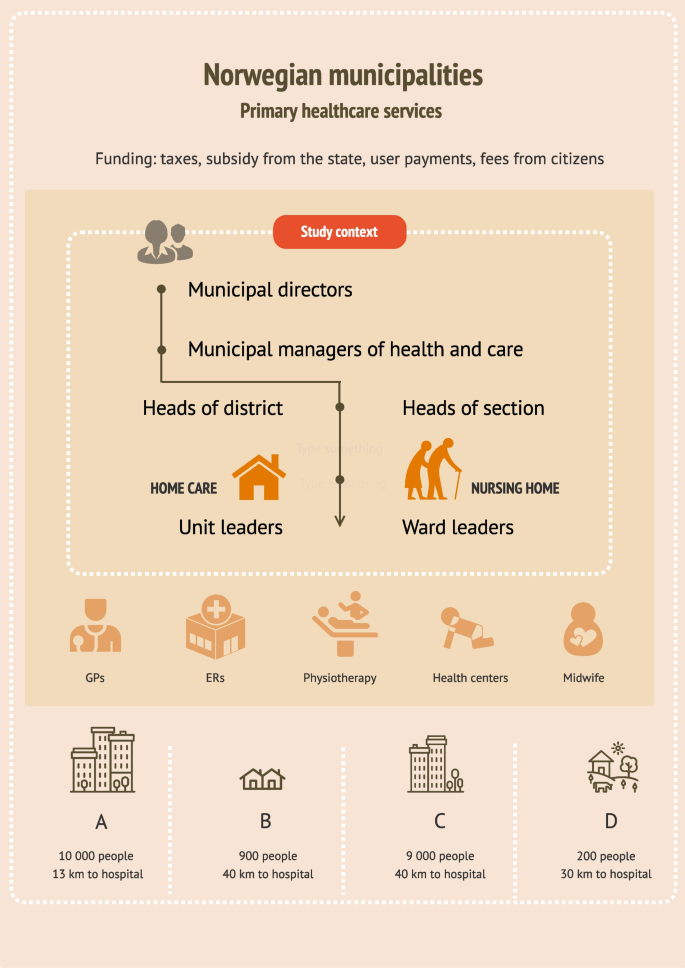
Brief overview of healthcare services provided by the Norwegian municipalities, comprising nursing homes and home care services, and the included municipalities
Recruitment and participants
Recruitment was anchored in the municipal management. The municipal manager of health and care in 11 municipalities across the Norwegian west coast were first contacted via email, then by telephone (se Fig. 1 ). Most managers who responded to our contact were positive, but many had to decline due to time constraints related to pandemic management. Four managers agreed to data collection in their municipality with the stipulation that the nursing home- and homecare leaders wanted to participate. All levels of leaders were eligible for inclusion due to the small size of the healthcare services. We contacted the leaders of nursing homes and home care services in the four municipalities, first by email, then by telephone. Nine leaders agreed to participate. One leader declined. All included leaders were female, registered nurses (RNs), and had long and broad experiences with working as RNs either in the healthcare service they now were leaders in, or in other healthcare settings. Some leaders stated that they had continued education or Master’s degrees, but more leader specific qualifications such as leader education, training or courses were not disclosed (Table 1 . Overview of participants and setting).
Data collection
Individual interviews were conducted from November 2021 to November 2022 by the first author (MKG). Leaders in one of the municipalities (municipality B) wished to do the interview in a group interview (three leaders), which we arranged. All but one interview was conducted at the leaders’ work premises (in their offices or in meeting rooms). One leader was interviewed via Zoom due to a temporary need for increased infection precautions. All interviews were guided by a predeveloped interview guide which was based on resilience in healthcare theory [ 50 , 51 ] and contained subject such as: Success factors and challenges with handling the COVID-19 pandemic; New solutions and how new knowledge and information was handled; and Lessons learned from the pandemic.
Data analysis
The interviews were audio recorded and transcribed. The analysis followed the steps in Braun and Clarkes thematic approach [ 52 ]. This involved reading through the transcripts multiple times to find meanings related to the overall research question. Text with meaning was inserted into a Word table which provided initial codes. After the coding process, which involved creating and continuously revising codes, there were 47 codes. The codes were then organized into categories and categories were sorted into initial main themes. Themes and categories were assessed to determine whether any of them should be merged, refined, split or eliminated [ 52 ] (see Table 2 for example of the analysis process). The author team reviewed and approved categories and themes to ensure that each theme illuminated its essence [ 52 ].
We analyzed the interviews and identified three main themes and eight categories (Table 3 ). The results are presented according to identified main themes.
Navigating the role of a leader during the pandemic
Overall, the leaders seemed to have two primary focuses when they talked about how they had experienced the COVID-19 pandemic. These were their personal coping, and how they managed the organizational challenges arising throughout the pandemic period. Particularly in the beginning, they reported feelings of fear and insecurity. Leaders dreaded the consequences which could result from mistakes, such as providing wrong, or missing essential information.
“Having such a responsibility is a burden, and even though you’re not alone, you still feel like you’re the one responsible for the safety of the employees and the patients. Ensuring the safety of everyone was the priority, which is why it was critical to make sure that the protocols we were distributing were the correct ones…” (L1 nursing home municipality C)
Additionally, several leaders stated that they were concerned about personnel who had contracted COVID-19 (some of whom had serious symptoms), and even felt responsible for their situation. Leaders of two of the municipalities reported feelings of frustration, and despair, and all leaders reported long working hours. Leaders expressed that they felt that they had been “on call” for the last two years, and described long working days, with limited consideration for evenings, nights, weekends, or vacations.
A range of organizational challenges was described (e.g., dealing with a stressed economy, experiencing task overload, working within an unprepared organization and the struggle to get a hold on enough personal protective equipment. One of the most prominent challenges in the data set, was the acquisition, interpretation, and distribution of information issued by the authorities. The leaders described that new information was issued frequently along with constantly changing routines. New routines where developed, distributed, and discarded nonstop in the attempt to “get the organization in line with the state authorities”.
“There was new information issued [from the Norwegian directorate of health] almost hourly… we had more than enough to, in a way, keep up with all these procedures that came, or all the new messages that came, and these [information and routines] had to be issued out to the employees and to the next of kin…” (L1 nursing home municipality A)
Despite the difficulties related to information flow, or lack thereof, the leaders devised a range of solutions to make information more accessible to their staff (e.g., informational e-mails, developing short information sheets, making information binders, and meeting up physically to go through new routines with their employees). The data indicated that it was hard to gauge how much information to make available to their staff, who were eager for knowledge, yet still found it hard to process everything. On occasion, the leaders desired assistance or someone to assume authority, or as one leader articulated: “someone to push the red button” (L1 homecare municipality C), due to their struggles to keep up with information, regulations, and routines in the face of rapid changes.
Not surprisingly, leaders felt a heightened need to take the lead during the COVID-19 pandemic. This was a long-running crisis, and they had to be present, approachable and a source of support for their staff, while also striving to gain the employees’ understanding. For example, in one healthcare service the employees wanted more strict rules than necessary and had strong opinions on how things should be done in “in their healthcare service”, while the leader was stringent with sticking to national regulations which were less strict. Another aspect was handling disagreement with measures among employees. Often measures were not in line with the employees’ wishes, which created friction.
The pandemic highlighted the importance of leaders taking on the task of creating a secure working environment for their employees. The leaders noted considerable anxiety among the staff, particularly in facilities that had not experienced any COVID-19 cases. Leaders came to understand the importance of tending to all wards, regardless of whether they had been affected by the infection, even though it was perceived as taxing. Overall, the leaders worked actively to make the situation in wards with infection outbreaks as best as possible. A leader from a healthcare service which had a major COVID-19 outbreak stated:
“We constantly tried to create new procedures to make it as easy as possible for them [So] that they didn’t have to think about anything. That they [didn’t have to think about] bringing food to work, that they had to [remember] this or that. That they were provided with everything they needed…” (L2 nursing home municipality C)
Another recurring topic in the dataset, was the constant challenges and changes the leaders had to overcome and adapt to during the COVID-19 pandemic. For example, there was a need to plan for all possible scenarios, particularly if they were to have a major infection outbreak among the staff (e.g., how to limit the infection outbreak, how to deal with staffing, how to arrange the wards in case of an outbreak). One healthcare service experienced such a scenario, which demanded a rapid response, when they had a major COVID-19 outbreak with over twenty infected employees almost overnight. The leaders were left with the impossible task of covering a range of shifts, and they were forced to adopt a strategy of reaching out to other healthcare services within their municipality (other wards, nursing homes, the home care services and psychiatric services) asking if they had any nurses “to spare.” Eventually, they managed to cover their staffing needs without using a temp agency.
The leaders of this nursing home also had to deal with numerous small, but important challenges such as how to deal with dirty laundry, what to do with food scraps, where to put decorations and knick-knacks, how to provide wardrobes and lunchrooms, and generally, how to handle an infection outbreak in facilities not designed for this purpose.
Leaders in all primary healthcare services implemented strategies to prevent infection or spread of infection. They introduced longer shifts, split up the personnel in teams, made cleaning routines for lunchrooms and on-call rooms, set up a temporary visiting room for next of kin, developed routines for patient visits, regularly debriefed personnel of infection routines, made temporary wardrobes, and removed unnecessary tasks from the work schedule. New digital tools were introduced, particularly for distributing instructional videos and information among employees, and to keep contact with other leaders.
Although many leaders described the situation as challenging, particularly in the beginning, many found themselves gaining increased control over the situation as time went by.
“Little by little, in some way, the routine of everyday life has become more settled… you can’t completely relax yet, but you can certainly feel a bit more organized, and more confident in your decisions, since we have been doing it for a while [ca 1 year]. (L1 nursing home municipality C)
The aftermath—management of covid-19 in rural primary healthcare services
Despite organizational as well as personal challenges, leaders’ overall impression of the COVID-19 management was positive. The leaders firmly believed that the quality of healthcare services had been preserved, and all the physical healthcare needs of the patients had been properly cared for. According to leaders, there was not a rise in adverse events (e.g., falls, wounds) and patients and next of kin were positive in their feedback. The one main concern regarding quality of care was, however, the aspect of the patients’ sociopsychological state. Patients became isolated and lonely when they could not receive visitors or had to be isolated in their rooms or their homes during COVID. Nevertheless, the leaders expressed admiration for the healthcare personnel's work in addressing psychosocial needs to the best of their capacity. Overall, the leaders were proud of how the front-line healthcare personnel had handled the pandemic, and the extraordinary effort they put in to keeping the healthcare services running.
Several leaders stated that they now felt better prepared for “a next pandemic”, but they also had multiple suggestions for organizational improvements. These suggestions included: set up a visit coordinator, develop a better pandemic plan, be better prepared nationally, develop local PPE storage sites, introduce digital supervision for isolation rooms (for example RoomMate [ 53 ]), provide more psychological help for employees who struggled in the aftermath of an infection outbreak, have designated staff on standby for emergency situations, establish clear communication channels for obtaining information and, when constructing new nursing homes and healthcare facilities, consider infection control measures.
The leaders also discussed the knowledge they had acquired during this period. Many talked about learning how to use digital tools, but mostly they talked about the experience they had gained in handling crisis:
“I believe we are equipped in a whole different way now. There’s no doubt about that. Both employees and leaders and the healthcare service in general, I think… I have no doubt about that… so… there have been lessons learned, no doubt about it….” (L1 nursing home municipality C)
Leaders also talked about what they experienced as success factors in handling the pandemic: Long shifts (11,5 h), with the same shift going 4 days in a row to avoid contacts between different shift, the use of Microsoft Teams and other communication tools to increased and ease intermunicipal cooperation, and the possibility to share experiences, making quick decisions and take action quickly, developing close cooperation with the municipality chief medical officer and the nursing home physician, the involvement of the occupational healthcare service (take the employees’ work situation seriously) and the conduct of “Risk, Vulnerability and Preparedness” analysis (a tool to identify possible threats in order to implement preventive measures and necessary emergency response). The leaders also talked about the advantages of getting input from employees (e.g., through close cooperation with the employee representatives).
The benefits and drawbacks of being small and rural during a pandemic
Aspects of being a small healthcare service within a small municipality were highlighted by several of the leaders. For example, the leader of one the smaller healthcare service included in the study, addressed the challenge of acquiring enough competent staff. To be able to fulfill their requirements for competent staff, the municipality needed to buy healthcare services from neighboring municipalities. Another drawback was that employees who had competence or healthcare education often lacked experience in infection control and infection control routines, because they had rarely or never had infectious outbreaks of any kind. This made it particularly challenging to implement infection control measures. In one of the larger municipalities in this study, they had worked targeted for years to increase the competence in their municipality by focusing on full time positions to all and educating assistants to become Licensed practical nurses (LPN). They benefited from these measures during the pandemic.
Another aspect which was emphasized as essential to survive a pandemic in a small municipality, was intermunicipal cooperation. Leaders of all four healthcare services stated that they built increased cooperation with nearby municipalities during the pandemic. Leaders from the different municipalities met often, sometimes several times a week, and helped each other, shared routines, and methods, asked each other questions, coordinated covid-19 testing and developed intermunicipal corona wards, kept each other updated on infection status locally, and relied on each other’s strengths.
“We established a very good intermunicipal cooperation within the health and care services. We helped each other. Shared both routines and procedures, and actually had Teams meetings twice a week, where I could ask questions…and… we all had different strengths in the roles we held, not all of them [group members] were healthcare personnel either, and they had a lot of questions regarding the practical [handling of the pandemic]. At the same time, they [people who were not healthcare personnel] were good at developing routines and procedures, which they shared with the rest. In other words, the cooperation between the municipalities was very good, and for a small municipality, it was worth its weight in gold”. (L1, nursing home/homecare Municipality D)
The same leader stated that they could not have managed the pandemic without support from other larger municipalities and advised closer cooperation following the pandemic as well. An advantage of being small was the ability to easily track and monitor the virus spread within the municipality. Moreover, it was easy to have close cooperation with the infectious disease physician, the municipal chief medical officer, and the nursing home physician, as one person often held several of these roles. Some leaders also had several roles themselves such as a combination of nursing home leader and homecare leader or a combination of nursing home leader and health and care manager (overseeing all health and care services in the municipality). This was perceived as both an advantage and a disadvantage. This was an advantage because they gained a full overview of the situation due to their multiple areas of responsibility, but a disadvantage because it was demanding for one person to handle everything alone, making the system vulnerable. Another challenging aspect was a lack of people to fill all the necessary roles. For example, in one municipality they did not have a public health officer (a physician in charge of the healthcare services in a municipality, and the municipal management’s medical adviser), and had to hire a private practicing physician, who was not resident in the municipality to take on this role.
The economy was also a continuous source of worry. Running a small healthcare service within a small municipality was stated as expensive because the municipalities were obligated to provide the same healthcare services as the larger municipalities, but with less income (e.g., tax payment per inhabitant). The pandemic led to new expenses such as overtime payment, and wage supplement for changed work hours. Leader had to continuously balance a sound use of resources, and responsible operation.
Table 4 provides and overview of the challenges leaders encountered, how they were handled, and leaders’ suggestions for further improvement.
We assessed how leaders in rural primary healthcare services coped with unprecedented challenges during the COVID-19 pandemic. On one hand, they had to manage personal struggles such as insecurity, guilt, and excessive workload. At the same time, they had to confront major organizational issues such as financial instability, lack of resources, and information overload. Moreover, their roles changed, and the need to lead, make more decisions and be more supportive was heightened. While adapting to these changing roles, the leaders continuously introduced new measures to handle pandemic induced challenges including development of new routines, distilled and distributed information, reorganized staffing plans and rearranged wards. Although patients’ safety and quality of care was perceived as safeguarded throughout the COVID-19 pandemic period, leaders had several suggestions for improvements in case of future crises.
Previous research on primary healthcare services during COVID-19 support several of the findings identified here. Similar challenges requiring leaders to adapt their ways of working such as insufficient contingency plans and infection control, lack of staffing, changing guidelines and routines and challenges related to information flow were found [ 17 , 31 , 54 , 55 , 56 ]. Leader strategies to handle these challenges included reallocation of staff, providing support, provide training and distill and distribute information [ 16 , 31 , 55 , 57 ]. Some findings in this study, particularly related to the rural context, has not been found elsewhere. We found that 1) the leaders’ and healthcare services’ increased their dependency on neighboring municipalities during the pandemic and 2) we identified both the advantages and drawbacks of leaders having to function in multiple roles during the pandemic. The heightened importance of cooperation within municipalities and healthcare services in rural areas as opposed to urban areas, has however, been highlighted both before and during the pandemic [ 17 , 23 ].
The pandemic prompted organizations like the World Health Organization (WHO), International Council of Nurses (ICN), and Organization for Economic Co-operation and Development (OECD) to advocate for the advancement of more resilient healthcare services to be able to overcome current and future health system challenges [ 3 , 58 , 59 ]. To achieve the goal of resilient healthcare services, a multi-focal perspective incorporating both individual, teams and systems, is needed. This is because health system organization and leadership on all levels will impact how resilience can be built on team and individual level and thereby reinforce resilience in organizations [ 12 , 51 , 60 , 61 , 62 ].
The multiple aspects of resilient leadership
Leadership style, leaders’ facilitation for flexibility and leaders’ management of resources, competence, and equipment, will affect the resilience of health personnel and thereby the organizational resilience [ 12 , 15 , 63 ]. However, resilient leadership is affected by multiple aspects. For one, leaders inherent individual resilience will influence how and if, they lead resiliently [ 64 ]. Individual resilience is a multifaceted concept consisting of the person’s determination, persistence, adaptability and recuperative capacity, and is impacted by their personal qualities, conduct and cultural outlook [ 12 ]. Similar to previous literature [ 65 , 66 ], the current study found that leaders had to cope with personal challenges such as fear, guilt, adapting to changed roles and increased workload, while performing their everyday tasks. Literature have shown that leaders' responses to challenges can be influenced by their unique personality traits, ultimately shaping their resilience and leadership style [ 67 , 68 ]. Personal qualities needed to “lead well” have also shown to vary between rural and urban healthcare services. For example, Doshi [ 69 ] found that being social, passionate and extrovert was more important in urban areas than in rural areas. This indicate that leaders’ personality traits affect resilience in healthcare, and that resilience promoting personality traits may vary across urban and rural areas. More research is needed to study these relationships.
Although measures to increase personal resilience can be effective (e.g., mindfulness, workshops/training, therapy) [ 70 , 71 , 72 , 73 ] it is not sufficient to base resilience building on these aspects alone [ 74 ]. There is a need to consider how leaders are influenced and supported by the system they are working within to become, and act more resiliently. This includes the support leaders have in their community (e.g., peer support, leader support and proper guidance), their access to resources and their freedom to make decisions [ 60 , 75 , 76 ]. In the current study, it appeared to be a connection between leaders’ coping and the amount of support they had from colleagues. In our interpretation, leaders who talked about their cooperation with others, also talked more positively of their COVID-19 experiences (e.g., how much they had learned or what they had accomplished, rather than how pressured and anxious they were). Similar results have previously been found. For example, leaders in Marshall and colleagues’ study [ 65 ] felt isolated and struggled to make sense of the situation (COVID-19 induced challenges), while leaders in Seljemo and colleagues’ study stated that support from other managers made it easier to cope with high workloads [ 31 ]. In smaller rural healthcare settings, obtaining support can be challenging due to the limited presence of leader colleagues in close proximity [ 77 ]. Additionally, Gray & Jones [ 78 ] suggests that resilient leaders are leaders who ask for help when needed. This indicates that leaders in more isolated areas may require more effort to form connections beyond their organization, and rural healthcare systems must afford greater attention to enabling peer networking (e.g., by providing time and resources).
Through recurrent intermunicipal, online meetings, leaders in the current study attained to initiate, and preserve contact with other leaders in other healthcare settings, much more than before the COVID-19 pandemic. This was particularly important for the smallest, most rural municipalities, where one leader held many roles, and was by one leader, stated as the main reason they were able to manage the COVID-19 pandemic in their primary healthcare service. The tendency to increase intermunicipal cooperation during this period, and the overall need for smaller, rural healthcare services to cooperate with others is found in other literature [ 23 , 79 ]. However, mostly as collaboration within primary healthcare services, and not across organizations. Although recommended by leaders, it is not clear if this close contact has been maintained after the pandemic.
The governance leaders are working under will affect leaders’ possibility to lead resiliently. The governance allows for effective coordination of financing, resource generation, and service delivery activities, ensuring optimal system performance [ 80 ]. Yet, governing for resilience has proven to be a major challenge, because it requires systems to be both flexible and stable at the same time [ 76 ]. Flexibility presupposes systems’, health personnel’, and leaders’ ability to adapt to current conditions, and is essential for systems to cope with unpredictable, non-linear, and ever-changing social and environmental conditions. Conversely, stability must also be implemented to ensure that new policies are sustained and effective, and to stabilize expectations and promote coordination over time [ 76 ]. This means that leaders need flexibility to make their own decisions, as well as the stability that proper guidelines and direction provides [ 81 ]. In this study, some leaders reported experiencing chaos and loss of control when routines and guidelines lacked in the beginning of the pandemic. Similar results have been found among other healthcare leaders, as well as healthcare personnel [ 32 , 66 ]. In contrast, the leaders’ need for flexibility to be able to adapt to the everchanging work environment brought on by the pandemic (examples in Table 3 ) was demonstrated in this, and other studies [ 16 , 17 ]. It can, however, be argued that the balance between flexibility and stability is often skewed more towards flexibility in rural regions. Rural leaders must make unsupported decisions more often than urban leaders as they face higher demands and fewer available resources (such as competence, staff, and funding) [ 77 ]. This requires rural leaders to be more innovative and adaptable to current circumstances [ 23 , 69 , 77 , 79 ]. That said, the availability of resources have shown to impact a system's flexibility, often by influencing the quality of its adaptations [ 2 ].
In low-resource healthcare settings across the globe, certain adaptations made to combat pandemic challenges ended up causing damage (e.g., reuse or misuse of PPE, overexploitation of healthcare personnel and the use of unconventional treatment methods) [ 2 , 82 ]. In high resource healthcare services, as included in this study, adaptations were often described as beneficial, and potential long-lasting solutions (Table 3 ) [ 16 , 17 , 31 ]. Although not comparable to low resource healthcare services, variation in resource availability and economy between the included healthcare services was also expressed in this study. Norwegian municipalities’ income is closely tied to their tax revenue and population size [ 83 ], and regardless of income, the municipalities are required to provide specific healthcare services to their inhabitants. Thus, the financial foundation of smaller more rural municipalities is not as strong as that of larger municipalities. These inequalities were expressed as notable by both leaders and by healthcare personnel in a preceding study exploring the same primary rural healthcare services as included here [ 32 ]. Since resilience in healthcare is also highly dependent on the competence and experience of employees and leaders, the combination of resource and financial deficiencies, more often experienced in rural healthcare services than in urban healthcare services, may pose particular challenges in resilience building in rural areas [ 23 , 84 ]. This is worth exploring further, along with the rural healthcare services’ particular need to be flexible versus the potential difficulty they may have in making beneficial adaptations because of a weaker financial foundation.
Resilience and leadership style
Providing support to employees was an important leader task during the pandemic [ 55 , 66 ] and have further, been found to be particularly vital in rural areas, where employees have a smaller network of colleagues to turn to [ 84 ]. Other vital leadership tasks, recognizable from crisis leadership literature and also found in this study, were the importance of organizing, directing and implementing actions, forging cooperation, enabling work- arounds or adaptation, direct and guide and the importance of communication and dissemination of information [ 85 , 86 ]. Although charismatic leadership Footnote 1 has been found to be most valuable during crisis [ 87 ], there is an ongoing discussion of what leadership style is best suited to promote resilience in healthcare [ 11 , 14 , 66 , 88 ]. For example, both transformational and transactional leadership 1 [ 89 ] have been stated as resilience promoting leadership styles [ 15 ]. However, as found in other literature [ 66 , 88 ], the results of this study indicated that leaders oscillated between different styles during the COVID-19 pandemic period. For example, in the beginning of the pandemic when uncertainty characterized the healthcare system, leaders became stricter with rules and regulations, demonstrating an authoritative leadership style 1 . Further, stepping in, lecturing about infection control procedures and use of PPE, indicated a coaching leadership 1 style and lastly, when the leaders went against employees wishes to ensure safe maintenance of operation, it showed similarities to a transformational leadership style 1 [ 90 ]. Interestingly, leaders did not speak directly about how their leadership styles changed, and seemed unaware of their leadership style adaptation. Similarly, in Sihvola et al. [ 66 ] leaders found it surprising how novel conditions could influence their leadership style.
On one side, these results, suggest that an adaptive leadership style can be necessary during crisis. On the other side, this and other studies [ 31 , 54 ] indicate that leaders need more knowledge on crisis leadership, for example, to be made aware of the potential need to oscillate between different leadership styles during a crisis, and the possible subsequent challenges. For example, a study conducted by Boyle og Mervin [ 91 ] found that being a “nurse leader” (all leaders in this study were nurses), showed challenging because the leaders were judged as a peer rather than a leader. This can cause challenges, particularly when stepping into an authoritative leadership style. Such conflicts were not reported in this study, however, these are all aspects which should be given more attention when investigating resilience in healthcare and leadership styles [ 88 ]. Furthermore, it is crucial to acquire further understanding on the distinctions between leading in rural and urban areas, and how various leadership approaches may be impacted by managing tight-knit employee teams, which is often the case in small rural nursing home and homecare services. And finally, there is a need to provide a deeper understanding of the factors that promote or impede resilience in rural primary healthcare services, and the influence of the contextual aspects on resilience in healthcare.
Limitations
This study has limitations which need to be addressed. A larger number of included primary healthcare leaders over a wider geographical area and across boarders would have provided a broader view of leader experiences during the COVID-19 pandemic. However, it was very difficult to get leaders to take time to reflect during this crisis. This study does provide insight into a variety of different municipalities of different sizes, organization and locations in the Norwegian context, providing a variety of rural primary healthcare leaders experiences during the pandemic. Interviews were conducted in different ways (focus group, digital and individually) this could have influenced leaders description of their experiences. Furthermore, interviews were held at different points throughout the pandemic phases, leading to a mix of leaders with both current and reflective experiences of navigating the pandemic. This should be taken into consideration when reading the results.
By exploring nursing home and home care leaders’ experiences with the COVID-19 pandemic in rural areas, we found that the leaders met a range of rapid onset challenges of different nature, many of which demanded fast decisions and solutions. Leaders handled these challenges and changes in a variety of ways in their different contexts. In addition to health system challenges, leaders also had to cope with rapidly changing roles, while managing their own and employees’ insecurities. This study’s results demonstrate the intricate nature of resilient leadership, encompassing individual resilience, personality, governance, resource availability, and the capability to adjust to organizational and employee requirements. In addition, there may be differences between how resilience in healthcare is built and progresses in rural healthcare services versus urban contexts. Further research to understand the interplay between these aspects is needed, and it is critical to consider context.

Availability of data and materials
Data are available from the corresponding author upon reasonable request.
Charismatic leadership : influence and persuasion of others to help the fulfill their mandate, also in face of adversity; Transformational leadership: pushing to work and think in new ways; Authoritative leadership : the leader in control, low autonomy; Coaching leadership : the leader support employee’s skill advancement; Transactional leadership : exchange of rewards for fulfilling expectations.
Abbreviations
International Council of Nurses
Licensed practical nurse
Organization for Economic Co-operation and Development
Personal protective equipment
Registered Nurse
The World Health Organization
WHO. COVID-19 continues to disrupt essential health services in 90% of countries WHO2021 [Available from: https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries .
Malin Knutsen G, Kristiana L, Siri W, et al. Resilience perspective on healthcare professionals’ adaptations to changes and challenges resulting from the COVID-19 pandemic: a meta-synthesis. BMJ Open. 2023;13(9):e071828.
Article Google Scholar
OECD. Ready for the Next Crisis? Investing in Health System Resilience. 2023.
Book Google Scholar
Franzosa E, Gorbenko K, Brody AA, et al. “At home, with care”: lessons from New York City home-based primary care practices managing COVID-19. J Am Geriatr Soc. 2021;69(2):300–6.
Article PubMed Google Scholar
Franchini L, Varani S, Ostan R, et al. Home palliative care professionals perception of challenges during the Covid-19 outbreak: a qualitative study. Palliat Med. 2021;35(5):862–74.
Damian AJ, Gonzalez M, Oo M, Anderson D. A national study of community health centers’ readiness to address COVID-19. J Am Board Fam Med. 2021;34(Suppl):S85-s94.
Zhao S, Yin P, Xiao LD, et al. Nursing home staff perceptions of challenges and coping strategies during COVID-19 pandemic in China. Geriatric Nursin. 2021;42(4):887–93.
Aalto UL, Pitkälä KH, Andersen-Ranberg K, et al. COVID-19 pandemic and mortality in nursing homes across USA and Europe up to October 2021. Eur Geriatr Med. 2022;13(3):705–9.
Article PubMed PubMed Central Google Scholar
Wiig S, Aase K, Billett S, et al. Defining the boundaries and operational concepts of resilience in the resilience in healthcare research program. BMC Health Serv Res. 2020;20(1):330.
Wiig S, Fahlbruch B. Exploring Resilience - An Introduction. In: Wiig S, Fahlbruch B, editors. Exploring Resilience : a scientific journey from practice to theory. Springer briefs in applied sciences and technology : safety management. Springer Open: Cham; 2019. p. 1–3.
Google Scholar
Barasa E, Mbau R, Gilson L. What is resilience and how can it be nurtured? A systematic review of empirical literature on organizational resilience. Int J Health Policy Manag. 2018;7(6):491–503.
Bowman A. Leadership and resilience: where the literature stands. J Leadersh Stud. 2022;16(2):33–41.
Akerjordet K, Furunes T, Haver A. Health-promoting leadership: an integrative review and future research agenda. J Adv Nurs. 2018;74(7):1505–16.
Eliot JL. Resilient leadership: the impact of a servant leader on the resilience of their followers. Adv Dev Hum Resour. 2020;22(4):404–18.
Ree E, Ellis LA, Wiig S. Managers’ role in supporting resilience in healthcare: a proposed model of how managers contribute to a healthcare system’s overall resilience. Int J Health Governance. 2021;26(3):266–80.
Lyng HB, Ree E, Wibe T, Wiig S. Healthcare leaders’ use of innovative solutions to ensure resilience in healthcare during the Covid-19 pandemic: a qualitative study in Norwegian nursing homes and home care services. BMC Health Serv Res. 2021;21(1):878.
Ree E, Wiig S, Seljemo C, et al. Managers’ strategies in handling the COVID-19 pandemic in Norwegian nursing homes and homecare services. Leadership in Health Services. (ahead-of-print). 2022;200–18.
Saleem J, Ishaq M, Zakar R, et al. Experiences of frontline Pakistani emigrant physicians combating COVID-19 in the United Kingdom: a qualitative phenomenological analysis. BMC Health Serv Res. 2021;21(1):291.
Glette MK, Bates DW, Dykes PC, et al. A resilience perspective on Healthcare Personnels’ Experiences of Managing the COVID-19 Pandemic: A qualitative study in Norwegian nursing homes and come care services. BMC Health Services Research. 2023 (in review).
Smedt SED, Mehus G. Sykepleieforskning i rurale områder i Norge; en scoping review (English title: Nursing research in rural areas in Norway; a scoping review). Norsk tidsskrift for helseforskning. 2017;13;2:1–27.
W P, L R. Rural, remote and at risk: Why rural health services face a steep climb to recovery from Covid-19. Nuffield Trust; 2020.
van Pijkeren N, Msc P, Wallenburg I, et al. Caring peripheries: How care practitioners respond to processes of peripheralisation. Sociologia Ruralis. 2023;64:64–81.
van de Bovenkamp H, van Pijkeren N, Ree E, et al. Creativity at the margins: a cross-country case study on how Dutch and Norwegian peripheries address challenges to quality work in care for older persons. Health Policy. 2023;127:66–73.
Melvin SC, Wiggins C, Burse N, et al. The role of public health in COVID-19 emergency response efforts from a Rural health perspective. Prev Chronic Dis. 2020;17:E70.
Segel JE, Ross HI, Edwards JL, et al. The unique challenges facing rural providers in the COVID-19 pandemic. Popul Health Manag. 2020;24(3):304–6.
Teixeira da Silva JA, Tsigaris P, Erfanmanesh M. Publishing volumes in major databases related to Covid-19. Scientometrics. 2021;126(1):831–42.
Article CAS PubMed Google Scholar
Gholami M, Fawad I, Shadan S, et al. COVID-19 and healthcare workers: a systematic review and meta-analysis. Int J Infect Dis. 2021;104:335–46.
Article CAS PubMed PubMed Central Google Scholar
Ferguson J, Rosser JI, Quintero O, et al. Characteristics and outcomes of coronavirus disease patients under nonsurge conditions, Northern California, USA, March-April 2020. Emerg Infect Dis. 2020;26(8):1679–85.
Helgeland J, Telle KE, Grøsland M, et al. Admissions to Norwegian hospitals during the COVID-19 pandemic. Scandinavian J Pub Health. 2021;49(7):681–8.
Moynihan R, Sanders S, Michaleff ZA, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3):e045343.
Seljemo C, Wiig S, Røise O, Ree E. The role of local context for managers’ strategies when adapting to the COVID-19 pandemic in Norwegian homecare services: a multiple case study. BMC Health Serv Res. 2023;23(1):492.
Glette MK, Bates DW, Dykes PC, et al. A resilience perspective on healthcare personnels’ experiences of managing the COVID-19 pandemic: a qualitative study in Norwegian nursing homes and come care services. BMC Health Serv Res. 2023;23(1):1177.
Iness AN, Abaricia JO, Sawadogo W, et al. The effect of hospital visitor policies on patients, their visitors, and health care providers during the COVID-19 pandemic: a systematic review. Am J Med. 2022;135(10):1158-67.e3.
Füszl A, Bouvier-Azula L, Van den Nest M, et al. Provision of safe patient care during the COVID-19 pandemic despite shared patient rooms in a tertiary hospital. Antimicrob Resist Infect Control. 2022;11(1):61.
Mohammadinia L, Saadatmand V, Khaledi Sardashti H, et al. Hospital response challenges and strategies during COVID-19 pandemic: a qualitative study. Front Public Health. 2023;11:1167411.
Samdal GB, Alpers LM, Sekse RJT, et al. Barriers and facilitators for leading nursing homes through the COVID-19 pandemic: a focus group study in Norway. Nurs Open. 2023;10(11):7154–67.
Abbas MJ, Kronenberg G, McBride M, et al. The early impact of the COVID-19 pandemic on acute care mental health services. Psychiatr Serv. 2021;72(3):242–6.
Nessler K, Van Poel E, Willems S, et al. The response of primary care practices in rural and urban settings in Poland to the challenges of the COVID-19 pandemic. Ann Agric Environ Med. 2022;29(4):575–81.
Anaraki NR, Mukhopadhyay M, Karaivanov Y, et al. Living and working in rural healthcare during the COVID-19 pandemic: a qualitative study of rural family physicians’ lived experiences. BMC Prim Care. 2022;23(1):335.
Pavloff M, Labrecque ME, Bally J, et al. Rural home care nursing during COVID-19. Can J Nurs Res. 2023;55(4):486–93.
OECD. Realising the Potential of Primary Health Care. OECD; 2020.
The World Bank. Rural population (% of total population) 2018. Available from: https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS . Cited 2023 18.12.
Ellis LA, Churruca K, Clay-Williams R, et al. Patterns of resilience: a scoping review and bibliometric analysis of resilient health care. Saf Sci. 2019;118:241–57.
Scott A, Braithwaite J, Melbourne Uo. Is COVID-19 opening the fault lines in our healthcare system? : Institute of Applied Economic and Social Research.; 2020 [Available from: http://nla.gov.au/nla.obj-2931172550 .
Creswell JW. Research design : qualitative, quantitative, and mixed methods approaches. 5th ed. ed. Los Angeles, Calif: SAGE; 2018.
Holloway I, Galvin K. Qualitative research in nursing and healthcare: Wiley Blackwell; 2017.
Lov om kommunal helse-og omsorgstjeneste (english title: Act on municipal health and care services), LOV-2011–06–24–30 (2011).
Lov om pasient- og brukerrettigheter (English title: Act on patient and user rights), LOV-1999-07-02-63.
Forskrift om kvalitet i pleie- og omsorgstjenestene (English title: Regulation on quality in nursing and care services for service provision), FOR-2003–06–27–792 (2003).
Hollnagel E, . Making Healthcare resilient: From safety-I to Safety-II. In: Hollnagel E, Braithwaite J, Wears RL, editors. Resilient health care. Ashgate studies in resilience engineering. 1. Farnham, Surrey, England: Ashgate; 2013.
Wiig S, Fahlbruch B. Exploring Resilience – An Introduction. In: Wiig S, Fahlbruch B, editors. Exploring Resilience: A Scientific Journey from Practice to Theory. Cham: Springer International Publishing; 2019. p. 1–5.
Chapter Google Scholar
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Sensio. RoomMate. Available from: https://www.sensio.io/no/produkter/roommate?utm_term=roommate&utm_campaign=S%C3%B8k+%7C+Produkter&utm_source=adwords&utm_medium=ppc&hsa_acc=5538158809&hsa_cam=20506326432&hsa_grp=159856433744&hsa_ad=672316590141&hsa_src=g&hsa_tgt=kwd-28346982&hsa_kw=roommate&hsa_mt=p&hsa_net=adwords&hsa_ver=3&gclid=EAIaIQobChMI3rHE6qPpgwMVOVKRBR124QjJEAAYASAAEgKR5vD_BwE . Cited 2024 19.01.
Alakeely M, Almutari A, Masud N, Altulaihi B. Preparedness of primary health care leaders during COVID-19 outbreak, Riyadh, Saudi Arabia: a qualitative study. Risk Manag Healthc Policy. 2021;14:4339–51.
Skagerström J, Fernemark H, Nilsen P, et al. Challenges of primary health care leadership during the COVID-19 pandemic in Sweden: a qualitative study of managers’ experiences. Leadersh Health Serv. 2023;36(3):389–401.
Dale JN, Morken T, Eliassen KE, et al. Preparedness and management during the first phase of the COVID-19 outbreak - a survey among emergency primary care services in Norway. BMC Health Serv Res. 2022;22(1):896.
Karreinen S, Paananen H, Kihlström L, et al. Living through uncertainty: a qualitative study on leadership and resilience in primary healthcare during COVID-19. BMC Health Serv Res. 2023;23(1):233.
ICN. ICN President calls for resilient health systems at UN High Level Meeting on Pandemic Prevention, Preparedness and Response: ICN; 2023 [updated 21.09.23. Available from: https://www.icn.ch/news/icn-president-calls-resilient-health-systems-un-high-level-meeting-pandemic-prevention .
World Health Organization. Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: a brief on the WHO position. Geneva: WHO; 2021. Available from: https://www.who.int/publications/i/item/WHO-UHL-PHC-SP-2021.02 .
Sagan A, Webb E, Rajan D, et al. Health system resilience during the pandemic: it’s mostly about governance. Eurohealth. 2021;27(1):10–5.
Wiig S, Lyng HB, Greenfield D, Braithwaite J. Care in the future—reconciling health system and individual resilience. Int J Qual Health Care. 2023;35(4):mzad082.
Tsandila-Kalakou F, Wiig S, Aase K. Factors contributing to healthcare professionals’ adaptive capacity with hospital standardization: a scoping review. BMC Health Serv Res. 2023;23(1):799.
Fagerdal B, Lyng HB, Guise V, et al. Exploring the role of leaders in enabling adaptive capacity in hospital teams - a multiple case study. BMC Health Serv Res. 2022;22(1):908.
Gröschke D, Hofmann E, Müller ND, Wolf J. Individual and organizational resilience—Insights from healthcare providers in Germany during the COVID-19 pandemic. Front Psychol. 2022;13:965380.
Marshall F, Gordon A, Gladman JRF, Bishop S. Care homes, their communities, and resilience in the face of the COVID-19 pandemic: interim findings from a qualitative study. BMC Geriatr. 2021;21(1):102.
Sihvola S, Kvist T, Nurmeksela A. Nurse leaders’ resilience and their role in supporting nurses’ resilience during the COVID-19 pandemic: a scoping review. J Nurs Manag. 2022;30(6):1869–80.
Haver A, Akerjordet K, Furunes T. Wise emotion regulation and the power of resilience in experienced hospitality leaders. Scand J Hosp Tour. 2014;14(2):152–69.
Kumari K, Ali SB, Batool M, et al. The interplay between leaders’ personality traits and mentoring quality and their impact on mentees’ job satisfaction and job performance. Front Psychol. 2022;13:937470.
Doshi D. Improving leadership of health services in rural areas: exploring traits and characteristics. Int J Healthcare Manag. 2020;13(sup1):183–91.
McKinley N, Karayiannis PN, Convie L, et al. Resilience in medical doctors: a systematic review. Postgrad Med J. 2019;95(1121):140–7.
Cleary M, Kornhaber R, Thapa DK, et al. The effectiveness of interventions to improve resilience among health professionals: a systematic review. Nurse Educ Today. 2018;71:247–63.
Huey CWT, Palaganas JC. What are the factors affecting resilience in health professionals? A synthesis of systematic reviews. Med Teach. 2020;42(5):550–60.
Joyce S, Shand F, Tighe J, et al. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. 2018;8(6):e017858.
Khalili H, Lising D, Kolcu G, et al. Advancing health care resilience through a systems-based collaborative approach: Lessons learned from COVID-19. J Interprof Care. 2021;35(6):809–12.
Kaul V, Shah VH, El-Serag H. Leadership during crisis: lessons and applications from the COVID-19 pandemic. Gastroenterology. 2020;159(3):809–12.
Beunen R, Patterson J, Van Assche K. Governing for resilience: the role of institutional work. Curr Opinion Environ Sustainability. 2017;28:10–6.
van de Bovenkamp H, van Pijkeren N, Ree E, et al. Creativity at the margins: a cross-country case study on how Dutch and Norwegian peripheries address challenges to quality work in care for older persons. Health Policy. 2022;127:66–73.
Gray D, Jones K. The resilience and wellbeing of public sector leaders. Int J Pub Leadership. 2018;14(3):138–54.
Bish M, Kenny A, Nay R. A scoping review identifying contemporary issues in rural nursing leadership. J Nurs Scholarsh. 2012;44(4):411–7.
Sagan A, Webb E, Azzopardi-Muscat N, et al. Health systems resilience during COVID-19. Lessons for building back better. Health policy series. 2021; 56:[1–136 pp.]. Available from: https://eurohealthobservatory.who.int/publications/i/health-systems-resilience-during-covid-19-lessons-for-building-back-better .
Grote G. Leadership in Resilient Organizations. In: Wiig S, Fahlbruch B, editors. Exploring Resilience : a scientific journey from practice to theory. 1. Springer Open: Cham; 2019. p. 59–67.
Poon YSR, Lin YP, Griffiths P, et al. A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: a systematic review with future directions. Human Resources Health. 2022;20(1):70.
NOU: 2022: no 10. Inntektssystemet for kommunene (English title: The revenue system for the municipalities). Oslo: Ministry of Local Government and Rural Affairs
Matheson C, Robertson HD, Elliott AM, et al. Resilience of primary healthcare professionals working in challenging environments: a focus group study. Br J Gen Pract. 2016;66(648):e507–15.
Boin A, Kuipers S, Overdijk W. Leadership in times of crisis: a framework for assessment. Int Rev Pub Administration. 2013;18(1):79–91.
Baker EL, Irwin R, Matthews G. Thoughts on adaptive leadership in a challenging time. J Public Health Manag Pract. 2020;26(4):378–9.
Ali BJ, Anwar G. Administrative crisis: the role of effective leadership styles in crisis management international journal of advanced engineering. Manag Sci. 2021;7(6):31–41.
Tvedt IM, Tommelein ID, Klakegg OJ, Wong J-M. Organizational values in support of leadership styles fostering organizational resilience: a process perspective. Int J Manag Proj Bus. 2023;16(2):258–78.
Grote G. Leadership in Resilient Organizations. In: Wiig S, Fahlbruch B, editors. Exploring Resilience: A Scientific Journey from Practice to Theory. Cham: Springer International Publishing; 2019. p. 59–69.
Jasper L. Building an adaptive leadership style. Strategic Finance. 2018;99(9):54–61.
Boyle TJ, Mervyn K. The making and sustaining of leaders in health care. J Health Organ Manag. 2019;33(2):241–62.
Download references
Acknowledgements
The authors would like to thank participating leaders for their contribution to the study. We would also like to acknowledge Ole-Jørn Borum for graphical design on fig. 1 .
Open access funding provided by University of Stavanger & Stavanger University Hospital The publication processing charge was covered by the University of Stavanger.
Author information
Authors and affiliations.
SHARE – Center for Resilience in Healthcare, Faculty of Health Sciences, University of Stavanger, Stavanger, Norway
Malin Knutsen Glette & Siri Wiig
Department of Health and Caring Sciences, Western Norway University of Applied Sciences, Haugesund, Norway
Malin Knutsen Glette & Tone Kringeland
Division of General Internal Medicine and Primary Care, Department of Medicine, Brigham & Women’s Hospital, Harvard Medical School, Boston, MA, USA
Lipika Samal & David W. Bates
Department of Health Policy and Management, Harvard T. H. Chan School of Public Health, Boston, MA, USA
You can also search for this author in PubMed Google Scholar
Contributions
MKG, SW, TK, and DWB was involved in discussions regarding the project’s development. MKG conducted interviews and led the analysis of the transcribed data. The manuscript was a collaborative effort between MKG, SW, TK, DWB and LS, where all authors provided feedback. The author team approved the manuscript before submission.
Corresponding author
Correspondence to Malin Knutsen Glette .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Norwegian Agency for Shared Services in Education and Research (SIKT) in 2022 and provides the ethical approval, information security and privacy services as a part of the HK-dir (Norwegian Directorate for Higher Education and Skills). An informed consent form was signed by all leaders prior to the interviews, and information about the aim of the study and their right to redraw was repeated immediately before the interviews started.
Consent for publication
Not applicable.
Competing interests
Dr. Bates reports grants and personal fees from EarlySense, personal fees from CDI Negev, equity from ValeraHealth, equity from Clew, equity from MDClone, personal fees and equity from AESOP, personal fees and equity from Feelbet-ter, equity from Guided Clinical Solutions, and grants from IBM Watson Health, outside the submitted work. Dr. Bates has a patent pending (PHC-028564 US PCT), on intraoperative clinical decision support. The other authors report no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Glette, M.K., Kringeland, T., Samal, L. et al. A qualitative study of leaders’ experiences of handling challenges and changes induced by the COVID-19 pandemic in rural nursing homes and homecare services. BMC Health Serv Res 24 , 442 (2024). https://doi.org/10.1186/s12913-024-10935-y
Download citation
Received : 22 January 2024
Accepted : 31 March 2024
Published : 09 April 2024
DOI : https://doi.org/10.1186/s12913-024-10935-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing home
- Resilience in healthcare
- Patient safety
- Quality of care
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,891,102 articles, preprints and more)
- Free full text
Epidemiology, Sociology, and the Social Sciences: Evaluating the Philippine Government’s Scientific Response to COVID-19
Author information, orcids linked to this article.
- Ballano V | 0000-0002-2013-6429
Preprint from SSRN , 08 Oct 2021 https://doi.org/10.2139/ssrn.3933290 PPR: PPR406335
Preprint Free full text in Europe PMC
Abstract
Free full text .
PPRID: PPR406335 EMSID: EMS136476 SSRN preprint, version 1, posted 2021 October 11 https://doi.org/10.2139/ssrn.3933290
Affiliations
- 1. Faculty Researcher, Research Institute for Human and Social Development (RISHD), Associate Professor V, Department of Sociology, Polytechnic University of the Philippines, Philippines
Copyright and license information
Copyright notice
This article examines the inadequacy of the Philippine government’s scientific response against the COVID19 pandemic, given the societal dimension of the virus. Applying sociological imagination and insights, specifically from Actor-Network Theory, and drawing from some secondary sources and previous research studies on COVID-19 pandemic, it argues that the Philippine government’s epidemiological approach is insufficient without the contribution of the holistic and qualitative approaches of sociology and the social sciences to fully understand and respond to the current crisis. COVID-19 pandemic is both a medical and social problem, thus, needing some sociological research and perspectives. It recommends that the Philippine government must include not only epidemiologists and health experts in its national response team, but also sociologists and social scientists in order to effectively address the social and cultural dimensions of the problem.
Keywords: COVID-19 Pandemic, Philippine Government, Sociology, Epidemiology, Social Sciences, Qualitative Research, Quantitative Research
Introduction
Undoubtedly, the greatest scourge that hit the world and the Philippines in recent times is the COVID-19 pandemic. The veteran pandemic researchers Reinhart (2020) and Rogoff (2009), who have analyzed similarities of various crises before COVID-19, have acknowledged that this current pandemic is truly different from past crises with respect to cause, scope, and severity. Compared to previous post-war pandemics, COVID-19 is already eight to nine times larger than the number of SARS cases ( Baldwin and Di Mauro 2020 ). Pisano, Sadun, and Zanini (2020) also noted that COVID-19 is not only similar with previous pandemics, but also quite unique in scope and effects to society: It overwhelms bureaucratic decisions and calls for a timely and scientific response in public administration. As of September 9, 2021, COVID-19 has already infected 223,733,507 people and killed 4,614,389 worldwide ( Wordometers 2021a ).
In the Philippines, COVID-19 the infection rate is one of the highest in the world with 2, 161,892 Filipinos infected to date and also one of the highest in Southeast Asia ( Wordometers 2021b ), with patients overcrowding hospitals and overwhelming the country’s fragile health care system. The pandemic has also contracted the local economy to a record-breaking 16.5 percent in the second quarter of 2020, throwing the country into a technical recession and brought social and economic hardships to a nation with a 16.7 percent poverty incidence ( Venson 2020 ). Despite longer and stricter community quarantines compared with its Asian neighbors and the government’s promise of “flattening the curve,” the Philippines is still struggling to control its surging COVID-19 infection. Turrini, Cristofoli, and Valotti claim that “while governments around the world struggle to combat the rapid escalation of the coronavirus disease 2019 (COVID-19) pandemic, scholars and practitioners are questioning what works and what does not” against the virus (2020, 1).
The Philippine government, however, seems convinced of what works against the current pandemic. As repeatedly expressed by its presidential spokesperson, Secretary Harry Roque ( Presidential Communications Operations Office 2020 ), the best strategy is said to be the science-based approach. He often assures the public that the government’s response to the COVID-19 pandemic will always be guided by sound science, implying that the government will utilize science’s traditional role of describing, explaining, and predicting phenomena, as well as enhancing public awareness and legitimizing governance capacity during crises ( Christensen, Lægreid, and Rykkja 2016 ). What is not clear, however, is the appropriateness and effectiveness of this science-based approach promised by the Philippine government against the current pandemic.
The global research on COVID-19 has focused on the medical and epidemiological aspects of the virus with little regard to their sociological significance. In particular, the Philippine government's response to the pandemic has been medicalized, reflecting the popular epidemiological approach of health experts and medical doctors worldwide. The aim of this article is to broadly evaluate the adequacy and limitations of the Philippine government’s scientific approach against the COVID-19 pandemic, given the highly social nature of the virus. It also explores the potential contribution of the sociological and social science approaches to the government’s ongoing pandemic response. It is structured into three main parts. The first part traces the role of the World Health Organization (WHO) and the country’s Department of Health (DOH) in shaping the Philippine government’s scientific response that adopts the epidemiological approach. The second part identifies the two major limitations of the government’s epidemiological model in dealing with the pandemic. The third part examines the social dimension of COVID-19 disease, explaining how the virus can form a complex network of humans and non-humans once it infects people. The last part explores the contribution of the sociological and social science approach in enhancing the Philippine government’s response against COVID-19.
Most scientific studies and commentaries on COVID-19, which are written by local epidemiologists, mathematicians, and health experts in the country, often deal with the pandemic’s medical and epidemiological aspects, but rarely on its social and sociological dimensions. This reflects Raewyn Connell’s observation that the discussion on COVID-19 is only limited among sociologists which does not directly affect public policy (2020). This article, therefore, aims to fill this gap and intends to incorporate sociological perspectives and methodologies in the current epidemiological strategies of the Philippine government in dealing with the current pandemic.
Conducting a systematic review of some scientific literature on COVID-19 and utilizing theoretical frameworks such as the sociological imagination and Actor-Network Theory (ANT), this article will analyze the government's overall response to the pandemic using the sociological lens. Overall, it argues that the Philippine government’s epidemiological approach needs the holistic and qualitative approaches of sociology and the social sciences in order to enhance the current response against the pandemic. COVID-19 is a highly social virus that thrives on people’s interactions, social networks, and global flows, thus needing the expertise of sociologists and social scientists. Once the virus infects people, it forms a complex social and material network that paralyzes people, public administration, and society. Philippine Government’s Epidemiological Approach to COVID-19 The existing network and cooperation between the WHO and the country’s DOH have made it easy for the Philippine government to adopt the epidemiological approach to contain the COVID-19 pandemic. At the beginning of the disease, the WHO helped the Philippines in enhancing its epidemiological strategy to defeat the virus. It closely working and coordinating with the DOH and other national stakeholders and partners to increase the country’s preparedness against COVID-19 in case of wider community transmission (WHO 2020). With this alliance, it is, therefore, apparent that the WHO-DOH's epidemiological approach has already determined the Philippines' overall strategy against the COVID-19 pandemic.
When the WHO defined COVID-19 as a disease and later as a pandemic on March 11, 2020 ( Zhou et al. 2020 ), the Philippines government had already utilized the fields of medical science and public health to control and eradicate the virus. Since COVID-19 is a disease, it primarily employed the expertise of medical doctors or health experts who are trained in the science of epidemiology, defined by McNeil as “the branch of Medicine concerned with understanding the factors that cause, prevent, and reduce diseases by studying associations between disease outcomes and their suspected determinants in human populations” (1996, 2).
As a branch of medicine, epidemiology is a natural science that enables medical doctors and disease experts to practice their profession. As part of medical science, it “rests on a human-biological (scientific) background” ( Zielhuis and Kiemeney 2001 , 43). Epidemiologists study biomedicine, the primary medical course for physicians ( Zielhuis and Kiemeney 2001 ). Although there is an emerging branch of epidemiology called social epidemiology that tries to incorporate the social sciences into the discipline, its legitimacy, however, is questioned by the mainstream clinical epidemiology which considers its approach as inopportune, unscientific, ideological, or too overreaching ( Kaplan 2004 ; Zielhuis and Kiemeney 2001 ). Clinical epidemiology remains the mainstream discipline that trains medical doctors and influences public health experts in dealing with diseases and pandemics in society ( Wemrell 2016 ).
Adopting the epidemiological strategy fundamentally implies listening to the advice of health experts and virologists rather than that of sociologists and social scientists. It also implies using the highly quantitative research method of epidemiology. Moreover, it necessitates the application of “two macroscopic strategies of action against the spread of the virus, namely, suppression (i.e. lockdown of whole cities like in Wuhan) and “flattening the curve” (by social distancing and contact tracing)” ( Jarynowski et al. 2020 , 10), as well as observing social distancing measures such as wearing face masks and face shields, social isolation, fourteen-day quarantine, lock-down, suspension of mass gatherings and public transport, and closure of some businesses.
Given the strong alliance between the WHO and the DOH, health experts and medical doctors can be considered hegemonic or very influential in disease control and pandemics in the Philippines. With the weak influence of sociology and the social sciences in the country’s policy making, it is not difficult to see why the Philippine government adopted the epidemiological approach, especially with the appointment of Dr. Francisco Duque III, a medical doctor and the DOH secretary, as the overall head of the country’s COVID-19 response team, the Inter-Agency Task Force on emerging Infectious Disease (IATF-EID). As the head of the IATF-EID, the health secretary has the power to call upon law enforcement agencies to assist in the implementation of quarantine and other measures to address the spread of disease. “The IATF-EID through Resolution No. 16 created a technical working group (TWG) consisting of representatives from the government departments and the Armed Forces of the Philippines” (Vallejo and Ong 2020, 2). This group, however, consists primarily of health experts and top bureaucrats and rather than social scientists.
When COVID-19 hit the Philippines in the early part of 2020, the Philippine government led by the President has already judged it a medical issue, thus relying heavily on the DOH’s biomedical and epidemiological prescriptions on how to deal with the pandemic. Sociology and other social sciences, which could offer a more holistic understanding of the social dimension of COVID-19, have been sidelined in the government’s scientific approach. The discussion in sociology on the current crisis is mainly among sociologists, “as sociology has not yet been much noticed in the public policy debates about COVID-19” compared to other disciplines, such as economics (Connell 2020, 1).
Major Limitations of the Epidemiological Approach
Lack of qualitative research strategy.
The highly quantitative discipline of epidemiology, as espoused by the DOH, primarily deals with medical knowledge itself ( Zielhuis and Kiemeney 2001 ). Epidemiology does not always recognize the contributions of the social sciences to the health sciences as such. Clinical epidemiologists assume that their discipline includes all relevant scientific methods, and that social science is largely based on qualitative research ( Wensing 2008 ). The adoption of the Philippine government of the epidemiological approach can have two major limitations in its fight against the COVID-19 pandemic.
The first limitation is the choice of research method in understanding the COVID-19 problem. Epidemiology as a discipline of medical science is known to use the statistical and numeral approach in handling and processing data: “Epidemiologists use vital statistics—that is, mortality and morbidity data-extensively” ( Lilienfeld 1980 , 483). What epidemiology shares with the social sciences is the use of quantitative and statistical method in handling data ( Zielhuis and Kiemeney 2001 ). Clinical epidemiologists have long resisted any attempts to mix their discipline with social dimensions ( Kaplan 2004 ). Thus, an emerging discipline called social epidemiology has challenged clinical epidemiology to include relevant methods from other sciences ( Wensing 2008 ).
The two cornerstones of epidemiological research are the observational and experimental studies that both rely on the statistical method ( McNeil 1996 ). Quantitative research techniques such as case-doubling rate, flattening the curve, and the like are prominently reported by the DOH in its regular press briefings in the mass media. Even some independent groups from the academe, such as the OCTA Research Team, which regularly publishes research papers and forecasts on the COVID-19, also uses the quantitative research techniques to understand the trend of infection (e.g., David et al. 2020 ). The qualitative research method, which is often used in the social sciences, particularly in sociology and anthropology, is apparently missing in the IATF and DOH’s research agenda against COVID-19 in order to analyze the progress and effectiveness of the country’s scientific approach.
Qualitative research…refers to the meanings, concepts, definitions, characteristics, metaphors, symbols, and descriptions of things. In contrast, quantitative research refers to counts and measures of things, the extent and distributions of our subject matter: how large a thing is, how many of them there are, or how likely we are to encounter one. ( Lune and Berg 2017 , 12)
If one wants to measure the quality of a thing such as the quality of the Philippine COVID-19 response, then qualitative research is appropriate for this objective. If one wants to count and know the extent of cases in COVID-19 infections, deaths, and recoveries, then the quantitative method of epidemiology, which is currently used by the country’s DOH against the virus, can be adequate. However, if one wants to know the effectiveness of the entire process of the government’s COVID-19 response, then a combination of the quantitative methods of epidemiology and qualitative research techniques of sociology and social sciences is desirable and holistic.
The Philippine pandemic response, which relies on the DOH and WHO’s strategies in handling the COVID-19 pandemic, prefers the highly quantitative methods in dealing with the crisis. Although the Philippine government emphasizes science as the guide to address the current pandemic, it is apparent that qualitative research methods of sociology and the social sciences are neglected in its scientific strategy to assist President Rodrigo Duterte and the IATF in crafting and implementing effective measures against COVID-19. Since the beginning of the Enhanced Community Quarantine (ECQ) for the entire Luzon last March 2020, the DOH and IATF have always emphasized the utilization of the statistical and qualitative method in their press briefings to understand the crisis and flatten the curve:
Flattening the curve refers to community isolation measures that keep the daily number of disease cases at a manageable level for medical providers. In epidemiology, the idea of slowing a virus’ spread so that fewer people need to seek treatment at any given time is known as “flattening the curve.” A flatter curve assumes the same number of people ultimately get infected, but over a longer period of time. A slower infection rate means a less stressed health care system, fewer hospital visits on any given day and fewer sick people being turned away. ( Hasab 2020 , 2)
Despite the assurance of the DOH that the flattening of the curve is near, the number of infections in the country continues to surge. As of this writing, the Philippines has already reached 2,161,892 infections with 34,733 deaths and is now joining the group of countries with the highest COVID-19 cases (Worldometers 2021). The DOH’s belief that the curve will flatten without qualitative research that documents and analyzes the entire COVID-19 process is unrealistic. Flattening the curve as a quantitative method is only a theoretical projection and construct on how infections would develop through time. The curve is the projected number of people who will contract COVID-19 in time. However, this is not a hard prediction on how people will get infected but a theoretical number that is used to model the virus’ spread ( Specktor 2020 ).
In fact, the flattening of the curve does not happen on paper using numerical computations, but on the effectiveness and efficiency of the government’s strategies and measures that are applied in concrete social settings, such as case testing, contact tracing, social distancing, and other measures to contain the virus. Thus, the actual reduction or flattening of cases is dependent on the quality of measures and their implementation against COVID-19. This can only be ascertained through qualitative research as a basis for the IATF to improve the process of its pandemic response.
Any social scientist knows that the basic advantage of a qualitative method is its ability to measure the process and to understand interventions outcomes (e.g., Arce 2001 ; Saksvik et al. 2002 ; Abildgaard, Saksvik, and Nielsen 2016 ). Moreover, the DOH’s quantitative assessment of COVID-19 is dependent on the transmission of numerical data and reports of COVID-19 cases by the various hospitals throughout the country. The current daily data collection of COVID-19 cases is not an assurance that the DOH has accurately gathered all the necessary figures to provide the public an accurate picture of the pandemic.
The great challenge of this method of data collection by the DOH is how to deal with unreported and undetected cases, which are not included in the national tally and statistical projection. Without qualitative research, the IATF would not fully understand how and why some infections escape government testing, quarantine, and case reporting protocols. The lack of qualitative assessment on the social and cultural factors that cause non-reporting or underreporting of COVID-19 cases can add more problems to the government’s scientific approach. Finally, knowing why some regions or places have more infections than others also need qualitative studies of the social sciences to understand the social and cultural networks of the place that facilitate surging of cases.
Using both quantitative and qualitative research methods to fully understand COVID-19 can be of great help to the government’s scientific strategy. Combining both methods can result in wider and deeper understanding of the phenomenon under study (cf. Olsen 2004 ) and enhanced triangulation of research data which increases the study’s accuracy and validity (Webb et. al. 1966). What is apparently lacking in the country’s pandemic response is a qualitative research strategy to make the IATF and DOH’s COVID-19 response more holistic and scientific.
Prioritizing the Medical over the Social and Cultural
Another limitation of the Philippine government’s epidemiological approach is the focusing on the medical aspect of COVID-19 at the expense of understanding of its societal dimension. Epidemiology, as a branch of biomedicine, is a natural science that primarily deals with the natural causes of diseases. Cockerhan argues:
The development of modern medicine had emphasized the microbiological and biochemical sciences…had long ignored the behavioral sciences. Modern medicine’s thinking was dominated by the search for drugs as “magic bullets” to be shot into the body to kill or control health disorders. (1981, 232-233)
Sociologists and social scientists generally contend that illnesses have societal roots. Health disorders are “problems of daily living,” and they involve multiple factors of causation which are not necessarily biological in nature ( Cockerham 1981 , 232). Sociologists specifically investigate the relationship between the physical and social dimensions of human life and their effects to illness ( Freund 1982 ; Freund and McGuire 1991 ; Lawler 1991). They oppose biological theories that explain differences in human behavior based on innate biological characteristics. They assert that the basis of understanding behavior is the social processes in culture and environment ( Cockerham 1981 ).
Following the popular epidemiological approach of many governments, such as the Philippines, against COVID-19 implies the adoption of a radical asociality, epitomized by lockdown and immobilization, whether enforced or voluntary ( Long 2020 ). But this runs counter to the real behavior of people as social beings who are always forming networks with people and material things in society. In COVID-19, infections do not only occur between people but also between people and material things. Some studies have indicated that infection can happen through human-to-human transmission via respiratory droplets, or human to infected surfaces (e.g., Shereen et al., 2020 ). Thus, a holistic understanding on how to deal with the virus requires knowing both its material and social nature. But the epidemiological approach primarily deals only with the natural dimension of the pandemic and ignores its social aspect. In medical sociology, one cannot really separate the natural from the social. This is also asserted by a recent sociological theory called the Actor-Network Theory (ANT): people cannot really separate the link between material or natural things from human beings in societies ( Latour 1996 , 1999 ).
Actor-Network Theory and the Social Nature of the COVID-19 Virus
The Actor-Network Theory, which is developed by the French sociologists of science Bruno Latour and Michel Callon, is one of the contemporary sociological theories that tries to reconcile the dualism between society and technology. “ANT which originated in poststructuralist French debates around the sociology of science and technology, offers insights into how things occur and, in particular, the nature of agency” (Mabrook and Singer 2019, 4). It is a recent theory in the history and sociology of science that aims to describe a society of human and non-humans as equal actors tied together into networks to achieve a particular goal.
ANT simply acknowledges the indispensable cooperation between non-humans or between material things and humans in agency. Human being cannot perform social actions without the cooperation and use of material things. Indeed, ANT is perhaps best known for its eradication of theoretical distinctions between humans and non-humans, as well as between far/near, inside/outside, and large/small components of a given phenomenon ( Latour 1996 ). ANT views all relevant components as actors, each exercising a level of agency and each holding comparable power ( Latour 2005 ). Whether or not they possess behavioral intentionality, all actors can promote, permit, or restrict results (Mabrook and Singer 2016). Using some elements of ANT, this study emphasizes “the essence of semiotic networks, stressing the agency of the biological viral factor affecting the behavior of people (actors)” ( Jarynowski et al. 2020 , 12).
In the case of COVID-19, the non-human virus forms a network with humans. When COVID-19 infects people, it forms a complex alliance with humans and other material things and infects the entire social order, affecting the economic, social, political, and cultural dimensions of life. Infected places, things, and surfaces can transmit the virus once touched by people. COVID-19 pandemic is an intricate system of material and human elements. Thus, it cannot easily be controlled using a purely epidemiological method without the involvement of sociology and the social sciences to handle the social aspects of the pandemic. Coronavirus disrupts society’s economy, business, worship, work, and social interaction.
COVID-19 affects public and social lives of people: family, jobs, participation in schools, churches, online networks, and their whole range of human activities and interactions in both spatiotemporal space and cyberspace. Thus, to contain it requires a networked and multidisciplinary approach that includes both natural and social sciences. Sociologists who apply the sociological imagination or holistic approach in their research endeavors are in the best position to lead in this effort to integrate the natural and the social to control the COVID-19 pandemic.
Furthermore, COVID-19 thrives on the growing integration of the current globalizing process to infect the world. Gössling, Scott, and Hall argues,
The main reasons for the increasing pandemic threat in the 21st century are: a rapidly growing and mobile world population; urbanization trends and the concentration of people; industrialized food production in global value chains; increased consumption of higher-order foods including meat; and, the development of global transport networks acting as vectors in the spread of pathogens. (2020, 3)
One of the major misconceptions of the COVID-19 pandemic is the popular view that this disease only needs a medical or epidemiological intervention to stop it from spreading. Medical researchers often overlook in the dynamics of the spread of infectious diseases such as COVID19 is the reality that viruses are also affected by social behavior ( Squazzoni et al. 2020 ). COVID-19 is more than just a disease and medical problem ( Ding et al. 2020 ); it is also a social problem that affects people's networks and economic lives. As De Silva (2020) contends, COVID-19 does not only affect human health. It also affects the economic health of countries: Its human cost is rapidly being matched by huge economic costs. To date, COVID-19 has already affected almost 200 countries (and still counting) globally and disturbed the entire human society, creating not just a “massive, global health crisis, but also a reconfiguration of the established forms of social life” ( Jarynowski et al, 2020 , 8).
The lack of dialogue between epidemiologists and social scientists, especially on how to deal with the COVID-19 pandemic, results in the unintended consequence of neglecting the social dimension of the disease ( Rangel et al. 2020 ). By adopting a predominantly epidemiological approach toward the pandemic, the Philippine government has overlooked the social and cultural aspects of the disease. The Philippines has a highly collectivist and personalistic culture; thus, it may become a breeding ground for the contagious virus. Van Bavel et al. argues, “while medical policies are different across societies, some differences in the response to the pandemic may be better described as cultural” (2020, 463). For instance, the priority given to obligations and duties in Asian societies to their communities may motivate individuals to remain committed to social norms, while North America and much of Western Europe, which tend to positively value the expressivity of the self, can explain why interpersonal transmission of the virus could be more likely in Western than in Asian cultures ( Van Bavel et al. 2020 ).
Philippine Collectivist Culture and COVID-19
Social ties are very important in the collectivist culture of the Philippines. Filipinos value family and kinship ties. They prioritize and cultivate relational bonds among friends, relatives, and family members ( Chao and Tseng 2002 ; Ho 1993 ; Hofstede 1980 ). This relates to their sense of collectivism and “smooth interpersonal relations” as well as their tendency to subordinate personal interests for the sake of their in-group ( Lynch 1973 ). Disease experts and medical doctors do have the expertise to understand the intricacy of the Filipino’s social and cultural behavior that can anticipate and detect the spread of the COVID-19 virus in cultural and social networks. Thus, the assistance of social scientists is essential.
In COVID-19, the virus can form a biological and social network with humans. Once COVID-19 infects people, it forms an intricate biosocial system that can affect the economic, social, political, and cultural spheres of society. This virus does not only infect people but also foods, food supply chains, surfaces, and environments (Rizou et al. 2020). In this case, the virus is aggressively forming material and social networks ready to infect the entire global network of people and things through travel, tourism, migration, and the growing globalization of the world. COVID-19 disease is an intricate system of material and human network that rides on the current globalization process. Thus, it cannot easily be controlled using only the epidemiological method of the natural or medical sciences, without the contribution of sociology and other branches of the social sciences to handle its social and behavioral aspects. To contain the current COVID-19 pandemic requires a networked and multidisciplinary approach that involves both the medical and the social sciences.
The Contribution of the Sociological and Social Science Approaches
One of major misconceptions on COVID-19 pandemic is the view that it is primarily a disease that calls for a medical or epidemiological intervention. But COVID-19 is more than just a disease. It affects the entire human society, creating not just a “massive, global health crisis, but also a reconfiguration of the established forms of social life” ( Jarynowski et al. 2020 , 8). For sociologists and other social scientists, diseases are not only biological phenomena but also social. Thus, addressing the COVID-19 pandemic implies studying social behavior, networks, and structures, to minimize its negative social impacts. COVID-19 is not just a health issue ( Ding et al. 2020 ). It is also a social and societal issue. Coronavirus is a subtle type of virus. It occurs as a natural phenomenon, but its impact is highly social as it thrives in social networks: the denser is the social network or grouping of people, the more it is highly contagious. Thus, the spread of Covid-19 is fundamentally related to human networks ( Long 2020 ).
COVID-19 is natural in origin but social in effects. For sociologists and other social scientists, who look at diseases and pandemics not only as biological phenomena but also social, addressing the COVID-19 pandemic implies studying social behavior, networks, and structures to minimize its local transmissions and negative social impacts. COVID-19 is more than just a health issue ( Ding et al. 2020 ) but also a societal problem. Complex social interactions have provided the virus remarkable opportunities for population growth, by colonizing multiple bodies and reproducing virally: “Human social contacts are precisely the coronavirus’s means of population growth” ( Ding et al. 2020 , 3).
Conversely, social behavior has consequences to the dynamics of infectious diseases such as COVID-19, but medical researchers have often disregarded the role of behavior in infectious illnesses ( Squazzoni et al. 2020 ). Van Bavel et al. explains that “while efforts to develop pharmaceutical interventions for COVID-19 are under way, the social and behavioral sciences can provide valuable insights for managing the pandemic and its impacts” (2020, 460). To sociologists and social scientists, diseases are primarily social. Viruses can become “social” agents once they are out from their habitat and infect people. As a virus, COVID-19 normally appears as a biological thing, but once it affects people through human networks, it becomes social: the denser is the social network, the deadlier it becomes as a virus. Thus, the spread of COVID-19 is fundamentally related to human networks ( Long 2020 ). Galea and Link (2013) claim that it would be hard to find an epidemiologist today in any leading academic department who would deny that social factors are not in the causal chain of factors that affect health.
Thus, if COVID-19 is a highly social virus, then sociology, which is the scientific study of society, culture, and social behavior, must play an important role in controlling the current virus. Jarynowski et al. contend that “although most aspects of COVID-19 fall into the research area of medical science, social science researchers such as sociologists, have not only data, resources and knowledge, but also a professional and moral responsibility to contribute to broadening our understanding of this phenomenon” (2020, 8–9). Sociology as a social science on human society can help the Philippine government’s IATF to contain the COVID-19 pandemic.
The sociological method, which applies a holistic approach in dealing with society, always aims to see the connections between the micro and macro or the global and local, biography and history. It looks at social patterns rather than the disjoint details of specific cases. Applying C. Wright Mills’s “sociological imagination,” the sociological approach aims to see reality as one interrelated system and study the relationships of social systems and networks in society ( Mills [1959] 2000 ). Karvonen, Kestila, and Maki-Opas argue that “sociological sensitivity provides perspectives for understanding the cultural backgrounds, norms, and behavioral traits, as well as their interlinks with social determinants…highlighting the importance of social structures in leading to ethnic health inequalities” (2018, 2).
In the case of COVID-19, applying the sociological imagination implies understanding the connections between the medical and the social, the biological and societal, as well as the epidemiological and sociological aspects of the virus. With its affinity with demographic patterns and social networks, sociology can guide the government’s response team in contact tracing, mapping infection trends, as well as understanding cultural dynamics and beliefs that contribute to the spread of the virus. Sociology of law, for instance, can enlighten law enforcers on how to implement the COVID-19 measures effectively according to social categories of people. Countries which are successful in controlling the pandemic appears to be holistic and sociological in their approach.
In addition, the sociological imagination can enable the government’s COVID-19 responders to see the connection between the growing integration of people and social networks of the global age and the swift increase of COVID-19 infections around the world. The growing integration of people in the current global age provides a perfect platform for the highly contagious Coronavirus to spread. Connell aptly painted a global picture which is highly conducive for COVID-19:
It is not hard to see how contemporary social patterns have worked in favour of SARSCoV-2 and its replication strategy. More humans are crowded into cities than ever before: the demographers tell us that the world total of urban populations passed the total of rural populations in 2008. Cities include huge informal settlements (Kibera, Khayelitsha, Dharavi, Nezahualcoyotl, Orangi, and many more) where “social distancing” is impossible, let alone the frequent hand washing recommended by the doctors. Air travel has massified: the global airline industry’s annual total of flights, already at 23.8 million in 2004, rose to 38.9 million in 2019 (Mazareanu 2020). (That is just the number of flights: in 2017 the industry carried 4.1 billion passengers on scheduled flights.) The speed of the COVID-19 epidemic has been one of its most disconcerting features. There has been little time for reflection and democratic decision-making. (Connell 2020, 4)
COVID-19 travels with people. Connell aptly argues that “social interaction has provided the virus remarkable opportunities for population growth…Human social contacts are precisely the coronavirus’s means of population growth” (2020, 3). “The integration of the global economy that enables people to travel around in large numbers over long distances at great speeds to meet and interact in closer ranges is providing this virus tremendous opportunities to multiply and infect large numbers of people” (Connell 2020, 2). Globalization as a transplanetary process or set of processes ( Ritzer 2010 ) has given the COVID-19 disease a unique platform which was not enjoyed by previous pandemics. With the “given global flows of goods and people the potential now exists for worldwide disasters” ( Matthewman and Huppatz 2020 , 5). Van Bavel et al. explains that “social networks can amplify the spread of behaviors that are both harmful and beneficial during an epidemic, and these effects may spread through the network to friends, friends’ friends and even friends’ friends’ friends” (2020, 463).
A strong scientific support of sociologists and social scientists to the government’s sciencebased approach could have averted the widespread growth of the virus in the Philippines. In the current age of globalization, tourism and travel are two of the COVID-19’s major drivers. It is already known in the media that because of the Philippines’ renewed ties with China under the Duterte administration, the DOH and the IATF could have anticipated the spread of the virus due to the increased arrivals of Chinese tourists into the country. If they tapped the expertise of sociologists and social scientists on how to address the social aspect of the COVID-19 disease, the community transmission could have been minimized. A sociological mind would be more discriminating in analyzing people’s travel history, social ties, and networks to prevent the spread of the virus.
Despite its great promise to address the current pandemic through its holistic approaches, sociology has not influenced the government’s current response against COVID-19 pandemic. Because of its academic mantle with the limited scope in the Philippine educational system, sociology has not really influenced policy making and public administration in the country. Unlike economics which has been the center in the debates about lockdowns and income support, sociology has not been noticed in the public policy arena against major disasters such as COVID-19 pandemic.
The president of the International Sociological Association (ISA), Sari Hannafi, believes that one urgent task of sociology for today’s pandemic is “to unpack the social origins and to understand the magnitude of the impacts COVID-19 has had, and continues to have, to understand how the upward curve of infection can be flattened” ( Hanafi 2020 , 2). To him, this implies a collaboration of scientists in all fields to fight the pandemic, as well as a sociological call for a cohesive, empirical, and multidisciplinary strategy to fight the virus. This article recommends that the Philippine government must involve sociologists and social scientists in its science-based approach against the current COVID-19 pandemic to help flatten the curve.
Conclusion and Recommendation
This article has shown that the Philippine government’s epidemiological response to the COVID19 disease is inadequate. It needs the assistance of sociology and the social sciences to address the social dimension of the disease. COVID-19 is a highly social disease, forming an inseparable and complex network with other material things and humans once it infects people and social networks. Adopting a purely epidemiological strategy would result in using a highly quantitative research approach against the virus and neglecting the qualitative research of sociology and social sciences that measures process and development of the government’s science-based approach against the pandemic. It also results in neglecting the study of social behavior, structure, and culture, which are essential in understanding the social nature and movement of the virus. COVID-19 disease is not just a medical issue but also a social one. Thus, sociology and its holistic approach is necessary to supplement the epidemiological approach of the government. The current pandemic is unique in scope and characteristics and rides on people’s interaction, social networks, and growing integration of the world due to globalization. For the Philippine government to be true to its promise to pursue a truly science-based approach, it must not only utilize the epidemiological approach of health experts, medical doctors, and epidemiologists but also the qualitative and holistic strategies of sociologists and social scientists, forming a multidisciplinary scientific team that advises the Philippine government on how to comprehensively understand and control the current COVID-19 pandemic.
In this regard, this study recommends that the government should replace the current members of the IATF with a composite team of top natural and social scientists in the country to advice the President on how to address the pandemic. The secretaries of the different departments who are currently members of the IATF must only act as implementers of the new scientific team's directives. Thus, scientific expertise must prevail in the current COVID-19 over administrative expertise to truly achieve the government’s alleged science-based approach against the pandemic. A special budget must be given to members of the new scientific team to enable them to design and commission sociological and social science research, both in qualitative and quantitative methods, to monitor and evaluate the process and progress of the government's response against COVID-19 pandemic.
Author Information
Correspondence: hp.ude.pup@onallabov .
About the Author
Dr. Vivencio O. Ballano: Faculty Researcher, Research Institute for Human and Social Development; and Associate Professor V, Department of Sociology and Anthropology, Polytechnic University of the Philippines), Manila, Philippines.
- Abildgaard Johan S , Saksvik Per O , Nielsen Karina . How to Measure the Intervention Process? An Assessment of Qualitative and Quantitative Approaches to Data Collection in the Process evaluation of Organizational Interventions . Frontiers in Psychology: Organizational Psychology . 2016 ; 22 ( 7 ): 1380 . https://doi.org/10.3389/fpsyg.2016.01380
- Arce Wilfredo . Systematic Qualitative Data Research: An Introduction for Filipino Practitioners . Quezon City: Office of Research and Publications, Ateneo de Manila University . 2001 .
- Baldwin Richard , Di Mauro Weder . How Behavioural Science Data Helps Mitigate the COVID-19 Crisis . Nature Human Behaviour . 2020 ; 4 : 438 . eds. 2020. Economics in the Time of COVID-19. London: CEPR Press. Betsch, Cornelia. 2020 https://doi.org/10.1038/s41562-020-0866-1
- Christensen Tom , Lægreid Per , Rykkja Lise H . Organizing for Crisis Management: Building Governance Capacity and Legitimacy . Public Administration Review . 2016 ; 76 ( 6 ): 887-997 . https://doi.org/10.1111/puar.12558
- Chao Ruth , Tseng Vivian . Parenting of Asians . In: Bornstein Marc H , editor. Handbook of Parenting . Mahwah : NJ: Erlbaum ; 2002 ; 56 ( 4 ). p. 745-751 . Connell, Raewyn. 2020. “COVID-19/Sociology.” Journal of Sociology 56 (4): 745–751. https://doi.org/10.1177/1440783320943262 https://doi.org/10.1177/1440783320943262
- Cockerham William C . Medical Sociology . International Review of Modern Sociology . 1981 ; 11 ( 1–2 ): 231-250 .
- David Guido , Rye Ranjit Singh , Agbulos Maria Patricia , Austriaco FrNicanor . COVID-19 Forecasts in the Philippines: NCR, Cebu and COVID-19 Hotspots as of July 10, 2020 . 2020 .
- De Silva Raymund . COVID-19: Its Impact on the Philippines–Parts I, II, III, and IV of V . Europe Solidaire Sans Frontières . 2020 May 4 .
- Ding Wenzhi , Levine Ross , Lin Chen , Xie Wensie . Corporate Immunity to COVID19 Pandemic, NBER Working Paper No. 27055 . 2020 .
- Freund Peter . The Civilized Body . Philadelphia : Temple University Press ; 1982 .
- Freund Peter , McGuire Meredith B . Health Illness and the Body: A Critical Sociology . NJ: Prentice Hall : Engelwood Cliffs ; 1991 .
- Kaplan George A . What’s Wrong with Social Epidemiology, and How can We Make it Better . Epidemiologic Review . 2004 ; 26 ( 1 ): 124-135 . https://doi.org/10.1093/epirev/mxh010
- Karvonen Sakari , Kestila Laura M , Maki-Opas Tomio E . Who Needs Sociology of Health and Illness? A New Agenda for Responsive and Interdisciplinary Sociology of Health and Medicine . Frontiers in Sociology: Medical Sociology . 2018 ; 4 : 1-5 . https://doi.org/10.3389/fsoc.2018.00004
- Galea Sandro , Link Bruce G . Six Paths for the Future of Social Epidemiology . American Journal of Epidemiology . 2013 ; 178 ( 6 ): 843-849 . https://doi.org/10.1093/aje/kwt148
- Gössling Stefan , Scott Daniel , Hall Michael . Pandemics, Tourism and Global Change: A Rapid Assessment of COVID-19 . Journal of Sustainable Tourism . 2020 ; 29 ( 1 ): 1-20 . https://doi.org/10.1080/09669582.2020.1758708
- Hanafi Sari . Global Sociology and the Coronavirus . ISA Digital Platform . 2020 . [Accessed January 5, 2020]
- Hasab Ali A . Flattening COVID-19 Curve in Egypt: An Epidemiological Modelling . Preprintsorg . 2020 May 20 .
- Ho David Yau-Fai . Relational Orientation in Asian Social Psychology . In: Kim Uichol , Berry John W , editors. Indigenous Psychologies: Research and Experience in Cultural Context . Newbury Park, CA : Sage Publications ; 1993 . p. 240-259 .
- Hofstede Geert . Culture’s Consequences: International Differences in Work-Related Values . Beverly Hills, CA : Sage ; 1980 .
- Jarynowski Andrzej M , Wojta-Kempa Monika , Platek Daniel , Czopek Karolina . Attempt to Understand Public Health-Relevant Social Dimensions of COVID-19 Outbreak in Poland . Society Register . 2020 ; 4 ( 3 ): 7-44 . https://doi.org/10.14746/sr.2020.4.3.01
- Latour Bruno . On Actor-Network Theory: A Few Clarifications . Soziale Welt . 1996 ; 47 ( 4 ): 369-381 .
- Latour Bruno . On Recalling Ant . Sociological Review . 1999 ; 47 ( 1 ): 15-25 . https://doi.org/10.1111/j.1467-954X.1999.tb03480.x
- Latour Bruno . Reassembling the Social: An Introduction to Actor-Network Theory . Behind the Screens: Somology and the Problem of the Body . Lawler, Jocalyn : Oxford: Oxford University Press ; 2005 . 1991, Edinburgh: Churchill Livingstone
- Lilienfeld Abraham M . Advances in Quantitative Methods in Epidemiology . Landmarks of American Epidemiology . 1980 ; 95 ( 5 ): 662-469 .
- Long Nicholas J . From Social Distancing to Social Containment: Reimagining Sociality for the Coronavirus Pandemic . Medicine Anthropology Theory . 2020 ; 7 ( 2 ): 247-260 .
- Lune Howard , Berg Bruce L . Qualitative Research Methods for the Social Sciences . 9. Harlow, England : Pearson ; 2017 .
- Lynch Frank . Social Acceptance Reconsidered . Lynch Frank , De Guzman Alfonso , editors. IPC Papers No.2: Four Readings on Philippine Values. Quezon City : Ateneo de Manila University Press ; 1973 . p. 1-68 .
- Matthewman Steve , Huppatz Kate . A Sociology of COVID-19 . Journal of Sociology . 2020 ; 56 ( 4 ): 675-683 . https://doi.org/10.1177/1440783320939416
- McNeil Donald . Epidemiological Research Methods . New York : John Wiley & Sons ; 1996 .
- Mills C . Wright. (1959) . The Sociological Imagination . Oxford : Oxford University Press ; 2000 .
- Olsen Wendy . Triangulation in Social Research: Qualitative and Quantitative Methods Can Really be Mixed . In: Holborn Martin , editor. Development in Sociology . Omskirk : Causeway Press ; 2004 . p. 1-30 .
- Pisano Gary P , Sadun Raffaella , Zanini Michele . Lessons from Italy’s Response to Coronavirus . Harvard Business Review . 2020 March 27 .
- Presidential Communications Operations Office . Science-Based Response to Fight COVID19--Palace . 2020 June 22 .
- Rangel JCristian , Ranade Sudit , Sutcliffe Penny , Mykhalovskiy Eric , Gastaldo Denise , Eakin Joan . COVID-19 Policy Measures-Advocating for the Inclusion of the Social Determinants of Health in Modelling and Decision Making . Journal of Evaluation in Clinical Practice . 2020 ; 26 ( 4 ): 1078-1080 . https://doi.org/10.1111/jep.13436
- Reinhart Carmen . This Time Truly is Different . Project Syndicate . 2020 March 23 .
- Ritzer George . Globalization: Basic Text . Hoboken, NJ : John Wiley & Sons ; 2010 .
- Rizou Myrto , Galanakis Ioananis M , Aldawould Turki MS , Galanakisa Charis M . Safety of Foods, Food Supply Chain and Environment within the COVID-19 Pandemic . Trends in Food Science & Technology . 2000 ; 102 : 293-299 . https://doi.org/10.1016/j.tifs.2020.06.008
- Rogoff Kenneth , Reihart Carmen . This Time is Different: Eight Centuries of Financial Folly . Princeton, New Jersey : Princeton University Press ; 2009 .
- Saksvik Per Øystein , Nytrø Kjell , Dahl-Jørgensen Carla , Mikkelsen Aslaug . A Process Evaluation of Individual and Organizational Occupational Stress and Health Interventions . Work & Stress . 2002 ; 16 ( 1 ): 37-57 . https://doi.org/10.1080/02678370110118744
- Shereen Muhammad Adnan , Khan Suliman , Kazmi Abeer , Bashir Nadia , Siddique Rabeea . COVID-19 Infection: Origin, Transmission, and Characteristics of Human Coronaviruses . Journal of Advanced Research . 2020 ; 24 : 91-98 . https://doi.org/10.1016/j.jare.2020.03.005
- Specktor Brandon . Coronavirus: What is “Flattening the Curve,’ and Will it Work? Live Science . 2020 March 16 .
- Squazzoni Flaminio J , Polhill Gareth , Edmonds Bruce , Ahrweiler Petra , Antosz Patrycja , Scholz Geeske , Chappin Émile , Borit Melania , Verhagen Harko , Giar-dini Francesca , Gilbert Nigel . Computational Models That Matter During a Global Pandemic Outbreak: A Call to Action . Journal of Artificial Societies and Social Simulation . 2020 ; 23 ( 2 ): 1-44 . https://doi.org/10.18564/jasss.4298
- Turrini Alex D , Cristofoli Daniela , Valloti Giovanni . Sense or Sensibility? Different Approaches to Cope with the COVID-19 Pandemic . American Review of Public Administration . 2020 ; 50 ( 6–7 ): 746-752 . https://doi.org/10.1177/0275074020942427
- Vallejo Benjamin M , Ong Rodrigo Angelo C . Policy Responses and Government Science Advice for the COVID 19 Pandemic in the Philippines: January to April 2020 . Progress in Disaster Science . 2020 ; 7 : 1-7 . https://doi.org/10.1016/j.pdisas.2020.100115
- Van Bavel , Jay J , Baicker Katherine , Boggio Paulo S , Capraro Valerio , Cichocka Aleksandra , Cikara Mina , Crockett Molly J , et al. Using Social and Behavioural Science to Support COVID-19 Pandemic Response . Nature Human Behaviour . 2020 ; 4 : 460-471 . https://doi.org/10.1038/s41562-020-0884-z
- Venson Cliff . Philippines Plunges into Recession as Economy Shrinks 16.5 in Q2 . Nikkei Asian Review . 2020 August 6 .
- Webb Eugene J , Campbell Donald T , Schwartz Richard D , Lee Sechrest . Unobtrusive Measures: Non-Reactive Research in the Social Sciences . Chicago : Rand McNally ; 1966 .
- Wemrell Maria , Merlo Juan , Mulinari Shai , Hornborg Anne-Christine . Contemporary Epidemiology: A Review of Critical Discussions within the Discipline and a Call for Further Dialogue with Social Theory . Sociology Compass . 2016 ; 10 ( 2 ): 153-171 . https://doi.org/10.1111/soc4.12345
- Wensing Michel . Research Methods from Social Science Can Contribute Much to the Health Sciences . Journal of Clinical Epidemiology . 2008 ; 61 ( 6 ): 519-520 . https://doi.org/10.1016/j.jclinepi.2007.12.014
- WHO (World Health Organization) . WHO Supports the Philippine Government in COVID-19 Response . 2020 February 13 .
- Wordometer . Coronavirus Cases . Wordometer . 2021a September 9 . 2021,
- Wordometer . Reported Cases by Country or Territory: Philippines . Wordometer . 2021b September 9 . 2021,
- Zhou Min , Zhang Xinxin , Jieming Qu J . Coronavirus Disease 2019 (COVID-19): A Clinical Update . Frontiers of Medicine . 2020 ; 14 : 126-135 . https://doi.org/10.1007/s11684-020-0767-8
- Zielhuis Gerhard A , Kiemeney Lambertus ALM . Social Epidemiology? No Way . International Journal of Epidemiology . 2001 ; 30 : 43-44 . https://doi.org/10.1093/ije/30.1.43
- Posted October 11, 2021.
Full text links
Read article at publisher's site: https://doi.org/10.2139/ssrn.3933290
Europe PMC is part of the ELIXIR infrastructure

Pipeline Disruption: The Impact of COVID-19 on the Next Generation of Teachers
- Aubrey Scheopner Torres Saint Anselm College
- Lisa D'Souza Assumption University
This qualitative study aims to provide insight into why teacher candidates, interested in pursuing K-12 teaching, made the decision to leave their traditional teacher preparation programs during the COVID-19 pandemic. The researchers utilized sociocultural theory as the framework to ground the research. The study finds the educational disruption caused by the pandemic added a layer of complexity to candidates’ experiences, including missed opportunities, limited clinical experience, and a general sense of uncertainty, which altered teacher candidates’ outlook on the teaching profession, impacted their education journeys, and ultimately shifted their immediate career trajectories. The results from this study indicate that clinical experiences are an important predictor of whether teacher candidates remain in their preparation programs. With this research study, we hope to support the development of a more robust teacher pipeline.
Author Biographies
Aubrey scheopner torres, saint anselm college.
Department of Education, Associate Professor
Lisa D'Souza, Assumption University
Department of Education, Professor
Active Minds. (2020). Covid-19 impact on college student mental health.
https://www.activeminds.org/studentsurvey/
Ahmad, F. Z., & Boser, U. (2014). America’s leaky pipeline for teachers of color: Getting
more teachers of color into the classroom. Center for American Progress. https://files.eric.ed.gov/fulltext/ED561065.pdf
American Association of Colleges for Teacher Education. (2020, May). AACTE state
policy tracking map: State actions to support EPPs and teacher candidates. https://aacte.org/state-actions-covid19/
Beck, J. S., Lunsmann, C., & Garza, T. (2020). “We need to be in the classroom more”:
Veteran teachers’ views on teacher preparation and retention. The Professional Educator, 43(1), 91-99. https://digitalcommons.odu.edu/teachinglearning_fac_pubs/142
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and
design. Harvard University Press.
Carver-Thomas, D., & Darling-Hammond, L. (2019). The trouble with teacher turnover:
How teacher attrition affects students and schools. Education Policy Analysis Archives, 27(36). http://dx.doi.org/10.14507/epaa.27.3699
Charmaz, K. (2000). Grounded theory: Objectivist and constructivist methods. In N. K.
Denzin & Y. S. Lincoln (Eds.), Handbook of qualitative research (2nd ed., pp. 509-535). Sage Publications.
Coffey, A., & Atkinson, P. (1996). Making sense of qualitative data: Complementary
research strategies. Sage Publications.
Dabrowski, A. (2021). Teacher wellbeing during a pandemic: Surviving or thriving?
Social Education Research, 2(1), 35-40. https://doi.org/10.37256/ser.212021588
Darling-Hammond, L. (2000). Solving the dilemmas of teacher supply, demand, and
standards: How we can ensure a competent, caring, and qualified teacher for every child. National Commission on Teaching and America’s Future. http://nctaf.org/wpcontent/uploads/2012/01/supply-demand-standards.pdf
Diliberti, M., & Kaufman, J. H. (2020). Will this school year be another casualty of the
pandemic?: Key findings from the American Educator Panels Fall 2020 COVID-19 surveys. Rand Corporation.
Eisenhart, M. (2001). Changing conceptions of culture and ethnographic methodology:
Recent thematic shifts and their implications for research on teaching. In V. Richardson (Ed.), Handbook of research on teaching (pp. 209-225). American Educational Research Association.
Glaser, B. G., & Strauss, A. L. (1967). The discovery of grounded theory: Strategies for
qualitative research. Aldine.
Goetz, J., & LeCompte, M. (1984). Ethnography and qualitative design in educational
research. Academic Press.
Heggeness, M. L., & Fields, J. M. (2020). Working moms bear brunt of home schooling
while working during Covid-19. U.S. Census Bureau. https://www.census.gov/library/stories/2020/08/parents-juggle-work-and-child-care-during-pandemic.html
Hill-Jackson, V., Ladson-Billings, G., & Craig, C. J. (2022). Teacher education and
“climate change”: In navigating multiple pandemics, is the field forever altered? Journal of Teacher Education, 73(1), 5-7. https://doi.org/10.1177/00224871211060138
Ingersoll, R. M., Merrill, L., & May, H. (2014). What are the effects of teacher education
and preparation on beginning teacher attrition. Consortium for Policy Research in Education.
Ingersoll, R., Merrill, E., Stuckey, D., & Collins, G. (2018). Seven trends: The
transformation of the teaching force – Updated October 2018 (#RR2018-2). Consortium for Policy Research in Education.
Irwin, V., Zhang, J., Wang, X., Hein, S., Wang, K. Robers, A., York, C., Barmer, A.,
Mann, F. B., Eilig, R., & Parker, S. (2021). Report on the condition of education 2021 (NCES 2021-144). U.S. Department of Education Institute of Education Sciences. https://nces.ed.gov/pubs2021/2021144.pdf
Kidd, W., & Murray, J. (2020). The Covid-19 pandemic and its effects on teacher
education in England: How teacher educators moved practicum learning online. European Journal of Teacher Education, 43(4), 542-558. https://doi.org/10/1080/02619768.2020.1820480
Kuhfeld, M., Soland, J., Tarasawa, B., Johnson, A., Ruzek, E., & Liu, J. (2020).
Projecting the potential impacts of COVID-19 school closures on academic achievement. Educational Researcher, 49(8), 549-565. https://doi.og/10.3102/0013189X20965918
Lortie, D. C. (1975). School-teacher: A sociological study. University of Chicago Press.
Massachusetts Educator Licensure and Preparation Program Approval Regulations (603
CMR 7.04(2) & 7.04(4)). https://www.doe.mass.edu/lawsregs/603cmr7.html?section=all
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis: An expanded
sourcebook (2nd ed.). Sage Publications.
Miles, M. B., Huberman, A. M., & Saldaña, J. (2014). Qualitative data analysis: A
methods sourcebook (3rd ed.). Sage Publications.
Natanson, H., & Balingit, M. (2022, June 16). Caught in the culture wars, teachers are
being forced from their jobs. Washington Post. https://www.washingtonpost.com/education/2022/06/16/teacher-resignations-firings-culture-wars/
New Hampshire Chapter ED 600 Approval of Professional Preparation Programs (ED
02 & ED 604.04). http://www.gencourt.state.nh.us/rules/state_agencies/ed600.html
Patton, M. Q. (2002). Qualitative evaluation and research methods (3rd ed.). Sage Publications.
Partelow, L. (2019). What to make of declining enrollment in teacher preparation
programs. Center for Education Progress.
Podolsky, A., Kini, T., Darling-Hammond, L., & Bishop, J. (2019). Strategies for
attracting and retaining educators: What does the evidence say? Education Policy Analysis Archives, 27(38). https://doi.org/10.14507/epaa/27/3722
Pressley, T. (2021). Factors contributing to teacher burnout during COVID-19.
Educational Researcher, 50(5), 325-327. https://doi.org/10.3102/0013189X211004138
Rondelft, M. (2021). Links among teacher preparation, retention, and teaching effectiveness.
National Academy of Education Committee on Evaluating and Improving Teacher Preparation Programs. https://naeducation.org/evaluating-and-improving-teacher-preparation-programs-commissioned-paper-series/
Rosenberg, D., & Anderson, T. (2021). Teacher turnover before, during, and after
COVID. Education Resource Strategies. https://files.eric.ed.gov/fulltext/ED614496.pdf
Sarason, S. B. (1971). The culture of school and the problem of change. Allyn and Bacon.
Sinclair, C., Dowson, M., & McInerney, D. M. (2006). Motivations to teach: Psychometric
perspectives across the first semester of teacher education. Teachers College Record, 108(6), 1132-1154. https://doi.org/10.1111/j.1467-9620.2006.00688.x
Stake, R. E. (2000). Case studies. In N. K. Denzin & Y. S. Lincoln (Eds.), Handbook of
qualitative research (2nd ed., pp. 435-454). Sage Publications.
Struyven, K., & Vanthournout, G. (2014). Teachers’ exit decisions: An investigation into
the reasons why newly qualified teachers fail to enter the teaching profession or why those who do enter do not continue teaching. Teaching and Teacher Education, 43, 37-45. https://doi.org/10.1016/j.tate.2014.06.002
Sutcher, L., Darling-Hammond, L., & Carver-Thomas, D. (2019). Understanding teacher
shortages: An analysis of teacher supply and demand in the United States. Education Policy Analysis Archives, 27(35). https://doi.org/10/14507/epaa.27.3696
U.S. Department of Education. (2021). Education in a pandemic: The disparate
impacts of COVID-19 on America’s students. Office for Civil Rights. https://www2.ed.gov/about/offices/list/ocr/docs/20210608-impacts-of-covid19.pdf
U.S. Department of Education. (2022a). Preparing and credentialing the nation’s
teachers: The secretary’s report on the teachers workforce. Office of Postsecondary Education. https://title2.ed.gov/Public/Title_II_Secretary's_Report_508.pdf
U.S. Department of Education. (2022b). Teacher shortage areas 2021-2022 school year.
Office of Postsecondary Education. https://tsa.ed.gov/#/home/
VanLone, J., Pansé-Barone, C., & Long, K. (2022). Teacher preparation and the COVID_19
disruption: Understanding the impact and implications for novice teachers. International Journal of Educational Research Open, 3. http://doi.org/10.1016/j.ijedro.2021.100120
Walker, N. T., & Ardell, A. (2020). Reconsidering preservice-mentor relationships in complex
times: New possibilities for collaboration and contribution. Issues in Teacher Education, 29(1-2), 132-141.
Watt, H. M. G., Richardson, P. W., Klusmann, T., Kunter, M., Beyer, B., Trautwein, U., &
Baumert, J. (2012). Motivations for choosing teaching as a career: An international comparison using the FIT-Choice scale. Teaching and Teacher Education, 28, 791-805. https://doi.org/10/1016/j.tate.2012.03.003
Wenger, E. (1998). Communities of practice: Learning, meaning, and identity. Cambridge
University Press.
Wilson, S. M., & Kelley, S. L. (2022). Landscape of teacher preparation programs and
teacher candidates. National Academy of Education Committee on Evaluating and Improving Teacher Preparation Programs. https://naeducation.org/evaluating-and-improving-teacher-preparation-programs-commissioned-paper-series/
Yin, R. K. (2006). Case study methods. In J. L. Green, G. Camilli, & P. B. Elmore (Eds.),
Handbook of complementary methods in education (pp. 111-122). American Educational Research Association. Lawrence Erlbaum Associates.’
Zamarro, G., Camp, A., Fuchsman, D., & McGee, J. B. (2021). How the pandemic has
changed teachers’ commitment to remaining in the classroom. Brookings Institute. https://www.brookings.edu/blog/brown-center-chalkboard/2021/09/08/how-the-pandemic-has-changed-teachers-commitment-to-remaining-in-the-classroom/
How to Cite
- Endnote/Zotero/Mendeley (RIS)
Copyright (c) 2024 Aubrey Scheopner Torres, Lisa D'Souza

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License .
Authors retain copyright without restrictions. Unless otherwise indicated, from 2021 all articles are published under the Creative Commons CC-BY-SA license. For more information visit https://creativecommons.org/licenses/by-sa/4.0/. Articles published prior to 2021 used a CC-BY-NC-SA license.
Make a Submission
Journal summary.
Current Issues in Education ( CIE; ISSN 1099-839X) is an open access, peer-reviewed academic education journal produced by doctoral students at the Mary Lou Fulton Teachers College of Arizona State University. The journal’s mission is to advance scholarly thought by publishing articles that promote dialogue, research, practice, and policy, and to advance a community of scholarship.
CIE publishes articles on a broad range of education topics that are timely and have relevance nationally and internationally. We seek innovative scholarship that tackles challenging issues facing education using various theoretical perspectives and methodological approaches. CIE welcomes original research, practitioner experience papers, and submissions in alternative formats.
Authors wishing to submit a manuscript for peer review must register for a journal account and should examine our author guidelines . As an open-access journal, authors maintain the copyright to their published work.
To enhance diversity and inclusion in scholarly publication, and support a greater global exchange of knowledge, CIE does not charge any fee to authors at any stage of the publication process.
Developed By

ORIGINAL RESEARCH article
Challenges and support needs in psychological and physical health among pilots: a qualitative study.

- 1 School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 2 Other, Shanghai, China
- 3 National Center For Global Health and Medicine, Shinjuku, Tokyo, Japan
- 4 School of Public Health, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 5 School of Nursing, Shanghai Jiao Tong University, Shanghai, Shanghai, China
- 6 International Peace Maternity and Child Health Hospital, Shanghai, Shanghai Municipality, China
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
Abstract Introduction Physical and mental health problems among pilots affect their working state and impact flight safety. Although pilots’ physical and mental health problems have become increasingly prominent, their health has not been taken seriously. This study aimed to clarify challenges and support needs related to psychological and physical health among pilots to inform development of a more scientific and comprehensive physical and mental health system for civil aviation pilots. Methods This qualitative study recruited pilots from nine civil aviation companies. Focus group interviews via an online conference platform were conducted in August 2022. Colaizzi analysis was used to derive themes from the data and explore pilots’ experiences, challenges, and support needs. Results The main sub-themes capturing pilots’ psychological and physical health challenges were: 1) imbalance between family life and work; 2) pressure from assessment and physical examination eligibility requirements; 3) pressure from worries about being infected with COVID-19; 4) nutrition deficiency during working hours; 5) changes in eating habits because of the COVID-19 pandemic; 6) sleep deprivation; 7) occupational diseases; 8) lack of support from the company in coping with stress; 9) pilots’ yearly examination standards; 10) support with sports equipment; 11) respecting planned rest time; and 12) isolation periods. Discussion The interviewed pilots experienced major psychological pressure from various sources, and their physical health condition was concerning. We offer several suggestions that could be addressed to improve pilots’ physical and mental health. However, more research is needed to compare standard health measures for pilots around the world in order to improve their physical and mental health and contribute to overall aviation safety.
Keywords: Occupational Health, Mental Health, physical health, qualitative study, Pilots and cabin crew, COVID-19
Received: 06 Dec 2023; Accepted: 05 Apr 2024.
Copyright: © 2024 Xu, Bao, Zhang, Li, Zhang, Li, Jin, Chen, Duan, Shi, Wang, Lu, Chen, Gao, Han, Ren, Su and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Yuyan Bao, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Lin Zhang, Other, Shanghai, China Qingqing Jin, Other, Shanghai, China Yan Chen, Other, Shanghai, China Qingqing Duan, Other, Shanghai, China Feng Shi, Other, Shanghai, China Linlin Wang, Other, Shanghai, China Ziyang Lu, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Xuhua Chen, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Qijing Gao, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Bin Ren, Other, Shanghai, China Ya Su, School of Nursing, Shanghai Jiao Tong University, Shanghai, Shanghai, China Mi Xiang, School of Public Health, School of Medicine, Shanghai Jiao Tong University, Shanghai, 200240, China
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Research on Quantitative Analysis of Multiple Factors Affecting COVID-19 Spread
1 Faculty of Information Technology, Beijing University of Technology, Beijing 100124, China; moc.361@39990183131 (Y.F.); moc.361@4131nawxav (Z.X.)
2 Beijing Institute of Smart City, Beijing University of Technology, Beijing 100124, China
The Corona Virus Disease 2019 (COVID-19) is spreading all over the world. Quantitative analysis of the effects of various factors on the spread of the epidemic will help people better understand the transmission characteristics of SARS-CoV-2, thus providing a theoretical basis for governments to develop epidemic prevention and control strategies. This article uses public data sets from The Center for Systems Science and Engineering at Johns Hopkins University (JHU CSSE), Air Quality Open Data Platform, China Meteorological Data Network, and WorldPop website to construct experimental data. The epidemic situation is predicted by Dual-link BiGRU Network, and the relationship between epidemic spread and various feature factors is quantitatively analyzed by the Gauss-Newton iteration Method. The study found that population density has the greatest positive correlation to the spread of the epidemic among the selected feature factors, followed by the number of landing flights. The number of newly diagnosed daily will increase by 1.08% for every 1% of the population density, the number of newly diagnosed daily will increase by 0.98% for every 1% of the number of landing flights. The results of this study show that the control of social distance and population movement has a high priority in epidemic prevention and control strategies, and it can play a very important role in controlling the spread of the epidemic.
1. Introduction
Since December 2019, The Corona Virus Disease 2019 (COVID-19) caused by the SARS-CoV-2, has spread rapidly around the world. On 11 March 2020, the WHO announced that COVID-19 has become a major issue in the world [ 1 , 2 , 3 , 4 ]. The spread of COVID-19 has had a serious impact on the medical and economic aspects of countries around the world [ 5 ]. Due to the complexity of the spread of COVID-19, existing models cannot accurately estimate the direction of the spread of the epidemic [ 6 ]. Therefore, we need to build a quantitative analysis model to deeply explore the spread and influencing factors of COVID-19 on a global scale. In the current research, the data-driven deep learning model has an outstanding performance in the task of modeling time series [ 7 ].
The symptoms of COVID-19 are fever, cough, shortness of breath, loss of consciousness and fatigue. Other symptoms include dyspnea and chest pain [ 8 ]. In order to prevent the spread of the epidemic, countries have adopted many measures, such as reducing gathering activities, controlling the movement of people, advocating the use of masks, and regular disinfection in public areas [ 9 ]. As of 31 December 2021, there have been more than 287 million confirmed cases of COVID-19 worldwide, and at least 5 million people have lost their lives [ 10 ]. In order to further grasp the factors affecting the spread of SARS-CoV-2, better support the decision-making of epidemic prevention and control, timely made targeted countermeasures, and control the further spread of the epidemic, it is very urgent to quantitatively analyze the relationship between various factors and the spread of SARS-CoV-2.
The remainder of this paper is arranged as follows. Section 2 comprehensively introduces the current research on COVID-19 and the transmission characteristics of the SARS-CoV-2. Section 3 introduces the data sources and presents our research methodology. Section 4 describes the experimental results and provides an analytical discussion, and Section 5 summarizes the conclusions of this study and proposes further research directions.
2. Related Research Work
2.1. research on covid-19 epidemic.
Since COVID-19 outbreak in December 2019, research on COVID-19 has attracted the attention of data scientists from all over the world. Duccio et al. [ 11 ] predicted that the maximum number of infections in Italy was about 26,000 and the death toll was about 18,000 through analysis of the spread of the epidemic in China and France. Ricardo et al. [ 12 ] proposed a regression of compressed space Gaussian processes based on chaotic dynamics system to predict the number of people infected with COVID-19 in the United States, and concluded that the number of infected people in the United States would reach more than one million on 14 June 2020. Rohit et al. [ 13 ] proposed Genetic Evolutionary Programming (GEP) to analyze and predict the amount of COVID-19 cases in India. They proposed a GEP model based on the use of a simple function, which was highly effective for the time series prediction of COVID-19 cases in India. Putra et al. [ 14 ] used Particle Swarm Optimization (PSO) to estimate the parameters in the Susceptible Infectives Recovered Model (SIR), and concluded that the parameter results of the PSO algorithm were more accurate and had lower errors than the traditional method. Mbuvha et al. [ 15 ] estimated the parameters of the SIR with data from Lombardy, Italy and Hubei, China, and used the SIR model to predict the number of COVID-19 cases in South Africa, and concluded that COVID-19 was still in the early stage in South Africa.
So far, some scholars have done excellent research, but if it is necessary to further study the transmission characteristics of the SARS-CoV-2, it is impossible to predict the number of patients only. It is necessary to collect data related to the spread of SARS-CoV-2, and to analyze the characteristics of SARS-CoV-2 to understand what factors are related to the spread of SARS-CoV-2 and the quantitative relationship between them, so as to support the more precise adoption of effective prevention, control and disposal measures.
2.2. Research on the Transmission Characteristics of the SARS-CoV-2 Virus
When COVID-19 became a global hot topic, people put forward many speculations that could affect the transmission characteristics of the SARS-CoV-2, such as temperature [ 16 , 17 , 18 ], humidity [ 19 , 20 ], population density [ 21 , 22 ], age [ 23 , 24 ], and so on. In this regard, scholars have also conducted a lot of research, which has a non-negligible inspiration for us to reveal the transmission characteristics of the SARS-CoV-2. Lin et al. [ 25 ] studied the relationship between climate and the spread of COVID-19 on a global scale, and concluded that the spread of COVID-19 was highly correlated with temperature and relative humidity. Roengrudee et al. [ 26 ] studied the relationship between smoking and the spread of COVID-19, and concluded that there was a significant correlation between the number of smokers and the spread of COVID-19. Kass et al. [ 27 ] analyzed the relationship between Body Mass Index (BMI) and age in the number of confirmed COVID-19 patients through a multiple linear regression model, and concluded that obesity may increase the infection rate of COVID-19. WU et al. [ 28 ] found that in the United States, areas with higher historical PM2.5 were positively correlated with higher COVID-19 mortality. Hamit et al. [ 29 ] found that population density was the main factor affecting the spread of the epidemic through research on the spread of the epidemic in Turkish cities.
The above-mentioned studies generally have the following problems: (1) The area covered by the data set is limited to local areas, and the propagation characteristics of SARS-CoV-2 cannot be analyzed from a global scale. (2) The conclusion is only a qualitative analysis, and it has not been able to quantify the effects of various factors on the impact of the spread of the SARS-CoV-2. In response to the above problems, this paper constructs a quantitative analysis model between COVID-19 and multiple factors. Firstly, we collect the required data on a global scale, and then build a Dual-link BiGRU prediction network to predict the number of new cases in each country every day, and quantitatively analyze the impact of different factors on the number of new cases per day of COVID-19. Compared with the above research, the model proposed in this paper is more helpful to analyze the development trend of the epidemic on a global scale, helps to grasp the characteristics of the SARS-CoV-2, and provides more clear theoretical support for the subsequent formulation of anti-epidemic policies by governments of various countries.
3. Data Sources
The data set in this paper is mainly divided into four parts including epidemic data, climate data, population and flight data, and air quality data.
- The source of the epidemic data is COVID-19 data set published by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. The data set was collected from all over the world from 22 January 2020, in the early stage of the epidemic. The experimental data in this article include the collected epidemic data from 22 January 2020 to 31 December 2021. The feature data elements include the cumulative number of confirmed cases, the cumulative number of cured people, the cumulative number of deaths, and the number of new cases per day.
- The climate data comes from the daily recorded data of weather stations around the world collected by the China Meteorological Data Network ( http://data.cma.cn/ ). This experiment selects the climate data of various regions from 22 January 2020 to 31 December 2021. The feature data elements include daily maximum temperature, daily minimum temperature, wind speed, precipitation, dew point temperature, atmospheric pressure, wind gust, altitude, absolute humidity and relative humidity.
- The population and flight data come from the Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. ( https://population.un.org/wpp/ ). This experiment selects population and flight data in various regions from 22 January 2020 to 31 December 2021. The feature data elements include total population, population density, the total number of flights, number of domestic flights, and international flights.
- The air quality data come from the open-source air quality website WAQI ( https://aqicn.org/data-platform/covid19/ ). This experiment selects air quality data in various regions from 22 January 2020 to 31 December 2021. The feature data elements include NO 2 , PM 10 , PM 2.5 , PM 1 , SO 2 , O 3 , CO content in the air, Air Quality Index(AQI), Suspended particle concentration(from NEPH), UV Index(UVI), Pollution(POL) and Wavelength Dominant(WD).
We collected 31-dimensional features of 81 countries to form a data set. Because we can get the data we need in these countries, we selected these 81 countries. In order to ensure that there was a sufficient amount of data to train the model, we selected the 9:1 segmentation ratio to divide the training set and test set, that is, the data from 22 January 2020 to 31 October 2021 was set as the training set and that from 1 November 2021 to 31 December 2021 as the test set.
4. Research Methods
The quantitative relationship model between COVID-19 spread and various characteristic factors proposed in this paper includes three steps: multi-source heterogeneous data preprocessing, constructing Dual-link BiGRU Network to prediction COVID-19 spread, and building a quantitative analysis model of multiple feature data relationships.
4.1. Multi-Source Heterogeneous Data Preprocessing
Because the data comes from a variety of public data sets, there are some problems among data sets, such as inaccurate data, missing data, inconsistent data format and etc. In the data preprocessing stage, this paper builds a dataset with the original data as the core. For inaccurate data, when the values of the same feature data in datasets from different sources are the same, we consider the data to be reasonable; otherwise, most of the data in datasets from different sources are selected as the final data. For missing data, the Cubic Spline Interpolation method is used to supplement the data. For inconsistent data format, feature level fusion method is adopted to extract the features of each source data set first, while the extracted feature information comes from the high-order representation of the original information, and then to aggregate and synthesize the multi-source data according to the feature information. The data with inconsistent scales are normalized by the linear normalization method to unify the data scale. This is also a commonly used data preprocessing method in the field of COVID-19 prediction. The information contained in the fused data is shown in Table 1 .
Feature display of fusion data set.
Tmax, Tmin, Wind_speed, Precipitation, DP_F, Pressure, Wind_gust, Altitude, Ab_humidity and Re_humidity represent daily maximum temperature, daily minimum temperature, daily average wind speed, daily rainfall, daily dew point temperature, atmospheric pressure, wind gust, altitude, absolute humidity and relative humidity. Pop, Density represent total population, population density. NO 2 , PM 10 , PM 2.5 , PM 1 , SO 2 , O 3 , CO and AQI, NEPH, UVI, POL, WD represent NO 2 , PM 10 , PM 2.5 , PM 1 , SO 2 , O 3 , CO content in the air, Air Quality Index(AQI), Suspended particle concentration(from NEPH), UV Index(UVI), Pollution(POL) and Wavelength Dominant(WD). Flight_total, Flight_domestic, and Flight_international represent the total number of flights, the number of domestic flights, and the number of international flights respectively.
4.2. Dual-Link BiGRU Network to Predict the Spread of COVID-19
In this paper, we construct Dual-link BiGRU Network to predict the spread of COVID-19. The task of Dual-link BiGRU is to regress and predict the number of new cases per day with input data. Dual-link BiGRU conducts parameter training through the relationship between daily different factors in the training set and the number of new cases. It inputs the values of the daily factors in the test set, and outputs the regression estimation of the number of new cases on that day. The network structure diagram of Dual-link BiGRU is shown in Figure 1 .

The network structure diagram of Dual-link BiGRU.
Dual-link BiGRU consists of a dual-link feature network and a fully connected network. In the feature network, Link 1 is composed of one-dimensional convolutional network, BiGRU network, and one-dimensional inverse convolutional network. Link 2 is composed of one-dimensional convolutional network, fully connected network, and one-dimensional inverse convolutional network. Link 1 is mainly responsible for learning the timing information in the data of multiple factors. The one-dimensional convolutional network in Link 2 provides a larger receptive field for the network with a larger size of convolution kernel to learn different feature information from Link 1. In this experiment, in order to obtain a larger receptive field and better features, we select the kernel size of 16. After the dual-link feature network is a fully connected network. The fully connected network’s main function is to change the output dimension of the entire Dual-link BiGRU network to the desired output dimension.
According to the prediction performance of the test set, the parameter settings of the prediction network are shown in Table 2 . The optimizer used for model training is Adam, the loss function is Mean Squared Error Loss Function (MSELoss), and the number of iterations is set to 500. In this paper, we selects BiLSTM [ 30 ], BiGRU [ 31 ], and CNN [ 32 ] for comparison at the same dataset which comes from Table 1 . BiLSTM, BiGRU, and CNN are connected by their respective models and fully connected layers. The hidden layer size and number of layers of BiLSTM and BiGRU are consistent with Dual-link BiGRU, and the parameter setting of CNN is consistent with 1-D Conv1 in Dual-link BiGRU.
Prediction network parameter settings.
4.3. The Quantitative Analysis Model of Multi Characteristic Data Relationships
In this paper, we sets the tolerance of the prediction error rate β ∈ [0, 1]. The model with a prediction error rate lower than β is called an effective model, otherwise it is called an invalid model. It is assumed that only effective models can participate in quantitative analysis. Therefore, the larger of β means the more effective models, and the quantitative analysis results have better generalization ability, but it also means that the results have larger errors; the smaller of β means the less effective the models and the poorer generalization ability of the quantitative analysis results, while the results have smaller errors within a limited range. This paper needs to have a small result errors on the basis of ensuring a certain generalization ability, so β = 0.2 is set in the experiment of this paper.
In this paper, the Gauss-Newton iterative method is used for quantitative analysis. The Gauss-Newton iterative method uses Taylor series expansion to approximately replace the nonlinear regression model. Through multiple iterations, the regression coefficient is modified many times, so that the regression coefficient continuously approaches the best regression coefficient of the nonlinear regression model, and finally the Residual Sum of Square of the original model is minimized.
According to the selected observation variable data, a multiple nonlinear regression model as in Equation ( 1 ) can be constructed.
where y is the dependent variable, which represents the number of newly diagnosed people every day in this experiment; X is the set of independent variables, which represents the data of each characteristic factor in this experiment; β is an unknown parameter; ϵ is an error term, and it is an unobservable random variable with a mean of zero and a variance of σ 2 > 0 . The above model can be used to predict the number of the newly diagnosed daily and determine the nonlinear quantitative relationship between each independent variable and the dependent variable. The Gauss-Newton iteration method estimates the to-be-regressed parameter β of the nonlinear regression model through continuous iteration.
The realization process of the quantitative analysis model includes the following steps:
- Construct multiple regression models and train through data;
- The prediction ability of the model is evaluated by modifying the determination coefficient;
- The quantitative relationship between multiple factors and the number of new cases per day was determined by a multiple regression model;
- Given different initial values for different factors x 0 ;
- For the k t h iteration, calculate the Jacobian matrix J , Hessian matrix H , B , and calculate the increment △ x k ;
- If △ x k is small enough, stop the iteration, otherwise, update x ( k + 1 ) = x k + △ x k ;
- Repeat steps (5) (6) until the maximum number of iterations is reached, or the termination condition of (6) is met;
- Complete the estimation of the unknown parameter β , and determine the quantitative relationship between different elements and the number of new cases per day;
- Complete for β to determine the quantitative relationship between different elements and the number of new cases per day.
5. Experimental Results and Discussion
5.1. dual-link bigru.
In this paper, the evaluation index is selected as the error rate ρ , and the error rate calculation formula is shown in Equation ( 2 ):
where y ^ i represents the model output, y i represents the label of the number of new cases per day, and m represents the total number of samples in the test set. This indicator can measure the gap between the model output and the label of the entire test set sample.
In this paper, we selects BiLSTM [ 30 ], BiGRU [ 31 ], and CNN [ 32 ] for comparison at the same dataset which comes from Table 1 . BiLSTM, BiGRU, and CNN are connected by their respective models and fully connected layers. The hidden layer size and number of layers of BiLSTM and BiGRU are consistent with Dual-link BiGRU in Table 2 , and the parameter setting of CNN is consistent with 1-D Conv1 in Dual-link BiGRU in Table 2 . Sets the prediction error tolerance β = 0.2, and uses the model error rate as the evaluation index. In the data of 81 countries, the model with an error rate lower than β is regarded as an effective model, and the difference in the number of effective models among different models is compared in the test dataset. The comparison experiment results are shown in Table 3 .
Comparison of model results.
Table 3 shows that (1) Dual-link BiGRU has a larger effective model ratio in the prediction network; (2) Compared with BiGRU, BiLSTM, and CNN, Dual-link BiGRU performs better in low error rate. Therefore, it is believed that the Dual-link BiGRU has better performance and generalization ability in predicting the daily number of new epidemics in various countries. Therefore, this paper selects the Dual-link BiGRU as the prediction network. Figure 2 shows the difference between the daily number of new cases predicted of the Dual-link BiGRU and the label value. Because showing the forecast results for all countries would make the paper extraordinarily long, in this paper, we select 6 countries with better results for display, including Canada, China, India, Indonesia, Russia, and United Kingdom.

Display of Dual-link BiGRU prediction results.
It can be seen from Figure 2 that in the selected 6 countries, the red solid line is the label of the number of new cases per day, and the green dashed line is the predicted value by the Dual-link BiGRU network. The two curves have a high degree of overlap. Therefore, the prediction network constructed in the experiment has a good fit with the real data. The trained prediction network can better predict the daily new cases and has a strong generalization ability. For different countries, the model can learn more appropriate parameters to predict the number of the daily new cases.
5.2. Quantitative Analysis Results of Multi-Characteristic Data Relationships
In this paper, we uses the method of Lin [ 25 ] and others to build a multiple regression model for the selected 44 effective national models and train them. Through the multiple regression model, the quantitative relationship between multiple factors and the number of new cases per day is determined, and the prediction ability of the model is evaluated by determining the Adjusted R Square (R). The larger R is, the stronger the prediction ability of the model is. If R is greater than 0.6, the model has strong epidemic prediction ability. Then, the initial value of the Gauss-Newton iterative method is selected through the model parameters. The quantitative relationship between multiple factors and the number of new cases per day is shown in Table 4 , and the initial values are shown in Table 5 .
Regression equation parameter.
Example of initial value of each characteristic coefficient.
In this paper, we uses the trained Dual-link BiGRU model of various countries to generate simulation data for quantitative analysis. The data generation method is as follows:
- Goal: To generate data for analyzing the quantitative relationship between x 1 and y , where x 1 is the maximum temperature per day and y is the number of new cases per day.
- To control other factors unchanged, adjust x 1 , and generate the predicted value of y .
- The simulation data is used as input, and training is performed with the Gauss-Newton method to obtain the coefficient between x 1 and y , so as to determine the quantitative relationship between them.
According to the above method, the coefficient equations between the number of new cases per day in each country and the characteristic factors in Table 1 are obtained respectively, and the quantitative relationship between the number of new cases per day and the characteristic factors in each country is determined. Then take the average of the quantitative relationship coefficients of the same feature in all countries, and finally get the quantitative relationship between each feature that is applicable in the selected country and the number of new cases per day with strong generalization performance, as shown in Table 6 .
Quantitative relationship between characteristic factors and daily number of new cases.
The influence >0, indicating that the factor has a positive correlation with the increase in the number of new cases per day. The influence <0, indicating that the factor has a negative correlation with the increase in the number of new cases per day.
As shown in Table 6 , among the selected features, the population density per unit land area has the largest positive correlation with the number of new cases per day, followed by the number of landing flights. The population density per square kilometer increases by 1%, and the number of new cases per day in the corresponding area increases by about 1.076%. For every 1% increase in the number of landing flights, the number of new cases per day in the corresponding area increases by about 0.98%. Among the selected features, the daily maximum temperature, daily minimum temperature and dew point temperature have negative correlations to the number of new cases per day. Within the range of 0–50 °C, each increase of 1 °C can reduce the number of new cases per day by 0.021%, 0.028% and 0.015% respectively.
Based on the above analysis, the following further inferences can be drawn:
- Population factors and flight factors has an obvious positive correlation impact on the spread of COVID-19. From the data of the selected 44 countries, it can be seen that population factors and flight factors have a greater impact on the spread of COVID-19. Every 1% increase in population factors will increase the spread of the epidemic by 1.044%. Every 1% increase in the number of arrival flights will increase the spread of the epidemic by 0.98%. Therefore it can be seen that population factors and flight factors have a more obvious impact on the increase in the spread of the epidemic. From the perspective of formulating epidemic prevention and control policies, controlling social distancing and population movement will have a more obvious positive correlation impact on epidemic prevention and control.
- The increase in temperature and relative humidity has a negative correlation impact on the spread of COVID-19.Among the climatic factors, the increase of temperature and humidity has a negative correlation impact on the spread of COVID-19. In this paper, the temperature range of 0–50 °C and the relative humidity range of 1–100% are selected for the experiment. It is obtained that within this range, temperature and relative humidity has a negative correlation impact on the spread of COVID-19, but the impact is not obvious. Since the correlation between population density and the speed of the epidemic is far greater than the correlation between temperature and the speed of the epidemic, it is speculated that in areas with higher temperatures and higher population densities, such as India and other countries, the speed of the epidemic still has a relatively rapid possibility.
- A larger AQI has a positive correlation impact on the spread of COVID-19.AQI represents the degree of air cleanliness or pollution and its impact on health. The higher the AQI, the more serious the air pollution in the region. This experiment shows that in the range of AQI value 100–200, the epidemic transmission speed of COVID-19 will increase by 0.013% every time AQI increases by 1. Some researchers have shown that SARS-CoV-2 can spread through aerosols [ 33 , 34 , 35 ]. Therefore, a higher AQI means a higher aerosol content in the air, which is not good for air circulation. Such an environment may promote the spread of COVID-19.
6. Discussion
Since the discovery of COVID-19 in 2019, countries have successively formulated epidemic prevention and control policies that suit their own national conditions [ 36 ]. According to the current development status of the world epidemic, a long-term coexistence with the virus has been formed, that is, even though the vaccine has been developed, it will take a long time to completely eliminate COVID-19 [ 37 , 38 ]. This paper carries out quantitative analysis and research on COVID-19 transmission by various factors all over the world and comes to the conclusion that the increase of population density, population flow, and flight times has a positively correlated impact on the epidemic transmission, and the increase of temperature, relative humidity, and dew point temperature has a negative correlation impact on the epidemic transmission. It can be concluded that the positive correlation effect of population density on the epidemic spread is much greater than the negative correlation effect of climate factors on the epidemic spread.
Therefore, according to the regional characteristics and national conditions, governments should formulate epidemic prevention and control policies to control population density and population flow in the climate environment with high local temperature and relative humidity, maximize the effect of epidemic prevention and control, and curb the spread of the epidemic from the aspects of transmission route and virus characteristics.
International organizations need to establish high, medium and low-risk epidemic spread levels globally. The faster the epidemic spread, the higher the epidemic spread level, and the more stringent prevention and control policies need to be adopted. For cities where the epidemic has spread, it is necessary to keep wearing masks, maintain proper social distancing, and reduce public recreational activities. For cities with large population density and serious epidemic spread, it is recommended to strictly control population flow, tighten restrictive measures for international flights, and take “city closure” measures when necessary, and other cities need to take more stringent entry epidemic prevention measures for personnel from high-risk countries and regions. For cities with slow epidemic spread, it is suggested to control the population flow within a certain range, allow international flights under the condition of good epidemic prevention measures, strictly control the flow of people from high-risk countries and regions, and be vigilant against the epidemic spread caused by climate change.
7. Conclusions and Future Work
In this paper, we fuses multi-source heterogeneous data, and makes predictions for the current COVID-19 epidemic based on the fusion data set, and quantitatively analyzes the model to obtain the quantitative relationship between various factors and the spread of the epidemic. The contributions of this paper are as follows:
- Compared with the CNN, LSTM, and GRU networks, the prediction accuracy of the Dual-link BiGRU network is improved by 35.03%, 31.41%, and 27.36%, respectively;
- Compared with the CNN, LSTM, and GRU networks, the generalization ability of the Dual-link BiGRU network is improved by 25.00%, 27.50%, and 28.75%, respectively.
- The increase in population factors and flight factors has an obvious positively correlated impact on the spread of COVID-19.
- The increase in AQI will has a minor positively correlated impact on the spread of COVID-19.
- The increase in temperature and relative humidity has a negative correlation impact on the spread of COVID-19.
Accordingly, this paper makes the following recommendations for global epidemic prevention and control:
- Countries should take appropriate or even stricter prevention and control measures according to their national conditions, such as demographic factors, climate factors, air quality factors, and the number of flights, to minimize the risk of outbreaks.
- Demographic factors have a strong positive relationship with the spread of COVID-19 epidemic. Governments can control the spread of the epidemic by strictly controlling the movement of people both within and outside the country.
- Since the impact of population and flight factors on the spread of the epidemic is much greater than that of climate factors, governments of various countries should not expect the epidemic to disappear after the temperature rises, and should actively control population movement.
This paper has completed the multi-factor quantitative analysis model affecting the spread of COVID-19. Due to the different detection coverage of COVID-19 in various countries, the number of confirmed cases is inevitably underestimated, and this paper does not evaluate the impact of changes in policies and local prevention and control strategies on the spread of COVID-19. Therefore, more detailed exploration is needed on these issues in the next step.
Author Contributions
Y.F. collected literature and wrote the manuscript; S.L. reviewed and edited the manuscript; Z.X. Put forward suggestions for revision of the article. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
COMMENTS
The Novel Coronavirus disease, also known as COVID-19, is considered one of the most devastating. outbreaks that have taken millions o f lives and have affected human spheres globally. The impact ...
3.5. Knowledge and concerns about COVID-19 and association with psychological impact. The proportions of respondents who perceive that the routes of transmission of the virus for COVID-19 were via droplets, via contaminated objects and airborne were 98.6%, 96.7% and 35.3%, respectively (Table 4). About 76.8% were satisfied to very satisfied ...
This may help us to understand the effect of contact among individuals and how transmits the virus more quickly. Recently, the serial interval has been calculated for the COVID-19, this estimates by 4.6 days . A reported study mentioned that the mean serial interval for COVID-19 was calculated as 3.96 days.
Introduction The SARS-CoV-2, virus that caused the COVID-19 global pandemic, possesses a neuroinvasive potential. Patients with COVID-19 infection present with neurological signs and symptoms aside from the usual respiratory affectation. Moreover, COVID-19 is associated with several neurological diseases and complications, which may eventually affect clinical outcomes. Objectives The ...
Low- and middle-income countries (LMICs) remained at elevated risk for the effects of the COVID-19 pandemic because of persistent stressors to their health systems. Simultaneously facing high infection rates, strict containment measures and natural disasters, the Philippines provides important grounds for health research in LMICs.
Providing English and native language quotes in qualitative research: a call to action. Nursing Open. 2022; 9: 168-174. Crossref; PubMed; ... Health Systems Impact of COVID-19 in the Philippines. Center for Global Development, Washington, DC 2021. View in Article Google Scholar; 6. World Health Organization ...
COVID-19 dynamics in the Philippines are driven by age, contact structure, mobility, and MHS adherence. Continued compliance with low-cost MHS should help the Philippines control the epidemic until vaccines are widely distributed, but disease resurgence may be occurring due to a combination of low population immunity and detection rates and new variants of concern.
Background: The 2019 coronavirus disease (COVID-19) pandemic poses a threat to societies' mental health. This study examined the prevalence of psychiatric symptoms and identified the factors contributing to psychological impact in the Philippines. Methods: A total of 1879 completed online surveys were gathered from March 28-April 12, 2020.
This study explores ways in which a non-governmental organization (NGO) in the Philippines protected their frontline workforce during the first year of the COVID-19 pandemic. Methods: Guided by a qualitative descriptive approach, 34 in-depth interviews were conducted with community-based health actors employed by the NGO between June 2020 and ...
IES-R and DASS-21 were previously used in research related to the COVID-19 ... in-depth analysis and studied the relationship between physical and mental outcomes and other variables related to COVID-19 in the Philippines and China. ... Bastani P, Bahrami MA. COVID-19 related misinformation on social media: a qualitative study from Iran. J Med ...
Introduction. The Philippine Development Plan for 2017-2023 highlights that children are among the most vulnerable population groups in society, including them in strategies for risk reduction and adaptive capacity strengthening. 1 Approximately 40% of the total Philippine population is comprised of Filipinos below 18 years of age. 2 Despite having a large portion of the Philippine population ...
Introduction The COVID-19 pandemic declared by the WHO has affected many countries rendering everyday lives halted. In the Philippines, the lockdown quarantine protocols have shifted the traditional college classes to online. The abrupt transition to online classes may bring psychological effects to college students due to continuous isolation and lack of interaction with fellow students and ...
COVID-19 in the Philippines Abstract Lockdowns and policy actions to curtail the transmission of COVID-19 have widespread health system, economic, and societal impacts. Health systems of low-to-middle-income countries may have fewer buffering resources and capacity against shocks from a pandemic. This paper presents
In this article, we draw on our experiences as qualitative researchers in the Philippines to present the unique challenges of conducting online research among vulnerable populations in the country during the pandemic. ... and on conducting qualitative research in the time of COVID-19. Then, we present data drawn from two multi-sited studies ...
Coronavirus (COVID-19) is known as an infectious disease caused by a newly discovered coronavirus (World Health Organization, 2020). According to the WHO's dashboard, globally, as of 2:45 pm CEST, October 22, 2020, there have been 41,104,946 confirmed cases of COVID-19, including 1,128,325 deaths (Khaliq, 2020).
Research Design In this qualitative research study, the Critical Discourse Analysis (CDA) was applied as both a theory and a study design. Procedure The Daily Guardian website, a local news source in Iloilo, Philippines, served as the source for the news stories for COVID-19. For the whole month of June 2020, one (1)
Online research COVID-19 Qualitative research Philippines . ABSTRACT Our article draws on two multi-sited studies to present the ethical and methodological challenges of conducting online qualitative research among vulnerable populations in the Philippines—specifically, among people who use drugs—during the COVID-19 pandemic.
As the COVID-19 pandemic has shown, setting up studies in time to gather relevant, real-world data enables researchers to capture current views and experiences, focus on practicalities on the ground, and deliver actionable results. Delivering high quality rapid studies in healthcare poses several challenges even in non-emergency situations. There is an expanding literature discussing benefits ...
Lasco G, Yu VG, Compra JM, Leuangvilay P, Suphanchaimat R, Zhang Y, Javier C. Nutrition in Times of Crisis: A Qualitative Study in Siargao Island, Philippines, during the COVID-19 Pandemic. Acta Med Philipp [Internet]. 2023May29 [cited 2024Apr.6];57(5).
A study of 1,210 respondents from 194 cities in China found that during the beginning of the COVID-19 outbreak, more than 50% had moderate to severe psychological impact, with ~30% reporting moderate to severe anxiety ( Wang et al., 2020a ). Mental patients displayed more serious symptoms relating to physical health and suicidal ideation ( Hao ...
The research base on COVID-19 has expanded extensively the past years , covering areas such as clinical risks and outcomes ... Bates DW, Dykes PC, et al. A resilience perspective on healthcare personnels' experiences of managing the COVID-19 pandemic: a qualitative study in Norwegian nursing homes and come care services. BMC Health Serv Res ...
In the Philippines, COVID-19 the infection rate is one of the highest in the world with 2, ... If one wants to measure the quality of a thing such as the quality of the Philippine COVID-19 response, then qualitative research is appropriate for this objective. If one wants to count and know the extent of cases in COVID-19 infections, deaths, and ...
As the COVID-19 pandemic disrupts everyday life, consumers encounter a complex institutional environment characterized by multiple incompatible logics that claim dominance for guiding action. ... Basics of Qualitative Research Techniques. Thousand Oaks: Sage. Google Scholar. Thornton PH, Ocasio W (1999) Institutional logics and the historical ...
This qualitative study aims to provide insight into why teacher candidates, interested in pursuing K-12 teaching, made the decision to leave their traditional teacher preparation programs during the COVID-19 pandemic. The researchers utilized sociocultural theory as the framework to ground the research. The study finds the educational disruption caused by the pandemic added a layer of ...
Qualitative examination of the impact of the COVID-19 pandemic on individuals with neuro-developmental disabilities and their families. J Child Fam Stud . (2022) 31:2202-14. doi: 10.1007/s10826-022-02336-8
Abstract. The COVID-19 pandemic has forced both quantitative and qualitative health researchers to adapt and strategize data collection strategies without causing any harm to the participants or researchers. This has resulted in utilizing various types of strategies such as online surveys and synchronous virtual platforms such as Zoom and Webex.
SOM 402 (FLEX) 13 Apr 2024 10:00 am - 13 Apr 2024 12:00 pm. The John Gokongwei School of Management (JGSOM) invites you to the. 3rd JGSOM Graduate Research Colloquium. Saturday, 13 April 2024, 10:00AM - 12:00NN. Onsite at SOMBA Room, SOM 402. Online via Zoom. Finalists for the JGSOM Outstanding Graduate Thesis Award: Silvestre D. Yraola III.
Results The main sub-themes capturing pilots' psychological and physical health challenges were: 1) imbalance between family life and work; 2) pressure from assessment and physical examination eligibility requirements; 3) pressure from worries about being infected with COVID-19; 4) nutrition deficiency during working hours; 5) changes in ...
2.2. Research on the Transmission Characteristics of the SARS-CoV-2 Virus. When COVID-19 became a global hot topic, people put forward many speculations that could affect the transmission characteristics of the SARS-CoV-2, such as temperature [16,17,18], humidity [19,20], population density [21,22], age [23,24], and so on.In this regard, scholars have also conducted a lot of research, which ...
The John Gokongwei School of Management invites you to a Brown Bag Session on "COVID-19 Blood Collection Volatility in the Philippines: A Data-Driven Disaster Preparedness and Recovery Policy Framework". Our presenter is Joel Patrick D. Caballa, Lecturer at the Department of Quantitative Methods and Information Technology.