Module 11: Schizophrenia Spectrum and Other Psychotic Disorders
Case studies: schizophrenia spectrum disorders, learning objectives.
- Identify schizophrenia and psychotic disorders in case studies

Case Study: Bryant
Thirty-five-year-old Bryant was admitted to the hospital because of ritualistic behaviors, depression, and distrust. At the time of admission, prominent ritualistic behaviors and depression misled clinicians to diagnose Bryant with obsessive-compulsive disorder (OCD). Shortly after, psychotic symptoms such as disorganized thoughts and delusion of control were noticeable. He told the doctors he has not been receiving any treatment, was not on any substance or medication, and has been experiencing these symptoms for about two weeks. Throughout the course of his treatment, the doctors noticed that he developed a catatonic stupor and a respiratory infection, which was identified by respiratory symptoms, blood tests, and a chest X-ray. To treat the psychotic symptoms, catatonic stupor, and respiratory infection, risperidone, MECT, and ceftriaxone (antibiotic) were administered, and these therapies proved to be dramatically effective. [1]
Case Study: Shanta
Shanta, a 28-year-old female with no prior psychiatric hospitalizations, was sent to the local emergency room after her parents called 911; they were concerned that their daughter had become uncharacteristically irritable and paranoid. The family observed that she had stopped interacting with them and had been spending long periods of time alone in her bedroom. For over a month, she had not attended school at the local community college. Her parents finally made the decision to call the police when she started to threaten them with a knife, and the police took her to the local emergency room for a crisis evaluation.
Following the administration of the medication, she tried to escape from the emergency room, contending that the hospital staff was planning to kill her. She eventually slept and when she awoke, she told the crisis worker that she had been diagnosed with attention-deficit/hyperactive disorder (ADHD) a month ago. At the time of this ADHD diagnosis, she was started on 30 mg of a stimulant to be taken every morning in order to help her focus and become less stressed over the possibility of poor school performance.
After two weeks, the provider increased her dosage to 60 mg every morning and also started her on dextroamphetamine sulfate tablets (10 mg) that she took daily in the afternoon in order to improve her concentration and ability to study. Shanta claimed that she might have taken up to three dextroamphetamine sulfate tablets over the past three days because she was worried about falling asleep and being unable to adequately prepare for an examination.
Prior to the ADHD diagnosis, the patient had no known psychiatric or substance abuse history. The urine toxicology screen taken upon admission to the emergency department was positive only for amphetamines. There was no family history of psychotic or mood disorders, and she didn’t exhibit any depressive, manic, or hypomanic symptoms.
The stimulant medications were discontinued by the hospital upon admission to the emergency department and the patient was treated with an atypical antipsychotic. She tolerated the medications well, started psychotherapy sessions, and was released five days later. On the day of discharge, there were no delusions or hallucinations reported. She was referred to the local mental health center for aftercare follow-up with a psychiatrist. [2]
Another powerful case study example is that of Elyn R. Saks, the associate dean and Orrin B. Evans professor of law, psychology, and psychiatry and the behavioral sciences at the University of Southern California Gould Law School.
Saks began experiencing symptoms of mental illness at eight years old, but she had her first full-blown episode when studying as a Marshall scholar at Oxford University. Another breakdown happened while Saks was a student at Yale Law School, after which she “ended up forcibly restrained and forced to take anti-psychotic medication.” Her scholarly efforts thus include taking a careful look at the destructive impact force and coercion can have on the lives of people with psychiatric illnesses, whether during treatment or perhaps in interactions with police; the Saks Institute, for example, co-hosted a conference examining the urgent problem of how to address excessive use of force in encounters between law enforcement and individuals with mental health challenges.
Saks lives with schizophrenia and has written and spoken about her experiences. She says, “There’s a tremendous need to implode the myths of mental illness, to put a face on it, to show people that a diagnosis does not have to lead to a painful and oblique life.”
In recent years, researchers have begun talking about mental health care in the same way addiction specialists speak of recovery—the lifelong journey of self-treatment and discipline that guides substance abuse programs. The idea remains controversial: managing a severe mental illness is more complicated than simply avoiding certain behaviors. Approaches include “medication (usually), therapy (often), a measure of good luck (always)—and, most of all, the inner strength to manage one’s demons, if not banish them. That strength can come from any number of places…love, forgiveness, faith in God, a lifelong friendship.” Saks says, “We who struggle with these disorders can lead full, happy, productive lives, if we have the right resources.”
You can view the transcript for “A tale of mental illness | Elyn Saks” here (opens in new window) .
- Bai, Y., Yang, X., Zeng, Z., & Yang, H. (2018). A case report of schizoaffective disorder with ritualistic behaviors and catatonic stupor: successful treatment by risperidone and modified electroconvulsive therapy. BMC psychiatry , 18(1), 67. https://doi.org/10.1186/s12888-018-1655-5 ↵
- Henning A, Kurtom M, Espiridion E D (February 23, 2019) A Case Study of Acute Stimulant-induced Psychosis. Cureus 11(2): e4126. doi:10.7759/cureus.4126 ↵
- Modification, adaptation, and original content. Authored by : Wallis Back for Lumen Learning. Provided by : Lumen Learning. License : CC BY: Attribution
- A tale of mental illness . Authored by : Elyn Saks. Provided by : TED. Located at : https://www.youtube.com/watch?v=f6CILJA110Y . License : Other . License Terms : Standard YouTube License
- A Case Study of Acute Stimulant-induced Psychosis. Authored by : Ashley Henning, Muhannad Kurtom, Eduardo D. Espiridion. Provided by : Cureus. Located at : https://www.cureus.com/articles/17024-a-case-study-of-acute-stimulant-induced-psychosis#article-disclosures-acknowledgements . License : CC BY: Attribution
- Elyn Saks. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Elyn_Saks . License : CC BY-SA: Attribution-ShareAlike
- A case report of schizoaffective disorder with ritualistic behaviors and catatonic stupor: successful treatment by risperidone and modified electroconvulsive therapy. Authored by : Yuanhan Bai, Xi Yang, Zhiqiang Zeng, and Haichen Yangcorresponding. Located at : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851085/ . License : CC BY: Attribution

Case study: treatment-resistant schizophrenia
WELLCOME CENTRE HUMAN NEUROIMAGING/SCIENCE PHOTO LIBRARY
Learning objectives
After reading this article, individuals should be able to:
- Describe the management of schizophrenia;
- Understand pharmaceutical issues that occur during treatment with antipsychotics, especially clozapine ;
- Explain how the Mental Health Act 1983 impacts on care;
- Understand the importance of multidisciplinary and patient-centred care in managing psychosis.
Around 0.5–0.7% of the UK population is living with schizophrenia. Of these individuals, up to one-third are classified as treatment-resistant. This is defined as schizophrenia that has not responded to two different antipsychotics [1,2] .
Clozapine is the most effective treatment for such patients [3] . It is recommended by the National Institute for Health and Care Excellence (NICE)[4], and is the only licensed medicine for this patient group [4,5] . For treatment-responsive patients, there should be a collaborative approach when choosing a treatment [4] . More information on the recognition and management of schizophrenia can be found in a previous article here , and in accompanying case studies here .
This case study aims to explore a patient’s journey in mental health services during a relapse of schizophrenia. It also aims to highlight good practice for communicating with patients with severe mental illness in all settings, and in explaining the role of clozapine.
Case presentation
Mr AT is a male, aged 26 years, who has been diagnosed with paranoid schizophrenia. He moved to the UK with his family from overseas five years ago. He lives with his parents in a small flat in London. His mother calls the police after he goes missing, finding his past two months’ medication untouched.
He is found at an airport, attempting to go through security without a ticket. He is confused and paranoid about the police asking him to come with them.
He is taken to A&E and is medically cleared (see Box 1) [6] .
Box 1: Common differentials for psychotic symptoms
Medical conditions can present as psychosis. These include:
- Intoxication/effects of drugs (cannabis, stimulants, opioids, corticosteroids);
- Cerebrovascular disease;
- Temporal lobe epilepsy.
Mr AT’s history is taken by a psychiatrist, and his crisis plan sought (as per NICE recommendations) but he does not have one [7] .
He has been under the care of mental health services for two years and disputes his diagnosis of paranoid schizophrenia. He was admitted to a psychiatric hospital 18 months ago where he was prescribed the antipsychotic amisulpride at 600mg daily.
He is teetotal, smokes ten cigarettes a day and smokes cannabis every day. His BMI is 26 and he has hypercholesterolaemia (total cholesterol = 6.1mmol/L, reference range <5mmol/L) but all other tests are normal.
He has no allergies. His only medication is amisulpride 600mg each morning, which he does not take.
Medicines reconciliation
Mr AT is transferred to a psychiatric ward and placed under Section 2 of the Mental Health Act , allowing detention for up to 28 days for assessment and treatment (see Box 2).
Box 2: The Mental Health Act 1983
This legislation allows for the detention and treatment of patients with serious mental illness, where urgent care is required. This is often referred to as “sectioning”.
It includes regulations about treatment against a patient’s consent to safeguard patients’ liberty, which become more stringent with longer detentions.
Patients may only be given medication to treat their mental illness without their consent and may refuse physical health treatment.
He denies any mental illness and tells the team they are conspiring with MI6. He is visibly experiencing auditory hallucinations: seen by him talking to himself and looking to empty corners of the room. Amisulpride is re-prescribed at 300mg, which he declines to take.
A pharmacy technician completes a medicines reconciliation and contacts the care coordinator. The technician provides information about Mr AT’s treatment and feels he is still unwell as he has continued to express paranoid beliefs about his neighbours and MI6.
The ward pharmacist speaks to the patient. As per NICE guidance on medicines adherence , they adopt a non-judgemental attitude [8] . Mr AT is provided with information on the benefits and side effects of the medication and is asked open questions regarding his reluctance to take it. For more information on non-adherence to medicines and mental illness, see Box 3 [9] .
Box 3: Medicines adherence and mental health
Adherence to medication is similar for both physical and mental health medicines: only about 50% of patients are adherent.
Side effects and lack of involvement in decision making often lead to poor adherence.
In mental illness, other factors are:
- Denial of illness (poor ‘insight’);
- Lack of contact by services;
- Cultural factors, such as family, religious or personal beliefs around mental illness or medication.
Mr AT reports gynaecomastia and impotence, and says that he will not take any antipsychotics as they are “poison designed by MI6”, although is unable to concentrate on the discussion owing to hearing voices.
He is prescribed clonazepam 1mg twice daily owing to his distress, which is to be reduced as treatment controls his psychosis. He is offered nicotine replacement therapy but decides to use an e-cigarette on the ward.
He is unable to weigh up information to make decisions owing to his chaotic thinking and is felt to not have capacity to make decisions on his treatment. The team debates what treatment to offer.
Patient preference
Mr AT refuses all options presented to him. A decision is made to administer against his will and aripiprazole is chosen as it is less likely to cause hyperprolactinaemia and sexual dysfunction. He then agrees to take tablets “if it will get me out of hospital”.
![mental health schizophrenia case study Table 1: Common side effects of antipsychotics[9]](https://pharmaceutical-journal.com/wp-content/uploads/2022/01/clozapine-schizophrenia-Table-1-Common-side-effects-WM.jpg)
After eight weeks of treatment with orodispersible aripiprazole 15mg, Mr AT is able have a more coherent conversation, but is hallucinating and distressed. He is clearly under treated. The pharmacist attempts to complete a side-effect rating scale ( Glasgow Antipsychotic Side-effect Scale [GASS] ) but he declines. He is pacing around the ward in circles: it is felt he may be experiencing akathisia (restlessness) — a common side effect of antipsychotics (see Table 1 ).
Treatment review
The team feels clozapine is the best option owing to the treatment failure of two antipsychotics.
The team suggests this to Mr AT. He refuses, stating the ward is experimenting on him with new medication and he refuses to take another antipsychotics.
The pharmacist meets the patient with an occupational therapist to discuss what his goals are. Mr AT states he wants to go to college to become a carpenter. They discuss routes to achieve this, which all involve the first step of leaving hospital and the conclusion that clozapine is the best way to achieve this. The pharmacist clarifies the patient’s aripiprazole will not continue once clozapine is established. They leave information about clozapine with the patient and offer to return to discuss it further.
Mr AT agrees to take clozapine a week later (see Box 4) [10–14] . Aripiprazole is tapered and stopped.
Box 4: Clozapine characteristics
Clozapine significantly prolongs life and improves quality of life [10] . Delaying clozapine is associated with poorer outcomes for patients [11] .
Clozapine is under-prescribed owing to healthcare professionals’ anxiety and unfamiliarity around its use [12–14] .
It causes neutropenia in up to 3% of patients so regular monitoring is required . Twice-weekly monitoring is needed if neutrophils are <2 x10 9 /L. Most patients should stop clozapine if neutrophils are <1.5×10 9 /L. These ranges can differ from some laboratory definitions of neutropenia.
Other side effects include sedation, hypersalivation and weight gain. See Table 2 for red flags for serious side effects.
Clozapine is titrated up slowly to avoid cardiovascular complications. A treatment break of >48 hours warrants specialist advice for a retitration plan.
The pharmacist meets with Mr AT to discuss clozapine. He is told that this is likely to be a long-term treatment. The pharmacist acknowledges that the patient disagrees with his diagnosis, but this treatment is likely to prevent him from returning to hospital.
He is started on clozapine at 12.5mg at night, which is slowly increased. Pre- and post-dose monitoring of his vital signs is completed.
On day nine of the titration, his pulse is 115bpm. He otherwise feels well and blood tests show no signs of myocarditis (see Table 2), so the titration is continued but slowed.
After 3 weeks he is taking 150mg twice daily of clozapine and his symptoms have significantly improved: he is regularly bathing, not visibly hallucinating and engaging with staff.
The pharmacy technician completes a GASS form. Mr AT reports constipation, hypersalivation and sedation.
A pharmacist meets the patient to reiterate important counselling points, and discuss questions he may have about his treatment and how to manage side effects. Medication changes are made with the patients’ input:
- His constipation is monitored with a stool chart and he is started on senna 15mg at night;
- He is started on hyoscine hydrobromide 300 micrograms at night for salivation;
- He is switched to clozapine 300mg once daily at night to simplify his regime and reduce daytime sedation. His clonazepam is reduced and stopped.
Smoking is discussed owing to tobacco’s role as an enzyme inducer (more information on tobacco smoking and its potential drug interactions can be found in a previous article here ). Mr AT states he will continue to use an e-cigarette for now. He is informed that if he starts smoking again, his clozapine may become less effective and he should immediately inform his team.
He is discharged a few weeks later via a home treatment team and attends a clinic once weekly. On each attendance, he has a full blood count taken and analysed on site. He is assessed by a pharmacy technician and nurse for side effects and adherence to treatment, and his smoking status is clarified.
The technician asks what he thinks the clozapine has done for him. Mr AT states he is still unsure about having a mental illness, but recognises that clozapine has helped him out of hospital and intends to continue taking it.
![mental health schizophrenia case study Table 2: Red flags with clozapine[9]](https://pharmaceutical-journal.com/wp-content/uploads/2022/01/clozapine-schizophrenia-Table-2-Red-flags-with-clozapine-WM.jpg)
Good practice in the pharmaceutical care of psychosis involves:
- Active patient involvement in discussions on treatment decisions;
- Regular review of treatment: discussing efficacy, side effects and the patient’s view and understanding of treatment;
- Multidisciplinary approaches to helping patients choose treatment;
- For patients who dispute their diagnosis and the need for treatment, open dialogue is important. Such discussions should involve the patient’s goals, which are likely to be shared by the team (rapid discharge, preventing admissions, reducing distress);
- Information about treatment should be provided regularly in both written and verbal form;
- Where appropriate, involve carers/next of kin in decision making and information sharing.
Important points
- Schizophrenia affects 1 in 200 people, meaning such patients will present regularly in all settings;
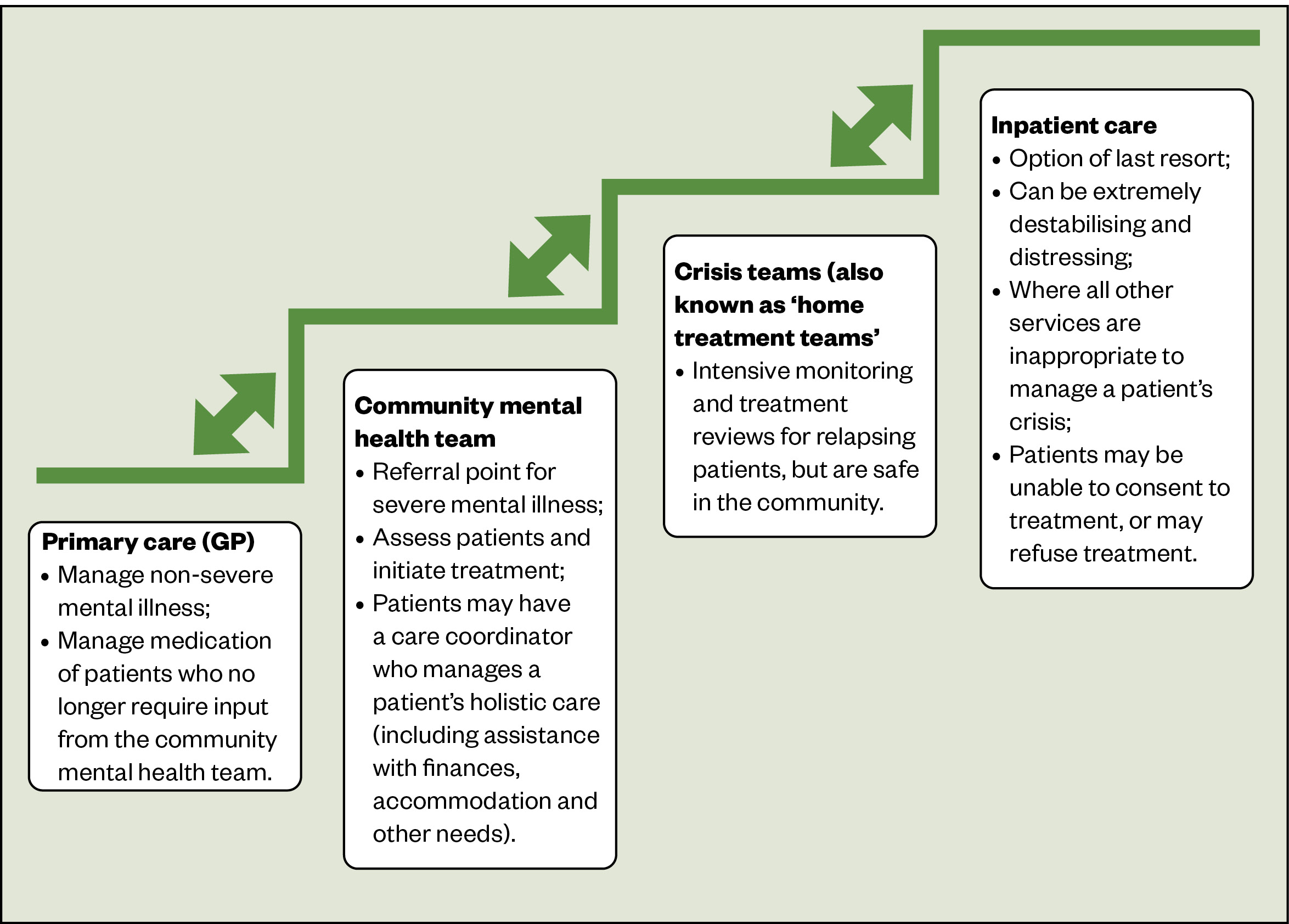
- Patients with acute psychosis, who are in recovery, may be managed by specialist teams, who are the best source of information for a patient’s care;
- Collaborating with the patient on a viable long-term treatment plan improves adherence;
- Clozapine is recommended where two antipsychotics have failed;
- Clozapine is a high-risk medicine, but the risks are manageable;
- Hydrocarbons produced by smoking (but not nicotine replacement therapy, e-cigarettes or chewing tobacco) induce the enzyme CYP1A2, which reduces clozapine levels markedly (up to 20–60%). Starting or stopping smoking could precipitate relapse or induce toxicity, respectively.
- 1 Conley RR, Kelly DL. Management of treatment resistance in schizophrenia. Biological Psychiatry. 2001; 50 :898–911. doi: 10.1016/s0006-3223(01)01271-9
- 2 Gillespie AL, Samanaite R, Mill J, et al. Is treatment-resistant schizophrenia categorically distinct from treatment-responsive schizophrenia? a systematic review. BMC Psychiatry. 2017; 17 . doi: 10.1186/s12888-016-1177-y
- 3 Taylor DM. Clozapine for Treatment-Resistant Schizophrenia: Still the Gold Standard? CNS Drugs. 2017; 31 :177–80. doi: 10.1007/s40263-017-0411-6
- 4 Psychosis and schizophrenia in adults: prevention and management. NICE. 2014. https://www.nice.org.uk/guidance/cg178/ (accessed Jan 2022).
- 5 Clozaril 25 mg tablets. Electronic medicines compendium. 2020. https://www.medicines.org.uk/emc/product/4411/smpc (accessed Jan 2022).
- 6 Psychosis and schizophrenia: what else might it be? NICE. 2020. https://cks.nice.org.uk/topics/psychosis-schizophrenia/diagnosis/differential-diagnosis/ (accessed Jan 2022).
- 7 Service user experience in adult mental health: improving the experience of care for people using adult NHS mental health services. NICE. 2011. https://www.nice.org.uk/guidance/cg136/ (accessed Jan 2022).
- 8 Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence . NICE. 2009. https://www.nice.org.uk/guidance/cg76/ (accessed Jan 2022).
- 9 Taylor D, Barnes T, Young A. The Maudsley Prescribing Guidelines in Psychiatry . 13th ed. Hoboken, New Jersey: : Wiley 2018.
- 10 Meltzer HY, Burnett S, Bastani B, et al. Effects of Six Months of Clozapine Treatment on the Quality of Life of Chronic Schizophrenic Patients. PS. 1990; 41 :892–7. doi: 10.1176/ps.41.8.892
- 11 Üçok A, Çikrikçili U, Karabulut S, et al. Delayed initiation of clozapine may be related to poor response in treatment-resistant schizophrenia. International Clinical Psychopharmacology. 2015; 30 :290–5. doi: 10.1097/yic.0000000000000086
- 12 Whiskey E, Barnard A, Oloyede E, et al. An Evaluation of the Variation and Underuse of Clozapine in the United Kingdom. SSRN Journal. 2020. doi: 10.2139/ssrn.3716864
- 13 Nielsen J, Dahm M, Lublin H, et al. Psychiatrists’ attitude towards and knowledge of clozapine treatment. J Psychopharmacol. 2009; 24 :965–71. doi: 10.1177/0269881108100320
- 14 Verdoux H, Quiles C, Bachmann CJ, et al. Prescriber and institutional barriers and facilitators of clozapine use: A systematic review. Schizophrenia Research. 2018; 201 :10–9. doi: 10.1016/j.schres.2018.05.046
- This article was corrected on 31 January 2022 to clarify that tobacco is an enzyme inducer, not an enzyme inhibitor
Useful structured introduction to the subject for clinical purposes
Thank you Amrit for your feedback, we are pleased that you found this article useful.
Michael Dowdall, Executive Editor, Research & Learning
Please note that smoking causes enzyme INDUCTION not INHIBITION as stated. (Via aromatic polyhydrocarbons, not nicotine)
Hi James. Thank you for bringing this to our attention. This has now been corrected. Hannah Krol, Deputy Chief Subeditor
Only with Herbal formula I was able to cure my schizophrenia Illness with the product I purchase from Dr Sims Gomez Herbs A Clinic in South Africa
Cancel reply
You must be logged in to post a comment.
You might also be interested in…

Test your knowledge on mental health

Pharmacist Support launches workplace wellbeing course for pharmacy leaders

Burnout among pharmacy professionals needs to be addressed at ‘systemic level’, RPS report finds

- Previous Article
- Next Article
INTRODUCTION
Clinical pearl i – pharmacokinetics, clinical pearl ii – clozapine and agranulocytosis, clinical pearl iii – hyperprolactinemia and associated complications, case based clinical pearls: a schizophrenic case study.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Guest Access
- Get Permissions
- Cite Icon Cite
- Search Site
O. Greg Deardorff , Stephanie A. Burton; Case Based Clinical Pearls: A schizophrenic case study. Mental Health Clinician 1 February 2012; 1 (8): 191–195. doi: https://doi.org/10.9740/mhc.n95632
Download citation file:
- Ris (Zotero)
- Reference Manager
Clinical pearls based on the treatment of a patient with schizophrenia who had stabbed a taxi cab driver are discussed in this case study. Areas explored include the pharmacokinetics of fluphenazine decanoate, strategies to manage clozapine-associated agranulocytosis, and approaches to addressing hyperprolactinemia.
Forensic psychiatry is a subspecialty in the field of psychiatry in which medicine and law collide. Practiced in many facilities such as hospitals, correctional institutions, private offices and courts, forensic psychiatry requires the cooperation of health care and legal professionals with the common goal of helping patients become competent of their legal charges and returning to a productive life in the community. In contrast to general psychiatric patients, the clients in this field have been referred through court systems instead of general practitioners and are evaluated not only for their symptoms but also their level of responsibility for their actions.
These patients can be some of the most challenging to treat because of factors such as non-compliance, an extensive history of failed medication trials, and the severity of their mental illness. Some of the most severe mentally ill patients reside in forensic psychiatric hospitals and have spent much of their lives institutionalized. Treatment refractory schizophrenia, defined as persistent psychotic symptoms after failing two adequate trials of antipsychotics, is a common occurrence in forensic psychiatric hospitals and often requires extensive manipulation of medication regimens to obtain a desired therapeutic response. Like other patients, these patients may present with barriers to using the most effective treatment such as agranulocytosis, inability to obtain and maintain therapeutic drug levels due to fast metabolism, or bothersome adverse effects such as hyperprolactinemia. In treatment resistant patients, it may still be necessary to use these medications even when barriers are present due to a lack of alternative therapeutic options not previously exhausted. In addition to complex regimens, treatment plans for these patients often require trials of multiple medication combinations or unique exploitation of interactions and biological phenomena.
We report a forensic case study that exemplifies multiple clinical pearls that may be useful in patients with treatment refractory schizophrenia. A 31-year-old African American female presented to the emergency room escorted by law enforcement after stabbing a cab driver with a pencil. The patient stated she was raped by the cab driver and while in the emergency room stated that “dirty cops brought me here.” She was admitted to the inpatient psychiatric unit to determine competency to stand trial for the assault of the cab driver. She had been in many previous correctional institutions with a known history of schizophrenia and additional diagnoses of amenorrhea, hyperprolactinemia, and obesity.
The patient's history was significant for auditory hallucinations and paranoid delusions beginning by age fourteen with a diagnosis of major depression with psychotic features. By age eighteen, she was diagnosed with schizophrenia, paranoid type. She had multiple previous hospitalizations and a history of poor compliance as an outpatient. There was no known history of tobacco, alcohol, or illicit drug use. Her family history was significant for schizophrenia, diabetes mellitus, and drug use. The patient reported abusive behavior by her grandmother, who was her primary caretaker as a child.
During hospitalization, the patient continued to report sexual assaults, accusing both patients and staff of rape, and declined to participate in groups. She denied any visual or auditory hallucinations but continued to exhibit paranoid delusions. The patient was later found to be permanently incompetent to stand trial and was committed to the state's department of mental health for long term treatment of her psychiatric illness.
The patient was previously treated with fluphenazine decanoate intermittently for two years with difficulty obtaining the desired therapeutic response. After approximately two months of therapy, the patient presumably at steady state (~14 day half-life) still failed to demonstrate any clinical response. There is no conclusive evidence that fluphenazine levels correlate with clinical outcomes, however the psychiatrist had worked with this patient in the past and felt the lack of response in this situation justified a fluphenazine level. 1 The fluphenazine level was shown to be 2.2ng/ml (therapeutic range 0.5–3 ng/ml) while taking fluphenazine decanoate 50mg intramuscularly (IM) every two weeks. Increasing the target drug level to the upper edge of the normal range was warranted in this patient due to the persistent positive symptoms and a desire to continue using a long-acting injectable agent, which can ensure the delivery of medication in uncooperative and noncompliant patients. Fluphenazine is a high potency first generation antipsychotic that can improve positive symptoms of schizophrenia; however it is not effective in treating the negative symptoms. It was decided that the addition of a CYP2D6 inhibitor such as fluoxetine would not only provide increased levels of fluphenazine, but would also improve the patient's negative symptoms such as flat affect, anhedonia, social isolation and amotivation. 2 Thus, fluoxetine was given as 20 mg orally (PO) daily resulting in an increase of the fluphenazine level by 0.9 ng/ml (40%) after twenty two days of therapy to 3.1 ng/ml. One month later the fluphenazine decanoate dose was increased to 125 mg IM every two weeks (max 100mg/dose), with continued fluoxetine treatment, resulting in a supratherapeutic level of 3.6 ng/ml. Positive and negative symptoms only showed minor improvement. A 6-week study by Goff, et al. demonstrated an increase of up to 65% in fluphenazine serum concentrations in patients administered concomitant fluoxetine 20 mg/day. 2 In this case, the addition of fluoxetine safely and effectively elevated fluphenazine blood levels. Addition of an inhibitor may be beneficial in patients who are CYP2D6 ultra-rapid metabolizers, as was suspected in this patient.
Many complications, including prolonged jail time, can arise from forensic clients being non-compliant with their medications, which is the reason long acting injectables are often warranted. Our patient had a history of non-compliance and continued to experience positive symptoms despite treatment with fluphenazine. Therefore, the decision was made to try another long-acting antipsychotic injection. After reviewing the patient's chart, it was noted that a previous trial of oral haloperidol 30mg/day showed moderate improvement. Thus, after tolerability and efficacy was determined with oral haloperidol the patient was converted to haloperidol decanoate 300 mg (10–15 x oral daily dose of haloperidol) administered every three weeks beginning two weeks after discontinuation of fluphenazine decanoate 125 mg IM every two weeks. Fluphenazine levels approximately six weeks after its discontinuation (and two weeks after the discontinuation of fluoxetine 20 mg PO daily) were still supratherapeutic. Given that this patient had a fluphenazine level of 3.6 ng/ml near the time of haloperidol decanoate administration, it would be questionable whether another high potency antipsychotic would be of any additional benefit in comparison to the increased risk of extrapyramidal side effects (EPS). Data provided in one study showed fluphenazine decanoate as being detectable for up to 48 weeks after discontinuation. 3 Because fluphenazine decanoate can be detected for such an extended period of time, it leaves the patient at a continued risk for extrapyramidal side effects, especially if another antipsychotic is added shortly thereafter. In the forensic population, many patients have treatment refractory schizophrenia and the use of antipsychotics will need to be life-long. It is often common for these patients to be on multiple concurrent agents, increasing the risk for developing long-term extrapyramidal side effects. Therefore, it is important to minimize the risk of these symptoms whenever possible.
Despite supratherapeutic levels of fluphenazine, the psychiatrist felt it would be beneficial to continue haloperidol decanoate 300 mg every three weeks with increased monitoring for signs and symptoms of EPS.
During the current admission the patient continued to exhibit paranoid behavior and lack of insight, expressed anger, and disliked attending or participating in groups. Her medication history included haloperidol, fluphenazine, quetiapine, aripiprazole, asenapine, olanzapine, paliperidone, and sixteen days of clozapine therapy before leukopenia warranted discontinuation. Due to her extensive history of failed antipsychotics and the known superior effectiveness of clozapine, this patient was an ideal candidate for clozapine therapy. Additionally, because of the poor quality of life a declaration of incompetency would lead to, using the most effective possible agent is an important priority in forensic patients. Clozapine is the most effective antipsychotic based on the U.S. Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) and the UK Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS). 4 , 5 In regards to the significant blood draws and monitoring that is continuously required, clozapine can be a challenging medication to use in treatment refractory patients.
One strategy we are currently working on in our hospital to help increase the number of patients on clozapine is using a point of care (POC) lab device which will allow a complete blood count (CBC) plus 5-part differential to be completed by finger stick, instead of weekly blood draws that our nurses, physicians and, especially, patients dislike. The cost of the POC lab device is approximately $20,000, although upon completion of a cost analysis it was found that five CBCs per day would pay for the cost of the machine after one year. Many times, these patients can become irritated and violent when having their blood drawn, especially, if on a consistent basis. Repetitive blood draws was noted by our physicians to be the largest obstacle in using clozapine in our treatment refractory patients.
Our primary challenge in using clozapine for this patient was finding a way to maintain the absolute neutrophil count (ANC) within acceptable limits (≥1500mm 3 ), which is not uncommon for many patients. The Clozaril Patient Monitoring Services revealed 0.4% of patients had pre-treatment white blood cell counts (WBC) too low to allow initiation of clozapine. Of these patients, 75% were of African or African-Caribbean descent, likely due to the increased leukocyte marginalization that has been shown to be more prominent in these populations. 6 Of all neutrophils in the body, 90% reside in the bone marrow and the remainder circulates freely in the blood or deposit next to vessel walls (margination). The addition of lithium has been shown to increase neutrophil counts by 2000/mm 3 through demarginalization of leukocytes. 7 This increase is not dose –related but may require a minimum lithium level of 0.4 mmol/L. 8 , 9 Lithium therapy used to increase neutrophil counts may be especially effective in patients of African or African-Caribbean descent due to demarginalization of leukocytes. In this patient case, lithium 300 mg by mouth three times daily was initiated for fifteen days to increase the absolute neutrophil count from 1200/mm 3 to ≥ 1500/mm 3 for continuation of clozapine while the white blood cells continued to stay within appropriate limits of ≥3000/mm 3 . It was soon realized that lithium was being cheeked, so liquid form was given, but discontinued after the patient continued to spit the medication out. Unfortunately, clozapine was discontinued thereafter as a result of noncompliance with the lithium causing failure to maintain appropriate white blood cell counts.
Another possible strategy for obtaining appropriate WBC and ANC levels that would enable clozapine continuation is to obtain blood samples later in the day. A study recently published compared the same set of patients having early morning blood draws to blood draws taken later in the day (mean sampling time - pre/post was 5 hours 24 minutes). 10 They showed a difference in the pre/post time change in WBC values being marginally significant (mean increase=667/mm 3 , p=.07), with a significant difference (mean increase=1,130/mm 3 , p=.003) between the pre/post time change in ANC values. ANC values were impacted to a greater extent by the time change than WBC values in this sample. Changing the time at which blood draws are taken during the day may allow for clozapine continuation by limiting the risk of pseudoneutropenia, however it remains the clinician's responsibility to discern between benign or malignant neutropenia. 10 It is recommended, for patients with WBC values trending down or below the predefined criteria, to have labs redrawn several hours after the morning lab before clozapine therapy is discontinued. 10 In this case study, obtaining the sample later in the day may have allowed our patient to continue clozapine therapy.
The patient in this case had additional diagnoses of amenorrhea and hyperprolactinemia. The diagnosis of amenorrhea prompted clinicians to obtain labs showing a prolactin level of 168.8 ng/ml (normal ranges: 3–20ng/ml for men; 4–25ng/ml for non-pregnant women; 30–400ng/ml for pregnant women). Lab monitoring of prolactin levels is not necessary if the patient is not exhibiting symptoms such as disturbances in the menstrual cycle, galactorrhea, gynecomastia, retrograde ejaculation, impotence, oligospermia, short luteal phase syndrome, diminished libido or hirsutism. Monitoring guidelines published in 2004 by APA recommend screening for symptoms of hyperprolactinemia at each visit for the first year and then yearly thereafter. Mt. Sinai Conference Physical Health Monitoring Guidelines for Antipsychotics published in 2004 recommended monitoring at every visit for the first twelve weeks and then yearly.
Occasionally, practitioners are confronted with the dilemma of whether treatment of hyperprolactinemia is warranted in asymptomatic patients. In answering that question, a few things should be considered, such as the patient's risk for osteoporosis and/or cardiovascular disorders. If there are no physical issues of concern, then psychological issues should be addressed. Estrogen deficiency, which may occur with increased prolactin, mediates mood, cognition and psychopathology. 11 Results of several studies conducted in women with hyperprolactinemia have demonstrated increased depression, anxiety, decreased libido and increased hostility. Men shared similar problems but did not exhibit an increase in hostility. 12 The authors hypothesized that women demonstrated increased hostility as a protective mechanism for their offspring.
Antipsychotic medications have differing potencies in regards to hyperprolactinemia, which may help guide product selection. The most potent inducer is risperidone, followed by haloperidol, olanzapine, and ziprasidone. 13 Clozapine and quetiapine are truly sparing, and aripiprazole has even been shown to reduce prolactin levels. 14 Aripiprazole may be a viable treatment option in some patients with hyperprolactinemia. In one study, females with risperidone induced hyperprolactinemia taking therapeutic doses of risperidone 2 to 15 mg/day showed significantly lower prolactin levels from weeks 8 to 16 compared to baseline when administered aripiprazole (3, 6, 9, or 12 mg daily). 15 The mean percent reductions in prolactin concentration at 3, 6, 9, and 12 mg daily were approximately 35%, 54%, 57%, and 63%; however, there was little variability in prolactin levels above 6 mg daily of aripiprazole. Therefore, unless giving liquid form, aripiprazole 5mg daily should be an optimal dose in lowering prolactin levels. In this case, the patient exhibited the clinical symptom of amenorrhea, which correlated with an elevated prolactin level. The addition of aripiprazole 10 mg by mouth once daily decreased this patient's prolactin level by 51 ng/mL (30.3%) after twelve days of treatment.
If an elevated prolactin level is incidentally found, the patient should be monitored for symptoms and labs may be repeated. In patients exhibiting symptoms of hyperprolactinemia with a serum level <200 ng/mL, the antipsychotic dose should be reduced or the agent changed to a more prolactin-sparing drug. 13 If switching the agent is not reasonable, the addition of a dopamine agonist such as bromocriptine or cabergoline may be beneficial, as well as the antiviral agent amantadine. 16 In patients with levels >200 ng/mL, or with persistently elevated levels despite changing to a more prolactin-sparing agent, an MRI of the sella turcica should be obtained to rule out a pituitary adenoma or parasellar tumor. 13 Practitioners should be aware that prolactin levels may remain elevated for significant periods of time following discontinuation of a long acting causative agent due to continued D 2 receptor antagonism. 1 One study found elevated prolactin levels in patients who discontinued fluphenazine decanoate as much as six months after the last injection. 1 , 3
In summary, we have discussed a few clinical pearls to be considered when working with treatment refractory patients with schizophrenia and outlined some unique aspects of treatment in forensic clients. First, we reviewed potential complications and concerns with using fluphenazine decanoate. In addition, we discussed that ultra-rapid CYP2D6 metabolizers may need an increase in dose when appropriate and/or an addition of an inhibitor. Secondly, patients with agranulocytosis that may benefit from clozapine may find improvement in WBC and ANC values with the administration of lithium and/or changing the time of day in which labs are drawn.
Lastly, hyperprolactinemia may result in not only physical symptoms but psychological symptoms as well. Also, health care providers should not only be cognizant regarding how and when to monitor for hyperprolactinemia, but also the various treatment options available, such as changing to less offensive agents, dopamine agonists, or adding low dose aripiprazole. This patient case exemplified multiple strategies that can be considered when managing treatment refractory patients in which alternative options for therapy are not readily available.
Recipient(s) will receive an email with a link to 'Case Based Clinical Pearls: A schizophrenic case study' and will not need an account to access the content.
Subject: Case Based Clinical Pearls: A schizophrenic case study
(Optional message may have a maximum of 1000 characters.)
Citing articles via
Get email alerts.
- Advertising
- Permissions
Affiliations
- eISSN 2168-9709
- Privacy Policy
- Get Adobe Acrobat Reader
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Schizophrenia
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may seem like they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective treatments are available. Learn more about schizophrenia .
Join A Study
For opportunities to participate in NIMH research on the NIH campus, visit the clinical research website . Travel and lodging assistance may be available.
Featured Studies
Featured studies include only those currently recruiting participants . Studies with the most recent start date appear first.
Anti-Inflammatory Challenge in Schizophrenia
Study Type: Interventional Start Date: March 31, 2024 Eligibility: 18 Years to 45 Years, Does Not Accept Healthy Volunteers Location(s): Grady Memorial Hospital, Atlanta, Georgia, United States; Emory University Hospital, Atlanta, Georgia, United States
This research project will explore negative symptoms of schizophrenia, such as motivational deficits, by examining the relationship between inflammation and reward-related brain regions. To accomplish this, we will administer a single infusion of either the anti-inflammatory medication infliximab or placebo (n=10 per group) to patients with high inflammation.
This study is important because schizophrenia can be a chronic and debilitating neuropsychiatric disorder and negative symptoms are some of the most difficult aspects of schizophrenia associated with worst functional outcomes. These symptoms do not typically respond to antipsychotic therapies, and as such, there are no current medications to treat negative symptoms.
Young Adults With Violent Behavior During Early Psychosis
Study Type: Interventional Start Date: February 29, 2024 Eligibility: 16 Years to 30 Years, Does Not Accept Healthy Volunteers Location(s): New York State Psychiatric Institute, New York, New York, United States
This study aims to provide an evidence-based behavioral intervention to reduce violent behavior for individuals experiencing early psychosis.
Tau Biomarkers in Late-onset Psychosis (LOP)
Study Type: Observational Start Date: February 16, 2024 Eligibility: 65 Years to 85 Years Location(s): The Feinstein Institutes for Medical Research, Manhasset, New York, United States
Hallucinations or delusions that occur for the first time in older people with no acute medical problems or mood symptoms may be related to impending dementia. This study aims to confirm this hypothesis using novel blood biomarkers and Positron Emission Tomography (PET) imaging tracers, as well as non-invasive testing.
Enhanced Coordinated Specialty Care for Early Psychosis
Study Type: Interventional Start Date: February 1, 2024 Eligibility: Age N/A, Does Not Accept Healthy Volunteers Location(s): McLean Hospital OnTrack Clinic, Belmont, Massachusetts, United States; Massachusetts General Hospital FEPP Clinic, Boston, Massachusetts, United States
The goal of this clinical trial is to compare engagement in treatment in coordinated specialty care (CSC) to five extra care elements (CSC 2.0) in first-episode psychosis. The main question it aims to answer is:
• Does the addition of certain elements of care increase the number of visits in treatment for first-episode psychosis?
Participants will either:
Receive care as usual (CSC) or
Receive care as usual (CSC) plus five additional care elements (CSC 2.0):
Individual peer support Digital outreach Care coordination Multi-family group therapy Cognitive remediation
Researchers will compare the standard of care (CSC) to CSC 2.0 to see if participants receiving CSC 2.0 have more visits to their clinic in their first year.
Accelerated Transcranial Magnetic Stimulation for People With Schizophrenia Treated With Clozapine
Study Type: Interventional Start Date: December 1, 2023 Eligibility: 18 Years to 50 Years, Does Not Accept Healthy Volunteers Location(s): UPMC Western Psychiatric Hospital/University of Pittsburgh, Pittsburgh, Pennsylvania, United States
In this study, the investigators will examine whether a type of repetitive transcranial magnetic stimulation called accelerated intermittent theta burst stimulation (iTBS) can augment neurocognition in individuals who receive treatment with clozapine. Following a baseline evaluation and magnetic resonance imaging (MRI), participants will undergo a session of iTBS +MRI and session of sham delivery + MRI. The order for these sessions will be blinded and randomized. The investigators predict that accelerated iTBS will enhance neurocognition relative to sham delivery.
Auditory Control Enhancement (ACE) in Schizophrenia
Study Type: Interventional Start Date: September 5, 2023 Eligibility: 18 Years to 40 Years, Does Not Accept Healthy Volunteers Location(s): Western Psychiatric Hospital of UPMC, Pittsburgh, Pennsylvania, United States
The purpose of this clinical trial is to investigate neural markers of target engagement to further develop auditory control enhancement (ACE) as a novel, inexpensive, and noninvasive intervention to address treatment-refractory auditory hallucinations. Here, we will address questions about the feasibility and acceptability of ACE, as well as the degree to which ACE results in measurable engagement of biophysical and neurophysiological targets.
Participants will complete:
Auditory Control Enhancement (ACE): Participants will be assigned by chance (such as a coin flip) into one of two groups to receive a different dosage or level of transcranial direct current stimulation (tDCS) during three sessions of cognitive training. tDCS is used to stimulate the brain for a short period of time. For tDCS one or two thin wet sponges are placed on the head and/or upper arm. The sponges will be connected to electrodes which will deliver a very weak electrical current. The Neuroelectrics Starstim 32 will be used to deliver tDCS. Interviews: Before and after ACE, in two separate sessions, participants will be asked questions about a) background; b) functioning in daily life and across different phases of your life and past, present and future medical records. Cognitive Tests: During the interview sessions, participants will also perform cognitive tests. Participants will be asked to complete computerized and pen-and-paper tests of attention, concentration, reading, and problem-solving ability. EEG scan: Participants will be asked to complete EEG (electroencephalography) studies before and after ACE training. EEG will be measured using the same Neuroelectrics Starstim 32 system used for tDCS. EEG measures the natural activity of the brain using small sensors placed on the scalp. These sensors use conductive gel to provide a connection suitable for recording brain activity. During EEG, participants will watch a silent video while sounds are played over headphones, or sometimes count the sounds. In addition to these auditory tasks, participants will also be asked to perform visual attention tasks, such pressing a button for a letter or image. Magnetic Resonance Imaging (MRI) Scan: Participants will also be asked to complete MRI studies before and after ACE training. An MRI is a type of brain scan that takes pictures of the brain that will later be used to create a 3D model of the brain. The MRI does not use radiation, but rather radio waves, a large magnet and a computer to create the images.
Researchers will compare individuals receiving ACE to those receiving sham tDCS during cognitive training to determine effects of ACE.
Restoring Spindle and Thalamocortical Efficiency in Early-Course Schizophrenia Patients Using Auditory Stimulation
Study Type: Interventional Start Date: July 20, 2023 Eligibility: 18 Years to 40 Years, Accepts Healthy Volunteers Location(s): University of Pittsburgh, Pittsburgh, Pennsylvania, United States
The purpose of this research is to identify differences in brain activity during sleep between health individuals and individuals with schizophrenia, schizophreniform, or schizoaffective disorder. This study will also investigate whether tones played during deep sleep can enhance specific features of sleep and whether enhancing such features is related to an improvement in cognitive performance.
EPI-MINN: Targeting Cognition and Motivation - National
Study Type: Interventional Start Date: May 30, 2023 Eligibility: 15 Years to 40 Years, Does Not Accept Healthy Volunteers Location(s): University of Minnesota Department of Psychiatry & Behavioral Sciences, Minneapolis, Minnesota, United States
The purpose of this study is to perform a practice-based research project designed to assess whether cognition and motivated behavior in early psychosis can be addressed as key treatment goals within real-world settings by using a 12-week mobile intervention program. Participants who are receiving care at coordinated specialty care (CSC) early psychosis clinics across the United States will be recruited to participate in this study. A qualifying CSC program will provide comprehensive clinical services such as psychotherapy, medication management, psychoeducation, and work or education support. This study will be conducted remotely, and participants can participate at home with their own electronic devices.
The aim of this study is to investigate a well-defined 12-week mobile intervention program specifically designed to target cognitive functioning and motivated behavior for individuals with early psychosis. Participants will complete a screening interview which will include diagnosis and symptom ratings, neurocognitive assessment, and self-reports of symptoms, behavior, and functioning. Then participants will be randomized to receive the 12-week mobile intervention, or an active control of treatment as usual. The investigators will test for differences in the clinical trajectories after training, and at two follow up appointments at 6 and 12 months post-training.
Improving Cognition Through Telehealth Aerobic Exercise and Cognitive Training After a First Schizophrenia Episode
Study Type: Interventional Start Date: May 23, 2023 Eligibility: 18 Years to 45 Years, Does Not Accept Healthy Volunteers Location(s): UCLA Aftercare Research Program, Los Angeles, California, United States
The participants in the study will receive psychiatric treatment at the UCLA Aftercare Research Program. All participants in this 12-month RCT will receive cognitive training. Half of the patients will also be randomly assigned to the aerobic exercise and strength training condition, and the other half will be randomly assigned to the Healthy Living Group condition. The primary outcome measures are improvement in cognition and level of engagement in the in-group and at-home exercise sessions. Increases in the level of the patient's serum brain-derived neurotropic factor (specifically Mature BDNF) which causes greater brain neuroplasticity and is indicator of engagement in aerobic exercise, will be measured early in the treatment phase in order to confirm engagement of this target. In order to demonstrate the feasibility and portability of this intervention outside of academic research programs, the interventions will be provided via videoconferencing. The proposed study will incorporate additional methods to maximize participation in the exercise condition, including the use of the Moderated Online Social Therapy (MOST) platform to enhance motivation for treatment based on Self-Determination Theory principles, and a "bridging" group to help the participants generalize gains to everyday functioning. In addition, the exercise group participants will receive personally tailored text reminders to exercise.
Deep Brain Stimulation in Treatment Resistant Schizophrenia
Study Type: Interventional Start Date: March 1, 2023 Eligibility: 22 Years to 65 Years, Does Not Accept Healthy Volunteers Location(s): The Johns Hopkins Hospital, Baltimore, Maryland, United States
The purpose of this pilot study is to investigate the use of deep brain stimulation (DBS) of the substantia nigra pars reticulata (SNr) in subjects with treatment-resistant schizophrenia. There is a subset of patients with schizophrenia who continue to have persistent psychotic symptoms (auditory hallucinations and delusions) despite multiple adequate medication trials with antipsychotic medications including clozapine. There are currently no available treatments for such patients who generally have poor function and are chronically disabled, unable to work, live independently or have meaningful social relationships. Neuroimaging studies in patients with schizophrenia have revealed information about pathological neural circuits that could be suitable targets using deep brain stimulation. Although not yet tested in patients with schizophrenia, DBS is in early phase clinical trials in other psychiatric disorders.
This pilot study will investigate the use of DBS in treatment-resistant schizophrenia subjects who have exhausted all other therapeutic alternatives but continue to have persistent disabling psychotic symptoms. Of note, DBS is not FDA approved for use in patients with schizophrenia. The method will be similar to that used in subthalamic nucleus stimulation in patients with Parkinson's Disease. However, the electrode will be advanced slightly inferior into the SNr, a major outflow nucleus of the basal ganglia, with the intention of causing local inhibition of SNr outflow resulting in disinhibition of the mediodorsal nucleus (MDN) of the thalamus. Hypofunction of the MDN has been implicated in the pathophysiology of schizophrenia in post-mortem as well as multiple structural and functional imaging studies. Evidence suggests that dysfunction of the MD is implicated in both positive and cognitive symptoms (such as working memory impairment) in schizophrenia. Frequent monitoring and clinical assessment with psychiatric scales will be used to monitor treatment response.
Song-making In a Group (SING)
Study Type: Interventional Start Date: October 14, 2022 Eligibility: 18 Years to 65 Years, Does Not Accept Healthy Volunteers Location(s): Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut, United States
The overarching aim of the proposed work is to align a promising treatment lead - Musical Intervention (MI) - with a promising mechanistic account of psychosis - Predictive Processing. This protocol focuses on the R33 phase, to optimize its administration (Is active participation more effective than passive listening? Does creation of new music help more than performing others' creations?). By tracking the interrelation between symptom mechanisms and MI, the investigators can use those metrics to prospectively assign patients to particular MI.
The R33 phase will examine the impact of SING on computational behavioral metrics of (Aim 1) Conditioned Hallucinations, (Aim 2) Social Reinforcement Learning, (Aim 3) Language Use, in 200 participants with voice hearing in the context of a psychotic illness (n=50per per group). Following a screening visit to determine eligibility, these computerized tasks will be administered behaviorally, and an interview will elicit speech, prior to and following the full SING intervention (in 10 groups of 5 participants, each facilitated by a trained musical interventionist, during the first two years of the project).
Participants will complete these tasks prior to and following randomization to four different conditions (facilitated by a SING team member) that will deconstruct the possible active ingredients of SING along two dimensions: Activity and Ownership: (a) SING (n=50, Activity + and Ownership +), participants produce and perform their own song; (b) Karaoke (n=50, Activity + and Ownership -), participants perform karaoke, singing along to others music; (c) Pop Music (n=50, Activity - and Ownership -), participants will listen to popular music chosen by the music interventionists; and (d) Curated Playlists (n=50, Activity -, Ownership +), participants will curate playlists of popular music and listen to them together.
This deconstruction will provide insights into the predictive processing framework, as applied to hallucinations and music, specifically, whether changes at higher, a-modal, hierarchical levels, particularly sense of self and active inference, influence precision weighted perceptual and social inferences more so than inactive experiences or experiences that do not engage sense of self.
This R33 portion of the study was originally included in NCT05537428, which now has results posted for the R61 phase of the study.
What the Nose Knows: Hedonic Capacity, Psychosocial Interventions and Outcomes in Schizophrenia
Study Type: Interventional Start Date: September 2, 2022 Eligibility: 18 Years to 65 Years, Does Not Accept Healthy Volunteers Location(s): Beth Israel Deaconess Medical Center, Boston, Massachusetts, United States
This project proposes to conduct the first study of the predictive utility of olfactory hedonic measurement for targeted psychosocial rehabilitation in schizophrenia. The information gathered from the project is of considerable public health relevance, in that, through simple, reliable olfactory assessment, it will provide knowledge about which individuals are most likely to benefit from these psychosocial interventions. Such information is crucial for tailoring existing interventions and developing new approaches to optimize outcomes in schizophrenia.
State Representation in Early Psychosis - Project 4
Study Type: Interventional Start Date: July 31, 2022 Eligibility: 15 Years to 45 Years, Accepts Healthy Volunteers Location(s): University of Minnesota, Minneapolis, Minnesota, United States
The purpose of this study is to examine state representation in individuals aged 15-45 who have been diagnosed with a psychotic illness, as well as young adults who do not have a psychiatric diagnosis. State Representation is our ability to process information about our surroundings. The investigators will complete a clinical trial examining two paradigms of cognitive training.
Remote State Representation in Early Psychosis
Study Type: Interventional Start Date: July 27, 2022 Eligibility: 18 Years to 30 Years, Does Not Accept Healthy Volunteers Location(s): University of Minnesota, Minneapolis, Minnesota, United States
The purpose of this study is to examine state representation in individuals aged 15-40 who have been diagnosed with a psychotic illness, as well as young adults who do not have a psychiatric diagnosis. State Representation is our ability to process information about our surroundings. The investigators will complete some observational tests as well as a cognitive training clinical trial.
Clozapine for the Prevention of Violence in Schizophrenia: a Randomized Clinical Trial
Study Type: Interventional Start Date: March 17, 2022 Eligibility: 18 Years to 65 Years, Does Not Accept Healthy Volunteers Location(s): New York State Psychiatric Institute, New York, New York, United States
Two-hundred and eighty individuals with schizophrenia who have a recent history of violent acts will be randomized in this 2-arm, parallel-group, 24-week, open-label, 7-site clinical trial to examine the effects of treatment with clozapine vs antipsychotic treatment as usual (TAU) for reducing the risk of violent acts in real-world settings
Academic-Community EPINET (AC-EPINET)
Study Type: Interventional Start Date: March 16, 2022 Eligibility: 16 Years to 35 Years, Does Not Accept Healthy Volunteers Location(s): Strong Ties Young Adults Program- University of Rochester Medical Center, Rochester, New York, United States; Program for Risk Evaluation and Prevention (PREP) - University of Michigan, Ann Arbor, Michigan, United States; Early Psychosis Intervention Clinic-New Orleans (EPIC-NOLA) - Tulane University, New Orleans, Louisiana, United States; Prevention and Recovery Center for Early Psychosis, Indianapolis, Indiana, United States; Vanderbilt's Early Psychosis Program - Vanderbilt University, Nashville, Tennessee, United States; The Early Psychosis Intervention Center (EPICENTER) at Ohio State, Columbus, Ohio, United States
The investigators propose to examine the effects of CSC services delivered via TH (CSC-TH) versus the standard clinic-based CSC model (CSC-SD) on engagement and outcomes in a 12-month, randomized trial.
Antipsychotic Response to Clozapine in B-SNIP Biotype-1 (Clozapine)
Study Type: Interventional Start Date: March 1, 2022 Eligibility: 18 Years to 60 Years, Does Not Accept Healthy Volunteers Location(s): UT Southwestern Medical Center, Dallas, Texas, United States
The CLOZAPINE study is designed as a multisite study across 5 sites and is a clinical trial, involving human participants who are prospectively assigned to an intervention. The study will utilize a stringent randomized, double-blinded, parallel group clinical trial design. B2 group will serve as psychosis control with risperidone as medication control. The study is designed to evaluate effect of clozapine on the B1 participants, and the effect that will be evaluated is a biomedical outcome. The study sample will be comprised of individuals with psychosis, including 1) schizophrenia, 2) schizoaffective disorder and 3) psychotic bipolar I disorder. The investigators plan to initially screen and recruit n=524 (from both the existing B-SNIP library and newly-identified psychosis cases, ~50% each) in order to enroll n=320 (B1 and B2) into the RCT.
State Representation in Early Psychosis
Study Type: Interventional Start Date: December 1, 2021 Eligibility: 15 Years to 45 Years, Accepts Healthy Volunteers Location(s): University of Minnesota, Minneapolis, Minnesota, United States
The purpose of this study is to examine state representation in individuals aged 15-45 who have been diagnosed with a psychotic illness, as well as young adults who do not have a psychiatric diagnosis. State Representation is our ability to process information about our surroundings. The investigators will complete some observational tests as well as a cognitive training clinical trial.
Enhancing Prefrontal Oscillations and Working Memory in Early-course Schizophrenia
Study Type: Interventional Start Date: November 5, 2021 Eligibility: 18 Years to 40 Years, Does Not Accept Healthy Volunteers Location(s): University of Pittsburgh, Pittsburgh, Pennsylvania, United States
This study will investigate the effects of intermittent Theta Burst Stimulation (iTBS) on natural oscillatory frequency of the dorsolateral prefrontal cortex (DLPFC) and working memory in early-course schizophrenia (EC-SCZ). Transcranial magnetic stimulation (TMS) will be used to evoke oscillatory activity, and EEG will record the responses of EC-SCZ participants. A working memory task will also be incorporated in order to determine how DLPFC natural frequency (NF) is related to working memory performance. iTBS (active or sham) will be administered, then the oscillatory activity of DLPFC and working memory performance will be reassessed. The overarching goal is to determine whether iTBS can acutely enhance the oscillatory activity of the DLPFC and to evaluate the relationship between changes in the DLPFC and working memory performance.
Targeting Processing Speed Deficits to Improve Social Functioning and Lower Psychosis Risk
Study Type: Interventional Start Date: October 28, 2021 Eligibility: 14 Years to 20 Years, Does Not Accept Healthy Volunteers Location(s): Northwell Health- The Zucker Hillside Hospital, Glen Oaks, New York, United States
This 10 week intervention, Specific Cognitive Remediation with Surround (or SCORES), is designed to target processing speed, a cognitive domain related directly to social functioning, which in turn, represents a vulnerability factor for psychosis. This remotely-delivered intervention combining targeted cognitive training exercises and group support was developed to directly impact processing speed, and at the same time, boost motivation and engagement in adolescents at risk for schizophrenia and other psychotic disorders.
Using Transcranial Magnetic Stimulation (TMS) to Understand Hallucinations in Schizophrenia
Study Type: Interventional Start Date: October 13, 2021 Eligibility: 18 Years to 55 Years, Does Not Accept Healthy Volunteers Location(s): McLean Hospital, Belmont, Massachusetts, United States
This study uses a noninvasive technique called transcranial magnetic stimulation (TMS) to study how hallucinations work in schizophrenia.
TMS is a noninvasive way of stimulating the brain, using a magnetic field to change activity in the brain. The magnetic field is produced by a coil that is held next to the scalp. In this study the investigators will be stimulating the brain to learn more about how TMS might improve these symptoms of schizophrenia.
Neurocognition After Perturbed Sleep
Study Type: Interventional Start Date: September 21, 2021 Eligibility: 18 Years to 60 Years, Does Not Accept Healthy Volunteers Location(s): Icahn School of Medicine at Mount Sinai, New York, New York, United States
Individuals with schizophrenia display a wide range of neurocognitive difficulties resulting in functional impairment and disability. Extensive evidence indicates insomnia and sleep disturbances play a substantial role in degrading cognitive functioning. However, the putative impact of insomnia and sleep disturbances on neurocognition and daily functioning has not been investigated in people with schizophrenia. The goal of this study is to characterize sleep in individuals with schizophrenia and quantify its impact on neurocognition and daily functioning.
A Translational and Neurocomputational Evaluation of a Dopamine Receptor 1 Partial Agonist for Schizophrenia
Study Type: Interventional Start Date: March 2, 2021 Eligibility: 18 Years to 45 Years, Does Not Accept Healthy Volunteers Location(s): Columbia University, New York, New York, United States; Stony Brook University, Stony Brook, New York, United States; University of Pennsylvania, Philadelphia, Pennsylvania, United States; Yale University, New Haven, Connecticut, United States
This study will test whether CVL-562 (PF-06412562), a dopamine 1 partial agonist novel compound, affects working memory neural circuits in patients with early episode schizophrenia. The overall aim is to establish neuroimaging biomarkers of the Dopamine Receptor 1/Dopamine Receptor 5 Family (D1R/D5R) target engagement to accelerate development of D1R/D5R agonists in humans to treat cognitive impairments that underlie functional disability in schizophrenia, a key unaddressed clinical and public health concern.
Family-Focused Therapy for Individuals at High Clinical Risk for Psychosis: A Confirmatory Efficacy Trial
Study Type: Interventional Start Date: January 15, 2021 Eligibility: 13 Years to 25 Years, Does Not Accept Healthy Volunteers Location(s): University of California, San Diego, San Diego, California, United States; University of California, San Francisco School of Medicine, San Francisco, California, United States; Yale University, New Haven, Connecticut, United States; Harvard University/Beth Israel Deconess Medical Center, Boston, Massachusetts, United States; Zucker Hillside Hospital, New York, New York, United States; University of Calgary, Calgary, Alberta, Canada; University of California, Los Angeles, Los Angeles, California, United States
The present study is a confirmatory efficacy trial of Family Focused Therapy for youth at clinical high risk for psychosis (FFT-CHR). This trial is sponsored by seven mature CHR clinical research programs from the North American Prodrome Longitudinal Study (NAPLS). The young clinical high risk sample (N = 220 youth ages 13-25) is to be followed at 6-month intervals for 18 months.
Medial-prefrontal Enhancement During Schizophrenia Systems Imaging
Study Type: Interventional Start Date: November 12, 2020 Eligibility: 18 Years to 64 Years, Accepts Healthy Volunteers Location(s): UCSF, San Francisco, California, United States
This randomized controlled trial in healthy controls (HC) and patients with schizophrenia (SZ) aims to examine 1) the underlying cognitive and neural cause of self-agency deficits in SZ; 2) the responsiveness to a novel navigated repetitive transcranial magnetic stimulation (nrTMS) target in the medial/superior prefrontal cortex (mPFC); and 3) how modulation of mPFC activity impacts the larger self-agency network to mediate changes in self-agency judgments. Our overall hypothesis is that increased mPFC excitability by active high-frequency nrTMS in HC and SZ will induce behavioral improvements in self-agency and neural changes in the larger self-agency network that will generalize to improvements in overall cognition, symptoms and daily functioning, and will likely lead to the development of new effective neuromodulation therapies in patients with schizophrenia.
Early-Phase Schizophrenia: Practice-based Research to Improve Outcomes
Study Type: Observational Start Date: April 1, 2020 Eligibility: 15 Years to 40 Years Location(s): Henderson Behavioral Health, Lauderdale Lakes, Florida, United States
The goal if the project is to develop a learning health network devoted to the treatment of first episode psychosis.
Multi-modal Assessment of Gamma-aminobutyric Acid (GABA) Function in Psychosis
Study Type: Interventional Start Date: January 16, 2020 Eligibility: 16 Years to 60 Years, Accepts Healthy Volunteers Location(s): University of Michigan, Ann Arbor, Michigan, United States
The purpose of this study is to better understand mental illness and will test the hypotheses that while viewing affective stimuli, patient groups will show increased blood oxygenation level dependent (BOLD) signal by fMRI after lorazepam.
This study will enroll participants between the ages of 16 and 60, who have a psychotic illness (such as psychosis which includes conditions like schizophrenia, schizoaffective disorder, and mood disorders). The study will also enroll eligible participants without any psychiatric illness, to compare their brains.
The study will require participants to have 3-4 sessions over a few weeks. The initial assessments (may be over two visits) will include a diagnostic interview and several questionnaires (qols) to assess eligibility. Subsequently, there will will be two separate functional magnetic resonance imaging (fMRI) sessions in which lorazepam or placebo will be given prior to the MRI. During the fMRI the participants will also be asked to answer questions. Additionally, the participants will have their blood drawn, women of child bearing potential will have a urine pregnancy test, vital signs taken, and asked to complete more qols.
Promoting Activity and Cognitive Enrichment in Schizophrenia (PACES)
Study Type: Interventional Start Date: October 1, 2019 Eligibility: 18 Years to 60 Years, Does Not Accept Healthy Volunteers Location(s): University of Pittsburgh, Pittsburgh, Pennsylvania, United States
This project will conduct a confirmatory efficacy trial of two novel psychosocial interventions, Cognitive Enhancement Therapy and Enriched Supportive Therapy, for the treatment of persistent negative symptoms in schizophrenia.
Remediation of Visual Perceptual Impairments in People With Schizophrenia
Study Type: Interventional Start Date: June 1, 2018 Eligibility: 18 Years to 60 Years, Does Not Accept Healthy Volunteers Location(s): New York Presbyterian Hospital, White Plains, New York, United States
The purpose of this study is to evaluate the effectiveness of a visual remediation intervention for people with schizophrenia. The intervention targets two visual functions that much research has shown are impaired in many people with the disorder, namely contrast sensitivity and perceptual organization. The first phase of the study will test the effects of interventions targeting each of these processes, as well as the effects of a combined package. A control condition of higher-level cognitive remediation is included as a fourth condition. The second phase of the study will evaluate the effectiveness of the most effective intervention from the first phase, but in a new and larger sample of individuals. Outcome measures include multiple aspects of visual functioning, as well as visual cognition and overall community functioning.
Neuronal Effects of Exercise in Schizophrenia
Study Type: Interventional Start Date: August 31, 2014 Eligibility: 21 Years to 70 Years, Does Not Accept Healthy Volunteers Location(s): University of Colorado Anschutz Medical Campus, Aurora, Colorado, United States
This study plans to learn more about how common drugs prescribed to individuals with schizophrenia contribute to weight gain, as well as how exercise and diet impact appetite and the brain's response to food. In this study, the investigators will be evaluating how participants' brains respond to food images as well as asking questions about their food preferences and intake and clinical symptoms. The investigators may also ask participants to complete an exercise or diet intervention to see how this changes brain responses or food preferences.
Imaging Cannabinoid Receptors Using Positron Emission Tomography (PET) Scanning
Study Type: Observational Start Date: July 31, 2010 Eligibility: Males, 18 Years to 55 Years, Accepts Healthy Volunteers Location(s): Connecticut Mental Health Center, Clinical Neuroscience Research Unit, New Haven, Connecticut, United States
The aim of the present study is to assess the availability of cannabinoid receptors (CB1R) in the human brain. CB1R are present in everyone's brain, regardless of whether or not someone has used cannabis. The investigators will image brain cannabinoid receptors using Positron Emission Tomography (PET) imaging and the radioligand OMAR, in healthy individuals and several conditions including 1) cannabis use disorders, 2) psychotic disorders, 3) prodrome of psychotic illness and 4) individuals with a family history of alcoholism, 5) Post-Traumatic Stress Disorder 6) Opioid Use Disorder using the PET imaging agent or radiotracer, [11C]OMAR. This will allow us to characterize the number and distribution of CB1R in these conditions. It is likely that the list of conditions will be expanded after the collection of pilot data and as new data on cannabinoids receptor function and psychiatric disorders becomes available.
Those in the cannabis us disorder arm of the study will have a PET scan on at least three occasions: once while smoking as usual, once after 48-hours of abstinence from cannabis, and a final time after 4 weeks of abstinence. Additional scans may be conducted within the 4 weeks and the last scan may be conducted well beyond 4 weeks. Similarly, while most schizophrenia patients may get scanned just once, a subgroup of patients may get scanned more than once. For example to tease out the effects of medications, unmedicated patients may get scanned while unmedicated and again after treatment with antipsychotic medications. Similarly prodromes may get scanned while in the prodromal stage off medications, on medications and after conversion to schizophrenia.
Functional Relevance of Dopamine Receptors in Healthy Controls and Patients With Schizophrenia: Characterization Through [11C]NNC-112 and [18F]Fallypride Positron Emission Tomography
Study Type: Observational Start Date: November 13, 2009 Eligibility: 18 Years to 90 Years, Accepts Healthy Volunteers Location(s): National Institutes of Health Clinical Center, Bethesda, Maryland, United States
Background:
Some illnesses, such as schizophrenia, have effects on brain cells called dopamine receptors, which are required for normal brain function. People with schizophrenia have difficulty thinking and experience hallucinations and delusions. Medications that change brain dopamine receptors can decrease these hallucinations and delusions. The cause of schizophrenia and its association with brain dopamine receptors is not known but may be clarified by studying dopamine receptors in people who have dopamine disorders (such as schizophrenia) and those who do not. Researchers are interested in studying the dopamine system to gain a better idea of how dopamine disorders develop, which may lead to better medical care for people with schizophrenia.
Objectives:
- To study the amount and distribution of two types of dopamine receptors.
Eligibility:
Individuals between the ages of 18 and 60 who have schizophrenia. Healthy volunteers between the ages of 18 and 90.
Participants will undergo a full screening, with physical and psychological history, a neurological examination, and blood and urine samples. Participants will have a blood flow map of the brain recorded with a positron emission tomography (PET) brain scan. A magnetic resonance imaging (MRI) scan will also be performed to determine brain anatomy. To study the amount and distribution of dopamine receptors in the brain, participants will receive a small amount of a radioactive chemical in the vein, followed by a PET scan. The procedure will be performed twice in two separate sessions, once for [18F]fallypride and once for [11C]NNC-112.
PET Scanning in Parkinson s Disease
Study Type: Observational Start Date: March 15, 2002 Eligibility: 18 Years to 90 Years, Accepts Healthy Volunteers Location(s): National Institutes of Health Clinical Center, Bethesda, Maryland, United States
This is an in vivo positron emission tomography (PET) study of regional cerebral dopamine and blood flow in normal volunteers, persons with Parkinson s disease (both familial and sporadic), and those with schizophrenia spectrum disorders. The latter also sign consent for NIH approved protocol 89-M-0160, "Inpatient Evaluation of Neuropsychiatric Patients," PI: Daniel Eisenberg, M.D. Using PET with 6-[F-18] Fluoro-L-dopa (FDOPA) and (15)0-H2O in a single scan session, both presynaptic dopaminergic function and regional cerebral blood flow (rCBF) are assessed. The kinetic rate constant (Ki) for presynaptic dopaminergic uptake in striatum and other regions is calculated. We compare Ki across subject groups and relate the findings to rCBF. Findings are also related to allelic variation in genes of interest, for determination of which participants sign separate consent for NIH approved protocol 95-M-0150 Neurobiological Investigation of Patients with Schizophrenia Spectrum Disorders and Their Siblings, PI: Karen F. Berman, MD. We also draw comparisons between subjects with inherited vs. sporadic Parkinson s disease to determine whether the PET phenotype is the same in both groups, and we compare system-level, circuit-based pathophysiology across PD and schizophrenia groups. Each subject is further screened with an MRI to rule out structural abnormalities and also to further delineate areas of interest in the PET scans.

Magnetic Resonance Imaging (MRI) of Neuropsychiatric Patients and Healthy Volunteers
Study Type: Observational Start Date: February 17, 2000 Eligibility: 18 Years and Older, Accepts Healthy Volunteers Location(s): National Institutes of Health Clinical Center, Bethesda, Maryland, United States
The purpose of this study is to use brain imaging technology to compare differences in brain structure, chemistry, and functioning in individuals with brain and mental disorders compared to healthy volunteers.
Schizophrenia is a brain disorder that results from subtle changes and abnormalities in neurons. These deficits likely occur in localized regions of the brain and may result in widespread, devastating consequences. The neuronal abnormalities are inherited through a complex combination of genetic and environmental factors. Brain imaging technologies can be used to better characterize brain changes in individuals with schizophrenia. This study will use magnetic resonance imaging (MRI) scans to identify predictable, quantifiable abnormalities in neurophysiology, neurochemistry and neuroanatomy that characterize schizophrenia and other neurological and neuropsychiatric disorders.
Genetic Study of Schizophrenia
Study Type: Observational Start Date: July 15, 1995 Eligibility: 18 Years to 55 Years, Accepts Healthy Volunteers Location(s): National Institutes of Health Clinical Center, Bethesda, Maryland, United States
This large ongoing study at NIMH investigates the neurobiology of schizophrenia by identifying susceptibility genes, evaluating their impact on brain function to better understand how to treat and prevent this illness.
Brain Imaging of Childhood Onset Psychiatric Disorders, Endocrine Disorders and Healthy Volunteers
Study Type: Observational Start Date: June 19, 1990 Eligibility: 3 Years and Older, Accepts Healthy Volunteers Location(s): National Institutes of Health Clinical Center, Bethesda, Maryland, United States
Magnetic Resonance Imaging (MRI) unlike X-rays and CT-scans does not use radiation to create a picture. MRI use as the name implies, magnetism to create pictures with excellent anatomical resolution. Functional MRIs are diagnostic tests that allow doctors to not only view anatomy, but physiology and function. It is for these reasons that MRIs are excellent methods for studying the brain.
In this study, researchers will use MRI to assess brain anatomy and function in X and Y chromosome variation, healthy volunteers, and patients with a variety of childhood onset psychiatric disorders. The disorders include attention deficit disorder, autism, congenital adrenal hyperplasia, childhood-onset schizophrenia, dyslexia, obsessive compulsive disorder, Sydenham's chorea, and Tourette's syndrome.
Results of the MRIs showing the anatomy of the brain and brain function will be compared across age, sex (gender), and diagnostic groups. Correlations between brain and behavioral measures will be examined for normal and clinical populations.
Inpatient Evaluation of Adults With Schizophrenia
Study Type: Observational Start Date: September 15, 1989 Eligibility: 18 Years to 120 Years, Does Not Accept Healthy Volunteers Location(s): National Institutes of Health Clinical Center, Bethesda, Maryland, United States
The purpose of this study is to understand the biologic basis of schizophrenia and to determine which symptoms are related to the illness itself and which are related to medications used to treat the illness.
Schizophrenia and related psychoses are chronic brain disorders whose prognosis is often poor and whose pathophysiology remains obscure. Brain imaging technologies such s positron emission tomography (PET), functional magnetic resonance imaging (fMRI), and magnetic resonance imaging (MRI) offer opportunities to study the pathophysiology of psychotic disorders by evaluating brain function. However, the use of anti-psychotic drugs may interfere with the results of such studies. In this study, psychotropic medication will be discontinued in patients for a short period of time to distinguish the effects of the illness on the brain without the interference of the medication's effects on the brain. Given that there is a risk that the patient's symptoms will increase, they are asked to stay on an inpatient unit where the NIMH clinical staff is available to help them 24 hours a day.
This study will be conducted in three phases. In Phase 1, participants will be admitted to the Clinical Center while continuing to take their medication and will undergo diagnostic interviews, physical and laboratory assessments, physiological monitoring, and neuropsychological testing. Behavioral ratings will also be performed and blood and urine samples will be collected. During Phase 2, participants will continue taking medications in a blinded fashion for 8 to 12 weeks. The active medications will be replaced with a placebo (an inactive pill) part of that time. PET, fMRI, and MRI scans will be used to monitor how the continuation or lack of medication affects the brain. Psychological tests will also be given to measure changes in cognition. In Phase 3, participants will have the opportunity for clinical stabilization.
- Case Report
- Open access
- Published: 29 March 2024
Clinical experiences of guided tapering of antipsychotics for patients with schizophrenia– a case series
- Sofie Norlin Mølgaard ORCID: orcid.org/0009-0008-6268-925X 1 ,
- Mette Ødegaard Nielsen ORCID: orcid.org/0000-0002-0780-7099 1 ,
- Kickan Roed ORCID: orcid.org/0000-0002-2926-6983 2 &
- Jimmi Nielsen ORCID: orcid.org/0000-0002-9868-7028 1
BMC Psychiatry volume 24 , Article number: 240 ( 2024 ) Cite this article
Metrics details
80% of patients value information on treatment options as an important part of recovery, further patients with a history of psychotic episodes feel excluded from decision making about their antipsychotic treatment, and on top of that, mental health staff is prone to be reluctant to support shared decision making and medication tapering for patients with schizophrenia. This case series aims to demonstrate the tapering of antipsychotic medication and how guided tapering affects the patient’s feeling of autonomy and psychiatric rehabilitation.
Case presentation
We present six patients diagnosed with schizophrenia (International Classification of Mental and Behavioral Disorders– 10th Edition codes F20.0–5, F20.7–9) who underwent professionally guided tapering in our clinic. The clinic aims to guide the patients to identify the lowest possible dose of antipsychotic medication in a safe setting to minimise the risk of severe relapse. Two patients completely discontinued their antipsychotic medication, two suffered a relapse during tapering, one chose to stop the tapering at a low dose, and one patient with treatment resistant schizophrenia, which is still tapering down.
Conclusions
Reducing the antipsychotic dose increased emotional awareness in some patients ( n = 4) helping them to develop better strategies to handle stress and increased feelings of recovery. Patients felt a greater sense of autonomy and empowerment during the tapering process, even when discontinuation was not possible. Increased awareness in patients and early intervention during relapse may prevent severe relapse.
Impact and implications
Some patients with schizophrenia might be over medicated, leading to unwanted side effects and the wish to reduce their medication. The patients in our study illustrate how guided tapering of antipsychotic medication done jointly with the patient can lead to improved emotional awareness and the development of effective symptom management strategies. This may in turn lead to a greater sense of empowerment and identity and give life more meaning, supporting the experience of personal recovery.
Peer Review reports
Antipsychotic medication remains a cornerstone in the management of psychotic symptoms [ 1 , 2 ]. With one in three patients possibly experiencing persistent symptoms despite antipsychotic treatment [ 3 ], the beneficial effect of long-term antipsychotic maintenance treatment for people with schizophrenia has been questioned [ 4 , 5 ]. Qualitative research shows that people with schizophrenia often have the desire to reduce or discontinue their antipsychotic medication [ 6 , 7 ]. Medication non-adherence among patients with schizophrenia is 41–49%, [ 8 ] and 47% of patients suffering from first-episode-schizophrenia will discontinue their antipsychotic medication within the first year of medication [ 9 ] despite sudden discontinuation possibly leading to exacerbation of symptoms, relapse, rehospitalisation, functional decline, and increased risk of death [ 10 ].
During recent years, an increased number of studies have focused on antipsychotic dose reduction [ 11 , 12 , 13 , 14 , 15 ] and deprescribing guidelines have also been published [ 16 , 17 ].
This has led to a slight shift in recommendations and clinical guidelines towards dose reduction or possibly discontinuation [ 18 ], however, discontinuation is still increasing the risk of clinical worsening significantly [ 19 ].
Although research shows that 80% of patients believe that having information about treatment options is a crucial aspect of recovery [ 20 ], individuals with a history of psychotic episodes often feel excluded from decision making about their antipsychotic treatment [ 7 ]. Moreover, mental health staff may be reluctant to support shared decision making and the tapering of medication for patients with schizophrenia [ 21 ]. Shared decision making, which is defined as two people, in this case a psychiatrist and a patient, sharing information to build consensus about the preferred treatment before agreeing on a treatment plan, [ 22 ] has been associated with the alleviation of symptoms, improved self-esteem, increased satisfaction with medical care, better treatment adherence, and lower rates of hospitalisation [ 23 ].
Currently, randomised controlled trials investigating the effect of antipsychotic medications largely focus on relapse prevention [ 24 ] but fail to incorporate outcomes that reflect personal recovery [ 25 ], which according to the CHIME framework comprises the five components its name stands for: connection to peers, hope, identity, meaning of life, and empowerment [ 26 ]. To our knowledge, there are no studies that describe how guided tapering unfolds in clinical practice. The case series presents how structured and closely monitored tapering can affect various life domains and how providers of psychiatric rehabilitation can support the decision to reduce medication with the least risk of relapse. Our discussion of the potential benefits and difficulties of tapering reflects that the patients in our study were diverse and had different outcomes.
Keywords: schizophrenia, antipsychotic medication, dose reduction, tapering, recovery, relapse.
In 2018, the health authorities in Denmark and the Capital Region of Denmark supported the establishment of a specialised outpatient clinic to meet the wishes of patients who wanted to taper their medication. The clinic offers guided tapering of antipsychotic medication for patients 18–64 years of age diagnosed with schizophrenia using International Classification of Mental and Behavioral Disorders– 10th Edition (ICD-10) codes F20.0–5, F20.7–9 [ 27 ] and works with patients to identify the lowest suitable dose of medication in a safe and professionally guided setting to minimise the risk of severe relapse.
Patients can be enrolled regardless of initial symptom load and level of function but to ensure the safe tapering of medication, patients must adhere to their medication and individual tapering schedule, as well as be available to speak by telephone weekly and to attend monthly appointments at the clinic. Further, we have a few exclusion criteria: Psychiatric hospitalization during the last 6 months, substance abuse to a degree which affect the possibility of participating in the regular assessments, and acutely increased risk of suicide or violence evaluated. In addition, the patient may be excluded if, following a comprehensive interview, the psychiatrist conclude that tapering is not recommended due to safety issue.
During the monthly visits, experienced and trained healthcare professionals evaluate symptoms based on the semi-structured interview using; the Positive and Negative Syndrome Scale (PANSS) [ 28 ]. We aim to reduce the antipsychotic dose monthly by 10%, and once half of the initial dose is reached, the dose is reduced monthly by approximately 5% until further reduction is no longer possible. Under the guidance of the staff, the patient decides whether to reduce the dose or not based on a thorough evaluation of their symptoms. When the patient decides to stop the tapering, or reach discontinuation, the patient is observed for additional 6 months. Although various models are available to ensure shared decision making [ 29 ], we do not adhere to any specific shared decision-making model.
Our unit’s staff strives to listen and comprehend the perspective and life circumstances of patients, while also connecting their experiences to past events and incorporating insights from other patients and scientific research. We are currently collecting data for a qualitative study on how our patients experience our approach during the tapering process.
The prescribing clinician collected data and case quotations at the monthly visits. The cases were meticulously selected to represent a broad range of tapering.
Patient presentation
Patient A is a 29-year-old male diagnosed with paranoid schizophrenia (ICD–10 code F20.0) at age 20 who has experienced anxiety and tics in stressful situations since age 10. His positive symptoms comprised vague evil thoughts that he did not see as his own, inner dialogue interpreted as internal hallucinations, self-referential thoughts, and the delusion of being persecuted. In addition to experiencing sleep disturbances and avolition, he was described with blunted affect. For several years he received long-acting injectable (LAI) aripiprazole and presented with no psychotic symptoms but continually had severe negative symptoms, e.g., a lack of energy, anhedonia, and avolition.
Patient A was enrolled in our clinic at his request because he had increasingly experienced a lack of energy and motivation over the past five years. At enrolment he had no psychotic symptoms but was severely affected by negative symptoms. He did not work or study but was living independently.
Patient A received LAI aripiprazole 400 mg/month and had a PANSS score of 70, dominated by negative symptoms with a score of 26. He followed the algorithm for dose reduction and did not experience any change in psychotic symptoms. After 10 months, he stated, “ I feel like I may have been stuck in a repetitive narrative of my symptoms. While answering your questions, it occurred to me that there are very few symptoms left. ” After 12 months the medication was discontinued after the last aripiprazole injection of 80 mg, and after an additional 6 months of observation, Patient A stated that his emotional life had returned since he could feel joy and sadness again (PANSS 38, P = 7, N = 11, G = 20).
During the observation period subsequent to discontinuing the medication, some of his tics reoccurred, e.g., clicking his tongue up to 20 times a minute, but he was not affected to a level that required treatment. He worked therapeutically to give his life more structure, especially by keeping a regular diurnal rhythm. At the final clinic visit, Patient A explained that he had been approved for an early retirement pension but that he volunteered at a computer repair shop twice a week and that his social life had expanded. He has currently been without medicine for 12 months and still does not have any psychotic symptoms.
Patient B is a 41-year-old man who was referred for tapering after > 10 years of treatment with aripiprazole. At the age of 28, he was diagnosed with depression and treated with citalopram 30 mg/day and aripiprazole 5 mg/day due to ruminating and racing thoughts. During the following two years, he suffered a severe loss of function, affective flattening, anhedonia, avolition, self-neglect, and social withdrawal, and only partial symptomatic improvement was observed. Patient B was enrolled in a specialised assertive early intervention program [ 30 ] with close contact for five years, during which time his diagnosis was changed from depression to unspecified schizophrenia (ICD–10 code F20.9) due to hypnogogic hallucinations.
The aripiprazole dose was increased to 30 mg/day and then switched to LAI aripiprazole 400 mg/month. Side effects continued, including increased sleep duration and a 13 kg weight gain. A general practitioner (GP) treated patient B for four years to help manage symptoms and reduced the dose to 300 mg/month, whereupon the patient was referred to further tapering at our clinic.
Patient B wanted to taper off medication because he did not feel sick and was in doubt about why he still received medication. In addition to feeling exceedingly tired and sleeping around 14 h a night, he found it impossible to lose weight while on medication. When enrolled in the tapering program, patient B’s PANSS total score was 66, with a negative symptom score of 20 and a general symptom score of 36. He followed the tapering plan, and his last aripiprazole injection of 80 mg was given 10 months after enrolment. His PANSS rating declined to 52 ( P = 9, N = 20, G = 23), mainly due to changes in general symptoms and he now slept only 9–10 h/night. He experienced that, “ the bell jar around him was removed ” and that he suddenly “ had to deal with his emotional life again ”, which worsened his tendency to ruminate about discussions with friends when going to sleep. To specifically address this issue, he was taught strategies in a focused therapeutic relationship before being discharged from the clinic. Patient B has now been without antipsychotic medication for 14 months and has no psychotic symptoms but has type 2 diabetes and hypertension. He regularly works out at a fitness center but continues to struggle with how to manage his emotional life and ruminating before he goes to sleep.
Patient C is a 35-year-old woman who was hospitalised at the age of 22 with visual and external auditory hallucinations with mixed second- and third-person perspective. She was diagnosed with paranoid schizophrenia (ICD–10 code F20.0) and treated with quetiapine 1600 mg/day, which was later changed to aripiprazole 30 mg/day and quetiapine 100 mg/day. After being stable for three years on LAI aripiprazole 400 mg/month, she resumed her education but experienced increased symptoms in terms of thought broadcasting, anxiety, and social isolation and had to interrupt her studies. The symptoms improved after adding quetiapine 200 mg/day, and after being stable for a period, quetiapine was changed to a pro re nata prescription, and aripiprazole was switched to an oral prescription, allowing her to resume her studies.
Patient C entered our clinic on her own initiative after being stable on aripiprazole 20 mg/day for one year. She was still hearing what she considered a good and supportive voice for the last 13 years, and she wanted to find out how well she could do with little or no medicine. Her PANSS baseline score was 40, with a positive symptom score of 10 resulting from a score of four at P3 (hallucinations). In the first week of tapering she said she was more emotional but that diminished before the next dose reduction. After six months, she was on a dose of aripiprazole 5 mg/day, which she chose to continue with even though she was about to move and had to terminate her treatment at the clinic. This decision was made after thorough consideration and discussion with the staff. Patient C explained that she was now “ more in touch with her feelings and her surroundings ” and her boyfriend said that she was also “ more emotionally available ”. Patient C appreciated having close contact with the staff while reducing her dose because it made her feel safer during the process. At this point, Patient C’s dose of aripiprazole 5 mg/day has been stable for four years. She is married and gave birth two years ago without her condition deteriorating. Patient C asserts that the dose reduction made her much more self-confident and “ in charge of her own life ”. She describes how being more in touch with her feelings makes it possible for her to have her own opinion, to judge what is good or bad for her, and that this has made her contact with reality stronger. She still hears a supportive voice in her head but it does not disturb her, and she no longer drifts into a psychotic reality. Her GP suggested stopping her medication completely, but she does not dare to do this without working closely with mental healthcare staff based on how safe and secure she felt while tapering her medication at the clinic.
Patient D was enrolled in the clinic at age 26 because he wanted to discontinue his antipsychotic medication. He was 18 years old when diagnosed with paranoid schizophrenia (ICD–10 code F20.0), and his positive symptoms included auditory hallucinations of second- and third-person perspectives, thought broadcasting, and persecutory delusions. At the time of enrolment, he did not have any symptoms of psychosis and had a total PANSS score of 34. He worked 32 h a week as a peer support worker and lived with his girlfriend. Patient D wished to discontinue the antipsychotic treatment mainly because he believed he had learned to cope with the symptoms through his recovery gains.
At enrolment, Patient D received aripiprazole 10 mg/day, which was reduced to aripiprazole 7.5 mg/day (P aripiprazole < 300 nmol/L, ref: 300–1700 nmol/L) during the first month. Patient D revealed that he had not been taking his medication regularly. To improve adherence, he agreed to switch to LAI aripiprazole 200 mg/month, which was tapered down to 120 mg/month over the next four months. Patient D started experiencing auditory and visual hallucinations, racing thoughts, and depressive delusions about being a hypocrite, his PANSS total score increased from 34 to 40. We practiced watchful waiting, i.e., we did not increase the antipsychotic dose unless symptoms increased, while Patient D went on sick leave.
At his next appointment at the clinic, we suggested adjusting the dose to LAI aripiprazole 300 mg/month. Patient D agreed that this was necessary, even though he was disheartened that he was unable to discontinue the medication, “ I thought I could do without. I tell the patients every day at work that to achieve recovery they need to fill their lives with meaningful things, but this shows that I just need to take the medication, nothing else matters ”.
The symptoms improved with the increased dose. After eight weeks, he was working 32 h a week again and had a PANSS total score of 31, which was lower than when he was enrolled at the clinic. Patient D told us that he felt he was “ functioning on a better level ” than when he began tapering. When we asked about his opinion on tapering, he replied: “ I think the time in the clinic has been good. I’m sad that I couldn’t do without medication, but now I know medication is important for me ”. He still receives and feels stable on LAI aripiprazole 300 mg/month.
Patient E is a 59-year-old woman who was diagnosed with paranoid schizophrenia (ICD–10 code F20.0) at the age of 27, presenting with persecutory delusions, auditory and visual hallucinations, sadness, and anxiety. She was enrolled in the clinic because she wanted to discontinue her medication since she questioned her need for antipsychotic treatment and whether her diagnosis was correct.
At the time of enrolment, Patient E had a PANSS total score of 59, her suspicion was easily aroused, she had trouble planning, and experienced anxiety. She lived on her own, had an adult daughter, and was working 11 h a week in a supermarket.
Patient E described her previous experience with treatment in the mental health services, “ I was hospitalised in Spain on a vacation, and they just injected me with medication. I don’t know which one. I was so scared, and now I don’t remember anything. ”
Patient E received LAI aripiprazole 200 mg/5th week at enrolment. We changed the dose to 160 mg/month, and Patient E began psychotherapy. After two months, her PANSS total score had increased to 62, mainly due to a five-point increase in the positive symptoms score, where P6 (suspiciousness) had increased by three points. She described her brain as stressed; she felt like she was being watched and was afraid of other people. Because of the minor increase in symptoms, we arranged an additional visit after 14 days and refrained from further dose reduction.
At the additional visit, she had a PANSS total score of 56 and told us that everything had cleared up but a week later she called and said that she needed additional medication. Patient E felt destabilised by intrusive thoughts about the time she got sick, a sense of derealisation, increased persecutory delusions, and a feeling of somebody speaking to her. As a result, we added aripiprazole 5 mg/day. At the next visit to the clinic, the PANSS total score had increased to 67 and the aripiprazole dose was increased to 300 mg/month plus 5 mg/day. She was nonetheless hospitalised in an open ward for 11 days without further changes in the medication. One month later, she started working again, and two months later she was stable, with a PANSS score of 48.
She concluded: “ Now I know that I need the medication and that I have a mental disorder. The relapse was very difficult, but it’s over now .” Even so, she asked for a further dose reduction the next month because she believed that the medication was causing pain in her legs. She still receives LAI aripiprazole and individual therapy with a psychodynamic focus to support her understanding of her symptoms related to her previous life experiences.
Patient F, a 30-year-old male diagnosed with paranoid schizophrenia (ICD–10 code F20.0) at the age of 20, was hospitalised after a sudden psychotic breakdown, after which he described delusions of self-reference and surveillance. Initially, he received an eight-week treatment of aripiprazole 20 mg/day, but due to lack of effect this was changed to risperidone 6 mg/day. The delusions disappeared gradually, and his positive symptom load was described as in remission after two years. Patient F experienced side effects such as weight gain (30 kg), increased sleep, apathy, akathisia, hyperprolactinemia, and sexual dysfunction. At his initiative, he discontinued the medication abruptly. Four months later, Patient F was hospitalised because he had covered his windows with oil, tomatoes, and flour to protect himself due to his delusions. Treatment with risperidone was resumed with some effect, but he refused treatment with long-acting antipsychotics. After a few months, Patient F discontinued the medical treatment and refused to have any contact with the mental health services. One year later, he was hospitalised after believing that he had clairvoyant and telepathic abilities. He initially received olanzapine 40 mg/day for two weeks, then zuclopenthixol 40 mg/day for six weeks, and after that, sertindole 24 mg/day for five months, all with insufficient effect. Subsequently, he received clozapine 600 mg/day (P-clozapine 2802 nmol/L, ref: 300-2000nmol/L) without any further improvement, which was augmented with amisulpride 400 mg/day. Since this did not change that he believed that he had clairvoyant abilities, he received 18 electroconvulsive therapy treatments, also without any effect. After being hospitalised for 20 months, Patient F was discharged to his apartment but with daily visits to ensure continuous medication adherence in the form of clozapine 425 mg/day and amisulpride 250 mg/day. During the following three years, he was stable, while clozapine was gradually reduced to 175 mg/day before he was referred for further dose reduction at our clinic.
Patient F wished to discontinue clozapine as he disagreed with the diagnosis and experienced side effects in terms of weight gain (body mass index of 33), newly diagnosed diabetes, and constantly feeling tired. He lived a quiet and socially isolated life, mainly filled with telepathic contacts, and he was still convinced that he had clairvoyant and telekinetic abilities. His initial PANSS total score was 85, with a positive symptom score of 27. After 16 months of enrolment at the clinic, his clozapine had been reduced to 12.5 mg/day without any increase in symptoms or decrease in level of function. Patient F has felt a slight improvement in that he experiences less emotional indifference, with a decrease in PANSS negative score from 26 to 22. Patient F still visits the clinic and aims to stop clozapine within the next four months, after which the plan is to follow him for six months on a stable dose of amisulpride 250 mg/day.
Discussion and conclusions
The benefits of tapering antipsychotic medication are under debate [ 31 ], but many patients request it, despite critics’ contention that it puts patients at unnecessary risk of relapse [ 32 , 33 ]. However, determining whether the current antipsychotic dose is still needed can only be ascertained by reducing the dose, and, as most side effects are dose dependent, treatment with the lowest effective dose is of crucial importance [ 34 ].
Our case series illustrates how diverse tapering, and its outcomes can be while also demonstrating how an increased feeling of autonomy during tapering may lead to an increased feeling of rehabilitation and recovery, despite the outcome. For example, Patient A and Patient B were able to discontinue antipsychotic medication completely with no worsening of positive symptoms but an improvement in negative symptoms and quality of life. Both patients have now been out of antipsychotic medication for more than a year with no signs of worsening, which is considered a favourable predictor [ 35 , 36 ], but as schizophrenia is seen upon as a life long condition the risk of relapsing after 12 months is still present. Many patients wish to reduce their dose or quit their medications entirely due to side effects, but this was only partly the case for Patient A and Patient B. When their antipsychotic medication was reduced and finally stopped, both patients experienced significantly more energy, initiative, pleasure, and emotional fluctuation. Although their files described them as “dominated by negative symptoms”, they appeared to be somewhat secondary to the medical treatment. Discriminating between primary and secondary negative symptoms can be almost impossible, but dose reduction can help to identify the negative symptoms medication causes. Patient A and Patient B increased their level of function and had a greater feeling of personal recovery in terms of hope, identity, the meaning of life, and empowerment [ 26 ]. Another important observation regarding the cases, especially Patient B, is that the level of symptoms led to long-lasting treatment with antipsychotic medication. Patient B’s files indicated that his medical treatment was initiated due to rumination and provided no evidence that he had suffered from delusions, hallucinations, or severe thought disorders. When guidelines recommend continuous antipsychotic treatment for all patients with schizophrenia, it categorises all patients as being at high risk for a severe psychotic episode. We argue that Patient B illustrates that this may not always be the case, underlining the importance of examining the individual patient’s history and evaluating the pros and cons of continuous treatment in collaboration with the patient to reach consensus.
Patient C, who had a similar outcome, decided to stay on 5 mg of aripiprazole with no signs of worsening. Although Patient C did not discontinue the antipsychotic drug completely, she experienced the benefits of the dose reduction and appreciated the tapering. Her decision to stop tapering her medications was partly due to moving to another part of Denmark, which required her to terminate treatment at our clinic. Patient C’s GP had suggested that she stop her antipsychotic treatment multiple times over the past years, but Patient C was aware that discontinuing the final dosage might worsen her symptoms and affect her overall level of functioning. As a result, she preferred to work with specialists to minimise any risks, which emphasises the importance of providing a safe and professional environment for tapering and shows that she felt that professional guidance in a specialised clinic decreased her risk of relapse. Consequently, although patients with no symptoms and no recurring symptoms during tapering seem to be the most suitable group for tapering, many other patients may benefit from a tapering trial.
Both Patient D and Patient E experienced relapses, the appearance of symptoms indicating that antipsychotic treatment was required. For Patient D, this led to psychologically accepting his psychiatric condition and the need for antipsychotic treatment. For Patient E, the impact on her perception of the necessity of medication may not be permanent. We are currently exploring whether a therapeutic relationship with a psychodynamic focus may be helpful to Patient E’s rehabilitation and lead to an increased feeling of personal recovery.
Patient F involved treatment-resistant schizophrenia; the various treatment strategies tried resulted in increased side effects rather than reduced psychotic symptoms. Often treatment is initiated during a worsening of symptoms, but disease fluctuations make evaluating the response difficult. In accordance with our experiences with this patient group, a Finnish study showed that olanzapine, combined with clozapine treatment, could be tapered with no worsening in symptoms [ 37 ]. Gradual tapering of antipsychotic drugs is not only relevant for patients with no symptoms but should also be considered for patients with treatment-resistant schizophrenia, where antipsychotic medication may not be efficient. In addition, treatment with clozapine may be associated with several troublesome side effects [ 38 ]. Today, only few existing guidelines address this issue [ 39 , 40 ].
Several patents in our clinic describe increased emotional awareness or emotional fluctuation during dose reduction. Although we did not monitor the emotional awareness using a rating scale, this is in line with recent findings [ 41 ]. This restoration of emotional reactivity during dose reduction can be a temporary state patients need to go through, but it can also be a warning sign of relapse. Frequent clinical assessment, psychoeducation and therapeutic support may be needed, and it is our experience that sometimes the patients want to resume antipsychotic treatment or increase the dose, even though no psychotic symptoms have occurred. Although tapering is associated with an increased risk of relapse [ 32 ], this case series shows that intensive follow-up can be used to identify relapse at an early stage before it becomes more severe and devastating. Before inclusion in the tapering program, we thoroughly inform patients that tapering is associated with an increased risk of relapse, which is a concern that most patients share with us. However, the desire to reduce their medications exceeds the fear of relapse and, through common agreement, we ensure a therapeutic alliance where patients recount being heard and understood.
Our tapering program is one example of how to reduce medication with the least risk of relapse. Our findings show that taking advantage of specialised mental health services with close contact during gradual tapering may reduce the risk of severe relapse, at least compared to patients who independently initiated abrupt discontinuation. While we have not encountered suicide attempts, violent actions, or other serious complications so far, it is crucial to remember that tapering down antipsychotics carries a risk and must be approached with the utmost precaution.
Regardless of the outcome of tapering, patients regularly visiting the clinic were often grateful for the opportunity to have their antipsychotic medication reduced and to be involved in decisions about their medical treatment, which created a greater feeling of autonomy. We are in the process of collecting data for a qualitative study on how our patients experience our approach during the tapering process. Likewise, well-designed future qualitative studies are required, to shed further light on the benefits of using specialised mental health services with close contact during tapering.
This case series has various limitations, but one in particular must be acknowledged. The cases presented were deliberately chosen from a pool of more than 100 patients from two tapering trials. The presented cases were chosen to achieve a diverse sample and to illustrate some of the various ways in which tapering can occur but are not necessarily quantitatively representative. (The full data and results will be published in the following years) Consequently, the results are not generalisable to all patients suffering from schizophrenia.
Research on antipsychotic tapering remains sparse, and additional quantitative and qualitative data are warranted. Some of the patients in our cases who reduced their antipsychotic dose increased their emotional awareness and seemed to develop better strategies for handling stress, which may have led to an increased feeling of empowerment, identity, and meaning in life. Future research may resolve whether this feeling of personal recovery is a factor that improves tapering outcomes. Notably, some of the patients in our clinic were increasingly open to antipsychotic treatment during stressful periods, indicating that treating schizophrenia more in terms of episodes is warranted.
The diagnoses of schizophrenia cover a heterogeneous group of patients, making it crucial to take an individualised approach to meet the specific treatment requirements of each patient. Also, antipsychotic associated benefits and sideeffects should be carefully and regularly evaluated with the patient. If guided tapering of antipsychotics is considered, the possible risk of relapse and consequences of this should also be discussed.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
International Classification of Mental and Behavioral Disorders– 10th Edition
The Positive and Negative Syndrome Scale
Long-acting injectable
General practitioner
Jibson MD, Waltham M, Marder S, UpToDAte. 2022. Second-generation antipsychotic medications: Pharmacology, administration, and side effects. Available from: https://www.uptodate.com/contents/second-generation-antipsychotic-medications-pharmacology-administration-and-side-effects .
Schneider-Thoma J, Chalkou K, Dörries C, Bighelli I, Ceraso A, Huhn M, et al. Comparative efficacy and tolerability of 32 oral and long-acting injectable antipsychotics for the maintenance treatment of adults with schizophrenia: a systematic review and network meta-analysis. Lancet. 2022;399(10327):824–36.
Article CAS PubMed Google Scholar
Potkin SG, Kane JM, Correll CU, Lindenmayer JP, Agid O, Marder SR, et al. The neurobiology of treatment-resistant schizophrenia: paths to antipsychotic resistance and a roadmap for future research. NPJ Schizophr. 2020;6(1):1.
Article PubMed PubMed Central Google Scholar
Harrow M, Jobe TH, Faull RN. Do all schizophrenia patients need antipsychotic treatment continuously throughout their lifetime? A 20-year longitudinal study. Psychol Med. 2012;42(10):2145–55.
Murray RM, Quattrone D, Natesan S, van Os J, Nordentoft M, Howes O, et al. Should psychiatrists be more cautious about the long-term prophylactic use of antipsychotics? Br J Psychiatry. 2016;209(5):361–5.
Article PubMed Google Scholar
Morant N, Azam K, Johnson S, Moncrieff J. The least worst option: user experiences of antipsychotic medication and lack of involvement in medication decisions in a UK community sample. J Ment Health. 2018;27(4):322–8.
Haugom EW, Stensrud B, Beston G, Ruud T, Landheim AS. Experiences of shared decision making among patients with psychotic disorders in Norway: a qualitative study. BMC Psychiatry. 2022;22(1):192.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909.
Cheng Z, Yuan Y, Han X, Yang L, Zeng X, Yang F, et al. Rates and predictors of one-year antipsychotic treatment discontinuation in first-episode schizophrenia: results from an open-label, randomized, real world clinical trial. Psychiatry Res. 2019;273:631–40.
Haddad P, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;43.
Moncrieff J, Crellin N, Stansfeld J, Cooper R, Marston L, Freemantle N, et al. Antipsychotic dose reduction and discontinuation versus maintenance treatment in people with schizophrenia and other recurrent psychotic disorders in England (the RADAR trial): an open, parallel-group, randomised controlled trial. Lancet Psychiatry. 2023;10(11):848–59.
Liu CC, Hsieh MH, Chien YL, Liu CM, Lin YT, Hwang TJ, et al. Guided antipsychotic reduction to reach minimum effective dose (GARMED) in patients with remitted psychosis: a 2-year randomized controlled trial with a naturalistic cohort. Psychol Med. 2023;53(15):7078–86.
Wunderink L, Nienhuis FJ, Sytema S, Slooff CJ, Knegtering R, Wiersma D. Guided discontinuation versus maintenance treatment in remitted first-episode psychosis: relapse rates and functional outcome. J Clin Psychiatry. 2007;68(5):654–61.
Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry. 2013;70(9):913–20.
Begemann MJH, Thompson IA, Veling W, Gangadin SS, Geraets CNW, Van ’T, Hag E, et al. To continue or not to continue? Antipsychotic medication maintenance versus dose-reduction/discontinuation in first episode psychosis: HAMLETT, a pragmatic multicenter single-blind randomized controlled trial. Trials. 2020;21(1):147.
Gupta S, Cahill JD, Miller R. Deprescribing antipsychotics: a guide for clinicians. BJPsych Adv. 2018;24(5):295–302.
Article Google Scholar
Horowitz MA, Jauhar S, Natesan S, Murray RM, Taylor D. A method for tapering antipsychotic treatment that May minimize the risk of Relapse. Schizophr Bull. 2021;47(4):1116–29.
Shimomura Y, Kikuchi Y, Suzuki T, Uchida H, Mimura M, Takeuchi H. Antipsychotic treatment in the maintenance phase of schizophrenia: an updated systematic review of the guidelines and algorithms. Schizophr Res. 2020;215:8–16.
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379(9831):2063–71.
Law H, Morrison AP. Recovery in psychosis: a Delphi study with experts by experience. Schizophr Bull. 2014;40(6):1347–55.
Roed K. Mental Health staffs’ perspectives on tapering of antipsychotic medication: a focus group study. Qual Health Res. 2023.
Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681–92.
Alguera-Lara V, Dowsey MM, Ride J, Kinder S, Castle D. Shared decision making in mental health: the importance for current clinical practice. Australasian Psychiatry. 2017;25(6):578–82.
Ostuzzi G, Vita G, Bertolini F, Tedeschi F, De Luca B, Gastaldon C, et al. Continuing, reducing, switching, or stopping antipsychotics in individuals with schizophrenia-spectrum disorders who are clinically stable: a systematic review and network meta-analysis. Lancet Psychiatry. 2022;9(8):614–24.
Zipursky RB, Agid O. Recovery, not progressive deterioration, should be the expectation in schizophrenia. World Psychiatry. 2015;14(1):94–6.
Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. 2011;199(6):445–52.
World health Organization. ICD-10 The international Classification of Mental and Behavioural Disorders [Internet]. 1992. Available from: https://icd.who.int/browse10/2019/en .
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76.
Stacey D, Légaré F, Pouliot S, Kryworuchko J, Dunn S. Shared decision making models to inform an interprofessional perspective on decision making: a theory analysis. Patient Educ Couns. 2010;80(2):164–72.
Secher RG, Hjorthøj CR, Austin SF, Thorup A, Jeppesen P, Mors O, et al. Ten-year follow-up of the OPUS specialized early intervention trial for patients with a first episode of psychosis. Schizophr Bull. 2015;41(3):617–26.
Potla S, Al Qabandi Y, Nandula SA, Boddepalli CS, Gutlapalli SD, Lavu VK, et al. A systematic review of the need for Guideline recommendations; slow tapering vs. maintenance dose in long-term antipsychotic treatment: 2022. Cureus. 2023;15(2):e34746.
PubMed PubMed Central Google Scholar
Højlund M, Kemp AF, Haddad PM, Neill JC, Correll CU. Standard versus reduced dose of antipsychotics for relapse prevention in multi-episode schizophrenia: a systematic review and meta-analysis of randomised controlled trials. Lancet Psychiatry. 2021;8(6):471–86.
Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry. 2018;17(2):149–60.
Leucht S, Bauer S, Siafis S, Hamza T, Wu H, Schneider-Thoma J, et al. Examination of dosing of Antipsychotic Drugs for Relapse Prevention in patients with stable Schizophrenia: a Meta-analysis. JAMA Psychiatry. 2021;78(11):1238–48.
Thompson A, Winsper C, Marwaha S, Haynes J, Alvarez-Jimenez M, Hetrick S, et al. Maintenance antipsychotic treatment versus discontinuation strategies following remission from first episode psychosis: systematic review. BJPsych Open. 2018;4(4):215–25.
Chen EYH, Hui CLM, Lam MML, Chiu CPY, Law CW, Chung DWS et al. Maintenance treatment with quetiapine versus discontinuation after one year of treatment in patients with remitted first episode psychosis: Randomised controlled trial. BMJ (Online). 2010;341(7770).
Repo-Tiihonen E, Hallikainen T, Kivistö P, Tiihonen J. Antipsychotic polypharmacy in Clozapine Resistant Schizophrenia: a randomized controlled trial of tapering antipsychotic co-treatment. Ment Illn. 2012;4(1):e1.
Dong S, Schneider-Thoma J, Bighelli I, Siafis S, Wang D, Burschinski A et al. A network meta-analysis of efficacy, acceptability, and tolerability of antipsychotics in treatment-resistant schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2023.
Baandrup L, Østrup Rasmussen J, Klokker L, Austin S, Bjørnshave T, Fuglsang Bliksted V, et al. Treatment of adult patients with schizophrenia and complex mental health needs - a national clinical guideline. Nord J Psychiatry. 2016;70(3):231–40.
Correll CU, Martin A, Patel C, Benson C, Goulding R, Kern-Sliwa J, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophrenia (Heidelberg Germany). 2022;8(1):5.
PubMed Google Scholar
Morant N, Long M, Jayacodi S, Cooper R, Akther-Robertson J, Stansfeld J, et al. Experiences of reduction and discontinuation of antipsychotics: a qualitative investigation within the RADAR trial. EClinicalMedicine. 2023;64:102135.
Download references
Acknowledgements
Not applicable.
No funding to declare.
Open access funding provided by Copenhagen University
Author information
Authors and affiliations.
Mental Health Center Glostrup, Copenhagen University Hospital, Unit for complicated schizophrenia, Glostrup, Denmark
Sofie Norlin Mølgaard, Mette Ødegaard Nielsen & Jimmi Nielsen
Mental Health Centre Glostrup, Copenhagen University Hospital– Mental Health Services CPH, Centre for Applied Research in Mental Health Care, Glostrup, Denmark
Kickan Roed
You can also search for this author in PubMed Google Scholar
Contributions
S.N.M and M.Ø.N., wrote the manuscript and designed the paper, with J.N. K.R. M.Ø.N and J.N have substantively revised it. All authors have approved the submitted version, and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Correspondence to Sofie Norlin Mølgaard .
Ethics declarations
Ethics approval and consent to participate.
Our study was conducted in accordance with the Declaration of Helsinki and approved by the Capital Region of Denmark’s ethics committee and the Danish Data Protection Agency (H-21047524).
Consent for publication
All participants provided written informed consent for publication of identifiable information/ images in open access journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mølgaard, S.N., Nielsen, M.Ø., Roed, K. et al. Clinical experiences of guided tapering of antipsychotics for patients with schizophrenia– a case series. BMC Psychiatry 24 , 240 (2024). https://doi.org/10.1186/s12888-024-05699-y
Download citation
Received : 15 January 2024
Accepted : 19 March 2024
Published : 29 March 2024
DOI : https://doi.org/10.1186/s12888-024-05699-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Schizophrenia
- Antipsychotic medication
- Dose reduction
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Frontiers in Psychiatry
- Schizophrenia
- Research Topics
Case Reports in Schizophrenia and Psychotic Disorders: 2023
Total Downloads
Total Views and Downloads
About this Research Topic
Frontiers in Psychiatry is proud to present our Case Reports series. Our case reports aim to highlight unique cases of patients that present with an unexpected/unusual diagnosis, including complexity and differential diagnosis and/or co-morbid diagnoses, treatment outcome, or clinical course. Case reports ...
Keywords : schizophrenia, case reports, psychotic, disorders
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines, participating journals.
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
If Faces Appear Distorted, You Could Have This Condition
Research presents a unique case of a patient with prosopometamorphopsia.
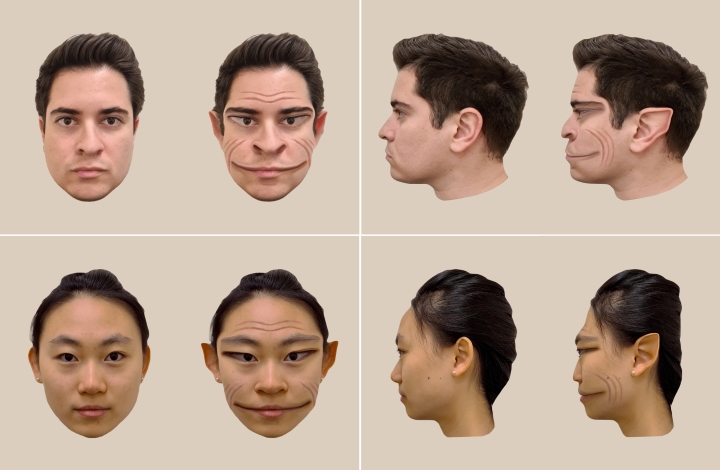
COVID-19 Can Cause 'Face Blindness'
Imagine if every time you saw a face, it appeared distorted. For those who have a very rare condition known as prosopometamorphopsia, which causes facial features to appear distorted, that is reality.
As the website on what is known as PMO explains, “‘Prosopo’ comes from the Greek word for face ‘prosopon’ while ‘metamorphopsia’ refers to perceptual distortions.” The distortions can affect the shape, size, color, and position of facial features, and PMO can last for days, weeks, or even years.
A new Dartmouth study published in the “Clinical Pictures” section of The Lancet reports on a unique case of a patient with PMO. The research is among the first to provide realistic visualizations of how a patient experienced facial distortions.
The patient, a 58-year-old male with PMO, sees faces without any distortions when viewed on a screen and on paper but sees distorted faces that appear “demonic” when viewed in-person. The case is especially rare because he does not see distortions of faces across all contexts.
For the study, the researchers took a photograph of a person’s face. Then, they showed the patient the photograph on a computer screen while he looked at the real face of the same person. The researchers obtained real-time feedback from the patient on how the face on the screen and the real face in front of him differed, as they modified the photograph using computer software to match the distortions perceived by the patient.
Through the process, we were able to visualize the patient’s real-time perception of the face distortions.
“In other studies of the condition, patients with PMO are unable to assess how accurately a visualization of their distortions represents what they see because the visualization itself also depicts a face, so the patients will perceive distortions on it too,” says lead author Antônio Mello , Guarini, a PhD student in the Department of Psychological and Brain Sciences .
In contrast, this patient doesn’t see distortions on a screen. This means that the researchers were able to modify the face in the photograph, and the patient could accurately compare how similar his perception of the real face was to the manipulated photograph. “Through the process, we were able to visualize the patient’s real-time perception of the face distortions,” says Mello.
In their research with other PMO cases, the co-authors state that some of their PMO participants have seen health professionals who wanted to help, but diagnosed them with another health condition, not PMO.
“We’ve heard from multiple people with PMO that they have been diagnosed by psychiatrists as having schizophrenia and put on anti-psychotics, when their condition is a problem with the visual system,” says senior author Brad Duchaine , a professor of psychological and brain sciences and principal investigator of the Social Perception Lab at Dartmouth.

“And it’s not uncommon for people who have PMO to not tell others about their problem with face perception because they fear others will think the distortions are a sign of a psychiatric disorder,” says Duchaine. “It’s a problem that people often don’t understand.”
Through their paper, the researchers hope to increase public awareness of what PMO is .
Daniel Stehr at Dartmouth and Professor of Neurology Krzysztof Bujarski at the Geisel School of Medicine also contributed to the study.
Amy Olson can be reached at [email protected] .
- Science & Health
- Innovation and Impact
- Arts and Sciences
- Press Release
- Guarini School of Graduate and Advanced Studies
- Geisel School of Medicine
- Department of Psychological and Brain Sciences
A Q&A With Film Critic and Theorist Vinzenz Hediger

After a Year of Turmoil, Harvard’s Applications Drop
Jump to content

Center for Continuing Medical Education
- Login with UCHAD or CNET ID
- Visitor login
- Create account
Bookmark/Search this post

You are here
Update on schizophrenia 2024: progressing from mental illness to mental health.
- Accreditation
- Get Started!
Target Audience
Learning objectives.
At the conclusion of this activity, participants will be able to:
- Recognize the gap between research advancements and improved outcomes for people with serious mental illness (SMI), the reasoning behind this gap, the stigma and bias in healthcare settings faced by people with SMI, and strategies to reduce stigma and improve compassion in healthcare;
- Define the three pillars of recovery by understanding the broader concept of health beyond healthcare, gaining familiarity with the deinstitutionalization movement and its impact, and understanding the lived experiences of patients with schizophrenia and their families;
- Apply knowledge about the neuroanatomical and neurodevelopmental models of Schizophrenia, understanding cognitive dysfunction in these patients through case studies.
You may also be interested in
Echo-chicago: suicide prevention in youth.

ECHO-Chicago: Suicide Prevention for Primary Care Providers
Echo-chicago: suicide prevention for behavioral health providers.
- 4.50 AMA PRA Category 1 Credit™
- 4.50 Participation
- Add to google calendar
- Add to yahoo calendar
- Add to iCalendar
- Add to Outlook
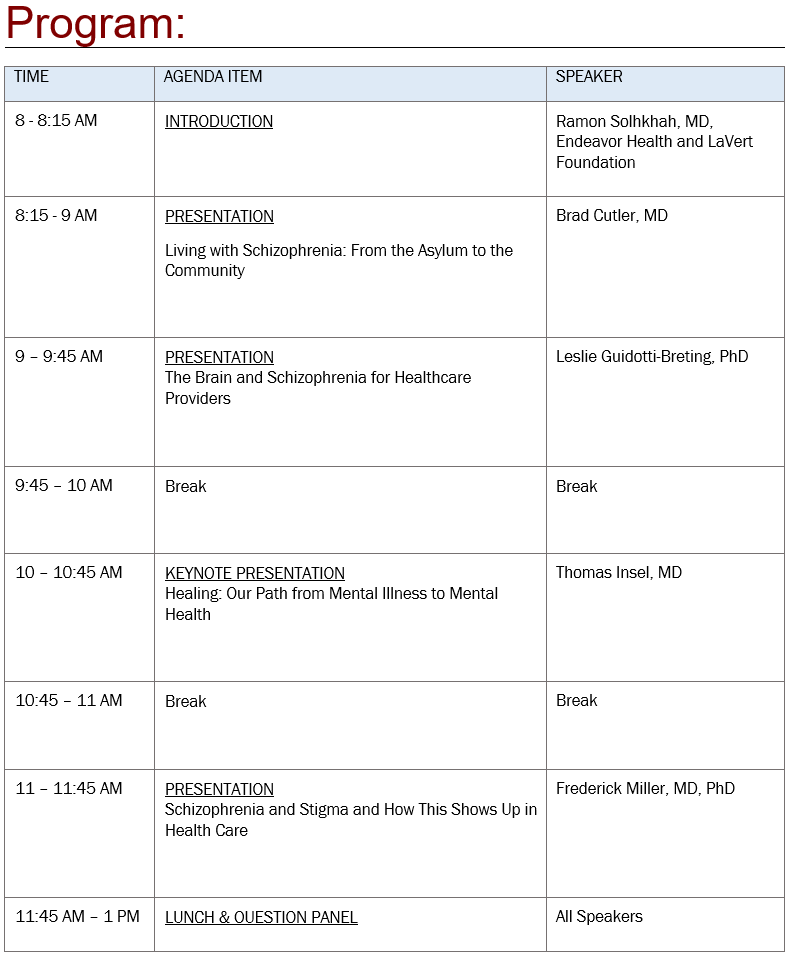
Agenda is subject to change.

WANT TO KNOW MORE?
Course director.

REGISTRATION
Claiming credit.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Physiother Can
- v.62(4); Fall 2010
Language: English | French
Case Report: Schizophrenia Discovered during the Patient Interview in a Man with Shoulder Pain Referred for Physical Therapy
Purpose: The purpose of this case report is to demonstrate the importance of a thorough patient interview. The case involves a man referred for physical therapy for a musculoskeletal dysfunction; during the patient interview, a psychiatric disorder was recognized that was later identified as schizophrenia. A secondary purpose is to educate physical therapists on the recognizable signs and symptoms of schizophrenia.
Client description: A 19-year-old male patient with chronic shoulder, elbow, and wrist pain was referred for physical therapy. During the interview, the patient reported that he was receiving signals from an electronic device implanted in his body.
Measures and outcome: The physical therapist's initial assessment identified a disorder requiring medical referral. Further management of the patient's musculoskeletal dysfunction was not appropriate at this time.
Intervention: The patient was referred for further medical investigation, as he was demonstrating signs suggestive of a psychiatric disorder. The patient was diagnosed with schizophrenia by a psychiatrist and was prescribed Risperdal.
Implications: This case study reinforces the importance of a thorough patient interview by physical therapists to rule out non-musculoskeletal disorders. Patients seeking neuromusculoskeletal assessment and treatment may have undiagnosed primary or secondary psychiatric disorders that require recognition by physical therapists and possible medical referral.
RÉSUMÉ
Objectif : L'objectif de cette étude de cas consiste à démontrer l'importance de réaliser des entrevues en profondeur avec les patients. Le cas étudié concerne un homme dirigé vers la physiothérapie en raison d'une dysfonction musculosquelettique. Au cours de l'entrevue avec ce patient, un problème psychiatrique a été décelé; par la suite, de la schizophrénie a été diagnostiquée. Le deuxième objectif de cette étude de cas est d'éduquer et de sensibiliser les physiothérapeutes aux signes et aux symptômes aisément reconnaissables de la schizophrénie.
Description du client : Le patient est un jeune homme de 19 ans qui souffre de douleurs chroniques à l'épaule, au coude et au poignet et qui avait été dirigé en physiothérapie. Au cours de l'entrevue, le patient a déclaré qu'il recevait des signaux provenant d'un appareil électronique implanté dans son corps.
Mesures et résultats : L'évaluation préliminaire du physiothérapeute a permis d'identifier un problème qui nécessitait que le patient soit redirigé vers un médecin. Une gestion plus poussée de la dysfonction musculosquelettique de ce patient a été jugée inappropriée à cette étape.
Intervention : Le patient a été dirigé vers une investigation médicale plus approfondie, puisqu'il manifestait des signes de possibles problèmes psychiatriques. Le patient a par la suite été diagnostiqué comme schizophrène et on lui a prescrit du Risperdal.
Implication : Cette étude de cas vient réaffirmer l'importance, pour le physiothérapeute, de procéder à des entrevues approfondies avec les patients pour s'assurer qu'il n'y a pas d'autres problèmes que les seules dysfonctions musculosquelettiques. Les patients qui souhaitent obtenir une évaluation et un traitement musculosquelettique peuvent souffrir aussi d'un problème psychiatrique primaire ou secondaire non diagnostiqué qui exige d'être reconnu par le physiothérapeute et qui nécessitera vraisemblablement une attention médicale ultérieure.
INTRODUCTION
A recent US study demonstrated that less than one-third of diagnoses provided to physical therapists by primary-care physicians are specific. 1 The same study illustrated that physical therapists must assume a greater diagnostic role and must routinely provide medical screening and differential diagnosis of pathology during the examination. 1 Similarly, studies conducted in Australia and Canada have concluded that the majority of referrals for physical therapy are not provided with a specific diagnosis. 2 , 3 Medical screening is important, since physical therapists are increasingly functioning as the primary contact for patients with neuromusculoskeletal dysfunctions, 4 , 5 which means a greater likelihood of encountering patients with non-musculoskeletal disorders, including psychiatric disorders.
As demonstrated by the World Health Organization's International Classification of Functioning, Disability and Health, it is imperative to take an individual's psychological state into account, since disorders in this area can lead to disability. 6 Many psychiatric conditions are commonly encountered in physical therapy practice; for example, depression, anxiety, and fear-avoidance have all been associated with low back, neck, and widespread musculoskeletal pain. 7 – 9 These psychiatric disorders have been identified both as risk factors for musculoskeletal dysfunction and as an important secondary psychosocial aspect of disablement. 7 – 10 It is therefore important for physical therapists to consider the primary and secondary roles of psychopathology in disability.
Although various models of primary-care physical therapy have demonstrated physical therapists' expertise in the realm of neuromusculoskeletal dysfunctions, there is a need for increased competencies in academic, clinical, and affective domains. 5 Few et al. propose a hypothesis-oriented algorithm for symptom-based diagnosis through which physical therapists can arrive at a diagnostic impression. 11 This algorithm takes into account the various causes of pathology, including psychogenic disorders. 11 Although additional research is necessary to validate Few et al.'s algorithm, it provides one model that considers underlying pathologies in determining the appropriateness of physical therapy intervention. 11 The present case report further illustrates the importance of considering the patient's affective and psychological state in order to more effectively screen for and identify psychiatric disorders that require medical referral.
The purpose of this case report is to demonstrate the importance of a thorough patient interview. We present the case of a man, referred for physical therapy for a musculoskeletal dysfunction, who was determined during the patient interview to have an undiagnosed psychiatric disorder, later identified as schizophrenia. In addition, this report is intended to educate physical therapists about the recognizable signs and symptoms of schizophrenia.
CASE DESCRIPTION
The patient was a 19-year-old male university student. His recreational activities included skateboarding, snowboarding, break dancing, and weight training. The patient first sought medical attention from a sport medicine physician in January 2006, when he reported right lateral wrist pain since falling and hitting the ulnar aspect of his wrist while skateboarding in October 2005. Plain film radiographs taken after the injury were negative, and the patient did not receive any treatment. The physician found no wrist swelling, minimal tenderness over the ulnar aspect of the right wrist, full functional strength, and minimally restricted range of motion (ROM). The patient was given ROM exercises and was diagnosed with a right wrist contusion.
Over the next 22 months, the patient returned to the same sport medicine clinic 10 times, reporting pain in his wrist, shoulder, elbow, knee, ankle, and neck. He stated that the elbow, wrist, and shoulder injuries were due to falls while skateboarding and snowboarding or to overuse during weight training; some injuries had no apparent cause. Over the course of his medical care, the patient followed up with three different physicians at the same clinic. He was diagnosed by these physicians, in order of occurrence, with (1) right wrist contusion and sprain; (2) right wrist impingement and left wrist strain; (3) right shoulder supraspinatus tendinopathy; (4) right peroneal overuse injury and strain; (5) disuse adhesions of the right peroneals and right hip adhesions; (6) right ankle neuropathic pain secondary to nerve injury and sprain and right-knee patellofemoral pain syndrome (PFPS); (7) neuropathic pain of the right peroneal nerve; (8) trauma-induced left-knee PFPS; (9) ongoing post-traumatic left-knee PFPS; and (10) right levator scapula strain, chronic right infraspinatus strain, right elbow ulnar ridge contusion, and right wrist chronic distal ulnar impingement secondary to malaligned triangular fibrocartilage complex (TFCC).
After his tenth visit to a physician, the patient was referred for physical therapy for chronic right levator scapula strain and right supraspinatus strain. During the interview, the patient stated that he had right shoulder pain because of a snowboarding injury sustained 1 year earlier and because of a fall onto the lateral right shoulder 2 years ago. Aggravating activities to the shoulder included pull-ups, rowing, and free weights. No position or movement alleviated his pain, and the pain did not fluctuate over the course of the day. His sleep was disturbed only when lying on the right shoulder. The patient was in generally good health, but he said that his right wrist and left knee occasionally felt cold for no apparent reason. He denied experiencing any loss of sensation, decreased blood flow, or numbness or tingling in the knee and wrist. The patient said he believed that his knee and wrist became cold as a result of electromagnetic impulses sent to the joint via an electrical implant in his body and that this device was the cause of his ongoing shoulder pain.
According to the patient, this device had been implanted into his body 2 years earlier by a government organization (the Central Intelligence Agency, the US government, or the US Army) to control his actions. Electromagnetic impulses generated by the implant had caused his falls and injuries; they also caused his joints to become cold or painful when he was doing something “they” did not want him to do, such as break dancing, snowboarding, skateboarding, or exercising. The patient also believed that many other people unknowingly had implants; he claimed that friends, neighbours, professors, and strangers were “working with them” and that they “emotionally abuse[d]” him by giving signs such as kicking a leg back to let him know he was being watched. Furthermore, he indicated that he often received commands telling him to harm his friends or family and that these orders came either from the electrical implant or from the people he claimed were emotionally abusing him. He therefore distanced himself from some friends because he did not want to follow through with these commands. I asked the patient if he felt he would harm himself or others because of his psychotic-like symptoms. He denied any desire to inflict harm on himself or others. Had he posed a threat to himself or others, he would have been “formed” (i.e., committed to a psychiatric facility by the appropriate medical professional).
The patient's past medical and family history were unremarkable. He did not use any prescription or over-the-counter medications, but he felt his thoughts about electrical implants were decreased by the use of marijuana, which he used socially. He was a non-smoker and a social consumer of alcohol. He had a normal gait and appeared comfortable in an unsupported seated position. He denied any weight changes, bowel or bladder problems, night pain, or difficulty breathing.
PHYSICAL EXAMINATION
The patient reported a maximum verbal numeric pain rating scale (NPRS) score of 8/10 and a minimum score of 0/10, with pain usually present in the shoulder. In a double-blind, placebo-controlled, multi-centre chronic pain study, when the baseline NPRS raw score fluctuated by 0 points, the sensitivity and specificity were 95.32% and 31.80% respectively; 12 , 13 when there was a 4-point raw score change, the sensitivity and specificity were 35.92% and 96.92% respectively. 12 The patient stated that when he experienced shoulder pain, it was located on the anterior, posterior, and lateral aspects of his shoulder and radiated down to his elbow and wrist. He reported 0/10 shoulder pain while seated.
Standing posture was assessed in the frontal and sagittal planes. 14 The patient had a mild forward head posture and internally rotated glenohumeral joints in the sagittal plane. The frontal-plane analysis revealed a slight elevation of the right shoulder and level iliac crests. Such visual assessment of cervical and lumbar lordosis has an intrarater reliability of k =0.50 but an interrater reliability of k =0.16. 15
In the frontal plane, the right scapula was abducted four finger-widths from the mid-thoracic spine, and the left scapula was abducted three finger-widths. The scapulas were superiorly rotated bilaterally. Surface palpation of the acromial angle, inferior angle, and spine of the scapula differed less than 0.98 cm, 0.46 cm, and 0.67 cm, respectively, from the actual bony location, with a 95% confidence interval. 16 There was visible hypertrophy of the pectoralis major muscle bilaterally. Active and passive ROM were tested for the shoulders as recommended by Magee. 14 The patient had full bilateral active ROM, with minimal pain at end-range flexion and abduction that was not increased with overpressure in accordance with Magee. 14 He had full passive ROM with no pain reported.
Manual muscle testing based on Hislop and Montgomery revealed 4/5 strength of external rotation at 0° and 45° of abduction, with pain reported along the anterolateral shoulder. 17 Testing also showed 3/5 strength and no pain with resisted abduction with the arm at the side at approximately 30° of abduction. 18 Manual muscle testing is a useful clinical assessment tool, although a recent literature review suggested that further testing is required for scientific validation. 18 Palpation of the shoulder, as described by Hoppenfeld, revealed slight tenderness over the greater tubercle, as well as along the length of the levator scapula muscle. 19
Special tests were negative for the sulcus sign, Speed's test, the drop arm test, and the empty can test, as described by Magee. 14 Research shows that Speed's test has a sensitivity and specificity of 32% and 61% for biceps and labral pathology respectively; 20 the drop arm test has a sensitivity of 27% and a specificity of 88% as a specific test for rotator cuff tears, and the empty can test has a sensitivity of 44% and a specificity of 90% in diagnosing complete or partial rotator cuff tears. 20 , 21 The Neer and Hawkins-Kennedy impingement tests were both negative. 14 According to a meta-analysis by Hegedus et al., the Neer test is 79% sensitive and 53% specific, while the Hawkins-Kennedy test is 79% sensitive and 59% specific, for impingement. 21
I (NS) diagnosed the patient with mild supraspinatus tendinosis, with no evidence of tearing of the rotator cuff muscles, based on the following findings drawn from the patient interview: shoulder pain aggravated by pull-ups, rowing, and free weights; increased pain when lying on the affected shoulder. Additional significant findings from the physical examination included full shoulder active ROM with minimal pain at end-range flexion and abduction; pain along the anterior lateral shoulder with resisted testing of external rotation at 0° and 45° of abduction; negative drop arm and empty can tests; and tenderness over the greater tubercle of the humerus. The musculoskeletal dysfunction did not explain the level of pain reported by the patient (maximum NPRS 8/10), nor was the physical examination able to reproduce the exact location of the reported shoulder pain or the elbow, wrist, and knee pain described by the patient.
I was concerned about a serious pathology or a psychological disorder, given that this 19-year-old had made 10 medical appointments over 22 months for 6 different regions of the body; in my experience of examining and treating patients between the ages of 18 and 25, the frequency of the appointments and the variation in afflicted body parts are not typical of a young patient. The patient's description of his shoulder pain, in terms of location and severity, was not reproducible by physical examination. Throughout our interview, the patient did not maintain good eye contact, spoke in a monotone voice, and had an overall flat affect. Even when he described his beliefs about implants and government control, his voice and demeanour remained expressionless. The patient described persecutory delusions, command hallucinations, and social isolation from friends and family, all of which are signs of psychosis according to the Diagnostic and Statistical Manual of Mental Health . 22
Based on the findings from the patient interview and the physical examination, the patient did have symptoms consistent with a known musculoskeletal dysfunction; however, the undiagnosed and uncontrolled psychiatric symptoms made it more appropriate to refer him back to the physician for evaluation and treatment of his psychosis than to provide physical therapy intervention for his shoulder dysfunction. Furthermore, because research shows that the rate of suicide among patients with schizophrenia can range from 2% or 4% to as high as 15% 23 , 24 and that the rate of suicide is highest among patients close to the date of diagnosis, early recognition is crucial. 23
INTERVENTION
Based on the findings from the patient interview and the signs and symptoms of psychiatric disorders, I explained to the patient that there was a need for further medical investigation. Although the patient did not agree with this initial assessment, he did consent to a follow-up with the referring physician.
I spoke to the referring physician in person and explained to him my findings from the patient interview, specifically the patient's belief that he had electrical implants in his body. I also pointed out the patient's affect and the limited physical findings during the physical examination. I provided the physician with some direct quotes from the patient to demonstrate the level of psychosis he was presenting with. I stated my conclusion that the patient was suffering from some form of psychosis that precluded physical therapy treatment for his shoulder at that time. The referring physician was quite concerned about the patient and called him during our meeting to arrange a follow-up medical appointment.
The physician examined the patient, made similar observations, concurred with my assessment, and concluded that the patient was experiencing some form of psychosis. The plan of care involved referral to a psychiatrist, follow-up with the physician, and explaining to the patient that physical therapy would not be appropriate at this time because of the presence of a serious psychiatric disorder. The patient did not believe that he had a psychiatric disorder, but he was willing to follow up with a psychiatrist. The physician noted that the patient was not a threat to himself or others and that he did not report having homicidal or suicidal thoughts.
The patient followed up with the psychiatrist 11 days after his appointment with the physician. He was diagnosed with schizophrenia and started on a daily dose of risperidone (Risperdal). The patient was also instructed to follow up with the psychiatrist every second week to ensure compliance with the medication and to discuss progress. Further details of the psychiatric assessment and treatment were not available for this case report. Outcomes are also unavailable for this case report, since follow-up by the physical therapist was not possible.
Case Summary
This case report describes a 19-year-old man referred to physical therapy with shoulder, wrist, and knee pain who was later diagnosed with a psychiatric disorder. After completing a thorough patient interview and physical examination, I concluded that the patient was suffering from an undiagnosed psychiatric disorder that required medical referral. The interview revealed that the patient had delusions about electrical devices' being implanted in his body and was experiencing various forms of hallucination. The patient was promptly referred for medical consult and was diagnosed with schizophrenia by a psychiatrist.
Patient Symptoms and Schizophrenia
Schizophrenia is a psychiatric disorder affecting between 0.5% and 1.5% of adults worldwide, with a slightly greater prevalence in men. 22 The age of onset may be from 5 to 60 years; however, more than 50% of first episodes occur between the ages of 15 and 24. 22 , 25 , 26 An earlier onset is more common among men, while later onset is more common among women. 25 Schizophrenia shows a higher incidence in individuals born in urban areas than in those born in rural areas. 22 , 25 Because the patient in the present case fell into several of these categories (male, born in an urban area, experienced onset of symptoms around age 17) and presented with clear symptoms of a psychiatric disorder (delusions, hallucinations), schizophrenia seemed the most likely diagnosis.
The signs and symptoms of schizophrenia are classified as either positive or negative. 22 Positive symptoms are an excess of normal function and include delusions, hallucinations, and disorganized speech; 22 , 27 negative symptoms are a deficiency of normal function and include limited goal-directed behaviour (avolition), limited fluency and productivity of speech and thought, and a flat affect. 22 , 27 The diagnosis of schizophrenia requires the presence of at least two of these positive or negative symptoms lasting at least 6 months. 22 , 27 In this case, the patient presented with delusions (e.g., electrical implants trying to control his and others' actions), including persecutory delusions (e.g., “they are emotionally abusing me”), hallucinations (e.g., hearing voices, seeing signs), and a flat affect. Since the patient was enrolled in university at the time of diagnosis, his cognitive function is assumed to be well preserved. The patient reported no change in symptoms for 2 years.
Schizophrenia is subdivided into five types: paranoid, disorganized, catatonic, undifferentiated, and residual (see Table Table1 1 ). 22 , 28 Based on these observations and on the literature, the patient's symptoms were suggestive of paranoid schizophrenia, 22 which is the most prevalent form of schizophrenia in most parts of the world. 22
Schizophrenia Subtypes 6
The aetiology of schizophrenia remains unknown. 29 , 30 There is a strong genetic predisposition. 29 , 30 Patients who experience the onset of schizophrenia before age 22 are 10 times more likely to have a history of a complicated caesarean birth than patients with a later onset of schizophrenia, which suggests a possible neurodevelopmental factor in early-onset schizophrenia. 31 Mild childhood head injuries may play a role in the expression of schizophrenia in families with a strong genetic predisposition to this disorder. 32 Psychological stress has also been implicated in the onset of schizophrenia, since it often precipitates the first psychotic episode or increases the likelihood of a relapse. 33 , 34 In this case, the patient described a family “break-up” which may have precipitated the onset of psychosis. Details about his childhood head injuries and the circumstances of his birth were not obtained. After being diagnosed with schizophrenia, the patient revealed to the referring physician that his father had experienced something similar when he was younger, which may point to a genetic predisposition.
There are no conclusive diagnostic tests for schizophrenia. 22 However, imaging studies have suggested neurophysiologic changes as an associated finding. Volumetric magnetic resonance imaging (MRI) studies of patients with schizophrenia have demonstrated an overall reduction in grey matter; an increase in white matter; decreased size of the amygdala, hippocampus, and parahippocampus; an overall reduction in brain volume; and larger lateral ventricles relative to a control group. 35 – 37
Psychiatric Disorders as They Relate to Musculoskeletal Dysfunction
As primary-care practitioners, physical therapists may encounter patients with possible psychiatric disorders such as schizophrenia. However, the physical therapy literature on psychiatric disorders as they relate to musculoskeletal disorders focuses mainly on low back pain (LBP). 7 , 8 In an examination of a large number of physical and psychological factors, one prospective case-control study points to the importance of psychological variables as a risk factor for chronic LBP and widespread musculoskeletal pain. 8 Previous research has also concurred with this study in implicating psychological variables as risk factors for LBP and neck pain. 9 , 10 These articles provide a link between psychological disorders and patients seeking physical therapy for musculoskeletal dysfunctions.
In this case report, the physical examination was suggestive of a mild supraspinatus tendinosis, but this did not explain the severity of pain reported by the patient or the referral of pain to the elbow, wrist, and knee. One of the limitations of the physical examination was that there was not sufficient time to perform physical examination of the elbow, wrist, and knee. The patient's undiagnosed and uncontrolled psychiatric symptoms took priority over the musculoskeletal dysfunction and required immediate medical referral without physical therapy intervention. Because of the inconsistencies between interview and physical examination, as well as the patient's perception that an electrical implant was causing his musculoskeletal pain, there is a possibility that at least some of his musculoskeletal symptoms may have been manifestations of his psychiatric disorder.
Effective Patient Interviews
The medical literature indicates that 50% of all mental illness is recognized during the interview process as part of medical assessment by the primary-care physician. 38 As physical therapists embrace their role as providers of primary care, 4 , 5 they must rely on their skills in patient interviewing and physical examination to rule out medical pathology. Improved assessment skills by the physical therapist may help to identify primary or secondary medical pathologies that have not previously been diagnosed. Within the peer-reviewed literature, a number of case studies demonstrate identification of non-musculoskeletal or visceral pathology that can manifest as musculoskeletal disorders; 39 – 41 these case studies are examples of how physical therapists can perform an initial assessment, identify a medical pathology that precludes treatment, and make an appropriate referral. During a patient interview, physical therapists must be well aware of the psychological and psychosocial aspects of the examination to identify relevant aspects of the patient's demeanour (e.g., appropriate self-care) and emotional state (e.g., inappropriate affect). The patient interview should consist of non-leading, open-ended questions about how pain in multiple areas is related and how it is caused. Furthermore, physical therapists should avoid rationalizing the patient's symptoms during the interview process. At a minimum, patients should be permitted to speak about and describe their symptoms in a way that is meaningful to them.
Schizophrenia and Primary Care
Schizophrenia is most often initially recognized by the primary-care physician. 42 Psychiatrists, psychologists, and even the lay community have also been noted in the literature as making the initial identification. 43 – 45 Although conspicuously absent from the literature on the initial identification of schizophrenia, physical therapists are in a position to be important first-contact care providers who can make the initial identification of schizophrenia, and other psychiatric disorders, through effective patient interviews. Although labelling patients as having a psychiatric disorder is outside physical therapists' scope of practice, the diagnostic process is not exclusive to any one profession. In this case, the process of diagnosis, which involves assessing the patient, grouping findings, interpreting the data, and identifying the patient's problems, led me to conclude that the primary dysfunction was psychiatric in nature. 46 This process, which Few et al. call “diagnostic reasoning,” is well within physical therapists' scope of practice and is something we constantly engage in during our daily clinical practice. 11 Diagnostic reasoning involves taking into account all of the possible pathological structures and determining the most likely cause of the patient's symptoms. In practice, expert clinicians do not follow standardized protocols; 46 rather, they pay attention to cues provided by the patient, recognize patterns, and test hypotheses to arrive at a probable cause for the patient's symptoms. 11
IMPLICATIONS AND FUTURE DIRECTIONs
The medical literature has identified gaps in the knowledge of primary-care physicians, specifically a lack of awareness of the symptoms and epidemiology of schizophrenia. 28 To facilitate early recognition, referral, and diagnosis of schizophrenia, the medical literature has suggested increased collaboration among family physicians and mental-health professionals, as well as ongoing mental-health training for family physicians. 47 , 48 Physical therapists should also heed these suggestions. A study in the physical therapy literature recommends mental-health training for recognizing the symptoms of depression in a population with LBP; 7 the same study, conducted in Australia, concluded that physical therapists' ability to recognize depressive symptoms in an outpatient setting was poor. 7
An initial step to address these gaps could be a position paper that draws on the medical literature to inform physical therapists about the presence, prevalence, signs, and symptoms of common psychiatric disorders. As well, future research needs to focus on the incidence of musculoskeletal signs and symptoms in patients with common psychiatric disorders.
KEY MESSAGES
What is already known on this topic.
To the authors' knowledge, there are no known studies in the literature describing a case of a patient referred to physical therapy for musculoskeletal dysfunction who was later diagnosed with schizophrenia.
What This Study Adds
This case report contributes to the existing literature on physical therapists functioning as competent providers of primary care who have the knowledge and skills needed to rule out non-musculoskeletal pathology. It also educates physical therapists about the signs and symptoms of schizophrenia.
Shah N, Nakamura Y. Case report: schizophrenia discovered during the patient interview in a man with shoulder pain referred for physical therapy. Physiother Can. 2010;62:308–315
Oral Health Status and Factors Related to Oral Health in Patients with Schizophrenia: A Matched Case-Control Observational Study
Affiliations.
- 1 Department of Oral Surgery, Faculty of Dentistry, University of Szeged, Tisza Lajos krt. 64-66., 6720 Szeged, Hungary.
- 2 Department of Psychiatry, Faculty of Medicine, University of Szeged, Korányi fasor 8-10., 6720 Szeged, Hungary.
- 3 Department of Prosthodontics, Faculty of Dentistry, University of Szeged, Tisza Lajos krt. 64-66., 6720 Szeged, Hungary.
- PMID: 38541811
- PMCID: PMC10970925
- DOI: 10.3390/jcm13061584
Background: Schizophrenia (SCZ) patients have disproportionately poor oral health outcomes owing to a multidimensional set of factors, such as pathophysiology of the disease, drug-related adverse effects and lower utilization rate of dental healthcare services. The aim of the present observational study was to compare the indicators of dental and periodontal health in patients with SCZ to those of nonaffected healthy controls; furthermore, the influence of various anamnestic factors and lifestyle habits on oral health status were also assessed. Methods: A total of 50 SCZ patients-in remission-receiving treatment at the Department of Psychiatry, University of Szeged, were compared with 50 age- and gender-matched healthy controls attending the Faculty of Dentistry, University of Szeged. Participants' dental (decayed, missing and filled surfaces [DMF-S] and decayed, missing and filled teeth [DMF-T]) and periodontal (plaque index [%], bleeding on probing [BOP%], pocket depth [PD] and attachment loss [AL]) status was measured according to the World Health Organization (WHO) criteria. Results: In total, 74.0%, 80.0% and 78.0% of SCZ patients received second-generation antipsychotics, benzodiazepines and mood stabilizers, respectively. Patients with SCZ had significantly higher DMFs (81.30 ± 40.16 vs. 61.64 ± 40.56; p = 0.010), D (8.18 ± 7.73 vs. 4.18 ± 4.22; p < 0.001) and DMF-T (18.20 ± 8.36 vs. 14.42 ± 8.21; p = 0.024) scores but significantly lower F (1.84 ± 0.29 vs. 4.62 ± 3.98; p < 0.001) scores compared to the controls; male subjects had significantly lower DMFs (74.52 ± 39.72 vs. 90.67 ± 39.1; p = 0.020) and DMF-T (16.52 ± 8.12 vs. 20.52 ± 8.32; p = 0.031) scores. Additionally, SCZ patients had significantly higher plaque indices (56.96 ± 23.19 vs. 27.44 ± 17.53; p < 0.001), BOP% (58.96 ± 22.89 vs. 23.56 ± 17.53; p < 0.001), PD (2.84 ± 0.67 vs. 2.19 ± 0.49; p = 0.024) and AL (3.39 ± 1.72 vs. 2.49 ± 0.76; p < 0.001) values compared to controls. Smoking > 10 cigarettes/day was associated with worse dental and periodontal indices, while consuming ≥ 4 units/week of alcohol was associated with worse periodontal indices, respectively ( p < 0.05 in all cases). In contrast, coffee consumption rates and vitamin supplementation status had no significant effect on oral health status indicators. Conclusions: Our study highlights the overall poor oral health status of individuals affected by SCZ and the need for targeted preventive interventions.
Keywords: DMF-T; case-control study; dental status; mental disorder; oral health; periodontal status; schizophrenia.
Grants and funding

IMAGES
VIDEO
COMMENTS
Schizophrenia is a chronic and severe mental disorder characterized by distortions in thinking, perception, emotions, language, sense of self, and behaviour. This report presents the role of clinical pharmacists in the management of a patient diagnosed with schizophrenia with symptoms of paranoia. A gainfully employed young African male adult reported to be roaming around town moving from one ...
Case 2: A woman with constipation. A woman aged 40 years* presents at the pharmacy. The pharmacist recognises her as she often comes in to collect medicine for her family. They are aware that she has a history of schizophrenia and that she was started on clozapine three months ago. She receives this from her mental health team on a weekly basis ...
Introduction. Schizophrenia is a chronic severe mental illness with heterogeneous clinical profile and debilitating course. Research shows that clinical features, severity of illness, prognosis, and treatment of schizophrenia vary depending on the age of onset of illness.[1,2] Hence, age-specific research in schizophrenia has been emphasized.Although consistency has been noted in ...
Case Study: Bryant. Thirty-five-year-old Bryant was admitted to the hospital because of ritualistic behaviors, depression, and distrust. At the time of admission, prominent ritualistic behaviors and depression misled clinicians to diagnose Bryant with obsessive-compulsive disorder (OCD). Shortly after, psychotic symptoms such as disorganized ...
1. Introduction. Schizophrenia is a severe mental disorder characterized by a debilitating progression in most cases. Despite its etiology not being completely understood, schizophrenia seems to result from a complex interaction of biological, genetic and environmental factors [].According to the DSM-5 criteria [], clinical features of schizophrenia comprise positive (delusions and ...
Background. Schizophrenia is a severe, chronic, and heterogeneous mental disorder that often has debilitating long-term outcomes. Its lifetime prevalence rate is estimated to be approximately 1% worldwide in the adult population (Lehman et al., 2010).Onset generally occurs in late adolescence or early adulthood, with an average age of 18 years for men and 25 years for women. 1 The term early ...
As per the recent systematic analysis for the Global Burden of Disease Study 2017, schizophrenia is one of the world's top 20 leading causes of ... the World Health Organization's Mental Health Action Plan and the World Psychiatric Association emphasized community-based mental health services ... Case studies of 72 programmes. PLoS One ...
Schizophrenia is considered one of the most severe psychiatric disorders (5). It is often associated with significant neurocognitive and social cognition deficits (6-8), daily functional impairment for many, high levels of internalized stigma (9, 10), and poor real-world outcomes (11-13). In this context, case reports and case series of ...
Schizophrenia symptoms can differ from person to person, but they generally fall into three main categories: psychotic, negative, and cognitive. Psychotic symptoms include changes in the way a person thinks, acts, and experiences the world. People with psychotic symptoms may lose a shared sense of reality with others and experience the world in ...
characterized by symptoms such as: hallucinations, delusions, disorganized communication, poor. planning, reduced motivation, and blunted a ffec t.(3) Genes and environment, and an altered ...
Schizophrenia is considered one of the most severe psychiatric disorders ( 5 ). It is often associated with significant neurocognitive and social cognition deficits ( 6 - 8 ), daily functional impairment for many, high levels of internalized stigma ( 9, 10 ), and poor real-world outcomes ( 11 - 13 ). In this context, case reports and case ...
18 Lysaker PH, Buck KD, Ringer JM: The recovery of metacognitive capacity in schizophrenia across 32 months of individual psychotherapy: a case study. Psychother Res 2007; 17:713-720Crossref, Google Scholar. 19 Anthony WA: Recovery from mental illness: the guiding vision of the mental health service system in the 1990s.
This case study aims to explore a patient's journey in mental health services during a relapse of schizophrenia. It also aims to highlight good practice for communicating with patients with severe mental illness in all settings, and in explaining the role of clozapine.
Mental Health Clinician (2012) 1 (8): 191-195. Clinical pearls based on the treatment of a patient with schizophrenia who had stabbed a taxi cab driver are discussed in this case study. Areas explored include the pharmacokinetics of fluphenazine decanoate, strategies to manage clozapine-associated agranulocytosis, and approaches to addressing ...
Case Illustration 2. YS is a 61-year-old woman with a medical history of schizophrenia diagnosed in her early 20s. After a decade of having very limited contact with family and experiencing homelessness as a result of discontinuing of her antipsychotic medication, YS was hospitalized and restarted on an antipsychotic, after which she resumed contact with her family.
1. INTRODUCTION. This paper reports a review of outcomes in schizophrenia in the twenty‐first century and is an extension of the work undertaken by the late Dr Richard Warner in his seminal book, "Recovery from Schizophrenia: Psychiatry and Political Economy" (1985 (Warner, 1985); 2004 (Warner, 2004)).The present work was started with Dr Warner's involvement, and the preliminary results ...
Mental health recovery involves an integration of clinical and psychosocial frameworks. The recovery journey of individuals diagnosed with schizophrenia and the factors that influence it have been extensively studied. Because the recovery journey is culturally influenced, we examined the recovery process expriences of individuals diagnosed with schizophrenia in China, focusing on the influence ...
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may seem like they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but ...
Background 80% of patients value information on treatment options as an important part of recovery, further patients with a history of psychotic episodes feel excluded from decision making about their antipsychotic treatment, and on top of that, mental health staff is prone to be reluctant to support shared decision making and medication tapering for patients with schizophrenia. This case ...
Case reports provide insight into the differential diagnosis, overlapping diagnoses and the increased complexity (such as treating schizophrenia and obsessive-compulsive disorder), decision-making, and clinical management of unusual cases as a valuable educational tool.Schizophrenia is a severe mental disorder, often associated with ...
Case Study Schizophrenia Keith RN unfolding clinical reasoning case study history of present problem: jeremy brown is caucasian male who was brought to the. ... Jeremy's mental health had been stable up until the last three months. He has been feeling more paranoid the past three months and experienced a dramatic increase in symptoms when he ...
Individually, they are some of the most complex and challenging psychiatric disorders to manage. This article reports on a case of an adolescent with co-morbid schizophrenia and OCD and the use of exposure and response prevention (ERP) for the treatment of OCD in the context of management of his schizophrenia and addressing developmental issues.
RN 222 Mental Health Exam 1 - Study Guide. Exam 2-1 - Study guide. MH Test 3 - Mental health practice quiz. N209 Exam 1 objectives. NUR 209 Final Exam Study Guide 2. Schizophrenia Case Study unfolding clinical reasoning case study history of present problem: jeremy brown is caucasian male who was brought to the emergency.
The patient, a 58-year-old male with PMO, sees faces without any distortions when viewed on a screen and on paper but sees distorted faces that appear "demonic" when viewed in-person. The case is especially rare because he does not see distortions of faces across all contexts. For the study, the researchers took a photograph of a person's ...
Psychotic-like experiences are highly prevalent in the general population, with figures of 20% or above being reported in some studies. 1 Major self-mutilation (or NSSI) is a rare but potentially catastrophic complication of severe mental illness. Most people who inflict NSSI have a psychotic disorder, usually a schizophrenia spectrum psychosis.
Northwest Community Hospital | Arlington Heights Hospital, IL This Psychiatry and Behavioral Health symposium tackles the complexities of schizophrenia within a fractured mental healthcare system. By uniting state and national leaders in psychiatry, we aim to bridge the gap between groundbreaking research and its accessibility for providers.
A man with a rare condition called prosopometamorphopsia, or PMO, in which faces are distorted shares his vision of the "demons" he sees when he looks at people's faces.
Schizophrenia is a psychiatric disorder affecting between 0.5% and 1.5% of adults worldwide, with a slightly greater prevalence in men. 22 The age of onset may be from 5 to 60 years; however, more than 50% of first episodes occur between the ages of 15 and 24. 22,25,26 An earlier onset is more common among men, while later onset is more common ...
Background: Schizophrenia (SCZ) patients have disproportionately poor oral health outcomes owing to a multidimensional set of factors, such as pathophysiology of the disease, drug-related adverse effects and lower utilization rate of dental healthcare services. The aim of the present observational study was to compare the indicators of dental and periodontal health in patients with SCZ to ...