- Patient Care & Health Information
- Diseases & Conditions
A member of your health care team will likely ask you for a description and history of your swallowing difficulties, perform a physical exam, and use various tests to find the cause of your swallowing problem.
Tests can include:
X-ray with a contrast material, called a barium X-ray. You drink a barium solution that coats the esophagus, making it easier to see on X-rays. A healthcare team can then see changes in the shape of the esophagus and can check the muscular activity.
You also may be asked to swallow solid food or a pill coated with barium. This allows the healthcare team to watch the muscles in the throat during swallowing or to look for blockages in the esophagus that the liquid barium solution might not show.
- Dynamic swallowing study. This study involves swallowing barium-coated foods of different consistencies. It provides an image of these foods as they travel down the throat. The images might show problems in the coordination of the mouth and throat muscles during swallowing. The images also can show if food is going into the breathing tube.
- Endoscopy. Endoscopy involves passing a thin, flexible lighted instrument, called an endoscope, down the throat. This allows your healthcare team to see your esophagus. Tissue samples, called biopsies, may be collected. The samples are studied to look for inflammation, eosinophilic esophagitis, narrowing or a tumor.
- Fiber-optic endoscopic evaluation of swallowing (FEES). During a FEES study, a healthcare professional examines the throat with an endoscope during swallowing.
- Esophageal muscle test, called manometry. In manometry (muh-NOM-uh-tree), a small tube is inserted into the esophagus and connected to a pressure recorder to measure the muscle contractions of the esophagus during swallowing.
- Imaging scans. These can include a CT scan, which combines a series of X-ray views and computer processing to create cross-sectional images of the body's bones and soft tissues, or an MRI scan, which uses a magnetic field and radio waves to create detailed images of organs and tissues.

FEES Swallowing Study
Hi, Addie. I'm Carrie. I'm a speech pathologist. I'm going to be helping out with the evaluation today. We're going to be doing a type of swallowing evaluation where we put a camera in your nose. We give you different consistencies of food items to swallow and watch you swallow those. This is the camera we're going to use. It goes in your nose about this far, just a little bit past that white line. There's not much space between your nose and your throat, so it doesn't have to go in very far. We're not in there very long. Just long enough to take a look around at the anatomy, give you a couple of things to eat and drink, watch you swallow those and then we come out, okay. So the different items we're going to be swallowing. We'd like to do an assortment of consistencies, so we do a thin liquid, a puree, and then a solid consistency. I put a little green food coloring in the liquid and the puree that just allows us to see it better when the cameras in place. Okay.
Proceduralist: Ready?
Assistant: Some slow deep breaths.
Carrie: That's the absolute worst part right there.
Assistant: Good job.
Proceduralist: Can you see?
Assistant: Can you see on the TV?
Carrie: Only if you want.
Proceduralist: We can show you afterwards too.
Carrie: Ready for me?
Assistant: Take a couple sips of juice.
Carrie: Go ahead and take a couple more for me. Good.
Assistant: Some applesauce.
Carrie: Your other hand. Go ahead and take a bite of one of those. And one more. You can move your head a little bit. All right. That's it.
Proceduralist: Are you done?
Carrie: I'm done.
Proceduralist: On the way out. Perfect.
Assistant: You did it! Good job.
- Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your dysphagia-related health concerns Start Here
More Information
Dysphagia care at Mayo Clinic
- Esophageal manometry
- Upper endoscopy
Treatment for dysphagia depends on the type or cause of your swallowing disorder.
Oropharyngeal dysphagia
For oropharyngeal dysphagia, you may be referred to a speech or swallowing therapist. Therapy might include:
- Learning exercises. Certain exercises might help coordinate your swallowing muscles or restimulate the nerves that trigger the swallowing reflex.
- Learning swallowing techniques. You also might learn ways to place food in your mouth or position your body and head to help you swallow. Exercises and new swallowing techniques might help if your dysphagia is caused by neurological problems such as Alzheimer's disease or Parkinson's disease.
Esophageal dysphagia
Treatment approaches for esophageal dysphagia might include:
- Esophageal dilation. Dilation involves placing an endoscope into the esophagus and inflating an attached balloon to stretch it. This treatment is used for achalasia, esophageal stricture, motility disorders, or an irregular ring of tissue at the junction of the esophagus and stomach, known as Schatzki ring. Long, flexible tubes of varying diameter also may be inserted through the mouth into the esophagus to treat strictures and rings.
- Surgery. For an esophageal tumor, achalasia or pharyngoesophageal diverticulum, you might need surgery to clear your esophageal path.
Medicines. Difficulty swallowing caused by GERD can be treated with prescription medicines to reduce stomach acid. You might need to take these medicines for a long time.
Corticosteroids might be recommended for eosinophilic esophagitis. For esophageal spasm, smooth muscle relaxants might help.
- Diet. You may be prescribed a special diet to help with your symptoms depending on the cause of the dysphagia. If you have eosinophilic esophagitis, diet might be used as treatment.
Severe dysphagia
If difficulty swallowing prevents you from eating and drinking enough and treatment doesn't allow you to swallow safely, a feeding tube may be recommended. A feeding tube provides nutrients without the need to swallow.
Surgery might be needed to relieve swallowing problems caused by throat narrowing or blockages. Blockages include bony outgrowths, vocal cord paralysis, pharyngoesophageal diverticula, GERD and achalasia. Surgery also can treat esophageal cancer. Speech and swallowing therapy is usually helpful after surgery.
The type of surgical treatment depends on the cause of dysphagia. Some examples are:
- Laparoscopic Heller myotomy. This involves cutting the muscle at the lower end of the esophagus, called the esophageal sphincter. In people who have achalasia, the esophageal sphincter fails to open and release food into the stomach. Heller myotomy helps correct this problem.
- Peroral endoscopic myotomy (POEM). The POEM procedure involves creating an incision in the inside lining of the esophagus to treat achalasia. Then, as in a Heller myotomy, the surgeon or gastroenterologist cuts the muscle at the lower end of the esophageal sphincter.
- Stent placement. A metal or plastic tube called a stent may be used to prop open a narrowed or blocked esophagus. Some stents are permanent, such as those for people with esophageal cancer, while others are removed later.
- OnabotulinumtoxinA (Botox). This can be injected into the muscle at the end of the esophagus, called the esophageal sphincter. This causes it to relax, improving swallowing in achalasia. Less invasive than surgery, this technique might require repeat injections. More study is needed.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
If you have trouble swallowing, be sure to see a healthcare professional. You also may try these approaches to help ease symptoms:
- Changing your eating habits. Try eating smaller, more frequent meals. Cut your food into smaller pieces, chew food thoroughly and eat more slowly. If you have difficulty swallowing liquids, there are products you can buy to thicken liquids.
- Trying foods with different textures to see if some cause you more trouble. Thin liquids, such as coffee and juice, are a problem for some people, and sticky foods, such as peanut butter or caramel, can make swallowing difficult. Avoid foods that cause you trouble.
- Limiting alcohol and caffeine. These can dry your mouth and throat, making swallowing more difficult.
Preparing for your appointment
See a healthcare professional if you're having problems swallowing. Depending on the suspected cause, you may be referred to an ear, nose and throat specialist; a doctor who specializes in treating digestive disorders, called a gastroenterologist; or a doctor who specializes in diseases of the nervous system, called a neurologist.
Here's some information to help you prepare for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet.
Make a list of:
- Your symptoms, including any that seem unrelated to the reason for which you scheduled the appointment, and when they began.
- Key personal information, including major stresses or recent life changes.
- All medicines, vitamins and supplements you take, including doses.
- Questions to ask your healthcare team.
For dysphagia, questions to ask include:
- What's the likeliest cause of my symptoms?
- What are other possible causes?
- What tests do I need?
- Is this condition temporary or long lasting?
- I have other health conditions. How can I best manage them together?
- Do I need to restrict my diet?
- Are there brochures or other printed material I can have? What websites do you recommend?
What to expect from your doctor
Your healthcare team is likely to ask you a number of questions, including:
- Have your symptoms been continuous or occasional?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms? For example, are certain foods harder to swallow than others?
- Do you have difficulty swallowing solids, liquids or both?
- Do you cough or gag when you try to swallow?
- Did you first have trouble swallowing solids and then develop difficulty swallowing liquids?
- Do you bring food back up after swallowing it?
- Do you ever vomit or bring up blood or black material?
- Have you lost weight?
What you can do in the meantime
Until your appointment, it might help to chew your food more slowly and thoroughly than usual. If you have heartburn or GERD , try eating smaller meals and not eating right before bedtime. Antacids that you can get without a prescription also might help temporarily.
- Fass R. Approach to the evaluation of dysphagia in adults. https://www.uptodate.com/contents/search. Accessed Aug. 4, 2023.
- Ferri FF. Dysphagia. In: Ferri's Clinical Advisor 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed Sept. 21, 2021.
- Dysphagia. National Institute on Deafness and Other Communication Disorders. https://www.nidcd.nih.gov/health/dysphagia. Accessed Aug. 4, 2023.
- Dysphagia. Merck Manual Professional Version https://www.merckmanuals.com/professional/gastrointestinal-disorders/esophageal-and-swallowing-disorders/dysphagia. Accessed Aug. 4, 2023.
- Lembo AJ. Oropharyngeal dysphagia: Clinical features, diagnosis, and management. https://www.uptodate.com/contents/search. Accessed Aug. 4, 2023.
- Dysphagia. American College of Gastroenterology. https://gi.org/topics/dysphagia/. Accessed Aug. 4, 2023.
- Panebianco M., et al. Dysphagia in neurological diseases: A literature review. Neurological Sciences. 2020; doi:10.1007/s10072-020-04495-2.
- Aging and swallowing. American Academy of Otolaryngology — Head and Neck Surgery. https://www.enthealth.org/conditions/aging-and-swallowing/. Accessed Aug. 4, 2023.
- Triggs J, et al. Recent advances in dysphagia management. F1000Research. 2019; doi:10.12688/f1000research.18900.1.
- Ami TR. Allscripts EPSi. Mayo Clinic. Aug. 8, 2023.
Associated Procedures
News from mayo clinic.
- Mayo Clinic Healthcare expert explains when swallowing issues are more than an accident Aug. 24, 2022, 04:01 p.m. CDT
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Speech Therapy for Swallowing Disorder Patients
Posted by Penn Medicine Becker ENT & Allergy
Swallowing disorders can affect a person’s daily life, and speech therapy is an effective treatment option. At Penn Medicine Becker ENT & Allergy, specialists have a strong knowledge of these issues and work with targeted exercises to help patients improve their ability to swallow.
Speech therapists are essential in treating swallowing disorders. They diagnose the condition and provide customized exercises and techniques to help people improve their swallowing function. The goal of speech therapy is to help patients return to as normal a swallowing ability as possible.

How Speech Therapy Helps With Swallowing Issues
- Speech therapy offers specialized techniques to help patients manage and improve swallowing disorders.
- Swallowing disorders, also known as dysphagia, can occur due to various health conditions and can affect people of all ages.
- In speech therapy, personalized exercises are designed to strengthen the muscles involved in swallowing.
- Techniques taught in speech therapy can also include strategies to make swallowing safer and prevent choking.
- Regular sessions with a speech therapist can significantly improve swallowing function and enhance the quality of life.
Understanding Swallowing Disorders and the Role of Speech Therapy
What are swallowing disorders.
Swallowing disorders, known as dysphagia, are medical conditions that make it difficult for individuals to swallow. These problems may be related to neurological disorders, or structural abnormalities, or could appear as part of a feeding disorder. Dysphagia is significant because it impacts both nutritional intake and respiratory health, making its effective management important.
How Can Speech Therapy Help?
Speech therapy, guided by a qualified speech therapist, is important in rehabilitation therapy for those with swallowing issues. Speech therapists use various strategies specifically designed to enhance swallowing function. Regular discussions between speech pathologists are instrumental in the continuous improvement of treatment techniques. The field of speech pathology includes numerous methods that assist individuals with disorders from speech pathology, helping them navigate the challenges associated with the condition.
Signs and Symptoms to Watch For
If someone has trouble swallowing, known as dysphagia, it’s important to recognize the signs early. Common symptoms include:
- Difficulty initiating a swallow
- Coughing while eating or afterward
- A sensation that food is stuck in the throat
- Unintentional weight loss
- Recurring pneumonia
These symptoms can indicate a neurological disease or gastroesophageal reflux disease that is affecting the swallowing process.
Professional Diagnosis
A thorough assessment by healthcare professionals is necessary to pinpoint the specific type of swallowing disorder , like Esophageal dysphagia. This often involves tools such as:
- Endoscopic assessment
The aim is to identify the exact disease causing the dysphagia. Specialists can create a targeted treatment plan with a proper diagnosis and management of swallowing physiology.
Step 1: Identifying the Type of Swallowing Disorder
Qualifications and specializations.
When choosing a speech therapist, confirm their qualifications:
- A master’s degree in speech-language pathology
- Certification from the American Speech-Language-Hearing Association (ASHA)
If you require specific expertise, such as for swallowing disorders, ensure the speech therapist has experience in that area to enhance the quality of care.
Preparing for Your First Appointment
Before your first speech therapy session:
- Collect all medical documents related to your speech condition.
- Collaborate with your entire healthcare team to provide your speech therapist with relevant information.
- This teamwork with your care team guarantees that your speech therapy is effective and customized to your needs.
Step 2: Finding a Qualified Speech Therapist
Short-term vs. long-term goals.
In speech therapy, goals are categorized into:
- Short-term Goals : Immediate targets for patients to aim toward.
- Long-term Goals : Ultimate achievements desired in the course of therapy.
The goals should be:
This framework ensures that patients and speech therapists are working towards a shared aim.
Working with Your Therapist to Set Realistic Expectations
Developing a realistic care plan involves:
- Collaboration : Working closely with your speech therapist is essential.
- Understanding : Knowing which outcomes are achievable allows therapy to be specifically tailored.
- Transparency : Fosters a clear relationship between patients and their treatment team.
- Trust : Establishes trust and ensures expectations are in line with what therapy can accomplish.
Step 3: Setting Goals for Therapy
Strengthening exercises.
Performing strengthening exercises is important to build up the muscles used in swallowing. These exercises are tailored to address muscle weakness and improve the functionality of the esophageal muscles.
- Consistent Practice : Helps patients build muscle strength and endurance for their swallowing mechanism.
Coordination and Timing Exercises
Swallowing exercises not only help strengthen but also enhance coordination and timing during each phase of swallowing.
- Precise Movements : Develops the movements needed between various muscle groups.
- Muscle Cooperation : Ensures muscles work together seamlessly during the phase of swallowing, reducing the risk of aspiration.
Step 4: Engaging in Therapeutic Exercises
Safe foods and textures.
- Blended or pureed foods : Easier to swallow and require less effort.
- Adjusted solid foods : Modified to a consistency that forms a cohesive bolus of food, aiding safer swallowing.
Strategies for Mealtime
- Smaller bites of food : Helps control the movement of food, reducing risks.
- Avoid crunchy food : Can be challenging and pose risks.
- Softer food alternatives : Important for nutrition and manageability of condition.
Step 5: Incorporating Dietary Modifications
Daily practice routines.
- Establish daily practice routines for strengthening muscles and improving coordination.
- Incorporate varying food textures during swallowing exercises as advised by speech therapists.
Tools and Devices That Can Help
- Utilize biofeedback devices to monitor muscle activity during swallowing.
- Employ simple implements for effective food positioning.
- Collaborate with speech therapists to select appropriate tools and devices.
Consistent practice of swallowing exercises, alongside the use of selected tools and devices, is essential for improvement. Speech therapists are pivotal in guiding the use and selection of aids to enhance swallowing function.
Step 6: Implementing Strategies to Improve Swallowing at Home
Keeping a progress journal.
Keeping a journal is important for tracking changes and noting achievements in speech therapy. It helps both patients and speech therapists see patterns and gives a clear measure of progress.
Collaborating with Your Therapist for Ongoing Adjustments
Working together with a speech therapist is a key part of care. Regular assessment, together with annual follow-up assessments, allows for the therapy goals to be updated as needed. This flexible approach ensures that the speech therapy continues to be relevant and successful as the patient’s needs change.
Step 7: Regularly Assessing Progress and Adjusting Goals
Additional advice and precautions, when to seek further medical advice.
If you notice new symptoms or if your condition deteriorates, it’s important to seek medical treatment immediately. Providing timely care to patients with swallowing disorders is important to prevent complications after treatment.
Coping with Emotional and Psychological Aspects
Swallowing disorders can impact emotional health, so it’s essential to manage mental well-being. Behavioral treatment, including therapy, can help. It can be part of a broader treatment plan that may also address cancer treatment if needed.
Steps to Improve Swallowing Through Speech Therapy
Speech therapy is instrumental in enhancing the swallowing process. It involves a series of targeted exercises that focus on:
- Strengthening the muscles involved in each phase of swallowing.
- Enhancing speech articulation that positively affects swallowing coordination.
- Customizing therapy to cater to individual patient needs, ensuring safe consumption of food.
The primary goal of speech therapy for those with swallowing difficulties is to establish secure and effective swallowing mechanisms as part of a comprehensive dysphagia treatment plan. This includes specific, effective treatment recommendations tailored to each patient’s unique situation.

If you or someone you know has trouble swallowing, it’s important to get help from experts. At Penn Medicine Becker ENT & Allergy, we’re committed to providing care for conditions like voice and swallowing problems. Our team works hard to make treatment plans that are tailored to each person, helping improve their life.
For professional advice and support, schedule a consultation by getting in touch with our offices in Central and Southern New Jersey, Philadelphia, PA, or Yardley, PA. Your well-being is our main concern, and we’re ready to assist you on your path to recovery.
The content, including but not limited to, text, graphics, images and other material contained on this website is for informational purposes only. No content on this website is intended to be a substitute for professional medical advice, diagnosis, or treatment, nor represent the opinion of our physicians. Always seek the guidance of a qualified healthcare provider for any medical condition or concern.
Book Your Consultation Today
Improve the quality of your life
" * " indicates required fields
Call now to schedule your appointment.
Same day and evening appointments available. Mon - Fri : 8 a.m. to 5 p.m.
COVID-19 Safety Updates
Freehold, NJ
732-375-9550
Hillsborough, NJ
908-271-2102
Lawrenceville, NJ
609-303-5163
609-831-0779
Mt. Laurel, NJ
856-724-4031
Mullica Hill, NJ
856-478-3111
Philadelphia, PA
215-671-6330
215-929-8301
Plainsboro, NJ
609-831-0807
Princeton, NJ
609-430-9200
609-759-8500
Robbinsville, NJ
609-436-5740
856-589-6673
Voorhees, NJ
856-772-1617
856-565-2900
Yardley, PA
267-399-4004
Woodbury, NJ
856-845-8300
Copyright © 2024. All Rights Reserved. The Rhinoplasty Center (opens in a new tab) | Schrader Facial Plastic Surgery (opens in a new tab) | Rhinoplasty Archive (opens in a new tab) | Lozada Facial Plastic Surgery (opens in a new tab) | Becker Plastic Surgery (opens in a new tab) | Rejuvenation Resource (opens in a new tab) | Kam Facial Plastic Surgery (opens in a new tab) Terms (opens in a new tab) . Privacy (opens in a new tab) . HIPAA (opens in a new tab) . Sitemap (opens in a new tab) .
910-862-8100

Can Speech Therapy Resolve Swallowing Problems?
Imagine not being able to eat without pain.
Consider the fact that thousands of Americans are barely able to swallow.
In certain cases, swallowing can even be impossible.
The medical term for difficulty swallowing is dysphagia, and working with a speech therapy clinic can help resolve these issues, enabling you to enjoy eating normally again.
Anyone at any age can have dysphagia, but it’s most common in older adults. Therefore, some residents at Balden East have this problem. This is one reason we provide certified speech therapists to help our residents return to the joy of eating without pain.

What Are the Signs of Dysphagia?
Everyone occasionally has some difficulty swallowing. This may come from eating too fast or not chewing thoroughly. It happens from time to time.
However, it’s when swallowing becomes a continual problem that you or your loved one may benefit from speech therapy.
In addition to difficulty swallowing, some of the signs of dysphagia are:
- Painful swallowing
- Feeling like food is stuck in the throat
- Feeling like food is behind your breastbone
- Spitting up food
- Repeated heartburn
- Losing weight unexpectedly
- Coughing or gagging
What Causes Dysphagia?
Anyone can have a swallowing disorder, but it is more common in older adults. It often happens when someone is affected by a disease that affects the nervous system.
This includes Parkinson’s disease and cerebral palsy.
Other disorders can contribute to difficulty swallowing. These include:
- GERD (gastroesophageal reflux disease)
- Other issues with the esophagus/throat
- Head injuries
- Problems or injuries to the spinal cord
- Head and neck cancers
In some instances, dysphagia can be effectively treated with medicines while other cases may require surgery.
What Is a Speech Therapist?
Speech therapists work closely with our residents in order to help them communicate effectively. This is important when someone has problems with both verbal and nonverbal communication.
Speech therapists work closely with those who have had a stroke or other disorder that has impaired their speech.
These therapists also help those who have swallowing problems. In many cases, they can “train” the muscles used in the throat and mouth to enable them to swallow without problems.
What Training Does a Speech Therapist Have?
Typically, speech language pathologists have a master’s degree and are licensed by the state. They may also have national certification from the Speech Language Therapy Association of America.
How Does Speech Therapy Help With Swallowing Problems?
Perhaps one of the biggest advantages of working with a speech therapy clinic is that they can tailor the treatment approach to your individual situation.
Speech therapists can show you methods to help. This can involve changing your diet or holding your head and neck in a certain way.
In other cases, speech therapy involves teaching your muscles how to effectively swallow. Often, this involves exercises. Most of these help with strengthening the tongue.
Swallowing is actually a complicated process. It involves coordination among several muscle groups used to push food down your throat and into the stomach. Speech therapy exercises help increase control over these muscles.
Swallowing Exercises for Dysphagia
There is no one swallowing exercise that works for everybody. However, during speech therapy, you may be asked to complete some of the following:
Take a straw and small pieces of paper. Place the straw in your mouth and suck on it, trying to pick up the pieces of paper. Keep sucking on the straw to hold the paper in place. Then, place the pieces in a cup.
Continue this exercise until you’re able to successfully place a certain number of pieces into the cup.
Another exercise involves dry swallowing (meaning you’re only swallowing your saliva). When you swallow, try to squeeze all muscles that are used in swallowing as tightly as possible. Eventually, repeating this action will strengthen these muscles.
Access to These Wonderful Services Is an Advantage of Living at Bladen East
Trouble swallowing can have a devastating effect on the quality of life for so many individuals. That’s why we only employ compassionate, friendly staff members who are experts in their field. Together, we work with you or your loved one’s entire health care team to provide the quality services you need and deserve.
Interested in learning more about rehabilitation at Bladen East? Contact us for more information.
Schedule a Tour
A speech-language pathologist is the obvious professional to visit for a communication problem. Not as many people realize they can also treat swallowing disorders, or dysphagia.
Johnna Johnson is the speech-language pathologist at Regional One Health’s East Campus Center for Rehabilitative Medicine . Johnson has special certification as a VitalStim provider to help patients who are experiencing dysphagia.

If you always feel like something “went down the wrong pipe,” you should consult with a speech-language pathologist to see if you have a swallowing disorder.
Johnson said there’s an easy way to tell if you should seek therapy.
“You should see a speech therapist if every time you eat or drink something you start coughing. That’s your body’s way of saying your swallow isn’t working right,” she said.
It’s especially concerning if your dysphagia is causing weight loss.
Johnson said everybody has something “go down the wrong pipe” now and then, usually if you eat too fast or don’t chew well enough. That’s actually a good description for what happens with a swallowing disorder.
Coughing is the body’s response when something incorrectly goes into the lungs. If that happens every time you drink or eat, something is wrong in the swallowing process.
Swallowing involves complex coordination between the mouth, tongue, throat and esophagus. A breakdown in any of those areas can cause dysphagia.
Johnson said there are several possible causes.

Patients with a swallowing disorder, or dysphagia, often cough after eating or drinking.
Esophageal dysphagia (which needs medical attention) may include the sensation of food being stuck in your throat. Causes may include:
- A problem with the esophageal muscle
- Spasms in the esophagus
- A narrowed esophagus due to tumors or scarring from acid reflux
- A foreign body partially blocking the throat or esophagus
Oropharyngeal dysphagia may involve weak throat muscles. This may be caused by neurological disorders such as stroke, multiple sclerosis, muscular dystrophy or Parkinson’s disease. Cancer and cancer treatment like radiation is another possible cause.
Older patients are at higher risk for dysphagia. Certain conditions also put patients at higher risk:
- Parkinson’s disease
- Multiple sclerosis
- Muscular dystrophy
- GERD (severe acid reflux)

Speech-language pathologist Johnna Johnson holds a special certification in VitalStim to help patients with swallowing disorders.
Johnson can help patients with weak musculature deficits that cause dysphagia. She focuses on helping patients strengthen the muscles that allow them to swallow properly.
Johnson uses proven exercises to improve strength, mobility and control of the muscles. She can also work with patients on diet modification and compensatory strategies.
Her special certification as a VitalStim provider is a huge benefit for her patients. VitalStim is a non-invasive therapy.
Small electrical currents stimulate the muscles used in swallowing. It is combined with traditional therapy to treat dysphagia.
Johnson said it is a safe and effective method that is proven to help patients with weakness in the pharyngeal muscle.
Johnson said there is hope for patients who are having difficulty swallowing. With a therapist’s help they can either reverse the problem or find ways to alleviate their difficulty.
Contact the Center for Rehabilitative Medicine at 901-515-5900 to learn more.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
The Benefits of Speech Therapy
What to expect, frequently asked questions.
A speech-language pathologist (SLP) can help you with speech, language, and swallowing. They provide speech therapy to children and adults who may have speech or language disorders.
People with certain medical conditions may also benefit from speech therapy. Medical conditions that may cause speech or swallowing impairment include traumatic brain injury , stroke (brain damage due to a blood vessel blockage or bleed), and dementia (decline in memory and thinking functions).
This article looks at the various uses for speech therapy, what to expect during a session, and the techniques involved in this type of therapy.
Verywell / Theresa Chiechi
Speech therapy can help with a variety of conditions.
Speech Disorders
Speech therapy may help with speech disorders like:
- Stuttering : Stuttering may involve repeating parts of words, prolonging words, or struggling to get out certain words. You may be more likely to have a stutter if you have a family history of stuttering.
- Apraxia : This motor speech disorder makes it difficult to move the tongue and lips to make sounds required for speech. In some cases, people with apraxia cannot speak at all. Causes for this disorder include brain tumors, dementia, stroke, and any other condition that causes brain injury.
- Voice : Voice disorders can be temporary or permanent and make it hard to speak. Chronic voice disorders include chronic cough, vocal fold paralysis, vocal polyps (growths on the vocal cords), and spasmodic dysphonia (vocal cord spasms).
- Dysarthria : People with this speech disorder have muscle weakness that makes it difficult to talk. They may slur or mumble their words. Dysarthria can happen due to brain injury or chronic degenerative conditions like Parkinson’s disease or Huntington’s disease .
Language Disorders
A language disorder ( aphasia ) is a condition that makes it difficult for a person to read, write, speak, or understand speech or other modes of communication.
Someone with this type of disorder may struggle to:
- Use incorrect words for things
- Say complete sentences
- Understand what other people say
- Understand jokes
- Read or spell
Brain tumors, traumatic brain injuries, and degenerative disorders that affect cognitive function can all cause aphasia.
Feeding and Swallowing Disorders
Feeding and swallowing disorders can occur in both children and adults. A feeding disorder involves trouble with eating, sucking, drinking from a cup, or chewing. The specific term for swallowing disorders is dysphagia . Children or adults with dysphagia have trouble swallowing food or drink.
Problems swallowing or feeding may or may not be related to a medical condition. Conditions that may cause a swallowing or feeding disorder include:
- Cleft palate or cleft lip
- Asthma and other breathing issues
- Heart disease
- Premature birth
- Nervous system disorders
- Reflux
- Muscle weakness
- Sensory issues
- Autism
- Behavior problems
- Certain medications
Speech therapy begins with an evaluation to assess your difficulties and whether any structural issues contribute to your speech, language, feeding, or swallowing problems. An evaluation may involve a standardized test to help determine what you most need help with. Informal conversations may also help figure out your needs.
A speech-language pathologist will then work with you to help improve your ability to speak, converse, or swallow. This may involve:
- Educating you on how to do certain things like articulating or pronouncing sounds
- Teaching you language skills
- Providing you with educational materials
- Giving you exercises to help strengthen your muscles
- Giving you exercises that help you breathe better
- Participation in group therapy sessions
You should also expect to practice the skills and exercises you learn in speech therapy sessions at home. Your speech-language pathologist may provide you with workbooks, worksheets, or virtual apps for at-home practice.
Speech Therapy for Adults
Depending on the reason you’re seeking out speech therapy, a speech-language pathologist may:
- Help you learn to move your muscles correctly to make sounds if you have apraxia or dysarthria
- Teach you how to use your breath to speak louder if you have dysarthria
- Help you learn to manage stuttering by teaching you to lower stress levels in certain situations
- Help you strengthen your mouth muscles to make it easier to swallow and eat if you have a feeding or swallowing disorder due to a brain injury or disease
Speech Therapy for Children
A speech-language pathologist’s approach will depend on the child. When working with a child who has a feeding or swallowing disorder, they might focus on:
- Strengthening the muscles of the mouth
- Helping the child with chewing
- Encouraging the child to try new food and drink
- Changing food texture to make it easier to swallow food
- Helping with sensory issues related to food
Other skills a speech-language pathologist may work on with a child include:
- Language complexity : For example, they might teach words like "and" and "or" to connect ideas within sentences.
- Conversation skills : This may include role-playing to help the child with socialization and improve their read of social cues.
- Vocabulary : They may use games or storytelling to help build the child’s vocabulary.
- Phonological awareness : This recognition of the sounds that make up words is an important skill for reading. The SLP may work on helping the child identify sounds and rhymes in words to build this skill.
Healthcare professionals will also test your child’s hearing to see if hearing loss may be contributing to language and speech issues.
If you or your child is getting speech therapy from a qualified speech-language pathologist, you might wonder how likely it is that you’ll see improvement in speech, language, or feeding.
Results will depend on the individual. It’s also essential to follow the exercises, tips, and strategies provided by the speech-language professional. Regular visits and keeping up with practice activities and exercises make it more likely to see an improvement in yourself or your child.
A speech-language pathologist works with children or adults who have speech, language, or feeding and swallowing disorders. Typically the first session will involve an evaluation to determine the areas that are causing you the most problems.
From there, they may teach you exercises and strategies to improve your speech, language, or ability to swallow and eat.

A Word From Verywell
Think you or your child would benefit from speech therapy? Get in touch with your primary healthcare provider and ask for a recommendation. You can also use the American Speech-Language-Hearing Association’s (ASHA) Find a Certified SLP Tool .
Not all children develop at the same rate, but if your child has issues understanding language, doesn’t use gestures, or doesn’t seem to be learning new words, you might consider having them evaluated by a speech therapist.
While this may depend on the individual and the cause of speech-related problems, research suggests that speech and language therapy can significantly improve speech and language issues.
One example of a typical speech therapy technique is articulation therapy. This technique teaches the person to make specific sounds, sometimes by showing them how to move their mouth or tongue.
A language delay is when a child has difficulty in speaking and understanding speech that is unusual for their age.
American Speech-Language-Hearing Association. Stuttering .
American Speech-Language-Hearing Association. Apraxia of speech in adults .
American Speech-Language-Hearing Association. Voice disorders .
American Speech-Language-Hearing Association. Dysarthria .
American Speech-Language-Hearing Association. Aphasia .
American Speech-Language-Hearing Association. Feeding and swallowing disorders in children .
Brainline. Speech therapy .
Understood for All. What is speech therapy .
Centers for Disease Control and Prevention. Languages and speech disorders in children .
Broomfield J, Dodd B. Is speech and language therapy effective for children with primary speech and language impairment? Report of a randomized control trial . Int J Lang Commun Disord . 2011;46(6):628-640. doi:10.1111/j.1460-6984.2011.00039.x
Nemours Children's Health. Speech-language therapy .
By Steph Coelho Steph Coelho is a freelance health and wellness writer and editor with nearly a decade of experience working on content related to health, wellness, mental health, chronic illness, fitness, sexual wellness, and health-related tech.She's written extensively about chronic conditions, telehealth, aging, CBD, and mental health. Her work has appeared in Insider, Healthline, WebMD, Greatist, Medical News Today, and more.
Ochsner Health is a system that delivers health to the people of Louisiana, Mississippi and the Gulf South with a mission to Serve, Heal, Lead, Educate and Innovate.
About Ochsner
- Mission & Vision
- Diversity, Equity and Inclusion
- Annual Report
- Outcomes & Honors
- News & Media
- Partnerships
- Ochsner Health Network
- Community Health Needs Assessment
- Community Benefit Report
- Serving Our Schools
- Discovery Health Sciences Academy
- Community Service
- Outreach by Region
- Classes & Events
- Sponsorships
Health Resources
- COVID-19 Information
- All Health Resources
- Healthy State
- To Your Health Blog
- Golden Opportunity
- Ochsner Magazine
Thank you for choosing Ochsner Health for your care. We are committed to making an ongoing difference in the health of our communities.
I need to…
- Find a Doctor
- Find a Location
- Find a Specialty Find a Specialty or Treatment
- Schedule an Appt. Schedule an Appointment
- Personalize Personalize My Content
Services & Resources
- Patient Services
- Visitor Policy
- Billing & Financial Services
- Insurance Information
- International Patients
- Language and Translation Services
- Share Your Story
- Read Patient Stories
- Request Medical Records
- About MyOchsner
- How to Use MyOchsner
- Patient Login
- New Patient? Sign Up
Connect to care at Ochsner. Click on a featured specialty on the list or search for a specialty.
Featured Specialties
- Primary Care (Internal Medicine)
- Urgent Care Services
- Connected Anywhere Virtual Visits
Women's Health
Men's Health
- Digital Medicine
- ER Locations
- Pharmacy & Wellness
- Psychiatry & Behavioral Health
- Smoking Cessation Services
- Heart & Vascular
- Cancer Care
- Neuroscience
- Organ Transplants
- Orthopedics
- Sports Medicine
- Therapy & Wellness
- Optical Shops
- Digestive Disorders
Ochsner is committed to a clinically-integrated research program with the ultimate goal of improving the health and wellness of our patients and communities. As the largest academic medical center in Louisiana, we are training the next generation of healthcare professionals to be leaders who can meet evolving healthcare challenges.
- Clinical Research
- Translational Research
- Outcomes Research
- Nursing Research
- Research Opportunities
- Investigator-Initiated Research Resources
- BioDesign Lab
- Ochsner-Xavier Institute for Health Equity and Research
- Browse All Programs
- UQ-Ochsner Clinical School
- Clinical Medical Education
- Graduate Medical Education
- Continuing Medical Education
- Medical Library
Discover Your Future At Ochsner! With unlimited growth potential, both professionally and personally, now is the time to start your future with Ochsner.
Find the Career for You
- Careers at Ochsner
- Why Work Here
- Search Jobs
Career Paths
- Allied Health
- Non-Medical Professional
- Management & Leadership
- Technology & Innovation
- Fellowships, Internships & Residencies
- Advanced Practice Providers
- Get Care Now
- Medical Professionals
- Food & Fitness
- Conditions & Treatment
- Health Trends
- Prevention & Wellness
- Women's Health
- Men's Health
Mental Health
Speech Therapy & Difficulty Swallowing: Causes and Symptoms
When people think about speech therapy, they may think about speech, phonation, articulation, even cognition and voice. But what about swallowing? Not only do we as speech-language pathologists address swallowing, but depending on the therapist and the setting, it may actually be a large focus of what we do each day.
Do you ever get that feeling that food or drink is "going down the wrong pipe?" It can actually happen and it's called aspiration. One “pipe” is the esophagus that goes to your stomach and one is the trachea which goes to your lungs. Aspiration is when food, drink, secretions, or any foreign material enters the trachea heading for the lungs.
How do you know if this has happened? The signs and symptoms can include coughing, throat clearing, wet/gurgly voice, choking, etc. while eating and drinking. A speech-language pathologist can typically determine if a person is aspirating and/or having difficulty swallowing. The speech therapist would proceed with a treatment plan and therapeutic exercises to target individual muscles of swallowing.
The individual may also be asked to participate in a Modified Barium Swallow Study, which is an x-ray of your throat while eating and drinking. The plan may include temporary or permanent modification of a person's diet and learning safe swallow strategies.
Modification to one's diet may include chopping up meats, cutting all food into small pieces, blending food to a puree or pudding consistency, thickening liquids, etc. Safe swallow strategies can include alternating small bites/sips, eliminating the use of straws, tucking your chin to chest while swallowing, turning your head towards one side while swallowing, slowing down, chewing thoroughly, avoiding talking with food in mouth, sitting upright 90 degrees for meals, etc.
People who may exhibit difficulty with swallowing include those with a stroke, Parkinson's disease, Alzheimer's disease, dementia, Traumatic Brain Injury, amyotrophic lateral sclerosis (ALS), spinal cord injury, multiple sclerosis, muscular dystrophy, cerebral palsy, cancer in the mouth/throat/esophagus, damage to the head or neck, etc.
Why does this happen? Typically the muscles of swallow have suffered some type of damage and are weak and unable to perform at full capacity. That is why diet modification, safe swallow strategies, and therapeutic exercises are important so that you can safely consume the Southern delicacies we all love.
If you or someone you know is experiencing difficulty swallowing, you should inform your doctor and inquire about visiting a speech-language pathologist for further assessment and/or treatment. Happy hearing and speech month!
You may also be interested in:
Rehabilitation: infants, children and adolescents, how can a speech pathologist help your child, speech development in children: when should you be concerned.
Subscribe to Our Newsletters
Select the newsletters you'd like to receive.

Food & Fitness

Pulse on Parenting

Please select at least one category to continue.
Curious about our newsletters?
Let us know where to send your newsletters.
You're all set!
We’ll send newsletters full of healthy living tips right to your inbox.
- Search the site GO Please fill out this field.
- Newsletters
- Health Conditions A-Z
- Neurological Disorders
What Is Speech Therapy?
:max_bytes(150000):strip_icc():format(webp)/ProfilePictureHealth.com-BrandiJones-07e01d5551a6465686eb5a69eeefdc6b.jpg)
FatCamera / Getty Images
Speech therapy is a form of healthcare that helps improve communication and speech. It can also help improve swallowing function and other behaviors related to feeding.
About one in 12 children in the United States has a speech or swallowing disorder. Disorders are most common in young children, but many adults have a related condition. For example, about one million adults in the United States have aphasia (difficulty expressing or comprehending written and verbal language).
Speech therapists (STs) or speech-language pathologists (SLPs) assess and treat people of all ages. They use various techniques to help people with challenges related to speech production, language comprehension, hearing, voice quality, fluency, and swallowing.
What Does Speech Therapy Treat?
Speech therapy treats various disorders involving hearing, speech, language, literacy, social communication, voice quality, executive functioning (for example, memory and problem-solving), feeding, and swallowing.
Specific speech disorders include:
- Articulation disorders: Difficulty pronouncing words or sounds such as the “s” sound (for example, saying “thun” rather than “sun”). This can occur during childhood language development or with structural problems like tongue-tie. A tongue tie is when a small band of skin connects the tip of the tongue to the bottom of the mouth. It is congenital, meaning it's present at birth.
- Dysarthria: Slow, slurred, or unclear speech. This occurs with oral (mouth) muscle control decline due to neurological conditions (related to the brain or nervous system), such as multiple sclerosis (MS) —a condition that occurs when the immune system attacks myelin, the covering wrapped around nerve cells.
- Apraxia: Knowing what you want to say but having difficulty producing the correct sounds or words. Apraxia can cause slow, error-prone speech or the need to intentionally move your tongue and lips in order to produce sounds and words. Apraxia can be present at birth, but it can also occur as a result of brain injuries, brain tumors , or a stroke .
- Fluency disorders: Speech flow disruptions like stuttering. Stuttering is experiencing interruptions in speech and repeating sounds, syllables, or words. Researchers are still exploring possible causes of dysfluency, but they seem to include genetics, developmental components, neurological factors (how the brain processes), and brain injury. Many children outgrow fluency disorders, but they can persist into adulthood.
- Voice disorders: Vocal cord spasming (choppy voice), hoarseness, pitch problems, or voice fatigue are examples of voice disorders. This can result from infection, overusing the vocal cords, or neurological disorders.
Language or communication disorders include:
- Aphasia : Aphasia is a language disorder in which you have difficulty expressing or comprehending written and verbal language. Receptive aphasia is difficulty understanding written or verbal words. Expressive aphasia is difficulty communicating thoughts and ideas with language components like vocabulary, grammar, and sentence formation. Aphasia can occur with childhood development, language impairment, autism spectrum disorder (ASD), brain injury, or neurological disorders.
- Pragmatic language disorder: This relates to social communication. Signs include misunderstanding social cues like eye contact, body language, and personal space. It can occur during childhood development or with underlying neurodivergence (brain variation), such as autism spectrum disorder (ASD) , a brain development condition that affects how a person perceives and socializes with other people.
- Accent or tone: While this is not a disorder, speech therapists can also work with people who wish to modify their accent or an unusual speech rhythm, pitch, or tone. For example, a high-pitched, sing-song, or robotic tone can occur with ASD.
- Executive functioning: Executive functioning challenges include difficulty with memory, planning, organization, problem-solving, and attention. This can occur due to brain injuries or conditions like ASD and attention-deficit hyperactivity disorder (ADHD) , a neurodevelopmental disorder characterized by inattention (being distracted), hyperactivity (feeling restless), and impulsivity (making hasty decisions).
- Auditory processing disorder: This is a neurological condition that makes it difficult to make sense of sounds.
Feeding and swallowing disorders affect how you suck, chew, and swallow food and drinks. Difficulty swallowing is also known as dysphagia , which can result in choking during meals—and lung infections if food or liquid enters the airways. It can occur with structural abnormalities, muscular weakness, or neurological conditions like a stroke.
How Does Speech Therapy Work?
Speech therapy involves techniques like language practice, pronunciation exercises, voice therapy, and swallowing exercises. It begins with a thorough assessment, including observation of communication strategies, challenges, and frustrations.
Speech therapy for infants, toddlers, and children involves fun and engaging activities like play, language exercises, reading, picture cards, and modeling correct sounds. This helps make learning more enjoyable.
Parents or caregivers often attend sessions and learn ways to support children at home. The ST or SLP will tailor the treatment plan to the child’s developmental stage. Early recognition and intervention (treatment) can help improve outcomes.
With adults, the ST or SLP will begin with an assessment to identify specific challenges. They will then create a specific care plan that addresses underlying concerns such as:
- Medical conditions
- Accent modification
- Voice challenges
- Pronunciation
- Conversational language
- Problem-solving
- Memory exercises
What To Expect During Speech Therapy
Speech therapy can occur in a class, small group, online, or one-on-one. Speech therapists typically assign exercises to practice at home in order to reinforce what you learn. Activities might include:
- Vocal warm-ups like humming
- Tongue twisters to improve articulation
- Breaking words into syllables to improve clarity
- Contrasting word exercises—for example, "ship" versus "sheep"
- “Pausing” practice (for stuttering)
- Repetition after listening to a native speaker
- Repetition exercises for sounds like “s”
- Speech rate control—for example, by tapping hands to a beat
- Pitch exercises
- Breathing and posture exercises
Receptive language exercises include:
- Memory or problem-solving exercises
- Reading comprehension (similar to a book report)
- Speech supplementation (written, gestural, voice amplifier, speech-generating devices)
- Word association
- Communication partner exercises, such as practicing eye contact and active listening
Exercises for swallowing and feeding include:
- Diet modification (pureed to solid foods)
- Oral muscle strengthening (like tongue “push-ups”)
- Swallowing exercises
Benefits of Speech Therapy
One of the main goals of speech therapy is to enhance a person’s ability to express thoughts, ideas, and emotions effectively. This can lead to a greater sense of self-expression, meaningful interactions with others, and less frustration. Other benefits include:
- Greater self-confidence: Gaining more control over language and communication can increase confidence and boost self-esteem. As a result, you might be more willing and excited to engage in social activities.
- Improved academic or professional performance: Clear speech and language can lead to enhanced skills in comprehension, reading, and writing. This can support academic success. Better articulation, language, and presentation abilities can help with career development.
- Greater independence: Speech therapy can lead to greater self-reliance, especially if you have severe communication challenges. For example, augmented and alternative communication (AAC) methods , such as speech-generating devices (SGDs), can allow you to express yourself more independently.
How Successful Is Speech Therapy?
Speech therapy's “success” depends on your goals. The meaning of success can vary based on your underlying communication or medical condition and its severity, as well as your motivation and commitment to therapy, the therapist's expertise, and your support systems. The time it takes to reach your goals also varies based on underlying factors like these.
For example, you may define success as improved pronunciation, or you may work towards more effective communication, more skilled accent modification, or swallowing without choking. If you stutter, your goal might be improved fluency or feeling more comfortable communicating openly with a stutter. For most people, what’s most important is to set realistic expectations and recognize that any improvement in communication is a success.
How To Find a Speech Therapist
A qualified speech therapist or speech-language pathologist holds a master's degree in speech-language pathology and state licensure to practice in your area. You can find speech therapists in settings like:
- Home health agencies
- Rehabilitation centers
- Private practice
- Telehealth (online)
You can also ask for recommendations from healthcare providers or school personnel who may know local speech therapists. The American Speech-Language-Hearing Association (ASHA) also offers an online directory of certified speech therapies to help you locate someone in your area.
Check with your health insurance provider to see if they cover speech therapy. They can provide you with information about your co-payments and deductibles. If your insurance doesn't cover the cost, the clinic or speech therapist may offer payment plans. Some children may also qualify for:
- Individualized education programs (IEPs) that cover speech therapy costs as a service from the school district
- Early intervention (EI) or Preschool on Preschool Special Education (CPSE) programs for infants and toddlers for little or no cost to families
- State and federal programs, like Medicaid
- Financial assistance programs from non-profit and advocate organizations
A Quick Review
Speech therapy is a specialized healthcare field in which trained professionals help improve speech, language, hearing, swallowing, and feeding for people of all ages. Speech therapists (STs) and speech-language pathologists (SLPs) thoroughly assess and develop specific treatment plans for a wide range of conditions including difficulty communicating or processing language, stuttering, and voice disorders.
Speech therapy takes place in locations like schools, hospitals, and private practice. It can be one-on-one or in a group setting. Success depends on underlying factors such as the severity of the condition. It also depends on personal goals and your definition of success—which can vary widely from person to person.
Many people who have speech therapy experience powerful benefits that affect them in nearly every aspect of life, including greater self-confidence and self-reliance.
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, language .
Houtrow A, Murphy N. Prescribing physical, occupational, and speech therapy services for children with disabilities . Pediatrics ; 143 (4): e20190285. doi:10.1542/peds.2019-0285
American Speech-Language-Hearing Association. Who are speech-language pathologists, and what do they do? .
National Institute on Deafness and Other Communication Disorders. Stuttering .
American Speech-Language-Hearing Association. Stuttering .
Law J, Dennis JA, Charlton JJ. Speech and language therapy interventions for children with primary speech and/or language disorders . The Cochrane Database of Systematic Reviews . 2017 (1). doi:10.1002/14651858.CD012490
Krekeler BN, Weycker JM, Connor NP. Effects of tongue exercise frequency on tongue muscle biology and swallowing physiology in a rat Model . Dysphagia . 2020; 35 (6):918. doi:10.1007/s00455-020-10105-2
National Institute of Deafness and Other Communication Disorders. Speech and language developmental milestones .
National Institute of Health Clinical Center. Speech and language pathology .
American Speech-Language-Hearing Association. Dysarthria in adult
Brady MC, Kelly H, Godwin J, Enderby P, Campbell P. Speech and language therapy for aphasia following stroke . The Cochrane Database of Systematic Reviews . 2016 (6). doi:10.1002/14651858.CD000425.pub4
American Speech-Language-Hearing Association. Scope of practice in speech-language pathology .
American Speech-Language-Hearing Association. Help finding a professional .
Related Articles
ALS Assocation
- Understanding ALS
- Newly Diagnosed
- FDA-Approved Drugs
- Maintaining Adequate Nutrition: A Continuing Challenge in ALS
- Nutrition & Feeding Tubes
- Mobility and ALS
- Respiratory Care
- Managing Speech & Swallowing Changes
- Assistive Technology
- Augmentative Communication
- Home Infusion
- Living Environment
- Adapting Your Environment
- Daily Living Activities
- Leisure Activities
- Participate in Research
- Medical Information Materials
- Informational Fact Sheets
- Resource Guides
- Coping with ALS
- For Caregivers
- Military Veterans
- Financial Information
- End of Life Plans
- My ALS Journey™
- Order Printed Materials
- Education For Healthcare Professionals
- Care Matters E-Newsletter
- Resources and Support
- Get Involved
Managing Speech and Swallowing Changes
One of the common symptoms of ALS is a gradual weakening and loss of control of the muscles in the mouth and throat. These muscles are known as “bulbar muscles,” and some of the “bulbar symptoms” of ALS include difficulty speaking or swallowing. Here are some tips on how to manage speaking and swallowing while living with ALS.
ALS can make it difficult to talk clearly and require extra effort by both the speaker and the listener. However, there are many things both people can do to make communication easier.
For someone living with ALS:
- Give speaking your full attention. Don’t try to eat or drink at the same time.
- Speak slowly and carefully. Pronounce all the syllables in each word.
- Repeat words if necessary. If that doesn’t work, spell them out.
- Be brief. Don’t add a lot of unnecessary words.
- Many speakers tend to trail off at the end of words or the end of sentences. Try to emphasize the ending sounds of each word.
- Taking a breath every few words will allow you to speak louder, making it easier to hear.
- Communication involves more than just speech. If you’re able, consider using gestures and facial expressions to help convey what you mean.
- If a word is difficult to say or understand, try substituting a different word or phrase. For example, if “book” is hard to say, substitute the name of the book or simply “thing you read.”
- It may be helpful to say or write down what the main topic of discussion is at the beginning of the conversation. Use a single keyword, like “lunch” or “medicine.” That way, listeners will know the overall theme of what you’re talking about and be better able to follow along.
- Some listeners may pretend to understand what you’ve said, even when they haven’t. If you think the listener didn’t hear you correctly, ask them to repeat back what you said.
ALS is progressive, so speaking will continue to get more difficult over time. Because of this, some people living with ALS choose to plan ahead by recording their own voices while they can still speak clearly.
They build up a “bank” of recorded words and phrases, which can later be programmed into an electronic device. This allows them to communicate using their own voice rather than a computer-generated one.
When speaking becomes too difficult, there are many tools and devices available that can help you communicate clearly. These range from low-tech alphabet boards to high-tech devices with speech-generating software.
Most people living with ALS with bulbar symptoms will go through a variety of communication aids as their needs and abilities change. A speech therapist can help you determine what techniques or tools will work best for you.
In any conversation, the listener’s role is just as important as the speaker’s role. When conversing with a person living with ALS who has bulbar symptoms, there are several things you can do to help:
- Give the speaker your full attention. Get rid of any unnecessary background noise and focus your eyes on the speaker so you can see any nonverbal cues.
- Check your hearing. If you have hearing loss, use a hearing aid or amplifier.
- If you don’t understand something that was said, ask the person to repeat it or spell it out. It may help for you to repeat what you did hear, so they can fill in the blanks: “You said you want to go somewhere, but I didn’t hear where.”
- Practice makes perfect. If you’re the caregiver, or a close friend or family member who speaks with the person regularly, you’ll probably be better at understanding what they say than a stranger would. So, you may be able to serve as a translator when the person living with ALS is talking with someone new.
Swallowing
The act of swallowing involves a number of muscles, including the tongue, lips, jaw and throat. Without all the muscles working together in harmony, swallowing becomes difficult. Food or liquid could end up “going down the wrong pipe” into the respiratory system, causing choking or other breathing difficulties .
There are several things people living with ALS can do to manage swallowing difficulties and maintain better overall health:
- Take smaller bites of food and smaller sips of liquids.
- Swallow two or three times with each mouthful to make sure all food is cleared from your throat.
- Changing the position of the head can help you swallow safely. For some people living with ALS, tilting the chin downwards helps prevent food from going down the windpipe. For others, tilting the head backward works better. Speech pathologists can recommend the best head position for you.
- When eating dry foods, moistening the food with sauce or gravy can help keep food pieces from getting stuck. Taking a sip of liquid between each bite can also help.
- People living with ALS may find it difficult to properly swallow foods that are a mix of solids and liquids, such as crunchy cereal with milk, or soup with chunks of meat or vegetables. Instead, substitute foods with a single consistency, like oatmeal or thick cream soups.
- If chewing and swallowing any solid food becomes too difficult, you may need to switch to pureed food, or naturally soft foods like mashed potatoes, canned fruit, or pudding.
- When drinking, thicker liquids are easier to control and swallow than thin liquids. For example, you may want to switch from milk to milkshakes, or from fruit juice to fruit nectar. There are also thickeners you can add to any beverage to make it easier to swallow.
- If swallowing saliva becomes a problem, there are medicines available that reduce the amount of saliva produced by the body. Suction machines can also be used to dispose of excess saliva, so it doesn’t have to be swallowed.
Eventually, swallowing enough food and drink to stay healthy may become impossible or impractical. When this happens, a feeding tube can be used to ensure you get the nutrition you need. You can learn more about ALS nutrition and feeding tubes here .

- See us on twitter
- See us on instagram
- See us on youtube
- See us on facebook
- See us on linkedin
Rehabilitation Program
Head & Neck Surgery
Appointments
(650) 498-6000
Press Option 2, then Option 3

Head and neck cancers and their treatments may impact a patient’s ability to eat and/or communicate. Many patients will benefit from speech and swallowing therapy to either address or prevent problems with communication and swallowing. Our head and neck cancer team includes expert speech-language pathologists (SLP’s) with specialized interest in the management of communication and swallowing disorders associated with head and neck cancer. Our goal is to preserve and optimize function and quality of life for all of our patients.
If you are diagnosed with head and neck cancer, you can expect to meet with a SLP before starting your treatment as well as during and after your treatment. Your comprehensive care plan will include evaluation of your current speech and swallowing function, education about changes you may experience during and after treatment, and a personalized therapy plan.
Speech & Swallowing Rehabilitation
Your Care Team
Director of the Head and Neck Speech and Swallowing Rehabilitation Program at Stanford Cancer Center

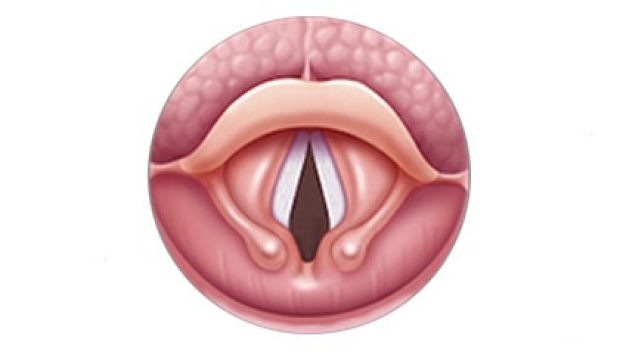
Our experts have extensive experience evaluating and treating swallowing disorders, sometimes referred to as dysphagia. Our speech-language pathologists use a number of tests to look at swallowing abilities. There are two primary tests we use to assess swallowing, video fluoroscopy and video endoscopy. Video fluoroscopy is a motion X-ray test where you will be given a variety of food consistencies mixed with barium, a white liquid that shows up clearly on an X-ray. The test measures swallowing ability from the mouth to the throat and to the esophagus if necessary. Video endoscopy is done using a small flexible endoscope that is passed through the nose to the throat. This allows us to look at the swallowing area from above. We can then watch as you swallow different foods and liquids to see how they go through the throat. These tests allow us to understand how your swallowing muscles are functioning so that we can customize your treatment plan.
- Swallowing Care
- Speech & Voice Care
- Head & Neck Lymphedema
Rehabilitation
This fluoroscopic video demonstrates a strong and efficient swallow that clears the dark liquid contrast through the throat into the esophagus (food pipe).
This fluoroscopic video demonstrates a swallow that lacks the strength to push the dark liquid contrast through the throat into the esophagus (food pipe). As a result, the contrast is seen to drip into the airway leading to aspiration.
This endoscopic evaluation demonstrates assessment of airway and swallowing following a supracricoid partial laryngectomy. This surgery involves removal of multiple structures of the voice box that typically offer airway protection during swallowing. By using a compensatory swallowing strategy taught by the speech and swallowing therapist, this patient was able to resume a nearly normal diet.

The anatomy of the swallowing system.
At the Stanford Cancer Center we believe in preventative medicine. Research and clinical experience has shown us that swallowing problems can be common after treatment. We also know that therapy during treatment reduces the chance of swallowing problems. Keeping your swallowing muscles strong and active during radiation therapy is the best way to ensure they continue to work for years to come. Strategies to rehabilitate swallowing function after treatment may include exercises that strengthen muscles or improve coordination, changes in posture while swallowing, or special swallowing techniques to make the food and liquid go down easier and safely. In some cases we will suggest specialty-designed utensils or drinking cups. Changes in food consistencies are sometimes suggested for safety or ease of swallowing.
Normal Swallowing

In the first stage of swallowing, the tongue pushes the food and liquid from the front to the back of the mouth. The lips must stay closed to prevent the food and liquid from spilling out of the front of the mouth. The cheek muscles must maintain tone so that the food and liquid does not spill into the space between the gums/teeth and the cheek.
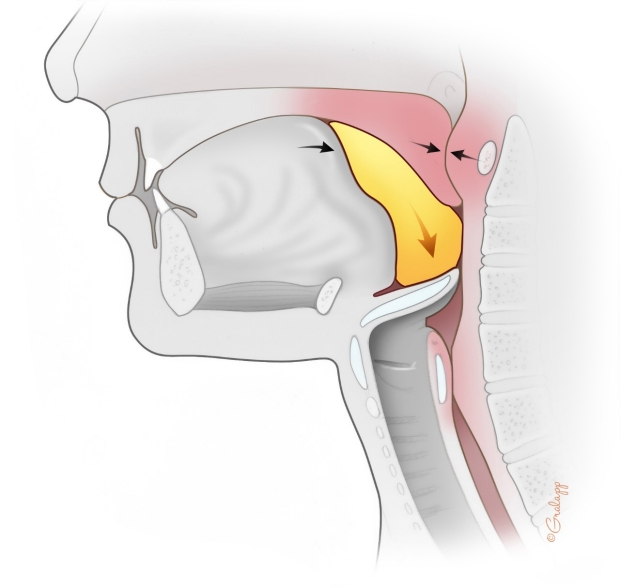
In the next phase of swallowing, the muscles of the upper throat and soft palate come together to prevent food and liquid from going up the nose. As the food and liquid enters the throat, the airway closes up to prevent food and liquid from entering the windpipe and lungs.

Towards the end of the swallow the muscles of the back of the tongue and throat come together to push the food out of the throat and into the food pipe (esophagus). The muscle at the top of the esophagus relaxes to allow the food and liquid through.
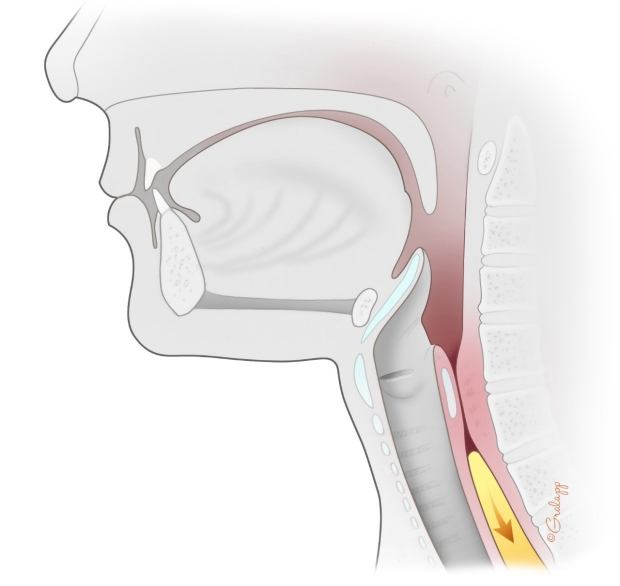
Once the food and liquid is fully within the esophagus, the airway opens back up and all muscles return to their resting position. The muscles of the esophagus then strip the food and liquid from the top of the esophagus into the stomach.
What is Dysphagia?

Dysphagia refers to difficulty in swallowing. Some symptoms of dysphagia include a sense of food/liquid getting caught in the mouth or throat, coughing/choking like things are going down the “wrong pipe”, difficulty chewing, and/or longer time needed to eat/drink. Dysphagia can lead to other problems like weight loss or pneumonia from food/liquids entering the lungs. Head and neck cancer and the treatments use to eliminate cancer are known risk factors for dysphagia. The speech language pathologist can provide preventative and rehabilitative intervention for dysphagia.
National Foundation of Swallowing Disorders
American Board of Swallowing and Swallowing Disorders
Dysphagia Research Society
What is Trismus?
Trismus occurs when a person has difficulty opening their mouth fully. Trismus can lead to difficulty with eating, dental care, and speech. Trismus often gets worse over time if not treated. Surgery and radiation to the head and neck region are known risk factors for trismus. Trismus prevention is an important part of the care provided by the speech language pathology team.
Speech & Swallowing Rehabilitation Pre-Radiation Education and Prophylactic Swallowing Exercise Guide
Managing side effects during radiation is important. The handout reviews the major side effects that can occur during radiation treatment for head and neck cancer and tips for managing them. The prophylactic swallowing exercises are designed primarily to reduce the potential for future swallowing problems.
Download Exercise Packet:
Pre Radiation Swallowing Exercise Packet (English)
Pre Radiation Swallowing Exercise Packet (Spanish)
Pre Radiation Swallowing Exercise Packet (Simplified Chinese)
Pre Radiation Swallowing Exercise Packet (Traditional Chinese)
Pre Radiation Swallowing Exercise Packet (Korean)
Pre Radiation Swallowing Exercise Packet (Vietnamese)
Pre Radiation Swallowing Exercise Packet (Tagalog)
Pre Radiation Swallowing Exercise Packet (Russian)
Pre Radiation Swallowing Exercise Packet (Nepali)
Pre Radiation Swallowing Exercise Packet (Japanese)
Pre Radiation Swallowing Exercise Packet (Arabic)
Pre Radiation Swallowing Exercise Packet (Dari)
Pre Radiation Swallowing Exercise Packet (Farsi)
Disclaimer: This website is an education and informational resource for speech-language pathologists. This website is not a substitute for consultation with a health care professional. If you have any health problems or health care-related questions, please call, or see your physician or other health care provider promptly. If you have an emergency medical condition, call 911.
Our speech-language pathologists have extensive experience in rehabilitation of speech and voice after treatment for head and neck cancers. Collaboration with other professionals such as surgeons and maxillofacial prosthedontists allows for individualized care. We understand the importance of maintaining functional communication after treatment. We offer comprehensive speech and voice care for all of our patients.
Our team has particular expertise in speech rehabilitation after removal of the voice box (total laryngectomy). We offer a full range of therapy options for patients who have had their voice box removed, including tracheoesophageal voice prostheses (TEP). Before your surgery you will meet with a speech-language pathologist to discuss the different communication options available after surgery and to decide what option is best for you. We also offer pulmonary and olfactory rehabilitation after laryngectomy to help improve breathing and taste/smell.
For patients with concerns regarding their voice, we offer comprehensive evaluation and treatment. To evaluate the vocal cords, a test called videostroboscopy is used to provide a magnified, slow-motion movie of the voice box during vibration. During the test, a small, angled telescope will be placed into your mouth or a flexible telescope may be placed through your nose. You will be asked to make specific sounds to make your vocal cords vibrate. These movies are recorded and can be reviewed later. Our team has extensive experience working with patients with voice problems and collaborates closely with our Laryngology team when medical or surgical interventions are necessary.
This video demonstrates the vibration of the vocal folds when creating voice. Our speech-language pathologists have expertise in the evaluation and treatment of voice disorders related to cancer and it's treatments.
What is Dysphonia?
Dysphonia is a change in voice. Dysphonia may present as hoarseness, rough voice, weak voice, changed pitch, or strained production of voice. Surgery and radiation to the voice box may lead to dysphonia. Voice treatment can be provided by the speech language pathologist in partnership with the laryngology team.
What is Aphonia?
Aphonia refers to total loss of voice. Aphonia is common after extensive surgery to the voice box or when the nerve to the voice box is damaged. The speech language pathology team can explore strategies and techniques to restore communication for patients with aphonia.
What is Dysarthria?
Dysarthria is a change in the ability to produce clear speech sounds. Though often associated with stroke and other neurological diseases, surgery and radiation to the head and neck can cause problems with the speech muscles and/or the nerves that connect the muscles to the speech centers in the brain. Dysarthria may be characterized by slurred speech, slowed speaking rate, and irregular speech. The speech language pathologist will help to combat dysarthria through speech intervention.
Laryngectomy

Web Whispers

International Association of laryngectomees

In Health Technologies

Atos Medical

Lauder - The Electrolarynx Company
Our speech pathology team can provide intervention for lymphedema of the head and neck region. Lymphedema is a type of swelling that occurs when the lymphatic system is damaged from surgery or radiation therapies. Lymphedema can cause discomfort and reduced movement in the affected areas. This may lead to cosmetic disfigurement but also functional problems with communication and swallowing as well as difficulties with breathing in some cases. Head and neck lymphedema therapy includes two primary treatments, manual lymphatic drainage and compression. Manual lymphatic drainage is a hands-on therapy that works to reestablish a new, more functional lymphatic drainage pattern. Our speech pathology team can train patients and caregivers to complete this treatment at home in between therapy sessions. Compression garments will be customized and fit according to patient need. Early intervention for lymphedema tends to be most successful rather than intervening once fibrosis develops.
What is Lymphedema?

Lymph nodes and vessels of the head and neck.
Lymphedema is chronic swelling in the head and/or neck due to damage to the lymphatic system. This is typically the result of either surgical or radiation changes. The normal drainage pathways are disrupted leading to pooling of protein rich fluid in the neck or face. The treatment for lymphedema includes skin care, manual lymph drainage, and compression therapy.
What Causes Lymphedema?

Place your hands over the sides of the neck. Alternate circling back and down toward the ear, one side at a time.
- The lymphatic system is an important part of your immune system and serves as a sort of waste disposal system, moving fluid, protein, and bacteria to the lymph nodes where the lymph fluid is processed.
- Damage to the lymphatic system can cause lymph fluid to collect in the tissues around the area of injury leading to swelling.
- Lymphedema may occur if the lymph nodes are removed or the lymph vessels are injured.
- This injury can occur during surgery or radiation treatment.
- It is also possible for a tumor to obstruct the normal lymphatic drainage system, resulting in lymphedema.
What Are the Symptoms of Lymphedema?
Symptoms of head and neck lymphedema include:
- Swollen eyes, face, lips, tongue, neck, or chin
- Swelling below the chin often described by patients as a “turkey waddle”
- A tight or heavy feeling in the neck or face
- Difficulty moving your neck or jaw
- Difficulty with swallowing, speaking, or breathing
How Common is Head & Neck Lymphedema?
Head and neck lymphedema may be seen in 50-75% of patients receiving surgery or radiation for head and neck cancer.
Symptoms may range from very mild to quite severe and the impact of lymphedema is often related to the severity of swelling.
How is Lymphedema Treated?

Place two fingers behind your ear and two in front of your ear. Circle back and down toward the ear.
Lymphedema is typically treated using complete decongestive therapy which includes:
- Manual lymph drainage - A massage like technique which moves lymph fluid from a congested area to a nearby functioning lymphatic drainage pathway.
- Compression - Use of tight fitting specialty garments which prevents fluid from back filling and promotes continued lymph drainage.
- Exercise - Moving the muscles in the region of swelling helps to promote fluid drainage.
- Skin care - Maintaining clean skin is important to prevent infection and breaks in the skin
Lymphedema therapy is most effective when performed daily, therefore home protocols are an important part of lymphedema treatment.
Who Can Help?
Lymphedema therapy may be provided by a specially trained physical therapist, occupational therapist, or speech pathologist. At the Stanford Cancer Center, head and neck lymphedema treatment is provided in our Speech and Swallowing clinic. To schedule a consultation, call 650-498-6000 (Press Option 2, then Option 3) and specify that you are requesting a head and neck lymphedema evaluation.
What If I Don’t Live Near Stanford?
Your lymphedema therapist may train you and your family or caregivers to do a good deal of the treatment at home. We recommend bringing a caregiver who may assist in your home care to your consultation for training.
If you need additional assistance closer to home, we recommend referring to the Lymphedema Association of Northern America as a starting point to locate a therapist.
Not all lymphedema therapists have experience working with the head and neck. We recommend asking the local center about their level of experience.
In addition to providing state of the art clinical care for communication and swallowing, our speech-language pathology team is engaged in clinical research to determine strategies to improve patient outcomes after a diagnosis of head and neck cancer. Our team recognizes the difficulties of going through cancer treatment and has particular interest in developing strategies to help patients make it through their treatment doing the therapies that will provide the best long-term outcomes. We collaborate closely with our surgeons, radiation oncologists, medical oncologists, and other team members to investigate how we can improve the patient experience of head and neck cancer care.
Annual Head & Neck Cancer Patient & Caregiver Education Symposium

Heather Starmer is passionate about providing patients and caregivers with support and education to help them along their cancer journey. In 2017 she established the annual Head & Neck Cancer Patient & Caregiver Education Symposium . This event brings patients and caregivers together experts in the field of head and neck cancer care to discuss important concepts for treatment and survivorship.
Presentations and Slides

Annual Swallowing Disorders Awareness Symposium
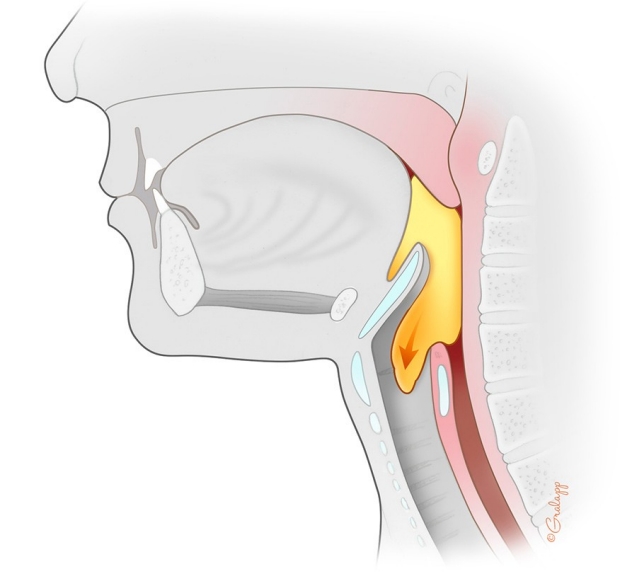
Swallowing disorders have the potential to impact the health and well-being of hundreds of thousands of people across the globe. Every other year, Stanford hosts the Swallowing Disorders Awareness Symposium in conjunction with Dysphagia Awareness month. On alternative years, the event is hosted by our colleagues at the University of California at Davis. This event provides learning opportunities for providers who care for patients with swallowing disorders as well as those who live with or love someone with swallowing difficulty.

June 10, 2020

June 20, 2018
Does Medicare cover physical therapy? Yes, and you might be eligible for more services, too

“Physical therapists are movement experts,” says Roger Herr, American Physical Therapy Association (APTA) president. They’re especially important to older adults given that about half of physical therapists’ patients are over the age of 65—and that number is expected to grow as the population ages.
As part of their scope of practice, physical therapists provide evaluation, consultation, education, and treatment to improve balance, mobility, strength and endurance, coordination, and flexibility, says Herr.
Common conditions treated by physical therapy include osteoarthritis , low back pain, and urinary incontinence.
“Physical therapy can also be useful as a preventative measure, such as when you feel shaky on your feet to prevent a fall, or it can assist in your recovery after a fall or surgery,” says Herr.
Medicare coverage of physical therapy services
Whether you’re staying in a facility, such as a hospital or nursing home, or at home, and need physical therapy, Medicare provides coverage to manage a chronic condition, such as multiple sclerosis (MS) , treat an injury or illness, or to ensure you can maintain your independence. Although an order or referral is not required under Medicare, a doctor, nurse practitioner, clinical nurse specialist, or physician assistant must certify that the services are medically necessary.
Medicare Part A will fully cover in-patient physical therapy for the first 60 days after a deductible is met , provided skilled nursing and/or rehabilitation services are required daily. After that, co-payments apply.
Outpatient coverage, which includes visits to a physical therapy clinic, or at home for older adults who are not homebound, is covered by Medicare Part B . After you meet the annual deductible, Medicare pays 80%, and you pay 20% of the Medicare-approved amount.
If you haven’t checked your coverage lately, you might be eligible for more services.
“Physical therapy coverage through Medicare changed in 2018,” says Diane Omdahl, author of Medicare for You and cofounder of the Medicare advisory firm 65 Incorporated .
“Before that, there were coverage limits. The rule changed to unlimited Medicare coverage for medically necessary outpatient physical therapy services each calendar year,” says Omdahl.
Medicare Advantage coverage of physical therapy services
“ Medicare Advantage plans may require prior authorization before approving your physical therapy treatment,” says Herr. Your physical therapist may need to perform an evaluation and submit a treatment plan to get approval for coverage, Herr explains.
Once approved, Medicare Advantage plans offer the same coverage as Medicare Parts A and B, with a few exceptions. Medicare Advantage plans may have different deductibles, require members to use physical therapy services from their networks and/or conduct more frequent audits or reviews to minimize costs and reduce over-utilization of services, says Herr.
Medicaid coverage of physical therapy services
Medicaid coverage of physical therapy services is an optional benefit depending on your state , so you’ll need to check to see what benefits your state offers .
Coverage of occupational therapy and speech-language pathology
In addition to physical therapy, Medicare, Medicare Advantage, and Medicaid generally provide the same coverage for other rehabilitation therapies as long as they are deemed medically necessary, says Herr.
This includes occupational therapy , or assistance helping you perform activities of daily living (such as bathing or dressing), home management, and community re-entry to maintain current capabilities or slow decline.
It also includes speech-language pathology , which offers support for help with speech and language skills, swallowing, and cognitive skills to maintain or improve current function or slow decline.
Outpatient physical therapy in a facility or at home—which is better?
All outpatient therapy is covered by Medicare Part B, but you may wonder if getting physical therapy at home is as useful as that provided at a facility.
“Physical therapy locations may have additional equipment and resources than what a physical therapist can provide in the home,” says Herr.
In addition, Herr says that the wait for physical therapy services at a facility may be less than those provided in the home.
“Going out to get physical therapy also helps with socialization, which may have been hindered when dealing with a mobility issue,” says Herr.
For some patients, however, home-based outpatient therapy provides an opportunity to address environmental challenges in the home and ensure that an individual can manage safely and independently in their own setting. Home-based therapy also serves to improve access to therapy for those without reliable transportation, says Herr.
Difficulty finding physical therapists
Even though Medicare covers physical therapy, it may be hard to find a physical therapist .
“The physical therapy shortage peaked during the pandemic, but we’re still seeing double-digit vacancies,” says Herr.
Other factors continue to contribute to the ongoing shortage, according to a KFF news report . One is that physical therapists are now required to have doctorates, so fewer students are entering the field. Another is that Medicare has cut physical therapy reimbursements by 9% over the last four years, which has led to lower staffing levels.
Most Popular


IMAGES
VIDEO
COMMENTS
having a wet or gurgly voice during or after eating or drinking. feeling like something is stuck in your throat or chest after eating or drinking. needing extra work or time to chew or swallow. having food or liquid leak from your mouth. food getting stuck in your mouth. having a hard time breathing after meals.
Overall, speech therapy is an essential component of dysphagia management and treatment. With the help of a skilled speech therapist, individuals with dysphagia can improve their swallowing function, reduce the risk of aspiration, and enjoy a better quality of life.
Surgery also can treat esophageal cancer. Speech and swallowing therapy is usually helpful after surgery. The type of surgical treatment depends on the cause of dysphagia. Some examples are: Laparoscopic Heller myotomy. This involves cutting the muscle at the lower end of the esophagus, called the esophageal sphincter.
Speech therapy offers specialized techniques to help patients manage and improve swallowing disorders. Swallowing disorders, also known as dysphagia, can occur due to various health conditions and can affect people of all ages. In speech therapy, personalized exercises are designed to strengthen the muscles involved in swallowing.
Speech therapists can show you methods to help. This can involve changing your diet or holding your head and neck in a certain way. In other cases, speech therapy involves teaching your muscles how to effectively swallow. Often, this involves exercises. Most of these help with strengthening the tongue. Swallowing is actually a complicated process.
A speech-language pathologist (speech therapist), treats speech and swallowing disorders. They work with babies, children and adults to help improve communication skills. They can help if you have a developmental disorder, neurological condition or injury that prevents you from communicating effectively or consuming food or drinks safely.
Speech-language pathologist Johnna Johnson holds a special certification in VitalStim to help patients with swallowing disorders. Johnson can help patients with weak musculature deficits that cause dysphagia. She focuses on helping patients strengthen the muscles that allow them to swallow properly.
The therapy is performed by speech-language pathologists - specialists trained in swallowing assessments and rehabilitation therapy. ... If removing the swallowing problem is not possible, changing what and how you eat can help make swallowing safer and more comfortable. Your speech-language pathologist may recommend:
A speech-language pathologist (SLP) can help you with speech, language, and swallowing. They provide speech therapy to children and adults who may have speech or language disorders. People with certain medical conditions may also benefit from speech therapy. Medical conditions that may cause speech or swallowing impairment include traumatic ...
The signs and symptoms can include coughing, throat clearing, wet/gurgly voice, choking, etc. while eating and drinking. A speech-language pathologist can typically determine if a person is aspirating and/or having difficulty swallowing. The speech therapist would proceed with a treatment plan and therapeutic exercises to target individual ...
Speech therapy can help you improve your: Early language skills (especially children learning to talk and communicate). ... They may have trouble with reading, writing, swallowing and other motor skills. Articulation disorder:People with articulation disorders are unable to produce certain word sounds. For example, they may substitute one sound ...
How long will speech and swallowing rehabilitation therapy take? The speech-language or swallowing evaluation is completed on a one-on-one basis and can typically last for one hour. If treatment is recommended, follow up visits range from 45 -60 minutes in length. The duration and frequency of treatment ranges for each individual person and ...
Speech-language pathologists or speech therapists can help when you are having problems speaking, communicating, or swallowing due to a wide range of conditions, including speech delays or strokes.
Speech therapy is a form of healthcare that helps improve communication and speech. It can also help improve swallowing function and other behaviors related to feeding. About one in 12 children in ...
With swallow therapy, a speech language pathologist (SLP) will work with a patient to help improve their ability to swallow safely, reducing the risk for aspiration. Techniques may include a combination of the following: Swallowing exercises and maneuvers. Positioning strategies. Modifications of foods and liquids.
Dysphagia and Swallowing Therapy. Call for appointment: 410-787-4433. Video unavailable. This video is unavailable. Swallowing disorders, also called dysphagia (dis-FAY-juh), can occur at different stages in the swallowing process: Oral phase - sucking, chewing, and moving food or liquid into the throat.
Speech therapy in Wooster, OH, helps children, teens, and adults with difficulties in communication, language, voice/speech, and even swallowing. When the tongue, oral cavity, or throat are damaged or malformed, a highly qualified speech therapist can assist in regaining lost skills or in learning new ways to speak, swallow, and more.
A speech therapist can help you determine what techniques or tools will work best for you. Listening In any conversation, the listener's role is just as important as the speaker's role. When conversing with a person living with ALS who has bulbar symptoms, there are several things you can do to help: Give the speaker your full attention.
People with multiple sclerosis, or MS, often have trouble swallowing, a problem called dysphagia. It can also lead to speech problems. ... A speech therapist can also help with swallowing problems.
Speech and language therapists (SALTs) assess difficulties with swallowing and communication. They can offer support through swallowing and speech exercises, dietary advice and changes to medication. Difficulties in swallowing, known as dysphagia, may arise from a number of medical causes. In dementia they may be caused by damage to parts of ...
Many patients will benefit from speech and swallowing therapy to either address or prevent problems with communication and swallowing. Our head and neck cancer team includes expert speech-language pathologists (SLP's) with specialized interest in the management of communication and swallowing disorders associated with head and neck cancer.
While a speech-language pathologist focuses on complications with language, speaking and swallowing, an occupational therapist helps patients gain, or remediate, the skills they need to perform daily functions, regardless of their age, condition or injury. ... Fortunately, USAHS can help you further navigate this OT-speech therapy decision.
Coverage of occupational therapy and speech-language pathology ... for help with speech and language skills, swallowing, ... equipment and resources than what a physical therapist can provide in ...