- Member Login

Oral Health Topics
The Oral Health Topics section on ADA.org is intended to provide dentists with clinically relevant, evidence-based science behind the issues that may affect their patients and their practice. Refer to the Oral Health Topics for current scientific reviews of subjects that relate to oral health, from amalgam separators and antibiotic prophylaxis to xerostomia and X-rays.
Featured oral health topics
Learn which oral analgesics are used for the management of acute dental pain.
Understand Occupational Safety and Health Administration (OSHA) safety standards.
Learn about special considerations for pregnant patients and pregnant dental personnel .
Efficacy information about whitening treatments for extrinsic and intrinsic staining.
- University of Michigan Library
- Research Guides
Dental Hygiene
- Creating a Well-Focused Question
- Databases & Journals
- E-Books & Print Books
- Web Resources
- Health Statistics
- EBDM Handbook
- Searching in PubMed
- Article Abstracts
- Accessing Full Articles with MGet It
- Information for Patients
- Special Populations
- Google Search Tips
- Clinical Scenario
You will usually begin your research with a clinical scenario:
Mark McGee – a 70-year-old male – is concerned about his bad breath. You tell him that he wouldn’t have much to be concerned about if he only brushed his teeth. He doesn’t believe you and says, “show me the evidence!”
Then you should use PICO , synonyms , & boolean operators to create a well-defined, searchable question.
The PICO model helps you create an answerable question from a clinical scenario by identifying search terms & their relationships so that you can conduct an effective literature search .
Based on the clinical scenario above:
- P = bad breath, male, adult
- I = toothbrushing
- C = doing nothing
- O = reduction in bad breath
Not all of these terms will be used directly in the search, but it's good to be aware of all potential search terms.
- Research Question
Here's the question that you'll base your search on.
Does toothbrushing, in comparison with doing nothing [i.e., what the patient is currently doing] , decrease bad breath in older male adults?
Synonyms , words that mean the same thing or are closely related to each other, can help expand your search appropriately.
For this search, the synonyms are:
You could also use terms such as mouth rinses or toothpaste .
- Boolean Operators
Boolean operators such as AND & OR are used to connect synonyms & concepts.
- Use OR to connect synonyms to appropriately expand your search for a concept. Your search results will contain citations for each term. Place parentheses around the search terms when you use OR so that the database searches them together.
- Use AND to connect concepts. This will narrow your search results, giving you just the articles that include all terms, that is, the intersection of the search terms you've used. Remember: Databases assume AND between terms, so you don't have to use it.
- Always capitalize boolean operators; if you don't, they'll be ignored.
- Putting It All Together
Here are the terms (also known as a "search string") that will be used to search the database:
(bad breath OR halitosis) AND (toothbrushing OR oral hygiene)
Bad breath & halitosis are synonyms for one concept, so they're connected by OR & placed within parentheses.
What's on this page?
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Other journals in brief
- Published: 26 July 2019
Which dental research topics are relevant to patients?
- Paul Hellyer 1
British Dental Journal volume 227 , page 113 ( 2019 ) Cite this article
231 Accesses
Metrics details
You have full access to this article via your institution.
Kakudate N, Yokoyama Y, Sumida F et al. Practice-based research agendas priorities selected by patients: findings from a practice-based research network. Int Dent J 2019; 69: 183−191.
Study shows priorities differ with age and gender.
'Public involvement in research is defined as research that is done with or by the public and not to, about or for them' (Involve www.invo.org.uk ) and many grant funders now require evidence of public and patient involvement in research projects. The research agenda, however, may still be being set by academics and not by patients. Relatively little research is based in general practice.
Using a questionnaire with patients in 11 dental clinics in Japan, Kakudate and colleagues have attempted to find out which research topics would be important and relevant to patients. Involving patients 'may provide opportunities to produce research which is valid, relevant, acceptable, sustainable and innovative.'
Following a pilot study, a 31 item questionnaire, divided into 11 categories was developed (orthodontic treatment, regular dental check ups, prognosis of dental treatment, dental implants, tooth brushing, diet and food, aesthetic dental care, topical fluoride application, social health insurance, bruxism and miscellaneous) and was completed by 482 patients (87.6% response rate).
The most commonly selected research agenda was 'age specific care to maintain oral health' (n = 84), followed closely by topics related to toothpastes and brushing, the durability of restorations and questions relating to diet, caries and periodontal disease. The least popular topic related to the use of interdental cleaning aids. In patients <40, selection of toothpaste was the most popular topic. Only responders <30 listed the timing of wisdom teeth extractions and orthodontic as topics. Only those aged >60 listed the durability of restorations in relation to treatment available under the national health insurance scheme.
Statistically significant age and gender differences were noted. Younger patients rated orthodontic treatment, aesthetic dental care and fluoride applications more frequently than older patients. Older patients rated regular dental check ups, implants, diet and health insurance as more interesting than younger ones. Females rated aesthetics as more important than did males, who rated toothbrushing as more interesting than did females.
Responses may be different from within a different culture. However, these results clearly show that different age groups have differing priorities with regard to research priorities. If research is to be patient centred and relevant, then shaping research questions around actual patients' concerns, needs and values assumes greater importance. These results may 'help research funders identify future priorities that have the greatest impact on patients and the clinicians who treat them.'
Author information
Authors and affiliations.
Honorary Teaching Fellow, University of Portsmouth Dental Academy, Portsmouth, UK
Paul Hellyer
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Hellyer, P. Which dental research topics are relevant to patients?. Br Dent J 227 , 113 (2019). https://doi.org/10.1038/s41415-019-0567-1
Download citation
Published : 26 July 2019
Issue Date : July 2019
DOI : https://doi.org/10.1038/s41415-019-0567-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Articles on Dental hygiene
Displaying all articles.

Caring for older Americans’ teeth and gums is essential, but Medicare generally doesn’t cover that cost
Frank Scannapieco , University at Buffalo and Ira Lamster , Stony Brook University (The State University of New York)

No, it’s not just sugary food that’s responsible for poor oral health in America’s children, especially in Appalachia
Daniel W. McNeil , West Virginia University and Mary L. Marazita , University of Pittsburgh

How did people clean their teeth in the olden days?
Jane Cotter , Texas A&M University
Related Topics
- Curious Kids US
- Dental care
- Dental insurance
- Health inequity
- Older people
- Oral health
- Periodontitis
- US Medicare
Top contributors
Professor and Chair of Oral Biology, University at Buffalo
Clinical Professor of Periodontics and Endodontics, Stony Brook University (The State University of New York)
Assistant Professor of Dental Hygiene, Texas A&M University
Director, Center for Craniofacial and Dental Genetics; Professor of Oral Biology and of Human Genetics, University of Pittsburgh
Eberly Distiniguished Professor Emeritus, Clinical Professor Emeritus of Dental Public Health & Professional Practice, West Virginia University
- X (Twitter)
- Unfollow topic Follow topic
Skip to content
Support the College of Dental Medicine
Community outreach.
Learn more about the College of Dental Medicine's community outreach programs.
Postdoctoral and Residency Programs
dds program.
Half of our graduates go directly into specialty training upon completion of the DDS degree.
Research Areas
Patient care, columbiadoctors dentistry, become a student.
Learn more about the admissions process and how you can apply.
Student Research Projects
Dental Hygiene
- Journals and Databases
- Books & eBooks
- Searching Tips
- Web Resources
- Streaming Videos
- Writing & Citing
- Your MCC Libraries
- PICO Worksheet
Use this handy worksheet for each topic you research. It will help you identify keywords, controlled vocabulary and the best databases to search for the topic.
What is PICO?
An essential part of evidence-based decision making involves asking a good question. A clinical or research question can generally be broken down into four components. 'PICO' is the acronym that identifies the four components of a good research question:
P opulation
I ntervention
C omparison
O utcome(s)
The PICO table on this page provides further explanation and examples for each of the four components.
The following links provide additional information and resources on PICO:
Introduction to PICO - UT Health, San Antonia
Forming Focused Questions with PICO - UNC Health Sciences Library
EBM Pico Tutorial: Forming a Clinical Question
PICO Explained
Pico search query.
Search Tips:
- Don't enter a question or sentence into the search box.
- Search by keywords or phrases
- Use Boolean operators (AND, OR, NOT) to help narrow or expand your search.
- Use Boolean operators to connect your PICO terms
Here are some examples:
AND - use to connect two separate concepts to narrow the search (AND finds articles that contain BOTH terms)
- periodontal disease AND pregnancy
OR - use to search for similar terms to expand the search (OR finds articles that contain EITHER term)
- wisdom teeth OR third molars
NOT - use to exclude terms to narrow the search (NOT find articles that contain one term but NOT the other)
- heart NOT lung
- << Previous: Searching Tips
- Next: Web Resources >>
- Last Updated: Jan 16, 2024 2:02 PM
- URL: https://mesacc.libguides.com/dental
121+ Interesting Dental Research Topics for Undergraduates

Did you know poor oral health can be linked to heart disease? It’s true! This surprising fact underscores the importance of dental research in maintaining overall health and well-being.
Understanding the intricate connections between oral health and systemic conditions like heart disease highlights the critical role of research in advancing our knowledge and improving patient outcomes.
In this blog, we will delve into various dental research topics tailored specifically for undergraduates, providing insights, resources, and inspiration to explore this fascinating field further.
Whether you’re passionate about dentistry or simply curious about the intersection of oral health and overall wellness, join us as we uncover the exciting possibilities in dental research for undergraduates.
What is Dental Research Topic?
Table of Contents
A dental research topic is a subject of study within the field of dentistry that aims to explore, investigate, and analyze various aspects related to oral health, dental care, and dental treatments.
These topics cover a wide range of areas, including but not limited to dental diseases, preventive measures, treatment methods, oral hygiene practices, dental technology advancements, and the impact of oral health on overall well-being.
Dental research topics provide opportunities for scholars, researchers, and students to contribute to the advancement of dental science, improve patient care, and address current challenges in oral health care.
Importance of Dental Research Topics for Undergraduates
Dental research topics are essential for undergraduates for several reasons:
Skill Development
Engaging in dental research topics helps undergraduates develop critical thinking, problem-solving, and analytical skills essential for their academic and professional growth.
Contribution to Knowledge
Undertaking research allows undergraduates to contribute to the existing body of knowledge in dentistry, advancing the field and addressing emerging challenges.
Career Preparation
Research experience enhances students’ competitiveness for dental school admissions, graduate programs, and future careers in academia, clinical practice, or research institutions.
Practical Application
Research topics offer undergraduates the opportunity to apply theoretical knowledge gained in the classroom to real-world scenarios, fostering a deeper understanding of dental concepts and techniques.
Professional Networking
Engaging in research exposes undergraduates to collaboration with peers, faculty, and professionals, facilitating valuable networking opportunities within the dental community.
Popular Dental Research Topics for Undergraduates
Dental research topics for undergraduates encompass a wide range of areas within dentistry. Here are some examples across different subfields:
Dental Diseases
- The role of genetics in the development of periodontal disease.
- Strategies for early detection and prevention of dental caries.
- Investigating the link between diabetes and periodontal disease.
- Factors influencing the prevalence of oral cancer among different demographics.
- Impact of dietary habits on the occurrence of enamel erosion.
- Effectiveness of fluoride in preventing dental decay.
- The role of saliva in maintaining oral health and preventing diseases.
- Trends in the prevalence of temporomandibular joint disorders.
- Oral manifestations of systemic diseases: A comprehensive review.
- Investigating the relationship between oral health and overall systemic health.
- The effectiveness of probiotics in preventing oral infections.
- Psychological factors influencing dental anxiety and its management.
Dental Treatments
- Comparison of different types of dental implants: Materials, techniques, and success rates.
- Advancements in minimally invasive techniques for dental restoration.
- Comparative analysis of traditional braces versus clear aligners in orthodontic treatment.
- The role of lasers in various dental procedures: Benefits and limitations.
- Innovations in endodontic treatment: From rotary instruments to regenerative techniques.
- Efficacy of different whitening agents in professional and over-the-counter dental bleaching.
- The impact of COVID-19 on dental practice: Adaptations, challenges, and future implications.
- Investigating the use of stem cells in dental tissue regeneration.
- Comparative study of different materials used in dental restorations: Strength, durability, and aesthetics.
- Exploring the potential of 3D printing technology in prosthodontics and oral surgery.
- Patient satisfaction and outcomes following different types of orthognathic surgeries.
- Long-term success rates of various techniques in root canal therapy.
Oral Health Promotion and Education
- Effectiveness of school-based oral health education programs in improving children’s oral hygiene.
- Strategies for promoting oral health in underserved communities: Challenges and solutions.
- Role of social media and technology in disseminating oral health information.
- Impact of community water fluoridation on dental caries prevention.
- The role of parents and caregivers in establishing children’s oral hygiene habits.
- Cultural influences on oral health beliefs and practices: Implications for public health campaigns.
- Effectiveness of motivational interviewing in promoting behavior change for better oral health.
- Investigating the efficacy of school-based dental sealant programs.
- Oral health literacy among different populations: Assessments and interventions.
- The role of dentists in advocating for policies promoting oral health equity.
- Strategies for improving oral health outcomes among elderly populations.
- Integrating oral health education into primary care settings: Opportunities and challenges.
Dental Materials and Biomaterials
- Biocompatibility of dental materials: Assessing safety and long-term effects.
- Development of antimicrobial dental materials to prevent biofilm formation.
- Investigating the mechanical properties of novel dental composites.
- Bioactive materials in dentistry: Applications and clinical implications.
- Biodegradable materials for temporary dental restorations.
- Nanotechnology in dentistry: Potential applications and future directions.
- Development of remineralizing agents for the management of dental caries.
- Investigating the properties and applications of dental ceramics.
- Biomimetic materials in dentistry: Mimicking natural tooth structure for improved outcomes.
- Sustainable practices in dental material manufacturing and disposal.
- Advances in adhesive systems for bonding dental restorations.
- Biomechanical properties of dental implant materials: Enhancing stability and osseointegration.
Oral Microbiology and Immunology
- Microbiome of the oral cavity: Composition, dynamics, and role in health and disease.
- Host-pathogen interactions in periodontal diseases: Insights into disease progression.
- Immunological responses to dental biofilms and their implications for treatment.
- Role of probiotics in modulating oral microbiota and preventing dental diseases.
- Viral infections in dentistry: From herpesviruses to SARS-CoV-2.
- Impact of antimicrobial resistance on dental infections and treatment outcomes.
- Microbial ecology of dental plaques in different oral environments.
- Oral manifestations of HIV/AIDS: Diagnosis, management, and implications.
- Biofilm formation on dental implant surfaces: Prevention and management strategies.
- Innate and adaptive immune responses in oral mucosal diseases.
- Virulence factors of oral pathogens and their role in disease progression.
- Immunomodulatory properties of dental materials and their impact on tissue response.
Dental Public Health
- Epidemiology of dental diseases: Trends, disparities, and risk factors.
- Health promotion strategies for improving access to dental care in rural areas.
- Oral health inequalities among different socioeconomic groups: Causes and solutions.
- Cost-effectiveness of preventive dental interventions: A systematic review.
- Integrating oral health into primary care: Models of collaborative practice.
- Tele-dentistry: Opportunities and challenges for improving access to dental care.
- Oral health surveillance systems: Monitoring trends and assessing needs.
- Assessing the effectiveness of community water fluoridation programs.
- Role of dental professionals in addressing oral health disparities.
- Impact of environmental factors on oral health outcomes: Pollution, climate change, and urbanization.
- Dental workforce issues: Distribution, shortages, and workforce diversity.
- Oral health policies and advocacy: Strategies for promoting legislative change.
Pediatric Dentistry
- Early childhood caries: Risk factors, prevention, and management strategies.
- Behavior management techniques in pediatric dentistry: Evidence-based approaches.
- Oral health outcomes of children with special healthcare needs: Challenges and interventions.
- Dental trauma in children: Prevention, diagnosis, and treatment.
- Assessment of dental fear and anxiety in pediatric patients: Tools and interventions.
- Maternal and child oral health: Prenatal factors influencing dental health outcomes.
- Dental developmental anomalies: Diagnosis, management, and long-term implications.
- Effectiveness of fluoride varnish application in preventing dental caries in children.
- Impact of nutrition and dietary habits on pediatric oral health.
- Pediatric sedation techniques in dentistry: Safety, efficacy, and guidelines.
- Orthodontic considerations in pediatric dentistry: Early intervention and treatment planning.
- Pediatric dental emergencies: Management and prevention strategies.
Oral and Maxillofacial Surgery
- Outcomes of orthognathic surgery in patients with skeletal discrepancies.
- Management of impacted third molars: Indications, techniques, and complications.
- Reconstruction of maxillofacial defects following trauma or tumor resection: Surgical options and outcomes.
- Temporomandibular joint disorders: Diagnosis, management, and surgical interventions.
- Bone grafting techniques in implant dentistry: Approaches and success rates.
- Surgical management of obstructive sleep apnea: Role of maxillomandibular advancement.
- Surgical treatment options for cleft lip and palate: Multidisciplinary approaches and long-term outcomes.
- Surgical management of oral and maxillofacial infections: Antibiotic therapy, drainage, and debridement.
- Soft tissue augmentation techniques in aesthetic and functional maxillofacial surgery.
- Advancements in minimally invasive techniques for orthognathic surgery.
- Surgical management of facial trauma: Emergency interventions and long-term rehabilitation.
- Digital planning and navigation in oral and maxillofacial surgery: Enhancing precision and outcomes.
Dental Education and Training
- Effectiveness of simulation-based training in dental education: Skill acquisition and retention.
- Integration of digital technology into dental curricula: Challenges and opportunities.
- Peer-assisted learning in dental education: Impact on student performance and satisfaction.
- Interprofessional education in dentistry: Collaborative approaches to patient care.
- Continuing education requirements for dental professionals: Trends and implications.
- Assessment methods in dental education: Moving beyond traditional exams.
- The role of mentorship in shaping the career trajectories of dental students.
- Global perspectives in dental education: Cross-cultural experiences and challenges.
- Incorporating evidence-based practice into dental curricula: Strategies and outcomes.
- Tele-education in dentistry: Remote learning platforms and their effectiveness.
- Student perceptions of clinical experiences in dental education: Barriers and facilitators.
- Innovations in competency-based dental education: Assessing clinical proficiency and readiness for practice.
Dental Technology and Innovation
- Artificial intelligence in dentistry: Applications in diagnosis, treatment planning, and outcomes prediction.
- Virtual reality and augmented reality in dental education and patient care.
- Robotics in dentistry: Automation of procedures and precision in surgical interventions.
- Wearable technology for monitoring oral health behaviors and conditions.
- 3D printing in dentistry: Customization of dental implants, prostheses, and surgical guides.
- Digital smile design: Utilizing technology for aesthetic treatment planning and communication.
- Smart materials in dentistry: Self-healing, self-cleaning, and bioactive properties.
- Teledentistry platforms for remote consultations, monitoring, and patient education.
- Biomimetic approaches in dental materials design: Mimicking natural tooth structure and function.
- Nanomaterials in oral healthcare products: Enhanced delivery systems and therapeutic applications.
- Bioprinting of dental tissues and organs: Advancements in regenerative dentistry.
- Energy-based devices in dentistry: Laser therapy, photobiomodulation, and electrosurgery applications.
- Development of a Smart Toothbrush with Artificial Intelligence Integration.
These topics offer a comprehensive overview of the diverse areas within the field of dental research and provide undergraduates with a plethora of options for exploring their interests and making meaningful contributions to the discipline.
Current Trends in Dental Research
Several trends were prevalent in dental research. While there may have been further developments since then, here are some prominent trends at that time:
Biomimetic Dentistry
Mimicking natural tooth structure and function using advanced materials and techniques.
Tele-dentistry
Utilizing technology for remote consultations, monitoring, and patient education, especially amidst the COVID-19 pandemic.
Regenerative Dentistry
Developing therapies to regenerate dental tissues and promote natural healing processes.
Personalized Dentistry
Tailoring treatment plans based on individual patient characteristics, genetics, and preferences.
Minimally Invasive Dentistry
Emphasizing conservative approaches to preserve tooth structure and improve patient comfort.
Digital Dentistry
Integration of digital technology for diagnostics, treatment planning, and fabrication of dental restorations.
Nanotechnology
Utilizing nanomaterials for improved dental materials, drug delivery systems, and diagnostic tools.
Challenges in Dental Research Topics
Dental research, like any scientific field, faces its share of challenges. These challenges can span various aspects of the research process, from funding and resources to methodological complexities and ethical considerations. Here are some common challenges in dental research:
Funding Constraints
Limited financial resources hinder the initiation and continuation of dental research projects.
Access to Resources
Inadequate access to specialized equipment, materials, and facilities poses a barrier to conducting comprehensive research.
Recruitment of Participants
Difficulty in recruiting diverse and representative study populations affects the generalizability of research findings.
Ethical Considerations
Navigating ethical complexities, such as informed consent and privacy concerns, adds challenges to dental research.
Interdisciplinary Collaboration
Facilitating collaboration between dental professionals, researchers, and other disciplines is essential but often challenging.
Translation of Research into Practice
Bridging the gap between research findings and clinical implementation remains a significant challenge in dental research.
The exploration of dental research topics holds immense promise for advancing oral health care and addressing multifaceted challenges within the field.
From unraveling the mysteries of oral diseases to pioneering innovative treatments and technologies, dental research serves as the cornerstone of progress and improvement in patient outcomes.
Despite facing various challenges such as funding constraints and ethical considerations, the pursuit of dental research remains crucial for enhancing preventive measures, refining treatment modalities, and promoting overall well-being.
By fostering interdisciplinary collaboration, embracing emerging trends, and prioritizing the translation of research findings into practice, the dental community can continue to drive impactful discoveries and advancements for the benefit of individuals worldwide.
1. How can I stay updated on the latest dental research?
Staying updated on the latest dental research can be as simple as subscribing to reputable dental journals, attending conferences, and following dental research institutions and experts on social media platforms.
2. What are some examples of emerging dental research topics?
Emerging dental research topics include genetics and oral health, biomaterials and tissue engineering, and microbiome studies, among others.
3. Why is dental research important for patients?
Dental research drives innovation in oral healthcare, leading to improved treatment outcomes, personalized care, and enhanced preventive strategies for patients.
Related Posts

Science Fair Project Ideas For 6th Graders
When it comes to Science Fair Project Ideas For 6th Graders, the possibilities are endless! These projects not only help students develop essential skills, such…

Java Project Ideas for Beginners
Java is one of the most popular programming languages. It is used for many applications, from laptops to data centers, gaming consoles, scientific supercomputers, and…
- Open access
- Published: 10 April 2024
Dental patients as partners in promoting quality and safety: a qualitative exploratory study
- Enihomo Obadan-Udoh 1 ,
- Vyshiali Sundararajan 1 ,
- Gustavo A. Sanchez 1 ,
- Rachel Howard 1 ,
- Siddardha Chandrupatla 2 &
- Donald Worley 3
BMC Oral Health volume 24 , Article number: 438 ( 2024 ) Cite this article
167 Accesses
Metrics details
Active patient involvement in promoting quality and safety is a priority for healthcare. We investigated how dental patients perceive their role as partners in promoting quality and safety across various dental care settings.
Focus group sessions were conducted at three dental practice settings: an academic dental center, a community dental clinic, and a large group private practice, from October 2018-July 2019. Patients were recruited through flyers or word-of-mouth invitations. Each session lasted 2.5 h and patients completed a demographic and informational survey at the beginning. Audio recordings were transcribed, and a hybrid thematic analysis was performed by two independent reviewers using Dedoose.
Forty-seven participants took part in eight focus group sessions; 70.2% were females and 38.3% were aged 45-64 years. Results were organized into three major themes: patients’ overall perception of dental quality and safety; patients’ reaction to an adverse dental event; and patients’ role in promoting quality and safety. Dental patients were willing to participate in promoting quality and safety by careful provider selection, shared decision-making, self-advocacy, and providing post-treatment provider evaluations. Their reactions towards adverse dental events varied based on the type of dental practice setting. Some factors that influenced a patient’s overall perception of dental quality and safety included provider credentials, communication skills, cleanliness, and durability of dental treatment.
The type of dental practice setting affected patients’ desire to work as partners in promoting dental quality and safety. Although patients acknowledged having an important role to play in their care, their willingness to participate depended on their relationship with their provider and their perception of provider receptivity to patient feedback.
Peer Review reports
Introduction
In recent years, there has been a surge in research related to dental quality and safety from various parts of the world [ 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 ]. These studies have investigated how adverse events occur in dentistry, identified methodologies for detecting adverse safety events, and focused on developing strategies to reduce the occurrence of adverse events [ 3 , 5 , 6 , 10 , 11 , 12 , 13 , 14 ].
Patient involvement in quality and safety-promoting activities is an emerging area of interest. Dentistry findings from several studies suggest that patient reports can provide meaningful insight and breadth regarding the quest to understand such adverse events [ 15 , 16 , 17 , 18 , 19 ]. In dentistry, previous studies have demonstrated that patients are apprehensive about safety at the dental office and are willing to participate in activities that promote quality and safety when properly engaged by providers [ 7 , 8 , 15 , 16 , 17 ]. However, majority of these studies focused solely on patients attending a single academic institution. We proposed a study that recruited patients from three different dental care settings to provide an array of diverse perspectives. Through this study, we assessed how dental patients perceive their role as partners in promoting quality and safety across various dental care settings.
Study sites
The study was conducted at three different dental practice settings: an academic dental center (Site U), a community dental clinic (Site I), and a large group dental private practice (Site H). Site H is in Minnesota, while both Sites U and I are located in Texas. The academic dental center (Site U) consists of a pre-doctoral teaching clinic, a resident/postgraduate clinic, and a faculty group practice. Patients visiting this center are from diverse racial and ethnic backgrounds. The community dental clinic (Site I) is comprised of a network of small to medium-sized dental offices scattered throughout the city. Affiliated with a religious non-profit organization, this site primarily serves low income and indigent families who lack access to health care. The large group dental private practice (Site H) encompasses over 70 dentists working across 21 dental office locations. The group serves a large range of patients from various demographic and socioeconomic backgrounds.
Study participants
Participants were recruited using a purposive sampling approach. Patients from the study sites were invited to participate through flyers and word-of-mouth invitations. Interested participants were screened by a local site coordinator to confirm that they met the following inclusion criteria: English-speaking, over 18 years of age, able to give informed consent, and attended at least one dental visit at a participating site. Enrolled participants selected one of eight focus group sessions: three of which were hosted at the academic dental center, three at the large group dental practice, and two at the community dental clinic. Ethical approval was obtained from the UCSF institutional review board (#18–25467). A unique participant’s ID was created for each participant using their site name and sex. Females were represented by “X” and males by “Y”.
Study procedures
Eight focus group sessions were held from October 2018 through July 2019. Researchers were provided with a quiet conference room within each dental site to host the sessions. Sessions lasted about 2.5 h and were recorded using two voice recorders. Participants completed an anonymous demographic questionnaire, an informational survey, and an evaluation form at the beginning or end of the session. Prior to the start of each session, ground rules were provided to participants about taking turns, refrainment from disclosure of comments to external parties, and the need to tolerate dissenting opinions. Name introductions were also done prior to starting the recording to ensure privacy. Participants provided verbal consent after reading the study information sheet. All audio recordings were stored safely on a password-protected laptop and de-identified for analysis. Participants received a $30 gift card along with food and beverage in appreciation of their time. The first author (EO-U) served as the lead facilitator/moderator for all the sessions. There were no conflicts of interest, given the authors do not provide patient care at any of the participating dental institutions.
Study instrument
A focus group discussion guide and informational survey were developed using questions from our previous qualitative study and publications by Davis et al. [ 8 , 16 , 17 ]. The discussion guide consisted of eight main topics with sub-topics and probing questions (see Additional file 1 ). The topics were:
Patients’ understanding about “patient safety” and “quality”
Current practices to ensure high quality care in dental care settings
Perceptions about dental patients contributing to dental quality and safety
Approaches to improve patient engagement in dental quality and safety activities
Factors affecting patients’ willingness to participate in dental quality and safety activities
Factors affecting the reporting of poor quality or adverse safety incidents
Features of a “safe” incident reporting system or platform
Patient considerations about the quality and safety of dental offices
The 45-item informational survey comprised six sections that assessed interactional and non-interactional behavior between patients and the dental care team including: asking factual or challenging questions, notifying the team, providing information, gaining information, and adverse event reporting.
Data analysis
Frequencies and descriptive statistics for demographic characteristics of the participants and survey responses were calculated, and audio recordings from the focus group discussions were professionally transcribed using Rev.com. The transcripts were verified against the original audio recordings for completeness by one co-author (VS).
Using Dedoose, two co-authors (VS, GS) independently analyzed each transcript using the following steps:
Repeated reading : After verifying the transcripts, data was read multiple times and memo writing was performed in Microsoft® Word. The research question served as a guide during this step.
Data coding : Bucket codes were created, and relevant texts from transcripts were selected for initial codes and coded for as many potential themes as feasible.
Exploring for themes : After completion of the initial coding process, a list of different codes identified across the data was generated. Within a code, common themes based on similarities, differences, topics, demographics, and approaches were extracted from the content of the focus group discussions. Opinions expressed by individuals that diverged from group consensus were also identified.
Discussing themes and sub-themes : Both primary coders discussed their initial codes. Similar or duplicate codes were merged into sub-themes. All codes were organized into three major themes based on the study objectives:
Patients’ overall perception of dental quality and safety (Theme 1)
Patients’ reaction to poor quality dental care and adverse events (Theme 2)
Patients’ perception of their role in promoting quality and safety (Theme 3)
Tie-breaking : Any code names or code applications that were discordant between both reviewers, were discussed with a third researcher (EO-U) who acted as a tiebreaker in finalizing the themes, sub-themes, and codes. This was only needed once in the study.
Demographic characteristics
A total of 47 patients ( n = 20 (Site I), n = 16 (Site H), n = 11 (Site U)) were successfully recruited to participate in eight focus group sessions (Table 1 ). Participants in the focus group sessions were mostly female (70.2%), and Caucasian (40.4%). Asians (23.4%) and Latinos (21.3%) were the second and third largest ethnicities represented, respectively. The educational level varied among participants, with nearly 50% having at least a bachelor’s degree. Most participants were aged between 25 – 64 years (68.1%).
Informational survey
The informational survey results were analyzed using descriptive statistics (Table 2 ). Patients were asked to assess willingness to engage in various activities at the dental office using a Likert scale (1 = “Definitely Will” through 7 = “Definitely Not”). Thus, lower mean scores represent patients’ willingness to play an active role in promoting quality and safety and higher scores represented an unwillingness to engage in that activity. While patients appeared willing and comfortable to ask factual questions from dental assistants/hygienists and dentists, patients were less willing to ask challenging questions of such providers unless the provider encouraged it (Table 2 ; Sections 1a, 1b, 2a, and 2b). Patients also reported feeling relatively willing to notify their providers as concerns arose regarding their care (Table 2 ; Sections 3a, 3b). Furthermore, while patients were willing to provide or gain pertinent information about their care or dental office, they were less willing to participate in reporting an adverse event occurrence unless it was encouraged by the dental care team (Table 2 ; Section 4, 5, and 6). We defined an adverse event as “the occurrence of any event that the patient perceived as negative or harmful while receiving care”. There was no significant difference between patients’ willingness to engage in safety behaviors with different members of the dental care team (i.e. dental assistant/ hygienist versus dentist).
Theme 1: patients’ overall perception of dental quality and safety (Table 3 , Section 1)
Provider training and qualifications.
Patients trusted that providers who possessed the proper dental licenses and credentials had received adequate training and education needed to provide high quality dental care. Patients found reassurance in public displays of the provider certificates and necessary clinic approvals, many of whom also inquired the names of their provider’s dental school and their experience performing certain procedures.
Patients at the private dental practice and community health center placed more value on the providers’ experience, years of practice, and reviews through websites, such as Yelp. These patients preferred providers who were not recent graduates; however, they also wanted providers to be familiar with recent clinical procedures and guidelines. In contrast, patients who received care at the academic center had tempered expectations about quality. These patients were comfortable with students’ performing treatments because supervising faculty oversaw every procedure.
Communication
Patients emphasized the importance of clear communication in promoting trust between patients and their dental providers. Participants also wanted providers to be honest about the necessary procedures, and their comfort level with performing those procedures. They preferred that providers educated them appropriately about their oral health and the necessary dental treatment using various methods (e.g., pictures, pre-visit videos, after-visit summaries) to facilitate informed decision making.
Unsurprisingly, exemplifying polite and courteous behavior (good chairside manners) as well as establishing a good rapport were often associated with high quality dental care. Older patients preferred more direct or in-person communication, while younger patients preferred more on-demand or virtual communication. Although the preferred communication methods varied, the theme of clear communication was unanimously expressed as a marker of quality dental care across all dental practice settings.
Cleanliness and clinic environment
Irrespective of the dental practice setting, most patients believed that cleanliness and sanitation were important indicators of dental quality and safety. Markers of cleanliness included: sterile instruments within sealed pouches, clean restrooms, clean floors and office space, constant use of gloves around patients, and the physical appearance of dental staff. Markers of uncleanliness included: foul smells, blood on syringes or instruments used for previous patients left lying around, opened sterilization pouches, and re-using dropped instruments.
Durability of dental treatment
Given patients expected their procedures to last, there was a perception of poor-quality care if patients needed to return for repeat procedures or treatment within a short time period.
Dental patients based their overall perception of dental quality and safety on the professional credentialing of providers, their individual dental care experience, the quality of provider-patient communication, the cleanliness of the dental office environment, and the durability of their treatments. Although patients from all dental settings emphasized the importance of cleanliness, perception of other sub-themes varied by dental practice setting. Whereas patients attending the academic dental center gave the benefit of doubt to the student providers and assumed a degree of risk with receiving poor quality dental care and experiencing adverse events, patients at the private dental office placed more emphasis on the quality of provider training and qualifications.
Theme 2: patients’ reaction to poor quality dental care and adverse events (Table 3 , Section 2)
Breach of trust.
When a patient visits a healthcare provider, they expect to receive adequate treatment to ensure good health. In the focus group sessions, patients expressed that experiencing an adverse event negatively impacted their ability to trust their providers, leaving them uncertain about how best to proceed. Some patients chose not to return to the culpable provider and looked for service elsewhere. Others decided to stop seeking dental treatment altogether due to the anxiety from the negative experience.

Fear and embarrassment
During the focus group sessions, some patients indicated that they were afraid to speak up after a perceived adverse event (i.e., received poor quality care or were harmed by dental treatment). Patients also reported feeling embarrassed for their lack of dental health literacy regarding the dental procedure when an incident occurred.
Clinic response to adverse events
Good communication and provider attitude influenced how patients reacted to adverse situations. Patients expressed the importance of dental practices providing a patient support advocate with whom patients can voice their concerns and/or opinions. However, some patients were concerned that speaking with a patient advocate could lead to provider backlash.
Patients had varying reactions to adverse events and receiving poor quality dental care. Most patients across all institutions expressed that they received adequate support from the provider/clinic team whereas others (predominantly from the community health center) described a reluctance to report their experience due to fear of retribution.
Theme 3: patients’ perception of their role in promoting quality and safety (Table 3 , Section 3)
Rationale for participation.
Dental patients had mixed reactions about their role in promoting dental quality and safety. Those who were positively disposed towards engagement activities believed that participation made them feel empowered about their care, stay informed about their choices, and play an active role in improving their oral health. Some believed reporting safety incidents helped make dental care safer for everyone. Patients who were hesitant about their role in promoting dental safety indicated they felt active participation was unnecessary unless they had received poor quality or unsafe dental care.
Timing of participation
Patient willingness to participate in different types of engagement activities depended on the dental care setting. For example, patients at the academic dental center preferred to deliver feedback immediately or shortly after receiving dental treatment, whereas patients at the private dental practice and community-based dental clinic preferred to wait until after they left the clinic or completed their procedure.
Format of participation
Quality and safety-promoting activities that patients were willing to participate in included: advocating for self when they felt that something was going awry, actively tracking their medical/dental health information, writing reviews, participating in dental research, educating themselves about their oral health conditions and dental procedures, and asking their dental providers questions about their dental procedures or safety practices (e.g., hand washing, sterilized instruments, post-procedural instructions). Patients were more hesitant to ask questions that could potentially appear confrontational. Conversely, patients indicated they were more comfortable speaking when providers invited and encouraged their feedback.
Patients also expressed willingness to participate in focus groups, which provide opportunities to voice opinions without fear of any repercussions from the dentist. Others preferred to have fill out surveys, provide comment cards, or speak directly with a dentist or office staff. Patients from the private practice setting appeared more willing to be involved in promoting the quality and safety of their experiences.
Patients preferred different types of communication based on their demographic information. Older patients with less experience using computers preferred printed materials. No comparable differences were observed between male and female participants in the focus groups; although males participated less often than females in the study.
Most patients, especially those at the academic institution, were willing to participate in activities that promote better dental quality and safety and offered various strategies for increasing patient engagement. However, a few patients from the private group practice expressed concerns about “over-engagement” and suggested that patients should be left alone unless they experienced an adverse event. Reactions varied by dental practice setting, with patients at the private dental office indicating that they received more support when things went wrong than patients at the community dental clinic or academic dental center.
This study investigates factors that influence dental patients’ perceptions of their role in promoting quality and safety across various dental care settings. We used multiple focus group sessions to define patients’ understanding of quality and safety and summarize their past experiences of receiving poor quality or unsafe dental care. Given the scarcity of literature on this topic, this study provides novel insight from three diverse dental care settings to jumpstart the conversation about quality of care from the patient’s perspective.
Although patient safety is a complex, multifactorial matter [ 1 , 18 ], our study and others have found that patients consider cleanliness a key component of patient safety. Congruent with our previous work [ 8 ], patients described the term safety using words associated with cleanliness such as “sterilized or clean instruments.” Wearing clean gloves and sterilizing instruments were perceived as important hygienic practices for practitioners to follow. Additional research has concluded that patients view the cleanliness of their units and sterilization protocols, along with maintaining a “clean clinical environment,” as crucial components of patient safety and quality of care [ 20 , 21 , 22 ]. Other studies have reported that patients deemed the use of state-of-the-art equipment as a necessary requirement for ensuring patient safety [ 20 ].
Patients’ expectations for quality of care from their practitioners varied depending on the dental setting they attended. Our previous work found that patients belonging to academic care settings were concerned about how the inexperience of student providers might impact the quality of dental care they received; however, such apprehensions were eased by faculty member oversight [ 8 ]. This finding aligns with results from our present study where patients expressed comfort in receiving care at the academic dental care setting and were more forgiving of mistakes. Another previous study [ 21 ] revealed that the perceived clinical ability of a dental student and the presence of supervisor oversight and assistance with procedures played a critical role in reducing patient anxiety. However, these opinions were not shared by patients at private practices and the community health center in this study, because they expected higher standards of care from their providers and were less forgiving of mistakes.
Our study revealed that patients from the private dental clinic focused on the credentials and training of their providers and only felt safe if the provider had years of experience and extensive training from top tier institutions. This finding is reinforced by prior research that concludes most patients prefer older practitioners whom they perceive as more experienced with refined communication skills [ 20 ]. On the contrary, a separate study found that some patients preferred younger dentists due to their utilization of technology and innovative methods during treatments [ 22 ]. This study also found that patients preferred female dentists because they believed that they had better interpersonal skills than their male counterparts. Together, these studies highlight how the perceived skills of dentists and their demographic characteristics can impact a patient’s perception of receiving quality dental services [ 23 ].
Dental practitioners have experienced a high volume of complaints over the years. Different studies have found that these complaints originate from various sources. While one study found most complaints were made by parents or relatives of patients [ 24 ], another reported that the majority of complaints received were about personal dental treatment [ 25 ]. Nonetheless, most complaints were made by women [ 25 ]. Reasons for complaints included: post-treatment symptoms like pain and eating issues, emotional trauma, unprofessional conduct, and communication breaches [ 25 ]. In the present study, patients expressed the importance of having a patient advocate who could help them discuss negative experiences with their dentists. Others preferred to seek an alternative dentist rather than return to the same practitioner following an adverse event. Fear played a major role as patients decided whether to report their experiences at the dentist. These findings are in accordance with other studies where patients reported losing trust in their dentist and changing providers due to adverse incidents or perceived risks. However, most patients were able to report incidents through advocate mediums that helped advocate for financial compensations and detect preventable injuries [ 25 ].
Our study also revealed that clear and concise communication was an important strategy for improving the quality of patient care. Participants recommended that practitioners engage in open conversations with patients and give honest opinions on their current oral health status and treatment recommendations. They noted that these strategies could encourage active patient participation in promoting quality and safety by enabling them to make informed decisions. Given the importance of conveying information pre-, during, and post-treatment, study participants viewed failure to properly communicate as a major cause for concern. Similar findings have been reported in other studies, Caltabiano et al [ 21 ].found that 50% of dental patients cited “interpersonal skills” of dental students as a factor that decreased anxiety among their dental patients. Simple descriptions of a patient’s diagnosis and the available treatment options are necessary to attain patient satisfaction and participation [ 26 ]. Research studies have shown that clear explanations during consultations and active listening to patients enable them to grasp the expected outcome of the proposed treatment. Miscommunication, rudeness, and inattentiveness can cause a breach in the relationship between dentists and patients [ 27 ]. Adequate communication is necessary to properly assess a patient’s medical condition or medication use before treatment and to help manage patient behavior during treatments to prevent adverse incidents [ 28 ]. Unclear explanations or indications by professionals can result in poor treatment adherence by patients, thereby compromising effectiveness [ 20 ]. Findings from other studies revealed that patients considered good dental services to include key communication strategies such as empathetic words of encouragement and comfort during the treatment process [ 23 ]. A prior study showed that 40% of patients undergoing dental radiographic treatments never had their dentist explain negative side effects and risk of treatment. More than half of these patients (55%) never or hardly ever made enquiries into the safety measures before undergoing radiography [ 29 ].
Involving patients in the monitoring and reporting process gives them a key role to play in enhancing patient safety, as they can provide provider feedback and report adverse incidents [ 28 ]. Patients in the current study expressed willingness to participate in focus groups that allow them to voice their opinions without fear of repercussions from dentists. Similarly, another study found that patients were willing to actively participate in their care and safety by advocating for themselves and being involved in the decision-making process regarding their conditions. Patients’ participation in care and patient safety measures were used as determinants to assess whether they felt safe or ignored [ 30 ].
Different patients preferred different forms of communication based on certain demographic factors. Older patients preferred to receive printed copies of ‘before’ and ‘after-visit’ summaries and were not comfortable using technological gadgets, while younger patients preferred iPads and other mobile devices, as they considered them to be more effective educational devices for patient engagement during treatment. Though most participants were female, there was no gender-based differences of opinions. A study of internal medicine patients found no difference in participation in patient safety activities based on age, gender, or profession [ 18 ]. However, an alternative study indicated that younger patients with advanced education were more willing to participate in the decision-making process regarding their treatments [ 20 ].
Although our findings have limited generalizability due to the use of convenience sampling, our study provides critical information on the willingness of dental patients across various dental care settings to participate in activities that promote the quality and safety of dental care. This study builds upon the findings from our previous work investigating patient participation at a single academic dental center. The conclusions confirm that dental patients react differently to working as partners depending on the dental care setting in which they receive care. Future studies assessing the patient’s perspective should also assess their oral health literacy, since their knowledge of dentistry may impact their perception. Such studies will help determine accessible and feasible methods for improving patient engagement in quality and safety.
Based on our findings, we offer several recommendations on how to facilitate patient participation in safety and quality care activities. “What to expect” summaries for pre-, during, and post-dental treatment periods need to be developed and customized for each dental procedure. Practices should consider employing patient advocates to handle patient concerns and make the feedback process more approachable. While employing a patient advocate might not be feasible in smaller dental offices, some alternatives could be to designate an administrative staff member to manage patient concerns or partner with other local dental offices to outsource the handling of patient grievances to a third-party patient advocacy or mediation group for resolution. Results from our study emphasize that dental practitioners should be approachable and deliver the necessary information at the right time using various modalities depending on the patient’s needs and preferences. Altogether, implementing these strategies will improve patient participation in quality and safety activities in dental care settings.
Our study revealed that dental patients care about the quality and safety of care that they receive. Their willingness to participate in quality and safety activities depended on their relationship with the provider and their perception regarding the receptiveness of providers to accept feedback. Patients were less willing to participate if an activity if it could potentially be perceived as confrontational. The type of dental care setting slightly impacted how patients perceived their role as partners in improving the quality and safety of dental care.
Availability of data and materials
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Bailey E, Tickle M, Campbell S, O’Malley L. Systematic review of patient safety interventions in dentistry. BMC Oral Health. 2015;15(1):152.
Article PubMed PubMed Central Google Scholar
Black I, Bowie P. Patient safety in dentistry: development of a candidate “never event” list for primary care. Br Dent J. 2017;222(10):782–8.
Article CAS PubMed Google Scholar
Kalenderian E, Obadan-Udoh E, Maramaldi P, et al. Classifying adverse events in the dental office. 2017.
Google Scholar
Kalenderian E, Obadan-Udoh E, Yansane A, et al. Feasibility of electronic health record–based triggers in detecting dental adverse events. Appl Clin Inform. 2018;9(3):646.
Maramaldi P, Walji MF, White J, et al. How dental team members describe adverse events. J Am Dent Assoc. 2016;147(10):803–11.
Obadan EM, Ramoni RB, Kalenderian E. Lessons learned from dental patient safety case reports. J Am Dent Assoc. 2015;146(5):318-326.e312.
Obadan-Udoh E, Panwar S, Yansane A-I, et al. Are dental patients concerned about safety? An exploratory study. J Evid Based Dent Pract. 2020;20(3):101424.
Article PubMed Google Scholar
Obadan-Udoh EM, Gharpure A, Lee JH, Pang J, Nayudu A. Perspectives of dental patients about safety incident reporting: a qualitative pilot study. J Patient Saf. 2021;17(8):e874–82.
Wright S, Ucer C, Speechley S. The perceived frequency and impact of adverse events in dentistry. Fac Dent J. 2017;9(1):14–9.
Article Google Scholar
Walji M, Yansane A, Hebballi N, et al. Finding dental harm to patients through electronic health record-based triggers. JDR Clin Transl Res. 2020;5(3):271–7.
CAS Google Scholar
Kalenderian E, Obadan-Udoh E, Maramaldi P, et al. Classifying adverse events in the dental office. J Patient Saf. 2021;17(6):e540–56.
Franklin A, Kalenderian E, Hebballi N, et al. Building consensus for a shared definition of adverse events: a case study in the profession of dentistry. J Patient Saf. 2022;18(5):470–4.
Kalenderian E, Lee JH, Obadan-Udoh EM, Yansane A, White JM, Walji MF. Development of an inventory of dental harms: methods and rationale. J Patient Saf. 2022;10:1097.
Yansane A, Lee J, Hebballi N, et al. Assessing the patient safety culture in dentistry. JDR Clin Transl Res. 2020;5(4):399–408.
Vincent CA, Coulter A. Patient safety: what about the patient? Qual Saf Health Care. 2002;11(1):76–80.
Article CAS PubMed PubMed Central Google Scholar
Davis RE, Sevdalis N, Pinto A, Darzi A, Vincent CA. Patients’ attitudes towards patient involvement in safety interventions: results of two exploratory studies. Health Expect. 2013;16(4):e164–76.
Davis RE, Sevdalis N, Vincent CA. Patient involvement in patient safety: How willing are patients to participate? BMJ Qual Saf. 2011;20(1):108–14.
Sahlström M, Partanen P, Azimirad M, Selander T, Turunen H. Patient participation in patient safety—an exploration of promoting factors. J Nurs Manag. 2019;27(1):84–92.
Weingart SN, Price J, Duncombe D, et al. Patient-reported safety and quality of care in outpatient oncology. Jt Comm J Qual Patient Saf. 2007;33(2):83–94.
PubMed Google Scholar
Henríquez-Tejo RB, Cartes-Velásquez RA. Patients’ perceptions about dentists: a literature review. Odontoestomatologia. 2016;18(27):15–22.
Caltabiano ML, Croker F, Page L, et al. Dental anxiety in patients attending a student dental clinic. BMC Oral Health. 2018;18(1):1–8.
Furnham A, Swami V. Patient preferences for dentists. Psychol Health Med. 2009;14(2):143–9.
Luo JYN, Liu PP, Wong MCM. Patients’ satisfaction with dental care: a qualitative study to develop a satisfaction instrument. BMC Oral Health. 2018;18(1):1–10.
Thomas L, Tibble H, Too L, Hopcraft M, Bismark M. Complaints about dental practitioners: an analysis of 6 years of complaints about dentists, dental prosthetists, oral health therapists, dental therapists and dental hygienists in Australia. Aust Dent J. 2018;63(3):285–93.
Hiivala N, Mussalo-Rauhamaa H, Murtomaa H. Can patients detect hazardous dental practice? A patient complaint study. Int J Health Care Qual Assur. 2015;28:274.
Iqbal W, Faran F, Yashfika A, Shoro F. Evaluation of dental care through patient satisfaction feedback–a cross sectional study at Dental Institute of OJHA Hospital, Karachi. Pakistan Adv Dent & Oral Health. 2018;8(4):0083–91.
Dental Protection Limited. Handling Compliants-England. https://www.dentalprotection.org/docs/librariesprovider4/dental-advice-booklets/dental-advice-booklet-complaints-handling-england.pdf . Published 2016. Accessed 25 July 2022.
Hiivala N. Patient safety incidents, their contributing and mitigating factors in dentistry. 2016.
Al Faleh W, Mubayrik AB, Al Dosary S, Almthen H, Almatrafi R. Public perception and viewpoints of dental radiograph prescriptions and dentists’ safety protection practice. Clin Cosmet Investig Dent. 2020;12:533.
Ringdal M, Chaboyer W, Ulin K, Bucknall T, Oxelmark L. Patient preferences for participation in patient care and safety activities in hospitals. BMC Nurs. 2017;16(1):1–8.
Download references
This project was funded by the UCSF Hellman Family Fund. The views presented here are strictly those of the authors and do not represent the views of the sponsoring organization.
Author information
Authors and affiliations.
Department of Preventive and Restorative Dental Sciences, University of California San Francisco, School of Dentistry, 707 Parnassus Avenue, D3214, Box #1361, San Francisco, CA, 94143, USA
Enihomo Obadan-Udoh, Vyshiali Sundararajan, Gustavo A. Sanchez & Rachel Howard
Ibn Sina Community Dental Clinic, Houston, TX, USA
Siddardha Chandrupatla
HealthPartners Institute, Bloomington, MN, USA
Donald Worley
You can also search for this author in PubMed Google Scholar
Contributions
E.O. was responsible for the study design, overall study execution, including obtaining IRB approvals, designing study instruments and recruitment flyers, data interpretation and manuscript, designing study instruments, recruitment flyers, data interpretation and man writing. V.S. assisted with data collection and analysis. G.S. performed data analysis and helped write the results section. RH revised the manuscript and prepared the tables. SC participated in patient recruitment. D.W. participated in study conceptualization, patient recruitment, and data collection. All authors reviewed and approved the final version of manuscript.
Corresponding author
Correspondence to Enihomo Obadan-Udoh .
Ethics declarations
Ethics approval and consent to participate.
Ethics Approval and Consent to Participate: The study was approved by the UCSF institutional review board (#18–25467). The verbal informed consent was obtained from all the participants which was approved by the UCSF IRB.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Obadan-Udoh, E., Sundararajan, V., Sanchez, G.A. et al. Dental patients as partners in promoting quality and safety: a qualitative exploratory study. BMC Oral Health 24 , 438 (2024). https://doi.org/10.1186/s12903-024-04030-1
Download citation
Received : 14 August 2023
Accepted : 14 February 2024
Published : 10 April 2024
DOI : https://doi.org/10.1186/s12903-024-04030-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dental care
- Healthcare quality
- Patient safety
- Qualitative study
- Patient engagement
BMC Oral Health
ISSN: 1472-6831
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Conserv Dent
- v.15(1); Jan-Mar 2012
Research methodology in Dentistry: Part I – The essentials and relevance of research
Jogikalmat krithikadatta.
Department of Conservative Dentistry and Endodontics, Mennakshi Ammal Dental College and Hospitals, Maduravoyal, Chennai – 600095, India
The need for scientific evidence should be the basis of clinical practice. The field of restorative dentistry and endodontics is evolving at a rapid pace, with the introduction of several materials, instruments, and equipments. However, there is minimal information of their relevance in clinical practice. On the one hand, material and laboratory research is critical, however; its translation into clinical practice is not being substantiated enough with clinical research. This four part review series focuses on methods to improve evidence-based practice, by improving methods to integrate laboratory and clinical research.
INTRODUCTION
The field of dental research in India has witnessed exponential growth in the last five years.[ 1 ] However, scientific publications in international peer-reviewed journals have been few.[ 2 ] The lacuna of Indian contribution to international scientific literature is probably a skewed understanding of research and its contribution in effecting improved patient care. The primary purpose of research is to produce new knowledge or find new ways of making the existing knowledge available to those who need it. Research is not a separate speciality which is practiced by a few but it is a systematic approach of reasoning, documenting, analysing and reporting unusual clinical observations that we come across in everyday clinical practice. Whether one is a “doer” or a “user” of research, a thorough understanding of the methodology is essential. In addition to individual practitioners, the “users” of research includes 1) professional organizations that set “practice guidelines”;2) policy makers (sometimes called as “decision makers”) and 3) program managers (for example, state or national government managers of dental health programs). While the academicians and research scholars (teaching institutions) have a unique position to be “Doers” of research. The value for research for its own sake is limited, and therefore understanding the essential concepts in Research Methodology is vital in producing dependable knowledge.
The purpose of this review series is to help the reader to organize the thought process when considering research needs and methods. It also aims to sensitize the mind to research avenues that would be beneficial to material and clinical research in particular and improving the quality of clinical care in general. This four-part review series encompasses topics on essentials of research, fundamentals in biostatistics, observational studies, and experimental studies in each part.
Conduct of research: The head start
Every action is first conceived in the mind and later executed. Planning a good research project forms the primary basis of meaningful publication. Certain fundamental requisites are listed in Table 1 . Focus in a particular area of interest is essential to build up a strong forte in academic excellence. Random choice of research projects dilutes the resource contribution in random directions and results in lack of identity of the person or faculty. Generating research hypothesis must aim at answering clinically relevant questions. The rationale for the choice of a particular stream could also result in a new concept of thinking or change the methods of treatment protocols.
Requisites of good research

It is prudent to decide apriori as to whom the results of a particular research question would be useful and will the results be applicable to patients in dental practices in the real world. Conventionally, in-vitro or laboratory research studies have good internal validity but poor external validity which means that the results obtained are only applicable to similar samples of the study. In other words, the results may not transfer to the clinical behaviour of the material. On the other hand, clinical studies have good external validity because they are tested on samples/ subjects that are closely related to the clinical condition and most often representative of all individuals with the condition; however they are more complex since so many other factors may influence the outcome of interest.
To understand validity, let us consider the research question on dentin bonding agents (DBA). In-vitro assessment of dentin bonding agents is usually measured in terms of bond strength and microleakage. In this scenario, all the samples and procedures are standardized to a specific methodology, that is, dentin cylinders 5 mm in height, with 4 mm of composite material, × N force at 0.5 cross-head speed, and so on. The bond strength values obtained can be best extrapolated to a similar set of conditions in the laboratory and may not deliver the same performance clinically to patients. On the contrary, if we conduct a clinical study to evaluate the performance of dentin bonding agents, the methodology would include a randomized controlled trial involving the restoration of non-carious cervical lesions ((NCCL), considered the ideal for bonding agent testing), the clinical evaluation criteria recommended by the United States Public Health System (USPHS), and followed over a period of time. The results of the study can be extrapolated to all similar patients requiring restoration of NCCLs. Hence, the valid method of testing the ultimate performance of DBA is by a clinical trial and not just bond strength testing. However, in-vitro studies provide an insight into which DBA is the best among the available, to be tested clinically. In-vitro studies provide internal validity , that is, they tell us if a particular drug or procedure works, but external validity questions if it is of use to the patient population at large, which can only be determined by clinical trials on patients.
Feasibility in terms of time, cost, samples, and infrastructure are vital to set a logistic time frame for the functioning and completion of the study. Finally, a study that does not adhere to ethical principles both for in-vitro and clinical designs, fails to answer clinically relevant questions. The principles of ethics are not restricted only to the handling of human participants, but also encompass the ethics followed in the methodology and reporting of results. The Indian Council of Medical Research (ICMR) has comprehensive guidelines for conducting experimental studies in India.[ 3 ]
Clinical epidemiology
The term Epidemiology refers to the study of the distribution and determinants of health-related states or events (including disease), and the application of these methods to the control of diseases and other health problems.[ 4 ] Erroneously in India, this science is often dissociated from dental clinical research and is regarded to be a practice under community dentistry. Hence research methods described under epidemiology have also not been used in answering many of our clinical research questions. David Sackett, in 1969, coined the term clinical epidemiology, which is the, “application, by a physician who provides direct patient care, of epidemiological and biometric methods, to the study of diagnostic and therapeutic processes, in order to effect an improvement in health.”[ 5 ] This concept identifies the clinician as the epidemiologist, which chiefly includes practitioners (general/specialist), students, and academicians, who are constantly involved in patient care. Almost four decades since this concept was introduced, our fraternity is waking up to this approach. It is important to note that knowledge of the disease process and treatment protocols constitute clinical knowledge. This forms only one essential part of clinical epidemiology. In order to understand the involvement of clinicians in clinical research, we need to be aware of certain disease manifestations in the community, with regard to the magnitude of the problem and measures to deliver dentalcare.
Consider this question being asked by the Head of Department of an institution, “What is the best endodontic regime for patients being treated in my department?” Traditionally, this question would be answered by schools of thought, textbook evidence, and findings reported in peer-reviewed literature. In reality, this simple question has the ability to raise meaningful research questions if we could apply this to the measurement iterative loop proposed by Tugwell et al .[ 6 ] [ Figure 1 ]. The measurement iterative loop breaks up the disease cycle into distinct component steps. It is iterative because, each step logically leads to the next, and thus comes back to the first step thus ‘closing’ the loop. Each step in the loop has the capacity to generate several research questions.

The measurement iterative loop
In this loop, the first step is to ascertain the burden of illness. The burden of illness (e.g., patients requiring root canal treatment) could be measured among the patients seeking dental care in the hospital or in a defined population. The former will provide an answer to the rate of occurrence of endodontic disease and the latter addresses the prevalence of endodontic disease, both of which would vary with place and time. The burden of illness could be subdivided into: (a) Unavoidable and (b) avoidable. Avoidable burden of illness comprises of disability, symptoms, and morbidity, for which efficacious caries preventive and intervention methods are present. The unavoidable burden of illness of disability comprises of symptoms and morbidity for which no efficacious prevention or cure exists. Eg if the tooth has been lost then root canal treatment is not possible.The focus on research in this area should be an effort to transfer the burden from unavoidable to avoidable.
Second is to identify and assess the possible cause of the burden of disease. The etiology and risk-factor assessment of a multifactorial disease like pulpal and periapical pathology in itself generates a lot of research avenues. This step also makes use of several traditional study designs to derive clinically significant conclusions. This step identifies the factors against which an intervention can reduce the burden of illness, for example, failure of primary endodontic treatment. To name a few obvious causes, inadequate cleaning and shaping, missed canals, and incomplete obturation. The risk factors in association to this failure could be: Vitality status of the pulp during initial endodontic treatment, amount of remaining tooth structure, and type of tooth.
Defining factors for causation also requires that there should be well-defined, specific, and reproducible definitions for both the disease state and the risk factors. Developing such criteria for defining disease and causative or risk factors contribute to increased diagnostic accuracy .
The third step of the loop is the most significant. Having identified the ‘intervenable’ factors, it is important to study if interventions against them will work. After identifying interventions, in vitro studies are carried out when necessary, and then the successful interventions are tried on humans. The initial trials should be to determine Efficacy . This means that it should be determined whether the intervention works if given in the right dose using the right methods, for the right duration, that is, Can it work in ideal circumstances ?
Once this is achieved, the intervention (preventive and restorative) methods are applied to the community, that is, patients seeking treatment for failed endodontic treatment or among the general population at a risk of developing failure of primary endodontic treatment. This step is Community effectiveness, which measures how well an intervention can work in real life . It assesses the benefit/harm ratio of potentially feasible interventions and estimates the reduction of burden of illness, if the program is successful. Community effectiveness is determined by five factors: (a) Efficacy , (b) Screening and diagnostic accuracy, (c) Evaluation of health care provider compliance, (d) Evaluation of patient compliance , and (e) Evaluation of coverage . To understand this better let us consider the question of treating symptomatic irreversible pulpitis with Mineral trioxide aggregate (MTA) pulpotomy in Department of Endodontics at a dental college and give hypothetical percentages of success for each factor and compute the community effectiveness.
- Efficacy: Will the current treatment do more good than harm in treating patients who are diagnosed correctly and fully comply with recommendations for treatment?(100%)
- Screening and diagnostic accuracy: Does the department have adequate diagnostic methods to identify patients with irreversible pulpitis and ensure methods to follow-up the disease/recovery status? (90%)
- Evaluation of health provider compliance: Is a postgraduate student competent enough to perform MTA pulpotomy? (80%)
- Evaluation of patient compliance: Will the patient comply with the treatment and follow-up for MTA pulpotomy compared to conventional endodontic treatment? As there are chances that postoperative pain with MTA pulpotomy could be a possibility, the patient suffering from this complication can resort to another dentist for relief. (80%)
- Evaluation of coverage: Is the treatment available to all potential patients who could benefit from the new method? Is there access to a dental college or knowledge of the treatment? (90%)
Now community effectiveness can be computed using the Multiplicative law of combining probabilities (P),[ 7 ] considering the probability of each of these factors
Community Effectiveness = P (Efficacy 100% × diagnostic accuracy 90% × health provider compliance 80% × patient compliance 80% × coverage 90%) = 52%
After determining an effective treatment plan for the community/patients, the efficiency of the same needs to be evaluated. This step determines the relationships between costs and effects of options within and across the program. Cost could be a major deterrent in MTA pulpotomy. This could propel ingenious preparations to match commercially available MTA, or allocate funds to deliver this treatment to indicated patients. This is followed by the synthesis and implementation of MTA pulpotomy as a standard of care for indicated patients with irreversible pulpitis. This is done after integration of the feasibility of community effectiveness and efficiency. Any program implemented needs to be followed up with systematic documentation and monitoring. It should include markers for success and failure on the basis short-term, intermediate, and long-term treatment outcomes.
With success data in hand, the burden of illness should again be re-assessed, to ascertain any modifications required within the existing program.
Era of evidence-based dentistry
Evidence-based practice is defined as, “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence-based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research.”[ 8 ] Individual clinical expertise is the proficiency and clinical judgment that is often a summation of clinical experience and clinical practice. This systematic clinical research in our field includes both in-vitro and clinical research, with equal importance. The sensible transition to clinical research by making use of the conclusions of in-vitro research will contribute evidence to various steps of the measurement iterative loop. It is often observed that the thrust for clinical research is feeble and as a result there is insufficient evidence from laboratory research translating to clinical practice. The ideal place to enable contribution to the best clinical evidence would undoubtedly be the institutional organization, which has the balance between clinical expertise from the teachers end and the requirement for research projects from the students’ end. The only missing link is a properly planned research , which can be fullfilled by employing the measurement iterativeloop.
The awareness of evidence-based dentistry is growing not only on the research/clinical front, but also from patients seeking quality dental care. Hence, the possibility of a research study being acknowledged in scientific literature is often driven by the relevance of evidence that a particular research study can deliver. There is a certain hierarchy termed as ‘Levels of Evidence,’ purely based on the reliability of information or from evidence derived from a scientific study,.[ 9 ]
There are five levels, and each level has sub-ranks as shown in Figure 2 .[ 7 ]

Levels of evidence
- Meta-Analysis
- Systematic review (SR) of Randomized Controlled Trials (RCT)
- Randomized Controlled Trials
- Systematic review of Cohort Studies
- Cohort Studies/Poor quality RCT
- Systematic review of Case-Control Studies
- Case-Control Studies
- In-vitro Studies
Case Series/Cross-sectional studies/Poor quality case control studies
Case Reports/Expert opinion/Literature review.
It must be noted, with caution, that the level of evidence is only a stratification based on the information that is obtained from each method, with minimal bias, and these levels in no way rank the study design. It is logical to perceive that study designs are chosen based on research questions. For example, even though Randomized Clinical Trials provide the best evidence, this study design is not meant to identify risk factors for occurrence of disease (determined by case-control study) or disease occurrence/prognosis (determined by Cohort study). Hence, levels of evidence are a logical ranking for evidence rather than a ranking for study designs.
What is your research question?
With the understanding of the measurement iterative loop and the significance to generate relevant evidence for clinical practice, the research question should aim at focusing on one primary issue at a time. The method to identify and prioritize research questions is given in Figure 3 .

Method used to identify and prioritize research questions
A well-built research question should include four parts, referred to as the PICO format, which includes Patient/Population/Problem, Intervention, Comparison, and Outcome (PICO).[ 10 ]
Patient/population/problem — Defines the condition of interest. This is usually derived from the patients’ chief complaint in a clinical situation (in particular or on a larger population) or is derived from the problem faced in a particular material research.
Intervention [ or ‘ exposure ’- making it PECO for causation questions ]— It is important to identify what has been planned for the patient or the problem . Depending on the problem, this may include the use of a specific diagnostic test, treatment, medication or the recommendation to the patient, to use a product or procedure. If the problem measures the causation of a particular disease, then the etiological agent is assumed as the intervention.
Comparison — It is an alternative to the intervention under study.
Outcome(s) — This pertains to the result of the study preferably outcomes that can be measured accurately that are important to the patient.
The PICO format can be used to generate a research question for determining the causation of disease, diagnosis of a disease or therapy and prognosis of particular condition/disease. Examples for each are given in Table 2 .
Use of PICO format to generate research questions

Although the PICO format is best applied to intervention studies and experimental designs, research questions for all other study designs can also be formulated using this approach.
Role of study designs
Both in-vitro and clinical study designs for various questions arising from clinical practice or knowledge can be determined by applying various sections of the iterative loop. Depending on the research question, the structure of each study design facilitates the derivation of appropriate answers. Prior to choosing the study design, there has to be a valid research question. The genesis of a research question should primarily focus on answering several aspects of a broader research interest. For example, if the research interest lies in stem cell research, then the best source of stem cells, ideal growth environment for stem cells, potential differentiation of stem cells into tissues, confluence of growth obtained by different processing methods, clinical application of laboratory-derived stem cells, storage of stem cells, potential for malignant transformation of stem cells, and so on, form the several aspects or avenues to generate research questions. The primary effort in research is not to focus on the research question, but to focus on your research interest . on study designs and its relevance in answering specific research question will be dealt with in detail in the subsequent articles of this review series on research methodology.
Role of biostatistics
The Role of Biostatistics is often overlooked and ignored in the current research work in our speciality. Biological systems form a dynamic continuum and variation between the units forming the biological systems (people, teeth, bacteria, etc.) is the norm. On account of this variability within the systems, it is often difficult to differentiate between groups within the system. The science of biostatistics helps us to quantify and evaluate its variability within and between groups that make up the biological systems. Statistics is not absolute; it is a measure of the probabilities of occurrence of an event.
Biostatistics is less mathematics and more a method of determining the relevance of the research findings by application of statistical methods. This retains equal importance in both in-vitro as well as clinical research, because this statistical inference lays a foundation for the evidence deduced from any study. Hence the role of the statistician and the clinical researcher are equivalent in finding answers to any research question. The next part on research methodology focuses on understanding biostatics for dental research.
The research processes both in-vitro and clinical studies can be best summarized by the flow chart in Figure 4 .

Anatomy of a research study
The need for good research is to find the best evidence for clinical practice, for specific problems, and to address methods in reducing the burden of illness on a larger scale. Research studies in Endodontic and Restorative dentistry are two dimensional. The first dimension is the laboratory research, which provides the best evidence on material science and the second dimension is clinical research, which provides the best evidence in dealing with the burden of illness, with efficient clinical practice. This increases the avenues for research studies in several directions. With an increasing requirement to publish, articles with good clinical evidence stand a definite chance to find their place in scientific literature.[ 11 ]
ACKNOWLEDGMENT
The author would like to thank Prof. Peter Tugwell, Professor of Medicine University of Ottawa, Canada, Prof. Emeritus. Vic Neufeld, Faculty of Health Sciences, McMaster University, Canada and Prof. Manjula Datta, Retd Prof & Head of Epidemiology, The Tamilnadu MGR Medical university for having accepted to review the manuscript and for their valuable inputs in the preparation of the same and Chennai Dental Research Foundation, Chennai for their support.
Source of Support: Nil
Conflict of Interest: None declared.
- Live CE Event – March 29, 2024
- Self-Study CE Courses
- Live Event CE Certificates
- Dental Quizzes
- Dental Hygiene
Dental Research
- Patient Care
- Life at Work
- Infection Control
- Students & New Grads
- Ask Kara RDH
- Curiosity Killed the Plaque
- Videos & Hygiene Chats
- Hygiene Chats: Kara & Emily
- Hygienist Spotlight
- Today’s RDH Honor Awards
- Submissions
- Mar. 29th Live CE Event

- Featured posts
- Most popular
- 7 days popular
- By review score

Researchers Find the Mechanism Behind Potential Anticancer Properties in Lidocaine

Oral Microbiome and Diet: Researchers Analyze DNA From Ancient “Chewing Gum”

Researchers Use Saliva Analysis to Help Diagnose Pain in Patients with Dementia

Research Reveals an Association Between Primary Teeth Biorhythm and Adolescent Weight Gain

Research Explores How Dietary Choices Affect the Oral Microbiome in Postmenopausal Women

The Mystery of Tooth Enamel Defects: A New Autoimmune Disorder Discovered

Research Suggests Association with Oral Infections and Metabolic Profiles

Researchers Find that Viking Age Dentistry Was Probably More Sophisticated than Previously Thought
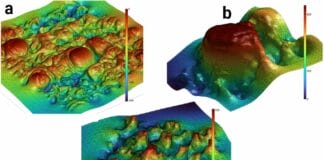
Research Using AI and 3D Imaging Unveils Unique Terrain of Individual Tongue Surfaces

Research Explores Innovative Tissue Regeneration for Endodontic Diseases With Potential Beyond Dentistry

Research Explores the Association Between Immune System’s Memory, Inflammatory Systemic Conditions, and Periodontitis

Systematic Review Analyzes the Association Between Daily Toothbrushing and Hospital-Acquired Pneumonia

Ancient Dental Calculus Reveals an Oral Microbiome Shift after the Black Death

Research Examines the Association Between Periodontal Care and Acute Myocardial Infarction Hospitalization

Research Finds a High Abundance of Previously Unknown Antibiotic-resistant Genes in Bacteria

Research Examines Fluoridated Water’s Impact on Child Emotional and Behavioral Development and Executive Functioning

Longitudinal Look at Tooth Loss and Cognitive Decline among Older Adults

Dental Health Improvement and Its Effects on Dentists’ and Hygienists’ Demand

Research Looks into the Unnecessary Prescribing of Antibiotics Among Dentists

Three-year Qualitative Study: A Life Was Changed by Dental Treatment
Trending now.

Nano-Hydroxyapatite Varnish: Does Research Support Caries Prevention Efficacy and Safety?

7 Ways Introverted Dental Hygienists Can Start Conversations with Patients

4 Simple Tips for Newly Graduated Dental Hygienists

Caviar Tongue: Are Dental Hygiene Patients Displaying Signs of “Aging?”
- Dental Hygiene 591
- Patient Care 319
- Dental Research 262
- Hygiene Chats & Videos 138
- Life at Work 121
- Healthy Smiles, Healthy Practices 86
- Students & New Grads 56
- COVID-19 53
- Hygienist Spotlight 48
Most Recent

Kiss and Tell: Variations of Normal and Pathology of the Lips

Dental Polishing and Cleansing Agents: A Quick Guide to Coronal Polishing...

How Hygienists Can Be the First Line of Defense Against Oral...
Don't miss.

A Hygienist’s Guide to Succeeding at Dental Conferences

The Topic of Topicals: Pain Management with Benzocaine Encourages Dental Patient...

Oil Pulling: Is it Effective?

Case Acceptance: Guiding Dental Patients through Treatment Planning via Imaging

IMAGES
VIDEO
COMMENTS
The ADHA regularly conducts research studies on various important topics within or affecting the practice of dental hygiene and the ADHA membership. ADHA also receives many requests for research or research support. Please view the ADHA's Policy on Requests for Research Support prior to soliciting support from ADHA for a research project.
Abstract. The field of dentistry is incredibly vast, with a seemingly endless array of research topics to choose from. In this book, author has compiled a list of 500+ research topics that are the ...
The content validity of the questions was established by using the Standards for Clinical Dental Hygiene Practice of the ADHA and previous DHDx research. 9,15 Using the guide ensured that all topics were covered in a valid and reliable manner during each interview. 18 Two members of the research team conducted a pilot interview to determine ...
PERSPECTIVES ON THE ADHA RESEARCH AGENDA. Dental hygiene and research have been linked since the early 1900s. In 1914, Dr. Fones' 5‐year study in public schools demonstrated that dental hygienists can positively impact oral disease using education and preventive methods.5 Dental hygienists today are increasingly becoming involved in ...
Roles of the dental hygienist. The key responsibilities of dental hygienists 1 include health promotion, education, clinical therapy, research, change agent, and administration. We are familiar ...
The National Center for Dental Hygiene Research was established through a 3-year grant from the Bureau of Health Professions (BHP), U.S. Department of Health and Human Services in ... • Stating the hypothesis or research question(s) • Selecting the research approach and potential valid and reliable measuring instruments • Seeking ...
dental hygiene research at the International ... 10.Salkind N J. 100 questions (and answers) about research methods. Sage, 2012. 11.Herr K, Anderson G L. ˛e action research
Featured oral health topics. Antibiotic prophylaxis. Infection control and sterilization. Treating Acute Dental Pain. Occupational Safety. Pregnancy. Whitening. The ADA Library & Archives also provides dental and oral health research and resources for members. Definitions, explanations and information about various oral health terms and dental ...
Boolean operators such as AND & OR are used to connect synonyms & concepts.. Use OR to connect synonyms to appropriately expand your search for a concept. Your search results will contain citations for each term. Place parentheses around the search terms when you use OR so that the database searches them together.; Use AND to connect concepts. This will narrow your search results, giving you ...
RESEARCH QUESTIONS. What is the comparative clinical evidence for dental examinations every 12 months compared with other intervals for the prevention of oral disease? ... RESEARCH QUESTIONS - Periodic Dental Examinations for Oral Health: A Review of Clinical Effectiveness, Cost Effectiveness, and Guidelines.
Dental providers possibly could influence parents and provide proper hygiene instruction and support for preschoolers at their first dental visits along with anticipatory guidance , yet this potential source of information and influence did not come up in interviews, perhaps due in part to the questions emphasizing oral hygiene behaviors. This ...
The least popular topic related to the use of interdental cleaning aids. In patients <40, selection of toothpaste was the most popular topic. Only responders <30 listed the timing of wisdom teeth ...
Assistant Professor of Dental Hygiene, Texas A&M University Mary L. Marazita Director, Center for Craniofacial and Dental Genetics; Professor of Oral Biology and of Human Genetics, University of ...
Project goal: Collect data at Harlem United using a questionnaire and perform statistical analysis. Students: Cheryn Amo-Adjei. Colleen Brophy. Jonathan Lomboy. Mentor: Dr. Burton Edelstein. Project title: Implementation of Dental Coverage in Affordable Care Act State-Facilitated Marketplaces. Research question: What decisions were made by each ...
A clinical or research question can generally be broken down into four components. 'PICO' is the acronym that identifies the four components of a good research question: Population. Intervention. Comparison. Outcome (s) The PICO table on this page provides further explanation and examples for each of the four components.
Question. 10 answers. Jun 20, 2014. Diseases of the teeth and the oral cavity can cause diabetes, heart disease, lung disease, rheumatoid arthritis, osteoporosis, atherosclerosis and a variety of ...
PICO is a framework for structuring clinical foreground questions, but its components are not clinical question types themselves. The question Type determines what types of primary study design provides stronger or weaker evidence for a particular question.. Take Note - Clinical guidelines based upon meta-analyses and systematic reviews, when available, often provide the best answers to ...
Questions are what drive scientific discovery. Big questions—the ones that keep us up at night—foster a desire for learning that never stops. They dare us to dream, to think differently. And they are how we transform our patient care. The School of Dentistry holds as a guiding principle a commitment to lifelong discovery through research that innovates the practice and study of dentistry ...
Dental research topics are essential for undergraduates for several reasons: Skill Development. Engaging in dental research topics helps undergraduates develop critical thinking, problem-solving, and analytical skills essential for their academic and professional growth. Contribution to Knowledge.
In recent years, there has been a surge in research related to dental quality and safety from various parts of the world [1,2,3,4,5,6,7,8,9,10,11].These studies have investigated how adverse events occur in dentistry, identified methodologies for detecting adverse safety events, and focused on developing strategies to reduce the occurrence of adverse events [3, 5, 6, 10,11,12,13,14].
It is prudent to decide apriori as to whom the results of a particular research question would be useful and will the results be applicable to patients in dental practices in the real world. Conventionally, in-vitro or laboratory research studies have good internal validity but poor external validity which means that the results obtained are only applicable to similar samples of the study.
Dental Research 262; Hygiene Chats & Videos 138; Life at Work 121; Healthy Smiles, Healthy Practices 86; Quizzes 67; Students & New Grads 56; COVID-19 53; Hygienist ... Today's RDH is an educational resource for Registered Dental Hygienists, dental hygiene students, and other dental professionals. It encompasses a daily digital publication ...