
Stay up to date with the latest in Practical Medical Imaging and Management with Applied Radiology.

Stay up to date
Create a new print or digital subscription to Applied Radiology.
Renew / Update
Renew or update your current subscription to Applied Radiology.
- Email Alert Manager
- Author Guidelines
- CME Credits
- CRA Credits

Everything you need to know about Computed Tomography (CT) & CT Scanning

Explore our numerous CT Scans, MRI, and X-Rays with the diagnosis in different anatomical regions and other Body CT topics. These case studies are designed for the education of medical professionals and radiologist.
Privacy Policy
CTisus uses cookies to collect information and enhance user experience. By clicking "Yes, I agree", you consent to our Privacy Policy and agree to its terms.

Case report
- Report problem with article
- View revision history
Citation, DOI, disclosures and article data
At the time the article was created Matt A. Morgan had no recorded disclosures.
At the time the article was last revised Matt A. Morgan had no recorded disclosures.
- Case reports
Case reports are a type of radiology research literature. They belong to the class of descriptive studies .
On this page:
- Related articles
The purpose of a radiology case report is to describe the patient history, clinical course, and imaging for a notable or unusual case. The case may be intended to aid other practitioners in interpretation, but frequently the oddity, rarity, and non-generalisibility of cases are meant more to amuse or entertain the reader.
A case report typically contains:
- a short introduction
- patient history and presentation
- a discussion of the imaging and other relevant interventions
- patient course
- summary/discussion
In radiology case reports, images from multiple imaging modalities are usually included, and gross pathology or histology is considered an excellent addition.
Case reports are generally considered the easiest and fastest radiology research paper to assemble.
Although debatable, the lack of "generalisibility" of case reports causes them to be regarded as lesser vehicles within research. Many journals will no longer accept case reports, for various reasons.
One disadvantage of case reports is that it may contribute to a type of recall bias in the reader. The attention the reader gives to a vanishingly rare case is held by the mind in a disproportionate regard compared with more common cases. The well-known maxim "an atypical presentation of a common disease is more likely than a typical presentation of a rare disease", is an effort to combat this type of bias.
Other disadvantages of case reports include:
- large numbers of case reports introduce an element of "noise" when searching the literature
- case reports claiming the first presentation of a case often find that they are actually not the first
- journals find that case reports do not get accessed as much as original research (it lowers their "impact factor")
That said, there are some advantages to case reports as well:
- the easier format allows junior researchers a chance to contribute to the literature, and helps them develop their skills
- a few case reports may develop into larger contributions to original research (for instance, in interventional radiology)
- they can be entertaining
- 1. Buckley O, Torreggiani WC. The demise of the case report. AJR Am J Roentgenol. 2007;189 (2): W54-5. doi:10.2214/AJR.07.2203 - Pubmed citation
- 2. Branstetter BF. Case reports: a premature demise. AJR Am J Roentgenol. 2008;190 (1): W80. doi:10.2214/AJR.07.2953 - Pubmed citation
Incoming Links
- BJR|case reports
- Case series
Related articles: Research
- case report
- case series
- Bayes' theorem
- Bayes' factor
- sensitivity
- specificity
- sensitivity and specificity of multiple tests
- positive predictive value (PPV)
- negative predictive value (NPV)
- incidence
- likelihood ratio (LR)
- standard error of the mean
- confidence interval (CI)
- retrospective studies
- prospective studies
- student t-test
- paired t-test
- one-way ANOVA
- factorial ANOVA
- repeated measures ANOVA
- multivariate ANOVA (MANOVA)
- single linear regression
- multiple linear regression analysis
- multiple logistic regression analysis
- chi-squared test
- automation bias
- length time bias
- lead time bias
- recall bias
- selection bias
Promoted articles (advertising)
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers


- Advanced Search
- Teaching Cases
- Submit a Case
Featured teaching case

Teaching cases

Featured selected case

Editors selection


Interesting Case Files
Submission of Radiology ICF’s to Yasin K. Jabir [email protected]
- Have your submission(s) reviewed by a faculty member.
- When your submission(s) receive final approval ask your reviewer(s) to send you an e-mail noting approval of your submission(s)
- Forward the approval e-mail(s) to me with the submission(s) attached to the forwarded message.
- If the files are too big to e-mail then forward the approval e-mail to me and provide me with CD or DVD containing your ICF’s
- I will notify you by e-mail that your submission(s) have been received.
- I will forward your submission(s) for posting to the web site.
- You will be notified when your submission(s) have been posted.
Search by Case Number :
- Education Home
- Medical Education Technology Support
- Graduate Medical Education
- Medical Scientist Training Program
- Public Health Sciences Program
- Continuing Medical Education
- Clinical Performance Education Center
- Center for Excellence in Education
- Research Home
- Biochemistry & Molecular Genetics
- Biomedical Engineering
- Cell Biology
- Microbiology, Immunology, & Cancer Biology (MIC)
- Molecular Physiology & Biological Physics
- Neuroscience
- Pharmacology
- Public Health Sciences
- Office for Research
- Clinical Research
- Clinical Trials Office
- Funding Opportunities
- Grants & Contracts
- Research Faculty Directory
- Cancer Center
- Cardiovascular Research Center
- Carter Immunology Center
- Center for Behavioral Health & Technology
- Center for Brain Immunology & Glia
- Center for Diabetes Technology
- Center for Immunity, Inflammation & Regenerative Medicine
- Center for Public Health Genomics
- Center for Membrane & Cell Physiology
- Center for Research in Reproduction
- Myles H. Thaler Center for AIDS & Human Retrovirus Research
- Child Health Research Center (Pediatrics)
- Division of Perceptual Studies
- Research News: The Making of Medicine
- Core Facilities
- Virginia Research Resources Consortium
- Center for Advanced Vision Science
- Charles O. Strickler Transplant Center
- Keck Center for Cellular Imaging
- Institute of Law, Psychiatry & Public Policy
- Translational Health Research Institute of Virginia
- Clinical Home
- Anesthesiology
- Dermatology
- Emergency Medicine
- Family Medicine
- Neurosurgery
- Obstetrics & Gynecology
- Ophthalmology
- Orthopaedic Surgery
- Otolaryngology
- Physical Medicine & Rehabilitation
- Plastic Surgery, Maxillofacial, & Oral Health
- Psychiatry & Neurobehavioral Sciences
- Radiation Oncology
- Radiology & Medical Imaging
- UVA Health: Patient Care
- Diversity Home
- Diversity Overview
- Student Resources
- GME Trainee Resources
- Faculty Resources
- Community Resources
- Medical Student Case Studies
Each student is required to prepare a teaching case to present to his/her colleagues and the course director. Past examples provided below.
General Diagnostic Case Studies
- Arteriovenous Fistula Secondary to Trauma
- Chylothorax, Cellulitis, Gas Gangrene
- Ectopic ACTH-Secreting Tumor
- Epiphrenic Diverticula
- Incidental Mediastinal Hilar Lymphadenopathy
- Liver Metastasis
- Neurocystercircosis
- Pneumoperitoneum
- Pneumothorax
- Posterior Urethralcutaneous Fistula
- Renal Cysts
- Rocky Mountain Spotted Fever
- Septic Emboli to the Brain
- Submassive Bilateral PE
- Tailgut Duplication Cyst
- Tension Pneumocephalus
- Tracheo-Esophageal Fistula
- Vestibular Schwannoma
Radiology Pathology Correlation Case Studies
- Adenoid Cystic Carcinoma
- Cholangiocarcinoma
- Cryptococcal PNA
- Disseminated Histoplasmosis
- Lung Adenocarcinoma
- Marginal Zone B-cell Lymphoma
- Metastatic Urothelial Carcinoma
- Mixed Clear Cell Papillary RCC
- Ovarian Carcinoma
- Pancreatic Adenocarcinoma
- Squamous Cell Carcinoma of the Lung
- Squamous Cell Carcinoma
- Uterine Leiomyosarcoma
- Cervical Adenosquamous Carcinoma
- Clear Cell Renal Cell Carcinoma
- Esophageal Adenocarcinoma
- Metastic Esophageal Gastrointestinal Stomal Tumor
- Ocular Melanoma with Mets to Liver
- Pancreatic Metatasis
- Papillary Thyroid Carcinoma
- Papillary Thyroid Carcinoma #2
- Renal Transplant Rejection
- Small Cell Lung Cancer
- Urothelial Carcinoma Lung Met
- Yolk Sac Tumor
- Burkitt’s Lymphoma
- Ewing Sarcoma
- Hepatocellular Carcinoma
- Hepatocellular Carcinoma #2
- High-grade Serous Ovarian Carcinoma
- Metastatic Duodenal Adenocarcinoma
- Metastatic Melanoma
- Ovarian Cancer
- Papillary Thyroid Carcinoma #3
- Papillary Thyroid Carcinoma with Nodal Involvement
- Well Differentiated Hepatocellular Carcinoma
- How to Apply
- Connor Sleeth, MD
- Eric Fromke, MD
- Hannah Clode, MD
- Jenna Pollock, MD
- Joshua Ravicz, MD
- Julia Kariher, MD
- Kaelin Cockrell, MD
- Nabeel Mirza, MD
- Samantha Epstein, MD
- Tyler Dalton, MD
- Vatsal Lal, MD
- Wayne Dell, MD
- Salary and Benefits
- Resident Lifestyle
- Early Specialization in Interventional Radiology (ESIR)
- Diagnostic Radiology/Nuclear Medicine (DR/NM) Pathway
- Diagnostic Radiology Research Track
- Current IR Residents
- Where Are They Now?
- Letter from the Chief Residents
- Former Residents
- Your UVA Interview Day
- Living in Charlottesville
- Participating Residents
- Program News and Updates
- Make a Gift
- Current Representatives
- Ladyologists – Supporting Each Other
- 4th-year Medical Students Scholarship
- Radiology Electives
- Radiology Interest Group
- Abdominal Imaging
- Breast Imaging
- Cardiothoracic Imaging
- Diagnostic Neuroradiology
- Musculoskeletal Imaging
- Nuclear Radiology
- Pediatric Radiology
- Angiography and Interventional Radiology Observership
- Breast Imaging International Visiting Scholars
- Why Choose Structured Education?
- Program Directors
- Verification of Graduate Medical Education Training and Faculty Appointment
- Online Training Resources

Radiology - Radiology Case Studies
Aquifer virtual patients, radiology case studies.
- Radiation Emergency Management
An educational platform providing virtual patient cases and clinical learning tools for medical students and educators, designed to enhance clinical training through realistic, peer-reviewed scenarios. It is widely used to support healthcare education by simulating real-life clinical experiences and ensuring the accuracy and relevance of its resources. To create an account, contact Jim Panacio .
Aquifer Vitutal Patient Cases are case-based clinical simulations designed to develop clinical reasoning and self-directed learning and self-assessment skills. CORE ( Case-based Online Radiology Education).
Register for a personal account using your PCOM email .
See How To Register for Institutional Subscribers . After registering, you’ll receive an email from i-InTIME with a subject line of i-InTIME New Account. Select the embedded link in the email to complete the registration process.
- Case in Point
- EuroRAD: Radiological Case Database
- Radiology Information Resources for Patients
- Radiology Today Magazine
- RadiologyInfo: Article Index
- Radiopaedia
- << Previous: Books
- Next: Radiation Emergency Management >>
Guide Information
- Educational Review
- Open access
- Published: 20 April 2021
Errors, discrepancies and underlying bias in radiology with case examples: a pictorial review
- Omer Onder 1 ,
- Yasin Yarasir 1 ,
- Aynur Azizova 1 ,
- Gamze Durhan 1 ,
- Mehmet Ruhi Onur 1 &
- Orhan Macit Ariyurek 1
Insights into Imaging volume 12 , Article number: 51 ( 2021 ) Cite this article
23k Accesses
26 Citations
2 Altmetric
Metrics details
Interpretation differences between radiologists and diagnostic errors are significant issues in daily radiology practice. An awareness of errors and their underlying causes can potentially increase the diagnostic performance and reduce individual harm. The aim of this paper is to review both the classification of errors and the underlying biases. Case-based examples are presented and discussed for each type of error and bias to provide greater clarity and understanding.
Errors, discrepancies and confounding biases are inseparable parts of radiology practice with various clinical consequences.
Radiological errors can occur before, during or after the reporting periods.
Effective communication between radiologists, radiology technicians, patients and clinicians is the key to proper patient management
Being familiar with the types of errors and underlying biases is essential for radiologists to cope with them.
Radiological imaging is an essential part of patient management. Despite significant technological developments, a radiological investigation is rarely definitive on its own, leading to discrepancies between radiological impressions and the ultimate outcome. Moreover, radiology reports, like all human endeavours, may contain errors or misunderstandings. The term "error" is described as no uncertainty about the correct finding, with no possibility for dispute or disagreement, while the word "discrepancy" stands for justifiable differences of opinion between colleagues [ 1 , 2 , 3 ].
Errors and discrepancies may cause direct or indirect, permanent, or temporary harmful effects because of a false, missed, or delayed diagnosis, or may not result in any harm if clinically insignificant, or feedback is received from clinicians or other radiologists [ 4 , 5 ].
In the literature, the classification of radiological errors and underlying biases has been discussed by different authors. Radiological errors can be classified according to the reporting process as pre-reporting, reporting or post-reporting errors. Pre-reporting errors consist of technical issues and procedure-related problems, whereas post-reporting errors are mainly caused by poor communication between radiologists and clinicians. Reporting errors are directly related to radiologists and can be categorized into two parts. "Perceptual errors" are more common and related to the fact that the present finding is not noticed, while "interpretative errors" are influenced by cognitive biases that can contribute to false reasoning. The classification of radiological error types according to the reporting process is shown in Table 1 [ 3 , 4 , 6 ].
According to the comprehensive classification system of Kim-Mansfield, there are 12 subgroups defined for radiological error types [ 7 ]. In this paper, the classifications are reviewed, and cases are presented related to those 12 types of radiological errors and underlying bias.
Definitions of “error” and “discrepancy”
Diagnostic error is a condition that could harm the patient, with no acceptable cause and no scientific data for defense, approved by all experts in this field (Fig. 1 ). Discrepancy refers to a reasonable difference of opinion between radiologists about a finding or diagnosis. It differs from error because discrepancies can be justified based on a range of scientific data, such as clinical information, laboratory results or radiological patterns [ 3 , 5 ] (Fig. 2 ).
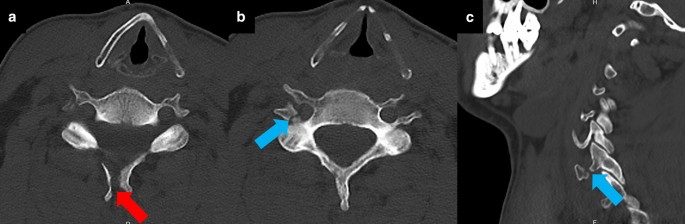
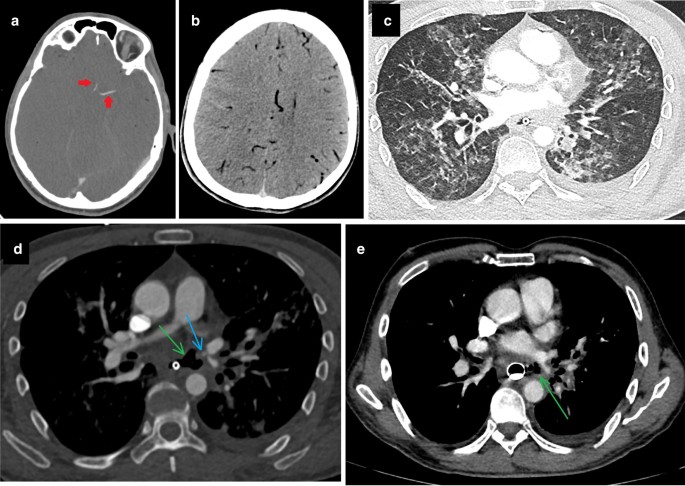
Diagnostic error. A 48-year-old male patient was admitted to the ER with head trauma after falling from a height of 2 m. The on-call radiologist reported a displaced fracture at the spinous process of the C6 vertebra (red arrow, a ). Another displaced fracture at the posterior and lateral wall of the right transverse foramen of the C6 vertebra was missed (blue arrows, b , c ). Emergency physicians were informed about the fractures after a second review of CT images. CT angiography performed to rule out vertebral artery injury, revealed no vascular injury
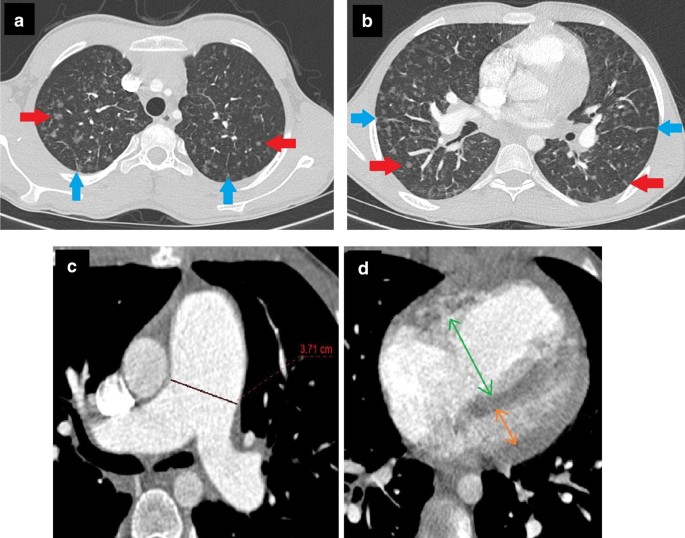
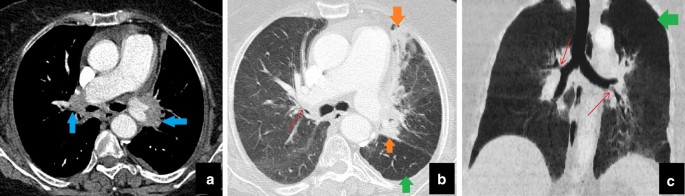
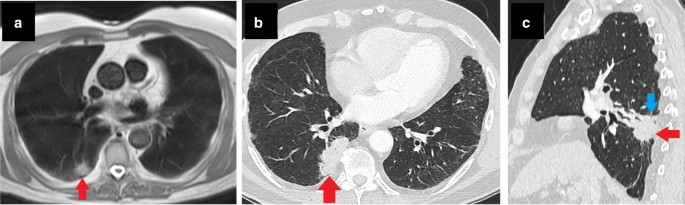
Discrepancy . A 13-year-old male patient with a history of pigeon-feeding presented at the Pediatric Department with the complaint of dyspnea. Clinicians suspected “hypersensitivity pneumonitis” as the first differential. The patient was hospitalized for further management. Serological tests proved the presence of antibodies against specific avian proteins. Thorax CT showed multiple ground-glass nodules (red arrows, a , b ). A radiologist interpreted these nodules in favor of "hypersensitivity pneumonia" considering the clinician’s opinion, patient history and serological test results. According to another radiologist, pulmonary veno-occlusive disease was more likely, because of accompanying interlobular septal thickening (blue arrows, a , b ), increased pulmonary artery diameter ( c ) and right ventricular dilatation ( d ). Although the radiologists were aware of each other’s opinions, both had plausible and supportive arguments for their provisional diagnosis. After a brief discussion, both possibilities were mentioned in the report, but both radiologists thought their own diagnosis was correct. After evaluating both possibilities in the multidisciplinary meeting, it was decided how to proceed with patient management
Common radiological error types
Diagnostic errors constitute a large and complex issue that needs to be addressed, as they can prevent proper patient management, and a delayed diagnosis could lead to important consequences. Different classifications have been proposed at various times for the classification of diagnostic errors to facilitate their comprehensibility. The most broadly accepted classification was developed by Kim and Mansfield. According to this classification, diagnostic errors are examined in 12 groups based on the cause of the error [ 3 , 4 , 6 , 7 ]:
False-positive or over-reading error In this scenario, an abnormality is noticed during the radiological examination. However, this finding is given more clinical value than it deserves and may consequently cause unnecessary diagnostic/therapeutic effort (Fig. 3 ) [ 6 , 7 ].
Faulty-reasoning error In this type of error, detected abnormal radiological findings are thought to be associated with a false clinical entity, mostly due to cognitive biases such as hindsight bias or attribution bias (Fig. 4 ) [ 6 , 7 , 8 ].
Lack of knowledge error This error type occurs when a pathological finding is noticed but cannot be interpreted correctly due to lack of adequate knowledge or experience of the radiologist about the finding, despite the availability of adequate clinical information (Fig. 5 ) [ 3 , 6 , 7 , 8 ].
Under-reading error This is the most common error type, in which an examination is reported as normal, although there is an undeniable and detectable abnormal finding. (Figs. 6 , 7 ) [ 3 , 6 , 7 ].
Poor communication-related error In this scenario, the abnormal finding is recognized and accurately reported. However, the diagnostic message is not delivered to the clinician because of communication-related problems. In some circumstances, referrers may not be aware of the importance of the reported findings in the radiology report due to individual failings in communication between radiologist and clinician or systemic issues such as lack of multidisciplinary meetings and teamwork, increased workload and understaffing. Poor communication errors may also result from referrers not understanding radiology reports, lack of knowledge about the meaning of radiological findings or their own biases. Last but not least, typing errors in the report may disrupt the communication between the radiologist and the referrer, irrespective of the quality of the information provided by radiologists or the competence of referrers (Fig. 8 , 9 ) (Table 1 ) [ 3 , 6 , 7 , 8 ].
Technique-related error This error occurs because of low technical quality, inaccuracies during the image acquisition process or selection of the wrong technique or modality, resulting in a decreased possibility of detecting abnormal findings and sometimes makes diagnosis impossible (Fig. 9 ) [ 1 , 6 , 7 ]
Prior examination-related error The underlying cause of this error is skipping the “comparison with previous exams” step, which is indispensable during radiological evaluation. Each evaluation must be compared with previous examinations to increase the likelihood of detecting pathological findings. However, when doing this, one must be careful about the ‘satisfaction of report’ error that will be explained later (Fig. 10 ) [ 6 , 7 ].
History-related error This error includes inaccurate reporting faults when the radiologist is not provided with adequate or correct information about the patient’s clinical history (Fig. 11 ) [ 3 , 6 , 7 , 8 ].
Location-related error Location-related error is characterized by the inability to recognize the pathological finding, which is seen within examination limits but falls outside the purposefully examined area, especially at the edges of the evaluated area (Fig. 12 ).
Satisfaction of search When the radiologist defines a pathological finding during the evaluation, other findings may be overlooked due to the satisfaction of the assessment and loss of motivation. Thus, accompanying findings may be under-read even if they are seen very clearly (Fig. 13 ) [ 6 , 7 ].
Complication As a general description, complications are the conditions that occur during or after the procedures and are directly related to the nature of the procedure. They are unanticipated occurrences and may happen even under ideal conditions, making it controversial to define them as errors (Fig. 14 ) [ 6 , 7 , 8 ]. However, according to the Kim-Mansfield classification, the term "complication," as an error type, refers to an adverse event related to invasive radiological procedures (Fig. 15 ) [ 6 ].
Satisfaction of report This results from having undue confidence in the patient’s prior reports. As a result, if a wrong assessment has been made in the previous report, it will be repeated. This type of error is closely related to alliterative bias (Fig. 10 ) [ 6 , 7 ].
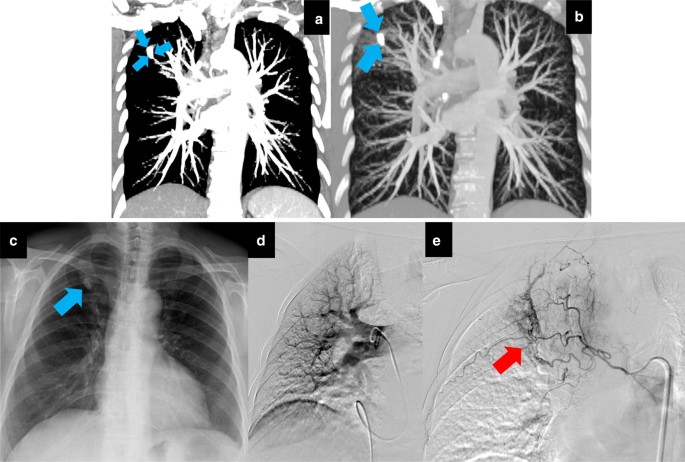
An over-reading (type 1) error with a positive effect on patient management . When evaluating contrast-enhanced CTs, failure to adjust the window settings may cause calcified lesions to be confused with vascular lesions (blue arrows, a , b ). A 67-year-old female patient presented with the complaint of hemoptysis to another hospital. Before that admission, she had been investigated several times for hemoptysis in different medical centers via CTA, which had shown no apparent causes and no dilated bronchial artery. The patient had been discharged each time because of negative imaging findings and regression of symptoms. Upon this last admission, pulmonary CTA was performed and reported as «Consistent with pulmonary artery aneurysm in the right lung apex.». The patient was referred urgently to our vascular interventional unit. Invasive pulmonary angiography revealed nothing abnormal ( d ). It was later understood that a calcified nodule at the right apex (blue arrow, c ) caused the over-reading error by mimicking an aneurysm. It was decided to perform bronchial arteriography following pulmonary angiography while the patient was already in the operating room because of the long-term recurrent hemoptysis history. Dilated, distorted and tortuous bronchial vessels detected on bronchial arteriography (red arrow, e ) were embolized. Throughout a one-year follow-up period, the patient had no recurrence of hemoptysis. As shown in this case, errors do not always cause patient harm. Occasionally, an error may have a positive effect on patient management. The diagnosis and treatment process of the underlying cause of the patient’s recurrent hemoptysis was accelerated owing to an over-reading error causing an urgent referral to our angiography unit
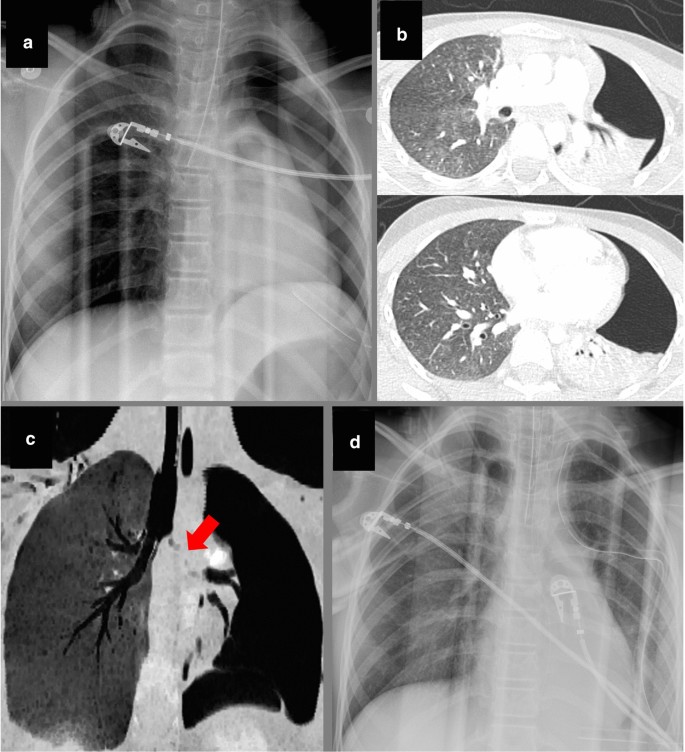
Faulty reasoning (type 2) error with anchoring and confirmation bias. A 10-year-old female patient was admitted to the ER after MVA. She had signs of severe head trauma and was intubated in the ER due to altered mental status. Following intubation, the absence of left lung ventilation was noticed, and a chest tube was placed in the left lung. Left-sided pneumothorax and misplaced intubation cannula extending to the bronchus intermedius were seen on the control chest radiograph ( a ). After stabilizing the vital signs, thorax and abdomen CTs were performed in the second hour of admission to assess the severity of the traumatic injury. Thorax CT showed “collapsed left lung with pneumothorax” ( b , c ) and “discontinuity of left main bronchus” (red arrow, c ). The on-call radiologist evaluated those findings in favor of “bronchial rupture” and “fallen lung sign.” After making a preliminary report, the radiologist was called by a clinician, who informed him that patient’s intubation was traumatic and difficult, and asked him whether these findings could be secondary to “acute bronchial obstruction and subsequent collapse.” The radiologist rejected this possibility without thinking and stated that the findings he saw were compatible with bronchial rupture. Following the telephone call, the radiologist scanned the literature and read that bronchial rupture is usually seen with severe accompanying thoracic injuries and is associated with pneumomediastinum and pneumothorax. Although the radiologist knew that the patient did not have any other thoracic injury or pneumomediastinum, he sought exceptional cases that supported his pre-diagnosis, and he stuck with his first decision. The patient’s poor general condition did not allow surgical intervention or bronchoscopy. She was followed up with chest tube drainage and bronchial aspiration. On the second day after admission, portable chest radiography showed that the left lung ventilation was markedly normalized ( d ). When the findings were evaluated retrospectively, it was understood that bronchial rupture was unlikely, and the diagnosis was compatible with “acute lung collapse and pneumothorax ex vacuo secondary to the traumatic intubation.” Thus, the radiologist, under the influence of anchoring confirmation bias, had falsely attributed the findings he detected in favor of a false pathology
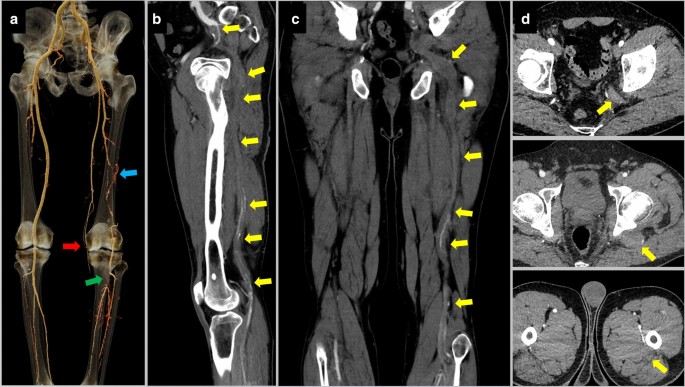
Lack of knowledge (type 3) error. A 55-year-old male patient underwent lower extremity CTA due to signs of peripheral artery disease in the left lower extremity. The radiology resident who examined the CTA for the preliminary results saw that the left superficial femoral artery was of thin caliber and ended at the knee level. He thought that it was chronically occluded (red arrow, a ). He also thought that collaterals between the left deep femoral artery and popliteal artery (blue arrow, a ) had developed secondary to the thrombi in the left popliteal artery (green arrow, a ). When the radiologist referred the CTA to the attending physician, he learned that the patient’s left internal iliac artery continued as the popliteal artery, which is a variation called persistent sciatic artery. The persistent sciatic artery of the patient was thrombosed throughout its course (yellow arrows, b , c , d ). The resident could not recognize this variation and the pathology due to the lack of knowledge. Although this is not a common variation that should be known by every radiologist, in this case, failure to recognize the thrombosed persistent sciatic artery could have adversely affected the possible interventional treatment plan
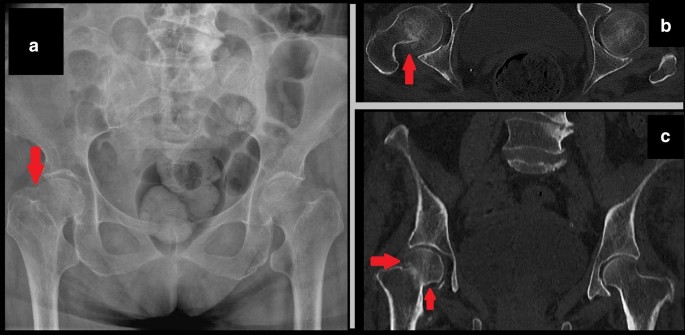
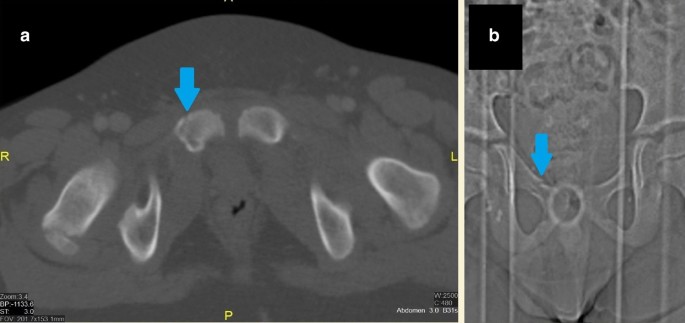
Under-reading (type 4) error with inattentional bias (Gorilla effect). A female patient was admitted to the emergency department with bilateral hip pain after falling down stairs. X-ray and pelvic CT were interpreted as “normal” by the on-call radiologist. However, shortening of the right femoral neck (red arrow, a ) and a hyperdense line due to impacted fracture (red arrows, b , c ) were missed. After retrospective detection of fracture, the radiologist was asked about the cause of missing these findings. He stated that he did not expect to see a hyperdense impaction fracture at all while evaluating that particular case. The prejudice of “fractures are seen as hypodense lines” caused inattentional blindness. A hyperdense fracture line is an uncommon finding, and due to its unexpected nature, may result in an under-reading error
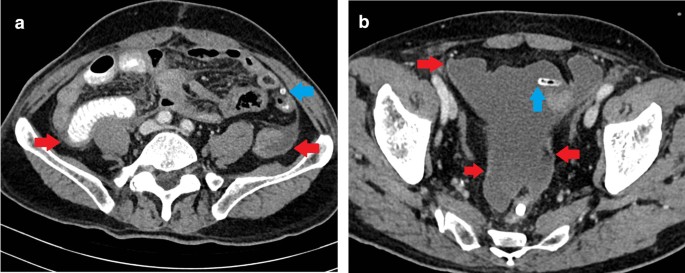
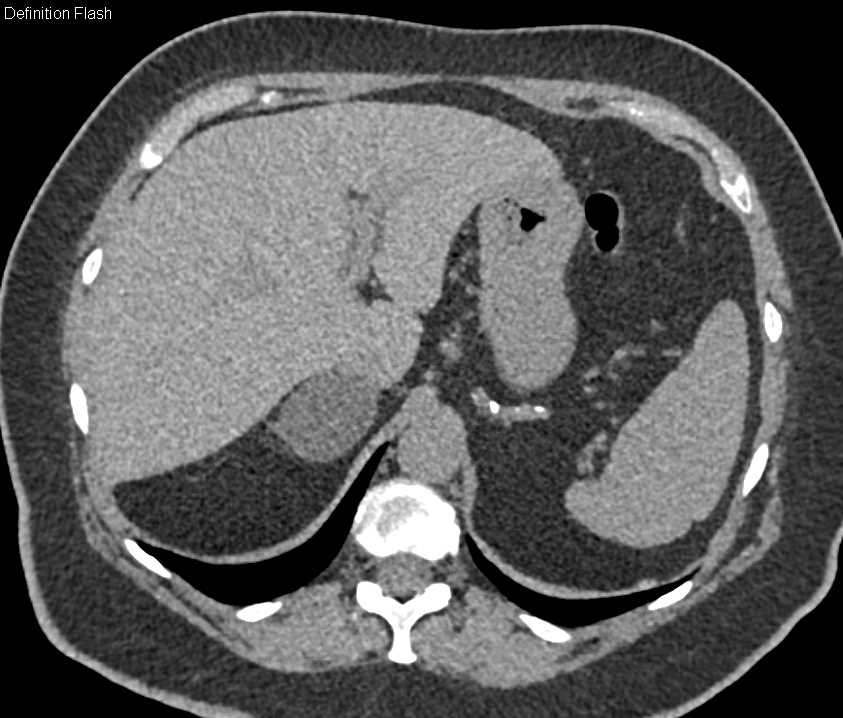
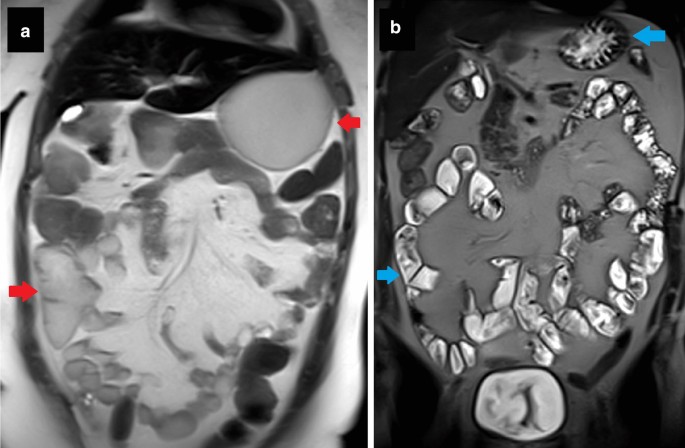
Premature closure bias causing an under-reading (type 4) error. A 52-year-old male patient with metastatic gastric cancer was brought to the emergency room due to abdominal pain, distension and discomfort. Abdominal CT showed thickened and enhanced peritoneal layers (red arrows a , b ) and accompanying pelvic-free fluid/mesenteric congestion. The radiologist prematurely jumped to the conclusion of “peritoneal carcinomatosis” because of the cancer history and did not think about other reasons that could cause those imaging findings. In the following period, it was retrospectively understood that there was a displaced jejunostomy catheter (blue arrows a , b ) into the peritoneal space. Due to premature closure bias, the radiologist did not pay enough attention to the rest of the examination and overlooked the displaced catheter. The patient was hospitalized and given long-term treatment. After removing the misplaced catheter and completing the appropriate treatment of peritonitis, induced by nutrients given through the jejunostomy, the patient’s complaints completely recovered
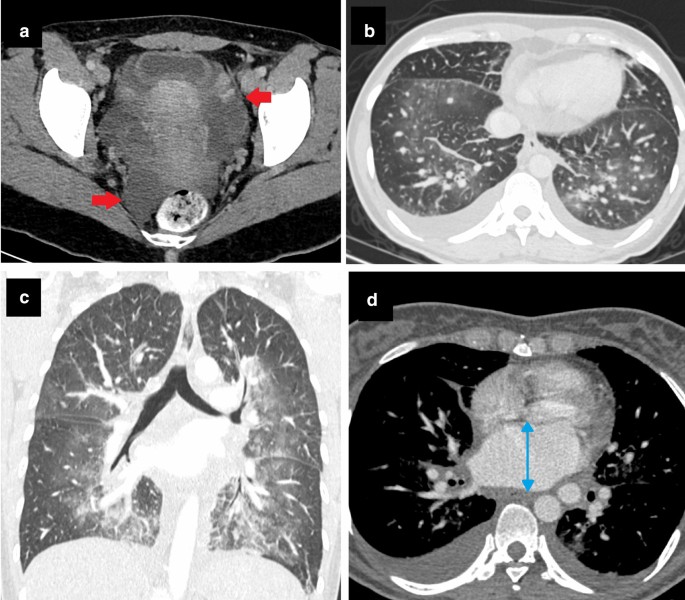
Poor communication (type 5) error with attribution bias. A 27-year-old female patient with no known disease presented at the Emergency Department with abdominal discomfort. After the first evaluation, an abdominal CECT was performed ( a , b ). Bilateral lung bases were also partially involved in abdominal CECT ( b ). CT was reported as “free fluid in the pelvis (red arrows a ), bilateral pleural effusion, interlobular septal thickenings, and bilateral central ground-glass opacities in lung bases” ( b ). Although these are well-known findings of cardiac congestion, they were not attributed to cardiogenic edema because of the patient’s age and clinical history. Instead, findings were only described without any comment or impression in the report, and clinicians were expected to read the report and evaluate findings. Six hours later, the patient became dyspneic and tachypneic. Contrast-enhanced thorax CT ( c , d ) revealed findings compatible with pulmonary edema ( c ) and enlarged left atrium (blue double-sided arrow, d ). Echocardiography, performed to rule out cardiac abnormality, showed severe mitral stenosis, possibly due to rheumatic heart disease. Attribution bias due to the “young age, clear medical history and irrelevant symptoms of the patient” caused the radiologist to avoid making any comments about the possibility of cardiac congestion in the report. As a result, poor communication between the radiologist and clinicians due to the lack of necessary interpretation in the report caused a delay in diagnosis
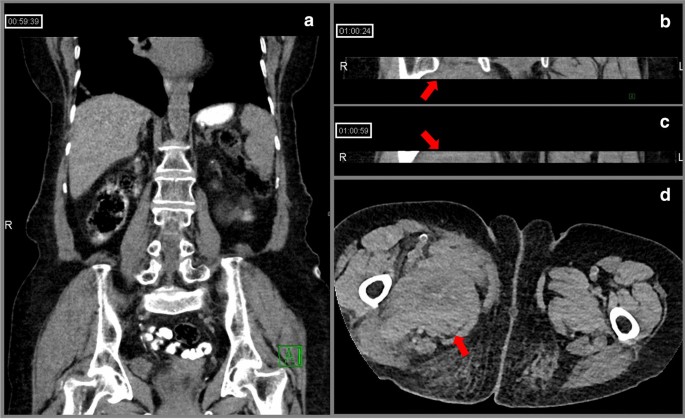
Technique-related (Type 6) error with poor communication. An 88-year-old female patient using an injectable anticoagulant was admitted to the emergency room with right lower quadrant pain. No finding to explain the symptom was observed on abdominal CT ( a ). Right inguinal swelling developed during follow-up and inguinal US revealed a large hematoma in this region. When the abdominal CT was evaluated retrospectively, it was noticed that, apart from the sections examined by the on-duty radiologists, two more series consisting of only 10–15 axial slices showing inguinal regions were separately uploaded to the PACS together with their coronal reformats ( b , c ). It was later learned that the CT technician had difficulty adjusting the field of view and had to take a few extra slices to cover the level of the symphysis pubis. However, he did not inform the on-call radiologists about this situation. Since the images were sent to the PACS piece by piece due to a technical error, and the radiologists were not informed about the problem due to lack of communication, the diagnosis of a clearly seen right inguinal hematoma was delayed (red arrows, b , c , d )
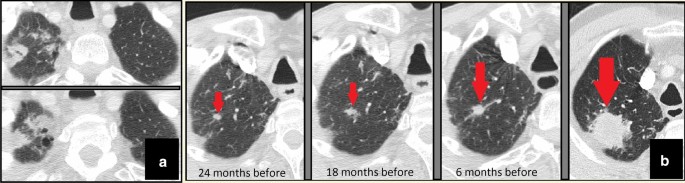
Prior examination (type 7) and satisfaction of report (type 12) errors. Follow-up images of a male patient with a history of larynx cancer showed that both lung apices were within the imaging field in all the control neck CTs. More prominently in the right apex, bilateral apical fibrotic changes were present and consistently reported ( a ). Due to reliance on previous reports, apical areas were not evaluated carefully. Consequently, a nodular lesion showing a gradual increase in size, located within right apical fibrotic changes, was repeatedly missed until it reached large dimensions (red arrows, b ). Percutaneous biopsy and subsequent histopathological examination confirmed the diagnosis of primary lung adenocarcinoma
History-related (type 8) error. A 75-year-old female patient presented at the Chest Clinic with a progressive cough. Thorax CT was reported as "bilateral residual tumoral soft tissue (blue arrows, a ) and parenchymal fibroatelectatic changes due to radiotherapy (orange arrows, b )." The referrer gave feedback to the radiologist about "the negative history of malignancy and radiotherapy," and intensive biomass exposure was mentioned. The CT was re-evaluated by the radiologist. Paramediastinal parenchymal changes (blue and orange arrows, a , b ) were interpreted as a result of “bronchial anthracofibrosis” after combining the associated air trapping (green arrows, b , c ) and bronchial narrowings (red arrows, b , c ). Although the radiologist made an unwarranted assumption about prior malignancy and treatment, the main reason for this reporting error was insufficient clinical information about “biomass exposure.” This case is a good example of “error with no harm” thanks to the effective communication between the radiologist and the clinician via the clinician’s feedback
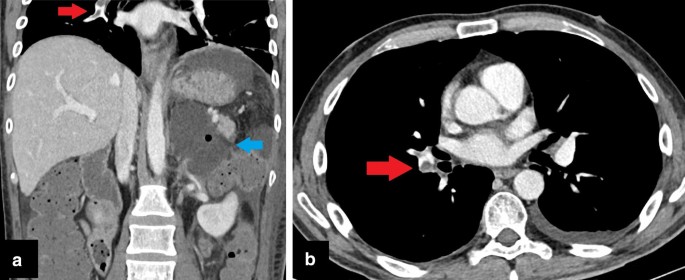
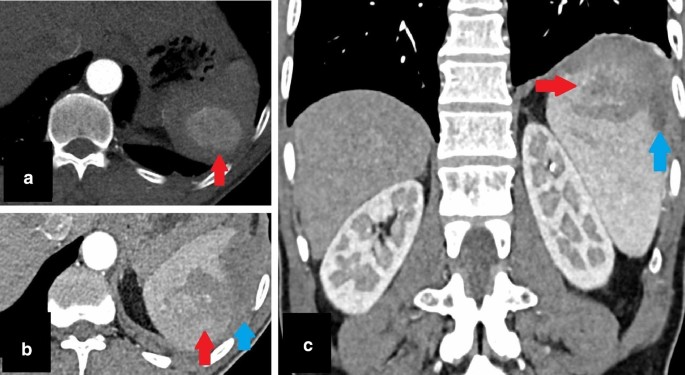
Location-related (type 9) error with under-reading. In a 28-year-old male patient with adrenalectomy, abdominal CECT was performed for evaluation of postoperative complications. Collection in the surgical area (blue arrow, a ) and postoperative changes were reported. Although filling defects in the right pulmonary artery were involved in upper CT slices, they could not be noticed due to their locations (red arrows, a , b ). As in this case, the marginal areas are prone to this type of error. There is also an accompanying under-reading error because the pulmonary emboli could be clearly seen and should have been reported
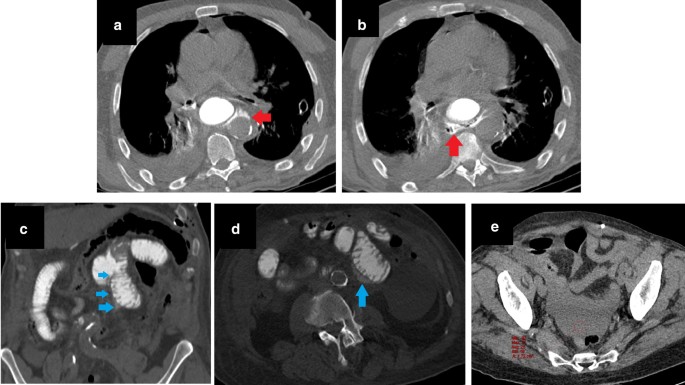
Satisfaction of search (type 10) error. A patient with gastric cardia tumor underwent total gastrectomy and distal esophagectomy. On the first postoperative day, dyspnea and abdominal pain developed. Anastomosis leakage was suspected, and thoracoabdominal CT with oral contrast agent was performed. The on-call radiologist noticed apparent contrast extravasation from esophagojejunostomy to the posterior mediastinum. The study was reported as “consistent with anastomosis leakage from esophagojejunostomy” (red arrows, a , b ). Due to the “satisfaction of search” effect of this significant finding, the remainder of the examination was reported as normal. However, the patient’s abdominal complaints progressed, and the general condition of the patient deteriorated, so the patient was re-operated on, and additional jejunojejunostomy leakage was detected. When the preoperative CT was retrospectively evaluated, apparent signs of leakage in the jejunojejunostomy area were noticed. Linear hyperdensity consistent with leakage extending inferiorly from the anastomosis (blue arrows, c ), extraluminal contrast material between jejunal loops (blue arrow, d ), and pelvic fluid with relatively high density (red ROI mark, e ) were overlooked findings
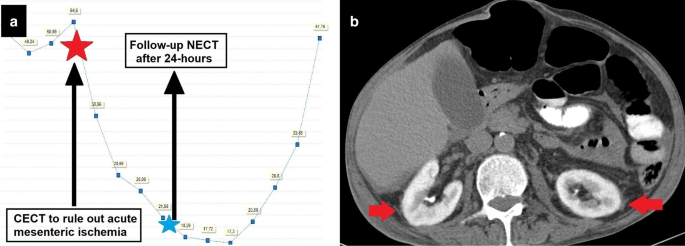
A complication developing under ideal conditions. A 64-year-old female patient with suspected sepsis was suffering from severe abdominal pain disproportionate to the clinical examination findings. Abdominal CECT was ordered to rule out “mesenteric vascular disease” after explaining all the risks of the procedure (including contrast-induced nephropathy) to the patient. Before the procedure, the glomerular filtration rate (GFR) was 54.5 ml/min/1.73 m2. After CECT, a progressive decline of GFR was observed. When the periprocedural GFR values were evaluated, it was clearly understood that contrast-induced nephropathy had developed ( a ). Follow-up NECT 24 h after the first examination revealed contrast retention of kidneys due to impaired filtration functions (red arrows, b )
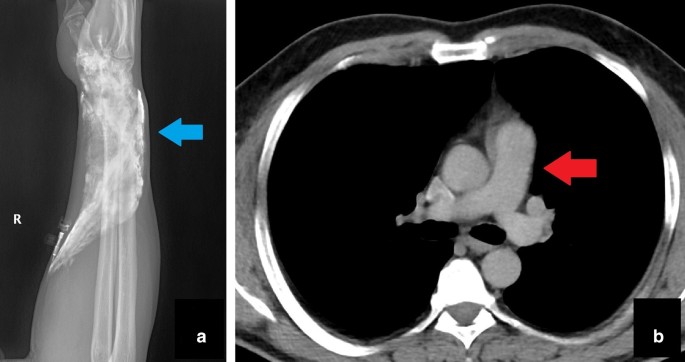
A complication (Type 11 error) causing acute harm to the patient and resulting in an insufficient examination. Thorax CT with pulmonary thromboembolism (PTE) protocol was performed for a dyspneic patient with a known breast cancer history. Just after the study, the patient complained of pain and swelling in the forearm. The X-ray of the upper extremity showed extravasated contrast agent to the wrist region (blue arrow, a ). It was noted that the amount of intravascular contrast media was not sufficient for the evaluation of PTE (red arrow, b ). Medical treatment was given, and the procedure was repeated. This case is a good example of “acute and temporary harm” caused by a periprocedural complication
Underlying bias types of radiological errors
Different biases are defined in the literature, which may affect the decision-making process when evaluating a radiological study. Biases may result in misinterpretation and different types of diagnostic errors, so awareness of certain types of biases can contribute to diagnostic accuracy. Biases can be classified as listed below [ 1 , 3 , 4 , 5 , 6 , 9 ]:
Attribution bias This is the tendency to attribute findings of a clinical condition by looking at specific characteristics of the patient; in other words, stereotyping (Fig. 8 ) [ 6 , 7 ].
Alliterative bias (Satisfaction of report) Alliterative bias occurs when previous interpretations of a study influence the decision-making process of the current study (Fig. 10 ) [ 2 , 4 , 5 ].
Availability bias This type of bias is characterized by an increased tendency to make the decision under the influence of recently seen cases (Fig. 16 ) [ 1 , 3 , 4 , 5 , 6 , 9 ].
Regret bias This happens when radiologists worry about underdiagnosing a possibility and thereby over-report it due to fear of missing a diagnosis (Fig. 16 ) [ 7 , 9 ].
Framing bias This bias type reflects the restriction of imaging assessment to the referral situation and clinical presentation framework (Fig. 17 ) [ 1 , 4 ].
Premature closure This results from accepting an initial impression as a final diagnosis without any verification. Radiologists may be cognitively satisfied after discovering the first finding and end the search. Therefore, premature closure bias may overlap with the “satisfaction of search” error (Fig. 7 ) [ 3 , 9 ].
Inattentional bias Inattentional bias, also named tunnel vision, may result in a diagnostic error due to an unusual appearance or location of findings (Fig. 6 ). This is also named the "Gorilla effect" after the famous study, in which a gorilla was inserted in a thorax CT by researchers and was overlooked by 83% of radiologists who were busy searching for lung nodules [ 10 ]. Inattentinal bias may cause devastating complications, even in cases with obvious imaging findings [ 3 , 5 , 9 ].
Hindsight bias This type of bias is characterized by believing that it would be easy to reach a correct diagnosis by ignoring or de-emphasizing the difficulties in making the initial diagnosis and discounting the scenario under which the decision making occurred. When specialists evaluate the findings retrospectively, they may have access to contributory information not available to the original reporters, and they tend to underestimate the difficulty of making an accurate diagnosis due to hindsight bias. In contrast to other types of bias, hindsight bias is retrospective in nature (Figs. 18 , 19 ) [ 3 , 4 , 8 , 9 ].
Zebra retreat The radiologist retreats from an accurate but unusual diagnosis due to a lack of confidence, despite the presence of supportive evidence. In one respect, this bias is the opposite of the previously described Regret bias (Fig. 19 ) [ 3 , 6 ].
Scout neglect The scout view is the preliminary image taken just before performing the imaging. Ignoring the scout view may result in a diagnostic error (Fig. 20 ) [ 4 ].
Anchoring bias This type of bias occurs when a radiologist becomes fixated on the first-sight diagnosis, although subsequently presented findings are incompatible with the first diagnosis. Anchoring bias is usually accompanied by confirmation bias, making it more dangerous (Fig. 4 ) [ 1 , 3 , 4 , 5 , 6 , 9 ].
Confirmation Bias Confirmation bias defines the active searching for more data to confirm the available hypothesis rather than seeking an alternative explanation (Fig. 4 ) [ 3 , 6 , 9 ].
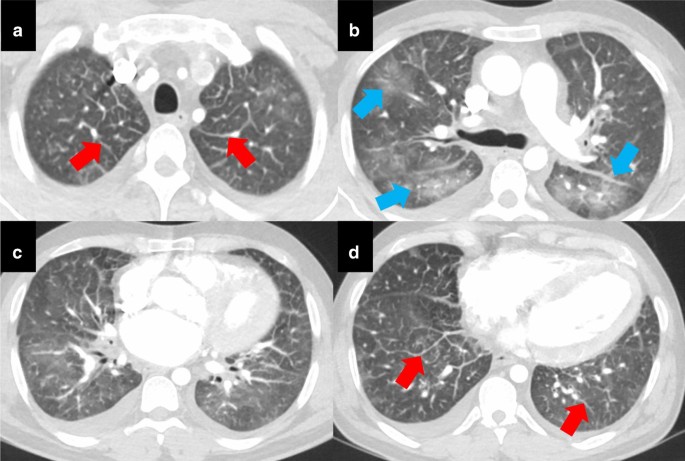
Availability and regret bias causing faulty reasoning error. A 41-year-old male patient with aortic valve stenosis was admitted to the Emergency Department with epigastric pain during the COVID-19 pandemic. A thoracoabdominal CT was ordered to assess the aortic stenosis, lung parenchyma and possible causes of epigastric pain. The on-call radiologist on the night-shift correctly described the CT findings as cardiomegaly, bilateral ground-glass opacities predominantly in the upper lobes of the lungs (blue arrows, b ), thickening of the interlobular septae (red arrows, a , d ) and bilateral pleural effusion. Before the CT of this patient, the radiologist had reported a large number of CTs compatible with viral pneumonia during the night-shift. In addition, he had overlooked a patient with positive chest CT finding for COVID-19 pneumonia on a previous night-shift, so he was overly sensitive about the diagnosis of COVID-19. Having been “burned once,” he did not want to underdiagnose the possibility of COVID-19. Therefore, these CT findings were attributed to pulmonary infection by indicating that COVID-19 pneumonia could not be excluded in the differential diagnosis. However, he did not mention the possibility of pulmonary edema. Viral pneumonia treatment was started due to the radiologist's opinion, and a reverse transcriptase polymerase chain reaction (RT-PCR) test for COVID-19 was ordered and reported as negative. On the following day, the attending emergency radiologist informed emergency physicians that the CT findings were primarily suggestive of cardiogenic pulmonary edema. The patient then showed a dramatic response to cardiogenic pulmonary edema treatment. As the frequency of viral pneumonia was greatly increased during the pandemic, and the radiologist had a lot of experience about this condition, availability bias resulted in misjudgment and faulty reasoning error. Although regret bias due to previous negative experience eliminated the possibility of overlooking another case of COVID-19 pneumonia for the radiologist, it also contributed to the error by affecting the thought process
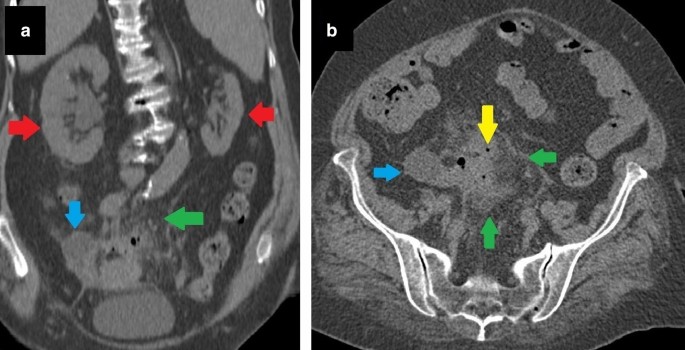
Framing bias causing an under-reading error. A 77-year-old female patient with a history of renal stone and recurrent urinary tract infections presented with lower abdominal pain. The patient’s symptoms did not regress under proper antibiotherapy. Non-enhanced CT was ordered for “evaluation of renal stones and urinary pathologies.” The CT was reported as “normal, except left atrophic kidney (red arrows, a ).” However, a collection (blue arrows, a , b ), free-air bubbles (yellow arrow, b ) and mesenteric fat stranding (green arrows, a , b ) adjacent to the sigmoid colon were overlooked due to the framing of clinical information. Although non-enhanced CT was technically inadequate to evaluate bowel pathologies, inflammatory changes were clearly visible on CT, and at least a suspicion should have been expressed. During follow-up, lower abdominal MRI revealed the final diagnosis as “perforated sigmoid colon malignancy” (not shown)
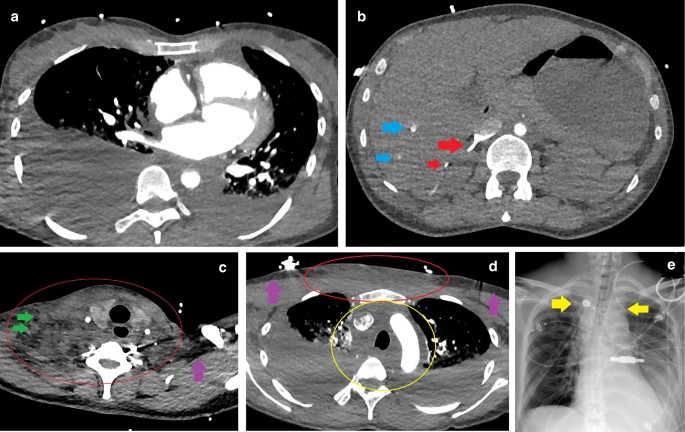
Hindsight bias. A 40-year-old female patient with no known disease history presented at the ER with complaints of chest pain, dyspnea and confusion. As severe back and neck pain had been ongoing for two days, aortic dissection was suspected. Triple rule-out CT showed bilateral massive pleural effusion ( a , d ) and severe contrast reflux into the inferior vena cava, right renal vein (red arrows, b ), and peripheral branches of hepatic veins (blue arrows, b ). These findings were suggestive of hemodynamic compromise. Pleural effusions were drained, and a significant amount of pus was observed. The patient was accepted as septic, and proper treatment was started. Microbiological evaluation of the pleural fluid was consistent with Streptococcus pyogenes, an unexpected pathogen bacteria in pleural samples. After feedback from the microbiologist, an ecchymotic area spreading from the neck to the anterior chest wall was noticed. Soft tissue infection was suspected. When the CT was retrospectively re-evaluated, it was understood that increased densities in subcutaneous fat tissues of the neck and anterior chest wall (red circles c , d ) were not noticed by the on-call radiologist ( purple arrows c , d : normal fat tissue as a reference). Lymphadenopathies within the affected areas (green arrows, c ), and obliteration of upper mediastinal fat tissues (yellow circle, d ) were other considerable findings. Moreover, mediastinal widening suggesting mediastinitis was detected retrospectively on the chest X-ray obtained after thoracentesis (yellow arrows, e ). Subsequently, the clinical situation rapidly deteriorated, the patient became hypotensive and a sharp myoglobin increase suggesting myonecrosis was observed. Acute kidney failure, acute respiratory distress and profound thrombocytopenia developed. After evaluating the clinical, radiological and microbiological findings altogether, the diagnosis of “streptococcal toxic shock” was made. The patient died three days after the onset of the complaints and one day after ER admission. With the knowledge of S.pyogenes presence in the pleura, history of neck pain and location of the ecchymotic area, it seems impossible to have overlooked changes in soft tissues and the upper mediastinum during retrospective evaluation (hindsight bias)
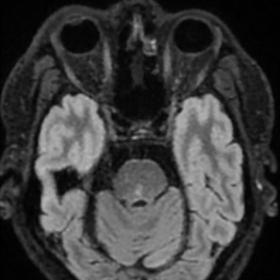
Zebra retreat and hindsight bias. A 75-year-old male patient with known tracheoesophageal fistula (green arrows, d , e ) suddenly lost consciousness. Brain CT and CT angiography revealed edematous brain tissue, diffuse air within brain vasculature ( b ), and contrast filling limited to just proximal segments of the left middle cerebral artery and anterior cerebral artery (red arrows, a ). Recent studies of the patient were re-evaluated to detect the etiology of cerebral air embolism. On thorax CT taken 3 days previously for hemoptysis, there was seen to be parenchymal ground glass opacities suggesting hemorrhage ( c ). In the mediastinal window, next to the fistula, there was an outpouching of the pulmonary vein (blue arrow, d ) that had not been present on the previous study ( e ). The on-call radiologist had also noticed this newly developed outpouching but did not feel confident enough to mention this finding in the report due to the absence of apparent contrast extravasation into the tracheal lumen. Moreover, the radiologist had thought that hemoptysis originating from a pulmonary vein was quite an unexpected situation. This phenomenon is called a “zebra retreat.” It seems to be impossible to overlook or underrate that outpouching with “a priori knowledge of diffuse cerebral air embolism” due to the hindsight bias during retrospective evaluation
Scout neglect bias. An abdominal CECT of a male patient was performed to evaluate solid organ injury after a motor vehicle accident. A right pubic fracture (blue arrows) was masked in routine abdominal CT images of 3 mm slice thickness with a soft filter ( a ). However, it was easily seen in the scout image without any doubt ( b )
The types of bias with a summary of the related thought processes of the radiologist are shown in Table 2 .
Possible clinical consequences caused by a radiological error
Errors in the assessment of the imaging examinations of patients are classified by Brady et al. based on the "durations of effect" and "severity of clinical consequences." According to this classification, errors causing no harm are considered "negligible," and errors with minimal ill-effects are accepted as "minor error." "Moderate" and "major errors" are distinguished based on the duration of the negative effects. "Moderate errors" have short-term effects, while "major errors" are defined by long-term undesirable effects. Finally, errors resulting in severe long-term or fatal effects are classified as “extreme errors” [ 8 ]. However, it should be kept in mind that this classification is only an example of a method intended to demonstrate how the effects of errors could be evaluated. It is neither a validated nor necessarily an accurate risk assessment tool, and it was not described as an absolute means of classifying the impact of radiological errors.
We can also classify errors according to their effects on patient management. Although some errors have a positive influence on patient management, these are rarely encountered and are the exception (Fig. 3 ). Apart from those, the most innocent errors are errors that are noticed before causing any effect on patient management. As expected, those errors cause no harm (Fig. 11 ).
Errors that affect patient management can be divided into two groups based on their impact on the patient. In the first group, the error reaches the patient but does not cause any harm. This error type may lead to unnecessary diagnostic effort and further examination (Fig. 21 ), or it may be clinically insignificant (Fig. 22 ). In the second group, the error reaches the patient and has a harmful effect. These errors may result in temporary or permanent clinical consequences, either directly or indirectly.
A technique error causing unnecessary effort. A 47-year-old female patient was investigated for inflammatory bowel disease, and MRI enterography was ordered. Before the procedure, the patient had drunk the gadolinium-containing contrast agent in the radiology department by mistake. Due to the paramagnetic feature of gadolinium, the required image quality for evaluation of the intestinal lumen could not be achieved. The MRI technician realized the problem and immediately informed the radiologist. After the radiologist’s evaluation, the study was rescheduled. Although the technical error caused unnecessary effort (repeated examination) in this case, the effective communication between the radiologist and MRI technician enabled them to recognize and correct the error earlier (red arrows, a intestinal lumen with gadolinium, blue arrows, b intestinal lumen with mannitol in another patient)
taken from the same slice levels of CTA ( c ) were less obvious to diagnose due to artifacts secondary to inadequate breath-holding. Higher spatial resolution with shorter imaging time of CTA enabled the radiologist to make an accurate diagnosis. As in this case, choosing the wrong technique or modality may decrease the possibility of detecting abnormal findings, cause a delay in diagnosis, and sometimes even make diagnosis impossible. However, in this particular case, the change in the diagnosis did not change the patient management to a great extent and did not cause any apparent harm
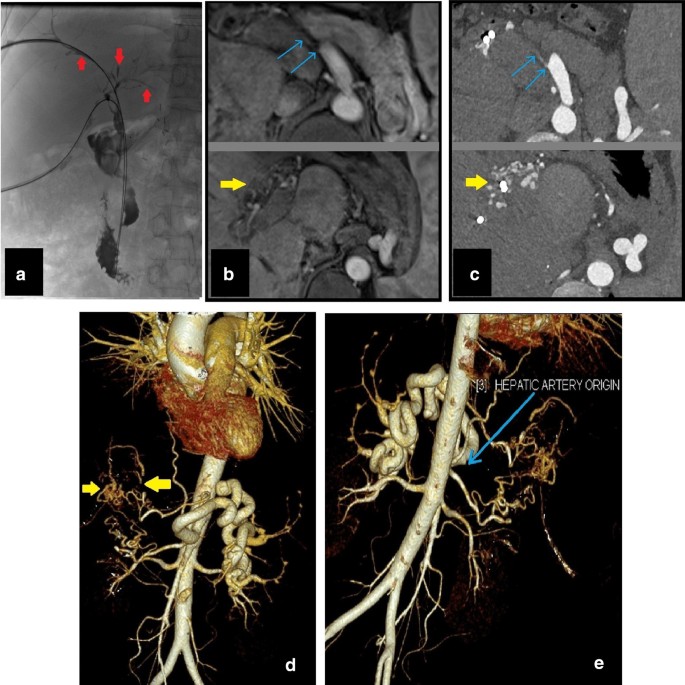
Delay in diagnosis with no apparent harm. A 45-year-old male patient presented at the clinic with jaundice and recurrent cholangitis history after liver transplantation. Due to persistent itching and progressive jaundice, percutaneous transhepatic cholangiography (PTC) was performed for biliary drainage. PTC showed multisegmental involvement with dilated and stenotic biliary ducts (red arrows, a ). Contrast-enhanced upper abdominal MRI and MRCP for evaluation of the biliary tree were reported as “Chronic cholangiopathic changes due to recurrent episodes of cholangitis” without any differential diagnoses. The clinicians suspected "ischemic cholangiopathy" due to liver transplant history and ordered abdominal CTA to rule out ischemic etiology. The CTA, which was performed two weeks after MRI, revealed hepatic artery occlusion (blue arrows, c , e ) and arterial collateralization (yellow arrows, c , d ). After confirmation of “ischemic biliopathy”, the previous MRI was evaluated retrospectively. The MRI images ( b )
The consequences of harmful errors can be examined in three groups. The first group is related to misdiagnosis or delay in the diagnosis. Thus, the imaging findings, which are essential for the patient's clinical condition, could be missed or inadvertently interpreted as an inaccurate diagnosis (Fig. 23 ).
Delay in diagnosis with indirect harm. Cardiac MRI of a 71-year-old male patient for evaluation of angina and left ventricle hypertrophy had shown a hyperintense lesion in the right lung, which had been seen in only one slice of black blood sequence with 8 mm slice thickness (red arrow, a ). This lesion had been overlooked due to the framing of clinical information and its location. A growing lung mass was detected three years later in the superior segment of the right lower lobe (red arrows, b , c ) on thorax CT. Percutaneous biopsy and subsequent histopathological examination confirmed primary lung cancer. Due to the major fissure invasion developed during the interval period (blue arrow, c ), the patient underwent right pneumonectomy instead of lobectomy
The second group is the errors causing a prolonged hospital stay, which leads to additional follow-up and sometimes the requirement for further treatment. This group of errors either results in acute injury (Fig. 15 ) or chronic/long-term unwanted situations (Fig. 7 ).
The third group is related to the overlooking or underestimating of significant and life-threatening findings. The latter can result in severe morbidity, even mortality (Fig. 24 ).
Delay in diagnosis with a life-threatening condition. A 47-year-old male patient presented with complaints of chest pain and abdominal discomfort. History and clinical examination suggested cardiovascular etiology as a possible underlying cause. Coronary CTA was ordered to evaluate the presence of coronary artery disease. The coronary arteries were reported as normal. However, a well-defined splenic hypervascular lesion was missed due to the “edge effect”. The lesion was seen only on the last few slices of “the CT images with a large field of view” (red arrow, a ). One week later, the patient was admitted to the ER with severe left upper quadrant pain. Abdominal CECT revealed a ruptured lesion (red arrows, B, c ) and subcapsular splenic hematoma (blue arrows, b , c ) with active extravasation (not shown)
Errors, discrepancies and confounding biases are integral parts of the daily routine for radiologists and can cause various unexpected clinical consequences. In this study, certain types of radiological errors and biases are explained with case-based examples. By so doing, it is aimed to increase awareness about radiological diagnostic errors and related biases. However, it is obvious that radiological assessment of imaging examinations is a part of overall patient management that may be limited due to the diagnostic utility of the imaging technique and referral information. Therefore, radiological reports should not be expected always to be complete and correct or be regarded as the only tool to catch, confirm, or exclude the diagnosis [ 1 , 3 ].
It should be kept in mind that effective communication between radiologists, radiology technicians, patients and clinicians is one of the key factors in reducing errors and thereby enabling proper patient management (Figs. 11 , 21 , 25 ). Finally, awareness of and familiarity with errors and underlying biases is essential for radiologists to be able to cope with them, avoid false interpretations and develop counter-measures [ 6 , 11 ].

Importance of effective communication. A 65-year-old female patient suffered from the new onset of dyspnea three days after mitral valve replacement. Thorax CT showed the intra-atrial location of the replaced mitral valve (red arrows, a , b ). When the abnormal valve location and new onset of dyspnea were considered, displacement of the replaced mitral valve was suspected. The cardiovascular surgery department was immediately called to report this situation. After a brief opinion exchange with the referrer, it was learned that this valve location is the expected location in patients who have undergone mitral valve replacement with the Chimney technique, which is preferred for patients with extensive mitral annular calcifications (blue arrows, a , b ) to prevent calcified embolism during the procedure. As a result, effective communication between the radiologist and the clinician overcame the possibility of “lack of knowledge and overreading errors”
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.

Abbreviations
Contrast-enhanced computed tomography
Computed tomography
Computed tomography angiography
Emergency room
Glomerular filtration rate
Hounsfield unit
Magnetic resonance cholangiopancreatography
Magnetic resonance imaging
Motor vehicle accident
Non-enhanced computed tomography
Percutaneous transhepatic cholangiography
Pulmonary thromboembolism
Region of interest
Fitzgerald R (2001) Error in radiology. Clin Radiol 56(12):938–946. https://doi.org/10.1053/crad.2001.0858
Article CAS PubMed Google Scholar
Donald JJ, Barnard SA (2012) Common patterns in 558 diagnostic radiology errors. J Med Imaging Radiat Oncol 56(2):173–178. https://doi.org/10.1111/j.1754-9485.2012.02348.x
Article PubMed Google Scholar
Brady AP (2016) Error and discrepancy in radiology: inevitable or avoidable? Insights Imaging 8(1):171–182. https://doi.org/10.1007/s13244-016-0534-1
Article PubMed PubMed Central Google Scholar
Itri JN, Tappouni RR, McEachern RO, Pesch AJ, Patel SH (2018) Fundamentals of diagnostic error in imaging. Radiographics 38(6):1845–1865. https://doi.org/10.1148/rg.2018180021
Waite S, Scott J, Gale B, Fuchs T, Kolla S, Reede D (2017) Interpretive error in radiology. AJR Am J Roentgenol 208(4):739–749. https://doi.org/10.2214/ajr.16.16963
Bruno MA, Walker EA, Abujudeh HH (2015) Understanding and confronting our mistakes: the epidemiology of error in radiology and strategies for error reduction. Radiographics 35(6):1668–1676. https://doi.org/10.1148/rg.2015150023
Kim YW, Mansfield LT (2014) Fool me twice: delayed diagnoses in radiology with emphasis on perpetuated errors. AJR Am J Roentgenol 202(3):465–470. https://doi.org/10.2214/AJR.13.11493
Brady AP, Laoide RO, McCarthy P, McDermott R (2012) Discrepancy and error in radiology: concepts. Causes Conseq Ulster Med J 81(1):3–9
Google Scholar
Busby LP, Courtier JL, Glastonbury CM (2018) Bias in radiology: the how and why of misses and misinterpretations. Radiographics 38(1):236–247. https://doi.org/10.1148/rg.2018170107
Drew T, Vo MLH, Wolfe JM (2013) The invisible gorilla strikes again: sustained inattentional blindness in expert observers. Physicol Sci 24(9):1848–1853. https://doi.org/10.1177/0956797613479386
Article Google Scholar
Go S, Furukawa T, Yamada K, Hiraoka T, Mochizuki S (2019) A case of supra-annular mitral valve replacement using chimney technique for severe mitral stenosis with extensive mitral annular calcification. Gen Thorac Cardiovasc Surg. https://doi.org/10.1007/s11748-019-01256-7
Download references
Acknowledgements
This paper was presented as a poster at ECR 2020 and was awarded with the Certificate of Merit.
Author information
Authors and affiliations.
Department of Radiology, Hacettepe University School of Medicine, Ankara, 06100, Turkey
Omer Onder, Yasin Yarasir, Aynur Azizova, Gamze Durhan, Mehmet Ruhi Onur & Orhan Macit Ariyurek
You can also search for this author in PubMed Google Scholar
Contributions
OO, YY and AA wrote the manuscript. GD, MRO and OMA edited the text. All of the authors read and approved the final manuscript.
Corresponding author
Correspondence to Orhan Macit Ariyurek .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Onder, O., Yarasir, Y., Azizova, A. et al. Errors, discrepancies and underlying bias in radiology with case examples: a pictorial review. Insights Imaging 12 , 51 (2021). https://doi.org/10.1186/s13244-021-00986-8
Download citation
Received : 26 December 2020
Accepted : 19 March 2021
Published : 20 April 2021
DOI : https://doi.org/10.1186/s13244-021-00986-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical errors
- Diagnostic errors
- Diagnostic ımaging
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Med Educ J
- v.9(2); 2018 May

Ethics in radiology: A case-based approach
Laura stiles-clarke.
1 Faculty of Education, St. Francis Xavier University, Nova Scotia, Canada
James Clarke
2 Department of Diagnostic Imaging, Dalhousie University, Nova Scotia, Canada
Ethics training is required for all radiology residents in Canada, but this may be difficult to provide as radiology departments may not have radiologists with formal ethics training, and may not have access to educational resources focussed on teaching ethics to radiologists. We describe the implementation of a case-based approach to teaching and learning ethics, designed for Canadian radiologists. This approach can be adapted for use in other specialties through development of specialty-specific ethics case scenarios.
Ethics case study rounds specific to Canadian radiologic practice were presented at two different institutions, and using two different methods within one institution. In one method, we requested that the residents read the case study and questions ahead of time; in the other, the rounds were presented without any expectation of residents doing prior preparation.
The participants, as a group, agreed with all seven survey statements describing the value of the experience. The opportunity to read the case ahead of time seemed helpful for some residents, but was not found to be overall more useful than discussing the case without prior review. Indeed, more than half of the resident participants in this group indicated that they did not make use of the advance materials at all.
Resident feedback indicates that ethics case study rounds are a useful and valuable experience, especially when the case is specifically tailored to their medical practice. Prior preparation was not necessary for residents to benefit from these rounds.
Introduction
Ethics education is important for the modern physician, as evidenced by the CanMEDS Professional 1 role requirement to “demonstrate a commitment to patients by applying best practices and adhering to high ethical standards.” 2 Unfortunately, medical ethics education can be difficult to provide as part of a residency education program, as discussed by Oljeski, Homer and Krackov:
[Residency] programs may not have faculty who possess formal training in the teaching of ethics. Even if a staff member has taken ethics courses at the undergraduate or graduate level, these courses may not have specifically addressed medical ethics. To compound the problem, we realize that even if the course pertained to medical ethics, the topics may not be relevant to ethics issues that are specific to the practice of radiology. 3
General medical ethics training is insufficient, as there are a variety of ethical dilemmas in radiology that are unique to the specialty. In addition, “medical ethics is decidedly more interesting and useful to study when it is appropriately tailored to the targeted audience.” 4
Ethics education is well suited to open-ended, discussion-based teaching, because ethical medical practice is tested in real-life situations as opposed to academic exams. Teaching ethics through lectures can also be problematic due to the unspoken “hidden curriculum”: in managing everyday ethical dilemmas, physicians tend to consult their own moral compasses before, or instead of, recalling what may have been extolled in lectures. Residents then watch and learn from how their staff behave in the real world and are influenced by those behaviours. Our case study rounds were designed to encourage resident engagement and participation, because “residents need to discuss and think about ethics issues in nonthreatening ways before a real, and not theoretic, need to do so arises.” 5 Shuman, Barnosky, and Koopmann agree that informal sessions work better for ethics education:
Challenging case studies provide a medium that facilitates participation among clinicians who can then hone these skills in an interactive format that is relevant to their practice. Departmental sessions provide an ideal setting whereby colleagues can discuss cases that relate directly to their own experience, while vetting opinions, management options, and perspectives from their coworkers, all within a nonjudgmental forum designed to educate and improve future care. 4
By presenting an open-ended ethics case study, we intended to encourage such discussions and sharing of experience in a way that lecture-based methods cannot do.
Study design and settings
A set of Canadian radiology-specific case studies was developed collaboratively between the departments of Diagnostic Imaging and Bioethics at Dalhousie University. JC, the second author of this paper and a staff radiologist, developed the case ideas, and a clinical bioethicist from Dalhousie University provided ethical analyses. Each case study presents an ethical challenge based on actual situations that have happened in Canadian radiology practices, and includes an ethical analysis, as well as a set of questions developed by the bioethicist to stimulate thoughtful discussion. The case used in this study has been published 6 and is available for others to use in their own contexts.
Here, we report on the implementation of ethics case study rounds to radiology residents at Dalhousie University and the University of Alberta, and explore using two different methods of presentation. Prior to these rounds presentations, there was no radiology-specific ethics training provided in either residency program. Residents in both programs would have had a heterogeneous background on non-radiology specific ethics training during their undergraduate and postgraduate medical training.
During rounds, residents were encouraged to place themselves in the shoes of the physician in the case study, and discuss their impressions and what subsequent actions they might take. JC facilitated the rounds, and stated up front that there would be no “correct answer” provided for the case study; the discussion and the participants’ various responses to the case were, in themselves, the purpose of the rounds.
Residents at Dalhousie were presented with two sets of rounds: during the first they were asked to read the case and associated questions before rounds, and during the second they were only presented with the case and questions at the start of the rounds. The intent of these two presentation methods was to determine whether the residents’ experiences of the sessions would be different if participants were given a chance to carefully consider their thoughts before rounds.
A third set of rounds was presented to radiology residents at the University of Alberta with the case and questions being provided ahead of time. Feedback on these rounds was analyzed to see whether the response would be different at a different university.
After each of these sessions, residents were invited to complete a questionnaire regarding the format of the rounds and utility of the rounds to their practice. The questionnaire contained seven statements, which participants rated on a five-point Likert scale (1 meaning “strongly disagree” and 5 meaning “strongly agree”), which was the same approach used by Oljeski, Homer, and Krackov. 3 Open-ended comments were also solicited. For the rounds where residents had been asked to read the case ahead of time, additional questions were asked about the experience of pre-reading the case.
Data analysis
All completed questionnaires were analyzed by entering both qualitative and quantitative responses into a Microsoft Excel spreadsheet. Descriptive statistics were used on all quantitative responses and thematic analysis 7 was carried out with the qualitative responses. The data from the two schools were compared and no significant difference between the two schools was found. Therefore, the data from the two schools were combined in order to create a larger data set.
Results and discussion
Quantitative results.
Forty-five participants submitted questionnaires for analysis (n=45). For all seven questions, there was a statistically significant difference between combined responses of “strongly agree” or “agree” as compared to combined responses of “neutral,” “disagree,” “strongly disagree,” or no response ( Table 1 ). The mean and standard deviation for the responses to each statement are shown in Table 1 .
Participant responses to feedback statements (n=45)
σ: standard deviation
Participants responded positively to six of the seven questions (Questions 1, 2, 4, 5, 6, and 7) in terms of their Likert scale ratings, as shown by the median values of 5, or “strongly agree”, for these questions. Responses to Question 3 were also positive, although the mean rating for this question was only 3.91 ± 1.16. Question 3, “The discussion questions brought to light issues that I hadn’t previously considered,” was rated lower than the other six survey questions, and its standard deviation was higher, but the participants still agreed with the statement. Although the responses to this question were less positive than the others, the rounds were simultaneously still felt to be beneficial, even by those students who disagreed with this question. This question addressed the discussion questions and not the cases themselves, and the slightly lower response may reflect that the residents had already experienced and thought about that scenario or that they did not believe guiding questions were required to stimulate discussion.
Qualitative results
A thematic analysis of open-text responses was carried out by LSC, the first author. The themes arising from the data included appreciation for the relevance of the case presented, enjoyment of the small group discussion format, and the desire to hear more cases of this type.
Participants appreciated that the case study had been chosen specifically to benefit their current and future medical practice. Among the many examples of resident comments on the specific relevance of the case are: “Excellent example of a relevant ethical situation,” and “One of the first ethics sessions I found truly applicable to my specialty.” This feedback points to the need for specialty-specific educational resources described by other researchers. 3 , 4
The participants also valued the small group discussion, commenting: “Small group discussion was critical, and thoroughly enjoyable!” and “Fun and insightful discussion in small groups. I feel like I actually learned something!”
Several participants stated that they would like to hear more cases of this type. Some of the comments included: “Maybe have more than one scenario,” and “If time permits, discuss additional challenging ethical scenarios.” Two residents requested a short introductory lecture on general ethical principles, and one requested additional references. Another requested a discussion of real-life example cases and their outcomes, similar to the format used by Shuman, Barnosky and Koopmann 4 . Clearly the participants expressed a strong desire to hear further cases tailored specifically to their needs.
More general constructive feedback was also received from all groups of participants. Some examples of these comments are: “Great case with excellent discussion” and “The discussion of what we would actually do vs. the ‘correct’ answer was useful.” No substantial negative feedback was received from any participant.
On the occasions when participants were provided with the case study and questions in advance, they were asked additional questions regarding their experience. Quantitative responses here were inconclusive ( Table 2 ); indeed, of those who were asked to read the case and questions ahead of time, fewer than half claimed to have actually done so. For this reason, we separated the group who stated that they read the materials before the rounds from those who were provided the materials, but did not read them. When comparing these two groups to each other and to the group that was not given the materials ahead of time, in terms of their responses to the first seven questions, we found no significant differences. The qualitative data analysis was similarly inconclusive: no participant commented that the opportunity to read the case ahead of time was detrimental, but some people did find it helpful, and others felt that advance preparation was unnecessary. This may reflect different preferred learning styles, a lack of time to prepare for rounds, or the fact that these rounds required a greater amount of self-introspection rather than memorized facts, as compared to more commonly presented types of rounds.
Pre-reading responses (n = 32)
Ethics rounds tailored for Canadian radiology residents were developed and presented using two different methods, to two different groups of residents. Quantitative feedback indicated that the participants found the experience to be quite valuable and effective. A thematic analysis of residents’ written comments showed both satisfaction with the ethics case study rounds experience and the desire to participate in further sessions of similar design. No differences were found between groups who had or had not read the preparatory material in advance of the rounds. Future research may include evaluation of faculty satisfaction with case study-based ethics teaching.
Acknowledgement
The authors thank the participants for their contribution to this study.
Conflicts of interest: No potential conflicts of interest were identified in the preparation of this work. There was no funding for this work.
- Introduction
- Conclusions
- Article Information
Standardized uptake value (SUV) ratios of the bilateral ACC and hippocampus were compared between patients with schizophrenia and healthy controls. Statistical significance was determined as a false discovery rate (FDR)–corrected P < .05. The center horizontal bars indicate means; the outer horizontal bars indicate 95% CIs.
Pearson correlation analysis between standardized uptake value (SUV) ratios of the bilateral anterior cingulate cortex (ACC) and positive symptom scores on the Positive and Negative Syndrome Scale (PANSS; range, 7-49, with higher scores indicating the greater severity of positive symptoms) was performed. Statistical significance was determined as a false discovery rate (FDR)–corrected P < .05.
The orange lines indicate regression lines.
eMethods. Sample Size Determination and Fluorine 18–Labeled THK 5351 Preparation
eTable 1. Pearson Correlation Analysis Between the Altered Standardized Uptake Ratio of Fluorine 18– Labeled THK5351 in Primary Regions of Interest and Positive Symptom Severity in Patients With Schizophrenia
eTable 2. Group Comparison Results of the Standardized Uptake Value Ratio of Fluorine 18– Labeled THK5351 in Secondary Regions of Interest
eTable 3. Pearson Correlation Analysis Between Altered Standardized Uptake Ratio of Fluorine 18– Labeled THK5351 in Primary Regions of Interest and Olanzapine-Equivalent Dose of Antipsychotics as Well as Duration of Illness in Patients With Schizophrenia
eFigure 1. Schematic Diagram of Fluorine 18– Labeled THK 5351 Positron Emission Tomography Analysis
eFigure 2. Group Comparison of Fluorine 18– Labeled THK5351 Standardized Uptake Value Ratios
eReferences
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Kim M , Choi W , Choi S, et al. In Vivo Reactive Astrocyte Imaging in Patients With Schizophrenia Using Fluorine 18–Labeled THK5351. JAMA Netw Open. 2024;7(5):e2410684. doi:10.1001/jamanetworkopen.2024.10684
Manage citations:
© 2024
- Permissions
In Vivo Reactive Astrocyte Imaging in Patients With Schizophrenia Using Fluorine 18–Labeled THK5351
- 1 Department of Neuropsychiatry, Seoul National University Hospital, Seoul, Republic of Korea
- 2 Department of Psychiatry, Seoul National University College of Medicine, Seoul, Republic of Korea
- 3 Department of Brain and Cognitive Sciences, Seoul National University College of Natural Sciences, Seoul, Republic of Korea
- 4 Department of Nuclear Medicine, Seoul National University College of Medicine, Seoul, Republic of Korea
- 5 Department of Radiology, Seoul National University College of Medicine, Seoul, Republic of Korea
- 6 Department of Public Health Medical Services, Seoul National University Bundang Hospital, Seongnam, Republic of Korea
- 7 Department of Psychiatry, Seoul Metropolitan Government–Seoul National University Boramae Medical Center, Seoul, Republic of Korea
- 8 Institute of Human Behavioral Medicine, Seoul National University–Medical Research Center, Seoul, Republic of Korea
Question Can region-specific reactive astrocytes in vivo associated with positive symptoms in patients with schizophrenia be measured using fluorine 18–labeled THK5351 ([ 18 F]THK5351) positron emission tomography?
Findings In this case-control study of 68 participants, standardized uptake value ratios (SUVrs) of [ 18 F]THK5351 in the bilateral anterior cingulate cortex and left hippocampus were greater in patients with schizophrenia than in healthy controls. Increased [ 18 F]THK5351 SUVrs were correlated with positive symptom severity in patients with schizophrenia.
Meaning Considering the role of astrocytes in brain development, neurotransmission, and immune reactions, reactive astrocytes in the bilateral anterior cingulate cortex and left hippocampus may be strong biomarkers for schizophrenia pathophysiology and treatment.
Importance In vivo imaging studies of reactive astrocytes are crucial for understanding the pathophysiology of schizophrenia because astrocytes play a critical role in glutamate imbalance and neuroinflammation.
Objective To investigate in vivo reactive astrocytes in patients with schizophrenia associated with positive symptoms using monoamine oxidase B (MAO-B)–binding fluorine 18 ([ 18 F])–labeled THK5351 positron emission tomography (PET).
Design, Setting, and Participants In this case-control study, data were collected from October 1, 2021, to January 31, 2023, from the internet advertisement for the healthy control group and from the outpatient clinics of Seoul National University Hospital in Seoul, South Korea, for the schizophrenia group. Participants included patients with schizophrenia and age- and sex-matched healthy control individuals.
Main Outcomes and Measures Standardized uptake value ratios (SUVrs) of [ 18 F]THK5351 in the anterior cingulate cortex (ACC) and hippocampus as primary regions of interest (ROIs), with other limbic regions as secondary ROIs, and the correlation between altered SUVrs and Positive and Negative Syndrome Scale (PANSS) positive symptom scores.
Results A total of 68 participants (mean [SD] age, 32.0 [7.0] years; 41 men [60.3%]) included 33 patients with schizophrenia (mean [SD] age, 32.3 [6.3] years; 22 men [66.7%]) and 35 healthy controls (mean [SD] age, 31.8 [7.6] years; 19 men [54.3%]) who underwent [ 18 F]THK5351 PET scanning. Patients with schizophrenia showed significantly higher SUVrs in the bilateral ACC (left, F = 5.767 [false discovery rate (FDR)–corrected P = .04]; right, F = 5.977 [FDR-corrected P = .04]) and left hippocampus ( F = 4.834 [FDR-corrected P = .04]) than healthy controls. Trend-level group differences between the groups in the SUVrs were found in the secondary ROIs (eg, right parahippocampal gyrus, F = 3.387 [ P = .07]). There were positive correlations between the SUVrs in the bilateral ACC and the PANSS positive symptom scores (left, r = 0.423 [FDR-corrected P = .03]; right, r = 0.406 [FDR-corrected P = .03]) in patients with schizophrenia.
Conclusions and Relevance This case-control study provides novel in vivo imaging evidence of reactive astrocyte involvement in the pathophysiology of schizophrenia. Reactive astrocytes in the ACC may be a future target for the treatment of symptoms of schizophrenia, especially positive symptoms.
Glutamatergic imbalance and neuroinflammation are believed to be important in schizophrenia pathophysiology. The glutamate hypothesis suggests that psychotic symptoms are caused by N -methyl- d -aspartate receptor hypofunction-mediated abnormal glutamatergic neurotransmission with a dysfunctional thalamic filter system. 1 - 3 Furthermore, excessive glutamate activity might lead to excitotoxic damage and oxidative stress–related neuroinflammation, which further explains the pathophysiology. 4 , 5 This finding is consistent with the immune hypothesis suggesting the involvement of neuroinflammation caused by microglial overactivation in the development and progression of schizophrenia. 6 - 9
Previous magnetic resonance (MR) spectroscopy studies have revealed that patients with schizophrenia exhibit altered glutamate and/or glutamine levels in several brain regions, including the anterior cingulate cortex (ACC) and hippocampus, although the direction and degree of alterations have been inconsistent. 10 - 13 Among individuals at clinically high risk for psychosis, the baseline hippocampal glutamate level was suggested to be associated with the transition to psychotic disorder. 14 In vivo microglial imaging studies using 18-kDa translocator protein positron emission tomography (PET) to detect neuroinflammation in the frontal cortex, ACC, temporal cortex, and hippocampus of patients with schizophrenia have also provided inconsistent results. 15 - 18 These inconsistencies may be due to the simple approach of using individual glutamate or neuroinflammation markers in a rather complex, mutually influencing system. However, investigations aimed at integrating glutamate imbalance and neuroinflammation in the pathophysiology of schizophrenia are limited, and only 1 study 5 has attempted to bridge the gap between the 2 hypotheses by showing that the levels of the antioxidant glutathione and excitotoxic glutamate and/or glutamine are lower in patients with schizophrenia who are in stable clinical condition.
Reactive astrocytes are promising candidates for achieving a comprehensive understanding of glutamate imbalance and neuroinflammation in the pathophysiology of schizophrenia because astrocytes play an important role in glutamate recycling, neurotransmission (including dopamine), and the neuroimmune system, in addition to their basic role in supporting neurons. 19 - 21 Reactive astrocytes are remodeled in response to injury, disease, or infection of the brain and can be measured in vivo by detecting overexpressed monoamine oxidase B (MAO-B) on the outer mitochondrial membrane. 22 In patients with schizophrenia, abnormal astrocyte-neuronal interactions have been suggested to be the mechanism of psychotic symptom development, 2 and alterations in the expression of astrocyte-related genes and their products in patients’ postmortem brains have been reported. 23 However, in vivo reactive astrocyte imaging has not yet been reported in patients with schizophrenia.
In this study, we investigated the in vivo imaging of reactive astrocytes and their association with positive symptoms in patients with schizophrenia using validated MAO-B–binding fluorine 18 ([ 18 F])–labeled THK5351 PET 24 - 26 to obtain a more comprehensive understanding of the role of reactive astrocytes in schizophrenia pathophysiology. The primary regions of interest (ROIs) were the ACC and hippocampus based on previous studies of glutamate imbalance, neuroinflammation, and positive symptom development in patients with schizophrenia. 10 , 13 , 16 , 27 The secondary ROIs included other limbic regions, such as the posterior cingulate cortex (PCC), parahippocampal gyrus, amygdala, insula, and nucleus accumbens, based on previous studies 28 , 29 that reported the association between glutamate alterations and positive symptoms in these regions in patients with schizophrenia.
This case-control study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline. All participants provided written informed consent after receiving a thorough explanation of the study procedure. The study was conducted in accordance with the Declaration of Helsinki 30 and was approved by the Institutional Review Board of Seoul National University Hospital.
A total of 33 patients with schizophrenia and 35 age- and sex-matched healthy controls participated in this study. All study participants were of East Asian descent. Information regarding the sample size calculation is provided in the eMethods in Supplement 1 . Patients with schizophrenia were recruited from the outpatient office of the Department of Neuropsychiatry at Seoul National University Hospital. The diagnosis of schizophrenia was confirmed using the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) Axis I Disorders (SCID-I) by board-certified psychiatrists (M.K., S.-Y.M., and S.K.L.). Psychotic symptoms were assessed using the Positive and Negative Syndrome Scale (PANSS). 31 The Hamilton Rating Scale for Depression 32 and the Hamilton Rating Scale for Anxiety 33 were used to measure the severity of depression and anxiety, respectively. The healthy controls were recruited via internet advertisement and were screened using the SCID-I Nonpatient Edition. Healthy controls were excluded if they had any past or current diagnosis of a psychiatric disorder and any first- to third-degree biological relatives with a psychotic disorder. In all participants, general functional status was evaluated using the modified Global Assessment of Functioning, and intelligent quotient (IQ) was measured with the Korean version of the Wechsler Adult Intelligence Scale. 34 The exclusion criteria included substance abuse or dependence (except nicotine), neurological disease or significant head trauma, medical illness that could accompany psychiatric symptoms, and intellectual disability (IQ < 70).
A PET-MR machine (Biograph mMR; Siemens Healthcare) was used to obtain dynamic 3-dimensional PET images. Immediately after an intravenous bolus injection of 185 MBq (5 mCi) of [ 18 F]THK5351, 27 frames of emission scans (8 × 15 seconds, 3 × 60 seconds, 5 × 120 seconds, and 11 × 300 seconds) and a total 70-minute PET scan were acquired while the participant was at rest. Fluorine 18–labeled THK5351 was synthesized and radiolabeled at Seoul National University Hospital, and details are provided in the eMethods in Supplement 1 . Each participant was fitted with an MR imaging coil and supporting cushion to reduce head motion during the PET scan, and the participants were asked to remain as still as possible during the scan.
Manufacturer’s software from the PET-MR device (e7tool; Siemens Healthcare) was used for the reconstruction of the PET data. The PET images were reconstructed using the ordered-subset expectation maximization algorithm with 24 subsets and 5 iterations. Images were filtered with a 4-mm full-width at half-maximum Gaussian filter at the center of the field of view (image matrix, 256 × 256; 127 sections; voxel size, 1.4 × 1.4 × 2.0 mm). Segmentation-based attenuation correction was conducted with a 3-tissue segmentation map acquired by an ultrashort echo time (TE) sequence (repetition time [TR], 11.9 milliseconds; TE 1, 0.07 milliseconds; TE 2, 2.46 milliseconds; flip angle, 10°; 192 × 192 matrix). A high-resolution structural T1 image (TE, 2.2 milliseconds; TR, 2400 milliseconds; flip angle, 8°; 0.85-mm section thickness) was also collected for each participant at the same time to rule out structural lesions in the brain and to provide an anatomical reference for the [ 18 F]THK5351 analysis.
All preprocessing was conducted using Statistical Parametric Mapping (SPM 12; Welcome Department of Imaging Neuroscience). The analysis flowchart and selected cerebellar lobules are presented in eFigure 1 in Supplement 1 .
For semiquantitative PET analysis, standardized uptake value ratios (SUVrs) were calculated in reference to the inferior cerebellar parcels of the cerebellar cortex. To delineate the inferior cerebellar ROI, the SUIT (spatially unbiased infratentorial template) toolbox, 35 which contains a high-resolution atlas template of the cerebellum and brainstem and individual T1 images, was used. The cerebellar structure was isolated from the cerebral structure and segmented into tissue types using the Dartel algorithm. Using the deformation field obtained during the Dartel procedure, the SUIT template was transferred to an individual PET space. The lobular ROIs that corresponded to the inferior cerebellar gray matter (bilateral Crus II, VIIb, VIIIa, VIIIb, and IX) were used to extract radioactivity from the PET image. After frame-by-frame motion correction of the PET image, the T1 images were coregistered to the mean images of 27 realigned PET frames.
The bilateral ACC and hippocampus, as primary ROIs, and other limbic regions (bilateral PCC, parahippocampal gyri, amygdala, insula, and nucleus accumbens), as secondary ROIs, were predefined using the Wake Forest University PickAtlas toolbox in SPM 12. 36 The predefined ROIs were transformed into PET standard space using the deformation matrix calculated from PET-coregistered T1 images, and SUVs were extracted for all PET frames to assess the time activity curve in each ROI. Finally, based on previous studies that tested the optimal time windows to estimate [ 18 F]THK5351 quantification, 37 the SUVr was calculated as the sum of 45- to 65-minute postinjection frames using the mean radioactivity of the inferior cerebellar ROI obtained by the SUIT procedure as a reference.
Data were collected from October 1, 2021, to January 31, 2023. Demographic and clinical characteristics were compared between patients with schizophrenia and healthy controls using an independent t test or a Welch t test if the variance was not equal and a χ 2 test or a Fisher exact test for categorical data. Group differences in the SUVr in the bilateral ACC and hippocampus (ie, primary ROIs) were tested using analysis of covariance, with age and sex as covariates. Pearson correlation analysis was performed to investigate the association between altered SUVrs in primary ROIs and PANSS positive symptom scores in patients with schizophrenia. To rule out the possible effect of the duration of illness or olanzapine-equivalent dose of antipsychotics prescribed at the time of study participation on the SUVrs of the primary ROIs, Pearson correlation analysis was performed. To account for multiple comparisons, a false discovery rate (FDR) correction was performed. Group differences in SUVrs in other limbic ROIs were assessed using repeated-measures analysis of variance (ANOVA), with brain regions (ie, bilateral PCC, parahippocampal gyri, amygdala, insula, and nucleus accumbens) as the within-participants factor and age and sex as covariates. All statistical analyses were performed in SPSS, version 25.0 for Windows (IBM Corporation), and the level of statistical significance was set at 2-sided P < .05.
A total of 68 participants (mean [SD] age, 32.0 [7.0] years; 41 men [60.3%] and 27 women 39.7%]) included 33 patients with schizophrenia (mean [SD] age, 32.3 [6.3] years; 22 men [66.7%] and 11 women [33.3%]) and 35 healthy controls (mean [SD] age, 31.8 [7.6] years; 19 men [54.3%] and 16 women [45.7%]). Table 1 summarizes the demographic and clinical characteristics of the participants. There were no significant group differences in age or sex, while mean (SD) IQ (107.2 [12.5] vs 116.7 [11.0]; P = .001) and modified Global Assessment of Functioning scores (54.1 [11.9] vs 87.3 [4.8]; P < .001) were lower in patients with schizophrenia than in healthy controls. There were no significant group differences in the amount of [ 18 F]THK5351 injected.
According to the group comparison of primary ROIs, patients with schizophrenia had significantly greater SUVrs in the bilateral ACC (left, F = 5.767 [FDR-corrected P = .04]; right, F = 5.977 [FDR-corrected P = .04]) and left hippocampus ( F = 4.834 [FDR-corrected P = .04]) than healthy controls ( Table 2 and Figure 1 ). There were positive correlations between the SUVrs in the bilateral ACC and the PANSS positive symptom scores (left, r = 0.423 [FDR-corrected P = .03]; right, r = 0.406 [FDR-corrected P = .03]) in patients with schizophrenia ( Figure 2 and eTable 1 in Supplement 1 ). Repeated-measures ANOVA revealed trend-level group differences in the SUVrs in the secondary ROIs (eg, right parahippocampal gyrus, F = 3.387 [ P = .07]) (eFigure 2 and eTable 2 in Supplement 1 ). There was no correlation between the duration of illness or olanzapine-equivalent dose of antipsychotics prescribed at the time of study participation and the SUVrs of the primary ROIs (eTable 3 in Supplement 1 ).
In this study, we investigated in vivo reactive astrocyte imaging using MAO-B–binding [ 18 F]THK5351 PET to reveal the role of reactive astrocytes, which are involved in both glutamate imbalance and neuroinflammation, in schizophrenia pathophysiology. Patients with schizophrenia had elevated SUVrs in the bilateral ACC and left hippocampus compared with healthy controls. In addition, positive correlations between the SUVrs in the bilateral ACC and the PANSS-positive symptom scores were found in patients with schizophrenia. There were trend-level group differences in the SUVrs in other limbic regions investigated as secondary ROIs. The results of this study not only provide in vivo neuroimaging evidence of the role of reactive astrocytes in schizophrenia pathophysiology but also highlight the region-specific association between reactive astrocytes in the ACC and positive symptoms in patients with schizophrenia.
Our findings of elevated MAO-B–binding [ 18 F]THK5351 uptake in patients with schizophrenia suggest a role for reactive astrocytes in the neurodevelopmental abnormalities of these patients. Astrocytes are known to be important in neurodevelopment and to play a critical role in synapse formation and function as well as neuronal survival and migration; thus, abnormal astrocytes can increase the vulnerability of the brain to neurodevelopmental disorders such as schizophrenia. 38 , 39 Windrem et al 40 showed that mice chimerized with induced pluripotent stem cells derived from patients with childhood-onset schizophrenia exhibited problems with glial cells, including astrocytes, suggesting that genetic abnormalities in schizophrenia produce abnormalities in astrocytes, which are critical for brain development and schizophrenia pathophysiology. Thus, the results of the present study support the vulnerability and neurodevelopmental model of schizophrenia and suggest the role of reactive astrocytes in schizophrenia pathophysiology by providing in vivo neuroimaging evidence of reactive astrocytes in patients with schizophrenia.
Furthermore, the results of this study provide integrative supporting evidence for the glutamate and immune hypotheses in schizophrenia pathophysiology. Previous studies aimed at measuring glutamate and/or glutamine levels in patients with schizophrenia 11 , 13 have produced inconsistent results, which may be due to the lack of consideration of interacting systems other than glutamate. Microglial imaging studies using translocator protein PET to show neuroinflammation in patients with schizophrenia 16 , 18 have also provided insufficient evidence that may be caused by subtle changes in microglial activity. Astrocytes not only play important roles in glutamate cycling and synaptic transmission but also undergo astrogliosis in reaction to neuroinflammation, as shown in neuroinflammatory diseases such as Wilson disease and multiple sclerosis. 2 , 6 , 25 , 41 Therefore, the results of the present study support that both the glutamate and immune hypotheses can provide a more comprehensive understanding of the interaction between glutamate and the immune system in the pathophysiology of schizophrenia by revealing reactive astrocytes in vivo in patients with schizophrenia.
In the present study, elevated [ 18 F]THK5351 uptake was detected in the bilateral ACC and left hippocampus of patients with schizophrenia compared with healthy controls. These findings are consistent with previous studies 23 , 42 reporting that elevated astrocyte-, glutamate-, and immune-related genes and gene products were found in the postmortem brains of patients with schizophrenia. Previous neuroimaging studies targeting the glutamate system or neuroinflammation 13 , 14 , 16 , 28 , 43 have also reported alterations in the ACC and hippocampus, which are known to be important brain regions involved in schizophrenia. In addition, an elevated SUVr of MAO-B–binding [ 18 F]THK5351 in the bilateral ACC was positively correlated with positive symptom severity, as measured by the PANSS, in patients with schizophrenia. The ACC is one of the limbic cortices, and its role in fundamental cognitive processes, such as motivation, decision-making, and social cognition, which are impaired in patients with schizophrenia in relation to psychotic symptoms, has been highlighted. 44 , 45 A previous study from Kim et al, 46 which revealed that thalamocortical dysrhythmia represented by elevated resting-state theta phase–gamma amplitude coupling in the ACC of patients with schizophrenia spectrum disorder was positively correlated with symptom severity, also supported the association of reactive astrocytes in the ACC with positive symptoms. 2
This study has several limitations. First, the current study participants were patients with schizophrenia who had more than 5 years of antipsychotic treatment, although there have been suggestions of an association between prolonged exposure to antipsychotics and increased MAO-B expression in animal studies. 47 , 48 However, there have been no reports regarding the association between chronic antipsychotic exposure and MAO-B elevation in patients with schizophrenia, and a recent study 49 suggested that MAO-B detected by PET imaging is a target for novel drug development in patients with schizophrenia. 23 , 50 In addition, we did not find any correlation between the duration of illness or olanzapine-equivalent dose of antipsychotics prescribed at the time of study participation and the SUVrs of the primary ROIs. The current study results should be interpreted with caution because we did not perform this study in patients who were drug naive or with first-episode psychosis who may experience a minimal effect of antipsychotics on MAO-B expression. Second, because of the limitations of the MAO-B–detecting PET method, this study could only provide indirect evidence of reactive astrocytes in schizophrenia pathophysiology, as in previous animal, postmortem brain, and neuroimaging studies. 13 , 21 , 23 , 40 Further studies with direct methods to investigate astrocytes in patients with schizophrenia are warranted to confirm the role of reactive astrocytes in the pathophysiology of schizophrenia. Third, the results of the present study are exploratory findings that need further validation in other studies due to the small effect size associated with the small sample size and other limitations mentioned above.
This case-control study provides novel in vivo imaging evidence of reactive astrocyte involvement in the pathophysiology of schizophrenia. Considering the role of astrocytes in brain development, neurotransmission, and immune reactions, reactive astrocytes can be a strong biomarker for schizophrenia treatment. In particular, reactive astrocytes in the ACC may be a future target of neuromodulation therapeutics for the positive symptoms of schizophrenia. To support the findings of the present study, a more direct investigation of astrocytes generated by the reverse differentiation of induced pluripotent stem cells derived from patients with schizophrenia is needed.
Accepted for Publication: March 3, 2024.
Published: May 9, 2024. doi:10.1001/jamanetworkopen.2024.10684
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Kim M et al. JAMA Network Open .
Corresponding Author: Jun Soo Kwon, MD, PhD, Department of Psychiatry, Seoul National University College of Medicine, 101 Daehak-no, Chongno-gu, Seoul 03080, Republic of Korea ( [email protected] ).
Author Contributions: Drs M. Kim and Kwon had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: M. Kim, Song, Lho, Kwon.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: M. Kim, Cho.
Critical review of the manuscript for important intellectual content: M. Kim, W. Choi, S. Choi, Oh, J. Kim, J. Lee, An, Hwang, Y.-S. Lee, Song, Moon, Lho, Kwon.
Statistical analysis: M. Kim, W. Choi, S. Choi, Cho.
Obtained funding: M. Kim, Kwon.
Administrative, technical, or material support: M. Kim, J. Lee, Y.-S. Lee, Song, Moon, Lho, Cho, Kwon.
Supervision: M. Kim, Song, Cho, Kwon.
Conflict of Interest Disclosures: None reported.
Funding/Support: This research was supported by the Basic Science Research Program, the Brain Pool Program, and the Brain Science Convergence Research Program through the National Research Foundation of Korea and the Basic Research Program of the Korea Brain Research Institute, funded by grants 2020M3E5D9079910, 2020H1D3A2A02085669, RS-2023-00266120, and 21-BR-03-01 from the Ministry of Science and Information and Communication Technology.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Integrating AI into the Clinical Workflow
Key takeaways.
The article you recommended will be added to the "what others are reading" feed on "My ACR".
The article you bookmarked will be added to the "my reading list" feed on "My ACR".
- Radiologists at Lahey Hospital & Medical Center have integrated six artificial intelligence (AI) algorithms into their clinical workflow.
- The algorithms help diagnose and triage imaging studies for potentially critical findings, prioritizing potentially positive studies and improving patient care.
- The Lahey team encourages all radiologists to familiarize themselves with AI. To help, the ACR Data Science Institute (DSI) has developed a web-based catalog called AI Central ™ , which radiologists can use to learn more about AI algorithms that have FDA approval.
Recognizing an Opportunity
Contracting with a vendor, integrating the algorithms, working with ai, understanding the benefits, adding more tools, creative commons, share your story.
Now It’s Your Turn Follow these steps to begin integrating AI algorithms into your own practice and tell us how you did at [email protected] or on Twitter with the hashtag #Imaging3.
- Identify a use case for AI in your practice, whether it’s workflow prioritization, finding detection, or quantitative analysis.
- Compare vendors using the AI Center to determine which one can best help you achieve your goals.
- Work with the vendor to integrate the algorithm into your existing workflow so that the tool is easy for radiologists to use.
Jenny Jones, Imaging 3.0 manager
Join the Discussion

Call for Case Studies


IMAGES
VIDEO
COMMENTS
Cases. By sharing our collective experience through interesting and classic patient cases, we can make a real difference in how people are imaged and diagnosed. Each case belongs to a contributing member and all cases are reviewed by our dedicated editors to ensure they reach quality standards and abide by privacy guidelines. Cases can public ...
Learn & Practice Radiology. Twelve courses and 1,500+ interactive cases covering "must-know" diagnoses. Learn efficiently with sample reports, focused discussions and annotated images. Try for FREE. watch video.
RSNA Case Collection is a collection of peer-reviewed radiology cases. Home | RSNA Case Collection To help offer the best experience possible, RSNA uses cookies on its site.
Hence, the art of good clinical case presentation is a skill that needs to be mastered. Case presentations are a part of most undergraduate and postgraduate training programs aimed at nurturing oratory and presentation design skills. This article is an attempt at providing a trainee in radiology a guideline to good case presentation skills.
Radiology Case Reports is an open-access journal publishing exclusively case reports that feature diagnostic imaging. Categories in which case reports can be placed include the musculoskeletal system, spine, central …. View full aims & scope. $550.
The Imaging 3.0 case studies series spotlights radiologists who are partnering with clinicians, other medical professionals, and patients to make the transition from a focus on the volume of scans read to the value of care provided. Each case study includes actionable steps that providers can follow to implement similar initiatives at their own ...
This case study focuses on Erie Shores Healthcare, a small Canadian hospital with a busy emergency department (ED) who acts as the sole provider of outpatient diagnostic imaging (DI) services to the community. ... who note that patient transport is an area where waste commonly occurs in radiology departments. Currently, porters are an issue to ...
Stay up to date with the latest in Practical Medical Imaging and Management with Applied Radiology. Stay up to date. Create a new print or digital subscription to Applied Radiology. Subscribe! Renew / Update. Renew or update your current subscription to Applied Radiology. Renew / Update. Resources. Email Alert Manager; Author Guidelines;
Case Studies in Medical Imaging. This book is written as a system-based clinical-radiological review providing images from the latest available imaging modalities and covers all major diseases that are encountered in everyday clinical practice. A problem-orientated approach is used. Each chapter contains a collection of clinical cases each ...
Information Technology. Radiology has always been at the forefront of medical technology. Imaging 3.0 encourages radiologists to continue pushing the technological envelope in ways that improve patient care.
These case studies are designed for the education of medical professionals and radiologist. Adrenal + 6,988 Teaching File Images + 9,934,658 Views + Most Recent Case: Right Adrenal Adenoma Body MR + 2,297 Teaching File Images + 3,928,825 Views
Purpose. The purpose of a radiology case report is to describe the patient history, clinical course, and imaging for a notable or unusual case. The case may be intended to aid other practitioners in interpretation, but frequently the oddity, rarity, and non-generalisibility of cases are meant more to amuse or entertain the reader.
Abstracting and Indexing. This journal's articles appear in a wide range of abstracting and indexing databases, and are covered by numerous other services that aid discovery and access. Find out more about where and how the content of this journal is available. Case Reports in Radiology publishes case reports and case series in all areas of ...
European Radiology. European Radiology Experimental. Insights into Imaging. ESOR. Eurorad is the largest database for peer-reviewed radiological case reports, operated by the European Society of Radiology (ESR).
Interesting Case Files. Submission of Radiology ICF's to Yasin K. Jabir [email protected]. ... Search by Case Number: Case # Title Category Faculty Reviewer Year; 0001: Choroid plexus cyst : 0002: ... 23 year old female with 6.5 cm adnexal cyst seen on outside study. Body Imaging: Joseph P. Hasapes, M.D. 2012:
General Diagnostic Case Studies. Arteriovenous Fistula Secondary to Trauma. Chylothorax, Cellulitis, Gas Gangrene. Ectopic ACTH-Secreting Tumor. Epiphrenic Diverticula. Incidental Mediastinal Hilar Lymphadenopathy. Liver Metastasis. Neurocystercircosis. Pneumoperitoneum.
Aquifer Vitutal Patient Cases are case-based clinical simulations designed to develop clinical reasoning and self-directed learning and self-assessment skills. CORE ( Case-based Online Radiology Education). Register for a personal account using your PCOM email. See How To Register for Institutional Subscribers.
Interpretation differences between radiologists and diagnostic errors are significant issues in daily radiology practice. An awareness of errors and their underlying causes can potentially increase the diagnostic performance and reduce individual harm. The aim of this paper is to review both the classification of errors and the underlying biases. Case-based examples are presented and discussed ...
Breast cancer remains a significant public health concern in the United States and globally (1,2). It is the most common cancer across both sexes, accounting for nearly 15.5% of all cancers and is the second leading cause for cancer deaths in the United States (1). Despite effective screening tools such as mammography, there remain wide disparities in utilization, outcome, and mortality rates ...
Information and case studies for your medical students. Image Wisely. Image Wisely ® is a joint initiative of the American College of Radiology, Radiological Society of North America, American Society of Radiological Technologists and American Association of Physicists in Medicine. It offers resources and information to radiologists, medical ...
The case used in this study has been published 6 and is available for others to use in their own contexts. Here, we report on the implementation of ethics case study rounds to radiology residents at Dalhousie University and the University of Alberta, and explore using two different methods of presentation.
Home / Practice Management, Quality, Informatics / Imaging 3.0 / Case Studies /Quality and Safety. Quality and Safety. Ensuring patients receive the highest quality care — from monitoring dose levels to encouraging radiologist participation in patient quality initiatives — is a top priority of Imaging 3.0.
Acad Radiol 2024; 31:338-342. From the University of Wisconsin School of Medicine and Public Health, 750 Highland Ave, Madison, WI 53705; University of Maryland School of Medicine, Baltimore, Maryland. Received July 17, 2023; revised August 8, 2023; accepted August 19, 2023.
5 Department of Radiology, Seoul National University College of Medicine, Seoul, Republic of Korea. ... This case-control study provides novel in vivo imaging evidence of reactive astrocyte involvement in the pathophysiology of schizophrenia. Considering the role of astrocytes in brain development, neurotransmission, and immune reactions ...
Radiologists at Lahey Hospital & Medical Center have integrated six artificial intelligence (AI) algorithms into their clinical workflow. The algorithms help diagnose and triage imaging studies for potentially critical findings, prioritizing potentially positive studies and improving patient care. The Lahey team encourages all radiologists to ...
Our study found that Black patients had 45% greater odds of false-positive case scores and 46% greater odds of false-positive risk scores than White patients. If radiologists normalize the adoption of AI recommendations based on White patients—the largest demographic group in the United States—then they risk inappropriately higher recall ...