Exploring the Mind–Body Connection Through Research

From ancient philosophers and religions to modern science, there have been different views on whether the mind and the body are related, if they can affect each other, and how that interaction can be possible.
Although mainstream contemporary science and healthcare practices tend to study and treat the mind and the body as separate entities, increasing research and evidence-based practices support the notion of a bidirectional relationship between the two.
This suggests that we might benefit more from acknowledging these interactions and adopting a more holistic approach to our health and wellbeing.
Before you continue, we thought you might like to download our three Positive Psychology Exercises for free . These science-based exercises will explore fundamental aspects of positive psychology including strengths, values, and self-compassion and will give you the tools to enhance the wellbeing of your clients, students, or employees.

This Article Contains:
Mind–body connection: a philosophical take, psychology theories on mind–body interaction, 2 examples of the mind–body connection, can the mind heal the body 3 research areas, 10 empirical ways to heal your mind through your body, a look at the mechanisms of mind–body therapy, a take-home message.
Throughout centuries, philosophers and scientists have hypothesized about the mind–body connection. However, far from reaching a definite solution, we have been left with what many refer to as the mind–body problem .
According to Westphal (2016), this is a logical problem with four statements about the nature and interaction of mind and body.
While considered to be true in isolation, they contradict each other when brought together, as illustrated below:
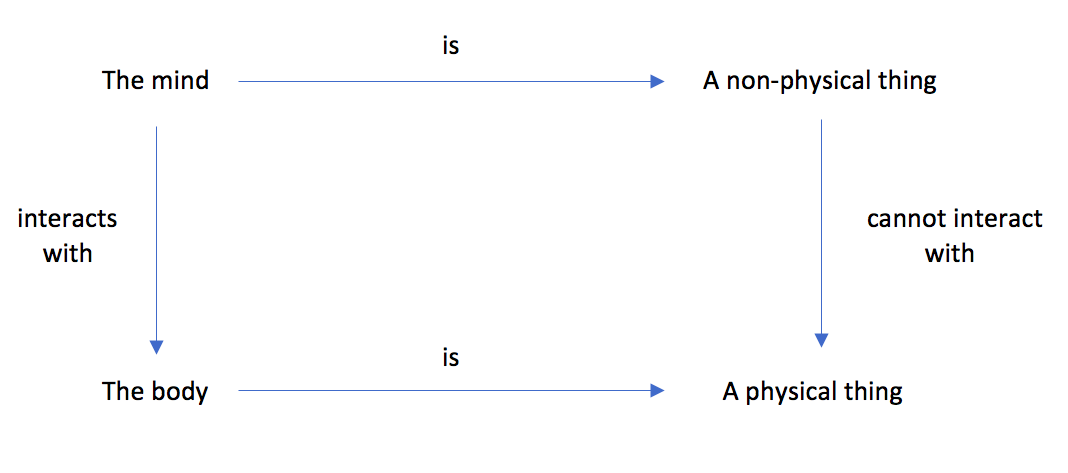
Figure 1. Illustration of the Mind–Body Problem. Adapted from “The Mind–Body Problem” by Westphal (2016). Copyright 2016 Massachusetts Institute of Technology.
Two main approaches within the philosophy of mind theorize about the mind–body connection by placing their attention in some of the statements above.
This approach posits that there is only one reality, composed only of either physical or non-physical substances (Kind, 2020).
Physicalism
This view assumes that everything existing is physical, including the mind. Here, the mind–body interaction is acknowledged only in the physical plane.
This is often related to traditional science, which tends to explain mental phenomena in terms of brain activities.
Using a metaphysical perspective, this standpoint sustains that reality is non-physical, and everything is either a mind or depends on the mind to exist.
In other words, this view proposes that reality depends on how our minds perceive and make sense of the world.
This philosophical standpoint theorizes that reality is composed of both physical and non-physical substances. Dualism posits that the body is physical, while the mind is not, treating mind and body as separate entities.
This worldview was developed by Rene Descartes during the 16th century, widely influencing modern science and compartmentalizing the study of body and mind (Descartes, 1960).
Dualism has evolved from views proposing that mind and body exist independently from one another without interaction, to ones that acknowledge a causal relationship between both.
According to Kind (2020), current views tend to be either interactionist property dualists or physicalists .
While physicalists would assert that the mind can be completely understood in terms of brain and neural networks, interactionist dualists would state that mental activities are rooted in the physical brain, yet are not reducible to these material properties (Westphal, 2016).
Non-dualism: Beyond the mind–body problem
This philosophical approach is often linked to several Eastern traditions and might provide further insight into the mind–body problem from a different angle.
Non-dualism proposes that the dualistic nature of things, such as mind/body, is an illusion.
Thus, there is no real separation between mind and body, as they are interdependent and need each other to exist (Loy, 1997).
Watch this short animated video by Embodied Philosophy to learn more about these approaches:
Interesting debate, but why and how is all this philosophical discussion relevant to mind–body research?
Although philosophy and empirical science may seem like independent silos, philosophy of mind is highly relevant to science and psychology in particular, as it informs the underlying assumptions and methods by which scientists conduct research and contribute to our understanding of mind–body interactions.

Behaviorists may hold a physicalist view, conceiving of the mind in terms of observable behavior expressed in or with the body.
While cognitivism acknowledges the body’s role, it tends to focus more on mental phenomena, reflecting a tendency towards dualism.
Finally, embodied approaches in psychology place equal value on the role of each, acknowledging their mutual interaction and adopting a more holistic view (Leitan & Murray, 2014).
Theories on emotions
These theories have evolved from considering emotions purely as physiological reactions to subjective interpretations to which we assign a valence depending on how they feel.
Cognitive appraisal theories
Pioneered by Magda Arnold and Richard Lazarus in the 1940s and 1950s respectively, the cognitive appraisal approach proposes that emotions result from the cognitive evaluation of an event in terms of their consequence as being pleasant or unpleasant (Shields & Kappas, 2006).
This is the background behind the use of the terms positive and negative emotions . Until the late 1990s, research on negative emotions broadly outnumbered studies on positive emotions, in part due to the perceived impact and relevance of negative emotions.
Broaden-and-build theory
Barbara Fredrickson (2000) posits that positive and negative affect complement each other and have the purpose of promoting the survival of the human species.
While negative emotions narrow our thought–action repertoire to respond more effectively to a threat, positive emotions expand this repertoire to build personal resources and pro-social behavior.
Remarkably, the broaden-and-build theory also states that “ positive emotions have an undoing effect on negative emotions ” (Fredrickson, 2000, p. 1).
Recent research in neuroscience has further supported this theory, suggesting that mindfulness and loving-kindness meditation can foster positive emotions and buffer against negative affect in a clinical population (Garland et al., 2010).
Cognitive theories
Although cognitive theories acknowledge the relationship between the mind (thoughts and subjective experiences of emotions) and the body (physical responses and behavior), they tend to place greater emphasis on the mental realm (Leitan & Murray, 2014).
This can be reflected in the lack of integration of the body within psychological interventions and psychotherapy (Hefferon, 2013).
Cognitive theory of psychopathology
Aaron Beck developed this model in the 1960s, contending that negative cognitions elicit unpleasant emotions, physical symptoms, and dysfunctional behavior.
He argues that these types of thoughts are the leading cause of depression, and therefore, psychotherapy should be aimed at addressing these mental processes to create positive change (Leitan & Murray, 2014).
Growth mindset theory
People with a growth mindset see challenges as opportunities to learn and grow, using their effort as a pathway to achieve mastery (Nussbaum & Dweck, 2008).
This involves mental processes grounded in the brain, such as increased awareness, attention, and the ability to adapt behavior to attain goals related to intrinsic motivation.
This framework is consistent with neuroplasticity, arguing that brain structures can reorganize, develop, and change according to our learning experiences (Ng, 2018).
Embodiment theories
This group of theories puts forward that bodily states and processes affect our psychological sphere and vice versa, contrasting with the disembodied view of the mind proposed by Descartes and early cognitivists.
Embodiment posits that our bodies mediate our interaction with the world and that mental symbols must be grounded in forms, such as words (Glenberg, 2010).
Embodied emotions
Considering previous theories on emotions, Prinz (2004) argues that although emotions are physical, they are essentially semantic too.
In other words, emotions can be conscious or unconscious perceptions of the body’s variations, but they are always grounded in language to an equal extent.
Embodied cognition (EC)
EC approaches generally agree that the type of body an organism has (e.g., human body) determines and shapes their perceptual and motor processes.
This means that the mind is grounded in the sensorimotor system, and that mind and body are equally relevant.
So rather than seeing the body as a server of the mind, EC posits that the body is actively and subjectively engaged in cognition (Leitan & Murray, 2014).
Embodiment theories allow bringing mind and body together into neuroscientific research, considering both participants’ subjective and physical experiences (Borghi & Caruana, 2015).
For example, a recent review of Beck’s Cognitive Theory considers neural and cognitive pathways to explain the effectiveness of Cognitive Therapy.
Research findings support the relationship between Cognitive Therapy and brain areas involved in initiating negative emotions and their cognitive control (Clark & Beck, 2010).

Download 3 Free Positive Psychology Exercises (PDF)
Enhance wellbeing with these free, science-based exercises that draw on the latest insights from positive psychology.
Download 3 Free Positive Psychology Tools Pack (PDF)
By filling out your name and email address below.
To support the psychology theories of mind-body interaction, we look at two examples.
The mind–body connection of trauma
The polyvagal theory describes and explains different mechanisms of neural regulation and their related behaviors when perceiving a threat, involving the brain cortex, immune response, hypothalamic-pituitary-adrenal, and gut-brain axes (Porges, 2001).
The chain reaction activated under these circumstances is called the defense cascade , comprising four different responses (Kozlowska, Walker, McLean, & Carrive, 2015):
- Arousal . Cardiac regulation response promotes either engagement or disengagement with the environment after perceiving a threat.
- Fight-or-flight response . The inhibition of the vagus nerve and the sympathetic nervous system’s activation lead to an increase in metabolic activity to mobilize the body to either escape or confront the threat.
- Freeze response . When facing an unavoidable threat, the vagus nerve is stimulated, the metabolic activity drops, and the body freezes.
- Quiescent immobility . After the threat is gone, the parasympathetic system overrides, and metabolic activity drops dramatically so the body can rest and heal.
Understanding the pattern of these responses can help us understand and heal trauma (Kozlowska et al., 2015).
Porges (2001) argues that the traumatic experience leaves an imprint in the body, getting stuck in a trauma-response mode.
Mind–body interventions can help people to release these imprints.
The mind–body connection of emotions and immunity
Research supports a strong relationship between affective states and immune system response.
Sustained negative emotional states such as stress, depression, and anxiety can worsen immunity functions and affect other bodily functions.
Recent studies show that positive emotions are associated with a range of health outcomes, such as reducing ill-health symptoms, reducing pain, and increasing longevity.
In terms of immunity and illness, positive emotions have been related to enhanced immunity outcomes in immune-depressive conditions, such as cancer and HIV, and also in the nonclinical population after being exposed to the flu virus (Pressman & Black, 2012).
But how is this possible? One possible pathway is that positive emotions buffer the stress response in the body and its consequences. This aligns with the undoing effect posited by the broaden-and-build theory.
Other pathways suggest that positive emotions promote social bonds and changes in lifestyle habits, such as clean eating, sleeping, and regular exercise, thus improving immunity (Pressman & Cohen, 2005).

A study exploring the effects of meditation on the brain compared novices to experienced meditators.
Functional MRI showed that experienced meditators had more brain activity in areas related to attention and inhibition response and less activation in regions related to discursive emotions and cognitions, suggesting a correlation between hours of practice and brain plasticity (Brefczynski-Lewis, Lutz, Schaefer, Levinson, & Davidson, 2007).
Loving-kindness meditation (LKM) is a type of meditation derived from Buddhist traditions, aiming at cultivating unconditional love and kindness for yourself and others, as well as compassion, joy, and equanimity.
A systematic review suggests that LKM is an effective intervention for increasing positive emotions and reducing pain (Zeng, Chiu, Wang, Oei, and Leung, 2015).
Mindfulness-based psychotherapy
Mindfulness can be used as a therapeutic tool to develop awareness and acceptance of feelings, thoughts, and bodily sensations, aligning to psychotherapy goals such as reducing ruminating thoughts or developing self-acceptance.
Applications linking the mind and the body can include mindful breathing and body scan exercises (Leitan & Murray, 2014).
A systematic review with meta-analysis found that mindfulness can help with depression, pain, weight management, schizophrenia, smoking, and anxiety (Goldberg et al., 2018).
Another study showed that a mindfulness program positively affects immunity and brain functions (Davidson et al., 2003).
Hypnotherapy
The American Psychological Association (2020) defines hypnosis as a therapeutic method used in clinical settings, where the client is induced into a state of relaxation by following suggestions from their psychotherapist.
It is hypothesized that in a relaxed state, the subconscious mind can more readily accept suggestions to change involuntary responses.
Clinical research evidence suggests that hypnosis can be useful for physical ailments such as managing pain and improving anxiety and depression.
One type of hypnosis is Gut-Directed Hypnotherapy , which has shown to effectively reduce irritable bowel syndrome symptoms and increase wellbeing (Peter et al., 2018).
Below are listed ten approaches believed to heal and improve the body and thereby heal and improve the mind.
1. Body psychotherapy
The body can be integrated as a central tool in psychotherapy by connecting bodily experiences to emotional and subjective experiences.
Body psychotherapy mainly uses body awareness of external and internal bodily sensations to accept and re-frame their meaning.
These mental health interventions can be beneficial not only for healing from trauma but also for wellbeing (Hefferon, 2013).
2. Exercise psychotherapy
Exercise can be used as a means to achieve psychotherapeutic goals, acknowledging that blending psychological and physical strategies can be more effective than using a standalone treatment.
This might include improving energy levels in clients with depression, reducing anxiety, or improving mastery and self-efficacy (Hefferon, 2013).
3. Somatic Experiencing (SE®)
SE® was developed by Dr. Peter Levine to regulate interrupted neuromuscular patterns due to trauma.
It consists of bringing awareness to physical sensations and reactions associated with a traumatic experience, helping clients describe physical patterns to integrate unconscious memories consciously.
Although there is limited empirical research, a systematic review including four studies on SE® suggests its effectiveness in improving post-traumatic stress disorder (PTSD) symptoms (Almeida, Gomez de Melo, & Cordeiro de Sousa, 2019).
4. Tension and trauma releasing exercises
Recently renamed as Self-induced Unclassified Therapeutic Tremor (SUTT), this method uses physical exercises to evoke natural tremor responses in the body to release tension associated with stress or trauma (Berceli, Salmon, Bonifas, & Ndefo, 2014).
Proposed by Dr. David Berceli, SUTT argues that although neuromuscular tremors are an innate response to events perceived as threatening, humans have learned to suppress them.
A pilot study (Berceli, et al. 2014) and a case study (Heath & Beattie, 2019) report that people experienced increased wellbeing and decreased stress at post-intervention measurements and follow-up.
Yoga is considered an ancient Eastern discipline integrating mind, body , and spirit through practices, typically including physical postures, breathing techniques, and meditation.
Yoga Chikitsa , or Yoga Therapy , refers to the use of yoga for improving ill-health conditions.
From a Western perspective, yoga has been used as an add-on therapy for improving symptoms of depression (Cramer, Lauche, Langhorst, & Dobos, 2013), anxiety (Cramer et al., 2018), PTSD (Nguyen-Feng, Clark, & Butler 2019), cancer (Cramer, Lange, Klose, Paul, & Dobos, 2012), and schizophrenia (Vancampfort et al., 2012).
Yoga benefits also relate to health and wellbeing outcomes in the general population (Hendriks, de Jong, & Cramer, 2017).
6. Dance therapy
Dance Movement Therapy (DMT) refers to “ the therapeutic use of movement aiming to further the emotional cognitive, physical, spiritual and social integration of the individual ” (European Association of Dance Movement Therapy, 2020, paragraph 1).
DMT seeks to understand and create new meanings from patterns of behavior by recognizing and exploring sensations, emotions, and stories emerging from the movement.
It is facilitated by a registered therapist, and it can be done individually or in a group setting (European Association of Dance Movement Therapy, 2020).
Studies suggest dance therapy ‘s effectiveness in improving ill health and trauma in clients with schizophrenia (Xia & Grant, 2009) and cancer (Bradt, Shim, & Goodill, 2015).
7. Progressive muscle relaxation (PMR)
Initially developed by Edmund Jacobson in the 1920s, PMR seeks to decrease anxiety levels by gradually contracting and relaxing muscle groups to reduce physical tension and physiological activation (Hefferon, 2013).
A systematic review with meta-analysis of relaxation intervention including 10 studies on PMR suggests this can be an efficacious treatment for anxiety in different clinical settings (Manzoni, Pagnini, Castelnuovo, & Molinari, 2008).
8. Deep breathing
Intentional breath regulation to increase pulmonary capacity while reducing the rate of breathing cycles has been acknowledged as an effective method to improve both physical and mental health .
By consciously engaging the diaphragm, the practice of slow-paced deep breathing activates the parasympathetic nervous system and inhibits the sympathetic nervous system, invoking a relaxation response and decreasing stress (Saoji, Raghavendra, & Manjunath, 2019).
Studies show that deep- breathing exercises can lower depressive and anxiety symptoms (Jerath, Crawford, Barnes, & Harden, 2015) and foster emotional wellbeing (Zaccaro et al., 2018).
9. Qigong and tai chi
Sharing the same philosophical roots, tai chi and qigong focus on the cultivation and enhancement of qi or life energy.
Along with yoga, they are considered meditative movement practices, and they include slow-paced and flow-like physical movements, as well as sitting, standing, or movement meditation; body shaking; and breathing techniques.
Underpinned by traditional Chinese medicine, they suggest that combining self-awareness with movement, meditation, and breath can promote mind–body balance and self-healing (Jahnke, Larkey, Rogers, Etnier, & Lin, 2010).
Several reviews have explored the effects of tai chi and qigong on different ill-health conditions such as cancer (Lee, Chen, Sancier, & Ernst, 2007), hypertension (Lee, Pittler, Guo, & Ernst, 2007), and cardiovascular disease (Lee, Pittler, Taylor-Piliae, & Ernst, 2007).
17 Top-Rated Positive Psychology Exercises for Practitioners
Expand your arsenal and impact with these 17 Positive Psychology Exercises [PDF] , scientifically designed to promote human flourishing, meaning, and wellbeing.
Created by Experts. 100% Science-based.
Mind–body Therapy (MBT) is an umbrella term for therapeutic approaches combining physical and mental elements, such as those mentioned above.
MBT has been gradually recognized as an effective add-on treatment to traditional approaches for improving physical and mental health outcomes.
Research in the field of genomics has shed light on the relationship between gene expression and emotional states.
Similarly, studies in neuroimaging and neurophysiology have examined the connections and pathways between emotions and thoughts (Muehsam et al., 2017).
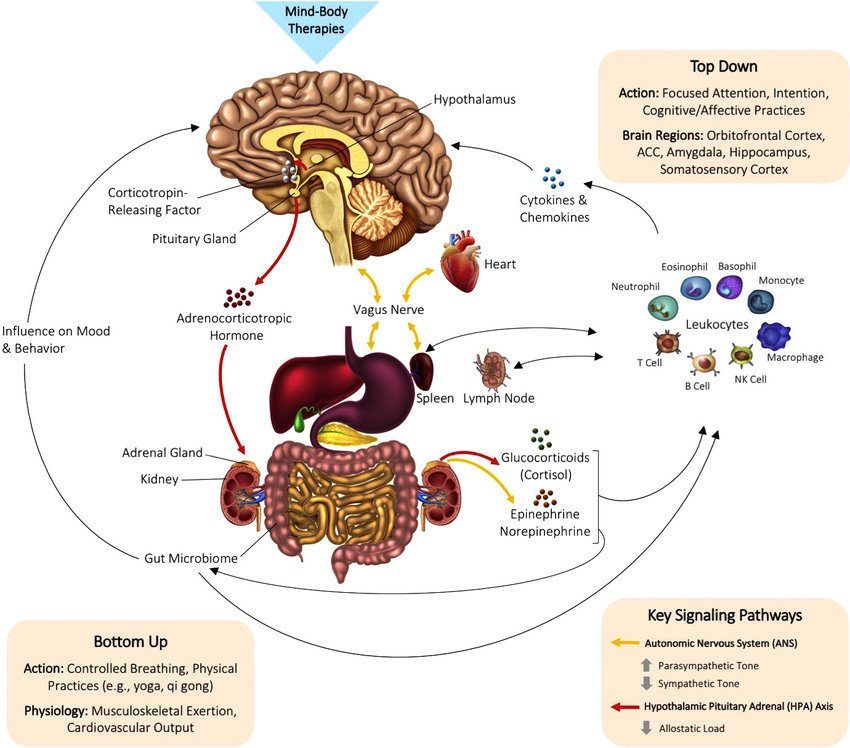
Figure 2. Biological Mechanisms of MBT. Extracted from “The embodied mind: a review on functional genomic and neurological correlates of mind-body therapies” by Muehsam, D., et al. (2017) Neuroscience & Biobehavioral Reviews, 73, p. 167. Copyright 2016 by Elsevier Ltd.
The diagram above illustrates how MBT works, including top-down and bottom-up pathways.
Top-down interventions like meditation or mindfulness focus on thoughts and emotions. Their neurological correlates in turn influence the endocrine and nervous system, with ulterior changes in the body.
Bottom-up interventions centered on breathing and physical movements such as yoga, tai chi, and qigong stimulate the nervous, immune, and endocrine systems, resulting in changes in psychological states.
The mind–body connection is undeniable, yet our understanding of how they interact is still limited.
The dualistic view of modern science has provided many advances in the knowledge of each, though in an isolated way.
Contemporary research urges the need to take a holistic approach to explore the mind and body as an integrated entity and continue to explore the potential of MBT for alleviating disease and enhancing wellbeing.
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free .
- Almeida, A. K., Gomez de Melo, S. C., & Cordeiro de Sousa, M. B. (2019). A systematic review of somatic intervention treatments in PTSD: Does Somatic Experiencing® (SE®) have the potential to be a suitable choice? Estudos de Psicologia , 24(3) , 237–246.
- American Psychological Association. (2020). Hypnosis. Retrieved on August 2020 from https://www.apa.org/topics/hypnosis.
- Berceli, D., Salmon, M., Bonifas, R., & Ndefo, N. (2014). Effects of self-induced unclassified therapeutic tremors on quality of life among non-professional caregivers: A pilot study. Global Advances in Health and Medicine , 3(5) , 45–48.
- Borghi, A.M., & Caruana, F. (2015). Embodiment theory. In: J.D. Wright (Ed.) International encyclopedia of the social & behavioral sciences, 2nd edition, Vol 6. (pp. 420–426). Oxford: Elsevier.
- Bradt, J., Shim, M., & Goodill, S. W. (2015). Dance/movement therapy for improving psychological and physical outcomes in cancer patients. Cochrane Database of Systematic Reviews, (1).
- Brefczynski-Lewis, J. A., Lutz, A., Schaefer, H. S., Levinson, D. B., & Davidson, R. J. (2007). Neural correlates of attentional expertise in long-term meditation practitioners. Proceedings of the National Academy of Sciences , 104(27) , 11483–11488.
- Clark, D. A., & Beck, A. T. (2010). Cognitive theory and therapy for anxiety and depression: Convergence with neurobiological findings. International Journal of Psychophysiology , 14(9) , 418–424.
- Cramer, H., Lauche, R., Anheyer, D., Pilkington, K., de Manincor, M., Dobos, G., & Ward, L. (2018). Yoga for anxiety: A systematic review and meta-analysis of randomized controlled trials. Depression and Anxiety , 35(9) , 830–843.
- Cramer H., Lange, S., Klose, P., Paul, A., & Dobos, G. (2012). Yoga for breast cancer patients and survivors: A systematic review and meta-analysis. BMC Cancer , 12 , 412–458.
- Cramer, H., Lauche, R., Langhorst, J., & Dobos, G. (2013). Yoga for depression: A systematic review and meta-analysis. Depression and Anxiety , 30 , 1068–1983.
- Davidson, R. J., Kabat-Zinn, J., Schumacher, J., Rosenkranz, M., Muller, D., Santorelli, S. F., … & Sheridan, J. F. (2003). Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine , 65(4) , 564–570.
- Descartes, R. (1960). Meditations on First Philosophy 1st Edition.
- European Association of Dance Movement Therapy. (2020). What is dance movement therapy? Retrieved on August 2020 from https://www.eadmt.com/?action=article&id=22.
- Fredrickson, B. L. (2000). Cultivating positive emotions to optimize health and wellbeing. Prevention and Treatment , 3(0001a) , 1–25.
- Garland, E. L., Fredrickson, B., Kring, A. M., Johnson, D. P., Meyer, P. S., & Penn, D. L. (2010). Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review , 30(7) , 849–864.
- Glenberg, A. M. (2010). Embodiment as a unifying perspective for psychology. Wiley Interdisciplinary Reviews: Cognitive Science , 1(4) , 586–596.
- Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review , 59 , 52–60.
- Heath, R., & Beattie, J. (2019). Case report of a former soldier using TRE (tension/trauma releasing exercises) for post- traumatic stress disorder self-care. Journal of Military and Veterans’ Health , 27(3) , 35–40.
- Hendriks, T., de Jong, J., & Cramer, H. (2017). The effects of yoga on positive mental health among healthy adults: A systematic review and meta-analysis. The Journal of Alternative and Complementary Medicine , 23(7) , 505–517.
- Hefferon, K. (2013). Positive psychology and the body: The somatopsychic side to flourishing . London: McGraw-Hill Education.
- Jahnke, R., Larkey, L., Rogers, C. Etnier, J., & Lin, F. (2010). A comprehensive review of health benefits of qigong and tai chi. American Journal of Health Promotion , 24(6) , 1–25.
- Jerath, R., Crawford, M. W., Barnes, V. A., & Harden, K. (2015). Self-regulation of breathing as a primary treatment for anxiety. Applications of Psychophysiological Feedback , 40 , 107–115.
- Kind, A. (2020). Philosophy of mind: The basics . New York: Routledge.
- Kozlowska, K., Walker, P., McLean, L., & Carrive, P. (2015). Fear and the defense cascade: Clinical implications and management. Harvard Review of Psychiatry , 23(4) , 263–287.
- Lee, M. S., Chen, K. W., Sancier, K. M., & Ernst, E. (2007) Qigong for cancer treatment: A systematic review of controlled clinical trials. Acta Oncologica , 46 , 717–722.
- Lee, M. S., Pittler, M. H., Guo, R., & Ernst, E. (2007). Qigong for hypertension: A systematic review of randomized clinical trials. Journal of Hypertension , 25 , 1525–32.
- Lee, M. S., Pittler, M. H., Taylor-Piliae, R. E., & Ernst, E. (2007). Tai chi for cardiovascular disease and its risk factors: A systematic review. Journal of Hypertension , 25 , 1974–1975.
- Leitan, N.D., & Murray, G. (2014). The mind-body relationship in psychotherapy: Grounded cognition as an explanatory framework. Frontiers In Psychology , 5(472) , 69–76.
- Loy, D. (1997). Nonduality: A study in comparative philosophy . New Jersey: Humanities Press.
- Manzoni, G. M., Pagnini, F., Castelnuovo, G., & Molinari, E. (2008). Relaxation training for anxiety: A ten-years systematic review with meta-analysis. BioMed Central Psychiatry , 8(41) , 1–12.
- Muehsam, D., Lutgendorf, S., Mills, P. J., Rickhi, B., Chevalier, G., Bat, N., … & Gurfein, B. (2017). The embodied mind: A review on functional genomic and neurological correlates of mind-body therapies. Neuroscience and Biobehavioral Reviews , 73 , 165–181.
- Nguyen-Feng, V. N., Clark, C. J., & Butler, M. E. (2019). Yoga as an intervention for psychological symptoms following trauma: A systematic review and quantitative synthesis. Psychological Services , 16(3) , 513–524.
- Ng, B. (2018). The neuroscience of growth mindset and intrinsic motivation. Brain Sciences , 8(2) , 20.
- Nussbaum, A. D., & Dweck, C. S. (2008). Defensiveness versus remediation: Self-theories and modes of self-esteem maintenance. Personality and Social Psychology Bulletin , 34(5) , 599–612.
- Peter, J., Fournier, C., Keip, B., Rittershaus, N., Stephanou-Rieser, N., Durdevic, M., … & Moser, G. (2018). Intestinal microbiome in irritable bowel syndrome: Before and after gut-directed hypnotherapy. International Journal of Molecular Sciences , 19 , 3619.
- Porges, S. W. (2001). The polyvagal theory: Phylogenetic substrates of a social nervous system. International Journal of Psychophysiology , 42(2) , 123–146.
- Pressman, S. D., & Black, L. L. (2012). Positive emotions and immunity. In S. C. Segerstrom (Ed.), The Oxford handbook of psychoneuroimmunology (pp. 92–104). New York: Oxford University Press.
- Pressman, S. D., & Cohen, S. (2005). Does positive affect influence health? Psychological Bulletin , 131(6) , 925–971.
- Prinz, J. (2004). Embodied emotions . In R. C. Solomon (Ed.), Thinking about feeling: Contemporary philosophers on emotions. Series in affective science. New York: Oxford University Press.
- Saoji, A. A., Raghavendra, B. R., & Manjunath, N. K. (2019). Effects of yogic breath regulation: A narrative review. Journal of Ayurveda and Integrative Medicine , 10(1) , 50–58.
- Shields, S. A., & Kappas, A. (2006). Magda B. Arnold’s contributions to emotions research. Cognition and Emotion , 20(7), 898–901.
- Vancampfort, D., Vansteelandt, K., Scheewe, T., Probst, M., Knapen, J., De Herdt, A., & De Hert, M. (2012). Yoga in schizophrenia: A systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica , 126(1) , 12–20.
- Westphal, J. (2016). The mind-body problem. Massachusetts Institute of Technology . Massachussets: MIT Press Books.
- Xia, J., & Grant, T. J. (2009). Dance therapy for schizophrenia. Cochrane Database of Systematic Reviews , 1 , 1–9.
- Zaccaro, A., Piarulli, A., Laurino, M., Garbella, E., Menicucci, D., Neri, B., & Gemignani, A. (2018). How breath control can change your life: A systematic review of psycho-physiological correlates of slow breathing. Frontiers of Human Neuroscience, 12 , 353 , 1–16.
- Zeng, X., Chiu, C. P., Wang, R., Oei, T. P., & Leung, F. Y. (2015). The effect of loving-kindness meditation on positive emotions: A meta-analytic review. Frontiers in Psychology, 6 , 1693, 1–14.
Share this article:
Article feedback
What our readers think.
Broad and concise amongs all the other sources. Thank you
Thanks for this very valuable research and proven work on the mind-body connection.
Thankyou for this wonderful article and your indepth research on recent studies. I’ll use this for my further research
Is an excellent article, the content is easy to read and very informative. It can be used as teaching resourcr
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

What Is the Health Belief Model? An Updated Look
Early detection through regular screening is key to preventing and treating many diseases. Despite this fact, participation in screening tends to be low. In Australia, [...]

Positive Pain Management: How to Better Manage Chronic Pain
Chronic pain is a condition that causes widespread, constant pain and distress and fills both sufferers and the healthcare professionals who treat them with dread. [...]

Mental Health in Teens: 10 Risk & Protective Factors
31.9% of adolescents have anxiety-related disorders (ADAA, n.d.). According to Solmi et al. (2022), the age at which mental health disorders most commonly begin to [...]
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (28)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (17)
- Positive Parenting (3)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (36)
- Self Awareness (21)
- Self Esteem (37)
- Strengths & Virtues (31)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
3 Positive Psychology Tools (PDF)
Our websites may use cookies to personalize and enhance your experience. By continuing without changing your cookie settings, you agree to this collection. For more information, please see our University Websites Privacy Notice .
Institute for Collaboration on Health, Intervention, and Policy (InCHIP)
Mind-body health research interest group.
The Mind-Body Health Research Interest Group (MBH RIG) is an interdisciplinary research collective that was established in 2015 and became part of InCHIP in 2019. Its mission is to further education, research, clinical/practical application, and community outreach with a focus on the emerging potential connections between the Mind and Body. The MBH RIG Directors are Drs. Melissa Bray, Mary Guerrera, Ana Verissimo, and Sandra Bushmich, and its members include students, faculty, and staff from UConn Health Center; UConn Hartford; College of Agriculture, Health, and Natural Resources; Neag School of Education; Operations and Information Management (OPIM) Department; and Student Health and Wellness. Non-UConn partners include Connecticut Children’s Medical Center, Copper Beech Institute, and Root Success Solutions™ LLC.
Leadership Team
Upcoming events:, the yes institute topic: supporting lgbtq+ youth health in today’s climate.
Towards a Fairer Future
When: March 6, 2024 | 6:30 to 7:30 PM EST University of Connecticut InCHIP Virtual – WebEx
Join us in learning from the YES Institute, a non-profit organization focused on the health of LGBTQ+ youth. They will be using both relevant research and vital personal experiences to help professionals, researchers, and allies improve health outcomes for this vulnerable population.
Our Speakers The YES Institute’s mission is toprevent suicide and ensure the healthydevelopment of all youth throughpowerful communication and education on gender and orientation.
Past Events:
“Hygge and Happiness,” Claus Elholm Andersen, Ph.D. “Introduction to Ayurveda,” Vanas hree Belgamwar, BAMS
Watch the recordings on InCHIP’s YouTube channel here .
“Go Outside, Go Within: Mindful Nature Connection for Surviving Zoom and Nature Deficit Disorder”
Watch the recording on InCHIP’s YouTube channel here .
“Connection: Exploring the Science of Mindfulness and Relationships”
Watch a recording on InCHIP’s YouTube channel here .

Mindfulness
How mindfulness affects the brain and body, interview with neuroscientist david vago..
Posted March 16, 2023 | Reviewed by Vanessa Lancaster
- What Is Mindfulness?
- Find a mindfulness-based therapist
- Despite its growing popularity, research on mindfulness presents methodological challenges.
- Mindfulness meditation can lower blood pressure, increase heart rate variability, improve inflammation, and help with pain management.
- Meditation can prevent age-related atrophy in the brain.

Neuroscientist David Vago begins each day with meditation. Like millions worldwide, Vago sees his mindfulness practice as good medicine holistically promoting health. Inspired by the staggering power of the human mind, Vago has studied the neurobiological mechanisms of mind-body practices for almost 15 years.
Mindfulness – a moment-to-moment, nonjudgmental awareness of one’s internal states and surroundings – boasts benefits ranging from stress reduction to enlightenment. However, scientific investigations of mindfulness paint a complex picture. Yes, it can boost physical and psychological well-being. But it is not a panacea and can even be counter-indicated for certain individuals. Despite significant progress over the past two decades, research on mindfulness is still riddled with various conceptual and methodological challenges. This is why, according to Vago, the question What does mindfulness really do? has no simple answer.
Mindfulness Is Far More Than Following Your Breath
Scientists like Vago study the effects of mindfulness by enrolling participants in eight-week interventions. There are four core practices in a mindfulness-based intervention:
- Focused attention . Mindfulness of breath or a body scan.
- Open monitoring . Being aware of thoughts arising and passing without attaching to them.
- Movement-based practices . Hatha yoga or walking meditation.
- Informal practices . Showing up with mindfulness in day-to-day life. Sometimes, the interventions can include constructive practices (loving-kindness meditation) that help individuals construct positive psychological states.
What about these practices that, moment by moment, begin to shift things for people? According to Vago, the possibilities are profound and consequential: people can get more insight into the workings of their minds; hone their ability to respond rather than to react to circumstances; gain glimpses of non-dual states; renew their understanding of the self and its place in the world; feel a deeper connection to others. “This is the Buddhist prescription for a flourishing life,” says Vago. “Everything else – the improved health and the calm – are merely side effects.”
The Gift of Paying Attention
One of the core faculties that mindfulness hinges on is attention. Attention might not have the buzzwordy flair of mindfulness . Yet, it’s one of our most precious resources. Attention, according to the father of modern psychology, William James, is somewhat of a curator of our lives (“My experience is what I agree to attend to.”) Poet Mary Oliver called paying attention “our endless and proper work.”
“Instructions for living a life: Pay attention. Be astonished. Tell about it.”
Philosopher Simone Weil considered attention “the rarest and purest form of generosity .” “Attention, taken to its highest degree, is the same as prayer. It presupposes faith and love , ” wrote Weil. Attention can even alter the perception of another limited human resource – time. As haste and demands leave many of us with the depleting feeling of weeks slipping by, attention can act as a salve to slow down the perceived passage of time (“ The best way to capture moments is to pay attention,” wrote Jon Kabat-Zinn, the founder of mindfulness-based stress reduction.)
Perhaps, then, one of the gifts of mindfulness can be found in nurturing our faculty of attention – to move it more nimbly, with more ease, between the micro and macro of our circumstances. To direct its precise lens on a single cherry blossom's pale, velvety petals and cast its vast reach beyond all boundaries . To discern content (thoughts, emotions) and context (relation to thoughts and emotions). To revel in the wonder that we are alive at this very moment, together with billions of other sentient beings near and far the blooming trees. This reminder will likely kindle a profound appreciation: for our impermanent existence and our affinity with others.
Here’s David Vago, on how mindfulness meditation affects the mind-brain-body.
MP: How does mindfulness benefit health?
DV: The most well-established health benefits of mindfulness meditation include a decrease in blood pressure and perceived stress , an increase in heart rate variability, and an improvement of inflammatory markers.
Mindfulness has also been shown to help with pain management . The experience of pain has physical and emotional components. While we can’t escape the physical effects of pain on the body, the emotional side (for example, catastrophizing pain) can be reduced through meditation. Namely, by impacting attentional biases, meditation can shift the way we attend to pain. For example, people with chronic pain conditions like fibromyalgia can begin to approach pain-related, fearful stimuli, which can help them become less hypervigilant, less avoidant, and less reactive to environmental pain-related signals.

In our lab, we are exploring the glymphatic system – a brain system associated with clearing metabolic waste. One of the ways that sleep benefits us is by eliminating toxins from our brains. Our findings show that by impacting the glymphatic system, mindfulness meditation – a low metabolic state – can act similarly to sleep and have restorative effects on brain functioning.
MP: How do mindfulness intervention outcomes compare to other treatments like therapy ?
DV: Overall, mindfulness improves various outcomes related to emotion , cognition , and the self (for example, rumination and empathy) – if we compare it to doing nothing else. Compared to treatments like SSRIs , anxiety drugs, or Cognitive Behavioral Therapy (CBT), mindfulness interventions work as well as these gold-standard treatment modalities but don’t often outperform them.
MP: Does mindfulness change the brain?
DV: Meditation instigates morphological changes in the brain. The challenge is quantifying them. Because the brain responds to every learning experience, it’s always changing. You’re always learning – no matter what you’re doing – thus, your brain is always changing. While there are different neuroscience methods to investigate how the brain changes shape and size, it’s difficult to show these changes in healthy individuals. In fact, it’s controversial what actually changes. However, for brains that have significant atrophy (for example, adults over 65 or brain trauma patients), morphological changes are detected more readily. This is in part because many atrophy processes are based on inflammation and meditation improves inflammation markers.
Functionally , brain imaging shows that mindfulness can activate the brain’s insula, the dorsal anterior cingulate, and the frontal-parietal network. The frontal parietal network is a group of brain structures that are critical for flexibly switching between processing the external world and the internal world. This helps us not get stuck in our thoughts. Often, our thoughts can have the quality of “stickiness.” For many of us, our most common thought is some version of “I’m not good enough.” We spend half of our lives in our heads, repeating to ourselves the various ways how we are not enough. These thoughts have us convinced that we are failing at some unachievable standard set by ourselves and society. As we elaborate on them, they start sticking. Hence our habit of rumination.
Mindfulness meditation helps develop the capacity to toggle between our thoughts and what’s happening in the world. The frontoparietal network also helps support meta-awareness – knowing where our mind is at any point. Moreover, research shows that individuals who develop high trait mindfulness can better regulate their emotions by increasing prefrontal activity and decreasing amygdala activity.
Whether or not meditation increases brain size has to do with preventing age-related atrophy in the brain. Most of meditation’s effects on cognition – executive functioning , attention, memory – don’t necessarily improve those skills in healthy individuals. It’s not like if you practice a lot of meditation. You’ll get super memory or outstanding decision-making abilities. Instead, brain areas that show increases in size with meditation are simply not atrophying in normal age-related ways.
After age 22, everyone’s cognitive capacities begin to decrease. We can see this as atrophy in specific regions in the brains of older adults. Thus, those older than 65 show the most increased brain size from an eight-week mindfulness course since meditation helps stabilize their cognition and prevents decline. The brains of older meditators don’t atrophy like most healthy, aging individuals because they are strengthening their abilities to keep those crucial brain areas active.
Many thanks to David Vago for his time and insights. Vago is an Associate Professor and visiting faculty at the University of Virginia’s Contemplative Sciences Center, Research Lead for the well-being app RoundGlass, and Director of Neurosciences for the International Society for Contemplative Research.
Ponte Márquez, P. H., Feliu-Soler, A., Solé-Villa, M. J., Matas-Pericas, L., Filella-Agullo, D., Ruiz-Herrerias, M., ... & Arroyo-Díaz, J. A. (2019). Benefits of mindfulness meditation in reducing blood pressure and stress in patients with arterial hypertension. Journal of Human Hypertension , 33 (3), 237-247.
Van Dam, N. T., Van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., ... & Meyer, D. E. (2018). Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science , 13 (1), 36-61.
Wittmann, M., & Schmidt, S. (2014). Mindfulness meditation and the experience of time. Meditation–neuroscientific approaches and philosophical implications , 199-209.
Hilton, L., Hempel, S., Ewing, B. A., Apaydin, E., Xenakis, L., Newberry, S., ... & Maglione, M. A. (2017). Mindfulness meditation for chronic pain: systematic review and meta-analysis. Annals of Behavioral Medicine , 51 (2), 199-213.
Nardi, W. R., Harrison, A., Saadeh, F. B., Webb, J., Wentz, A. E., & Loucks, E. B. (2020). Mindfulness and cardiovascular health: Qualitative findings on mechanisms from the mindfulness-based blood pressure reduction (MB-BP) study. PLoS One , 15 (9), e0239533.
Zollars, I., Poirier, T. I., & Pailden, J. (2019). Effects of mindfulness meditation on mindfulness, mental well-being, and perceived stress. Currents in Pharmacy Teaching and Learning , 11 (10), 1022-1028.
Christodoulou, G., Salami, N., & Black, D. S. (2020). The utility of heart rate variability in mindfulness research. Mindfulness , 11 , 554-570.
Bower, J. E., & Irwin, M. R. (2016). Mind–body therapies and control of inflammatory biology: A descriptive review. Brain, Behavior, and Immunity , 51 , 1-11.
Klimecki, O., Marchant, N. L., Lutz, A., Poisnel, G., Chetelat, G., & Collette, F. (2019). The impact of meditation on healthy ageing—the current state of knowledge and a roadmap to future directions. Current Opinion in Psychology , 28 , 223-228.

Marianna Pogosyan, Ph.D. , is a lecturer in Cultural Psychology and a consultant specialising in cross-cultural transitions.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- About UniSA
Professor Lorimer Moseley AO
- Bradley Distinguished Professor UniSA Allied Health & Human Performance
- City East Campus (C7-35)
- tel +61 8 830 21416
- email [email protected]
Alternative contact
- Available for media comment
- Research Degree Supervisor
Alternative contact details
Administrative Officer (Research) Tracy Jones: +61 8 8302 2454 Works - Monday, Tuesday, Thursday, Friday
- External engagement & recognition
- Teaching & student supervision
I am fascinated by humans. That fascination has led me to become a physiotherapist, then a neuroscientist, a pain scientist and a science educator. After working as a physiotherapist for seven years, I combined my clinical work with research - a PhD at the University of Sydney Pain Management Research Institute and research positions at the University of Queensland, University of Sydney and Oxford University, UK. My official qualifications are: DSc, PhD, FAAHMS, FACP, HonFFPMANZCA, HonMAPA, BAppSc(Phty)(Hons). In 2020, I was made an Officer of the Order of Australia, for "distinguished service to medical research and science communication, to education, to the study of pain and its management, and to physiotherapy, ... Read more

UniSA Allied Health & Human Performance
Focused on shaping community wellbeing, UniSA Allied Health & Human Performance educates future health professionals and delivers solutions-based research that addresses global health needs.
- Google Scholar
- ResearcherID
I am fascinated by humans. That fascination has led me to become a physiotherapist, then a neuroscientist, a pain scientist and a science educator. After working as a physiotherapist for seven years, I combined my clinical work with research - a PhD at the University of Sydney Pain Management Research Institute and research positions at the University of Queensland, University of Sydney and Oxford University, UK. My official qualifications are: DSc, PhD, FAAHMS, FACP, HonFFPMANZCA, HonMAPA, BAppSc(Phty)(Hons). In 2020, I was made an Officer of the Order of Australia, for "distinguished service to medical research and science communication, to education, to the study of pain and its management, and to physiotherapy, to humanity at large."
I was appointed University of South Australia's Inaugural Chair in Physiotherapy, and Professor of Clinical Neurosciences, in 2011 and was honoured to be appointed a Bradley Distinguished Professor in 2021.
I have been supported by NHMRC Fellowship/Investigator funding since my return to Australia in 2009.
I am the Chair of PainAdelaide Stakeholders' Consortium , which brings together Adelaide's pain researchers, clinicians and consumers to 'put our heads together' for persistent pain. I established and lead the non-profit grassroots movement called Pain Revolution , which is committed to a bold but realistic vision that all Australians will have access to the knowledge, skills and local support to prevent and overcome persistent pain. Our annual Flagship Event is the Pain Revolution Rural Outreach Tour. Our awareness and fund-raising challenge 'Go the Distance!' encourages pepole to walk, run or ride to meet their own personal challenge, raising awareness of the problem of persistent pain and the possibilities that are emerging with each new scientific discovery. Our ongoing capacity-building programs - Local Pain Educator Program and Local Pain Collectives Project , aim to (i) embed in rural and regional communities the capacity to prevent and overcome persistent pain, and (ii) develop local pain networks to provide sustainable capacity. Learn about Pain Revolution here: painrevolution.org.
I led the establishment of UniSA's Innovation, Implementation & Clinical Translation in Health ('IIMPACT in Health') and was Director from inception until 2023. IIMPACT has grown to about 100 researchers, publishing over 500 scientific articles a year, with a research income of about $2m a year. The research in IIMPACT centres around taking a truly 'biopsychosocial' to a range of significant health conditions, and the primary role that allied health professionals play in discovery and treatment. Central to IIMPACT has been an 'innovation to implementation' approach, led by clinical and consumer needs, with both playing important roles in every phase of the research journey.
I lead the Body in Mind Research Group within IIMPACT. This research group investigates the role of the brain and mind in chronic pain. Pain is a huge problem - it affects 20% of the population and costs western societies about as much as diabetes and cancer combined. We have a major public engagement and education focus, with our articles and videos attracting over 13 million reads/views, including being on repeat in hospitals and community health centres in several countries. Body in Mind, or 'BIM', research is supported by MRFF and NHMRC Grants and industry funding, and many BIMsters have NHMRC scholarship or fellowship support. We have eight nationalities and several disciplines represented.
For those of you keen on 'metrics' , my main metrics are: Total number of papers - about 400; Google scholar H-index - 95; Average Field-weighted citation index - 1.9 - 2.6 in the fields in which I am most active; competitive grant funding - about $22 million over 20 years.
I supervise PhD students and host post-doctoral fellows for between 1 - 3 years. Expressions of interest in joining our group should be directed in the first instance to [email protected]. We have many such expressions of interest each year so it is best to make contact at least 12 months in advance.
I co-developed, with David Moen and Sam Chisolm, a consumer facing resource called Tame the Beast - go to tamethebeast.org.
I established bodyinmind.org in 2009 and was Chief Editor until we handed it to the IASP. This library of over 900 blog posts is now hosted on their consumer/clinician facing website called RELIEF. You can visit that library here: https://relief.news/relief-to-provide-body-in-mind-content-as-a-free-resource/
Pain revolution is revamping our website , but until then you can find some factsheets you can download and print in a range of languages here: https://www.painrevolution.org/factsheets
I have authored or co-authored several books. You can find them here: https://www.noigroup.com/shop/
Please note that I receive royalties for these books. I have no financial interest in the publisher noigroup.com. I do however, have relevant disclosures - in the last five years, I have received support from the following entities: Reality Health, Kaiser Permanente, ConnectHealth UK, workers compensation agencies in Australia and abroad, AIA Australia, Arsenal Football Club, the International Olympic Committee. Professional and scientific bodies have reimbursed me for travel costs related to presentation of research on pain at scientific conferences/symposia.
I am on the Board of Pain Australia.
I live and work on Kaurna Country.
Professional Associations
Australian Academy of Health & Medical Science
Australian Physiotherapy Association
Faculty of Pain Medicine, Australia New Zealand College of Anaesthetists
International Association for the Study of Pain
Australian Pain Society
Qualifications
Doctor of Philosophy University of Sydney
Bachelor of Applied Sciences University of Sydney
- Professional associations
Research focus
- Clinical Sciences
- Neurosciences
- Human Movement and Sports Science
- Medical and Health Sciences
Excludes commercial-in-confidence projects.
Targeting unhelpful pain beliefs to promote physical activity in people with knee osteoarthritis: a multicentre, randomised controlled trial with cost-effectiveness analysis, NHMRC - Project Grant, 01/10/2019 - 31/10/2024
Gippsland Local Pain Educator Program, Gippsland Lakes Community Health, 01/11/2019 - 31/12/2021
Does targeting pain-related beliefs in people with knee osteoarthritis increase physical activity?, Arthritis Australia - Project Grants, 01/01/2018 - 30/06/2020
The role of the brain and mind in chronic pain, NHMRC - Research Fellowship, 01/01/2014 - 31/12/2019
Resolve: A new treatment - sensorimotor retaining with Explaining pain - for chronic low back pain, NHMRC - Project Grant, 01/01/2015 - 31/12/2019
Central Adelaide Local Health Network Incorporated Scholarship, Central Adelaide Local Health Network Incorporated, 01/03/2016 - 31/12/2017
Testing the imprecision hypothesis of chronic pain, NHMRC - Project Grant, 01/01/2013 - 31/12/2016
Joint pain without a joint? An investigation into the nature of postsurgical pain following joint replacement, Arthritis Australia, 01/01/2014 - 30/07/2016
Research outputs for the last seven years are shown below. Some long-standing staff members may have older outputs included. To see earlier years visit ORCID , ResearcherID or Scopus
Open access indicates that an output is open access.
Journal Articles
Conferences, non traditional outputs.
- Collaborations

Teaching & student supervision
Pain Sciences:
Lorimer gives lectures on pain sciences to undergraduate and post-graduate courses
- Courses and programs
Courses I teach
- SCALH 90001 Pain Education SC (2023)
- Research degree supervision
Supervisions from 2010 shown
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- March 1, 2024 | VOL. 19, NO. 3 CURRENT ISSUE pp.2-13
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Neurological Evidence of a Mind-Body Connection: Mindfulness and Pain Control
- Raymond St. Marie , M.D. ,
- Kellie S. Talebkhah , M.S.
Search for more papers by this author
Chronic pain is commonly defined as an unpleasant experience felt in any part of the body that persists longer than 3 months and that may or may not be associated with a well-defined illness process ( 1 ). Chronic pain affects up to 28%–65% of the U.S. population and often leads to reduced occupational activity and subsequent economic loss ( 2 ). In 2008, the costs of chronic pain in the United States ranged from $560 to $635 billion ( 3 ). In addition to health care costs, chronic pain results in lost economic productivity, as well as exorbitant financial compensation for persons unable to work ( 3 ). Providing pain relief that is clinically significant and sustained and that has few adverse effects is the goal of chronic pain management ( 4 ). Here, we assess the role of the mind-body connection (i.e., social, emotional, and behavioral factors influencing physical health) and how it relates to mindfulness techniques that can alleviate chronic pain ( 5 ).
Currently, the most commonly used and most widely available treatment modality for chronic pain is medication, with the goal of maximizing efficacy with the fewest toxic side effects ( 6 , 7 ). The most commonly prescribed agents are opioid-based medications, nonopioid agents (nonsteroidal anti-inflammatory drugs and acetaminophen), and adjuvant medications (anticonvulsants, muscle relaxants, corticosteroids, topical-numbing agents, and antidepressants) ( 8 ). However, there are nonpharmacologic treatment modalities, including mindfulness techniques, exercise programs, brain and spinal cord stimulation, and virtual-reality hypnosis ( 9 ). The most effective results are typically seen in multidisciplinary pain clinics, but these clinic services are not widely available to all patients ( 10 ).
Numerous studies have demonstrated the inadequacy of current pain management modalities and the need for newer, more widely available interventions ( 6 , 11 ). Physicians should consider supplementing or replacing medications with nonpharmacologic modalities such as mindfulness ( 12 , 13 ). Dr. Jon Kabat-Zinn, founder of the Center for Mindfulness in Medicine, defines mindfulness as "paying attention to something, in a particular way, on purpose, in the present moment, non-judgmentally" ( 14 ). The goal of mindfulness in the treatment of chronic pain is to cultivate a quality of openness and experiential acceptance of pain, rather than rejecting or avoiding the pain ( 14 ). In this way, mindfulness can be beneficial in treating chronic pain through a noninvasive approach via the mind-body connection ( 11 ).
The Role of Mindfulness
Mindfulness has been used as a supplement to medication for various conditions, including cancer, diabetes, and eating disorders ( 15 – 17 ). Dr. Kabat-Zinn describes mindfulness as being "more in touch with the fullness of [one's] being through a systematic process of self-observation, self-inquiry, and mindful action" ( 18 ). For many patients who experience chronic pain, these concepts of inward reflection may not appear to be possible, helpful, or preferable to medication. Furthermore, such patients may not associate the pervasive, intense nature of their condition with a psychological or spiritual idea ( 18 ). However, there is a growing body of evidence suggesting that mindfulness can be effective in the treatment of chronic pain ( 19 ).
Many studies have independently examined the effectiveness of mindfulness in pain reduction, the neurological effects of mindfulness, and the neurophysiology of pain ( 20 – 22 ). However, few studies have examined these aspects simultaneously while also investigating the relevant neurophysiological processes in relation to pain reduction ( 23 ).
Brain Regions Involved in Pain Processing
The various brain regions involved in central pain processing have specific, understood roles in the anticipation, evaluation, and response to pain. The lateral thalamus and primary somatosensory cortex are associated with the sensory processing and discriminative aspects of painful stimuli ( 24 ). The anterior cingulate and insular cortices have been shown to play a role in the emotional and arousal responses to pain, as well as in attentional processing, which is the way a person's brain filters relevant information from distractions in order to appropriately respond to a stimulus ( 24 – 26 ). The hippocampus and amygdala, alternatively, are involved in the anticipation of pain, while the thalamus modifies afferent input to these limbic structures ( 25 , 27 ) ( Figure 1 ).
FIGURE 1. Brain Regions Involved in Pain Processing a
a The open circles represent the specific role of a brain region in pain processing, and the small black squares represent neurological changes associated with mindfulness in conjunction with decreasing pain.
Structural Brain Changes
Neuroplasticity can occur within the nociceptive pathways involving the aforementioned brain regions in people who practice mindfulness-based stress reduction ( 24 ). Mindfulness-based stress reduction is a structured, weekly meditation program that has standardized guidelines and involves a combination of mindfulness meditation, body awareness, and yoga ( 19 ). Su et al. ( 28 ) examined functional MRI (fMRI) scans of the brains of persons who completed a 6-week mindfulness-based-stress-reduction course. fMRI was conducted at baseline and 6 weeks after completion of the course. Participants who completed the course experienced significantly less subjective pain elicited by a thermal stimulus compared with control subjects who did not complete the course. Attenuation of pain was associated with increased neuronal connectivity from the anterior insular cortex and dorsal anterior mid-cingulate cortex. These results suggest that mindfulness plays a role in the modulation of brain connections and networks that underlie the subjective experience of pain ( 28 ).
Grant et al. ( 20 ) used structural MRI scans to examine a group of individuals who were experts (defined as >10,000 hours of practice) in meditation techniques. Compared with control subjects, the expert meditators had a decreased sensitivity to pain, which was associated with significantly thicker dorsal anterior cingulate cortex and significantly thicker secondary somatosensory cortex. These results suggest that long-term mindfulness practice may affect cortical thickness in pain-related brain areas, thus causing changes in pain sensitivity ( 20 ).
Signal-Processing Changes
Changes in the processing of pain signals, specifically in areas involved in pain anticipation and attentional processing, have been reported ( 25 ). Lutz et al. ( 25 ) used fMRI in a study demonstrating that mindfulness techniques can modulate neural brain processes before (anticipation) and during (attentional) painful stimuli. In this study, expert meditators (compared with control subjects) reported significantly less unpleasantness from a painful stimulus elicited during meditation, which was associated with enhanced activity in the dorsal anterior insula and the anterior mid-cingulate, two areas of the brain associated with attentional processing. Meditators also had significantly less activity in the amygdala, an area associated with pain anticipation. These findings support the mindfulness principle, which suggests that openness of oneself to an experience of pain (attentional processing) rather than avoidance (anticipation) may reduce the mind's tendency toward anxiety, which can further exacerbate pain ( 25 ).
In another fMRI study, Zeidan et al. ( 29 ) reported that subjective decreases in pain sensation were associated with increased activity in the anterior cingulate cortex and anterior insula, two areas involved in the emotional regulation of pain processing as well as attentional processing. Increased activation in the orbitofrontal cortex, an area known to reframe contextual evaluation of sensory events similar to attentional processing, was also observed. Additionally, reductions in pain unpleasantness were associated with thalamic deactivation ( 29 ).
The aforementioned studies demonstrated that there are neurological changes involved in differentiating between the sensory experience of pain (subjective intolerance to pain) and the emotional response to pain (hopelessness and fear) ( 20 , 24 , 25 , 29 ). Identifying these experiences as separate, or "uncoupling" them from the emotional response via mindfulness techniques, allows one to distinguish between unpleasant sensations and secondary emotions in the context of pain, thus reducing the body's sensitivity to the unpleasant experience ( 18 ).

Autonomic Nervous System Process Changes
The autonomic nervous system plays a role in the anticipation of and response to pain ( 30 ). Through its integration with structures in the upper brainstem, hypothalamus, anterior cingulate cortex, insula, and amygdala, the autonomic nervous system integrates bodily sensation with emotion and generates homeostatic autonomic responses ( 30 ). Lush et al. ( 31 ) reported that women with fibromyalgia who completed a mindfulness-based stress-reduction program had decreases in basal sympathetic tone. Sympathetic nervous system responses typically exacerbate the physical symptoms of illness ( 30 ). Therefore, mindfulness-based stress reduction appears to play a role in attenuating autonomic nervous system responses, which can reduce chronic pain ( 31 ).
Braden et al. ( 32 ) reported that mindfulness-based stress-reduction practices were linked to alterations in the autonomic nervous system, specifically an increase in regional frontal-lobe blood flow, which was associated with the attenuation of chronic back pain and affective depression symptoms ( 32 ). The frontal lobe plays a role in reframing the contextual evaluation of an event ( 25 ). Therefore, this increase in hemodynamic activity is presumably associated with the reevaluation and awareness of changes in emotional state, a key concept of mindfulness ( 32 ). Being consciously aware of pain and uncoupling it from negative emotion are keys to decreasing the subjective experience of pain ( 18 , 32 ).
Conclusions
Although mindfulness has been well studied as an effective supplement or augmentation for pain management, few studies have simultaneously examined the neuroanatomical and neurophysiological alterations that can occur as a result of mindfulness to actively reduce pain. There are some contradictory studies that have demonstrated the potential ineffectiveness of mindfulness; however, it is important to consider that mindfulness is a modality that has minimal risks and can be beneficial. Further studies are needed to expand our understanding of the neurophysiological and psychological mechanisms underlying the effects of mindfulness on pain processing and perception.
Key Points/Clinical Pearls
Chronic pain affects up to 65% of the U.S. population and often leads to reduced occupational activity and subsequent economic loss.
Current pain management modalities are inadequate, leaving opportunity for nonpharmacological modalities such as mindfulness.
Mindfulness involves nonjudgmental observation of and present-moment engagement with one's physical, emotional, and mental states.
There are proven neuroanatomical and neurophysiological changes associated with mindfulness in reducing the subjective experience of pain.
1. Anand K, Craig K: New perspectives on the definition of pain . Pain 1996 ; 67:3–6 Google Scholar
2. Gerdle B, Bjork J, Henriksson C, et al. : Prevalence of current and chronic pain and their influences upon work and healthcare- seeking: a population study . J Rheumatol 2004 ; 31(7):1399–1406 Google Scholar
3. Gaskin J, Richard P: The Economic Costs of Pain in the United States: Relieving Pain in America: A Blueprint for Transofming Prevention, Care, Education, and Research . Washington, DC, National Academies Press, 2011 Google Scholar
4. Finnerup N, Sindrup S, Jensen T: The evidence for pharmacological treatment of neuropathic pain . Pain 2010 ; 150:573–581 Crossref , Google Scholar
5. Ray O: How the mind hurts and heals the body . Am Psychol 2004 ; 59(1):29–40 Crossref , Google Scholar
6. Falope E, Appel S: Substantive review of the literature of medication treatment of chronic low back pain among adults . J Am Assoc Nurse Pract 2015 ; 27(5):270–279 Google Scholar
7. Gilron I, Jensen T, Dickenson A: Combination pharmacotherapy for management of chronic pain: from bench to bedside . Lancet Neurol 2013 ; 12:1084–1095 Crossref , Google Scholar
8. Fine P: Pharmacological management of persistent pain in older patients . Clin J Pain 2004 ; 20(4):220–226 Crossref , Google Scholar
9. Turk D, McCarberg B: Non-pharmacological treatments for chronic pain: a disease management context . Dis Manag Health Outcomes 2005 ; 13(1):19–30 Crossref , Google Scholar
10. Okifuji A, Turk A, Kalauokalani D, et al. : Clinical outcome and economic evaluation of multidisciplinary pain centers , in Handbook of Pain Syndromes: Biopsychosocial Perspectives . Edited by Block A,Kremer E,Fernandez E. Mahwah, NJ, Lawrence Erlbaum Associates Publishers, 1999 , pp 77–97 Google Scholar
11. Lee C, Crawford C, Hickey A: Mind-body therapies for the self-management of chronic pain symptoms . Pain Med 2014 ; 15:S21–S39 Crossref , Google Scholar
12. Lynch M, Watson C: The pharmacotherapy of chronic pain: a review . Pain Res Manag 2006 ; 11(1):11–38 Crossref , Google Scholar
13. Burdick D: Mindfulness Skills Workbook for Clinicians and Clients: 111 Tools, Techniques, Activities, and Worksheets . Eau Claire, Wisc, PESI Publishing and Media, 2013 , p9 Google Scholar
14. Kabat-Zinn J: The clinical use of mindfulness meditation for the self-regulation of chronic pain . J Behav Med 1985 ; 8(2):163–190 Crossref , Google Scholar
15. Zhang J, Zhou Y, Feng Z, et al. : Randomized controlled trial of mindfulness-based stress reduction (MBSR) on posttraumatic growth of Chinese breast cancer survivors . Psychol Health Med 2017 ; 22(1):94–109 Crossref , Google Scholar
16. Caluyong M, Zambrana A, Romanow H, et al. : The relationship between mindfulness, depression, diabetes self-care, and health-related quality of life in patients with type 2 diabetes . Mindfulness 2015 ; 6(6):1313–1321 Crossref , Google Scholar
17. Cook-Cottone C: Incorporating positive body image into the treatment of eating disorders: a model for attunement and mindful self-care . Body Image 2015 ; 14:158–167 Crossref , Google Scholar
18. Kabat-Zinn J: Wherever you go, there you are . New York, MJF Books, 1994 , p 6 Google Scholar
19. Wong S, Chan F, Wong R, et al. : Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain: a randomized comparative trial . Clin J Pain 2011 ; 27:724–734 Crossref , Google Scholar
20. Grant J, Courtemanche J, Duerden E, et al. : Cortical thickness and pain sensitivity in Zen meditators . Emotion 2010 ; 10(1):43–53 Crossref , Google Scholar
21. Grossman P, Niemann L, Schmidt S, et al. : Mindfulness-based stress reduction and health benefits: a meta-analysis . J Psychosom Res 2004 ; 57:35–43 Crossref , Google Scholar
22. Shapiro S, Carlson L, Astin J, et al. : Mechanisms of mindfulness . J Clin Psychol 2006 ; 62(3):373–386 Crossref , Google Scholar
23. Greeson J, Eisenlohr-Moul T: Mindfulness-based stress reduction for chronic pain , in Mindfulness-Based Treatment Approaches . Edited by Baer R . San Diego, Academic Press, 2014 , pp269–292 Google Scholar
24. Nakata H, Sakamoto K, Kakigi R: Meditation reduces pain-related neural activity in the anterior cingulate cortex, insula, secondary somatosensory cortex, and thalamus . Front Psychol 2014 ; 5:1489. doi: 10.3389/fpsyg.2014.01489 Crossref , Google Scholar
25. Lutz A, McFarlin D, Perlman D, et al. : Altered anterior insula activation during anticipation and experience of painful stimuli in expert meditators . Neuroimage 2013 ; 64:538–546 Crossref , Google Scholar
26. Apkarian A, Bushnell M, Treede R, et al. : Human brain mechanisms of pain perception and regulation in health and disease . Eur J Pain 2005 ; 9(4):463–484 Crossref , Google Scholar
27. Ploghaus A, Narain C, Tracey I, et al. : Exacerbation of pain by anxiety is associated with activity in a hippocampal network . J Neurosci 2001 ; 21(24):9896–9903 Crossref , Google Scholar
28. Su I, Liang K, Cheng K, et al. : Pain perception can be modulated by mindfulness training: a resting-state fMRI study . Front Hum Neurosci 2016 ; 10:570 Crossref , Google Scholar
29. Zeidan F, Martucci K, Kraft R, et al. : Brain mechanisms supporting the modulation of pain by mindfulness meditation . J Neurosci 2011 ; 31(14):5540–5548 Crossref , Google Scholar
30. Cortelli P, Giannini G, Favoni V, et al. : Nociception and autonomic nervous system . Neurol Sci 2013 ; 34:S41–S46 Crossref , Google Scholar
31. Lush E, Salmon P, Floyd A, et al. : Mindfulness meditation for symptom reduction in fibromyalgia: psychophysiological correlates . J Clin Psychol Med Settings 2009 ; 16(2):200–207 Crossref , Google Scholar
32. Braden BB, Pipe TB, Smith R, et al. : Brain and behavior changes associated with an abbreviated 4-week mindfulness-based stress reduction course in back pain patients . Brain Behav 2016 ; 6(3):e00443 Google Scholar
- Biomarkers of stress as mind–body intervention outcomes for chronic pain: an evaluation of constructs and accepted measurement 2 April 2024 | Pain, Vol. 1
- Oxytocin Modulation in Mindfulness-Based Pain Management for Chronic Pain 15 February 2024 | Life, Vol. 14, No. 2
- Physical Pain as a Source of Spiritual and Artistic Inspiration in Jackson Hlungwani’s Work 1 November 2023 | Pharos Journal of Theology, No. 104(5)
- Sikhism and Its Contribution to Well-Being 1 August 2023
- Amy Gillespie , Ph.D. , and
- Catherine J. Harmer , D.Phil.
- Unlocking Performance Excellence: Review of Evidence-Based Mindful Meditation 8 August 2022 | Plastic & Reconstructive Surgery, Vol. 150, No. 4
- The intersection between integrative medicine and neuropathic pain: A case report EXPLORE, Vol. 18, No. 2
- Proprioceptive afferents differentially contribute to effortful perception of object heaviness and length 4 February 2021 | Experimental Brain Research, Vol. 239, No. 4

- Issue 1 Editorial
- Issue 1 Research 1
- Issue 1 Research 2
- Issue 1 Research 3
- Issue 1 The MBMRC
- Issue 2 Editorial I
- Issue 2 Editorial II
- Issue 2 Research 1
- Issue 2 Research 2
- Issue 2 Research 3
- Issue 2 Student´s corner
- Issue 3 Editorial
- Issue 3 Research 1
- Issue 3 Research 2
- Issue 3 Research 3
- Issue 3 Student´s corner
- Pre-Conference Workshops
The MBMRC Team
Curious who is behind the mbmrc let us introduce ourselves to you..

Tobias Esch, M.D.
Tobias Esch , M.D., MBMRC-Co-Chair , is a tenured Professor of Medicine and Director of the Institute of Integrative Health Care and Health Promotion at Witten/Herdecke University, Germany. He is a former Visiting Professor of Medicine at Harvard Medical School, and Harkness Fellow in Health Care Policy and Practice (The Commonwealth Fund, New York). With his background in neurobiology/neuroscience and health psychology and primary care, Esch focuses his work on integrative health promotion, especially Mind-Body Medicine, and patient empowerment.

George Stefano, Ph.D.
George Stefano , Ph.D., MBMRC-Co-Chair , Department of Psychiatry, First Faculty of Medicine, Charles University and General University Hospital in Prague, Czech Republic and Distinguished Prof. Emeritus at State University of New York. He also acted as the former Director of Basic Research at the Mind/Body Medical Institute (now Benson-Henry Institute) at Harvard Medical School. He has an outstanding expertise and highest accomplishments particularly in the field of neurobiology and behavioral neuroscience.

Prof. PhDr. Radek Ptáček, Ph.D., MBA
Prof. PhDr. Radek Ptáček , Ph.D., MBA clinical psychologist and the first professor of medical psychology in the Czech Republic. He also worked as a forensic psychologist for many years. His research is focused on the broadest issues of health psychology and medical psychology. He works as a professor at the Psychiatric Clinic of the 1st Faculty of Medicine of Charles University and the General Hospital in Prague. His research group has a long-term focus on the issue of lifestyle and mental disorders, burnout syndrome. ADHD is also a major research topic in the context of topics such as physical growth, diet and lifestyle, perception of time and sleep. He is the author of the most extensive series of monographs in the field of medical ethics and psychology, which as of this year has 13 monographs.

Dr. rer. medic. Dr. rer. oec. Maren M. Michaelsen
Dr. Dr. Maren M. Michaelsen, MBMRC Project Lead , is postdoctoral researcher and head of research at the Institute of Integrative Health Care and Health Promotion at Witten/Herdecke University, Germany. She is an active meditator und teacher of mind-body practices. With her background in health economics and behavioral sciences, Michaelsen focuses on health behavior change and mindfulness as elements of integrative health promotion. She conducts theoretical and empirical research in the field of Mind-Body Medicine with the aim to strengthen health competence in various population groups.

Dr. rer. nat. Franziska Melanie Collmann
Dr. Franziska Melanie Collmann, MBMRC Conference Organization , is postdoctoral researcher at the Institute of Integrative Health Care and Health Promotion at Witten/Herdecke University, Germany. She is the main point of contact in the organization of the upcoming International MBM Conference.
With her background in Biomedicine, Franziska is passionate about holistic approaches for a healthy life – both with regards to the fascinating aspect of the body and the mind. As a certified Yoga teacher and Systemic Coach, she combines mindfulness, body and mind into her daily work. Based on her fascination for the Mind-Body Medicine she is grateful to deepen her knowledge by contributing to related research projects.

Jil Herker, MSc
Jil Herker, MSc, MBMRC Web Management , is researcher at the Institute of Integrative Health Care and Health Promotion at Witten/Herdecke University, Germany.
As a psychologist, she is interested in the psychological perspective on health promotion. Additionally, she maintains our website and newsletter.

Helena Müller-Peters, BSc Helena Müller-Peters, BSc, is working as a student assistant in the preparation of the upcoming International Congress on MBM Research. After completing her Bachelor's degree in Organic Agriculture, she is currently studying Psychology at the University of Witten/Herdecke.
Within MBM research, she is particularly fascinated by the investigation of the effects of nutrition and mindfulness practice on health care.
Maja Figura, Bsc
MBMRC intern text and coordination ( March & April 2023)
Maja Figura, Bsc, is a mind-body medicine therapist currently finishing her MScPH.
Her area of interest is to make the latest scientific findings of mind-body medicine available to the public. She draws on many years of experience in teaching mindfulness techniques such as Yoga.
The Hosting Institute
The Mind-Body Medicine Research Concil has been founded by the Insitute for Integrative Health Care and Health Promotion
The Institute for Integrative Health Care and Health Promotion (IGVF), Faculty of Health/School of Medicine at Witten/Herdecke University, Germany focuses its attention on improving primary health care and increasing the effectiveness of health promotion efforts for patients. While the implications of our research findings certainly contribute to improving health outcomes at the population level, our focus remains on the individual and his or her personal resources and the pathways through which protective (salutogenetic) factors – including, but not limited to, resilience, self-efficacy, self-care and -healing, and the motivation to improve one’s personal health behaviors – can be activated and strengthened.
For this, we apply basic and applied sciences, from neurobiology to general health research, including integrative as well as mind/body medicine (MBM). Tobias Esch, a university professor, researcher, and physician, serves as the institute’s director and has founded the university’s outpatient clinic in general medicine, thus closing the gap between rigorous research and patient-focused practice, and ensuring that the research conducted remains clinically relevant to patients.
Our research efforts are driven by a team of researchers and health care practitioners from a wide spectrum of disciplines who work closely and effectively with one another. Witnessing the successful fusion of research and practice at the institute has led us to pursue additional and similarly fruitful collaborations.
Recent publications of MBMRC members
Büttiker, P., Weissenberger, S., Esch, T., Anders, M., Raboch, J., Ptacek, R., Kream,& R. M., & Stefano, G.B. (2023). Dysfunctional mitochondrial processes contribute to energy perturbations in the brain and neuropsychiatric symptoms. Front. Pharmacol. 13 :1095923. https://doi.org/10.3389/fphar.2022.1095923
Esch, T., Welzer, H., Utsch, M., & Donner, S. (2023). PSYCHOLOGIE HEUTE - Bei sich ankommen. 13-21. https://www.researchgate.net/publication/370471634_PSYCHOLOGIE_HEUTE_-_Bei_sich_ankommen
Michaelsen, M. M., Ecken, T. S., Herker, J. & Esch, T. (2023). Achtsamkeit & Ernährung - Neurobiologische Mechanismen achtsamen Essens. Sportärztezeitung , 4 , 90–95. https://sportaerztezeitung.com/rubriken/psychologie/15096/achtsamkeit-ernaehrung/
Michaelsen, M. M., & Esch, T. (2023). Understanding health behavior change by motivation and reward mechanisms: a review of the literature. Frontiers in Behavioral Neuroscience, 17 . https://doi.org/10.3389/fnbeh.2023.1151918
Michaelsen, M. M., Graser, J., Onescheit, M., Tuma, M. P., Werdecker, L., Pieper, D., & Esch, T. (2023). Mindfulness-based and mindfulness-informed interventions at the workplace: A systematic review and meta-regression analysis of RCTS. Mindfulness . https://doi.org/10.1007/s12671-023-02130-7
Poslt Königová, M., Sebalo Vňuková, M., Řehořková, P., Anders, M., & Ptáček, R. (2023). The effectiveness of gluten-free dietary interventions: A systematic review. Frontiers in Psychology , 14 , 1107022.
Sebalo Vňuková, M., Sebalo, I., Anders, M., Ptáček, R., & Surman, C. (2023). Psychometric Properties of the Czech Version of the Vanderbilt ADHD Diagnostic Parent Rating Scale. Journal of Attention Disorders , 10870547231167567.
Smetackova, I., Ptacek, R., Vnukova, M., & Dechterenko, F. (2023). The impact of ADHD in an individual's daily life on planning, coping and time perspective. Ceskoslovenska Psychologie , 67 (1), 15-29.
Stefano, G. B. (2023). Artificial Intelligence as a Tool for the Diagnosis and Treatment of Neurodegenerative Diseases. Brain Sciences , 13 (6), 938. https://doi.org /10.3390/brainsci13060938
Stefano, G. B., Büttiker, P., Weissenberger, S., Anders, M., Raboch, J., Ptacek, R., & Kream, R. M. (2023). Potential Prion Involvement in Long COVID-19 Neuropathology, Including Behavior. Cellular and Molecular Neurobiology , 1-6. https://doi.org/10.1007/s10571-023-01342-8
Stefano, G. B., Büttiker, P., Weissenberger, S., Esch, T., Anders, M., Raboch, J., Kream, R. M., & Ptacek, R. (2023). Independent and sensory human mitochondrial functions reflecting symbiotic evolution. Frontiers in Cellular and Infection Microbiology, 13 . https://doi.org/10.3389/fcimb.2023.1130197
Stefano, G. B., Büttiker, P. Weissenberger, S., Esch, T., Michaelsen, M., Anders, M., Raboch, J., & Ptacek, R. (2023). Artificial Intelligence: Deciphering the links between psychiatric disorders and neurodegenerative disease. Brain Sciences, 13 (7), 1055. https://doi.org/10.3390/brainsci13071055
Stefano, G. B., Kream, R. M., & Esch, T. (2023). Mobility Coupled with Motivation Promotes Survival: The Evolution of Cognition as an Adaptive Strategy. Biology , 12 (1). https://doi.org/10.3390/biology12010080
Urbanová, L., Vňuková, M. S., Anders, M., Ptáček, R. & Bušková, J. (2023). The Updating and Individualizing of Sleep Hygiene Rules for Non-clinical Adult Populations. Prague Medical Report, 124 (4), 329-343. https://doi.org/10.14712/23362936.2023.26
Vňuková, M., Děchtěrenko, F., Weissenberger, S., Anders, M., & Ptáček, R. (2023). Childhood School performance in adults diagnosed with attention-deficit/hyperactivity disorder. Journal of Attention Disorders , 27 (3), 307-312.
Vňuková, M., Ptáček, R., Děchtěrenko, F., Weissenberger, S., Ptáčková, H., Braaten, E., Raboch, J., Anders, M., Klicperová-Baker, M., & Goetz, M. (2021). Prevalence of ADHD symptomatology in adult population in the Czech Republic–A National Study. Journal of Attention Disorders , 25 (12), 1657-1664.
Vňuková, M. S., Sebalo, I., Brečka, T., Anders, M., & Ptáček, R. (2023). Burnout syndrome in the Czech Republic: The decreasing trend over the years. Frontiers in Public Health , 11 , 1099528.
Altmann, N., Scheer, L. & Esch, T. (2022). Digitale Kommunikation in der Praxis: Chancen, Risiken, Tipps und Tools. In M. Henningsen, P. Stachwitz, S. Fahimi-Weber, B. Afzali & N. Altmann (Hrsg.), Die digitale Arztpraxis: Technik, Tools und Tipps zur Umsetzung. Medizinisch Wissenschaftliche Verlagsgesellschaft.
Büttiker, P., Stefano, G. B., Weissenberger, S., Ptacek, R., Anders, M., Raboch, J. & Kream, R. M. (2022). HIV, HSV, SARS-CoV-2 and Ebola Share Long-Term Neuropsychiatric Sequelae. Neuropsychiatric Disease and Treatment , 18 , 2229–2237. https://doi.org/10.2147/NDT.S382308
Esch, T. (2022). The ABC Model of Happiness-Neurobiological Aspects of Motivation and Positive Mood, and Their Dynamic Changes through Practice, the Course of Life. Biology , 11 (6). https://doi.org/10.3390/biology11060843
Esch, T. & Brinkhaus, B. (2022). Die Bedeutung der Selbstregulation in der Integrativen und Mind-Body-Medizin. In A. Mollik (Hrsg.), Mindful Doctor: Next Generation Leadership in Medizin und Gesundheit. Medizinisch Wissenschaftliche Verlagsgesellschaft.
Esch, T. & Stefano, G. B. (2022). The BERN Framework of Mind-Body Medicine: Integrating Self-Care, Health Promotion, Resilience, and Applied Neuroscience. Frontiers in Integrative Neuroscience , 16 , 913573. https://doi.org/10.3389/fnint.2022.913573
Henningsen, M., Stachwitz, P., Fahimi-Weber, S., Afzali, B. & Altmann, N. (Hrsg.). (2022). Die digitale Arztpraxis: Technik, Tools und Tipps zur Umsetzung . Medizinisch Wissenschaftliche Verlagsgesellschaft.
Jacobs, A., Flägel, K., Werdecker, L. & Esch, T. (2022). Peak Moments im Ärzt*innen-Patient*innen-Kontakt der hausärztlichen Praxis–eine qualitative Studie mit Allgemeinmediziner*innen in Deutschland [Peak moments in physician-patient consultations in general practice: A qualitative study among primary care physicians in Germany]. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen , 172 , 31–39. https://doi.org/10.1016/j.zefq.2022.04.028
Karwetzky, C., Michaelsen, M. M., Werdecker, L. & Esch, T. (2022). The U-Curve of Happiness Revisited: Correlations and Differences in Life Satisfaction Over the Span of Life-An Empirical Evaluation Based on Data From 1,597 Individuals Aged 12-94 in Germany. Frontiers in Psychology , 13 , 837638. https://doi.org/10.3389/fpsyg.2022.837638
Koch, S., Esch, T. & Werdecker, L. (2022). Effects of a Yoga-Based Stress Intervention Program on the Blood Pressure of Young Police Officers: A Randomized Controlled Trial. Journal of Integrative and Complementary Medicine , 28 (3), 234–240. https://doi.org/10.1089/jicm.2021.0294
Michaelsen, M. M. & Esch, T. (2022). Functional Mechanisms of Health Behavior Change Techniques: A Conceptual Review. Frontiers in Psychology , 13 , 725644. https://doi.org/10.3389/fpsyg.2022.725644
Michaelsen, M. M. & Esch, T. (2022). Meditations- und Achtsamkeitsinterventionen zur Förderung psychischer Ressourcen in der supportiven onkologischen Behandlung. Onkologische Welt , 13 (03), 157–161. https://doi.org/10.1055/a-1729-9464
Schönfeld, S., Rathmer, I., Michaelsen, M. M., Hoetger, C., Onescheit, M., Lange, S., Werdecker, L. & Esch, T. (2022). Effects of a Mindfulness Intervention Comprising an App, Web-Based Workshops, and a Workbook on Perceived Stress Among Nurses and Nursing Trainees: Protocol for a Randomized Controlled Trial. JMIR research protocols , 11 (8), e37195. https://doi.org/10.2196/37195
Schwarz, J. & Esch, T. (2022). OpenNotes in Mental Health? Pro . Der Nervenarzt , 93 (11), 1163–1164. https://doi.org/10.1007/s00115-022-01357-4
Stefano, G. B., Büttiker, P. & Kream, R. M. (2022). Reassessment of the blood-brain barrier: a potential target for viral entry into the immune-privileged brain. Germs , 12 (1), 99–101. https://doi.org/10.18683/germs.2022.1310
Stefano, G. B., Büttiker, P., Weissenberger, S., Ptacek, R., Wang, F., Esch, T., Bilfinger, T. V., Raboch, J. & Kream, R. M. (2022). Biomedical Perspectives of Acute and Chronic Neurological and Neuropsychiatric Sequelae of COVID-19. Current Neuropharmacology , 20 (6), 1229–1240. https://doi.org/10.2174/1570159X20666211223130228
Stefano, G. B. & Kream, R. M. (2022). Mitochondrial DNA Heteroplasmy as an Informational Reservoir Dynamically Linked to Metabolic and Immunological Processes Associated with COVID-19 Neurological Disorders. Cellular and Molecular Neurobiology , 42 (1), 99–107. https://doi.org/10.1007/s10571-021-01117-z.
Stefano, G. B. & Kream, R. M. (2022). Viruses Broaden the Definition of Life by Genomic Incorporation of Artificial Intelligence and Machine Learning Processes. Current Neuropharmacology , 20 (10), 1888–1893. https://doi.org/10.2174/1570159X20666220420121746
Esch, T. (2022). The ABC Model of Happiness. Encyclopedia . https://encyclopedia.pub/entry/24683 ; (accessed on 30 June 2022)
Werdecker, L. & Esch, T. (2022). Glück in der Hausarztpraxis – Ergebnisse einer qualitativen Studie unter Praxisteams. Zeitschrift für Allgemeinmedizin , 98 (1), 24–29. https://doi.org/10.53180/zfa.2022.0024-0029
Werdecker, L. & Esch, T. (2022). Stress und Gesundheit. In R. Haring (Hrsg.), Gesundheitswissenschaften. Springer Berlin Heidelberg.
- Scroll to top
Control group design: enhancing rigor in research of mind-body therapies for depression
Affiliation.
- 1 Virginia Commonwealth University, School of Nursing, 1100 East Leigh Street, Richmond, VA 23298, USA.
- PMID: 23662111
- PMCID: PMC3638639
- DOI: 10.1155/2013/140467
Although a growing body of research suggests that mind-body therapies may be appropriate to integrate into the treatment of depression, studies consistently lack methodological sophistication particularly in the area of control groups. In order to better understand the relationship between control group selection and methodological rigor, we provide a brief review of the literature on control group design in yoga and tai chi studies for depression, and we discuss challenges we have faced in the design of control groups for our recent clinical trials of these mind-body complementary therapies for women with depression. To address the multiple challenges of research about mind-body therapies, we suggest that researchers should consider 4 key questions: whether the study design matches the research question; whether the control group addresses performance, expectation, and detection bias; whether the control group is ethical, feasible, and attractive; and whether the control group is designed to adequately control for nonspecific intervention effects. Based on these questions, we provide specific recommendations about control group design with the goal of minimizing bias and maximizing validity in future research.
Grants and funding
- M01 RR000065/RR/NCRR NIH HHS/United States
- R01 CA114718/CA/NCI NIH HHS/United States
- T32 AT000052/AT/NCCIH NIH HHS/United States
Christy Collins
Body in Mind & Lorimer Moseley
Body in Mind is a really interesting group of neuroscience researchers based in Australia. They study pain and what happens when the body’s pain processing system begins to malfunction. According to the “ Who We Are ” section of their website, Body in Mind is:
“…exploring how the brain and its representation of the body change when pain persists, how the mind influences physiological regulation of the body, how the changes in the brain and mind can be normalised via treatment, and how we can teach people about it all in a way that is both interesting and accurate.”
Lorimer Moseley is one of the driving forces behind Body in Mind. He does research focusing on the idea that pain is not an accurate indicator of tissue damage: sometimes we feel pain when there’s nothing wrong, and sometimes something can be very wrong and yet we feel no pain.
One of the things I really appreciate about Moseley’s approach is that he works a lot of witty anecdotes and stories into his explanations of pain, making them easy to understand (and also less depressing!).
He tells some of those same stories in this TEDx talk .
Scientific Articles
Lorimer Moseley– Reconceptualising pain according to modern pain science
Leave a Reply Cancel
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Frontiers in Psychology
- Cognitive Science
- Research Topics
Body in Mind
Total Downloads
Total Views and Downloads
About this Research Topic
The sense of touch is vital in development, and for how we perceive the world and interact with others. The skin envelopes our body and is our largest organ providing us with information about our immediate environment. In addition to this ‘surface’ information our somatosensory system also processes ...
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Appointments at Mayo Clinic
- Consumer health
- Mindfulness exercises
See how mindfulness helps you live in the moment.
If you've heard of or read about mindfulness meditation — also known as mindfulness — you might be curious about how to practice it. Find out how to do mindfulness exercises and how they might benefit you.
What is mindfulness?
Mindfulness is a type of meditation in which you focus on being intensely aware of what you're sensing and feeling in the moment, without interpretation or judgment. Practicing mindfulness involves breathing methods, guided imagery, and other practices to relax the body and mind and help reduce stress.
Spending too much time planning, problem-solving, daydreaming, or thinking negative or random thoughts can be draining. It can also make you more likely to experience stress, anxiety and symptoms of depression. Practicing mindfulness exercises can help you direct your attention away from this kind of thinking and engage with the world around you.
What are the benefits of meditation?
Meditation has been studied in many clinical trials. The overall evidence supports the effectiveness of meditation for various conditions, including:
- High blood pressure (hypertension)
Preliminary research indicates that meditation can also help people with asthma and fibromyalgia.
Meditation can help you experience thoughts and emotions with greater balance and acceptance. Meditation also has been shown to:
- Improve attention
- Decrease job burnout
- Improve sleep
- Improve diabetes control
What are some examples of mindfulness exercises?
There are many simple ways to practice mindfulness. Some examples include:
- Pay attention. It's hard to slow down and notice things in a busy world. Try to take the time to experience your environment with all of your senses — touch, sound, sight, smell and taste. For example, when you eat a favorite food, take the time to smell, taste and truly enjoy it.
- Live in the moment. Try to intentionally bring an open, accepting and discerning attention to everything you do. Find joy in simple pleasures.
- Accept yourself. Treat yourself the way you would treat a good friend.
- Focus on your breathing. When you have negative thoughts, try to sit down, take a deep breath and close your eyes. Focus on your breath as it moves in and out of your body. Sitting and breathing for even just a minute can help.
You can also try more structured mindfulness exercises, such as:
- Body scan meditation. Lie on your back with your legs extended and arms at your sides, palms facing up. Focus your attention slowly and deliberately on each part of your body, in order, from toe to head or head to toe. Be aware of any sensations, emotions or thoughts associated with each part of your body.
- Sitting meditation. Sit comfortably with your back straight, feet flat on the floor and hands in your lap. Breathing through your nose, focus on your breath moving in and out of your body. If physical sensations or thoughts interrupt your meditation, note the experience and then return your focus to your breath.
- Walking meditation. Find a quiet place 10 to 20 feet in length, and begin to walk slowly. Focus on the experience of walking, being aware of the sensations of standing and the subtle movements that keep your balance. When you reach the end of your path, turn and continue walking, maintaining awareness of your sensations.
When and how often should I practice mindfulness exercises?
It depends on what kind of mindfulness exercise you plan to do.
Simple mindfulness exercises can be practiced anywhere and anytime. Research indicates that engaging your senses outdoors is especially beneficial.
For more structured mindfulness exercises, such as body scan meditation or sitting meditation, you'll need to set aside time when you can be in a quiet place without distractions or interruptions. You might choose to practice this type of exercise early in the morning before you begin your daily routine.
Aim to practice mindfulness every day for about six months. Over time, you might find that mindfulness becomes effortless. Think of it as a commitment to reconnecting with and nurturing yourself.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Bystritsky A. Complementary and alternative treatments for anxiety symptoms and disorders: Physical, cognitive, and spiritual interventions. https://uptodate.com/contents/search. Accessed June 14, 2018.
- Seaward BL. Meditation and mindfulness. In: Managing Stress: Principles and Strategies for Health and Well-being. 9th ed. Burlington, Mass.: Jones & Bartlett Learning; 2018.
- Shapiro SL, et al. The Art and Science of Mindfulness: Integrating Mindfulness into Psychology and the Helping Professions. 2nd ed. Washington, D.C.: American Psychological Association; 2017.
- Lymeus F, et al. Building mindfulness bottom-up: Meditation in natural settings supports open monitoring and attention restoration. Consciousness and Cognition. 2018;59:40.
- Blanck P, et al. Effects of mindfulness exercises as stand-alone interventions on symptoms of anxiety and depression: Systematic review and meta-analysis. Behaviour Research and Therapy. 2018;102:25.
- AskMayoExpert. Meditation. Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2018.
- Khoury B, et al. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research. 2015;78:519.
- Practice mindfulness and relaxation. Springboard Beyond Cancer. https://survivorship.cancer.gov/springboard/stress-mood/practice-mindfulness. Accessed June 14, 2018.
Products and Services
- A Book: The Mayo Clinic Diet Bundle
- The Mayo Clinic Diet Online
- A Book: Mayo Clinic Guide to Pain Relief
- A very happy brain
- Alternative cancer treatments: 11 options to consider
- Candida cleanse diet
- Colloidal silver supplements
- Colon cleansing
- Detox foot pads
- Diabetes treatment: Can cinnamon lower blood sugar?
- Do infrared saunas have any health benefits?
- Prickly pear cactus
- Herbal supplements and heart drugs
- Kombucha tea
- Kratom: Unsafe and ineffective
- Kratom for opioid withdrawal
- Learn to reduce stress through mindful living
- Medical marijuana
- Meditation 2.0: A new way to meditate
- Natural remedies for depression: Are they effective?
- Tai Chi and Cardiac Rehab
- Valerian: A safe and effective herbal sleep aid?
- Alternative psoriasis treatments
- Do zinc supplements shorten colds?
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
6 Common Leadership Styles — and How to Decide Which to Use When
- Rebecca Knight

Being a great leader means recognizing that different circumstances call for different approaches.
Research suggests that the most effective leaders adapt their style to different circumstances — be it a change in setting, a shift in organizational dynamics, or a turn in the business cycle. But what if you feel like you’re not equipped to take on a new and different leadership style — let alone more than one? In this article, the author outlines the six leadership styles Daniel Goleman first introduced in his 2000 HBR article, “Leadership That Gets Results,” and explains when to use each one. The good news is that personality is not destiny. Even if you’re naturally introverted or you tend to be driven by data and analysis rather than emotion, you can still learn how to adapt different leadership styles to organize, motivate, and direct your team.
Much has been written about common leadership styles and how to identify the right style for you, whether it’s transactional or transformational, bureaucratic or laissez-faire. But according to Daniel Goleman, a psychologist best known for his work on emotional intelligence, “Being a great leader means recognizing that different circumstances may call for different approaches.”
- RK Rebecca Knight is a journalist who writes about all things related to the changing nature of careers and the workplace. Her essays and reported stories have been featured in The Boston Globe, Business Insider, The New York Times, BBC, and The Christian Science Monitor. She was shortlisted as a Reuters Institute Fellow at Oxford University in 2023. Earlier in her career, she spent a decade as an editor and reporter at the Financial Times in New York, London, and Boston.
Partner Center
Moscow Lexical Typology group
Seminar seminars of the student research group “typological studies in lexicon”.
In 2014-2016 seminars of the Student Research Group “Typological Studies in Lexicon” were held every fortnight in the School of Linguistics, NRU Higher School of Economics.
In 2014, the group investigated animal sounds in lexical typological perspective. Students presented analyses of this semantic field in different languages. As a result, a database containig the data of 20 languages was created and a collection of papers with detailed descriptions of the semantic systems in question was published.
In 2015, the focus of the research shifted to the zone of falling. Fundamental components of this field were discoverd: (1) object of falling, (2) starting point of falling, (3) end point of falling. These components served as the basis for the semantic map, which summarized similarities and differences in the organization of this field in languages of the world. A database visualizing connections between frames of falling in different languages was created and published on-line .
- Work & Careers
- Life & Arts
Become an FT subscriber
Try unlimited access Only $1 for 4 weeks
Then $75 per month. Complete digital access to quality FT journalism on any device. Cancel anytime during your trial.
- Global news & analysis
- Expert opinion
- Special features
- FirstFT newsletter
- Videos & Podcasts
- Android & iOS app
- FT Edit app
- 10 gift articles per month
Explore more offers.
Standard digital.
- FT Digital Edition
Premium Digital
Print + premium digital, digital standard + weekend, digital premium + weekend.
Today's FT newspaper for easy reading on any device. This does not include ft.com or FT App access.
- 10 additional gift articles per month
- Global news & analysis
- Exclusive FT analysis
- Videos & Podcasts
- FT App on Android & iOS
- Everything in Standard Digital
- Premium newsletters
- Weekday Print Edition
- FT Weekend newspaper delivered Saturday plus standard digital access
- FT Weekend Print edition
- FT Weekend Digital edition
- FT Weekend newspaper delivered Saturday plus complete digital access
- Everything in Preimum Digital
Essential digital access to quality FT journalism on any device. Pay a year upfront and save 20%.
- Everything in Print
- Everything in Premium Digital
Complete digital access to quality FT journalism with expert analysis from industry leaders. Pay a year upfront and save 20%.
Terms & Conditions apply
Explore our full range of subscriptions.
Why the ft.
See why over a million readers pay to read the Financial Times.
International Edition
MOSCOW - RUSSIA
Icb - indicator group, moscow.
Moscow Aurora Business Park, 2nd Dl., 82 Sadovnicheskaya St., Building 2, 115035 Moscow, Russia
- Phone: +7 (495) 225 9353
- Fax: +7 (495) 225 9300
- email: [email protected]
- web: www.indicatorgroup.com
Company Profile
- LIST WITH US
To: ICB - INDICATOR GROUP, MOSCOW
Enter the security code:
+7 (495) 225 9300
+7 (495) 225 9353
Directory of Freight Forwarders, Cargo Agents, Shipping Companies, Air, Ocean, Land, Logistics and Transportation Brokers
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Focus (Am Psychiatr Publ)
- v.19(2); Spring 2021

Mind-Body Interventions for Anxiety Disorders: A Review of the Evidence Base for Mental Health Practitioners
Mind-body interventions have gained increasing popularity for use with anxiety symptoms; however, it is unclear what role they play in the treatment of anxiety disorders, such as generalized anxiety disorder, panic disorder, and social anxiety disorder. Although psychopharmacology and psychotherapy treatment interventions are available, mind-body interventions may be low-stigma options that can serve as effective alternatives. The goal of this review is to provide clinicians with an overview of high-quality studies for the most well researched mind-body interventions. This review involved a search of the primary literature, including meta-analyses, systematic reviews, and randomized controlled trials (RCTs), that evaluated mind-body interventions for the treatment of anxiety disorders. When published evidence was limited, lower-quality studies were reviewed. Overall, data were limited on the efficacy of most mind-body modalities for anxiety disorders. The highest-quality data existed for yoga, mindfulness-based interventions, and applied relaxation for anxiety disorders. However, findings were sometimes inconsistent across studies, and some studies were limited by small sample sizes, poorly defined randomization and blinding procedures, and inadequate control groups. Although not enough data exist to recommend mind-body interventions as primary treatment options, they may be considered as part of a larger treatment plan given their relatively low levels of risk. Future steps for researchers include conducting additional RCTs with adequate control groups, comparing mind-body treatments with existing treatments, and examining long-term effects of mind-body interventions.
Mind-body interventions, such as yoga and mindfulness meditation, are an area of exponential growth and increased interest of the general population; yet clear clinical guidelines are limited concerning which interventions are evidenced based and appropriate for general psychiatric practice. Furthermore, it is unclear what role these interventions play in the treatment of anxiety disorders. The most common anxiety disorders are panic disorder, specific phobia, generalized anxiety disorder, and social anxiety disorder. These disorders often cause significant impairment in social, interpersonal, or occupational functioning, with a lifetime prevalence of nearly 33.7% ( 1 ); economic costs of these disorders, estimated at $42.3 billion per year ( 2 ), are attributed to treatment, lost productivity, and poor quality of life ( 3 ). Psychiatrists may be asked by their patients about whether any of these mind-body interventions are appropriate for them. The purpose of this review is to summarize the high-quality literature on effective mind-body interventions for anxiety disorders to better inform general psychiatric practice.
This review involved a search of the primary literature, including articles from the Ovid MEDLINE, PsycArticles, and PsycINFO databases; additional studies cited in prior literature reviews and meta-analyses were also added. Studies that included patients with a diagnosed anxiety disorder, such as social anxiety, general anxiety, panic disorder, or specific phobia, were reviewed as well as studies that utilized a validated anxiety severity questionnaire with a predefined cutoff score thought to represent the likely presence of an anxiety disorder. For mind-body interventions with limited data on anxiety disorders, we reviewed their effect on anxiety symptoms if a cutoff score was used to indicate likely presence of the disorder. Studies that consisted of an intervention that was not given through a formally trained teacher or developed and designed by a trained teacher or practitioner were excluded. In addition, literature that focused on mind-body interventions for a primary diagnosis of obsessive-compulsive disorder, posttraumatic stress disorder, or substance use disorder were excluded. High-quality data from meta-analyses, systematic reviews, and randomized controlled trials (RCTs) were given priority; however, for mind-body interventions with limited data, lower-quality studies were included. Studies that included comorbid depression were included if thought to be useful to the general psychiatrist, given the high comorbidity with anxiety disorders and depression.
Mind-Body Interventions and Evidence
Meditation and mindfulness-based interventions (mbis).
Meditation practices have received increased interest as possible interventions for psychological distress and anxiety. Mindfulness meditation is a type of meditation that has been widely researched in studies using adapted, manualized MBIs to improve emotional coping and physical well-being. The focus of MBI is on the practice of mindfulness, which involves paying attention to one’s thoughts, feelings, and physical sensations and adopting a nonjudgmental stance toward them ( 4 ). We examined studies that were close approximations of the established MBI formats (i.e., mindfulness-based stress reduction [MBSR], mindfulness-based cognitive therapy [MBCT]) and included patients whose primary diagnosis was an anxiety disorder such as generalized anxiety disorder, panic disorder, and social anxiety disorder.
The more well-studied MBIs included MBSR and MBCT. These formats are both standardized, manualized, 8-week programs that include group sessions and individual home practices. Classes are 2–2.5 hours weekly and led by a trained instructor; they include a 1-day “retreat” as well as daily audio-guided individual home practice for about 45 minutes per day ( 5 ). MBSR was created by Jon Kabat-Zinn in 1979 to assist patients with chronic pain, but it has since been applied to many other physical and emotional problems ( 6 ). MBSR teaches mindfulness meditation techniques, including breath awareness, body scanning, and mindful movement, which are used to help patients be aware of internal and external stimuli, notice habitual thought processes, and recognize maladaptive responses to stressors and more easily choose their reactions with intention and awareness.
MBCT was developed in 2002 by Teasdale et al. ( 7 ) with the goal to prevent relapses of major depression. It combines concepts and elements from MBSR and adds cognitive-behavioral therapy (CBT) principles. Just as in CBT, patients are taught to recognize automatic thoughts and associated emotional states but without passing judgment. The goal is to change their relationship with those thoughts rather than necessarily change the thoughts themselves. The “3-minute breathing space” is a key MBCT technique used to help bring attention to the breath and body after becoming aware of thoughts and feelings. Both programs encourage incorporating mindfulness into daily activities as well as group-based discussions of individual experience with mindfulness ( 5 – 7 ).
The use of MBIs for treatment of psychiatric conditions is relatively new compared with other forms of psychotherapy ( 5 ). Although many studies have investigated the overall effect of MBIs, they vary in their methods, objectives, and targeted patient populations. Khoury et al. ( 8 ) performed a comprehensive meta-analysis of 209 studies that examined the effects of MBIs on a range of physical and psychological conditions. They found generally moderate effect sizes across a mixture of pre-post comparisons, comparison with waitlist control groups, and comparison with active treatment. They also reported no significant differences between MBIs and CBT, behavioral therapies, or pharmacological treatments in several conditions. Despite this plethora of research, few high-quality studies have focused on MBI treatment specifically for formally diagnosed anxiety disorders.
With regard to MBSR, Kabat-Zinn et al. ( 6 ) performed an early pilot study with patients who had generalized anxiety disorder or panic disorder, which showed improvement in anxiety on the basis of the Hamilton Anxiety Rating Scale (HAM-A) and the Beck Anxiety Inventory (BAI) after treatment with the standardized MBSR program; however, no control group was used in this initial study. We found five RCTs that focused on MBSR for one or more diagnosed anxiety disorders ( 9 – 13 ). Notably, two of the studies included clinician-rated scales, which may be more objective ( 14 – 16 ). Although anxiety disorders were the primary diagnoses, most did not exclude comorbid depression. They had slight variation in exclusion criteria, but the majority excluded for psychosis, bipolar disorder, acute safety concerns, recent substance use, and participation in other forms of therapy.
Overall, these studies showed significant improvement in anxiety symptoms after the MBSR programs; however, several limitations were found, such as small sample size and reliance on self-report scales (such as the BAI and the Penn State Worry Questionnaire). Most of the studies did not examine long-term, follow-up data, with the longest time to follow-up being 6 months ( 10 ). Hoge et al. ( 11 ) had the only RCT that used an attention control group, an internally designed stress management education course that followed the same structure and time requirements of MBSR but did not contain any elements of mindfulness; this design allowed for control of nonspecific effects included in MBSR, such as instructor attention and group support. The MBSR group was found to have significantly larger reduction in anxiety symptoms in most clinical outcome measures (Severity and Improvement subscales of Clinical Global Impressions scale; BAI) but not in the primary outcome (HAM-A).
Two of the RCTs compared MBSR with active comparator groups. Arch et al. ( 9 ) found that patients in both their MBSR and CBT groups had a moderate-to-large effect sizes; however, the CBT group had significantly greater improvements in anxious arousal symptoms, whereas the MBSR group had greater improvements in worry and comorbid emotional disorders. Jazaieri et al. ( 12 ) compared MBSR with aerobic exercise of similar duration and format for patients with social anxiety disorder. They found significant improvements in both groups compared with untreated control groups, although randomization was not used for the nontreatment group. Jazaieri et al. also found significant differences between groups on symptoms of social anxiety, mood, and overall well-being, although the study was not powered to do formal equivalence testing.
Although several RCTs have demonstrated the effectiveness of MBCT on the prevention of relapse in major depressive disorder, only two high-quality studies used MBCT for diagnosed anxiety disorders ( 5 , 17 ). Zemestani and Fazeli Nikoo ( 18 ) studied pregnant women with depression or anxiety disorders. Although they reported that MBCT was associated with greater improvements in BAI scores in the MBCT group immediately after treatment, no significant differences were found at 3-month follow-up ( 18 ). Furthermore, given that patients with anxiety and depressive disorders were combined in all analyses, it is difficult to apply these findings to patients with anxiety disorders specifically or to nonpregnant patients. Kim et al. ( 19 ) included patients with generalized anxiety disorder or panic disorder; however, this study was unblinded, nonrandomized, and had no long-term follow-up data. Both studies had small sample sizes (N=33, N=46, respectively). Although both studies included education control groups, they were significantly less intensive with regard to time, attention, and effort than the MBCT group; thus, they did not adequately control for nonspecific effects of treatment.
The currently available RCTs using MBSR and MBCT specifically for anxiety disorders are encouraging, along with the preliminary findings in the larger body of research for comorbid disorders and other psychological outcomes. At the same time, limited data have targeted anxiety disorders specifically, and the current evidence has several limitations. One of the most significant limitations is the lack of robust control groups; however, the few studies that did implement control groups were still positive ( 11 , 18 , 19 ). Long-term data contributing to the understanding of the clinical efficacy of these treatments are minimal. Future studies for both MBSR and MBCT would benefit from improved power and use of active control groups that closely match the format of these interventions, but without the mindfulness components, and follow-up with patients over time.
Interestingly, adding an MBI to CBT may enhance the effectiveness and adherence to CBT, which suggests another way that MBIs could be used in treatment planning. In the future, it may also be useful to see what attracts patients with anxiety to these alternative treatment formats, as concepts of mindfulness may make it easier for patients to engage in treatment, which alone could be a benefit to these therapies over other options. Overall, the current research points to MBIs being potentially useful tools for patients with anxiety disorders, but additional research could help clarify the best type of MBI, format, and timing to optimize treatment outcomes.
Meditation Studies (Nonmindfulness)
We also attempted to find studies that examined meditation practices, separate from mindfulness, for anxiety disorders. One meta-analytic review compared the effectiveness of meditation versus relaxation therapies in the treatment of anxiety disorders ( 20 ). Fourteen RCTs were reviewed (N=862), 10 of which focused on anxiety symptoms in some way (e.g., trait anxiety, high anxiety sensitivity, social anxiety); however, only three focused specifically on anxiety disorders, such as generalized anxiety disorder. The effect size demonstrated that meditation was slightly more effective (g=−0.23, with the number needed to treat=7.74). Overall, RCT studies and reviews on meditation as an intervention for anxiety disorders were limited. We did not find any studies on patients diagnosed as having an anxiety disorder in which a meditation intervention (which was also separate from previously mentioned mindfulness and yoga interventions) was clearly described and patients were randomly assigned to two groups.
Yoga originated from India thousands of years ago ( 21 ), but the modern form practiced in Western countries is an innovation of the 19th century ( 22 ). Modern yoga is heterogeneous, including many subtypes designed to link mind and body (e.g., Hatha, Iyengar, Sudarshan Kriya) ( 21 ), and may include elements of static postures (asanas), flowing movements (vinyasas), patterns of breathing (pranayama), and mindfulness ( 22 , 23 ). Its benefits for mood and anxiety symptoms have been documented in the literature since the 1970s ( 21 , 24 , 25 ). Yoga has become popular among the general population for its purported health benefits, with more than 10% of U.S. adults having practiced yoga at least once in their lifetime ( 26 ).
A large body of research has investigated the impact of yoga on stress and anxiety symptoms among a variety of populations, including healthy adults as well as patients with obesity, arthritis, breast cancer, and migraines. In a recent meta-analysis, Zoogman et al. ( 27 ) found a large effect size (d=0.80) for yoga interventions on anxiety levels across these populations. However, relatively few yoga studies have investigated psychiatric clinical populations with formally diagnosed anxiety disorders.
Two recent meta-analyses focused on yoga for anxiety disorders. Cramer et al. ( 23 ) included eight RCTs studying yoga among participants with formal anxiety diagnoses or anxiety levels exceeding predefined cutoffs on questionnaires suggesting a diagnosis (e.g., BAI, HAM-A). They found a small effect size for yoga compared with no treatment (standard mean difference [SMD]=−0.43) and, interestingly, a larger effect size when compared with an active control group (SMD=−0.86). However, no significant difference was found between yoga and either no treatment or an active control group when including only studies with formally diagnosed anxiety disorders.
Vollbehr et al. ( 28 ) included five RCTs studying Hatha yoga for anxiety disorders and found no significant effect on anxiety symptoms. However, they commented that included studies had small sample sizes and therefore limited power.
We looked for additional studies in the literature and found seven RCTs that measured the effects of yoga on anxiety disorders. One well-designed RCT ( 29 ) with a relatively large sample (N=90) demonstrated benefits of both Hatha yoga and mindfulness meditation on anxiety symptoms among a group of patients with anxiety and depressive disorders compared with a nontreatment control group. No difference was identified between participants in the yoga versus the meditation groups. Given the lack of an attention control group, it is unclear whether these improvements reflect specific benefits of yoga and mindfulness independently, a shared factor of these two interventions (e.g., both include elements of meditation and mindful breathing), or nonspecific effects of any treatment (e.g., time spent with a mental health provider, attention from research staff).
In a recent study, Simon et al. ( 30 ) compared CBT, Kundalini yoga, and an educational attention control group for patients with generalized anxiety disorder. They found that the yoga group had a statistically significant greater response rate than the control group. However, when the yoga response rate was compared with CBT, yoga was less efficacious than CBT.
One small RCT with an active control group consisting of massage, steam, diaphragmatic breathing, and acupressure ( 31 ) found improvements in anxiety symptoms in both groups, with a nonsignificant trend favoring yoga over the active control group among patients with generalized anxiety disorder. Another RCT ( 32 ) comparing yoga alone with a combined yoga+CBT intervention for panic disorder demonstrated improvements in anxiety over time with a trend favoring the combined condition. However, both studies were potentially underpowered to identify group differences (both with n≤20). RCTs assessing the effect of yoga on anxiety symptoms among patients with nonspecific diagnoses of psychoneurosis ( 33 , 34 ) and anxiety disorder ( 35 ) showed greater decreases in anxiety symptoms versus control groups undergoing “pseudo-yoga” and no treatment, respectively; however these studies have limited methodological information available, and so their impact is unclear.
Although the impact is limited by the study design, several nonrandomized studies concluded that yoga interventions improved anxiety disorder symptoms. In one such study, Gabriel et al. ( 36 ) used statistical techniques (e.g., propensity score matching) to reduce bias from lack of randomization; they found that patients with generalized anxiety disorder showed substantial reductions in anxiety symptoms after yoga, with moderate to large effect sizes, relative to participants in an active control condition receiving individual psychotherapy, who showed no symptom reduction. However, the meaning of these findings is unclear because patients chose their treatment group. In other nonrandomized studies, when compared with treatment as usual, patients with mixed anxiety disorders (but mostly generalized anxiety disorder) showed reduced symptoms after a 2-week yogic breathing intervention ( 37 ) but not after a single-session intervention at a partial hospitalization program ( 38 ). In the absence of randomization, these studies carry high risk of bias. Several uncontrolled studies demonstrated improvements in anxiety symptoms over time after completing yoga interventions among patients with generalized anxiety disorder in particular ( 39 , 40 ) and a diverse array of anxiety diagnoses in general ( 6 , 36 , 41 , 42 ); but again, in the absence of a control group, whether these changes are caused by or merely correlated with participation in a yoga intervention is unclear.
In addition to the paucity of robust RCTs, the studies reviewed have two significant limitations. First, only four studies reviewed present any follow-up data ( 29 , 39 , 41 , 43 ); thus, the largely positive results demonstrated immediately after completion of a yoga intervention may not persist in the long term. Second, the yoga interventions used are highly heterogenous, with variation in their components (i.e., postures, breathing, and meditation), length (ranging from a single session to 12 weeks), and frequency (ranging from daily to weekly).
In summary, some promising findings suggest that yoga may be effective in reducing anxiety among clinical populations, with the strongest evidence for generalized anxiety disorder. However, with few RCTs (which themselves are limited by small sample sizes and diverse diagnostic populations), it is difficult to establish a firm causal link between yoga and improved anxiety. With limited follow-up data, it is difficult to conclude whether any benefits after yoga interventions persist in the long term. Furthermore, the heterogeneity of interventions studied makes it difficult to “prescribe” yoga with confidence in any specific form, frequency, or duration. Although yoga is unlikely to have adverse effects ( 23 , 27 ) and may benefit people without psychiatric conditions, evidence is currently insufficient to recommend the routine practice of yoga as primary treatment for patients with anxiety disorders.
Applied Relaxation (AR)
AR was widely studied in anxiety disorders during the 1980s, particularly for generalized anxiety disorder, for which it is now considered an established treatment ( 44 ). In AR, patients are trained in psychotherapy sessions to use relaxation techniques to interrupt or prevent anxiety symptoms. Patients are first taught to recognize the onset of anxiety symptoms; they then apply specific skills such as progressive relaxation training, which involves slow, paced diaphragmatic breathing or imagery techniques ( 45 ).
A recent review and meta-analysis ( 46 ) examined 16 clinical trials using relaxation therapy for anxiety disorders. Although the majority of the trials were for generalized anxiety disorder (k=6), panic disorder (k=4) and social anxiety disorder (k=2) were also represented; in addition, four trials were for mixed anxiety disorders. The authors concluded that the overall effect size was 0.62 (Hedges’ g), representing a medium-high effect; this finding indicates that good research support exists for the effectiveness of relaxation training for anxiety disorders.
Since that review, a few more recent studies have been published. For example, in a three-arm trial involving 116 patients, Milrod et al. ( 47 ) compared AR, CBT, and psychodynamic psychotherapy for the treatment of panic disorder. They reported that the three treatments were equally effective in reducing anxiety symptoms but that patients who were more severely ill found AR less acceptable. Another study compared AR with a newly developed psychotherapy, acceptance-based behavior therapy, in a sample of 81 people with generalized anxiety disorder ( 48 ). The authors reported that both treatments were associated with clinically meaningful change.
Swedish Massage (SM) is one of the most commonly used forms of massage treatments in the community ( 49 ). It consists of rhythmic long strokes, kneading, and percussive touch ( 49 ). SM has also been found to be effective for the treatment of anxiety disorders, as demonstrated in one study by Rapaport et al. ( 49 ). This RCT consisted of 47 untreated patients, diagnosed with generalized anxiety disorder by DSM-IV criteria and a HAM-A score greater than 14, who were assigned to either SM twice a week or a control intervention of light touch for 6 weeks. A statistically significant reduction was found in HAM-A scores with SW compared with the control group, with an effect size of −0.69.
In another study, Sherman et al. ( 50 ) evaluated 68 patients with generalized anxiety disorder who were randomly assigned to therapeutic massage, thermotherapy, or relaxing room therapy control groups for 10 sessions over 12 weeks. Although the massage group and both control groups showed improvements at the end of treatment and maintained improvements at 26-week follow-up, the study did not show any statistically significant differences between groups ( 50 ).
Tai chi has been used as a therapeutic tool for multiple conditions for centuries in China. Although originally developed as a martial art, tai chi evolved into a form of mind-body exercise involving a series of synergistic and deliberate movements while shifting weight accompanied by deep relaxation and visual concentration ( 51 ).
Although data are limited, one RCT (N=32) suggests that in older patients (ages 60–75) with an anxiety disorder, the combination of tai chi with paroxetine had greater improvements in anxiety compared with paroxetine alone (as assessed by the HAM-A) after 45 days of treatment, with lower rates of recurrence after paroxetine was discontinued (9.09% vs. 42.86%) ( 51 ).
A recent assessor-blinded, randomized controlled feasibility study examined the effect of a 10-week tai chi chuan (TCC) intervention on anxiety and sleep quality in a young adult college student population; these students reported mild to severe levels of anxiety on the seven-item Generalized Anxiety Disorder Assessment (GAD-7) but were not formally diagnosed as having an anxiety disorder ( 51 – 53 ). Participants were randomly assigned to one of three arms: 10 weeks of TCC meetings occurring twice a week (N=28), 10 weeks of TCC meetings plus an out-of-class practice aid (N=28), and a control group receiving an anxiety management handout (N=19). Anxiety was measured by the 20 state anxiety questions of the Spielberger State-Trait Anxiety Inventory ( 54 ). Results showed that levels of anxiety decreased for the TCC and combined TCC groups, whereas no reductions in anxiety were found in the control group. Although the difference in anxiety symptom reduction was not statistically significant between the control group and the TCC groups, the effect size suggests that TCC had a small but increasingly positive effect on anxiety levels over time compared with the control group, with a Hedges’ g between the two groups of 0.3 at 4 weeks, 0.4 at 10 weeks, and 0.4 at 2-month follow-up.
In another study, Hoffmann-Smith et al. ( 55 ) evaluated the effects of tai chi within an ambulatory population with high levels of anxiety by clinicians utilizing the HAM-A. They used a pretest-posttest design in which all participants completed a 10-week tai chi program. After the program, an 11-point drop occurred on the HAM-A, demonstrating a meaningful drop in anxiety symptoms.
Multiple systematic reviews have evaluated the effects of tai chi on anxiety symptoms but without clearly defined anxiety disorders or cutoffs for anxiety scales ( 56 – 58 ). The conclusions of these studies are consistent; tai chi has been positively associated with anxiety reduction, but the quality of studies published in the literature is modest.
Taken together, although it appears through preliminary research that tai chi may be beneficial for individuals with anxiety symptoms, more RCTs with rigorous designs are necessary to establish the efficacy of tai chi in treating anxiety disorders.
Reiki has been utilized as a treatment for a variety of ailments since being developed in Japan in the mid-19th century. It is a form of energy therapy involving laying hands “on or just above a person, with the goal of directing energy to help facilitate the person’s own healing response” ( 59 ). Although several studies looked at anxiety symptoms, we did not find any that included patients diagnosed as having anxiety disorders.
A recent Cochrane review identified three RCTs that evaluated the effects of reiki on anxiety symptom reduction (but not for anxiety disorders) ( 60 ). One study assigned men with prostate cancer to one of three groups: reiki, relaxation, and waitlist control. Following the intervention, individuals with anxiety in the reiki group had reduced anxiety, but the differences between reiki and the other two groups were not statistically significant ( 61 ). Another study assigned older adults to either reiki or waitlist control; no statistically significant differences were found in anxiety change scores between groups ( 62 ). In a third study, university students were randomly assigned to reiki and relaxation-treated control groups; but again, changes with treatment were not significant between the groups ( 63 ).
A 2008 systematic review on reiki found four RCTs that included anxiety symptom reduction as an outcome ( 64 ). One study, which evaluated the effect of reiki on pain and anxiety in patients who were chronically ill, found a significant reduction in anxiety symptoms in the reiki group compared with the sham control group ( 65 ). The other three trials did not find intergroup differences compared with the control group ( 66 – 68 ). A few other RCTs evaluated reiki in reducing stress and anxiety in various populations and found a significantly greater drop in anxiety in the reiki group compared with the control group ( 69 , 70 ).
In sum, the existing data on reiki for anxiety are limited. Systematic reviews on reiki in anxiety symptom reduction across a variety of populations have demonstrated inconsistent findings, and vary widely in methodology, making it difficult to compare and generalize. Although two more recent RCTs mentioned here ( 69 , 70 ) found evidence of anxiety symptom reduction, the studies were not conducted among patients with a diagnosed anxiety disorder. Thus, no high-quality evidence exists showing that reiki is beneficial for the treatment of anxiety disorders.
Therapeutic Touch
Therapeutic touch is a Western form of energy therapy developed in the early 1970s that has been described as the practitioner moving one’s
hands around the patient’s body, at a distance of two to five inches, encountering and assessing the energy field by feeling for changes in temperature, pressure, rhythm or a tingling sensation . . . and redirecting and rebalancing energy through the use of hand movements . . . to bring the two energy fields into a harmonic resonance. ( 71 )
To date, no RCTs have been conducted to evaluate the effectiveness of therapeutic touch for anxiety disorders ( 71 ). Although uncontrolled, some studies have suggested that therapeutic touch can have a positive effect on anxiety among patients with cancer ( 72 ), individuals in nursing homes ( 73 ), patients with burns ( 74 ), and a variety of other populations ( 75 ). Furthermore, a recent systematic review concluded that this intervention might reduce anxiety levels among patients with various disease conditions, including heart disease and stroke ( 76 ). However, we do not have enough evidence to recommend therapeutic touch as treatment for patients with anxiety disorders.
Guided Imagery
Guided imagery is an ancient relaxation technique that focuses on the interaction between brain, mind, body, and behavior using the patient’s own imagination and mental processing to form a pleasing mental representation of an object, place, event, or situation to replace negative or stressful feelings ( 77 , 78 ). Guided imagery can be self-directed or conducted by a professional or a recording ( 78 ).
In a series of RCTs assessing the effects of guided imagery on symptoms of anxiety among nonclinical populations, we find a growing body of literature that may support this intervention. These studies assessed the effects of guided imagery among populations of nonclinical adults seeking general stress and anxiety relief, parents of children hospitalized with malignancies, adults with work-related stress, patients receiving hemodialysis, patients with irritable bowel syndrome, adults and children with preoperative anxiety, and patients with acrophobia or fear of heights ( 78 – 85 ). In each of these studies, anxiety outcomes were significantly reduced following the guided imagery intervention compared with control groups.
Qigong is a traditional Chinese mind-body exercise that could be used as a stress management intervention technique that provides skills for relaxation, reduction of stressors, and coping with stress ( 86 ). Qigong involves mind-body exercises that integrate body, breath, and mind adjustments into one, addressing both psychological and physiological aspects of health by integrating both dynamic (movement) and static (still) forms; both of these forms usually incorporate the meditative state, in which the body, breath, and mind are one ( 77 ). Several types of Qigong practice are commonly practiced, including self-healing Qigong and “Baduanjin” ( 77 , 87 ).
Several RCTs assessed the effects of Qigong on symptoms of anxiety among nonclinical groups, including a distressed Korean population, first-year nursing and midwifery students, as well as adults with burnout and anxiety symptoms ( 86 , 88 – 90 ). In three of these studies, anxiety outcomes were statistically significant following the Qigong intervention compared with the control groups ( 86 , 88 , 90 ). In one study comparing Qigong with cognitively oriented behavioral rehabilitation with Qigong, no significant differences were found, although both treatments significantly reduced symptoms of anxiety from pre- to posttreatment ( 89 ).
Meta-analyses examining Qigong have supported the efficacy of Qigong across various populations for reducing anxiety symptoms, although in the majority of these studies, anxiety was a secondary outcome measure ( 77 , 91 – 94 ). Qigong has been shown to be effective in reducing anxiety and depression among older adults ( 93 ) as well as reducing stress and anxiety among healthy adults ( 94 ) and people with varying physical and mental illnesses ( 91 ).
More RCTs with rigorous research designs are needed to establish the efficacy of Qigong as an intervention for populations with clinically diagnosed anxiety. However, as evidence for Qigong continues to develop, promising results from multiple RCTs are encouraging ( 77 , 91 , 92 ).
Laughter Therapy
Laughter therapy is a combination of mimicking laughter and yoga-like movements and breathing styles, in which the patient is encouraged to focus on the experience of laughter and the associated bodily sensations. This practice creates a resulting focus on the present moment, which is hypothesized to provide temporary relief from negative thoughts and rumination while providing an opportunity for a release of negative emotions ( 95 , 96 ). Laughter therapy or humor training is generally done in a group setting, over several weeks, and focuses on different humor behaviors such as spontaneous and simulated laughter ( 97 , 98 ). During this practice, patients are encouraged to engage in simulated laughter, which may lead to spontaneous or genuine laughter among group members and instructors, thus creating greater connections among group members ( 96 , 97 ).
Laughter therapy is a relatively new field of research that has yet to reach maturity, although reviews have found a growing body of support for laughter therapy as an intervention for anxiety symptoms ( 97 ). Several RCTs assessed the effects of laughter therapy among populations of people postmastectomy, people receiving in-vitro fertilization, and adults undergoing dialysis; these RCTs found that symptoms of anxiety were significantly reduced compared with the control groups receiving treatment as usual ( 99 – 101 ). One study found that among adults with diagnosed depression with stress or anxiety symptoms, reductions in symptoms of anxiety did not reach significance ( 96 ). Other studies found no significant effect of laughter therapy compared with a control group, including one with people diagnosed as having anxiety disorders ( 98 , 100 ).
In their meta-analysis, van der Wal and Kok ( 97 ) found that laughter-inducing therapies may improve anxiety symptoms among patients undergoing dialysis, elderly populations, healthy populations, people experiencing chronic pain, and people who are pregnant, although the overall quality of this evidence was low and the field has yet to reach maturity. Interestingly, they suggested that simulated or nonhumorous laughter may have more of a positive effect on depression and anxiety compared with spontaneous or genuine laughter.
Humor and laughter interventions are safe and convenient and can promote interpersonal relationships in both patients and clinicians. Therefore, these interventions have great feasibility and potential to be used as an aspect of psychotherapy to improve anxiety, depression, and sleep quality among adults ( 102 ).
Underlying Mechanisms
Underlying mechanisms for mind-body interventions have not been clearly worked out. However, various possibilities have been proposed for mindfulness meditation and yoga, which may also be applicable to other mind-body treatment approaches. For example, both Hölzel et al. ( 103 ) and Shapiro et al. ( 104 ) have suggested that these mind-body practices increase “reperceiving,” “decentering,” and “reappraisal,” which allows an individual to experience their thoughts differently. This practice allows them to partake in a larger perspective and not be as closely identified with the experience, creating a path to greater flexibility in reacting to experiences and improved emotion regulation. Another proposed mechanism is exposure, by which a person allows themselves to be “exposed” to previously avoided stimuli (such as memories or thoughts) while practicing nonreactivity; this practice leads to greater acceptance and nonjudgment, which, in turn, makes the stimuli less provocative over time. Greater research into underlying mechanisms for mind-body interventions is needed.
Practical Considerations for Mind-Body Interventions in Anxiety Disorders
Overall, the data supporting the use of mind-body interventions for anxiety disorders are limited. RCTs are limited, and many available studies have small sample sizes that limit statistical power, include patients with mixed depression and anxiety, and do not utilize control groups that adequately control for attention and expectation effects; these limitations make it difficult to establish firm causal links between interventions and reductions in anxiety. However, stronger evidence exists for some interventions with certain anxiety disorders, such as AR for generalized anxiety disorder, increasingly promising but still limited outcomes for yoga for generalized anxiety disorder, and MBSR and MBCT for several disorders. It is worth noting that studies on the latter two treatments sometimes included comorbid depression in their populations, which could have affected anxiety outcomes given the overlap in symptoms. Although we often see both depression and anxiety in our clinical populations and a broad effect on psychiatric symptoms might be desirable, it is difficult scientifically to distinguish the effects of MBSR and MBCT on anxiety versus depression in mixed samples.
The question of researcher allegiance (RA) was raised in several of the reviewed studies and must also be considered because it can contribute to bias. RA refers to the experimenter’s “belief in the superiority of a treatment [and] . . . the superior validity of the theory of change that is associated with the treatment” ( 105 , 106 ). Researchers are motivated by personal beliefs or experiences that lead them to pursue research in complementary and alternative medicine ( 107 ). Given the limitation that blinding cannot be adequately performed in mind-body intervention trials, RA can contribute to optimism bias and serve as a form of nonfinancial conflict of interest ( 108 ). A recent meta-analysis found that RA may contribute to bias in MBI studies across a variety of psychiatric conditions ( 109 ). RA should be considered when interpreting results of these mind-body studies.
Studies varied dramatically from one another in terms of frequency of intervention, duration of treatment, and length of follow-up, if included at all. For example, the longest follow-up periods reported in the studies that we evaluated for MBSR and yoga for anxiety disorders were both 6 months ( 13 , 30 ). Recent findings, however, suggest that although Kundalini yoga may have short-term efficacy for generalized anxiety disorder, these improvements may not be persistent ( 30 ). The next step for researchers is to look more closely at long-term effects of mind-body interventions, in addition to further RCTs with adequate control groups and further comparisons with existing treatments.
Cost and access to these interventions are a consideration when considering options. Various types of yoga have become more accessible across the country and can be found in most cities in health care settings, gyms, private studios, and wellness centers. MBIs, however, tend to be less common and may be more costly. Most important, mind-body treatments are often not reimbursed by health insurance companies, although there are exceptions. Especially relevant in the context of the coronavirus (SARS-CoV-2) pandemic, we also do not know whether online versions or patient-led versions of these interventions are equivalent in efficacy.
Potential risks and side effects of mind-body treatments must also be considered. According to the then director of the National Center for Complementary and Integrative Medicine at the National Institutes of Health, complementary treatments can pose harms to be patients because of “unjustified claims of benefit, possible adverse effects . . . and the possibility that vulnerable patients with serious diseases may be misled” ( 110 ). Although most class-based, mind-body interventions are safe and well-tolerated, studies have sometimes reported depersonalization, anxiety, panic, and reexperiencing of trauma-related memories; moreover, in overnight retreat settings, psychosis and mania have been reported ( 111 ). Few studies evaluating yoga for anxiety reported on adverse events; for those that did, no adverse events were found ( 23 ).
Conclusions
Weighing the limited data against the overall low risk for these mind-body interventions, we cannot recommend these methods for primary treatment of an anxiety disorder; however, these interventions, especially MBIs and yoga, may serve a role as part of an overall treatment plan. The strongest evidence for treatment efficacy exists for AR for generalized anxiety disorder, yoga for generalized anxiety disorder, and MBSR and MBCT for several disorders. We recommend that the general psychiatrist consider cost, patient preference, and potential synergy with traditional treatments when evaluating mind-body interventions for their patients. These therapies could be potentially added to either pharmacotherapy and psychotherapy as part of a larger treatment plan; they could also be used in cases in which symptoms are mild or when patients strongly desire nonpharmacologic treatments.
Dr. Bandealy and Dr. Sheth contributed equally to this article.
The authors report no financial relationships with commercial interests.
Watch CBS News
Why is looking at a solar eclipse dangerous without special glasses? Eye doctors explain.
By Sara Moniuszko
Edited By Allison Elyse Gualtieri
Updated on: April 8, 2024 / 8:54 AM EDT / CBS News
The solar eclipse will be visible for millions of Americans on April 8, 2024, making many excited to see it — but how you watch it matters, since it can be dangerous for your eyes.
A solar eclipse occurs when the moon passes between the sun and Earth, blocking the sun's light . When the moon blocks some of the sun, it's a partial solar eclipse, but when moon lines up with the sun, blocking all of its light, a total solar eclipse occurs, NASA explains . Either way, you need eye protection when viewing.
"The solar eclipse will be beautiful, so I hope that everyone experiences it — but they need to experience it in the right way," said Dr. Jason P. Brinton, an ophthalmologist and medical director at Brinton Vision in St. Louis.
Here's what to know to stay safe.
Why is looking at a solar eclipse dangerous?
Looking at the sun — even when it's partially covered like during an eclipse — can cause eye damage.
There is no safe dose of solar ultraviolet rays or infrared radiation, said Dr. Yehia Hashad , an ophthalmologist, retinal specialist and the chief medical officer at eye health company Bausch + Lomb.
"A very small dose could cause harm to some people," he said. "That's why we say the partial eclipse could also be damaging. And that's why we protect our eyes with the partial as well as with the full sun."
Some say that during a total eclipse, it's safe to view the brief period time when the moon completely blocks the sun without eye protection. But experts warn against it.
"Totality of the eclipse lasts only about 1 to 3 minutes based on geographic location, and bright sunlight suddenly can appear as the moon continues to move," notes an eclipse viewing guide published in JAMA , adding, "even a few seconds of viewing the sun during an eclipse" can temporarily or permanently damage your vision.
Do I need special glasses for eclipse viewing?
Yes. Eclipse glasses are needed to protect your eyes if you want to look at the eclipse.
Regular sunglasses aren't protective enough for eclipse viewing — even if you stack more than one.
"There's no amount of sunglasses that people can put on that will make up for the filtering that the ISO standard filters and the eclipse glasses provide," Brinton said.
You also shouldn't look at the eclipse through a camera lens, phone, binoculars or telescope, according to NASA, even while wearing eclipse glasses. The solar rays can burn through the lens and cause serious eye injury.
Eclipse glasses must comply with the ISO 12312-2 international safety standard , according to NASA, and should have an "ISO" label printed on them to show they comply. The American Astronomical Society has a list of approved solar viewers.
Can't find these, or they're sold out near you? You can also make homemade viewers , which allow you to observe the eclipse indirectly — just don't accidentally look at the sun while using one.
How to keep kids safe during the solar eclipse
Since this eclipse is expected to occur around the time of dismissal for many schools across the country, it may be tempting for students to view it without the proper safety precautions while getting to and from their buses. That's why some school districts are canceling classes early so kids can enjoy the event safely with their families.
Dr. Avnish Deobhakta, vitreoretinal surgeon at New York Eye and Ear Infirmary at Mount Sinai, said parents should also be careful because it can be difficult for children to listen or keep solar eclipse glasses on.
"You want to actually, in my opinion, kind of avoid them even looking at the eclipse, if possible," he said. "Never look directly at the sun, always wear the right eclipse sunglasses if you are going to look at the sun and make sure that those are coming from a reliable source."
Brinton recommends everyone starts their eclipse "viewing" early, by looking at professional photos and videos of an eclipse online or visiting a local planetarium.
That way, you "have an idea of what to expect," he said.
He also recommends the foundation Prevent Blindness , which has resources for families about eclipse safety.
What happens if you look at a solar eclipse without eclipse glasses?
While your eyes likely won't hurt in the moment if you look at the eclipse without protection, due to lowered brightness and where damage occurs in the eye, beware: The rays can still cause damage .
The harm may not be apparent immediately. Sometimes trouble starts to appear one to a few days following the event. It could affect just one or both eyes.
And while some will regain normal visual function, sometimes the damage is permanent.
"Often there will be some recovery of the vision in the first few months after it, but sometimes there is no recovery and sometimes there's a degree to which it is permanent," Brinton said.
How long do you have to look at the eclipse to damage your eyes?
Any amount of time looking at the eclipse without protection is too long, experts say.
"If someone briefly looks at the eclipse, if it's extremely brief, in some cases there won't be damage. But damage can happen even within a fraction of a second in some cases," Brinton said. He said he's had patients who have suffered from solar retinopathy, the official name for the condition.
Deobhakta treated a patient who watched the 2017 solar eclipse for 20 seconds without proper eye protection. She now has permanent damage in the shape of a crescent that interferes with her vision.
"The crescent that is burned into the retina, the patient sees as black in her visual field," he said. "The visual deficit that she has will never go away."
How to know if you've damaged your eyes from looking at the eclipse
Signs and symptoms of eye damage following an eclipse viewing include headaches, blurred vision, dark spots, changes to how you see color, lines and shapes.
Unfortunately, there isn't a treatment for solar retinopathy.
"Seeing an eye care professional to solidify the diagnosis and for education I think is reasonable," Brinton said, but added, "right now there is nothing that we do for this. Just wait and give it time and the body does tend to heal up a measure of it."
Sara Moniuszko is a health and lifestyle reporter at CBSNews.com. Previously, she wrote for USA Today, where she was selected to help launch the newspaper's wellness vertical. She now covers breaking and trending news for CBS News' HealthWatch.
More from CBS News

Denver Health teaching orthopedic surgeons from around the world

DU fans excited about Frozen Four semi-final watch party at Magness Arena

Back-to-school night prompts kidney donation, changing lives of 2 women forever

Watch: Car smashes into gas station pump in Colorado, takes off

IMAGES
VIDEO
COMMENTS
Although helpful for assessing feasibility and initial effect sizes, research on mind-body interventions should apply the gold-standard randomized controlled trial approach. Yet this approach can face practical and ethical challenges when working within communities, such as lack of clear blinding and a control group.
The mind-body connection of emotions and immunity. Research supports a strong relationship between affective states and immune system response. Sustained negative emotional states such as stress, depression, and anxiety can worsen immunity functions and affect other bodily functions.
Historical Perspective. Mind-body medicine (MBM) was founded by late Harvard cardiologist Herbert Benson in the context of modern meditation research that emerged in the 1970s (Benson and Klipper, 2000).Right from the start, there was the observation that connections and interactions between the brain, mind, body, and behavior can activate psychophysiological changes and a health-promoting ...
The Mind-Body Health Research Interest Group (MBH RIG) is an interdisciplinary research collective that was established in 2015 and became part of InCHIP in 2019. Its mission is to further education, research, clinical/practical application, and community outreach with a focus on the emerging potential connections between the Mind and Body. ...
Facing these kinds of illnesses, Sulmasy might reason a spiritual experience; such an experience "grasps persons by the soul as well as by the body and disturbs both" (Sulmasy, 2006, p. 17). Recent years have seen increasing interest in spirituality in medical research, and important efforts to address the spiritual needs of patients in ...
Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science , 13 (1), 36-61. Wittmann, M., & Schmidt, S. (2014).
Affiliations 1 Body in Mind Research Group, Sansom Institute for Health Research, University of South Australia, Adelaide, Australia; Recover Injury Research Centre, Menzies Health Institute Queensland, Griffith University, Gold Coast, Australia. Electronic address: [email protected]. 2 Body in Mind Research Group, Sansom Institute for Health Research, University of South Australia ...
The debate, which is far from being recent, on the mind-body problem arises from the attempt to explain the nature of the relationship between what we commonly define as "mind" and the "body" we use to interact with the physical world. After the contribution of eminent philosophers on this issue over the past centuries, the issue got popular again in recent decades both thanks to the ...
These unexpected findings triggered a large body of research into mind-body interventions—such as group therapy, stress-reduction techniques and cognitive-behavioural therapy (CBT)—and whether they can affect survival and pain in cancer, AIDS and bone-marrow transplant patients, with findings split between positive and negative for life ...
research techniques allows scientists, psychologists, and counselors to address questions ... mind-body skills group, which included meditation, guided imagery, breathing techniques, autogenic training, biofeedback, genograms, and self-expression through drawings and movement. The most interesting finding was that even after seven months,
I lead the Body in Mind Research Group within IIMPACT. This research group investigates the role of the brain and mind in chronic pain. Pain is a huge problem - it affects 20% of the population and costs western societies about as much as diabetes and cancer combined. We have a major public engagement and education focus, with our articles and ...
Chronic pain is commonly defined as an unpleasant experience felt in any part of the body that persists longer than 3 months and that may or may not be associated with a well-defined illness process ().Chronic pain affects up to 28%-65% of the U.S. population and often leads to reduced occupational activity and subsequent economic loss ().In 2008, the costs of chronic pain in the United ...
The team of the Mind-Body Medicine Research Council and the idea of THE MIND explained, including an introduction of the founders Tobias Esch, M.D., and George Stefano, ... His research group has a long-term focus on the issue of lifestyle and mental disorders, burnout syndrome. ADHD is also a major research topic in the context of topics such ...
Abstract. Although a growing body of research suggests that mind-body therapies may be appropriate to integrate into the treatment of depression, studies consistently lack methodological sophistication particularly in the area of control groups. In order to better understand the relationship between control group selection and methodological ...
Body in Mind is a really interesting group of neuroscience researchers based in Australia. They study pain and what happens when the body's pain processing system begins to malfunction. ... Lorimer Moseley is one of the driving forces behind Body in Mind. He does research focusing on the idea that pain is not an accurate indicator of tissue ...
The sense of touch is vital in development, and for how we perceive the world and interact with others. The skin envelopes our body and is our largest organ providing us with information about our immediate environment. In addition to this 'surface' information our somatosensory system also processes information regarding body position and internal bodily states. This research topic aims ...
These unexpected findings triggered a large body of research into mind-body interventions—such as group therapy, stress‐reduction techniques and cognitive‐behavioural therapy (CBT)—and whether they can affect survival and pain in cancer, AIDS and bone‐marrow transplant patients, with findings split between positive and negative for ...
You can also try more structured mindfulness exercises, such as: Body scan meditation. Lie on your back with your legs extended and arms at your sides, palms facing up. Focus your attention slowly and deliberately on each part of your body, in order, from toe to head or head to toe. Be aware of any sensations, emotions or thoughts associated ...
Much has been written about common leadership styles and how to identify the right style for you, whether it's transactional or transformational, bureaucratic or laissez-faire. But according to ...
Control Group Design in Mind-Body Research. The design of control groups in clinical trials with nonpharmacological, psychosocial, and/or behavioral interventions is often much more complex than those of drug studies. Researchers investigating mind-body complementary interventions for clinical conditions have a number of challenges in optimal ...
In 2014, the group investigated animal sounds in lexical typological perspective. Students presented analyses of this semantic field in different languages. As a result, a database containig the data of 20 languages was created and a collection of papers with detailed descriptions of the semantic systems in question was published.
DeepMind is also using AI to explore other areas of biology and accelerate research into drug discovery and delivery, material science, mathematics, weather prediction and nuclear fusion technology.
Home / News / Live recording of Lunch and Learn held on April 10th: Dr. Chad Danyluck - Harmonizing mind and body: Simple strategies for stress and wellness. Live recording of Lunch and Learn held on April 10th: Dr. Chad Danyluck - Harmonizing mind and body: Simple strategies for stress and wellness Friday, April 12, 2024
ICB - INDICATOR GROUP, MOSCOW. Moscow Aurora Business Park, 2nd Dl., 82 Sadovnicheskaya St., Building 2, 115035 Moscow, Russia. Phone: +7 (495) 225 9353
Mind-body interventions, such as yoga and mindfulness meditation, are an area of exponential growth and increased interest of the general population; yet clear clinical guidelines are limited concerning which interventions are evidenced based and appropriate for general psychiatric practice. ... manualized, 8-week programs that include group ...
Thai-Na: Relaxation for Body and Mind, Moscow, Russia. 14 likes · 5 were here. Ощутите гармонию, легкость тела и разума в ...
The hotel offers its guests unlimited access to the gym. Our bowling facility sports 6 Brunswick tracks and our fitness class offers both individual and group programs. Beauticians at the PRIMORYE Wellness centre offer body sculpting procedures, treating skin conditions of the face and body using the latest beauty machines.
While your eyes likely won't hurt in the moment if you look at the eclipse without protection, due to lowered brightness and where damage occurs in the eye, beware: The rays can still cause damage ...