The Cersonsky Lab at UW-Madison
The Cersonsky Lab is a research group based at the University of Wisconsin - Madison, Department of Chemical and Biological Engineering

8 Tips for a Literature Review Presentation
by Caleb Youngwerth
Literature reviews for research are very different from any other presentation you may have done before, so prepare to relearn how to present. The goals of research literature reviews are different, the style is different, even the pacing is different. Even if you have previously done a literature review in an academic setting, you will still want to know these tips. I found this out the hard way, so you don’t have to. Also, to clarify, these tips are meant for a literature review of a topic, not a singular study or paper, though many of the tips do apply to both.
1. Highlight current research
The point of a literature review for research is to highlight the current state of research related to your topic, not to simply give background information. Background information is important and should be included, but the focus of the presentation should be showing some current studies that either confirm or challenge the topic you are studying. As much as textbooks from 30 years ago might seem to have all the information you need for your presentation, a research study from this decade does a far better job representing the current state of the topic, which is the end goal of the presentation. Also, since the new research should be the focal point of the presentation, as a general piece of advice, try to give each research study a minimum of one full slide, so you can give a fuller picture of what the study actually concluded and how they reached their conclusion.
2. Alternate old and new
The best way to keep people listening to your presentation is to vary what you include in your presentation. Rather than trying to give all of the background information first and then showcase all the flashy new research, try to use the two interchangeably. Organize the presentation by idea and give all the background needed for the idea, then develop the idea further by using the new research studies to help illustrate your point. By doing this, you not only avoid having to backtrack and reteach the background for each and every new study, but also help keep the presentation interesting for the audience. This method also helps the audience avoid being overwhelmed since only a little bit of new information is introduced at a time. Obviously, you may need to include a brief introductory section that contains nothing but textbook information that is absolutely necessary to understand anything about the topic, but the more varied the presentation, the better.
3. Use complete sentences
Every presentation class up to this point probably has taught you that slides with full sentences are harmful to your presentation because it is distracting to the listener. Unlearn all that information for this style of presentation. Bullet points are still good, but you should have complete ideas (which usually means complete sentences) for every single point. If someone would be able to read your slides and not hear you, and still be able to understand most of your presentation, your literature review is perfect in a research setting. The point of this presentation is to share all the new information you have learned, so hiding it is helping no one. You still do not want to be reading your slides verbatim and can absolutely add information beyond the slides, but all your main ideas should be on the slides.
4. Read smart
I will admit that I stole this tip from Rosy, but it is a very good tip, so I decided to include it. When you read, you want to read as much as you can, but wasting time reading an irrelevant research study is helping no one. When finding a new study, read the abstract, then the conclusion, then the pictures. If it looks like a good study from those three parts, or you personally find it interesting, you then can go over the actual paper and read it, but by reading the less dense parts first, you can get a general idea of the study without actually having to take a lot of time to read the entire paper. Though textbooks and review papers generally are a little more difficult to read using this method, you can still look at the introduction, pictures, and conclusion and save time reading the rest if the source ends up not being interesting or important.
5. Reading is good for you
As much as you want to read smart when you can, the more you read, the more knowledgeable you become. The goal of the presentation is to become an expert on you topic, so the only way you can do that is by reading as much as you can. You should read more information than you present, since many sources you read probably will not fit in a time-constrained presentation. As Rosy likes to say, in anything research, only about 10% of what you know should actually be shared with the world. By reading more, you are better-suited to answer questions, and you also just generally are able to understand what you are studying better because, chances are, the main purpose of this presentation for you is to help you better understand your research. If something looks interesting and is vaguely related to your topic, read it; it will be beneficial to you, even if you do not end up presenting the information.
6. Let pictures talk for you
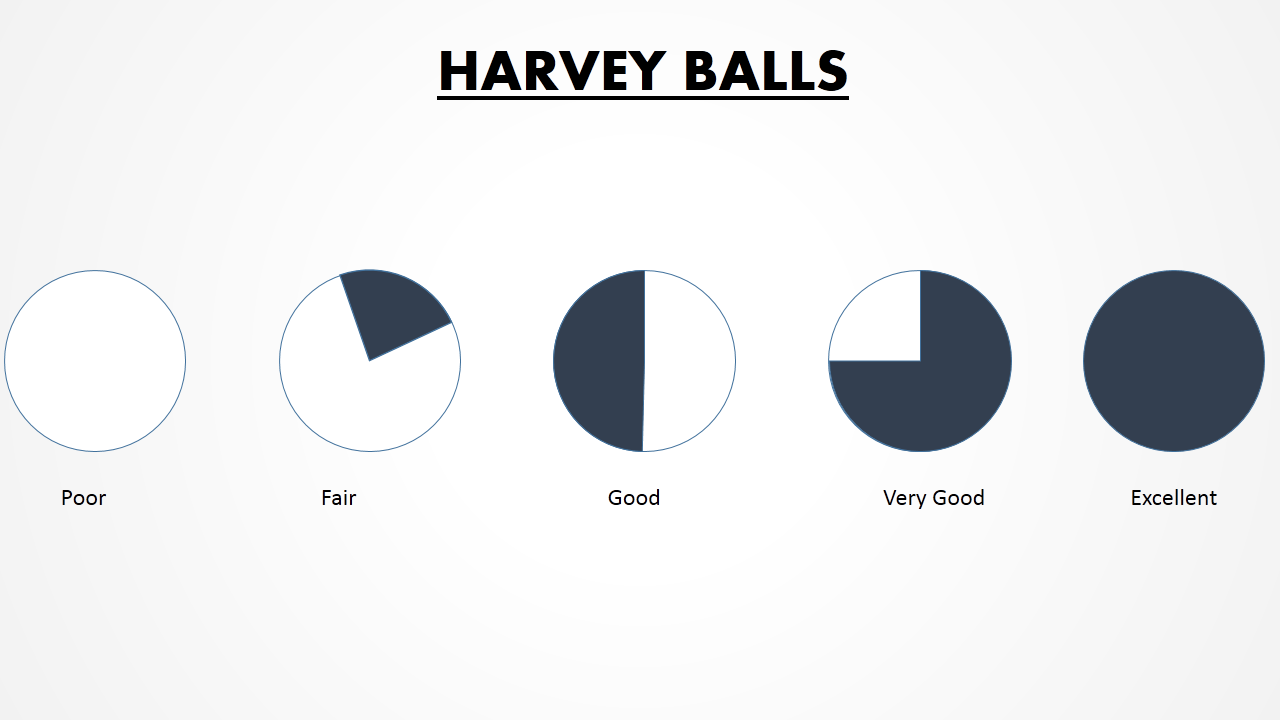
When reading research papers, the pictures are usually the best part. Your presentation should be the same way. The best way to be able to show the concept you are trying to explain is to literally show it. The best way to show the results of a research study is usually by showing a graph or infographic, so if the paper has a graph that shows the results, you should absolutely use it. Charts, diagrams, and even videos can also help illustrate a piece of background information that might be difficult to put into words. That being said, you should know and be able to explain every single part of the graphic. Otherwise, it loses meaning and makes the audience even more confused. Captions can and should be used to help explain the graphic, not only to remind you, but also let your audience know what the general idea of the graphic is. Since they keep slides interesting, you should probably have some sort of picture on every slide, otherwise the slides will be not only bland, but also likely less informative.
7. Avoid overcrowded slides
Just because you should have a lot of information in your presentation does not mean that your slides need to show that. In fact, a slide with too much information will only harm your presentation since your audience will be distracted trying to read all of a long slide while you are trying to explain it. Doing anything to make slides less dense will help avoid having the audience focused on the slide, so they focus on you more. Transitions that only show one point at a time or wait to reveal an image can be helpful in breaking up an overcrowded slide. Also, simply adding more slides can help since it accomplishes the purpose of putting less information on your slides while still keeping the exact same amount of information. You still want to share as much information as you can with the audience, but overcrowded slides do not accomplish this purpose.
8. Expect questions
Another thing that might be slightly different about a research presentation is questions. Most presentations have the question section after the presenter has finished. Research presentations are different because they allow for questions during the presentation (assuming it is a presentation to a small group). If you get any questions in the middle of the presentation, it is not someone being rude, but simply a fellow researcher who is legitimately curious about your topic. Of course, there will be a question period after the presentation, but you may be asked questions during the presentation. If you read enough information on the topic, you should be able to answer any question easily, but if the question is completely unrelated to anything you read, then it is perfectly reasonable to answer that you did not research the specific area in question. Overall, the questions related to your presentation should not be your biggest worry, but you should definitely be ready.
These are not all the rules for a literature review presentation nor are they set in stone. These are just some tips that I was told or learned that were the most helpful for me, so I hope they will help you too. I had to rewrite my presentation entirely my first literature review because I did not understand some of these differences, so if you give the presentation when you are scheduled to go, you are already better off than I was. Also, do not be afraid to ask anyone in the research group, even Rosy, if you need help. Chances are everyone in the group has given a literature review presentation at some point, so we would be more than happy to help you if you are confused about something. That being said, we are not experts on your topic, so specific questions about organization and content are going to have to be figured out by yourself. Either way, no matter what you do, do not stress out about this presentation. The goal of the presentation is mostly just to help improve your knowledge on a topic, and the presentation is simply to share with the group some of the information you have learned. Best of luck with the presentation, and I hope these tips help clear up what exactly the goal of a literature review presentation in a research setting is.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
memorial day
12 templates

66 templates
american history
75 templates

music video
21 templates
150 templates
Literature Review
It seems that you like this template, literature review presentation, free google slides theme, powerpoint template, and canva presentation template.
Whether you're a student or an academic, mastering the literature review is a key skill in scholarly writing. This fully customizable Google Slides and PowerPoint template can assist you in structuring your review seamlessly. Featuring a vibrant yellow design with captivating book illustrations, this template is designed to facilitate the organization and presentation of your research. Navigate your audience through chapters, themes, and references with ease and clarity using this versatile academic tool. Utilize this tool to craft an impressive literature review that leaves a lasting impression!
Features of this template
- 100% editable and easy to modify
- 35 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

Register for free and start editing online

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Literature Review: Introduction and Notes
Published by Virginia Hampton Modified over 6 years ago
Similar presentations
Presentation on theme: "Literature Review: Introduction and Notes"— Presentation transcript:
Critical Reading Strategies: Overview of Research Process
Project Proposal.
Literature review Cindy Wee Te Puna Ako Learning centre.

Writing a Research Paper
Thesis Project Nirvana
WRITING the Research Problem.
Literature Review.

Dr. MaLinda Hill Advanced English C1-A Designing Essays, Research Papers, Business Reports and Reflective Statements.

DR. AHMAD SHAHRUL NIZAM ISHA
How to Write a Literature Review
Soc 3306a Lecture 4 The Research Report and the Literature Review.
Northcentral University The Graduate School February 2014

Literature Review. What is a literature review? A literature review discusses published information in a particular subject area, and sometimes information.
Experimental Research Methods in Language Learning Chapter 16 Experimental Research Proposals.

Science Fair How To Get Started… (

How to write a professional paper. 1. Developing a concept of the paper 2. Preparing an outline 3. Writing the first draft 4. Topping and tailing 5. Publishing.
Literature Review. Outline of the lesson Learning objective Definition Components of literature review Elements of LR Citation in the text Learning Activity.
Literature review IBC 464
Literature Review Taken From: University of Washington Psychology Writing Center.
OK. So I’ve Submitted My Proposal
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Harvey Cushing/John Hay Whitney Medical Library
- Collections
- Research Help
YSN Doctoral Programs: Steps in Conducting a Literature Review
- Biomedical Databases
- Global (Public Health) Databases
- Soc. Sci., History, and Law Databases
- Grey Literature
- Trials Registers
- Data and Statistics
- Public Policy
- Google Tips
- Recommended Books
- Steps in Conducting a Literature Review
What is a literature review?
A literature review is an integrated analysis -- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question. That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
A literature review may be a stand alone work or the introduction to a larger research paper, depending on the assignment. Rely heavily on the guidelines your instructor has given you.
Why is it important?
A literature review is important because it:
- Explains the background of research on a topic.
- Demonstrates why a topic is significant to a subject area.
- Discovers relationships between research studies/ideas.
- Identifies major themes, concepts, and researchers on a topic.
- Identifies critical gaps and points of disagreement.
- Discusses further research questions that logically come out of the previous studies.
APA7 Style resources
APA Style Blog - for those harder to find answers
1. Choose a topic. Define your research question.
Your literature review should be guided by your central research question. The literature represents background and research developments related to a specific research question, interpreted and analyzed by you in a synthesized way.
- Make sure your research question is not too broad or too narrow. Is it manageable?
- Begin writing down terms that are related to your question. These will be useful for searches later.
- If you have the opportunity, discuss your topic with your professor and your class mates.
2. Decide on the scope of your review
How many studies do you need to look at? How comprehensive should it be? How many years should it cover?
- This may depend on your assignment. How many sources does the assignment require?
3. Select the databases you will use to conduct your searches.
Make a list of the databases you will search.
Where to find databases:
- use the tabs on this guide
- Find other databases in the Nursing Information Resources web page
- More on the Medical Library web page
- ... and more on the Yale University Library web page
4. Conduct your searches to find the evidence. Keep track of your searches.
- Use the key words in your question, as well as synonyms for those words, as terms in your search. Use the database tutorials for help.
- Save the searches in the databases. This saves time when you want to redo, or modify, the searches. It is also helpful to use as a guide is the searches are not finding any useful results.
- Review the abstracts of research studies carefully. This will save you time.
- Use the bibliographies and references of research studies you find to locate others.
- Check with your professor, or a subject expert in the field, if you are missing any key works in the field.
- Ask your librarian for help at any time.
- Use a citation manager, such as EndNote as the repository for your citations. See the EndNote tutorials for help.
Review the literature
Some questions to help you analyze the research:
- What was the research question of the study you are reviewing? What were the authors trying to discover?
- Was the research funded by a source that could influence the findings?
- What were the research methodologies? Analyze its literature review, the samples and variables used, the results, and the conclusions.
- Does the research seem to be complete? Could it have been conducted more soundly? What further questions does it raise?
- If there are conflicting studies, why do you think that is?
- How are the authors viewed in the field? Has this study been cited? If so, how has it been analyzed?
Tips:
- Review the abstracts carefully.
- Keep careful notes so that you may track your thought processes during the research process.
- Create a matrix of the studies for easy analysis, and synthesis, across all of the studies.
- << Previous: Recommended Books
- Last Updated: Jan 4, 2024 10:52 AM
- URL: https://guides.library.yale.edu/YSNDoctoral
DEAN’S BOOK w/ Prof. CONNIE GRIFFIN
Honors291g-cdg’s blog, literature review/poster presentation guide.
Literature Review & Poster/Visual Presentation Guide GIVING & GETTING EFFECTIVE PRESENTATIONS PRESENTATIONS In many disciplines presentations are given at academic conferences, symposia, and other places where scholars share their work with one another (including the Massachusetts Undergraduate Research Conference). It can be very challenging to display and communicate all of one’s research findings in a synthesized manner and short timeframe. Following are some thoughts about both preparing your presentation and also how to maximize your experience as an audience member. I. PRESENTER’S ROLE: The overall purpose of your presentation is to share your research process and findings with the class. In all cases, whatever topic you choose for your research, the objective is to stimulate in your listeners an understanding of that topic and how you went about developing that understanding for yourself as a researcher. The purpose of your talk is to present your research. Keep that goal in mind as you consider what to include and how to organize it.. In the visual portion of your presentation, be sure to include the following:
1) Title 2) Your research question 3) Examples of what you found (results) including a. Visual and quantitative information b. Important quotes 4) Your conclusion
Remember to keep your presentation (and your visual material) concise. It is very easy to overwhelm an audience with too much text. Also, be sure to use a font size that is large enough to read from several feet away. Presentation considerations. Five minutes go fast! Therefore, stick with the most important points (details can come in the Q&A session), and be sure to organize your presentation logically. Be sure to practice. Nothing will prepare you better than giving your presentation several times to an audience. Speak slowly, clearly, expressively. Make eye contact. Also make sure your visual really does support your oral presentation and aid your audience! Concluding your presentation. End your presentation with a quick summary or suggestion of what’s been gained by your research. Then be prepared for questions. Be ready with a question of your own in case the audience needs prompting. A crucial part of your presentation is thinking about how to engage the audience. Listen closely, be sure you understand each questioner’s intent, and then answer as directly as possible. II. AUDIENCE’S ROLE: Even when not presenting, you play a crucial role in the presentation and determining its quality. As a listener, demonstrate your interest: make eye contact with the presenter as you listen closely, and take notes so you can ask informed, pertinent, and helpful questions during the Q&A period. Putting a presenter at ease can go a long way to ensuring an effective presentation.
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Writing a Literature Review

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays). When we say “literature review” or refer to “the literature,” we are talking about the research ( scholarship ) in a given field. You will often see the terms “the research,” “the scholarship,” and “the literature” used mostly interchangeably.
Where, when, and why would I write a lit review?
There are a number of different situations where you might write a literature review, each with slightly different expectations; different disciplines, too, have field-specific expectations for what a literature review is and does. For instance, in the humanities, authors might include more overt argumentation and interpretation of source material in their literature reviews, whereas in the sciences, authors are more likely to report study designs and results in their literature reviews; these differences reflect these disciplines’ purposes and conventions in scholarship. You should always look at examples from your own discipline and talk to professors or mentors in your field to be sure you understand your discipline’s conventions, for literature reviews as well as for any other genre.
A literature review can be a part of a research paper or scholarly article, usually falling after the introduction and before the research methods sections. In these cases, the lit review just needs to cover scholarship that is important to the issue you are writing about; sometimes it will also cover key sources that informed your research methodology.
Lit reviews can also be standalone pieces, either as assignments in a class or as publications. In a class, a lit review may be assigned to help students familiarize themselves with a topic and with scholarship in their field, get an idea of the other researchers working on the topic they’re interested in, find gaps in existing research in order to propose new projects, and/or develop a theoretical framework and methodology for later research. As a publication, a lit review usually is meant to help make other scholars’ lives easier by collecting and summarizing, synthesizing, and analyzing existing research on a topic. This can be especially helpful for students or scholars getting into a new research area, or for directing an entire community of scholars toward questions that have not yet been answered.
What are the parts of a lit review?
Most lit reviews use a basic introduction-body-conclusion structure; if your lit review is part of a larger paper, the introduction and conclusion pieces may be just a few sentences while you focus most of your attention on the body. If your lit review is a standalone piece, the introduction and conclusion take up more space and give you a place to discuss your goals, research methods, and conclusions separately from where you discuss the literature itself.
Introduction:
- An introductory paragraph that explains what your working topic and thesis is
- A forecast of key topics or texts that will appear in the review
- Potentially, a description of how you found sources and how you analyzed them for inclusion and discussion in the review (more often found in published, standalone literature reviews than in lit review sections in an article or research paper)
- Summarize and synthesize: Give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: Don’t just paraphrase other researchers – add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically Evaluate: Mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: Use transition words and topic sentence to draw connections, comparisons, and contrasts.
Conclusion:
- Summarize the key findings you have taken from the literature and emphasize their significance
- Connect it back to your primary research question
How should I organize my lit review?
Lit reviews can take many different organizational patterns depending on what you are trying to accomplish with the review. Here are some examples:
- Chronological : The simplest approach is to trace the development of the topic over time, which helps familiarize the audience with the topic (for instance if you are introducing something that is not commonly known in your field). If you choose this strategy, be careful to avoid simply listing and summarizing sources in order. Try to analyze the patterns, turning points, and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred (as mentioned previously, this may not be appropriate in your discipline — check with a teacher or mentor if you’re unsure).
- Thematic : If you have found some recurring central themes that you will continue working with throughout your piece, you can organize your literature review into subsections that address different aspects of the topic. For example, if you are reviewing literature about women and religion, key themes can include the role of women in churches and the religious attitude towards women.
- Qualitative versus quantitative research
- Empirical versus theoretical scholarship
- Divide the research by sociological, historical, or cultural sources
- Theoretical : In many humanities articles, the literature review is the foundation for the theoretical framework. You can use it to discuss various theories, models, and definitions of key concepts. You can argue for the relevance of a specific theoretical approach or combine various theorical concepts to create a framework for your research.
What are some strategies or tips I can use while writing my lit review?
Any lit review is only as good as the research it discusses; make sure your sources are well-chosen and your research is thorough. Don’t be afraid to do more research if you discover a new thread as you’re writing. More info on the research process is available in our "Conducting Research" resources .
As you’re doing your research, create an annotated bibliography ( see our page on the this type of document ). Much of the information used in an annotated bibliography can be used also in a literature review, so you’ll be not only partially drafting your lit review as you research, but also developing your sense of the larger conversation going on among scholars, professionals, and any other stakeholders in your topic.
Usually you will need to synthesize research rather than just summarizing it. This means drawing connections between sources to create a picture of the scholarly conversation on a topic over time. Many student writers struggle to synthesize because they feel they don’t have anything to add to the scholars they are citing; here are some strategies to help you:
- It often helps to remember that the point of these kinds of syntheses is to show your readers how you understand your research, to help them read the rest of your paper.
- Writing teachers often say synthesis is like hosting a dinner party: imagine all your sources are together in a room, discussing your topic. What are they saying to each other?
- Look at the in-text citations in each paragraph. Are you citing just one source for each paragraph? This usually indicates summary only. When you have multiple sources cited in a paragraph, you are more likely to be synthesizing them (not always, but often
- Read more about synthesis here.
The most interesting literature reviews are often written as arguments (again, as mentioned at the beginning of the page, this is discipline-specific and doesn’t work for all situations). Often, the literature review is where you can establish your research as filling a particular gap or as relevant in a particular way. You have some chance to do this in your introduction in an article, but the literature review section gives a more extended opportunity to establish the conversation in the way you would like your readers to see it. You can choose the intellectual lineage you would like to be part of and whose definitions matter most to your thinking (mostly humanities-specific, but this goes for sciences as well). In addressing these points, you argue for your place in the conversation, which tends to make the lit review more compelling than a simple reporting of other sources.
Researched by Consultants from Top-Tier Management Companies

Powerpoint Templates
Icon Bundle
Kpi Dashboard
Professional
Business Plans
Swot Analysis
Gantt Chart
Business Proposal
Marketing Plan
Project Management
Business Case
Business Model
Cyber Security
Business PPT
Digital Marketing
Digital Transformation
Human Resources
Product Management
Artificial Intelligence
Company Profile
Acknowledgement PPT
PPT Presentation
Reports Brochures
One Page Pitch
Interview PPT
All Categories
Top 10 Literature Review Templates with Samples and Examples
Hanisha Kapoor
The Harry Potter series has massively impacted pop culture. It marks the terminal moment of modernity. It has also showed that children are ready to read longer works.
If you have seen the Harry Potter movie or read the series, you would agree with the above example of a literature review. And if you have not, these observations will have created enough curiosity in you to encourage your children to watch Harry Potter movies or give JK Rowling’s book a workout.
A literary review is the amalgamation of extensive knowledge and understanding of the subject matter. A literature review, for all our purposes, needs to a critique that helps take the entire subject matter forward. It has to be a well-meaning critique.
A Literature Review Example for Better Understanding
An example where literature review could be done is on Malcolm Gladwell’s works on success and thinking, in the two books titled ‘Outliers’ and ‘Blink’.
As a sample literary review for these two works, one has to create a problem statement and then show how or why you take the discussion forward to a higher plane. In this case, a literary review could start by saying that success and the factors that influence it are always on the human mind.
The problem statement could be that does luck play a bigger part in success or is your talent and hard work are the major contributors? Then, one may also give examples of previous works that said the same or supported the opposite.
The key elements to a good literary review are balance, poise and evidence.
Scholars, professors, and researchers dig deeper, find scientific or literary relevance to the subject, and help readers widen their horizons. Having done this, literature reviews also give us a window into works that we should read.
This blog will take you deep into literature reviews and how these need to be structured and delivered for greater impact.
As the first step, we have to be mindful that literature reviews are not a cakewalk. It involves a lot of work: From finding suitable material to evaluating it, critical thinking, paraphrasing, citation skills, creating a methodology, etc.
Conducting an ethical and structured research needs a systematic methodology to put forth your arguments and ideas. Read this blog to showcase your research in an effective manner.
What's even more challenging for a reviewer is to present his/her study without the right visuals.
To bridge this gap, SlideTeam brings you a collection of beautiful, jaw-dropping literature review PowerPoint Templates to showcase your research in a concise and easy manner. Browse the PPT Slides below and use them to present your scholarly review!
Template 1: Literature Review PowerPoint Template
This is a well-designed PowerPoint Template to help you highlight your literature review. Incorporate this state-of-the-art PPT design and present your analysis on the specific topic. This customizable PowerPoint slide shows the findings and your evaluation of a subject. Download this PPT layout and grab your audience’s attention with your balanced review.

Download this template
Template 2: Literature Review PPT Graphic
Here is another beautiful preset for showcasing your analysis on the subject. Support your research scope and evaluation with this actionable PowerPoint template. Deploying this fully editable PPT diagram helps you professionally showcase your knowledge on the topic. Use this ready-made PowerPoint Template and justify your thesis or research questions in detail. Grab this template now!
Want to organize and present your research to get under the spotlight? Explore this blog to find suitable thesis templates to document your dissertation.
Grab this slide
Template 3: Literature Review PowerPoint Slide
Want to elaborate on your literature study? Get access to this content-ready PowerPoint Template and help your audience get your point straightaway. This PPT Design comprises an illustration to capture your viewer’s attention. List down your points on the right side of the layout and confidently present your literature review. It is a custom-made template. You can use it as per requirement. Download now!
Template 4: Literature Review PPT Template
Grab another ready-to-use PowerPoint diagram to present your summary of the published work. Use this visually appealing PPT slide to discuss your contributions in the field. Narrow down your finding and showcase proof of rational investigation to impress your audience with this custom-made PowerPoint Template. Download now!
Template 5: Literature Review PowerPoint Diagram
Wish to exhibit your literature review? Get this exclusive PPT Template to discuss the topic's strengths and weaknesses. Incorporate this ready-made PowerPoint diagram to make a point with your critical analysis and objective evaluation. Use this PPT slide to present an executive summary of your research topic. Download this fully customizable PowerPoint design now!
Grab this template
Template 6: Literature Review PowerPoint Template
Looking for ways to showcase the steps to writing a professional literature review? Deploy this content-ready PowerPoint Template and walk your audience through the steps of writing a gripping research report. This PPT slide comprises an illustration demonstrating the ways of a research methodology. Use this pre-designed preset and help your audience write some striking research findings. Download now!
Template 7: Literature Review PowerPoint Graphic
Do you want to summarize your arguments on a particular topic? Incorporate this content-ready PowerPoint template and present your research on a chosen subject. Use this ready-made PPT graphic and provide an overview of the key findings and unresolved problems that your research has addressed. It is a custom-made PPT template. Download now!
Template 8: Literature Review PPT Slide
Here is another well-crafted PowerPoint Template for you to exhibit your theoretical framework for your research. This fully editable PPT diagram is perfect to help you highlight past work related to the topic. Walk your audience through your research study analysis using this ready-made PowerPoint template. Grab this preset now!
It is difficult to prove your plan of work in front of the audience. You might find our one-page research proposal templates useful to convince your readers the value of your project.

Template 9: Literature Review PowerPoint Template
Use this one-page literature review PowerPoint Slide and showcase your audience with a description, summary, and critical evaluation of your work. Incorporate this actionable PPT design and provide your audience with an overview of sources you have explored while studying the topic. Deploy this custom-made PowerPoint Template to demonstrate how and where your research fits within the broader field of investigation and research.
Template 10: Literature Review PPT Diagram
This is another well-designed one-page literature review PowerPoint Template to present your research on a particular topic. Give your audience a brief introduction on the subject and highlight its strengths and weaknesses using this actionable PPT Design. Showcase your research within the context of existing literature with this customizable PowerPoint diagram. Click the link below to grab this ready-made PPT slide.
Finally, the gist
Citing research is not enough. It is essential to bring your study into notice to make a point in public. Thus, deploy SlideTeam’s ready-made literature review PowerPoint Templates to justify and support your research. These PPT slides are easy to use and can be downloaded with just one click. Get access to these ready-made and premium PowerPoint Slides from our monthly, semi-annual, annual, annual + custom design subscriptions here .
PS: Wish to showcase your past research experience? Explore this exclusive guide replete with research statement PPT templates to communicate your findings in a clear and concise manner.
Literature Review FAQs
What are the important parts of literature review.
Like most academic papers, literature reviews also comprise three basic elements:
- An introduction or background information section
- The body of the review containing the discussion of sources
- Conclusion and/or recommendations section to end the paper.
What is reviewed in a literature review?
A literature review is a academic writing providing audience with the knowledge and understanding literature on a specific topic. A literature review includes a critical analysis of the material; this is why it is called a literature review rather than a literature report.
What are the characteristics of a good literature review?
An effective literature review provides an overview of an existing research in the following ways:
- Outlining research trends
- Evaluating strengths and weaknesses of the subject
- Identifying potential gaps in the topic
- Establishing the need for current/future research projects
Why is literature review important?
Literature review helps in gaining an understanding of the existing research. It expands your knowledge relevant to a particular topic or area of study. It is also important as literature reviews showcase improvements needed in a piece of literature. The key word to remember in speaking about literature reviews is critique. We critique to produce better body of literature the next time.
Why do we need literature review?
The purpose of any literature review is to summarize the arguments and ideas of existing knowledge on a particular subject without adding any new contribution. Being built on existing knowledge, literature review helps the researcher to bring new insights and even bring a fresh, unique perspective to view the original topic of research.
Related posts:
- How to Design the Perfect Service Launch Presentation [Custom Launch Deck Included]
- Quarterly Business Review Presentation: All the Essential Slides You Need in Your Deck
- [Updated 2023] How to Design The Perfect Product Launch Presentation [Best Templates Included]
- 99% of the Pitches Fail! Find Out What Makes Any Startup a Success
Liked this blog? Please recommend us

Top 20 Research and Innovation PPT Templates To Get A Competitive Edge
![lit review presentation Top 10 Research Roadmap Templates To Trace Your Journey of Innovations and Expeditions [Free PDF Attached]](https://www.slideteam.net/wp/wp-content/uploads/2022/03/1013x441no-button-20-1013x441.jpg)
Top 10 Research Roadmap Templates To Trace Your Journey of Innovations and Expeditions [Free PDF Attached]
This form is protected by reCAPTCHA - the Google Privacy Policy and Terms of Service apply.

Digital revolution powerpoint presentation slides

Sales funnel results presentation layouts
3d men joinning circular jigsaw puzzles ppt graphics icons
Business Strategic Planning Template For Organizations Powerpoint Presentation Slides
Future plan powerpoint template slide

Project Management Team Powerpoint Presentation Slides

Brand marketing powerpoint presentation slides

Launching a new service powerpoint presentation with slides go to market

Agenda powerpoint slide show
Four key metrics donut chart with percentage

Engineering and technology ppt inspiration example introduction continuous process improvement

Meet our team representing in circular format


Literature Reviews
- Getting started
What is a literature review?
Why conduct a literature review, stages of a literature review, lit reviews: an overview (video), check out these books.
- Types of reviews
- 1. Define your research question
- 2. Plan your search
- 3. Search the literature
- 4. Organize your results
- 5. Synthesize your findings
- 6. Write the review
- Artificial intelligence (AI) tools
- Thompson Writing Studio This link opens in a new window
- Need to write a systematic review? This link opens in a new window

Contact a Librarian
Ask a Librarian
Definition: A literature review is a systematic examination and synthesis of existing scholarly research on a specific topic or subject.
Purpose: It serves to provide a comprehensive overview of the current state of knowledge within a particular field.
Analysis: Involves critically evaluating and summarizing key findings, methodologies, and debates found in academic literature.
Identifying Gaps: Aims to pinpoint areas where there is a lack of research or unresolved questions, highlighting opportunities for further investigation.
Contextualization: Enables researchers to understand how their work fits into the broader academic conversation and contributes to the existing body of knowledge.

tl;dr A literature review critically examines and synthesizes existing scholarly research and publications on a specific topic to provide a comprehensive understanding of the current state of knowledge in the field.
What is a literature review NOT?
❌ An annotated bibliography
❌ Original research
❌ A summary
❌ Something to be conducted at the end of your research
❌ An opinion piece
❌ A chronological compilation of studies
The reason for conducting a literature review is to:

Literature Reviews: An Overview for Graduate Students
While this 9-minute video from NCSU is geared toward graduate students, it is useful for anyone conducting a literature review.

Writing the literature review: A practical guide
Available 3rd floor of Perkins


Writing literature reviews: A guide for students of the social and behavioral sciences
Available online!

So, you have to write a literature review: A guided workbook for engineers

Telling a research story: Writing a literature review

The literature review: Six steps to success

Systematic approaches to a successful literature review
Request from Duke Medical Center Library

Doing a systematic review: A student's guide
- Next: Types of reviews >>
- Last Updated: May 17, 2024 8:42 AM
- URL: https://guides.library.duke.edu/litreviews

Services for...
- Faculty & Instructors
- Graduate Students
- Undergraduate Students
- International Students
- Patrons with Disabilities
- Harmful Language Statement
- Re-use & Attribution / Privacy
- Support the Libraries

Home Collections Education Literature Review PowerPoint Presentations
Literature Review PowerPoint Presentations And Google Slides

Literature Review Presentation Slides
A literature review in research is a critical and systematic analysis of existing literature, scholarly articles, books, and other relevant sources that are pertinent to a particular research topic or question. Incorporating a literature review in research is essential for contextualizing the study within existing knowledge, identifying research gaps, and guiding the research design and This Presentation simplifies complex ideas, making your presentation both engaging and informative. This Presentation is explain detailed with Literature images. This template is fully created by green based theme. The template empowers you to concisely convey the essence of your literature review, capturing attention and fostering understanding. This Presentation is fully customized and It is used for researchers, academics, students, and professionals engaged in various fields of study.
Features of the templates:
- 100% customizable slides and easy to download.
- Slides are available in different nodes & colors.
- The slide contained 16:9 and 4:3 formats.
- Easy to change the slide colors quickly.
- It is a well-crafted template with an instant download facility.
- Highly compatible with PowerPoint and Google Slides.
- Literature Review
- Review Of Literature
- Literature Survey
- Literature Reviews
- Google Slides
43+ Templates
177+ Templates
1297+ Templates
179+ Templates
Animals and birds
269+ Templates
Country Flags
46+ Templates

415+ Templates
Galaxy or Space
124+ Templates

30+ Templates
You May Also Like These PowerPoint Templates

What’s Included: Literature Review Template
This template is structure is based on the tried and trusted best-practice format for formal academic research projects such as dissertations and theses. The literature review template includes the following sections:
- Before you start – essential groundwork to ensure you’re ready
- The introduction section
- The core/body section
- The conclusion /summary
- Extra free resources
Each section is explained in plain, straightforward language , followed by an overview of the key elements that you need to cover. We’ve also included practical examples and links to more free videos and guides to help you understand exactly what’s required in each section.
The cleanly-formatted Google Doc can be downloaded as a fully editable MS Word Document (DOCX format), so you can use it as-is or convert it to LaTeX.
PS – if you’d like a high-level template for the entire thesis, you can we’ve got that too .
FAQs: Literature Review Template
What format is the template (doc, pdf, ppt, etc.).
The literature review chapter template is provided as a Google Doc. You can download it in MS Word format or make a copy to your Google Drive. You’re also welcome to convert it to whatever format works best for you, such as LaTeX or PDF.
What types of literature reviews can this template be used for?
The template follows the standard format for academic literature reviews, which means it will be suitable for the vast majority of academic research projects (especially those within the sciences), whether they are qualitative or quantitative in terms of design.
Keep in mind that the exact requirements for the literature review chapter will vary between universities and degree programs. These are typically minor, but it’s always a good idea to double-check your university’s requirements before you finalize your structure.
Is this template for an undergrad, Master or PhD-level thesis?
This template can be used for a literature review at any level of study. Doctoral-level projects typically require the literature review to be more extensive/comprehensive, but the structure will typically remain the same.
Can I modify the template to suit my topic/area?
Absolutely. While the template provides a general structure, you should adapt it to fit the specific requirements and focus of your literature review.
What structural style does this literature review template use?
The template assumes a thematic structure (as opposed to a chronological or methodological structure), as this is the most common approach. However, this is only one dimension of the template, so it will still be useful if you are adopting a different structure.
Does this template include the Excel literature catalog?
No, that is a separate template, which you can download for free here . This template is for the write-up of the actual literature review chapter, whereas the catalog is for use during the literature sourcing and sorting phase.
How long should the literature review chapter be?
This depends on your university’s specific requirements, so it’s best to check with them. As a general ballpark, literature reviews for Masters-level projects are usually 2,000 – 3,000 words in length, while Doctoral-level projects can reach multiples of this.
Can I include literature that contradicts my hypothesis?
Yes, it’s important to acknowledge and discuss literature that presents different viewpoints or contradicts your hypothesis. So, don’t shy away from existing research that takes an opposing view to yours.
How do I avoid plagiarism in my literature review?
Always cite your sources correctly and paraphrase ideas in your own words while maintaining the original meaning. You can always check our plagiarism score before submitting your work to help ease your mind.
Do you have an example of a populated template?
We provide a walkthrough of the template and review an example of a high-quality literature research chapter here .
Can I share this literature review template with my friends/colleagues?
Yes, you’re welcome to share this template in its original format (no editing allowed). If you want to post about it on your blog or social media, all we ask is that you reference this page as your source.
Do you have templates for the other dissertation/thesis chapters?
Yes, we do. You can find our full collection of templates here .
Can Grad Coach help me with my literature review?
Yes, you’re welcome to get in touch with us to discuss our private coaching services , where we can help you work through the literature review chapter (and any other chapters).

University of Washington Links
- College of Arts & Sciences
- Directories
- Concentrations
- Photo/Media
- Painting + Drawing
- 3D4M: ceramics + glass + sculpture
- Field Studies
- Student Work
- Study Abroad
- Art History BA
- Art History Minor
- Art History MA Thesis
- Art History MA Practicum
- Art History PhD
- Student Research
- Interaction Design
- Visual Communication Design
- Industrial Design
- Laptop Requirement
- Master of Design
- BDes/MDes Shows
- COVID-19 Updates
- Voicing a Concern
- News + Events
- Exhibitions
Mobile Menu
- Graduate Students
- Visiting Artists + Lecturers
- Seattle Arts + Culture
- Jobs, Internships, and Opportunities
- First Day Attendance
- Final Exam Attendance
- Career Fair
- Design Travel Award Application
- Finding an Internship
- Finding a Job
- Portfolio Advice
- Resume Advice
- Alumni Blog
- Alumni Statistics
- Prevention Plan
- For Students
- Press Releases
- Stay Connected
- Undergraduate Students
- Jobs + Opportunities
- Academic Advising
- Student Voice Project
- Scholarships + Awards
- Advisory Board
- A-Z Directory
- Recent News
- News Archive
- Technology + Equipment
- Rome Center
- Exhibitions, 2022-2023
- Exhibitions, 2021-2022
- Exhibitions, 2020-2021
- Exhibitions, 2019–2020
- Exhibitions, 2018–2019
- Exhibitions, 2017–2018
- Exhibitions, 2016–2017
- Exhibitions, 2015–2016
- Exhibitions, 2014–2015
- Jacob Lawrence Legacy Residency
- The Black Embodiments Studio
- BIPOC Graduate Student Curatorial Fellowship
- Critical Art Writing Group

You are here
- Autumn 2024
DESIGN 496 A: Directed Research in Interaction Design
- Open access
- Published: 21 May 2024
A modern way to teach and practice manual therapy
- Roger Kerry 1 ,
- Kenneth J. Young ORCID: orcid.org/0000-0001-8837-7977 2 ,
- David W. Evans 3 ,
- Edward Lee 1 , 4 ,
- Vasileios Georgopoulos 1 , 5 ,
- Adam Meakins 6 ,
- Chris McCarthy 7 ,
- Chad Cook 8 ,
- Colette Ridehalgh 9 , 10 ,
- Steven Vogel 11 ,
- Amanda Banton 11 ,
- Cecilia Bergström 12 ,
- Anna Maria Mazzieri 13 ,
- Firas Mourad 14 , 15 &
- Nathan Hutting 16
Chiropractic & Manual Therapies volume 32 , Article number: 17 ( 2024 ) Cite this article
2025 Accesses
109 Altmetric
Metrics details
Musculoskeletal conditions are the leading contributor to global disability and health burden. Manual therapy (MT) interventions are commonly recommended in clinical guidelines and used in the management of musculoskeletal conditions. Traditional systems of manual therapy (TMT), including physiotherapy, osteopathy, chiropractic, and soft tissue therapy have been built on principles such as clinician-centred assessment , patho-anatomical reasoning, and technique specificity. These historical principles are not supported by current evidence. However, data from clinical trials support the clinical and cost effectiveness of manual therapy as an intervention for musculoskeletal conditions, when used as part of a package of care.
The purpose of this paper is to propose a modern evidence-guided framework for the teaching and practice of MT which avoids reference to and reliance on the outdated principles of TMT. This framework is based on three fundamental humanistic dimensions common in all aspects of healthcare: safety , comfort , and efficiency . These practical elements are contextualised by positive communication , a collaborative context , and person-centred care . The framework facilitates best-practice, reasoning, and communication and is exemplified here with two case studies.
A literature review stimulated by a new method of teaching manual therapy, reflecting contemporary evidence, being trialled at a United Kingdom education institute. A group of experienced, internationally-based academics, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through reviews of contemporary literature and discussions in an iterative process. Public presentations were made to multidisciplinary groups and feedback was incorporated. Consensus was achieved through repeated discussion of relevant elements.
Conclusions
Manual therapy interventions should include both passive and active, person-empowering interventions such as exercise, education, and lifestyle adaptations. These should be delivered in a contextualised healing environment with a well-developed person-practitioner therapeutic alliance. Teaching manual therapy should follow this model.
Musculoskeletal (MSK) conditions are leading contributors to the burden of global disability and healthcare [ 1 ]. Amongst other interventions, manual therapy (MT) has been recommended for the management of people with MSK conditions in multiple clinical guidelines, for example [ 2 , 3 ].
MT has been described as the deliberate application of externally generated force upon body tissue, typically via the hands, with therapeutic intent [ 4 ]. It includes touch-based interventions such as thrust manipulation, joint mobilisation, soft-tissue mobilisation, and neurodynamic movements [ 5 ]. For people with MSK conditions, this therapeutic intent is usually to reduce pain and improve movement, thus facilitating a return to function and improved quality of life [ 6 ]. Patient perceptions of MT are, however, vague and sit among wider expectations of treatment including education, self-efficacy and the role of exercise, and prognosis [ 7 ].
Although the teaching and practice of MT has invariably changed over time, its foundations arguably remain unaltered and set in biomedical and outdated principles. This paper sets out to review contemporary literature and propose a revised model to inform the teaching and practice of MT.
The aim of this paper is to stimulate debate about the future teaching and practice of manual therapy through the proposal of an evidence-informed re-conceptualised model of manual therapy. The new model dismisses traditional elements of manual therapy which are not supported by research evidence. In place, the model offers a structure based on common humanistic principles of healthcare.
Consenus methodology
We present the literature synthesis and proposed framework as a consensus document to motivate further professional discussion developed through a simple three-stage iterative process over a 5-year period. The consensus methodology was classed as educational development which did not require ethical approval. Stage 1: a change of teaching practice was adopted by some co-authors (VG, RK, EL) on undergraduate and postgraduate Physiotherapy programmes at a UK University in 2018. This was a result of standard institutional teaching practice development which includes consideration of evidence-informed teaching. Stage 2: Input from a broader spectrum of stakeholders was sought, so a group of experienced, internationally-based educators, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through discussions in an iterative process. Stage 3: Presentations were made by some of the co-authors (VG, RK, SV, KY) to multidisciplinary groups (UK, Europe, North America) and feedback via questions and discussions was incorporated into further co-author discussions on the development of the framework. Consensus was achieved through repeated discussion of relevant elements. Figure 1 summarises the consensus methodology.
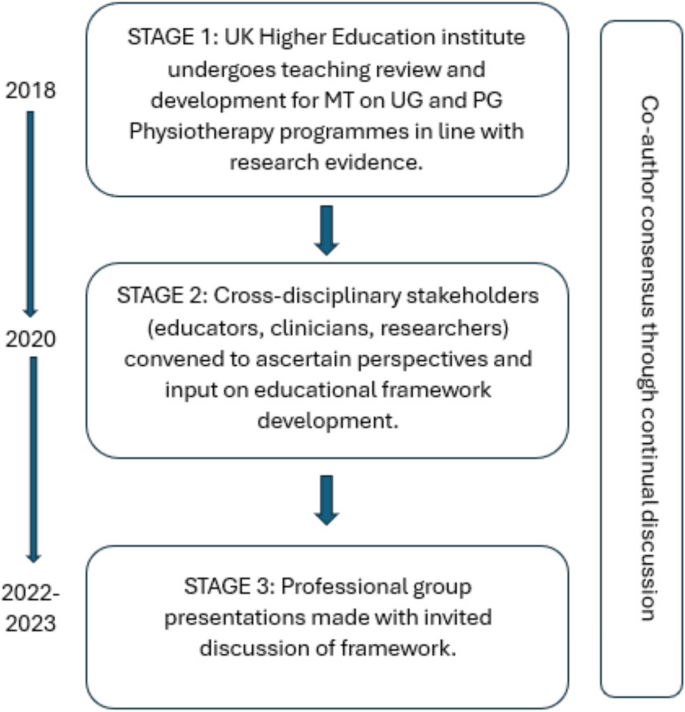
Summary and timeline of iterative consensus process for development of framework (MT: Manual Therapy; UG: Undergraduate; PG: Postgraduate)
Clinical & cost effectiveness of manual therapy
Manual therapy has been suggested to be a valuable part of a multimodal approach to managing MSK pain and disability, for example [ 8 ]. The majority of recent systematic reviews of clinical trials report a beneficial effect of MT for a range of MSK conditions, with at least similar effect sizes to other recommended approaches, for example [ 9 ]. Some systematic reviews report inconclusive findings, for example [ 10 ], and a minority report effects that were no better than comparison or sham treatments, for example [ 11 ].
Potential benefits must always be weighed against potential harms, of course. Mild to moderate adverse events from MT (e.g. mild muscle soreness) are common and generally considered acceptable [ 12 ], whilst serious adverse events are very rare and their risk may be mitigated by good practice [ 13 ]. MT has been reported by people with MSK disorders as a preferential and effective treatment with accepted levels of post-treatment soreness [ 14 ].
MT is considered cost-effective [ 15 ] and the addition of MT to exercise packages has been shown to increase clinical and cost-effectiveness compared to exercise alone in several MSK conditions [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 ]. Further, manual therapy has been shown to be less costly and more beneficial than evidence-based advice to stay active [ 24 ].
In summary, MT is considered a useful evidence-based addition to care packages for people experiencing pain and disability associated with MSK conditions. As such, MT continues to be included in national and international clinical guidelines for a range of MSK conditions as part of multimodal care.
Principles of traditional manual therapy (TMT)
Manual therapy has been used within healthcare for centuries [ 4 ] with many branches of MT having appeared (and disappeared) over time [ 25 ]. In developed nations today, MT is most commonly utilised by the formalised professional groups of physiotherapy, osteopathy, chiropractic, as well as groups such as soft tissue therapists. All of these groups have a history that borrows heavily from traditional healers and bone-setters [ 26 ].
Although there are many elements of MT, three principles appear to have become ubiquitous within what we shall now refer to as ‘traditional manual therapy’ (TMT): clinician-centred assessment , patho-anatomical reasoning , and technique specificity [ 27 , 28 , 29 , 30 ]. These principles continue to influence the teaching and practice of manual therapy over recent years, for example [ 31 ].
However, they have become increasingly difficult to defend given a growing volume of empirical evidence to the contrary.
Traditional manual therapy (TMT) principles: origins and problems
Clinician-centred assessment.
TMT has long had an emphasis on what we shall refer to as clinician-centred assessments . Within this, we claim, is an assumption that clinical information is both highly accurate and diagnostically important, for example [ 32 ]. Clinician-centred assessments include, for example, routine imaging, the search for patho-anatomical 'lesions’ and asymmetries, and specialised palpation. Although the focus of this paper is on the ‘hands-on’ examples of client-centred assessment, the notion of imaging is presented below to expose some of the flaws in the underlying belief system for TMT.
The emphasis on clinician-centred assessments has probably been driven, in part, by a desire for objective diagnostic tests which align well with gold-standard imaging. Indeed, since the discovery of x-rays, radiological imaging been used as an assessment for spinal pain – and a justification for using spinal manipulation – particularly in the chiropractic profession [ 33 ]. Contrary to many TMT claims, X-ray imaging is not without risk [ 34 ]. Additionally, until relatively recently (with the advent of magnetic resonance imaging) it was not widely appreciated that patho-anatomical ‘lesions’ believed to explain MSK pain conditions were nearly as common in pain-free individuals as those with pain [ 35 ]. Accordingly, the rates of unnecessary treatments, including surgery, are known to increase when imaging is used routinely [ 36 ]. For patients with non-specific low back pain, for example, imaging does not improve outcomes and risks overdiagnosis and overtreatment [ 37 ]. Hence, despite being objective in nature, the value of imaging for many MSK pain conditions (particularly spinal pain) has reduced drastically with clinical guidelines across the globe recommending against routine imaging for MSK pain of non-traumatic origin [ 38 ]. Even so, the practice of routine imaging continues [ 39 ].
Hands-on interventions are inextricably related to hands-on assessment [ 40 ], and often associated with claims of ‘specialisation’ [ 41 ]. By this we mean where a great level of training and precision are claimed to be necessary for influencing the interpretation of assessment findings, treatment decisions, and/or treatment outcomes. Implicit within this claim is that therapists who are unable to achieve such precision are not able to perform MT to an acceptable level (and thereby are not able to provide benefit to patients).
There are numerous studies that cast doubt over claims of highly specialised palpation skills. Palpation of anatomical landmarks does not reach a clinically acceptable level of validity [ 42 ]. Specialised motion palpation does not appear to be a good method for differentiating people with or without low back pain [ 43 ]. Poor content validity of specialised motion tests have been reported, in line with a lack of acceptable reference standards [ 44 ]. Palpable sensations reported by therapists are unlikely to be due to tissue deformation [ 45 ]. Furthermore, the delivery of interventions based on specialised palpatory findings is no better than non-specialised palpation [ 46 ]. Generally poor reliability of motion palpation skills has been reported, for example [ 47 ] and appear to be independent of clinician experience or training, for example [ 48 ]. Notably, person-centred palpation—for pain and tenderness for example—has slightly higher reliability, but is still fair at best [ 49 ].
This does not mean that palpation is of no use at all though; just that effective manual therapy does not depend upon it. For example, expert therapists can display high levels of interrater reliability during specialised motion palpation [ 50 ]. Focused training can improve the interrater reliability of specialised skills [ 51 ]. However, the validity of the phenomenon remains poor. Given the weight of the evidence and consistency of data over recent decades, we suggest that the role of clinician-centred hands-on assessment is no longer central to contemporary manual therapy.
Patho-anatomical reasoning
The justification for selecting particular MT interventions has historically been based upon the patho-anatomical status of local peripheral tissue [ 52 , 53 , 54 , 55 ]. Patho-anatomical reasoning, we propose, is the framework that links clinician-centred assessments to the desire for highly specific delivery of MT interventionsKey to this is the relationship between a patho-anatomic diagnosis and the assumed mechanisms of action of the intervention employed.
Theories for the mechanisms of action of MT interventions are many. Some of the most prominent include reductions of disc herniations [ 56 ], re-positioning of a bone or joint [ 32 ], removal of intra-articular adhesions [ 57 ], changes in the biomechanical properties of soft tissues [ 58 ], central pain modulation [ 59 ], and biochemical changes [ 60 ]. These theories have been used to justify the choice of certain interventions: a matching of diagnosis (i.e., existence of a lesion) to the effect of treatment takes place. However, most of these mechanistic theories either lack evidence or have been directly contested [ 61 ].
The causal relationship between proposed tissue-based factors such as posture, ergonomic settings, etc. and painful experience has also been disputed [ 62 ]. Although local tissue stiffness has been observed in people with pain, this is typically associated with neuromuscular responses, rather than patho-anatomical changes at local tissue level [ 63 , 64 , 65 , 66 ]. Overall, although some local tissue adaptions have been identified in people with recurrent MSK pain, this is inconsistent and the evidence is currently of low quality [ 67 ] are generally limited to short-term follow-up measures [ 68 ].
Technique specificity
TMT techniques have been taught with an emphasis that a particular direction, ‘grade’ of joint movement, or deformation of tissue at a very specific location in a certain way, is required to achieve a successful treatment outcome.
One problem with a demand for technique specificity in manual therapy is that an intervention does not always result in the intended effect. For example, posteroanterior forces applied during spinal mobilization consistently induce sagittal rotation, as opposed to the assumed posteroanterior translation, for example [ 69 ]. Furthermore, irrespective of the MT intervention chosen, restricting movements to a particular spinal segment is difficult and a regional, non-specific motion is typically induced, for example [ 70 ].
To support technique specificity, comparative data must repeatedly and reproducibly show superiority of outcome from specific MT interventions over non-specific MT, which is consistently not observed [ 71 , 72 , 73 ]. Some studies have demonstrated localised effects of targeted interventions [ 74 ] but there appears to be no difference in outcome related to: the way in which techniques are delivered [ 75 ]; whether technique selection is random or clinician-selected [ 41 ]; or variations in the direction of force or targeted spinal level [ 76 ]. Conversely, there is evidence that non-specific technique application may improve outcomes [ 77 , 78 , 79 ]. Further, sham techniques produce comparable results to specialised approaches [ 11 ].
Passive movement and localised touch have been associated with significant analgesic responses [ 80 ]. These data indicate the presence of an analgesic mechanism. Unfortunately, mechanistic explanation for the therapeutic effects of MT upon pain and disability still remain largely in a ‘black box’ state [ 81 ]. Nevertheless, there are several plausible mechanisms of action to explain the analgesic action of MT interventions, including the activation of modulatory spinal and supraspinal responses [ 82 , 83 , 84 , 85 ]. In support of this, MT interventions have been associated with a variety of neurophysiological responses [ 61 ]. However, it must be acknowledged that these studies provide mechanistic evidence based on association, which is insufficient to make causal claims [ 86 ]. Importantly, none of these neurophysiological responses have been directly related to either the analgesic mechanisms or clinical outcome and may therefore be incidental.
There is evidence that MT does not provide analgesia in injured tissues [ 87 , 88 ]. Conversely, MT has been shown to decrease inflammatory biomarkers [ 89 , 90 , 91 , 92 , 93 ], although these changes have not been evaluated in the longer-term, nor associated with clinical outcomes.
A modern framework for manual therapy
We propose a new direction for the future of MT in which the teaching and practice of this core dimension of MSK care are no longer based on the traditional principles of clinician-centred assessment , patho-anatomical reasoning , and technique specificity .
In doing so, this framework places MT more explicitly as part of person-centred care and appeals to common principles of healthcare, best available evidence, and contemporary theory which avoids unnecessary and over-complicated explanations of observed effects. The framework is simple in terms of implementation and delivery and contextualised by common elements of best practice for healthcare, in line with regulated standard of practice, e.g., [ 94 , 95 , 96 , 97 ]. Our proposal simply illustrates the operationalisation of these common elements through manual therapy.
Too much emphasis has been given to clinician-centred assessments and this should be rebalanced with an increased use of patient-centred assessments, such as a thorough case history, the use of validated patient-reported outcome measures (PROMS), and real-time patient feedback during assessments.
The new framework considers fundamental and humanistic dimensions of touch-based therapies, such as non-specific neuromodulation, communication and sense-making, physical education, and contextual clinical effectiveness. This aligns to contemporary ideas regarding therapeutic alliance and a move towards genuinely holistic healthcare [ 98 , 99 ]. The framework needs to be “open” in order to represent and allow expression of the complexity of the therapeutic encounter. However, to prevent the exploitation of this openness the framework is underpinned by evidence, and any manual therapy approaches without plausible and measurable mechanisms are not supported.
To provide the best care, common healthcare elements such as the safety and comfort of the person seeking help and therapist must be considered, and care should be provided as efficiently as possible. Our framework embraces these dimensions and employs an integration of current evidence. It is transdisciplinary in nature and may be adopted by all MT professions. Figure 1 provides a graphical representation of the framework. It is acknowledged that all components overlap, relate, and influence each. There are two main components: the practical elements on the inside, comprised of safety, comfort, and efficiency, and the conceptual themes on the outer regions, consisting of communication, context, and person-centred care Fig. 2 .
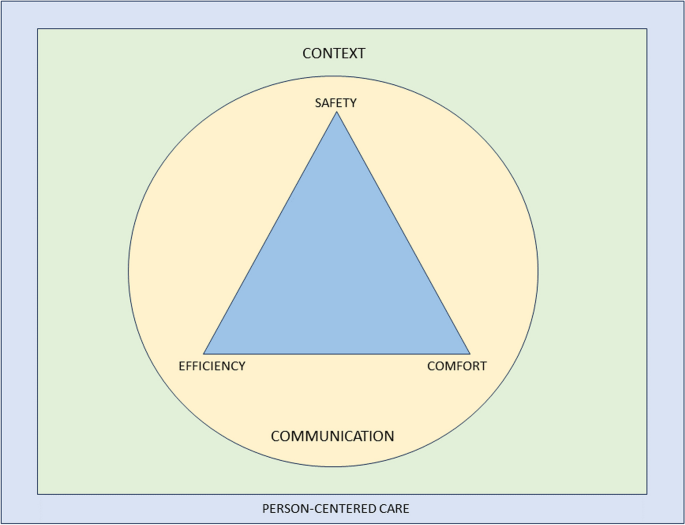
Representation of a modern teaching and practice framework for manual therapy. The image is purposefully designed to be simple, and has been developed primarily to be used as a teaching aid. When displayed in a learning environment, learners and clinicians can quickly refer to the image to check their practice against each element. To keep the image clear, each element of the image is described in detail in the text below”
Practical elements
Safety for people seeking help is a primary concern for all healthcare providers, with the aims to “ prevent and reduce risks, errors and harm that occur to patients [sic] during provision of health care… and to deliver quality essential health services ” [ 100 ]. This, and the notion of safety more generally (including that of the therapist), should be central to way MT is taught and practised.
A fundamentally safe context should be created where there is an absence of any obvious danger or risk of harm to physical or mental health. Consideration should be given to ensuring that communication and consent processes are orientated towards the safety of both the person seeking help and the therapist. The therapist should pay attention to any sense of threat that could be present in the physical, emotional, cognitive and environmental domains of the clinical encounter, and use skilful communication to mitigate anxiety about the assessment or therapeutic process.
Safety should also be considered in the clinical context of the assessment and treatment approach, ensuring that relevant and meaningful safety screenings have been undertaken [ 67 , 101 ]. There remains a need for good, skilful practice and development of manually applied techniques, but this can be achieved without reference to the principles of TMT and without the dogma of a proprietary therapeutic approach.
Comfort suggests that both the person seeking help and the therapist are physically and emotionally content during the assessment and therapeutic process. For example, the person seeking help is agreeable with any necessary state of dress (sociocultural difference should be considered); the person is relaxed and untroubled in whatever position they are in, and is adequately supported whether sitting, standing or recumbent during assessment and treatment; the therapist is comfortable with their positioning and posture; any discomfort produced by the therapeutic process is negotiated and agreed. Any physical mobilisation or touch should be applied with respect to the feedback from the person in relation to their comfort, rather than a pre-determined force based on the notion of resistance. This process requires clinical phronesis, sensitivity, responsivity, dexterity, and embodied communication [ 102 ].
The therapeutic process should be undertaken in a well-organised, competent manner aiming to achieve maximum therapeutic benefit with minimum waste of effort, time, or expense. To enhance the efficiency dimension, the assessment and therapeutic process should be an integral part of a holistic educational and/or activity-based approach to the management of the people which might also address psychological, nutritional, or ergonomic aspects of care, while being aware of social determinants to health. Recommendations exist which serve as a useful guide for enhancing care and promoting self-management in an efficient way [ 103 ].
A principle of this new model of MT is that therapists should not lose sight of the goals they develop with the people they help and ensure that there is coherence between their management aims and their techniques. Therapists should aim to support a person’s self-efficacy and use active approaches to empower them in their recovery. The overall number of therapeutic applications should be made in the context of fostering therapeutic alliance and supporting people to make sense of their situation and symptoms. This should be informed by contemporary views of the effects of manual therapy, emphasising a “physical education process” to promote sense-making and self-efficacy in alliance with the people they aim to help.
Clinical interactions need to be reproducible under a person’s own volition, serving to enhance self-empowerment. For example, someone could be taught how to “self-mobilise” if a positive effect is found with a particular therapeutic application. This should be appropriately scaffolded with behavioural change principles and functional contextualism that promote autonomy and self-management, rather than inappropriate reliance on the therapist [ 103 , 104 ].
An important and emergent notion from the proposed model is to question what constitutes indications for MT given that the model excludes traditional factors which would have informed whether manual therapy is indicated or not for a particular person. The response to this sits within the efficiency and safety dimensions: MT can be beneficial as part of a multi-dimensional approach to management across a broad population of people with musculoskeletal dysfunction, with no evidence to suggest any clinician-centered or patho-anatomical finding influences outcomes. The choice of whether or not to include MT as part of a management strategy should therefore be a product of a lack of contraindications and shared-decision making.
This framework aligns with evidence-based propositions that effectiveness and efficiency in assessment, diagnosis, and outcomes are not reliant on the therapist’s skill set of specialised elements of TMT, but rather other factors—for example variations in pain phenotypes [ 5 ].
Conceptual themes
Communication.
Communication is the overriding critical dimension to the whole therapeutic process and should be aimed at addressing peoples’ fundamental needs to make sense of their symptoms and path to recovery. The delivery and uptake of the therapy should therefore be operationalised in a communication process that meaningfully represents shared-decision making and the best possible attempt to contextualise the therapy in positive and evidence-informed explanations of the process and desired effects [ 105 ].
Within a therapeutic encounter, practitioners must give the time to listen to peoples’ accounts and explanations of their symptoms, including their ideas about their cause [ 106 ]. The assessment and diagnostic process should be a shared endeavour, for example, the negotiation of symptom reproduction. This should be done in a manner that facilitates sense-making, and which simultaneously encourages people to move on from unhelpful beliefs about their symptoms [ 107 , 108 ], encouraging understanding of the uncertain nature of pain and injury. Person-centered communication requires attention to what we communicate and how we communicate across the entire clinical interaction including interview, examination, and management planning [ 109 ]. Therapists need to be open, reflective, aware and responsive to verbal and non-verbal cues, and demonstrate a balance between engaging with people (e.g. eye-gaze) and writing/typing notes during the interview [ 110 , 111 , 112 ].
People should be given the opportunity to discuss their understanding of the diagnosis and options for treatment and rehabilitation. The decision-making process is dialogical, in which alternative options to the offered therapy should also be discussed with the comparative risks and benefits of all available management options, including doing nothing [ 113 , 114 ].
The therapist must fully appreciate the potential consequences of touch without consent. Continual dialogue should ensure that all parties are moving towards mutually agreed goals. The context of the therapy should be explicitly communicated to give appropriate context for any particular intervention as part of a holistic, evidence-based approach [ 115 , 116 , 117 ]. Therapists should be aware that their own beliefs can affect the way they communicate with their people; in the same way, a person’s context affects how they communicate what they expect from their treatment [ 107 , 118 , 119 , 120 ]. The construction of contextual healing scenarios which support positive outcomes, whilst minimising nocebic effects, is critical to effective healthcare [ 121 , 122 , 123 ].
There is a growing academic interest in the nature, role, and purpose of social and affective touch, and any re-framing of MT should consider touch as a means of communication to develop and enhance cooperative communications and strengthen the therapeutic relationship [ 124 , 125 , 126 , 127 , 128 , 129 ]. It can be soothing for a person in pain to experience the caring touch of a professional therapist [ 130 ]; on the other hand, probing, diagnostic, and touch can be experienced as alienating [ 131 , 132 , 133 ]. Touch can alter a person’s sense of body ownership and their ability to recognise and process their emotions by modulating interoceptive precision [ 129 , 134 , 135 ], and intentional touch may be perceived differently from casual, unfocussed touch [ 136 , 137 ]. There is also a thesis that touch generates shared understanding and meaning [ 138 , 139 , 140 ]. This wider appreciation of touch should be embedded in modern MT communication.
The contextual quality of a person’s experience of the therapeutic encounter can affect satisfaction and clinical outcomes [ 141 , 142 , 143 , 144 , 145 ]. The context in which therapeutic care takes place should therefore be developed to enhance this experience. There could be very local, practical aspects of the context, such as the type of passive information available in the clinical space, e.g. replacing biomedical and pathological imagery and objects with positive, active artefacts; judicious and thoughtful organisation and use of treatment tables to discourage a sense of passivity and disempowerment; allocating a comfortable space where communication can take place; colour schemes and light sources which facilitate positivity; ensuring consistency through all clinical and administrative staff promoting encouraging and non-nocebic messages. Importantly, the way the therapist dresses influences peoples’ perception of their healthcare experience [ 146 , 147 ], and that in turn should be contextually and culturally sensitive [ 148 , 149 , 150 ].
Beyond the local clinical space is the broader social environment. The undertaking of MT should serve a role in a person’s engagement with their social environment. For example, someone returning home after engaging with their therapist and disseminating positive health messages within their home and social networks; people acting as advocates for self-empowered healthcare. Furthermore, early data have demonstrated that aligning treatment with the beliefs and values of culturally and linguistically diverse communities enhances peoples’ engagement with their healthcare [ 151 ].
Person-centred care
Here we borrow directly from one of the most established and clinically useful definitions of Person-Centered Medicine [ 152 ]:
“(Person-Centered Medicine is) an affordable biomedical and technological advance to be delivered to patients [sic] within a humanistic framework of care that recognises the importance of applying science in a manner that respects the patients [sic] as a whole person and takes full account of [their] values, preferences, aspirations, stories, cultural context, fears, worries and hopes and thus that recognises and responds to [their] emotional, social and spiritual necessities in addition to [their] physical needs” [ 152 ] , p219.
Person-centred care incorporates a person’s perspective as part of the therapeutic process. In practice, therapists need to communicate in a manner that creates adequate conversational space to elicit a person’s agenda (i.e. understanding, impact of pain, concerns, needs, and goals), which guides clinical interactions. This approach encourages greater partnership in management [ 109 , 153 , 154 ].
A roadmap outlining key actions to implement person-centeredness in clinical practice has been outlined in detail elsewhere [ 155 ]. This includes screening for serious pathology, health co-morbidities and psychosocial factors; adopting effective communication; providing positive health education; coaching and supporting people towards active self-management; and facilitating and managing co-care (when needed) [ 154 ].
It is critical and necessary now to make these features explicit and central to the revised model of MT proposed in this paper. We wish to identify common ground across all MT professions in order to achieve a trans-disciplinary understanding of the evidence supporting the use of MT.
We acknowledge that our arguments here are rooted in empiricism and deliberately based on available research data from within the health science disciplines. We also acknowledge that there is a wider debate about future directions in person-centred care arising from the current evolution of the evidence-based health care movement, which has pointed to the need to learn more about peoples’ lived experiences, to redefine the model of the therapeutic relationship. Although beyond the scope of this paper, a full exploration of modern health care provision involves reconsideration of the ethics and legal requirements of communication and shared decision-making [ 156 , 157 , 158 , 159 ]. The authors envision this paper as a stimulus for self-reflection, stakeholder discussions, and ultimately change that can positively impact outcomes for people who seek manual therapy interventions.
Manual therapy has long been part of MSK healthcare and, given that is likely to continue. Current evidence suggests that effectiveness does not rely on the traditional principles historically developed in any of the major manual therapies. Therefore, the continued teaching and practice based on the principles of clinician-centred palpation , patho-anatomical reasoning , and technique specificity are no longer justified and may well even limit the value of MT.
A revised and reconceptualised framework of MT, based on the humanistic domains of safety, comfort and efficiency and underpinned by the dimensions of communication, context and person-centred care will ensure an empowering, biopsychosocial, evidence-informed approach to MSK care. We propose that the future teaching and practice of MT in physiotherapy, osteopathy, chiropractic, and all associated hands-on professions working within the healthcare field should be based on this new framework.
Availability of data and materials
Young C, Argáez C. CADTH Rapid Response Reports. Manual Therapy for Chronic Non-Cancer Back and Neck Pain: A Review of Clinical Effectiveness. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. Copyright © 2020 Canadian Agency for Drugs and Technologies in Health.; 2020.
Blanpied PR, Gross AR, Elliott JM, Devaney LL, Clewley D, Walton DM, et al. Neck Pain: Revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1-a83.
Article PubMed Google Scholar
NICE. Low back pain and sciatica in over 16s: assessment and management. NICE guideline [NG59]. 2016.
Pettman E. A history of manipulative therapy. J Man Manip Ther. 2007;15(3):165–74.
Article PubMed PubMed Central Google Scholar
Damian K, Chad C, Kenneth L, David G. Time to evolve: the applicability of pain phenotyping in manual therapy. J Man Manip Ther. 2022;30(2):61–7.
McCarthy CJ. Combined Movement Theory: Rational Mobilization and Manipulation of the Vertebral Column. London, UK: Churchill Livingstone; 2010.
Google Scholar
Subialka JA, Smith K, Signorino JA, Young JL, Rhon DI, Rentmeester C. What do patients referred to physical therapy for a musculoskeletal condition expect? A qualitative assessment. Musculoskel Sci Pract. 2022;59:102543.
Article Google Scholar
Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017;25(3):160–8.
Wilhelm M, Cleland J, Carroll A, Marinch M, Imhoff M, Severini N, et al. The combined effects of manual therapy and exercise on pain and related disability for individuals with nonspecific neck pain: A systematic review with meta-analysis. J Man Manip Ther. 2023;31(6):393–407.
Schenk R, Donaldson M, Parent-Nichols J, Wilhelm M, Wright A, Cleland JA. Effectiveness of cervicothoracic and thoracic manual physical therapy in managing upper quarter disorders - a systematic review. J Man Manipulative Therap. 2021:1–10.
Lavazza C, Galli M, Abenavoli A, Maggiani A. Sham treatment effects in manual therapy trials on back pain patients: a systematic review and pairwise meta-analysis. BMJ Open. 2021;11(5):e045106.
Funabashi M, Pohlman KA, Goldsworthy R, Lee A, Tibbles A, Mior S, et al. Beliefs, perceptions and practices of chiropractors and patients about mitigation strategies for benign adverse events after spinal manipulation therapy. Chiropr Man Therap. 2020;28(1):46.
Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for Examination of the Cervical Region for Potential of Vascular Pathologies of the Neck Prior to Musculoskeletal Intervention: International IFOMPT Cervical Framework. J Orthop Sports Phys Ther. 2022;53(1):7–22.
Thomas M, Thomson OP, Kolubinski DC, Stewart-Lord A. The attitudes and beliefs about manual therapy held by patients experiencing low back pain: a scoping review. Musculoskelet Sci Pract. 2023;65:102752.
Lilje S, van Tulder M, Wykman A, Aboagye E, Persson U. Cost-effectiveness of specialised manual therapy versus orthopaedic care for musculoskeletal disorders: long-term follow-up and health economic model. Ther Adv Musculoskelet Dis. 2023;15:1759720x221147751.
Article CAS PubMed PubMed Central Google Scholar
Abbott JH, Robertson MC, Chapple C, Pinto D, Wright AA, Leon de la Barra S, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: clinical effectiveness. Osteoarthritis Cartilage. 2013;21(4):525–34.
Article CAS PubMed Google Scholar
Bove AM, Smith KJ, Bise CG, Fritz JM, Childs JD, Brennan GP, et al. Exercise, Manual Therapy, and Booster Sessions in Knee Osteoarthritis: Cost-Effectiveness Analysis From a Multicenter Randomized Controlled Trial. Phys Ther. 2018;98(1):16–27.
Leininger B, McDonough C, Evans R, Tosteson T, Tosteson AN, Bronfort G. Cost-effectiveness of spinal manipulative therapy, supervised exercise, and home exercise for older adults with chronic neck pain. Spine J. 2016;16(11):1292–304.
Tsertsvadze A, Clar C, Court R, Clarke A, Mistry H, Sutcliffe P. Cost-effectiveness of manual therapy for the management of musculoskeletal conditions: a systematic review and narrative synthesis of evidence from randomized controlled trials. J Manipulative Physiol Ther. 2014;37(6):343–62.
UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ. 2004;329(7479):1377.
Article PubMed Central Google Scholar
UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: cost effectiveness of physical treatments for back pain in primary care. BMJ (Clinical research ed). 2004;329(7479):1381.
van Dongen JM, Groeneweg R, Rubinstein SM, Bosmans JE, Oostendorp RA, Ostelo RW, et al. Cost-effectiveness of manual therapy versus physiotherapy in patients with sub-acute and chronic neck pain: a randomised controlled trial. Eur Spine J. 2016;25(7):2087–96.
Woods B, Manca A, Weatherly H, Saramago P, Sideris E, Giannopoulou C, et al. Cost-effectiveness of adjunct non-pharmacological interventions for osteoarthritis of the knee. PLoS ONE. 2017;12(3):e0172749.
Aboagye E, Lilje S, Bengtsson C, Peterson A, Persson U, Skillgate E. Manual therapy versus advice to stay active for nonspecific back and/or neck pain: a cost-effectiveness analysis. Chiropr Man Therap. 2022;30(1):27.
Paris SV. A History of Manipulative Therapy Through the Ages and Up to the Current Controversy in the United States. J Man Manipulative Ther. 2000;8(2):66–77.
MacDonald CW, Osmotherly PG, Parkes R, Rivett DA. The current manipulation debate: historical context to address a broken narrative. J Man Manipulative Therap. 2019;27(1):1–4.
Fryer G. Intervertebral dysfunction: a discussion of the manipulable spinal lesion. J Am Osteopath Assoc. 2003;6(2):64–73.
McCarthy CJ. Spinal manipulative thrust technique using combined movement theory. Man Ther. 2001;6(4):197–204.
Vickers A, Zollman C. ABC of complementary medicine Massage therapies. BMJ (Clinical research ed). 1999;319(7219):1254–7.
Evans DW. Osteopathic principles: More harm than good? Int J Osteopath Med. 2013;16(1):46–53.
Mourad F, Yousif MS, Maselli F, Pellicciari L, Meroni R, Dunning J, et al. Knowledge, beliefs, and attitudes of spinal manipulation: a cross-sectional survey of Italian physiotherapists. Chiropr Man Therap. 2022;30(1):38.
Cyriax JH, Cyriax PJ. Cyriax's Illustrated Manual of Orthopaedic Medicine. 3rd ed: Butterworth-Heinemann; 1996.
Young KJ. Words matter: the prevalence of chiropractic-specific terminology on Australian chiropractors’ websites. Chiropr Man Therap. 2020;28(1):18.
Jenkins HJ, Downie AS, Moore CS, French SD. Current evidence for spinal X-ray use in the chiropractic profession: a narrative review. Chiropr Man Therap. 2018;26:48.
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–6.
Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573–81.
Hall AM, Aubrey-Bassler K, Thorne B, Maher CG. Do not routinely offer imaging for uncomplicated low back pain. BMJ (Clinical research ed). 2021;372:n291.
PubMed Google Scholar
Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79.
Hall AM, Scurrey SR, Pike AE, Albury C, Richmond HL, Matthews J, et al. Physician-reported barriers to using evidence-based recommendations for low back pain in clinical practice: a systematic review and synthesis of qualitative studies using the Theoretical Domains Framework. Implement Sci. 2019;14(1):49.
Eriksson L, Ekenberg L, Melander-Wikman A. The concept of palpation of the shoulder – A basic element of physiotherapy practice: A focus group study with physiotherapists. Adv Physiother. 2012;14(4):183–93.
Nim CG, Downie A, O’Neill S, Kawchuk GN, Perle SM, Leboeuf-Yde C. The importance of selecting the correct site to apply spinal manipulation when treating spinal pain: Myth or reality? A systematic review. Sci Rep. 2021;11(1):23415.
Alexander N, Rastelli A, Webb T, Rajendran D. The validity of lumbo-pelvic landmark palpation by manual practitioners: A systematic review. Int J Osteopath Med. 2021;39:10–20.
Leboeuf-Yde C, van Dijk J, Franz C, Hustad SA, Olsen D, Pihl T, et al. Motion palpation findings and self-reported low back pain in a population-based study sample. J Manipulative Physiol Ther. 2002;25(2):80–7.
Najm WI, Seffinger MA, Mishra SI, Dickerson VM, Adams A, Reinsch S, et al. Content validity of manual spinal palpatory exams - A systematic review. BMC Complement Altern Med. 2003;3:1.
Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, Findley T. Three-dimensional mathematical model for deformation of human fasciae in manual therapy. J Am Osteopath Assoc. 2008;108(8):379–90.
Gabriel A, Konrad A, Roidl A, Queisser J, Schleip R, Horstmann T, et al. Myofascial Treatment Techniques on the Plantar Surface Influence Functional Performance in the Dorsal Kinetic Chain. J Sports Sci Med. 2022;21(1):13–22.
PubMed PubMed Central Google Scholar
Nolet PS, Yu H, Côté P, Meyer A-L, Kristman VL, Sutton D, et al. Reliability and validity of manual palpation for the assessment of patients with low back pain: a systematic and critical review. Chiropr Man Therap. 2021;29(1):33.
Seffinger MA, Najm WI, Mishra SI, Adams A, Dickerson VM, Murphy LS, et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004;29(19):E413–25.
Beynon AM, Hebert JJ, Walker BF. The interrater reliability of static palpation of the thoracic spine for eliciting tenderness and stiffness to test for a manipulable lesion. Chiropr Man Therap. 2018;26:49.
Petersen EJ, Thurmond SM, Shaw CA, Miller KN, Lee TW, Koborsi JA. Reliability and accuracy of an expert physical therapist as a reference standard for a manual therapy joint mobilization trial. J Man Manip Ther. 2021;29(3):189–95.
Petersen EJ, Thurmond SM, Buchanan SI, Chun DH, Richey AM, Nealon LP. The effect of real-time feedback on learning lumbar spine joint mobilization by entry-level doctor of physical therapy students: a randomized, controlled, crossover trial. J Man Manip Ther. 2020;28(4):201–11.
Abbott JH, Flynn TW, Fritz JM, Hing WA, Reid D, Whitman JM. Manual physical assessment of spinal segmental motion: intent and validity. Man Ther. 2009;14(1):36–44.
Bialosky JE, Simon CB, Bishop MD, George SZ. Basis for spinal manipulative therapy: a physical therapist perspective. J Electromyogr Kinesiol. 2012;22(5):643–7.
Henderson CN. The basis for spinal manipulation: chiropractic perspective of indications and theory. J Electromyogr Kinesiol. 2012;22(5):632–42.
Sizer PS Jr, Felstehausen V, Sawyer S, Dornier L, Matthews P, Cook C. Eight critical skill sets required for manual therapy competency: a Delphi study and factor analysis of physical therapy educators of manual therapy. J Allied Health. 2007;36(1):30–40.
Ombregt L. A System of Orthopaedic Medicine: Elsevier; 2013.
Cramer GD, Henderson CN, Little JW, Daley C, Grieve TJ. Zygapophyseal joint adhesions after induced hypomobility. J Manipulative Physiol Ther. 2010;33(7):508–18.
George JW, Tunstall AC, Tepe RE, Skaggs CD. The Effects of Active Release Technique on Hamstring Flexibility: A Pilot Study. J Manipulative Physiol Ther. 2006;29(3):224–7.
Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–8.
Plaza-Manzano G, Molina-Ortega F, Lomas-Vega R, Martínez-Amat A, Achalandabaso A, Hita-Contreras F. Changes in biochemical markers of pain perception and stress response after spinal manipulation. J Orthop Sports Phys Ther. 2014;44(4):231–9.
Zusman M. Mechanism of mobilization. Physical Therapy Reviews. 2011;16(4):233–6.
De Carvalho DE, de Luca K, Funabashi M, Breen A, Wong AYL, Johansson MS, et al. Association of Exposures to Seated Postures With Immediate Increases in Back Pain: A Systematic Review of Studies With Objectively Measured Sitting Time. J Manipulative Physiol Ther. 2020;43(1):1–12.
Colloca CJ, Keller TS. Stiffness and neuromuscular reflex response of the human spine to posteroanterior manipulative thrusts in patients with low back pain. J Manipulative Physiol Ther. 2001;24(8):489–500.
Colloca CJ, Keller TS, Gunzburg R. Biomechanical and neurophysiological responses to spinal manipulation in patients with lumbar radiculopathy. J Manipulative Physiol Ther. 2004;27(1):1–15.
Reed WR, Long CR, Kawchuk GN, Sozio RS, Pickar JG. Neural Responses to Physical Characteristics of a High-velocity, Low-amplitude Spinal Manipulation: Effect of Thrust Direction. Spine. 2018;43(1):1–9.
Reed WR, Pickar JG, Sozio RS, Liebschner MAK, Little JW, Gudavalli MR. Characteristics of Paraspinal Muscle Spindle Response to Mechanically Assisted Spinal Manipulation: A Preliminary Report. J Manipulative Physiol Ther. 2017;40(6):371–80.
Devecchi V, Rushton AB, Gallina A, Heneghan NR, Falla D. Are neuromuscular adaptations present in people with recurrent spinal pain during a period of remission? a systematic review. PLoS ONE. 2021;16(4):e0249220.
Pagé I, Nougarou F, Lardon A, Descarreaux M. Changes in spinal stiffness with chronic thoracic pain: Correlation with pain and muscle activity. PLoS ONE. 2018;13(12):e0208790.
Lee RY, McGregor AH, Bull AM, Wragg P. Dynamic response of the cervical spine to posteroanterior mobilisation. Clin Biomech (Bristol, Avon). 2005;20(2):228–31.
Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific? Spine. 2004;29(13):1452–7.
Donaldson M, Petersen S, Cook C, Learman K. A Prescriptively Selected Nonthrust Manipulation Versus a Therapist-Selected Nonthrust Manipulation for Treatment of Individuals With Low Back Pain: A Randomized Clinical Trial. J Orthop Sports Phys Ther. 2016;46(4):243–50.
McCarthy CJ, Potter L, Oldham JA. Comparing targeted thrust manipulation with general thrust manipulation in patients with low back pain. A general approach is as effective as a specific one. A randomised controlled trial. BMJ Open Sport Exerc Med. 2019;5(1):e000514.
Sutlive TG, Mabry LM, Easterling EJ, Durbin JD, Hanson SL, Wainner RS, et al. Comparison of short-term response to two spinal manipulation techniques for patients with low back pain in a military beneficiary population. Mil Med. 2009;174(7):750–6.
Tuttle N, Evans K, Sperotto dos Santos Rocha C. Localised manual therapy treatment has a preferential effect on the kinematics of the targeted motion segment. Musculoskelet Sci Pract. 2021;56:102457.
Ali MN, Sethi K, Noohu MM. Comparison of two mobilization techniques in management of chronic non-specific low back pain. J Bodyw Mov Ther. 2019;23(4):918–23.
de Oliveira RF, Costa LOP, Nascimento LP, Rissato LL. Directed vertebral manipulation is not better than generic vertebral manipulation in patients with chronic low back pain: a randomised trial. J Physiother. 2020;66(3):174–9.
Gevers-Montoro C, Provencher B, Northon S, Stedile-Lovatel JP, Ortega de Mues A, Piché M. Chiropractic Spinal Manipulation Prevents Secondary Hyperalgesia Induced by Topical Capsaicin in Healthy Individuals. Front Pain Res (Lausanne, Switzerland). 2021;2:702429.
Provencher B, Northon S, Piché M. Segmental Chiropractic Spinal Manipulation Does not Reduce Pain Amplification and the Associated Pain-Related Brain Activity in a Capsaicin-Heat Pain Model. Front Pain Res (Lausanne, Switzerland). 2021;2:733727.
Watanabe N, Piché M. Editorial: Mechanisms and Effectiveness of Complementary and Alternative Medicine for Pain Management. Front Pain Res (Lausanne, Switzerland). 2022;3:863751.
Muhsen A, Moss P, Gibson W, Walker B, Jacques A, Schug S, et al. The Association Between Conditioned Pain Modulation and Manipulation-induced Analgesia in People With Lateral Epicondylalgia. Clin J Pain. 2019;35(5):435–42.
Howick J, Glasziou P, Aronson JK. Evidence-based mechanistic reasoning. J Roy Soc Med. 2010;103(11):433–41.
Haavik Taylor H, Murphy B. The effects of spinal manipulation on central integration of dual somatosensory input observed after motor training: a crossover study. J Manipulative Physiol Ther. 2010;33(4):261–72.
Haavik-Taylor H, Murphy B. Cervical spine manipulation alters sensorimotor integration: a somatosensory evoked potential study. ClinNeurophysiol. 2007;118(2):391–402.
Ogura T, Tashiro M, Masud M, Watanuki S, Shibuya K, Yamaguchi K, et al. Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain. Altern Ther Health Med. 2011;17(6):12–7.
Sparks C, Cleland JA, Elliott JM, Zagardo M, Liu WC. Using functional magnetic resonance imaging to determine if cerebral hemodynamic responses to pain change following thoracic spine thrust manipulation in healthy individuals. J Orthop Sports Phys Ther. 2013;43(5):340–8.
Evans DW. How to gain evidence for causation in disease and therapeutic intervention: from Koch’s postulates to counter-counterfactuals. Med Health Care Philos. 2022;25(3):509–21.
Lascurain-Aguirrebeña I, Newham D, Critchley DJ. Mechanism of Action of Spinal Mobilizations: A Systematic Review. Spine. 2016;41(2):159–72.
Parravicini G, Bergna A. Biological effects of direct and indirect manipulation of the fascial system Narrative review. J Bodyw Mov Ther. 2017;21(2):435–45.
Crane JD, Ogborn DI, Cupido C, Melov S, Hubbard A, Bourgeois JM, et al. Massage therapy attenuates inflammatory signaling after exercise-induced muscle damage. Sci Transl Med. 2012;4(119):119ra13.
Degenhardt BF, Darmani NA, Johnson JC, Towns LC, Rhodes DC, Trinh C, et al. Role of osteopathic manipulative treatment in altering pain biomarkers: a pilot study. J Am Osteopath Assoc. 2007;107(9):387–400.
Kovanur-Sampath K, Mani R, Cotter J, Gisselman AS, Tumilty S. Changes in biochemical markers following spinal manipulation-a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;29:120–31.
Lohman EB, Pacheco GR, Gharibvand L, Daher N, Devore K, Bains G, et al. The immediate effects of cervical spine manipulation on pain and biochemical markers in females with acute non-specific mechanical neck pain: a randomized clinical trial. J Man Manip Ther. 2019;27(4):186–96.
Teodorczyk-Injeyan JA, McGregor M, Triano JJ, Injeyan SH. Elevated Production of Nociceptive CC Chemokines and sE-Selectin in Patients With Low Back Pain and the Effects of Spinal Manipulation: A Nonrandomized Clinical Trial. Clin J Pain. 2018;34(1):68–75.
Council GC. The Code: Standards of conduct, performance and ethics for chiropractors. GCC; 2019.
Council HaCP. Standards of Proficiency - Physiotherapists. HCPC; 2013.
Council GO. Osteopathic Practice Standards. GOC; 2023.
Therapies TCfST. GCMT Code of Practice, Ethics and Proficiency for Professional Associations. GCMT; 2023.
Daluiso-King G, Hebron C. Is the biopsychosocial model in musculoskeletal physiotherapy adequate? An evolutionary concept analysis. Physiotherapy theory and practice. 2020:1–17.
Søndenå P, Dalusio-King G, Hebron C. Conceptualisation of the therapeutic alliance in physiotherapy: is it adequate? Musculoskelet Sci Pract. 2020;46:102131.
World Health Organisation. Patient Safety 2019 [Available from: https://www.who.int/news-room/fact-sheets/detail/patient-safety#:~:text=Patient%20Safety%20is%20a%20health,during%20provision%20of%20health%20care .
Vogel S, Mars T, Keeping S, Barton T, Marlin N, Froud R, et al. Clinical Risk Osteopathy and Management Scientific Report. 2012.
Ekerholt K, Bergland A. Learning and knowing bodies: Norwegian psychomotor physiotherapists’ reflections on embodied knowledge. Physiother Theory Pract. 2019;35(1):57–69.
Hutting N, Johnston V, Staal JB, Heerkens YF. Promoting the Use of Self-management Strategies for People With Persistent Musculoskeletal Disorders: The Role of Physical Therapists. J Orthop Sports Phys Ther. 2019;49(4):212–5.
Kongsted A, Ris I, Kjaer P, Hartvigsen J. Self-management at the core of back pain care: 10 key points for clinicians. Braz J Phys Therap. 2021.
Elwyn G, Durand MA, Song J, Aarts J, Barr PJ, Berger Z, et al. A three-talk model for shared decision making: multistage consultation process. BMJ (Clinical research ed). 2017;359:j4891.
Broom B. The Practice of Whole Person-Centred Healthcare. In: Anjum RL, Copeland S, Rocca E, editors. Rethinking Causality, Complexity and Evidence for the Unique Patient: A CauseHealth Resource for Healthcare Professionals and the Clinical Encounter. Cham: Springer International Publishing; 2020. p. 215–26.
Chapter Google Scholar
Darlow B, Dowell A, Baxter GD, Mathieson F, Perry M, Dean S. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med. 2013;11(6):527–34.
Stewart M, Loftus S. Sticks and Stones: The Impact of Language in Musculoskeletal Rehabilitation. J Orthop Sports Phys Ther. 2018;48(7):519–22.
Lin I, Wiles L, Waller R, Caneiro JP, Nagree Y, Straker L, et al. Patient-centred care: the cornerstone for high-value musculoskeletal pain management. Br J Sports Med. 2020;54(21):1240–2.
Cowell I, O’Sullivan P, O’Sullivan K, Poyton R, McGregor A, Murtagh G. Perceptions of physiotherapists towards the management of non-specific chronic low back pain from a biopsychosocial perspective: A qualitative study. Musculoskelet Sci Pract. 2018;38:113–9.
Edmond SN, Keefe FJ. Validating pain communication: current state of the science. Pain. 2015;156(2):215–9.
O’Keeffe M, Cullinane P, Hurley J, Leahy I, Bunzli S, O’Sullivan PB, et al. What Influences Patient-Therapist Interactions in Musculoskeletal Physical Therapy? Qualitative Systematic Review and Meta-Synthesis. Phys Ther. 2016;96(5):609–22.
Copnell G. Informed consent in physiotherapy practice: it is not what is said but how it is said. Physiotherapy. 2018;104(1):67–71.
Lee A. Bolam’ to “Montgomery” is result of evolutionary change of medical practice towards ’patient-centred care. Postgrad Med J. 2017;93(1095):46–50.
Lewis J, O’Sullivan P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med. 2018;52(24):1543–4.
Lewis J, Ridehalgh C, Moore A, Hall K. This is the day your life must surely change: Prioritising behavioural change in musculoskeletal practice. Physiotherapy. 2021.
Lewis JS, Stokes EK, Gojanovic B, Gellatly P, Mbada C, Sharma S, et al. Reframing how we care for people with persistent non-traumatic musculoskeletal pain. Suggestions for the rehabilitation community. Physiotherapy. 2021.
Bishop A, Foster NE, Thomas E, Hay EM. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain. 2008;135(1–2):187–95.
Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain (London, England). 2012;16(1):3–17.
Article CAS Google Scholar
Lakke SE, Soer R, Krijnen WP, van der Schans CP, Reneman MF, Geertzen JH. Influence of Physical Therapists’ Kinesiophobic Beliefs on Lifting Capacity in Healthy Adults. Phys Ther. 2015;95(9):1224–33.
Howe LC, Leibowitz KA, Crum AJ. When Your Doctor “Gets It” and “Gets You”: The Critical Role of Competence and Warmth in the Patient-Provider Interaction. Front Psych. 2019;10:475.
Newell D, Lothe LR, Raven TJL. Contextually Aided Recovery (CARe): a scientific theory for innate healing. Chiropr Man Therap. 2017;25:6.
Rossettini G, Camerone EM, Carlino E, Benedetti F, Testa M. Context matters: the psychoneurobiological determinants of placebo, nocebo and context-related effects in physiotherapy. Arch Physiother. 2020;10:11.
Gallace A. Social Touch. In: Olausson H, Wessberg J, Morrison I, McGlone F, editors. Affective Touch and the Neurophysiology of CT Afferents: Springer; 2016.
Gallace A, Spence C. The science of interpersonal touch: an overview. Neurosci Biobehav Rev. 2010;34(2):246–59.
Kelly MA, Nixon L, McClurg C, Scherpbier A, King N, Dornan T. Experience of Touch in Health Care: A Meta-Ethnography Across the Health Care Professions. Qual Health Res. 2018;28(2):200–12.
McGlone F, Cerritelli F, Walker S, Esteves J. The role of gentle touch in perinatal osteopathic manual therapy. Neurosci Biobehav Rev. 2017;72:1–9.
Olausson H, Wessberg J, Morrison I, McGlone F. Affective Touch and the Neurophysiology of CT Afferents: Springer; 2016.
McParlin Z, Cerritelli F, Rossettini G, Friston KJ, Esteves JE. Therapeutic Alliance as Active Inference: The Role of Therapeutic Touch and Biobehavioural Synchrony in Musculoskeletal Care. Front Behav Neurosci. 2022;16:897247.
Meijer LL, Ruis C, van der Smagt MJ, Scherder EJA, Dijkerman HC. Neural basis of affective touch and pain: A novel model suggests possible targets for pain amelioration. J Neuropsychol. 2021.
Allen-Collinson J, Pavey A. Touching moments: phenomenological sociology and the haptic dimension in the lived experience of motor neurone disease. Sociol Health Illn. 2014;36(6):793–806.
Bjorbækmo WS, Mengshoel AM. “A touch of physiotherapy” - the significance and meaning of touch in the practice of physiotherapy. Physiother Theory Pract. 2016;32(1):10–9.
Nummenmaa L, Tuominen L, Dunbar R, Hirvonen J, Manninen S, Arponen E, et al. Social touch modulates endogenous μ-opioid system activity in humans. Neuroimage. 2016;138:242–7.
Calsius J, De Bie J, Hertogen R, Meesen R. Touching the Lived Body in Patients with Medically Unexplained Symptoms. How an Integration of Hands-on Bodywork and Body Awareness in Psychotherapy may Help People with Alexithymia. Front Psychol. 2016;7:253.
Gentsch A, Crucianelli L, Jenkinson P, Fotopoulou A. The touched self: Affective touch and body awareness in health and disease. Affective touch and the neurophysiology of CT afferents Springer; 2016.
Cerritelli F, Chiacchiaretta P, Gambi F, Ferretti A. Effect of Continuous Touch on Brain Functional Connectivity Is Modified by the Operator’s Tactile Attention. Front Hum Neurosci. 2017;11:368.
Tramontano M, Cerritelli F, Piras F, Spanò B, Tamburella F, Piras F, et al. Brain Connectivity Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Brain Sci. 2020;10(12):969.
Øberg GK, Blanchard Y, Obstfelder A. Therapeutic encounters with preterm infants: interaction, posture and movement. Physiother Theory Pract. 2014;30(1):1–5.
Øberg GK, Normann B, Gallagher S. Embodied-enactive clinical reasoning in physical therapy. Physiother Theory Pract. 2015;31(4):244–52.
Consedine S, Standen C, Niven E. Knowing hands converse with an expressive body – An experience of osteopathic touch. Int J Osteopath Med. 2016;19:3–12.
Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48.
Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41–8.
Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201–3.
Sherriff B, Clark C, Killingback C, Newell D. Musculoskeletal practitioners’ perceptions of contextual factors that may influence chronic low back pain outcomes: a modified Delphi study. Chiropr Man Therap. 2023;31(1):12.
Sherriff B, Clark C, Killingback C, Newell D. Impact of contextual factors on patient outcomes following conservative low back pain treatment: systematic review. Chiropr Manual Therap. 2022;30(1):20.
Mercer E, Mackay-Lyons M, Conway N, Flynn J, Mercer C. Perceptions of outpatients regarding the attire of physiotherapists. Physiother Can. 2008;60(4):349–57.
Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature— targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578.
Beach MC, Fitzgerald A, Saha S. White Coat Hype: Branding Physicians With Professional Attire. JAMA Intern Med. 2013;173(6):467–8.
Bearman G, Bryant K, Leekha S, Mayer J, Munoz-Price LS, Murthy R, et al. Healthcare Personnel Attire in Non-Operating-Room Settings. Infect Control Hosp Epidemiol. 2014;35(2):107–21.
Rehman SU, Nietert PJ, Cope DW, Kilpatrick AO. What to wear today? Effect of doctor’s attire on the trust and confidence of patients. Am J Med. 2005;118(11):1279–86.
Brady B, Veljanova I, Schabrun S, Chipchase L. Integrating culturally informed approaches into physiotherapy assessment and treatment of chronic pain: a pilot randomised controlled trial. BMJ Open. 2018;8(7):e021999.
Miles A, Mezzich JE. The care of the patient and the soul of the clinic: person-centered medicine as an emergent model of clinical practice. Int J Person Centred Med. 2012;1(2):207–22.
Cowell I, McGregor A, O’Sullivan P, O’Sullivan K, Poyton R, Schoeb V, et al. How do physiotherapists solicit and explore patients’ concerns in back pain consultations: a conversation analytic approach. Physiother Theory Pract. 2021;37(6):693–709.
Hutting N, Caneiro JP, Ong'wen MO, Miciak M, Roberts LE. Patient-centered care in musculoskeletal practice: key elements to support clinicians to focus on the person. 2021.
Caneiro JP, Roos EM, Barton CJ, O’Sullivan K, Kent P, Lin I, et al. It is time to move beyond “body region silos” to manage musculoskeletal pain: five actions to change clinical practice. Br J Sports Med. 2020;54(8):438–9.
Greenhalgh T, Howick J, Maskrey N, EBM Renaissance Group. Evidence based medicine: a movement in crisis? Brit Med J. 2014;348:g3725.
Greenhalgh T, Snow R, Ryan S, Rees S, Salisbury H. Six ‘biases’ against patients and carers in evidence-based medicine. Bmc Med. 2015;13(1):200.
Loughlin M, Fuller J, Bluhm R, Buetow S, Borgerson K. Theory, experience and practice. J Eval Clin Pract. 2016;22(4):459–65.
Simpson JK, Innes S. Informed consent, duty of disclosure and chiropractic: where are we? Chiropr Man Therap. 2020;28(1):60.
Download references
Acknowledgements
Use of any animal or human data or tissue.
No funding was received for this paper.
Author information
Authors and affiliations.
School of Health Sciences, Queens Medical Centre, University of Nottingham, Nottingham, NG7 2HA, UK
Roger Kerry, Edward Lee & Vasileios Georgopoulos
Allied Health Research Unit, University of Central Lancashire, Preston, PR1 2HE, UK
Kenneth J. Young
Centre of Precision Rehabilitation for Spinal Pain, School of Sport, Exercise and Rehabilitation Sciences, University of Birmingham, Edgbaston, Birmingham, B15 2TT, UK
David W. Evans
Nottingham CityCare Partnership, Bennerley Rd, Nottingham, NG6 8WR, UK
School of Medicine, University of Nottingham, Queens Medical Centre, Nottingham, NG7 2HA, UK
Vasileios Georgopoulos
Department of Orthopaedics, West Herts Hospitals Trust, Watford, WD18 0HB, UK
Adam Meakins
School of Physiotherapy, Manchester Metropolitan University, Manchester, M15 6GX, UK
Chris McCarthy
Department of Orthopaedics, Duke University, 200 Morris Street, Durham, NC, 27701, USA
School of Sport and Health Sciences, University of Brighton, Darley Rd, Eastbourne, BN20 7UR, UK
Colette Ridehalgh
Clinical Neuroscience, Trafford Building, Brighton and Sussex Medical School, University of Sussex, Brighton, BN1 9PX, UK
University College of Osteopathy, 275 Borough High St, London, SE1 1JE, UK
Steven Vogel & Amanda Banton
Department of Clinical Sciences, Obstetrics and Gynecology, Umeå University, S-90187, Umeå, Sweden
Cecilia Bergström
The School of Soft Tissue Therapy, Exmouth, Devon, EX8 1DQ, UK
Anna Maria Mazzieri
Department of health, LUNEX, Differdange, 4671, Luxembourg
Firas Mourad
Luxembourg Health & Sport Sciences Research Institute A.s.b.l., 50, Avenue du Parc des Sports, Differdange, 4671, Luxembourg
Department of Occupation and Health, School of Organization and Development, HAN University of Applied Sciences, Nijmegen, the Netherlands
Nathan Hutting
You can also search for this author in PubMed Google Scholar
Contributions
Concept and research design: RK, KJY, DWE, EL, AM, VG. Data collection: All authors. Data analysis: All authors. Writing and editing of the manuscript: All authors.
Corresponding author
Correspondence to Kenneth J. Young .
Ethics declarations
Ethics approval and consent to participate.
All participants are co-authors. Ethical approval was not necessary.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kerry, R., Young, K.J., Evans, D.W. et al. A modern way to teach and practice manual therapy. Chiropr Man Therap 32 , 17 (2024). https://doi.org/10.1186/s12998-024-00537-0
Download citation
Received : 18 October 2023
Accepted : 17 April 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s12998-024-00537-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Manual Therapy
- Evidence-based healthcare
- Person-centred healthcare
- Physiotherapy
- Chiropractic
- Soft-tissue therapy
Chiropractic & Manual Therapies
ISSN: 2045-709X
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Neuroblastoma in Adults: A Scoping Review of Presentations, Genetics and Therapies
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- For correspondence: [email protected]
- Info/History
- Preview PDF
Purpose: As a scoping review, evaluate the literature on the presentations, genetics, and therapies for neuroblastoma in adult patients. Methods: We searched four databases for studies reporting adults with neuroblastoma. Cohort studies, case series, and case reports were synthesized qualitatively. Progression-free and overall survival were compared amongst cohort studies. Results: Of 2287 unique records, 136 studies published in 141 articles were included. A total of 679 patients were included. On review of individual patient-level data, the adrenal gland and retroperitoneum were the most common primary site (47.3%). MYCN was rarely amplified: seven studies reported zero patients with MYCN amplified, two studies with a single patient, and one study with 3/7 patients. Adult patients appear to show a high frequency of somatic mutations, specifically ALK (42%) and ATRX (58%). Registry data of included studies showed 5-year overall survival to be 36.3% in adults aged ≥20 years. Conclusion: Of nearly 700 cases of adult neuroblastoma published in the literature, the most common primary site is the adrenals or retroperitoneum. Relative to pediatric cases, adult cases demonstrate a considerable rate of somatic mutations such as ALK and ATRX. Registry data showed 5-year survival of 36%. Future studies evaluating targeted therapies in larger samples are needed.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
This study did not receive any funding
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
Only publicly available human data from published studies were used for this review. All published studies were cited in the manuscript of the study.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
All data produced in the present study are available upon reasonable request to the authors
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
- Addiction Medicine (324)
- Allergy and Immunology (632)
- Anesthesia (168)
- Cardiovascular Medicine (2397)
- Dentistry and Oral Medicine (289)
- Dermatology (207)
- Emergency Medicine (381)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (848)
- Epidemiology (11791)
- Forensic Medicine (10)
- Gastroenterology (705)
- Genetic and Genomic Medicine (3765)
- Geriatric Medicine (350)
- Health Economics (637)
- Health Informatics (2407)
- Health Policy (938)
- Health Systems and Quality Improvement (904)
- Hematology (342)
- HIV/AIDS (785)
- Infectious Diseases (except HIV/AIDS) (13339)
- Intensive Care and Critical Care Medicine (769)
- Medical Education (367)
- Medical Ethics (105)
- Nephrology (401)
- Neurology (3521)
- Nursing (199)
- Nutrition (528)
- Obstetrics and Gynecology (678)
- Occupational and Environmental Health (667)
- Oncology (1831)
- Ophthalmology (538)
- Orthopedics (220)
- Otolaryngology (287)
- Pain Medicine (234)
- Palliative Medicine (66)
- Pathology (447)
- Pediatrics (1036)
- Pharmacology and Therapeutics (426)
- Primary Care Research (424)
- Psychiatry and Clinical Psychology (3186)
- Public and Global Health (6176)
- Radiology and Imaging (1288)
- Rehabilitation Medicine and Physical Therapy (751)
- Respiratory Medicine (832)
- Rheumatology (380)
- Sexual and Reproductive Health (372)
- Sports Medicine (324)
- Surgery (403)
- Toxicology (50)
- Transplantation (172)
- Urology (147)
- Search Menu
- Sign in through your institution
- Volume 2024, Issue 5, May 2024 (In Progress)
- Volume 2024, Issue 4, April 2024
- Case of the Year
- MSF Case Reports
- Audiovestibular medicine
- Cardiology and cardiovascular systems
- Critical care medicine
- Dermatology
- Emergency medicine
- Endocrinology and metabolism
- Gastroenterology and hepatology
- Geriatrics and gerontology
- Haematology
- Infectious diseases and tropical medicine
- Medical ophthalmology
- Medical disorders in pregnancy
- Paediatrics
- Palliative medicine
- Pharmacology and pharmacy
- Radiology, nuclear medicine, and medical imaging
- Respiratory disorders
- Rheumatology
- Sexual and reproductive health
- Sports medicine
- Substance abuse
- Author Guidelines
- Submission Site
- Open Access
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case presentation, acknowledgements, conflict of interest statement.
- < Previous
A peculiar foreign body ingestion in 2-year-old girl complicated by esophageal perforation: case report and review of the literature
- Article contents
- Figures & tables
- Supplementary Data
Danah Albarrak, Suliman Alrajhi, Mohammed Naeem, A peculiar foreign body ingestion in 2-year-old girl complicated by esophageal perforation: case report and review of the literature, Oxford Medical Case Reports , Volume 2024, Issue 5, May 2024, omae040, https://doi.org/10.1093/omcr/omae040
- Permissions Icon Permissions
Foreign body ingestion is a common pediatric gastrointestinal emergency, which should be suspected in all patients who present with signs of airway obstruction or upper GI bleeding, especially if it developed after the child was left unwitnessed for a while. The most common foreign bodies identified in the literature are button batteries or coins. Early identification and management of suspected foreign body ingestion is crucial as it can lead to devastating complications including bleeding, fistula formation, perforation, mediastinitis, or abscess. Here we report a case of a peculiar foreign body ingestion resulting in esophageal perforation in a 2-year-old girl.
Foreign body (FB) ingestion is considered a common gastrointestinal (GI) emergency in the pediatric population with the majority of cases occurring in children aged 6 months to 5 years [ 1 , 2 ]. The most common FB identified are coins, however, button batteries, magnets, toys, jewelry, and less commonly sharp objects have been reported in the literature [ 1 , 2 ]. Based on the 2021 Annual American Association of Poison Control Center report, FB ingestion in children less than 5 years accounted for approximately 55 000 cases with higher rates observed among boys [ 3 ]. Clinical presentation varies depending on the type and location of the FB ingested however common symptoms may include drooling, vomiting, dysphagia, throat, or chest pain [ 4 ]. Fortunately, the mortality rate is low and the majority of FBs ingested are spontaneously passed [ 1 ]. However, based on current guidelines endoscopic retrieval is indicated if the FB is impacted in the esophagus within 2hrs in case of battery ingestion with or without symptoms. A coin, magnet, or sharp foreign bodies impacted in the esophagus in an asymptomatic patient can be removed within 24hrs [ 5 ]. Any long foreign (more than 6-cm) in the esophagus should be removed within 24hrs even if the patient is asymptomatic. Only < 1% of patients may require further surgical intervention [ 1 ]. Possible complications of FB ingestion include the development of ulceration, bleeding, fistula formation, perforation, mediastinitis, or abscess [ 1 ]. Here we report a case of esophageal perforation caused by FB ingestion in a 2-year-old girl.
A 2-year-old developmentally normal girl with no significant past medical or surgical history presented to the emergency department (ED) with a three-day history of vomiting large amounts of fresh blood with clots and a single episode of dark stool. The family denied any history of fever, abdominal pain, upper respiratory tract symptoms, bleeding from other sites, easy bruising, or trauma. Two days prior to this presentation the family sought medical attention in another hospital, the patient was found to have a low hemoglobin (Hb) level of 5 g/dl. She was suspected to have foreign body ingestion and was recommended to proceed with an endoscopy. However, the family refused and the patient was discharged against medical advice.
Upon physical examination, vital signs were as follows HR 127 beats/minute, BP 84/39 mmHg, RR 26 breaths/minute, afebrile, and oxygen saturation 98% on room air. The patient was alert and active, with intact pulses, and warm extremities with no bleeding, bruises, or skin changes; the rest of the physical examination was unremarkable. The repeated Hb level was 4 g/dl, thus the patient received 10 ml/kg (-O) packed red blood cells (PRBC) transfusion. Initial chest x-ray (CXR) revealed a round radiolucent object seen lateral to the trachea on the left side with mild widening of the mediastinum, and lung fields were clear ( Fig. 1 ). The patient was anticipated to have a difficult airway and therefore was intubated to proceed with imaging safely, CXR was repeated revealing an opacity in the right upper lung likely due to aspiration ( Fig. 1 ). Computed tomography (CT) showed a hyperdense object measuring 18.1 mm, seen in the posterior mediastinum, consolidation in the right upper lobe due to aspiration and mediastinal hematoma ( Fig. 2 ).

( A ) initial CXR in the ED: reveals a round radiolucent object seen lateral to the trachea on the left side with mild widening of the mediastinum and clear lung fields. ( B ) Repeated CXR 4hrs after, an endotracheal tube is observed and there is an opacity in the right upper lung likely due to aspiration.

Findings of chest CT on the day of patient presentation (red arrows). ( A ) axial view: shows hyperdense object seen in the posterior mediastinum likely within the esophagus. ( B ) Axial and lung window view: hyperdense subject seen in the posterior mediastinum and there is consolidation in the right upper lobe (aspiration). ( C ) Coronal view: hyperdense object (FB) seen in the posterior mediastinum. ( D ) Sagittal view: hyperdense FB seen in the posterior mediastinum. Maximum intensity projection (MIP) imaging revealed a round hyperdense FB measure it 18.1 mm seen in the posterior mediastinum in multiple views, ( E ) Coronal view, ( F ) sagittal view.
The patient was rushed for exploratory thoracotomy and FB retrieval with concurrent esophagogastroduodenoscopy (EGD). Initially, rigid endoscopy was performed and revealed pooling of blood inside the esophageal lumen with bulging of the mucosa, there was no active bleeding. Left thoracotomy revealed multiple perforated feeding vessels to the pleura, which were ligated using a clip. There was no evidence of fistula, active bleeding, or inflammatory process in that area. The esophagus was skeletonized and showed no pus collection, hematoma, or cyst. However, it couldn’t be skeletonized more proximally as the arch of the aorta was intervening. The area was reexamined using rigid endoscopy and there was no evidence of perforation or active bleeding: therefore; proceeded with a fluoroscopic esophagogram which showed an esophageal pouch at the left second rib, suspicious of esophageal duplication cyst. The gastrology department was consulted to perform flexible endoscopy, which revealed a cystic-like lesion in the esophagus at almost 15 cm from the mouth with no evidence of perforation, guidewire was inserted in the cyst for the surgeon to continue.
Left thoracotomy was closed and converted to right thoracotomy which revealed a cystic-like structure, esophageal pouch, which was flimsy and macerated. An enterotomy was performed in the anterior esophageal wall almost 3 cm in length. The esophageal lumen was examined from the inside, and old digested blood coming from the esophageal lumen was noted: however; there was no active bleeding. Additionally, the cyst was followed to its origin and proximal to the enterotomy made, upon closer inspection and dissection the FB was found eroding the esophagus coming from the esophageal mucosa which was easily retrieved ( Fig. 3 ). The operation was concluded by a primary repair of the esophageal side perforation and repair of the esophageal enterotomy.

Picture of the foreign body after retrieval.
Following the surgery, the patient was admitted to PICU for close monitoring. Initially, the patient was doing well: however; on the third day she suddenly developed emesis and epistaxis and had systolic hypotension, tachycardia, and tachypnea. She improved after being managed with 20 ml/kg stat bolus, PRPCs, and platelet transfusion. Additionally, she developed left followed by right-sided pneumothorax which improved the next day. Moreover, the patient’s blood culture came back positive for gram cocci in chains (anginosus group), infectious disease department was consulted and recommended treatment with tazocin. Fluoroscopy was performed seven days postop revealing a narrowing of the upper esophagus with passing contrast to the lower esophagus and stomach ( Fig. 4 ). On day 12, the patient improved clinically and was discharged.

Fluoroscopy on day 7 post-op: revealed a narrowing of the upper esophagus (white arrows) with passing contrast to the lower esophagus and stomach.
FB ingestion is frequently encountered in pediatric emergencies, patients might present with a wide array of symptoms including drooling, dysphagia, vomiting, or emesis [ 4 ]. Timely identification of FB and management is essential to avoid possible complications which can include but are not limited to esophageal ulceration, bleeding, fistula formation, and perforation [ 1 ].
Based on the review of the literature 12 cases reported esophageal perforation secondary to FB ingestion in children aged 24 months or less ( Table 1 ). The most common FBs were button batteries and metal objects, none of the FBs identified was similar to the one retrieved from our patient. Delayed presentation and prolonged duration of impaction, especially > 1 week resulted in the development of multiple complications. Most patients were alive and well on follow-up with no complications, 2 lost follow-up, and 2 developed complications including vocal cord paralysis and intermittent croup [ 6–11 ].
Literature review of esophageal perforation secondary to FB ingestion in children aged 24 months or less
In our case, the patient had delayed presentation of FB ingestion as she started to develop signs of Upper GI bleeding 3 days prior. CT confirmed the presence of a round hyperdense FB in the posterior mediastinum. Flexible endoscopy was only able to identify a spot in the esophagus that looked cystic-like lesion. An emergency thoracotomy retrieved the FB that had eroded the esophagus. This foreign body was found to be a cork that is widely used in the caps of disposable bottles. Postoperatively the patient was admitted to the PICU for close monitoring and later discharged once she was clinically stable.
FB ingestion should be suspected in all pediatric patients who present with signs of airway obstruction or upper GI bleeding, especially if it developed after the child was left unwitnessed for a while. Parental education regarding prevention, signs and symptoms of FB ingestion is imminent in order to prevent delayed presentation and the development of devastating complications.
Primary care and emergency healthcare workers should consider FB ingestion as a differential diagnosis in any pediatric patient presenting with symptoms of airway compromise or GI bleeding, especially if there is a history of leaving the child unchaperoned. Additionally, community education on the topic is recommended to allow early recognition, and treatment and to avoid the development of any complications.
Not applicable.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
The patient provided informed consent for publication of the case report.
Eisen GM , Baron TH , Dominitz JA , Faigel DO , Goldstein JL , Johanson JF . et al. Guideline for the management of ingested foreign bodies . Gastrointest Endosc 2002 ; 55 : 802 – 6 .
Google Scholar
Dorterler ME , Günendi T . Foreign body and caustic substance ingestion in childhood . Open Access Emerg Med 2020 ; 12 : 341 – 52 .
Gummin DD , Mowry JB , Beuhler MC , Spyker DA , Rivers LJ , Feldman R . et al. 2021 annual report of the national poison data system© (npds) from america’s poison centers: 39th annual report . Clin Toxicol (Phila) 2022 ; 60 : 1381 – 643 .
Rybojad B , Niedzielska G , Niedzielski A , Drozak ER , Rybojad P . Esophageal foreign bodies in pediatric patients: a thirteen-year retrospective study . ScientificWorldJournal 2012 ; 2012 : 102642 .
Kramer RE , Lerner DG , Lin T , Manfredi M , Shah M , Stephen TC . et al. Management of ingested foreign bodies in children: a clinical report of the naspghan endoscopy committee . J Pediatr Gastroenterol Nutr 2015 ; 60 : 562 – 74 .
Leinwand K , Brumbaugh DE , Kramer RE . Button battery ingestion in children: a paradigm for management of severe pediatric foreign body ingestions . Gastrointest Endosc Clin N Am 2016 ; 26 : 99 – 118 .
Shah PV , Wathen J , Keyes J , Osborne C , Messacar K , Stence N . et al. Foreign body esophageal perforation leading to multifocal brain abscesses: a case report . J Emerg Med 2020 ; 59 : 131 – 5 .
Chang MY , Chang ML , Wu CT . Esophageal perforation caused by fish vertebra ingestion in a seven-month-old infant demanded surgical intervention: a case report . World J Gastroenterol 2006 ; 12 : 7213 – 5 .
Kimball SJ , Park AH , Rollins MD , Grimmer JF , Muntz H . A review of esophageal disc battery ingestions and a protocol for management . Arch Otolaryngol Head Neck Surg 2010 ; 136 : 866 – 71 .
Panella NJ , Kirse DJ , Pranikoff T , Evans AK . Disk battery ingestion: case series with assessment of clinical and financial impact of a preventable disease . Pediatr Emerg Care 2013 ; 29 : 165 – 9 .
Oliveros L , McIntosh C , Wilsey A , Karjoo S , Wilsey M . "Jingle all the way!": sharp foreign bodies embedded within the esophageal mucosa during the holiday season . Cureus 2022 ; 26 : e24493 .
Email alerts
Citing articles via, affiliations.
- Online ISSN 2053-8855
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Case Report
- Open access
- Published: 14 May 2024
Motor polyradiculoneuropathy as an unusual presentation of neurobrucellosis: a case report and literature review
- Ahmad Alikhani 1 ,
- Noushin Ahmadi 1 ,
- Mehran Frouzanian 2 &
- Amirsaleh Abdollahi 2
BMC Infectious Diseases volume 24 , Article number: 491 ( 2024 ) Cite this article
173 Accesses
Metrics details
Brucellosis, a zoonotic disease caused by Brucella species, poses a significant global health concern. Among its diverse clinical manifestations, neurobrucellosis remains an infrequent yet debilitating complication. Here, we present a rare case of neurobrucellosis with unusual presentations in a 45-year-old woman. The patient’s clinical course included progressive lower extremity weakness, muscle wasting, and double vision, prompting a comprehensive diagnostic evaluation. Notable findings included polyneuropathy, elevated brucella agglutination titers in both cerebrospinal fluid and blood, abnormal EMG-NCV tests, and resolving symptoms with antibiotic therapy. The clinical presentation, diagnostic challenges, and differentiation from other neurological conditions are discussed. This case underscores the importance of considering neurobrucellosis in regions where brucellosis is prevalent and highlights this rare neurological complication’s distinctive clinical and radiological features. Early recognition and appropriate treatment are crucial to mitigate the significant morbidity associated with neurobrucellosis.
Peer Review reports
Introduction
Brucellosis, caused by Brucella species, is an infectious ailment recognized by various names such as remitting, undulant, Mediterranean, Maltese, Crimean, and goat fever. Humans contract it through the consumption of unpasteurized milk and dairy products, undercooked meat, or skin contact with infected livestock [ 1 , 2 , 3 ]. Various Brucella species, including Brucella melitensis (primarily sourced from sheep and goats), Brucella abortus (found in cattle), Brucella suis (associated with pigs/hogs), and Brucella canis (linked to dogs), can lead to illness in humans [ 3 , 4 , 5 ]. While brucellosis in humans is rarely fatal, it can lead to disability [ 6 ]. Brucellosis ranks among the most prevalent zoonotic diseases, impacting approximately 500,000 individuals yearly [ 7 ]. The combined estimate for the prevalence of brucellosis was 15.53% [ 8 ].
Neurobrucellosis, a rare complication of systemic brucellosis, can occur in adult and pediatric cases [ 9 ], and can manifest at any stage of the disease. They can present in various clinical presentations such as meningitis, encephalitis, meningoencephalitis, myelitis, radiculopathy, polyneuropathy, stroke, cerebral venous thrombosis, and occasionally psychiatric symptoms [ 10 , 11 ]. Although the mortality rate is low, patients often experience persistent neurological issues following neurobrucellosis [ 12 ]. Studies suggest that around 20% of neurobrucellosis cases result in lasting neurological problems [ 13 ]. It is uncommonly considered in cases of meningoencephalitis or polyneuropathy, making it crucial for clinicians to have a high suspicion of it in patients displaying such symptoms, especially in endemic regions, to prevent severe clinical outcomes. In this study, we present a rare case of neurobrucellosis with unusual clinical presentations in a patient admitted to our center.
Case presentation
A 45-year-old female patient, with no prior medical history, presented to our center after enduring distal pain and weakness in her lower extremities for approximately 10 months. Over this period, the muscle weakness progressed, affecting proximal muscles of upper and lower limbs, and leading to a substantial weight loss of 25–30 kg despite maintaining appetite. Initially dismissive of the limb weakness and pain, the patient sought medical attention six months after symptom onset due to the worsening symptoms and gait impairment. Over the subsequent four months, she underwent multiple medical evaluations and tests, including a lumbar X-ray. Following these initial investigations and due to low serum vitamin D levels, vitamin D and calcium supplements were prescribed, and lumbar MRI were requested for further evaluation. (Table 1 )
Upon referral to an infectious disease specialist, the patient’s history of local dairy consumption and positive serologic test for brucellosis prompted treatment with rifampin and doxycycline. However, the patient’s condition deteriorated significantly five days after starting this treatment. She experienced severe gait disorder, lower extremity weakness, diplopia, and blurred vision that had gradually worsened over two weeks. Subsequently, she presented to our center for further assessment.
Upon admission, the patient was unable to stand even with assistance and exhibited diplopia. Cranial nerve examination revealed no abnormalities, except for the II, III, and IV cranial nerves, which could not be thoroughly examined due to the presence of diplopia. The patient tested negative for Kernig and Brudzinski signs. There were no palpable supraclavicular or inguinal lymph nodes. Physical examinations of the breast, axilla, lungs, heart, and abdomen were unremarkable. Muscle strength was reduced in the lower extremities, and deep tendon reflexes of the knee and Achilles were absent. The plantar reflex was non-responsive, and certain reflexes, including biceps, triceps, and brachioradialis, were absent despite normal movement of the upper extremities. Anorectal muscle tone and anal reflex were normal.
Further investigations included normal urinalysis and abdominal and pelvic ultrasound. Chest X-ray and brain CT were also ordered. Due to the patient’s refusal of lumbar puncture, a suspicion of neurobrucellosis led to the initiation of a three-drug regimen (Table 2 ); ceftriaxone 2 g IV twice daily, rifampin 600 mg PO daily, and doxycycline 100 mg PO twice daily. The ophthalmology consultation did not reveal any ocular pathology, and the neurologist ordered brain MRI and EMG-NCV tests. The patient’s brain MRI was unremarkable, but EMG-NCV showed sensory and motor polyneuropathy. Consequently, intravenous immunoglobulin (IVIG) therapy was initiated at a daily dose of 25 g. After five days, the patient consented to lumbar puncture, confirming the diagnosis of brucellosis. Co-trimoxazole 960 mg PO three times daily was added to her treatment regimen, and IVIG therapy continued for seven days. Following a 3-day course of IVIG treatment, the neuropathy symptoms showed significant improvement. By the seventh day, there was a notable enhancement in limb strength, particularly in the upper limbs, reaching a 2-point improvement. After undergoing three weeks of intravenous therapy, the patient transitioned to oral medication. Despite disagreement regarding the necessity of a second CSF examination, the patient was discharged with a prescription for doxycycline, rifampin, and cotrimoxazole. Upon discharge, the patient could walk with the aid of a walker. However, within a month, a slight limp persisted, and by the third-month post-discharge, all symptoms had resolved completely.
Brucellosis is widely spread globally, with more than half a million reported human cases annually [ 14 , 15 ]. Countries like Kenya, Yemen, Syria, Greece, and Eritrea have experienced high rates of brucellosis. The situation of brucellosis has shown signs of improvement in many epidemic regions. However, new areas with high occurrences of this disease continue to emerge, particularly in Africa and the Middle East, where the incidence of the disease varies [ 16 ]. Brucellosis is linked to various neurological complications collectively known as neurobrucellosis, which is an uncommon condition, and only a few cases have been reported globally [ 17 , 18 , 19 , 20 , 21 ]. Our patient exhibited muscle weakness, polyneuropathy, and inability to walk, which are often not regarded as indicative of a brucella infection by many physicians. While the diagnosis of neurobrucellosis can typically be confirmed through classical clinical signs, radiological examinations, and serological tests, patients might not always display typical symptoms, as observed in our case. Hence, in regions where the disease is prevalent, clinicians should maintain a high level of suspicion if patients do not show improvement with standard treatment. Additionally, the lack of awareness among healthcare professionals and limited access to advanced laboratory facilities can lead to misdiagnosis.
The frequent manifestations of neurobrucellosis include meningitis or meningoencephalitis. Typically, it starts with a sudden headache, vomiting, and altered mental state, which can progress to unconsciousness, with or without seizures [ 22 ]. Additionally, brucellosis can lead to several central nervous system issues such as inflammation of cerebral blood vessels, abscesses in the brain or epidural space, strokes, and cerebellar ataxia. Peripheral nerve problems may include nerve damage or radiculopathy, Guillain-Barré syndrome, and a syndrome resembling poliomyelitis [ 13 ]. Nevertheless, the patient exhibited no indications of seizures, brain hemorrhage, stroke, or focal neurological impairments. Instead, the observed symptoms were consistent with radiculopathy and muscular weakness.
In only 7% of neurobrucellosis cases, the peripheral nervous system is affected. Remarkably, our case falls within this rare category, adding to its unique and intriguing nature. Previous case studies have detailed polyradiculoneuropathies, manifesting as acute, subacute, or chronic forms [ 23 ]. Our patient’s condition aligns with chronic motor polyradiculopathy. Interestingly, some of these cases exhibit sensory deficits or resemble Guillain-Barré syndrome [ 23 , 24 ]. In a prior case study conducted by Abuzinadah and colleagues, a comparable case was described as a subacute motor polyradiculopathy. The patient exhibited gradual bilateral lower limb weakness over three weeks, eventually leading to loss of mobility within seven weeks. Brucella was isolated from the cerebrospinal fluid after a two-week incubation period, and high antibody titers were detected in the patient’s serum [ 23 ]. In another study led by Alanazi and colleagues, a 56-year-old man initially diagnosed with Guillain-Barré syndrome experienced worsening symptoms despite appropriate treatment. Following plasma exchange and antibiotics, his condition improved temporarily, only to relapse, raising suspicion of chronic inflammatory demyelinating polyneuropathy, and treatment with IVIG resulted in substantial improvement. Upon further investigation, he was diagnosed with brucellosis [ 24 ]. This highlights the importance of recognizing GBS-like symptoms in regions where brucellosis is prevalent, prompting clinicians to consider the possibility of brucellosis in their diagnosis.
While there are no established criteria for diagnosing neurobrucellosis [ 25 ], certain articles have suggested several methods for its diagnosis. These methods include the presence of symptoms aligning with neurobrucellosis, isolating brucella from cerebrospinal fluid (CSF) or detecting a positive brucella agglutination titer in CSF, observing lymphocytosis, elevated protein, and decreased glucose levels in CSF, or identifying specific diagnostic indicators in cranial imaging such as magnetic resonance imaging or computed tomography (MRI or CT) [ 13 , 26 , 27 , 28 ]. Neurobrucellosis does not present a distinct clinical profile or specific CSF characteristics. Imaging observations of neurobrucellosis fall into four categories: normal, inflammatory (indicated by granulomas and enhanced meninges, perivascular spaces, or lumbar nerve roots), alterations in white matter, and vascular changes [ 29 ]. We suspected neurobrucellosis based on the patient’s clinical symptoms, geographic correlation, high brucella agglutination test titers in both cerebrospinal fluid and blood, symptom resolution following treatment, and the exclusion of other common causes.
In Iran, one differential diagnosis often confused with brucellosis is tuberculosis, as both chronic granulomatous infectious diseases are prevalent here [ 30 , 31 ]. Neurobrucellosis and tuberculosis exhibit significant similarities in clinical symptoms, lab results, and neuroimaging findings. However, deep grey matter involvement and widespread white matter lesions seen in neuroimaging, resembling demyelinating disorders, appear to be distinctive to brucellosis [ 32 ]. There is a noticeable similarity in the clinical symptoms and laboratory findings of brucellosis and tuberculosis [ 33 ]. It is crucial to thoroughly eliminate the possibility of tuberculosis in any suspected or confirmed brucellosis cases before starting antibiotic treatment.
Due to the challenging nature of treating brucellosis and the likelihood of experiencing relapses, it is crucial to provide an extended course of treatment [ 27 ]. This treatment approach should involve a combination of antibiotics that can easily penetrate the cell wall and effectively reach the central nervous system [ 27 , 34 ]. Neurobrucellosis is treated with 3 to 6 months of combination therapy comprising doxycycline, rifampicin, and ceftriaxone or trimethoprim-sulfamethoxazole [ 35 ], similar to the treatment administered to our patient. For patients allergic to cephalosporins, quinolones are recommended, which are considered to be effective in treating brucellosis [ 36 , 37 ]. In complicated situations such as meningitis or endocarditis, streptomycin or gentamicin is administered in the initial 14 days of treatment, in addition to the previously mentioned regimen. Timely and proper treatment results in a positive prognosis, with a less than 1% fatality rate for such complex cases [ 17 , 38 ]. Our patient experienced a highly positive outcome following the prescribed therapy. Initially relying on a walker, a slight limp endured for a month, and by the third month after discharge, all symptoms completely disappeared.
The present study underscores the significance of considering neurobrucellosis as a potential diagnosis when evaluating muscle weakness and radiculopathy, especially in regions where the disease is prevalent. A comprehensive patient history, precise clinical examination, positive serology in blood or cerebrospinal fluid, imaging results, or cerebrospinal fluid analysis can contribute to establishing a conclusive diagnosis.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to our team’s privacy concerns but are available from the corresponding author on reasonable request.
Galińska EM, Zagórski J. Brucellosis in humans–etiology, diagnostics, clinical forms. Ann Agric Environ Med. 2013;20(2):233–8.
PubMed Google Scholar
Głowacka P, Żakowska D, Naylor K, Niemcewicz M, Bielawska-Drózd A. Brucella - Virulence factors, Pathogenesis and treatment. Pol J Microbiol. 2018;67(2):151–61.
Article PubMed PubMed Central Google Scholar
Khurana SK, Sehrawat A, Tiwari R, Prasad M, Gulati B, Shabbir MZ, et al. Bovine brucellosis - a comprehensive review. Vet Q. 2021;41(1):61–88.
Article CAS PubMed PubMed Central Google Scholar
Yagupsky P, Morata P, Colmenero JD. Laboratory diagnosis of human brucellosis. Clin Microbiol Rev. 2019;33(1).
Kurmanov B, Zincke D, Su W, Hadfield TL, Aikimbayev A, Karibayev T et al. Assays for identification and differentiation of Brucella species: a review. Microorganisms. 2022;10(8).
Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. Lancet Infect Dis. 2007;7(12):775–86.
Article CAS PubMed Google Scholar
Mantur BG, Amarnath SK, Shinde RS. Review of clinical and laboratory features of human brucellosis. Indian J Med Microbiol. 2007;25(3):188–202.
Khoshnood S, Pakzad R, Koupaei M, Shirani M, Araghi A, Irani GM, et al. Prevalence, diagnosis, and manifestations of brucellosis: a systematic review and meta-analysis. Front Vet Sci. 2022;9:976215.
Dhar D, Jaipuriar RS, Mondal MS, Shunmugakani SP, Nagarathna S, Kumari P et al. Pediatric neurobrucellosis: a systematic review with case report. J Trop Pediatr. 2022;69(1).
Mahajan SK, Sharma A, Kaushik M, Raina R, Sharma S, Banyal V. Neurobrucellosis: an often forgotten cause of chronic meningitis. Trop Doct. 2016;46(1):54–6.
Article PubMed Google Scholar
Dreshaj S, Shala N, Dreshaj G, Ramadani N, Ponosheci A. Clinical manifestations in 82 neurobrucellosis patients from Kosovo. Mater Sociomed. 2016;28(6):408–11.
Gul HC, Erdem H, Bek S. Overview of neurobrucellosis: a pooled analysis of 187 cases. Int J Infect Dis. 2009;13(6):e339–43.
Guven T, Ugurlu K, Ergonul O, Celikbas AK, Gok SE, Comoglu S, et al. Neurobrucellosis: clinical and diagnostic features. Clin Infect Dis. 2013;56(10):1407–12.
Alkahtani AM, Assiry MM, Chandramoorthy HC, Al-Hakami AM, Hamid ME. Sero-prevalence and risk factors of brucellosis among suspected febrile patients attending a referral hospital in southern Saudi Arabia (2014–2018). BMC Infect Dis. 2020;20(1):26.
Pappas G, Papadimitriou P, Akritidis N, Christou L, Tsianos EV. The new global map of human brucellosis. Lancet Infect Dis. 2006;6(2):91–9.
Liu Z, Gao L, Wang M, Yuan M, Li Z. Long ignored but making a comeback: a worldwide epidemiological evolution of human brucellosis. Emerg Microbes Infect. 2024;13(1):2290839.
Naderi H, Sheybani F, Parsa A, Haddad M, Khoroushi F. Neurobrucellosis: report of 54 cases. Trop Med Health. 2022;50(1):77.
Farhan N, Khan EA, Ahmad A, Ahmed KS. Neurobrucellosis: a report of two cases. J Pak Med Assoc. 2017;67(11):1762–3.
Karsen H, Tekin Koruk S, Duygu F, Yapici K, Kati M. Review of 17 cases of neurobrucellosis: clinical manifestations, diagnosis, and management. Arch Iran Med. 2012;15(8):491–4.
Türel O, Sanli K, Hatipoğlu N, Aydoğmuş C, Hatipoğlu H, Siraneci R. Acute meningoencephalitis due to Brucella: case report and review of neurobrucellosis in children. Turk J Pediatr. 2010;52(4):426–9.
Guney F, Gumus H, Ogmegul A, Kandemir B, Emlik D, Arslan U, et al. First case report of neurobrucellosis associated with hydrocephalus. Clin Neurol Neurosurg. 2008;110(7):739–42.
Corbel MJ. Brucellosis: an overview. Emerg Infect Dis. 1997;3(2):213–21.
Abuzinadah AR, Milyani HA, Alshareef A, Bamaga AK, Alshehri A, Kurdi ME. Brucellosis causing subacute motor polyradiculopathy and the pathological correlation of pseudomyopathic electromyography: a case report. Clin Neurophysiol Pract. 2020;5:130–4.
Alanazi A, Al Najjar S, Madkhali J, Al Malik Y, Al-Khalaf A, Alharbi A. Acute Brucellosis with a Guillain-Barre Syndrome-Like Presentation: a Case Report and Literature Review. Infect Dis Rep. 2021;13(1):1–10.
Raina S, Sharma A, Sharma R, Bhardwaj A, Neurobrucellosis. A Case Report from Himachal Pradesh, India, and review of the literature. Case Rep Infect Dis. 2016;2016:2019535.
PubMed PubMed Central Google Scholar
McLean DR, Russell N, Khan MY. Neurobrucellosis: clinical and therapeutic features. Clin Infect Dis. 1992;15(4):582–90.
Bouferraa Y, Bou Zerdan M, Hamouche R, Azar E, Afif C, Jabbour R. Neurobrucellosis: brief review. Neurologist. 2021;26(6):248–52.
Aygen B, Doğanay M, Sümerkan B, Yildiz O, Kayabaş Ü. Clinical manifestations, complications and treatment of brucellosis: a retrospective evaluation of 480 patients. Méd Mal Infect. 2002;32(9):485–93.
Article Google Scholar
Kizilkilic O, Calli C, Neurobrucellosis. Neuroimaging Clin N Am. 2011;21(4):927–37. ix.
Chalabiani S, Khodadad Nazari M, Razavi Davoodi N, Shabani M, Mardani M, Sarafnejad A, et al. The prevalence of brucellosis in different provinces of Iran during 2013–2015. Iran J Public Health. 2019;48(1):132–8.
Doosti A, Nasehi M, Moradi G, Roshani D, Sharafi S, Ghaderi E. The pattern of tuberculosis in Iran: A National Cross-sectional Study. Iran J Public Health. 2023;52(1):193–200.
Rajan R, Khurana D, Kesav P. Deep gray matter involvement in neurobrucellosis. Neurology. 2013;80(3):e28–9.
Dasari S, Naha K, Prabhu M. Brucellosis and tuberculosis: clinical overlap and pitfalls. Asian Pac J Trop Med. 2013;6(10):823–5.
Ko J, Splitter GA. Molecular host-pathogen interaction in brucellosis: current understanding and future approaches to vaccine development for mice and humans. Clin Microbiol Rev. 2003;16(1):65–78.
Zhao S, Cheng Y, Liao Y, Zhang Z, Yin X, Shi S. Treatment efficacy and risk factors of Neurobrucellosis. Med Sci Monit. 2016;22:1005–12.
Hasanain A, Mahdy R, Mohamed A, Ali M. A randomized, comparative study of dual therapy (doxycycline-rifampin) versus triple therapy (doxycycline-rifampin-levofloxacin) for treating acute/subacute brucellosis. Braz J Infect Dis. 2016;20(3):250–4.
Falagas ME, Bliziotis IA. Quinolones for treatment of human brucellosis: critical review of the evidence from microbiological and clinical studies. Antimicrob Agents Chemother. 2006;50(1):22–33.
Budnik I, Fuchs I, Shelef I, Krymko H, Greenberg D. Unusual presentations of pediatric neurobrucellosis. Am J Trop Med Hyg. 2012;86(2):258–60.
Download references
This research did not receive any funding or financial support.
Author information
Authors and affiliations.
Infectious Diseases Department and Antimicrobial Resistance Research Center and Transmissible Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran
Ahmad Alikhani & Noushin Ahmadi
Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
Mehran Frouzanian & Amirsaleh Abdollahi
You can also search for this author in PubMed Google Scholar
Contributions
A.A oversaw and treated the case, including the entire revision process. N.A. contributed to the article’s composition. M.F. authored the discussion section, along with the complete revision. AS.A. played a role in crafting the case report discussion and participated in the entire revision process.
Corresponding author
Correspondence to Amirsaleh Abdollahi .
Ethics declarations
Ethics approval and consent to participate.
In adherence to ethical standards, rigorous protocols were followed to obtain approval from the relevant ethics committee and secure informed consent from all participants involved in the study.
Consent for publication
informed consent was obtained from the patient for both study participation AND publication of identifying information/images in an online open-access publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Alikhani, A., Ahmadi, N., Frouzanian, M. et al. Motor polyradiculoneuropathy as an unusual presentation of neurobrucellosis: a case report and literature review. BMC Infect Dis 24 , 491 (2024). https://doi.org/10.1186/s12879-024-09365-2
Download citation
Received : 04 December 2023
Accepted : 29 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12879-024-09365-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Neurobrucellosis
- EMG-NCV tests
- Polyradiculoneuropathy
- Antibiotic therapy
- Intravenous immunoglobulin therapy
- Zoonotic disease
- Gait disorder
- Lower extremity weakness
- Blurred vision
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
a description of the publication. a summary of the publication's main points. an evaluation of the publication's contribution to the topic. identification of critical gaps, points of disagreement, or potentially flawed methodology or theoretical approaches. indicates potential directions for future research.
Examples of literature reviews. Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review.
A good literature review is a critical appraisal of narrowly focused, selected and truly relevant work that provides the current status (perspective) of the topic. This presentation basically is a brief guide on the process of doing and writing a literature review for a thesis, research proposal, research paper, etc. Doing a Literature Review
14. Final checklist (1/2) Choose the right topic Check the literature you have chosen The topic must be interesting to you; it should also be well-defined and important to the field. Monitor the papers you have chosen to review, make changes to your bibliography, if required; prepare a complete reference list.
1. Highlight current research. The point of a literature review for research is to highlight the current state of research related to your topic, not to simply give background information. Background information is important and should be included, but the focus of the presentation should be showing some current studies that either confirm or ...
Literature Review Presentation . Multi-purpose . Free Google Slides theme, PowerPoint template, and Canva presentation template . Whether you're a student or an academic, mastering the literature review is a key skill in scholarly writing. This fully customizable Google Slides and PowerPoint template can assist you in structuring your review ...
The Literature Review Process. 1. The Literature Review Process Annie Downey. 2. Purpose of the Literature Review "A substantive, thorough, sophisticated literature review is a precondition for doing substantive, thorough, sophisticated research.". - Boote and Beile, 2005 "you join [ing] the conversation -first by listening to what is ...
1. Outline and identify the purpose of a literature review. As a first step on how to write a literature review, you must know what the research question or topic is and what shape you want your literature review to take. Ensure you understand the research topic inside out, or else seek clarifications.
Demonstrate your knowledge of the research topic. Identify the gaps in the literature and show how your research links to these. Provide the foundation for your conceptual framework (if you have one) Inform your own methodology and research design. To achieve this, your literature review needs a well-thought-out structure.
Point out: and areas or issue pertinent to future study. As you read, try to see the "big picture"—your literature review should provide an overview of the state of research. Include only source materials that help you shape your argument. Resist the temptation to include everything you've read! Balance summary and analysis as you write.
As mentioned above, writing your literature review is a process, which I'll break down into three steps: Finding the most suitable literature. Understanding, distilling and organising the literature. Planning and writing up your literature review chapter. Importantly, you must complete steps one and two before you start writing up your chapter.
Presentation on theme: "Literature Review: Introduction and Notes"— Presentation transcript: 1 Literature Review: Introduction and Notes. 2 Goal of a Literature Review. The ultimate goal of literature review is To become an expert of something Or, if not, at least pretend to be one. 3 Writing a Literature Review.
A literature review is an integrated analysis-- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question.That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
Template 4: Comprehensive Literature Review PPT Slide. Download this tried-and-true literature review template to present a descriptive summary of your research topic statement. The given PPT layout is replete with relevant content to help you strike a balance between supporting and opposing aspects of an argument.
Literature Review & Poster/Visual Presentation Guide GIVING & GETTING EFFECTIVE PRESENTATIONS PRESENTATIONS In many disciplines presentations are given at academic conferences, symposia, and other places where scholars share their work with one another (including the Massachusetts Undergraduate Research Conference).
literature review in academia, at this point it might be useful to state what a literature review is not, before looking at what it is. It is not: § A list or annotated bibliography of the sources you have read § A simple summary of those sources or paraphrasing of the conclusions § Confined to description of the studies and their findings
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis).The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays).
Template 1: Literature Review PowerPoint Template. This is a well-designed PowerPoint Template to help you highlight your literature review. Incorporate this state-of-the-art PPT design and present your analysis on the specific topic. This customizable PowerPoint slide shows the findings and your evaluation of a subject.
What is a literature review? Definition: A literature review is a systematic examination and synthesis of existing scholarly research on a specific topic or subject. Purpose: It serves to provide a comprehensive overview of the current state of knowledge within a particular field. Analysis: Involves critically evaluating and summarizing key findings, methodologies, and debates found in ...
How to do a Literature Review. Mar 7, 2018 • Download as PPTX, PDF •. 13 likes • 8,367 views. E. Elizabeth Moll-Willard. This presentation is to assist students and graduates in conducting an academic literature review, with step by step help, including some tips for academic reading and writing. Read more. Education. Slideshow view.
Literature Review Presentation Slides. A literature review in research is a critical and systematic analysis of existing literature, scholarly articles, books, and other relevant sources that are pertinent to a particular research topic or question. Incorporating a literature review in research is essential for contextualizing the study within ...
The literature review template includes the following sections: Before you start - essential groundwork to ensure you're ready. The introduction section. The core/body section. The conclusion /summary. Extra free resources. Each section is explained in plain, straightforward language, followed by an overview of the key elements that you ...
Working in teams under supervision of faculty members, students review relevant literature, pose research questions, design and conduct studies, and present the results in papers prepared either for submission to a professional journal or for presentation at a professional conference. Offered: AWSp.
A literature review stimulated by a new method of teaching manual therapy, reflecting contemporary evidence, being trialled at a United Kingdom education institute. A group of experienced, internationally-based academics, clinicians, and researchers from across the spectrum of manual therapy was convened. ... Public presentations were made to ...
Purpose: As a scoping review, evaluate the literature on the presentations, genetics, and therapies for neuroblastoma in adult patients. Methods: We searched four databases for studies reporting adults with neuroblastoma. Cohort studies, case series, and case reports were synthesized qualitatively. Progression-free and overall survival were compared amongst cohort studies. Results: Of 2287 ...
Clinical presentation varies depending on the type and location of the FB ingested however common symptoms may include drooling, vomiting, dysphagia, throat, ... Based on the review of the literature 12 cases reported esophageal perforation secondary to FB ingestion in children aged 24 months or less . The most common FBs were button batteries ...
2. INTRODUCTION Review of literature is one of the most important steps in the research process. It is an account of what is already known about a particular phenomenon. The main purpose of literature review is to convey to the readers about the work already done & the knowledge & ideas that have been already established on a particular topic ...
Brucellosis, a zoonotic disease caused by Brucella species, poses a significant global health concern. Among its diverse clinical manifestations, neurobrucellosis remains an infrequent yet debilitating complication. Here, we present a rare case of neurobrucellosis with unusual presentations in a 45-year-old woman. The patient's clinical course included progressive lower extremity weakness ...
Lit review powerpoint - Download as a PDF or view online for free. Submit Search. Upload. Lit review powerpoint ... Sample Dissertation Defense Presentation Powerpoint Presentation Slides.
and neuroradiological presentation of Erdheim-Chester disease: Report of 6 cases and systematic review of the literature. J Neurol. 2006;253(10):1267-77 13. Chasset F, Barete S, Charlotte F, et al. Cutaneous manifestations of Erdheim-Chester disease (ECD): Clinical, pathological, and molecular features in a monocentric series of 40 patients.