Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- JME Commentaries
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 47, Issue 2
- Good reasons to vaccinate: mandatory or payment for risk?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1691-6403 Julian Savulescu 1 , 2 , 3
- 1 Faculty of Philosophy , University of Oxford , Oxford , UK
- 2 Murdoch Childrens Research Institute , Parkville , Victoria , Australia
- 3 Melbourne Law School , University of Melbourne , Melbourne , Victoria , Australia
- Correspondence to Professor Julian Savulescu, Faculty of Philosophy, University of Oxford, Oxford, UK; julian.savulescu{at}philosophy.ox.ac.uk
Mandatory vaccination, including for COVID-19, can be ethically justified if the threat to public health is grave, the confidence in safety and effectiveness is high, the expected utility of mandatory vaccination is greater than the alternatives, and the penalties or costs for non-compliance are proportionate. I describe an algorithm for justified mandatory vaccination. Penalties or costs could include withholding of benefits, imposition of fines, provision of community service or loss of freedoms. I argue that under conditions of risk or perceived risk of a novel vaccination, a system of payment for risk in vaccination may be superior. I defend a payment model against various objections, including that it constitutes coercion and undermines solidarity. I argue that payment can be in cash or in kind, and opportunity for altruistic vaccinations can be preserved by offering people who have been vaccinated the opportunity to donate any cash payment back to the health service.
- behaviour modification
- technology/risk assessment
- philosophical ethics
- public health ethics
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/medethics-2020-106821
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
We are in the midst of a global pandemic with COVID-19 and there is a race to develop a vaccine. At the time of writing, there are 53 vaccines in clinical trials on humans (plus five that have bypassed the full trial process) and at least 92 preclinical vaccines under active investigation in animals. There are a number of different approaches: (1) genetic—using mRNA to cause the body to produce viral proteins; (2) viral vector—using genetically modified viruses such as adenovirus to carry sections of coronavirus genetic material; (3) protein—delivering viral proteins (but not genetic material) to provoke an immune response; (4) inactivated or attenuated coronavirus; (5) repurposing existing vaccines, eg, BCG (bacillus Calmette–Guérin). 1
Given the mounting number of deaths globally, and the apparent failure of many countries to contain the pandemic without severely damaging or problematic lockdowns and other measures, there have been calls to make a vaccine, if it were approved, mandatory. 2 Mandatory vaccination has not been ruled out within the UK. 3
The first part of this article asks when, if ever, a vaccine should be mandatory. I will create a set of criteria and a decision algorithm for mandatory vaccination. I will argue that in the case of COVID-19, some of these criteria may not be satisfied. The second part of the article argues that in the case of COVID-19, it may be ethically preferable to incentivise vaccine uptake. I will justify incentivisation and discuss different kinds of incentives.
Ethics of mandatory COVID-19 vaccination
There is a large body of literature on the justification for the use of coercion in public health and infectious disease in particular. Mandatory vaccination is typically justified on Millian grounds: harm to others. According to John Stuart Mill, the sole ground for the use of state coercion (and restriction of liberty) is when one individual risks harming others. 4 The most prominent arguments from bioethicists appeal to preventing harm to others. 5–7 In the case of children, significant risk of harm to the child is also a ground for state protection. Bambery et al 8 give the example of a child taking a box of toxic bleach to school, potentially harming himself and other children. Teachers are entitled to restrain the child and remove the poison both because of risk to the child and to other children. 8 Flanigan uses a similar example of a person shooting a gun into a crowd. 5
The Nuffield Council of Bioethics produced an influential report on public health which considers when coercion and mandatory vaccination might be justified:
When assessing whether more directive policies are acceptable, the following factors should be taken into account: the risks associated with the vaccination and with the disease itself, and the seriousness of the threat of the disease to the population. In the case of incentivised policies, the size of the incentive involved should be appropriate so that it would not unduly compromise the voluntariness of consent. We identified two circumstances in which quasi-mandatory vaccination measures are more likely to be justified. First, for highly contagious and serious diseases, for example with characteristics similar to smallpox. Second, for disease eradication if the disease is serious and if eradication is within reach. 9
I will elaborate on these brief suggestions and provide a novel structured algorithm for when vaccination should be mandatory.
COVID-19 is almost unique because of the gravity of the problem at the global level: not only is there cost in terms of lives from COVID-19, there is also the extraordinary economic, health and well-being consequences of various virus-control measures, including lockdown, which will extend into the future. Probably never before has a vaccine been developed so rapidly and the pressure to use it so great, at least at the global level.
There is a strong case for making any vaccination mandatory (or compulsory) if four conditions are met:
There is a grave threat to public health
The vaccine is safe and effective
Mandatory vaccination has a superior cost/benefit profile compared with other alternatives
The level of coercion is proportionate.
Each of these conditions involves value judgements.
Grave threat to public health
So far, there have been over 1 million deaths attributed to COVID-19 globally (as of 30 September 2020). 10 In the UK alone, it was predicted in influential early modelling that 500 000 would have died if nothing was done to prevent its spread. Even with the subsequent introduction of a range of highly restrictive lockdown measures (measures which could themselves come at a cost of 200 000 non-COVID-19 lives according to a recent UK government report), 11 more than 42 000 (as of 30 September 2020) 12 have died in the UK within 28 days of a positive test.
The case fatality rate was originally estimated to be as high as 11%, but (as is typical with new diseases) this was quickly scaled down to 1.5% or even lower. 13 The infection fatality rate (IFR, which accounts for asymptomatic and undiagnosed cases) is lower still as it has become clear that there are a large number of asymptomatic and mild cases. For example, the Centre for Evidence Based Medicine reports that “In Iceland, where the most testing per capita has occurred, the IFR lies somewhere between 0.03% and 0.28%”. 14
Of course, how you define “grave” is a value judgement. One of the worst-affected countries in the world in terms of COVID-19-attributed deaths per million is Belgium. The mortality is (at the time of writing) around 877 per million population, which is still under 0.1%, and the average age of death is 80. Of course, Belgium and most other countries have taken strict measures to control the virus and so we are not seeing the greatest possible impact the virus could have. Yet others such as Brazil and Sweden have intervened to a much lesser degree, yet (currently) have rates of 687 and 578 deaths per million respectively. Sweden’s April all-cause deaths and death rate at the peak of its pandemic so far, while extremely high, were surpassed by months in 1993 and 2000. 15
The data are complex and difficult to compare with different testing rates, and ways of assigning deaths and collecting data differing from country to country. For example, Belgium counts deaths in care homes where there is a suspicion that COVID-19 was the cause (without the need for a positive test) and, until recently, the UK counted a death which followed any time from a COVID-19 positive test as a COVID-19 death. Moreover, there have been huge behavioural changes even in countries without legally enforced lockdowns. Furthermore, the IFR varies wildly by age-group and other factors. Even among survivors, there is emerging evidence that there may be long-term consequences for those who have been infected but survived. Long COVID-19 health implications may present a grave future public health problem. Nevertheless, some might still argue that this disease has not entered the “grave” range that would warrant mandatory vaccination. The Spanish influenza killed many more (50–100 million), 16 and it afflicted younger rather than older people, meaning even more “life years” were lost. It is not difficult to imagine a Superflu, or bioengineered bug, which killed 10% across all ages. This would certainly be a grave public health emergency where it is likely mandatory vaccination would be employed.
Deciding whether COVID-19 is sufficiently grave requires both more data than we have and also a value judgement over the gravity that would warrant this kind of intervention. But let us grant for the sake of argument that COVID-19 is a grave public health emergency.
Vaccine is safe and effective
There are concerns that testing has been rushed and the vaccine may not be safe or effective. 17
First, although the technology being used in many of these vaccine candidates has been successfully used in other vaccines, no country has ever produced a safe and effective vaccine against a coronavirus. So in one way, we are all in uncharted waters.
Second, any vaccine development will be accelerated in the context of a grave public health emergency.The inherent probabilistic nature of the development of any biologic means that no vaccine could be said to be 100% safe. There will be risks and those risks are likely to be greater than with well-established vaccines.
Thirdly, some side effects may take time to manifest.
This is not to support the anti-vaccination movement. Vaccines are one of the greatest medical accomplishments and a cornerstone of public health. There are robust testing procedures in place in most jurisdictions to ensure that licensed COVID-19 vaccines are both effective and safe. It is only to acknowledge that everything, including vaccination, has risks. Perhaps the biggest challenge in the development of a vaccine for COVID-19 will be to be honest about the extent of those risks and convey the limitations of confidence in safety and efficacy relative to the evidence accrued.
There is an ethical balance to be struck: introducing a vaccine early and saving more lives from COVID-19, but risking side effects or ineffectiveness versus engaging in longer and more rigorous testing, and having more confidence in safety and efficacy, but more people dying of COVID-19 while such testing occurs. There is no magic answer and, given the economic, social and health catastrophe of various anti-COVID-19 measures such as lockdown, there will be considerable pressure to introduce a vaccine earlier.
To be maximally effective, particularly in protecting the most vulnerable in the population, vaccination would need to achieve herd immunity (the exact percentage of the population that would need to be immune for herd immunity to be reached depends on various factors, but current estimates range up to 82% of the population). 18
There are huge logistical issues around finding a vaccine, proving it to be safe, and then producing and administering it to the world’s population. Even if those issues are resolved, the pandemic has come at a time where there is another growing problem in public health: vaccine hesitancy.
US polls “suggest only 3 in 4 people would get vaccinated if a COVID-19 vaccine were available, and only 30% would want to receive the vaccine soon after it becomes available.” 18
Indeed, vaccine refusal appears to be going up. A recent Pew survey suggested 49% of adults in the USA would refuse a COVID-19 vaccine in September 2020. 19
If these results prove accurate then even if a safe and effective vaccine is produced, at best, herd immunity will be significantly delayed by vaccine hesitancy at a cost both to lives and to the resumption of normal life, and at worst, it may never be achieved.
There remain some community concerns about the safety of all pre-existing vaccines, including many that have been rigorously tested and employed for years.
In the case of COVID-19, the hesitancy may be exacerbated by the accelerated testing and approval process which applies not only to Sputnik V (the controversial “Russian vaccine”). Speaking about America’s vaccine programme, Warp Speed, Donald Trump applauded its unprecedented pace:
…my administration cut through every piece of red tape to achieve the fastest-ever, by far, launch of a vaccine trial for this new virus, this very vicious virus. And I want to thank all of the doctors and scientists and researchers involved because they’ve never moved like this, or never even close. 20
The large impact on society means the vaccine will be put to market much more quickly than usual, perhaps employing challenge studies or other innovative designs, or by condensing or running certain non-safety critical parts of the process in parallel (for example, creating candidate vaccines before its approval).
While the speed is welcomed by politicians and some members of the public, the pressure to produce a candidate vaccine, and the speed at which it has been done, may be also perceived (perhaps unfairly) to increase the likelihood of the kind of concerns that lead to vaccine hesitancy: concerns over side-effects that are unexpected or rare, or that take longer to appear than the testing process allows for, or that for another reason may be missed in the testing process.
The job to be done will not only be to prove scientifically that the vaccine is safe and effective, but also to inform and reassure the public, especially the group who are willing to take the vaccine in theory—but only after others have tried it out first.
The question remains of how safe is safe enough to warrant mandatory vaccination. It is vanishingly unlikely that there will be absolutely no risk of harm from any biomedical intervention, and the disease itself has dramatically different risk profiles in different groups of the population. In an ideal world, the vaccine would be proven to be 100% safe. But there will likely be some risk remaining. Any mandatory vaccination programme would therefore need to make a value judgement about what level of safety and what level of certainty are safe and certain enough. Of course, it would need to be very high, but a 0% risk option is very unlikely.
A COVID-19 vaccine may be effective in reducing community spread and/or preventing disease in individuals. Mandatory vaccination is most justifiable when there are benefits to both the individual and in terms of preventing transmission. If the benefits are only to individual adults, it is more difficult to support mandatory vaccination. One justification would be to prevent exhaustion of healthcare services in an emergency (eg, running out of ventilators), which has been used a basis of restriction of liberty (it was the main justification for lockdown). It could also be justified in the case of protection of children and others who cannot decide for themselves, and of other adults who either cannot be vaccinated for medical reasons.
Better than the alternatives
It is a standard principle of decision theory that the expected utility of a proposed option must be compared with the expected utility of relevant alternatives. There are many alternatives to mandatory vaccination. See figure 1 for a summary of the range of strategies for preventing infectious disease.
- Download figure
- Open in new tab
- Download powerpoint
Strategies for prevention of infectious disease.
A popular position, especially among medical professionals, 7 is that we don’t need mandatory vaccination because people are self-interested or altruistic enough to come forward for vaccination. We can reach herd immunity without mandatory vaccination.
If this were true, all well and good, but the surveys mentioned above cast doubt on this claim with regard to the future COVID-19 vaccine. Moreover, reaching herd immunity is not good enough.
First, how fast we reach herd immunity is also important. In a pandemic, time is lives. If it takes a year to reach herd immunity, that could be thousands or tens of thousands of lives in one country.
Second, herd immunity is necessary because some people cannot be vaccinated for medical reasons: they have allergies, immune problems, or other illnesses. The elderly often don’t mount a strong immune response (that is why it is better to vaccinate children for influenza because they are the biggest spreaders of that disease 7 —although COVID-19 appears to be different on the current evidence). And immunity wanes over time—so even people previously vaccinated may become vulnerable.
Even when national herd immunity is achieved, local areas can fall below that level over time, causing outbreaks, as happened with measles recently. This is especially likely to happen where people opposed to vaccines tend to cluster toghether—for example, in the case of certain religious communities. So ideally we need better than herd immunity to ensure that people are protected both over time and in every place.
These are thus reasons to doubt whether a policy of voluntary vaccination will be good enough, though it remains to be seen.
There are other policies that might obviate the need for mandatory vaccination. South Korea has kept deaths down to about 300 (at the time of writing) with a population of 60 000 000 with a vigorous track and trace programme (although it was criticised for exposing extra-marital affairs and other stigmatised behaviours). 21 Other countries have enforced quarantine with tracking devices. There could be selective lockdown of certain groups, 22 or for intermittent periods of time.
The long-term costs and benefits of such policies would have to be evaluated. That is, we should calculate the expected utility of mandatory vaccination (in combination with other policies) and compare it to alternative strategies (or some other combination of these). How utility should be evaluated is an ethical question. Should we count deaths averted (no matter how old), life years lost or lost well-being (perhaps measured by quality adjusted life years)? 23 Should we count loss of liberty or privacy into the other side the equation?
It may be that a one-off mandatory vaccination is a significantly smaller loss of well-being or liberty than these other complex resource intensive strategies.
So we cannot say whether a mandatory policy of COVID-19 vaccination is ethically justified until we can assess the nature of the vaccine, the gravity of the problem and the likely costs/benefit of alternatives. But it is certainly feasible that it could be justified.
It is important to recognise that coercive vaccination can be justified. This is easy to see by comparing it to other coercive interventions in the public interest.
Conscription in war
In the gravest emergencies, where the existence and freedom of the whole population is at stake, people are conscripted to serve their country, often with high risk of death or permanent injury. We often analogise the pandemic to a war: we are fighting the virus. If people can be sent to war against their will, in certain circumstances some levels of coercion are justified in the war on the virus. Notably, in conditions of extreme emergency in past wars (graver than currently exist for COVID-19), imprisonment or compulsion have even been employed. 24
A more mundane example is the payment of taxes. Taxes benefit individuals because tax revenue allows the preservation of public goods. But if sufficient numbers of others are paying their taxes, it is in a person’s self-interest to free ride and avoid taxes. Indeed, paying taxes may result in harm in some circumstances. 24 In the USA, where there is a large private healthcare sector, paying your taxes may mean you cannot pay for lifesaving medical care that you would otherwise have been able to afford. Still, taxes are mandatory based on considerations of fairness and utility.
Seat belts are mandatory in the UK and many other countries, whereas they were previously voluntary. Interestingly, 50% or so of Americans initially opposed making seat belts mandatory, but now 70% believe mandatory laws are justified. 25
Seat belts reduce the chance of death if you are involved in a car accident by 50%. They are very safe and effective. Notably, they do cause injuries (seat belt syndrome) and even, very occasionally, death. But the chances of being benefitted by wearing them vastly outweigh these risks, so they are mandatory, with enforcement through fines . I have previously likened vaccination to wearing a seat belt. 25
Pre-existing mandatory vaccination
Mandatory vaccination policies are already in place in different parts of the world. Mandatory vaccination policies are those that include a non-voluntary element to vaccine consent and impose a penalty or cost for unjustified refusal (justified refusal includes those who have a contraindicating medical condition, or those who already have natural immunity). There are a range of possible penalties or costs which can coerce people. Australia has the “No Jab, No Pay” scheme which withholds child benefits if the child is not vaccinated, and a “No Jab, No Play” scheme which withholds kindergarten childcare benefits. Italy introduced fines for unvaccinated children who attend school. In the USA, state regulations mandate that children cannot attend school if they are not vaccinated, and healthcare workers are required to vaccinate. Some US states (eg, Michigan) make exemptions difficult to obtain by requiring parents to attend immunisation education courses 26 (see also 27 28 ).
Figure 2 summarises the range of coercive policies that can constitute mandatory vaccination.
Cost of mandatory/coercive vaccination.
Coercion is proportionate
In public health ethics, there is a familiar concept of the “least restrictive alternative”. 28 The least restrictive alternative is the option which achieves a given outcome with the least coercion (and least restriction of liberty).
This is a very weak principle: it uses liberty as tie breaker between options with the same expected utility. More commonly, however, we need to weigh utility against liberty. That is, a more restrictive policy will achieve more expected utility—but is it justified?
According to a principle of proportionality, the additional coercion or infringement in liberty is justified if it is proportionate to the gain in expected utility of the more coercive intervention compared with next best option. That is, additional coercion is justified when the restriction of liberty is both minimised and proportionate to the expected advantages offered by the more coercive policy.
As we can see from the previous section and figure 2, there are a variety of coercive measures. (The Nuffield Council has created a related “Intervention Ladder”, 29 though this includes education and incentives, as well as coercive measures.) Penalties can be high. In war, those who conscientiously objected to fighting went to jail or were forced to perform community service (or participate in medical research). In France, parents were given a suspended prison sentence for refusing to vaccinate their child. 30
While there are legitimate concerns that the effectiveness of these policies in different contexts has been inadequately investigated, a number of these policies have been shown to increase vaccination rates. 31
Notably, the fine or punishment for avoiding taxes varies according to the gravity of the offence. The fine for not wearing a seat belt is typically small. A modest penalty for not being vaccinated in a grave public health emergency could be justifiable. For example, a fine or restriction of movement might be justified.
Figure 3 combines these four factors into an algorithm for justified mandatory vaccination.
Algorithm for mandatory vaccination.
These four factors can be justified in several ways. They represent a distillation and development of existing principles in public health ethics, for example, the least restrictive alternative. They can also be justified by the four principles of biomedical ethics.
For example, justice is about the distribution of benefits and burdens across a population in a fair manner. Justice and beneficence, in the context of vaccination policies, both require that the problem addressed is significant and vaccination is an effective means of addressing it. Non-maleficence requires that the risk imposed on individuals be small. Respect for autonomy and justice both require that coercion be applied only if necessary and that it be proportionate to additional utility of mandatory vaccination (and that such coercion be minimised, which is a feature of proportionality).
It is important to recognise that vaccines may have benefits both to the individual and to others (the community). If the vaccine has an overall net expected utility for the individual, beneficence supports its administration.
How great a sacrifice (loss of liberty or risk) can be justified? The most plausible account is provided by a duty of easy rescue: when the cost to an individual is small of some act, but the benefit or harm to another is large, then there is a moral obligation to perform that act. I have elsewhere argued for a collective duty of easy rescue: where the cost of some act to an individual is small, and the benefit of everyone doing that act to the collective is large, there is a collective duty of easy rescue. 32 Such a principle appropriately balances respect for autonomy with justice.
Whether mandatory vaccination for any disease can be justified will depend on precise facts around the magnitude of the problem, the nature of the disease and vaccination, the availability and effectiveness of alternative strategies and the level of coercion. Elsewhere I compare mandatory vaccination for influenza and COVID-19 in more detail. 27
Better than coercion? Payment for risk
Given the risks, or perceived risks, of a novel COVID-19 vaccine, it would be practically and perhaps ethically problematic to introduce a mandatory policy, at least initially (when uncertainty around safety will be greater). Is there a more attractive alternative?
The arguments in favour of vaccination, particularly for those at lower risk (children, young people and those previously infected) can be based on a principle of solidarity. After all, “We are in this together” has been a recurrent slogan supporting pandemic measures in different countries. Those at low risk are asked to do their duty to their fellow citizens, which is a kind of community service. Yet they have little to personally gain from vaccination. The risk/benefit profile looms large for those at lowest risk.
However, another way of looking at this is that those at low risk are being asked to do a job which entails some risk., so they should be paid for the risk they are taking for the sake of providing a public good. And although it may be unlikely to influence so-called 'anti-vaxxers', it may influence a good portion of the 60% of American adults who responded in a March 2020 poll that they would either delay vaccination or didn’t know about vaccination. 33
I have previously argued that we should reconceive live organ donation and participation in risky research, including challenge studies, 34 as jobs where risk should be remunerated, much like we pay construction workers and other dangerous professions both for the job and for the risk involved. 35 36 While the risk profile for approved vaccinations means that it differs from these examples, it could be compared to a job such as social work as a further argument in favour of payment. People may legitimately be incentivised to take on risks, as the Nuffield Council recognises in its Intervention Ladder. 29
The advantage of payment for risk is that people are choosing voluntarily to take it on. As long as we are accurate in conveying the limitations in our confidence about the risks and benefits of a vaccine, then it is up to individuals to judge whether they are worth payment.
Of course, that is a big ask. It would require government to be transparent, explicit and comprehensive in disclosure of data, what should be inferred and the limitations on the data and confidence. This has often not been the case—one only has to remember the denial of the risks of bovine spongiform encephalopathy (BSE) at the height of the crisis by the British government, when in 1990 the Minister for Agriculture, Fisheries and Food, John Gummer proudly fed his 4-year-old daughter, Cordelia, a hamburger in front of the world’s media, declaring British beef safe. (Gummer was awarded a peerage in 2010 and is now Lord Deben.) 37
There is also a danger that payment might signal lack of confidence in safety. That is a real risk and one that I will address in the “payment in kind” section below.
But the basic ethical point (public acceptability aside) is that, if a vaccine is judged to be safe enough to be used without payment, then it is safe enough to be used with payment. 36 Payment itself does not make a vaccine riskier. If a vaccine is considered too risky to be administered to the population, then it should not be administered, no matter whether coercively, through incentives, or through some other policy.
A standard objection to payment for risk (whether it is risky research or live organ donation) is that it is coercive: it forces people to take risks against their better judgement. In Macklin’s words:
The reason for holding that it is ethically inappropriate to pay patients to be research subjects is that it is likely to be coercive, violating the ethical requirement that participation in research should be fully voluntary. 38
As I have previously argued, 39 this demonstrates deep conceptual confusion. Coercion exists when an option which is either desired or good is removed or made very unappealing. The standard example is a robber who demands “Your money or your life”. This removes the most desired and best option: your money and your life. The Australian “No Jab, No Pay”scheme arguably does constitute coercion as it removes an option that one is entitled to, that is, non-vaccination with the “Pay”. So too is the Italian scheme of fines coercive.
However, paying people is not coercive. Adding an option, like payment, without affecting the status quo is not coercive. If a person chooses that option, it is because they believe that overall their life will go better with it, in this case, with the vaccination and the payment. The gamble may not pay off: some risk might eventuate and then it wasn’t worth it. But that is life—and probability.
It is true that the value of the option might exercise force over our rational capacities, but that is no different from offering a lot of money to attract a favoured job applicant.
What can be problematic about offers is exploitation. Exploitation exists where one offers less than a fair deal and a person only accepts it because of vulnerability from background injustice.
There are two ways to prevent exploitation. First, we can correct any background injustice that might cause it. In this case, the person would have little reason to accept the offer. Second, we can pay a fair minimum price for risk, as when we pay construction workers danger money. Paradoxically, this requires paying more, rather than less. 40
But there is an important additional feature of vaccination. If a vaccine were deemed to be safe enough to offer on a voluntary basis without payment, it must be safe enough to incentivise with payment because the risks are reasonable. It may be that those who are poorer may be more inclined to take the money and the risk, but this applies to all risky or unpleasant jobs in a market economy. It is not necessarily exploitation if there are protections in place such as a minimum wage or a fair price is paid to take on risk.
So payment for vaccination which passes independent safety standards (and could reasonably be offered without payment) is not exploitation, if the payment is adequate.
Undue influence?
A related concern is undue influence. Undue influence means that because of the attractiveness of the offer, I can’t autonomously and rationally weigh up the risks and benefits. It is sometimes understood as “were it not for the money, he would not do it”.
But that formulation is too broad—were it not for the money, many people would not go to work. Rather what the concept of ‘undue influence’ intends to capture is that the offer, usually money, bedazzles a person so that he or she makes a mistake in weighing up the risks and benefits. Someone offers Jones a million dollars to take on a risk of 99.99% of dying in a dangerous experiment. He just focuses on the money and takes a deal which is unfair and unreasonable. However, taking such an offer might be rational. If Jones’ daughter is about to die without a million dollars and he values her life more than his own, it might be both autonomous and rational to take the deal.
Because we cannot get into people’s minds, it is difficult in practice to unravel whether undue influence is occurring—how can you differentiate it from a rational decision? In practice, if it would be acceptable to be vaccinated for nothing, it is acceptable to do it for money. Concerns about undue influence are best met by implementing procedures to minimise bias and irrational decision making, such as cooling off periods, information reframing, and so on.
There remains a lurking concern that a decision where payment is involved may not be fully autonomous or authentic. For example, racial and ethnic minorities are among the groups most gravely affected by COVID-19, but given concerns about systemic racism in research and medicine, these communities may have good reason to distrust the medical machine. Is it acceptable to use payment to get over those concerns?
All we can do practically to address concerns about autonomy and authenticity is to redouble efforts: to ensure we do know the risks and they are reasonable (and that the underpinning research is not itself subject to concerns about systemic racism), and try to foster trust with such public education campaigns. This can work alongside a payment scheme. People still need to understand what the facts are. They still need to make as autonomous and authentic a decision as possible.
Practical advantages
A payment model could also be superior to a mandatory model from a practical point of view. There may be considerable resistance to a mandatory model which may make it difficult, expensive and time-consuming to implement, with considerable invasion of liberty. In a payment model, people are doing what they want to do.
A payment model could also be very cheap, compared with the alternatives. The cost of the UK’s furlough scheme is estimated to reach £60 billion by its planned end in October, 41 and the economic shut down is likely to cost many billions more, as well as the estimated 200 000 lives expected to be lost as a result. 11 It would make economic sense to pay people quite a lot to incentivise them to vaccinate sooner rather than later—which, for example, would speed up their full return to work.
It may be that payment is only required to incentivise certain groups. For example, it may be that young people require incentivising because they are at lower risk from the disease itself. On the other hand, justice might require payment for all taking the risk. Although the elderly and those at higher risk have more to gain personally, they are also providing a service by being vaccinated and not using limited health resources. (There is an enormous backlog of patients in the NHS—another grave threat to public health.)
One particularly difficult case is paying parents to vaccinate their children. It is one thing to pay people to take on risk for themselves; it is quite another to pay them to enable their children to take on risks, particularly when the children have little to gain as they are at lowest risk. In part, the answer to this issue is determined by how safe the vaccine is and how confident we can be in that assessment. If it were safe, to a level that even a mandatory programme would be justified, it may be appropriate to instead incentivise parents to volunteer their children for vaccination. If safety is less certain, payment for risk in this group is the most problematic.
It is true that some mandatory vaccination programmes already fine parents for failure to vaccinate their children. However, in those cases vaccination is clearly in the child’s best interest, as the child receives the benefit of immunity to diseases such as measles, that pose a greater risk to that child than we currently believe COVID-19 does. Moreover, they are for vaccines that have been in place for many years and have a well-established safety profile.
A standard objection to paying people to do their duty, particularly civic duty, is that it undermines solidarity, trust, reciprocity and other community values. This is the argument given by Richard Titmuss for a voluntary blood donation scheme. 42
The UK does not pay donors for blood or blood products, but does purchase blood products from other countries, including Austria where donors are paid a “travel allowance” for plasma donation. In Australia, which runs a donor system, more than 50% of the plasma comes from paid donors in the USA. 43 Altruism is insufficient. Germany recently moved to paying for plasma donors. It does not appear to have undermined German society.
In the end, the policy we should adopt towards COVID-19 vaccination will depend on the precise risks and benefits of the vaccine (and our confidence in them), the state of the pandemic, the nature of the alternatives, and particularly the public appetite for a vaccine.
In the right circumstances, mandatory vaccination could be ethically justified, if the penalty is suitably proportionate.
Payment for vaccination, perhaps, has even more to be said for it.
For those attached to the gift of altruism, the vaccinated could be offered the opportunity to donate their fee back to the NHS (or similar health service provider). This combined “payment-donation” model would be a happy marriage of ethics and economics. It would give altruists a double chance to be altruistic: first by vaccinating and second by donating the fee. It would also couple self-interest with morality for free-riders (as they would have greater self-interest to do what is moral), and it would give those who face obstacles to vaccination an additional reason to overcome these.
Payment in kind
Of course, benefits can come in cash or kind. An alternative “payment” model is to pay those who vaccinate in kind. This could take the form of greater freedom to travel, opportunity to work or socialise. With some colleagues, I have given similar arguments in favour of immunity passports. 44
One attractive benefit would be the freedom to not wear a mask in public places if you carried a vaccination certificate, and not to socially distance. Currently, everyone has to wear a mask and practise social distancing. Relaxing this requirement for those who have been vaccinated (or otherwise have immunity) would be an attractive benefit. Moreover, it would help ameliorate the risks the unvaccinated would pose to others.
Payment in kind has one advantage over cash in that it might not send the signal that vaccination is perceived to be unsafe. A cash payment may paradoxically undermine vaccination uptake by introducing unwarranted suspicion (though this is an intuition that may need to be tested). Benefits in kind are less susceptible to this concern because they are directly linked to the benefit provided by the vaccine itself: the vaccinated person is no longer a threat to others.
Some might object that this represents a form of shaming the non-vaccinators (some of whom might be excluded from vaccination for health reasons), just as presenting those who evaded conscription with a white feather was a method of shaming perceived free-riders. But this could be managed through an education campaign about the justification for face covering requirements. There is a good reason to require the non-vaccinated to continue to wear masks and practice social distancing, regardless of whether their refusal is justified—they do represent a greater direct threat to others.
It is quite possible that some mixture of altruism, financial and non-financial benefits will obviate the need to introduce mandatory vaccination. It is better that people voluntarily choose on the basis of reasons to act well, rather than being forced to do so. Structuring the rewards and punishments in a just and fair way is one way of giving people reasons for action.
Mandatory vaccination can be ethically justified (see figure 3), but when risks are more uncertain, payment for vaccination (whether in cash or kind) may be an ethically superior option.
Acknowledgments
This piece builds on a previous piece I published on the JME blog, Good Reasons to Vaccinate: COVID19 Vaccine, Mandatory or Payment Model? [ https://blogs.bmj.com/medical-ethics/2020/07/29/good-reasons-to-vaccinate-covid19-vaccine-mandatory-or-payment-model/ ]. I would like to thank an anonymous reviewer for very many helpful and constructive comments. I would also like to thank Alberto Giubilini for his help.
- Zimmer C , et al
- Bambery B ,
- Douglas T ,
- Selgelid MJ , et al
- Selgelid M ,
- Maslen H , et al
- Nuffield Council on Bioethics
- Worldometer
- ↵ Gov.uk. coronavirus (COVID-19) in the UK . Available: https://coronavirus.data.gov.uk/ [Accessed 30 Sep 2020 ].
- Rajgor DD ,
- Archuleta S , et al
- Johnson S ,
- Greenberger M
- Schaffer DeRoo S ,
- Pudalov NJ ,
- Johnson C ,
- Whitehouse.gov
- Savulescu J ,
- Persson I ,
- Wilkinson D
- Giubilini A
- Giubilini A ,
- Savulescu J
- Sabin Vaccine Institute
- MacDonald NE ,
- Dube E , et al
- LX Morning Consult
- Weijer C , et al
- Anomaly J ,
- Grimwade O ,
- Giubilini A , et al
- Brown RCH ,
- Williams B , et al
Supplementary materials
- Press release
Contributors Sole authorship.
Funding JS is supported by the Uehiro Foundation on Ethics and Education. He received funding from the Wellcome Trust WT104848 and WT203132. Through his involvement with the Murdoch Children’s Research Institute, he has received funding through from the Victorian State Government through the Operational Infrastructure Support (OIS) Program.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement No data are available.
Linked Articles
- Response Persuasion, not coercion or incentivisation, is the best means of promoting COVID-19 vaccination Susan Pennings Xavier Symons Journal of Medical Ethics 2021; 47 709-711 Published Online First: 27 Jan 2021. doi: 10.1136/medethics-2020-107076
Read the full text or download the PDF:
Other content recommended for you.
- Spoonful of honey or a gallon of vinegar? A conditional COVID-19 vaccination policy for front-line healthcare workers Owen M Bradfield et al., Journal of Medical Ethics, 2021
- The unintended consequences of COVID-19 vaccine policy: why mandates, passports and restrictions may cause more harm than good Kevin Bardosh et al., BMJ Global Health, 2022
- Exploring vaccine hesitancy in care home employees in North West England: a qualitative study Amelia Dennis et al., BMJ Open, 2022
- Persuasion, not coercion or incentivisation, is the best means of promoting COVID-19 vaccination Susan Pennings et al., Journal of Medical Ethics, 2021
- COVID-19 vaccine boosters for young adults: a risk benefit assessment and ethical analysis of mandate policies at universities Kevin Bardosh et al., Journal of Medical Ethics, 2022
- Vaccine mandates for healthcare workers beyond COVID-19 Alberto Giubilini et al., Journal of Medical Ethics, 2022
- No Jab, No Job? Ethical Issues in Mandatory COVID-19 Vaccination of Healthcare Personnel Rachel Gur-Arie et al., BMJ Global Health, 2021
- Evaluating potential unintended consequences of COVID-19 vaccine mandates and passports Maxwell J Smith, BMJ Global Health, 2022
- Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review Mei Li et al., Postgraduate Medical Journal, 2021
- Covid-19: Is the UK heading towards mandatory vaccination of healthcare workers? Jacqui Wise, BMJ, 2021
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 14 May 2021
Public attitudes toward COVID-19 vaccination: The role of vaccine attributes, incentives, and misinformation
- Sarah Kreps 1 ,
- Nabarun Dasgupta 2 ,
- John S. Brownstein 3 , 4 ,
- Yulin Hswen 5 &
- Douglas L. Kriner ORCID: orcid.org/0000-0002-9353-2334 1
npj Vaccines volume 6 , Article number: 73 ( 2021 ) Cite this article
19k Accesses
72 Citations
43 Altmetric
Metrics details
- Health care
- Translational research
While efficacious vaccines have been developed to inoculate against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; also known as COVID-19), public vaccine hesitancy could still undermine efforts to combat the pandemic. Employing a survey of 1096 adult Americans recruited via the Lucid platform, we examined the relationships between vaccine attributes, proposed policy interventions such as financial incentives, and misinformation on public vaccination preferences. Higher degrees of vaccine efficacy significantly increased individuals’ willingness to receive a COVID-19 vaccine, while a high incidence of minor side effects, a co-pay, and Emergency Use Authorization to fast-track the vaccine decreased willingness. The vaccine manufacturer had no influence on public willingness to vaccinate. We also found no evidence that belief in misinformation about COVID-19 treatments was positively associated with vaccine hesitancy. The findings have implications for public health strategies intending to increase levels of community vaccination.
Similar content being viewed by others
Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA
Sahil Loomba, Alexandre de Figueiredo, … Heidi J. Larson
Vaccine hesitancy and monetary incentives
Ganesh Iyer, Vivek Nandur & David Soberman
Providing normative information increases intentions to accept a COVID-19 vaccine
Alex Moehring, Avinash Collis, … Dean Eckles
Introduction
In less than a year, an array of vaccines was developed to bring an end to the SARS-CoV-2 pandemic. As impressive as the speed of development was the efficacy of vaccines such as Moderna and Pfizer, which are over 90%. Despite the growing availability and efficacy, however, vaccine hesitancy remains a potential impediment to widespread community uptake. While previous surveys indicate that overall levels of vaccine acceptance may be around 70% in the United States 1 , the case of Israel may offer a cautionary tale about self-reported preferences and vaccination in practice. Prospective studies 2 of vaccine acceptance in Israel showed that about 75% of the Israeli population would vaccinate, but Israel’s initial vaccination surge stalled around 42%. The government, which then augmented its vaccination efforts with incentive programs, attributed unexpected resistance to online misinformation 3 .
Research on vaccine hesitancy in the context of viruses such as influenza and measles, mumps, and rubella, suggests that misinformation surrounding vaccines is prevalent 4 , 5 . Emerging research on COVID-19 vaccine preferences, however, points to vaccine attributes as dominant determinants of attitudes toward vaccination. Higher efficacy is associated with greater likelihood of vaccinating 6 , 7 , whereas an FDA Emergency Use Authorization 6 or politicized approval timing 8 is associated with more hesitancy. Whether COVID-19 misinformation contributes to vaccine preferences or whether these attributes or policy interventions such as incentives play a larger role has not been studied. Further, while previous research has focused on a set of attributes that was relevant at one particular point in time, the evidence and context about the available vaccines has continued to shift in ways that could shape public willingness to accept the vaccine. For example, governments, employers, and economists have begun to think about or even devise ways to incentivize monetarily COVID-19 vaccine uptake, but researchers have not yet studied whether paying people to receive the COVID-19 vaccine would actually affect likely behavior. As supply problems wane and hesitancy becomes a limiting factor, understanding whether financial incentives can overcome hesitancy becomes a crucial question for public health. Further, as new vaccines such as Johnson and Johnson are authorized, knowing whether the vaccine manufacturer name elicits or deters interest in individuals is also important, as are the corresponding efficacy rates of different vaccines and the extent to which those affect vaccine preferences. The purpose of this study is to examine how information about vaccine attributes such as efficacy rates, the incidence of side effects, the nature of the governmental approval process, identity of the manufacturers, and policy interventions, including economic incentives, affect intention to vaccinate, and to examine the association between belief in an important category of misinformation—false claims concerning COVID-19 treatments—and willingness to vaccinate.
General characteristics of study population
Table 1 presents sample demographics, which largely reflect those of the US population as a whole. Of the 1335 US adults recruited for the study, a convenience sample of 1100 participants consented to begin the survey, and 1096 completed the full questionnaire. The sample was 51% female; 75% white; and had a median age of 43 with an interquartile range of 31–58. Comparisons of the sample demographics to those of other prominent social science surveys and U.S. Census figures are shown in Supplementary Table 1 .
Vaccination preferences
Each subject was asked to evaluate a series of seven hypothetical vaccines. For each hypothetical vaccine, our conjoint experiment randomly assigned values of five different vaccine attributes—efficacy, the incidence of minor side effects, government approval process, manufacturer, and cost/financial inducement. Descriptions of each attribute and the specific levels used in the experiment are summarized in Table 2 . After seeing the profile of each vaccine, the subject was asked whether she would choose to receive the vaccine described, or whether she would choose not to be vaccinated. Finally, subjects were asked to indicate how likely they would be to take the vaccine on a seven-point likert scale.
Across all choice sets, in 4419 cases (58%) subjects said they would choose the vaccine described in the profile rather than not being vaccinated. As shown in Fig. 1 , several characteristics of the vaccine significantly influenced willingness to vaccinate.
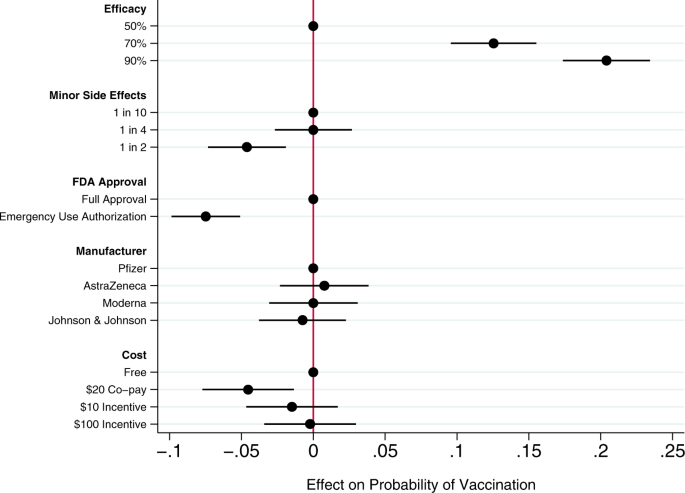
Circles present the estimated effect of each attribute level on the probability of a subject accepting vaccination from the attribute’s baseline level. Horizontal lines through points indicate 95% confidence intervals. Points without error bars denote the baseline value for each attribute. The average marginal component effects (AMCEs) are the regression coefficients reported in model 1 of Table 3 .
Efficacy had the largest effect on individual vaccine preferences. An efficacy rate of 90% increased uptake by about 20% relative to the baseline at 50% efficacy. Even a high incidence of minor side effects (1 in 2) had only a modest negative effect (about 5%) on willingness to vaccinate. Whether the vaccine went through full FDA approval or received an Emergency Use Authorization (EUA), an authority that allows the Food and Drug Administration mechanisms to accelerate the availability and use of treatments or medicines during medical emergencies 9 , significantly influenced willingness to vaccinate. An EUA decreased the likelihood of vaccination by 7% compared to a full FDA authorization; such a decline would translate into about 23 million Americans. While a $20 co-pay reduced the likelihood of vaccination relative to a no-cost baseline, financial incentives did not increase willingness to vaccinate. Lastly, the manufacturer had no effect on vaccination attitudes, despite the public pause of the AstraZeneca trial and prominence of Johnson & Johnson as a household name (our experiment was fielded before the pause in the administration of the Johnson & Johnson shot in the United States).
Model 2 of Table 3 presents an expanded model specification to investigate the association between misinformation and willingness to vaccinate. The primary additional independent variable of interest is a misinformation index that captures the extent to which each subject believes or rejects eight claims (five false; three true) about COVID-19 treatments. Additional analyses using alternate operationalizations of the misinformation index yield substantively similar results (Supplementary Table 4 ). This model also includes a number of demographic control variables, including indicators for political partisanship, gender, educational attainment, age, and race/ethnicity, all of which are also associated with belief in misinformation about the vaccine (Supplementary Table 2 ). Finally, the model also controls for subjects’ health insurance status, past experience vaccinating against seasonal influenza, attitudes toward the pharmaceutical industry, and beliefs about vaccine safety generally.
Greater levels of belief in misinformation about COVID-19 treatments were not associated with greater vaccine hesitancy. Instead, the relevant coefficient is positive and statistically significant, indicating that, all else being equal, individuals who scored higher on our index of misinformation about COVID-19 treatments were more willing to vaccinate than those who were less susceptible to believing false claims.
Strong beliefs that vaccines are safe generally was positively associated with willingness to accept a COVID-19 vaccine, as were past histories of frequent influenza vaccination and favorable attitudes toward the pharmaceutical industry. Women and older subjects were significantly less likely to report willingness to vaccinate than men and younger subjects, all else equal. Education was positively associated with willingness to vaccinate.
This research offers a comprehensive examination of attitudes toward COVID-19 vaccination, particularly the role of vaccine attributes, potential policy interventions, and misinformation. Several previous studies have analyzed the effects of vaccine characteristics on willingness to vaccinate, but the modal approach is to gauge willingness to accept a generic COVID-19 vaccine 10 , 11 . Large volumes of research show, however, that vaccine preferences hinge on specific vaccine attributes. Recent research considering the influence of attributes such as efficacy, side effects, and country of origin take a step toward understanding how properties affect individuals’ intentions to vaccinate 6 , 7 , 8 , 12 , 13 , but evidence about the attributes of actual vaccines, debates about how to promote vaccination within the population, and questions about the influence of misinformation have moved quickly 14 .
Our conjoint experiment therefore examined the influence of five vaccine attributes on vaccination willingness. The first category of attributes involved aspects of the vaccine itself. Since efficacy is one of the most common determinants of vaccine acceptance, we considered different levels of efficacy, 50%, 70%, and 90%, levels that are common in the literature 7 , 15 . Evidence from Phase III trials suggests that even the 90% efficacy level in our design, which is well above the 50% threshold from the FDA Guidance for minimal effectiveness for Emergency Use Authorization 16 , has been exceeded by both Pfizer’s and Moderna’s vaccines 17 , 18 . The 70% efficacy threshold is closer to the initial reports of the efficacy of the Johnson & Johnson vaccine, whose efficacy varied across regions 19 . Our analysis suggests that efficacy levels associated with recent mRNA vaccine trials increases public vaccine uptake by 20% over a baseline of a vaccine with 50% efficacy. A 70% efficacy rate increases public willingness to vaccinate by 13% over a baseline vaccine with 50% efficacy.
An additional set of epidemiological attributes consisted of the frequency of minor side effects. While severe side effects were plausible going into early clinical trials, evidence clearly suggests that minor side effects are more common, ranging from 10% to 100% of people vaccinated depending on the number of doses and the dose group (25–250 mcg) 20 . Since the 100 mcg dose was supported in Phase III trials 21 , we include the highest adverse event probability—approximating 60% as 1 in 2—and 1 in 10 as the lowest likelihood, approximating the number of people who experienced mild arthralgia 20 . Our findings suggest that a the prevalence of minor side effects associated with recent trials (i.e. a 1 in 2 chance), intention to vaccinate decreased by about 5% versus a 1 in 10 chance of minor side effects baseline. However, at a 25% rate of minor side effects, respondents did not indicate any lower likelihood of vaccination compared to the 10% baseline. Public communications about how to reduce well-known side effects, such as pain at the injection site, could contribute to improved acceptance of the vaccine, as it is unlikely that development of vaccine-related minor side effects will change.
We then considered the effect of EUA versus full FDA approval. The influenza H1N1 virus brought the process of EUA into public discourse 22 , and the COVID-19 virus has again raised the debate about whether and how to use EUA. Compared to recent studies also employing conjoint experimental designs that showed just a 3% decline in support conditional on EUA 6 , we found decreases in support of more than twice that with an EUA compared to full FDA approval. Statements made by the Trump administration promising an intensely rapid roll-out or isolated adverse events from vaccination in the UK may have exacerbated concerns about EUA versus full approval 8 , 23 , 24 , 25 . This negative effect is even greater among some subsets of the population. As shown in additional analyses reported in the Supplementary Information (Supplementary Fig. 5 ), the negative effects are greatest among those who believe vaccines are generally safe. Among those who believe vaccines generally are extremely safe, the EUA decreased willingness to vaccinate by 11%, all else equal. This suggests that outreach campaigns seeking to assure those troubled by the authorization process used for currently available vaccines should target their efforts on those who are generally predisposed to believe vaccines are safe.
Next, we compared receptiveness as a function of the manufacturer: Moderna, Pfizer, Johnson and Johnson, and AstraZeneca, all firms at advanced stages of vaccine development. Vaccine manufacturers in the US have not yet attempted to use trade names to differentiate their vaccines, instead relying on the association with manufacturer reputation. In other countries, vaccine brand names have been more intentionally publicized, such as Bharat Biotech’s Covaxin in India and Gamaleya Research Institute of Epidemiology and Microbiology Sputnik V in Russia. We found that manufacturer names had no impact on willingness to vaccinate. As with hepatitis and H. influenzae vaccines 26 , 27 , interchangeability has been an active topic of debate with coronavirus mRNA vaccines which require a second shot for full immunity. Our research suggests that at least as far as public receptiveness goes, interchangeability would not introduce concerns. We found no significant differences in vaccination uptake across any of the manufacturer treatments. Future research should investigate if a manufacturer preference develops as new evidence about efficacy and side effects becomes available, particularly depending on whether future booster shots, if needed, are deemed interchangeable with the initial vaccination.
Taking up the question of how cost and financial incentives shape behavior, we looked at paying and being paid to vaccinate. While existing research suggests that individuals are often willing to pay for vaccines 28 , 29 , some economists have proposed that the government pay individuals up to $1,000 to take the COVID-19 vaccine 30 . However, because a cost of $300 billion to vaccinate the population may be prohibitive, we posed a more modest $100 incentive. We also compared this with a $10 incentive, which previous studies suggest is sufficient for actions that do not require individuals to change behavior on a sustained basis 31 . While having to pay a $20 co-pay for the vaccine did deter individuals, the additional economic incentives had no positive effect although they did not discourage vaccination 32 . Consistent with past research 31 , 33 , further analysis shows that the negative effect of the $20 co-pay was concentrated among low-income earners (Supplementary Fig. 7 ). Financial incentives failed to increase vaccination willingness across income levels.
Our study also yields important insights into the relationship between one prominent category of COVID-19 misinformation and vaccination preferences. We find that susceptibility to misinformation about COVID-19 treatments—based on whether individuals can distinguish between factual and false information about efforts to combat COVID-19—is considerable. A quarter of subjects scored no higher on our misinformation index than random guessing or uniform abstention/unsure responses (for the full distribution, see Supplementary Fig. 2 ). However, subjects who scored higher on our misinformation index did not exhibit greater vaccination hesitancy. These subjects actually were more likely to believe in vaccine safety more generally and to accept a COVID-19 vaccine, all else being equal. These results run counter to recent findings of public opinion in France where greater conspiracy beliefs were negatively correlated with willingness to vaccinate against COVID-19 34 and in Korea where greater misinformation exposure and belief were negatively correlated with taking preventative actions 35 . Nevertheless, the results are robust to alternate operationalizations of belief in misinformation (i.e., constructing the index only using false claims, or measuring misinformation beliefs as the number of false claims believed: see Supplementary Table 4 ).
We recommend further study to understand the observed positive relationship between beliefs in COVID-19 misinformation about fake treatments and willingness to receive the COVID-19 vaccine. To be clear, we do not posit a causal relationship between the two. Rather, we suspect that belief in misinformation may be correlated with an omitted factor related to concerns about contracting COVID-19. For example, those who believe COVID-19 misinformation may have a higher perception of risk of COVID-19, and therefore be more willing to take a vaccine, all else equal 36 . Additional analyses reported in the Supplementary Information (Supplementary Fig. 6 ) show that the negative effect of an EUA on willingness to vaccinate was concentrated among those who scored low on the misinformation index. An EUA had little effect on the vaccination preferences of subjects most susceptible to misinformation. This pattern is consistent with the possibility that these subjects were more concerned with the disease and therefore more likely to vaccinate, regardless of the process through which the vaccine was brought to market.
We also observe that skepticism toward vaccines in general does not correlate perfectly with skepticism toward the COVID-19 vaccine. Therefore, it is important not to conflate people who are wary of the COVID-19 vaccine and those who are anti-vaccination, as even medically informed individuals may be hesitant because of the speed at which the COVID-19 vaccine was developed. For example, older people are more likely to believe vaccines are safe but less willing to receive the COVID-19 vaccine in our survey, perhaps following the high rates of vaccine skepticism among medical staff expressing concerns regarding the safety of a rapidly-developed vaccine 2 . This inverse relationship between age and willingness to vaccinate is also surprising. Most opinion surveys find older adults are more likely to vaccinate than younger adults 37 . However, most of these survey questions ask about willingness to take a generic vaccine. Two prior studies, both recruiting subjects from the Lucid platform and employing conjoint experiments to examine the effects of vaccine attributes on public willingness to vaccinate, also find greater vaccine hesitancy among older Americans 6 , 7 . Future research could explore whether these divergent results are a product of the characteristics of the sample or of the methodological design in which subjects have much more information about the vaccines when indicating their vaccination preferences.
An important limitation of our study is that it necessarily offers a snapshot in time, specifically prior to both the election and vaccine roll-out. We recommend further study to understand more how vaccine perceptions evolve both in terms of the perceived political ownership of the vaccine—now that President Biden is in office—and as evidence has emerged from the millions of people who have been vaccinated. Similarly, researchers should consider analyzing vaccine preferences in the context of online vaccine controversies that have been framed in terms of patient autonomy and right to refuse 38 , 39 . Vaccination mandates may evoke feelings of powerlessness, which may be exacerbated by misinformation about the vaccines themselves. Further, researchers should more fully consider how individual attributes such as political ideology and race intersect with vaccine preferences. Our study registered increased vaccine hesitancy among Blacks, but did not find that skepticism was directly related to misinformation. Perceptions and realities of race-based maltreatment could also be moderating factors worth exploring in future analyses 40 , 41 .
Overall, we found that the most important factor influencing vaccine preferences is vaccine efficacy, consistent with a number of previous studies about attitudes toward a range of vaccines 6 , 42 , 43 . Other attributes offer potential cautionary flags and opportunities for public outreach. The prospect of a 50% likelihood of mild side effects, consistent with the evidence about current COVID-19 vaccines being employed, dampens likelihood of uptake. Public health officials should reinforce the relatively mild nature of the side effects—pain at the injection site and fatigue being the most common 44 —and especially the temporary nature of these effects to assuage public concerns. Additionally, in considering policy interventions, public health authorities should recognize that a $20 co-pay will likely discourage uptake while financial incentives are unlikely to have a significant positive effect. Lastly, belief in misinformation about COVID-19 does not appear to be a strong predictor of vaccine hesitancy; belief in misinformation and willingness to vaccinate were positively correlated in our data. Future research should explore the possibility that exposure to and belief in misinformation is correlated with other factors associated with vaccine preferences.
Survey sample and procedures
This study was approved by the Cornell Institutional Review Board for Human Participant Research (protocol ID 2004009569). We conducted the study on October 29–30, 2020, prior to vaccine approval, which means we captured sentiments prospectively rather than based on information emerging from an ongoing vaccination campaign. We recruited a sample of 1096 adult Americans via the Lucid platform, which uses quota sampling to produce samples matched to the demographics of the U.S. population on age, gender, ethnicity, and geographic region. Research has shown that experimental effects observed in Lucid samples largely mirror those found using probability-based samples 45 . Supplementary Table 1 presents the demographics of our sample and comparisons to both the U.S. Census American Community Survey and the demographics of prominent social science surveys.
After providing informed consent on the first screen of the online survey, participants turned to a choice-based conjoint experiment that varied five attributes of the COVID-19 vaccine. Conjoint analyses are often used in marketing to research how different aspects of a product or service affect consumer choice. We build on public health studies that have analyzed the influence of vaccine characteristics on uptake within the population 42 , 46 .
Conjoint experiment
We first designed a choice-based conjoint experiment that allowed us to evaluate the relative influence of a range of vaccine attributes on respondents’ vaccine preferences. We examined five attributes summarized in Table 2 . Past research has shown that the first two attributes, efficacy and the incidence of side effects, are significant drivers of public preferences on a range of vaccines 47 , 48 , 49 , including COVID-19 6 , 7 , 13 , 50 . In this study, we increased the expected incidence of minor side effects from previous research 6 to reflect emerging evidence from Phase III trials. The third attribute, whether the vaccine received full FDA approval or an EUA, examines whether the speed of the approval process affects public vaccination preferences 6 . The fourth attribute, the manufacturer of the vaccine, allows us to examine whether the highly public pause in the AstraZeneca trial following an adverse event, and the significant differences in brand familiarity between smaller and less broadly known companies like Moderna and household name Johnson & Johnson affects public willingness to vaccinate. The fifth attribute examines the influence of a policy tool—offsetting the costs of vaccination or even incentivizing it financially—on public willingness to vaccinate.
Attribute levels and attribute order were randomly assigned across participants. A sample choice set is presented in Supplementary Fig. 1 . After viewing each profile individually, subjects were asked: “If you had to choose, would you choose to get this vaccine, or would you choose not to be vaccinated?” Subjects then made a binary choice, responding either that they “would choose to get this vaccine” or that they “would choose not to be vaccinated.” This is the dependent variable for the regression analyses in Table 3 . After making a binary choice to take the vaccine or not be vaccinated, we also asked subjects “how likely or unlikely would you be to get the vaccine described above?” Subjects indicated their vaccination preference on a seven-point scale ranging from “extremely likely” to “extremely unlikely.” Additional analyses using this ordinal dependent variable reported in Supplementary Table 3 yield substantively similar results to those presented in Table 3 .
To determine the effect of each attribute-level on willingness to vaccinate, we followed Hainmueller, Hopkins, and Yamamoto and employed an ordinary least squares (OLS) regression with standard errors clustered on respondent to estimate the average marginal component effects (AMCEs) for each attribute 51 . The AMCE represents the average difference in a subject choosing a vaccine when comparing two different attribute values—for example, 50% efficacy vs. 90% efficacy—averaged across all possible combinations of the other vaccine attribute values. The AMCEs are nonparametrically identified under a modest set of assumptions, many of which (such as randomization of attribute levels) are guaranteed by design. Model 1 in Table 3 estimates the AMCEs for each attribute. These AMCEs are illustrated in Fig. 1 .
Analyzing additional correlates of vaccine acceptance
To explore the association between respondents’ embrace of misinformation about COVID-19 treatments and vaccination willingness, the survey included an additional question battery. To measure the extent of belief in COVID-19 misinformation, we constructed a list of both accurate and inaccurate headlines about the coronavirus. We focused on treatments, relying on the World Health Organization’s list of myths, such as “Hand dryers are effective in killing the new coronavirus” and true headlines such as “Avoiding shaking hands can help limit the spread of the new coronavirus 52 .” Complete wording for each claim is provided in Supplementary Appendix 1 . Individuals read three true headlines and five myths, and then responded whether they believed each headline was true or false, or whether they were unsure. We coded responses to each headline so that an incorrect accuracy assessment yielded a 1; a correct accuracy assessment a -1; and a response of unsure was coded as 0. From this, we created an additive index of belief in misinformation that ranged from -8 to 8. The distribution of the misinformation index is presented in Supplementary Fig. 2 . A possible limitation of this measure is that because the survey was conducted online, some individuals could have searched for the answers to the questions before responding. However, the median misinformation index score for subjects in the top quartile in terms of time spent taking the survey was identical to the median for all other respondents. This may suggest that systematic searching for correct answers is unlikely.
To ensure that any association observed between belief in misinformation and willingness to vaccinate is not an artifact of how we operationalized susceptibility to misinformation, we also constructed two alternate measures of belief in misinformation. These measures are described in detail in the Supplementary Information (see Supplementary Figs. 3 and 4 ). Additional regression analyses using these alternate measures of misinformation beliefs yield substantively similar results (see Supplementary Table 4 ). Additional analyses examining whether belief in misinformation moderates the effect of efficacy and an FDA EUA on vaccine acceptance are presented in Supplementary Fig. 6 .
Finally, model 2 of Table 3 includes a range of additional control variables. Following past research, it includes a number of demographic variables, including indicator variables identifying subjects who identify as Democrats or Republicans; an indicator variable identifying females; a continuous variable measuring age (alternate analyses employing a categorical variable yield substantively similar results); an eight-point measure of educational attainment; and indicator variables identifying subjects who self-identify as Black or Latinx. Following previous research 6 , the model also controlled for three additional factors often associated with willingness to vaccinate: an indicator variable identifying whether each subject had health insurance; a variable measuring past frequency of influenza vaccination on a four-point scale ranging from “never” to “every year”; beliefs about the general safety of vaccines measured on a four-point scale ranging from “not at all safe” to “extremely safe”; and a measure of attitudes toward the pharmaceutical industry ranging from “very positive” to “very negative.”
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data and statistical code to reproduce the tables and figures in the manuscript and Supplementary Information are published at the Harvard Dataverse via this link: 10.7910/DVN/ZYU6CO.
Hamel, L., Kirzinger, A., Munana, C. & Brodie, M. KFF COVID-19 Vaccine Monitor: December 2020 | KFF (2020).
Dror, A. A. et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur. J. Epidemiol. 35 , 775–779 (2020).
Article CAS PubMed Google Scholar
Scharf, I. & Ben Zion, I. As Vaccinations Lag, Israel Combats Online Misinformation. AP2 (21AD).
Nyhan, B. & Reifler, J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine 33 , 459–464 (2015).
Article PubMed Google Scholar
Hussain, A., Ali, S., Ahmed, M. & Hussain, S. The anti-vaccination movement: a regression in modern medicine. Cureus 10 , e2919 (2018).
PubMed PubMed Central Google Scholar
Kreps, S. et al. Factors Associated With US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw. open 3 , (2020).
Motta, M. Can a COVID-19 vaccine live up to Americans’ expectations? A conjoint analysis of how vaccine characteristics influence vaccination intentions. Soc. Sci. Med . 113642, https://doi.org/10.1016/j.socscimed.2020.113642 (2021).
Bokemper, S. E., Huber, G. A., Gerber, A. S., James, E. K. & Omer, S. B. Timing of COVID-19 vaccine approval and endorsement by public figures. Vaccine , https://doi.org/10.1016/j.vaccine.2020.12.048 (2021).
Quinn, S. C., Jamison, A. M. & Freimuth, V. Communicating effectively about emergency use authorization and vaccines in the COVID-19 pandemic. Am. J. Public Health e1–e4 (2020).
Malik, A. A., McFadden, S. A. M., Elharake, J. & Omer, S. B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 26 , 100495 (2020).
Article PubMed PubMed Central Google Scholar
Fisher, K. A. et al. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann. Intern. Med. 173 , 964–973 (2020).
Lazarus, J. V. et al . A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med . 1–4 (2020).
Schwarzinger, M., Watson, V., Arwidson, P., Alla, F. & Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Heal ., https://doi.org/10.1016/s2468-2667(21)00012-8 (2021).
Wood, S. & Schulman, K. Beyond politics—promoting Covid-19 vaccination in the United States. N. Engl. J. Med . NEJMms2033790, https://doi.org/10.1056/NEJMms2033790 (2021).
Marshall, H. S., Chen, G., Clarke, M. & Ratcliffe, J. Adolescent, parent and societal preferences and willingness to pay for meningococcal B vaccine: a discrete choice experiment. Vaccine 34 , 671–677 (2016).
Administration, F. and D. Development and Licensure of Vaccines to Prevent COVID-19: Guidance for Industry . (2020).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 383 , 2603–2615 (2020).
Baden, L. R. et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med ., https://doi.org/10.1056/nejmoa2035389 (2020).
Johnson & Johnson. Johnson & Johnson Announces Single-Shot Janssen COVID-19 Vaccine Candidate Met Primary Endpoints in Interim Analysis of its Phase 3 ENSEMBLE Trial. (2020). Available at: https://www.jnj.com/johnson-johnson-announces-single-shot-janssen-covid-19-vaccine-candidate-met-primary-endpoints-in-interim-analysis-of-its-phase-3-ensemble-trial . (Accessed 28 Feb 2021).
Jackson, L. A. et al. An mRNA vaccine against SARS-CoV-2—preliminary report. N. Engl. J. Med. 383 , 1920–1931 (2020).
Anderson, E. J. et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N. Engl. J. Med. 383 , 2427–2438 (2020).
Quinn, S. C., Kumar, S., Freimuth, V. S., Kidwell, K. & Musa, D. Public willingness to take a vaccine or drug under emergency use authorization during the 2009 H1N1 pandemic. Biosecurity Bioterrorism 7 , 275–290 (2009).
Holden Thorp, H. A dangerous rush for vaccines. Science 369 , 885 (2020).
Limaye, R. J., Sauer, M. & Truelove, S. A. Politicizing public health: the powder keg of rushing COVID-19 vaccines. Hum. Vaccines Immunother ., https://doi.org/10.1080/21645515.2020.1846400 (2020).
Feuer, W. Trump Says ‘No President’s Ever Pushed’ the FDA Like Jim, Vaccine Coming ‘Very Shortly’. CNBC (2020).
Soysal, A., Gokçe, I., Pehlivan, T. & Bakir, M. Interchangeability of a hepatitis A vaccine second dose: Avaxim 80 following a first dose of Vaqta 25 or Havrix 720 in children in Turkey. Eur. J. Pediatr. 166 , 533–539 (2007).
Greenberg, D. P. & Feldman, S. Vaccine interchangeability. Clin. Pediatrics 42 , 93–99 (2003).
Article Google Scholar
Bishai, D., Brice, R., Girod, I., Saleh, A. & Ehreth, J. Conjoint analysis of French and German parents’ willingness to pay for meningococcal vaccine. PharmacoEconomics 25 , 143–154 (2007).
Cameron, M. P., Newman, P. A., Roungprakhon, S. & Scarpa, R. The marginal willingness-to-pay for attributes of a hypothetical HIV vaccine. Vaccine 31 , 3712–3717 (2013).
Litan, R. Want herd immunity? Pay people to take the vaccine. Brookings (2020).
Kane, R. L., Johnson, P. E., Town, R. J. & Butler, M. A structured review of the effect of economic incentives on consumers’ preventive behavior. Am. J. Preventive Med. 27 , 327–352 (2004).
Volpp, K. G., Loewenstein, G. & Buttenheim, A. M. Behaviorally informed strategies for a National COVID-19 vaccine promotion program. JAMA - J. Am. Med. Assoc. 325 , 125–126 (2020).
Google Scholar
Nowalk, M. P. et al. Improving influenza vaccination rates in the workplace. A randomized trial. Am. J. Prev. Med. 38 , 237–246 (2010).
Bertin, P., Nera, K. & Delouvée, S. Conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: a conceptual replication-extension in the COVID-19 pandemic context. Front. Psychol. 11 , 2471 (2020).
Lee, J. J. et al. Associations between COVID-19 misinformation exposure and belief with COVID-19 knowledge and preventive behaviors: cross-sectional online study. J. Med. Internet Res. 22 , e22205 (2020).
Reyna, V. F. Risk perception and communication in vaccination decisions: a fuzzy-trace theory approach. Vaccine 30 , 3790–3797 (2012).
Lin, C., Tu, P. & Beitsch, L. M. Confidence and receptivity for covid‐19 vaccines: a rapid systematic review. Vaccines 9 , 1–32 (2021).
Broniatowski, D. A. et al. Facebook pages, the ‘Disneyland’ measles outbreak, and promotion of vaccine refusal as a civil right, 2009–2019. Am. J. Public Health 110 , S312–S318 (2020).
Moon, K., Riege, A., Gourdon-Kanhukamwe, A. & Vallée-Tourangeau, G. The Moderating Effect of Autonomy on Promotional Health Messages Encouraging Flu Vaccination Uptake Among Healthcare Professionals . (PsyArXiv, 2020), https://doi.org/10.31234/OSF.IO/AJV4Q .
Ferdinand, K. C., Nedunchezhian, S. & Reddy, T. K. The COVID-19 and influenza “Twindemic”: barriers to influenza vaccination and potential acceptance of SARS-CoV2 vaccination in African Americans. J. Natl. Med. Assoc. 112 , 681–687 (2020).
PubMed Google Scholar
Jaiswal, J., LoSchiavo, C. & Perlman, D. C. Disinformation, misinformation and inequality-driven mistrust in the time of COVID-19: lessons unlearned from AIDS denialism. AIDS Behav. 24 , 2776–2780 (2020).
Determann, D. et al. Acceptance of vaccinations in pandemic outbreaks: a discrete choice experiment. PLoS ONE 9 , e102505 (2014).
Simpson, C. R., Ritchie, L. D., Robertson, C., Sheikh, A. & McMenamin, J. Effectiveness of H1N1 vaccine for the prevention of pandemic influenza in Scotland, UK: A retrospective observational cohort study. Lancet Infect. Dis. 12 , 696–702 (2012).
Remmel, A. COVID vaccines and safety: what the research says. Nature 590 , 538–540 (2021).
Coppock, A. & McClellan, O. A. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Res. Polit. 6 , 1–14 (2019).
de Bekker-Grob, E. W. et al. The impact of vaccination and patient characteristics on influenza vaccination uptake of elderly people: A discrete choice experiment. Vaccine 36 , 1467–1476 (2018).
Determann, D. et al. Public preferences for vaccination programmes during pandemics caused by pathogens transmitted through respiratory droplets–A discrete choice experiment in four European countries, 2013. Eurosurveillance 21 , 1–13 (2016).
de Bekker-Grob, E. W. et al. Girls’ preferences for HPV vaccination: A discrete choice experiment. Vaccine 28 , 6692–6697 (2010).
Guo, N., Zhang, G., Zhu, D., Wang, J. & Shi, L. The effects of convenience and quality on the demand for vaccination: results from a discrete choice experiment. Vaccine 35 , 2848–2854 (2017).
Kaplan, R. M. & Milstein, A. Influence of a COVID-19 vaccine’s effectiveness and safety profile on vaccination acceptance. Proc. Natl. Acad. Sci. USA 118 , 2021726118 (2021).
Hainmueller, J., Hopkins, D. J. & Yamamoto, T. Causal inference in conjoint analysis: Understanding multidimensional choices via stated preference experiments. Polit. Anal. 22 , 1–30 (2014).
Organization, W. H. Coronavirus disease (COVID-19) advice for the public: Mythbusters. (2020). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters . (Accessed 14 Jan 2021).
Download references
Acknowledgements
S.K. and D.K. would like to thank the Cornell Atkinson Center for Sustainability for financial support.
Author information
Authors and affiliations.
Department of Government, Cornell University, Ithaca, NY, USA
Sarah Kreps & Douglas L. Kriner
Injury Prevention Research Center, University of North Carolina, Chapel Hill, NC, USA
Nabarun Dasgupta
Department of Pediatrics, Harvard Medical School, Boston, MA, USA
John S. Brownstein
Computational Epidemiology Lab, Boston Children’s Hospital, Boston, MA, USA
Epidemiology and Biostatistics, University of California, San Francisco, CA, USA
Yulin Hswen
You can also search for this author in PubMed Google Scholar
Contributions
S.K. and D.K. designed the experiment/survey instrument and conducted the statistical analysis. S.K., N.D., J.B., Y.H., and D.K. all contributed to the conceptual design of the research and to the writing of the paper.
Corresponding author
Correspondence to Douglas L. Kriner .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Kreps, S., Dasgupta, N., Brownstein, J.S. et al. Public attitudes toward COVID-19 vaccination: The role of vaccine attributes, incentives, and misinformation. npj Vaccines 6 , 73 (2021). https://doi.org/10.1038/s41541-021-00335-2
Download citation
Received : 25 January 2021
Accepted : 06 April 2021
Published : 14 May 2021
DOI : https://doi.org/10.1038/s41541-021-00335-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Progress with covid vaccine development and implementation.
- Richard W. Titball
- David I. Bernstein
- Alan D. T. Barrett
npj Vaccines (2024)
A synthesis of evidence for policy from behavioural science during COVID-19
- Kai Ruggeri
- Friederike Stock
- Robb Willer
Nature (2024)
The rapid progress in COVID vaccine development and implementation
- Nicolas V. J. Fanget
npj Vaccines (2022)
COVID-19 Vaccine Acceptability and Financial Incentives among Unhoused People in Los Angeles County: a Three-Stage Field Survey
- Allison D. Rosen
- Jacqueline Beltran
- Chelsea L. Shover
Journal of Urban Health (2022)
The shot, the message, and the messenger: COVID-19 vaccine acceptance in Latin America
- Pablo Argote
- Elena Barham
- Oscar Pocasangre
npj Vaccines (2021)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- Open access
- Published: 20 October 2020
A qualitative analysis of vaccine decision makers’ conceptualization and fostering of ‘community engagement’ in India
- Tapati Dutta ORCID: orcid.org/0000-0002-3272-1115 1 ,
- Beth E. Meyerson 2 ,
- Jon Agley 3 ,
- Priscilla A. Barnes 4 ,
- Catherine Sherwood-Laughlin 5 &
- Jill Nicholson-Crotty 6
International Journal for Equity in Health volume 19 , Article number: 185 ( 2020 ) Cite this article
4462 Accesses
14 Citations
28 Altmetric
Metrics details
Globally, and in India, research has highlighted the importance of community engagement in achieving national vaccination goals and in promoting health equity. However, community engagement is not well-defined and remains an underutilized approach. There is also paucity of literature on community engagement’s effectiveness in achieving vaccination outcomes. To address that gap, this study interviewed Indian vaccination decision makers to derive a shared understanding of the evolving conceptualization of community engagement, and how it has been fostered during India’s Decade of Vaccines (2010-2020).
Semi-structured interviews were conducted with 25 purposefully sampled national-level vaccine decision makers in India, including policymakers, immunization program heads, and vaccine technical committee leads. Participants were identified by their ‘elite’ status among decisionmakers in the Indian vaccination space. Schutz’ Social Phenomenological Theory guided development of an a priori framework derived from the Social Ecological Model. The framework helped organize participants’ conceptualizations of communities, community engagement, and related themes. Inter-rater reliability was computed for a subsample of coded interviews, and findings were validated in a one-day member check-in meeting with study participants and teams.
The interviews successfully elucidated participants’ understanding of key terminology (“community”) and approaches to community engagement propagated by the vaccine decision makers. Participants conceptualized ‘communities’ as vaccine-eligible children, their parents, frontline healthcare workers, and vaccination influencers. Engagement with those communities was understood to mean vaccine outreach, capacity-building of healthcare workers, and information dissemination. However, participants indicated that there were neither explicit policy guidelines defining community engagement nor pertinent evaluation metrics, despite awareness that community engagement is complex and under-researched. Examples of different approaches to community engagement ranged from vaccine imposition to empowered community vaccination decision-making. Finally, participants proposed an operational definition of community engagement and discussed concerns related to implementing it.
Conclusions
Although decision makers had different perceptions about what constitutes a community, and how community engagement should optimally function, the combined group articulated its importance to ensure vaccination equity and reiterated the need for concerted political will to build trust with communities. At the same time, work remains to be done both in terms of research on community engagement as well as development of appropriate implementation and outcome metrics.
The Global Vaccine Action Plan 2011–2020 lists equity as one of its six guiding principles [ 1 ]. Resonating this ethos, various national vaccination policies and programs have acknowledged vaccines’ contribution to preventing high-cost treatments and averting medical impoverishment, while striving to extend the benefits of immunization to all [ 2 , 3 ]. Correspondingly, community engagement (CE) for vaccinations has increasingly been recognized by decision makers [ 4 ] as a core component of working toward health equity, with a focus on community-based participatory research [ 5 , 6 , 7 ]. CE has been lauded for its facilitation of research translation [ 8 ] and for fostering positive perceptions of vaccines and immunization-related interventions [ 9 ], while decreasing the likelihood of therapeutic misconception [ 10 ]. CE also has been recognized for its assertion that research and interventions with people but without their input is unethical [ 11 ]. Further, recurring incidents of vaccine backlash by communities, as demonstrated by skepticism, resistance, and lack of vaccine support, are often attributed to ‘inappropriate CE’ [ 12 ]. Despite this salutogenic understanding of CE, which has been hypothesized to be a pathway through which population health goals related to public health equity can be met [ 13 ], several studies have suggested that CE has not been clearly defined or explicated in the context of vaccination programs [ 14 , 15 ]. It is important to understand how CE may be utilized to ensure that vaccines are translated into affordable and globally accessible public health solutions, which are acceptable by all communities [ 16 , 17 , 18 ].
To do so, this study examined CE in the context of India’s Universal Immunization Program. India has made tremendous progress during the “Decade of Vaccines” (2010-2020) by introducing multiple new vaccines along with striving to increase access to new and underused vaccines in the country [ 19 ]. The National Vaccine Policy of India mentions ethical use and equitable access as its basic mantra (Ch 5, p 28). However, vaccine decisionmakers are increasingly concerned with the 62% vaccination uptake prevalence among vaccine-eligible children (12-23 months), compared to the 90% target set under government’s Universal Immunization Program, to be achieved by the end of 2020 [ 20 ].
Vaccine studies also indicate the need to embed CE within India’s immunization programs [ 19 , 21 , 22 ]. This growing sensitization about CE among Indian vaccine decision makers has been bolstered by the Supreme Court advisory which recommends meaningful dialogue with communities to accelerate vaccination uptake [ 21 ]. CE is also perceived to be an important step in addressing communities’ vaccine resistance, which leads to delays that inhibit timely vaccination. For example, the cervical cancer-preventing human papilloma virus vaccine was suspended by the Supreme Court of India in 2010. Later, the country's right-wing groups wrote to the Prime Minister expressing concerns about pharmaco-governance and asserting that foreign companies were pushing the vaccine onto an unsuspecting public. Through July 2020, despite advice by the National Technical Advisory Group on Immunization, the Federation of Obstetric & Gynecological Societies of India, and the Indian Academy of Pediatrics for its inclusion in the Universal Immunization Program, substantial community resistance remains. As a result, the vaccine has been sporadically rolled out in three (Sikkim, Punjab and Delhi) out of 36 states and Union Territories [ 23 , 24 ].
Community skepticism about vaccines has a long history in India, evidenced by covert and overt vaccine resistance. As early as the mid 1800’s, some Hindus resisted the smallpox vaccine on religious grounds, because the material used for vaccines was drawn from the lymph of a cow, which is considered a sacred animal by the community [ 25 ]. During the National Polio Surveillance Program, community resistance ranged from people closing their doors and windows when they heard vaccinators approaching their houses, to vaccine backlash such as physical conflict between vaccinators and communities [ 26 ]. Recently, in 2017, there was decreased uptake of measles-rubella vaccination in certain Indian states amidst community uproar following social media rumors of political conspiracy and safety concerns about the vaccine [ 27 , 28 ]. Thus, work to articulate a shared conceptualization of CE is critical at this juncture to establish concerted and strategic CE that can facilitate transparent vaccine communication between communities and decisionmakers and build on existing technology, interventions, and healthcare systems to address inequities in vaccination coverage, especially among under-reached and underserved populations. This may be especially useful in overcoming communities’ myths and fears about new vaccines, which are often considerably more expensive than existing ones, and target relatively ‘hidden’ diseases [ 21 , 23 ]. However, current CE evidence is limited to a few systematic examinations focused on community counselling and vaccination campaigns, often in pockets of high vaccine resistance and low vaccination coverage [ 29 , 30 ]. These reviews have also focused on public opposition rather than involvement, and no data have been collected to indicate ‘if’ and ‘how’ communities are engaged beyond individuals’ decisions to vaccinate themselves and their children [ 31 , 32 , 33 ]. The wider body of academic literature attributes this dearth of CE related studies to the variously premised and sometimes conflicting definitions of and rationales for CE [ 34 ] and the absence of CE metrics [ 35 ]. Other studies mention that evaluating CE is challenging, as such activities often occur in the context of ongoing work and throughout the process of adopting more collaborative engagement approaches [ 36 , 37 ].
It is our perception that typifying an understanding of CE may lead to contextual and ethical application of CE within a complex system of relationships among researchers, policymakers, implementation scientists, and vaccine users. It may also prevent erroneous assumptions about its value and utility, or lack thereof, and inform research and data needs related to CE. This may, in turn, trigger a policy dialogue focused on robust measures to assess what works, how it works, and, over time, if CE efforts have improved vaccination rates and thereby bolstered national efforts to reach out to every vaccine eligible child and adult. Therefore, this study aimed to examine elite Indian vaccine decision makers’ individual perspectives and collective understanding about CE, the circumstances in which CE has been implemented, and how they have fostered CE for effective vaccination.
Schutz’s Social Phenomenology Theory was used as an underlying approach because it is consistent with the belief that ‘conceptualizations’ are socially constructed and appropriated to explore participatory action [ 38 ]. This theory also helped direct attention toward considering the dynamic contexts in which CE was conceived and operationalized [ 39 ]. Social Phenomenology further helped to treat CE conceptualization and its fostering as intersubjective, integral to institutions and systems, all embedded in history, time, and space [ 40 ]. The lead author’s (TD) professional role was that of a translational researcher, supporting evidence-based programs and policy through examination of ecological frameworks using a community-based participatory approach. Her a priori assumption was that community engagement can foster social, relational, and ethical progress toward health equity [ 41 ]. However, few assumptions were made about how decisionmakers would conceptualize CE and community, as these issues infrequently are described in formal, written documents and must instead be intuited from distally related activities.
In preparing for this study, the lead author (TD) purposefully identified 30 individuals who had authoritative roles related to vaccine discovery, development and delivery, such as national-level vaccine decision makers who were policymakers, program heads and/or associates in the government, private sector, non-governmental organizations, and country-offices of international donor and UN agencies. Thus, these individuals, by virtue of their knowledge and positions, were the ‘elites’ [ 42 ] and were able to provide a unique ‘big-picture perspective’ [ 43 ] about CE strategizing and implementation during India’s Decade of Vaccines. Interviewees were approached with this status differential in mind [ 44 ]. In keeping with the assumptions and beliefs of social phenomenology, a two-step participatory approach for data collection was used: (1) semi-structured elite interviews followed by (2) a member check-in meeting [ 42 ]. All interactions used a community-engaged approach, including emphasis on mutual respect and recognition of the knowledge and expertise of study participants. This included adhering to participants’ preferred meeting dates on December 25 and January 1, even though these were national holidays. Further, the member check-in meeting was democratically conducted rather than using the researcher as a moderator. In addition, the researcher was sensitive that issues related to vaccine resistance were occurring in real time, wherein trust building with the study participants was necessary to obtain ‘good data’ and completion of the project.
Access to participants (distinct from identification of the sample) was obtained using a snowball methodology, beginning from the professional network of the principal investigator (TD). Recruitment emails were sent by TD in December 2017 to each of the 30 potential participants, followed up with phone calls to identify interest and availability for an in-person interview. Interviews were conducted by TD with 25 individuals who agreed to participate in the study from December 2017 to February 2018. Each interview lasted for 50 to 90 minutes, was carried out in English, and conducted in the country-offices of the respective agencies, institutions, and organizations located in or around New Delhi, the capital city of India. Interviews were audio recorded and transcribed verbatim. All personalized information was anonymized. Data also included field-notes written within 24 hours of each interview. The interview topics drew from earlier studies focusing on CE as a strategic tool for vaccine research and rollout [ 45 , 46 ]. Accordingly, the inquiries explored participants’: (i) conceptualization of community and CE, (ii) evolution of CE, (iii) fostering support for CE, (iv) resources available for CE, (v) partnerships for CE, (vi) enablers to CE, and (vii) barriers to actualize CE. The interview guide used for this study, including questions and probes, is available as a digital supplement ( 1 ) to this article.
Once a preliminary analysis of the interview data was completed, TD presented the findings in a one-day member check-in meeting among the study participants and their teams (who held second-line leadership positions) in January 2018. Study participants and their team members who participated in the member check-in meeting were knowledgeable about the issue and were comfortable validating and candidly critiquing the primary findings. All study participants and their teams were nationally known; thus, in order to maintain confidentiality, identities, names, and organizational affiliations were not used in reporting the findings. Therefore, although participants in the follow-up meeting knew each other, no specific responses were linked to any individual or organization. This meeting ensured that the overall summation and meaning making of the findings prepared by TD and the research team conformed with what the study participants had mentioned in their interviews and made sense to both the vaccine decision makers and their teams in India (e.g., validity). This was a participatory way to verify both data saturation and completeness of the findings, as well as archival document review (part of the overall project, but not of this study). The study was approved by Indiana University’s Institutional Review Board.
Data analysis
First, all data were transcribed verbatim and entered in NVivo12 (QSR International, Melbourne, Australia) for qualitative data management.
An a priori coding structure was used to categorize individual participants’ conceptualization of CE, how their interests in CE for vaccination evolved by overcoming barriers and optimizing facilitators, while integrating 'policy push for vaccine uptake' and 'generating vaccination demand pull' approaches for different vaccines under the UIP. Based on the interpretive analysis used in social phenomenology, first-level broad construction of CE was done, followed by second-level typical constructs, deliberated through critical events or performance of CE ‘duties’ and ‘responsibilities’ throughout the tenure of the decision makers [ 47 ]. Categories conceptually corresponded with the Social Ecological Model, which has been used to study vaccination uptake and health disparities [ 41 ]. Given this loose pre-existing framework, a general inductive approach was used [ 46 ]. To reach intercoder-reliability (>90%), two coders joined TD, iteratively reviewed, and re-reviewed data for existing and emerging themes and/or patterns, and ultimately crystallized a holistic interpretation through multiple coding conferences. Thereafter the three coders independently coded five interviews to test, reject, accept, or refine the codes [ 43 ]. The final coding structure contained 7 multi-dimensional CE themes with 42 nodes. Exemplar interview excerpts illustrate the findings, although the analysis drew from the entire dataset. The coding structure is available in full as a digital supplemental ( 2 ) file.
All study participants held national and multi-regional leadership roles in vaccine policymaking, financing, and/or program planning and management across vaccine research, development, and roll-out stages for at least ten years in India. In addition to their roles in India, five participants reported managing programs in multiple countries in Asia, Africa, and Latin America. Table 1 describes the study participants.
This section sequentially shares results organized by the following categories and subcategories. Because the results are extensive, we list many of the key themes in brief here as well.
conceptualization of community, and how stakeholders define community;
community was typically understood to be one or more of the following: vaccine-eligible children and their parents and vaccine-eligible adults, frontline healthcare providers, local-level stakeholders, vaccine gatekeepers, and local-level implementing organizations.
conceptualization of CE, with particular attention to analyzing extant efforts, which generally fell into three categories:
capacity building of frontline stakeholders as CE;
capacity building most often was expressed as training, training-of-trainers, and course offerings;
vaccine-related information dissemination as CE;
participants described a wide variety of different communication methods, as well as perceived benefits and disadvantages to each;
targeted community interventions as CE;
participants provided examples of ways in which community
interventions had been carried out;
different tangible ways in which CE might be fostered;
fostering CE was viewed on a broad spectrum that ranged from highly participatory approaches to direct imposition of vaccination services;
evolution and transformation of CE;
all participants acknowledged the need for a better understanding of CE and, in the member check-in meeting, came to a consensus on a definition of CE.
Conceptualization of community
Most participants defined communities as ‘beneficiaries of the UIP,’ with a notion of transactional exchange of vaccine related information between the providers and the communities, always with the aim of vaccination uptake. Communities consisted of the following categories of people: (1) vaccine-eligible children, vaccine-eligible young adults, and their parents and guardians who make vaccination-decisions for the former; (2) healthcare providers who deliver vaccines and sensitize vaccine-eligible populations and their guardians for improved vaccination rates and herd immunity; (3) local-level stakeholders who disseminate information to encourage vaccination uptake; (4) gatekeepers who resist a particular vaccine or vaccination per se , and; (5) local-level implementing organizations of community health workers, groups that includes what are known in India as the 3As. These are Auxiliary Nurse Midwifes who are based at a sub-center and are multipurpose workers responsible for administering vaccines among communities of < 5000 people; Accredited Social Health Activists, who are local women trained to act as health educators in their communities, catering to 700 people in tribal areas and 1000 in rural villages; and Anganwadi Workers, resident workers in the village rural child care centers in India who are responsible for promoting maternal and child health, including interpersonal communication for full immunization coverage, among communities of <1000 people. A few participants took a broader perspective: “ It is the whole communities in which those individuals were living.”
Most of the participants acknowledged their distance from the community, mentioning “if I went to the community nobody will accept me,” while comparing the sense of community with local organizations because they “help raise community demand for routine immunization. ” These organizations included grassroots non-profit organizations (NPOs), community-based organizations (CBOs) like women’s self-help groups, local-level representatives of occupational groups like brick-kiln workers and barbers, and the local-chapters of technical and youth organizations such as the Indian Association of Pediatricians and Nehru Yuva Kendras Sangathan (autonomous organization for youth development under the Government of India, Ministry of Youth Affairs and Sports). Several NGO heads identified themselves as ‘communities’ for their people-centric approach, though, in most of these expressions, fractious relationships and issues of incompatibility between decision makers [mostly government or donors] and NPOs were evident.
“ … .they [Government or donors] want to clip our wings. This is very sad because we [NPOs] bring up issues [local issues of the communities] , which you [Government or donors because of being at the national-level] might never know.”
Some participants identified vaccine-gatekeepers, people who were suspicious that vaccination is a political agenda against minority groups, as communities. Interventions targeting their positive vaccination decisions came across as an area of CE.
“ … in Mallapuram the mother generally said ‘no’ to vaccination because their husband lived in the Middle East [who was proxy decision-makers for their child’s vaccination] .”
Finally, it was unclear whether the media was part of the community, or a driver of communities’ vaccination decisions. Most participants indicated that the media spread misinformation and promulgated negative sentiments among vaccine priority populations about vaccines, and thus expressed the need “to stop negative media so that they [media] do not “blindly publish” , or “ over-sensationalize when it is not an Adverse Event Following Immunization.”
Conceptualization of CE
The participants perceived CE both as a strategy and tool in implementation terms, and variously defined CE as segments of processes comprising of: (1) vaccine policy and program formulation; (2) capacity-building of frontline stakeholders; (3) vaccine information dissemination among communities to promote vaccination uptake, and; (4) targeted community-level interventions to curtail the recurring incidents of vaccine-related community backlash. There was evidence of relational goals of CE, like “longer-term trust building” [between the vaccine decision makers and the communities], and “ … .understand what is going on in people’s minds [regarding vaccinations] ” .
Intuitively, all the participants proposed ongoing and early instantiation of CE for better vaccination outcomes:
“We always go to the communities earlier and have media campaigns, and interpersonal communications to sensitize people on what [vaccine] we would give to their children.”
However, several participants critiqued that CE interventions came in waves, mostly during vaccine introductions, before and during vaccine trials, and in response to a disease outbreak. They also noted that there were no tools or metrics to measure its impact. They speculated that these deficits may be because:
“The Immunization Technical Unit was not built with a CE model [CE frame] for immunization. Like, you [Government] compensate Accredited Social Health Activists for fully immunizing children and trainings attended, but not for doing CE.”
Participants described a top-down and decentralized vaccine governance structure where vaccine policy formulation and vaccine introductions were conducted at the Ministry, considering disease burden, vaccine cost, cold-chain, and supply chain issues. These efforts were completely funded by the Ministry of Health and Family Welfare (MoHFW) and international donors.
“ … . [CE is like] a chandelier, the [MoHFW] is the hook. The different lights are the different partners, they are held at right distances in the right manner. In immunization, the roles and partnerships [of national level decisionmakers] are clearly defined .”
The development of vaccine policies and operational guidelines in English and Hindi (one of the 22 scheduled languages of the Republic of India, and also one of the official languages of India which is understood, spoken, and read by more people than English) by the technical bodies of MoHFW, such as the Immunization Technical Support Unit, and the Mission Steering Group, was conceptualized as CE too. Participants mentioned that the “ state translated and modified [these documents] if they think that something is to be added or deleted,” though no such example of any such revisions incorporated based on communities’ recommendations was cited.
Except the Vaccine Policy (2011), which recommended enhancing communities’ vaccination acceptance and confidence, and vaccine-specific Operational Guidelines, which recommended community-facing strategies, participants did not identify any sub-population-based CE-specific policy. Almost half of the participants cited the Communication Strategy for Polio Eradication , published by the UNICEF and USAID CORE Group, detailing intensive outreach for polio vaccination, as nearest to any CE guideline. Three participants, considering India’s diversity where “every mile the language changes, the culture changes” suggested having a “village-level communication strategy.” Participants noted strategic programs like Mission Indradhanush and Intensified Mission Indradhanush to achieve 90% immunization “to the last child” as CE.
The heads of organizations and technical bodies often criticized chasms in this one-way, top-down approach as “ working in silos” and “not real CE,” and feared that it would ultimately “hinder an integrated approach.” A few participants identified CE as activities occurring in spaces like Village Nutrition and Sanitation Days, which are organized monthly at rural childcare centers. There, communities can ask questions about vaccines and vaccination strategies. However, these participants were doubtful that communities possessed any emancipated voice beyond seeking or resisting vaccines.
Capacity building of frontline stakeholders
Some participants mentioned ‘cascade training of trainers’ for the 3As and local Master Trainers as CE, since the goal is to motivate communities for full immunization. Notably, the CE roles of the 3As and other local stakeholders were different. The Auxiliary Nurse Midwives and Anganwadi Workers are salaried staff for vaccine administration among communities and the Accredited Social Health Activists receive honoraria for counselling and escorting the communities to vaccinations. However, the local NPOs and CBOs appeared to be instrumental in carrying out community-based activities to motivate each community’s vaccination decisions, and, in the case of vaccine trial conducting organizations, act as conduits between researchers and vaccine clinical trial participants.
Participants conceptualized the 18 months training for ANMs, and 3–4 weeks trainings for AWWs and ASHA workers respectively, with additional trainings such as the 3-day Boosting Routine Immunization Demand Generation course for the 3As, and vaccination sensitization trainings for the local-level vaccine-champions (community advisory boards, local religious leaders, barbers, and CBO members), as CE. In these instances, it appeared that some interpersonal tactics were imparted to frontline stakeholders, and tasks were later delegated to them. However, a few participants questioned the ‘quality of CE outcomes’ from these trainings:
“So, you [Government] piggy back everything on the Community Healthcare Worker, who talks to communities about everything: immunization, family planning, maternal health, school health, adolescent health, non-communicable diseases, and cancer … [but] you are not actually engaging or doing CE.”
Vaccine-related information dissemination
Most respondents mentioned “ bilateral information transfer [interpersonal and behavior change communication] sent down to communities” as CE. In the same vein, most participants denoted the Communications Officer as the CE human resource. In fact, one participant said, “The role of communication, I mean CE, sorry using the wrong word again.”
Some participants highlighted the need to be creative and explore web-based media, considering its ease of use, cost-effectiveness, and penetration to interior locations:
“Nobody is interested to read your mobile texts. So, use GIF messaging.”
There were a few examples where bottom-up information, going from the community to the government which facilitated realizing the vaccine program goals, was acknowledged:
“In a construction site we [participant’s organization] did the mapping. But when we reached the community after a fortnight, they [community] have already migrated. The local person would tell us the whereabouts of the mobile community and we could then reach them through the Accredited Social Health Activist network.”
Some participants highlighted campaign-related booklets like the area-based ‘ Underserved Strategy,’ developed after a polio outbreak in Uttar Pradesh in 2002 among the Muslim populations, the ‘ Social Mobilization Network’ formed in 2001 to sensitize families to polio immunization, ‘ My Village my Home’ , a pictographic vaccination tracking method in the shape of a hut, where each column of the hut contains vaccination details of each new-born in the village, and media trainings of “State Immunization Officers on how to handle the media and stop negative media,” as CE.
Vaccine champion engagement and celebrity engagement to motivate communities’ vaccination decisions came across as another form of CE, though there were mixed reactions regarding this strategy.
“Our communication campaigns are pathetic. What is the point in having [a film star in his 70s ] there? We have no way of measuring CE. Does he convey safety of the product? To sell a toothpaste or a phone we spend hundreds of millions of dollars. How much is going into selling something far more important as vaccines?”
Targeted community interventions
Some participants perceived CE as a [right of the communities], “communities want the leadership to come to them. … just sit with them [communities], work with them and that is CE. The leader needs to go to the community at least once or twice. It really increases the communities’ motivation and trust.”
Others suggested a more emancipatory understanding of CE:
“[Vaccine] demand generation is another thing [than CE] . It means that you [government/vaccine providers] are giving and we [vaccine-eligible community] are accepting. Policy influencing is that where the [empowered] community thinks that certain things needs to be changed [and advocates for that] .”
Intervention programs reflected a range, between vaccine imposition and respectful engagement with community stakeholders, where participants’ responses reflected balanced trade-offs between CE’s time and resource investments and feasibility, emphasizing that it is a “ marathon, and not a sprint,” “an expensive process” and “took 20 years to learn about community and how to do CE.”
“In XXXX district community was very resistant and started beating the vaccination team. Then we had to contact a local muscleman, briefed him that this [carrying on with the vaccination drive] is important, and then told him to make an announcement that vaccination is not a bad thing.”
“We engaged with the staff of Aligarh Muslim University, Jamia Milia Islamia and Jamia Hamdard [institutions of higher education that were created to manifest indigenous ethos and spirit of diversity in India] , who went to the field. That helped to address the issue of vaccine hesitancy among religious leaders [especially the Muslim religious leaders] .”
Later, in the member check-in meeting, participants reiterated that effective CE conceptualization and conduct will require developing CE performance and outcome indicators and advocating for their incorporation in immunization surveillance instruments in India. Herein, all the participants emphasized the need to document CE effectiveness and its relational gains:
“ … as a country, I will be ashamed … ., very poor in documentation. You will hardly see any papers from the learnings of polio eradication. This is so because the people who are doing CE do not have the time to document.”
Range of approaches to fostering CE
Though a strict categorization of responses by organizations would not be accurate, participants endorsed a wide variety of types of approaches to fostering CE. These methods generally fell on a spectrum ranging from empowered (‘1’) to disempowered (‘7’). Table 2 provides exemplar quotes illustrating efforts or actions that might be categorized into these different levels.
All participants acknowledged “ decision makers’ good intention for CE but they were not matched with recipes of successful CE models.” Most of the CE interventions reported occurred during the National Polio Surveillance Program (a campaign of the World Health Organization and MoHFW initiated in 1995 to ensure polio eradication through house-to-house poliovirus vaccine delivery), with minimal evidence of institutionalization, replication, or scale-up of these during introduction of other vaccines.
Evolution and transformation of CE
All participants indicated that CE was still a “very poorly understood space,” “complex,” and there were “several gaps to understand this puzzle.” Three participants from NPOs critiqued that it is “ offhand,” “ad-hoc practices to douse the fire,” “firefight,” or “control big chaos and help put things back to normal” and recommended “real community engagement” and a “scientific approach to CE.” Recollecting CE’s evolution, participants noted that the earlier paternalistic prevention impositions has built a negative community memory, and jeopardized communities’ trust on vaccine authorities:
“..the vaccine fear was connected to the family planning program wherein women were forcibly sterilized.”
There was some evidence of pragmatic pressures by global provider/donor organizations (e.g., “GAVI funding went partly for community mobilization” ) that reinforced renewed systems-thinking and inclusive bottom-up- models, like:
“We were not really very serious and formed a small community group. [Initially, the community group ] came, had some snacks and went off. CE really didn’t go beyond that. But by then the NIH and USAID wanted Community Advisory Boards or CABs … and then we learnt how necessary it was.”
Consequently, several participants described recent and direct interactions between vaccine decisionmakers and communities while referring to “ The Prime Minister’s Office invites suggestion from the public” and “ Health Minister issues letters to each Accredited Social Health Activist and Auxiliary Nurse Midwife encouraging them to vaccinate every child.”
In the day-long member check-in meeting, the summary of analysis from the interviews was presented. Study participants and their teams agreed with the findings, and jointly came up with a robust definition of CE, which can be summarized as:
“CE is an upstream policy imperative rather than downstream interventions to build trustworthy relationships between vaccine decisionmakers and communities. It involves demystifying vaccine science and transparent communication for empowered community agency. This would enable communities to critically analyze vaccine related myths and misinformation and enable knowledge co-production in building community sensitive vaccine policies and programs. [CE] is incumbent to sustained political-will and resources to ensure evidence-informed, tailored, vaccine policies and programs, providing equitable, quality, and tangible vaccination and capacity building benefits to community members.”
Meeting participants recognized the need to carry out interventions in ways such that trustworthy relationships between communities and decision makers are established. There were comments reflecting realizations like “If we [decisionmakers] close the doors once again to the community, we might lose their trust, and not get the communities back, ever again.” They also recommended creating more opportunities for relationship-building and group discussions between community healthcare workers and vaccine decision makers. Meeting participants were especially interested in addressing inequities in vaccination coverage by building on the existing range of interventions while innovating newer mechanisms such as community mobilization for vaccination, strategic interventions with vaccine gatekeepers, providing immunization information using traditional, digital, and social media, and dispelling vaccine misinformation and disinformation while formulating rumor management strategies.
This study was able to identify elite decision makers’ core conceptualizations of community, CE, and both extant and aspirational approaches to CE related to vaccination programs in India. In reviewing these findings with study participants, a core definition of CE emerged, focused on upstream relationships (bidirectional), fostering trust, transparent communication, capacity building, and political will to ensure such approaches. Participants indicated that much of the extant work being conceptualized as CE is primarily downstream delivery and even imposition of services for vaccination uptake. While such things can be beneficial (e.g., vaccination), it likely matters to whom they done, in what way, and with what level of community voice (e.g., changing “to whom” to “with whom”). Given that direct imposition has resulted in community backlash against vaccination campaigns both in India and other parts of the world, including violence and hiding children from vaccinators, achieving national policy goals and fostering equitable distribution of public health outcomes may be difficult without a revised approach to CE. Concomitant to this must be an increased focus on CE metrics to promote greater understanding of processes and goals. Importantly, each of the different approaches to CE, including direct imposition, appeared to have been done with the primary goal of increasing equitable access to vaccinations (e.g., supporting community immunization). Thus, the underlying question discussed in this study did not focus on whether individuals should have equitable access to vaccinations, but rather on how such an outcome might best be achieved – that is, the degree to which a revised understanding of CE can support bilateral improvements in both vaccination dissemination by the government and vaccine confidence among communities.
Notably, being an Indian but performing the research at an American university, mitigated reflexivity issues and gave TD the identity of an 'informed outsider,' which allowed her to gain increased access to elites [ 43 ]. Being an implementation researcher allowed TD to deeply engage in analyzing the data while utilizing NVivo predominately as a data management tool. The member check-in meeting facilitated a participatory approach to the interviews, providing considerable interpretive latitude, and probing opportunities. It also allowed participants to critically review CE in UIP with a diversity-equity-inclusion focus. This was particularly important because studies on ‘elite interviewing’ mention that such access can be rare, because such people are hard to reach, surrounded by gatekeepers, and have power and ability to protect themselves from intrusion and criticism [ 44 , 48 ].
This study also benefited from the fact that none of the CE strategies/interventions were ranked as ‘best practice’ over another by institutional mandate or leadership, unlike the traditional ranking of engagement models in Holland Matrix (1997) [ 49 ], or Arnestein’s Ladder [ 50 ]. This helped reduce social desirability issues among the participants, who would not be perceived as ignoring a best-practice approach when answering honestly about CE.
In most cases, decision makers did not identify themselves or their families as ‘community’, and in some cases only a section of the public was perceived as ‘community’. Ensuring full immunization to communities under UIP was considered the most important CE goal and a step toward equitable health outcomes. However, as noted in other literature [ 35 , 51 ], a non-immersive and reductionist approach to conceptualizing communities may inhibit formation of trusted collaborations with the communities, ultimately compromising the creation of communities’ agency [ 52 ]. Some authors have described this as ‘conservative corporatism’ which, contrary to the ‘whole community approach’ [ 53 ], can lead to fragmented health governance, introduce barriers to building comprehensive people-centered vaccine policy reform [ 36 ], and risk defining communities as internally homogenous entities, which is unlikely to be the case given the diversities prevalent in India [ 54 ]. This may also undermine tailored CE strategies for particular sub-populations, leading to reductions in their trust of vaccinators and empowered vaccination decision making, especially among those for whom vaccine hesitancies are high, and/or vaccination uptake is low [ 55 , 56 ].
While findings supported current iterations of CE in making substantive contributions to vaccine demand generation and disease eradication, communities were often seen as offering ‘passive demand.’ Ideally, communities would actively seek vaccines and there would be community demand reflecting social support for vaccination as a norm [ 11 ]. Head’s research goes so far as to suggest that utilitarian CE may foster health inequities [ 57 ]. Gopichandran’s work looks at the relational gains (more intrinsic in nature, rather than transactional relationship building) from CE and posits development of trust between vaccine decision makers and communities as a result of shared CE goals integrated into vaccination targets [ 56 ]. Accordingly, doing empowered CE may require a paradigm-shift to perceive communities as integral parts of the policy and delivery systems, incorporate CE metrics into vaccine surveillance, and create new roles with a focused responsibility to coordinate CE.
It appears that many facets of the national-level CE response were an equilibrating reaction to appease community outrage rather than an integral approach set in place a priori . Adhikari et. al. has defined such CE as 'short-hand' [ 31 ], often resulting in wasted resources, with the potential to create mistrust rather than enhance benefits, create legitimacy, or share responsibility [ 31 , 56 ]. Other authors have envisaged that such CE can eventually give rise to communities as agents of the government, and CE becoming an ‘involvement industry’ ‘procured from external organizations’ [ 57 , 58 ]. To alleviate this, Folayan et. al. (2019) have recommended memoranda signed between the government and local partner organizations at the study design stage [ 54 ]. That noted, Webber seems to doubt whether national government-based public health initiatives might ever be able to stray too far from a top-down approach, postulated as the ‘two-community thesis’ [ 58 ]. Other authors suggest that deviation from this paradigm will require transformative leadership which is difficult to achieve in the public service sector with the prevailing traditional organizational thinking, policies, and management techniques [ 59 ].
While frontline local stakeholders played a role in Indian vaccination efforts as two-way conduits between decision makers and the community, more studies are recommended to examine complex issues derived thereof, such as internal chasms and accountability mechanisms between the 3As, and motivational erosion when CE work is not compensated financially (adequately). Prior research would not suggest, though, that social media could replace this in-person work. Ramsbottom’s et al.’s study found that, although social-media messaging is a cost-effective mechanism for vaccine information dissemination, it might not be the best approach for India, and could leave out social media illiterate populations, those with erratic and sporadic internet connectivity, and areas where vaccine communication needs to be translated to local dialects [ 53 ].
Limitations
Ensuring open discussion with vaccine decision makers and their team members on a potentially controversial topic like CE for vaccination was not always easy; it took time to convince the potential participants to participate. Some of the elites were difficult to access because of the ongoing community uproars around Measles-Rubella and HPV vaccines which were playing out in real time in the country during the study’s time period [ 60 , 61 ]. Despite these structural impediments, theoretical saturation was ensured by virtue of interviewing nearly the entire group of elite vaccine decision makers in the country. This was achieved by utilizing TD’s professional networking and familiarity with some of the study participants, use of a sensitive mix of knowledge and intercultural humility, flexibility to re-schedule appointments after office hours or on national holidays, and use appropriately persuasive multiple communication channels like Facebook Messenger, or WhatsApp [ 43 ], in addition to emails and phone calls. Nonetheless, the study findings were limited by the inherent limitations of a qualitative study design. However, generalizability within India might be more strongly inferred than would be typical given the high percentage of decision makers who provided data. In addition, all the study participants were interviewed in or around New Delhi. While the individuals who were interviewed each had a national or international scope to their decision making, this centrality may have influenced the findings in some way. Finally, some of the findings related to intended actions in the future rather than things that had already been completed; this hampered the ability to ascribe definite actions in some cases. However, existing literature demonstrates that intentions are moderately good predictors of future behavior [ 62 , 63 ].
The results from this study can be used both to understand past CE challenges and successes and to prospectively plan community-led, tailored CE initiatives for better vaccination outcomes. Of note, there appears to be conceptual tension between multiple vaccination-related goals, such that each can be perceived as CE for health equity; namely, top-down vaccination programs may be successful in achieving some short-term immunization, but there may be backlash, and longer-term increases in immunization rates may suffer as a result. At this stage, it will be critical to devise CE process and outcome indicators for vaccination programs in India, and to advocate for their incorporation in vaccination surveillance datasets. As of now, the suggestions herein are theoretical – and evaluation metrics would allow for demonstrations of how CE impacts a variety of important outcomes, and, ultimately, foster replicability of successful efforts within India and internationally.
Availability of data and materials
All twenty-five qualitative interviews (audio recording and transcripts) are available from the lead author (TD) and can be shared on request.
Plan WG. Plan 2011–2020. Geneva: World Health Organization. 2013. http://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/ .
Boyce T, Gudorf A, de Kat C, Muscat M, Butler R, Habersaat KB. Towards equity in immunisation. Eurosurveillance. 2019;24(2):1800204.
Article PubMed Central Google Scholar
Chang AY, Riumallo-Herl C, Perales NA, Clark S, Clark A, Constenla D, Garske T, Jackson ML, Jean K, Jit M, Jones EO. The equity impact vaccines may have on averting deaths and medical impoverishment in developing countries. Health Affairs. 2018;37(2):316–24.
Article PubMed Google Scholar
Boxelaar, L, Paine, M, Beilin, R. Community Engagement: for Whom? Proceedings of International Conference on Engaging Communities. Brisbane: Queensland Department of Main Roads, 2005.
Boston PQ, Mitchell MM, Collum K, Gravlee CC. Community engagement and health equity. Practicing Anthropol. 2015;37(4):28–32.
Article Google Scholar
Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(S1):S40–6.
Article PubMed PubMed Central Google Scholar
Wallerstein NB, Yen IH, Syme SL. Integration of social epidemiology and community-engaged interventions to improve health equity. Am J Public Health. 2011;101(5):822–30.
Sariola S, Reynolds L. The Ethics and Politics of Community Engagement in Global Health Research. Crit Public Health. 2018;28(3):257–68.
Pramanik S, Ghosh A, Nanda RB, De Rouw M, Forth P, Albert S. Impact evaluation of a community engagement intervention in improving childhood immunization coverage: a cluster randomized controlled trial in Assam, India. BMC Public Health. 2018;18(1):1–3.
Fregonese F. Community involvement in biomedical research conducted in the global health context; what can be done to make it really matter? BMC Medical Ethics. 2018;19(1):44.
Gibson A, Britten N, Lynch J. Theoretical directions for an emancipatory concept of patient and public involvement. Health. 2012;16(5):531–47.
Larson HJ, De Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301.
Fawcett S, Schultz J, Watson-Thompson J, Fox M, Bremby R. Peer reviewed: Building multisectoral partnerships for population health and healthequity. Prev Chronic Dis. 2010;7(6):1–7.
Kagee A, De Wet A, Kafaar Z, Lesch A, Swartz L, Newman PA. Caveats and pitfalls associated with researching community engagement in the context of HIV vaccine trials. J Health Psychol. 2020;25(1):82–91.
Tindana P, de Vries J, Campbell M, Littler K, Seeley J, Marshall P, Troyer J, Ogundipe M, Alibu VP, Yakubu A, Parker M. Community engagement strategies for genomic studies in Africa: a review of the literature. BMC Medical Ethics. 2015;16(1):24.
Pratt B, de Vries J. Community engagement in global health research that advances health equity. Bioethics. 2018;32(7):454–63.
Goldstein S, MacDonald NE, Guirguis S. SAGE Working Group on Vaccine Hesitancy. Health communication and vaccine hesitancy. Vaccine. 2015;33(34):4212–4.
Obregón R, Chitnis K, Morry C, Feek W, Bates J, Galway M, Ogden E. Achieving polio eradication: a review of health communication evidence and lessons learned in India and Pakistan. Bull World Health Organization. 2009;87:624–30.
Paul S, Sahoo J. Four new vaccines for routine immunization in India: What about hemophilus influenza B and pneumococcal vaccine? J Family Med Primary Care. 2015;4(1):9.
IIPS I. National Family Health Survey (NFHS-4), 2015–16. International Institute for Population Sciences (IIPS), Mumbai, India. 2017.
Gurnani V, Haldar P, Aggarwal MK, Das MK, Chauhan A, Murray J, Arora NK, Jhalani M, Sudan P. Improving vaccination coverage in India: lessons from Intensified Mission Indradhanush, a cross-sectoral systems strengthening strategy. BMJ. 2018;363.
Laxminarayan R, Ganguly NK. India’s vaccine deficit: why more than half of Indian children are not fully immunized, and what can—and should—be done. Health Affairs. 2011;30(6):1096–103.
Zimet GD, Meyerson BE, Dutta T, Forster A, Corcoran B, Hanley S. Political and Public Responses to Human Papillomavirus Vaccination. InHuman Papillomavirus 2020 Jan 1 (pp. 363-377). Academic Press.
Sankaranarayanan R, Basu P, Kaur P, Bhaskar R, Singh GB, Denzongpa P, Grover RK, Sebastian P, Saikia T, Oswal K, Kanodia R. Current status of human papillomavirus vaccination in India's cervical cancer prevention efforts. Lancet Oncol. 2019;20(11):e637–44.
Lahariya C. A brief history of vaccines & vaccination in India. Indian J Med Res. 2014;139(4):491.
PubMed PubMed Central Google Scholar
Solomon R. Involvement of civil society in India’s polio eradication program: lessons learned. Am J Tropical Med Hygiene. 2019;101(4_Suppl):15–20.
Das MK, Singh D. Vaccine news in India: trend and content analysis of online mass media. Int J Community Med Public Health. 2018;5(9):3951.
Rao M & Govindarajan V, Scroll in, Feb 24, 2017 WhatsApp rumours about vaccinations hamper India's drive to halt measles and rubella. Accessed 1 Mar 2017. https://scroll.in/pulse/830129/rumours-about-measles-rubella-vaccine-hit-coverage . Accessed on July 25, 2020.
Dimala CA, Kika BT, Kadia BM, Blencowe H. Current challenges and proposed solutions to the effective implementation of the RTS, S/AS01 Malaria Vaccine Program in sub-Saharan Africa: A systematic review. PloS one. 2018;13(12):e0209744.
Article CAS PubMed PubMed Central Google Scholar
Sarrami-Foroushani P, Travaglia J, Debono D, Braithwaite J. Implementing strategies in consumer and community engagement in health care: results of a large-scale, scoping meta-review. BMC Health Services Research. 2014;14(1):402.
Adhikari B, James N, Newby G, Von Seidlein L, White NJ, Day NP, Dondorp AM, Pell C, Cheah PY. Community engagement and population coverage in mass anti-malarial administrations: a systematic literature review. Malaria J. 2016;15(1):523.
Farmer J, Taylor J, Stewart E, Kenny A. Citizen participation in health services co-production: a roadmap for navigating participation types and outcomes. Australian Journal of Primary Health. 2018;23(6):509–15.
Ministry of Health and Family Welfare. Government of India Drugs and Cosmetics (First Amendment) Rules. New Delhi: Government of India Press; 2013.
Google Scholar
Enria L, Lees S, Smout E, Mooney T, Tengbeh AF, Leigh B, Greenwood B, Watson-Jones D, Larson H. Power, fairness and trust: understanding and engaging with vaccine trial participants and communities in the setting up the EBOVAC-Salone vaccine trial in Sierra Leone. BMC Public Health. 2016;16(1):1140.
MacQueen KM, Bhan A, Frohlich J, Holzer J, Sugarman J, Ethics Working Group of the HIV Prevention Trials Network. Evaluating community engagement in global health research: the need for metrics. BMC Medical Ethics. 2015;16(1):44.
Martin GP, Carter P, Dent M. Major health service transformation and the public voice: conflict, challenge or complicity? J Health Services Res Policy. 2018;23(1):28–35.
Forsythe LP, Carman KL, Szydlowski V, Fayish L, Davidson L, Hickam DH, Hall C, Bhat G, Neu D, Stewart L, Jalowsky M. Patient engagement in research: early findings from the Patient-Centered Outcomes Research Institute. Health Affairs. 2019;38(3):359–67.
Schutz A. The problem of personality in the social world. InCollected papers VI. Literary reality and relationships 2013 (pp. 199-240). Springer, Dordrecht.
Uddin J, Sarma H, Bari TI, Koehlmoos TP. Introduction of new vaccines: decision-making process in Bangladesh. J Health Population Nutrition. 2013;31(2):211.
Weston C, Gandell T, Beauchamp J, McAlpine L, Wiseman C, Beauchamp C. Analyzing interview data: The development and evolution of a coding system. Qualitative Sociol. 2001;24(3):381–400.
McElfish PA, Post J, Rowland B. A social ecological and community-engaged perspective for addressing health disparities among Marshallese in Arkansas. International Journal of Nursing & Clinical Practices. 2016;30:2016.
Aberbach JD, Rockman BA. Conducting and coding elite interviews. Political Science and Politics. 2002;35(4):673–6.
Harvey WS. Strategies for conducting elite interviews. Qualitative Res. 2011;11(4):431–41.
Lancaster K. Confidentiality, anonymity and power relations in elite interviewing: conducting qualitative policy research in a politicised domain. Int J Soc Res Methodol. 2017;20(1):93–103.
Kumar S, Quinn SC, Kim KH, Musa D, Hilyard KM, Freimuth VS. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Education Behavior. 2012;39(2):229–43.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Res. 2005;15(9):1277–88.
Elo S, Kyngäs H. The qualitative content analysis process. J Advanced Nurs. 2008;62(1):107–15.
Hochschild JL. Conducting intensive interviews and elite interviews. InWorkshop on interdisciplinary standards for systematic qualitative research 2009. National Science Foundation. .
Holland B. Factors and strategies that influence faculty involvement in public service. Building the Field of Higher Education Engagement: Foundational Ideas and Future Directions. 2019.
Arnstein SR. A ladder of citizen participation. City Reader. 2015;279.
O'Mara-Eves A, Brunton G, McDaid G, Oliver S, Kavanagh J, Jamal F, Matosevic T, Harden A, Thomas J. Community engagement to reduce inequalities in health: a systematic review, meta-analysis and economic analysis. Pub Health Res. 2013;1(4). https://doi.org/10.3310/phr01040 .
Kuhlmann E, Burau V. Strengthening stakeholder involvement in health workforce governance: why we need to talk about power. J Health Services Res Policy. 2018;23(1):66–8.
Ramsbottom A, O’Brien E, Ciotti L, Takacs J. Enablers and barriers to community engagement in public health emergency preparedness: a literature review. J Community Health. 2018;43(2):412–20.
Folayan MO, Oyedeji KS, Fatusi OA. Community members' engagement with and involvement in genomic research: Lessons to learn from the field. Developing World Bioethics. 2015;15(1):1–7.
Howard-Grabman L, Miltenburg AS, Marston C, Portela A. Factors affecting effective community participation in maternal and newborn health programme planning, implementation and quality of care interventions. BMC Pregnancy Childbirth. 2017;17(1):268.
Gopichandran V. Public trust in vaccination: an analytical framework. Indian J Med Ethics. 2017;2(2):98–104.
PubMed Google Scholar
Head BW. Community engagement: participation on whose terms? Australian J Political Sci. 2007;42(3):441–54.
Webber DJ. Explaining policymakers' use of policy information: The relative importance of the two-community theory versus decision-maker orientation. Knowledge. 1986;7(3):249–90.
Newman PA, Rubincam C. Advancing community stakeholder engagement in biomedical HIV prevention trials: principles, practices and evidence. Expert Review Vaccines. 2014;13(12):1553–62.
Article CAS Google Scholar
Firstpost, Nair N, 2017 Won't take Modi-RSS vaccine’: Myths, quacks derail Malappuram vaccination drive putting lakhs of children at risk. Accessed 20 Mar 2018. https://www.firstpost.com/india/wont-take-modi-rss-vaccine-myths-quacks-derail-malappuram-vaccination-drive-putting-lakhs-of-children-at-risk-4236543.html .
Cheatham A, February 26, 2018, Duke Global Reproductive Health, Despite Government Policy, Cervical Cancer Progress Stalls in India. Accessed 20 Mar 2018. http://dukecenterforglobalreproductivehealth.org/2018/02/26/despite-government-policy-cervical-cancer-progress-stalls-in-india/ .
Frew PM, Archibald M, Martinez N, del Rio C, Mulligan MJ. Promoting HIV vaccine research in African American communities: does the theory of reasoned action explain potential outcomes of involvement? Challenge (Atlanta, Ga.). 2007;13(2):61.
Albarracin D, Wyer RS Jr. The cognitive impact of past behavior: influences on beliefs, attitudes, and future behavioral decisions. J Personality Social Psychol. 2000;79(1):5.
Download references
Acknowledgements
We thank all the study participants and their teams for providing the information and data used in this study and for hosting the member check-in in meeting in New Delhi, India.
The lead author (TD) received a scholarship from Dhar India Studies Program, Indiana University, to undertake travel to India for the member check-in meeting.
Author information
Authors and affiliations.
Room No. 469, Berndt Hall, Public Health Department, Health Sciences Division, Fort Lewis College, Durango, CO, 81301, USA
Tapati Dutta
Southwest Institute for Research on Women, College of Social & Behavioral Sciences, Family & Community Medicine, College of Medicine, University of Arizona, Tucson, USA
Beth E. Meyerson
Department of Applied Health Science, Prevention Insights, Indiana University School of Public Health-Bloomington, 809 E 9th Street, Room 101, Bloomington, IN, 47405, USA
Department of Applied Health Science, Indiana University School of Public Health-Bloomington, 809 E 9th Street, Room 203, Bloomington, IN, 47405, USA
Priscilla A. Barnes
Department of Applied Health Science, Indiana University School of Public Health-Bloomington, 801 E 7th Street, Room 102, Bloomington, IN, 47405, USA
Catherine Sherwood-Laughlin
School of Public and Environmental Affairs, Indiana University, Room 351, 1315 E 10th Street, Bloomington, IN, 47405, USA
Jill Nicholson-Crotty
You can also search for this author in PubMed Google Scholar
Contributions
As the first and corresponding author, TD was primarily responsible for conceptualizing the study, conducting the data collection and analysis, coordinating and facilitating the check-in validation meetings, writing the manuscript, and adding the revisions addressing the reviewer comments in this version of the manuscript. Other authors (dissertation committee members) offered extensive input at the proposal and study design stages and throughout the dissertation (BEM, JA, PB, CSL, JNC). JA additionally contributed intensively to revisions and preparation of this manuscript for publication, and revisions addressing reviewer comments. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Tapati Dutta .
Ethics declarations
Ethics approval and consent to participate.
This manuscript is one of the papers from the lead author’s (TD) doctoral dissertation. That study, and all related manuscripts, were reviewed and approved under the 'Exempt' category by the Indiana University's Institutional Review Board (protocol 1710654732). Consent to participate was obtained from all study participants via email.
Consent for publication
The co-authors here are the former Dissertation Committee members (BEM, JA, PB, CSL, JNC) of the lead author (TD), and have consented to be co-authors for this manuscript.
Competing interests
The study does not have any conflict of interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Supplementary information
Additional file 1., additional file 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dutta, T., Meyerson, B.E., Agley, J. et al. A qualitative analysis of vaccine decision makers’ conceptualization and fostering of ‘community engagement’ in India. Int J Equity Health 19 , 185 (2020). https://doi.org/10.1186/s12939-020-01290-5
Download citation
Received : 28 May 2020
Accepted : 24 September 2020
Published : 20 October 2020
DOI : https://doi.org/10.1186/s12939-020-01290-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

41 templates

el salvador
32 templates
49 templates

21 templates
16 templates

28 templates
Vaccinations Thesis Statement
Vaccinations thesis statement presentation, free google slides theme and powerpoint template.
There is a lot of information about vaccines and, sadly also a lot of misinformation. It is in health worker’s hands to select only proven information and share it in a clear, understandable way that makes people who don’t understand the subject feel safer and more open to get their shot. A presentation can be the perfect way of speaking about it, since giving visual information, as well as references and medical data will make every listener feel trust in the speaker. If you want to give the presentation a creative touch, you can rely on this creative template for medical issues!
Features of this template
- 100% editable and easy to modify
- 23 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the free resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

- Open access
- Published: 08 March 2022
WHO-led consensus statement on vaccine delivery costing: process, methods, and findings
- Ann Levin 1 ,
- Laura Boonstoppel 2 na1 ,
- Logan Brenzel 3 na1 ,
- Ulla Griffiths 4 na1 ,
- Raymond Hutubessy 5 na1 ,
- Mark Jit 6 na1 ,
- Vittal Mogasale 7 na1 ,
- Sarah Pallas 8 na1 ,
- Stephen Resch 9 na1 ,
- Christian Suharlim 9 na1 &
- Karene Hoi Ting Yeung 5 na1
BMC Medicine volume 20 , Article number: 88 ( 2022 ) Cite this article
2550 Accesses
10 Citations
2 Altmetric
Metrics details
Differences in definitions and methodological approaches have hindered comparison and synthesis of economic evaluation results across multiple health domains, including immunization. At the request of the World Health Organization’s (WHO) Immunization and Vaccines-related Implementation Research Advisory Committee (IVIR-AC), WHO convened an ad hoc Vaccine Delivery Costing Working Group, comprising experts from eight organizations working in immunization costing, to address a lack of standardization and gaps in definitions and methodological guidance. The aim of the Working Group was to develop a consensus statement harmonizing terminology and principles and to formulate recommendations for vaccine delivery costing for decision making. This paper discusses the process, findings of the review, and recommendations in the Consensus Statement.
The Working Group conducted several interviews, teleconferences, and one in-person meeting to identify groups working in vaccine delivery costing as well as existing guidance documents and costing tools, focusing on those for low- and middle-income country settings. They then reviewed the costing aims, perspectives, terms, methods, and principles in these documents. Consensus statement principles were drafted to align with the Global Health Cost Consortium costing guide as an agreed normative reference, and consensus definitions were drafted to reflect the predominant view across the documents reviewed.
The Working Group identified four major workstreams on vaccine delivery costing as well as nine guidance documents and eleven costing tools for immunization costing. They found that some terms and principles were commonly defined while others were specific to individual workstreams. Based on these findings and extensive consultation, recommendations to harmonize differences in terminology and principles were made.
Conclusions
Use of standardized principles and definitions outlined in the Consensus Statement within the immunization delivery costing community of practice can facilitate interpretation of economic evidence by global, regional, and national decision makers. Improving methodological alignment and clarity in program costing of health services such as immunization is important to support evidence-based policies and optimal resource allocation. On the other hand, this review and Consensus Statement development process revealed the limitations of our ability to harmonize given that study designs will vary depending upon the policy question that is being addressed and the country context.
Peer Review reports
Immunization has been shown to provide a high return on investment across low- and middle-income countries [ 1 ]. Nevertheless, disparities in immunization access persist within and between countries. With the launch of the new Immunization Agenda 2030 [ 2 ], many low- and middle-income countries (LICs and MICs) are considering introducing new vaccines or vaccine-related technologies, life-course immunization programs, and improving the effectiveness and efficiency of their immunization programs. To determine the feasibility of doing so, estimation of vaccine procurement and delivery costs is of considerable interest to policymakers, program managers, researchers, and other stakeholders concerned with improving immunization programs. In particular, results from delivery cost studies can help countries in decision-making and planning on introducing new infant and life-course vaccines and technologies, preparation of budgets and financing for rollout of vaccines, and evaluation of alternative service delivery approaches.
Recent reviews of immunization delivery cost literature identified a lack of standardization in methods and reporting, making cross-study comparison and synthesis difficult [ 3 ]. These discrepancies limit the interpretability and utility of immunization cost study evidence for immunization program decision-making. In light of these challenges, the World Health Organization (WHO) Immunization and Vaccines-related Implementation Research Advisory Committee (IVIR-AC) recommended at their March 2018 meeting that the WHO Guidance on Vaccine Delivery Costing be updated [ 4 ]. An ad hoc Working Group comprising vaccine delivery costing experts Footnote 1 was therefore convened by the WHO secretariat to review guidance documents and tools on vaccine delivery costing, focused on low- and middle-income country settings. This initial review found that several groups were already developing methodological guidance to address the disparate definitions and approaches in the field, which partly address the original IVIR-AC’s request. In March 2019, IVIR-AC modified its request to instead review guidance documents and costing tools, assess their similarities and differences, and identify gaps in guidance [ 5 ]. In addition, the Working Group recommended that a Consensus Statement be developed to harmonize the differences in costing terminology and principles for groups working in vaccine delivery costing.
For the purpose of this paper, vaccine delivery costing is defined as “costs associated with delivering immunizations to target populations, exclusive of vaccine procurement costs” [ 6 ].
This paper describes the history and process involved to develop the Consensus Statement on Vaccine Delivery Costing, the methods used and the findings of the review of guidance documents and costing tools, and terms and principles as well as recommendations agreed upon by the Working Group.
Process of developing the consensus statement
The consultation process of coming to agreement on a Consensus Statement included setting up a time-limited Working Group of staff of organizations working in vaccine delivery costing (who are also the authors of this paper), conducting a review of guidance documents, costing tools, and other documents and the costing terms, methods, and principles used in these, agreeing upon the costing terminologies and principles, making recommendations to harmonize their differences, writing the text of the Consensus Statement and Annexes (Additional file 1 ). Figure 1 shows a timeline of the meetings and activities that led to the development of the Consensus Statement.
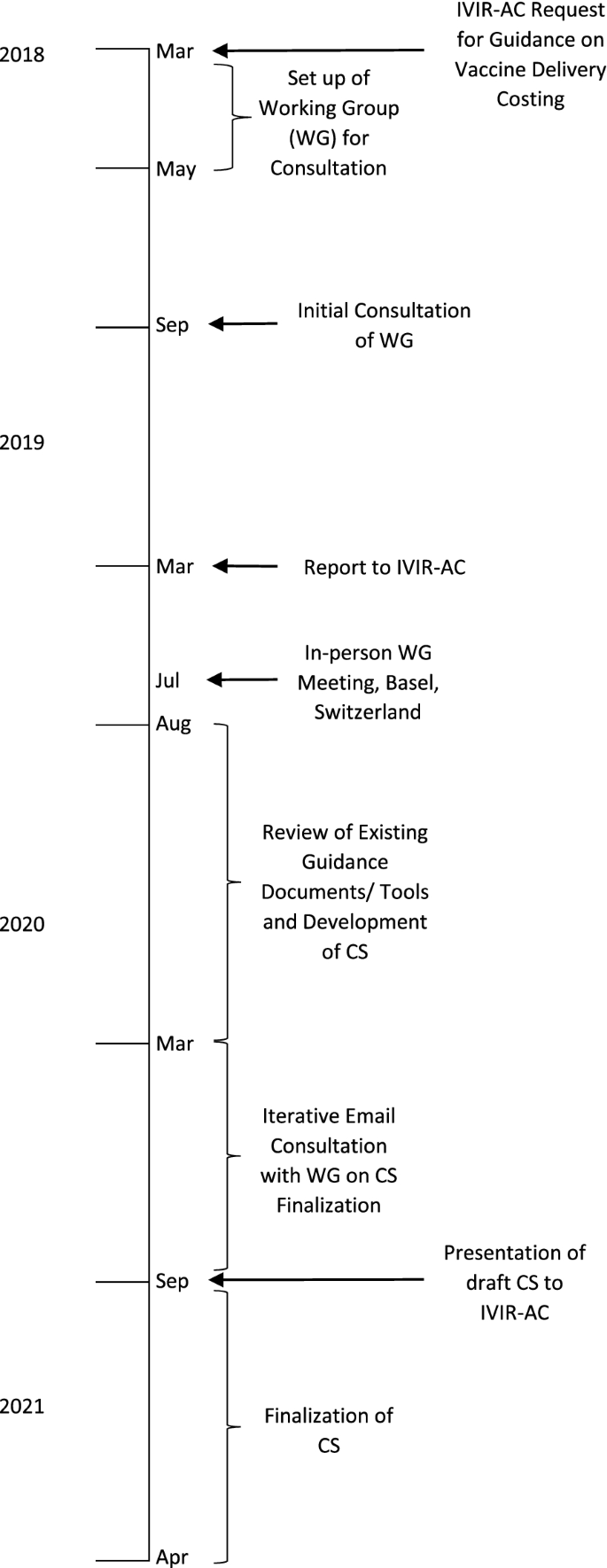
Timeline of the consultation process to develop a Consensus Statement (CS) on vaccine delivery costs
In March 2018, the IVIR-AC initiated the process and requested that WHO update its guidance for conducting vaccine delivery costing in LICs and MICs so that methods used in costing tools and guidance documents could be standardized among WHO and other organizations.
As a follow-up, the WHO secretariat set up a Working Group of Experts comprising staff of organizations conducting research and policy advice on vaccine delivery costing in LICs and MICs to ensure that no parallel efforts were taking place. The initial Working Group comprised of technical experts from the Bill & Melinda Gates Foundation (BMGF), International Vaccine Institute (IVI), Levin & Morgan LLC, UNICEF, and WHO, and two members of IVIR-AC. The group noted that there are several ongoing workstreams conducting cost studies and developing guidance documents and/or costing tools, with different purposes and approaches to costing. In addition, some of these workstreams had developed guidance documents specific to their approach, which were already in the public domain. Thus, a review of these would be required to determine if an additional vaccine delivery costing guidance would be necessary. The Working Group also suggested that a presentation be made at the IVIR-AC meeting in March 2019 to present the findings on the different workstreams to determine the next steps.
In March 2019, the WHO team and the BMGF-funded ThinkWell project (Immunization Costing Action Network [ICAN]) presented to IVIR-AC on findings from the discussion with the Working Group [ 2 ]. Footnote 2 IVIR-AC recommended that an in-person workshop meeting be held with other groups working on vaccine delivery costing so that a consensus could be reached on the best way to standardize costing terms and principles.
In July 2019, WHO and the BMGF convened a meeting with eleven experts from different organizations and institutions in immunization economics during an International Health Economics Association (iHEA) meeting in Basel, Switzerland. The Working Group was expanded to include technical experts from other organizations involved in vaccine delivery costing such as Harvard (Expanded Programme on Immunization Costing [EPIC] studies) and the United States Centers for Disease Control and Prevention (CDC). Based on the subject matter knowledge and professional experience of the Working Group members, the different purposes of the workstreams were discussed and a matrix of costing tools listing out the characteristics of each was created. The Working Group agreed that it would be useful to develop a Consensus Statement that presents the different purposes of each workstream, a review of existing vaccine delivery costing guidance documents and tools, and agreed-upon costing terms and principles.
As a follow-up from the meeting in Basel, from August 2019 to March 2020, an analysis of guidance documents and tools was conducted for each of the four workstreams identified by the Working Group. The Group identified similarities and differences in costing methods, terms and principles among the approaches and in guidance documents, and gaps where further guidance was needed.
Based on these findings, the WHO team developed a proposed draft Consensus Statement report with recommendations for costing terms and principles that could be adhered to for future vaccine delivery costing work and accompanying annexes that summarized the findings from the review on costing terms, costing principles, and methods for vaccine delivery costing. After extensive consultation within the Working Group and several rounds of written revisions to reach consensus on the statement, the findings and recommendations were presented to IVIR-AC in September 2020. The IVIR-AC commended the process to create the Consensus Statement (Additional file 1 ) [ 7 ].
Review of vaccine delivery costing guidance documents and tools
The first step was to conduct a landscape analysis of the organizations involved in vaccine delivery costing and their workstreams, and the available guidance documents and tools on vaccine delivery costs. This landscape analysis was conducted through discussions between the Working Group members during teleconferences and an in-person meeting as well as internet searches of websites of organizations working in the field (e.g., ICAN, Immunization Economics) between August 2019 and March 2020. It was not a systematic literature review and did not aim to include general health service costing tools and guidance documents beyond those with known use for costing immunization in LICs and MICs. However, the analysis built on the recent systematic review and reporting guidance for immunization costing studies conducted by some working group member organizations [ 3 ].
The second step was to compare the characteristics of the guidance documents and tools for immunization costing identified in terms of (1) how costing terms were defined in the guidance documents and costing tools; (2) whether data collection, sampling, and analysis were described in the guidance documents; and (3) whether costing principles were specified in guidance documents.
To review the costing terms in the guidance documents, the definitions were extracted from the source documents and entered into a table so that similarities and differences could be compared qualitatively and recommendations could be made for harmonized definitions for key terms. The costing principles and the guidance text, including on data collection, sampling, and analysis, were also compared and entered into a table by workstreams to assess the similarities, differences, and gaps. To do so, the costing principles in the guidance documents were compared to the ones in the checklist in the Global Health Cost Consortium (GHCC) [ 8 ] that has become a normative reference standard for global health costing work. These principles are similar to those found in the CHEERS checklist [ 9 ]. Recommendations were then made for harmonized principles in the Consensus Statement.
Existing immunization delivery costing workstreams
The Working Group identified four major current workstreams on vaccine delivery costing in LICs and MICs. These include the following: (1) retrospective routine immunization (multiple vaccines) cross-sectional costing, (2) retrospective single-vaccine costing, (3) new vaccine introduction cost projection, and (4) national immunization program cost projection (Fig. 2 ). Although the workstreams had involvement from particular organizations at the time of the review, they are defined by their different objectives and corresponding methodologies and constitute a typology of immunization delivery costing work to which other organizations and practitioners beyond those listed contribute.
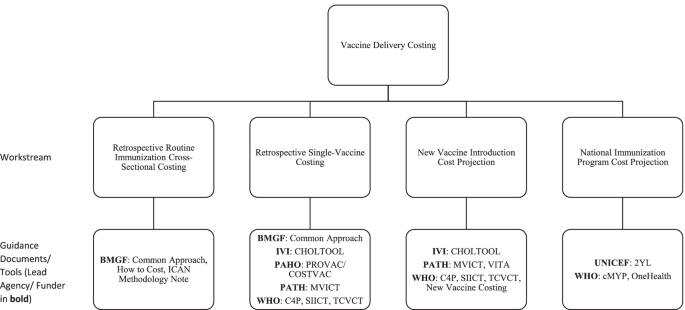
Major current workstreams in vaccine delivery costing identified by the Working Group. Note: 2YL, 2nd Year of Life; BMGF, Bill & Melinda Gates Foundation; C4P, Cervical Cancer Prevention and Control Costing; CDC, United States Centers for Disease Control and Prevention; CHOLTOOL, Oral Cholera Vaccine Costing Tool; cMYP, comprehensive multi-year plan; EPIC, Expanded Programme on Immunization Costing; ICAN, Immunization Costing Action Network; IVI, International Vaccine Institute; MVICT, Malaria Vaccine Immunization Costing Tool; SIICT, Seasonal Influenza Immunization Costing Tool; TCVCT, Typhoid Conjugate Vaccine Costing Tool; VTIA, Vaccine Technology Costs and Health Impact Assessment Tool; WHO, World Health Organization
The first workstream is focused on estimating retrospective (i.e., already incurred) routine immunization cross-sectional costs of service delivery units at a single point in time for multiple vaccines delivered through the routine immunization program. These analyses focus on estimating routine immunization costs incurred at the facility, district, and higher administrative levels in the health system. Such analyses typically estimate unit costs (cost per dose, cost per person, or cost per fully immunized person [FIP]). Some examples of this work include the EPIC studies [ 10 ] and other work by institutes, such as the Harvard T.H. Chan School of Public Health, Wits University, Curatio Foundation, PAHO, ThinkWell, UNICEF, Johns Hopkins University, and PATH. The objectives of research within this workstream are to develop benchmarks for costs to be used in future studies, to analyze variation in unit costs, and to compare the findings with data from other costing studies [ 4 ].
The second workstream is to estimate retrospective costs for a specific vaccine or campaign, typically using incremental costing. That is, it usually aims to measure the value of additional resources employed to introduce a new vaccine or conduct a vaccination campaign. This is often done through data collection at a single point in time (post-campaign or post-introduction) with reference to documents and recall by key informants to estimate which resource use was specifically incremental. Examples of such studies include those conducted by groups such as EPIC, ThinkWell, CDC, and IVI. This workstream includes retrospective cost studies of vaccine implementation using vaccine-specific costing tools (e.g., Cervical Cancer Prevention and Control Costing [C4P], Oral Cholera Vaccine Costing Tool [CHOLTOOL], Malaria Vaccine Immunization Costing Tool [MVICT], Seasonal Influenza Immunization Costing Tool [SIICT], and Typhoid Conjugate Vaccine Costing Tool [TCVCT]). These studies yield results that will assist countries with comparing budgeted amounts to actual implementation resource use, budgeting for future immunization activities, and conducting cost-effectiveness analyses that compare the incremental resource use for a specific vaccine introduction or campaign with its incremental health impacts.
The third workstream is focused on estimating new vaccine introduction costs through projection of the value of resources or ingredients (e.g., time, equipment, training, and vaccines) needed for vaccine introduction, typically using incremental costing for a specific period. Data for these analyses are obtained through interviews with program managers and facility visits to obtain current information on personnel time, supplies, equipment, and other resources as well as retrospective cost data from other vaccine introduction. These analyses are often conducted using costing tools, including some of the same tools used for retrospective single-vaccine costing (e.g., C4P, CHOLTOOL, MVICT, SIICT, and TCVCT). These studies produce cost estimates that will assist countries with planning and decision-making on new vaccines during the introduction period.
The fourth workstream is projection of immunization program costs. Some costing tools used to produce these estimates include the comprehensive multi-year plan (cMYP), 2nd Year of Life (2YL), and OneHealth tool where the activities of a national program and related cost is entered for a baseline year and then the future years are projected. These analyses are an integral part of strategic planning for budgeting and resource mobilization over a specific period of time such as 5 years. Whereas work under the first three workstreams may produce estimates of financial, economic, or undepreciated financial costs, projections under the fourth workstream are intended to estimate undepreciated financial costs (i.e., undiscounted monetary outlays).
In practice, projects may combine elements of multiple workstreams (e.g., retrospective single vaccine costing in one country may be used to help inform estimates of new vaccine introduction costs for a different vaccine or delivery strategy).
Existing guidance documents on vaccine delivery costing
Table 1 shows the nine guidance documents on vaccine delivery costing identified by the Working Group. Some of these provide guidance for more than one type of costing. Three are for estimation of retrospective routine immunization cross-sectional costs, five are for estimation of retrospective single-vaccine costs, five are for projection of new vaccine introduction costs, and one for projection of immunization program costs. The list of costing tools for vaccine delivery identified by the Working Group is shown in Additional file 1 : Table A2b.
Table 2 shows a comparison of costing term definitions among the various guidance documents. It shows that among the different guidance documents, definitions are generally similar but have differences in wording, e.g., vaccine delivery cost, economic cost, start-up/ introduction cost, and prospective cost. Also, some terms (retrospective costing, cost projections, bottom-up and top-down costing) are only defined in the Global Health Costing Consortium reference case. Note that some guidance documents have been grouped together since they were developed by the same teams; i.e., (i) EPIC documents and (ii) WHO vaccine-specific costing tool user manuals.
Figure 3 shows the percentage of guidance documents with definitions of individual costing terms. As can be seen, most documents had definitions of financial cost, economic cost, capital cost, recurrent cost, incremental cost, and vaccine delivery cost, and about half of these defined start-up/introduction cost. Fewer than half of the guidance documents had definitions of perspective, micro-costing (ingredients costing), full costing, retrospective costing, or cost projection.
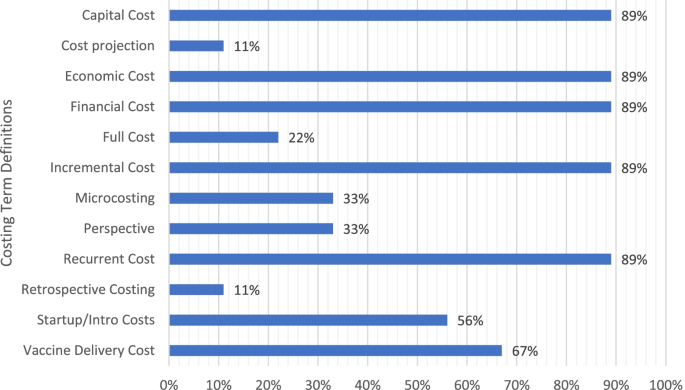
Percentage of guidance documents with definitions of costing terms ( N = 9)
Several gaps were noted from the review. Most guidance documents did not go into detail about some methodological decision points in costing, such as how the choice of perspective will affect which costs are included as financial costs, which may limit the comparability of such costs across studies. For example, if a payer or provider perspective is used, the organizations included in the study definition as “payers” or “providers” will determine whose monetary outlays are considered as financial costs. If a donor (e.g., Gavi) provides funding to a UNICEF country office for social mobilization for a new vaccine introduction, expenditures of those funds will be included as financial costs only if the study perspective is defined as including UNICEF (e.g., a provider perspective defined as all partners “providing” the new vaccine introduction activities, or a health sector perspective including all health sector partners); however, if the study is conducted from a perspective that does not include UNICEF (e.g., a provider perspective defined as only the government “providing” the new vaccine introduction activities, or a government perspective), these resources from UNICEF would not be counted as financial costs but only as economic costs as an in-kind contribution from UNICEF.
Also, most guidance documents did not address whether to include economic costs of existing capital such as equipment or building space, or how to make or assess assumptions for slackness (i.e., available unused capacity) of existing capital goods. Also, vaccine delivery costing definitions differ on whether actual vaccine product costs should be included or not. If not, which specific aspects of the vaccine product costs should be excluded (e.g., vaccine only, diluent, syringes, safety boxes, freight, and insurance). For financial costs, the guidance review suggested whether to include existing personnel costs will depend on whether the costing is incremental or full.
Figure 4 shows the percentage of documents that recommended key costing principles (details in Additional file 1 : Table A3). As can be seen, most guidance documents recommended principles on stating objectives, defining units, describing time horizon, methods and data sources, and annualizing capital costs, while less than half recommend specifying the perspective, scope, sampling, data collection timing, discount rates, shadow prices, exploring variation, analyzing uncertainty, and methods of communicating results.
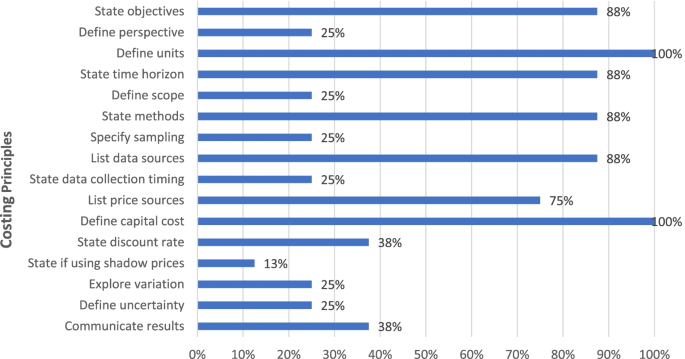
Percentage of costing principles recommended by guidance documents ( N = 9)
In Table 3 , the recommendations of guidance documents on data collection and analysis are disaggregated by workstream. While guidance is given on some aspects in all documents, in other cases, no guidance is provided. Specifically, guidance is given on data collection for all of the workstreams with the exception of projection of new vaccine introduction costs.
Recommended costing terminology and principles
After reviewing the definitions of costing terms, the following definitions of costing terms are recommended:
Vaccine delivery costs
Costs associated with delivering immunization programs to target populations, exclusive of vaccine costs.
Vaccine cost
At a minimum includes the cost of the vaccine and diluent (if applicable); the analysis should include accounting for wastage rates; the analyst should specify whether this also includes injection supplies (syringes), international shipment, insurance, and customs/duties.
Financial cost
Monetary outlays, with straight-line depreciation for capital goods; does not include opportunity costs for use of resources or donated goods and services from sources other than the payer(s) defined in the analysis. Definition is dependent on perspective since monetary outlays are specific to the payer(s) defined in the analysis.
Economic cost
The value of all resources utilized, regardless of the source of financing. Includes opportunity costs for use of existing resources and any donated goods or services from any source. Capital costs are annualized and discounted.
Undepreciated financial cost
Financial costs without depreciation of capital costs (note: such costs have been termed “initial investment” in some costing tools and referred to as fiscal costs in previous analyses.)
Recurrent cost
Value of resources that last less than one year. Start-up activity costs may include recurrent costs.
Capital cost
Value of resources lasting more than one year such as equipment, buildings, and trainings. Start-up activity costs may include capital costs.
Incremental cost
Cost of adding a new service/intervention or a package of services/interventions over and above an existing program; inclusion of existing resources will depend on assumptions made about excess capacity (i.e., whether resources are underemployed; if there are no slack resources (e.g., all personnel time is fully allocated before the addition of the new service/intervention), then their use for the new service or intervention incurs an opportunity cost that should be included—either by measurement or assumption).
Baseline cost as well as the additional/incremental cost of the new intervention, including vaccine cost.
Cost projection
Estimation of future costs of both recurrent and capital inputs.
Prospective data collection
Direct observation of resource use during intervention implementation; i.e., data are collected concurrently with intervention implementation.
Retrospective data collection
Data collection after resource use is completed.
Start-up cost
Cost of initial one-time programmatic activities. Examples may include initial micro-planning, initial training activities, and initial sensitization/social mobilization/information, education, and communication (IEC); does not include routine or repeated programmatic activities such as refresher training or annual microplanning. Start-up activities may include both recurrent and capital costs; they are defined by the non-repeating nature of the activity, not the type of input.
Micro-costing
Focuses on granular accounting of input prices and quantities; disaggregates costs of particular output into specific goods and services consumed.
Bottom-up costing
Measures input quantities at the client (e.g., per vaccination administered) or activity level.
Top-down costing
Divides overall program cost or expenditures, often including those at administrative levels above service delivery level, by number of outputs to calculate unit cost.
Perspective
The point of view considered for costs (and benefits, if included) in a costing study, by whom the costs were incurred. Payers are the disbursing agents for a good or service, and may differ from the original source of funding. A provider perspective includes costs incurred by health service providers (can be limited to the government), a payer perspective includes costs to the payer(s), such as government or an external partner, while the societal perspective includes all costs incurred by providers as well as clients.
Shared cost
Shared resources that are not used only for immunization, but also for other productive activities.
The recommended costing principles include the following.
Definitions of terms used in studies of vaccine delivery costing should conform closely to the recommended definitions in this Consensus Statement.
The study scope in terms of its purpose, audience, target population, time horizon, and service/output should be clearly stated. It should also state whether data collection will be prospective or retrospective, and whether the analysis will be retrospective or a cost projection.
The perspective of the cost estimation should be stated and justified.
Types of costs to be generated should be clearly defined in terms of start-up/introduction or non-start-up/introduction (sometimes called operating costs), recurrent and capital, undepreciated financial, financial or economic, and incremental or full. Capital costs should be appropriately annualized and depreciated for financial and economic costs and the discount rate justified.
The scope of the inputs to be estimated should be defined, justified, and if needed referenced. For example, do the costs include national and sub-national costs or only facility-level service delivery costs? Are non-immunization costs included?
The “units” in the unit costs for strategies, services, and interventions should be defined, e.g., cost per dose administered.
If incremental costing is conducted, any assumptions made regarding existing health system capacity should be described (see GHCC reference case, pg. 64).
The selection of the data sources, including any adjustments to price data (e.g., inflation or currency conversion) should be described and referenced.
The methods for estimating the quantity of inputs should be described—whether top-down or bottom-up, methods of allocation, use of shadow prices and the opportunity cost of time, and methods for excluding research and evaluation costs.
Costs should be mapped and reported as either inputs or activities:
Resource inputs include, for example, personnel time, vaccines, injection and safety supplies, vehicles, fuel, per diem and travel allowances, cold chain equipment, stationery, laboratory equipment, and buildings;
Program activities include, for example, vaccine procurement, service delivery, training, micro-planning, social mobilization, and advocacy and communication, monitoring and evaluation, surveillance, adverse event following immunization monitoring, and supervision.
Some boundaries around costs included in the analysis may be employed to keep the costing scope feasible and will depend on the purpose of the costing study, with the rationale for any exclusions provided; use discretion about including one-time costs that are unique or unlikely to be replicated or transferable across settings (for example, new vaccine launches with the President). Clarify definition and threshold for including or excluding small costs that have expected small contribution (e.g., <$25) to total costs in aggregate across all sampled units, such as the use of existing office supplies by health facility staff.
The sampling strategy employed should aim for internal and external validity of the data Footnote 3 . Sampling strategy should be stated, described, and justified, depending on the workstream and costing objectives. Sampling of different service delivery units is desirable as it provides a more representative picture of costs and highlights cost variation and cost drivers for a strategy or vaccine.
Variation in the cost of the intervention by site/organization, sub-population, or by other drivers of heterogeneity should be explored and reported for retrospective analyses when possible.
The uncertainty around the cost estimates should be appropriately characterized when feasible, (e.g., sensitivity analyses; ranges of results for different input parameter scenarios for cost projections; mean and standard deviation for non-representative samples with multiple units; and confidence intervals or credible intervals for retrospective analyses).
Inclusion and exclusion criteria: “stopping rules” Footnote 4 should be defined, explaining which costs are included and the respective rationale.
Cost estimates should be communicated clearly and transparently to enable decision-makers to interpret and use the results relevant to the original policy and/or programmatic question.
The lack of standardization in terminology, implementation, and principles for vaccine delivery costing has resulted in difficulties in making comparisons among studies, reducing the potential for synthesis of economic evidence across studies for immunization program policy, planning, budgeting, and implementation. As noted earlier, governments need to know the cost of vaccine delivery in order to make decisions on introducing new infant and life-course vaccines, budgeting, and for making improvements in service delivery. The review indicates that existing guidance documents differ somewhat in the inclusion and definitions, of costing terms and costing principles that are recommended, reflecting in part differences in the aims and scope of the costing study.
The review of guidance documents and tools on vaccine delivery costing and iterative discussions among the Working Group members revealed considerable agreement among the different groups working in vaccine delivery costing. Most of the documents made the distinction between economic and financial costs as well as recurrent and capital costs. However, fewer went into detail about the perspective to choose, definition of some costing terms such as start-up costs, micro-costing, and bottom-up/top-down costing, and in some cases, recommended approaches for data collection and analyses. The review also identified gaps in guidance for some analyses, e.g., such as how perspective affects financial costs calculation.
The review revealed that different workstreams focus on distinct aspects of immunization costing with different purposes. These require different types of data collection and analyses. For example, retrospective costing of vaccination focuses on estimating actual resource use, benchmarking of costs, and investigation of variation at the facility and other levels. Cost projections, on the other hand, focus on estimation of (typically incremental) costs to assist in decision-making, preparation of budgets, and evaluating different approaches to a new technology, vaccine, or service delivery strategy.
The process to achieve a consensus statement of vaccine delivery costing methods was facilitated by having extensive consultations with different organizations conducting this work. It also was facilitated by conducting reviews of the guidance documents and costing tools so that similarities, differences, and gaps could be identified. Other strengths of the process include broad and ongoing engagement of experts across various workstreams, including members of the Immunization Economics Community of Practice [ 18 ], as well as dedicated support for facilitation, review, and write-up.
The process to develop a consensus statement provides lessons for developing agreement among other organizations and researchers on types of research methods and tools in other study areas. It requires the potential to bring together organizations working on similar research and then having the time and resources to develop consensus. In addition, it is useful to have some teleconferences and in-person (or virtual meetings with break-out sessions) meetings to have sufficient time to come to consensus.
One limitation of the exercise was that a systematic review was not conducted and some guidelines and costing tools may have been missed. More engagement of country-level practitioners and data and analysis experts outside of those directly involved in the workstreams, as well as a systematic literature search for any methodology documents beyond those known to the workstream participants, would have strengthened the process.
The work on immunization costing is extensive but some gaps were identified. The guidance documents, mostly user manuals for costing tools and the 2002 WHO guidance on introducing new vaccines for cost projections of new vaccines, are not sufficiently detailed regarding data collection and analyses. That is, these do not include instructions on methods of data collection and sampling and analysis methods, when required. Researchers that have piloted the costing tools have also noted that the manuals need to provide more instructions on perspective (see [ 19 ], for example). For example, there is a need for more guidance on how to treat perspective when there is more than one source of financing of vaccines, how to handle slack, etc. As a result, it would be useful to add to current user manuals or develop a new guidance document for cost projections for both single vaccines, multiple vaccines, and immunization programs.
This review and Consensus Statement development process revealed the limitations of our ability to harmonize given that study designs will vary depending upon the policy question that is being addressed and the country context. The Working Group hopes that the consensus statement will contribute to the development of costing guidelines and tools for new vaccines (single or multiple) and immunization programs that are better aligned in terms of definitions, methods, and reporting.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its additional file.
The experts in the Working Group were from the World Health Organization, UNICEF, US Centers for Disease Control and Prevention, the Bill & Melinda Gates Foundation, Harvard T.H. Chan School of Public Health, International Vaccine Institute, ThinkWell, and the London School of Hygiene and Tropical Medicine.
Two presentations were made: (1) the WHO team’s Ann Levin presented on WHO/IVI/PATH’s work conducting vaccine delivery cost projections with costing tools and the lack of standardization with other workstreams; and (2) ThinkWell’s Annette Ozaltin, representing the BMGF portfolio, presented their work on vaccine costing and the repository of vaccine delivery costs known as the Vaccine Cost Catalogue.
Internal validity refers to the extent of systematic bias in an estimate while external validity is the extent to which the cost estimate can be directly applied to other programmatic setting. (GHCC, pg. A15–A16).
A “stopping rule” defines and explains which costs are included, and how the line is drawn between inclusions and exclusions. (GHCC reference case, pg. B-2)
Abbreviations
2nd Year of Life
Bill & Melinda Gates Foundation
Cervical Cancer Prevention and Control Costing
United States Centers for Disease Control and Prevention
Oral Cholera Vaccine Costing Tool
Comprehensive multi-year plan
- Consensus statement
Expanded Programme on Immunization Costing
Fully immunized person
Global Health Cost Consortium
Immunization Costing Action Network
Information, education, and communication
International Health Economics Association
International Vaccine Institute
Immunization and Vaccines-related Implementation Research Advisory Committee
Low-income country
Middle-income country
Malaria Vaccine Immunization Costing Tool
Seasonal Influenza Immunization Costing Tool
Typhoid Conjugate Vaccine Costing Tool
Vaccine Technology Costs and Health Impact Assessment Tool
World Health Organization
Johns Hopkins University, International Vaccine Access Center. Methodology report: decade of vaccines economics (DOVE). Return on investment analysis. Medford: Immunization Economics; 2019. https://static1.squarespace.com/static/556deb8ee4b08a534b8360e7/t/5d56d54c6dae8d00014ef72d/1565971791774/DOVE-ROI+Methodology+Report+16AUG19.pdf . Accessed March 2020.
Google Scholar
WHO. Immunization agenda 2030: a global strategy to leave no one behind; 2019.
Vaughan K, Ozaltin A, Moi F, Griffiths UK, Mallow M, Brenzel L. 2020 reporting gaps in immunization costing studies: recommendations for improving the practice. Vaccine X. 2020;5:100069.
Article Google Scholar
WHO 2018. Immunization and vaccine-related implementation research advisory committee (IVIR-AC): executive summary, 6-8 march 2018, vol. 93. Chamonix: WHO Weekly Epidemiological Record, No 24; 2018. p. 345–56.
WHO 2019. Immunization and Vaccine-related Implementation Research Advisory Committee (IVIR-AC) recommendations. WHO Wkly Epidemiol Record No 24. 2019;94:225–32.
Immunization Costing Action Network (ICAN). Immunization delivery costs in low- and middle-income countries: a methodology note for the systematic review, cost catalogue, and analytics. Washington, DC: ThinkWell; 2018.
WHO, 2020. Immunization and Vaccine-related Implementation Research Advisory Committee (IVIR-AC): summary and recommendations, September 2019. WHO Wkly Epidemiol Record No 49. 2020;95:609–28.
Vassall A, Sweeney S, Kahn J, Gomez G, Bollinger L, Marseille E, et al. Reference case for estimating the costs of Global Health services and interventions; 2017.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. BMJ. 2013;346:f1049. https://doi.org/10.1136/bmj.f1049 .
Article PubMed Google Scholar
ImmunizationEconomics.org. 2021. EPIC projects. The Bill & Melinda Gates Foundation. https://immunizationeconomics.org/epic . Accessed 24 Jan 2022.
Brenzel L. 2013. Common approach for the costing and financing analyses of routine immunization and new vaccine introduction costs. Working Paper. Bill & Melinda Gates Foundation.
Harvard T. H. Chan School of Public Health. 2019. How to cost immunization programs: a practical guide on primary data collection and analysis.
International Vaccine Institute and WHO, Choltool: Planning and Costing User’s Guide. Seoul, South Korea.
WHO. Guidelines for estimating costs of introducing new vaccines into the national immunization system. Geneva: Switzerland; 2002.
WHO, WHO Cervical Cancer Prevention and Control Costing Tool (C4P) User’s Guide. Geneva, Switzerland. https://cdn.who.int/media/docs/default-source/immunization/hpv/who-cervical-cancer-prevention-and-control-costing.pdf?sfvrsn=b56c33cb_7 . Accessed 1 Feb 2022.
World Health Organization. Immunization Costing & Financing: a tool and user guide for comprehensive multi-year planning (cMYP). Geneva: WHO; 2006.
WHO, WHO Seasonal Influenza Immunization Costing Tool: Planning and Costing User’s Guide. Geneva, Switzerland.
ImmunizationEconomics.org. 2021. Community of practice. The Bill & Melinda Gates Foundation. https://immunizationeconomics.org/community . Accessed 24 Jan 2022.
Pallas S, Ahmeti A, Morgan W, Preza I, Nelaj E, Ebama M, et al. Program cost analysis of influenza vaccination of health care workers in Albania. Vaccine. 2020;38(2):220–7. https://doi.org/10.1016/j.vaccine.2019.10.027.Epub 2019 Oct 25.
Download references
Acknowledgements
We thank Xiao Xian Huang and Stéphane Verguet, two Working Group members, for their contributions to and review of the consensus statement. We also thank Shuoning Huang for her coordination and contribution to the first draft of the consensus statement. We acknowledge comments received on earlier versions of the consensus statement from Taiwo Abimbola, Anna Hidle, Timothy Brennan, Nelly Mejia, and Carlo Davila Payan of the CDC.
The views in this manuscript are those of the authors in their individual capacities and do not represent the official positions of the authors’ organizations.
The WHO provided funding for the consultant that led the working group.
Author information
Laura Boonstoppel, Logan Brenzel, Ulla Griffiths, Raymond Hutubessy, Mark Jit, Vittal Mogasale, Sarah Pallas, Stephen Resch, Christian Suharlim, and Karene Hoi Ting Yeung contributed equally and are listed in alphabetical order.
Authors and Affiliations
Levin & Morgan LLC, Bethesda, USA
ThinkWell, Geneva, Switzerland
Laura Boonstoppel
Bill & Melinda Gates Foundation, Seattle, USA
Logan Brenzel
UNICEF, New York, USA
Ulla Griffiths
Department of Immunization, Vaccines and Biologicals, World Health Organization, Geneva, Switzerland
Raymond Hutubessy & Karene Hoi Ting Yeung
London School of Hygiene & Tropical Medicine, London, UK
International Vaccine Institute, Seoul, South Korea
Vittal Mogasale
Centers for Disease Control and Prevention, Atlanta, USA
Sarah Pallas
Harvard T.H. Chan School of Public Health, Boston, USA
Stephen Resch & Christian Suharlim
You can also search for this author in PubMed Google Scholar
Contributions
AL reviewed the guidance documents and costing tools and was the lead author. All authors contributed to the data interpretation and critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Raymond Hutubessy .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. .
Consensus Statement on Vaccine Delivery Costs which includes a review of vaccine delivery cost guidance documents and costing tools as well as a consensus statement on the terminology and methodological principles to be used for vaccine delivery costing. It includes two figures and 6 tables. Figure S1. Major current workstreams in vaccine delivery costing identified by working group. Figure A1 – Timeline for developing a Consensus Statement on Vaccine Delivery Costs. Table A2a. List of guidelines by publication year, target interventions, and purposes. Table A2b. List of costing tools for vaccine delivery or immunization program. Table A3. Definitions of costing terms in guidance documents. Table A4. Comparison of costing principles among guidance. Table A5. Characteristics of costing workstreams. Table 6A. Data sources, sampling and characterization of uncertainty, and terminology by workstreams.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Levin, A., Boonstoppel, L., Brenzel, L. et al. WHO-led consensus statement on vaccine delivery costing: process, methods, and findings. BMC Med 20 , 88 (2022). https://doi.org/10.1186/s12916-022-02278-4
Download citation
Received : 18 October 2021
Accepted : 27 January 2022
Published : 08 March 2022
DOI : https://doi.org/10.1186/s12916-022-02278-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Delivery cost
- Immunization
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
POV: Policymakers Are Entitled to Their Own Opinions. But Should They Be Entitled to Their Own Science?
Republicans are less likely to cite research than democrats and more likely to cite misleading science when they do.

Photo via iStock/wellesenterprises
Policymakers Are Entitled to Their Own Opinions. But Should They Be Entitled to Their Own Science?
Matthew motta.
Scientific research is playing an increasingly prominent role in the policymaking process. That’s according to a new working paper , which finds that policymakers have become increasingly likely to cite scientific research when producing policy documents (e.g., congressional committee reports) on topics related to infectious disease threats, climate change, the costs of health insurance, and much more.
Reliance on scientific research in the policymaking process is, in my view, a very positive development.
That’s because the United States increasingly faces a wide range of complex policy challenges, including mitigating the effects of a changing climate, developing sustainable artificial intelligence regulations, and responding to emerging infectious disease threats. Crafting effective policy solutions that address these concerns requires specialized knowledge that most members of Congress simply cannot be expected to have.
Still, I believe that there is some cause for concern.
Some policymakers are more likely than others to defer to scientific expertise when informing their efforts to combat some of the most pressing issues facing the country today. Specifically, Republican members of Congress are less likely than Democrats to cite scientific research papers in conference proceedings. Republican elected officials at many levels of government are also less likely than Democrats to exhibit deference and respect for scientific experts.
I refer to this phenomenon as the asymmetric polarization of scientific expertise.
Asymmetric polarization in deference to scientific authority mirrors two complementary developments that I describe in my forthcoming book, Anti-Scientific Americans: The Prevalence, Origins, and Political Consequences of Anti-Intellectualism in the United States (Oxford University Press). There, I demonstrate that self-identified Republicans have become increasingly likely to hold negative views toward scientists as people—a phenomenon I and others refer to as “anti-intellectualism.”
In my book, I show that the resentment of scientific authorities tends to coincide with the election of anti-science candidates to political office. This includes Donald Trump’s rise to the White House in 2016, which was characterized by hostility toward science in many forms, such as efforts to defund scientific agencies, prevent government climate scientists from presenting the results of their research, and undermine the public health recommendations of his own administration’s public health advisors throughout the COVID-19 pandemic.
Partisan asymmetries in public anti-intellectual attitude endorsement provide an electoral incentive for GOP policymakers to forgo soliciting the advice of scientific experts. Correspondingly, my book shows that lawmakers tend to be less likely to invite scientists to testify before congressional committees in periods of high public anti-intellectual attitude endorsement.
This dynamic may help explain the pattern of effects documented in that working paper. Republicans are less likely to defer to scientific expertise, because they see doing so as politically advantageous.
Of course, Republicans do not completely forgo citing scientific research in the policymaking process. Anecdotally, though, we do observe differences in the types of experts that partisans solicit when gathering the information necessary to inform evidence-based policy.
Consider, for example, the House Select Subcommittee on the Coronavirus Pandemic’s recent hearings on the origins of COVID-19. Ostensibly, information from a fact-finding mission like this one could be used to inform policy efforts to prevent future pandemics—such as a bill sponsored by Congresswoman Rosa DeLauro (D-Conn.) and US Senator Edward Markey (D-Mass.) aimed at investing in the development of a universal influenza vaccine.
Indeed, Democrats on the subcommittee used the hearings as an opportunity to seek out sworn testimony from research scientists who authored a scientific study documenting that the origins of the COVID-19 pandemic were more likely to be the result of animal-to-human transmission than a “leak” from a virology research lab in Wuhan, China—and that the scientists reached these conclusions independently of potential political pressures.
Nevertheless, these hearings were, at times, focused on anything but the facts.
For example, subcommittee member Representative Marjorie Taylor Greene (R-Ga.), who described herself as “having a PhD in recognizing bullshit,” cited data from the Vaccine Adverse Event Reporting System (VAERS) in order to cast doubt on COVID-19 vaccine safety. As my colleague Dominik Stecula (assistant professor of political science at Colorado State University) and I have written elsewhere, VAERS data are self-reported vaccine injury claims. While these data can be useful for identifying side effects warranting further scientific study, they can nevertheless be subject to misreporting.
So, even the most extreme members of the GOP caucus seek the trappings of science for their arguments. Greene’s comments co-opt the language of science by drawing on government data to levy her anti-science claims, weaponizing science in service of casting doubt on scientific consensus. Her concerns were echoed by other GOP members of the subcommittee, including Representative Brad Wenstrup (R-Ohio).
More generally, the asymmetric polarization of scientific expertise implies that, in periods where Republicans control the legislature, science may play a less pronounced role in informing public policy. This is concerning, as the policy challenges facing our nation are not subject to biannual election cycles.
That’s why I believe that members of Congress should be entitled to their own opinions—not their own facts.
Still, I think there is plenty of reason for optimism.
If members of the American public place greater trust in science and scientists, policymakers will have less of an incentive to embrace anti-science views in Washington. I believe it is incumbent on all of us to defend the rigors of scientific peer review and scientists’ nonpartisan intentions to produce sound research, when discussing current affairs with friends and family.
All of us can play a role in combating the asymmetric polarization of science.
Matthew Motta , assistant professor of health law, policy, and management at Boston University’s School of Public Health, can be reached at [email protected] . His book, Anti-Scientific Americans: The Prevalence, Origins, and Political Consequences of Anti-Intellectualism in the United States , is to be published by Oxford University Press in September.
“POV” is an opinion page that provides timely commentaries from students, faculty, and staff on a variety of issues: on-campus, local, state, national, or international. Anyone interested in submitting a piece, which should be about 700 words long, should contact John O’Rourke at [email protected] . BU Today reserves the right to reject or edit submissions. The views expressed are solely those of the author and are not intended to represent the views of Boston University.
Explore Related Topics:
- Public Policy
- Share this story
- 0 Comments Add
Matthew Motta Profile
Matthew Motta, assistant professor of health law, policy, and management at Boston University’s School of Public Health, can be reached at [email protected]. His book, Anti-Scientific Americans: The Prevalence, Origins, and Political Consequences of Anti-Intellectualism in the United States, is to be published by Oxford University Press in September.
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
Latest from BU Today
Learn more about bu spark bu’s innovation and experiential learn lab, bu student-slash-amateur aviator soars to new heights, bu falls 2-1 in overtime in 2024 ncaa semifinal, bu ras authorize four-day strike over contract negotiations, ai task force report recommends critical embrace of technology and cautious use of ai-detector apps, a wrinkle in time closes out wheelock family theatre’s 2023–2024 season, bu softball hosts holy cross in 2024 patriot league home opener, six bu runners share their boston marathon charity stories, join the citywide festivities for one boston day: discover events across town, seven things to know as bu begins the 2024 frozen four, the weekender: april 11 to 15, school of visual arts mfa thesis exhibitions feature work by 61 artists, bu’s sargent college named nation’s top occupational therapy program in u.s. news 2024 best graduate schools rankings, rats does boston need a “rat czar”, pov: you’re using the wrong door—and there’s a reason, your everything guide to living off campus, bu marks 50 years of changing lives behind bars, $100,000 awarded to student entrepreneurs at sha’s annual hospitality leadership summit, bu’s earth day celebrations.
Assessment of Risk for Sudden Cardiac Death Among Adolescents and Young Adults After Receipt of COVID-19 Vaccine — Oregon, June 2021–December 2022
Weekly / April 11, 2024 / 73(14);317–320
Juventila Liko, MD 1 ; Paul R. Cieslak, MD 1 ( View author affiliations )
What is already known about this topic?
In April 2021, cases of myocarditis after COVID-19 vaccination, particularly among young male vaccine recipients, were reported to the Vaccine Adverse Event Reporting System.
What is added by this report?
To determine risk for sudden cardiac death among adolescents and young adults after COVID-19 vaccination, investigators examined June 2021–December 2022 Oregon death certificate data for decedents aged 16–30 years. Of 40 deaths that occurred among persons who had received an mRNA COVID-19 vaccine dose, three occurred ≤100 days after vaccination. Among these, two occurred in persons with underlying illness, and one decedent had an undetermined cause of death.
What are the implications for public health practice?
The data do not support an association of COVID-19 vaccination with sudden cardiac death among previously healthy young persons. COVID-19 vaccination is recommended for all persons aged ≥6 months to prevent COVID-19 and complications, including death.
- Article PDF
- Full Issue PDF
COVID-19 vaccination has been associated with myocarditis in adolescents and young adults, and concerns have been raised about possible vaccine-related cardiac fatalities in this age group. In April 2021, cases of myocarditis after COVID-19 vaccination, particularly among young male vaccine recipients, were reported to the Vaccine Adverse Event Reporting System. To assess this possibility, investigators searched death certificates for Oregon residents aged 16–30 years who died during June 2021–December 2022 for cardiac or undetermined causes of death. For identified decedents, records in Oregon’s immunization information system were reviewed for documentation of mRNA COVID-19 vaccination received ≤100 days before death. Among 1,292 identified deaths, COVID-19 was cited as the cause for 30. For 101 others, a cardiac cause of death could not be excluded; among these decedents, immunization information system records were available for 88, three of whom had received an mRNA COVID-19 vaccination within 100 days of death. Of 40 deaths that occurred among persons who had received an mRNA COVID-19 vaccine dose, three occurred ≤100 days after vaccination. Two of these deaths were attributed to chronic underlying conditions; the cause was undetermined for one. No death certificate attributed death to vaccination. These data do not support an association between receipt of mRNA COVID-19 vaccine and sudden cardiac death among previously healthy young persons. COVID-19 vaccination is recommended for all persons aged ≥6 months to prevent COVID-19 and complications, including death.
Introduction
In December 2020, the Food and Drug Administration authorized two COVID-19 mRNA vaccines for use in the United States. Early vaccine supplies were prioritized for health care personnel and long-term care facility residents, with phased vaccination of other persons, beginning with those who were older or had high-risk medical conditions, and concluding with healthy younger persons ( 1 ). In Oregon, healthy persons aged ≥16 years became eligible for COVID-19 vaccination on April 19, 2021. In April 2021, reports of myocarditis after COVID-19 vaccination, particularly among young male vaccine recipients, began to appear.* , † Investigators in Israel estimated that the risk for myocarditis associated with receipt of mRNA COVID-19 vaccine was 2.13 per 100,000 among vaccine recipients, and was highest among adolescents and young adult males (10.69 per 100,000) ( 2 ). Published accounts suggest that postvaccination myocarditis is typically mild and associated with good outcomes after brief hospitalization ( 3 , 4 ). As of July 17, 2023, no fatal cases of myocarditis in Oregon had been reported to the federal Vaccine Adverse Event Reporting System (VAERS); however, because VAERS is a passive reporting system, adverse events after vaccination are likely underestimated. In late 2022, reports of sudden deaths among previously healthy young athletes, with suggested attribution to COVID-19 vaccination, appeared in the lay press § and then in the medical literature ( 5 , 6 ). To ascertain whether young persons in Oregon might be dying from cardiac causes shortly after having received a COVID-19 vaccine dose, Oregon death certificate data were reviewed.
Data Sources
Oregon law requires that a certificate of death be completed for each death in Oregon. Oregon’s vital records system abides by CDC’s National Center for Health Statistics’ data-quality standards ¶ , including extensive quality-assurance review. An independent source of data for assessing the completeness of death certificate reporting is not available. Data on Oregon resident deaths occurring outside the state are also collected through interstate exchange agreements. The ALERT Immunization Information System (IIS) is Oregon’s statewide and lifespan immunization registry. During the COVID-19 pandemic, reporting of all COVID-19 vaccinations to ALERT IIS was mandated in Oregon.
Data Analysis
To ascertain the occurrence of sudden cardiac deaths among adolescents or young adults that might plausibly be attributed to recent COVID-19 vaccination, investigators searched the Oregon death certificate database to identify persons aged 16–30 years who died during June 1, 2021–December 31, 2022 with “sudden death,” “arrhythmia,” “dysrhythmia,” “asystole,” “cardiac arrest,” “myocarditis,” “congestive heart failure,” “unknown,” “undetermined,” or “pending” cited among the immediate or four possible entries for underlying causes of death and other significant conditions contributing to death. Among the subset of decedents for whom death from a cardiac cause could not be ruled out by accompanying information in the death certificate database, records of mRNA COVID-19 vaccination within 100 days ( 7 ) before the date of death were retrieved from ALERT(IIS. Findings were stratified by sex. This activity was reviewed by the Oregon Health Authority, deemed not research, and was conducted consistent with applicable federal law and Oregon Health Authority policy.**
In Oregon, during June 2021–December 2022, a total of 1,292 deaths among persons aged 16–30 years were identified. These decedents included 925 (72%) males and 367 (28%) females ( Figure ).
Male Decedents
Among the 925 male decedents, no death certificate listed vaccination either as the immediate or as a contributing cause of death. Overall, 17 (2%) deaths among males were attributed to COVID-19. Death certificates cited noncardiac causes of death or other conditions contributing to death for 842 (91%) of the male decedents. Among the remaining 66 (7%) male decedents, excluding a cardiac cause of death based on the death certificate was not possible. Among these 66 decedents, IIS vaccination records were available for 58 (88%); receipt of at least one mRNA COVID-19 vaccination was recorded for 24 (41%).
Among the 24 male decedents with an mRNA COVID-19 vaccination record in IIS, two (8%) died within 100 days of having received the vaccine. The first death was recorded as having occurred in a natural manner 21 days after COVID-19 vaccination. The immediate cause of death noted on the death certificate was congestive heart failure attributed to hypertension; other significant conditions included morbid obesity, type 2 diabetes, and obstructive sleep apnea. The second decedent had received a COVID-19 vaccine dose 45 days before the date of death; the cause of death was recorded as “undetermined natural cause.” Toxicology results were negative for alcohol, cannabinoids, methamphetamine, and opiates; aripiprazole, ritalinic acid, and trazodone were detected. Follow-up with the medical examiner could neither confirm nor exclude a vaccine-associated adverse event as a cause of death for this decedent.
Female Decedents
Among the 367 female decedents, no death certificate listed vaccination as either the immediate or a contributing cause of death. Thirteen (4%) deaths were attributed to COVID-19. Noncardiac causes were recorded on the death certificates for 319 (87%) decedents. Among the remaining 35 (10%) female decedents, IIS records for 30 (86%) were identified, 16 (53%) of whom had documentation of receipt of at least 1 mRNA COVID-19 vaccine dose. Only one of these deaths occurred within 100 days of having received an mRNA COVID-19 vaccine dose; the decedent died 4 days after COVID-19 vaccination. The manner of death was recorded as natural, and the immediate cause was listed as undetermined but as a consequence of chronic respiratory failure with hypoxia attributed to mitral stenosis.
Electronic health record data from 40 U.S. health care systems during January 2021–January 2022, showed that the risk for cardiac complications was significantly higher after COVID-19 infection than after mRNA COVID-19 vaccination among persons aged ≥5 years ( 8 ). Data from CDC’s National Center for Health Statistics show a background mortality rate from diseases of the heart among Oregonians aged 15–34 years of 2.9 and 4.1 deaths per 100,000, during 2019 and 2021, respectively. Although the rate was higher during the pandemic year of 2021, myocarditis remained an infrequent cause of death among persons in this age group. †† Detection of a small difference in mortality rate from myocarditis would require a larger sample size.
In this study of 1,292 deaths among Oregon residents aged 16–30 years during June 2021–December 2022, none could definitively be attributed to cardiac causes within 100 days of receipt of an mRNA COVID-19 vaccine dose; one male died from undetermined causes 45 days after receipt of a COVID-19 vaccine. During May 1, 2021–December 31, 2022, a total of 979,289 doses of COVID-19 vaccines were administered to Oregonians aged 16–30 years (unpublished data, ALERT IIS, 2024.)
During the same period, COVID-19 was cited as the cause of death for 30 Oregon residents in this age group. Among these 30 decedents, ALERT IIS had records for 22 (73%), only three of whom had received any COVID-19 vaccination. Studies have shown significant reductions in COVID-19–related mortality among vaccinated persons; during the first 2 years of COVID-19 vaccine availability in the United States, vaccination prevented an estimated 18.5 million hospitalizations and 3.2 million deaths ( 9 ).
Limitations
The findings in this report are subject to at least two limitations. First, this report cannot exclude the possibility of vaccine-associated cardiac deaths >100 days after COVID-19 vaccine administration. However, published data indicate that potential adverse events associated with vaccinations tend to occur within 42 days of vaccine receipt ( 10 ). Second, small population size made it less likely that Oregon would see a rare event such as sudden cardiac death among adolescents and young adults.
Implications for Public Health Practice
These data do not support an association between receipt of mRNA COVID-19 vaccine and sudden cardiac death among previously healthy young persons. COVID-19 vaccination is recommended for all persons aged ≥6 months to prevent COVID-19 and complications, including death.
Acknowledgments
Michael Day, Tasha Martin, Anne Vancuren, Center for Health Statistics, Oregon Public Health Division; Rebecca Millius, Office of the Chief Medical Examiner, Medical Examiner Division, Oregon State Police.
Corresponding author: Juventila Liko, [email protected] .
1 Public Health Division, Oregon Health Authority, Portland, Oregon
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* www.cdc.gov/vaccines/acip/work-groups-vast/report-2021-05-17.html
† https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-06/04-COVID-Lee-508.pdf
§ https://www.nytimes.com/2022/01/28/technology/covid-vaccines-misinformation.html
¶ https://www.oregon.gov/oha/PH/BirthDeathCertificates/VitalStatistics/death/Pages/index.aspx
** 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
†† https://wonder.cdc.gov/ucd-icd10-expanded.html (Accessed February 12, 2024).
- Dooling K, Marin M, Wallace M, et al. The Advisory Committee on Immunization Practices’ updated interim recommendation for allocation of COVID-19 vaccine—United States, December 2020. MMWR Morb Mortal Wkly Rep 2021;69:1657–60. https://doi.org/10.15585/mmwr.mm695152e2 PMID:33382671
- Witberg G, Barda N, Hoss S, et al. Myocarditis after COVID-19 vaccination in a large health care organization. N Engl J Med 2021;385:2132–9. https://doi.org/10.1056/NEJMoa2110737 PMID:34614329
- Power JR, Keyt LK, Adler ED. Myocarditis following COVID-19 vaccination: incidence, mechanisms, and clinical considerations. Expert Rev Cardiovasc Ther 2022;20:241–51. https://doi.org/10.1080/14779072.2022.2066522 PMID:35414326
- Behers BJ, Patrick GA, Jones JM, et al. Myocarditis following COVID-19 vaccination: a systematic review of case reports. Yale J Biol Med 2022;95:237–47. PMID:35782472
- Polykretis P, McCullough PA. Rational harm-benefit assessments by age group are required for continued COVID-19 vaccination. Scand J Immunol 2022;98:e13242. https://doi.org/10.1111/sji.13242 PMID:38441161
- Sun CLF, Jaffe E, Levi R. Increased emergency cardiovascular events among under-40 population in Israel during vaccine rollout and third COVID-19 wave. Sci Rep 2022;12:6978. https://doi.org/10.1038/s41598-022-10928-z PMID:35484304
- Sexson Tejtel SK, Munoz FM, Al-Ammouri I, et al. Myocarditis and pericarditis: case definition and guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine 2022;40:1499–511. https://doi.org/10.1016/j.vaccine.2021.11.074 PMID:35105494
- Block JP, Boehmer TK, Forrest CB, et al. Cardiac complications after SARS-CoV-2 infection and mRNA COVID-19 vaccination—PCORnet, United States, January 2021–January 2022. MMWR Morb Mortal Wkly Rep 2022;71:517–23. https://doi.org/10.15585/mmwr.mm7114e1 PMID:35389977
- Fitzpatrick M, Moghadas S, Pandey A, Galvani A. Two years of U.S. COVID-19 vaccines have prevented millions of hospitalizations and deaths. New York, NY: The Commonwealth Fund; 2022. https://www.commonwealthfund.org/blog/2022/two-years-covid-vaccines-prevented-millions-deaths-hospitalizations https://doi.org/10.26099/whsf-fp90
- CDC. Update: vaccine side effects, adverse reactions, contraindications, and precautions. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 1996;45(No. RR-12):1–35. PMID:8801442
FIGURE . Deaths* among persons aged 16–30 years, by sex, cause of death, † and mRNA COVID-19 vaccination status §,¶, ** (N = 1,292) — Oregon, June 2021–December 2022
* Coded on the death certificate as sudden death, arrhythmia, dysrhythmia, asystole, cardiac arrest, myocarditis, congestive heart failure, unknown, undetermined, or pending.
† Cardiac versus noncardiac.
§ Six of the 34 males who did not receive mRNA COVID-19 vaccine received Janssen (Johnson & Johnson) vaccine.
¶ An alternative plausible cause of death was identified for one of the males who had been vaccinated ≤100 days before death. After review of death certificate and medical examiner findings, an adverse event from COVID‐19 vaccination could neither be confirmed nor excluded as the cause for the other decedent.
** The only female decedent vaccinated ≤100 days before death was vaccinated 4 days before death. The manner of death was recorded as natural, and the immediate cause was “undetermined” as a consequence of chronic respiratory failure with hypoxia due to mitral stenosis.
Suggested citation for this article: Liko J, Cieslak PR. Assessment of Risk for Sudden Cardiac Death Among Adolescents and Young Adults After Receipt of COVID-19 Vaccine — Oregon, June 2021–December 2022. MMWR Morb Mortal Wkly Rep 2024;73:317–320. DOI: http://dx.doi.org/10.15585/mmwr.mm7314a5 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Work & Careers
- Life & Arts
Become an FT subscriber
Try unlimited access Only $1 for 4 weeks
Then $75 per month. Complete digital access to quality FT journalism on any device. Cancel anytime during your trial.
- Global news & analysis
- Expert opinion
- Special features
- FirstFT newsletter
- Videos & Podcasts
- Android & iOS app
- FT Edit app
- 10 gift articles per month
Explore more offers.
Standard digital.
- FT Digital Edition
Premium Digital
Print + premium digital, digital standard + weekend, digital premium + weekend.
Today's FT newspaper for easy reading on any device. This does not include ft.com or FT App access.
- 10 additional gift articles per month
- Global news & analysis
- Exclusive FT analysis
- Videos & Podcasts
- FT App on Android & iOS
- Everything in Standard Digital
- Premium newsletters
- Weekday Print Edition
- FT Weekend newspaper delivered Saturday plus standard digital access
- FT Weekend Print edition
- FT Weekend Digital edition
- FT Weekend newspaper delivered Saturday plus complete digital access
- Everything in Preimum Digital
Essential digital access to quality FT journalism on any device. Pay a year upfront and save 20%.
- Everything in Print
- Everything in Premium Digital
Complete digital access to quality FT journalism with expert analysis from industry leaders. Pay a year upfront and save 20%.
Terms & Conditions apply
Explore our full range of subscriptions.
Why the ft.
See why over a million readers pay to read the Financial Times.
International Edition
- The Power of mRNA
- Responsibility
Statements & Perspectives Details
Statement on Kenya Manufacturing Facility
Moderna has paused its efforts to build an mRNA manufacturing facility in Kenya while it determines future demand for mRNA vaccines on the African continent. The demand in Africa for COVID-19 vaccines has declined since the pandemic and is insufficient to support the viability of the factory planned in Kenya. Moderna has not received any vaccine orders for Africa since 2022 and has faced the cancellation of previous orders, resulting in more than $1 billion in losses and write-downs. Despite these challenges, Moderna is committed to ensuring equitable access and meeting emerging demands from African nations for its COVID-19 vaccine through its global manufacturing network.
Moderna is actively working on the development of public health vaccines, including those for diseases that predominantly affect the African continent, such as HIV and malaria. These initiatives are part of our broader commitment to help address global health challenges through our innovative mRNA technology. However, these investigational vaccines are at an early development stage. Given this, and in alignment with our strategic planning, Moderna believes it is prudent to pause its efforts to build an mRNA manufacturing facility in Kenya. This approach will allow Moderna to better align its infrastructure investments with the evolving healthcare needs and vaccine demand in Africa.
Moderna appreciates the strong support received from the governments of the United States and Kenya on this journey. We look forward to a continuing dialogue about future options to support the Kenyan healthcare ecosystem, including as we advance other mRNA vaccines and therapeutics of importance to the African continent through our pipeline.
Forward-Looking Statement Disclaimer
This statement contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995, as amended, including statements regarding: Moderna’s plans for meeting the evolving healthcare needs and vaccine demand in Africa, and ensuring equitable access; and Moderna’s development of public health vaccines to help address global health challenges. The forward-looking statements in this post are neither promises nor guarantees, and you should not place undue reliance on these forward-looking statements because they involve known and unknown risks, uncertainties and other factors, many of which are beyond Moderna’s control and which could cause actual results to differ materially from those expressed or implied by these forward-looking statements. These risks, uncertainties and other factors include, among others, those risks and uncertainties described under the heading “Risk Factors” in Moderna’s Annual Report on Form 10-K for the fiscal year ended December 31, 2023, filed with the U.S. Securities and Exchange Commission (SEC), and in subsequent filings made by Moderna with the SEC, which are available on the SEC’s website at www.sec.gov . Except as required by law, Moderna disclaims any intention or responsibility for updating or revising any forward-looking statements contained in this presentation in the event of new information, future developments or otherwise. These forward-looking statements are based on Moderna’s current expectations and speak only as of the date of this statement.
Quick Links
- SEC Filings
- Investor FAQs
- Information Request Form
Investor Email Alerts
To opt-in for investor email alerts, please enter your email address in the field below and select at least one alert option. After submitting your request, you will receive an activation email to the requested email address. You must click the activation link in order to complete your subscription. You can sign up for additional alert options at any time.
At Moderna, we promise to treat your data with respect and will not share your information with any third party. You can unsubscribe to any of the investor alerts you are subscribed to by visiting the ‘unsubscribe’ section below. If you experience any issues with this process, please contact us for further assistance.
By providing your email address below, you are providing consent to Moderna to send you the requested Investor Email Alert updates.
Email Alert Sign Up Confirmation
Investor overview
Press releases
Media Center
Partnerships.
Strategic collaborators
Company culture
People behind the science
Join our team
Innovation Incubator
New venture labs
- Terms of Use
- Privacy Policy
- Contact Moderna
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

COVID‐19 vaccine research and development: ethical issues
1 Department of Microbiology, Faculty of Medicine Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta Indonesia
2 Medical and Health Research Ethics Committee, Faculty of Medicine Public Health and Nursing, Universitas Gadjah Mada / Dr. Sardjito General Hospital, Yogyakarta Indonesia
The achievements of vaccine research and development bring a hope to our societies that we may cope with the COVID‐19 pandemic. There are two aspects that should be maintained in balance: the immediate necessity for speed of vaccine research and the inherent need for protection of research subjects, which is the foremost concern of research ethics. This narrative review highlights ethical issues in COVID‐19 vaccine research and development that every stakeholder needs to be aware of and to consider.
Introduction
COVID‐19 is a deadly disease which continues to affect many countries in the world. The incidence is higher in the Americas (14 117 714 cases and 486 843 deaths) and Europe (4 515 514 cases and 222 624 deaths) than in South East Asia (4 786 594 cases and 84 541 deaths), Africa (1 088 093 cases and 23 101 deaths) and the Western Pacific (520 012 cases and 11 306 deaths) [ 1 ].
Vaccines are the most important public health measure to protect people from COVID‐19 worldwide, since SARS‐CoV‐2 is highly contagious and infects populations widely and globally [ 2 ]. Traditionally, vaccine development takes years, even decades: from about 40 years for polio to 5 years for Ebola,most vaccines took 15 years on average [ 3 , 4 ]. The trial process for vaccines consists of several steps which need to be conducted systematically and in a measurable stride. The length of this process is correlated with the nature of the vaccine itself, which is to protect healthy people from being infected by pathogens. Adverse events and deleterious effects will not be tolerated, vaccines are not the same as drugs that are consumed by the sick. The risk–benefit analysis for prescription drugs and vaccine administration is different.
The invention of a successful and widely available COVID‐19 vaccine will be a great leap forward for humankind, but there are several challenges to overcome: (1) a lack of understanding of the pathogenesis and the predictive role of vaccines in the clinical pathway of persons being infected by SARS‐CoV‐2 [ 5 , 6 , 7 ], (2) a huge disagreement among experts about how to determine the most immunogenic epitopes and antigens of SARS‐CoV‐2 [ 8 , 9 ], (3) the finding that antibody‐dependent enhancement (ADE) may contribute to the exaggeration of SARS‐CoV‐2 disease [ 10 , 11 ], (4) the lack of established animal models for COVID‐19 vaccine challenge testing, which raises the speculation of using controlled human infection (CHI) as a potential approach [ 3 ], and finally, (5) speculation that the duration of protection by immune response in natural infection is not long enough [ 12 ].
The race for COVID‐19 vaccine invention and development against the spread and catastrophic effects of the disease is real. WHO released a draft list of COVID‐19 candidate vaccines on 3 September 2020. At least 34 vaccine candidates are in clinical evaluation to date [ 13 ]. Several new technologies are used as COVID‐19 vaccine development platforms. Conventional techniques for the development of vaccines such as inactivated, inactivated with adjuvant and live attenuated are still being used. However, reversed vaccinology approaches are also being emplyed, such as a recombinant subunit vaccine, and a more advanced approach using vector delivery systems, along with RNA‐ and DNA‐based vaccines (Table 1 ) [ 4 , 9 , 13 ].
Candidate COVID‐19 Vaccines in Clinical Trial Phases*
The attempts to accelerate vaccine development are associated with efforts to streamline the process. Unfortunately, streamlining may have consequences for the traditional ethics of vaccine research and development, especially the long‐held principles of beneficence and non‐maleficence. This short narrative review summarises the ethical issues that may emerge from the current directions in COVID‐19 vaccine research and development during the pandemic.
Vaccine candidates must fulfil several requirements: safety, efficacy and quality. Because of the current escalation of the global COVID‐19 pandemic, some aspects may change. The speed of vaccine development may push public health ministers, heads of states and the pharmaceutical industry to change their strategy for bulk budget investment for vaccine research. They must decide to prepare mass production events based on the limited data of promising vaccine candidates [ 14 ]. The need to protect billions of earth’s inhabitants pushes governments and societies of the world to a ‘great expectation’ for the new vaccine. The overriding expectation, although with diverse interests, may influence the objective judgement typically required of candidate vaccine safety. Protecting human lives should be the priority.
mRNA‐ [ 15 ] and DNA‐based vaccine technologies [ 9 , 16 ] are being implemented in humans, especially as vaccine candidates. Several concerns about mRNA vaccine safety have been identified besides its promising potential advantages. The most important risks include the possibility that mRNA vaccines may generate strong type I interferon responses that could lead to inflammation and autoimmune conditions [ 17 ]. The safety concerns of DNA‐based vaccines involve the possibility that the targeting of DNA into the chromosomal DNA of the acceptor will trigger mutagenic effects in the functional gene located in the insertion loci [ 18 ]. At present, there are no mRNA‐ and DNA‐based vaccines against any disease authorised to be marketed.
The strategy of DNA vaccines is similar to gene therapy in that a delivery system, such as plasmid, delivers targeted DNA into cells, where it is translated into proteins that induce the acceptors’ immune response to generate targeted T‐cell and antibody responses [ 19 ]. We have experience in using DNA for several gene therapies mostly related to inherited diseases or familial predispositions. Mainstream gene therapy scientists have stated that gene therapy is only suitable for terminally ill patients because the risks are very high [ 20 ]. Vaccine administration is completely different from interventions with gene therapy since the vaccine is for healthy human subjects, and the risk–benefit consideration would be completely different too. Both terminally ill and healthy persons have the same risk for the introduction of foreign DNA into their body, but terminally ill persons may benefit through having a chance to recover from their deadly disease, whereas healthy individuals may not have any benefit because they have never encountered the particular pathogen.
When we perform the risk assessment of new technology, it is based on a theoretical framework without direct evidence concerning to what extent the probability of the risk may occur. Theoretically, DNA vaccine may be able to induce autoimmune diseases and can be inserted into any part of the chromosomes [ 21 ]. Scientists know how the mechanism works and are able to predict the risk if it might happen. But nobody knows for certain how great the probability is of producing mutagenic and deleterious effects in one part of a gene sequence when inserted into another. For example, when a test subject named Jessie Gelsinger was injected with adeno‐associated viruses (AAVs), nobody expected the deadly risk that ultimately occurred in this research subject [ 22 ]. Accordingly, the risk–benefit assessment in the use of new technology should be done carefully. It is true that sometimes we have to deal with a risk possibility that is not immediately present but theoretically possible, and vice versa. Mitigation to the deleterious effect could be started prior to the clinical trial. However, there is always the possible existence of risks that have not been identified yet and will only show in the later phases of clinical trials.
In the current pandemic, all societies expect a breakthrough in medical and health technology. In a situation where understanding of the new disease is poor and no satisfactory medical technology is available for prevention and treatment yet, it is natural to think that ‘doing something is better than nothing’. This is going to make safety judgement among stakeholders more prone to deterioration.
Controlled human infection (CHI)
One of the crucial steps of vaccine development is the challenge test, which is used to measure the potential protection of the candidate. The challenge test is usually part of the pre‐clinical study in an animal model. However, in the case of COVID‐19 and some other diseases, an animal model is not available, although there are candidates that need to be verified [ 3 , 23 , 24 , 25 ]. It seems the pathogen does not produce a similar clinical course in common animal models, which excludes safety and efficacy data from animal models alone. There was a proposal of human challenge testing to replace the pre‐clinical challenge test in animal models, with the use of controlled human infection (CHI). It will solve the problem of the animal models’ unreliability and gain time for the developers especially in phase III [ 3 , 26 ].
To some extent, it is possible to perform these challenge tests with human volunteers. It sounds like an unsafe experimentation, but the choices are extremely limited. The next question is how can we do this experiment with the current ethical review process? The WHO has issued a guideline for CHI [ 27 ]. The guideline is broad and needs local ethics committee approval for its implementation. Considerations of the pros and cons of CHI are widely discussed in COVID‐19 vaccine development. Previously, CHI was used to develop vaccines against malaria [ 28 ], typhoid [ 29 ] and cholera [ 30 ], which are diseases with established treatment [ 31 ]. Subjects who suffered from deleterious effects after experimentation could be rescued by the established treatment. Application of CHI in COVID‐19 is a very different story because there is no standard treatment for this new and highly contagious disease. Nevertheless, there have been thousands of volunteers from 162 countries who declared their willingness to be participants in this CHI [ 32 ]. The need for a vaccine is prevalent in people’s minds and equally necessary from the public health point of view. Without any precedents, it is going to be difficult to judge the risks benefits in this matter [ 33 ].
Controlled human infection could be done in a situation where there is an attenuated virus strain available, for example, using an artificial mutant virus. This approach is to prevent fatal outcomes in trial subjects. But the challenge test results from attenuated virus may not be generalisable – the attenuated strain may not be similar enough to the naturally circulating virus. In addition, producing the attenuated virus may require another step that will take almost as much time to perform as the regular phase III in typical controlled clinical trials. This additional step in an already complicated process will render futile the main purpose to gain more time to develop an effective vaccine [ 34 ].
Location and population
Development sites of COVID‐19 vaccines are involving research subjects from many countries, for example USA, Russia, Argentina, Brazil, Germany, India, Saudi Arabia, Pakistan and others [ 35 ]. The need of multi‐centred research is obvious in the vaccine development. The safety, tolerability, and efficacy of the vaccines should be obtained from different geographic areas, ethnicities, prevalence and varieties of the virus circulating in the areas [ 36 ]. The attempt to fulfil this requirement may result in the involvement of countries with limited resources and whose underdeveloped infrastructure would make the people involved become even more vulnerable as research subjects from the ethical and humane point of view. The possible exploitation of vulnerable people from less developed countries should be reviewed thoroughly. The vaccine trial should give them equitable advantages in trade, such as capacity building, transfer of technology and access to the vaccine during the current pandemic of COVID‐19.
Another concern is the availability of an adequate health facility and system to ensure that trial subjects and their families and/or communities have access to treatment and proper care in case of serious adverse events related to the trial outcomes. This must be assessed before any clinical trials begin. Providing the most comprehensive health services to the trial population will be an added value for population involvement in the trial. The best practice of vaccine clinical trials should have direct benefits for the community, such as improvement and availability of basic health facilities [ 37 ]
Vaccine acceptors are sometimes segmented into target groups, which is related to the host distribution of the target disease, for example by gender, age and specific population in the endemic area. A vaccine clinical trial is usually started in adult subjects and continued to more vulnerable subjects such as infants, young children, the elderly and women. Clinical vaccine trials will recruit vulnerable subjects. Protection measures to safeguard the vulnerable and marginalised populations should be carefully scrutinised during review. Ethical considerations must be adjusted to the individual situation to protect these vulnerable subjects from exploitation and later abandonment [ 38 ].
However, in an emergency pandemic situation, the definition of vulnerability needs to be openly discussed, and emergency calls for exceptions. The exclusion of vulnerable groups may diminish trial validity because of selection bias, so they should not be excluded without reasonable scientific and ethical justification [ 39 ].
Post‐trial access
After clinical vaccine trials, the subjects should have access to the developed vaccine. This is part of their direct advantage for their involvement in the research. While it is mentioned in the international ethical guidelines, not all researchers know and are aware of this important obligation [ 40 ]. The current COVID‐19 vaccine development involves multi‐country and intercontinental research recruiting subjects from different countries and regions. The post‐trial access to COVID‐19 vaccines should be expanded beyond the community where the trial is performed to include the country and region.
Post‐trial access is a matter which must be addressed from the very beginning of research design. Community engagement should be considered prior to the trial and involve all stakeholders: sponsors, industries, developers, investigators, subjects of the trial, communities and the government where the trial is performed.
In summary, the current COVID‐19 vaccine research and development involves people from many countries, which raises ethical issues that must be addressed by all stakeholders. Even in the emergency of a pandemic, the urgency of providing an effective COVID‐19 vaccine for humankind must be balanced with the exigency of research ethics that must be maintained. In any event, the safety and well‐being of research subjects must be protected, especially that of vulnerable subjects.
Sustainable Development Goals (SDGs): SDG 3 (good health and well‐being)

IMAGES
VIDEO
COMMENTS
Thesis Summary . Vaccines are one of the world's most impactful medical therapies. They are cost-effective, successfully proven, and one of the quickest treatment options available today (Clark et al., 2016). They save millions of lives every year and have eliminated certain diseases on a
Thesis Statement: Research shows that the benefits of vaccination outweigh the risks because vaccines can prevent serious illness and disease in individuals, vaccinations can also prevent widespread outbreaks of diseases in populations and the side effect of vaccinations, though occasionally serious, are vary rare. Don't use plagiarized sources.
There is a strong case for making any vaccination mandatory (or compulsory) if four conditions are met: There is a grave threat to public health. The vaccine is safe and effective. Mandatory vaccination has a superior cost/benefit profile compared with other alternatives. The level of coercion is proportionate.
Risks and Benefits of Vaccination. The factual bases for vaccine refusal have largely been scientifically refuted. There is no scientific support for the notion that vaccines overwhelm the infant immune system. 18 Most additives in vaccines are safe in the absence of anaphylaxis to a component ingredient. 19 No reputable study has suggested a link between autism and any vaccine. 20
State of the World's Vaccine and Immunizations (in the press) Feudtner, C. & Marcuse, E. K. Ethics and immunization policy: promoting dialogue to sustain consensus. Pediatrics 107, 1158-1164 (2001).
Vaccine hesitancy is a major threat to the success of COVID-19 vaccination programs. The present cross-sectional online survey of adult Poles (n = 1020) expressing a willingness to receive the COVID-19 vaccine was conducted between February and March 2021 and aimed to assess (i) the general trust in different types of vaccines, (ii) the level of acceptance of the COVID-19 vaccines already in ...
While efficacious vaccines have been developed to inoculate against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; also known as COVID-19), public vaccine hesitancy could still ...
Perception of the COVID-19 Vaccine Compared to Previous Historic ...
The Global Vaccine Action Plan 2011-2020 lists equity as one of its six guiding principles [].Resonating this ethos, various national vaccination policies and programs have acknowledged vaccines' contribution to preventing high-cost treatments and averting medical impoverishment, while striving to extend the benefits of immunization to all [2, 3].
These included; (1) knowledge of. the primary series immunization schedule in both a child on time and delinquent, (2) knowledge of timing between diptheria, tetanus, and pertussis boosters, and (3) knowledge of the contraindications to vaccinate. The results showed an 89% correct response rate for knowledge of the.
Immunization is reported to prevent an estimated 2 to 3 million deaths each year worldwide (WHO, 2009). The year 2014 marked the 40th anniversary of the WHO's Expanded Program on Immunization (EPI), which was established to ensure equitable access to routine immunization (RI) services (CDC, 2015). The WHO (2009) has stated
While others (especially Brennan, 2018) have argued that vaccine mandates do not violate general constraints against government restriction, we take our advance to be framing the defense of mandates in the very language of rights and consent most commonly used by their opponents. For purposes of this paper, we begin with three assumptions.
Thesis/Problem Statement In this thesis, I will investigate the basis and prevalence of the controversies surrounding vaccines and examine the data and claims based on this data that brings forth the controversy of vaccines. Specifically, I will address the following research questions. Why do controversies of vaccines exist?
uncertainty around the virus and consequently the vaccine. This thesis aims to explore nurses' decision-making around COVID-19 vaccination, with a specific focus on the role of uncertainty both about the pandemic and available vaccines. In what follows, this study first reviews the state of the COVID-19 pandemic, and specifically the
Schmitz, M. (2020). Human Papillomavirus (HPV) infection and vaccine knowledge and attitudes among university students [Master's thesis, Minnesota State University, Mankato]. Cornerstone: A Collection of Scholarly and Creative Works for Minnesota State University, Mankato. https://cornerstone.lib.mnsu.edu/ etds/1031
Vaccine too new, want to wait and see how it works for others (53%) Politics has played too large of a role in vaccine development (51%) Risk of COVID-19 is exaggerated (43% total, but 57% among hesitant Republicans) Source: KFF COVID-19 Vaccine Monitor (KFF Health Tracking Poll, Nov. 30-Dec. 8, 2020).
THESIS STATEMENT Parents should follow the American Pediatric Association's vaccination schedule because vaccines reduce drastically once prevalent and devastating disease, do not impact brain development or function, reduce the risk for those who cannot be given the vaccine, and are cost effective when compared to the cost of treatment.
Background. Since the development of the first U.S. Food and Drug Administration-approved vaccine for the prevention of serious disease and death associated with the SARS-CoV-2 virus, health care workers have been expected to comply with mandatory immunization requirements or face potential termination of employment and censure by their state medical boards.
Our analyses indicate that vaccine effectiveness generally decreases over time against SARS-CoV-2 infections, hospitalisations, and mortality. The baseline vaccine effectiveness levels for the omicron variant were notably lower than for other variants. Therefore, other preventive measures (eg, face-mask wearing and physical distancing) might be necessary to manage the pandemic in the long term.
Vaccinations Thesis Statement Presentation . Education . Free Google Slides theme and PowerPoint template . There is a lot of information about vaccines and, sadly also a lot of misinformation. It is in health worker's hands to select only proven information and share it in a clear, understandable way that makes people who don't understand ...
Process of developing the consensus statement. The consultation process of coming to agreement on a Consensus Statement included setting up a time-limited Working Group of staff of organizations working in vaccine delivery costing (who are also the authors of this paper), conducting a review of guidance documents, costing tools, and other documents and the costing terms, methods, and ...
Scientific research is playing an increasingly prominent role in the policymaking process. That's according to a new working paper, which finds that policymakers have become increasingly likely to cite scientific research when producing policy documents (e.g., congressional committee reports) on topics related to infectious disease threats, climate change, the costs of health insurance, and ...
Introduction. It is widely recognized that immunization is one of the most successful public health interventions in medical history. Immunization programs have been credited with reducing morbidity and mortality from several pathogens, including the complete or near eradication of infectious diseases such as smallpox and polio. 1 However, to continue making progress in the face of an ...
Introduction. In December 2020, the Food and Drug Administration authorized two COVID-19 mRNA vaccines for use in the United States. Early vaccine supplies were prioritized for health care personnel and long-term care facility residents, with phased vaccination of other persons, beginning with those who were older or had high-risk medical conditions, and concluding with healthy younger persons ...
Sales of its Covid-19 mRNA vaccine, its only approved product, are projected to total $3.9bn this year, according to a consensus of analysts' estimates, down 79 per cent from peak sales of $18 ...
This paper evaluates and reviews the origins of the anti-vaccination movement, the reasons behind the recent strengthening of the movement, role of the internet in the spread of anti-vaccination ideas, and the repercussions in terms of public health and safety. Keywords: vaccination, mmr vaccine, measles outbreak, virus, anti-vaccine movement.
Statement on Kenya Manufacturing Facility Moderna has paused its efforts to build an mRNA manufacturing facility in Kenya while it determines future demand for mRNA vaccines on the African continent. The demand in Africa for COVID-19 vaccines has declined since the pandemic and is insufficient to support the viability of the factory planned in Kenya.
The achievements of vaccine research and development bring a hope to our societies that we may cope with the COVID‐19 pandemic. There are two aspects that should be maintained in balance: the immediate necessity for speed of vaccine research and the inherent need for protection of research subjects, which is the foremost concern of research ethics.