An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Neuropsychiatr Dis Treat

Recognizing Depression in the Elderly: Practical Guidance and Challenges for Clinical Management
Maria devita.
1 Department of General Psychology (DPG), University of Padua, Padua, Italy
2 Geriatrics Division, Department of Medicine (DIMED), University of Padua, Padua, Italy
Rossella De Salvo
Adele ravelli, marina de rui, alessandra coin, giuseppe sergi, daniela mapelli.
Depression is one of the most common mood disorders in the late-life population and is associated with poor quality of life and increased morbidity, disability and mortality. Nevertheless, in older adults, it often remains undetected and untreated. This narrative review aims at giving an overview on the main definitions, clinical manifestations, risk and protective factors for depression in the elderly, and at discussing the main reasons for its under/misdiagnosis, such as cognitive decline and their overlapping symptomatology. A practical approach for the global and multidisciplinary care of the older adult with depression, derived from cross-checking evidence emerging from the literature with everyday clinical experience, is thus provided, as a short and flexible “pocket” guide to orient clinicians in recognizing, diagnosing and treating depression in the elderly.
Introduction
Depression is one of the most common mood disorders in the late-life population. 1 , 2 The prevalence of depressive disorder in the over 60 years old population is about 5.7%. 3 However, it increases with age, to reach the peak of 27% in over-85 individuals. 1 Interestingly, the prevalence still increases and reaches the 49% in those living in communities or nursing homes, 4 , 5 regardless of the severity or the definition of depression considered. 1
Late-life depression (LLD) can be distinguished according to the age at which the first depression occurred. Early-onset depression (EOD) identifies the persistence or recurrence in old age of a depression previously diagnosed throughout adulthood, while late-onset depression (LOD) represents a depressive disorder developed de novo in old age. 6
DSM 5 identifies a cluster of depressive symptoms, namely depressed mood, loss of interest and pleasure, weight loss or gain, fatigue, insomnia or hypersomnia, psychomotor agitation or retardation, decreased concentration, thoughts of death and/or suicide and worthlessness. 3
However, LLD is characterized by an atypical cluster of symptoms, ie somatic symptoms which are predominant compared to mood symptoms, so it is important to be aware of this particular clinical presentation in order to not underestimate LLD.
Moreover, the complex spectrum of Late-Life Depression (LLD) goes beyond the main diagnostic entities of unipolar depressive disorders, such as Major Depressive Disorder (MDD) and persistent depressive disorder. 7 Relevant depressive symptoms which do not fulfill the criteria for a diagnosis of depression have nevertheless a significant clinical relevance, because of their association with poorer quality of life and increased disability; however, they are often undetected and untreated, despite a very small chance of spontaneous remission. 8
Depressive symptoms produce clinically significant distress and impairment in daily life, notching social, familiar, and occupational areas of functioning. Depression is entangled in a bidirectional relationship with somatic morbidity finally resulting in an increase in patients’ burden of disability and frailty and augmenting mortality. 9 In fact, besides being a risk factor and a predictor of poor prognosis for many conditions, like diabetes, cancer, cardiovascular diseases, dementia, 10–12 depression can be precipitated and perpetuated by chronic medical conditions typical of the aging process. A longitudinal study of 3214 healthy elderly individuals proved that Mild Cognitive Impairment (MCI), as well as smoking and mobility, vision, and subjective memory impairments, can significantly increase the risk of depression. 13
Thus, the diagnosis of depression is challenging in elderly people, since it often presents with multifaceted and more somatic symptoms compared to adults, 14 thus resembling a “real” medical organic disease. 5
Also, treatment is demanding, because of the complexity of older patients, who more frequently have a pharmacological-resistant depression and require a multidimensional and, possibly, a multi-professional equipe taking charge.
The objective of this review is, on the one hand, to explain the strong impact of geriatric depression on individual and caregivers’ quality of life and the difficulties in recognizing and prescribing the adequate treatment and, on the other hand, to propose a practical approach for the global and multi-disciplinary care of the older adult with depression, from diagnosis up to the definition of a customized treatment. In order to do so, a short and flexible “pocket” guide is here proposed as a tool to orient clinicians in recognizing, diagnosing and treating depression in the elderly. To the best of our knowledge, there is no tool currently available, such as the here proposed pocket guide, thought to be flexible and easily adaptable to the most disparate clinical contexts.
Reviewing the Literature on Geriatric Depression: Definitions, Risk and Protective Factors, Symptomatology and Clinical Variants
Geriatric depression syndrome: characterization and symptomatology.
While the depression severity appears to remain stable across the lifespan, what really differentiates depression in middle and old age concerns qualitative differences in the clinical presentation of the symptomatology ( Table 1 ).
Depression Symptoms in Younger and Older Adults: Typical and Atypical Presentation
Abbreviations : *DSM, Diagnostic and Statistical Manual of Mental disorders; **GI, gastrointestinal.
As an example, considering depressed mood (sadness or dysphoria) and loss of interest (anhedonia), which are the two core symptoms of Major Depressive Disorder (MDD) according to the DSM 5, they can be manifested differently in older adults compared younger people, 15 as well as inappropriate guilt or feelings of worthlessness. 16 Notably, regarding the first of these two core symptoms (ie depressed mood), feelings of dysphoria or sadness are frequently absent in older adults, 7 underlying a specific variant of geriatric depression indicated as “depression without sadness”, 17 characterized by lack of interest, sleep difficulties, lack of hope, loss of appetite and thoughts of death.
On the contrary, symptoms like lack of vigor and withdrawal, which are referred to the second core symptom of MDD, are usually more pronounced. In fact, “loss of interest” is usually pronounced, since older adults tend to be more apathetic. 18 Suicidal thoughts are frequent in LLD, together with state of anxiety, especially in the morning. 19
What characterizes even more LLD is a shift towards somatic symptoms, 18 which become prominent and vary in their manifestations compared to early onset depression, although the criteria symptoms remain the same. For example, while increased appetite and overeating may frequently occur in younger individuals, loss of appetite and weight are more common in late life. 20 Similarly, considering that sleep duration declines with age, decreased sleep is more common in LLD compared to hypersomnia, which is more typically experienced by younger depressed adults. 18 Fatigue is expressed both as physical tiring and lack of energy rather than a mental symptom, while the “poor concentration” symptom could be manifested more as a broader cognitive impairment where memory loss is related to executive dysfunction. 21 In general, older people manifest more vague and gastrointestinal somatic complaints, together with hypochondriasis. 22 Lastly, psychomotor retardation is more common in LLD than agitation, leading to disturbances in speech, facial expression, fine motor behavior, and gross locomotor activity, which exceed the general slowdown observed in normal aging. 23
It is therefore clear that one of the main challenges in recognizing the diagnostic features of geriatric depression is the overlap of its typical symptoms with those of other comorbid physical or neurologic conditions and, in general, with the typical signs of frailty (ie, weight loss, psychomotor slowing and exhaustion).
In fact, the somatic symptoms that in younger adults are indicative of depression, in the elderly may be correlated with aging and may not be indicative of a specific pathology, as well as could be due to other comorbid conditions. Thus, while including somatic symptoms in geriatric screening for depression regardless of their etiology (inclusive approach) may lead to false positives, 24 it remains true that they cannot be completely excluded from the diagnostic framework (as the exclusive approach, instead, proposes), as aging and its associated conditions do not necessarily justify all these aspects. An alternative is represented by the aetiological approach, in which somatic symptoms are considered only if they are not primarily due to another medical condition. 25 In general, a good clinical practice is to ask people about their mood when they refer to non-specific physical complaints, as to assess the presence of mood problems that older adults tend not to autonomously express, as previously stated.
Geriatric Depression Syndromes
Because of its peculiar features and complexity, different specific variants of geriatric depression have been proposed to better frame its presentations.
Among these, the “depletion syndrome”, 26 characterized by lack of interest, sleep difficulties, lack of hope, loss of appetite and thoughts of death, described the common condition of “depression without sadness” seen in older adults.
Another condition is referred to as “reversible dementia”. In some cases, in fact, older patients suffering from a severe depression development with marked cognitive impairment can induce the clinicians to misdiagnose dementia. 27 However, in these patients, the cognitive symptomatology recedes with the remission of depression, even if a part of them subsequently develops a proper dementia. 28 The label of “pseudodementia” this condition was addressed as, is no longer used, because of the complex relationship between depression and dementia, which represents an interaction between pathological processes, with more than one illness masquerading as another. 29
In fact, the complex entanglement involving aging-related processes, network dysfunction and depressive symptoms is also supported by the fact that two distinct syndromes regarding LOD can be recognized, ie the “depression-executive dysfunction syndrome” (DED) and vascular depression. DED 30 develops in patients whose fronto-striatal pathways are affected by aging-related or pathological changes. It is marked by psychomotor retardation, loss of interest, suspiciousness, lack of insight and pronounced disability, but rather mild vegetative symptoms and less prominent depressive ideation. 31 Moreover, individuals affected by this syndrome have impaired performance in tests of executive functioning (namely verbal fluency, response inhibition, problem solving, cognitive flexibility, working memory and ideomotor planning). 32 Vascular depression, instead, is characterized by psychomotor slowing, lack of initiative and apathy, and it is typically observed in patients with a medical history of hypertension and cognitive impairment. 31 The “vascular depression” hypothesis postulates that cerebrovascular disease may predispose, precipitate, or perpetuate some geriatric depressive disorders, 31 disrupting networks supporting affective and cognitive functions. 32
Risk and Protective Factors
The identification of factors that can increase or protect from the risk of developing depression in the elderly population is crucial in order to promote prevention strategies, but also for the best comprehensive approach to this disease. The literature has shown that suffering from a chronic disorder 4 , 33–35 or cognitive impairment, 36 having a weak social, emotional and supportive network, 5 , 37 living isolated, taking care of relatives with chronic disease, 38 losing a partner, 39 can facilitate the rising of depressive symptoms. Furthermore, gender differences, well known in younger patients, persists also into late life, so being a woman can represent a risk factor. 40 On the other hand, having a high level of self-esteem, 41 resilience 42 and sense of control, 41 keeping a healthy lifestyle 43 and having a medium/high level of cognitive reserve 44 represent protective factors for the rising of depression in elderly age. Table 2 provides a detailed overview of the main risk and protective factors involved in geriatric depression.
Risk and Protective Factors for Depression in Elderly
Recognizing Geriatric Depression in the Elderly: A Current Challenge
Depression in older adults is often under- or misdiagnosed and thus undertreated or inappropriately treated. Reasons for underdiagnosis are several and include psychosocial factors too. The first issue concerns the prejudice that depression is a normal phase of aging, because of the medical and situational conditions typical of older age, such as the limitations imposed by functional disability, health concerns and psychological stressors as decreasing social contacts, transitions in key social roles (ie, retirement) and grief. 15 Although, mood deflection is certainly understandable, it does not imply that it should be neglected, nor that it is not treatable, especially when it is a source of suffering and impairs functioning. Another barrier for depression recognition involves stigmatization. In fact, some individuals are reluctant to accept a diagnosis of depression, and often both patients and clinicians may hope to find a “medical illness” in order to avoid the stigma of a psychiatric diagnosis. 20 Moreover, older adults are less likely to express mood problems, like dysphoria or worthlessness, and may describe their symptoms in a more “somatic” way. 7 In general, older adults often find physical illness to be more acceptable than psychiatric illness. 45 At the same time, physicians may lack screening for depression because of more urgent physical problems or because they wrongly attribute depressive symptoms to comorbid medical illness. 46
In addition to underdiagnosis, another factor that contributes to undertreatment is misdiagnosis. As previously stated ( Table 1 ), in the elderly depression has an atypical presentation, including persistent complaints of pain, headache, fatigue, apathy, agitation, insomnia, weight loss, low attention and other nonspecific symptoms which can overlap with or be confused with other physical illnesses and dementia. This can lead clinicians to pursue an expensive medical workup, when they may not be able to recognize these problems as being part of a depressive episode. At the same time, older adults may relate their symptoms to a medical condition, thus not seeking the proper help. 18 Thus, it is necessary to gain insight on variability in the presentation of specific depressive symptoms across the lifespan.
Confounding Factors: Cognitive Impairment and Depression in Older Adults
Another specific challenge in the accurate diagnosis of depression concerns its entanglement with cognitive impairment and dementia. In fact, there is a substantial overlapping in the clinical presentation of late-life depression and early-stage dementia: a subjective perception of memory loss, as well as psychomotor retardation and a lack of motivation in answering at cognitive tests are typically observed in depressed older adults, and can be interpreted as signs of dementia. 47 Moreover, in older adults, depression is commonly accompanied by cognitive deficits, which are present in 20 to 50% of cases. 48 , 49 On the other hand, depressive symptoms are a common neuropsychiatric symptom of Alzheimer’s Disease (AD). 50 Still, given the prevalence of both syndromes in the older population, they can also independently co-occur, and the two diagnoses are not mutually exclusive. 36
Geriatric depression is characterized by cognitive deficits involving executive functions, such as problem solving, planning, decision-making and inhibition, along with selective and sustained attention and working memory impairment. 51 Other deficits, involving some aspects of episodic memory and visuospatial functions, may be secondary to executive dysfunction. 28 These symptoms remain significant even after the remission of the depressive symptomatology. 52 In a 10-year longitudinal study, Ly et al 53 have shown that depressed older adults perform worse than compared healthy controls in cognitive tasks, maybe for the neurotoxic effects of depression and reduced cognitive reserve.
The relationship between late-life depression and cognitive decline is even more complex, considering that, besides mimicking each other, they also can coexist and be mutually a risk factor.
On the one hand, in fact, older adults with dementia can develop pure depressive symptoms. Clinical depression in these cases can be either reactive to the diagnosis or a relapse of a previously diagnosed depression. 54 Olin et al proposed diagnostic criteria for “depression of Alzheimer’s disease”, including the presence of at least three significant depressive symptoms during the same two-week period that represents a significant perturbation from previous functioning, when all the criteria of AD are fulfilled. 55
On the other hand, Ly et al 53 found that late-onset depression, but not EOD, was associated with a more rapid cognitive decline over time. These findings suggest that EOD, whose symptoms are persistent or recurrent in old age, is a vulnerability factor that alters cognitive abilities even in healthy aging, representing a risk factor for dementia. 21 On the contrary, LOD could be a real harbinger of dementia. In particular, highly educated people are more likely to show depressive symptoms as initial presentation of dementia, probably because cognitive reserve may delay the onset of cognitive, but not depressive, symptomatology. 56
Reviewing the Literature on Therapeutic Approaches to Depression in the Elderly
The effective management of geriatric depression builds upon different strategies, involving both pharmacological and non-pharmacological options that have to be considered based on the patient’s characteristics and psychosocial environment, in order to shape a tailored and comprehensive intervention. In fact, the most effective approach is the biopsychosocial one, combining pharmacotherapy, psychotherapy and an array of lifestyle and social environment’s personalized modifications. These therapies and good practices have shown to be effective, resulting in improved quality of life, enhanced functional capacity, possible improvement in medical health status, increased longevity, and lower health care costs. 14
Pharmacological Treatment of Depression in Older Adults
Late-life depression compared with that of younger patients shows a lower response rate to antidepressants, nonetheless several treatment options exist.
When prescribing drugs, including psychotropic drugs, to older adults’ attention should be paid to pharmacokinetic and pharmacodynamic changes associated with aging. In fact, drug distribution varies, due to the increase in body fat that leads to an increasing distribution volume and elimination of half-life for lipophilic drugs. Renal filtration rate decrease enhances the problem of drug elimination. In addition, hepatic metabolism, besides being affected by aging, is also influenced by other concomitant drugs that induce or inhibit cytochrome P-450 metabolic enzymes.
In the choice of antidepressant treatment, the patient’s previous response to treatment should be considered, as well as his/her other comorbidities and medications, in order to minimize the risk of side effects and drug–drug interactions. In addition, somatic symptoms associated with depression like anxiety, psychotic symptoms, insomnia/hypersomnia, hyperphagia/poor nutrition should be considered.
The second-generation antidepressants, ie Selective Serotonin Reuptake Inhibitors (SSRIs) and Selective Norepinephrine Reuptake Inhibitors (SNRIs), are considered the first-line treatment options for depression in the elderly, because of their efficacy, 57 tolerability and safety profile. Except for paroxetine, they have lower anticholinergic effects than older antidepressants (ie tricyclics) and are thus well tolerated by patients with cognitive impairment or cardiovascular disease. SSRIs are also good for improving cognition, 58 while SNRIs are a good first choice in comorbid neuropathic pain. Most frequent SSRIs and SNRIs side effects include hyponatremia, 59 nausea and gastro-intestinal bleeding, 60 so periodic blood exams are recommended. Another second-generation antidepressant is mirtazapine that improves appetite being useful for anorexia, 61 and whose sedative side effect can be useful for insomnia. 62 A novel antidepressant, vortioxetine, a multimodal serotonin modulator, seems to be promising for elderly people since it also has a positive effect on cognition, independently of the improvement in depression. 63
When psychotic symptoms coexist, the addition of antipsychotics to antidepressants may be more effective than antipsychotics or antidepressants monotherapy, as reported by Meyers et al, 64 who found that the combination treatment of olanzapine plus sertraline was not only more effective than monotherapy but also equally tolerated.
Psychotherapy in Geriatric Depression
As for younger adults, also for older people psychotherapeutic approaches are to be encouraged, even in the presence of cognitive decline, since that treatment’s versatility gives the therapist the opportunity to adapt it to the patient’s needs and characteristics and to his/her physical and emotional environment.
In the following paragraphs a brief overview of the principal psychotherapy approaches available for older persons with depression is shortly provided.
Problem Adaptation Therapy (PATH)
PATH is a home-delivered psychosocial intervention, which has shown to lead to significant positive results in elderly with depression, by providing help in emotional regulation. 65 , 66 This kind of therapy puts the focus on strategies personalized on each patient’s needs (ie memory and organizational deficits, behavioral/functional limitations, interpersonal tension, social isolation and anhedonia). 65 PATH looks to lessen the negative impact of emotions by improving pleasurable activities, using a problem-solving approach and integrating environmental adaptations and compensatory strategies, for instance using calendars, checklists and strategies to sustain or shift attention.
Engage Therapy
This stepped therapy targets behavioral domains grounded on neurobiological constructs using simple and efficient behavioral techniques. 31 The intervention aims at modulating patient’s response using the “reward exposure” strategy, working on three main behavioral domains, ie “negativity bias” (negative valence system dysfunction), “apathy” (arousal system dysfunction), and “emotional dysregulation” (cognitive control dysfunction), and add strategies targeting these domains.
Problem Solving Therapy (PST)
PST is an 8-week intervention that consists in a seven-step process to solve problems, including problem orientation that directs patient attention to one problem at a time, problem definition that helps patients select relevant information to determine what the root problem is, goal setting that focuses attention to the desired outcome, brainstorming that helps patients consider different ways for reaching the goal, decision-making, to evaluate the alternative solutions likelihood and picking the best choice, and action planning that involves a step-by-step plan for the patient to implement his/her solution. 67
Supportive Therapy
This home-delivered psychotherapy focuses on nonspecific therapeutic factors as facilitating expression of affect, conveying empathy, highlighting successful experiences, and imparting optimism. Supportive Therapy reduces depression and disability in older patients with major depression, cognitive impairment, and disability. 65
Interpersonal Therapy
Interpersonal Therapy is a psychodynamic therapy that focuses on complicated grief, role transition, role dispute/interpersonal conflicts, and interpersonal deficits. 68 During the first phase of treatment, therapists help patients to explore and understand depressive symptoms through a psychoeducational approach. In later phases, problems are identified and understood in the interpersonal context. In the final phase, the therapist focuses on the gains and limitations of therapy and the prevention of relapses. 68
Computerized Cognitive Remediation (CCR)
CCR has demonstrated improvements in mood and self-reported function in depressed patients similar to those obtained through the Problem Solving Therapy. 81 CCR is suitable for patients with an MMSE score of at least 24/30. 68 It makes use of a video game to treat depression (EVO), personalized, self-administered and continuously adapted to the patients’ aptitude both at baseline and progress in treatment. 67 Unlike Problem Solving Therapy, the EVO participants showed generalization to untrained measures of working memory and attention, as well as negativity bias. CCR is relatively inexpensive and can be used at the patients’ homes, thus minimizing barriers to access of care, common in older adults. 31
Electroconvulsive Therapy (ECT)
An effective treatment for depression in elderly population, available from mental health specialists, is electroconvulsive therapy (ECT). 69 In ECT, an electrical stimulus is given for a brief period to produce a generalized seizure. The treatment is effective especially for psychotic depression, severe suicidality, treatment-refractory depression, catatonia, and depression with severe weight loss and anorexia, moreover, is indicated for older old (≥80 years). 70 A meta-analysis of the cognitive effects of ECT suggests its relative safety and the transient character of its effects on cognition. 71 Compared to antidepressants, ECT induces a higher speed of remission. 72
Practical Guidance for Depression Diagnosis and Treatment in the Elderly: A Pocket Guide for the Daily Clinical Management
If the proper recognition of geriatric depression remains at current challenge, the key aspects and main evidence presented here, along with a long interdisciplinary team clinical experience, lead to the identification of some guidelines to optimize the recognition and the adequate differential diagnosis of depression in the elderly. All the contents discussed below are summarized in the pocket guide, as a practical reference for a comprehensive diagnostic procedure in everyday clinical practice (see Figure 1 ).

Pocket guide for the assessment and management of geriatric depression in everyday clinical practice.
Clinicians should carefully consider depression among possible differential diagnosis, particularly when: patients refer to their attention with vague complaints as pain, fatigue and diffuse symptoms and/or suffer from anxiety or sleep disturbances; some clues are evident, such as poor personal hygiene, flat affect and slumped posture; the patient tends to frequently use healthcare resources, as calls or visits to practitioners. 46 , 48
In these cases, an accurate screening for the underlying risk factors and a collection of anamnestic data, which include medical, psychological and cognitive remote and recent history, is crucial to evaluate all potential contributing or protecting factors. Furthermore, to assess the individual’s protective factors (that mainly deal with aspects related to social network, hobbies, physical activity or personal interests) will also have a positive clinical implication in the management and treatment of depressive symptoms from a non-pharmacological point of view, by knowing the activities that could be pleasant and stimulating, as well as his or her personal resources.
Moreover, caregivers and families can be helpful, since they may provide information about the patient’s mood, behavior and general functioning. In fact, they could notice relevant changes that are not reported by the patient, especially if she or he has poor insight, as in the case of the co-occurrence of cognitive impairment.
When talking to patients, instead, it is important to adequate to the social and cultural background of older adults. As discussed in the previous sections, they are not used to deal with mental health issues and to verbally express concerns about their mood. Thus, the clinician should prefer to use expressions such as “Are you feeling low/down?” instead of directly asking “Are you depressed?” in order to address the stigma, and discuss mental health referral in the broader context of other medical conditions to increase the acceptability. 38 At the same time, all the healthcare professionals should promote the sensitization of the elderly to mood disorders and more generally to mental health, so that they can themselves become more attentive and aware in recognizing their emotional and psychological difficulties.
Clinicians can count on several validated tools to quantitatively assess the presence and severity of depression, namely self-report scales, clinician rating scales and structured interviews. Despite their popularity and their clear advantages, some considerations have to be taken into account when dealing with older adults. First of all, these tools were mostly developed for young adults, so they do not always catch the appropriate features for the elderly. 73 This also falls on their validity and reliability, which are strictly related to the population they are based on. 74 Self-reports are widely used because of their quickness and ease of administration. However, they are susceptible to some respondent’s characteristics, such as low educational attainment or cognitive impairment, which can influence the true comprehension of questions or of the response format. 75 In general, in the case of older adults with cognitive impairment, it is preferable to avoid self-reports and use alternative assessment methods that include direct observation and family reports. 7 Moreover, especially for patients with comorbidities, items with somatic content may need further clarifications, since somatic symptoms could be misattributed to depression. 76 Lastly, visual impairment can obstacle the completion of self-report scales: in these cases, the clinician can either propose an enlarged copy of the scale or administrate it orally. The use of clinician rating scales overcomes some of these issues, since they are based on the direct observation of a trained professional. If clinician rating scales offer a more accurate measurement of depression, it has been found that they are less sensitive in detecting changes in mild forms of depression. 77 Structured interviews offer the possibility to facilitate the comprehension of questions, as well as to deeper investigate aspects that need to be better clarified, as the nature of somatic symptoms; however, because of the time and skills requested for their administration, their utility is limited. 78 Overall, there is no single superior assessment method; rather, it is important that clinicians are aware of their strengths and shortcomings and informed about the psychometric properties of the main tools, so that they can choose the most appropriate instrument depending on the characteristics of the individuals. Moreover, using multiple methods and sources of information (ie, multidimensional assessment) has been shown to be the most effective approach. 78
When depressive symptoms are detected and a diagnosis of LLD is probable, among all the other factors, also the domestic and family context has to be looked at, that is, whether there are dynamics that can exacerbate the depressive symptomatology of the patient. This could be the case, for example, of a dysfunctional interaction in the patient-caregiver dyad or of some psycho-affective characteristics of the caregiver himself (for example, if he or her is depressed as well), likewise tensions in family relationships or other health or financial issue of relevant psychological impact.
Lastly, it is important to exclude somatic causes of depression and to characterize a depressive episode or symptoms through patient history, clinical examination, laboratory tests, and/or imaging. In fact, LLD can per se be distinguished into a proper LOD or the recurrence of an EOD and, as stated, this has some clinical implications. Alternatively, depression can be secondary to a general medical condition or to a substance or medication use, considering that multimorbidity and polypharmacy are extremely common conditions among older adults. 79 Moreover, depressive symptoms could be the manifestation of a cerebrovascular disease or of a prodromal stage of AD, thus having a primarily organic origin. It is also important, in any case, to repeat when possible both the instrumental examinations (namely imaging techniques for the investigation of regional brain glucose metabolism, as FDG-PET) and the administration of cognitive and/or psychological screening tools in order to re-evaluate the overall diagnosis at a follow-up after 6–9 months. In fact, since LLD is a treatable and reversible condition, when a diagnosis of depression is made and a pharmacological or non-pharmacological treatment has been proposed, there should be evidence of efficacy. Otherwise, the question arises if the depressive symptoms observed were secondary to another cause (so, the diagnosis was incorrect) or the therapeutic approach chosen was not the most suitable one.
Depression and Cognitive Impairment: How to Address Differential Diagnosis?
Whereas depressive and cognitive disorders often coexist in the elderly, it is crucial to distinguish a geriatric depression that includes cognitive deficits from a mild dementia with depressive symptoms. What needs to be determined from a clinical point of view, in particular, is whether or not the picture observed will evolve into dementia.
Time is a first important criterion: while in the case of dementia symptoms will develop with a slow progression over several years, depressive symptomatology onset can be dated with more precision and the progression of symptoms is more rapid. 48 , 80 Another relevant cue concerns awareness. Patients with reversible dementia complain more about their cognitive disturbances, highlighting their failures and disability and precisely describing the pattern of their deficits; older adults with dementia, on the contrary, usually lack insight and their description of cognitive loss is vague. 80
From a neuropsychological point of view, evidence has been described about a different characterization of cognitive profiles of patients with AD and depression that can be striking in the differential diagnosis.
First of all, patients with LLD show a prominent dysexecutive profile, with a slight impairment in global cognition. 21 Conversely, a broader cognitive impairment, with significant deficits of orientation, language, praxis and memory is typical of AD. 81 Secondly, although a memory disturbance is visible in both AD and LLD, they have a different functional origin. The episodic memory impairment of AD, due to hippocampal damage, is defined by a recall deficit that does not improve with cueing or recognition testing, since storage processes are primarily affected. 82 Depression, instead, leads to an insufficient allocation of attentional resources and executive dysfunction that affect encoding or retrieval strategies, 83 without a pure storage deficit. Thus, a differential diagnosis can be made with specific memory testing based on effective and specific encoding of information and retrieval facilitation with cueing. 82 Inefficacy of cueing and a flat learning curve despite exposure is typical of AD, while an improvement with exposure and a normal recall with retrieval cues are distinctive features of depression. 36
In general, patients with depression have a suboptimal cognitive performance due to poor motivation that leads them to give up the task more easily, not pay enough attention and use ineffective strategies, so their overall performance is more influenced by the cognitive load of the task and the extent to which it relies on executive functions. 83
In addition to all the steps that have to be gone through, and the factors that have to be taken into account for a comprehensive assessment that includes depression among the differential hypothesis, some general guidelines are here suggested about organizational aspects that can be implemented to improve the detection of depressive symptoms in the elderly.
First, given the predominance of somatic symptoms in late-life depression, as well as their tendency to focus more on their physical (rather than mental) issues, it is plausible that older adults who suffer from depression do not spontaneously refer to a mental health professional at first, but to other figures, such as general practitioners, physicians or other health professionals. For this reason, it would be important to improve the knowledge about late-life depression presentation, as well as the capacity to carry out screening activities, of specialists of other disciplines. In fact, although a formal diagnosis of depression is not part of their role, they could improve the detection of potential cases because of their position, as it is the case of occupational and physical therapists, nurses or general practitioners. 45
Furthermore, different professional figures, as psychiatrists, geriatricians, psychologists and neuropsychologists, often have to interface with older adults’ depressive symptoms in the presence of multimorbidity and/or cognitive deficits, and thus answer questions concerning the differential diagnosis of depression. It is of paramount importance for each specialist to evaluate individuals in their whole complexity. In this regard, a multidimensional assessment should always be provided, in order to take into account all the aspects discussed above, such as risk and protective factors, medical and psychological history, social context and recent life events. Moreover, when appropriate, specialists should choose a multidisciplinary approach, referring patients to other professionals that can have a role in the differential diagnosis or in identifying the most appropriate therapeutic option. When possible, it would be a valuable resource for figures with different and complementary competences to work together.
For example, in the specific case of older adults with depressive symptoms with a subjective perception or signs of cognitive impairment, geriatricians and neuropsychologists could manage outpatient visits and consultations in wards together, considering the tangled characteristics of LLD discussed above. In this way, these professional figures can provide a first screening of cognitive functioning and the characterization of some deficits that will help in the differential diagnosis between depression and dementia. Moreover, this synergy can help to consciously investigate the presence of a mood disorder and, where necessary, to offer to the patient a more accurate psychological and cognitive assessment, targeted medical investigations and therefore a tailored treatment.
In case older adults are aware of having a mood problem, they mainly refer to the psychiatrist. Notwithstanding the crucial role and competence of psychiatrists in this context, it is still important for them to consider older adults in their whole complexity. In this regard, they should provide a multidimensional assessment that takes into account all the aspects previously stated (ie, risk and protective factor, medical and psychological history, social context, recent life events…) and, when appropriate, have a multidisciplinary approach, referring patients to other professionals that can have a role in the differential diagnosis or in identifying the most appropriate therapeutic approach.
Another professional figure that frequently has to cope with the differential diagnosis of depression are geriatricians, since in their clinical practice they consult with patients who show signs or have a subjective perception of cognitive or neuropsychiatric problems. Both in outpatient visits and in consultations in wards, it could be a valuable resource for the geriatricians to be assisted by a neuropsychologist. For the characteristics of LLD discussed above, it would be beneficial for patients if the geriatrician and the psychologist/neuropsychologist could work together in the assessment of older adults, both for the outpatient visits and for the consultation inwards.
In this way, these professional figures can synergistically provide a first screening of cognitive functioning and the characterization of some deficits that will help in the differential diagnosis between depression and dementia. Moreover, it can help to consciously investigate the presence of a mood disorder and, where necessary, to offer the patient a more accurate psychological and cognitive assessment, targeted medical investigations and therefore a tailored treatment.
In conclusion, as a general indication, it is overall important to periodically screen older adults for depression. Furthermore, patients who already are in treatment for depression need to be periodically re-evaluated, since the persistence of a depressive symptomatology suggests that the therapeutic approach chosen (pharmacological or not) should be revised.
Conclusions
This review, beyond reviewing depression, its clinical main characterizations and current challenges had the goal to propose a few guidelines born from the “every-day” clinical activity carried-out on this population. A “pocket guide” has been produced in order to hopefully orient clinicians in their daily clinical management of depression and in sensitizing different professionals to a comprehensive, global and multidisciplinary assessment of a complex disorder affecting complex individuals such as the elderly are. Shortly, after a first multidimensional assessment, clinicians are provided with clinical cues orienting their diagnostic process. Whereas the diagnosis of depression is confirmed, by also excluding other co-occurrent/different pathologies (ie cognitive decline), a first- and second-line therapeutic approaches are suggested, including both pharmacological and non-pharmacological options. Lastly, follow-ups and periodic clinical assessments are strongly recommended to monitor individuals over time.
Finally, by considering not only the risk, but also the protective factors that may help people in facing depression along late life, this review also indirectly encourages clinicians in promoting active social, cognitive and psycho-affective lifestyles in the elderly, as crucial, modifiable factors that may significantly influence the natural course of their aging.
The authors report no conflicts of interest in this work.
Depression and Aging
Depression is not a normal part of growing older.
Depression is a true and treatable medical condition, not a normal part of aging. However older adults are at an increased risk for experiencing depression. If you are concerned about a loved one, offer to go with him or her to see a health care provider to be diagnosed and treated.
Depression is not just having “the blues” or the emotions we feel when grieving the loss of a loved one. It is a true medical condition that is treatable, like diabetes or hypertension.
- How do I know if it's Depression?
- How is depression different for older adults?
- How many older adults are depressed?
- How do I find help?
- Additional Resources
How do I know if it’s Depression?
Someone who is depressed has feelings of sadness or anxiety that last for weeks at a time. He or she may also experience–
- Feelings of hopelessness and/or pessimism
- Feelings of guilt, worthlessness and/or helplessness
- Irritability, restlessness
- Loss of interest in activities or hobbies once pleasurable
- Fatigue and decreased energy
- Difficulty concentrating, remembering details and making decisions
- Insomnia, early–morning wakefulness, or excessive sleeping
- Overeating or appetite loss
- Thoughts of suicide, suicide attempts
- Persistent aches or pains, headaches, cramps, or digestive problems that do not get better, even with treatment
How is Depression Different for Older Adults?
- Older adults are at increased risk. We know that about 80% of older adults have at least one chronic health condition, and 50% have two or more. Depression is more common in people who also have other illnesses (such as heart disease or cancer) or whose function becomes limited.
- Older adults are often misdiagnosed and undertreated. Healthcare providers may mistake an older adult’s symptoms of depression as just a natural reaction to illness or the life changes that may occur as we age, and therefore not see the depression as something to be treated. Older adults themselves often share this belief and do not seek help because they don’t understand that they could feel better with appropriate treatment.

How Many Older Adults are Depressed?
The good news is that the majority of older adults are not depressed.
Some estimates of major depression in older people living in the community range from less than 1% to about 5% but rise to 13.5% in those who require home healthcare and to 11.5% in older hospitalized patients.
How do I Find Help?
Most older adults see an improvement in their symptoms when treated with antidepression drugs, psychotherapy, or a combination of both. If you are concerned about a loved one being depressed, offer to go with him or her to see a health care provider to be diagnosed and treated.
If you or someone you care about is in crisis, please seek help immediately.

Visit a nearby emergency department or your health care provider’s office
Call the toll-free, 24-hour hotline of the national suicide prevention lifeline at 988 to talk to a trained counselor.
- National Institute on Aging, Depression and Older Adults
- National Institute on Mental Health, Older Adults, and Depression
- PEARLS Toolkit (Program to Encourage Active, Rewarding Lives), CDC University of Washington Prevention Research Center [PDF – 588 KB]
- SAMHSA (Substance Abuse and Mental Health Services Administration) Toolkit for Treatment of Depression in Older Adults
- Loneliness and Social Isolation in Older Adults
To receive email updates about Alzheimer's Disease and Healthy Aging, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

- Current Issue
- Upcoming Issue
- Guidance to Authors
- Editorial Executive Board
- Individual Details
- Become a Peer Reviewer
- Proof Readers
- Terms & Conditions
- Submit a Manuscript
- Manuscript Guidance
- Add Conference
- Add Job Advert
Depression in older adults
Claire Pocklington
Introduction
Depression is a clinical syndrome. The International Classification of Diseases (ICD) diagnostic classification systems describe three core symptoms of depression; low mood, anhedonia and reduced energy levels 1 . Other symptoms include impaired concentration, loss of confidence, suicidal ideation, disturbances in sleep and changes in appetite. Symptoms must have been present for at least a period of two weeks for a diagnosis of depression to be made. Major depression refers to the presence of all three core symptoms and, in accordance with ICD criteria, at least the presence of a further five other symptoms 1 . See Table 1 for severity criteria of a depressive episode according to ICD criteria.
Table 1: Severity criteria of a depressive episode according to ICD-10 1
Depressive symptoms, which can be clinically significant, can be present in the absence of a major depressive episode. Depressive symptoms are those that do not fulfil diagnostic criteria for a diagnosis of depression to be made. Depressive symptoms can be collectively referred to as sub-threshold depression, sub-syndromal depression or minor depression 2 .
It has been proposed that there are two types of depression; early-onset and late-onset depression. Late-onset depression refers to a new diagnosis in individuals aged 65 years of age or older. Over half of all cases of depression in older adults are newly arising (i.e. the individual has never experienced depression before) and thus late-onset type depression. Late-onset type depression is associated more with structural brain changes, vascular risk factors and cognitive deficits. It has been suggested that late-onset depression could be prodromal to dementia 3 .
The Kings Fund has estimated that by 2032 the proportion of older adults aged 65-84 years old will have increased by 39% whereas the proportion over the age of 85 years will have increased by 106% 4 . This increase in population will consequently see the incidence and prevalence of depression rise. By 2020 it is estimated that depression will be the second leading cause of disability in the world regardless of age 5 . Recognising, and so diagnosing, depression in older adults will become more important because of a greater demand on existing healthcare services and provisions, due to physical health consequences, impact upon healthcare utilisation and greater economic healthcare costs.
Presentation of depression in older adults
The presentation of depression in older adults is markedly different to that in younger adults. The most significant and fundamental difference in presentation in older adults is that depression can be present with the absence of an affect component, i.e. subjective feelings of low mood or sadness are not experienced 3,6-9 . The absence of an affective component is referred to as ‘depression without sadness’ 8-9 . It is common instead for older adults to report a lack of feeling or emotion when depressed 8-9 .
Anhedonia is also less prevalent in this population. However, reduced energy levels and fatigue are frequently reported 8-9 .
Compared to younger adults, psychological symptoms of depression occur more frequently and are more prevalent in older adults 10 . Such psychological symptoms include feelings of guilt, poor motivation, low interest levels, anxiety related symptoms and suicidal ideation. The presence of irritability and agitation are key features as well 7 . Hallucinations and delusions are also more common in older adults, particularly nihilistic delusions (i.e. a person believing their body is dead or a part of their body is not working properly or rotting).
Cognitive deficits are characteristic of depression in older adults 7,11 and are described as ‘substantial and disabling’ 12 . Such deficits mainly concern executive function 13-14 . Pseudodementia is a phenomenon seen in older adults 15 . The term refers to cognitive impairment secondary to a psychiatric condition, most commonly depression 16 . Pseudodementia has become synonymous with depression. Pseudodementia can be mistaken for an organic dementia and so older adults who are depressed can present primarily to mental health services with memory problems. Pseudodementia is classically associated with ‘don’t know’ answers, whereas older adults with a true dementia will often respond with incorrect answers 17 .
‘Depression-executive dysfunction syndrome’ is a more specific and descriptive term to describe the cognitive deficits found in older adults with depression 14 . It is associated with psychomotor retardation, which can be a core feature of depression in this population 7,14,18 . Psychomotor retardation describes a slowing of movement and mental activity 19 . Like pure cognitive deficits, psychomotor retardation contributes significantly to functional impairment 19 . Both executive dysfunction and psychomotor retardation have been found to be related to underlying structural changes in the frontal lobes 14, 20-21 . Psychomotor retardation is further related to white matter changes in the motor system, which leads to impaired motor planning 21 . There is conflicting evidence of whether the presence of psychomotor retardation is related to depression severity 18-19 .
Somatisation and hypochondriasis are associated with depression in older adults and increasing age in general 22-23 . Somatisation is often overlooked in older adults by healthcare professional who actively search to attribute such symptoms to a physical cause. Somatisation is more common in those who have physical comorbidities. Somatisation in older adults is associated with structural brain changes and cognitive deficits 24 .
Depression in older adults is associated with functional impairment cognitively, physically and socially 7,12,25 . Such functional impairment is linked to loss of independent function and increased rates of disability 26 . Withdrawal from normal social and leisure activities can be marked 7,25 . Social avoidance reduces interaction with others and is often a maintaining factor for depression 25 .
Self-neglect is a classical feature of depression 7 , with the presence of depressive symptoms in older adults being predictive of it 27 . Behavioural disturbances can be a common mode of presentation, especially for older adults living in institutionalised care 6-7 . Behavioural disturbances include incontinence, food refusal, screaming, falling and violence towards others 7 .
Diagnostic difficulties
Depression in older adults has been a condition that has constantly been under-recognised. Several issues account for this. Firstly, phenomenological differences are present. Many have argued that phenomenological issues contribute heavily to diagnostic difficulties 28 ; both the DSM and ICD classification systems do not have specific diagnostic criteria for depression in older adults. Potentially invalid diagnostic criteria for depression in older adults could result in fundamental difficulties in understanding, with consequent impact on both clinical practice and research.
Diagnostic difficulties are also encountered because depression in older adults can present with vague symptoms, which do not correspond to the classical triad of low mood, low energy levels and anhedonia, which can all be cardinal symptoms in a younger population. Reports of fatigue, poor sleep and reduced appetite can be attributed to a host of causes other than depression and therefore it is no surprise that a diagnosis of depression is overlooked and goes undetected by healthcare professionals 29 .
The absence of an affective component (i.e. low mood) can lead to healthcare professionals disregarding the potential for the presence of depression and consequently not exploring for other symptoms.
Furthermore, symptoms of depression, especially somatic ones, are often attributed to physical illnesses. Depressive somatic symptoms often lead to a diagnosis of depression being over looked; such symptoms ‘mask’ the clinical diagnosis of depression and hence the term ‘masked depression’ 30 . Depressive somatic symptoms – e.g. low energy levels, insomnia, poor appetite and weight loss - are often attributed to physical illness and/or frailty by both the individual and healthcare professional 7-8, 31 .
Further complicating diagnostic difficulties and under-recognition is the fact that older adults are less likely to report any symptoms associated with mental health problems and ask for help in the first place 7,10,32 ; explanations for this include older adults being less emotionally open, having a sense of being a burden or nuisance, and believing symptoms are a normal part of ageing or secondary to physical illness 7,10,29,33 .Older adults also have a reluctance to report mental health problems due to their perception of associated stigma; many older adults hold the view the mental health problems are shameful, represents personal failure and leads to a loss of autonomy 7 .
There is an overlap between symptoms of depression and symptoms of dementia. It is quite common for older adults with dementia to initially present with depressive symptoms. Depression has a high incidence in those with dementia, especially those with vascular dementia. Depression is particularly difficult to diagnose in dementia due to communication difficulties; diagnosis is often based on observed behaviours 8,33 .
Depression and comorbidity in older adults
In those with pre-existing physical health problems, depression is associated with deterioration, impaired recovery and overall worse outcomes 34 . For example, the relative risk of increased morbidity related to coronary heart disease is 3.3 in comparison to individuals without depression 35 . Mykletun et al. established that a diagnosis of depression in older adults increased mortality by 70% 36 . Several causative routes account for poor physical illness outcomes. Older adults with depression are less likely to report worsening health. Depressive symptomatology indirectly affects physical illness through reduced motivation (often secondary to feelings of helplessness and hopelessness) and engagement with management. Poor compliance with management advice, notably adherence to medications is observed 37 . Feelings of hopelessness, helplessness and negativity will contribute to the failure to seek medical attention in the first place or report worsening health when seen by a healthcare professional.
Depression affects biological pathways directly, which impairs physical recovery. Such biological effects include pro-inflammatory factors, metabolic factors, impact upon the hypothalamic-pituitary axis and autonomic nervous system changes 38 .
Older adults who are depressed are more likely to have existing physical health conditions and more likely to develop physical health conditions 15 . Depression is particularly associated with specific physical illnesses; cardiovascular disease and diabetes mellitus. A study by Win et al . found that cardiovascular mortality is higher in older adults with depression because of physical inactivity; the study established that physical inactivity was accountable for a 25% increased risk in cardiovascular disease 39 . The relationships between depression and cardiovascular disease and depression and diabetes have been described as “bidirectional” 38 .
Higher incidents of cardiovascular disease and diabetes mellitus are seen in people with depression regardless of age. A study by Brown et al. found that older adults with depression had a 1.46 relative risk increase for developing coronary heart disease compared to those without depression 40 . The hypothalamic-pituitary axis dysfunction found in depression leads to increased levels of cortisol, which in turn, increases visceral fat. Increased visceral fat is associated with increased insulin resistance, promoting diabetes mellitus, and increased cardiovascular pathology 38 .
Depression is a risk factor for the subsequent development of dementia; this is especially so if an older adult has no previous history of depression (i.e. depression is late-onset) 13 .
Healthcare utilisation and economic impacts
Older adults are less likely to report depressive symptoms to healthcare professionals explaining the under-utilisation of mental health services for depression 32,41 . Despite older adults under-utilising mental health services they over utilise other healthcare services 26,41 . For example, those presenting with non-specific medical complaints or somatisation have been found to have an increase use of healthcare services. Non-specific medical complaints and somatisation lead to an unnecessary use of resources, such as unnecessary consultations with healthcare professionals and investigations 41 . Increase in service utilisation means an increase in the associated economic cost of depression in older adults 41-43 .
Healthcare costs of older adults with a comorbid physical illness and depression are far greater than those without depression – findings in diabetes mellitus are a good example 43 . The majority of the increased healthcare costs are associated with the chronic physical disease and not the care and treatment of the depression 44 . Poor compliance with physical illness management is associated with missed appointments and a greater number of hospital admissions, which both have financial implications.
Aetiology and associations of depression in older adults
Late-onset type depression in older adults has been associated with the term ‘vascular depression’ 45-47 . Studies have found a significant higher rate and severity of white matter hyperintensities on MRI imaging in older adults with depression compared to those without depression 46,48,50 . White matter hyperintensities represent damage to the nerve cells; such damage is a result of hypo-perfusion of the cells secondary to small blood vessel damage 49 . White hyperintensities are associated with vascular risk factors (e.g. age, hypertension, hypercholesterolaemia, obesity, diabetes mellitus, smoking) and are linked to cerebrovascular disease, such as stroke, vascular dementia. A relationship has been found between psychosocial stress and consequent development of vascular risk factors, which further supports the hypothesis of ‘vascular depression’ 46 . Clinically, ‘depression-executive dysfunction syndrome’ and psychomotor retardation are associated with vascular changes 48 .
In older adults with depression, white matter hyperintensities are associated with structural changes to corticostriatal circuits and subsequent executive functional deficits. Loss of motivation or interest and cognitive impairment in depression are hallmark features of structural brain changes associated with the frontal lobes, which in turn are associated with a vascular pathology 20 . A study by Hickie et al. established that white matter hyperintensities in older adults with depression are associated with greater neurological impairment and poorer response to antidepressant treatment 50 . It is not fully understood why vascular depression responds less well to antidepressants; poor response has been linked directly to vascular factors but has also been associated with deficits in executive function 46-47 .
The relationship between cerebrovascular disease and depression is described as ‘bi-directional’ 45,51 ; depression has been found to cause cardiovascular disease and vice versa 51 . Baldwin et al. direct the reader to the presence of post-stroke depression and the occurrence of depression in vascular dementia 45 .
Younger and older adults share a number of fundamental risk factors for depression; such as female gender, personal history and family history 7 . Older adults have additional risk factors related to ageing, which are not just physiological in nature.
Age related changes:
Age related changes occurring in the endocrine, cardiovascular, neurological, inflammatory and immune systems have been directly linked to depression in older adults 3 .
The normal ageing process sees changes to sleep architecture and circadian rhythms with resultant changes to sleep patterns 52 . Thus sleep disturbances are common in older adults and positively correlated to advancing age 52 ; over a quarter of adults over the age of 80 years report insomnia, and research has well-established that this is a risk factor for depression 53-54 . A meta-analysis by Cole et al . found sleep disturbances to be a significant risk factor for the development of depression in older adults 53 .
Sensory impairment:
Sensory impairments, whether secondary to the ageing or a disease process, are risk factors 53,55 . Research has found that hearing and vision impairments are linked to depression 56 . A sensory impairment can lead to social isolation and withdrawal, which, in turn, are further risk factors for depression.
Physical illness:
Physical illness, regardless of age, is a risk factor for depression. Older adults are more likely to have physical illnesses and so in turn are more at risk of depression. See Table 2. Physical illness is associated with sensory impairments, reduced mobility, impairment in activities of daily living and impaired social function, all of which can lead to depression. Physical illnesses associated with chronicity, pain and disability pose the greatest risk for the subsequent development of depression 7,53,55 . Physical illness affecting particular systems of the body, such as the cardiovascular, cerebrovascular and neurological, are more likely to cause depression 3 . Essentially, however, any serious or chronic illness can lead to the development of depression. It should be noted that a large proportion of older adults have physical illness but do not experience depression symptoms, therefore other factors must be at play 5,57 .
Treatments of physical illness are directly linked to aetiology in depression, for example, certain medications are known to cause depression; cardiovascular drugs (e.g. Propranolol, thiazide diuretics), anti-Parkinson drugs (e.g. levodopa), anti-inflammatories (e.g. NSAIDs), antibiotics (e.g. Penicillin, Nitrofurantoin), stimulants (e.g. caffeine, cocaine, amphetamines), antipsychotics (e.g. Haloperidol), anti-anxiolytics (e.g. benzodiazepines), hormones (e.g. corticosteroids), and anticonvulsants (e.g. Phenytoin, Carbamazepine) 7,29 . Polypharmacy is present in many older adults further increasing the risk of depression. Pharmacokinetic and pharmacodynamic age related changes also contribute to an increased risk of medication induced depression in older adults.
Table 2: Table of physical illnesses associated with depression 3,7
Dementia is common in old age and those with dementia are at higher risk of developing depression compared to those who do not have it 58 . 20-30% of older adults with Alzheimer’s disease have depression 59 . Depression is a risk factor for the subsequent onset of dementia.
Psychosocial:
When compared to younger adults, older adults are at a greater risk of developing depression due to the increased likelihood of experiencing particular psychosocial stressors, in particular adverse life events. Stressors include lack of social support, social isolation, loneliness and financial hardship. Financial hardship and functional impairment often sees older adults downsizing in property. Deteriorating physical health often sees older adults no longer being able to manage living independently at home necessitating a move into institutional living. Bereavement, especially spousal, and the associated role change that follows this are risk factors for depression 3 .
Sub-threshold depression:
Sub-threshold depression is an established risk factor for major depression.
Prevalence and epidemiology
The prevalence of depression in older adults in England and Wales was found to be 8.7% in 2007; however, if those with dementia are included this figure rises to 9.7% 60 . A meta-analysis by Luppa et al. established a 7.2% point prevalence of major depression and a 17.1% point prevalence of depressive disorder in older adults 61 . The projected lifetime risk of an older adult developing major depression by the age of 75 years old is 23% 62 .
Sub-threshold depression is 2-3 times more prevalent than major depression in older adults 26,63 . These depressive symptoms are often clinically relevant 26,29 . 8-10% of older adults per year with sub-threshold depressive symptoms go onto develop a major depressive episode 63 .
Incidence and prevalence are greater in women; 10.4% of women over the age of 65 years have depression compared to 6.5% of men 60 . Older women are more likely to experience recurrent episodes of depression compared to older men 62 . The gender gap in incidence and prevalence becomes narrower with increasing age 3 . It should be acknowledged however that women are more likely to present to healthcare services and seek help in comparison to men 64-65 .
The prevalence of major depression in older adults varies by setting 66 . Highest rates are seen in long-term institutional care and inpatient hospital settings 67 . Table 3 summaries prevalence rates of major depression by setting.
Table 3: Prevalence rate of major depression by setting 7, 67
Prognosis of depression in older adults
Depression in older adults is associated with a slower rate of recovery 9 , worse clinical outcomes compared to younger adults 3 and is associated with higher relapse rates 68 . Worse prognosis in older adults correlates with advancing age, physical comorbidities and functional impairment 70 . The structural brain changes associated with depression in older adults are linked, as discussed, to poorer treatment response.
Morbidity and mortality associated with depression can be described as primary or secondary; primary morbidity and mortality arises directly from the depressive illness; whereas secondary morbidity and mortality arises from physical health problems, which are secondary to depression.
Outcomes from sub-threshold depression are on par with those of major depression; however sub-threshold depression which develops into major depression is associated with worse outcomes 2 .
Proportionally more people over the age of 65 years commit suicide compared to younger people 71 . Depression is the leading cause of suicide in older adults 29,71 ; one study reports that 75% of older adults who killed themselves were depressed 72 .
The vast majority of older adults who commit suicide have had contact with a health professional within the preceding month 9 ; this figure has been quoted as high as 70% 3 . This further supports and suggests the fact the depression is under-detected. Unlike younger adults, older adults are less likely to report suicidal ideation and can experience suicidal ideation without feeling low in mood 3,7 . Older adults have few suicide attempts, compared to younger adults, because their suicide methods are more lethal 13 .
- World Health Organization (WHO) 2001a. The World Health Report. Mental Health: New understanding, new hope., WHO.
- Cherubini, A., Nistico, G., Rozzini, R., Liperoti, R., Di Bari, M., Zampi, E., Ferrannini, L., Aguglia, E., Pani, L and Bernabei, R. 2012. Subthreshold depression in older subjects: An unmet therapeutic need. The journal of nutrition, health & aging, 16 , 909-913.
- Fiske, A., Wetherell, J. L. & Gatz, M. 2009. Depression in older adults. Annual review of clinical psychology, 5 , 363-389.
- The Kings Fund. 2014. Ageing Population [Online]. Available: http://www.kingsfund.org.uk/time-to-think-differently/trends/demography/ageing-population [Accessed October 1st 2014].
- Mathers, C. D. & Loncar, D. 2006. Projections of global mortality and burden of disease from 2002 to 2030. PLoS medicine, 3 , e442.
- Evans, M. 1995. Detection and management of depression in the elderly physically ill patient. Human Psychopharmacology: Clinical and Experimental, 10 , S235-S241.
- Evans, M. & Mottram, P. 2000. Diagnosis of depression in elderly patients. Advances in Psychiatric Treatment, 6 , 49-56.
- Alexopoulos, G. S. 2005. Depression in the elderly. The Lancet, 365 , 1961-1970.
- Arean, P. A. & Ayalon, L. 2005. Assessment and treatment of depressed older adults in primary care. Clinical Psychology: Science and Practice, 12 , 321-335.
- Mitchell, A. J., Rao, S. & Vaze, A. 2010. Do primary care physicians have particular difficulty identifying late-life depression? A meta-analysis stratified by age. Psychotherapy & Psychosomatics, 79 , 285-94.
- Butters, M. A., Mulsant, B. H., Houck, P. R., Dew, M. A., Nebes, R. D., Reynolds, C. F., Bhalla, R. K., Mazumdar, S., Begley, A. E., Pollock, B. G & Becker, J. T. 2004. Executive Functioning, Illness Course, and Relapse/Recurrence in Continuation and Maintenance Treatment of Late-life Depression: Is There a Relationship? The American Journal of Geriatric Psychiatry, 12 , 387-394.
- Butters, M., A, Whyte, E. M., Nebes, R. D., Bebley, A. E., Dew, M. A., Mulsant, B. H., Zmuda, M. D., Bhalla, R., Meltzer, C. C. & Pollock, B. G. 2004. The Nature and Determinants of Neuropsychological Functioning in Late-LifeDepression. Archives of General Psychiatry, 61 , 587-595.
- Alexopoulos, G. S., Meyers, B. S., Young, R. C., Kalayam, B., Kakuma, T., Gabrille, M., Sirey, J. A. & Hull, J. 2000. Executive dysfunction and long-term outcomes of geriatric depression. Archives of General Psychiatry, 57 , 285-290.
- Lockwood, K., A., Alexopoulos, G. S., Kakuma, T. & Van Gorp, W. G. 2000. Subtypes of cognitive impairment in depressed older adults. The American Journal of Geriatric Psychiatry, 8 , 201-208.
- Chapman, D. P & Perry, G. S. 2008. Depression as a major component of public health for older adults. Centres for Disease Control and Prevention, 7.
- Kang, H., Zhao, F., You, L., Giorgetta, C., Venkatesh, D., Sarkhel, S. & Prakash, R. 2014. Pseudo-dementia: A neuropsychological review. Annals of Indian Academy of Neurology, 17 , 147-154.
- Bieliauskas, L. A. & Drag, L. 2013. Differential Diagnosis of Depression and Dementia, New York, Springer.
- Beheydt, L., Schrijvers, D., Docx, L., Bouckart, F., Hulstijn, W. & Sabbe, B. 2014. Psychomotor retardation in elderly untreated depressed patients. Frontiers in Psychiatry, 5 , 196.
- Bennabi, D., Vandel, P., Papaxanthis, C., Pozzo, T. & Haffen, E. 2013. Psychomotor retardation in depression: a systematic review of diagnostic, pathophysiologic and therapeutic implications. BioMed Research International.
- Rapp, M. A., Dahlman, K., Sano, M., Grossman, H. T., Haroutunian, V. & Gorman, J. M. 2005. Neuropsychological differences between late-onset and recurrent geriatric major depression. American Journal of Psychiatry, 162 , 691-698.
- Walthers, S., Hofle, O., Federspiel, A., Horn, H., Hugli, S., Wiest, R., Strik, W. & Muller, T. J. 2012. Neural correlates of disbalanced motor control in major depression. Journal of Affective Disorders, 136 , 124-133.
- El-Gabalawy, R., Mackenzie, C., Thibodeau, M., Asmundson, G. & Sareen, J. 2013. Health anxiety disorders in older adults: conceptualizing complex conditions in late life. Clinical Psychology Review, 33 , 1096-1105.
- Shahpesandy, H. 2005. Different manifestation of depressive disorder in the elderly. Neuroendocrinology Letters, 26 , 691-5.
- Inamura, K., Tsuno., N., Shinagawa, S., Nagata, K & Nakayaman, K. 2015. Correlation between cognition and symptomatic severity in patients with late-life somatoform disorders. Aging and Mental Health, 19 , 169-174.
- Polenick, C. A. 2013. Behavioral activation for depression in older adults: theoretical and practical considerations. Association for Behavioral Analysis International, 36 , 35-55.
- Rinaldi, P., Mecocci, P., Benedetti, C., Ercolani, S., Bregnocchi, M., Menculini, G., Catani, M., Senin, U & Cherubini, A. 2003. Validation of the Five‐Item Geriatric Depression Scale in Elderly Subjects in Three Different Settings. Journal of the American Geriatrics Society, 51 , 694-698.
- Abraams, R. C., Lachs, M., Mcavay, G., Keohane, D. J., Bruce, M. L. 2002. Predictors of self-neglect in community-dwellings elders. American Journal of Psychiatry, 159 , 1724-30.
- Prakash, O., Gupta, L. N., Singh, V. B & Nagarajarao, G. 2009. Applicability of 15-item Geriatric Depression Scale to detect depression in elderly medical outpatients. Asian journal of psychiatry, 2 , 63-65.
- Birrer, R. B. & Vemuri, S. P. 2004. Depression in later life: a diagnostic and therapeutic challenge. American Family Physician, 69.
- Small, G. W. 1991. Recognition and treatment of depression in the elderly. The Journal of Clinical Psychiatry, 52, 11-22.
- Friedman, B., Conwell, Y., Delavan, R. R., Wamsley, B. R & Eggert, G. M. 2005. Depression and suicidal behaviors in Medicare primary care patients under age 65. Journal of general internal medicine, 20 , 397-403.
- Crabb, R. & Hunsley, J. 2006. Utilization of mental health care services among older adults with depression. Journal of Clinical Psychology, 62 , 299-312.
- Alexopoulos, G. S., Kiosses, D. N., Heo, M., Murphy, C. F., Shanmugham, B. & Gunning-Dixon, F.2005. Executive dysfunction and the course of geriatric depression. Biological Psychiatry, 58 , 204-10.
- Aroma, A., Raitasalo, A., Reunanen, O., Impivaara, M., Heliovaara, P. & Knekt, P. 1994. Depression and cardiovascular diseases. Acta Psychiatr Scand. Supple, 377, 77-82.
- Mykletun, A., Bjerkeset, O. & Overland, S. 2009. Levels of anxiety and depression as predictors of mortality: the HUNT study. British Journal of Psychiatry. 195: 118-125.
- Evans, M., Hammond, M., Wilson, K., Lye, M. & Copeland, J. 1997. Treatment of depression in the elderly: effect of physical illness on response. International Journal of Geriatric Psychiatry, 12 , 1189-94.
- Katon, W. J. 2011. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues in Clinical Neuroscience, 13 , 7-23.
- Win, S., Parakh, K., Eze-Nillam, C. M., Gottdiener, J. S., Kop, W. J. & Ziegeistein, R. C. 2011. Depressive symptoms, physical inactivity and risk of cardiovascular mortality in older adults: the cardiovascular health study. Heart, 97 , 500-505.
- Brown, J. M., Steward, J. C., Stump, T. E. & Callahan, C. M. 2011. Risk of coronary heart disease events over 15 years among older adults with depressive symptoms. The American Journal of Geriatric Psychiatry, 19 , 721-729.
- Speed, D. C. & Schneider, M. G. 2003. Mental health needs of older adults and primary care: Opportunity for interdisciplinary geriatric team practice. Clinical Psychology: Science and Practice, 10 , 85-101.
- Weeks, S. K., Mcgann, P. E., Michaels, T. K. & Penninx, B. W. 2003. Comparing Various Short‐Form Geriatric Depression Scales Leads to the GDS‐5/15. Journal of Nursing Scholarship, 35 , 133-137.
- Finkelstein, E. A., Bray, J. W., Chen, H., Larson, M. J., Miller, K., Tompkins, C., Keme, A. & Manderscheid, R. 2003. Prevalence and costs of major depression among elderly claimants with diabetes. Diabetes care, 26 , 415-420.
- Unutzer, J. & Schoenbaum, M. 2009. Healthcare costs associated with depression in medically ill fee-for-service Medicare participants. Journal of the American Geriatric Society, 57 , 375-584.
- Baldwin, R. C. 2000. Poor prognosis of depression in elderly people: causes and actions. Annals of Medicine, 32 , 252-6.
- Sneed, J. R., Culang-Reinlieb, M. E., Brickman, A. M., Gunning-Dixon, F. M., Johnert, L., Garcon, E. & Roose, S. P. 2011. MRI signal hyperintensities and failure to remit following antidepressant treatment. Journal of affective disorders, 135 , 315-20.
- Sneed, J. R., Rindskopf, D., Steffens, D. C., Krishnan, K. R. R. & Roose, S. P. P. 2008. The vascular depression subtype: evidence of internal validity. Biological Psychiatry, 64 , 491-7.
- Hickie, L., Simons, L., Naismith, S., Simons, J., Mccallum, J. & Pearson, K. 2003. Vascular risk to late-life depression: evidence from a longitudinal community study. Australian & New Zealand Journal of Psychiatry, 37 , 62-65.f
- Debette, S. & Markus, H. S. 2010. The clinical importance of white matter hyper intensities on brain magnetic resonance imaging; systematic review and meta-analysis. BMJ, 341.
- Hickie, I., Scott, E., Wilhelm, K. & Broadaty, H. 1997. Subcortical hyperintensities on magnetic resonance imaging in patients with severe depression--a longitudinal evaluation. Biological Psychiatry, 42 , 367-74.
- Gothe, F., Enache, D., Wahlund, L, O., Winblad, B., Crisby, M., Lokk, J. & Aarsland, D. 2012. Cerebrovascular diseases and depression: epidemiology, mechanisms and treatment. Panminerva Medica, 54 , 161-170.
- Van Someren, E. 2000. Circadian and sleep disturbances in the elderly. Experimental gerontology, 35 , 1229-1237.
- Cole, M. G. & Dendukuri, N. 2003. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. American Journal of Psychiatry, 160 , 1147-1156.
- Pigeon, W. R., Hegel, M., Unutzer, J., Fan, M. Y., Sateia, M. J., Lyness, J. M., Phillips, C. & Perlis, M. L. 2008. Is insomnia a perpetuating factor for late-life depression in the IMPACT cohort? Sleep, 31 , 481.
- Huang, C. Q., Dong, B, R., Zu, Z. C., Yue, J. R. & Liu, Q. X. 2010. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing research reviews, 9 , 131-141.
- Bernabei, V., Morini, V., Moretti, F., Marchiori, A., Ferrari, B., Dalmonte, E., De Ronchi, D. & Rita, A. 2011. Vision and hearing impairments are associated with depressive-anxiety syndrome in Italian elderly. Aging Mental Health, 15(4), 467-74
- Harpole, L. H., Williams, J. W., Olsen, M. K., Stechuchak, K. M., Oddone, E., Callahan, C. M., Katon, W. J., Lin, E. H., Grypma, L. M. & Unutzer, J. 2005. Improving depression outcomes in older adults with comorbid medical illness. General Hospital Psychiatry, 27 , 4-12.
- Conradsson, M., Rosendahl, E., Littbrand, H., Gustafson, Y., Olofsson, B. & Lovheim, H. 2013. Usefulness of the Geriatric Depression Scale 15-item version among very old people with and without cognitive impairment. Aging & mental health, 17 , 638-645.
- Tsuno, N. & Homma, A. 2009. What is the association between depression and Alzheimer's disease? Expert review of neurotherapeutics, 9 , 1667-1676.
- Mcdougall, F. A., Kvaal, K., Matthews, F. E., Paykel, E., Jones, P. B., Dewey, M. E., Brayne, C. 2007. Prevalence of depression in older people in England and Wales: the MRC CFA Study.[Erratum appears in Psychol Med. 2007 Dec;37(12):1796]. Psychological medicine, 37 , 1787-95.
- Luppa, M., Sikorski, C., Luck, T., Ehreke, L., Konnopka, A., Wiese, B., Weyerer, S., Konig, H. H. & Riedel-Heller, S. 2012. Age-and gender-specific prevalence of depression in latest-life–systematic review and meta-analysis. Journal of affective disorders, 136 , 212-221.
- Kessler, R. C., Mcgonagle, K. A., Nelson, C. B., Hughes, M., Swartz, M. & Blazer, D. G. 1994. Sex and depression in the National Comorbidity Survey. II: Cohort effects. Journal of affective disorders, 30 , 15-26.
- Meeks, T., Vahia, I., Lavretsky, H., Kulkarni, G. & Jeste, D. 2011. A tune in 'A minor' can be 'B major': A review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. Journal of Affective Disorders, 129 , 126-142.
- Oliver, M. I., Pearson, N., Coe, N. & Gunnell, D. 2005. Help-seeking behaviour in men and wmen with common mental health problems: cross-sectional study. The British Journal of Psychiatry, 186(4), 297-301.
- Mackenzie, C. S., Gekoski, W. L. & Knox, V. J. 2006. Age, gender and the underutilization of mental health services: The influence of help-seeking attitudes. Aging and Mental Health, 10, 574-582.
- Gellis, Z. D. & Mccracken, S. G. 2014. Depressive Disorders in Older Adults. Mental Health and Older Adults. Chicago: Council on Social Work Education.
- Djernes, J. K. 2006. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatrica Scandinavica, 113 , 372-387.
- Mitchell, A. J. & Subramaniam, H. 2005. Prognosis of depression in old age compared to middle age: a systematic review of comparative studies. American Journal of Psychiatry, 162 , 1588-1601.
- Licht-Strunk, E., Van der Kooij, K. G., Van Schaik, D. J., Van Marwijk, H. W., Van Hout, H. P., De Haan, M. & Beekman, A. T. 2005. Prevalence of depression in older patients consulting their general practitioner in The Netherlands. International Journal of Geriatric Psychiatry, 20 , 1013-1019.
- Rodda, J., Walker, Z. & Carter, J. 2011. Depression in older adults. BMJ: British Medical Journal (Overseas & Retired Doctors Edition), 343 , 683-687.
- Sawyer, P. 2012. Counselling Older Adults at Risk of Suicide: Recognizing Barriers, Reviewing Strategies, and Exploring Opportunities for Intervention. Alabama Counseling Association Journal, 38 , 80-103.

- Disclaimers
- Patient Care & Health Information
- Diseases & Conditions
- Depression (major depressive disorder)
- What is depression? A Mayo Clinic expert explains.
Learn more about depression from Craig Sawchuk, Ph.D., L.P., clinical psychologist at Mayo Clinic.
Hi, I'm Dr. Craig Sawchuk, a clinical psychologist at Mayo Clinic. And I'm here to talk with you about depression. Whether you're looking for answers for yourself, a friend, or loved one, understanding the basics of depression can help you take the next step.
Depression is a mood disorder that causes feelings of sadness that won't go away. Unfortunately, there's a lot of stigma around depression. Depression isn't a weakness or a character flaw. It's not about being in a bad mood, and people who experience depression can't just snap out of it. Depression is a common, serious, and treatable condition. If you're experiencing depression, you're not alone. It honestly affects people of all ages and races and biological sexes, income levels and educational backgrounds. Approximately one in six people will experience a major depressive episode at some point in their lifetime, while up to 16 million adults each year suffer from clinical depression. There are many types of symptoms that make up depression. Emotionally, you may feel sad or down or irritable or even apathetic. Physically, the body really slows down. You feel tired. Your sleep is often disrupted. It's really hard to get yourself motivated. Your thinking also changes. It can just be hard to concentrate. Your thoughts tend to be much more negative. You can be really hard on yourself, feel hopeless and helpless about things. And even in some cases, have thoughts of not wanting to live. Behaviorally, you just want to pull back and withdraw from others, activities, and day-to-day responsibilities. These symptoms all work together to keep you trapped in a cycle of depression. Symptoms of depression are different for everyone. Some symptoms may be a sign of another disorder or medical condition. That's why it's important to get an accurate diagnosis.
While there's no single cause of depression, most experts believe there's a combination of biological, social, and psychological factors that contribute to depression risk. Biologically, we think about genetics or a family history of depression, health conditions such as diabetes, heart disease or thyroid disorders, and even hormonal changes that happen over the lifespan, such as pregnancy and menopause. Changes in brain chemistry, especially disruptions in neurotransmitters like serotonin, that play an important role in regulating many bodily functions, including mood, sleep, and appetite, are thought to play a particularly important role in depression. Socially stressful and traumatic life events, limited access to resources such as food, housing, and health care, and a lack of social support all contribute to depression risk. Psychologically, we think of how negative thoughts and problematic coping behaviors, such as avoidance and substance use, increase our vulnerability to depression.
The good news is that treatment helps. Effective treatments for depression exist and you do have options to see what works best for you. Lifestyle changes that improve sleep habits, exercise, and address underlying health conditions can be an important first step. Medications such as antidepressants can be helpful in alleviating depressive symptoms. Therapy, especially cognitive behavioral therapy, teaches skills to better manage negative thoughts and improve coping behaviors to help break you out of cycles of depression. Whatever the cause, remember that depression is not your fault and it can be treated.
To help diagnose depression, your health care provider may use a physical exam, lab tests, or a mental health evaluation. These results will help identify various treatment options that best fit your situation.
Help is available. You don't have to deal with depression by yourself. Take the next step and reach out. If you're hesitant to talk to a health care provider, talk to a friend or loved one about how to get help. Living with depression isn't easy and you're not alone in your struggles. Always remember that effective treatments and supports are available to help you start feeling better. Want to learn more about depression? Visit mayoclinic.org. Do take care.
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. Also called major depressive disorder or clinical depression, it affects how you feel, think and behave and can lead to a variety of emotional and physical problems. You may have trouble doing normal day-to-day activities, and sometimes you may feel as if life isn't worth living.
More than just a bout of the blues, depression isn't a weakness and you can't simply "snap out" of it. Depression may require long-term treatment. But don't get discouraged. Most people with depression feel better with medication, psychotherapy or both.
Depression care at Mayo Clinic
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Although depression may occur only once during your life, people typically have multiple episodes. During these episodes, symptoms occur most of the day, nearly every day and may include:
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Angry outbursts, irritability or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies or sports
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy, so even small tasks take extra effort
- Reduced appetite and weight loss or increased cravings for food and weight gain
- Anxiety, agitation or restlessness
- Slowed thinking, speaking or body movements
- Feelings of worthlessness or guilt, fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts or suicide
- Unexplained physical problems, such as back pain or headaches
For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities or relationships with others. Some people may feel generally miserable or unhappy without really knowing why.
Depression symptoms in children and teens
Common signs and symptoms of depression in children and teenagers are similar to those of adults, but there can be some differences.
- In younger children, symptoms of depression may include sadness, irritability, clinginess, worry, aches and pains, refusing to go to school, or being underweight.
- In teens, symptoms may include sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, using recreational drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression symptoms in older adults
Depression is not a normal part of growing older, and it should never be taken lightly. Unfortunately, depression often goes undiagnosed and untreated in older adults, and they may feel reluctant to seek help. Symptoms of depression may be different or less obvious in older adults, such as:
- Memory difficulties or personality changes
- Physical aches or pain
- Fatigue, loss of appetite, sleep problems or loss of interest in sex — not caused by a medical condition or medication
- Often wanting to stay at home, rather than going out to socialize or doing new things
- Suicidal thinking or feelings, especially in older men
When to see a doctor
If you feel depressed, make an appointment to see your doctor or mental health professional as soon as you can. If you're reluctant to seek treatment, talk to a friend or loved one, any health care professional, a faith leader, or someone else you trust.
When to get emergency help
If you think you may hurt yourself or attempt suicide, call 911 in the U.S. or your local emergency number immediately.
Also consider these options if you're having suicidal thoughts:
- Call your doctor or mental health professional.
- Contact a suicide hotline.
- In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
- U.S. veterans or service members who are in crisis can call 988 and then press “1” for the Veterans Crisis Line . Or text 838255. Or chat online .
- The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
More Information
Depression (major depressive disorder) care at Mayo Clinic
- Male depression: Understanding the issues
- Nervous breakdown: What does it mean?
- Pain and depression: Is there a link?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It's not known exactly what causes depression. As with many mental disorders, a variety of factors may be involved, such as:
- Biological differences. People with depression appear to have physical changes in their brains. The significance of these changes is still uncertain, but may eventually help pinpoint causes.
- Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that likely play a role in depression. Recent research indicates that changes in the function and effect of these neurotransmitters and how they interact with neurocircuits involved in maintaining mood stability may play a significant role in depression and its treatment.
- Hormones. Changes in the body's balance of hormones may be involved in causing or triggering depression. Hormone changes can result with pregnancy and during the weeks or months after delivery (postpartum) and from thyroid problems, menopause or a number of other conditions.
- Inherited traits. Depression is more common in people whose blood relatives also have this condition. Researchers are trying to find genes that may be involved in causing depression.
- Marijuana and depression
- Vitamin B-12 and depression
Risk factors
Depression often begins in the teens, 20s or 30s, but it can happen at any age. More women than men are diagnosed with depression, but this may be due in part because women are more likely to seek treatment.
Factors that seem to increase the risk of developing or triggering depression include:
- Certain personality traits, such as low self-esteem and being too dependent, self-critical or pessimistic
- Traumatic or stressful events, such as physical or sexual abuse, the death or loss of a loved one, a difficult relationship, or financial problems
- Blood relatives with a history of depression, bipolar disorder, alcoholism or suicide
- Being lesbian, gay, bisexual or transgender, or having variations in the development of genital organs that aren't clearly male or female (intersex) in an unsupportive situation
- History of other mental health disorders, such as anxiety disorder, eating disorders or post-traumatic stress disorder
- Abuse of alcohol or recreational drugs
- Serious or chronic illness, including cancer, stroke, chronic pain or heart disease
- Certain medications, such as some high blood pressure medications or sleeping pills (talk to your doctor before stopping any medication)
Complications
Depression is a serious disorder that can take a terrible toll on you and your family. Depression often gets worse if it isn't treated, resulting in emotional, behavioral and health problems that affect every area of your life.
Examples of complications associated with depression include:
- Excess weight or obesity, which can lead to heart disease and diabetes
- Pain or physical illness
- Alcohol or drug misuse
- Anxiety, panic disorder or social phobia
- Family conflicts, relationship difficulties, and work or school problems
- Social isolation
- Suicidal feelings, suicide attempts or suicide
- Self-mutilation, such as cutting
- Premature death from medical conditions
- Depression and anxiety: Can I have both?
There's no sure way to prevent depression. However, these strategies may help.
- Take steps to control stress, to increase your resilience and boost your self-esteem.
- Reach out to family and friends, especially in times of crisis, to help you weather rough spells.
- Get treatment at the earliest sign of a problem to help prevent depression from worsening.
- Consider getting long-term maintenance treatment to help prevent a relapse of symptoms.
- Brown AY. Allscripts EPSi. Mayo Clinic, Rochester, Minn. Nov. 17, 2016.
- Research report: Psychiatry and psychology, 2016-2017. Mayo Clinic. http://www.mayo.edu/research/departments-divisions/department-psychiatry-psychology/overview?_ga=1.199925222.939187614.1464371889. Accessed Jan. 23, 2017.
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Jan. 23, 2017.
- Depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/depression/index.shtml. Accessed Jan. 23, 2017.
- Depression. National Alliance on Mental Illness. http://www.nami.org/Learn-More/Mental-Health-Conditions/Depression/Overview. Accessed Jan. 23, 2017.
- Depression: What you need to know. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/depression-what-you-need-to-know/index.shtml. Accessed Jan. 23, 2017.
- What is depression? American Psychiatric Association. https://www.psychiatry.org/patients-families/depression/what-is-depression. Accessed Jan. 23, 2017.
- Depression. NIH Senior Health. https://nihseniorhealth.gov/depression/aboutdepression/01.html. Accessed Jan. 23, 2017.
- Children’s mental health: Anxiety and depression. Centers for Disease Control and Prevention. https://www.cdc.gov/childrensmentalhealth/depression.html#depression. Accessed. Jan. 23, 2017.
- Depression and complementary health approaches: What the science says. National Center for Complementary and Integrative Health. https://nccih.nih.gov/health/providers/digest/depression-science. Accessed Jan. 23, 2017.
- Depression. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/databases/medical-conditions/d/depression.aspx. Accessed Jan. 23, 2017.
- Natural medicines in the clinical management of depression. Natural Medicines. http://naturaldatabase.therapeuticresearch.com/ce/CECourse.aspx?cs=naturalstandard&s=ND&pm=5&pc=15-111. Accessed Jan. 23, 2017.
- The road to resilience. American Psychological Association. http://www.apa.org/helpcenter/road-resilience.aspx. Accessed Jan. 23, 2017.
- Simon G, et al. Unipolar depression in adults: Choosing initial treatment. http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Stewart D, et al. Risks of antidepressants during pregnancy: Selective serotonin reuptake inhibitors (SSRIs). http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Kimmel MC, et al. Safety of infant exposure to antidepressants and benzodiazepines through breastfeeding. http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Bipolar and related disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Jan. 23, 2017.
- Hirsch M, et al. Monoamine oxidase inhibitors (MAOIs) for treating depressed adults. http://www.uptodate.com/home. Accessed Jan. 24, 2017.
- Hall-Flavin DK (expert opinion). Mayo Clinic, Rochester, Minn. Jan. 31, 2017.
- Krieger CA (expert opinion). Mayo Clinic, Rochester, Minn. Feb. 2, 2017.
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Antidepressants: Which cause the fewest sexual side effects?
- Atypical antidepressants
- Clinical depression: What does that mean?
- Depression in women: Understanding the gender gap
- Depression, anxiety and exercise
- Depression: Supporting a family member or friend
- MAOIs and diet: Is it necessary to restrict tyramine?
- Monoamine oxidase inhibitors (MAOIs)
- Natural remedies for depression: Are they effective?
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
Associated Procedures
- Complete blood count (CBC)
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
News from Mayo Clinic
- Mayo Clinic Q and A: How to support a loved one with depression Oct. 23, 2022, 11:00 a.m. CDT
- Mayo study lays foundation to predict antidepressant response in people with suicide attempts Oct. 03, 2022, 03:30 p.m. CDT
- Science Saturday: Researchers validate threshold for determining effectiveness of antidepressant treatment Aug. 27, 2022, 11:00 a.m. CDT
- Mayo Clinic expert explains differences between adult and teen depression May 24, 2022, 12:19 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Psychiatry hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

The Assessment of Depression Among Older Adults
In this CME article, learn about the best ways to assess depression in the geriatric population.

Khunatorn/AdobeStock

CATEGORY 1 CME
Premiere Date: March 20, 2022
Expiration Date: September 20, 2023
ACTIVITY GOAL
The goal of this activity is to review the epidemiology, risk factors, and evidence-based assessment of depression among older adults.
LEARNING OBJECTIVES
1. To describe the epidemiology and risk factors for depression among older adults
2. To discuss the assessment of depression among older adults
TARGET AUDIENCE
This accredited continuing education (CE) activity is intended for psychiatrists, psychologists, primary care physicians, physician assistants, nurse practitioners, and other health care professionals seeking to improve the care of patients with mental health disorders.
ACCREDITATION/CREDIT DESIGNATION/FINANCIAL SUPPORT
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Physicians’ Education Resource®, LLC, and Psychiatric Times™. Physicians’ Education Resource®, LLC, is accredited by the ACCME to provide continuing medical education for physicians.
Physicians’ Education Resource®, LLC, designates this enduring material for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
This activity is funded entirely by Physicians’ Education Resource®, LLC. No commercial support was received.
OFF-LABEL DISCLOSURE/DISCLAIMER
This accredited CE activity may or may not discuss investigational, unapproved, or off-label use of drugs. Participants are advised to consult prescribing information for any products discussed. The information provided in this accredited CE activity is for continuing medical education purposes only and is not meant to substitute for the independent clinical judgment of a physician relative to diagnostic or treatment options for a specific patient’s medical condition. The opinions expressed in the content are solely those of the individual faculty members and do not reflect those of Physicians’ Education Resource®, LLC.
FACULTY, STAFF, AND PLANNERS’ DISCLOSURES AND CONFLICT OF INTEREST (COI) MITIGATION
The peer reviewer and staff members of Physicians’ Education Resource®, LLC, and Psychiatric Times™ have no relevant financial relationships with commercial interests.
None of the staff of Physicians’ Education Resource®, LLC, or Psychiatric Times TM , or the planners of this educational activity, have relevant financial relationship(s) to disclose with ineligible companies whose primary business is producing, marketing, selling, reselling, or distributing health care products used by or on patients. The authors do not have any conflicts of interest to disclose for this article.
For content-related questions, email us at [email protected] . For questions concerning the accreditation of this CE activity or how to claim credit, please contact [email protected] and include “ The Assessment of Depression Among Older Adults ” in the subject line.
HOW TO CLAIM CREDIT
Once you have read the article, please use the following URL to evaluate and request credit: https://education.gotoper.com/activity/ptcme22mar . If you do not already have an account with Physicians’ Education Resource®, LLC, you will be prompted to create one. You must have an account to evaluate and request credit for this activity.
(This is part 1 of a 2-part CME activity discussing depression in older adults. Part 2 appears in the April issue—Ed.)
According to the DSM-5, major depressive disorder (MDD) is a condition that is characterized by the presence of depressed mood or marked loss of interest or pleasure in activities. 1 Other symptoms associated with MDD include changes in sleep, energy, concentration, appetite, weight (changes in 5% of total body weight), and psychomotor activity. Additionally, individuals present with feelings of inappropriate guilt or worthlessness and recurrent thoughts of death or suicide . Furthermore, these symptoms should cause clinically significant distress or impairments in social, occupational, or other areas of functioning. Also, these episodes of depression should not be attributable to the psychological effects of substances or medical conditions. To meet the criteria for an MDD, an individual should have depressed mood or marked loss of interest or pleasure in activities, plus 4 associated symptoms. These symptoms should have occurred during the same 2-week period.
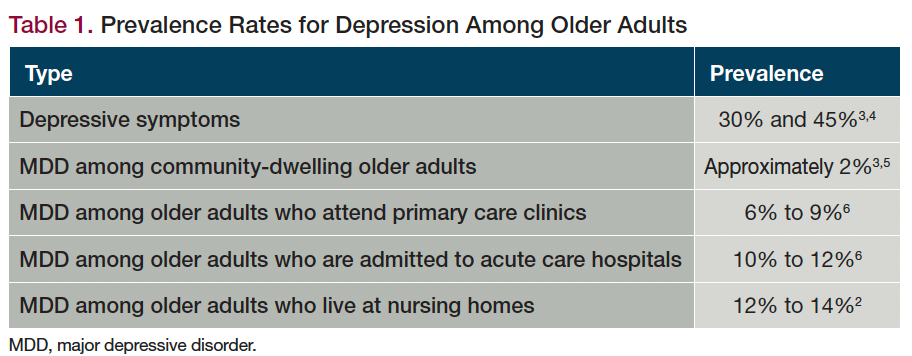
Table 1. Prevalence Rates for Depression Among Older Adults
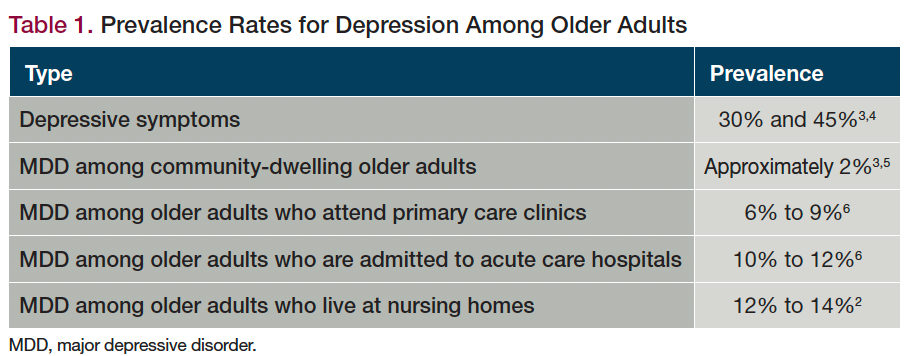
The term late-life depression (LLD) is specifically used to describe depression that occurs among individuals 65 years or older who do not have a previous history of depression. 2 Table 1 describes the prevalence rates for depression among older adults. 3-6
Presentation
The presentation of MDD in older adults differs from the presentation of MDD among younger adults. 3,7 Table 2 highlights the differences between MDD in older adults vs younger adults. 3,7-9
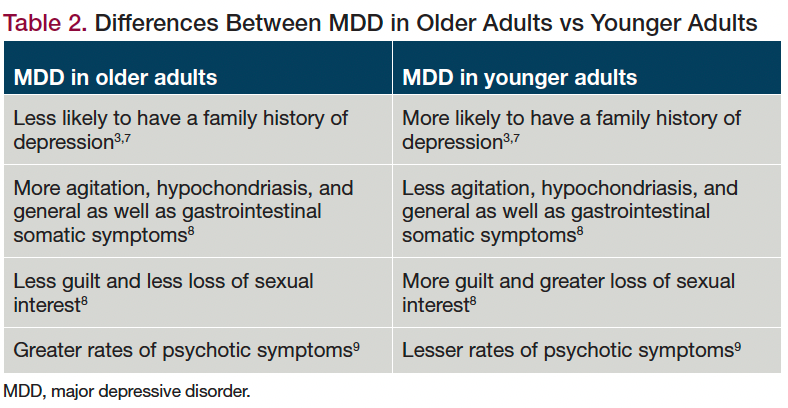
Table 2. Differences Between MDD in Older Adults vs Younger Adults
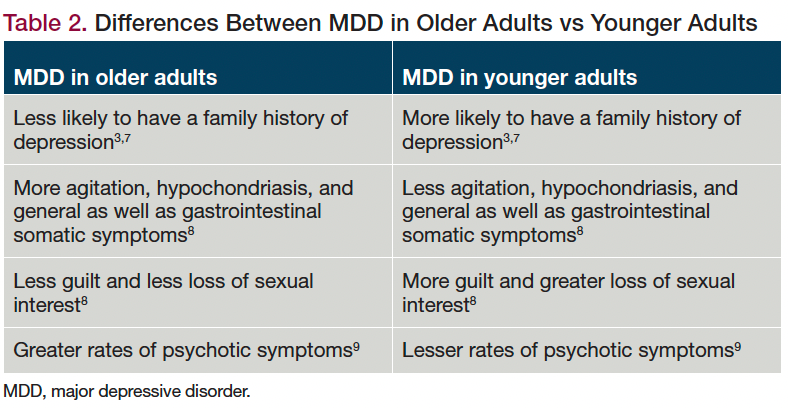
Psychotic Depression
MDD with psychotic symptoms accounts for approximately 25% to 50% of admissions to inpatient geriatric psychiatry units. 10 Nihilistic, somatic, or poverty-based delusions are often seen among older adults with MDD. These individuals also have greater rates of insomnia , somatic symptoms, diurnal variation of mood, and poor insight into their illness. 3,10 Among older individuals with MDD, hallucinations appear to occur less frequently than delusions.
The risk factors for the development of psychotic symptoms among older adults with MDD include being single, widowed, or living alone. 10 The presence of psychotic symptoms in older patients with MDD is a poor prognostic factor. These individuals present with frequent recurrences of symptoms that result in hospitalizations. 3 Age-related deterioration of the cortical areas of the brain, neurochemical changes commonly seen with aging, comorbid medical conditions, social isolation, sensory deficits, cognitive decline, and polypharmacy are all considered possible reasons for the occurrence of psychotic symptoms among older adults with MDD. 9
Relationship Between Depression and Dementia
Depression and dementia in older adults have a similar presentation and share an important relationship. 11,12 Older adults with MDD are more likely to develop cognitive deficits when compared with their age- and education-matched counterparts without depression. 13-15 Approximately 20% to 50% of older adults with depression develop cognitive deficits, including executive dysfunction and deficits in information processing and visuospatial functioning. 13-15 Depressive pseudodementia or depression-associated dementia are the reversible cognitive deficits that are often seen during an episode of depression and that tend to improve with the treatment of the depressive episode. 2,4
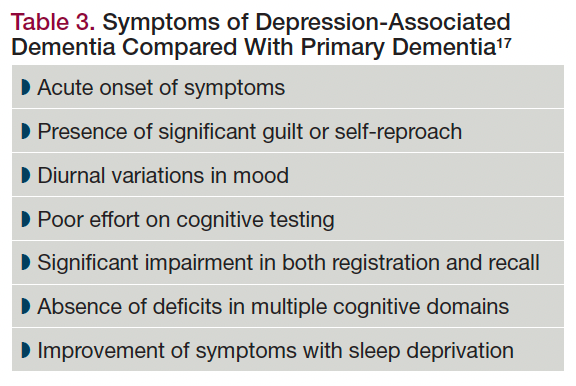
Table 3. Symptoms of Depression-Associated Dementia Compared With Primary Dementia 17
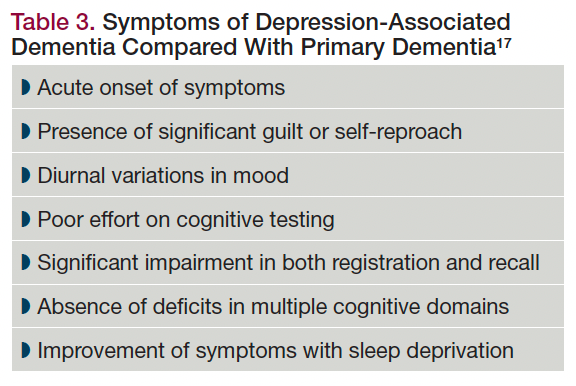
Often, the occurrence of depressive symptoms can be the presenting symptom of dementia in this patient population. It is still unclear from available evidence whether an episode of depression is a prodrome for the onset of dementia, a risk factor for dementia, or an independent event. 16 Table 3 describes the symptoms that primarily occur among individuals with depression-associated dementia when compared with a primary dementia. 17
Neurobiology
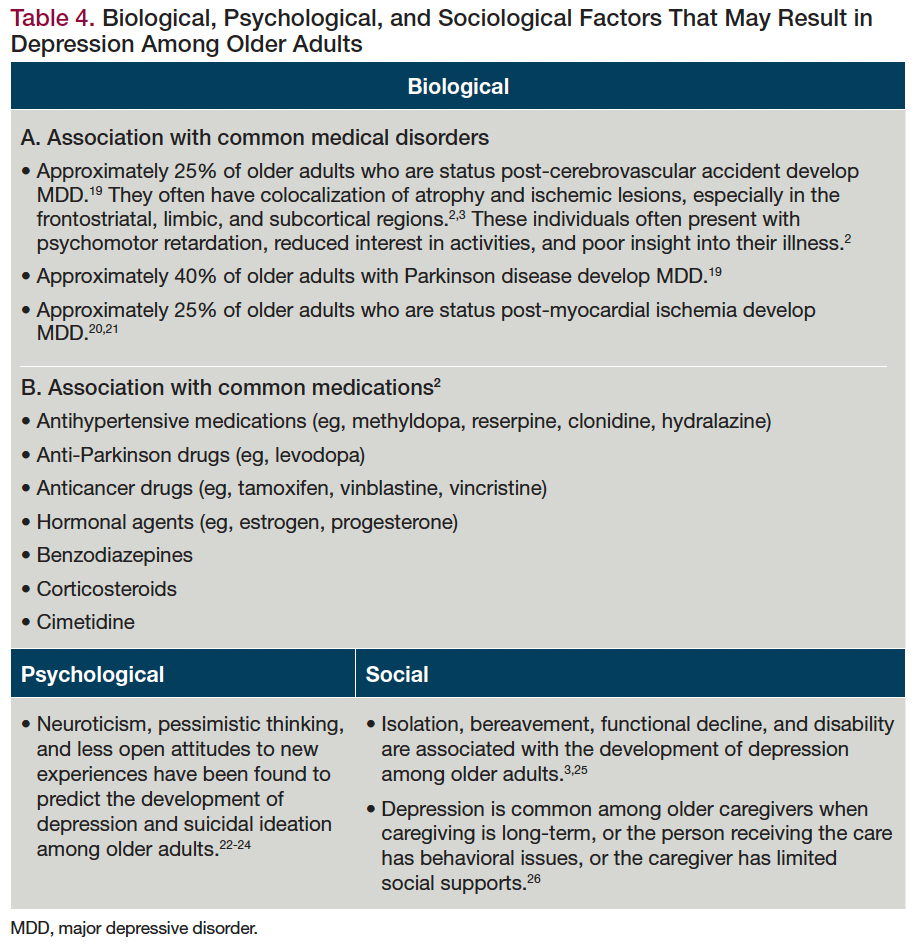
Table 4. Biological, Psychological, and Sociological Factors That May Result in Depression Among Older Adults
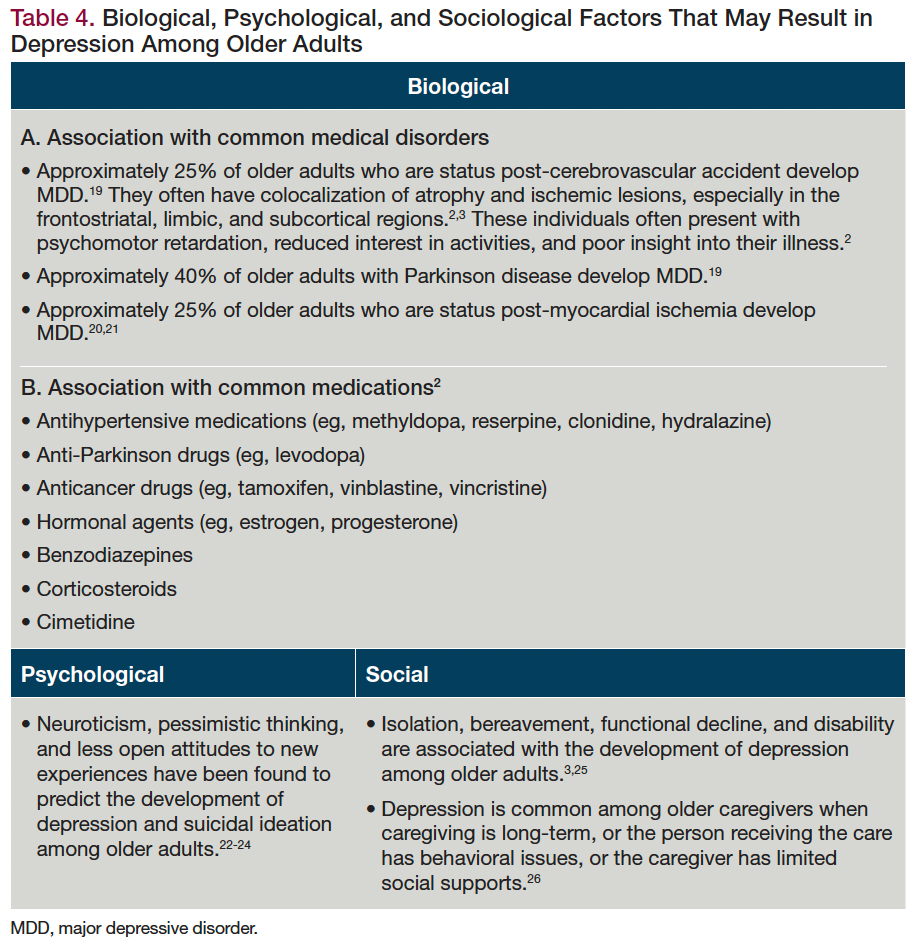
Current evidence indicates that LLD occurs due to the complex interactions among the various biological, psychological, and sociological factors seen among older adults. 18 Table 4 describes the various biological, psychological, and sociological factors that result in the development of depression among older adults. 19-26
Available evidence indicates that the impact of psychosocial risk factors on depression among older adults can be altered by personal or environmental factors. 26 One meta-analysis noted that the important risk factors for the development of depression among older community-dwelling individuals include a prior history of depression, female gender, sleep disturbance , bereavement, and the presence of disability. 27
Consequences
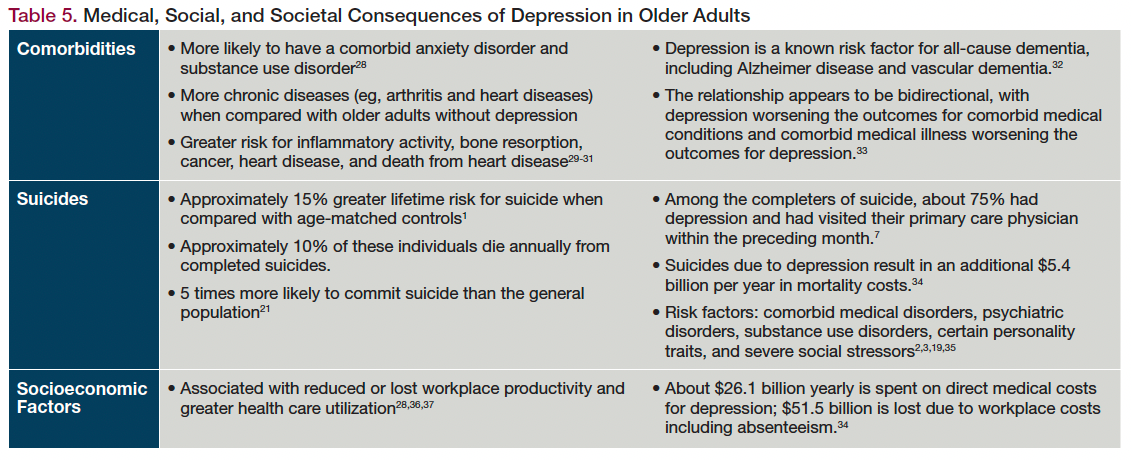
Table 5. Medical, Social, and Societal Consequences of Depression in Older Adults
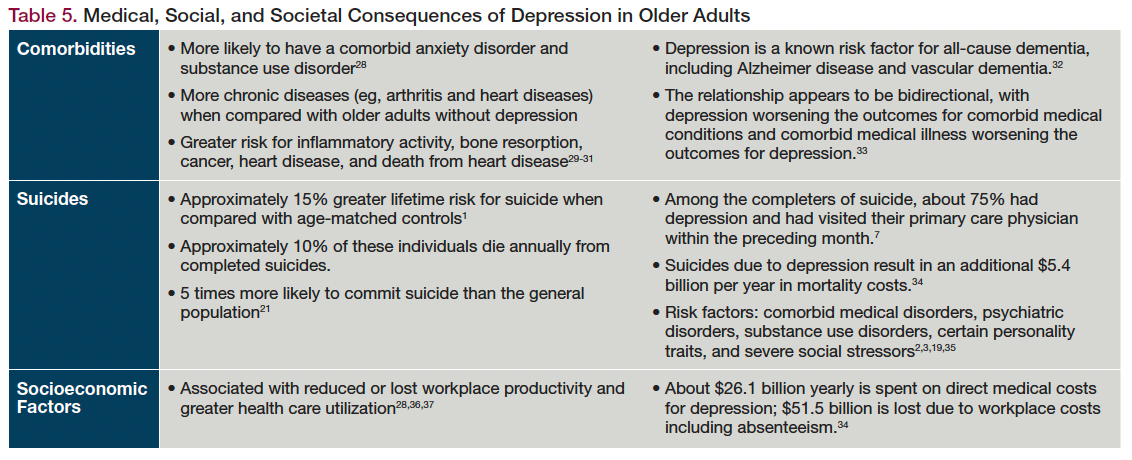
As with younger patients, depression among older adults can result in various poor outcomes. Older adults with depression have 1.5 to 3 times greater morbidity when compared with older adults without depression. 1 Table 5 describes the medical, social, and societal consequences of depression in older adults. 28-37
Current evidence indicates that almost 50% of older adults who have MDD go undiagnosed; a major reason for this is that the initial evaluation of these individuals for psychiatric symptoms is often completed by their primary physician rather than a psychiatrist. 38,39 Additionally, many of these individuals do not report depressive symptoms; instead, they present with somatic complaints, cognitive difficulties, and/or functional changes. 33 Any older adult who presents with these symptoms should always be screened for possible depression.
The assessment of depression among older adults starts with a thorough history, which should be obtained from the patient and, if possible, a knowledgeable informant. 3 In addition, these individuals should have a comprehensive medical and psychosocial assessment. There should also be a suicide risk assessment, a cognitive screening, and a functional evaluation.
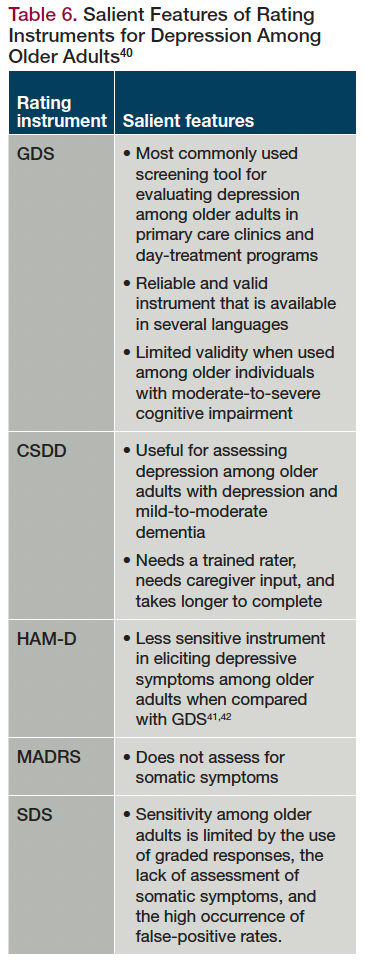
Table 6. Salient Features of Rating Instruments for Depression Among Older Adults 40
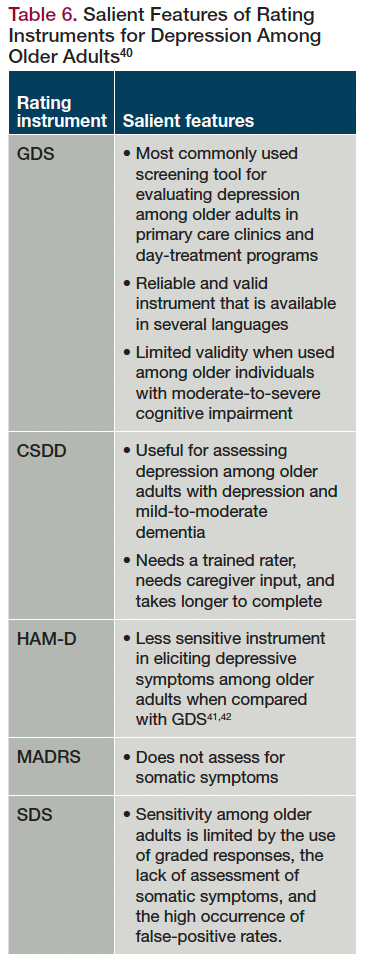
The use of standardized screening instruments can assist with the diagnosis of depression and the screening for suicide. 40 In addition, these instruments can help with assessing the severity of depression, identifying psychotic symptoms, and assessing treatment responses. The common screening tools for depression in older adults are the Geriatric Depression Scale (GDS), the Cornell Scale for Depression in Dementia (CSDD), the Hamilton Rating Scale for Depression (HAM-D), the Montgomery-Asberg Depression Rating Scale (MADRS), and the Zung Self-Rating Depression Scale (SDS). The Brief Psychiatric Rating Scale is the most commonly used scale to detect and rate the severity of psychopathology among older adults with depression and psychotic symptoms. Table 6 discusses the salient features of these rating instruments. 40-42
A thorough physical examination is an important part of the assessment, as these individuals have greater rates of medical comorbidities when compared with age-matched controls. 37 Table 7 specifies the medical workup for older adults with depression. 43-45
Evidence indicates that depression is a chronic and relapsing illness. 46 Although approximately 25% of older adults with depression will achieve full remission with or without any treatment, another 25% will never achieve any treatment response. 3 The remaining 50% will have a waxing-and-waning course. Poor prognostic factors include the presence of psychotic features, comorbid medical illness, physical disability, and a lack of social supports. 3,10 The presence of medical comorbidities is a major risk factor for poor treatment response and poor antidepressant tolerability among these individuals. 46
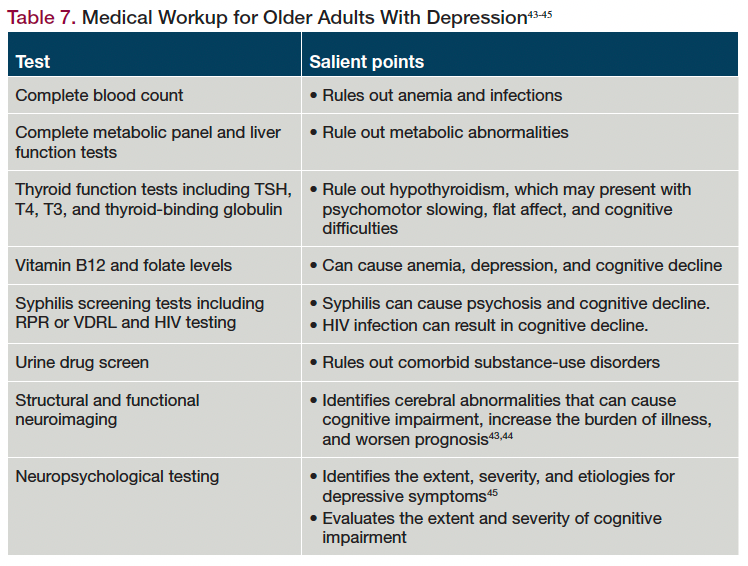
Table 7. Medical Workup for Older Adults With Depression 43-45
Conclusions
Evidence indicates that depression is not an uncommon condition among older adults. Depression is often underdiagnosed in this patient population and is associated with poorer outcomes, including greater rates of morbidity and mortality. A thorough history should include ruling out medical causes and drug effects; a focused physical examination; and appropriate laboratory studies, including neuroimaging and neuropsychological testing when necessary, as these are important in identifying depression among older adults.
Depression remains a chronic and relapsing illness, with approximately half of the individuals having a waxing-and-waning course. The presence of psychotic symptoms, medical comorbidities, and physical disability, and the absence of social supports, worsen prognosis for depression among older adults.
Dr Tampi is professor and chairman, Department of Psychiatry, Creighton University School of Medicine and Catholic Health Initiatives (CHI) Health Behavioral Health Services, Omaha, Nebraska. He is also an adjunct professor of psychiatry at Yale School of Medicine . Ms Tampi is cofounder and managing principal, Behavioral Health Advisory Group, Princeton, New Jersey.
1. Depressive disorders. In: American Psychiatric Association. Desk Reference to the Diagnostic Criteria From DSM-5. American Psychiatric Publishing; 2013:93-114.
2. Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961-1970.
3. Fountoulakis KN, O’Hara R, Iacovides A, et al. Unipolar late-onset depression: a comprehensive review. Ann Gen Hosp Psychiatry. 2003;2(1):11.
4. Alexopoulos GS. New concepts for prevention and treatment of late-life depression. Am J Psychiatry. 2001;158(6):835-838.
5. Harman JS, Schulberg HC, Mulsant BH, Reynolds CF III. The effect of patient and visit characteristics on diagnosis of depression in primary care. J Fam Pract. 2001;50(12):1068.
6. Taylor WD, Doraiswamy PM. A systematic review of antidepressant placebo-controlled trials for geriatric depression: limitations of current data and directions for the future. Neuropsychopharmacology. 2004;29(12):2285-2299.
7. Dunner DL. Treatment considerations for depression in the elderly. CNS Spectr. 2003;8(12 Suppl 3):14-19.
8. Hegeman JM, Kok RM, van der Mast RC, Giltay EJ. Phenomenology of depression in older compared with younger adults: meta-analysis. Br J Psychiatry. 2012;200(4):275-281.
9. Thorpe L. The treatment of psychotic disorders in late life. Can J Psychiatry. 1997;42 Suppl 1:19S-27S.
10. Gournellis R, Lykouras L, Fortos A, et al. Psychotic (delusional) major depression in late life: a clinical study. Int J Geriatr Psychiatry. 2001;16(11):1085-1091.
11. Raskind MA. The clinical interface of depression and dementia. J Clin Psychiatry. 1998;59 Suppl 10:9-12.
12. Wang S, Blazer DG. Depression and cognition in the elderly. Annu Rev Clin Psychol. 2015;11:331-360.
13. Yaffe K, Blackwell T, Gore R, et al. Depressive symptoms and cognitive decline in nondemented elderly women: a prospective study. Arch Gen Psychiatry. 1999;56(5):425-430.
14. Comijs HC, Jonker C, Beckman AT, Deeg DJ. The association between depressive symptoms and cognitive decline in community-dwelling elderly persons. Int J Geriatr Psychiatry. 2001;16(4):361-367.
15. Wilson RS, Barnes LL, Mendes de Leon CF, et al. Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology. 2002;59(3):364-370.
16. Bennett S, Thomas AJ. Depression and dementia: cause, consequence or coincidence? Maturitas. 2014;79(2):184-190.
17. Reynolds CF III, Smith GS, Dew MA, et al. Accelerating symptom-reduction in late-life depression: a double-blind, randomized, placebo-controlled trial of sleep deprivation. Am J Geriatr Psychiatry. 2005;13(5):353-358.
18. Weisenbach SL, Kumar A. Current understanding of the neurobiology and longitudinal course of geriatric depression. Curr Psychiatry Rep. 2014;16(9):463.
19. Alexopoulos GS, Katz IR, Reynolds CF III, et al. Pharmacotherapy of depression in older patients: a summary of the expert consensus guidelines. J Psychiatr Pract. 2001;7(6):361-376.
20. Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. impact on 6-month survival. JAMA . 1993;270(15):1819-1825.
21. Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiatry. 2003;54(3):241-247.
22. Katon W, Lin E, von Korff M, et al. The predictors of persistence of depression in primary care. J Affect Disord. 1994;31(2):81-90.
23. Lynch TR, Johnson CS, Mendelson T, et al. New onset and remission of suicidal ideation among a depressed adult sample. J Affect Disord. 1999;56(1):49-54.
24. Duberstein PR. Openness to experience and completed suicide across the second half of life. Int Psychogeriatr. 1995;7(2):183-198.
25. Bruce ML. Psychosocial risk factors for depressive disorders in late life. Biol Psychiatry. 2002;52(3):175-184.
26. Clyburn LD, Stones MJ, Hadjistavropoulos T, Tuokko H. Predicting caregiver burden and depression in Alzheimer’s disease. J Gerontol B Psychol Sci Soc Sci. 2000;55(1):S2-S13.
27. Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160(6):1147-1156.
28. Goff VV. Depression: a decade of progress, more to do. NHPF Issue Brief . 2002;(786):1-14.
29. Hall CA, Reynolds CF III. Late-life depression in the primary care setting: challenges, collaborative care, and prevention. Maturitas. 2014;79(2):147-152.
30. Michelson D, Stratakis C, Hill L, et al. Bone mineral density in women with depression. N Engl J Med. 1996;335(16):1176-1181.
31. Ferketich AK, Schwartzbaum JA, Frid DJ, Moeschberger ML. Depression as an antecedent to heart disease among women and men in the NHANES I study. National Health and Nutrition Examination Survey. Arch Intern Med. 2000;160(9):1261-1268.
32. Diniz BS, Butters MA, Albert SM, et al. Late-life depression and risk of vascular dementia and Alzheimer’s disease: systematic review and meta-analysis of community-based cohort studies. Br J Psychiatry. 2013;202(5):329-335.
33. Glover J, Srinivasan S. Assessment of the person with late-life depression. Psychiatr Clin North Am. 2013;36(4):545-560.
34. Greenberg PE, Kessler RC, Birnbaum HG, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry. 2003;64(12):1465-1475.
35. Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10(4):398-406.
36. Johnson J, Weissman MM, Klerman GL. Service utilization and social morbidity associated with depressive symptoms in the community. JAMA. 1992;267(11):1478-1483.
37. Croghan TW, Obenchain RL, Crown WE. What does treatment of depression really cost? Health Aff (Millwood). 1998;17(4):198-208.
38. Mulsant BH, Ganguli M. Epidemiology and diagnosis of depression in late life. J Clin Psychiatry. 1999;60 Suppl 20:9-15.
39. Unützer J, Katon W, Russo J, et al. Patterns of care for depressed older adults in a large-staff model HMO. Am J Geriatr Psychiatry. 1999;7(3):235-243.
40. Mulkeen A, Zdanys K, Muralee S, Tampi RR. Screening tools for late-life depression: a review. Depression: Mind and Body. 2008;3(4):150-157.
41. Lichtenberg PA, Marcopulos BA, Steiner DA, Tabscott JA. Comparison of the Hamilton Depression Rating Scale and the Geriatric Depression Scale: detection of depression in dementia patients. Psychol Rep. 1992;70(2):515-521.
42. Clayton A, Holroyd S, Sheldon-Keller A. Geriatric Depression Scale vs Hamilton Rating Scale for Depression in a sample of anxiety patients. Clin Gerontologist. 1997;17:3-13.
43. Benjamin S, Steffens DC. Structural neuroimaging of geriatric depression. Psychiatr Clin North Am. 2011;34(2):423-435, ix.
44. Gunning FM, Smith GS. Functional neuroimaging in geriatric depression. Psychiatr Clin North Am . 2011;34(2):403-422, viii.
45. McClintock SM, Minto L, Denney DA, et al. Clinical neuropsychological evaluation in older adults with major depressive disorder. Curr Psychiatry Rep. 2021;23(9):55.
46. Mitchell AJ, Subramaniam H. Prognosis of depression in old age compared to middle age: a systematic review of comparative studies. Am J Psychiatry. 2005;162(9):1588-1601. ❒
Managing Suicidal Thoughts, Behaviors, and Risk in Treatment-Resistant Depression

Blue Light Blockers: A Behavior Therapy for Mania
First Patient Dosed in Phase 2 Clinical Trial of NBI-1070770 for MDD

Treating ‘Morally Objectionable’ Patients

Rejoyn Becomes First Prescription Digital Therapeutic Authorized for Treatment of MDD

From the Pages of Psychiatric Times: March 2024
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


- Upload Ppt Presentation
- Upload Pdf Presentation
- Upload Infographics
- User Presentation
- Related Presentations

Emotion and Memory Changes in Aging Adults
By: medhelp Views: 377

Congenital Heart Diseases
By: medhelp Views: 333

Neurotransmission
By: medhelp Views: 287

Why Oral Health
By: medhelp Views: 2186

Pre-cancer and Malignant Disease of Vulva
By: medhelp Views: 401


Diagnosis and Management of Syncope
By: JenniferDwayne Views: 1213

Diseases of the Nervous System
By: medhelp Views: 421

Disorders of Childhood
By: KhushbuSG Views: 560

Guidelines for the Management of Severe Traumatic Brain Injury
By: drdwayn Views: 1279

By: marlonlbs Views: 1065

- About : Designer
- Occupation : Medical Professional
- Specialty : Other Health Professionals
- Country : India
HEALTH A TO Z
- Eye Disease
- Heart Attack
- Medications
DEPRESSION IN THE ELDERLY
Feb 12, 2012
750 likes | 1.82k Views
DEPRESSION IN THE ELDERLY. CCSMH NATIONAL GUIDELINES-INFORMED INTERACTIVE CASE-BASED TUTORIAL. BASED ON TEACHING MODULE BY: DR. M. BOSMA MODIFIED BY: DRS. KL. CASSIDY, C. MURPHY, M. BOSMA, C. HICKEY, & M. RITCHIE (RN). INTRODUCTION.
Share Presentation
- mental status examination
- see ccsmh depression guidelines
- nice depression tool
- ccsmh depression guidelines pp

Presentation Transcript
DEPRESSION IN THE ELDERLY CCSMH NATIONAL GUIDELINES-INFORMEDINTERACTIVE CASE-BASED TUTORIAL BASED ON TEACHING MODULE BY: DR. M. BOSMA MODIFIED BY: DRS. KL. CASSIDY, C. MURPHY, M. BOSMA, C. HICKEY,& M. RITCHIE (RN)
INTRODUCTION • Guidelines have been developed by the Canadian Coalition for Seniors Mental Health for the diagnosis and management of depression in the elderly • Please refer to the handout you have been given to work through the following case example
CASE: REFERRAL You have been asked to see Mrs. D. Pressed. She is a 78 year old woman whose husband died suddenly of a heart attack one month ago. Her family doctor reports that since the death, she has appeared sad-looking, with low energy and trouble falling asleep. She has spoken of “feeling his presence” and hearing his voice call her name. She is accompanied by one of her daughters.
NICE DEPRESSION TOOL You recently received a tool on depression assessment for older adults from NICE, or National Institute for the Care of the Elderly. After reviewing it, you decide to take it with you as it may be helpful in assessing Mrs. Pressed.
What else would you like to know? 1. Past psychiatric history • Past medical history • Medications and substances • Family history • Personal history See CCSMH Depression Guidelines p 22
What do you think is going on? 1. Bereavement • Adjustment Disorder with depressed mood • Major Depression (?with psychotic features) See CCSMH Depression Guidelines pp 23-26
What else would you like to know? • Estimate of severity: presence of catatonic or psychotic symptoms • Suicide risk assessment • Level of functioning or disability • Review DSM Criteria for depression See CCSMH Depression Guidelines p 22
CRITERIA FOR DEPRESSION SIGECAPS Sleep disturbance Loss of Interest Inappropriate or excessive feelings of Guilt Decreased Energy and increased fatigue Diminished ability to think or Concentrate Appetite change Psychomotor agitation or retardation Suicidal ideation See CCSMH Depression Guidelines p 10, 19, and 22 NICE Brochure
CASE: HISTORY OF PRESENT ILLNESS Mrs. Pressed reports the following information: She feels “down” with poor sleep and energy, and hasn’t been enjoying usual activities like knitting or playing bridge with friends. Her appetite and concentration are normal, and she denies hopelessness or suicidal ideation. She sometimes hears her husband’s voice calling her name, but knows he has died. She does not report symptoms of anxiety or psychosis. She has not been drinking alcohol. There is no impairment in cognition or functioning.
CASE: PAST PSYCHIATRIC HISTORY She had a postpartum depression after the birth of her youngest child. She was treated successfully for two years with Amitriptyline 150 mg OD.
CASE: PAST MEDICAL HISTORY • Hypertension • Osteoarthritis • 2003 – fracture right wrist from fall • 1955 – appendectomy
CASE: MEDICATIONS • Hydrochlorthiazide 25 mg OD • Tylenol plain daily for arthritis pain • Gravol 1-2x/week to help sleep
CASE: FAMILY HISTORY Mrs. Pressed is the middle child of a sibship of 7. Her mother had “bad nerves”. Two of her brothers had alcohol problems.
CASE: PERSONAL HISTORY Mrs. Pressed was born in Windsor, NS. Her childhood was unremarkable. She finished Grade 10 and then worked as a waitress. She married at age 18 and moved to Halifax with her husband. She stayed at home to raise their three daughters, and then worked as the church secretary for 15 years until she retired at age 60. Her husband retired from his job at the bank at age 65. They moved into a seniors’ apartment five years ago, and usually spend the winter in Florida. Only one of her daughters still lives in Halifax.
What is the most likely diagnosis? Bereavement
BEREAVEMENT What is bereavement? • Reaction to the death/loss of a loved one • May present with symptoms characteristic of major depression • Typically seen as “normal” See CCSMH Depression Guidelines pp 20-21
BEREAVEMENT When is bereavement “abnormal”? • If it is prolonged • DSM-IV suggests 2 months as cutoff • If symptoms are severe • Certain abnormal characteristics suggest major depression See CCSMH Depression Guidelines pp 20-21
BEREAVEMENT What symptoms suggest “abnormal” grief? • Guilt about things other than actions taken or not taken at the time of the death • Thoughts of death other than feeling that he/she should have died with the deceased • Intense worthlessness • Marked psychomotor retardation • Marked and prolonged functional impairment • Hallucinatory experiences other than transiently hearing or seeing the deceased person See CCSMH Depression Guidelines pp 20-21
What is your management plan? You agree to see her in one month for a follow up appointment. You refer her to an upcoming grief group. You ask her daughter to “keep an eye on her”. See CCSMH Depression Guidelines pp 20-21
CASE: MRS. PRESSED Mrs. Pressed does not attend her follow-up appointment. Two months later you see her in the emergency department after she has taken an overdose of Gravol. She has significantly deteriorated and rarely gets out of bed. She stopped eating and drinking one week ago and has lost 20 pounds. She rarely bathes, and doesn’t clean the house. She is very quiet, but often speaks of having headaches. She believes this is from “brain cancer”, and that she is dying. She wishes she had died from the overdose.
CASE: MENTAL STATUS EXAMINATION The previous information is confirmed by MSE including assessment for cognitive function. Mrs. Pressed does not appear to have insight into her condition. On MMSE she scores 18/30, often answering “I don’t know”. See CCSMH Depression Guidelines pp 10 and 22
What is your diagnosis? Major depression, Severe, With psychotic features
CASE: MRS. PRESSED Mrs. Pressed’s daughter is shocked that her mother attempted suicide. She didn’t think that “old people killed themselves”.
SUICIDE Is suicide common in the elderly? • Older men • 5x greater in white men >65 • 60% of completers are men • Hanging and firearms most common • 75% of attempters are women • Drug overdose, hanging, cutting most common See CCSMH Suicide Guidelines p 14 See CCSMH Depression Guidelines p 21
SUICIDE: LADDER ASSESSMENT Screening for Suicide in the Elderly In those with risk factors assess for: • Suicidal ideation and death ideation • Presence of suicidal intent • Presence of a suicide plan • Review current or past suicidal behaviour • Be vigilant: ask about it regularly, get collateral • Consider hospitalization for severe suicidal ideation or plan See CCSMH Suicide Guidelines p 15
SUICIDE What can we do? • Patients with suicidal thoughts are often suffering an unrecognized 1st episode of depression • Depression is treatable! • Most communicate suicidal thoughts first • 75% see GP in month before • For general medical or somatic complaints
SUICIDE What are non-modifiable risk factors of suicide in the elderly? • Old age • Male gender • Caucasian • Widowed/ Divorced • Previous attempt • Losses • Personality factors: rigid, non-adaptive See CCSMH Suicide Guidelines pp 16-17 See CCSMH Depression Guidelines p 21 See NICE Brochure
SUICIDE What are some potentially modifiable risk factors of suicide in the elderly? • Medical illness: present or perceived, including chronic painful conditions • Social isolation • Substance abuse/misuse • Presence and severity of depression • Presence of hopelessness • Access to means (especially firearms) See CCSMH Suicide Guidelines pp 16-17 See CCSMH Depression Guidelines p 21 See NICE Brochure
SUICIDE What are protective factors for suicide in the elderly? • Sense of meaning and purpose • Enhanced social support and interpersonal activities • Good physical health See CCSMH Suicide Guidelines p 17
What is your management plan and why? Admission to acute care Medical investigations Treatment
CASE: MEDICAL INVESTIGATIONS What test will you order? • CBC • Electrolytes • BUN/creatinine • ALT/AST/GGT • Glucose • TSH • B12/Folate • Urinalysis • CT Head (WHY?) See CCSMH Depression Guidelines p 10
CASE: MEDICAL INVESTIGATIONS Test Results • Na 146 • BUN 10.5 • CT Head – Age-associated atrophy • Other results normal • What do Na and BUN results suggest? }dehydration
CASE: MRS. PRESSED Mrs. Pressed is admitted to an acute care ward for treatment of psychotic depression. You meet with her daughter to discuss treatment options. Before discussing treatment, her daughter requests education on depression in the elderly. She asks, “Isn’t it normal to be sad when you’re old? Why does she need treatment?”
Is depression a normal response to the aging process? NO How common is depression in the elderly compared to a younger cohort? See CCSMH Depression Guidelines p 16
EPIDEMIOLOGY Prevalence over 65 • 1.4% ♀ • 0.4% ♂ • 1% overall • 2% dysthymia • 4% adjustment disorder with depressed mood • 15% depressive symptoms • Higher in institutional setting: Up to 25-40% in a general hospital setting and in long term care See CCSMH Depression Guidelines p 16 Serby et al 2003 Konstantinos et al 2003
DIAGNOSIS Depression is under-reported: WHY? • Communication issues (eg. hearing impairment) • Presence of dementia • Symptom overlap • Stigma of aging • Depression is “normal” • Symptoms “masked” by co-morbid illness • Cohort effect • Older persons less likely to report depression THEREFORE YOU MUST SCREEN IN THOSE AT HIGHER RISK! See CCSMH Depression Guidelines p 16
RISK FACTORS What are risk factors for depression in the elderly? • Recently bereaved • Female gender • Single/widowed (recently) • Stressful life events (eg. prolonged hospitalization, recent move to nursing home) • Social isolation • Persistent complaints of memory difficulties, diagnosis of dementia • Chronic disabling illness or recent major physical illness (eg. Parkinson’s disease, stroke) • Chronic sleep problems or anxiety See CCSMH Depression Guidelines pp 9 and 22
CLINICAL CHARACTERISTICS Does depression look different in the elderly? • “Depressed mood” may be less prominent • More anxiety • More likely to express somatic complaints • 65% have hypochondriacal symptoms • Less likely to report guilt feelings • Cognitive impairment more common • Psychosis more common • Typical delusions – more common • Somatic, persecution, nihilism, poverty See CCSMH Depression Guidelines p 19
CLINICAL CHARACTERISTICS Late-onset depression may differ from early onset depression: • More likely to have • Cognitive impairment • Cerebral atrophy • Deep white matter changes • Medical comorbidity • Higher mortality • Less likely to have family history of depression See CCSMH Depression Guidelines, Special Populations p 45 Nelson 2001
CLINICAL CHARACTERISTICS “Vascular Depression” Subtype • Marked apathy • Lack of insight into depression • Less depressed ideation • Executive dysfunction • Cortical and subcortical white matter changes • Treatment resistance (controversial) See CCSMH Depression Guidelines, Special Populations p 45 Nelson 2001
TREATMENT What are your treatment options? Medication ECT Psychotherapy WHICH ONE WILL YOU CHOOSE? See CCSMH Depression Guidelines p 24-26
ECT Why choose ECT? • Elderly are more sensitive to side effects of psychotropic medications • Psychotic features are more common • Vulnerable to physical and functional complications • Dehydration • Malnutrition • Sustained inactivity See CCSMH Depression Guidelines p 26
ECT CONSIDERATIONS IN THE ELDERLY • Average number of treatments is 6 – 12 • Cognitive deficits are not permanent • Patients with co-morbid dementia or other neurological disorders are more likely to be confused
CASE: MRS. PRESSED After 12 treatments with ECT Mrs. Pressed is free of depressive and psychotic symptoms. What is the next step of her treatment?
What are the treatment options for this patient? Antidepressant Maintenance ECT Psychotherapy Combination Which will you choose? TRY TO AVOID THE USE OF BENZODIAZEPINES See CCSMH Depression Guidelines pp 34 and 40
ANTIDEPRESSANTS What are the classes of antidepressants? Tricyclics (TCA’s) SSRI’s “Others” How will you choose? See CCSMH Depression Guidelines pp 33 and 34 NICE Brochure
ANTIDEPRESSANTS Guidelines on choosing an antidepressant: • Previous response to treatment • Type of depression • Other medical problems • Other medications* • Potential for risk of overdose *Caution: Wellbutrin (bupropion) could increase anxiety See CCSMH Depression Guidelines p 34
ANTIDEPRESSANT CONSIDERATIONS IN THE ELDERLY Monitoring for Side Effects • Drug – drug interactions are common • S/E’s are more likely to occur, even for SSRI’s • S/E’s have more serious consequences- avoid anticholinergic medications • Hip fractures are more frequent with ALL antidepressants See CCSMH Depression Guidelines p 36
ANTIDEPRESSANTS What are side effects of TCA’s? • Anticholinergic • Orthostatic hypotension • Sedation • Cardiotoxicity Which TCA’s might you use in the elderly? • Nortriptyline (least alpha-adrenergic blockade) • Desipramine (least anticholinergic) See CCSMH Depression Guidelines Table 5.1 p 33
ANTIDEPRESSANTS Anticholinergic side effects of TCA’s • Dry mouth • Urinary retention • Constipation • Blurred vision • Confusion See CCSMH Depression Guidelines Table 5.1 p 33, and p 34
- More by User
TREATMENT OF DEPRESSION IN THE ELDERLY
TREATMENT OF DEPRESSION IN THE ELDERLY. Jackie L. Neel, D.O. OSU Center for Health Sciences College of Osteopathic Medicine (Revised 9/2002). “It is not enough for a great nation merely to have added new years to life--our objective must also be to add new life to those years.”.
1.97k views • 46 slides
SAVING LIVES: Understanding Depression And Suicide In The Elderly
ElderCare Gatekeeper Training. 2.
1.07k views • 83 slides
Depression in Elderly
Depression in Elderly. Kalpana P. Padala, MD, MS Research Geriatrician Assistant Professor Dept. of Family Medicine University of Nebraska Medical Center Email: [email protected]. Disclosures. None. Goals and Objectives.
1.7k views • 53 slides
Delirium in the Elderly
Case Study. Mrs. M. is a 70 year old woman with a history of thalamic CVA, bipolar illness, chronic pain, and osteoarthritis. She takes tylenol with codeine, valproate, lithium, conjugated estrogens with progesterone, and aspirin. Two months ago, her daughter died unexpectedly, and she has been more depressed. One week ago, she became agitated and uncooperative. She was seen in the ER, where labs and CXR were normal. A consulting psychiatrist recommended clonezapam..
1.15k views • 43 slides
Treating Elderly Persons with Depression
Objectives. Discuss epidemiological and other relevant data regarding depression in geriatric populations.Discuss a clinical formulation of elderly persons regarding depression.Cover questions PCPs can ask of elderly patients to assess the presence of depression.Talking with elderly people about
628 views • 18 slides
Delirium in the Elderly. Kirsten M. Wilkins, MD Assistant Professor of Psychiatry Yale School of Medicine VA CT Healthcare System. Case 1:.
2.27k views • 49 slides
Update on Elderly Depression and Suicide
Update on Elderly Depression and Suicide . Dr. E Cheung Associate Consultant Psychogeriatric Team Castle Peak Hospital. Depression in the Elderly. Common Treatable Under-diagnosed & under-treated > 60% treated inappropriately Disease burden Morbidity & mortality.
1.74k views • 89 slides

Pharmacotherapy in the Elderly
Pharmacotherapy in the Elderly. Judy Wong [email protected]. The percentage of population with prescriptions, and the number of medications per individual, increase with age. Pharmacological Principles.
909 views • 22 slides
Overview of Dementia, Depression and Schizophrenia in the Elderly
Overview of Dementia, Depression and Schizophrenia in the Elderly. Peter Betz, M.D. Hierarchical Levels of Human Mental Life. Components of Modes of Treatment Psychological Life Mental Disorder Initiatives Personal Chronicle Disruptive Life Stories Rescript
697 views • 42 slides
Treating Elderly Persons with Depression. Scott J. Adams, Psy.D. WICHE Mental Health Program. Objectives. Discuss epidemiological and other relevant data regarding depression in geriatric populations. Discuss a clinical formulation of elderly persons regarding depression.
430 views • 18 slides
FALLS in THE ELDERLY
FALLS in THE ELDERLY. Vania L. Yu, MD. INCIDENCE. 25% at 70 years of age 35% after 75 years of age 40% after 80 years of age Women fall twice as much as men until the age of 75; after which the frequency equalizes.
5.48k views • 62 slides
Pharmacology in the Elderly
Pharmacology in the Elderly. Pharmacological Challenges in the Elderly. Pharmacokinetic changes Pharmacodynamic changes Multiple co-morbidities Polypharmacy More adverse effects Adherence problems/cognition Reduced diagnostic precision Few well designed trials in this population.
474 views • 9 slides
SAVING LIVES: Understanding Depression And Suicide In The Elderly. Sponsored by the Ohio Department of Mental Health in Partnership with the ADAMH Board of Franklin County and the Ohio Suicide Prevention Team Developed by Ellen Anderson, Ph.D., PCC, 2003-2006.
1.11k views • 86 slides
Arthritis in the Elderly
Quality of Life. Arthritis in the Elderly. Arthritis in the Elderly. Making a difference in 46 million lives in the United States. Our GOAL is to improve the quality of life, decrease pain and suffering, and increase the patient’s ability to live life to it’s fullest.
1.04k views • 25 slides
Hypertension in the Elderly
Hypertension in the Elderly. Debra L. Bynum, MD. Outline . Defining Systolic Hypertension Risks of SH in older persons Preventing stroke, CHF, CV events, dementia Review of major trials Choice of treatment Pulse Pressure Specific treatment groups: Stage 1 SH
789 views • 52 slides
Dialysis in the Elderly
Dialysis in the Elderly. Zalman Suldan MD, PhD. Dialysis in the Elderly What is “Elderly”. Merriam Webster’s Online Dictionary: Main Entry: 1 el·der·ly Pronunciation: ˈel- dər - lē Function: adjective Date: 1611
652 views • 37 slides
Depression in the Elderly: Recognition, Diagnosis, and Treatment
Depression in the Elderly: Recognition, Diagnosis, and Treatment. LOUIS A. CANCELLARO, PhD, MD, EFAC Psych Professor Emeritus and Interim Chair ETSU Department of Psychiatry & Behavioral Sciences. Diagnosis. Diagnosing depression in elderly Use family + patient for history
693 views • 27 slides
Diabetes in the Elderly
In this 21st century, we get to see that both average life expectancy and the prevalence of diabetes are at a rise on a regular basis. Amongst the elderly population, type 2 of the diabetes has turned out to be a growing problem and it is found that a larger portion of the newly diagnosed diabetes patients are older.
462 views • 3 slides
Know the Signs of Depression in the Elderly
The identification of depression on time can open the doors to effective treatment. Even something like socialization on a daily basis might be useful. Several Senior Citizen Homes encourage volunteers working for them to understand more deeply about the problem so that they can provide help for the elderly who live in an NGO-supported Old Age Home.
47 views • 2 slides
673 views • 66 slides

10 of the most common signs of depression in older adults
Posted: July 27, 2023 | Last updated: July 27, 2023

Depression is not an inherent part of aging: Here are 10 of the most common signs in older adults
The American Psychiatric Association defines depression as "a common and serious medical illness that negatively affects how you feel, the way you think, and how you act," resulting in, among other symptoms, "feelings of sadness and/or a loss of interest in activities you once enjoyed."
Mental illnesses should be approached with the same seriousness and urgency as any physical disease. Unfortunately, depression in older adults is frequently misdiagnosed, undertreated, or mistaken as a natural sign of a person's "slowing down" with age or enduring chronic age-related physical ailments , of which an estimated 80% of older adults have at least one.
Stacker compiled a list of 10 of the most common signs of depression in older adults using information from the National Institute on Aging and other scientific and medical sources. Identifying these symptoms and seeking timely professional help can significantly improve the quality of life of older adults.
While depression rates among older adults are lower than among younger people, a lack of access to accurate information greatly increases the likelihood that older adults do not understand what is happening to them or how to ask for help. Depression in older people is often tied to cognitive changes, changes in sleep patterns, and a general loss of interest , all of which can contribute to a significantly higher risk of isolation. Family members, friends, caregivers, and health professionals in contact with seniors must therefore be aware of the warning signs in order to offer support and treatment options.
According to the Centers for Disease Control and Prevention, most older adults do not report feeling depressed , though living conditions and a person's degree of social interaction play a major role. While cases of depression among the elderly living within a community range from less than 1% to 5%, 11.5% of hospitalized patients and 13.5% of those who receive home health care have reported depressive symptoms.
Most elderly patients suffering from depression do respond to anti-depressive drugs, psychotherapy, or a combination thereof. Symptoms are usually different in seniors than in younger adults—they are less likely to develop cognitive-affective symptoms, such as dysphoria, worthlessness, or guilt than younger patients, while insomnia, fatigue, psychomotor lethargy, loss of interest in living, and hopelessness tend to be more prevalent.

Extended periods of feeling sad, anxious, or 'empty'
Grief and sadness due to the loss of a loved one or other life events are normal at all ages, but can become especially acute among seniors who outlive their siblings and friends. If the older adult is sad, anxious, or mentions feeling empty for a long period of time—more than a few months—they might be experiencing dysthymia or depression.
![Consistent feelings of hopelessness, helplessness, worthlessness, or guilt <p>According to a study published by the<a href="https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9160466/"> National Library of Medicine,</a> "self-worthlessness [or] inadequacy is a distinctive and consistent symptom of major depression across all cultures." The onset of these feelings is also a distinct reproducible predictor of a person's risk of recurrence after overcoming an initial bout of depression.</p>](https://img-s-msn-com.akamaized.net/tenant/amp/entityid/AA1eqF9k.img)
Consistent feelings of hopelessness, helplessness, worthlessness, or guilt
According to a study published by the National Library of Medicine, "self-worthlessness [or] inadequacy is a distinctive and consistent symptom of major depression across all cultures." The onset of these feelings is also a distinct reproducible predictor of a person's risk of recurrence after overcoming an initial bout of depression.

Restlessness or irritability
Seniors may show signs of being agitated, busy, or short-tempered by manifesting consistent nervous behaviors. They can repeatedly tap their fingers against a table, fidget, or repeat movements. They may also fixate on specific daily tasks such as cleaning and organizing, moving objects from one place to another, or making up excuses to try to leave the house. These and other demonstrations of restlessness, while a common symptom in Alzheimer's patients, can also be a sign of depression, especially when combined with episodes of irritability.

Loss of interest in hobbies and other pleasurable activities
Social withdrawal and a loss of interest in hobbies and other activities previously found pleasurable is called anhedonia, a core symptom of depression. Anhedonia can present as a social or physical symptom; social anhedonia is a progressive disinterest in interpersonal relationships and a lack of comfort in social situations, while physical anhedonia is the inability to feel tangible pleasures such as eating or touching.

Loss of energy or fatigue
Fatigue can make simple daily activities, such as getting out of bed or getting dressed, too hard to perform. It can be a consequence of suffering one or several other symptoms of depression, such as sleeping problems, indigestion due to bad food choices, or stress. It can also be a symptom on its own. One 2018 study found that more than 90% of patients with depression report feeling fatigued .

Sluggishness or moving and talking more slowly
While fatigue is the feeling of being exhausted even after sleeping or resting, sluggishness or lethargy can be a mental condition that compromises the capacity to move nimbly, even if the patient is physically able and healthy. It can affect speech, movement, and reflexes.

Memory and decision-making issues
In older adults, the loss of executive functions, memory, and the ability to make decisions can be symptoms of different diseases or just a normal part of the aging process. A health professional must accurately diagnose the patient to discard brain conditions such as dementia, infectious diseases, and chronic illnesses before attributing these symptoms to depression .

Sleep irregularity, including waking up too early or sleeping too late
According to the Sleep Foundation : "People with depression may find it difficult to fall asleep and stay asleep during the night or experience periods of excessive daytime sleepiness." The organization states that sleep problems and vice versa can exacerbate depression; sleep problems can bring on depression. Either way, there is an undeniable link between depression and sleeping. The sleeping habits of seniors must be closely supervised to prevent mental and physical health problems.

Change in appetite, especially with unintentional weight gain or loss
It is common for older adults to have less appetite since they have lower energy requirements due to less physical activity. There are several reasons for the elderly to lose their appetite: dental issues, difficulty chewing and swallowing, side effects of prescription medications, and depression. A mental health exam is recommended if a senior loses their appetite and weight for no apparent reason. On the other hand, if the person starts eating excessively, it might be a sign of stress or anxiety, conditions often linked to depression as well.

Suicide ideation or suicide attempts
A 2021 primer on the relationship between suicide ideation and suicide attempts pointed to, among other sources, a study by the World Health Organization that found "two‐thirds of individuals with suicidal ideation never make a suicide attempt." Mental conditions, such as depression, are strongly linked to suicidal ideation, but are not necessarily associated with suicide attempts. Constantly monitoring the elderly and providing them with adequate care and medical help is critical, especially if they have ever expressed suicidal thoughts.
Additional research by Emilia Ruzicka. Story editing by Brian Budzynski. Copy editing by Kristen Wegrzyn. Photo selection by Clarese Moller.
More for You
J.K. Rowling says 'Harry Potter' stars who've criticized her anti-trans views 'can save their apologies'
Vietnam sentences real estate tycoon to death in its largest-ever fraud case
This Is How Long You Can Leave Butter On the Counter, According to Land O'Lakes
K-pop singer Park Bo-ram dies aged 30, investigation into death underway
NASA Solves Moon-Crossing Object Mystery
30 trans celebrities who broke barriers
Coast Guard, Navy rescue 3 stranded men after spotting 'HELP' sign made with palm leaves
A major Burger King franchisee in California says he can't roll out order kiosks fast enough due to the state's new $20 fast-food minimum wage
Paramount shows 'Gladiator 2' as Disney goes R-rated
This common trait is a red flag of a toxic boss, says ex-IBM CEO: 'I used to think it was a great skill'
Private Japanese Moon Lander's View Of Solar Eclipse Shadow And Earth
European Union's Only Nuclear-Powered Navy Is Getting Ready for War
78 Riddles for Adults That Will Test Your Smarts
Department store closes its doors after 201 years
Burger King's menu adds a new twist on a British classic
New 'Beetlejuice Beetlejuice' Footage Introduces Jenna Ortega's New Character
Space Rock Slammed Into Moon - The Explosion Was Seen From Japan
Donald Trump and Marjorie Taylor Greene Are on a Collision Course
Why Do People Add Plywood Under Their Countertops, And Do You Need To Do It?
Masters neighbor refuses to sell home despite millions in offers from Augusta golf club

Health | Research shows older adults have higher risk of…
Share this:.
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to print (Opens in new window)
- Coronavirus
Health | Research shows older adults have higher risk of developing depression

Older people – those between 65 and 80 – tended to cope better with anxiety and other mental health challenges during the COVID pandemic, according to a University of Michigan survey.
In fact, they adapt better to crises than younger folks in general.
“It’s resilience, wisdom, the ability to put current stressors in the context of past things we’ve been able to get through,” says Dr. Lauren Gerlach, a geriatric psychiatrist and assistant professor at UM. Gerlach was the author of a paper that interpreted the results of the Healthy Aging Poll.
Yet, research shows that older adults have a higher risk of developing depression, which is defined as feelings of sadness, anxiety and/or lack of interest in activities for at least two weeks that impact a person’s ability to function normally. Chronic illness, the loss of loved ones, post-retirement financial worries, and reduced mobility are a few common causes. Depression also goes undiagnosed in older people, meaning that many of them are left to struggle on their own.
Gone untreated, depression can lead to drug and alcohol misuse and suicide, both of which have increased among older adults in the last decade.
Depression amplifies other problems, like physical illness, and interferes with treatment and rehab after injury. Some of the risk factors for depression – social isolation, declining health and grief – also can lead to substance use disorders like excessive drinking and using opioids.
Gerlach says about half of older adults will have their first episode of depression after the age of 65.
Some research has shown that older adults who have late-onset depression are likelier to have a history of cerebrovascular disease (e.g., stroke, brain aneurysms, blood clots). More research has shown a link between late-onset depression and cognitive problems, especially in the ability to organize, plan, make decisions, solve problems and control behavior.
Depression looks different in older adults — one reason it can often be missed.
A study published in the journal Neuropsychiatric Disease and Treatment in 2022 found that depression in older adults is characterized by a lack of interest, less sleep, weight loss, fatigue, poor concentration, a lack of hope, a loss of appetite and thoughts of death rather than sadness.
Doctors may view these symptoms as age-related frailty rather than a mental health condition.
To make a correct diagnosis, it is important to consider depression but also to rule out other reversible causes such as the use of prescription drugs like opioids, steroids and benzodiazepines (Xanax, Valium, etc.) that can cause symptoms that mimic depression, Gerlach says. Over-the-counter drugs like Benadryl can affect memory. Untreated illnesses like thyroid disease and sleep apnea can impact a person’s mood and ability to think.
Depression in older adults is often accompanied by changes in memory or difficulty in concentration, which can be difficult to distinguish from dementia. Treating a person for depression can often help to improve concentration and focus, Gerlach says.
First-line treatment for depression often includes a combination of medications and therapy.
Antidepressants work well for the treatment of depression in older adults, as long as they don’t interact with other medicines the patient is taking. And it’s important to remember that it takes four to six weeks for the drug to start having an effect, Gerlach says.
Research shows that behavioral therapy, cognitive behavioral therapy, problem-solving therapy, brief psychodynamic therapy, and life review/reminiscence therapy are highly effective, but not used enough in older adults.
“Establishing a daily routine, getting exercise, maintaining a regular sleep schedule, avoiding drugs and alcohol, and socializing can all be helpful, too,” Gerlach says.
While some stigma remains surrounding mental health treatment, “the current generation of older adults is more willing to engage in care — which can have a tremendous impact on improving quality of life and happiness. Talking to your primary care physician is a great first step,” Gerlach says. “The pandemic has really shined a light on the prevalence of mental health concerns and the importance of recognizing mental health as an integral part of physical health.”
Protect your mental health
• Get enough sleep: Lack of sleep can cause depressed feelings as well as irritability. Aim to get seven to nine hours each night.
• Stay active: Exercise can help improve your mood and strengthen your heart and lungs. Activities like brisk walking, swimming and light yard work are all great choices for older adults.
• Be social: Make an effort to stay in touch with friends and family to keep those connections alive. Consider volunteering at a local animal shelter or food pantry to help gain a greater sense of purpose while meeting new people.
• Eat right: Eating a heart-healthy diet can help you have more energy and prevent medical conditions that may indirectly increase your risk for depression.
• Limit the use of recreational drugs: Marijuana and alcohol are depressants.
• Discuss your concerns: Talk to your primary care doctor if you feel sad or depressed. They are trained to help you.
• Manage your illness: If you have an illness like diabetes or even cancer, keep it under control by working with your doctors.
This content is provided by AgeWays Nonprofit Senior Services (the new name for the Area Agency on Aging 1-B), a nonprofit that serves older adults and family caregivers in Livingston, Macomb, Monroe, Oakland, St. Clair and Washtenaw counties. We provide services, programs and resources that are designed to help seniors age safely and independently. Call us at 800-852-7795 to get connected.
More in Health

SUBSCRIBER ONLY
Health | end of internet subsidies for low-income households threatens telehealth access.

Health | ACA plans are being switched without enrollees’ OK

Health | Feds join ranks of employers with generous fertility benefits

Health | For-profit companies open psychiatric hospitals in areas clamoring for care
Brain stimulation treatment may improve depression, anxiety in older adults
A noninvasive brain stimulation treatment improved depression and anxiety symptoms among older adults in a new University of Florida-led study.
Improvements in depression and anxiety symptoms were greatest among patients who reported higher symptom levels before treatment. Among participants who experienced moderate to severe state anxiety -- or anxiety associated with stressful situations or events -- the treatment benefits persisted at a one-year followup.
The findings, published in the journal Brain Stimulation , suggest the treatment, known as transcranial direct current stimulation, or tDCS, holds promise as a noninvasive, drug-free option to treat depression and anxiety symptoms, which affect 1 in 4 older adults.
"Depression and anxiety can impact our overall mental health, cognitive function and ability to function independently as we age," said the study's senior author Adam Woods, Ph.D., the associate dean for research and a professor of clinical and health psychology at the UF College of Public Health and Health Professions and co-director of UF's Center for Cognitive Aging and Memory Clinical Translational Research. "Often, front-line treatments involve medication and/or therapy, which can both be effective. However, there is also a pressing need for accessible and noninvasive options that can be deployed in people who are either nonresponsive to pharmaceutical treatment, unable to access or participate in clinic-based intensive treatment programs, or for a variety of other reasons."
Treatment benefits in the UF-led study were seen among participants with subclinical depression and anxiety, meaning their symptoms may not meet the criteria for diagnosis. Yet, even subclinical depression and anxiety can be associated with cognitive decline in older adults, the researchers say.
The tDCS treatment is delivered by a safe and weak electrical current passed through electrodes placed on a person's head. Researchers targeted the prefrontal cortex, an area of the brain associated with cognition and emotion regulation.
The new study was conducted as part of the National Institute on Aging-funded Augmenting Clinical Training in Older Adults Study, the largest study of its kind with older adults participating at UF and University of Arizona study sites. Nearly 400 older adults were randomly assigned to one of two groups: 12 weeks of tDCS paired with cognitive training designed to improve working memory and processing speed, or 12 weeks of cognitive training paired with a placebo version of tDCS.
Investigators also collected a wealth of data from cognitive, functional and neuroimaging tests as well as self-report measures of psychological symptoms, including depression and anxiety.
After controlling for factors such as prescription drugs that may impact depression and anxiety symptoms, the study team found that participants who received the tDCS treatment had significant improvements in mild depression and moderate to severe state anxiety, compared with the group that did not receive tDCS.
"Extensive research has demonstrated the efficacy of active stimulation to this area of the brain in reducing psychological symptoms in individuals with diagnosed psychiatric disorders," said Hanna Hausman, the study's lead author and a UF PHHP clinical psychology Ph.D. student in neuropsychology. "It was an unexpected yet welcome surprise to witness similar effects in our sample of older adults without significant psychiatric histories, especially on a large scale. Demonstrating this therapeutic effect is important because even subclinical depression and anxiety symptoms in older adults are associated with adverse outcomes."
Next steps for this research should include a phase 3 randomized clinical trial designed to assess the effect of tDCS and cognitive training on anxiety among a large and diverse group of older adults, the investigators say. The Korea Food and Drug Administration has approved tDCS as an at-home treatment for depression for adults in South Korea, and with additional study, it could become an accessible and easy-to-use treatment in the U.S. once sufficient evidence is available for U.S. Food and Drug Administration approval.
"tDCS treatment is cost-effective, portable and can be seamlessly integrated with existing mental health therapies or used as a standalone intervention," Hausman said. "Its potential for at-home self-administration would further expand accessibility and reduce personnel costs, making it a promising intervention for individuals who may experience barriers accessing face-to-face clinical care."
- Mental Health Research
- Psychology Research
- Mental Health
- Postpartum depression
- Deep brain stimulation
- Adult attention-deficit disorder
- Methamphetamine
- Psychopathology
- Antidepressant
Story Source:
Materials provided by University of Florida . Original written by Jill Pease. Note: Content may be edited for style and length.
Journal Reference :
- Hanna K. Hausman, Gene E. Alexander, Ronald Cohen, Michael Marsiske, Steven T. DeKosky, Georg A. Hishaw, Andrew O'Shea, Jessica N. Kraft, Yunfeng Dai, Samuel Wu, Adam J. Woods. tDCS reduces depression and state anxiety symptoms in older adults from the augmenting cognitive training in older adults study (ACT) . Brain Stimulation , 2024; 17 (2): 283 DOI: 10.1016/j.brs.2024.02.021
Cite This Page :
Explore More
- Ozone Removes Mating Barriers Between Fly ...
- Parkinson's: New Theory On Origins and Spread
- Clash of Stars Solves Stellar Mystery
- Secure Quantum Computing at Home
- Ocean Currents: Collapse of Antarctic Ice ...
- Pacific Cities Much Older Than Previously ...
- The Milky Way in Ancient Egyptian Mythology
- Physical Activity Best in the Evening
- How the Body Switches out of 'Fight' Mode
- New Drug Prevents Flu-Related Lung Damage
Trending Topics
Strange & offbeat.

Depression May Lead to Faster Cognitive Decline among Black, Latino Adults

Rats! Does Boston Need a “Rat Czar”?
Depression may lead to faster cognitive decline among black, latino adults ..

Depression May Lead to Faster Cognitive Decline among Black, Latino Adults
The findings suggest that black and latino adults are more susceptible to the negative effects of depressive symptoms later in life, even if they experience these symptoms less often than white adults., jillian mckoy.
Although multiple studies have linked depression to cognitive decline, there remains a gap in knowledge in the different ways depression affects cognition, and whether this association differs across racial/ethnic groups.
A study led by researchers at the School of Public Health found that depressive symptoms were associated with worse cognition among all racial/ethnic groups, but were particularly harmful among Black and Latino older adults.
Published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association , the results showed that depression spurred faster cognitive decline among Black and Latino older adults. Associations between depression and cognitive decline were especially significant for Latino individuals—at several times the magnitude than in White individuals. These declines were less apparent among both Asian and White older adults.
“As there are no cures for dementia, and because dementia is a long-term disease, it is important to identify risk factors earlier in the life course that can be intervened to slow down cognitive decline later in life,” says study lead and corresponding author Marcia Pescador Jimenez , assistant professor of epidemiology. “Our study suggests that treating depressive symptoms, particularly among Black and Latino older adults could delay cognitive decline.”
For the study, Pescador Jimenez and colleagues utilized data on cognition and depressive symptoms among 2,227 Asian, Black, Latino, or White adults ages 50 and older who completed up to three cognitive assessments over a four-year period.
Among all participants, depressive symptoms were associated with worse scores in executive function—skills that enable people to manage planning, organization, time management, self-control, and other fundamental functions—as well as semantic memory (the capacity to recall words and concepts).
Higher depressive symptoms were also linked to lower scores in verbal episodic memory (memory of events and experiences), among Black and Latino participants, but not among Asian or White participants. The decline was especially high among Black participants.
Consistent with prior research, Asian and Black adults had lower scores of depressive symptoms at baseline than their Latino and White counterparts. The fact that Black adults showed lower scores of depression but higher rates of cognitive decline could reflect racial disparities in healthcare access, which may affect how depression is diagnosed and treated among Black patients, the researchers note.
“We know through the ‘Minority Stress Theory’ that exposure to racial discrimination and acculturative stress constitutes a hostile psychological environment leading to negative health consequences,” Pescador Jimenez says. “Based on this, we were interested in the different experience of depressive symptoms by race and ethnicity and how this difference could be associated with cognitive health. For our next steps, we aim to examine how the effects of individual factors, such as depression, are potentially shaped by environment conditions that may be especially important for Black and Latino adults living in communities affected by unequal opportunities due to decades of systemic racism.”
The study was coauthored by researchers at SPH, Kaiser Permanente, Columbia University, the University of California Irvine School of Medicine, and the University of California, Davis.
Explore Related Topics:
- alzheimer's
- Alzheimer’s disease
- alzheimer’s/dementia
- mental and behavioral health
- mental health
- mental health disorders
- racial disparities
- strategic direction
- Share this story
- 0 Comments Add
Senior Writer and Editor
Jillian McKoy is the senior writer and editor at the School of Public Health. Profile
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *

IMAGES
VIDEO
COMMENTS
In fact, there is a substantial overlapping in the clinical presentation of late-life depression and early-stage dementia: a subjective perception of memory loss, as well as psychomotor retardation and a lack of motivation in answering at cognitive tests are typically observed in depressed older adults, and can be interpreted as signs of ...
Distance themselves from communities, activities and other social groups they used to be part of. Shower less often and/or stop caring about their appearance. Stop taking their medications or ...
For that reason, it's important to make sure that an older adult you are concerned about is evaluated and treated, even if the depression is mild. Older people may not have the obvious symptoms ...
Hoover DR, Siegel M, Lucas J, Kalay E, Gaboda D, Devanand DP, Crystal S. Depression in the first year of stay for elderly long-term nursing home residents in the USA. Int Psychogeriatr. 2010 Nov;22(7):1161-71. doi: 10.1017/S1041610210000578.
Depression is a true and treatable medical condition, not a normal part of aging. However older adults are at an increased risk for experiencing depression. If you are concerned about a loved one, offer to go with him or her to see a health care provider to be diagnosed and treated. Depression is not just having "the blues" or the emotions ...
The Clinical Problem. Late-life depression is the occurrence of major depressive disorder in adults 60 years of age or older. Major depressive disorder occurs in up to 5% of community-dwelling ...
Depression in older adults Joanne Rodda, Zuzana Walker, Janet Carter Depression is a major contributor to healthcare costs and is projected to be the leading cause of disease burden in middle and higher income countries by the year 2030.w1 Depression in later life, traditionally defined as age older
According to the Centers for Disease Control and Prevention (CDC), depression affects about 1%-5% of the general elderly population, 13.5% in elderly who require home healthcare, and 11.5% in older hospital patients.¹. Older adults are at risk of misdiagnosis and lack of treatment because some of their symptoms can mimic normal age-related issues.
The presentation of depression in older adults is markedly different to that in younger adults. The most significant and fundamental difference in presentation in older adults is that depression can be present with the absence of an affect component, i.e. subjective feelings of low mood or sadness are not experienced 3,6-9.
Depression is a mood disorder that causes feelings of sadness that won't go away. Unfortunately, there's a lot of stigma around depression. Depression isn't a weakness or a character flaw. It's not about being in a bad mood, and people who experience depression can't just snap out of it. Depression is a common, serious, and treatable condition.
Depression and dementia in older adults have a similar presentation and share an important relationship. 11,12 Older adults with MDD are more likely to develop cognitive deficits when compared with their age- and education-matched counterparts without depression. 13-15 Approximately 20% to 50% of older adults with depression develop cognitive ...
The entire range of clinical symptoms of early onset depression also occurs in the elderly. Historical notions of a unique presentation of late life depression -the hypochondriacal depressive or the neurovegetative depressive - are largely discounted today. However, recognizing depression in the elderly can require special skills and experience.
7 likes • 4,368 views. K. Katie Brandner. Depression in the elderly. Healthcare. 1 of 22. Download Now. Download to read offline. Depression in the elderly - Download as a PDF or view online for free.
Depression in people 65 and older is a major public health problem, according to the NIMH.-Advancing age is often accompanied by loss of social support systems due to death of a spouse or siblings, retirement, or relocation of residence. -Because it can be hard to recognize symptoms of depression in the elderly, effective treatment is often ...
Check out this medical PowerPoint presentation titled "Depression in the elderly" by James T. Birch, Jr., MD, MSPH.<break><break>This medical PowerPoint presentation is about the issue of depression in the elderly.<break><break>Depression is a common mental health condition that affects people of all ages, including the elderly. In fact, depression in the elderly is a significant public ...
A noninvasive brain stimulation treatment improved depression and anxiety symptoms among older adults in a new University of Florida College of Public Health and Health Professions-led study. Improvements in depression and anxiety symptoms were greatest among patients who reported higher symptom levels before treatment. Among participants who ...
Depression in Elderly Kalpana P. Padala, MD, MS Research Geriatrician Assistant Professor Dept. of Family Medicine University of Nebraska Medical Center Email: [email protected]. Disclosures • None. Goals and Objectives Identify the variation in presentation of depression in various age groups Overview of assessment of depression along with use of common rating scale Selection of ...
TREATMENT OF DEPRESSION IN THE ELDERLY Jackie L. Neel, D.O. OSU Center for Health Sciences College of Osteopathic Medicine (Revised 9/2002) "It is not enough for a great nation merely to have added new years to life--our objective must also be to add new life to those years." ---John F. Kennedy Depression of the Elderly - - Jackie L. Neel, D.O.. Our population is Aging! • 2/3 of all the ...
An Image/Link below is provided (as is) to download presentation Download Policy: ... Diagnosing depression in elderly Use family + patient for history. 693 views • 27 slides. Diabetes in the Elderly. In this 21st century, we get to see that both average life expectancy and the prevalence of diabetes are at a rise on a regular basis. Amongst ...
The findings, published in the journal Brain Stimulation, suggest the treatment, known as transcranial direct current stimulation, or tDCS, holds promise as a noninvasive, drug-free option to treat depression and anxiety symptoms, which affect 1 in 4 older adults. "Depression and anxiety can impact our overall mental health, cognitive ...
Depression in older people is often tied to cognitive changes, changes in sleep patterns, and a general loss of interest, all of which can contribute to a significantly higher risk of isolation ...
Gerlach says about half of older adults will have their first episode of depression after the age of 65. Some research has shown that older adults who have late-onset depression are likelier to ...
tDCS reduces depression and state anxiety symptoms in older adults from the augmenting cognitive training in older adults study (ACT). Brain Stimulation , 2024; 17 (2): 283 DOI: 10.1016/j.brs.2024 ...
Although multiple studies have linked depression to cognitive decline, there remains a gap in knowledge in the different ways depression affects cognition, and whether this association differs across racial/ethnic groups.. A study led by researchers at the School of Public Health found that depressive symptoms were associated with worse cognition among all racial/ethnic groups, but were ...