Loading metrics
Open Access
Peer-reviewed
Research Article

A Systematic Review of the Prevalence of Schizophrenia
Affiliation Queensland Centre for Mental Health Research, The Park Centre for Mental Health, Wacol, Australia
Affiliations Queensland Centre for Mental Health Research, The Park Centre for Mental Health, Wacol, Australia, Department of Psychiatry, University of Queensland, St. Lucia, Australia
* To whom correspondence should be addressed. E-mail: [email protected]
- Sukanta Saha,
- David Chant,
- Joy Welham,
- John McGrath

- Published: May 31, 2005
- https://doi.org/10.1371/journal.pmed.0020141
- Reader Comments
Understanding the prevalence of schizophrenia has important implications for both health service planning and risk factor epidemiology. The aims of this review are to systematically identify and collate studies describing the prevalence of schizophrenia, to summarize the findings of these studies, and to explore selected factors that may influence prevalence estimates.
Methods and Findings
Studies with original data related to the prevalence of schizophrenia (published 1965–2002) were identified via searching electronic databases, reviewing citations, and writing to authors. These studies were divided into “core” studies, “migrant” studies, and studies based on “other special groups.” Between- and within-study filters were applied in order to identify discrete prevalence estimates. Cumulative plots of prevalence estimates were made and the distributions described when the underlying estimates were sorted according to prevalence type (point, period, lifetime, and lifetime morbid risk). Based on combined prevalence estimates, the influence of selected key variables was examined (sex, urbanicity, migrant status, country economic index, and study quality).
A total of 1,721 prevalence estimates from 188 studies were identified. These estimates were drawn from 46 countries, and were based on an estimated 154,140 potentially overlapping prevalent cases. We identified 132 core studies, 15 migrant studies, and 41 studies based on other special groups. The median values per 1,000 persons (10%–90% quantiles) for the distributions for point, period, lifetime, and lifetime morbid risk were 4.6 (1.9–10.0), 3.3 (1.3–8.2), 4.0 (1.6–12.1), and 7.2 (3.1–27.1), respectively. Based on combined prevalence estimates, we found no significant difference (a) between males and females, or (b) between urban, rural, and mixed sites. The prevalence of schizophrenia in migrants was higher compared to native-born individuals: the migrant-to-native-born ratio median (10%–90% quantile) was 1.8 (0.9–6.4). When sites were grouped by economic status, prevalence estimates from “least developed” countries were significantly lower than those from both “emerging” and “developed” sites ( p = 0.04). Studies that scored higher on a quality score had significantly higher prevalence estimates ( p = 0.02).
Conclusions
There is a wealth of data about the prevalence of schizophrenia. These gradients, and the variability found in prevalence estimate distributions, can provide direction for future hypothesis-driven research.
Citation: Saha S, Chant D, Welham J, McGrath J (2005) A Systematic Review of the Prevalence of Schizophrenia. PLoS Med 2(5): e141. https://doi.org/10.1371/journal.pmed.0020141
Academic Editor: Steven E. Hyman, Harvard University, United States of America
Received: February 15, 2005; Accepted: March 29, 2005; Published: May 31, 2005
Copyright: © 2005 Saha et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: LMR, lifetime morbid risk; NOS, not otherwise specified
Introduction
Schizophrenia is a disabling group of brain disorders characterized by symptoms such as hallucinations, delusions, disorganized communication, poor planning, reduced motivation, and blunted affect. While the incidence of the disorder is relatively low (median value 15.2 per 100,000 persons per year) [ 1 ], the condition is one of the major contributors to the global burden of disease [ 2 ]. The substantial burden of disease is a reflection of two features of schizophrenia: (a) the disorder usually has its onset in early adulthood, and (b) despite optimal treatment, approximately two-thirds of affected individuals have persisting or fluctuating symptoms [ 3 ].
Understanding the “epidemiological landscape” of schizophrenia requires many different types of descriptive studies [ 4 ]. Studies that estimate the incidence of schizophrenia are required in order to identify gradients across time and/or place. These gradients allow us to generate candidate risk factors that may underlie variations in the disorder. However, studies that report the prevalence of a disorder are also important. Estimating the proportion of a population affected with schizophrenia is central to health service planning. With respect to estimating the burden of disorder, prevalence proportions can provide insights into how incidence rates are refracted via different trajectories (e.g., recovery, chronicity, or early death). The statement “prevalence = incidence + course of illness” oversimplifies the dynamic matrix of factors influencing each component of the equation. Nevertheless, prevalence proportions can help us chart contours on the still-incomplete epidemiological map of schizophrenia.
Several scholarly narrative reviews of the prevalence of schizophrenia have been published in recent decades [ 4 – 8 ]. The sheer volume of data available on the prevalence of schizophrenia now requires a more systematic and orderly approach. As with many fields of medical knowledge, there is a growing appreciation that reviews should be based on data that are as complete and as free of bias as possible [ 9 ]. Systematic reviews have prespecified methods for locating studies and for extracting and synthesizing the data. Not all systematic reviews are accompanied by meta-analysis (i.e., pooling the data to provide one summary value) [ 10 ]. Even without pooling of data, the orderly sorting of data using meta-analytic techniques can provide useful insights into the structure of the relevant literature [ 11 ].
One systematic review of the prevalence of schizophrenia has been published to date [ 12 ]. This review (based solely on census and/or community survey data) identified 18 studies that provided estimates of either period and/or lifetime prevalence of schizophrenia. Goldner and colleagues reported pooled estimates for 1-y and lifetime prevalence of 3.4 and 5.5 per 1,000 persons, respectively. The authors commented on the heterogeneity of the data and suggested that this reflected “real variation” in the distribution of schizophrenia around the world.
Recently, we published a systematic review of the incidence of schizophrenia [ 1 ]. In brief, we found that the incidence of schizophrenia varied widely between sites (persons, media n = 15.2 per 100,000; 10%–90% quantiles = 7.7–43.0). In addition, the study identified that (a) males were more likely to develop schizophrenia than females (median male:female risk ratio = 1.4); (b) migrants were more likely to develop schizophrenia than native-born individuals (median risk ratio = 4.6); and (c) individuals in urban sites had a higher risk of developing schizophrenia than those in mixed urban/rural sites. Regardless of the factors that underpin these incidence gradients, would these same gradients also be found in the prevalence of schizophrenia? If so, then it might suggest, for example, that factors influencing the course of the illness were more evenly distributed across these groups than factors influencing the incidence of the disorder. If the prevalence gradients are not congruent with the incidence gradients, then we are faced with the challenging task of unraveling the factors that could influence the differential course of schizophrenia between risk groups.
In this paper we continue our cartography of the epidemiological landscape of schizophrenia by presenting a systematic review of the prevalence of this disorder.
Ways to Measure the Prevalence of Schizophrenia
Prevalence measures the proportion of individuals who manifest a disorder at a specified time, or during a specified period. Generally prevalence estimates are calculated as a proportion, by dividing the total number of individuals who manifest a disorder (the numerator) by the total population at risk, including those with the disorder (the denominator). Prevalence proportions vary according to temporal criteria (e.g., point, period, or lifetime), but are not reported as an index of events over time (i.e., they are not like incidence rates that report the number of new cases per background population per year). Prevalence proportions are often loosely referred to as “rates”; however, in this review we will refer to them as “prevalence estimates” or “estimates.” Tables S1 and S2 define the types of prevalence estimates used in this study, and provide descriptions of the variables that we have used to describe the studies.
Point prevalence is the proportion of individuals who manifest a disorder at a given point in time (e.g., 1 d or 1 wk), while period prevalence measures the proportion of individuals who manifest a disorder during a specified period of time (e.g., 1 y). Given that the course of schizophrenia extends over months to decades, estimates of point prevalence based on 1 d are comparable to those based on 1 mo [ 5 ]. Thus, in this review we have combined all estimates based on temporal criteria of 1 mo or less in “point prevalence,” while studies that reported prevalence estimates between 1 mo and 12 mo are included under the heading “period prevalence.”
“Lifetime prevalence” is the proportion of individuals in the population who have ever manifested a disorder, who are alive on a given day. It is important to emphasize that lifetime prevalence needs to be clearly distinguished from “lifetime morbid risk” (LMR; also described elsewhere as morbid risk or expectancy). LMR differs from lifetime prevalence in that it attempts to include the entire lifetime of a birth cohort both past and future, and includes those deceased at the time of the survey [ 13 ]. LMR is the probability of a person developing the disorder during a specified period of their life or up to a specified age. There are various ways to calculate LMR [ 14 , 15 ]. The reviews of Odegaard [ 15 ], and Larsson and Sjogren [ 16 ] noted that, for low-incidence disorders such as schizophrenia, summation of age-specific incidence rates gives almost the same result as other more complicated methods of calculation [ 17 ]. The World Health Organization ten-country study [ 18 ] used this so-called “summation method” for the approximation of LMR. If one were to apply Linnean principles in order to design a taxonomy of frequency measures of disease, prevalence measures such as point, period, and lifetime would be closely related species within the same genus. However, there is a case to allocate LMR to the Genus “Incidence” rather than the Genus “Prevalence.” Conceptually (but not mathematically), LMR is closely related to cumulative incidence proportions derived from birth cohort studies [ 19 ].
Traditional prevalence studies (henceforth referred to as “core” studies) generate an estimate based on the population residing within a defined catchment area. However, it should be noted that the boundaries chosen for epidemiological studies (e.g., health districts, cities, states, or nations) may not be optimal for the detection of variations of the disorder within or between various populations. Lumping populations into large but convenient administrative areas can obscure informative, fine-grained gradients. With respect to prevalence estimates, factors such as the age structure of the population, mortality rates, and migration patterns can influence the estimates, and these may vary within and between sites.
Apart from catchment-area-based studies of the general population, there are many studies that report prevalence estimates for subgroups of the population. These may include groups defined by narrow age strata (e.g., the elderly or children), migrant status, ethnic or religious status, or twin status, to name but a few. A recent paper has systematically reviewed the prevalence of schizophrenia in prison settings [ 20 ]; however, this will not be included in this review. Migrant studies will be collated separately for analysis , while the remaining subgroup prevalence estimates will be included in “other special groups.”
Some studies report inpatient census data over a period of time (e.g., 1 y) and use the count of unique individuals with schizophrenia to generate a proportion based on general population figures. While these studies may be useful for administrative purposes, it is important not to mistake these estimates as “true” prevalence proportions. Very few patients require prolonged and continuous inpatient care; therefore, prevalence proportions based on inpatient data alone grossly underestimate true prevalence proportions. This review will collate these studies separately (henceforth referred to as “inpatient-census-derived” data); however, they will not be included in any of the main analyses.
Key Research Questions about the Prevalence of Schizophrenia
First there is a need to examine the degree of variation in the prevalence estimates of schizophrenia between sites. The companion review on the incidence of schizophrenia [ 1 ] found that within the central 80% of incidence rates, the difference ranged from 7.7 to 43 per 100,000 (over a 5-fold difference). While there has been debate within the schizophrenia research community about whether this range of rates is “narrow” or “prominent” (see review [ 21 ]), variations in prevalence estimates have not been a focus of controversy. The World Health Organization ten-country study commented that the prognosis of schizophrenia [ 18 ] was better in developing than in developed nations, a finding that has been “clear and consistent” in general [ 22 ]. The present review will describe the distribution of the different types of prevalence rates, and specifically examine whether the “developed versus developing” status of the sites influences the distribution of estimates.
Are the gradients that were identified in the incidence of schizophrenia also reflected in the prevalence of the disorder? For example, based on the previous finding that males have a significantly higher incidence of schizophrenia [ 1 , 23 ], it would be predicted that this sex difference might also be reflected in prevalence estimates. In addition, a recent study from China [ 24 , 25 ] highlighted an apparently unusual higher prevalence of schizophrenia in females in this country. In light of this issue, the male:female prevalence ratio will also be compared when the sites are sorted by a measure of “developed versus developing” status. Similarly, the incidence review identified significantly higher rates for (a) urban place of residence when compared to mixed urban/rural sites, and (b) migrant groups when compared to native-born individuals. These gradients will also be explored regarding the prevalence of schizophrenia.
Finally, systematic reviews can explore possible sources of heterogeneity in data by sorting the data according to methodological features. We will compare the distributions of estimates based on the quality of the study (as assessed by design features and thoroughness of reporting).
Identification of Studies
This systematic review conforms to the guidelines outlined by the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) recommendations [ 26 ]. The search methodology for this review was identical to that of our previous review paper on incidence of schizophrenia [ 1 ]. As a first step, a broad (free text) search string ([schizo* OR psych*] AND [incidence OR prevalence]) was used in MEDLINE, PsychINFO, EMBASE, and LILACS. Potentially relevant papers (in all languages) were accessed in order to review the full text. The references cited by each potentially relevant paper, review, and book chapter were scrutinized in order to locate additional potential papers. Posters were presented at two international schizophrenia conferences [ 27 , 28 ] in order to encourage researchers to contribute studies, especially studies from the “grey literature” (e.g., conference reports, theses, government reports, and unpublished studies). Subsequently, letters or E-mails were sent to the senior authors of papers that met the inclusion criteria. These authors were provided with an interim list of included papers and asked to nominate missing studies.
Included Studies
We included studies that reported primary data on the prevalence of schizophrenia first published between January 1965 and December 2002. Where multiple publications presented identical data, the most “informative version” of the study was included. Studies published in a language other than English were translated, and relevant papers were included.
Excluded Studies
Studies that reported prevalence data on prison or forensic populations were excluded (see recent systematic review of these studies [ 20 ]). We did not include genetic epidemiological studies that reported prevalence estimates in family members of affected (index) probands. Some studies report the LMR within large, multiplex families. These were not included; however, if the prevalence estimates were based on the entire population within a catchment area (e.g., an isolated population living in a village), then they were included.
Potential studies that had not been located at the time of submission were allocated to the “awaiting assessment” category. Studies based on inpatient-census-derived proportions are presented in the tables and summarized for comparative purposes, but were excluded from the main analyses.
Data Extraction
Once a study was included, data were extracted and entered into a three-level normalized database (i.e., only the unique prevalence estimate identifier was allowed to occur in more than one level) that included study-level variables (e.g., authors, year of publication, and site), middle-level variables (e.g., urban/rural status, age group, recruitment duration, case finding method, and diagnostic criteria), and rate-level variables (e.g., sex-specific rates for persons, males, and females). Two or more of the authors checked all data used in the analysis. When disagreements arose, these were resolved by consensus. If required, we contacted the original authors for clarification of issues. The full electronic dataset is available as Dataset 1 .
Consistent with our previous systematic review of the incidence of schizophrenia [ 1 ], studies were given “quality points” based on operationalized features related to (a) optimal research design (e.g., higher scores for greater coverage, face-to-face interview versus chart diagnosis, and reliability of instruments), and (b) quality of reporting (e.g., provision of numerator and denominator, and description of diagnostic criteria). Details of the quality scores used in this review are provided in Table S3 .
Sorting Prevalence Estimates by the Application of Sequential Filters
In systematic reviews, it is important that individuals are not “double counted” by the same or different studies. Thus, a key feature of this study is the application of sequential filters in order to identify discrete prevalence estimates. We applied a similar sorting algorithm as in our previous review of incidence of schizophrenia [ 1 ]. Briefly, the first filter parsed prevalence estimates from the included studies into three groups: core, migrant, and other special groups. Next, as the second filter, the estimates were sorted into six main types: point (1 mo or less), period (between 1 and 12 mo), lifetime, LMR, not otherwise specified (NOS), and inpatient-census-derived data.
A third, study-level filter was applied in order to isolate discrete data from multiple studies that overlapped in both time and place. This third filter was used to select one representative prevalence estimate for inclusion in the cumulative distribution using the “most informative” rule. For example, if one study presented multiple overlapping estimates, the estimate based on the largest sample was preferred (e.g., the widest age range was preferred over narrower age strata). Furthermore, filter rules were defined in order to select discrete estimates such that they allowed the greatest number of estimates to be included.
Presentation and Analyses of the Data
Key details of the included studies are presented in tables sorted by country, year of publication and first author (Tables S4 , S5 , and S6 ). The distributions of prevalence estimates are presented in cumulative plots, with every estimate contributing to the distribution. The distribution of the data is shown in rank order for prevalence estimate (lowest to highest ranks) with the cumulative percent of estimates shown on the vertical axis. The plots show horizontal reference lines indicating the 50% (median), and 25% and 75% quantiles (between which lies the interquartile range). In order to aid visual interpretation, some plots have been truncated, excluding very high estimates. Key features of these distributions are presented in tables (e.g., median, mean, harmonic mean, standard deviation, and quantiles at 10%, 25%, 50%, 75%, and 90%). These summary characteristics are based on the entire distributions. Results are presented as prevalence estimates per 1,000. In plots of prevalence ratios (e.g., male:female ratio), a vertical reference at the line of unity is shown.
We wish to draw attention to several features of the graphs used in this review. First, the central, near-linear segment of the cumulative distributions may extend beyond the interquartile range (e.g., from the 10%–90% quantiles), thus shape features (where the tails start or the range of the linear central segment) can be more informative than traditional interquartile ranges. Second, steeper segments of the cumulative plots are underpinned by estimates that have a narrow distribution, while flatter (i.e., more horizontal) segments of the distribution are underpinned by data that are relatively more dispersed. Finally, some distributions are derived from more data than others. Regardless of slope (i.e., steep or flat), if many estimates underpin segments of the distributions, then inferences based on these segments are probably more reliable than those based on segments underpinned by less data.
Meta-analyses often display data points with confidence intervals, and formal tests of heterogeneity are usually applied before combining data. For several reasons, the data in this review do not lend themselves to this type of analysis. Among the discrete core studies (see below), no study provided confidence limits to accompany the prevalence estimate. One study, which was allocated to “other special groups,” did provide confidence limits [ 29 ]. Where studies provided the corresponding numerator and denominator for a prevalence estimate, we were able to derive standard errors. However, we were able to impute standard errors for only 26% of the prevalence estimates, which were drawn from less than half (45%) of the discrete core studies. Faced with such a restricted pool of standard errors, the ability to assess the heterogeneity of the estimates in a manner generalizable across all core studies is compromised. In addition, the issues that underlie the decision to combine data from randomized controlled trials or risk factor epidemiological studies are of less relevance to prevalence estimates, where estimates based on very large populations should not necessarily carry more weight than estimates based on small populations. Based on first principles, there is no reason to assume that prevalence estimates for a disease remain static across time or place. Thus, forcing individual prevalence estimates into one pooled estimate loses important information. In this review we wish to draw attention to several characteristics of the distribution of estimates (e.g., central tendency, shape and width of the distribution, and density of data), rather than provide one pooled estimate.
In keeping with our systematic review of the incidence of schizophrenia [ 1 ], we supplement the graphical presentation of the prevalence estimates with statistical analyses. These analyses take into account (a) the need to control for within-study variation (estimates drawn from the same study tend to be more alike than estimates drawn from different studies), and (b) the use of a log transformation of the data in order to analyze distributions that are often positively skewed. Note that the median value is more informative than the arithmetic mean to assess central tendency in a skewed distribution, as is the harmonic mean (which is calculated as the exponential of the arithmetic mean of the log-transformed data, also known as the geometric mean). The analyses were carried out in SAS 9.1 using proc univariate (for medians and other quantiles of the raw data) and proc mixed for comparisons of harmonic means (because one study may provide more than one estimate, it is important to control for within-study variation).
Faced with a large quantity of data, systematic reviewers need to keep a tight rein on the number of comparisons undertaken on the data [ 30 ]. While it is tempting to reanalyze data in the light of findings that emerge from the data, such reanalyses should be kept to a minimum. The analysis of prevalence estimates is particularly challenging because of the many different prevalence types (e.g., point, period, lifetime, and LMR). Thus, in order to minimize the number of statistical comparisons in the current review, we restricted the analyses to a limited set of planned sensitivity analyses, each with a priori directional hypotheses, and, for post hoc analyses, applied multiple comparison corrections to the nominal significance levels by a Bonferroni correction. Furthermore, these analyses were based on hybrid distributions, which merged four different prevalence estimate types (point, period, lifetime, and NOS; henceforth referred to as “combined prevalence estimates”). Apart from the specific analyses related to sex differences, we undertook these analyses on distributions for persons only (i.e., males and females combined).
Based on first principles, we predicted that the estimates for known prevalence types that include different temporal criteria would be significantly different. More specifically, we predicted the following: (a) prevalence estimates for persons would differ between lifetime, period and point (point being the lowest), and (b) LMR estimates would be higher than lifetime estimates.
There is now strong evidence that males have an increased risk of developing schizophrenia [ 1 , 23 ]. We compared the distribution for males versus females on the combined prevalence estimates, predicting that males would have distributions derived from higher estimates (i.e., distributions for males would be right-shifted compared to distributions for females).
In order to explore the influence of urbanicity of site on the prevalence of schizophrenia, we divided the combined prevalence estimates for persons into three categories (urban, rural, and mixed urban/rural). Allocation was based on the study descriptions of the area or, in the absence of these descriptors, the review authors' best estimate of this variable. There are several reasons to predict that the prevalence of schizophrenia would be higher in urban regions than in rural regions. First, the incidence of schizophrenia is higher in urban sites than mixed urban/rural sites [ 1 ]. Second, the “social drift” hypothesis suggests that the individuals with schizophrenia are more likely to move into urban regions in response to various factors related to poverty, the availability of services, and easier access to cheap accommodation [ 31 ]. Finally, some commentators suggest that less industrialized settings (e.g., rural regions and/or developing countries) may facilitate recovery via social connectedness and easier access to work [ 32 ]. Thus, we predicted that the prevalence of schizophrenia would be higher in urban sites than in rural or mixed urban/rural.
Migrants have a significantly increased risk of developing schizophrenia [ 1 , 33 ]. Assuming that the course of the illness does not vary according to migrant status, based on combined prevalence estimates for persons, we predicted that the prevalence of schizophrenia would be higher in migrants than in native-born individuals.
While there is a lack of evidence addressing whether the incidence of schizophrenia varies with the economic status of nations, there is solid evidence showing that people with schizophrenia from developing countries tend to have better outcomes than individuals in developed nations [ 18 , 22 ]. Mindful that there is a lack of consensus on how best to define the multidimensional concept of economic development, we have sorted prevalence estimates according to the per capita gross national product of the study site (2004 data) [ 34 ], and used standard World Bank definitions [ 35 ]: (a) least developed countries, = mean income of less than US$2,995; (b) emerging economy countries, = mean income between US$2,995 and $9,266; and (c) developed countries, = mean income of greater than US$9,266. Thus, based on combined prevalence estimates for persons, we predicted that the prevalence of schizophrenia would be significantly different across the three economic categories, and that the prevalence of schizophrenia would be significantly lower in least developed countries than in developed countries. Furthermore, a recent commentary drew attention to the apparent female excess in the prevalence of schizophrenia in developing nations, in contrast to the male excess thought to characterize the developed world [ 25 ]. Thus, based on combined prevalence estimates, we compared the male:female ratio when the prevalence estimates were classified by the three economic categories. We predicted that the ratio would be significantly different between the three economic levels, and specifically, that the male:female ratio in developed nations would be significantly higher than that of least developed countries.
Finally, methodological features can influence prevalence estimates. For example, studies that use comprehensive case ascertainment methods (e.g., “door-knock” surveys, inpatient and outpatient records, general practitioner surveys, and/or surveys based on other community sources), should identify more cases than those that rely on fewer recruitment sources. Based on the combined prevalence estimates for persons, we divided the estimates into quality score terciles. We predicted that the prevalence estimates would be significantly different when assessed by quality score. More specifically, we predicted that prevalence estimates from studies with the highest quality score tercile would be higher than those from the lowest tercile.
The “Epidemiology” of Prevalence Estimates
The results of the search strategy, including source of the studies, subsequent culling, and final distribution of the papers, are shown in Figure 1 . The electronic search identified 1,112 papers (85% of the total papers included in the study), while manual reference checking identified an additional 142 references (11%). We received responses from 31 authors (see Acknowledgments for full list), who provided an additional 53 references (4%). We identified 98 studies that were published in languages other than English. After translation 17 of these studies were included in this review.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Double asterisk indicates exclusion categories (number studies excluded in parentheses). Double asterisk indicates numbers that are not mutually exclusive. A few studies provided rates for more than one group (11 studies provided data for both core and migrant [ n = 3] or both core and other special groups [ n = 8]; details in Results). LOTE, language other than English.
https://doi.org/10.1371/journal.pmed.0020141.g001
The list of references arranged by various criteria can be found in Tables 1 – 4 . The systematic review identified 188 studies that provided prevalence estimates [ 18 , 29 , 36 – 223 ]. These studies provided 1,721 estimates and were drawn from 46 countries. There were 132 core studies, 15 migrant studies (of which three overlap with discrete core), and 41 studies that reported the prevalence of schizophrenia in other special groups.
https://doi.org/10.1371/journal.pmed.0020141.t001
https://doi.org/10.1371/journal.pmed.0020141.t004
https://doi.org/10.1371/journal.pmed.0020141.t002
https://doi.org/10.1371/journal.pmed.0020141.t003
Key features of these core, migrant, and special groups are provided in Tables S4 – S6 . We excluded 26 studies that were completely overlapping by time and place, and 19 studies that reported prevalence data on prison populations (see Figure 1 ). However, ten partially overlapping studies were included that provided at least one discrete rate for this review [ 37 , 40 , 45 , 60 , 64 , 100 , 148 , 153 , 187 , 220 ].
The prevalence estimates were based on an estimated total of 154,140 potentially overlapping cases. The 132 core studies provided from one to 13 prevalence estimates per study. Four studies [ 59 , 120 , 169 , 224 ] reported prevalence only within narrow age strata without providing an overall rate. These studies were not included in the discrete core analyses.
Of the 132 core studies, we identified 21 studies for point prevalence, 34 studies for period prevalence, and 24 studies for lifetime prevalence. Thirty-two studies provided no information on the type of prevalence they reported—these were allocated to NOS prevalence. There were nine studies that reported LMR. Finally there were 44 studies that reported inpatient-census-derived data.
The Distribution of Prevalence Estimates
Figures 2 – 7 and Tables 5 – 7 show the distribution of the different types of prevalence estimates, and quantiles and moments for persons, males, and females.
https://doi.org/10.1371/journal.pmed.0020141.g002
https://doi.org/10.1371/journal.pmed.0020141.g007
https://doi.org/10.1371/journal.pmed.0020141.t005
https://doi.org/10.1371/journal.pmed.0020141.t007
https://doi.org/10.1371/journal.pmed.0020141.g003
https://doi.org/10.1371/journal.pmed.0020141.g004
https://doi.org/10.1371/journal.pmed.0020141.g005
https://doi.org/10.1371/journal.pmed.0020141.g006
The median point prevalence for persons (based on 23 estimates) was 4.6 per 1,000, and the 10% and 90% quantiles ranged from 1.9 to 10.0 per 1,000 (a 5-fold difference). The median period prevalence for persons (based on 42 estimates) was 3.3 per 1,000, and the 10% and 90% quantiles ranged from 1.3 to 8.2 per 1,000 (a 6.5-fold difference). The median lifetime prevalence for persons (based on 29 estimates) was 4.0 per 1,000, and the 10% and 90% quantiles ranged from 1.8 to 11.6 per 1,000 (a 6.4-fold difference).
There were 32 prevalence estimates that could not be classified to the above criteria (NOS). Based on the distribution of these prevalence estimates, the median prevalence was 2.7 per 1,000 for persons, and the 10% and 90% quantiles ranged from 1.4 to 4.8 per 1,000 (a 3.4-fold difference).
The median LMR for persons (based on 27 estimates) was 7.2 per 1,000, and the 10% and 90% quantiles ranged from 3.1 to 27.1 per 1,000 (a 8.7-fold difference) (see Table 6 ).
https://doi.org/10.1371/journal.pmed.0020141.t006
The review identified 108 estimates based on inpatient-census-derived data. Based on the distribution of these estimates for persons, the median value was 2.4 per 1,000, and the 10% and 90% quantiles ranged from 0.07 to 10.0 per 1,000 (a 154-fold difference) (see Table 7 ). Inpatient-census-derived prevalence is not included for any subsequent analyses.
When point, period, and lifetime estimates were compared, the distributions were not significantly different ( F 2,75 = 2.48, p = 0.09) . Estimates based on LMR were significantly higher than estimates based on lifetime estimates ( F 1,25 = 4.53, p = 0.04).
Male Versus Female Prevalence
Table 8 shows the moments and quantiles for the combined prevalence estimates for persons, males, and females, and for a ratio derived from male:female estimates. Figure 8 shows the distribution of these data for males and females—these distributions were not significantly different ( F 1,72 = 0.68, p = 0.41). For the male:female estimate ratio (based on 57 ratios), the median value was 1.11, and the 10% and 90% quantiles were 0.50 to 1.70 (approximately a 3.4-fold difference) (see Figure 9 ).
https://doi.org/10.1371/journal.pmed.0020141.g008
https://doi.org/10.1371/journal.pmed.0020141.g009
https://doi.org/10.1371/journal.pmed.0020141.t008
Urbanicity of Sites
We identified 31 discrete-core studies with 73 rates from urban sites (see Table 4 ), 24 studies with 48 rates from rural sites, and 45 studies with 137 mixed urban/rural rates. There were four discrete-core studies providing rates for both urban ( n = 12) and rural ( n = 10) categories. Figure 10 and Table 9 show the distribution of overall prevalence based on rural, urban, and mixed urbanicity status for persons. While the mixed urban/rural estimates were higher than urban and rural rates, this difference was not statistically significant ( F 2,235 = 1.63, p = 0.20), nor were urban estimates significantly different from rural estimates ( F 1,120 = 0.95, p = 0.33).
https://doi.org/10.1371/journal.pmed.0020141.g010
https://doi.org/10.1371/journal.pmed.0020141.t009
https://doi.org/10.1371/journal.pmed.0020141.t010
https://doi.org/10.1371/journal.pmed.0020141.t011
Migrant Status
We identified 15 migrant studies from eight countries: Australia ( n = 2; [ 55 , 207 ]), Germany ( n = 1; [ 92 ]), India ( n = 1; [ 175 ]), Israel ( n = 1; [ 200 ]), Taiwan ( n = 1; [ 129 ]), the Netherlands ( n = 1; [ 173 ]); United Kingdom ( n = 7; [ 39 , 43 , 65 – 68 , 133 ]); and United States ( n = 1; [ 180 ]).
Table S5 presents a detailed list of migrant studies with key descriptive variables, prevalence rates, and within-study migrant:native-born estimate ratios.
The number of different migrant groups in one study ranged between one and 38. There were six studies that derived data from inpatient-census-derived prevalence [ 43 , 55 , 65 – 67 , 92 ] and thus could not used in this analysis. In addition, four migrant studies did not present data for native-born populations [ 92 , 133 , 173 , 200 ]. Therefore, our analysis was limited to five papers only [ 39 , 129 , 175 , 180 , 207 ]. Based on 22 prevalence ratios, the median migrant:native-born prevalence ratio was 1.84 and the 10% and 90% quantiles were 0.86 to 6.41 (approximately a 7.5-fold difference) (see Table 1 0; Figure 11 ). When the migrant versus the native-born prevalence estimates were compared, there was a significant difference ( F 1,2 = 5.57, p = 0.04).
https://doi.org/10.1371/journal.pmed.0020141.g011
Economic Status of Sites
Based on the three economic categories, we identified 19 estimates from least developed countries, 22 estimates from emerging economy countries, and 96 estimates from developed countries (see Table 1 1; Figure 12 ). When divided by this criterion, the prevalence estimate distributions were significantly different ( F 2,85 = 3.57, p = 0.03), with the difference attributed to the lower prevalence estimate distribution for the less developed economies (developed versus least developed, F 1,74 = 6.55, p = 0.04). Table 12 also shows the male:female prevalence estimate ratio when subdivided by economic status. The distributions of these ratios (see Figure 13 ) , were not significantly different ( F 2,42 = 0.44, p = 0.44).
https://doi.org/10.1371/journal.pmed.0020141.g012
https://doi.org/10.1371/journal.pmed.0020141.g013
https://doi.org/10.1371/journal.pmed.0020141.t012
Quality Score
When the combined prevalence estimates for persons were divided into quality score terciles, the prevalence estimate distributions were significantly different ( F 2,105 = 4.79 , p = 0.01), with the highest quality studies reporting significantly higher prevalence estimates than the other two terciles (highest versus lowest quality scores, p = 0.02) ( Table 13 ; Figure 14 ).
https://doi.org/10.1371/journal.pmed.0020141.g014
https://doi.org/10.1371/journal.pmed.0020141.t013
Other Special Group Studies
Details of these studies can be found in Table S6 . We identified 41 studies that reported the prevalence of schizophrenia in other special groups. These studies came from 14 countries: Australia ( n = 4), Canada ( n = 4), Denmark ( n = 3), Finland ( n = 1), Germany ( n = 3), India ( n = 2), Israel ( n = 1), Japan ( n = 3), Romania ( n = 1), Spain ( n = 1), Sweden ( n = 2), Taiwan ( n = 1), United Kingdom ( n = 2), and United States ( n = 5).
Prevalence estimates were obtained from a range of population subgroups including elderly individuals ( n = 10; [ 52 , 70 , 71 , 101 , 108 , 121 , 149 – 151 , 159 ]), ethnic groups ( n = 8; [ 58 , 134 , 139 , 140 , 166 , 199 , 213 , 218 ]), Aborigines ( n = 4; [ 105 , 106 , 115 , 164 ]), religious groups ( n = 5; [ 29 , 80 , 128 , 182 , 191 ]), homeless individuals ( n = 4; [ 118 , 161 , 192 , 194 ]), children and adolescents ( n = 3; [ 57 , 185 , 189 ]), students ( n = 2; [ 147 , 178 ]), twins ( n = 1; [ 61 ]), industrial workers ( n = 1; [ 172 ]), different castes ( n = 1; [ 145 ]), and an isolate pedigree ( n = 1; [ 99 ]).
The marked heterogeneity of these data does not make them suitable for combining. However, we note that prevalence estimates in some homeless populations were very high—300 per 1,000 persons for Sydney homeless individuals [ 194 ] and 131 per 1,000 persons for Los Angeles homeless individuals [ 118 ]. Conversely, some religious groups had very low prevalence estimates—0.36 per 1,000 persons for Amish individuals [ 80 ] and 1.29 per 1,000 persons for Hutterite individuals [ 29 ].
There is a wealth of data available on the prevalence of schizophrenia—a total of 1,721 estimates from 188 studies were identified in this systematic review. These estimates were drawn from 46 countries, and were based on an estimated 154,140 potentially overlapping prevalent cases.
The median prevalence estimates for persons were 4.6 per 1,000 for point prevalence, 3.3 for period prevalence, 4.0 for lifetime prevalence, and 7.2 for LMR. These estimates are congruent with an earlier narrative review of 70 studies by Torrey [ 8 ], who reported an overall prevalence estimate of 4.6 per 1,000. Key policy documents have correctly estimated the point prevalence of schizophrenia at about four per 1,000 [ 2 , 225 ]; however, the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) [ 3 ], reported that the lifetime prevalence of schizophrenia is “usually estimated to be between 0.5% and 1%.” This overestimate is often repeated in textbooks [ 226 ]. As with the misunderstandings about the incidence of schizophrenia [ 21 ], this is another example where the research community needs to review their belief systems in the face of data. It is reasonable to assume that lifetime prevalence estimates for schizophrenia would be higher than point estimates. Surprisingly, the data in this review do not support this assumption. While outside the scope of the current review, the findings raise interesting research questions about factors that may influence prevalence (e.g., recovery, suicide, or other forms of early mortality). Indeed, it is curious that the identification of the onset of psychotic disorders has received so much recent attention [ 227 , 228 ], while we still struggle to understand the offset of schizophrenia. Point and period prevalence estimates assume that we can identify when someone has recovered from an illness. Recovery from schizophrenia clearly occurs [ 229 – 231 ], but it is unclear whether those who are free of positive symptoms but who have mild residual disability should be counted as “active” cases or not. The definitions of recovery versus persistence are multidimensional, and future prevalence studies will benefit if these definitions can be operationalized.
The median LMR estimate was 7.2 per 1,000, which is consistent with two other narrative reviews. Fremming [ 232 ], who reviewed 18 studies conducted in central Europe between 1926 and 1938, reported a mean LMR of 7.4 per 1,000, while Gottesman and Shields [ 233 ] reported a mean LMR of 8.0 per 1,000 in their classic review. As predicted, LMR estimates were significantly higher than lifetime estimates, which reflects the different heritage of these two indices. It is reasonable to assume that the oft-quoted statistic that “schizophrenia affects about one in a hundred” derives from LMR data (see [ 234 ]). However, one in a hundred is an overestimate—our systematic review agrees with two previous reviews showing that the LMR for schizophrenia is between seven and eight per 1,000. While the arithmetic mean value of 11.9 per 1,000 is more consistent with the “one in a hundred” dogma, the median is a more appropriate measure of central tendency for this skewed distribution. If we wish to provide the general public with a measure of the likelihood that individuals will develop schizophrenia during their lifetime, then a more accurate statement would be that “about seven to eight individuals per 1,000 will be affected.”
While there has been considerable debate about whether or not the incidence of schizophrenia varies between sites [ 21 ], there is a tacit understanding that the prevalence of schizophrenia is variable. For example, in an earlier review by Eaton [ 5 ], a 12-fold variation in point and a 10-fold variation in lifetime prevalence were noted. A recent systematic review by Goldner et al. [ 12 ] also observed a 13-fold variation in lifetime prevalence of schizophrenia. Based on the central 80% of the estimates (10% to 90% quantiles), the present review found that the different types of prevalence estimates had from 3.4-fold (point) to 4.6-fold (period) variation. The use of the 10% and 90% quantiles to define the central segment of the distribution means that our reporting of the variability of estimates is more conservative than other commentators (i.e., we have ignored 20% of the distribution in the tails). If we had included all data points, the range of prevalence estimates would have been much higher. Regardless of whether this variability is labeled “narrow” or “prominent,” the task for the researchers is to determine how much of this variation is a function of measurement error versus “true” underlying variation. With respect to measurement error, it should be noted that this study found that quality of the study does significantly influence prevalence estimates. Future studies could explore the impact of quality on the variation in prevalence estimates.
Sex and Schizophrenia
One of the unexpected findings of this review was that there was no statistically significant difference in prevalence estimates between males and females. In our previous study of incidence of schizophrenia we found a male:female risk ratio of 1.40 [ 1 ]. Because narrative reviews conclude that the course of the illness tends to be more severe in men than in women [ 235 ], we assumed that this would be reflected in a higher prevalence in males than females. The lack of coherence between (a) the sex differences found in the incidence of schizophrenia, (b) the presumed difference in course of illness, and (c) the identified lack of difference in prevalence warrants closer scrutiny.
Economic Status and Schizophrenia
In keeping with our hypothesis, the prevalence of schizophrenia is lower in developing nations than in developed nations. However, we urge caution in the interpretation of these data. The use of a single economic variable is a crude way to assess a complex and multidimensional concept. Furthermore, the median prevalence estimates for emerging economies are numerically higher than those for the richest countries. While not statistically significant, the results did identify many prevalence studies from the developing world where females outnumbered males. Recently, a study from China examined whether this unexpected sex ratio was due to differential suicide rates in males with schizophrenia [ 24 ]; however, this did not seem to explain the female excess. Our findings lend weight to the commentary by Ran and Yu-Hai Chen [ 25 ], drawing attention to the different features of schizophrenia in the developing world. Overall, the findings suggest that factors that influence the course of illness of schizophrenia in men and women differ around the world. Regardless of the mechanisms underlying this possibility, the findings highlight the importance of using systematic techniques to identify data; 17 studies included in this review were only available in languages other than English. We speculate that the results of past narrative reviews may have been biased towards data from developed nations. From a wider perspective, the findings reinforce the importance of encouraging more research from poorer countries [ 236 ].
Urbanicity and the Prevalence of Schizophrenia
In the previous systematic review of the incidence of schizophrenia, we found that urban sites had significantly higher incidence rates of schizophrenia than mixed urban/rural sites (there were too few pure rural sites to make the direct urban versus rural comparison) [ 1 ]. Contrary to our expectations, the prevalence of schizophrenia did not differ according to urbanicity. While Figure 10 suggests that mixed urban/rural sites have higher prevalence estimates than pure urban and rural sites, this study found, in fact, that there was no significant difference between urban, rural, and mixed sites. Perhaps the inclusion of many sites from the developing world in this review has confounded the expected urban/rural gradient. This will be examined in more detail in future analyses.
Migrant Status and the Prevalence of Schizophrenia
As predicted, prevalence estimates for migrant groups tend to be higher than estimates for native-born populations. This finding is consistent with past systematic reviews of the incidence of schizophrenia [ 1 , 33 ]. Migrant studies are prone to a range of methodological issues (e.g., differential pathways to care, diagnostic inaccuracies due to language and cultural practices, and uncertainty about the denominator required for the calculation of proportions). While the prevalence estimates included in this systematic review may share common biases, the increased prevalence of schizophrenia in migrant groups found in this study adds weight to the argument that migrant status is an important risk factor for schizophrenia.
Quality Scores and Other Special Groups
Reassuringly, studies that had higher overall quality scores tended to identify more cases, and thus generate higher prevalence estimates than lower quality studies. Future studies will explore whether the findings based on the overall studies persist in the subgroup of studies in the highest quality tercile.
With respect to the studies included in the category “other special groups,” the estimates are not readily comparable, but it is interesting to note that these studies reported a wide range of prevalence estimates (e.g., high in homeless populations and low in certain religious groups). Future publications will examine these groups in more detail.
Based on our experience with previous systematic reviews, we acknowledge that we may have missed studies and/or made data entry errors. We encourage readers to inform us of missing studies or errors in the data. Updated lists of relevant studies and raw data will be available from the authors. Furthermore, in the absence of clear guidelines on how to synthesize descriptive studies [ 26 , 237 ], many of the rules we used to filter studies and extract data were necessarily ad hoc. In the future, researchers may wish to reanalyze the dataset using different criteria, and perform sensitivity analyses related to these choices.
Two of the prevalence types (LMR and inpatient-census-derived data) had distributions for persons that were higher than distributions for both males and females separately. This pattern, which is difficult to explain, was also noted in some of the previously published incidence distributions [ 1 ]. The impact of quality scores on this pattern will be assessed in future studies.
The planned sensitivity analyses were conducted on combined data, a strategy that reduced the number of comparisons substantially (one combined analysis versus five analyses on each of point, period, lifetime, LMR, and NOS data). However, the combined prevalence estimate included studies that contributed more than one prevalence type (e.g., one study could contribute both point and period prevalence estimates). Of the 94 studies, eight contributed more than one prevalence type to the combined prevalence estimates. While the analytic technique controlled for within-study variance, the combined dataset is not based on discrete data (in contrast to the prevalence-type-specific analyses).
It was disappointing that standard errors could be allocated to so few prevalence estimates (26%). Despite this, in the future we plan to undertake a traditional meta-analysis based on this subset of estimates in order to compare the pooled estimate values with those presented in the current study.
Concerning the analyses for urbanicity, the estimates from mixed urban/rural studies are likely to be very heterogeneous. Indeed, we allocated studies to the mixed category if there was any possibility that rural sectors were included. This bias would have made any true difference between urban versus mixed urban/rural more difficult to detect. There are good reasons to review the findings for both urbanicity and sex ratio more closely when categorized by economic status. Such analyses may help generate hypotheses for future analyses, but researchers need to be extremely cautious when systematic reviews are subjected to excessive data analyses (i.e., “data torturing” [ 238 ]). The contributing studies were not designed to test many of the hypotheses examined in this review, therefore researchers must be frugal in the use of planned sensitivity analyses, and cautious in the interpretation of the results. However, researchers are encouraged to freely explore the full data to examine additional research questions.
While there is substantial variation between sites, generally the prevalence of schizophrenia ranges from four to seven per 1,000 persons, depending on the type of prevalence estimate used. Countries from the developing world have a lower prevalence of schizophrenia. Overall, the prevalence of schizophrenia does not vary between the sexes; however, the data suggest that sex ratio of prevalence estimates may vary between sites more than previously believed. While the incidence of schizophrenia is higher in urban than rural settings, this is not reflected in the overall prevalence data. The prevalence of schizophrenia is higher in migrants than native-born individuals.
Regardless of the exact magnitude and precision of prevalence estimates, the numbers speak to a deeper, human dimension. Many people with schizophrenia have persisting symptoms, despite the best mix of interventions we can offer. This sobering reality has also emerged from research about “best buys” with respect to the cost of averting disability [ 239 ]. For schizophrenia, with the current mix of interventions we can only reduce 13% of the burden. If we improve efficiencies within the current services, we can do somewhat better (22%). In a utopian world, even if unlimited funding were available, three-quarters of the burden of schizophrenia would remain unavoidable [ 240 ]. This is a powerful argument for investing in applied and basic research.
As with its companion study on the incidence of schizophrenia [ 1 ], we hope that the current review will populate the “epidemiological landscape” with data, and that this enriched environment will select the fittest (most heuristic) hypotheses [ 21 ]. The epidemiological landscape of schizophrenia is no longer terra incognita—many of its contours have been mapped out. We can gain traction on this landscape and use the identified gradients to generate candidate risk factors for future research [ 241 ]. Equally, these systematic reviews have brought into focus the gaps in our knowledge—parts of the map “do not fit.” Paradoxes such as these can be powerful catalysts for advancing knowledge.
Supporting Information
Dataset s1. access dataset of prevalence studies.
https://doi.org/10.1371/journal.pmed.0020141.sd001
(272 KB ZIP).
Table S1. Definitions of Prevalence Estimate Types
https://doi.org/10.1371/journal.pmed.0020141.st001
(32 KB DOC).
Table S2. Definitions for the Variables Used to Characterize the Prevalence Studies
https://doi.org/10.1371/journal.pmed.0020141.st002
(43 KB DOC).
Table S3. Quality Score Criteria
https://doi.org/10.1371/journal.pmed.0020141.st003
(38 KB DOC).
Table S4. Characteristics of Core Prevalence Studies
https://doi.org/10.1371/journal.pmed.0020141.st004
(644 KB DOC).
Table S5. Characteristics of Migrant Prevalence Studies
https://doi.org/10.1371/journal.pmed.0020141.st005
(136 KB DOC).
Tables S6. Characteristics of Other Special Groups Prevalence Studies
https://doi.org/10.1371/journal.pmed.0020141.st006
(243 KB DOC).
Acknowledgments
The authors wish to express their gratitude to the following colleagues who assisted in the search for data and translation of the studies: R. C. Bland, D. Blazer, S. Caleo, G. Canino, B. Cooper, J. Copeland, J. Cullberg, H. Dominique, O. El Saadi, M. Fichter, R. Grawe, S. C. Gupta, H. Herrman, A. Isailovic, E. Jacko, F. Jacobi, H. Katchadourian, K. Kendler, B. Moreno-Kustner, I. Levav, C. MacCauley, D. McLean, R. McCreadie, P. Munk-Jorgensen, A. Preti, P. Rabins, J. Robertson, A. Robinson, S. Scheurer, P. Shrout, L. Teplin, P. Thomsen, E. F. Torrey, M. Von Korff, J. Waddington, A. Weeke, M. Weingarten, M. Weissman, Z. Welham, E. Wells, and H. Wittchen. The Stanley Medical Research Institute supported this project. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author Contributions
JM designed the study. SS, DC, JW, and JM analyzed the data and contributed to writing the paper.
- View Article
- Google Scholar
- 2. Murray CJ, Lopez AD, editors. (1996) The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Boston: Harvard School of Public Health. 990 p.
- 3. American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders: DSM-IV, 4th ed. Washington (DC): American Psychiatric Association. 886 p.
- 4. Jablensky A (2003) Schizophrenia: The epidemiological horizon. Hirsch SR, Weinberger DR, editors. Schizophrenia Oxford: Blackwell Science. pp. 203–231.
- 6. Eaton WW, Tien AY, Poeschla BDDen Boer JA, Westenberg HGM, van Praag HM (1995) Epidemiology of schizophrenia. Advances in the neurobiology of schizophrenia. Chichester (New York): John Wiley and Sons. 469 p.
- 13. Kleinbaum DG, Kupper LL, Morgenstern H (1982) Epidemiologic research: Principles and quantitative methods. Belmont (California): Lifetime Learning Publications. 560 p.
- 19. Cox DR, Oakes D (1984) Analysis of survival data. London: Chapman and Hall. 201 p.
- 22. Bresnahan M, Menezes P, Varma V, Susser EMurray RM>, Jones PB, Susser E, van Os J, Cannon M (2003) Geographical variation in incidence, course and outcome of schiozphrenia: A comparison of developing and developed countries. The epidemiology of schizophrenia. Cambridge: Cambridge University Press. pp. 18–33.
- 32. Warner R (1985) Recovery from schizophrenia: Psychiatry and political economy. London: Routledge and Kegan Paul. 380 p.
- 34. Central Intelligence Agency (2004) CIA World Factbook, 2004. Washington (DC): Central Intelligence Agency, Office of Public Affairs. 730 p.
- 35. Soubbotina TP (2004) Beyond economic growth: An introduction to sustainable development, 2nd ed. Washington (DC): World Bank. 205 p.
- 38. Babigian HKaplan H, Freedman A, Sadock B (1980) Schizophrenia: Epidemiology. Comprehensive textbook of psychiatry III. Baltimore: Williams and Wilkins. pp. 1113–1121.
- 59. Statistics Canada (1979) Mental Health Statistics, Volume II. Ottawa: Ministry of Industry, Trade and Commerce. 123 p.
- 103. Jayasundera MGLin WCT (1969) Mental health surveys in Ceylon. Mental health research in Asia and the Pacific. Honolulu: East-West Center Press. pp. 54–64.
- 123. Leaf PJ, Myers JK, McEvoy LTRobins LN, Regier DA (1991) Procedures used in the epidemiologic catchment area study. Psychiatric disorders in America. New York: The Free Press. pp. 11–32.
- 129. Lin TY, Rin H, Yeh EK, Hsu CC, Chu HM (1969) Mental disorders in Taiwan, fifteen years later. In: Caudill W, Lin T, editors. Mental health research in Asia and the Pacific. Honolulu: East-West Center Press. pp. 66–91.
- 184. Sundaram D, Sathyavathi K, Murthy HN (1967) Ecological aspects in schizophrenia. Transactions of All-India Institute of Mental Health. Bangladore: India Institute of Mental Health. pp. 43–53.
- 224. O'Hare A, Walsh D (1972) Activities of Irish Psychiatric Hospitals and Units 1965–1969, and 1970. Dublin: The Medico-Social Research Board. 33 p.
- 226. Murray RMMurray R, Hill P, McGuffin P (1997) Schizophrenia. The essentials of postgraduate psychiatry, 3rd ed. Cambridge: Cambridge University Press. pp. 281–309.
- 232. Fremming KH (1947) Morbidity risk of mental disease and other mental abnormalities in an average Danish population. Copenhagen: Munksgaard. 278 p.
- 233. Gottesman II, Shields J (1982) Schizophrenia: The epi-genetic puzzle. Cambridge: Cambridge University Press. 258 p.
Patient Summary
Background..
Schizophrenia is a very serious mental illness and a major contributor to the global burden of disease. The topic of this study is the question of how common schizophrenia is among different groups and in different countries around the world. “Prevalence” means the number of people who have the disease at a particular time. The study itself is a so-called systematic review, which means the researchers used prespecified methods for finding individual studies and for extracting and summarizing the data from these individual studies in as objective a way as possible.
Why Was This Study Done?
Health care planning is based on prevalence estimates, and as a result, many studies on schizophrenia prevalence have been done by researchers around the world. The authors decided to do a systematic review of these studies to come up with a scientifically sound view of the big picture.
What Did the Researchers Do?
They looked at a total of 1,721 estimates of the prevalence of schizophrenia from 188 studies and covering 46 countries. They then calculated median prevalence estimates (that is, the middle value of all estimates) over a variety of time periods (see below).
What Did They Find?
The take-home message from their study is that about seven to eight individuals out of 1,000 will be affected by schizophrenia. To be more precise, the researchers found the following median estimates for the prevalence of schizophrenia: 4.6 out of 1,000 people have the disease at a specific time point; 3.3 per 1,000 have the disease within a surveillance period one to 12 months long; the lifetime prevalence (the number of people in the population who have ever manifested the disease) is 4.0 per 1,000; and the lifetime morbid risk (the likelihood that a particular individual will develop schizophrenia in their lifetime) is 7.2 per 1,000. While previous research has shown that men have a higher risk of developing schizophrenia, the researchers found that the prevalence of schizophrenia was the same in men and women (suggesting that the course of the illness differs between the sexes). The prevalence of schizophrenia was lower in poorer countries than in richer countries.
What Does This Mean?
Based on these estimates, our textbook numbers on lifetime prevalence and overall risk for an individual to develop schizophrenia are probably too high. Taken together with estimates on the incidence of schizophrenia (that is, the annual number of new cases), it is also clear that current treatments fail to cure most patients with schizophrenia.
More Information Online.
Additional information on schizophrenia can be found at the following sources.
United States National Institutes of Mental Health (search for “schizophrenia”): http://www.nimh.nih.gov/
Schizophrenia.com, a not-for-profit Web site providing information and education on schizophrenia: http://www.schizophrenia.com
For an explanation of systematic reviews: http://www.shef.ac.uk/scharr/ir/units/systrev/definitions.htm ; http://www.cochrane.org/index0.htm
For definitions of incidence and prevalence: http://www.wrongdiagnosis.com/admin/preval.htm
For more information about the systematic reviews of the incidence and prevalence of schizophrenia: http://www.qcmhr.uq.edu.au/epi/
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
On the Origins of Schizophrenia
- René S. Kahn , M.D., Ph.D.
Search for more papers by this author
What have we accomplished for schizophrenia patients since the introduction of chlorpromazine in 1952 ( 1 )? Have we really made a difference in the outcome of schizophrenia? When we examine objective and clinically meaningful “hard” outcomes, the answer appears to be negative. Still only about 10% of schizophrenia patients will find (or hold) gainful employment ( 2 ). Life expectancy in schizophrenia is reduced by almost 15 years, and this has not improved over recent decades ( 3 ). Patients with schizophrenia are rarely able to establish a family, at least when judged by reproductive fitness or fecundity ( 4 ). The reason is not that antipsychotics are ineffective; in fact, they are highly successful in what they were designed to accomplish, which is to reduce psychosis (at least during the initial phase of the illness). Almost two-thirds of first-episode schizophrenia patients reach remission after 4 to 10 weeks of antipsychotic treatment ( 5 ); even after 1 year of treatment, two-thirds are doing well ( 6 ).
So why have these medications not been able to significantly improve the long-term prognosis of schizophrenia patients? One of the reasons is that patients fail to continue treatment. Indeed, when antipsychotics are used uninterruptedly, mortality is reduced ( 7 ) and outcome, expressed as rehospitalization, improves ( 8 ). However, I propose that the principal reason that we have not been able to materially ameliorate the outcome in schizophrenia is that we have been barking up the wrong tree; we have mistakenly focused on psychosis.
Neither Kraepelin nor Bleuler considered psychosis as the core symptom of what we now call schizophrenia; neither defined schizophrenia on the basis of it. Kraepelin delineated the illness on the cognitive decline preceding the onset of psychosis—which he therefore named dementia praecox. Indeed, when Kraepelin first described the disorder, in the 4th edition of his textbook (which has never been translated into English), he starts the narrative with the slow but steady cognitive decline during adolescence ( 9 ). His account of the cognitive (and social) decline precedes the first mention of psychotic symptoms by six pages, indicating the relative priority—both in chronology and in relevance—he attributed to cognition rather than psychosis. Bleuler ( 10 ) viewed delusions and hallucinations as accessory symptoms as well; the basis of the illness was, according to him, determined by disturbance in affect, cognition (associative thinking), social interaction (autism), and volition (ambivalence). So why has research—and drug development—focused so much on that one symptom, or syndrome, in schizophrenia, even to the extent that schizophrenia and psychosis are seen as one and the same? Could the reason be just because our medications are so effective in treating this aspect of schizophrenia? Indeed, it is the treatability of psychosis and, conversely, the stigma associated with the poor outcome of schizophrenia, that is—mistakenly ( 11 )—used as an argument to question the validity of the schizophrenia concept ( 12 ). Focusing on psychosis instead of on the defining phenotype of schizophrenia may well be the reason the field has made little material progress in improving its outcome.
Cognitive Decline in Adolescence: Renewed Focus on a Century-Old Observation
The emphasis on psychosis has permeated our textbooks; consequently our students are still taught that schizophrenia debuts in early adulthood—because that is indeed when the first signs of psychosis usually present themselves to the health care provider. However, several well-designed retrospective and prospective studies show that the first signs of the illness precede the onset of psychosis by a decade or more. Entirely consistent with Kraepelin’s original observations, abundant evidence has accumulated that schizophrenia does not debut with psychosis but with much more subtle deviations from the norm, expressed in motor, social, and cognitive behavior ( 13 , 14 ). The data on cognition are most compelling. Linking cognitive testing results from the Israeli draft board with those of the National Psychiatric Hospitalization Case Registry, Reichenberg et al. ( 15 ) found significant premorbid deficits on intellectual measures during the draft assessment (at ages 16–17) in those who later developed schizophrenia. This was confirmed, using school achievement as an indication of intellectual performance, in a population-wide study relating data from the Swedish National School Register (also acquired at age 16) to the Swedish Hospital Discharge Register ( 16 ). Among psychiatric disorders, lower IQ as a premorbid marker of illness appears to be specific to this disorder; a recent review concluded that individuals who later develop schizophrenia, but not those who develop related psychotic illnesses such as bipolar disorder, exhibit an IQ deficit prior to presentation of the first psychosis ( 17 ). It was estimated, again using data from the Israeli draft board, that poor school performance precedes the onset of the illness by almost a decade ( 18 ). This is consistent with results from our study comparing scholastic aptitude in twins discordant for schizophrenia, where the twin who would go on to develop schizophrenia showed poorer school performance more than a decade before psychosis onset ( 19 ).
Prospective studies assessing participants from birth—and therefore able to identify changes much earlier than the aforementioned retrospective studies—found the first signs of schizophrenia to occur during the early teens, if not earlier. Specifically, studies of birth cohorts from New Zealand and the United Kingdom find poorer cognitive performance at age 13 ( 20 , 21 ) and possibly even at age 4 or age 8 ( 21 ) in those who are later diagnosed with schizophrenia. Also, cognitive function is lower than would be expected on the basis of the educational attainment of their first-degree relatives ( 22 ), suggesting that this underperformance is related to the risk of developing the illness. Thus, there is little doubt that cognitive function starts to decline many years before the first psychotic symptoms manifest themselves in the context of schizophrenia. Equally relevant, this phenomenon is related to the development of schizophrenia and not to psychosis per se.
Lower Cognitive Function Preceding the Onset of Psychosis
The realization that schizophrenia debuts well before patients present with psychosis or are hospitalized has led to the concept of studying individuals who have some psychotic symptoms but do not (yet) fulfill the full criteria for psychosis, let alone schizophrenia. The concept goes by various names and acronyms, such as at-risk mental state (ARMS), ultra high risk (UHR), and, when help seeking, clinical high risk (CHR) ( 23 ). All have in common that the patients are defined by so-called attenuated psychotic symptoms with the outcome defined as “conversion” or “transition” to full psychosis—not necessarily schizophrenia. One of the more problematic, although interesting, issues with the CHR concept is that even in this subsyndromal population, transition to full psychosis is rare: about 15% (e.g., reference 24 ). Moreover, the concept of transition itself is criticized on the basis of the selective sampling of these cohorts and the fact that transition is a binary outcome defined as a higher score on the continuous scale that selected the population in the first place ( 25 )—although recently suggestions have been made for improving sampling strategies ( 26 ). Nevertheless, the exclusive focus on psychosis (both at baseline and as outcome) in the CHR concept may be inherently flawed ( 25 ). Also, it is important to realize that the age range of the subjects included in these studies is usually very wide (from 12 to 35 years), with the upper end far too old to be credibly related to the development of schizophrenia. Nevertheless, the CHR studies have the potential to provide, if indirectly, interesting clues on the risk factors of schizophrenia: in the largest single study to date, including almost 700 CHR patients, cognitive impairment was present in the entire sample but was most pronounced in those who developed full psychosis—although here, as in most CHR studies, schizophrenia as an outcome was not reported ( 27 ). Studies examining the longitudinal course of cognitive development in CHR—essential to reliably draw conclusions on cognitive development in those cohorts—have not been published to date.
Abnormal Brain Maturation Preceding the Onset of Psychosis
The finding that cognitive decline in schizophrenia starts at, if not before, adolescence is consistent with studies examining brain structure in schizophrenia. More than four decades ago, Johnstone et al. ( 28 ) published their seminal paper reporting for the first time reduced brain volume (or, more precisely, increased lateral ventricle volume) in schizophrenia patients on the basis of CT scans. Since this concerned a cross-sectional study in chronic patients, the question remained as to when these changes manifest themselves. Since then, multiple studies in medication-naive patients with first-episode schizophrenia have shown that brain volumes are smaller at the first presentation of psychosis than those of matched control subjects ( 29 ). Consistently, CHR subjects who go on to develop a full psychotic episode exhibit smaller brain volumes before they receive antipsychotic medication ( 24 ). The fact that brain volumes are smaller in schizophrenia before the emergence of the first psychosis suggests that, contrary to what is sometimes suggested ( 30 ), the brain loss cannot be attributed to antipsychotic medication. Although the results from MRI studies in first-episode schizophrenia and CHR subjects suggest that brain loss is present at or before the first psychosis, they do not clarify at what time point the decreases in brain volume first become apparent. However, there is compelling evidence that the process leading to decreased brain volume starts well before the onset of psychosis. This conclusion is based on a simple but often overlooked variable: intracranial volume (ICV), or more simply put, skull size. ICV is a highly reliable measure that is often not assessed, or goes unreported, in neuroimaging studies in schizophrenia. Nevertheless, it is relevant because ICV directly reflects brain growth, as cranial growth is driven by the expansion of the brain. Although the exact age when the brain reaches it maximum size is somewhat variable, it is generally considered to be at the start of puberty ( 31 ). Thus, an ICV that is smaller in schizophrenia patients than in matched healthy control subjects must be due to stunted brain growth (at any point in time) before that age. Since the effect size is small and therefore often, if reported, is not significant in single studies, the results of our meta-analysis in over 18,000 subjects show a small (d=0.2) but highly significant reduction in ICV ( 29 ). These results indicate that some of the brain loss in schizophrenia is developmental in nature and must occur before the early teens—that is, long before there is any indication of psychosis, let alone schizophrenia.
A relatively novel way to study brain development is the so-called brain-age gap—the difference between the “age” of the brain and the chronological age of a person. For instance, a 20-year-old may have a brain that resembles that of a 25-year-old person, in which case the brain-age gap is 5 years. We reported, examining brain age in a longitudinal study across a 50-year age span (16–67 years), that brain age was significantly higher (by 3.6 years) than chronological age in schizophrenia patients ( 32 ). Similarly, when the brain-age gap was studied in a CHR population, albeit in a cross-sectional study, it was found to significantly deviate from the norm in those who transitioned to psychosis ( 33 ). Thus, it appears from the available evidence, which admittedly is still scarce, that abnormal brain maturation starting before the mid-teens is related to the development of schizophrenia. However, large longitudinal studies focusing on young adolescents and using schizophrenia (in contrast to psychosis) as outcome are sorely needed.
Cognitive and Brain Abnormalities and the Genetic Risk for Schizophrenia
Cognitive function is related to brain structure in the healthy population: intelligence positively correlates with global brain volume, explaining a little over 6% of the variance ( 34 ). However, brain volume is not static, nor is IQ. Indeed, in a longitudinal study in 504 healthy subjects, we reported that intelligence is more related to the magnitude and timing of changes in brain structure than to brain structure per se ( 35 ), especially in early adolescence ( 36 ).
In medication-naive first-episode schizophrenia patients, lower IQ was related to smaller brain volumes ( 37 ), with most of the brain volume loss over time confined to the group of patients showing cognitive decline over the first years of illness ( 38 ). Thus, there is growing evidence that changes in IQ are related to (maturational) changes in the cortex, both in healthy subjects and in patients with schizophrenia. Intriguingly, this relationship seems itself age dependent and to present itself predominantly at the onset of puberty. What is more, it appears that genes that increase the risk of developing schizophrenia may drive the changes in both the brain and in cognition.
That schizophrenia is heritable has been suspected since the first days the illness was conceptualized; indeed, it was recently estimated that genetic variation contributes up to 85% of the risk of developing the illness ( 39 ). Brain volume and intelligence are highly heritable as well, with estimates up to 90% for total brain volume ( 40 ) and 80% for IQ ( 41 ). Thus, one may assume that if there is a genetic relationship between risk for schizophrenia and cognition, this risk may also be expressed in brain volume loss. Indeed, on the basis of 1,243 twins, using mathematical models, we concluded that 25% of the total risk variance for schizophrenia is explained by lower IQ, and 4% of this variance is explained by smaller brain volume ( 42 ). Taken together with the early onset of cognitive changes and the smaller intracranial volume found in schizophrenia, these results suggest that part of the genetic risk of developing the illness may be related to an abnormal early development of the brain leading to cognitive deficits. The brain changes appear to be primarily expressed in cortical thickness and white matter integrity ( 43 ). However, it is more likely that the substrate in the brain underlying the cognitive changes in the development of schizophrenia is related to abnormal connectivity rather than gross volume decreases.

Brain Networks and Cognitive Changes in Schizophrenia
Schizophrenia has been conceptualized as a disorder of brain connectivity since the illness was first defined ( 9 , 10 , 44 ), and this idea was revived a century later using more modern techniques ( 45 ). Consistent with these hypotheses, we have shown that white matter connectivity is disrupted in schizophrenia, particularly in those areas that form the hubs for the main connections in the brain ( 46 , 47 ). In view of their rich interconnectedness, these hubs are sometimes collectively called the “rich club” ( 46 ). These networks, also called the “connectome” of the brain ( 48 ), are under genetic control ( 43 , 49 ) and are already being formed in the second trimester of pregnancy ( 50 ). The efficiency of this network—defined as the optimal relationship between functional connectivity and distance between brain areas ( 51 )—is highly related to intelligence ( 52 ), as are the observed changes in this network’s efficiency during adolescence ( 49 ). Not only are brain networks under considerable genetic control, and not only are the abnormalities related to some of the genes conferring increased risk for schizophrenia, but also important changes in these networks crucially occur during early adolescence. In general, the cortex becomes thinner during adolescence (e.g., 53 ), with its connecting white matter fibers increasing in volume ( 54 ). The cortical changes are genetically controlled and are related to cognitive development during adolescence ( 55 ). Crucially, the brain networks become increasingly more efficiently organized during this period ( 49 ), with their efficiency increasing in adolescence between ages 10 and 13 ( 56 ) and the effect leveling off between ages 13 and 18. The connectome’s efficiency itself and the relationship between intelligence and network efficiency are under genetic control (47% and 87%, respectively) ( 54 ). Thus, abnormal development of the brain’s network appears to be a plausible candidate for the neuroanatomical and functional substrate of the cognitive changes that precede the onset of psychosis in schizophrenia. Moreover, in view of the high heritability, abnormalities in the networks’ efficiency could possibly be related to the genetic risk of schizophrenia. Indeed, abnormal network efficiency in the rich club has been found in siblings ( 57 ) and offspring of schizophrenia patients ( 58 ). Interestingly, this effect in the rich club hubs appears to be specific for schizophrenia—it has not been found in patients with bipolar disorder ( 59 ) or their offspring ( 58 ). Since the abnormalities are also observed in medication-naive schizophrenia patients, they cannot be attributed to the use of medication and are most likely present before illness onset ( 60 ). Moreover, connectome organization has been found to be related to functional outcome and decreases in IQ over time in schizophrenia patients ( 61 ). Importantly, the macroscopic hub areas of the brain, as identified with MRI, can also be determined on a cellular, microscopic level, and they are highly related to higher-order cognitive functions, such as IQ ( 62 , 63 ). Moreover, when combining transcriptional profiles of schizophrenia risk genes with data on the decreased hub connectivity, we found that the expression profile of risk genes across cortical regions was significantly correlated with the regional dysconnectivity ( 64 ). In addition, effects were found to be potentially specific to schizophrenia, with transcriptional profiles not related to cortical dysconnectivity in patients with bipolar illness. Especially fascinating is the finding that brain connections present in humans but not in chimpanzees—those predominantly involved in semantic comprehension and language processing—are those affected in schizophrenia and not in other psychiatric disorders, such as autism, obsessive-compulsive disorder, and major depression ( 65 ), suggesting that the same areas that have evolved in humans to acquire higher-order cognitive capabilities, such as language, are those that are particularly vulnerable to being affected in the development of schizophrenia. Another line of evidence suggesting that brain development during adolescence is a crucial factor in the path to schizophrenia is derived from genetic studies.
Brain Networks and The Genetics of Schizophrenia
Currently more than 200 genome-wide significant loci have been associated with the risk of schizophrenia in Caucasian populations ( 66 ). The strongest genetic relationship is that across the major histocompatibility complex (MHC) locus on chromosome 6, which is known for its role in immunity. Sekar et al. ( 67 ) identified alleles of the complement component 4 (C4 genes) in the MHC region as underlying the MHC signal. Also, allelic variation in C4 was related to increased risk for schizophrenia in proportion to its promotion of expression of C4A mRNA. Sekar et al. also found increased levels of C4 mRNA expression in postmortem brain from individuals with schizophrenia compared with matched control subjects. This discovery was recently replicated in a transcriptomic study by the PsychEncode consortium that included 559 schizophrenia case subjects and 936 healthy control subjects ( 68 ). Relevant for the development of schizophrenia during adolescence, Stevens et al. ( 69 ) have shown that proteins of the complement system are involved in activity-dependent synaptic pruning: weak synapses are tagged by these complement proteins and eliminated by microglia. Similar properties were recently found for C4 ( 67 ). In a human in vitro model with induced neurons and microglia, Sellgren et al. ( 70 ) showed that microglia generated from stem cells of schizophrenia patients eliminated more synaptic structures, with both neuronal and microglial factors contributing. These studies have revitalized the hypothesis that schizophrenia may result from abnormalities in brain maturation ( 71 ), specifically abnormalities in the synaptic pruning of prefrontal and temporal cerebral cortex that normally characterizes adolescent brain maturation ( 72 ). Indeed, excessive loss of gray matter and abnormally low numbers of synapses on cortical neurons in these brain regions (i.e., excessive synaptic pruning) are well-replicated pathological findings in schizophrenia ( 73 ). The hypothesis on the role of increased complement activity as a pathogenic mechanism in schizophrenia elegantly links genetic, neuroanatomical, and phenotypical findings ( 74 ). Although it still needs to be properly tested, it provides an inspiring example of how data from various sources can help elucidate the causes of schizophrenia.
Translating Old Findings to New Initiatives
In order to understand schizophrenia, its causes, development, and outcome, and in order to define new subgroups of patients who may be differentially responsive to treatment or, hopefully, prevention interventions, we will need to switch our focus from psychosis to cognition and the related brain development during childhood and early adolescence. It is clear that cognitive decline before the onset of psychosis is an important marker, if not a harbinger, of impending schizophrenia with the possibility, if identified appropriately early, that interventions can be developed to halt this decline and prevent psychosis ( 75 ). Thus, research efforts that target the second decade of life are essential if we are to find mechanisms for intervention and cure. These studies are costly and time-consuming, but there is an example that is rapidly providing some of this information: the UK Biobank, a unique initiative, is an open source of data that is producing the information that will help resolve the issues described above. For instance, in a study using UK Biobank data from more than 2,800 participants from the general population, a relationship was found between the polygenic risk score for schizophrenia and cortical thinning on MRI ( 76 ). These findings confirm—in the general population—the reported association between genetic vulnerability to the disorder and brain pathology in those at increased genetic risk for schizophrenia ( 77 ). Equally important, and showing the need for such large samples, individuals with rare copy number variants (CNVs) were identified in a study of over 400,000 subjects in the UK Biobank reporting a relationship between CNVs that are associated with an increased risk for schizophrenia and lower cognitive performance on neuropsychological tests ( 78 ). Finally, researchers using UK Biobank data were able to identify new loci related to cognitive function ( 79 ) and the related variable of educational attainment ( 80 ) in the general population—information that will be, for reasons outlined here, potentially relevant for the study of schizophrenia. A comparable program in the United States is the Million Veteran Program (MVP), which is expected to be as informative and successful as the UK Biobank; indeed, recently Harvey et al. ( 81 ), using data from the MVP, reported robust associations between greater polygenic loading for schizophrenia risk and poorer cognitive performance.
Clearly, more of such large-scale initiatives will be needed, and they need to longitudinal. Although some cohorts are being followed—the Adolescent Brain and Cognitive Development study comes to mind ( 82 )—their numbers will still be too low to detect causes for relatively rare disorders such as schizophrenia (of the 10,000 subjects included, only 100 are expected to develop schizophrenia).
In addition to these large population-based studies, subjects can be followed who are at greatly increased risk for schizophrenia, which requires, given the large relative risk ratios, much smaller numbers. Schizophrenia risk is probably increased through a combination of many common variants, more of which are being identified as sample sizes are increasing ( 83 ). However, the explained risk is very low for each of these variants, and even these variants in combination. Much larger effects are seen in the people who carry very rare CNVs. Although results obtained from following these subjects will be difficult to interpret in view of their scarcity in the population and less generalizable than results from samples from the general population, they are helpful in studying mechanistic questions. One promising example is the identification of SETD1A as a schizophrenia susceptibility gene ( 84 ). Loss of function in this gene was recently shown to negatively affect the brain connectome in mice, which in turn was related to cognitive deficits in these animals ( 85 ).
The usefulness of examining the role of rare variants has also proven its merit in human studies, such as adolescents with the 22q11.2 deletion syndrome (22q11DS), who have a 25-fold increased risk of developing schizophrenia ( 86 ). When cognitive function was assessed longitudinally in a group of 829 children and adolescents with this syndrome, cognitive performance declined in the entire group of patients, but it was most pronounced in those who went on to develop schizophrenia ( 87 ). Since the 22q11DS is rare—1:4,000 for deletions and 1:1,600 for duplications in the 22q11.2 area ( 88 )—this study could only be successful because all researchers working in this field shared their data. Finally, studying another high-risk group, the offspring of patients with schizophrenia, is a good possibility for enriching samples for the development of schizophrenia. Indeed, long-term follow-up of offspring of patients with bipolar disorder has provided important information on the highly heterogeneous pathways to bipolar illness ( 89 ). Following offspring of schizophrenia patients, although more difficult given the decreased fecundity of schizophrenia patients ( 4 ), would be expected to be as informative.
Conclusions
Despite an enormous expansion in our knowledge on the etiology, pathophysiology, and illness course of schizophrenia, so far we have not been able to materially improve the outcome of this highly incapacitating illness. One of the reasons may be that we have been focusing on psychosis, which is a relatively late-occurring, and nonspecific, symptom of schizophrenia. It has become abundantly clear that schizophrenia debuts with cognitive decline years before the onset of the first psychosis. Cognitive and brain development are highly linked, especially during early adolescence, and both are, independently as well as their interaction, under substantial genetic control. A growing body of evidence suggests that abnormal brain maturation during the early teen years, especially that of the hub areas in the brain, may be causally related to the development of the disorder. These changes can be linked to specific genetic loci that have been found to increase the risk for schizophrenia and can be attributed to abnormal synaptic pruning during this developmental period. Large collaborative longitudinal (population based and high-risk) studies focusing on early adolescence and linking cognition, phenomenology, brain imaging, biomarkers, and genetics may be the path forward to elucidate the causes of schizophrenia. We should then be able to develop the tools to finally improve outcomes for the patients suffering from this devastating disorder.
Dr. Kahn has served as a consultant for Alkermes, Janssen-Cilag, Luye Pharma, Otsuka, and Sunovion.
1 Delay J, Deniker P : Neuroleptic effects of chlorpromazine in therapeutics of neuropsychiatry . J Clin Exp Psychopathol 1955 ; 16:104–112 Medline , Google Scholar
2 Davidson M, Kapara O, Goldberg S, et al. : A nation-wide study on the percentage of schizophrenia and bipolar disorder patients who earn minimum wage or above . Schizophr Bull 2016 ; 42:443–447 Crossref , Medline , Google Scholar
3 Hjorthøj C, Stürup AE, McGrath JJ, et al. : Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis . Lancet Psychiatry 2017 ; 4:295–301 Crossref , Medline , Google Scholar
4 Haukka J, Suvisaari J, Lönnqvist J : Fertility of patients with schizophrenia, their siblings, and the general population: a cohort study from 1950 to 1959 in Finland . Am J Psychiatry 2003 ; 160:460–463 Link , Google Scholar
5 Kahn RS, Winter van Rossum I, Leucht S, et al. : Amisulpride and olanzapine followed by open-label treatment with clozapine in first-episode schizophrenia and schizophreniform disorder (OPTiMiSE): a three-phase switching study . Lancet Psychiatry 2018 ; 5:797–807 Crossref , Medline , Google Scholar
6 Kahn RS, Fleischhacker WW, Boter H, et al. : Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial . Lancet 2008 ; 371:1085–1097 Crossref , Medline , Google Scholar
7 Tiihonen J, Mittendorfer-Rutz E, Torniainen M, et al. : Mortality and cumulative exposure to antipsychotics, antidepressants, and benzodiazepines in patients with schizophrenia: an observational follow-up study . Am J Psychiatry 2016 ; 173:600–606 Link , Google Scholar
8 Tiihonen J, Mittendorfer-Rutz E, Majak M, et al. : Real-world effectiveness of antipsychotic treatments in a nationwide cohort of 29 823 patients with schizophrenia . JAMA Psychiatry 2017 ; 74:686–693 Crossref , Medline , Google Scholar
9 Kraepelin E: Ein kurzes Lehrbuch für Studirende und Aerzte, 4th ed. Leipzig, Abel, 1893, pp 435–445 Google Scholar
10 Bleuler E : Dementia Praecox oder die Gruppe der Schizophrenien . Leipzig, Deuticke, 1911 Google Scholar
11 Kahn RS : Why the concept of schizophrenia is still alive and kicking . Psychol Med 2018 ; 48:247–248 Crossref , Medline , Google Scholar
12 Guloksuz S, van Os J : The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum . Psychol Med 2018 ; 48:229–244 Crossref , Medline , Google Scholar
13 Dickson H, Laurens KR, Cullen AE, et al. : Meta-analyses of cognitive and motor function in youth aged 16 years and younger who subsequently develop schizophrenia . Psychol Med 2012 ; 42:743–755 Crossref , Medline , Google Scholar
14 Woodberry KA, Giuliano AJ, Seidman LJ : Premorbid IQ in schizophrenia: a meta-analytic review . Am J Psychiatry 2008 ; 165:579–587 Link , Google Scholar
15 Reichenberg A, Weiser M, Rabinowitz J, et al. : A population-based cohort study of premorbid intellectual, language, and behavioral functioning in patients with schizophrenia, schizoaffective disorder, and nonpsychotic bipolar disorder . Am J Psychiatry 2002 ; 159:2027–2035 Link , Google Scholar
16 Kendler KS, Ohlsson H, Mezuk B, et al. : A Swedish national prospective and co-relative study of school achievement at age 16, and risk for schizophrenia, other nonaffective psychosis, and bipolar illness . Schizophr Bull 2016 ; 42:77–86 Medline , Google Scholar
17 Mollon J, Reichenberg A : Cognitive development prior to onset of psychosis . Psychol Med 2018 ; 48:392–403 Crossref , Medline , Google Scholar
18 Velthorst E, Reichenberg A, Kapra O, et al. : Developmental trajectories of impaired community functioning in schizophrenia . JAMA Psychiatry 2016 ; 73:48–55 Crossref , Medline , Google Scholar
19 van Oel CJ, Sitskoorn MM, Cremer MPM, et al. : School performance as a premorbid marker for schizophrenia: a twin study . Schizophr Bull 2002 ; 28:401–414 Crossref , Medline , Google Scholar
20 Reichenberg A, Caspi A, Harrington H, et al. : Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-year study . Am J Psychiatry 2010 ; 167:160–169 Link , Google Scholar
21 Mollon J, David AS, Zammit S, et al. : Course of cognitive development from infancy to early adulthood in the psychosis spectrum . JAMA Psychiatry 2018 ; 75:270–279 Crossref , Medline , Google Scholar
22 Keefe RSE, Eesley CE, Poe MP : Defining a cognitive function decrement in schizophrenia . Biol Psychiatry 2005 ; 57:688–691 Crossref , Medline , Google Scholar
23 Fusar-Poli P : The Clinical High-Risk State for Psychosis (CHR-P), Version II . Schizophr Bull 2017 ; 43:44–47 Crossref , Medline , Google Scholar
24 Cannon TD, Chung Y, He G, et al. : Progressive reduction in cortical thickness as psychosis develops: a multisite longitudinal neuroimaging study of youth at elevated clinical risk . Biol Psychiatry 2015 ; 77:147–157 Crossref , Medline , Google Scholar
25 van Os J, Guloksuz S : A critique of the “ultra-high risk” and “transition” paradigm . World Psychiatry 2017 ; 16:200–206 Crossref , Medline , Google Scholar
26 Fusar-Poli P, Sullivan SA, Shah JL, et al. : Improving the detection of individuals at clinical risk for psychosis in the community, primary and secondary care: an integrated evidence-based approach . Front Psychiatry 2019 ; 10:774 Crossref , Medline , Google Scholar
27 Seidman LJ, Shapiro DI, Stone WS, et al. : Association of neurocognition with transition to psychosis: baseline functioning in the second phase of the North American Prodrome Longitudinal Study . JAMA Psychiatry 2016 ; 73:1239–1248 Crossref , Medline , Google Scholar
28 Johnstone EC, Crow TJ, Frith CD, et al. : Cerebral ventricular size and cognitive impairment in chronic schizophrenia . Lancet 1976 ; 2:924–926 Crossref , Medline , Google Scholar
29 Haijma SV, Van Haren N, Cahn W, et al. : Brain volumes in schizophrenia: a meta-analysis in over 18 000 subjects . Schizophr Bull 2013 ; 39:1129–1138 Crossref , Medline , Google Scholar
30 Fusar-Poli P, Smieskova R, Kempton MJ, et al. : Progressive brain changes in schizophrenia related to antipsychotic treatment? A meta-analysis of longitudinal MRI studies . Neurosci Biobehav Rev 2013 ; 37:1680–1691 Crossref , Medline , Google Scholar
31 Libby J, Marghoub A, Johnson D, et al. : Modelling human skull growth: a validated computational model . J R Soc Interface 2017 ; 14: 20170202 Crossref , Medline , Google Scholar
32 Schnack HG, van Haren NEM, Nieuwenhuis M, et al. : Accelerated brain aging in schizophrenia: a longitudinal pattern recognition study . Am J Psychiatry 2016 ; 173:607–616 Link , Google Scholar
33 Chung Y, Addington J, Bearden CE, et al. : Use of machine learning to determine deviance in neuroanatomical maturity associated with future psychosis in youths at clinically high risk . JAMA Psychiatry 2018 ; 75:960–968 Crossref , Medline , Google Scholar
34 Pietschnig J, Penke L, Wicherts JM, et al. : Meta-analysis of associations between human brain volume and intelligence differences: how strong are they and what do they mean? Neurosci Biobehav Rev 2015 ; 57:411–432 Crossref , Medline , Google Scholar
35 Schnack HG, van Haren NEM, Brouwer RM, et al. : Changes in thickness and surface area of the human cortex and their relationship with intelligence . Cereb Cortex 2015 ; 25:1608–1617 Crossref , Medline , Google Scholar
36 Brouwer RM, van Soelen ILC, Swagerman SC, et al. : Genetic associations between intelligence and cortical thickness emerge at the start of puberty . Hum Brain Mapp 2014 ; 35:3760–3773 Crossref , Medline , Google Scholar
37 Rais M, Cahn W, Schnack HG, et al. : Brain volume reductions in medication-naive patients with schizophrenia in relation to intelligence quotient . Psychol Med 2012 ; 42:1847–1856 Crossref , Medline , Google Scholar
38 Kubota M, van Haren NEM, Haijma SV, et al. : Association of IQ changes and progressive brain changes in patients with schizophrenia . JAMA Psychiatry 2015 ; 72:803–812 Crossref , Medline , Google Scholar
39 Kahn RS, Sommer IE, Murray RM, et al. : Schizophrenia . Nat Rev Dis Primers 2015 ; 1:15067 Crossref , Medline , Google Scholar
40 van Haren NEM, Rijsdijk F, Schnack HG, et al. : The genetic and environmental determinants of the association between brain abnormalities and schizophrenia: the Schizophrenia Twins and Relatives Consortium . Biol Psychiatry 2012 ; 71:915–921 Crossref , Medline , Google Scholar
41 Posthuma D, de Geus EJ, Boomsma DI : Perceptual speed and IQ are associated through common genetic factors . Behav Genet 2001 ; 31:593–602 Crossref , Medline , Google Scholar
42 Toulopoulou T, van Haren N, Zhang X, et al. : Reciprocal causation models of cognitive vs volumetric cerebral intermediate phenotypes for schizophrenia in a pan-European twin cohort . Mol Psychiatry 2015 ; 20:1386–1396 Crossref , Medline , Google Scholar
43 Bohlken MM, Mandl RCW, Brouwer RM, et al. : Heritability of structural brain network topology: a DTI study of 156 twins . Hum Brain Mapp 2014 ; 35:5295–5305 Crossref , Medline , Google Scholar
44 Wernicke C : Grundrisse der Psychiatrie . Leipzig, Thieme, 1906 Google Scholar
45 Friston KJ, Frith CD : Schizophrenia: a disconnection syndrome? Clin Neurosci 1995 ; 3:89–97 Medline , Google Scholar
46 van den Heuvel MP, Kahn RS, Goñi J, et al. : High-cost, high-capacity backbone for global brain communication . Proc Natl Acad Sci USA 2012 ; 109:11372–11377 Crossref , Medline , Google Scholar
47 van den Heuvel MP, Sporns O, Collin G, et al. : Abnormal rich club organization and functional brain dynamics in schizophrenia . JAMA Psychiatry 2013 ; 70:783–792 Crossref , Medline , Google Scholar
48 de Reus MA, Saenger VM, Kahn RS, et al. : An edge-centric perspective on the human connectome: link communities in the brain . Philos Trans R Soc Lond B Biol Sci 2014 ; 369: 20130527 Crossref , Medline , Google Scholar
49 Koenis MMG, Brouwer RM, van den Heuvel MP, et al. : Development of the brain’s structural network efficiency in early adolescence: a longitudinal DTI twin study . Hum Brain Mapp 2015 ; 36:4938–4953 Crossref , Medline , Google Scholar
50 Turk E, van den Heuvel MI, Benders MJ, et al. : Functional connectome of the fetal brain . J Neurosci 2019 ; 39:9716–9724 Crossref , Medline , Google Scholar
51 Bullmore E, Sporns O : The economy of brain network organization . Nat Rev Neurosci 2012 ; 13:336–349 Crossref , Medline , Google Scholar
52 van den Heuvel MP, Stam CJ, Kahn RS, et al. : Efficiency of functional brain networks and intellectual performance . J Neurosci 2009 ; 29:7619–7624 Crossref , Medline , Google Scholar
53 Brown TT, Kuperman JM, Chung Y, et al. : Neuroanatomical assessment of biological maturity . Curr Biol 2012 ; 22:1693–1698 Crossref , Medline , Google Scholar
54 Brouwer RM, Mandl RCW, Schnack HG, et al. : White matter development in early puberty: a longitudinal volumetric and diffusion tensor imaging twin study . PLoS One 2012 ; 7: e32316 Crossref , Medline , Google Scholar
55 Teeuw J, Brouwer RM, Koenis MMG, et al. : Genetic influences on the development of cerebral cortical thickness during childhood and adolescence in a Dutch longitudinal twin sample: the Brainscale Study . Cereb Cortex 2019 ; 29:978–993 Crossref , Medline , Google Scholar
56 Koenis MMG, Brouwer RM, Swagerman SC, et al. : Association between structural brain network efficiency and intelligence increases during adolescence . Hum Brain Mapp 2018 ; 39:822–836 Crossref , Medline , Google Scholar
57 Collin G, Kahn RS, de Reus MA, et al. : Impaired rich club connectivity in unaffected siblings of schizophrenia patients . Schizophr Bull 2014 ; 40:438–448 Crossref , Medline , Google Scholar
58 Collin G, Scholtens LH, Kahn RS, et al. : Affected anatomical rich club and structural-functional coupling in young offspring of schizophrenia and bipolar disorder patients . Biol Psychiatry 2017 ; 82:746–755 Crossref , Medline , Google Scholar
59 Collin G, van den Heuvel MP, Abramovic L, et al. : Brain network analysis reveals affected connectome structure in bipolar I disorder . Hum Brain Mapp 2016 ; 37:122–134 Crossref , Medline , Google Scholar
60 Chung Y, Haut KM, He G, et al. : Ventricular enlargement and progressive reduction of cortical gray matter are linked in prodromal youth who develop psychosis . Schizophr Res 2017 ; 189:169–174 Crossref , Medline , Google Scholar
61 Collin G, de Nijs J, Hulshoff Pol HE, et al. : Connectome organization is related to longitudinal changes in general functioning, symptoms, and IQ in chronic schizophrenia . Schizophr Res 2016 ; 173:166–173 Crossref , Medline , Google Scholar
62 Seidlitz J, Váša F, Shinn M, et al. : Morphometric similarity networks detect microscale cortical organization and predict inter-individual cognitive variation . Neuron 2018 ; 97:231–247.e7 Crossref , Medline , Google Scholar
63 van den Heuvel MP, Scholtens LH, de Reus MA, et al. : Associated microscale spine density and macroscale connectivity disruptions in schizophrenia . Biol Psychiatry 2016 ; 80:293–301 Crossref , Medline , Google Scholar
64 Romme IAC, de Reus MA, Ophoff RA, et al. : Connectome disconnectivity and cortical gene expression in patients with schizophrenia . Biol Psychiatry 2017 ; 81:495–502 Crossref , Medline , Google Scholar
65 van den Heuvel MP, Scholtens LH, de Lange SC, et al. : Evolutionary modifications in human brain connectivity associated with schizophrenia . Brain 2019 ; 142:3991–4002 Crossref , Medline , Google Scholar
66 Schizophrenia Working Group of the Psychiatric Genomics Consortium : Biological insights from 108 schizophrenia-associated genetic loci . Nature 2014 ; 511:421–427 Crossref , Medline , Google Scholar
67 Sekar A, Bialas AR, de Rivera H, et al. : Schizophrenia risk from complex variation of complement component 4 . Nature 2016 ; 530:177–183 Crossref , Medline , Google Scholar
68 Gandal MJ, Zhang P, Hadjimichael E, et al. : Transcriptome-wide isoform-level dysregulation in ASD, schizophrenia, and bipolar disorder . Science 2018 ; 362: eaat8127 Crossref , Medline , Google Scholar
69 Stevens B, Allen NJ, Vazquez LE, et al. : The classical complement cascade mediates CNS synapse elimination . Cell 2007 ; 131:1164–1178 Crossref , Medline , Google Scholar
70 Sellgren CM, Gracias J, Watmuff B, et al. : Increased synapse elimination by microglia in schizophrenia patient-derived models of synaptic pruning . Nat Neurosci 2019 ; 22:374–385 Crossref , Medline , Google Scholar
71 Feinberg I : Schizophrenia: caused by a fault in programmed synaptic elimination during adolescence? J Psychiatr Res 1982–1983 ; 17:319–334 Crossref , Medline , Google Scholar
72 McGlashan TH, Hoffman RE : Schizophrenia as a disorder of developmentally reduced synaptic connectivity . Arch Gen Psychiatry 2000 ; 57:637–648 Crossref , Medline , Google Scholar
73 Berdenis van Berlekom A, Muflihah CH, Snijders GJLJ, et al. : Synapse pathology in schizophrenia: a meta-analysis of postsynaptic elements in postmortem brain studies . Schizophr Bull 2019 ; sbz060 Crossref , Google Scholar
74 Johnson MB, Stevens B : Pruning hypothesis comes of age . Nature 2018 ; 554:438–439 Crossref , Google Scholar
75 Keefe RSE, Kahn RS : Cognitive decline and disrupted cognitive trajectory in schizophrenia . JAMA Psychiatry 2017 ; 74:535–536 Crossref , Medline , Google Scholar
76 Neilson E, Shen X, Cox SR, et al. : Impact of polygenic risk for schizophrenia on cortical structure in UK Biobank . Biol Psychiatry 2019 ; 86:536–544 Crossref , Medline , Google Scholar
77 de Zwarte SMC, Brouwer RM, Agartz I, et al. : The association between familial risk and brain abnormalities is disease specific: an ENIGMA-Relatives study of schizophrenia and bipolar disorder . Biol Psychiatry 2019 ; 86:545–556 Crossref , Medline , Google Scholar
78 Kendall KM, Bracher-Smith M, Fitzpatrick H, et al. : Cognitive performance and functional outcomes of carriers of pathogenic copy number variants: analysis of the UK Biobank . Br J Psychiatry 2019 ; 214:297–304 Crossref , Medline , Google Scholar
79 Davies G, Marioni RE, Liewald DC, et al. : Genome-wide association study of cognitive functions and educational attainment in UK Biobank (N=112 151) . Mol Psychiatry 2016 ; 21:758–767 Crossref , Medline , Google Scholar
80 Okbay A, Beauchamp JP, Fontana MA, et al. : Genome-wide association study identifies 74 loci associated with educational attainment . Nature 2016 ; 533:539–542 Crossref , Medline , Google Scholar
81 Harvey PD, Sun N, Bigdeli TB, et al. : Genome-wide association study of cognitive performance in US veterans with schizophrenia or bipolar disorder . Am J Med Genet B Neuropsychiatr Genet (Epub ahead of print, December 24, 2019) Google Scholar
82 Casey BJ, Cannonier T, Conley MI, et al. : The Adolescent Brain Cognitive Development (ABCD) study: imaging acquisition across 21 sites . Dev Cogn Neurosci 2018 ; 32:43–54 Crossref , Medline , Google Scholar
83 Lam M, Chen C-Y, Li Z, et al. : Comparative genetic architectures of schizophrenia in East Asian and European populations . Nat Genet 2019 ; 51:1670–1678 Crossref , Medline , Google Scholar
84 Takata A, Xu B, Ionita-Laza I, et al. : Loss-of-function variants in schizophrenia risk and SETD1A as a candidate susceptibility gene . Neuron 2014 ; 82:773–780 Crossref , Medline , Google Scholar
85 Mukai J, Cannavò E, Crabtree GW, et al. : Recapitulation and reversal of schizophrenia-related phenotypes in Setd1a-deficient mice . Neuron 2019 ; 104:471–487.e12 Crossref , Medline , Google Scholar
86 Tang SX, Gur RE : Longitudinal perspectives on the psychosis spectrum in 22q11.2 deletion syndrome . Am J Med Genet A 2018 ; 176:2192–2202 Crossref , Medline , Google Scholar
87 Vorstman JAS, Breetvelt EJ, Duijff SN, et al. : Cognitive decline preceding the onset of psychosis in patients with 22q11.2 deletion syndrome . JAMA Psychiatry 2015 ; 72:377–385 Crossref , Medline , Google Scholar
88 Olsen L, Sparsø T, Weinsheimer SM, et al. : Prevalence of rearrangements in the 22q11.2 region and population-based risk of neuropsychiatric and developmental disorders in a Danish population: a case-cohort study . Lancet Psychiatry 2018 ; 5:573–580 Crossref , Medline , Google Scholar
89 Mesman E, Nolen WA, Reichart CG, et al. : The Dutch bipolar offspring study: 12-year follow-up . Am J Psychiatry 2013 ; 170:542–549 Link , Google Scholar
- Ned H. Kalin , M.D.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Research articles

Association of cytokines levels, psychopathology and cognition among CR-TRS patients with metabolic syndrome
- Yeqing Dong
- Minghuan Zhu
Racial disparities with PRN medication usage in inpatient psychiatric treatment
- Areef S. Kassam
- Peter Karalis
- E. Ann Cunningham
Variations to plasma H 2 O 2 levels and TAC in chronical medicated and treatment-resistant male schizophrenia patients: Correlations with psychopathology
- Haidong Yang
- Xiaobin Zhang

Transplantation of gut microbiota derived from patients with schizophrenia induces schizophrenia-like behaviors and dysregulated brain transcript response in mice
- Mingliang Ju
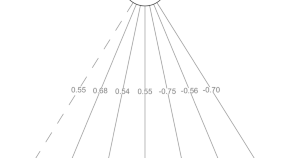
The Ethiopian Cognitive Assessment battery in Schizophrenia (ECAS): a validation study
- Yohannes Gebreegziabhere
- Kassahun Habatmu
- Atalay Alem
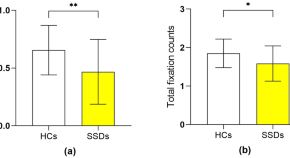
Further clarification of cognitive processes of prospective memory in schizophrenia by comparing eye-tracking and ecologically-valid measurements
- Chuan-Yue Wang
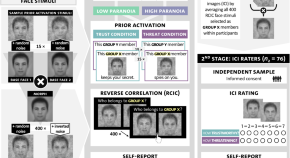
Visualizing threat and trustworthiness prior beliefs in face perception in high versus low paranoia
- Antonia Bott
- Hanna C. Steer
- Tania M. Lincoln
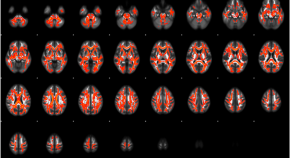
Association of homocysteine with white matter dysconnectivity in schizophrenia
- Koichi Tabata
- Shuraku Son
- Makoto Arai
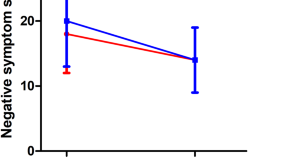
Smoking affects symptom improvement in schizophrenia: a prospective longitudinal study of male patients with first-episode schizophrenia
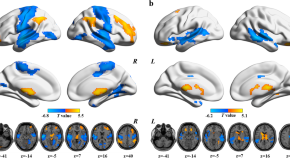
Exploring functional dysconnectivity in schizophrenia: alterations in eigenvector centrality mapping and insights into related genes from transcriptional profiles
- Mengjing Cai
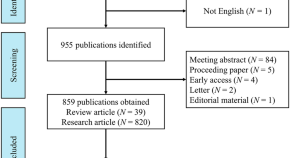
Mapping the landscape: a bibliometric analysis of resting-state fMRI research on schizophrenia over the past 25 years
- Remilai Aximu
Cortical white matter microstructural alterations underlying the impaired gamma-band auditory steady-state response in schizophrenia
- Daisuke Koshiyama
- Ryoichi Nishimura
- Kiyoto Kasai
Genetic overlap between schizophrenia and cognitive performance
- Jianfei Zhang
- Yanmin Peng
The relationship between visual hallucinations, functioning, and suicidality over the course of illness: a 10-year follow-up study in first-episode psychosis
- Isabel Kreis
- Kristin Fjelnseth Wold
- Ingrid Melle
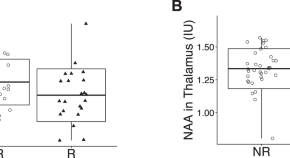
Reduction of N-acetyl aspartate (NAA) in association with relapse in early-stage psychosis: a 7-Tesla MRS study
- Marina Mihaljevic
- Yu-Ho Chang
Changes in kynurenine metabolites in the gray and white matter of the dorsolateral prefrontal cortex of individuals affected by schizophrenia
- Nico Antenucci
- Giovanna D’Errico
- Giuseppe Battaglia

Parkinson’s disease and schizophrenia interactomes contain temporally distinct gene clusters underlying comorbid mechanisms and unique disease processes
- Kalyani B. Karunakaran
- Sanjeev Jain
- Madhavi K. Ganapathiraju
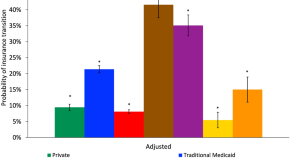
Transitions in health insurance among continuously insured patients with schizophrenia
- Brittany L. Ranchoff
- Chanup Jeung
- Kimberley H. Geissler
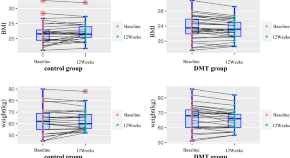
Dance/movement therapy for improving metabolic parameters in long-term veterans with schizophrenia
- Zhaoxia Zhou
- Hengyong Guan
- Fengchun Wu

Linking childhood trauma to the psychopathology of schizophrenia: the role of oxytocin
- Yuan-Jung Chen
- Mong-Liang Lu
- Kah Kheng Goh
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment
Schizophrenia: A Very Short Introduction
Author webpage
- Cite Icon Cite
- Permissions Icon Permissions
Schizophrenia: A Very Short Introduction considers a common mental disorder that has a devastating effect on sufferers and their families. While patients typically hear voices in their heads and hold bizarre beliefs, the schizophrenic patient presented to the public in sensational press reports and lurid films bears little resemblance to the reality of the illness. This VSI describes what schizophrenia is really like, how the illness progresses, and the treatments that have been applied. It summarizes the most up-to-date knowledge about the biological bases of schizophrenia and attempts to convey what it is like to suffer from it and what this disorder reveals about the relationship between mind and brain.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
External resource
- In the OUP print catalogue
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Schizophrenia Research Paper

This sample schizophrenia research paper features: 6600 words (approx. 22 pages), an outline, and a bibliography with 6 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Schizophrenia is a psychotic disorder characterized by disturbances in thought, emotion, and behavior. This research paper discusses the symptoms, etiology, treatment, and other pertinent issues concerning this mental illness.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code, i. description and classification, a. symptoms, 1. delusions, 2. hallucinations, 3. disorganized speech, 4. disorganized or catatonic behavior, 5. negative symptoms, b. variability of symptoms among patients, c. subtypes of schizophrenia, ii. history, iii. demographic characteristics of schizophrenia, a. sex differences, b. social class differences, iv. life functioning and prognosis, a. long-term course, b. premorbid characteristics of schizophrenia, v. etiology: theories and research findings, a. brain abnormalities in schizophrenia, b. biochemical factors, c. genetics, d. obstetrical complications, e. viral infection, f. diathesis-stress model, vi. treatment and therapy, a. antipsychotic medication, b. psychological treatment, vii. summary.

Delusions are the primary example of abnormal thought content in schizophrenia. Delusional beliefs conflict with reality and are tenaciously held, despite evidence to the contrary. There are several types of delusions. Delusions of control is the belief that one is being manipulated by an external force, often a powerful individual or organization (e.g., the FBI) that has malevolent intent. Delusions of grancleur refers to patients’ beliefs that they are especially important and have unique qualities or powers (e.g., the capacity to influence weather conditions). In contrast, some patients express the conviction that they are victims of persecution or an organized plot, and these beliefs are referred to as delusions of persecution. Examples of more specific delusions include thought broadcasting, the patient’s belief that his or her thoughts are transmitted so that others know them, and thought withdrawal, the belief that an external force has stolen one’s thoughts.
Hallucinations are among the most subjectively distressing symptoms experienced by schizophrenia patients. These perceptual distortions vary among patients and can be auditory, visual, olfactory, gustatory, or tactile. The majority of hallucinations are auditory in nature and typically involve voices. Examples include the patient hearing someone threatening or chastising him or her, a voice repeating the patient’s own thoughts, two or more voices arguing, and voices commenting. The second most common form of hallucination is visual. Visual hallucinations often entail the perception of distortions in the physical environment, especially in the faces and bodies of other people.
Other perceptual distortions that are commonly reported by schizophrenia patients include feeling as if parts of the body are distorted in size or shape, feeling as if an object is closer or farther away than it actually is, feeling numbness, tingling, or burning, being hypersensitive to sensory stimuli, and perceiving objects as flat and colorless. In addition to these distinctive perceptual abnormalities, persons suffering from schizophrenia often report difficulties in focusing their attention or sustaining concentration on a task.
It is important to note that in order for an unsubstantiated belief or sensory experience to quality as a delusion or hallucination, the individual must experience it within a clear sensorium (e.g., unsubstantiated sensory experiences that occur only upon awaking from sleep or when falling asleep would not qualify as delusions). Thus, for example, if a patient reports hearing something that sounds like voices when alone, but adds that he or she is certain that this is a misinterpretation of a sound, such as the wind blowing leaves, this would not constitute an auditory hallucination.
The DSM uses the term disorganized speech to refer to abnormalities in the form or content of the individual’s verbalizations. It is assumed that these abnormalities reflect underlying distortions in the patient’s thought processes. Thus the term thought disorder is frequently used by researchers and practitioners to refer to the disorganized speech that often occurs in schizophrenia.
Problems in the form of speech are reflected in abnormalities in the organization and coherent expression of ideas to others. One common abnormality of form, incoherent speech, is characterized by seemingly unrelated images or fragments of thoughts that are incomprehensible to the listener. The term loose association refers to the tendency to abruptly shift to a topic that has no apparent association with the previous topic. In general, the overall content of loosely associated speech may be easier to comprehend than incoherent speech. In perseverative speech, words, ideas, or both are continuously repeated, as if the patient is unable to shift to another idea. Clang association is the utterance of rhyming words that follow each other (e.g., “a right, bright kite”). Patients choose words for their similarity in sound rather than their syntax, often producing a string of rhyming words.
The overt behavioral symptoms of schizophrenia fall in two general areas: motor functions and interpersonal behavior. Motor abnormalities, including mannerisms, stereotyped movements, and unusual posture, are common among schizophrenia patients. Other common signs include bizarre facial expressions, such as repeated grimacing or staring, and repeated peculiar gestures that often involve complex behavioral sequences. As with other symptoms of the psychosis, the manifestation of motor abnormalities varies among individuals. Schizophrenia patients sometimes mimic the behavior of others, known as echopraxia, or repeat their own movements, known as stereotyped behaviors. Although a subgroup of patients demonstrate heightened levels of activity, including motoric excitement (e.g., agitation or flailing of the limbs), others suffer from a reduction of movement. At the latter extreme, some exhibit catatonic immobility and assume unusual postures that are maintained for extended periods of time. Some may also demonstrate waxy flexibility, a condition in which patients do not resist being placed into strange positions that they then maintain. Catatonia has decreased dramatically in recent decades, so that it is now rare. Several researchers have attributed this decline to the introduction of antipsychotic medication (described later).
In the domain of interpersonal interactions, schizophrenia patients frequently demonstrate behaviors that are perceived as bizarre or inappropriate by others. For example, it is not uncommon for patients to use socially unacceptable language and unusual tones of voice, or to show overly dependent or intrusive behavior. Another common symptom, inappropriate affect, involves unusual emotional reactions to events and experiences. For example, patients may laugh at a sad or somber occasion, or be enraged by insignificant events. Finally, many patients manifest increasingly poor hygiene as their illness progresses. Their appearance may also be marked by disheveled clothing or inappropriate clothing, such as gloves and coats in the summer.
The symptoms of schizophrenia can be classified into the general categories of positive and negative. Positive symptoms involve behavioral excesses and most of the symptoms described earlier fall in to this category (e.g., delusions, hallucinations, and bizarre behaviors). In contrast, negative symptoms involve behavioral deficits. Examples include fiat affect (blunted expressions of emotion), apathy, and social withdrawal. In the domain of verbal expression, schizophrenia patients who manifest a very low rate of verbal output are described as showing poverty of speech. Patients whose speech is normal in quantity, but lacks meaning, suffer from poverty of content. Recently, some researchers have suggested that positive and negative symptoms may be caused by different neural mechanisms.
It is important to mention that a reduction in overt displays of emotion does not necessarily imply that patients have less intense subjective emotional experiences than the average person. In fact, recent findings indicate that blunted emotional expressions can coexist with intense subjective feelings of emotion.
According to DSM-IV, patients must show two or more of the preceding five symptoms to meet the diagnostic criteria for schizophrenia. Thus, no one of these symptoms is required for the diagnosis. Furthermore, the following four criteria must also be met: (1) the patient shows marked deterioration in occupational, interpersonal, or domestic functioning; (2) the patient manifests continuous signs of symptoms or dysfunction for at least 6 months; (3) the patient does not manifest predominant signs of mood disturbance (e.g., depression or mania); and (4) the symptoms are not caused by substance abuse or a primary medical condition.
Because the diagnostic criteria for schizophrenia are relatively broad, with no one essential symptom, there is a great deal of variability among patients in their symptom profiles. It has therefore been proposed that schizophrenia is a heterogeneous disorder with multiple causes. It is also the case, however, that patients must show a marked and persistent impairment to meet the diagnostic criteria for schizophrenia. Thus, those who meet criteria for the diagnosis are significantly impaired in everyday functioning. For many individuals who are diagnosed with schizophrenia, independent functioning is never achieved.
The DSM lists five subtypes of schizophrenia. In schizophrenia of the paranoid type, delusional concerns about persecution and/or preoccupation with threat dominate the clinical presentation, although delusions of grandeur are also often present. Disorganized schizophrenia is distinguished by extremely incoherent speech and behavior, as well as blunted or inappropriate affect. In catatonic schizophrenia, the clinical picture is dominated by abnormalities in movement and posture, such as those described earlier. Patients classified as having undifferentiated schizophrenia do not meet criteria for any of the previous subtypes. Finally, the diagnosis of residual schizophrenia is applied to patients who have had at least one episode of schizophrenia and who continue to show functional impairment, but who do not currently manifest any positive symptoms.
During the late 1800s and early 1900s, Emil Kraepelin and Eugen Bleuler provided the first conceptualizations of schizophrenia. Kraepelin defined “dementia praecox,” the original term for schizophrenia, as an endogenous psychosis characterized by intellectual deterioration (dementia) and early onset (praecox). Kraepelin included negativism, hallucinations, delusions, stereotyped behaviors, attentional difficulties, and emotional dysfunction as major symptoms of the disorder. Kraepelin’s work focused on description and phenomenology, leaving subsequent researchers to investigate the cause or causes of the disorder.
In contrast to Kraepelin, Eugen Bleuler, a Swiss psychiatrist, proposed a broader view of dementia praecox, with a more theoretical emphasis. Bleuler contested two of Kraepelin’s defining assumptions: specifically, that the psychosis was typically characterized by early onset and intellectual deterioration. Bleuler attempted to identify an underlying commonality among the diverse variations of what Kraepelin referred to as dementia praecox and concluded that all of the patients suffered from a “breaking of associative threads,” causing a disharmony among communicative and thought processes. He believed this abnormality accounted for the problems of thought, emotional expression, decision making, and social interaction associated with schizophrenia. Guided by the defining principle of disharmonious mental structures, Bleuler renamed the disorder “schizophrenia,” meaning “split mind.”
In the early to mid-1900s, American psychiatrists continued to use a broad definition of schizophrenia. The distinction between process and reactive schizophrenia was considered important, however, because it was assumed to distinguish between cases characterized by gradual deterioration (process) and cases that were precipitated by acute stress (reactive).
During this time, some clinicians and researchers viewed the specific diagnostic criteria for the major mental illnesses (schizophrenia, bipolar disorder, major depression) as artificial and discretionary, and used instead flexible and inconsistent standards for diagnoses. Studies that compared the rates of disorder across nations revealed that schizophrenia was diagnosed at a much higher rate in the United States than in Great Britain and some other countries. This national difference resulted from the use of broader criteria for diagnosing schizophrenia in the United States. Many patients who were diagnosed as having depression or bipolar disorder in Britain were diagnosed with schizophrenia in the United States. Because subsequent revisions in the DSM have included more restrictive criteria for schizophrenia, U.S. diagnostic rates are now comparable with other countries.
In addition to a more restrictive definition of schizophrenia, subsequent editions of the DSM have included additional diagnostic categories that contain similar symptoms. Thus the range of “schizophrenia spectrum disorders” continue to broaden with the description of variants of schizophrenia, such as schizoaffective disorder, which is characterized by a mix of affective and psychotic symptoms. The diagnostic category of schizophreniform disorder was also added. This diagnosis is given when the patient shows the typical symptoms of schizophrenia, but does not meet the criterion of 6 months of continuous illness.
Estimates of the prevalence of schizophrenia converge at around 1% of the population. Although there is evidence of cross-national differences in the rate of schizophrenia, the differences are not large (i.e., 1 to 2% difference). It is, in fact, striking that the rate of occurrence is so consistent across cultures.
The modal age at onset of schizophrenia is in early adulthood, usually before 25 years of age. Thus most patients have not had the opportunity to marry or establish a stable work history before the onset of the illness. As a result of this, and the often chronic nature of the illness, many patients never attain financial independence. It is relatively rare for preadolescent children to receive a diagnosis of schizophrenia. Similarly, it is rare for individuals beyond the age of 40 to experience a first episode of the illness.
Although it has traditionally been assumed that there is no sex difference in the rates of schizophrenia, some recent research findings indicate that a somewhat larger proportion of males than females meet the DSM-IV criteria for the disorder. Nonetheless, the overall rates do not differ dramatically for men and women. It is well established, however, that women are more likely to have a later onset of illness, as well as a better prognosis. Women also show a higher level of interpersonal and occupational functioning during the period prior to illness onset. The reasons for this sex difference are not known, but it has been proposed by several theorists that the female sex hormone, estrogen, may function in attenuating the severity of the illness.
Compared with the general population averages, schizophrenia patients tend to have significantly lower incomes and educational levels. Poor urban inner city districts, inhabited by the lowest socioeconomic class, contain the largest proportion of schizophrenia patients. There is a sharp contrast between the rates of schizophrenia in the lowest socioeconomic class and all other levels, including the next higher level. Findings from various cultures suggest that rates of schizophrenia are almost two times higher in the lowest social class group compared with the next lowest.
These social class differences appear to be a partial consequence of the debilitating nature of the illness. The social-drift theory suggests that during the development of schizophrenia, people drift into poverty. When the incomes and educational levels of the parents of patients are compared with those of the general population, the differences are not as striking.
There is, nonetheless, evidence that patients do come from families where the incomes and educational backgrounds of the parents are slightly below the average. These findings have led researchers to conclude that there may be a causal link between social class and risk for the illness. The sociogenic hypothesis posits that situational factors associated with low social class, such as degrading treatment from society, low levels of education, and few opportunities for achievement and reward, produce stress that contributes to the risk for schizophrenia.
Before the introduction of antipsychotic medications in 1950, the majority of patients spent most of their lives in institutional settings. There was little in the way of programs for rehabilitation. But contemporary, multifaceted treatment approaches have made it possible for most patients to live in community settings.
Of course, during active episodes of the illness, schizophrenia patients are usually seriously functionally impaired. They are typically unable to work or maintain a social network, and often require hospitalization. Even when in remission, some patients find it challenging to hold a job or to be self-sufficient. This is partially due to residual symptoms, as well as to the interruptions in educational attainment and occupational progress that result from the illness. However, there are many patients who are able to lead productive lives, hold stable jobs, and raise families. With the development of greater community awareness of mental illness, some of the stigma that kept patients from pursuing work or an education has diminished.
For about one third of patients, the illness is chronic and is characterized by episodes of severe symptoms with intermittent periods when the symptoms subside but do not disappear. For others, there are multiple episodes with periods of substantial symptom remission. About one third of those who receive the diagnosis eventually show a partial or complete recovery after one or two episodes.
Several factors have been linked with a more favorable prognosis for schizophrenia. Early treatment seems to be important in that the shorter the period between the onset of the patient’s symptoms and the first prescribed medication, the better the clinical outcome. Another indicator of better prognosis is a high level of occupational and interpersonal functioning in the premorbid period. Also, as noted earlier, women and patients who have a later onset of symptoms have a better long-term outcome.
Some of the difficulties experienced by individuals with schizophrenia can be observed before the onset of the clinical symptoms. Deficits in social skills, concentration, emotional expression, motivation, and occupational or academic performance often precede the first clinical symptoms. This period of gradual decline in functioning before the first illness episode is referred to as the prodromal phase.
However, there are often more subtle signs of dysfunction long before the onset of the prodromal period. Controlled studies using archival data sources, such as medical and school records or childhood home-movies, indicate that subtle differences are discernible as early as infancy in some patients. Individuals who succumb to schizophrenia in adulthood sometimes have abnormal motor development and show deficits in emotional expression and interpersonal relationships in early childhood. Cognitive impairment and difficult temperament have also been observed. During middle childhood and adolescence, researchers have found evidence of neurological abnormality, poor emotional control, social immaturity, and academic performance deficits. Premorbid behavioral problems often become marked through the adolescent years, and many exhibit behavioral disturbances and cognitive abnormalities that resemble the clinical symptoms of schizophrenia.
The causes of schizophrenia are unknown, but it is now widely accepted by both researchers and clinicians that schizophrenia is biologically determined. This is in striking contrast to the early and mid-1900s, when many subscribed to the theory that faulty parenting, especially cold and rejecting mothers, caused schizophrenia in offspring.
There are several sources of evidence for the assumption that schizophrenia involves an abnormality in brain function. First, studies of schizophrenia patients have revealed a variety of behavioral signs of central nervous system impairment, including motor and cognitive dysfunctions. Second, when the brains of patients are examined with in vivo imaging techniques, such as magnetic resonance imaging (MRI), many show abnormalities in brain structure. Similarly, postmortem studies of brain tissue have revealed irregularities in nerve cell formation and interconnections.
Laboratory studies of schizophrenia patients have revealed a variety of abnormalities, including irregularities in smooth pursuit eye movements, psychophysiological responses to sensory stimuli, and concentration. Research on the neuropsychological performance of schizophrenia patients was first conducted in the 1950s and continues to the present time. Individual neuropsychological tests are designed to measure functions subserved by specific regions or systems of the brain. An early finding in this area was that schizophrenia patients were the one psychiatric group whose performance on neuropsychological tests was indistinguishable from people with known brain damage. The findings suggested a generalized cerebral dysfunction in schizophrenia. However, patients show the most consistent deficits on tests of attention and memory, indicating dysfunction of the frontal and temporal lobes and the hippocampus. Further evidence of dysfunction in these brain regions is derived from poor performance on tests of executive functions: the ability to formulate, maintain, and adapt appropriate responses to the environment.
Brain-imaging studies of schizophrenia have yielded results that mirror those obtained from neuropsychological research. Some relatively consistent findings are that the brains of schizophrenia patients have abnormal frontal lobes and enlarged ventricles. Enlarged ventricles suggest decreased brain mass, particularly in the limbic regions, which are intimately involved in emotional processing. Furthermore, ventricular size correlates with negative symptoms, performance deficits on neuropsychological tests, poor response to medication, and poor premorbid adjustment. These associations between ventricular enlargement and both premorbid and postmorbid characteristics suggest that the brain abnormalities are long-standing, perhaps congenital.
In addition to brain structure, investigators have examined biological indices of brain function in schizophrenia. Functional brain-imaging studies, with procedures such as positron emission tomography (PET) and measurement of regional cerebral blood flow, reveal that schizophrenia patients have decreased levels of blood flow to the frontal lobes, especially while performing cognitive tasks.
Researchers are now pursuing the question of what causes the brain abnormalities observed in schizophrenia. Although as yet there are no definitive answers, investigators have made continuous progress in identifying factors that are associated with risk for the disorder.
The structural brain abnormalities that have been observed in schizophrenia support the assumption that it is a disorder of the central nervous system. But it has also been shown that similar structural abnormalities (i.e., ventricular enlargement and volume reductions) are present in other disorders, both neurological and psychiatric. It is therefore assumed that specific abnormalities in brain biochemistry may play a role in schizophrenia.
The functioning of the central nervous system is dependent on a host of chemicals that serve as the “messenger substances” among neurons. These chemicals or neurotransmitters have been the subject of intense investigation. Among the various neurotransmitters that have been implicated in the neuropathophysiology of schizophrenia is dopamine. Dopamine is viewed as a likely candidate for two main reasons: (1) drugs that act to enhance the release or activity of dopamine can produce psychotic symptoms, and (2) drugs that have been established to have antipsychotic properties (i.e., reduce psychotic symptoms) reduce the activity of dopamine in the brain. Current theories of the role of dopamine in schizophrenia have focused on dopamine receptors. There is evidence that there may be an abnormality in the number or sensitivity of certain dopamine receptors in the brains of schizophrenia patients. To date, however, this evidence remains inconclusive.
Several other neurotransmitters have also been hypothesized to play a role in schizophrenia. Current theories under investigation include a malfunction of the receptors for a neurotransmitter called glutamate and an abnormality in the balance between dopamine and serotonin (another neurotransmitter which, like dopamine, has been implicated in the pathogenesis of schizophrenia). As research findings on the biochemical aspects of schizophrenia accumulate, it increasingly appears that the illness may involve multiple neurotransmitters, with different biochemical profiles for different patients.
A convincing body of research supports the notion of a genetic predisposition to schizophrenia. Behavioral genetic studies of families, twins, and adopted offspring of schizophrenia patients indicate that an inherited vulnerability is involved in at least some cases of the disorder.
There is an elevated risk of schizophrenia for individuals with a biological relative who suffers from the disorder, and the risk rates increase as a function of the genetic closeness of the relationship. For example, it has been estimated that children of schizophrenia patients have a 9 to 15 % likelihood of developing the illness, siblings of patients have an 8 to 14% likelihood, and cousins have a 2 to 6% likelihood of being diagnosed with schizophrenia. Given the general population rate of approximately 1%, relatives of patients are at statistically increased risk. It must be noted, however, that relatives share common experiences as well as common genes. Therefore, examinations of the prevalence of schizophrenia in the relatives of patients cannot elucidate the relative contributions of environmental and genetic factors.
Some investigators have studied the development of adopted children whose biological mothers had schizophrenia. This approach has the potential to provide more conclusive information than family studies. The results of these investigations show that when biological offspring of schizophrenic mothers are reared from infancy in adoptive homes they are more likely to develop schizophrenia than are adopted children from healthy mothers. Furthermore, these children also exhibit a higher rate of other adjustment problems when compared with controls. Studies of this type have clearly illustrated that vulnerability to schizophrenia can be inherited.
Research on twins examines differences in concordance rates between identical (monozygotic or MZ) and fraternal (dizygotic or DZ) twins. Twin studies rely on the fact that MZ twins essentially share 100% of their genes. Thus, environmental influences account for any behavioral differences between MZ twins. In contrast, DZ twins are no more genetically similar than regular siblings; DZ twins do, however, share more similar environmental factors than do nontwin siblings. To date, the results of twin studies have consistently shown that MZ twins are significantly more likely to be concordant for schizophrenia than are DZ twins.
At the same time, it is important to note that in at least 50% of the cases in which one member of an MZ twin pair has schizophrenia, the other does not. Such “discordant” pairs have been the subject of a recent, comprehensive investigation in the United States. Among the most important findings from this research project are those from the MRI scans conducted on the twins. The ill twins in the pairs showed significantly more brain abnormalities than the healthy twins. Most notable were reductions in the volume of certain brain regions, especially the hippocampus, and increases in the size of the ventricles. These results clearly indicate the importance of environmental factors in the etiology of schizophrenia.
As is the case with many other disorders that involve brain dysfunction, there is evidence that schizophrenia is associated with exposure to prenatal and delivery complications. Obstetrical complications (OCs) are defined as physical deviations from the normal course of events during pregnancy, labor, or the neonatal period. Estimates of OCs in schizophrenics have been as high as 67%, significantly higher than the rate of OCs found in normal controls.
Among the prenatal factors that have been found to be associated with increased risk for schizophrenia are prenatal maternal nutritional deficiency, viral infection, bleeding, and toxemia. Complications of delivery that can result in hypoxia have also been linked with heightened risk for the disorder. Hypoxia, a deficiency in the amount of oxygen available to the fetus, can affect the development of various parts of the brain. Some researchers argue that hypoxia results in hippocampal damage, thus contributing to vulnerability for schizophrenia. Low birth weight, a neonatal complication, is another potential early factor contributing to schizophrenia. There is evidence that low birth weight is related to increased ventricular size, which is a common characteristic of schizophrenia patients.
The findings on prenatal complications support the notion that fetal brain development may be disrupted in individuals who later manifest schizophrenia. A central question raised by these findings concerns the nature of the etiologic role of OCs. Some hypothesize that OCs produce the neural predisposition to schizophrenia, whereas others posit that OCs exacerbate or interact with an existing genetic predisposition.
Findings from prospective, high-risk research projects lend support to the hypothesis that OCs interact with genetic vulnerabilities in the etiology of schizophrenia. High-risk studies involve the repeated assessment of children of schizophrenia patients, based on the expectation that a larger percentage of these children will eventually develop the illness than individuals in the general population. The high-risk method offers some advantages when compared with retrospective studies of the precursors of schizophrenia. One advantage is that it allows for the direct assessment of subjects in the premorbid period, as well as the selection and study of variables that are thought to have prognostic relevance. Furthermore, because a significant portion of the data collection takes place during the premorbid period, this reduces confounds that often occur in the study of diagnosed patients (e.g., medication and institutionalization).
Studies using the high-risk method have shown an interactive effect of genetic risk and exposure to OCs in predicting adult psychiatric outcome. In other words, the correlation between OCs and adult psychiatric symptoms was greater for offspring of schizophrenia parents than for children of healthy parents. The same pattern was apparent for the relation between OCs and adult brain morphology, suggesting that pre- and perinatal factors contribute to brain abnormalities.
As noted earlier, prenatal exposure to maternal viral infection has also been linked with schizophrenia. Specifically, the rate of schizophrenia is increased for cohorts who were in the second trimester during flu epidemics. Another source of evidence for the viral hypothesis is the finding that the births of schizophrenia patients do not seem to be randomly distributed throughout the course of the year. Instead, the births of schizophrenia patients occur more frequently in winter months.
Some researchers have suggested that postnatal viral infection may also be relevant to schizophrenia, and that the illness may be caused by a long-acting virus. This hypothesis claims that “slow viruses,” which are active over a long period of time, interact with a genetic predisposition to produce schizophrenia. Various findings are cited in support of this hypothesis. Some researchers have identified a viral infection in fatal catatonia, a disorder characterized by schizophrenia-like symptoms, suggesting that a similar viral infection may be found for schizophrenia. Other researchers have found signs of viral activity in the cerebrospinal fluid of patients with schizophrenia.
The diathesis-stress model has dominated theories about the etiology of schizophrenia for several decades. This model assumes that certain individuals inherit or acquire a vulnerability to schizophrenia (the diathesis), and that the behavioral expression of this vulnerability is determined or triggered by environmental stressors. Although “stress” was originally conceptualized as psychosocial in origin, contemporary versions of this model broaden the definition of stress to include prenatal and postnatal insults to the central nervous system. Thus the diathesis, combined with exposure to environmental stressors, can produce schizophrenia.
Exposure to stress within the context of the family has been the focus of researchers in the field. Families in which there is a schizophrenia patient show more conflict and abnormalities in communication than do other families. However, it has also been shown that there is greater conflict and more abnormalities of communication in families in which any member has a severe debilitating illness. Thus, family communication styles are unlikely to play a unique causal role in schizophrenia.
There is good evidence, however, that exposure to high levels of criticism from family members can increase the likelihood of relapse in schizophrenia patients. The number of critical comments, expressions of hostility, and emotional overinvolvement comprise a construct referred to as expressed emotion (EE). Recovering schizophrenia patients in families high in EE are much more likely to have a relapse compared with patients in families low in EE. There is also evidence from studies of the adopted offspring of schizophrenia patients suggesting that familial stress can hasten the onset of symptoms.
Before 1900, knowledge of the nature and causes of mental disorders was limited. Individuals with psychiatric symptoms, particularly psychotic symptoms, were typically viewed by others with disdain or amusement. However, social trends and advances in medical knowledge converged to produce greater sympathy for those with mental illness. This led, especially during the early part of the century, to the construction of public and private hospitals devoted to the care of the mentally ill.
Today, most schizophrenia patients experience at least one period of inpatient treatment. This is typically precipitated by the first psychotic episode. During this initial hospitalization, an extensive assessment is usually conducted to determine the most appropriate diagnosis. Treatment is then initiated to reduce symptoms and stabilize patients so that they can return to the community as soon as possible.
In the past, periods of hospitalization were longer in duration than they are today. This is due, in part, to the availability today of better medical treatments. Another factor that has contributed to shorter hospital stays is the deinstitutionalization movement. Initially spurred by concerns that too many of the mentally ill were becoming “institutionalized” and were losing their ability to function in the community, financial support for state psychiatric hospitals was gradually cut. But community support services and transitional living arrangements were not readily available to many patients. As a result, former psychiatric inpatients now constitute a substantial proportion of the homeless found in U.S. cities.
Introduced in the 1950s, antipsychotic medication has since become the most effective and widely used treatment for schizophrenia. Research indicated that the “typical” antipsychotics, such as haloperidol, decreased the symptoms of schizophrenia, especially positive symptoms, and reduced the risk of relapse. However, they were not as effective in reducing the negative symptoms. Furthermore, some patients showed no response to antipsychotic drugs.
Chlorpromazine (Thorazine) was among the first antipsychotic commonly used to treat schizophrenia. Since the 1950s, many other antipsychotic drugs have been introduced. Like chlorpromazine, these drugs reduce hallucinations, delusions, and thought disorder, and engender more calm, manageable, and socially appropriate behavior. As mentioned, all currently used antipsychotic drugs block dopamine neurotransmission. Thus it has been assumed that their efficacy is due to their capacity to reduce the overactivation of dopamine pathways in the brain.
Unfortunately, the benefits of standard or typical antipsychotic drugs are often mitigated by side effects. Minor side effects include sensitivity to light, dryness of mouth, and drowsiness. The more severe effects are psychomotor dysfunction, skin discoloration, visual impairment, and tardive dyskinesia (an involuntary movement disorder that can appear after prolonged use of antipsychotics). It is especially unfortunate that tardive dyskinesia is sometimes irreversible when patients are withdrawn from neuroleptics. Many of these physical signs are known to be caused by chronic blockade of dopamine pathways. Although additional medications can counter some of the negative effects of the typical antipsychotics, schizophrenia patients often resist taking them because of an aversion to the side effects.
Within the past decade, some new, “atypical” antipsychotic drugs have been introduced. It was hoped that these drugs would be effective in treating patients who had not responded to standard antipsychotics. Also, researchers hoped to identify medications that had fewer side effects. One example is Clozapine, released in 1990, which seems to reduce negative symptoms more effectively than typical antipsychotic drugs. Clozapine not only offers hope for patients who are nonresponsive to other medications, but it also has fewer side effects than typical antipsychotics. However, clozapine can produce one rare, but potentially fatal, side effect, agranulocytosis, a blood disorder. Consequently, patients who are on this medication must be monitored on a regular basis. It is fortunate that several other new antipsychotic medications have recently become available, and some of these appear to have no serious side effects.
It appears that it is important to begin pharmacological treatment of schizophrenia as soon as possible after the symptoms are recognized. The longer patients go without treatment of illness episodes, the worse the long-term prognosis. Medication also has the benefit of lowering the rate of mortality, particularly suicide, among schizophrenia patients. Patients who are treated with antipsychotic medication generally require maintenance of the medication to obtain continued relief from symptoms. Medication withdrawal often results in relapse. At the same time, the associated long- and short-term side effects of antipsychotics, especially the typical antipsychotics, are of continuing concern to patients, their families, and physicians. It is possible that future research on the neural mechanisms involved in schizophrenia will lead to the development of novel treatments that eliminate the need for maintenance medication.
Many schizophrenia patients also suffer from depression and, as noted, are at elevated risk for suicide. The reason or reasons for the high rate of co-occurance of depression with schizophrenia is not known. Given the debilitating and potentially chronic nature of schizophrenia, however, it is likely that some patients experience depressive symptoms in response to their condition. For others, depressive symptoms may be medication side effects or a manifestation of a biologically based vulnerability to depression.
Clinicians have used various forms of psychological therapy in an effort to treat schizophrenia patients. Early attempts to provide therapy for schizophrenia patients relied on insight-oriented or psychodynamic techniques. The chief goal was to foster introspection and self-understanding in patients. Research findings provided no support for the efficacy of these therapies in the treatment of schizophrenia.
It has been shown, however, that supportive therapy can be a useful adjunct to medication in the treatment of patients. Similarly, psychoeducational approaches that emphasize providing information about symptom management have proven effective in reducing relapse. Among the most beneficial forms of psychological treatment is behavioral therapy. Some psychiatric hospitals have established programs in which patients earn credits or “tokens” for appropriate behavior and then redeem these items for privileges or tangible rewards. These programs can increase punctuality, hygiene, and other socially acceptable behaviors in patients.
In recent years, family therapy has become a standard component of the treatment of schizophrenia. These family therapy sessions are psychoeducational in nature and are intended to provide the family with support, information about schizophrenia, and constructive guidance in dealing with the illness in a family member. In this way, family members become a part of the treatment process and learn new ways to help their loved one cope with schizophrenia.
Another critical component of effective treatment is the provision of rehabilitative services. These services take the form of structured residential settings, independent life-skills training, and vocational programs. Such programs often play a major role in helping patients recover from their illness.
It is now firmly established that schizophrenia is caused by an abnormality of brain function that in most cases has its origin in early brain insults, inherited vulnerabilities, or both. But the identification of the causal agents and the specific neural substrates responsible for schizophrenia must await the findings of future research. There is reason to be optimistic about future research progress. New technologies are available for examining brain structure and function. In addition, dramatic advances in neuroscience have expanded our understanding of the brain and the impact of brain abnormalities on behavior. We are likely to witness great strides in our understanding of the causes of all mental illnesses within the coming decades.
It is hoped that advances will also be made in the treatment of schizophrenia. New drugs are being developed at a rapid pace, and more effective medications are likely to result. At the same time, advocacy efforts on the part of patients and their families have resulted in improvements in services. But a further expansion of services is greatly needed to provide patients with the structured living situations and work environments they need to make the transition into independent community living.
Bibliography:
- Breier, A. (Ed.). (1996). The new pharmacotherapy of schizophrenia. Washington DC: American Psychiatric Press.
- Keefe, R. S., & Harvey, P. (1994). Understanding schizophrenia: A guide to the new research on causes and treatment. New York: Free Press.
- Miller, G. A. (Ed.). (1995). The behavioral high-risk paradigm in psychopathology. New York: Springer.
- Shriqui, C. L., & Nasrallah, H. A. (Eds.). (1995). Contemporary issues in the treatment of schizophrenia. Washington DC: American Psychiatric Press.
- Torrey, E. F. (1994). Schizophrenia and manic-depressive disorder: The biological roots of mental illness as revealed by the landmark study of identical twins. New York: Basic Books.
- Walker, E. F. (1991). Schizophrenia: A life-course developmental perspective. New York: Academic Press.
ORDER HIGH QUALITY CUSTOM PAPER

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
McDonagh MS, Dana T, Selph S, et al. Treatments for Schizophrenia in Adults: A Systematic Review [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2017 Oct. (Comparative Effectiveness Reviews, No. 198.)

Treatments for Schizophrenia in Adults: A Systematic Review [Internet].
Introduction.
Schizophrenia is a chronic mental health condition that most often presents in early adulthood and can lead to disabling outcomes. The most recent version of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 5th Edition ( DSM-5 ), 1 has continued the trend of clarifying and simplifying the diagnostic criteria for schizophrenia from the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition ( DSM-III ) through DSM-IV without changing the defined patient population among the editions. 2 Currently, DSM-5 defines schizophrenia as: the presence of two or more of the five core symptoms (delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms); at least one of the symptoms being delusions, hallucinations, or disorganized speech; and, symptoms being present for at least 6 months. Lifetime prevalence is approximately 0.3 to 0.7 percent, with onset most commonly between late adolescence through the third decade. 3 Differential diagnosis is broad and includes delineation from mood disorders (bipolar disorder or major depressive disorder) with psychotic features and substance/medication-induced psychotic disorders. The course of schizophrenia varies. Approximately 20 percent of individuals may experience significant improvement including, in some cases, full recovery; 4 however, the majority tend to experience some degree of social and occupational difficulty as well as need for daily living supports. That said, more recent research and practice has focused on early intervention with first episode psychosis, demonstrating promise toward improving outcomes sooner and reducing longer-term disability. 5 , 6
Treatment Strategies
Antipsychotic medications (primarily effective via dopaminergic antagonism) and nonpharmacological treatments are typically used together when treating individuals with schizophrenia. Both approaches can result in meaningful improvements in a variety of outcome areas, including psychiatric symptoms, functioning (e.g., employment, social), service utilization (e.g., hospitalization, crisis services), legal system involvement, quality of life, self-harm and aggressive behaviors, treatment engagement and retention, and co-occurring substance abuse. Ideally, improvements in symptoms translate to long-term, clinically relevant, positive changes in other outcome areas, with limited and manageable adverse effects. While pivotal trials of antipsychotic efficacy are limited to measurement of symptom reduction, measurement of other important recovery-oriented outcomes that reflect improvement in social and occupational functioning are necessary to describe benefits of treatments on overall quality of life and functional ability.
Historically, the wide array of antipsychotic drug treatments has had uncertain impact on long-term patient-centered outcomes, such as the ability to have consistent employment and successful interpersonal relationships, as well as maintenance in independent living, and includes serious concerns about adverse effects (e.g., tardive dyskinesia, weight gain, diabetes, and dyslipidemia) for some treatments. Many patients prescribed an antipsychotic discontinue it. Discontinuation rates and time to discontinuation vary by treatment and patient characteristics. Older, first-generation antipsychotics (FGAs), such as haloperidol, have proven efficacy but adverse effects such as extrapyramidal symptoms ( EPS ) and in some cases tardive dyskinesia, often limit long-term adherence. Second-generation antipsychotics (SGAs), beginning with clozapine, were introduced as having equal or better efficacy, specifically potentially better effects on negative symptoms, and the hope of fewer EPS and lower risk of tardive dyskinesia. But SGAs also have potentially serious adverse effects (e.g., cardiovascular and endocrinologic adverse effects) that make their overall risk/benefit profile less clear-cut than anticipated.
Although there are a large number of treatments for schizophrenia, it is not clear whether they afford long-term benefits on employment and social relationships and improve the likelihood of recovery, and the most effective duration of treatment is unclear. Equally important in selecting among competing interventions for a specific patient is consideration of patient-level characteristics that may affect the outcomes (including age, duration of symptoms, severity, and other psychiatric or medical comorbidities) across a diverse group of possible interventions. For example, treatment of negative symptoms (e.g., diminished emotional response and lack of interest) may differ from treatment of positive symptoms (e.g., hallucinations and delusions). Most psychosocial interventions have specific targets for the patient population and outcome measure. Patients and providers are also interested in other patient-centered health outcomes.
While the success of any given treatment depends on the balance of benefit and harm, specific treatment considerations will vary across the lifespan. Treating patients aggressively early in the disease is thought to improve long-term outcomes although overly aggressive treatments, particularly drug treatments, may result in adverse effects. Additionally, substance abuse (e.g., tobacco, alcohol, illicit drugs) may begin early on for individuals with schizophrenia, and in these patients successful treatment of schizophrenia involves consideration of this comorbidity as well. 7 – 10 The metabolic effects related to both the disease and drug treatments are concerning across age groups, starting in adolescence or early adulthood. 11 Epidemiologic studies have found an association with obesity, elevated lipids, and shorter lifespan, and several antipsychotic drugs are known to increase these risks. 12 – 18 Older patients may have increased risk of mortality 19 – 22 and require antipsychotic dosing changes with age. 23 , 24 Across all age groups, primary goals include diminishing core illness symptoms and reducing relapses of acute psychosis; however, physical health comorbidities can present challenges requiring modification of the treatment plan.
- Scope and Key Questions
Scope of the Review
In this systematic review, we evaluate the current evidence to inform treatment options for individuals with schizophrenia. The review synthesizes evidence on the comparative effectiveness of pharmacological treatments and the effectiveness of common psychosocial and other nonpharmacological treatment strategies for individuals with schizophrenia, points out areas of controversy, and highlights future research needed.
Due to a very large number of studies and interventions, the scope of the review focuses on specific types of evidence. For pharmacological interventions, we limited to the most commonly used FGA drugs (fluphenazine, haloperidol, and perphenazine), but included all United States Food and Drug Administration ( FDA )-approved SGA drugs. For the pharmacological interventions, the focus was on comparative evidence, directly comparing drugs to each other. This decision was based in part on the availability of sufficient evidence on general efficacy of the drugs to treat schizophrenia in the form of studies used to gain FDA approval, that is, placebo-controlled trials. For psychosocial and nonpharmacological interventions, we limited to the most commonly-used interventions relevant to United States practices. In doing this, we excluded single studies of unique interventions, and studies conducted in countries with cultural, social, and health care environments that are very different from the United States. We limited to studies comparing a psychosocial or other nonpharmacological intervention to “usual care” as a common comparator. This decision was made largely due to the heterogeneity of interventions and comparators across studies, the existence of many studies comparing these interventions to usual care, and to provide a common comparator across the interventions.
We limited the outcomes to those that are patient centered health outcomes (rather than intermediate outcomes), which were arranged according to their priority from the perspective of the patient, their family, and their clinicians. We considered advice from our experts in selecting and prioritizing the outcomes. We did not include two outcomes that are sometimes evaluated. First, we excluded rehospitalization, because: (1) there is important variation in the indications for and length of psychiatric hospitalizations across time, in different localities, and with different financial contexts; and (2) there is important variation across trials in how rehospitalization is measured/evaluated, which may confound study interpretation. For assertive community treatment, where decreasing rehospitalization is the target of the intervention, we included rehospitalization as an outcome. Second, we excluded changes in neurocognitive test results, as these were viewed as an intermediate outcome. Instead, we have prioritized measures of functioning that include neurocognition as part of a set of broader patient-centered health outcomes. The Analytic Framework for the review appears in Figure 1 .
Analytic framework. Pharmacological treatments: At least 90 percent of patients must have been diagnosed with schizophrenia. For studies specifically on harms of antipsychotic drugs, populations can be mixed-diagnoses, as the harms are not diagnosis-specific (more...)
Key Questions
What are the comparative benefits and harms of pharmacological treatments for adults with schizophrenia?
How do the benefits and harms of pharmacological treatments for adults with schizophrenia vary by patient characteristics? a
What are the benefits and harms of psychosocial and other nonpharmacological treatments for adults with schizophrenia?
How do the benefits and harms of psychosocial and other nonpharmacological treatments for adults with schizophrenia vary by patient characteristics? a
Patient characteristics include age, sex, race, ethnicity, socioeconomic status, time since illness onset, prior treatment history, co-occurring psychiatric disorders, pregnancy, etc.
- Cite this Page McDonagh MS, Dana T, Selph S, et al. Treatments for Schizophrenia in Adults: A Systematic Review [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2017 Oct. (Comparative Effectiveness Reviews, No. 198.) Introduction.
- PDF version of this title (8.3M)
- Disable Glossary Links
In this Page
Other titles in these collections.
- AHRQ Comparative Effectiveness Reviews
- Health Services/Technology Assessment Texts (HSTAT)
Recent Activity
- Introduction - Treatments for Schizophrenia in Adults: A Systematic Review Introduction - Treatments for Schizophrenia in Adults: A Systematic Review
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
schizophrenia is a mental disorder that is. characterized by delusions, hallucinations, disorganized speech, grossly disorganized or. catatonic behavior, and negative symptoms. including ...
Schizophrenia is a debilitating mental illness which involves three groups of symptoms, i.e., positive, negative and cognitive, and has major public health implications. According to various sources, it affects up to 1% of the population. The pathomechanism of schizophrenia is not fully understood and current antipsychotics are characterized by ...
The prevalence of schizophrenia is between 0.6% and 1.9% in the U.S. population. 10 Moreover, a claims analysis has estimated that the annual prevalence of diagnosed schizophrenia in the U.S. is 5.1 per 1,000 lives. 11 The prevalence of the disorder seems to be equal in males and females, although the onset of symptoms occurs at an earlier age ...
Introduction and background. Schizophrenia is a chronic illness that causes psychosis with a decline in functioning. It is a multifactorial disorder affecting millions worldwide. ... The findings from GWAS studies allow us to identify possible genes for targeted treatment and future research regarding the immune mechanisms of schizophrenia ...
Neurochemical disturbance, involving dopamine function and glutamatergic N-methyl-D-aspartate receptor function, is supported by indirect and direct evidence. The genetic contribution to schizophrenia is now recognised to be largely polygenic. Birth and early life factors also have an important aetiological role.
Introduction. Schizophrenia is an often debilitating, chronic, ... (CINP 22, Italian guidelines 41, NICE 34, NJDMHS 32, Schizophrenia Patient Outcomes Research Team [PORT] 30,31).
Advances in schizophrenia research: first special issue, 2020 ... I will introduce here the outstanding papers on this major psychiatric disorder of immense public health relevance.
schizophrenia include overt delusions, auditory, visual, and tactile hallucinations, thought disorder, and behavior. that is bizarre when compared to norm al behavior in the culture where it ...
Therefore, due to the growing knowledge in schizophrenia research and the under-pinned mechanisms, we aimed to provide some insights into and a viewpoint on the recently investigated schizophrenia research fields in order to discuss the potential future research directions in schizophrenia research, including the overview of recently developed
Introduction. Schizophrenia is a disabling group of brain disorders characterized by symptoms such as hallucinations, delusions, disorganized communication, poor planning, reduced motivation, and blunted affect. ... the elderly or children), migrant status, ethnic or religious status, or twin status, to name but a few. A recent paper has ...
What have we accomplished for schizophrenia patients since the introduction of chlorpromazine in 1952 ... published their seminal paper reporting for the first time reduced brain volume (or, more precisely, increased lateral ventricle volume) in ... research efforts that target the second decade of life are essential if we are to find ...
1. INTRODUCTION. This paper reports a review of outcomes in schizophrenia in the twenty‐first century and is an extension of the work undertaken by the late Dr Richard Warner in his seminal book, "Recovery from Schizophrenia: Psychiatry and Political Economy" (1985 (Warner, 1985); 2004 (Warner, 2004)).The present work was started with Dr Warner's involvement, and the preliminary results ...
Abstract. Schizophrenia is a mental disorder characterized by disruptions in thought processes, perceptions, emotional responsiveness, and social interactions. Schizophrenia affects approx. 24 million people or 1 in 300 people (0.32%) worldwide. This rate is 1 in 222 people (0.45%) among adults.
1. Introduction 2. Diagnostic issues 2.1 Relevance of diagnostic issues for epidemiological research 2.2 ICD-I0 classification of schizophrenia 2.3 DSM-111-R and DSM-IV classifications of schizophrenia 2.4 Similarities and dissimilarities between ICD-10, DSM-111-R and DSM-IV 2.5 Assessment methods 2.6 Case-finding methods 3.
Read the latest Research articles from Schizophrenia. Variations to plasma H 2 O 2 levels and TAC in chronical medicated and treatment-resistant male schizophrenia patients: Correlations with ...
Introduction. Schizophrenia is the major mental illness of our time. It was first described by. Kraepelin (1896) as "dementia praecox" and later given the name "schizophrenia" by. Bleuler ...
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may seem as though they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but ...
Pathophysiology and etiology. Schizophrenia has a substantial genetic component, with a high heritability (up to 80%), indicating that about 80% of the variation in the trait of schizophrenia may be attributed to genetic factors [].Genome-wide association studies (GWASs), which compare the genomes of thousands of healthy and affected individuals, have found several genes associated with ...
Abstract. Schizophrenia: A Very Short Introduction considers a common mental disorder that has a devastating effect on sufferers and their families. While patients typically hear voices in their heads and hold bizarre beliefs, the schizophrenic patient presented to the public in sensational press reports and lurid films bears little resemblance to the reality of the illness.
Schizophrenia is a chronic psychiatric disorder with a heterogeneous genetic and neurobiological background that influences early brain development and is expressed as a combination of psychotic symptoms such as hallucinations, delusions and disorganization and motivational and cognitive dysfunctions. Although Schizophrenia afects men and women ...
This sample schizophrenia research paper features: 6600 words (approx. 22 pages), an outline, and a bibliography with 6 sources. Browse other research paper exa ... Before the introduction of antipsychotic medications in 1950, the majority of patients spent most of their lives in institutional settings. There was little in the way of programs ...
Schizophrenia is a chronic mental health condition that most often presents in early adulthood and can lead to disabling outcomes. The most recent version of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5),1 has continued the trend of clarifying and simplifying the diagnostic criteria for schizophrenia from the American ...
Research suggests that one of the causes of schizophrenia may be changes in the levels of the neurotransmitters dopamine and serotonin. Altering the levels of these neurotransmitters with the use of medications may alleviate the symptoms of schizophrenia and is the basis of the pharmacological treatment of the disorder.6 ENVIRONMENTAL FACTORS