Essay on Cancer for Students and Children
500+ words essay on cancer.
Cancer might just be one of the most feared and dreaded diseases. Globally, cancer is responsible for the death of nearly 9.5 million people in 2018. It is the second leading cause of death as per the world health organization. As per studies, in India, we see 1300 deaths due to cancer every day. These statistics are truly astonishing and scary. In the recent few decades, the number of cancer has been increasingly on the rise. So let us take a look at the meaning, causes, and types of cancer in this essay on cancer.
Cancer comes in many forms and types. Cancer is the collective name given to the disease where certain cells of the person’s body start dividing continuously, refusing to stop. These extra cells form when none are needed and they spread into the surrounding tissues and can even form malignant tumors. Cells may break away from such tumors and go and form tumors in other places of the patient’s body.


Types of Cancers
As we know, cancer can actually affect any part or organ of the human body. We all have come across various types of cancer – lung, blood, pancreas, stomach, skin, and so many others. Biologically, however, cancer can be divided into five types specifically – carcinoma, sarcoma, melanoma, lymphoma, leukemia.
Among these, carcinomas are the most diagnosed type. These cancers originate in organs or glands such as lungs, stomach, pancreas, breast, etc. Leukemia is the cancer of the blood, and this does not form any tumors. Sarcomas start in the muscles, bones, tissues or other connective tissues of the body. Lymphomas are the cancer of the white blood cells, i.e. the lymphocytes. And finally, melanoma is when cancer arises in the pigment of the skin.
Get the huge list of more than 500 Essay Topics and Ideas
Causes of Cancer
In most cases, we can never attribute the cause of any cancer to one single factor. The main thing that causes cancer is a substance we know as carcinogens. But how these develop or enters a person’s body will depend on many factors. We can divide the main factors into the following types – biological factors, physical factors, and lifestyle-related factors.
Biological factors involve internal factors such as age, gender, genes, hereditary factors, blood type, skin type, etc. Physical factors refer to environmental exposure of any king to say X-rays, gamma rays, etc. Ad finally lifestyle-related factors refer to substances that introduced carcinogens into our body. These include tobacco, UV radiation, alcohol. smoke, etc. Next, in this essay on cancer lets learn about how we can treat cancer.
Treatment of Cancer
Early diagnosis and immediate medical care in cancer are of utmost importance. When diagnosed in the early stages, then the treatment becomes easier and has more chances of success. The three most common treatment plans are either surgery, radiation therapy or chemotherapy.
If there is a benign tumor, then surgery is performed to remove the mass from the body, hence removing cancer from the body. In radiation therapy, we use radiation (rays) to specially target and kill the cancer cells. Chemotherapy is similar, where we inject the patient with drugs that target and kill the cancer cells. All treatment plans, however, have various side-effects. And aftercare is one of the most important aspects of cancer treatment.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Ernest and Isadora Rosenbaum Library

The Will to Live
Ernest H. Rosenbaum, M.D. Isadora R. Rosenbaum, M.A.
As medical professionals, we have always been fascinated by the power of the will to live. Like all creatures in the animal world, human beings have a fierce instinct for survival. The will to live is a force within all of us to fight for survival when our lives are threatened by a disease such as cancer. Yet this force is stronger in some people than in others.
Many physicians have seen how two patients of similar ages and with the same diagnosis, degree of illness, and treatment program experience vastly different results.
Sometimes the biology of a cancer will dictate the course of events regardless of the patient’s attitude and fighting spirit. These events are often beyond our control. But patients with positive attitudes are better able to cope with disease-related problems and may respond better to therapy. Many physicians have seen how two patients of similar ages and with the same diagnosis, degree of illness, and treatment program experience vastly different results. One of the few apparent differences is that one patient is pessimistic and the other optimistic.
We have known for over 2,000 years— from the writings of Plato and Galen— that there is a direct correlation between the mind, the body, and one’s health. “The cure of many diseases is unknown to physicians,” Plato concluded, “because they are ignorant of the whole. For the part can never be well unless the whole is well.”
Recently there has been a shift in health care toward recognizing this wisdom, namely that the psychological and the physical elements of a body are not separate, isolated, and unrelated, but are vitally linked elements of a total system. Health is increasingly being recognized as a balance of many inputs, including physical and environmental factors, emotional and psychological states, and nutritional habits and exercise patterns.
Researchers are now experimenting with methods of actively enlisting the mind in the body’s combat with cancer, using techniques such as meditation, biofeedback, and visualization (creating in the mind positive images about what is occurring in the body). Some doctors and psychologists now believe that the proper attitude may even have a direct effect on cell function and consequently may be used to arrest, if not cure, cancer. This new field of scientific study, called psychoneuroimmunology, focuses on the effect that mental and emotional activity have on physical well-being, indicating that patients can play a much larger role in their recovery.
It will be many years before we know whether it is possible for the mind to control the immune defense system. Experiments with biofeedback and visualization are helpful in that they encourage positive thinking and provide relaxation, thereby increasing the will to live. But they can also be damaging if a patient puts all of his or her faith in them and ignores conventional therapy.
The Power of the Mind
The mind’s role in causing and curing disease has been debated endlessly. Speculation abounds, particularly in the case of cancer. But no studies have proven in a scientifically valid way that a person can control the course of his or her cancer with the mind, although patients often believe otherwise. There are many individual cases that attest to the power of positive attitudes and emotions. One patient with high-risk cancer had a mastectomy at age twentynine. At thirty-one, she had advanced Stage IV cancer with widespread massive liver and bone involvement and, subsequently, extensive lung metastases. She also had an amazingly strong will to live.
“I would get out of bed every morning as if nothing was wrong,” she once said. “I may have known I was going to have to face things and could feel sick during the day, but I never got out of bed that way. There was a lot I was fighting for. I had a three-year-old child, a wonderful life, and a magical love affair with my husband.” Thirty years later, she is still alive, still on chemotherapy, and still living an active life.
We often ask our patients to explain how they are able to transcend their problems. We have found that however diverse they are in ethnic or cultural background, age, educational level, or type of illness, they have all gone through a similar process of psychological recovery.
We often ask our patients to explain how they are able to transcend their problems. We have found that however diverse they are in ethnic or cultural background, age, educational level, or type of illness, they have all gone through a similar process of psychological recovery. They all consciously made a “decision to live.” After an initial period of feeling devastated, they simply decided to assess their new reality and make the most of each day.
Their “will to live” means that they really want to live, whether or not they’re afraid to die. They want to enjoy life, they want to get more out of life, they believe that their life is not over, and they’re willing to do whatever they can to squeeze more out of it.
The threat of death often renews our appreciation of the importance of life, love, friendship, and all there is to enjoy. We open up to new possibilities and begin taking risks we didn’t have the courage to take before. Many patients say that facing the uncertainties of living with an illness makes life more meaningful. The smallest pleasures are intensified and much of the hypocrisy in life is eliminated. When bitterness and anger begin to dissipate, there is still a capacity for joy.
One patient wrote, “I love living, I love nature. Being outdoors, feeling the sun on my skin or the wind blowing against my body, hearing birds sing, breathing in the spray of the ocean. I never lose hope that I may somehow stumble upon or be graced with a victory against this disease.”
Strengthening Your Will to Live
Unfortunately, and quite understandably, many patients react to the diagnosis of cancer in the same way that people in primitive cultures react to the imposition of a curse or spell: as a sentence to a ghastly death. This phenomenon, known as “bone pointing,” results in a paralytic fear that causes the victim to simply withdraw from the world and await the inevitable end. In modern medical practice, a similar phenomenon may occur when, out of ignorance or superstition, a patient believes the diagnosis of cancer to be a death sentence. However, the phenomenon of self-willed death is only effective if the person believes in the power of the curse.
In the treatment of cancer, we’ve seen patients fail on their first course of chemotherapy, fail again on the second and third treatments, then—with more advanced disease—a fourth treatment is highly successful.
In all things, you have to take a risk if you want to win, to get a remission or recover with the best quality of life. Just the willingness to take a risk seems to generate hope and a positive atmosphere in which the components of the will to live are enhanced. There are many other ways of strengthening the will to live.
Getting Involved The best thing a patient can do to strengthen the will to live is to get involved as an active participant in combating his or her disease. When patients approach their disease in an aggressive fighting posture, they are no longer helpless victims. Instead, they become active partners with their medical support team in the fight for improvement, remission, or cure. This partnership must be based on honesty, open communication, shared responsibility, and education about the nature of the disease, therapy options, and rehabilitation. The result of this partnership is an increased ability to cope that, in turn, nurtures the will to live.
Helping and Sharing with Others – A way to strengthen this partnership is to extend the relationship to others. The emotional experience of sharing and enjoying your family and partnerships supports your love for life and your will to survive.
As you make the transition from helpless victim to activist, one of the most important realizations is that you have everything to do with how others perceive you and treat you. If you can accept your condition and hold self-pity at bay, others won’t feel sorry for you. If you can discuss your disease and medical therapy in a matter-of-fact manner, they’ll respond in kind without fear or awkwardness. You are in charge. You can subtly and gently put your family, friends, and coworkers at ease by being frank about what you want to talk about or not talk about and by being explicit about whether and when you want their help.
Sharing your life with others and receiving aid or support from friends and family will improve your ability to cope and help you fight for your life. A person who is lonely or alone often feels like a helpless victim. There is a need to share your own problems, but helping others find solutions to or cope better with the problems of daily living gives strength to both the giver and the receiver. There are few more satisfying experiences in life than helping a person in need.
Patients can also take part in psychological support programs, either through private counseling or through group therapy. Sharing frustrations with others in similar circumstances often relieves the sense of isolation, terror, and despair cancer patients often feel.
Those who must live with cancer can live to the maximum of their capacity by
- living in the present, not the past,
- setting realistic goals and being willing to compromise,
- regaining control of their lives and maintaining a sense of independence and self-esteem,
- trying to resolve negative emotions and depression by actively doing things to help themselves and others, and
- following an improved diet and exercising regularly.
Nurturing Hope
Of all the ingredients in the will to live, hope is the most vital. Hope is the emotional and mental state that motivates you to keep on living, to accomplish things, and to succeed. A person who lacks hope can give up on life and lose the will to live. Without hope, there is little to live for. But with hope, a positive attitude can be maintained, determination strengthened, coping skills sharpened, and love and support more freely given and received.
Even if a diagnosis is such that the future seems limited, hope must be maintained. Hope is what people have to live on. Take away hope, and you take away a chance for the future, which leads to depression. When people fall to that low emotional state, their bodies simply turn off.
Hope can be maintained as long as there is even a remote chance for survival. It can be kindled and nurtured by minor improvements or a remission and maintained when crises or reversals occur. There may be times when you will feel exhausted and drained by never-ending problems and feel ready to give up the struggle to survive. All too often it seems easier to give up than to keep on fighting. Frustrations and despair can sometimes feel overwhelming. Determination or dogged persistence is needed to accomplish the difficult task of fighting for your health.
The experience of cancer not only is destructive in a physical way, but can be a major deterrent to your fighting attitude and will to live. But even during the roughest times, there are often untapped reserves of physical and emotional strength to call upon to help you survive one more day. These reserves can add meaning to your life as well as serve as a lighthouse that leads you to a safe haven during a turbulent storm.
Hope has different meanings for each person. It is a component of a positive attitude and acceptance of our fate in life. We use our strengths to gain success to live life to the fullest. Circumstances often limit our hopes of happiness, cure, remission, or increased longevity. We also live with fears of poverty, pain, a bad death, or other unhappy experiences.
You may worry so much that you lose sight of the possibility of recovery and lose your sense of optimism. On the other hand, you may become so hopeful and confident that you lose sight of reality. Your main challenge is balancing your worry and your hope.
Hope is nourished by the way we live our lives. Achieving the best quality of life requires settling old problems, quarrels, and family strife as well as completing current tasks. Problems that have not been resolved need to have completion. New tasks should be undertaken. If the future seems limited, you can achieve the satisfaction of knowing that you have taken care of your affairs and not left the burden to your family or others. By doing so, you can achieve peace of mind, which will also help strengthen your will to live. With each passing day, try to complete what you can and have that satisfaction that you have done your best.
Be bold, be venturesome, and be willing to experience each day to the fullest to enhance your enjoyment of life. As long as fear, suffering, and pain can be controlled, life can be lived fully until the last breath. Each of us has the capacity to live each day a little better, but we need to focus on both purpose and goals and set into action a realistic daily plan—often altered many times—to help us achieve them. These resources are the foundation of the will to live. Only by using the power of the will to live—nourished by hope—can we achieve the sublime feelings of knowing and experiencing the wonders of life and appreciate its meanings through vital living.
Related Articles

The Role of the Clergy
Religion and Spirituality

The Art of Forgiveness

Coping with Cancer

Coping with Depression

When Your Spouse Has Cancer

The Waiting Process

Patient Stories

One Patients Way of Coping

Feeling Right When Things Go Wrong

I Live a Disease-Threatening Life

The Scent of an Orange

In Touch with My Dream

I Don't Have Time Not to Live

A Cup of Breath

One in a Million

Expedition Inspiration

To Call Forth That Spark
Ernest h. rosenbaum, m.d..
Clinical Professor of Medicine, University of California, San Francisco, Comprehensive Cancer Center; Adjunct Clinical Professor, Department of Medicine, Stanford University Medical Center; Director, Stanford Cancer Supportive Care Programs National/International, Stanford Complementary Medicine Clinic, Stanford University Medical Center, Stanford, California. More
Ernest H. Rosenbaum’s career has included a fellowship at the Blood Research Laboratory of Tufts University School of Medicine (New England Center Hospital) and MIT. He teaches at the University of California, San Francisco, Comprehensive Cancer Center, was the cofounder of the Northern California Academy of Clinical Oncology, and founded the Better Health Foundation and the Cancer Supportive Care Program at the Stanford Complementary Medicine Clinic, Stanford University Medical Center.
His passionate interest in clinical research and developing ways to improve patient care and communication with patients and colleagues has resulted in over fifty articles on cancer and hematology in various medical journals. He has also participated in many radio and television programs and frequently lectures to medical and public groups.
He has written numerous books, including Living with Cancer: A Home Care Training Program for Cancer Patients; Decisions for Life: You Can Live Ten Years Longer with Better Health; Cancer Supportive Care: A Comprehensive Guide for Cancer Patients and Their Families; Nutrition for the Cancer Patient; Everyone’s Guide to Cancer Therapy; and Everyone’s Guide to Cancer Survivorship. For Everyone’s Guide to Cancer Therapy, Ernest Rosenbaum, M.D., Malin Dollinger, M.D., and Greg Cable received and Honorable Mention in 1991 from the American Medical Writers Association for Excellence in Medical Publications. Ernest and Isadora Rosenbaum received the same award in 1982 for their book, A Comprehensive Guide for Cancer Patients and Their Families.
Isadora Rosenbaum, M.A.
Isadora Rosenbaum is a medical assistant who worked in immunology research and is currently at an oncology practice at the UCSF Comprehensive Cancer Center offering advice and psychosocial support. She coauthored Nutrition for the Cancer Patient and The Comprehensive Guide for Cancer Patients and Their Families. She has written chapters in Everyone’s Guide to Cancer Therapy, Living with Cancer, and You Can Live 10 Years Longer with Better Health.
The Unique Hell of Getting Cancer as a Young Adult

W hen I got diagnosed with Stage 3b Hodgkin Lymphoma at age 32, it was almost impossible to process. Without a family history or lifestyle risk factors that put cancer on my radar, I stared at the emergency room doctor in utter disbelief when he said the CT scan of my swollen lymph node showed what appeared to be cancer—and lots of it. A few days away from a bucket list trip to Japan, I’d only gone to the emergency room because the antibiotics CityMD prescribed to me when I was sick weren’t working.I didn’t want to be sick in a foreign country. So when the doctor told me of my diagnosis, the only question I could conjure was: “So Tokyo is a no-go?”
Around the world, cancer rates in people under 50 are surging, with a recent study in BMJ Oncology showing that new cases for young adults have risen 79% overall over the past three decades. In the U.S. alone, new cancer diagnoses in people under 50 hit 3.26 million, with the most common types being breast, windpipe, lung, bowel, and stomach. A new feature in the Wall Street Journal highlights the mad dash among doctors and researchers to determine what’s causing this troubling rise. Strangely, overall cancer rates in the U.S. have dropped over the past three decades, while young people—particularly with colorectal cancers—are increasingly diagnosed at late stages. “We need to make it easier for adolescents and young adults to participate in clinical trials to improve outcomes and study the factors contributing to earlier onset cancers so we can develop new cures,” says Julia Glade Bender, MD, co-lead of the Stuart Center for Adolescent and Young Adult (AYA) Cancers at Memorial Sloan Kettering in New York City (where I am currently a patient.)
Doctors suspect that lifestyle factors and environmental elements, from microplastics to ultra-processed foods, could be to blame. But many adults in their 20s and 30s, such as myself, were otherwise healthy before their diagnoses. It felt like all those years of forcing myself to run, eat high-fiber foods, and choke down kombucha were for nothing.
Cancer is hell at any age, but the challenges facing young adults are especially steep, as the disease disrupts a formative period for building a career, family, and even healthy self-esteem, from body image to gender identity. It’s critical that our approach to treating and supporting these patients reflects the severity of this disruption. In recent years, a growing number of cancer hospitals have developed young adult-specific programming like support groups, information sessions on dating and sexual health, and even mobile apps to help counter social alienation. But there is still a long way to go.
Read more: Why I Stopped Being A “Good” Cancer Patient
Shockingly enough, canceling my trip to Japan was the least of my worries. Beyond the excruciating physical side effects of high-dose chemotherapy and a number of life-threatening complications, cancer pulverized my self-esteem into nothingness, as I watched peers get married and promoted from my bed. Thankfully, after switching to a new hospital, I found support groups that connected me with a community of peers who got it, as well as social workers who work exclusively with young adults and thus recognized many of my biggest challenges, like social isolation, financial strain, the dating nightmare, and hating my bald head.
Perhaps the biggest reason I resented cancer was for disrupting a milestone I’d worked for my whole life: a book launch. (My diagnosis came two months before my first book was published.) Young adulthood is meant to be littered with these kinds of professional and personal benchmarks, many of which are hard enough to accomplish without tumors; dating, for instance, is impossible for me even as a healthy person. Now I have to re-enter the pool older, weaker, and more traumatized?
“Young adult patients may be trying to assert independence from parents, establish a career or intimate relationship, or even be parents themselves,” says Bender. “Most will be naïve to the medical system or a serious health condition.” And so they require flexible, creative clinicians who can help navigate them “to and through the best available therapy and back to their lives, inevitably ‘changed’ but intact.” Not only do these patients need specialized psychosocial support, but research initiatives should prioritize developing treatments that minimize long-term toxicities.
Given that many young patients haven’t yet built financial stability and are often in some form of debt, organizations like Young Adults Survivors United (YASU) have emerged to support young adult survivors and patients through the financial overwhelm. Stephanie Samolovitch, MSW and founder of YASU, says that there’s still an enormous need for resources supporting young adult cancer patients and survivors.
“Cancer causes a young adult to be dependent again, whether it’s moving back in with parents, getting rides to appointments, or asking for financial help,” says Samolovitch, who was diagnosed with leukemia in 2005, two weeks before her 20th birthday. “Young adults never expect to apply for Medicaid or Social Security Disability during our twenties or thirties, yet cancer doesn't give us a choice sometimes. That causes stress, shame, depression, and anxiety when trying to navigate the healthcare system.”
Read more: How to Create an Action Plan After a Cancer Diagnosis
When Ana Calderone, a 33-year-old magazine editor, was diagnosed with stage 2 breast cancer at 30, the most challenging part of getting diagnosed so young was “everything.”
“I felt like it set my whole life back, which sounds stupid because I was literally fighting for my life,” she says. “Who cares if I had to delay my wedding a year because I was still getting radiation treatment? But it was really hard at the time. Everything was delayed, and still is.”
During chemo, Calderone’s doctors gave her a shot that she still receives to try and preserve her ovaries, and she’s been able to try IVF twice. She says she had to proactively advocate for those things with her care team. While Calderone is currently cancer free, she still must take medication that has further delayed her plans to build a family. “I’m fairly confident I’d have a child by now if I didn’t get cancer. That’s been the most devastating part,” she says. “My oncologist would consider letting me get pregnant in two more years, which would be 4.5 years post-diagnosis, and even that is still a risk.”
For 32-year-old Megan Koehler, whose son was one and a half when she was diagnosed with Hodgkin Lymphoma, the hardest part “was knowing the world continued on while I spent days in bed,” she says. “My coworkers still worked on projects I was supposed to be part of, and the worst was knowing my son was growing up, learning to speak sentences, and just becoming a toddler without me – or so it felt that way.”
She remembers crying for most of his second birthday because she was in bed post chemo, feeling devastated that she didn’t have the energy to spend the day with him. During a 50-plus day hospital stay caused by an adverse reaction to a chemotherapy drug, she would Facetime him and cry when he spoke in sentences, because he wasn’t doing that before she was admitted. While she’s grateful for the support she had from her husband and mother, she felt alienated. “I spoke to a few people my age via social media, but no one in person. My center mostly catered to the older generations, so it was somewhat isolating. I did have a great relationship with a few of the infusion nurses who were around my age.”
While oncologists may be rightly focused on saving patients’ lives, there must be more consideration for quality of life during and after treatment – both physical and mental. “More questions need to be asked about their relationships, fertility options, and any mental health concerns or symptoms,” says Samolovitch. From a research perspective, initiatives must expand to pinpoint not only the reason for the rise of cancer in young adults, but find ways to screen and diagnose earlier.
Towards the beginning of my treatment, before I switched hospitals, my oncologist seemed to treat my concerns about self-esteem and hair loss as trivial compared to the real work of saving my life. At my weakest, I had to advocate repeatedly to get accurate information on cold capping, a process of scalp cooling that can preserve most of your hair during chemotherapy, and I had to beg again and again for a social worker to reach out to me, which took weeks.
It’s a beautiful thing that more young adults with cancer are surviving their illnesses. But that means they’ll have decades of life ahead of them. Providers must do a better job supporting young adult patients through all the collateral damage that comes with cancer and its treatment.
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- The Revolution of Yulia Navalnaya
- 6 Compliments That Land Every Time
- What's the Deal With the Bitcoin Halving?
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]

I’ll Tell You the Secret of Cancer
It’s been almost 20 years since my diagnosis, and I’ve learned quite a bit.
Are you someone who enjoys the unsolicited opinions of strangers and acquaintances? If so, I can’t recommend cancer highly enough. You won’t even have the first pathology report in your hands before the advice comes pouring in. Laugh and the world laughs with you; get cancer and the world can’t shut its trap.
Stop eating sugar; keep up your weight with milkshakes. Listen to a recent story on NPR; do not read a recent story in Time magazine. Exercise—but not too vigorously; exercise— hard , like Lance Armstrong. Join a support group, make a collage, make a collage in a support group, collage the shit out of your cancer. Do you live near a freeway or drink tap water or eat food microwaved on plastic plates? That’s what caused it. Do you ever think about suing? Do you ever wonder whether, if you’d just let some time pass, the cancer would have gone away on its own?
Before I got cancer, I thought I understood how the world worked, or at least the parts that I needed to know about. But when I got cancer, my body broke down so catastrophically that I stopped trusting what I thought and believed. I felt that I had to listen when people told me what to do, because clearly I didn’t know anything.
Much of the advice was bewildering, and all of it was anxiety-producing. In the end, because so many people contradicted one another, I was able to ignore most of them. But there was one warning I heard from a huge number of people, almost every day, and sometimes two or three times a day: I had to stay positive. People who beat cancer have a great positive attitude . It’s what distinguishes the survivors from the dead.
There are books about how to develop the positive attitude that beats cancer, and meditation tapes to help you visualize your tumors melting away. Friends and acquaintances would send me these books and tapes—and they would send them to my husband, too. We were both anxious and willing to do anything in our control.
But after a terrible diagnosis, a failed surgery, a successful surgery, and the beginning of chemotherapy, I just wasn’t feeling very … up. At the end of another terrible day, my husband would gently ask me to sit in the living room so that I could meditate and think positive thoughts. I was nauseated from the drugs, tired, and terrified that I would leave my little boys without a mother. All I wanted to do was take my Ativan and sleep. But I couldn’t do that. If I didn’t change my attitude, I was going to die.
P eople get diagnosed with cancer in different ways. Some have a family history, and their doctors monitor them for years. Others have symptoms for so long that the eventual diagnosis is more of a terrible confirmation than a shock. And then there are people like me, people who are going about their busy lives when they push open the door of a familiar medical building for a routine appointment and step into an empty elevator shaft.
The afternoon in 2003 that I found out I had aggressive breast cancer, my boys were almost 5. The biggest thing on my mind was getting the mammogram over with early enough that I could pick up some groceries before the babysitter had to go home. I put on the short, pink paper gown and thought about dinner. And then everything started happening really fast. Suddenly there was the need for a second set of films, then a sonogram, then the sharp pinch of a needle. In my last fully conscious moment as the person I once was, I remember asking the doctor if I should have a biopsy. The reason I asked was so that he could look away from the screen, realize that he’d scared me, and reassure me. “No, no,” he would say; “it’s completely benign.” But he didn’t say that. He said, “That’s what we’re doing right now.”
Later I would wonder why the doctor hadn’t asked my permission for the needle biopsy. The answer was that I had already passed through the border station that separates the healthy from the ill. The medical community and I were on new terms.
Read: I thought Stage IV cancer was bad enough
The doctor could see that I was in shock, and he seemed pretty rattled himself. He kept saying that he should call my husband. “You need to prepare yourself,” he said, twice. And once: “It’s aggressive.” But I didn’t want him to call my husband. I wanted to tear off my paper gown and never see that doctor, his office, or even the street where the building was located ever again. I had a mute, animal need to get the hell out of there. The news was so bad, and it kept getting worse. I couldn’t think straight. My little boys were so small. They were my life, and they needed me.
Three weeks later, I was in the infusion center. Ask Google “What is the worst chemotherapy drug?” and the answer is doxorubicin. That’s what I got, as well as some other noxious pharmaceuticals. That oncologist filled me and my fellow patients up with so much poison that the sign on the bathrooms said we had to flush twice to make sure every trace was gone before a healthy person—a nurse, or a family member—could use the toilet. I was not allowed to hug my children for the first 24 hours after treatment, and in the midst of this absolute hell—in the midst of the poison and the crying and the sorrow and the terror—I was supposed to get a really great positive attitude.
The book we were given several copies of, which was first published in 1986 and has been reissued several times since, is titled Love, Medicine and Miracles and was written by a pediatric surgeon named Bernie Siegel. He seems less interested in exceptional scientific advances than in “exceptional patients.” To be exceptional, you have to tell your body that you want to live; you have to say “No way” to any doctor who says you have a fatal illness. You have to become a channel of perfect self-love, and remember that “the simple truth is, happy people generally don’t get sick.” Old angers or disappointments can congeal into cancer. You need to get rid of those emotions, or they will kill you.
In 1989 a Stanford psychiatrist named David Spiegel published a study of women with metastatic breast cancer. He created a support group for half the women, whom he taught self-hypnosis. The other women got no extra social support. The results were remarkable: Spiegel reported that the women in the group survived twice as long as the other women. This study was hugely influential in modern beliefs about meditation and cancer survival. It showed up in the books my husband read to me, which were filled with other stories of miraculous healings, of patients defying the odds though their own emotional work. But I was so far behind. From the beginning I couldn’t stop crying. I began to think I was hopeless and would never survive.
I needed help, and I remembered a woman my husband and I had talked to in the first week after my diagnosis. Both of us had found in those conversations our only experience of calm, our only reassurance that we were doing the right things. Anne Coscarelli is a clinical psychologist and the founder of the Simms/Mann-UCLA Center for Integrative Oncology , which helps patients and their families cope with the trauma of cancer. We had reached out to her when we were trying to understand my diagnosis. Now I needed her for much more.
For the first half hour in her office, we just talked about how sick I felt and how frightened I was. Then—nervously—I confessed: I wasn’t doing the work of healing myself. I wasn’t being positive.
“Why do you need to be positive?” she asked in a neutral voice.
I thought it should be obvious, but I explained: Because I didn’t want to die!
Coscarelli remained just as neutral and said, “There isn’t a single bit of evidence that having a positive attitude helps heal cancer.”
What? That couldn’t possibly be right. How did she know that?
“They study it all the time,” she said. “It’s not true.”
David Spiegel was never able to replicate his findings about metastatic breast cancer. The American Cancer Society and the National Center for Complementary and Integrative Health say there’s no evidence that meditation or support groups increase survival rates. They can do all sorts of wonderful things, like reducing stress and allowing you to live in the moment instead of worrying about the next scan. I’ve learned, whenever I start to get scared, to do some yoga-type breathing with my eyes closed until I get bored. If I’m bored, I’m not scared, so then I open my eyes again. But I’m not alive today because of deep breathing.
When I began to understand that attitude doesn’t have anything to do with survival, I felt myself coming up out of deep water. I didn’t cause my cancer by having a bad attitude, and I wasn’t going to cure it by having a good one.
And then Coscarelli told me the whole truth about cancer. If you’re ready, I will tell it to you.
Cancer occurs when a group of cells divide in rapid and abnormal ways. Treatments are successful if they interfere with that process.
That’s it, that’s the whole equation.
Everyone with cancer has a different experience, and different beliefs about what will help. I feel strongly that these beliefs should be respected—including the feelings of those who decide not to have any treatment at all. It’s sadism to learn that someone is dangerously ill and to impose upon her your own set of unproven assumptions, especially ones that blame the patient for getting sick in the first place.
That meeting with Anne Coscarelli took place 18 years ago, and never once since then have I worried that my attitude was going to kill me. I’ve had several recurrences, all of them significant, but I’m still here, typing and drinking a Coke and not feeling super upbeat.
Before I left that meeting, I asked her one last question: Maybe I couldn’t think my way out of cancer, but wasn’t it still important to be as good a person as I could be? Wouldn’t that karma improve my odds a little bit?
Coscarelli told me that, over the years, many wonderful and generous women had come to her clinic, and some of them had died very quickly. Yikes. I had to come clean: Not only was I un-wonderful. I was also kind of a bitch.
God love her, she came through with exactly what I needed to hear: “I’ve seen some of the biggest bitches come in, and they’re still alive.”
And that, my friends, was when I had my very first positive thought. I imagined all those bitches getting healthy, and I said to myself, I think I’m going to beat this thing.
What Is Cancer?
Get email updates from NCI on cancer health information, news, and other topics
Get email updates from NCI
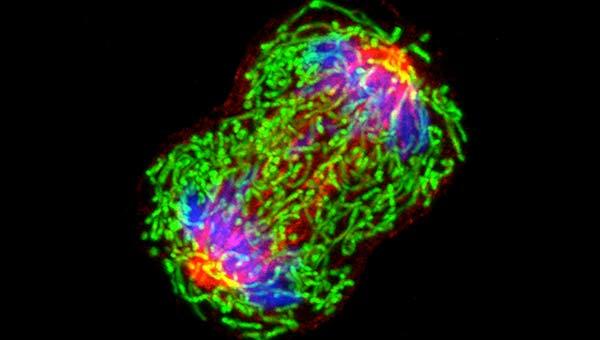
A dividing breast cancer cell.
The Definition of Cancer
Cancer is a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body.
Cancer can start almost anywhere in the human body, which is made up of trillions of cells. Normally, human cells grow and multiply (through a process called cell division) to form new cells as the body needs them. When cells grow old or become damaged, they die, and new cells take their place.
Sometimes this orderly process breaks down, and abnormal or damaged cells grow and multiply when they shouldn’t. These cells may form tumors, which are lumps of tissue. Tumors can be cancerous or not cancerous ( benign ).
Cancerous tumors spread into, or invade, nearby tissues and can travel to distant places in the body to form new tumors (a process called metastasis ). Cancerous tumors may also be called malignant tumors. Many cancers form solid tumors, but cancers of the blood, such as leukemias , generally do not.
Benign tumors do not spread into, or invade, nearby tissues. When removed, benign tumors usually don’t grow back, whereas cancerous tumors sometimes do. Benign tumors can sometimes be quite large, however. Some can cause serious symptoms or be life threatening, such as benign tumors in the brain.
Differences between Cancer Cells and Normal Cells

Get Answers >
Have questions? Connect with a Cancer Information Specialist for answers.
Cancer cells differ from normal cells in many ways. For instance, cancer cells:
- grow in the absence of signals telling them to grow. Normal cells only grow when they receive such signals.
- ignore signals that normally tell cells to stop dividing or to die (a process known as programmed cell death , or apoptosis ).
- invade into nearby areas and spread to other areas of the body. Normal cells stop growing when they encounter other cells, and most normal cells do not move around the body.
- tell blood vessels to grow toward tumors. These blood vessels supply tumors with oxygen and nutrients and remove waste products from tumors.
- hide from the immune system . The immune system normally eliminates damaged or abnormal cells.
- trick the immune system into helping cancer cells stay alive and grow. For instance, some cancer cells convince immune cells to protect the tumor instead of attacking it.
- accumulate multiple changes in their chromosomes , such as duplications and deletions of chromosome parts. Some cancer cells have double the normal number of chromosomes.
- rely on different kinds of nutrients than normal cells. In addition, some cancer cells make energy from nutrients in a different way than most normal cells. This lets cancer cells grow more quickly.
Many times, cancer cells rely so heavily on these abnormal behaviors that they can’t survive without them. Researchers have taken advantage of this fact, developing therapies that target the abnormal features of cancer cells. For example, some cancer therapies prevent blood vessels from growing toward tumors , essentially starving the tumor of needed nutrients.
How Does Cancer Develop?
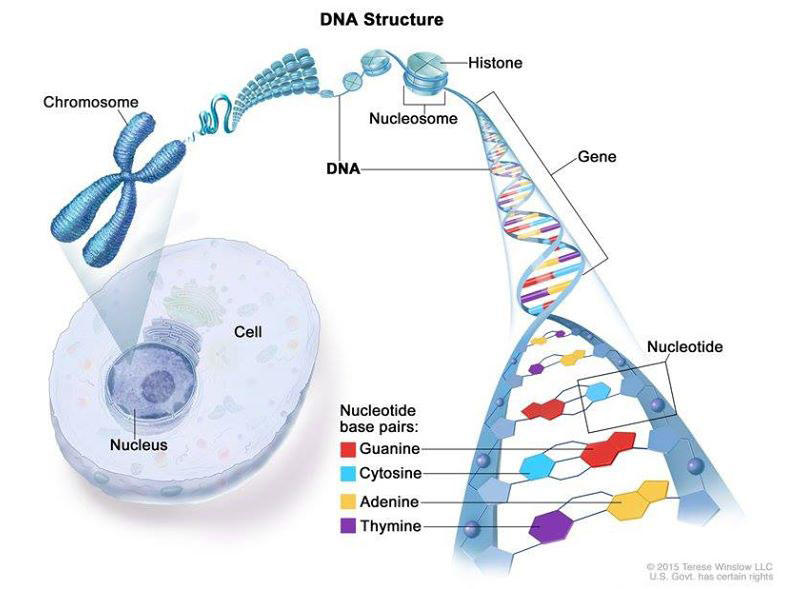
Cancer is caused by certain changes to genes, the basic physical units of inheritance. Genes are arranged in long strands of tightly packed DNA called chromosomes.
Cancer is a genetic disease—that is, it is caused by changes to genes that control the way our cells function, especially how they grow and divide.
Genetic changes that cause cancer can happen because:
- of errors that occur as cells divide.
- of damage to DNA caused by harmful substances in the environment, such as the chemicals in tobacco smoke and ultraviolet rays from the sun. (Our Cancer Causes and Prevention section has more information.)
- they were inherited from our parents.
The body normally eliminates cells with damaged DNA before they turn cancerous. But the body’s ability to do so goes down as we age. This is part of the reason why there is a higher risk of cancer later in life.
Each person’s cancer has a unique combination of genetic changes. As the cancer continues to grow, additional changes will occur. Even within the same tumor, different cells may have different genetic changes.
Fundamentals of Cancer
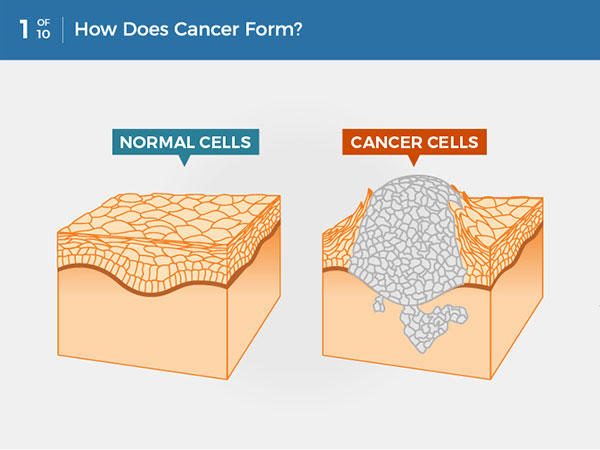
Cancer is a disease caused when cells divide uncontrollably and spread into surrounding tissues.
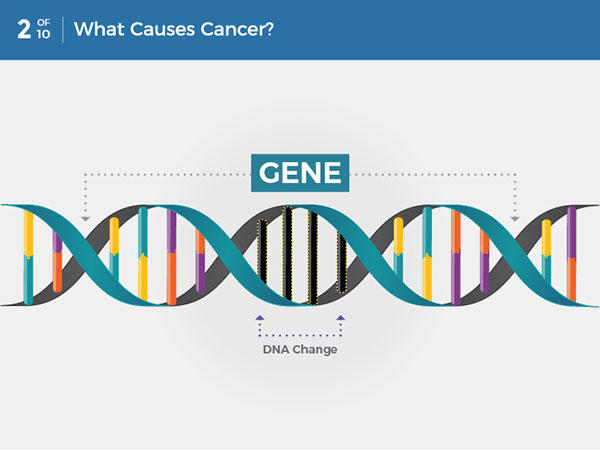
Cancer is caused by changes to DNA. Most cancer-causing DNA changes occur in sections of DNA called genes. These changes are also called genetic changes.
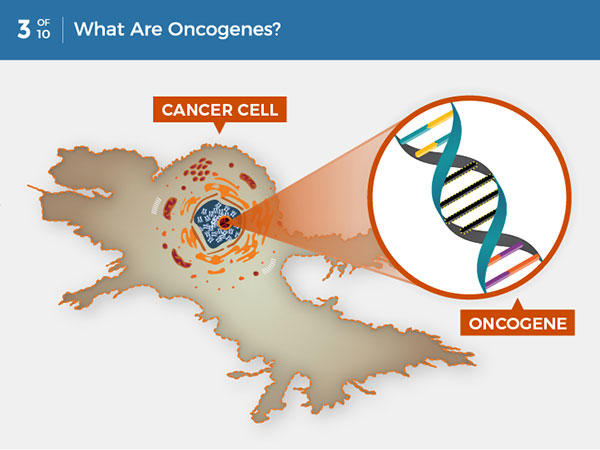
A DNA change can cause genes involved in normal cell growth to become oncogenes. Unlike normal genes, oncogenes cannot be turned off, so they cause uncontrolled cell growth.
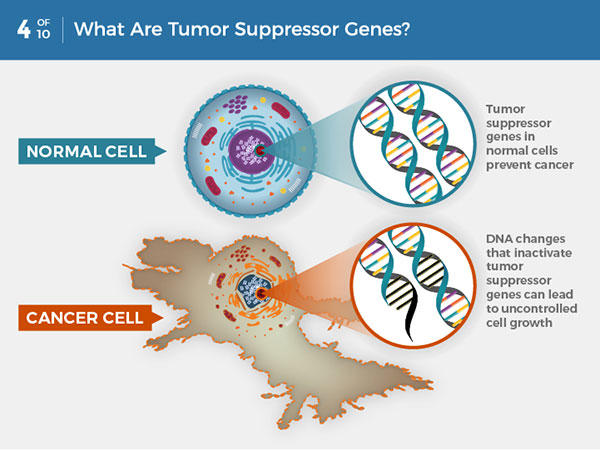
In normal cells, tumor suppressor genes prevent cancer by slowing or stopping cell growth. DNA changes that inactivate tumor suppressor genes can lead to uncontrolled cell growth and cancer.
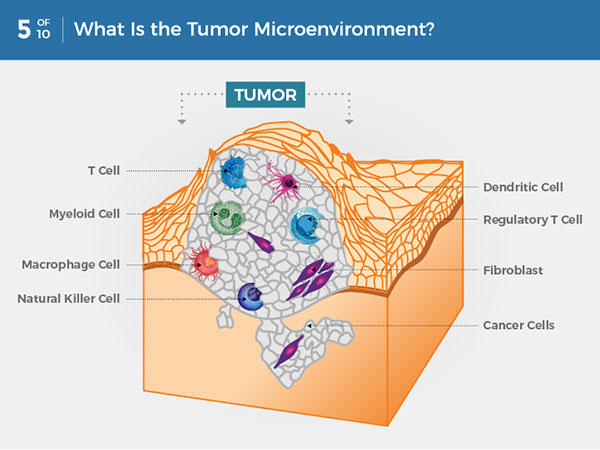
Within a tumor, cancer cells are surrounded by a variety of immune cells, fibroblasts, molecules, and blood vessels—what’s known as the tumor microenvironment. Cancer cells can change the microenvironment, which in turn can affect how cancer grows and spreads.
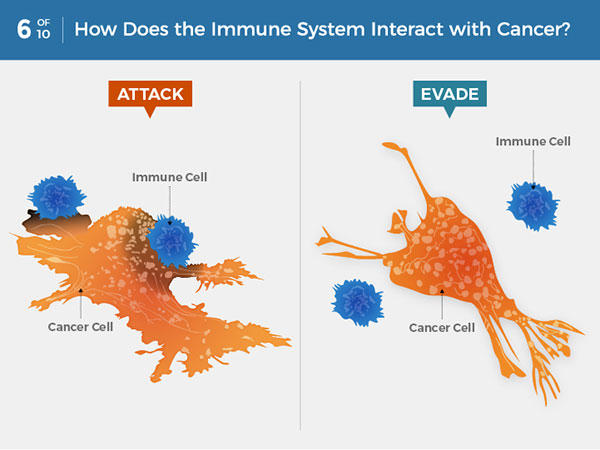
Immune system cells can detect and attack cancer cells. But some cancer cells can avoid detection or thwart an attack. Some cancer treatments can help the immune system better detect and kill cancer cells.
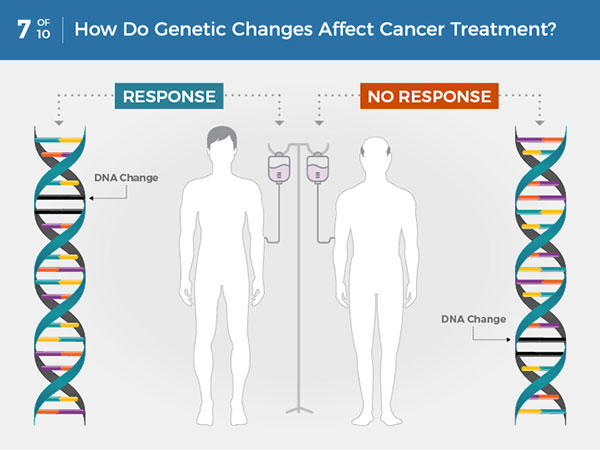
Each person’s cancer has a unique combination of genetic changes. Specific genetic changes may make a person’s cancer more or less likely to respond to certain treatments.
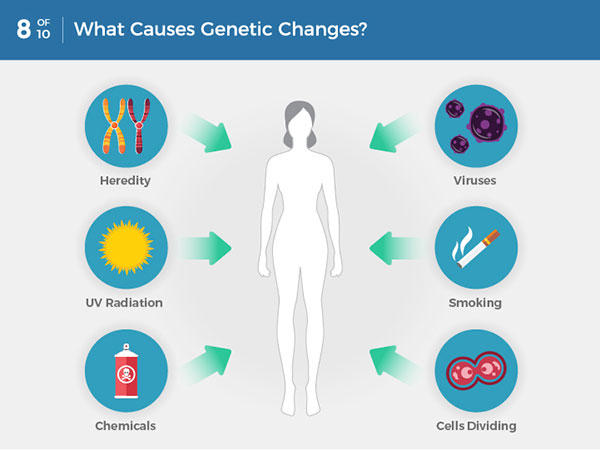
Genetic changes that cause cancer can be inherited or arise from certain environmental exposures. Genetic changes can also happen because of errors that occur as cells divide.
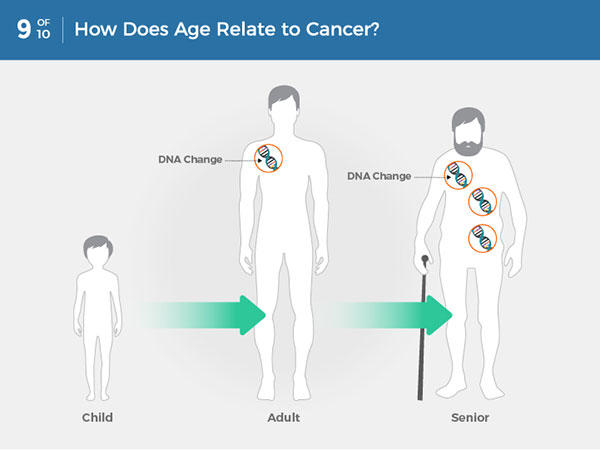
Most often, cancer-causing genetic changes accumulate slowly as a person ages, leading to a higher risk of cancer later in life.
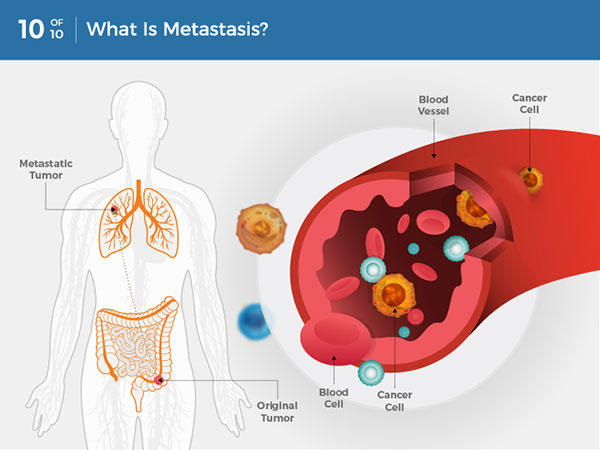
Cancer cells can break away from the original tumor and travel through the blood or lymph system to distant locations in the body, where they exit the vessels to form additional tumors. This is called metastasis.
Types of Genes that Cause Cancer
The genetic changes that contribute to cancer tend to affect three main types of genes— proto-oncogenes , tumor suppressor genes , and DNA repair genes. These changes are sometimes called “drivers” of cancer.
Proto-oncogenes are involved in normal cell growth and division. However, when these genes are altered in certain ways or are more active than normal, they may become cancer-causing genes (or oncogenes), allowing cells to grow and survive when they should not.
Tumor suppressor genes are also involved in controlling cell growth and division. Cells with certain alterations in tumor suppressor genes may divide in an uncontrolled manner.
DNA repair genes are involved in fixing damaged DNA. Cells with mutations in these genes tend to develop additional mutations in other genes and changes in their chromosomes, such as duplications and deletions of chromosome parts. Together, these mutations may cause the cells to become cancerous.
As scientists have learned more about the molecular changes that lead to cancer, they have found that certain mutations commonly occur in many types of cancer. Now there are many cancer treatments available that target gene mutations found in cancer . A few of these treatments can be used by anyone with a cancer that has the targeted mutation, no matter where the cancer started growing .
When Cancer Spreads
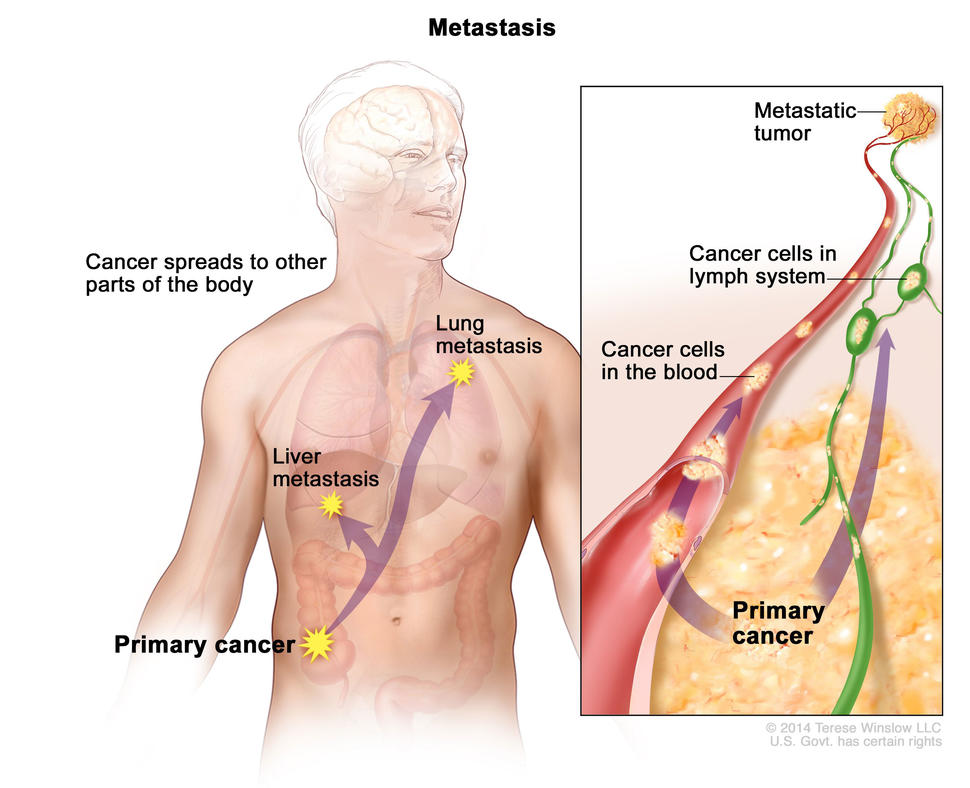
In metastasis, cancer cells break away from where they first formed and form new tumors in other parts of the body.
A cancer that has spread from the place where it first formed to another place in the body is called metastatic cancer. The process by which cancer cells spread to other parts of the body is called metastasis.
Metastatic cancer has the same name and the same type of cancer cells as the original, or primary, cancer. For example, breast cancer that forms a metastatic tumor in the lung is metastatic breast cancer, not lung cancer.
Under a microscope, metastatic cancer cells generally look the same as cells of the original cancer. Moreover, metastatic cancer cells and cells of the original cancer usually have some molecular features in common, such as the presence of specific chromosome changes.
In some cases, treatment may help prolong the lives of people with metastatic cancer. In other cases, the primary goal of treatment for metastatic cancer is to control the growth of the cancer or to relieve symptoms it is causing. Metastatic tumors can cause severe damage to how the body functions, and most people who die of cancer die of metastatic disease.
Tissue Changes that Are Not Cancer
Not every change in the body’s tissues is cancer. Some tissue changes may develop into cancer if they are not treated, however. Here are some examples of tissue changes that are not cancer but, in some cases, are monitored because they could become cancer:
- Hyperplasia occurs when cells within a tissue multiply faster than normal and extra cells build up. However, the cells and the way the tissue is organized still look normal under a microscope. Hyperplasia can be caused by several factors or conditions, including chronic irritation.
- Dysplasia is a more advanced condition than hyperplasia. In dysplasia, there is also a buildup of extra cells. But the cells look abnormal and there are changes in how the tissue is organized. In general, the more abnormal the cells and tissue look, the greater the chance that cancer will form. Some types of dysplasia may need to be monitored or treated, but others do not. An example of dysplasia is an abnormal mole (called a dysplastic nevus ) that forms on the skin. A dysplastic nevus can turn into melanoma, although most do not.
- Carcinoma in situ is an even more advanced condition. Although it is sometimes called stage 0 cancer, it is not cancer because the abnormal cells do not invade nearby tissue the way that cancer cells do. But because some carcinomas in situ may become cancer, they are usually treated.
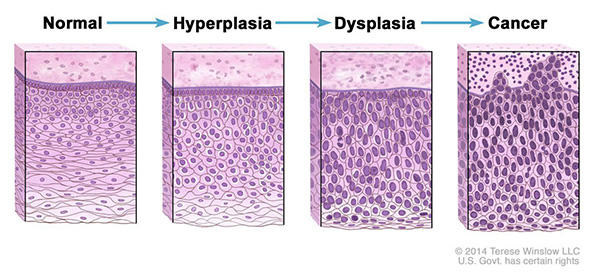
Normal cells may become cancer cells. Before cancer cells form in tissues of the body, the cells go through abnormal changes called hyperplasia and dysplasia. In hyperplasia, there is an increase in the number of cells in an organ or tissue that appear normal under a microscope. In dysplasia, the cells look abnormal under a microscope but are not cancer. Hyperplasia and dysplasia may or may not become cancer.
Types of Cancer
There are more than 100 types of cancer. Types of cancer are usually named for the organs or tissues where the cancers form. For example, lung cancer starts in the lung, and brain cancer starts in the brain. Cancers also may be described by the type of cell that formed them, such as an epithelial cell or a squamous cell .
You can search NCI’s website for information on specific types of cancer based on the cancer’s location in the body or by using our A to Z List of Cancers . We also have information on childhood cancers and cancers in adolescents and young adults .
Here are some categories of cancers that begin in specific types of cells:
Carcinomas are the most common type of cancer. They are formed by epithelial cells, which are the cells that cover the inside and outside surfaces of the body. There are many types of epithelial cells, which often have a column-like shape when viewed under a microscope.
Carcinomas that begin in different epithelial cell types have specific names:
Adenocarcinoma is a cancer that forms in epithelial cells that produce fluids or mucus. Tissues with this type of epithelial cell are sometimes called glandular tissues. Most cancers of the breast, colon, and prostate are adenocarcinomas.
Basal cell carcinoma is a cancer that begins in the lower or basal (base) layer of the epidermis, which is a person’s outer layer of skin.
Squamous cell carcinoma is a cancer that forms in squamous cells, which are epithelial cells that lie just beneath the outer surface of the skin. Squamous cells also line many other organs, including the stomach, intestines, lungs, bladder, and kidneys. Squamous cells look flat, like fish scales, when viewed under a microscope. Squamous cell carcinomas are sometimes called epidermoid carcinomas.
Transitional cell carcinoma is a cancer that forms in a type of epithelial tissue called transitional epithelium, or urothelium. This tissue, which is made up of many layers of epithelial cells that can get bigger and smaller, is found in the linings of the bladder, ureters, and part of the kidneys (renal pelvis), and a few other organs. Some cancers of the bladder, ureters, and kidneys are transitional cell carcinomas.
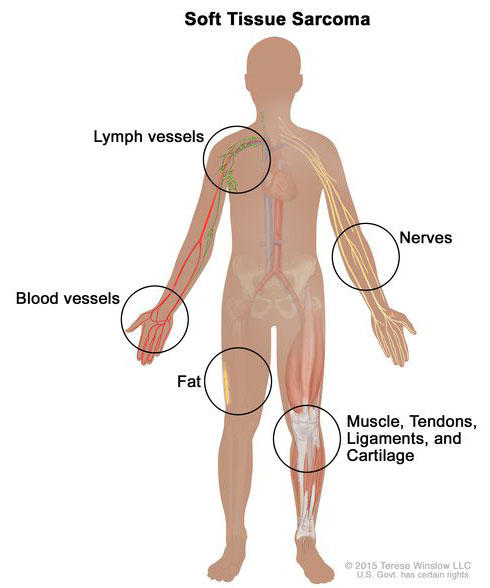
Soft tissue sarcoma forms in soft tissues of the body, including muscle, tendons, fat, blood vessels, lymph vessels, nerves, and tissue around joints.
Sarcomas are cancers that form in bone and soft tissues, including muscle, fat, blood vessels, lymph vessels , and fibrous tissue (such as tendons and ligaments).
Osteosarcoma is the most common cancer of bone. The most common types of soft tissue sarcoma are leiomyosarcoma , Kaposi sarcoma , malignant fibrous histiocytoma , liposarcoma , and dermatofibrosarcoma protuberans .
Our page on soft tissue sarcoma has more information.
Cancers that begin in the blood-forming tissue of the bone marrow are called leukemias. These cancers do not form solid tumors. Instead, large numbers of abnormal white blood cells (leukemia cells and leukemic blast cells) build up in the blood and bone marrow, crowding out normal blood cells. The low level of normal blood cells can make it harder for the body to get oxygen to its tissues, control bleeding, or fight infections.
There are four common types of leukemia, which are grouped based on how quickly the disease gets worse (acute or chronic) and on the type of blood cell the cancer starts in (lymphoblastic or myeloid). Acute forms of leukemia grow quickly and chronic forms grow more slowly.
Our page on leukemia has more information.
Lymphoma is cancer that begins in lymphocytes (T cells or B cells). These are disease-fighting white blood cells that are part of the immune system. In lymphoma, abnormal lymphocytes build up in lymph nodes and lymph vessels, as well as in other organs of the body.
There are two main types of lymphoma:
Hodgkin lymphoma – People with this disease have abnormal lymphocytes that are called Reed-Sternberg cells. These cells usually form from B cells.
Non-Hodgkin lymphoma – This is a large group of cancers that start in lymphocytes. The cancers can grow quickly or slowly and can form from B cells or T cells.
Our page on lymphoma has more information.
Multiple Myeloma
Multiple myeloma is cancer that begins in plasma cells , another type of immune cell. The abnormal plasma cells, called myeloma cells, build up in the bone marrow and form tumors in bones all through the body. Multiple myeloma is also called plasma cell myeloma and Kahler disease.
Our page on multiple myeloma and other plasma cell neoplasms has more information.
Melanoma is cancer that begins in cells that become melanocytes, which are specialized cells that make melanin (the pigment that gives skin its color). Most melanomas form on the skin, but melanomas can also form in other pigmented tissues, such as the eye.
Our pages on skin cancer and intraocular melanoma have more information.
Brain and Spinal Cord Tumors
There are different types of brain and spinal cord tumors. These tumors are named based on the type of cell in which they formed and where the tumor first formed in the central nervous system. For example, an astrocytic tumor begins in star-shaped brain cells called astrocytes , which help keep nerve cells healthy. Brain tumors can be benign (not cancer) or malignant (cancer).
Our page on brain and spinal cord tumors has more information.
Other Types of Tumors
Germ cell tumors.
Germ cell tumors are a type of tumor that begins in the cells that give rise to sperm or eggs. These tumors can occur almost anywhere in the body and can be either benign or malignant.
Our page of cancers by body location/system includes a list of germ cell tumors with links to more information.
Neuroendocrine Tumors
Neuroendocrine tumors form from cells that release hormones into the blood in response to a signal from the nervous system. These tumors, which may make higher-than-normal amounts of hormones, can cause many different symptoms. Neuroendocrine tumors may be benign or malignant.
Our definition of neuroendocrine tumors has more information.
Carcinoid Tumors
Carcinoid tumors are a type of neuroendocrine tumor. They are slow-growing tumors that are usually found in the gastrointestinal system (most often in the rectum and small intestine). Carcinoid tumors may spread to the liver or other sites in the body, and they may secrete substances such as serotonin or prostaglandins, causing carcinoid syndrome .
Our page on gastrointestinal neuroendocrine tumors has more information.
Talk to our experts
1800-120-456-456
- National Cancer Awareness Day: Empowering Hope and Health

Coveted as one of the most notorious diseases in the world, cancer has known to be one of the leading causes of death across the world. Cancer in any form is life-threatening and people often shy away from discussing it. However, cancer awareness can be of great benefit to the common people.
Long Essay on Cancer
In this long essay on cancer, we are providing you with cancer meaning, speech on cancer awareness. Go through this cancer essay to get a complete overview of this deadly disease.
In a recent study conducted in 2018, it was found that around 9.5 million people died that year owing to cancer. The World Health Organisation has revealed that cancer is the second leading cause of death across the world. The statistics in India are also no better and as per recent figures about 1300 people die every day owing to cancer of different types. Cancer types and causes have seen a steady increase in the past decade which does not bode well for the world population.
Meaning of Cancer
Before we proceed in this essay on cancer, we must understand cancer's meaning or what exactly is cancer? Cancer is the term given collectively to any and all forms of unregulated cell growth. Normally, the cells inside our body follow a definitive cycle from generation to death. However, in a person suffering from cancer, this cycle is unchecked and hence the cell cycle passes through the checkpoints unhinged and the cells continue to grow.
Types of Cancer
Now, that we have a preliminary understanding of the meaning of cancer, let us proceed to the cancer types or specifications. Cancer types are usually named after the area they affect in the body - usually like skin, lung, pancreas, blood, stomach among the others. However, if classified biologically, there are primarily five types of cancer. These include - leukemia, melanoma, carcinoma, sarcoma, and lymphoma.
Leukemia is the type of cancer that originates in the blood marrow and is a cancer of the blood. In this cancer type, no tumors are formed. Melanoma is regarded as one of the most dangerous types of cancer as in this, the skin coloring pigment or melanin becomes cancerous in nature. Carcinomas are cancers of the various types of glands or organs such as the breasts, stomach, lungs, pancreas, etc. Cancers of the connective tissues such as the bones, muscles, etc are classified as sarcomas. Lymphomas, on the other hand, are cancers of the white blood cells. Among the most diagnosed types of cancers are carcinomas.
Cancer Causes
In the present day living environment, a number of factors are liable to cause cancer. However, in many cases, one single factor cannot be attributed or held responsible for causing cancer in an individual. The substances that are known to be cancer-causing or increasing the risks of cancer are known as carcinogens. Carcinogens can range from anything from pollutants to tobacco to something as simple as processed meats.
The effect of carcinogens, however, on different individuals is different and it is also dependent on a number of factors, be it physical, lifestyle-choice, or biological. The physical factors enabling the effect of carcinogens include exposure to different environmental conditions such as UV rays, X-rays, etc. Cancer among mining workers because of their constant exposure to asbestos and fine silicone dust is common. Biological factors generally include hereditary factors, such as the passing of a mutated BRCA1 or 2 mutations from mother to daughter in case of breast cancer. In addition, they also include factors such as age, gender, blood type, etc. Lifestyle choice refers to habits such as smoking, drinking, radiation exposure, etc, which can act as triggers for carcinogens.
Cancer Treatment
In this segment of our essay on cancer, we will discuss the various types of cancer treatments involved and their applicability. The most commonly applied cancer treatments include surgery, chemotherapy, and radiation therapy. Often, these treatments are given in a combination of one with the other. Surgery is usually performed in the case of benign tumors usually followed by a short cycle of preventive chemotherapy. The treatment of chemotherapy includes a combination of drugs targeted to kill cancer cells. Radiation therapy, on the other hand, makes use of radiations to kill cancerous cells. All these treatments are usually known to have side effects, so after-care for cancer survivors is also equally important.
The kind of treatment best suited for a patient is usually determined by the physician. The most important aspect of cancer treatment is early diagnosis and immediate medical intervention. The chances of surviving or beating cancer increase by a paramount value if diagnosed in the early stages.
Cancer Awareness
In India, and many other countries, speaking or discussing cancer is still considered taboo and this perception is in dire need of a change. Always remember cancer awareness is the first step towards cancer prevention. You must come across survivors sharing their journey by means of speech of cancer awareness. It can be of great benefit to know about the disease beforehand as it will keep you wary of any signs or symptoms you might come across and bring the same to the notice of your physician immediately. This will help in preventing or fighting cancer more effectively.
Short Essay on Cancer
To provide you with a grasp on the subject matter, we have provided a short essay on cancer here. Cancer is a disease in which the cells in specified or different parts of the body start dividing continuously. Cancer is usually caused by specific substances that affect several factors in our body. These specific substances are called carcinogens.
Cancer can be caused owing to exposure to pollution, radiation, harmful substances, poor lifestyle choices, etc. Cancer is best treated when detected early. Usually, surgery as well as other treatments such as chemotherapy, radiation therapy, etc. are used to treat cancer.
Cancer awareness is one of the best means that help in preventing and fighting the disease.
Points to Remember About Cancer
Students are recommended to remember the point of facts so it can be helpful for the students to write an essay with ease. Below are listed a few quick points for the convenience of students who are opting to write an essay on Cancer—
Cancer is a condition in which the cells divide in vast numbers uncontrollably which results in impairment and other damage to the body.
Excessive alcohol consumption, poor nutrition or physical inactivity and, excess weight of the body are some of the causes of Cancer.
Genetic factors can be responsible for the development of cancer.
Some genetic malfunctions occur after birth and factors like exposure to the sun and smoking can increase the risks.
A person can also inherit a certain predisposition for a particular type of cancer.
Chemotherapy is one of the treatments for cancer that targets the dividing cells, it can cure cancer but the side effects can be fatal.
Hormone Therapy is another way for treating cancer where the medication targets certain hormones that interfere with the human body. Hormones are essential in breast cancer and prostate cancer.
Immunotherapy is another way where the medication and treatment target the immune system to boost it.
Personalized medication is one of the newer developments where the treatment is more personalized depending on the person’s body and gene. It is believed that this kind of treatment can cure all types of cancer.
Radiation therapy is the treatment in which a high dose of radiation is given out to kill the cancerous cells. It can be used for shrinking the tumors before the surgery.
Stem cell transplant is essential for blood-related cancer like leukemia and lymphoma. In this treatment, the blood cells are removed that are destroyed by chemotherapy and radiation and then the cells are put back into the body after being developed by the doctors.
Surgery is also a part of the treatment.
Leukemia, Breast cancer, thyroid cancer, melanoma, non-Hodgkin’s lymphoma, pancreatic, endometrial, colon, liver, and bladder cancer are the types of cancer that people are diagnosed with every year.
The most common types of cancer are lung cancer and melanoma.
Cancer is classified by doctors in two ways.
First, by the location of the cancerous cells.
And secondly, by the tissues that are affected by it.
Metastasis is a condition where cancerous cells spread to different parts of the body.
Improvements in the rate of cancer have been seen over the years after a significant drop in tobacco consumption and smoking.
The outlook of cancer depends on the severity, type, and location of the cancerous cells.
Some cancer can exhibit symptoms while others don’t so it is always advised to report anything to the medical expert if something is wrong. Cancer doesn’t exhibit many symptoms unless it is in an advanced stage so it is usually better to go for regular checkups.
Tumors can be caused in the brain and spinal that can be cancerous in nature.
Germ cell tumors give rise to sperm and eggs in the body and it can be caused in any part of the body.
Quick Ways to Remember and Write an Essay on Cancer
Do the research
It is essential to write the valid points and present them in this essay as it is based on Cancer. An essay on Cancer must be comprehensive and should ideally contain the context related to this topic hence, it is very important for a student to know about this topic thoroughly in order to write the essay brilliantly.
Analyze the question
A student must understand the intention of the essay and know the terms that are needed to be used. It will clearly form an essay that consists of all the valid points related to cancer.
Remembering the information on Cancer
Cancer as a topic is vast because there are several types of Cancer and writing about all of them is not possible in a condensed essay so it is important to understand and remember the points which are more essential than the others to be mentioned in the essay.
Defining the terms and theories
It is essential for a student to explain the terms being used in the essay. For example, writing the names of the types of Cancer is not enough, it also has to be explained by the student on how it affects and how it may be treated.
Organize a structured essay
Students must write the essay in a coherent manner which must begin with the introduction to cancer, followed by the body of the essay that must contain the types of cancer, treatment, and other information regarding the topic of Cancer. It must be well concluded later to tie everything up neatly.
Cancer is, undoubtedly, one of the most life-shattering diseases. Together, let us make an effort to take on this disease with more care and hope.

FAQs on National Cancer Awareness Day: Empowering Hope and Health
1. Differentiate Between Cancerous and Non-Cancerous Tumours.
The unregulated cell mass inside the body is known as a tumour and can be specified to a particular area or the uninhibited cell growth may spread to the surrounding tissues. Based on this, tumours are majorly classified into two types:
Benign Tumours: This type of tumours are usually regarded as non-cancerous as they are specified to a particular area and can be surgically removed without causing damage to the surrounding tissue.
Malignant Tumours: These tumours, on the other hand, have broken free from their site of origin and spread to other tissues, usually through the bloodstream. These tumours are cancerous in nature and usually require other treatments.
- Patient Care & Health Information
- Tests & Procedures
- Chemotherapy
Chemotherapy is a drug treatment that uses powerful chemicals to kill fast-growing cells in your body.
Chemotherapy is most often used to treat cancer, since cancer cells grow and multiply much more quickly than most cells in the body.
Many different chemotherapy drugs are available. Chemotherapy drugs can be used alone or in combination to treat a wide variety of cancers.
Though chemotherapy is an effective way to treat many types of cancer, chemotherapy treatment also carries a risk of side effects. Some chemotherapy side effects are mild and treatable, while others can cause serious complications.

Products & Services
- Mayo Clinic Comprehensive Cancer Center
- Sign up for Email: Get Your Free Resource – Coping with Cancer
Why it's done
Chemotherapy is used to kill cancer cells in people with cancer.
There are a variety of settings in which chemotherapy may be used in people with cancer:
- To cure the cancer without other treatments. Chemotherapy can be used as the primary or sole treatment for cancer.
- After other treatments, to kill hidden cancer cells. Chemotherapy can be used after other treatments, such as surgery, to kill any cancer cells that might remain in the body. Doctors call this adjuvant therapy.
- To prepare you for other treatments. Chemotherapy can be used to shrink a tumor so that other treatments, such as radiation and surgery, are possible. Doctors call this neoadjuvant therapy.
- To ease signs and symptoms. Chemotherapy may help relieve signs and symptoms of cancer by killing some of the cancer cells. Doctors call this palliative chemotherapy.
Chemotherapy for conditions other than cancer
Some chemotherapy drugs have proved useful in treating other conditions, such as:
- Bone marrow diseases. Diseases that affect the bone marrow and blood cells may be treated with a bone marrow transplant, also known as a stem cell transplant. Chemotherapy is often used to prepare for a bone marrow transplant.
- Immune system disorders. Lower doses of chemotherapy drugs can help control an overactive immune system in certain diseases, such as lupus and rheumatoid arthritis.
Side effects of chemotherapy drugs can be significant. Each drug has different side effects, and not every drug causes every side effect. Ask your doctor about the side effects of the particular drugs you'll receive.
Side effects that occur during chemotherapy treatment
Common side effects of chemotherapy drugs include:
- Loss of appetite
- Mouth sores
- Constipation
- Easy bruising
Many of these side effects can be prevented or treated. Most side effects subside after treatment ends.
Long-lasting and late-developing side effects
Chemotherapy drugs can also cause side effects that don't become evident until months or years after treatment. Late side effects vary depending on the chemotherapy drug but can include:
- Damage to lung tissue
- Heart problems
- Infertility
- Kidney problems
- Nerve damage (peripheral neuropathy)
- Risk of a second cancer
Ask your doctor if you have a risk of any late side effects. Ask what signs and symptoms you should be aware of that may signal a problem.
How you prepare
How you prepare for chemotherapy depends on which drugs you'll receive and how they'll be administered. Your doctor will give you specific instructions to prepare for your chemotherapy treatments. You may need to:
- Have a device surgically inserted before intravenous chemotherapy. If you'll be receiving your chemotherapy intravenously — into a vein — your doctor may recommend a device, such as a catheter, port or pump. The catheter or other device is surgically implanted into a large vein, usually in your chest. Chemotherapy drugs can be given through the device.
- Undergo tests and procedures to make sure your body is ready to receive chemotherapy. Blood tests to check kidney and liver functions and heart tests to check for heart health can determine whether your body is ready to begin chemotherapy. If there's a problem, your doctor may delay your treatment or select a different chemotherapy drug and dosage that's safer for you.
- See your dentist. Your doctor may recommend that a dentist check your teeth for signs of infection. Treating existing infections may reduce the risk of complications during chemotherapy treatment, since some chemotherapy may reduce your body's ability to fight infections.
- Plan ahead for side effects. Ask your doctor what side effects to expect during and after chemotherapy and make appropriate arrangements. For instance, if your chemotherapy treatment will cause infertility, you may wish to consider your options for preserving your sperm or eggs for future use. If your chemotherapy will cause hair loss, consider planning for a head covering.
Make arrangements for help at home and at work. Most chemotherapy treatments are given in an outpatient clinic, which means most people are able to continue working and doing their usual activities during chemotherapy. Your doctor can tell you in general how much the chemotherapy will affect your usual activities, but it's difficult to predict exactly how you'll feel.
Ask your doctor if you'll need time off work or help around your home after treatment. Ask your doctor for the details of your chemotherapy treatments so that you can make arrangements for work, children, pets or other commitments.
Prepare for your first treatment. Ask your doctor or chemotherapy nurses how to prepare for chemotherapy. It may be helpful to arrive for your first chemotherapy treatment well rested. You might wish to eat a light meal beforehand in case your chemotherapy medications cause nausea.
Have a friend or family member drive you to your first treatment. Most people can drive themselves to and from chemotherapy sessions. But the first time you may find that the medications make you sleepy or cause other side effects that make driving difficult.
What you can expect
Determining which chemotherapy drugs you'll receive.
Your doctor chooses which chemotherapy drugs you'll receive based on several factors, including:
- Type of cancer
- Stage of cancer
- Overall health
- Previous cancer treatments
- Your goals and preferences
Discuss your treatment options with your doctor. Together you can decide what's right for you.
How chemotherapy drugs are given
Chemotherapy drugs can be given in different ways, including:
- Chemotherapy infusions. Chemotherapy is most often given as an infusion into a vein (intravenously). The drugs can be given by inserting a tube with a needle into a vein in your arm or into a device in a vein in your chest.
- Chemotherapy pills. Some chemotherapy drugs can be taken in pill or capsule form.
- Chemotherapy shots. Chemotherapy drugs can be injected with a needle, just as you would receive a shot.
- Chemotherapy creams. Creams or gels containing chemotherapy drugs can be applied to the skin to treat certain types of skin cancer.
- Chemotherapy drugs used to treat one area of the body. Chemotherapy drugs can be given directly to one area of the body. For instance, chemotherapy drugs can be given directly in the abdomen (intraperitoneal chemotherapy), chest cavity (intrapleural chemotherapy) or central nervous system (intrathecal chemotherapy). Chemotherapy can also be given through the urethra into the bladder (intravesical chemotherapy).
- Chemotherapy given directly to the cancer. Chemotherapy can be given directly to the cancer or, after surgery, where the cancer once was. As an example, thin disk-shaped wafers containing chemotherapy drugs can be placed near a tumor during surgery. The wafers break down over time, releasing chemotherapy drugs. Chemotherapy drugs may also be injected into a vein or artery that directly feeds a tumor.
How often you receive chemotherapy treatments
Your doctor determines how often you'll receive chemotherapy treatments based on what drugs you'll receive, the characteristics of your cancer and how well your body recovers after each treatment. Chemotherapy treatment schedules vary. Chemotherapy treatment can be continuous, or it may alternate between periods of treatment and periods of rest to let you recover.
Where you receive chemotherapy treatments
Where you'll receive your chemotherapy treatments depends on your situation. Chemotherapy treatments can be given:
- In an outpatient chemotherapy unit
- In a doctor's office
- In the hospital
- At home, such as when taking chemotherapy pills
You'll meet with your cancer doctor (oncologist) regularly during chemotherapy treatment. Your oncologist will ask about any side effects you're experiencing, since many can be controlled.
Depending on your situation, you may also undergo scans and other tests to monitor your cancer during chemotherapy treatment. These tests can give your doctor an idea of how your cancer is responding to treatment, and your treatment may be adjusted accordingly.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Chemotherapy care at Mayo Clinic
- Chemotherapy and you: Support for people with cancer. National Cancer Institute. https://www.cancer.gov/publications/patient-education/chemo-and-you. Accessed Oct. 1, 2019.
- Niederhuber JE, et al., eds. Cancer pharmacology. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Sept. 26, 2019.
- What to expect when having chemotherapy. Cancer.Net. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/chemotherapy/what-expect-when-having-chemotherapy. Accessed Oct. 1, 2019.
- Cyclophosphamide (Cytoxan). American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Treatments/Cyclophosphamide-Cytoxan. Accessed Oct. 1, 2019.
- Warner KJ. Allscripts EPSi. Mayo Clinic. Nov. 25, 2019.
- Acute lymphocytic leukemia
- Acute myelogenous leukemia
- Anal cancer
- Bladder cancer
- Bone cancer
- Bone metastasis
- Brain tumor
- Breast cancer
- Cancer treatment myths
- Carcinoid syndrome
- Castleman disease
- Cervical cancer
- Chemo targets
- Chemotherapy and hair loss: What to expect during treatment
- Chemotherapy and sex: Is sexual activity OK during treatment?
- Chemotherapy nausea and vomiting: Prevention is best defense
- Chemotherapy side effects: A cause of heart disease?
- Cholangiocarcinoma (bile duct cancer)
- Choroid plexus carcinoma
- Chronic lymphocytic leukemia
- Chronic myelogenous leukemia
- Colon cancer
- Cutaneous T-cell lymphoma
- Eating during cancer treatment: Tips to make food tastier
- Embryonal tumors
- Endometrial cancer
- Esophageal cancer
- Ewing sarcoma
- Fertility preservation
- Floor of the mouth cancer
- Gallbladder cancer
- Glioblastoma
- Hairy cell leukemia
- Head and neck cancers
- Hodgkin's lymphoma (Hodgkin's disease)
- Inflammatory breast cancer
- Invasive lobular carcinoma
- Liver cancer
- Lung cancer
- Magic mouthwash
- Male breast cancer
- Merkel cell carcinoma
- Mesothelioma
- Mouth cancer
- Multiple myeloma
- Myelofibrosis
- Nasopharyngeal carcinoma
- Neuroblastoma
- Neuroendocrine tumors
- Neurofibromatosis
- Non-Hodgkin's lymphoma
- Oligodendroglioma
- Osteosarcoma
- Ovarian cancer
- Paget's disease of the breast
- Pancreatic cancer
- Peripheral nerve tumors
- Pheochromocytoma
- PICC line placement
- Pineoblastoma
- Prostate cancer
- Rectal cancer
- Recurrent breast cancer
- Retinoblastoma
- Salivary gland tumors
- Scrotal masses
- Self-Image During Cancer
- Skin cancer
- Soft tissue sarcoma
- Spinal cord tumor
- Stage 4 prostate cancer
- Stomach cancer
- Testicular cancer
- Throat cancer
- Thyroid cancer
- Treatment options for biliary tract cancer
- Vaginal cancer
- Vertebral tumor
- Vulvar cancer
- Wilms tumor
- Zollinger-Ellison syndrome
News from Mayo Clinic
- Mayo Clinic Minute: The right way to talk with someone who has cancer Dec. 18, 2023, 05:30 p.m. CDT
- Mayo Clinic Q&A podcast: Hot chemotherapy for late-stage cancers Oct. 18, 2022, 12:30 p.m. CDT
- 9 common questions about genetic testing for cancer July 27, 2022, 01:03 p.m. CDT
- Diet tips during cancer treatment April 27, 2022, 03:05 p.m. CDT
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

5 Reflections on Living a Long Life With Cancer
Reflections on living with cancer from a fellow traveler on this journey..
Posted August 25, 2022 | Reviewed by Jessica Schrader
- Sc(anxiety) is a feature, not a bug, of living with cancer.
- Families and friends are important parts of the cancer journey, long after treatment is complete.
- Evidence shows that having a health care team you trust is essential to quality of life post-cancer treatment.
This month marks my sixth year since being diagnosed with colorectal cancer (which I’ve written about here ).
Since that initial diagnosis in August 2016, I have marked the passage of time with an additional calendar layer dictated by the doctors and nurses that were working to save my life. Initially, this calendar was quite packed and each event felt like a major turning point where I could fall off course: Days of pre-operative assessments, day of surgery, days of hospitalization, visits from the home health care nurse every three days, four weeks until the post-operative assessment, etc.
Then, once the most acute phase of my care was over, the calendar settled into one of surveillance, watching for potentially ominous changes: quarterly blood draws and doctor visits, annual colonoscopies, and—most terrifying to me—annual CT scans to look for metastases to my liver, lung, or something else that it is difficult to live without.
For five years, from August 2016 to August 2021, that was my clock. This is the first August in five years that I have not had to drink 32 ounces of a “mocha shake” ( narrator note: tastes nothing like a mocha shake but will ruin frappucinos for you forever ) of barium sulfate to prepare for the scan. The first August in five years when I have not felt the terror of waiting alone in the small, cold room—trying to not pass out from fear —after changing into a far-too-large hospital gown. The first August in five years I have not heard the “voice” of the incredible machine that allows my doctors to see what is otherwise impossible for them to assess until it is too late telling me to “Hold my breath ... Breathe” as radiation moves through me. The first August in five years when I have struggled to stay present and think positive as I await the call from my doctor telling me what the scan showed—which for five years was the best news a cancer patient can ask for: “No evidence of disease.”
After five years of such surveillance, the evidence (or, perhaps more cynically, the cost-savings to the health care system) that ongoing scans are worth it from a risk-benefit ratio isn’t needed. And so you get discharged from your cancer care team. Your time and how you mark it, such as it is, is yours again. In the parlance of some (I do not use nor do I like this term), you are a “survivor.”

And so, in recognition of that time and the lessons I’ve learned during it, I am offering five reflections on living with cancer, intended for others who are on this journey and the people who love them. This reflection embodies much of the empirical research in psycho-oncology that has developed over the past 30 years, summarized earlier this year in an editorial by David Kissane.
- Sc( anxiety ) is a feature, not a bug, of living with cancer.
The medical profession loves jargon. The term they have coined for the intense fear that most cancer patients who have completed their treatment feel about their disease, especially during those regular blood tests and scans that make up the surveillance component of care, is “fear of cancer recurrence” (FCR), defined as “fear, worry, or concern relating to the possibility that cancer will come back or progress.” The acronym and definition do not even remotely reflect the existential terror that I experienced whenever I would lay down for my CT scan, which bordered on depersonalization.
With the caveat that most studies of “FCR” have been limited to people who have experienced breast cancer, researchers estimate that about two-thirds of individuals report unmet needs related to fears around cancer recurrence, unmet needs regarding information about their health post-treatment, and negative expectations about their lives going forward, etc. The loudness and obtrusiveness of these existential questions (e.g., What will happen to my family if the cancer comes back? What does it mean to be a "cancer survivor"? ) that only emerge after treatment is complete are a part of the journey that can be difficult to process, especially because at the beginning the entire purpose of the journey appears to be to complete treatment. But that is a false peak : completing surgery, chemotherapy, or radiation is not the true destination of the experience of living with cancer. They are simply sights along the way. Appreciating that sc(anxiety) is an expected, rational part of the journey is an important component of adjusting to living with cancer.
2. You are not going through this alone.
You are not the only one who is terrified of the cancer returning. Your partner, your parents, your children, your friends, and even your doctors are also fearful of that.
Of course, friends and families—even when they mean well—may not be able to provide the kind of support you need. You may even be angry at them for not “showing up” in the way you wanted them to. And if your relationships were challenging before cancer, they will likely also be challenging—potentially to the breaking point—after cancer.
Even if your family and friends are supporting you, it doesn’t mean you wouldn’t benefit from talking to others who know exactly what it is like to walk in your shoes. Support groups are not just for people who are in the thick of cancer treatment—they also serve to support people dealing with the aforementioned existential questions that cancer lays on your table. I only started attending support groups when I was about 12-18 months out from completing my treatment. Most of the people in my group were similarly “seasoned” in their journeys, and many of them were several years out from completing treatment.

3. Hope is a verb.
Getting a cancer diagnosis is traumatic . And we know that trauma can be harmful for mental and physical health. However, we also know that adversity can also spur incredibly meaningful personal growth, compassion for oneself and others, and deep, positive reflection and connections with others.
Research shows that factors that support such positive changes include being physically active and having a health care support team that is engaged and informative. These are modifiable determinants, and should be the focus of post-treatment cancer surveillance care. As someone who was failed by the health care system ( by being misdiagnosed for nine months ) before I was saved by it, I have a deep appreciation for the importance of having a health care team that sees you as a person, not a patient or a case. And if you do not have that, it may be time to fire them and find a new one.
4. There will come a day when your experience with cancer is not the first thing you think of when you wake up.
For me, that took about 65 months from the time I was diagnosed, but I am finally here.
5. Make peace with your body.
Yes, technically , your body tried to kill you. Cancer cells aren’t foreign invaders: they are your cells, with your (mutant) DNA , growing with impunity in ways and in places they shouldn’t for other parts of your body to work. And as a result, for a long time after my diagnosis I didn’t trust my body. That is to say, I believed it was still trying to kill me, even though my doctors had told me I was NED. Any moment of light-headedness when standing signaled to me that the cancer had spread to my brain. Any shortness of breath from climbing the stairs meant that it had spread to my lungs. For the first few years after my diagnosis, I lived in fear of my body, and what it was capable of.
And then, for the first time in my life, I started running. Not because my doctors told me to or because I had read that it was important for post-traumatic growth , but because—for me—running was one of the few things that helped me form connections between my (fearful) mind and my (recovering) body. I couldn’t think about how afraid I was when I was so focused on keeping my legs moving. After a year, I ran 5 miles, which was farther than I had ever thought possible. The next year I ran a half-marathon. And then a second. And today I don’t run, but I do pilates and strength training, and through movement I have made peace with my body. It is capable of amazing things—of carrying me further and faster than I ever thought possible.
Your body will likely carry markers of your cancer journey forever. Some of those markers are visible to others (I tell people who ask that the round 2-inch scar on my abdomen, a leftover from when my intestines were literally re-routed outside my body via an ostomy, is from the time that I was shot, because that was how acute my diagnosis felt when I first received it), and some of them are not. Those scars, pains, etc. are part of your story, but they are not your whole story—and making peace with my body is what has helped me distinguish the two.
I hope to live a long life, and I look forward to the same milestones that I did before I got sick. I am more intentional about pursuing them now, because I also know that there are no guarantees that I will have the life I hope for. And I work every day to make peace with that fact, using the tools I described here. I hope my fellow travelers on this journey and their families will find this helpful, and I wish you all many years of love, peace, and health as you reset your clocks for the years ahead.
Lebel S., Ozakinci G., Humphris G., Mutsaers B., Thewes B., Prins J., et al.. (2016). From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support. Care Cancer 24, 3265–3268. 10.1007/s00520-016-3272-5
Shanafelt, Tait, Alex Adjei, and Frank L. Meyskens. "When your favorite patient relapses: physician grief and well-being in the practice of oncology." Journal of clinical oncology 21.13 (2003): 2616-2619.
Urbutienė E, Pukinskaitė R. Fear of Cancer Recurrence as Reminder About Death: Lived Experiences of Cancer Survivors' Spouses. Omega (Westport). 2022 Aug 22:302228221123152. doi: 10.1177/00302228221123152.
Soriano EC, Perndorfer C, Siegel SD, Laurenceau JP. Threat sensitivity and fear of cancer recurrence: a daily diary study of reactivity and recovery as patients and spouses face the first mammogram post-diagnosis. J Psychosoc Oncol. 2019 Mar-Apr;37(2):131-144. doi: 10.1080/07347332.2018.1535532.
Evans C, Saliba-Serre B, Préau M, Bendiane MK, Gonçalves A, Signoli M, Bouhnik AD. Post-traumatic growth 5 years after cancer: identification of associated actionable factors. Support Care Cancer. 2022 Jul 12. doi: 10.1007/s00520-022-07253-6. Epub ahead of print. PMID: 35821449.
Jewett PI, Vogel RI, Galchutt P, Everson-Rose SA, Teoh D, Radomski M, Blaes AH. Associations between a sense of connection and existential and psychosocial outcomes in gynecologic and breast cancer survivors. Support Care Cancer. 2022 Apr;30(4):3329-3336. doi: 10.1007/s00520-021-06784-8. Epub 2022 Jan 5. PMID: 34985561; PMCID: PMC8727470.

Briana Mezuk, Ph.D. , is a Professor of Epidemiology and Director of the Center for Social Epidemiology and Population Health at the University of Michigan's School of Public Health.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Premium Content
- MIND, BODY, WONDER
Can aspirin help protect against colorectal cancers?
A new study details how a daily dose could prevent or delay the progression of the world’s third most common type of cancer.

Aspirin is well known for its ability to ease pain from muscle aches and headaches; it reduces fevers; and low doses can thin blood, reducing the chance of clots that cause strokes and heart attacks. Now a new study suggests it may also play a role in colorectal cancer prevention.
Colorectal cancer, a cancer of either the large intestine or rectum, is the third most common type of cancer, and the second most common cause of death from cancer , worldwide. There were 1.9 million new cases diagnosed across the globe in 2020, according to the World Health Organization, and these numbers are expected to grow. In the United States, the rates of colorectal cancers have been rising in people younger than age 50 since the 1990s, which includes more young people dying from the disease, according to the National Cancer Institute .
Now a new study published in the journal Cancer shows that colorectal cancer patients who took a daily dose of aspirin had a lower rate of metastasis to the lymph nodes and stronger immune response to their tumors. The research suggests that aspirin may be boosting the ability of the immune system to hunt for cancer cells.
“It is a rather unexpected effect, because aspirin is mainly used as an anti-inflammatory drug,” says Marco Scarpa, a researcher at the University of Padova, and one of the authors of the study. As Scarpa notes, this study suggests that aspirin may be playing a slightly different role by stimulating the immune system’s surveillance response, which can then prevent or delay the progression of colorectal cancer.
Your immune system is always surveilling the body for cells that just aren’t right. When they find such cancer cells, they will kill them just as they would kill invading bacteria or viruses, says Cindy Kin , a surgeon at Stanford University, who specializes in colon and rectal surgery.

“The data about aspirin and cancer is really evolving,” says Maen Abdelrahim , an oncologist at Houston Methodist Hospital, who specializes in treating colorectal cancers. However, there are still a lot of unanswered questions about how aspirin can prevent and delay the progression of these cancers, as well as which subset of patients would benefit from a daily aspirin.
( Colon cancer is rising among young adults. Here are signs to watch for. )
People who take a consistent use of aspirin have a lower risk of colorectal cancer, “but it has to be balanced with the risks,” which includes the possibility of bleeding in the gastrointestinal tract, says Jeff Meyerhardt , an oncologist and co-director of the Colon and Rectal Cancer Center at the Dana-Farber Cancer Institute, in Boston.
Aspirin protects against colorectal cancer
There are several studies that suggest a link between aspirin and colorectal cancer prevention and delay. However, the mechanism by which aspirin does this is still unknown. That makes it hard to predict which patients will benefit the most.
In a 2020 meta-analysis , which analyzed the results of 45 observational studies, researchers found that regular aspirin use was associated with less incidence of colorectal cancer.
A low dose, between 75 and 100 milligrams, was associated with a 10 percent reduction in the risk of developing colorectal cancer; a regular dose of 325 milligrams was associated with a 35 percent decline.
Other studies have shown a link between daily aspirin and a delayed progression , including a lower risk of dying in patients who had already been diagnosed with colorectal cancer.
“What has been seen in multiple studies for colorectal cancers is that having a more robust immune reaction does seem to have a better outcome,” Meyerhardt says. “This is looking at how aspirin may interact with that.”
Study suggests mechanism
In the study, researchers obtained tissue samples from 238 patients who had undergone surgery for the colorectal cancers. Of these patients, 12 percent were taking a daily low dose of aspirin for the prevention of heart disease. When compared to patients who were not taking aspirin, the researchers found a lower rate of metastasis to the lymph nodes, and higher numbers of immune cells that had infiltrated the tumors.
This higher level of infiltration is thought to be linked to slower cancer progression—including the lower rate of spread to the lymph nodes—by allowing immune cells to enter the tumor mass and fight the cancerous cells more effectively.
( Why is stomach cancer rising in young women? )
The researchers also found higher levels of immune markers that are responsible for triggering the immune system surveillance response. “It’s boosting the immune system, and it’s helping the immune system inside the tumor,” Abdelrahim says.
In recent years, the immune system’s role in protecting against the development of cancer has become recognized.
Patients with suppressed immune systems are at higher risk for developing cancers , compared to patients with a fully functional immune system. As these results suggest, aspirin may increase the vigilance of the immune system when it comes to the detection of colorectal cancers.
“Your immune system is doing all of these things in the background, that you’re not even aware of,” Kin says. “It’s not just the tumor’s behavior and how aggressive it’s going to be, but it’s your body versus the tumor.”
Related Topics
- INFLAMMATION
- DIGESTIVE SYSTEM
You May Also Like

Why is stomach cancer rising in young women?

These 4 medicinal herbs may help keep men healthy

How exercise can help—or hurt—your digestion

These microbes found in tumors promote cancer. What if we just kill them?

Turkey tail. Chaga. Lion’s mane. Do these mushroom supplements really help you?
- Environment
- Perpetual Planet
- History & Culture
- Paid Content
History & Culture
- Mind, Body, Wonder
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
Francis Collins: Why I’m going public with my prostate cancer diagnosis
I served medical research. now it’s serving me. and i don’t want to waste time..
Over my 40 years as a physician-scientist, I’ve had the privilege of advising many patients facing serious medical diagnoses. I’ve seen them go through the excruciating experience of waiting for the results of a critical blood test, biopsy or scan that could dramatically affect their future hopes and dreams.
But this time, I was the one lying in the PET scanner as it searched for possible evidence of spread of my aggressive prostate cancer . I spent those 30 minutes in quiet prayer. If that cancer had already spread to my lymph nodes, bones, lungs or brain, it could still be treated — but it would no longer be curable.
Why am I going public about this cancer that many men are uncomfortable talking about? Because I want to lift the veil and share lifesaving information, and I want all men to benefit from the medical research to which I’ve devoted my career and that is now guiding my care.
Five years before that fateful PET scan, my doctor had noted a slow rise in my PSA, the blood test for prostate-specific antigen. To contribute to knowledge and receive expert care, I enrolled in a clinical trial at the National Institutes of Health, the agency I led from 2009 through late 2021.
At first, there wasn’t much to worry about — targeted biopsies identified a slow-growing grade of prostate cancer that doesn’t require treatment and can be tracked via regular checkups, referred to as “active surveillance.” This initial diagnosis was not particularly surprising. Prostate cancer is the most commonly diagnosed cancer in men in the United States, and about 40 percent of men over age 65 — I’m 73 — have low-grade prostate cancer . Many of them never know it, and very few of them develop advanced disease.
Why am I going public about this cancer that many men are uncomfortable talking about? Because I want to lift the veil and share lifesaving information.
But in my case, things took a turn about a month ago when my PSA rose sharply to 22 — normal at my age is less than 5. An MRI scan showed that the tumor had significantly enlarged and might have even breached the capsule that surrounds the prostate, posing a significant risk that the cancer cells might have spread to other parts of the body.
New biopsies taken from the mass showed transformation into a much more aggressive cancer. When I heard the diagnosis was now a 9 on a cancer-grading scale that goes only to 10, I knew that everything had changed.
Thus, that PET scan, which was ordered to determine if the cancer had spread beyond the prostate, carried high significance. Would a cure still be possible, or would it be time to get my affairs in order? A few hours later, when my doctors showed me the scan results, I felt a rush of profound relief and gratitude. There was no detectable evidence of cancer outside of the primary tumor.
Later this month, I will undergo a radical prostatectomy — a procedure that will remove my entire prostate gland. This will be part of the same NIH research protocol — I want as much information as possible to be learned from my case, to help others in the future.
While there are no guarantees, my doctors believe I have a high likelihood of being cured by the surgery.
My situation is far better than my father’s when he was diagnosed with prostate cancer four decades ago. He was about the same age that I am now, but it wasn’t possible back then to assess how advanced the cancer might be. He was treated with a hormonal therapy that might not have been necessary and had a significant negative impact on his quality of life.
Because of research supported by NIH, along with highly effective collaborations with the private sector, prostate cancer can now be treated with individualized precision and improved outcomes.
As in my case, high-resolution MRI scans can now be used to delineate the precise location of a tumor. When combined with real-time ultrasound, this allows pinpoint targeting of the prostate biopsies. My surgeon will be assisted by a sophisticated robot named for Leonardo da Vinci that employs a less invasive surgical approach than previous techniques, requiring just a few small incisions.
Advances in clinical treatments have been informed by large-scale, rigorously designed trials that have assessed the risks and benefits and were possible because of the willingness of cancer patients to enroll in such trials.
I feel compelled to tell this story openly. I hope it helps someone. I don’t want to waste time.
If my cancer recurs, the DNA analysis that has been carried out on my tumor will guide the precise choice of therapies. As a researcher who had the privilege of leading the Human Genome Project , it is truly gratifying to see how these advances in genomics have transformed the diagnosis and treatment of cancer.
I want all men to have the same opportunity that I did. Prostate cancer is still the No. 2 cancer killer among men. I want the goals of the Cancer Moonshot to be met — to end cancer as we know it. Early detection really matters, and when combined with active surveillance can identify the risky cancers like mine, and leave the rest alone. The five-year relative survival rate for prostate cancer is 97 percent, according to the American Cancer Society , but it’s only 34 percent if the cancer has spread to distant areas of the body.
But lack of information and confusion about the best approach to prostate cancer screening have impeded progress. Currently, the U.S. Preventive Services Task Force recommends that all men age 55 to 69 discuss PSA screening with their primary-care physician, but it recommends against starting PSA screening after age 70.
Other groups, like the American Urological Association , suggest that screening should start earlier, especially for men with a family history — like me — and for African American men, who have a higher risk of prostate cancer. But these recommendations are not consistently being followed.
Our health-care system is afflicted with health inequities. For example, the image-guided biopsies are not available everywhere and to everyone. Finally, many men are fearful of the surgical approach to prostate cancer because of the risk of incontinence and impotence, but advances in surgical techniques have made those outcomes considerably less troublesome than in the past. Similarly, the alternative therapeutic approaches of radiation and hormonal therapy have seen significant advances.
A little over a year ago, while I was praying for a dying friend, I had the experience of receiving a clear and unmistakable message. This has almost never happened to me. It was just this: “Don’t waste your time, you may not have much left.” Gulp.
Having now received a diagnosis of aggressive prostate cancer and feeling grateful for all the ways I have benefited from research advances, I feel compelled to tell this story openly. I hope it helps someone. I don’t want to waste time.
Francis S. Collins served as director of the National Institutes of Health from 2009 to 2021 and as director of the National Human Genome Research Institute at NIH from 1993 to 2008. He is a physician-geneticist and leads a White House initiative to eliminate hepatitis C in the United States, while also continuing to pursue his research interests as a distinguished NIH investigator.
An earlier version of this article said prostate cancer is the No. 2 killer of men. It is the No. 2 cause of cancer death among men. The article has been updated.
- Does eating too much sugar really make kids hyper? We asked researchers. April 21, 2024 Does eating too much sugar really make kids hyper? We asked researchers. April 21, 2024
- Spouse’s stroke could boost partner’s depression risk, study suggests April 20, 2024 Spouse’s stroke could boost partner’s depression risk, study suggests April 20, 2024
- How to revive hair that thins, grays or gets out of control as you age April 15, 2024 How to revive hair that thins, grays or gets out of control as you age April 15, 2024

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

The biological and clinical effects of smoking by patients with cancer and strategies to implement evidence-based tobacco cessation support
Associated data.
Tobacco use is an established risk factor for the development of several cancers; however, far less work has been done to understand the effects of continued smoking on cancer treatment outcomes, and structured tobacco cessation efforts are not well incorporated into the standard care for patients with cancer. In this Review we discuss the known biological effects of smoking on cancer cell biology and emphasise the clinical effects of continued smoking in patients with cancer treated with chemotherapy or radiotherapy. Although evidence supports the need for inclusion of dedicated tobacco cessation efforts for patients with cancer, clinicians should consider the methods used to provide evidence-based tobacco cessation support and the available resources to deliver and maintain consistent tobacco cessation support. We also address the variables to consider in the design and implementation of a sustainable tobacco cessation programme.
Introduction
Tobacco is a well established cause of at least 13 cancers; 1 however, until recently there have been no large evidence-based assessments of the effects of smoking on cancer treatment outcomes. The 2014 Surgeon General’s Report 1 is the “first large evidence review to report a causal association between tobacco use and adverse clinical outcomes for patients with cancer”. These findings provide the evidence base to effectively change clinical practice by justifying the need to address tobacco use in patients with cancer ( panel 1 ).
Conclusions of the 2014 Surgeon General’s Report 1
Smoking causes adverse health outcomes in patients with cancer and survivors.
- In cancer patients and survivors, the evidence is sufficient to infer a causal relationship between cigarette smoking and adverse health outcomes. Quitting smoking improves the prognosis of cancer patients.
- In cancer patients and survivors, the evidence is sufficient to infer a causal relationship between cigarette smoking and increased all-cause mortality and cancer-specific mortality.
- In cancer patients and survivors, the evidence is sufficient to infer a causal relationship between cigarette smoking and increased risk for second primary cancers known to be caused by cigarette smoking, such as lung cancer.
- In cancer patients and survivors, the evidence is suggestive but not sufficient to infer a causal relationship between cigarette smoking and the risk of recurrence, poorer response to treatment, and increased treatment-related toxicity.
Although the evidence-base is now sufficient to infer a causal relation between tobacco use and adverse clinical outcomes, there are substantial deficits in how we address tobacco use in patients with cancer. First, there are no standard recommendations for the accurate assessment of tobacco use in patients with cancer, which limits the ability of clinicians to accurately identify patients who are at risk from continued tobacco use and to infer relationships between tobacco use and cancer treatment outcomes. 2 Second, many oncologists do not regularly provide tobacco cessation assistance to patients with cancer who smoke and most do not feel adequately trained to deliver evidence-based tobacco cessation support. 3 , 4 Third, no dedicated attempt has been made to fully address the dynamic effects of tobacco use or tobacco cessation on cancer treatment outcomes. Although smoking adversely affects cancer treatment and the effects of former smoking on outcomes are less damaging 1 we do not yet know the optimum period for, or magnitude of benefits from, quitting smoking that would have most benefit for patients with cancer. Fourth, provision of tobacco cessation support in clinical cancer care and clinical research needs efficient design and delivery.
The aim of this Review is to provide a concise overview of the biological and clinical effects of smoking on cancer treatment with emphasis on patients who are treated with chemotherapy and radiotherapy. We provide specific and practical guidance for implementation of changes to improve cancer treatment outcomes for patients through tobacco cessation support in cancer care and research.
The biological effect of tobacco and tobacco products on cancer
Cigarette smoke and cell signalling in cancer.
Tremendous work and evidence supports the carcinogenic effects of tobacco for various cancers. Detailed reviews are presented in the 2014 Sugeon General’s Report on the carcinogenic properties of tobacco. 1 Far less work has been done, however, to understand the biological effects of tobacco on existing cancer cells.
Cigarette smoke is a complex mixture of 7000 different aerosolised chemicals and tobacco components, including more than 60 known carcinogens in gaseous or particulate phases. 4 The gaseous phase is associated with chronic pulmonary disease and lung toxicity, whereas the particulate phase is most frequently associated with cancer. 5 The Federal Trade Commission has made attempts to standardise smoke conditions for use in the research setting, but there is substantial variation in the chemical composition of cigarette smoke including cigarette brand, composition, and cigarette usage behaviour. 6 As a result, evaluation of the biological effects of cigarette smoke on cancer cells is complicated and largely unexplored at this time.
A summary of the known effects of cigarette smoke and constituents of cigarette smoke on cancer cells is shown in the figure . Immediate effects stimulate the immune system and activate cellular receptors leading to activation of intermediate signalling pathways such as Src, Wnt, mitochondrial, arachidonic acid, and other unknown pathways including activation of phase I and phase II drug metabolising enzymes. Intermediate signalling leads to a broad range of downstream signals that promote tumour growth and decrease the response to cytotoxic treatments. Importantly, many downstream signals generate feedback mechanisms that continue to promote a tumorigenic environment. Although some of the effects of cigarette smoke on cancer cells are known ( figure ), substantial work is needed to clarify the effects and cross-signalling that occurs with exposure to the thousands of compounds in cigarette smoke. Furthermore, the well-established carcinogenic effects of cigarette smoke on non-cancer cells 1 are mostly untested with respect to oncogenic mutations across a range of cancer disease sites. The effects of cigarette smoke on tumour biology are far from fully understood.

ROS=reactive oxygen species. β-AR=β-adrenergic receptor. nAChR=nicotinic acetylcholine receptor. AHR=aryl hydrocarbon receptor. EGFR=epidermal growth factor receptor. PKC=protein kinase C. PLA2=phospholipase A2. PLC=phosphoinositide phospholipase C. LRP=lipoprotein receptor-related protein. COX=cyclo-oxygenase. LOX=lipoxygenase. MEK=mitogen activated kinase kinase. ERK=extracellular signal related kinase. CYP=cytochrome P450. MRP=multidrug resistance-associated protein. TGF=transforming growth factor. STAT=signal transducer and activator of transcription. JAK=janus kinase. MUC4=mucin 4, cell surface associated. NFKB1=nuclear factor of kappa light polypeptide gene enhancer in B-cells 1. XIAP=x-linked inhibitor of apoptosis. MMP=matrix metalloproteinase. Bcl-xl=B-cell lymphoma extra large. HIF-1α=hypoxia inducible factor 1-α. EGF=epidermal growth factor. EGFR=epidermal growth factor receptor. VEGF=vascular endothelial growth factor. VEGFR=vascular endothelial growth factor receptor. NOS=nitric oxide. synthase. Bcl-2=B-cell lymphoma 2.
Exposure of cancer cells to cigarette smoke increases proliferation and tumorigenesis through the activation of many cellular signalling pathways. The components of cigarette smoke benzo(a)pyrene and polycyclic aromatic hydrocarbons can act as ligands and bind directly to the aryl hydrocarbon receptor, a transcription factor, leading to expression of CYP450 enzymes, multidrug resistance-associated proteins, ABCG2 and adrenomedullin 7 – 10 that in turn increase tumour growth and potential clonal expansion of cancer stem cells. Exposure to cigarette smoke downregulates DKK1 and leads to activation of Wnt signalling. 11 Cigarette smoke also downregulates microRNA-487b, which mediates cell cycle arrest and senescence in lung cancer cells, by targeting WNT5A, a non-conical Wnt ligand, and components PRC1 and PRC2 of the polycomb repressive complex. 12 Furthermore, cigarette smoke activates the arachidonic acid cascade through β1-adrenergic receptors and β2-adrenergic receptors and the subsequent expression of COX2, 5-lipoxygenase, VEGF, and matrix metalloproteinases. 13 – 16 Additionally, cigarette smoke modulates canonical ligand-dependent EGFR signalling through reactive oxygen species induced autocrine shedding of the EGFR ligands HBEGF, AREG, and TGF-α. 17 – 19 Oxidative stress due to cigarette smoke induces non-canonical EGFR autophosphorylation at Src-dependent phos phorylation sites leading to recruitment of Src to EGFR, which triggers the Ras/Raf/MEK/ERK and PI3K/AKT signalling cascades and contributes to tyrosine-kinase inhibitor resistance in tyrosine-kinase inhibitor sensitive lung cancer cells. 20 – 21
Evidence shows that cigarette smoke contributes to the ability of cancer cells to evade several cell death pathways by altering SMAD3–SMAD4 complex formation, which upregulates Bcl-2 and reduces TGF-β induced apoptosis in lung cancer cells. 22 Exposure to cigarette smoke induces cisplatin resistance in bladder cancer cells by reducing the expression of mitochondrial matrix protein AK3, altering mitochondrial membrane potential, increasing levels of intracellular reactive oxygen species, and elevating Bcl-xl and Bcl-2 expression. 23 Studies have also suggested that cigarette smoke might be involved in modulating the NOS pathway and autophagic response in head and neck cancer cells. 24
Several studies have also examined the role cigarette smoke has in mediating invasion and metastasis of cancer cells. Long-term exposure of breast cancer cells to cigarette smoke enhances the invasion and metastatic potential of cells. 25 Exposure of non-small-cell lung carcinoma lines to cigarette smoke increased the expression of MTA1, which is involved in mediating epithelial to mesenchymal transition. 26 Cigarette smoke has also been shown to reduce activity of the Na + /K + -ATPase 27 leading to disruption of tight junctions and altered cell polarity that might be involved in early epithelial to mesenchymal transition events.
Effects of nicotinic acetylcholine receptor activation on cancer cells
Nicotine is the primary addictive component of tobacco. 1 Several recent reviews have discussed the tumour-promoting activity of nicotine and of the nicotine-derived 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol, and N′-nitrosonornicotine. 28 – 31 There are several excellent reviews on the effects of these tobacco products to stimulate cell proliferation, migration, invasion, angiogenesis, and resistance to cell death pathways such as apoptosis. 28 – 31
Overall, cigarette smoke is distributed throughout the lungs and metabolites of cigarette smoke are present in virtually all peripheral tissues. Nicotine and its metabolites are distributed in almost all tissues of the body. In peripheral tissues, these substances activate systemically expressed nicotinic acetylcholine receptors (nAChRs) and β-adrenergic receptors that in turn activate several pathways, including the Ras/Raf/MEK/MAPK and PI3K/Akt oncogenic pathways causing substantial cross-activation of these pathways leading to a tumour-promoting phenotype. In relation to chemotherapy and radiotherapy, nicotine and activation of nAChRs have been shown to decrease the therapeutic response to chemotherapy and radiotherapy both in vitro and in vivo. 32 – 34 Collectively, these data suggest that activation of systemic nAChRs might be one mechanism associated with cigarette smoke-induced tumour promotion.
The preclinical data showing the tumour-promoting activities of nicotine are a subject of discussion among some oncologists; however, we are not aware of any studies or reports on the safety of nicotine-replacement therapy in patients with cancer with respect to mortality, toxicity, or cancer recurrence. Nicotine-replacement therapy is evidence-based, and increases the effectiveness of smoking cessation 35 advocated for use in patients with cancer by both ASCO 36 and AACR. 37 Although there is little evidence on the potential effects of nicotine-replacement therapy on cancer treatment outcomes at this time there is now strong evidence that smoking causes adverse outcomes in patients with cancer. Unless evidence suggests that nicotine-replacement therapy has any adverse effects in patients with cancer we advise clinicians to consider nicotine-replacement therapy as an effective means to promote tobacco cessation for these patients.
The clinical effects of smoking on patients with cancer
The findings described in the 2014 Surgeon General’s Report warrant a paradigm shift in the standard clinical care for patients with cancer. 1 On the basis of evidence in the 2014 Surgeon General’s Report, smoking by patients with cancer should now be viewed as a cause of increased overall mortality and cancer-specific mortality and a cause of second primary cancer. A full review of the clinical effects of smoking on patients with cancer is beyond the scope of this Review and broad ranging data have been provided in the 2014 Surgeon General’s Report. 1 For our purposes, large studies reporting one or more clinical effects of current smoking in patients treated with chemotherapy and radiotherapy are highlighted.
The diversity of studies, treatments, disease sites, disease stage, and definitions of tobacco use do not allow an overall comparative analysis to estimate the magnitude of the associations between smoking and outcome. However, 22 (81%) of 27 studies show one or more significant negative associations between current smoking and treatment outcome ( table ). 38 – 64 Two studies 42 , 60 show near significant negative associations and the results of three studies show no association. 40 , 43 , 63 No studies reported a positive effect of smoking on outcome, but it is important to note that a recent meta-analysis of smaller studies suggests that smoking decreases the risk of radiation-induced pneumonitis. 65 Lung cancer studies represented the largest disease site (ten), prostate cancer (six), head and neck cancer (four), and breast cancer (three) with one study each of cervical cancer, Hodgkin’s disease, colon cancer, and male cancer patients.
Effects of current smoking on mortality, recurrence, cancer treatment toxicity, and second primary cancer in patients treated with chemotherapy or radiotherapy
95% CI given when available.
NA=not available. ADT=androgen deprivation therapy. RR=relative risk. CaPSURE=Cancer of the Prostate Strategic Urologic Research Endeavor. NHIC=national health insurance corporation. NSCLC=non-small cell lung cancer. HR=hazard ratio. RTOG=Radiation Therapy Oncology Group. NS=not statistically significant. PPD=pack per day. SCLC=small-cell lung cancer. WHEAL=Women’s Healthy Eating and Living Study. ER=oestrogen receptor.
The effect of current smoking on mortality in patients with cancer was reported in 15 studies with 12 (80%) showing that smoking increases overall mortality 38 , 39 , 44 , 46 , 48 – 51 , 53 , 55 – 57 and three showing no association ( table ). 40 , 43 , 63 Several other studies show that mortality is increased in patients who are current smokers compared with patients who are former smokers and those who were never smokers combined. The relative risk (RR) of mortality was increased for patients with head and neck cancer who were current smokers (2·34, 95% CI 1·56–3·50) compared with all other patients in a report on 504 patients with stage III–IV head and neck cancer treated in one of two phase 3 randomised trials. 49 Khuri and colleagues 50 showed increased risk of mortality in patients who were current smokers compared with those who were former smokers (RR 1·6, 95% CI 1·23–2·07) and those who had never smoked (2·51, 95% CI 1·54–4·10). 50 In patients with prostate cancer who are current smokers, mortality is increased compared with those who are former smokers 55 , 57 and in comparison with patients who are former smokers or who have never smoked combined. 56 The effects of smoking on mortality are perhaps best shown in a series of 1354 patients with prostate cancer who received radiotherapy with or without androgen deprivation therapy, and in whom current smoking increased the risk of death due to heart disease (relative risk [RR] 3·05, p=0·007), non-prostate cancer related mortality (RR 5·52, p=0·002), and other causes (RR 4·09, p=0·002) with no significant effect on prostate cancer mortality. 53 However, deaths not caused by prostate cancer accounted for 92% of overall mortality. The authors of the study note that high rates of cancer control are possible, but that implementation of healthy lifestyle programmes including smoking cessation is important to consider in prostate cancer management.
Current smoking also increases the risk of recurrence and cancer-specific mortality. 49 , 55 , 56 Increased recurrence and cancer-related mortality are probably closely linked to changes in tumour biology leading to a decreased response to cytotoxic therapy ( figure ). Smoking can alter cancer-drug metabolism that might lead to changes in therapeutic efficacy or toxicity. 66 As cigarette smoke is potently tumorigenic, several studies have shown that current smoking significantly increases the risk of the patient developing a second primary cancer, 45 , 47 , 54 , 59 , 62 particularly second tobacco-related primary cancers. 64 Notably, some studies suggest that smoking confers an additive or synergistic risk of development of a second primary cancer when combined with chemotherapy or radiotherapy. 54 As a result, patients who are smokers are at increased risk of mortality from recurrence and progression of both primary and secondary cancers.
Quitting smoking seems to improve outcomes in patients with cancer. Those with lung cancer who quit smoking at, or after, diagnosis have a reduced risk of developing a second cancer compared with patients who continue smoking. 45 , 47 Patients who quit smoking after diagnosis also have reduced toxicity associated with cancer treatment. 52 Data indicate that patients who smoke less have reduced toxicity due to radiotherapy compared with those who are current heavy smokers. 61 Substantial work is needed to clarify the time-dependent and dose-dependent benefits of smoking cessation. However, in 205 patients with head or neck cancer receiving radiotherapy, 43% of patients who smoked and were treated in the morning had grade 3 or higher mucositis compared with 76% of patients who smoked who were treated in the afternoon (p=0·04), suggesting that some of the effects of smoking on toxicity might be reduced within hours. 67
Addressing tobacco use in patients
Clinical guidelines and clinical practice.
Recent statements from the American Society of Clinical Oncology (ASCO) 36 and American Association for Cancer Research (AACR) 37 provide strong support and guidance ( panel 2 ).
AACR guidelines for addressing tobacco use in patients with cancer 37
“Patients with cancer from all clinical settings, participants in therapeutic cancer clinical trials, and cancer screening patients who use tobacco or have recently quit (past 30 days) should be provided with evidence-based tobacco cessation assistance. Ideally, that assistance capacity should be within or associated with the oncology practice. Even if the assistance is provided through an external service, the cancer patient’s oncology service provider should assume responsibility for ensuring that the patient receives appropriate care. That capacity can also be supplemented by telephone cessation quitlines in all 50 states that can be reached via a common toll-free telephone number (800-QUIT-NOW). Tobacco use should be comprehensively and repeatedly documented for all patients so that the confounding effects of tobacco on cancer treatment, disease progression, comorbid events, and survival can be evaluated in all oncology clinical trials, from registration to survival endpoints, and in all clinical cancer settings.”
AACR=American Association for Cancer Research
The Tobacco Cessation Guide for Oncology Providers was recently released by ASCO 68 to provide guidelines for tobacco cessation support in patients with cancer based on the 5-As model of tobacco cessation from the 2008 Public Health Service (PHS) guidelines. 35 In brief, ASCO recommends that clinicians should ask patients about tobacco use at every visit, advise patients of the benefits of tobacco cessation, assess the patient for willingness to quit, assist patients in quitting tobacco use with evidence-based support approaches, and arrange follow-up. Unfortunately, two large recent surveys show that although roughly 90% of oncologists ask patients about tobacco use and about 80% advise patients, only about 40% of oncologists regularly provide assistance to patients to quit smoking. 3 , 4 In view of the recent evidence from the 2014 Surgeon General’s Report, this unfortunate lack of tobacco cessation support for patients with cancer can now be viewed as a deficit in addressing evidence-based medicine.
There are several important considerations in the design and implementation of a sustainable clinical tobacco cessation programme. Variables in a tobacco cessation programme can be integrated into the design and implementation of a structured tobacco-use assessment and cessation approach for patients with cancer ( panel 3 ). Clinicians should consider how tobacco cessation can be delivered, including methods of screening patients for tobacco use, methods of tobacco cessation support, which health-care providers will deliver tobacco-cessation support, and in what setting support can be delivered. Clinicians could further consider a partnership with institutional and community resources. All patients should be screened and we advise that all at-risk patients should receive tobacco cessation support, but this needs participation and support from physicians, clinical staff, and administrators to facilitate the development of a structured tobacco cessation programme to merge with ongoing clinical efforts. This strategy would allow clinicians to then implement tobacco cessation support and tailor a tobacco cessation plan for each patient. We also suggest that clinicians move away from a so-called one size fits all approach and that building a sustainable treatment strategy will need the design of an efficient and clinically effective tobacco cessation programme that integrates well with other aspects of clinical cancer treatment.
Conceptual design of a tobacco cessation programme for patients with cancer: creation of a tobacco-cessation support approach
Method of screening.
- By physicians or support sta3
- Biochemical testing
Method of tobacco cessation support
- Behavioural counselling
- Pharmacotherapy
Delivery of tobacco cessation support
- By phone, web, or in-person
- In-person in a cancer clinic
- In-person in a separate clinic
Providers for tobacco cessation support
- Non-physician health-care professionals
- Dedicated tobacco cessation specialists
Obtaining institutional support
- Screening for all patients
- Treatment or referral of all patients for evidence-based tobacco cessation support
- Support for referring physicians, clinical staff, and administrators
- Financial support for tobacco cessation programme
- Incorporating tobacco-use assessment and tobacco cessation into standard clinical practice
- Communication among administrators, clinicians, cessation providers, and patients
Considerations for implementing the 5-As in patients with cancer
- Ask about tobacco use repeatedly at initial consultation, treatment, and follow-up
- Recommend an immediate quit or choose a quit date in the near future
- Prepare patient
- Cite adverse effects of tobacco on cancer treatment outcomes
- Remind patient of adverse health effects of tobacco on non-cancer outcomes such as heart disease, stroke, wound healing, pulmonary disease, etc
- Tailor to needs of the patient; consider the treatment plan, diagnosis, and expected outcome
- Motivational interviews, behavioural counselling, and evidence-based pharmacotherapy
- Direct tobacco cessation assistance
- Referral to a tobacco cessation specialist
- By phone or in-person
- Consider cancer treatment plan and urgency of cancer treatment
- Consistent communication among patients, clinicians, and referring physicians
Behavioural counselling, pharmacotherapy, and electronic cigarettes
Methods of tobacco cessation support for the general population have been discussed extensively, and are systematically reviewed and defined in the 2008 Public Health Service Guidelines. 35 The core elements of tobacco cessation support for patients rely on repeatedly addressing tobacco use through motivational and behavioural counselling, accompanied by pharmacotherapy to promote behavioural change. Patient counselling sessions that consist of brief interventions and counselling sessions that involve more detailed and intense counselling are effective, although more intense counselling is generally associated with high tobacco cessation rates. Pharmacotherapy is a proven method to improve the efficacy of tobacco cessation programmes, and many patients will need several attempts to successfully quit smoking. Nicotine-replacement therapy is the most common pharmacotherapy used in the USA in the form of lozenges, nasal sprays, gum, inhalers, and longacting patches. The proper use of these medications is important to promote effective pharmacological replacement. For example, nicotine gum should be chewed slowly to allow absorption of nicotine in the appropriate dose and timeframe. Varenicline, bupropion, and cytisine have also been used with efficacious results, although cytisine is not currently used for tobacco cessation in the USA. 69
The use of electronic cigarettes is increasing among the general population and in patients with cancer. There are several brands and designs of these products designed to deliver nicotine through a device that may resemble the shape and feel of a cigarette. However, these products are not well regulated and the true nicotine content and nicotine delivery rate vary substantially. 70 Electronic cigarettes have serious implications for worldwide tobacco use as a potential substitute for combustible tobacco, but could also be potentially addictive for non-smokers who begin to use them. The results of a trial of electronic cigarettes versus nicotine patches in aiding tobacco cessation were recently published, 71 suggesting that electronic cigarettes have the potential to help patients to quit smoking, 71 but the authors of the study noted that the power of the study and analyses were limited, yielding quit rates lower than those commonly associated with a structured tobacco cessation support programme using PHS guidelines. 35
A recent publication from the Tobacco Control Committee of IASLC has provided guidance for clinicians regarding e-cigarette use in patients with cancer. 72 Currently, there are no clear data supporting the use of electronic cigarettes as an aid to tobacco cessation in patients with cancer. The effects of electronic cigarettes on cancer-cell biology, treatment efficacy, therapy-related toxicity, and patient survival have not been evaluated and there are no published data to confirm that electronic cigarettes are more or less toxic for patients with cancer than are tobacco products. However, the broad adverse effects of smoking on cancer treatment are now well documented. 1 Clinicians are urged to consider the recommendations from IASLC 72 for patients with cancer ( panel 4 ).
IASLC guidance on e-cigarettes for patients with cancer 72
“There are currently no evidence-based guidelines to support the recommendation of e-cigarettes. Whereas evidence-based cessation strategies should be used wherever possible, clinicians should consider the strong need for cancer patients to stop smoking as soon as possible to promote the most effective outcomes of cancer therapy. In the absence of sufficient evidence that e-cigarettes are effective and safe for treating nicotine dependence in cancer patients, the International Association for the Study of Lung Cancer advises against recommending their use at this time. However, this recommendation may change if new data become available. The International Association for the Study of Lung Cancer does recommend that research be done to evaluate the safety and efficacy of e-cigarettes as a cessation treatment in cancer patients to help guide clinical practice. For individual patients who are either using or planning to use e-cigarettes despite advice not to do so, they should be offered evidence-based stop smoking treatments while monitoring for any adverse effect of e-cigarette use.”
IASLC=International Association for the Study of Lung Cancer
Assessment of tobacco use in patients with cancer
An estimated 30–50% of patients with cancer are smokers at the time of cancer diagnosis, with higher rates of smoking among patients with disease sites for traditionally tobacco-related cancers such as head and neck or lung cancer and lower rates of smoking among patients with disease sites for traditionally non-tobacco-related cancer such as breast or prostate cancer. 73 There are no current standardised national or international recommendations for the assessment of tobacco use in patients with cancer, thus these estimates probably reflect some bias in the method of assessment. Guidance has been provided for the inclusion of specific questions to assess a patient’s history of tobacco use and their current tobacco use status in patients with cancer. 74 – 75 We recommend that patients should be asked questions that specifically define their current tobacco use status (current, former, never), their history of tobacco use, amount and frequency of tobacco use, the degree of tobacco dependence, and current use of tobacco cessation medications. In clinical practice, however, patients might be reluctant to answer a broad base of questions about previous tobacco use and might be reluctant to accurately report tobacco use patterns in the presence of family members or friends. Studies also show that patients can be stigmatised due to tobacco use and specific cancer diagnoses such as lung cancer. 76 A recent study 77 of tobacco use screening questions in nearly 12 000 patients with cancer shows that just a few questions at diagnosis and in follow-up can yield effective referral rates to dedicated tobacco cessation programmes. Moreover, repetition of assessments monthly at follow-up seemed to result in few delayed referrals to a dedicated tobacco cessation programme. This recent study has yet to be duplicated, but suggests that clinically efficient systems can be developed to accurately screen patients for tobacco use and refer patients to dedicated tobacco cessation support programmes.
Consideration of the intensity of tobacco cessation support
Several notable programmes in the USA have developed rigorous tobacco cessation support services, including programmes at the MD Anderson Cancer Center, Mayo Clinic, and the Memorial Sloan Kettering Cancer Center, with commendable quit rates seen in patients with cancer. These programmes generally incorporate intensive assessments, behavioural counselling, pharmacotherapy, and follow-up to achieve quit rates of greater than 30%. 78 , 79 Importantly, these successful programmes have removed clinical tobacco cessation support from the duties of the treating oncologist and placed that responsibility within a centralised and dedicated programme designed specifically to treat tobacco dependence. These effective specialised and intensive programmes have highly trained individuals and are integrated into existing clinical cancer care programmes.
Many institutions might not be able to provide resources for dedicated tobacco cessation support. Clinicians could take on the role of providing tobacco cessation support directly or identifying available external resources. This approach, however, should not deter clinicians from providing evidence-based tobacco cessation support. For example, behavioural counselling even for a few minutes can significantly increase quit rates in smokers. 35 In general, more intensive tobacco cessation support yields higher quit rates, as evidenced in the general population by numerous publications. 1 , 35 The results of a meta-analysis 80 of tobacco cessation in patients admitted to hospital showed that high-intensity, long-term behavioural inter ventions initiated during hospital stay increased the rate of smoking cessation whereas low-intensity, short-duration interventions did not. In another meta-analysis 81 of smoking cessation interventions compared with usual care in patients with cancer, the results did not show a significant difference with either short-term or long-term follow-up (pooled odds ratio [OR] 1·54, 95% CI 0·909–2·64, and pooled OR 1·31, 95% CI 0·93–1·84, respectively). However, studies using combination therapy (pharmacological and non-pharmacological) improved quit rates (pooled OR 1·4, 95% CI 1·06–1·87) and perioperative interventions also showed a strong effect favouring the perioperative period compared with the clinic (pooled OR 2·31, 95% CI 1·32–4·07). 81 Despite heterogeneous patient populations and study designs, data support the recommendation that all patients should have access to structured tobacco cessation support beginning at the time of cancer diagnosis. Clinicians who refer patients to external tobacco cessation support programmes should ideally receive updates on tobacco cessation activities from patients and note progress by patients to reduce and ultimately eliminate their use of tobacco.
For patients with cancer treated in a community environment, rather than in a comprehensive cancer treatment centre or other large institution, tobacco cessation programmes might be even more difficult to access. In the USA, the state quitlines are resources that are available by calling 1-800-QUIT-NOW, whereby individuals are automatically connected to tobacco cessation support resources in any state. Unfortunately, many international community oncology practices might not have access to universally available tobacco cessation resources. Community oncologists could also consider obtaining continuing medical education credits in tobacco cessation support, which is offered on-line or in-person. Large group-oncology practices could consider pooling resources to establish a specialist tobacco cessation unit within their management group, local hospital, or in the community for a direct referral resource. Panel 3 and the ASCO toolkit 68 provide information to consider in the development and implementation of community-based tobacco cessation support resources for patients with cancer.
Discussion of tobacco use and tobacco cessation with patients
We recommend that clinicians explain empathetically to patients why tobacco cessation is important for their treatment and survival. The 2014 Surgeon General’s Report concludes that continued smoking causes adverse outcomes in patients with cancer, specifically, increased overall mortality, cancer-specific mortality, and second primary cancer. 1 Evidence suggests that smoking increases the risk of cancer recurrence and treatment toxicity. However, the clinical toxicity and expected outcomes of cancer treatment varies substantially according to the diagnosis. For example, breast cancer treatment is very different from treatment for head and neck cancer, but patients with either cancer are at an increased risk of mortality, comorbid disease, poor surgical wound healing, adverse effects from systemic therapy, risk of second primary cancer, and poor cosmetic outcome. Patients with breast cancer can tolerate treatment with few adverse effects, are generally able to maintain nutritional requirements, can usually continue daily activities such as a regular work schedule, and might not feel any stigma associated with their diagnosis. By contrast, patients with head and neck cancer might have severe adverse effects from treatment, which causes deficits in maintaining nutrition, absence from work, substantial augmentation of pain, and patients might experience stigmatisation from a seemingly tobacco-related cancer diagnosis. Psychiatric comorbidities (anxiety, depression) and substance use (alcohol) might also differ in patient populations. Clinicians can personalise and tailor the approach to tobacco use and cessation in patients with cancer for whom different clinical outcomes are anticipated.
Search strategy and selection criteria
A comprehensive review of the literature is given in the 2014 Surgeon General’s Report. 1 We used the same general criteria used to identify studies evaluating the effect of current smoking at cancer diagnosis on mortality, toxicity, and risk of second primary cancer in patients treated with chemotherapy and radiotherapy. Published manuscripts that reported the effect of current smoking on one or more of mortality, recurrence, toxicity, second primary cancer were identified. PubMed was searched for studies using the search terms “smoking” and “cancer” with additional search terms according to disease site ( appendix ). A total of 622 works published between 1990–2012 that reported on the effects of smoking on one or more clinical outcomes in patients with cancer (mortality, toxicity, second primary cancer) were identified. Papers that did not clearly define current smoking, report on any clinical effects of current smoking (as opposed to ever smoking), or specify chemotherapy or radiotherapy were excluded. Studies with fewer than 500 patients were also excluded, a total of 27 studies, reporting on more than 54 000 patients met the criteria ( table ).
Clinicians might also wish to consider how the message is delivered. So-called gain-framed statements are based on presentation of the benefits and positive aspects associated with a treatment or change in behaviour, and loss-framed statements present the negative aspects of treatment or behavioural change. For example, a statement such as, “quitting smoking will improve your chances of survival” is a gain-framed approach whereas a statement such as, “if you don’t quit smoking, you may have a poor cancer outcome” is a loss-framed approach. Messaging is largely untested in patients with cancer with respect to tobacco use, but loss-framed messaging is a common tool to motivate people in the general population to stop smoking. 82 Though gain-framed versus loss-framed messaging has not been explored in relation to tobacco use in patients with cancer, gain-framed messaging might be important to consider in the screening and treatment of these patients. 83
Clinicians might feel that patients with cancer with either early stage or curable disease are the ideal groups on whom smoking cessation efforts should be focussed. The 2014 Surgeon Gerneral’s Report reviews a wealth of studies, showing that smoking increases mortality in patients with both early and advanced or metastatic cancer. 1 Several studies show that smoking increases the risk of hospital admission, infection, pulmonary complications, wound infections, and decreases patients’ quality of life. The studies presented in the 2014 Surgeon General’s Report might cover several disease sites and modalities of cancer treatment, but these data also suggest that smoking affects clinical outcomes in the care of patients with advanced and metastatic cancer. We are not aware of any studies that provide a comprehensive assessment of the benefits of tobacco cessation across disease sites, disease stage, and stage of treatment. However, clinicians should consider the potential benefits of smoking cessation even in patients with metastatic and recurrent cancers possibly to improve survival, but also possibly to reduce complications in cancer care at the end of life.
Design of tobacco cessation support in clinical practice and research
All patients should receive tobacco cessation support to improve therapeutic outcomes, but clinicians could also consider the integration of tobacco use assessment and tobacco cessation into research programmes. 37 Screening patients using paper-based systems that capture subjective tobacco use responses might be useful to encourage referrals for tobacco cessation, but the integration of tobacco use assessments and tobacco cessation support using computerised systems (eg, through the electronic medical record) can substantially increase efficiency in identification of forms of tobacco use, referral of patients to dedicated tobacco cessation support programmes, and tracking of the efficacy of tobacco cessation in patients. Examples of annotated design systems have been recommended and implemented in clinical practice for patients with cancer. 74 , 77 We also suggest that clinicians consider the imple mentation of assessment of tobacco use and tobacco cessation approaches that promote effective tobacco cessation, yet also maintain efficient clinical workflow for other aspects of cancer care. An understanding that smoking cessation is a crucial part of the overall effectiveness of cancer treatment is important for patients.
Societal influences on tobacco cessation support
An often overlooked variable to consider is the social and medical environment in which tobacco cessation is approached. The WHO Framework Convention on Tobacco Control (FCTC) is an effort started in 2003 to reduce the international health burden attributed to tobacco. A summary of the FCTC is provided in a recent review, 84 in which the efforts of the tobacco industry to manipulate worldwide tobacco control are highlighted. In some countries, tobacco is increasingly regulated, resulting in a decrease in the prevalence of tobacco use and changes in social norms with smoking no longer seen as socially acceptable but as unacceptable. 1 The prevalence of tobacco use, however, is increasing in low-income and middle-income countries. Approaches to tobacco cessation in specific countries, regions, cities, and even clinics might necessitate knowledge of the effect of the tobacco industry on social and medical resources. Reimbursement might be important in medical systems in which there is third party billing. High rates of tobacco use by physicians in some high-income and low-income or middle-income countries might deter implementation of tobacco cessation programmes as standard clinical care for patients with cancer. 85 In low-income and middle-income countries, tobacco cessation is only now becoming a priority in the general population, and has yet to be seen as the main target in patients with cancer or other chronic illness. Integration of tobacco cessation into tuberculosis and HIV care has been called for as a priority on the basis of a parallel set of adverse medical and survival outcomes. 86 , 87
Oncology clinicians should champion tobacco cessation as a method to improve clinical cancer treatment outcomes for patients. Clinicians are also encouraged to partner with institutional and community resources to develop a unified approach to the assessment of tobacco use and cessation for patients with cancer at diagnosis, during treatment, and throughout follow-up.
Conclusions
The evidence presented in the 2014 Surgeon General’s Report warrants a substantial change in evidence-based cancer care. Smoking causes adverse outcomes in patients with cancer, in part through the activation of tumorigenic pathways and in part through alterations in physiology that lead to complications associated with cancer treatment and continued development of comorbid disease. There are currently no cancer treatments shown to produce superior results in patients with cancer who smoke compared with those who do not smoke and there are no biomarkers to predict adverse outcomes in patients with cancer who continue to smoke. Tobacco use by patients with cancer should be accurately identified and all at-risk patients should be offered structured tobacco cessation support. On the basis of the findings in the 2014 Surgeon General’s Report, addressing tobacco use in patients with cancer has the potential to substantially improve overall cancer treatment outcomes through reduced treatment-related toxicity, treatment failure, and comorbid disease and improved survival.
Supplementary Material
Acknowledgments.
This work was supported in part by the American Cancer Society (MRSG-11-031-01-CCE to GWW) and the National Cancer Institute (P30-CA16672 to ERG).
Contributors
Declaration of interests
We declare no competing interests.
See Online for appendix
- Skip to main content
- Keyboard shortcuts for audio player
Medical Treatments
Why former nih director francis collins went public with his cancer diagnosis.
NPR's Scott Detrow spoke with the former director of the National Institutes of Health, Dr. Francis Collins, about his recent prostate cancer diagnosis.
SCOTT DETROW, HOST:
Throughout the coronavirus pandemic, we heard from a lot of people on this show, people who helped us try to understand what was going on and how to keep ourselves safe and how to get through a really challenging time. One of those people was Dr. Francis Collins. At the time, he was the director of the National Institutes of Health. Well, we learned on Friday that Dr. Collins is going through his own health crisis right now. He's been diagnosed with an aggressive form of prostate cancer, and he wrote all about it in an article published at The Washington Post. Dr. Collins, welcome back to ALL THINGS CONSIDERED.
FRANCIS COLLINS: Thanks, Scott. Nice to be with you.
DETROW: I just want to start off - I was really sorry to hear about this diagnosis. How are you doing?
COLLINS: I'm doing OK. Not exactly what I would have hoped to be experiencing right now, but I'm feeling pretty fortunate that, thanks to a lot of surveillance and early detection, I'm in a good position with the surgery that's now coming up soon to expect that this cancer can be cured. And that is a lot different than if I hadn't had all of this attention to make sure that we were watching this closely.
DETROW: What was your first response to the news that not only did you have cancer, but a pretty serious form of it?
COLLINS: It's one of those moments that I guess we all have once in a while, where the words come at you and you realize my life is now different than it was five seconds ago.
DETROW: Yeah.
COLLINS: When they said that this cancer - having been previously a very slow-growing, not-much-to-see-here kind of version - now in the latest biopsies had switched into high gear, something called a Gleason 9 - and it only goes to 10 on that scale - I knew that it was going to be time for action - serious action, and everything that I had maybe planned for the coming weeks, months and years was going to be affected.
DETROW: You mentioned a surgery. Can you tell us about how you're treating this?
COLLINS: So because the cancer does seem to be completely still contained within the prostate, after much searching to be sure of that, then the best way to avoid a downstream outcome, which I really would like to avoid - where the cancer spreads elsewhere, like to bones or to lymph nodes or to liver, lungs or brain - is to actually get the prostate removed. If you want to use an analogy, if the horse is the cancer and the barn is the prostate, we're not just going to get rid of the horse, we're going to get rid of the barn, too, because...
COLLINS: ...We're just not quite sure how big that horse is. So the surgery is what's called a radical prostatectomy. It's done using a robot as well as a surgeon to try to limit the amount of recovery time, but also to be very precise in terms of how one does this, trying not to injure the other structures nearby, like the nerves and the vessels that can be kind of important.
DETROW: Are you worried about the treatment at all? I mean, this is to be blunt, surgery in a pretty intimate part of your body. And I think more broadly with cancer, a lot of people worry about the treatment. How - my dad's around your age. He's battling cancer right now. The treatment's working, but I see how much it takes out of him.
COLLINS: No, Scott, you're quite right, and I am worried about that. The surgery has gotten a lot better, but there's still plenty of opportunities for some men, and maybe that will be me, to end up with incontinence or with impotence because this is, as you say, a rather sensitive part of the male anatomy. And as hard as the surgeons try to try to take out the prostate and the cancer, there's a lot of other things nearby that can be temporarily or sometimes even permanently affected. And one has to have a realistic expectation walking into this that that could happen.
DETROW: Yeah. What are you hoping to gain by being so public about your diagnosis?
COLLINS: You know, maybe it feels like it would be a good thing to have more of a discussion about two things. One is doing this kind of regular early detection for cancers of all sorts - not just prostate cancer, but breast cancer, colon cancer. We fell way behind on a lot of those screens during COVID, for obvious reasons. People just weren't able to necessarily go in and have them done. We need to kick back in there because this is how you detect cancer early and save lives from lots of different areas of the body. So that was one reason.
The other is prostate cancer is particularly one of those that makes men uncomfortable, and I get that. And talking about it openly has not always been easy. And we need to get over that. And particularly men who have reached the point of age 50 or so, really need to think about what they can do to take care of themselves with the kind of screening that I had. I honestly think if I hadn't been in this circumstance of detecting something five years ago that said, ooh, there's something happening, following it closely with what we call active surveillance, and then discovering rather quickly the cancer had taken a bad turn, I probably wouldn't have known about this for several more years, at which point it might have presented by metastatic disease, which could not then be cured. So there's a message here. This kind of surveillance - even though a lot of people put it off, this can be lifesaving. And if there's some little part of my story that gets somebody interested in doing that for themselves, then it's worth being out there in the public.
DETROW: I imagine you've had health problems before over the course of your life, but probably nothing this serious. I'm wondering, being in this position, being on the other side of the conversation with a medical professional, have you learned something about medicine that maybe you didn't realize when you were the expert, when you were the person walking somebody through their options, as opposed to being the person listening to what your options are?
COLLINS: Oh yeah. It's one thing to be imagining what somebody is experiencing as you're giving them news that might be really serious and maybe even life-threatening. It's another to be the person in that spot. As many times as I have thought about what that feels like to be given a diagnosis of cancer, it's just a little different when it is coming at you. And I realize I had some of those same difficulties at first about being able to absorb this and listen carefully and get my head around exactly what was being said and what the consequences would be. So yeah, I think I will - when I next have the chance to be involved in this kind of circumstance as a physician, I'll have a different perspective.
DETROW: You know, you mentioned a couple times in the article where you talked about this news - you mentioned gratitude. Can you tell me what exactly you're grateful for?
COLLINS: I'm grateful that I had the opportunity to take part in this kind of early detection, which should be now available to everybody but hasn't broadly been accomplished in a lot of instances. And we have health inequities in our country that contribute to that. Without that access, I would not be in the place of being able to anticipate that this disease can be cured. I'm grateful to have the expertise of people at the NIH. I'm part of a clinical trial there, and therefore I'm hoping that whatever is learned about me can be widely shared and can teach people about other ways to deal with this disease.
I'm grateful with all the people that are around me who have been so supportive. Scott, I can't tell you that when this came out publicly, I just had this deluge of information and outreach from people, some of whom I haven't been around for a while, people who I have had wonderful, friendly relationships with. But just in the last day or so, all of these people that I considered friends have somehow crossed a line in being very comfortable saying, Francis, I love you. The word love has just come forward in a dramatically positive way. Maybe that's what it takes - is for something like this to get people to say the word. That's pretty touching. That's pretty amazing. I have...
DETROW: Well...
COLLINS: (Laughter) My heart is full of gratitude for that.
DETROW: That's a nice feeling. But let me actually - let me ask about that because, at the same time, I know that it's also a widespread feeling of when you hear that somebody, you know, has gotten a really serious diagnosis or something has really taken a bad turn with their health, sometimes people feel like, gosh, I don't even know what to say. I want to reach out, but I don't know what to say. You're being reached out to right now. What would you tell people who kind of wrestle with that?
COLLINS: Oh, I think what some of the people are reaching out to me with is a great example - to say, you know, I'm really supportive of you. I know you're going through a tough time. I just want you to know I love you. That was just astounding. That's a whole lot better than my thoughts and prayers are with you, which was sort of the old way of saying it. These are very genuine statements of affection that I have very much cherished.
DETROW: Speaking of praying, though, I did want to ask about how you ended your essay. I'm going to read a quote from the end of it. You write...
(Reading) A little over a year ago, when I was praying for a dying friend, I had the experience of receiving a clear and unmistakable message. This has almost never happened to me. It was just this - don't waste your time. You may not have much left.
You are getting treated. You are moving forward. You feel like you have a clear path to beat this cancer, to keep going. But tell me how you're thinking about that sentiment now, what you want to do with the time you've got left.
COLLINS: Well, getting a cancer diagnosis does focus your mind on that a bit, doesn't it?
COLLINS: I am a person of faith, and even before this diagnosis, I had that particular revelation that you just read about that I don't know - quite know how to interpret. And in fact, of course, that's true of all of us. We don't know how much time we have left, and we shouldn't be wasting that time. But it feels more acutely true right now that if there are things I am doing that are not necessarily contributing much to bettering the people around me or the world, maybe those things ought to be deprioritized. And I had to really think about, how do I want to focus my time on giving the most I can to my family, to my friends, to my profession, to my faith, so that I won't look back and say, oh, I really kind of wasted that? That feels like a moment to pay attention to, especially when you have a significant cancer that's just landed in the middle of your life course.
DETROW: Yeah. That's Dr. Francis Collins. He was the director of the National Institutes of Health from 2009 to 2021. Thanks for talking to us, and we'll be thinking about you as you go through with this.
COLLINS: Well, thanks a lot, Scott. It's a pleasure to talk with you today.
Copyright © 2024 NPR. All rights reserved. Visit our website terms of use and permissions pages at www.npr.org for further information.
NPR transcripts are created on a rush deadline by an NPR contractor. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of NPR’s programming is the audio record.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 10 April 2024
How to supercharge cancer-fighting cells: give them stem-cell skills
- Sara Reardon 0
Sara Reardon is a freelance journalist based in Bozeman, Montana.
You can also search for this author in PubMed Google Scholar
A CAR T cell (orange; artificially coloured) attacks a cancer cell (green). Credit: Eye Of Science/SPL
You have full access to this article via your institution.
Bioengineered immune cells have been shown to attack and even cure cancer , but they tend to get exhausted if the fight goes on for a long time. Now, two separate research teams have found a way to rejuvenate these cells: make them more like stem cells .
Both teams found that the bespoke immune cells called CAR T cells gain new vigour if engineered to have high levels of a particular protein. These boosted CAR T cells have gene activity similar to that of stem cells and a renewed ability to fend off cancer . Both papers were published today in Nature 1 , 2 .
The papers “open a new avenue for engineering therapeutic T cells for cancer patients”, says Tuoqi Wu, an immunologist at the University of Texas Southwestern in Dallas who was not involved in the research.
Reviving exhausted cells
CAR T cells are made from the immune cells called T cells, which are isolated from the blood of person who is going to receive treatment for cancer or another disease. The cells are genetically modified to recognize and attack specific proteins — called chimeric antigen receptors (CARs) — on the surface of disease-causing cells and reinfused into the person being treated.
But keeping the cells active for long enough to eliminate cancer has proved challenging, especially in solid tumours such as those of the breast and lung. (CAR T cells have been more effective in treating leukaemia and other blood cancers.) So scientists are searching for better ways to help CAR T cells to multiply more quickly and last longer in the body.
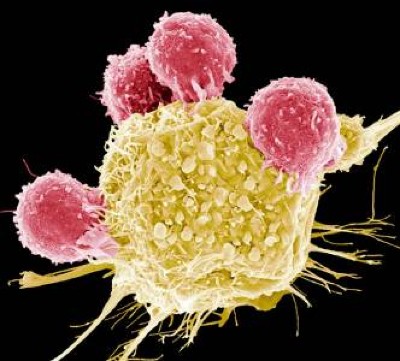
Cutting-edge CAR-T cancer therapy is now made in India — at one-tenth the cost
With this goal in mind, a team led by immunologist Crystal Mackall at Stanford University in California and cell and gene therapy researcher Evan Weber at the University of Pennsylvania in Philadelphia compared samples of CAR T cells used to treat people with leukaemia 1 . In some of the recipients, the cancer had responded well to treatment; in others, it had not.
The researchers analysed the role of cellular proteins that regulate gene activity and serve as master switches in the T cells. They found a set of 41 genes that were more active in the CAR T cells associated with a good response to treatment than in cells associated with a poor response. All 41 genes seemed to be regulated by a master-switch protein called FOXO1.
The researchers then altered CAR T cells to make them produce more FOXO1 than usual. Gene activity in these cells began to look like that of T memory stem cells, which recognize cancer and respond to it quickly.
The researchers then injected the engineered cells into mice with various types of cancer. Extra FOXO1 made the CAR T cells better at reducing both solid tumours and blood cancers. The stem-cell-like cells shrank a mouse’s tumour more completely and lasted longer in the body than did standard CAR T cells.
Master-switch molecule
A separate team led by immunologists Phillip Darcy, Junyun Lai and Paul Beavis at Peter MacCallum Cancer Centre in Melbourne, Australia, reached the same conclusion with different methods 2 . Their team was examining the effect of IL-15, an immune-signalling molecule that is administered alongside CAR T cells in some clinical trials. IL-15 helps to switch T cells to a stem-like state, but the cells can get stuck there instead of maturing to fight cancer.
The team analysed gene activity in CAR T cells and found that IL-15 turned on genes associated with FOXO1. The researchers engineered CAR T cells to produce extra-high levels of FOXO1 and showed that they became more stem-like, but also reached maturity and fought cancer without becoming exhausted. “It’s the ideal situation,” Darcy says.
Stem-cell and genetic therapies make a healthy marriage
The team also found that extra-high levels of FOXO1 improved the CAR T cells’ metabolism, allowing them to last much longer when infused into mice. “We were surprised by the magnitude of the effect,” says Beavis.
Mackall says she was excited to see that FOXO1 worked the same way in mice and humans. “It means this is pretty fundamental,” she says.
Engineering CAR T cells that overexpress FOXO1 might be fairly simple to test in people with cancer, although Mackall says researchers will need to determine which people and types of cancer are most likely to respond well to rejuvenated cells. Darcy says that his team is already speaking to clinical researchers about testing FOXO1 in CAR T cells — trials that could start within two years.
And Weber points to an ongoing clinical trial in which people with leukaemia are receiving CAR T cells genetically engineered to produce unusually high levels of another master-switch protein called c-Jun, which also helps T cells avoid exhaustion. The trial’s results have not been released yet, but Mackall says she suspects the same system could be applied to FOXO1 and that overexpressing both proteins might make the cells even more powerful.
Nature 628 , 486 (2024)
doi: https://doi.org/10.1038/d41586-024-01043-2
Doan, A. et al. Nature https://doi.org/10.1038/s41586-024-07300-8 (2024).
Article Google Scholar
Chan, J. D. et al. Nature https://doi.org/10.1038/s41586-024-07242-1 (2024).
Download references
Reprints and permissions
Related Articles
- Medical research

Bacteria deploy umbrella toxins against their competitors
News & Views 17 APR 24

Brain endothelial GSDMD activation mediates inflammatory BBB breakdown
Article 17 APR 24
ROS-dependent S-palmitoylation activates cleaved and intact gasdermin D
Article 10 APR 24

AI traces mysterious metastatic cancers to their source
News 17 APR 24

Biological age surges in survivors of childhood cancer
Research Highlight 11 APR 24

FOXO1 is a master regulator of memory programming in CAR T cells

AI’s keen diagnostic eye
Outlook 18 APR 24

Refining the impact of genetic evidence on clinical success
Analysis 17 APR 24
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Share full article
Advertisement
Supported by
Guest Essay
We Regulate a Tiny Fraction of the 12,000 ‘Forever Chemicals.’ There’s a Better Way.

By Kathleen Blackburn
Dr. Blackburn teaches creative nonfiction writing at the University of Chicago.
When I was 12 years old, I sat inside a raucous tent revival in West Texas, gripping my seat in fear that a traveling evangelist would accuse me of killing my father.
A healthy former Air Force pilot who’d averaged an eight-minute mile in the New York City Marathon, my father had just been diagnosed with advanced colorectal cancer and been given a short time to live. Nothing about his predicament made sense to our family at the time. He was 38, a nonsmoker and nondrinker, with no history of cancer in his family.
My parents were conservative evangelicals deeply skeptical of the medical industry, and his diagnosis kicked their beliefs into high gear. When doctors couldn’t answer our questions — Why did Dad have cancer? What could we do? — we sought out faith healers who did. Traveling evangelists and local preachers claimed that the cancer was, in fact, a satanic attack. This gave us a way out: We simply had to muster enough faith to believe a miracle was possible and God would heal him.
What no one in my family knew at the time was that for most of his life my father had been exposed to perfluoroalkyl and polyfluoroalkyl substances, the synthetic compounds known collectively as PFAS, which have been linked to increased risk of certain cancers . His fallow muscle, jaundiced skin and weight loss were very likely because of the decades-long accumulation of carcinogenic chemicals in the drinking water at the military sites where he had lived and worked since his childhood.
The environmental violence exacted by PFAS, like the effects of radiation and polychlorinated biphenyls, or PCBs, can be difficult to prove. Only a few studies have examined the relationship between PFAS exposure and colorectal cancer (though the Yale School of Public Health has estimated that around 80 percent of cases are linked to environmental exposure). But on April 10 the Environmental Protection Agency announced the first federal mandate to limit the level of six PFAS in tap water. Going forward, water systems where they are detected will be required to remove them. Michael Regan, the E.P.A. administrator, called the announcement “life-changing,” and for me it was — it validated what I’d long suspected, that exposure to these chemicals can be devastating.
But if six PFAS sounds like a small number, that’s because it is. At this point, more than 12,000 formulations of PFAS exist and only a fifth of Americans’ PFAS exposure comes from drinking water. That means additional PFAS that have not been targeted for regulation persist in our water, soil and consumer products, leaving many Americans vulnerable to exposure. To reduce the risk they pose, we need far more comprehensive mandates that test, monitor and limit the entire class of PFAS chemicals.
In the 1930s and ’40s, manufacturing companies like DuPont and 3M began developing these substances for use as repellent in nonstick items including Teflon pans, Scotchgard and firefighting foams. But the chemical bonds that make them so useful as a repellent also make PFAS nearly indestructible; it’s why they have been labeled “forever chemicals.” They don’t break down once they enter the environment, and instead they accumulate in water, soil and our bodies.
Firefighting foams have been a major source of PFAS contamination since their development in the 1960s. In collaboration with the U.S. Navy, 3M produced foams that the Defense Department sprayed in routine fire drills and emergencies around the country. The chemicals eventually leached into groundwater at military sites like the ones where my father lived and water sources surrounding them. In 2000, 3M began phasing out its use of perfluorooctanyl sulfonate, a component of PFAS-containing firefighting foam, citing health concerns. Still, it was not until 2023 that the Department of Defense was banned from purchasing foams containing PFAS.
The E.P.A.’s move this month to regulate PFAS is a significant next step, but even in places where the groundwater is not highly contaminated, we will all still be exposed to unregulated PFAS without further government action. The chemicals are used in a staggering number of consumer products, including carpet, pizza boxes, microwave popcorn, yoga pants, bags and toiletries like dental floss, shampoo and cosmetics. They are still key ingredients in some firefighting foams; many fire departments still use these foams in emergencies like chemical plant fires. And in Texas, thousands of pounds of PFAS are being shot into the ground to lubricate drill bits for fracking.
We already know that high levels of exposure to PFAS have been linked to disastrous health impacts like birth defects, liver damage and many kinds of cancer. Yet the rate at which PFAS are being released into the environment far outpaces toxicologists’ ability to study their consequences for human health. Some 31 percent of groundwater samples in places with no known source of PFAS have shown contamination levels that exceed E.P.A. limits. And in some locations with established sources, like military and industrial sites, the levels of PFAS are far higher than the standard set by the new rule.
We now need a federal ban on firefighting foams containing PFAS and regulations that are enforceable by law to limit not just specific compounds in our water, but the whole class of highly pervasive chemicals. Mandates should identify the historical sources of pollution to hold industries accountable and avoid further straining the communities exposed to PFAS with the additional cost of their cleanup. On Friday, the E.P.A. helpfully put two PFAS compounds under its Superfund authority, shifting accountability for cleanup from taxpayers to polluters.
I am now 39, the age my father was when he died from cancer in 1998. Nearly 20 years passed before I discovered that the Defense Department is responsible for a significant portion of the PFAS pollution in the United States and that dangerously high levels of PFAS have been confirmed or are suspected of contaminating the drinking water at military sites from Guam to Universal City, Texas, including where my father had lived as a child and worked as an Air Force officer. My father was no longer an officer when he was diagnosed, but the reality of PFAS exposure shows that we carry the traces of each place we’ve lived even after we’ve left.
This month’s federal announcement cannot resurrect the dead. Still, it gives context to tragedies that made no sense at the time and sent my family into a desperate search for a miracle that never came.
I would never wish such a revelation on my 2-year-old son’s generation. I would not have them blindly searching for answers that first manifest, as so often quests through oblivion do, in blaming one’s self. This is exactly what companies like 3M and DuPont hope will continue happening — that those of us who were first exposed will still bear the burden of proof.
We should not have to risk repeated exposure to the most powerful bonds in organic chemistry caused by the willful negligence of industry each time we place our faith in a glass of water. Let’s not wait for more long-term effects on our health before we act.
Kathleen Blackburn teaches creative nonfiction writing at the University of Chicago. She is the author of “Loose of Earth.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .

IMAGES
VIDEO
COMMENTS
500+ Words Essay on Cancer. Cancer might just be one of the most feared and dreaded diseases. Globally, cancer is responsible for the death of nearly 9.5 million people in 2018. It is the second leading cause of death as per the world health organization.
The will to live is a force within all of us to fight for survival when our lives are threatened by a disease such as cancer. Yet this force is stronger in some people than in others. Many physicians have seen how two patients of similar ages and with the same diagnosis, degree of illness, and treatment program experience vastly different results.
The Biology of Cancer. Cancer is a disease that begins with genetic and epigenetic alterations occurring in specific cells, some of which can spread and migrate to other tissues. 4 Although the biological processes affected in carcinogenesis and the evolution of neoplasms are many and widely different, we will focus on 4 aspects that are particularly relevant in tumor biology: genomic and ...
Around the world, cancer rates in people under 50 are surging, with a recent study in BMJ Oncology showing that new cases for young adults have risen 79% overall over the past three decades. In ...
Cancer brought about many stops and starts in my personal life and career. My friends and family would be going about life in a forward-looking and normal way, starting their families and advancing their careers.
You need to get rid of those emotions, or they will kill you. In 1989 a Stanford psychiatrist named David Spiegel published a study of women with metastatic breast cancer. He created a support ...
The Definition of Cancer. Cancer is a disease in which some of the body's cells grow uncontrollably and spread to other parts of the body. Cancer can start almost anywhere in the human body, which is made up of trillions of cells. Normally, human cells grow and multiply (through a process called cell division) to form new cells as the body ...
Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020, or nearly one in six deaths. The most common cancers are breast, lung, colon and rectum and prostate cancers. Around one-third of deaths from cancer are due to tobacco use, high body mass index, alcohol consumption, low fruit and vegetable intake, and ...
Outlook: measuring population dynamics. Cancer was recognized as an evolutionary process more than 60 years ago 5 and, since then, evolutionary ideas have had an important role in cancer research ...
Chemo is considered a systemic treatment because the drugs travels throughout the body, and can kill cancer cells that have spread (metastasized) to parts of the body far away from the original (primary) tumor. This makes it different from treatments like surgery and radiation. Surgery removes a tumor from a part of the body where cancer has ...
Chemo kills cancer cells, plain and simple. It is a drug in the anticancer tool kit. As a survivor of Stage 4 testicular cancer diagnosed 15 years ago, I know how such a diagnosis turns your world ...
The T lymphocyte, especially its capacity for antigen-directed cytotoxicity, has become a central focus for engaging the immune system in the fight against cancer. Basic science discoveries ...
March 4, 2024. "This disease is incurable, it's terminal, and it will eventually kill you. Tell your children, tell your family, they need to know the truth.". Dr. Phil Stieg's verdict ...
Radiation therapy and cell death. Radiation therapy can kill cancer cells by a variety of mechanisms. The main goal of radiation therapy is to deprive cancer cells of their multiplication potential and eventually kill the cancer cells. Cancer cells whose DNA is damaged beyond repair stop dividing and die.
Long Essay on Cancer. In this long essay on cancer, we are providing you with cancer meaning, speech on cancer awareness. ... The treatment of chemotherapy includes a combination of drugs targeted to kill cancer cells. Radiation therapy, on the other hand, makes use of radiations to kill cancerous cells. All these treatments are usually known ...
Cancer is a global health problem responsible for one in six deaths worldwide. Treating cancer has been a highly complex process. Conventional treatment approaches, such as surgery, chemotherapy, and radiotherapy, have been in use, while significant advances are being made in recent times, including stem cell therapy, targeted therapy, ablation therapy, nanoparticles, natural antioxidants ...
Chemotherapy is used to kill cancer cells in people with cancer. There are a variety of settings in which chemotherapy may be used in people with cancer: To cure the cancer without other treatments. Chemotherapy can be used as the primary or sole treatment for cancer. After other treatments, to kill hidden cancer cells.
Cytotoxic T lymphocytes (CTL) are the cells that recognize and destroy cancer cells, and they're first activated in tumor-draining lymph nodes. From there, they enter the bloodstream to reach tumors and battle malignant cells. Tumors, however, are hostile environments for CTLs. When researchers used imaging techniques to examine what goes on ...
Appreciating that sc (anxiety) is an expected, rational part of the journey is an important component of adjusting to living with cancer. 2. You are not going through this alone. You are not the ...
The new approach capitalizes on cancer cells' self-homing ability—the process by which cancer cells can track the cells of their kind that have spread within the same organ or to other parts of the body. Harnessing this power could overcome drug delivery challenges, helping to get therapeutics to tumor sites that may otherwise be difficult ...
6. Essay on Cancer Treatment: (Around 400 Words) Radiation Therapy Kills Cancer Cells by Triggering Apoptosis or Mitotic Death: If a tumor has invaded into surrounding tissues and possibly metastasized to distant sites, surgery may not be able to remove all cancer cells from the body. In some cases, surgery is not even practical.
Cancer is one of the most important non-infectious or non-communicable diseases. "Cancer is referred to as an ailment characterised by an unrestrained growth of abnormal cells which if untreated and unchecked eventually kills the patient." In India nearly four lakhs of people are affected by cancer every year. Out of them two lakhs of ...
Colorectal cancer, a cancer of either the large intestine or rectum, is the third most common type of cancer, and the second most common cause of death from cancer, worldwide. There were 1.9 ...
The best way to reduce your risk is to avoid unnecessary exposure to UV light. The sun's rays are strongest between 10 a.m. and 4 p.m., so limit your time outside during those hours.
Prostate cancer is still the No. 2 cancer killer among men. I want the goals of the Cancer Moonshot to be met — to end cancer as we know it. Early detection really matters, and when combined ...
Introduction. Tobacco is a well established cause of at least 13 cancers; 1 however, until recently there have been no large evidence-based assessments of the effects of smoking on cancer treatment outcomes. The 2014 Surgeon General's Report 1 is the "first large evidence review to report a causal association between tobacco use and adverse clinical outcomes for patients with cancer".
COLLINS: So because the cancer does seem to be completely still contained within the prostate, after much searching to be sure of that, then the best way to avoid a downstream outcome, which I ...
The bioengineered immune players called CAR T cells last longer and work better if pumped up with a large dose of a protein that makes them resemble stem cells. The papers "open a new avenue for ...
Guest Essay. We Regulate a Tiny Fraction of the 12,000 'Forever Chemicals.' There's a Better Way. ... my father had just been diagnosed with advanced colorectal cancer and been given a short ...
Nasopharyngeal carcinoma (NPC) is one of the deadliest cancers in the world. In treating NPC, Intensity Modulated Radiation Therapy (IMRT) uses radiation fields from several directions to kill cancer cells and shrink tumours. IMRT requires accurate planning using the Treatment Planning System (TPS) to avoid organs at risk (OARs) around the nasopharyngeal cavity. The purpose of this study is to ...