Update: RaDonda Vaught Sentenced to 3 Years Supervised Probation
On May 13, 2022, RaDonda Vaught was sentenced to three years supervised probation with judicial diversion. The diversion option allows first-time offenders to have charges dropped and their records expunged once they successfully complete probation. Vaught faced a potential sentence of up to eight years imprisonment.
Davidson County Criminal Court Judge Jennifer Smith noted that there “have been consequences to the defendant.” Although Vaught will not be imprisoned unless she violates the probation conditions, she was fired and lost her nursing license.
Nurses and other healthcare workers attended the trial to protest the criminalization of nursing mistakes. After the verdict was announced, many applauded.
Joelle Y. Jean, RN, FNP-C, feels very happy with the sentencing. Along with the sentencing, Jean feels even happier nurses rallied together to support Vaught.
“We need to keep this same energy when other nurses find themselves in situations like this,” Jean says. “We need to continue to have each other’s backs and fight for what’s right and speak up, even if it’s through social media or writing to our legislators.”
Organizations including the American Nurses Association (ANA) and the Institute for Healthcare Improvement (IHI) spoke out on the trial overall:
- “While we are relieved that Ms. RaDonda Vaught did not receive a prison sentence, we remain disappointed and deeply concerned about the criminalization of error in medicine, which offers no remedy for improving patient safety. In fact, Ms. Vaught’s arrest and conviction makes patients less safe,” the IHI said in a statement.
- “We are grateful to the judge for demonstrating leniency in the sentencing of Nurse Vaught. Unfortunately, medical errors can and do happen, even among skilled, well-meaning, and vigilant nurses and healthcare professionals,” the ANA said in a statement.
In March 2022, a jury found former Tennessee nurse RaDonda Vaught guilty of criminally negligent homicide and gross neglect of an impaired adult after injecting a patient with the wrong medication, bypassing several safeguards and system warnings. The Vaught trial brings public attention to how medical errors happen in nursing and how safeguards can fail.
Healthcare providers, especially nurses, have been watching events closely due to the rarity of criminal trials for nursing mistakes. Instead, most nursing errors are addressed through nursing boards for professional discipline and civil courts for legal consequences.
“This case is a nurse’s worst nightmare,” family nurse practitioner Joelle Jean says.
Some nurses fear that as a result of this nurse trial:
- Medical mistakes will be increasingly criminalized.
- Nurses will be the scapegoats for overall failures to create a culture of safety.
- Nurses will be afraid to admit to medical errors or to report others’ errors.
“The criminalization of medical errors is unnerving, and this verdict sets into motion a dangerous precedent,” the American Nurses Association said in a statement in response to the conviction of Vaught.
This article explains what happened and the steps nurses and nurse leaders can take to support safety at an individual and organizational level.

What Happened in the Vaught Case: In Brief
On Dec. 24, 2017, Charlene Murphey was admitted with a brain injury to Vanderbilt University Medical Center, where DeRonda Vaught worked as a nurse. To prepare her for a brain scan, Murphey was prescribed Versed, a benzodiazepine used to help patients relax.
The fatal medical error resulted from Vaught’s interactions with an electronic medication cabinet, where nurses must enter the first part of the medication’s generic name to withdraw a drug. Vaught attempted to withdraw Versed by typing “VE” into the system without realizing she should be searching for “midazolam,” the generic name for Versed.
When the cabinet did not dispense Versed, Vaught triggered an override of the machine and withdrew vecuronium, a paralyzing medication, overlooking at least five warnings.
She administered the vecuronium and left Murphey to be scanned. Murphey died, and Vaught testified in a hearing that she was at fault because she had been “distracted” and “complacent.”
The state board of nursing rescinded her nursing license, and Vaught was later charged with reckless homicide. She was acquitted of that charge but convicted of gross neglect of an impaired adult and negligent homicide, both lesser charges.
When Medical Mistakes Happen in Healthcare
Medical error is a leading cause of illness, injury, and death. Medication errors are one of the most common types. The numbers show how serious the situation is.
- The Food and Drug Administration receives more than 100,000 reports of medication errors annually.
- About four out of 10 Americans (41%) have experienced or known somebody affected by a medical error.
- More than 7 million Americans are affected each year by medication errors, and the total annual cost is $40 billion .
- The estimated medication error rate is between 8% and 25% .
As in any field, medical errors are especially likely to happen when staff is overworked, either through fatigue, distraction, or not having enough time to check and recheck safety measures.
“My thoughts are very similar to nurses and healthcare providers who are overworked, tired, and burnt out,” Jean says. “This could happen to any one of us at any point in our career.”
She adds that the consequences for nurses can be especially grave. Jean encourages nurses to seek ways to protect their license.
“I hope this case is also a wake-up call for nurses, your job is to care for patients, but you must always protect your license no matter what,” Jean says.
Safeguards and When They Fail
The role of safeguards played a major role in the Vaught trial.
Vaught performed manual overrides when accessing the medication and saw, but did not act upon, several warning messages. The prosecution argued that this was so reckless that Vaught’s behavior qualified as a homicide. In contrast, the defense and many nurses argued that the safeguards were so faulty that nurses routinely overrode them to access the correct drugs.
State investigators found that Vanderbilt University Medical Center carried a “heavy burden of responsibility,” but only Vaught faced criminal charges.
“For this unfortunate event to occur, many systems were broken, and many people were involved,” Jean states.
Creating a Culture of Safety as Nurses and Nurse Leaders
Administering medication safely requires five “rights”:
- The right patient
- The right medication
- The right time
- The right dose
- The right route
All parties, including hospital or provider administrators, the healthcare team, nurse leaders, and frontline nurses, can and must foster a culture of safety to ensure these five rights and prevent medical errors.
What Nurses Can Do
In addition to being sure to perform safety checks as individuals, nurses can act to sustain a culture of safety to prevent medical errors. Here are six ways nurses can ensure a culture of safety and protect themselves.
1. If You See Something, Say Something
Nurses can help prevent medical errors by speaking up if they notice a potential error in any of the five rights. This may sometimes require speaking up about a physician’s or supervisor’s potential error, but the ability to do so safely is a must for a true culture of safety.
2. Understand Your Limits
Healthcare workers are in a bind when they are overworked. While they know they need to rest to perform effectively, the nursing shortage has forced many to work even when they don’t have enough rest.
If you’re tired, put extra effort into checking and rechecking to avoid medical errors. Alert a supervisor if you’re aware that you can’t perform safely.
3. Report Issues With Systems That Require Overrides
The prosecution emphasized that Vaught performed several overrides to access the wrong medication during the trial. The defense countered that nurses routinely performed overrides to access correct medications.
Nurses can address this issue by reporting false alarms and excessive overrides to superiors. They can document the number of overrides they must perform to access the correct medications. The Vaught trial may make administrators more aware of the importance of accurate warnings.
4. Pay Attention to Alerts and Alarms
During the Vaught trial, both parties agreed that Vaught saw several warnings as she prepared the incorrect medication. They disagreed on whether this was a case of a professional mistakenly ignoring “the boy who cried wolf” or reckless misconduct.
During the aftermath of this nurse trial, nurses should demand support for taking the extra time it takes to mentally process each alarm message and determine if it is valid or a false alarm. Like overrides, nurses can support safety by reporting false alarms and unnecessary alerts, both for the sake of efficiency and avoiding medical errors.
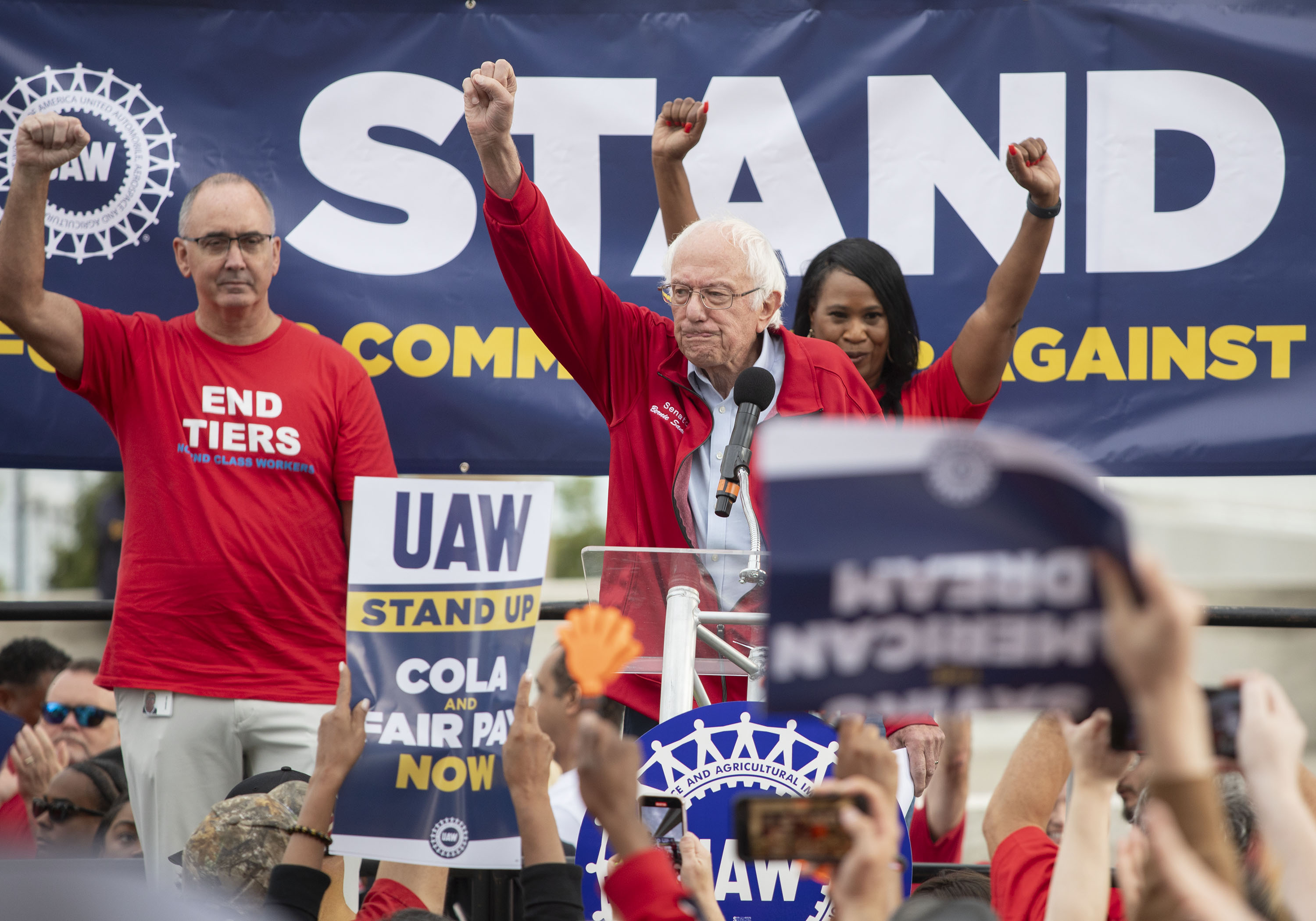
5. Unionize the Workplace
While there are pros and cons to nurse union membership , unions can strengthen the voices of individual nurses. Unions can require staffing ratios and mandate working conditions that include enough rest between shifts.
“Nurses need more protection, and that can be in the form of a nursing union,” Jean says.
6. Protect Yourself
A history of speaking out about errors can help document that you actively promote patient safety. Consider getting your own nurse malpractice insurance to protect yourself and your license as well.
What Nurse Leaders Can Do
Beyond nurses, nurse leaders and hospitals have a role in protecting nurses and creating a culture of safety. Protecting nurses fosters a culture of safety that protects patients.
“Nursing leaders and healthcare institutions have the responsibility to create, measure, and reevaluate the systems that are in place to protect the nurse as well as the patient,” Jean says.
1. Advocate for Their Staff
Nurse leaders must ensure that their staff are equipped to prevent errors, both their own potential errors and those of others. This includes adequate staffing, tools, and education.
They must protect nurses from retaliation for reporting errors and model speaking up when they notice potential medical errors.
2. Create an Environment of Accountability
Jean says that many nurses feel unsupported and that if things go wrong, they will be “thrown under the bus.”
Nurse leaders can create a culture of accountability by ensuring that the organization’s emphasis is on preventing medical errors at a systems and an individual level, rather than punishment after the fact, and that everybody is held responsible for preventing errors.
When nurses believe that the culture of accountability permits them to speak up and that everybody takes responsibility for their actions, they feel they can speak up. They might also recommend improvements and act as a team to prevent medical errors.
3. Ensure Proper Staffing Ratios
Nurse staffing levels affect how much time nurses can dedicate to safety checks and how likely they are to be distracted or functioning without enough rest. Studies consistently associate higher staffing ratios with better patient outcomes.
4. Incorporating Rounds and Debriefs as Daily Practices
Rounds and debriefs ensure that all providers know and communicate about patient conditions and prescribed treatments. They allow all participants to ask and answer questions in real time.
Rounds and debriefs also foster a habit of communication. They can develop professional relationships that help care providers communicate more effectively. Jean also urges providers to implement hourly huddles to share important information.
5. Encourage Writing and Reporting Incident Reports
Incident reports allow healthcare providers to understand what happened in the case of medical errors. Nurse leaders and administrators can use incident reports to look for patterns or potential failure points leading to medical errors.
6. Constantly Look for Ways to Improve Safety
Jean urges nurse leaders to perform root cause analysis to foster a culture of safety and recommends “creating hard stops and performing ‘time outs’ for all procedures.”
A culture where nurses and all staff feel as though they will be listened to means that they will share ideas for improving safety.
7. Build Multidisciplinary Collaborations
Every team in a hospital has a role to play in preventing medical errors, not just clinicians. Human resources can support education, informatics teams can collect and analyze data, technology teams can carry out or recommend software and systems improvements, and clinicians at all levels can share ideas on improving safety and reducing medical errors.
Process, Culture, and Communications
As we saw in the Vaught trial, medical errors often stem from a series of potential risks. Poor judgments at the point of care play a part and did so in this case. But systemic issues are also at play, including tools that generate so many false alarms that it’s difficult to decipher real warnings from warnings that don’t trigger specific actions.
In other cases of medical errors, nurses being overworked and fatigued, poor internal communications, especially during handoffs, and a culture of working around problems rather than addressing them all contribute.
Nurses and nurse leaders can, and usually do, prevent medical errors at the individual and systemic levels and must be given the tools and access to do even more.
Meet Our Contributor

Joelle Y. Jean, RN, FNP-BC
Joelle Jean has been a nurse for more than 10 years and family nurse practitioner for over three years. She has a background in pediatric emergency room, labor and delivery, and primary care medicine. Her passion for the nursing profession and writing led her to her current role as a senior writer for NurseJournal .
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
Public Health
As a nurse faces prison for a deadly error, her colleagues worry: could i be next.
Brett Kelman

RaDonda Vaught, with her attorney, Peter Strianse, is charged with reckless homicide and felony abuse of an impaired adult after a medication error killed a patient. Mark Humphrey/AP hide caption
RaDonda Vaught, with her attorney, Peter Strianse, is charged with reckless homicide and felony abuse of an impaired adult after a medication error killed a patient.
Four years ago, inside the most prestigious hospital in Tennessee, nurse RaDonda Vaught withdrew a vial from an electronic medication cabinet, administered the drug to a patient and somehow overlooked signs of a terrible and deadly mistake.
The patient was supposed to get Versed, a sedative intended to calm her before being scanned in a large, MRI-like machine. But Vaught accidentally grabbed vecuronium, a powerful paralyzer, which stopped the patient's breathing and left her brain-dead before the error was discovered.
Vaught, 38, admitted her mistake at a Tennessee Board of Nursing hearing last year, saying she became "complacent" in her job and "distracted" by a trainee while operating the computerized medication cabinet. She did not shirk responsibility for the error, but she said the blame was not hers alone.
"I know the reason this patient is no longer here is because of me," Vaught said, starting to cry. "There won't ever be a day that goes by that I don't think about what I did."

Shots - Health News
Former nurse found guilty in accidental injection death of 75-year-old patient.
If Vaught's story had followed the path of most medical errors, it would have been over hours later, when the Tennessee Board of Nursing revoked her license and almost certainly ended her nursing career.
But Vaught's case is different: This week, she goes on trial in Nashville on criminal charges of reckless homicide and felony abuse of an impaired adult for the killing of Charlene Murphey, the 75-year-old patient who died at Vanderbilt University Medical Center in late December 2017. If convicted of reckless homicide, Vaught faces up to 12 years in prison.
Prosecutors do not allege in their court filings that Vaught intended to hurt Murphey or was impaired by any substance when she made the mistake, so her prosecution is a rare example of a health care worker facing years in prison for a medical error. Fatal errors are generally handled by licensing boards and civil courts. And experts say prosecutions like Vaught's loom large for a profession terrified of the criminalization of such mistakes — especially because her case hinges on an automated system for dispensing drugs that many nurses use every day.
The Nashville District Attorney's Office declined to discuss Vaught's trial. Vaught's lawyer, Peter Strianse, did not respond to requests for comment. Vanderbilt University Medical Center has repeatedly declined to comment on Vaught's trial or its procedures.
Vaught's trial will be watched by nurses nationwide, many of whom worry a conviction may set a precedent — as the coronavirus pandemic leaves countless nurses exhausted, demoralized and likely more prone to error.
Janie Harvey Garner, a St. Louis registered nurse and founder of Show Me Your Stethoscope , a nurses group with more than 600,000 members on Facebook, said the group has closely watched Vaught's case for years out of concern for her fate — and their own.

A Doctor Confronts Medical Errors — And Flaws In The System That Create Mistakes
Garner said most nurses know all too well the pressures that contribute to such an error: long hours, crowded hospitals, imperfect protocols and the inevitable creep of complacency in a job with daily life-or-death stakes.
Garner said she once switched powerful medications just as Vaught did and caught her mistake only in a last-minute triple-check.
"In response to a story like this one, there are two kinds of nurses," Garner said. "You have the nurses who assume they would never make a mistake like that, and usually it's because they don't realize they could. And the second kind are the ones who know this could happen, any day, no matter how careful they are. This could be me. I could be RaDonda."
As the trial begins, Nashville prosecutors will argue that Vaught's error was anything but a common mistake any nurse could make. Prosecutors will say she ignored a cascade of warnings that led to the deadly error.
The case hinges on the nurse's use of an electronic medication cabinet, a computerized device that dispenses a range of drugs. According to documents filed in the case , Vaught initially tried to withdraw Versed from a cabinet by typing "VE" into its search function without realizing she should have been looking for its generic name, midazolam. When the cabinet did not produce Versed, Vaught triggered an override that unlocked a much larger swath of medications, then searched for "VE" again. This time, the cabinet offered vecuronium.
Vaught then overlooked or bypassed at least five warnings or pop-ups saying she was withdrawing a paralyzing medication, documents state. She also did not recognize that Versed is a liquid but vecuronium is a powder that must be mixed into liquid, documents state.
Finally, just before injecting the vecuronium, Vaught stuck a syringe into the vial, which would have required her to "look directly" at a bottle cap that read "Warning: Paralyzing Agent," the DA's documents state.
The DA's office points to this override as central to Vaught's reckless homicide charge. Vaught acknowledges she performed an override on the cabinet. But she and others say overrides are a normal operating procedure used daily at hospitals.
While testifying before the nursing board last year, foreshadowing her defense in the upcoming trial, Vaught said that at the time of Murphey's death, Vanderbilt was instructing nurses to use overrides to overcome cabinet delays and constant technical problems caused by an ongoing overhaul of the hospital's electronic health records system.
Murphey's care alone required at least 20 cabinet overrides in just three days, Vaught said.
"Overriding was something we did as part of our practice every day," Vaught said. "You couldn't get a bag of fluids for a patient without using an override function."
Overrides are common outside of Vanderbilt, too, according to experts following Vaught's case.
Michael Cohen, president emeritus of the Institute for Safe Medication Practices, and Lorie Brown, past president of the American Association of Nurse Attorneys, each said it is common for nurses to use an override to obtain medication in a hospital.
But Cohen and Brown stressed that even with an override, it should not have been so easy to access vecuronium.
"This is a medication that you should never, ever, be able to override to," Brown said. "It's probably the most dangerous medication out there."
Cohen said that in response to Vaught's case, manufacturers of medication cabinets modified the devices' software to require up to five letters to be typed when searching for drugs during an override, but not all hospitals have implemented this safeguard. Two years after Vaught's error, Cohen's organization documented a "strikingly similar" incident in which another nurse swapped Versed with another drug, verapamil, while using an override and searching with just the first few letters. That incident did not result in a patient's death or criminal prosecution, Cohen said.
Maureen Shawn Kennedy, the editor-in-chief emerita of the American Journal of Nursing , wrote in 2019 that Vaught's case was "every nurse's nightmare."
In the pandemic, she said, this is truer than ever.
"We know that the more patients a nurse has, the more room there is for errors," Kennedy said. "We know that when nurses work longer shifts, there is more room for errors. So I think nurses get very concerned because they know this could be them."
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. It is an editorially independent operating program of KFF (Kaiser Family Foundation).
- criminal case
- Newsletters
Site search
- Israel-Hamas war
- 2024 election
- TikTok’s fate
- Supreme Court
- All explainers
- Future Perfect
Filed under:
- Health Care
A nurse was just sentenced to 3 years of probation for a lethal medical error
RaDonda Vaught’s conviction set a dangerous precedent for patient safety, but is also driving a push for better protections for nurses.
Share this story
- Share this on Facebook
- Share this on Twitter
- Share this on Reddit
- Share All sharing options
Share All sharing options for: A nurse was just sentenced to 3 years of probation for a lethal medical error
/cdn.vox-cdn.com/uploads/chorus_image/image/70867034/AP22133571694690.0.jpg)
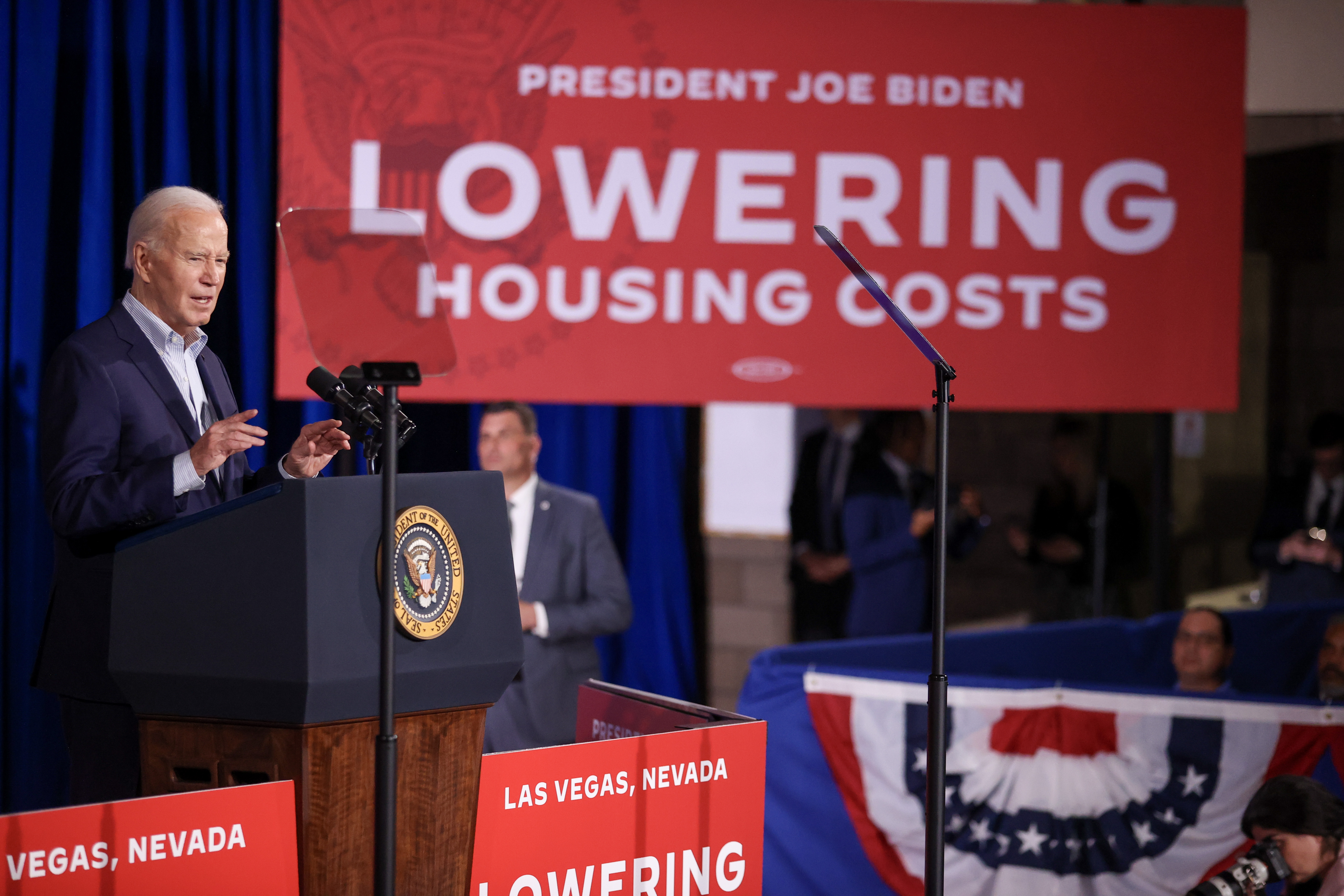
RaDonda Vaught, whose criminal prosecution for a fatal medical error made her case a flashpoint in national conversations about nursing shortages and patient safety, was sentenced on Friday to three years of probation in a Nashville criminal court. After the probationary period, she could ultimately have her conviction dismissed .
Vaught had been convicted of criminally negligent homicide and gross neglect of an impaired adult, which together carried a potential prison sentence of up to eight years .
In late 2017, Vaught, a nurse, mistakenly administered the wrong medication to patient Charlene Murphey while Murphey awaited a radiologic study at Vanderbilt University Medical Center. Murphey died as a consequence of the error, and an investigation later found that multiple patient safeguards that should have existed in the hospital had been absent or failing at the time of the event and were partially responsible for her death.
Vaught’s errors included removing the wrong medication from one of the hospital’s electronic prescribing cabinets, overlooking several warnings on the medication vial, and not monitoring Murphey’s vital signs after administering the medication.
What made Vaught’s case notable was that she was prosecuted in criminal court, a decision made by the Nashville district attorney. Most nursing malpractice cases are disciplined through state nursing boards, which can revoke professional licenses. If legal action is taken in nursing errors, it is generally through civil courts, where patients and families can obtain financial compensation.
Vaught’s case was also notable because while she was charged with a crime, her employer — Vanderbilt University Medical Center — faced fewer consequences.
A federal investigation found that at the time Vaught made the error, gaps in the hospital’s patient safety policies and systems constituted an immediate threat to patients .
While the hospital settled a civil case out of court with Murphey’s family, it has not been held criminally liable. And while the Tennessee health department revoked Vaught’s license, it did not punish the hospital, although the Tennessee Bureau of Investigation found multiple instances of wrongdoing and cover-ups on the hospital’s part.
Although the sentencing was lenient, patient safety advocates and nursing groups are upset about the case, and say it sets a bad precedent: because Vaught individually took the fall for a systematic failure.
Punishing individuals for systemic safety failures is concerning to patient safety advocates because it is ultimately detrimental to patient safety.
Why punishing nurses for medication errors can make patients less safe
For decades , scholars have understood that keeping patients safe requires continually improving the systems that prevent and catch medical errors before they happen. Critically, those systems cannot improve if the people within them don’t feel safe reporting problems.
One of the biggest concerns among patient safety experts is that severe punishment for medical errors — as in Vaught’s case — will lead to reduced error reporting by other nurses due to fear of being fired, or fear of prosecution. That could lead systemic problems to persist unfixed, which would be worse for patient safety.
In an April interview , Robert Gatter, a health law expert at Saint Louis University, said Vaught’s prosecution was a smokescreen that distracted from her employer’s inadequate safety systems. “They can forever now point to this person and say, ‘Wow, she is so bad,’” he said, rather than being held accountable for having a broken patient safety infrastructure.
Vaught’s case is one of several recent cases in which criminal charges were levied against nurses in settings ranging from jails to nursing homes. Many nurses say this trend, combined with the stresses of the pandemic and preexisting nursing shortages , has exacerbated already low morale among nurses.
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/23463067/AP22133548366774.jpg)
Anecdotally, their disillusionment is leading many nurses to leave patient care roles. But there are signs Vaught’s verdict might be an inflection point for broader patient safety efforts.
Kedar Mate, a physician who is president of the Institute for Healthcare Improvement , recalls a recent anecdotal example of the case’s potential chilling effect among medical professionals. He was in an audience for a talk on patient safety in a room full of doctors and nurses. When the speaker asked how many of the attendees had reported a medical error, most of the hands in the room went up — and when he asked how many would do it now, in light of the Vaught case, most of the hands went down. “It’s had a very significant effect,” he said, although there isn’t hard data to cite here.
Mate said several hospital CEOs — for example, the leadership of Northern Virginia’s Inova Health — are trying to head off that concern by communicating directly with employees. “Health system leaders are issuing statements, supporting their staff to come forward transparently to report — in essence, saying that ‘We hear and see what’s going on in Tennessee. In our system, we value transparent, candid, open, honest reporting of near misses and adverse events.’”
It’s hard to know what the outcome of that outreach will be. Rates of medical errors — and measures of staff willingness to report them — are only revealed over time.
“We’re not going to know for a little while whether this is going to have an effect,” said Mate of Vaught’s case.
The case is inspiring calls for policies that support nurses, and patients
American nurses are under enormous strain , and Vaught’s sentencing is unlikely to help. However, the case has directed attention to policies and legislations that would help prevent medical errors in the first place.
For one, the case has energized efforts to establish a National Patient Safety Board (NPSB), which would function much the way the National Transportation Safety Board does by reviewing data on medical errors and close calls with the highest likelihood of causing patient harm. The NPSB would then make recommendations for solutions and corrective actions that would prevent further bad outcomes for patients.
Karen Feinstein, leader of the advocacy coalition supporting the board’s creation, said she now uses Vaught’s case as an example of why the agency is necessary. “If you had an NPSB,” she said, “I don’t believe an accident like this would happen.”
An estimated 7,000 to 9,000 people die in the US each year as a result of a medication error. With a national board in place, many factors that contributed to the error that killed Charlene Murphey could have been identified in advance, including persistent software problems that weakened automated safety checks during medication dispensing, and Vaught’s distraction by an orientee (Vaught had been multitasking when the error occurred, helping with nursing needs across her unit and orienting a new employee).
Nurse-to-patient ratios are an important determinant of patient safety , and bills aimed at ensuring safer staffing ratios are making their way through the House and Senate . At the National Nurses March in Washington, DC, yesterday, many of those marching expressed support for the bills. The powerful hospital lobby is likely to oppose the legislation, lowering its chances of success, said a senior congressional staffer who requested anonymity to speak candidly about the bill. But nurses and nurses unions in several states are advocating for its passage.
On the day of the sentencing, hundreds of nurses gathered across the street from the Nashville municipal courthouse to support Vaught, a purple banner reading “We are nurses not criminals” on display. They held hands as they listened to a live broadcast of Judge Jennifer Smith’s decision, and erupted in cheers as the sentence was read.
Julie Griffin, a Florida nurse who was fired in 2018 after making complaints about unsafe staffing and monitoring procedures at the medical center where she worked, attended the rally. After the sentence was handed down, she said she felt ambivalent. “I mean, it’s a great verdict,” she said, “on a charge that should never have been imposed.”
The sentence notwithstanding, the case had already done damage to the nursing profession, said Griffin. Nurses were walking away from the profession before Vaught’s April verdict, but the case has intensified the sense of alienation for many, she said.
“The health care system needs to look in towards itself and start promoting a culture where nurses are allowed to speak up — to effect change before these things happen,” she said.
Will you help keep Vox free for all?
At Vox, we believe that clarity is power, and that power shouldn’t only be available to those who can afford to pay. That’s why we keep our work free. Millions rely on Vox’s clear, high-quality journalism to understand the forces shaping today’s world. Support our mission and help keep Vox free for all by making a financial contribution to Vox today.
We accept credit card, Apple Pay, and Google Pay. You can also contribute via
Next Up In Science
Sign up for the newsletter today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
Thanks for signing up!
Check your inbox for a welcome email.
Oops. Something went wrong. Please enter a valid email and try again.

Why is there so much lead in American food?

Multigenerational housing is coming back in a big way
You can’t afford to buy a house. Biden knows that.
Want a 32-hour workweek? Give workers more power.

The harrowing “Quiet on Set” allegations, explained

The chaplain who doesn’t believe in God
- Visit Nurse.com on Facebook
- Visit Nurse.com on YouTube
- Visit Nurse.com on Instagram
- Visit Nurse.com on LinkedIn
Nurse.com by Relias . © Relias LLC 2024. All Rights Reserved.
Jump to navigation

Bookmark/Search this post

Mayo Clinic School of Continuous Professional Development
You are here, a criminal case against a nurse for medication error: lessons learned from the radonda vaught case.
- Accreditation

Nurses and clinicians have been criminally prosecuted for medication errors and negligence leading to patient deaths. Listen to the lessons learned from these cases and learn strategies to reduce liability in nursing practice. A must for every nurse.
Target Audience
This course series is designed for nurses in all practice settings.
Learning Objectives
Upon completion of this activity, participants should be able to:
- Identify the potential for criminal and civil liability in clinical nursing practice.
- Describe two strategies to reduce civil liability in nursing care.
- Summarize three lessons learned from a criminal medication error case against a nurse.
Attendance at any Mayo Clinic course does not indicate or guarantee competence or proficiency in the skills, knowledge or performance of any care or procedure(s) which may be discussed or taught in this course.
- 1.00 Attendance
Faculty Elizabeth G. Rudolph, JD, MSN, RN, PLNC Founder and CEO JurexNurse.com
Course Director Denise Rismeyer, MSN, RN, NPD-BC Nursing Education Specialist-Continuing Nursing Education Program Assistant Professor of Nursing, Mayo Clinic College of Medicine and Science Department of Nursing Mayo Clinic, Rochester, MN
Credit Statements ANCC Mayo Clinic College of Medicine and Science designates this enduring activity for a maximum of 1.00 ANCC contact hours.

Other Healthcare Professionals A record of attendance will be provided to all registrants for requesting credits in accordance with state nursing boards, specialty societies or other professional associations.
Available Credit
Cancellation and Refund Policy
Request for cancellations must be submitted in writing to [email protected] .
If the cancellation is made prior to the start of the activity, a refund less an administration fee of $25 will be issued. If the cancellation is made after the start of the activity, no refund will be issued. All refunds will be made using the same method as the original payment.
Any use of this site constitutes your agreement to the Terms and Conditions of Online Registration.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Ethics Hist Med
Ethical and legal aspects of patient’s safety: a clinical case report
Maliheh kadivar.
1 Professor, Division of Neonatology, Department of Pediatrics, Children’s Medical Center, Tehran University of Medical Sciences, Tehran, Iran.
Arpi Manookian
2 Assistant Professor, School of Nursing & Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
Fariba Asghari
3 Associate Professor, Medical Ethic s and History of Medicine Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Nikoo Niknafs
4 Assistant Professor, Division of Neonatology, Department of Pediatrics, Vali-e-Asr Hospital, Tehran University of Medical Sciences, Tehran, Iran.
Arash Okazi
5 Assistant Professor, Department of Forensic Medicine, Tehran University of Medical Sciences, Tehran, Iran.
Asal Zarvani
6 Nursing Student, School of Nursing & Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
Since patient safety is multidimensional and grounded in ethical and legal imperatives, both ethical and legal challenges should be taken into account. In this regard, a falling incident case of a 12-day-old newborn was raised in the monthly ethics round in the Children's Medical Center of Tehran University of Medical Sciences, Iran, and the ethical and legal dimensions of patient safety were discussed by experts in various fields.
This report presents different aspects of patient safety in terms of root cause analysis (RCA) and risk management, the role of human resources, the role of professionalism, the necessity of informing the parents (disclosure of medical errors), and forensic medicine with focus on ethical aspects.
Introduction
According to the non-maleficence principle of medical ethics, ensuring patients’ safety and preventing any injury or damage to them is a major priority for healthcare providers ( 1 ). Thus, it has been the most emphasized component of the quality of health care services all around the world. The Institute of Medicine (IOM) released a report in 1999 entitled "Man is fallible: create a safe health system" in relation to the incidence of medical errors in United States, and consequently, initiated widespread international change in the field of patient safety ( 2 ). Correspondingly, the Iranian health care system implemented special plans purposed to deliver standard health care services and prevent any mistakes and an organized approach to risk management, systematic deficiency, and patient safety improvement ( 3 ). One of these programs is clinical governance which was introduced by the Ministry of Health and Medical Education (MOHME) and initiated since November 2009. Although great emphasis has been placed on the importance of clinical governance by the MOHME, there are some challenges in achieving the desired outcomes ( 4 ). This could be the result of healthcare providers’ inadequate understanding about the importance of clinical governance and lack of organizational safety culture ( 5 , 6 ).
Studies showed that a non-negligible percentage of patients are exposed to health care-related injuries. Based on World Health Organization (WHO) report, the possibility of harming patients in the process of providing health care services is 1 out of 300, whereas the possibility of aviation accidents is 1 out of 100,000. Since 2004, with the beginning of the patient safety project, so far 140 countries have attempted to improve their patients' safety plans in their own health system ( 7 ). The most common cause of injury is medication errors and falling. Although falling includes 21% of total incidents, only 4% of them are serious. Meanwhile the neonatal falling statistics in the USA is 1.6-4.4 in 10,000 live births, an estimated 600-1600 falling incidents in a year. These cases are often the result of shortcomings in systems and processes, organizational complexity and ambiguity, and poor communication ( 8 , 9 ).
Despite various patient safety guidelines and standards, less attention is paid to the ethical and legal aspects of this issue. From a moral perspective, the main goal of patient safety in the health system can be studied from two aspects. It can be studied as a practical value, in the sense that the main focus is its positive outcomes and benefits. It can also be studied as a moral value by focusing on the protection and promotion of humanity and human dignity. It should be emphasized that both aspects are important in the health system. From a professional point of view, moral values in patient safety are not separated from basic medical obligations, but are so central that they may be the source of other moral values emphasized in medicine. This means that patient safety is closely related to the concept of human dignity and all patient safety measures taken must insure the protection of human’s dignity ( 10 ). In other words, the responsibility of the health care staff and professional commitment, in general, are closely related to human dignity ( 11 ).
This case was raised in the monthly ethics round in the Children's Medical Center of Tehran University of Medical Sciences, Iran, and ethical dimensions of patient safety were discussed by experts in various fields. The opinions expressed in this article are a summary of the views of experts in various fields including neonatology, medical law, ethics, and nursing.
It is worth mentioning that the ethics round has been held every month for more than 5 years in the Children's Medical Center. A complicated case is discussed in each session with the presence of different relevant experts.
The clinical case
A 12-day old newborn infant was hospitalized in the neonatal intensive care unit (NICU) because of multiple seizures. He was the first child of the family. The mother’s and family history was negative for seizures or any other disease. Seizures were controlled by medications, and diagnostic assessments including electroencephalography (EEG) were ordered. As the infant was stable and had tolerated breast feeding, it was planned to transfer him to the level II NICU, but it was postponed due to lack of available beds.
On the evening shift of the third day of admission, his nurse heard a sudden noise and noticed that the incubator door was open and the baby was on the floor. The in-charge nurse immediately announced the incident to the on-call physician. The newborn was examined thoroughly and no physical injuries were found. Moreover, the incident was reported to the chief physician of the department and the record of this incident was immediately sent to the hospital officials. Later, all other incubators were inspected to make sure they were secure enough.
When the staff informed the newborn’s father of the falling, he accused the mother of neglecting the child, although she had said that she was resting at the time of the incident.
The questions raised in the meeting were as follows:
What are the factors leading to this incident? How could this incident been prevented? What is the responsibility of the staff in dealing with this incident? Based on professional commitments, what is the duty of medical and nursing staff in such events? What are the ethical issues of patient safety in this case? What are the legal obligations and consequences of this case?
Root cause analysis and risk management
Searching for the causes and finding the right solution, in other words, the basic analysis of the incident is one of the initial and essential measures taken to decrease the incidence of patient injuries. It should be noted that the mentioned process must be free of any bias and should focus on finding the main cause and resolving it instead of identifying the responsible person. One way of preventing such events is to have a special guideline for reporting the event in a suitable organized ethical atmosphere without accusing anyone. Indeed, fear of blame, penalties, limited organizational support, inadequate feedback, and lack of knowledge about the associated factors are some of the barriers to reporting medical errors in hospitals ( 12 ).
Assessment and reduction of patients’ risk of injury, or risk management in the clinical setting is influenced by several factors. One way is the establishment of an organizational culture based on mutual trust and effective communication in all hospital levels ( 13 , 14 ).
From an ethical perspective, the value of trustworthiness is a prerequisite of successful risk management. This value is connected to safety culture since it refers to physical safety, psychological safety, and cultural safety. Thus, the managers’ responsibility is to create mental and physical safety settings based on openness in order to promote patient safety and care quality. Furthermore, it is important for the managers to encourage multidisciplinary collaboration to facilitate transparent reporting ( 10 ).
In this case, the apparent reason was that the incubator door was left open by someone or was not correctly closed. Questions raised in this context include the following: Was the nurse occupied with other emergency and essential actions? Was the incubator door latch broken? Why would the nurse forget to accurately examine the door? Is it possible that lack of guidelines for patient safety led to this incident?
The most important step to reduce the possibility of such events in clinical settings is to establish policies and procedures that work best for each ward. Furthermore, the continuous training of the personnel in patient safety, steady supervision, and controlling the efficacy level of the performed actions are some other steps that can be taken in this regard. For instance, in this case, frequent checking of the incubator door, the use of two locks, and explanation of safety tips regarding the incubator to the staff are also important. Furthermore, evaluation and constant controlling of compliance with patient safety rules, and feedback are also necessary.
The role of human resources
The quantity of human resources is also noteworthy in the field of patient safety. In other words, quality assurance depends on the quantity of manpower. Therefore, in order to prevent similar incidents, providing an adequate number of staff at the bedside is essential ( 12 ).
The role of professionalism
Professional ethics and patient safety are intertwined fundamental concepts in medicine. Patient safety is grounded in ethical principles which are considered as care quality indicators ( 15 ). The realization of patient safety requires the provision and implementation of a professional code of ethics. Based on the Iranian healthcare professional code of conduct, it is expected that all patients be treated with dignity and be protected from any possible harm ( 16 ). Accordingly, adherence to ethical principles requires healthcare providers to identify potential safety failures to prevent falling incidents ( 15 ).
The establishment of patient safety has different individual, professional, and organizational aspects with a special focus on ethics. Professional and organizational commitment leads to detecting and reporting of both one’s own and others’ errors ( 10 ).
From an ethical view, the following actions are recommended:
Following professional and institutional guidelines (if any exist) related to falling incidents; Taking basic actions to assess the patient’s physical health and rescue his/her life; Informing the in-charge staff; Punctual assessment of the situation, and complete documentation and reporting of the event (important data such as the time of the incident, the infant’s position, level of consciousness, vital signs, those present at the scene, actions taken in the process, and etc.) should be documented; Informing the parents and providing them with emotional support.
Informing parents (Disclosure of medical errors)
It seems in case of any error made by the care team, the event must be announced to the parents honestly without blaming the care providers. Moreover, irritating phrases such as “It happens” and “Nothing has happened though” should not be used.
Under circumstances in which errors were caused by inappropriate pattern of providing hospital services, parents should be reassured that all services will be paid for by the hospital. It would be better if the parents were informed by the chief physician or the head nurse and given enough time to express their concern or anger.
Although anger under such circumstances is a natural reaction, we cannot hide medical errors because of fear of parents’ reaction. Moreover, parents’ anger would be more severe if they found out that the hospital personnel have concealed the truth.
It should be considered that knowing the truth is one of the basic rights of patients and their family members. According to similar studies, explaining the error to the patients could be a stressful situation combined with intense emotional reactions from patient/family members or the care team. Generally, the person who committed the error has a sense of guilt or fear of punishment, and patient/family members experience feelings such as anger and anxiety. Furthermore, it should be noticed that primary conversations usually take place when there is not accurate and comprehensive information about the event, so recognizing, understanding, and explaining all the details in complicated clinical situations is not possible. Thus, it is suggested that in such situations, information be given in several stages and by providing psychological support for the patient. Furthermore, while they may need supportive interventions, the patient's family can be considered as an important source of information in the process of root cause analysis (RCA) of similar incidents ( 17 - 20 ). Since creating ethical patient safety is a multidimensional accomplishment, it should be considered that actively partnering with the patient’s family may be a high-yield approach to detecting and preventing medical errors ( 10 ).
In addition, regarding the presented case, the father should be ensured that hospitalizing the newborn was necessary and the mother should not be blamed. In fact, he should be ensured that the incident was entirely due to system error and not by the mother. Basically, maintaining the integrity of the family is essential and medical staff must consider family support at all stages, especially in such circumstances.
Indeed, an important ethical point in this case is the necessity of offering an honest apology. It is not always as simple as saying: “We are sorry”. The way of informing the parents is a sensitive issue and there is an urgent need for training healthcare providers in sensitive interpersonal relationships and related skills to facilitate honest and proper communication with the patient’s family ( 20 ).
Forensic medicine aspect
Laws and regulations related to patient safety, which may vary based on the legislation system of each country, should encourage the disclosure of medical errors while supporting the implementation of the ethical imperatives of patient safety. In general, based on the medical law, the patient who is a victim of negligence is supposed to be fairly compensated. In addition, these rules provide possibilities for promotion of transparency and open communications in all levels. Reaching this goal requires regarding all stakeholders in the healthcare system ( 21 ).
In the mentioned case, some questions could be raised. Either the falling was in the presence of the mother or not. If it was in her presence, the hypothesis is that she dropped the baby intentionally. However, if there is no sign of any apparent trauma, it seems there was no specific hurtful force or he fell from his mother’s arms, and it shows the mother’s lack of experience.
Accordingly, it should be considered that maternal postpartum sleepiness is one of the major risk factors for falling of newborns. Half of all newborn falling incidents in hospitals have occurred while the mother was holding the infant in a hospital bed. Therefore, recognizing the risks of neonatal falling during mother–baby care situations and teaching the mothers is a major nursing responsibility ( 22 ).
If the mother is incapable of taking care of the hospitalized baby, she should be under supervision of the care team and should be educated. Furthermore, notifying the father is an appropriate act if the complaint was raised by the father.
The main task of the physician or nurse after a detailed examination and treatment is the detailed registration and description of all events without any assumptions. If the examinations found evidence of neglect, it would be a completely different discussion and calling the social services would be absolutely necessary.
The question might also be raised that “if nothing happened to the child and we did all the assessments to insure his health, are we obligated to inform the parents?”
There is an obligation to inform the patient or the family about every unwanted event in healthcare settings. The idea that there is no need to disclose errors which did not affect the patient is based on the traditional stance of the law. Furthermore, today, it is well known that such disclosures will enhance patients’ trust to healthcare professionals while making them aware of that which is going on around them. In addition, through this approach, healthcare professionals can respect the patients’ autonomy and dignity ( 21 , 23 ).
Despite increased attention toward the quality of health care services, there are still numerous threats to patient safety in healthcare settings. Since patient safety is multidimensional and grounded in ethical and legal imperatives, both ethical and legal challenges should be taken into account.
Reaching the ultimate goal of the healthcare system, which is to ensure quality and safety of the services, requires structured policies and processes to foster the safety settings based on mutual trust. This can be facilitated by encouraging multidisciplinary collaboration for the transparent reporting of medical errors and also active participation of the patients and their families in detecting medical errors. Furthermore, the provision of emotional support and legal protection of the staffs by the organization is essential to encourage voluntary reporting of incidents.
Moreover, training and emphasizing on the professional code of ethics can be effective on deepening the understanding of and belief in the moral foundations of patient safety.
Conflict of interest
The authors declare that there is no conflict of interest.
6 sisters called to study nursing pursue their dreams together
NEW YORK (WCBS) - The family that studies together stays together could be the motto for six sisters from New York all studying nursing together.
The six Lawrence sisters – Nathalia, Danielle, Dominique, Alexsandria, Lauren and Gabriella – can predict what will happen when their professors at Adelphi University call attendance.
“‘Cousins? Are you friends?’ We’re sisters. ‘Sisters?’” Alexsandria Lawrence said.
“‘Oh yeah, ‘cause you guys are like sorority sisters?’ No, we’re biological sisters. ‘All of you?’ Yeah, all of us,” Danielle Lawrence said.
Two years apart, the siblings – by all accounts, inseparable – are all studying nursing.
“It’s a whole support system that I thank God for. I’m just really happy to be with my sisters,” Nathalia Lawrence said.
The Lawrences can be spotted running down hallways and racing up steps with contagious energy, which they say was instilled by their parents. Their father is a former minor league baseball player.
“We went to regular school and home school. So, when we went to home school, he said, ‘You know what? You guys go take the GED, so we can put you in college,’ and that’s how the whole thing started,” Dominique Lawrence said.
The sisters received degrees in public health from State University of New York schools then, based on their good grades, earned scholarships together to Adelphi.
“I am very proud of them. They have faced great adversity, so they really are wonderful role models and mentors for other students,” said Deborah Hunt, the dean of nursing at Adelphi.
The sisters’ obstacles included overcoming homelessness and housing insecurity. They are now living temporarily with relatives in Brooklyn.
Blessed with a strong faith, the siblings say nursing and helping others is their calling.
“You give that sense of calm to the family members. You’re the middleman, and you’re that road to healing,” Gabriella Lawrence said.
The sisters have four more semesters to go. They might begin their nursing careers in an intensive care unit or emergency room, but they vow to be together until they open what they hope will be the Lawrence Sisters Nursing Center.
Copyright 2024 WCBS via CNN Newsource. All rights reserved.

Heavy Snow Overnight; Becoming Sunny & Warm This Week

Vandal spray paints derogatory words on elementary school in Rapid City

‘It’s all gone’: 81-year-old veteran and cancer survivor loses everything in house fire

Gypsy Rose Blanchard announces separation from husband 3 months after her prison release

Author uncovers family tragedy: ‘Death on St Charles Street’ reveals decades-old mystery
Latest news.

Former Oglala Sioux Tribe president denied request for new counsel ahead of federal trial

Judge expands Trump’s gag order after ex-president’s social media posts about judge’s daughter

Warmer air settles in

2-year-old boy drowns in pond while at family gathering, police say

404 Not Found
We can't find the page you're looking for...
Five-star Bayern roll over Rostov
Tuesday, September 13, 2016
Article summary
Robert Lewandowski's penalty was added to by Thomas Müller, Juan Bernat and two Joshua Kimmich strikes as Bayern won 5-0 to give Russian newcomers Rostov a harsh introduction.
Article top media content
Article body.
Bayern München produced a five-star display to dispatch group stage debutants FC Rostov, setting a new UEFA Champions League record with a 13th successive home win.
- Barcelona and Bayern begin in style
- Also in Group D: PSV 0-1 Atlético
Rostov did not help their own cause by giving away two soft goals in the first half, the first a Robert Lewandowski penalty and the second on the stroke of half-time to Thomas Müller, on his 27th birthday.
Bayern had hardly broken sweat in the first 45 minutes, but began to press harder in the second. The impressive Joshua Kimmich scored twice in quick succession before Juan Bernat added a fifth in stoppage time.
Key Player: Joshua Kimmich (Bayern) When Ancelotti announced that Joshua Kimmich would be in the starting XI, many assumed he would replace Philipp Lahm at right-back. Instead, the Italian put him in the heart of his midfield and the 21-year-old didn't disappoint. Not disheartened by two failed attempts on goal in the first half, the Bayern youngster continued to push forward to exploit the space afforded him and was rewarded with his first UEFA Champions League goals.

Bayern's depth Being able to rest key players like Philipp Lahm, Franck Ribéry and Xabi Alonso for a UEFA Champions League match is not a luxury many teams enjoy, but Bayern have quality in abundance. Kimmich has clearly given Carlo Ancelotti something to think about, while the Italian still has to fit Jérôme Boateng into a defence that is yet to concede this season. Kingsley Coman and Arjen Robben are also yet to return to bolster an already devastating attack.
Rostov's rude awakening Rostov discovered just how big the gulf in class is in the UEFA Champions League, as they were outplayed in Munich. Naivety as much as anything cost the Russian side as they gave away an unnecessary penalty, which was converted by the prolific Robert Lewandowski, but the sucker punch was to come on the stroke of half time when poor defending presented Thomas Müller with a simple finish to effectively end the contest.
UEFA.com team reporters' views
Jordan Maciel, Bayern ( @UEFAcomJordanM ) A good start to the campaign for Bayern, who never really had to get out of first gear. Rostov gave a good account of themselves in the first half and will rue conceding the opener from a penalty and then again so close to half-time. Ancelotti will have no complaints as his side claimed all three points and a healthy goal difference ahead of another meeting with Atlético.
Richard van Poortvliet, Rostov ( @UEFAcomRichVP ) Rostov offered little in attack, which is understandable given the size of the task of playing against one of the best sides in Europe. However, it's imperative the side from the south of Russia become more streetwise in their remaining games if they are to have any hope of qualifying.
Match reaction
Carlo Ancelotti, Bayern coach It was a good start to our Champions League campaign. It was difficult to score early on, we didn't have many chances. We got there. At the moment the team is in good condition, both physically and mentally.
Ivan Danilyants, Rostov coach We have never played against a team that played like Bayern today. We tried hard to hold them off and stay organised then the first goal came from an unfortunate penalty. The rest from quick counters. This side is different to the one under Pep Guardiola: they are much more direct.


VIDEO
COMMENTS
Update: On May 13, 2022, RaDonda Vaught was sentenced to three years supervised probation with judicial diversion. The diversion option allows first-time offenders to have charges dropped and their records expunged once they successfully complete probation. Vaught faced a potential sentence of up to eight years imprisonment.
Former nurse RaDonda Vaught is on trial on charges of reckless homicide. Her case raises consequential questions about how nurses use computerized medication-dispensing cabinets.
In late 2017, Vaught, a nurse, mistakenly administered the wrong medication to patient Charlene Murphey while Murphey awaited a radiologic study at Vanderbilt University Medical Center.
Nurse Case Study: Deviation from the standard of care. This case involves a registered nurse working in an ambulatory surgery setting. Total incurred payments and expenses: Greater than $375,000. (Monetary amounts represent only the payment made on behalf of the insured registered nurse and do not reflect payments made on behalf of the other ...
An 80 year-old male was transported by ambulance to the emergency department (ED) for evaluation after experiencing an unwitnessed fall in a local nursing home. The patient resided at the nursing home and had a medical history of severe dementia and osteoporosis. The patient arrived to the ED alone without family or staff from the local nursing ...
April 11, 2019. An RN's careful note-taking protects hospital from liability. This month we look at a case in which a nurse's careful documentation of a patient's neurologic examination ...
Inadequate Nurse's Notes Lead to Lawsuit. Mrs. H was a 71-year-old long-term resident of a skilled nursing facility. Her medical history was significant for severe malnutrition, pneumonia, urinary tract infection, and brittle diabetes mellitus. She was unable to ambulate and required assistance with multiple activities of daily living.
This case study involves a registered nurse working in an operating room setting, who treated a 70-year-old male who presented for a cystoscopy and transurethral resection of the prostate procedure due to urinary retention and benign prostate hyperplasia. Indemnity Settlement Payment: Greater than $250,000. Legal Expenses: More than $25,000.
Legal nurse consulting practice brings medical and legal facts to light using CaseMap® software CASE STUDY— LITIGATION SOLUTIONS The 200+ legal nurse consultants working with P.J. West & Associates (PJWA) provide expert medical consultation to the legal community based on the foundations of ethics, competence and excellence. Their work helps
A historical single-case study was selected for this research because this methodology allows for an in-depth, focused analysis of a nursing home chain. A case study is ideal for examining "what" and "why" questions about a contemporary set of events and allows investigators to analyze real-life events. 43 Standard case study procedures ...
However, it was precisely the nurse's documentation that allowed the court to be able to dismiss the case. Without her documentation, the case would have had to go to trial for a jury to decide ...
tem, and the judicial process; the role of the nurse in legal matters; and the importance of case law in developing standards of nursing care. Part 2 outlines ethical theories and principles, the role of ethics committees and organi-zational ethics, and addresses the application of ethics in nursing settings, including moral distress, moral ...
Dr. Joseph S. Barr, Jr. (Orthopaedic Surgery): Most of what I currently do is review medical legal cases. Mistakes must be documented in the medical record, and the medical record can never be ...
The case against the hospital and the surgeon who admitted her to the second hospital went before a jury. The jury returned a verdict for the son, finding that the professional negligence of the hospital nurses caused the deceased patient's death, and awarded him $500,000. However, the trial court later granted judgment as a matter of law (JMOL ...
This case study attempted to present to the reader a systematic ethical and legal analysis of a specific practice issue in physical therapy. The use of a multi-step process as presented in this paper may be used by other practitioners as a template for analyzing practice issues involving their respective professions.
Nurses and clinicians have been criminally prosecuted for medication errors and negligence leading to patient deaths. Listen to the lessons learned from these cases and learn strategies to reduce liability in nursing practice. A must for every nurse.
Key judgments and application of legislation in key medical negligence cases are discussed. Relevant medicolegal issues and negligence statistics are discussed. The civil tort of negligence is elaborately discussed, step-by-step, with relevant Common Law and legislation relevant to NSW. The watershed cases of Hadiza Bawa-Garba and Nurse Amaro ...
Jonathan S. Towner, PhD, Luke Nyakarahuka, PhD, MPH, BVM, and Patrick Atimnedi, BVM. Marburg virus is carried by the Egyptian rousette bat, a common cave-dwelling fruit bat endemic to sub-Saharan Africa, where populations can exceed 50 000. AMA J Ethics. 2024;26 (2):E109-115. doi: 10.1001/amajethics.2024.109. Case and Commentary.
Abstract. Since patient safety is multidimensional and grounded in ethical and legal imperatives, both ethical and legal challenges should be taken into account. In this regard, a falling incident case of a 12-day-old newborn was raised in the monthly ethics round in the Children's Medical Center of Tehran University of Medical Sciences, Iran ...
MEDSURG Nursing—August 2007—Vol. 16/No. 4 275 Ethics, Law, and Policy Vicki D. Lachman Moral Courage in Action: Case Studies riences cardiac arrest before the discussion occurs and you watch helplessly as members of the Code Blue Team perform resuscitation. Mr. T. is now on a ventilator and the son has dissolved into tears with cries of ...
After graduating, the sisters hope to open their own nursing center together. (WCBS via CNN) NEW YORK (WCBS) - The family that studies together stays together could be the motto for six sisters ...
The facts of the case, as submitted by the applicant, may be summarised as follows. On 9 February 2007 the applicant was arrested on suspicion of drug offences. On 16 February 2007 he was charged with attempted drug trafficking. On 10 February 2007 Bataysk Town Court, Rostov region, ("the Town Court") ordered to place the applicant in ...
Prelate Dimitry of Rostov. Oct. 4 (Sept. 21 old calendar). Prelate Dimitry (Daniel Tuptalo in the world) came from the village Makarovo of the Kiev region.He was born into a Kazak family in 1651. He had to give up his studies at the Kiev academy, because of war and finished his education studying by himself.
Robert Lewandowski's penalty was added to by Thomas Müller, Juan Bernat and two Joshua Kimmich strikes as Bayern won 5-0 to give Russian newcomers Rostov a harsh introduction.