- Open access
- Published: 27 March 2023

The effect of music therapy on cognitive functions in patients with Alzheimer’s disease: a systematic review of randomized controlled trials
- Malak Bleibel 1 ,
- Ali El Cheikh 2 ,
- Najwane Said Sadier 1 , 3 &
- Linda Abou-Abbas ORCID: orcid.org/0000-0001-9185-3831 1 , 4
Alzheimer's Research & Therapy volume 15 , Article number: 65 ( 2023 ) Cite this article
41k Accesses
14 Citations
51 Altmetric
Metrics details
The use of music interventions as a non-pharmacological therapy to improve cognitive and behavioral symptoms in Alzheimer’s disease (AD) patients has gained popularity in recent years, but the evidence for their effectiveness remains inconsistent.
To summarize the evidence of the effect of music therapy (alone or in combination with pharmacological therapies) on cognitive functions in AD patients compared to those without the intervention.
A systematic literature search was performed in PubMed, Cochrane library, and HINARI for papers published from 1 January 2012 to 25 June 2022. All randomized controlled trials that compared music therapy with standard care or other non-musical intervention and evaluation of cognitive functions are included. Cognitive outcomes included: global cognition, memory, language, speed of information processing, verbal fluency, and attention. Quality assessment and narrative synthesis of the studies were performed.
A total of 8 studies out of 144 met the inclusion criteria (689 participants, mean age range 60.47–87.1). Of the total studies, 4 were conducted in Europe (2 in France, 2 in Spain), 3 in Asia (2 in China, 1 in Japan), and 1 in the USA. Quality assessment of the retrieved studies revealed that 6 out of 8 studies were of high quality. The results showed that compared to different control groups, there is an improvement in cognitive functions after music therapy application. A greater effect was shown when patients are involved in the music making when using active music intervention (AMI).
The results of this review highlight the potential benefits of music therapy as a complementary treatment option for individuals with AD and the importance of continued investigation in this field. More research is needed to fully understand the effects of music therapy, to determine the optimal intervention strategy, and to assess the long-term effects of music therapy on cognitive functions.
Introduction
Alzheimer’s disease (AD) is a progressive, incurable neurological illness that is the most common cause of dementia, affecting an estimated 5% of men and 6% of women over the age of 60 worldwide [ 1 ]. The prevalence of AD increases exponentially with age, with 1% of those aged 60 to 64 years old and 24% to 33% of those aged 85 years or older affected [ 2 ]. As the global population ages, it is anticipated that the number of individuals with Alzheimer’s disease will increase.
Neuropsychiatric symptoms, such as apathy, depression, and agitation, are commonly observed in individuals with AD, in addition to the more well-known cognitive symptoms such as memory loss, visuospatial problems, and difficulties with executive functions [ 3 , 4 ]. These symptoms can cause a significant burden to patients, caregivers, and society as a whole [ 5 ]. While pharmacological therapies have been used to manage these symptoms, they have not always been effective in achieving long-term clinical efficacy [ 6 ]. As a result, non-pharmacological interventions have gained increasing attention as a complementary treatment option for managing neuropsychiatric symptoms in AD. Such therapies include cognitive training and music therapy which have been used for decades to improve symptoms of dementia [ 7 ].
Music Therapy is the use of music to address the physical, emotional, cognitive, and social needs of individuals [ 8 ]. The American Music Therapy Association describes music therapy as the use of music interventions in a clinical and evidence-based manner to achieve specific goals, which are tailored to the individual, by a professional who is credentialed and has completed an approved music therapy program [ 8 ]. Music therapy incorporates a crucial aspect of the interaction between the client and therapist through an evidence-based model [ 9 ]. It can include both active techniques, such as improvisation, singing, clapping, or dancing, and receptive techniques, where the client listens to music with the intention of identifying its emotional content [ 9 ]. In music listening approaches, the therapist creates a personalized playlist for the client, which can either be an individualized program or chosen by the therapist [ 9 , 10 ]. Generalized music interventions use music without a therapist present, with the goal of enhancing the patient’s well-being, and can include both active and music listening protocols. Music listening is used to stimulate memories, verbalization, or encourage relaxation [ 9 ].
For many years, music therapy has been used to help manage symptoms of dementia [ 9 , 11 ]. Music therapy can improve mood, cognitive functions, memory, and provide a sense of connection and socialization for patients who may be isolated [ 12 , 13 ]. Studies have found that musical training may help mitigate the effects of age-related cognitive impairments, and the capacity of persons to remember music makes it a good stimulus that engages AD patients [ 7 , 14 , 15 ]. After listening to music, AD patients showed improvement in categorical word fluency [ 16 ], autobiographical memory [ 17 , 18 ], and the memory of the lyrics [ 15 ]. Additionally, it can provide an opportunity for caregivers to participate in therapy sessions, which can improve the overall caregiving experience by giving them the opportunity for self-expression allowing them to depict their thoughts and emotions [ 19 ].
The specific mechanisms by which music therapy is beneficial are not fully understood. In 2003, research indicates that music may activate neural networks that remain intact in individuals with AD [ 20 ]. A recent study by Jacobsen et al. [ 21 ] used 7 T functional magnetic resonance imaging to examine the brain’s response to music and identify regions involved in encoding long-term musical memory. When these regions were evaluated for Alzheimer’s biomarkers, such as amyloid accumulation, hypometabolism, and cortical atrophy, the results showed that, although amyloid disposition was not significantly lower in the AD group compared to the control group, there was a substantial reduction in cortical atrophy and glucose metabolism disruption in AD patients [ 21 ]. These findings suggest that musical memory regions are largely spared and well-preserved in AD, which could help explain why music therapy is so effective in retrieving verbal and musical memories in individuals with the disease [ 21 ].
One experimental paradigm used to study the effects of music therapy in AD is the use of live music performances, in which a music therapist plays live music for individuals with the disease in a group setting [ 22 ]. Another paradigm is the use of individualized music, in which a music therapist creates a playlist of personalized music for an individual with the disease to listen to at home [ 23 ]. Both paradigms have been shown to be effective in improving mood and reducing agitation in individuals with AD [ 22 , 23 ].
The advantages of music therapy for AD patients include its non-invasive nature and lack of side effects, its ability to address multiple symptoms at once, and its cost-effectiveness and ease of implementation [ 9 , 18 , 24 , 25 ]. However, there are also some limitations to its application. Music therapy may not be suitable for patients with severe dementia [ 26 ] as their cognitive and physical abilities may be too impaired to fully participate in therapy sessions. Additionally, it requires trained therapists [ 8 , 9 ], who may not be easily accessible in some areas. In this review, we aimed to summarize the evidence of the effect of music therapy (alone or in combination with pharmacological therapies) on cognitive functions in AD patients compared to those without the intervention.
This systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA 2009) guidelines [ 27 ]. The protocol of this study was registered in PROSPERO. A statement of ethics was not required.
We used the PICO framework (population, intervention, comparator, and outcome) as follows:
P: Alzheimer patients
I: Music therapy (alone or in combination with pharmacological therapies)
C: Alzheimer patients with and without the intervention
O: Cognitive functions
Search strategy and databases
A systematic literature search of PubMed, Cochrane, and HINARI was performed for studies published in peer-reviewed journals from 1 January 2012 up to 25 June 2022. The databases were searched using the keywords of “Alzheimer’s Disease,” “AD,” “music therapy,” “music intervention,” “cognitive functions,” and “cognition.” Keywords were combined using the Boolean operators “OR” and “AND.”
Study selection and eligibility criteria
All randomized controlled trials (RCTs) published between 2012 and 2022 in the English language and providing quantitative measures of the association between AD and music therapy and its effect on cognitive functions were included in our review. Studies that assess the effect of music therapy on patients with a probable diagnosis of AD or studies where the music therapy was combined with another non-pharmacological therapy are excluded.
Data extraction
Search and identification of eligibility according to inclusion criteria and extraction of data were performed by the two reviewers MB and AC. For each paper, detailed information was collected on: study information (author’s name, publication year, and location), sample characteristics (sample size, age, and gender), study design, intervention details (description, duration) the control group, and the cognitive outcome measures.
Methodological quality assessment
A methodological quality assessment of all included studies was performed by two independent reviewers (MB and AC) using the Jadad scale for RCTs [ 28 ]. Although not used as a criterion for study inclusion or exclusion. Jadad scale is developed to assess randomized controlled trials on the bases of 3 essential items: (1) randomization, 1 point if randomization is mentioned 1 additional point if the method of randomization is appropriate and deduct 1 point if the method of randomization is inappropriate,(2) blinding 1 point if blinding is mentioned, 1 additional point if the method of blinding is appropriate, deduct 1 point if the method of blinding is inappropriate; (3) an account of all patients, the fate of all patients in the trial is known. If there are no data, the reason is stated. It is commonly considered that a study is of “high quality” if it scores 3 points or more.
Study selection
The flowchart of the study selection process is presented in Fig. 1 . The literature search identified a total of 144 records. After the exclusion of duplicate records and non-relevant abstracts, 57 studies were retained. After reviewing the full text, 49 studies were excluded according to our inclusion and exclusion criteria. In the end, a total of 8 full-text studies were included in the qualitative synthesis.
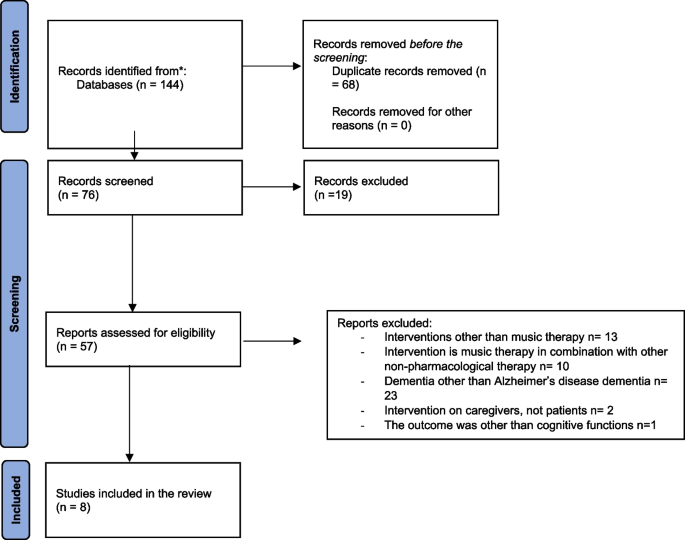
PRISMA flow diagram of the selection procedure
Study characteristics
Characteristics of included studies are presented in Table 1 . The final sample was composed of 8 RCTs, 4 studies were conducted in Europe (2 in France, 2 in Spain), 3 studies in Asia (2 in China, 1 in Japan), and one in the USA. All these studies were published in the English language in peer-reviewed journals. Included trials showed a total of 689 participants (300 females, 43.54%). Sample sizes ranged from 39 [ 29 ] to 298 [ 30 ]. Mean ages ranged from 60.47 [ 31 ] to 87.1 [ 26 ]. Participants’ stages of AD dementia varied from mild to severe. Mean Mini-Mental State Examination (MMSE) [ 32 ] at baseline is assessed in 7 trials out of 8 and varied from 4.65 [ 29 ] to 25.07 [ 33 ].
Intervention characteristics
Music therapy approach.
Music therapy methods were heterogeneous across the included studies. In one study, the active music therapy approach used was singing with the played songs [ 33 ]. Two other studies used the receptive (passive) music therapy approach which consists in listening to music and songs played on a CD player [ 31 , 35 ]. The remaining five studies were based on a combination of both active and receptive music approaches [ 26 , 29 , 30 , 34 , 36 ].
Comparators
In four studies, music therapy intervention was compared to standard care [ 29 , 30 , 34 , 35 , 36 ], while in the four remaining studies, different interventions other than music therapy were used as comparators such as: watching nature videos [ 36 ], painting [ 33 ], cooking [ 26 ], and practicing meditation [ 31 ].
Application of the intervention
Only three trials were conducted by a music therapist [ 29 , 34 , 36 ], 1 trial was conducted by a professional choir conductor [ 33 ], 1 by musicians [ 30 ] and the 3 remaining trials were conducted with facilitators with no musical expertise [ 26 , 31 , 35 ].
Types of applied music
Seven trials out of 8 were based on individualized songs (chosen according to patient’s preferences or songs that are used to evoke positive emotions in them) [ 29 , 30 , 31 , 33 , 34 , 35 , 36 ]. The remaining trial was based on familiar songs chosen without considering the patient’s preferences [ 26 ].
Outcome characteristics
The included studies assessed different outcomes, but we focused on domains directly related to outcome inclusion criteria: global cognition, memory, language, speed of information processing, verbal fluency, and attention. All cognitive outcomes and measurement tools used across studies are listed in Table 1 .
Risk of bias
The quality of trials was assessed by Jadad scales [ 28 ]. Studies with scores ≥ 3 were classified as high-quality studies and those of ≤ 2 were classified as “low-quality” studies. [ 26 , 29 , 30 , 31 , 33 , 36 ] studies were considered high-quality studies while [ 34 , 35 ] studies were considered of low-quality. Blinding of participants was not possible due to the nature of the intervention considered in this review. Randomization was mentioned in all studies except one study [ 34 ]. Results of the quality assessment of all studies using the Jadad scales are summarized in Table 2 .
Results of individual studies
Sakamoto et al. [ 29 ] studied the effect of music intervention (active and passive) on patients with severe dementia. Results showed that there is a short-term improvement in emotional state assessed by the facial scale which is a tool commonly used by psychologists and healthcare professionals to assess and code facial expressions, both positive and negative, to determine a patient’s emotional state [ 37 , 38 ]. In addition to eliciting positive emotions, music therapy has been shown to have long-term benefits in reducing behavioral and psychological symptoms of dementia assessed by the Behavioral Pathology in Alzheimer’s Disease (BEHAVE-AD) Rating Scale, a well-established instrument to assess and evaluate behavioral symptoms in AD patients, as well as to evaluate treatment outcomes and identify potentially remediable symptoms [ 39 ].
The study by Narme et al. [ 26 ] was conducted to evaluate the effectiveness of music and cooking interventions in improving the emotional, cognitive, and behavioral well-being of AD and mixed dementia patients. The study lasted 4 weeks and involved 48 patients, who received two 1-h sessions of either music or cooking interventions per week. Both interventions showed positive results, such as improved emotional state and reduced the severity of behavioral disorders, as well as reduced caregiver distress. However, there was no improvement in the cognitive status of the patients. Although the study did not find any specific benefits of music interventions, it suggests that these non-pharmacological treatments can improve the quality of life for patients with moderate to severe dementia and help to ease caregiver stress [ 26 ].
The study by Gómez Gallego and Gómez García [ 34 ] showed a significant increase in MMSE scores, especially in the domains of orientation, language and memory [ 34 ]. Subsequent study from the same author aiming to compare the benefits from active music therapy versus receptive music therapy or usual care on 90 AD patients showed impressive results of active music intervention improving cognitive deficits and behavioral symptoms [ 36 ]. Other supportive data revealed an increase of MMSE and MoCA scores over the study duration in the intervention group, in comparison to the control group [ 35 ].
The study by Pongan et al. [ 33 ] examined the effects of singing versus painting on 50 AD patients over a period of 12 weeks. Results showed that both therapies elicited benefits in reducing depression, anxiety, and pain. The only advantage that the singing group had over the painting group is the stabilization of verbal memory (assessed using FCRT) over time [ 33 ].
Lyu et al. [ 30 ] study aimed to investigate the effects of music therapy on cognitive functions and mental well-being in AD patients. The study utilized the World Health Organization University of California-Los Angeles Auditory Verbal Learning Test (WHO-UCLA AVLT) to assess the short-term and long-term memory of the participants. Subjects were tested on their ability to recall 15 verbal words immediately and after a delay of 30 min. The results showed that music therapy was more effective in improving verbal fluency and alleviating psychiatric symptoms and caregiver distress than lyric reading in AD patients. The stratified analysis revealed that music therapy improved memory and language ability in mild AD patients and reduced psychiatric symptoms (delusions, hallucinations, agitation/aggression, dysphoria, anxiety, euphoria, apathy, disinhibition, irritability/lability, and aberrant motor activity) and caregiver distress in moderate or severe AD patients. However, no significant effect was found on daily activities in any group of patients [ 30 ].
Innes et al. [ 31 ] study consisted of testing music listening therapy over a period of 12 weeks. Cognitive functions were assessed through various measures, including memory (using the Memory Functioning Questionnaire MFQ), executive function (using the Trail Making Test (TMT) Parts A and B), and psychomotor speed, attention, and working memory (using the 90-s Wechsler Digit-Symbol Substitution Test). The scores assessed at baseline, 3 months, and 6 months after therapy showed an improvement in measures of memory function, psychological status, and cognitive performance including executive functions, working memory, processing speed, and attention [ 31 ].
Neurodegenerative diseases, such as dementia, pose a major challenge to global health and will continue to increase in impact with the aging population. AD is a widespread form of dementia affecting a large number of elderly individuals globally and may contribute to 60–70% of cases [ 40 ]. Despite efforts to find effective treatments through pharmacological means, the results have been disappointing in recent decades. As a result, non-pharmacological therapies have gained more attention as a way to improve cognitive, behavioral, social, and emotional functions in AD patients.
Music therapy has been shown to induce plastic changes in some brain networks [ 41 ], facilitate brain recovery processes, modulate emotions, and promote social communication [ 42 ], making it a promising rehabilitation approach. Thus, the present systematic review aimed to systematically synthesize the impact of music therapy on cognitive functions in AD patients. Out of the eight studies reviewed, totaling 689 subjects, seven studies found a significant and positive effect of music therapy on enhancing cognitive functions in individuals with AD. However, one study by Narme et al. [ 26 ] did not find evidence of the efficacy of music therapy on cognitive functions [ 26 ]. This result may be due to the use of music that was chosen by the therapist, rather than being based on the patient’s preferences, and the use of cooking as a control group rather than a standard group to test the efficacy of the intervention. Furthermore, Narme et al. [ 26 ] suggested that a larger sample size would be beneficial in conducting parametric analysis, which could provide more robust results [ 26 ]. These findings highlight the potential benefits of music therapy as a non-pharmacological intervention for AD patients.
Six out of eight studies revealed that patients who underwent Active Music Intervention (AMI) had better outcomes compared to those who underwent Receptive Music Intervention (RMI) [ 29 , 30 , 33 , 34 , 35 , 36 ]. On the other hand, the findings of the studies by Innes et al. [ 31 ] and Wang et al. [ 35 ] that used only the RMI approach, showed a positive impact on cognitive functions in AD patients [ 31 , 35 ].
In the study by Innes et al. [ 31 ], both the meditation and music listening groups showed significant improvements in cognitive functions, without a significant difference between the two groups. In the study by Wang et al. [ 35 ], music therapy was found to be an effective adjuvant to support pharmacological interventions in AD, leading to significant improvements in the MMSE and MoCA scores. It is worth noting that AMI and RMI differ in terms of the level of patient involvement and the objectives of the therapy. AMI involves the direct participation of patients in musical activities such as singing, playing an instrument, or moving to the beat, whereas RMI consists of passive listening to music. From a functional and physiological perspective, AMI may have a greater impact on cognitive and emotional processes due to the increased level of engagement and interaction with the music [ 36 ]. AMI has been shown to activate brain regions involved in auditory processing, motor control, and emotional regulation, leading to improved cognitive functions and reduced agitation and anxiety [ 41 ]. On the other hand, RMI may have a more relaxing effect, as it can induce changes in heart rate and breathing, reducing stress levels and improving sleep quality [ 42 ]. Based on our systematic review, it is not possible to draw conclusions about the optimal music types (classic music, familiar songs, individualized songs…) for music therapy in patients with AD. This is due to the heterogeneity of the studies included in our review, including differences in the types of music used and the methods of exposure. Therefore, it is not possible to determine with certainty which type of music is most effective for improving cognitive functions in AD patients. Further research is needed to establish the optimal music types and optimal duration of music therapy in this population. Our findings also revealed that individualized music playlists, consisting of songs chosen based on the patient’s preferences, showed improvement in cognitive functions, particularly in memory. A study by [ 31 ] used relaxing music in the intervention group, chosen according to patients’ preferences. The music listening CD to be heard by patients in this study contained selections from Bach, Beethoven, Debussy, Mozart, Pachelbel, and Vivaldi, which resulted in an improvement in cognitive functions. This is consistent with the [ 43 ] study which showed that listening to classical music, specifically selections from Mozart, could result in a temporary improvement in certain cognitive tasks such as abstract/spatial reasoning tests. While the “Mozart Effect” has been linked more to the acute arousal brought on by the pleasure of listening to music, rather than a direct impact on cognitive ability [ 44 ], both studies highlight the potential for listening to classical music to have a positive impact on cognitive functions.
The improvement in orientation, language, and memory domains in individuals with AD, as reported in the studies by [ 34 , 36 ], can be attributed to several factors such as the use of an individualized playlist or the presence of a music therapist to perform the sessions. The study by [ 30 ] suggests that music intervention has a positive effect on verbal fluency, memory, and language in individuals with AD. The rhythmic and repetitive elements of music regulate brain function, and musical activities such as singing and playing instruments can activate neural networks involved in memory and language processing.
Further beneficial effects other than improved cognitive behaviors, memory, language, and orientation, the study by [ 29 ] showed a positive impact on the emotional state of the patients. This is consistent with the idea that several cognitive processes such as perception, attention, learning, memory, reasoning, and problem-solving, are all influenced by emotions [ 45 ]. However, the positive effects observed in the emotional state of the patients disappeared 3 weeks after the intervention period. The effects of the intervention lasted after the follow-up for a period that varied between studies [ 29 , 30 , 31 , 33 , 35 ], from 1 month [ 33 ] to 6 months [ 30 , 31 ]. Further research is needed to determine the most effective and optimal duration for music therapy interventions.
Our review has some limitations including differences in participant characteristics (participant age/severity of illness/cognitive ability…), outcome measures, and intervention methods, that may have influenced the results. Additionally, the music therapy interventions used in the studies differed, with activities ranging from singing to playing instruments. These factors, combined with the small number of studies included in the review, limit the power of our findings. Furthermore, the heterogeneity of the interventions and outcome measures used in the studies makes it difficult to perform a meta-analysis and combine the data in a meaningful way. The varying methods of music selection and exposure also pose challenges in synthesizing the results.
The findings of this review suggest that music therapy could have a positive impact on cognitive functions in patients with AD. This supports the growing body of evidence that targets music therapy as a promising cognitive rehabilitating process aiming to improve cognitive functions in individuals with AD dementia like memory, executive functions, or attention. Improvements in these cognitive functions can, in turn, enhance the quality of life of both the patients and their caregivers. However, more research is needed to fully understand the mechanisms behind these effects and to determine the optimal approach to music therapy for this population, including the time frame for follow-up evaluations. Nevertheless, the results of this review highlight the potential benefits of music therapy as a treatment option for individuals with AD and the importance of continued investigation in this field, including long-term follow-up assessments to determine the sustained impact of music therapy on cognitive functions.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- Alzheimer’s disease
Active music therapy
Behavior Pathology in Alzheimer’s Disease
Digit Symbol Substitution Test
Frontal assessment battery
Free and Cued Recall Test
Memory Functioning Questionnaire
Mini-Mental State Examination
Montreal Cognitive Assessment
Positron emission tomography
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
Randomized controlled trials
Receptive music therapy
Severe impairment battery
Trail Making Test
United States of America
World Health Organization University of California-Los Angeles Auditory Verbal Learning test
World Health Organisation (WHO). World Health Organisation. Summary: World report on disability 2011 (6099570705). 2011. Retrieved from: https://apps.who.int/iris/handle/10665/44575 .
Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–7.
Article PubMed PubMed Central Google Scholar
Geda YE, Schneider LS, Gitlin LN, Miller DS, Smith GS, Bell J, et al. Neuropsychiatric symptoms in Alzheimer’s disease: past progress and anticipation of the future. Alzheimer’s Dement. 2013;9(5):602–8.
Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA. 2002;288(12):1475–83.
Article PubMed Google Scholar
Burns A. The burden of Alzheimer’s disease. Int J Neuropsychopharmacol. 2000;3(7):31–8. https://doi.org/10.1017/s1461145700001905 .
Berg-Weger M, Stewart DB. Non-pharmacologic interventions for persons with dementia. Missouri Med. 2017;114(2):116.
PubMed PubMed Central Google Scholar
Särkämö T, Tervaniemi M, Laitinen S, Numminen A, Kurki M, Johnson JK, Rantanen P. Cognitive, emotional, and social benefits of regular musical activities in early dementia: randomized controlled study. Gerontologist. 2014;54(4):634–50. https://doi.org/10.1093/geront/gnt100 .
American Music Therapy Association AMTA member sourcebook. The Association (1998). retrieved from: https://www.musictherapy.org/ .
Raglio A, Oasi O. Music and health: what interventions for what results? Front Psychol. 2015;6:230. https://doi.org/10.3389/fpsyg.2015.00230 .
Tang H-YJ, Vezeau T. The use of music intervention in healthcare research: a narrative review of the literature. J Nurs Res. 2010;18(3):174–90.
McDermott O, Crellin N, Ridder HM, Orrell M. Music therapy in dementia: a narrative synthesis systematic review. Int J Geriatr Psychiatry. 2013;28(8):781–94.
Koelsch S. Brain correlates of music-evoked emotions. Nat Rev Neurosci. 2014;15(3):170–80.
Article CAS PubMed Google Scholar
Raglio A, Attardo L, Gontero G, Rollino S, Groppo E, Granieri E. Effects of music and music therapy on mood in neurological patients. World J Psych. 2015;5(1):68–78. https://doi.org/10.5498/wjp.v5.i1.68 .
Article Google Scholar
Schellenberg EG, Hallam S. Music listening and cognitive abilities in 10-and 11-year-olds: The blur effect. Ann N Y Acad Sci. 2005;1060(1):202–9.
Simmons-Stern NR, Budson AE, Ally BA. Music as a memory enhancer in patients with Alzheimer’s disease. Neuropsychologia. 2010;48(10):3164–7.
Thompson RG, Moulin C, Hayre S, Jones R. Music enhances category fluency in healthy older adults and Alzheimer’s disease patients. Exp Aging Res. 2005;31(1):91–9.
Irish M, Cunningham CJ, Walsh JB, Coakley D, Lawlor BA, Robertson IH, Coen RF. Investigating the enhancing effect of music on autobiographical memory in mild Alzheimer’s disease. Dement Geriatr Cogn Disord. 2006;22(1):108–20.
Peck KJ, Girard TA, Russo FA, Fiocco AJ. Music and memory in Alzheimer’s disease and the potential underlying mechanisms. J Alzheimers Dis. 2016;51(4):949–59.
Popa LC, Manea MC, Velcea D, Şalapa I, Manea M, & Ciobanu AM. Impact of Alzheimer's dementia on caregivers and quality improvement through art and music therapy. Healthcare (Basel). 2021;9(6). https://doi.org/10.3390/healthcare9060698
Platel H, Baron J-C, Desgranges B, Bernard F, Eustache F. Semantic and episodic memory of music are subserved by distinct neural networks. Neuroimage. 2003;20(1):244–56.
Jacobsen J-H, Stelzer J, Fritz TH, Chételat G, La Joie R, Turner R. Why musical memory can be preserved in advanced Alzheimer’s disease. Brain. 2015;138(8):2438–50.
Cox E, Nowak M, Buettner P. Managing agitated behaviour in people with Alzheimer’s disease: the role of live music. Br J Occup Ther. 2011;74(11):517–24.
Park H, Pringle Specht JK. Effect of individualized music on agitation in individuals with dementia who live at home. J Gerontol Nurs. 2009;35(8):47–55.
Leggieri M, Thaut MH, Fornazzari L, Schweizer TA, Barfett J, Munoz DG, Fischer CE. Music Intervention Approaches for Alzheimer’s Disease: A Review of the Literature. Front Neurosci. 2019;13:132. https://doi.org/10.3389/fnins.2019.00132 .
Van der Steen JT, Smaling HJ, Van der Wouden JC, Bruinsma MS, Scholten RJ, Vink AC. Music-based therapeutic interventions for people with dementia. Cochr Database Syst Rev. 2018. (7).
Narme P, Clément S, Ehrlé N, Schiaratura L, Vachez S, Courtaigne B, et al. Efficacy of musical interventions in dementia: evidence from a randomized controlled trial. J Alzheimer’s Dis. 2014;38(2):359–69.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):1–11.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Sakamoto M, Ando H, Tsutou A. Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int Psychogeriatr. 2013;25(5):775–84.
Lyu J, Zhang J, Mu H, Li W, Champ M, Xiong Q, et al. The effects of music therapy on cognition, psychiatric symptoms, and activities of daily living in patients with Alzheimer’s disease. J Alzheimer’s Dis. 2018;64(4):1347–58.
Innes KE, Selfe TK, Brundage K, Montgomery C, Wen S, Kandati S, et al. Effects of meditation and music-listening on blood biomarkers of cellular aging and Alzheimer’s disease in adults with subjective cognitive decline: An exploratory randomized clinical trial. J Alzheimer’s Dis. 2018;66(3):947–70.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Pongan E, Tillmann B, Leveque Y, Trombert B, Getenet JC, Auguste N, et al. Can musical or painting interventions improve chronic pain, mood, quality of life, and cognition in patients with mild Alzheimer’s disease? Evidence from a randomized controlled trial. J Alzheimer’s Dis. 2017;60(2):663–77.
Gómez Gallego M, Gómez García J. Music therapy and Alzheimer’s disease: Cognitive, psychological, and behavioural effects. Neurologia. 2017;32(5):300–8. https://doi.org/10.1016/j.nrl.2015.12.003 .
Wang Z, Li Z, Xie J, Wang T, Yu C, An N. Music therapy improves cognitive function and behavior in patients with moderate Alzheimer’s disease. Int J Clin Exp Med. 2018;11(5):4808–14.
Google Scholar
Gómez-Gallego M, Gómez-Gallego JC, Gallego-Mellado M, García-García J. Comparative efficacy of active group music intervention versus group music listening in Alzheimer’s disease. Int J Environ Res Public Health. 2021;18(15):8067.
McKinley S, Coote K, Stein-Parbury J. Development and testing of a faces scale for the assessment of anxiety in critically ill patients. J Adv Nurs. 2003;41(1):73–9.
Pautex S, Michon A, Guedira M, Emond H, Lous PL, Samaras D, et al. Pain in severe dementia: Self-assessment or observational scales? J Am Geriatr Soc. 2006;54(7):1040–5.
Monteiro IM, Boksay I, Auer SR, Torossian C, Ferris SH, Reisberg B. Addition of a frequency-weighted score to the Behavioral Pathology in Alzheimer’s Disease Rating Scale: the BEHAVE-AD-FW: methodology and reliability. Eur Psychiatry. 2001;16(Suppl 1):5s–24s. https://doi.org/10.1016/s0924-9338(00)00524-1 .
World Health Organisation (WHO). World Health Organisation. Dementia. 2022. Retrieved from: https://www.who.int/en/news-room/fact-sheets/detail/dementia .
Schlaug G. Part VI Introduction. Ann N Y Acad Sci. 2009;1169(1):372–3.
Thompson W, Schlaug G. Music can heal the brain. Scientific American: MIND. 2015.
Rauscher FH, Shaw GL, Ky CN. Music and spatial task performance. Nature. 1993;365(6447):611–611.
Thompson WF, Schellenberg EG, Husain G. Arousal, mood, and the Mozart effect. Psychol Sci. 2001;12(3):248–51. https://doi.org/10.1111/1467-9280.00345 .
Tyng CM, Amin HU, Saad MNM, Malik AS. The Influences of Emotion on Learning and Memory. Front Psychol. 2017;8:1454. https://doi.org/10.3389/fpsyg.2017.01454 .
Download references
Acknowledgements
Not applicable.
This research received no external funding.
Author information
Authors and affiliations.
Faculty of Medical Sciences, Neuroscience Research Centre, Lebanese University, Beirut, Lebanon
Malak Bleibel, Najwane Said Sadier & Linda Abou-Abbas
Pierre and Marie Curie Campus, Sorbonne University, Paris, France
Ali El Cheikh
College of Health Sciences, Abu Dhabi University, Abu Dhabi, United Arab Emirates
Najwane Said Sadier
INSPECT-LB (Institut National de Santé Publique Epidémiologie Clinique Et Toxicologie-Liban), Beirut, Lebanon
Linda Abou-Abbas
You can also search for this author in PubMed Google Scholar
Contributions
Conception or design of the work: MB and LAA, Data collection, extraction, and quality assessment MB and AC, supervision, LAA, writing—original draft preparation, MB; Critical revision of the article: LAA and NSS; all authors read and approved the final manuscript.
Corresponding author
Correspondence to Linda Abou-Abbas .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Neuroscience Research Committee.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bleibel, M., El Cheikh, A., Sadier, N.S. et al. The effect of music therapy on cognitive functions in patients with Alzheimer’s disease: a systematic review of randomized controlled trials. Alz Res Therapy 15 , 65 (2023). https://doi.org/10.1186/s13195-023-01214-9
Download citation
Received : 26 August 2022
Accepted : 15 March 2023
Published : 27 March 2023
DOI : https://doi.org/10.1186/s13195-023-01214-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cognitive functions
- Music therapy
- Music intervention
Alzheimer's Research & Therapy
ISSN: 1758-9193
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Managing...
Music as a person-centred intervention for dementia
Rapid response to:
Managing neuropsychiatric symptoms in patients with dementia
- Related content
- Article metrics
- Rapid responses
Rapid Response:
Dear Editor
In their timely review of person-centred interventions for managing neuropsychiatric symptoms in dementia, Watt and colleagues do not foreground an intervention of high relevance to many people living with dementia: music.
Evidence from meta-analyses of randomised controlled trials [1,2] suggests that music-based therapeutic interventions in dementia can reduce depressive symptoms and ameliorate behavioural disturbance and may also reduce anxiety and improve emotional well-being and quality of life. Benefits may be further enhanced by ‘personalised playlists’ holding particular resonance for the individual living with dementia [3], potentially even in the later stages of the illness when opportunities for intervention are often limited. Music is a source of meaningful occupation in dementia [4] – a cornerstone of wellbeing in the delivery of person-centred care. By facilitating communication, it may also reduce the frustration and helplessness that contribute significantly to challenging behaviours.
As a therapeutic intervention, music is innocuous, accessible, flexible and relatively easy to implement. Over and above its beneficial effects on standard neuropsychiatric symptom indices of dementia, music is a lifelong source of pleasure and resilience for a great many people, and may help to maintain social connectedness in ways that are difficult to quantify. Music is a unique source of solace against the loneliness and despair that too often attend dementia: a lesson that the Covid-19 pandemic has poignantly affirmed.
Laura M Bolton, Music Therapist, Older People Mental Health, NHS Lothian Arts Therapies Service, United Kingdom [email protected]
Jessica Jiang, Research Psychologist, Dementia Research Centre, University College London, London, United Kingdom [email protected]
Jason D Warren, Professor of Neurology, Dementia Research Centre, University College London, London, United Kingdom [email protected]
Disclaimer: The views expressed here are the authors’ own and do not represent the NHS or other affiliated organisations.
Acknowledgments. Our research in music and dementia is supported by the Alzheimer’s Society, the Royal National Institute for Deaf People, a Frontotemporal Dementia Research Studentship in Memory of David Blechner (funded through The National Brain Appeal) and UCL Music Futures.
1. Van der Steen JT, Smaling HJ, van der Wouden JC, Bruinsma MS, Scholten RJ, Vink AC. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2018; 7: CD003477. doi: 10.1002/14651858.CD003477.pub4
2. Dorris JL, Neely S, Terhorst L, VonVille HM, Rodakowski J. Effects of music participation for mild cognitive impairment and dementia: A systematic review and meta-analysis. J Am Geriatr Soc. 2021; 69: 2659-2667. doi: 10.1111/jgs.17208.
3. Lineweaver TT, Bergeson TR, Ladd K, Johnson H, Braid D, Ott M, Hay DP, Plewes J, Hinds M, LaPradd ML, Bolander H, Vitelli S, Lain M, Brimmer T. The effects of individualized music listening on affective, behavioral, cognitive, and sundowning symptoms of dementia in long-term care residents. J Aging Health. 2022; 34(1): 130-143. doi: 10.1177/08982643211033407.
4. Travers C, Brooks D, Hines S, O'Reilly M, McMaster M, He W, MacAndrew M, Fielding E, Karlsson L, Beattie E. Effectiveness of meaningful occupation interventions for people living with dementia in residential aged care: a systematic review. JBI Database System Rev Implement Rep. 2016; 14(12): 163-225. doi: 10.11124/JBISRIR-2016-003230.
Competing interests: No competing interests
SYSTEMATIC REVIEW article
Music therapy in the treatment of dementia: a systematic review and meta-analysis.

- 1 Department of Inorganic Chemistry, Organic Chemistry and Biochemistry, Faculty of Environmental Sciences and Biochemistry, University of Castilla-La Mancha, Toledo, Spain
- 2 School of Nursing and Physiotherapy, University of Castilla-La Mancha, Toledo, Spain
- 3 Regional Centre for Biomedical Research, University of Castilla-La Mancha, Albacete, Spain
Background: Dementia is a neurological condition characterized by deterioration in cognitive, behavioral, social, and emotional functions. Pharmacological interventions are available but have limited effect in treating many of the disease's features. Several studies have proposed therapy with music as a possible strategy to slow down cognitive decline and behavioral changes associated with aging in combination with the pharmacological therapy.
Objective: We performed a systematic review and subsequent meta-analysis to check whether the application of music therapy in people living with dementia has an effect on cognitive function, quality of life, and/or depressive state.
Methods: The databases used were Medline, PubMed Central, Embase, PsycINFO, and the Cochrane Library. The search was made up of all the literature until present. For the search, key terms, such as “music,” “brain,” “dementia,” or “clinical trial,” were used.
Results: Finally, a total of eight studies were included. All the studies have an acceptable quality based on the score on the Physiotherapy Evidence Database (PEDro) and Critical Appraisal Skills Program (CASP) scales. After meta-analysis, it was shown that the intervention with music improves cognitive function in people living with dementia, as well as quality of life after the intervention and long-term depression. Nevertheless, no evidence was shown of improvement of quality of life in long-term and short-term depression.
Conclusion: Based on our results, music could be a powerful treatment strategy. However, it is necessary to develop clinical trials aimed to design standardized protocols depending on the nature or stage of dementia so that they can be applied together with current cognitive-behavioral and pharmacological therapies.
• Music therapy is used as a treatment for the improvement of cognitive function in people with dementia.
• The intervention based on listening to music presents the greatest effect on patients with dementia followed by singing.
• Music therapy improved the quality of life of people with dementia.
• Music has a long-term effect on depression symptoms associated with dementia.
Introduction
Approximately 50 million people worldwide have dementia, and it is projected to almost triple by 2050 ( 1 ). Dementia is an overall term for diseases and conditions characterized by progressive affectation of cognitive alterations, such as memory and language, as well as behavioral alterations including depression and anxiety ( 2 , 3 ). In order to ameliorate the symptoms of dementia, different intervention approaches, both pharmacological and non-pharmacological, have been trialed. Pharmacological interventions, such as acetylcholinesterase inhibitors, are mainly aimed to treat cognitive symptoms but without avoiding the course of the disease. Unfortunately, these therapies have limited effect on alleviating behavioral and psychological symptoms of dementia ( 2 , 4 ). On the other hand, non-pharmacological interventions can provide complementary therapy, offering versatile approaches to improve outcomes for people living with dementia and minimize behavioral occurrences as well as to improve or sustain quality of life ( 2 , 5 – 9 ). There are many types of non-pharmacological approaches, such as psychosocial and educational therapies (either with individuals or in groups) and physical or sensorial activities (music, therapeutic touch, and multisensory stimuli) ( 7 , 10 – 12 ). In particular, music therapy is thoroughly used in daily clinical practice in case of dementia ( 13 , 14 ). Many authors emphasize the positive effects of music on the brain. In this sense, several studies showed that people with dementia enjoy music, and their ability to respond to it is preserved even when verbal communication is no longer possible. These studies claimed that interventions based on musical activities have positive effects on behavior, emotion and cognition ( 2 , 15 , 16 ). Therefore, studying and playing music alter brain function and can improve cognitive areas, such as the neural mechanisms for speech ( 17 ), learning, attention ( 18 ), and memory ( 19 ). Music can also activate subcortical circuits, the limbic system, and the emotional reward system, provoking sensations of welfare and pleasure ( 14 ). In this regard, long-term musical training and learning of associated skills can be a strong stimulus for neuroplastic changes, in both the developing brain and the adult brain. These findings suggest the great capacity of music to enhance cerebral plasticity ( 13 , 16 , 20 ). Contrariwise, there are studies that question the specific effect of music therapy on people with dementia ( 21 ). With this background, the aim of this study is to analyze from an unbiased approach the effect of music therapy on the cognitive function, quality of life, and/or depressive state in people living with dementia.
Search Strategy and Selection Criteria
A systematic review was conducted following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) ( Figure 1 and Searching procedure of Supplementary Data ) ( 22 ). An independent literature search was conducted across Medline, PubMed Central, Embase, PsycINFO, and Cochrane library databases. We carried out the systematic review of the literature following a series of criteria as detailed below.
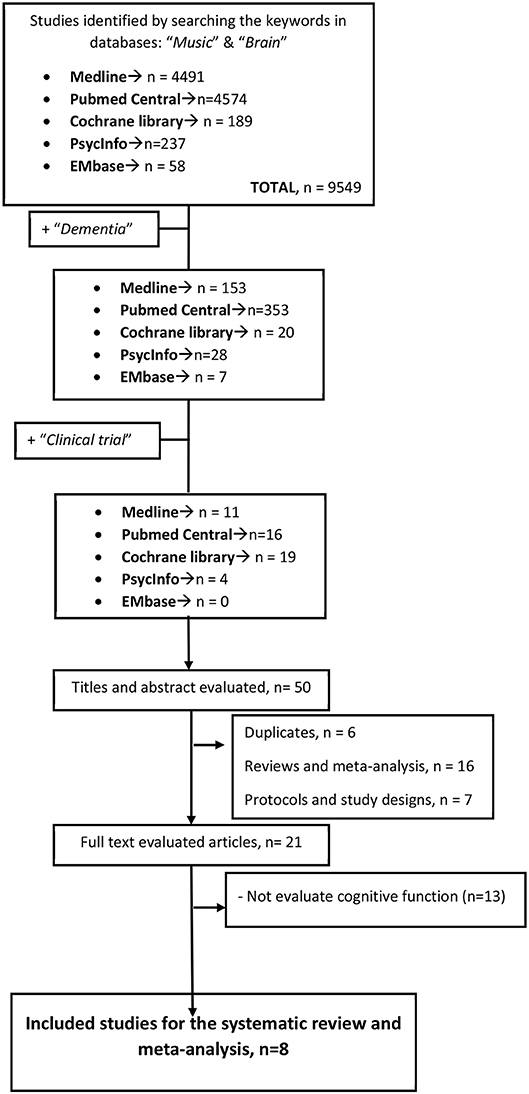
Figure 1 . Flow of studies through the review process for systematic review and meta-analysis.
Initially, the search began with the terms “brain” and “music.” Later, “dementia” was added, and finally, “clinical trial” was included. The search period used was from 1990 to present. Next, a more in-depth study of selected trials was carried out. Duplicate studies were removed. All studies that compared any form and method of musical intervention with an intervention without music were evaluated. Lastly, those studies that were systematic analysis, reviews, and study protocols and those which do not evaluate cognitive function were excluded. All the trials chosen were designed as randomized controlled trials (RCTs).
Data Collection, Extraction, and Quality Assessment
Two authors (CMM and PMM) independently assessed publications for eligibility. Discrepancies or difficulties were discussed with a third review author (CP). Data were collected independently using a standardized data extraction form in order to summarize the characteristics of the studies and outcome data ( 23 ).
From each individual study, we extracted baseline information: publication and year, study design, participants (number, age, and sex ratio), Mini-Mental Status Examination (MMSE) score, and Clinical Dementia Rating (CDR) (clinical evaluation of dementia) when possible, as well as the design of each individual study (intervention method, frequency, duration, and time of evaluation of the results) ( Table 1 ).

Table 1 . Characteristics of the studies.
In addition, at the beginning of the study, we assessed the quality of meta-analysis-included studies using the Physiotherapy Evidence Database (PEDro) scale and the Critical Appraisal Skills Program (CASP) scale ( Supplementary Tables 1 , 2 of the Supplementary Data ) ( 23 , 32 , 33 ).
Outcome Measures
The primary outcome defined to be compared was cognitive function evaluated through MMSE ( 34 ), Alzheimer's Disease Assessment Scale-cognitive subscale (ADAS-Cog) ( 35 ), Revised Memory and Behavior Problems Checklist (RMBPC) ( 36 ), or Immediate and Deferred Prose Memory test (MPI and MPD, respectively) ( 37 ). Other comparative results, named as secondary outcomes, were quality of life, assessed through Quality of Life in Alzheimer's Disease (QOL-AD) ( 38 ), and depression, evaluated through Cornell–Brown Scale for Quality of Life in Dementia (CBS) and Geriatric Depression Scale (GDS) ( 39 , 40 ).
Statistical Analysis: Meta-Analysis
First, a comparison was made using the random-effects model. All outcomes were continuous variables [mean ± standard deviation (SD) of the change in the score before and after the therapy in the different diagnostic tests], and the standardized mean difference (SMD) was analyzed. All the analyses were carried out considering a confidence interval (CI) of 95%. Statistical heterogeneity was also tested by I 2 . I 2 <25% was identified as low heterogeneity ( 41 , 42 ). Finally, the publication bias was evaluated using funnel plot graphs ( 43 , 44 ). To further investigate the heterogeneity, meta-regression and subgroup analyses were performed to assess the primary outcome data and associations according to the method of intervention (interactive and passive), trial period, number of sessions per week, and effect of evaluation method used. The P values in the meta-regression revealed the overall significance of the influence factors.
Meta-analysis, heterogeneity study, and graphical representations were performed using R with the Metafor package ( 44 ). To digitize graphics and obtain numerical data from those trials that did not provide them, the GetData Graph Digitizer program ( Getdata-graph-digitizer.com ) was used.
Baseline Characteristics
Results of initial search and exclusions are shown in Figure 1 . A thorough reading of each article was carried out, and a summary of each of them is shown in Table 1 . Therefore, we finally stayed for the systematic review and meta-analysis with eight articles. The size of the studies was between 30 and 201 subjects, with a total of 816 subjects with mild to severe dementia, assigned randomly to both the intervention and control groups. All the people in the trials stayed in nursing homes or hospitals. Särkämö et al. divided the participants into three groups, an active group that sang, a passive group that listened to music, and a control group ( 24 , 25 ). On the other hand, Doi et al. evaluated two cognitive programs of leisure activities: dancing and playing musical instruments ( 26 ). Furthermore, Han et al. tested a multimodal cognitive improvement therapy (MCET) consisting of cognitive training, cognitive stimulation, reality orientation, physical, reminiscence, and music therapy against a sham therapy without music ( 27 ). In this line, Ceccato et al. tried the program Sound Training for Attention and Memory in Dementia (STAM-Dem), a manualized music-based protocol designed to be used in the rehabilitation of cognitive functions in people with dementia. Those in the control group continued with the normal “standard care” provided ( 28 ). While Lyu et al. compared the effect of singing on cognitive function and mood, Chu et al. assessed a protocol that includes playing an instrument, dancing, and listening to music. The effect size of all those studies reveals a general improvement in the results of the experimental group ( 29 , 30 ). Finally, Guétin et al. did not find a significant difference between the experimental and control groups when evaluating the cognitive function after an 18-month therapy based on listening to music ( 31 ).
All the studies had an acceptable quality as confirmed after applying the PEDro and CASP scales ( Supplementary Tables 1 , 2 , respectively, of the Supplementary Data ).
In case of medication (dementia, antipsychotic, and antidepressant medication and sedative or sleeping medication), it must have been stable prior to the trial. Since participants were randomized, there were no significant differences between the control and music-treated groups with regard to medication. Likewise, there were no significant differences between groups in the dementia severity and/or demographic variables.
Efficacy of Musical Intervention in Cognitive Function
Figure 2 summarizes the relevant results of the quantitative synthesis of the effect of music therapy for people living with dementia. First, we evaluated the effect of music therapy on cognitive function by analyzing eight studies (816 cases) ( Figure 2A ). In the random-effects model, SMD was −0.23 (95% CI: −0.44, −0.02), which suggested that musical intervention could be beneficial to improve cognitive function in people living with dementia. However, the trials showed very high heterogeneity [ I 2 value = 72% ( P < 0.0001)].
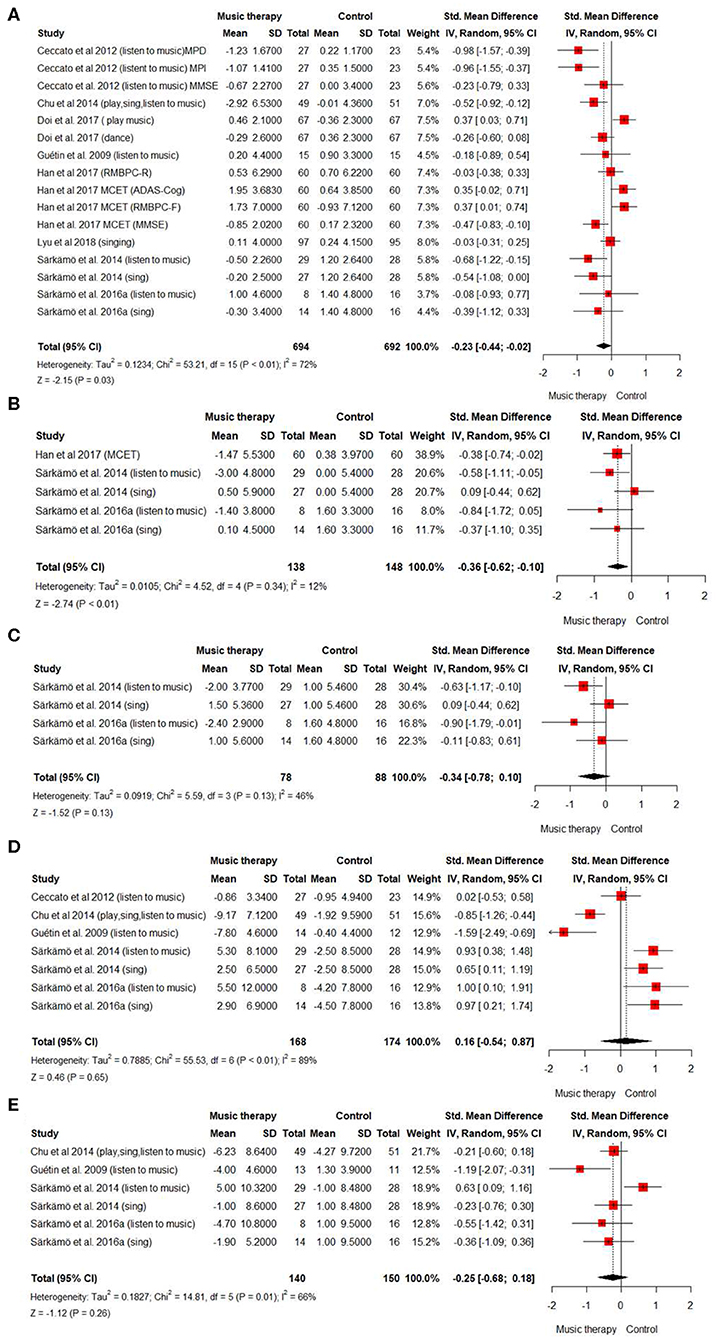
Figure 2 . Summary of efficacy of music intervention on cognitive function and secondary outcomes. Forest plot. Overall efficacy of music intervention in people with dementia (A) on cognitive function. (B) on quality of life. (C) on quality of life of people after 6 months of treatment. (D) on depressive state (E) on depressive state after 6 months.
Subgroup analyses and meta-regression were used to further explore this source of heterogeneity ( Table 2 ). Two significant sources of heterogeneity were detected: the trial period and the intervention method (coefficient = 7.43, P = 0.006 and coefficient = 3.981; P = 0.046, respectively). Interestingly, we observed that shorter intervention periods (<20 weeks) and passive interventions methods (listening to music) had greater effect on people living with dementia than longer intervention periods or interactive interventions, such as singing and dancing ( Figure 2A ; Table 2 ). On the other hand, to play an instrument does not seem to have a positive effect on cognitive function. Nevertheless, it appears to be effective when it is combined with singing and listening to music, without improving the effect of just listening to music ( Figure 2A ). The funnel plot on the publication bias across cognitive studies appeared symmetrically low ( Supplementary Figure 1 of the Supplementary Data ).
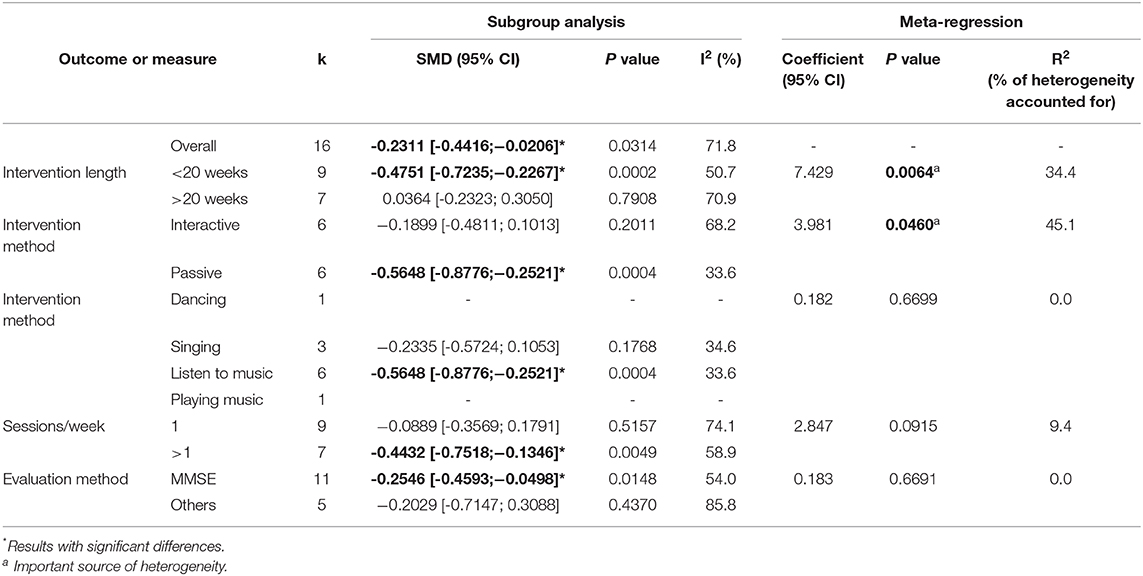
Table 2 . Meta-regression for the effect of music intervention vs. control on cognitive function.
Efficacy of Musical Intervention in Quality of Life
A meta-analysis about the quality of life of people living with dementia after the intervention with music therapy was designed. The analysis included three studies (286 cases). The results suggested that there was an effect on the quality of life of patients once the intervention is finished (SMD = −0.36, 95% CI: −0.62, 0.10) ( Figure 2B ). On the other hand, no significant effect of music therapy was observed when carrying out the analysis (two studies; 166 cases) of the quality of life of people living with dementia 6 months after the intervention (SMD = −0.34, 95% CI: −0.78, 0.10) ( Figure 2C ). The heterogeneity of the studies was small in the short-term analysis but >25 in the long term ( I 2 = 12 and I 2 = 42, respectively).
Supplementary Figures 1B,C in the Supplementary Data represent the funnel plot about the quality of life measured after the intervention and 6 months later. Data indicate that there is no publication bias.
Efficacy of Musical Intervention in the Depressive State
Finally, in order to evaluate the influence of music therapy on the depressive state associated with dementia, in both the short and long terms, we analyzed its effect when the intervention had just ended and 6 months after the treatment. The result of the meta-analysis (5 studies, 342 cases) suggested that there was no short-term effect on the depressive state of the patients (SMD = 0.16, 95% CI: −0.54, 0.87) ( Figure 2D ). However, when studying the depressive state of patients 6 months after the intervention to know if there is a long-term effect (4 studies, 290 cases), the result indicated that music therapy could have a positive effect on the depressive state of people living with dementia (SMD = −0.25, 95% CI: −0.68, 0.18) ( Figure 2E ). In both cases, the heterogeneity of the studies was high [ I 2 = 89% ( P < 0.0001) in the short term; I 2 = 66% ( P < 0.01) in the long term]. The funnel plot of the depressive state after the intervention and about the depressive state at 6 months denotes that there is no publication bias ( Supplementary Figures 1D,E in the Supplementary Data ).
The main objective of this work was to study through systematic review and meta-analysis whether the application of music as a therapy has an effect on cognitive function, quality of life, and/or depressive state in a group of specific diseases such as dementia. Nowadays, there is a growing incidence of this pathology in the population ( 1 ), and therefore, it is necessary to develop treatments and activities to relieve its symptoms. In addition, there is not enough scientific evidence about the efficacy of music as a therapy on the cognitive and behavioral states of these patients.
Our results suggest that music therapy has a positive effect on cognitive function for people living with dementia. To reach that assumption, we performed a comprehensive systematic review that includes eight studies with 816 subjects. We observed that listening to music is the intervention type with the greatest positive effect on cognitive function. This could be explained because listening to music integrates perception of sounds, rhythms, and lyrics and the response to the sound and requires attention to an environment, which implies that our brain has many areas activated. Those events are linked to wide cortical activation ( 14 , 15 , 45 ). In addition, music training is a strong stimulus for neuroplastic changes. So music could decrease neuronal degeneration by enhancing cerebral plasticity and inducing the creation of new connections in the brain ( 46 , 47 ). However, the heterogeneity presented by the different studies included in the meta-analysis does not allow us to reach reliable conclusions ( I 2 = 75%). This heterogeneity may be due to the design of each study, the difference in the type of intervention carried out, and the number of participants among other variables ( 41 ). Meta-regression showed that the intervention method, interactive or passive, is a significant source of heterogeneity accounting for 45.1% of the total heterogeneity detected ( Table 2 ). We observed a significant effect on cognitive function in the passive intervention group ( P = 0.0004). This result is in agreement with our previous analysis where listening to music has the greatest effect. Other sources of heterogeneity found when we analyzed the effect of music therapy on the cognitive function were the intervention length and the number of sessions per week (34.4 and 9.4%, respectively), the latter not being significant ( Table 2 ). Based on the literature, there is a huge diversity in the scheduling of music treatment duration. In our case, sessions varied from 90 min once a week during 10 or 20 weeks to 60 min during 40 weeks. It seems that the length for the entire music intervention procedure might be a crucial element for successful results and seems to be associated with the intervention type ( 48 – 50 ). We observed that shorter intervention periods (<20 weeks) had a greater effect on people living with dementia than longer intervention ones. This finding is not enough to draw further conclusion due to the heterogeneity found. According to our results, although the number of sessions per week seems not to have an impact on music therapy effectiveness, a greater frequency of therapy seems to be of particular importance ( 48 ).
Xu et al. and Roman-Caballero et al. showed similar results in two meta-analysis studies conducted on musical intervention in cognitive dysfunction in healthy older adults ( 18 , 23 ). In fact, as in our study, the level of heterogeneity found was also very wide. Van der Steen et al. also analyzed music-based therapeutic intervention on cognition in people with dementia ( 51 ). They found low-quality evidence that music-based therapeutic interventions may have little or no effect on cognition. Nevertheless, they did not analyze the effects in relation to the overall duration of the treatment, the number of sessions, and the type of music intervention.
After analysis of the secondary outcomes, music therapy surprisingly did not have a marked effect. Regarding quality of life, our data suggested a positive effect once the therapy is finished, but it was not durable after 6 months of music intervention. On the other hand, the study evaluating the effect of music therapy on the depressive state of people living with dementia showed no improvement in the state of these patients when they were evaluated after the intervention. However, if the depressive state was evaluated after 6 months from treatment, a shift in favor of music therapy was observed. This result suggests that the effects of music are not immediate and that the design of progressive and continuous interventions is necessary in order to obtain successful results as has also been discussed by Leubner and Hinterberger ( 49 ).
Xu et al. observed that, both in the analysis of the depressive state and in the quality of life, music therapy does not have a positive effect ( 23 ). These data corroborate the results obtained in the short term in our study. However, they did not measure the effects of long-term music therapy. Furthermore, Dyer et al. found that music as a non-pharmacological intervention improves behavioral and psychological symptoms of dementia but concluded that further research is required ( 2 , 52 ). Van der Steen et al. also compared the effect music-based therapeutic intervention versus usual care or versus other activities on depression and emotional well-being ( 51 ). Likewise, at the end of treatment, they found low-quality evidence that the musical interventions may improve emotional well-being and quality of life.
Music is a pleasant stimulus, especially when it is adapted to one's personal preferences, and it can evoke positive emotions. Some studies have demonstrated that music therapy had an influence on levels of hormones such as cortisol. It also affects the autonomic nervous systems by decreasing stress-related activation ( 53 , 54 ). At the same time, some studies suggest that music promotes several neurotransmitters, such as endorphins, endocannabinoids, dopamine, and nitric oxide. This implies that music takes part in reward, stress, and arousal processes ( 55 ). However, the lack of standardized methods for musical stimulus selection is a common feature in the studies we have reviewed. Additionally, the absence of a suitable control of the intervention to match levels of arousal, attentional engagement, mood state modification, or emotional qualities between participants may be a reason for the differences between studies ( 55 ). Furthermore, our results have likely been influenced by the type of test used to evaluate depression symptoms. Most studies used questionnaires that were based on self-assessment. However, it is unclear whether this approach is valid to detect changes regarding symptom improvement. Future approaches should add measurements of physiological body reactions, such as skin conductance and heart rate, for more objectivity ( 49 ).
Conclusions
This study shows evidence with a positive trend supporting music therapy for the improvement of cognitive function in people living with dementia. Additionally, the study reveals a positive result for treatment of long-term depression, without showing an effect on short-term depression in these patients. Furthermore, music therapy seems to improve quality of life of people with dementia once the intervention is finished, but it does not have a long-lasting effect.
Limitations And Potential Explanations
This meta-analysis had several limitations. First, there are many clinical trials in development like NCT03496675 and NCT03271190 ( Clinicaltrials.gov ), whose completion is estimated to be in 2024 and 2022, respectively, which could not be included in this analysis ( 56 , 57 ). Secondly, there are several important limitations in the design of the trials included. First, some of the studies included had a very small sample size (<100 participants), which means that they may lack enough participants to detect differences between groups. Also, the musical interventions and the method used to evaluate the cognitive function and depression were diverse and make it difficult to state clearly their benefit when compared to usual care. The lack of standardized methods for musical stimulus selection is a common drawback in the studies we reviewed and a probable contributor to inconsistencies across studies ( 55 ).
Finally, we could not perform a subgroup analysis regarding dementia severity to evaluate when music intervention would be more appropriate in the disease trajectory. This was due to the fact that in all studies selected, participants with different dementia stage were randomly assigned to the intervention or control group. Besides, almost all trials in the literature were focused on the mild or moderate stage of dementia, and there were few studies about people living with severe dementia. However, those studies do not evaluate cognitive function ( 58 ).
Future Research Recommendation
Despite the limitations, music is a non-pharmacological intervention, noninvasive, and without side effects, and its application is economical ( 53 , 54 ). For this reason, in order to confirm the effect of musical interventions, more clinical trials on the effect of music therapy should be promoted. The tests should include a high number of participants, be robust, and be randomized. As explained, music therapy methods and techniques used in clinical practice are diverse. Therefore, it is necessary to design standardized clinical trials that evaluate cognitive function and the disease behavioral features through the same battery of tests to obtain comparable results. On the other hand, there were no high-quality longitudinal studies that demonstrated long-term benefits of music therapy. It is also important to develop study designs that will be sensitive to the nature and severity of dementia. Future music therapy studies need to define a theoretical model, include better-focused outcome measures, and discuss how the findings may improve the well-being of people with dementia as discussed by McDermott et al. ( 45 ). and many others ( 49 , 54 , 55 ).
The investment in research in this novel therapy could lead to its implementation as a new and alternative intervention together with current cognitive-behavioral and pharmacological therapies.
Data Availability Statement
All datasets generated for this study are included in the article/ Supplementary Material .
Author Contributions
CM-M and PM-M: did systematic review and review the manuscript. CM-M and RC: meta-analysis. RC: meta-regression and sub-group analysis and review the manuscript. CP: design the study, conceptualization, supervision, wrote the paper.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.

Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2020.00160/full#supplementary-material
1. WHO. Global Action Plan on the Public Health Response to Dementia 2017–2025 . Geneva: World Health Organization (2017). p. 52. Retrieved from: http://www.who.int/mental_health/neurology/dementia/action_plan_2017_2025/en/
2. Dyer SM, Harrison SL, Laver K, Whitehead C, Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int Psychogeriatrics. (2018) 30:295–309. doi: 10.1017/S1041610217002344
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Kolanowski A, Boltz M, Galik E, Gitlin LN, Kales HC, Resnick B, et al. Determinants of behavioral and psychological symptoms of dementia: a scoping review of the evidence. Nurs Outlook . (2017) 65:515–29. doi: 10.1016/j.outlook.2017.06.006
4. Laver K, Dyer S, Whitehead C, Clemson L, Crotty M. Interventions to delay functional decline in people with dementia: a systematic review of systematic reviews. BMJ Open. (2016) 6:10767. doi: 10.1136/bmjopen-2015-010767
5. Olazarán J, Cruz BR, Isabel LC, Cruz I, Peña-Casanova J, Del Ser T, et al. Nonpharmacological therapies in Alzheimer's disease: a systematic review of efficacy. Dement Geriatr Cogn Disord. (2010) 30:161–78. doi: 10.1159/000316119
6. Chalfont G, Milligan C, Simpson J. A mixed methods systematic review of multimodal non-pharmacological interventions to improve cognition for people with dementia. Dementia. (2018) 19:9. doi: 10.1177/1471301218795289
7. Lorusso LN, Bosch SJ. Impact of multisensory environments on behavior for people with dementia: a systematic literature review. Gerontologist. (2018) 58:e168–e79. doi: 10.1093/geront/gnw168
8. Oliveira AM de, Radanovic M, Mello PCH de, Buchain PC, Vizzotto AD, Celestino DL, et al. Nonpharmacological interventions to reduce behavioral and psychological symptoms of dementia: a systematic review. Biomed Res Int. (2015) 2015:1–9. doi: 10.1155/2015/218980
9. Cations M, May N, Crotty M, Low LF, Clemson L, Whitehead C, et al. Health professional perspectives on rehabilitation for people with dementia. Gerontologist. (2019) 60:503–12. doi: 10.1093/geront/gnz007
10. Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ. (2015) 350(mar02 7):h369. doi: 10.1136/bmj.h369
11. Tak SH, Zhang H, Patel H, Hong SH. Computer activities for persons with dementia. Gerontologist. (2015) 55:S140–S9. doi: 10.1093/geront/gnv003
12. Regier NG, Hodgson NA, Gitlin LN. Characteristics of activities for persons with dementia at the mild, moderate, and severe stages. Gerontologist. (2017) 57:987–97. doi: 10.1093/geront/gnw133
13. Altenmüller E, Schlaug G. Apollo's gift: new aspects of neurologic music therapy. Prog Brain Res. (2015) 217:237–52. doi: 10.1016/bs.pbr.2014.11.029
14. Soria-Urios G, Duque P, García-Moreno JM. Music and brain. Rev Neurol. (2011) 53:739–46. doi: 10.33588/rn.5312.2011475
15. Gaser C, Schlaug G. Brain structures differ between musicians and non-musicians. J Neurosci. (2003) 23:9240–5. doi: 10.1016/23/27/9240
16. Schlaug G. Musicians and music making as a model for the study of brain plasticity. Prog Brain Res . (2015) 217: 37–55. doi: 10.1016/bs.pbr.2014.11.020
17. Musacchia G, Sams M, Skoe E, Kraus N. Musicians have enhanced subcortical auditory and audiovisual processing of speech and music. Proc Natl Acad Sci USA . (2007) 104:15894–8. doi: 10.1073/pnas.0701498104
18. Román-Caballero R, Arnedo M, Triviño M, Lupiáñez J. Musical practice as an enhancer of cognitive function in healthy aging - a systematic review and meta-analysis. PLoS ONE. (2018) 13:e207957. doi: 10.1371/journal.pone.0207957
19. Gooding LF, Abner EL, Jicha GA, Kryscio RJ, Schmitt FA. Musical training and late-life cognition. Am J Alzheimers Dis Other Demen. (2014) 29:333–43. doi: 10.1177/1533317513517048
20. Perrone-Capano C, Volpicelli F, di Porzio U. Biological bases of human musicality. Rev Neurosci. (2017) 28:235–45. doi: 10.1515/revneuro-2016-0046
21. Baird A, Samson S. Music and dementia. Prog Brain Res. (2015) 217:207–35. doi: 10.1016/bs.pbr.2014.11.028
22. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
23. Xu B, Sui Y, Zhu C, Yang X, Zhou J, Li L, et al. Music intervention on cognitive dysfunction in healthy older adults: a systematic review and meta-analysis. Neurol Sci. (2017) 38:983–92. doi: 10.1007/s10072-017-2878-9
24. Särkämö T, Tervaniemi M, Laitinen S, Numminen A, Kurki M, Johnson JK, et al. Cognitive, emotional, and social benefits of regular musical activities in early dementia: Randomized controlled study. Gerontologist. (2014) 54:634–50. doi: 10.1093/geront/gnt100
25. Särkämö T, Laitinen S, Numminen A, Kurki M, Johnson JK, Rantanen P. Pattern of emotional benefits induced by regular singing and music listening in dementia. J Am Geriatr Soc. (2016) 64:439–40. doi: 10.1111/jgs.13963
26. Doi T, Verghese J, Makizako H, Tsutsumimoto K, Hotta R, Nakakubo S, et al. Effects of cognitive leisure activity on cognition in mild cognitive impairment: results of a randomized controlled trial. J Am Med Dir Assoc. (2017) 18:686–91. doi: 10.1016/j.jamda.2017.02.013
27. Han JW, Lee H, Hong JW, Kim K, Kim T, Byun HJ, et al. Multimodal cognitive enhancement therapy for patients with mild cognitive impairment and mild dementia: a multi- center, randomized, controlled, double-blind, crossover trial. J Alzheimer's Dis. (2017) 55:787–96. doi: 10.3233/JAD-160619
28. Ceccato E, Vigato G, Bonetto C, Bevilacqua A, Pizziolo P, Crociani S, et al. STAM protocol in dementia: A multicenter, single-blind, randomized, and controlled trial. Am J Alzheimers Dis Other Demen. (2012) 27:301–10. doi: 10.1177/1533317512452038
29. Lyu J, Zhang J, Mu H, Li W, Champ M, Xiong Q, et al. The effects of music therapy on cognition, psychiatric symptoms, and activities of daily living in patients with Alzheimer's disease. J Alzheimers Dis. (2018) 64:1347–58. doi: 10.3233/JAD-180183
30. Chu H, Yang CY, Lin Y, Ou KL, Lee TY, O'Brien AP, et al. The impact of group music therapy on depression and cognition in elderly persons with dementia: a randomized controlled study. Biol Res Nurs. (2014) 16:209–17. doi: 10.1177/1099800413485410
31. Guétin S, Portet F, Picot MC, Pommié C, Messaoudi M, Djabelkir L, et al. Effect of music therapy on anxiety and depression in patients with Alzheimer's type dementia: randomised, controlled study. Dement Geriatr Cogn Disord. (2009) 28:36–46. doi: 10.1159/000229024
32. de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. (2009) 55:129–33. doi: 10.1016/S0004-9514(09)70043-1
33. Hyde M, Higgs P, Wiggins RD, Blane D. A decade of research using the CASP scale: Key findings and future directions. Aging Ment Heal. (2015) 19:571–5. doi: 10.1080/13607863.2015.1018868
34. Arevalo-Rodriguez I, Smailagic N, Roqué i Figuls M, Ciapponi A, Sanchez-Perez E GA, Pedraza OL, et al. Mini-Mental State Examination (MMSE) for the detection of Alzheimer's disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev. (2015) 2015:CD010783. doi: 10.1002/14651858.CD010783.pub2
CrossRef Full Text | Google Scholar
35. Kueper JK, Speechley M, Montero-odasso M. The Alzheimer's disease assessment scale – cognitive subscale (ADAS-Cog): modifications and responsiveness in pre-dementia population. A narrative review. J Alzheimer's Dis. (2018) 63:423–44. doi: 10.3233/JAD-170991
36. Roth DL, Burgio LD, Gitlin LN, Gallagher-Thompson D, Coon DW, et al. Psychometric analysis of the revised memory and behavior problems checklist: factor structure of occurrence and reaction ratings. Psychol Aging. (2003) 18:906–15. doi: 10.1037/0882-7974.18.4.906
37. Volpi L, Pagni C, Radicchi C, Cintoli S, Miccoli M, Bonuccelli U, et al. Detecting cognitive impairment at the early stages: the challenge offirst line assessment. J Neurol Sci. (2017) 377:12–8. doi: 10.1016/j.jns.2017.03.034
38. Hoe J, Katona C, Roch B, Livingston G. Use of the QOL-AD for measuring quality of life in people with severe dementia - The LASER-AD study. Age Ageing. (2005) 34:130–5. doi: 10.1093/ageing/afi030
39. Ready RE, Ott BR, Grace J, Fernandez I. The cornell-brown scale for quality of life in dementia. Alzheimer Dis Assoc Disord. (2002) 16:109–15. doi: 10.1097/00002093-200204000-00008
40. Lucas-Carrasco R, Gómez-Benito J, Rejas J, Ott BR. The cornell-brown scale for quality of life in dementia: Spanish adaptation and validation. Alzheimer Dis Assoc Disord. (2013) 27:44–50. doi: 10.1097/WAD.0b013e318242040b
41. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
42. Higgins JP, Thompson SG, Deeks JJ AD. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
43. Sedgwick P, Marston L. How to read a funnel plot in a meta-analysis. BMJ. (2015) 351:1–3. doi: 10.1136/bmj.h4718
44. Viechtbauer. Conducting meta-analyses in R with the metafor Package. J Stat Softw . (2010) 36:3. doi: 10.18637/jss.v036.i03
45. McDermott O, Crellin N, Ridder HM, Orrell M. Music therapy in dementia: A narrative synthesis systematic review. Int J Geriatr Psychiatry. (2013) 28:781–94. doi: 10.1002/gps.3895
46. Habibi A, Damasio A, Ilari B, Veiga R, Joshi AA, Leahy RM, et al. Childhood music training induces change in micro and macroscopic brain structure: results from a longitudinal study. Cereb Cortex. (2017) 28:1–12. doi: 10.1093/cercor/bhx286
47. Hyde KL, Lerch J, Norton A, Forgeard M, Winner E, Evans AC, et al. The effects of musical training on structural brain development: a longitudinal study. Ann N Y Acad Sci. (2009) 1169:182–6. doi: 10.1111/j.1749-6632.2009.04852.x
48. Carr C, Odell-Miller H, Priebe S. A systematic review of music therapy practice and outcomes with acute adult psychiatric in-patients. PLoS ONE. (2013) 8:70252. doi: 10.1371/journal.pone.0070252
49. Leubner D, Hinterberger T. Reviewing the effectiveness of music interventions in treating depression. Front Psychol. (2017) 8:1109. doi: 10.3389/fpsyg.2017.01109
50. Vink A, Hanser S. Music-based therapeutic interventions for people with dementia: a mini-review. Medicines. (2018) 5:109. doi: 10.3390/medicines5040109
51. van der Steen JT, Smaling HJA, van der Wouden JC, Bruinsma MS, Scholten RJPM, Vink AC. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. (2018) 2018:7. doi: 10.1002/14651858.CD003477.pub4
52. Lyketsos CG, Steinberg M, Tschanz JAT, Norton MC, Steffens DC, Breitner JCS. Mental and behavioral disturbances in dementia: Findings from the cache county study on memory in aging. Am J Psychiatry. (2000) 157:708–14. doi: 10.1176/appi.ajp.157.5.708
53. Gómez Gallego M, Gómez García J. Music therapy and Alzheimer's disease: cognitive, psychological, and behavioural effects. Neurology. (2017) 32:300–8. doi: 10.1016/j.nrleng.2015.12.001
54. Fang R, Ye S, Huangfu J, Calimag DP. Music therapy is a potential intervention for cognition of Alzheimer's Disease: A mini-review. Transl Neurodegener. (2017) 6:1–8. doi: 10.1186/s40035-017-0073-9
55. Chanda ML, Levitin DJ. The neurochemistry of music. Trends Cogn Sci. (2013) 17:179–93. doi: 10.1016/j.tics.2013.02.007
56. Belleville S, Moussard A, Ansaldo AI, Belchior P, Bherer L, Bier N, et al. Rationale and protocol of the ENGAGE study: A double-blind randomized controlled preference trial using a comprehensive cohort design to measure the effect of a cognitive and leisure-based intervention in older adults with a memory complaint. Trials. (2019) 20:1–18. doi: 10.1186/s13063-019-3250-6
57. Gold C, Eickholt J, Assmus J, Stige B, Wake JD, Baker FA, et al. Music interventions for dementia and depression in elderly care (MIDDEL): Protocol and statistical analysis plan for a multinational cluster-randomised trial. BMJ Open. (2019) 9:1–14. doi: 10.1136/bmjopen-2018-023436
58. Sakamoto M, Ando H, Tsutou A. Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. (2013) 2013:775–84. doi: 10.1017/S1041610212002256
Keywords: systematic review, meta-analysis, dementia, music therapy, cognitive function, quality of life, depressive state
Citation: Moreno-Morales C, Calero R, Moreno-Morales P and Pintado C (2020) Music Therapy in the Treatment of Dementia: A Systematic Review and Meta-Analysis. Front. Med. 7:160. doi: 10.3389/fmed.2020.00160
Received: 28 January 2020; Accepted: 09 April 2020; Published: 19 May 2020.
Reviewed by:
Copyright © 2020 Moreno-Morales, Calero, Moreno-Morales and Pintado. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cristina Pintado, cristina.pintado@uclm.es
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Diseases & Diagnoses
Issue Index
- Case Reports
Music and Dementia: An Overview
Music appears to be a unique and powerful stimulus for reaffirming personal identity and social connectedness in individuals with dementia..
Ronald Devere, MD
Among the most significant artistic expressions, music is embedded in the fabric of human culture and identity. We have all been exposed to music in some way, whether by listening to recordings, playing an instrument, attending concerts, or dancing. It provides a unique emotional experience that takes on personal and social meaning in endless respects. As a neurologist specializing in dementia, I have long wondered about the connections of music and memory and the relationship of music to cognition. Do individuals with dementia, for example, get any benefit from exposure to music? If so, what are those benefits, and how do they work?
Over the last 25 years, many published reports and studies have examined and attempted to shed light on the relationship of music to cognitive impairment. Ahead, I will offer a broad overview of several notable studies.
PRACTICAL POINTER
Music can elicit emotions and memories and help provide a link to a person’s past and promote interconnection with caregivers and others with dementia. Recent findings suggest that that musical training delays cognitive decline and promotes brain plasticity in the elderly brain. More studies are needed to confirm the specific benefits of music therapy.
Understanding Procedural Memory
Despite the level of brain impairment and severity in dementia, certain activities remain preserved in most instances and are very resistant to decline. These include activities such as pedaling an indoor bicycle, enjoying music, dancing, and throwing a baseball. The person doing these activities may not know who you are or who they are, but these activities were learned and engrained in their younger years and remain. The memory for these activities is called Procedural Memory (PM). Memory for events, knowledge, and reasoning, known as Explicit Memory (EM), gradually disappears as dementia worsens.
What does the literature say about the value of music in people with dementia and other categories of cognitive impairment? Let’s first look at individuals with predominantly moderate to severe memory impairment. In his famous book Musicology , published in 2007, the late Oliver Sacks discussed a few patients with severe memory impairment only. 1 In particular, he discussed the English musician Clive Wearing, who developed Herpes Encephalitis in his 40s. It predominantly damaged his medial temporal lobes responsible for normal memory function. His memory span was less than 15 seconds. He could not preserve new memories and had loss of almost his entire past. His wife Deborah stated that it was as if every waking moment was the first waking moment. “He always feels he just emerged from unconsciousness and arising from the dead,” she said.
Dr. Sacks interviewed Clive in his home and noted some Bach music sitting on top of the piano and asked him to play it. Clive said he had never played it or seen it before. He then started playing “Prelude 9 in E major” and remembered playing it before. His memory for that particular piece only occurred while he played it. With this music he was able to improvise, joke, and play with any piece of music. His general knowledge or semantic memory was greatly affected along with his episodic and day-to-day memories. Clive was safe enough in his home but would get immediately lost if he went out alone. His musical powers, however, were totally intact. He was able to automatically read music, sing the notes, play the keyboard, and sing with his wife and create his own world. Clive did not lose any skills he acquired in the past before his encephalitis and he was able to learn new skills with training and practice, even if he would retain no memory for the practice sessions. Without any intact explicit memory, Clive could not remember from day to day which piece he chose to work on previously, or that he ever worked on it before. Without close direction from someone else, he was incapable of undertaking the process of learning any new piece irrespective of his considerable technical skills. Twenty years after his encephalitis, Clive had dropped out of space and time, but when seen at the keyboard alone or with his wife, he was himself again and wholly alive. His life revolved around filling the present—the now—and that only occurred when he was totally immersed in his music.
Interestingly, the response to music is preserved even when the dementia is advanced, such as when patients have impairment of executive function (judgment, planning, reasoning and insight), speech, and language.
Music and Dementia: Looking at the Data
Musical perception, musical emotion, and musical memory can survive long after other forms of memory and cognitive function have disappeared. In non-demented Parkinson’s disease, music therapy can lead to fluent motor flow, such as dancing. But once the music stops, so does the improvement in motor function. In dementia it can improve mood, behavior, and in some cases cognitive function, which can persist for hours and days after the music stops. Music also does not need to be familiar to exert these improvements and one does not need to have any formal knowledge of music or be musically inclined to enjoy music and respond to it at the deepest level.
Music and Agitation
Agitation is one of the most common behavioral concerns in dementia and present in more than 50 percent of cases. There are at least three subtypes of agitation that occur in Dementia: 1. Physically nonaggressive behavior such as wandering. 2. Physically aggressive behavior such as hitting and kicking. 3. Verbal vocal agitation such as shouting, repeating words and demanding attention. This agitation, regardless of type, leads to caregiver distress and predicts nursing home placement and greater use of restraints and psychotropic drugs, causing increased cognitive decline, stroke and death. This has triggered the important need for non-pharmacologic therapies, such as music, to manage agitation. It is important to know that music therapy can help agitation but it is not necessarily better than other recreational activities, such as playing with puzzles, robotic animals, and squeezing a ball. Dementia patients respond better with individualized activities including personally preferred music.
Listening to familiar music can elicit pleasurable responses such as smiling or moving/dancing even when communication is lost. 2 Singing has also been shown to improve behavior, mood, and cognitive function in some dementia cases. 3 From a physiological standpoint, music can also increase the heart rate and hormone levels in cognitively impaired patients. 4 Moreover, playing a musical instrument can delay the onset of future cognitive decline and reduce the risk of dementia. 5 Thus, music appears to be a necessity for dementia patients.
Of note, most of the studies discussing music and dementia come from patients with AD. Much less is known about its impact on other causes of dementia, however, studies have shown that singing, playing a musical instrument, and composing music are often well preserved in severe AD as well as frontotemporal dementia (FTD). 6-7 Some studies have shown that musicians with AD can learn to play new tunes. 8 People with AD showed preserved recognition of familiar tunes similar to normal healthy individuals, but learning and recognition after 24-hour delay was impaired in familiar and unfamiliar melodies. In a 2009 study, AD patients exposed repeatedly to new melodies were able to recognize these songs for up to eight weeks. 9 This did not occur with music repeated less frequently.
Familiar tunes and lyrics can be recognized across all stages of AD. 10 Due to bonds formed early in life between highly familiar tunes and lyrics, the ability to recognize such information is very functional in individuals with AD. The ability to detect pitch distortion or recall songs from spoken lyrics is usually impaired. Also noted is that the sense of familiarity in AD is preserved, whereas recollection that involves retrieval of information is impaired. In a study of two musicians, one with AD and one with FTD (behavioral variant), investigators found that the FTD case showed preserved recognition of musical composition, but the AD case showed deficits in this area compared to healthy musicians. 11
Behavior and Cognition. A large number of studies claim that music intervention has positive effects on behavior, agitation, mood, and cognition in dementia. For example, short-term music therapy has been found to reduce mood symptoms, such as depression and anxiety, 12 while longer music therapy (over three months) has also been shown to be very effective. 13 Another study found that the beneficial effects of individual music therapy on anxiety and depression lasted up to eight weeks. 14
In a study comparing standard care to regular singing or music listening sessions over 10 weeks in 89 people with dementia (type not specified), music sessions improved general cognition (MMSE score), attention, and executive function compared to standard care. 15 Singing appeared to evoke personal remote memories by increasing recall of names of children, friends, and immediate short story recall.
Music in the form of a song has been shown to be an effective verbal memory aid in mild AD. Verbal information presented as lyrics in an unfamiliar song rather than the spoken word is better recognized in forced choice testing. Several studies have reported that music listening facilitates recall of personal memories (involuntary autobiographical memory) in people with AD. It’s worth noting, however, that cafeteria noise can yield the same result, suggesting any type of auditory stimulation could produce this effect. In AD, personally selected music (music rated high on familiarity and emotion) has led to more specific memories, is recalled more quickly, and is rated higher in emotional content. The memories recalled were more positive than negative in feelings compared to younger and older healthy adults.
It is worth noting that the experimental rigor of many of these trials is lacking, and biases have interfered with results. Some of the limitations of these studies include small sample sizes, lack of randomization, group dissimilarity, and no control groups. The results of many of these studies, therefore, need to be interpreted with some caution. Nevertheless, music appears to be a unique and powerful stimulus for reaffirming personal identity and social connectedness in persons with dementia, which is crucial for optimal well being, despite severe memory impairment as in AD.
Music Expertise, Aging Cognition, and Dementia Risk
Music can have a significant impact on memory and cognition beyond merely listening to it. In fact, musicians have been shown to have greater volume of the auditory cortex (surface), premotor regions, cerebellum, and anterior corpus callosum compared to non-musicians. Musicians are likely to recruit both halves of the brain when performing music tasks (such as detection of pitch) and use multiple rather than single strategies to perform music cognition tasks. Studies have shown that elderly musicians outperform non-musicians on tasks assessing auditory processing, cognitive control, and comprehension of speech in noisy environments. 16-17 This has also been shown to occur in elderly persons with minimal early music training and even after a short period of music training in those with no previous music training. In addition, music training early in life was associated with faster neural responses to speech in elderly individuals.
In one study, musically naïve participants (ages 30-85) who received six months of piano lessons compared with no treatment control group showed improved performance on specific cognitive tasks that represent executive function, such as speed of processing information, verbal fluency, and enhanced mood. 18 These studies suggest that music training may have a protective effect in the face of age-related mild cognitive changes and can occur even after short periods of training in the elderly. This raises the question of whether music expertise gives rise to greater cognitive reserve and access to different strategies in the musician brain and may potentially reduce the risks of dementia. 19,5 Lending further weight to this notion is a study in which researchers interviewed 23 elderly former orchestra members (mean age 77 years old) and found that no participant was aware of current or former members of the orchestra with dementia. 20 Findings from a five-year prospective study evaluating frequency of engagement of leisure activities in 469 people over 75 years of age who did not have dementia revealed that playing a musical instrument was one of several leisure activities associated with reduced risk of dementia. 5 While these results are encouraging, the potential protective effect of musical expertise in the face of neuropathology requires more investigation.
Music and Dementia: Key Considerations
Recent randomized controlled studies have shown the efficacy of music intervention in improving the well-being of individuals with dementia and their caregivers.
— Music abilities are not completely spared in dementia.
— Different dementias likely respond differently to music intervention (Alzheimer’s disease versus frontotemporal dementia), and more studies are needed in other dementias, including vascular, Parkinson’s disease dementia, and Lewy Body dementia.
— Musical training appears to delay cognitive decline and promote brain plasticity in the elderly brain, but more studies with pathology are needed.
— The development and use of the MiDAS assessment scale has provided insight into who is likely to show improved quality of life or reduction in psychiatric symptoms in response to music therapy.
Musical composing in the presence of cognitive impairment has been studied in the famous French composer Maurice Ravel, who is especially known for his musical piece “Bolero,” amongst others. In October 1932, Ravel was involved in a car accident and suffered facial and chest injuries. He also developed progressive cognitive decline, 21 having difficulty writing and even signing his name. In addition to trouble writing music, he could no longer conduct an orchestra (even his own music). Partially intact were his perceptual auditory abilities, and he was able to recognize his own composed works. He could also recognize slight mistakes when someone was playing his music.
When Ravel died, no autopsy was performed. In reviewing his case, neurologists have suggested that he had a progressive neurodegenerative disease, such as the primary progressive aphasia variant of frontal temporal dementia, which causes inability to carry out speech and the normal use of the left upper extremity (he was right-handed). Ravel underwent brain surgery on the right side and the neurosurgeon noted a very shrunken brain size and dilated ventricles in the brain. Other neurologists considered Alzheimer’s disease, stroke, etc., but the exact cause was not proven. Most neurologists believe his car accident was not the cause of his disorder but was perhaps the proverbial straw that broke the camel’s back, allowing a neurodegenerative disorder to start showing itself.
Whether Ravel’s brain disorder influenced his musical writings is difficult to say, but there is strong evidence that the composer had a brain disorder that predominantly affected the left side of his brain. The speech and language centers are predominantly on the left side of the brain, which explains his impaired speech, writing and reading difficulties, and the use and control of the right hand. Moreover, his ability to recognize his music and errors played by other musicians suggest the right side of his brain was still functional. Studies by musicians and neurologists have suggested that Ravel was impaired with his illness in the late 1920s and early 1930s when he was composing “Bolero” and “Concerto for the Left Hand.” “Bolero” turned out to be a very different composition than his other works, suggesting a possible imbalance of both sides of the brain. “Concerto for the Left Hand” consists of one movement and greater use of wind instruments, while themes and phrases are much shorter and less elaborate. Music experts stated that this composition avoids the difficulty of elaborating a complex structured theme, which was not the usual standard of his previous music. They believe when this was written his disease was already very active and the piece was based predominantly on the right side of the brain. This information and other studies in normal individuals strongly suggest that music-related functions are not lateralized to one side of the brain as language, speech, and following commands in a normal limb.
Benefits of Music Therapy
The aim of music therapy in people with dementia is to address emotions, cognitive powers, thoughts, and memories—to stimulate them and bring them to the fore. It aims to enrich and give freedom, stability, organization, and focus. Evaluation of music therapy and its impact is a complex task. Clinically significant changes are often highly individual and standardized outcome measures may not always portray what matters most. No studies before 2014 used dementia-specific validated music therapy outcome measures. In an articled entitled “The Development of Music in Dementia Assessment Scales (MiDAS),” investigators sought to obtain a deeper understanding on the meaning and value of music for people with Dementia. 22 They elected to engage three focus groups—family caregivers, care home staff, and music therapists—in addition to dementia patients, who play an important role in giving an opinion on how music plays a role in dementia. The focus groups and interviews aimed to investigate the meaning and experience of music for people with dementia and observed the effects of music. The key questions asked in these groups were:
To people with dementia: What does music mean to you? What do you think of your music therapy/music activities? In what way is music important to you?
To families, staff, and therapists : What changes and responses do you observe in your families/clients following music therapy or music activities? How do you know if music is meaningful to the person?
One dementia patient observes: “Medications have horrible side effects such as sleepiness, and music focuses me different from reading a newspaper. I get carried away singing you don’t want to stop.”
A staff member noted about a dementia patient: “Before music therapy he was often withdrawn, wander around the corridor, or stuck in a wheelchair. During a music session, there is a real sense of group interaction and humor.”
After evaluation of these focus groups and getting detailed input, the authors decided that five important areas had to be included in any music scale: Interest, Response, Initiation, Involvement, and Enjoyment. Importantly, MiDAS was not developed for a specific music therapy and has been used in active music making, singing, and dancing with music. This scale system is based on individual optimal levels (the best score the individual can achieve), rather than a uniform pre-determined set of scores. The optimum score will be different in each individual and may change as the dementia progresses. When the MiDAS system is used, it can also be compared with cognitive tests or quality of life.
Further analysis of the qualitive data revealed that the effects of music for people with dementia goes beyond reduction of behavioral and psychological symptoms. They also noted that individual preference of music is closely linked to personal identity and personal history. Moreover, sustaining “here and now” musical and interpersonal connectedness helps value the uniqueness of an individual and help maintain the quality of his/her life.
How and why music is beneficial to cognitive impaired individuals and the extent to which efficacy of music surpasses that of other pleasant activities remains to be further clarified. 23 Nevertheless, it’s clear from the available data that music plays a role in cognition and that music therapy can be potentially beneficial for some dementia patients.
Ronald Devere, MD is director of the Alzheimer’s Disease and Memory Disorders Center in Austin, Texas.
1. Sacks, O. MUSICOLOGY. Alfred A Knopf publisher 2007
2. Cuddy L.L., Duffin J et al. Music Memory and Alzheimer’s Disease : Is music recognition spared in Dementia and How can it be assessed. Med. Hypothesis 2005, 64, 229-235
3. Narme P., Clement S. et al Efficacy of Music Intervention in Dementia, evidence from a randomized control study. Journal Alzheimer’s Disease 2014, 38, 359-369
4. Suzuki M, Kanamori M et al Behavioral and Endocrinological evaluation of music therapy for elderly patients with Dementia. 2004, Nursing Health Science 6. 11-18
5. Verghese J. et al Leisure activities and the risk of Dementia in the elderly. NEJM 2003, 348: 2508-2516.
6. Beatty, W. et al. Autopsy proven Alzheimer’s Disease in a patient with Dementia who retained Musical Skills in Life. 1997: Archives of Neurology 54: 1448.
7. Warren, J.D. et al, Nothing to say, Something to sing: Primary progressive dynamic aphasia. Neurocase 9, 140-155
8. Fornazzari, L. et al. Preservation of Episodic Musical Memory in a pianist with Alzheimer’s Disease. 2006; Neurology 66, 610-611.
9. Samson S. et al. Emotional Power of Music in Patients with Memory Disorders : Clinical Implications of Cognitive Neuroscience. Annals of The New York Academy of Science. 2009; 1169; p. 245-255.
10. Cuddy L.L. et al. Music, memory and Alzheimer’s Disease: Is music recognition spared in dementia and how is it assessed. 2005; Med Hypothesis 64; 229-235.
11. Omar R et al, The cognitive organization of music analysis; a clinical analysis Brain 2010; 133; p1200-1230.
12. Chu, H. et al The impact of group music therapy on depression and cognition in elderly persons with Dementia; a randomized control study. Biol. Res. Nurs. 2014 16: 209-217.
13. Ueda T. et al, Effects of Music Therapy on Behavioral and psychological symptoms of Dementia: A systemic review and Metanalysis. 2013 Aging Research Review 12; 628-641.
14. Guetin S. et al; Effect of music therapy on anxiety and depression in patients with Alzheimer type dementia: randomized controlled study. 2009 Dement. Geriatr. Cogn. Disord. 28; 36-46
15. Sarkamo, T. et al, Cognitive, emotional and social benefits of regular musical activities in early Dementia: randomized control study. Gerontologist 2014; 54, 634-650.
16. Hanna-Pladdy, B.et al, The relation between instrumental musical activity and cognitive aging. 2011, Neuropsychology 25, 378-86
17. Amer, T.L. et al. Do older professional musicians have cognitive advantages? PLoS ONE 8 (8), e71630 2013
18. White-Schwoch, T et al, Older adults benefit from music training early in life; Biological evidence for long term training driven plasticity. 2013 J. Neuroscience 33, 17667-17674
19. Omigie, D. et al. A protective effect of Musical Expertise on cognitive outcome following Brain Damage? 2014 Neuropsychological Review. 24, 455-460
20. Grant, M.D. et al. Musical experience and Dementia. Hypothesis. Aging Clin. Exp. Res. 2004, 16; 403-405
21. Amaducci, L. et al. Maurice Ravel and right hemisphere musical creativity: influence of disease on his last musical works. European Journal of Neurology 2002, 9: 75-82.
22. McDermott O. et al. The Development of Music in Dementia Assessment Scales (MiDAS). Nordic Journal of Music Therapy. 2015, 24; (3); pp.
23. Baird A., Severine Sampson. Music and Dementia Progress in Brain Research 2015. Volume 217 pp 207-235.
The Rapidly Evolving Front in Alzheimer's Diagnosis
With Ronald C. Petersen, MD, PhD, a Q&A
Telemedicine Outcomes and Performance: The Next Phase in Stroke Care
with Lawrence Wechsler, MD, a Q&A
This Month's Issue
Ana C. Pereira, MD; and Suzanne E. Schindler, MD, PhD
Jonathan Ogulnick, MD; and Mary Hahn, MD, MS

Related Articles
Daniel C. Potts, MD, FAAN
James E. Galvin, MD, MPH
Sign up to receive new issue alerts and news updates from Practical Neurology®.
Related News
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu
- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Effects of music therapy on patients with dementia—a systematic review.

1. Introduction
2. materials and methods, 3.1. cognition, 3.1.1. overall cognition, 3.1.2. memory, 3.1.3. language, 3.2. behavioral and psychological symptoms of dementia (bpsds), 3.2.1. overall bpsd, 3.2.2. anxiety and depression, 3.2.3. agitation, 3.3. apathy, 3.4. daily functioning, 3.5. physiological outcomes, 3.6. quality of life, 4. discussion, 5. conclusions, author contributions, conflicts of interest.
- Department of Economic and Social Affairs; United Nations. World Population Prospects 2019: Highlights. 2019. Available online: https://population.un.org/wpp/Publications/Files/WPP2019_10KeyFindings.pdf (accessed on 24 July 2020).
- Fiest, K.M.; Jetté, N.; Roberts, J.I.; Maxwell, C.J.; Smith, E.E.; Black, S.E.; Hogan, D.B. The Prevalence and Incidence of Dementia: A Systematic Review and Meta-analysis. Can. J. Neurol. Sci. 2016 , 43 , S3–S50. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Alzheimer’s Society. Risk Factors for Dementia (Factsheet 450LP). 2016. Available online: https://www.alzheimers.org.uk/sites/default/files/pdf/factsheet_risk_factors_for_dementia.pdf (accessed on 24 July 2020).
- Kalaria, R.N.; Maestre, G.E.; Arizaga, R.; Friedland, R.P.; Galasko, D.; Hall, K.; Antuono, P. Alzheimer’s disease and vascular dementia in developing countries: Prevalence, management, and risk factors. Lancet Neurol. 2008 , 7 , 812–826. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Blanco-Silvente, L.; Castells, X.; Saez, M.; Barceló, M.A.; Garre-Olmo, J.; Vilalta-Franch, J.; Capellà, D. Discontinuation, Efficacy, and Safety of Cholinesterase Inhibitors for Alzheimer’s Disease: A Meta-Analysis and Meta-Regression of 43 Randomized Clinical Trials Enrolling 16 106 Patients. Int. J. Neuropsychopharmacol. 2014 , 20 , 519–528. [ Google Scholar ] [ CrossRef ]
- Raglio, A.; Filippi, S.; Bellandi, D.; Stramba-Badiale, M. Global music approach to persons with dementia: Evidence and practice. Clin. Interv. Aging 2014 , 9 , 1669. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Davis, W.B.; Gfeller, K.E.; Thaut, M. An Introduction to Music Therapy: Theory and Practice ; American Music Therapy Association: Silver Spring, MD, USA, 2008. [ Google Scholar ]
- Definition and Quotes about Music Therapy. Available online: https://www.musictherapy.org/about/quotes/ (accessed on 10 August 2020).
- Bruscia, K.E. Defining Music Therapy ; Gilsum, N.H., Ed.; Barcelona: New Braunfels, TX, USA, 1998. [ Google Scholar ]
- Li, C.; Liu, C.; Yang, Y.; Chou, M.; Chen, C.; Lai, C. Adjunct effect of music therapy on cognition in Alzheimer’s disease in Taiwan: A pilot study. Neuropsychiatr. Dis. Treat. 2015 , 11 , 291. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Hong, I.S.; Choi, M.J. Songwriting oriented activities improve the cognitive functions of the aged with dementia. Arts Psychother. 2011 , 38 , 221–228. [ Google Scholar ] [ CrossRef ]
- Raglio, A.; Bellelli, G.; Traficante, D.; Gianotti, M.; Ubezio, M.C.; Villani, D.; Trabucchi, M. Efficacy of Music Therapy in the Treatment of Behavioral and Psychiatric Symptoms of Dementia. Alzheimer Dis. Assoc. Disord. 2008 , 22 , 158–162. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Lyu, J.; Zhang, J.; Mu, H.; Li, W.; Champ, M.; Xiong, Q.; Li, M. The Effects of Music Therapy on Cognition, Psychiatric Symptoms, and Activities of Daily Living in Patients with Alzheimer’s Disease. J. Alzheimers Dis. 2018 , 64 , 1347–1358. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Chu, H.; Yang, C.; Lin, Y.; Ou, K.; Lee, T.; O’Brien, A.P.; Chou, K. The Impact of Group Music Therapy on Depression and Cognition in Elderly Persons with Dementia. Biol. Res. Nurs. 2013 , 16 , 209–217. [ Google Scholar ] [ CrossRef ]
- Särkämö, T.; Tervaniemi, M.; Laitinen, S.; Numminen, A.; Kurki, M.; Johnson, J.K.; Rantanen, P. Cognitive, Emotional, and Social Benefits of Regular Musical Activities in Early Dementia: Randomized Controlled Study. Gerontologist 2013 , 54 , 634–650. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Ceccato, E.; Vigato, G.; Bonetto, C.; Bevilacqua, A.; Pizziolo, P.; Crociani, S.; Barchi, E. STAM Protocol in Dementia. Am. J. Alzheimers Dis. Other Dement. 2012 , 27 , 301–310. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lord, T.R.; Garner, J.E. Effects of Music on Alzheimer Patients. Percept. Mot. Skills 1993 , 76 , 451–455. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Suzuki, M.; Kanamori, M.; Watanabe, M.; Nagasawa, S.; Kojima, E.; Ooshiro, H.; Nakahara, D. Behavioral and endocrinological evaluation of music therapy for elderly patients with dementia. Nurs. Health Sci. 2004 , 6 , 11–18. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, Z.; Li, Z.; Xie, J.; Wang, T.; Yu, C.; An, N. Music therapy improves cognitive function and behavior in patients with moderate Alzheimer’s disease. Int. J. Clin. Exp. Med. 2018 , 11 , 4808–4814. [ Google Scholar ]
- Choi, A.; Lee, M.S.; Cheong, K.; Lee, J. Effects of Group Music Intervention on Behavioral and Psychological Symptoms in Patients with Dementia: A Pilot-Controlled Trial. Int. J. Neurosci. 2009 , 119 , 471–481. [ Google Scholar ] [ CrossRef ]
- Svansdottir, H.B.; Snaedal, J. Music therapy in moderate and severe dementia of Alzheimer’s type: A case–control study. Int. Psychogeriatr. 2006 , 18 , 613–621. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Pongan, E.; Tillmann, B.; Leveque, Y.; Trombert, B.; Getenet, J.C.; Auguste, N.; Rouch, I. Can Musical or Painting Interventions Improve Chronic Pain, Mood, Quality of Life, and Cognition in Patients with Mild Alzheimer’s Disease? Evidence from a Randomized Controlled Trial. J. Alzheimers Dis. 2017 , 60 , 663–677. [ Google Scholar ] [ CrossRef ]
- Nair, B.K.; Heim, C.; Krishnan, C.; D’este, C.; Marley, J.; Attia, J. The effect of Baroque music on behavioural disturbances in patients with dementia. Australas. J. Ageing 2011 , 30 , 11–15. [ Google Scholar ] [ CrossRef ]
- Raglio, A.; Bellelli, G.; Traficante, D.; Gianotti, M.; Ubezio, M.; Gentile, S.; Trabucchi, M. Efficacy of music therapy treatment based on cycles of sessions: A randomised controlled trial. Aging Ment. Health 2010 , 14 , 900–904. [ Google Scholar ] [ CrossRef ]
- Tang, Q.; Zhou, Y.; Yang, S.; Thomas, W.K.; Smith, G.D.; Yang, Z.; Chung, J.W. Effect of music intervention on apathy in nursing home residents with dementia. Geriatr. Nurs. 2018 , 39 , 471–476. [ Google Scholar ] [ CrossRef ]
- Lin, Y.; Chu, H.; Yang, C.; Chen, C.; Chen, S.; Chang, H.; Chou, K. Effectiveness of group music intervention against agitated behavior in elderly persons with dementia. Int. J. Geriatr. Psychiatry 2010 , 26 , 670–678. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- De la Rubia Ortí, J.E.; García-Pardo, M.P.; Iranzo, C.C.; Madrigal, J.J.; Castillo, S.S.; Rochina, M.J.; Gascó, V.J. Does Music Therapy Improve Anxiety and Depression in Alzheimer’s Patients? J. Altern. Complement. Med. 2018 , 24 , 33–36. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Okada, K.; Kurita, A.; Takase, B.; Otsuka, T.; Kodani, E.; Kusama, Y.; Atarashi, H.; Mizuno, K. Effects of Music Therapy on Autonomic Nervous System Activity, Incidence of Heart Failure Events, and Plasma Cytokine and Catecholamine Levels in Elderly Patients with Cerebrovascular Disease and Dementia. Int. Heart J. 2009 , 50 , 95–110. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Sánchez, A.; Maseda, A.; Marante-Moar, M.P.; Labra, C.D.; Lorenzo-López, L.; Millán-Calenti, J.C. Comparing the Effects of Multisensory Stimulation and Individualized Music Sessions on Elderly People with Severe Dementia: A Randomized Controlled Trial. J. Alzheimers Dis. 2016 , 52 , 303–315. [ Google Scholar ] [ CrossRef ]
- Shiltz, D.L.; Lineweaver, T.T.; Brimmer, T.; Cairns, A.C.; Halcomb, D.S.; Juett, J.; Plewes, J. “Music First” An Alternative or Adjunct to Psychotropic Medications for the Behavioral and Psychological Symptoms of Dementia. GeroPsych 2018 , 31 , 17–30. [ Google Scholar ] [ CrossRef ]
- Narme, P.; Clément, S.; Ehrlé, N.; Schiaratura, L.; Vachez, S.; Courtaigne, B.; Samson, S. Efficacy of Musical Interventions in Dementia: Evidence from a Randomized Controlled Trial. J. Alzheimers Dis. 2013 , 38 , 359–369. [ Google Scholar ] [ CrossRef ]
- Ho, R.T.; Fong, T.C.; Sing, C.; Lee, P.H.; Leung, A.B.; Chung, K.S.; Kwok, J.K. Managing behavioral and psychological symptoms in Chinese elderly with dementia via group-based music intervention: A cluster randomized controlled trial. Dementia 2018 , 18 , 2785–2798. [ Google Scholar ] [ CrossRef ]
- Sakamoto, M.; Ando, H.; Tsutou, A. Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int. Psychogeriatr. 2013 , 25 , 775–784. [ Google Scholar ] [ CrossRef ]
- Kwak, J.; Anderson, K.; Valuch, K.O. Findings from a Prospective Randomized Controlled Trial of an Individualized Music Listening Program for Persons With Dementia. J. Appl. Gerontol. 2018 , 39 , 567–575. [ Google Scholar ] [ CrossRef ]
- Raglio, A.; Bellandi, D.; Baiardi, P.; Gianotti, M.; Ubezio, M.C.; Zanacchi, E.; Stramba-Badiale, M. Effect of Active Music Therapy and Individualized Listening to Music on Dementia: A Multicenter Randomized Controlled Trial. J. Am. Geriatr. Soc. 2015 , 63 , 1534–1539. [ Google Scholar ] [ CrossRef ]
- Guétin, S.; Portet, F.; Picot, M.; Pommié, C.; Messaoudi, M.; Djabelkir, L.; Touchon, J. Effect of Music Therapy on Anxiety and Depression in Patients with Alzheimer’s Type Dementia: Randomised, Controlled Study. Dement. Geriatr. Cogn. Disord. 2009 , 28 , 36–46. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Maseda, A.; Cibeira, N.; Lorenzo-López, L.; González-Abraldes, I.; Buján, A.; Labra, C.D.; Millán-Calenti, J.C. Multisensory Stimulation and Individualized Music Sessions on Older Adults with Severe Dementia: Effects on Mood, Behavior, and Biomedical Parameters. J. Alzheimers Dis. 2018 , 63 , 1415–1425. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Ragneskog, H.; Bråne, G.; Karlsson, I.; Kihlgren, M. Influence of Dinner Music on Food Intake and Symptoms Common in Dementia. Scand. J. Caring Sci. 1996 , 10 , 11–17. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sung, H.; Chang, A.M.; Lee, W. A preferred music listening intervention to reduce anxiety in older adults with dementia in nursing homes. J. Clin. Nurs. 2010 , 19 , 1056–1064. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Clarkson, K.A.; Cassidy, K.; Eskes, G.A. Singing Soothes: Music Concerts for the Management of Agitation in Older Adults with Dementia. Can. J. Geriatr. 2007 , 10 , 80–87. [ Google Scholar ]
- Sung, H.; Lee, W.; Li, T.; Watson, R. A group music intervention using percussion instruments with familiar music to reduce anxiety and agitation of institutionalized older adults with dementia. Int. J. Geriatr. Psychiatry 2011 , 27 , 621–627. [ Google Scholar ] [ CrossRef ]
- Cooke, M.L.; Moyle, W.; Shum, D.H.; Harrison, S.D.; Murfield, J.E. A randomized controlled trial exploring the effect of music on agitated behaviours and anxiety in older people with dementia. Aging Ment. Health 2010 , 14 , 905–916. [ Google Scholar ] [ CrossRef ]
- Cooke, M.; Moyle, W.; Shum, D.; Harrison, S.; Murfield, J. A Randomized Controlled Trial Exploring the Effect of Music on Quality of Life and Depression in Older People with Dementia. J. Health Psychol. 2010 , 15 , 765–776. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Chang, F.; Huang, H.; Lin, K.; Lin, L. The effect of a music programme during lunchtime on the problem behaviour of the older residents with dementia at an institution in Taiwan. J. Clin. Nurs. 2010 , 19 , 939–948. [ Google Scholar ] [ CrossRef ]
- Garland, K.; Beer, E.; Eppingstall, B.; O’connor, D.W. A Comparison of Two Treatments of Agitated Behavior in Nursing Home Residents with Dementia: Simulated Family Presence and Preferred Music. Am. J. Geriatr. Psychiatry 2007 , 15 , 514–521. [ Google Scholar ] [ CrossRef ]
- Ragneskog, H.; Asplund, K.; Kihlgren, M.; Norberg, A. Individualized music played for agitated patients with dementia: Analysis of video-recorded sessions. Int. J. Nurs. Pract. 2001 , 7 , 146–155. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jennings, B.; Vance, D. The Short-Term Effects of Music Therapy on Different Types of Agitation in Adults with Alzheimer’s. Act. Adapt. Aging 2002 , 26 , 27–33. [ Google Scholar ] [ CrossRef ]
- Ridder, H.M.; Stige, B.; Qvale, L.G.; Gold, C. Individual music therapy for agitation in dementia: An exploratory randomized controlled trial. Aging Ment. Health 2013 , 17 , 667–678. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Ledger, A.J.; Baker, F.A. An investigation of long-term effects of group music therapy on agitation levels of people with Alzheimer’s Disease. Aging Ment. Health 2007 , 11 , 330–338. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vink, A.C.; Zuidersma, M.; Boersma, F.; Jonge, P.D.; Zuidema, S.U.; Slaets, J.P. The effect of music therapy compared with general recreational activities in reducing agitation in people with dementia: A randomised controlled trial. Int. J. Geriatr. Psychiatry 2012 , 28 , 1031–1038. [ Google Scholar ] [ CrossRef ]
- Holmes, C.; Knights, A.; Dean, C.; Hodkinson, S.; Hopkins, V. Keep music live: Music and the alleviation of apathy in dementia subjects. Int. Psychogeriatr. 2006 , 18 , 623–630. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Takahashi, T.; Matsushita, H. Long-Term Effects of Music Therapy on Elderly with Moderate/Severe Dementia. J. Music Ther. 2006 , 43 , 317–333. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, Y.; Cai, J.; An, L.; Hui, F.; Ren, T.; Ma, H.; Zhao, Q. Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing Res. Rev. 2017 , 35 , 1–11. [ Google Scholar ] [ CrossRef ]
- Gómez-Romero, M.; Jiménez-Palomares, M.; Rodríguez-Mansilla, J.; Flores-Nieto, A.; Garrido-Ardila, E.M.; González López-Arza, M.V. Benefits of music therapy on behaviour disorders in subjects diagnosed with dementia: A systematic review. Neurologia 2017 , 32 , 253–263. [ Google Scholar ] [ CrossRef ]
- Peretz, I.; Gagnon, L.; Hébert, S.; Macoir, J. Singing in the Brain: Insights from Cognitive Neuropsychology. Music Percept. 2004 , 21 , 373–390. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Steinke, W.R.; Cuddy, L.L.; Jakobson, L.S. Dissociations among functional subsystems governing melody recognition after right-hemisphere damage. Cogn. Neuropsychol. 2001 , 18 , 411–437. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bradt, J.; Dileo, C.; Magill, L.; Teague, A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst. Rev. 2016 , 8 . [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kühlmann, A.Y.R.; De Rooij, A.; Kroese, L.F.; Van Dijk, M.; Hunink, M.G.M.; Jeekel, J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br. J. Surg. 2018 , 105 , 773–783. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Li, H.C.; Wang, H.H.; Lu, C.Y.; Chen, T.B.; Lin, Y.H.; Lee, I. The effect of music therapy on reducing depression in people with dementia: A systematic review and meta-analysis. Geriatr. Nurs. 2019 , 40 , 510–516. [ Google Scholar ] [ CrossRef ]
- Tsoi, K.K.F.; Chan, J.Y.C.; Ng, Y.M.; Lee, M.M.Y.; Kwok, T.C.Y.; Wong, S.Y.S. Receptive Music Therapy Is More Effective than Interactive Music Therapy to Relieve Behavioral and Psychological Symptoms of Dementia: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2018 , 19 , 568–576. [ Google Scholar ] [ CrossRef ]
- Sihvonen, A.J.; Särkämö, T.; Leo, V.; Tervaniemi, M.; Altenmüller, E.; Soinila, S. Music-based interventions in neurological rehabilitation. Lancet Neurol. 2017 , 16 , 648–660. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- American Music Therapy Association. Scope of Music Therapy Practice. Available online: https://www.musictherapy.org/about/scope_of_music_therapy_practice/ (accessed on 22 August 2020).
- Moreira, S.V.; Justi, F.R.R.; Moreira, M. Can musical intervention improve memory in Alzheimer’s patients? Evidence from a systematic review. Dement. Neuropsychol. 2018 , 12 , 133–142. [ Google Scholar ] [ CrossRef ]
- Pedersen, S.K.A.; Lugo, R.G.; Andreassen, M.; Sütterlin, S. Effects of Music on Agitation in Dementia: A Meta-Analysis. Front. Psychol. 2017 , 8 , 742. [ Google Scholar ] [ CrossRef ]
- Schumann, C.; Alexopoulos, P.; Perneczky, R. Determinants of self- and carer-rated quality of life and caregiver burden in Alzheimer disease. Int. J. Geriatr. Psychiatry 2019 , 34 , 1378–1385. [ Google Scholar ] [ CrossRef ]
- Birks, J.S.; Grimley Evans, J. Rivastigmine for Alzheimer’s disease. Cochrane Database Syst. Rev. 2015 , 4 . [ Google Scholar ] [ CrossRef ]
- Birks, J.S.; Harvey, R.J. Donepezil for dementia due to Alzheimer’s disease. Cochrane Database Syst. Rev. 2018 , 6 . [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Modalities [ ] | Description |
|---|---|
| Song writing | Usually under the guidance of a music therapist in a group session; patients write lyrics for a melody. |
| Directed music listening | Music is played to patients in individualized sessions, sometimes according to their preference. |
| Music and relaxation exercises | Patients stretch and breathe to the rhythm of music. |
| Lyric discussion | A group-based session where patients discuss the lyrics of a song with each other, often in the presence of a music therapist. |
| Singing/Toning | Patients sing to accompany a given melody with lyrics. |
| Moving to music | Patients move or dance to songs. |
| Recording and video creation | Patients participate in producing a music recording or video. |
| Adapted instrument lessons | Patients learn to play musical instruments with the difficulty adapted to their personal condition. |
| Inclusion Criteria of Study: | Exclusion Criteria of Study: |
|---|---|
| Types of study: Randomized controlled trials (RCTs), cohort studies, case-control studies, case reports and case series, systematic reviews and meta analyses | Studies with music therapy combined with another intervention (e.g., cognitive enhancement therapies) |
| English full-text articles only | Studies with patients with unclear/possible clinical diagnosis of dementia, or patients with mild cognitive impairment |
| Study intervention: music therapy | Interventions of rhythmic auditory stimulation |
| Study population: patients clinically diagnosed with dementia |
| Modality of Music Therapy | Singing | Music Listening | Playing Musical Instruments | Song-Writing | Lyric Reading | Combined (2 or More Modalities) | |
|---|---|---|---|---|---|---|---|
| Outcomes | |||||||
| Cognition | |||||||
| Improved overall cognition | Y: Two studies [ , ] N: One study [ ] | Y: One study [ ] Mixed: One study [ ] * N: Two studies [ , ] | N: One study [ ] | Y: One study [ ] | N: One study [ ] | Y: One study [ ] N: Three studies [ , , ] | |
| Improved memory | Y: One study [ ] N: One study [ ] | – | – | Y: One study [ ] | N: One study [ ] | Y: Two studies [ , ] | |
| Improved language or verbal fluency | Y: One study [ ] | – | – | Y: One study [ ] | Y: One study [ ] | Y: One study [ ] | |
| Behavioral and Psychological Symptoms of Dementia (BPSD) | |||||||
| Reduced overall BPSD (lower NPI score) | Y: Two studies [ , ] | Y: Two studies [ , ] N: Three studies [ , , ] | Y: One study [ ] N: One study [ ] | – | Y: One study [ ] | Y: Two studies [ , ] | |
| Reduced anxiety or depression | Mixed: One study [ ] ** | Y: Five studies [ , , , , ] N: Two studies [ , ] | N: One study [ ] | – | – | Y: Six studies [ , , , , , ] N: One study [ , ] **** | |
| Reduced agitation | – | Y: Six studies [ , , , , , ] N: Two studies [ , ] | Y: One study [ ] | – | – | Y: Five studies [ , , , , ] N: Four studies [ , , , ] | |
| Apathy | |||||||
| Reduced apathy | – | Mixed: One study [ ] *** | Y: One study [ ] | – | – | Y: One study [ ] | |
| Daily Functioning | |||||||
| Improved daily functioning (improved Barthel Index) | N: One study [ ] | – | N: One study [ ] | – | N: One study [ ] | Y: One study [ ] | |
| Physiological outcomes | |||||||
| Reduced congested heart failure events | – | – | – | – | – | Y: One study [ ] | |
| Reduced pain | Y: One study [ ] | – | – | – | – | – | |
| Increased appetite | – | Y: One study [ ] | – | – | – | – | |
| Lowered blood pressure | – | – | – | – | – | Y: One study [ ] | |
| Decreased IL-6 and catecholamines | – | – | – | – | – | Y: One study [ ] | |
| Reduction in salivary cortisol | – | – | – | – | – | Y: One study [ ] N: Two studies [ , ] | |
| Quality of life | |||||||
| Improved quality of life | Y: One study [ ] | Y: One study [ ] N: One study [ ] | – | – | – | Y: Two studies [ , ] N: Two studies [ , ] | |
Share and Cite
Lam, H.L.; Li, W.T.V.; Laher, I.; Wong, R.Y. Effects of Music Therapy on Patients with Dementia—A Systematic Review. Geriatrics 2020 , 5 , 62. https://doi.org/10.3390/geriatrics5040062
Lam HL, Li WTV, Laher I, Wong RY. Effects of Music Therapy on Patients with Dementia—A Systematic Review. Geriatrics . 2020; 5(4):62. https://doi.org/10.3390/geriatrics5040062
Lam, Hei Long, Wai Tak Victor Li, Ismail Laher, and Roger Y. Wong. 2020. "Effects of Music Therapy on Patients with Dementia—A Systematic Review" Geriatrics 5, no. 4: 62. https://doi.org/10.3390/geriatrics5040062
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Jump to navigation
- Bahasa Malaysia

Music-based therapeutic interventions for people with dementia
People with dementia gradually develop difficulties with memory, thinking, language and daily activities. Dementia is often associated with emotional and behavioural problems and may decrease a person's quality of life. In the later stages of dementia it may be difficult for people to communicate with words, but even when they can no longer speak they may still be able to hum or play along with music. Therapy involving music may therefore be especially suitable for people with dementia. Music therapists are specially qualified to work with individuals or groups of people, using music to try to help meet their physical, psychological and social needs. Other professionals may also be trained to provide similar treatments.
Purpose of this review
We wanted to see if we could find evidence that treatments based on music improve the emotional well-being and quality of life of people with dementia. We were also interested in evidence about effects on emotional, behavioural, social or cognitive (e.g. thinking and remembering) problems in people with dementia.
What we did
We searched for clinical trials that measured these effects and in which people with dementia were randomly allocated to a music-based treatment or to a comparison group. The comparison groups might have had no special treatment, or might have been offered a different activity. We required at least five sessions of treatment because we thought fewer sessions than five were unlikely to have much effect. We combined results of trials to estimate the effect of the treatment as accurately as possible. The evidence is current to 19 June 2017.
What we found
We found 22 trials to include in the review and we were able to combine results for at least some outcomes from 890 people. All of the people in the trials stayed in nursing homes or hospitals. Some trials compared music-based treatments with usual care, and some compared them with other activities, such as cooking or painting. The quality of the trials and how well they were reported varied, and this affected our confidence in the results. First, we looked at outcomes immediately after a course of therapy ended. From our results, we could be moderately confident that music-based treatments improve symptoms of depression and overall behavioural problems, but not specifically agitated or aggressive behaviour. They may also improve anxiety and emotional well-being including quality of life, although we were less confident about these results. They may have little or no effect on cognition. We had very little confidence in our results on social interaction. Some studies also looked to see whether there were any lasting effects four weeks or more after treatment ended. However, there were few data and we were uncertain or very uncertain about the results. Further trials are likely to have a significant impact on what we know about the effects of music-based treatments for people with dementia, so continuing research is important.
Providing people with dementia who are in institutional care with at least five sessions of a music-based therapeutic intervention probably reduces depressive symptoms and improves overall behavioural problems at the end of treatment. It may also improve emotional well-being and quality of life and reduce anxiety, but may have little or no effect on agitation or aggression or on cognition. We are uncertain about effects on social behaviour and about long-term effects. Future studies should examine the duration of effects in relation to the overall duration of treatment and the number of sessions.
Dementia is a clinical syndrome with a number of different causes which is characterised by deterioration in cognitive, behavioural, social and emotional functions. Pharmacological interventions are available but have limited effect to treat many of the syndrome's features. Less research has been directed towards non-pharmacological treatments. In this review, we examined the evidence for effects of music-based interventions.
To assess the effects of music-based therapeutic interventions for people with dementia on emotional well-being including quality of life, mood disturbance or negative affect, behavioural problems, social behaviour and cognition at the end of therapy and four or more weeks after the end of treatment.
We searched ALOIS , the Specialized Register of the Cochrane Dementia and Cognitive Improvement Group (CDCIG) on 19 June 2017 using the terms: music therapy, music, singing, sing, auditory stimulation. Additional searches were carried out on 19 June 2017 in the major healthcare databases MEDLINE, Embase, PsycINFO, CINAHL and LILACS; and in trial registers and grey literature sources.
We included randomised controlled trials of music-based therapeutic interventions (at least five sessions) for people with dementia that measured any of our outcomes of interest. Control groups either received usual care or other activities with or without music.
Two review authors worked independently to screen the retrieved studies against the inclusion criteria and then to extract data and assess methodological quality of the included studies. If necessary, we contacted trial authors to ask for additional data, including relevant subscales, or for other missing information. We pooled data using random-effects models.
We included 22 studies with 1097 randomised participants. Twenty-one studies with 890 participants contributed data to meta-analyses. Participants in the studies had dementia of varying degrees of severity, and all were resident in institutions. Seven studies delivered an individual music intervention; the other studies delivered the intervention to groups of participants. Most interventions involved both active and receptive musical elements. The methodological quality of the studies varied. All were at high risk of performance bias and some were at high risk of detection or other bias.
At the end of treatment, we found low-quality evidence that the interventions may improve emotional well-being and quality of life (standardised mean difference (SMD) 0.32, 95% confidence interval (CI) 0.02 to 0.62; 9 studies, 348 participants) and reduce anxiety (SMD –0.43, 95% CI –0.72 to –0.14; 13 studies, 478 participants). We found low-quality evidence that music-based therapeutic interventions may have little or no effect on cognition (SMD 0.15, 95% CI –0.06 to 0.36; 7 studies, 350 participants). There was moderate-quality evidence that the interventions reduce depressive symptoms (SMD –0.27, 95% CI –0.45 to –0.09; 11 studies, 503 participants) and overall behaviour problems (SMD –0.23, 95% CI –0.46 to –0.01; 10 studies, 442 participants), but do not decrease agitation or aggression (SMD –0.07, 95% CI –0.24 to 0.10; 14 studies, 626 participants). The quality of the evidence on social behaviour was very low, so effects were very uncertain.
The evidence for long-term outcomes measured four or more weeks after the end of treatment was of very low quality for anxiety and social behaviour, and for the other outcomes, it was of low quality for little or no effect (with small SMDs, between 0.03 and 0.34).
- Search Menu
- Sign in through your institution
- Advance articles
- Author Guidelines
- Submission Site
- Open Access Options
- COPE guidelines for peer review
- Fair Editing and Peer Review
- Promoting your article
- About Journal of Music Therapy
- About the American Music Therapy Association
- Editorial Board
- Advertising and Corporate Services
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, limitations, conclusions, conflicts of interest.
- < Previous
Influence of Music Therapy and Music-Based Interventions on Dementia: A Pilot Study
- Article contents
- Figures & tables
- Supplementary Data
Rebecca Dahms, Cornelia Eicher, Marten Haesner, Ursula Mueller-Werdan, Influence of Music Therapy and Music-Based Interventions on Dementia: A Pilot Study, Journal of Music Therapy , Volume 58, Issue 3, Fall 2021, Pages e12–e36, https://doi.org/10.1093/jmt/thab005
- Permissions Icon Permissions
According to national dementia plan in many countries, the music implementation into the daily routine as an adjunctive therapy to medication treatment is common. However, the ability of long-term care facilities to implement individualized music therapy (MT) and music-based interventions is not sufficiently taken into account. This pilot study examined the frequency of use and acceptance of MT and technology-based music interventions (TBMI) as well as the influence of high and low usage of both interventions of dementia on behavioral and psychological symptoms (BPSD) at two timepoints. Furthermore, the influence on the combination of MT and TBMI of dementia within the nursing home setting on BPSD with a focus on agitation, apathy, depression, and quality of life at all timepoints was considered. In the present study, data from 30 people with dementia (PwD) aged on average 81 years were analyzed within an eight-week noncontrolled intervention study, including four-week follow-up. Initial outcome data indicated significant decreases at times T2 and T3 in agitation and apathy among PwD with a high usage of MT and TBMI than among those with a low usage. In general, reductions were obtained from all observed BPSD at all timepoints. Significant results were found only for agitation over time. Considering the demonstrated results, a long-term implementation of music within daily routines in nursing homes for PwD should be strived for.
Dementia and Therapeutic Treatments
Dementia, depending on its characteristics, negatively affects different cognitive domains—“memory, thinking, orientation, understanding, calculation, ability to learn, language, and judgment” ( World Health Organization [WHO], 2020a ). Approximately, 50 million people worldwide currently suffer from dementia, caused by Alzheimer’s disease or related diseases. In addition, the content and the intervention effort of the respective therapy methods vary depending on the severity and course of the disease.
Music Therapy and Music-Based Interventions
The American Music Therapy Association (AMTA) defines music therapy (MT) as “the clinical and evidence-based use of music interventions to accomplish individualized goals within a therapeutic relationship by an certified individual who has completed an approved music therapy program” ( AMTA, 2020 ). Music therapy can be used as an alternative therapy and can function as a medium for people with dementia (PwD) to engage more actively with their environment and to better express their emotions ( Elliott & Gardner, 2018 ; Götell et al., 2009 ). Although dementia is characterized in particular by a disturbance of higher cortical functions (such as memory, thinking, and judgment) ( WHO, 2020b ), PwD can often still remember the lyrics of songs they learned as children ( Hubbard et al., 2002 ). Long-term music memory is still intact for a long time in PwD and is less affected by the typical metabolic disorders and nerve cell loss. Long-term music memory is not located in the hippocampal area, where ordinary memories are stored, but in the supplementary motor cortex, which is responsible for complex, motor movements ( Jacobsen et al., 2015 ). The results of the study by Jacobsen et al. (2015) also suggest that long-term music memory is better preserved than short-term memory, autobiographical long-term memory, or language.
In addition, the use of MT in people with cognitive impairments and dementia can help improve the perceived quality of life and well-being ( Cho, 2018 ; Liesk et al., 2015 ) and may delay the progress of the disorder ( Kampragkou et al., 2017 ).
Furthermore, there are nursing homes that provide music-based interventions (MBI) additionally to MT. These MBI provide music with or without the credentialed therapist; however, they are not always individualized. Some studies mention the terms “individualized MT” and “group MT,” although they are in fact MBI ( Sakamoto et al., 2013 ; Sung et al., 2006 ). Since MBI are considered more a leisure activity than a therapeutic intervention, those services are not adapted to the individual needs and musical preferences of the PwD ( van der Geer et al., 2009 ). Individualized music is not only important in MT but also in MBI. Benefits of individualized MBI also show positive effects in terms of physiological, psychological, and emotional impacts ( Hebert et al., 2018 ; Huber et al., 2020 ; Ray & Mittelman, 2017 ; Thomas et al., 2017 ; Weise et al., 2020 ).
With regard to the music implementation in the daily structure of nursing homes, some European countries (such as the Netherlands, Luxembourg, Belgium, Great Britain, France, Norway, Denmark, and Finland) as well as other countries in the world (such as Australia and the United States) act according to the National Dementia Plan, which provided guidelines for this music implementation ( Alzheimer’s Disease International, 2020 ). The majority of music intervention studies within this setting of nursing homes consist of active MT and receptive MT ( Narme et al., 2014 ; Raglio et al., 2015 ), without including MBI. However, there is a lack of studies investigating the influence of technology-based music interventions (TBMI), for example, via mobile devices or TV, on Behavioral and Psychological Symptoms of Dementia (BPSD). In summary, little is known about the impacts of the use, acceptance, and interaction of MT and TBMI by PwD with BPSD in the context of long-term care settings.
Research Questions
Both the frequency of use and acceptance, as well as the impact of music therapy (active and receptive) in the context of TBMI on behavioral symptoms in PwD within nursing homes are rarely considered in the literature.
What was the frequency of use and acceptance of the different music interventions (MT and TBMI) offered to PwD in nursing homes?
This basic research question suggests the investigation of secondary research questions:
What is the relationship between use/acceptance and sociodemographic data (age, gender, and dementia)?
Does high versus low usage impact observed BPSD exhibited by persons with dementia?
What influence do the music interventions have on the BPSD such as agitation, apathy, depression, and quality of life over time?
Due to our focus on evaluating the influence of MT and TBMI for nursing home residents, the researcher (certified study director and study staff according to the international GCP guidelines) conducted a bicentric study to question PwD and their related persons (RPs). An RP is defined as a person who has maintained a social relationship with the PwD in daily life and is informed about his or her physical and cognitive limitations. Since the majority of PwD had few or no relatives, most of the RPs were professional caregivers.
Over a period of 14 weeks, the pilot study was conducted in three nursing homes with 30 PwD. Three nursing homes, two in Berlin and one in Stuttgart, Germany, took part in the study (1. nursing home in city area, no focus on specific diseases, 74 PwD in total; 2. nursing home in city area, focus on PwD with higher support and security needs, 69 PwD in total; and 3. nursing home in city area, closed gerontopsychiatry, focus on mental illness in old age, 69 PwD in total).
Inclusion criteria of PwD were a minimum age of 65 years, extensive independence (had to be able to participate independently in the musical interventions), and a clinically diagnosed dementia. The exclusion criterion was a lack of verbal expression (should be able to express music preferences or dislikes toward music songs).
All participants, the RP and the PwD themselves, in the case of the ability to consent or in the presence of relatives, were informed about the course and content of the study by providing written and oral study information. After that, all participants gave written informed consent. The selection of the PwD, who took part in the study, was made by the caregivers in the nursing homes. Due to the limited ability of all participated PwD to consent due to the severity of their disorder, the questionnaires were answered by an RP (external assessment questionnaires).
The study protocol was prepared in accordance with the standards of the Declaration of Helsinki and approved by the Ethics Review Committee and the Data Protection Committee of the Charité. All participants gave their written informed consent to take part in the study. In addition, the study is listed in the German Clinical Trials Register under the number DRKS00011552.
Treatment fidelity
The study team, the credentialed music therapists, the fitness trainer, as well as the caregivers were informed about the course of the study, the content, their tasks, and the goal of the pilot study before the study. The adherence and the fidelity to these general conditions for the music intervention were ensured before the study by manualized study protocols and manuscripts for each stakeholder, during and after the study by personal consultations and monitoring. The monitoring in terms of adherence to the fidelity of the protocol manual took place as part of the Dementia Care Mapping (DCM) observation (not part of this paper, submitted elsewhere).
An instruction session was prepared and conducted for the caregivers prior to the study, in which they were informed about the overall duration of the study, the content, the intervals, and the location of the music interventions. In addition, the caregivers were taught the exact use of the TBMI as well as the corresponding on and off times of the music devices (e.g., background music and music program in common room). In addition, the caregivers were able to ask questions during the training course and to relieve fears and concerns about the study.
After the instruction session, flyers were put up in the rooms where the regularly occurring music interventions were displayed. A study folder with all important details about the study and contact addresses for the study team was kept in the caregivers’ room. If necessary, questions and problems of the caregivers were clarified by telephone or in person. In addition, the functionalities of the music devices were tested and recorded at least 2–3 times per week.
The study was divided into four study phases. The baseline phase T1 (two weeks), followed by the eight-week intervention phase (T2 and T3), and the four-week follow-up phase (T4).
In T1, the Mini-Mental-Status Examination was conducted with the PwD. Moreover, sociodemographic data of the residents (e.g., age, gender, degree of care, and date of the first diagnosis of dementia) were recorded with questionnaires. In addition, information on the state of health was obtained from the attending physician. All questionnaires filled in by the RP for the PwD in the subsequent study phases (from T2 to T4) included questions on the following topics: instrumental activities of daily life that influence the behavior of PwD (e.g., disruptive behavior/agitation and social behavior/apathy, measured by the subscale of the Nurses’ Observation Scale for Geriatric Patients [NOSGER]; Wahle et al., 1996 ), depression (Cornell Depression Scale [CDS]; Alexopoulos et al., 1988 ), and quality of life (QUALIDEM; Dichter et al., 2016 ). Additionally in T2, questions were asked about expectations of MT and TBMI. In T3, questions were asked about the frequency of use and acceptance of MT and TBMI. To examine the influence of high and low usage on observed BPSD, calculations were made using data from the variable “frequency of use” at timepoints T2 and T3 (see Data Analysis). In fact, at timepoint T4, no music interventions took place. Moreover, in T4, data on the sustainability of MT and TBMI were collected.
Disruptive behavior/agitation and social behavior/apathy (NOSGER)
On a 5-point Likert scale ( never , occasionally , often , mostly , and always ), the RP evaluated the frequency of occurrence of the corresponding behavioral symptoms. A minimum score of 5 and a maximum score of 25 could be achieved for each dimension. Thus, low dimension scores meant no or only minor losses or disturbances, whereas high values meant significant losses or disturbances in the respective areas. The subscale “Social behavior” of the NOSGER questionnaire was used within this study to calculate the influence on apathy and the subscale “Disruptive behavior” for calculating the influence on agitation. In the following, disruptive behavior is used synonymously for agitation and social behavior synonymously for apathy. The NOSGER questionnaire has good psychometric characteristics in terms of reliability (test–retest reliability: rank correlation coefficient r s = .84 ≤ r s ≤ .92) and validity (criterion validity: sensitivity ≥ 48% and specificity ≥ 69%) ( Spiegel et al., 1991 ; Wahle et al., 1996 ).
Depression (CDS)
The occurrence of depression among the residents was measured by the CDS, in which a maximum score of 38 points can be achieved. A value of 8 points or more indicates an existing depressive disorder. Overall, the CDS has very good psychometric properties in terms of reliability (e.g., internal consistency: Cronbach’s α = .86) ( Amuk et al., 2003 ) and validity (e.g., criterion validity: sensitivity = 93%, sensitivity = 93%, and specificity = 97%) ( Kørner et al., 2006 ).
Quality of life (QUALIDEM)
The assessment of the quality of life was measured using the validated QUALIDEM instrument, which consists of a total of nine subscales (in a heterogeneous sample, as in this study). The higher the value of the subscale (whereby the scales can reach different scores from min. 12 points to max. 42 points), the higher the quality of life of the person with dementia in each dimension. The QUALIDEM questionnaire has good psychometric characteristics. In terms of reliability, a strong internal consistency was measured in numerous studies (Cronbach’s α > 0.7) ( Bouman et al., 2011 ; Dichter et al., 2011 ; Gräske et al., 2014 ). With regard to validity, studies showed good to very good scalability up to three subscales (Loevinger’s H = 0.31 ≤ H ≤ 0.65) ( Dichter et al., 2013 ).
Intervention
The main goal of all provided music interventions was to investigate their usage by PwD in nursing homes and to examine the related influence on BPSD over time. A total of six different types of music interventions (MT and TBMI) were offered to meet the individual preferences and likings of each study participant. These music interventions were interventions that were compatible with both the spatial, organizational, and staffing conditions of the nursing homes.
This type of active MT was performed once a week for 45 minutes by a credentialed, certified, and experienced (with the target group) music therapist. The planned group size of the MT group was five study participants. However, other nursing home residents occasionally participated in the sessions by random chance, so that the group size varied (max. 10 participants). The music was improvised, mainly played by the music therapist with a guitar or accordion. In addition, singing bowls and percussion instruments were sometimes used to support the experience of rhythm, which were played by some participants in the study.
Individual MT
The individual MT was conducted in the context of receptive MT. This music intervention was performed every two weeks (alternating weeks with group music with movements) for 30 minutes by a credentialed, certified, and experienced (with the target group) music therapist for only one study participant each. The music was played by the music therapist using a guitar.
Background music
This TBMI was played by caregivers daily during each meal (breakfast, lunch, 3:00 p.m. tea, and dinner) for all study participants for approx. 4 minutes via CD player. It was standardized and suitable music for the respective meals.
Group music with movements
This TBMI was performed every two weeks (alternating weeks with individual MT) for 60 minutes by a certified fitness trainer for physical activation. The planned group size was 10 study participants, which was not exceeded. The music was a prepared music playlist that was transmitted via TV. The music selection was based on a biographically relevant approach.
Music program in common room
This TBMI in the common room was turned on and off by caregivers and was made available to each study participant every day from 10:00 a.m. to 04:00 p.m. via TV and an external hard disk. Other nursing home residents also took advantage of this offer. On days when other MBI or MT were offered in the common room (e.g., group music with movements), the music program was turned off at this time. The following music program was played: karaoke (both with traditional continuous text and with text sung by an older person), pictures/videos accompanied by music, and provided instruments.
Individual radio
This TBMI was played automatically twice per day for a maximum of 30 minutes in the resident’s own room at an individual volume. The automatic playing time varied according to the needs of the study participants. All music songs were played at an appropriate volume for the PwD, and the playing speed was adjusted (slowing down). Further information on the interventions (e.g., theoretical reference) can be found in Supplementary Tables 2 and 3 .
Data Analysis
The data from the questionnaires were collected paper-based within the clinical study and afterward transformed into digital data using Microsoft Excel. The analysis for the evaluation of the questionnaires was carried out using the statistical program IBM SPSS Statistics 27 (IBM Corp, Armonk, New York).
In order to investigate the influence of high usage or low usage to timepoints T2 and T3, bivariate and multivariable analyses with the variable “Frequency of use on MT and TBMI” (collected at T3), a total sum of all these variables (e.g., group music therapy and karaoke) was calculated. Accordingly, low values reflected a high usage of MT and TBMI and high values reflected a low usage of MT and TBMI (“1” = “very much used,” “4” = “very less used,” “5” = “not used,” “6” = “don’t know”). Values 5 and 6 and missing values were excluded from the calculations. In order to carry out further calculations, this new variable was dichotomized to distinguish the sample between “residents with high usage” and “residents with low usage.” A median was calculated ( Mdn = 27, min = 9, and max = 45). To calculate the influence of MT and TBMI usage on agitation, apathy, and depression, nonparametric Mann–Whitney U -tests were performed on the change scores between T2 and T3. For the variable quality of life, independent samples t- test was used.
Correlations of acceptance and use of MT and TBMI in relation to gender were calculated using a univariate analysis of variance. For the variables age and Mini-Mental State Examination correlations according to Pearson were calculated.
A Friedman test was conducted to investigate the influence of MT and TBMI on agitation ( N = 24), apathy ( N = 24), and depression ( N = 23) on the raw scores at different timepoints ( k = 3). In the case of normal distribution (only with variable quality of life), a one-way Analysis of Variance with repeated measures ( p -values corrected according to Bonferroni) ( N = 11) was performed.
Participants
The total sample of PwD (see Table I ) included 30 persons ( n = 18; 60.0% female and 60.0% widowed) aged 52 to 97 years ( M = 81.4 years) from three different nursing homes. The average MMSE score was 8.5 points ( SD = 7.4 points), which corresponds to severe dementia. With regard to musical activities, the RP stated that 83.3% ( n = 25) of the interviewed PwD regularly listened to music, 16.7% ( n = 5) of the residents still handled this independently, while the majority ( n = 25; 83.3%) of PwD were dependent on support for it (e.g., to turn on a music player). Therefore, it seems plausible that 96.7% ( n = 29) did not play an instrument anymore. In addition, the residents preferred to listen to folk music and pop songs ( n = 26; 86.7%), followed by classical music and opera ( n = 10; 33.3%) as well as pop music/musicals ( n = 7; 23.3%) and rock ( n = 3; 10.0%), according to the RP. The number of PwDs interviewed decreased over the measurement timepoints (T1–T4). One of the reasons for this was the death of five PwD during the study (see Figure 1 ).
Sociodemographic Data of the PwD and RP
| Characteristics . | Forms . | PwD . | RP . |
|---|---|---|---|
| Sample size ( ) | Total | 30 | 9 |
| Female | 18 | 7 | |
| Male | 12 | 2 | |
| Age (Ø years, ± SD) | Total | 81.4 ± 9.0 | 48.7 ± 8.2 |
| Female | 82.7 ± 8.1 | 48.5 ± 8.9 | |
| Male | 79.5 ± 10.3 | 49.6 ± 5.9 | |
| MMSE (Ø points, ± SD) | Total | 8.5 ± 7.4 | N.A. |
| Frequency of contact PwD & RP (in %) | Less than once a month | 0.0 | |
| Once a month | 0.0 | ||
| Weekly | 0.0 | ||
| More than once a week | 10.0 | ||
| Daily | 56.7 | ||
| Several times a day | 33.3 | ||
| Favorite music genre (in %) | Folk music | 86.7 | |
| Classic songs/Opera | 33.3 | ||
| Pop music | 23.3 | ||
| Rock music | 10.0 | ||
| Jazz/Blues | 0.0 |
| Characteristics . | Forms . | PwD . | RP . |
|---|---|---|---|
| Sample size ( ) | Total | 30 | 9 |
| Female | 18 | 7 | |
| Male | 12 | 2 | |
| Age (Ø years, ± SD) | Total | 81.4 ± 9.0 | 48.7 ± 8.2 |
| Female | 82.7 ± 8.1 | 48.5 ± 8.9 | |
| Male | 79.5 ± 10.3 | 49.6 ± 5.9 | |
| MMSE (Ø points, ± SD) | Total | 8.5 ± 7.4 | N.A. |
| Frequency of contact PwD & RP (in %) | Less than once a month | 0.0 | |
| Once a month | 0.0 | ||
| Weekly | 0.0 | ||
| More than once a week | 10.0 | ||
| Daily | 56.7 | ||
| Several times a day | 33.3 | ||
| Favorite music genre (in %) | Folk music | 86.7 | |
| Classic songs/Opera | 33.3 | ||
| Pop music | 23.3 | ||
| Rock music | 10.0 | ||
| Jazz/Blues | 0.0 |
Note. PwD = people with dementia; RP, related person; SD, standard deviation. Multiple answers were possible for the item “favorite music genre.”

CONSORT diagram.
The sample of RP ( n = 9) included nurses ( n = 8) and an occupational therapist ( n = 1) (77.8% female) with an average age of 48.7 years. The majority of the RP ( n = 20; 90.0%) had daily or even several times a day contact to the residents.
Frequency of Use and Acceptance of MT and TBMI
As shown in Figure 2 , the frequency of use of MT and TBMI was surveyed on a 6-point Likert scale (“1” = very often and “6” = do not know ). Frequent use of group music with movements ( n = 19; 70.3%), group MT ( n = 18; 66.6%), and individual MT ( n = 15; 55.5%) was also reported by the caregivers. The frequency of use of the technically supported music interventions, for example, karaoke and biography-specific favorite music, was lower than the frequency of use of the personnel-guided music interventions (similar to the acceptance of the music interventions). According to the RP, the reasons for nonuse were mainly health problems of the residents ( n = 11; 42.3%), memory about the existence of the music interventions ( n = 9; 34.6%), tendency to retreat ( n = 3; 11.5%), and motor restlessness ( n = 1; 3.8%). More than half of the RPs felt the common music room with its alternating music program (e.g., karaoke, music accompanied by pictures, and musicals) as appropriately equipped for older people ( n = 16; 59.3%) and for PwD ( n = 17; 62.9%). In addition, the RPs reported that 63.0% ( n = 17) of the residents to have liked the choice of music interventions pretty much or very much. No significant correlation was found with regard to the frequency of use on MT and TBMI with gender ( F (1, 28) = 0,67, p = .42, partial η 2 = .02), age ( r = .29, p = .13), and MMSE ( r = .21, p = .29).

Frequency of use on music interventions.
As shown in Figure 3 , the frequency of acceptance of MT and TBMI was surveyed on a 6-point Likert scale (“1” = very good and “6” = do not know ). With regard to the acceptance of the PwD toward individual music interventions, group MT ( n = 22; 81.4% good or very good) was rated best, along with the group music with movements ( n = 21; 77.7% good or very good) and individual MT ( n = 19; 70.3% good or very good) (see Figure 7 ). No significant correlation was determined with regard to acceptance of MT and TBMI with gender ( F (1, 28) = 0,60, p = .45, partial η 2 = .02) and MMSE ( r = .26, p = .18). A significant correlation was found only with regard to age ( r = .40, p < .05).

Frequency of acceptance on music interventions.
Agitation and Apathy
Considering the influence of MT and TBMI on agitation at times T2 and T3, agitation was found to decrease more strongly among the residents with a high usage of MT and TBMI ( Mdn = −4.5, Q1 = −7.5, Q3 = −1.5) than among those with a low usage of MT and TBMI ( Mdn = 0.0, Q1 = −2.5, Q3 = 1.5; U = 41.00, p < .05).
Figure 4 shows a reduction of agitation at time T3 ( Mdn = 6.0 points, Q1 = 5.0, Q3 = 11.0) compared with T2 ( Mdn = 10.5 points, Q1 = 7.3, Q3 = 12.8). In addition, the median value of agitation after the intervention at time T4 increased slightly to 9.0 points ( Q1 = 6.0, Q3 = 11.0). The overall influence of time was significant (Friedman test: Chi square = 7.35, p < .05, n = 24).

Distribution of agitation scores over time.
The comparison between T2 and T3 shows that the apathetic behavioral symptoms of residents with a high usage of MT and TBMI ( Mdn = −6.0, Q1 = −9.0, Q3 = −2.5) decrease more than those with a low usage of MT and TBMI ( Mdn = 1.0, Q1 = −2.0, Q3 = 3.0; U = 36.50, p < .01).
Figure 5 shows the same tendencies for apathy scores. The median apathy score in T2 decreased from 13.0 points ( Q1 = 11.0, Q3 = 18.0) to 11.0 points ( Q1 = 5.0, Q3 = 14.8) in T3 and increased slightly to a total of 13.5 points ( Q1 = 8.0, Q3 = 19.8) at time T4. However, the overall influence of time was not significant (Friedman test: Chi square = .886, p = .64, n = 24).

Distribution of apathy scores over time.
No significant differences in depressive symptoms at times T2 and T3 in PwD with high usage of MT and TBMI ( Mdn = −8.0, Q1 = −11.5, Q3 = −0.5) compared with PwD with low usage of MT and TBMI ( Mdn = −2.0, Q1 = −4.0, Q3 = 0.5) were detected (U = 63.00, p = .20).
As shown in Figure 6 , at time T2 ( Mdn = 7.0 points, Q1 = 3.0, Q3 = 11.0) of the noncontrolled intervention study, depressive disorders were observed on median in PwD. At time T3 ( Mdn = 2.0 points, Q1 = 0.0, Q3 = 8.0), a decrease of the median value in depressive symptoms of the residents was observed, which increased slightly to a median depression score of 5.0 points ( Q1 = 2.0, Q3 = 8.0) in the follow-up phase in T4. However, there were no significant differences between these measurement points (Friedman test: Chi square = 4.57, p = .10, n = 23).

Distribution of depression scores over time.
Quality of life
Comparing the changes in quality of life in T2 and T3 between residents by means with a high usage of MT and TBMI ( M = 6.0, SD = 4.6) and those with a low usage of MT and TBMI ( M = 4.3, SD = 13.1), no significant differences were observed ( t (13) =. 21 , p = .84).
The results of the subscales of the quality of life measuring instrument (see Figure 7 ) were summarized as a total average score. The one-way ANOVA with repeated measures shows an improvement in quality of life with MT and TBMI. The quality of life of PwD increased on average from time T2 from 138.9 points ( SD = 23.4) to 141.4 points ( SD = 27.1) in T3. However, at time T4, it decreased again on average by 7.9 points ( M = 133.5, SD = 19.0). There was no statistically significant difference for all timepoints ( F (2,20) = 3.18, p = .06, partial η 2 = .24).

Average quality of life scores over time.
The purpose of this nonrandomized and noncontrolled 14-week pilot study was to assess the impact of frequency of use and acceptance of individual-based MT and TBMI in nursing homes on PwD. The focus was to consider (1) the relationship between use/acceptance of music interventions and sociodemographic data, (2) influence of high/low usage of music interventions on PwD’s BPSD, and (3) influence of music interventions on PwD’s BPSD over time.
Results Reflection
Descriptive results showed higher frequencies of use and acceptance of the music interventions delivered during personnel-guided MT and TBMI (such as individual MT, group MT, and group music with movements) compared with the music interventions that were only technology based and played without guidance. This result seems to indicate that actively guided and individual-based music interventions delivered by qualified personnel are better accepted by PwD than technique-based music interventions only. Furthermore, these results imply that the integration of individual-based music into the standard patient care of an inpatient nursing home setting can succeed despite the involvement of external staff (music therapists and fitness trainers) and the disadvantages that may be associated with this (e.g., lack of knowledge about the facility and residents and negative working atmosphere/unrest in the internal team).
In addition to song selection for individual-based and biographically relevant implementation of the music interventions, caregivers were also responsible to turn music on and off (except for the automatic individual radio). The results of nonuse of the different music interventions indicate that, despite multiple training courses, it appears that there were challenges in using technology. The music devices used were not adapted to the operability of the target population of PwD (e.g., to the requirements of progressive dementia)/caregivers (e.g., to the requirements for the level of technical knowledge) nor were they adapted for use within the nursing home setting. This issue was indicated by Ruggiano et al. (2019) in their study. Therefore, according to this study by Ruggiano et al., having providers of such technologies assist in the selection process to assess and meet the specific needs of each stakeholder and provide solutions to problems can be a solution. For example, instruction sessions, consultations, and monitorings with all those persons involved (including external music therapists) who are engaged in the implementation of the music interventions are indispensable in order to prevent technical anxieties, problems, and difficulties. In order to increase use and acceptance, providers of TBMI should always consider the individual functional, cognitive and emotional needs, and activities of users in the development, whether they are caregivers or PwD ( Langley et al., 2020 ). Therefore, in the future, MT and TBMI should ensure to use musical instruments, music devices, and music programs in a user-friendly, intuitive manner that focuses on the individual needs of persons with dementia ( Gerdner, 2019 ). For people (e.g., relatives) who assist PwD in the use of TBMI, continuous further training is necessary ( Hahna et al., 2012 ) to ensure that they have the skills to use the latest technology and to promote their own readiness and acceptance of technology.
However, although the relationship between use and age was not statistically demonstrated, significance was found between acceptance and age. As other studies have found ( Czaja et al., 2006 ; Venkatesh & Davis, 2000 ; Venkatesh et al., 2003 ), the results (age: M = 81.4 years; MMSE: M = 8.5 points) of this study also indicate that certain factors, such as age, have an impact on technology acceptance. However, future studies using a larger sample would need to investigate, for example, the strength of the association of age and cognitive status of PwD on the use and acceptance of technology and TBMI.
Furthermore, the results found that agitation and apathy decreased significantly more with high usage of MT and TBMI compared with low usage. Similar to numerous studies demonstrating improvement in BPSD with MT ( Lam et al., 2020 ), this study demonstrated a positive impact entirely of these observed outcomes. Although MT and TBMI were not considered separately in the context of high/low usage, there were no negative abnormalities among PwD that could be attributed to TBMI. In the future, further research and developments in TBMI will make it easier to integrate these technologies into nursing home settings. Furthermore, TBMI always enables individual-based ( Hebert et al., 2018 ; Huber et al., 2020 ; Thomas et al., 2017 ; Weise et al., 2020 ), autonomous, and time-independent access to music, even for those PwD who do not wish to or cannot participate in community offerings such as group MT. To have an exact view of the influence of high/low usage of MT and TBMI on BPSD, further studies are needed that consider both music interventions separately.
Methodological Reflection
The results showed that MT and TBMI exclusively had a significant effect on the observed outcome of agitation over time. In contrast to other studies, no significant effects were found in this study in relation to BPSD outcomes, such as apathy ( Tang et al., 2018 ), depression ( Biasutti & Mangiacotti, 2021 ), and quality of life ( Cho, 2018 ). One reason could be the selection of measurement instruments, for example, the NOSGER scale, which measures apathy and agitation with a few items. The study team had to pay attention to the length of the questionnaires and the duration of the interviews. Therefore, short questionnaires with fewer items per outcome were chosen. In subsequent studies, efforts should be made to ensure that meaningful, reputable, and valid measurement instruments are used for each outcome, such as the Agitated Behavior in Dementia Scale ( Logsdon et al., 1999 ), the Cohen-Mansfield Agitation Inventory ( Cohen-Mansfield et al., 1989 ), and the Pittsburgh Agitation Scale ( Rosen et al., 1994 ).
To obtain valid data, the study team decided to have the questionnaires filled out by other persons instead of the study participants themselves. This was due to the fact that to answer the questionnaires, certain information of the long-term memory needed to be retrieved (e.g., taste in music and abnormalities of the BPSD). One limiting effect is that it leads to certain discrepancies between the subjective perception of the caregivers and the actual feelings and mood of the PwD. There are also ways of dealing with these discrepancies and proxy bias in dementia research ( Lacey et al., 2015 ; Robertson et al., 2020 ). Future studies should consider interviewing PwD and caregivers. To obtain additional first-person information, it should be considered to track participation and attendance at music interventions. For example, objective observation through video analysis might give more insight into the individual and complex emotional processes and behavior change during MT and TBMI.
Overall, the implementations should be investigated not only by quantitative studies but also by qualitative studies considering all participants (e.g., caregivers) through observations (e.g., DCM) and evaluations in order to identify and validate quality identifying music interventions. Controlled studies with reference to biographically relevant and individualized MBI and TBMI should also be considered in order to compare efficiency with conventional pharmacological studies and studies on active and receptive MT. In addition, long-term effects and larger investigations should be examined in further studies as well as considering other settings, such as outpatient-cared PwD.
This study is a novel study to examine the influence involving MT and TBMI on BPSD in dementia. Although this study supports previous research, there are a number of limitations that highlight further recommendations for future research.
When interpreting the results, it should be noted that in this sample PwD were heterogeneous with regard to the progression of the disease, for which a self-assessment of the questions was no longer possible. With regard to this, no individual technical acceptance of the residents in the use of MT and TBMI was measured. Based on the exclusion criteria, the transferability of the results for severe cases of dementia and nonverbal patients seems unclear although MT and music intervention often are highly valued. In addition, no conclusions can be drawn either about the influence of individual music interventions, for example, on the quality of life, or about the influence of TBMI in comparison to conventional methods of MT (group MT). Furthermore, the duration of the eight-week intervention phase of this pilot study seems not sufficient enough to detect long-term effects in PwD with respect to the parameters studied.
The results of this pilot study provide initial evidence that the use and acceptance of personnel-guided music interventions (MT, group music with movements) in nursing homes of PwD are higher than for TBMI (karaoke, pictures/videos with music, and individual radio). In addition, there is evidence that both music interventions decreased agitation and apathy, with greater changes observed in the group of high usage on MT and TBMI. This is the first pilot study that combined both MT and TBMI with each other for PwD in several nursing homes and examined the impact of use and acceptance on different behavioral symptoms. Although changes were demonstrated, further research with larger samples and separate analysis consideration of MT and TBMI is needed to examine the effectiveness of these different music interventions. Nevertheless, the use of TBMI offers a good supplement as a psychosocial intervention for PwD in nursing homes. A major advantage of TBMI is that it can be used in a personal, time-independent, and non-binding manner, and individual music preferences can be accommodated, even when nursing home staff or a music therapist is not available.
The author know none declared conflicts of interest associated with this publication.
The responsibility for the contents of this publication lies with the authors. The aim of the wider project was to develop a musical system for people with dementia. This was a joint project that ended in September 2018.
This study was supported by the German Federal Ministry of Education and Research (BMBF) under grant number 16SV7371. This research received a specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
We know of none declared conflicts of interest associated with this publication.
Alexopoulos , G. S. , Abrams , R. C. , Young , R. C. , & Shamoian , C. A . ( 1988 ). Cornell Scale for Depression in Dementia . Biological Psychiatry, 23 ( 3 ), 271 – 284 . doi: 10.1016/0006-3223(88)90038-8
Google Scholar
Alzheimer’s Disease International . ( 2020 ). Dementia plans | Alzheimer’s Disease International . Dementia Plans . Retrieved from https://www.alz.co.uk/dementia-plans
AMTA . ( 2020 ). What is Music Therapy? Retrieved from https://www.musictherapy.org/
Amuk , T. , Karadağ , F. , Oğuzhanoğlu , N. , & Oğuzhanoğlu , A . ( 2003 ). Reliability and validity of the Cornell Scale for Depression in Dementia in an elderly Turkish population . Turk Psikiyatri Dergisi = Turkish Journal of Psychiatry, 14 ( 4 ), 263 – 271 .
Biasutti , M. , & Mangiacotti , A . ( 2021 ). Music training improves depressed mood symptoms in elderly people: A randomized controlled trial . International Journal of Aging & Human Development, 92 ( 1 ), 115 – 133 . doi: 10.1177/0091415019893988
Bouman , A. I. E. , Ettema , T. P. , Wetzels , R. B. , van Beek , A. P. A. , de Lange , J. , & Dröes , R. M . ( 2011 ). Evaluation of Qualidem: A dementia-specific quality of life instrument for persons with dementia in residential settings; scalability and reliability of subscales in four Dutch field surveys . International Journal of Geriatric Psychiatry, 26 ( 7 ), 711 – 722 . doi: 10.1002/gps.2585
Cho , H. K . ( 2018 ). The effects of music therapy-singing group on quality of life and affect of persons with dementia: A randomized controlled trial . Frontiers in Medicine, 5 , 1 – 13 . doi: 10.3389/fmed.2018.00279
Cohen-Mansfield , J. , Marx , M. S. , & Rosenthal , A. S . ( 1989 ). A description of agitation in a nursing home . Journal of Gerontology, 44 ( 3 ), M77 – M84 . doi: 10.1093/geronj/44.3.m77
Czaja , S. J. , Charness , N. , Fisk , A. D. , Hertzog , C. , Nair , S. N. , Rogers , W. A. , & Sharit , J . ( 2006 ). Factors predicting the use of technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE) . Psychology and Aging, 21 ( 2 ), 333 – 352 . doi: 10.1037/0882-7974.21.2.333
Dichter , M. , Bartholomeyczik , S. , Nordheim , J. , Achterberg , W. , & Halek , M . ( 2011 ). Validity, reliability, and feasibility of a quality of life questionnaire for people with dementia . Zeitschrift Fur Gerontologie Und Geriatrie, 44 ( 6 ), 405 – 410 . doi: 10.1007/s00391-011-0235-9
Dichter , M. N. , Dortmann , O. , Halek , M. , Meyer , G. , Holle , D. , Nordheim , J. , & Bartholomeyczik , S . ( 2013 ). Scalability and internal consistency of the German version of the dementia-specific quality of life instrument QUALIDEM in nursing homes – A secondary data analysis . Health and Quality of Life Outcomes, 11 ( 1 ), 91 . doi: 10.1186/1477-7525-11-91
Google Preview
Dichter , M. N. , Ettema , T. P. , Schwab , C. G. G. , Meyer , G. , Bartholomeyczik , S. , Halek , M. , & Dröes , R.-M . ( 2016 ). QUALIDEM. User-Guide . Retrieved from https://www.dzne.de/fileadmin/Dateien/editors/images/Standorte/Witten/Projekte/QoL-Dem/QUALIDEM_User_Guide_2016_final_30_06_2016_01.pdf
Elliott , M. , & Gardner , P . ( 2018 ). The role of music in the lives of older adults with dementia ageing in place: A scoping review . Dementia (London, England), 17 ( 2 ), 199 – 213 . doi: 10.1177/1471301216639424
Gerdner , L. A . ( 2019 ). Evidence-Based Guideline: Individualized Music in Persons with Dementia (6 th Edition) . ResearchGate. Retrieved from https://www.researchgate.net/publication/330545192_Evidence-Based_Guideline_Individualized_Music_in_Persons_with_Dementia_6_th_Edition
Götell , E. , Brown , S. , & Ekman , S. L . ( 2009 ). The influence of caregiver singing and background music on vocally expressed emotions and moods in dementia care: A qualitative analysis . International Journal of Nursing Studies, 46 ( 4 ), 422 – 430 . doi: 10.1016/j.ijnurstu.2007.11.001
Gräske , J. , Verbeek , H. , Gellert , P. , Fischer , T. , Kuhlmey , A. , & Wolf-Ostermann , K . ( 2014 ). How to measure quality of life in shared-housing arrangements? A comparison of dementia-specific instruments . Quality of Life Research, 23 ( 2 ), 549 – 559 . doi: 10.1007/s11136-013-0504-8
Hahna , N. D. , Hadley , S. , Miller , V. H. , & Bonaventura , M . ( 2012 ). Music technology usage in music therapy: A survey of practice . The Arts in Psychotherapy, 39 ( 5 ), 456 – 464 . doi: 10.1016/j.aip.2012.08.001
Hebert , C. A. , Hancock , K. , & McConnell , E. S . ( 2018 ). Implementation of individualized music in long-term care: Application of the PARiHS framework . Journal of Gerontological Nursing, 44 ( 8 ), 29 – 38 . doi: 10.3928/00989134-20180626-01
Hubbard , G. , Cook , A. , Tester , S. , & Downs , M . ( 2002 ). Beyond words—Older people with dementia using and interpreting nonverbal behaviour . Journal of Aging Studies, 16 ( 2 ), 155 – 167 . doi: 10.1016/S0890-4065(02)00041-5
Huber , A. , Oppikofer , S. , Meister , L. , Langensteiner , F. , Meier , N. , & Seifert , A . ( 2020 ). Music & memory: The impact of individualized music listening on depression, agitation, and positive emotions in persons with dementia . Activities, Adaptation & Aging, 45 ( 1 ), 70 – 84 . doi: 10.1080/01924788.2020.1722348
Jacobsen , J. H. , Stelzer , J. , Fritz , T. H. , Chételat , G. , La Joie , R. , & Turner , R . ( 2015 ). Why musical memory can be preserved in advanced Alzheimer’s disease . Brain, 138 ( Pt 8 ), 2438 – 2450 . doi: 10.1093/brain/awv135
Kampragkou , C. , Iakovidis , P. , Kampragkou , E. , & Kellis , E . ( 2017 ). Effects of a 12-week aerobic exercise program combined with music therapy and memory exercises on cognitive and functional ability in people with middle type of Alzheimer’s disease . International Journal of Physiotherapy, 4 ( 5 ), 262 – 268 . doi: 10.15621/ijphy/2017/v4i5/159420
Kørner , A. , Lauritzen , L. , Abelskov , K. , Gulmann , N. , Marie Brodersen , A. , Wedervang-Jensen , T. , & Marie Kjeldgaard , K . ( 2006 ). The Geriatric Depression Scale and the Cornell Scale for Depression in Dementia. A validity study . Nordic Journal of Psychiatry, 60 ( 5 ), 360 – 364 . doi: 10.1080/08039480600937066
Lacey , L. , Bobula , J. , Rüdell , K. , Alvir , J. , & Leibman , C . ( 2015 ). Quality of life and utility measurement in a large clinical trial sample of patients with mild to moderate Alzheimer’s disease: Determinants and level of changes observed . Value in Health, 18 ( 5 ), 638 – 645 . doi: 10.1016/j.jval.2015.03.1787
Lam , H. L. , Victor , W. T. , Laher , I. , & Wong , R. Y . ( 2020 ). Effects of music therapy on patients with dementia—A systematic review . Geriatrics, 5 ( 4 ), 62 . doi: 10.3390/geriatrics5040062
Langley , J. , Wheeler , G. , Partridge , R. , Bec , R. , Wolstenholme , D. , & Sproson , L . ( 2020 ). Designing with and for older people. In A. Woodcock , L. Moody , D. McDonagh , A. Jain , & L. C. Jain (Eds.), Design of assistive technology for ageing populations (S. 3–19). Springer International Publishing .
Liesk , J. , Hartogh , T. , & Kalbe , E . ( 2015 ). Kognitive Stimulation und Musikintervention bei stationär versorgten Menschen mit Demenz: Eine Pilotstudie, Probleme und Perspektiven . Zeitschrift für Gerontologie und Geriatrie, 48 ( 3 ), 275 – 281 . doi: 10.1007/s00391-014-0661-6
Logsdon , R. G. , Teri , L. , Weiner , M. F. , Gibbons , L. E. , Raskind , M. , Peskind , E. , Grundman , M. , Koss , E. , Thomas , R. G. , & Thal , L. J . ( 1999 ). Assessment of agitation in Alzheimer’s disease: The agitated behavior in Dementia Scale. Alzheimer’s Disease Cooperative Study . Journal of the American Geriatrics Society, 47 ( 11 ), 1354 – 1358 . doi: 10.1111/j.1532-5415.1999.tb07439.x
Narme , P. , Clément , S. , Ehrlé , N. , Schiaratura , L. , Vachez , S. , Courtaigne , B. , Munsch , F. , & Samson , S . ( 2014 ). Efficacy of musical interventions in dementia: Evidence from a randomized controlled trial . Journal of Alzheimer’s Disease, 38 ( 2 ), 359 – 369 . doi: 10.3233/JAD-130893
Raglio , A. , Bellandi , D. , Baiardi , P. , Gianotti , M. , Ubezio , M. C. , Zanacchi , E. , Granieri , E. , Imbriani , M. , & Stramba-Badiale , M . ( 2015 ). Effect of active music therapy and individualized listening to music on dementia: A multicenter randomized controlled trial . Journal of the American Geriatrics Society, 63 ( 8 ), 1534 – 1539 . doi: 10.1111/jgs.13558
Ray , K. D. , & Mittelman , M. S . ( 2017 ). Music therapy: A nonpharmacological approach to the care of agitation and depressive symptoms for nursing home residents with dementia . Dementia (London, England), 16 ( 6 ), 689 – 710 . doi: 10.1177/1471301215613779
Robertson , S. , Cooper , C. , Hoe , J. , Lord , K. , Rapaport , P. , Marston , L. , Cousins , S. , Lyketsos , C. G. , & Livingston , G . ( 2020 ). Comparing proxy rated quality of life of people living with dementia in care homes . Psychological Medicine, 50 ( 1 ), 86 – 95 . doi: 10.1017/S0033291718003987
Rosen , J. , Burgio , L. , Kollar , M. , Cain , M. , Allison , M. , Fogleman , M. , Michael , M. , & Zubenko , G. S . ( 1994 ). The Pittsburgh Agitation Scale: A user-friendly instrument for rating agitation in dementia patients . The American Journal of Geriatric Psychiatry, 2 ( 1 ), 52 – 59 . doi: 10.1097/00019442-199400210-00008
Ruggiano , N. , Brown , E. L. , Shaw , S. , Geldmacher , D. , Clarke , P. , Hristidis , V. , & Bertram , J . ( 2019 ). The potential of information technology to navigate caregiving systems: Perspectives from dementia caregivers . Journal of Gerontological Social Work, 62 ( 4 ), 432 – 450 . doi: 10.1080/01634372.2018.1546786
Sakamoto , M. , Ando , H. , & Tsutou , A . ( 2013 ). Comparing the effects of different individualized music interventions for elderly individuals with severe dementia . International Psychogeriatrics, 25 ( 5 ), 775 – 784 . doi: 10.1017/S1041610212002256
Spiegel , R. , Brunner , C. , Ermini-Fünfschilling , D. , Monsch , A. , Notter , M. , Puxty , J. , & Tremmel , L . ( 1991 ). A new behavioral assessment scale for geriatric out- and in-patients: The NOSGER (Nurses’ Observation Scale for Geriatric Patients) . Journal of the American Geriatrics Society, 39 ( 4 ), 339 – 347 . doi: 10.1111/j.1532-5415.1991.tb02897.x
Sung , H. C. , Chang , S. M. , Lee , W. L. , & Lee , M. S . ( 2006 ). The effects of group music with movement intervention on agitated behaviours of institutionalized elders with dementia in Taiwan . Complementary Therapies in Medicine, 14 ( 2 ), 113 – 119 . doi: 10.1016/j.ctim.2006.03.002
Tang , Q. , Zhou , Y. , Yang , S. , Thomas , W. K. S. , Smith , G. D. , Yang , Z. , Yuan , L. , & Chung , J. W . ( 2018 ). Effect of music intervention on apathy in nursing home residents with dementia . Geriatric Nursing (New York, N.Y.), 39 ( 4 ), 471 – 476 . doi: 10.1016/j.gerinurse.2018.02.003
Thomas , K. S. , Baier , R. , Kosar , C. , Ogarek , J. , Trepman , A. , & Mor , V . ( 2017 ). Individualized music program is associated with improved outcomes for U.S. nursing home residents with dementia . The American Journal of Geriatric Psychiatry, 25 ( 9 ), 931 – 938 . doi: 10.1016/j.jagp.2017.04.008
van der Geer , E. R. , Vink , A. C. , Schols , J. M. , & Slaets , J. P . ( 2009 ). Music in the nursing home: hitting the right note! The provision of music to dementia patients with verbal and vocal agitation in Dutch nursing homes . International Psychogeriatrics, 21 ( 1 ), 86 – 93 . doi: 10.1017/S104161020800793X
Venkatesh , V. , Morris , M. G. , Davis , G. B. , & Davis , F. D . ( 2003 ). User acceptance of information technology: Toward a unified view . MIS Quarterly, 27 ( 3 ), 425 – 478 .
Venkatesh , V. , & Davis , F. D . ( 2000 ). A theoretical extension of the technology acceptance model: Four longitudinal field studies . Management Science, 46 ( 2 ), 186 – 204 . doi: 10.1287/mnsc.46.2.186.11926
Wahle , M. , Häller , S. , & Spiegel , R . ( 1996 ). Validation of the NOSGER (Nurses’ Observation Scale for Geriatric Patients): Reliability and validity of a caregiver rating instrument . International Psychogeriatrics, 8 ( 4 ), 525 – 547 . doi: 10.1017/s1041610296002864
Weise , L. , Töpfer , N. F. , Deux , J. , & Wilz , G . ( 2020 ). Feasibility and effects of individualized recorded music for people with dementia: A pilot RCT study . Nordic Journal of Music Therapy, 29 ( 1 ), 39 – 56 . doi: 10.1080/08098131.2019.1661507
World Health Organization (WHO) . ( 2020a ). Dementia . Retrieved from https://www.who.int/news-room/fact-sheets/detail/dementia
World Health Organization (WHO) . ( 2020b ). ICD-11—Mortality and Morbidity Statistics . ICD-11 for Mortality and Morbidity Statistics . Retrieved from https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f795022044
Supplementary data
| Month: | Total Views: |
|---|---|
| May 2021 | 519 |
| June 2021 | 409 |
| July 2021 | 428 |
| August 2021 | 383 |
| September 2021 | 814 |
| October 2021 | 1,149 |
| November 2021 | 984 |
| December 2021 | 669 |
| January 2022 | 658 |
| February 2022 | 972 |
| March 2022 | 1,382 |
| April 2022 | 1,243 |
| May 2022 | 1,018 |
| June 2022 | 552 |
| July 2022 | 489 |
| August 2022 | 365 |
| September 2022 | 725 |
| October 2022 | 912 |
| November 2022 | 906 |
| December 2022 | 587 |
| January 2023 | 796 |
| February 2023 | 885 |
| March 2023 | 1,040 |
| April 2023 | 1,090 |
| May 2023 | 833 |
| June 2023 | 446 |
| July 2023 | 480 |
| August 2023 | 432 |
| September 2023 | 723 |
| October 2023 | 972 |
| November 2023 | 918 |
| December 2023 | 617 |
| January 2024 | 826 |
| February 2024 | 1,017 |
| March 2024 | 1,166 |
| April 2024 | 1,054 |
| May 2024 | 872 |
| June 2024 | 584 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 2053-7395
- Copyright © 2024 American Music Therapy Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(3); 2023 Mar
- PMC10151115

Music Therapy in the Treatment of Dementia: A Review Article
Apurv shirsat.
1 Anatomy, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Roshan K Jha
2 Biochemistry, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Priyanshu Verma
The etiology of depression is the degeneration of the brain cells involved in cognitive function before the other brain cells. It is characterized by a neurological condition that causes a reduction in terms of physical, social, and cognitive impairment and has no cure presently. These nonpharmacological approaches, such as music therapy, enhance living outcomes for those dealing with dementia and also reduce behavioral incidence. Among these strategies is music therapy, and individual or gap-time psychological and educational counseling. Many scientists believe in the advantages of music for the brain. The brain is affected by music function and enhances some cognitive abilities, including the mechanism of speech, alteration, memory, and learning. Music can activate the limbic system, subcortical circuits, and emotionally related systems, inducing the sensation of well-being. The music itself is quite effective at increasing cerebral plasticity. Music therapy has powerful stimulation for neuroplastic alterations in the adult and developing brain. Dementia can be cured by music therapy and music-based intervention (nonpharmacological intervention) rather than by medication. This study highlights dementia therapy utilizing the music therapy method.
Introduction and background
The usage of customized music playlists in medical settings to address mental and behavioral issues and symptoms of patients affected by dementia is on the rise. However, little is known about how individuals with various histories of mental illness and symptoms respond to music in various ways [ 1 ]. There has been an uptick in recent years sharp rise in the interest of the public in the healing results of music for patients affected by dementia. A music therapist's duties typically involve helping and instructing staff members, families, volunteers, and even certain teachers in the use of music-therapeutic approaches in addition to dealing with clients on a clinical level. Six researchers in music therapy (MT) from six different nations concurred that the time was right to host a roundtable where they could exchange their expertise in dementia care, or skill sharing in dementia care, and their indirect MT practice [ 2 - 7 ]. Music is frequently included in everyday routine as an adjuvant therapy to drug treatment, per national dementia plans in many different nations. However, facilities for long-term care capacity to characterize music-based interventions and treatment therapies is not given enough consideration [ 3 ]. An important global public health concern is dementia care. One of the toughest tasks in this situation is managing behavioral psychological symptoms of dementia (BPSD). Nonpharmacological approaches like music-based interventions, which are regarded as low-risk, accessible, and inclusive, appear like promising choices. This scoping research intended to map every music-based intervention utilized in dementia care, with a focus on BPSD, and debrief its elements, framework, and logic. Activities involving therapeutic music, such as MT, were included [ 4 ]. Degeneration in cognitive, behavioral, and emotional functioning characterizes rearrangement interventions for dementia as a clinical condition with several underlying causes. Pharmaceutical treatments are accessible to treat some of the symptoms of the syndrome, notwithstanding their limited efficacy. Very few studies were reported in the past on nonpharmacological remedies [ 5 ]. People with severe dementia have proven that multisensory stimulation and custom music are effective at managing their psychological and behavioral symptoms.
Due to the physical, psychological, financial, and social effects that dementia has on the elderly, their families, and their carers, it is regarded as a public health concern. Healthcare professionals might use MT as an additional treatment to address this problem [ 6 ]. Dementia, a major cognitive disability, is characterized by reminiscence loss. It has an impact on a person's behavior and emotions, which can harm their well-being and quality of life. According to studies, there's been an upsurge in motivation using music as a newer kind of treatment for dementia during the past few decades [ 7 ]. The term dementia overall includes conditions marked by advancement rearrangement that affects cognitive processes like remembering and language, in addition to behavioral changes like anxiety and sadness. To be able to treat dementia, both pharmacological and nonpharmacological interventions are used by consultants worldwide. Pharmacological interventions such as acetylcholinesterase inhibitors are used in such cases. Although there is medication for dementia, its potential benefits are minimal, especially in noncognitive outcomes. There is an increasing prevalence of dementia. MT, for example, is a nondrug approach that might produce superior outcomes [ 8 ]. The most common cause of disability in aged persons on a global scale is dementia. Treatment of patients affected by dementia may be difficult for clinicians due to the illness's various psychological and behavioral signs (BPSD). To control BPSD and prevent side effects linked to antipsychotic medication, the dementia action network along with the Beers Criteria of the American Geriatrics Society advocates nonpharmacological and behavioral interventions as a first-line treatment [ 9 ].
Methodology
We undertook a systematic search through PubMed and CENTRAL in November 2020 using keywords such as "Music Therapy" and "Dementia" ([Title/Abstract]) OR ((Music Therapy(Title/Abstract))) OR (MT*[Title/Abstract]) OR ("Music Therapy" [MeSH Terms]) AND (" Dementia" [Title/Abstract]) OR (Dementia [Title/Abstract]) OR ("Dementia" [MeSH Terms]). We additionally searched for key references from bibliographies of the relevant studies. The search was updated in February 2022. One reviewer independently monitored the retrieved studies against the inclusion criteria, in the beginning, based on the title and abstract and then on full texts. Another reviewer also reviewed approximately 20% of these studies to validate the inclusion of studies (Figure 1 ).

Figure credits: Apurv Shirsat.
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Effects of dementia on the elderly population
A neurological disorder called dementia is defined as a decline in emotional, social, behavioral, and cognitive abilities. Although pharmaceutical treatments are available, many of their effects on symptoms are brief to the disease. Numerous research has suggested using MT along with pharmaceutical treatment to lessen the effects of aging-related cognitive decline and behavioral disorders [ 10 - 13 ]. Agitation is a general term that denotes a variety of actions, such as behavior, agitation, wandering, and aggressive actions, which are the signs of common concern in people affected by dementia. Agitation decreases the likelihood of fruitful social interaction, which enhances organizational and mental exhaustion. Despite the prevalence of medical therapies, complementary or alternative approaches are still necessary. A possible approach to lessen agitation in people affected by dementia is music intervention [ 11 ]. Both domestically and globally, MT is frequently utilized informally in a residential setting facility to strengthen the communication and emotional, cognitive, and behavioral abilities of older patients having dementia [ 12 ]. Dementia is a catch-all word for numerous chronic conditions, including Alzheimer's, which has an impact on problem-solving, language, memory, and thinking ability, and interferes with daily activities. People affected by dementia frequently struggle with social and communication skills, which significantly affects both their quality of life and that of others around them (Figure (Figure2 2 ).

In the past, Indians, Arabs, and Greeks knew about MT. In India, the literature on this technique is found in the Gandharva, Tattvas, and Raga Chikitsa (meaning raga treatment). Similar to how western music affects emotions, Indian classical culture is also available in Sangit Sudha. The first record of MT dates to a 1789 article in a Colombian journal titled Music Physically Considered . It was conducted in the 1800s. Wilhelm van de wall was the first to utilize MT in state-funded facilities (in 1936). At the University of Alberta, researchers took 42 children on trial aged 3 to 11 years and discovered that in individuals who listened to soothing music, the pain was reduced and distress was less compared with the patients who did not listen to music. People affected by dementia respond best to music when individualized music or melodies have resonance with them and are meaningful to them personally.
The study reported that musicians were 64% less likely to develop mild cognitive impairment (MCI) or dementia. The impact of these investigations on cognitive and physiological studies is minimal, despite the fact that some limitations of the results are consistent with MT's effectiveness in treating behavioral and psychological symptoms of dementia (BPSD), which are common. Dementia is already a critical issue worldwide where the human race is super-aging. This circumstance necessitates the development of rehabilitative strategies for relieving the symptoms of the patients. The goal of this study was to conduct a meta-analysis of the effects of MT on cognitive capacities in people affected by dementia [ 13 ]. According to reports, personalized music improves attitude and mood in people affected by dementia [ 14 ].
This study compared the behavioral expressions of passing happiness and pleasant behavior toward important people in MT and normal social situations [ 15 ]. Several studies were conducted to determine whether MT in people with dementia affects cognitive function, life quality, and depression. The impact of performing music therapies was assessed in randomized controlled trials on cognitive performance, psychological health, and social engagement in older persons with likely MCI or dementia [ 16 ]. A few studies also aimed to assess whether MT is beneficial in lowering distress in people with dementia [ 17 ].
People with dementia are increasingly using music as a therapeutic aid. Numerous aspects of music are responsible for its positive impacts. We developed the Music, Memory, and Movement (MMM) course and assessed its effectiveness based on the recognition of seven therapeutic qualities of music. Utilizing music as a form of therapy for people with dementia has three key benefits. First, making use of music in treatment is convenient. Music is more accessible today than ever before, especially with recent technological advancements. In a variety of circumstances, from private music listening on iPods to public music listening, individuals have access to millions of songs spanning cultures and time. As people can participate in the experience (either through listening, moving, or generating music) regardless of their degree of performance, music is suitable for the dementia population (Figure 3 ).

People with dementia are as diverse as those who do not have dementia, and they each have their own life experiences, preferences, and histories. Each person's identity, history, and significant moments from their past are discovered to be intimately correlated with their musical tastes [ 18 ]. The standard of interaction between both the dementia patient and their family caregiver can be severely compromised by dementia progression, which can worsen feelings of loneliness and isolation. The findings of this comprehensive analysis show how music can enhance a caring relationship [ 19 ]. The belief that music is merely for enjoyment rather than being a useful and important instrument in the treatment of dementia was one of the biggest obstacles to the program's implementation. However, the straightforward form used to record mood and responsiveness to progressive multifocal leukoencephalopathy (PML) gave each MT a chance to consider the efficacy of the intervention, which encouraged widespread use [ 20 ].
Two simultaneous cluster randomized controlled trials are being carried out in this study using an adaptive study design. Three main aspects of the adaptive design are tested: different implementation methods, boosting enrollment of residents for whom the intervention will probably be beneficial, and smoothly running a stage three/four trial [ 21 ]. Although more work is required to take into account the disease's clinical complexity and build stronger evidence capable of addressing rehabilitative techniques, the protocol for the use of music played by the individual to bring back memories of past may represent an initial application of personalized medicine in dementia [ 22 ]. Unfortunately, a few characterizations are utilizing musical interventions, especially regarding the training of the practitioner and specifics regarding the use of music, in different studies and systematic opinions on the impacts of music like MT [ 23 ].
Although there is no direct evidence that MT has efficacy on the cognitive and behavioral condition of these patients, the results of some studies assert that listening to music has a beneficial impact on people with dementia [ 24 , 25 ]. Systematic reviews show that the only nonpharmacological interventions shown to greatly reduce behavioral disturbances (including depressive symptoms) in people affected by dementia are MT and behavioral therapy techniques, such as caregiver reinforcing desired behavior combined with appropriate training [ 24 ]. In this study, communication within the music-for-life group intervention for people with dementia in residential care was conceptualized. In doing so, it made an effort to comprehend how people with dementia communicate throughout an eight-week music-based activity [ 25 ].
Understanding how music-based therapies affect cognitive function favorably requires taking into account the different sorts of interventions. The concept of receptive and active music-based interventions could be used to categorize all music-based interventions. Participants in receptive interventions were required to listen to music, while those in active interventions were required to play percussion music, play instruments, or move to the music [ 26 ]. According to the literature, patients affected by Alzheimer's dementia may be able to avoid or delay the development of decreased quality of life by using unorthodox, nonpharmacological therapies as alternative therapies [ 27 ]. The main objective of this study is whether MT affects cognitive ability, general well-being, and melancholy state of mind. Compared to the therapies assessed in earlier studies, our study additionally includes a higher dose of tailored music-listening sessions, continual playlist review, and systematic selection of self-relevant music with each participant. By carefully observing the implementation process and assessing the implementation's performance, we also overcome the shortcomings of earlier studies [ 28 ].
The results showed that compared to the MT listening group or television control group, the brief group singing for MT directed by a music therapist had a greater impact on the quality of life and people with dementia [ 29 ]. This study's objective was to determine if the carers of people affected by dementia would accept and consider a personalized music-based intervention useful when it was introduced by a community-based organization [ 30 ]. The study's findings provide the first proof that the Modigliani-Miller theorem personalized music program may be linked to lowered levels of antipsychotic and sedative drug use as well as a decrease in BPSD among null hypothesis (NH) citizens with Alzheimer's disease and related dementia (ADRD) [ 31 ].
In line with previous research, older adults who engaged in interactive music assistance that included personalized music and activities, like clapping and dancing, experienced a greater reduction in the psychological and behavioral signs of dementia than older adults in a control group who received no music [ 32 , 33 ]. We examined how a musical dual-task training (MDTT) program affected those who have moderate-to-mild dementia. We created the MDTT with the expectation that focusing participants' attention during dual-task situations will enhance their cognitive and physical abilities. Our main findings showed that compared to the control intervention, eight separate MDTT sessions, each lasting 60 minutes, significantly improved attention regulation [ 34 ]. The majority of the research utilized tests to evaluate particular cognitive skills like memory and attention; executive function, language, and visuomotor skills; as well as general cognitive screening evaluations. Additionally, multifunctional batteries with measures for assessing behavior, mood, and particular protocols for MT evaluation were used [ 35 ].
We have detailed an innovative program that includes both caregivers and those who have younger-onset dementia (YOD). It combines online delivery of psychological approaches and evidence-based therapeutic songwriting strategies with trained facilitators to enhance social ties and mental health. We anticipate that if the program is a success, it will be simple to scale up and be able to help additional YOD dyads [ 36 ]. Dementia is already a serious problem worldwide, and society ages extremely quickly. The development of rehabilitation strategies is necessary for this situation of relieving the symptoms of patients. Psychiatric outcomes and cognitive functioning were the questions asked most frequently in the research, and global quality of life was based on general outcomes.
Conclusions
Music could be a powerful treatment strategy. It is much needed to develop a clinical trial aimed to design standards based on the severity of dementia and methods that are compatible with existing pharmacological, cognitive behavioral, and behavioral therapy. Even while several studies have shown that music and social connection can improve dementia symptoms, just nine studies have coupled music with other activities to accomplish. These other activities included playing games, performing crossword puzzles, gardening, and engaging in physical and mental activities. This study has demonstrated that integrating social interactions can be enhanced by MT.
The authors have declared that no competing interests exist.

IMAGES
VIDEO
COMMENTS
Background: Dementia is a neurological condition characterized by deterioration in cognitive, behavioral, social, and emotional functions. Pharmacological interventions are available but have limited effect in treating many of the disease's features. Several studies have proposed therapy with music as a possible strategy to slow down cognitive decline and behavioral changes associated with ...
was concluded that music therapy is more beneficial in decreasing depressive symptoms in. dementia patients than recreational singing (2017). Chu et al. (2014) found that group music. therapy may be appropriate for those with mild and moderate dementia, as the Cornell Scale for.
1. Introduction. Between 1990 and 2016, the number of people affected by dementia has seen a rising global tendency of 117%, probably due to an aging population [].Currently, this rise presents an estimated increase of 57.4 to 152.8 million cases from 2019 to 2050 [].Additionally, in 2019, 5% of all deaths in the European Union were related to Alzheimer's and other dementias [].
Background: Dementia, a significant cognitive impairment, is characterized by a decline in memory. It affects an individual's mood and behavior, which can impair their quality of life and well-being. Studies show that the demand for applying music as a new therapy method for dementia has increased during the last decades.
The use of music interventions as a non-pharmacological therapy to improve cognitive and behavioral symptoms in Alzheimer's disease (AD) patients has gained popularity in recent years, but the evidence for their effectiveness remains inconsistent. To summarize the evidence of the effect of music therapy (alone or in combination with pharmacological therapies) on cognitive functions in AD ...
Music is a source of meaningful occupation in dementia [4] - a cornerstone of wellbeing in the delivery of person-centred care. By facilitating communication, it may also reduce the frustration and helplessness that contribute significantly to challenging behaviours. As a therapeutic intervention, music is innocuous, accessible, flexible and ...
r side efects and music therapy has been efective in reducing BPSD (2015). Research on music therapy in the treatment of memory disorders has shown the following benefits: ♦ Decreased depression & improved mood ♦ Decreased anxiety & agitation ♦ Decreased medication ♦ Increased alertness & orientation ♦ Enhanced cognition & memory ...
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by The University of Arizona. Running head: MUSIC THERAPY AND PATIENTS WITH DEMENTIA 1 ... and agitation in patients with dementia through music therapy. Recommendations for best practice will be created in this thesis using evidence-based research
Background: Dementia is a neurological condition characterized by deterioration in cognitive, behavioral, social, and emotional functions. Pharmacological interventions are available but have limited effect in treating many of the disease's features. Several studies have proposed therapy with music as a possible strategy to slow down cognitive decline and behavioral changes associated with ...
Supporting all of the above is a wealth of clinical research evidencing the ways in which music therapy can help people living with dementia, including: Reducing depression, stress, anxiety and blood pressure levels. Decreasing agitated and aggressive behaviours. Reducing the use of medication. Eliciting positive changes in mood and emotional ...
The aim of music therapy in people with dementia is to address emotions, cognitive powers, thoughts, and memories—to stimulate them and bring them to the fore. It aims to enrich and give freedom, stability, organization, and focus. Evaluation of music therapy and its impact is a complex task. Clinically significant changes are often highly ...
A new study shows that music therapy interventions may improve social interactions between people with dementia and their caregivers. The findings indicate that music therapy may also decrease ...
2017 were included for the review (n=15). The literature indicates the use of music therapy as an adjuvant therapy for the treatment of dementia in older adults may be beneficial in decreasing symptoms of aggression, anxiety, agitation and depression. Music therapy is used in varying settings, but more specifically in long term care facilities.
This might suggest that lyrics in pieces used for music therapy could play an important role in memory formation activation, and hence improve verbal fluency in patients living with dementia. The ability of music therapy to alleviate anxiety and depression is apparent in the selected groups of patients [, ].
those with Alzheimer's/dementia. Of those 67%, types of music therapy used over the. course of a year were varied: 30% used singing, 23% used the radio, 20% used live. music, 10% used a music therapist, 10% used a musical instrument, and 7% used an iPod. or other music-playing device.
Dementia is an increasingly common syndrome and while pharmacotherapy is available, its potential benefit is limited, especially in non-cognitive outcomes. Non-pharmacotherapy such as music therapy is potentially associated with improved outcomes. We assessed the effects of music therapy on patients with dementia to evaluate its potential benefits on dementia.
Music therapy is often informally used in residential care units to. enhance communication, emotional, co gnitive and beha vioural skills. in elderly patients diagnosed with dementia both ...
Authors' conclusions: Providing people with dementia who are in institutional care with at least five sessions of a music-based therapeutic intervention probably reduces depressive symptoms and improves overall behavioural problems at the end of treatment. It may also improve emotional well-being and quality of life and reduce anxiety, but may ...
The main result of this study was that music has positive benefits to dementia. In particular, appropriate, relaxing or individualized music significantly lowers agitation. Music was also found to have positive effects in mood, socialization, cooperation, and communication and enhanced interaction.
Introduction Dementia and Therapeutic Treatments. Dementia, depending on its characteristics, negatively affects different cognitive domains—"memory, thinking, orientation, understanding, calculation, ability to learn, language, and judgment" (World Health Organization [WHO], 2020a).Approximately, 50 million people worldwide currently suffer from dementia, caused by Alzheimer's disease ...
The effects of music when applied can bring psychological symptoms and the behaviours in people with dementia by affecting the physiological parameters like the autonomic nervous system for example the heart rate variability and the plasma cytokine and catcholaine levels. (Raglio et al 2010) and Okada et al 2009.
Music Therapy And Dementia Essay. Dementia is an extremely common disease among the elderly, with 4 million Americans currently suffering from the Alzheimer's type alone. Figures show that 3% of people between the ages of 65-74 suffer from the disease, rapidly increasing to 19% for the 75-84 age bracket, and as high as 47% for the over 85s.
This study highlights dementia therapy utilizing the music therapy method. Keywords: quality of life, depressive state, dementia, music therapy, meta-analysis. Introduction and background. The usage of customized music playlists in medical settings to address mental and behavioral issues and symptoms of patients affected by dementia is on the rise.
Music Therapy And Dementia Essay. According to Geretsegger et al. (2014), music therapy is an effective clinical intervention for a varied of medical conditions, which are profoundly supported by strong scientific evidence on their significance for mood enhancement and stress relief. The five conditions for which music therapy has been studied ...