
More results...

Browse Articles
Diagnostic Radiology, Pictorial Essay
Intraperitoneal anatomy with the aid of pathologic fluid and gas: An imaging pictorial review
Matthew Montanarella, Kimberly Boldig, Mayur Virarkar, Sindhu Kumar, Sherif Elsherif, Chandana Lall, Dheeraj Reddy Gopireddy
J Clin Imaging Sci 13 (13) (19th May, 2023)
Dual-energy computed tomography of the abdomen: A reliable trouble-shooter
Viswanath Anand Chidambaram, Mindy Chu Ming Choong, Chaitra Dhiraj Goud
J Clin Imaging Sci 13 (12) (21st April, 2023)
Vascular and Interventional Radiology, Pictorial Essay
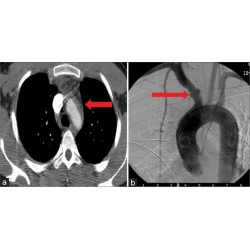
Imaging of penetrating vascular trauma of the body and extremities secondary to ballistic and stab wounds
Dheeraj Reddy Gopireddy, Joanna W. Kee-Sampson, Sai Swarupa Reddy Vulasala, Rachel Stein, Sindhu Kumar, Mayur Virarkar
J Clin Imaging Sci 13 (1) (3rd January, 2023)
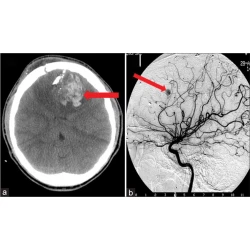
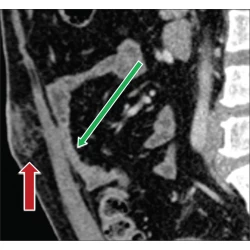
Neuroradiology Head and Neck Imaging, Pictorial Essay
Role of imaging in penetrating vascular injuries of the craniocervical region
Joanna W. Kee-Sampson, Dheeraj Reddy Gopireddy, Sai Swarupa Reddy Vulasala, Rachel Stein, Sindhu Kumar, Mayur Virarkar
J Clin Imaging Sci 12 (63) (3rd December, 2022)
Catheter-directed computed tomography angiography: A pictorial essay
Abheek Ghosh, Ellen Moxley, Suneet Waghmarae, James Stoner, Sheena Anand, Nabeel M. Akhter
J Clin Imaging Sci 12 (49) (18th August, 2022)
Musculoskeletal Imaging, Pictorial Essay
Chordoma at the skull base, spine, and sacrum: A pictorial essay
Sin Hang Lee, Kai Yan Kwok, Sin Man Wong, Chik Xing Jason Chan, Yu Ting Wong, Man Lung Tsang
J Clin Imaging Sci 12 (44) (5th August, 2022)
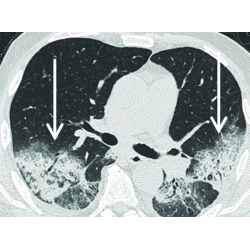
The many faces of cryptogenic organizing pneumonia (COP)
Christopher Kloth, Wolfgang Maximilian Thaiss, Meinrad Beer, Hans Bösmüller, Karolin Baumgartner, Jan Fritz, Marius Horger
J Clin Imaging Sci 12 (29) (3rd June, 2022)
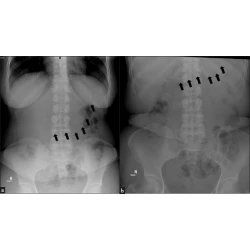
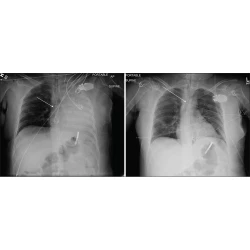
Plain X-ray findings of post sleeve gastrectomy gastric leak
Sultan R Alharbi
J Clin Imaging Sci 12 (28) (12th May, 2022)
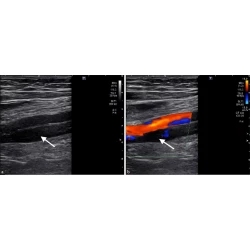
Imaging findings and interventional management of deep venous thrombosis
Hussam Hindi, Gauthier Dongmo, Alyssa Goodwin, Sean Jones, Kristian Loveridge
J Clin Imaging Sci 12 (26) (12th May, 2022)
Cardiopulmonary Imaging, Pictorial Essay
Pictorial review of computed tomography features of diffuse cystic lung disease
Yi Lam Priscilla Chan, Chun Hung Kevin Yu, Wing Ho Chong, Kai Yan Kwok, Allen Li
J Clin Imaging Sci 12 (11) (17th March, 2022)
Different facets of intracranial central nervous system lymphoma and its imaging mimics
Hoi Ming Kwok, Kwok Yan Li, Rois L. S. Chan, Chi Hin Chan, Stephen Ka Hon Wong, Chiu Man Lee, Lik Fai Cheng, Johnny Ka Fai Ma
J Clin Imaging Sci 12 (4) (4th February, 2022)
Neuroradiology, Pictorial Essay
A myriad spectrum of seizures on magnetic resonance imaging – A pictorial essay
Rahul Karthik Lingutla, Ajit Mahale, Akshatha R. Bhat, Sonali Ullal
J Clin Imaging Sci 12 (3) (21st January, 2022)
Gastrointestinal Imaging, Pictorial Essay
Added value of iodine-specific imaging and virtual non-contrast imaging for gastrointestinal assessment using dual-energy computed tomography
Madison R. Kocher, Mark D. Kovacs, William Stewart, Brian P. Flemming, Shaun Hinen, Andrew D. Hardie
J Clin Imaging Sci 11 (68) (23rd December, 2021)
Pediatric Imaging, Pictorial Essay
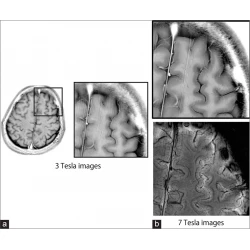
Application of 7 tesla magnetic resonance imaging for pediatric neurological disorders: Early clinical experience
Kenichi Yamada, Junichi Yoshimura, Masaki Watanabe, Kiyotaka Suzuki
J Clin Imaging Sci 11 (65) (2nd December, 2021)
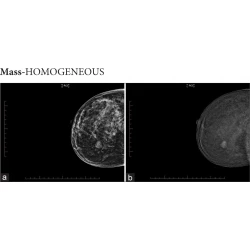
Breast Imaging, Pictorial Essay
Enhancement patterns in contrast mammography – A pictorial essay
Gesine Peters, Anne Margaret Lynch, Johannes Peters
J Clin Imaging Sci 11 (63) (26th November, 2021)
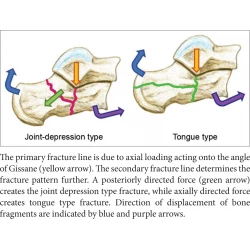
Computed Tomography for Calcaneal Fractures: Adding Value to the Radiology Report
Hoi Ming Kwok, Nin Yuan Pan, Fung Him Ng
J Clin Imaging Sci 11 (59) (9th November, 2021)
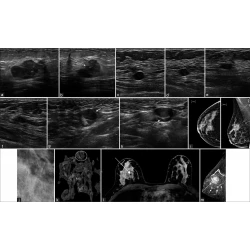
Pregnancy Associated Breast Cancer
Frances Perez, Ashley Bragg, Gary Whitman
J Clin Imaging Sci 11 (49) (21st September, 2021)
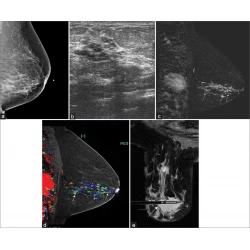
Imaging of Noncalcified Ductal Carcinoma
Ashley Bragg, Rosalind Candelaria, Beatriz Adrada, Monica Huang, Gaiane Rauch, Lumarie Santiago, Marion Scoggins, Gary Whitman
J Clin Imaging Sci 11 (34) (16th June, 2021)
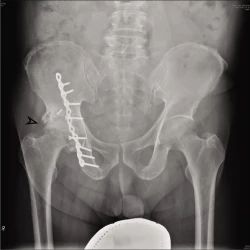
Hybrid Magnetic Resonance Imaging with Single Photon Emission Computed Tomography/Computed Tomography Bone Scan for Diagnosis Of Avascular Necrosis of Femoral Head
Fung Him Ng, Terence Kin Bong Lai, Sun Yu Lam, Nin Yuan Pan, Wing Hang Luk
J Clin Imaging Sci 11 (2) (12th January, 2021)
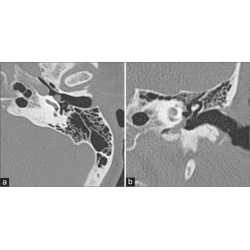
Imaging in Pulsatile Tinnitus: Case Based Review
Girish Bathla, Amogh Hegde, Prashant Nagpal, Amit Agarwal
J Clin Imaging Sci 10 (84) (20th December, 2020)
Abdominal Radiology, Pictorial Essay
Spectrum of CT Findings Related to Bowel Adhesions Without Bowel Obstruction: A Comprehensive Imaging Review
Dheeraj Reddy Gopireddy, Erik Soule, Hina Arif-Tiwari, Smita Sharma, Devaraju Kanmaniraja, Kapila Jain, Haley Letter, Chandana Lall
J Clin Imaging Sci 10 (80) (10th December, 2020)
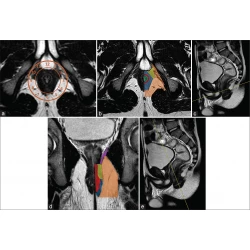
Magnetic Resonance Imaging of the Anal Region: Clinical Applications
Giuseppe Cicero, Giorgio Ascenti, Alfredo Blandino, Socrate Pallio, Claudia Abate, Tommaso D’Angelo, Silvio Mazziotti
J Clin Imaging Sci 10 (76) (21st November, 2020)
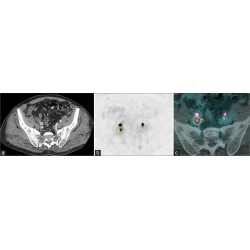
Nuclear Medicine, Pictorial Essay
Combined Intravenous Urogram and 68Ga-PSMA PET/ CT for Improved Staging and Restaging of Prostate Cancer
Rhiannon McBean, Anisa Kumari, Louise McEwan, James Walters, David Wong
J Clin Imaging Sci 10 (67) (24th October, 2020)
Malpositioned Lines and Tubes on Chest Radiograph – A Concise Pictorial Review
Muthu Kumar Sakthivel, Thangavijayan Bosemani, Leon Bacchus, Ertan Pamuklar
J Clin Imaging Sci 10 (66) (22nd October, 2020)
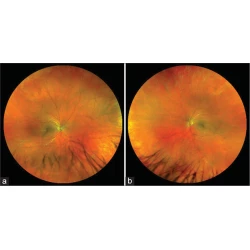
Lipemia Retinalis in a Patient with Familial Hypertriglyceridemia
Patrick Wang, Eric K. Chin, David R. P. Almeida
J Clin Imaging Sci 10 (64) (17th October, 2020)
Vascular Trauma in the Head and Neck and Endovascular Neurointerventional Management
Jeet Patel, Thien J. Huynh, Dinesh Rao, Grzegorz Brzezicki
J Clin Imaging Sci 10 (44) (30th July, 2020)
PICTORIAL ESSAY
Adverse Events in Coronavirus Disease Patients Management: A Pictorial Essay
Salvatore Alessio Angileri, Mario Petrillo, Letizia Di Meglio, Antonio Arrichiello, Giovanni Maria Rodà, Anna Maria Ierardi, Raman Uberoi, Gianpaolo Carrafiello
J Clin Imaging Sci 10 (42) (21st July, 2020)
Magnetic Resonance Imaging of the Diaphragm: From Normal to Pathologic Findings
Giuseppe Cicero, Silvio Mazziotti, Alfredo Blandino, Francesca Granata, Michele Gaeta
J Clin Imaging Sci 10 (1) (13th January, 2020)

Nonconventional Options for Tumor Localization in Breast and Axillary Lymph Nodes: A Pictorial How-To
Naziya Samreen, Christine U Lee, Asha A Bhatt
J Clin Imaging Sci 8 (54) (12th December, 2018)

Tomosynthesis-Guided Core Biopsy of the Breast: Why and How to Use it
Kyungmin Shin, Davis Teichgraeber, Sarah Martaindale, Gary J Whitman
J Clin Imaging Sci 8 (28) (31st July, 2018)

Incremental Value of Magnetic Resonance Imaging in Further Characterizing Hypodense Mediastinal and Paracardiac Lesions Identified on Computed Tomography
Abhishek Chaturvedi, Chris Gange, Hakan Sahin, Apeksha Chaturvedi
J Clin Imaging Sci 8 (10) (12th March, 2018)
Computed Tomography-guided Pulmonary Nodule Microcoil Localization Technique, Misplacement Errors, and Complications: A Pictorial Essay
J Clin Imaging Sci 8 (8) (9th March, 2018)

Magnetic Resonance Imaging Appearance of Schwannomas from Head to Toe: A Pictorial Review
Jamie Crist, Jacob R Hodge, Matthew Frick, Fiona P Leung, Eugene Hsu, Ming Tye Gi, Sudhakar K Venkatesh
J Clin Imaging Sci 7 (38) (3rd October, 2017)

Anatomic Variations of the Right Portal Vein: Prevalence, Imaging Features, and Implications for Successful Transjugular Intrahepatic Portosystemic Shunt Creation
Senthil S Gunasekaran, Ron C Gaba
J Clin Imaging Sci 7 (14) (28th March, 2017)
Different Sonographic Faces of Ectopic Pregnancy
Charu Chanana, Nishant Gupta, Itisha Bansal, Kusum Hooda, Pranav Sharma, Mohit Gupta, Darshan Gandhi, Yogesh Kumar
J Clin Imaging Sci 7 (6) (20th February, 2017)

Unexpected Angiography Findings and Effects on Management
Matthew Neill, Hearns W Charles, Jonathan S Gross, Sean Farquharson, Amy R Deipolyi
J Clin Imaging Sci 6 (33) (1st September, 2016)
Thoracic Presentations of Small Round Blue Cell Tumors
Annalice Chang, Kyle Pfeifer, Peter Chen, Vivek Kalra, Myung Soo Shin
J Clin Imaging Sci 6 (25) (23rd June, 2016)

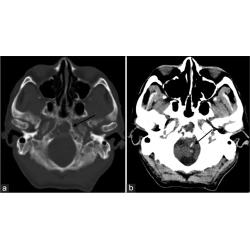
Sinonasal Fungal Infections and Complications: A Pictorial Review
Jose Gavito-Higuera, Carola Birgit Mullins, Luis Ramos-Duran, Hugo Sandoval, Nassim Akle, Ramon Figueroa
J Clin Imaging Sci 6 (23) (14th June, 2016)

Sonographic Appearance of the Median Nerve Following Revision Carpal Tunnel Surgery
Shane A Shapiro, Ashkan Alkhamisi, George G A Pujalte
J Clin Imaging Sci 6 (11) (30th March, 2016)

3D-Printing in Congenital Cardiology: From Flatland to Spaceland
Sébastien Deferm, Bart Meyns, Dirk Vlasselaers, Werner Budts
J Clin Imaging Sci 6 (8) (30th March, 2016)

Uncommon Causes of Acute Abdominal Pain – A Pictorial Essay
Mahesh Hariharan, Rajan Balasubramaniam, Sharath Kumar Shetty, Shanthala Yadavalli, Mohammed Ahetasham, Sravya Devarapalli
J Clin Imaging Sci 6 (4) (26th February, 2016)

Gastroesophageal Variceal Filling and Drainage Pathways: An Angiographic Description of Afferent and Efferent Venous Anatomic Patterns
Ron C Gaba, Patrick M Couture, Janesh Lakhoo
J Clin Imaging Sci 5 (61) (30th November, 2015)
Rare Malignant Tumors of the Breast
Trevor Miller, Constance Albarracin, Selin Carkaci, Gary J Whitman, Beatriz E Adrada
J Clin Imaging Sci 5 (58) (30th October, 2015)
Back to Basics – ‘Must Know’ Classical Signs in Thoracic Radiology
Athiyappan Kumaresh, Mitesh Kumar, Bhawna Dev, Rajani Gorantla, PM Venkata Sai, Vijayalakshmi Thanasekaraan
J Clin Imaging Sci 5 (43) (31st July, 2015)

Magnetic Resonance Imaging of Non-ischemic Cardiomyopathies: A Pictorial Essay
Cristina I Olivas-Chacon, Carola Mullins, Kevan Stewart, Nassim Akle, Jesus E Calleros, Luis R Ramos-Duran
J Clin Imaging Sci 5 (37) (30th June, 2015)

Assessment of Ischemic Cardiomyopathy Using Cardiovascular Magnetic Resonance Imaging: A Pictorial Review
Cristina Ivette Olivas-Chacon, Carola Mullins, Agnieszka Solberg, Nassim Akle, Jesus E Calleros, Luis R Ramos-Duran
J Clin Imaging Sci 5 (28) (22nd May, 2015)

Unusual Benign Tumors of the Breast
Beatriz E Adrada, Savitri Krishnamurthy, Selin Carkaci, Flavia E Posleman-Monetto, Adesuwa Ewere, Gary J Whitman
J Clin Imaging Sci 5 (27) (22nd May, 2015)

Cross-sectional Imaging Features of Primary Retroperitoneal Tumors and Their Subsequent Treatment
Turker Acar, Mustafa Harman, Serkan Guneyli, Kazim Gemici, Duran Efe, Ibrahim Guler, Melda Yildiz
J Clin Imaging Sci 5 (24) (30th April, 2015)

Incidentally Detected Mediastinal Vascular Anatomical Variants on PET-CT: A Pictorial Essay
Kathyayini Gopalkrishna Murthy Paidipati, Raghava Kashyap, Hima Tadimeti, Mahidhar Peyyeti
J Clin Imaging Sci 5 (19) (31st March, 2015)
Congenital Absence of the Right Pericardium: Embryology and Imaging
Chi Wan Koo, Adrienne Newburg
J Clin Imaging Sci 5 (12) (27th February, 2015)

Radiography of Cardiac Conduction Devices: A Pictorial Review of Pacemakers and Implantable Cardioverter Defibrillators
Stephanie C Torres-Ayala, Guido Santacana-Laffitte, José Maldonado
J Clin Imaging Sci 4 (74) (31st December, 2014)

MRI of Uncommon Lesions of the Large Bowel: A Pictorial Essay
Christine U Lee, James F Glockner
J Clin Imaging Sci 4 (71) (31st December, 2014)
Blood Pool Contrast-enhanced Magnetic Resonance Angiography with Correlation to Digital Subtraction Angiography: A Pictorial Review
Martha-Grace Knuttinen, Jillian Karow, Winnie Mar, Margaret Golden, Karen L Xie
J Clin Imaging Sci 4 (63) (29th November, 2014)

Revisiting Ectopic Pregnancy: A Pictorial Essay
Artemis Petrides, Cheryl Dinglas, Martin Chavez, Sharon Taylor, Sabrina Mahboob
J Clin Imaging Sci 4 (37) (31st July, 2014)
Imaging Features of AlloDerm Used in Postmastectomy Breast Reconstructions
Christine U. Lee, Allison J. Clapp, Steven R. Jacobson
J Clin Imaging Sci 4 (19) (29th April, 2014)

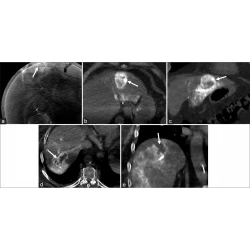
Adrenal Lesions: Spectrum of Imaging Findings with Emphasis on Multi-Detector Computed Tomography and Magnetic Resonance Imaging
Antonino Guerrisi, Daniele Marin, Mahbubeh Baski, Pietro Guerrisi, Federica Capozza, Carlo Catalano
J Clin Imaging Sci 3 (61) (31st December, 2013)

Magnetic Resonance Imaging of Benign Cardiac Masses: A Pictorial Essay
Thomas J. Ward, Michael A. Kadoch, Adam H. Jacobi, Pablo P. Lopez, Javier Sanz Salvo, Matthew D. Cham
J Clin Imaging Sci 3 (34) (31st August, 2013)

Angiographic Patterns of Transjugular Intrahepatic Portosystemic Shunt Dysfunction and Interventional Approaches to Shunt Revision
Ahmad Parvinian, Benedictta O. Omene, James T. Bui, Martha Grace Knuttinen, Jeet Minocha, Ron C. Gaba
J Clin Imaging Sci 3 (19) (30th April, 2013)

Radiological Features of Metastatic Gastrointestinal Stromal Tumors
Sujata Patnaik, Yarlagadda Jyotsnarani, Susarla Rammurti
J Clin Imaging Sci 2 (43) (28th July, 2012)

Shoulder Ultrasonography: Performance and Common Findings
Diana Gaitini
J Clin Imaging Sci 2 (38) (28th July, 2012)

Prenatal and Postnatal Schizencephaly Findings by 2D and 3D Ultrasound: Pictorial Essay
Lívia Teresa Moreira Rios, Edward Araujo, Luciano Marcondes Machado Nardozza, Ana Carolina Rabachini Caetano, Antonio Fernandes Moron, Marília da Glória Martins
J Clin Imaging Sci 2 (30) (23rd May, 2012)

Radiological Imaging Features of Infection – A Pictorial Review
Abdurrahim Dusak, Mehmet R. Onur, Mutalip Cicek, Ugur Firat, Tianbo Ren, Vikram S. Dogra
J Clin Imaging Sci 2 (2) (27th January, 2012)


Non-Coronary Cardiac Findings and Pitfalls in Coronary Computed Tomography Angiography
Noriko Oyama-Manabe, Teppei Sugaya, Takayoshi Yamaguchi, Satoshi Terae
J Clin Imaging Sci 1 (51) (25th October, 2011)

Multimodality Imaging of Normal Hepatic Transplant Vasculature and Graft Vascular Complications
Jeffrey H Roberts, Fernanda S Mazzariol, Susan J Frank, Sarah K Oh, Mordecai Koenigsberg, Marjorie W Stein
J Clin Imaging Sci 1 (50) (25th October, 2011)

Magnetic Resonance Enterography Findings in Crohn′s disease in the Pediatric Population and Correlation with Fluoroscopic and Multidetector Computed Tomographic Techniques
Parul Patel, Margaret Ormanoski, Kim M. Hoadley
J Clin Imaging Sci 1 (41) (30th July, 2011)
Angiogenesis Imaging in Neoplasia
David J. Bowden, Tristan Barrett
J Clin Imaging Sci 1 (38) (27th July, 2011)
Crohn’s disease: Multimodality Imaging of Surgical Indications, Operative Procedures, and Complications
B Kolar, J Speranza, S Bhatt, V Dogra
J Clin Imaging Sci 1 (37) (14th July, 2011)

Imaging Features of the Pleuropulmonary Manifestations of Rheumatoid Arthritis: Pearls and Pitfalls
Harbir S Sidhu, Gauraang Bhatnagar, Pervinder Bhogal, Richard Riordan
J Clin Imaging Sci 1 (32) (21st June, 2011)

Image-guided Percutaneous Drainage in the Pediatric Population: A Primer for Radiologists
Keerthi Arani, Kiran Nandalur, Christina M Tucker, David A Bloom
J Clin Imaging Sci 1 (31) (21st June, 2011)

The Fetal Magnetic Resonance Imaging Experience in a Large Community Medical Center
Peter M Ghobrial, Rebecca A Levy, Stephen C O’Connor
J Clin Imaging Sci 1 (29) (31st May, 2011)

Diffusion-weighted Magnetic Resonance Imaging: What Makes Water Run Fast or Slow?
Francesca Fornasa
J Clin Imaging Sci 1 (27) (19th May, 2011)

Imaging of the Bursae
Zameer Hirji, Jaspal S Hunjun, Hema N Choudur
J Clin Imaging Sci 1 (22) (2nd May, 2011)

Imaging of Mechanical Cardiac Assist Devices
Daniel Ginat, Howard Todd Massey, Shweta Bhatt, Vikram S Dogra
J Clin Imaging Sci 1 (21) (2nd May, 2011)

Sonographic Upper Gastrointestinal Series in the Vomiting Infant: How We Do It
Thaddeus W Herliczek, Deepak Raghavan, Kathleen McCarten, Michael Wallach
J Clin Imaging Sci 1 (19) (31st March, 2011)
Magnetic Resonance Imaging of Neurosarcoidosis
Daniel T Ginat, Gurpreet Dhillon, Jeevak Almast
J Clin Imaging Sci 1 (15) (11th February, 2011)

X-ray Digital Linear Tomosynthesis Imaging for Artificial Pulmonary Nodule Detection
Tsutomu Gomi
J Clin Imaging Sci 1 (16) (10th February, 2011)

Sonographic Spectrum of Tunica Albuginea Cyst
Daniel M. Alvarez, Shweta Bhatt, Vikram S. Dogra
J Clin Imaging Sci 1 (5) (1st January, 2011)
ISSN (Print): 2156-7514 ISSN (Online): 2156-5597

Privacy Overview

Wanted: Emergencies in head and neck radiology; pictorial essay.

Learning objectives
There is a perception as little as emergencies can occur in head and radiology. Whereas there are many emergencies in head and neck radiology, they can threaten the life because of the anatomical proximity of vital organs.
We aimed to describe and identify radiological findings of the most common emergencies in head and neck radiology. In these situations, radiologist plays an essential role in a patient’s outcome. Fig. 2 : Introduction summary. References: https://www.imdb.com/title/tt0114814/mediaviewer/rm1975465472" title="Fig. 2: Introduction summary. References: https://www.imdb.com/title/tt0114814/mediaviewer/rm1975465472" href="https://epos.myesr.org/posterimage/esr/ecr2020/156057/mediagallery/869618">Fig. 2

Gastrointestinal Emergency in Neonates and Infants: A Pictorial Essay
Affiliations.
- 1 Department of Radiology, Korea University Ansan Hospital, Ansan, Korea.
- 2 Department of Radiology, Korea University Ansan Hospital, Ansan, Korea. [email protected].
- 3 Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- PMID: 34983099
- PMCID: PMC8743148
- DOI: 10.3348/kjr.2021.0111
Gastrointestinal (GI) emergencies in neonates and infants encompass from the beginning to the end of the GI tract. Both congenital and acquired conditions can cause various GI emergencies in neonates and infants. Given the overlapping or nonspecific clinical findings of many different neonatal and infantile GI emergencies and the unique characteristics of this age group, appropriate imaging is key to accurate and timely diagnosis while avoiding unnecessary radiation hazard and medical costs. In this paper, we discuss the radiological findings of essential neonatal and infantile GI emergencies, including esophageal atresia and tracheoesophageal fistula, hypertrophic pyloric stenosis, duodenal atresia, malrotation, midgut volvulus for upper GI emergencies, and jejunoileal atresia, meconium ileus, meconium plug syndrome, meconium peritonitis, Hirschsprung disease, anorectal malformation, necrotizing enterocolitis, and intussusception for lower GI emergencies.
Keywords: Anorectal malformation; Gastrointestinal emergency; Hirschsprung disease; Imaging; Infant; Intestinal atresia; Intussusception; Meconium plug syndrome; Midgut volvulus; Necrotizing enterocolitis; Neonate; Tracheoesophageal fistula.
Copyright © 2022 The Korean Society of Radiology.
Publication types
- Diagnostic Imaging
- Duodenal Obstruction*
- Infant, Newborn
- Intestinal Atresia*
- Intussusception*
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Imaging Sci Dent
- v.46(1); 2016 Mar

Formation of ghost images due to metal objects on the surface of the patient's face: A pictorial essay
Bárbara couto ramos.
1 Department of Oral Radiology, School of Dentistry, Pontifical Catholic University of Minas Gerais, Belo Horizonte, Brazil.
Bruna Raquel da Silva Izar
Jéssica lourdes costa pereira, priscilla sena souza, claudia scigliano valerio, fabrício mesquita tuji.
2 Department of Oral Radiology, School of Dentistry, Federal University of Pará, Belém do Pará, Brazil.
Flávio Ricardo Manzi
Panoramic radiographs are a relatively simple technique that is commonly used in all dental specialties. In panoramic radiographs, in addition to the formation of real images of metal objects, ghost images may also form, and these ghost images can hinder an accurate diagnosis and interfere with the accuracy of radiology reports. Dentists must understand the formation of these images in order to avoid making incorrect radiographic diagnoses. Therefore, the present study sought to present a study of the formation of panoramic radiograph ghost images caused by metal objects in the head and neck region of a dry skull, as well as to report a clinical case n order to warn dentists about ghost images and to raise awareness thereof. An understanding of the principles of the formation of ghost images in panoramic radiographs helps prevent incorrect diagnoses.
Introduction
Radiographs are an important method of diagnosing and monitoring oral diseases, dentofacial development, and the progress or prognosis of therapy. 1 Panoramic radiography is recommended for patients in several age ranges: children with transitional dentition (after eruption of the first permanent tooth); adolescents with permanent dentition (prior to the eruption of the third molars); and adults who are dentate or partially edentulous. Panoramic radiographs are also recommended in new patients being evaluated for oral diseases and in patients undergoing follow-up, based on clinical signs, symptoms, and treatment plans. 1 Intraoral radiographs are more accurate than panoramic radiographs; however, panoramic examinations may be advantageous because they involve a reduced radiation dosage, cost less, and allow a larger area to be imaged. Thus, although these issues have been addressed in prior studies, it is important that dentists understand the mechanisms associated with the formation of real and ghost images in panoramic radiographs.
The panoramic radiograph technique is based on the principle of computed tomography, since both techniques involve synchronized rotation between an X-ray source and an image receptor around the patient's head that remains stationary. 2 This is a radiological technique that is relatively simple and is commonly used in all dental specialties, 3 , 4 since patients have shown a good tolerance to this technique, it is fast and comfortable, and, most importantly, it includes the entire maxillomandibular structure (dental arches, temporomandibular joint, and associated structures) in a single film. 4 , 5 , 6 It is used in a broad range of clinical settings, including the evaluation of deciduous and permanent teeth; orthodontic evaluations; the evaluation of bone lesions, erupted teeth, periodontal bone supports, third molars, lesions in the maxillary sinus, and fractures of the mandible; and evaluations of foreign bodies and the loss of bone mineral density (osteopenia and osteoporosis); among others. 4 , 6 , 7 , 8 However, this technique also presents certain disadvantages, such as the overlap of the images of certain anatomical structures, the amplification and reduction of images (geometric distortion), and the production of ghost images. 3 , 5 , 6 , 9 , 10
Ghost images, or artifacts, are created by anatomical structures or objects that are located outside of the zone of focus or image layer but have a sufficient density to attenuate the X-ray beams, in turn producing distorted radiographic images. 2 Although panoramic radiographs play a crucial role in diagnosis, these ghost images complicate the use of panoramic radiographs, since they may closely resemble the lesions themselves, be confounded with dental structures in inappropriate locations, or mask anomalies by obstructing the view of subjacent anatomical structures. 4
Panoramic radiographs of a patient with earrings inserted in his or her earlobe are one of the most common examples of how ghost images of non-anatomic origin may be formed. 2 In such cases, one can observe images of the earrings in the molar region, the coronoid process, the mandibular notch, and/or the mandibular condyle, resembling an impacted tooth or a cyst, among other abnormalities. It is therefore important to understand the appearance of anatomical structures and their variations in panoramic radiographs, 4 with the additional challenge of identifying structures that fall outside of the standards of normality in order to make correct and coherent diagnoses.
Since many patients have piercings or other metal objects in their facial region, and as these objects can impair the quality of the panoramic radiograph image and its interpretation, it is important to understand the errors and artifacts that accompany this radiological technique. Therefore, the aim of the present study was to present a study of the formation of ghost images in panoramic radiographs caused by metal objects in different regions of the skull, as well as to report a clinical case, in an attempt to aid dentists in understanding the mechanisms associated with the formation of real and ghost images in panoramic radiographs.
Materials and Methods
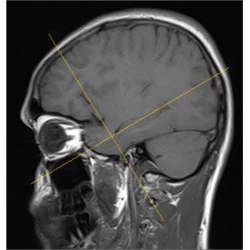
After having received approval for the present study from our institution's Ethics Committee (CAE: 45441815.4.0000.5137), we conducted this study using a macerated adult skull placed in a Kodak 9000C three-dimensional panoramic device (Eastman Kodak Company, Rochester, New York, USA). The skull was positioned in the X-ray device according to standard procedures, with its sagittal plane placed in the center of the zone of focus of the X-ray unit and perpendicular to the horizontal plane and the Frankfurt plane parallel to the horizontal plane. According to the bitewing of the device, the top teeth were arranged to place the dental arches in the zone of focus or image layer.
A round metal object was attached in various areas of the skull to assess the formation of real and ghost images (the region around tooth 46, the upper region of the ear, the anterior nasal spine, the nasal wing, the lateral pole of the temporomandibular joint, the region around tooth 18, the mandibular angle, the earlobe, the hyoid bone, and the dorsum of the tongue). One image was taken with no metal object, which was defined as the control radiograph. The radiographs were taken using the following exposure factors: 60 kV, 2.0 mA, and 14.3 s of exposure.
The present study mapped the maxillomandibular areas according to the diagram proposed by Reuter et al., 11 who demonstrated the formation of one, two, or three similar images after the strategic positioning of a metal object in different anatomic structures of the face. Reuter et al. 11 referred to the zones where the test object was portrayed once as zone 1A and zone 1B, the zone where the test object was portrayed twice as zone 2, and the zone where the test object was portrayed three times as zone 3 ( Fig. 1 ). In the areas corresponding to zone 1A, which comprises the anterior regions of the mandible and the maxilla, the formation of one single real image occurs. In zone 1B, which includes the most posterior portion of the zone of focus or image layer (i.e., the regions of the occipital bone and the foramen magnum), the production of a single ghost image occurs. The mandibular ramus and angle, the mandibular condyles, the hard palate, and the earlobes are located in the areas corresponding to zone 2, where two images are produced: one ghost image and one real image. In zone 3, comprising the spine and hyoid bone, the formation of a triple image can be observed, including two real images lateral to the film and one ghost image in the center of the film.

In this study, the images obtained from the skull were examined directly in the Kodak Dental Imaging Software (Kodak Dental Systems, Rochester, NY, USA) by two trained oral radiologists, one with ten years of experience and the other with eight years of experience. They used a computer with a GeForce 9500 GT graphics card (Nvidia Corporation Santa Clara, CA, USA), and an LED LG Flatron E2241 monitor (LG Electronics, Seoul, Korea), with a resolution of 1920×1080 pixels and the brightness and contrast levels of the monitor set to the default configuration. The analysis of the images was performed following the schematic design of zones 1A, 1B, 2, and 3. Disagreements were resolved by discussion, and a final consensus was reached.
In order to exemplify the importance of the anatomic and technical knowledge of the formation of panoramic radiographic images, we also report the clinical case of a 24-year-old male patient referred to the radiology clinic to undergo dental exams necessary for orthodontic treatment. Panoramic and lateral cephalometric radiographs were taken using the Orthopantomograph® OP 100 (Instrumentarium Imaging, Tuusula, Finland). For the panoramic radiograph, the X-ray tube was operated with settings of 57 kVp, 3.2 mA, and an exposure time of 17.6 s. For the lateral cephalometric radiograph, the X-ray tube was operated with settings of 80 kVp, 10 mA, and an exposure time of 0.7 s. After radiographic exposure, all films were processed in a Macrotec MX-2 automatic processor (Macrotec, São Paulo, Brazil) with Picker RP type-S processing chemistry (Eastman Kodak Company, Rochester, NY, USA).
First, a panoramic radiograph was taken of the macerated skull with a metal sphere attached in the region where tooth 46 was missing. This region was located within the focal plane, corresponding to the formation of images in zone 1A. The result was a single real image of the metal sphere ( Fig. 2 ).

Figure 3 presents a panoramic radiograph taken with a metal sphere that was attached to the crown of tooth 18. This region is located in the focal plane but corresponds to image formation in zone 2. The result was the production of a real image in the region of the crown of tooth 18 (ipsilateral) and a ghost image on the opposite side (contralateral). The ghost image was located at a higher position and was sharper.

Figure 4 shows another example of a panoramic radiograph taken with a metal sphere located in zone 2. In this case, the metal sphere was attached in the region of the right earlobe, producing a real ipsilateral image and a distorted contralateral ghost image.

In the last panoramic radiograph, the metal sphere was attached in the region of the hyoid bone ( Fig. 5 ). This region corresponds to image formation in zone 3. Thus, three images were formed, with two real and bilateral images projected in the region of the right and left mandibular angle and one ghost image in the center of the film, overlapping the region of the inferior incisors.

In this case report, the panoramic radiograph presented a radiopaque image overlapping the roots of the molars, premolars, and canines, located in the upper right hemiarch ( Fig. 6A ). The lateral cephalometric radiograph was analyzed to evaluate the existence of a metal object that could explain the formation of the radiopaque band observed in the panoramic radiograph ( Fig. 6B ).

This study demonstrated the formation of real and ghost images in panoramic radiographs through the placement of metallic objects in different maxillomandibular regions of a macerated adult skull. The images were analyzed using the schematic design of zones where the test object was portrayed once (zone 1A and 1B), twice (zone 2), and three times (zone 3).
Panoramic radiographs may contain single or double real images, as well as ghost images. A real image is formed when the object is located between the rotation center of the X-ray beam and the image receptor, and the image is taken with high definition and sharpness when the object is near the central layer of the zone of focus ( Fig. 7 ). 12 , 13 The central ray of the X-ray beam must also be perpendicular to the object and image detector. 14 The shape of the panoramic radiograph zone of focus or image layer is similar to that of the dental arch. Figure 2 shows the formation of a single real image in a panoramic radiograph taken with one metal sphere attached in the region where tooth 46 was missing (zone 1A).

A ghost image occurs when the object or anatomic structure is located between the X-ray source and the center of rotation, and has a density that is sufficient to attenuate the X-ray beams. 2 , 12 This image subsequently presents the same morphology as the object, but with distortion, and appears on the opposite side and at a higher point than the corresponding real object. The image appears in a vertically expanded form. but may or may not be expanded horizontally. 10 The ghost image also contains a corresponding real image, which may or may not be visible in the panoramic radiograph. 12 Figures 3 and and4, 4 , as well as the case report, illustrate the formation of a real ipsilateral image and a distorted contralateral ghost image in panoramic radiographs with a metal object located in zone 2.
A double image consists of a pair of real images. The double image is formed when an object or anatomic structure is located between the center of rotation of the X-ray beams and the image receptor, but is intercepted twice during the exposure cycle. 2 , 12 The distance of the object to the image receptor is the same in both instances in which the object is exposed. 2 The double images are as sharp as the real images. 2 , 11 Double images are caused by objects or anatomic structures that are located in the midline. Figure 5 demonstrates the formation of a double image caused by a metal sphere placed in the region of the hyoid bone (zone 3). This figure shows two real bilateral images projected upon the mandibular angle. Another clinical example is the cervical spine, from which a real image is portrayed bilaterally at the extreme sides of the radiograph. 12
Triple images can consist of two lateral images and a central ghost, as in case of the cervical spine and hyoid bone. 11 In this situation, a real image is portrayed bilaterally at the extreme sides of the radiograph, and the central image is a ghost. 11 , 12 Figure 5 exemplifies the formation of a triple image caused by the placement of a metal sphere in the region of the hyoid bone (zone 3).
In this case report, the panoramic radiograph presented a radiopaque image located in the upper right hemiarch. Also observed was a voluminous metal restoration in the occlusal region of tooth 28. The lateral cephalometric radiograph showed no metal object in the upper right hemiarch. Therefore, it was confirmed that the radiopaque image formed in the region of the maxilla on the right side of the panoramic radiograph was in fact a ghost image caused by the restoration of the amalgam present in the maxillary left third molar. The metal restoration was located in zone 2 and produced an ipsilateral real image (restoration in tooth 28) and a distorted contralateral ghost image (radiopaque band).
In conclusion, knowledge of the principles of the formation of ghost images in panoramic radiographs, as well as of normal anatomy, prevents incorrect diagnoses that could result in inappropriate prognoses and treatment plans. It is recommended that, whenever possible, all metal objects should be removed from the head and neck region in order to prevent the formation of ghost images created by these objects.
This project was supported by the Foundation for Research Support of the State of Minas Gerais (Fundação de Amparo a Pesquisa do Estado de Minas Gerais - FAPEMIG), and the CAPES Foundation.
- Educational Review
- Open access
- Published: 02 October 2023
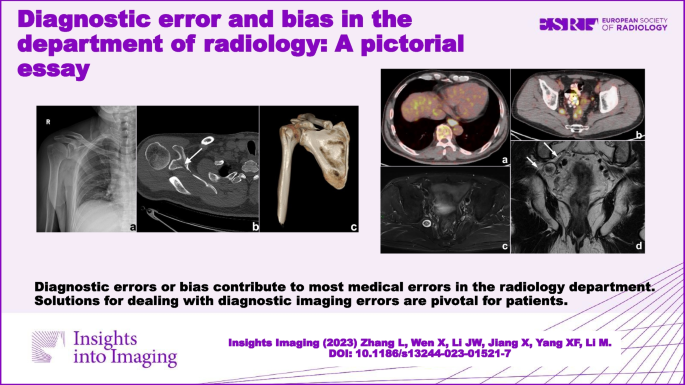
Diagnostic error and bias in the department of radiology: a pictorial essay
- Li Zhang 1 na1 ,
- Xin Wen 1 na1 ,
- Jian-Wei Li 1 ,
- Xu Jiang 1 ,
- Xian-Feng Yang 2 &
- Meng Li ORCID: orcid.org/0000-0001-7592-2091 1
Insights into Imaging volume 14 , Article number: 163 ( 2023 ) Cite this article
5764 Accesses
12 Altmetric
Metrics details
Diagnostic imaging is an essential and indispensable part of medical diagnosis and treatment, and diagnostic errors or biases are also common in the department of radiology, sometimes even having a severe impact on the diagnosis and treatment of patients. There are various reasons for diagnostic errors or biases in imaging. In this review, we analyze and summarize the causes of diagnostic imaging errors and biases based on practical cases. We propose solutions for dealing with diagnostic imaging errors and reducing their probability, thereby helping radiologists in their clinical practice.
Critical relevance statement Diagnostic errors or bias contribute to most medical errors in the radiology department. Solutions for dealing with diagnostic imaging errors are pivotal for patients.
• Diagnostic errors or bias contribute to most medical errors in radiology department.
• Solutions for dealing with diagnostic imaging errors are pivotal for patients.
• This review summarizes the causes of diagnostic errors and offers solutions to them.
Graphical Abstract
Introduction
Quality assurance is the key component of the modern healthcare system; the structure, processes, and results of clinical work are the major elements of quality management and measurement. Low-quality medical care may result in medical errors, including errors in diagnosis, treatment, prevention, and other types. Medical errors are an important cause of mortality, leading to unnecessary health expenditure [ 1 , 2 ]. Among them, the percentage of diagnostic errors, including misdiagnoses, missed diagnoses, and delayed diagnoses, is as high as 10–26% of all cases [ 3 , 4 ]. According to the Committee on Diagnostic Error in Health Care of the Institute of Medicine, diagnostic error is defined as “the failure to (a) establish an accurate and timely explanation of the patient’s health problem(s) or (b) communicate that explanation to the patient” [ 5 ]. In addition, medical errors can lead to patient concern, with one study reporting that 38% of patients attending emergency departments had concerns about medical errors, the most common being misdiagnosis (22%) [ 6 ]. In the radiology department, most medical errors are classified as diagnostic errors or other errors, such as information failure. Approximately 75% of malpractice lawsuits filed against radiologists relate to diagnostic imaging errors [ 7 ].
Diagnostic imaging is the professional interpretation of images; it is a series of uncertain and intricate task processes. The diagnostic process mainly contains 6 steps: assessing the pretest probability of a disease, ensuring the patient’s identity, perception to differentiate negative/positive situations, pattern recognition for the positive findings in radiological diagnosis, differential diagnosis and categorization of the findings, and timely communication of the results in an actionable and reliable format. Therefore, at every step of the process, we are likely to make mistakes due to multiple factors. In addition, the high variability and complexity of imaging techniques and the inherent limitations of the diagnostic capabilities of various imaging modalities also affect the diagnosis. The study of imaging interpretation errors began in the 1940s. At that time, Professor Chamberlain lectured on fluoroscopic errors, including image quality and dark adaptation [ 8 ], and presented what may be the earliest traceable study of radiological errors. In 1959, Garland’s research made radiologists aware of the high rate of diagnostic errors in radiology [ 9 ]. Subsequent studies have shown that the diagnostic imaging error rate remains, although researchers have performed research and intervention in that area for decades, and the data do not improve compared with Garland’s results. More specifically, if only the number of abnormal imaging results is used as the denominator, the error rate is approximately 30%, but if the number of all imaging results (including abnormal and normal cases) is used as the denominator, the error rate is 3.5–4.5% [ 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ]. With the development of modern imaging, although advanced imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) have greatly improved the diagnostic accuracy in the detection of diseases, there are still numerous radiological diagnostic errors due to increased amounts of data and diagnostic information.
These studies suggest that errors in radiology are common and even inevitable. However, to avoid harming the patients primarily, there is a requirement for us to minimize the error rate. This review presents an overview of the common causes and classifications of diagnostic errors in imaging based on our experience and clinical cases. In addition, we also develop some preliminary proposals about how to cope with errors, improve the quality, and help radiologists learn from mistakes. The structure of the error type categorization and the related error management strategies are summarized in Supplementary Table 1 .
Professional causes of diagnostic errors in radiology
The causes of imaging diagnostic errors are complicated and often coexist for multiple reasons. In this article, we mainly discuss two types: perceptual error and cognitive error. A perceptual error can be referred to as a “miss,” which means an important finding is not observed. Similarly, cognitive errors can be considered “misunderstanding,” which means an unusual image is found but subjected to faulty reasoning, or the diagnostic classification of the imaging abnormality is generally correct, but there is inadequate interpretation or complacency due to cognitive bias. Perceptual errors account for approximately 60 to 80% of diagnostic reporting errors, and the proportion of cognitive mistakes is approximately 20 to 40% [ 10 , 18 ]. Next, we will detail the common causes and examples of these two types of errors based on clinical practice.
- Perceptual errors
Images are the basis of diagnosis, so inappropriate or incomplete scan protocols, image artifacts, and low-quality images caused by limitations of equipment and post-processing software are important objective causes of image reporting errors. In radiology department, quality control focuses on technical performance (artifacts, selection of the study region, etc.) and diagnostic performance (detection of pathology, terminological errors, etc.) [ 19 ]. Solutions to these errors include the increasing investment of time and effort in scan and equipment development and routine image quality control, thereby reducing diagnostic errors caused by equipment issues. Apart from that, most perception errors occur when doctors fail to find a meaningful lesion in images (search error), when a lesion is noted for a short time but not given sufficient attention (recognition error), or when doctors attach importance to the lesions but do not provide the correct diagnosis (decision error) [ 20 , 21 ]. Based on our clinical experience and literature published, we categorize perceptual errors into the following causes.
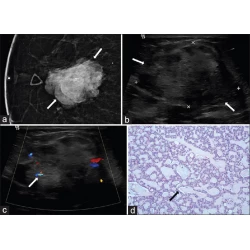
Perceptual errors related to lesion size and density/signal
This is probably one of the most common causes of search errors or missed diagnoses: the lesion is too small to attract the radiologist’s attention. Among such errors, search errors due to small lesions may be the most common; clinically, they include missing small pulmonary nodules, fractures, small liver foci (Fig. 1 ), and abdominal lymphadenopathy. Moreover, the similarity of the density/signal of the lesion to that of the surrounding tissue also contributes to the omission of lesions. The solutions include increased time for careful reading, bilateral contrast, and postprocessing methods such as maximum intensity projection (MIP), multiplanar reformation (MPR), and three-dimensional (3D) reconstruction.
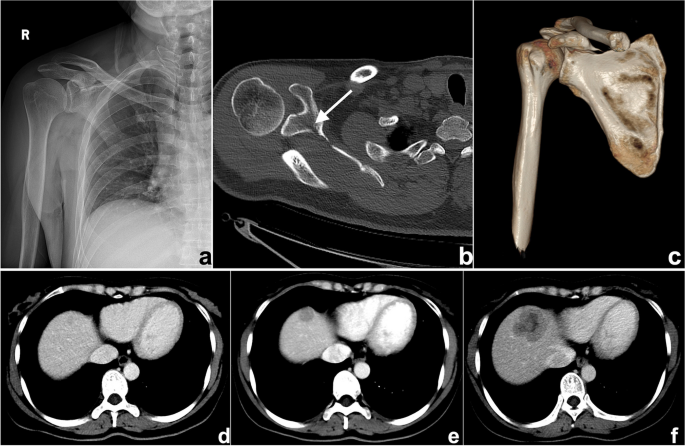
a – c A 47-year-old man suffering from right shoulder pain for 3 days after trauma. a Plain radiography was reported to be normal because the radiologist missed the subtle low-density fracture line due to the overlapping position and careless reading. Axial computed tomography (CT) image ( b ) and three-dimensional (3D) reconstruction ( c ) showed scapular fractures below the coracoid (arrow). d – f Gradually enlarged low-density liver metastasis in a 32-year-old woman after radical resection and chemotherapy of sigmoid cancer. The images demonstrated an ill-defined margin and heterogeneous enhancement. The lesion was not detected and reported in a timely manner from the first two CT scans ( d , e ) because it was small and located at the top of the liver
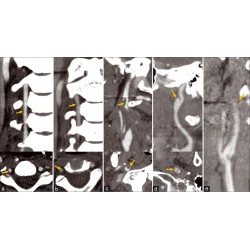
Perceptual errors related to the location/type of lesions
Whether the lesion is missed is also dependent on its location. If it exists in blind spots or outside the regions of interest (ROIs), such as unique anatomical sites, structural overlaps, the last slice of the scanning field of view (SFOV), the edge of the image, or a corner that is hard to notice, its location may lead to it being missed. This kind of error is known as the location error, and some researchers call it the inattentional bias. For instance, these locations in the chest include the apex of the lung, cardiophrenic angle, parahilar and paraaortic regions, bones, and pulmonary artery. Imaging reading blind spots are a common objective cause of perceptual errors, accounting for 7% of radiological diagnostic errors [ 10 ] (Fig. 2 ). There are some disease entities that can be easily missed. A retrospective study of 122 imaging reports over 2 years demonstrated that the most easily missed types were lymph node metastases of the abdominal and pelvic cavities, bone metastases, malignant lesions of the abdomen and pelvis, fractures, pulmonary nodules, and pulmonary embolism [ 22 ] (Fig. 2 ). This may be due to the high prevalence of these diseases themselves or the fact that these lesions tend to be small or in anatomical blind spots. In addition, bone metastases are often missed because the bone window is not analyzed during body CT reading (Fig. 3 ). Solutions to this problem include increasing time for comprehensive imaging reading and being more familiar with common blind areas, easily missed lesion types, and the metastatic pattern of neoplastic diseases.
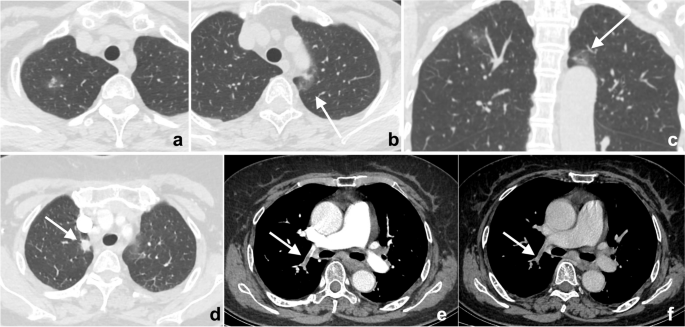
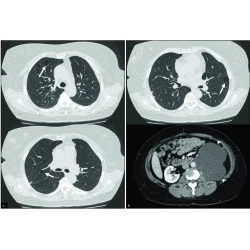
a – c Double primary lung adenocarcinoma in a 60-year-old woman. a Radiologists stopped searching for other lesions after detecting the subsolid nodule in the tip of the right upper lobe, missing another subsolid nodule (arrows) in the posterior apical segment of the left upper lobe, above the aortic arch and next to the mediastinum. Multiplanar reformation (MPR) demonstrated that the nodule (arrow) was above the aortic arch where there was a blind area commonly encountered in image reading. d – f A 72-year-old woman affected by COVID-19. The enhanced CT presented a description of the nodule (arrows) in the right upper lobe along with the burr sign of lobes, thus prompting the consideration of lung cancer. However, the low-density filling defect in the right upper pulmonary artery, which was a sign of pulmonary artery embolism, was missed
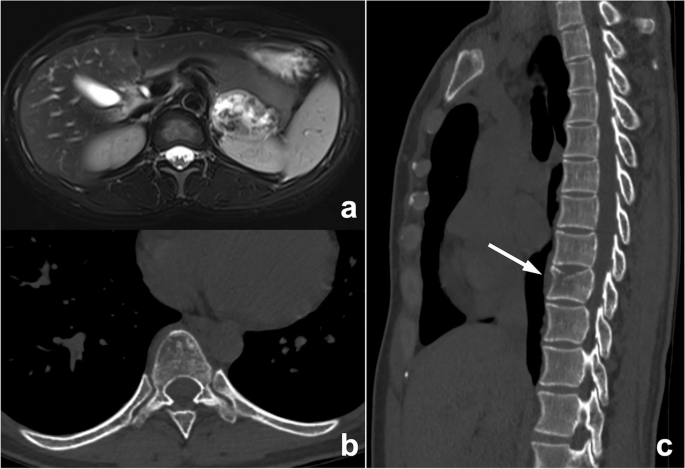
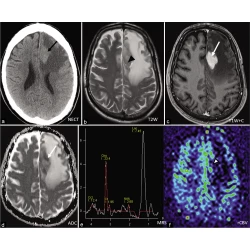
An abnormal signal mass of the left adrenal gland presented by abdominal MRI in a 39-year-old woman. In the routine preoperative chest CT scan ( b , c ), bone metastasis (arrow) was missed because radiologists mainly observed the pulmonary and mediastinal window but ignored the bone window. The diagnosis of postoperative pathology was left adrenocortical adenocarcinoma
Insufficiency of clinical information
A clinically provided request form is often the only way to obtain a history. If the radiologist fails to read the request form carefully or the clinician does not write the information clearly on the request form or update the patient’s clinical status promptly, missed diagnosis or misdiagnosis may ensue. For example, postoperative complications are likely to be missed for postoperative patients because the medical history is usually not updated in time, and radiologists are usually less sensitive to postoperative complications (Fig. 4 ). Solutions to this problem include improving hospital information systems to ensure adequate clinical and pathological information and increasing the sensitivity of radiologists toward complications following surgery.
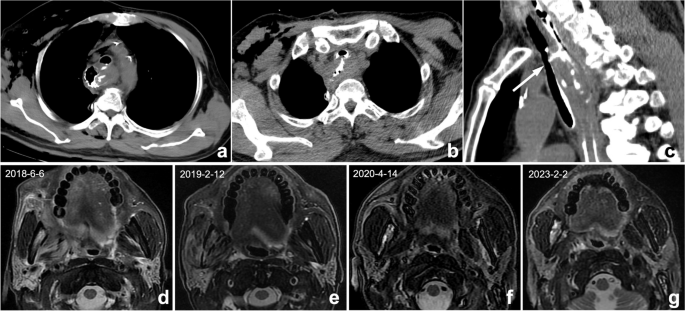
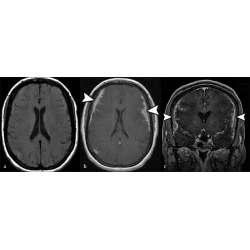
a – c Postoperative changes in esophageal cancer in a 67-year-old man. a , b Axial CT showed the postoperative changes in esophageal cancer. However, because the clinical request form did not provide a reminder, radiologists only described postoperative changes and failed to mention tracheoesophageal fistula. Multiplanar reformation (MPR) can better display the fistula (arrow). According to the administration of oral contrast agent, radiologists should understand that the doctor wants to observe if a fistula occurs. ( d - g ) A 56-year-old man with right oropharyngeal carcinoma after radiotherapy. Four MRIs at different times showed abnormal signals in the right mandible. The first two reports ( d , e ) did not mention abnormal signals, illustrating a perceptual error. In the third exam ( f ), the radiologist found but mistook it as bone metastasis, illustrating a cognitive error. The patient’s frequent swollen gums since 2018 were omitted, and this syndrome improved substantially after anti-inflammatory therapy. The diagnosis should be right mandibular osteoradionecrosis with osteomyelitis, but radiologists misdiagnosed it because they were not familiar with radiotherapy complications and diagnostic bias
Perceptual errors related to thinking bias
Some perceptual errors are related to the thinking bias of the human brain, the most common being the satisfaction of search, which refers to decreased vigilance to other abnormalities after detecting the first lesion, resulting in the termination of reading and the omission of other vital lesions (Fig. 2 ). This is a common cause of errors, contributing approximately 22% [ 10 ]. All of these situations have been well documented in the musculoskeletal system [ 23 ]. Solutions include reading images systematically, initiating a secondary search to continue looking for others after finding the first abnormality, and having a comprehensive knowledge of common diagnostic combinations.
- Cognitive errors
Cognitive errors have more subjective elements; therefore, they are more complicated. Researchers have most frequently classified the causes of imaging diagnosis or cognitive errors by using the Kim-Mansfield Radiologic Error Classification System [ 10 ]. It should be pointed out that careless terminological errors such as reversing left and right writing and misspellings and huge measurement errors are also common reporting errors that are likely to be misunderstood by patients, which may shake patient confidence and lead to unpleasant arguments; in particular, reversing left and right writing errors can sometimes result in severe medical errors and disputes. This type of error is not included in this review.
Cognitive errors related to lack of professional knowledge
Errors due to a lack of knowledge often occur among medical students and junior physicians. The insufficiency of experience and expertise can easily lead to the misdiagnosis of lesions. For example, beginners may easily mislocate frontal lobe lesions to the parietal lobe in transverse axial brain CT or MRI images. Alternatively, in chest CT diagnosis, the pericardial recess is easily misdiagnosed as enlarged lymph nodes. Moreover, if pivotal signs are missed, the diagnosis of two similar lesions can also be confused (Fig. 5 ). Solutions include attaching importance to the training of professional knowledge by report writing training and continuing education for radiologists.
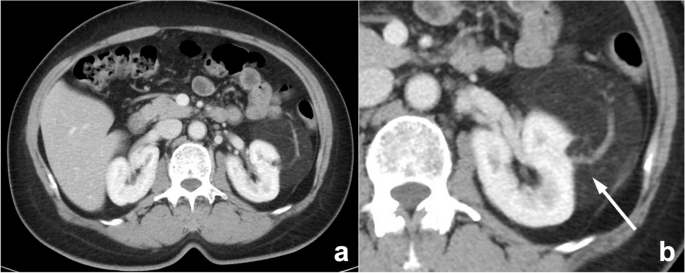
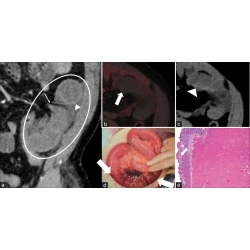
A mass revealed by physical examination in the left kidney of a 58-year-old woman. a An enhanced, axial abdominal CT image showed a left pararenal fat-density mass, which was diagnosed as liposarcoma. However, this lesion should have been diagnosed as angiomyolipoma instead of liposarcoma. The misdiagnosis may be due to missing key signs such as large blood vessels (arrow) in the tumor and the renal cortical “split sign”
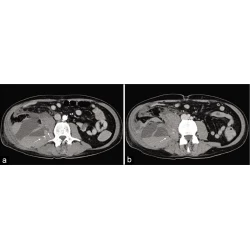
Cognitive errors related to the prior examination and report
References to previous reports and comparison of lesions are of great necessity in patients undergoing follow-up or response evaluation. When comparing lesions, it is better to compare them with an earlier or baseline examination rather than just the previous examination; otherwise, the error of comparison will occur (Fig. 6 ). Moreover, a lack of reference to earlier reports can sometimes lead to misdiagnosis, and excessive trust or reliance on previously reported diagnoses can also lead to diagnostic biases or errors. Some researchers call it prior report bias, alliterative error, or satisfaction of report bias (Fig. 7 ). Solutions include reading the images carefully and making a diagnosis before reviewing previous reports, revisiting and refining previous reports, and considering a second diagnosis.
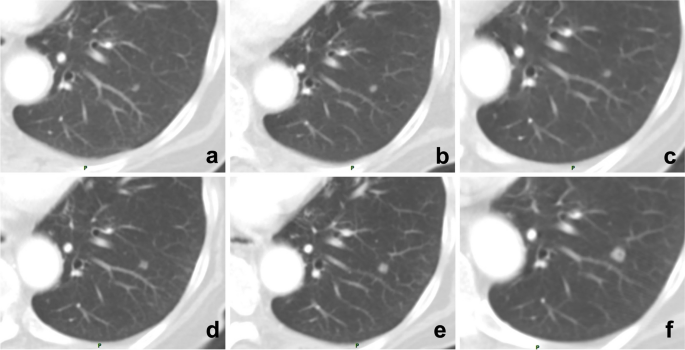
A 71-year-old man underwent multiple follow-up visits after colon cancer surgery. a – f Images showed a small nodule in the lower lobe of the left lung, but the radiologist only compared the current CT image with that of the last examination and reported no changes. By comparing each CT image, the gradually enlarging nodule was recognized, and follow-up imaging confirmed it as a metastatic tumor
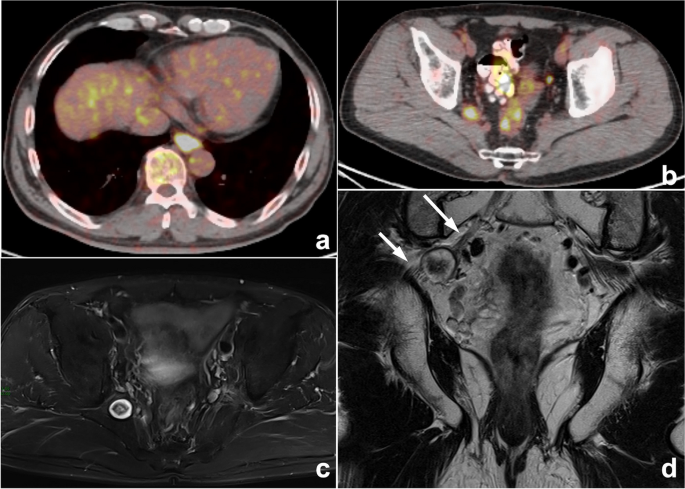
Esophageal carcinoma with multiple systemic metastases reported by PET-CT in a 60-year-old man with dysphagia for 1 month. a , b PET-CT images showed a mildly elevated pelvic uptake nodule in the right pelvis, which was suspected to be metastasis. c , d Therefore, the radiologist was influenced by the previous esophageal carcinoma and PET-CT reports, ignoring typical neurogenic tumor signs such as the “target sign” and the close association with the sacral plexus nerve (arrows). Eventually, the right pelvic nodule was misdiagnosed as metastasis in the MRI report. This is a typical example of prior report bias
Cognitive errors related to clinical information
The clinical history is crucial to the diagnosis. Because the request form does not provide a complete or accurate clinical history or is not sensitive enough to specific clinical histories, such as side effects after treatment, radiologists often make false decisions (Fig. 4 ). Therefore, when the diagnosis is difficult, it is important for radiologists to ask for the clinical history or physical examination in person.
Cognitive errors related to thinking cognitive bias
Thinking biases are tendencies of our cognitive functions to obey certain patterns that are not always productive. Various cognitive biases can keep us “locked” on an irrelevant finding, leading to a wrong diagnosis and preventing an objective interpretation. The most frequent and important cognitive biases in our work include anchoring bias, confirmation bias, availability bias, and attribution bias [ 24 ].
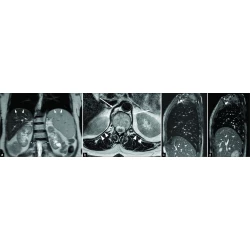
Anchoring bias and confirmation bias can be considered fixed mindset bias. Anchoring bias means that a doctor fixes on his or her initial diagnostic impression too early and ignores subsequently acquired new signs or signs that conflict with the initial impression. Confirmation bias refers to the situation in which when a particular point of view is subjectively supported, we tend to seek information that can help the original point of view but ignore information that may overthrow the original point of view. Regarding the solutions, before the final diagnosis is made, all available evidence should be reviewed and gathered, especially evidence supporting a different opinion, and then we can consider a second diagnosis. For instance, when we find vertebral compression fractures in patients with a history of malignancy, we are likely to consider metastatic tumors, and signs supporting benign diseases may be ignored (Fig. 8 ).
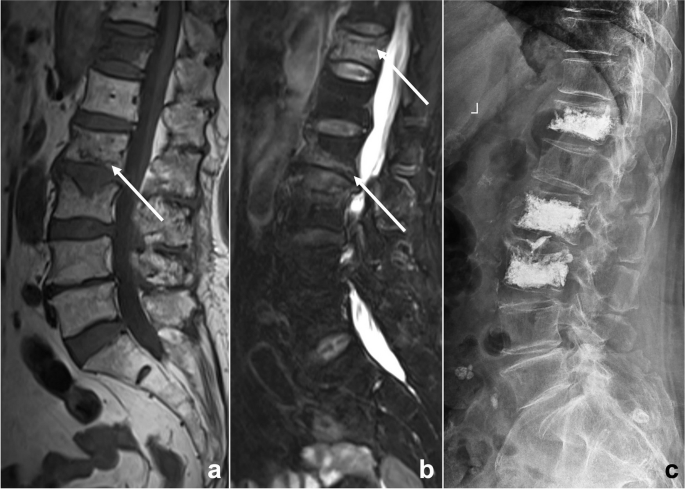
An 81-year-old woman suffered from low back pain for a week after lymphoma chemotherapy. Lumbar MRI T 1 WI ( a ) and T 2 WI/FS ( b ) illustrated multiple abnormal vertebral signals with mild compression fractures. The radiologist misdiagnosed it as a malignant lesion because of the patient’s clinical history of malignant tumor, missing some signs of benign compression fracture such as linear low signal under the endplate, strip-like abnormal signal (arrows), and Schmorl’s nodes. This diagnostic bias is classified as anchoring bias and confirmation bias. After the patient underwent vertebral biopsy and arthroplasty ( c ), no evidence of malignant tumor was found by pathology, and a benign compression fracture was diagnosed
The definition of availability bias is judging the possibility of an event based on how easily and frequently it comes to mind. Another similar cognitive bias is called zebra retreat bias, which refers to a condition in which the patient’s history and imaging findings support a rare diagnosis, but the radiologist is afraid to make the correct diagnosis because of its rarity [ 25 ] (Fig. 9 ). Solutions include using objective data of the disease incidence to correlate with the radiologist’s diagnostic rates and make a differential diagnosis.
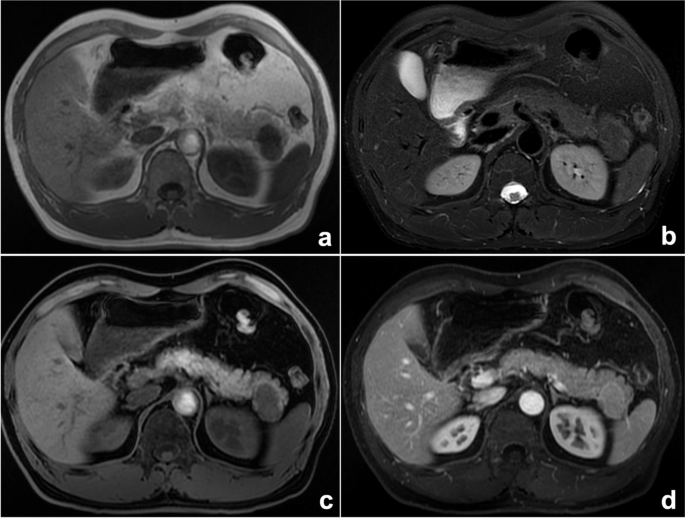
A space-occupying lesion of the pancreatic tail in a 52-year-old man. Axial MRI T 1 WI ( a ), T 2 WI/FS ( b ), T 1 WI/FS ( c ), and enhanced ( d ) sequences all showed that the lesion’s signal was similar to that of the spleen, but our radiologist’s diagnosis was pancreatic neuroendocrine tumor, which was relatively common, rather than a rarely occurring ectopic spleen. Finally, the surgical pathology confirmed an ectopic spleen in the pancreas. This thinking bias is classified as zebra retreat bias
Attribution bias means that some specialist doctors are more willing to favor the diagnosis of diseases in their specialty. For radiologists, disease stereotypes are often based on information provided by the department where the patient is seen or the request form. Other analogical biases, such as framing bias, draw different conclusions from the same information because of the different ways or order in which information is presented. For radiologists, misdiagnosis often occurs due to the preconception of clinical information (Fig. 10 ). Solutions include realizing that initial clinical impressions can sometimes be wrong and reviewing the images before checking the clinical history.
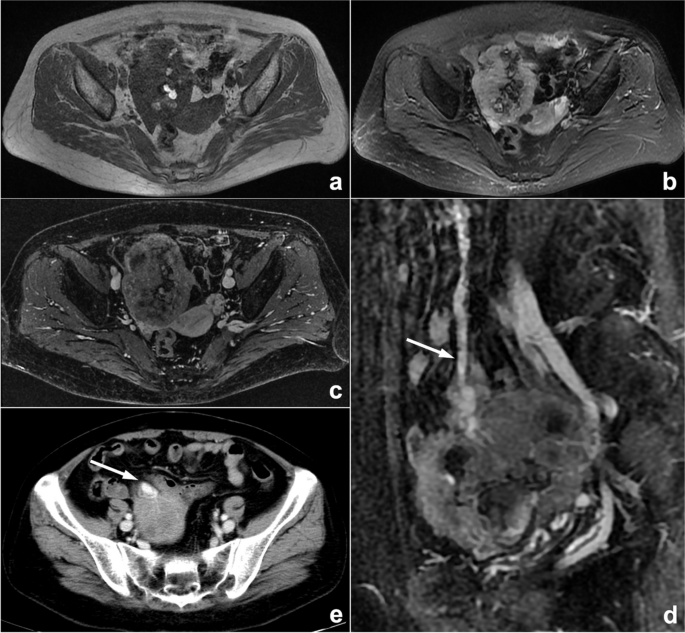
A palpable pelvic mass that was diagnosed as an ovarian tumor by the gynecologist in a 57-year-old woman who presented in gynecological clinics. MRI scan ( a – c ) showed a pelvic mass with hemorrhage-like confounding hyperintensity on T 1 WI and hypointensity on T 2 WI/FS internally. An enhanced scan represented heterogeneous enhancement. The mass was closely related to the small intestine, and blood supply by large mesenteric vessels (arrows) could also be observed on enhanced sagittal MRI ( d ) and axial CT ( e ) images, suggesting intestinal original disease. However, the radiologist mistook small intestinal stromal tumors as ovarian tumors because of the gynecologist’s diagnosis. This is classified as attribution bias
Other cognitive biases include outcome bias and premature closure. The former refers to the tendency of doctors to prefer diagnostic decisions that lead to a better outcome for the patient [ 25 ], and the latter refers to regarding a preliminary diagnosis as the premature conclusion [ 26 ]. The above errors often occur in multiple combinations (Fig. 4 ). Solutions include realizing the above cognitive biases that can influence our diagnosis and conducting a complete and accurate diagnosis with a correct attitude.
Non-professional causes of diagnostic errors in radiology
Many non-professional causes can affect the accuracy of reports during the workflow of radiologists, and fatigue is one of the most important causes [ 20 , 27 ]. For instance, fatigue from lack of sleep has been identified as a contributing factor in many severe accidents [ 28 , 29 ]. Some studies have shown that the error rate in diagnosis reports is higher during the night shift, especially after midnight [ 30 ]. More importantly, the workload of radiologists has relentlessly increased and is a frequent reason for burnout. Burnout is “a syndrome resulting from chronic workplace stress that has not been successfully managed.” A recent Medscape survey found that 47% of radiologists suffer from burnout [ 31 , 32 ]. In addition, the rapid reading of images is unavoidable in real work due to the inevitable increase in workload [ 33 ]. Under these circumstances, errors the radiologists make will be regarded as reckless readings in the case of medical lawsuits, and these lawsuits will allege that missed diagnoses are due to radiologists spending insufficient time analyzing images. Although the authors of a recent article advocated putting limits on shift hours and workload for radiologists, there is a lack of scientific measures to weigh the workload [ 34 ], responsibilities, and reading speed of radiologists.
Another common reason is the inadequate attention of the readers. Currently, radiologists are involved in multidisciplinary teams (MDTs) and scientific teaching meetings in addition to reading images. It has been demonstrated that additional interruptions can lead to a 12% decrease in report correctness [ 35 ]. In addition, as a profession requiring intense attention, high visual perception, and cognitive demands, radiologists need optimal physiological conditions. However, approximately 58% of radiologists suffer neck and shoulder pain, back pain, carpal tunnel syndrome, eye strain, headache, and other symptoms that may interfere with work [ 36 , 37 ]. Solutions to cope with these non-professional factors include taking regular breaks to avoid fatigue, moving and standing from time to time when reading images, minimizing interruptions in the diagnostic process caused by phone calls, using height-adjustable desks and ergonomic chairs, adjusting the brightness of indoor lighting and screens, and reducing ambient noise [ 38 ].
Judgment and systematic strategies for diagnostic errors in radiology
Defining diagnostic errors is a difficult task due to the inherent subjectivity of image interpretation, especially for cognitive errors. First, it is crucial to distinguish between “errors” and observer “discrepancy” when discussing errors in diagnostic radiology. The term “error” implies that there is no potential for argument about what is “correct” and that the reporting radiologist should have been able to make the proper diagnosis or report but was unable to do so. The word “discrepancy” stands for justifiable differences of opinion between colleagues [ 39 , 40 ]. Second, radiological reports not only accurately convey the presence of abnormalities but also the radiologist’s opinion and the level of diagnostic confidence that expresses a particular level of certainty in the suggested diagnoses [ 41 ]. However, because imaging findings are often nonspecific, radiological conclusions usually cannot be clear or definite in clinical work. Sometimes, radiologists will adopt protective measures such as vague or descriptive diagnoses and lengthy differential diagnoses when they want to avoid mistakes and disputes. In general, the interpretation of diagnostic imaging studies relies on consensus expert opinion to determine diagnostic errors [ 42 ]. In the process of determining errors in radiology, there are also certain thinking or cognitive biases, such as hindsight bias, which means experts retrospectively downplay or underestimate the difficulties and challenges of the initial diagnosis after the diagnosis of a lesion has been confirmed or additional information has been added, especially if fatality discussions or medical errors/disputes discussions [ 7 , 26 , 43 , 44 ].
Previous errors in radiological diagnosis are often attributed to individual carelessness, negligence, or poor performance. Therefore, the solutions for reducing the error rate often focus on improving individual ability and responsibility, as illustrated by earlier descriptions in this article of countermeasures to strengthen the influencing factors. However, there is growing recognition of the limitations of radiologists in image perception and cognition involving a series of complex diagnostic decisions that cause the inevitability of errors. Developing systematic policies and approaches to reduce errors is an effective measure and may involve several approaches, such as multiple reviewer report system, using structured reporting templates and reporting and data system (RADS), error measurement or detection strategies such as electronic trigger tools and checklists to detect “wrong-side” misidentification errors [ 45 ], report writing training and continuing education for radiologists, holding radiology quality control meetings and providing peer feedback learning, improving hospital information systems to ensure adequate clinical and pathological information, enhancing communication with doctors or patients, matching workload to staffing, and promoting the application of artificial intelligence (AI).
Multiple reviewer report system can ensure diagnostic accuracy, but they may increase human labor costs. However, in the double-reviewer report system, the reviewers are mainly medical students and junior radiologists; therefore, the application of this system is the most feasible way to balance labor costs and report quality, which also has educational significance for junior reviewers. In difficult cases, we can hold more MDTs with several senior doctors to make correct diagnoses. Moreover, with its rapid development, artificial intelligence (AI) is bound to help doctors reduce missed diagnoses of lesions, improve diagnostic efficiency, and decrease human labor costs. For individual difficult cases, group discussions with wide participation are needed, which can help reduce the diagnostic bias of senior doctors and contribute to residents’ education. For radiology quality control meetings, near misses are potential learning opportunities that should be used to promote quality controls and radiologists’ self-improvement in an attempt to prevent future accidents. In addition, an unbiased “no blame” culture should be introduced and ensured as a method to focus attention on understanding case error instead of individual radiologists and improve the quality of care by learning from mistakes [ 46 , 47 ].
In summary, this review presents an analysis of the causes of diagnostic errors in imaging and provides solutions for them with the objective of helping radiologists reduce errors in clinical practice. Quality control of imaging diagnosis is a challenging problem that will need to be addressed by more efforts and research in the future.
Availability of data and materials
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
Abbreviations
Three-dimensional
Artificial intelligence
Computed tomography
Multidisciplinary team
Maximum intensity projection
Multiplanar reformation
Magnetic resonance imaging
Reporting and data system
Region of interest
Scanning field of view
Kohn LT, Corrigan JM, Donaldson MS et al (2000) In: To Err is Human: Building a Safer Health System. National Academies Press (US), Washington
Google Scholar
Blendon RJ, DesRoches CM, Brodie M et al (2002) Views of practicing physicians and the public on medical errors. N Engl J Med 347:1933–1940. https://doi.org/10.1056/NEJMsa022151
Article PubMed Google Scholar
Berner ES, Graber ML (2008) Overconfidence as a cause of diagnostic error in medicine. Am J Med 121:S2–23. https://doi.org/10.1016/j.amjmed.2008.01.001
Roosen J, Frans E, Wilmer A et al (2000) Comparison of premortem clinical diagnoses in critically ill patients and subsequent autopsy findings. Mayo Clin Proc 75:562–567. https://doi.org/10.4065/75.6.562
Article CAS PubMed Google Scholar
Balogh EP, Miller BT, Ball JR (eds) (2015) Improving diagnosis in health care. National Academies Press (US), Washington
Burroughs TE, Waterman AD, Gallagher TH et al (2005) Patient concerns about medical errors in emergency departments. Acad Emerg Med 12:57–64. https://doi.org/10.1197/j.aem.2004.08.052
Lee CS, Nagy PG, Weaver SJ, Newman-Toker DE (2013) Cognitive and system factors contributing to diagnostic errors in radiology. AJR Am J Roentgenol 201:611–617. https://doi.org/10.2214/AJR.12.10375
Chamberlain WE (1942) Fluoroscopes and fluoroscopy. Radiology 38:383–413. https://doi.org/10.1148/38.4.383
Article Google Scholar
Garland LH (1959) Studies on the accuracy of diagnostic procedures. Am J Roentgenol Radium Ther Nucl Med 82:25–38
CAS PubMed Google Scholar
Kim YW, Mansfield LT (2014) Fool me twice: delayed diagnoses in radiology with emphasis on perpetuated errors. AJR Am J Roentgenol 202:465–470. https://doi.org/10.2214/AJR.13.11493
Berlin L (2007) Accuracy of diagnostic procedures: has it improved over the past five decades? AJR Am J Roentgenol 188:1173–1178. https://doi.org/10.2214/AJR.06.1270
Lehr JL, Lodwick GS, Farrell C et al (1976) Direct measurement of the effect of film miniaturization on diagnostic accuracy. Radiology 118:257–263. https://doi.org/10.1148/118.2.257
Brady AP, Stevenson GW, Stevenson I (1994) Colorectal cancer overlooked at barium enema examination and colonoscopy: a continuing perceptual problem. Radiology 192:373–378. https://doi.org/10.1148/radiology.192.2.8029400
Saunders CG, MacEwen DW (1971) Delay in diagnosis of colonic cancer–a continuing challenge. Radiology 101:207–208. https://doi.org/10.1148/101.1.207
Siegle RL, Baram EM, Reuter SR et al (1998) Rates of disagreement in imaging interpretation in a group of community hospitals. Acad Radiol 5:148–154. https://doi.org/10.1016/s1076-6332(98)80277-8
Borgstede JP, Lewis RS, Bhargavan M, Sunshine JH (2004) RADPEER quality assurance program: a multifacility study of interpretive disagreement rates. J Am Coll Radiol 1:59–65. https://doi.org/10.1016/S1546-1440(03)00002-4
Soffa DJ, Lewis RS, Sunshine JH, Bhargavan M (2004) Disagreement in interpretation: a method for the development of benchmarks for quality assurance in imaging. J Am Coll Radiol 1:212–217. https://doi.org/10.1016/j.jacr.2003.12.017
Berlin L (1996) Malpractice issues in radiology. Perceptual errors. AJR Am J Roentgenol 167:587–590. https://doi.org/10.2214/ajr.167.3.8751657
Morozov S, Guseva E, Ledikhova N et al (2018) Telemedicine-based system for quality management and peer review in radiology. Insights Imaging 9:337–341. https://doi.org/10.1007/s13244-018-0629-y
Article PubMed PubMed Central Google Scholar
Degnan AJ, Ghobadi EH, Hardy P et al (2019) Perceptual and interpretive error in diagnostic radiology-causes and potential solutions. Acad Radiol 26:833–845. https://doi.org/10.1016/j.acra.2018.11.006
Kundel HL, Nodine CF, Carmody D (1978) Visual scanning, pattern recognition and decision-making in pulmonary nodule detection. Invest Radiol 13:175–181. https://doi.org/10.1097/00004424-197805000-00001
Owens EJ, Taylor NR, Howlett DC (2016) Perceptual type error in everyday practice. Clin Radiol 71:593–601. https://doi.org/10.1016/j.crad.2015.11.024
Ashman CJ, Yu JS, Wolfman D (2000) Satisfaction of search in osteoradiology. AJR Am J Roentgenol 175:541–544. https://doi.org/10.2214/ajr.175.2.1750541
Mansi L (2021) Haris Chrysikopoulos: Errors in Imaging. Eur J Nucl Med Mol Imaging 48:1271–1271. https://doi.org/10.1007/s00259-020-05159-1
Bruno MA, Walker EA, Abujudeh HH (2015) Understanding and confronting our mistakes: the epidemiology of error in radiology and strategies for error reduction. Radiographics 35:1668–1676. https://doi.org/10.1148/rg.2015150023
Busby LP, Courtier JL, Glastonbury CM (2018) Bias in radiology: the how and why of misses and misinterpretations. Radiographics 38:236–247. https://doi.org/10.1148/rg.2018170107
Ricci JA, Chee E, Lorandeau AL, Berger J (2007) Fatigue in the U.S. workforce: prevalence and implications for lost productive work time. J Occup Environ Med 49:1–10. https://doi.org/10.1097/01.jom.0000249782.60321.2a
Leape LL (1994) Error in medicine. JAMA 272:1851–1857
Dinges DF (1995) An overview of sleepiness and accidents. J Sleep Res 4:4–14. https://doi.org/10.1111/j.1365-2869.1995.tb00220.x
Patel AG, Pizzitola VJ, Johnson CD, Zhang N, Patel MD (2020) Radiologists make more errors interpreting off-hours body CT studies during overnight assignments as compared with daytime assignments. Radiology 297:374–379. https://doi.org/10.1148/radiol.2020201558
Bailey CR, Bailey AM, McKenney AS, Weiss CR (2022) Understanding and appreciating burnout in radiologists. Radiographics 42:E137–E139. https://doi.org/10.1148/rg.220037
European Society of Radiology (ESR) (2022) The role of radiologist in the changing world of healthcare: a White Paper of the European Society of Radiology (ESR). Insights Imaging 13:100. https://doi.org/10.1186/s13244-022-01241-4
Alexander R et al (2022) Mandating limits on workload, duty, and speed in radiology. Radiology 304:274–282. https://doi.org/10.1148/radiol.212631
Lexa FJ (2021) Duty hour limits for radiologists: it’s about time. J Am Coll Radiol 18:208–21038
Balint BJ et al (2014) Do telephone call interruptions have an impact on radiology resident diagnostic accuracy? Acad Radiol 21:1623–1628
Boiselle PM, Levine D, Horwich PJ et al (2008) Repetitive stress symptoms in radiology: prevalence and response to ergonomic interventions. J Am Coll Radiol 5:919–923. https://doi.org/10.1016/j.jacr.2008.01.014
Seidel RL, Krupinski EA (2017) The Agony of It All: Musculoskeletal Discomfort in the Reading Room. J Am Coll Radio 14:1620–1625. https://doi.org/10.1016/j.jacr.2017.07.024
Prabhu SP, Gandhi S, Goddard PR (2005) Ergonomics of digital imaging. Br J Radiol 78:582–586. https://doi.org/10.1259/bjr/51650129
Brady AP (2017) Error and discrepancy in radiology: inevitable or avoidable? Insights Imaging 8:171–182. https://doi.org/10.1007/s13244-016-0534-1
Onder O, Yarasir Y, Azizova A et al (2021) Errors, discrepancies and underlying bias in radiology with case examples: a pictorial review. Insights Imaging 12:51. https://doi.org/10.1186/s13244-021-00986-8
Rosenkrantz AB, Kiritsy M, Kim S (2014) How “consistent” is “consistent”? A clinician-based assessment of the reliability of expressions used by radiologists to communicate diagnostic confidence. Clin Radiol 69:745–749. https://doi.org/10.1016/j.crad.2014.03.004
Waite S, Scott J, Gale B et al (2017) Interpretive error in radiology. AJR Am J Roentgenol 208:739–749. https://doi.org/10.2214/AJR.16.16963
Croskerry P (2003) (2003) The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med 78:775–780. https://doi.org/10.1097/00001888-200308000-00003
Gunderman RB (2009) Biases in radiologic reasoning. AJR Am J Roentgenol 192:561–564. https://doi.org/10.2214/AJR.08.1220
Sheehan SE, Safdar N, Singh H et al (2020) Detection and remediation of misidentification errors in radiology examination ordering. Appl Clin Inform 11:79–87. https://doi.org/10.1055/s-0039-3402730
Elmqvist KO, Rigaudy MT, Vink JP (2016) Creating a no-blame culture through medical education: a UK perspective. J Multidiscip Healthc 9:345–346. https://doi.org/10.2147/JMDH.S111813
Parker J, Davies B (2020) No blame no gain? From a no blame culture to a responsibility culture in medicine. J Appl Philos 37:646–660. https://doi.org/10.1111/japp.12433
Download references
No funding.
Author information
Li Zhang and Xin Wen contributed equally to this work.
Authors and Affiliations
Department of Diagnostic Radiology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100021, China
Li Zhang, Xin Wen, Jian-Wei Li, Xu Jiang & Meng Li
Department of Radiology, Drum Tower Hospital Affiliated to Medical School of Nanjing University, Nanjing, China
Xian-Feng Yang
You can also search for this author in PubMed Google Scholar
Contributions
ML conceived this study and modified the draft. LZ and XW performed manuscript drafting and image collection. JWL, XJ, and XFY reviewed the literature and prepared figures. All authors critically edited the manuscript. All authors read and approved the submitted version.
Corresponding author
Correspondence to Meng Li .
Ethics declarations
Ethics approval and consent to participate.
Images in this review article are published under study permission granted by the hospital district. Informed consent was waived due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: supplementary table 1..
Summarized errors’ types categorization and related errors management strategies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhang, L., Wen, X., Li, JW. et al. Diagnostic error and bias in the department of radiology: a pictorial essay. Insights Imaging 14 , 163 (2023). https://doi.org/10.1186/s13244-023-01521-7
Download citation
Received : 27 April 2023
Accepted : 03 September 2023
Published : 02 October 2023
DOI : https://doi.org/10.1186/s13244-023-01521-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Diagnostic imaging
Advertisement
Spiral head CT in the evaluation of acute intracranial pathology: a pictorial essay
- Pictorial Essay
- Published: 13 October 2010
- Volume 18 , pages 81–91, ( 2011 )
Cite this article
- Aaron Sodickson 1 ,
- Heitor Okanobo 1 &
- Stephen Ledbetter 1
348 Accesses
6 Citations
Explore all metrics
The purpose of this pictorial essay is to review the benefits of spiral head computed tomography (CT) with routine multiplanar reformations in the evaluation of acute intracranial pathology. This technique is particularly useful in trauma patients for detection of skull base or calvarial fractures, thin tentorial subdural hematomas, or for more specific characterization of intracranial hemorrhage. The benefits of multiplanar reformations have been described for a variety of other diagnoses in the chest, abdomen, extremities, and spine, and their routine use continues to grow with the widespread availability of multi-slice CT scanners. In this article, we describe spiral head CT technique with multiplanar reformations as an alternative to the routinely used sequential technique. Subtle findings and lesions aligned predominantly in the axial plane can often be visualized to better advantage with multiplanar reformations. We also address technical factors for optimizing spiral technique.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price excludes VAT (USA) Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Multiplanar reconstructed ct images increased depiction of intracranial hemorrhages in pediatric head trauma.
Stacey Langford, Ashok Panigrahy, … Giulio Zuccoli
Reformatted images improve the detection rate of acute traumatic subdural hematomas on brain CT compared with axial images alone
Timothy J. Amrhein, William Mostertz, … Peter G. Kranz

Dual Energy CT: Basic Principles
Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM (2000) Indications for computed tomography in patients with minor head injury. N Engl J Med 343:100–105
Article CAS PubMed Google Scholar
Cassidy JD, Carroll LJ, Peloso PM et al (2004) Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO collaborating centre task force on mild traumatic brain injury. J Rehabil Med (43 Suppl):28–60
Google Scholar
Aschoff AJ (2006) MDCT of the abdomen. Eur Radiol 16(Suppl 7):M54–M57
PubMed Google Scholar
Fanucci E, Fiaschetti V, Rotili A, Floris R, Simonetti G (2007) Whole body 16-row multislice CT in emergency room: effects of different protocols on scanning time, image quality and radiation exposure. Emerg Radiol 13:251–257
Article PubMed Google Scholar
Jaffe TA, Martin LC, Thomas J, Adamson AR, DeLong DM, Paulson EK (2006) Small-bowel obstruction: coronal reformations from isotropic voxels at 16-section multi-detector row CT. Radiology 238:135–142
Jayashankar A, Udayasankar U, Sebastian S, Lee EK, Kalra M, Small W (2008) MDCT of thoraco-abdominal trauma: an evaluation of the success and limitations of primary interpretation using multiplanar reformatted images vs axial images. Emerg Radiol 15:29–34
Kim HC, Yang DM, Jin W (2008) Identification of the normal appendix in healthy adults by 64-slice MDCT: the value of adding coronal reformation images. Br J Radiol 81:859–864
Lucey BC, Stuhlfaut JW, Hochberg AR, Varghese JC, Soto JA (2005) Evaluation of blunt abdominal trauma using PACS-based 2D and 3D MDCT reformations of the lumbar spine and pelvis. AJR Am J Roentgenol 185:1435–1440
Mirvis SE, Shanmuganagthan K (2007) Imaging hemidiaphragmatic injury. Eur Radiol 17:1411–1421
Zangos S, Steenburg SD, Phillips KD et al (2007) Acute abdomen: added diagnostic value of coronal reformations with 64-slice multidetector row computed tomography. Acad Radiol 14:19–27
Sliker CW (2008) Blunt cerebrovascular injuries: imaging with multidetector CT angiography. Radiographics 28:1689–1708, discussion 1709–1610
Hernalsteen D, Cosnard G, Robert A, Grandin C, Vlassenbroek A, Duprez T (2007) Suitability of helical multislice acquisition technique for routine unenhanced brain CT: an image quality study using a 16-row detector configuration. Eur Radiol 17:975–982
Ptak T, Rhea JT, Novelline RA (2003) Radiation dose is reduced with a single-pass whole-body multi-detector row CT trauma protocol compared with a conventional segmented method: initial experience. Radiology 229:902–905
Wei SC, Ulmer S, Lev MH, Pomerantz SR, Gonzalez RG, Henson JW (2010) Value of coronal reformations in the CT evaluation of acute head trauma. AJNR Am J Neuroradiol 31:334–339
Zacharia TT, Nguyen DT (2009) Subtle pathology detection with multidetector row coronal and sagittal CT reformations in acute head trauma. Emerg Radiol 17:97–102
Depreitere B, Van Lierde C, Sloten JV et al (2006) Mechanics of acute subdural hematomas resulting from bridging vein rupture. J Neurosurg 104:950–956
Servadei F, Murray GD, Teasdale GM et al (2002) Traumatic subarachnoid hemorrhage: demographic and clinical study of 750 patients from the European brain injury consortium survey of head injuries. Neurosurgery 50:261–267, discussion 267–269
Gentry LR (1994) Imaging of closed head injury. Radiology 191:1–17
CAS PubMed Google Scholar
Mattioli C, Beretta L, Gerevini S et al (2003) Traumatic subarachnoid hemorrhage on the computerized tomography scan obtained at admission: a multicenter assessment of the accuracy of diagnosis and the potential impact on patient outcome. J Neurosurg 98:37–42
Strub WM, Leach JL, Tomsick T, Vagal A (2007) Overnight preliminary head CT interpretations provided by residents: locations of misidentified intracranial hemorrhage. AJNR Am J Neuroradiol 28:1679–1682
Laine FJ, Shedden AI, Dunn MM, Ghatak NR (1995) Acquired intracranial herniations: MR imaging findings. AJR Am J Roentgenol 165:967–973
New PF, Aronow S, Hesselink JR (1980) National Cancer Institute study: evaluation of computed tomography in the diagnosis of intracranial neoplasms. IV. Meningiomas. Radiology 136:665–675
Smirniotopoulos JG, Murphy FM, Rushing EJ, Rees JH, Schroeder JW (2007) Patterns of contrast enhancement in the brain and meninges. Radiographics 27:525–551
Hofman PA, Nelemans P, Kemerink GJ, Wilmink JT (2000) Value of radiological diagnosis of skull fracture in the management of mild head injury: meta-analysis. J Neurol Neurosurg Psychiatry 68:416–422
Turner BG, Rhea JT, Thrall JH, Small AB, Novelline RA (2004) Trends in the use of CT and radiography in the evaluation of facial trauma, 1992–2002: implications for current costs. AJR Am J Roentgenol 183:751–754
Download references
Author information
Authors and affiliations.
Department of Radiology, Brigham and Women’s Hospital–Harvard Medical School, 75 Francis St., Boston, MA, 02115, USA
Aaron Sodickson, Heitor Okanobo & Stephen Ledbetter
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Aaron Sodickson .
Rights and permissions
Reprints and permissions
About this article
Sodickson, A., Okanobo, H. & Ledbetter, S. Spiral head CT in the evaluation of acute intracranial pathology: a pictorial essay. Emerg Radiol 18 , 81–91 (2011). https://doi.org/10.1007/s10140-010-0914-7
Download citation
Received : 03 July 2010
Accepted : 28 September 2010
Published : 13 October 2010
Issue Date : January 2011
DOI : https://doi.org/10.1007/s10140-010-0914-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Spiral head CT
- Helical head CT
- Multiplanar reformations
- Head trauma
- Intracranial hemorrhage
- Calvarial fracture
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Emergency Radiology. A Journal of Practical Imaging Official Journal of the American Society of Emergency Radiology. Publishing model: Hybrid. Submit your manuscript (this opens in a new tab) ... Pictorial Essays - 1500 words, 15 figures including all figure parts, 2 tables, 20 references.
Vascular and Interventional Radiology, Pictorial Essay. Catheter-directed computed tomography angiography: A pictorial essay. Abheek Ghosh, Ellen Moxley, Suneet Waghmarae, James Stoner, Sheena Anand, Nabeel M. Akhter. J Clin Imaging Sci 12 (49) (18th August, 2022) DOI: 10.25259/JCIS_76_2022. 0.
Familiarity with the imaging appearances of these disorders helps the radiologists to establish the correct diagnosis in the emergency setting, which contributes to timely clinical management. This pictorial essay provides a description of the clinical presentation and imaging findings of nontraumatic orbital emergencies.
Whereas there are many emergencies in head and neck radiology, they can threaten the life because of the anatomical proximity of vital organs. We aimed to describe and identify radiological ...
Pathologies with educative value and risk of severe morbidity and mortality in lack of rapid diagnosis were selected for this pictorial essay. Fig. 3 Pathologies that clinician cannot distinguish, where radiologist plays an important role were classified as traumatic and inflammatory; and one patient included despite nonbeing trauma or ...
Familiarity with the imaging appearances of these disorders helps the radiologists to establish the correct diagnosis in the emergency setting, which contributes to timely clinical management. This pictorial essay provides a description of the clinical presentation and imaging findings of nontraumatic orbital emergencies.
Emergency Radiology. A Journal of Practical Imaging Official Journal of the American Society of Emergency Radiology. Publishing model: Hybrid. ... Pictorial Essay 17 September 2021 Pages: 207 - 213 Inguinal ovarian hernia on point of care ultrasound: case reports and review of the literature ...
Interventional radiology in renal emergencies: a pictorial essay. Emerg Radiol2022 Apr;29 (2):409-424. doi: 10.1007/s10140-021-02004-2. Epub 2022 Jan 10. Renal emergencies necessitate prompt diagnosis and management to stop active bleeding and retain kidney function. Causes of renal emergencies can be classified into traumatic, atraumatic ...
Abstract. Use of a systematic approach to orbital emergencies will assist the radiologist with identifying immediate threats to vision and facilitate prompt clinical management. Imaging of the orbit plays an important role in the workup of orbital emergencies. Orbital imaging is particularly useful in the emergency department, where clinical ...
Indications for IR depend on the CT evidence of vascular injuries and, therefore, a robust CT protocol and the radiologist's expertise are crucial. Emergency and IR radiologists form an integral part of the trauma team and are crucial for tailored management of traumatic injuries. Keywords: motor vehicle crash, trauma, major trauma, high ...
Abstract. Diagnostic imaging is an essential and indispensable part of medical diagnosis and treatment, and diagnostic errors or biases are also common in the department of radiology, sometimes even having a severe impact on the diagnosis and treatment of patients. There are various reasons for diagnostic errors or biases in imaging.
There is a perception as little as emergencies can occur in head and radiology. Whereas there are many emergencies in head and neck radiology, they can threaten the life because of the anatomical proximity of vital organs. We aimed to describe and identify radiological findings of the most common emergencies in head and neck radiology.
Patients often present to the emergency department with a wide variety of nontraumatic infectious, inflammatory, and neoplastic conditions of the head and neck. Because the use of cervical and neck computed tomography (CT) has become routine in the emergency setting, knowledge of the imaging findings of common acute conditions of the head and neck is essential to ensure an accurate diagnosis ...
Wanted: Emergencies in head and neck radiology; pictorial essay. Poster No.: C-14700 Congress: ECR 2020 ... Fig. 4: A 32-year-old woman admitted to the emergency department with dysphagia and
Gastrointestinal Emergency in Neonates and Infants: A Pictorial Essay Korean J Radiol. 2022 Jan;23(1):124-138. doi: 10.3348/kjr.2021.0111. ... Affiliations 1 Department of Radiology, Korea University Ansan Hospital, Ansan, Korea. 2 Department of Radiology, Korea University Ansan Hospital, Ansan, Korea. [email protected].
Formation of ghost images due to metal objects on the surface of the patient's face: A pictorial essay. ... we also report the clinical case of a 24-year-old male patient referred to the radiology clinic to undergo dental exams necessary for orthodontic treatment. Panoramic and lateral cephalometric radiographs were taken using the ...
actors such as bradykinin, histamine, and various cytokines. The recognition of hyperechoic fat on sonography may be an important indicator of the primary source of pathology. In addition, it often reflects a more advanced degree of transmural pathology, such as "walled-off" perforation of a hollow viscus. This pictorial essay will present a variety of examples of hyperechoic inflamed fat ...
Hero K. Hussain. Roula Hourani. Original Article 18 October 2023 Pages: 699 - 709. 1. 2. …. 53. Next. Emergency Radiology informs its readers about the radiologic aspects of emergency care, thereby the journal acts as a resource body on emergency radiology for ...
Abnormal uterine bleeding (AUB) poses a multifaceted challenge in women's health, necessitating an integrated approach that addresses its diverse etiologies and clinical presentations. The International Federation of Gynecology and Obstetrics PALM-COEIN classification system provides a systematic approach to the diagnosis of AUB in non-pregnant women, based on clinical and imaging-based ...
Diagnostic imaging is an essential and indispensable part of medical diagnosis and treatment, and diagnostic errors or biases are also common in the department of radiology, sometimes even having a severe impact on the diagnosis and treatment of patients. There are various reasons for diagnostic errors or biases in imaging. In this review, we analyze and summarize the causes of diagnostic ...
Emergency Department. Gender Health Center. Neurosurgery. Orthopedic Surgery. Pediatrics. Post Acute Care Transition. Rehabilitation Center. Sobrato Cancer Center. ... (Radiology) Valley Health Center Bascom Diagnostic Imaging (Radiology) Sunday: Closed. Monday: 7:40 am — 7:00 pm. Tuesday: 7:40 am — 7:00 pm. Wednesday:
The purpose of this pictorial essay is to review the benefits of spiral head computed tomography (CT) with routine multiplanar reformations in the evaluation of acute intracranial pathology. This technique is particularly useful in trauma patients for detection of skull base or calvarial fractures, thin tentorial subdural hematomas, or for more specific characterization of intracranial ...
Diagnostic imaging technologists at Santa Clara Valley Medical Center work within a fully digital imaging department in one of California's newest clinical facilities. The Diagnostic Imaging Department utilizes an advanced Picture Archiving and Communication System (PACS). PACS is linked to the hospital's information infrastructure and enables ...