- Open access
- Published: 27 June 2015

Medical professionalism: what the study of literature can contribute to the conversation
- Johanna Shapiro 1 ,
- Lois L. Nixon 2 ,
- Stephen E. Wear 3 &
- David J. Doukas 4
Philosophy, Ethics, and Humanities in Medicine volume 10 , Article number: 10 ( 2015 ) Cite this article
15k Accesses
26 Citations
21 Altmetric
Metrics details
Medical school curricula, although traditionally and historically dominated by science, have generally accepted, appreciated, and welcomed the inclusion of literature over the past several decades. Recent concerns about medical professional formation have led to discussions about the specific role and contribution of literature and stories. In this article, we demonstrate how professionalism and the study of literature can be brought into relationship through critical and interrogative interactions based in the literary skill of close reading. Literature in medicine can question the meaning of “professionalism” itself (as well as its virtues), thereby resisting standardization in favor of diversity method and of outcome. Literature can also actively engage learners with questions about the human condition, providing a larger context within which to consider professional identity formation. Our fundamental contention is that, within a medical education framework, literature is highly suited to assist learners in questioning conventional thinking and assumptions about various dimensions of professionalism.
Introduction
Over the past fifty years the study of literature has become a generally accepted aspect of medical education. As thoughtful scholars have recently considered how to teach professionalism effectively and meaningfully, questions have arisen about the role of stories, essays, first-person narratives, and poetry in facilitating the professional identity formation of medical students. Those who argue affirmatively imply that exposing students to literature will inculcate professionalism virtues and attributes [ 1 ]. Those who disagree assert that the study of literature has goals and purposes unrelated to professionalism [ 2 ]. In this article, we investigate definitions of medical professionalism, and frame its inclusion in the competency framework as an effort to anchor its abstract virtues in behavioral specificity. Next we consider how literature can advance our understanding of medical professionalism through a different kind of singularity grounded in the literary method of close reading. Ultimately, we contend that the development of medical professionalism will benefit from the critical and interrogative methods of literature.
This article is a result of the Project to Rebalance and Integrate Medical Education (PRIME), sponsored by the Patrick and Edna Romanell Foundation. PRIME focused on how medical ethics and humanities education are prerequisite to professionalism formation in medical school and residency training [ 3 , 4 ]. PRIME, in turn, resulted in the creation of the Academy for Professionalism in Health Care as an organization devoted to professionalism education [ 5 ].
The conundrum of professionalism in medical education
There are at least two significant issues to consider in discussing medical professionalism. One has to do with the content of professionalism itself, i.e., how it is defined. The second is essentially an implementation issue, i.e., the methods which establish how professionalism is achieved. These issues, and their implications for professionalism education, are discussed below.
Defining medical professionalism
The Medical Professionalism Project initiated by the American Board of Internal Medicine Foundation, the American College of Physicians Foundation, and the European Federation of Internal Medicine resulted in a professionalism charter consisting of virtue-based attributes such as altruism, trust, honesty, patient empowerment, and commitment to social justice [ 6 ]. Medical educatorshave also argued for a virtue-based definition, including qualities of compassion, integrity; truth-telling; respect for others; self-effacement; and fidelity to patients [ 7 – 10 ]. Prior PRIME publications acknowledged the importance of scientific and clinical competence using established rigorous evidence-based medicine; while emphasizing promotion of patients’ best interests as the clinician’s primary moral consideration (with self-interest as a subservient claim) and honoring the exercise of the public trust , as a necessary obligation to carry forth the fiduciary traditions of medicine (as opposed to guild-like self-interest) [ 4 ]. Other definitions also support the commitment to and reinforcement of moral values and ethical principles [ 11 , 12 ].
These definitions, while valuable, highlighted primarily general, abstract virtues and attributes that have proved difficult to translate into daily actions. Recent considerations of professionalism and professional identity formation have stressed the necessity of moving from abstraction to practice [ 13 , 14 ], highlighting what is often referred to as phronesis or practical wisdom [ 15 ]. Medical educators have wrestled with this challenge for the past decade, most notably through the effort to incorporate medical professionalism into the competency framework.
Professionalism as a competency
Indeed, it could be argued that the rise of the competency movement in medical education [ 16 ] has been an effort to anchor generalities of training in specific, concrete, measurable behaviors. In terms of professionalism specifically, attempting to inculcate values and virtues often struck both learners and educators as threatening and potentially implying character defects in students [ 17 ]. Thus, professionalism moved from the conceptual realm to become one of six essential medical education competencies, sometimes viewed as a “meta”- or “ordering” contextual competency for more technical competencies [ 18 , 19 ]. In this respect, competency-based education appeared to offer a “solution” to the abstract nature of earlier approaches to conceptualizing professionalism, precisely because of its behavioral specificity. Many medical educators found the notion of professional competencies appealing because they seemed to offer the promise of transforming amorphous, ill-defined, and difficult-to-measure qualities into instrumental behaviors that were observable and assessable. Recently more detailed “milestones” have been added to supplement and refine the six competencies, but these remainrooted in the establishment of measurable behavior [ 20 ]. Whether discussing milestones or competencies, the language employed reflects a tendency in these guidelines to prescribe, control, and shape learners in specific, reductive directions.
Challenging a behavioral approach to medical professionalism
Even as professionalism became identified as an area of medical competence, some medical educators’ reflections on the topic continued to reveal a discomfort with behavioral pedagogical approaches, instead advocating for developing, reinforcing, and sustaining deeply held attitudes and values [ 17 , 21 ]. As Hanna and Fins write, medical students must learn how to “ be good doctors, rather than merely to act like good doctors [ 18 , 22 , 23 ]”.
Others also assert that behavioral professionalism tempts students to behave in ways that fulfill others’ expectations of professionalism without actually believing in the virtues or principles that underpin these behaviors [ 24 ], resulting in an emphasis on surface impression management [ 25 ]. Others complain that in clinical settings, professionalism is simplistically and narrowly defined as a technical problem, with most solutions offered being prescriptive, mechanical, and rule-bound [ 26 ].
Setbacks in teaching professionalism
With some notable exceptions, such as small group reflection-based sessions [ 27 , 28 ] that have shown promise most approaches to teaching professionalism, implicitly or explicitly rooted in the competency model, have not documented significant success. An article by two medical students claims that medical educators are more likely to evaluate appearance, formality, and conformity as “professional” than they are to pay attention to traits of honor, altruism, and responsibility. This “view from the trenches” suggests that adherence to hospital etiquette, respecting academic hierarchy, and subservience to authority are valued more than patient-centered virtues [ 29 ]. A survey study examining student attitudes toward professionalism found that almost a third of respondents felt professionalism education was patronizing and demeaning [ 30 ], while a more in-depth qualitative study concluded that medical students made a distinction between “good” doctors and “professional” doctors, and perceived professionalism as an external and imposed construct [ 31 ].
One troubling study found that, despite required professionalism training, unprofessional behavior in students actually increased during their clinical years [ 32 ]. These and similar concerns suggest that students see professionalism training as little more than a tool of governance [ 33 ] wielded by supervisors promoting exterior and often trivial performance, rather than emphasizing virtue.
The dilemma is clear. Medical educators have agreed to define professionalism as a competency to be achieved by measurable behaviors. They simultaneously recognize it to be a deeper, more meaningful sense of identity that incorporates a set of humanistic attitudes, behaviors, and critical thinking skills. Some medical educators hope that the study of literature can help resolve this educational impasse by contributing a new perspective to our understanding of professionalism that, like the competency model, attempts to bridge the gap between theory and practice, but does so in a radically different way. Our argument is that the study of literature is where we learn, in an emotionally and critically engaged way, to see how characters face moral dilemmas, how they resolve them, and the consequences of those resolutions.
Implications of the Study of Literature for Medical Professionalism
If competencies have not provided a meaningful format for teaching medical professionalism, nevertheless it is a fundamental contention of the PRIME scholars that professionalism must involve the application of virtues to the practice of medicine [ 34 ]. We believe that the study of literature, with its emphasis on the discreteness of specific texts, has an important role to play in assisting learners in professionalism formation. One crucial way in which this occurs is by developing in learners the habit of close reading, a fundamental literary skill.
How close reading relates to medical professionalism
Close reading has been defined as a disciplined reading and rereading of complex texts to identify layers of meaning that lead to more nuanced interpretation and deeper, more subtle understanding [ 35 ]. It is not difficult to imagine the translational relevance of close reading for developing a meaningful medical professionalism tied to the particulars of each patient’s care. Like a patient encounter, close reading first requires attentive observation – what does the reader notice about the text? What does the doctor notice about the patient? Interpretation follows observation – what is the meaning of the reader’s – or the doctor’s - observations [ 36 ]? Close reading requires a wariness of superficial and facile interpretations, a clinical position that helps the clinician avoid bias, assumptions, and judgmentalness.
A fundamental premise of close reading is the revisiting of texts to investigate alternative or complementary meanings while recognizing that there are not necessarily any right answers. Similarly, physicians trained in close reading may be more likely to continue to think about their patients and to remain open to new interpretations of their actions and attitudes. In close reading, students must not only “feel” a certain way in response to the text, but they must know how to defend their conclusions through reference to particular words and passages [ 37 ]. In the clinical context, physicians must be ready to question their initial emotional responses to patients in favor of more nuanced and complex responses that are based in evidence emerging from the clinical encounter.
Close reading interrogates the structure of a particular narrative. Why is a story told in a certain way? Who is telling the story? Who else might tell this story? How might different tellings change the nature of the story? Who is the intended audience for this story? Why are certain words selected and not others? Why are certain metaphors employed? What seems to be important or striking in the story? Are there contradictions or discrepancies in the story? Is the author trying to persuade the listener of something? What has been omitted from the story? Are there repetitions? What is the predominant tone of the story? Does it shift, and if so why? What patterns emerge in the text [ 38 ]? Such an approach, translated into the clinical encounter, is likely to result in a critical professionalism through respect, engaged attention, and critical thinking within a very specific context.
The implications of close reading for medical professionalism are far-reaching. In the remainder of this article, we discuss how close reading leads to a different and more critical way of understanding medical professionalism that is grounded in the specifics of each clinical encounter as well as the contextual specifics of race, gender, culture, and history. It is a method that questions conventional thinking about professionalism, complicates accepted virtues, and emphasizes individual variation.
Asking meaningful questions rather than inculcating behavior
Although some scholars have suggested that studying literature can help medical students learn to better attend to and understand their patients’ stories [ 39 ], cultivate emotional resonance in patient care [ 40 , 41 ], and address burn-out through supporting more examined, fulfilled professional lives [ 42 ], no educational process can guarantee or compel virtues, self-awareness, or wellbeing in learners. In the real world, medical educators are not always certain how such ineffable qualities or attributes can be meaningfully “demonstrated”. In these circumstances, what literature can do is help learners engage in critical thinking about what the virtues and values of medical professionalism might be; and how these actually might occur in particular situations influenced by culture, race, disability, gender, sexual orientation, and historical consideration.
Many professionalism issues are complicated, convoluted, and resist a simple behavioral solution (e.g., maintaining eye contact, touching a shoulder, employing rote expressions of empathy ). Rather, questions about how to think, feel, and behave professionally in a given circumstance are best approached as complex conundrums in which there will likely be disagreement among those involved about the nature of the problem, the desired resolution (if any), and the steps required to achieve it [ 26 ]. Studying literature can help prepare learners to grapple with these situations because stories suggest various responses without dictating them, urge consideration of different behaviors without ordering them, and illuminate values without oversimplifying them. Such approaches offer learners methods for exploring professionalism values that honor the distinctive, irreducible human qualities of each patient and each circumstance embedded in larger social and cultural contexts [ 43 ].
The countercultural perspective
Although competencies by definition require instrumental goals, literary scholars are generally more comfortable advocating non-instrumental aims for the role of literature in medical education. One such overarching aim is the cultivation of a critical and questioning attitude toward conventional wisdom, a so-called “countercultural” [ 44 ] perspective on medicine that implicates both personal and professional moral development while situating medicine within a larger sociocultural framework [ 45 , 46 ]. In this view, integrating literature into the curriculum should not blindly support the status quo in medicine, but instead should help learners question their own and the system’s preconceptions and prejudgments [ 47 ] to make transparent the values, culture, and ideology of medicine [ 48 ].
Drawing on critical theory, many health humanities scholars call for literature to open a “discursive space” that critiques conventional assumptions about medicine and the healthcare system [ 49 , 50 ]. Dror argues that teaching literature offers a way of rethinking medicine, not instilling standards [ 48 ]. This approach emphasizes “catalyz[ing] emancipatory insights” [ 51 ] and creating an environment of “sustained critical reflection [ 52 ]”. Engaging with literature will not produce a set of measurable professionalism-specific behaviors in learners, but it is well-suited to facilitating a critical consciousness of self, others, and the world [ 53 ]. By stimulating critical thinking, literature enables learners to question established ways of understanding relationships between doctors and patients, doctors and other healthcare professionals and staff, and doctors and society. This standpoint asserts that, properly executed, literature should provoke discomfort and resistance in learners and disrupt their reflexive participation in healthcare [ 54 , 55 ]. Kumagai and Wear call this process “making strange” taken-for granted assumptions and beliefs that may compromise humanistic care [ 56 ].
Developing moral imagination
One way in which the study of literature can result in productive discomfort for students (and teachers!) is by critically interrogating the meaning of professionalism itself. Is professionalism primarily about protecting the “guild” of medicine? Is it about endorsing adherence to abstract virtues? Does it have to do with translating virtuous concepts into observable and measurable behaviors? Is it about a moral relationship between two (or more – often many more) people under trying circumstances? Working with a wide range of literary texts in a medical education context can help learners discover how to frame such questions and debate different answers.
Precisely how this happens is not fully circumscribed, but some scholars have argued that in part students become adept at both asking questions and exploring answers through the development of moral imagination, defined by Carson [ 57 ]as the heightened capacity to envision experience, whether one’s own or someone else’s, from a different perspective. Importantly, examination of literary texts reveals that in any given situation there are multiple ways of understanding and prioritizing events, thus making the privileging of any one perspective suspect. Charon refers to this as the capacity to visualize others’ narrative worlds [ 58 ]. Appreciation of differing points of view engages critical thinking through honing learner awareness of different, often contradictory but co-existing understandings [ 46 ]. It also facilitates empathetic orientation by encouraging emotional connection with or recognition of characters different from oneself and health-related roles different from one’s own [ 59 , 60 ].
In discussing moral imagination, the psychiatrist Robert Coles [ 61 ] observes that stories admonish us, point us in new directions, and sometimes inspire us to lead lives of greater moral integrity. We should note that such aspirations are quite different from acquisition of standardized behaviors to be performed regardless of the particular situation and circumstance. Rather, selected stories stimulate moral imagination in medical learners by enabling them to step back from and become critically aware of their own values, beliefs, and assumptions about professionalism and how these are influenced by the dominant culture and other systems of influence in which they participate. From this beginning, learners can then imagine new possibilities for attitudes and action based on consideration of others’ values, perspectives, and priorities, especially those of disempowered and marginalized individuals, as well as their own. The critical thinking that emerges from the study of literature can help medical learners evaluate from a moral point of view both their original assumptions and dominating models of what professionalism is, as well as new possibilities they now envision in collaboration with their patients from a wider social perspective [ 62 ].
The complication of professionalism values
Studying literature and reading stories reveal that even such enshrined professionalism values as compassion do not necessarily always serve moral ends; and point out ways in which such values need to be interrogated more critically to understand how they might go astray. Apparently beneficial qualities such as empathy, the ability to engender trust, and good communication skills all can be employed to encourage docility and compliance in less powerful individuals (i.e., patients) [ 2 ]. Some scholars have criticized the empathic skills trained in medical school for their potential as a tool to manipulate care, rather than as a virtue of care [ 63 – 65 ]. Similarly, compassion may devolve into a patronizing and demeaning position that approaches pity when not carefully and respectfully placed within the context of understanding the patient’s subjective experience of suffering within her culture, personal history, and values. Respect can be undermined through a mindless allegiance to autonomy in which physicians essentially abandon patients and families by expecting them to make medical decisions for which they have not been sufficiently prepared. Altruism can deteriorate into rigid self-sacrifice in physicians who think patients’ wellbeing requires a persistent neglect of personal wellbeing and life balance. By encouraging awareness of such nuances, reading literature critically and thoughtfully has the intriguing capacity to both challenge and deepen the virtues and attributes that comprise medical professionalism
Standardization of professionalism?
The National Board of Medical Examiners calls for the “standardization” of professionalism in medicine [ 66 ]. From a literary perspective, with its emphasis on multiple, often contradictory perspectives and the importance of acknowledging the specifics of every situation, a “standardized” approach to professional attitudes, behaviors, and identity may not be possible. While elements of both standardization and diversity are likely important in formulating sufficiently complex views of professionalism [ 67 ], literature’s forte is to challenge “standardized” views of professionalism by invoking nuance and context. The role of literature is to cultivate a thoughtful examination of the implications and consequences of a spectrum of different attitudes, behaviors, and identities; and to situate these within a larger socioeconomic, cultural, and political context of power and privilege. Recalling Hanna and Fins’ concerns, we believe that literature offers a way to help students understand what it means to be, rather than merely act like, a humane professional. In this way, literature urges the opposite of “one size fits all” standardization by emphasizing the intrinsic value of diversity in how professionalism manifests filtered through each unique interaction of individuals (doctors, medical team, patients, and families), circumstances, and dominant discourses.
Widening the lens
Competency involves standardized achievement of “correct” behaviors, a necessary narrowing to obtain reliability and consistency of assessment. Literature, on the other hand, offers a plethora of models and possibilities for being in the world and eschews the one right answer. Instead, the study of literature leads learners in directions that are open-ended, unpredictable, and self-determining. It can both widen the lens and provide insight into the complexities of the human condition, suffering, personhood, and our responsibility to each other [ 68 ]. Instead of compelling learners to narrow their focus to concrete behaviors, literature can help them realize that professionalism cannot be separated from an understanding of their own humanity and that of their patients. This is why students may learn more about professionalism from reading War and Peace than from an ACGME manual on professionalism milestones. Footnote 1
Assessment of professionalism
In contemplating the influence of the study of literature on students’ understanding of medical professionalism, how do we ascertain whether learners have actively engaged with what this concept might mean for them personally in different clinical situations? How do we achieve insight into what capacities and habits of mind they have developed as a result of their studies? In medicine, assessment approaches are often quantitative and numerical. Such an approach has little to propose in determining what happens to students as a result of critically reading a story or writing a reflective essay.
Assessment of the understanding of professionalism that students glean from literature will be better achieved through qualitative, narrative means [ 69 ]. Longitudinal evaluation by instructors, to allow for the maturation of professional identity, that examines both individual and collaborative student writing and creative projects [ 70 ] reflecting on professional formation issues and dilemmas, as well as narrative self-assessment of professional development might be considered according to criteria listed in Fig. 1 . In considering such student work, pedagogical theory in the humanities suggests that what is important is transparency in how the student thinks , rather than the specific nature of the conclusions they reach [ 71 , 72 ].
How we know students have engaged with professional formation through the study of literature
Following this line of reasoning, we suggest that projects, essays, and other relevant products should be examined for their ability to make students’ thinking about professionalism formation and dilemmas visible and plain. This might mean, for example, attending to how a student both develops and questions an argument, considers multiple perspectives, understands emotional sequelae for both self and others, and has some sense of the relevant cultural, historical, familial, and personal factors implicated. Further, research suggests that professionalism decisions in medicine are highly context dependent [ 73 ], are influenced by a wide range of considerations, and are surprisingly shifting and malleable depending on the input of peers [ 74 ]. These findings suggest that assessment of professionalism cannot be global and general, but must be situation specific.
Since it is impossible to anticipate all professionalism dilemmas, it is particularly important to nurture habits of mind such as are outlined above that can be brought to bear on unique clinical encounters. For example, Kuper suggests that students’ increasing emotional awareness, self-reflection, and capacity to grasp ambiguity might be considered as proxy outcomes for actual patient interaction skills [ 75 ]. Here again, such qualities cannot be measured through a Likert scale, but might be explored through an evaluative process that explores students’ growth on these dimensions, and explores how these qualities can be translated into real-world situations. Charon talks about “narrative evidence”, or the insights and sensibility offered through careful attentiveness to the patient’s story [ 76 ]. We might do well to refer to this concept in assessing what medical students learn from exposure to literature – i.e., what have they discovered about how to access the person of the patient in a medical interview? How has their understanding evolved regarding the ways in which a patient’s cultural background, class, family and community affect her response to illness? Within this framework, evaluation of learners might best be understood as a kind of conversation between faculty and student rather than a definitive, top-down assessment.
Charon also points out that the true metrics of success have to do with clinicians’ attitudes, behavior and interactions in the clinical arena, and the effects these have on their patients [ 77 ]. Following Charon’s lead, we suggest that the gold standard of professionalism is patient and family assessment of these dimensions of care in their student doctors. By this we do not mean yet more patient satisfaction measures of learners. Rather, time-consuming as it would be, obtaining narrative responses from patients and families about how they experience the trustworthiness, respectfulness, non-judgmentalism of learners, their capacity to listen and care and to demonstrate compassion in action by thinking outside the box, would be a truly meaningful form of assessment. Such an approach is an essential way to reveal to what extent nuanced scrutiny of stories, poetry, and essays by patients and physicians affects the way learners interact with and behave toward actual patients and families. By making such inquiries of patients and their family members, we would learn how students translate the professionalism values, attitudes, and interactive skills they have discovered in literature into each unique of clinical encounters.
In summary, we suggest that literature is an essential element of medical education that, through the method of close reading, contributes intellectual inquiry, emotional awareness, sociocultural context, and a countercultural perspective to questions regarding medical professionalism. Narrative and storytelling broaden and make more complex the ethical context of care provided by students and faculty. They assist learners in rigorously and feelingly examining, in specific evocative contexts, what it means to be a doctor in relationship with patients and families within a framework of larger social dynamics and discourses. Literature can deepen the understanding of medical professionalism, as many medical educators desire; but it cannot simultaneously promote assessment practices that rely on facile quantitative behavioral responses. If medical education can not only tolerate but embrace the opportunity to challenge the assumptions and beliefs its learners hold about the profession, literature has much to offer professionalism formation.
Some examples of short stories and poems that encourage self-examination and broader thinking include: "Laundry" by Susan Mates, "Touching" by David Hellerstein, "Carnal Knowledge" by Danny Abse, "Skin for Ricky" by DL Scheidermayer, "Baptism by Rotation" by Mikhail Bulgakov, "Imelda" by Richard Selzer, and "Talking to the Family" by John Stone. While doctors are not the only or the most important storytellers, such texts are especially useful entry points for medical learners uncertain as to the value of studying narratives as part of their medical education.
Holmgren L, Fuks A, Bourdreau D, Sparks T, Kreiswirth M. Terminology and praxis: clarifying the scope of narrative in medicine. Lit Med. 2012;29(2):246–73.
Article Google Scholar
Bishop JP. Rejecting medical humanism: Medical humanities and the metaphysics of medicine. J Med Humanit. 2008;29:15–25.
Doukas DJ, McCullough LB, Wear S, Project to Rebalance and Integrate Medical Education (PRIME) Investigators. Medical education in medical ethics and humanities as the foundation for developing medical professionalism. Acad Med. 2012;87:334–41.
Doukas DJ, McCullough LB, Wear S, et al. Perspective: The challenge of promoting professionalism through medical ethics and humanities education. Acad Med. 2013;88:1624–9.
Available at: http://academy-professionalism.org . Accessed July 22, 2014.
American Board of Internal Medicine Foundation. American College of Physicians–American Society of Internal Medicine Foundation. European Federation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med. 2002;136(3):243–6.
Little JM. Humanistic medicine or values-based medicine…what's in a name? Med J Aust. 2002;177:319–21.
Google Scholar
Giordano J. Quo vadis? Philosophy, ethics, and humanities in medicine: preserving the humanistic character of medicine in a biotechnological future. Philos Ethics Humanit Med. 2009;14(4):12.
Markakis KM, Beckman HB, Suchman AL, Frankel RM. The path to professionalism: cultivating humanistic values and attitudes in residency training. Acad Med. 2000;75:141–50.
Doukas DJ. Where is the virtue in professionalism? Camb Q Healthc Ethics. 2003;12(2):147–54.
Holden M, Buck E, Clark M, Szauter K, Trumble J. Professional identity formation in medical education: the convergence of multiple domains. HEC Forum. 2012;24:245–55.
Wilson I, Cowin LS, Johnson M, Young H. Professional identity in medical students: Pedagogical challenges to medical education. Teach Learn Med. 2013;25:369–73.
Wald HS, Anthony D, Hutchinson TA, Liben S, Smilovitch M, Donato AA. Professional identity formation in medical education for humanistic, resilient physicians: pedagogic strategies for bridging theory to practice. Acad Med. 2015;90(6):753–60.
Doukas DJ, Kirch DG, Brigham TP, Barzansky BM, Wear S, Carrese JA, et al. Transforming educational accountability in medical ethics and humanities education toward professionalism. Acad Med. 2015;90(6):738–43.
Kumagai AK. From competencies to human interests: ways of knowing and understanding in medical education. Acad Med. 2014;89(7):978–83.
Long DM. Competency-based residency training: The next advance in graduate medical education. Acad Med. 2000;75(12):1178–83.
Kirk LM. Professionalism in medicine: definitions and considerations for teaching. Proc (Bayl Univ Med Cent). 2007;20(1):13–6.
The core competencies as described by the Outcome Project. Chicago, IL: Accreditation Council for Graduate Medical Education; updated 2001 [cited 2004 Jun 11]. Available from: www.acgme.org/acgmeweb .
Batalden P, Leach D, Swing S, Dreyfus H, Dreyfus S. General competencies and accreditation in graduate medical education. Health Aff (Millwood). 2002;21(5):103–11.
https://www.acgme.org/acgmeweb/tabid/430/ProgramandInstitutionalAccreditation/NextAccreditationSystem/Milestones.aspx
Hafferty F. Measuring professionalism: a commentary. J Eval in Clin Pract. 2002;8:281–306.
Hanna M, Fins JJ. Power and communication: why simulation training ought to be complemented by experiential and humanist learning. Acad Med. 2006;81:265–70.
Jarvis-Selinger S, Pratt DD, Regehr G. Competency is not enough: Integrating identity formation into the medical education discourse. Acad Med. 2012;87:1185–90.
Cohen JJ. Linking professionalism to humanism: what it means, why it matters. Acad Med. 2007;82:1029–32.
Rees CE, Knight LV. The trouble with assessing students’ professionalism: theoretical insights from sociocognitive psychology. Acad Med. 2007;82:46–50.
Lucey C, Souba W. The problem with the problem of professionalism. Acad Med. 2010;85:1018–24.
Branch Jr WT. The road to professionalism: reflective practice and reflective learning. Patient Educ Couns. 2010;80(3):327–32.
Sharpless J, Baldwin N, Cook R, Kofman A, Morley-Fletcher A, Slotkin R, et al. The becoming: students' reflections on the process of professional identity formation in medical education. Acad Med. 2015;90(6):713–7.
Brainard AH, Brislen HC. Learning professionalism: a view from the trenches. Acad Med. 2007;82:1010–4.
Baernstein A, Amies Oelschlager A-ME, Chang TA, Wenrich MD. Learning professionalism: perspectives of preclinical medical students. Acad Med. 2009;84:574–81.
Cuesta-Briand B, Auret K, Johnson P, Playford D. A world of difference': a qualitative study of medical students' views on professionalism and the 'good doctor. BMC Med Educ. 2014;14:77.
Humphrey HJ, Smith K, Reddy S, Scott D, Madara JL, Arora VM. Promoting an environment of professionalism: the University of Chicago “roadmap.”. Acad Med. 2007;82:1098–107.
Petersen A, Bleakley A, Brömer R, Marshall R. The medical humanities today: humane health care or tool of governance? J Med Humanit. 2008;29(1):1–4.
Brody H, Doukas D. Professionalism: a framework to guide medical education. Med Educ. 2014;48(10):980–7.
Fisher D, Frey N. Text complexity and close readings. International Reading Association: Newark DE; 2012.
Kain P. How to do a close reading. Writing Center: Harvard University. www.fas.harvard.edu ; 1998.
Beers K, Probst RE. Notice and note: Strategies for close reading. Portsmouth NH: Heinemann; 2012.
Paul R, Elder L. How to read a paragraph: The art of close reading. Dillon Beach, CA: Foundation for Critical Thinking Press; 2008.
Charon R. Narrative medicine: Honoring the stories of illness. Oxford: Oxford University Press; 2008.
Shapiro J: The feeling physician: Educating the emotions in medical training. European Journal of Patient-Centered Medicine 2013, 1(2)
Shapiro J. Does medical education promote professional alexithymia? A call for attending to the emotions of patients and self in medical training. Acad Med. 2011;86(3):326–32.
McEntyre MC. Getting from how to why: a pause for reflection on professional life. Acad Med. 1997;72(12):1051–5.
Wear D, Nixon LL. Literary inquiry and professional development in medicine: Against abstractions. Perspect Biol Med. 2002;45(1):104–24.
Stephens GG. Family medicine as counterculture. Fam Med. 1998;30(9):629–36.
Macnaughton J. The humanities in medical education: context, outcomes and structures. Med Humanit. 2000;26:23–30.
Doukas DJ, McCullough LB, Wear S for the Project to Rebalance and Integrate Medical Education (PRIME) Investigators. Perspective: Medical education in medical ethics and humanities as the foundation for developing medical professionalism. Acad Med. 2012;87:334–41.
Kirklin D. Medical humanities and the ongoing search for reliability, authenticity and humility. Med Humanit. 2011;37(2):67.
Dror OE. De-medicalizing the medical humanities. The European Legacy. 2011;16:317–26.
Squier SM. Beyond nescience: The intersectional insights of health humanities. Perspect Biol Med. 2007;50(3):334–7.
Waitzkin H. A critical theory of medical discourse: Ideology, social control, and the processing of social context in medical encounters. J Hlth Soc Behav. 1989;30(2):220–39.
Kester GH. Conversation pieces: Community and communication in modern art. Berkeley: University of California Press; 2004.
Broderick S. Arts practices in unreasonable doubt? Reflections on understandings of arts practices in healthcare contexts. Arts Health. 2011;3:95–109.
Kumagai AK, Lypson ML. Beyond cultural competence: critical consciousness, social justice, and multicultural education. Acad Med. 2009;84:782–7.
Wear D, Aultman JM. Creating difficulties everywhere. Perspect Biol Med. 2007;50(3):348–62.
Belling C. Sharper instruments: on defending the humanities in undergraduate medical education. Acad Med. 2010;85:936–94.
Kumagai AK, Wear D. "Making strange": a role for the humanities in medical education. Acad Med. 2014;89(7):973–7.
Carson RA. Educating the moral imagination. In: Carson RA, Burns CR, TR Cole TR, editors. Practicing the medical humanities: Engaging physicians and patients. Hagerstown, MD: University Publishing Group; 2003. p. 25–38.
Charon R. Narrative evidence based medicine. The Lancet. 2008;371(9609):296–7.
Shapiro J. Walking a mile in their patients' shoes: empathy and othering in medical students' education. Philos Ethics Humanit Med. 2008;3:10.
Wear D. The medical humanities: toward a renewed praxis. J Med Humanit. 2009;30:209–20.
Coles R. The call of stories: Teaching and the moral imagination. New York: Houghton Mifflin; 1990.
Brody H. Defining the medical humanities: three conceptions and three narratives. J Med Humanit. 2011;32(1):1–7.
Case GA, Brauner DJ. The doctor as performer: a proposal for change based on a performance studies paradigm. Acad Med. 2010;85:159–63.
Garden R. Sympathy, disability, and the nurse: Female power in Edith Wharton’s The Fruit of the Tree. J Med Humanit. 2010;31:223–42.
Garden R. The problem of empathy: Medicine and the humanities. New Literary History. 2007;38:551–67.
National Board of Medical Examiners: Assuring quality of the healthcare practitioner workforce: An essential ingredient of a high quality health system. Policies of the National Board of Medical Examiners® regarding health system reform. April, 2011. http://www.nbme.org/PDF/Health-System-Reform/health-system-reform-policies.pdf
Frost HD, Regehr G. “I am a doctor”: negotiating the discourses of standardization and diversity in professional identity construction. Acad Med. 2013;88:1570–7.
Avrahami E. Bridging the divides. The European Legacy. 2011;16:299–306.
Krupat E, Pelletier SR, Chernicky DW. The third year in the first person: medical students report on their principle clinical year. Acad Med. 2011;86:90–7.
Kumagai AK. Acts of interpretation: a philosophical approach to using creative arts in medical education. Acad Med. 2012;87:1138–44.
Chick NL: Beyond the essay: Making student thinking visible in the humanities. http://cft.vanderbilt.edu/guides-sub-pages/beyond-the-essay/
Chick NL, Haynie A, Gurung RAR, Regan AR: From generic to signature pedagogies: teaching disciplinary understandings. In Exploring signature pedagogies: Approaching disciplinary habits of mind. Edited by Gurung C, Haynie A. Sterling, WV: Stylus;2009:1–16.
Goldie J. Assessment of professionalism: a consolidation of current thinking. Med Teach. 2013;35(2):e952–6.
Ginsburg S, Bernabeo E, Ross KM, Holmboe ES. "It depends": results of a qualitative study investigating how practicing internists approach professional dilemmas. Acad Med. 2012;87(12):1685–93.
Kuper A. Literature and medicine: a problem of assessment. Acad Med. 2006;81:S128–37.
Charon R. At the membranes of care: stories in narrative medicine. Acad Med. 2012;87:342–7.
Charon R. Calculating the contributions of humanities to medical practice – motives, methods, and metrics. Acad Med. 2010;85:935–7.
Download references
Acknowledgments
We gratefully acknowledge Delese Wear, Ph.D. for her reading of an earlier version of this paper; and all the PRIME conference participants for their thoughtful perspectives on the issues addressed in the article.
Author information
Authors and affiliations.
Family Medicine and Director of the Program in Medical Humanities & Arts, University of California-Irvine, School of Medicine, 101 City Dr. South, Rte 81, Bldg 200, Ste 835, Orange, CA, 92868, USA
Johanna Shapiro
Internal Medicine, Division of Ethics and Humanities, University of South Florida School of Medicine, 12901 Bruce B Downs Blvd, Tampa, FL, 33612, USA
Lois L. Nixon
Center for Clinical Ethics and Humanities in Healthcare, Departments of Medicine, Gynecology-Obstetrics, and Philosophy, University at Buffalo SUNY School of Medicine, Buffalo, NY, USA
Stephen E. Wear
William Ray Moore Endowed Chair of Family Medicine and Medical Humanism, and Division of Medical Humanism and Ethics, Department of Family and Geriatric Medicine, University of Louisville, 2301S 3rd St, Louisville, KY, 40292, USA
David J. Doukas
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Johanna Shapiro .
Additional information
Competing interests.
All authors declare that they have no competing interests.
Authors’ contributions
JS was primarily responsible for the review of the literature and the conceptualization of the paper. LLN provided conceptual guidance, supplemented the citations, and was a major contributor to the writing of the paper. SW contributed to the development of the paper’s conclusions, the interpretation of the literature, and the writing of the paper. DJD contributed to the literature analysis and the writing of the paper. In addition, his establishing and organizing a series of PRIME conferences (Project to Rebalance and Integrate Medical Education) provided the necessary intellectual impetus for this work. All authors read and approved the final amnuscript.
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/4.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Shapiro, J., Nixon, L.L., Wear, S.E. et al. Medical professionalism: what the study of literature can contribute to the conversation. Philos Ethics Humanit Med 10 , 10 (2015). https://doi.org/10.1186/s13010-015-0030-0
Download citation
Received : 10 September 2014
Accepted : 23 June 2015
Published : 27 June 2015
DOI : https://doi.org/10.1186/s13010-015-0030-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical professionalism
- Professional identity formation
- Health humanities
- Medical humanities
Philosophy, Ethics, and Humanities in Medicine
ISSN: 1747-5341
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Palgrave Encyclopedia of the Health Humanities pp 1–7 Cite as
Reflective Practice in Medical Education
- Rachel Conrad Bracken 3
- Living reference work entry
- First Online: 23 November 2021
95 Accesses
Critical reflection ; Reflection ; Reflective writing
“Practice” refers both to the repeated exercise of a skill or activity in order to achieve proficiency and the application of a method, skill, or belief. Accordingly, “reflective practice” refers to the ways in which reflection, as a skill and a habit of mind, is first acquired and then utilized by professionals. Within the fields of medicine and medical education, reflective practice encompasses both a praxis – to do the work of healing patients guided by ongoing reflective thought – and the curricular interventions through which medical trainees hone their reflective capacity. As it pertains to reflective practice, “reflection” is “the process of analyzing, questioning, and reframing an experience in order to make an assessment of it for the purposes of learning (reflective learning) and/or to improve practice (reflective practice)” (Aronson, 2011 : 200–201). The capacity for reflection as “an epistemology of...
This is a preview of subscription content, log in via an institution .
Aronson, L. (2011). Twelve tips for teaching reflection at all levels of medical education. Medical Teacher, 33 (3), 200–205. https://doi.org/10.3109/0142159X.2010.507714
Article Google Scholar
Belling, C. (2010). Sharper instruments: On defending the humanities in undergraduate medical education. Academic Medicine, 85 (6), 938–940.
Bolton, G. (1999). Stories at work: Reflective writing for practitioners. Lancet, 354 , 243–245.
Charon, R. (2006). Narrative medicine: Honoring the stories of illness . Oxford University Press.
Google Scholar
Charon, R., & Hermann, N. (2012). A sense of story, or why teach reflective writing? Academic Medicine, 87 (1), 5–7. https://doi.org/10.1097/ACM.0b013e31823a59c7
Clandinin, D. J., & Cave, M. T. (2008). Creating pedagogical spaces for developing doctor professional identity. Medical Education, 42 , 765–770. https://doi.org/10.1111/j.1365-2923.2008.03098.x
Clará, M. (2015). What is reflection? Looking for clarity in an ambiguous notion. Journal of Teacher Education, 66 (3), 261–271.
DasGupta, S. & Charon, R. (2004). Personal illness narratives: Using reflective writing to teach empathy. Academic Medicine, 79 (4), 351–356.
de la Croix, A., & Veen, M. (2018). The reflective zombie: Problematizing the conceptual framework of reflection in medical education. Perspectives on Medical Education, 7 (6), 394–400. https://doi.org/10.1007/s40037-018-0479-9
Engel, J. D., Zarconi, J., Pethtel, L. L., & Missimi, S. A. (2008). Narrative in health care: Healing patients, practitioners, profession, and community . Radcliffe Publishing Ltd.
Fragkos, K. C. (2016). Reflective practice in healthcare education: An umbrella review. Education Sciences, 6 (27). https://doi.org/10.3390/educsci6030027
Hafferty, F. W. (1998). Beyond curriculum reform: Confronting medicine’s hidden curriculum. Academic Medicine, 73 (4), 403–407. https://doi.org/10.1097/00001888-199804000-00013
Jennings, M. L. (2009). Medical student burnout: Interdisciplinary exploration and analysis. Journal of Medical Humanities, 30 , 253–269. https://doi.org/10.1007/s10912-009-9093-5
Kumagai, A. K., & Naidu, T. (2015). Reflection, dialogue, and the possibilities of space. Academic Medicine, 90 , 283–288.
Mann, K., Gordon, J., & MacLeod, A. (2009). Reflection and reflective practice in health professions education: A systematic review. Advances in Health Sciences Education, 14 , 595–621. https://doi.org/10.1007/s10459-007-9090-2
Murphy, J. W., Franz, B. A., & Schlaerth, C. (2018). The role of reflection in narrative medicine. Journal of Medical Education and Curricular Development, 5 , 1–5. https://doi.org/10.1177/2382120518785301
Ng, S. L., Kinsella, E. A., Friesen, F., & Hodges, B. (2015). Reclaiming a theoretical orientation to reflection in medical education research: A critical narrative review. Medical Education, 49 , 461–475. https://doi.org/10.1111/medu.12680
Ng, S. L., Wright, S. R., & Kuper, A. (2019). The divergence and convergence of critical reflection and critical reflexivity: Implications for health professions education. Academic Medicine, 94 , 1122–1128.
Nguyen, Q. D., Fernandez, N., Karsenti, T., & Charlin, B. (2014). What is reflection? A conceptual analysis of major definitions and a proposal of a five-component model. Medical Education, 48 , 1176–1189. https://doi.org/10.1111/medu.12583
Platt, L. (2014). The ‘wicked problem’ of reflective practice: A critical literature review. Innovations in Practice, 9 (1), 44–53.
Rodgers, C. R. (2002). Defining reflection: Another look at John Dewey and reflective thinking. Teachers College Record, 104 (4), 842–866.
Sandars, J. (2009). The use of reflection in medical education: AMEE guide no. 44. Medical Teacher, 31 (8), 685–695. https://doi.org/10.1080/01421590903050374
Shapiro, J., Kasman, D., & Shafer, A. (2006). Words and wards: A model of reflective writing and its uses in medical education. Journal of Medical Humanities, 27 , 231–244. https://doi.org/10.1007/s10912-006-9020-y
Shemtob, L. (2016). Reflecting on reflection: A medical student’s perspective. Academic Medicine, 91 (9), 1190–1191.
Wald, H. S. (2015). Refining a definition of reflection for the being as well as doing the work of a physician. Medical Teacher, 37 , 696–699.
Wald, H. S., & Reis, S. P. (2010). Beyond the margins: Reflective writing and development of reflective capacity in medical education. Journal of General Internal Medicine, 25 (7), 746–749.
Wald, H. S., Davis, S. W., Reis, S. P., Monroe, A. D., & Borkan, J. M. (2009). Reflecting on reflection: Enhancement of medical education curriculum with structured field notes and guided feedback. Academic Medicine, 84 (7), 830–836.
Wald, H. S., Borkan, J. M., Taylor, J. S., Anthony, D., & Reis, S. P. (2012). Fostering and evaluating reflective capacity in medical education: Developing the REFLECT rubric for assessing reflective writing. Academic Medicine, 87 (1), 41–50.
Wass, V., & Harrison, C. (2014). Empowering the learner to reflect: Do we need another approach? Medical Education, 48 (12), 1146–1147.
Wear, D., Zarconi, J., Garden, R., & Jones, T. (2012). Reflection in/and writing: Pedagogy and practice in medical education. Academic Medicine, 87 (5), 603–609. https://doi.org/10.1097/ACM.0b013e31824d22e9
Whiting, E., Wear, D., Aultman, J. M., & Zupp, L. (2012). Teaching softly in hard environments: Meanings of small-group reflective teaching to clinical faculty. Journal for Learning through the Arts, 8 (1). https://doi.org/10.21977/D9812654
Download references
Author information
Authors and affiliations.
Family and Community Medicine, Northeast Ohio Medical University, Rootstown, OH, USA
Rachel Conrad Bracken
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Rachel Conrad Bracken .
Editor information
Editors and affiliations.
School of Health Sciences, The University of Nottingham, Derby, UK
Paul Crawford
University of Global Health Equity, Kigali, Rwanda
Paul Kadetz
Section Editor information
No affiliation provided
Paul I. Kadetz
Kira Hopkins
Jamie Crawford
Rights and permissions
Reprints and permissions
Copyright information
© 2021 The Author(s), under exclusive licence to Springer Nature Switzerland AG
About this entry
Cite this entry.
Bracken, R.C. (2021). Reflective Practice in Medical Education. In: Crawford, P., Kadetz, P. (eds) Palgrave Encyclopedia of the Health Humanities. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-26825-1_203-1
Download citation
DOI : https://doi.org/10.1007/978-3-030-26825-1_203-1
Received : 19 December 2020
Accepted : 10 April 2021
Published : 23 November 2021
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-26825-1
Online ISBN : 978-3-030-26825-1
eBook Packages : Springer Reference Literature, Cultural and Media Studies Reference Module Humanities and Social Sciences Reference Module Humanities
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Libr Assoc
- v.97(4); 2009 Oct
The health sciences librarian in medical education: a vital pathways project task force
Diane g. schwartz.
Director, Libraries, Kaleida Health, 100 High Street, Buffalo, NY 14203 gro.htlaehadielak@ztrawhcsd
Paul M. Blobaum
Associate Professor, College of Health and Human Services, and Librarian, Library, Governors State University, One University Parkway, University Park, IL 60466 ude.tsvog@muabolb-p
Jean P. Shipman
Director, Spencer S. Eccles Health Sciences Library, University of Utah, 10 North 1900 East, Building 589, Salt Lake City, UT, 84121 [email protected]
Linda Garr Markwell
Head, Branch Library Services, Grady Branch, Woodruff Health Sciences Center Library, Emory University, 69 Jesse Hill Jr. Drive Southeast, Atlanta, GA 30303 ude.yrome@mglbil

Joanne Gard Marshall
Alumni Distinguished Professor, School of Information and Library Science, University of North Carolina at Chapel Hill, 100 Manning Hall, CB#3360, Chapel Hill, NC 27599-3360 ude.cnu.sli@llahsram
Associated Data
Objectives:.
The Medical Education Task Force of the Task Force on Vital Pathways for Hospital Librarians reviewed current and future roles of health sciences librarians in medical education at the graduate and undergraduate levels and worked with national organizations to integrate library services, education, and staff into the requirements for training medical students and residents.
Standards for medical education accreditation programs were studied, and a literature search was conducted on the topic of the role of the health sciences librarian in medical education.
Expectations for library and information services in current standards were documented, and a draft standard prepared. A comprehensive bibliography on the role of the health sciences librarian in medical education was completed, and an analysis of the services provided by health sciences librarians was created.
Conclusion:
An essential role and responsibility of the health sciences librarian will be to provide the health care professional with the skills needed to access, manage, and use library and information resources effectively. Validation and recognition of the health sciences librarian's contributions to medical education by accrediting agencies will be critical. The opportunity lies in health sciences librarians embracing the diverse roles that can be served in this vital activity, regardless of accrediting agency mandates.
In response to reported closings of and staff reductions at hospital libraries, the Medical Library Association (MLA) and the Hospital Libraries Section of MLA agreed to study the state of hospital libraries and librarians under the auspices of the Task Force on Vital Pathways for Hospital Librarians. The task force's Health Sciences Librarian in Medical Education Task Force (METF) * was charged with reviewing the accreditation standards regarding libraries for residency programs and with working with national organizations to integrate library services, education, and staff into the requirements for training medical students and residents.
Standards review
The Accreditation Council on Graduate Medical Education (ACGME) accredits graduate medical education (GME) training programs in the United States and Canada. ACGME is responsible for establishing standards for residency and postgraduate fellowship programs in twenty-six specialties and approximately one hundred subspecialty programs [ 1 ]. The Residency Review Committees (RRCs) are a subset of the ACGME.
Medical librarians have always served a vital role in educating residents and medical students. So as libraries in teaching hospitals closed, questions regarding the impact of the closures on the accreditation of residency programs surfaced. In 2005, an METF member conducted an assessment and analysis of RRC requirements for libraries with the goal of understanding the impact of the closures on residency training programs. The 2004–2005 edition of the Graduate Medical Education Directory (Green Book) [ 2 ] published by the ACGME was the primary source for the review.
In the fall of 2006, an METF member conducted an analysis of library-related RRC requirements, using the ACGME website rather than the printed version of the Green Book. The analysis was compiled to identify the similarities and differences among the twenty-two medical specialties. Concurrently, the METF considered the work of the ACGME Outcome Project [ 3 ] and its “Minimum Program Requirements” that described the six competency skill sets expected of residents upon completion of the resident's training program. Other documents informed the METF's research, including “Standards for Hospital Libraries 2007” [ 4 ], the “Building on Success: Charting the Future of Knowledge Management within the Academic Health Sciences Center” by the Association of Academic Health Sciences Libraries (AAHSL) [ 5 ], and the Medical School Objectives Project (MSOP) of the Association of American Medical Colleges (AAMC) [ 6 ]. To ensure a comprehensive understanding of the issues, METF also reviewed standards for libraries issued by the American Osteopathic Association (AOA), the AAMC, and the American Medical Association's (AMA's) Liaison Committee on Medical Education (LCME). Each organization's website and publications related to accreditation standards were reviewed for statements concerning medical libraries or medical librarians.
Hospital librarian roles
To codify and document the changing array of services that are being performed by health sciences librarians, many of which go unreported and unrecognized, the METF created an initial list of services based on their own experiences and observations. The list was further augmented by searching the library science literature. Librarians participating in the MLA Hospital Libraries Section email discussion list also contributed to this list. The goal was to create a list of services that could be modified and updated over time to reflect changes occurring as the health care environment evolves.
The bibliography
A comprehensive but selective bibliography of materials related to the role of health sciences librarians and libraries in medical education was first prepared in 2006. An initial literature review produced an interesting array of articles on current and future roles for librarians. The list of articles was expanded with the writing of this article. Four databases were searched: Library, Information Science & Technology Abstracts (LISTA), Library Literature & Information Science, Ovid MEDLINE, and PubMed. The initial search strategy was
“'librar* AND (health OR medical OR hospital) AND (future OR role* OR “21st century”)”
The bibliography covers the years 1987 through 2008.
Accreditation Council on Graduate Medica Education
The results of the analysis of ACGME requirements were a cause for concern. In the preface to the Green Book , the “Institutional Requirements” section stated, “Residents must have access to adequate communication resources and technological support. This should include, at a minimum, computers and access to the Internet” [ 2 ]. No mention was made of the role of libraries. The RRCs followed the ACGME's lead ( Table 1 ).
Residency standards

Most RRCs stipulated that a training program must provide access to a convenient library where residents could be trained or an onsite library; however, only one required a physical onsite library. The keyword in this statement is “or”; also significant is the word “convenient.” The Green Book did not define the meaning of “convenient” and did not require a professional health sciences librarian be available onsite to participate in the educational programs being offered to residents. The following terms were used by the RRCs to describe acceptable library services: department or program-based library, hospital-based library, onsite or sponsoring institution library, arrangements with a convenient nearby institution, and electronic library. Most RRC statements focused on the library as a place and required access to a major medical library, either onsite or at a nearby institution. Only the Anesthesiology RRC required a department library.
Electronic library services were not required with the exception of database searching, although five residency programs also specified availability of Internet access. The majority of RRCs required night and weekend access, as well as access to electronic medical databases and reference tools, but did not specifically require the expertise of a professional librarian. The preventive medicine specialty was the only RRC to require an on-site reference librarian.
In 1999, all RRCs incorporated the six competencies into their program requirements: patient care, medical knowledge, practice-based learning, interpersonal communication skills, professionalism, and systems-based practice. The METF determined that “medical knowledge” and “practice-based learning” were two competencies that would benefit from educational intervention by health sciences librarians and the resources of medical libraries. Based on these findings, a draft “standard” library statement was prepared, based on ACGME standards:
- Faculty and residents must have ready access to adequate communication resources and technology supported by a health sciences librarian with an American Library Association–accredited degree.
- Residents must have twenty-four-hour, seven-day-a-week access to authoritative specialty- or subspecialty-specific knowledge-based information resources and reference materials at the hospital. Comprehensive electronic medical literature databases, including MEDLINE, and document delivery services must be available. A health sciences librarian holding an American Library Association–accredited degree must manage the library.
American Osteopathic Association
AOA accredits postdoctoral training programs in eighteen specialty areas, but graduates of osteopathic medical schools can also receive postgraduate training at allopathic hospital residency programs that are accredited by the ACGME. Standards set forth in AOA's Accreditation Document for Osteopathic Training Institutions (OPTI) and The Basic Document for Postdoctoral Training Programs were both substantive and extensive regarding expectations for library services and professional librarian support [ 7 ]. Table 2 shows standards for libraries from the AOA's OPTI and The Basic Document for Postdoctoral Training Programs , prepared in 2005.
American Osteopathic Association (AOA) accreditation documents

Roles of health sciences libraries and librarians in medical education
The final bibliography on the roles of health sciences libraries and librarians in medical education consisted of 329 references ( Appendix, online ). It was conceived as a research resource and companion piece to the “Services Performed by Health Sciences Librarians” ( Table 3 ). The long-term goal is to expand the bibliography over time so that the information contained in it can be used to create standards for libraries and the role of the professional librarian in the future.
List of services performed by health sciences librarians

DISCUSSION AND OUTCOMES
Health sciences librarians working in hospitals and academic medical centers have served an active role in educating medical students, residents, and attending physicians, as well as other health care professionals, over the years. Nevertheless, the standards issued by the agencies that accredit these training programs generally do not recognize the roles and contributions of health sciences librarians.
As the clinical practice environment becomes increasingly technology driven as the result of widespread implementation of electronic medical records, health care professionals will require information management and informatics knowledge and skills to function effectively. In addition to the impact of technology on clinical decision making, professional development activities will also increasingly require knowledge and skill in using many different technological resources. Facilitating the advancement of these skills among health care provider trainees—whether at the undergraduate, graduate, or postgraduate level—will remain an essential role and responsibility of the health sciences librarian. Several accrediting organizations have provided leadership in delineating the role of the librarian in information management education and informatics skill development, including the AOA and the LCME.
In late 2006, MLA sent a letter to the executive director of the Institutional Review Committee of the ACGME, the group that sets the RRC standards. The letter requested that the RRCs consider adopting the proposed library standard statement created by METF when they update residency requirements, which is mandated every five years. In response, ACGME requested a more generic statement, one that would meet the needs of many different teaching hospitals. ACGME requested the change because they believed that small hospitals might not be able to afford a hospital library. As of early 2009, further action is pending regarding these activities with ACGME.
In fall 2006, MLA headquarters staff met with AOA representatives and discussed updates to AOAs health care facility accreditation standards. The standards were published in the AOA's Accreditation Document for Osteopathic Training Institutions (OPTI) and The Basic Document for Postdoctoral Training Programs [ 7 ]. A revised set of standards will be published in fall 2009. The standards include comprehensive support for the role of the health sciences librarian in the education of osteopathic physicians. Due to the scope and comprehensiveness of the AOA standards, it is clear that the standards could serve as a model that MLA could use as an advocacy tool for distribution to other accrediting agencies. While this was an important achievement, it was not directly a result of METF's work.
At the same time that these events were occurring, an AAHSL task force was charged with recommending changes and additions to “Section V–Educational Resource, Subsection D–Information Resources and Library Services” of the LCME self-study database [ 8 ]. The objective was to reflect digital and remote library resources and services. A revised document, based on input from AAHSL, was accepted in 2007. As a result of these efforts, AAHSL succeeded in changing the standards. The revision emphasized the role of the professional librarian in training medical students in information management skills rather than in the use of library resources and services [ 9 ].
As part of its work, METF conducted a thorough review of the literature on the role of health sciences librarians in medical education. The literature search demonstrated that librarians have wide-ranging roles and responsibilities in the area of education. Nevertheless, accrediting agencies have not recognized the contributions of the professional health sciences librarian in this domain. For example, ACGME recognizes that all residents need to acquire information management skills during their graduate medical education training. However, no mention appears in ACGME's general competencies of the important role that librarians serve in achieving this goal. The standards for residency programs issued by each RRC vary greatly with regard to libraries. Some RRC standards require that residents have access to a library, while other RRCs do not mention the need for library services or the role of the professional librarian. Those RRC standards that do mention access to library materials or services do not provide either definitions or guidelines on how to meet the requirements. The AAMC also identified informatics skills as a core competency in its MSOP report II [ 6 ] and clearly delineated the skills that medical students should master by the time of graduation. A number of the objectives, such as information and knowledge management and informatics skills, are examples of the training that has traditionally been provided by librarians, but MSOP report II did not specify that the skills should be taught by health sciences librarians.
CONCLUSIONS
The health care environment continues to be one of the most rapidly changing sectors in society. The need to disseminate and use quality health information to support patient care, education, and research has never been greater, and the way in which information is stored and used will continue to change. Librarians have already developed new roles for themselves, as demonstrated by METF's “List of Services Performed by Health Sciences Librarians.” With support from MLA, health sciences librarians must enhance their advocacy and communication activities with accrediting agencies to ensure that recognition of their roles, responsibilities, and contributions remains strong.
MLA should continue to partner with ACGME, AOA, and LCME to strengthen the library-related standards of these organizations. The outcome will be enhanced involvement of the professional health sciences librarian in medical education.
Electronic Content
EC A supplemental appendix is available with the online version of this journal.
* Diane G. Schwartz, AHIP, FMLA, chair, Jean Shipman, AHIP, FMLA, board liaison, Paul Blobaum, Linda Garr Markwell, AHIP, Joanne Gard Marshall, FMLA, and Laurie Thompson, AHIP.
- MHC's currently closed. MHC will open Wed at 9:00 AM
- More Library Hours
- Visit the Library
- Today’s Hours: 8:00 am - 8:00 pm
Ask a Librarian
- MHC Blog Home
Digitizing Medical Illustrations from the Heart Bulletin + The Role of Art in the Medical Field
![role of literature in medical education [Illustration, p. 74: “Cardiac Clinic: Renal Hypertension” drawing, July/August, 1957, Box 11, Folder 37, IC 094 Medical Arts Publishing Foundation, McGovern Historical Center, Texas Medical Center Library]](https://library.tmc.edu/mcgovern/wp-content/uploads/sites/5/2024/04/IC094-heart-illustrations-0604-074_banner-1024x501.jpg)
By Johana Canales, Archives Intern.
As archivists discussed recently , the Houston-based Medical Arts Publishing Foundation produced illustrated medical publications like the Cancer Bulletin , Heart Bulletin , and Psychiatric Bulletin .
The Foundation’s records began arriving at the McGovern Historical Center in 1992. Since then some of the collection’s medical illustrations had already been digitized, including several complete issues of the Psychiatric Bulletin from 1950-1960. The great folks here at the MHC allowed me to digitize Box 11 of the collection, belonging to the Heart Bulletin ’s medical illustrations series. This was such a fun box to digitize because of the creative and sometimes wacky original illustrations it contained, but also because I got to read original publication notes used in the creation of the Heart Bulletin between 1951 and 1964. During this project, I was able to think deeply about the archival practice of appraisal, as well as the important role that art plays in the medical field. Here are some of my main takeaways:
Informational characteristics
These original medical illustrations are informative to the medical field in their own separate and unique ways. First of all, they are informative in the most obvious way, which is that they offer visual representations corresponding to the information discussed in the articles. A lot of the images depict diagrams and drawings of medical tools, technology, treatment, and rehabilitation. An article discussing chronic pericarditis has a radiographic image displaying just that. However, what is unique about this archival image is the fact that publication notes are present. These notes highlight the communication between the creators and editors, which gives more insight about the publication process in the 1950s and 1960s.
![role of literature in medical education [Illustration, p. 111: “Pericardiectomy for Relief of Chronic Constrictive Pericarditis” X-ray image, November/December, 1955, Box 11, Folder 9, IC 094 Medical Arts Publishing Foundation, McGovern Historical Center, Texas Medical Center Library]](https://library.tmc.edu/mcgovern/wp-content/uploads/sites/5/2024/04/IC094-heart-illustrations-0406-111.jpg)
The original illustrations also depict coloring techniques that provide more insight into how colors were planned and implemented in medical journals at the time such as overlaying tinted plastic sheets on top of drawings to achieve a different color hue on the published image. It was also nice to see the imperfections that these seemingly perfect illustrations had and the white-out techniques used to edit and clean them on the spot.
![role of literature in medical education [Illustration, p. 24: “Taxi cab” drawing with red overlay, January/February, 1957, Box 11, Folder 32, IC 094 Medical Arts Publishing Foundation, McGovern Historical Center, Texas Medical Center Library]](https://library.tmc.edu/mcgovern/wp-content/uploads/sites/5/2024/04/IC094-heart-illustrations-0602-024-rotated.jpg)
Medical illustrations are such a niche field within both the arts and medical fields. Thankfully, the signatures on multiple pieces from Jo Spier and Joseph F. Schwarting, allow us to track and credit the appropriate artists with their art as well as follow their work and how it has changed and developed throughout their careers. Tracking these changes could also reveal greater changes that happened in the medical illustrations field as a whole.
![role of literature in medical education [Illustration, p. 84: “Doctor examining child” drawing by Jo Spier, September/October, 1956, Box 11, Folder 30, IC 094 Medical Arts Publishing Foundation, McGovern Historical Center, Texas Medical Center Library]](https://library.tmc.edu/mcgovern/wp-content/uploads/sites/5/2024/04/IC094-heart-illustrations-0505-084-rotated.jpg)
Medical illustrations as abstract representations of health, medicine, and medical tools
I was pleasantly surprised to digitize many illustrations that were not one-to-one representations of reality such as a drawing of a sphygmomanometer wrapped around a kidney ureter, or a drawing of a kidney combined with a beaker with a straw and electrical plugs sticking out of it to represent an artificial kidney. These drawings were not meant to be accurate representations of reality. Rather, they serve as visual metaphors that help the viewer quickly grasp the essence of the article by relating it to something they are familiar with. This is a clear indication of how medical illustrations can significantly enhance the information derived from medical publications and the helpful role that art and artists play in the medical field.
![role of literature in medical education [Illustration, p. 74: “Cardiac Clinic: Renal Hypertension” drawing, July/August, 1957, Box 11, Folder 37, IC 094 Medical Arts Publishing Foundation, McGovern Historical Center, Texas Medical Center Library]](https://library.tmc.edu/mcgovern/wp-content/uploads/sites/5/2024/04/IC094-heart-illustrations-0604-074-rotated.jpg)
All of the original Heart Bulletin illustrations found in Box 11 of the Medical Arts Publishing Foundation records are now available to view online !
The Texas Medical Center Library. 1133 John Freeman Blvd, Houston, TX 77030
More results...
- Open access
- Published: 15 April 2024
Implementing spiritual care education into the teaching of palliative medicine: an outcome evaluation
- Yann-Nicolas Batzler 1 ,
- Nicola Stricker 2 , 3 ,
- Simone Bakus 4 ,
- Manuela Schallenburger 1 , 6 ,
- Jacqueline Schwartz 1 &
- Martin Neukirchen 1 , 5
BMC Medical Education volume 24 , Article number: 411 ( 2024 ) Cite this article
335 Accesses
Metrics details
The concept of “total pain” plays an important role in palliative care; it means that pain is not solely experienced on a physical level, but also within a psychological, social and spiritual dimension. Understanding what spirituality entails, however, is a challenge for health care professionals, as is screening for the spiritual needs of patients.
This is a novel, interprofessional approach in teaching undergraduate medical students about spiritual care in the format of a seminar. The aim of this study is to assess if an increase in knowledge about spiritual care in the clinical context is achievable with this format.
In a mandatory seminar within the palliative care curriculum at our university, both a physician and a hospital chaplain teach strategies in symptom control from different perspectives (somatic domain – spiritual domain). For evaluation purposes of the content taught on the spiritual domain, we conducted a questionnaire consisting of two parts: specific outcome evaluation making use of the comparative self-assessment (CSA) gain and overall perception of the seminar using Likert scale.
In total, 52 students participated. Regarding specific outcome evaluation, the greatest gain was achieved in the ability to define total pain (84.8%) and in realizing its relevance in clinical settings (77.4%). The lowest, but still fairly high improvement was achieved in the ability to identify patients who might benefit from spiritual counselling (60.9%). The learning benefits were all significant as confirmed by confidence intervals. Overall, students were satisfied with the structure of the seminar. The content was delivered clearly and comprehensibly reaching a mean score of 4.3 on Likert scale (4 = agree). The content was perceived as overall relevant to the later work in medicine (mean 4.3). Most students do not opt for a seminar solely revolving around spiritual care (mean 2.6).
Conclusions
We conclude that implementing spiritual care education following an interprofessional approach into existing medical curricula, e.g. palliative medicine, is feasible and well perceived among medical students. Students do not wish for a seminar which solely revolves around spiritual care but prefer a close link to clinical practice and strategies.
Peer Review reports
Introduction
Education in palliative care was introduced in 2009 as a compulsory subject in German medical curricula. In the 1960s, Dame Cicely Saunders established palliative medicine and hospices as we know them today. Back then, Cicely Saunders propagated the concept of “total pain”, which means that pain or suffering in general is not solely experienced on a physical level, but also within a psychological, social and spiritual dimension (see. Fig. 1 ) [ 1 , 2 , 3 , 4 ]. Understanding the importance of spirituality in everyday clinical practice and what it entails, however, is a challenge for health care professionals (HCP) in all medical disciplines across the world [ 5 , 6 ]. Palliative care is a relatively young medical discipline which oftentimes is not sufficiently taught in medical curricula [ 1 , 7 ] and, therefore, knowledge regarding the importance of spirituality, which at many faculties is integrated into palliative care education, is scarce [ 1 , 7 ]. As a result, HCP tend to neglect the spiritual needs of patients [ 7 , 8 ]. But, if there is no fundamental knowledge in regards of spirituality and spiritual care among physicians, how can they target total pain adequately?
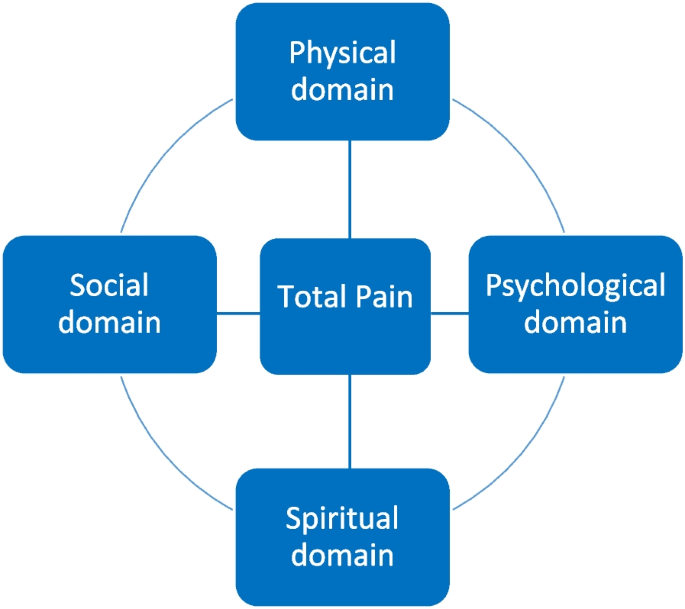
The European Association of palliative care (EAPC) describes spirituality as following:
“Spirituality is the dynamic dimension of human life that relates to the way persons (individual and community) experience, express and/or seek meaning, purpose and transcendence, and the way they connect to the moment, to self, to others, to nature, to the significant and/or the sacred.” [ 1 , 9 ].
It must be clear to all HCP that spirituality is a unique and subjective phenomenon that differs substantially from patient to patient [ 2 , 10 ]. Furthermore, to fully address the spiritual needs of patients, self-reflection, thorough consideration of one’s own attitude towards death, and finding meaning in life, are essential [ 8 , 9 ]. Several studies have shown the impact which the addressing of spiritual needs in the context of total pain can have on ameliorating the symptoms of patients, leading to a better quality of life and care [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 ]. Thus, once spiritual needs become imminent, it is necessary to engage in an interdisciplinary and multi-professional collaboration with specially trained professionals in the field of spiritual care [ 8 , 10 , 14 , 15 , 19 ]. Summing up, it is very important to raise awareness about the positive impact of spiritual care among HCPs [ 8 , 15 ]. To increase such knowledge and accrue such skills, the teaching of spiritual care in medical curricula is essential [ 20 ]. Throughout different regions in the world, in-person didactic teaching on spiritual care is the most commonly used technique [ 5 ]. Usually, the teaching is based on case studies and many include screening strategies assessing spiritual needs [ 5 ]. Often, education on spirituality and spiritual care is part of curricula in palliative care [ 5 , 21 ]. In German medical curricula, there is no compulsory subject solely revolving around spiritual care [ 22 ]. However, regarding the concept of total pain, implementing spiritual care into palliative care teaching, however, seems like a plausible proposition.
This study was conducted in order to assess the way medical students perceive the concept of implementing spiritual care into the teaching on symptom control in palliative care. Furthermore, we aimed to determine whether an actual increase of knowledge about spiritual care in the clinical context was achievable within this seminar.
Material and methods
This study is a single-centre prospective study conducted at University Hospital Duesseldorf, Germany. Ethical approval was obtained by the local ethics committee (reference number 2022–2274).
Curricular structure
At our facility, palliative care education is structured as followed: Five lectures (somatic symptoms, psychological symptoms, social symptoms and advance care planning, spiritual symptoms and end-of-life care and care for relatives, clinical ethics) and four seminars (symptom control, breaking bad news, clinical ethics I and II). Since 2022, the lecture on spiritual symptoms and end-of-life-care is held by both a physician and a hospital chaplain within the palliative care curriculum at Düsseldorf medical faculty. Beforehand, this lecture was solely held by a hospital chaplain. As internal evaluations implied, this concept was not well perceived by medical students as the relevance to daily clinical work was not apparent to them. They did not understand how spiritual care can support somatic strategies of symptom control and how both approaches are intertwined. Furthermore, they were unsure of how to assess patients’ spiritual needs. We therefore opted for the above-mentioned approach which allows lecturing relevant medical implications alongside spiritual care. As evaluations showed, this embeds spiritual care in a more clinical and tangible manner and students seem to better realize the relevance that spiritual care has in daily clinical practice. For example, students repeatedly stated that they were now able to understand the importance of ongoing collaborations for patients’ comfort care, e.g., in more sufficiently relieving anxiety or social distress.
Since this novel concept was perceived positively by medical students, we transposed it to our seminar titled “symptom control” which is now also held by a hospital chaplain and a physician. In the seminars, content from the lectures is further deepened and there is more room for discussions, e.g. concerning assessment of spiritual needs, possibilities of spiritual care, and inter-professional collaboration. There is also an emphasis on determining which patients might benefit from spiritual care making use of the SPIR tool (patient’s self-description as a S piritual person— P lace of spirituality in patient’s life – patient’s I ntegration in a spiritual community – R ole of health care professional in the domain of spirituality), which tackles different dimensions of spirituality [ 23 ].
In the seminar, a 33-year-old fictitious patient (inspired by a real patient) served as an example case. Her situation is used to address strategies for symptom control on both somatic and spiritual domains. To achieve this, a reflective question is discussed with the students followed by a joint development of possible therapeutic strategies on both the somatic and spiritual domain (see Fig. 2 ).
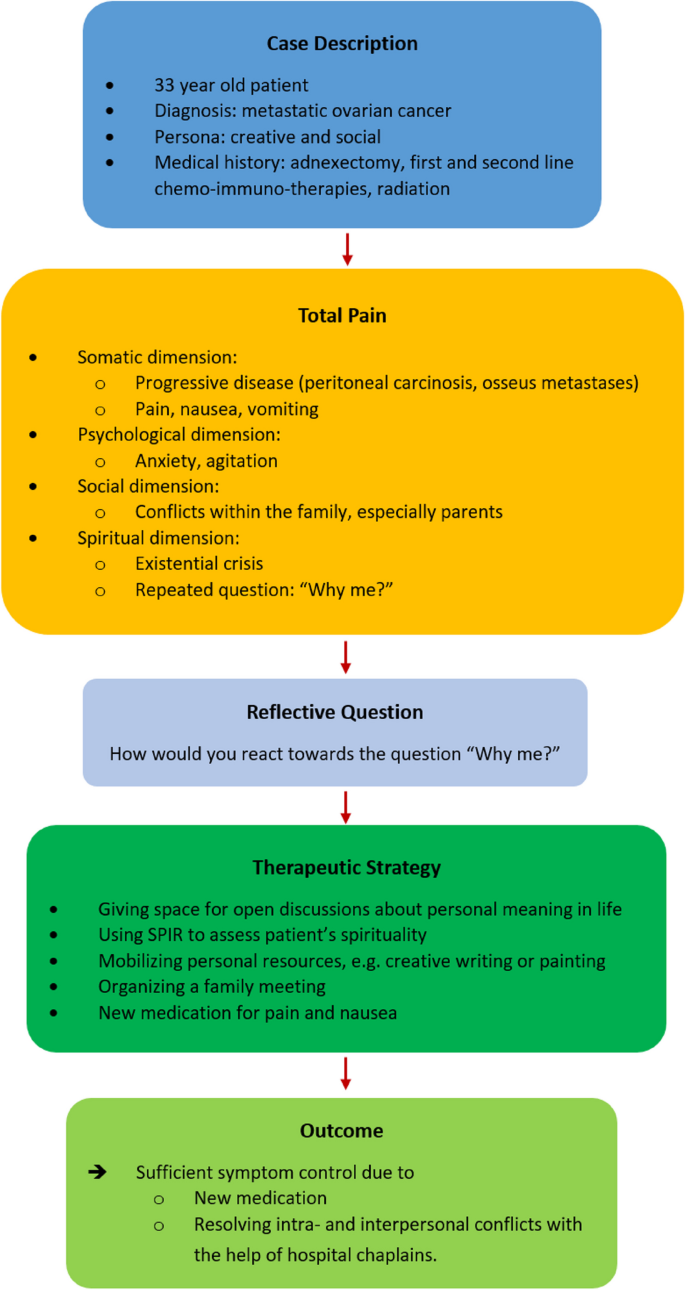
Case discussion in the seminar
Our approach can be described as novel, since training in spiritual care often involves the mere shadowing of chaplains [ 5 , 24 , 25 , 26 ]. An interprofessional, educational approach was mainly used with physicians or nurses in training [ 5 , 27 , 28 , 29 ], but not with medical students.
Evaluation methods
A structured, paper-based questionnaire was developed in repeated interdisciplinary and multi-professional discussions in the Interdisciplinary Centre for Palliative Care Medicine, University Hospital Düsseldorf, Germany. The basis for the questionnaire were the learning goals that are to be achieved within the seminar, as well as a didactic evaluation. The questionnaire was pretested among medical students, and unclear statements were altered. The questionnaire consists of two parts. The first part is made up of five statements regarding knowledge about total pain, assessing spiritual needs, and defining spiritual care (see Table 1 ) on both the knowledge and skills level. These statements cover the field of specific outcome evaluation. Making use of the comparative self-assessment (CSA) method to determine if a gain in knowledge was achieved, each student evaluated their knowledge before and after the seminar using the German school grading system (1 = “excellent” to 6 = “unsatisfactory”). The CSA gain is a well described and implemented method in evaluating actual knowledge gains in education [ 30 , 31 , 32 , 33 , 34 ]. This evaluation tool has the benefit of not taking into account experiences made beforehand as they are not contributing to the effect size [ 31 ]. CSA gain is calculated as followed:
Furthermore, CSA gain was calculated with a 95% confidence interval and standard error using individual learning gain (ILG) values. These values were calculated using the following formulas:
ILG = 0 if pre = post and
ILG = (pre − post)/(pre − 1) × 100 if pre > post [ 31 ].
The second part of the questionnaire consists of four questions regarding the perception of the seminar (structure, teaching spiritual care alongside symptom control in palliative care). A 5-Point-Likert scale was used for evaluation (1 = strongly disagree, 2 = disagree, 3 = neither, 4 = agree, 5 = strongly agree).
Study participation and analysis
Participation in the study was anonymous, voluntary, and could be withdrawn at any time without explanation. Eligible participants were undergraduate medical students at the beginning of their fifth year of medical education (Germany: total of min. six years), who completed the mandatory palliative care course. The purpose and content of the study were presented orally, and, furthermore, written information and consent documents were handed out. After completion of the seminar, the questionnaire was handed out making use of a post-then design in which the students were asked to retrospectively rate their knowledge before and after the seminar. There were no exclusion criteria other than refusing to participate. Due to the small number of students per seminar ( n = 15–20), no demographic characteristics besides sex were assessed.
Data analysis was performed using Microsoft Excel 2020 (version 16.42, Microsoft Corp., Redmond, WA, USA) and IBM SPSS Statistic version 28.0.1.1 (IBM, Armonk, NY, USA).
Throughout the course of one semester in 2023, the questionnaires were rolled out in each of six separate seminars. Out of 108 eligible attending students, 52 students participated in total (48.1%). 25% ( n = 13) of the participants were of female, 75% ( n = 39) of male sex. Within the answered questionnaires, there was no missing data.
Regarding the specific outcome evaluation, CSA gains showed a relevant increase especially in the field of knowledge (see Table 2 and Fig. 3 ). The greatest improvement (84.8%) was achieved in the ability of defining total pain and realizing its importance in clinical settings (77.4%). After the seminar, medical students were increasingly able to name tools such as SPIR in order to engage in spiritual needs assessment (CSA gain 68,8%). A lower increase in knowledge was achieved in realizing how spiritual care itself can benefit patients’ needs (66.7%). The lowest gain was detected in actually identifying patients who might benefit from spiritual care (60.9%), which represents a skill to be learned rather than knowledge to be gained.
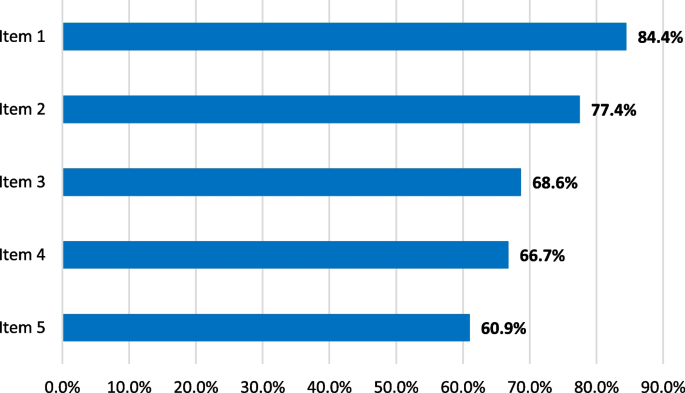
CSA gains for each item
Statistical analysis using 95% confidence intervals confirmed the gains in knowledge, which were significant for all items (Table 2 ).
In regard to the second part of the questionnaire, students were overall satisfied with the new structure of the seminar (Table 3 and Fig. 4 ). The content was comprehensible and delivered clearly gaining a mean score of 4.3 (median 4, SD 0.6, min. 2, max. 5). The content was perceived as overall relevant to the later work in medicine (mean 4.3, median 4, SD 0.6, min. 3, max. 5). It seems as if medical students regard the implementation of spiritual care education into the seminar “symptom control”, which focuses on alleviating symptoms on multidimensional levels, as expedient. They feel that implementing education on spiritual care into this seminar makes sense (mean 4.2, median 4, SD 0.8, min. 1, max. 5). Furthermore, most students do not opt for a seminar solely revolving around spiritual care (mean 2.6, median 2, SD 1.3, min. 1, max. 5).
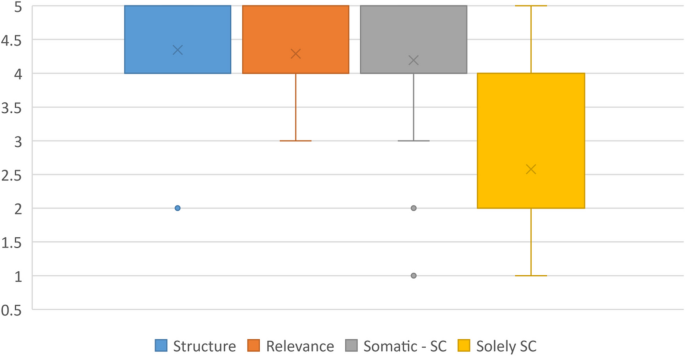
Perception of the seminar, Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither, 4 = agree, 5 = strongly agree)
Our data show that implementing spiritual care education into existing medical curricula, in our example palliative care, is feasible and well perceived among medical students. The timing of our seminar is in accordance to other studies that found that spiritual care should be implemented in mandatory undergraduate courses [ 6 ]. Students do not wish for a seminar solely revolving around spiritual care but prefer a connection to clinical practice and strategies in symptom management. This enables them to understand the relevance of spiritual care in a daily clinical setting.
To evaluate training programs, Kirkpatrick proposed a four-level approach (level 1: reaction, level 2: learning, level 3: behaviour, level 4: results) [ 35 ]. We followed levels 1 (reaction—satisfaction) and 2 (learning—gains in knowledge) making use of the conducted questionnaire. Level 3 (change in behaviour – acquired skills) was briefly addressed with item 5 in the first part of the questionnaire. As level 4 is an indicator of direct results of the training at an organizational level, we were not able to incorporate items on this level. A different study among undergraduate nursing students assessed the effectiveness of teaching spiritual care in mandatory classes: There was an increase in knowledge, e.g., in defining spirituality, compared to students who obtained no information on spiritual care [ 36 ]. This is comparable to our study, as there were gains in knowledge after completing the mandatory seminar. We reached higher individual learning gains on the knowledge level than on the skills level, as was also the case in a number of other studies we conducted [ 31 ]. This is mainly because, due to the format of the seminar, no bedside teaching takes place and scenarios that might occur in everyday clinical practice can only be discussed and serve as examples.
The concept of total pain is essential in palliative care; however, it should not only be taken into consideration in a palliative setting, but whenever patients experience high burdens on various dimensions such as pain, anxiety, grief or existential distress [ 2 , 4 , 17 , 37 , 38 ]. We were able to thoroughly educate students on total pain and its relevance in clinical settings. Spirituality plays an important role in a holistic approach. However, literature shows that HCP often don’t know how to implement spiritual assessments and how to deal with spiritual needs [ 1 , 5 , 6 , 8 ]. A systematic review on teaching methods found the usage of practical tools and the involvement of chaplains to be effective facilitators in the teaching of spiritual care [ 5 ]. A scoping review found that spiritual care should be taught in both mono- and multi-disciplinary educational settings [ 6 ]. With our multi-professional approach, we were able to introduce students to tools in assessing spiritual needs, such as SPIR [ 23 ]. Within this item, there was a definite gain in knowledge of these tools which make assessing spiritual needs of patients more feasible. This is in accordance with findings of a number other studies [ 5 ]. In our study, however, students are still unsure if they are fully able to determine which patients might actually benefit from spiritual care, even though this item still reached a learning gain of 60.9%. As concluded by other authors, there is need for ongoing education [ 5 ].
Even though our seminar entails many different aspects of the total pain concept (somatic symptom management, spirituality, and spiritual care) medical students found the content to be clearly structured and comprehensible. More importantly, they understood the relevance of spirituality for their future clinical work and perceived the multi-professional teaching as highly satisfactory. In sensitizing them in this, we hope that they keep in mind the importance of ongoing collaborations between different professions.
Our study has some limitations. Even though the questionnaire was pretested among medical students before the actual study, no validated questionnaire was used. The response rate of almost 50% is relatively low and it can be assumed that those who participated were mostly students who were interested in the topic. This might have led to bias as positive effects might have been overestimated. Due to the small study population and to protect the privacy of participating students, no demographic data besides sex was collected. Demographic data, however, might contribute to a better understanding of spirituality or palliative medicine beforehand such as age, professional expertise, or own spiritual resources. This also meant that adjusting for confounding factors was not possible. This study solely dealt with medical students and no patients were involved. It would be of interest to assess as to whether the content taught in this seminar ultimately impacts the wellbeing or stress levels of patients in everyday clinical practice. A study focusing on patients would complement the findings of this study, as suggested by other researchers [ 5 ]. Furthermore, the study was only performed in one centre; therefore, it can only serve as an example on how spiritual care education might be successfully implemented into medical curricula.
Spirituality plays an important role for many people and should always be taken into consideration when treating patients. This especially applies to palliative care where the addressing of spiritual needs is of crucial importance [ 18 ]. However, many HCP don’t know how to address topics revolving around spirituality which makes it hard to determine which patients might benefit from spiritual care. Therefore, education on the nature of spiritual care, on what it entails and on how it can support patients in everyday clinical practice should be thoroughly integrated into medical curricula. We opted to implement spirituality and spiritual care into an existing seminar and lecture within the medical curriculum at our faculty. This was well received among students. As a result, we found a clear increase in knowledge about total pain and about the tools one might use to assess spiritual needs. This knowledge needs to be further strengthened in practical clinical scenarios.
Availability of data and materials
All data and materials are available within this publication.
Abbreviations
Health care professional
European Association of palliative care
- Spiritual care
Best M, Leget C, Goodhead A, Paal P. An EAPC white paper on multi-disciplinary education for spiritual care in palliative care. BMC Palliat Care. 2020;19(1):9.
Article Google Scholar
Goebel JR, Doering LV, Lorenz KA, Maliski SL, Nyamathi AM, Evangelista LS. Caring for special populations: total pain theory in advanced heart failure: applications to research and practice. Nurs Forum (Auckl). 2009;44(3):175–85.
Krok D, Telka E, Zarzycka B. Total Pain and Illness Acceptance in Pelvic Cancer Patients: Exploring Self-Efficacy and Stress in a Moderated Mediation Model. Int J Environ Res Public Health. 2022;19(15):9631.
Rettke H, Naef R, Rufer M, Peng-Keller S. Spirituality and health care. The perspective of patients with chronic pain. Schmerz. 2021;35(5):333–42.
Jones KF, Paal P, Symons X, Best MC. The Content, Teaching Methods and Effectiveness of Spiritual Care Training for Healthcare Professionals: A Mixed-Methods Systematic Review. J Pain Symptom Manage. 2021;62(3):e261–78.
Rykkje L, Søvik MB, Ross L, McSherry W, Cone P, Giske T. Educational interventions and strategies for spiritual care in nursing and healthcare students and staff: A scoping review. J Clin Nurs. 2022;31(11–12):1440–64.
Puchalski CM, Sbrana A, Ferrell B, Jafari N, King S, Balboni T, et al. Interprofessional spiritual care in oncology: A literature review, vol. 4. ESMO Open: BMJ Publishing Group; 2019.
Google Scholar
Willemse S, Smeets W, van Leeuwen E, Nielen-Rosier T, Janssen L, Foudraine N. Spiritual care in the intensive care unit: An integrative literature research. J Crit Care. 2020;1(57):55–78.
Chahrour WH, Hvidt NC, Hvidt EA, Viftrup DT. Learning to care for the spirit of dying patients: the impact of spiritual care training in a hospice-setting. BMC Palliat Care. 2021;20(1):115.
Gomes-Ferraz CA, Rezende G, Fagundes AA, De Carlo MMR do P. Assessment of total pain in people in oncologic palliative care: integrative literature review. Palliat Care Soc Pract. 2022;16:26323524221125244 SAGE Publications Ltd.
Evangelista CB, Lopes MEL, Costa SFG da, Batista PS de S, Batista JBV, Oliveira AM de M. Palliative care and spirituality: an integrative literature review. Rev Bras Enferm. 2016;69(3):591–601.
Gijsberts MJHE, Liefbroer AI, Otten R, Olsman E. Spiritual Care in Palliative Care: A Systematic Review of the Recent European Literature. Medical Sciences. 2019;7(2):25.
Bai J, Brubaker A, Meghani SH, Bruner DW, Yeager KA. Spirituality and Quality of Life in Black Patients With Cancer Pain. J Pain Symptom Manage. 2018;56(3):390–8.
Grossoehme DH, Friebert S, Baker JN, Tweddle M, Needle J, Chrastek J, et al. Association of Religious and Spiritual Factors With Patient-Reported Outcomes of Anxiety, Depressive Symptoms, Fatigue, and Pain Interference Among Adolescents and Young Adults With Cancer. JAMA Netw Open. 2020;3(6): e206696.
Klop HT, Koper I, Schweitzer BPM, Jongen E, Onwuteaka-Philipsen BD. Strengthening the spiritual domain in palliative care through a listening consultation service by spiritual caregivers in Dutch PaTz-groups: An evaluation study. BMC Palliat Care. 2020;19(1):92.
Phenwan T. Relieving total pain in an adolescent: A case report. BMC Res Notes. 2018;11(1):265.
Wisesrith W, Sukcharoen P, Sripinkaew K. Spiritual Care Needs of Terminal Ill Cancer Patients. Asian Pac J Cancer Prev. 2021;22(12):3773–9.
Fegg MJ, Brandstätter M, Kramer M, Kögler M, Haarmann-Doetkotte S, Borasio GD. Meaning in Life in Palliative Care Patients. J Pain Symptom Manage. 2010;40(4):502–9.
Arrieira IC de O, Thofehrn MB, Porto AR, Moura PMM, Martins CL, Jacondino MB. Spirituality in palliative care: Experiences of an interdisciplinary team. Revista da Escola de Enfermagem. 2018;52:e03312.
Pieters J, Dolmans DHJM, Verstegen DML, Warmenhoven FC, Courtens AM, Van Den Beuken-Van Everdingen MHJ. Palliative care education in the undergraduate medical curricula: Students’ views on the importance of, their confidence in, and knowledge of palliative care. BMC Palliat Care. 2019;18(1):72.
Paal P, Roser T, Frick E. Developments in spiritual care education in German - Speaking countries. BMC Med Educ. 2014;14(1):112.
MFT Medizinischer Fakultätentag der Bundesrepublik Deutschland e.V., editor Nationaler Kompetenzbasierter Lernzielkatalog Medizin (NKLM) [Internet]. 2015 [cited 2024 Mar 11]. Available from: http://www.nklm.de/
Frick E, Riedner C, Fegg M, Hauf S, Borasio G. A clinical interview assessing cancer patients’ spiritual needs and preferences. Eur J Cancer Care (Engl). 2006;15:238–43.
Gomez S, White B, Browning J, DeLisser HM. Medical Students’ Experience in a Trauma Chaplain Shadowing Program: A Mixed Method Analysis. Med Educ Online. 2020;25(1):1710896.
Bell D, Harbinson M, Toman G, Crawford V, Cunningham H. Wholeness of Healing: An Innovative Student-Selected Component Introducing United Kingdom Medical Students to the Spiritual Dimension in Healthcare. South Med J. 2010;103(12):1204–9.
Hemming P, Teague PJ, Crowe T, Levine R. Chaplains on the Medical Team: A Qualitative Analysis of an Interprofessional Curriculum for Internal Medicine Residents and Chaplain Interns. J Relig Health. 2016;55(2):560–71.
Robinson MR, Thiel MM, Shirkey K, Zurakowski D, Meyer EC. Efficacy of Training Interprofessional Spiritual Care Generalists. J Palliat Med. 2016;19(8):814–21.
Huehn SL, Kuehn MB, Fick KE. Integrating Spiritual Care During Interprofessional Simulation for Baccalaureate Nursing Students. J Holist Nurs. 2019;37(1):94–9.
Anandarajah G, Roseman J, Lee D, Dhandhania N. A 10-Year Longitudinal Study of Effects of a Multifaceted Residency Spiritual Care Curriculum: Clinical Ability, Professional Formation, End of Life, and Culture. J Pain Symptom Manage. 2016;52(6):859-872.e1.
Raupach T, Münscher C, Beißbarth T, Burckhardt G, Pukrop T. Towards outcome-based programme evaluation: Using student comparative self-assessments to determine teaching effectiveness. Med Teach. 2011;33(8):e446-53.
Schwartz J, Schallenburger M, Tenge T, Batzler YN, Schlieper D, Kindgen-Milles D, et al. Palliative Care e-Learning for Physicians Caring for Critically Ill and Dying Patients during the COVID-19 Pandemic: An Outcome Evaluation with Self-Assessed Knowledge and Attitude. Int J Environ Res Public Health. 2022;19(19):12377.
Laupichler MC, Hadizadeh DR, Wintergerst MWM, von der Emde L, Paech D, Dick EA, et al. Effect of a flipped classroom course to foster medical students’ AI literacy with a focus on medical imaging: a single group pre-and post-test study. BMC Med Educ. 2022;22(1):803.
Thyson T, Schallenburger M, Scherg A, Leister A, Schwartz J, Neukirchen M. Communication in the face of death and dying - how does the encounter with death influence the patient management competence of medical students? An outcome-evaluation. BMC Med Educ. 2022;22(1):25.
Seifert T, Becker T, Büttcher AF, Herwig N, Raupach T. Restructuring the clinical curriculum at University Medical Center Göttingen: effects of distance teaching on students’ satisfaction and learning outcome. GMS J Med Educ. 2021;38(1):Doc1.
Kirkpatrick DL. Evaluating Training Programs. San Francisco, CA, USA: Berret-Koehler Publishers, Inc.; 1994.
Yilmaz M, Gurler H. The efficacy of integrating spirituality into undergraduate nursing curricula. Nurs Ethics. 2014;21(8):929–45.
Faria C, Branco V, Ferreira P, Gouveia C, Trevas S. Total Pain Management and a Malignant Wound: The Importance of Early Palliative Care Referral. Cureus. 2021;13(12):e20678.
Best M, Aldridge L, Butow P, Olver I, Webster F. Conceptual analysis of suffering in cancer: a systematic review. Psychooncology. 2015;24(9):977–86.
Download references
Acknowledgements
We thank Dr Jessica JT Fischer for excellent English language editing.
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Interdisciplinary Center for Palliative Care, University Hospital, Heinrich Heine University, Duesseldorf, Germany
Yann-Nicolas Batzler, Manuela Schallenburger, Jacqueline Schwartz & Martin Neukirchen
Evangelical Church in the Rhineland, Duesseldorf, Germany
Nicola Stricker
Institut Protestant de Théologie, Paris, France
Evangelical Hospital Chaplaincy (Pastoral Care), University Hospital, Heinrich Heine University, Duesseldorf, Germany
Simone Bakus
Department of Anesthesiology, University Hospital, Heinrich Heine University, Düsseldorf, Germany
Martin Neukirchen
Interdisciplinary Centre for Palliative Medicine, Medical Faculty, Heinrich Heine University Duesseldorf, Moorenstr. 5, 40225, Düsseldorf, Germany
Manuela Schallenburger
You can also search for this author in PubMed Google Scholar
Contributions
YB, NS, MS, JS, MN designed the study. YB analysed and interpreted the data. YB drafted the first version of the manuscript, which was critically revised by NS, MS, JS, and MN in several rounds of feedback. All authors have approved the submitted version and have agreed to be accountable for their contributions as well as for accuracy and integrity for any part of the work.
Corresponding author
Correspondence to Manuela Schallenburger .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Ethics Committee of Heinrich-Heine-University Düsseldorf (Study No. 2022–2274). Written informed consent was obtained from all participants, which were all over 18 years and informed about the study before starting the questionnaire. Researchers assured participants that the contents of the surveys would be used solely for research purposes.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Heinrich Heine University Duesseldorf (reference number 2022-2274).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Batzler, YN., Stricker, N., Bakus, S. et al. Implementing spiritual care education into the teaching of palliative medicine: an outcome evaluation. BMC Med Educ 24 , 411 (2024). https://doi.org/10.1186/s12909-024-05415-0
Download citation
Received : 23 August 2023
Accepted : 11 April 2024
Published : 15 April 2024
DOI : https://doi.org/10.1186/s12909-024-05415-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Spirituality
- Palliative medicine
- Medical students
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
COLUMBIA UNIVERSITY IN THE CITY OF NEW YORK

Clinical Research Coordinator
- Ophthalmology
- Columbia University Medical Center
- Opening on: Apr 23 2024
- Job Type: Officer of Administration
- Regular/Temporary: Regular
- Hours Per Week: 35
- Salary Range: $62,400 - $65,000
Position Summary
Under the direction of the Director of the Clinical Trials Unit (CTU) and Principal Investigators, the Clinical Research Coordinator will conduct clinical research studies (industry-sponsored and investigator-initiated) within the Columbia University Irving Medical Center (CUIMC) Department of Ophthalmology in adherence with assigned study protocols and manuals of operation and in accordance with clinical research principles.
Responsibilities
- Serve as the contact person for those interested in study participation and assist with recruitment activities including pre-screening electronic medical records for eligibility, contacting potential subjects, explaining all study procedures, and consenting eligible subjects or assenting parents or guardians for children enrolled in research studies.
- Coordinate day-to-day aspects of study related procedures, including, but not limited to scheduling visits and procedures, data entry, preparing for research visits, research visit documentation, maintenance of regulatory binders and study files, creation and/or maintenance of source documentation, preparation for monitoring visits, site initiation/closeout visits and audits as needed.
- Be able to coordinate and perform research testing and imaging for clinical research studies including but not limited to visual acuity, refraction, dark adaptation, visual field, microperimetry, fluorescein angiography, fundus photography, optical coherence tomography (OCT), ICG angiography, slit lamp photography, MP1, corneal mapping, specular biomicroscopy including confocal imaging, HRT Analyzer (glaucoma), and ERGs.
- Be able to administer surveys, such as the National Eye Institute Vision Function Questionnaire (NEI-VFQ-25), EuroQOL-5 Dimension, Reading speed, Health Utilities Index.
- Work with the research team and ocular photography department to ensure that all required eye exams and ocular testing are scheduled and completed according to protocol.
- Obtain and maintain study certifications for ETDRS, OCT, and photography for clinical trials.
- Obtain access to sponsors’ electronic data capture (EDC) systems, complete EDC trainings, and enter data into the EDC within 5 days of seeing the study patient.
- Maintain and organize study-related documentation and records using the EDC platforms, including capturing adverse events and serious adverse events and preparing for monitoring visits.
- Respond to all sponsor-related queries in a timely manner.
- Ensure that all aspects of Good Clinical Practice are followed at all times by developing and ensuring adherence with Standard Operating Procedure (SOP) for clinical studies being conducted in the Ophthalmology Clinical Trials Unit.
- Work with the Regulatory Manager to gain CUIMC Institutional Review Board (IRB) approval in a timely manner by creating informed consent forms using sponsors’ templates, responding to IRB correspondents, submitting amendments, renewals, modifications, and other regulatory documents required by the sponsor and FDA, including progress reports.
- Ensure that all appropriate Institutional, State, and Federal regulations are followed throughout the course of the study according to study-related protocols and manuals.
- Work directly with sponsors’ designated Clinical Research Organizations (CRO) to complete all required study start-up documents including FDA 1572 forms, investigator signatures, CVs, medical licenses, Conflict of Interest, HIPAA, and Human Subjects Trainings in a timely manner.
- Complete feasibility forms requested by sponsors in a timely manner to assess ophthalmic equipment and examination rooms to conduct the studies.
Minimum Qualifications
- Bachelor’s degree or equivalent in education and experience, plus minimum of 1 to 2 years of related experience.
- Conform to all applicable HIPAA, billing compliance and safety requirements.
- Must be able to work effectively with minimal supervision.
- Prior research experience to include recruiting study participants, conducting standardized protocol visits and data entry.
- Excellent verbal and written communication skills and attention to detail required.
- Computer skills (Word, Excel) required.
- Excellent interpersonal skills.
- Willingness to travel to different sites.
Preferred Qualifications
- Working knowledge of Spanish
- Phlebotomy license
- Prior experience in ophthalmology
Equal Opportunity Employer / Disability / Veteran
Columbia University is committed to the hiring of qualified local residents.
Commitment to Diversity
Columbia university is dedicated to increasing diversity in its workforce, its student body, and its educational programs. achieving continued academic excellence and creating a vibrant university community require nothing less. in fulfilling its mission to advance diversity at the university, columbia seeks to hire, retain, and promote exceptionally talented individuals from diverse backgrounds. , share this job.
Thank you - we'll send an email shortly.
Other Recently Posted Jobs
Assistant Director of Strategic Partnerships
Assistant manager, assistant director-human resources.
Refer someone to this job

- ©2022 Columbia University
- Accessibility
- Administrator Log in
Wait! Before you go, are you interested in a career at Columbia University? Sign up here!
Thank you, for sharing your information. A member of our team will reach out to you soon!
This website uses cookies as well as similar tools and technologies to understand visitors' experiences. By continuing to use this website, you consent to Columbia University's usage of cookies and similar technologies, in accordance with the Columbia University Website Cookie Notice .

IMAGES
VIDEO
COMMENTS
The role of literature in medical education. A commentary on the poem: Roswell, Hanger 84. - PMC. Journal List. J Med Ethics. v.25 (6); 1999 Dec. PMC479308. As a library, NLM provides access to scientific literature. Inclusion in an NLM database does not imply endorsement of, or agreement with, the contents by NLM or the National Institutes of ...
For Craice de Benedetto, Gatti, and Lima da Costa (2011), the most important role the study of literature has for medical students is the fact that it can help them to better understand how empathy is perceived, i.e., they better comprehend the life and experiences of their patients and can use this understanding to help put their patients at ...
In conclusion, literature plays a critical role in medical education. It has the power to enhance patient care by fostering empathy and understanding, creating more humane and complete doctors. As healthcare continues to evolve, it is essential to recognize and harness the transformative power of literature in shaping the future of healthcare.
Roles for literature in medical education Martyn Evans Martyn Evans is Professor of Humanities in Medicine at the Centre for Arts and Humanities in Health and Medicine, University of Durham (14/15 Old Elvet, Durham DH1 3HP, UK. E-mail: [email protected]). He is a philosopher, who from 1986
Evans, M. (2003) Roles for literature in medical education. Advances in Psychiatric Treatment, 9, 380-385. General Medical Council (1993) Tomorrow's Doctors: recommendations on undergraduate medical education. London: GMC. --- (2002) Tomorrow's Doctors: Recommendations on Under-graduate Medical Education (Revised). London: GMC.
a study, from conception and design, to implemen-tation and analysis, to manuscript preparation and submission. Planning the literature review requires understand-ing of journal requirements, which vary greatly by journal (TABLE 1). Authors are advised to take note of common problems with reporting results of the literature review.
Medicine. 1920. 1,619. PDF. The sustained study of literary texts and, to a lesser extent, of techniques of literary analysis offers a number of educational 'goods' to the medical curriculum, to medical students and to the clinical practitioners they will one day become. In addition to the intrinsic goods of literature - the intense and ...
The nature of medicine decides the pivotal role of the humanities in medical education.More than thirty years of literature teaching in American medical schools demonstrated that literature was an important vehicle for medical humanities education.Narrative medicine,which was gaining more and more momentum in the past decade,had materialized ...
The potential role of literature in medical education has also been explored, with an emphasis on the importance of the broader concept of 'medical education' rather than simply 'medical training ...
Being a doctor requires continuous learning, unlearning, and relearning and being able to formulate good questions, put disparate concepts together, and innovate. Arts and humanities learning in medical education may afect the ability to learn in a truly integrative fashion.
Glossary. Narrative- (based) medicine: The practice of medicine with these skills of recognizing, absorbing, interpreting by the stories of illness; as a new frame for health care, it aims to create an effective health-care system than recognizing and respecting the persons undergoing care. Marini MG. 2015.
The roles that patients currently play in medical education are considered, along with aims, benefits, and potential drawbacks of involvement for patients, students, and medical educators. A review of current literature and the limitations thereof is included. The gap between policy and practice is considered, and potential reasons for this gap ...
Medical school curricula, although traditionally and historically dominated by science, have generally accepted, appreciated, and welcomed the inclusion of literature over the past several decades. Recent concerns about medical professional formation have led to discussions about the specific role and contribution of literature and stories. In this article, we demonstrate how professionalism ...
It is shown that literature (and the arts more generally) have a value for medical education and the practice of health care wider than their instrumental use in medicine. The use of the arts in health care is increasing in the UK. More specifically, there are three main strands to the movement: the use of the arts as therapy; as an aid to health promotion in commu nities, and in medical ...
Medical students may experience this phenomenon when exposed to depictions of healing in literature or film, or through exposure to a positive role model. Shapiro and Rucker note the effect as regards movies, but the experience can be harnessed as a learning tool through stories, songs, and art (Kumagai Citation 2008 ).
The capacity for reflection as "an epistemology of practice" and "a critical approach to inquiry" (Ng et al., 2015: 263) is considered essential for the provision of competent and compassionate healthcare. Integrating reflective practice into medical education is, therefore, critical to medical trainees' personal and professional ...
Abstract. The sustained study of literary texts and, to a lesser extent, of techniques of literary analysis offers a number of educational 'goods' to the medical curriculum, to medical students and to the clinical practitioners they will one day become. In addition to the intrinsic goods of literature - the intense and direct experience of ...
As part of its work, METF conducted a thorough review of the literature on the role of health sciences librarians in medical education. The literature search demonstrated that librarians have wide-ranging roles and responsibilities in the area of education. Nevertheless, accrediting agencies have not recognized the contributions of the ...
Perspectives on Medical Education's mission is to support and enrich collaborative scholarship between education researchers and clinical educators, and to advance new knowledge regarding clinical education practices.. The journal is the official journal of the The Netherlands Association of Medical Education (NVMO), which sponsors the journal as an Open Access journal that is free to read ...
By Johana Canales, Archives Intern. As archivists discussed recently, the Houston-based Medical Arts Publishing Foundation produced illustrated medical publications like the Cancer Bulletin, Heart Bulletin, and Psychiatric Bulletin.. The Foundation's records began arriving at the McGovern Historical Center in 1992. Since then some of the collection's medical illustrations had already been ...
Background The concept of "total pain" plays an important role in palliative care; it means that pain is not solely experienced on a physical level, but also within a psychological, social and spiritual dimension. Understanding what spirituality entails, however, is a challenge for health care professionals, as is screening for the spiritual needs of patients. Objective This is a novel ...
Job Type: Officer of Administration Regular/Temporary: Regular Hours Per Week: 35 Salary Range: $62,400 - $65,000 The salary of the finalist selected for this role will be set based on a variety of factors, including but not limited to departmental budgets, qualifications, experience, education, licenses, specialty, and training. The above hiring range represents the University's good faith ...