Competencies for Public Health Professionals
- Core Competencies for Public Health Professionals
- Use of the Core Competencies
- Select Public Health Workforce Competency Frameworks
Competencies are the knowledge, skills, abilities, and behaviors that contribute to individual and organizational performance. In public health, successful mastery of competencies is vital to developing a strong workforce that can support community and program needs. Public health agencies and organizations can use competencies to
- Develop job descriptions
- Assess knowledge and skills that contribute to job performance
- Identify critical gaps in training
- Create career paths
- Inform workforce development plans
- Support efforts to meet accreditation standards
The Core Competencies for Public Health Professionals (Core Competencies) are a framework for workforce development planning and action. The Core Competencies are defined as “a consensus set of knowledge and skills for the broad practice of public health, defined by the 10 Essential Public Health Services .” They can serve as a starting point for public health professionals and organizations working to better understand and meet workforce development needs, improve performance, prepare for accreditation, and enhance the health of the communities they serve.
The Core Competencies have a long history in supporting workforce efforts in public health practice and academic settings. They were initially developed in 1991 by the Council on Linkages Between Academia and Public Health Practice (Council on Linkages), a collaborative of national public health practice-based and academic organizations . The current version of the Core Competencies was adopted by the Council on Linkages on October 21, 2021, following a yearlong review and revision process.
The Healthy People Public Health Infrastructure Topic Area —coordinated by CDC’s National Center for State, Tribal, Local, and Territorial Public Health Infrastructure and Workforce ( Public Health Infrastructure Center ) and the Health Resources and Services Administration—includes objectives focused on use of the Core Competencies by state, local, territorial, and tribal health departments. These objectives were included in Healthy People 2020 and have been retained as Public Health Infrastructure core objectives in Healthy People 2030 .

Competency sets are often used by learning management systems and training platforms to help users identify offerings that meet their needs. TRAIN is a learning management platform supported by the Public Health Foundation and used by CDC via CDC TRAIN and other public health agencies and organizations. TRAIN users can find trainings based on a specific tier or domain of the Core Competencies and other select competencies sets using the “Competencies and Capabilities” feature.
Public health agencies and organizations use the Core Competencies to better understand, assess, and meet their education, training, and other workforce development needs. Some of these uses include
- Identifying and meeting training gaps
- Assessing workforce development needs
- Determining competency strengths and areas for improvement in organizational and individual performance evaluations
- Developing quality trainings
- Identifying mentoring and coaching opportunities
- Writing job and position descriptions
- Addressing workforce-related national accreditation standards (see Domain 8 of Public Health Accreditation Board Standards & Measures)
The Public Health Foundation’s website provides many tools that can be adapted and includes examples of how organizations use the Core Competencies.
Public health organizations use a variety of discipline-specific competency frameworks in addition to the Core Competencies. The list below is not exhaustive but includes many competency models that support and advance public health workforce efforts.
- Core Competencies for Public Health Professionals Council on Linkages between Academia and Public Health Practice (Council on Linkages) (Latest edition: 2021)
- Competencies for Performance Improvement Professionals in Public Health (PI Competencies) Council on Linkages (Latest edition: 2018)
- Public Health Law Competency Model: Version 1.0 [PDF – 1.406 KB] CDC’s Public Health Law Program (Latest edition: 2016)
- Legal Epidemiology Competency Model Version 1.0 CDC’s Public Health Law Program (Latest edition: 2018)
- Public Health Emergency Law Competency Model Version 1.0 CDC’s Center for Preparedness and Response and CDC’s Public Health Law Program (Latest edition: 2013)
- Applied Epidemiology Competencies CDC and the Council of State and Territorial Epidemiologists (Latest edition: 2023)
- Community/Public Health Nursing Competencies [PDF – 668 KB] The Council of Public Health Nursing Organizations (Latest edition: 2018)
- Competencies for Population Health Professionals Association for Community Health Improvement, Catholic Health Association, Council on Linkages, Association of American Medical Colleges, and Association of State and Territorial Health Officials (Latest edition: 2019)
- Environmental Health Competencies The American Public Health Association with support from CDC’s National Center for Environmental Health (Latest edition: 2020)
- Applied Public Health Informatics Competency Model [PDF – 399 KB] The Informatics Academy at the Public Health Informatics Institute (Latest edition: 2016)
- Immunization Information System (IIS) Core Competency Model Public Health Informatics Institute with support from CDC (Latest edition: 2021)
- Including People with Disabilities: Public Health Workforce Competencies A national committee comprised of disability and public health experts with support from CDC (Latest edition: 2016)
- Responsibilities and Competencies for Health Education Specialists The National Commission for Health Education Credentialing, Inc. (Latest edition: 2020)
- Competency Guidelines for Public Health Laboratory Professionals CDC and the Association of Public Health Laboratories (Latest edition: 2015)
- Public Health Associate Program (PHAP) Cohort Competencies CDC’s Public Health Infrastructure Center (Latest edition: 2020)
- Accreditation Criteria: Schools of Public Health & Public Health Programs – includes MPH and DrPH foundational competencies The Council on Education for Public Health (Latest edition: 2021)
- Racial Justice Competencies for Public Health Professionals The Public Health Training Center Network in partnership with the National Network of Public Health Institutes (Latest edition: 2022)
To receive email updates about this page, enter your email address:

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

- Health Communication
- Healthcare Management
- Global Health
- Artificial Intelligence in Healthcare
- Choose a Public Health Degree Based on Your Personality
- Public Health vs. Medicine vs. Nursing
- What is Online Learning
- Master’s in Health Informatics vs. Health Information Management
- MPH vs. MSPH vs. MHS
- Online MPH programs with no GRE requirements
- Accelerated Online MPH
- Online Executive MPH
- Online DrPH
- Biostatistics
- Community Health and Health Promotion
- Environmental Health
- MPH in Epidemiology vs. Biostatistics
- Generalist Public Health
- Health Equity
- Health Science
- Health & Human Services
- Infectious Disease
- Maternal & Child Health
- Occupational Health
- Social and Behavioral Health
- What Can You Do With a Public Health Degree?
- How to Be a Good Candidate for a Public Health Job
- How to Become a Biostatistician
- How to Become an Emergency Management Specialist
- How to Become an Environmental Health Specialist
- How to Become a Health Educator
- Healthcare Administration Certifications
- Healthcare Administrator Salary
- Types of Epidemiologists and Salary
- How to Become an Occupational Health and Safety Specialist
- How to Become a Public Health Nurse
- Nutritionist vs Dietitian
- Registration Examination for Dietitians (CDR Exam)
- Internships for MPH Students
- Health Informatics Careers and Jobs
- Health Informatics vs. Bioinformatics
- Guide to CDC Jobs
- Massachusetts
- North Carolina
Home » Resources
Public Health Core Competencies
September 14, 2020
Public health professionals focus on making the lives of other people and their communities better. They concern themselves with many factors that play a role in the health of humans, such as the environment, public policy, health care and laws. If you are interested in taking on a public health role and are looking for an appropriate graduate program, a master’s degree might be an ideal way to achieve your goal.
As an MPH student, you will be guided by 22 foundational core public health competencies (PDF, 406 KB) set forth by the Council on Education for Public Health (CEPH). Here is a closer look at these core competencies for public health professionals and why they are essential.

Simmons University
Department of public health.
Women with 17+ prior college credits or an associate degree: Complete your bachelor’s degree in a supportive women’s online public health BS program.
- Up to 96 transfer credits accepted, plus credit for life experience
- Degree programs are designed for working professionals and can be completed part time
- CEPH-accredited
info SPONSORED
Definition of Core Competencies
Core competencies are difficult to mimic. They are the fundamental knowledge, skills and attributes a person or organization holds that allow an individual or company to succeed and grow. What are core competencies in public health?
In the public health sector, core public health competencies allow the workforce to operate effectively and carry out the core functions of public health , including population health assessment, monitoring, health promotion, disease and injury prevention, health protection and emergency preparedness.
Some public health employers may refer to the core competencies to develop job descriptions in postings, performance objectives and assessment, and workforce development plans to ensure a skilled workforce . Plus, for students who are about to enter the job market, knowing the core competencies is a great way to understand your own strengths/weaknesses and evaluate your professional capabilities.
What are the 5 Core Competencies of Public Health?
A master’s in public health program, such as Master of Public Health(MPH) or Master’s in Healthcare Administration , advances a graduate student’s understanding of the following five public health disciplines.
Biostatistics
Competencies in biostatistics enable public health professionals to address and solve problems in public health by analyzing and interpreting data and applying statistical reasoning and methods.
Environmental Health Sciences
This competency focuses on how biological, physical and chemical environmental factors affect human health.
Epidemiology
Often associated with public health and public health degree programs, the epidemiology competency is the ability to study diseases and injury within populations.
Health Policy and Management
It’s the ability to use both a managerial and a policy perspective to focus on the delivery, accessibility, quality, organization and health care costs for individuals and populations.
Social and Behavioral Sciences
This competency in public health examines how behavioral, social, and cultural matters contribute to public health issues.
What are the 22 CEPH Competencies of Public Health?
Built on the conventional public health core knowledge areas (biostatistics, environmental health sciences, epidemiology, health policy and management, and social and behavioral sciences), as well as multisector and emerging public health areas; these CEPH competencies must be demonstrated by all graduates and are critical to the success of public health professionals.
Evidence-based approaches to public health
1. Apply epidemiological methods to the breadth of settings and situations in public health practice.
2. Select quantitative and qualitative data collection methods appropriate for a given public health context.
3. Analyze quantitative and qualitative data using biostatistics, informatics, computer-based programming and software, as appropriate.
4. Interpret the results of data analysis for public health research, policy, or practice.
Public health a n d health care systems
5. Compare the organization, structure, and function of health care, public health and regulatory systems across national and international settings.
6. Discuss how structural bias, social inequities and racism undermine health and create challenges for achieving health equity at the organizational, community and societal levels.
Planning and management to promote health
7. Assess population needs, assets and capacities that affect communities’ health.
8. Apply awareness of cultural values and practices to the design or implementation of public health policies or programs.
9. Design a population-based policy, program, project or intervention.
10. Explain the basic principles and tools of budget and resource management.
11. Select methods to evaluate public health programs.
Policy in public health
12. Discuss multiple dimensions of the policy-making process, including the roles of ethics and evidence.
13. Propose strategies to identify stakeholders and build coalitions and partnerships for influencing public health outcomes.
14. Advocate for political, social or economic policies and programs that will improve health in diverse populations.
15. Evaluate policies for their impact on public health and health equity.
16. Apply principles of leadership, governance, and management, which include creating a vision, empowering others, fostering collaboration and guiding decision making.
17. Apply negotiation and mediation skills to address organizational or community challenges.
Communication
18. Select communication strategies for different audiences and sectors.
19. Communicate audience-appropriate public health content, in writing and through oral presentation.
20. Describe the importance of cultural competence in communicating public health content.
Interprofessional practice
21. Perform effectively on interprofessional teams.
Systems thinking
22. Apply systems thinking tools to a public health issue.
While both are necessary for effective public health work, they are distinct in that core competencies of public health are the knowledge, skills and abilities needed to successfully perform “critical work functions,” whereas public health specializations are a narrow or defined area of expertise in which to apply core competencies.
There may be numerous ways to improve depending on your needs and career goals. You might consider advancing your education. Many online programs have been launched catering to students who don’t want to commute to campus, such as online MPH programs , online MHI programs , online MHA programs and more. There are also other ways to continue developing your competencies after graduation from school. Read our Resources for Continuing Professional Development in Public Health to learn more.
Information last updated in July 2020
Career Guide: Public Health
- Search for Organizations
- Prep for Your Interview - Research The Industry
- Career Sites
Core Competencies
Data analytics, policy development & program planning skills, communications, health equity, community partnership skills, management & finance, public health leadership & systems thinking.
- More Guides
The Council on Linkages Between Academia and Public Health Practice has developed the Core Competencies for Public Health Professionals , which are used by hundreds of health departments across the U.S. The core competencies are organized into 8 domains representing skill areas within public health:
- Data Analytics & Assessment Skills
- Communication Skills
- Health Equity Skills
- Public Health Sciences Skills
- Management & Finance Skills
- Leadership & Systems Thinking Skills
Many jobs and careers related to public health will involve using some combination of these skill domains. The MPH Career Services Program recommends students explore and identify the skill domains they are most interested in further developing and utilizing in their careers. In addition, it can also be helpful to use the skill domains as an organizing principle for one's job search and as a marketing tool.
The resources below provide a starting point for exploring opportunities within the skill domains. If you have a recommended resource to add, please contact Career Services Manager, Chandlee Bryan .
- Data for Health Impact Program Bloomberg Philanthropies, Data for Health Initiative
- Lessons in Leadership: Using Data to Drive Public Health Decisions McKinsey
- What's the Difference between a Data Analyst and a Data Scientist? Career Foundry
Python, R, and Stata are three common programming languages used in data analytics. Here are library guides to provide you with resources for learning each of them
- Python Bites Workshop Series - Research Guides at Dartmouth College
- R Koujue - Statistical Software - Research Guides at Dartmouth College
- Stata Koujue - Statistical Software - Research Guides at Dartmouth College
- Public Policy Development Public Health Institute
- National Conference of State Legislatures
- Public Health Communications Collaborative Communications resources for public health professionals
- Health Communications Strategies and Resources National Prevention Information Network
- Usability.gov
- Health Equity Assessment Tool Kit World Health Organization
- Health Equity Curricular Toolkit American Academy of Family Physicians
- Health Equity Toolkit for COVID-19 Big Cities Health Coalition and Human Impact Partners
- Rural Health Equity Toolkit RHIhub
- Sources for Data on Social Determinants of Health CDC
- Indian Health Service Community Health Tools
- Institute for Healthcare Improvement (IHI)
- Public Health Toolbox
- Rural Health Data Sources & Tools Ruralhealthinfo.org
- Urban Health World Health Organization
- Public Health Finance National Association of County and City Health Officials
- Public Health Finance & Management Bootcamp
- Health Systems Governance and Financing World Health Organization
- National Leadership Academy for the Public's Health CDC - Public Health Professionals Gateway
- Center for Health Leadership and Practice Public Health Institute
- Systems Thinking Resources New England Public Health Training Center
- << Previous: Career Sites
- Next: More Guides >>
- Last Updated: Feb 8, 2024 3:47 PM
- URL: https://researchguides.dartmouth.edu/mph-career
- Open access
- Published: 13 November 2023
Developing public health competency statements and frameworks: a scoping review and thematic analysis of approaches
- Melissa MacKay 1 ,
- Caitlin Ford 1 ,
- Lauren E. Grant 1 ,
- Andrew Papadopoulos 1 &
- Jennifer E. McWhirter 1
BMC Public Health volume 23 , Article number: 2240 ( 2023 ) Cite this article
1710 Accesses
1 Citations
3 Altmetric
Metrics details
Competencies ensure public health students and professionals have the necessary knowledge, skills, values, and behaviours to do their jobs effectively. Public health is a dynamic and complex field requiring robust competency statements and frameworks that are regularly renewed. Many countries have public health competencies, but there has been no evidence synthesis on how these are developed. Our research aim was to synthesize the extent and nature of the literature on approaches and best practices for competencies statement and framework development in the context of public health, including identifying the relevant literature on approaches for developing competency statements and frameworks for public health students and professionals using a scoping review; and, synthesizing and describing approaches and best practices for developing public health competency statements and frameworks using a thematic analysis of the literature identified by the scoping review. We conducted a scoping review and thematic analysis of the academic and grey literature to synthesize and describe approaches and best practices for developing public health competency statements and frameworks. A systematic search of six databases uncovered 13 articles for inclusion. To scope the literature, articles were assessed for characteristics including study aim, design, methods, key results, gaps, and future research recommendations. Most included articles were peer-reviewed journal articles, used qualitative or mixed method design, and were focused on general, rather than specialist, public health practitioners. Thematic analysis resulted in the generation of six analytical themes that describe the multi-method approaches utilized in developing competency statements and frameworks including literature reviews, expert consultation, and consensus-building. There was variability in the transparency of competency framework development, with challenges balancing foundational and discipline-specific competencies. Governance, and intersectoral and interdisciplinary competency, are needed to address complex public health issues. Understanding approaches and best practices for competency statement and framework development will support future evidence-informed iterations of public health competencies.
Peer Review reports
Competencies are defined as the knowledge, skills, values, and behaviours required to perform well within a profession and an organization [ 1 ]. Knowledge can be acquired through education and experience [ 1 ]. Skills result from the repeated application of knowledge, and behaviours reflect how individuals perform in various contexts [ 1 ]. Attitudes and values form the context in which competencies are practiced and are the beliefs that motivate people to act in different ways [ 2 ]. Competencies required for professional practice depend on many factors including an individual’s position within an organization and an organization’s needs [ 1 , 3 ]. Within education, curriculum and pedagogical approaches provide students with opportunities to advance their knowledge and skills through didactic and experiential training [ 4 , 5 ]. For both professional development and education, defining the competencies needed and creating development opportunities explicitly linked to them is essential.
There are various conceptualizations of competencies, including behavioural, performance continuum, and integrated or holistic approaches. Each conceptualization has strengths and weaknesses based on the complexity and interconnectedness of the approach, its focus on tasks or job performance, and how competencies are developed within individuals during their careers [ 6 ]. The holistic approach to competence conveys the interrelationship of knowledge, skills, behaviours, and attitudes/values [ 6 , 7 ]. Frameworks and approaches to competencies are context-dependent and developmental, where there is progressive interaction between an individual’s tasks, abilities, and the systems and environments in which they perform [ 6 ]. Thus, establishing an integrated competency framework for any discipline or sector, including public health, provides clarity and professional standards, promotes reflective practice, and requires a clear understanding of the interconnectedness of the attributes required.
Competency statements for public health ensure students and practitioners have the necessary knowledge, skills, behaviours, and values to effectively perform [ 2 , 8 ]. This promotes standardization in the field and provides a benchmark for capable personnel, allowing for a consistent approach to organizational planning and performance measurement, which in turn improves the quality of public health programs and services [ 5 ]. Competency frameworks define a set of competency statements and support their implementation through describing public health practice expectations and informing workforce planning and development [ 9 ]. There are a number of frameworks for public health competencies around the world, including the Core Competencies for Public Health in Canada [ 2 ], the United States (US) Core Competencies for Public Health Professionals [ 8 ], the WHO-ASPHER Competency Framework for the Public Health Workforce in the European Region [ 10 ], the Public Health Competencies and Impact Variables for Low- and Middle-Income Countries [ 11 ], the Asia-Pacific Academic Consortium for Public Health Competency Framework [ 12 ], and the Core Competencies for Public Health: A Regional Framework for the Americas [ 13 ].Although each framework consists of different conceptualizations of competencies for different countries and sociopolitical regions, they are all based on a need for a tool that facilitates development of a knowledgeable and skilled public health workforce able to effectively address complex public health challenges [ 4 ].
Current public health challenges include multiple crises including climate change [ 14 ], mental health [ 15 ], and opioid use disorder [ 16 ], which overlap many sectors and disciplines. The COVID-19 pandemic exacerbated existing global health issues including health inequities, mental health, social isolation, and addictions [ 17 , 18 ]. Additionally, declining trust in public health resulted from ineffective crisis communication and management [ 19 ], and a complex information ecosystem where mis/disinformation is widely circulating [ 20 ]. More than ever, public health needs competency frameworks that reflect the current multifaceted and overlapping public health challenges to ensure the workforce is adequately equipped to address them.
Core competency frameworks in public health are usually developed through collaboration with a range of public health experts and professionals. Public health competency frameworks are developed at various levels including the country level, organizational level, and discipline-specific public health practice to support workforce development planning, professional development, and improved public health action. For example, within Canada, the Core Competencies for Public Health were released in 2008 by the Public Health Agency of Canada in collaboration and consultation with public health practitioners, government, and experts [ 2 ]. Similarly in the US, the Core Competencies for Public Health Professionals are developed and updated through extensive consultation and revision with the public health and population health sectors across the country [ 21 ]. This work also occurs on an organizational level within academia to develop programs and curriculum matched to public health competency frameworks [ 22 ], as well as for specific disciplines within public health such as implementation science [ 5 ], public health preparedness and response [ 23 ], and environmental public health [ 24 ].
The field of public health is dynamic and complex; thus, competency frameworks must be regularly updated to remain relevant. Approaches for developing public health competency statements and frameworks must be optimized and mobilized to ensure they are relevant and have impact within public health [ 25 ]. Renewal of public health competency frameworks varies globally, with some countries regularly updating their competencies, such as the US (considers renewal three years after the prior release), while others, such as Canada, do not currently have a systematic approach to updating competencies, though there are calls for renewal and efforts are underway to revisit this. Identifying and describing approaches for the development of public health competency statements and frameworks will support future evidence-informed iterations, but no previous evidence synthesis has been conducted.
To address this gap, our goal is to synthesize the extent and nature of the literature on approaches and best practices for public health competencies statement and framework development. The objectives are:
Identify relevant literature on approaches for developing competency statements and frameworks for public health students and professionals using a scoping review; and,
Synthesize and describe approaches and best practices for developing public health competency statements and frameworks using a thematic analysis of the literature identified in the scoping review.
Review approach and team
The scoping review methods were based on the framework outlined by Arskey and O’Malley [ 26 ] and updated by Levac et al. [ 27 ]. A research team with expertise in the subject matter and methods was established to develop and guide the scoping review protocol and thematic analysis [ 26 , 27 ]. A specialist research librarian with expertise in public health and research synthesis was consulted for the scoping review protocol. This scoping review is reported in accordance with the PRISMA statement for scoping reviews [ 28 ].
Review scope
Articles were included if they were published in English. There were no geographic or date restrictions. Peer-reviewed journal articles with qualitative, quantitative, and/or mixed methods study designs, dissertations, and grey literature were included. Literature was included when it focused on developing competency statements and frameworks for public health students and practitioners. Competency development in other disciplines (e.g., medicine, dentistry, etc.) was excluded unless it was explicitly public health focused (e.g., public health nursing).
Search strategy
In collaboration with the research team and a specialist research librarian, the search strategy was developed by exploring the relevant literature for keywords and controlled vocabulary. Originally, our review intended to focus on communication-related competencies for public health specifically, so controlled vocabulary and keywords were included to reflect this focus. During the screening process, it became apparent there was not enough literature focused on public health communication. The search strategy was expanded to focus across all competencies relevant to public health, including communication.
The search strategy was tested in Ovid via MEDLINE and refined to ensure the results were relevant to the review scope. The search strategy was then translated for use in other databases by modifying syntax, as needed. The final search was carried out on November 24, 2022, in the following databases: Ovid via MEDLINE (Table 1 ), PsycINFO, Web of Science, Communication and Mass Media Complete, ERIC, and CAB Direct. These databases were selected to provide a comprehensive coverage of public health, education, and communication sources.
To supplement the database search, we hand-searched the following journals: Journal of Public Health Management and Practice, American Journal of Public Health, Journal of Health Communication, Health Promotion Practice , and Health Communication . The journals were identified by examining the most frequently cited journals in the database search results. Additional peer-reviewed articles were also identified during the grey literature search. Grey literature was searched using Google through appropriate combinations of concepts (e.g., “core competencies” AND “public health”) and pages 1–10 were screened for relevant results.
Relevance screening
The results of the search were imported into DistillerSR review software [ 29 ] to facilitate screening by independent reviewers and track all steps. Deduplication of results occurred in DistillerSR after all relevant citations were imported from Mendeley [ 30 ]. Title and abstract, and full-text screening were also conducted in DistillerSR. Reviewers (MM and CF) pilot tested ten random articles to ensure understanding of the inclusion criteria. Two independent reviewers (MM and CF) screened the title and abstract of each article using a screening form and any conflicts were resolved through discussion. Kappa was 0.81 for title and abstract screening, indicating high agreement [ 31 ].
The full text of articles deemed potentially relevant during the title and abstract screening were obtained and screened independently by the same two reviewers. Steps were taken to obtain the full text of all articles including searching within the University of Guelph Library, using Google and Google Scholar, and contacting the author directly through ResearchGate or their publicly available institutional email. A screening form was developed in collaboration with the research team and pre-tested before implementation. The form assessed each article’s eligibility for inclusion in the review by the following criteria: literature type, language, population, and measurement, evaluation, or detailed report of competency statement or framework development in public health students and/or the workforce. After completion of full-text screening, Kappa was 0.80, indicating high agreement [ 31 ]. Conflicts were resolved through discussion to the point of reaching agreement for inclusion or exclusion in the review.
Data extraction
Two researchers conducted data extraction for the included articles (MM and CF). Each researcher acted as the primary data extractor for half of the dataset and validated the other half as the secondary data extractor. Key information was extracted using an Excel form developed in collaboration with the research team [ 32 ]. The following information was extracted from each included article: title, author(s), year, article type, country of origin, study design, study aim, methods, theories or frameworks included, institutions involved in developing competency statements, existing competency frameworks included, focus of competency framework (e.g., general or discipline-specific), process used to develop competency statements or framework, level of competency development focus (e.g., nation-wide, organizational, etc.), target population (e.g., graduate student, general public health practitioner), transparency of the process, lessons learned, implementing and adoption of competency statements or framework, evaluation of the process, bias identified, and future research directions.
The results of the data extraction were thematically analyzed following the method outlined by Arskey and O’Malley [ 26 ] and updated by Levac et al. [ 27 ]. First, the research team developed key areas to capture results for data extraction to answer objective 2, including transparency of methods and results, evaluation of the process, lessons learned, and implementation/adoption of the competencies. One researcher (MM) coded the extracted data line-by-line, as well as revisited the full text articles, to develop an initial thematic framework that described approaches and best practices for developing competency frameworks in public health. Codes were inductively created based on the key areas of data extraction outlined above and refined into larger concepts where data overlapped to generate initial themes. Significant outliers were captured in the coding and incorporated into themes where appropriate. Approaches for developing competency statements and frameworks described any methods undertaken and/or key recommendations for generating competency statements for public health that outline the values, knowledge, skills, and behaviours needed to effectively perform in various public health roles. Best practices describe areas of significant overlap in the data that reported successful methods or recommendations for developing, implementing, and/or evaluating competency statements and frameworks for public health. The research team collaboratively discussed and refined the themes to provide perspective and triangulation of results, ultimately developing six analytical themes. The research team also identified any areas of ambiguity during discussion and/or revisions and MM revisited the extracted and coded data, as well as full text articles, to add detail. The research team then collaboratively discussed, refined, and finalized the analytical thematic framework.
Search and selection of articles
A total of 3,716 articles were screened at the title and abstract stage following deduplication. Next, 373 full-text articles were reviewed for relevance, with 13 studies identified for inclusion. Figure 1 depicts the PRISMA flow diagram of the article screening and inclusion process.
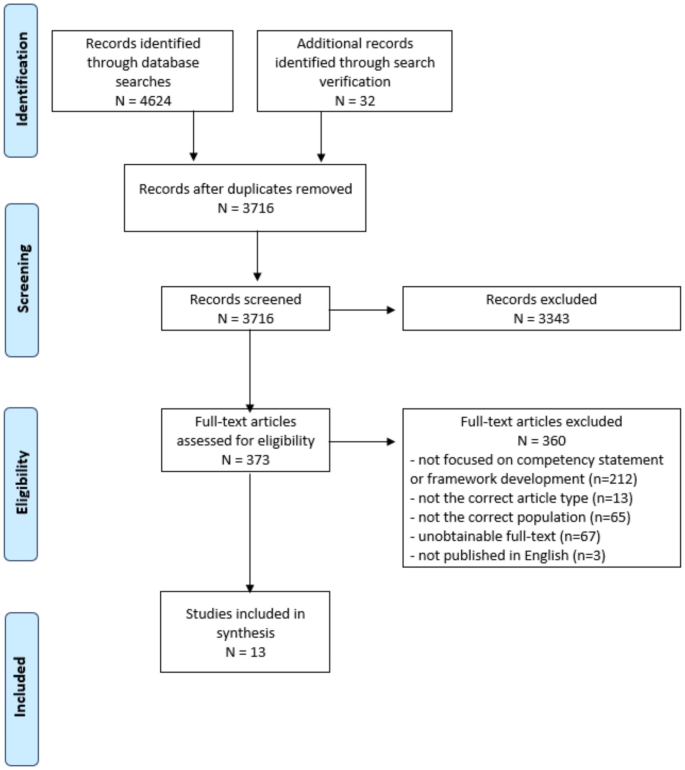
PRISMA flow diagram of scoping review process
Characterization of Articles included
Most included articles were peer-reviewed journal articles, used qualitative or mixed method design, and were targeted towards generalist public health practitioners (Table 2 ). See Supplementary Table 1 for the data extraction results.
Thematic analysis
Six themes were generated to describe the approaches and best practices for developing competency statements and frameworks for public health. The themes related to the approaches include initial methods used, building consensus, and transparency in reporting. Themes related to best practices include governance and coordination and a multifaceted approach for addressing complex public health challenges. The theme describing developing foundational and discipline-specific competencies and those that apply to varying levels of expertise included approaches and best practices.
Initial competency statements are developed using literature reviews and expert consultations
Literature reviews [ 33 , 34 , 35 , 36 , 37 ], expert consultation [ 38 , 39 , 40 , 41 ], or a combination of both [ 35 , 36 , 42 , 43 ] were used to develop initial competency statements.
As a first step, a literature review was often completed to identify competencies, including for public health physicians [ 43 ], health communicators [ 42 ], global public health practitioners [ 35 ], and for health literacy for public health professionals [ 34 ]. Grey literature, including existing country-level public health competencies (e.g., USA, Europe, Canada, New Zealand, Spain), existing competency frameworks (e.g., Emergency Preparedness Core Competencies for Public Health Workers), textbooks, and public health education curricula was frequently included in literature reviews for competency list development [ 33 , 35 , 37 , 39 , 43 ]. Less frequently, expert consultation was used as a first step in developing competency statements, including for emergency preparedness and response [ 37 ], public health epidemiology [ 44 ], and for senior public health officials [ 39 ]. Additional methods for getting started included conducting an environmental scan, which was used to develop Indigenous public health core competencies [ 36 ].
As a second step, expert consultations took place using interviews and surveys to gather information relevant to competency framework development, including feedback on competency statements, contextual factors, and responsibilities of and gaps in the workforce, including at various levels of public health practice [ 42 , 43 ] and within academia [ 35 ]. Exemplar practitioners who demonstrate the competencies within well-established practices can model the knowledge, skills, and abilities required within a particular context [ 40 , 41 ]; however, expert consultations are not an appropriate first step when the area of practice is emerging and there is no history of exemplar practitioners [ 34 , 40 ]. Representation is important for expert consultations: Indigenous peoples’ leadership in creating an Indigenous competency framework ensured their beliefs, values, and knowledge were central [ 36 ]. Context, including culture, geography, experience, and education must be considered when identifying evidence and theory for competency list development [ 37 ].
While some of the included literature identified potential challenges in gathering and synthesizing diverse expert opinions within their methods [ 34 , 36 , 39 , 41 ], no insights on how these were addressed during the research were shared in the results or discussion. One exception was that participants of a consensus-building process with less expertise had some difficulty understanding more complex competencies [ 41 ]. The authors did not elaborate on how this may have impacted the results or how they addressed this issue during the research, other than recommending that further research in this area is needed.
Public health competency statement development is consensus-driven with practitioners and researchers
Expert consultation and validation by experts and practitioners must be included to increase the impact of competency frameworks [ 34 , 40 , 41 , 42 , 43 , 44 ]. Expert consultation that provides repeated assessment of the competency statements increases the validity of the results [ 43 ], convergence of findings [ 34 , 39 , 44 ], and comprehensiveness of the framework [ 41 ]. Modified Delphi technique was frequently used to facilitate discussion between experts and allow for successive feedback of the group opinion on competency statements [ 34 , 37 , 39 , 40 ]. For example, a Delphi technique to build competencies for bioterrorism and emergency readiness in public health gathered experts from food safety, epidemiology, occupational health, and Indigenous health and included various levels of expertise and roles, including Directors, staff, and community leaders [ 37 ].
Other techniques to develop consensus on competency frameworks included focus groups [ 37 , 41 ], workshops [ 44 , 45 ], a survey [ 42 , 43 ], interviews with expert practitioners [ 43 ], an advisory committee [ 33 ], and a conference with experts [ 38 ]. The size of the consensus-building expert group should reflect the uncertainty in the literature, resources available, and the topic area within public health [ 34 ]. For example, an expert panel for developing health literacy competencies aimed to include at least 20 individuals from across a network of schools of health professionals, educators, and experts in health literacy to attend an in-person two-day meeting to ensure a variety and breadth of perspectives included [ 34 ].
Purposive sampling of experts to gather various levels of experience and expertise within various public health disciplines was frequently used [ 34 , 37 , 41 , 42 , 43 , 44 ]. Participants were recruited via professional association listservs [ 34 , 42 , 44 ], relevant government and community-based organizations [ 37 ], and public health agencies [ 41 ]. In terms of number of participants, studies did not include any information on a priori sample sizes for quantitative methods, however, qualitative methods were guided by the achievement of data saturation [ 41 , 44 ].
As part of the consensus-building process, surveys are often used to gather feedback on agreement [ 34 , 37 , 42 , 44 ] and importance [ 34 , 35 , 37 , 40 , 42 ] of competencies. Likert scales were used, including a 4-point scale of importance ranging from 1 (very important) to 4 (not important) [ 34 ], a 5-point scale of importance ranging from 0 (not used at all) to 4 (essential) [ 42 ], and a 5-point agreement scale ranging from 1 (strongly disagree) to 5 (strongly agree) [ 44 ]. Competency statement acceptance, rejection, or clarification based on feedback through surveys were sometimes reported [ 34 , 44 ].
Transparency of consensus-building processes for developing competency frameworks varied
Reporting transparency regarding how consensus on competency frameworks was reached varied. Some studies were very detailed [ 34 , 39 , 41 , 42 ] while others less so [ 35 , 38 , 45 ].
Studies often reported response rates and agreement for all competency items included [ 34 , 35 , 39 , 44 ]. Statistical analysis, usually as associations between agreement ratings, and agreement levels for included competency statements, were also reported [ 39 , 42 , 43 , 44 ]. Statistical analysis included a factor analysis to reduce and synthesize the overall number of behavioural traits identified for public health physicians [ 43 ], means and standard deviations to identify participant characteristics and the importance of the competence statements [ 42 ], and bivariate analyses to determine if the level of agreement differed by participant characteristics [ 44 ]. A pre-determined threshold of acceptance was used by Coleman et al. [ 34 ] to increase the validity of findings.
Overall results of the process to build consensus on a final competency framework were reported by some studies but details were often lacking on how agreement was assessed [ 33 , 37 ].
Competency frameworks varied across foundational and discipline-specific competencies and levels of expertise
Competency frameworks must balance comprehensiveness with being targeted to various disciplines and roles within public health [ 39 , 40 , 41 , 45 ]. While specialist competency frameworks are necessary, a coherent and unifying public health competency framework is needed to provide structure, guidance, and a common understanding of public health more broadly [ 39 , 40 , 41 , 45 ]. There is overlap between competency skills, knowledge, and behaviours within competency domains and between foundational and discipline-specific frameworks [ 25 , 46 ], making it more difficult to assess agreement or importance during consensus-building [ 34 , 44 ].
Foundational competencies to address systemic factors related to colonialism and incorporate non-Western knowledge and Indigenous governance structures in public health are also necessary [ 36 ]. For example, community health workers are excluded from needing to have all the core competencies in the Core Competencies for Public Health in Canada 1.0 release [ 36 ]. However, these public health practitioners play a central role in Indigenous health and lack of proficiency in all the competencies can significantly impact Ingenious health [ 36 ].
Discipline-specific competencies define the roles within public health and guide professional development and education within the specialty [ 39 , 40 , 41 , 42 , 43 , 44 ]. In discipline-specific areas, such as emergency preparedness and response, competency development must reflect all potential public health areas of action and interdisciplinary and intersectoral action [ 37 , 40 ]. Working collaboratively across sectors, disciplines, and at different levels of service enhances the impact of public health action and must be reflected in competencies for public health in discipline specific frameworks [ 38 ], as well as foundational frameworks.
Coordination across levels of jurisdiction, as well as credentialing practitioners from novice to expert levels of competence, facilitates integration of competencies into practice [ 37 ]. A model for lifelong learning for bioterrorism and emergency management is used to credential practitioners at varying levels of expertise from novice to expert, which combines education, practical experience, and learning outcomes to assess the level of expertise [ 37 ]. Similarly, competencies for public health can be approached at various levels of expertise including basic, advanced, and expert [ 37 , 39 , 41 ]. For example, verb changes can be made to competency statements to make them more appropriate for varying levels of expertise (e.g., understand vs. analyze vs. create) [ 41 ]. Competency theory can be used in combination with a foundational approach to create competency frameworks for public health where statements are interpreted for different functions in public health (e.g., communication, leadership, policy) [ 41 ].
Recognition and integration of competence acquired through experience, professional development, and strategic development toward organizational goals must be recognized, along with those acquired through formal education [ 37 , 41 , 44 ] and different forms of knowledge, including Indigenous ways of knowing [ 36 ]. Bhandari et al. [ 39 ] also note the distinction between competencies for public health students -- those that are expected to be obtained by the end of the education program and organized around academic disciplines – and professional competencies which reflect the needs of the workforce. The two are intricately related as professional competencies, or those needed to effectively perform on the job, should guide and inform educational competencies [ 39 ].
Governance ensures competency frameworks are current, integrated into practice, and connected to professional development
Funding to establish indicators or performance measures for competencies to ensure their integration into practice is needed [ 38 , 45 ]. Professional development in the competency areas is necessary for integration into practice and requires dedicated, ongoing funding [ 38 , 45 ]. Common methods of competency assessment should be a key area of governance and funded programming within professional development [ 41 ]. Quality assurance mechanisms for professional development are needed that reflect the local context and should be implemented by training organizations and institutions [ 38 ]. Ideally, an independent administrative body should be instituted to develop and implement standards and quality assurance mechanisms [ 38 ].
Competency lists must be revisited and revitalized on a consistent basis in partnership with various sectors such as healthcare and academia [ 38 , 40 , 41 , 42 ]. Discipline-specific competency frameworks must be reviewed and updated more regularly compared to general frameworks [ 40 ]. Competency frameworks that have not been updated for five years or more should be used with caution, especially in curriculum design, health communication, and organizational planning [ 40 ]. Overall, renewal should be planned for as part of the overall initial development of any framework and should include a survey of current practices to understand strengths and areas of opportunity [ 40 ].
A comprehensive plan for communicating the results of developing competency frameworks ensures competencies are adopted by public health organizations [ 38 ] and the work is not duplicated [ 40 ]. Various formats for competency frameworks were used, including Tables (33,34,39,42,43), lists [ 35 , 37 , 38 , 41 ], visual models [ 36 , 43 , 45 ], and concept maps [ 44 ]. Only one study included any evaluation of the usefulness of the design and found simple and concise layouts were preferred [ 41 ].
Competency frameworks provide organizations and policymakers with a tool by which they can address their specific context and needs through workforce planning, including developing job descriptions, performance indicators, and professional development opportunities [ 39 , 40 ]. New and revitalized frameworks should be mapped against job descriptions in public health to identify gaps [ 39 ]. Practitioners were apprehensive around competency frameworks being used for accreditation and performance evaluation [ 44 ]. Training programs should be designed and assessed to ensure they are able to develop the competencies that are outlined within frameworks [ 39 , 40 , 41 , 42 ]. Professional development for the current public health workforce must be integrated within the development and implementation of public health competency frameworks [ 34 , 39 , 41 , 42 , 44 , 45 ].
Values underpin and support competency frameworks to enable public health to address complex public health challenges
Values should be reflected in competency statements, although these are the most difficult to develop and measure [ 36 , 38 , 43 ]. A reflexive practice to identify the values and beliefs that guide public health practice would contribute to intercultural competency [ 36 ]. Values must include a commitment to health equity, social justice, intercultural competency, climate justice, and others that are rooted in the social ecological model of health and the social determinants of health [ 35 , 36 , 38 , 42 ].
Although many frameworks highlight the importance of reducing health inequities (e.g., in the preamble), they varied in terms of the emphasis placed within competency statements on reducing health inequities and culturally appropriate approaches to public health [ 36 , 39 ]. Competencies for providing culturally appropriate public health and healthcare for Indigenous peoples are vital and can contribute to overcoming misunderstanding, discrimination, and racism [ 36 ]. The explicit recognition of Indigenous peoples, colonialism and the impact on health, and related health inequities throughout the public health core competencies, including integration within definitions in the glossary and practice examples, is necessary [ 36 ].
Public health competencies are necessary to facilitate shared understanding of expectations and actions required to address complex public health issues that are intersectoral and interdisciplinary [ 38 , 41 , 45 ]. The ability to influence policy and develop partnerships can be negatively influenced by predominant culture and requires political will and in some cases governmental reform to ensure competencies to address complex public health issues are included in public health frameworks and practice [ 36 , 38 , 41 , 43 ]. A flexible, action-oriented, and regulated public health workforce is needed to address serious and complex public health challenges, including climate change and health inequities [ 45 ]. Greater integration of competency frameworks with relevant legislation, programs, and guidelines for the specific jurisdiction, as well as within global health, to address complex public health issues is recommended [ 44 ].
Overall, thirteen articles were identified related to approaches for developing competency statements and frameworks for public health, just one of which focused on communication competence. Most of the included literature was original, peer-reviewed research using qualitative or mixed-methods approaches. The main target population for competency framework development was generalist public health practitioners and the process was largely driven by academia. Foundational competency frameworks for general public health practice at the country level were the most commonly developed in the included studies. A range of approaches, especially in combination, were taken for developing competency statements frameworks, with consensus-building through modified Delphi techniques, expert consultation, and surveys commonly used. Below, we summarize the six themes described in the results and discuss these approaches and their importance for developing public health competency statements and frameworks (Table 3 ). In Table 3 , the content within the Actions to Achieve Recommendation column summarizes key aspects of the results and discussion that relate to the success and impact of the approaches and best practices for developing competency statements and frameworks identified. We compare and contrast our findings to similar literature in veterinary medicine and healthcare to put the recommendations into a wider context and body of knowledge.
A strong evidence-informed foundation for developing competency statements bridges the research-practice interface. The quality of the evidence used to generate findings is key to the reliability and validity of the resulting competency frameworks [ 47 , 48 ]. Literature reviews, expert consultations, review of existing competency frameworks, and environmental scans can be used as a first step to gather evidence [ 48 , 49 ] that can close the gap between research and practical knowledge and provides contextual evidence about the public health system in Canada. Within healthcare, a similar process is used where literature reviews [ 50 ], surveys [ 51 ], and interviews [ 52 ] were used to develop the initial list of competency statements for further consensus-building [ 49 ]. This approach is consistent with the steps outlined in the Delphi and modified Delphi techniques [ 48 , 49 ].
Multi-step processes for consensus-building, including expert consultation and iterative methods, increase the validity of results through the incorporation expert knowledge and research findings [ 49 ]. Expert consultation is a key step in the consensus-building process to ensure a strong basis in the evidence [ 47 , 48 ]. Practitioners and researchers are most often included in consensus-building processes in the included public health literature and within healthcare [ 50 , 51 , 52 ] and veterinary medicine [ 53 , 54 ]. Consensus-building processes to develop competency frameworks in the included literature were most often academia-led and conducted via expert consultations, surveys, and modified Delphi technique with public health academics and practitioners. However, public health goes beyond the public health sector and the consensus-building process should include community-based organizations, government, and other stakeholders to ensure community needs and values are being met [ 45 ]. The inclusion of other actors ensures competencies are reflective of collaborative, intersectoral, community-based public action.
Transparent and comprehensive reporting of the methods and results of consensus-building processes for public health competencies and frameworks is needed so that the research can be repeated, or similar processes can be implemented, and understood. The details of the consensus-building process were lacking in some studies – a similar trend has found for competency framework development in the healthcare [ 50 , 51 , 52 ] and veterinary medicine [ 53 , 54 ]. This is also true across health research in general where lack of transparent reporting makes interpreting the methods, evaluating the reliability and validity of results, and comparing to the wider body of knowledge difficult [ 55 ]. Research with low transparency has implications for use including possible harms and unintended consequences and reducing the possibility of benefits, contributing to lower overall public health impact [ 56 ]. Competency theory and validated instruments that guide consensus-building and ensure reliable and accurate results were identified as lacking by included studies. A threshold for agreement has also not been validated, making it difficult for studies to select an a priori level of agreement [ 34 , 39 ]. The focus on validated instruments within competency framework research tends to be for measuring perceived competence development in education [ 57 ] or professional development [ 58 ] rather than the process itself of developing consensus when building competency frameworks. Pilot testing of instruments for measuring agreement during consensus-building can help to ensure validity before the process begins. The CONFRED-HP (COmpeteNcy FramEwork Development in health professions) recommendations for reporting provides researchers with clear descriptions of vital areas for reporting the development of competency frameworks to increase the transparency and trustworthiness of the research and allow for informed decision-making around its use [ 59 ]. The EQUATOR (Enhancing the Quality and Transparency Of health Research) Network guidelines can be used for increasing the transparency and trustworthiness of research on building competencies in public health students and practitioners [ 55 ]. Reporting guidelines are important tools that support best practices in research reporting, contributing to increased transparency and research impact [ 56 ].
Public health effectiveness relies on how practitioners combine their individual values, knowledge, skills, and behaviours to address community needs. The effectiveness of a public health team and workforce results from this combination across individuals, levels, and disciplines [ 60 ], although interdisciplinary teamwork is difficult [ 61 ]. Foundational competencies lay the groundwork for a common understanding of what is required to do good work in public health. Discipline-specific competencies allow for public health practitioners to have opportunities to learn and build on foundational competencies for additional mastery [ 62 ]. Despite this, diversity of competency frameworks and levels of competencies (expert and foundational vs. specialized) are key challenges in developing competency frameworks [ 63 ]. The diversity in competencies and the subsequent difficulties have implications for workforce planning and development and education [ 63 ]. Frameworks that combine different ways of knowing, including theory and practice-based knowledge, and practical examples can help contextualize the competencies [ 63 ] to different expertise levels and specializations within public health. Competencies related to communication and interdisciplinarity can assist with the challenges of multiple levels of expertise and foundational and discipline-specific competencies as well [ 25 , 60 , 64 ].
Integrating competency frameworks into practice requires governance and coordinated efforts, as identified by the included literature. Governance of public health core competencies is necessary to ensure competency frameworks are up-to-date, appropriately resourced, and reflective of current public health needs and values. Within a governance structure, funding, standards and quality assurance, and a comprehensive framework rollout plan were also identified as necessary. A lack of resources and infrastructure to support the development, implementation, evaluation, and ongoing refresh of competencies are key contextual factors influencing the success of competency frameworks [ 46 ]. This complements findings from another review indicating that a comprehensive and coordinated implementation strategy, including resources, governance, and collaboration, is associated with the use and impact of competency frameworks [ 25 ].
Design and readability of competency frameworks impacts their use and effectiveness. Competency statements should be written in clear language and be reasonable in number, and frameworks should be user-friendly, use tables, and be translated where applicable [ 25 , 65 , 66 , 67 ]. Although there were a range of presentations in the included literature, most did not evaluate the usefulness of the design, with the exception of Shickle et al. [ 41 ], which found clear language was preferred.
Finally, a multifaceted approach to developing and measuring competencies is needed to address complex public health challenges. Complex public health issues including climate change, global health, health inequities, and racism/discrimination must be addressed, reflected, and integrated into public health competencies. Values that guide our research, practice, and community interactions must also be reflected in competency statements and frameworks to address these complex issues. Values are most often geared at individual practitioners but should also be extended to organizational values, as these create a culture and context for individual values to guide practice [ 68 ]. In the context of Indigenous health and reconciliation, it is imperative to explicitly integrate decolonization, anti-racist, and culturally appropriate public health practice into the public health competencies [ 36 ]. Within other disciplines, including midwifery [ 69 ] and healthcare [ 70 ], core competencies have been proposed to guide providers working to address health disparities and ensure culturally safe and effective services for Indigenous Peoples. Structural factors, including power dynamics, current and historical relationships, and needs and resources of marginalized groups must be incorporated into competency frameworks and directly influence use [ 25 , 46 ]. Competency frameworks should be flexible enough to serve as practice guidelines that can be adapted to suit the specific context, complexity, and population requirements in which it is being applied [ 25 ].
Limitations
Within the current study, the results could be limited by the selection of databases; however, we used a number of diverse databases and supplemented the search by hand searching and grey literature. Further, our research intended to focus on health communication, but found the literature to be greatly lacking, rendering a more focused review impossible. The inclusion of health communication as a key concept within the search strategy may have limited the results to those public health competency frameworks that included communication. Communication is identified across many disciplines, including public health, as a key competency, so this aspect may not have had a great impact on the results. The results may also be limited by language bias as studies were only included if they were published in English. Although we had no date or geographic restrictions, this language bias may have limited articles globally, especially those that are low or low-middle income countries, impacting the overall generalizability of results.
Biases created by study design of the included articles also result in limitations, including participant recruitment and the methods used to understand their perspectives. Information bias was present as most studies employ purposive sampling to select consensus-building groups [ 34 , 35 , 37 , 41 , 44 ]. There is also no established target number of participants for consensus-building processes for developing competency frameworks (Coleman et al., 2013) and sample sizes can be small [ 35 , 41 , 42 ]. The nature of participant experience and breadth of perspective could also be limited by the sampling [ 34 , 37 , 39 , 41 , 42 , 44 ]. Further, many studies relied on expert knowledge and the literature to develop competency frameworks, but many areas of public health are rapidly expanding and changing [ 34 ] and/or lack the theoretical underpinning necessary to ensure reliable and valid results [ 34 , 39 , 41 ]. Some studies reported an a priori cut-off point for agreement [ 34 , 39 ]; however, this threshold is not validated in the research [ 34 , 39 ].
Future research directions
Research is needed to distinguish between competencies required for core public health roles versus those for specialized roles. Research specific to the various disciplines, including public health communication, is needed to determine best practices for developing, implementing, and evaluating competency frameworks. Research reporting on the implementation and evaluation of foundational and discipline-specific competency frameworks is needed to help understand best practices and challenges in harmonizing varying competency frameworks in practice. The creation and implementation, reliability, and validity of a competency assessment instrument should also be explored. Some areas of literature related to competency statements and frameworks, such as health literacy, are heavily skewed towards healthcare and medicine, and more work is needed centring different topics within public health so that the focus is at the population level rather than the patient/individual level. Research to strengthen the connection between competency frameworks and the learning outcomes of public health graduate training and professional development would be valuable. Finally, research is needed to evaluate consensus-building processes from the perspective of participants and the utility and impact of the final framework, including design considerations. Literature in this area is largely focused on competency framework development and not on the evaluation of the process of development, implementation, use, or impact of the frameworks in practice.
The review scopes and analyzes the literature on developing competency statements and frameworks for public health. The findings highlight the similarities in approaches for developing competency statements and frameworks across studies, including using a multi-step process that involves literature reviews, expert consultations, and consensus-building. Foundational and discipline-specific competency frameworks, as well those that are role- and expertise-specific, including for students, new practitioners, and leaders, are needed. Variation in transparency of reporting the process of developing competency statements and frameworks exists, with some studies including very detailed methods and results while others only high-level overviews. High transparency and multi-step processes are necessary to ensure the validity, reliability, and utility of competency statements and frameworks. Governance and comprehensive plans for implementation and renewal are necessary to ensure integration of competencies into professional standards and professional development. Values that reflect culture and social justice when addressing complex public health needs must be integrated into public health competency statements and frameworks.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
National Institutes of Health. Office of Human Resources. 2017 [cited 2023 Mar 16]. What are competencies? Available from: https://hr.nih.gov/about/faq/working-nih/competencies/what-are-competencies .
Public Health Agency of Canada. Core Competencies for Public Health in Canada. Government of Canada [Internet]. Government of Canada. 2008. Available from: https://www.canada.ca/content/dam/phac-aspc/documents/services/public-health-practice/skills-online/core-competencies-public-health-canada/cc-manual-eng090407.pdf .
Public Health Association of BC. Public Health Core Competency Development [Internet]. 2023. Available from: https://phabc.org/public-health-core-competency-development/ .
Hunter MB, Ogunlayi F, Middleton J, Squires N. Strengthening capacity through competency-based education and training to deliver the essential public health functions: reflection on roadmap to build public health workforce. BMJ Glob Health. 2023;8(3):e011310.
Article PubMed PubMed Central Google Scholar
Schultes MT, Aijaz M, Klug J, Fixsen DL. Competences for implementation science: what trainees need to learn and where they learn it. Adv Health Sci Educ Theory Pract. 2021;26(1):19–35.
Article PubMed Google Scholar
Belita E. Development and Psychometric Assessment of the Evidence-Informed Decision-Making Competence Measure for Public Health Nursing [Internet]. [Hamilton, Ontario, Canada]: McMaster University; 2020. Available from: http://hdl.handle.net/11375/25765 .
Cheetham G, Chivers G. The reflective (and competent) practitioner: a model of professional competence which seeks to harmonise the reflective practitioner and competence-based approaches. J Eur Industrial Train. 1998;22(7):267–76.
Article Google Scholar
Public Health Foundation. PHF. 2023 [cited 2023 Mar 16]. Core Competencies for Public Health Professionals: Domains. Available from: https://www.phf.org/programs/corecompetencies/Pages/Core_Competencies_Domains.aspx .
Batt A, Williams B, Rich J, Tavares W. A Six-Step Model for Developing Competency Frameworks in the Healthcare Professions. Frontiers in Medicine [Internet]. 2021 [cited 2023 May 4];8. Available from: https://www.frontiersin.org/articles/ https://doi.org/10.3389/fmed.2021.789828 .
World Health Organization. WHO-ASPHER Competency Framework for the Public Health Workforce in the European Region [Internet], Copenhagen. Denmark: WHO Regional Office for Europe; 2020. Available from: https://www.euro.who.int/__data/assets/pdf_file/0003/444576/WHO-ASPHER-Public-Health-Workforce-Europe-eng.pdf .
Zwanikken PA, Alexander L, Huong NT, Qian X, Valladares LM, Mohamed NA, et al. Validation of public health competencies and impact variables for low- and middle-income countries. BMC Public Health. 2014;14(1):55.
Karunathilake IM, Liyanage CK. Accreditation of Public Health Education in the Asia-Pacific Region. Asia Pac J Public Health. 2015;27(1):38–44.
Pan American Health Organization. Pan American Health Organization. 2013 [cited 2023 Oct 23]. Core Competencies for Public Health: A Regional Framework for the Americas - PAHO/WHO. Available from: https://www.paho.org/en/documents/core-competencies-public-health-regional-framework-americas .
World Health Organization. World Health Organization. 2023 [cited 2023 Oct 23]. Climate change. Available from: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health .
Kuehn BM. WHO: Pandemic sparked a push for global Mental Health Transformation. JAMA. 2022;328(1):5–7.
Americas TLRH. Opioid crisis: addiction, overprescription, and insufficient primary prevention. The Lancet Regional Health – Americas [Internet]. 2023 Jul 1 [cited 2023 Oct 23];23. Available from: https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(23)00131-X/fulltext .
Canada PHA. of. aem. 2020 [cited 2020 Nov 3]. From risk to resilience: An equity approach to COVID-19 – The Chief Public Health Officer of Canada’s Report on the State of Public Health in Canada 2020. Available from: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html?utm_source=Canadian+Public+Health+Assocation&utm_campaign=cedbc06deb-EMAIL_CAMPAIGN_2020_10_30_02_02&utm_medium=email&utm_term=0_1f88f45ba0-cedbc06deb-181652396 .
Health TLP. COVID-19 pandemic: what’s next for public health? The Lancet Public Health. 2022;7(5):e391.
Leslie J, Council on Foreign Relations. 2023 [cited 2023 Oct 23]. The Crisis of Trust in Public Health | Think Global Health. Available from: https://www.thinkglobalhealth.org/article/crisis-trust-public-health .
Illari L, Restrepo NJ, Johnson NF. Rise of post-pandemic resilience across the distrust ecosystem. Sci Rep. 2023;13(1):15640.
Article CAS PubMed PubMed Central Google Scholar
Public Health Foundation. PHF. 2021 [cited 2023 Mar 16]. 2021 Revision of the Core Competencies for Public Health Professionals. Available from: http://www.phf.org/programs/corecompetencies/Pages/2021_Revision_of_the_Core_Competencies_for_Public_Health_Professionals.aspx .
Calhoun JG, Ramiah K, Weist EM, Shortell SM. Development of a core competency model for the Master of Public Health Degree. Am J Public Health. 2008;98(9):1598–607.
Ablah E, Elizabeth McGean Weist MA, John E, McElligott MPH, Laura A, Biesiadecki M, Audrey R, Gotsch D, William Keck C. Public health preparedness and response competency model methodology. Am J Disaster Med. 2013;8(1):49–56.
Wallar LE, McEwen SA, Sargeant JM, Mercer NJ, Papadopoulos A. Prioritizing professional competencies in environmental public health: a best–worst scaling experiment. Environ Health Rev. 2018;61(2):50–63.
Lebrun-Pare F, Malai D, Gervais MJ. Advisory on the Use of Competency Frameworks in Public Health: Literature Review, Exploratory Interviews and Courses of Action [Internet]. Quebec: INSPQ Center for Expertise and Reference in Public Health; 2021. Available from: https://www.inspq.qc.ca/publications/2827 .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
DistillerSR [Internet], Ottawa C. 2023. Available from: https://www.distillersr.com/ .
Mendeley. Mendeley Reference Manager [Internet]. 2023. Available from: https://www.mendeley.com/reference-management/reference-manager .
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82.
Microsoft Corporation. Microsoft Excel [Internet]. 2018. Available from: https://office.microsoft.com/excel .
Baseman JG, Marsden-Haug N, Holt VL, Stergachis A, Goldoft M, Gale JL. Epidemiology Competency Development and Application To Training for Local and Regional Public Health Practitioners. Public Health Rep. 2008;123(1suppl):44–52.
Coleman CA, Hudson S, Maine LL. Health Literacy Practices and Educational Competencies for Health professionals: a Consensus Study. J Health Communication. 2013;18(sup1):82–102.
Hagopian A, Spigner C, Gorstein JL, Mercer MA, Pfeiffer J, Frey S, et al. Developing competencies for a Graduate School Curriculum in International Health. Public Health Rep. 2008;123(3):408–14.
Hunt S, Review of Core Competencies for Public Health. An Aboriginal Public Health Perspective [Internet]. National Collaborating Centre for Aboriginal health; 2015. Available from: https://www.nccih.ca/docs/context/RPT-CoreCompentenciesHealth-Hunt-EN.pdf .
Olson D, Hoeppner M, Larson S, Ehrenberg A, Leitheiser AT. Lifelong Learning for Public Health Practice Education: a Model Curriculum for Bioterrorism and Emergency Readiness. Public Health Rep. 2008;123(2suppl):53–64.
Allegrante JP, Barry MM, Airhihenbuwa CO, Auld ME, Collins JL, Lamarre MC et al. Domains of Core Competency, Standards, and Quality Assurance for Building Global Capacity in Health Promotion: The Galway Consensus Conference Statement. Health Educ Behav. 2009;36(3):476–82.
Bhandari S, Wahl B, Bennett S, Engineer CY, Pandey P, Peters DH. Identifying core competencies for practicing public health professionals: results from a Delphi exercise in Uttar Pradesh, India. BMC Public Health. 2020;20(1):1737.
Gebbie KM. Competency-To-Curriculm Toolkit [Internet]. Columbia University School of Nursing and Association for Prevention Teaching and Research; 2008 Mar. Available from: https://www.phf.org/resourcestools/Documents/Competency_to_Curriculum_Toolkit08.pdf .
Shickle D, Stroud L, Day M, Smith K. The applicability of the UK Public Health Skills and Knowledge Framework to the practitioner workforce: lessons for competency framework development. J Public Health. 2019;41(1):e109–17.
Park SY, Harrington NG, Crosswell LH, Parvanta C. Competencies for Health communication specialists: Survey of Health communication educators and practitioners. J Health Communication. 2021;1–21.
Shi L, Fan L, Xiao H, Chen Z, Tong X, Liu M, et al. Constructing a general competency model for Chinese public health physicians: a qualitative and quantitative study. Eur J Pub Health. 2019;29(6):1184–91.
Bondy SJ, Johnson I, Cole DC, Bercovitz K. Identifying Core Competencies for Public Health Epidemiologists. Can J Public Health. 2008;99(4):246–51.
Wright J, Rao M, Walker K. The UK Public Health Skills and Career Framework—could it help to make public health the business of every workforce? Public Health. 2008;122(6):541–4.
Battel-Kirk B, Barry MM. Has the Development of Health Promotion Competencies Made a difference? A scoping review of the literature. Health Educ Behav. 2019;46(5):824–42.
Barrett D, Heale R. What are Delphi studies? Evid Based Nurs. 2020;23(3):68–9.
Staykova MPS. Rediscovering the Delphi Technique: A Review of the Literature. 2019 Jan 31 [cited 2023 Mar 28];6(1). Available from: http://scholarpublishing.org/index.php/ASSRJ/article/view/5959 .
Arifin MA. Applying modified e-Delphi technique: Guideline for HR researchers and practitioners for developing competency profiles during Covid-19 pandemic. IJARBSS. 2021;11(9):Pages746–754.
Mitsuyama T, Son D, Eto M, Kikukawa M. Competency lists for urban general practitioners/family physicians using the modified Delphi method. BMC Prim Care. 2023;24(1):21.
Taylor RM, Feltbower RG, Aslam N, Raine R, Whelan JS, Gibson F. Modified international e-Delphi survey to define healthcare professional competencies for working with teenagers and young adults with cancer. BMJ Open. 2016;6(5):e011361.
Janke KK, Kelley KA, Sweet BV, Kuba SE. A modified Delphi process to define competencies for Assessment leads supporting a doctor of Pharmacy Program. AJPE. 2016;80(10):167.
Bell MA, Cake MA, King LT, Mansfield CF. Identifying the capabilities most important for veterinary employability using a modified Delphi process. Veterinary Record [Internet]. 2022 Apr [cited 2023 Mar 22];190(7). Available from: https://onlinelibrary.wiley.com/doi/ https://doi.org/10.1002/vetr.777 .
Duijn CCMA, ten Cate O, Kremer WDJ, Bok HGJ. The development of Entrustable Professional activities for Competency-Based Veterinary Education in Farm Animal Health. J Vet Med Educ. 2019;46(2):218–24.
Simera I, Moher D, Hirst A, Hoey J, Schulz KF, Altman DG. Transparent and accurate reporting increases reliability, utility, and impact of your research: reporting guidelines and the EQUATOR Network. BMC Med. 2010;8(1):24.
Nicholls SG, Langan SM, Benchimol EI, Moher D. Reporting transparency: making the ethical mandate explicit. BMC Med. 2016;14(1):44.
Chan CKY, Luk LYY. Development and validation of an instrument measuring undergraduate students’ perceived holistic competencies. Assess Evaluation High Educ. 2021;46(3):467–82.
Miranda FBG, Mazzo A, Alves Pereira-Junior G. Construction and validation of competency frameworks for the training of nurses in emergencies. Rev Latino-Am Enfermagem [Internet]. 2018 Oct 25 [cited 2023 Mar 22];26(0). Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692018000100368&lng=en&tlng=en .
Batt AM, Tavares W, Horsley T, Rich JV, Williams B, Collaborators CONFERD-HP, et al. CONFERD-HP: recommendations for reporting COmpeteNcy FramEwoRk Development in health professions. Br J Surg. 2023;110(2):233–41.
Kozlowski SWJ, Ilgen DR. Enhancing the effectiveness of work groups and teams. Psychol Sci Public Interest. 2006;7(3):77–124.
Zumstein-Shaha M, Grace PJ. Competency frameworks, nursing perspectives, and interdisciplinary collaborations for good patient care: delineating boundaries. Nurs Philos. 2023;24(1):e12402.
National Collaborating Centre for Determinants of Health. Do public health discipline-specific competencies provide guidance for equity-focused practice? [Internet]. Antigonish, NS: St Francis Xavier University. 2015. Available from: https://nccdh.ca/resources/entry/do-public-health-discipline-specific-competencies-provide-guidance-for-equi .
Coombe L, Severinsen CA, Robinson P. Mapping competency frameworks: implications for public health curricula design. Aust N Z J Public Health. 2022;46(5):564–71.
Canadian Interprofessional Health Collaborative. A National Interprofessional Competency Framework [Internet]. University of British Columbia. 2010 Feb. Available from: https://phabc.org/wp-content/uploads/2015/07/CIHC-National-Interprofessional-Competency-Framework.pdf .
Burnett E, Curran E, Loveday H, Kiernan M, Tannahill M. The outcome competency framework for practitioners in Infection prevention and control: use of the outcome logic model for evaluation. J Infect Prev. 2014;15(1):14–21.
Article CAS PubMed Google Scholar
Cotter C. Review of the Public Health Skills and Knowledge Framework (PHSKF) Report on a series of consultations [Internet]. London, England: Public Health England; 2015. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/449309/PHSKF_Review_spring_2015.pdf .
Nash RE, Chalmers L, Stupans I, Brown N. Knowledge, use and perceived relevance of a profession’s competency standards; implications for Pharmacy Education. Int J Pharm Pract. 2016;24(6):390–402.
Standford N. Designing competency frameworks [Internet]. Naomi Stanford. 2020 [cited 2023 May 5]. Available from: https://naomistanford.com/2020/06/30/designing-competency-frameworks/ .
Lavallee B, Neville A, Anderson M, Shore B, Diffey L, First Nations, Inuit. Métis Health CORE COMPETENCIES [Internet]. Indigenous Physicians Association of Canada and the Association of Faculties of Medicine Canada; 2009 Apr. Available from: www.ipac-amic.org; www.afmc.ca/social-aboriginal-health-e.php.
Baba L. Cultural Safety in Frist Nations, Inuit and Metis Public Health. Price George, BC: National Collaborating Centre for Aboriginal Health; 2013.
Google Scholar
Download references
Acknowledgements
Not applicable.
Funding for this research was provided by the Canadian Institutes for Health Research (CIHR) in the form of a CIHR Catalyst Grant (FRN 184647).
Author information
Authors and affiliations.
Department of Population Medicine, University of Guelph, Guelph, ON, N1G 2W1, Canada
Melissa MacKay, Caitlin Ford, Lauren E. Grant, Andrew Papadopoulos & Jennifer E. McWhirter
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, M.M., J.E.M., L.E.G., and A.P.; methodology, M.M., J.E.M.,; formal analysis, M.M., J.E.M, and C.F.; investigation, M.M., C.F.; writing—original draft preparation, M.M.; writing—review and editing, M.M., C.F., L.E.G., J.E.M., and A.P.; supervision J.E.M.; validation; M.M. and J.E.M.; visualization; M.M.; project administration, J.E.M.; funding acquisition, J.E.M., M.M., L.E.G., and A.P. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Jennifer E. McWhirter .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
Consent for publication, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
MacKay, M., Ford, C., Grant, L.E. et al. Developing public health competency statements and frameworks: a scoping review and thematic analysis of approaches. BMC Public Health 23 , 2240 (2023). https://doi.org/10.1186/s12889-023-17182-6
Download citation
Received : 04 August 2023
Accepted : 07 November 2023
Published : 13 November 2023
DOI : https://doi.org/10.1186/s12889-023-17182-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Public health
- Competencies
- Competency frameworks
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Skip to content
Read the latest news stories about Mailman faculty, research, and events.
Departments
We integrate an innovative skills-based curriculum, research collaborations, and hands-on field experience to prepare students.
Learn more about our research centers, which focus on critical issues in public health.
Our Faculty
Meet the faculty of the Mailman School of Public Health.
Become a Student
Life and community, how to apply.
Learn how to apply to the Mailman School of Public Health.
Skills for Health and Research Professionals (SHARP) Training
Registration is open for summer trainings check out this year's topics below..
Our SHARP Program consists of short, intensive boot camps led by field experts to teach in-demand research skills and methods to investigators at all career levels and from any organization. Check out the official flyer with all 2024 topics to share with your colleagues.
SHARP trainings will be offered in-person, livestream virtual, or hybrid (in-person and livestream virtual). The format of each training is different, and specific workshop location details can be found on each respective training page. All trainings regardless of location are live, and are not self-paced, pre-recorded courses. Additional details about training formats, locations, transportation, and hotels are provided on our Location Details page .
Scholarships
Several scholarships are available for our summer trainings! The application deadline is February 29, 2024 at 11:59pm ET.
SHARP Trainings
Join the Columbia SHARP Training Program's email list to be the first to hear about new trainings, registration opening, and scholarship deadlines! Share your suggestions for future trainings.
New Training Topics for 2024
- Better Presentations Workshop
- Data, Designed Workshop
K Awards Training: A Path to Success
- The Scientist and the Storyteller Workshop
Summer 2024 Trainings
Single cell analysis boot camp: systems biology methods for analysis of single cell rna-seq, may 20-21, 2024 | livestream, virtual, google earth engine boot camp: methods for using satellite and geospatial data for environmental exposure science, gis workshop: visualizing and analyzing health data, may 30-31, 2024 | livestream, virtual, the scientist and the storyteller workshop: training for scientists and journalists to effectively communicate science to the public, may 30-31, 2024 | in-person training, python data wrangling boot camp: introduction to data wrangling, cleaning and manipulation with the python programming language, june 6-7, 2024 | in-person training, pi crash course: skills for future or new lab leaders, june 10-11, 2024 | in-person training, multi-omics boot camp: analysis of omics data for research studies, june 12-14, 2024 | livestream, virtual, climate change and health boot camp: building skills and knowledge for effective engagement, statistical analysis with missing data workshop: methods and applications in health studies, june 17-18, 2024 | in-person training, microbiome data analytics boot camp: planning, generating, and analyzing 16s rrna gene sequencing surveys, june 20-21, 2024 | livestream, virtual, quantitative genomics training: methods and tools for whole-genome and transcriptome analyses, june 24-25, 2024 | livestream, virtual, sql boot camp: building and querying databases, june 26-28, 2024 | hybrid training, code rigor and reproducibility with r boot camp, july 1-2, 2024 | in-person training, nih grant writing boot camp: building a strong foundation for funding success, july 8-9, 2024 | livestream, virtual training, creating compelling research narrative workshop: strategies for effectively presenting your science, july 11, 2024 | livestream, virtual, the pi's business of research boot camp: ins and outs of budgets, personnel and project management, july 15-16, 2024 | livestream, virtual training, data, designed workshop: develop your creative process to create better, more effective data visualizations, the exposome boot camp: measuring exposures on an omic scale, july 18-19, 2024 | in-person training, radiation safety officer (rso) training, july 19-21 and july 26-28, 2024 | hybrid training, better presentations workshop: from design to delivery, july 22-23, 2024 | livestream, virtual training, environmental mixtures workshop: applications in environmental health studies, july 22-23, 2024 | in-person training, epigenetics boot camp: planning and analyzing dna methylation studies for human populations, july 29-30, 2024 | hybrid training, causal mediation analysis training: methods and applications using health data, july 29-31, 2024 | livestream, virtual, mendelian randomization boot camp: a practical guide to study design and implementation, august 5-6, 2024 | hybrid training, exposure modeling boot camp: traditional and machine learning methods in environmental epidemiology, august 8-9, 2024 | in-person training, life cycle assessment boot camp: lca for the health sector, august 12-13 and september 23-24, 2024 | livestream, virtual training, environmental justice boot camp: theory and methods to study environmental health disparities, august 15-16, 2024 | hybrid training at harvard chan school in boston, august 19, 2024 | livestream, virtual training, bayesian modeling for environmental health workshop: concepts and computational tools for spatial, temporal, and spatiotemporal modeling relevant to public health, august 21-22, 2024 | in-person training, electronic medical records boot camp: biostatistical methods for analyzing emr data, august 22-23, 2024 | livestream, virtual, machine learning boot camp: analyzing biomedical and health data, returning summer 2025 | hybrid training, indigenous environmental health research workshop: methods, ethics and practice to collaborate with communities, returning summer 2025 | livestream, virtual.

10 Emerging Skills Public Health Professionals Need to Stay Competitive

Industry Advice Public Health & Public Policy
Obtaining a job in public health requires much more than health and science coursework. It demands experience in the field as well as specialized skills that enable prospective professionals to focus on the preventative and educational aspects of healthcare.
To stand out from the competition, aspiring public health professionals should familiarize themselves with the skills required in the field, and understand why they’re so important to their long-term success.
Is Public Health a Competitive Industry?
Like most healthcare professions, public health is a thriving industry that has become a highly competitive job market. An increasing number of young people are becoming interested in improving others’ lives and creating the foundation for long-term, sustainable public health—especially at the local level. This draw couldn’t come at a better time as there’s a noticeable decline in sufficient healthcare personnel.
According to the World Health Organization (WHO), there will be a shortage of around 18 million health workers by 2030 to meet the requirements of their sustainable development goals unless more people enter the field. This shortage makes the preventative side of healthcare even more crucial.
To ensure you find the right career in public health, you’ll need to obtain the right skills. For example, those interested in becoming public health program managers need specific experience and competencies to succeed.
Here’s everything a prospective public health program manager should know about the current job skill requirements.
Top Skills Every Public Health Program Manager Should Have
While there are important skills to highlight for prospective public health program managers, it’s crucial to first examine changing skills trends over the years.
According to a Lightcast report, there’s been a considerable shift in the list of required skills for public health program managers. Skills like program management, communications, leadership, and research have increased by over 100 percent. Even more impressive is the increase in skills like program development, advocacy, and marketing, which were virtually non-existent in job postings as recent as 2020.
According to Emily Grilli-Scott, assistant program director of the Master of Public Health (MPH) program at Northeastern University, this trend isn’t that surprising. “I can see why there’s an increased need for advocacy, marketing, communications, and leadership skills. We’re acknowledging as a field that there is no ‘one size fits all’ approach to [a field whose responsibilities range from] distributing free COVID-19 tests nationally to something more local like communicating to folks in densely populated areas about rising summer temperatures and the urban heat island effect.”
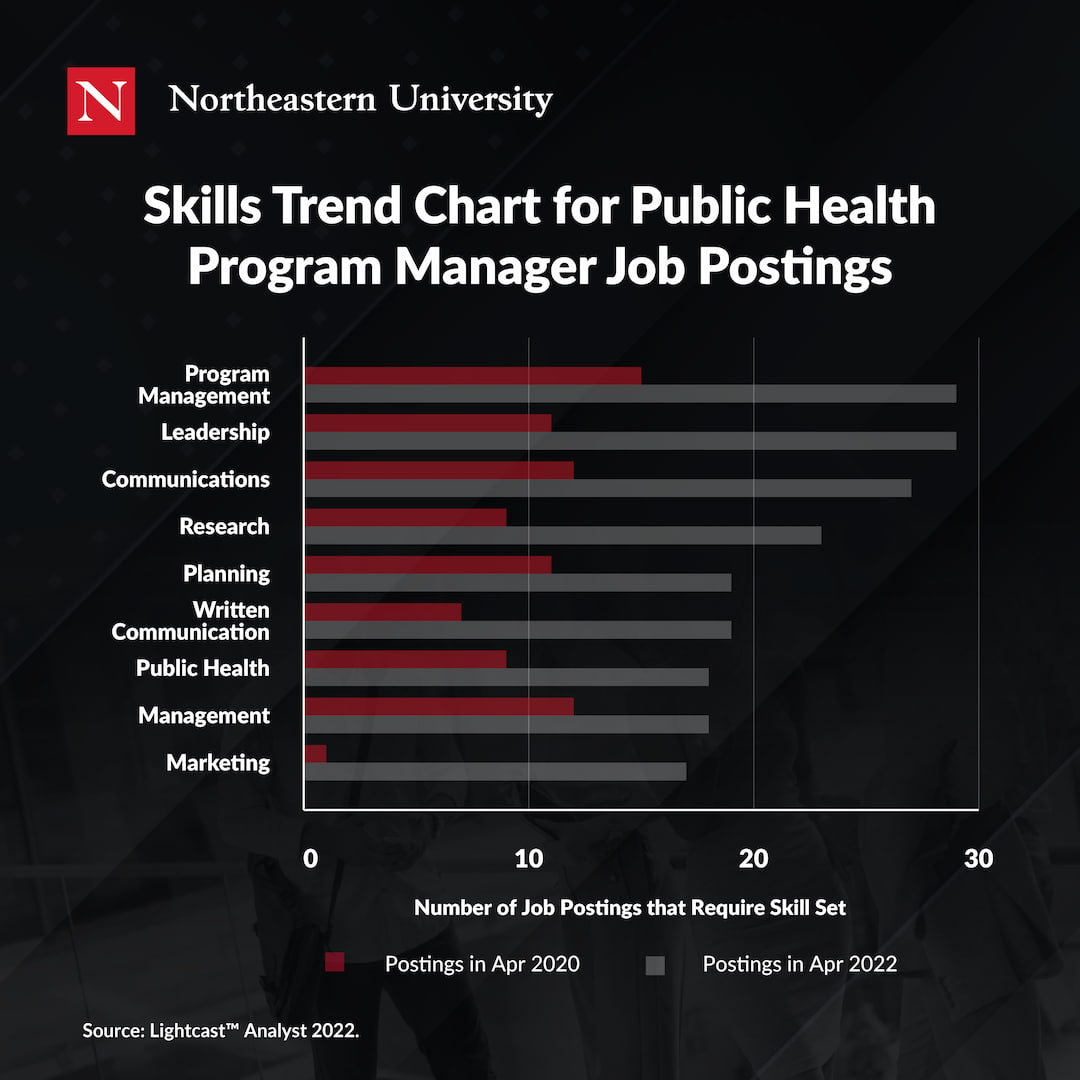
Specialized Skills
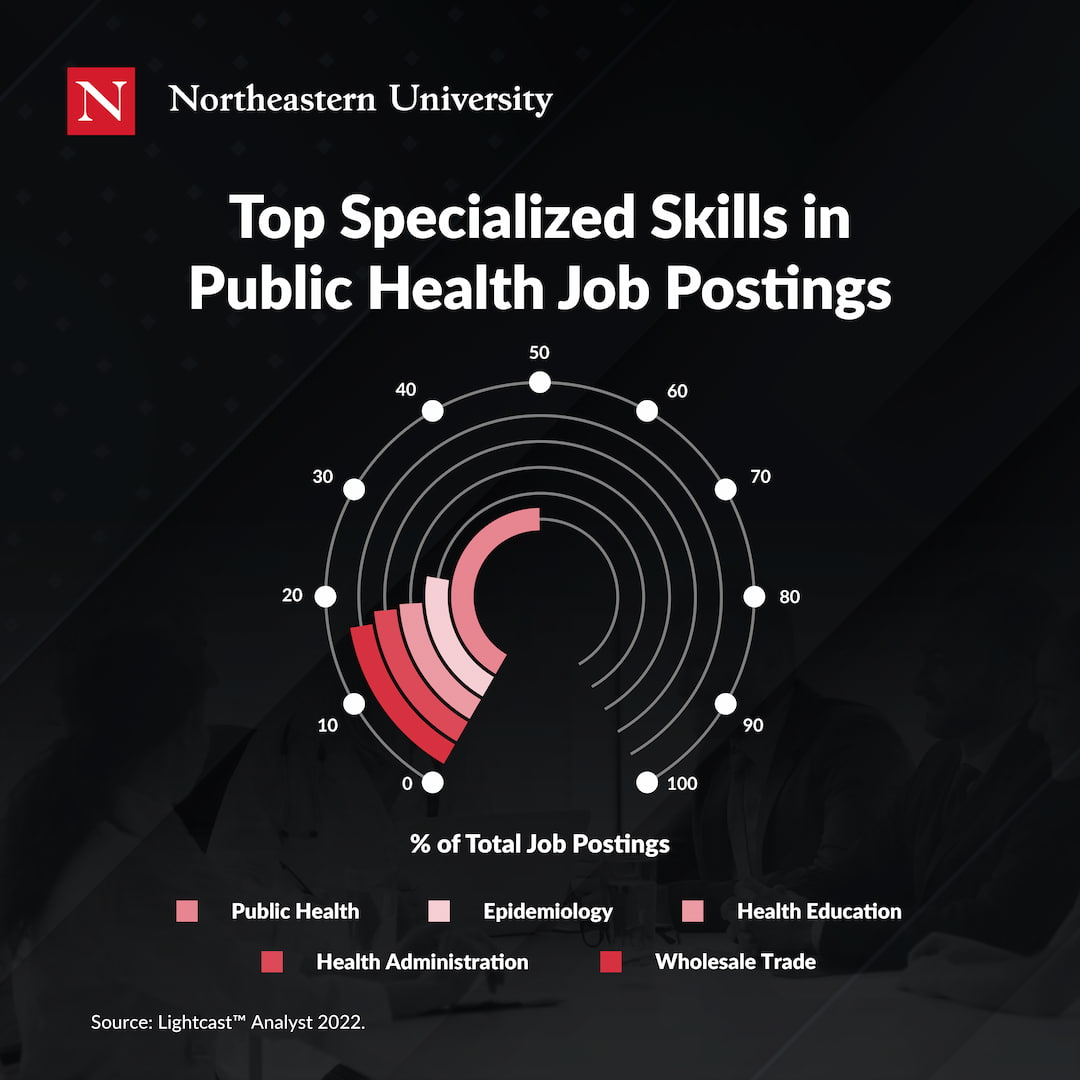
1. Public Health
Individuals interested in pursuing a career in public health need to have an in-depth understanding of the fundamentals of the field, such as social determinants of health , biostatistics and research methods, and program planning. In addition, they should recognize the key goals of public health: preventing diseases and injuries within a community by promoting healthy lifestyles through the implementation of developed educational programs, policies, and services.
2. Epidemiology
While this skill is highly specialized, it’s helpful for public health program managers to have a foundational knowledge of the subject. Epidemiology—studying how often diseases occur in different groups of people and why—offers a plethora of useful data that aids the planning and evaluation of illness prevention strategies in the future. Due to the emergence of the COVID-19 pandemic, there’s a raised awareness of communicable disease prevention and the resources needed to combat it. A basic understanding of epidemiology can only help advance your career as a public health program manager.
3. Health Education
Health education is a fundamental aspect of many public health positions, including a program manager. A public health program manager must be able to leverage this tool to present information to target populations on specific health topics and provide the necessary tools needed to support community behavioral changes. Prospective public health educators should have experience with the following activities:
4. Health Administration
Experience in health administration is an incredibly valuable skill to have when pursuing a career in public health. Those with administrative experience have improved the lives of people within the community they serve by dealing with the day-to-day operations in work settings such as government health agencies, non-profit organizations, and educational institutions. Public health program manager candidates with health administration skills should be able to complete the following responsibilities:
- Creating budgets
- Hiring staff
- Writing grant proposals and reports
- Obtaining necessary equipment
5. Data Analysis
Since public health program managers collect and interpret a lot of data, analysis skills are crucial. If you’re interested in the public health technology industry, this skill is particularly important. Several public health positions, including public health program managers and data analysts, look closely at current and historical industry data to predict trends, enhance community outreach, and improve disease management.
Common Skills
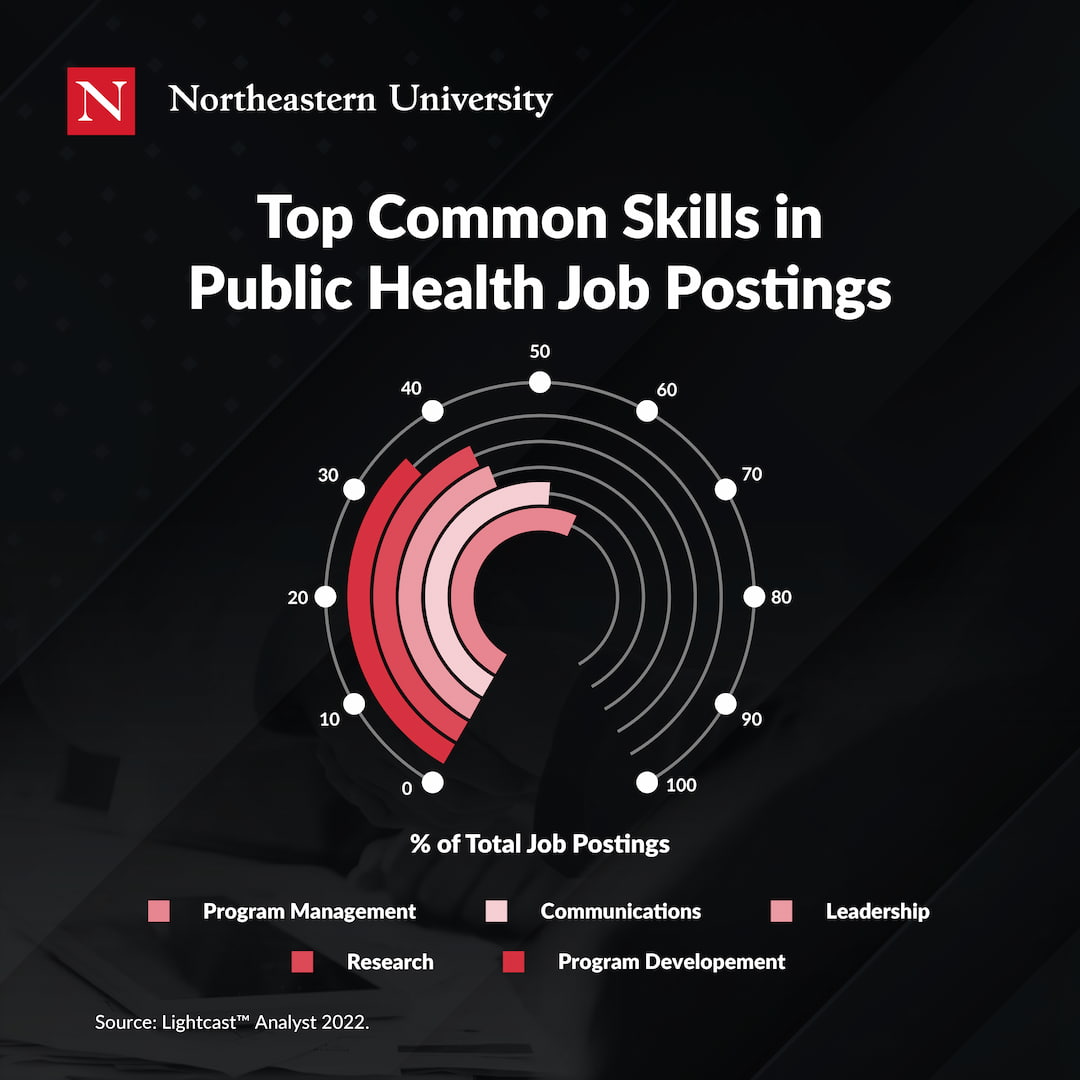
6. Program Management
As a program manager, it only makes sense that program and project management are vital skills. As a public health program manager, you’ll need management skills to stay on top of the various working parts of a health initiative or campaign. According to the Centers for Disease Control and Prevention , there are ten essential services that public health professionals provide. While many deal with assessing gaps in community health, public health also builds and maintains a strong organizational infrastructure for public health. This requires a great deal of program management to organize.
7. Communications
All managers are required to communicate, and public health program managers are no exception. They need to convey vital information to various groups, such as key stakeholders, coworkers, and community members. “All types of communications—written or verbal—are important because public health folks need to understand how to interpret findings, materials, data, and then make it digestible to the audience they’re serving,” Grilli-Scott adds.
8. Leadership
Successful public health program managers need effective leadership skills. Not only do they lead a team of public health professionals, but they also hold a leadership role within the community they serve. A health program or campaign is only as strong as the team that helped build it and the messaging relayed to the target audience.
9. Research
Public health is a preventative healthcare sector that mainly deals with research. Understanding the various research methods performed by public health program managers, such as case-control studies, cross-cutting studies, and medical administrative databases can give you a leg up compared to other candidates.
10. Program Development
Program development is a vital public health program management skill. While leadership and management skills are crucial elements of this position, a well-developed program plan is the foundation of a public health program manager’s responsibilities. Employers look for candidates that not only have the capacity to take on this responsibility but have experience doing so with proven success.
How to Develop Public Health Skills
Many prospective healthcare professionals gain the required skill set through a traditional advanced degree. For example, public health professionals must obtain a Master of Public Health (MPH) in order to gain employment post-graduation. Northeastern University’s accredited, one-year experiential master’s program can take your public health skills to the next level.
“There’s an experiential field component to all MPH degrees that are accredited,” says Grilli-Scott. “But with this one-year, accelerated program, you’re getting experiential opportunities, both in your coursework and through the traditional MPH practicum experience.” Most of these experiences expose students to the positive effects that successful local public health can have on a global scale.
So whether you’re a recent college graduate or a career changer, it’s important to find a program that gives you experience with the right skills in the field.
To learn more about advancing your public health career, download our free guide below.
Subscribe below to receive future content from the Graduate Programs Blog.
About kate gibson, related articles.

Jackney Prioly Joseph on How Her MPA Helped Her Career


Master’s in Nonprofit Management vs. Public Administration

How an MPH Clarified One Alumna’s Career Path
Did you know.
Advanced degree holders earn a salary an average 25% higher than bachelor's degree holders. (Economic Policy Institute, 2021)
Northeastern University Graduate Programs
Explore our 200+ industry-aligned graduate degree and certificate programs.
Most Popular:
Tips for taking online classes: 8 strategies for success, public health careers: what can you do with an mph, 7 international business careers that are in high demand, edd vs. phd in education: what’s the difference, 7 must-have skills for data analysts, in-demand biotechnology careers shaping our future, the benefits of online learning: 8 advantages of online degrees, how to write a statement of purpose for graduate school, the best of our graduate blog—right to your inbox.
Stay up to date on our latest posts and university events. Plus receive relevant career tips and grad school advice.
By providing us with your email, you agree to the terms of our Privacy Policy and Terms of Service.
Keep Reading:
5 Homeland Security Careers for the Future

The Top 3 Job Requirements For a Homeland Security Career

What Are Security Studies?

Should I Go To Grad School: 4 Questions to Consider
- CONSULTING & TRAINING SERVICES

Related Categories: Council on Linkages , Workforce Development
Download this File
- Core Competencies Tools
- Examples of Core Competencies Use
- Upcoming Events featuring the Core Competencies
- Recent News and Blog Discussion about the Core Competencies
- Tailored Technical Assistance related to the Core Competencies
Add A Comment
Great information and very applicable.
Josephine Ekong
Very informative
JUDITH SPENCER-COLE
very good content
Carol Bristow
Good information
Tom Johnson
Valuable information!
H. David Moss
I found it very informative and useful.
Very good information,mostly upto date and relevant to my work experience. May need one or two classes changed to include more current health concerns and safety trainings.
Rafael Portillo
Very good information
Why am I only seeing Data and Analytics as the core competencies?
Ruth Greenslade
I am looking for the 2020 revisions to the Core Competencies. Can you add a link to the new version to this page?
Michelle Hutchinson
Thank you for your long and hard work on the updates to the Core Competencies for Public Health Professionals. I feel I would be remiss, however, if I didn't mention how disappointed I am to see that revisions contain nothing about organizational health literacy skills (https://www.cdc.gov/healthliteracy/learn/index.html, also called responsive health literacy skills), or at the very least, plain language skills. One of the 10 Essential Public Health Services (Revised 2020, https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html) is "Communicate effectively to inform and educate people about health, factors that influence it, and how to improve it." How can public health professionals communicate effectively if they don't know how to use health literacy practices (https://www.cdc.gov/healthliteracy/planact/steps/index.html), or at the very least, use plain language standards (https://www.plainlanguage.gov/guidelines/)?
Ida Bradley
The content of this information and the accessment is very rewarding. Learning about the program, can have a impact on pimproving my skills and project development.
A very interesting overview for public health.
The information provide is very useful on improving certain areas of weakness relating to public health field. The information also has helped me build ans specialize on my area of expertise.
Migdalia torres Velazquez
Wonderful and interesting
Loraine Cooper
How do I get to the core competencies assesment from here?
The information given was very informative
Uke Patience
Very informative page, it's important to understand basic training ideas that are relevant for understanding what you want and how it can impact on areas of interest and practice for an improved work performance.
Linda Bayless
Great information
Anthony chukwunwike ogorchukwu
Thanks I'm so much delighted to work in the future of our public health organization and I believe our goal is to achieve a common goal in the future to impacts More information about the public on health and safety which can improve our services and innovation of building a community and Nation
Crosswalk of the 2014 Core Competencies for Public Health Professionals and the Essential Public Health Services
Crosswalk of the Core Competencies for Public Health Professionals and the Essential Public Health Services
Crosswalk of the 2014 and 2010 Core Competencies for Public Health Professionals
ASTHO and PHF Present: 2014 Core Competencies for Public Health Professionals (Webinar)
ASTHO Virtual Town Hall Meeting: Core Competencies for Public Health Professionals
Subscribe to PHF

Master These Public Health Skills with an MPH
Advanced public health professionals work in a field that requires specialized training, under job titles like Epidemiologist, Sanitarian, Biostatician, Disaster and Emergency Specialist, and Public Health Director or Educator. Roles like these require a specific set of public health skills that can only be attained through a Master’s in Public Health ( MPH ) program.
What does it take to succeed in the world of public health? Goodwin University’s MPH curriculum offers what you need to develop and enhance these public health skill areas, and forge a rewarding career.
1. Research and Analytical Skills
In the public health profession, you will be expected to draw on your abilities to conduct thorough and sound research. Even more, you will need to possess analytical skills to interpret your research and turn it into action! You see, methodology is not enough in an advanced public health career. In this field, leaders must use their research to make decisions, address public health needs, allocate resources, and affect large populations of people. Therefore, accuracy in your assessments is of the utmost importance.
In your second semester at Goodwin University’s MPH program, you will dive right into two required courses designed to help hone your research and analytical skills: one on methods , and the second on ethical issues .
2. Ethics and Empathy
Speaking of ethical issues—if you want to be working in public health, your standard of ethics should be sky-high. Whether you’re working with biohazards, vulnerable populations, or infectious diseases, the integrity of your actions will go hand-in-hand with mitigating risk. In fact, there is an entire 34-page Public Health Code of Ethics, published by the American Public Health Association (APHA), which is an important resource for all public health practitioners. The APHA includes the following “core ethical values” in no particular rank or order:
- Professionalism and Trust
- Health and Safety
- Health Justice and Equity
- Interdependence and Solidarity
- Human Rights and Civil Liberties
- Inclusivity and Engagement
Each of these points are inter-dependent on one another, if the promotion of public health is to succeed and do good for our communities. Sensitive public health situations require an ethically sound and empathetic public health professional.
3. Effective Communication
No matter your specific role in public health, communication skills are going to be absolutely essential in order to do your job well. As one Forbes says of “competent and confident” communication, “…there may be no skill more fundamentally important for realizing progress.” And isn’t “progress” the entire point of public health work?
An MPH curriculum is built to give you the confidence and decisiveness in your technical skills and education, to make you an efficient communicator and leader. After all, public health leaders must communicate with a range of individuals and teams, communities and populations. Communication is at the heart of their career.
You can beef up the talk to your walk, as well, with Career Services from your University. At Goodwin, these include benefits like mock interviews and employer networking events. Showing your strength as a communicator will start when you first shake the hand of your prospective new boss. Striding into the hiring process with a support system like Goodwin University at your back should put you at ease.
4. Critical Thinking
People who like problems are often attracted to the field of public health. Well, people who like solving them, anyway! The electives offered in the MPH program at Goodwin University teach real-life public health skills, such as: U.S. Healthcare Delivery Systems , Public Health and an Aging Society , and Introduction to Maternal and Child Health .
Learning what the core public health issues are in specific populations — including rural or dense communities, aging groups of people, and family health — will help you assess and diagnose problems, draw up a plan for action, and implement health programs that fit the population’s needs. This is a key area where you’ll want to demonstrate your strong critical thinking skills through specificity. Different populations require different solutions, and as a leader in public health, you will want to display and embody an attentiveness to diversity and cultural competency.
5. Politics and Policy Management
Whether you’re working in the field and collecting data, analyzing biohazardous materials in the lab, or creating reports for government organizations, politics and policy management are essential public health skills for your career. In fact, you will most certainly be touching policy in one way or another. You might be writing policy, implementing policy, evaluating policy, or actively trying to improve policy. All of the work that public health workers do is scaled for systems, and therefore, policy must be put in place in order for populations to receive the intended assistance. The course Public Health Policy will provide a strong foundation for your career, which you may build on with electives like Public Health Administration , Environmental Health Policy , and Public Health Economics .
The MPH degree at Goodwin University is focused on producing scholars who are equipped with the most important public health skills—the skills required for today’s competitive workforce. Working in public health is a dynamic way to make an impact on the world, and develop a rewarding career. Learn more about the advantages of Goodwin University’s Master’s in Public Health program online.

Goodwin University is a nonprofit institution of higher education and is accredited by the New England Commission of Higher Education (NECHE), formerly known as the New England Association of Schools and Colleges (NEASC). Goodwin University was founded in 1999, with the goal of serving a diverse student population with career-focused degree programs that lead to strong employment outcomes.
- Open access
- Published: 02 April 2018
Population health intervention research training: the value of public health internships and mentorship
- Anne-Marie Hamelin 1 &
- Gilles Paradis 1
Public Health Reviews volume 39 , Article number: 6 ( 2018 ) Cite this article
4889 Accesses
11 Citations
25 Altmetric
Metrics details
Better alignment between academia and public health practice and policies are critical to improve public health actions. Training of future researchers to address complex issues and to conduct transdisciplinary and collaborative research will help improve this alignment. In this paper, we describe the role of internship placements and mentorship for trainees’ skills development in population health intervention research and the benefits of embedding research trainees within public health organizations.
This qualitative descriptive study assessed the perceptions of the role and benefits of internships and mentorship for population health intervention research training among former doctoral and postdoctoral students, public health mentors, and senior public health managers who participated in the 4P Program, a research training program which bridges academic training and the public health system in Quebec, Canada. Two types of interviews were conducted: telephone semi-structured interviews by an external evaluator and face-to-face trainee “exit” interviews by the Program co-director. Semi-annual evaluation reports from each trainee were also reviewed. Qualitative data were subjected to a thematic analysis.
Internships provided trainees with a working knowledge of the public health system and the context in which decisions and public health interventions are implemented. It was an opportunity for trainees to interact with knowledge-user partners and assess the gap between research and practice. Effective mentorship was key to help trainees interpret the public health reality and develop population health intervention research skills. Trainees learned to ask the “how” questions that are critical for in-depth understanding of complex interventions and the conditions under which they can be best implemented. Conditions of success of internships and mentorship for population health intervention research included the alignment of the interests between the trainee, the mentor and the public health organization, quality mentoring, and the acquisition of specific population health intervention skills, especially collaborative research skills.
Conclusions
The findings suggest that public health internships and mentorship facilitate trainee engagement in applied public health research.
Increasing research capacity in population health intervention research (PHIR) requires better alignment between academia and public health practice [ 1 , 2 , 3 ] and a greater ability of researchers to conduct transdisciplinary and collaborative research [ 4 , 5 , 6 , 7 , 8 , 9 ]. Internships and mentorship are perceived to be important aspects of training and career development for researchers [ 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 ]. However, whether and how they enhance research training in public health is poorly understood.
Our objectives are to examine (1) the role of internship placements and mentorship for trainees’ skills development in PHIR and (2) the benefits of embedding research trainees within public health organizations (PHOs), based on the perspective of trainees and mentors who participated in the 4P Program, a university-public health partnership research training program [ 19 ].
Program description
The main objective of the 4P Program [ 19 ] was to prepare doctoral and post-doctoral students from Quebec universities to conduct applied research on population and public health interventions (PHI) in PHOs. Over 12 years (2003–2015), 63 doctoral and post-doctoral trainees were funded to participate in the Program. It offered training based on core competencies development, including (1) foundational knowledge of public health, (2) transdisciplinary research, (3) intervention research ethics, (4) development of research networks and partnerships, (5) knowledge translation, and (6) research career management.
A unique component of this Program involved embedding trainees into a PHO under the supervision of a public health mentor. Doctoral candidates were required to spend 60% of their time for 3 years in a PHO and post-doctoral fellows, 80% of their time for 2 years. Internship objectives were to (1) provide a public health field experience to trainees; (2) increase their understanding of the public health system, its values and its needs; (3) understand how public health problems are conceptualized, researched, and solved in PHOs; and (4) develop cross-disciplinary working relationships with practitioners while appreciating the challenges of collaborative work and knowledge translation in implementing evidence-informed interventions.
Ten PHOs hosted trainees. A total of 37 departments from seven universities and 31 disciplines were represented among trainees and mentors. Sixty percent of mentors who supervised trainees were employed by PHOs, 47% had a PhD, 44% were MDs, and 38% mentored more than one 4P trainee. Mentorship took place through regular in-person meetings. The roles and responsibilities of mentors are presented in Table 1 . Each trainee was expected to play an important role in the activities of the mentor’s public health team, while maintaining progress in their graduate studies. The placements’ specific experiences and topics of study were varied and reflected current public health priorities.
The Program’s overall evaluation has been described [ 19 ]. For the current qualitative study, we assessed the perceptions of Program participants on the role and benefits of internships and mentorship for PHIR training through multiple means (Table 2 ; see also a timeline of the evaluation in Fig. 1 ). Telephone semi-structured interviews (TI) were conducted by an external evaluator with former trainees, mentors, and senior public health managers to assess their perceptions of the Program’s contributions to trainee outcomes. For these interviews, 18 out of a total of 44 trainees who had completed the Program by January 2014 were randomly selected, ensuring balance across PHOs (local, regional, national level), disciplinary field of origin (social sciences and humanities, natural and life sciences, other), and research areas (prevention, health promotion, organization of health care and services, public policies). Six public health mentors (out of ten sampled) and two senior PHO managers (out of five sampled) were also interviewed. Interviews were recorded and summary notes transcribed for thematic analyses. From 2009 onward, trainees had face-to-face, end-of-Program “exit interviews” (EI) that lasted between 90 and 120 min with the Program co-director to assess the attainment of learning objectives and perceived impact of the Program on their training. Thematic analyses were conducted from detailed notes from 33 exit interviews (out of 37). In addition, the semiannual trainee self-reported internship evaluations (SAER, 2003–2014) were reviewed. Finally, online surveys completed by 38 out of a total of 63 former trainees and 41 out of a total of 55 mentors provided additional information for the acquisition of skills in PHIR and were used to add to the triangulation of methods and cross verify the convergence of the results.
Timeline of different evaluation components of the 4P Program
We examined the role of internships and mentorship based on the unique features of PHIR [ 20 ] in which PHIs are conceived as complex systems in continuous interaction within a changing environment [ 21 ]. PHIR questions of interest emphasize the “how” and revolve around the relevance, coherence, responsiveness, achievements, and impact of interventions [ 20 ]. We therefore paid attention to the broad knowledge and particular competencies needed by researchers to address the complexity of public health problems, programs, and policy interventions and to understand the “process of designing and testing solutions” [ 20 ].
We drew on the literature on effective research mentoring [ 12 , 13 , 22 , 23 ] to examine the mentoring relationship [ 13 , 24 ]. Research mentorship was defined as: “…a complex and multidimensional process through which emerging scientists acquire the norms and standards, values and attitudes, and knowledge, skills and behaviors to develop into successful independent researchers” [ 24 ]. The literature on training in public health research [ 5 , 11 , 25 , 26 , 27 , 28 ] was also used to examine learning processes that foster skills development in PHIR.
The role of internships and mentorship
In interviews and in semiannual reports, a majority of trainees and mentors stated that embedding students in PHOs had been positive, which reflects the results of the online survey [ 19 ]. First and foremost, they reported that the placements provided a unique opportunity for trainees to acquire an understanding of the role and functions of the public health system and to connect with the reality of conducting public health research “on the ground.”
According to exit interviews, the placements enabled trainees to interact with public health practitioners and to understand PHIs. Embedding of trainees in PHOs created the opportunity to experience the development, implementation, and evaluation of interventions: “I was able to reflect and question public health interventions thanks to my internship and my mentor's team that showed me what effective interventions are and how to evaluate them” (EI-17). Likewise, trainees and mentors in telephone interviews reported: “the possibility of experiencing public health” ... “to know the conditions for the implementation of the action” (TI-T8), “to understand priorities” (TI-T6). Trainees gained an understanding of patterns of interactions and relationships within PHO: “My internship allowed me to better understand the situation on the ground, the necessary conditions for innovations, coalitions and changes” (SAER-16).
The placements allowed trainees to appreciate the range of research activities in PHOs and the finality of PHIR: “I saw what can be done in population health research” (EI-27). It also permitted trainees to identify the multidimensionality (e.g., contextual, ethical dimensions) of public health research problems and understand what research questions are of interest to practitioners, according to interviews with mentors. Trainees acquired a knowledge of the processes involved in PHIR and how research informed programs: “I gained a deeper understanding of the structure of public health research, how the evidence is constructed, how decisions are made: all this was new to me” (EI-25). Trainees learned to get closer to decision-makers and to invite knowledge users on their teams from the research onset. Indeed, in exit and in telephone interviews, trainees characterized placements as thought-provoking and formative experiences in public health research.
Simultaneously, the placement was an opportunity to assess the gap between research and practice, and experience intersectorality, which one trainee defined as “the needed reconciliation of the public health practice and the research practice” (EI-27). By being in the practice environment, trainees discovered that they had to learn how to do research in relation with partners, to develop intersectoral working relationships with practitioners (EI-10), to focus research on a common goal with decision-makers (EI-11).
For trainees, mentorship was key to penetrate the field of public health: “The main quality of mentoring is getting us into the public health environment to conduct our projects” (EI-5). This integration was critical for internship success:
“Insertion into a research team makes it possible to engage in learning about research. Mentoring provided me with access to the senior researchers who helped me with my learning, such as how to coordinate a project, make a budget, acquire methodological knowledge, manage a database, and so on. I had access to several researchers who were open and who stimulated the learning of early career researchers. … I have greatly benefited from the leadership of these researchers and their contacts with productive external members” (EI-35).
A successful mentorship involved a reciprocal commitment between mentor and mentee. Engaged and available mentors, who were skilled in PHIR, respectful of trainees, and who drew upon trainees’ strengths, were perceived as successful. For example, one trainee said:
“Not only were my learning objectives and career goals present in all discussions with my mentor, but also the public health vision and purpose. ... The exchanges contributed to the further elaboration and application of public health concepts in my research work” (EI-11).
An engaged trainee whose project fitted the PHO’s priority was seen as stimulating by mentors. Altogether, a good fit between the mentor and the trainee, immersion of the trainee in the mentor’s research team, and productive mentoring dialogs set the conditions for success.
Mentors helped trainees refine their competencies, develop research methods applied to the local context, and provided opportunities for networking and research partnerships. Beyond the mentoring relationship, trainees noted the importance of the research capacity at the PHO and of the leadership of the mentor.
Benefits of internships and mentorship
The internships and mentorship allowed trainees to apply research skills in context and integrate learning. Integration of learning about PHIR happened in multiple ways: changes in attitudes, a recognition of the complexity of PHIs, a gradual deepening of PHIR, and the development of cross cutting competencies, as shown below.
The confrontation with the realities of the public health field affected trainees’ attitudes towards research. It was a shock for some trainees: “I changed my research topic” (TI-T8). Internships and mentorship encouraged openness: “The program forced us to open up to the world and take a systemic approach; it permitted to get out the dominant train of thought” (EI-16). Trainees became more critical of their research and asked “what is the use of what we do?” (e.g., EI-16, EI-19). Trainees said that they gained maturity and confidence: “I gained more insights as I progressed through my internships” (EI-34); “I built my capacity to ask questions and discuss public health problems” (EI-17). Trainees alluded to a “process of maturation” (EI-16, EI-35) in the ways of seeing things and looking for solutions to public health challenges. Internships and mentorship strengthened trainees’ perspectives on population health intervention research. They said: “The program brought a refreshing perspective by bringing together researchers and decision-makers; without the Program, I would not have had the potential to influence practice” (TI-T6); “It expanded my knowledge and the range of what I thought I could do” (EI-2); “[It] made me realize the importance of knowledge translation” (EI-27). Trainees spoke of becoming more open to the realities of core public health functions and to the need for research to inform practice and have an impact: “I quickly learned this: to change things, it is not sufficient to have knowledge but you need the know-how to put it in practice” (EI-37); “How can we attract attention of decision-makers, how can we measure change?” (EI-3).
Trainees discovered the complexity of real-world public health problems and interventions. They experienced the influence of context on PHIs, including the power relationships between various stakeholders engaged in PHIs (e.g., practitioners; managers): “Now I see the importance of taking into account the realities on the ground” (EI-11).
Many trainees said that they felt better equipped to understand complexity, health equity, and the need for knowledge translation; they also developed critical thinking skills. Trainees started to ask questions like “so what” and “how and under which conditions” can an intervention be successfully implemented.
“Now I ask myself: “what’s the point?”, “what’s it for?”, “what do we do next?”, “what will the managers who work at the Agency do with this?” Thanks to my internship, I familiarized myself with the milieu and saw how, with my mentor, I could get managers and decision-makers to listen. Now I know that my thesis will serve in practical ways the development of healthy public policies” (EI-19).
Trainees gained research experience: “[The internship] ... allowed me to develop a more complex research plan” (EI-3). This is also reflected in their willingness to revisit their conceptual frameworks and adopt a more transdisciplinary approach to research. In some instances, trainees revised their research protocol to more effectively respond to public health priorities. One trainee made this statement:
“The approach to intervention research was a discovery. This changed the way I look at the research process, and got me to think about research in terms of how it should be led in order to influence intervention and be used by decision-makers. Addressing ethics, considering the complexity of evaluation of interventions, all this knowledge has changed my way of thinking and influenced the choice of the theoretical framework of my thesis. This has influenced my way of seeing my research topic. I now have a more systematic view of innovation” (EI-16).
The mentors corroborated in interviews, and in internships reports, that the internships permitted trainees to reorient their research according to their observations.
Throughout their internships, trainees experienced the challenges of applying the principles of intervention research and developed cross-cutting competencies essential to PHIR such as interdisciplinary and intersectoral communication, partnerships, networking, and knowledge translation. Trainees improved their capacity to interact with researchers and knowledge-user partners from different disciplinary perspectives. They expressed comments such as this one:
“I developed an openness to other disciplinary horizons, learned to adjust my language, to involve various actors to address a particular issue, how to work in partnership. I would not have done this so thoroughly without the 4P” (EI-23).
Mentorship in applied public health settings enabled trainees to learn about processes of knowledge translation, including exchange between researchers and decision-makers, and sharing of knowledge “in an appropriate and effective manner” (SAER-30). Trainees also learned to produce research results useful to public health. Summing up her experience, one trainee said:
“My mentor put me in close contact with the stakeholders at the regional level. ... My ability to produce useful results was enhanced. ... The 4P Program brings legitimacy to the trainee, which translates into an authorization to observe, engage in dialogue with practitioners and key decision makers in public health, be heard and considered. This legitimacy and the quality of the knowledge exchanges are linked, and this shapes things to come, i.e. the translation of knowledge into action. The trainee presence in the public health milieu shaped a reciprocal relationship with the mentor” (EI-5).
A majority of trainees spoke of placements as having broadened their research network and facilitated professional connections with practitioners and decision-makers. Networking and knowledge exchange practices with mentors and knowledge users represented the starting point in learning to engage in collaborative PHIR with members of PHOs.
Overall, former trainees said they acquired competencies not taught in doctoral programs. Field placements acted as catalysts for achieving mastery of the 4P Program core competencies. One trainee put it this way:
“The 4P Program acted as a buffer zone between doctoral studies and the reality of the practical environment. It has shown its full worth in accompanying us in the milieu and by facilitating linkages with this milieu” (EI-26).
Nevertheless, many trainees mentioned they had less than perfect public health internships and mentorship experiences in both exit (about 12 out of 33 trainees since 2009) and telephone interviews (about 7 out of 18; sample of trainees since 2003). For example, trainees said: “my mentor was not available” (EI-19; TI-T3; TI-T14; TI-T16); “It was difficult to establish a good mentoring relationship with my mentor” (EI-19); “I don’t think my mentor understood her role” (EI-27); “My research topic was not a priority for the PHO. I didn’t work with the mentor’s team. As a result, I couldn’t develop my skills in collaborative research as I expected” (EI-13); “My mentor’s team was dynamic but there was no opportunity to exchange with other research teams” (EI-06). In telephone interviews, one trainee explained that her/his internship fell short of her/his expectations for a number of reasons: she/he was not asked by her/his mentor to participate in regular team meetings, there were no real opportunities to develop collaborative projects, and no opportunity to be integrated as a full researcher in a PHO after her/his placement (TI-T3).
Internships and mentorship influenced trainees’ career path. Trainees reported that internships opened doors to employment opportunities outside academia and enabled opportunities for collaboration. However, unfavorable experiences could reorient research careers away from public health. Trainees and mentors alike identified characteristics of successful placements, including the volume of research activity in the PHO, the dynamism of the PHO’s sector of activity to which the trainee was attached, and the PHO focus on intervention research.
Public health managers, for their part, felt that three conditions had to be met for successful internships: (1) integration of the trainee within the organizational framework of the PHO, (2) alignment of the trainee research topic with the PHO’s and the research team priorities, and (3) contributions of trainees to innovative research, practice, and evaluation within the PHO. In their eyes, the contribution of the Program was through the insertion of trainees in cutting-edge research and emerging initiatives in public health.
The mentors, trainees, and public health managers provided advice for how to strengthen the quality and improve the impact of research internships. They advised to improve (1) the fit between the trainee, the mentor, and the PHO (ensure the best alignment of the interests of each, make explicit the aspects of the collaboration, and establish the basis for a successful milieu-trainee relationship); (2) the skill sets of mentors (train mentors in PHIR skills, and support them to fulfill their mentoring role); and (3) the development of PHIR skills (a combination of an increased exposure of trainees to PHIR, a stronger intervention focus in trainees’ research, and a more structured mentoring process focusing on the acquisition of specific PHIR skills).
The consistency of findings across methods and sources of data conveys a clear message on the conditions of success of internships and mentorship for PHIR.
Through prolonged internship and mentorship, 4P trainees explored the functional and relational characteristics of the public health system and developed a working knowledge of complex organizations, including structure, staff, activities, and context. This was seen by the Program designers as a prerequisite for the development of PHIR competencies. This is congruent with the observations of Bachrach and Daley [ 29 ] who noted a need for “experience-based training and mentoring in the skills needed to lead and collaborate in interdisciplinary teams” (p. 252). Interdisciplinary collaboration skills were one of three core domains, along with knowledge acquisition and knowledge translation, identified by these authors as critical in developing outstanding interdisciplinary population health scientists [ 10 ].
Building on social theory [ 30 , 31 ], Potvin and colleagues provided conceptual grounds to reflect on PHIs and the role of PHIR in supporting innovation and transformation of practices in the “social-health space” [ 21 , 32 ]. Bilodeau and Potvin [ 21 ] argue that “conceiving PHIs as systems, [which] provides a framework for problematizing relationships between interventions and their contexts, and how such relationships transform them both” (p.2), is strategic since “this leads to examining the connections between the various elements of the intervention and context, the network they form and the evolution of that network” (p.2).
In this vein, PHOs represent important research training laboratories to understand the “social-health space.” Indeed, internships in PHOs and mentorships opened a window on the “sociotechnical network,” a hybrid collection of social actors from various sectors (e.g., public administration, civil society, private sector) that connect with knowledge on activities and services and with resources and constraints from the environment [ 21 ]. In this vibrant context, the trainee may (1) observe the dynamic context in which decisions are made and interventions are implemented, (2) witness the interactions between these social actors, and (3) experience interdisciplinary research partnerships.
Becoming part of this network meant access to the “black box of PHIs” [ 21 ]. The trainee could link intervention “processes, conditions, context, and effects” [ 33 ] (p.14). The mentor acted as an operator that permitted the trainee to observe the inner working of the black box of interventions and learn, for example, how an intervention is decided upon and implemented; how it produces its effects; how actors relate to each other, share information, negotiate, connect, and influence intervention design and implementation; how decision-makers manage changing circumstances; and how their decisions impact intervention outcomes. In sum, the “how” questions are critical to a more comprehensive view of the complexity of PHI [ 21 ] and are needed to accelerate the effective implementation of evidence-informed public health practice and decision-making [ 34 ]. Immersion in the public health milieu promoted a collaborative research workspace in which trainees interacted with knowledge-user partners and experienced the co-construction of knowledge, including issues of transdisciplinarity and partnerships [ 35 ], as well as challenges and opportunities for knowledge translation [ 36 , 37 ].
Consistent with twenty-first century goals for public health training [ 28 ] and adult learning principles [ 38 ], trainees who benefited most from their internships were exposed to learning situations that engaged them actively in a complex and changing public health system to develop and apply new knowledge relevant to PHIs. Such applied training appears to be valuable in developing the field of PHIR [ 39 ], creating the evidence base for population health, and addressing the demand for consequential science [ 10 , 29 , 33 , 40 ].
The internship experience was not the same for all trainees and was directly linked to the quality of mentorship. Observed challenges in mentoring coincided fully with the scientific literature regarding the need for an adequate match between mentor and mentee [ 24 ], explicit communication strategies and clarification of expectations [ 14 , 22 ], and formal training in mentoring practices [ 12 , 14 , 22 , 24 , 41 , 42 ] and skills to implement PHIR [ 26 ]. The need to better structure mentorship and objectives around PHIR learning (e.g., to introduce focused discussions around designing and testing the effectiveness of PHIs) was identified as key to program improvements. As per the literature on mentorship [ 12 , 14 , 42 , 43 ], mentors should be provided with the tools and resources to initiate discussions as well as guide trainees’ observations and research skills development, and mentors should be evaluated.
Successful mentoring also requires immersion in a facilitative environment [ 13 , 43 ] with an excellent research capacity [ 22 , 42 ], and that promotes the integration of contributions from diverse disciplines [ 10 ]. There is also a role for institutions to oversee mentorship [ 24 , 42 ] and to promote collaborations between practice, policy, and research [ 44 ].
From the Program’s perspective, challenges to creating successful mentored internships in public health include structuring the learning environment and measuring the efficacy of the mentoring process, sustaining a steady engagement of mentors in the Program, and ensuring comprehensive training in collaborative research [ 25 , 29 , 35 , 37 , 45 , 46 , 47 ]. More broadly, challenges also include maintaining training program funding and supporting new PHIR researchers who completed the Program. Another issue concerns the interface between public health and university. The difficulties involved in bringing together two entities whose mission, vision of research, and priorities are different require clarification and strengthening of collaborations and partnerships [ 46 ].
This study suggests that our program created a successful learning environment that allowed the opening of the “black box” of PHIs and was conducive to the development of PHIR competencies among PhD and post-doctoral trainees. Public health internships and mentorship prepared trainees to engage in “public health research of consequence” [ 40 ]. Indeed, quality internships gave trainees the opportunity to experience the development, implementation, and evaluation of public health programs and policy interventions while quality mentorship was conducive to asking consequential questions like “so what” and “how and under which conditions” an intervention could be successful.
Future research to improve PHIR training include (1) identifying which aspects of mentorship are most conducive to meaningful, long-term integration of researchers in PHOs and to orienting the research career of young investigators towards transdisciplinary collaborative research; (2) understanding the dynamic context in which trainees, mentors, and institutions produce innovative research, practice, and policies; and (3) measuring the conditions in which academia and the public health system can work durably to bridge research and practice in public health.
Green LW. Public health asks of systems science: to advance our evidence-based practice, can you help us get more practice-based evidence? Am J Pub Health. 2006;96:406–9.
Article Google Scholar
Institute of Medicine. Who will keep the public healthy? Educating public health professionals for the 21st century. Washington: The National Academies Press; 2002.
Brownson RC, Fielding JE, Green LW. Building-capacity for evidence-based public health: reconciling the pulls of practice and the push of research. Annu Rev Public Health. 2018; First posted on November 20 2017;39:1–27.
Jayasinghe S. Conceptualizing population health: from mechanistic thinking to complexity science. Emerg Themes Epidemiol. 2011;8:2–7.
Article PubMed PubMed Central Google Scholar
Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am J Public Health. 2012;102:1274–81.
Jones C, Clavier C, Potvin L. Adapting public policy theory for public health research: a framework to understand the development of national policies on global health. Soc Sci Med. 2017;177:69–77.
Article PubMed Google Scholar
Mitrany M, Stokols D. Gauging the transdisciplinary qualities and outcomes of doctoral training programs. J Plan Educ Res. 2005;24:437–49.
Lang DJ, Wiek A, Bergmann M, Stauffacher M, Martens P, Moll P, Swilling M, Thomas CJ. Transdisciplinary research in sustainability science: practice, principles, and challenges. Sustain Sci. 2012;7:25–43.
Lee LM, Zarowsky C. Foundational values for public health. Public Health Rev. 2015;36:1–9.
CAS Google Scholar
Bachrach CA, Robert S, Thomas Y. Training in interdisciplinary health science: current successes and future needs. Institute of Medicine Roundtable on Population Health Improvement of the National Academies of Sciences, Engineering and Medicine edition; 2016.
McGartland Rubio D, Schoenbaum EE, Lee LS, Schteingart DE, Marantz PR, Anderson KE, Platt LD, Baez A, Esposito K. Defining translational research: implications for training. Acad Med. 2010;85:470–5.
Jeste DV, Twamley EW, Cardenas V, Lebowitz B, Reynolds CF III. A call for training the trainers: focus on mentoring to enhance diversity in mental health research. Am J Public Health. 2009;99:S31–7.
Sambunjak D, Strauss SE, Marusic A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med. 2009;25:72–8.
Johnson MO, Ghandi M. A mentor training program improves mentoring competency for researchers working with early-career investigators from underrepresented backgrounds. Adv Health Sci Educ. 2015;20:683–9.
Gourevitch MN, Jay MR, Goldfrank LR, Mendelsohn AL, Dreyer BP, Foltin GL, Lipkin M, Schwartz MD. Training physician investigators in medicine and public health research. Am J Public Health. 2012;102:e39–45.
Paglis L, Green SG, Bauer TN. Does adviser mentoring add value? A longitudinal study of mentoring and doctoral student outcomes. Res High Educ. 2006;47:451–74.
Thornicroft G, Cooper S, van Bortel T, Kakuma R, Lund C. Capacity building in global mental health. Harv Rev Psychiatry. 2012;20:13–24.
Cole DC, Jonhson N, Mejia R, McCullough H, Turcotte-Tremblay A-M, Barnoya J, Luco SFM. Mentoring health researchers globally: diverse experiences, programmes, challenges and responses. Glob Public Health. 2016;11:1093–108.
Paradis G, Hamelin A-M, Malowany M, Levy J, Rossignol M, Bergeron P, Kishchuk N. The university-public health partnership for public health research training in Quebec, Canada. Am J Public Health. 2017;107:100–4.
Hawe P, Potvin L. What is population health intervention research? Can J Public Health. 2009;100:I8–I14.
Google Scholar
Bilodeau A, Potvin L. Unpacking complexities in population health interventions with the actor-network theory. Health Promot Int. 2016:1–9.
Sopher CJ, Adamson BJS, Andrasik MP, Flood DF, Wakefield SF, Stoff DM, Cook RS, Kublin JG, Fuchs JD. Enhancing diversity in the public health research workforce: the research and mentorship program for future HIV vaccine scientists. Am J Public Health. 2015;105:823–30.
Kalichman M. Mentoring . In Responsible conduct of research: an introductory guide . Edited by the Office of Research Integrity at the University of California; 2001. http://ccnmtl.columbia.edu/projects/rcr/rcr_mentoring/foundation/index.html
Keyser DJ, Lakoski JM, Lara-Cinisomo S, Schultz DJ, Williams VL, Zellers DF, Pincus HA. Advancing institutional efforts to support research mentorship: a conceptual framework and self-assessment tool. Acad Med. 2008;83
Hall KL, Feng AX, Moser RP, Stokols D, Taylor BK. Moving the science of team science forward: collaboration and creativity. Am J Prev Med. 2008;35:S243–9.
Israel BA, Coombe CM, Cheezum RR, Schulz AJ, McGranaghan RJ, Lichtenstein R, Reyes AG, Clement J, Burris A. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health. 2010;100:2094–102.
Lyall C, Meagher LR. A masterclass in interdisciplinarity: research into practice in training the next generation of interdisciplinary researchers. Futures. 2012;44:608–17.
McKee M. Seven goals for public health training in the 21st century. Eur J Pub Health. 2012;23:186–7.
Bachrach CA, Daley DM. Shaping a new field: three key challenges for population health science. Am J Public Health. 2017;107:251–2.
Potvin L, Gendron S, Bilodeau A, Chabot P. Integrating social theory into public health practice. Am J Public Health. 2005;95:591–5.
Potvin L, Clavier C. La théorie de l'acteur-réseau. In: Aubry F, Potvin L, editors. Construire l'espace socio-sanitaire. Montréal: Les Presses de l’Université de Montréal; 2012.
Potvin L. Repères conceptuels pour réfléchir sur l'action dans l'espace socio-sanitaire . In Construire l'espace socio-sanitaire . Edited by Aubry F, Potvin L. Montréal: Les Presses de l’Université de Montréal; 2012.
Potvin L, Di Ruggiero E, Shoveller J. Pour une science des solutions : la recherche interventionnelle en santé des populations. La santé en action. 2013:13–5.
Potvin L. Wishful thinking will not do it! Practitioners and decision-makers need tools to implement evidence-informed public health. Int J Public Health. 2013;58:491–2.
Aubry F, Clavier C, Jones CM, Mantoura P, Bisset S, Gough M. La formation des chercheurs en santé publique. In Construire l’espace socio-sanitaire. Edited by Aubry F, Potvin L. Montreal: Presses de l'Université de Montréal; 2012.
Hobin EP, Hayward S, Riley B, Di Ruggiero E, Birdsell J. Maximising the use of evidence: exploring the intersection between population health intervention research and knowledge translation from a Canadian perspective. Evid & Policy: A Journal of Research, Debate and Practice. 8(1):97–115.
Clavier C, Sénéchal Y, Vibert S, Potvin L. A theory-based model of translation practices in public health participatory research. Sociol Health Illn. 2012;34:791–805.
Bryan RL, Kreuter MW, Brownson RC. Integrating adult learning principles into training for public health practice. Health Promot Pract. 2009;10:557–63.
Di Ruggiero E, Potvin L, Allegrante JP, Dawson A, Verweij M, De Leeuw E, Dunn JR, Franco E, Frohlich KL, Geneau R, et al. Ottawa statement from the sparking solutions summit on population health intervention research. Can J Public Health. 2016;107:e492–6.
Rimer BK. Preparing students to engage in public health research of consequence. Am J Public Health. 2016;106:1546–7.
Steiner JF. Promoting mentorship in translational research: should we hope for Athena or train mentor? Acad Med. 2014;89:702–4.
Kalichman M, Rescuing RCR. Education. Account Res. 2014;21:68–83.
Jokelainen M. The elements of effective student nurse mentorship in placement learning environments: systematic review and Finnish and British mentors´ conceptions. Kuopio: University of Eastern Finland, Faculty of Health Sciences; 2013.
Jansen MW, De Vries NK, Kok G, Van Oers HA. Collaboration between practice, policy and research in local public health in the Netherlands. Health Policy. 2008;86:295–307.
Potvin L, Aumaître F. Les partenariats: espaces négociés de controverses et d’innovations. In: Potvin L, Moquet M-J, Jones C, editors. Réduire les inégalités sociales en santé. Saint-Denis: INPES; 2010. p. 318–25.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202.
Article CAS PubMed Google Scholar
Jessani N, Kennedy C, Bennett S. The human capital of knowledge brokers: an analysis of attributes, capacities and skills of academic teaching and research faculty at Kenyan schools of public health. Health Res Policy and Syst. 2016;14:1–13.
Download references
Acknowledgements
We wish to thank Dr. Maureen Malowany from the Braun School of Public Health and Community Medicine of The Hebrew University of Jerusalem-Hadassah; Dr. Pierre Bergeron, who was an expert at the Institut national de santé publique du Québec, but who is now retired; Dr. Michel Rossignol from the Institut national d’excellence en santé et services sociaux (Montréal, Québec); and Dr. Joseph Levy from the Université du Québec à Montréal for their contributions to the development of the 4P Program.
The 4P Research Training Program was funded by the Canadian Institutes of Health Research (grant TGF 63304) and the Fonds de recherche du Québec – Santé (grant 5225) through the Quebec Population Health Research Network.
Availability of data and materials
Data are available from the authors upon request.
Author information
Authors and affiliations.
Department of Epidemiology, Biostatistics and Occupational Health, McGill University, Montreal, Quebec, Canada
Anne-Marie Hamelin & Gilles Paradis
You can also search for this author in PubMed Google Scholar
Contributions
GP designed the 4P Program, obtained funding, and supervised all aspects of the 4P Program. AMH contributed to the design of the 4P Program and was responsible for implementing the Program and its evaluation. She analyzed the data and wrote the manuscript with substantive contributions from GP. Both authors approved the final manuscript.
Corresponding author
Correspondence to Anne-Marie Hamelin .
Ethics declarations
Ethics approval and consent to participate.
The study falls under the definition of program evaluation in the Canadian “Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans,” and therefore, institutional review board approval was not needed.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Telephone interviews with trainees. Telephone interviews with mentors. Exit interviews - template. Semiannual evaluation reports. Online Survey - trainees. Online Survey - mentors with trainees. (ZIP 999 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Hamelin, AM., Paradis, G. Population health intervention research training: the value of public health internships and mentorship. Public Health Rev 39 , 6 (2018). https://doi.org/10.1186/s40985-018-0084-9
Download citation
Received : 23 August 2017
Accepted : 19 January 2018
Published : 02 April 2018
DOI : https://doi.org/10.1186/s40985-018-0084-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Population health intervention research
- Internships
- Competency-based research training
- Capacity building
- University-public health partnership
Public Health Reviews
ISSN: 2107-6952
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 23 October 2023
What are the research priorities for strengthening public health emergency preparedness and response in Africa?
- Obinna Onwujekwe 1 , 2 ,
- Chinyere Mbachu ORCID: orcid.org/0000-0003-3936-6184 1 , 3 ,
- Joseph Okeibunor 4 ,
- Godwin Uchenna Ezema 1 , 2 , 5 ,
- Nonso Ejiofor 4 ,
- Fiona Braka 4 ,
- Adama Thiam 4 ,
- Etien Luc Koua 4 ,
- Dick Chamla 4 &
- Abdou Salam Gueye 4
Health Research Policy and Systems volume 21 , Article number: 107 ( 2023 ) Cite this article
1438 Accesses
1 Citations
1 Altmetric
Metrics details
Research evidence is needed to strengthen capacities in emergency preparedness and response (EPR). However, the absence of a clear research agenda limits the optimal use of research evidence. This paper reports on the prioritization of research questions and topics that could contribute to evidence-informed strengthening of EPR capacities in the African region.
The priority-setting consisted of desk review and stakeholder consultation workshop. Twenty-nine people participated in the workshop, including representatives from WHO regional office and EPR focal points in Africa, representatives of research institutions, and partners from Science for Africa Foundation, United Nations Children's Fund and Africa Center for Disease Control. Modified Delphi technique was used to systematically arrive at specific and cross-cutting research priorities in the three broad areas of the EPR, which are program Implementation, Clinical and Epidemiology. The research questions/topics were ranked on five-point Likert scale (1 = very low to 5 = very high) based on seven agreed-on criteria. Research priority score was calculated for each question as the mean of the criteria scores.
A total of 123 research questions comprising, 29 on Epidemiology, 22 on Clinical, 23 on program Implementation, and 49 on cross-cutting issues were ranked. The top ten research priorities were: knowledge and skills of healthcare workers in detecting and responding effectively to disease outbreaks; quality of data (accuracy, timeliness, completeness) for epidemic prone diseases; determinants of vaccine hesitancy; determinants of infection transmission among health care workers during PHE; effective measures for protecting health workers from highly infectious pathogens in PHE; strategies to improve the effectiveness of contact tracing for epidemic prone diseases; effectiveness of current case definitions as screening tools for epidemic and pandemic prone diseases; measures to strengthen national and sub-national laboratory capacity for timely disease confirmation within the Integrated Diseases Surveillance and Response framework; factors affecting prompt data sharing on epidemic-prone diseases; and effective strategies for appropriate community participation in EPR.
Conclusions
The collaborative multi-stakeholder workshop produced a starting list of priority research questions and topics for strengthening EPR capacities in Africa. Action needs to be taken to continuously update the research agenda and support member States to contextualize the research priorities and commission research for timely generation and uptake of evidence.
Peer Review reports
Globally, there are multiple health emergencies comprising disease outbreaks and humanitarian conflicts and often in challenging settings. The African region especially reports over 100 public health events/emergencies (PHEs) annually [ 1 ], of which approximately 80% are emerging and re-emerging infectious diseases, events, and conditions [ 2 ]. We define PHE as “any situation whose health consequences have the potential to overwhelm routine capabilities to address them due to the scale, timing or unpredictability of the situation” [ 3 ]. PHEs could be of national or international concern depending on geographic spread. Recent public health emergencies in the region include infectious disease outbreaks such as Ebola, COVID-19, and the ongoing Cholera outbreak; man-made disasters such as conflicts and wars in the central African region and the Horn of African; and natural disasters such as cyclones, flooding and drought in the southern African region and the Horn of Africa [ 4 , 5 ]. These events have significant implications for global health security and universal health coverage gains [ 6 ], and are often associated with high morbidity, mortality, and significant socio-economic disruptions.
The impact of unexpected public health events can be significantly minimized if national capacities for emergency preparedness and response (EPR) are strengthened. The International Health Regulations (IHR) stipulates 13 core capacities that are required by countries to be able to effectively detect and respond to public health risks and emergencies. They are: National legislation, policy and financing; Coordination and National Focal Point communications; Surveillance; Response; Preparedness; Risk communication; Human resources; Laboratory; Points of entry; Zoonotic events; Food safety; Chemical events; and Radionuclear emergencies [ 7 ]. Although the World Health Organization (WHO) has made significant efforts to facilitate the attainment of the core capacities required under the IHR, many countries in the African region still lack the minimum capacities necessary to predict, plan for, rapidly detect and respond to and recover from public health emergencies.
Evidence from research is needed to understand the drivers of public health emergencies in the African region, and to support the discovery, design and delivery of effective interventions that will contribute to strengthening capacities in EPR [ 8 , 9 ]. National Health Research Systems are disposed to generate context-specific and relevant knowledge in a timely manner [ 10 ]. Entrenching research agenda on health emergencies such as pandemics and stimulating the generation of evidence, translation and dissemination of valuable knowledge will help in enhancing emergency preparedness and response (EPR) to health emergencies. The unpredictability of the events makes it more challenging to rely on old knowledge and systems to contain them. Improving our response to these events requires information and research, this calls for a robust research agenda.
Well-defined health research priorities provide useful guidance in the strategic allocation of research resources, such that the benefits of research investment can be maximized [ 11 ]. Although there could be an endless list of research questions that could contribute to strengthening EPR capacities in SSA, the resources to undertake health research are limited. It therefore becomes necessary to identify the research questions that will generate relevant contextual evidence for programme improvements.
Failure to prioritize research questions and topics for ensuring evidence-based decision making will result in the persistence of poor health and weak preparedness against health emergencies in the region. Also, it could lead to misinterpretation of the drivers of poor health, poor articulation of the soundest interventions for strengthening country EPR capacities, and a failure to understand the strategies for optimizing the effectiveness of these interventions [ 10 ]. Such failures can accentuate the current state of weak EPR capacities in the region.
This paper reports on the prioritization of research questions and topics that provide the required evidence for evidence-informed strengthening of EPR in sub-Sahara Africa (SSA). It provides new knowledge on the research priorities for strengthening EPR capacities in SSA. It also contributes to existing literature on health system research priority setting.
Study context and design
The WHO AFRO EPR Cluster launched three flagship programmes namely, Promoting Resilience of Systems for Emergencies (PROSE), Transforming African Surveillance Systems (TASS), and Strengthening and Utilizing Response Groups for Emergencies (SURGE) in early 2022. The overarching goal of the programmes is to promote health security in the African Region and contribute to the achievement of the Sustainable Development Goal 3. The specific objectives are to support Member States to prepare for and prevent disease outbreaks and health emergencies; promptly detect, speedily report, and confirm outbreaks; strengthen and sustain capacity to promptly respond to and recover from the negative effects of outbreaks and health emergencies. To achieve these objectives, each flagship programme proposed a set of activities and plans that are aligned to the 5-year goal of rolling out all three flagships to the entire African continent. For PROSE, the goal for 2022 was to determine a clear roadmap with each of the 17 countries and begin implementation of activities. For TASS the goal was to assess the needs of the targeted countries, define implementation modalities and provide laboratory strengthening services. And for SURGE, the goal was to make sure countries have the workforce, operations, and logistics support, and the coordination mechanism needed to stop the next pandemic. An initial set of 17 countries were targeted for the roll out in 2022 with the intent to scale up to the whole of the continent. To this end, there is the need to answer some broad questions, (i) How effective are the flagships; (ii) What combinations of flagship interventions have a maximum impact on preparedness, detection, response, and health systems resilience—the game changers; (iii) What enabling environment required for implementation of flagships; and (iv) What is missing (that could have more impact).
In line with WHO’s Core Function of Leadership and support for research in health EPR, and Transformation focus area of Strengthening capacity in use of evidence for health policy and action, the process of setting the agenda for EPR research in Africa was initiated with three broad areas of focus namely implementation, clinical and epidemiological. This would ensure that there are clear research priorities that would contribute to strengthening EPR capacities in the region.
The research priority setting was implemented through a systematic process of a consensus building. The methodology of the Child Health and Nutrition Research Initiative [ 12 ] was used in the prioritization exercise. This systematic process of research priority setting comprises 15 steps that begin with the selection of stakeholders/participants and span through choosing a limited set of the most useful and important criteria, listing of a large number of proposed health research options, scoring of the health research options using the chosen set of criteria, and calculating overall priority scores and assigning ranks. This methodology has been used extensively in research prioritization exercises with demonstrated practicality at institutional, regional, national, international, or global levels, and it has a general appeal among policy makers, development partners and researchers, and it supports the participation of a wide range of stakeholders [ 13 , 14 ].
The specific methods that were used in the priority setting were desk review and a stakeholder workshop. The purpose of the desk review was to identify various criteria that have been used to set research priorities and how these criteria were operationalized (defined and applied). The aims of the stakeholder workshop were to identify issues in EPR to be addressed through research, and to select the research priorities based on an agreed set of assessment criteria. The entire process from participant selection to data analysis is highlighted in Fig. 1 .
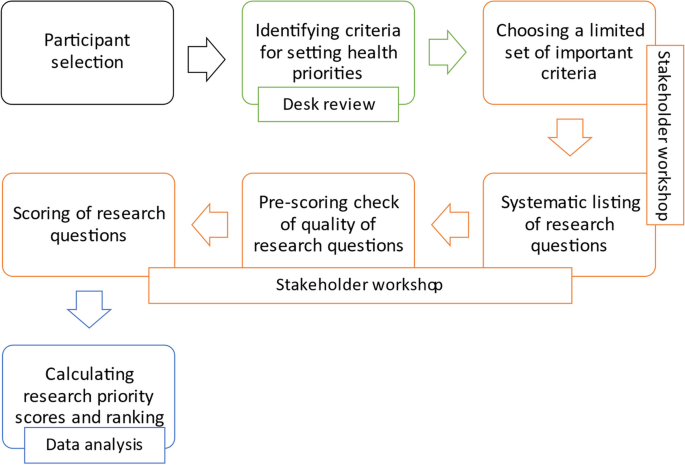
Flow chart of the methodological process of research priority setting for EPR in Africa
Desk review
A rapid review of documents was conducted. The search algorithm included various combinations of the following key terms: criteria, research priority, research prioritization, research agenda, public health emergency, preparedness, response. Searches were performed on Google for relevant documents including articles, reports of expert meetings, official/public documents, and programme reports. Minutes and reports of previous research priority setting meetings were also retrieved through email exchange from experts.
The criteria for assessment of research questions were compiled with a working definition for each criterion. The starting list was adapted from relevant documents (articles and reports) on research priority setting including the guidelines that were developed by CHNRI for priority setting in health research investment and the WHO global research agenda for family planning [ 12 , 15 , 16 ]. Both activities involved systematic processes of ranking and consensus-building among experts. The need for a systematic approach to the specification of the research prioritization criteria is well documented in literature [ 12 , 17 , 18 , 19 , 20 ]. Table 1 shows the names and definitions of the assessment criteria.
Stakeholder consultation workshop
The stakeholder consultation workshop was a five-day hybrid event that lasted from 17 to 21 October 2022. Online participants joined the workshop through Zoom. Unique meeting invite links were sent to registered participants. To ensure meaningful participation of online participants, the virtual meeting room was unmuted during the workshop and each in-person attendee had access to a micro-phone and headset. Remote participants were intentionally and personally invited to speak or comment during the workshop, and questions or comments posted in the chat were read out by the facilitators. To give remote participants a greater presence in the room, two monitors were set up in the room and the main screen was used to project life size images of remote participants.
Three stages of consensus building were conducted: (i) Structured brainstorming to select the criteria for ranking of research questions/topics and a list of research questions based on identified needs; (ii) Two-round modified Delphi exercise to establish consensus on the most relevant/suitable criteria for assessing the research questions; and (iii) Two-round modified Delphi exercise to establish consensus on research priorities. The steps are discussed in detail in the next paragraphs.
A total of 29 experts participated in the workshop, which was held in Brazzaville, Congo (Table 2 ). The workshop participants were technical focal points from the different programme areas in EPR and the Assistant Regional Director Cluster of WHO AFRO. Others were EPR focal points from country offices, representatives of WHO EPR hubs in Dakar and Nairobi, representatives from five ministries of Health (Nigeria, Senegal, Democratic Republic of Congo, Kenya, and Ethiopia), representatives from Africa Center for Disease Control, the WHO Headquarters in New York, United Nation’s Children Fund and from research institutions in SSA. The activities that were undertaken in each of the three stages of consensus building are presented in the ensuing sub-sections.
Structured brainstorming
Structured brainstorming is a systematic process which encourages active participation in contributing ideas towards a specific goal, in a non-critical or non-evaluative environment. Participants are given a fair chance to voice their ideas such that the discussion is not dominated by one person or a few people. In this workshop, structured brainstorming was used to: (i) identify (from experience or knowledge) the challenges and knowledge gaps in EPR in SSA; and (ii) generate a starting list of research questions that can contribute to addressing the challenges and gaps in the three broad research areas of the EPR.
Group work: The brainstorming exercise began with a random assignment of participants into four groups. Each group was asked to reflect on the three broad areas of the EPR programme in SSA, and identify from their experiences and/or knowledge, (i) the challenges (problems, capacity needs, etc.) that the programme faces in each broad areas; and (ii) the knowledge (research and development) gaps that need to be filled—to better understand current and future challenges, effective interventions for strengthening country EPR capacities, and potential strategies for optimizing the effectiveness of interventions.
Having generated ideas on challenges and knowledge gaps, each group was asked to articulate specific research questions (or topics) that will generate answers or solutions to the challenges identified and contribute to filling the gaps in knowledge in EPR in the region. The ideas were recorded in a uniform Microsoft Word template with comprising four broad areas—Epidemiology, Clinical, programme Implementation and Cross-cutting.
Plenary discussion: Outputs from each group were projected and presented for critical review and feedback from facilitators and participants, and for discussion in plenary. Groups received comments and suggestions for refining their ideas and research questions. Revised outputs from each group were submitted and circulated to all the participants for collation and synthesis.
Thematic collation and synthesis of ideas: Participants were reassigned to three groups—Epidemiology, Clinical and Implementation—based on their expertise, interest and/or area of work. Each group was tasked with the responsibility to collate (assemble) all challenges, knowledge gaps and research questions that are recorded in the templates for their assigned broad area (theme), and to removing any duplicates. They were additionally requested to record any cross-cutting issues and research questions that were not captured on the lists.
Generation of consolidated list of research questions: An initial list of research questions was generated by merging the updated list of research questions from each broad area. Excluding duplicates, all research questions that were generated and adopted/adapted by participants were retained.
Prioritization of assessment criteria using the Delphi technique
The Delphi technique is a consensus-building method of eliciting and refining judgements from a group of people, in order to generate knowledge that is currently not available [ 21 ]. The three main features of the technique—anonymous response, iteration and controlled feedback, and statistical group response—are designed to minimize the influence of dominant individuals in group interactions, and the biasing effects of irrelevant communication, and group pressure towards conformity. In this workshop, modified Delphi technique was used to achieve the consensus opinion of participants on, (i) the set of criteria to be used to assess research questions, and (ii) the research priorities in EPR for SSA.
Although there are several criteria that can be used to define health research priorities, stakeholders should carefully select the most suitable ones for the context of prioritization[ 17 , 22 , 23 ]. The key considerations in the study were the programme context of EPR in SSA, to ensure that the research priorities were aligned to the needs of the programme and the values of the key stakeholders in the programme.
Two rounds of Delphi exercise were undertaken to establish consensus on the most relevant/suitable criteria for assessing research questions. In round one, the starting list of 14 criteria was presented and participants were asked to rank the criteria from the most relevant or suitable to the least relevant or suitable for assessing research questions in EPR. The first round of ranking was followed by plenary discussions on the rationale for ranking the criteria.
In the second round of the modified Delphi, participants got a second chance to re-rank the 14 criteria in order of relevance or suitability. The first and second ranking exercises were through live online polling. Seventeen [ 12 ] participants voted in the first-round while 29 voted in the second round.
Prioritization of research questions
In the first round of the modified Delphi, the initial list of research questions was shown to participants (in thematic groups) and they were asked to vote to keep, remove or modify the research questions based on their assessment of the quality and relevance of the question to EPR capacities in the region. The voting was through live online polling. Research questions were ranked high (to keep), medium (to modify) and low (to remove). Consensus was set a priori at 50% agreement with any of the available options. Percent agreement is the basis for definition of consensus for many studies that adopt the Delphi method [ 24 ]. The decision for 50% consensus was made based on the suggestions of participants and the agreement that this was an acceptable cut-off for deciding which research questions should be kept, modified, or dropped before the ranking exercise.
In the second round of the modified Delphi, the condensed list of research questions was coded on the Open Data Kit software and each research question was ranked from 1 to 5 in each of the selected assessment criterion. Table 3 shows the ranking/scoring template. (A rank of 1 meant that for that criterion the research question was considered to rank very low; a score of 2 signified low ranking; a score of 3 signified moderate ranking; 4 signified high ranking; and 5 signified very high ranking) . Scores assigned to each question were tallied, by criterion and the question with the highest score was given the highest priority. Research priority score (RPS) was calculated for each research question as the mean of the criteria scores for 29 participants. The maximum achievable RPS per question is 145 (5*29) and the minimum is 29 (1*29).
Ranking of assessment criteria
The results of the ranking and re-ranking of the assessment criteria are shown in Figs. 2 and 3 , respectively. The top seven ranked criteria from the first round were feasibility, potential to have impact, answerability, public health benefits, potential for translation, affordability, and equity. After the second round of voting, feasibility, and potential to have impact retained their positions as the top two ranked criteria. Potential for translation also retained its position as the fifth criteria. General public health benefits moved up to the third ranked criteria while answerability moved down to 6 th position. Affordability and equity moved down to the bottom half of the ranks while ethical aspects and involvement of end-users occupied the 4 th and 7 th positions, respectively.
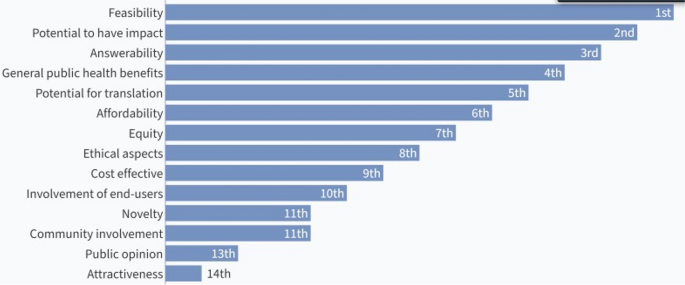
Results of the first ranking of criteria for assessing research questions
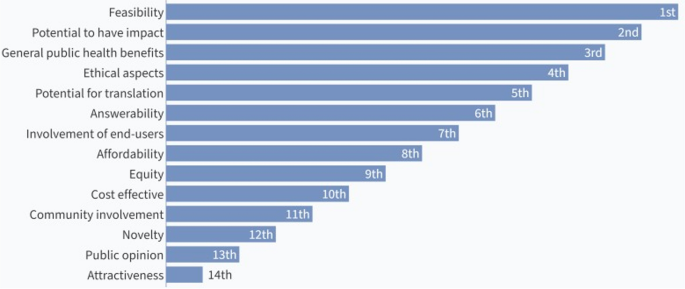
Results of the re-ranking of criteria for assessing research questions
Participants decided that since potential to have impact encompasses public health benefits, the latter should be considered a part of the former, and affordability should be included in the list of seven criteria that will be used to assess the research questions.
Generation and ranking of priority research questions.
A total of 123 research questions were generated. This comprised 29 questions on the Epidemiology broad area, 22 on the Clinical area, 23 on Implementation, and 49 on cross-cutting issues. The highest ranked question achieved a research priority score of 123.0 while the least ranked question had a score of 89.0. The condensed list of priority research questions with their corresponding RPS is attached as a supplementary file [see Additional file 1 ]. Also attached as a supplementary file is the disaggregated list of the research questions by the EPR broad areas [see Additional file 2 ].
Table 4 shows the research priority scores of the top 25 research questions and the corresponding broad areas. Nine of the questions were on the clinical broad area, and eight each were on the Epidemiology and Implementation broad areas. None of the top 25 questions was on a cross-cutting issue.
The top ten research priorities were on issues around the knowledge and skills of healthcare workers in detecting and responding effectively to disease outbreaks; quality of data (accuracy, timeliness, completeness) for epidemic prone diseases; determinants of vaccine hesitancy; determinants of infection transmission among health care workers during PHE; effective measures for protecting health workers from highly infectious pathogens in PHE; strategies to improve the effectiveness of contact tracing for epidemic prone diseases; effectiveness of current case definitions as screening tools for epidemic and pandemic prone diseases; measures to strengthen national and sub-national laboratory capacity for timely disease confirmation within the Integrated Diseases Surveillance and Response framework; factors affecting prompt data sharing on epidemic-prone diseases; and effective strategies for appropriate community participation in EPR. Other top research priorities are as shown in Table 4 .
Table 5 shows the disaggregated and total proportions of research questions that achieved ≥ 75% (high), 50–75% (medium) or < 50% (low) research priority scores out of the maximum achievable research priority score (which is 145).
A total of 52 (42.28%) research questions had research priority scores that were at least 75% of the maximum achievable score. Most of the research questions on the clinical broad area (72.73%) and the implementation broad area (60.87%) had high research priority scores. Whereas 42.28% of the questions on epidemiology had high research priority scores. Only 16.33% of the cross-cutting research questions achieved high research priority scores. None of the research questions had a research priority score that was less than 50% of the maximum achievable score. This implies that all the research questions were judged to be of above average priority to the stakeholders.
Our findings show that within the context of WHO AFRO’s Emergency Preparedness Programme, stakeholders generated a long list of research questions and topics that they adjudged to be relevant for strengthening capacities for EPR within the African region. However, to provide valuable direction for the allocation of public and private research funds, the stakeholders had to decide, through consensus-building, which research questions were more or less important.
Our study shows that consulting with a diverse group of stakeholders ensures that differing and distinct views and perceptions are brought to the fore. The importance of stakeholder engagement in setting research priorities as also reported elsewhere [ 12 , 23 ]. It is important that the key stakeholders are involved in the research priority setting and that their interests are taken into consideration in the prioritization process. However, the difficult task of managing the often-conflicting interests of stakeholders is acknowledged, particularly when there is uneven distribution of power among the stakeholders. Hence, in setting the EPR research priorities, the facilitators employed a mix of strategies for effective stakeholder engagement, including, the purposive selection of participants, and consensus-building through iterations of group creativity activities and individual ranking exercises.
The process of determining the strategic importance of research questions could be tedious for stakeholders if there are no clear criteria for assessment. The specification of criteria enables a more rational process of priority setting, particularly where the research questions are brand new [ 20 , 22 ]. In our research priority setting exercise, the use of a systematic and transparent approach of consensus-building to define the set of criteria for assessing the newly formed EPR research questions was a plausible approach to ensure widespread consensus and ownership of the final research priorities by all the participants. Adopting a methodologically transparent approach in consensus-building aligns with existing literature on stakeholder management [ 25 ]. Methodological transparency is closely tied to trust and credibility in consensus-building processes [ 25 ]. Stakeholders are more likely to trust the outcomes of a consensus-building effort when they can clearly understand and evaluate the methods used and can see how decisions are made.
The top twenty-five research questions that were prioritized for strengthening EPR capacities in the African region align with the global capacity needs for effective EPR [ 26 , 27 ]. Other research priorities that resonate with exiting literature include understanding the determinants of vaccine hesitancy, strengthening community participation in EPR, protection of health workers from highly infectious pathogens during PHE, and strengthening national and sub-national laboratory capacity for timely disease confirmation.
These research priorities address some of the demand- and supply-side barriers to effective EPR in the African region, the knowledge gaps in EPR, and some recommended strategies for effective management of PHE [ 28 , 29 , 30 , 31 , 32 ]. Although the Emergency Preparedness Programme of WHO AFRO aims to strengthen country capacities in emergency preparedness and response across the three broad areas of the Programme, attention should also be paid to fundamental health systems issues that underline overall health system resilience and responsiveness during public health emergencies.
The major limitations of research priority setting are, (i) the likelihood of excluding some key stakeholders in the prioritization process and missing some relevant research questions; (ii) the potential influence of dominant individuals; (iii) the biasing effects of irrelevant reflections from dominant speakers; and (iv) the potential to conform to the popular opinion. In this prioritization exercise, stakeholders at the frontlines of EPR in the AFRO member states were not included in the exercise. The EPR office of WHO AFRO is planning some webinar sessions to get additional inputs on research priorities from more stakeholders and all member states. A face-to-face validation workshop is also being planned and this will engage a wider range of stakeholders. The use of modified Delphi technique minimized the effects of the other limitations and ensured that each participant’s opinion contributed to the final research priorities.
The stakeholder consultation workshop was successful in developing a starting set of research priorities for EPR in Africa. The prioritization exercise led to the selection of the most useful research questions for strengthening EPR capacities in SSA. The next steps would be to get the WHO member countries in the region to buy into these research priorities, and to subsequently develop context-specific research agenda, implementation frameworks and operational guidelines. Action needs to be taken to continuously update the research agenda so that the research priorities are time and context sensitive.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
African Regional Office
- Emergency preparedness and response
Public health events/emergencies
Sub-Saharan Africa
Zafar A, Talati C, Graham E. 2014–2015 West Africa Ebola crisis: impact update. Washington: Banco Mundial; 2016.
Google Scholar
Huber C, Finelli L, Stevens W. The economic and social burden of the 2014 Ebola outbreak in West Africa. J Infect Dis. 2018;218(Supplement 5):S698–704.
Article PubMed Google Scholar
Nelson C, Lurie N, Wasserman J, Zakowski S. Conceptualizing and defining public health emergency preparedness. Am J Public Health. 2007;97(Suppl 1):S9-11.
Article PubMed PubMed Central Google Scholar
Nnaji ND, Onyeaka H, Reuben RC, Uwishema O, Olovo CV, Anyogu A. The deuce-ace of Lassa Fever, Ebola virus disease and COVID-19 simultaneous infections and epidemics in West Africa: clinical and public health implications. Trop Med Health. 2021;49(1):102.
World Health Organization. Cholera in the WHO African Region. World Health Organization; 2023.
World Bank. The economic impact of the 2014 Ebola epidemic: short- and medium-term estimates for West Africa: The World Bank; 2014. 106 p.
World Health Organization. International health regulations. 3rd ed. Geneva: World Health Organization; 2005.
Lozano R, Fullman N, Abate D, Abay SM, Abbafati C, Abbasi N, et al. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. The lancet. 2018;392(10159):2091–138.
Article Google Scholar
Kinyanjui S, Fonn S, Kyobutungi C, Vicente-Crespo M, Bonfoh B, Ndung’u T, et al. Enhancing science preparedness for health emergencies in Africa through research capacity building. BMJ Specialist J. 2020. https://doi.org/10.1136/bmjgh-2020-003072 .
Rusakaniko S, Makanga M, Ota MO, Bockarie M, Banda G, Okeibunor J, et al. Strengthening national health research systems in the WHO African Region—progress towards universal health coverage. Glob Health. 2019;15(1):50.
de Haan S, Kingamkono R, Tindamanyire N, Mshinda H, Makandi H, Tibazarwa F, et al. Setting research priorities across science, technology, and health sectors: the Tanzania experience. Health Res Policy Syst. 2015;13(1):14.
Rudan I, Gibson JL, Ameratunga S, Arifeen SE, Bhutta ZA, Black M, et al. Setting priorities in global child health research investments: guidelines for implementation of CHNRI method. Croat Med J. 2008;49(6):720–33.
Rudan I, Kapiriri L, Tomlinson M, Balliet M, Cohen B, Chopra M. Evidence-based priority setting for health care and research: tools to support policy in maternal, neonatal, and child health in Africa. PLoS Med. 2010;7(7): e1000308.
Tomlinson M, Yasamy MT, Emerson E, Officer A, Richler D, Saxena S. Setting global research priorities for developmental disabilities, including intellectual disabilities and autism. J Intellect Disabil Res. 2014;58(12):1121–30.
Article CAS PubMed PubMed Central Google Scholar
Ali M, Seuc A, Rahimi A, Festin M, Temmerman M. A global research agenda for family planning: results of an exercise for setting research priorities. Bull World Health Organ. 2014;92(2):93–8.
Viergever RF, Olifson S, Ghaffar A, Terry RF. A checklist for health research priority setting: nine common themes of good practice. Health Res Policy Syst. 2010;8(1):1–9.
Viergever RF, Olifson S, Ghaffar A, Terry RF. A checklist for health research priority setting: nine common themes of good practice. Health Res Policy Syst. 2010;8(1):36.
World Health O. A systematic approach for undertaking a research priority-setting exercise: guidance for WHO staff. Geneva: World Health Organization; 2020. p. 2020.
Chanda-Kapata P, Ngosa W, Hamainza B, Kapiriri L. Health research priority setting in Zambia: a stock taking of approaches conducted from 1998 to 2015. Health Res Policy Syst. 2016;14(1):1–9.
Badakhshan A, Arab M, Rashidian A, Gholipour M, Mohebbi E, Zendehdel K. Systematic review of priority setting studies in health research in the Islamic Republic of Iran. East Mediterr Health J. 2018;24(8):753–69.
Dalkey NC. The Delphi method: an experimental study of group opinion. Santa Monica: RAND Corporation; 1969.
Tong A, Synnot A, Crowe S, Hill S, Matus A, Scholes-Robertson N, et al. Reporting guideline for priority setting of health research (REPRISE). BMC Med Res Methodol. 2019;19(1):243.
Sibbald SL, Singer PA, Upshur R, Martin DK. Priority setting: what constitutes success? A conceptual framework for successful priority setting. BMC Health Serv Res. 2009;9(1):1–12.
Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401–9.
Aguinis H, Ramani RS, Alabduljader N. What you see is what you get? Enhancing methodological transparency in management research. Acad Manag Ann. 2018;12(1):83–110.
World Health Organization. Global assessment of national health sector emergency preparedness and response. Geneva: Switzerland; 2008.
Laura N, Sydney Morgan B, Alexia C, Sharanya K, Mays S, Luis H, et al. Global health security preparedness and response: an analysis of the relationship between joint external evaluation scores and COVID-19 response performance. BMJ Open. 2021;11(12): e050052.
Ayenew T, Tassew SF, Workneh BS. Level of emergency and disaster preparedness of public hospitals in Northwest Ethiopia: a cross-sectional study. Afr J Emerg Med. 2022;12(3):246–51.
Marston C, Renedo A, Miles S. Community participation is crucial in a pandemic. The Lancet. 2020;395(10238):1676–8.
Article CAS Google Scholar
Johnson BW, Demanou M, Fall G, Betoulle JL, Obiekea C, Basile AJ, et al. Laboratory capacity assessments in 25 African countries at high risk of yellow fever, August-December 2018. Pan Afr Med J. 2021;38:402.
Nkengasong JN, Tessema SK. Africa needs a new public health order to tackle infectious disease threats. Cell. 2020;183(2):296–300.
Wiysonge CS, Ndwandwe D, Ryan J, Jaca A, Batouré O, Anya B-PM, et al. Vaccine hesitancy in the era of COVID-19: could lessons from the past help in divining the future? Hum Vaccin Immunother. 2022;18(1):1–3.
Article CAS PubMed Google Scholar
Download references
Acknowledgements
Not applicable.
The research priority setting workshop was funded by the Emergency Preparedness Flagship Programme of the WHO. The views expressed in the manuscript are solely of the authors and not of the funder.
Author information
Authors and affiliations.
Health Policy Research Group, Department of Pharmacology and Therapeutics, College of Medicine, University of Nigeria, Enugu, 400001, Nigeria
Obinna Onwujekwe, Chinyere Mbachu & Godwin Uchenna Ezema
Department of Health Administration and Management, College of Medicine, University of Nigeria, Enugu, 400001, Nigeria
Obinna Onwujekwe & Godwin Uchenna Ezema
Department of Community Medicine, College of Medicine, University of Nigeria, Enugu, 400001, Nigeria
Chinyere Mbachu
World Health Organisation Regional Office for Africa (AFRO), Brazzaville, Congo
Joseph Okeibunor, Nonso Ejiofor, Fiona Braka, Adama Thiam, Etien Luc Koua, Dick Chamla & Abdou Salam Gueye
Enugu State Primary Healthcare Development Agency, Enugu, Nigeria
Godwin Uchenna Ezema
You can also search for this author in PubMed Google Scholar
Contributions
OO and CM designed the techniques. OO, CM and GUE analyzed and interpreted the data. OO, CM, JO and NE contributed to the production of the first draft of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chinyere Mbachu .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Comprehensive list of research questions and topics and corresponding Research Priority Scores in descending order of ranking
Additional file 2.
Disaggregated list of research questions and topics by EPR broad areas, and corresponding Research Priority Scores
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Onwujekwe, O., Mbachu, C., Okeibunor, J. et al. What are the research priorities for strengthening public health emergency preparedness and response in Africa?. Health Res Policy Sys 21 , 107 (2023). https://doi.org/10.1186/s12961-023-01059-6
Download citation
Received : 24 March 2023
Accepted : 06 October 2023
Published : 23 October 2023
DOI : https://doi.org/10.1186/s12961-023-01059-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Prioritization
- Research priority-setting
- African region
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Mindful Eating

What Is It?
Mindful eating stems from the broader philosophy of mindfulness, a widespread, centuries-old practice used in many religions. Mindfulness is an intentional focus on one’s thoughts, emotions, and physical sensations in the present moment. Mindfulness targets becoming more aware of, rather than reacting to, one’s situation and choices. Eating mindfully means that you are using all of your physical and emotional senses to experience and enjoy the food choices you make. This helps to increase gratitude for food, which can improve the overall eating experience. Mindful eating encourages one to make choices that will be satisfying and nourishing to the body. However, it discourages “judging” one’s eating behaviors as there are different types of eating experiences. As we become more aware of our eating habits, we may take steps towards behavior changes that will benefit ourselves and our environment.
How It Works
Mindful eating focuses on your eating experiences, body-related sensations, and thoughts and feelings about food, with heightened awareness and without judgment. Attention is paid to the foods being chosen, internal and external physical cues, and your responses to those cues. [1] The goal is to promote a more enjoyable meal experience and understanding of the eating environment. Fung and colleagues described a mindful eating model that is guided by four aspects: what to eat , why we eat what we eat , how much to eat , and how to eat . [1]
Mindful eating:
- considers the wider spectrum of the meal: where the food came from, how it was prepared, and who prepared it
- notices internal and external cues that affect how much we eat
- notices how the food looks, tastes, smells, and feels in our bodies as we eat
- acknowledges how the body feels after eating the meal
- expresses gratitude for the meal
- may use deep breathing or meditation before or after the meal
- reflects on how our food choices affect our local and global environment
Seven practices of mindful eating
- Honor the food . Acknowledge where the food was grown and who prepared the meal. Eat without distractions to help deepen the eating experience.
- Engage all senses . Notice the sounds, colors, smells, tastes, and textures of the food and how you feel when eating. Pause periodically to engage these senses.
- Serve in modest portions . This can help avoid overeating and food waste. Use a dinner plate no larger than 9 inches across and fill it only once.
- Savor small bites, and chew thoroughly . These practices can help slow down the meal and fully experience the food’s flavors.
- Eat slowly to avoid overeating . If you eat slowly, you are more likely to recognize when you are feeling satisfied, or when you are about 80% full, and can stop eating.
- Don’t skip meals . Going too long without eating increases the risk of strong hunger, which may lead to the quickest and easiest food choice, not always a healthful one. Setting meals at around the same time each day, as well as planning for enough time to enjoy a meal or snack reduces these risks.
- Eat a plant-based diet, for your health and for the planet . Consider the long-term effects of eating certain foods. Processed meat and saturated fat are associated with an increased risk of colon cancer and heart disease . Production of animal-based foods like meat and dairy takes a heavier toll on our environment than plant-based foods.
Watch: Practicing mindful eating
The Research So Far
The opposite of mindful eating, sometimes referred to as mindless or distracted eating, is associated with anxiety, overeating, and weight gain. [3] Examples of mindless eating are eating while driving, while working, or viewing a television or other screen (phone, tablet). [4] Although socializing with friends and family during a meal can enhance an eating experience, talking on the phone or taking a work call while eating can detract from it. In these scenarios, one is not fully focused on and enjoying the meal experience. Interest in mindful eating has grown as a strategy to eat with less distractions and to improve eating behaviors.
Intervention studies have shown that mindfulness approaches can be an effective tool in the treatment of unfavorable behaviors such as emotional eating and binge eating that can lead to weight gain and obesity, although weight loss as an outcome measure is not always seen. [5-7] This may be due to differences in study design in which information on diet quality or weight loss may or may not be provided. Mindfulness addresses the shame and guilt associated with these behaviors by promoting a non-judgmental attitude. Mindfulness training develops the skills needed to be aware of and accept thoughts and emotions without judgment; it also distinguishes between emotional versus physical hunger cues. These skills can improve one’s ability to cope with the psychological distress that sometimes leads to binge eating. [6]
Mindful eating is sometimes associated with a higher diet quality, such as choosing fruit instead of sweets as a snack, or opting for smaller serving sizes of calorie-dense foods. [1]
- A literature review of 68 intervention and observational studies on mindfulness and mindful eating found that these strategies improved eating behaviors such as slowing down the pace of a meal and recognizing feelings of fullness and greater control over eating. [8] Slower eating was associated with eating less food, as participants felt fuller sooner. Mindfulness and mindful eating interventions appeared most successful in reducing binge eating and emotional eating. However, the review did not show that these interventions consistently reduced body weight. Limitation of the studies included small sample sizes, limited durations of about 6 months or less, lack of focus on diet quality, and lack of follow-up so that longer-term success was not determined.
- A randomized controlled trial following 194 adults with obesity (78% were women) for 5.5 months looked at the effects of a mindfulness intervention on mindful eating, sweets consumption, and fasting glucose levels. The participants were randomly assigned to one of two groups: a diet and exercise program with mindfulness concepts (stress reduction, chair yoga, meditation, affirmations) or the same program but without mindfulness concepts. After 12 months, the mindfulness group showed a decreased intake of sweets and maintenance of fasting blood glucose, as opposed to the control group showing increased fasting blood glucose. [9] The research authors also evaluated weight loss with these participants, but did not find a significant difference in weight changes between the mindfulness group and control group. [10]
- A small controlled trial of 50 adults with type 2 diabetes were randomized to either a 3-month mindful eating intervention that was focused on reducing overeating and improving eating regulation or to a diabetes self-management education (DSME) intervention that was focused on improving food choices. Both groups showed significant improvements in measures of depression, nutrition self-efficacy, and controlling overeating behaviors. Both groups lost weight during the intervention but there was no difference in amount of weight loss between groups. [11]
It is important to note that currently there is no standard for what defines mindful eating behavior, and there is no one widely recognized standardized protocol for mindful eating. Research uses a variety of mindfulness scales and questionnaires. Study designs often vary as well, with some protocols including a weight reduction component or basic education on diet quality, while others do not. Additional research is needed to determine what behaviors constitute a mindful eating practice so that a more standardized approach can be used in future studies. [1] Standardized tools can help to determine the longer-term impact of mindful eating on health behaviors and disease risk and prevention, and determine which groups of people may most benefit from mindfulness strategies. [1]
Mindfulness is a strategy used to address unfavorable eating behaviors in adults, and there is emerging interest in applying this method in adolescents and children due to the high prevalence of unhealthy food behaviors and obesity in younger ages. More than one-third of adolescents in the U.S. have overweight or obesity. Youth who have overweight/obesity are likely to experience weight-related stigma and bullying by their peers, which in turn can negatively affect eating behaviors and lead to eating disorders. [12] Studies have found that eating disorders are developing at younger ages, with an increased number of children younger than 12 years of age presenting for treatment. [12]
- A review of 15 studies of mindfulness-based interventions in adolescents found that mindfulness techniques were associated with reduced concerns about body shape, less dietary restraint, decreased weight, and less binge eating. [12] However, interestingly, the overall acceptability of the mindfulness-related interventions was rated low by the participants, compared with general health education. It is likely that the way mindful strategies are presented to younger ages needs better understanding as it may be different than in adults. An example could be using new online technologies that are specific to their developmental age and learning ability. The review also found that mindfulness in the form of meditation and mindful breathing can have significant effects on disordered eating through better stress management and reduced overeating caused by depression and anxiety.
- Studies are still scarce in children, but novel programs are emerging. A pilot mindful eating intervention was tested in a low-income school in California involving third-through-fifth grade children including Hispanic and non-Hispanic children. [13] The goal was to foster healthy eating behaviors in the children and their parents. The program included topics such as “Master Mindless Munching,” “Getting to Know Hunger and Fullness,” and “Sensational Senses,” and provided take-home activities to do with their parents. Surveys at the end of the program showed that the children and parents liked the activities, and there was an increase in parents serving nutritious meals and practicing mindfulness during meals (e.g., recognizing when hungry vs. full).
Potential Pitfalls
- Mindful eating is not intended to replace traditional treatments for severe clinical conditions such as eating disorders . Neurochemical imbalances are a risk factor for developing eating disorders such as bulimia and anorexia nervosa, and although mindfulness may be an effective component of a treatment plan, it should not be used as a sole treatment.
- May not be effective as a weight loss strategy on its own, but rather a complement to a weight loss program. Mindful eating embraces making food choices that promote well-being and increasing enjoyment of the eating experience. Traditional weight loss regimens focus on following a structured meal plan that may not necessarily be satisfying or enjoyable. Combining mindfulness with a meal plan under the guidance of a registered dietitian may reduce the risk of emotional overeating or binge eating. [14] Research has not consistently shown that mindfulness strategies lead to weight loss, but this may be due to the study design not including education on healthy eating choices as part of the mindfulness intervention.

Bottom Line
Mindful eating is an approach to eating that can complement any eating pattern. Research has shown that mindful eating can lead to greater psychological wellbeing, increased pleasure when eating, and body satisfaction. Combining behavioral strategies such as mindfulness training with nutrition knowledge can lead to healthful food choices that reduce the risk of chronic diseases, promote more enjoyable meal experiences, and support a healthy body image. More research is needed to examine whether mindful eating is an effective strategy for weight management.
Mindful eating in context of COVID-19
In the meantime, individuals may consider incorporating any number of mindful eating strategies in their daily lives alongside other important measures to help stay healthy during COVID-19 . For example:
- If you’re working from home and find that “office” time blends into all hours of the day, schedule times in your calendar to only eat : a lunch break away from your computer, a reserved time for dinner with your family, etc.
- If you find yourself standing in your pantry or staring in your refrigerator, pause and ask yourself: “am I truly hungry, or am I just bored or stressed?” If hungry, eat. If boredom or stress is the source, reroute your attention to an activity you enjoy, call a friend, or simply spend some time breathing.
- If you have a craving for comfort foods, pause and take a few in-breaths and out-breaths to be fully present with your craving. Take a portion of the food from the container (a handful of chips, a scoop of ice cream) and put it on a plate. Eat mindfully, savoring each bite.
A note about eating disorders : The COVID-19 pandemic may raise unique challenges for individuals with experience of eating disorders. [17] In the U.S., the National Eating Disorders Association has reported a significant increase in calls and messages for help as compared to a year ago. As noted, mindful eating is not intended to replace traditional treatments for severe clinical conditions such as eating disorders. If you or someone you know is struggling with an eating disorder, you can call the National Eating Disorders Association Helpline at 1-800-931-2237, or text “NEDA” to 741-741.
A note about food insecurity : Many individuals may be facing food shortages because of unemployment or other issues related to the pandemic. If you (or someone you know) are struggling to access enough food to keep yourself or your family healthy, there are several options to help. Learn more about navigating supplemental food resources .
- Healthy Weight
- The Best Diet: Quality Counts
- Diet Reviews
- Fung TT, Long MW, Hung P, Cheung LW. An expanded model for mindful eating for health promotion and sustainability: issues and challenges for dietetics practice. Journal of the Academy of Nutrition and Dietetics . 2016 Jul 1;116(7):1081-6.
- Hanh TN, Cheung L. Savor: Mindful Eating, Mindful Life . HarperCollins Publishers. 2010.
- Stanszus LS, Frank P, Geiger SM. Healthy eating and sustainable nutrition through mindfulness? Mixed method results of a controlled intervention study. Appetite . 2019 Oct 1;141:104325.
- Ogden J, Coop N, Cousins C, Crump R, Field L, Hughes S, Woodger N. Distraction, the desire to eat and food intake. Towards an expanded model of mindless eating. Appetite . 2013 Mar 1;62:119-26.
- Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eating behaviors . 2014 Apr 1;15(2):197-204.
- O’Reilly GA, Cook L, Spruijt‐Metz D, Black DS. Mindfulness‐based interventions for obesity‐related eating behaviours: a literature review. Obesity reviews . 2014 Jun;15(6):453-61.
- Ruffault A, Czernichow S, Hagger MS, Ferrand M, Erichot N, Carette C, Boujut E, Flahault C. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obesity research & clinical practice . 2017 Sep 1;11(5):90-111.
- Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutrition research reviews . 2017 Dec;30(2):272-83. *Disclosure: Study was funded by Mondelez International.
- Mason AE, Epel ES, Kristeller J, Moran PJ, Dallman M, Lustig RH, Acree M, Bacchetti P, Laraia BA, Hecht FM, Daubenmier J. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the SHINE randomized controlled trial. Journal of behavioral medicine . 2016 Apr 1;39(2):201-13.
- Daubenmier J, Moran PJ, Kristeller J, Acree M, Bacchetti P, Kemeny ME, Dallman M, Lustig RH, Grunfeld C, Nixon DF, Milush JM. Effects of a mindfulness‐based weight loss intervention in adults with obesity: A randomized clinical trial. Obesity . 2016 Apr;24(4):794-804.
- Miller CK, Kristeller JL, Headings A, Nagaraja H. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a randomized controlled trial. Health Education & Behavior . 2014 Apr;41(2):145-54.
- Omiwole M, Richardson C, Huniewicz P, Dettmer E, Paslakis G. Review of mindfulness-related interventions to modify eating behaviors in adolescents. Nutrients . 2019 Dec;11(12):2917.
- Wylie A, Pierson S, Goto K, Giampaoli J. Evaluation of a mindful eating intervention curriculum among elementary school children and their parents. Journal of nutrition education and behavior . 2018 Feb 1;50(2):206-8.
- Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite . 2009 Apr 1;52(2):396-404.
- Bhutani S, Cooper JA. COVID‐19 related home confinement in adults: weight gain risks and opportunities. Obesity . 2020 May 19.
- Clemmensen C, Petersen MB, Sørensen TI. Will the COVID-19 pandemic worsen the obesity epidemic?. Nature Reviews Endocrinology . 2020 Sep;16(9):469-70.
- Branley-Bell D, Talbot CV. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. Journal of Eating Disorders . 2-2020 Aug;8(44).
Last reviewed September 2020
Terms of Use
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Lee KM, Bosold A, Alvarez C, et al.; Mathematica. Surging the Public Health Workforce: Lessons Learned from the COVID-19 Response at State, Tribal, Local, and Territorial Public Health Agencies: ASPE Report [Internet]. Washington (DC): Office of the Assistant Secretary for Planning and Evaluation (ASPE); 2023 Sep.

Surging the Public Health Workforce: Lessons Learned from the COVID-19 Response at State, Tribal, Local, and Territorial Public Health Agencies: ASPE Report [Internet].
Appendix a research questions.
- What was the baseline status (numbers, roles, competencies) of the STLT public health workforce before the pandemic? What were the gaps?
- What was the status of the public health workforce during the peak of the pandemic? How many new staff were engaged, and of what type? To what extent were staff reassigned from their existing roles to roles within the COVID-19 response (either part or full-time)?
- Which were most effective and efficient?
- What barriers to hiring did these mechanisms help overcome, and how?
- Which strategies were most suitable for specific types of staff?
- Why were certain mechanisms more effective in certain jurisdictions?
- Were there any pipeline strategies already in place that were able to deliver new staff? Were there any pipeline strategies newly put into place during the COVID-19 response that were able to deliver new staff?
- Were any forecasting or workforce models or surge planning handbooks used and how were they helpful, if at all? What data were used to inform hiring decisions? How did the lack of robust data hinder effective hiring?
- What are the lessons learned from staffing during the COVID-19 pandemic that will inform (1) federal and state or local strategies for effective use of current investments in the public health workforce and (2) planning for workforce surge for future pandemics? Specifically, what resources (such as toolkits, planning guides, and models), programs, and partnerships can the U.S. government provide that will support state and local preparedness for a future pandemic and staffing surges during a pandemic?
- Cite this Page Lee KM, Bosold A, Alvarez C, et al.; Mathematica. Surging the Public Health Workforce: Lessons Learned from the COVID-19 Response at State, Tribal, Local, and Territorial Public Health Agencies: ASPE Report [Internet]. Washington (DC): Office of the Assistant Secretary for Planning and Evaluation (ASPE); 2023 Sep. Appendix A, Research Questions.
- PDF version of this title (788K)
Other titles in this collection
- HHS ASPE Reports
Recent Activity
- Research Questions - Surging the Public Health Workforce: Lessons Learned from t... Research Questions - Surging the Public Health Workforce: Lessons Learned from the COVID-19 Response at State, Tribal, Local, and Territorial Public Health Agencies
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
National Cancer Institute - Cancer.gov
Postdoctoral Fellow - endocrine, cancer research
Job description.
Come join our friendly, collaborative group and help us improve treatments for patients with endocrine cancers!
A Postdoctoral position is available beginning in mid-to-late summer in the Surgical Oncology Program, CCR, NCI. Our group, the Laboratory of Neuro-Endocrine Cancer Diagnostics and Therapy is seeking a motivated Postdoctoral fellow interested in working at the interface of the application of novel therapeutic development and primary model development. Our laboratory program is dedicated to studying the behavior and growth of aggressive endocrine cancer and identifying novel and effective targeted therapies for personalized treatment of metastatic endocrine cancers.
Applicants will gain experience in protein signaling, cancer cell genome modification, single-cell cancer genomics, cell and molecular assays, and preclinical drug development. One particular group of endocrine cancers, gastroenteropancreatic neuroendocrine tumors (GEP-NETs), have limited models available despite an increasing public health burden. These models are limited to only the most aggressive cancer phenotypes, which limits our ability to treat tumors early enough to provide benefit to patients. New models can be derived from patient tissues, and our early work has shown promise in the development of several new study systems including cell lines, organoids, and patient derived xenografts. Some of our current therapeutic work has involved SSTR2 expression modification using epigenetic modifying therapeutics. By changing the expression of SSTR2, the opportunity to treat patients with more aggressive cancers is improved, providing a safer and more effective alternative to toxic chemotherapy regimens. We are currently using advanced analyses including cell line therapeutic sensitivity screening, bioinformatic based single-cell “multiomic” interrogation, functional genomic CRISPR inhibition and activation screens and genetic modeling of primary tumors to further explore new therapeutic targets. Fellows would be exposed to all areas of current research in the lab and multiple projects and techniques would be available to explore.
Endocrine Oncology at NIH encompasses unique patient cohorts of rare endocrine cancers, and our multi-disciplinary program has the capacity to translate preclinical findings into clinical trials, with the purpose of improving patient outcomes.
Training opportunities are augmented by collaborations with colleagues and physicians from the intramural and extramural communities. Fellows are encouraged to take advantage of formal, focused courses (e.g., training in bioinformatics and translational research), actively engage and participate in a variety of activities such as journal clubs within the Surgical Oncology Branch.
Qualifications and Job Details
Required and preferred skills.
- Candidates must have a PhD and/or MD degree or equivalent that includes training in molecular biology, cell biology, bioinformatics, or biochemistry, with laboratory experience.
- Strong background in genetics/genomics, bioinformatic analysis, tissue culture, and molecular biological techniques (e.g., cloning, western blot, qPCR, protein expression/purification).
- Excellent written and verbal communication, organizational, and time management skills are preferred, and with an ability to work independently as well as collaborate as a valued team member.
This position is subject to a background investigation.
- Some experience with R or another coding language preferred, but not required.
About the NCI Center for Cancer Research
The Center for Cancer Research (CCR) is home to nearly 250 basic and clinical research groups located on two campuses just outside of Washington, D.C. CCR is part of the National Cancer Institute (NCI) and makes up the largest component of the research effort at the National Institutes of Health (NIH). Centrally supported by long-term funding and a culture of complete intellectual freedom, CCR scientists are able to pursue the most important and challenging problems in cancer research. We collaborate with academic and commercial partners and advocacy groups across the world in efforts to prevent, diagnose and treat cancer and HIV/AIDS. The CCR research portfolio covers the full spectrum of biological and biomedical research. Our work ranges from basic to translational and clinical, and our clinical trials are conducted in the NIH Clinical Center, the world’s largest hospital dedicated to clinical research that offers a robust infrastructure to support CCR’s patients on an estimated 250 open studies. The success of CCR is grounded in an exceptionally strong discovery research program that provides the foundation for the seamless translation of insights from bench to bedside. Read more about CCR , the benefits of working at CCR and hear from our staff on their CCR experiences.
Bethesda is one of the most highly educated communities in the United States and has a nationally renowned school system. The city is a thriving suburban center close to Washington, D.C., and home to many restaurants, retailers and a flourishing arts and entertainment district.
- Statement of Research Goals
- 3 References
- Cover Letter
Please send your personal statement, CV/Resume, statement of research goals, and 3 letters of reference to Ms. Anna Coxen at [email protected] and Dr. Samira Sadowski at [email protected].
You may also like
Postdoctoral fellow - pericytes, metastatic microenvironment, postdoctoral fellow - dna damage, dna repair, postdoctoral fellow - immunology, developmental biology.

IMAGES
VIDEO
COMMENTS
public health agency, academic institution, community-based organization, health system, or other setting, these competencies apply to professionals who practice, teach, and research public health. Specific knowledge and skills related to these competency statements differ based on the responsibilities of an individual within an organization.
Developed by the Council on Linkages Between Academia and Public Health Practice (Council on Linkages), the Core Competencies reflect foundational skills desirable for professionals engaging in the practice, education, and research of public health. The Core Competencies support workforce development within public health and can serve as a ...
People entering the public health research field can expect rewarding work. The job outlook for these positions is promising. According to the U.S. Bureau of Labor Statistics (BLS), the number of public health research positions is projected to grow 8 percent by 2028. The median public health researcher salary was $88,790 in May 2019.
The Core Competencies for Public Health Professionals (Core Competencies) are a framework for workforce development planning and action. The Core Competencies are defined as "a consensus set of knowledge and skills for the broad practice of public health, defined by the 10 Essential Public Health Services."They can serve as a starting point for public health professionals and organizations ...
Public Health Core Competencies. September 14, 2020. Public health professionals focus on making the lives of other people and their communities better. They concern themselves with many factors that play a role in the health of humans, such as the environment, public policy, health care and laws. If you are interested in taking on a public ...
The Core Competencies for Public Health Professionals (Core Competencies) are organized into eight domains representing skill areas within public health. Each domain contains between 4 and 13 competency statements. In addition, the Core Competencies include three tiers, which describe different types of responsibilities within public health ...
The Core Competencies for Public Health Professionals (Core Competencies) are a consensus set of knowledge and skills for the broad practice of public health, as defined by the 10 Essential Public Health Services.Developed by the Council on Linkages Between Academia and Public Health Practice (Council on Linkages), the Core Competencies reflect foundational or crosscutting knowledge and skills ...
Collect and manage your data. 5. Analyze and interpret your data. 6. Write and present your report. 7. Disseminate and apply your results. Research skills are essential for public health ...
The Council on Linkages Between Academia and Public Health Practice has developed the Core Competencies for Public Health Professionals, which are used by hundreds of health departments across the U.S. The core competencies are organized into 8 domains representing skill areas within public health: Data Analytics & Assessment Skills
Competencies ensure public health students and professionals have the necessary knowledge, skills, values, and behaviours to do their jobs effectively. Public health is a dynamic and complex field requiring robust competency statements and frameworks that are regularly renewed. Many countries have public health competencies, but there has been no evidence synthesis on how these are developed.
Overview. This comprehensive guide to health research reaches out to a wide spectrum of people: students who wish to learn the basic principles of health research and how to conduct it, field researchers, and those involved in teaching and training of health research methodologies. It seeks to develop practical skills, starting with defining ...
A public health researcher is responsible for conducting surveys and analyzing data and lab results in order to gain a better perspective of a population's health. They uncover trends, risks, and other factors, such as whether biology, behavior, society, or the environment play a role in a population's health.
Training for public health professionals in omics, data science, environmental health, and professional development. Open to researchers at all career levels and from any organization. Skills for Health and Research Professionals (SHARP) Training | Columbia University Mailman School of Public Health
Role of public health in overall health system. 4. Cultural Competency. Cultural Competency Skills focus on understanding and responding to diverse needs, assessing organizational cultural diversity and competence, assessing effects of policies and programs on different populations, and taking action to support a diverse public health workforce.*.
This course is part of Qualitative Research Design and Methods for Public Health Specialization. Taught in English. 21 languages available ... It outlines a step-by-step approach to qualitative research design that begins by identifying a public health topic of interest, works to hone in on a specific research problem, and then specifies ...
In a recent study on essential skills for using research evidence in public health policy, Ziam et al. (2021) identified only three empirical studies that used the ACAP model in the health field ...
According to a Lightcast report, there's been a considerable shift in the list of required skills for public health program managers. Skills like program management, communications, leadership, and research have increased by over 100 percent. Even more impressive is the increase in skills like program development, advocacy, and marketing ...
Introduction. Public health is critical to a healthy, fair, and sustainable society. Public health's role in this vision stems from its foundational values of social justice and collectivity (Rutty and Sullivan 2010) and—we argue—from its position at the interface of research, practice, and policy.. Realizing this vision requires imagining a public health community that can maintain that ...
Skill 5Strategic Thinking. Strategic thinking involves knowing your goals and creating a plan for achieving them. This mindset is essential for public health coursework like health services administration, which involves program planning and evaluation, quality control, and much more.
The Core Competencies for Public Health Professionals (Core Competencies) are a consensus set of knowledge and skills for the broad practice of public health, as defined by the 10 Essential Public Health Services. Developed by the Council on Linkages Between Academia and Public Health Practice (Council on Linkages), the Core Competencies ...
1. Research and Analytical Skills. In the public health profession, you will be expected to draw on your abilities to conduct thorough and sound research. Even more, you will need to possess analytical skills to interpret your research and turn it into action! You see, methodology is not enough in an advanced public health career.
Methods. Since 2015, faculty and staff from a midwestern College of Public Health have conducted a cross-sectional assessment of the education and training needs of local public health departments in following the principles of practice-based systems research [].The Institutional Review Board considers the assessments to be a quality improvement activity and not human subjects research ...
Better alignment between academia and public health practice and policies are critical to improve public health actions. Training of future researchers to address complex issues and to conduct transdisciplinary and collaborative research will help improve this alignment. In this paper, we describe the role of internship placements and mentorship for trainees' skills development in population ...
A focus on consequential health threats and risks should be met with a parallel emphasis on measurement, metrics and methods, including assessment of costs. These are knowledge and skill areas that students should master and practice. If students are to be prepared to engage in public health scholarship of consequence, they must see faculty ...
Background Research evidence is needed to strengthen capacities in emergency preparedness and response (EPR). However, the absence of a clear research agenda limits the optimal use of research evidence. This paper reports on the prioritization of research questions and topics that could contribute to evidence-informed strengthening of EPR capacities in the African region. Methods The priority ...
AP Seminar and AP Research students to submit performance tasks as final and their presentations to be scored by their AP Seminar or AP Research teachers. AP Computer Science Principles students to submit their Create performance task as final. Late Testing . Occasionally, circumstances make it necessary for students to test late.
Ruffault A, Czernichow S, Hagger MS, Ferrand M, Erichot N, Carette C, Boujut E, Flahault C. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obesity research & clinical practice. 2017 Sep 1;11(5):90-111. Warren JM, Smith N, Ashwell M.
This study addressed the following research questions: What was the baseline status (numbers, roles, competencies) of the STLT public health workforce before the pandemic? What were the gaps?What was the status of the public health workforce during the peak of the pandemic? How many new staff were engaged, and of what type? To what extent were staff reassigned from their existing roles to ...
About the NCI Center for Cancer Research. The Center for Cancer Research (CCR) is home to nearly 250 basic and clinical research groups located on two campuses just outside of Washington, D.C. CCR is part of the National Cancer Institute (NCI) and makes up the largest component of the research effort at the National Institutes of Health (NIH).
Sonila Dubare. Sonila Dubare, a third-year Ph.D. student in the department of epidemiology, recently delivered a guest lecture on "Machine Learning Applications in Clinical Settings" at The Military Medical Center in Guatemala.She presented with M.D. residents and fourth-year medical students of Mariano Gálvez University of Guatemala.